User login
IMDC model mirrors mRCC clinical outcomes
In hindsight, a widely used prognostic model for patients with metastatic renal cell carcinoma (mRCC) has been shown to be effective at stratifying patient risk, and may inform the design of future clinical trials.
By retrospectively comparing clinical outcomes with risk categories determined by the International Metastatic Renal Cell Carcinoma Database Consortium (IMDC) model, Brian I Rini, MD, of the Cleveland Clinic, and his colleagues found notable differences in progression-free survival, overall survival, and objective response rates between the different risk categories among patients with mRCC treated with sunitinib (Sutent) in a major clinical trial.
“These benchmark values can aid current and future design and interpretation of clinical trials in mRCC. Results of this analysis demonstrate clear differences in patient outcomes based on IMDC prognostic risk group,” they wrote. The report was published in Clinical Genitourinary Cancer.
They also found that the Memorial Sloan Kettering Cancer Center (MSKCC) model appeared to be similar in prognostic utility to the IMDC model, and that either model could be useful for counseling patients about prognosis and treatment options.
They based their conclusions on an analysis of data from a phase 3 clinical trial comparing sunitinib with interferon alfa in patients with mRCC. Patients in this study were grouped according to prognostic risk category by the MSKCC criteria, which overlap with the IMDC criteria in five of six areas.
In the current study, Dr. Rini and his associates applied the IMDC criteria to the same population, and derived benchmark values for outcomes by IMDC risk groups based on radiologic tumor progression measurements performed by independent reviewers on images of patients in the intention-to-treat population.
They also conducted an analysis of data from investigator measurements of tumor progression, and compared the results with the independently reviewed radiologic data for patients outcomes according to the MSKCC model.
They found that for sunitinib-treated patients in the IMDC favorable-risk group, median PFS was 14.1 months, compared with 10.7 months for those in the intermediate-risk group, 2,4 months in the poor-risk group, and 10.6 months for the combined intermediate and poor-risk groups.
The respective objective response rates were 53%, 33.7%, 11.8%, and 30.5%.
Median overall survival for favorable-risk patients was not reached, with more than 50% of patients alive at the time of data cutoff. The respective median overall survival for the intermediate-, poor-, and intermediate-plus-poor–risk groups were 23, 5.1, and 20.3 months.
“Results of this study suggest there may be significant prognostic differences between the intermediate-1 and intermediate-2 IMDC risk groups and that this should be considered when counseling patients identified to be in one of these groups,” the investigators wrote.
Medical writing for the study was supported by Pfizer. Dr. Rini and his coauthors disclosed research funding and/or consulting fees from Pfizer and other companies. Four of the coauthors are Pfizer employees and stockholders.
SOURCE: Rini B et al. Clin Genitourin Cancer. 2018 May 3. doi: 10.1016/j.clgc.2018.04.005.
In hindsight, a widely used prognostic model for patients with metastatic renal cell carcinoma (mRCC) has been shown to be effective at stratifying patient risk, and may inform the design of future clinical trials.
By retrospectively comparing clinical outcomes with risk categories determined by the International Metastatic Renal Cell Carcinoma Database Consortium (IMDC) model, Brian I Rini, MD, of the Cleveland Clinic, and his colleagues found notable differences in progression-free survival, overall survival, and objective response rates between the different risk categories among patients with mRCC treated with sunitinib (Sutent) in a major clinical trial.
“These benchmark values can aid current and future design and interpretation of clinical trials in mRCC. Results of this analysis demonstrate clear differences in patient outcomes based on IMDC prognostic risk group,” they wrote. The report was published in Clinical Genitourinary Cancer.
They also found that the Memorial Sloan Kettering Cancer Center (MSKCC) model appeared to be similar in prognostic utility to the IMDC model, and that either model could be useful for counseling patients about prognosis and treatment options.
They based their conclusions on an analysis of data from a phase 3 clinical trial comparing sunitinib with interferon alfa in patients with mRCC. Patients in this study were grouped according to prognostic risk category by the MSKCC criteria, which overlap with the IMDC criteria in five of six areas.
In the current study, Dr. Rini and his associates applied the IMDC criteria to the same population, and derived benchmark values for outcomes by IMDC risk groups based on radiologic tumor progression measurements performed by independent reviewers on images of patients in the intention-to-treat population.
They also conducted an analysis of data from investigator measurements of tumor progression, and compared the results with the independently reviewed radiologic data for patients outcomes according to the MSKCC model.
They found that for sunitinib-treated patients in the IMDC favorable-risk group, median PFS was 14.1 months, compared with 10.7 months for those in the intermediate-risk group, 2,4 months in the poor-risk group, and 10.6 months for the combined intermediate and poor-risk groups.
The respective objective response rates were 53%, 33.7%, 11.8%, and 30.5%.
Median overall survival for favorable-risk patients was not reached, with more than 50% of patients alive at the time of data cutoff. The respective median overall survival for the intermediate-, poor-, and intermediate-plus-poor–risk groups were 23, 5.1, and 20.3 months.
“Results of this study suggest there may be significant prognostic differences between the intermediate-1 and intermediate-2 IMDC risk groups and that this should be considered when counseling patients identified to be in one of these groups,” the investigators wrote.
Medical writing for the study was supported by Pfizer. Dr. Rini and his coauthors disclosed research funding and/or consulting fees from Pfizer and other companies. Four of the coauthors are Pfizer employees and stockholders.
SOURCE: Rini B et al. Clin Genitourin Cancer. 2018 May 3. doi: 10.1016/j.clgc.2018.04.005.
In hindsight, a widely used prognostic model for patients with metastatic renal cell carcinoma (mRCC) has been shown to be effective at stratifying patient risk, and may inform the design of future clinical trials.
By retrospectively comparing clinical outcomes with risk categories determined by the International Metastatic Renal Cell Carcinoma Database Consortium (IMDC) model, Brian I Rini, MD, of the Cleveland Clinic, and his colleagues found notable differences in progression-free survival, overall survival, and objective response rates between the different risk categories among patients with mRCC treated with sunitinib (Sutent) in a major clinical trial.
“These benchmark values can aid current and future design and interpretation of clinical trials in mRCC. Results of this analysis demonstrate clear differences in patient outcomes based on IMDC prognostic risk group,” they wrote. The report was published in Clinical Genitourinary Cancer.
They also found that the Memorial Sloan Kettering Cancer Center (MSKCC) model appeared to be similar in prognostic utility to the IMDC model, and that either model could be useful for counseling patients about prognosis and treatment options.
They based their conclusions on an analysis of data from a phase 3 clinical trial comparing sunitinib with interferon alfa in patients with mRCC. Patients in this study were grouped according to prognostic risk category by the MSKCC criteria, which overlap with the IMDC criteria in five of six areas.
In the current study, Dr. Rini and his associates applied the IMDC criteria to the same population, and derived benchmark values for outcomes by IMDC risk groups based on radiologic tumor progression measurements performed by independent reviewers on images of patients in the intention-to-treat population.
They also conducted an analysis of data from investigator measurements of tumor progression, and compared the results with the independently reviewed radiologic data for patients outcomes according to the MSKCC model.
They found that for sunitinib-treated patients in the IMDC favorable-risk group, median PFS was 14.1 months, compared with 10.7 months for those in the intermediate-risk group, 2,4 months in the poor-risk group, and 10.6 months for the combined intermediate and poor-risk groups.
The respective objective response rates were 53%, 33.7%, 11.8%, and 30.5%.
Median overall survival for favorable-risk patients was not reached, with more than 50% of patients alive at the time of data cutoff. The respective median overall survival for the intermediate-, poor-, and intermediate-plus-poor–risk groups were 23, 5.1, and 20.3 months.
“Results of this study suggest there may be significant prognostic differences between the intermediate-1 and intermediate-2 IMDC risk groups and that this should be considered when counseling patients identified to be in one of these groups,” the investigators wrote.
Medical writing for the study was supported by Pfizer. Dr. Rini and his coauthors disclosed research funding and/or consulting fees from Pfizer and other companies. Four of the coauthors are Pfizer employees and stockholders.
SOURCE: Rini B et al. Clin Genitourin Cancer. 2018 May 3. doi: 10.1016/j.clgc.2018.04.005.
FROM CLINICAL GENITOURINARY CANCER
Key clinical point: The IMDC model is prognostic for responses and survival in patients with mRCC treated with sunitinib.
Major finding: Median progression-free survival for favorable, intermediate, and poor-risk patients was 14.1, 10.7, and 2.4 months, respectively.
Study details: Retrospective analysis of 375 sunitinib-treated patients in a randomized clinical trial.
Disclosures: Medical writing for the study was supported by Pfizer. Dr. Rini and his coauthors disclosed research funding and/or consulting fees from Pfizer and other companies. Four of the coauthors are Pfizer employees and stockholders.
Source: Rini B et al. Clin Genitourin Cancer. 2018 May 3. doi: 10.1016/j.clgc.2018.04.005.
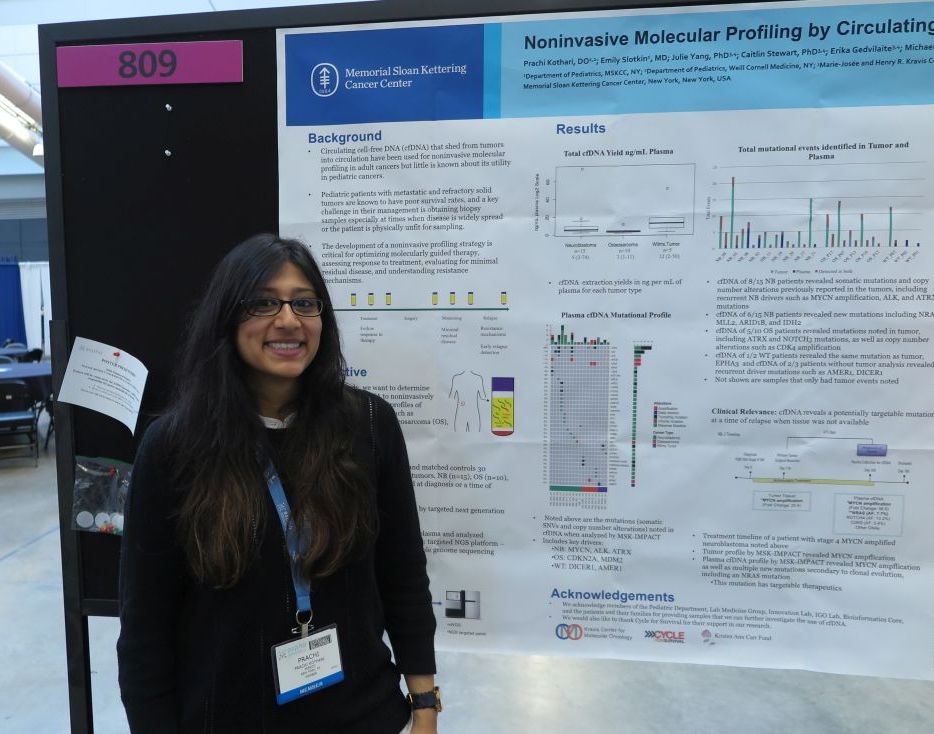
cfDNA reveals targetable mutations in pediatric neuroblastoma, sarcoma
PITTSBURGH – Genetic analysis of circulating free DNA (cfDNA) from pediatric solid tumors can noninvasively identify somatic mutations and copy number alterations that could be used to identify therapeutic targets, investigators reported.
An analysis of tumor specimens and plasma samples from children with neuroblastoma, osteosarcoma, and Wilms tumor revealed in cfDNA both somatic mutations and copy number alterations that had already been detected in the solid tumors, and new, potentially targetable mutations, reported Prachi Kothari, DO, and her colleagues from Memorial Sloan Kettering Cancer Center in New York.
“Circulating free DNA is much less invasive than a tumor biopsy, and you can do it throughout the patient’s entire timeline of treatment, so you get real-time information or after they relapse to see what’s going on if you’re not able to get a tumor biopsy,” Dr. Kothari said at annual meeting of the American Society of Pediatric Hematology/Oncology.
So-called “liquid biopsy” using cfDNA has been used for molecular profiling of adults malignancies, but there are few data on its use in pediatric tumors, Dr. Kothari said.
To see whether the technique could provide useful clinical information for the management of pediatric tumors, the investigators examined tumor samples taken at diagnosis or at the time of disease progression from 15 patients with neuroblastoma, 10 with osteosarcoma, and 5 with Wilms tumor. They analyzed the tumor samples using targeted next-generation sequencing (NGS), and cfDNA using three different genomic analysis techniques, including NGS, MSK-IMPACT (Integrated Mutation Profiling of Actionable Cancer Targets), and shallow whole genome sequencing.
For each of the tumor types studies, cfDNA analysis with the MSK-IMPACT platform identified key drivers of malignancy, including MYCN, ALK, and ATRX in neuroblastoma; CDKN2A and MDM2 in osteosarcoma; and DICER1 and AMER1 in Wilms tumor.
The cfDNA samples also revealed somatic mutations and copy number alterations previously reported in the tumors of 8 of the 15 patients with neuroblastoma, as well as potentially targetable new mutations in 6 of the 15 patients, including NRAS, MLL2, ARID1B, and IDH2.
For example, in one patient with stage 4 MYCN-amplified neuroblastoma, both tumor analysis and cfDNA revealed MYCN amplification, but cfDNA also show multiple new mutations, including a targetable NRAS mutation, secondary to clonal mutation.
In 5 of the 10 patients with osteosarcoma, cfDNA detected mutations that had been seen in the tumor samples, including mutations in ATRX and NOTCH3, and copy number alterations such as CDK4 amplification,
Of the five patients with Wilms tumors, cfDNA analysis was performed on two samples, one of which showed the same mutation as the tumor. Additionally, for the three patients without tumor analysis, cfDNA showed recurrent driver mutations such as AMER1 and DICER1.
The investigators have used the data from this study to create a genome-wide z score derived from shallow whole genome sequencing profiles and cfDNA, and found that a high genomewide z score, compared with a low score was significantly associated a more than four-fold greater risk for worse survival (hazard ratio, 4.42; P = .049).
“Establishing a platform using cfDNA to identify molecular profiles of these tumors can serve as a powerful tool for guiding treatment and monitoring response to treatment,” the investigators concluded.
The study was supported by Cycle for Survival and the Kristen Ann Carr Fund. The investigators reported having no conflicts of interest.
SOURCE: Kothari P et al. ASPHO 2018. Abstract #809.
PITTSBURGH – Genetic analysis of circulating free DNA (cfDNA) from pediatric solid tumors can noninvasively identify somatic mutations and copy number alterations that could be used to identify therapeutic targets, investigators reported.
An analysis of tumor specimens and plasma samples from children with neuroblastoma, osteosarcoma, and Wilms tumor revealed in cfDNA both somatic mutations and copy number alterations that had already been detected in the solid tumors, and new, potentially targetable mutations, reported Prachi Kothari, DO, and her colleagues from Memorial Sloan Kettering Cancer Center in New York.
“Circulating free DNA is much less invasive than a tumor biopsy, and you can do it throughout the patient’s entire timeline of treatment, so you get real-time information or after they relapse to see what’s going on if you’re not able to get a tumor biopsy,” Dr. Kothari said at annual meeting of the American Society of Pediatric Hematology/Oncology.
So-called “liquid biopsy” using cfDNA has been used for molecular profiling of adults malignancies, but there are few data on its use in pediatric tumors, Dr. Kothari said.
To see whether the technique could provide useful clinical information for the management of pediatric tumors, the investigators examined tumor samples taken at diagnosis or at the time of disease progression from 15 patients with neuroblastoma, 10 with osteosarcoma, and 5 with Wilms tumor. They analyzed the tumor samples using targeted next-generation sequencing (NGS), and cfDNA using three different genomic analysis techniques, including NGS, MSK-IMPACT (Integrated Mutation Profiling of Actionable Cancer Targets), and shallow whole genome sequencing.
For each of the tumor types studies, cfDNA analysis with the MSK-IMPACT platform identified key drivers of malignancy, including MYCN, ALK, and ATRX in neuroblastoma; CDKN2A and MDM2 in osteosarcoma; and DICER1 and AMER1 in Wilms tumor.
The cfDNA samples also revealed somatic mutations and copy number alterations previously reported in the tumors of 8 of the 15 patients with neuroblastoma, as well as potentially targetable new mutations in 6 of the 15 patients, including NRAS, MLL2, ARID1B, and IDH2.
For example, in one patient with stage 4 MYCN-amplified neuroblastoma, both tumor analysis and cfDNA revealed MYCN amplification, but cfDNA also show multiple new mutations, including a targetable NRAS mutation, secondary to clonal mutation.
In 5 of the 10 patients with osteosarcoma, cfDNA detected mutations that had been seen in the tumor samples, including mutations in ATRX and NOTCH3, and copy number alterations such as CDK4 amplification,
Of the five patients with Wilms tumors, cfDNA analysis was performed on two samples, one of which showed the same mutation as the tumor. Additionally, for the three patients without tumor analysis, cfDNA showed recurrent driver mutations such as AMER1 and DICER1.
The investigators have used the data from this study to create a genome-wide z score derived from shallow whole genome sequencing profiles and cfDNA, and found that a high genomewide z score, compared with a low score was significantly associated a more than four-fold greater risk for worse survival (hazard ratio, 4.42; P = .049).
“Establishing a platform using cfDNA to identify molecular profiles of these tumors can serve as a powerful tool for guiding treatment and monitoring response to treatment,” the investigators concluded.
The study was supported by Cycle for Survival and the Kristen Ann Carr Fund. The investigators reported having no conflicts of interest.
SOURCE: Kothari P et al. ASPHO 2018. Abstract #809.
PITTSBURGH – Genetic analysis of circulating free DNA (cfDNA) from pediatric solid tumors can noninvasively identify somatic mutations and copy number alterations that could be used to identify therapeutic targets, investigators reported.
An analysis of tumor specimens and plasma samples from children with neuroblastoma, osteosarcoma, and Wilms tumor revealed in cfDNA both somatic mutations and copy number alterations that had already been detected in the solid tumors, and new, potentially targetable mutations, reported Prachi Kothari, DO, and her colleagues from Memorial Sloan Kettering Cancer Center in New York.
“Circulating free DNA is much less invasive than a tumor biopsy, and you can do it throughout the patient’s entire timeline of treatment, so you get real-time information or after they relapse to see what’s going on if you’re not able to get a tumor biopsy,” Dr. Kothari said at annual meeting of the American Society of Pediatric Hematology/Oncology.
So-called “liquid biopsy” using cfDNA has been used for molecular profiling of adults malignancies, but there are few data on its use in pediatric tumors, Dr. Kothari said.
To see whether the technique could provide useful clinical information for the management of pediatric tumors, the investigators examined tumor samples taken at diagnosis or at the time of disease progression from 15 patients with neuroblastoma, 10 with osteosarcoma, and 5 with Wilms tumor. They analyzed the tumor samples using targeted next-generation sequencing (NGS), and cfDNA using three different genomic analysis techniques, including NGS, MSK-IMPACT (Integrated Mutation Profiling of Actionable Cancer Targets), and shallow whole genome sequencing.
For each of the tumor types studies, cfDNA analysis with the MSK-IMPACT platform identified key drivers of malignancy, including MYCN, ALK, and ATRX in neuroblastoma; CDKN2A and MDM2 in osteosarcoma; and DICER1 and AMER1 in Wilms tumor.
The cfDNA samples also revealed somatic mutations and copy number alterations previously reported in the tumors of 8 of the 15 patients with neuroblastoma, as well as potentially targetable new mutations in 6 of the 15 patients, including NRAS, MLL2, ARID1B, and IDH2.
For example, in one patient with stage 4 MYCN-amplified neuroblastoma, both tumor analysis and cfDNA revealed MYCN amplification, but cfDNA also show multiple new mutations, including a targetable NRAS mutation, secondary to clonal mutation.
In 5 of the 10 patients with osteosarcoma, cfDNA detected mutations that had been seen in the tumor samples, including mutations in ATRX and NOTCH3, and copy number alterations such as CDK4 amplification,
Of the five patients with Wilms tumors, cfDNA analysis was performed on two samples, one of which showed the same mutation as the tumor. Additionally, for the three patients without tumor analysis, cfDNA showed recurrent driver mutations such as AMER1 and DICER1.
The investigators have used the data from this study to create a genome-wide z score derived from shallow whole genome sequencing profiles and cfDNA, and found that a high genomewide z score, compared with a low score was significantly associated a more than four-fold greater risk for worse survival (hazard ratio, 4.42; P = .049).
“Establishing a platform using cfDNA to identify molecular profiles of these tumors can serve as a powerful tool for guiding treatment and monitoring response to treatment,” the investigators concluded.
The study was supported by Cycle for Survival and the Kristen Ann Carr Fund. The investigators reported having no conflicts of interest.
SOURCE: Kothari P et al. ASPHO 2018. Abstract #809.
REPORTING FROM ASPHO 2018
Key clinical point: Circulating free DNA analysis is a noninvasive method for detecting potential therapeutic targets.
Major finding: cfDNA revealed potentially targetable new mutations in 6 of 15 patients with neuroblastoma.
Study details: Retrospective analysis of tumor and plasma samples in 30 patients with neuroblastoma, osteosarcoma, or Wilms tumor.
Disclosures: The study was supported by Cycle for Survival and the Kristen Ann Carr Fund. The investigators reported having no conflicts of interest.
Source: Kothari P et al. ASPHO 2018. Abstract #809.
Pediatric cancers are on the rise
PITTSBURGH – The incidence of many pediatric cancers are on the rise, and the increase is occurring in nearly all demographic groups studied, according to the latest data from the U.S. Centers for Disease Control and Prevention.
Pediatric cancers that increased significantly in incidence from 2001 through 2014, compared with previous time periods, include thyroid carcinoma, hepatic tumors, lymphomas, renal tumors, and brain tumors. Other cancer types remained unchanged, except malignant melanoma, which saw a significant decline in incidence over the same period, reported David A. Siegel, MD, of the Epidemic Intelligence Service at the CDC in Atlanta.
Recent studies of trends in pediatric cancer have either used data from before 2010 or covered less than a third of the U.S. population, the investigators noted.
To get a more accurate estimate of current trends, the investigators relied on the United States Cancer Statistics, which combines data from the Surveillance, Epidemiology, and End Results (SEER) program and the National Program of Cancer Registries. Together, the combined databases cover 100% of the U.S. population.
Dr. Siegel and his colleagues looked at cancer incidence rates and trends among individuals younger than 20 years of age from across 48 states from 2001 to 2014 – Mississippi, Nevada, and the District of Columbia were not included.
They used a joinpoint regression method to calculate average annual percent change (AAPC) in rates, then stratified rates and trends by sex, age, and race/ethnicity; location; economic status; and cancer type.
During the 14-year period of the study, there were a total of 196,200 incident cases of pediatric cancer, for an overall cancer incidence rate of 173 per million. The pediatric cancer with the highest incident rate was leukemia of any type (45.6 per million), brain tumors (30.8), and lymphomas (26.0).
Incidence rates were highest among males, patients from infancy through age 4, non-Hispanic whites, children who live in the Northeast region, those who live in the wealthiest counties, and those who live in urban/metropolitan counties. The overall pediatric cancer incidence rate increased, with an AAPC of 0.7 (95% confidence interval, 0.5-0.8).
“Rates increased in each stratum of sex, age, and race/ethnicity (except non-Hispanic American Indian/Alaska Native), region, economic status, and rural/urban classification,” the investigators wrote.
Cancers with significantly increased AAPC included thyroid carcinomas (AAPC, 4.8), hepatic tumors (2.5), lymphomas (1.7), renal tumors (0.6), and brain tumors (all types, 0.4).
There were no significant changes in the incidence of either germ cell cancer, retinoblastoma, leukemia, neuroblastoma, soft-tissue sarcomas, or bone tumors.
The only significant decrease over the study period was in the incidence of melanoma in children (–2.6).
“Possible causes of increasing rates might include changes in diagnostic, coding, and reporting standards, increased detection, population-based changes (such as increasing obesity), and environmental exposures,” they wrote.
Public health campaigns about the dangers of UV exposure and promoting the use of sunscreens may account for the decline in the incidence of malignant melanoma, they suggested.
The study was supported by the CDC. Dr. Siegel and coauthors are CDC employees. They reported having no conflicts of interest.
SOURCE: Siegel DA et al. ASPHO 2018, Abstract 605.
PITTSBURGH – The incidence of many pediatric cancers are on the rise, and the increase is occurring in nearly all demographic groups studied, according to the latest data from the U.S. Centers for Disease Control and Prevention.
Pediatric cancers that increased significantly in incidence from 2001 through 2014, compared with previous time periods, include thyroid carcinoma, hepatic tumors, lymphomas, renal tumors, and brain tumors. Other cancer types remained unchanged, except malignant melanoma, which saw a significant decline in incidence over the same period, reported David A. Siegel, MD, of the Epidemic Intelligence Service at the CDC in Atlanta.
Recent studies of trends in pediatric cancer have either used data from before 2010 or covered less than a third of the U.S. population, the investigators noted.
To get a more accurate estimate of current trends, the investigators relied on the United States Cancer Statistics, which combines data from the Surveillance, Epidemiology, and End Results (SEER) program and the National Program of Cancer Registries. Together, the combined databases cover 100% of the U.S. population.
Dr. Siegel and his colleagues looked at cancer incidence rates and trends among individuals younger than 20 years of age from across 48 states from 2001 to 2014 – Mississippi, Nevada, and the District of Columbia were not included.
They used a joinpoint regression method to calculate average annual percent change (AAPC) in rates, then stratified rates and trends by sex, age, and race/ethnicity; location; economic status; and cancer type.
During the 14-year period of the study, there were a total of 196,200 incident cases of pediatric cancer, for an overall cancer incidence rate of 173 per million. The pediatric cancer with the highest incident rate was leukemia of any type (45.6 per million), brain tumors (30.8), and lymphomas (26.0).
Incidence rates were highest among males, patients from infancy through age 4, non-Hispanic whites, children who live in the Northeast region, those who live in the wealthiest counties, and those who live in urban/metropolitan counties. The overall pediatric cancer incidence rate increased, with an AAPC of 0.7 (95% confidence interval, 0.5-0.8).
“Rates increased in each stratum of sex, age, and race/ethnicity (except non-Hispanic American Indian/Alaska Native), region, economic status, and rural/urban classification,” the investigators wrote.
Cancers with significantly increased AAPC included thyroid carcinomas (AAPC, 4.8), hepatic tumors (2.5), lymphomas (1.7), renal tumors (0.6), and brain tumors (all types, 0.4).
There were no significant changes in the incidence of either germ cell cancer, retinoblastoma, leukemia, neuroblastoma, soft-tissue sarcomas, or bone tumors.
The only significant decrease over the study period was in the incidence of melanoma in children (–2.6).
“Possible causes of increasing rates might include changes in diagnostic, coding, and reporting standards, increased detection, population-based changes (such as increasing obesity), and environmental exposures,” they wrote.
Public health campaigns about the dangers of UV exposure and promoting the use of sunscreens may account for the decline in the incidence of malignant melanoma, they suggested.
The study was supported by the CDC. Dr. Siegel and coauthors are CDC employees. They reported having no conflicts of interest.
SOURCE: Siegel DA et al. ASPHO 2018, Abstract 605.
PITTSBURGH – The incidence of many pediatric cancers are on the rise, and the increase is occurring in nearly all demographic groups studied, according to the latest data from the U.S. Centers for Disease Control and Prevention.
Pediatric cancers that increased significantly in incidence from 2001 through 2014, compared with previous time periods, include thyroid carcinoma, hepatic tumors, lymphomas, renal tumors, and brain tumors. Other cancer types remained unchanged, except malignant melanoma, which saw a significant decline in incidence over the same period, reported David A. Siegel, MD, of the Epidemic Intelligence Service at the CDC in Atlanta.
Recent studies of trends in pediatric cancer have either used data from before 2010 or covered less than a third of the U.S. population, the investigators noted.
To get a more accurate estimate of current trends, the investigators relied on the United States Cancer Statistics, which combines data from the Surveillance, Epidemiology, and End Results (SEER) program and the National Program of Cancer Registries. Together, the combined databases cover 100% of the U.S. population.
Dr. Siegel and his colleagues looked at cancer incidence rates and trends among individuals younger than 20 years of age from across 48 states from 2001 to 2014 – Mississippi, Nevada, and the District of Columbia were not included.
They used a joinpoint regression method to calculate average annual percent change (AAPC) in rates, then stratified rates and trends by sex, age, and race/ethnicity; location; economic status; and cancer type.
During the 14-year period of the study, there were a total of 196,200 incident cases of pediatric cancer, for an overall cancer incidence rate of 173 per million. The pediatric cancer with the highest incident rate was leukemia of any type (45.6 per million), brain tumors (30.8), and lymphomas (26.0).
Incidence rates were highest among males, patients from infancy through age 4, non-Hispanic whites, children who live in the Northeast region, those who live in the wealthiest counties, and those who live in urban/metropolitan counties. The overall pediatric cancer incidence rate increased, with an AAPC of 0.7 (95% confidence interval, 0.5-0.8).
“Rates increased in each stratum of sex, age, and race/ethnicity (except non-Hispanic American Indian/Alaska Native), region, economic status, and rural/urban classification,” the investigators wrote.
Cancers with significantly increased AAPC included thyroid carcinomas (AAPC, 4.8), hepatic tumors (2.5), lymphomas (1.7), renal tumors (0.6), and brain tumors (all types, 0.4).
There were no significant changes in the incidence of either germ cell cancer, retinoblastoma, leukemia, neuroblastoma, soft-tissue sarcomas, or bone tumors.
The only significant decrease over the study period was in the incidence of melanoma in children (–2.6).
“Possible causes of increasing rates might include changes in diagnostic, coding, and reporting standards, increased detection, population-based changes (such as increasing obesity), and environmental exposures,” they wrote.
Public health campaigns about the dangers of UV exposure and promoting the use of sunscreens may account for the decline in the incidence of malignant melanoma, they suggested.
The study was supported by the CDC. Dr. Siegel and coauthors are CDC employees. They reported having no conflicts of interest.
SOURCE: Siegel DA et al. ASPHO 2018, Abstract 605.
REPORTING FROM ASPHO 2018
Key clinical point: Major finding: From 2001 to 2014, there were 196,200 incident cases of pediatric cancer for an overall cancer incidence rate of 173 per 1 million.
Study details: A review of data from the United States Cancer Statistics for children under age 20.
Disclosures: The CDC supported the study. Dr. Siegel and his coauthors are CDC employees. They reported having no conflicts of interest.
Source: Siegel DA et al. ASPHO 2018, Abstract 605.
Multiple solid tumors targeted by concept CAR T
PITTSBURGH – Call it the CAR of the future – an investigational chimeric antigen receptor–T cell construct targeted against an antigen highly expressed on pediatric solid tumors has shown promising efficacy in preclinical studies.
Investigators found that the antigen, labeled B7-H3, was expressed on 84% of microarrays of pediatric solid tumors. More importantly, a single dose of CAR targeted to B7-H3 caused complete regression of osteosarcoma and Ewing sarcoma xenografts and improved survival over an untransduced, CD19-targeted CAR in mice, Robbie Majzner, MD, reported at the annual meeting of the American Society of Pediatric Hematology/Oncology.
Dr. Majzner was the recipient of an ASPHO young investigator award for his team’s research into developing a CAR T that could be as effective against solid tumors as other CAR Ts have been against hematologic malignancies such as acute lymphoblastic leukemia.
Solid tumors are more challenging to target than leukemias or lymphomas because of the small number of antigens expressed on most pediatric tumors, he said.
“Over 95% of tumors have a very low rate of mutations, which means that they have very few neoantigens which the immune system can recognize in order to attack,” he said.
In the Children’s Oncology Group ADVL1412 trial, single-agent immunotherapy with the anti–programmed death protein 1 (PD-1) inhibitor nivolumab (Opdivo) showed no evidence of efficacy against either Ewing sarcoma, osteosarcoma, rhabdomyosarcoma, or measurable neuroblastoma. PD–ligand 1 was found to be expressed in only a few of the 43 tumors studied, suggesting that checkpoint inhibitor therapy is unlikely to work in these solid tumors, he said.
In contrast, B7-H3 is highly expressed on many different pediatric solid tumors, including rhabdomyosarcoma (95% of tumors stained), Ewing sarcoma (89%), Wilms tumor (100%), neuroblastoma (82%), ganglioneuroblastoma and ganglioneuroma (53%), medulloblastoma (96%), glioblastoma multiforme (84%), and diffuse intrinsic pontine glioma (100%).
To see whether CAR T therapy might have better efficacy than checkpoint inhibitors in this population, the investigators created a B7-H3 CAR using the B7-H3 tumor–specific monoclonal antibody MGA271, which has been shown to be safe in both adults and children in early clinical trials.
In human tumor xenograft models of osteosarcoma, all mice who received a single dose of the B7-H3 CAR survived at least 70 days after tumor engraftment, whereas all control mice, who received the CD19 CAR, died by day 60 (P = .0067). Similarly, in a model of Ewing sarcoma, all mice treated with B7-H3 survived at least 100 days, whereas all controls were dead by day 50 (P = .0015).
The B7-H3 construct also showed good activity against a model of medulloblastoma, showing that it was capable of crossing the blood-brain barrier.
Since B7-H3 has been reported to be expressed on both myeloid and lymphoid leukemia cells, the investigators also tested the CAR against a murine model of leukemia generated by injection of K562, a well-characterized line of myeloid leukemia cells.
“While we found some increase in survival in the mice that received the B7-H3 CAR T cells, compared to mice that received untransduced CAR T cells, this clearly is not as effective as in our solid tumor models,” Dr. Majzner said.
Going back to the cell line, they discovered that expression of B7-H3 was considerably lower in the K562 cells than in either the osteosarcoma or medulloblastoma cell lines used in their other models.
They found that both in vitro and in vivo, high levels of B7-H3 expression were necessary to provoke the immune system into releasing cytokines necessary for an adequate antitumor response.
The investigators are currently planning clinical trials using the B7-H3 CAR T-cell construct in patients with solid tumors.
The work is supported by the Sarcoma Alliance for Research through Collaboration, the St. Baldrick’s Foundation, and Stand Up to Cancer. Dr. Majzner reported having no financial disclosures.
SOURCE: Majzner RG et al. ASPHO 2018, Abstract #PS2003.
PITTSBURGH – Call it the CAR of the future – an investigational chimeric antigen receptor–T cell construct targeted against an antigen highly expressed on pediatric solid tumors has shown promising efficacy in preclinical studies.
Investigators found that the antigen, labeled B7-H3, was expressed on 84% of microarrays of pediatric solid tumors. More importantly, a single dose of CAR targeted to B7-H3 caused complete regression of osteosarcoma and Ewing sarcoma xenografts and improved survival over an untransduced, CD19-targeted CAR in mice, Robbie Majzner, MD, reported at the annual meeting of the American Society of Pediatric Hematology/Oncology.
Dr. Majzner was the recipient of an ASPHO young investigator award for his team’s research into developing a CAR T that could be as effective against solid tumors as other CAR Ts have been against hematologic malignancies such as acute lymphoblastic leukemia.
Solid tumors are more challenging to target than leukemias or lymphomas because of the small number of antigens expressed on most pediatric tumors, he said.
“Over 95% of tumors have a very low rate of mutations, which means that they have very few neoantigens which the immune system can recognize in order to attack,” he said.
In the Children’s Oncology Group ADVL1412 trial, single-agent immunotherapy with the anti–programmed death protein 1 (PD-1) inhibitor nivolumab (Opdivo) showed no evidence of efficacy against either Ewing sarcoma, osteosarcoma, rhabdomyosarcoma, or measurable neuroblastoma. PD–ligand 1 was found to be expressed in only a few of the 43 tumors studied, suggesting that checkpoint inhibitor therapy is unlikely to work in these solid tumors, he said.
In contrast, B7-H3 is highly expressed on many different pediatric solid tumors, including rhabdomyosarcoma (95% of tumors stained), Ewing sarcoma (89%), Wilms tumor (100%), neuroblastoma (82%), ganglioneuroblastoma and ganglioneuroma (53%), medulloblastoma (96%), glioblastoma multiforme (84%), and diffuse intrinsic pontine glioma (100%).
To see whether CAR T therapy might have better efficacy than checkpoint inhibitors in this population, the investigators created a B7-H3 CAR using the B7-H3 tumor–specific monoclonal antibody MGA271, which has been shown to be safe in both adults and children in early clinical trials.
In human tumor xenograft models of osteosarcoma, all mice who received a single dose of the B7-H3 CAR survived at least 70 days after tumor engraftment, whereas all control mice, who received the CD19 CAR, died by day 60 (P = .0067). Similarly, in a model of Ewing sarcoma, all mice treated with B7-H3 survived at least 100 days, whereas all controls were dead by day 50 (P = .0015).
The B7-H3 construct also showed good activity against a model of medulloblastoma, showing that it was capable of crossing the blood-brain barrier.
Since B7-H3 has been reported to be expressed on both myeloid and lymphoid leukemia cells, the investigators also tested the CAR against a murine model of leukemia generated by injection of K562, a well-characterized line of myeloid leukemia cells.
“While we found some increase in survival in the mice that received the B7-H3 CAR T cells, compared to mice that received untransduced CAR T cells, this clearly is not as effective as in our solid tumor models,” Dr. Majzner said.
Going back to the cell line, they discovered that expression of B7-H3 was considerably lower in the K562 cells than in either the osteosarcoma or medulloblastoma cell lines used in their other models.
They found that both in vitro and in vivo, high levels of B7-H3 expression were necessary to provoke the immune system into releasing cytokines necessary for an adequate antitumor response.
The investigators are currently planning clinical trials using the B7-H3 CAR T-cell construct in patients with solid tumors.
The work is supported by the Sarcoma Alliance for Research through Collaboration, the St. Baldrick’s Foundation, and Stand Up to Cancer. Dr. Majzner reported having no financial disclosures.
SOURCE: Majzner RG et al. ASPHO 2018, Abstract #PS2003.
PITTSBURGH – Call it the CAR of the future – an investigational chimeric antigen receptor–T cell construct targeted against an antigen highly expressed on pediatric solid tumors has shown promising efficacy in preclinical studies.
Investigators found that the antigen, labeled B7-H3, was expressed on 84% of microarrays of pediatric solid tumors. More importantly, a single dose of CAR targeted to B7-H3 caused complete regression of osteosarcoma and Ewing sarcoma xenografts and improved survival over an untransduced, CD19-targeted CAR in mice, Robbie Majzner, MD, reported at the annual meeting of the American Society of Pediatric Hematology/Oncology.
Dr. Majzner was the recipient of an ASPHO young investigator award for his team’s research into developing a CAR T that could be as effective against solid tumors as other CAR Ts have been against hematologic malignancies such as acute lymphoblastic leukemia.
Solid tumors are more challenging to target than leukemias or lymphomas because of the small number of antigens expressed on most pediatric tumors, he said.
“Over 95% of tumors have a very low rate of mutations, which means that they have very few neoantigens which the immune system can recognize in order to attack,” he said.
In the Children’s Oncology Group ADVL1412 trial, single-agent immunotherapy with the anti–programmed death protein 1 (PD-1) inhibitor nivolumab (Opdivo) showed no evidence of efficacy against either Ewing sarcoma, osteosarcoma, rhabdomyosarcoma, or measurable neuroblastoma. PD–ligand 1 was found to be expressed in only a few of the 43 tumors studied, suggesting that checkpoint inhibitor therapy is unlikely to work in these solid tumors, he said.
In contrast, B7-H3 is highly expressed on many different pediatric solid tumors, including rhabdomyosarcoma (95% of tumors stained), Ewing sarcoma (89%), Wilms tumor (100%), neuroblastoma (82%), ganglioneuroblastoma and ganglioneuroma (53%), medulloblastoma (96%), glioblastoma multiforme (84%), and diffuse intrinsic pontine glioma (100%).
To see whether CAR T therapy might have better efficacy than checkpoint inhibitors in this population, the investigators created a B7-H3 CAR using the B7-H3 tumor–specific monoclonal antibody MGA271, which has been shown to be safe in both adults and children in early clinical trials.
In human tumor xenograft models of osteosarcoma, all mice who received a single dose of the B7-H3 CAR survived at least 70 days after tumor engraftment, whereas all control mice, who received the CD19 CAR, died by day 60 (P = .0067). Similarly, in a model of Ewing sarcoma, all mice treated with B7-H3 survived at least 100 days, whereas all controls were dead by day 50 (P = .0015).
The B7-H3 construct also showed good activity against a model of medulloblastoma, showing that it was capable of crossing the blood-brain barrier.
Since B7-H3 has been reported to be expressed on both myeloid and lymphoid leukemia cells, the investigators also tested the CAR against a murine model of leukemia generated by injection of K562, a well-characterized line of myeloid leukemia cells.
“While we found some increase in survival in the mice that received the B7-H3 CAR T cells, compared to mice that received untransduced CAR T cells, this clearly is not as effective as in our solid tumor models,” Dr. Majzner said.
Going back to the cell line, they discovered that expression of B7-H3 was considerably lower in the K562 cells than in either the osteosarcoma or medulloblastoma cell lines used in their other models.
They found that both in vitro and in vivo, high levels of B7-H3 expression were necessary to provoke the immune system into releasing cytokines necessary for an adequate antitumor response.
The investigators are currently planning clinical trials using the B7-H3 CAR T-cell construct in patients with solid tumors.
The work is supported by the Sarcoma Alliance for Research through Collaboration, the St. Baldrick’s Foundation, and Stand Up to Cancer. Dr. Majzner reported having no financial disclosures.
SOURCE: Majzner RG et al. ASPHO 2018, Abstract #PS2003.
REPORTING FROM ASPHO 2018
Key clinical point:
Major finding: A single dose of the B7-H3 CAR caused complete regression of osteosarcoma and Ewing sarcoma xenografts and extended survival in mice.
Study details: Preclinical research.
Disclosures: The work is supported by the Sarcoma Alliance for Research through Collaboration, St. Baldrick’s Foundation, and Stand Up to Cancer. Dr. Majzner reported having no financial disclosures.
Source: Majzner RG et al. ASPHO 2018, Abstract #PS2003.
Children with Down syndrome and ALL have good outcomes today
PITTSBURGH – In the current era, children with Down syndrome who have standard risk B-cell precursor acute lymphoblastic leukemia have event-free and overall survival rates nearly as good as those of other children with standard-risk B–ALL, results of a Children’s Oncology Group study show.
Among 5,311 children enrolled in the COG AALL0331 trial, a study of combination chemotherapy for young patients with newly diagnosed ALL, the 5-year event-free survival (EFS) rate for children with Down syndrome was 86%, compared with 89% for children without Down syndrome (P = .025).
Although the differences in EFS and OS were significant, ”overall in this study, Down syndrome ALL had an excellent outcome that was similar to those patients without Down syndrome,” she said at the annual meeting of the American Society of Pediatric Hematology/Oncology.
The trial confirmed her group’s previous finding that there is a low rate of favorable cytogenetic features in patients with Down syndrome ALL; nonetheless, in the current study, 5-year continuous complete remission rates for standard-risk average, low, and high in patients with Down syndrome were similar to those for patients without Down syndrome, she said.
In the trial, patients were treated with a three-drug induction regimen, and following induction were assigned to standard-risk low, average, or high groups based on leukemia genetics and initial response to therapy.
Of the 5,311 children enrolled, 141 (2.7%) had Down syndrome, and these patients received risk-stratified therapy with additional supportive care guidelines, including leucovorin rescue after intrathecal methotrexate until maintenance. The care team strongly encouraged hospitalizations during high-risk blocks for this subgroup of patients until they experienced neutrophil recovery.
At the end of induction, patients who were judged to be standard-risk average were then randomized in a 2x2 design to either standard or intensified consolidation, and to standard interim maintenance with delayed intensification, or to intensified interim maintenance with delayed intensification.
The intensified interim maintenance with delayed intensification randomization was closed in 2008 because of superior results with escalating intravenous methotrexate during interim maintenance for standard-risk ALL patients treated in the CCG 1991 trial. Subsequently, all patients enrolled in AALL0331 received escalating intravenous methotrexate during interim maintenance.
Also in AALL0331, patients with Down syndrome who had standard-high ALL were given intensified consolidation and a single vs. double intensified interim maintenance with delayed intensification; patients without Down syndrome and standard risk high received the double intensified interim maintenance regimen.
Standard-risk low Down syndrome patients and non–Down syndrome patients participated in a randomization to additional pegaspargase doses during consolidation and interim maintenance.
There were no significant differences between patients with or without Down syndrome in the proportion of either rapid or slow early responses. Significantly fewer patients with Down syndrome had standard-risk low disease, and significantly more had average or high-risk disease.
Patients with Down syndrome initially had 11.5% excess risk for death during induction, but following additional treatment modifications, the excess risk decreased to 1.7%.
Among patients with Down syndrome, one died during intensive consolidation, and two died during delayed intensification. All three deaths were due to infections. No patients with Down syndrome died during maintenance.
Patients with Down syndrome also had a significantly increased risk for infection during induction (P less than .0001).
For patients with standard-risk low disease, 5-year EFS was 100% for those with Down syndrome, compared with 95.35% for patients without. Respective rates for standard risk average and high disease were 88.07% vs. 89.63%. and 82.35% vs. 86.18%.
Down syndrome was not an independent risk factor for survival in multivariate analyses accounting for risk group, Dr. Maloney said.
COG AALL0331 was supported by the National Cancer Institute. Dr. Maloney reported having no financial disclosures.
SOURCE: Maloney K et al. ASPHO 2018, Abstract PP 2001.
PITTSBURGH – In the current era, children with Down syndrome who have standard risk B-cell precursor acute lymphoblastic leukemia have event-free and overall survival rates nearly as good as those of other children with standard-risk B–ALL, results of a Children’s Oncology Group study show.
Among 5,311 children enrolled in the COG AALL0331 trial, a study of combination chemotherapy for young patients with newly diagnosed ALL, the 5-year event-free survival (EFS) rate for children with Down syndrome was 86%, compared with 89% for children without Down syndrome (P = .025).
Although the differences in EFS and OS were significant, ”overall in this study, Down syndrome ALL had an excellent outcome that was similar to those patients without Down syndrome,” she said at the annual meeting of the American Society of Pediatric Hematology/Oncology.
The trial confirmed her group’s previous finding that there is a low rate of favorable cytogenetic features in patients with Down syndrome ALL; nonetheless, in the current study, 5-year continuous complete remission rates for standard-risk average, low, and high in patients with Down syndrome were similar to those for patients without Down syndrome, she said.
In the trial, patients were treated with a three-drug induction regimen, and following induction were assigned to standard-risk low, average, or high groups based on leukemia genetics and initial response to therapy.
Of the 5,311 children enrolled, 141 (2.7%) had Down syndrome, and these patients received risk-stratified therapy with additional supportive care guidelines, including leucovorin rescue after intrathecal methotrexate until maintenance. The care team strongly encouraged hospitalizations during high-risk blocks for this subgroup of patients until they experienced neutrophil recovery.
At the end of induction, patients who were judged to be standard-risk average were then randomized in a 2x2 design to either standard or intensified consolidation, and to standard interim maintenance with delayed intensification, or to intensified interim maintenance with delayed intensification.
The intensified interim maintenance with delayed intensification randomization was closed in 2008 because of superior results with escalating intravenous methotrexate during interim maintenance for standard-risk ALL patients treated in the CCG 1991 trial. Subsequently, all patients enrolled in AALL0331 received escalating intravenous methotrexate during interim maintenance.
Also in AALL0331, patients with Down syndrome who had standard-high ALL were given intensified consolidation and a single vs. double intensified interim maintenance with delayed intensification; patients without Down syndrome and standard risk high received the double intensified interim maintenance regimen.
Standard-risk low Down syndrome patients and non–Down syndrome patients participated in a randomization to additional pegaspargase doses during consolidation and interim maintenance.
There were no significant differences between patients with or without Down syndrome in the proportion of either rapid or slow early responses. Significantly fewer patients with Down syndrome had standard-risk low disease, and significantly more had average or high-risk disease.
Patients with Down syndrome initially had 11.5% excess risk for death during induction, but following additional treatment modifications, the excess risk decreased to 1.7%.
Among patients with Down syndrome, one died during intensive consolidation, and two died during delayed intensification. All three deaths were due to infections. No patients with Down syndrome died during maintenance.
Patients with Down syndrome also had a significantly increased risk for infection during induction (P less than .0001).
For patients with standard-risk low disease, 5-year EFS was 100% for those with Down syndrome, compared with 95.35% for patients without. Respective rates for standard risk average and high disease were 88.07% vs. 89.63%. and 82.35% vs. 86.18%.
Down syndrome was not an independent risk factor for survival in multivariate analyses accounting for risk group, Dr. Maloney said.
COG AALL0331 was supported by the National Cancer Institute. Dr. Maloney reported having no financial disclosures.
SOURCE: Maloney K et al. ASPHO 2018, Abstract PP 2001.
PITTSBURGH – In the current era, children with Down syndrome who have standard risk B-cell precursor acute lymphoblastic leukemia have event-free and overall survival rates nearly as good as those of other children with standard-risk B–ALL, results of a Children’s Oncology Group study show.
Among 5,311 children enrolled in the COG AALL0331 trial, a study of combination chemotherapy for young patients with newly diagnosed ALL, the 5-year event-free survival (EFS) rate for children with Down syndrome was 86%, compared with 89% for children without Down syndrome (P = .025).
Although the differences in EFS and OS were significant, ”overall in this study, Down syndrome ALL had an excellent outcome that was similar to those patients without Down syndrome,” she said at the annual meeting of the American Society of Pediatric Hematology/Oncology.
The trial confirmed her group’s previous finding that there is a low rate of favorable cytogenetic features in patients with Down syndrome ALL; nonetheless, in the current study, 5-year continuous complete remission rates for standard-risk average, low, and high in patients with Down syndrome were similar to those for patients without Down syndrome, she said.
In the trial, patients were treated with a three-drug induction regimen, and following induction were assigned to standard-risk low, average, or high groups based on leukemia genetics and initial response to therapy.
Of the 5,311 children enrolled, 141 (2.7%) had Down syndrome, and these patients received risk-stratified therapy with additional supportive care guidelines, including leucovorin rescue after intrathecal methotrexate until maintenance. The care team strongly encouraged hospitalizations during high-risk blocks for this subgroup of patients until they experienced neutrophil recovery.
At the end of induction, patients who were judged to be standard-risk average were then randomized in a 2x2 design to either standard or intensified consolidation, and to standard interim maintenance with delayed intensification, or to intensified interim maintenance with delayed intensification.
The intensified interim maintenance with delayed intensification randomization was closed in 2008 because of superior results with escalating intravenous methotrexate during interim maintenance for standard-risk ALL patients treated in the CCG 1991 trial. Subsequently, all patients enrolled in AALL0331 received escalating intravenous methotrexate during interim maintenance.
Also in AALL0331, patients with Down syndrome who had standard-high ALL were given intensified consolidation and a single vs. double intensified interim maintenance with delayed intensification; patients without Down syndrome and standard risk high received the double intensified interim maintenance regimen.
Standard-risk low Down syndrome patients and non–Down syndrome patients participated in a randomization to additional pegaspargase doses during consolidation and interim maintenance.
There were no significant differences between patients with or without Down syndrome in the proportion of either rapid or slow early responses. Significantly fewer patients with Down syndrome had standard-risk low disease, and significantly more had average or high-risk disease.
Patients with Down syndrome initially had 11.5% excess risk for death during induction, but following additional treatment modifications, the excess risk decreased to 1.7%.
Among patients with Down syndrome, one died during intensive consolidation, and two died during delayed intensification. All three deaths were due to infections. No patients with Down syndrome died during maintenance.
Patients with Down syndrome also had a significantly increased risk for infection during induction (P less than .0001).
For patients with standard-risk low disease, 5-year EFS was 100% for those with Down syndrome, compared with 95.35% for patients without. Respective rates for standard risk average and high disease were 88.07% vs. 89.63%. and 82.35% vs. 86.18%.
Down syndrome was not an independent risk factor for survival in multivariate analyses accounting for risk group, Dr. Maloney said.
COG AALL0331 was supported by the National Cancer Institute. Dr. Maloney reported having no financial disclosures.
SOURCE: Maloney K et al. ASPHO 2018, Abstract PP 2001.
REPORTING FROM ASPHO 2018
Key clinical point:
Major finding: The 5-year event-free survival rate for children with Down syndrome was 86% vs. 89% for children without Down syndrome (P = .025).
Study details: Follow-up of 5,311 children with newly diagnosed ALL in the COG AALL0331 trial.
Disclosures: COG AALL0331 was supported by the National Cancer Institute. Dr. Maloney reported having no financial disclosures.
Source: Maloney K et al. ASPHO 2018, Abstract PP 2001.
Patients with CF at increased risk for GI cancers
Patients with cystic fibrosis have a significantly greater risk for developing cancers of the gastrointestinal tract compared with the general population, results of a systematic review and meta-analysis indicate.
Among persons with cystic fibrosis (CF) the standardized incidence ratio (SIR) for any gastrointestinal cancer compared with the general population was 8.13 (P less than .0001). Patients with CF were at significantly elevated risk for cancers of the small bowel, colon, biliary tract, and pancreas, reported Atsushi Sakuraba, MD, PhD, of the University of Chicago, and his colleagues.
“Additionally, our findings suggest that patients who had an organ transplant have a higher risk of developing gastrointestinal cancer than those who did not. Although further studies are needed to monitor gastrointestinal cancer incidence over time in patients with cystic fibrosis, the development of a screening strategy for gastrointestinal cancer in these patients is warranted,” they wrote in Lancet Oncology.
As patients with CF live longer because of improvements in therapies and management of comorbidities, their risks for cancer and other diseases will increase, the authors noted.
To get a more accurate estimate of the degree of risk than what smaller cohort studies could provide, the investigators conducted a systematic review and meta-analysis. They narrowed their search to six cohort studies including 99,925 patients with CF followed for a total of 5,444,695 person-years.
As noted, patients with CF overall had an eightfold higher risk for gastrointestinal cancers compared with the general population, and for the subgroup of patients who had undergone a lung transplant, the SIR was 21.13 compared with 4.18 for those with CF but no lung transplant (P less than .0001).
- The SIRs for site-specific gastrointestinal cancers were as follows:
- Small bowel: SIR= 18.94 (P less than .0001).
- Colon: SIR = 10.91 (P less than .0001).
- Biliary tract: SIR = 17.87 (P less than .0001).
- Pancreas: SIR = 6.18 (P = .022).
The investigators recommend screening for gastrointestinal cancers in patients with CF in general, and especially for patients who have undergone lung transplantation and are receiving immunosuppressive therapies.
Because of the elevated risk of pancreatic and biliary tract cancers, the authors propose a screening program including magnetic resonance cholangiopancreatography, endoscopic ultrasound, or abdominal ultrasound and measurement of cancer antigen 19-9.
The authors reported that the study had no funding source, and they declared no competing interests.
SOURCE: Yamada A et al. Lancet Oncol. 2018 Apr 26. doi: 10.1016/S1470-2045(18)30188-8.
The emergence of gastrointestinal cancer as a clinical complication in adults with cystic fibrosis is a consequence of the substantial improvement in life expectancy. Novel CFTR modulator therapies, which correct the malfunctioning protein and increase its expression at the apical surface, might decrease the incidence of gastrointestinal cancers in patients with cystic fibrosis.
In conclusion, the meta-analysis by Yamada and colleagues shows that cystic fibrosis can be considered a gastrointestinal cancer syndrome, for which screening and surveillance protocols should be implemented. Oncologists and gastroenterologists managing patients with cystic fibrosis should consider the best methods for screening of the small bowel, biliary tract, pancreas, and colon to prevent gastrointestinal malignancies in these patients.
Mordechai Slae, MD, and Michael Wilschanski, MD, are with the Hadassah Medical Center in Jerusalem. These comments are condensed from their editorial in The Lancet Oncology.
The emergence of gastrointestinal cancer as a clinical complication in adults with cystic fibrosis is a consequence of the substantial improvement in life expectancy. Novel CFTR modulator therapies, which correct the malfunctioning protein and increase its expression at the apical surface, might decrease the incidence of gastrointestinal cancers in patients with cystic fibrosis.
In conclusion, the meta-analysis by Yamada and colleagues shows that cystic fibrosis can be considered a gastrointestinal cancer syndrome, for which screening and surveillance protocols should be implemented. Oncologists and gastroenterologists managing patients with cystic fibrosis should consider the best methods for screening of the small bowel, biliary tract, pancreas, and colon to prevent gastrointestinal malignancies in these patients.
Mordechai Slae, MD, and Michael Wilschanski, MD, are with the Hadassah Medical Center in Jerusalem. These comments are condensed from their editorial in The Lancet Oncology.
The emergence of gastrointestinal cancer as a clinical complication in adults with cystic fibrosis is a consequence of the substantial improvement in life expectancy. Novel CFTR modulator therapies, which correct the malfunctioning protein and increase its expression at the apical surface, might decrease the incidence of gastrointestinal cancers in patients with cystic fibrosis.
In conclusion, the meta-analysis by Yamada and colleagues shows that cystic fibrosis can be considered a gastrointestinal cancer syndrome, for which screening and surveillance protocols should be implemented. Oncologists and gastroenterologists managing patients with cystic fibrosis should consider the best methods for screening of the small bowel, biliary tract, pancreas, and colon to prevent gastrointestinal malignancies in these patients.
Mordechai Slae, MD, and Michael Wilschanski, MD, are with the Hadassah Medical Center in Jerusalem. These comments are condensed from their editorial in The Lancet Oncology.
Patients with cystic fibrosis have a significantly greater risk for developing cancers of the gastrointestinal tract compared with the general population, results of a systematic review and meta-analysis indicate.
Among persons with cystic fibrosis (CF) the standardized incidence ratio (SIR) for any gastrointestinal cancer compared with the general population was 8.13 (P less than .0001). Patients with CF were at significantly elevated risk for cancers of the small bowel, colon, biliary tract, and pancreas, reported Atsushi Sakuraba, MD, PhD, of the University of Chicago, and his colleagues.
“Additionally, our findings suggest that patients who had an organ transplant have a higher risk of developing gastrointestinal cancer than those who did not. Although further studies are needed to monitor gastrointestinal cancer incidence over time in patients with cystic fibrosis, the development of a screening strategy for gastrointestinal cancer in these patients is warranted,” they wrote in Lancet Oncology.
As patients with CF live longer because of improvements in therapies and management of comorbidities, their risks for cancer and other diseases will increase, the authors noted.
To get a more accurate estimate of the degree of risk than what smaller cohort studies could provide, the investigators conducted a systematic review and meta-analysis. They narrowed their search to six cohort studies including 99,925 patients with CF followed for a total of 5,444,695 person-years.
As noted, patients with CF overall had an eightfold higher risk for gastrointestinal cancers compared with the general population, and for the subgroup of patients who had undergone a lung transplant, the SIR was 21.13 compared with 4.18 for those with CF but no lung transplant (P less than .0001).
- The SIRs for site-specific gastrointestinal cancers were as follows:
- Small bowel: SIR= 18.94 (P less than .0001).
- Colon: SIR = 10.91 (P less than .0001).
- Biliary tract: SIR = 17.87 (P less than .0001).
- Pancreas: SIR = 6.18 (P = .022).
The investigators recommend screening for gastrointestinal cancers in patients with CF in general, and especially for patients who have undergone lung transplantation and are receiving immunosuppressive therapies.
Because of the elevated risk of pancreatic and biliary tract cancers, the authors propose a screening program including magnetic resonance cholangiopancreatography, endoscopic ultrasound, or abdominal ultrasound and measurement of cancer antigen 19-9.
The authors reported that the study had no funding source, and they declared no competing interests.
SOURCE: Yamada A et al. Lancet Oncol. 2018 Apr 26. doi: 10.1016/S1470-2045(18)30188-8.
Patients with cystic fibrosis have a significantly greater risk for developing cancers of the gastrointestinal tract compared with the general population, results of a systematic review and meta-analysis indicate.
Among persons with cystic fibrosis (CF) the standardized incidence ratio (SIR) for any gastrointestinal cancer compared with the general population was 8.13 (P less than .0001). Patients with CF were at significantly elevated risk for cancers of the small bowel, colon, biliary tract, and pancreas, reported Atsushi Sakuraba, MD, PhD, of the University of Chicago, and his colleagues.
“Additionally, our findings suggest that patients who had an organ transplant have a higher risk of developing gastrointestinal cancer than those who did not. Although further studies are needed to monitor gastrointestinal cancer incidence over time in patients with cystic fibrosis, the development of a screening strategy for gastrointestinal cancer in these patients is warranted,” they wrote in Lancet Oncology.
As patients with CF live longer because of improvements in therapies and management of comorbidities, their risks for cancer and other diseases will increase, the authors noted.
To get a more accurate estimate of the degree of risk than what smaller cohort studies could provide, the investigators conducted a systematic review and meta-analysis. They narrowed their search to six cohort studies including 99,925 patients with CF followed for a total of 5,444,695 person-years.
As noted, patients with CF overall had an eightfold higher risk for gastrointestinal cancers compared with the general population, and for the subgroup of patients who had undergone a lung transplant, the SIR was 21.13 compared with 4.18 for those with CF but no lung transplant (P less than .0001).
- The SIRs for site-specific gastrointestinal cancers were as follows:
- Small bowel: SIR= 18.94 (P less than .0001).
- Colon: SIR = 10.91 (P less than .0001).
- Biliary tract: SIR = 17.87 (P less than .0001).
- Pancreas: SIR = 6.18 (P = .022).
The investigators recommend screening for gastrointestinal cancers in patients with CF in general, and especially for patients who have undergone lung transplantation and are receiving immunosuppressive therapies.
Because of the elevated risk of pancreatic and biliary tract cancers, the authors propose a screening program including magnetic resonance cholangiopancreatography, endoscopic ultrasound, or abdominal ultrasound and measurement of cancer antigen 19-9.
The authors reported that the study had no funding source, and they declared no competing interests.
SOURCE: Yamada A et al. Lancet Oncol. 2018 Apr 26. doi: 10.1016/S1470-2045(18)30188-8.
FROM THE LANCET ONCOLOGY
Key clinical point: Patients with cystic fibrosis, especially those who have received a lung transplant, are at increased risk for gastrointestinal tract cancers.
Major finding: The standard incidence ratio for GI cancers among patients with CF was 8.13 compared with the general population.
Study details: Systematic review and meta-analysis of published studies including 99,925 patients with CF followed for 5,444,695 person-years.
Disclosures: The authors reported that the study had no funding source, and they declared no competing interests.
Source: Yamada A et al. Lancet Oncol 2018 Apr 26. doi: 10.1016/S1470-2045(18)30188-8.
Hydroxyurea in infancy yields better SCD outcomes
PITTSBURGH – Children with sickle cell disease (SCD) who were started on hydroxyurea in infancy had significantly better outcomes than do children started on the drug as toddlers, researchers report.
Among 65 children with SCD, those who started on hydroxyurea before age 1 year had significantly fewer hospitalizations, pain crises, and transfusions in the first 2 years of life, compared with patients started on the drug during 1-2 years of age or after age 2 years, found Sarah B. Schuchard, PharmD, from the SSM Health Cardinal Glennon Children’s Hospital in St. Louis and her colleagues.
At the Children’s Hospital and Clinics of Minnesota in Minneapolis, where Dr. Schuchard recently completed her training and conducted the research, the goal is to initiate all infants with sickle cell anemia and sickle-beta0-thalassemia on hydroxyurea within this first year of life.
To evaluate outcomes associated with this practice, the investigators conducted a retrospective review of all children with SCD who began hydroxyurea therapy at their center during 2008-2016.
They divided the population into three cohorts. Patients in cohort 1 were started on hydroxyurea before age 1 year (35 patients; mean age, 7.2 months), those in cohort 2 started between 1 and 2 years of age (13 patients; mean age, 19.5 months) and those in cohort 3 were started after 2 years of age (three patients; mean age, 35.5 months).
All patients had been diagnosed with either sickle cell anemia or sickle-beta0-thalassemia, and all had at least two laboratory assessments at 6 months, 12 months, 18 months, or 24 months of age.
For the coprimary endpoint of laboratory data, the investigators found that patients in cohort 1, the early starters, had significantly higher hemoglobin (P = .0003), lower absolute reticulocyte counts (P = .0304), and mean corpuscular volume (P = .0199) than did the patients in cohort 3.
Infants in cohort 1 had significantly lower white blood cell counts than did the patients in either cohorts 2 or 3 (P = .0007 and P less than .0001, respectively) and lower absolute neutrophil counts (P = .0364 and .0025, respectively), although no patients required hydroxyurea therapy to be held because of low ANC.
Clinical events, the other coprimary endpoint, were also significantly better among patients in cohort 1, who had significantly fewer hospitalizations (P = .0025), a trend toward fewer painful events (P = .0618), and significantly fewer transfusions (P = .0426) than did patients in the other two cohorts.
“Early hydroxyurea also appears to contribute to fewer pain crises requiring admission,” the investigators noted.
They noted that in their study, the hematologic response was greater than that seen in the BABY HUG study, which studied the protective effects of hydroxyurea in children aged 9-18 months. The mean age of hydroxyurea initiation was 13.6 months in that study, compared with 7.2 months in the study by Dr. Schuchard and her colleagues.
“It would be interesting to see if the splenic and renal function (the unmet primary endpoints of BABY HUG) are preserved in patients starting hydroxyurea at this younger age,” they wrote.
The study was internally funded. Dr. Schuchard reported having no conflicts of interest.
SOURCE: Schuchard S et al. ASPHO 2018, Poster 342.
PITTSBURGH – Children with sickle cell disease (SCD) who were started on hydroxyurea in infancy had significantly better outcomes than do children started on the drug as toddlers, researchers report.
Among 65 children with SCD, those who started on hydroxyurea before age 1 year had significantly fewer hospitalizations, pain crises, and transfusions in the first 2 years of life, compared with patients started on the drug during 1-2 years of age or after age 2 years, found Sarah B. Schuchard, PharmD, from the SSM Health Cardinal Glennon Children’s Hospital in St. Louis and her colleagues.
At the Children’s Hospital and Clinics of Minnesota in Minneapolis, where Dr. Schuchard recently completed her training and conducted the research, the goal is to initiate all infants with sickle cell anemia and sickle-beta0-thalassemia on hydroxyurea within this first year of life.
To evaluate outcomes associated with this practice, the investigators conducted a retrospective review of all children with SCD who began hydroxyurea therapy at their center during 2008-2016.
They divided the population into three cohorts. Patients in cohort 1 were started on hydroxyurea before age 1 year (35 patients; mean age, 7.2 months), those in cohort 2 started between 1 and 2 years of age (13 patients; mean age, 19.5 months) and those in cohort 3 were started after 2 years of age (three patients; mean age, 35.5 months).
All patients had been diagnosed with either sickle cell anemia or sickle-beta0-thalassemia, and all had at least two laboratory assessments at 6 months, 12 months, 18 months, or 24 months of age.
For the coprimary endpoint of laboratory data, the investigators found that patients in cohort 1, the early starters, had significantly higher hemoglobin (P = .0003), lower absolute reticulocyte counts (P = .0304), and mean corpuscular volume (P = .0199) than did the patients in cohort 3.
Infants in cohort 1 had significantly lower white blood cell counts than did the patients in either cohorts 2 or 3 (P = .0007 and P less than .0001, respectively) and lower absolute neutrophil counts (P = .0364 and .0025, respectively), although no patients required hydroxyurea therapy to be held because of low ANC.
Clinical events, the other coprimary endpoint, were also significantly better among patients in cohort 1, who had significantly fewer hospitalizations (P = .0025), a trend toward fewer painful events (P = .0618), and significantly fewer transfusions (P = .0426) than did patients in the other two cohorts.
“Early hydroxyurea also appears to contribute to fewer pain crises requiring admission,” the investigators noted.
They noted that in their study, the hematologic response was greater than that seen in the BABY HUG study, which studied the protective effects of hydroxyurea in children aged 9-18 months. The mean age of hydroxyurea initiation was 13.6 months in that study, compared with 7.2 months in the study by Dr. Schuchard and her colleagues.
“It would be interesting to see if the splenic and renal function (the unmet primary endpoints of BABY HUG) are preserved in patients starting hydroxyurea at this younger age,” they wrote.
The study was internally funded. Dr. Schuchard reported having no conflicts of interest.
SOURCE: Schuchard S et al. ASPHO 2018, Poster 342.
PITTSBURGH – Children with sickle cell disease (SCD) who were started on hydroxyurea in infancy had significantly better outcomes than do children started on the drug as toddlers, researchers report.
Among 65 children with SCD, those who started on hydroxyurea before age 1 year had significantly fewer hospitalizations, pain crises, and transfusions in the first 2 years of life, compared with patients started on the drug during 1-2 years of age or after age 2 years, found Sarah B. Schuchard, PharmD, from the SSM Health Cardinal Glennon Children’s Hospital in St. Louis and her colleagues.
At the Children’s Hospital and Clinics of Minnesota in Minneapolis, where Dr. Schuchard recently completed her training and conducted the research, the goal is to initiate all infants with sickle cell anemia and sickle-beta0-thalassemia on hydroxyurea within this first year of life.
To evaluate outcomes associated with this practice, the investigators conducted a retrospective review of all children with SCD who began hydroxyurea therapy at their center during 2008-2016.
They divided the population into three cohorts. Patients in cohort 1 were started on hydroxyurea before age 1 year (35 patients; mean age, 7.2 months), those in cohort 2 started between 1 and 2 years of age (13 patients; mean age, 19.5 months) and those in cohort 3 were started after 2 years of age (three patients; mean age, 35.5 months).
All patients had been diagnosed with either sickle cell anemia or sickle-beta0-thalassemia, and all had at least two laboratory assessments at 6 months, 12 months, 18 months, or 24 months of age.
For the coprimary endpoint of laboratory data, the investigators found that patients in cohort 1, the early starters, had significantly higher hemoglobin (P = .0003), lower absolute reticulocyte counts (P = .0304), and mean corpuscular volume (P = .0199) than did the patients in cohort 3.
Infants in cohort 1 had significantly lower white blood cell counts than did the patients in either cohorts 2 or 3 (P = .0007 and P less than .0001, respectively) and lower absolute neutrophil counts (P = .0364 and .0025, respectively), although no patients required hydroxyurea therapy to be held because of low ANC.
Clinical events, the other coprimary endpoint, were also significantly better among patients in cohort 1, who had significantly fewer hospitalizations (P = .0025), a trend toward fewer painful events (P = .0618), and significantly fewer transfusions (P = .0426) than did patients in the other two cohorts.
“Early hydroxyurea also appears to contribute to fewer pain crises requiring admission,” the investigators noted.
They noted that in their study, the hematologic response was greater than that seen in the BABY HUG study, which studied the protective effects of hydroxyurea in children aged 9-18 months. The mean age of hydroxyurea initiation was 13.6 months in that study, compared with 7.2 months in the study by Dr. Schuchard and her colleagues.
“It would be interesting to see if the splenic and renal function (the unmet primary endpoints of BABY HUG) are preserved in patients starting hydroxyurea at this younger age,” they wrote.
The study was internally funded. Dr. Schuchard reported having no conflicts of interest.
SOURCE: Schuchard S et al. ASPHO 2018, Poster 342.
REPORTING FROM ASPHO 2018
Key clinical point: Early initiation of hydroxyurea is associated with better SCD outcomes.
Major finding: Patients started on hydroxyurea at a mean of 7.2 months had significantly fewer admissions, pain crises, and transfusions than did patients started after age 1 year.
Study details: Retrospective review of data on 65 children with SCD in a single center.
Disclosures: The study was internally funded. Dr. Schuchard reported having no conflicts of interest.
Source: Schuchard S et al. ASPHO 2018, Poster 342.
Screening tool IDs older NSCLC patients suitable for SBRT
A validated screening tool may help to identify older adults with early-stage non–small cell lung cancer who could benefit from stereotactic body radiotherapy with curative intent, investigators contend,
Among 43 patients aged 65-89 years (median age 78) with stage T1 or T2 non–small cell lung cancer tumors who underwent stereotactic body radiotherapy (SBRT), scores of 13 or higher on the Geriatric 8 (G8) screening tool were associated with high 2- and 5-year survival rates, reported Toshiya Maebayashi, MD, PhD, from Nihon University in Tokyo, and colleagues.
“Regardless of age, the G8 screening tool may enable us to identify relatively healthy seniors who would be likely to have longer survival times after SBRT for early lung cancer,” they wrote in a study published in the Journal of Geriatric Oncology.
The G8 Screening tool assesses the health status of older patients according to their food intake, recent weight loss, mobility, neuropsychological problems, body mass index, prescription drug use, and age. Higher scores on the scale, which can range from 0 to 17, are indicative of better health status.
To see whether the G8 tool could predict the benefits of SBRT, the investigators performed a retrospective study of long-term outcomes in older patients with early-stage non–small cell lung cancer.
They included 34 patients with T1 tumors and 9 patients with T2 tumors who underwent SBRT from 2004 to 2011 at their center. The median follow-up was 46 months (range, 3-112 months).
Patients with T1 tumors had G8 scores ranging from 9 to 16 (median 13). Patients with T2 tumors had scores ranging from 8 to 15 (median 12).
For patients with G8 scores of 12 or lower, the overall survival rate after 2 years was 56.1%, and 28% after 5 years. In contrast, the respective 2- and 5-year overall survival rates for patients with G8 scores of 13 or higher were 94.1% and 68.4% (P = .0014).
In univariate analysis, factors significantly associated with survival included T-stage (P = .034), pathology (P = .004), and G8 score (P = .001). G8 score was also significantly associated with overall survival in multivariate analysis (P = .006).
Adverse events included rib fractures in nine patients, grade 2 pneumonitis in four and grade 3 pneumonitis in two patients. There were no cases of hemoptysis. Neither G8 score nor age were related to adverse events.
“We anticipate that functional evaluation of older patients will allow us to actively recommend SBRT [an approach less likely than other current treatments to cause adverse events] to older patients who are in relatively good condition but hesitant to receive treatment,” the investigators wrote.
The authors did not receive special funding for the study, and had no conflicts of interest.
SOURCE: Maebayashi T et al. J Geriatr Oncol. 2018 Mar 22. doi: 10.1016/j.jgo.2018.03.005.
A validated screening tool may help to identify older adults with early-stage non–small cell lung cancer who could benefit from stereotactic body radiotherapy with curative intent, investigators contend,
Among 43 patients aged 65-89 years (median age 78) with stage T1 or T2 non–small cell lung cancer tumors who underwent stereotactic body radiotherapy (SBRT), scores of 13 or higher on the Geriatric 8 (G8) screening tool were associated with high 2- and 5-year survival rates, reported Toshiya Maebayashi, MD, PhD, from Nihon University in Tokyo, and colleagues.
“Regardless of age, the G8 screening tool may enable us to identify relatively healthy seniors who would be likely to have longer survival times after SBRT for early lung cancer,” they wrote in a study published in the Journal of Geriatric Oncology.
The G8 Screening tool assesses the health status of older patients according to their food intake, recent weight loss, mobility, neuropsychological problems, body mass index, prescription drug use, and age. Higher scores on the scale, which can range from 0 to 17, are indicative of better health status.
To see whether the G8 tool could predict the benefits of SBRT, the investigators performed a retrospective study of long-term outcomes in older patients with early-stage non–small cell lung cancer.
They included 34 patients with T1 tumors and 9 patients with T2 tumors who underwent SBRT from 2004 to 2011 at their center. The median follow-up was 46 months (range, 3-112 months).
Patients with T1 tumors had G8 scores ranging from 9 to 16 (median 13). Patients with T2 tumors had scores ranging from 8 to 15 (median 12).
For patients with G8 scores of 12 or lower, the overall survival rate after 2 years was 56.1%, and 28% after 5 years. In contrast, the respective 2- and 5-year overall survival rates for patients with G8 scores of 13 or higher were 94.1% and 68.4% (P = .0014).
In univariate analysis, factors significantly associated with survival included T-stage (P = .034), pathology (P = .004), and G8 score (P = .001). G8 score was also significantly associated with overall survival in multivariate analysis (P = .006).
Adverse events included rib fractures in nine patients, grade 2 pneumonitis in four and grade 3 pneumonitis in two patients. There were no cases of hemoptysis. Neither G8 score nor age were related to adverse events.
“We anticipate that functional evaluation of older patients will allow us to actively recommend SBRT [an approach less likely than other current treatments to cause adverse events] to older patients who are in relatively good condition but hesitant to receive treatment,” the investigators wrote.
The authors did not receive special funding for the study, and had no conflicts of interest.
SOURCE: Maebayashi T et al. J Geriatr Oncol. 2018 Mar 22. doi: 10.1016/j.jgo.2018.03.005.
A validated screening tool may help to identify older adults with early-stage non–small cell lung cancer who could benefit from stereotactic body radiotherapy with curative intent, investigators contend,
Among 43 patients aged 65-89 years (median age 78) with stage T1 or T2 non–small cell lung cancer tumors who underwent stereotactic body radiotherapy (SBRT), scores of 13 or higher on the Geriatric 8 (G8) screening tool were associated with high 2- and 5-year survival rates, reported Toshiya Maebayashi, MD, PhD, from Nihon University in Tokyo, and colleagues.
“Regardless of age, the G8 screening tool may enable us to identify relatively healthy seniors who would be likely to have longer survival times after SBRT for early lung cancer,” they wrote in a study published in the Journal of Geriatric Oncology.
The G8 Screening tool assesses the health status of older patients according to their food intake, recent weight loss, mobility, neuropsychological problems, body mass index, prescription drug use, and age. Higher scores on the scale, which can range from 0 to 17, are indicative of better health status.
To see whether the G8 tool could predict the benefits of SBRT, the investigators performed a retrospective study of long-term outcomes in older patients with early-stage non–small cell lung cancer.
They included 34 patients with T1 tumors and 9 patients with T2 tumors who underwent SBRT from 2004 to 2011 at their center. The median follow-up was 46 months (range, 3-112 months).
Patients with T1 tumors had G8 scores ranging from 9 to 16 (median 13). Patients with T2 tumors had scores ranging from 8 to 15 (median 12).
For patients with G8 scores of 12 or lower, the overall survival rate after 2 years was 56.1%, and 28% after 5 years. In contrast, the respective 2- and 5-year overall survival rates for patients with G8 scores of 13 or higher were 94.1% and 68.4% (P = .0014).
In univariate analysis, factors significantly associated with survival included T-stage (P = .034), pathology (P = .004), and G8 score (P = .001). G8 score was also significantly associated with overall survival in multivariate analysis (P = .006).
Adverse events included rib fractures in nine patients, grade 2 pneumonitis in four and grade 3 pneumonitis in two patients. There were no cases of hemoptysis. Neither G8 score nor age were related to adverse events.
“We anticipate that functional evaluation of older patients will allow us to actively recommend SBRT [an approach less likely than other current treatments to cause adverse events] to older patients who are in relatively good condition but hesitant to receive treatment,” the investigators wrote.
The authors did not receive special funding for the study, and had no conflicts of interest.
SOURCE: Maebayashi T et al. J Geriatr Oncol. 2018 Mar 22. doi: 10.1016/j.jgo.2018.03.005.
FROM THE JOURNAL OF GERIATRIC ONCOLOGY
Key clinical point: The Geriatric 8 screening tool may identify older patients with non–small cell lung cancer who could benefit from stereotactic body radiotherapy.
Major finding: Geriatric 8 scores of 13 or higher were associated with better 2- and 5-year overall survival.
Study details: A retrospective analysis of 43 patients aged 65-89 years with stage T1 or T2 non–small cell lung cancer.
Disclosures: The authors did not receive special funding for the study, and had no conflicts of interest to disclose.
Source: Maebayashi T et al. J Geriatr Oncol. 2018 Mar 22. doi: 10.1016/j.jgo.2018.03.005.
Hormone therapy raises diabetes risk in breast cancer survivors
Hormone therapy for breast cancer more than doubles a woman’s risk for developing type 2 diabetes, results of a case-cohort study suggest.
Hormone therapy with tamoxifen was associated with a more than twofold increase in risk of diabetes, and aromatase inhibitors were associated with a more than fourfold increase, reported Hatem Hamood, MD, of Leumit Health Services in Karmiel, Israel, and colleagues.
Among 2,246 women with breast cancer and no diabetes at baseline, followed for a mean of 5.9 years (longest follow-up 13 years), the crude cumulative lifetime incidence rate of diabetes was 20.9%, the investigators wrote. The report was published in the Journal of Clinical Oncology.
“[Hormone therapy] is a significant risk factor of diabetes among breast cancer survivors. The underlying mechanism is unclear, and additional research is warranted. Although cessation of treatment is not recommended and progression of breast cancer often is inevitable, devised strategies aimed at lifestyle modifications in patients at high risk of diabetes could at least preserve the natural history of breast cancer,” they wrote.
Diabetes has previously been identified as a possible risk factor for breast cancer, but the potential for breast cancer therapy as a precipitating factor for diabetes is uncertain, the authors said.
“Given the detrimental impact of diabetes on breast cancer survival, additional exploration of the role of breast cancer treatment in the development of diabetes is important not only because it would add valuable information on the etiology of diabetes but also because it would help to identify high-risk patients in need of accentuated clinical care,” they wrote.
To explore the possible association between hormone therapy and diabetes risk, the investigators performed a retrospective case-cohort study of 2,246 women who had been diagnosed with primary nonmetastatic breast cancer treated with hormone therapy from 2002 through 2012.
They examined data on a randomly selected cohort of 448 breast cancer survivors and all patients in the parent (no diabetes at baseline) cohort who developed diabetes during the study period (324 patients).
They found that the prevalence of diabetes among their source population of 2,644 breast cancer survivors (including those with baseline diabetes) increased “drastically” from 6% in 2002 to 28% in 2015. The prevalence exceeded Israeli national norms from 2010 through 2013, with standardized prevalence ratios of 1.61 to 1.81 (P less than .001).
As noted, in the population without baseline diabetes, the crude cumulative incidence rate of diabetes in the presence of death as a competing risk factor was 20.9%.
In multivariate analyses controlling for demographic and socioeconomic factors, and for chemotherapy type, hypertension, outpatient visits, use of corticosteroids, thiazide diuretics, beta-blockers, statins, and year of breast cancer diagnosis, factors significantly associated with diabetes risk were use of hormone therapy (adjusted hazard ratio [HR] 2.40, P = .008), tamoxifen (aHR 2.25, P = .013), aromatase inhibitors (aHR 4.27, P = .013), therapy duration more than 1 year (aHR 2.36, P = .009), and 1 year or less (aHR 6.48, P = .004).
The investigators noted that although other reports have found no association between aromatase inhibitors and diabetes risk, those studies had small samples or offered no explanation of the lack of association.
In contrast, a 2016 joint ACS/ASCO breast cancer survivorship-care guideline notes that aromatase inhibitors may raise the risk of diabetes, the investigators noted.
The study was supported by grants from the Israeli Council for Higher Education. The investigators reported no conflicts of interest.
SOURCE: Hamood H et al. J Clin Oncol. 2018 Apr 24. doi: 10.1200/JCO.2017.76.3524.
Hormone therapy for breast cancer more than doubles a woman’s risk for developing type 2 diabetes, results of a case-cohort study suggest.
Hormone therapy with tamoxifen was associated with a more than twofold increase in risk of diabetes, and aromatase inhibitors were associated with a more than fourfold increase, reported Hatem Hamood, MD, of Leumit Health Services in Karmiel, Israel, and colleagues.
Among 2,246 women with breast cancer and no diabetes at baseline, followed for a mean of 5.9 years (longest follow-up 13 years), the crude cumulative lifetime incidence rate of diabetes was 20.9%, the investigators wrote. The report was published in the Journal of Clinical Oncology.
“[Hormone therapy] is a significant risk factor of diabetes among breast cancer survivors. The underlying mechanism is unclear, and additional research is warranted. Although cessation of treatment is not recommended and progression of breast cancer often is inevitable, devised strategies aimed at lifestyle modifications in patients at high risk of diabetes could at least preserve the natural history of breast cancer,” they wrote.
Diabetes has previously been identified as a possible risk factor for breast cancer, but the potential for breast cancer therapy as a precipitating factor for diabetes is uncertain, the authors said.
“Given the detrimental impact of diabetes on breast cancer survival, additional exploration of the role of breast cancer treatment in the development of diabetes is important not only because it would add valuable information on the etiology of diabetes but also because it would help to identify high-risk patients in need of accentuated clinical care,” they wrote.
To explore the possible association between hormone therapy and diabetes risk, the investigators performed a retrospective case-cohort study of 2,246 women who had been diagnosed with primary nonmetastatic breast cancer treated with hormone therapy from 2002 through 2012.
They examined data on a randomly selected cohort of 448 breast cancer survivors and all patients in the parent (no diabetes at baseline) cohort who developed diabetes during the study period (324 patients).
They found that the prevalence of diabetes among their source population of 2,644 breast cancer survivors (including those with baseline diabetes) increased “drastically” from 6% in 2002 to 28% in 2015. The prevalence exceeded Israeli national norms from 2010 through 2013, with standardized prevalence ratios of 1.61 to 1.81 (P less than .001).
As noted, in the population without baseline diabetes, the crude cumulative incidence rate of diabetes in the presence of death as a competing risk factor was 20.9%.
In multivariate analyses controlling for demographic and socioeconomic factors, and for chemotherapy type, hypertension, outpatient visits, use of corticosteroids, thiazide diuretics, beta-blockers, statins, and year of breast cancer diagnosis, factors significantly associated with diabetes risk were use of hormone therapy (adjusted hazard ratio [HR] 2.40, P = .008), tamoxifen (aHR 2.25, P = .013), aromatase inhibitors (aHR 4.27, P = .013), therapy duration more than 1 year (aHR 2.36, P = .009), and 1 year or less (aHR 6.48, P = .004).
The investigators noted that although other reports have found no association between aromatase inhibitors and diabetes risk, those studies had small samples or offered no explanation of the lack of association.
In contrast, a 2016 joint ACS/ASCO breast cancer survivorship-care guideline notes that aromatase inhibitors may raise the risk of diabetes, the investigators noted.
The study was supported by grants from the Israeli Council for Higher Education. The investigators reported no conflicts of interest.
SOURCE: Hamood H et al. J Clin Oncol. 2018 Apr 24. doi: 10.1200/JCO.2017.76.3524.
Hormone therapy for breast cancer more than doubles a woman’s risk for developing type 2 diabetes, results of a case-cohort study suggest.
Hormone therapy with tamoxifen was associated with a more than twofold increase in risk of diabetes, and aromatase inhibitors were associated with a more than fourfold increase, reported Hatem Hamood, MD, of Leumit Health Services in Karmiel, Israel, and colleagues.
Among 2,246 women with breast cancer and no diabetes at baseline, followed for a mean of 5.9 years (longest follow-up 13 years), the crude cumulative lifetime incidence rate of diabetes was 20.9%, the investigators wrote. The report was published in the Journal of Clinical Oncology.
“[Hormone therapy] is a significant risk factor of diabetes among breast cancer survivors. The underlying mechanism is unclear, and additional research is warranted. Although cessation of treatment is not recommended and progression of breast cancer often is inevitable, devised strategies aimed at lifestyle modifications in patients at high risk of diabetes could at least preserve the natural history of breast cancer,” they wrote.
Diabetes has previously been identified as a possible risk factor for breast cancer, but the potential for breast cancer therapy as a precipitating factor for diabetes is uncertain, the authors said.
“Given the detrimental impact of diabetes on breast cancer survival, additional exploration of the role of breast cancer treatment in the development of diabetes is important not only because it would add valuable information on the etiology of diabetes but also because it would help to identify high-risk patients in need of accentuated clinical care,” they wrote.
To explore the possible association between hormone therapy and diabetes risk, the investigators performed a retrospective case-cohort study of 2,246 women who had been diagnosed with primary nonmetastatic breast cancer treated with hormone therapy from 2002 through 2012.
They examined data on a randomly selected cohort of 448 breast cancer survivors and all patients in the parent (no diabetes at baseline) cohort who developed diabetes during the study period (324 patients).
They found that the prevalence of diabetes among their source population of 2,644 breast cancer survivors (including those with baseline diabetes) increased “drastically” from 6% in 2002 to 28% in 2015. The prevalence exceeded Israeli national norms from 2010 through 2013, with standardized prevalence ratios of 1.61 to 1.81 (P less than .001).
As noted, in the population without baseline diabetes, the crude cumulative incidence rate of diabetes in the presence of death as a competing risk factor was 20.9%.
In multivariate analyses controlling for demographic and socioeconomic factors, and for chemotherapy type, hypertension, outpatient visits, use of corticosteroids, thiazide diuretics, beta-blockers, statins, and year of breast cancer diagnosis, factors significantly associated with diabetes risk were use of hormone therapy (adjusted hazard ratio [HR] 2.40, P = .008), tamoxifen (aHR 2.25, P = .013), aromatase inhibitors (aHR 4.27, P = .013), therapy duration more than 1 year (aHR 2.36, P = .009), and 1 year or less (aHR 6.48, P = .004).
The investigators noted that although other reports have found no association between aromatase inhibitors and diabetes risk, those studies had small samples or offered no explanation of the lack of association.
In contrast, a 2016 joint ACS/ASCO breast cancer survivorship-care guideline notes that aromatase inhibitors may raise the risk of diabetes, the investigators noted.
The study was supported by grants from the Israeli Council for Higher Education. The investigators reported no conflicts of interest.
SOURCE: Hamood H et al. J Clin Oncol. 2018 Apr 24. doi: 10.1200/JCO.2017.76.3524.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Consider screening survivors of nonmetastatic breast cancer for diabetes.
Major finding: The crude lifetime incidence of diabetes following hormone therapy for breast cancer was 20.9%.
Study details: Case-cohort study of 2,246 women with nonmetastatic breast cancer and no baseline diabetes treated with hormone therapy.
Disclosures: The study was supported by grants from the Israeli Council for Higher Education. The investigators reported no conflicts of interest.
Source: Hamood H et al. J Clin Oncol. 2018 Apr 24. doi: 10.1200/JCO.2017.76.3524.
Venetoclax shows muscle against CLL relapsed after idelalisib
For patients with relapsed or refractory chronic lymphocytic leukemia despite therapy with idelalisib (Zydelig), venetoclax (Venclexta) was associated with relatively high overall response and progression-free survival rates, results of a phase 2 study show.
Among 36 patients with relapsed/refractory CLL who had received idelalisib as their most recent B-cell receptor pathway inhibitor (BCRi), the overall response rate (ORR) was 67%, and median progression-free and overall survival (PFS and OS) had not been reached after 14 months of follow-up, reported Steven Coutre, MD, of Stanford (Calif.) University, and his colleagues.
“[V]enetoclax monotherapy is active and well-tolerated in patients with CLL progression after therapy with idelalisib, including a significant number of patients who also received prior therapy with ibrutinib [Imbruvica]. These results from the first prospective trial in this high-risk population provide evidence that venetoclax should be considered as a treatment option for such patients,” the investigators wrote. The report was published in Blood.
In clinical trials with idelalisib, approximately one-third of patients with CLL experienced disease progression on therapy, and other patients had to discontinue the drug, an inhibitor of the delta isoform of phosphoinositide 3-kinase (PI3K), because of toxicities, the investigators noted.
“The optimal treatment of patients with CLL progressing after idelalisib has not been well characterized,” they wrote. “Outcomes in patients who discontinued idelalisib treatment early are poor, with one retrospective analysis reporting a median overall survival (OS) after idelalisib discontinuation of approximately 2 months (range, 0-10 months).”
Venetoclax, an inhibitor of the apoptotic BCL-2 protein, has been shown to have activity against CLL, including in patients with high-risk features such as the chromosome 17p deletion (del17p), prompting the investigators to evaluate it as a follow-on in patients with relapsed/refractory CLL treated with a B-cell receptor pathway inhibitor.
They reported on the idelalisib cohort in a phase 2 trial in which patients with CLL that progressed on either idelalisib or ibrutinib were subsequently treated with venetoclax. The patients in this analysis included those treated with idelalisib in the main study cohort or an expansion cohort.
Patients were started on venetoclax 20 mg daily, followed by weekly dose escalations to a target of 400 mg daily by week 5, or to a maximum of 600 mg for patients who did not have a response by the week 12 assessment.
The overall response rate – the primary efficacy endpoint – was 67%. There were two complete remissions (CR) and one CR with incomplete bone marrow recovery. The remaining 21 patients with responses had partial responses.
At a median of 14 months of follow-up, neither median PFS, duration of response, or OS had been reached.
The investigator-estimated 12-month PFS rate was 79%.
The most common grade 3 or 4 adverse events were neutropenia in 50% of patients, thrombocytopenia in 25%, and anemia in 17%. There were no cases of clinical tumor lysis syndrome, which has been known to occur when venetoclax is initiated at full dose without a ramp-up.
The most common adverse events of any grade included neutropenia, diarrhea, upper respiratory tract infection, thrombocytopenia, nausea, fatigue, cough, rash, and anemia.
“The low number of CRs reported at the time of analysis may be a result of the follow-up time, particularly for patients in the expansion cohort, as other clinical studies with venetoclax report CR occurring after 1 year on therapy. Patients with prior ibrutinib exposure who had progressed on idelalisib as their most recent therapy before study entry had similar efficacy results,” the investigators wrote.
Genentech and AbbVie funded the study. Dr. Coutre is an advisory board member for both companies and others, and receives institutional funding from AbbVie and others. Multiple coauthors disclosed financial relationships with AbbVie, Genentech, or both, as well as other companies.
SOURCE: Coutre S et al. Blood. 2018;131(15):1704-11.
For patients with relapsed or refractory chronic lymphocytic leukemia despite therapy with idelalisib (Zydelig), venetoclax (Venclexta) was associated with relatively high overall response and progression-free survival rates, results of a phase 2 study show.
Among 36 patients with relapsed/refractory CLL who had received idelalisib as their most recent B-cell receptor pathway inhibitor (BCRi), the overall response rate (ORR) was 67%, and median progression-free and overall survival (PFS and OS) had not been reached after 14 months of follow-up, reported Steven Coutre, MD, of Stanford (Calif.) University, and his colleagues.
“[V]enetoclax monotherapy is active and well-tolerated in patients with CLL progression after therapy with idelalisib, including a significant number of patients who also received prior therapy with ibrutinib [Imbruvica]. These results from the first prospective trial in this high-risk population provide evidence that venetoclax should be considered as a treatment option for such patients,” the investigators wrote. The report was published in Blood.
In clinical trials with idelalisib, approximately one-third of patients with CLL experienced disease progression on therapy, and other patients had to discontinue the drug, an inhibitor of the delta isoform of phosphoinositide 3-kinase (PI3K), because of toxicities, the investigators noted.
“The optimal treatment of patients with CLL progressing after idelalisib has not been well characterized,” they wrote. “Outcomes in patients who discontinued idelalisib treatment early are poor, with one retrospective analysis reporting a median overall survival (OS) after idelalisib discontinuation of approximately 2 months (range, 0-10 months).”
Venetoclax, an inhibitor of the apoptotic BCL-2 protein, has been shown to have activity against CLL, including in patients with high-risk features such as the chromosome 17p deletion (del17p), prompting the investigators to evaluate it as a follow-on in patients with relapsed/refractory CLL treated with a B-cell receptor pathway inhibitor.
They reported on the idelalisib cohort in a phase 2 trial in which patients with CLL that progressed on either idelalisib or ibrutinib were subsequently treated with venetoclax. The patients in this analysis included those treated with idelalisib in the main study cohort or an expansion cohort.
Patients were started on venetoclax 20 mg daily, followed by weekly dose escalations to a target of 400 mg daily by week 5, or to a maximum of 600 mg for patients who did not have a response by the week 12 assessment.
The overall response rate – the primary efficacy endpoint – was 67%. There were two complete remissions (CR) and one CR with incomplete bone marrow recovery. The remaining 21 patients with responses had partial responses.
At a median of 14 months of follow-up, neither median PFS, duration of response, or OS had been reached.
The investigator-estimated 12-month PFS rate was 79%.
The most common grade 3 or 4 adverse events were neutropenia in 50% of patients, thrombocytopenia in 25%, and anemia in 17%. There were no cases of clinical tumor lysis syndrome, which has been known to occur when venetoclax is initiated at full dose without a ramp-up.
The most common adverse events of any grade included neutropenia, diarrhea, upper respiratory tract infection, thrombocytopenia, nausea, fatigue, cough, rash, and anemia.
“The low number of CRs reported at the time of analysis may be a result of the follow-up time, particularly for patients in the expansion cohort, as other clinical studies with venetoclax report CR occurring after 1 year on therapy. Patients with prior ibrutinib exposure who had progressed on idelalisib as their most recent therapy before study entry had similar efficacy results,” the investigators wrote.
Genentech and AbbVie funded the study. Dr. Coutre is an advisory board member for both companies and others, and receives institutional funding from AbbVie and others. Multiple coauthors disclosed financial relationships with AbbVie, Genentech, or both, as well as other companies.
SOURCE: Coutre S et al. Blood. 2018;131(15):1704-11.
For patients with relapsed or refractory chronic lymphocytic leukemia despite therapy with idelalisib (Zydelig), venetoclax (Venclexta) was associated with relatively high overall response and progression-free survival rates, results of a phase 2 study show.
Among 36 patients with relapsed/refractory CLL who had received idelalisib as their most recent B-cell receptor pathway inhibitor (BCRi), the overall response rate (ORR) was 67%, and median progression-free and overall survival (PFS and OS) had not been reached after 14 months of follow-up, reported Steven Coutre, MD, of Stanford (Calif.) University, and his colleagues.
“[V]enetoclax monotherapy is active and well-tolerated in patients with CLL progression after therapy with idelalisib, including a significant number of patients who also received prior therapy with ibrutinib [Imbruvica]. These results from the first prospective trial in this high-risk population provide evidence that venetoclax should be considered as a treatment option for such patients,” the investigators wrote. The report was published in Blood.
In clinical trials with idelalisib, approximately one-third of patients with CLL experienced disease progression on therapy, and other patients had to discontinue the drug, an inhibitor of the delta isoform of phosphoinositide 3-kinase (PI3K), because of toxicities, the investigators noted.
“The optimal treatment of patients with CLL progressing after idelalisib has not been well characterized,” they wrote. “Outcomes in patients who discontinued idelalisib treatment early are poor, with one retrospective analysis reporting a median overall survival (OS) after idelalisib discontinuation of approximately 2 months (range, 0-10 months).”
Venetoclax, an inhibitor of the apoptotic BCL-2 protein, has been shown to have activity against CLL, including in patients with high-risk features such as the chromosome 17p deletion (del17p), prompting the investigators to evaluate it as a follow-on in patients with relapsed/refractory CLL treated with a B-cell receptor pathway inhibitor.
They reported on the idelalisib cohort in a phase 2 trial in which patients with CLL that progressed on either idelalisib or ibrutinib were subsequently treated with venetoclax. The patients in this analysis included those treated with idelalisib in the main study cohort or an expansion cohort.
Patients were started on venetoclax 20 mg daily, followed by weekly dose escalations to a target of 400 mg daily by week 5, or to a maximum of 600 mg for patients who did not have a response by the week 12 assessment.
The overall response rate – the primary efficacy endpoint – was 67%. There were two complete remissions (CR) and one CR with incomplete bone marrow recovery. The remaining 21 patients with responses had partial responses.
At a median of 14 months of follow-up, neither median PFS, duration of response, or OS had been reached.
The investigator-estimated 12-month PFS rate was 79%.
The most common grade 3 or 4 adverse events were neutropenia in 50% of patients, thrombocytopenia in 25%, and anemia in 17%. There were no cases of clinical tumor lysis syndrome, which has been known to occur when venetoclax is initiated at full dose without a ramp-up.
The most common adverse events of any grade included neutropenia, diarrhea, upper respiratory tract infection, thrombocytopenia, nausea, fatigue, cough, rash, and anemia.
“The low number of CRs reported at the time of analysis may be a result of the follow-up time, particularly for patients in the expansion cohort, as other clinical studies with venetoclax report CR occurring after 1 year on therapy. Patients with prior ibrutinib exposure who had progressed on idelalisib as their most recent therapy before study entry had similar efficacy results,” the investigators wrote.
Genentech and AbbVie funded the study. Dr. Coutre is an advisory board member for both companies and others, and receives institutional funding from AbbVie and others. Multiple coauthors disclosed financial relationships with AbbVie, Genentech, or both, as well as other companies.
SOURCE: Coutre S et al. Blood. 2018;131(15):1704-11.
FROM BLOOD
Key clinical point:
Major finding: The overall response rate was 67%, including two complete responses (CRs) and one CR with incomplete bone marrow recovery.
Study details: Cohort of 36 patients with relapsed/refractory CLL previously treated with idelalisib.
Disclosures: Genentech and AbbVie funded the study. Dr. Coutre is an advisory board member for both companies and others, and receives institutional funding from AbbVie and others. Multiple coauthors disclosed financial relationships with AbbVie, Genentech, or both, as well as other companies.
Source: Coutre S et al. Blood. 2018;131(15):1704-11.