User login
Case Report
A 54-year-old Hispanic woman with a history of type 2 diabetes mellitus and hyperlipidemia presented with recurrent painful plaques and nodules on the bilateral lower extremities and a severe burning sensation on the feet of 3 years’ duration. The patient denied experiencing any associated fevers, chills, night sweats, weight loss, joint aches, cough, or shortness of breath. She had a history of pustular psoriasis and reported a positive purified protein derivative (PPD)(tuberculin) skin test approximately 40 years prior.
She presented with a 4×4-cm, poorly defined, tender, indurated plaque on the middle of the left shin and a 2×3-cm, red-brown plaque on the dorsal aspect of the left foot (Figure 1). No lymphadenopathy or any other abnormalities were noted. The clinical differential diagnosis included various panniculitides, such as erythema nodosum, erythema induratum of Bazin (EIB), and lupus panniculitis, as well as other conditions, including polyarteritis nodosa, sarcoidosis, Sweet disease, deep fungal and mycobacterial infections, and cutaneous lymphoma.


|
| Figure 1. Erythematous indurated plaques on the middle of the left shin (A) and on the dorsal aspect of the left foot (B). |
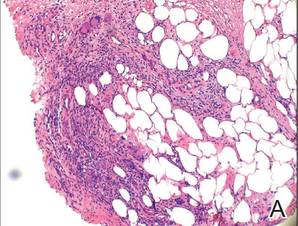
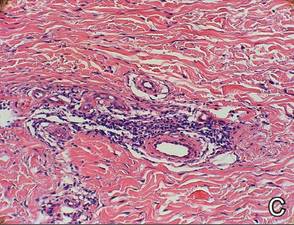
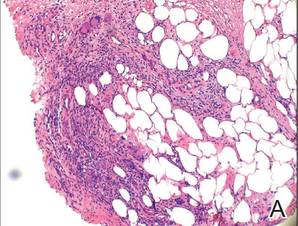
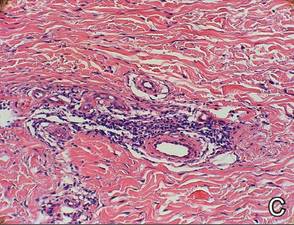
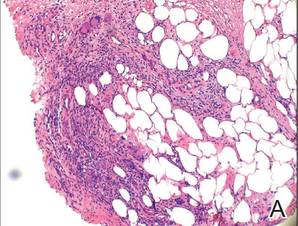
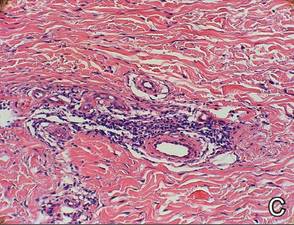
Two skin biopsies taken for histopathologic evaluation revealed primarily granulomatous lobular panniculitis with foci of microthrombi and vasculitis (Figure 2). These findings were consistent with nodular vasculitis. Acid-fast bacillus and Gomori methenamine-silver stains were negative for mycobacterial or fungal organisms. Tissue cultures also were negative. Results from a complete blood cell count, chemistry panel, thyroid and liver function tests, hepatitis panel, and rapid plasma reagin test were unremarkable. Immunologic markers, including antinuclear antibody, antineutrophil cytoplasmic antibody, rheumatoid factor, and cryoglobulins, also revealed no abnormalities. A chest radiograph showed scarring in the suprahilar region of the upper lobe of the left lung consistent with a prior case of pulmonary tuberculosis, and exposure to Mycobacterium tuberculosis was confirmed with an IFN-γ release assay (IGRA) result of 1.49 IU/mL (>0.34 IU/mL indicates positive test). These findings from clinical and histopathologic examination as well as laboratory tests were consistent with a diagnosis of EIB.

|
Figure 2. Granulomatous lobular panniculitis (A)(H&E, original magnification ×40) with foci of microthrombi and vasculitis (B and C)(both H&E, original magnifications ×200). |
Standard antituberculosis therapy with rifampin, isoniazid, pyrazinamide, and ethambutol (RIPE) was simplified to rifampin and isoniazid due to her inability to tolerate the full regimen because of gastrointestinal tract upset and diarrhea. After 6 months of therapy, a repeat IGRA decreased to 0.43 IU/mL, and the painful plaques and nodules on the lower extremities and burning sensation in the feet completely resolved.
Comment
Our case of EIB associated with peripheral neuropathy is a unique presentation of lesions on the pretibial area of the bilateral legs and dorsal aspect of the feet. We confirmed the presence of latent tuberculosis infection with a chest radiograph and an IGRA. Symptoms of peripheral neuropathy resolved after antituberculosis treatment, which suggests an immune-mediated mechanism of neuronal damage from circulating tuberculosis antigens.
Pathogenesis
Although erythema induratum was first described by Ernest Bazin in 1861, it was not until the early 1900s that the link between tuberculosis and erythema induratum was made by French dermatologists.1,2 Around the same time, similar cases of erythema induratum were discovered in England with no evidence of tuberculosis, which led to the distinct classification of erythema induratum of Whitfield (EIW). This classification described these nontuberculoid cases.1,2 In 1945, Montgomery et al3 in the United States coined the term nodular vasculitis for EIW and categorized its clinical features and histopathology as separate from EIB.3 Today, some authors use EIB, EIW, and nodular vasculitis interchangeably and believe they all are the same entity.2 We use EIB for all cases related to tuberculosis and nodular vasulitis when referring to all other etiologies, including nontuberculoid bacterial infections, chronic hepatitis B and C virus, thrombophlebitis, hypothyroidism, and rheumatoid arthritis.4,5
Erythema induratum of Bazin, lichen scrofulosorum, and papulonecrotic tuberculids are considered tuberculid diseases and are thought to be caused by hypersensitivity reactions to mycobacterial antigens rather than local mycobacterial infections. Tuberculids are believed to be a reaction to an id reaction of circulating mycobacterial antigens in the setting of latent or active tuberculosis infection. The basis for this view is that mycobacteria cannot be cultured or visualized from lesions in tuberculid diseases.6 Cutaneous tuberculosis, such as scrofuloderma, miliary tuberculosis, tuberculosis chancre, lupus vulgaris, and gummatous tuberculosis, differ from EIB and other tuberculid diseases in that mycobacteria can be cultured and visualized on histologic examination with Ziehl-Neelsen staining.6 The pathology of cutaneous tuberculosis results from a mycobacterial infection of the skin, and cutaneous tuberculosis diseases are categorized as multibacillary or paucibacillary based on the number of organisms visualized in biopsies.
The absence of M tuberculosis organisms in skin lesions has led some to doubt the causal relationship between M tuberculosis and EIB.7 However, the advent of polymerase chain reaction (PCR) and specific DNA primers for M tuberculosis has allowed for the detection of M tuberculosis DNA in biopsy specimens, which has further established the relationship between tuberculosis and EIB.5 Some authors have suggested that the absence of mycobacteria in EIB and other tuberculid lesions may be due to small numbers of bacilli in the lesions or early destruction of mycobacteria organisms before biopsy.8,9 These authors consider cutaneous tuberculosis and tuberculids as diseases on the same spectrum, with tuberculids representing one extreme in which there are few mycobacteria organisms present in the lesions.
Presentation
Erythema induratum commonly affects middle-aged women and presents with recurrent crops of tender nodules on the lower extremities.10-13 Nodules often are most commonly found on the lower calves but also can present on the arms, thighs, feet, or buttocks.10 Our patient’s presentation was atypical in that lesions were distributed on the pretibial area of the legs and dorsal aspect of the feet. Obesity and venous insufficiency of the lower extremities are believed to be predisposing factors to the development of EIB nodules.2 The nodules develop over several weeks and heal over several months with possible ulceration and hyperpigmented scarring.10,11 Ulcerated nodules often are irregular and shallow with an overlying crust and a bluish border.11,13 Nodules often are precipitated by cold weather or venostasis.1,11,12
Silva et al14 reported a case of EIB on the lower legs associated with a burning sensation on the feet and paresthesia; all known causes of peripheral neuropathy were excluded by a comprehensive laboratory workup. The burning sensation on the feet resolved after several weeks of antituberculosis therapy. Our patient also presented with a burning sensation on the feet that remarkably improved after 6 months of antituberculosis therapy. Peripheral neuropathy could have been a consequence of diabetes mellitus in our patient, though neuronal damage also could be a consequence of hypersensitivity to tuberculosis antigens. Silva et al14 proposed that macrophages activated by M tuberculosis antigens produce lytic enzymes that can cause tissue necrosis and nerve damage if released into surrounding tissue.
Diagnosis
The diagnosis of EIB is made based on clinical presentation, evidence of prior or current tuberculosis infection, histopathologic findings, and response to antituberculosis therapy.15 Evidence of active or latent tuberculosis infection typically is gathered by patient history, chest radiograph, tuberculin skin tests, interferon-releasing assays, and PCR of skin biopsies. Tuberculin skin tests in patients with EIB result in reactive induration that is typically more than 20 mm.8 In vitro T-lymphocyte proliferation assays in response to PPD have further supported the suggestion that there is a markedly enhanced T-lymphocyte response to M tuberculosis antigens in patients with EIB.16
IFN-γ release assays have provided useful methods for the detection of latent tuberculosis infection.17 The IGRA is effective when the tuberculin skin test yields a suspected false-negative or in the context of prior bacille Calmette-Guérin vaccination.17 IFN-γ release assays also may be preferred to tuberculin skin tests because it provides less discomfort to the patient in the event of a positive hypersensitive reaction to the PPD.
Before the advent of IGRAs, PCR was used to detect M tuberculosis DNA in skin biopsies and to confirm the diagnosis of EIB. Some researchers believe PCR can be an important tool for confirming a diagnosis of EIB, especially in cases and countries where results from the Mantoux test do not have great value.15,18 A PCR assay for detecting M tuberculosis DNA in blood and urine samples also was found helpful in confirming a diagnosis of EIB when skin biopsies were unavailable.8,19 However, PCR has been shown to have low sensitivity for the diagnosis of EIB because of its ability to detect M tuberculosis DNA ranging from 0% to 77% of skin biopsy specimens.20,21 Therefore, a negative PCR for the detection of M tuberculosis DNA in nodules does not exclude a diagnosis of erythema induratum.
Treatment
The mainstay of EIB treatment is a multidrug antituberculosis regimen.5,8,10-12 Our patient was successfully treated with rifampin and isoniazid and a repeat IGRA was used as a laboratory marker of response to therapy. Single-drug therapy with isoniazid has been shown to result in greater likelihood of EIB relapse in comparison to multidrug regimens.22 Other treatments include potassium iodide and gold, but they are not well-studied.23-25 Treatment of venous insufficiency with bed rest and nonsteroidal anti-inflammatory drugs for pain also may be helpful.2 In cases of nodular vasulitis that are not associated with tuberculosis infection, treatment should be targeted at the underlying cause of the immune response. For example, a case of nodular vasculitis associated with hepatitis C virus did not respond to antituberculosis multidrug therapy, but skin lesions did improve with pegylated interferon and ribavirin.4
1. Segura S, Pujol RM, Trindade F, et al. Vasculitis in erythema induratum of Bazin: a histopathologic study of 101 biopsy specimens from 86 patients. J Am Acad Dermatol. 2008;59:839-851.
2. Requena L, Sánchez Yus E. Panniculitis. part II. mostly lobular panniculitis. J Am Acad Dermatol. 2001;45:325-361.
3. Montgomery H, O’Leary PA, Barker NW. Nodular vascular disease of the legs: erythema induratum and allied conditions. JAMA. 1945;128:335-342.
4. Fernandes SS, Carvalho J, Leite S, et al. Erythema induratum and chronic hepatitis C infection [published online ahead of print February 23, 2009]. J Clin Virol. 2009;44:333-336.
5. Gilchrist H, Patterson JW. Erythema nodosum and erythema induratum (nodular vasculitis): diagnosis and management. Dermatol Ther. 2010;23:320-327.
6. Frankel A, Penrose C, Emer J. Cutaneous tuberculosis: a practical case report and review for the dermatologist. J Clin Aesthet Dermatol. 2009;2:19-27.
7. Schneider JW, Jordaan HF, Geiger DH, et al. Erythema induratum of Bazin. a clinicopathological study of 20 cases and detection of Mycobacterium tuberculosis DNA in skin lesions by polymerase chain reaction. Am J Dermatopathol. 1995;17:350-356.
8. Lighter J, Tse DB, Li Y, et al. Erythema induratum of Bazin in a child: evidence for a cell-mediated hyper-response to Mycobacterium tuberculosis. Pediatr Infect Dis J. 2009;28:326-328.
9. Bravo FG, Gotuzzo E. Cutaneous tuberculosis. Clin Dermatol. 2007;25:173-180.
10. Rademaker M, Lowe DG, Munro DD. Erythema induratum (Bazin’s disease). J Am Acad Dermatol. 1989;21 (4, pt 1):740-745.
11. Sharon V, Goodarzi H, Chambers CJ, et al. Erythema induratum of Bazin. Dermatol Online J. 2010;16:1.
12. Feiwel M, Munro DD. Diagnosis and treatment of erythema induratum (Bazin). Br Med J. 1965;1:1109-1111.
13. Lebel M, Lassonde M. Erythema induratum of Bazin. J Am Acad Dermatol. 1986;14(5, pt 1):738-742.
14. Silva MT, Antunes SL, Rolla VC, et al. Distal painful peripheral neuropathy associated with erythema induratum of Bazin. Eur J Neurol. 2006;13:e5-e6.
15. Jacinto SS, Nograles KB. Erythema induratum of bazin: role of polymerase chain reaction in diagnosis. Int J Dermatol. 2003;42:380-381.
16. Ollert MW, Thomas P, Korting HC, et al. Erythema induratum of Bazin. evidence of T-lymphocyte hyperresponsiveness to purified protein derivative of tuberculin: report of two cases and treatment. Arch Dermatol. 1993;129:469-473.
17. Angus J, Roberts C, Kulkarni K, et al. Usefulness of the QuantiFERON test in the confirmation of latent tuberculosis in association with erythema induratum [published online ahead of print October 10, 2007]. Br J Dermatol. 2007;157:1293-1294.
18. Seckin D, Hízel N, Demirhan B, et al. The diagnostic value of polymerase chain reaction in erythema induratum of Bazin. Br J Dermatol. 1997;137:1011-1012.
19. Cannas A, Goletti D, Girardi E, et al. Mycobacterium tuberculosis DNA detection in soluble fraction of urine from pulmonary tuberculosis patients. Int J Tuberc Lung Dis. 2008;12:146-151.
20. Tan SH, Tan BH, Goh CL, et al. Detection of Mycobacterium tuberculosis DNA using polymerase chain reaction in cutaneous tuberculosis and tuberculids. Int J Dermatol. 1999;38:122-127.
21. Baselga E, Margall N, Barnadas MA, et al. Detection of Mycobacterium tuberculosis DNA in lobular granulomatous panniculitis (erythema induratum-nodular vasculitis). Arch Dermatol. 1997;133:457-462.
22. Cho KH, Lee DY, Kim CW. Erythema induratum of Bazin. Int J Dermatol. 1996;35:802-808.
23. Schulz EJ, Whiting DA. Treatment of erythema nodosum and nodular vasculitis with potassium iodide. Br J Dermatol. 1976;94:75-78.
24. Horio T, Imamura S, Danno K, et al. Potassium iodide in the treatment of erythema nodosum and nodular vasculitis. Arch Dermatol. 1981;117:29-31.
25. Shaffer N, Kerdel FA. Nodular vasculitis (erythema induratum): treatment with auranofin. J Am Acad Dermatol. 1991;25(2, pt 2):426-429.
Case Report
A 54-year-old Hispanic woman with a history of type 2 diabetes mellitus and hyperlipidemia presented with recurrent painful plaques and nodules on the bilateral lower extremities and a severe burning sensation on the feet of 3 years’ duration. The patient denied experiencing any associated fevers, chills, night sweats, weight loss, joint aches, cough, or shortness of breath. She had a history of pustular psoriasis and reported a positive purified protein derivative (PPD)(tuberculin) skin test approximately 40 years prior.
She presented with a 4×4-cm, poorly defined, tender, indurated plaque on the middle of the left shin and a 2×3-cm, red-brown plaque on the dorsal aspect of the left foot (Figure 1). No lymphadenopathy or any other abnormalities were noted. The clinical differential diagnosis included various panniculitides, such as erythema nodosum, erythema induratum of Bazin (EIB), and lupus panniculitis, as well as other conditions, including polyarteritis nodosa, sarcoidosis, Sweet disease, deep fungal and mycobacterial infections, and cutaneous lymphoma.


|
| Figure 1. Erythematous indurated plaques on the middle of the left shin (A) and on the dorsal aspect of the left foot (B). |
Two skin biopsies taken for histopathologic evaluation revealed primarily granulomatous lobular panniculitis with foci of microthrombi and vasculitis (Figure 2). These findings were consistent with nodular vasculitis. Acid-fast bacillus and Gomori methenamine-silver stains were negative for mycobacterial or fungal organisms. Tissue cultures also were negative. Results from a complete blood cell count, chemistry panel, thyroid and liver function tests, hepatitis panel, and rapid plasma reagin test were unremarkable. Immunologic markers, including antinuclear antibody, antineutrophil cytoplasmic antibody, rheumatoid factor, and cryoglobulins, also revealed no abnormalities. A chest radiograph showed scarring in the suprahilar region of the upper lobe of the left lung consistent with a prior case of pulmonary tuberculosis, and exposure to Mycobacterium tuberculosis was confirmed with an IFN-γ release assay (IGRA) result of 1.49 IU/mL (>0.34 IU/mL indicates positive test). These findings from clinical and histopathologic examination as well as laboratory tests were consistent with a diagnosis of EIB.

|
Figure 2. Granulomatous lobular panniculitis (A)(H&E, original magnification ×40) with foci of microthrombi and vasculitis (B and C)(both H&E, original magnifications ×200). |
Standard antituberculosis therapy with rifampin, isoniazid, pyrazinamide, and ethambutol (RIPE) was simplified to rifampin and isoniazid due to her inability to tolerate the full regimen because of gastrointestinal tract upset and diarrhea. After 6 months of therapy, a repeat IGRA decreased to 0.43 IU/mL, and the painful plaques and nodules on the lower extremities and burning sensation in the feet completely resolved.
Comment
Our case of EIB associated with peripheral neuropathy is a unique presentation of lesions on the pretibial area of the bilateral legs and dorsal aspect of the feet. We confirmed the presence of latent tuberculosis infection with a chest radiograph and an IGRA. Symptoms of peripheral neuropathy resolved after antituberculosis treatment, which suggests an immune-mediated mechanism of neuronal damage from circulating tuberculosis antigens.
Pathogenesis
Although erythema induratum was first described by Ernest Bazin in 1861, it was not until the early 1900s that the link between tuberculosis and erythema induratum was made by French dermatologists.1,2 Around the same time, similar cases of erythema induratum were discovered in England with no evidence of tuberculosis, which led to the distinct classification of erythema induratum of Whitfield (EIW). This classification described these nontuberculoid cases.1,2 In 1945, Montgomery et al3 in the United States coined the term nodular vasculitis for EIW and categorized its clinical features and histopathology as separate from EIB.3 Today, some authors use EIB, EIW, and nodular vasculitis interchangeably and believe they all are the same entity.2 We use EIB for all cases related to tuberculosis and nodular vasulitis when referring to all other etiologies, including nontuberculoid bacterial infections, chronic hepatitis B and C virus, thrombophlebitis, hypothyroidism, and rheumatoid arthritis.4,5
Erythema induratum of Bazin, lichen scrofulosorum, and papulonecrotic tuberculids are considered tuberculid diseases and are thought to be caused by hypersensitivity reactions to mycobacterial antigens rather than local mycobacterial infections. Tuberculids are believed to be a reaction to an id reaction of circulating mycobacterial antigens in the setting of latent or active tuberculosis infection. The basis for this view is that mycobacteria cannot be cultured or visualized from lesions in tuberculid diseases.6 Cutaneous tuberculosis, such as scrofuloderma, miliary tuberculosis, tuberculosis chancre, lupus vulgaris, and gummatous tuberculosis, differ from EIB and other tuberculid diseases in that mycobacteria can be cultured and visualized on histologic examination with Ziehl-Neelsen staining.6 The pathology of cutaneous tuberculosis results from a mycobacterial infection of the skin, and cutaneous tuberculosis diseases are categorized as multibacillary or paucibacillary based on the number of organisms visualized in biopsies.
The absence of M tuberculosis organisms in skin lesions has led some to doubt the causal relationship between M tuberculosis and EIB.7 However, the advent of polymerase chain reaction (PCR) and specific DNA primers for M tuberculosis has allowed for the detection of M tuberculosis DNA in biopsy specimens, which has further established the relationship between tuberculosis and EIB.5 Some authors have suggested that the absence of mycobacteria in EIB and other tuberculid lesions may be due to small numbers of bacilli in the lesions or early destruction of mycobacteria organisms before biopsy.8,9 These authors consider cutaneous tuberculosis and tuberculids as diseases on the same spectrum, with tuberculids representing one extreme in which there are few mycobacteria organisms present in the lesions.
Presentation
Erythema induratum commonly affects middle-aged women and presents with recurrent crops of tender nodules on the lower extremities.10-13 Nodules often are most commonly found on the lower calves but also can present on the arms, thighs, feet, or buttocks.10 Our patient’s presentation was atypical in that lesions were distributed on the pretibial area of the legs and dorsal aspect of the feet. Obesity and venous insufficiency of the lower extremities are believed to be predisposing factors to the development of EIB nodules.2 The nodules develop over several weeks and heal over several months with possible ulceration and hyperpigmented scarring.10,11 Ulcerated nodules often are irregular and shallow with an overlying crust and a bluish border.11,13 Nodules often are precipitated by cold weather or venostasis.1,11,12
Silva et al14 reported a case of EIB on the lower legs associated with a burning sensation on the feet and paresthesia; all known causes of peripheral neuropathy were excluded by a comprehensive laboratory workup. The burning sensation on the feet resolved after several weeks of antituberculosis therapy. Our patient also presented with a burning sensation on the feet that remarkably improved after 6 months of antituberculosis therapy. Peripheral neuropathy could have been a consequence of diabetes mellitus in our patient, though neuronal damage also could be a consequence of hypersensitivity to tuberculosis antigens. Silva et al14 proposed that macrophages activated by M tuberculosis antigens produce lytic enzymes that can cause tissue necrosis and nerve damage if released into surrounding tissue.
Diagnosis
The diagnosis of EIB is made based on clinical presentation, evidence of prior or current tuberculosis infection, histopathologic findings, and response to antituberculosis therapy.15 Evidence of active or latent tuberculosis infection typically is gathered by patient history, chest radiograph, tuberculin skin tests, interferon-releasing assays, and PCR of skin biopsies. Tuberculin skin tests in patients with EIB result in reactive induration that is typically more than 20 mm.8 In vitro T-lymphocyte proliferation assays in response to PPD have further supported the suggestion that there is a markedly enhanced T-lymphocyte response to M tuberculosis antigens in patients with EIB.16
IFN-γ release assays have provided useful methods for the detection of latent tuberculosis infection.17 The IGRA is effective when the tuberculin skin test yields a suspected false-negative or in the context of prior bacille Calmette-Guérin vaccination.17 IFN-γ release assays also may be preferred to tuberculin skin tests because it provides less discomfort to the patient in the event of a positive hypersensitive reaction to the PPD.
Before the advent of IGRAs, PCR was used to detect M tuberculosis DNA in skin biopsies and to confirm the diagnosis of EIB. Some researchers believe PCR can be an important tool for confirming a diagnosis of EIB, especially in cases and countries where results from the Mantoux test do not have great value.15,18 A PCR assay for detecting M tuberculosis DNA in blood and urine samples also was found helpful in confirming a diagnosis of EIB when skin biopsies were unavailable.8,19 However, PCR has been shown to have low sensitivity for the diagnosis of EIB because of its ability to detect M tuberculosis DNA ranging from 0% to 77% of skin biopsy specimens.20,21 Therefore, a negative PCR for the detection of M tuberculosis DNA in nodules does not exclude a diagnosis of erythema induratum.
Treatment
The mainstay of EIB treatment is a multidrug antituberculosis regimen.5,8,10-12 Our patient was successfully treated with rifampin and isoniazid and a repeat IGRA was used as a laboratory marker of response to therapy. Single-drug therapy with isoniazid has been shown to result in greater likelihood of EIB relapse in comparison to multidrug regimens.22 Other treatments include potassium iodide and gold, but they are not well-studied.23-25 Treatment of venous insufficiency with bed rest and nonsteroidal anti-inflammatory drugs for pain also may be helpful.2 In cases of nodular vasulitis that are not associated with tuberculosis infection, treatment should be targeted at the underlying cause of the immune response. For example, a case of nodular vasculitis associated with hepatitis C virus did not respond to antituberculosis multidrug therapy, but skin lesions did improve with pegylated interferon and ribavirin.4
Case Report
A 54-year-old Hispanic woman with a history of type 2 diabetes mellitus and hyperlipidemia presented with recurrent painful plaques and nodules on the bilateral lower extremities and a severe burning sensation on the feet of 3 years’ duration. The patient denied experiencing any associated fevers, chills, night sweats, weight loss, joint aches, cough, or shortness of breath. She had a history of pustular psoriasis and reported a positive purified protein derivative (PPD)(tuberculin) skin test approximately 40 years prior.
She presented with a 4×4-cm, poorly defined, tender, indurated plaque on the middle of the left shin and a 2×3-cm, red-brown plaque on the dorsal aspect of the left foot (Figure 1). No lymphadenopathy or any other abnormalities were noted. The clinical differential diagnosis included various panniculitides, such as erythema nodosum, erythema induratum of Bazin (EIB), and lupus panniculitis, as well as other conditions, including polyarteritis nodosa, sarcoidosis, Sweet disease, deep fungal and mycobacterial infections, and cutaneous lymphoma.


|
| Figure 1. Erythematous indurated plaques on the middle of the left shin (A) and on the dorsal aspect of the left foot (B). |
Two skin biopsies taken for histopathologic evaluation revealed primarily granulomatous lobular panniculitis with foci of microthrombi and vasculitis (Figure 2). These findings were consistent with nodular vasculitis. Acid-fast bacillus and Gomori methenamine-silver stains were negative for mycobacterial or fungal organisms. Tissue cultures also were negative. Results from a complete blood cell count, chemistry panel, thyroid and liver function tests, hepatitis panel, and rapid plasma reagin test were unremarkable. Immunologic markers, including antinuclear antibody, antineutrophil cytoplasmic antibody, rheumatoid factor, and cryoglobulins, also revealed no abnormalities. A chest radiograph showed scarring in the suprahilar region of the upper lobe of the left lung consistent with a prior case of pulmonary tuberculosis, and exposure to Mycobacterium tuberculosis was confirmed with an IFN-γ release assay (IGRA) result of 1.49 IU/mL (>0.34 IU/mL indicates positive test). These findings from clinical and histopathologic examination as well as laboratory tests were consistent with a diagnosis of EIB.

|
Figure 2. Granulomatous lobular panniculitis (A)(H&E, original magnification ×40) with foci of microthrombi and vasculitis (B and C)(both H&E, original magnifications ×200). |
Standard antituberculosis therapy with rifampin, isoniazid, pyrazinamide, and ethambutol (RIPE) was simplified to rifampin and isoniazid due to her inability to tolerate the full regimen because of gastrointestinal tract upset and diarrhea. After 6 months of therapy, a repeat IGRA decreased to 0.43 IU/mL, and the painful plaques and nodules on the lower extremities and burning sensation in the feet completely resolved.
Comment
Our case of EIB associated with peripheral neuropathy is a unique presentation of lesions on the pretibial area of the bilateral legs and dorsal aspect of the feet. We confirmed the presence of latent tuberculosis infection with a chest radiograph and an IGRA. Symptoms of peripheral neuropathy resolved after antituberculosis treatment, which suggests an immune-mediated mechanism of neuronal damage from circulating tuberculosis antigens.
Pathogenesis
Although erythema induratum was first described by Ernest Bazin in 1861, it was not until the early 1900s that the link between tuberculosis and erythema induratum was made by French dermatologists.1,2 Around the same time, similar cases of erythema induratum were discovered in England with no evidence of tuberculosis, which led to the distinct classification of erythema induratum of Whitfield (EIW). This classification described these nontuberculoid cases.1,2 In 1945, Montgomery et al3 in the United States coined the term nodular vasculitis for EIW and categorized its clinical features and histopathology as separate from EIB.3 Today, some authors use EIB, EIW, and nodular vasculitis interchangeably and believe they all are the same entity.2 We use EIB for all cases related to tuberculosis and nodular vasulitis when referring to all other etiologies, including nontuberculoid bacterial infections, chronic hepatitis B and C virus, thrombophlebitis, hypothyroidism, and rheumatoid arthritis.4,5
Erythema induratum of Bazin, lichen scrofulosorum, and papulonecrotic tuberculids are considered tuberculid diseases and are thought to be caused by hypersensitivity reactions to mycobacterial antigens rather than local mycobacterial infections. Tuberculids are believed to be a reaction to an id reaction of circulating mycobacterial antigens in the setting of latent or active tuberculosis infection. The basis for this view is that mycobacteria cannot be cultured or visualized from lesions in tuberculid diseases.6 Cutaneous tuberculosis, such as scrofuloderma, miliary tuberculosis, tuberculosis chancre, lupus vulgaris, and gummatous tuberculosis, differ from EIB and other tuberculid diseases in that mycobacteria can be cultured and visualized on histologic examination with Ziehl-Neelsen staining.6 The pathology of cutaneous tuberculosis results from a mycobacterial infection of the skin, and cutaneous tuberculosis diseases are categorized as multibacillary or paucibacillary based on the number of organisms visualized in biopsies.
The absence of M tuberculosis organisms in skin lesions has led some to doubt the causal relationship between M tuberculosis and EIB.7 However, the advent of polymerase chain reaction (PCR) and specific DNA primers for M tuberculosis has allowed for the detection of M tuberculosis DNA in biopsy specimens, which has further established the relationship between tuberculosis and EIB.5 Some authors have suggested that the absence of mycobacteria in EIB and other tuberculid lesions may be due to small numbers of bacilli in the lesions or early destruction of mycobacteria organisms before biopsy.8,9 These authors consider cutaneous tuberculosis and tuberculids as diseases on the same spectrum, with tuberculids representing one extreme in which there are few mycobacteria organisms present in the lesions.
Presentation
Erythema induratum commonly affects middle-aged women and presents with recurrent crops of tender nodules on the lower extremities.10-13 Nodules often are most commonly found on the lower calves but also can present on the arms, thighs, feet, or buttocks.10 Our patient’s presentation was atypical in that lesions were distributed on the pretibial area of the legs and dorsal aspect of the feet. Obesity and venous insufficiency of the lower extremities are believed to be predisposing factors to the development of EIB nodules.2 The nodules develop over several weeks and heal over several months with possible ulceration and hyperpigmented scarring.10,11 Ulcerated nodules often are irregular and shallow with an overlying crust and a bluish border.11,13 Nodules often are precipitated by cold weather or venostasis.1,11,12
Silva et al14 reported a case of EIB on the lower legs associated with a burning sensation on the feet and paresthesia; all known causes of peripheral neuropathy were excluded by a comprehensive laboratory workup. The burning sensation on the feet resolved after several weeks of antituberculosis therapy. Our patient also presented with a burning sensation on the feet that remarkably improved after 6 months of antituberculosis therapy. Peripheral neuropathy could have been a consequence of diabetes mellitus in our patient, though neuronal damage also could be a consequence of hypersensitivity to tuberculosis antigens. Silva et al14 proposed that macrophages activated by M tuberculosis antigens produce lytic enzymes that can cause tissue necrosis and nerve damage if released into surrounding tissue.
Diagnosis
The diagnosis of EIB is made based on clinical presentation, evidence of prior or current tuberculosis infection, histopathologic findings, and response to antituberculosis therapy.15 Evidence of active or latent tuberculosis infection typically is gathered by patient history, chest radiograph, tuberculin skin tests, interferon-releasing assays, and PCR of skin biopsies. Tuberculin skin tests in patients with EIB result in reactive induration that is typically more than 20 mm.8 In vitro T-lymphocyte proliferation assays in response to PPD have further supported the suggestion that there is a markedly enhanced T-lymphocyte response to M tuberculosis antigens in patients with EIB.16
IFN-γ release assays have provided useful methods for the detection of latent tuberculosis infection.17 The IGRA is effective when the tuberculin skin test yields a suspected false-negative or in the context of prior bacille Calmette-Guérin vaccination.17 IFN-γ release assays also may be preferred to tuberculin skin tests because it provides less discomfort to the patient in the event of a positive hypersensitive reaction to the PPD.
Before the advent of IGRAs, PCR was used to detect M tuberculosis DNA in skin biopsies and to confirm the diagnosis of EIB. Some researchers believe PCR can be an important tool for confirming a diagnosis of EIB, especially in cases and countries where results from the Mantoux test do not have great value.15,18 A PCR assay for detecting M tuberculosis DNA in blood and urine samples also was found helpful in confirming a diagnosis of EIB when skin biopsies were unavailable.8,19 However, PCR has been shown to have low sensitivity for the diagnosis of EIB because of its ability to detect M tuberculosis DNA ranging from 0% to 77% of skin biopsy specimens.20,21 Therefore, a negative PCR for the detection of M tuberculosis DNA in nodules does not exclude a diagnosis of erythema induratum.
Treatment
The mainstay of EIB treatment is a multidrug antituberculosis regimen.5,8,10-12 Our patient was successfully treated with rifampin and isoniazid and a repeat IGRA was used as a laboratory marker of response to therapy. Single-drug therapy with isoniazid has been shown to result in greater likelihood of EIB relapse in comparison to multidrug regimens.22 Other treatments include potassium iodide and gold, but they are not well-studied.23-25 Treatment of venous insufficiency with bed rest and nonsteroidal anti-inflammatory drugs for pain also may be helpful.2 In cases of nodular vasulitis that are not associated with tuberculosis infection, treatment should be targeted at the underlying cause of the immune response. For example, a case of nodular vasculitis associated with hepatitis C virus did not respond to antituberculosis multidrug therapy, but skin lesions did improve with pegylated interferon and ribavirin.4
1. Segura S, Pujol RM, Trindade F, et al. Vasculitis in erythema induratum of Bazin: a histopathologic study of 101 biopsy specimens from 86 patients. J Am Acad Dermatol. 2008;59:839-851.
2. Requena L, Sánchez Yus E. Panniculitis. part II. mostly lobular panniculitis. J Am Acad Dermatol. 2001;45:325-361.
3. Montgomery H, O’Leary PA, Barker NW. Nodular vascular disease of the legs: erythema induratum and allied conditions. JAMA. 1945;128:335-342.
4. Fernandes SS, Carvalho J, Leite S, et al. Erythema induratum and chronic hepatitis C infection [published online ahead of print February 23, 2009]. J Clin Virol. 2009;44:333-336.
5. Gilchrist H, Patterson JW. Erythema nodosum and erythema induratum (nodular vasculitis): diagnosis and management. Dermatol Ther. 2010;23:320-327.
6. Frankel A, Penrose C, Emer J. Cutaneous tuberculosis: a practical case report and review for the dermatologist. J Clin Aesthet Dermatol. 2009;2:19-27.
7. Schneider JW, Jordaan HF, Geiger DH, et al. Erythema induratum of Bazin. a clinicopathological study of 20 cases and detection of Mycobacterium tuberculosis DNA in skin lesions by polymerase chain reaction. Am J Dermatopathol. 1995;17:350-356.
8. Lighter J, Tse DB, Li Y, et al. Erythema induratum of Bazin in a child: evidence for a cell-mediated hyper-response to Mycobacterium tuberculosis. Pediatr Infect Dis J. 2009;28:326-328.
9. Bravo FG, Gotuzzo E. Cutaneous tuberculosis. Clin Dermatol. 2007;25:173-180.
10. Rademaker M, Lowe DG, Munro DD. Erythema induratum (Bazin’s disease). J Am Acad Dermatol. 1989;21 (4, pt 1):740-745.
11. Sharon V, Goodarzi H, Chambers CJ, et al. Erythema induratum of Bazin. Dermatol Online J. 2010;16:1.
12. Feiwel M, Munro DD. Diagnosis and treatment of erythema induratum (Bazin). Br Med J. 1965;1:1109-1111.
13. Lebel M, Lassonde M. Erythema induratum of Bazin. J Am Acad Dermatol. 1986;14(5, pt 1):738-742.
14. Silva MT, Antunes SL, Rolla VC, et al. Distal painful peripheral neuropathy associated with erythema induratum of Bazin. Eur J Neurol. 2006;13:e5-e6.
15. Jacinto SS, Nograles KB. Erythema induratum of bazin: role of polymerase chain reaction in diagnosis. Int J Dermatol. 2003;42:380-381.
16. Ollert MW, Thomas P, Korting HC, et al. Erythema induratum of Bazin. evidence of T-lymphocyte hyperresponsiveness to purified protein derivative of tuberculin: report of two cases and treatment. Arch Dermatol. 1993;129:469-473.
17. Angus J, Roberts C, Kulkarni K, et al. Usefulness of the QuantiFERON test in the confirmation of latent tuberculosis in association with erythema induratum [published online ahead of print October 10, 2007]. Br J Dermatol. 2007;157:1293-1294.
18. Seckin D, Hízel N, Demirhan B, et al. The diagnostic value of polymerase chain reaction in erythema induratum of Bazin. Br J Dermatol. 1997;137:1011-1012.
19. Cannas A, Goletti D, Girardi E, et al. Mycobacterium tuberculosis DNA detection in soluble fraction of urine from pulmonary tuberculosis patients. Int J Tuberc Lung Dis. 2008;12:146-151.
20. Tan SH, Tan BH, Goh CL, et al. Detection of Mycobacterium tuberculosis DNA using polymerase chain reaction in cutaneous tuberculosis and tuberculids. Int J Dermatol. 1999;38:122-127.
21. Baselga E, Margall N, Barnadas MA, et al. Detection of Mycobacterium tuberculosis DNA in lobular granulomatous panniculitis (erythema induratum-nodular vasculitis). Arch Dermatol. 1997;133:457-462.
22. Cho KH, Lee DY, Kim CW. Erythema induratum of Bazin. Int J Dermatol. 1996;35:802-808.
23. Schulz EJ, Whiting DA. Treatment of erythema nodosum and nodular vasculitis with potassium iodide. Br J Dermatol. 1976;94:75-78.
24. Horio T, Imamura S, Danno K, et al. Potassium iodide in the treatment of erythema nodosum and nodular vasculitis. Arch Dermatol. 1981;117:29-31.
25. Shaffer N, Kerdel FA. Nodular vasculitis (erythema induratum): treatment with auranofin. J Am Acad Dermatol. 1991;25(2, pt 2):426-429.
1. Segura S, Pujol RM, Trindade F, et al. Vasculitis in erythema induratum of Bazin: a histopathologic study of 101 biopsy specimens from 86 patients. J Am Acad Dermatol. 2008;59:839-851.
2. Requena L, Sánchez Yus E. Panniculitis. part II. mostly lobular panniculitis. J Am Acad Dermatol. 2001;45:325-361.
3. Montgomery H, O’Leary PA, Barker NW. Nodular vascular disease of the legs: erythema induratum and allied conditions. JAMA. 1945;128:335-342.
4. Fernandes SS, Carvalho J, Leite S, et al. Erythema induratum and chronic hepatitis C infection [published online ahead of print February 23, 2009]. J Clin Virol. 2009;44:333-336.
5. Gilchrist H, Patterson JW. Erythema nodosum and erythema induratum (nodular vasculitis): diagnosis and management. Dermatol Ther. 2010;23:320-327.
6. Frankel A, Penrose C, Emer J. Cutaneous tuberculosis: a practical case report and review for the dermatologist. J Clin Aesthet Dermatol. 2009;2:19-27.
7. Schneider JW, Jordaan HF, Geiger DH, et al. Erythema induratum of Bazin. a clinicopathological study of 20 cases and detection of Mycobacterium tuberculosis DNA in skin lesions by polymerase chain reaction. Am J Dermatopathol. 1995;17:350-356.
8. Lighter J, Tse DB, Li Y, et al. Erythema induratum of Bazin in a child: evidence for a cell-mediated hyper-response to Mycobacterium tuberculosis. Pediatr Infect Dis J. 2009;28:326-328.
9. Bravo FG, Gotuzzo E. Cutaneous tuberculosis. Clin Dermatol. 2007;25:173-180.
10. Rademaker M, Lowe DG, Munro DD. Erythema induratum (Bazin’s disease). J Am Acad Dermatol. 1989;21 (4, pt 1):740-745.
11. Sharon V, Goodarzi H, Chambers CJ, et al. Erythema induratum of Bazin. Dermatol Online J. 2010;16:1.
12. Feiwel M, Munro DD. Diagnosis and treatment of erythema induratum (Bazin). Br Med J. 1965;1:1109-1111.
13. Lebel M, Lassonde M. Erythema induratum of Bazin. J Am Acad Dermatol. 1986;14(5, pt 1):738-742.
14. Silva MT, Antunes SL, Rolla VC, et al. Distal painful peripheral neuropathy associated with erythema induratum of Bazin. Eur J Neurol. 2006;13:e5-e6.
15. Jacinto SS, Nograles KB. Erythema induratum of bazin: role of polymerase chain reaction in diagnosis. Int J Dermatol. 2003;42:380-381.
16. Ollert MW, Thomas P, Korting HC, et al. Erythema induratum of Bazin. evidence of T-lymphocyte hyperresponsiveness to purified protein derivative of tuberculin: report of two cases and treatment. Arch Dermatol. 1993;129:469-473.
17. Angus J, Roberts C, Kulkarni K, et al. Usefulness of the QuantiFERON test in the confirmation of latent tuberculosis in association with erythema induratum [published online ahead of print October 10, 2007]. Br J Dermatol. 2007;157:1293-1294.
18. Seckin D, Hízel N, Demirhan B, et al. The diagnostic value of polymerase chain reaction in erythema induratum of Bazin. Br J Dermatol. 1997;137:1011-1012.
19. Cannas A, Goletti D, Girardi E, et al. Mycobacterium tuberculosis DNA detection in soluble fraction of urine from pulmonary tuberculosis patients. Int J Tuberc Lung Dis. 2008;12:146-151.
20. Tan SH, Tan BH, Goh CL, et al. Detection of Mycobacterium tuberculosis DNA using polymerase chain reaction in cutaneous tuberculosis and tuberculids. Int J Dermatol. 1999;38:122-127.
21. Baselga E, Margall N, Barnadas MA, et al. Detection of Mycobacterium tuberculosis DNA in lobular granulomatous panniculitis (erythema induratum-nodular vasculitis). Arch Dermatol. 1997;133:457-462.
22. Cho KH, Lee DY, Kim CW. Erythema induratum of Bazin. Int J Dermatol. 1996;35:802-808.
23. Schulz EJ, Whiting DA. Treatment of erythema nodosum and nodular vasculitis with potassium iodide. Br J Dermatol. 1976;94:75-78.
24. Horio T, Imamura S, Danno K, et al. Potassium iodide in the treatment of erythema nodosum and nodular vasculitis. Arch Dermatol. 1981;117:29-31.
25. Shaffer N, Kerdel FA. Nodular vasculitis (erythema induratum): treatment with auranofin. J Am Acad Dermatol. 1991;25(2, pt 2):426-429.
Practice Points
- Erythema induratum of Bazin (EIB) is a type of nodular vasculitis related to tuberculosis and commonly presents with plaques and nodules on the lower extremities.
- Peripheral neuropathy may manifest as a result of a hypersensitivity reaction to tuberculosis antigens causing tissue and nerve damage.
- Treatment of EIB and other cases of nodular vasculitis should be directed at the underlying cause of the immune response.
