User login
Bullets no match for dual-energy CT scrutiny
CHICAGO – Dual-energy computed tomography may have a role in clearing patients with embedded bullets and other metallic objects for magnetic resonance imaging who would otherwise be excluded because of safety concerns.
A Swiss analysis of bullets and shotgun pellets found that dual-energy CT had a high discriminatory power to distinguish between projectiles with and without ferromagnetic properties. MR safety depends on whether a metallic object has ferromagnetic properties – something that most patients don’t know or may be unable to communicate during an emergency evaluation, study author Dr. Sebastian Winklhofer said at the annual meeting of the Radiological Society of North America.
"Dual-energy measurements may contribute to MR safety and allow for MR imaging of patients with retained projectiles," he said.
Retained metallic objects such as bullets, shrapnel, and medical devices are frequently contraindicated for MRI, because they might move, dislodge, or accelerate at dangerously high velocities toward the scanner’s magnet. This has led to patient injury, and in some cases death, if the object is located near or in a critical anatomic structure.
Session comoderator Dr. Seppo Koskinen of Helsinki University Central Hospital, Finland, said he recently had to forgo MR imaging in a patient with a bullet lodged in the spinal canal because the patient didn’t know if it was lead or steel.
"We didn’t do an MR, but maybe with this system we could have," he said in an interview. "So it has a real clinical impact."
Unsafe exams and misinformed refusals to refer or scan a patient are also occurring as a result of confusion over the ever increasing number of metallic orthopedic and cardiovascular implants. For example, a device that is known to be safe on a 1.5 tesla scanner may be contraindicated on a more powerful 3T scanner or on other scanners using different settings.
When the American College of Radiology penned its Safe MR Practices guidelines in 2007, no cardiac pacemakers or implantable defibrillators were labeled as safe or conditionally safe for MR imaging, prompting the college to recommend that routine MRI is inadvisable in patients with these devices.
In its scientific statement on the controversial topic, the American Heart Association says data are available to support MR imaging in patients with cardiovascular devices, but recommends a series of precautions, including careful patient screening and an accurate determination of the device and its properties (Circulation 2007:116:2878-91).
Dual-energy CT has been used in research and clinical settings to assess the composition of various objects, said Dr. Winklhofer of University Hospital Zurich, Switzerland. He highlighted one study showing that dual-energy CT had a 98% specificity in differentiating between urinary stones that did or did not contain uric acid (Invest. Radiology 2010;45:1-6).
In the current study, nine bullets and two shotgun pellets were scanned in an ex vivo chest phantom using second-generation dual-source CT (SOMATOM Definition Flash, Siemens Healthcare), with tube voltages set at 80, 100, 120, and 140 kVp. Two readers, blinded to the ferromagnetic properties of the projectiles, independently assessed CT numbers on 44 images reconstructed using the extended CT scale technique, which helps overcome artifacts arising from metallic objects. A CT number is the density assigned to a voxel in a CT scan.
Dual-energy indices (DEI) were calculated from 80/140 kVP and 100/140 kVP pairs, and receiver operating characteristics analyses were fitted to predict ferromagnetic properties by means of DEI and CT numbers.
The bullets/pellets ranged in diameter from 2 mm to 14 mm; five were ferromagnetic and six nonferromagnetic.
Intrareader agreement was significantly correlated with mean CT number measurements (P less than .001), with excellent intraclass correlation coefficient agreement (Reader 1: ICC = 0.998; Reader 2: ICC = 0.963), Dr. Winklhofer said.
Interreader agreement was also significantly correlated (P less than .001), and again, there was excellent ICC agreement (both readers ICC = 0.988).
In contrast, when the same projectiles were scanned with single-energy CT, no significant differences in CT numbers for ferromagnetic vs. nonferromagnetic projectiles were observed, said Dr. Winklhofer, who received the RSNA Trainee Research prize for his work.
"Single-energy does not allow for differentiation between those types of projectiles, whereas the dual-energy results show it is possible to differentiate between ferromagnetic and nonferromagnetic projectiles," he said.
Finally, the dual-energy indices of ferromagnetic projectiles were significantly higher than were those of nonferromagnetic projectiles for both the 80/140 kVP and 100/140 kVP energy pairs (at a P value less than .10).
Before dual-energy CT is ready for prime time, however, additional studies are needed to prove that the technique is valid in phantoms of other body regions and in humans, Dr. Winklhofer said in an interview. The prospective study is currently underway.
Dr. Winklhofer and Dr. Koskinen reported no conflicts of interest.
CHICAGO – Dual-energy computed tomography may have a role in clearing patients with embedded bullets and other metallic objects for magnetic resonance imaging who would otherwise be excluded because of safety concerns.
A Swiss analysis of bullets and shotgun pellets found that dual-energy CT had a high discriminatory power to distinguish between projectiles with and without ferromagnetic properties. MR safety depends on whether a metallic object has ferromagnetic properties – something that most patients don’t know or may be unable to communicate during an emergency evaluation, study author Dr. Sebastian Winklhofer said at the annual meeting of the Radiological Society of North America.
"Dual-energy measurements may contribute to MR safety and allow for MR imaging of patients with retained projectiles," he said.
Retained metallic objects such as bullets, shrapnel, and medical devices are frequently contraindicated for MRI, because they might move, dislodge, or accelerate at dangerously high velocities toward the scanner’s magnet. This has led to patient injury, and in some cases death, if the object is located near or in a critical anatomic structure.
Session comoderator Dr. Seppo Koskinen of Helsinki University Central Hospital, Finland, said he recently had to forgo MR imaging in a patient with a bullet lodged in the spinal canal because the patient didn’t know if it was lead or steel.
"We didn’t do an MR, but maybe with this system we could have," he said in an interview. "So it has a real clinical impact."
Unsafe exams and misinformed refusals to refer or scan a patient are also occurring as a result of confusion over the ever increasing number of metallic orthopedic and cardiovascular implants. For example, a device that is known to be safe on a 1.5 tesla scanner may be contraindicated on a more powerful 3T scanner or on other scanners using different settings.
When the American College of Radiology penned its Safe MR Practices guidelines in 2007, no cardiac pacemakers or implantable defibrillators were labeled as safe or conditionally safe for MR imaging, prompting the college to recommend that routine MRI is inadvisable in patients with these devices.
In its scientific statement on the controversial topic, the American Heart Association says data are available to support MR imaging in patients with cardiovascular devices, but recommends a series of precautions, including careful patient screening and an accurate determination of the device and its properties (Circulation 2007:116:2878-91).
Dual-energy CT has been used in research and clinical settings to assess the composition of various objects, said Dr. Winklhofer of University Hospital Zurich, Switzerland. He highlighted one study showing that dual-energy CT had a 98% specificity in differentiating between urinary stones that did or did not contain uric acid (Invest. Radiology 2010;45:1-6).
In the current study, nine bullets and two shotgun pellets were scanned in an ex vivo chest phantom using second-generation dual-source CT (SOMATOM Definition Flash, Siemens Healthcare), with tube voltages set at 80, 100, 120, and 140 kVp. Two readers, blinded to the ferromagnetic properties of the projectiles, independently assessed CT numbers on 44 images reconstructed using the extended CT scale technique, which helps overcome artifacts arising from metallic objects. A CT number is the density assigned to a voxel in a CT scan.
Dual-energy indices (DEI) were calculated from 80/140 kVP and 100/140 kVP pairs, and receiver operating characteristics analyses were fitted to predict ferromagnetic properties by means of DEI and CT numbers.
The bullets/pellets ranged in diameter from 2 mm to 14 mm; five were ferromagnetic and six nonferromagnetic.
Intrareader agreement was significantly correlated with mean CT number measurements (P less than .001), with excellent intraclass correlation coefficient agreement (Reader 1: ICC = 0.998; Reader 2: ICC = 0.963), Dr. Winklhofer said.
Interreader agreement was also significantly correlated (P less than .001), and again, there was excellent ICC agreement (both readers ICC = 0.988).
In contrast, when the same projectiles were scanned with single-energy CT, no significant differences in CT numbers for ferromagnetic vs. nonferromagnetic projectiles were observed, said Dr. Winklhofer, who received the RSNA Trainee Research prize for his work.
"Single-energy does not allow for differentiation between those types of projectiles, whereas the dual-energy results show it is possible to differentiate between ferromagnetic and nonferromagnetic projectiles," he said.
Finally, the dual-energy indices of ferromagnetic projectiles were significantly higher than were those of nonferromagnetic projectiles for both the 80/140 kVP and 100/140 kVP energy pairs (at a P value less than .10).
Before dual-energy CT is ready for prime time, however, additional studies are needed to prove that the technique is valid in phantoms of other body regions and in humans, Dr. Winklhofer said in an interview. The prospective study is currently underway.
Dr. Winklhofer and Dr. Koskinen reported no conflicts of interest.
CHICAGO – Dual-energy computed tomography may have a role in clearing patients with embedded bullets and other metallic objects for magnetic resonance imaging who would otherwise be excluded because of safety concerns.
A Swiss analysis of bullets and shotgun pellets found that dual-energy CT had a high discriminatory power to distinguish between projectiles with and without ferromagnetic properties. MR safety depends on whether a metallic object has ferromagnetic properties – something that most patients don’t know or may be unable to communicate during an emergency evaluation, study author Dr. Sebastian Winklhofer said at the annual meeting of the Radiological Society of North America.
"Dual-energy measurements may contribute to MR safety and allow for MR imaging of patients with retained projectiles," he said.
Retained metallic objects such as bullets, shrapnel, and medical devices are frequently contraindicated for MRI, because they might move, dislodge, or accelerate at dangerously high velocities toward the scanner’s magnet. This has led to patient injury, and in some cases death, if the object is located near or in a critical anatomic structure.
Session comoderator Dr. Seppo Koskinen of Helsinki University Central Hospital, Finland, said he recently had to forgo MR imaging in a patient with a bullet lodged in the spinal canal because the patient didn’t know if it was lead or steel.
"We didn’t do an MR, but maybe with this system we could have," he said in an interview. "So it has a real clinical impact."
Unsafe exams and misinformed refusals to refer or scan a patient are also occurring as a result of confusion over the ever increasing number of metallic orthopedic and cardiovascular implants. For example, a device that is known to be safe on a 1.5 tesla scanner may be contraindicated on a more powerful 3T scanner or on other scanners using different settings.
When the American College of Radiology penned its Safe MR Practices guidelines in 2007, no cardiac pacemakers or implantable defibrillators were labeled as safe or conditionally safe for MR imaging, prompting the college to recommend that routine MRI is inadvisable in patients with these devices.
In its scientific statement on the controversial topic, the American Heart Association says data are available to support MR imaging in patients with cardiovascular devices, but recommends a series of precautions, including careful patient screening and an accurate determination of the device and its properties (Circulation 2007:116:2878-91).
Dual-energy CT has been used in research and clinical settings to assess the composition of various objects, said Dr. Winklhofer of University Hospital Zurich, Switzerland. He highlighted one study showing that dual-energy CT had a 98% specificity in differentiating between urinary stones that did or did not contain uric acid (Invest. Radiology 2010;45:1-6).
In the current study, nine bullets and two shotgun pellets were scanned in an ex vivo chest phantom using second-generation dual-source CT (SOMATOM Definition Flash, Siemens Healthcare), with tube voltages set at 80, 100, 120, and 140 kVp. Two readers, blinded to the ferromagnetic properties of the projectiles, independently assessed CT numbers on 44 images reconstructed using the extended CT scale technique, which helps overcome artifacts arising from metallic objects. A CT number is the density assigned to a voxel in a CT scan.
Dual-energy indices (DEI) were calculated from 80/140 kVP and 100/140 kVP pairs, and receiver operating characteristics analyses were fitted to predict ferromagnetic properties by means of DEI and CT numbers.
The bullets/pellets ranged in diameter from 2 mm to 14 mm; five were ferromagnetic and six nonferromagnetic.
Intrareader agreement was significantly correlated with mean CT number measurements (P less than .001), with excellent intraclass correlation coefficient agreement (Reader 1: ICC = 0.998; Reader 2: ICC = 0.963), Dr. Winklhofer said.
Interreader agreement was also significantly correlated (P less than .001), and again, there was excellent ICC agreement (both readers ICC = 0.988).
In contrast, when the same projectiles were scanned with single-energy CT, no significant differences in CT numbers for ferromagnetic vs. nonferromagnetic projectiles were observed, said Dr. Winklhofer, who received the RSNA Trainee Research prize for his work.
"Single-energy does not allow for differentiation between those types of projectiles, whereas the dual-energy results show it is possible to differentiate between ferromagnetic and nonferromagnetic projectiles," he said.
Finally, the dual-energy indices of ferromagnetic projectiles were significantly higher than were those of nonferromagnetic projectiles for both the 80/140 kVP and 100/140 kVP energy pairs (at a P value less than .10).
Before dual-energy CT is ready for prime time, however, additional studies are needed to prove that the technique is valid in phantoms of other body regions and in humans, Dr. Winklhofer said in an interview. The prospective study is currently underway.
Dr. Winklhofer and Dr. Koskinen reported no conflicts of interest.
AT THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Intrareader agreement was significantly correlated with mean CT number measurements (P less than .001), with excellent intraclass correlation coefficient agreement.
Data Source: Prospective analysis of ballistic projectiles.
Disclosures: Dr. Winklhofer and Dr. Koskinen reported no conflicts of interest.
Marshall score better predictor of early TBI death
CHICAGO – The Marshall CT classification system is a better predictor of early death in patients with traumatic brain injury than is the Rotterdam score, an award-winning study found.
As observed in previous reports, higher scores on both computed tomography–based scoring systems were significantly associated with early death among patients with mild to severe traumatic brain injury, or TBI (both P values less than .0001).
In a logistic regression analysis, however, only the Marshall scoring system was significantly associated with early death, defined as death at hospital discharge (P less than .002), Dr. Daddy Mata Mbemba reported at the annual meeting of the Radiological Society of North America.
This is likely because the two strongest independent predictors of early death – the absence of basal cistern and positive midline shift – are included in both CT scoring systems, while the next strongest predictor, hemorrhagic mass, is included in the Marshall score only, he explained.
Marshall and Rotterdam are the two most commonly used radiologic scoring systems, according to Dr. Mbemba, but they group CT findings differently. The Marshall score includes the status of basal cisterns, midline shift greater than 5 mm, and hemorrhagic mass, whereas the Rotterdam score includes basal cisterns, midline shift greater than 5 mm, subarachnoid hemorrhage and/or intraventricular hemorrhage, and epidural hemorrhage, but not hemorrhagic mass, explained Dr. Mbemba, a radiologist at Tohoku University, Sendai City, Japan.
He noted that several studies have suggested that increased intracranial pressure may lead to early death, while vasospasm associated with subarachnoid hemorrhage and/or intraventricular hemorrhage that decrease intracerebral circulation is associated with a worsening clinical outcome.
To assess whether the Marshall or Rotterdam scores are related to death at hospital discharge, investigators in the current study reviewed the initial CT scans and status at hospital discharge of 245 consecutive patients with mild to severe TBI. Mild cases, defined by a Glasgow Coma Scale score of 13-15, were included if a CT examination was recommended according to New Orleans Criteria and/or the Canadian CT Head Rule. Patients’ mean age was 49 years (range, 15-93 years), and 67% were men.
At hospital discharge, 25 patients had died and 220 were alive. The median time to death was 3 days (range, 1-83 days), said Dr. Mbemba, who earned a trainee research award from RSNA for his study.
In a logistic regression analysis, CT findings independently related to early death were basal cistern status (odds ratio, 771.5; P less than .001), positive midline shift (OR, 56.2; P = .0011), hemorrhagic mass (OR, 12.9; P = .0065), and subarachnoid hemorrhage and/or intraventricular hemorrhage (OR 3.8; P = .0394), Dr. Mbemba said. The presence or absence of an epidural hemorrhage was not a significant predictor.
In a recently published study, initial Marshall and Rotterdam scores were significantly associated with mortality after severe TBI, while Glasgow Coma Scale scores on admission were not (Neurosurgery 2012;70:1095-105). No relationship was observed, however, between any of the three scoring systems and ICU intracranial pressure or brain tissue oxygen tension, suggesting that factors associated with outcome, may not always predict a patient’s ICU course, especially intracranial physiology.
Dr. Mbemba and his coauthors reported no relevant financial disclosures.
computed tomography–based scoring systems, TBI, Dr. Daddy Mata Mbemba, Radiological Society of North America, vasospasm, associated with subarachnoid hemorrhage, intraventricular hemorrhage, intracerebral circulation,
CHICAGO – The Marshall CT classification system is a better predictor of early death in patients with traumatic brain injury than is the Rotterdam score, an award-winning study found.
As observed in previous reports, higher scores on both computed tomography–based scoring systems were significantly associated with early death among patients with mild to severe traumatic brain injury, or TBI (both P values less than .0001).
In a logistic regression analysis, however, only the Marshall scoring system was significantly associated with early death, defined as death at hospital discharge (P less than .002), Dr. Daddy Mata Mbemba reported at the annual meeting of the Radiological Society of North America.
This is likely because the two strongest independent predictors of early death – the absence of basal cistern and positive midline shift – are included in both CT scoring systems, while the next strongest predictor, hemorrhagic mass, is included in the Marshall score only, he explained.
Marshall and Rotterdam are the two most commonly used radiologic scoring systems, according to Dr. Mbemba, but they group CT findings differently. The Marshall score includes the status of basal cisterns, midline shift greater than 5 mm, and hemorrhagic mass, whereas the Rotterdam score includes basal cisterns, midline shift greater than 5 mm, subarachnoid hemorrhage and/or intraventricular hemorrhage, and epidural hemorrhage, but not hemorrhagic mass, explained Dr. Mbemba, a radiologist at Tohoku University, Sendai City, Japan.
He noted that several studies have suggested that increased intracranial pressure may lead to early death, while vasospasm associated with subarachnoid hemorrhage and/or intraventricular hemorrhage that decrease intracerebral circulation is associated with a worsening clinical outcome.
To assess whether the Marshall or Rotterdam scores are related to death at hospital discharge, investigators in the current study reviewed the initial CT scans and status at hospital discharge of 245 consecutive patients with mild to severe TBI. Mild cases, defined by a Glasgow Coma Scale score of 13-15, were included if a CT examination was recommended according to New Orleans Criteria and/or the Canadian CT Head Rule. Patients’ mean age was 49 years (range, 15-93 years), and 67% were men.
At hospital discharge, 25 patients had died and 220 were alive. The median time to death was 3 days (range, 1-83 days), said Dr. Mbemba, who earned a trainee research award from RSNA for his study.
In a logistic regression analysis, CT findings independently related to early death were basal cistern status (odds ratio, 771.5; P less than .001), positive midline shift (OR, 56.2; P = .0011), hemorrhagic mass (OR, 12.9; P = .0065), and subarachnoid hemorrhage and/or intraventricular hemorrhage (OR 3.8; P = .0394), Dr. Mbemba said. The presence or absence of an epidural hemorrhage was not a significant predictor.
In a recently published study, initial Marshall and Rotterdam scores were significantly associated with mortality after severe TBI, while Glasgow Coma Scale scores on admission were not (Neurosurgery 2012;70:1095-105). No relationship was observed, however, between any of the three scoring systems and ICU intracranial pressure or brain tissue oxygen tension, suggesting that factors associated with outcome, may not always predict a patient’s ICU course, especially intracranial physiology.
Dr. Mbemba and his coauthors reported no relevant financial disclosures.
CHICAGO – The Marshall CT classification system is a better predictor of early death in patients with traumatic brain injury than is the Rotterdam score, an award-winning study found.
As observed in previous reports, higher scores on both computed tomography–based scoring systems were significantly associated with early death among patients with mild to severe traumatic brain injury, or TBI (both P values less than .0001).
In a logistic regression analysis, however, only the Marshall scoring system was significantly associated with early death, defined as death at hospital discharge (P less than .002), Dr. Daddy Mata Mbemba reported at the annual meeting of the Radiological Society of North America.
This is likely because the two strongest independent predictors of early death – the absence of basal cistern and positive midline shift – are included in both CT scoring systems, while the next strongest predictor, hemorrhagic mass, is included in the Marshall score only, he explained.
Marshall and Rotterdam are the two most commonly used radiologic scoring systems, according to Dr. Mbemba, but they group CT findings differently. The Marshall score includes the status of basal cisterns, midline shift greater than 5 mm, and hemorrhagic mass, whereas the Rotterdam score includes basal cisterns, midline shift greater than 5 mm, subarachnoid hemorrhage and/or intraventricular hemorrhage, and epidural hemorrhage, but not hemorrhagic mass, explained Dr. Mbemba, a radiologist at Tohoku University, Sendai City, Japan.
He noted that several studies have suggested that increased intracranial pressure may lead to early death, while vasospasm associated with subarachnoid hemorrhage and/or intraventricular hemorrhage that decrease intracerebral circulation is associated with a worsening clinical outcome.
To assess whether the Marshall or Rotterdam scores are related to death at hospital discharge, investigators in the current study reviewed the initial CT scans and status at hospital discharge of 245 consecutive patients with mild to severe TBI. Mild cases, defined by a Glasgow Coma Scale score of 13-15, were included if a CT examination was recommended according to New Orleans Criteria and/or the Canadian CT Head Rule. Patients’ mean age was 49 years (range, 15-93 years), and 67% were men.
At hospital discharge, 25 patients had died and 220 were alive. The median time to death was 3 days (range, 1-83 days), said Dr. Mbemba, who earned a trainee research award from RSNA for his study.
In a logistic regression analysis, CT findings independently related to early death were basal cistern status (odds ratio, 771.5; P less than .001), positive midline shift (OR, 56.2; P = .0011), hemorrhagic mass (OR, 12.9; P = .0065), and subarachnoid hemorrhage and/or intraventricular hemorrhage (OR 3.8; P = .0394), Dr. Mbemba said. The presence or absence of an epidural hemorrhage was not a significant predictor.
In a recently published study, initial Marshall and Rotterdam scores were significantly associated with mortality after severe TBI, while Glasgow Coma Scale scores on admission were not (Neurosurgery 2012;70:1095-105). No relationship was observed, however, between any of the three scoring systems and ICU intracranial pressure or brain tissue oxygen tension, suggesting that factors associated with outcome, may not always predict a patient’s ICU course, especially intracranial physiology.
Dr. Mbemba and his coauthors reported no relevant financial disclosures.
computed tomography–based scoring systems, TBI, Dr. Daddy Mata Mbemba, Radiological Society of North America, vasospasm, associated with subarachnoid hemorrhage, intraventricular hemorrhage, intracerebral circulation,
computed tomography–based scoring systems, TBI, Dr. Daddy Mata Mbemba, Radiological Society of North America, vasospasm, associated with subarachnoid hemorrhage, intraventricular hemorrhage, intracerebral circulation,
AT THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: In a logistic regression analysis, only the Marshall score was significantly associated with early death, defined as death at hospital discharge (P less than .002).
Data Source: Retrospective analysis involving 245 patients with traumatic brain injury.
Disclosures: Dr. Mbemba and his coauthors reported no relevant financial disclosures.
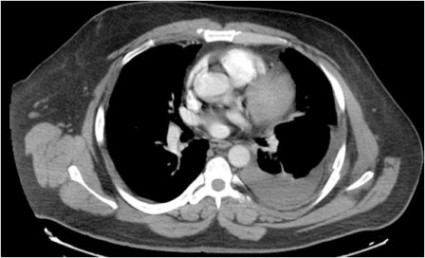
Two-Step Rule Sizes Up CT Pleural Effusions
CHICAGO – Researchers have developed and validated a simple two-step rule to quantify pleural effusion size on computed tomography – something currently not standardized.
Use of the rule significantly improved interobserver agreement, from a kappa coefficient of 0.56 to 0.79 (P less than .0001), among nine physicians ranging in skill from cardiothoracic radiologists and pulmonologists to radiology residents.
"It’s practical for any physician with access to the images and the referent tool, and conveys relevant information in terms of comparing effusion size and possibly guiding therapy," Dr. Matthew Moy said at the annual meeting of the Radiological Society of North America.
Computed tomography (CT) is highly sensitive for detecting small effusions, and differentiating pleural and parenchymal disease. The problem lies in the subjective grading of pleural effusion size and the wide variation in terminology between radiologists. These issues lead to confusion among physicians when reading CT reports or comparing effusions based on different reports, he said.
To illustrate his point, Dr. Moy showed three CT images of pleural effusions reported as being "small-moderate" to "moderate" to "large," although all three were similar in size.
In an effort to improve this communication, investigators at the Albert Einstein College of Medicine, New York, selected 34 adult CT scans, representing a wide range of pleural effusion sizes, and measured the volume of each effusion and ipsilateral hemithorax using a morphometric segmentation tool. The effusion and ipsilateral hemithorax were then manually traced on each axial slice, and the effusion volume calculated as a percent of the volume of the hemithorax to account for differences in body habitus, explained Dr. Moy.
The mean effusion volume was 37.42% of the hemithorax (range, 5.59%-89.05%). The patients’ mean age was 64 years, and 74% had undergone noncontrast CT.
Two cardiothoracic fellowship–trained radiologists then reviewed the CTs to identify qualitative and quantitative features that correlated with effusion volume. Several features emerged, but only anteroposterior (AP) quartile, maximum AP depth, and degree of atelectasis remained significant in multivariate analysis. The last was dropped, however, because it was not found to be useful for differentiating large effusions, said Dr. Moy, now with Massachusetts General Hospital in Boston.
AP quartile is calculated using the axial image where the effusion appears largest cephalad to the dome of the hemidiaphragm. The hemithorax is divided into four quartiles, and the AP quartile is then measured as the anterior-most quartile in which the effusion is seen, he explained. Maximum AP depth is measured in centimeters at the midclavicular line.
A classification rule was then developed in which first AP quartile (0%-25%) effusions are small, second quartile (25%-50%) effusions are moderate, and third or fourth AP quartile (50%-75% or 75%-100%) effusions are large. In borderline cases where it’s not easy to assess the quartile, AP depth can be measured using cutoffs of less than 3 cm (small), 3-10 cm (moderate), and more than 10 cm (large), Dr. Moy suggested.
To validate the rule, the 34 CT scans were then assessed by the nine physicians, who were not involved in the initial CT analysis. Interobserver agreement improved from a kappa of 0.59 to a kappa of 0.73 for radiology residents, 0.54 to 0.76 for pulmonologists, and 0.74 to 0.85 for cardiothoracic radiologists.
"This rule can elevate the level of agreement and consistency of both the novice radiologist and clinician to the level of cardiothoracic radiologists," Dr. Moy observed.
Session comoderator Dr. Reginald Munden, a professor of diagnostic radiology at the University of Texas M.D. Anderson Cancer Center in Houston, said in an interview, "I like anything we can do to standardize our reports, because we’re all over the place. This is particularly important, because a lot of smalls are insignificant and we don’t need to do anything with them.
"In our setting, with patients on chemotherapy, we see pleural effusions all the time," he added. "So it’s important when an effusion becomes large enough that it needs to be drained or it might be symptomatic for some other issue."
Dr. Munden went on to say that the grading scale needs to be validated in a larger population and should include a fourth subcategory, "present, but normal," to distinguish small effusions from those that are normal, but may be only 15 cc.
All effusions characterized as small in the analysis were less than 328 mL in absolute volume, Dr. Moy said in an interview. This is significant because malignant pleural effusions less than 1 cm in thickness on a lateral decubitus radiograph are a relative contraindication to thoracentesis, per American Thoracic Society guidelines (Am. J. Respir. Crit. Care Med. 2000;162:1987-2001). Pleural effusions greater than 1 cm on a lateral decubitus view have been shown to measure more than 300 mL in volume (Radiology 1994;191:681-4), he noted.
The new two-step rule is currently in use at Albert Einstein, and has been published online (Chest 2012 Nov. 8 [doi: 10.1378/chest.12-1292]).
Dr. Moy reported no conflicts of interest. A coauthor reported investments in Ortho Space and Kryon Systems.
CHICAGO – Researchers have developed and validated a simple two-step rule to quantify pleural effusion size on computed tomography – something currently not standardized.
Use of the rule significantly improved interobserver agreement, from a kappa coefficient of 0.56 to 0.79 (P less than .0001), among nine physicians ranging in skill from cardiothoracic radiologists and pulmonologists to radiology residents.
"It’s practical for any physician with access to the images and the referent tool, and conveys relevant information in terms of comparing effusion size and possibly guiding therapy," Dr. Matthew Moy said at the annual meeting of the Radiological Society of North America.
Computed tomography (CT) is highly sensitive for detecting small effusions, and differentiating pleural and parenchymal disease. The problem lies in the subjective grading of pleural effusion size and the wide variation in terminology between radiologists. These issues lead to confusion among physicians when reading CT reports or comparing effusions based on different reports, he said.
To illustrate his point, Dr. Moy showed three CT images of pleural effusions reported as being "small-moderate" to "moderate" to "large," although all three were similar in size.
In an effort to improve this communication, investigators at the Albert Einstein College of Medicine, New York, selected 34 adult CT scans, representing a wide range of pleural effusion sizes, and measured the volume of each effusion and ipsilateral hemithorax using a morphometric segmentation tool. The effusion and ipsilateral hemithorax were then manually traced on each axial slice, and the effusion volume calculated as a percent of the volume of the hemithorax to account for differences in body habitus, explained Dr. Moy.
The mean effusion volume was 37.42% of the hemithorax (range, 5.59%-89.05%). The patients’ mean age was 64 years, and 74% had undergone noncontrast CT.
Two cardiothoracic fellowship–trained radiologists then reviewed the CTs to identify qualitative and quantitative features that correlated with effusion volume. Several features emerged, but only anteroposterior (AP) quartile, maximum AP depth, and degree of atelectasis remained significant in multivariate analysis. The last was dropped, however, because it was not found to be useful for differentiating large effusions, said Dr. Moy, now with Massachusetts General Hospital in Boston.
AP quartile is calculated using the axial image where the effusion appears largest cephalad to the dome of the hemidiaphragm. The hemithorax is divided into four quartiles, and the AP quartile is then measured as the anterior-most quartile in which the effusion is seen, he explained. Maximum AP depth is measured in centimeters at the midclavicular line.
A classification rule was then developed in which first AP quartile (0%-25%) effusions are small, second quartile (25%-50%) effusions are moderate, and third or fourth AP quartile (50%-75% or 75%-100%) effusions are large. In borderline cases where it’s not easy to assess the quartile, AP depth can be measured using cutoffs of less than 3 cm (small), 3-10 cm (moderate), and more than 10 cm (large), Dr. Moy suggested.
To validate the rule, the 34 CT scans were then assessed by the nine physicians, who were not involved in the initial CT analysis. Interobserver agreement improved from a kappa of 0.59 to a kappa of 0.73 for radiology residents, 0.54 to 0.76 for pulmonologists, and 0.74 to 0.85 for cardiothoracic radiologists.
"This rule can elevate the level of agreement and consistency of both the novice radiologist and clinician to the level of cardiothoracic radiologists," Dr. Moy observed.
Session comoderator Dr. Reginald Munden, a professor of diagnostic radiology at the University of Texas M.D. Anderson Cancer Center in Houston, said in an interview, "I like anything we can do to standardize our reports, because we’re all over the place. This is particularly important, because a lot of smalls are insignificant and we don’t need to do anything with them.
"In our setting, with patients on chemotherapy, we see pleural effusions all the time," he added. "So it’s important when an effusion becomes large enough that it needs to be drained or it might be symptomatic for some other issue."
Dr. Munden went on to say that the grading scale needs to be validated in a larger population and should include a fourth subcategory, "present, but normal," to distinguish small effusions from those that are normal, but may be only 15 cc.
All effusions characterized as small in the analysis were less than 328 mL in absolute volume, Dr. Moy said in an interview. This is significant because malignant pleural effusions less than 1 cm in thickness on a lateral decubitus radiograph are a relative contraindication to thoracentesis, per American Thoracic Society guidelines (Am. J. Respir. Crit. Care Med. 2000;162:1987-2001). Pleural effusions greater than 1 cm on a lateral decubitus view have been shown to measure more than 300 mL in volume (Radiology 1994;191:681-4), he noted.
The new two-step rule is currently in use at Albert Einstein, and has been published online (Chest 2012 Nov. 8 [doi: 10.1378/chest.12-1292]).
Dr. Moy reported no conflicts of interest. A coauthor reported investments in Ortho Space and Kryon Systems.
CHICAGO – Researchers have developed and validated a simple two-step rule to quantify pleural effusion size on computed tomography – something currently not standardized.
Use of the rule significantly improved interobserver agreement, from a kappa coefficient of 0.56 to 0.79 (P less than .0001), among nine physicians ranging in skill from cardiothoracic radiologists and pulmonologists to radiology residents.
"It’s practical for any physician with access to the images and the referent tool, and conveys relevant information in terms of comparing effusion size and possibly guiding therapy," Dr. Matthew Moy said at the annual meeting of the Radiological Society of North America.
Computed tomography (CT) is highly sensitive for detecting small effusions, and differentiating pleural and parenchymal disease. The problem lies in the subjective grading of pleural effusion size and the wide variation in terminology between radiologists. These issues lead to confusion among physicians when reading CT reports or comparing effusions based on different reports, he said.
To illustrate his point, Dr. Moy showed three CT images of pleural effusions reported as being "small-moderate" to "moderate" to "large," although all three were similar in size.
In an effort to improve this communication, investigators at the Albert Einstein College of Medicine, New York, selected 34 adult CT scans, representing a wide range of pleural effusion sizes, and measured the volume of each effusion and ipsilateral hemithorax using a morphometric segmentation tool. The effusion and ipsilateral hemithorax were then manually traced on each axial slice, and the effusion volume calculated as a percent of the volume of the hemithorax to account for differences in body habitus, explained Dr. Moy.
The mean effusion volume was 37.42% of the hemithorax (range, 5.59%-89.05%). The patients’ mean age was 64 years, and 74% had undergone noncontrast CT.
Two cardiothoracic fellowship–trained radiologists then reviewed the CTs to identify qualitative and quantitative features that correlated with effusion volume. Several features emerged, but only anteroposterior (AP) quartile, maximum AP depth, and degree of atelectasis remained significant in multivariate analysis. The last was dropped, however, because it was not found to be useful for differentiating large effusions, said Dr. Moy, now with Massachusetts General Hospital in Boston.
AP quartile is calculated using the axial image where the effusion appears largest cephalad to the dome of the hemidiaphragm. The hemithorax is divided into four quartiles, and the AP quartile is then measured as the anterior-most quartile in which the effusion is seen, he explained. Maximum AP depth is measured in centimeters at the midclavicular line.
A classification rule was then developed in which first AP quartile (0%-25%) effusions are small, second quartile (25%-50%) effusions are moderate, and third or fourth AP quartile (50%-75% or 75%-100%) effusions are large. In borderline cases where it’s not easy to assess the quartile, AP depth can be measured using cutoffs of less than 3 cm (small), 3-10 cm (moderate), and more than 10 cm (large), Dr. Moy suggested.
To validate the rule, the 34 CT scans were then assessed by the nine physicians, who were not involved in the initial CT analysis. Interobserver agreement improved from a kappa of 0.59 to a kappa of 0.73 for radiology residents, 0.54 to 0.76 for pulmonologists, and 0.74 to 0.85 for cardiothoracic radiologists.
"This rule can elevate the level of agreement and consistency of both the novice radiologist and clinician to the level of cardiothoracic radiologists," Dr. Moy observed.
Session comoderator Dr. Reginald Munden, a professor of diagnostic radiology at the University of Texas M.D. Anderson Cancer Center in Houston, said in an interview, "I like anything we can do to standardize our reports, because we’re all over the place. This is particularly important, because a lot of smalls are insignificant and we don’t need to do anything with them.
"In our setting, with patients on chemotherapy, we see pleural effusions all the time," he added. "So it’s important when an effusion becomes large enough that it needs to be drained or it might be symptomatic for some other issue."
Dr. Munden went on to say that the grading scale needs to be validated in a larger population and should include a fourth subcategory, "present, but normal," to distinguish small effusions from those that are normal, but may be only 15 cc.
All effusions characterized as small in the analysis were less than 328 mL in absolute volume, Dr. Moy said in an interview. This is significant because malignant pleural effusions less than 1 cm in thickness on a lateral decubitus radiograph are a relative contraindication to thoracentesis, per American Thoracic Society guidelines (Am. J. Respir. Crit. Care Med. 2000;162:1987-2001). Pleural effusions greater than 1 cm on a lateral decubitus view have been shown to measure more than 300 mL in volume (Radiology 1994;191:681-4), he noted.
The new two-step rule is currently in use at Albert Einstein, and has been published online (Chest 2012 Nov. 8 [doi: 10.1378/chest.12-1292]).
Dr. Moy reported no conflicts of interest. A coauthor reported investments in Ortho Space and Kryon Systems.
AT THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Use of the rule significantly improved interobserver agreement from a kappa coefficient of 0.56 to 0.79 among nine cardiothoracic radiologists, pulmonologists, and radiology residents (P less than .0001).
Data Source: Analysis of 34 adult chest CT scans.
Disclosures: Dr. Moy reported no conflicts of interest. A coauthor reported investments in Ortho Space and Kryon Systems.
Targeted CT follow-up proposed for incidental lung nodules
CHICAGO – Limiting CT follow-up of incidental pulmonary nodules to a small area around the suspicious nodule may help resolve a common clinical dilemma and an Achilles heel of lung cancer screening, researchers suggest.
It could also reduce the radiation dose by more than 80%.
"Why should we radiate the entire thorax on follow-up?" Dr. Gregory D. Pearson asked rhetorically at the annual meeting of the Radiological Society of North America.
In the pivotal National Lung Cancer Screening Trial, annual low-dose CT reduced lung cancer deaths by 20% and all-cause mortality by 6.7% among heavy smokers, compared with traditional X-rays. Approximately 40% of the CT group, however, had findings of small, indeterminate pulmonary nodules considered suspicious for lung cancer on at least one scan, with 1.4% experiencing a complication as a result of additional testing (N. Engl. J. Med. 2011;365:395-409).
Several societies are working to devise the best protocol for further workup of detected nodules, but none have come up with the solution. The Fleischner Society, an international society for thoracic radiology, previously proposed serial follow-up imaging at intervals of less than 1 year for solid nodules smaller than 8 mm detected incidentally at nonscreening CT (Radiology 2005;237:395-400). For all semisolid nodules and ground-glass nodules at least 5 mm in size, researchers recommended a 3-month follow-up (Radiology 2005;237:395-400).
Follow-up CT scans, however, add costs and contribute to a patient’s cumulative radiation burden, said Dr. Pearson, a thoracic radiologist at New York-Presbyterian Hospital/Columbia University in New York City.
In an effort to develop a more practical solution, Dr. Pearson and his colleagues analyzed the variability in nodule location among 50 patients with subcentimeter nodules identified on CT screening for lung cancer and emphysema, and then devised a protocol for targeted CT follow-up that was validated in 50 additional patients.
Two experts and one novice reader, a medical student, independently measured the distances of the nodules from two anatomical landmarks, the lung apex and carina, on baseline and follow-up scans by cross-referencing the axial images with the CT scanogram on a PACS (picture archiving and communication system) workstation.
The interobserver variability was quite low, with mean differences of just 2-3 mm when the two experts were paired together or individually paired with the novice reader, Dr. Pearson said. Results were significantly better measuring from the apex than from the carina for two of the three reader pairings (P = .005 and .03), although the absolute difference was just 1 mm.
Interscan variability between the baseline and follow-up scans was slightly larger, averaging 5.3 mm from the apex and 6.2 mm from the carina. The maximal difference in nodule location between the two scans was 24 mm from the apex and 29 mm from the carina. Both outcomes significantly favored the measurement from the apex (P = .01).
"The measurements were highly reproducible, [there was] no benefit in measuring from the carina, and we figured that if the nodules were normally distributed throughout the lungs, that 99% of nodules should range between the mean plus 3 standard deviations, which would be about a 38-mm range," Dr. Pearson said.
To allow for a greater margin of error, measurements in the validation phase of the study were only from the ipsilateral lung apex and covered a 60-mm range. At baseline, the expert identified the nodule and placed a cut line on the scan to measure the distance from the apex. Medical students then measured the distance of the nodule from the apex on the follow-up scan, and reviewed a region of about 6 cm to determine whether the nodule would have been included in its entirety if the range of the CT scan had been narrowed to just 60 mm.
"The results here are pretty simple; 100% of the nodules in follow-up were scanned in their entirety," Dr. Pearson said.
The average craniocaudal coverage on follow-up CT was 363 mm.
By using a targeted 60-mm range, the average craniocaudal coverage and radiation dose would be reduced by 83%, although the actual dose reduction will depend on the location of the nodules, he added.
In addition, use of targeted CTs would cut interpretation and report times due to the decreased anatomical coverage, would not disrupt work flow, and would require minimal technologist training.
Still, the technique needs to be validated prospectively in larger groups, and would require buy-in from radiologists, medical societies, and Medicare and private insurers, Dr. Pearson said.
Session comoderator Dr. H. Page McAdams, division chief of cardiac and thoracic imaging at Duke University in Durham, N.C., said in an interview that the concept is intriguing, but raises a number of potential societal, reimbursement, and medical-legal issues. For example, what happens if a physician does a limited follow-up CT and misses a new nodule? The other question is, how many patients in these screening populations really have a simple nodule? If most of them have multiple nodules, it would obviate the benefits of targeted CT.
"I think it’s a great idea, but there’s a lot of work that still needs to be done in terms of answering those particular questions," Dr. McAdams said.
Roughly 75% of the 100 consecutive patients in the study had a single nodule, Dr. Pearson told this publication.
Dr. McAdams reported a research grant from General Electric, serving as a consultant for American College of Radiology Image Metrix, and working as an author for Reed Elsevier and UpToDate Inc.
CHICAGO – Limiting CT follow-up of incidental pulmonary nodules to a small area around the suspicious nodule may help resolve a common clinical dilemma and an Achilles heel of lung cancer screening, researchers suggest.
It could also reduce the radiation dose by more than 80%.
"Why should we radiate the entire thorax on follow-up?" Dr. Gregory D. Pearson asked rhetorically at the annual meeting of the Radiological Society of North America.
In the pivotal National Lung Cancer Screening Trial, annual low-dose CT reduced lung cancer deaths by 20% and all-cause mortality by 6.7% among heavy smokers, compared with traditional X-rays. Approximately 40% of the CT group, however, had findings of small, indeterminate pulmonary nodules considered suspicious for lung cancer on at least one scan, with 1.4% experiencing a complication as a result of additional testing (N. Engl. J. Med. 2011;365:395-409).
Several societies are working to devise the best protocol for further workup of detected nodules, but none have come up with the solution. The Fleischner Society, an international society for thoracic radiology, previously proposed serial follow-up imaging at intervals of less than 1 year for solid nodules smaller than 8 mm detected incidentally at nonscreening CT (Radiology 2005;237:395-400). For all semisolid nodules and ground-glass nodules at least 5 mm in size, researchers recommended a 3-month follow-up (Radiology 2005;237:395-400).
Follow-up CT scans, however, add costs and contribute to a patient’s cumulative radiation burden, said Dr. Pearson, a thoracic radiologist at New York-Presbyterian Hospital/Columbia University in New York City.
In an effort to develop a more practical solution, Dr. Pearson and his colleagues analyzed the variability in nodule location among 50 patients with subcentimeter nodules identified on CT screening for lung cancer and emphysema, and then devised a protocol for targeted CT follow-up that was validated in 50 additional patients.
Two experts and one novice reader, a medical student, independently measured the distances of the nodules from two anatomical landmarks, the lung apex and carina, on baseline and follow-up scans by cross-referencing the axial images with the CT scanogram on a PACS (picture archiving and communication system) workstation.
The interobserver variability was quite low, with mean differences of just 2-3 mm when the two experts were paired together or individually paired with the novice reader, Dr. Pearson said. Results were significantly better measuring from the apex than from the carina for two of the three reader pairings (P = .005 and .03), although the absolute difference was just 1 mm.
Interscan variability between the baseline and follow-up scans was slightly larger, averaging 5.3 mm from the apex and 6.2 mm from the carina. The maximal difference in nodule location between the two scans was 24 mm from the apex and 29 mm from the carina. Both outcomes significantly favored the measurement from the apex (P = .01).
"The measurements were highly reproducible, [there was] no benefit in measuring from the carina, and we figured that if the nodules were normally distributed throughout the lungs, that 99% of nodules should range between the mean plus 3 standard deviations, which would be about a 38-mm range," Dr. Pearson said.
To allow for a greater margin of error, measurements in the validation phase of the study were only from the ipsilateral lung apex and covered a 60-mm range. At baseline, the expert identified the nodule and placed a cut line on the scan to measure the distance from the apex. Medical students then measured the distance of the nodule from the apex on the follow-up scan, and reviewed a region of about 6 cm to determine whether the nodule would have been included in its entirety if the range of the CT scan had been narrowed to just 60 mm.
"The results here are pretty simple; 100% of the nodules in follow-up were scanned in their entirety," Dr. Pearson said.
The average craniocaudal coverage on follow-up CT was 363 mm.
By using a targeted 60-mm range, the average craniocaudal coverage and radiation dose would be reduced by 83%, although the actual dose reduction will depend on the location of the nodules, he added.
In addition, use of targeted CTs would cut interpretation and report times due to the decreased anatomical coverage, would not disrupt work flow, and would require minimal technologist training.
Still, the technique needs to be validated prospectively in larger groups, and would require buy-in from radiologists, medical societies, and Medicare and private insurers, Dr. Pearson said.
Session comoderator Dr. H. Page McAdams, division chief of cardiac and thoracic imaging at Duke University in Durham, N.C., said in an interview that the concept is intriguing, but raises a number of potential societal, reimbursement, and medical-legal issues. For example, what happens if a physician does a limited follow-up CT and misses a new nodule? The other question is, how many patients in these screening populations really have a simple nodule? If most of them have multiple nodules, it would obviate the benefits of targeted CT.
"I think it’s a great idea, but there’s a lot of work that still needs to be done in terms of answering those particular questions," Dr. McAdams said.
Roughly 75% of the 100 consecutive patients in the study had a single nodule, Dr. Pearson told this publication.
Dr. McAdams reported a research grant from General Electric, serving as a consultant for American College of Radiology Image Metrix, and working as an author for Reed Elsevier and UpToDate Inc.
CHICAGO – Limiting CT follow-up of incidental pulmonary nodules to a small area around the suspicious nodule may help resolve a common clinical dilemma and an Achilles heel of lung cancer screening, researchers suggest.
It could also reduce the radiation dose by more than 80%.
"Why should we radiate the entire thorax on follow-up?" Dr. Gregory D. Pearson asked rhetorically at the annual meeting of the Radiological Society of North America.
In the pivotal National Lung Cancer Screening Trial, annual low-dose CT reduced lung cancer deaths by 20% and all-cause mortality by 6.7% among heavy smokers, compared with traditional X-rays. Approximately 40% of the CT group, however, had findings of small, indeterminate pulmonary nodules considered suspicious for lung cancer on at least one scan, with 1.4% experiencing a complication as a result of additional testing (N. Engl. J. Med. 2011;365:395-409).
Several societies are working to devise the best protocol for further workup of detected nodules, but none have come up with the solution. The Fleischner Society, an international society for thoracic radiology, previously proposed serial follow-up imaging at intervals of less than 1 year for solid nodules smaller than 8 mm detected incidentally at nonscreening CT (Radiology 2005;237:395-400). For all semisolid nodules and ground-glass nodules at least 5 mm in size, researchers recommended a 3-month follow-up (Radiology 2005;237:395-400).
Follow-up CT scans, however, add costs and contribute to a patient’s cumulative radiation burden, said Dr. Pearson, a thoracic radiologist at New York-Presbyterian Hospital/Columbia University in New York City.
In an effort to develop a more practical solution, Dr. Pearson and his colleagues analyzed the variability in nodule location among 50 patients with subcentimeter nodules identified on CT screening for lung cancer and emphysema, and then devised a protocol for targeted CT follow-up that was validated in 50 additional patients.
Two experts and one novice reader, a medical student, independently measured the distances of the nodules from two anatomical landmarks, the lung apex and carina, on baseline and follow-up scans by cross-referencing the axial images with the CT scanogram on a PACS (picture archiving and communication system) workstation.
The interobserver variability was quite low, with mean differences of just 2-3 mm when the two experts were paired together or individually paired with the novice reader, Dr. Pearson said. Results were significantly better measuring from the apex than from the carina for two of the three reader pairings (P = .005 and .03), although the absolute difference was just 1 mm.
Interscan variability between the baseline and follow-up scans was slightly larger, averaging 5.3 mm from the apex and 6.2 mm from the carina. The maximal difference in nodule location between the two scans was 24 mm from the apex and 29 mm from the carina. Both outcomes significantly favored the measurement from the apex (P = .01).
"The measurements were highly reproducible, [there was] no benefit in measuring from the carina, and we figured that if the nodules were normally distributed throughout the lungs, that 99% of nodules should range between the mean plus 3 standard deviations, which would be about a 38-mm range," Dr. Pearson said.
To allow for a greater margin of error, measurements in the validation phase of the study were only from the ipsilateral lung apex and covered a 60-mm range. At baseline, the expert identified the nodule and placed a cut line on the scan to measure the distance from the apex. Medical students then measured the distance of the nodule from the apex on the follow-up scan, and reviewed a region of about 6 cm to determine whether the nodule would have been included in its entirety if the range of the CT scan had been narrowed to just 60 mm.
"The results here are pretty simple; 100% of the nodules in follow-up were scanned in their entirety," Dr. Pearson said.
The average craniocaudal coverage on follow-up CT was 363 mm.
By using a targeted 60-mm range, the average craniocaudal coverage and radiation dose would be reduced by 83%, although the actual dose reduction will depend on the location of the nodules, he added.
In addition, use of targeted CTs would cut interpretation and report times due to the decreased anatomical coverage, would not disrupt work flow, and would require minimal technologist training.
Still, the technique needs to be validated prospectively in larger groups, and would require buy-in from radiologists, medical societies, and Medicare and private insurers, Dr. Pearson said.
Session comoderator Dr. H. Page McAdams, division chief of cardiac and thoracic imaging at Duke University in Durham, N.C., said in an interview that the concept is intriguing, but raises a number of potential societal, reimbursement, and medical-legal issues. For example, what happens if a physician does a limited follow-up CT and misses a new nodule? The other question is, how many patients in these screening populations really have a simple nodule? If most of them have multiple nodules, it would obviate the benefits of targeted CT.
"I think it’s a great idea, but there’s a lot of work that still needs to be done in terms of answering those particular questions," Dr. McAdams said.
Roughly 75% of the 100 consecutive patients in the study had a single nodule, Dr. Pearson told this publication.
Dr. McAdams reported a research grant from General Electric, serving as a consultant for American College of Radiology Image Metrix, and working as an author for Reed Elsevier and UpToDate Inc.
AT THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: By using a targeted 60-mm range during CT follow-up of suspicious nodules, the average craniocaudal coverage and radiation dose would be reduced by 83%.
Data Source: Two-phase validation study in 100 consecutive patients with incidental subcentimeter lung nodules.
Disclosures: Dr. McAdams reported a research grant from General Electric, serving as a consultant for American College of Radiology Image Metrix, and working as an author for Reed Elsevier and UpToDate Inc.
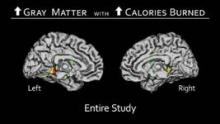
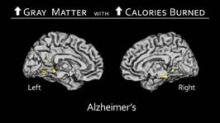
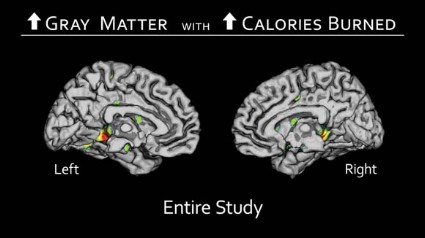
PET/CT Pinpoints Physiological Evidence of Chemo Brain
CHICAGO – PET/CT scans routinely used in the care of oncology patients may prove useful in pinpointing physiological changes associated with chemo brain.
An analysis of 18F-fluorodeoxyglucose (18F-FDG) PET/CT images taken before and after chemotherapy in breast cancer patients revealed significant declines in glucose metabolism in two key regions of the brain. The affected areas were the superior medial frontal gyrus and temporal operculum, which are responsible for mental agility, problem solving, daily decision making, sequencing, and long-term memory, Dr. Rachel Lagos reported at the annual meeting of the Radiological Society of North America.
Interestingly, no changes in metabolism were observed in 61 other regions of the brain studied.
"If we can come up with an answer to explain why that is, or to reverse this, then we can solve the problem," Dr. Lagos said in an interview. "The good news is that we already know what these two areas do, so we know at a social level what to prepare women and their families for. We can give them some tools for coping, rather than just a pat on the hand."
Although many cancer patients complain of a mental fog or loss of coping skills, some clinicians remain skeptical without definitive scientific evidence. Previous studies have used magnetic resonance imaging, but this modality only allows clinicians to see anatomic details such as small losses in brain volume. With PET/CT, one can see the effects of chemotherapy on brain function over time, explained Dr. Lagos, a diagnostic radiology resident at West Virginia University in Morgantown.
The retrospective analysis involved PET/CT scans taken at the time of initial cancer staging and 12 months after chemotherapy from 116 women with advanced breast cancer, all of whom also received tamoxifen (Nolvadex, Soltamox). The investigators compared the scans to identify areas of reduced 18F-FDG uptake, representing lower glucose metabolism, and then plotted the changes as Z-score values. One patient with brain metastases was excluded from the analysis.
Statistically significant declines in glucose metabolism were observed post chemotherapy in the superior medial frontal gyrus as a whole (P = .025), when it was evaluated from left to right (P = .023), and in the temporal operculum (P = .036), Dr. Lagos said.
The investigators did not calculate an average value for the change in Z scores, but the decline in values ranged from 2.5 to 8.0 points, she said.
In 21 patients, the affected regions of the brain regained their metabolism, which corresponds to anecdotal information from patients that chemo brain lifts about 1-2 years after treatment.
"With the small data I’ve been able to accumulate so far, it’s hopeful that this kind of brain phenomenon is temporary," Dr. Lagos said.
The next step is to prospectively assess brain function starting at the time of cancer diagnosis and continuing throughout long-term follow-up, which potentially could lead to improved treatments or prevention, she said. In the meantime, the results provide physiologic evidence for chemo brain, and may prompt peers and counselors to use simple interventions such as creating lists for patients of their daily activities or meal plans to compensate for the mental fog.
Dr. Patrick J. Peller, a radiologist with the Mayo Clinic in Rochester, Minn., who hosted the poster session, said the study provides an understanding of the substrate for the often frustrating symptoms that patients experience, and could facilitate interventions to prevent chemo brain.
"Once you have a way to measure something, it sometimes drives your ability to treat it," he said in an interview. "We don’t have that treatment right now, just like we don’t have treatment for Alzheimer’s disease, but my sense is that it’s possible that our treatment for Alzheimer’s might work in some of these patients because it helps in compensation and not actually changing the underlying disease.
"If it improves the patient’s memory function, it might work in this situation, and you might be able to measure if it’s working with this technique."
Dr. Lagos and Dr. Peller reported no relevant financial disclosures.
CHICAGO – PET/CT scans routinely used in the care of oncology patients may prove useful in pinpointing physiological changes associated with chemo brain.
An analysis of 18F-fluorodeoxyglucose (18F-FDG) PET/CT images taken before and after chemotherapy in breast cancer patients revealed significant declines in glucose metabolism in two key regions of the brain. The affected areas were the superior medial frontal gyrus and temporal operculum, which are responsible for mental agility, problem solving, daily decision making, sequencing, and long-term memory, Dr. Rachel Lagos reported at the annual meeting of the Radiological Society of North America.
Interestingly, no changes in metabolism were observed in 61 other regions of the brain studied.
"If we can come up with an answer to explain why that is, or to reverse this, then we can solve the problem," Dr. Lagos said in an interview. "The good news is that we already know what these two areas do, so we know at a social level what to prepare women and their families for. We can give them some tools for coping, rather than just a pat on the hand."
Although many cancer patients complain of a mental fog or loss of coping skills, some clinicians remain skeptical without definitive scientific evidence. Previous studies have used magnetic resonance imaging, but this modality only allows clinicians to see anatomic details such as small losses in brain volume. With PET/CT, one can see the effects of chemotherapy on brain function over time, explained Dr. Lagos, a diagnostic radiology resident at West Virginia University in Morgantown.
The retrospective analysis involved PET/CT scans taken at the time of initial cancer staging and 12 months after chemotherapy from 116 women with advanced breast cancer, all of whom also received tamoxifen (Nolvadex, Soltamox). The investigators compared the scans to identify areas of reduced 18F-FDG uptake, representing lower glucose metabolism, and then plotted the changes as Z-score values. One patient with brain metastases was excluded from the analysis.
Statistically significant declines in glucose metabolism were observed post chemotherapy in the superior medial frontal gyrus as a whole (P = .025), when it was evaluated from left to right (P = .023), and in the temporal operculum (P = .036), Dr. Lagos said.
The investigators did not calculate an average value for the change in Z scores, but the decline in values ranged from 2.5 to 8.0 points, she said.
In 21 patients, the affected regions of the brain regained their metabolism, which corresponds to anecdotal information from patients that chemo brain lifts about 1-2 years after treatment.
"With the small data I’ve been able to accumulate so far, it’s hopeful that this kind of brain phenomenon is temporary," Dr. Lagos said.
The next step is to prospectively assess brain function starting at the time of cancer diagnosis and continuing throughout long-term follow-up, which potentially could lead to improved treatments or prevention, she said. In the meantime, the results provide physiologic evidence for chemo brain, and may prompt peers and counselors to use simple interventions such as creating lists for patients of their daily activities or meal plans to compensate for the mental fog.
Dr. Patrick J. Peller, a radiologist with the Mayo Clinic in Rochester, Minn., who hosted the poster session, said the study provides an understanding of the substrate for the often frustrating symptoms that patients experience, and could facilitate interventions to prevent chemo brain.
"Once you have a way to measure something, it sometimes drives your ability to treat it," he said in an interview. "We don’t have that treatment right now, just like we don’t have treatment for Alzheimer’s disease, but my sense is that it’s possible that our treatment for Alzheimer’s might work in some of these patients because it helps in compensation and not actually changing the underlying disease.
"If it improves the patient’s memory function, it might work in this situation, and you might be able to measure if it’s working with this technique."
Dr. Lagos and Dr. Peller reported no relevant financial disclosures.
CHICAGO – PET/CT scans routinely used in the care of oncology patients may prove useful in pinpointing physiological changes associated with chemo brain.
An analysis of 18F-fluorodeoxyglucose (18F-FDG) PET/CT images taken before and after chemotherapy in breast cancer patients revealed significant declines in glucose metabolism in two key regions of the brain. The affected areas were the superior medial frontal gyrus and temporal operculum, which are responsible for mental agility, problem solving, daily decision making, sequencing, and long-term memory, Dr. Rachel Lagos reported at the annual meeting of the Radiological Society of North America.
Interestingly, no changes in metabolism were observed in 61 other regions of the brain studied.
"If we can come up with an answer to explain why that is, or to reverse this, then we can solve the problem," Dr. Lagos said in an interview. "The good news is that we already know what these two areas do, so we know at a social level what to prepare women and their families for. We can give them some tools for coping, rather than just a pat on the hand."
Although many cancer patients complain of a mental fog or loss of coping skills, some clinicians remain skeptical without definitive scientific evidence. Previous studies have used magnetic resonance imaging, but this modality only allows clinicians to see anatomic details such as small losses in brain volume. With PET/CT, one can see the effects of chemotherapy on brain function over time, explained Dr. Lagos, a diagnostic radiology resident at West Virginia University in Morgantown.
The retrospective analysis involved PET/CT scans taken at the time of initial cancer staging and 12 months after chemotherapy from 116 women with advanced breast cancer, all of whom also received tamoxifen (Nolvadex, Soltamox). The investigators compared the scans to identify areas of reduced 18F-FDG uptake, representing lower glucose metabolism, and then plotted the changes as Z-score values. One patient with brain metastases was excluded from the analysis.
Statistically significant declines in glucose metabolism were observed post chemotherapy in the superior medial frontal gyrus as a whole (P = .025), when it was evaluated from left to right (P = .023), and in the temporal operculum (P = .036), Dr. Lagos said.
The investigators did not calculate an average value for the change in Z scores, but the decline in values ranged from 2.5 to 8.0 points, she said.
In 21 patients, the affected regions of the brain regained their metabolism, which corresponds to anecdotal information from patients that chemo brain lifts about 1-2 years after treatment.
"With the small data I’ve been able to accumulate so far, it’s hopeful that this kind of brain phenomenon is temporary," Dr. Lagos said.
The next step is to prospectively assess brain function starting at the time of cancer diagnosis and continuing throughout long-term follow-up, which potentially could lead to improved treatments or prevention, she said. In the meantime, the results provide physiologic evidence for chemo brain, and may prompt peers and counselors to use simple interventions such as creating lists for patients of their daily activities or meal plans to compensate for the mental fog.
Dr. Patrick J. Peller, a radiologist with the Mayo Clinic in Rochester, Minn., who hosted the poster session, said the study provides an understanding of the substrate for the often frustrating symptoms that patients experience, and could facilitate interventions to prevent chemo brain.
"Once you have a way to measure something, it sometimes drives your ability to treat it," he said in an interview. "We don’t have that treatment right now, just like we don’t have treatment for Alzheimer’s disease, but my sense is that it’s possible that our treatment for Alzheimer’s might work in some of these patients because it helps in compensation and not actually changing the underlying disease.
"If it improves the patient’s memory function, it might work in this situation, and you might be able to measure if it’s working with this technique."
Dr. Lagos and Dr. Peller reported no relevant financial disclosures.
AT THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Statistically significant declines in glucose metabolism were observed post chemotherapy in the superior medial frontal gyrus as a whole (P = .025), when it was evaluated from left to right (P = .023), and in the temporal operculum (P = .036).
Data Source: This was a retrospective analysis of PET/CT scans from 115 patients with advanced breast cancer.
Disclosures: Dr. Lagos and Dr. Peller reported no relevant financial disclosures.
Mammograms Dip in Wake of USPSTF Recommendations
CHICAGO – There has been a clear and abrupt decline in screening mammography in the wake of the controversial breast cancer screening recommendations by the U.S. Preventive Services Task Force.
After climbing steadily at a rate of about 1% per year since 2001, breast mammography among women on Medicare declined 4.3% in 2010, the first full year after the USPSTF recommendations came out.
The reasons for the decline aren’t entirely clear, but it may be that women over age 74 years began to follow the task force recommendations and no longer got screened, or that women aged 50-74 years extended their screening interval from 1 to 2 years, again according to task force recommendations, lead author Dr. David C. Levin said at the annual meeting of the Radiological Society of North America.
"What is clear is that the introduction of those recommendations in late 2009 had a chilling effect on the willingness of women to get screened," he said. "It remains to be seen whether this trend is going to continue and whether it will affect breast cancer mortality."
For the analysis, Dr. Levin reviewed film and digital screening mammography codes in the Medicare Part B Physician/Supplier Procedure Summary Master Files for 2005 to 2010. The database provides volumes for each code each year.
From these data, he calculated that the screening mammography rate per 1,000 female Medicare beneficiaries had been growing in small increments each year from 311.6 in 2005 to 312.4 in 2006, 316.2 in 2007, 320.1 in 2008, and 322.9 in 2009. This represents a compound annual growth rate of 0.9%.
After the recommendations came out, the screening mammography rate fell to 309.1/1,000 women in 2010, representing a decline of 4.3% in a single year, said Dr. Levin, a radiologist and founder of the center for research on utilization of imaging services at Thomas Jefferson University Hospital in Philadelphia.
He pointed out that earlier this year, Mayo Clinic researchers reported a 5.7% decline in screening mammography in 2010 among women aged 40-64, based on data from almost 7.9 million women enrolled in nearly 100 health plans.
In a separate presentation at the meeting, investigators analyzed the outcomes of 43,351 screening mammograms performed between 2007 and 2010 to determine how the new USPSTF recommendations against screening in women 40-49 years could impact this age group.
The cross-sectional analysis included all patients presenting for a screening mammogram without clinical findings at New York Presbyterian Hospital–Weill Cornell Medical College (NYPH-WCMC) in New York City. Women aged 40-49 comprised 33.5% of the screening population.
During the 4 years, 205 breast cancers were detected (4.7/1,000). Women in their forties accounted for 19% of the cancers found, which would represent a substantial degree of underdiagnoses if they had been missed, reported Dr. Elizabeth Arleo, a radiologist at NYPH-WCMC.
Notably, only three of the women in their forties with screen-detected breast cancer had a first-degree relative with premenopausal breast cancer, thereby placing them at higher risk. More than half of the cancers in this subgroup, however, were invasive (21/39).
If the USPSTF recommendations had been enforced during the study years, these cancers may not have been detected until the patients’ baseline screening at age 50 or until the cancers had progressed to clinically evident, palpable disease, Dr. Arleo coauthors said.
Dr. Levin reported relationships with HealthHelp and Outpatient Imaging Affiliates. Dr. Arleo said she had no relevant financial disclosures.
CHICAGO – There has been a clear and abrupt decline in screening mammography in the wake of the controversial breast cancer screening recommendations by the U.S. Preventive Services Task Force.
After climbing steadily at a rate of about 1% per year since 2001, breast mammography among women on Medicare declined 4.3% in 2010, the first full year after the USPSTF recommendations came out.
The reasons for the decline aren’t entirely clear, but it may be that women over age 74 years began to follow the task force recommendations and no longer got screened, or that women aged 50-74 years extended their screening interval from 1 to 2 years, again according to task force recommendations, lead author Dr. David C. Levin said at the annual meeting of the Radiological Society of North America.
"What is clear is that the introduction of those recommendations in late 2009 had a chilling effect on the willingness of women to get screened," he said. "It remains to be seen whether this trend is going to continue and whether it will affect breast cancer mortality."
For the analysis, Dr. Levin reviewed film and digital screening mammography codes in the Medicare Part B Physician/Supplier Procedure Summary Master Files for 2005 to 2010. The database provides volumes for each code each year.
From these data, he calculated that the screening mammography rate per 1,000 female Medicare beneficiaries had been growing in small increments each year from 311.6 in 2005 to 312.4 in 2006, 316.2 in 2007, 320.1 in 2008, and 322.9 in 2009. This represents a compound annual growth rate of 0.9%.
After the recommendations came out, the screening mammography rate fell to 309.1/1,000 women in 2010, representing a decline of 4.3% in a single year, said Dr. Levin, a radiologist and founder of the center for research on utilization of imaging services at Thomas Jefferson University Hospital in Philadelphia.
He pointed out that earlier this year, Mayo Clinic researchers reported a 5.7% decline in screening mammography in 2010 among women aged 40-64, based on data from almost 7.9 million women enrolled in nearly 100 health plans.
In a separate presentation at the meeting, investigators analyzed the outcomes of 43,351 screening mammograms performed between 2007 and 2010 to determine how the new USPSTF recommendations against screening in women 40-49 years could impact this age group.
The cross-sectional analysis included all patients presenting for a screening mammogram without clinical findings at New York Presbyterian Hospital–Weill Cornell Medical College (NYPH-WCMC) in New York City. Women aged 40-49 comprised 33.5% of the screening population.
During the 4 years, 205 breast cancers were detected (4.7/1,000). Women in their forties accounted for 19% of the cancers found, which would represent a substantial degree of underdiagnoses if they had been missed, reported Dr. Elizabeth Arleo, a radiologist at NYPH-WCMC.
Notably, only three of the women in their forties with screen-detected breast cancer had a first-degree relative with premenopausal breast cancer, thereby placing them at higher risk. More than half of the cancers in this subgroup, however, were invasive (21/39).
If the USPSTF recommendations had been enforced during the study years, these cancers may not have been detected until the patients’ baseline screening at age 50 or until the cancers had progressed to clinically evident, palpable disease, Dr. Arleo coauthors said.
Dr. Levin reported relationships with HealthHelp and Outpatient Imaging Affiliates. Dr. Arleo said she had no relevant financial disclosures.
CHICAGO – There has been a clear and abrupt decline in screening mammography in the wake of the controversial breast cancer screening recommendations by the U.S. Preventive Services Task Force.
After climbing steadily at a rate of about 1% per year since 2001, breast mammography among women on Medicare declined 4.3% in 2010, the first full year after the USPSTF recommendations came out.
The reasons for the decline aren’t entirely clear, but it may be that women over age 74 years began to follow the task force recommendations and no longer got screened, or that women aged 50-74 years extended their screening interval from 1 to 2 years, again according to task force recommendations, lead author Dr. David C. Levin said at the annual meeting of the Radiological Society of North America.
"What is clear is that the introduction of those recommendations in late 2009 had a chilling effect on the willingness of women to get screened," he said. "It remains to be seen whether this trend is going to continue and whether it will affect breast cancer mortality."
For the analysis, Dr. Levin reviewed film and digital screening mammography codes in the Medicare Part B Physician/Supplier Procedure Summary Master Files for 2005 to 2010. The database provides volumes for each code each year.
From these data, he calculated that the screening mammography rate per 1,000 female Medicare beneficiaries had been growing in small increments each year from 311.6 in 2005 to 312.4 in 2006, 316.2 in 2007, 320.1 in 2008, and 322.9 in 2009. This represents a compound annual growth rate of 0.9%.
After the recommendations came out, the screening mammography rate fell to 309.1/1,000 women in 2010, representing a decline of 4.3% in a single year, said Dr. Levin, a radiologist and founder of the center for research on utilization of imaging services at Thomas Jefferson University Hospital in Philadelphia.
He pointed out that earlier this year, Mayo Clinic researchers reported a 5.7% decline in screening mammography in 2010 among women aged 40-64, based on data from almost 7.9 million women enrolled in nearly 100 health plans.
In a separate presentation at the meeting, investigators analyzed the outcomes of 43,351 screening mammograms performed between 2007 and 2010 to determine how the new USPSTF recommendations against screening in women 40-49 years could impact this age group.
The cross-sectional analysis included all patients presenting for a screening mammogram without clinical findings at New York Presbyterian Hospital–Weill Cornell Medical College (NYPH-WCMC) in New York City. Women aged 40-49 comprised 33.5% of the screening population.
During the 4 years, 205 breast cancers were detected (4.7/1,000). Women in their forties accounted for 19% of the cancers found, which would represent a substantial degree of underdiagnoses if they had been missed, reported Dr. Elizabeth Arleo, a radiologist at NYPH-WCMC.
Notably, only three of the women in their forties with screen-detected breast cancer had a first-degree relative with premenopausal breast cancer, thereby placing them at higher risk. More than half of the cancers in this subgroup, however, were invasive (21/39).
If the USPSTF recommendations had been enforced during the study years, these cancers may not have been detected until the patients’ baseline screening at age 50 or until the cancers had progressed to clinically evident, palpable disease, Dr. Arleo coauthors said.
Dr. Levin reported relationships with HealthHelp and Outpatient Imaging Affiliates. Dr. Arleo said she had no relevant financial disclosures.
AT THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Breast mammography among women on Medicare declined 4.3% in 2010, the first full year after the USPSTF recommendations came out.
Data Source: Findings are based on two retrospective analyses of women undergoing screening mammography.
Disclosures: Dr. Levin reported relationships with HealthHelp and Outpatient Imaging Affiliates. Dr. Arleo said she had no relevant financial disclosures.
Active lifestyle boosts brain structure in older adults
CHICAGO – An active lifestyle positively influences brain volume in older adults with or without Alzheimer’s disease, a magnetic resonance imaging study revealed.
Among 876 individuals, the average gray matter volume was 663 mL in those with an active lifestyle, compared with 628 mL in those with an inactive lifestyle. That equates to a significant 5% difference (P value less than .05).
"That is a large number difference when you consider the tremendous biologic forces that have to be at work for gray matter volume to decrease," lead author Dr. Cyrus Raji said in a press briefing at the annual meeting of the Radiological Society of North America.
Prior research has looked at the influence of individual lifestyle factors such as obesity or walking on brain structure, but not a variety of activities, as was done in the current study. Improving lifestyle could reduce the risk for Alzheimer’s disease by 50%, resulting in 1.1 million fewer cases in the United States, said Dr. Raji, a radiology resident at the University of California, Los Angeles.
"In the United States, the lack of physical activity is the No. 1 most powerful lifestyle factor, contributing to 21% of cases of Alzheimer’s disease," he said. "Worldwide, it is the third most powerful risk factor after low educational attainment and smoking."
To determine how lifestyle influences brain structure, the investigators used MRI scans and clinical data collected over 20 years from 876 individuals enrolled at four sites in the Cardiovascular Health Study. The Minnesota Leisure Time Physical Activity Questionnaire was used to assess caloric expenditure during 15 different aerobic activities: swimming, hiking, aerobics, jogging, tennis, racquetball, walking, gardening, mowing, raking, golfing, bicycling, dancing, calisthenics, and riding an exercise bike. A technique called voxel-based morphology was used to quantify the amount of brain matter in the MRI scans.
The participants expended an average of 1,093 kcal/week. Overall, 42% were men, 88% were white, and about 25% had been diagnosed with Alzheimer’s disease or mild cognitive impairment (MCI). The cohort was largely overweight, with an average body mass index of 27 kg/m2. Their average age was 78 years.
The analysis controlled for head size; age; gender; body mass index, which has been related to brain structure and atrophy; small vessel ischemic disease, which reflects processes like diabetes and hypertension that can affect the brain; Alzheimer’s or mild cognitive impairment (MCI) status; and study site.
The most active participants burned an average of 3,434 kcal/week, compared with 348 kcal/week in the least active participants.
There was larger bilateral gray matter volume in the cingulate gyrus, hippocampus, and temporal lobes – areas responsible for memory and learning – among individuals who burned the most calories per week, compared with those who burned the fewest, Dr. Raji said.
"That means the areas of the brain that are benefiting the most from this active lifestyle are also the areas affected in Alzheimer’s disease and are also responsible for cognition," he explained.
The same findings were observed in participants with Alzheimer’s disease or MCI. "People with Alzheimer’s who were more physically active in our study weren’t cured, but they had less deterioration in their brain matter volume, compared with the sedentary individuals," said Dr. Raji, who described the study as one of the largest voxel-based imaging studies of humans ever done.
Press briefing moderator Dr. Candice A. Johnstone of the Medical College of Wisconsin in Milwaukee said in an interview that what’s unique about the study is that it shows that physical activity actually changes brain volume and that this benefit can be obtained through a variety of activities. This is especially important when counseling patients who may have difficulty walking.
What the study fails to address, however, is whether an active lifestyle will have an impact on the symptoms of Alzheimer’s or MCI.
"Whether physical activity can significantly alter the course remains to be seen," she said. "It may be that people with changes in brain volume may be more likely to have [fewer] symptoms because their brain’s actively working to enhance those areas, but that’s the subject of future research. We do not know that."
Dr. Raji and Dr. Johnstone reported no conflicts of interest.
CHICAGO – An active lifestyle positively influences brain volume in older adults with or without Alzheimer’s disease, a magnetic resonance imaging study revealed.
Among 876 individuals, the average gray matter volume was 663 mL in those with an active lifestyle, compared with 628 mL in those with an inactive lifestyle. That equates to a significant 5% difference (P value less than .05).
"That is a large number difference when you consider the tremendous biologic forces that have to be at work for gray matter volume to decrease," lead author Dr. Cyrus Raji said in a press briefing at the annual meeting of the Radiological Society of North America.
Prior research has looked at the influence of individual lifestyle factors such as obesity or walking on brain structure, but not a variety of activities, as was done in the current study. Improving lifestyle could reduce the risk for Alzheimer’s disease by 50%, resulting in 1.1 million fewer cases in the United States, said Dr. Raji, a radiology resident at the University of California, Los Angeles.
"In the United States, the lack of physical activity is the No. 1 most powerful lifestyle factor, contributing to 21% of cases of Alzheimer’s disease," he said. "Worldwide, it is the third most powerful risk factor after low educational attainment and smoking."
To determine how lifestyle influences brain structure, the investigators used MRI scans and clinical data collected over 20 years from 876 individuals enrolled at four sites in the Cardiovascular Health Study. The Minnesota Leisure Time Physical Activity Questionnaire was used to assess caloric expenditure during 15 different aerobic activities: swimming, hiking, aerobics, jogging, tennis, racquetball, walking, gardening, mowing, raking, golfing, bicycling, dancing, calisthenics, and riding an exercise bike. A technique called voxel-based morphology was used to quantify the amount of brain matter in the MRI scans.
The participants expended an average of 1,093 kcal/week. Overall, 42% were men, 88% were white, and about 25% had been diagnosed with Alzheimer’s disease or mild cognitive impairment (MCI). The cohort was largely overweight, with an average body mass index of 27 kg/m2. Their average age was 78 years.
The analysis controlled for head size; age; gender; body mass index, which has been related to brain structure and atrophy; small vessel ischemic disease, which reflects processes like diabetes and hypertension that can affect the brain; Alzheimer’s or mild cognitive impairment (MCI) status; and study site.
The most active participants burned an average of 3,434 kcal/week, compared with 348 kcal/week in the least active participants.
There was larger bilateral gray matter volume in the cingulate gyrus, hippocampus, and temporal lobes – areas responsible for memory and learning – among individuals who burned the most calories per week, compared with those who burned the fewest, Dr. Raji said.
"That means the areas of the brain that are benefiting the most from this active lifestyle are also the areas affected in Alzheimer’s disease and are also responsible for cognition," he explained.
The same findings were observed in participants with Alzheimer’s disease or MCI. "People with Alzheimer’s who were more physically active in our study weren’t cured, but they had less deterioration in their brain matter volume, compared with the sedentary individuals," said Dr. Raji, who described the study as one of the largest voxel-based imaging studies of humans ever done.
Press briefing moderator Dr. Candice A. Johnstone of the Medical College of Wisconsin in Milwaukee said in an interview that what’s unique about the study is that it shows that physical activity actually changes brain volume and that this benefit can be obtained through a variety of activities. This is especially important when counseling patients who may have difficulty walking.
What the study fails to address, however, is whether an active lifestyle will have an impact on the symptoms of Alzheimer’s or MCI.
"Whether physical activity can significantly alter the course remains to be seen," she said. "It may be that people with changes in brain volume may be more likely to have [fewer] symptoms because their brain’s actively working to enhance those areas, but that’s the subject of future research. We do not know that."
Dr. Raji and Dr. Johnstone reported no conflicts of interest.
CHICAGO – An active lifestyle positively influences brain volume in older adults with or without Alzheimer’s disease, a magnetic resonance imaging study revealed.
Among 876 individuals, the average gray matter volume was 663 mL in those with an active lifestyle, compared with 628 mL in those with an inactive lifestyle. That equates to a significant 5% difference (P value less than .05).
"That is a large number difference when you consider the tremendous biologic forces that have to be at work for gray matter volume to decrease," lead author Dr. Cyrus Raji said in a press briefing at the annual meeting of the Radiological Society of North America.
Prior research has looked at the influence of individual lifestyle factors such as obesity or walking on brain structure, but not a variety of activities, as was done in the current study. Improving lifestyle could reduce the risk for Alzheimer’s disease by 50%, resulting in 1.1 million fewer cases in the United States, said Dr. Raji, a radiology resident at the University of California, Los Angeles.
"In the United States, the lack of physical activity is the No. 1 most powerful lifestyle factor, contributing to 21% of cases of Alzheimer’s disease," he said. "Worldwide, it is the third most powerful risk factor after low educational attainment and smoking."
To determine how lifestyle influences brain structure, the investigators used MRI scans and clinical data collected over 20 years from 876 individuals enrolled at four sites in the Cardiovascular Health Study. The Minnesota Leisure Time Physical Activity Questionnaire was used to assess caloric expenditure during 15 different aerobic activities: swimming, hiking, aerobics, jogging, tennis, racquetball, walking, gardening, mowing, raking, golfing, bicycling, dancing, calisthenics, and riding an exercise bike. A technique called voxel-based morphology was used to quantify the amount of brain matter in the MRI scans.
The participants expended an average of 1,093 kcal/week. Overall, 42% were men, 88% were white, and about 25% had been diagnosed with Alzheimer’s disease or mild cognitive impairment (MCI). The cohort was largely overweight, with an average body mass index of 27 kg/m2. Their average age was 78 years.
The analysis controlled for head size; age; gender; body mass index, which has been related to brain structure and atrophy; small vessel ischemic disease, which reflects processes like diabetes and hypertension that can affect the brain; Alzheimer’s or mild cognitive impairment (MCI) status; and study site.
The most active participants burned an average of 3,434 kcal/week, compared with 348 kcal/week in the least active participants.
There was larger bilateral gray matter volume in the cingulate gyrus, hippocampus, and temporal lobes – areas responsible for memory and learning – among individuals who burned the most calories per week, compared with those who burned the fewest, Dr. Raji said.
"That means the areas of the brain that are benefiting the most from this active lifestyle are also the areas affected in Alzheimer’s disease and are also responsible for cognition," he explained.
The same findings were observed in participants with Alzheimer’s disease or MCI. "People with Alzheimer’s who were more physically active in our study weren’t cured, but they had less deterioration in their brain matter volume, compared with the sedentary individuals," said Dr. Raji, who described the study as one of the largest voxel-based imaging studies of humans ever done.
Press briefing moderator Dr. Candice A. Johnstone of the Medical College of Wisconsin in Milwaukee said in an interview that what’s unique about the study is that it shows that physical activity actually changes brain volume and that this benefit can be obtained through a variety of activities. This is especially important when counseling patients who may have difficulty walking.
What the study fails to address, however, is whether an active lifestyle will have an impact on the symptoms of Alzheimer’s or MCI.
"Whether physical activity can significantly alter the course remains to be seen," she said. "It may be that people with changes in brain volume may be more likely to have [fewer] symptoms because their brain’s actively working to enhance those areas, but that’s the subject of future research. We do not know that."
Dr. Raji and Dr. Johnstone reported no conflicts of interest.
AT THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: There was larger bilateral gray matter volume in the cingulate gyrus, hippocampus, and temporal lobes – areas responsible for memory and learning – among individuals who burned the most calories per week (3,434 kcal), compared with those who burned the least (348 kcal).
Data Source: This study reviewed MRI scans and clinical data collected over 20 years from 876 individuals with normal cognition, Alzheimer’s disease, or mild cognitive impairment who were enrolled at four sites in the Cardiovascular Health Study.
Disclosures: Dr. Raji and Dr. Johnstone reported no conflicts of interest.