User login
HDAC/aromatase inhibitor combo shows promise for HR+/HER2- advanced breast cancer
MUNICH – For patients with HR-positive (HR+) and human epidermal growth factor receptor 2 (HER2)–advanced breast cancer who have progressed after endocrine therapy, a combination of the oral histone deacetylase (HDAC) inhibitor chidamide and exemestane appears safe and more effective than exemestane alone, according to results from the phase 3 ACE trial.
“This is the first phase 3 trial to demonstrate that an HDAC inhibitor plus endocrine blockade improves progression-free survival, compared to endocrine blockade alone in hormone receptor positive advanced breast cancer patients who have progressed after prior endocrine therapy,” said lead author, Zefei Jiang, MD, at the European Society for Medical Oncology Congress.
HDAC inhibitors have historically been used for psychiatric and neurologic applications, but interest in their antineoplastic potential has increased over the past decade. Chidamide is approved for T-cell lymphoma in China, but not in the United States, where three other HDAC inhibitors are labeled for T-cell lymphoma, and a fourth is approved for multiple myeloma.
Although no HDAC inhibitors are clinically available for breast cancer, the future may tell a different story. The HDAC inhibitor entinostat received a breakthrough therapy designation by the Food and Drug Administration after the phase 2 ENCORE 301 trial showed clinical benefit (also with exemestane for advanced breast cancer). Ongoing studies are also evaluating the potential for HDAC inhibitors in combination with immunotherapy.
“Histone modulation by HDACs is a very important mechanism for epigenetic regulation,” said Dr. Jiang, of the 307th Hospital of Chinese People’s Liberation Army in Beijing, highlighting associations with breast cancer drug resistance. HDAC inhibition may be able to overcome this obstacle by resensitizing tumors to estrogen modulator therapy.
ACE was a double-blind, placebo-controlled study involving 362 patients with HR+/HER2–advanced breast cancer who failed endocrine therapy. Patients had previously received no more than one round of chemotherapy for advanced disease, and no more than four therapies total. The treatment group received either chidamide 30 mg twice weekly with exemestane 25 mg daily (n = 241) or exemestane with placebo (n = 121). Tumor assessments were performed every 8 weeks, and the primary endpoint was progression-free survival (PFS).
The addition of chidamide nearly doubled PFS (7.4 months vs. 3.8 months) and provided a hazard ratio of .75 (P = .0336). Objective response and clinical benefit rates also were increased. At the time of presentation, data were too immature for an overall survival rate.
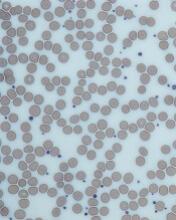
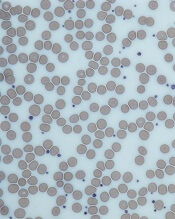
The most common grade 3 or higher adverse events were hematologic: neutropenia (50.8%), thrombocytopenia (27.5%), and leukopenia (18.8%), all considerably higher than 2.5% for each in the placebo group.
These tolerability issues were expected, however, based on previous chidamide findings.
“Not surprisingly ... 33% of patients had their dose reduced, 50% their dose interrupted, and this is despite the biweekly schedule,” said invited discussant Rebecca Dent, MD, of the National Cancer Centre in Singapore. Despite these issues, Dr. Dent concluded that chidamide otherwise “appears to be quite well tolerated,” and showed meaningful results.
“We now have a second trial demonstrating ... clinical benefit from the addition of HDAC inhibitors to endocrine therapy in [HR+] advanced breast cancer,” Dr. Dent said. “HDAC inhibitors clearly warrant further investigation in earlier settings of [HR+] advanced breast cancer and ... yet to be defined ... subgroups, and obviously we anxiously await the phase 3 results of entinostat.”
In consideration of the future, Dr. Dent suggested that more studies are needed to develop subgroup-targeted therapies and optimize sequencing. “We’ve really underestimated the selective pressure of these treatments and how they impact our subsequent therapies,” she said.
Dr. Dent noted how these factors limit predictive relevance of study findings in clinical practice, in which patients with different treatment histories may have completely different responses to the same agent.
To overcome these obstacles, Dr. Dent encouraged development of biomarker-driven strategies that can identify unique patterns of drug resistance and sensitivity. “This will allow us to ... identify which patients, which drug, and at which time.”
The ACE trial was funded by Chipscreen Biosciences.
SOURCE: Jiang Z et al. ESMO 2018, Abstract 283O.
MUNICH – For patients with HR-positive (HR+) and human epidermal growth factor receptor 2 (HER2)–advanced breast cancer who have progressed after endocrine therapy, a combination of the oral histone deacetylase (HDAC) inhibitor chidamide and exemestane appears safe and more effective than exemestane alone, according to results from the phase 3 ACE trial.
“This is the first phase 3 trial to demonstrate that an HDAC inhibitor plus endocrine blockade improves progression-free survival, compared to endocrine blockade alone in hormone receptor positive advanced breast cancer patients who have progressed after prior endocrine therapy,” said lead author, Zefei Jiang, MD, at the European Society for Medical Oncology Congress.
HDAC inhibitors have historically been used for psychiatric and neurologic applications, but interest in their antineoplastic potential has increased over the past decade. Chidamide is approved for T-cell lymphoma in China, but not in the United States, where three other HDAC inhibitors are labeled for T-cell lymphoma, and a fourth is approved for multiple myeloma.
Although no HDAC inhibitors are clinically available for breast cancer, the future may tell a different story. The HDAC inhibitor entinostat received a breakthrough therapy designation by the Food and Drug Administration after the phase 2 ENCORE 301 trial showed clinical benefit (also with exemestane for advanced breast cancer). Ongoing studies are also evaluating the potential for HDAC inhibitors in combination with immunotherapy.
“Histone modulation by HDACs is a very important mechanism for epigenetic regulation,” said Dr. Jiang, of the 307th Hospital of Chinese People’s Liberation Army in Beijing, highlighting associations with breast cancer drug resistance. HDAC inhibition may be able to overcome this obstacle by resensitizing tumors to estrogen modulator therapy.
ACE was a double-blind, placebo-controlled study involving 362 patients with HR+/HER2–advanced breast cancer who failed endocrine therapy. Patients had previously received no more than one round of chemotherapy for advanced disease, and no more than four therapies total. The treatment group received either chidamide 30 mg twice weekly with exemestane 25 mg daily (n = 241) or exemestane with placebo (n = 121). Tumor assessments were performed every 8 weeks, and the primary endpoint was progression-free survival (PFS).
The addition of chidamide nearly doubled PFS (7.4 months vs. 3.8 months) and provided a hazard ratio of .75 (P = .0336). Objective response and clinical benefit rates also were increased. At the time of presentation, data were too immature for an overall survival rate.
The most common grade 3 or higher adverse events were hematologic: neutropenia (50.8%), thrombocytopenia (27.5%), and leukopenia (18.8%), all considerably higher than 2.5% for each in the placebo group.
These tolerability issues were expected, however, based on previous chidamide findings.
“Not surprisingly ... 33% of patients had their dose reduced, 50% their dose interrupted, and this is despite the biweekly schedule,” said invited discussant Rebecca Dent, MD, of the National Cancer Centre in Singapore. Despite these issues, Dr. Dent concluded that chidamide otherwise “appears to be quite well tolerated,” and showed meaningful results.
“We now have a second trial demonstrating ... clinical benefit from the addition of HDAC inhibitors to endocrine therapy in [HR+] advanced breast cancer,” Dr. Dent said. “HDAC inhibitors clearly warrant further investigation in earlier settings of [HR+] advanced breast cancer and ... yet to be defined ... subgroups, and obviously we anxiously await the phase 3 results of entinostat.”
In consideration of the future, Dr. Dent suggested that more studies are needed to develop subgroup-targeted therapies and optimize sequencing. “We’ve really underestimated the selective pressure of these treatments and how they impact our subsequent therapies,” she said.
Dr. Dent noted how these factors limit predictive relevance of study findings in clinical practice, in which patients with different treatment histories may have completely different responses to the same agent.
To overcome these obstacles, Dr. Dent encouraged development of biomarker-driven strategies that can identify unique patterns of drug resistance and sensitivity. “This will allow us to ... identify which patients, which drug, and at which time.”
The ACE trial was funded by Chipscreen Biosciences.
SOURCE: Jiang Z et al. ESMO 2018, Abstract 283O.
MUNICH – For patients with HR-positive (HR+) and human epidermal growth factor receptor 2 (HER2)–advanced breast cancer who have progressed after endocrine therapy, a combination of the oral histone deacetylase (HDAC) inhibitor chidamide and exemestane appears safe and more effective than exemestane alone, according to results from the phase 3 ACE trial.
“This is the first phase 3 trial to demonstrate that an HDAC inhibitor plus endocrine blockade improves progression-free survival, compared to endocrine blockade alone in hormone receptor positive advanced breast cancer patients who have progressed after prior endocrine therapy,” said lead author, Zefei Jiang, MD, at the European Society for Medical Oncology Congress.
HDAC inhibitors have historically been used for psychiatric and neurologic applications, but interest in their antineoplastic potential has increased over the past decade. Chidamide is approved for T-cell lymphoma in China, but not in the United States, where three other HDAC inhibitors are labeled for T-cell lymphoma, and a fourth is approved for multiple myeloma.
Although no HDAC inhibitors are clinically available for breast cancer, the future may tell a different story. The HDAC inhibitor entinostat received a breakthrough therapy designation by the Food and Drug Administration after the phase 2 ENCORE 301 trial showed clinical benefit (also with exemestane for advanced breast cancer). Ongoing studies are also evaluating the potential for HDAC inhibitors in combination with immunotherapy.
“Histone modulation by HDACs is a very important mechanism for epigenetic regulation,” said Dr. Jiang, of the 307th Hospital of Chinese People’s Liberation Army in Beijing, highlighting associations with breast cancer drug resistance. HDAC inhibition may be able to overcome this obstacle by resensitizing tumors to estrogen modulator therapy.
ACE was a double-blind, placebo-controlled study involving 362 patients with HR+/HER2–advanced breast cancer who failed endocrine therapy. Patients had previously received no more than one round of chemotherapy for advanced disease, and no more than four therapies total. The treatment group received either chidamide 30 mg twice weekly with exemestane 25 mg daily (n = 241) or exemestane with placebo (n = 121). Tumor assessments were performed every 8 weeks, and the primary endpoint was progression-free survival (PFS).
The addition of chidamide nearly doubled PFS (7.4 months vs. 3.8 months) and provided a hazard ratio of .75 (P = .0336). Objective response and clinical benefit rates also were increased. At the time of presentation, data were too immature for an overall survival rate.
The most common grade 3 or higher adverse events were hematologic: neutropenia (50.8%), thrombocytopenia (27.5%), and leukopenia (18.8%), all considerably higher than 2.5% for each in the placebo group.
These tolerability issues were expected, however, based on previous chidamide findings.
“Not surprisingly ... 33% of patients had their dose reduced, 50% their dose interrupted, and this is despite the biweekly schedule,” said invited discussant Rebecca Dent, MD, of the National Cancer Centre in Singapore. Despite these issues, Dr. Dent concluded that chidamide otherwise “appears to be quite well tolerated,” and showed meaningful results.
“We now have a second trial demonstrating ... clinical benefit from the addition of HDAC inhibitors to endocrine therapy in [HR+] advanced breast cancer,” Dr. Dent said. “HDAC inhibitors clearly warrant further investigation in earlier settings of [HR+] advanced breast cancer and ... yet to be defined ... subgroups, and obviously we anxiously await the phase 3 results of entinostat.”
In consideration of the future, Dr. Dent suggested that more studies are needed to develop subgroup-targeted therapies and optimize sequencing. “We’ve really underestimated the selective pressure of these treatments and how they impact our subsequent therapies,” she said.
Dr. Dent noted how these factors limit predictive relevance of study findings in clinical practice, in which patients with different treatment histories may have completely different responses to the same agent.
To overcome these obstacles, Dr. Dent encouraged development of biomarker-driven strategies that can identify unique patterns of drug resistance and sensitivity. “This will allow us to ... identify which patients, which drug, and at which time.”
The ACE trial was funded by Chipscreen Biosciences.
SOURCE: Jiang Z et al. ESMO 2018, Abstract 283O.
REPORTING FROM ESMO 2018
Key clinical point: For patients with HR+/HER2–advanced breast cancer who have progressed after endocrine therapy, a combination of oral HDAC inhibitor chidamide and exemestane appears safe and more effective than exemestane alone.
Major finding: Chidamide + exemestane combination therapy increased progression-free survival by about 4 months compared with exemestane monotherapy (7.4 months vs 3.8 months).
Study details: ACE was a phase 3, double-blind, placebo-controlled trial involving 362 patients with HR+/HER2–advanced breast cancer who failed endocrine therapy.
Disclosures: The study was funded by Chipscreen Biosciences.
Source: Jiang Z et al. ESMO 2018, Abstract 283O.
High systemic inflammation at midlife portends cognitive changes in later life
ATLANTA – results from a long-term analysis showed.
“There is considerable evidence suggesting that abnormal immune functioning and inflammation may influence cognitive functioning and promote dementia,” lead study author Keenan Walker, PhD, said in an interview in advance of the annual meeting of the American Neurological Association. “For example, several studies have found higher levels of inflammatory markers in the blood and cerebral spinal fluid of patients with dementia, compared to nondemented individuals of a comparable age. What is less clear, however, is whether inflammation actually promotes cognitive decline or occurs simply as a result of the brain changes underlying dementia.”
To help answer this question, Dr. Walker, of Johns Hopkins University, Baltimore, and his colleagues evaluated blood biomarkers of inflammation in 12,727 middle-aged participants during visits one and two of the Atherosclerosis Risk in Communities (ARIC) study, a prospective epidemiologic analysis conducted in four U.S. communities and funded by the National Heart, Lung, and Blood Institute. Visit one occurred between 1987 and 1989, while visit two took place between 1990 and 1992. The researchers related these markers to cognitive change over the subsequent decades. Specifically, they used four biomarkers (fibrinogen, white blood cell count, von Willebrand factor, and Factor VIII) to create an inflammation composite score at visit one, and measured C-reactive protein (CRP) at visit two. Next, they used measures of memory, executive function, and language assess cognition over three visits spanning 20 years.
The average age of study participants at first cognitive assessment was 57 years, 56% were women, and 21% were black. After controlling for differences in demographic variables, vascular risk factors and comorbidities, the researchers observed that each standard deviation (SD) increase in the midlife inflammation composite score was associated with an additional 20-year global cognitive decline of –0.035 SD (P less than .01). They found a similar association between each SD higher midlife CRP level and additional 20-year decline in global cognition (–0.038 SD; P less than .01). In addition, study participants with a midlife inflammation composite score in the top quartile had a 7.6% steeper decline in global cognition, compared with participants in the lowest quartile; a similar association was observed for CRP.
“We were surprised at what we found when we looked at inflammation’s effect on individual cognitive domains,” Dr. Walker said. “Specifically, we found that inflammation was associated with declines in memory, but not declines in other domains, such as executive function or language. One possible interpretation for these findings is that inflammation may selectively influence brain regions such as the hippocampus, which are necessary for memory consolidation and are also most vulnerable to Alzheimer’s disease.” He added that the current findings “provide support for the idea that systemic inflammation may have an early pathogenic role in the cognitive decline that occurs in the decades leading up to older adulthood.”
Dr. Walker acknowledged certain limitations of the study, including the attrition of participants because of deaths and dropouts over the 20-year follow-up period. “Because high levels of inflammation and comorbid disease are related to death and risk of study dropout, the sample of participants who completed the entirety of the study may represent a group that is healthier overall than the general population,” he said. “However, we took several steps to reduce any potential attrition bias using advanced statistical techniques.”
Dr. Walker disclosed that he receives funding support from the National Institutes of Health.
Source: Walker et al. ANA 2018, Abstract 305.
ATLANTA – results from a long-term analysis showed.
“There is considerable evidence suggesting that abnormal immune functioning and inflammation may influence cognitive functioning and promote dementia,” lead study author Keenan Walker, PhD, said in an interview in advance of the annual meeting of the American Neurological Association. “For example, several studies have found higher levels of inflammatory markers in the blood and cerebral spinal fluid of patients with dementia, compared to nondemented individuals of a comparable age. What is less clear, however, is whether inflammation actually promotes cognitive decline or occurs simply as a result of the brain changes underlying dementia.”
To help answer this question, Dr. Walker, of Johns Hopkins University, Baltimore, and his colleagues evaluated blood biomarkers of inflammation in 12,727 middle-aged participants during visits one and two of the Atherosclerosis Risk in Communities (ARIC) study, a prospective epidemiologic analysis conducted in four U.S. communities and funded by the National Heart, Lung, and Blood Institute. Visit one occurred between 1987 and 1989, while visit two took place between 1990 and 1992. The researchers related these markers to cognitive change over the subsequent decades. Specifically, they used four biomarkers (fibrinogen, white blood cell count, von Willebrand factor, and Factor VIII) to create an inflammation composite score at visit one, and measured C-reactive protein (CRP) at visit two. Next, they used measures of memory, executive function, and language assess cognition over three visits spanning 20 years.
The average age of study participants at first cognitive assessment was 57 years, 56% were women, and 21% were black. After controlling for differences in demographic variables, vascular risk factors and comorbidities, the researchers observed that each standard deviation (SD) increase in the midlife inflammation composite score was associated with an additional 20-year global cognitive decline of –0.035 SD (P less than .01). They found a similar association between each SD higher midlife CRP level and additional 20-year decline in global cognition (–0.038 SD; P less than .01). In addition, study participants with a midlife inflammation composite score in the top quartile had a 7.6% steeper decline in global cognition, compared with participants in the lowest quartile; a similar association was observed for CRP.
“We were surprised at what we found when we looked at inflammation’s effect on individual cognitive domains,” Dr. Walker said. “Specifically, we found that inflammation was associated with declines in memory, but not declines in other domains, such as executive function or language. One possible interpretation for these findings is that inflammation may selectively influence brain regions such as the hippocampus, which are necessary for memory consolidation and are also most vulnerable to Alzheimer’s disease.” He added that the current findings “provide support for the idea that systemic inflammation may have an early pathogenic role in the cognitive decline that occurs in the decades leading up to older adulthood.”
Dr. Walker acknowledged certain limitations of the study, including the attrition of participants because of deaths and dropouts over the 20-year follow-up period. “Because high levels of inflammation and comorbid disease are related to death and risk of study dropout, the sample of participants who completed the entirety of the study may represent a group that is healthier overall than the general population,” he said. “However, we took several steps to reduce any potential attrition bias using advanced statistical techniques.”
Dr. Walker disclosed that he receives funding support from the National Institutes of Health.
Source: Walker et al. ANA 2018, Abstract 305.
ATLANTA – results from a long-term analysis showed.
“There is considerable evidence suggesting that abnormal immune functioning and inflammation may influence cognitive functioning and promote dementia,” lead study author Keenan Walker, PhD, said in an interview in advance of the annual meeting of the American Neurological Association. “For example, several studies have found higher levels of inflammatory markers in the blood and cerebral spinal fluid of patients with dementia, compared to nondemented individuals of a comparable age. What is less clear, however, is whether inflammation actually promotes cognitive decline or occurs simply as a result of the brain changes underlying dementia.”
To help answer this question, Dr. Walker, of Johns Hopkins University, Baltimore, and his colleagues evaluated blood biomarkers of inflammation in 12,727 middle-aged participants during visits one and two of the Atherosclerosis Risk in Communities (ARIC) study, a prospective epidemiologic analysis conducted in four U.S. communities and funded by the National Heart, Lung, and Blood Institute. Visit one occurred between 1987 and 1989, while visit two took place between 1990 and 1992. The researchers related these markers to cognitive change over the subsequent decades. Specifically, they used four biomarkers (fibrinogen, white blood cell count, von Willebrand factor, and Factor VIII) to create an inflammation composite score at visit one, and measured C-reactive protein (CRP) at visit two. Next, they used measures of memory, executive function, and language assess cognition over three visits spanning 20 years.
The average age of study participants at first cognitive assessment was 57 years, 56% were women, and 21% were black. After controlling for differences in demographic variables, vascular risk factors and comorbidities, the researchers observed that each standard deviation (SD) increase in the midlife inflammation composite score was associated with an additional 20-year global cognitive decline of –0.035 SD (P less than .01). They found a similar association between each SD higher midlife CRP level and additional 20-year decline in global cognition (–0.038 SD; P less than .01). In addition, study participants with a midlife inflammation composite score in the top quartile had a 7.6% steeper decline in global cognition, compared with participants in the lowest quartile; a similar association was observed for CRP.
“We were surprised at what we found when we looked at inflammation’s effect on individual cognitive domains,” Dr. Walker said. “Specifically, we found that inflammation was associated with declines in memory, but not declines in other domains, such as executive function or language. One possible interpretation for these findings is that inflammation may selectively influence brain regions such as the hippocampus, which are necessary for memory consolidation and are also most vulnerable to Alzheimer’s disease.” He added that the current findings “provide support for the idea that systemic inflammation may have an early pathogenic role in the cognitive decline that occurs in the decades leading up to older adulthood.”
Dr. Walker acknowledged certain limitations of the study, including the attrition of participants because of deaths and dropouts over the 20-year follow-up period. “Because high levels of inflammation and comorbid disease are related to death and risk of study dropout, the sample of participants who completed the entirety of the study may represent a group that is healthier overall than the general population,” he said. “However, we took several steps to reduce any potential attrition bias using advanced statistical techniques.”
Dr. Walker disclosed that he receives funding support from the National Institutes of Health.
Source: Walker et al. ANA 2018, Abstract 305.
REPORTING FROM ANA 2018
Key clinical point: Inflammation was associated with declines in memory, but not declines in other domains, such as executive function or language.
Major finding: Each standard deviation (SD) increase in the midlife inflammation composite score was associated with an additional 20-year global cognitive decline of –0.035 SD (P less than .01).
Study details: An evaluation of blood biomarkers of inflammation in 12,727 middle-aged participants in the Atherosclerosis Risk in Communities Study.
Disclosures: Dr. Walker disclosed that he receives funding support from the National Institutes of Health.
Source: Walker et al. ANA 2018, Abstract 305.
PALOMA-3: Overall survival better for endocrine-sensitive patients only
MUNICH – The combination of the cyclin-dependent kinase 4/6 inhibitor palbociclib (Ibrance) and fulvestrant (Faslodex) was associated with longer overall survival of women with hormone receptor–positive, human epidermal growth factor receptor 2 (HER2)–negative advanced breast cancer in the PALOMA-3 trial.
But the benefit seemed to be almost entirely limited to women with sensitivity to previous endocrine therapy; differences in overall survival among the entire cohort were not statistically significant, reported Massimo Cristofanilli, MD, of Northwestern University in Chicago, and his colleagues.
“These findings confirm that the use of palbociclib plus fulvestrant is a standard for care in patients with previously treated hormone receptor–positive, HER2-negative advanced breast cancer, he said in a briefing held prior to his presentation of the data at the European Society for Medical Oncology Congress.
The results were published simultaneously online in the New England Journal of Medicine.
Briefing discussant Nadia Harbeck, MD, is a breast cancer specialist with the University of Munich Medical Center, who is a coinvestigator of PALOMA-3, noted that there are currently three marketed cyclin-dependent kinase (CDK) 4/6 inhibitors and that all three have been shown to be associated with prolonged progression-free survival (PFS).
Yet, “there’s still a lot of uncertainty out there in the community whether to give these drugs, when to give these drugs, and also from the payers’ perspective, because there’s no overall survival, and I think this is now going to change,” she said.
“Ten months overall survival benefit in a CDK 4/6 inhibitor study in the second-line setting I think is unprecedented, and I think will change people’s hearts who weren’t quite sure, and I think we can now confidently say to our patients that this is the drug to take,” she added.
Dr. Cristofanilli discussed results of a prespecified analysis of overall survival from the previously reported trial.
Investigators enrolled 521 patients with HR-positive, HER2-negative advanced breast cancer who had progression or relapse during previous endocrine therapy, and randomly assigned them to fulvestrant plus palbociclib or placebo.
In addition to looking at overall survival, the analysis included evaluation of the effects of palbociclib in women both with and without sensitivity to endocrine therapy, the presence or absence of visceral metastatic disease, and menopausal status. In addition, the analysis looked at the efficacy of therapies after disease progression, and safety of the respective regimens.
The median overall survival at a median follow-up of 44.8 months was 34.9 months with palbociclib/fulvestrant vs. 28 months for placebo/fulvestrant, translating into a stratified hazard ratio (HR) for death in the palbociclib arm of 0.81, but this difference was not statistically significant (P = .09). The unstratified HR was 0.79 (P = .05; the prespecified significance threshold was a two-sided P value of .047).
When they looked at the 410 patients with documented sensitivity to previous endocrine therapy, however, the investigators found a median OS of 39.7 months with palbociclib vs. 29.7 months with placebo. The HR for death with palbociclib in this subgroup was 0.72, with a 95% confidence interval indicating statistical significance.
In contrast, among 111 patients with documented intrinsic endocrine resistance, the median OS with palbociclib was actually lower than in the placebo group, albeit not significantly, at 20.2 vs. 26.2 months, respectively (HR, 1.14; P = .012 for interaction).
The median time to starting chemotherapy was 17.6 months in the palbociclib/fulvestrant group vs. 8.8 months in the placebo/fulvestrant group (HR, 0.58; P less than .001).
The safety profile of the combination was similar to that seen in the primary analysis of PALOMA-3. Grade 3 or 4 neutropenia occurred in 70% of patients on palbociclib vs. none of the patients on placebo. Other grade 3 or 4 events included anemia in 4% vs. 2%, thrombocytopenia in 3% vs. none, and febrile neutropenia in 1% vs. none.
Other grade 3 or greater events occurring with palbociclib in more than 2% of patients were infections, fatigue, and elevated aspartate aminotransferase levels.
Invited discussant Fatima Cardoso, MD, director of the breast unit of the Champalimaud Clinical Center in Lisbon, commented that PALOMA-3 was adequately powered for the primary endpoint of PFS, but not for a secondary overall survival endpoint.
She also raised questions that still need to be answered about the use of CDK 4/6 inhibitors with endocrine therapy in this population, including how to better identify which patients might benefit from the combination, whether the combination should be used in the first line or in subsequent lines of therapy, and whether it should be used in patients with or without prior endocrine therapy exposure.
Another unanswered question is whether disease progression accelerates after CDK 4/6 inhibitors are stopped.
“We need to confirm if this problem of post progression is true or not, and there may be a rationale to explore continuing beyond progression. This was a paradigm that changed in the HER2-positive population, and we now know that we need to continue to block the HER2 pathway, because if we don’t, the progression is faster. Will that apply here as well?,” she asked.
Hope S. Rugo, MD, a clinical professor of medicine and director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center, commented that patients in PALOMA-3 were allowed to have had chemotherapy, and there is evidence to suggest that prior chemotherapy is a risk factor for resistance to other therapies as well.
“So looking at patients with hormone-sensitive disease who have done their chemotherapy, seeing a survival benefit in any subset of patients with hormone receptor–positive disease getting a targeted agent is already pretty exciting,” she said in an interview.
Dr. Rugo was not involved in PALOMA-3.
PALOMA-3 was supported by Pfizer. Dr. Cristofanilli disclosed personal fees from Pfizer, Novartis, and Merus. Dr. Harbeck disclosed honoraria for consulting and lecturing for Pfizer and others. Dr. Cardoso has disclosed consulting fees and institutional support from Pfizer and others. Dr. Rugo has received fees/honoraria and other support for activities for Pfizer and others.
SOURCE: Turner NC et al. N Engl J Med. 2018 Oct 20. doi: 10.1056/NEJMoa1810527.
MUNICH – The combination of the cyclin-dependent kinase 4/6 inhibitor palbociclib (Ibrance) and fulvestrant (Faslodex) was associated with longer overall survival of women with hormone receptor–positive, human epidermal growth factor receptor 2 (HER2)–negative advanced breast cancer in the PALOMA-3 trial.
But the benefit seemed to be almost entirely limited to women with sensitivity to previous endocrine therapy; differences in overall survival among the entire cohort were not statistically significant, reported Massimo Cristofanilli, MD, of Northwestern University in Chicago, and his colleagues.
“These findings confirm that the use of palbociclib plus fulvestrant is a standard for care in patients with previously treated hormone receptor–positive, HER2-negative advanced breast cancer, he said in a briefing held prior to his presentation of the data at the European Society for Medical Oncology Congress.
The results were published simultaneously online in the New England Journal of Medicine.
Briefing discussant Nadia Harbeck, MD, is a breast cancer specialist with the University of Munich Medical Center, who is a coinvestigator of PALOMA-3, noted that there are currently three marketed cyclin-dependent kinase (CDK) 4/6 inhibitors and that all three have been shown to be associated with prolonged progression-free survival (PFS).
Yet, “there’s still a lot of uncertainty out there in the community whether to give these drugs, when to give these drugs, and also from the payers’ perspective, because there’s no overall survival, and I think this is now going to change,” she said.
“Ten months overall survival benefit in a CDK 4/6 inhibitor study in the second-line setting I think is unprecedented, and I think will change people’s hearts who weren’t quite sure, and I think we can now confidently say to our patients that this is the drug to take,” she added.
Dr. Cristofanilli discussed results of a prespecified analysis of overall survival from the previously reported trial.
Investigators enrolled 521 patients with HR-positive, HER2-negative advanced breast cancer who had progression or relapse during previous endocrine therapy, and randomly assigned them to fulvestrant plus palbociclib or placebo.
In addition to looking at overall survival, the analysis included evaluation of the effects of palbociclib in women both with and without sensitivity to endocrine therapy, the presence or absence of visceral metastatic disease, and menopausal status. In addition, the analysis looked at the efficacy of therapies after disease progression, and safety of the respective regimens.
The median overall survival at a median follow-up of 44.8 months was 34.9 months with palbociclib/fulvestrant vs. 28 months for placebo/fulvestrant, translating into a stratified hazard ratio (HR) for death in the palbociclib arm of 0.81, but this difference was not statistically significant (P = .09). The unstratified HR was 0.79 (P = .05; the prespecified significance threshold was a two-sided P value of .047).
When they looked at the 410 patients with documented sensitivity to previous endocrine therapy, however, the investigators found a median OS of 39.7 months with palbociclib vs. 29.7 months with placebo. The HR for death with palbociclib in this subgroup was 0.72, with a 95% confidence interval indicating statistical significance.
In contrast, among 111 patients with documented intrinsic endocrine resistance, the median OS with palbociclib was actually lower than in the placebo group, albeit not significantly, at 20.2 vs. 26.2 months, respectively (HR, 1.14; P = .012 for interaction).
The median time to starting chemotherapy was 17.6 months in the palbociclib/fulvestrant group vs. 8.8 months in the placebo/fulvestrant group (HR, 0.58; P less than .001).
The safety profile of the combination was similar to that seen in the primary analysis of PALOMA-3. Grade 3 or 4 neutropenia occurred in 70% of patients on palbociclib vs. none of the patients on placebo. Other grade 3 or 4 events included anemia in 4% vs. 2%, thrombocytopenia in 3% vs. none, and febrile neutropenia in 1% vs. none.
Other grade 3 or greater events occurring with palbociclib in more than 2% of patients were infections, fatigue, and elevated aspartate aminotransferase levels.
Invited discussant Fatima Cardoso, MD, director of the breast unit of the Champalimaud Clinical Center in Lisbon, commented that PALOMA-3 was adequately powered for the primary endpoint of PFS, but not for a secondary overall survival endpoint.
She also raised questions that still need to be answered about the use of CDK 4/6 inhibitors with endocrine therapy in this population, including how to better identify which patients might benefit from the combination, whether the combination should be used in the first line or in subsequent lines of therapy, and whether it should be used in patients with or without prior endocrine therapy exposure.
Another unanswered question is whether disease progression accelerates after CDK 4/6 inhibitors are stopped.
“We need to confirm if this problem of post progression is true or not, and there may be a rationale to explore continuing beyond progression. This was a paradigm that changed in the HER2-positive population, and we now know that we need to continue to block the HER2 pathway, because if we don’t, the progression is faster. Will that apply here as well?,” she asked.
Hope S. Rugo, MD, a clinical professor of medicine and director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center, commented that patients in PALOMA-3 were allowed to have had chemotherapy, and there is evidence to suggest that prior chemotherapy is a risk factor for resistance to other therapies as well.
“So looking at patients with hormone-sensitive disease who have done their chemotherapy, seeing a survival benefit in any subset of patients with hormone receptor–positive disease getting a targeted agent is already pretty exciting,” she said in an interview.
Dr. Rugo was not involved in PALOMA-3.
PALOMA-3 was supported by Pfizer. Dr. Cristofanilli disclosed personal fees from Pfizer, Novartis, and Merus. Dr. Harbeck disclosed honoraria for consulting and lecturing for Pfizer and others. Dr. Cardoso has disclosed consulting fees and institutional support from Pfizer and others. Dr. Rugo has received fees/honoraria and other support for activities for Pfizer and others.
SOURCE: Turner NC et al. N Engl J Med. 2018 Oct 20. doi: 10.1056/NEJMoa1810527.
MUNICH – The combination of the cyclin-dependent kinase 4/6 inhibitor palbociclib (Ibrance) and fulvestrant (Faslodex) was associated with longer overall survival of women with hormone receptor–positive, human epidermal growth factor receptor 2 (HER2)–negative advanced breast cancer in the PALOMA-3 trial.
But the benefit seemed to be almost entirely limited to women with sensitivity to previous endocrine therapy; differences in overall survival among the entire cohort were not statistically significant, reported Massimo Cristofanilli, MD, of Northwestern University in Chicago, and his colleagues.
“These findings confirm that the use of palbociclib plus fulvestrant is a standard for care in patients with previously treated hormone receptor–positive, HER2-negative advanced breast cancer, he said in a briefing held prior to his presentation of the data at the European Society for Medical Oncology Congress.
The results were published simultaneously online in the New England Journal of Medicine.
Briefing discussant Nadia Harbeck, MD, is a breast cancer specialist with the University of Munich Medical Center, who is a coinvestigator of PALOMA-3, noted that there are currently three marketed cyclin-dependent kinase (CDK) 4/6 inhibitors and that all three have been shown to be associated with prolonged progression-free survival (PFS).
Yet, “there’s still a lot of uncertainty out there in the community whether to give these drugs, when to give these drugs, and also from the payers’ perspective, because there’s no overall survival, and I think this is now going to change,” she said.
“Ten months overall survival benefit in a CDK 4/6 inhibitor study in the second-line setting I think is unprecedented, and I think will change people’s hearts who weren’t quite sure, and I think we can now confidently say to our patients that this is the drug to take,” she added.
Dr. Cristofanilli discussed results of a prespecified analysis of overall survival from the previously reported trial.
Investigators enrolled 521 patients with HR-positive, HER2-negative advanced breast cancer who had progression or relapse during previous endocrine therapy, and randomly assigned them to fulvestrant plus palbociclib or placebo.
In addition to looking at overall survival, the analysis included evaluation of the effects of palbociclib in women both with and without sensitivity to endocrine therapy, the presence or absence of visceral metastatic disease, and menopausal status. In addition, the analysis looked at the efficacy of therapies after disease progression, and safety of the respective regimens.
The median overall survival at a median follow-up of 44.8 months was 34.9 months with palbociclib/fulvestrant vs. 28 months for placebo/fulvestrant, translating into a stratified hazard ratio (HR) for death in the palbociclib arm of 0.81, but this difference was not statistically significant (P = .09). The unstratified HR was 0.79 (P = .05; the prespecified significance threshold was a two-sided P value of .047).
When they looked at the 410 patients with documented sensitivity to previous endocrine therapy, however, the investigators found a median OS of 39.7 months with palbociclib vs. 29.7 months with placebo. The HR for death with palbociclib in this subgroup was 0.72, with a 95% confidence interval indicating statistical significance.
In contrast, among 111 patients with documented intrinsic endocrine resistance, the median OS with palbociclib was actually lower than in the placebo group, albeit not significantly, at 20.2 vs. 26.2 months, respectively (HR, 1.14; P = .012 for interaction).
The median time to starting chemotherapy was 17.6 months in the palbociclib/fulvestrant group vs. 8.8 months in the placebo/fulvestrant group (HR, 0.58; P less than .001).
The safety profile of the combination was similar to that seen in the primary analysis of PALOMA-3. Grade 3 or 4 neutropenia occurred in 70% of patients on palbociclib vs. none of the patients on placebo. Other grade 3 or 4 events included anemia in 4% vs. 2%, thrombocytopenia in 3% vs. none, and febrile neutropenia in 1% vs. none.
Other grade 3 or greater events occurring with palbociclib in more than 2% of patients were infections, fatigue, and elevated aspartate aminotransferase levels.
Invited discussant Fatima Cardoso, MD, director of the breast unit of the Champalimaud Clinical Center in Lisbon, commented that PALOMA-3 was adequately powered for the primary endpoint of PFS, but not for a secondary overall survival endpoint.
She also raised questions that still need to be answered about the use of CDK 4/6 inhibitors with endocrine therapy in this population, including how to better identify which patients might benefit from the combination, whether the combination should be used in the first line or in subsequent lines of therapy, and whether it should be used in patients with or without prior endocrine therapy exposure.
Another unanswered question is whether disease progression accelerates after CDK 4/6 inhibitors are stopped.
“We need to confirm if this problem of post progression is true or not, and there may be a rationale to explore continuing beyond progression. This was a paradigm that changed in the HER2-positive population, and we now know that we need to continue to block the HER2 pathway, because if we don’t, the progression is faster. Will that apply here as well?,” she asked.
Hope S. Rugo, MD, a clinical professor of medicine and director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center, commented that patients in PALOMA-3 were allowed to have had chemotherapy, and there is evidence to suggest that prior chemotherapy is a risk factor for resistance to other therapies as well.
“So looking at patients with hormone-sensitive disease who have done their chemotherapy, seeing a survival benefit in any subset of patients with hormone receptor–positive disease getting a targeted agent is already pretty exciting,” she said in an interview.
Dr. Rugo was not involved in PALOMA-3.
PALOMA-3 was supported by Pfizer. Dr. Cristofanilli disclosed personal fees from Pfizer, Novartis, and Merus. Dr. Harbeck disclosed honoraria for consulting and lecturing for Pfizer and others. Dr. Cardoso has disclosed consulting fees and institutional support from Pfizer and others. Dr. Rugo has received fees/honoraria and other support for activities for Pfizer and others.
SOURCE: Turner NC et al. N Engl J Med. 2018 Oct 20. doi: 10.1056/NEJMoa1810527.
AT ESMO 2018
Key clinical point: The combination of a CDK 4/6 inhibitor and a selective estrogen receptor modifier is associated with longer overall survival in some patients.
Major finding: Median OS 39.7 months with palbociclib/fulvestrant vs. 29.7 months with placebo/fulvestrant.
Study details: Prespecified survival analysis of 521 patients in the PALOMA-3 trial.
Disclosures: PALOMA-3 was supported by Pfizer. Dr. Cristofanilli disclosed personal fees from Pfizer, Novartis, and Merus. Dr. Harbeck disclosed honoraria for consulting and lecturing for Pfizer and others. Dr. Cardoso has disclosed consulting fees and institutional support from Pfizer and others. Dr. Rugo has received fees/honoraria and other support for activities for Pfizer and others.
Source: Turner NC et al. N Engl J Med. 2018 Oct 20. doi: 10.1056/NEJMoa1810527.
Prior TIA proves less risky than stroke in AF patients
MONTREAL – Stroke and transient ischemic attack, usually joined at the hip as related histories that each flag a similar need for anticoagulation may in fact not be nearly as equivalent as conventional wisdom says.
Analysis of 2-year follow-up data from the GARFIELD-AF registry of more than 52,000 patients with newly diagnosed atrial fibrillation (AF) showed that, while patients with a history of stroke had significantly elevated rates of both all-cause mortality and stroke, those with just a history of a transient ischemic attack (TIA) had mortality and stroke rates virtually identical to AF patients with no history of a cerebrovascular event.
“A history of TIA only is not a reliable predictor of an increased risk for events,” Werner Hacke, MD, said at the World Stroke Congress. “A history of TIA should be removed from scores estimating the risk for stroke and systemic embolism in AF patients,” said Dr. Hacke, professor and chairman of the department of neurology at the University of Heidelberg (Germany).
“The weak predictive power of a history of TIA is probably caused by the relatively low reliability of establishing the diagnosis of TIA,” especially when the diagnosis is made by someone who’s not a neurologist. “It’s a very fuzzy diagnosis,” even for a neurologist, and it consistently confounds other clinicians, he said in an interview. “I’d be really careful of deciding to anticoagulate a patient [with AF] based on a history of TIA.” In the GARFIELD-AF registry, “I’m convinced that most people with a history of TIA actually never had a TIA.”
Dr. Hacke has been unable to find a good explanation of why, years ago, TIAs began to get routinely lumped with stroke. “I asked all the old AF guys when did TIA start coming in and why, and none of them could remember,” he said. “At first, they talked about a history of ‘cerebrovascular events,’ but then that became stroke and TIA, and it was as if it was one word,” always said in the same breath. Both the CHADS2 score (JAMA. 2001 Jun 13;285[22]:2864-70) and the CHA2DS2-VASc score (Chest. 2010 Feb;137[2]:263-72) make a history of stroke or TIA, as well as thromboembolism, coequal risk factors that count for 2 points when calculating the thrombotic risk score for a patient with AF.
To test whether this really made sense, Dr. Hacke and his associates decided to look at the separate consequences of a history of stroke only, compared with a history of a TIA only. They used data collected in GARFIELD-AF (Global Anticoagulant Registry in the Field), a multinational registry with 51,670 patients newly diagnosed with AF, followed for 2 years, and with complete information on their stroke and TIA history. This included 5,617 patients with a history of at least one diagnosed cerebrovascular event, including 3,362 diagnosed with stroke only, 1,788 diagnosed with TIA only, and the remaining patients diagnosed with both types of events.
When compared with AF patients without a history of any type of cerebrovascular event, those with a history of a stroke only had a statistically significant 29% increased rate of all-cause death and a 2.3-fold higher rate of stroke after adjustment for baseline demographic and clinical differences. In contrast, the patients with a history of TIA only had mortality and stroke rates during follow-up that did not differ significantly from the comparator group.
Source: Hacke W et al. World Stroke Congress, Abstract.
MONTREAL – Stroke and transient ischemic attack, usually joined at the hip as related histories that each flag a similar need for anticoagulation may in fact not be nearly as equivalent as conventional wisdom says.
Analysis of 2-year follow-up data from the GARFIELD-AF registry of more than 52,000 patients with newly diagnosed atrial fibrillation (AF) showed that, while patients with a history of stroke had significantly elevated rates of both all-cause mortality and stroke, those with just a history of a transient ischemic attack (TIA) had mortality and stroke rates virtually identical to AF patients with no history of a cerebrovascular event.
“A history of TIA only is not a reliable predictor of an increased risk for events,” Werner Hacke, MD, said at the World Stroke Congress. “A history of TIA should be removed from scores estimating the risk for stroke and systemic embolism in AF patients,” said Dr. Hacke, professor and chairman of the department of neurology at the University of Heidelberg (Germany).
“The weak predictive power of a history of TIA is probably caused by the relatively low reliability of establishing the diagnosis of TIA,” especially when the diagnosis is made by someone who’s not a neurologist. “It’s a very fuzzy diagnosis,” even for a neurologist, and it consistently confounds other clinicians, he said in an interview. “I’d be really careful of deciding to anticoagulate a patient [with AF] based on a history of TIA.” In the GARFIELD-AF registry, “I’m convinced that most people with a history of TIA actually never had a TIA.”
Dr. Hacke has been unable to find a good explanation of why, years ago, TIAs began to get routinely lumped with stroke. “I asked all the old AF guys when did TIA start coming in and why, and none of them could remember,” he said. “At first, they talked about a history of ‘cerebrovascular events,’ but then that became stroke and TIA, and it was as if it was one word,” always said in the same breath. Both the CHADS2 score (JAMA. 2001 Jun 13;285[22]:2864-70) and the CHA2DS2-VASc score (Chest. 2010 Feb;137[2]:263-72) make a history of stroke or TIA, as well as thromboembolism, coequal risk factors that count for 2 points when calculating the thrombotic risk score for a patient with AF.
To test whether this really made sense, Dr. Hacke and his associates decided to look at the separate consequences of a history of stroke only, compared with a history of a TIA only. They used data collected in GARFIELD-AF (Global Anticoagulant Registry in the Field), a multinational registry with 51,670 patients newly diagnosed with AF, followed for 2 years, and with complete information on their stroke and TIA history. This included 5,617 patients with a history of at least one diagnosed cerebrovascular event, including 3,362 diagnosed with stroke only, 1,788 diagnosed with TIA only, and the remaining patients diagnosed with both types of events.
When compared with AF patients without a history of any type of cerebrovascular event, those with a history of a stroke only had a statistically significant 29% increased rate of all-cause death and a 2.3-fold higher rate of stroke after adjustment for baseline demographic and clinical differences. In contrast, the patients with a history of TIA only had mortality and stroke rates during follow-up that did not differ significantly from the comparator group.
Source: Hacke W et al. World Stroke Congress, Abstract.
MONTREAL – Stroke and transient ischemic attack, usually joined at the hip as related histories that each flag a similar need for anticoagulation may in fact not be nearly as equivalent as conventional wisdom says.
Analysis of 2-year follow-up data from the GARFIELD-AF registry of more than 52,000 patients with newly diagnosed atrial fibrillation (AF) showed that, while patients with a history of stroke had significantly elevated rates of both all-cause mortality and stroke, those with just a history of a transient ischemic attack (TIA) had mortality and stroke rates virtually identical to AF patients with no history of a cerebrovascular event.
“A history of TIA only is not a reliable predictor of an increased risk for events,” Werner Hacke, MD, said at the World Stroke Congress. “A history of TIA should be removed from scores estimating the risk for stroke and systemic embolism in AF patients,” said Dr. Hacke, professor and chairman of the department of neurology at the University of Heidelberg (Germany).
“The weak predictive power of a history of TIA is probably caused by the relatively low reliability of establishing the diagnosis of TIA,” especially when the diagnosis is made by someone who’s not a neurologist. “It’s a very fuzzy diagnosis,” even for a neurologist, and it consistently confounds other clinicians, he said in an interview. “I’d be really careful of deciding to anticoagulate a patient [with AF] based on a history of TIA.” In the GARFIELD-AF registry, “I’m convinced that most people with a history of TIA actually never had a TIA.”
Dr. Hacke has been unable to find a good explanation of why, years ago, TIAs began to get routinely lumped with stroke. “I asked all the old AF guys when did TIA start coming in and why, and none of them could remember,” he said. “At first, they talked about a history of ‘cerebrovascular events,’ but then that became stroke and TIA, and it was as if it was one word,” always said in the same breath. Both the CHADS2 score (JAMA. 2001 Jun 13;285[22]:2864-70) and the CHA2DS2-VASc score (Chest. 2010 Feb;137[2]:263-72) make a history of stroke or TIA, as well as thromboembolism, coequal risk factors that count for 2 points when calculating the thrombotic risk score for a patient with AF.
To test whether this really made sense, Dr. Hacke and his associates decided to look at the separate consequences of a history of stroke only, compared with a history of a TIA only. They used data collected in GARFIELD-AF (Global Anticoagulant Registry in the Field), a multinational registry with 51,670 patients newly diagnosed with AF, followed for 2 years, and with complete information on their stroke and TIA history. This included 5,617 patients with a history of at least one diagnosed cerebrovascular event, including 3,362 diagnosed with stroke only, 1,788 diagnosed with TIA only, and the remaining patients diagnosed with both types of events.
When compared with AF patients without a history of any type of cerebrovascular event, those with a history of a stroke only had a statistically significant 29% increased rate of all-cause death and a 2.3-fold higher rate of stroke after adjustment for baseline demographic and clinical differences. In contrast, the patients with a history of TIA only had mortality and stroke rates during follow-up that did not differ significantly from the comparator group.
Source: Hacke W et al. World Stroke Congress, Abstract.
REPORTING FROM THE WORLD STROKE CONGRESS
Key clinical point:
Major finding: The adjusted rate of stroke in patients with a TIA history was not significantly different from patients with no history.
Study details: GARFIELD-AF, a multinational registry of 52,014 patients newly diagnosed with atrial fibrillation.
Disclosures: GARFIELD-AF is funded by Bayer. Dr. Hacke has been an adviser to Boehringer Ingelheim and Cerenovus and he has received research funding from Boehringer Ingelheim.
Source: Hacke W et al. World Stroke Congress, Abstract.
Study explores link between GERD and poor sleep quality
ATLANTA – results from an ongoing longitudinal analysis demonstrated.
“We have little longitudinal information on GERD in the general population; the last published article on GERD incidence was 20 years ago,” lead study author Maurice M. Ohayon, MD, DSc, PhD, said in an interview in advance of the annual meeting of the American Neurological Association. “As a sleep specialist, I am always interested to see how a specific medical condition may affect the sleep quality of the individuals with that condition. How we live our day has an impact on our night; it works together.”
In an effort to examine the long-term effects of GERD on sleep disturbances, Dr. Ohayon, director of the Stanford (Calif.) Sleep Epidemiology Research Center, and his colleagues used U.S. Census data to identify a random sample of adults in Arizona, California, Colorado, Idaho, New York, Oregon, Pennsylvania, and Texas. The researchers conducted two waves of phone interviews with the subjects 3 years apart, beginning in 2004. They limited their analysis to 10,930 subjects with a mean age of 43 years who participated in both interviews.
Between wave 1 and wave 2 of phone interviews, the proportion of adults who reported having GERD rose from 10.6% to 12.4% and the prevalence of new GERD cases was 8.5% per year, while the incidence was 3.2% per year. Chronic GERD, defined as that present during both interview periods, was observed in 3.9% of the sample.
The researchers found that 77.3% of GERD subjects were taking a treatment to alleviate their symptoms, mostly proton-pump inhibitors. Those with chronic GERD were more likely to report being dissatisfied with their sleep during wave 2 of the study, compared with wave 1 (24.2% vs. 13.5%; P less than .001). In addition, compared with their non-GERD counterparts, those with chronic GERD were more likely to wake up at night (33.9% vs. 28.3%; P less than .001) and to have nonrestorative sleep (15.6% vs. 10.5%; P less than .001).
“Discomfort related to GERD may happen while you are sleeping,” said Dr. Ohayon, who is also a professor of psychiatry and behavioral sciences at Stanford University. “It may wake you up and, if not, it may make you feel unrested when you wake up. We observed both of these symptoms in our GERD participants. Insomnia disorders were also rampant in the chronic GERD group (24.5%, compared with 14.4% in non-GERD participants). An insomnia disorder is more than just having difficulty falling asleep or waking up at night, it means that your daytime functioning is affected by the poor quality of your night.”
Dr. Ohayon said other findings from the study were “rather alarming.” For example, individuals with GERD, especially those with the chronic form, weighed much more than those with no GERD did. “Over a 3-year period, the chronic GERD individuals gained one point in the body mass index, which for a 6-foot tall man translates into a weight gain of 30 pounds,” he said. “Of course, with that follows high blood pressure, high cholesterol, diabetes, chronic pain, and heart disease.”
He concluded that GERD has its main manifestations when affected individuals are sleeping on their backs. “The impact of GERD on the quality of sleep is major,” he said. “Sleepiness and fatigue during the day are the consequences impacting work, family, and quality of life.”
Dr. Ohayon acknowledged certain limitations of the study, including the fact that GERD was based on self-report. The study was supported by an unrestricted grant from Takeda.
Source: Oyahon et al. ANA 2018, Abstract 625.
ATLANTA – results from an ongoing longitudinal analysis demonstrated.
“We have little longitudinal information on GERD in the general population; the last published article on GERD incidence was 20 years ago,” lead study author Maurice M. Ohayon, MD, DSc, PhD, said in an interview in advance of the annual meeting of the American Neurological Association. “As a sleep specialist, I am always interested to see how a specific medical condition may affect the sleep quality of the individuals with that condition. How we live our day has an impact on our night; it works together.”
In an effort to examine the long-term effects of GERD on sleep disturbances, Dr. Ohayon, director of the Stanford (Calif.) Sleep Epidemiology Research Center, and his colleagues used U.S. Census data to identify a random sample of adults in Arizona, California, Colorado, Idaho, New York, Oregon, Pennsylvania, and Texas. The researchers conducted two waves of phone interviews with the subjects 3 years apart, beginning in 2004. They limited their analysis to 10,930 subjects with a mean age of 43 years who participated in both interviews.
Between wave 1 and wave 2 of phone interviews, the proportion of adults who reported having GERD rose from 10.6% to 12.4% and the prevalence of new GERD cases was 8.5% per year, while the incidence was 3.2% per year. Chronic GERD, defined as that present during both interview periods, was observed in 3.9% of the sample.
The researchers found that 77.3% of GERD subjects were taking a treatment to alleviate their symptoms, mostly proton-pump inhibitors. Those with chronic GERD were more likely to report being dissatisfied with their sleep during wave 2 of the study, compared with wave 1 (24.2% vs. 13.5%; P less than .001). In addition, compared with their non-GERD counterparts, those with chronic GERD were more likely to wake up at night (33.9% vs. 28.3%; P less than .001) and to have nonrestorative sleep (15.6% vs. 10.5%; P less than .001).
“Discomfort related to GERD may happen while you are sleeping,” said Dr. Ohayon, who is also a professor of psychiatry and behavioral sciences at Stanford University. “It may wake you up and, if not, it may make you feel unrested when you wake up. We observed both of these symptoms in our GERD participants. Insomnia disorders were also rampant in the chronic GERD group (24.5%, compared with 14.4% in non-GERD participants). An insomnia disorder is more than just having difficulty falling asleep or waking up at night, it means that your daytime functioning is affected by the poor quality of your night.”
Dr. Ohayon said other findings from the study were “rather alarming.” For example, individuals with GERD, especially those with the chronic form, weighed much more than those with no GERD did. “Over a 3-year period, the chronic GERD individuals gained one point in the body mass index, which for a 6-foot tall man translates into a weight gain of 30 pounds,” he said. “Of course, with that follows high blood pressure, high cholesterol, diabetes, chronic pain, and heart disease.”
He concluded that GERD has its main manifestations when affected individuals are sleeping on their backs. “The impact of GERD on the quality of sleep is major,” he said. “Sleepiness and fatigue during the day are the consequences impacting work, family, and quality of life.”
Dr. Ohayon acknowledged certain limitations of the study, including the fact that GERD was based on self-report. The study was supported by an unrestricted grant from Takeda.
Source: Oyahon et al. ANA 2018, Abstract 625.
ATLANTA – results from an ongoing longitudinal analysis demonstrated.
“We have little longitudinal information on GERD in the general population; the last published article on GERD incidence was 20 years ago,” lead study author Maurice M. Ohayon, MD, DSc, PhD, said in an interview in advance of the annual meeting of the American Neurological Association. “As a sleep specialist, I am always interested to see how a specific medical condition may affect the sleep quality of the individuals with that condition. How we live our day has an impact on our night; it works together.”
In an effort to examine the long-term effects of GERD on sleep disturbances, Dr. Ohayon, director of the Stanford (Calif.) Sleep Epidemiology Research Center, and his colleagues used U.S. Census data to identify a random sample of adults in Arizona, California, Colorado, Idaho, New York, Oregon, Pennsylvania, and Texas. The researchers conducted two waves of phone interviews with the subjects 3 years apart, beginning in 2004. They limited their analysis to 10,930 subjects with a mean age of 43 years who participated in both interviews.
Between wave 1 and wave 2 of phone interviews, the proportion of adults who reported having GERD rose from 10.6% to 12.4% and the prevalence of new GERD cases was 8.5% per year, while the incidence was 3.2% per year. Chronic GERD, defined as that present during both interview periods, was observed in 3.9% of the sample.
The researchers found that 77.3% of GERD subjects were taking a treatment to alleviate their symptoms, mostly proton-pump inhibitors. Those with chronic GERD were more likely to report being dissatisfied with their sleep during wave 2 of the study, compared with wave 1 (24.2% vs. 13.5%; P less than .001). In addition, compared with their non-GERD counterparts, those with chronic GERD were more likely to wake up at night (33.9% vs. 28.3%; P less than .001) and to have nonrestorative sleep (15.6% vs. 10.5%; P less than .001).
“Discomfort related to GERD may happen while you are sleeping,” said Dr. Ohayon, who is also a professor of psychiatry and behavioral sciences at Stanford University. “It may wake you up and, if not, it may make you feel unrested when you wake up. We observed both of these symptoms in our GERD participants. Insomnia disorders were also rampant in the chronic GERD group (24.5%, compared with 14.4% in non-GERD participants). An insomnia disorder is more than just having difficulty falling asleep or waking up at night, it means that your daytime functioning is affected by the poor quality of your night.”
Dr. Ohayon said other findings from the study were “rather alarming.” For example, individuals with GERD, especially those with the chronic form, weighed much more than those with no GERD did. “Over a 3-year period, the chronic GERD individuals gained one point in the body mass index, which for a 6-foot tall man translates into a weight gain of 30 pounds,” he said. “Of course, with that follows high blood pressure, high cholesterol, diabetes, chronic pain, and heart disease.”
He concluded that GERD has its main manifestations when affected individuals are sleeping on their backs. “The impact of GERD on the quality of sleep is major,” he said. “Sleepiness and fatigue during the day are the consequences impacting work, family, and quality of life.”
Dr. Ohayon acknowledged certain limitations of the study, including the fact that GERD was based on self-report. The study was supported by an unrestricted grant from Takeda.
Source: Oyahon et al. ANA 2018, Abstract 625.
REPORTING FROM ANA 2018
Key clinical point: GERD has a major impact on quality of sleep.
Major finding: Study participants with chronic GERD were more likely to report being dissatisfied with their sleep during wave 2 of the study, compared with wave 1 (24.2% vs. 13.5%; P less than .001).
Study details: A telephone-based survey of 10,930 U.S. adults who were interviewed during two waves 3 years apart.
Disclosures: The study was supported by an unrestricted grant from Takeda.
Source: Oyahon et al. ANA 2018, Abstract 625.
Finally, immunotherapy shows benefit in TNBC
MUNICH – For the first time, a combination of an immune checkpoint inhibitor and a taxane has shown significant clinical benefit in patients with metastatic triple-negative breast cancer in a phase 3 trial, but the benefit was seen only in patients positive for programmed death-ligand 1 (PD-L1), investigators reported.
Among 902 patients with untreated metastatic triple-negative breast cancer (mTNBC) randomly assigned to receive the PD-L1 inhibitor atezolizumab (Tecentriq) plus nanoparticle albumin-bound (nab)-paclitaxel or placebo plus nab-paclitaxel, atezolizumab was associated with a 38% improvement in median overall survival among patients with PD-L1–positive disease in an interim analysis of the IMpassion 130 trial.
However, although there was a significant progression-free survival (PFS) benefit with atezolizumab in an intention-to-treat (ITT) analysis that included patients with PD-L1 negative tumors, there was no significant difference in median overall survival (OS) when all patients were considered together, said Peter Schmid, MD, PhD, Barts Cancer Institute, Queen Mary University of London.
“For patients with PD-L1–positive tumors, these data establish atezolizumab and nab-paclitaxel as a new standard of care,” he said at the European Society for Medical Oncology Congress.
The results were published online in the New England Journal of Medicine to coincide with the presentation of the data.
At a briefing prior to presentation of the data in a symposium, discussant Nadia Harbeck, MD, of the University of Munich Medical Center, a breast cancer specialist, confessed to being of envious of her colleagues in other oncology specialties in which immunotherapy has made great inroads.
“We have a lot of patients out there right now in clinical trials with immune therapy, but so far in breast cancer, we have not seen the tremendous effects we have seen in melanoma or lung cancer, so this is the first time we have a phase 3 trial proving that immune therapy in triple-negative breast cancer improves survival, and I think this is something that will change the way we practice in triple-negative breast cancer,” she said.
The rationale for using a PD-L1 inhibitor comes from the discovery that PD-L1 expression occurs primarily on tumor-infiltrating cells in TNBC rather than on tumor cells, which can inhibit immune responses directed against tumors.
The investigators enrolled 902 patients with previously untreated mTNBC and randomly assigned them to receive nab-paclitaxel 100 mg/m2 intravenously on days 1, 8, and 15 of each 28-day cycle, plus either atezolizumab 804 mg intravenously or placebo on days 1 and 15 of each cycle.
Patients were stratified according to whether they received neoadjuvant or adjuvant taxane therapy, the presence of liver metastases at baseline, and PD-L1 expression at baseline.
Treatment was continued until disease progression or unacceptable toxicity.
The primary endpoints were PFS and OS in both the ITT and PD-L1–positive population.
In the ITT analysis, 1-year PFS rate was significantly improved in the atezolizumab arm, at 24% vs. 18% in the placebo arm. This translated into a stratified hazard ratio of 0.80 (P = .0025).
In the analysis restricted to the PD-L1-positive population (369 patients), the 1-year PFS rates were 29% for atezolizumab vs. 16% for placebo, translating into to an HR of 0.62 (P less than .0001).
As noted before, the interim OS analysis in the PD-L1 population showed a clinical benefit with atezolizumab, with a 2-year OS rate of 54% vs. 37%, respectively. The median OS in this analysis was 25 months with atezolizumab, vs. 15.5 months with placebo. The stratified HR favoring the PD-L1 inhibitor was 0.62, but because of the hierarchical statistical analysis design of the trial, formal testing of OS was not performed for the interim analysis.
Adverse events of any kind occurred in 99.3% of patients assigned to atezolizumab/nab-paclitaxel and 97.9% of those assigned to placebo/nab-paclitaxel.
Grade 1 or 2 immune-related hypothyroidism occurred more frequently with atezolizumab (17.3% vs. 4.3%), but none led to discontinuation of the drug regimen.
Six patients assigned to atezolizumab and three assigned to placebo died. Four of the deaths were deemed by investigators to be related to the trial regimen, include three deaths in the atezolizumab arm (from autoimmune hepatitis, mucosal inflammation, and septic shock), and one death in the placebo arm (from hepatic failure).
“A benefit with atezolizumab/nab-paclitaxel in patients with PD-L1–positive tumors that was shown in our trial provides evidence of the efficacy of immunotherapy in at least a subset of patients. It is important for patients’ PD-L1 expression status on tumor-infiltrating immune cells to be taken into consideration to inform treatment choices for patients with metastatic triple-negative breast cancer,” Dr. Schmid and his colleagues wrote in the study’s conclusion.
“I really do think that these results are going to make a very big difference,” said coinvestigator Hope S. Rugo, MD, a clinical professor of medicine and director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center.
“We believed from the phase 1 data and the less-than-exciting phase 2 data that there was clearly some role for immunotherapy in breast cancer but were really struggling as to what that role was. We knew for example that if they had a response, patients lived longer and really dramatically longer,” she said in an interview.
But unlike the clinical revolution brought about by the introduction of trastuzumab, in which clinicians had a biomarker and a large number of patients benefited, “here we have no biomarker and a small number of patients benefited, but the benefit is huge,” she said.
Giuseppe Curigliano, MD, PhD, from the University of Milan and European Cancer Institute, Italy, the invited discussant at the symposium, agreed that the study “brings breast cancer into the immunotherapy era.”
Dr. Curigliano added, however, that the study was missing an arm – atezolizumab alone, which might be a good option for a subset of patients.
He also questioned whether nab-paclitaxel was the best partner for atezolizumab, vs. other drugs with known immunogenic effects, such as doxorubicin, cyclophosphamide, other taxanes, gemcitabine, or platinum salts.
The study was supported by F. Hoffmann–La Roche/Genentech. Dr. Schmid reported grant and nonfinancial support from Roche. Multiple coauthors reported financial relationships with Roche/Genentech and others. Dr. Harbeck has disclosed honoraria from and serving as a consultant for Roche and others. Dr. Rugo disclosed grants and nonfinancial support from F. Hoffmann–La Roche. Dr. Curigliano disclosed consulting/advising, speakers bureau participation, and travel/accommodations from Roche/Genentech.
SOURCE: Schmid P et al. N Engl J Med. 2018 Oct 20. doi: 10.1056/NEJMoa1809615.
MUNICH – For the first time, a combination of an immune checkpoint inhibitor and a taxane has shown significant clinical benefit in patients with metastatic triple-negative breast cancer in a phase 3 trial, but the benefit was seen only in patients positive for programmed death-ligand 1 (PD-L1), investigators reported.
Among 902 patients with untreated metastatic triple-negative breast cancer (mTNBC) randomly assigned to receive the PD-L1 inhibitor atezolizumab (Tecentriq) plus nanoparticle albumin-bound (nab)-paclitaxel or placebo plus nab-paclitaxel, atezolizumab was associated with a 38% improvement in median overall survival among patients with PD-L1–positive disease in an interim analysis of the IMpassion 130 trial.
However, although there was a significant progression-free survival (PFS) benefit with atezolizumab in an intention-to-treat (ITT) analysis that included patients with PD-L1 negative tumors, there was no significant difference in median overall survival (OS) when all patients were considered together, said Peter Schmid, MD, PhD, Barts Cancer Institute, Queen Mary University of London.
“For patients with PD-L1–positive tumors, these data establish atezolizumab and nab-paclitaxel as a new standard of care,” he said at the European Society for Medical Oncology Congress.
The results were published online in the New England Journal of Medicine to coincide with the presentation of the data.
At a briefing prior to presentation of the data in a symposium, discussant Nadia Harbeck, MD, of the University of Munich Medical Center, a breast cancer specialist, confessed to being of envious of her colleagues in other oncology specialties in which immunotherapy has made great inroads.
“We have a lot of patients out there right now in clinical trials with immune therapy, but so far in breast cancer, we have not seen the tremendous effects we have seen in melanoma or lung cancer, so this is the first time we have a phase 3 trial proving that immune therapy in triple-negative breast cancer improves survival, and I think this is something that will change the way we practice in triple-negative breast cancer,” she said.
The rationale for using a PD-L1 inhibitor comes from the discovery that PD-L1 expression occurs primarily on tumor-infiltrating cells in TNBC rather than on tumor cells, which can inhibit immune responses directed against tumors.
The investigators enrolled 902 patients with previously untreated mTNBC and randomly assigned them to receive nab-paclitaxel 100 mg/m2 intravenously on days 1, 8, and 15 of each 28-day cycle, plus either atezolizumab 804 mg intravenously or placebo on days 1 and 15 of each cycle.
Patients were stratified according to whether they received neoadjuvant or adjuvant taxane therapy, the presence of liver metastases at baseline, and PD-L1 expression at baseline.
Treatment was continued until disease progression or unacceptable toxicity.
The primary endpoints were PFS and OS in both the ITT and PD-L1–positive population.
In the ITT analysis, 1-year PFS rate was significantly improved in the atezolizumab arm, at 24% vs. 18% in the placebo arm. This translated into a stratified hazard ratio of 0.80 (P = .0025).
In the analysis restricted to the PD-L1-positive population (369 patients), the 1-year PFS rates were 29% for atezolizumab vs. 16% for placebo, translating into to an HR of 0.62 (P less than .0001).
As noted before, the interim OS analysis in the PD-L1 population showed a clinical benefit with atezolizumab, with a 2-year OS rate of 54% vs. 37%, respectively. The median OS in this analysis was 25 months with atezolizumab, vs. 15.5 months with placebo. The stratified HR favoring the PD-L1 inhibitor was 0.62, but because of the hierarchical statistical analysis design of the trial, formal testing of OS was not performed for the interim analysis.
Adverse events of any kind occurred in 99.3% of patients assigned to atezolizumab/nab-paclitaxel and 97.9% of those assigned to placebo/nab-paclitaxel.
Grade 1 or 2 immune-related hypothyroidism occurred more frequently with atezolizumab (17.3% vs. 4.3%), but none led to discontinuation of the drug regimen.
Six patients assigned to atezolizumab and three assigned to placebo died. Four of the deaths were deemed by investigators to be related to the trial regimen, include three deaths in the atezolizumab arm (from autoimmune hepatitis, mucosal inflammation, and septic shock), and one death in the placebo arm (from hepatic failure).
“A benefit with atezolizumab/nab-paclitaxel in patients with PD-L1–positive tumors that was shown in our trial provides evidence of the efficacy of immunotherapy in at least a subset of patients. It is important for patients’ PD-L1 expression status on tumor-infiltrating immune cells to be taken into consideration to inform treatment choices for patients with metastatic triple-negative breast cancer,” Dr. Schmid and his colleagues wrote in the study’s conclusion.
“I really do think that these results are going to make a very big difference,” said coinvestigator Hope S. Rugo, MD, a clinical professor of medicine and director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center.
“We believed from the phase 1 data and the less-than-exciting phase 2 data that there was clearly some role for immunotherapy in breast cancer but were really struggling as to what that role was. We knew for example that if they had a response, patients lived longer and really dramatically longer,” she said in an interview.
But unlike the clinical revolution brought about by the introduction of trastuzumab, in which clinicians had a biomarker and a large number of patients benefited, “here we have no biomarker and a small number of patients benefited, but the benefit is huge,” she said.
Giuseppe Curigliano, MD, PhD, from the University of Milan and European Cancer Institute, Italy, the invited discussant at the symposium, agreed that the study “brings breast cancer into the immunotherapy era.”
Dr. Curigliano added, however, that the study was missing an arm – atezolizumab alone, which might be a good option for a subset of patients.
He also questioned whether nab-paclitaxel was the best partner for atezolizumab, vs. other drugs with known immunogenic effects, such as doxorubicin, cyclophosphamide, other taxanes, gemcitabine, or platinum salts.
The study was supported by F. Hoffmann–La Roche/Genentech. Dr. Schmid reported grant and nonfinancial support from Roche. Multiple coauthors reported financial relationships with Roche/Genentech and others. Dr. Harbeck has disclosed honoraria from and serving as a consultant for Roche and others. Dr. Rugo disclosed grants and nonfinancial support from F. Hoffmann–La Roche. Dr. Curigliano disclosed consulting/advising, speakers bureau participation, and travel/accommodations from Roche/Genentech.
SOURCE: Schmid P et al. N Engl J Med. 2018 Oct 20. doi: 10.1056/NEJMoa1809615.
MUNICH – For the first time, a combination of an immune checkpoint inhibitor and a taxane has shown significant clinical benefit in patients with metastatic triple-negative breast cancer in a phase 3 trial, but the benefit was seen only in patients positive for programmed death-ligand 1 (PD-L1), investigators reported.
Among 902 patients with untreated metastatic triple-negative breast cancer (mTNBC) randomly assigned to receive the PD-L1 inhibitor atezolizumab (Tecentriq) plus nanoparticle albumin-bound (nab)-paclitaxel or placebo plus nab-paclitaxel, atezolizumab was associated with a 38% improvement in median overall survival among patients with PD-L1–positive disease in an interim analysis of the IMpassion 130 trial.
However, although there was a significant progression-free survival (PFS) benefit with atezolizumab in an intention-to-treat (ITT) analysis that included patients with PD-L1 negative tumors, there was no significant difference in median overall survival (OS) when all patients were considered together, said Peter Schmid, MD, PhD, Barts Cancer Institute, Queen Mary University of London.
“For patients with PD-L1–positive tumors, these data establish atezolizumab and nab-paclitaxel as a new standard of care,” he said at the European Society for Medical Oncology Congress.
The results were published online in the New England Journal of Medicine to coincide with the presentation of the data.
At a briefing prior to presentation of the data in a symposium, discussant Nadia Harbeck, MD, of the University of Munich Medical Center, a breast cancer specialist, confessed to being of envious of her colleagues in other oncology specialties in which immunotherapy has made great inroads.
“We have a lot of patients out there right now in clinical trials with immune therapy, but so far in breast cancer, we have not seen the tremendous effects we have seen in melanoma or lung cancer, so this is the first time we have a phase 3 trial proving that immune therapy in triple-negative breast cancer improves survival, and I think this is something that will change the way we practice in triple-negative breast cancer,” she said.
The rationale for using a PD-L1 inhibitor comes from the discovery that PD-L1 expression occurs primarily on tumor-infiltrating cells in TNBC rather than on tumor cells, which can inhibit immune responses directed against tumors.
The investigators enrolled 902 patients with previously untreated mTNBC and randomly assigned them to receive nab-paclitaxel 100 mg/m2 intravenously on days 1, 8, and 15 of each 28-day cycle, plus either atezolizumab 804 mg intravenously or placebo on days 1 and 15 of each cycle.
Patients were stratified according to whether they received neoadjuvant or adjuvant taxane therapy, the presence of liver metastases at baseline, and PD-L1 expression at baseline.
Treatment was continued until disease progression or unacceptable toxicity.
The primary endpoints were PFS and OS in both the ITT and PD-L1–positive population.
In the ITT analysis, 1-year PFS rate was significantly improved in the atezolizumab arm, at 24% vs. 18% in the placebo arm. This translated into a stratified hazard ratio of 0.80 (P = .0025).
In the analysis restricted to the PD-L1-positive population (369 patients), the 1-year PFS rates were 29% for atezolizumab vs. 16% for placebo, translating into to an HR of 0.62 (P less than .0001).
As noted before, the interim OS analysis in the PD-L1 population showed a clinical benefit with atezolizumab, with a 2-year OS rate of 54% vs. 37%, respectively. The median OS in this analysis was 25 months with atezolizumab, vs. 15.5 months with placebo. The stratified HR favoring the PD-L1 inhibitor was 0.62, but because of the hierarchical statistical analysis design of the trial, formal testing of OS was not performed for the interim analysis.
Adverse events of any kind occurred in 99.3% of patients assigned to atezolizumab/nab-paclitaxel and 97.9% of those assigned to placebo/nab-paclitaxel.
Grade 1 or 2 immune-related hypothyroidism occurred more frequently with atezolizumab (17.3% vs. 4.3%), but none led to discontinuation of the drug regimen.
Six patients assigned to atezolizumab and three assigned to placebo died. Four of the deaths were deemed by investigators to be related to the trial regimen, include three deaths in the atezolizumab arm (from autoimmune hepatitis, mucosal inflammation, and septic shock), and one death in the placebo arm (from hepatic failure).
“A benefit with atezolizumab/nab-paclitaxel in patients with PD-L1–positive tumors that was shown in our trial provides evidence of the efficacy of immunotherapy in at least a subset of patients. It is important for patients’ PD-L1 expression status on tumor-infiltrating immune cells to be taken into consideration to inform treatment choices for patients with metastatic triple-negative breast cancer,” Dr. Schmid and his colleagues wrote in the study’s conclusion.
“I really do think that these results are going to make a very big difference,” said coinvestigator Hope S. Rugo, MD, a clinical professor of medicine and director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center.
“We believed from the phase 1 data and the less-than-exciting phase 2 data that there was clearly some role for immunotherapy in breast cancer but were really struggling as to what that role was. We knew for example that if they had a response, patients lived longer and really dramatically longer,” she said in an interview.
But unlike the clinical revolution brought about by the introduction of trastuzumab, in which clinicians had a biomarker and a large number of patients benefited, “here we have no biomarker and a small number of patients benefited, but the benefit is huge,” she said.
Giuseppe Curigliano, MD, PhD, from the University of Milan and European Cancer Institute, Italy, the invited discussant at the symposium, agreed that the study “brings breast cancer into the immunotherapy era.”
Dr. Curigliano added, however, that the study was missing an arm – atezolizumab alone, which might be a good option for a subset of patients.
He also questioned whether nab-paclitaxel was the best partner for atezolizumab, vs. other drugs with known immunogenic effects, such as doxorubicin, cyclophosphamide, other taxanes, gemcitabine, or platinum salts.
The study was supported by F. Hoffmann–La Roche/Genentech. Dr. Schmid reported grant and nonfinancial support from Roche. Multiple coauthors reported financial relationships with Roche/Genentech and others. Dr. Harbeck has disclosed honoraria from and serving as a consultant for Roche and others. Dr. Rugo disclosed grants and nonfinancial support from F. Hoffmann–La Roche. Dr. Curigliano disclosed consulting/advising, speakers bureau participation, and travel/accommodations from Roche/Genentech.
SOURCE: Schmid P et al. N Engl J Med. 2018 Oct 20. doi: 10.1056/NEJMoa1809615.
AT ESMO 2018
Key clinical point: IMpassion 130 is the first phase 3 trial to show a benefit of immunotherapy in triple-negative breast cancer.
Major finding: Progression-free and overall survival were significantly improved with atezolizumab in the PD-L1–positive population.
Study details: Randomized phase 3 trial in 902 patients with triple-negative breast cancer.
Disclosures: The study was supported by F. Hoffmann–La Roche/Genentech. Dr. Schmid reported grant and nonfinancial support from Roche. Multiple coauthors reported financial relationships with Roche/Genentech and others. Dr. Harbeck has disclosed honoraria from and serving as a consultant for Roche and others. Dr. Rugo disclosed grants and nonfinancial support from F. Hoffmann–La Roche. Dr. Curigliano disclosed consulting/advising, speakers bureau participation, and travel/accommodations from Roche/Genentech.
Source: Schmid P et al. N Engl J Med. 2018 Oct 20. doi: 10.1056/NEJMoa1809615.
Computer program credited with cognitive stability in Alzheimer’s
NEW YORK – As part of a comprehensive support program, a computer program administered to patients with cognitive impairment, including those with Alzheimer’s disease, has been associated with preserved cognitive function.
“Based on this series of cases, we believe that the brain in patients with dementia can maintain cognitive function for up to 8 years when an integrative rehabilitation program is employed,” reported Valentin I. Bragin, MD, PhD, of the Stress and Pain Relief Memory Training Center, New York.
While the integrative program involves other types of supportive care, including physical exercises and pharmacologic treatments, the focus of this case series was on the contribution of a computer program for cognitive training. As described by Dr. Bragin, it consists of tasks aimed at training working memory, selective attention, visual field expansion, and eye-hand coordination.
The computer program is designed to improve or maintain motor speed and reaction time. The aim is a rehabilitation process to activate the brain via sensory motor and other bodily systems to prevent patients with Alzheimer’s disease from decline, according to Dr. Bragin. He explained that the computer program is augmented with pen and paper tasks, such as clock drawing, that also stimulate cognitive function.
“The theory behind this treatment is the notion that increased cerebral blood flow is a highly modifiable factor in the risk of cognitive decline,” Dr. Bragin explained at the International Conference on Parkinson’s Disease and Movement Disorders. This premise is supported by a case series of four patients. The shortest duration of treatment was 4 years, but two patients were treated for 7 years and one for 8 years. In this series, motor speed has remained stable in all four patients throughout follow-up. Reaction time remained stable over the period of study in three of four patients, while working memory remained stable in two of the four. Although there was no control group, this persistence of cognitive function is longer than that expected in patients with progressive dementia, according to Dr. Bragin.
“Previously, we demonstrated an improvement and stabilization of cognitive functions in people with mild dementia and depression for periods of up to 6 years by using pen and paper tests,” Dr. Bragin reported. He explained that the computer program expands on this approach.
“We believe that cerebral blood flow is a highly modifiable factor that is a crucial element for reducing hypoxia, improving energy production, and increasing protein synthesis to prevent dementia,” Dr. Bragin said.
Although Dr. Bragin acknowledged that the findings from this case series are preliminary and need to be replicated in a large and controlled trial, he considers it a reasonable empirical strategy, particularly when employed as part of an integrative rehabilitation program like the one now in place at his center.
“This could be a feasible treatment option for dementia patients to stabilize their cognition and improve their quality of life until newer effective approaches become available,” Dr. Bragin said. He noted in the absence of a clear understanding of the pathology of Alzheimer’s disease and other progressive disorders involving cognitive decline, “the most successful treatment model is integrative care.”
NEW YORK – As part of a comprehensive support program, a computer program administered to patients with cognitive impairment, including those with Alzheimer’s disease, has been associated with preserved cognitive function.
“Based on this series of cases, we believe that the brain in patients with dementia can maintain cognitive function for up to 8 years when an integrative rehabilitation program is employed,” reported Valentin I. Bragin, MD, PhD, of the Stress and Pain Relief Memory Training Center, New York.
While the integrative program involves other types of supportive care, including physical exercises and pharmacologic treatments, the focus of this case series was on the contribution of a computer program for cognitive training. As described by Dr. Bragin, it consists of tasks aimed at training working memory, selective attention, visual field expansion, and eye-hand coordination.
The computer program is designed to improve or maintain motor speed and reaction time. The aim is a rehabilitation process to activate the brain via sensory motor and other bodily systems to prevent patients with Alzheimer’s disease from decline, according to Dr. Bragin. He explained that the computer program is augmented with pen and paper tasks, such as clock drawing, that also stimulate cognitive function.
“The theory behind this treatment is the notion that increased cerebral blood flow is a highly modifiable factor in the risk of cognitive decline,” Dr. Bragin explained at the International Conference on Parkinson’s Disease and Movement Disorders. This premise is supported by a case series of four patients. The shortest duration of treatment was 4 years, but two patients were treated for 7 years and one for 8 years. In this series, motor speed has remained stable in all four patients throughout follow-up. Reaction time remained stable over the period of study in three of four patients, while working memory remained stable in two of the four. Although there was no control group, this persistence of cognitive function is longer than that expected in patients with progressive dementia, according to Dr. Bragin.
“Previously, we demonstrated an improvement and stabilization of cognitive functions in people with mild dementia and depression for periods of up to 6 years by using pen and paper tests,” Dr. Bragin reported. He explained that the computer program expands on this approach.
“We believe that cerebral blood flow is a highly modifiable factor that is a crucial element for reducing hypoxia, improving energy production, and increasing protein synthesis to prevent dementia,” Dr. Bragin said.
Although Dr. Bragin acknowledged that the findings from this case series are preliminary and need to be replicated in a large and controlled trial, he considers it a reasonable empirical strategy, particularly when employed as part of an integrative rehabilitation program like the one now in place at his center.
“This could be a feasible treatment option for dementia patients to stabilize their cognition and improve their quality of life until newer effective approaches become available,” Dr. Bragin said. He noted in the absence of a clear understanding of the pathology of Alzheimer’s disease and other progressive disorders involving cognitive decline, “the most successful treatment model is integrative care.”
NEW YORK – As part of a comprehensive support program, a computer program administered to patients with cognitive impairment, including those with Alzheimer’s disease, has been associated with preserved cognitive function.
“Based on this series of cases, we believe that the brain in patients with dementia can maintain cognitive function for up to 8 years when an integrative rehabilitation program is employed,” reported Valentin I. Bragin, MD, PhD, of the Stress and Pain Relief Memory Training Center, New York.
While the integrative program involves other types of supportive care, including physical exercises and pharmacologic treatments, the focus of this case series was on the contribution of a computer program for cognitive training. As described by Dr. Bragin, it consists of tasks aimed at training working memory, selective attention, visual field expansion, and eye-hand coordination.
The computer program is designed to improve or maintain motor speed and reaction time. The aim is a rehabilitation process to activate the brain via sensory motor and other bodily systems to prevent patients with Alzheimer’s disease from decline, according to Dr. Bragin. He explained that the computer program is augmented with pen and paper tasks, such as clock drawing, that also stimulate cognitive function.
“The theory behind this treatment is the notion that increased cerebral blood flow is a highly modifiable factor in the risk of cognitive decline,” Dr. Bragin explained at the International Conference on Parkinson’s Disease and Movement Disorders. This premise is supported by a case series of four patients. The shortest duration of treatment was 4 years, but two patients were treated for 7 years and one for 8 years. In this series, motor speed has remained stable in all four patients throughout follow-up. Reaction time remained stable over the period of study in three of four patients, while working memory remained stable in two of the four. Although there was no control group, this persistence of cognitive function is longer than that expected in patients with progressive dementia, according to Dr. Bragin.
“Previously, we demonstrated an improvement and stabilization of cognitive functions in people with mild dementia and depression for periods of up to 6 years by using pen and paper tests,” Dr. Bragin reported. He explained that the computer program expands on this approach.
“We believe that cerebral blood flow is a highly modifiable factor that is a crucial element for reducing hypoxia, improving energy production, and increasing protein synthesis to prevent dementia,” Dr. Bragin said.
Although Dr. Bragin acknowledged that the findings from this case series are preliminary and need to be replicated in a large and controlled trial, he considers it a reasonable empirical strategy, particularly when employed as part of an integrative rehabilitation program like the one now in place at his center.
“This could be a feasible treatment option for dementia patients to stabilize their cognition and improve their quality of life until newer effective approaches become available,” Dr. Bragin said. He noted in the absence of a clear understanding of the pathology of Alzheimer’s disease and other progressive disorders involving cognitive decline, “the most successful treatment model is integrative care.”
REPORTING FROM ICPDMD 2018
Key clinical point: Patients with cognitive impairment can prevent loss with a computerized program with cognitive tasks.
Major finding: In all but one patient in a small series, reaction time remains stable throughout at least four years of follow-up.
Study details: Case series.
Disclosures: Dr. Bragin reported no financial relationships relevant to this study.
Objective studies help identify Parkinson’s patients at risk for falls
NEW YORK – There are numerous clinical factors and objective tools for identifying patients with Parkinson’s disease who have an increased risk of falls, according to data from a prospective study and an overview of this topic that was presented at the International Conference on Parkinson’s Disease and Movement Disorders
“Identifying risk of falls, which can produce complications beyond the acute injury, is one of the most important unmet needs in Parkinson’s disease,” reported A.V. Srinivasan, MD, PhD, DSc, of the Tamil Nadu Dr. MGR Medial University, Chennai, India.
Falls pose a risk of complications beyond acute injury because of the potential domino effect, according to Dr. Srinivasan. He maintained that when aging Parkinson’s disease patients are confined to bed for an extended period of recovery, a host of adverse health consequences can follow, including such life-threatening events as aspiration pneumonia.
“A serious fall can be the start of a downward clinical slope,” according to Dr. Srinivasan, who cited data suggesting that 40%-70% of Parkinson’s disease patients will have a serious fall at advanced stages of disease.
To identify those at greatest risk, a number of objective studies were shown to be useful in a study undertaken at the Institute of Neurology of Madras (India) Medical College, according to Dr. Srinivasan, where he was a professor when the study was conducted. In this study, 112 patients were evaluated with more than 15 months of follow-up. The 57 (51%) who experienced a fall were compared with the 55 who did not.
Between these groups, there was no difference in mean age (approximately 57 years in both) or in gender (approximately 70% male in both), according to Dr. Srinivasan. However, those who fell were significantly more likely to be obese (P = .009), to be on two or more anti-Parkinson’s medication (P = .01), and to be hypertensive (P = .018). Disease duration was significantly longer and disease severity significantly greater in those who fell relative to those who did not, according to Dr. Srinivasan.
However, Dr. Srinivasan placed particular emphasis on the objective studies that predicted risk of falls.
“When we compared baseline characteristics, Tinetti balance score, episodes of freezing gait, and the Get-Up-And-Go Test [GAGT], were all significant predictors of falls [all P less than .001],” Dr. Srinivasan said.
Of clinical studies, he suggested that GAGT is particularly simple and helpful. In GAGT, the time for a patient to rise from a chair, walk 10 feet, and return to their original sitting position, is timed. According to Dr. Srinivasan, an interval of 12 seconds or greater is a measure of impaired mobility and a signal for increased risk of falls.
Other patient characteristics or disease features that predicted increased risk of falls included the presence of dyskinesias and treatment with relatively high doses of levodopa. All of these factors should be considered when conducting a comprehensive risk assessment.
“A formal evaluation should be conducted routinely in all patients because there are a number of simple and effective strategies to reduce falls in patients at high risk,” Dr. Srinivasan said. These include teaching patients to avoid abrupt movements and modifying therapies to avoid gait freezing and other symptoms associated with falls. He cited a 2014 review article by Canning et al. (Neurodegen Dis Manag. 2014;4:203-21) as one source of clinically useful approaches.
“Early prevention is important. One of the most significant risks of falls is a previous fall. Control of disease symptoms lowers risk, but motor symptoms are not the only concern,” Dr. Srinivasan said. He suggested nonmotor issues, including inadequate sleep, impaired cognitive function, and attention deficits, can all be addressed in order to prevent falls and the risks they pose to quality of life and outcome.
NEW YORK – There are numerous clinical factors and objective tools for identifying patients with Parkinson’s disease who have an increased risk of falls, according to data from a prospective study and an overview of this topic that was presented at the International Conference on Parkinson’s Disease and Movement Disorders
“Identifying risk of falls, which can produce complications beyond the acute injury, is one of the most important unmet needs in Parkinson’s disease,” reported A.V. Srinivasan, MD, PhD, DSc, of the Tamil Nadu Dr. MGR Medial University, Chennai, India.
Falls pose a risk of complications beyond acute injury because of the potential domino effect, according to Dr. Srinivasan. He maintained that when aging Parkinson’s disease patients are confined to bed for an extended period of recovery, a host of adverse health consequences can follow, including such life-threatening events as aspiration pneumonia.
“A serious fall can be the start of a downward clinical slope,” according to Dr. Srinivasan, who cited data suggesting that 40%-70% of Parkinson’s disease patients will have a serious fall at advanced stages of disease.
To identify those at greatest risk, a number of objective studies were shown to be useful in a study undertaken at the Institute of Neurology of Madras (India) Medical College, according to Dr. Srinivasan, where he was a professor when the study was conducted. In this study, 112 patients were evaluated with more than 15 months of follow-up. The 57 (51%) who experienced a fall were compared with the 55 who did not.
Between these groups, there was no difference in mean age (approximately 57 years in both) or in gender (approximately 70% male in both), according to Dr. Srinivasan. However, those who fell were significantly more likely to be obese (P = .009), to be on two or more anti-Parkinson’s medication (P = .01), and to be hypertensive (P = .018). Disease duration was significantly longer and disease severity significantly greater in those who fell relative to those who did not, according to Dr. Srinivasan.
However, Dr. Srinivasan placed particular emphasis on the objective studies that predicted risk of falls.
“When we compared baseline characteristics, Tinetti balance score, episodes of freezing gait, and the Get-Up-And-Go Test [GAGT], were all significant predictors of falls [all P less than .001],” Dr. Srinivasan said.
Of clinical studies, he suggested that GAGT is particularly simple and helpful. In GAGT, the time for a patient to rise from a chair, walk 10 feet, and return to their original sitting position, is timed. According to Dr. Srinivasan, an interval of 12 seconds or greater is a measure of impaired mobility and a signal for increased risk of falls.
Other patient characteristics or disease features that predicted increased risk of falls included the presence of dyskinesias and treatment with relatively high doses of levodopa. All of these factors should be considered when conducting a comprehensive risk assessment.
“A formal evaluation should be conducted routinely in all patients because there are a number of simple and effective strategies to reduce falls in patients at high risk,” Dr. Srinivasan said. These include teaching patients to avoid abrupt movements and modifying therapies to avoid gait freezing and other symptoms associated with falls. He cited a 2014 review article by Canning et al. (Neurodegen Dis Manag. 2014;4:203-21) as one source of clinically useful approaches.
“Early prevention is important. One of the most significant risks of falls is a previous fall. Control of disease symptoms lowers risk, but motor symptoms are not the only concern,” Dr. Srinivasan said. He suggested nonmotor issues, including inadequate sleep, impaired cognitive function, and attention deficits, can all be addressed in order to prevent falls and the risks they pose to quality of life and outcome.
NEW YORK – There are numerous clinical factors and objective tools for identifying patients with Parkinson’s disease who have an increased risk of falls, according to data from a prospective study and an overview of this topic that was presented at the International Conference on Parkinson’s Disease and Movement Disorders
“Identifying risk of falls, which can produce complications beyond the acute injury, is one of the most important unmet needs in Parkinson’s disease,” reported A.V. Srinivasan, MD, PhD, DSc, of the Tamil Nadu Dr. MGR Medial University, Chennai, India.
Falls pose a risk of complications beyond acute injury because of the potential domino effect, according to Dr. Srinivasan. He maintained that when aging Parkinson’s disease patients are confined to bed for an extended period of recovery, a host of adverse health consequences can follow, including such life-threatening events as aspiration pneumonia.
“A serious fall can be the start of a downward clinical slope,” according to Dr. Srinivasan, who cited data suggesting that 40%-70% of Parkinson’s disease patients will have a serious fall at advanced stages of disease.
To identify those at greatest risk, a number of objective studies were shown to be useful in a study undertaken at the Institute of Neurology of Madras (India) Medical College, according to Dr. Srinivasan, where he was a professor when the study was conducted. In this study, 112 patients were evaluated with more than 15 months of follow-up. The 57 (51%) who experienced a fall were compared with the 55 who did not.
Between these groups, there was no difference in mean age (approximately 57 years in both) or in gender (approximately 70% male in both), according to Dr. Srinivasan. However, those who fell were significantly more likely to be obese (P = .009), to be on two or more anti-Parkinson’s medication (P = .01), and to be hypertensive (P = .018). Disease duration was significantly longer and disease severity significantly greater in those who fell relative to those who did not, according to Dr. Srinivasan.
However, Dr. Srinivasan placed particular emphasis on the objective studies that predicted risk of falls.
“When we compared baseline characteristics, Tinetti balance score, episodes of freezing gait, and the Get-Up-And-Go Test [GAGT], were all significant predictors of falls [all P less than .001],” Dr. Srinivasan said.
Of clinical studies, he suggested that GAGT is particularly simple and helpful. In GAGT, the time for a patient to rise from a chair, walk 10 feet, and return to their original sitting position, is timed. According to Dr. Srinivasan, an interval of 12 seconds or greater is a measure of impaired mobility and a signal for increased risk of falls.
Other patient characteristics or disease features that predicted increased risk of falls included the presence of dyskinesias and treatment with relatively high doses of levodopa. All of these factors should be considered when conducting a comprehensive risk assessment.
“A formal evaluation should be conducted routinely in all patients because there are a number of simple and effective strategies to reduce falls in patients at high risk,” Dr. Srinivasan said. These include teaching patients to avoid abrupt movements and modifying therapies to avoid gait freezing and other symptoms associated with falls. He cited a 2014 review article by Canning et al. (Neurodegen Dis Manag. 2014;4:203-21) as one source of clinically useful approaches.
“Early prevention is important. One of the most significant risks of falls is a previous fall. Control of disease symptoms lowers risk, but motor symptoms are not the only concern,” Dr. Srinivasan said. He suggested nonmotor issues, including inadequate sleep, impaired cognitive function, and attention deficits, can all be addressed in order to prevent falls and the risks they pose to quality of life and outcome.
REPORTING FROM ICPDMD 2018
Key clinical point: Patients with Parkinson’s disease at high risk for falls can be identified in order to initiate preventive strategies.
Major finding: For predicting falls, the Tinetti balance score and the Get-Up-And-Go test are both highly significant predictors (both P less than .001).
Study details: Observational study.
Disclosures: Dr. Srinivasan reports no financial relationships relevant to this study.
Inhibitor receives orphan designation for ITP
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to PRN1008 for the treatment of patients with immune thrombocytopenia (ITP).
PRN1008 is an oral, reversible, covalent Bruton’s tyrosine kinase (BTK) inhibitor being developed by Principia Biopharma, Inc.
Principia is conducting a phase 1/2 trial (NCT03395210) to evaluate the safety and efficacy of PRN1008 in patients with ITP.
Results of preclinical research with PRN1008 in ITP were presented at the 2017 ASH Annual Meeting.
There, researchers reported that PRN1008 significantly reduced platelet loss in a mouse model of ITP.
The team found the BTK inhibitor could diminish platelet loss in two ways:
- By reducing platelet destruction via inhibition of autoantibody/FcγR signaling in splenic macrophages
- By reducing autoantibody generation through inhibition of B-cell activation and maturation.
The researchers also assessed the effects of PRN1008 and ibrutinib on platelet function in samples from healthy volunteers and ITP patients.
Samples were treated with one of the two BTK inhibitors, and platelet aggregation was induced by platelet agonists.
Unlike ibrutinib, PRN1008 did not impact platelet aggregation in healthy volunteer or ITP patient samples.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to PRN1008 for the treatment of patients with immune thrombocytopenia (ITP).
PRN1008 is an oral, reversible, covalent Bruton’s tyrosine kinase (BTK) inhibitor being developed by Principia Biopharma, Inc.
Principia is conducting a phase 1/2 trial (NCT03395210) to evaluate the safety and efficacy of PRN1008 in patients with ITP.
Results of preclinical research with PRN1008 in ITP were presented at the 2017 ASH Annual Meeting.
There, researchers reported that PRN1008 significantly reduced platelet loss in a mouse model of ITP.
The team found the BTK inhibitor could diminish platelet loss in two ways:
- By reducing platelet destruction via inhibition of autoantibody/FcγR signaling in splenic macrophages
- By reducing autoantibody generation through inhibition of B-cell activation and maturation.
The researchers also assessed the effects of PRN1008 and ibrutinib on platelet function in samples from healthy volunteers and ITP patients.
Samples were treated with one of the two BTK inhibitors, and platelet aggregation was induced by platelet agonists.
Unlike ibrutinib, PRN1008 did not impact platelet aggregation in healthy volunteer or ITP patient samples.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to PRN1008 for the treatment of patients with immune thrombocytopenia (ITP).
PRN1008 is an oral, reversible, covalent Bruton’s tyrosine kinase (BTK) inhibitor being developed by Principia Biopharma, Inc.
Principia is conducting a phase 1/2 trial (NCT03395210) to evaluate the safety and efficacy of PRN1008 in patients with ITP.
Results of preclinical research with PRN1008 in ITP were presented at the 2017 ASH Annual Meeting.
There, researchers reported that PRN1008 significantly reduced platelet loss in a mouse model of ITP.
The team found the BTK inhibitor could diminish platelet loss in two ways:
- By reducing platelet destruction via inhibition of autoantibody/FcγR signaling in splenic macrophages
- By reducing autoantibody generation through inhibition of B-cell activation and maturation.
The researchers also assessed the effects of PRN1008 and ibrutinib on platelet function in samples from healthy volunteers and ITP patients.
Samples were treated with one of the two BTK inhibitors, and platelet aggregation was induced by platelet agonists.
Unlike ibrutinib, PRN1008 did not impact platelet aggregation in healthy volunteer or ITP patient samples.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
Investigational BTK inhibitor for relapsing MS advances on positive phase 2 data
BERLIN – Evobrutinib, an investigational inhibitor of Bruton’s tyrosine kinase (BTK), significantly reduced the number of new T1 gadolinium-enhancing lesions at 24 weeks compared with placebo in patients with relapsing multiples sclerosis (MS).
However, the molecule was also associated with grade 3 and 4 elevations in alanine aminotransferase – a troubling finding, Xavier Montalban, MD, said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
“Fortunately, all patients were asymptomatic, and the elevations were completely reversible. The results of this trial do support further development of this molecule,” said Dr. Montalban, director of the Multiple Sclerosis Centre of Catalonia at the Vall d’Hebron University Hospital in Barcelona.
Evobrutinib exerts a dual action in MS, Dr. Montalban said. By inhibiting BTK, the drug blocks B-cell activation and interaction between B and T cells. It also inhibits macrophage survival and dampens cytokine release, he said.
The study randomized 213 patients with relapsing MS to placebo or to evobrutinib in three daily doses: 25 mg, 75 mg, or 150 mg. A control arm of 54 additional patients received treatment with dimethyl fumarate. After 24 weeks of randomized treatment, patients who got placebo switched to 25 mg per day; everyone else continued in their assigned groups for another 24 weeks. The study concluded with an open-label extension phase during which everyone took 75 mg daily.
Dr. Montalban reported the primary 24-week analysis. The remainder of the data has not been analyzed yet, he said. The primary endpoint was the total number of T1 gadolinium-enhancing lesions at weeks 12, 16, 20, and 24. Secondary endpoints included the 24-week annualized relapse rate and safety signals. Patients were a mean of 41 years old, with a mean disease duration of 10 years. They had experienced a mean of two relapses in the prior 2 years. About 20% had gadolinium-enhancing lesions at baseline.
Compared with placebo and with the 25-mg dose, evobrutinib 75 mg and 150 mg significantly reduced the number of new enhancing lesions at 24 weeks. There was evidence of a dose-response effect, Dr. Montalban said. Patients taking placebo developed a mean of 3.8 new lesions, while those on 75 mg developed a mean of 1.69 and those taking 150 mg, a mean of 1.15. Patients in the 25-mg group developed a mean of four new lesions – not significantly different than placebo.
Both the 75-mg and 150-mg doses decreased the annualized relapse rate, compared with placebo but missed statistical significance, with P values of 0.90 and 0.63, respectively.
These two doses also conferred significant benefit on two other secondary endpoints, significantly reducing the number of new or enlarging T2 lesions and reducing the total T2 lesion volume, compared with placebo.
The safety profile was relatively benign, with no infections, including no opportunistic infections, and no neoplasms. About 7% of the highest-dose group experienced nausea, and the same number, arthralgia. Seven patients taking evobrutinib experienced grade 1 lymphopenia, compared with three patients taking placebo; grade 2 lymphopenia developed in one patient in the highest-dose group.
ALT elevation was the most concerning adverse event, Dr. Montalban said. Grade 1 elevations developed in 17% of the low-dose group and about 22% of the other two active groups (11 patients each), compared with 7% of the placebo group. Grade 2 elevations developed in three placebo patients and in two taking the highest dose of evobrutinib. There was one grade 3 elevation, which occurred in a patient in the highest-dose group. These were asymptomatic and resolved after discontinuing the medication. Lipase and aspartate transaminase elevations were also associated with evobrutinib, but Dr. Montalban did not provide these details.
He has been a paid consultant for Merck Serono, which is developing evobrutinib.
SOURCE: Montalban X et al. ECTRIMS 2018. Abstract 322.
BERLIN – Evobrutinib, an investigational inhibitor of Bruton’s tyrosine kinase (BTK), significantly reduced the number of new T1 gadolinium-enhancing lesions at 24 weeks compared with placebo in patients with relapsing multiples sclerosis (MS).
However, the molecule was also associated with grade 3 and 4 elevations in alanine aminotransferase – a troubling finding, Xavier Montalban, MD, said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
“Fortunately, all patients were asymptomatic, and the elevations were completely reversible. The results of this trial do support further development of this molecule,” said Dr. Montalban, director of the Multiple Sclerosis Centre of Catalonia at the Vall d’Hebron University Hospital in Barcelona.
Evobrutinib exerts a dual action in MS, Dr. Montalban said. By inhibiting BTK, the drug blocks B-cell activation and interaction between B and T cells. It also inhibits macrophage survival and dampens cytokine release, he said.
The study randomized 213 patients with relapsing MS to placebo or to evobrutinib in three daily doses: 25 mg, 75 mg, or 150 mg. A control arm of 54 additional patients received treatment with dimethyl fumarate. After 24 weeks of randomized treatment, patients who got placebo switched to 25 mg per day; everyone else continued in their assigned groups for another 24 weeks. The study concluded with an open-label extension phase during which everyone took 75 mg daily.
Dr. Montalban reported the primary 24-week analysis. The remainder of the data has not been analyzed yet, he said. The primary endpoint was the total number of T1 gadolinium-enhancing lesions at weeks 12, 16, 20, and 24. Secondary endpoints included the 24-week annualized relapse rate and safety signals. Patients were a mean of 41 years old, with a mean disease duration of 10 years. They had experienced a mean of two relapses in the prior 2 years. About 20% had gadolinium-enhancing lesions at baseline.
Compared with placebo and with the 25-mg dose, evobrutinib 75 mg and 150 mg significantly reduced the number of new enhancing lesions at 24 weeks. There was evidence of a dose-response effect, Dr. Montalban said. Patients taking placebo developed a mean of 3.8 new lesions, while those on 75 mg developed a mean of 1.69 and those taking 150 mg, a mean of 1.15. Patients in the 25-mg group developed a mean of four new lesions – not significantly different than placebo.
Both the 75-mg and 150-mg doses decreased the annualized relapse rate, compared with placebo but missed statistical significance, with P values of 0.90 and 0.63, respectively.
These two doses also conferred significant benefit on two other secondary endpoints, significantly reducing the number of new or enlarging T2 lesions and reducing the total T2 lesion volume, compared with placebo.
The safety profile was relatively benign, with no infections, including no opportunistic infections, and no neoplasms. About 7% of the highest-dose group experienced nausea, and the same number, arthralgia. Seven patients taking evobrutinib experienced grade 1 lymphopenia, compared with three patients taking placebo; grade 2 lymphopenia developed in one patient in the highest-dose group.
ALT elevation was the most concerning adverse event, Dr. Montalban said. Grade 1 elevations developed in 17% of the low-dose group and about 22% of the other two active groups (11 patients each), compared with 7% of the placebo group. Grade 2 elevations developed in three placebo patients and in two taking the highest dose of evobrutinib. There was one grade 3 elevation, which occurred in a patient in the highest-dose group. These were asymptomatic and resolved after discontinuing the medication. Lipase and aspartate transaminase elevations were also associated with evobrutinib, but Dr. Montalban did not provide these details.
He has been a paid consultant for Merck Serono, which is developing evobrutinib.
SOURCE: Montalban X et al. ECTRIMS 2018. Abstract 322.
BERLIN – Evobrutinib, an investigational inhibitor of Bruton’s tyrosine kinase (BTK), significantly reduced the number of new T1 gadolinium-enhancing lesions at 24 weeks compared with placebo in patients with relapsing multiples sclerosis (MS).
However, the molecule was also associated with grade 3 and 4 elevations in alanine aminotransferase – a troubling finding, Xavier Montalban, MD, said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
“Fortunately, all patients were asymptomatic, and the elevations were completely reversible. The results of this trial do support further development of this molecule,” said Dr. Montalban, director of the Multiple Sclerosis Centre of Catalonia at the Vall d’Hebron University Hospital in Barcelona.
Evobrutinib exerts a dual action in MS, Dr. Montalban said. By inhibiting BTK, the drug blocks B-cell activation and interaction between B and T cells. It also inhibits macrophage survival and dampens cytokine release, he said.
The study randomized 213 patients with relapsing MS to placebo or to evobrutinib in three daily doses: 25 mg, 75 mg, or 150 mg. A control arm of 54 additional patients received treatment with dimethyl fumarate. After 24 weeks of randomized treatment, patients who got placebo switched to 25 mg per day; everyone else continued in their assigned groups for another 24 weeks. The study concluded with an open-label extension phase during which everyone took 75 mg daily.
Dr. Montalban reported the primary 24-week analysis. The remainder of the data has not been analyzed yet, he said. The primary endpoint was the total number of T1 gadolinium-enhancing lesions at weeks 12, 16, 20, and 24. Secondary endpoints included the 24-week annualized relapse rate and safety signals. Patients were a mean of 41 years old, with a mean disease duration of 10 years. They had experienced a mean of two relapses in the prior 2 years. About 20% had gadolinium-enhancing lesions at baseline.
Compared with placebo and with the 25-mg dose, evobrutinib 75 mg and 150 mg significantly reduced the number of new enhancing lesions at 24 weeks. There was evidence of a dose-response effect, Dr. Montalban said. Patients taking placebo developed a mean of 3.8 new lesions, while those on 75 mg developed a mean of 1.69 and those taking 150 mg, a mean of 1.15. Patients in the 25-mg group developed a mean of four new lesions – not significantly different than placebo.
Both the 75-mg and 150-mg doses decreased the annualized relapse rate, compared with placebo but missed statistical significance, with P values of 0.90 and 0.63, respectively.
These two doses also conferred significant benefit on two other secondary endpoints, significantly reducing the number of new or enlarging T2 lesions and reducing the total T2 lesion volume, compared with placebo.
The safety profile was relatively benign, with no infections, including no opportunistic infections, and no neoplasms. About 7% of the highest-dose group experienced nausea, and the same number, arthralgia. Seven patients taking evobrutinib experienced grade 1 lymphopenia, compared with three patients taking placebo; grade 2 lymphopenia developed in one patient in the highest-dose group.
ALT elevation was the most concerning adverse event, Dr. Montalban said. Grade 1 elevations developed in 17% of the low-dose group and about 22% of the other two active groups (11 patients each), compared with 7% of the placebo group. Grade 2 elevations developed in three placebo patients and in two taking the highest dose of evobrutinib. There was one grade 3 elevation, which occurred in a patient in the highest-dose group. These were asymptomatic and resolved after discontinuing the medication. Lipase and aspartate transaminase elevations were also associated with evobrutinib, but Dr. Montalban did not provide these details.
He has been a paid consultant for Merck Serono, which is developing evobrutinib.
SOURCE: Montalban X et al. ECTRIMS 2018. Abstract 322.
REPORTING FROM ECTRIMS 2018
Key clinical point: Evobrutinib reduced the number of new T1 gadolinium-enhancing lesions.
Major finding: At 24 weeks, the 150-mg group had a mean of 1.15 new lesions vs. 3.8 in the placebo group.
Study details: The phase 2 study randomized 213 patients.
Disclosures: Dr. Montalban has been a paid consultant for Merck Serono, which is developing the molecule.
Source: Montalban X et al. ECTRIMS 2018.Abstract 322.