User login
Two new tests can detect CJD

Credit: Elise Amendola
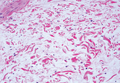
Two groups of scientists have developed new tests to diagnose Creutzfeldt-Jakob disease (CJD).
One test uses samples collected from nasal passages to detect sporadic CJD, and the other uses urine samples to identify variant CJD.
The researchers said these tests provide simple methods for differentiating CJD from other diseases and could help prevent the transmission of CJD via blood
transfusions, transplants, or contaminated surgical instruments.
Both tests are described in The New England Journal of Medicine.
Nasal test for sporadic CJD
In one NEJM article, Byron Caughey, PhD, of the National Institute of Allergy and Infectious Diseases in Rockville, Maryland, and his colleagues detailed their results with the nasal test.
The researchers collected 31 nasal samples from patients with sporadic CJD and 43 samples from patients who had other neurologic diseases or no neurologic disease. The team brushed the inside of a subject’s nose to collect olfactory neurons connected to the brain.
Testing these samples allowed the researchers to correctly identify 30 of the 31 sporadic CJD patients (97% sensitivity). The tests also correctly showed negative results for all 43 of the non-CJD patients (100% specificity).
By comparison, tests using cerebral spinal fluid, which is currently used to detect sporadic CJD, were 77% sensitive and 100% specific. And these results took twice as long to obtain.
While continuing to validate the new testing method in CJD patients, the scientists are looking to expand their research to diagnose forms of prion diseases in sheep, cattle, and wildlife. The team also hopes to replace the nasal brush with an even simpler swabbing approach.
Urine test for variant CJD
In another NEJM article, Fabio Moda, PhD, of the University of Texas Medical School at Houston, and his colleagues described results observed with their urine test.
The team noted that the infectious agent in transmissible spongiform encephalopathies appears to be composed exclusively of the misfolded form of the prion protein, PrPSc. So they set out to determine if they could detect PrPSc in the urine of patients with CJD.
The researchers analyzed urine samples from healthy individuals (n=52) and patients with variant CJD (n=68), sporadic CJD (n=14), genetic forms of prion disease (n=4), other neurodegenerative disorders (n=50), and nondegenerative neurologic disorders (n=50).
The group found they could only detect PrPSc in samples from patients with variant CJD. They found “minute quantities” of PrPSc in 13 of the 14 urine samples from variant CJD patients, but PrPSc was not present in any of the samples from the other patients or the healthy individuals.
This suggests the test has a sensitivity of 92.9% and a specificity of 100%. ![]()

Credit: Elise Amendola
Two groups of scientists have developed new tests to diagnose Creutzfeldt-Jakob disease (CJD).
One test uses samples collected from nasal passages to detect sporadic CJD, and the other uses urine samples to identify variant CJD.
The researchers said these tests provide simple methods for differentiating CJD from other diseases and could help prevent the transmission of CJD via blood
transfusions, transplants, or contaminated surgical instruments.
Both tests are described in The New England Journal of Medicine.
Nasal test for sporadic CJD
In one NEJM article, Byron Caughey, PhD, of the National Institute of Allergy and Infectious Diseases in Rockville, Maryland, and his colleagues detailed their results with the nasal test.
The researchers collected 31 nasal samples from patients with sporadic CJD and 43 samples from patients who had other neurologic diseases or no neurologic disease. The team brushed the inside of a subject’s nose to collect olfactory neurons connected to the brain.
Testing these samples allowed the researchers to correctly identify 30 of the 31 sporadic CJD patients (97% sensitivity). The tests also correctly showed negative results for all 43 of the non-CJD patients (100% specificity).
By comparison, tests using cerebral spinal fluid, which is currently used to detect sporadic CJD, were 77% sensitive and 100% specific. And these results took twice as long to obtain.
While continuing to validate the new testing method in CJD patients, the scientists are looking to expand their research to diagnose forms of prion diseases in sheep, cattle, and wildlife. The team also hopes to replace the nasal brush with an even simpler swabbing approach.
Urine test for variant CJD
In another NEJM article, Fabio Moda, PhD, of the University of Texas Medical School at Houston, and his colleagues described results observed with their urine test.
The team noted that the infectious agent in transmissible spongiform encephalopathies appears to be composed exclusively of the misfolded form of the prion protein, PrPSc. So they set out to determine if they could detect PrPSc in the urine of patients with CJD.
The researchers analyzed urine samples from healthy individuals (n=52) and patients with variant CJD (n=68), sporadic CJD (n=14), genetic forms of prion disease (n=4), other neurodegenerative disorders (n=50), and nondegenerative neurologic disorders (n=50).
The group found they could only detect PrPSc in samples from patients with variant CJD. They found “minute quantities” of PrPSc in 13 of the 14 urine samples from variant CJD patients, but PrPSc was not present in any of the samples from the other patients or the healthy individuals.
This suggests the test has a sensitivity of 92.9% and a specificity of 100%. ![]()

Credit: Elise Amendola
Two groups of scientists have developed new tests to diagnose Creutzfeldt-Jakob disease (CJD).
One test uses samples collected from nasal passages to detect sporadic CJD, and the other uses urine samples to identify variant CJD.
The researchers said these tests provide simple methods for differentiating CJD from other diseases and could help prevent the transmission of CJD via blood
transfusions, transplants, or contaminated surgical instruments.
Both tests are described in The New England Journal of Medicine.
Nasal test for sporadic CJD
In one NEJM article, Byron Caughey, PhD, of the National Institute of Allergy and Infectious Diseases in Rockville, Maryland, and his colleagues detailed their results with the nasal test.
The researchers collected 31 nasal samples from patients with sporadic CJD and 43 samples from patients who had other neurologic diseases or no neurologic disease. The team brushed the inside of a subject’s nose to collect olfactory neurons connected to the brain.
Testing these samples allowed the researchers to correctly identify 30 of the 31 sporadic CJD patients (97% sensitivity). The tests also correctly showed negative results for all 43 of the non-CJD patients (100% specificity).
By comparison, tests using cerebral spinal fluid, which is currently used to detect sporadic CJD, were 77% sensitive and 100% specific. And these results took twice as long to obtain.
While continuing to validate the new testing method in CJD patients, the scientists are looking to expand their research to diagnose forms of prion diseases in sheep, cattle, and wildlife. The team also hopes to replace the nasal brush with an even simpler swabbing approach.
Urine test for variant CJD
In another NEJM article, Fabio Moda, PhD, of the University of Texas Medical School at Houston, and his colleagues described results observed with their urine test.
The team noted that the infectious agent in transmissible spongiform encephalopathies appears to be composed exclusively of the misfolded form of the prion protein, PrPSc. So they set out to determine if they could detect PrPSc in the urine of patients with CJD.
The researchers analyzed urine samples from healthy individuals (n=52) and patients with variant CJD (n=68), sporadic CJD (n=14), genetic forms of prion disease (n=4), other neurodegenerative disorders (n=50), and nondegenerative neurologic disorders (n=50).
The group found they could only detect PrPSc in samples from patients with variant CJD. They found “minute quantities” of PrPSc in 13 of the 14 urine samples from variant CJD patients, but PrPSc was not present in any of the samples from the other patients or the healthy individuals.
This suggests the test has a sensitivity of 92.9% and a specificity of 100%. ![]()
Gene plays crucial role in cancer development, team says

Credit: Beth A. Sullivan
New research suggests DNA ligase 3 is crucial for the evolutionary processes that drive cancer.
“We have identified a gene that, as cells age, seems to regulate whether the cells become cancerous or not,” said Eric A. Hendrickson, PhD, of the University of Minnesota in Minneapolis.
“This gene has never been identified before in this role, so this makes it a potentially very important therapeutic target.”
Dr Hendrickson and his colleagues recounted this discovery in Cell Reports.
The researchers noted that short, dysfunctional telomeres can fuse, thereby generating dicentric chromosomes and initiating breakage-fusion-bridge cycles. The cells that manage to escape the subsequent crisis have genomic rearrangements that drive clonal evolution and malignant progression.
The team wanted to determine exactly what allows these malignant cells to escape telomere-driven crisis and avoid death.
To find out, the group disabled certain genes in human cells and then studied the impact this had on telomere fusion.
They found that cells escaped death when ligase 3 was active but not when its action, which appears to promote fusion within like chromosomes rather than between different chromosomes, was inhibited.
“Telomere dysfunction has been identified in many human cancers,” said study author Duncan Baird, PhD, of Cardiff University in the UK.
“And, as we have shown previously, short telomeres can predict the outcome of patients with [chronic lymphocytic leukemia] and probably many other tumor types. Thus, the discovery that ligase 3 is required for this process is fundamentally important.”
This research was made possible by a chance meeting between Dr Baird and Dr Hendrickson at an international conference. The pair discovered they were both looking at the role of ligase 3 in cancer and decided to collaborate.
“The collaboration paid off, as we were able to uncover something that neither one of us could have done on our own,” Dr Hendrickson said.
Additional studies are already underway. The researchers are investigating the discovery that the reliance on ligase 3 appears to be dependent upon the activity of another key DNA repair gene, p53.
“Since p53 is the most commonly mutated gene in human cancer, it now behooves us to discover how these two genes are interacting and to see if we can’t use that information to develop synergistic treatment modalities,” Dr Hendrickson concluded. ![]()

Credit: Beth A. Sullivan
New research suggests DNA ligase 3 is crucial for the evolutionary processes that drive cancer.
“We have identified a gene that, as cells age, seems to regulate whether the cells become cancerous or not,” said Eric A. Hendrickson, PhD, of the University of Minnesota in Minneapolis.
“This gene has never been identified before in this role, so this makes it a potentially very important therapeutic target.”
Dr Hendrickson and his colleagues recounted this discovery in Cell Reports.
The researchers noted that short, dysfunctional telomeres can fuse, thereby generating dicentric chromosomes and initiating breakage-fusion-bridge cycles. The cells that manage to escape the subsequent crisis have genomic rearrangements that drive clonal evolution and malignant progression.
The team wanted to determine exactly what allows these malignant cells to escape telomere-driven crisis and avoid death.
To find out, the group disabled certain genes in human cells and then studied the impact this had on telomere fusion.
They found that cells escaped death when ligase 3 was active but not when its action, which appears to promote fusion within like chromosomes rather than between different chromosomes, was inhibited.
“Telomere dysfunction has been identified in many human cancers,” said study author Duncan Baird, PhD, of Cardiff University in the UK.
“And, as we have shown previously, short telomeres can predict the outcome of patients with [chronic lymphocytic leukemia] and probably many other tumor types. Thus, the discovery that ligase 3 is required for this process is fundamentally important.”
This research was made possible by a chance meeting between Dr Baird and Dr Hendrickson at an international conference. The pair discovered they were both looking at the role of ligase 3 in cancer and decided to collaborate.
“The collaboration paid off, as we were able to uncover something that neither one of us could have done on our own,” Dr Hendrickson said.
Additional studies are already underway. The researchers are investigating the discovery that the reliance on ligase 3 appears to be dependent upon the activity of another key DNA repair gene, p53.
“Since p53 is the most commonly mutated gene in human cancer, it now behooves us to discover how these two genes are interacting and to see if we can’t use that information to develop synergistic treatment modalities,” Dr Hendrickson concluded. ![]()

Credit: Beth A. Sullivan
New research suggests DNA ligase 3 is crucial for the evolutionary processes that drive cancer.
“We have identified a gene that, as cells age, seems to regulate whether the cells become cancerous or not,” said Eric A. Hendrickson, PhD, of the University of Minnesota in Minneapolis.
“This gene has never been identified before in this role, so this makes it a potentially very important therapeutic target.”
Dr Hendrickson and his colleagues recounted this discovery in Cell Reports.
The researchers noted that short, dysfunctional telomeres can fuse, thereby generating dicentric chromosomes and initiating breakage-fusion-bridge cycles. The cells that manage to escape the subsequent crisis have genomic rearrangements that drive clonal evolution and malignant progression.
The team wanted to determine exactly what allows these malignant cells to escape telomere-driven crisis and avoid death.
To find out, the group disabled certain genes in human cells and then studied the impact this had on telomere fusion.
They found that cells escaped death when ligase 3 was active but not when its action, which appears to promote fusion within like chromosomes rather than between different chromosomes, was inhibited.
“Telomere dysfunction has been identified in many human cancers,” said study author Duncan Baird, PhD, of Cardiff University in the UK.
“And, as we have shown previously, short telomeres can predict the outcome of patients with [chronic lymphocytic leukemia] and probably many other tumor types. Thus, the discovery that ligase 3 is required for this process is fundamentally important.”
This research was made possible by a chance meeting between Dr Baird and Dr Hendrickson at an international conference. The pair discovered they were both looking at the role of ligase 3 in cancer and decided to collaborate.
“The collaboration paid off, as we were able to uncover something that neither one of us could have done on our own,” Dr Hendrickson said.
Additional studies are already underway. The researchers are investigating the discovery that the reliance on ligase 3 appears to be dependent upon the activity of another key DNA repair gene, p53.
“Since p53 is the most commonly mutated gene in human cancer, it now behooves us to discover how these two genes are interacting and to see if we can’t use that information to develop synergistic treatment modalities,” Dr Hendrickson concluded. ![]()
Interim data appear positive for MM drug
Interim results of the phase 3 ASPIRE trial suggest carfilzomib can improve progression-free survival (PFS) in patients with relapsed multiple myeloma (MM).
Patients who received carfilzomib, lenalidomide, and dexamethasone lived 8.7 months longer without progression than patients who received only lenalidomide and dexamethasone.
The companies developing carfilzomib, Amgen and its subsidiary, Onyx Pharmaceuticals, Inc., recently shared these results.
They said additional results will be submitted for presentation at the 56th Annual ASH Meeting in December.
The companies also said data from the ASPIRE trial will form the basis for regulatory submissions for carfilzomib throughout the world.
In the US, the data may support the conversion of accelerated approval to full approval and expand the current indication for carfilzomib.
The ASPIRE trial includes 792 patients with relapsed MM who were randomized to treatment at sites in North America, Europe, and Israel. Prior to study treatment, the patients had received 1 to 3 therapeutic regimens.
The patients were randomized to receive carfilzomib (20 mg/m2 on days 1 and 2 of cycle 1 only, then 27 mg/m2), in addition to a standard dosing schedule of lenalidomide (25 mg per day for 21 days on, 7 days off) and low-dose dexamethasone (40 mg per week in 4-week cycles), or lenalidomide and low-dose dexamethasone alone.
The primary endpoint was PFS, and secondary endpoints included overall survival, overall response rate, duration of response, disease control rate, health-related quality of life, and safety.
At a planned interim analysis, patients in the carfilzomib arm had a significantly longer median PFS than patients in the other arm—26.3 months and 17.6 months, respectively (P<0.0001).
The data for overall survival are not yet mature, but the analysis showed a trend in favor of carfilzomib that did not reach statistical significance, according to Amgen and Onyx.
The companies said the safety profile in this study is consistent with previous studies, including the rate of cardiac events.
Treatment discontinuation due to adverse events and on-study deaths were comparable between the 2 arms, and researchers did not identify any new safety signals. ![]()
Interim results of the phase 3 ASPIRE trial suggest carfilzomib can improve progression-free survival (PFS) in patients with relapsed multiple myeloma (MM).
Patients who received carfilzomib, lenalidomide, and dexamethasone lived 8.7 months longer without progression than patients who received only lenalidomide and dexamethasone.
The companies developing carfilzomib, Amgen and its subsidiary, Onyx Pharmaceuticals, Inc., recently shared these results.
They said additional results will be submitted for presentation at the 56th Annual ASH Meeting in December.
The companies also said data from the ASPIRE trial will form the basis for regulatory submissions for carfilzomib throughout the world.
In the US, the data may support the conversion of accelerated approval to full approval and expand the current indication for carfilzomib.
The ASPIRE trial includes 792 patients with relapsed MM who were randomized to treatment at sites in North America, Europe, and Israel. Prior to study treatment, the patients had received 1 to 3 therapeutic regimens.
The patients were randomized to receive carfilzomib (20 mg/m2 on days 1 and 2 of cycle 1 only, then 27 mg/m2), in addition to a standard dosing schedule of lenalidomide (25 mg per day for 21 days on, 7 days off) and low-dose dexamethasone (40 mg per week in 4-week cycles), or lenalidomide and low-dose dexamethasone alone.
The primary endpoint was PFS, and secondary endpoints included overall survival, overall response rate, duration of response, disease control rate, health-related quality of life, and safety.
At a planned interim analysis, patients in the carfilzomib arm had a significantly longer median PFS than patients in the other arm—26.3 months and 17.6 months, respectively (P<0.0001).
The data for overall survival are not yet mature, but the analysis showed a trend in favor of carfilzomib that did not reach statistical significance, according to Amgen and Onyx.
The companies said the safety profile in this study is consistent with previous studies, including the rate of cardiac events.
Treatment discontinuation due to adverse events and on-study deaths were comparable between the 2 arms, and researchers did not identify any new safety signals. ![]()
Interim results of the phase 3 ASPIRE trial suggest carfilzomib can improve progression-free survival (PFS) in patients with relapsed multiple myeloma (MM).
Patients who received carfilzomib, lenalidomide, and dexamethasone lived 8.7 months longer without progression than patients who received only lenalidomide and dexamethasone.
The companies developing carfilzomib, Amgen and its subsidiary, Onyx Pharmaceuticals, Inc., recently shared these results.
They said additional results will be submitted for presentation at the 56th Annual ASH Meeting in December.
The companies also said data from the ASPIRE trial will form the basis for regulatory submissions for carfilzomib throughout the world.
In the US, the data may support the conversion of accelerated approval to full approval and expand the current indication for carfilzomib.
The ASPIRE trial includes 792 patients with relapsed MM who were randomized to treatment at sites in North America, Europe, and Israel. Prior to study treatment, the patients had received 1 to 3 therapeutic regimens.
The patients were randomized to receive carfilzomib (20 mg/m2 on days 1 and 2 of cycle 1 only, then 27 mg/m2), in addition to a standard dosing schedule of lenalidomide (25 mg per day for 21 days on, 7 days off) and low-dose dexamethasone (40 mg per week in 4-week cycles), or lenalidomide and low-dose dexamethasone alone.
The primary endpoint was PFS, and secondary endpoints included overall survival, overall response rate, duration of response, disease control rate, health-related quality of life, and safety.
At a planned interim analysis, patients in the carfilzomib arm had a significantly longer median PFS than patients in the other arm—26.3 months and 17.6 months, respectively (P<0.0001).
The data for overall survival are not yet mature, but the analysis showed a trend in favor of carfilzomib that did not reach statistical significance, according to Amgen and Onyx.
The companies said the safety profile in this study is consistent with previous studies, including the rate of cardiac events.
Treatment discontinuation due to adverse events and on-study deaths were comparable between the 2 arms, and researchers did not identify any new safety signals. ![]()
Combative Behavior and Delirium
Delirium affects up to 82% of critical‐care patients and 29% to 64% of general medical patients, resulting in medical morbidity, decreased function, and mortality.[1, 2, 3, 4, 5] Delirium is associated with specific, adverse hospital outcomes, including falls, aspiration pneumonia, pressure ulcers, and restraint use.[6, 7] As a consequence of delirium, individuals may be transformed from independent and active at the time of admission to requiring skilled nursing supervision at discharge, in some cases resulting in permanent cognitive disability for the remainder of the person's life.[4, 8]
Combative behavior in hospitalized patients can be a threat to self or others, including other patients and staff. An emergency alert to staff regarding the presence of a combative patient requiring intervention is known as a behavioral code or Code Gray.[9] Guidelines addressing this particular hospital emergency typically refer to de‐escalation methods and implementation of security measures. Ideally, however, at‐risk patients would be identified prior to development into a full behavioral code. Unfortunately, the medical literature on the causes, prevention, and interventions for combative behavior requiring intervention is limited. Interventions published to date focus on patients living with severe and persistent mental illness, such as schizophrenia or bipolar disorder.[9, 10, 11, 12]
We hypothesized that delirium contributes to combative behavior in hospitalized patients, leading to the adverse outcome of behavioral codes. Delirium identification would therefore provide an opportunity for prevention and early identification of patients at risk, thereby improving safety for patients and staff. However, no studies published to date address the impact of delirium on the likelihood of a patient hospitalized in a general medical/surgical setting becoming combative and requiring intervention such as a behavioral code. The purpose of this article is to determine the strength of the association between delirium and combative behavior requiring intervention.
METHODS
This study was conducted as part of a quality improvement project, resulting in a waiver by the institutional review board of the hospital. All data with patient‐specific information were securely handled and deidentified prior to analysis. The setting is a 336‐bed, nonuniversity, teaching hospital serving adults in the Pacific Northwest, with approximately 16,000 admissions per year, and 31 critical‐care beds. Delirium prevention has been identified as an institutional priority, and we have been screening for delirium on admission and with twice‐daily Confusion Assessment Method (CAM) scores since 2010.
The study design was a retrospective case control study of hospital inpatients. Consecutive patients experiencing combative behavior requiring a specific behavioral code intervention (n=125) between January 1, 2011 to December 31, 2011 were identified using security reports and operator code logs. Five patients were excluded because the combative behavior requiring intervention occurred prior to hospital admission, in the emergency department or short‐stay observation unit. Interventions for combative behavior are institution specific. At our institution, a behavioral code is called when a patient or visitor is disruptive and exhibiting behavior that, if not controlled immediately, may result in serious injury to self or others, in line with the approach recommended by the Washington State Hospital Association.[9] When this situation arises, a staff member calls the hospital operator and an alert is paged overhead. Security staff then comes to the area to assist the clinical staff in determining the proper response.
The sample of 120 patients with behavioral codes was compared to a control group of 159 inpatients from the same year, randomly selected from all hospital discharges. For both groups, patients under the age of 18 and patients who were cared for only in the emergency department or short stay observation unit were excluded.
The presence or absence of delirium, the primary exposure of interest, was determined using a combined reference standard. First, by institutional protocol, all inpatients underwent nursing administration of the CAM[13] or the CAM for the Intensive Care Unit[14] on admission and every 12 hours thereafter. Patients with a positive CAM score within the 48 hours preceding the behavioral code event in cases, or anytime during the hospitalization in controls, were considered to have delirium. The CAM was performed as part of routine care at our institution by clinical nurses. However, when used outside of the research setting, untrained nurses using the CAM may substantially underestimate the incidence of delirium.[15, 16] Therefore, as a second reference standard, among patients who did not have delirium by the CAM criteria above, chart review was performed to identify delirium. Though chart review is also imperfect for the determination of both delirium and potential confounders, given the limitations of CAM scores in clinical rather than research settings, the use of this combined reference standard improves detection of delirium. Our chart review method is based on the previously reported work by Lakatos et al. and Inouye et al., identifying delirium from key words in the medical record demonstrating the diagnostic criteria for delirium.[6, 16] The Lakatos et al. study provided the specific key words used in our chart review.[6]
For each case and control subject, 1 of 2 experienced chart reviewers abstracted data from the electronic medical record retrospectively. The abstractors were not informed as to whether or not the patients were cases or controls, but could not be blinded as this information may be clear from the medical record. (The chart abstraction tool, with the key words mapped to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition criteria for delirium and the CAM is included in the Supporting Information, Appendix, in the online version of this article). We assessed interobserver agreement for delirium diagnosis through double review of 20% of charts. The presence or absence of potential confounders, including dementia, substance use or other psychiatric illness, and use of drugs associated with delirium specific (opiates, sedatives, anticholinergics, and antihistamines), and demographic information, including time of admission; hospital length of stay; any intensive care unit (ICU) visit; and discharge disposition was also determined from the electronic medical record.
Bivariate statistics were completed comparing patients with a behavioral code to the control group. Categorical variables were compared using 2, and continuous variables were compared using the t test. Logistic regression using stepwise regression, threshold of 0.1, dependent variable of behavioral code, and independent variable of delirium was performed to determine the association of delirium with behavioral codes after adjustment for confounders. In the multivariate model, use of any medication associated with delirium (Table 1) was considered as a single binary variable, regardless of drug type or class. Agreement was assessed through the kappa statistic. All statistics were performed using Stata MP v.12 (StataCorp, College Station, TX).
| Patients With Behavioral Code, N=120 | Patients Without Behavioral Code, N=159 | P Value | |
|---|---|---|---|
| |||
| Narcotic analgesics (%) | 78 (65) | 111 (70) | 0.40 |
| Fentanyl (%) | 47 (39) | 84 (53) | 0.024 |
| Hydromorphone (%) | 51 (43) | 78 (49) | 0.28 |
| Oxycodone (%) | 34 (28) | 46 (29) | 0.91 |
| Sedative hypnotics (%) | 76 (63) | 84 (53) | 0.08 |
| Midazolam (%) | 35 (29) | 70 (44) | 0.011 |
| Lorazepam (%) | 58 (48) | 15 (9) | <0.001 |
| No. of different drugs/person, mean (SD), range 010 | 2.6 (2.2) | 2.3 (1.9) | 0.27 |
RESULTS
Patients experiencing combative behavior requiring intervention through a behavioral code were significantly more likely to be male, admitted overnight, require an ICU stay during their hospitalization, and have a diagnosis of dementia or substance‐use disorder (Table 2). Patients with a behavioral code demonstrated an increased hospital length of stay (9.4 vs 4.5 days) and were significantly more likely to be discharged to a skilled nursing facility (31/120, 26% vs 16/159, 10%), or leave against medical advice (10% 12/120 vs 0%, P<0.001). Of the patients leaving against medical advice, none had evidence of delirium or dementia in the record; 92% (11/12) had International Classification of Disease9th Revision codes reflecting alcohol and/or drug abuse or dependence. Exposure to medications commonly associated with delirium was common in both groups, with differences in usage patterns for different drugs (Table 1).
| Characteristic | Patients With Behavioral Code, N=120 | Patients Without Behavioral Code, N=159 | P Value |
|---|---|---|---|
| |||
| Age, y, mean (SD) | 64.8 (19.5) | 63.9 (16.7) | 0.66 |
| Female (%) | 39 (33) | 78 (49) | 0.006 |
| Race/ethnicity (%) | 0.68 | ||
| White non‐Hispanic | 95 (79) | 129 (81) | |
| Other or unknown | 25 (21) | 30 (19) | |
| Patient Diagnosis Related Group (%) | 0.017 | ||
| Medical | 69 (57) | 69 (43) | |
| Gynecological or surgical | 51 (43) | 90 (57) | |
| Hospital admit between 6 pm and 6 am (%) | 63 (53) | 54 (34) | 0.002 |
| Any intensive care unit visit (%) | 43 (36) | 26 (16) | <0.001 |
| Any positive Confusion Assessment Method score | 70 (58) | 16 (10) | 0.002 |
| Delirium (%)a | 87 (73) | 26 (16) | <0.001 |
| Mental disorders as any discharge diagnosis code (%) | 110 (92) | 58 (36) | <0.001 |
| Dementia and other persistent (%) | 29 (24) | 9 (6) | <0.001 |
| Alcohol/drugs (%) | 61 (51) | 23 (14) | <0.001 |
Although combative behavior requiring intervention occurred throughout the stay, the majority (84/120, 70%) of behavioral codes occurred during the first 72 hours of hospital admission. Behavioral codes occurred throughout all nursing shifts, with 27% (32/120) between 7:00 am and 3:00 pm, 32% (39/120) between 3:00 pm and 11:00 pm, and 41% (49/120) between 11:00 pm and 7:00 am. Psychiatric consultation occurred in only 17% (20/120) of patients prior to the behavioral code.
Delirium was evident in the 48 hours preceding the behavioral code event in 50% (60/120) of cases, and was present overall in 16% of the comparison group. In the cases, delirium prior to behavioral code was identified by positive CAM scores in 23% (28/120) and by chart review in 27% (32/120). In the control subjects, delirium was identified by CAM scores in 10% (16/159) and by chart review in 10% (16/159). The chart review delirium assessment demonstrated high interobserver reliability (kappa=0.71). Among patients with behavioral codes, only 28/60 (46.7%) of delirium cases were identified by the CAM score.
The unadjusted odds ratio (OR) for having a behavioral code in the setting of delirium (within 48 hours prior to the code) was 5.1 (95% confidence interval [CI]: 2.9‐8.9, P<0.001), with the combined reference standard of positive CAM or delirium by chart review. Because each reference standard (chart review or CAM) only identified some of the delirium, the OR with only a single reference standard was lower. The risk of behavioral code in the setting of delirium when only CAM scores are considered for the diagnosis of delirium, the OR for behavioral code was 2.7 (95% CI: 1.4‐ 5.3, P=0.003), and when only chart review was used for delirium diagnosis, the OR was 2.7 (95% CI: 1.5‐5.0, P=0.001).
In the stepwise logistic regression model (using the composite reference standard of positive CAM score or delirium on chart review), the odds of having a behavioral code was 3.8 times greater in the setting of delirium (OR: 3.8, 95% CI: 2.07.3, P<0.001), after adjustment for substance abuse (OR: 5.3, 95% CI: 2.810.2, P<0.001), dementia (OR: 6.5, 95% CI: 2.616.1, P<0.001), other mental health diagnosis (OR: 3.2, 95% CI: 1.7‐6.1, P<0.001), and gender (OR male gender: 2.4, 95% CI: 1.34.5, P=0.006). Other potential confounders (age, use of delirium‐associated medications, ICU stay, time of admission) were not significant and so were not included in the final multivariate model.
DISCUSSION
In this study, we identify a 3.8‐fold increased odds of combative behavior requiring a behavioral code intervention in hospitalized patients with delirium. Although a previous association between delirium and restraint use among mechanically ventilated patients in the ICU has been published,[6] this is the first article to describe the strong, statistically significant association between combative patient behavior and delirium in the general medical/surgical acute‐care setting. This association raises the possibility that prevention, early identification, and treatment of delirium in hospitalized patients can decrease the incidence of such combative behavior, and may lead to shorter length of stay and less institutionalization after discharge.
In the multivariate model, we did identify other predictors of combative behavior requiring intervention, including substance abuse, dementia, and other psychiatric diagnoses. Our results do not support age as predictive of combative behavior after adjustment for other predictors. However, our hospital population is relatively old (mean age in controls, 63.9 years). In populations different from ours, age may still be an important predictor. We also did not identify use of medications potentially associated with delirium as a predictor of combative behavior requiring intervention, after adjustment for other predictors. We did, however, consider all medications together, and are not able to differentiate the potential predictive ability of any single drug or class. Finally, we report relatively high rates of opiate and sedative use in our sample, likely because we included short‐acting agents (ie, midazolam, fentanyl) that are commonly used for procedures and perioperative care.
Our study also highlights the challenges of accurately identifying delirium for quality improvement interventions. The CAM is a validated and widely accepted method of prospective screening for delirium, but in relatively untrained hands outside of research settings (as in our institution) does underestimate the true incidence of delirium.[15, 16, 17] Further, both CAM assessment and chart review may underestimate the incidence of hypoactive delirium. In our study, we note that the CAM scores only identified 46.7% of the behavioral code patients with delirium. Chart review also has limitations, identified by Inouye et al.,[16] particularly in the setting of comorbid dementia, high baseline delirium risk, and other comorbid conditions. Comorbidities as defined by APACHE II (Acute Physiology and Chronic Health Evaluation II) score may contribute to false positives, and poor documentation may result in false negatives. Our use of a combined reference standard of CAM assessment and chart review for delirium is supported by the fact that the incidence of delirium we report in the control group is similar to the published literature.[5]
Combative behavior in the hospital setting may be a threat to patients, staff, and visitors, and multiple state hospital associations have called for standardized responses, including the calling of behavioral codes when such circumstances arise.[9] In general, de‐escalation techniques and security measures are sufficient for patients exhibiting combative behavior. However, in cases of delirium‐associated combative behavior, clinical evaluation of root causes and both pharmacological and nonpharmacological interventions, including proactive psychiatric consultation, may also be beneficial.[18, 19, 20, 21] Many nonpharmacological interventions may need to be multicomponent in nature, as has been described previously.[18, 19, 20, 21]
We acknowledge the limitations of this article. First, we identify a strong association between combative behavior requiring intervention and delirium, but cannot prove causality. Second, though the chart reviewers where not told if reviewing cases or controls, we were not able to blind them to information on combative behavior that might have been present in the medical record. The use of unblinded reviewers could lead to overestimation of the presence of delirium in cases, and overestimation of the association between delirium and combative behavior requiring intervention. Third, chart review methods may underestimate the prevalence of dementia, which can confound the diagnosis of delirium. Finally, we defined delirium in the behavioral code cases as occurring in the 48 hours prior to the code event. However, as no such event occurred in the controls, we considered delirium as present if identified any time during the hospitalization. This could potentially lead to underestimation of the true association of delirium with combative behavior requiring intervention. It is also worth noting that many of the identified predictors for combative behavior are also predictors for delirium and may be identifying a subset of combative behavior related to agitated delirium. Overall, however, the strength of the association we report does strongly support identification and treatment of delirium in the context of combative behavior.
In this article, we identify a strong association between delirium and combative behavior requiring intervention, even after adjustment for other predictors. Understanding this association can help providers consider delirium as a potential cause of combative behavior in a medical/surgical setting, beyond behavioral issues associated with community violence, serious mental illness, progressive dementia, or substance use. Overall, therefore, delirium risk assessment, screening, prevention, and early intervention may potentially decrease combative behavior, and contribute to improving patient and staff safety in hospital settings.
Disclosures: C. Craig Blackmore, MD, reports royalties from the Springer Verlag publishing company for a textbook series on evidence‐based imaging, which is not relevant to this article. None of the authors report any conflicts of interest.
- Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000.
- , , , et al. Delirium as a predictor of mortality in mechanically ventilated patients in the ICU. JAMA. 2004;291:1753–1762.
- , , . Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care. Am J Med. 1999;106:565–573.
- , , , et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization and dementia. JAMA. 2010;304:443–451.
- , , . Delirium in elderly people. Lancet. 2014;383(9920):911–922.
- , , , et al. Falls in the general hospital: association with delirium, advanced age, and specific surgical procedures. Psychosomatics. 2009;50:218–226.
- , , , , . Delirium as detected by the CAM‐ICU predicts restraint use among mechanically ventilated patients. Crit Care Med. 2005;33:226–229.
- , , . Delirium: prevention, treatment and outcome studies. J Geriatr Psychiatry Neurol. 1998;11:126–137.
- Washington State Hospital Association. Standardization of emergency code calls in Washington: implementation toolkit. Available at: http://www.wsha.org/files/82/EmergencyCodesExceutiveSummary.pdf. Accessed October 23, 2013.
- . Words for the wise: defusing combative patient behavior through verbal intervention. J Healthc Prot Manage. 2005;21:81–88.
- , , , . Rapid response team for behavioral emergencies. J Am Psychiatric Nurses Assoc. 2010;16:93–100.
- , . Physical and chemical restraints. Emerg Med Clin N Am. 2009;27:655–667.
- , , , , , . Clarifying confusion: the Confusion Assessment Method. Ann Int Med. 1990;113:941–948.
- , , , et al. Delirium in mechanically ventilated patients: validity and reliability of the Confusion Assessment Method for the Intensive Care Unit (CAM‐ICU). JAMA. 2001;286:2703–2710.
- , , , , , . A researchh algorithm to improve detection of delirium in the intensive care unit. Crit Care. 2006;10:R121.
- , , , , , . A chart‐based method for identification of delirium: validation compared with interviewer ratings using the Confusion Assessment Method. J Am Geriatic Soc. 2005;53:312–318.
- , , , , . Nurses' recognition of delirium and its symptoms. Arch Int Med. 2001;161:2467–2473.
- , , , et al. A multi‐component intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340:669–676.
- , , . Delirium: screening, prevention and diagnosis—a systematic review of the evidence. Evidence‐based Synthesis Program (ESP). Washington, DC: Department of Veterans Affairs; 2011.
- , , , , , . A longitudinal study of motor subtypes in delirium: frequency and stability during episodes. J Psychsom Res. 2012;72:236–241.
- , , , et al. Pharmacologic management of delirium in hospitalized adults—a systematic evidence review. J Gen Intern Med. 2009;24:848–853.
Delirium affects up to 82% of critical‐care patients and 29% to 64% of general medical patients, resulting in medical morbidity, decreased function, and mortality.[1, 2, 3, 4, 5] Delirium is associated with specific, adverse hospital outcomes, including falls, aspiration pneumonia, pressure ulcers, and restraint use.[6, 7] As a consequence of delirium, individuals may be transformed from independent and active at the time of admission to requiring skilled nursing supervision at discharge, in some cases resulting in permanent cognitive disability for the remainder of the person's life.[4, 8]
Combative behavior in hospitalized patients can be a threat to self or others, including other patients and staff. An emergency alert to staff regarding the presence of a combative patient requiring intervention is known as a behavioral code or Code Gray.[9] Guidelines addressing this particular hospital emergency typically refer to de‐escalation methods and implementation of security measures. Ideally, however, at‐risk patients would be identified prior to development into a full behavioral code. Unfortunately, the medical literature on the causes, prevention, and interventions for combative behavior requiring intervention is limited. Interventions published to date focus on patients living with severe and persistent mental illness, such as schizophrenia or bipolar disorder.[9, 10, 11, 12]
We hypothesized that delirium contributes to combative behavior in hospitalized patients, leading to the adverse outcome of behavioral codes. Delirium identification would therefore provide an opportunity for prevention and early identification of patients at risk, thereby improving safety for patients and staff. However, no studies published to date address the impact of delirium on the likelihood of a patient hospitalized in a general medical/surgical setting becoming combative and requiring intervention such as a behavioral code. The purpose of this article is to determine the strength of the association between delirium and combative behavior requiring intervention.
METHODS
This study was conducted as part of a quality improvement project, resulting in a waiver by the institutional review board of the hospital. All data with patient‐specific information were securely handled and deidentified prior to analysis. The setting is a 336‐bed, nonuniversity, teaching hospital serving adults in the Pacific Northwest, with approximately 16,000 admissions per year, and 31 critical‐care beds. Delirium prevention has been identified as an institutional priority, and we have been screening for delirium on admission and with twice‐daily Confusion Assessment Method (CAM) scores since 2010.
The study design was a retrospective case control study of hospital inpatients. Consecutive patients experiencing combative behavior requiring a specific behavioral code intervention (n=125) between January 1, 2011 to December 31, 2011 were identified using security reports and operator code logs. Five patients were excluded because the combative behavior requiring intervention occurred prior to hospital admission, in the emergency department or short‐stay observation unit. Interventions for combative behavior are institution specific. At our institution, a behavioral code is called when a patient or visitor is disruptive and exhibiting behavior that, if not controlled immediately, may result in serious injury to self or others, in line with the approach recommended by the Washington State Hospital Association.[9] When this situation arises, a staff member calls the hospital operator and an alert is paged overhead. Security staff then comes to the area to assist the clinical staff in determining the proper response.
The sample of 120 patients with behavioral codes was compared to a control group of 159 inpatients from the same year, randomly selected from all hospital discharges. For both groups, patients under the age of 18 and patients who were cared for only in the emergency department or short stay observation unit were excluded.
The presence or absence of delirium, the primary exposure of interest, was determined using a combined reference standard. First, by institutional protocol, all inpatients underwent nursing administration of the CAM[13] or the CAM for the Intensive Care Unit[14] on admission and every 12 hours thereafter. Patients with a positive CAM score within the 48 hours preceding the behavioral code event in cases, or anytime during the hospitalization in controls, were considered to have delirium. The CAM was performed as part of routine care at our institution by clinical nurses. However, when used outside of the research setting, untrained nurses using the CAM may substantially underestimate the incidence of delirium.[15, 16] Therefore, as a second reference standard, among patients who did not have delirium by the CAM criteria above, chart review was performed to identify delirium. Though chart review is also imperfect for the determination of both delirium and potential confounders, given the limitations of CAM scores in clinical rather than research settings, the use of this combined reference standard improves detection of delirium. Our chart review method is based on the previously reported work by Lakatos et al. and Inouye et al., identifying delirium from key words in the medical record demonstrating the diagnostic criteria for delirium.[6, 16] The Lakatos et al. study provided the specific key words used in our chart review.[6]
For each case and control subject, 1 of 2 experienced chart reviewers abstracted data from the electronic medical record retrospectively. The abstractors were not informed as to whether or not the patients were cases or controls, but could not be blinded as this information may be clear from the medical record. (The chart abstraction tool, with the key words mapped to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition criteria for delirium and the CAM is included in the Supporting Information, Appendix, in the online version of this article). We assessed interobserver agreement for delirium diagnosis through double review of 20% of charts. The presence or absence of potential confounders, including dementia, substance use or other psychiatric illness, and use of drugs associated with delirium specific (opiates, sedatives, anticholinergics, and antihistamines), and demographic information, including time of admission; hospital length of stay; any intensive care unit (ICU) visit; and discharge disposition was also determined from the electronic medical record.
Bivariate statistics were completed comparing patients with a behavioral code to the control group. Categorical variables were compared using 2, and continuous variables were compared using the t test. Logistic regression using stepwise regression, threshold of 0.1, dependent variable of behavioral code, and independent variable of delirium was performed to determine the association of delirium with behavioral codes after adjustment for confounders. In the multivariate model, use of any medication associated with delirium (Table 1) was considered as a single binary variable, regardless of drug type or class. Agreement was assessed through the kappa statistic. All statistics were performed using Stata MP v.12 (StataCorp, College Station, TX).
| Patients With Behavioral Code, N=120 | Patients Without Behavioral Code, N=159 | P Value | |
|---|---|---|---|
| |||
| Narcotic analgesics (%) | 78 (65) | 111 (70) | 0.40 |
| Fentanyl (%) | 47 (39) | 84 (53) | 0.024 |
| Hydromorphone (%) | 51 (43) | 78 (49) | 0.28 |
| Oxycodone (%) | 34 (28) | 46 (29) | 0.91 |
| Sedative hypnotics (%) | 76 (63) | 84 (53) | 0.08 |
| Midazolam (%) | 35 (29) | 70 (44) | 0.011 |
| Lorazepam (%) | 58 (48) | 15 (9) | <0.001 |
| No. of different drugs/person, mean (SD), range 010 | 2.6 (2.2) | 2.3 (1.9) | 0.27 |
RESULTS
Patients experiencing combative behavior requiring intervention through a behavioral code were significantly more likely to be male, admitted overnight, require an ICU stay during their hospitalization, and have a diagnosis of dementia or substance‐use disorder (Table 2). Patients with a behavioral code demonstrated an increased hospital length of stay (9.4 vs 4.5 days) and were significantly more likely to be discharged to a skilled nursing facility (31/120, 26% vs 16/159, 10%), or leave against medical advice (10% 12/120 vs 0%, P<0.001). Of the patients leaving against medical advice, none had evidence of delirium or dementia in the record; 92% (11/12) had International Classification of Disease9th Revision codes reflecting alcohol and/or drug abuse or dependence. Exposure to medications commonly associated with delirium was common in both groups, with differences in usage patterns for different drugs (Table 1).
| Characteristic | Patients With Behavioral Code, N=120 | Patients Without Behavioral Code, N=159 | P Value |
|---|---|---|---|
| |||
| Age, y, mean (SD) | 64.8 (19.5) | 63.9 (16.7) | 0.66 |
| Female (%) | 39 (33) | 78 (49) | 0.006 |
| Race/ethnicity (%) | 0.68 | ||
| White non‐Hispanic | 95 (79) | 129 (81) | |
| Other or unknown | 25 (21) | 30 (19) | |
| Patient Diagnosis Related Group (%) | 0.017 | ||
| Medical | 69 (57) | 69 (43) | |
| Gynecological or surgical | 51 (43) | 90 (57) | |
| Hospital admit between 6 pm and 6 am (%) | 63 (53) | 54 (34) | 0.002 |
| Any intensive care unit visit (%) | 43 (36) | 26 (16) | <0.001 |
| Any positive Confusion Assessment Method score | 70 (58) | 16 (10) | 0.002 |
| Delirium (%)a | 87 (73) | 26 (16) | <0.001 |
| Mental disorders as any discharge diagnosis code (%) | 110 (92) | 58 (36) | <0.001 |
| Dementia and other persistent (%) | 29 (24) | 9 (6) | <0.001 |
| Alcohol/drugs (%) | 61 (51) | 23 (14) | <0.001 |
Although combative behavior requiring intervention occurred throughout the stay, the majority (84/120, 70%) of behavioral codes occurred during the first 72 hours of hospital admission. Behavioral codes occurred throughout all nursing shifts, with 27% (32/120) between 7:00 am and 3:00 pm, 32% (39/120) between 3:00 pm and 11:00 pm, and 41% (49/120) between 11:00 pm and 7:00 am. Psychiatric consultation occurred in only 17% (20/120) of patients prior to the behavioral code.
Delirium was evident in the 48 hours preceding the behavioral code event in 50% (60/120) of cases, and was present overall in 16% of the comparison group. In the cases, delirium prior to behavioral code was identified by positive CAM scores in 23% (28/120) and by chart review in 27% (32/120). In the control subjects, delirium was identified by CAM scores in 10% (16/159) and by chart review in 10% (16/159). The chart review delirium assessment demonstrated high interobserver reliability (kappa=0.71). Among patients with behavioral codes, only 28/60 (46.7%) of delirium cases were identified by the CAM score.
The unadjusted odds ratio (OR) for having a behavioral code in the setting of delirium (within 48 hours prior to the code) was 5.1 (95% confidence interval [CI]: 2.9‐8.9, P<0.001), with the combined reference standard of positive CAM or delirium by chart review. Because each reference standard (chart review or CAM) only identified some of the delirium, the OR with only a single reference standard was lower. The risk of behavioral code in the setting of delirium when only CAM scores are considered for the diagnosis of delirium, the OR for behavioral code was 2.7 (95% CI: 1.4‐ 5.3, P=0.003), and when only chart review was used for delirium diagnosis, the OR was 2.7 (95% CI: 1.5‐5.0, P=0.001).
In the stepwise logistic regression model (using the composite reference standard of positive CAM score or delirium on chart review), the odds of having a behavioral code was 3.8 times greater in the setting of delirium (OR: 3.8, 95% CI: 2.07.3, P<0.001), after adjustment for substance abuse (OR: 5.3, 95% CI: 2.810.2, P<0.001), dementia (OR: 6.5, 95% CI: 2.616.1, P<0.001), other mental health diagnosis (OR: 3.2, 95% CI: 1.7‐6.1, P<0.001), and gender (OR male gender: 2.4, 95% CI: 1.34.5, P=0.006). Other potential confounders (age, use of delirium‐associated medications, ICU stay, time of admission) were not significant and so were not included in the final multivariate model.
DISCUSSION
In this study, we identify a 3.8‐fold increased odds of combative behavior requiring a behavioral code intervention in hospitalized patients with delirium. Although a previous association between delirium and restraint use among mechanically ventilated patients in the ICU has been published,[6] this is the first article to describe the strong, statistically significant association between combative patient behavior and delirium in the general medical/surgical acute‐care setting. This association raises the possibility that prevention, early identification, and treatment of delirium in hospitalized patients can decrease the incidence of such combative behavior, and may lead to shorter length of stay and less institutionalization after discharge.
In the multivariate model, we did identify other predictors of combative behavior requiring intervention, including substance abuse, dementia, and other psychiatric diagnoses. Our results do not support age as predictive of combative behavior after adjustment for other predictors. However, our hospital population is relatively old (mean age in controls, 63.9 years). In populations different from ours, age may still be an important predictor. We also did not identify use of medications potentially associated with delirium as a predictor of combative behavior requiring intervention, after adjustment for other predictors. We did, however, consider all medications together, and are not able to differentiate the potential predictive ability of any single drug or class. Finally, we report relatively high rates of opiate and sedative use in our sample, likely because we included short‐acting agents (ie, midazolam, fentanyl) that are commonly used for procedures and perioperative care.
Our study also highlights the challenges of accurately identifying delirium for quality improvement interventions. The CAM is a validated and widely accepted method of prospective screening for delirium, but in relatively untrained hands outside of research settings (as in our institution) does underestimate the true incidence of delirium.[15, 16, 17] Further, both CAM assessment and chart review may underestimate the incidence of hypoactive delirium. In our study, we note that the CAM scores only identified 46.7% of the behavioral code patients with delirium. Chart review also has limitations, identified by Inouye et al.,[16] particularly in the setting of comorbid dementia, high baseline delirium risk, and other comorbid conditions. Comorbidities as defined by APACHE II (Acute Physiology and Chronic Health Evaluation II) score may contribute to false positives, and poor documentation may result in false negatives. Our use of a combined reference standard of CAM assessment and chart review for delirium is supported by the fact that the incidence of delirium we report in the control group is similar to the published literature.[5]
Combative behavior in the hospital setting may be a threat to patients, staff, and visitors, and multiple state hospital associations have called for standardized responses, including the calling of behavioral codes when such circumstances arise.[9] In general, de‐escalation techniques and security measures are sufficient for patients exhibiting combative behavior. However, in cases of delirium‐associated combative behavior, clinical evaluation of root causes and both pharmacological and nonpharmacological interventions, including proactive psychiatric consultation, may also be beneficial.[18, 19, 20, 21] Many nonpharmacological interventions may need to be multicomponent in nature, as has been described previously.[18, 19, 20, 21]
We acknowledge the limitations of this article. First, we identify a strong association between combative behavior requiring intervention and delirium, but cannot prove causality. Second, though the chart reviewers where not told if reviewing cases or controls, we were not able to blind them to information on combative behavior that might have been present in the medical record. The use of unblinded reviewers could lead to overestimation of the presence of delirium in cases, and overestimation of the association between delirium and combative behavior requiring intervention. Third, chart review methods may underestimate the prevalence of dementia, which can confound the diagnosis of delirium. Finally, we defined delirium in the behavioral code cases as occurring in the 48 hours prior to the code event. However, as no such event occurred in the controls, we considered delirium as present if identified any time during the hospitalization. This could potentially lead to underestimation of the true association of delirium with combative behavior requiring intervention. It is also worth noting that many of the identified predictors for combative behavior are also predictors for delirium and may be identifying a subset of combative behavior related to agitated delirium. Overall, however, the strength of the association we report does strongly support identification and treatment of delirium in the context of combative behavior.
In this article, we identify a strong association between delirium and combative behavior requiring intervention, even after adjustment for other predictors. Understanding this association can help providers consider delirium as a potential cause of combative behavior in a medical/surgical setting, beyond behavioral issues associated with community violence, serious mental illness, progressive dementia, or substance use. Overall, therefore, delirium risk assessment, screening, prevention, and early intervention may potentially decrease combative behavior, and contribute to improving patient and staff safety in hospital settings.
Disclosures: C. Craig Blackmore, MD, reports royalties from the Springer Verlag publishing company for a textbook series on evidence‐based imaging, which is not relevant to this article. None of the authors report any conflicts of interest.
Delirium affects up to 82% of critical‐care patients and 29% to 64% of general medical patients, resulting in medical morbidity, decreased function, and mortality.[1, 2, 3, 4, 5] Delirium is associated with specific, adverse hospital outcomes, including falls, aspiration pneumonia, pressure ulcers, and restraint use.[6, 7] As a consequence of delirium, individuals may be transformed from independent and active at the time of admission to requiring skilled nursing supervision at discharge, in some cases resulting in permanent cognitive disability for the remainder of the person's life.[4, 8]
Combative behavior in hospitalized patients can be a threat to self or others, including other patients and staff. An emergency alert to staff regarding the presence of a combative patient requiring intervention is known as a behavioral code or Code Gray.[9] Guidelines addressing this particular hospital emergency typically refer to de‐escalation methods and implementation of security measures. Ideally, however, at‐risk patients would be identified prior to development into a full behavioral code. Unfortunately, the medical literature on the causes, prevention, and interventions for combative behavior requiring intervention is limited. Interventions published to date focus on patients living with severe and persistent mental illness, such as schizophrenia or bipolar disorder.[9, 10, 11, 12]
We hypothesized that delirium contributes to combative behavior in hospitalized patients, leading to the adverse outcome of behavioral codes. Delirium identification would therefore provide an opportunity for prevention and early identification of patients at risk, thereby improving safety for patients and staff. However, no studies published to date address the impact of delirium on the likelihood of a patient hospitalized in a general medical/surgical setting becoming combative and requiring intervention such as a behavioral code. The purpose of this article is to determine the strength of the association between delirium and combative behavior requiring intervention.
METHODS
This study was conducted as part of a quality improvement project, resulting in a waiver by the institutional review board of the hospital. All data with patient‐specific information were securely handled and deidentified prior to analysis. The setting is a 336‐bed, nonuniversity, teaching hospital serving adults in the Pacific Northwest, with approximately 16,000 admissions per year, and 31 critical‐care beds. Delirium prevention has been identified as an institutional priority, and we have been screening for delirium on admission and with twice‐daily Confusion Assessment Method (CAM) scores since 2010.
The study design was a retrospective case control study of hospital inpatients. Consecutive patients experiencing combative behavior requiring a specific behavioral code intervention (n=125) between January 1, 2011 to December 31, 2011 were identified using security reports and operator code logs. Five patients were excluded because the combative behavior requiring intervention occurred prior to hospital admission, in the emergency department or short‐stay observation unit. Interventions for combative behavior are institution specific. At our institution, a behavioral code is called when a patient or visitor is disruptive and exhibiting behavior that, if not controlled immediately, may result in serious injury to self or others, in line with the approach recommended by the Washington State Hospital Association.[9] When this situation arises, a staff member calls the hospital operator and an alert is paged overhead. Security staff then comes to the area to assist the clinical staff in determining the proper response.
The sample of 120 patients with behavioral codes was compared to a control group of 159 inpatients from the same year, randomly selected from all hospital discharges. For both groups, patients under the age of 18 and patients who were cared for only in the emergency department or short stay observation unit were excluded.
The presence or absence of delirium, the primary exposure of interest, was determined using a combined reference standard. First, by institutional protocol, all inpatients underwent nursing administration of the CAM[13] or the CAM for the Intensive Care Unit[14] on admission and every 12 hours thereafter. Patients with a positive CAM score within the 48 hours preceding the behavioral code event in cases, or anytime during the hospitalization in controls, were considered to have delirium. The CAM was performed as part of routine care at our institution by clinical nurses. However, when used outside of the research setting, untrained nurses using the CAM may substantially underestimate the incidence of delirium.[15, 16] Therefore, as a second reference standard, among patients who did not have delirium by the CAM criteria above, chart review was performed to identify delirium. Though chart review is also imperfect for the determination of both delirium and potential confounders, given the limitations of CAM scores in clinical rather than research settings, the use of this combined reference standard improves detection of delirium. Our chart review method is based on the previously reported work by Lakatos et al. and Inouye et al., identifying delirium from key words in the medical record demonstrating the diagnostic criteria for delirium.[6, 16] The Lakatos et al. study provided the specific key words used in our chart review.[6]
For each case and control subject, 1 of 2 experienced chart reviewers abstracted data from the electronic medical record retrospectively. The abstractors were not informed as to whether or not the patients were cases or controls, but could not be blinded as this information may be clear from the medical record. (The chart abstraction tool, with the key words mapped to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition criteria for delirium and the CAM is included in the Supporting Information, Appendix, in the online version of this article). We assessed interobserver agreement for delirium diagnosis through double review of 20% of charts. The presence or absence of potential confounders, including dementia, substance use or other psychiatric illness, and use of drugs associated with delirium specific (opiates, sedatives, anticholinergics, and antihistamines), and demographic information, including time of admission; hospital length of stay; any intensive care unit (ICU) visit; and discharge disposition was also determined from the electronic medical record.
Bivariate statistics were completed comparing patients with a behavioral code to the control group. Categorical variables were compared using 2, and continuous variables were compared using the t test. Logistic regression using stepwise regression, threshold of 0.1, dependent variable of behavioral code, and independent variable of delirium was performed to determine the association of delirium with behavioral codes after adjustment for confounders. In the multivariate model, use of any medication associated with delirium (Table 1) was considered as a single binary variable, regardless of drug type or class. Agreement was assessed through the kappa statistic. All statistics were performed using Stata MP v.12 (StataCorp, College Station, TX).
| Patients With Behavioral Code, N=120 | Patients Without Behavioral Code, N=159 | P Value | |
|---|---|---|---|
| |||
| Narcotic analgesics (%) | 78 (65) | 111 (70) | 0.40 |
| Fentanyl (%) | 47 (39) | 84 (53) | 0.024 |
| Hydromorphone (%) | 51 (43) | 78 (49) | 0.28 |
| Oxycodone (%) | 34 (28) | 46 (29) | 0.91 |
| Sedative hypnotics (%) | 76 (63) | 84 (53) | 0.08 |
| Midazolam (%) | 35 (29) | 70 (44) | 0.011 |
| Lorazepam (%) | 58 (48) | 15 (9) | <0.001 |
| No. of different drugs/person, mean (SD), range 010 | 2.6 (2.2) | 2.3 (1.9) | 0.27 |
RESULTS
Patients experiencing combative behavior requiring intervention through a behavioral code were significantly more likely to be male, admitted overnight, require an ICU stay during their hospitalization, and have a diagnosis of dementia or substance‐use disorder (Table 2). Patients with a behavioral code demonstrated an increased hospital length of stay (9.4 vs 4.5 days) and were significantly more likely to be discharged to a skilled nursing facility (31/120, 26% vs 16/159, 10%), or leave against medical advice (10% 12/120 vs 0%, P<0.001). Of the patients leaving against medical advice, none had evidence of delirium or dementia in the record; 92% (11/12) had International Classification of Disease9th Revision codes reflecting alcohol and/or drug abuse or dependence. Exposure to medications commonly associated with delirium was common in both groups, with differences in usage patterns for different drugs (Table 1).
| Characteristic | Patients With Behavioral Code, N=120 | Patients Without Behavioral Code, N=159 | P Value |
|---|---|---|---|
| |||
| Age, y, mean (SD) | 64.8 (19.5) | 63.9 (16.7) | 0.66 |
| Female (%) | 39 (33) | 78 (49) | 0.006 |
| Race/ethnicity (%) | 0.68 | ||
| White non‐Hispanic | 95 (79) | 129 (81) | |
| Other or unknown | 25 (21) | 30 (19) | |
| Patient Diagnosis Related Group (%) | 0.017 | ||
| Medical | 69 (57) | 69 (43) | |
| Gynecological or surgical | 51 (43) | 90 (57) | |
| Hospital admit between 6 pm and 6 am (%) | 63 (53) | 54 (34) | 0.002 |
| Any intensive care unit visit (%) | 43 (36) | 26 (16) | <0.001 |
| Any positive Confusion Assessment Method score | 70 (58) | 16 (10) | 0.002 |
| Delirium (%)a | 87 (73) | 26 (16) | <0.001 |
| Mental disorders as any discharge diagnosis code (%) | 110 (92) | 58 (36) | <0.001 |
| Dementia and other persistent (%) | 29 (24) | 9 (6) | <0.001 |
| Alcohol/drugs (%) | 61 (51) | 23 (14) | <0.001 |
Although combative behavior requiring intervention occurred throughout the stay, the majority (84/120, 70%) of behavioral codes occurred during the first 72 hours of hospital admission. Behavioral codes occurred throughout all nursing shifts, with 27% (32/120) between 7:00 am and 3:00 pm, 32% (39/120) between 3:00 pm and 11:00 pm, and 41% (49/120) between 11:00 pm and 7:00 am. Psychiatric consultation occurred in only 17% (20/120) of patients prior to the behavioral code.
Delirium was evident in the 48 hours preceding the behavioral code event in 50% (60/120) of cases, and was present overall in 16% of the comparison group. In the cases, delirium prior to behavioral code was identified by positive CAM scores in 23% (28/120) and by chart review in 27% (32/120). In the control subjects, delirium was identified by CAM scores in 10% (16/159) and by chart review in 10% (16/159). The chart review delirium assessment demonstrated high interobserver reliability (kappa=0.71). Among patients with behavioral codes, only 28/60 (46.7%) of delirium cases were identified by the CAM score.
The unadjusted odds ratio (OR) for having a behavioral code in the setting of delirium (within 48 hours prior to the code) was 5.1 (95% confidence interval [CI]: 2.9‐8.9, P<0.001), with the combined reference standard of positive CAM or delirium by chart review. Because each reference standard (chart review or CAM) only identified some of the delirium, the OR with only a single reference standard was lower. The risk of behavioral code in the setting of delirium when only CAM scores are considered for the diagnosis of delirium, the OR for behavioral code was 2.7 (95% CI: 1.4‐ 5.3, P=0.003), and when only chart review was used for delirium diagnosis, the OR was 2.7 (95% CI: 1.5‐5.0, P=0.001).
In the stepwise logistic regression model (using the composite reference standard of positive CAM score or delirium on chart review), the odds of having a behavioral code was 3.8 times greater in the setting of delirium (OR: 3.8, 95% CI: 2.07.3, P<0.001), after adjustment for substance abuse (OR: 5.3, 95% CI: 2.810.2, P<0.001), dementia (OR: 6.5, 95% CI: 2.616.1, P<0.001), other mental health diagnosis (OR: 3.2, 95% CI: 1.7‐6.1, P<0.001), and gender (OR male gender: 2.4, 95% CI: 1.34.5, P=0.006). Other potential confounders (age, use of delirium‐associated medications, ICU stay, time of admission) were not significant and so were not included in the final multivariate model.
DISCUSSION
In this study, we identify a 3.8‐fold increased odds of combative behavior requiring a behavioral code intervention in hospitalized patients with delirium. Although a previous association between delirium and restraint use among mechanically ventilated patients in the ICU has been published,[6] this is the first article to describe the strong, statistically significant association between combative patient behavior and delirium in the general medical/surgical acute‐care setting. This association raises the possibility that prevention, early identification, and treatment of delirium in hospitalized patients can decrease the incidence of such combative behavior, and may lead to shorter length of stay and less institutionalization after discharge.
In the multivariate model, we did identify other predictors of combative behavior requiring intervention, including substance abuse, dementia, and other psychiatric diagnoses. Our results do not support age as predictive of combative behavior after adjustment for other predictors. However, our hospital population is relatively old (mean age in controls, 63.9 years). In populations different from ours, age may still be an important predictor. We also did not identify use of medications potentially associated with delirium as a predictor of combative behavior requiring intervention, after adjustment for other predictors. We did, however, consider all medications together, and are not able to differentiate the potential predictive ability of any single drug or class. Finally, we report relatively high rates of opiate and sedative use in our sample, likely because we included short‐acting agents (ie, midazolam, fentanyl) that are commonly used for procedures and perioperative care.
Our study also highlights the challenges of accurately identifying delirium for quality improvement interventions. The CAM is a validated and widely accepted method of prospective screening for delirium, but in relatively untrained hands outside of research settings (as in our institution) does underestimate the true incidence of delirium.[15, 16, 17] Further, both CAM assessment and chart review may underestimate the incidence of hypoactive delirium. In our study, we note that the CAM scores only identified 46.7% of the behavioral code patients with delirium. Chart review also has limitations, identified by Inouye et al.,[16] particularly in the setting of comorbid dementia, high baseline delirium risk, and other comorbid conditions. Comorbidities as defined by APACHE II (Acute Physiology and Chronic Health Evaluation II) score may contribute to false positives, and poor documentation may result in false negatives. Our use of a combined reference standard of CAM assessment and chart review for delirium is supported by the fact that the incidence of delirium we report in the control group is similar to the published literature.[5]
Combative behavior in the hospital setting may be a threat to patients, staff, and visitors, and multiple state hospital associations have called for standardized responses, including the calling of behavioral codes when such circumstances arise.[9] In general, de‐escalation techniques and security measures are sufficient for patients exhibiting combative behavior. However, in cases of delirium‐associated combative behavior, clinical evaluation of root causes and both pharmacological and nonpharmacological interventions, including proactive psychiatric consultation, may also be beneficial.[18, 19, 20, 21] Many nonpharmacological interventions may need to be multicomponent in nature, as has been described previously.[18, 19, 20, 21]
We acknowledge the limitations of this article. First, we identify a strong association between combative behavior requiring intervention and delirium, but cannot prove causality. Second, though the chart reviewers where not told if reviewing cases or controls, we were not able to blind them to information on combative behavior that might have been present in the medical record. The use of unblinded reviewers could lead to overestimation of the presence of delirium in cases, and overestimation of the association between delirium and combative behavior requiring intervention. Third, chart review methods may underestimate the prevalence of dementia, which can confound the diagnosis of delirium. Finally, we defined delirium in the behavioral code cases as occurring in the 48 hours prior to the code event. However, as no such event occurred in the controls, we considered delirium as present if identified any time during the hospitalization. This could potentially lead to underestimation of the true association of delirium with combative behavior requiring intervention. It is also worth noting that many of the identified predictors for combative behavior are also predictors for delirium and may be identifying a subset of combative behavior related to agitated delirium. Overall, however, the strength of the association we report does strongly support identification and treatment of delirium in the context of combative behavior.
In this article, we identify a strong association between delirium and combative behavior requiring intervention, even after adjustment for other predictors. Understanding this association can help providers consider delirium as a potential cause of combative behavior in a medical/surgical setting, beyond behavioral issues associated with community violence, serious mental illness, progressive dementia, or substance use. Overall, therefore, delirium risk assessment, screening, prevention, and early intervention may potentially decrease combative behavior, and contribute to improving patient and staff safety in hospital settings.
Disclosures: C. Craig Blackmore, MD, reports royalties from the Springer Verlag publishing company for a textbook series on evidence‐based imaging, which is not relevant to this article. None of the authors report any conflicts of interest.
- Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000.
- , , , et al. Delirium as a predictor of mortality in mechanically ventilated patients in the ICU. JAMA. 2004;291:1753–1762.
- , , . Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care. Am J Med. 1999;106:565–573.
- , , , et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization and dementia. JAMA. 2010;304:443–451.
- , , . Delirium in elderly people. Lancet. 2014;383(9920):911–922.
- , , , et al. Falls in the general hospital: association with delirium, advanced age, and specific surgical procedures. Psychosomatics. 2009;50:218–226.
- , , , , . Delirium as detected by the CAM‐ICU predicts restraint use among mechanically ventilated patients. Crit Care Med. 2005;33:226–229.
- , , . Delirium: prevention, treatment and outcome studies. J Geriatr Psychiatry Neurol. 1998;11:126–137.
- Washington State Hospital Association. Standardization of emergency code calls in Washington: implementation toolkit. Available at: http://www.wsha.org/files/82/EmergencyCodesExceutiveSummary.pdf. Accessed October 23, 2013.
- . Words for the wise: defusing combative patient behavior through verbal intervention. J Healthc Prot Manage. 2005;21:81–88.
- , , , . Rapid response team for behavioral emergencies. J Am Psychiatric Nurses Assoc. 2010;16:93–100.
- , . Physical and chemical restraints. Emerg Med Clin N Am. 2009;27:655–667.
- , , , , , . Clarifying confusion: the Confusion Assessment Method. Ann Int Med. 1990;113:941–948.
- , , , et al. Delirium in mechanically ventilated patients: validity and reliability of the Confusion Assessment Method for the Intensive Care Unit (CAM‐ICU). JAMA. 2001;286:2703–2710.
- , , , , , . A researchh algorithm to improve detection of delirium in the intensive care unit. Crit Care. 2006;10:R121.
- , , , , , . A chart‐based method for identification of delirium: validation compared with interviewer ratings using the Confusion Assessment Method. J Am Geriatic Soc. 2005;53:312–318.
- , , , , . Nurses' recognition of delirium and its symptoms. Arch Int Med. 2001;161:2467–2473.
- , , , et al. A multi‐component intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340:669–676.
- , , . Delirium: screening, prevention and diagnosis—a systematic review of the evidence. Evidence‐based Synthesis Program (ESP). Washington, DC: Department of Veterans Affairs; 2011.
- , , , , , . A longitudinal study of motor subtypes in delirium: frequency and stability during episodes. J Psychsom Res. 2012;72:236–241.
- , , , et al. Pharmacologic management of delirium in hospitalized adults—a systematic evidence review. J Gen Intern Med. 2009;24:848–853.
- Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000.
- , , , et al. Delirium as a predictor of mortality in mechanically ventilated patients in the ICU. JAMA. 2004;291:1753–1762.
- , , . Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care. Am J Med. 1999;106:565–573.
- , , , et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization and dementia. JAMA. 2010;304:443–451.
- , , . Delirium in elderly people. Lancet. 2014;383(9920):911–922.
- , , , et al. Falls in the general hospital: association with delirium, advanced age, and specific surgical procedures. Psychosomatics. 2009;50:218–226.
- , , , , . Delirium as detected by the CAM‐ICU predicts restraint use among mechanically ventilated patients. Crit Care Med. 2005;33:226–229.
- , , . Delirium: prevention, treatment and outcome studies. J Geriatr Psychiatry Neurol. 1998;11:126–137.
- Washington State Hospital Association. Standardization of emergency code calls in Washington: implementation toolkit. Available at: http://www.wsha.org/files/82/EmergencyCodesExceutiveSummary.pdf. Accessed October 23, 2013.
- . Words for the wise: defusing combative patient behavior through verbal intervention. J Healthc Prot Manage. 2005;21:81–88.
- , , , . Rapid response team for behavioral emergencies. J Am Psychiatric Nurses Assoc. 2010;16:93–100.
- , . Physical and chemical restraints. Emerg Med Clin N Am. 2009;27:655–667.
- , , , , , . Clarifying confusion: the Confusion Assessment Method. Ann Int Med. 1990;113:941–948.
- , , , et al. Delirium in mechanically ventilated patients: validity and reliability of the Confusion Assessment Method for the Intensive Care Unit (CAM‐ICU). JAMA. 2001;286:2703–2710.
- , , , , , . A researchh algorithm to improve detection of delirium in the intensive care unit. Crit Care. 2006;10:R121.
- , , , , , . A chart‐based method for identification of delirium: validation compared with interviewer ratings using the Confusion Assessment Method. J Am Geriatic Soc. 2005;53:312–318.
- , , , , . Nurses' recognition of delirium and its symptoms. Arch Int Med. 2001;161:2467–2473.
- , , , et al. A multi‐component intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340:669–676.
- , , . Delirium: screening, prevention and diagnosis—a systematic review of the evidence. Evidence‐based Synthesis Program (ESP). Washington, DC: Department of Veterans Affairs; 2011.
- , , , , , . A longitudinal study of motor subtypes in delirium: frequency and stability during episodes. J Psychsom Res. 2012;72:236–241.
- , , , et al. Pharmacologic management of delirium in hospitalized adults—a systematic evidence review. J Gen Intern Med. 2009;24:848–853.
© 2014 Society of Hospital Medicine
BEST PRACTICES IN: Acne Vulgaris
A Best Practices Supplement to Skin & Allergy News®. This supplement was sponsored by Valeant Dermatology, a division of Valeant Pharmaceuticals.
- Introduction
- ACANYA (clindamycin phosphate and benzoyl peroxide) Gel Indication and Mechanisms
- ACANYA Gel Efficacy
- ACANYA Gel Tolerability
- IMPORTANT SAFETY INFORMATION
Faculty/Faculty Disclosures
Hilary Baldwin, MD
SUNY Downstate Medical Center
Brooklyn, NY
Dr. Baldwin discloses that she serves as a member on the advisory board for Valeant Pharmaceuticals.
Copyright © by Frontline Medical Communications Inc.
A Best Practices Supplement to Skin & Allergy News®. This supplement was sponsored by Valeant Dermatology, a division of Valeant Pharmaceuticals.
- Introduction
- ACANYA (clindamycin phosphate and benzoyl peroxide) Gel Indication and Mechanisms
- ACANYA Gel Efficacy
- ACANYA Gel Tolerability
- IMPORTANT SAFETY INFORMATION
Faculty/Faculty Disclosures
Hilary Baldwin, MD
SUNY Downstate Medical Center
Brooklyn, NY
Dr. Baldwin discloses that she serves as a member on the advisory board for Valeant Pharmaceuticals.
Copyright © by Frontline Medical Communications Inc.
A Best Practices Supplement to Skin & Allergy News®. This supplement was sponsored by Valeant Dermatology, a division of Valeant Pharmaceuticals.
- Introduction
- ACANYA (clindamycin phosphate and benzoyl peroxide) Gel Indication and Mechanisms
- ACANYA Gel Efficacy
- ACANYA Gel Tolerability
- IMPORTANT SAFETY INFORMATION
Faculty/Faculty Disclosures
Hilary Baldwin, MD
SUNY Downstate Medical Center
Brooklyn, NY
Dr. Baldwin discloses that she serves as a member on the advisory board for Valeant Pharmaceuticals.
Copyright © by Frontline Medical Communications Inc.
Product News: 08 2014
Acticlate
Aqua Pharmaceuticals, LLC, announces US Food and Drug Administration approval of the new drug application for Acticlate (doxycycline hyclate) tablets. Acticlate is a tetracycline-class antibacterial indicated for the treatment of a number of infections, including adjunctive therapy in severe acne. Acticlate is available in round 75-mg tablets and oval-shaped, dual-scored 150-mg tablets. Utilizing the latest manufacturing technology, the 150-mg tablets are formulated in a substantially reduced tablet size for Acticlate, allowing for dosing flexibility and making it easier for the patient to swallow. For more information, visit www.aquapharm.com.
ATX-101
Kythera Biopharmaceuticals, Inc, announces that its new drug application for ATX-101 (deoxycholic acid) has been accepted for filing by the US Food and Drug Administration. ATX-101 is an injectable treatment for the reduction of submental fat. The treatment contours the area under the chin by destroying fat cells while leaving surrounding tissue largely unaffected. The new drug application review should be completed by May 13, 2015. For more information, visit www.kytherabiopharma.com/pipeline/ATX-101.
EpiCeram Airless Pump
PuraCap Pharmaceutical LLC adds the EpiCeram 225-g airless pump to its product line. This airless pump gives patients more EpiCeram to treat any size area of atopic dermatitis with twice-daily application. The convenient and portable pump dispenser gives patients more control in applying EpiCeram. A 90-g tube is already available. The EpiCeram Controlled Release Skin Barrier Emulsion helps to relieve the burning and itching associated with skin conditions such as atopic dermatitis and eczema. For more information, visit www.epiceram-us.com.
Hair Regrowth System
brandMD Skin Care introduces the Hair Regrowth System, a 3-step daily regimen to prevent and improve signs of hair loss. The regimen includes the Replenish Shampoo, Restorative Conditioning Treatment, and Rapid Growth Serum. By reducing the production of dihydrotestosterone, the system stimulates hair growth and improves hair follicle anchoring. Both men and women can use the Hair Regrowth System. For more information, visit www.brandMDskincare.com.
Rasuvo
Medac Pharma Inc obtains US Food and Drug Administration approval for Rasuvo, a subcutaneous injectable methotrexate therapy delivered in a single-dose autoinjector for rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, and psoriasis. Rasuvo is available in 10 dosage strengths ranging from 7.5 to 30 mg in 2.5-mg increments. Because of the possibility of serious toxic reactions, Rasuvo should be used only in patients with psoriasis or rheumatoid arthritis with severe, recalcitrant, disabling disease that is not adequately responsive to other forms of therapy. For more information, visit www.rasuvo.com.
Restylane Silk
Valeant Pharmaceuticals International, Inc, obtains US Food and Drug Administration marketing clearance for Restylane Silk injectable gel with 0.3% lidocaine, which is indicated for submucosal implantation for lip augmentation and dermal implantation for correction of perioral rhytides in patients older than 21 years. Restylane Silk is composed of hyaluronic acid and is free from animal protein. Allergy pretesting is not necessary. Restylane Silk should not be used in patients with prior hypersensitivity to local anesthetics of the amide type, such as lidocaine. For more information, visit www.valeant.com.
Zenatane Provider Portal
Promius Pharma, LLC, launches a Web-based provider portal to follow a patient taking Zenatane (isotretinoin). It is designed to allow any authorized prescriber using the Promius Promise pharmacy program to obtain instant access to secure patient data. This portal is valuable for dermatologists to track patient adherence to guidelines for using isotretinoin. It will provide patient demographics, dates of prescriptions received and shipped, and information on pending prescription shipments. A messaging tool also allows health care providers to send questions and receive answers within the portal itself. It maintains strict privacy in accordance with the Health Insurance Portability and Accountability Act.
If you would like your product included in Product News, please e-mail a press release to the Editorial Office at cutis@frontlinemedcom.com.
Acticlate
Aqua Pharmaceuticals, LLC, announces US Food and Drug Administration approval of the new drug application for Acticlate (doxycycline hyclate) tablets. Acticlate is a tetracycline-class antibacterial indicated for the treatment of a number of infections, including adjunctive therapy in severe acne. Acticlate is available in round 75-mg tablets and oval-shaped, dual-scored 150-mg tablets. Utilizing the latest manufacturing technology, the 150-mg tablets are formulated in a substantially reduced tablet size for Acticlate, allowing for dosing flexibility and making it easier for the patient to swallow. For more information, visit www.aquapharm.com.
ATX-101
Kythera Biopharmaceuticals, Inc, announces that its new drug application for ATX-101 (deoxycholic acid) has been accepted for filing by the US Food and Drug Administration. ATX-101 is an injectable treatment for the reduction of submental fat. The treatment contours the area under the chin by destroying fat cells while leaving surrounding tissue largely unaffected. The new drug application review should be completed by May 13, 2015. For more information, visit www.kytherabiopharma.com/pipeline/ATX-101.
EpiCeram Airless Pump
PuraCap Pharmaceutical LLC adds the EpiCeram 225-g airless pump to its product line. This airless pump gives patients more EpiCeram to treat any size area of atopic dermatitis with twice-daily application. The convenient and portable pump dispenser gives patients more control in applying EpiCeram. A 90-g tube is already available. The EpiCeram Controlled Release Skin Barrier Emulsion helps to relieve the burning and itching associated with skin conditions such as atopic dermatitis and eczema. For more information, visit www.epiceram-us.com.
Hair Regrowth System
brandMD Skin Care introduces the Hair Regrowth System, a 3-step daily regimen to prevent and improve signs of hair loss. The regimen includes the Replenish Shampoo, Restorative Conditioning Treatment, and Rapid Growth Serum. By reducing the production of dihydrotestosterone, the system stimulates hair growth and improves hair follicle anchoring. Both men and women can use the Hair Regrowth System. For more information, visit www.brandMDskincare.com.
Rasuvo
Medac Pharma Inc obtains US Food and Drug Administration approval for Rasuvo, a subcutaneous injectable methotrexate therapy delivered in a single-dose autoinjector for rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, and psoriasis. Rasuvo is available in 10 dosage strengths ranging from 7.5 to 30 mg in 2.5-mg increments. Because of the possibility of serious toxic reactions, Rasuvo should be used only in patients with psoriasis or rheumatoid arthritis with severe, recalcitrant, disabling disease that is not adequately responsive to other forms of therapy. For more information, visit www.rasuvo.com.
Restylane Silk
Valeant Pharmaceuticals International, Inc, obtains US Food and Drug Administration marketing clearance for Restylane Silk injectable gel with 0.3% lidocaine, which is indicated for submucosal implantation for lip augmentation and dermal implantation for correction of perioral rhytides in patients older than 21 years. Restylane Silk is composed of hyaluronic acid and is free from animal protein. Allergy pretesting is not necessary. Restylane Silk should not be used in patients with prior hypersensitivity to local anesthetics of the amide type, such as lidocaine. For more information, visit www.valeant.com.
Zenatane Provider Portal
Promius Pharma, LLC, launches a Web-based provider portal to follow a patient taking Zenatane (isotretinoin). It is designed to allow any authorized prescriber using the Promius Promise pharmacy program to obtain instant access to secure patient data. This portal is valuable for dermatologists to track patient adherence to guidelines for using isotretinoin. It will provide patient demographics, dates of prescriptions received and shipped, and information on pending prescription shipments. A messaging tool also allows health care providers to send questions and receive answers within the portal itself. It maintains strict privacy in accordance with the Health Insurance Portability and Accountability Act.
If you would like your product included in Product News, please e-mail a press release to the Editorial Office at cutis@frontlinemedcom.com.
Acticlate
Aqua Pharmaceuticals, LLC, announces US Food and Drug Administration approval of the new drug application for Acticlate (doxycycline hyclate) tablets. Acticlate is a tetracycline-class antibacterial indicated for the treatment of a number of infections, including adjunctive therapy in severe acne. Acticlate is available in round 75-mg tablets and oval-shaped, dual-scored 150-mg tablets. Utilizing the latest manufacturing technology, the 150-mg tablets are formulated in a substantially reduced tablet size for Acticlate, allowing for dosing flexibility and making it easier for the patient to swallow. For more information, visit www.aquapharm.com.
ATX-101
Kythera Biopharmaceuticals, Inc, announces that its new drug application for ATX-101 (deoxycholic acid) has been accepted for filing by the US Food and Drug Administration. ATX-101 is an injectable treatment for the reduction of submental fat. The treatment contours the area under the chin by destroying fat cells while leaving surrounding tissue largely unaffected. The new drug application review should be completed by May 13, 2015. For more information, visit www.kytherabiopharma.com/pipeline/ATX-101.
EpiCeram Airless Pump
PuraCap Pharmaceutical LLC adds the EpiCeram 225-g airless pump to its product line. This airless pump gives patients more EpiCeram to treat any size area of atopic dermatitis with twice-daily application. The convenient and portable pump dispenser gives patients more control in applying EpiCeram. A 90-g tube is already available. The EpiCeram Controlled Release Skin Barrier Emulsion helps to relieve the burning and itching associated with skin conditions such as atopic dermatitis and eczema. For more information, visit www.epiceram-us.com.
Hair Regrowth System
brandMD Skin Care introduces the Hair Regrowth System, a 3-step daily regimen to prevent and improve signs of hair loss. The regimen includes the Replenish Shampoo, Restorative Conditioning Treatment, and Rapid Growth Serum. By reducing the production of dihydrotestosterone, the system stimulates hair growth and improves hair follicle anchoring. Both men and women can use the Hair Regrowth System. For more information, visit www.brandMDskincare.com.
Rasuvo
Medac Pharma Inc obtains US Food and Drug Administration approval for Rasuvo, a subcutaneous injectable methotrexate therapy delivered in a single-dose autoinjector for rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, and psoriasis. Rasuvo is available in 10 dosage strengths ranging from 7.5 to 30 mg in 2.5-mg increments. Because of the possibility of serious toxic reactions, Rasuvo should be used only in patients with psoriasis or rheumatoid arthritis with severe, recalcitrant, disabling disease that is not adequately responsive to other forms of therapy. For more information, visit www.rasuvo.com.
Restylane Silk
Valeant Pharmaceuticals International, Inc, obtains US Food and Drug Administration marketing clearance for Restylane Silk injectable gel with 0.3% lidocaine, which is indicated for submucosal implantation for lip augmentation and dermal implantation for correction of perioral rhytides in patients older than 21 years. Restylane Silk is composed of hyaluronic acid and is free from animal protein. Allergy pretesting is not necessary. Restylane Silk should not be used in patients with prior hypersensitivity to local anesthetics of the amide type, such as lidocaine. For more information, visit www.valeant.com.
Zenatane Provider Portal
Promius Pharma, LLC, launches a Web-based provider portal to follow a patient taking Zenatane (isotretinoin). It is designed to allow any authorized prescriber using the Promius Promise pharmacy program to obtain instant access to secure patient data. This portal is valuable for dermatologists to track patient adherence to guidelines for using isotretinoin. It will provide patient demographics, dates of prescriptions received and shipped, and information on pending prescription shipments. A messaging tool also allows health care providers to send questions and receive answers within the portal itself. It maintains strict privacy in accordance with the Health Insurance Portability and Accountability Act.
If you would like your product included in Product News, please e-mail a press release to the Editorial Office at cutis@frontlinemedcom.com.
Pretibial Myxedema
Pretibial myxedema (PM) is a cutaneous mucinosis associated with thyroid dysfunction. It most commonly presents in the setting of Graves disease and is seen less often in patients with hypothyroidism and euthyroidism.1 The anterior tibia is most frequently affected, but lesions also may present on the feet, thighs, and upper extremities. Physical examination generally demonstrates skin thickening, hyperkeratosis, hyperpigmentation, yellow-red discoloration, and hyperhidrosis. Classically, the term peau d’orange has been used to characterize these clinical features.1 Histologic examination of PM typically reveals marked deposition of mucin throughout the reticular dermis with sparing of the papillary dermis (Figure 1) and may be accompanied by overlying hyperkeratosis. Collagen fibers are splayed and appear decreased in density (Figure 2). Alcian blue, periodic acid–Schiff, colloidal iron, and toluidine blue staining can be used to highlight dermal mucin.
 | 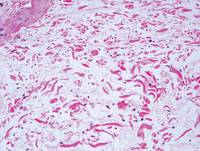 |
Figure 1. Prominent mucin deposition throughout the reticular dermis in pretibial myxedema (H&E, original magnification ×40). | Figure 2. Increased mucin deposition and collagen fiber splaying in pretibial myxedema (H&E, original magnification ×200). |
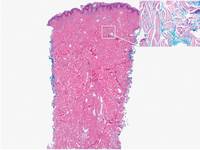 | 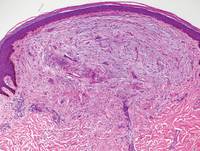 |
Figure 3. Scleredema with increased dermal thickness (H&E, original magnification ×20) and interstitial mucin on colloidal iron–stained sections (inset in upper right corner, original magnification ×400). | Figure 4. Scleromyxedema with mucin deposition primarily in the superficial dermis as well as increased cellularity and fibrosis (H&E, original magnification ×200). |
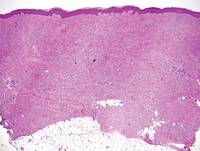 | 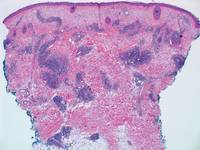 |
Figure 5. Nephrogenic systemic fibrosis with prominent mucinous fibrosis (H&E, original magnification ×40). | Figure 6. Tumid lupus erythematosus with a superficial and perivascular lymphoid infiltrate as well as increased dermal mucin (H&E, original magnification ×40). |
Similar to PM, histologic examination of scleredema and scleromyxedema usually demonstrate prominent mucin deposition. In scleredema, mucin primarily is visualized in the deep dermis between thick collagen bundles and typically is localized to the back (Figure 3). Scleromyxedema is distinguished by mucin deposition in the superficial dermis with associated fibroblast proliferation and fibrosis (Figure 4).
Nephrogenic systemic fibrosis is characterized by proliferation of CD34+ dermal spindle cells, fibroblasts, interstitial mucin, altered elastic fibers, and thickened collagen bundles that involve the dermis and subcutaneous septa (Figure 5).2 Tumid lupus erythematosus classically demonstrates perivascular and periadnexal superficial and deep lymphocytic inflammation (Figure 6). Similar to scleredema and PM, mucin deposition in tumid lupus erythematosus is interspersed between collagen bundles in the reticular dermis.3
1. Fatourechi V. Pretibial myxedema: pathophysiology and treatment options. Am J Clin Dermatol. 2005;6:295-309.
2. Cowper SE, Lyndon DS, Bhawan J, et al. Nephro-genic fibrosing dermopathy. Am J Dermatopathol.2001;23:383-393.
3. Kuhn A, Dagmar RH, Oslislo C, et al. Lupus erythematosus tumidus: a neglected subset of cutaneous lupus erythematosus: report of 40 cases. Arch Dermatol. 2000;136:1033-1041.
Pretibial myxedema (PM) is a cutaneous mucinosis associated with thyroid dysfunction. It most commonly presents in the setting of Graves disease and is seen less often in patients with hypothyroidism and euthyroidism.1 The anterior tibia is most frequently affected, but lesions also may present on the feet, thighs, and upper extremities. Physical examination generally demonstrates skin thickening, hyperkeratosis, hyperpigmentation, yellow-red discoloration, and hyperhidrosis. Classically, the term peau d’orange has been used to characterize these clinical features.1 Histologic examination of PM typically reveals marked deposition of mucin throughout the reticular dermis with sparing of the papillary dermis (Figure 1) and may be accompanied by overlying hyperkeratosis. Collagen fibers are splayed and appear decreased in density (Figure 2). Alcian blue, periodic acid–Schiff, colloidal iron, and toluidine blue staining can be used to highlight dermal mucin.
 | 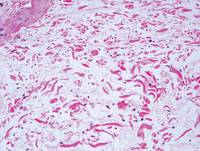 |
Figure 1. Prominent mucin deposition throughout the reticular dermis in pretibial myxedema (H&E, original magnification ×40). | Figure 2. Increased mucin deposition and collagen fiber splaying in pretibial myxedema (H&E, original magnification ×200). |
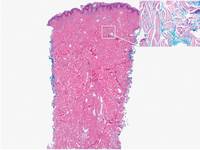 | 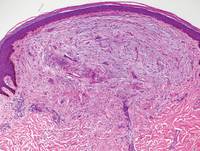 |
Figure 3. Scleredema with increased dermal thickness (H&E, original magnification ×20) and interstitial mucin on colloidal iron–stained sections (inset in upper right corner, original magnification ×400). | Figure 4. Scleromyxedema with mucin deposition primarily in the superficial dermis as well as increased cellularity and fibrosis (H&E, original magnification ×200). |
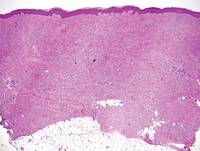 | 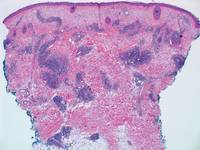 |
Figure 5. Nephrogenic systemic fibrosis with prominent mucinous fibrosis (H&E, original magnification ×40). | Figure 6. Tumid lupus erythematosus with a superficial and perivascular lymphoid infiltrate as well as increased dermal mucin (H&E, original magnification ×40). |
Similar to PM, histologic examination of scleredema and scleromyxedema usually demonstrate prominent mucin deposition. In scleredema, mucin primarily is visualized in the deep dermis between thick collagen bundles and typically is localized to the back (Figure 3). Scleromyxedema is distinguished by mucin deposition in the superficial dermis with associated fibroblast proliferation and fibrosis (Figure 4).
Nephrogenic systemic fibrosis is characterized by proliferation of CD34+ dermal spindle cells, fibroblasts, interstitial mucin, altered elastic fibers, and thickened collagen bundles that involve the dermis and subcutaneous septa (Figure 5).2 Tumid lupus erythematosus classically demonstrates perivascular and periadnexal superficial and deep lymphocytic inflammation (Figure 6). Similar to scleredema and PM, mucin deposition in tumid lupus erythematosus is interspersed between collagen bundles in the reticular dermis.3
Pretibial myxedema (PM) is a cutaneous mucinosis associated with thyroid dysfunction. It most commonly presents in the setting of Graves disease and is seen less often in patients with hypothyroidism and euthyroidism.1 The anterior tibia is most frequently affected, but lesions also may present on the feet, thighs, and upper extremities. Physical examination generally demonstrates skin thickening, hyperkeratosis, hyperpigmentation, yellow-red discoloration, and hyperhidrosis. Classically, the term peau d’orange has been used to characterize these clinical features.1 Histologic examination of PM typically reveals marked deposition of mucin throughout the reticular dermis with sparing of the papillary dermis (Figure 1) and may be accompanied by overlying hyperkeratosis. Collagen fibers are splayed and appear decreased in density (Figure 2). Alcian blue, periodic acid–Schiff, colloidal iron, and toluidine blue staining can be used to highlight dermal mucin.
 | 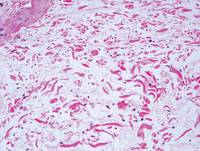 |
Figure 1. Prominent mucin deposition throughout the reticular dermis in pretibial myxedema (H&E, original magnification ×40). | Figure 2. Increased mucin deposition and collagen fiber splaying in pretibial myxedema (H&E, original magnification ×200). |
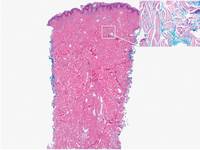 | 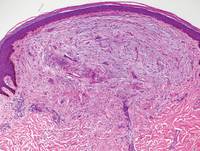 |
Figure 3. Scleredema with increased dermal thickness (H&E, original magnification ×20) and interstitial mucin on colloidal iron–stained sections (inset in upper right corner, original magnification ×400). | Figure 4. Scleromyxedema with mucin deposition primarily in the superficial dermis as well as increased cellularity and fibrosis (H&E, original magnification ×200). |
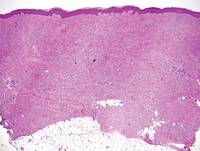 | 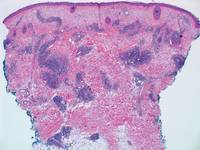 |
Figure 5. Nephrogenic systemic fibrosis with prominent mucinous fibrosis (H&E, original magnification ×40). | Figure 6. Tumid lupus erythematosus with a superficial and perivascular lymphoid infiltrate as well as increased dermal mucin (H&E, original magnification ×40). |
Similar to PM, histologic examination of scleredema and scleromyxedema usually demonstrate prominent mucin deposition. In scleredema, mucin primarily is visualized in the deep dermis between thick collagen bundles and typically is localized to the back (Figure 3). Scleromyxedema is distinguished by mucin deposition in the superficial dermis with associated fibroblast proliferation and fibrosis (Figure 4).
Nephrogenic systemic fibrosis is characterized by proliferation of CD34+ dermal spindle cells, fibroblasts, interstitial mucin, altered elastic fibers, and thickened collagen bundles that involve the dermis and subcutaneous septa (Figure 5).2 Tumid lupus erythematosus classically demonstrates perivascular and periadnexal superficial and deep lymphocytic inflammation (Figure 6). Similar to scleredema and PM, mucin deposition in tumid lupus erythematosus is interspersed between collagen bundles in the reticular dermis.3
1. Fatourechi V. Pretibial myxedema: pathophysiology and treatment options. Am J Clin Dermatol. 2005;6:295-309.
2. Cowper SE, Lyndon DS, Bhawan J, et al. Nephro-genic fibrosing dermopathy. Am J Dermatopathol.2001;23:383-393.
3. Kuhn A, Dagmar RH, Oslislo C, et al. Lupus erythematosus tumidus: a neglected subset of cutaneous lupus erythematosus: report of 40 cases. Arch Dermatol. 2000;136:1033-1041.
1. Fatourechi V. Pretibial myxedema: pathophysiology and treatment options. Am J Clin Dermatol. 2005;6:295-309.
2. Cowper SE, Lyndon DS, Bhawan J, et al. Nephro-genic fibrosing dermopathy. Am J Dermatopathol.2001;23:383-393.
3. Kuhn A, Dagmar RH, Oslislo C, et al. Lupus erythematosus tumidus: a neglected subset of cutaneous lupus erythematosus: report of 40 cases. Arch Dermatol. 2000;136:1033-1041.
Findings support endovascular-first approach for ruptured VAAs
BOSTON – Endovascular interventions for ruptured visceral artery aneurysms are associated with reduced morbidity and mortality, compared with open interventions, according to findings from a retrospective chart review.
Both endovascular and open repairs are safe and durable for intact visceral artery aneurysms, Dr. Ankur J. Shukla reported at a the 2014 Vascular Annual Meeting.
Of 261 patients who presented with visceral artery aneurysms (VAAs), 174 underwent repair: 74 who presented with ruptured VAA and 100 who presented with intact VAA. The majority – 73% of ruptured VAA and 62% of intact VAA – were repaired with an endovascular approach.
Among those with ruptured VAA, 30-day mortality was 7.4% following endovascular repair, compared with 28.6% following open repair, a significant difference, said Dr. Shukla of the University of Pittsburgh Medical Center.
Survival at 3 years of ruptured VAA was about 70% vs. 46.4% in the endovascular and open repair groups, respectively, he said.
About 65% of patients with ruptured VAA presented with pain, and about 30% presented in hemodynamic shock. The most commonly identified etiology was "inflammatory/pancreatitis inflammatory," and 80% of the aneurysms were pseudoaneurysmal in nature.
A large proportion of the aneurysms were in the splenic and arterial beds, but 26% were located in the pancreaticoduodenal arcade, and those had a mean size of 12.7 mm. Most (95%) were pseudoaneurysms.
The outcomes with ruptured VAA were quite good, Dr. Shukla said, noting that the technical success rate was 98.7%.
Although the 30-day reintervention rate with endovascular repair was higher, the difference between the groups was not statistically significant, and there was a trend toward a lower rate of major complications with endovascular repair.
Factors found to be predictors of mortality risk were older age and steroid use, while endovascular repair was found to be protective.
As for the patients with intact VAA, most presented without symptoms, and the most common etiology was atherosclerosis.
"When we looked at the distribution, this was very consistent with what has been reported in the literature, with the splenic and arterial beds really making up the lion’s share of this group. Notable is the fact that 6.7% of our patients had intact aneurysms in the pancreaticoduodenal arcade," he said.
Outcomes in those with intact aneurysms were good. A slightly higher 30-day reintervention rate in those who underwent endovascular repair did not reach statistical significance, and both the endovascular and open repair groups had low rates of major complications.
Survival at 3 years for intact aneurysms did not differ in the endovascular and open repair groups. This was partly due to a 0% 30-day mortality, and – despite the fact that the overall mortality in those with intact aneurysms was 10% – there was zero overall aneurysm-related mortality, he said.
Patients in the study were treated at a single institution between 2003 and 2013. Most were in their mid to late 50s, and there were more men and more individuals on immunosuppressive therapy in the ruptured VAA group. However, comorbidities were similar in the ruptured and intact VAA groups.
Visceral artery aneurysms occur only rarely, affecting 0.1% to 2% of the general population, but because of the increasing use of noninvasive imaging, more of these aneurysms are being detected incidentally.
When they are not found incidentally, they often go undetected and present when they rupture, Dr. Shukla said.
"Because of the increasing utilization and improvement of endovascular technology, we now have a lot of options to fix these aneurysms. But the outcomes are not well defined. Even less well defined is the outcome of ruptured visceral artery aneurysms," he said, noting that most studies have a small sample size or look only at endovascular or open repairs.
Overall, the current study showed that there is "an acute and sharp drop-off in survival with open repair," related, most likely, to operative mortality, he said.
"Based on the findings, we recommend aggressive treatment of pseudoaneurysms and true aneurysms in the pancreaticoduodenal arcade, and advocate for an endovascular-first approach to treating ruptured visceral artery aneurysms, acknowledging that success in this is really predicated on good planning based on advanced imaging and endovascular set-up," he concluded.
Dr. Shukla reported having no disclosures
Visceral Artery Aneurysms (VAA) can be challenging to treat from an open approach especially when the aneurysm is adherent to the surrounding pancreatic, visceral or retroperitoneal tissue. In most areas of vascular disease endovascular therapy is easier. But, endovascular therapy for VAA can be as challenging as the open surgical repair because of vessel tortuosity and access, imaging challenges, and the few options available for durable aneurysm treatment. Dr. Shukla and colleagues reviewed their outcomes in treating VAA over a 10-year period and report high rates of technical success, low morbidity and mortality using endovascular means for both intact and ruptured VAA. The results for endovascular therapy for ruptured VAA were particularly promising. These results indicate that coils and other ablative maneuvers may suffice in the setting of hemorrhage and be preferable to open surgical repair or ligation. This study provides important information on a rare problem and reassures us that the mid-term durability of ablative techniques for VAA is acceptable.
Dr. Vikram Kashyap is professor of surgery, Case Western Reserve University and chief, Division of Vascular Surgery and Endovascular Therapy, and co-director, Harrington Heart & Vascular Institute, University Hospitals Case Medical Center,Cleveland.
Visceral Artery Aneurysms (VAA) can be challenging to treat from an open approach especially when the aneurysm is adherent to the surrounding pancreatic, visceral or retroperitoneal tissue. In most areas of vascular disease endovascular therapy is easier. But, endovascular therapy for VAA can be as challenging as the open surgical repair because of vessel tortuosity and access, imaging challenges, and the few options available for durable aneurysm treatment. Dr. Shukla and colleagues reviewed their outcomes in treating VAA over a 10-year period and report high rates of technical success, low morbidity and mortality using endovascular means for both intact and ruptured VAA. The results for endovascular therapy for ruptured VAA were particularly promising. These results indicate that coils and other ablative maneuvers may suffice in the setting of hemorrhage and be preferable to open surgical repair or ligation. This study provides important information on a rare problem and reassures us that the mid-term durability of ablative techniques for VAA is acceptable.
Dr. Vikram Kashyap is professor of surgery, Case Western Reserve University and chief, Division of Vascular Surgery and Endovascular Therapy, and co-director, Harrington Heart & Vascular Institute, University Hospitals Case Medical Center,Cleveland.
Visceral Artery Aneurysms (VAA) can be challenging to treat from an open approach especially when the aneurysm is adherent to the surrounding pancreatic, visceral or retroperitoneal tissue. In most areas of vascular disease endovascular therapy is easier. But, endovascular therapy for VAA can be as challenging as the open surgical repair because of vessel tortuosity and access, imaging challenges, and the few options available for durable aneurysm treatment. Dr. Shukla and colleagues reviewed their outcomes in treating VAA over a 10-year period and report high rates of technical success, low morbidity and mortality using endovascular means for both intact and ruptured VAA. The results for endovascular therapy for ruptured VAA were particularly promising. These results indicate that coils and other ablative maneuvers may suffice in the setting of hemorrhage and be preferable to open surgical repair or ligation. This study provides important information on a rare problem and reassures us that the mid-term durability of ablative techniques for VAA is acceptable.
Dr. Vikram Kashyap is professor of surgery, Case Western Reserve University and chief, Division of Vascular Surgery and Endovascular Therapy, and co-director, Harrington Heart & Vascular Institute, University Hospitals Case Medical Center,Cleveland.
BOSTON – Endovascular interventions for ruptured visceral artery aneurysms are associated with reduced morbidity and mortality, compared with open interventions, according to findings from a retrospective chart review.
Both endovascular and open repairs are safe and durable for intact visceral artery aneurysms, Dr. Ankur J. Shukla reported at a the 2014 Vascular Annual Meeting.
Of 261 patients who presented with visceral artery aneurysms (VAAs), 174 underwent repair: 74 who presented with ruptured VAA and 100 who presented with intact VAA. The majority – 73% of ruptured VAA and 62% of intact VAA – were repaired with an endovascular approach.
Among those with ruptured VAA, 30-day mortality was 7.4% following endovascular repair, compared with 28.6% following open repair, a significant difference, said Dr. Shukla of the University of Pittsburgh Medical Center.
Survival at 3 years of ruptured VAA was about 70% vs. 46.4% in the endovascular and open repair groups, respectively, he said.
About 65% of patients with ruptured VAA presented with pain, and about 30% presented in hemodynamic shock. The most commonly identified etiology was "inflammatory/pancreatitis inflammatory," and 80% of the aneurysms were pseudoaneurysmal in nature.
A large proportion of the aneurysms were in the splenic and arterial beds, but 26% were located in the pancreaticoduodenal arcade, and those had a mean size of 12.7 mm. Most (95%) were pseudoaneurysms.
The outcomes with ruptured VAA were quite good, Dr. Shukla said, noting that the technical success rate was 98.7%.
Although the 30-day reintervention rate with endovascular repair was higher, the difference between the groups was not statistically significant, and there was a trend toward a lower rate of major complications with endovascular repair.
Factors found to be predictors of mortality risk were older age and steroid use, while endovascular repair was found to be protective.
As for the patients with intact VAA, most presented without symptoms, and the most common etiology was atherosclerosis.
"When we looked at the distribution, this was very consistent with what has been reported in the literature, with the splenic and arterial beds really making up the lion’s share of this group. Notable is the fact that 6.7% of our patients had intact aneurysms in the pancreaticoduodenal arcade," he said.
Outcomes in those with intact aneurysms were good. A slightly higher 30-day reintervention rate in those who underwent endovascular repair did not reach statistical significance, and both the endovascular and open repair groups had low rates of major complications.
Survival at 3 years for intact aneurysms did not differ in the endovascular and open repair groups. This was partly due to a 0% 30-day mortality, and – despite the fact that the overall mortality in those with intact aneurysms was 10% – there was zero overall aneurysm-related mortality, he said.
Patients in the study were treated at a single institution between 2003 and 2013. Most were in their mid to late 50s, and there were more men and more individuals on immunosuppressive therapy in the ruptured VAA group. However, comorbidities were similar in the ruptured and intact VAA groups.
Visceral artery aneurysms occur only rarely, affecting 0.1% to 2% of the general population, but because of the increasing use of noninvasive imaging, more of these aneurysms are being detected incidentally.
When they are not found incidentally, they often go undetected and present when they rupture, Dr. Shukla said.
"Because of the increasing utilization and improvement of endovascular technology, we now have a lot of options to fix these aneurysms. But the outcomes are not well defined. Even less well defined is the outcome of ruptured visceral artery aneurysms," he said, noting that most studies have a small sample size or look only at endovascular or open repairs.
Overall, the current study showed that there is "an acute and sharp drop-off in survival with open repair," related, most likely, to operative mortality, he said.
"Based on the findings, we recommend aggressive treatment of pseudoaneurysms and true aneurysms in the pancreaticoduodenal arcade, and advocate for an endovascular-first approach to treating ruptured visceral artery aneurysms, acknowledging that success in this is really predicated on good planning based on advanced imaging and endovascular set-up," he concluded.
Dr. Shukla reported having no disclosures
BOSTON – Endovascular interventions for ruptured visceral artery aneurysms are associated with reduced morbidity and mortality, compared with open interventions, according to findings from a retrospective chart review.
Both endovascular and open repairs are safe and durable for intact visceral artery aneurysms, Dr. Ankur J. Shukla reported at a the 2014 Vascular Annual Meeting.
Of 261 patients who presented with visceral artery aneurysms (VAAs), 174 underwent repair: 74 who presented with ruptured VAA and 100 who presented with intact VAA. The majority – 73% of ruptured VAA and 62% of intact VAA – were repaired with an endovascular approach.
Among those with ruptured VAA, 30-day mortality was 7.4% following endovascular repair, compared with 28.6% following open repair, a significant difference, said Dr. Shukla of the University of Pittsburgh Medical Center.
Survival at 3 years of ruptured VAA was about 70% vs. 46.4% in the endovascular and open repair groups, respectively, he said.
About 65% of patients with ruptured VAA presented with pain, and about 30% presented in hemodynamic shock. The most commonly identified etiology was "inflammatory/pancreatitis inflammatory," and 80% of the aneurysms were pseudoaneurysmal in nature.
A large proportion of the aneurysms were in the splenic and arterial beds, but 26% were located in the pancreaticoduodenal arcade, and those had a mean size of 12.7 mm. Most (95%) were pseudoaneurysms.
The outcomes with ruptured VAA were quite good, Dr. Shukla said, noting that the technical success rate was 98.7%.
Although the 30-day reintervention rate with endovascular repair was higher, the difference between the groups was not statistically significant, and there was a trend toward a lower rate of major complications with endovascular repair.
Factors found to be predictors of mortality risk were older age and steroid use, while endovascular repair was found to be protective.
As for the patients with intact VAA, most presented without symptoms, and the most common etiology was atherosclerosis.
"When we looked at the distribution, this was very consistent with what has been reported in the literature, with the splenic and arterial beds really making up the lion’s share of this group. Notable is the fact that 6.7% of our patients had intact aneurysms in the pancreaticoduodenal arcade," he said.
Outcomes in those with intact aneurysms were good. A slightly higher 30-day reintervention rate in those who underwent endovascular repair did not reach statistical significance, and both the endovascular and open repair groups had low rates of major complications.
Survival at 3 years for intact aneurysms did not differ in the endovascular and open repair groups. This was partly due to a 0% 30-day mortality, and – despite the fact that the overall mortality in those with intact aneurysms was 10% – there was zero overall aneurysm-related mortality, he said.
Patients in the study were treated at a single institution between 2003 and 2013. Most were in their mid to late 50s, and there were more men and more individuals on immunosuppressive therapy in the ruptured VAA group. However, comorbidities were similar in the ruptured and intact VAA groups.
Visceral artery aneurysms occur only rarely, affecting 0.1% to 2% of the general population, but because of the increasing use of noninvasive imaging, more of these aneurysms are being detected incidentally.
When they are not found incidentally, they often go undetected and present when they rupture, Dr. Shukla said.
"Because of the increasing utilization and improvement of endovascular technology, we now have a lot of options to fix these aneurysms. But the outcomes are not well defined. Even less well defined is the outcome of ruptured visceral artery aneurysms," he said, noting that most studies have a small sample size or look only at endovascular or open repairs.
Overall, the current study showed that there is "an acute and sharp drop-off in survival with open repair," related, most likely, to operative mortality, he said.
"Based on the findings, we recommend aggressive treatment of pseudoaneurysms and true aneurysms in the pancreaticoduodenal arcade, and advocate for an endovascular-first approach to treating ruptured visceral artery aneurysms, acknowledging that success in this is really predicated on good planning based on advanced imaging and endovascular set-up," he concluded.
Dr. Shukla reported having no disclosures
AT THE 2014 VASCULAR ANNUAL MEETING
Key clinical point: The researchers recommend aggressive treatment of visceral artery pseudoaneurysms and true aneurysms, with an endovascular-first approach to treating ruptured aneurysms.
Major finding: Thirty-day mortality was 7.4% vs. 26% with endovascular vs. open repair of ruptured VAAs.
Data source: A retrospective chart review involving 174 cases.
Disclosures: Dr. Shukla reported having no disclosures.
Self-care for the weary
"Try and be nice to people, avoid eating fat, read a good book every now and then get some walking in, and try and live together in peace and harmony with people of all creeds and nations."
–Monty Python, "The Meaning of Life"
1. Set boundaries. This is arguably the most important aspect of the physician-patient relationship. A relationship like this is inherently fertile ground for such Freudian defenses as transference and projection. It’s important to recognize, too, that the process is not necessarily a one-way street. Freud was, after all, flawed like his subjects.
2. Don’t sweat the small stuff. This is self-evident, yet surprisingly difficult to remember.
3. Keep a journal. You’ll want to remember the good times, and keeping track of the bad times just shows you how far you’ve come.
4. Nourish your spirit – church, yoga, meditation. Take your pick. The best life advice I’ve ever received is that the mind needs structured space for quiet because otherwise you are never alone; there is always that voice in your head, constantly narrating your life and probably judging you for it.
5. There is a whole world outside of medicine. How easy is it to let our lives be consumed by our profession? How much happier would it make us to be reminded that music and literature and art exist? For my birthday this year, I asked my sister to give me a book that she thinks I should own.
6. Related to #5: Learn something outside of medicine. There are brilliant podcasts on science, the economy, politics. There are audio courses on great books or philosophy. Pick up a new instrument or a new language.
7. Indulge in the experiences that make you happy, whether that’s going to the beach, or eating out, throwing parties, or traveling. In the arguably dubious field of happiness research, studies show that spending money on experiences leads to happiness much more so than spending money on objects. (Of course, there may be a selection bias problem, in that it is entirely possible that people who are likely to buy experiences are happier at baseline than people who are likely to buy objects. But you get my meaning.)
8. Exercise. Run, take bike rides, walk your dog. Go for hikes. Take rowing lessons.
9. Sleep is crucial. We are not teenagers any longer, and it is a losing proposition to think that you can still get away with barely sleeping. If I get 8 hours of sleep, I am almost guaranteed to not be as grumpy at work. I feel refreshed, my mind is clearer, and I feel better equipped to deal with the challenges of the workday.
10. Forgive yourself – for the grumpiness, for mistakes, for bad outcomes that you could not possibly have done anything about.
11. Bonus: Mental health therapy, if done right, is a fantastic investment in yourself.
Dr. Chan practices rheumatology in Pawtucket, R.I.
"Try and be nice to people, avoid eating fat, read a good book every now and then get some walking in, and try and live together in peace and harmony with people of all creeds and nations."
–Monty Python, "The Meaning of Life"
1. Set boundaries. This is arguably the most important aspect of the physician-patient relationship. A relationship like this is inherently fertile ground for such Freudian defenses as transference and projection. It’s important to recognize, too, that the process is not necessarily a one-way street. Freud was, after all, flawed like his subjects.
2. Don’t sweat the small stuff. This is self-evident, yet surprisingly difficult to remember.
3. Keep a journal. You’ll want to remember the good times, and keeping track of the bad times just shows you how far you’ve come.
4. Nourish your spirit – church, yoga, meditation. Take your pick. The best life advice I’ve ever received is that the mind needs structured space for quiet because otherwise you are never alone; there is always that voice in your head, constantly narrating your life and probably judging you for it.
5. There is a whole world outside of medicine. How easy is it to let our lives be consumed by our profession? How much happier would it make us to be reminded that music and literature and art exist? For my birthday this year, I asked my sister to give me a book that she thinks I should own.
6. Related to #5: Learn something outside of medicine. There are brilliant podcasts on science, the economy, politics. There are audio courses on great books or philosophy. Pick up a new instrument or a new language.
7. Indulge in the experiences that make you happy, whether that’s going to the beach, or eating out, throwing parties, or traveling. In the arguably dubious field of happiness research, studies show that spending money on experiences leads to happiness much more so than spending money on objects. (Of course, there may be a selection bias problem, in that it is entirely possible that people who are likely to buy experiences are happier at baseline than people who are likely to buy objects. But you get my meaning.)
8. Exercise. Run, take bike rides, walk your dog. Go for hikes. Take rowing lessons.
9. Sleep is crucial. We are not teenagers any longer, and it is a losing proposition to think that you can still get away with barely sleeping. If I get 8 hours of sleep, I am almost guaranteed to not be as grumpy at work. I feel refreshed, my mind is clearer, and I feel better equipped to deal with the challenges of the workday.
10. Forgive yourself – for the grumpiness, for mistakes, for bad outcomes that you could not possibly have done anything about.
11. Bonus: Mental health therapy, if done right, is a fantastic investment in yourself.
Dr. Chan practices rheumatology in Pawtucket, R.I.
"Try and be nice to people, avoid eating fat, read a good book every now and then get some walking in, and try and live together in peace and harmony with people of all creeds and nations."
–Monty Python, "The Meaning of Life"
1. Set boundaries. This is arguably the most important aspect of the physician-patient relationship. A relationship like this is inherently fertile ground for such Freudian defenses as transference and projection. It’s important to recognize, too, that the process is not necessarily a one-way street. Freud was, after all, flawed like his subjects.
2. Don’t sweat the small stuff. This is self-evident, yet surprisingly difficult to remember.
3. Keep a journal. You’ll want to remember the good times, and keeping track of the bad times just shows you how far you’ve come.
4. Nourish your spirit – church, yoga, meditation. Take your pick. The best life advice I’ve ever received is that the mind needs structured space for quiet because otherwise you are never alone; there is always that voice in your head, constantly narrating your life and probably judging you for it.
5. There is a whole world outside of medicine. How easy is it to let our lives be consumed by our profession? How much happier would it make us to be reminded that music and literature and art exist? For my birthday this year, I asked my sister to give me a book that she thinks I should own.
6. Related to #5: Learn something outside of medicine. There are brilliant podcasts on science, the economy, politics. There are audio courses on great books or philosophy. Pick up a new instrument or a new language.
7. Indulge in the experiences that make you happy, whether that’s going to the beach, or eating out, throwing parties, or traveling. In the arguably dubious field of happiness research, studies show that spending money on experiences leads to happiness much more so than spending money on objects. (Of course, there may be a selection bias problem, in that it is entirely possible that people who are likely to buy experiences are happier at baseline than people who are likely to buy objects. But you get my meaning.)
8. Exercise. Run, take bike rides, walk your dog. Go for hikes. Take rowing lessons.
9. Sleep is crucial. We are not teenagers any longer, and it is a losing proposition to think that you can still get away with barely sleeping. If I get 8 hours of sleep, I am almost guaranteed to not be as grumpy at work. I feel refreshed, my mind is clearer, and I feel better equipped to deal with the challenges of the workday.
10. Forgive yourself – for the grumpiness, for mistakes, for bad outcomes that you could not possibly have done anything about.
11. Bonus: Mental health therapy, if done right, is a fantastic investment in yourself.
Dr. Chan practices rheumatology in Pawtucket, R.I.
Drugs can increase risk of MDS and AML

A class of immunosuppressive agents appear to increase the risk of acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) in patients with inflammatory bowel disease (IBD).
In an observational study of more than 19,000 IBD patients, past exposure to the agents—thiopurines—increased the risk of developing AML or MDS nearly 7-fold, when compared to the general population.
However, the absolute risk to an individual patient was about 1 in 10,000.
The researchers reported these results in Clinical Gastroenterology and Hepatology.
Thiopurines are an established treatment for IBD patients, but the drugs are also used to prevent rejection after a kidney transplant, to treat rheumatoid arthritis, as maintenance therapy for acute lymphocytic leukemia, and to induce remission in patients with AML.
Previous research showed that long-term use of thiopurines can increase a person’s risk of developing lymphoma.
“In order to make appropriate, informed decisions about thiopurines, patients and providers need to be well-educated about the risks and benefits of this treatment,” said study author Laurent Peyrin-Biroulet, MD, PhD, of the University Hospital of Nancy-Brabois in France.
“According to our research, the risk of myeloid disorders was not increased among the overall IBD population, compared with the general population. However, it was increased amongst those taking thiopurines. We hope these findings encourage other researchers to investigate more about the drug and its potentially harmful effects.”
The researchers analyzed 19,486 patients who were enrolled in the Cancers Et Surrisque Associé aux Maladies inflammatoires intestinales En France study from May 2004 through June 2005.
At study entry, 10,810 patients had never received thiopurines, 2810 patients had discontinued such drugs, and 5866 patients were still receiving them.
After 3 years of follow up, 5 patients were diagnosed with incident myeloid disorders—2 with AML and 3 with MDS. Four of these patients had been exposed to thiopurines—1 with ongoing treatment and 3 with past exposure.
The risk of myeloid disorders was not increased among the overall IBD population, compared with the general population. The standardized incidence ratio (SIR) was 1.80.
Similarly, the risk of myeloid disorders was not increased among IBD patients still receiving thiopurine treatment. The SIR was 1.54.
However, patients with prior exposure to thiopurines did have a significantly increased risk of myeloid disorders, with an SIR of 6.98.
The researchers noted that, although these findings provide evidence of a connection between thiopurines and myeloid disorders in IBD patients, the absolute risk to an individual patient was low.
So it seems the link between thiopurines and myeloid disorders remains complex. And physicians must balance the risk against the known benefits of thiopurines in the management of IBD.
The American Gastroenterological Association has developed a guideline-based clinical decision support tool to help providers determine when to use thiopurines in these patients. ![]()

A class of immunosuppressive agents appear to increase the risk of acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) in patients with inflammatory bowel disease (IBD).
In an observational study of more than 19,000 IBD patients, past exposure to the agents—thiopurines—increased the risk of developing AML or MDS nearly 7-fold, when compared to the general population.
However, the absolute risk to an individual patient was about 1 in 10,000.
The researchers reported these results in Clinical Gastroenterology and Hepatology.
Thiopurines are an established treatment for IBD patients, but the drugs are also used to prevent rejection after a kidney transplant, to treat rheumatoid arthritis, as maintenance therapy for acute lymphocytic leukemia, and to induce remission in patients with AML.
Previous research showed that long-term use of thiopurines can increase a person’s risk of developing lymphoma.
“In order to make appropriate, informed decisions about thiopurines, patients and providers need to be well-educated about the risks and benefits of this treatment,” said study author Laurent Peyrin-Biroulet, MD, PhD, of the University Hospital of Nancy-Brabois in France.
“According to our research, the risk of myeloid disorders was not increased among the overall IBD population, compared with the general population. However, it was increased amongst those taking thiopurines. We hope these findings encourage other researchers to investigate more about the drug and its potentially harmful effects.”
The researchers analyzed 19,486 patients who were enrolled in the Cancers Et Surrisque Associé aux Maladies inflammatoires intestinales En France study from May 2004 through June 2005.
At study entry, 10,810 patients had never received thiopurines, 2810 patients had discontinued such drugs, and 5866 patients were still receiving them.
After 3 years of follow up, 5 patients were diagnosed with incident myeloid disorders—2 with AML and 3 with MDS. Four of these patients had been exposed to thiopurines—1 with ongoing treatment and 3 with past exposure.
The risk of myeloid disorders was not increased among the overall IBD population, compared with the general population. The standardized incidence ratio (SIR) was 1.80.
Similarly, the risk of myeloid disorders was not increased among IBD patients still receiving thiopurine treatment. The SIR was 1.54.
However, patients with prior exposure to thiopurines did have a significantly increased risk of myeloid disorders, with an SIR of 6.98.
The researchers noted that, although these findings provide evidence of a connection between thiopurines and myeloid disorders in IBD patients, the absolute risk to an individual patient was low.
So it seems the link between thiopurines and myeloid disorders remains complex. And physicians must balance the risk against the known benefits of thiopurines in the management of IBD.
The American Gastroenterological Association has developed a guideline-based clinical decision support tool to help providers determine when to use thiopurines in these patients. ![]()

A class of immunosuppressive agents appear to increase the risk of acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) in patients with inflammatory bowel disease (IBD).
In an observational study of more than 19,000 IBD patients, past exposure to the agents—thiopurines—increased the risk of developing AML or MDS nearly 7-fold, when compared to the general population.
However, the absolute risk to an individual patient was about 1 in 10,000.
The researchers reported these results in Clinical Gastroenterology and Hepatology.
Thiopurines are an established treatment for IBD patients, but the drugs are also used to prevent rejection after a kidney transplant, to treat rheumatoid arthritis, as maintenance therapy for acute lymphocytic leukemia, and to induce remission in patients with AML.
Previous research showed that long-term use of thiopurines can increase a person’s risk of developing lymphoma.
“In order to make appropriate, informed decisions about thiopurines, patients and providers need to be well-educated about the risks and benefits of this treatment,” said study author Laurent Peyrin-Biroulet, MD, PhD, of the University Hospital of Nancy-Brabois in France.
“According to our research, the risk of myeloid disorders was not increased among the overall IBD population, compared with the general population. However, it was increased amongst those taking thiopurines. We hope these findings encourage other researchers to investigate more about the drug and its potentially harmful effects.”
The researchers analyzed 19,486 patients who were enrolled in the Cancers Et Surrisque Associé aux Maladies inflammatoires intestinales En France study from May 2004 through June 2005.
At study entry, 10,810 patients had never received thiopurines, 2810 patients had discontinued such drugs, and 5866 patients were still receiving them.
After 3 years of follow up, 5 patients were diagnosed with incident myeloid disorders—2 with AML and 3 with MDS. Four of these patients had been exposed to thiopurines—1 with ongoing treatment and 3 with past exposure.
The risk of myeloid disorders was not increased among the overall IBD population, compared with the general population. The standardized incidence ratio (SIR) was 1.80.
Similarly, the risk of myeloid disorders was not increased among IBD patients still receiving thiopurine treatment. The SIR was 1.54.
However, patients with prior exposure to thiopurines did have a significantly increased risk of myeloid disorders, with an SIR of 6.98.
The researchers noted that, although these findings provide evidence of a connection between thiopurines and myeloid disorders in IBD patients, the absolute risk to an individual patient was low.
So it seems the link between thiopurines and myeloid disorders remains complex. And physicians must balance the risk against the known benefits of thiopurines in the management of IBD.
The American Gastroenterological Association has developed a guideline-based clinical decision support tool to help providers determine when to use thiopurines in these patients. ![]()