User login
Early career considerations for gastroenterologists interested in diversity, equity, and inclusion roles

Highlighting the importance of DEI across all aspects of medicine is long overdue, and the field of gastroenterology is no exception. Diversity in the gastroenterology workforce still has significant room for improvement with only 12% of all gastroenterology fellows in 2018 identifying as Black, Latino/a/x, American Indian or Alaskan Native, or Native Hawaiian or Pacific Islander.1 Moreover, only 4.4% of practicing gastroenterologists identify as Black, 6.7% identify as Latino/a/x, 0.1% as American Indian or Alaskan Native, and 0.003% as Native Hawaiian or Pacific Islander.2
The intensified focus on diversity in GI is welcomed, but increasing physician workforce diversity is only one of the necessary steps. If our ultimate goal is to improve health outcomes and achieve health equity for historically marginalized racial, ethnic, and socioeconomically disadvantaged communities, we must critically evaluate the path beyond just enhancing workforce diversity.
Black and Latino/a/x physicians are more likely to care for historically marginalized communities,3 which has been shown to improve all-cause mortality and reduce racial disparities.4 Additionally, diverse work teams are more innovative and productive.5 Therefore, expanding diversity must include 1) providing equitable policies and access to opportunities and promotions; 2) building inclusive environments in our institutions and practices; and 3) providing space for all people to feel like they can belong, feel respected at work, and genuinely have their opinions and ideas valued. What diversity, equity, inclusion, and belonging provide for us and our patients are avenues to thrive, solve complex problems, and tackle prominent issues within our institutions, workplaces, and communities.
To this end, many academic centers, hospitals, and private practice entities have produced a flurry of new DEI initiatives coupled with titles and roles. Some of these roles have thankfully brought recognition and economic compensation to the people doing this work. Still, as an early career gastroenterologist, you may be offered or are considering taking on a DEI role during your early career. As two underrepresented minority women in medicine who took on DEI roles with their first jobs, we wanted to highlight a few aspects to think about during your early career:
Does the DEI role come with resources?
Historically, DEI efforts were treated as “extra work,” or an activity that was done using one’s own personal time. In addition, this work called upon the small number of physicians underrepresented in medicine, largely uncompensated and with an exorbitant minority tax during a critical moment in establishing their early careers. DEI should no longer be seen as an extracurricular activity but as a vital component of an institution’s success.
If you are considering a DEI role, the first question to ask is, “Does this role come with extra compensation or protected time?” We highly recommend not taking on the role if the answer is no. If your institution or employer is only offering increased minority tax, you are being set up to either fail, burn out, or both. Your employer or institution does not appear to value your time or effort in DEI, and you should interpret their lack of compensation or protected time as such.
If the answer is yes, then here are a few other things to consider: Is there institutional support for you to be successful in your new role? As DEI work challenges you to come up with solutions to combat years of historic marginalization for racial and ethnic minorities, this work can sometimes feel overwhelming and isolating. The importance of the DEI community and mentorship within and outside your institution is critical. You should consider joining DEI working groups or committees through GI national societies, the Association of American Medical Colleges, or the Accreditation Council for Graduate Medical Education. You can also connect with a fantastic network of people engaged in this work via social media and lean on friends and colleagues leading similar initiatives across the country.
Other critical logistical questions are if your role will come with administrative support, whether there is a budget for programs or events, and whether your institution/employer will support you in seeking continued professional development for your DEI role.6
Make sure to understand the “ask” from your division, department, or company.
Before confirming you are willing to take on this role, get a clear vision of what you are being asked to accomplish. There are so many opportunities to improve the DEI landscape. Therefore, knowing what you are specifically being asked to do will be critical to your success.
Are you being asked to work on diversity?
Does your institution want you to focus on and improve the recruitment and retention of trainees, physicians, or staff underrepresented in medicine? If so, you will need to have access to all the prior work and statistics. Capture the landscape before your interventions (% underrepresented in medicine [URiM] trainees, % URiM faculty at each level, % of URiM trainees retained as faculty, % of URiM faculty being promoted each year, etc.) This will allow you to determine the outcomes of your proposed improvements or programs.
Is your employer focused on equity?
Are you being asked to think about ways to operationalize improved patient health equity, or are you being asked to build equitable opportunities/programs for career advancement for URiMs at your institution? For either equity issue, you first need to understand the scope of the problem to ask for the necessary resources for a potential solution. Discuss timeline expectations, as equity work is a marathon and may take years to move the needle on any particular issue. This timeline is also critical for your employer to be aware of and support, as unrealistic timelines and expectations will also set you up for failure.
Or, are you being asked to concentrate on inclusion?
Does your institution need an assessment of how inclusive the climate is for trainees, staff, or physicians? Does this assessment align with your division or department’s impression, and how do you plan to work toward potential solutions for improvement?
Although diversity, equity, and inclusion are interconnected entities, they all have distinct objectives and solutions. It is essential to understand your vision and your employer’s vision for this role. If they are not aligned, having early and in-depth conversations about aligning your visions will set you on a path to success in your early career.
Know your why or more importantly, your who?
Early career physicians who are considering taking on DEI work do so for a reason. Being passionate about this type of work is usually born from a personal experience or your deep-rooted values. For us, experiencing and witnessing health disparities for our family members and people who look like us are what initially fueled our passion for this work. Additional experiences with trainees and patients keep us invigorated to continue highlighting the importance of DEI and encourage others to be passionate about DEI’s huge value added. As DEI work can come with challenges, remembering and re-centering on why you are passionate about this work or who you are engaging in this work for can keep you going.
There are several aspects to consider before taking on a DEI role, but overall, the work is rewarding and can be a great addition to the building blocks of your early career. In the short term, you build a DEI community network of peers, mentors, colleagues, and friends beyond your immediate institution and specialty. You also can demonstrate your leadership skills and potential early on in your career. In the long-term, engaging in these types of roles helps build a climate and culture that is conducive to enacting change for our patients and communities, including advancing healthcare equity and working toward recruitment, retention, and expansion efforts for our trainees and faculty. Overall, we think this type of work in your early career can be an integral part of your personal and professional development, while also having an impact that ripples beyond the walls of the endoscopy suite.
Dr. Fritz is an assistant professor of medicine in the division of gastroenterology at Washington University School of Medicine, St. Louis. Dr. Rodriguez is a gastroenterologist with Brigham and Women’s Hospital in Boston. Neither Dr. Rodriguez nor Dr. Fritz disclosed no conflicts of interest.
References
1. Santhosh L,Babik JM. Trends in racial and ethnic diversity in internal medicine subspecialty fellowships from 2006 to 2018. JAMA Network Open 2020;3:e1920482-e1920482.
2. Colleges AoAM. Physician Specialty Data Report/Active physicians who identified as Black or African-American, 2021. 2022.
3. Komaromy M et al. The role of black and Hispanic physicians in providing health care for underserved populations. New England Journal of Medicine 1996;334:1305-10.
4. Snyder JE et al. Black representation in the primary care physician workforce and its association with population life expectancy and mortality rates in the US. JAMA Network Open 2023;6:e236687-e236687.
5. Page S. Diversity bonuses and the business case. The Diversity Bonus: Princeton University Press, 2017:184-208.
6. Vela MB et al. Diversity, equity, and inclusion officer position available: Proceed with caution. Journal of Graduate Medical Education 2021;13:771-3.
Helpful resources
Diversity and Inclusion Toolkit Resources, AAMC
Blackinggastro.org, The Association of Black Gastroenterologists and Hepatologists (ABGH)
Podcast: Clinical Problem Solvers: Anti-Racism in Medicine

Highlighting the importance of DEI across all aspects of medicine is long overdue, and the field of gastroenterology is no exception. Diversity in the gastroenterology workforce still has significant room for improvement with only 12% of all gastroenterology fellows in 2018 identifying as Black, Latino/a/x, American Indian or Alaskan Native, or Native Hawaiian or Pacific Islander.1 Moreover, only 4.4% of practicing gastroenterologists identify as Black, 6.7% identify as Latino/a/x, 0.1% as American Indian or Alaskan Native, and 0.003% as Native Hawaiian or Pacific Islander.2
The intensified focus on diversity in GI is welcomed, but increasing physician workforce diversity is only one of the necessary steps. If our ultimate goal is to improve health outcomes and achieve health equity for historically marginalized racial, ethnic, and socioeconomically disadvantaged communities, we must critically evaluate the path beyond just enhancing workforce diversity.
Black and Latino/a/x physicians are more likely to care for historically marginalized communities,3 which has been shown to improve all-cause mortality and reduce racial disparities.4 Additionally, diverse work teams are more innovative and productive.5 Therefore, expanding diversity must include 1) providing equitable policies and access to opportunities and promotions; 2) building inclusive environments in our institutions and practices; and 3) providing space for all people to feel like they can belong, feel respected at work, and genuinely have their opinions and ideas valued. What diversity, equity, inclusion, and belonging provide for us and our patients are avenues to thrive, solve complex problems, and tackle prominent issues within our institutions, workplaces, and communities.
To this end, many academic centers, hospitals, and private practice entities have produced a flurry of new DEI initiatives coupled with titles and roles. Some of these roles have thankfully brought recognition and economic compensation to the people doing this work. Still, as an early career gastroenterologist, you may be offered or are considering taking on a DEI role during your early career. As two underrepresented minority women in medicine who took on DEI roles with their first jobs, we wanted to highlight a few aspects to think about during your early career:
Does the DEI role come with resources?
Historically, DEI efforts were treated as “extra work,” or an activity that was done using one’s own personal time. In addition, this work called upon the small number of physicians underrepresented in medicine, largely uncompensated and with an exorbitant minority tax during a critical moment in establishing their early careers. DEI should no longer be seen as an extracurricular activity but as a vital component of an institution’s success.
If you are considering a DEI role, the first question to ask is, “Does this role come with extra compensation or protected time?” We highly recommend not taking on the role if the answer is no. If your institution or employer is only offering increased minority tax, you are being set up to either fail, burn out, or both. Your employer or institution does not appear to value your time or effort in DEI, and you should interpret their lack of compensation or protected time as such.
If the answer is yes, then here are a few other things to consider: Is there institutional support for you to be successful in your new role? As DEI work challenges you to come up with solutions to combat years of historic marginalization for racial and ethnic minorities, this work can sometimes feel overwhelming and isolating. The importance of the DEI community and mentorship within and outside your institution is critical. You should consider joining DEI working groups or committees through GI national societies, the Association of American Medical Colleges, or the Accreditation Council for Graduate Medical Education. You can also connect with a fantastic network of people engaged in this work via social media and lean on friends and colleagues leading similar initiatives across the country.
Other critical logistical questions are if your role will come with administrative support, whether there is a budget for programs or events, and whether your institution/employer will support you in seeking continued professional development for your DEI role.6
Make sure to understand the “ask” from your division, department, or company.
Before confirming you are willing to take on this role, get a clear vision of what you are being asked to accomplish. There are so many opportunities to improve the DEI landscape. Therefore, knowing what you are specifically being asked to do will be critical to your success.
Are you being asked to work on diversity?
Does your institution want you to focus on and improve the recruitment and retention of trainees, physicians, or staff underrepresented in medicine? If so, you will need to have access to all the prior work and statistics. Capture the landscape before your interventions (% underrepresented in medicine [URiM] trainees, % URiM faculty at each level, % of URiM trainees retained as faculty, % of URiM faculty being promoted each year, etc.) This will allow you to determine the outcomes of your proposed improvements or programs.
Is your employer focused on equity?
Are you being asked to think about ways to operationalize improved patient health equity, or are you being asked to build equitable opportunities/programs for career advancement for URiMs at your institution? For either equity issue, you first need to understand the scope of the problem to ask for the necessary resources for a potential solution. Discuss timeline expectations, as equity work is a marathon and may take years to move the needle on any particular issue. This timeline is also critical for your employer to be aware of and support, as unrealistic timelines and expectations will also set you up for failure.
Or, are you being asked to concentrate on inclusion?
Does your institution need an assessment of how inclusive the climate is for trainees, staff, or physicians? Does this assessment align with your division or department’s impression, and how do you plan to work toward potential solutions for improvement?
Although diversity, equity, and inclusion are interconnected entities, they all have distinct objectives and solutions. It is essential to understand your vision and your employer’s vision for this role. If they are not aligned, having early and in-depth conversations about aligning your visions will set you on a path to success in your early career.
Know your why or more importantly, your who?
Early career physicians who are considering taking on DEI work do so for a reason. Being passionate about this type of work is usually born from a personal experience or your deep-rooted values. For us, experiencing and witnessing health disparities for our family members and people who look like us are what initially fueled our passion for this work. Additional experiences with trainees and patients keep us invigorated to continue highlighting the importance of DEI and encourage others to be passionate about DEI’s huge value added. As DEI work can come with challenges, remembering and re-centering on why you are passionate about this work or who you are engaging in this work for can keep you going.
There are several aspects to consider before taking on a DEI role, but overall, the work is rewarding and can be a great addition to the building blocks of your early career. In the short term, you build a DEI community network of peers, mentors, colleagues, and friends beyond your immediate institution and specialty. You also can demonstrate your leadership skills and potential early on in your career. In the long-term, engaging in these types of roles helps build a climate and culture that is conducive to enacting change for our patients and communities, including advancing healthcare equity and working toward recruitment, retention, and expansion efforts for our trainees and faculty. Overall, we think this type of work in your early career can be an integral part of your personal and professional development, while also having an impact that ripples beyond the walls of the endoscopy suite.
Dr. Fritz is an assistant professor of medicine in the division of gastroenterology at Washington University School of Medicine, St. Louis. Dr. Rodriguez is a gastroenterologist with Brigham and Women’s Hospital in Boston. Neither Dr. Rodriguez nor Dr. Fritz disclosed no conflicts of interest.
References
1. Santhosh L,Babik JM. Trends in racial and ethnic diversity in internal medicine subspecialty fellowships from 2006 to 2018. JAMA Network Open 2020;3:e1920482-e1920482.
2. Colleges AoAM. Physician Specialty Data Report/Active physicians who identified as Black or African-American, 2021. 2022.
3. Komaromy M et al. The role of black and Hispanic physicians in providing health care for underserved populations. New England Journal of Medicine 1996;334:1305-10.
4. Snyder JE et al. Black representation in the primary care physician workforce and its association with population life expectancy and mortality rates in the US. JAMA Network Open 2023;6:e236687-e236687.
5. Page S. Diversity bonuses and the business case. The Diversity Bonus: Princeton University Press, 2017:184-208.
6. Vela MB et al. Diversity, equity, and inclusion officer position available: Proceed with caution. Journal of Graduate Medical Education 2021;13:771-3.
Helpful resources
Diversity and Inclusion Toolkit Resources, AAMC
Blackinggastro.org, The Association of Black Gastroenterologists and Hepatologists (ABGH)
Podcast: Clinical Problem Solvers: Anti-Racism in Medicine

Highlighting the importance of DEI across all aspects of medicine is long overdue, and the field of gastroenterology is no exception. Diversity in the gastroenterology workforce still has significant room for improvement with only 12% of all gastroenterology fellows in 2018 identifying as Black, Latino/a/x, American Indian or Alaskan Native, or Native Hawaiian or Pacific Islander.1 Moreover, only 4.4% of practicing gastroenterologists identify as Black, 6.7% identify as Latino/a/x, 0.1% as American Indian or Alaskan Native, and 0.003% as Native Hawaiian or Pacific Islander.2
The intensified focus on diversity in GI is welcomed, but increasing physician workforce diversity is only one of the necessary steps. If our ultimate goal is to improve health outcomes and achieve health equity for historically marginalized racial, ethnic, and socioeconomically disadvantaged communities, we must critically evaluate the path beyond just enhancing workforce diversity.
Black and Latino/a/x physicians are more likely to care for historically marginalized communities,3 which has been shown to improve all-cause mortality and reduce racial disparities.4 Additionally, diverse work teams are more innovative and productive.5 Therefore, expanding diversity must include 1) providing equitable policies and access to opportunities and promotions; 2) building inclusive environments in our institutions and practices; and 3) providing space for all people to feel like they can belong, feel respected at work, and genuinely have their opinions and ideas valued. What diversity, equity, inclusion, and belonging provide for us and our patients are avenues to thrive, solve complex problems, and tackle prominent issues within our institutions, workplaces, and communities.
To this end, many academic centers, hospitals, and private practice entities have produced a flurry of new DEI initiatives coupled with titles and roles. Some of these roles have thankfully brought recognition and economic compensation to the people doing this work. Still, as an early career gastroenterologist, you may be offered or are considering taking on a DEI role during your early career. As two underrepresented minority women in medicine who took on DEI roles with their first jobs, we wanted to highlight a few aspects to think about during your early career:
Does the DEI role come with resources?
Historically, DEI efforts were treated as “extra work,” or an activity that was done using one’s own personal time. In addition, this work called upon the small number of physicians underrepresented in medicine, largely uncompensated and with an exorbitant minority tax during a critical moment in establishing their early careers. DEI should no longer be seen as an extracurricular activity but as a vital component of an institution’s success.
If you are considering a DEI role, the first question to ask is, “Does this role come with extra compensation or protected time?” We highly recommend not taking on the role if the answer is no. If your institution or employer is only offering increased minority tax, you are being set up to either fail, burn out, or both. Your employer or institution does not appear to value your time or effort in DEI, and you should interpret their lack of compensation or protected time as such.
If the answer is yes, then here are a few other things to consider: Is there institutional support for you to be successful in your new role? As DEI work challenges you to come up with solutions to combat years of historic marginalization for racial and ethnic minorities, this work can sometimes feel overwhelming and isolating. The importance of the DEI community and mentorship within and outside your institution is critical. You should consider joining DEI working groups or committees through GI national societies, the Association of American Medical Colleges, or the Accreditation Council for Graduate Medical Education. You can also connect with a fantastic network of people engaged in this work via social media and lean on friends and colleagues leading similar initiatives across the country.
Other critical logistical questions are if your role will come with administrative support, whether there is a budget for programs or events, and whether your institution/employer will support you in seeking continued professional development for your DEI role.6
Make sure to understand the “ask” from your division, department, or company.
Before confirming you are willing to take on this role, get a clear vision of what you are being asked to accomplish. There are so many opportunities to improve the DEI landscape. Therefore, knowing what you are specifically being asked to do will be critical to your success.
Are you being asked to work on diversity?
Does your institution want you to focus on and improve the recruitment and retention of trainees, physicians, or staff underrepresented in medicine? If so, you will need to have access to all the prior work and statistics. Capture the landscape before your interventions (% underrepresented in medicine [URiM] trainees, % URiM faculty at each level, % of URiM trainees retained as faculty, % of URiM faculty being promoted each year, etc.) This will allow you to determine the outcomes of your proposed improvements or programs.
Is your employer focused on equity?
Are you being asked to think about ways to operationalize improved patient health equity, or are you being asked to build equitable opportunities/programs for career advancement for URiMs at your institution? For either equity issue, you first need to understand the scope of the problem to ask for the necessary resources for a potential solution. Discuss timeline expectations, as equity work is a marathon and may take years to move the needle on any particular issue. This timeline is also critical for your employer to be aware of and support, as unrealistic timelines and expectations will also set you up for failure.
Or, are you being asked to concentrate on inclusion?
Does your institution need an assessment of how inclusive the climate is for trainees, staff, or physicians? Does this assessment align with your division or department’s impression, and how do you plan to work toward potential solutions for improvement?
Although diversity, equity, and inclusion are interconnected entities, they all have distinct objectives and solutions. It is essential to understand your vision and your employer’s vision for this role. If they are not aligned, having early and in-depth conversations about aligning your visions will set you on a path to success in your early career.
Know your why or more importantly, your who?
Early career physicians who are considering taking on DEI work do so for a reason. Being passionate about this type of work is usually born from a personal experience or your deep-rooted values. For us, experiencing and witnessing health disparities for our family members and people who look like us are what initially fueled our passion for this work. Additional experiences with trainees and patients keep us invigorated to continue highlighting the importance of DEI and encourage others to be passionate about DEI’s huge value added. As DEI work can come with challenges, remembering and re-centering on why you are passionate about this work or who you are engaging in this work for can keep you going.
There are several aspects to consider before taking on a DEI role, but overall, the work is rewarding and can be a great addition to the building blocks of your early career. In the short term, you build a DEI community network of peers, mentors, colleagues, and friends beyond your immediate institution and specialty. You also can demonstrate your leadership skills and potential early on in your career. In the long-term, engaging in these types of roles helps build a climate and culture that is conducive to enacting change for our patients and communities, including advancing healthcare equity and working toward recruitment, retention, and expansion efforts for our trainees and faculty. Overall, we think this type of work in your early career can be an integral part of your personal and professional development, while also having an impact that ripples beyond the walls of the endoscopy suite.
Dr. Fritz is an assistant professor of medicine in the division of gastroenterology at Washington University School of Medicine, St. Louis. Dr. Rodriguez is a gastroenterologist with Brigham and Women’s Hospital in Boston. Neither Dr. Rodriguez nor Dr. Fritz disclosed no conflicts of interest.
References
1. Santhosh L,Babik JM. Trends in racial and ethnic diversity in internal medicine subspecialty fellowships from 2006 to 2018. JAMA Network Open 2020;3:e1920482-e1920482.
2. Colleges AoAM. Physician Specialty Data Report/Active physicians who identified as Black or African-American, 2021. 2022.
3. Komaromy M et al. The role of black and Hispanic physicians in providing health care for underserved populations. New England Journal of Medicine 1996;334:1305-10.
4. Snyder JE et al. Black representation in the primary care physician workforce and its association with population life expectancy and mortality rates in the US. JAMA Network Open 2023;6:e236687-e236687.
5. Page S. Diversity bonuses and the business case. The Diversity Bonus: Princeton University Press, 2017:184-208.
6. Vela MB et al. Diversity, equity, and inclusion officer position available: Proceed with caution. Journal of Graduate Medical Education 2021;13:771-3.
Helpful resources
Diversity and Inclusion Toolkit Resources, AAMC
Blackinggastro.org, The Association of Black Gastroenterologists and Hepatologists (ABGH)
Podcast: Clinical Problem Solvers: Anti-Racism in Medicine
Selecting therapies in moderate to severe inflammatory bowel disease: Key factors in decision making
Despite new advances in treatment, head to head clinical trials, which are considered the gold standard when comparing therapies, remain limited. Other comparative effectiveness studies and network meta-analyses are the currently available substitutes to guide decision making.1
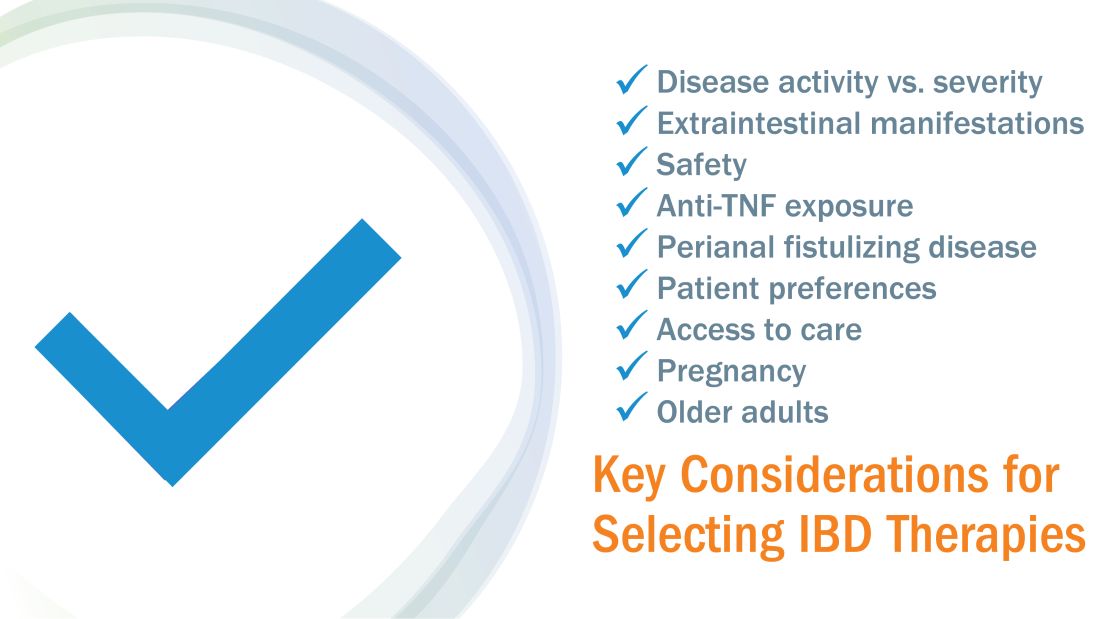
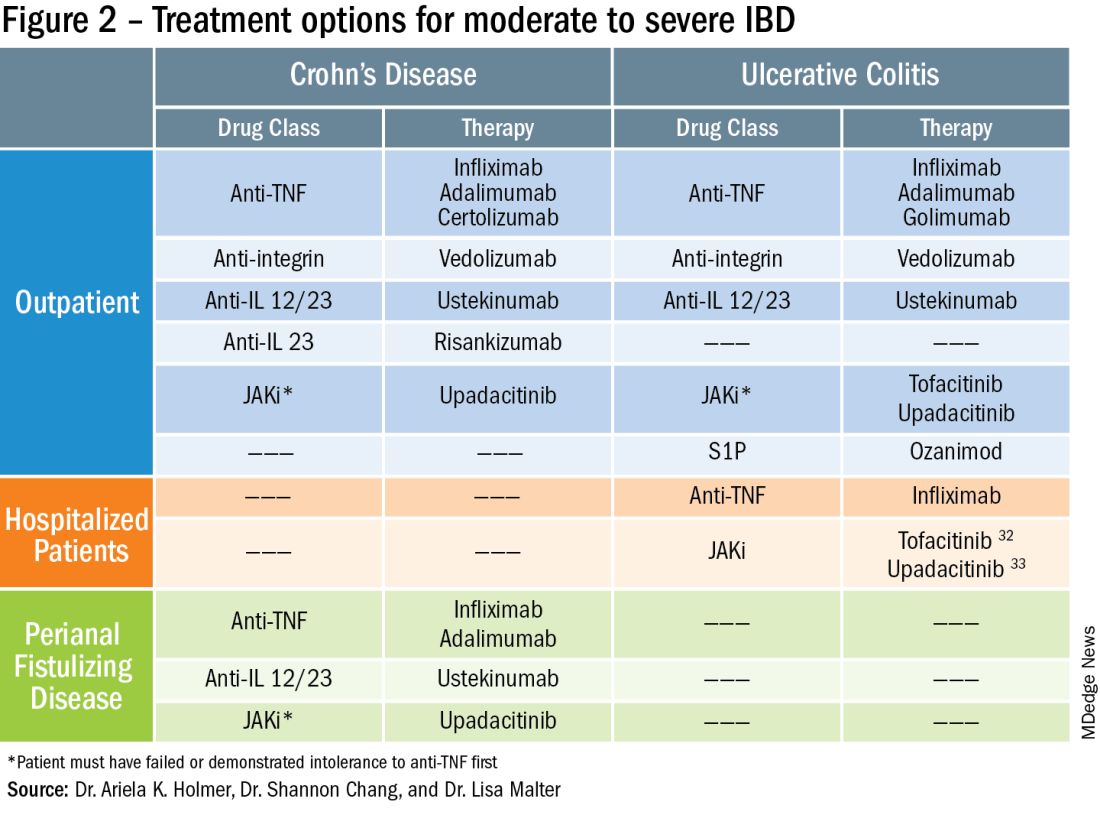
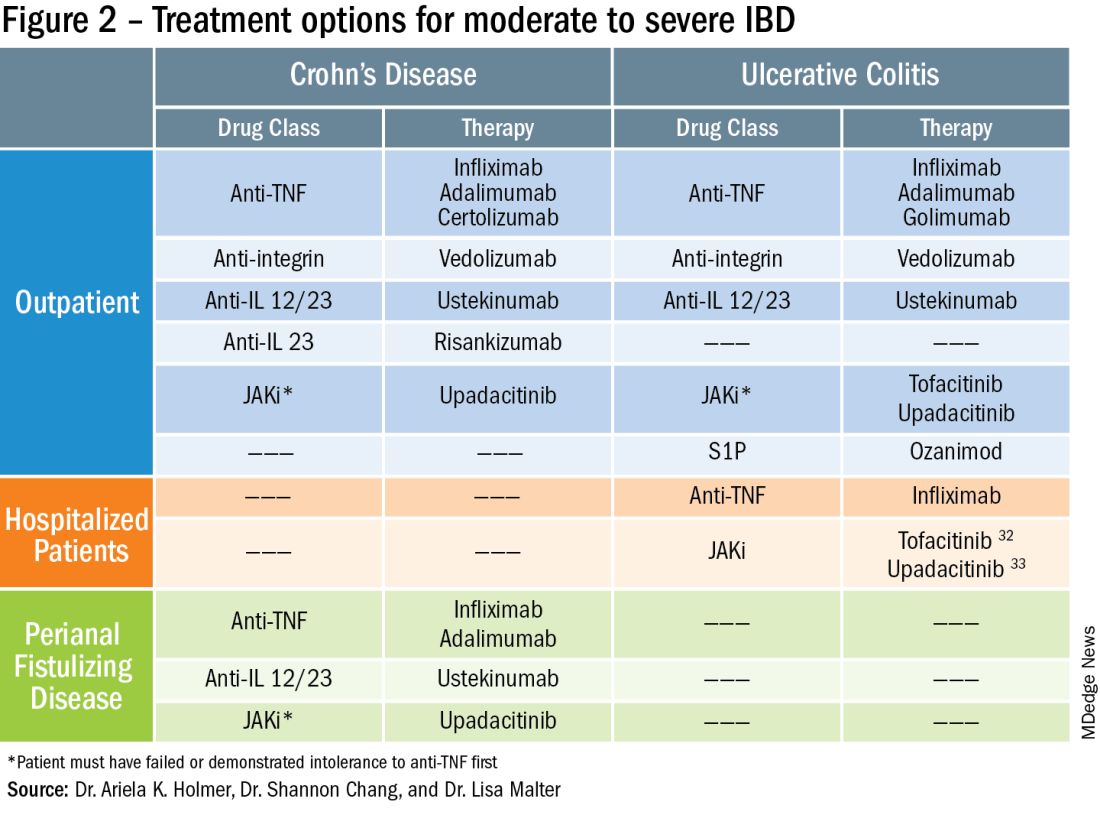
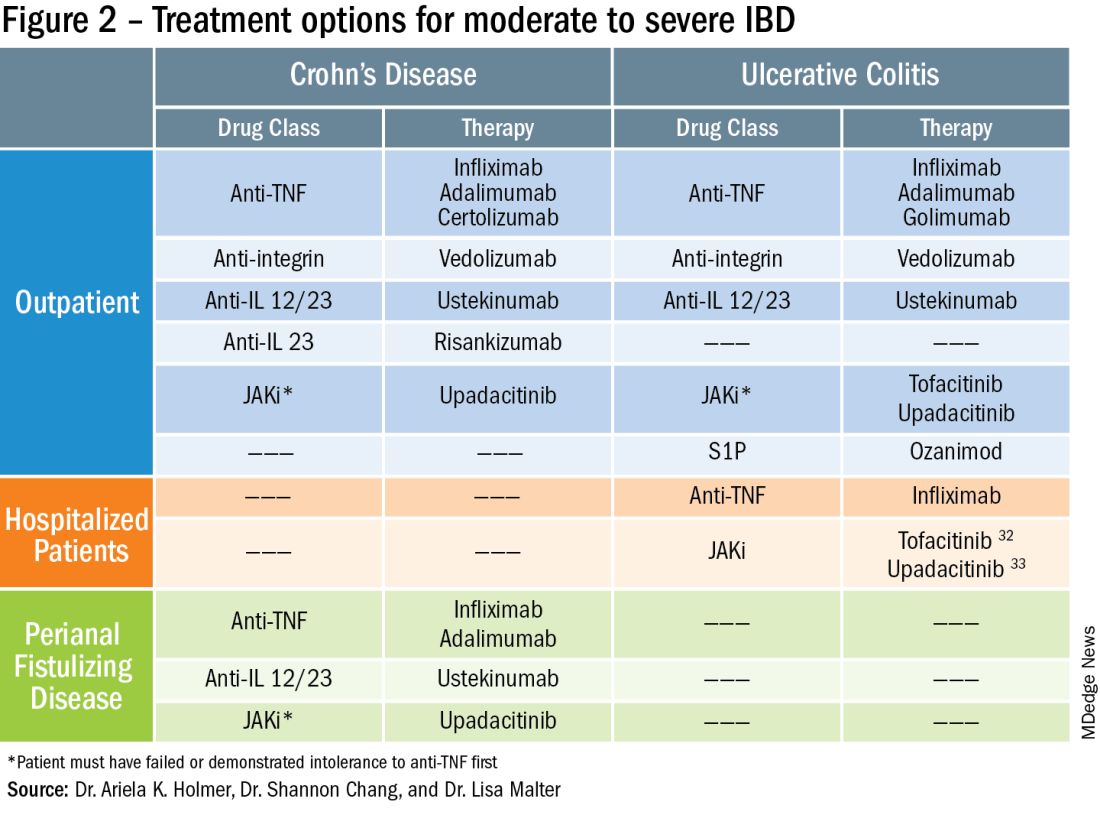
While efficacy is often considered first when choosing a drug, other critical factors play a role in tailoring a treatment plan. This article focuses on key considerations to help guide clinical decision making when treating patients with moderate to severe IBD (Figure 1).
Disease activity versus severity
Both disease activity and disease severity should be considered when evaluating a patient for treatment. Disease activity is a cross-sectional view of one’s signs and symptoms which can vary visit to visit. Standardized indices measure disease activity in both Crohn’s disease (CD) and ulcerative colitis (UC).2,3 Disease severity encompasses the overall prognosis of disease over time and includes factors such as the presence or absence of high risk features, prior medication exposure, history of surgery, hospitalizations and the impact on quality of life.4
To prevent disease complications, the goals of treatment should be aimed at both reducing active symptoms (disease activity) but also healing mucosal inflammation, preventing disease progression (disease severity) and downstream sequelae including cancer, hospitalization or surgery.5 Determining the best treatment option takes disease activity and severity into account, in addition to the other key factors listed below (Figure 2).
Extraintestinal manifestations
Inflammation of organs outside of the gastrointestinal tract is common and can occur in up to 50% of patients with IBD.6 The most prevalent extraintestinal manifestations (EIMs) involve the skin and joints, which will be the primary focus in this article. We will also focus on treatment options with the most evidence supporting their use. Peripheral arthritis is often associated with intestinal inflammation, and treatment of underlying IBD can simultaneously improve joint symptoms. Conversely, axial spondyloarthritis does not commonly parallel intestinal inflammation. Anti–tumor necrosis factor (TNF) agents including infliximab and adalimumab are effective for the treatment of both peripheral and axial disease.6
Ustekinumab, an interleukin (IL)-12/23 inhibitor, may be effective for peripheral arthritis, however is ineffective for the treatment of axial spondyloarthritis.6 Janus kinase (JAK) inhibitors which include tofacitinib and upadacitinib are oral small molecules used to treat peripheral and axial spondyloarthritis and have more recently been approved for moderate to severe IBD.6,7
Erythema nodosum (EN) and pyoderma gangrenosum (PG) are skin manifestations seen in patients with IBD. EN appears as subcutaneous nodules and parallels intestinal inflammation, while PG consists of violaceous, ulcerated plaques, and presents with more significant pain. Anti-TNFs are effective for both EN and PG, with infliximab being the only biologic studied in a randomized control trial of patients with PG.8 In addition, small case reports have described some benefit from ustekinumab and upadacitinib in the treatment of PG.9,10
Safety
The safety of IBD therapies is a key consideration and often the most important factor to patients when choosing a treatment option. It is important to note that untreated disease is associated with significant morbidity, and should be weighed when discussing risks of medications with patients. In general, anti-TNFs and JAK inhibitors may be associated with an increased risk of infection and malignancy, while ustekinumab, vedolizumab, risankizumab and ozanimod offer a more favorable safety profile.11 In large registries and observational studies, infliximab was associated with up to a two times greater risk of serious infection as compared to nonbiologic medications, with the most common infections being pneumonia, sepsis and herpes zoster.12 JAK inhibitors are associated with an increased risk of herpes zoster infection, with a dose dependent effect seen in the maintenance clinical trials with tofacitinib.7
Ozanimod may be associated with atrioventricular conduction delays and bradycardia, however long-term safety data has reported a low incidence of serious cardiac related adverse events.13 Overall, though risks of infection may vary with different therapies, other consistent risk factors associated with greater rates of serious infection include prolonged corticosteroid use, combination therapy with thiopurines, and disease severity. Anti-TNFs have also been associated with a somewhat increased risk of lymphoma, increased when used in combination with thiopurines. Reassuringly, however, in patients with a prior history of cancer, anti-TNFs and non-TNF biologics have not been found to increase the risk of new or recurrent cancer.14
Ultimately, in patients with a prior history of cancer, the choice of biologic or small molecule should be made in collaboration with a patient’s oncologist.
Anti-TNF exposure
Anti-TNFs were the first available biologics for the treatment of IBD. After the approval of vedolizumab in 2014, the first non-TNF biologic, many patients enrolled in clinical trials thereafter had already tried and failed anti-TNFs. In general, exposure to anti-TNFs may reduce the efficacy of a future biologic. In patients treated with vedolizumab, endoscopic and clinical outcomes were negatively impacted by prior anti-TNF exposure.15 However, in VARSITY, a head-to-head clinical trial where 20% of patients with UC were previously exposed to anti-TNFs other than adalimumab, vedolizumab had significantly higher rates of clinical remission and endoscopic improvement compared to adalimumab.16 Clinical remission rates with tofacitinib were not impacted by exposure to anti-TNF treatment, and similar findings were observed with ustekinumab.7,17 Risankizumab, a newly approved selective anti-IL23, also does not appear to be impacted by prior anti-TNF exposure by demonstrating similar rates of clinical remission regardless of biologic exposure status.18 Therefore, in patients with prior history of anti-TNF use, consideration of ustekinumab, risankizumab or JAK inhibitors as second line agents may be more favorable as compared to vedolizumab.
Perianal fistulizing disease
Perianal fistulizing disease can affect up to one-third of patients with CD and significantly impact a patient’s quality of life.19 The most robust data for the treatment of perianal fistulizing disease includes the use of infliximab with up to one-third of patients on maintenance therapy achieving complete resolution of fistula drainage. While no head-to-head trials compare combination therapy with infliximab plus immunomodulators versus infliximab alone for this indication specifically, one observational study demonstrated higher rates of fistula closure with combination therapy as compared to infliximab mono-therapy.19 In a post hoc analysis, higher infliximab concentrations at week 14 were associated with greater fistula response and remission rates.20 In patients with perianal disease, ustekinumab and vedolizumab may also be an effective treatment option by promoting resolution of fistula drainage.21
More recently, emerging data demonstrate that upadacitinib may be an excellent option as a second-line treatment for perianal disease in patients who have failed anti-TNF therapy. Use of upadacitinib was associated with greater rates of complete resolution of fistula drainage and higher rates of external fistula closure (Figure 2).22 Lastly, as an alternative to medical therapy, mesenchymal stem cell therapy has also shown to improve fistula drainage and improve external fistula openings in patients with CD.23 Stem cell therapy is only available through clinical trials at this time.
Patient preferences
Overall, data are lacking for evaluating patient preferences in treatment options for IBD especially with the recent increase in therapeutic options. One survey demonstrated that patient preferences were most impacted by the possibility of improving abdominal pain, with patients accepting additional risk of treatment side effects in order to reduce their abdominal pain.24 An oral route of administration and improving fatigue and bowel urgency were similarly important to patients. Patient preferences can also be highly variable with some valuing avoidance of corticosteroid use while others valuing avoidance of symptoms or risks of medication side effects and surgery. It is important to tailor the discussion on treatment strategies to each individual patient and inquire about the patient’s lifestyle, medical history, and value system, which may impact their treatment preferences utilizing shared decision making.
Access to treatment including the role of social determinants of health
The expanded therapeutic armamentarium has the potential to help patients achieve the current goals of care in IBD. However, these medications are not available to all patients due to numerous barriers including step therapy payer policies, prohibitive costs, insurance prior authorizations, and the role of social determinants of health and proximity to IBD expertise.25 While clinicians work with patients to determine the best treatment option, more often than not, the decision lies with the insurance payer. Step therapy is the protocol used by insurance companies that requires patients to try a lower-cost medication and fail to respond before they approve the originally requested treatment. This can lead to treatment delays, progression of disease, and disease complications. The option to incorporate the use of biosimilars, currently available for anti-TNFs, and other biologics in the near future, will reduce cost and potentially increase access.26 Additionally, working with a clinical pharmacist to navigate access and utilize patient assistance programs may help overcome cost related barriers to treatment and prevent delays in care.
Socioeconomic status has been shown to impact IBD disease outcomes, and compliance rates in treatment vary depending on race and ethnicity.27 Certain racial and ethnic groups remain vulnerable and may require additional support to achieve treatment goals. For example, disparities in health literacy in patients with IBD have been demonstrated with older black men at risk.28 Additionally, the patient’s proximity to their health care facility may impact treatment options. Most IBD centers are located in metropolitan areas and numerous “IBD deserts” exist, potentially limiting therapies for patients from more remote/rural settings.29 Access to treatment and the interplay of social determinants of health can have a large role in therapy selection.
Special considerations: Pregnancy and older adults
Certain patient populations warrant special consideration when approaching treatment strategies. Pregnancy in IBD will not be addressed in full depth in this article, however a key takeaway is that planning is critical and providers should emphasize the importance of steroid-free clinical remission for at least 3 months before conception.30 Additionally, biologic use during pregnancy has not been shown to increase adverse fetal outcomes, thus should be continued to minimize disease flare. Newer novel small molecules are generally avoided during pregnancy due to limited available safety data.
Older adults are the largest growing patient population with IBD. Frailty, or a state of decreased reserve, is more commonly observed in older patients and has been shown to increase adverse events including hospitalization and mortaility.31 Ultimately reducing polypharmacy, ensuring adequate nutrition, minimizing corticosteroid exposure and avoiding undertreatment of active IBD are all key in optimizing outcomes in an older patient with IBD.
Conclusion
When discussing treatment options with patients with IBD, it is important to individualize care and share the decision-making process with patients. Goals include improving symptoms and quality of life while working to achieve the goal of healing intestinal inflammation. In summary, this article can serve as a guide to clinicians for key factors in decision making when selecting therapies in moderate to severe IBD.
Dr. Holmer is a gastroenterologist with NYU Langone Health specializing in inflammatory bowel disease. Dr. Chang is director of clinical operations for the NYU Langone Health Inflammatory Bowel Disease Center. Dr. Malter is director of education for the Inflammatory Bowel Disease Center at NYU Langone Health and director of the inflammatory bowel disease program at Bellevue Hospital Center. Follow Dr. Holmer on X (formerly Twitter) at @HolmerMd and Dr. Chang @shannonchangmd. Dr. Holmer disclosed affiliations with Pfizer, Bristol Myers Squibb, and AvevoRx. Dr. Chang disclosed affiliations with Pfizer and Bristol Myers Squibb. Dr. Malter disclosed receiving educational grants form Abbvie, Janssen, Pfizer and Takeda, and serving on the advisory boards of AbbVie, Bristol Myers Squibb, Celltrion, Janssen, Merck, and Takeda.
References
1. Chang S et al. Am J Gastroenterol. 2023 Aug 24. doi: 10.14309/ajg.0000000000002485.
2. Harvey RF et al. The Lancet. 1980;1:514.
3. Lewis JD et al. Inflammatory Bowel Diseases. 2008;14:1660-1666.
4. Siegel CA et al. Gut. 2018;67(2):244-54.
5. Peyrin-Biroulet L et al. Am J Gastroenterol. 2015;110:1324-38
6. Rogler G et al. Gastroenterology. 2021;161:1118-32.
7. Sandborn WJ et al. N Engl J Med. 2017;376:1723-36.
8. Brooklyn TN et al. Gut. 2006;55:505-9.
9. Fahmy M et al. Am J Gastroenterol. 2012;107:794-5.
10. Van Eycken L et al. JAAD Case Rep. 2023;37:89-91.
11. Lasa JS et al. Lancet Gastroenterol Hepatol. 2022;7:161-70.
12. Lichtenstein GR et al. Inflamm Bowel Dis. 2018;24:490-501.
13. Long MD et al. Gastroenterology. 2022;162:S-5-S-6.
14. Holmer AK et al. Clin Gastroenterol Hepatol.2023;21:1598-1606.e5.
15. Sands BE et al. Gastroenterology. 2014;147:618-27.e3.
16. Sands BE et al. N Engl J Med. 2019;381:1215-26.
17. Sands BE et al. N Engl J Med. 2019;381:1201-14.
18. D’Haens G et al. Lancet. 2022;399:2015-30.
19. Bouguen G et al. Clin Gastroenterol Hepatol. 2013;11:975-81.e1-4.
20. Papamichael K et al. Am J Gastroenterol. 2021;116:1007-14.
21. Shehab M et al. Inflamm Bowel Dis. 2023;29:367-75.
22. Colombel JF et al. J Crohns Colitis. 2023;17:i620-i623.
23. Garcia-Olmo D et al. Dis Colon Rectum. 2022;65:713-20.
24. Louis E et al. J Crohns Colitis. 2023;17:231-9.
25. Rubin DT et al. Inflamm Bowel Dis. 2017;23:224-32.
26. Gulacsi L et al. Curr Med Chem. 2019;26:259-69.
27. Cai Q et al. BMC Gastroenterol. 2022;22:545.
28. Dos Santos Marques IC et al. Crohns Colitis 360. 2020 Oct;2(4):otaa076.
29. Deepak P et al. Gastroenterology. 2023;165:11-15.
30. Mahadevan U et al. Gastroenterology. 2019;156:1508-24.
31. Faye AS et al. Inflamm Bowel Dis. 2022;28:126-32.
32. Berinstein JA et al. Clin Gastroenterol Hepatol. 2021;19:2112-20.e1.
33. Levine J et al. Gastroenterology. 2023;164:S103-S104.
Despite new advances in treatment, head to head clinical trials, which are considered the gold standard when comparing therapies, remain limited. Other comparative effectiveness studies and network meta-analyses are the currently available substitutes to guide decision making.1
While efficacy is often considered first when choosing a drug, other critical factors play a role in tailoring a treatment plan. This article focuses on key considerations to help guide clinical decision making when treating patients with moderate to severe IBD (Figure 1).
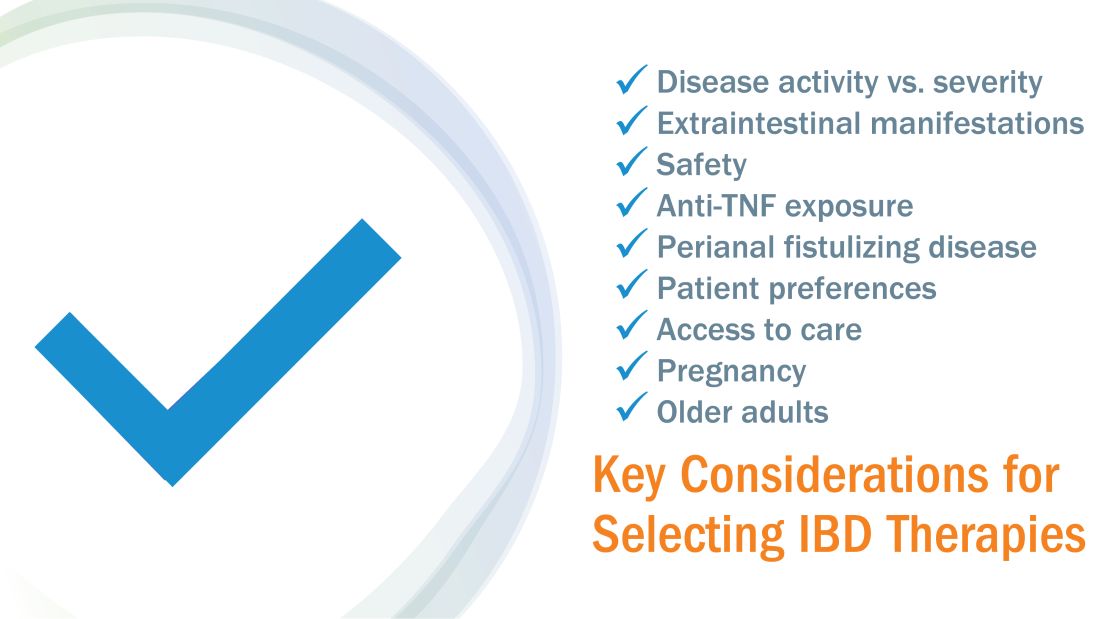
Disease activity versus severity
Both disease activity and disease severity should be considered when evaluating a patient for treatment. Disease activity is a cross-sectional view of one’s signs and symptoms which can vary visit to visit. Standardized indices measure disease activity in both Crohn’s disease (CD) and ulcerative colitis (UC).2,3 Disease severity encompasses the overall prognosis of disease over time and includes factors such as the presence or absence of high risk features, prior medication exposure, history of surgery, hospitalizations and the impact on quality of life.4
To prevent disease complications, the goals of treatment should be aimed at both reducing active symptoms (disease activity) but also healing mucosal inflammation, preventing disease progression (disease severity) and downstream sequelae including cancer, hospitalization or surgery.5 Determining the best treatment option takes disease activity and severity into account, in addition to the other key factors listed below (Figure 2).
Extraintestinal manifestations
Inflammation of organs outside of the gastrointestinal tract is common and can occur in up to 50% of patients with IBD.6 The most prevalent extraintestinal manifestations (EIMs) involve the skin and joints, which will be the primary focus in this article. We will also focus on treatment options with the most evidence supporting their use. Peripheral arthritis is often associated with intestinal inflammation, and treatment of underlying IBD can simultaneously improve joint symptoms. Conversely, axial spondyloarthritis does not commonly parallel intestinal inflammation. Anti–tumor necrosis factor (TNF) agents including infliximab and adalimumab are effective for the treatment of both peripheral and axial disease.6
Ustekinumab, an interleukin (IL)-12/23 inhibitor, may be effective for peripheral arthritis, however is ineffective for the treatment of axial spondyloarthritis.6 Janus kinase (JAK) inhibitors which include tofacitinib and upadacitinib are oral small molecules used to treat peripheral and axial spondyloarthritis and have more recently been approved for moderate to severe IBD.6,7
Erythema nodosum (EN) and pyoderma gangrenosum (PG) are skin manifestations seen in patients with IBD. EN appears as subcutaneous nodules and parallels intestinal inflammation, while PG consists of violaceous, ulcerated plaques, and presents with more significant pain. Anti-TNFs are effective for both EN and PG, with infliximab being the only biologic studied in a randomized control trial of patients with PG.8 In addition, small case reports have described some benefit from ustekinumab and upadacitinib in the treatment of PG.9,10
Safety
The safety of IBD therapies is a key consideration and often the most important factor to patients when choosing a treatment option. It is important to note that untreated disease is associated with significant morbidity, and should be weighed when discussing risks of medications with patients. In general, anti-TNFs and JAK inhibitors may be associated with an increased risk of infection and malignancy, while ustekinumab, vedolizumab, risankizumab and ozanimod offer a more favorable safety profile.11 In large registries and observational studies, infliximab was associated with up to a two times greater risk of serious infection as compared to nonbiologic medications, with the most common infections being pneumonia, sepsis and herpes zoster.12 JAK inhibitors are associated with an increased risk of herpes zoster infection, with a dose dependent effect seen in the maintenance clinical trials with tofacitinib.7
Ozanimod may be associated with atrioventricular conduction delays and bradycardia, however long-term safety data has reported a low incidence of serious cardiac related adverse events.13 Overall, though risks of infection may vary with different therapies, other consistent risk factors associated with greater rates of serious infection include prolonged corticosteroid use, combination therapy with thiopurines, and disease severity. Anti-TNFs have also been associated with a somewhat increased risk of lymphoma, increased when used in combination with thiopurines. Reassuringly, however, in patients with a prior history of cancer, anti-TNFs and non-TNF biologics have not been found to increase the risk of new or recurrent cancer.14
Ultimately, in patients with a prior history of cancer, the choice of biologic or small molecule should be made in collaboration with a patient’s oncologist.
Anti-TNF exposure
Anti-TNFs were the first available biologics for the treatment of IBD. After the approval of vedolizumab in 2014, the first non-TNF biologic, many patients enrolled in clinical trials thereafter had already tried and failed anti-TNFs. In general, exposure to anti-TNFs may reduce the efficacy of a future biologic. In patients treated with vedolizumab, endoscopic and clinical outcomes were negatively impacted by prior anti-TNF exposure.15 However, in VARSITY, a head-to-head clinical trial where 20% of patients with UC were previously exposed to anti-TNFs other than adalimumab, vedolizumab had significantly higher rates of clinical remission and endoscopic improvement compared to adalimumab.16 Clinical remission rates with tofacitinib were not impacted by exposure to anti-TNF treatment, and similar findings were observed with ustekinumab.7,17 Risankizumab, a newly approved selective anti-IL23, also does not appear to be impacted by prior anti-TNF exposure by demonstrating similar rates of clinical remission regardless of biologic exposure status.18 Therefore, in patients with prior history of anti-TNF use, consideration of ustekinumab, risankizumab or JAK inhibitors as second line agents may be more favorable as compared to vedolizumab.
Perianal fistulizing disease
Perianal fistulizing disease can affect up to one-third of patients with CD and significantly impact a patient’s quality of life.19 The most robust data for the treatment of perianal fistulizing disease includes the use of infliximab with up to one-third of patients on maintenance therapy achieving complete resolution of fistula drainage. While no head-to-head trials compare combination therapy with infliximab plus immunomodulators versus infliximab alone for this indication specifically, one observational study demonstrated higher rates of fistula closure with combination therapy as compared to infliximab mono-therapy.19 In a post hoc analysis, higher infliximab concentrations at week 14 were associated with greater fistula response and remission rates.20 In patients with perianal disease, ustekinumab and vedolizumab may also be an effective treatment option by promoting resolution of fistula drainage.21
More recently, emerging data demonstrate that upadacitinib may be an excellent option as a second-line treatment for perianal disease in patients who have failed anti-TNF therapy. Use of upadacitinib was associated with greater rates of complete resolution of fistula drainage and higher rates of external fistula closure (Figure 2).22 Lastly, as an alternative to medical therapy, mesenchymal stem cell therapy has also shown to improve fistula drainage and improve external fistula openings in patients with CD.23 Stem cell therapy is only available through clinical trials at this time.
Patient preferences
Overall, data are lacking for evaluating patient preferences in treatment options for IBD especially with the recent increase in therapeutic options. One survey demonstrated that patient preferences were most impacted by the possibility of improving abdominal pain, with patients accepting additional risk of treatment side effects in order to reduce their abdominal pain.24 An oral route of administration and improving fatigue and bowel urgency were similarly important to patients. Patient preferences can also be highly variable with some valuing avoidance of corticosteroid use while others valuing avoidance of symptoms or risks of medication side effects and surgery. It is important to tailor the discussion on treatment strategies to each individual patient and inquire about the patient’s lifestyle, medical history, and value system, which may impact their treatment preferences utilizing shared decision making.
Access to treatment including the role of social determinants of health
The expanded therapeutic armamentarium has the potential to help patients achieve the current goals of care in IBD. However, these medications are not available to all patients due to numerous barriers including step therapy payer policies, prohibitive costs, insurance prior authorizations, and the role of social determinants of health and proximity to IBD expertise.25 While clinicians work with patients to determine the best treatment option, more often than not, the decision lies with the insurance payer. Step therapy is the protocol used by insurance companies that requires patients to try a lower-cost medication and fail to respond before they approve the originally requested treatment. This can lead to treatment delays, progression of disease, and disease complications. The option to incorporate the use of biosimilars, currently available for anti-TNFs, and other biologics in the near future, will reduce cost and potentially increase access.26 Additionally, working with a clinical pharmacist to navigate access and utilize patient assistance programs may help overcome cost related barriers to treatment and prevent delays in care.
Socioeconomic status has been shown to impact IBD disease outcomes, and compliance rates in treatment vary depending on race and ethnicity.27 Certain racial and ethnic groups remain vulnerable and may require additional support to achieve treatment goals. For example, disparities in health literacy in patients with IBD have been demonstrated with older black men at risk.28 Additionally, the patient’s proximity to their health care facility may impact treatment options. Most IBD centers are located in metropolitan areas and numerous “IBD deserts” exist, potentially limiting therapies for patients from more remote/rural settings.29 Access to treatment and the interplay of social determinants of health can have a large role in therapy selection.
Special considerations: Pregnancy and older adults
Certain patient populations warrant special consideration when approaching treatment strategies. Pregnancy in IBD will not be addressed in full depth in this article, however a key takeaway is that planning is critical and providers should emphasize the importance of steroid-free clinical remission for at least 3 months before conception.30 Additionally, biologic use during pregnancy has not been shown to increase adverse fetal outcomes, thus should be continued to minimize disease flare. Newer novel small molecules are generally avoided during pregnancy due to limited available safety data.
Older adults are the largest growing patient population with IBD. Frailty, or a state of decreased reserve, is more commonly observed in older patients and has been shown to increase adverse events including hospitalization and mortaility.31 Ultimately reducing polypharmacy, ensuring adequate nutrition, minimizing corticosteroid exposure and avoiding undertreatment of active IBD are all key in optimizing outcomes in an older patient with IBD.
Conclusion
When discussing treatment options with patients with IBD, it is important to individualize care and share the decision-making process with patients. Goals include improving symptoms and quality of life while working to achieve the goal of healing intestinal inflammation. In summary, this article can serve as a guide to clinicians for key factors in decision making when selecting therapies in moderate to severe IBD.
Dr. Holmer is a gastroenterologist with NYU Langone Health specializing in inflammatory bowel disease. Dr. Chang is director of clinical operations for the NYU Langone Health Inflammatory Bowel Disease Center. Dr. Malter is director of education for the Inflammatory Bowel Disease Center at NYU Langone Health and director of the inflammatory bowel disease program at Bellevue Hospital Center. Follow Dr. Holmer on X (formerly Twitter) at @HolmerMd and Dr. Chang @shannonchangmd. Dr. Holmer disclosed affiliations with Pfizer, Bristol Myers Squibb, and AvevoRx. Dr. Chang disclosed affiliations with Pfizer and Bristol Myers Squibb. Dr. Malter disclosed receiving educational grants form Abbvie, Janssen, Pfizer and Takeda, and serving on the advisory boards of AbbVie, Bristol Myers Squibb, Celltrion, Janssen, Merck, and Takeda.
References
1. Chang S et al. Am J Gastroenterol. 2023 Aug 24. doi: 10.14309/ajg.0000000000002485.
2. Harvey RF et al. The Lancet. 1980;1:514.
3. Lewis JD et al. Inflammatory Bowel Diseases. 2008;14:1660-1666.
4. Siegel CA et al. Gut. 2018;67(2):244-54.
5. Peyrin-Biroulet L et al. Am J Gastroenterol. 2015;110:1324-38
6. Rogler G et al. Gastroenterology. 2021;161:1118-32.
7. Sandborn WJ et al. N Engl J Med. 2017;376:1723-36.
8. Brooklyn TN et al. Gut. 2006;55:505-9.
9. Fahmy M et al. Am J Gastroenterol. 2012;107:794-5.
10. Van Eycken L et al. JAAD Case Rep. 2023;37:89-91.
11. Lasa JS et al. Lancet Gastroenterol Hepatol. 2022;7:161-70.
12. Lichtenstein GR et al. Inflamm Bowel Dis. 2018;24:490-501.
13. Long MD et al. Gastroenterology. 2022;162:S-5-S-6.
14. Holmer AK et al. Clin Gastroenterol Hepatol.2023;21:1598-1606.e5.
15. Sands BE et al. Gastroenterology. 2014;147:618-27.e3.
16. Sands BE et al. N Engl J Med. 2019;381:1215-26.
17. Sands BE et al. N Engl J Med. 2019;381:1201-14.
18. D’Haens G et al. Lancet. 2022;399:2015-30.
19. Bouguen G et al. Clin Gastroenterol Hepatol. 2013;11:975-81.e1-4.
20. Papamichael K et al. Am J Gastroenterol. 2021;116:1007-14.
21. Shehab M et al. Inflamm Bowel Dis. 2023;29:367-75.
22. Colombel JF et al. J Crohns Colitis. 2023;17:i620-i623.
23. Garcia-Olmo D et al. Dis Colon Rectum. 2022;65:713-20.
24. Louis E et al. J Crohns Colitis. 2023;17:231-9.
25. Rubin DT et al. Inflamm Bowel Dis. 2017;23:224-32.
26. Gulacsi L et al. Curr Med Chem. 2019;26:259-69.
27. Cai Q et al. BMC Gastroenterol. 2022;22:545.
28. Dos Santos Marques IC et al. Crohns Colitis 360. 2020 Oct;2(4):otaa076.
29. Deepak P et al. Gastroenterology. 2023;165:11-15.
30. Mahadevan U et al. Gastroenterology. 2019;156:1508-24.
31. Faye AS et al. Inflamm Bowel Dis. 2022;28:126-32.
32. Berinstein JA et al. Clin Gastroenterol Hepatol. 2021;19:2112-20.e1.
33. Levine J et al. Gastroenterology. 2023;164:S103-S104.
Despite new advances in treatment, head to head clinical trials, which are considered the gold standard when comparing therapies, remain limited. Other comparative effectiveness studies and network meta-analyses are the currently available substitutes to guide decision making.1
While efficacy is often considered first when choosing a drug, other critical factors play a role in tailoring a treatment plan. This article focuses on key considerations to help guide clinical decision making when treating patients with moderate to severe IBD (Figure 1).
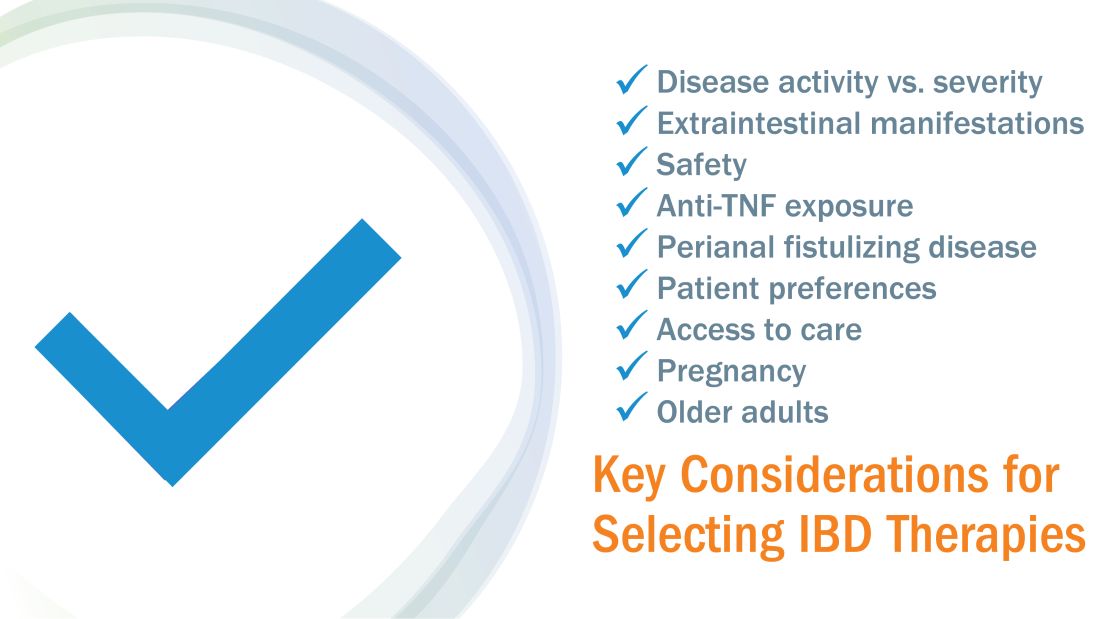
Disease activity versus severity
Both disease activity and disease severity should be considered when evaluating a patient for treatment. Disease activity is a cross-sectional view of one’s signs and symptoms which can vary visit to visit. Standardized indices measure disease activity in both Crohn’s disease (CD) and ulcerative colitis (UC).2,3 Disease severity encompasses the overall prognosis of disease over time and includes factors such as the presence or absence of high risk features, prior medication exposure, history of surgery, hospitalizations and the impact on quality of life.4
To prevent disease complications, the goals of treatment should be aimed at both reducing active symptoms (disease activity) but also healing mucosal inflammation, preventing disease progression (disease severity) and downstream sequelae including cancer, hospitalization or surgery.5 Determining the best treatment option takes disease activity and severity into account, in addition to the other key factors listed below (Figure 2).
Extraintestinal manifestations
Inflammation of organs outside of the gastrointestinal tract is common and can occur in up to 50% of patients with IBD.6 The most prevalent extraintestinal manifestations (EIMs) involve the skin and joints, which will be the primary focus in this article. We will also focus on treatment options with the most evidence supporting their use. Peripheral arthritis is often associated with intestinal inflammation, and treatment of underlying IBD can simultaneously improve joint symptoms. Conversely, axial spondyloarthritis does not commonly parallel intestinal inflammation. Anti–tumor necrosis factor (TNF) agents including infliximab and adalimumab are effective for the treatment of both peripheral and axial disease.6
Ustekinumab, an interleukin (IL)-12/23 inhibitor, may be effective for peripheral arthritis, however is ineffective for the treatment of axial spondyloarthritis.6 Janus kinase (JAK) inhibitors which include tofacitinib and upadacitinib are oral small molecules used to treat peripheral and axial spondyloarthritis and have more recently been approved for moderate to severe IBD.6,7
Erythema nodosum (EN) and pyoderma gangrenosum (PG) are skin manifestations seen in patients with IBD. EN appears as subcutaneous nodules and parallels intestinal inflammation, while PG consists of violaceous, ulcerated plaques, and presents with more significant pain. Anti-TNFs are effective for both EN and PG, with infliximab being the only biologic studied in a randomized control trial of patients with PG.8 In addition, small case reports have described some benefit from ustekinumab and upadacitinib in the treatment of PG.9,10
Safety
The safety of IBD therapies is a key consideration and often the most important factor to patients when choosing a treatment option. It is important to note that untreated disease is associated with significant morbidity, and should be weighed when discussing risks of medications with patients. In general, anti-TNFs and JAK inhibitors may be associated with an increased risk of infection and malignancy, while ustekinumab, vedolizumab, risankizumab and ozanimod offer a more favorable safety profile.11 In large registries and observational studies, infliximab was associated with up to a two times greater risk of serious infection as compared to nonbiologic medications, with the most common infections being pneumonia, sepsis and herpes zoster.12 JAK inhibitors are associated with an increased risk of herpes zoster infection, with a dose dependent effect seen in the maintenance clinical trials with tofacitinib.7
Ozanimod may be associated with atrioventricular conduction delays and bradycardia, however long-term safety data has reported a low incidence of serious cardiac related adverse events.13 Overall, though risks of infection may vary with different therapies, other consistent risk factors associated with greater rates of serious infection include prolonged corticosteroid use, combination therapy with thiopurines, and disease severity. Anti-TNFs have also been associated with a somewhat increased risk of lymphoma, increased when used in combination with thiopurines. Reassuringly, however, in patients with a prior history of cancer, anti-TNFs and non-TNF biologics have not been found to increase the risk of new or recurrent cancer.14
Ultimately, in patients with a prior history of cancer, the choice of biologic or small molecule should be made in collaboration with a patient’s oncologist.
Anti-TNF exposure
Anti-TNFs were the first available biologics for the treatment of IBD. After the approval of vedolizumab in 2014, the first non-TNF biologic, many patients enrolled in clinical trials thereafter had already tried and failed anti-TNFs. In general, exposure to anti-TNFs may reduce the efficacy of a future biologic. In patients treated with vedolizumab, endoscopic and clinical outcomes were negatively impacted by prior anti-TNF exposure.15 However, in VARSITY, a head-to-head clinical trial where 20% of patients with UC were previously exposed to anti-TNFs other than adalimumab, vedolizumab had significantly higher rates of clinical remission and endoscopic improvement compared to adalimumab.16 Clinical remission rates with tofacitinib were not impacted by exposure to anti-TNF treatment, and similar findings were observed with ustekinumab.7,17 Risankizumab, a newly approved selective anti-IL23, also does not appear to be impacted by prior anti-TNF exposure by demonstrating similar rates of clinical remission regardless of biologic exposure status.18 Therefore, in patients with prior history of anti-TNF use, consideration of ustekinumab, risankizumab or JAK inhibitors as second line agents may be more favorable as compared to vedolizumab.
Perianal fistulizing disease
Perianal fistulizing disease can affect up to one-third of patients with CD and significantly impact a patient’s quality of life.19 The most robust data for the treatment of perianal fistulizing disease includes the use of infliximab with up to one-third of patients on maintenance therapy achieving complete resolution of fistula drainage. While no head-to-head trials compare combination therapy with infliximab plus immunomodulators versus infliximab alone for this indication specifically, one observational study demonstrated higher rates of fistula closure with combination therapy as compared to infliximab mono-therapy.19 In a post hoc analysis, higher infliximab concentrations at week 14 were associated with greater fistula response and remission rates.20 In patients with perianal disease, ustekinumab and vedolizumab may also be an effective treatment option by promoting resolution of fistula drainage.21
More recently, emerging data demonstrate that upadacitinib may be an excellent option as a second-line treatment for perianal disease in patients who have failed anti-TNF therapy. Use of upadacitinib was associated with greater rates of complete resolution of fistula drainage and higher rates of external fistula closure (Figure 2).22 Lastly, as an alternative to medical therapy, mesenchymal stem cell therapy has also shown to improve fistula drainage and improve external fistula openings in patients with CD.23 Stem cell therapy is only available through clinical trials at this time.
Patient preferences
Overall, data are lacking for evaluating patient preferences in treatment options for IBD especially with the recent increase in therapeutic options. One survey demonstrated that patient preferences were most impacted by the possibility of improving abdominal pain, with patients accepting additional risk of treatment side effects in order to reduce their abdominal pain.24 An oral route of administration and improving fatigue and bowel urgency were similarly important to patients. Patient preferences can also be highly variable with some valuing avoidance of corticosteroid use while others valuing avoidance of symptoms or risks of medication side effects and surgery. It is important to tailor the discussion on treatment strategies to each individual patient and inquire about the patient’s lifestyle, medical history, and value system, which may impact their treatment preferences utilizing shared decision making.
Access to treatment including the role of social determinants of health
The expanded therapeutic armamentarium has the potential to help patients achieve the current goals of care in IBD. However, these medications are not available to all patients due to numerous barriers including step therapy payer policies, prohibitive costs, insurance prior authorizations, and the role of social determinants of health and proximity to IBD expertise.25 While clinicians work with patients to determine the best treatment option, more often than not, the decision lies with the insurance payer. Step therapy is the protocol used by insurance companies that requires patients to try a lower-cost medication and fail to respond before they approve the originally requested treatment. This can lead to treatment delays, progression of disease, and disease complications. The option to incorporate the use of biosimilars, currently available for anti-TNFs, and other biologics in the near future, will reduce cost and potentially increase access.26 Additionally, working with a clinical pharmacist to navigate access and utilize patient assistance programs may help overcome cost related barriers to treatment and prevent delays in care.
Socioeconomic status has been shown to impact IBD disease outcomes, and compliance rates in treatment vary depending on race and ethnicity.27 Certain racial and ethnic groups remain vulnerable and may require additional support to achieve treatment goals. For example, disparities in health literacy in patients with IBD have been demonstrated with older black men at risk.28 Additionally, the patient’s proximity to their health care facility may impact treatment options. Most IBD centers are located in metropolitan areas and numerous “IBD deserts” exist, potentially limiting therapies for patients from more remote/rural settings.29 Access to treatment and the interplay of social determinants of health can have a large role in therapy selection.
Special considerations: Pregnancy and older adults
Certain patient populations warrant special consideration when approaching treatment strategies. Pregnancy in IBD will not be addressed in full depth in this article, however a key takeaway is that planning is critical and providers should emphasize the importance of steroid-free clinical remission for at least 3 months before conception.30 Additionally, biologic use during pregnancy has not been shown to increase adverse fetal outcomes, thus should be continued to minimize disease flare. Newer novel small molecules are generally avoided during pregnancy due to limited available safety data.
Older adults are the largest growing patient population with IBD. Frailty, or a state of decreased reserve, is more commonly observed in older patients and has been shown to increase adverse events including hospitalization and mortaility.31 Ultimately reducing polypharmacy, ensuring adequate nutrition, minimizing corticosteroid exposure and avoiding undertreatment of active IBD are all key in optimizing outcomes in an older patient with IBD.
Conclusion
When discussing treatment options with patients with IBD, it is important to individualize care and share the decision-making process with patients. Goals include improving symptoms and quality of life while working to achieve the goal of healing intestinal inflammation. In summary, this article can serve as a guide to clinicians for key factors in decision making when selecting therapies in moderate to severe IBD.
Dr. Holmer is a gastroenterologist with NYU Langone Health specializing in inflammatory bowel disease. Dr. Chang is director of clinical operations for the NYU Langone Health Inflammatory Bowel Disease Center. Dr. Malter is director of education for the Inflammatory Bowel Disease Center at NYU Langone Health and director of the inflammatory bowel disease program at Bellevue Hospital Center. Follow Dr. Holmer on X (formerly Twitter) at @HolmerMd and Dr. Chang @shannonchangmd. Dr. Holmer disclosed affiliations with Pfizer, Bristol Myers Squibb, and AvevoRx. Dr. Chang disclosed affiliations with Pfizer and Bristol Myers Squibb. Dr. Malter disclosed receiving educational grants form Abbvie, Janssen, Pfizer and Takeda, and serving on the advisory boards of AbbVie, Bristol Myers Squibb, Celltrion, Janssen, Merck, and Takeda.
References
1. Chang S et al. Am J Gastroenterol. 2023 Aug 24. doi: 10.14309/ajg.0000000000002485.
2. Harvey RF et al. The Lancet. 1980;1:514.
3. Lewis JD et al. Inflammatory Bowel Diseases. 2008;14:1660-1666.
4. Siegel CA et al. Gut. 2018;67(2):244-54.
5. Peyrin-Biroulet L et al. Am J Gastroenterol. 2015;110:1324-38
6. Rogler G et al. Gastroenterology. 2021;161:1118-32.
7. Sandborn WJ et al. N Engl J Med. 2017;376:1723-36.
8. Brooklyn TN et al. Gut. 2006;55:505-9.
9. Fahmy M et al. Am J Gastroenterol. 2012;107:794-5.
10. Van Eycken L et al. JAAD Case Rep. 2023;37:89-91.
11. Lasa JS et al. Lancet Gastroenterol Hepatol. 2022;7:161-70.
12. Lichtenstein GR et al. Inflamm Bowel Dis. 2018;24:490-501.
13. Long MD et al. Gastroenterology. 2022;162:S-5-S-6.
14. Holmer AK et al. Clin Gastroenterol Hepatol.2023;21:1598-1606.e5.
15. Sands BE et al. Gastroenterology. 2014;147:618-27.e3.
16. Sands BE et al. N Engl J Med. 2019;381:1215-26.
17. Sands BE et al. N Engl J Med. 2019;381:1201-14.
18. D’Haens G et al. Lancet. 2022;399:2015-30.
19. Bouguen G et al. Clin Gastroenterol Hepatol. 2013;11:975-81.e1-4.
20. Papamichael K et al. Am J Gastroenterol. 2021;116:1007-14.
21. Shehab M et al. Inflamm Bowel Dis. 2023;29:367-75.
22. Colombel JF et al. J Crohns Colitis. 2023;17:i620-i623.
23. Garcia-Olmo D et al. Dis Colon Rectum. 2022;65:713-20.
24. Louis E et al. J Crohns Colitis. 2023;17:231-9.
25. Rubin DT et al. Inflamm Bowel Dis. 2017;23:224-32.
26. Gulacsi L et al. Curr Med Chem. 2019;26:259-69.
27. Cai Q et al. BMC Gastroenterol. 2022;22:545.
28. Dos Santos Marques IC et al. Crohns Colitis 360. 2020 Oct;2(4):otaa076.
29. Deepak P et al. Gastroenterology. 2023;165:11-15.
30. Mahadevan U et al. Gastroenterology. 2019;156:1508-24.
31. Faye AS et al. Inflamm Bowel Dis. 2022;28:126-32.
32. Berinstein JA et al. Clin Gastroenterol Hepatol. 2021;19:2112-20.e1.
33. Levine J et al. Gastroenterology. 2023;164:S103-S104.
Working with industry in private practice gastroenterology
In this video, Dr. Nadeem Baig of Allied Digestive Health in West Long Branck, N.J., discusses why he chose private practice gastroenterology and how his organization works with industry to support its mission of providing the best care for patients.
He has no financial conflicts relative to the topics in this video.

In this video, Dr. Nadeem Baig of Allied Digestive Health in West Long Branck, N.J., discusses why he chose private practice gastroenterology and how his organization works with industry to support its mission of providing the best care for patients.
He has no financial conflicts relative to the topics in this video.

In this video, Dr. Nadeem Baig of Allied Digestive Health in West Long Branck, N.J., discusses why he chose private practice gastroenterology and how his organization works with industry to support its mission of providing the best care for patients.
He has no financial conflicts relative to the topics in this video.

AGA patient and physician advocates visit Capitol Hill to push for prior authorization reform

In our first in-person Advocacy Day on Capitol Hill since 2019, AGA leaders and patient advocates from 22 total states met with House and Senate offices to educate members of Congress and their staff about policies affecting GI patient care such as prior authorization and step therapy. Federal research funding and Medicare reimbursement were also on the agenda.
In the meetings, the patient shared their stories of living with various gastrointestinal diseases, including ulcerative colitis and Crohn’s disease, and the struggles they’ve gone through to get treatments approved by their insurers. AGA physicians shared the provider perspective of how policies like prior authorization negatively impact practices. According to a 2023 AGA member survey, 95% of respondents say that prior authorization restrictions have impacted patient access to clinically appropriate treatments and patient clinical outcomes and 84% described that the burden associated with prior authorization policies have increased “significantly” or “somewhat” over the last 5 years. AGA’s advocacy day came not long after UnitedHealthcare’s announcement of a new “Gold Card” prior authorization policy to be implemented in 2024, which will impact most colonoscopies and endoscopies for its 27 million commercial beneficiaries. The group expressed serious concerns about the proposed policy to lawmakers. 
“It was a wonderful and empowering experience to share my personal story with my Representative/Senator and know that they were really listening to my concerns about insurer overreach,” said Aaron Blocker, a Crohn’s disease patient and advocate. “I hope Congress acts swiftly on passing prior authorization reform, so no more patients are forced to live in pain while they wait for treatments to be approved.” As gastroenterologists, too much administrative time is spent submitting onerous prior authorization requests on a near daily basis. We hope Congress takes our concerns seriously and comes together to rein in prior authorization.
AGA thanks the patient and physician advocates who participated in this year’s Advocacy Day and looks forward to continuing our work to ensure timely access to care.

In our first in-person Advocacy Day on Capitol Hill since 2019, AGA leaders and patient advocates from 22 total states met with House and Senate offices to educate members of Congress and their staff about policies affecting GI patient care such as prior authorization and step therapy. Federal research funding and Medicare reimbursement were also on the agenda.
In the meetings, the patient shared their stories of living with various gastrointestinal diseases, including ulcerative colitis and Crohn’s disease, and the struggles they’ve gone through to get treatments approved by their insurers. AGA physicians shared the provider perspective of how policies like prior authorization negatively impact practices. According to a 2023 AGA member survey, 95% of respondents say that prior authorization restrictions have impacted patient access to clinically appropriate treatments and patient clinical outcomes and 84% described that the burden associated with prior authorization policies have increased “significantly” or “somewhat” over the last 5 years. AGA’s advocacy day came not long after UnitedHealthcare’s announcement of a new “Gold Card” prior authorization policy to be implemented in 2024, which will impact most colonoscopies and endoscopies for its 27 million commercial beneficiaries. The group expressed serious concerns about the proposed policy to lawmakers. 
“It was a wonderful and empowering experience to share my personal story with my Representative/Senator and know that they were really listening to my concerns about insurer overreach,” said Aaron Blocker, a Crohn’s disease patient and advocate. “I hope Congress acts swiftly on passing prior authorization reform, so no more patients are forced to live in pain while they wait for treatments to be approved.” As gastroenterologists, too much administrative time is spent submitting onerous prior authorization requests on a near daily basis. We hope Congress takes our concerns seriously and comes together to rein in prior authorization.
AGA thanks the patient and physician advocates who participated in this year’s Advocacy Day and looks forward to continuing our work to ensure timely access to care.

In our first in-person Advocacy Day on Capitol Hill since 2019, AGA leaders and patient advocates from 22 total states met with House and Senate offices to educate members of Congress and their staff about policies affecting GI patient care such as prior authorization and step therapy. Federal research funding and Medicare reimbursement were also on the agenda.
In the meetings, the patient shared their stories of living with various gastrointestinal diseases, including ulcerative colitis and Crohn’s disease, and the struggles they’ve gone through to get treatments approved by their insurers. AGA physicians shared the provider perspective of how policies like prior authorization negatively impact practices. According to a 2023 AGA member survey, 95% of respondents say that prior authorization restrictions have impacted patient access to clinically appropriate treatments and patient clinical outcomes and 84% described that the burden associated with prior authorization policies have increased “significantly” or “somewhat” over the last 5 years. AGA’s advocacy day came not long after UnitedHealthcare’s announcement of a new “Gold Card” prior authorization policy to be implemented in 2024, which will impact most colonoscopies and endoscopies for its 27 million commercial beneficiaries. The group expressed serious concerns about the proposed policy to lawmakers. 
“It was a wonderful and empowering experience to share my personal story with my Representative/Senator and know that they were really listening to my concerns about insurer overreach,” said Aaron Blocker, a Crohn’s disease patient and advocate. “I hope Congress acts swiftly on passing prior authorization reform, so no more patients are forced to live in pain while they wait for treatments to be approved.” As gastroenterologists, too much administrative time is spent submitting onerous prior authorization requests on a near daily basis. We hope Congress takes our concerns seriously and comes together to rein in prior authorization.
AGA thanks the patient and physician advocates who participated in this year’s Advocacy Day and looks forward to continuing our work to ensure timely access to care.
Scrubs & Heels Summit 2023: Filling a void for women in GI
.1-3 This gender disparity arises from a multitude of factors including lack of effective mentoring, unequal leadership and career advancement opportunities, and pay inequity. In this context, The Scrubs & Heels Leadership Summit (S&H) was launched in 2022 focused on the professional and personal development of women in gastroenterology.
I had the great pleasure and honor of attending the 2023 summit which took place in February in Rancho Palos Verdes, Calif. There were nearly 200 attendees ranging from trainees to midcareer and senior gastroenterologists and other health care professionals from both academia and private practices across the nation. The weekend course was directed by S&H cofounders, Dr. Aline Charabaty and Dr. Anita Afzali, and cochaired by Dr. Amy Oxentenko and Dr. Aja McCutchen.
The 2-day summit opened with a presentation by Sally Helgesen, author of How Women Rise, describing the 12 common habits that often hold women back in career advancement, promotion, or opportunities. Dr. Aline Charabaty addressed the myth of women needing to fulfill the role of superwoman or have suprahuman abilities. Attendees were challenged to reframe this societal construct and begin to find balance and the reasonable choice to switch to part-time work and, as Dr. Aja McCutch emphasized, dial-down responsibilities to maintain wellness when life has competing priorities.
Dr. Amy Oxentenko shared her personal journey to success and instilled the importance of engaging with community and society at large. We then heard from Dr. Neena Abraham on how to gracefully embrace transitions in our professional lives, whether intentionally sought or natural progressions of a career. She encouraged attendees to control our own narrative and seek challenges that promote growth. We explored different practice models with Dr. Caroline Hwang and learned strategies of switching from academics to private practice or vice versa. We also heard from cofounder Dr. Anita Afzali on becoming a physician executive and the importance of staying connected to patient care when rising in ranks of leadership.
The second day opened with a keynote address delivered by Dr. Marla Dubinsky detailing her journey of becoming a CEO of a publicly-traded company while retaining her role as professor and chief of pediatric gastroenterology in a large academic institution. Attendees were provided with a master class on discovering ways to inspire our inner entrepreneur and highlighted the benefit of physicians, especially women, in being effective business leaders. This talk was followed by a talk by Phil Schoenfeld, MD, FACS, editor-in-chief of Evidence-Based GI for the American College of Gastroenterology. He spoke on the importance of male allyship for women in GI and shared his personal experiences and challenges with allyship.
The summit included a breakout session by Dr. Rashmi Advani designed for residents to hear tips on how to have a successful fellowship match and for fellows to embrace a steep learning curve when starting and included tips for efficiency. Additional breakout sessions included learning ergonomic strategies for positioning and scope-holding, vocal-cord exercises before giving oral presentations, and how to formulate a business plan and negotiate a contract.
We ended the summit with uplifting advice from executive coaches Sonia Narang and Dr. Dawn Sears who taught us the art of leaning into opportunities, mansizing aspirations, finding coconspirators for amplification of female GI leaders, and supporting our colleagues personally and professionally.
Three key takeaway messages:
- Recognize your self-worth and the contributions you bring to your patients and community as a whole.
- Lean into the importance of vocalizing your asks, advocating for yourself, building your brand, and showcasing your accomplishments.
- Be mindful of the balance between the time and energy you dedicate towards goals that bring you recognition and fuel your passion and your mental, physical, and emotional health.
As a trainee, I benefited tremendously from attending and expanding my professional network of mentors, sponsors and colleagues. I am encouraged by this programming and hope to see more of it in the future.
Contributors to this article included: Rashmi Advani, MD2; Anita Afzali, MD3; Aline Charabaty, MD.4
Neither Dr. Syed, nor the article contributors, had financial conflicts of interest associated with this article. The AGA was represented at the Scrubs and Heels Summit as a society partner committed to the advancement of women in GI. AGA is building on years of efforts to bolster leadership, mentorship, and sponsorship among women in GI through its annual women’s leadership conference and most recently with its 2022 regional women in GI workshops held around the country that led to the development of a comprehensive gender equity strategy designed to build an environment of gender equity in the field of GI so that all can thrive.
Institutions and social media handle
1. Santa Clara Valley Medical Center (San Jose, Calif), @noorannemd
2. Cedars Sinai (Los Angeles), @AdvaniRashmiMD
3. University of Cincinnati, @IBD_Afzali
4. Johns Hopkins Medicine (Washington), @DCharabaty
References
Advani R et al. Gender-specific attitudes of internal medicine residents toward gastroenterology. Dig Dis Sci. 2022 Nov;67(11):5044-52.
American Association of Medical Colleges. Diversity in Medicine: Facts and Figures (2019).
Elta GH. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
Burke CA et al. Gender disparity in the practice of gastroenterology: The first 5 years of a career. Am J Gastroenterol 2005;100:259-64
David, Yakira N. et al. Gender-specific factors influencing gastroenterologists to pursue careers in advanced endoscopy: perceptions vs reality. Journal of the American College of Gastroenterology, ACG 116.3 (2021):539-50.
Rabinowitz LG et al. Gender dynamics in education and practice of gastroenterology. Gastrointest Endosc. 2021;93:1047-56.
Rabinowitz LG et al. Survey finds gender disparities impact both women mentors and mentees in gastroenterology. Journal of the American College of Gastroenterology, ACG 2021;116:1876-84.
.1-3 This gender disparity arises from a multitude of factors including lack of effective mentoring, unequal leadership and career advancement opportunities, and pay inequity. In this context, The Scrubs & Heels Leadership Summit (S&H) was launched in 2022 focused on the professional and personal development of women in gastroenterology.
I had the great pleasure and honor of attending the 2023 summit which took place in February in Rancho Palos Verdes, Calif. There were nearly 200 attendees ranging from trainees to midcareer and senior gastroenterologists and other health care professionals from both academia and private practices across the nation. The weekend course was directed by S&H cofounders, Dr. Aline Charabaty and Dr. Anita Afzali, and cochaired by Dr. Amy Oxentenko and Dr. Aja McCutchen.
The 2-day summit opened with a presentation by Sally Helgesen, author of How Women Rise, describing the 12 common habits that often hold women back in career advancement, promotion, or opportunities. Dr. Aline Charabaty addressed the myth of women needing to fulfill the role of superwoman or have suprahuman abilities. Attendees were challenged to reframe this societal construct and begin to find balance and the reasonable choice to switch to part-time work and, as Dr. Aja McCutch emphasized, dial-down responsibilities to maintain wellness when life has competing priorities.
Dr. Amy Oxentenko shared her personal journey to success and instilled the importance of engaging with community and society at large. We then heard from Dr. Neena Abraham on how to gracefully embrace transitions in our professional lives, whether intentionally sought or natural progressions of a career. She encouraged attendees to control our own narrative and seek challenges that promote growth. We explored different practice models with Dr. Caroline Hwang and learned strategies of switching from academics to private practice or vice versa. We also heard from cofounder Dr. Anita Afzali on becoming a physician executive and the importance of staying connected to patient care when rising in ranks of leadership.
The second day opened with a keynote address delivered by Dr. Marla Dubinsky detailing her journey of becoming a CEO of a publicly-traded company while retaining her role as professor and chief of pediatric gastroenterology in a large academic institution. Attendees were provided with a master class on discovering ways to inspire our inner entrepreneur and highlighted the benefit of physicians, especially women, in being effective business leaders. This talk was followed by a talk by Phil Schoenfeld, MD, FACS, editor-in-chief of Evidence-Based GI for the American College of Gastroenterology. He spoke on the importance of male allyship for women in GI and shared his personal experiences and challenges with allyship.
The summit included a breakout session by Dr. Rashmi Advani designed for residents to hear tips on how to have a successful fellowship match and for fellows to embrace a steep learning curve when starting and included tips for efficiency. Additional breakout sessions included learning ergonomic strategies for positioning and scope-holding, vocal-cord exercises before giving oral presentations, and how to formulate a business plan and negotiate a contract.
We ended the summit with uplifting advice from executive coaches Sonia Narang and Dr. Dawn Sears who taught us the art of leaning into opportunities, mansizing aspirations, finding coconspirators for amplification of female GI leaders, and supporting our colleagues personally and professionally.
Three key takeaway messages:
- Recognize your self-worth and the contributions you bring to your patients and community as a whole.
- Lean into the importance of vocalizing your asks, advocating for yourself, building your brand, and showcasing your accomplishments.
- Be mindful of the balance between the time and energy you dedicate towards goals that bring you recognition and fuel your passion and your mental, physical, and emotional health.
As a trainee, I benefited tremendously from attending and expanding my professional network of mentors, sponsors and colleagues. I am encouraged by this programming and hope to see more of it in the future.
Contributors to this article included: Rashmi Advani, MD2; Anita Afzali, MD3; Aline Charabaty, MD.4
Neither Dr. Syed, nor the article contributors, had financial conflicts of interest associated with this article. The AGA was represented at the Scrubs and Heels Summit as a society partner committed to the advancement of women in GI. AGA is building on years of efforts to bolster leadership, mentorship, and sponsorship among women in GI through its annual women’s leadership conference and most recently with its 2022 regional women in GI workshops held around the country that led to the development of a comprehensive gender equity strategy designed to build an environment of gender equity in the field of GI so that all can thrive.
Institutions and social media handle
1. Santa Clara Valley Medical Center (San Jose, Calif), @noorannemd
2. Cedars Sinai (Los Angeles), @AdvaniRashmiMD
3. University of Cincinnati, @IBD_Afzali
4. Johns Hopkins Medicine (Washington), @DCharabaty
References
Advani R et al. Gender-specific attitudes of internal medicine residents toward gastroenterology. Dig Dis Sci. 2022 Nov;67(11):5044-52.
American Association of Medical Colleges. Diversity in Medicine: Facts and Figures (2019).
Elta GH. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
Burke CA et al. Gender disparity in the practice of gastroenterology: The first 5 years of a career. Am J Gastroenterol 2005;100:259-64
David, Yakira N. et al. Gender-specific factors influencing gastroenterologists to pursue careers in advanced endoscopy: perceptions vs reality. Journal of the American College of Gastroenterology, ACG 116.3 (2021):539-50.
Rabinowitz LG et al. Gender dynamics in education and practice of gastroenterology. Gastrointest Endosc. 2021;93:1047-56.
Rabinowitz LG et al. Survey finds gender disparities impact both women mentors and mentees in gastroenterology. Journal of the American College of Gastroenterology, ACG 2021;116:1876-84.
.1-3 This gender disparity arises from a multitude of factors including lack of effective mentoring, unequal leadership and career advancement opportunities, and pay inequity. In this context, The Scrubs & Heels Leadership Summit (S&H) was launched in 2022 focused on the professional and personal development of women in gastroenterology.
I had the great pleasure and honor of attending the 2023 summit which took place in February in Rancho Palos Verdes, Calif. There were nearly 200 attendees ranging from trainees to midcareer and senior gastroenterologists and other health care professionals from both academia and private practices across the nation. The weekend course was directed by S&H cofounders, Dr. Aline Charabaty and Dr. Anita Afzali, and cochaired by Dr. Amy Oxentenko and Dr. Aja McCutchen.
The 2-day summit opened with a presentation by Sally Helgesen, author of How Women Rise, describing the 12 common habits that often hold women back in career advancement, promotion, or opportunities. Dr. Aline Charabaty addressed the myth of women needing to fulfill the role of superwoman or have suprahuman abilities. Attendees were challenged to reframe this societal construct and begin to find balance and the reasonable choice to switch to part-time work and, as Dr. Aja McCutch emphasized, dial-down responsibilities to maintain wellness when life has competing priorities.
Dr. Amy Oxentenko shared her personal journey to success and instilled the importance of engaging with community and society at large. We then heard from Dr. Neena Abraham on how to gracefully embrace transitions in our professional lives, whether intentionally sought or natural progressions of a career. She encouraged attendees to control our own narrative and seek challenges that promote growth. We explored different practice models with Dr. Caroline Hwang and learned strategies of switching from academics to private practice or vice versa. We also heard from cofounder Dr. Anita Afzali on becoming a physician executive and the importance of staying connected to patient care when rising in ranks of leadership.
The second day opened with a keynote address delivered by Dr. Marla Dubinsky detailing her journey of becoming a CEO of a publicly-traded company while retaining her role as professor and chief of pediatric gastroenterology in a large academic institution. Attendees were provided with a master class on discovering ways to inspire our inner entrepreneur and highlighted the benefit of physicians, especially women, in being effective business leaders. This talk was followed by a talk by Phil Schoenfeld, MD, FACS, editor-in-chief of Evidence-Based GI for the American College of Gastroenterology. He spoke on the importance of male allyship for women in GI and shared his personal experiences and challenges with allyship.
The summit included a breakout session by Dr. Rashmi Advani designed for residents to hear tips on how to have a successful fellowship match and for fellows to embrace a steep learning curve when starting and included tips for efficiency. Additional breakout sessions included learning ergonomic strategies for positioning and scope-holding, vocal-cord exercises before giving oral presentations, and how to formulate a business plan and negotiate a contract.
We ended the summit with uplifting advice from executive coaches Sonia Narang and Dr. Dawn Sears who taught us the art of leaning into opportunities, mansizing aspirations, finding coconspirators for amplification of female GI leaders, and supporting our colleagues personally and professionally.
Three key takeaway messages:
- Recognize your self-worth and the contributions you bring to your patients and community as a whole.
- Lean into the importance of vocalizing your asks, advocating for yourself, building your brand, and showcasing your accomplishments.
- Be mindful of the balance between the time and energy you dedicate towards goals that bring you recognition and fuel your passion and your mental, physical, and emotional health.
As a trainee, I benefited tremendously from attending and expanding my professional network of mentors, sponsors and colleagues. I am encouraged by this programming and hope to see more of it in the future.
Contributors to this article included: Rashmi Advani, MD2; Anita Afzali, MD3; Aline Charabaty, MD.4
Neither Dr. Syed, nor the article contributors, had financial conflicts of interest associated with this article. The AGA was represented at the Scrubs and Heels Summit as a society partner committed to the advancement of women in GI. AGA is building on years of efforts to bolster leadership, mentorship, and sponsorship among women in GI through its annual women’s leadership conference and most recently with its 2022 regional women in GI workshops held around the country that led to the development of a comprehensive gender equity strategy designed to build an environment of gender equity in the field of GI so that all can thrive.
Institutions and social media handle
1. Santa Clara Valley Medical Center (San Jose, Calif), @noorannemd
2. Cedars Sinai (Los Angeles), @AdvaniRashmiMD
3. University of Cincinnati, @IBD_Afzali
4. Johns Hopkins Medicine (Washington), @DCharabaty
References
Advani R et al. Gender-specific attitudes of internal medicine residents toward gastroenterology. Dig Dis Sci. 2022 Nov;67(11):5044-52.
American Association of Medical Colleges. Diversity in Medicine: Facts and Figures (2019).
Elta GH. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
Burke CA et al. Gender disparity in the practice of gastroenterology: The first 5 years of a career. Am J Gastroenterol 2005;100:259-64
David, Yakira N. et al. Gender-specific factors influencing gastroenterologists to pursue careers in advanced endoscopy: perceptions vs reality. Journal of the American College of Gastroenterology, ACG 116.3 (2021):539-50.
Rabinowitz LG et al. Gender dynamics in education and practice of gastroenterology. Gastrointest Endosc. 2021;93:1047-56.
Rabinowitz LG et al. Survey finds gender disparities impact both women mentors and mentees in gastroenterology. Journal of the American College of Gastroenterology, ACG 2021;116:1876-84.
Navigating NAFLD: Unveiling the approach to mitigate the impact of NAFLD
Burden of NAFLD in the U.S.
NAFLD is a manifestation of systemic metabolic abnormalities, including insulin resistance, dyslipidemia, central obesity, and hypertension. In this short review, we summarize data on the burden of NAFLD in the U.S. and its prognostic determinants and review what clinical and public health approaches may be needed to mitigating its impact.
Epidemiology of NAFLD
Worldwide, the prevalence of NAFLD is estimated at 6% to 35%, with biopsy-based studies reporting NASH in 3% to 5%.1 U.S. estimates for the prevalence of NAFLD range from 10% to 46%.2 In our own analysis of the National Health and Nutrition Examination Survey (NHANES) data, transient elastography-detected steatosis was found in 36%, which projected to a minimum of 73 million American adults.3
NAFLD represents a spectrum of disorders ranging from simple steatosis to nonalcoholic steatohepatitis (NASH), the latter leading, in some cases, to progressive hepatic fibrosis and cirrhosis.4 Out of a large number of subjects with NAFLD, the proportions of NASH patients that develop severe liver problems such as end-stage liver disease (ESLD) or hepatocellular carcinoma (HCC) are progressively smaller. For example, we recently reported that less than 2,000 liver-related deaths are attributable to NAFLD in the U.S. per annum, which corresponds to a crude case fatality rate of < 0.005% per year.5
According to the Centers for Disease Control and Prevention (CDC), there have been substantial increases in liver-related deaths over the last 2 decades. Mortality from liver disease including hepatobiliary cancers more than doubled from 41,966 deaths (including 15,321 women and 26,645 men) in 2000 to 85,884 deaths (33,000 women and 52,884 men) in 2020. The proportion of deaths specifically attributed to NAFLD among liver-related deaths was miniscule in 2000, accounting for 1.1% in women and 0.7% in men. By 2020, the proportions increased several folds in both sexes (7.4% in women and 2.7% in men).6 Moreover, it is likely that a substantial portion of deaths from chronic liver disease from unknown causes (“cryptogenic”) are likely end-stage NAFLD, making these figures underestimates of the true impact of NAFLD in the U.S.
From a comparative epidemiologic perspective, there are significant racial and ethnic and socioeconomic disparities in NAFLD prevalence, wherein Hispanic persons and individuals experiencing food insecurity – independent of poverty status, education level, race and ethnicity – are disproportionately more affected by NAFLD.7,8 Furthermore, these disparities persist when examining long-term complications of NAFLD, such as developing HCC.
Prognosis in NAFLD: NASH versus fibrosis
Given the enormous prevalence and increasing public health burden of NAFLD, systematic interventions to mitigate its impact are urgently needed. Clearly, patients who already have developed advanced liver disease need to be directed to specialty care so the disease progression may be halted and complications of ESLD may be prevented or managed. On the other hand, in order to mitigate the future impact of ESLD, prompt identification of at-risk patients and proactive interventions to improve liver health are needed.
In the assessment of disease progression, prior data have shown that the presence of NASH and increasing stages of liver fibrosis are important predictors of disease progression. Fibrosis is a component of NASH, while NASH is thought to be a prerequisite for fibrosis. In a prospective, multicenter follow-up study of NAFLD evaluated by liver biopsies (n = 1,773), over a median follow-up of 4 years, 37 (2%) developed hepatic decompensation, while 47 (3%) died from any cause, which included ESLD (n = 12), cardiovascular complications (n = 4), and malignancies (n = 12), including HCC (n = 9).9 It is not entirely surprising that advanced fibrosis and cirrhosis was highly associated with the development of hepatic decompensation. In their multivariable analysis, patients with F3-4 had a 13.8-fold (95% confidence interval [CI]: 4.6, 41.0) increase in the hazard of reaching a MELD score of 15 compared to those with F0-2. In addition, all-cause mortality was 17.2-fold (95% CI: 5.2, 56.6) higher with F3-4 compared to F0-2.
These data have been borne out by a larger body of literature on the topic. In a recent meta-analysis assessing the relation between liver fibrosis and future mortality, which included 17,301 subjects with NAFLD, patients with at least stage 2 fibrosis experience a significantly increased risk of liver-related and overall mortality, a trend that accelerates at higher fibrosis stages.10 These point to liver fibrosis as the singular determinant of long-term prognosis, in comparison, for example, with the diagnosis of NASH. Hagström conducted a retrospective cohort study of patients with biopsy-proven NAFLD in Sweden. When fibrosis stage and histological diagnosis of NASH were considered together, NASH did not have an impact on overall mortality (hazard ratio [HR] = 0.83, P = .29) or liver morbidity (HR = 0.62, P = .25).11
On an individual level, factors that affect fibrosis progression are not as well studied. It is commonly believed that demographic factors (e.g., age, sex and race), genetic polymorphisms (e.g., PNPLA3, TM6SF2), clinical comorbidities (e.g., obesity, DM, and sleep apnea), and environmental factors (e.g., smoking) may accelerate fibrosis and disease outcomes, although prospective data are sparse to estimate the extent these individual variables affect progression.12 Recent guidelines remain silent about whether and how these data may be incorporated in screening for NAFLD in the population.
Assessment of liver fibrosis
The traditional means to detect liver fibrosis is liver histology, which also assesses steatosis, individual components of NASH and, often importantly, other concomitant liver pathology. In reality, however, liver biopsies have several limitations including the risk of complications, patient discomfort, economic costs, and sampling variability. Increasingly, “noninvasive” methods have been used to estimate liver fibrosis in patients with NAFLD. Liver elastography estimates the physical stiffness of the organ, which may be measured by MRI or ultrasound. Among ultrasound-based technologies, vibration-controlled transient elastography (VCTE) is more widely accepted and affordable although it may not be as accurate as MR elastography.13
In general, these elastographic tests are not readily accessible to most physicians outside hepatology specialty practices. Instead, blood test-based markers have been developed and widely recommended as the initial modality to assess liver fibrosis. Figure 1 represents a partial list of blood test-based markers. Traditionally, FIB-4 and NFS have been considered the most widely recommended by society guidelines. The AGA Pathway for evaluation of patients with NAFLD recommends first to apply the FIB-4 score and, in patients considered to be at intermediate risk of fibrosis for advanced fibrosis (stage 3 or 4, FIB-4 = 1.3-2.67), to assess liver stiffness by VCTE.14
More recently, the accumulating natural history data have highlighted the inflection in the risk of future outcomes coinciding with F2 and therapeutic trials that target patients with “at risk NASH,” thus more attention has been paid to the identification of patients with stage 2 (or higher). The steatosis-associated fibrosis estimator (SAFE) was developed for this specific purpose. The score has been validated in multiple data sets, in all of which SAFE outperformed FIB-4 and NFS (Figure 1). When the score was applied to assess overall survival in participants of the NHANES, patients with NAFLD deemed to be high risk (SAFE > 100) had significantly lower survival (37% Kaplan-Meier survival at 20 years), compared to those with intermediate (SAFE 0-100, 61% survival) and low (SAFE < 0, 86% survival). In comparison, the 20-year survival of subjects without NAFLD survival was 79%.15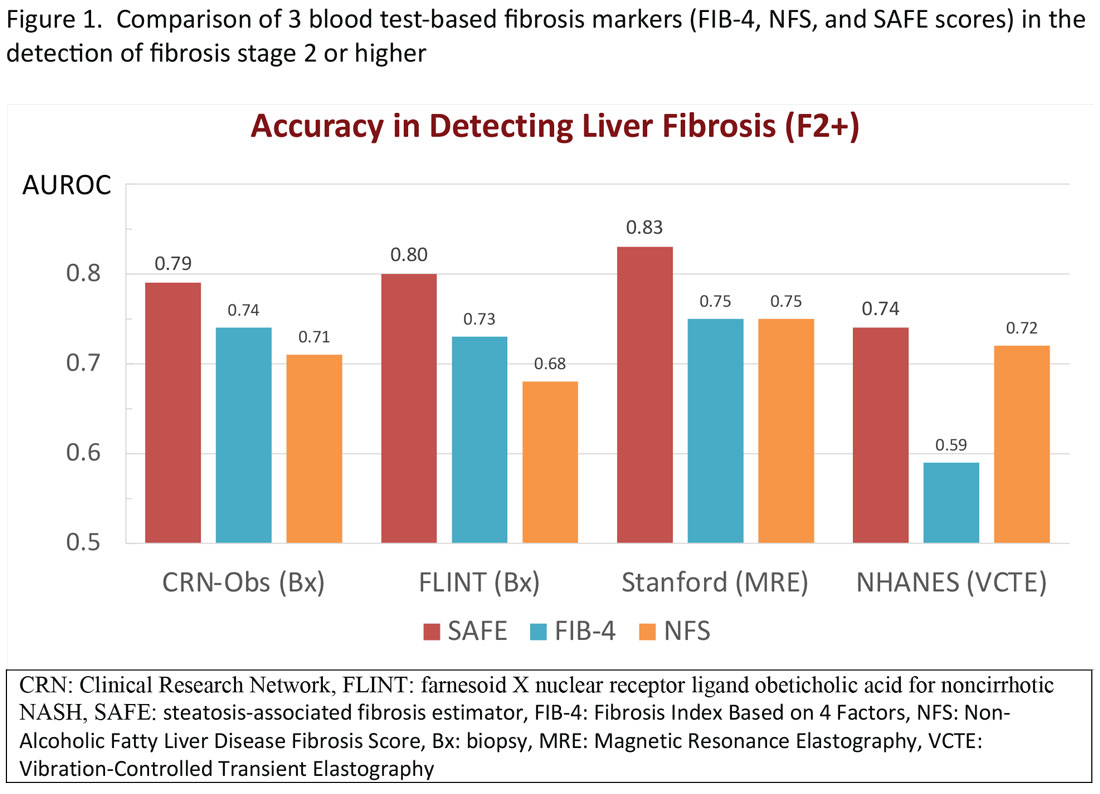
Regardless of the modality for initial stratification, it is widely accepted that mechanical elastography constitutes the next step in prognosticating the patient. In the AGA Pathway, liver stiffness of < 8 kPa is considered low risk, which corresponds in most analysis with lack of stage 2 fibrosis, whereas stiffness of > 12 kPa may be indicative of stage 3 or 4. These recommendations are consistent with those from the latest Baveno Consensus Conference (“Baveno 7”). Figure 2 expands on the so-called “rule of 5” from the consensus document and correlates liver stiffness (by VCTE) with progression of liver fibrosis as well as clinical presentation. For example, liver stiffness < 15 kPa is associated with a low risk of clinically significant portal hypertension (CSPH). Similarly, in patients with a normal platelet count (>150,000/mm3) and liver stiffness < 20 kPa, the probability of gastroesophageal varices is sufficiently low that a screening endoscopy may be avoided. On the other hand, liver stiffness > 25 kPa is associated with increasing risk of decompensated cirrhosis and portal hypertension.16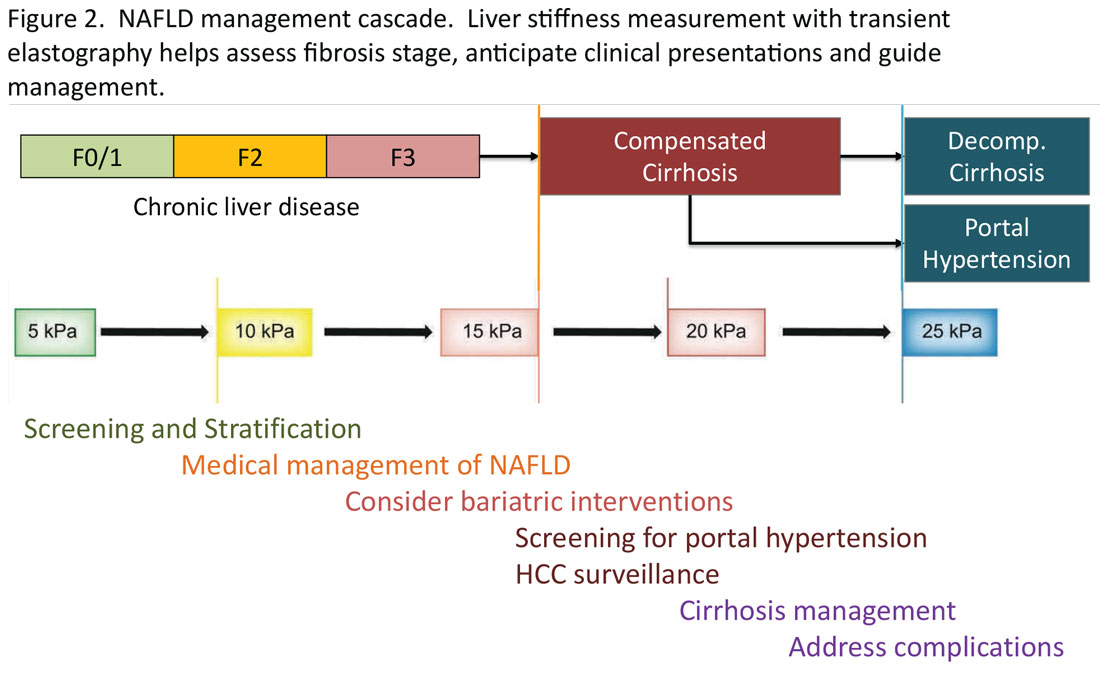
Partnership between primary care and specialty
The insights expressed in Figure 2 can be utilized to guide management decisions. In patients without evidence of liver fibrosis, emphasis may primarily be on screening, stratification and management of metabolic syndrome. For patients with evidence of incipient liver fibrosis, medical management of NAFLD needs to be implemented including lifestyle changes and pharmacological interventions as appropriate. For patients unresponsive to medical therapy, an endoscopic or surgical bariatric procedure should be considered. Management of patients with evidence of cirrhosis includes screening for portal hypertension, surveillance for HCC, medical management of cirrhosis, and finally, in suitable cases, referral for liver transplant evaluation. The reader is referred to the latest treatment guidelines for detailed discussion of these individual management modalities [ref, AGA and AASLD guidelines].14,17
Given the spectrum of management modalities needed to successfully manage patients with NAFLD, it is unrealistic to expect that hepatologists and gastroenterologists are able to manage the large number of patients with NAFLD. In general, clinical activities on the left side of the figure are in the domain of primary care providers, whereas management of patients with progressive liver fibrosis is conducted by the specialist. An important aspect of the overall management of these patients is risk management in terms of the metabolic syndrome, including cardiovascular risk reduction and diabetes management, as appropriate. Many patients with NAFLD are burdened with several comorbidities and likely to benefit from a multidisciplinary team consisting of primary care, endocrinology, preventive cardiology, pharmacy, nutrition/dietetics, social services, and addiction specialists, as well as hepatology and gastroenterology. Prospective, high-quality data to define these teams and their function are yet to be generated.
Conclusion
NAFLD is an important and increasing public health concern in the U.S. Once diagnosed, assessing liver fibrosis and evaluating the presence of the components of metabolic syndrome in these patients, constitute the key components in the care in terms of risk stratification, medical management, and referral decisions. Noninvasive tests have been increasingly utilized including liver stiffness measurements and various blood test-based indicators. For patients in specialty GI/hepatology care, transient elastography is a widely accepted tool, with which standardized recommendations may be made for screening, stratification, and medical and surgical interventions in patients with NAFLD.
Mai Sedki, MD, MPH, is a doctoral candidate at the University of California, San Francisco. W. Ray Kim, MD, is professor of medicine (gastroenterology and hepatology) at Stanford (Calif.) University. Address correspondence to: wrkim@stanford.edu. The authors disclosed no conflicts of interest. Twitter: @SedkiMD and @WRayKimMD.
References
1. Younossi ZM et al. Epidemiology of chronic liver diseases in the USA in the past three decades. Gut. 2020 Mar;69(3):564-8.
2. Lazo M et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Epidemiol. 2013 Jul 1;178(1):38-45.
3. Kim D et al. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology. 2013 Apr;57:1357-65.
4. Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002 Apr 18;346:1221-31.
5. Kim D et al. Changing trends in etiology-based annual mortality from chronic liver disease, from 2007 through 2016. Gastroenterology. 2018;155(4):1154-63.e3.
6. FastStats. Chronic Liver Disease and Cirrhosis. Centers for Disease Control and Prevention.
7. Rich NE et al. Racial and ethnic disparities in nonalcoholic fatty liver disease prevalence, severity, and outcomes in the United States: A systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2018;16(2):198-210. e2.
8. Coleman-Jensen A et al. Household food security in the United States in 2020 (ERR-298). Washington, DC: U.S. Department of Agriculture; Sep 2021.
9. Sanyal AJ et al. Prospective study of outcomes in adults with nonalcoholic fatty liver disease. N Engl J Med. 2021 Oct 21;385(17):1559-69.
10. Ng CH et al. Mortality outcomes by fibrosis stage in nonalcoholic fatty liver disease: A systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2023 Apr;21(4):931-9.e5.
11. Hagström H et al. Fibrosis stage but not NASH predicts mortality and time to development of severe liver disease in biopsy-proven NAFLD. J Hepatol. 2017;67(6):1265-73.
12. Rinella ME et al. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology. 2023 May 1;77(5):1797-835.
13. Singh S et al. Diagnostic performance of magnetic resonance elastography in staging liver fibrosis: A systematic review and meta-analysis of individual participant data. Clin Gastroenterol Hepatol. 2015 Mar;13(3):440-51.e6.
14. Kanwal F et al. Clinical Care Pathway for the risk stratification and management of patients with nonalcoholic fatty liver disease. Gastroenterology. 2021 Nov;161(5):1657-69.
15. Sripongpun P et al. The steatosis-associated fibrosis estimator (SAFE) score: A tool to detect low-risk NAFLD in primary care. .
16. de Franchis R et al. Baveno VII: Renewing consensus in portal hypertension. J Hepatol. 2022 Apr;76(4):959-74.
17. Rinella ME et al. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology. 2023 May 1;77(5):1797-835.
Burden of NAFLD in the U.S.
NAFLD is a manifestation of systemic metabolic abnormalities, including insulin resistance, dyslipidemia, central obesity, and hypertension. In this short review, we summarize data on the burden of NAFLD in the U.S. and its prognostic determinants and review what clinical and public health approaches may be needed to mitigating its impact.
Epidemiology of NAFLD
Worldwide, the prevalence of NAFLD is estimated at 6% to 35%, with biopsy-based studies reporting NASH in 3% to 5%.1 U.S. estimates for the prevalence of NAFLD range from 10% to 46%.2 In our own analysis of the National Health and Nutrition Examination Survey (NHANES) data, transient elastography-detected steatosis was found in 36%, which projected to a minimum of 73 million American adults.3
NAFLD represents a spectrum of disorders ranging from simple steatosis to nonalcoholic steatohepatitis (NASH), the latter leading, in some cases, to progressive hepatic fibrosis and cirrhosis.4 Out of a large number of subjects with NAFLD, the proportions of NASH patients that develop severe liver problems such as end-stage liver disease (ESLD) or hepatocellular carcinoma (HCC) are progressively smaller. For example, we recently reported that less than 2,000 liver-related deaths are attributable to NAFLD in the U.S. per annum, which corresponds to a crude case fatality rate of < 0.005% per year.5
According to the Centers for Disease Control and Prevention (CDC), there have been substantial increases in liver-related deaths over the last 2 decades. Mortality from liver disease including hepatobiliary cancers more than doubled from 41,966 deaths (including 15,321 women and 26,645 men) in 2000 to 85,884 deaths (33,000 women and 52,884 men) in 2020. The proportion of deaths specifically attributed to NAFLD among liver-related deaths was miniscule in 2000, accounting for 1.1% in women and 0.7% in men. By 2020, the proportions increased several folds in both sexes (7.4% in women and 2.7% in men).6 Moreover, it is likely that a substantial portion of deaths from chronic liver disease from unknown causes (“cryptogenic”) are likely end-stage NAFLD, making these figures underestimates of the true impact of NAFLD in the U.S.
From a comparative epidemiologic perspective, there are significant racial and ethnic and socioeconomic disparities in NAFLD prevalence, wherein Hispanic persons and individuals experiencing food insecurity – independent of poverty status, education level, race and ethnicity – are disproportionately more affected by NAFLD.7,8 Furthermore, these disparities persist when examining long-term complications of NAFLD, such as developing HCC.
Prognosis in NAFLD: NASH versus fibrosis
Given the enormous prevalence and increasing public health burden of NAFLD, systematic interventions to mitigate its impact are urgently needed. Clearly, patients who already have developed advanced liver disease need to be directed to specialty care so the disease progression may be halted and complications of ESLD may be prevented or managed. On the other hand, in order to mitigate the future impact of ESLD, prompt identification of at-risk patients and proactive interventions to improve liver health are needed.
In the assessment of disease progression, prior data have shown that the presence of NASH and increasing stages of liver fibrosis are important predictors of disease progression. Fibrosis is a component of NASH, while NASH is thought to be a prerequisite for fibrosis. In a prospective, multicenter follow-up study of NAFLD evaluated by liver biopsies (n = 1,773), over a median follow-up of 4 years, 37 (2%) developed hepatic decompensation, while 47 (3%) died from any cause, which included ESLD (n = 12), cardiovascular complications (n = 4), and malignancies (n = 12), including HCC (n = 9).9 It is not entirely surprising that advanced fibrosis and cirrhosis was highly associated with the development of hepatic decompensation. In their multivariable analysis, patients with F3-4 had a 13.8-fold (95% confidence interval [CI]: 4.6, 41.0) increase in the hazard of reaching a MELD score of 15 compared to those with F0-2. In addition, all-cause mortality was 17.2-fold (95% CI: 5.2, 56.6) higher with F3-4 compared to F0-2.
These data have been borne out by a larger body of literature on the topic. In a recent meta-analysis assessing the relation between liver fibrosis and future mortality, which included 17,301 subjects with NAFLD, patients with at least stage 2 fibrosis experience a significantly increased risk of liver-related and overall mortality, a trend that accelerates at higher fibrosis stages.10 These point to liver fibrosis as the singular determinant of long-term prognosis, in comparison, for example, with the diagnosis of NASH. Hagström conducted a retrospective cohort study of patients with biopsy-proven NAFLD in Sweden. When fibrosis stage and histological diagnosis of NASH were considered together, NASH did not have an impact on overall mortality (hazard ratio [HR] = 0.83, P = .29) or liver morbidity (HR = 0.62, P = .25).11
On an individual level, factors that affect fibrosis progression are not as well studied. It is commonly believed that demographic factors (e.g., age, sex and race), genetic polymorphisms (e.g., PNPLA3, TM6SF2), clinical comorbidities (e.g., obesity, DM, and sleep apnea), and environmental factors (e.g., smoking) may accelerate fibrosis and disease outcomes, although prospective data are sparse to estimate the extent these individual variables affect progression.12 Recent guidelines remain silent about whether and how these data may be incorporated in screening for NAFLD in the population.
Assessment of liver fibrosis
The traditional means to detect liver fibrosis is liver histology, which also assesses steatosis, individual components of NASH and, often importantly, other concomitant liver pathology. In reality, however, liver biopsies have several limitations including the risk of complications, patient discomfort, economic costs, and sampling variability. Increasingly, “noninvasive” methods have been used to estimate liver fibrosis in patients with NAFLD. Liver elastography estimates the physical stiffness of the organ, which may be measured by MRI or ultrasound. Among ultrasound-based technologies, vibration-controlled transient elastography (VCTE) is more widely accepted and affordable although it may not be as accurate as MR elastography.13
In general, these elastographic tests are not readily accessible to most physicians outside hepatology specialty practices. Instead, blood test-based markers have been developed and widely recommended as the initial modality to assess liver fibrosis. Figure 1 represents a partial list of blood test-based markers. Traditionally, FIB-4 and NFS have been considered the most widely recommended by society guidelines. The AGA Pathway for evaluation of patients with NAFLD recommends first to apply the FIB-4 score and, in patients considered to be at intermediate risk of fibrosis for advanced fibrosis (stage 3 or 4, FIB-4 = 1.3-2.67), to assess liver stiffness by VCTE.14
More recently, the accumulating natural history data have highlighted the inflection in the risk of future outcomes coinciding with F2 and therapeutic trials that target patients with “at risk NASH,” thus more attention has been paid to the identification of patients with stage 2 (or higher). The steatosis-associated fibrosis estimator (SAFE) was developed for this specific purpose. The score has been validated in multiple data sets, in all of which SAFE outperformed FIB-4 and NFS (Figure 1). When the score was applied to assess overall survival in participants of the NHANES, patients with NAFLD deemed to be high risk (SAFE > 100) had significantly lower survival (37% Kaplan-Meier survival at 20 years), compared to those with intermediate (SAFE 0-100, 61% survival) and low (SAFE < 0, 86% survival). In comparison, the 20-year survival of subjects without NAFLD survival was 79%.15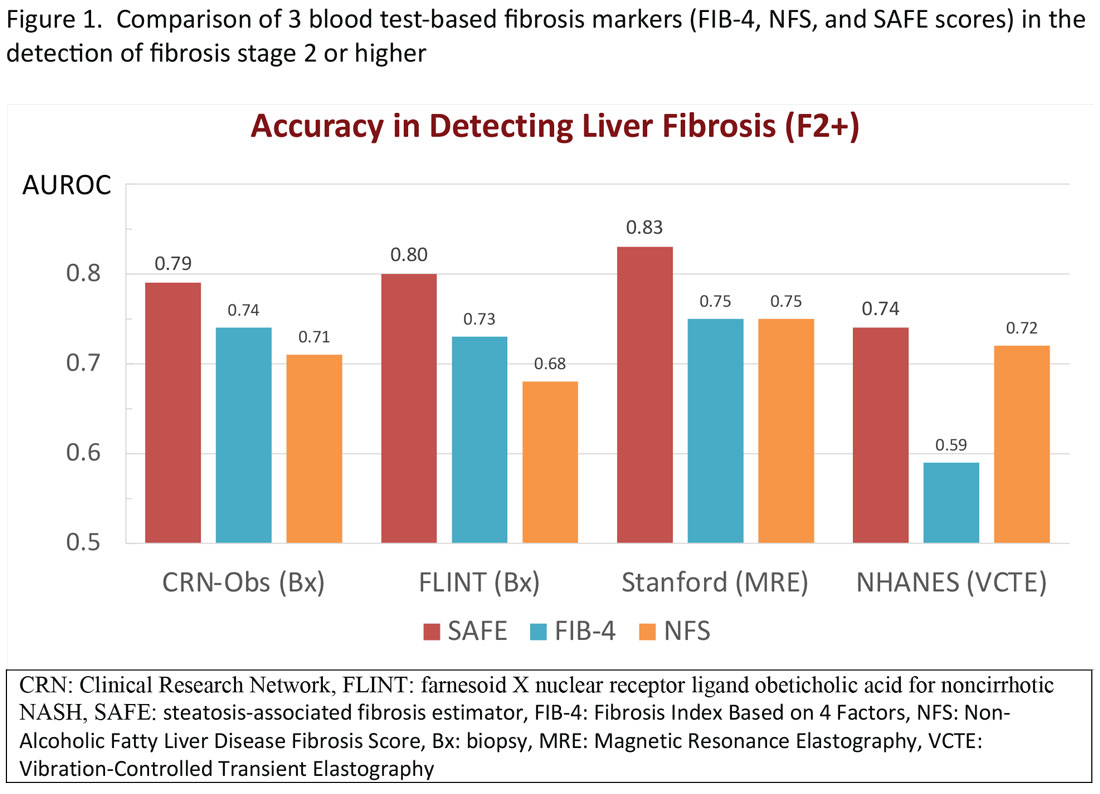
Regardless of the modality for initial stratification, it is widely accepted that mechanical elastography constitutes the next step in prognosticating the patient. In the AGA Pathway, liver stiffness of < 8 kPa is considered low risk, which corresponds in most analysis with lack of stage 2 fibrosis, whereas stiffness of > 12 kPa may be indicative of stage 3 or 4. These recommendations are consistent with those from the latest Baveno Consensus Conference (“Baveno 7”). Figure 2 expands on the so-called “rule of 5” from the consensus document and correlates liver stiffness (by VCTE) with progression of liver fibrosis as well as clinical presentation. For example, liver stiffness < 15 kPa is associated with a low risk of clinically significant portal hypertension (CSPH). Similarly, in patients with a normal platelet count (>150,000/mm3) and liver stiffness < 20 kPa, the probability of gastroesophageal varices is sufficiently low that a screening endoscopy may be avoided. On the other hand, liver stiffness > 25 kPa is associated with increasing risk of decompensated cirrhosis and portal hypertension.16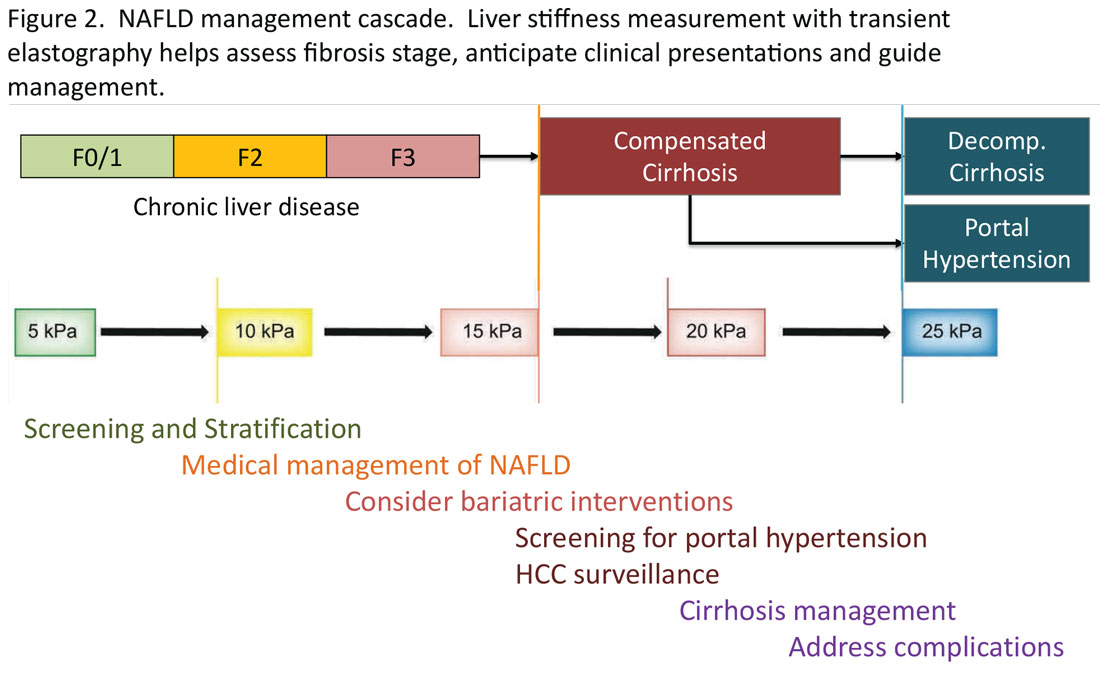
Partnership between primary care and specialty
The insights expressed in Figure 2 can be utilized to guide management decisions. In patients without evidence of liver fibrosis, emphasis may primarily be on screening, stratification and management of metabolic syndrome. For patients with evidence of incipient liver fibrosis, medical management of NAFLD needs to be implemented including lifestyle changes and pharmacological interventions as appropriate. For patients unresponsive to medical therapy, an endoscopic or surgical bariatric procedure should be considered. Management of patients with evidence of cirrhosis includes screening for portal hypertension, surveillance for HCC, medical management of cirrhosis, and finally, in suitable cases, referral for liver transplant evaluation. The reader is referred to the latest treatment guidelines for detailed discussion of these individual management modalities [ref, AGA and AASLD guidelines].14,17
Given the spectrum of management modalities needed to successfully manage patients with NAFLD, it is unrealistic to expect that hepatologists and gastroenterologists are able to manage the large number of patients with NAFLD. In general, clinical activities on the left side of the figure are in the domain of primary care providers, whereas management of patients with progressive liver fibrosis is conducted by the specialist. An important aspect of the overall management of these patients is risk management in terms of the metabolic syndrome, including cardiovascular risk reduction and diabetes management, as appropriate. Many patients with NAFLD are burdened with several comorbidities and likely to benefit from a multidisciplinary team consisting of primary care, endocrinology, preventive cardiology, pharmacy, nutrition/dietetics, social services, and addiction specialists, as well as hepatology and gastroenterology. Prospective, high-quality data to define these teams and their function are yet to be generated.
Conclusion
NAFLD is an important and increasing public health concern in the U.S. Once diagnosed, assessing liver fibrosis and evaluating the presence of the components of metabolic syndrome in these patients, constitute the key components in the care in terms of risk stratification, medical management, and referral decisions. Noninvasive tests have been increasingly utilized including liver stiffness measurements and various blood test-based indicators. For patients in specialty GI/hepatology care, transient elastography is a widely accepted tool, with which standardized recommendations may be made for screening, stratification, and medical and surgical interventions in patients with NAFLD.
Mai Sedki, MD, MPH, is a doctoral candidate at the University of California, San Francisco. W. Ray Kim, MD, is professor of medicine (gastroenterology and hepatology) at Stanford (Calif.) University. Address correspondence to: wrkim@stanford.edu. The authors disclosed no conflicts of interest. Twitter: @SedkiMD and @WRayKimMD.
References
1. Younossi ZM et al. Epidemiology of chronic liver diseases in the USA in the past three decades. Gut. 2020 Mar;69(3):564-8.
2. Lazo M et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Epidemiol. 2013 Jul 1;178(1):38-45.
3. Kim D et al. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology. 2013 Apr;57:1357-65.
4. Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002 Apr 18;346:1221-31.
5. Kim D et al. Changing trends in etiology-based annual mortality from chronic liver disease, from 2007 through 2016. Gastroenterology. 2018;155(4):1154-63.e3.
6. FastStats. Chronic Liver Disease and Cirrhosis. Centers for Disease Control and Prevention.
7. Rich NE et al. Racial and ethnic disparities in nonalcoholic fatty liver disease prevalence, severity, and outcomes in the United States: A systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2018;16(2):198-210. e2.
8. Coleman-Jensen A et al. Household food security in the United States in 2020 (ERR-298). Washington, DC: U.S. Department of Agriculture; Sep 2021.
9. Sanyal AJ et al. Prospective study of outcomes in adults with nonalcoholic fatty liver disease. N Engl J Med. 2021 Oct 21;385(17):1559-69.
10. Ng CH et al. Mortality outcomes by fibrosis stage in nonalcoholic fatty liver disease: A systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2023 Apr;21(4):931-9.e5.
11. Hagström H et al. Fibrosis stage but not NASH predicts mortality and time to development of severe liver disease in biopsy-proven NAFLD. J Hepatol. 2017;67(6):1265-73.
12. Rinella ME et al. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology. 2023 May 1;77(5):1797-835.
13. Singh S et al. Diagnostic performance of magnetic resonance elastography in staging liver fibrosis: A systematic review and meta-analysis of individual participant data. Clin Gastroenterol Hepatol. 2015 Mar;13(3):440-51.e6.
14. Kanwal F et al. Clinical Care Pathway for the risk stratification and management of patients with nonalcoholic fatty liver disease. Gastroenterology. 2021 Nov;161(5):1657-69.
15. Sripongpun P et al. The steatosis-associated fibrosis estimator (SAFE) score: A tool to detect low-risk NAFLD in primary care. .
16. de Franchis R et al. Baveno VII: Renewing consensus in portal hypertension. J Hepatol. 2022 Apr;76(4):959-74.
17. Rinella ME et al. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology. 2023 May 1;77(5):1797-835.
Burden of NAFLD in the U.S.
NAFLD is a manifestation of systemic metabolic abnormalities, including insulin resistance, dyslipidemia, central obesity, and hypertension. In this short review, we summarize data on the burden of NAFLD in the U.S. and its prognostic determinants and review what clinical and public health approaches may be needed to mitigating its impact.
Epidemiology of NAFLD
Worldwide, the prevalence of NAFLD is estimated at 6% to 35%, with biopsy-based studies reporting NASH in 3% to 5%.1 U.S. estimates for the prevalence of NAFLD range from 10% to 46%.2 In our own analysis of the National Health and Nutrition Examination Survey (NHANES) data, transient elastography-detected steatosis was found in 36%, which projected to a minimum of 73 million American adults.3
NAFLD represents a spectrum of disorders ranging from simple steatosis to nonalcoholic steatohepatitis (NASH), the latter leading, in some cases, to progressive hepatic fibrosis and cirrhosis.4 Out of a large number of subjects with NAFLD, the proportions of NASH patients that develop severe liver problems such as end-stage liver disease (ESLD) or hepatocellular carcinoma (HCC) are progressively smaller. For example, we recently reported that less than 2,000 liver-related deaths are attributable to NAFLD in the U.S. per annum, which corresponds to a crude case fatality rate of < 0.005% per year.5
According to the Centers for Disease Control and Prevention (CDC), there have been substantial increases in liver-related deaths over the last 2 decades. Mortality from liver disease including hepatobiliary cancers more than doubled from 41,966 deaths (including 15,321 women and 26,645 men) in 2000 to 85,884 deaths (33,000 women and 52,884 men) in 2020. The proportion of deaths specifically attributed to NAFLD among liver-related deaths was miniscule in 2000, accounting for 1.1% in women and 0.7% in men. By 2020, the proportions increased several folds in both sexes (7.4% in women and 2.7% in men).6 Moreover, it is likely that a substantial portion of deaths from chronic liver disease from unknown causes (“cryptogenic”) are likely end-stage NAFLD, making these figures underestimates of the true impact of NAFLD in the U.S.
From a comparative epidemiologic perspective, there are significant racial and ethnic and socioeconomic disparities in NAFLD prevalence, wherein Hispanic persons and individuals experiencing food insecurity – independent of poverty status, education level, race and ethnicity – are disproportionately more affected by NAFLD.7,8 Furthermore, these disparities persist when examining long-term complications of NAFLD, such as developing HCC.
Prognosis in NAFLD: NASH versus fibrosis
Given the enormous prevalence and increasing public health burden of NAFLD, systematic interventions to mitigate its impact are urgently needed. Clearly, patients who already have developed advanced liver disease need to be directed to specialty care so the disease progression may be halted and complications of ESLD may be prevented or managed. On the other hand, in order to mitigate the future impact of ESLD, prompt identification of at-risk patients and proactive interventions to improve liver health are needed.
In the assessment of disease progression, prior data have shown that the presence of NASH and increasing stages of liver fibrosis are important predictors of disease progression. Fibrosis is a component of NASH, while NASH is thought to be a prerequisite for fibrosis. In a prospective, multicenter follow-up study of NAFLD evaluated by liver biopsies (n = 1,773), over a median follow-up of 4 years, 37 (2%) developed hepatic decompensation, while 47 (3%) died from any cause, which included ESLD (n = 12), cardiovascular complications (n = 4), and malignancies (n = 12), including HCC (n = 9).9 It is not entirely surprising that advanced fibrosis and cirrhosis was highly associated with the development of hepatic decompensation. In their multivariable analysis, patients with F3-4 had a 13.8-fold (95% confidence interval [CI]: 4.6, 41.0) increase in the hazard of reaching a MELD score of 15 compared to those with F0-2. In addition, all-cause mortality was 17.2-fold (95% CI: 5.2, 56.6) higher with F3-4 compared to F0-2.
These data have been borne out by a larger body of literature on the topic. In a recent meta-analysis assessing the relation between liver fibrosis and future mortality, which included 17,301 subjects with NAFLD, patients with at least stage 2 fibrosis experience a significantly increased risk of liver-related and overall mortality, a trend that accelerates at higher fibrosis stages.10 These point to liver fibrosis as the singular determinant of long-term prognosis, in comparison, for example, with the diagnosis of NASH. Hagström conducted a retrospective cohort study of patients with biopsy-proven NAFLD in Sweden. When fibrosis stage and histological diagnosis of NASH were considered together, NASH did not have an impact on overall mortality (hazard ratio [HR] = 0.83, P = .29) or liver morbidity (HR = 0.62, P = .25).11
On an individual level, factors that affect fibrosis progression are not as well studied. It is commonly believed that demographic factors (e.g., age, sex and race), genetic polymorphisms (e.g., PNPLA3, TM6SF2), clinical comorbidities (e.g., obesity, DM, and sleep apnea), and environmental factors (e.g., smoking) may accelerate fibrosis and disease outcomes, although prospective data are sparse to estimate the extent these individual variables affect progression.12 Recent guidelines remain silent about whether and how these data may be incorporated in screening for NAFLD in the population.
Assessment of liver fibrosis
The traditional means to detect liver fibrosis is liver histology, which also assesses steatosis, individual components of NASH and, often importantly, other concomitant liver pathology. In reality, however, liver biopsies have several limitations including the risk of complications, patient discomfort, economic costs, and sampling variability. Increasingly, “noninvasive” methods have been used to estimate liver fibrosis in patients with NAFLD. Liver elastography estimates the physical stiffness of the organ, which may be measured by MRI or ultrasound. Among ultrasound-based technologies, vibration-controlled transient elastography (VCTE) is more widely accepted and affordable although it may not be as accurate as MR elastography.13
In general, these elastographic tests are not readily accessible to most physicians outside hepatology specialty practices. Instead, blood test-based markers have been developed and widely recommended as the initial modality to assess liver fibrosis. Figure 1 represents a partial list of blood test-based markers. Traditionally, FIB-4 and NFS have been considered the most widely recommended by society guidelines. The AGA Pathway for evaluation of patients with NAFLD recommends first to apply the FIB-4 score and, in patients considered to be at intermediate risk of fibrosis for advanced fibrosis (stage 3 or 4, FIB-4 = 1.3-2.67), to assess liver stiffness by VCTE.14
More recently, the accumulating natural history data have highlighted the inflection in the risk of future outcomes coinciding with F2 and therapeutic trials that target patients with “at risk NASH,” thus more attention has been paid to the identification of patients with stage 2 (or higher). The steatosis-associated fibrosis estimator (SAFE) was developed for this specific purpose. The score has been validated in multiple data sets, in all of which SAFE outperformed FIB-4 and NFS (Figure 1). When the score was applied to assess overall survival in participants of the NHANES, patients with NAFLD deemed to be high risk (SAFE > 100) had significantly lower survival (37% Kaplan-Meier survival at 20 years), compared to those with intermediate (SAFE 0-100, 61% survival) and low (SAFE < 0, 86% survival). In comparison, the 20-year survival of subjects without NAFLD survival was 79%.15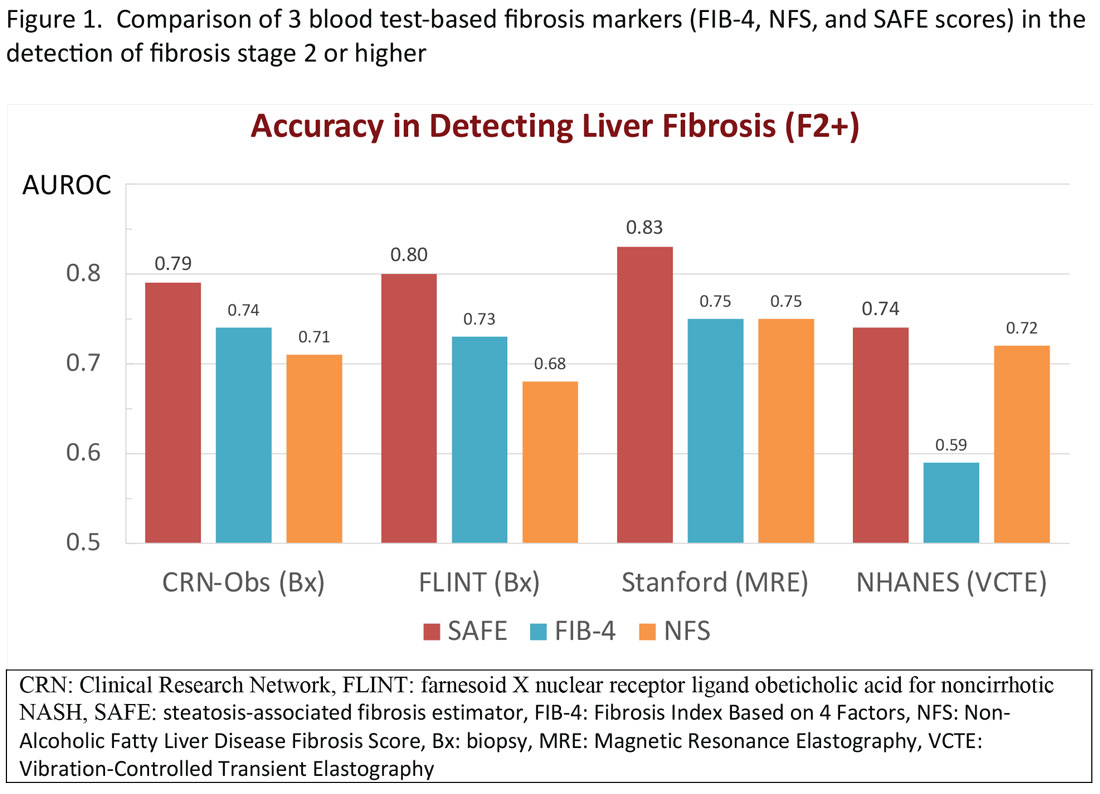
Regardless of the modality for initial stratification, it is widely accepted that mechanical elastography constitutes the next step in prognosticating the patient. In the AGA Pathway, liver stiffness of < 8 kPa is considered low risk, which corresponds in most analysis with lack of stage 2 fibrosis, whereas stiffness of > 12 kPa may be indicative of stage 3 or 4. These recommendations are consistent with those from the latest Baveno Consensus Conference (“Baveno 7”). Figure 2 expands on the so-called “rule of 5” from the consensus document and correlates liver stiffness (by VCTE) with progression of liver fibrosis as well as clinical presentation. For example, liver stiffness < 15 kPa is associated with a low risk of clinically significant portal hypertension (CSPH). Similarly, in patients with a normal platelet count (>150,000/mm3) and liver stiffness < 20 kPa, the probability of gastroesophageal varices is sufficiently low that a screening endoscopy may be avoided. On the other hand, liver stiffness > 25 kPa is associated with increasing risk of decompensated cirrhosis and portal hypertension.16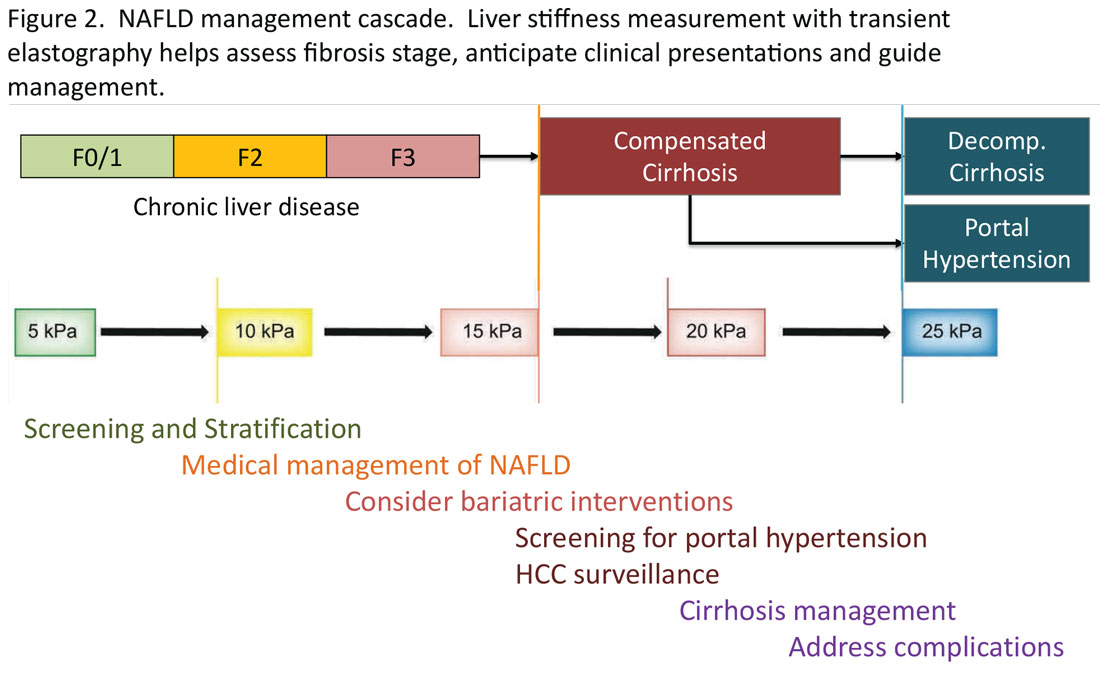
Partnership between primary care and specialty
The insights expressed in Figure 2 can be utilized to guide management decisions. In patients without evidence of liver fibrosis, emphasis may primarily be on screening, stratification and management of metabolic syndrome. For patients with evidence of incipient liver fibrosis, medical management of NAFLD needs to be implemented including lifestyle changes and pharmacological interventions as appropriate. For patients unresponsive to medical therapy, an endoscopic or surgical bariatric procedure should be considered. Management of patients with evidence of cirrhosis includes screening for portal hypertension, surveillance for HCC, medical management of cirrhosis, and finally, in suitable cases, referral for liver transplant evaluation. The reader is referred to the latest treatment guidelines for detailed discussion of these individual management modalities [ref, AGA and AASLD guidelines].14,17
Given the spectrum of management modalities needed to successfully manage patients with NAFLD, it is unrealistic to expect that hepatologists and gastroenterologists are able to manage the large number of patients with NAFLD. In general, clinical activities on the left side of the figure are in the domain of primary care providers, whereas management of patients with progressive liver fibrosis is conducted by the specialist. An important aspect of the overall management of these patients is risk management in terms of the metabolic syndrome, including cardiovascular risk reduction and diabetes management, as appropriate. Many patients with NAFLD are burdened with several comorbidities and likely to benefit from a multidisciplinary team consisting of primary care, endocrinology, preventive cardiology, pharmacy, nutrition/dietetics, social services, and addiction specialists, as well as hepatology and gastroenterology. Prospective, high-quality data to define these teams and their function are yet to be generated.
Conclusion
NAFLD is an important and increasing public health concern in the U.S. Once diagnosed, assessing liver fibrosis and evaluating the presence of the components of metabolic syndrome in these patients, constitute the key components in the care in terms of risk stratification, medical management, and referral decisions. Noninvasive tests have been increasingly utilized including liver stiffness measurements and various blood test-based indicators. For patients in specialty GI/hepatology care, transient elastography is a widely accepted tool, with which standardized recommendations may be made for screening, stratification, and medical and surgical interventions in patients with NAFLD.
Mai Sedki, MD, MPH, is a doctoral candidate at the University of California, San Francisco. W. Ray Kim, MD, is professor of medicine (gastroenterology and hepatology) at Stanford (Calif.) University. Address correspondence to: wrkim@stanford.edu. The authors disclosed no conflicts of interest. Twitter: @SedkiMD and @WRayKimMD.
References
1. Younossi ZM et al. Epidemiology of chronic liver diseases in the USA in the past three decades. Gut. 2020 Mar;69(3):564-8.
2. Lazo M et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Epidemiol. 2013 Jul 1;178(1):38-45.
3. Kim D et al. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology. 2013 Apr;57:1357-65.
4. Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002 Apr 18;346:1221-31.
5. Kim D et al. Changing trends in etiology-based annual mortality from chronic liver disease, from 2007 through 2016. Gastroenterology. 2018;155(4):1154-63.e3.
6. FastStats. Chronic Liver Disease and Cirrhosis. Centers for Disease Control and Prevention.
7. Rich NE et al. Racial and ethnic disparities in nonalcoholic fatty liver disease prevalence, severity, and outcomes in the United States: A systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2018;16(2):198-210. e2.
8. Coleman-Jensen A et al. Household food security in the United States in 2020 (ERR-298). Washington, DC: U.S. Department of Agriculture; Sep 2021.
9. Sanyal AJ et al. Prospective study of outcomes in adults with nonalcoholic fatty liver disease. N Engl J Med. 2021 Oct 21;385(17):1559-69.
10. Ng CH et al. Mortality outcomes by fibrosis stage in nonalcoholic fatty liver disease: A systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2023 Apr;21(4):931-9.e5.
11. Hagström H et al. Fibrosis stage but not NASH predicts mortality and time to development of severe liver disease in biopsy-proven NAFLD. J Hepatol. 2017;67(6):1265-73.
12. Rinella ME et al. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology. 2023 May 1;77(5):1797-835.
13. Singh S et al. Diagnostic performance of magnetic resonance elastography in staging liver fibrosis: A systematic review and meta-analysis of individual participant data. Clin Gastroenterol Hepatol. 2015 Mar;13(3):440-51.e6.
14. Kanwal F et al. Clinical Care Pathway for the risk stratification and management of patients with nonalcoholic fatty liver disease. Gastroenterology. 2021 Nov;161(5):1657-69.
15. Sripongpun P et al. The steatosis-associated fibrosis estimator (SAFE) score: A tool to detect low-risk NAFLD in primary care. .
16. de Franchis R et al. Baveno VII: Renewing consensus in portal hypertension. J Hepatol. 2022 Apr;76(4):959-74.
17. Rinella ME et al. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology. 2023 May 1;77(5):1797-835.
Transitions and growth
Dear friends,
This fall, I will also be starting my first position out of fellowship. I look forward to many opportunities and challenges to come.
This month in In Focus, Dr. Mai Sedki and Dr. W. Ray Kim unpack the nuances of assessing and risk-stratifying patients with nonalcoholic fatty liver disease by using non-invasive testing in daily practice. Beyond daily practice, it is important to know where our field is advancing to offer patients more options. In Short Clinical Reviews, Dr. Aileen Bui and Dr. James Buxbaum review how the field of endohepatology is expanding into endoscopic ultrasound–guided liver biopsies, portal pressure measurements, and interventions of gastric varices.
In our Early Career feature, Dr. Corlan Eboh, Dr. Victoria Jaeger, and Dr. Dawn Sears describe how gastroenterologists are uniquely positioned for burnout and what can be done to prevent and treat it, particularly among new and transitioning gastroenterologists. In post-COVID era, practices have experienced an increase in portal messages and other non-face-to-face patient care, which may be contributing burnout.
In our Finance section this month, Dr. Luis Nieto and Dr. Jami Kinnucan review the types of patient encounters and billing options to optimize your compensation for time spent.
In Private Practice Perspectives, Dr. David Ramsey discusses why he joined a private practice and how understanding your own goals and values can guide you to a good fit in different practice models. Lastly, Dr. Dan Kroch describes his unique journey in becoming a third-space endoscopist without an advanced fellowship year and why dedicated training is the future of advanced endoscopic resection and third-space endoscopy.
If you are interested in contributing or have ideas for future TNG topics, please contact me (jtrieu23@gmail.com), or Jillian Schweitzer (jschweitzer@gastro.org), managing editor of TNG.
Until next time, I leave you with a historical fun fact: The first endoscopic retrograde cholangiopancreatography (ERCP) was first performed by an obstetrician, Dr. William McCune in 1968, and achieved by taping an external accessory channel to a duodenoscope.
Yours truly,
Judy A Trieu, MD, MPH
Editor-in-Chief
Advanced Endoscopy Fellow
Division of Gastroenterology & Hepatology
University of North Carolina at Chapel Hill
Dear friends,
This fall, I will also be starting my first position out of fellowship. I look forward to many opportunities and challenges to come.
This month in In Focus, Dr. Mai Sedki and Dr. W. Ray Kim unpack the nuances of assessing and risk-stratifying patients with nonalcoholic fatty liver disease by using non-invasive testing in daily practice. Beyond daily practice, it is important to know where our field is advancing to offer patients more options. In Short Clinical Reviews, Dr. Aileen Bui and Dr. James Buxbaum review how the field of endohepatology is expanding into endoscopic ultrasound–guided liver biopsies, portal pressure measurements, and interventions of gastric varices.
In our Early Career feature, Dr. Corlan Eboh, Dr. Victoria Jaeger, and Dr. Dawn Sears describe how gastroenterologists are uniquely positioned for burnout and what can be done to prevent and treat it, particularly among new and transitioning gastroenterologists. In post-COVID era, practices have experienced an increase in portal messages and other non-face-to-face patient care, which may be contributing burnout.
In our Finance section this month, Dr. Luis Nieto and Dr. Jami Kinnucan review the types of patient encounters and billing options to optimize your compensation for time spent.
In Private Practice Perspectives, Dr. David Ramsey discusses why he joined a private practice and how understanding your own goals and values can guide you to a good fit in different practice models. Lastly, Dr. Dan Kroch describes his unique journey in becoming a third-space endoscopist without an advanced fellowship year and why dedicated training is the future of advanced endoscopic resection and third-space endoscopy.
If you are interested in contributing or have ideas for future TNG topics, please contact me (jtrieu23@gmail.com), or Jillian Schweitzer (jschweitzer@gastro.org), managing editor of TNG.
Until next time, I leave you with a historical fun fact: The first endoscopic retrograde cholangiopancreatography (ERCP) was first performed by an obstetrician, Dr. William McCune in 1968, and achieved by taping an external accessory channel to a duodenoscope.
Yours truly,
Judy A Trieu, MD, MPH
Editor-in-Chief
Advanced Endoscopy Fellow
Division of Gastroenterology & Hepatology
University of North Carolina at Chapel Hill
Dear friends,
This fall, I will also be starting my first position out of fellowship. I look forward to many opportunities and challenges to come.
This month in In Focus, Dr. Mai Sedki and Dr. W. Ray Kim unpack the nuances of assessing and risk-stratifying patients with nonalcoholic fatty liver disease by using non-invasive testing in daily practice. Beyond daily practice, it is important to know where our field is advancing to offer patients more options. In Short Clinical Reviews, Dr. Aileen Bui and Dr. James Buxbaum review how the field of endohepatology is expanding into endoscopic ultrasound–guided liver biopsies, portal pressure measurements, and interventions of gastric varices.
In our Early Career feature, Dr. Corlan Eboh, Dr. Victoria Jaeger, and Dr. Dawn Sears describe how gastroenterologists are uniquely positioned for burnout and what can be done to prevent and treat it, particularly among new and transitioning gastroenterologists. In post-COVID era, practices have experienced an increase in portal messages and other non-face-to-face patient care, which may be contributing burnout.
In our Finance section this month, Dr. Luis Nieto and Dr. Jami Kinnucan review the types of patient encounters and billing options to optimize your compensation for time spent.
In Private Practice Perspectives, Dr. David Ramsey discusses why he joined a private practice and how understanding your own goals and values can guide you to a good fit in different practice models. Lastly, Dr. Dan Kroch describes his unique journey in becoming a third-space endoscopist without an advanced fellowship year and why dedicated training is the future of advanced endoscopic resection and third-space endoscopy.
If you are interested in contributing or have ideas for future TNG topics, please contact me (jtrieu23@gmail.com), or Jillian Schweitzer (jschweitzer@gastro.org), managing editor of TNG.
Until next time, I leave you with a historical fun fact: The first endoscopic retrograde cholangiopancreatography (ERCP) was first performed by an obstetrician, Dr. William McCune in 1968, and achieved by taping an external accessory channel to a duodenoscope.
Yours truly,
Judy A Trieu, MD, MPH
Editor-in-Chief
Advanced Endoscopy Fellow
Division of Gastroenterology & Hepatology
University of North Carolina at Chapel Hill
New and transitioning gastroenterologists face burnout too
The field of gastroenterology can be challenging, both professionally and personally, leading to burnout, especially for new and transitioning gastroenterologists. Burnout is a state of emotional, physical, and mental exhaustion caused by prolonged or excessive stress.1 It is characterized by emotional fatigue, depersonalization, and a reduced sense of personal accomplishment.2,3 This condition can have severe consequences for physicians and their patients.
More than 50% of physicians report meeting the criteria for burnout, which is pervasive in all medical professions.3 Survey results of 7,288 U.S. physicians showed that burnout and dissatisfaction with work-life balance are significantly higher than among other working U.S. adults.3
The long and often irregular work hours expected of gastroenterologists significantly contribute to burnout within our field. The physically, intellectually, and technically demanding reality of managing complex patients and making high stakes decisions at all hours has far-reaching consequences.3 Most gastroenterologists work between 55 and 60 hours per week.4 This sharply contrasts the average 43-hour work week for full-time employees in the United States.5 Gastroenterologists may experience inaccurate perceptions of their commitment to patients, education, and their families based solely on time observed on each activity.4 Higher education and professional degrees usually protect against burnout.3 However, a degree in medicine (MD or DO) increases the burnout risk.3
New gastroenterologists are learning a wide range of intricate procedures and becoming proficient in diagnosing and managing gastrointestinal disorders. Extensive career demands often coincide with intense family-forming years, creating tension for a physician’s finite time and energy. The culture of medicine demanding “patients come first” while attempting to be fully human can sometimes feel irreconcilable, leading to feelings of inadequacy and anxiety.3 Gastroenterology training takes 3 years because of the complexity, danger, and need for thousands of procedures to gain proficiency and competence to recognize when complications occur. Oversight is ubiquitous during training, making this the ideal time to learn from mistakes and formulate lifelong habits of constant improvement. However, perfectionist tendencies and the Hippocratic Oath can create unrealistic self expectations.6 The risk of potential litigation, simply missing a diagnosis, or causing actual patient harm is never far from a proceduralist’s mind.
The diversity of gastroenterology requires high clinical knowledge, expertise, and emotional intelligence. Leading potentially intense end-of-life, cancer, fertility, and risk-factor discussions can be all-consuming. Keeping up with the latest research, treatments, and techniques in the field can be daunting. Furthermore, gastroenterologists spend many hours each day on electronic medical records. Constant re-documentation of interactions, seemingly endless prior authorizations, disability forms, referrals, and simply re-addressing patient and family concerns can feel low value. This uncompensated work also creates moral injury as it takes away from direct patient care.
Striking a work-life balance
New gastroenterologists are advised to find work-life balance. However, they are also plagued by the massive professional demands being constantly placed on them. The desire to find the mythical “balance” may create a mindset of significant sacrifices in their private lives as the only way to achieve professional successes.7 When gastroenterologists do not prioritize time for personal activities, including exercise, health checks, hobbies, rest, relaxation, family, and friends, they can get caught in a vicious cycle of continuing to feel poorly, resulting in overcompensating by working more in order to feel “accomplished.” The perfectionist pressure to maintain high productivity and patient satisfaction can also further contribute to burnout.
Gastroenterology burnout can severely affect physicians’ health status, job performance, and patient satisfaction.9 It may erode professionalism, negatively influence the quality of care, increase the risk of medical errors, and promote early retirement.3 Burnout may also correlate with adverse personal consequences for physicians, such as broken relationships, problematic alcohol use, and suicidal ideation.3 Physician burnout and professional satisfaction have strategic importance to health care organizations.10 Less burned-out physicians have patient panels with higher adherence and satisfaction with medical care.10 With more physicians becoming employees, there are opportunities for accountability of organizational leadership.10 Interestingly, healthy well-being or burnout is contagious from leaders to their teams.10 A 2015 study by Shanafelt et al. found that at the work unit level, 11% and 47% of the variation in burnout and satisfaction, correlated with the leader’s relative scores.10
So, what can be done to prevent and treat burnout in new and transitioning gastroenterologists? The gastroenterologist may implement several strategies. It is essential for individuals to take responsibility for their well-being and to prioritize self-care by setting boundaries, practicing stress management techniques, and seeking support from colleagues and mental health professionals when needed. 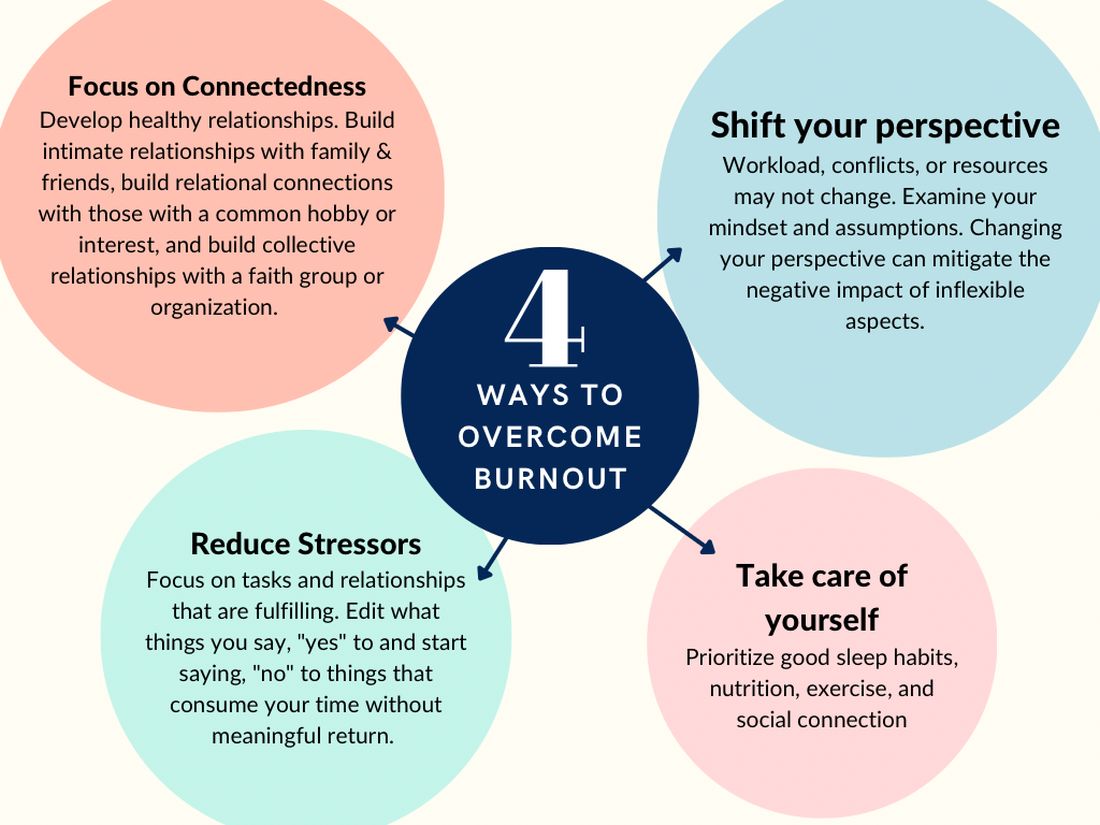
According to Dave et al. (2020), engagement in self-care practices such as mindfulness may offer advantages to gastroenterologists’ well-being and improved patient care.11
Burnout is not due to an individuals’ need for more resiliency. Instead, it developed from a systemic overwhelming of a health system near its breaking point. Recognizing that by 2033, there is a projected shortage of nearly 140,000 physicians in the United States, the U.S. Surgeon General, Dr. Vivek H. Murthy, issued a crisis advisory.12 This advisory highlights the urgent need to address the health worker burnout crisis nationwide that outlined “whole of society” efforts.12 Key components of the advisory on building a thriving health workforce included empowering health care workers, changing policies, reducing administrative burdens, prioritizing connections, and investing in our workforce.12
Provide access to mental health services
Institutions and practices would greatly benefit from providing access to mental health services, counseling, educational opportunities, potential mental health days, and mentorship programs. While the literature indicates that both individual-focused and structural or organizational strategies can result in clinically meaningful reductions in burnout among physicians, a meta-analysis revealed that corporate-led initiatives resulted in larger successes.12,13 Physicians who received support and resources from their institutions report lower levels of burnout and higher job satisfaction.2,3
New strategies to select and develop physician leaders who motivate, inspire, and effectively manage physicians may result in positive job satisfaction while decreasing employee burnout. Therefore, increased awareness of the importance of frontline leadership well-being and professional fulfillment of physicians working for a large health care organization is necessary.13 Robust and continual leadership training can ensure the entire team’s well-being, longevity, and success.13
Addressing the root causes of systemic burnout is imperative. Leadership could streamline administrative processes, optimize electronic medical records, delegate prior authorizations, and ensure staffing levels are appropriate to meet patient care demands. In a survey by Rao et al. (2017), the authors found that physicians who reported high levels of administrative burden and work overload were more likely to experience burnout.14
Institutions and practices should promote a culture of work-life balance by implementing flexible scheduling, promoting time off and vacation time, and encouraging regular exercise and healthy habits. The current compensation structure disincentivizes physicians from taking time away from patient care – this can be re-designed. Community and support mitigate burnout. Therefore, institutions and practices will benefit by intentionally providing opportunities for social connection and team building.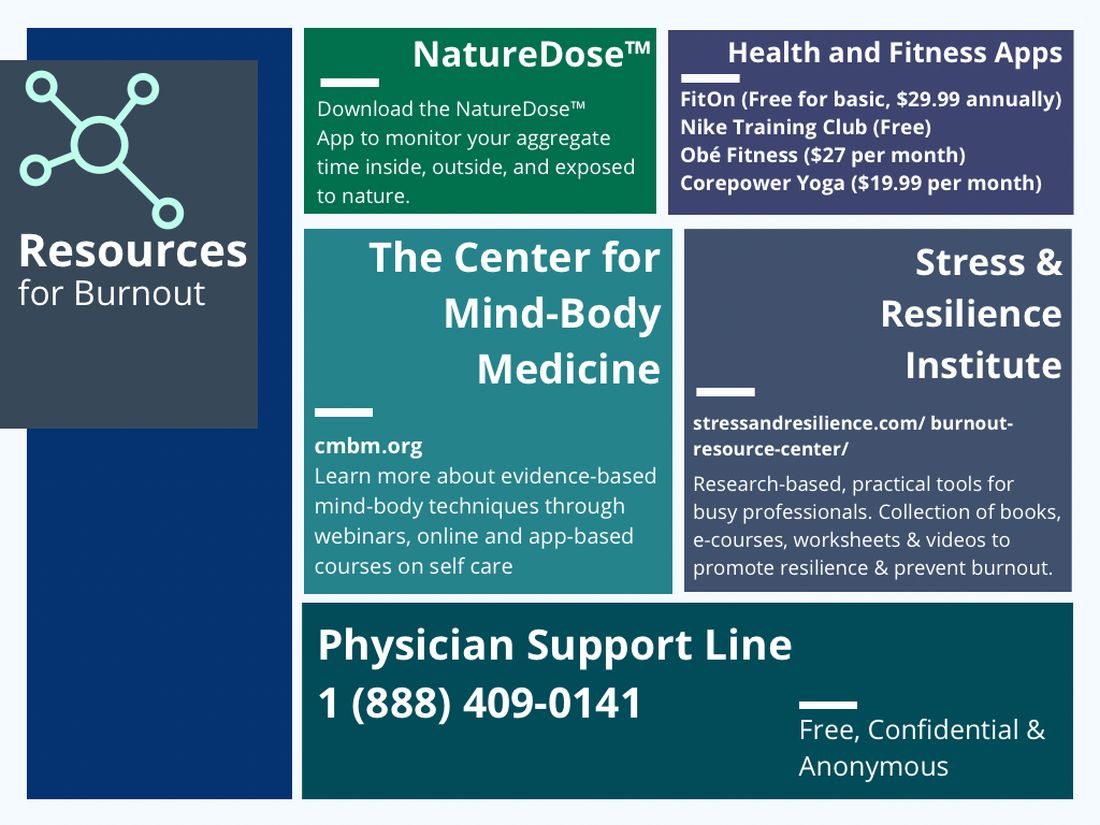
In reflection of the U.S. Surgeon General’s call for all of society to be part of the solution, we are pleased to see the Accreditation Council for Graduate Medical Education (ACGME) create mandatory 6 weeks of parental or caregiver leave for trainees.15 Continued positive pressure on overseeing agencies to minimize paperwork, preauthorizations, and non–value-added tasks to allow physicians to continue to provide medical services instead of documentation and auditing services would greatly positively impact all of health care. Therefore, communicating with legislators, policy makers, system leadership, and all health care societies to continue these improvements would be a wise use of time of resources.
In conclusion, burnout among new and transitioning gastroenterologists is a prevalent and concerning issue that can have severe consequences for both the individual and the health care system. Similar to the ergonomic considerations of being an endoscopist, A multifaceted approach to the well-being of all medical staff can help ensure the delivery of the highest quality patient care. By taking a proactive approach to preventing burnout, we can have a strong future for ourselves, our patients, and our profession.
Dr. Eboh is a gastroenterologist with Atrium Health, Charlotte, N.C.; Dr. Jaeger is with Baylor Scott & White Medical Center in Dallas. She is a gastroenterology fellow with Temple University Hospital, Philadelphia. Dr. Sears is clinical professor at Texas A&M University School of Medicine, and chief of gastroenterology at VA Central Texas Healthcare System. Dr. Sears owns GutGirlMD Consulting LLC, where she offers institutional and leadership coaching for physicians. Dr. Eboh on Instagram @Polyp.picker_EbohMD and on Twitter @PolypPicker_MD. Dr. Jaeger on Instagram @Doc.Tori.Fit and Twitter @DrToriJaeger. Dr. Sears is on Twitter @GutGirlMD.
References
1. Maslach C and Jackson S E. Maslach burnout inventory manual. Palo Alto, Calif: Consulting Psychologists Press, 1986.
2. Shanafelt TD et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015 Dec 12;90:1600-13.
3. Shanafelt TD et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012 Oct 8;172(18):1377-85.
4. Elta G. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
5. Gallup. Work and Workplace. 2023.
6. Gawande A. When doctors make mistakes. The New Yorker. 1999 Feb 1.
7. Buscarini E et al. Burnout among gastroenterologists: How to manage and prevent it. United European Gastroenterol J. 2020 Aug;8(7):832-4.
8. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016 Nov 5;388(10057):2272-81.
9. Adarkwah CC et al. Burnout and work satisfaction are differentially associated in gastroenterologists in Germany. F1000Res. 2022 Mar 30;11:368. doi: 10.12688/f1000research.110296.3. eCollection 2022.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015 Apr;90(4):432-40.
11. Umakant D et al. Mindfulness in gastroenterology training and practice: A personal perspective. Clin Exp Gastroenterol. 2020 Nov 4;13:497-502.
12. Murthy VH. Addressing Health Worker Burnout: The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. The U.S. Department of Health and Human Services: Office of the U.S. Surgeon General, 2022.
13. Panagioti M et al. Controlled interventions to reduce burnout in physicians: A systematic review and meta-analysis. JAMA Intern Med. 2017 Feb 1;177(2):195-205.
14. Rao SK et al. The impact of administrative burden on academic physicians: Results of a hospital-wide physician survey. Acad Med. 2017 Feb;92(2):237-43.
15. ACGME. ACME Institutional Requirements 2021.
The field of gastroenterology can be challenging, both professionally and personally, leading to burnout, especially for new and transitioning gastroenterologists. Burnout is a state of emotional, physical, and mental exhaustion caused by prolonged or excessive stress.1 It is characterized by emotional fatigue, depersonalization, and a reduced sense of personal accomplishment.2,3 This condition can have severe consequences for physicians and their patients.
More than 50% of physicians report meeting the criteria for burnout, which is pervasive in all medical professions.3 Survey results of 7,288 U.S. physicians showed that burnout and dissatisfaction with work-life balance are significantly higher than among other working U.S. adults.3
The long and often irregular work hours expected of gastroenterologists significantly contribute to burnout within our field. The physically, intellectually, and technically demanding reality of managing complex patients and making high stakes decisions at all hours has far-reaching consequences.3 Most gastroenterologists work between 55 and 60 hours per week.4 This sharply contrasts the average 43-hour work week for full-time employees in the United States.5 Gastroenterologists may experience inaccurate perceptions of their commitment to patients, education, and their families based solely on time observed on each activity.4 Higher education and professional degrees usually protect against burnout.3 However, a degree in medicine (MD or DO) increases the burnout risk.3
New gastroenterologists are learning a wide range of intricate procedures and becoming proficient in diagnosing and managing gastrointestinal disorders. Extensive career demands often coincide with intense family-forming years, creating tension for a physician’s finite time and energy. The culture of medicine demanding “patients come first” while attempting to be fully human can sometimes feel irreconcilable, leading to feelings of inadequacy and anxiety.3 Gastroenterology training takes 3 years because of the complexity, danger, and need for thousands of procedures to gain proficiency and competence to recognize when complications occur. Oversight is ubiquitous during training, making this the ideal time to learn from mistakes and formulate lifelong habits of constant improvement. However, perfectionist tendencies and the Hippocratic Oath can create unrealistic self expectations.6 The risk of potential litigation, simply missing a diagnosis, or causing actual patient harm is never far from a proceduralist’s mind.
The diversity of gastroenterology requires high clinical knowledge, expertise, and emotional intelligence. Leading potentially intense end-of-life, cancer, fertility, and risk-factor discussions can be all-consuming. Keeping up with the latest research, treatments, and techniques in the field can be daunting. Furthermore, gastroenterologists spend many hours each day on electronic medical records. Constant re-documentation of interactions, seemingly endless prior authorizations, disability forms, referrals, and simply re-addressing patient and family concerns can feel low value. This uncompensated work also creates moral injury as it takes away from direct patient care.
Striking a work-life balance
New gastroenterologists are advised to find work-life balance. However, they are also plagued by the massive professional demands being constantly placed on them. The desire to find the mythical “balance” may create a mindset of significant sacrifices in their private lives as the only way to achieve professional successes.7 When gastroenterologists do not prioritize time for personal activities, including exercise, health checks, hobbies, rest, relaxation, family, and friends, they can get caught in a vicious cycle of continuing to feel poorly, resulting in overcompensating by working more in order to feel “accomplished.” The perfectionist pressure to maintain high productivity and patient satisfaction can also further contribute to burnout.
Gastroenterology burnout can severely affect physicians’ health status, job performance, and patient satisfaction.9 It may erode professionalism, negatively influence the quality of care, increase the risk of medical errors, and promote early retirement.3 Burnout may also correlate with adverse personal consequences for physicians, such as broken relationships, problematic alcohol use, and suicidal ideation.3 Physician burnout and professional satisfaction have strategic importance to health care organizations.10 Less burned-out physicians have patient panels with higher adherence and satisfaction with medical care.10 With more physicians becoming employees, there are opportunities for accountability of organizational leadership.10 Interestingly, healthy well-being or burnout is contagious from leaders to their teams.10 A 2015 study by Shanafelt et al. found that at the work unit level, 11% and 47% of the variation in burnout and satisfaction, correlated with the leader’s relative scores.10
So, what can be done to prevent and treat burnout in new and transitioning gastroenterologists? The gastroenterologist may implement several strategies. It is essential for individuals to take responsibility for their well-being and to prioritize self-care by setting boundaries, practicing stress management techniques, and seeking support from colleagues and mental health professionals when needed. 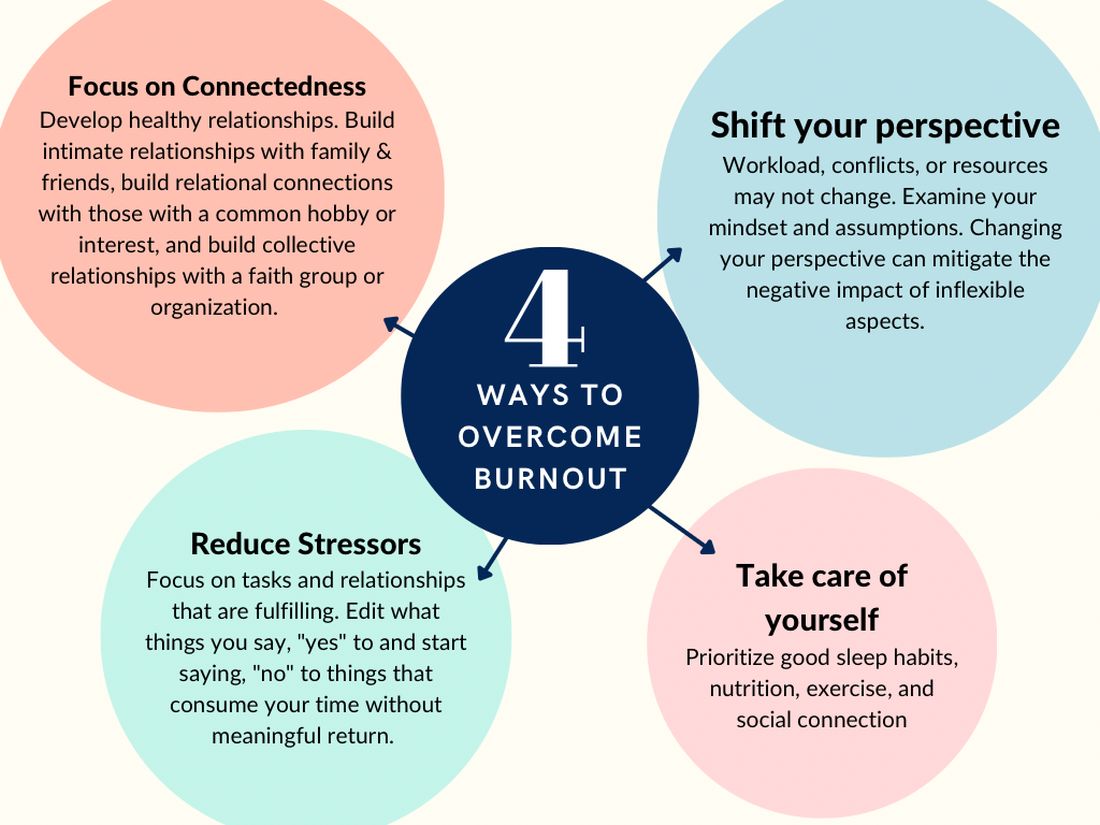
According to Dave et al. (2020), engagement in self-care practices such as mindfulness may offer advantages to gastroenterologists’ well-being and improved patient care.11
Burnout is not due to an individuals’ need for more resiliency. Instead, it developed from a systemic overwhelming of a health system near its breaking point. Recognizing that by 2033, there is a projected shortage of nearly 140,000 physicians in the United States, the U.S. Surgeon General, Dr. Vivek H. Murthy, issued a crisis advisory.12 This advisory highlights the urgent need to address the health worker burnout crisis nationwide that outlined “whole of society” efforts.12 Key components of the advisory on building a thriving health workforce included empowering health care workers, changing policies, reducing administrative burdens, prioritizing connections, and investing in our workforce.12
Provide access to mental health services
Institutions and practices would greatly benefit from providing access to mental health services, counseling, educational opportunities, potential mental health days, and mentorship programs. While the literature indicates that both individual-focused and structural or organizational strategies can result in clinically meaningful reductions in burnout among physicians, a meta-analysis revealed that corporate-led initiatives resulted in larger successes.12,13 Physicians who received support and resources from their institutions report lower levels of burnout and higher job satisfaction.2,3
New strategies to select and develop physician leaders who motivate, inspire, and effectively manage physicians may result in positive job satisfaction while decreasing employee burnout. Therefore, increased awareness of the importance of frontline leadership well-being and professional fulfillment of physicians working for a large health care organization is necessary.13 Robust and continual leadership training can ensure the entire team’s well-being, longevity, and success.13
Addressing the root causes of systemic burnout is imperative. Leadership could streamline administrative processes, optimize electronic medical records, delegate prior authorizations, and ensure staffing levels are appropriate to meet patient care demands. In a survey by Rao et al. (2017), the authors found that physicians who reported high levels of administrative burden and work overload were more likely to experience burnout.14
Institutions and practices should promote a culture of work-life balance by implementing flexible scheduling, promoting time off and vacation time, and encouraging regular exercise and healthy habits. The current compensation structure disincentivizes physicians from taking time away from patient care – this can be re-designed. Community and support mitigate burnout. Therefore, institutions and practices will benefit by intentionally providing opportunities for social connection and team building.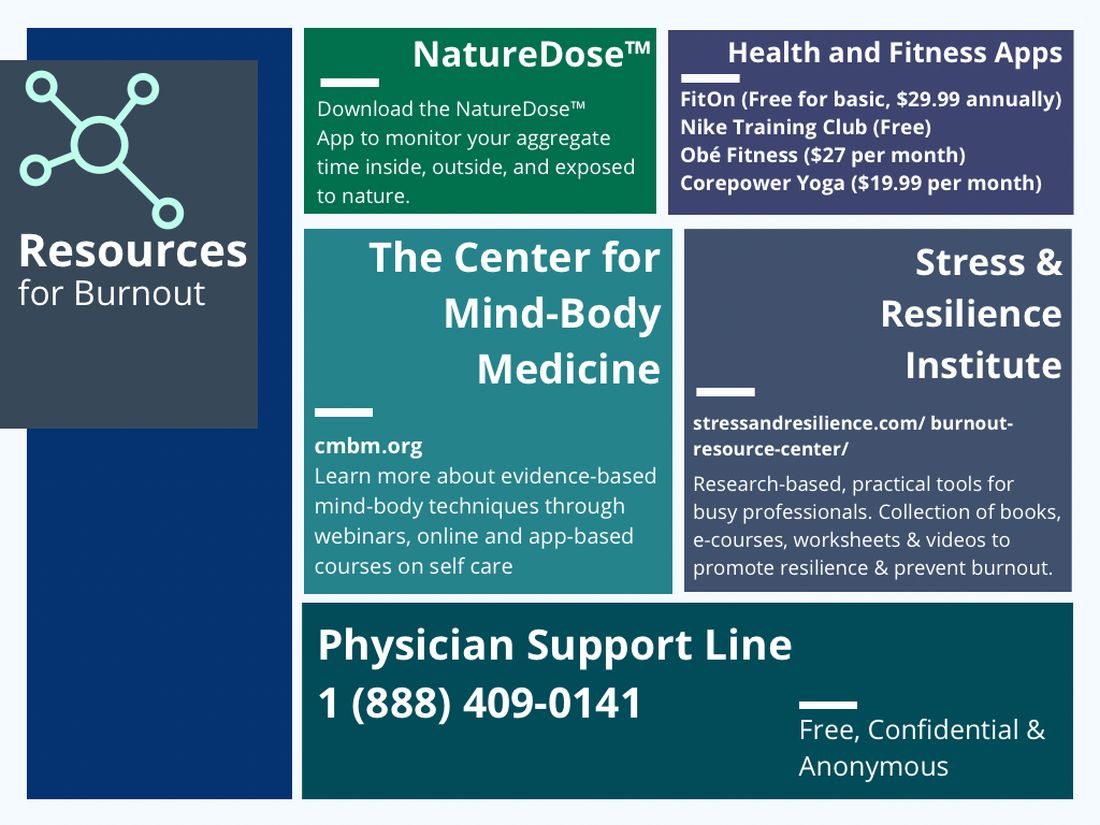
In reflection of the U.S. Surgeon General’s call for all of society to be part of the solution, we are pleased to see the Accreditation Council for Graduate Medical Education (ACGME) create mandatory 6 weeks of parental or caregiver leave for trainees.15 Continued positive pressure on overseeing agencies to minimize paperwork, preauthorizations, and non–value-added tasks to allow physicians to continue to provide medical services instead of documentation and auditing services would greatly positively impact all of health care. Therefore, communicating with legislators, policy makers, system leadership, and all health care societies to continue these improvements would be a wise use of time of resources.
In conclusion, burnout among new and transitioning gastroenterologists is a prevalent and concerning issue that can have severe consequences for both the individual and the health care system. Similar to the ergonomic considerations of being an endoscopist, A multifaceted approach to the well-being of all medical staff can help ensure the delivery of the highest quality patient care. By taking a proactive approach to preventing burnout, we can have a strong future for ourselves, our patients, and our profession.
Dr. Eboh is a gastroenterologist with Atrium Health, Charlotte, N.C.; Dr. Jaeger is with Baylor Scott & White Medical Center in Dallas. She is a gastroenterology fellow with Temple University Hospital, Philadelphia. Dr. Sears is clinical professor at Texas A&M University School of Medicine, and chief of gastroenterology at VA Central Texas Healthcare System. Dr. Sears owns GutGirlMD Consulting LLC, where she offers institutional and leadership coaching for physicians. Dr. Eboh on Instagram @Polyp.picker_EbohMD and on Twitter @PolypPicker_MD. Dr. Jaeger on Instagram @Doc.Tori.Fit and Twitter @DrToriJaeger. Dr. Sears is on Twitter @GutGirlMD.
References
1. Maslach C and Jackson S E. Maslach burnout inventory manual. Palo Alto, Calif: Consulting Psychologists Press, 1986.
2. Shanafelt TD et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015 Dec 12;90:1600-13.
3. Shanafelt TD et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012 Oct 8;172(18):1377-85.
4. Elta G. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
5. Gallup. Work and Workplace. 2023.
6. Gawande A. When doctors make mistakes. The New Yorker. 1999 Feb 1.
7. Buscarini E et al. Burnout among gastroenterologists: How to manage and prevent it. United European Gastroenterol J. 2020 Aug;8(7):832-4.
8. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016 Nov 5;388(10057):2272-81.
9. Adarkwah CC et al. Burnout and work satisfaction are differentially associated in gastroenterologists in Germany. F1000Res. 2022 Mar 30;11:368. doi: 10.12688/f1000research.110296.3. eCollection 2022.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015 Apr;90(4):432-40.
11. Umakant D et al. Mindfulness in gastroenterology training and practice: A personal perspective. Clin Exp Gastroenterol. 2020 Nov 4;13:497-502.
12. Murthy VH. Addressing Health Worker Burnout: The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. The U.S. Department of Health and Human Services: Office of the U.S. Surgeon General, 2022.
13. Panagioti M et al. Controlled interventions to reduce burnout in physicians: A systematic review and meta-analysis. JAMA Intern Med. 2017 Feb 1;177(2):195-205.
14. Rao SK et al. The impact of administrative burden on academic physicians: Results of a hospital-wide physician survey. Acad Med. 2017 Feb;92(2):237-43.
15. ACGME. ACME Institutional Requirements 2021.
The field of gastroenterology can be challenging, both professionally and personally, leading to burnout, especially for new and transitioning gastroenterologists. Burnout is a state of emotional, physical, and mental exhaustion caused by prolonged or excessive stress.1 It is characterized by emotional fatigue, depersonalization, and a reduced sense of personal accomplishment.2,3 This condition can have severe consequences for physicians and their patients.
More than 50% of physicians report meeting the criteria for burnout, which is pervasive in all medical professions.3 Survey results of 7,288 U.S. physicians showed that burnout and dissatisfaction with work-life balance are significantly higher than among other working U.S. adults.3
The long and often irregular work hours expected of gastroenterologists significantly contribute to burnout within our field. The physically, intellectually, and technically demanding reality of managing complex patients and making high stakes decisions at all hours has far-reaching consequences.3 Most gastroenterologists work between 55 and 60 hours per week.4 This sharply contrasts the average 43-hour work week for full-time employees in the United States.5 Gastroenterologists may experience inaccurate perceptions of their commitment to patients, education, and their families based solely on time observed on each activity.4 Higher education and professional degrees usually protect against burnout.3 However, a degree in medicine (MD or DO) increases the burnout risk.3
New gastroenterologists are learning a wide range of intricate procedures and becoming proficient in diagnosing and managing gastrointestinal disorders. Extensive career demands often coincide with intense family-forming years, creating tension for a physician’s finite time and energy. The culture of medicine demanding “patients come first” while attempting to be fully human can sometimes feel irreconcilable, leading to feelings of inadequacy and anxiety.3 Gastroenterology training takes 3 years because of the complexity, danger, and need for thousands of procedures to gain proficiency and competence to recognize when complications occur. Oversight is ubiquitous during training, making this the ideal time to learn from mistakes and formulate lifelong habits of constant improvement. However, perfectionist tendencies and the Hippocratic Oath can create unrealistic self expectations.6 The risk of potential litigation, simply missing a diagnosis, or causing actual patient harm is never far from a proceduralist’s mind.
The diversity of gastroenterology requires high clinical knowledge, expertise, and emotional intelligence. Leading potentially intense end-of-life, cancer, fertility, and risk-factor discussions can be all-consuming. Keeping up with the latest research, treatments, and techniques in the field can be daunting. Furthermore, gastroenterologists spend many hours each day on electronic medical records. Constant re-documentation of interactions, seemingly endless prior authorizations, disability forms, referrals, and simply re-addressing patient and family concerns can feel low value. This uncompensated work also creates moral injury as it takes away from direct patient care.
Striking a work-life balance
New gastroenterologists are advised to find work-life balance. However, they are also plagued by the massive professional demands being constantly placed on them. The desire to find the mythical “balance” may create a mindset of significant sacrifices in their private lives as the only way to achieve professional successes.7 When gastroenterologists do not prioritize time for personal activities, including exercise, health checks, hobbies, rest, relaxation, family, and friends, they can get caught in a vicious cycle of continuing to feel poorly, resulting in overcompensating by working more in order to feel “accomplished.” The perfectionist pressure to maintain high productivity and patient satisfaction can also further contribute to burnout.
Gastroenterology burnout can severely affect physicians’ health status, job performance, and patient satisfaction.9 It may erode professionalism, negatively influence the quality of care, increase the risk of medical errors, and promote early retirement.3 Burnout may also correlate with adverse personal consequences for physicians, such as broken relationships, problematic alcohol use, and suicidal ideation.3 Physician burnout and professional satisfaction have strategic importance to health care organizations.10 Less burned-out physicians have patient panels with higher adherence and satisfaction with medical care.10 With more physicians becoming employees, there are opportunities for accountability of organizational leadership.10 Interestingly, healthy well-being or burnout is contagious from leaders to their teams.10 A 2015 study by Shanafelt et al. found that at the work unit level, 11% and 47% of the variation in burnout and satisfaction, correlated with the leader’s relative scores.10
So, what can be done to prevent and treat burnout in new and transitioning gastroenterologists? The gastroenterologist may implement several strategies. It is essential for individuals to take responsibility for their well-being and to prioritize self-care by setting boundaries, practicing stress management techniques, and seeking support from colleagues and mental health professionals when needed. 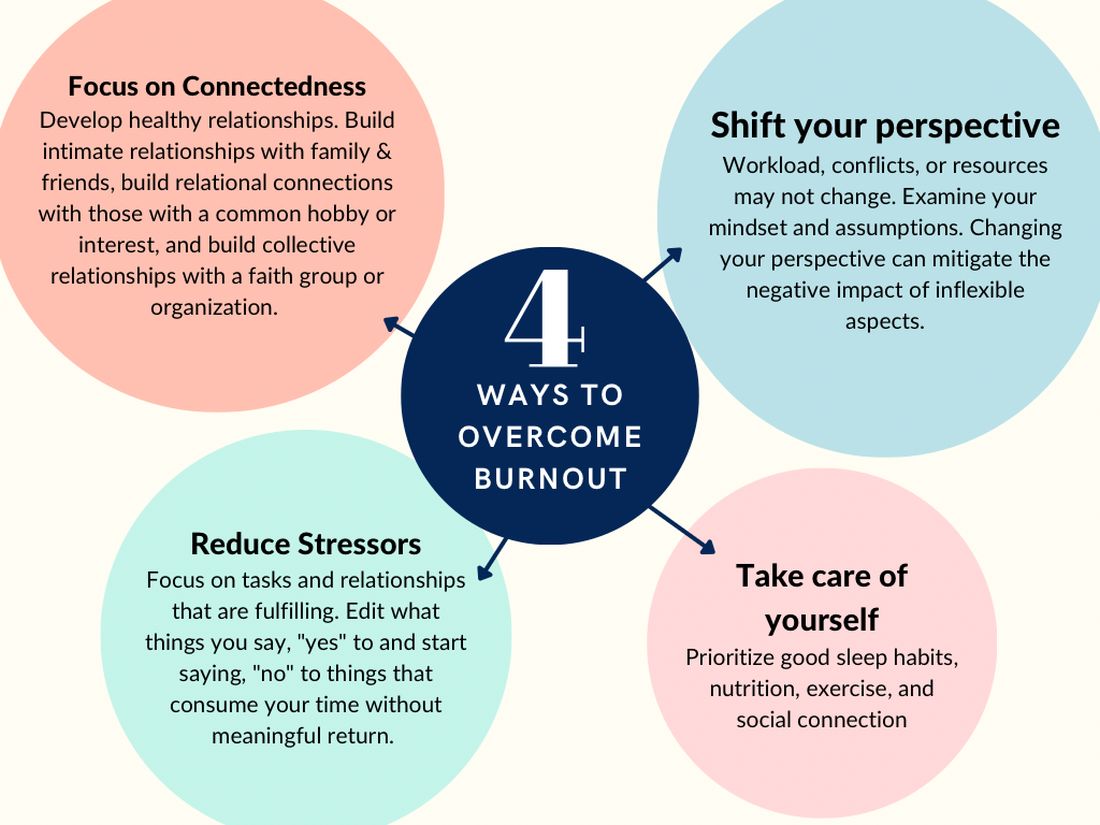
According to Dave et al. (2020), engagement in self-care practices such as mindfulness may offer advantages to gastroenterologists’ well-being and improved patient care.11
Burnout is not due to an individuals’ need for more resiliency. Instead, it developed from a systemic overwhelming of a health system near its breaking point. Recognizing that by 2033, there is a projected shortage of nearly 140,000 physicians in the United States, the U.S. Surgeon General, Dr. Vivek H. Murthy, issued a crisis advisory.12 This advisory highlights the urgent need to address the health worker burnout crisis nationwide that outlined “whole of society” efforts.12 Key components of the advisory on building a thriving health workforce included empowering health care workers, changing policies, reducing administrative burdens, prioritizing connections, and investing in our workforce.12
Provide access to mental health services
Institutions and practices would greatly benefit from providing access to mental health services, counseling, educational opportunities, potential mental health days, and mentorship programs. While the literature indicates that both individual-focused and structural or organizational strategies can result in clinically meaningful reductions in burnout among physicians, a meta-analysis revealed that corporate-led initiatives resulted in larger successes.12,13 Physicians who received support and resources from their institutions report lower levels of burnout and higher job satisfaction.2,3
New strategies to select and develop physician leaders who motivate, inspire, and effectively manage physicians may result in positive job satisfaction while decreasing employee burnout. Therefore, increased awareness of the importance of frontline leadership well-being and professional fulfillment of physicians working for a large health care organization is necessary.13 Robust and continual leadership training can ensure the entire team’s well-being, longevity, and success.13
Addressing the root causes of systemic burnout is imperative. Leadership could streamline administrative processes, optimize electronic medical records, delegate prior authorizations, and ensure staffing levels are appropriate to meet patient care demands. In a survey by Rao et al. (2017), the authors found that physicians who reported high levels of administrative burden and work overload were more likely to experience burnout.14
Institutions and practices should promote a culture of work-life balance by implementing flexible scheduling, promoting time off and vacation time, and encouraging regular exercise and healthy habits. The current compensation structure disincentivizes physicians from taking time away from patient care – this can be re-designed. Community and support mitigate burnout. Therefore, institutions and practices will benefit by intentionally providing opportunities for social connection and team building.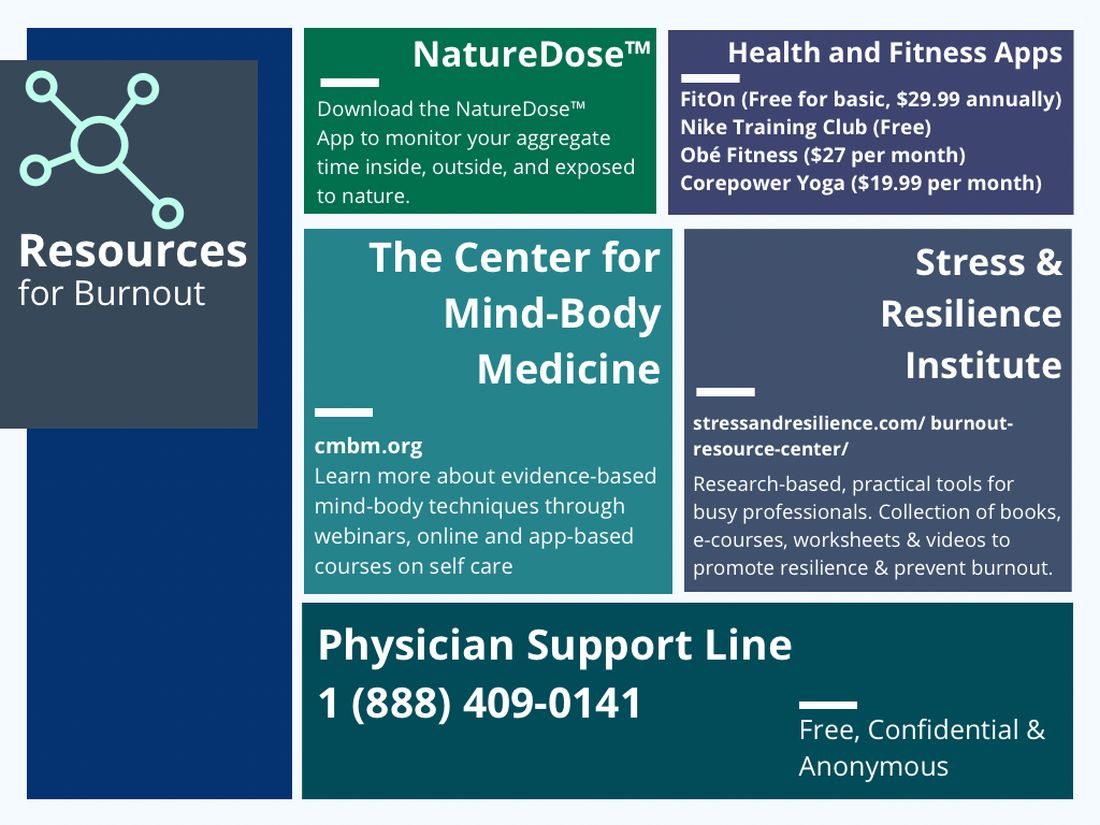
In reflection of the U.S. Surgeon General’s call for all of society to be part of the solution, we are pleased to see the Accreditation Council for Graduate Medical Education (ACGME) create mandatory 6 weeks of parental or caregiver leave for trainees.15 Continued positive pressure on overseeing agencies to minimize paperwork, preauthorizations, and non–value-added tasks to allow physicians to continue to provide medical services instead of documentation and auditing services would greatly positively impact all of health care. Therefore, communicating with legislators, policy makers, system leadership, and all health care societies to continue these improvements would be a wise use of time of resources.
In conclusion, burnout among new and transitioning gastroenterologists is a prevalent and concerning issue that can have severe consequences for both the individual and the health care system. Similar to the ergonomic considerations of being an endoscopist, A multifaceted approach to the well-being of all medical staff can help ensure the delivery of the highest quality patient care. By taking a proactive approach to preventing burnout, we can have a strong future for ourselves, our patients, and our profession.
Dr. Eboh is a gastroenterologist with Atrium Health, Charlotte, N.C.; Dr. Jaeger is with Baylor Scott & White Medical Center in Dallas. She is a gastroenterology fellow with Temple University Hospital, Philadelphia. Dr. Sears is clinical professor at Texas A&M University School of Medicine, and chief of gastroenterology at VA Central Texas Healthcare System. Dr. Sears owns GutGirlMD Consulting LLC, where she offers institutional and leadership coaching for physicians. Dr. Eboh on Instagram @Polyp.picker_EbohMD and on Twitter @PolypPicker_MD. Dr. Jaeger on Instagram @Doc.Tori.Fit and Twitter @DrToriJaeger. Dr. Sears is on Twitter @GutGirlMD.
References
1. Maslach C and Jackson S E. Maslach burnout inventory manual. Palo Alto, Calif: Consulting Psychologists Press, 1986.
2. Shanafelt TD et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015 Dec 12;90:1600-13.
3. Shanafelt TD et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012 Oct 8;172(18):1377-85.
4. Elta G. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
5. Gallup. Work and Workplace. 2023.
6. Gawande A. When doctors make mistakes. The New Yorker. 1999 Feb 1.
7. Buscarini E et al. Burnout among gastroenterologists: How to manage and prevent it. United European Gastroenterol J. 2020 Aug;8(7):832-4.
8. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016 Nov 5;388(10057):2272-81.
9. Adarkwah CC et al. Burnout and work satisfaction are differentially associated in gastroenterologists in Germany. F1000Res. 2022 Mar 30;11:368. doi: 10.12688/f1000research.110296.3. eCollection 2022.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015 Apr;90(4):432-40.
11. Umakant D et al. Mindfulness in gastroenterology training and practice: A personal perspective. Clin Exp Gastroenterol. 2020 Nov 4;13:497-502.
12. Murthy VH. Addressing Health Worker Burnout: The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. The U.S. Department of Health and Human Services: Office of the U.S. Surgeon General, 2022.
13. Panagioti M et al. Controlled interventions to reduce burnout in physicians: A systematic review and meta-analysis. JAMA Intern Med. 2017 Feb 1;177(2):195-205.
14. Rao SK et al. The impact of administrative burden on academic physicians: Results of a hospital-wide physician survey. Acad Med. 2017 Feb;92(2):237-43.
15. ACGME. ACME Institutional Requirements 2021.
Developing training pathways in advanced endoscopic resection and third-space endoscopy in the U.S.
As a gastroenterology and hepatology fellow, choosing a career path was a daunting prospect. Despite the additional specialization, there seemed to be endless career options to consider. Did I want to join an academic, private, or hybrid practice? Should I subspecialize within the field? Was it important to incorporate research or teaching into my practice? What about opportunities to take on administrative or leadership roles?
Fellowship training at a large academic research institution provided me the opportunity to work with expert faculty in inflammatory bowel disease, esophageal disease, motility and functional gastrointestinal disease, pancreaticobiliary disease, and hepatology. I enjoyed seeing patients in each of these subspecialty clinics. But, by the end of my second year of GI fellowship, I still wasn’t sure what I wanted to do professionally.
A career in academic general gastroenterology seemed to be a good fit for my personality and goals. Rather than focusing on research, I chose to position myself as a clinician educator. I knew that having a subspecialty area of expertise would help improve my clinical practice and make me a more attractive candidate to academic centers. To help narrow my choice, I looked at the clinical enterprise at our institution and assessed where the unmet clinical needs were most acute. Simultaneously, I identified potential mentors to support and guide me through the transition from fellow to independent practitioner. I decided to focus on acquiring the skills to care for patients with anorectal diseases and lower-GI motility disorders, as this area met both of my criteria – excellent mentorship and an unmet clinical need. Under the guidance of Dr. Yolanda Scarlett, I spent my 3rd year in clinic learning to interpret anorectal manometry tests, defecograms, and sitz marker studies and treating patients with refractory constipation, fecal incontinence, and anal fissures.
With a plan to develop an expertise in anorectal diseases and low-GI motility disorders, I also wanted to focus on improving my endoscopic skills to graduate as well rounded a clinician as possible. To achieve this goal, I sought out a separate endoscopy mentor, Dr. Ian Grimm, the director of endoscopy at the University of North Carolina at Chapel Hill. Dr. Grimm, a classically trained advanced endoscopist performing endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP), had a burgeoning interest in endoscopic mucosal resection (EMR) and had just returned from a few months in Japan learning to perform endoscopic submucosal dissection (ESD) and peroral endoscopic myotomy (POEM).
When I began working with Dr. Grimm, I had not even heard the term third-space endoscopy and knew nothing about ESD or POEM. I spent as much time as possible watching and assisting Dr. Grimm with complex endoscopic mucosal resection (EMR) during the first few months of my 3rd year. Soon after my exposure to advanced endoscopic resection, it was clear that I wanted to learn and incorporate this into my clinical practice. I watched Dr. Grimm perform the first POEM at UNC in the fall of 2016 and by that time I was hooked on learning third-space endoscopy. I observed and assisted with as many EMR, ESD, and POEM cases as I could that year. In addition to the hands-on and cognitive training with Dr. Grimm, I attended national meetings and workshops focused on learning third-space endoscopy. In the spring of my 3rd year I was honored to be the first fellow to complete the Olympus master class in ESD – a 2-day hands-on training course sponsored by Olympus. By the end of that year, I was performing complex EMR with minimal assistance and had completed multiple ESDs and POEMs with cognitive supervision only.
After fellowship, I joined the UNC faculty as a general gastroenterologist with expertise in anorectal disease and lower-GI motility disorders. While I was comfortable performing complex EMR, I still needed additional training and supervision before I felt ready to independently perform ESD or POEM. With the gracious support and encouragement of our division chief, I continued third-space endoscopy training with Dr. Grimm during dedicated protected time 2 days each month. Over the ensuing 4 years, I transitioned to fully independent practice performing all types of advanced EMR and third-space endoscopy including complex EMR, ESD, endoscopic full-thickness resection (EFTR), submucosal tunnel endoscopic resection (STER), esophageal POEM, gastric POEM, and Zenker’s POEM.
As one of the first gastroenterologists in the United States to perform third-space endoscopy without any formal training in advanced pancreaticobiliary endoscopy, I believe learning advanced endoscopic resection and third-space endoscopy is best achieved through a training pathway separate from the conventional advanced endoscopy fellowship focused on teaching EUS and ERCP. Although there are transferable skills learned from EUS and ERCP to the techniques used in third-space endoscopy, there is nothing inherent to performing EUS or ERCP that enables one to learn how to perform an ESD or a POEM.
There is a robust training pathway to teach advanced pancreaticobiliary endoscopy, but no formal training pathway exists to teach third-space endoscopy in the United States. Historically, a small number of interested and motivated advanced pancreaticobiliary endoscopists sought out opportunities to learn third-space endoscopy after completion of their advanced endoscopy fellowship, in some cases many years after graduation. For these early adopters in the United States, the only training opportunities required travel to Japan or another Eastern country with arrangements made to observe and participate in third-space endoscopy cases with experts there. With increased recognition of the benefits of ESD and POEM over the past 5-10 years in the United States, there has been greater adoption of third-space endoscopy and with it, more training opportunities. Still, there are very few institutions with formalized training programs in advanced endoscopic resection and third-space endoscopy in the United States to date.
Proof that this model works
In Eastern countries such as Japan, training endoscopists to perform ESD and POEM has been successfully achieved through an apprenticeship model whereby an expert in third-space endoscopy closely supervises a trainee who gains greater autonomy with increasing experience and skill over time. My personal experience is proof that this model works. But, adopting such a model more widely in the United States may prove difficult. We lack a sufficient number of experienced third-space endoscopy operators and, given the challenges to appropriate reimbursement for third-space endoscopy in the United States, there is understandable resistance to accepting the prolonged training period necessary for technical mastery of this skill.
In part, a long training period is needed because of a relative paucity of appropriate target lesions for ESD and the rarity of achalasia in the United States. While there is consensus among experts regarding the benefits of ESD for resection of early gastric cancer (EGC), relatively few EGCs are found in the United States and indications for ESD outside resection of EGC are less well defined with less clear benefits over more widely performed piecemeal EMR. Despite these challenges, it is critical that we continue to develop dedicated training pathways to teach advanced endoscopic resection and third-space endoscopy in the United States. My practice has evolved considerably since completion of fellowship nearly 6 years ago, and I now focus almost exclusively on advanced endoscopic resection and third-space endoscopy. Recently, Dr. Grimm and I began an advanced endoscopic resection elective for the general GI fellows at UNC and we are excited to welcome our first advanced endoscopic resection and third-space endoscopy fellow to UNC this July.
While there are many possible avenues to expertise in advanced endoscopic resection, few will likely follow the same path that I have taken. Trainees who are interested in pursuing this subspecialty should seek out supportive mentors in a setting where there is already a robust case volume of esophageal motility disorders and endoscopic resections. Success requires the persistent motivation to seek out diverse opportunities for self-study, exposure to experts, data on developments in the field, and hands-on exposure to as many ex-vivo and in-vivo cases as possible.
Dr. Kroch is assistant professor of medicine in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. He disclosed having no conflicts of interest.
As a gastroenterology and hepatology fellow, choosing a career path was a daunting prospect. Despite the additional specialization, there seemed to be endless career options to consider. Did I want to join an academic, private, or hybrid practice? Should I subspecialize within the field? Was it important to incorporate research or teaching into my practice? What about opportunities to take on administrative or leadership roles?
Fellowship training at a large academic research institution provided me the opportunity to work with expert faculty in inflammatory bowel disease, esophageal disease, motility and functional gastrointestinal disease, pancreaticobiliary disease, and hepatology. I enjoyed seeing patients in each of these subspecialty clinics. But, by the end of my second year of GI fellowship, I still wasn’t sure what I wanted to do professionally.
A career in academic general gastroenterology seemed to be a good fit for my personality and goals. Rather than focusing on research, I chose to position myself as a clinician educator. I knew that having a subspecialty area of expertise would help improve my clinical practice and make me a more attractive candidate to academic centers. To help narrow my choice, I looked at the clinical enterprise at our institution and assessed where the unmet clinical needs were most acute. Simultaneously, I identified potential mentors to support and guide me through the transition from fellow to independent practitioner. I decided to focus on acquiring the skills to care for patients with anorectal diseases and lower-GI motility disorders, as this area met both of my criteria – excellent mentorship and an unmet clinical need. Under the guidance of Dr. Yolanda Scarlett, I spent my 3rd year in clinic learning to interpret anorectal manometry tests, defecograms, and sitz marker studies and treating patients with refractory constipation, fecal incontinence, and anal fissures.
With a plan to develop an expertise in anorectal diseases and low-GI motility disorders, I also wanted to focus on improving my endoscopic skills to graduate as well rounded a clinician as possible. To achieve this goal, I sought out a separate endoscopy mentor, Dr. Ian Grimm, the director of endoscopy at the University of North Carolina at Chapel Hill. Dr. Grimm, a classically trained advanced endoscopist performing endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP), had a burgeoning interest in endoscopic mucosal resection (EMR) and had just returned from a few months in Japan learning to perform endoscopic submucosal dissection (ESD) and peroral endoscopic myotomy (POEM).
When I began working with Dr. Grimm, I had not even heard the term third-space endoscopy and knew nothing about ESD or POEM. I spent as much time as possible watching and assisting Dr. Grimm with complex endoscopic mucosal resection (EMR) during the first few months of my 3rd year. Soon after my exposure to advanced endoscopic resection, it was clear that I wanted to learn and incorporate this into my clinical practice. I watched Dr. Grimm perform the first POEM at UNC in the fall of 2016 and by that time I was hooked on learning third-space endoscopy. I observed and assisted with as many EMR, ESD, and POEM cases as I could that year. In addition to the hands-on and cognitive training with Dr. Grimm, I attended national meetings and workshops focused on learning third-space endoscopy. In the spring of my 3rd year I was honored to be the first fellow to complete the Olympus master class in ESD – a 2-day hands-on training course sponsored by Olympus. By the end of that year, I was performing complex EMR with minimal assistance and had completed multiple ESDs and POEMs with cognitive supervision only.
After fellowship, I joined the UNC faculty as a general gastroenterologist with expertise in anorectal disease and lower-GI motility disorders. While I was comfortable performing complex EMR, I still needed additional training and supervision before I felt ready to independently perform ESD or POEM. With the gracious support and encouragement of our division chief, I continued third-space endoscopy training with Dr. Grimm during dedicated protected time 2 days each month. Over the ensuing 4 years, I transitioned to fully independent practice performing all types of advanced EMR and third-space endoscopy including complex EMR, ESD, endoscopic full-thickness resection (EFTR), submucosal tunnel endoscopic resection (STER), esophageal POEM, gastric POEM, and Zenker’s POEM.
As one of the first gastroenterologists in the United States to perform third-space endoscopy without any formal training in advanced pancreaticobiliary endoscopy, I believe learning advanced endoscopic resection and third-space endoscopy is best achieved through a training pathway separate from the conventional advanced endoscopy fellowship focused on teaching EUS and ERCP. Although there are transferable skills learned from EUS and ERCP to the techniques used in third-space endoscopy, there is nothing inherent to performing EUS or ERCP that enables one to learn how to perform an ESD or a POEM.
There is a robust training pathway to teach advanced pancreaticobiliary endoscopy, but no formal training pathway exists to teach third-space endoscopy in the United States. Historically, a small number of interested and motivated advanced pancreaticobiliary endoscopists sought out opportunities to learn third-space endoscopy after completion of their advanced endoscopy fellowship, in some cases many years after graduation. For these early adopters in the United States, the only training opportunities required travel to Japan or another Eastern country with arrangements made to observe and participate in third-space endoscopy cases with experts there. With increased recognition of the benefits of ESD and POEM over the past 5-10 years in the United States, there has been greater adoption of third-space endoscopy and with it, more training opportunities. Still, there are very few institutions with formalized training programs in advanced endoscopic resection and third-space endoscopy in the United States to date.
Proof that this model works
In Eastern countries such as Japan, training endoscopists to perform ESD and POEM has been successfully achieved through an apprenticeship model whereby an expert in third-space endoscopy closely supervises a trainee who gains greater autonomy with increasing experience and skill over time. My personal experience is proof that this model works. But, adopting such a model more widely in the United States may prove difficult. We lack a sufficient number of experienced third-space endoscopy operators and, given the challenges to appropriate reimbursement for third-space endoscopy in the United States, there is understandable resistance to accepting the prolonged training period necessary for technical mastery of this skill.
In part, a long training period is needed because of a relative paucity of appropriate target lesions for ESD and the rarity of achalasia in the United States. While there is consensus among experts regarding the benefits of ESD for resection of early gastric cancer (EGC), relatively few EGCs are found in the United States and indications for ESD outside resection of EGC are less well defined with less clear benefits over more widely performed piecemeal EMR. Despite these challenges, it is critical that we continue to develop dedicated training pathways to teach advanced endoscopic resection and third-space endoscopy in the United States. My practice has evolved considerably since completion of fellowship nearly 6 years ago, and I now focus almost exclusively on advanced endoscopic resection and third-space endoscopy. Recently, Dr. Grimm and I began an advanced endoscopic resection elective for the general GI fellows at UNC and we are excited to welcome our first advanced endoscopic resection and third-space endoscopy fellow to UNC this July.
While there are many possible avenues to expertise in advanced endoscopic resection, few will likely follow the same path that I have taken. Trainees who are interested in pursuing this subspecialty should seek out supportive mentors in a setting where there is already a robust case volume of esophageal motility disorders and endoscopic resections. Success requires the persistent motivation to seek out diverse opportunities for self-study, exposure to experts, data on developments in the field, and hands-on exposure to as many ex-vivo and in-vivo cases as possible.
Dr. Kroch is assistant professor of medicine in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. He disclosed having no conflicts of interest.
As a gastroenterology and hepatology fellow, choosing a career path was a daunting prospect. Despite the additional specialization, there seemed to be endless career options to consider. Did I want to join an academic, private, or hybrid practice? Should I subspecialize within the field? Was it important to incorporate research or teaching into my practice? What about opportunities to take on administrative or leadership roles?
Fellowship training at a large academic research institution provided me the opportunity to work with expert faculty in inflammatory bowel disease, esophageal disease, motility and functional gastrointestinal disease, pancreaticobiliary disease, and hepatology. I enjoyed seeing patients in each of these subspecialty clinics. But, by the end of my second year of GI fellowship, I still wasn’t sure what I wanted to do professionally.
A career in academic general gastroenterology seemed to be a good fit for my personality and goals. Rather than focusing on research, I chose to position myself as a clinician educator. I knew that having a subspecialty area of expertise would help improve my clinical practice and make me a more attractive candidate to academic centers. To help narrow my choice, I looked at the clinical enterprise at our institution and assessed where the unmet clinical needs were most acute. Simultaneously, I identified potential mentors to support and guide me through the transition from fellow to independent practitioner. I decided to focus on acquiring the skills to care for patients with anorectal diseases and lower-GI motility disorders, as this area met both of my criteria – excellent mentorship and an unmet clinical need. Under the guidance of Dr. Yolanda Scarlett, I spent my 3rd year in clinic learning to interpret anorectal manometry tests, defecograms, and sitz marker studies and treating patients with refractory constipation, fecal incontinence, and anal fissures.
With a plan to develop an expertise in anorectal diseases and low-GI motility disorders, I also wanted to focus on improving my endoscopic skills to graduate as well rounded a clinician as possible. To achieve this goal, I sought out a separate endoscopy mentor, Dr. Ian Grimm, the director of endoscopy at the University of North Carolina at Chapel Hill. Dr. Grimm, a classically trained advanced endoscopist performing endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP), had a burgeoning interest in endoscopic mucosal resection (EMR) and had just returned from a few months in Japan learning to perform endoscopic submucosal dissection (ESD) and peroral endoscopic myotomy (POEM).
When I began working with Dr. Grimm, I had not even heard the term third-space endoscopy and knew nothing about ESD or POEM. I spent as much time as possible watching and assisting Dr. Grimm with complex endoscopic mucosal resection (EMR) during the first few months of my 3rd year. Soon after my exposure to advanced endoscopic resection, it was clear that I wanted to learn and incorporate this into my clinical practice. I watched Dr. Grimm perform the first POEM at UNC in the fall of 2016 and by that time I was hooked on learning third-space endoscopy. I observed and assisted with as many EMR, ESD, and POEM cases as I could that year. In addition to the hands-on and cognitive training with Dr. Grimm, I attended national meetings and workshops focused on learning third-space endoscopy. In the spring of my 3rd year I was honored to be the first fellow to complete the Olympus master class in ESD – a 2-day hands-on training course sponsored by Olympus. By the end of that year, I was performing complex EMR with minimal assistance and had completed multiple ESDs and POEMs with cognitive supervision only.
After fellowship, I joined the UNC faculty as a general gastroenterologist with expertise in anorectal disease and lower-GI motility disorders. While I was comfortable performing complex EMR, I still needed additional training and supervision before I felt ready to independently perform ESD or POEM. With the gracious support and encouragement of our division chief, I continued third-space endoscopy training with Dr. Grimm during dedicated protected time 2 days each month. Over the ensuing 4 years, I transitioned to fully independent practice performing all types of advanced EMR and third-space endoscopy including complex EMR, ESD, endoscopic full-thickness resection (EFTR), submucosal tunnel endoscopic resection (STER), esophageal POEM, gastric POEM, and Zenker’s POEM.
As one of the first gastroenterologists in the United States to perform third-space endoscopy without any formal training in advanced pancreaticobiliary endoscopy, I believe learning advanced endoscopic resection and third-space endoscopy is best achieved through a training pathway separate from the conventional advanced endoscopy fellowship focused on teaching EUS and ERCP. Although there are transferable skills learned from EUS and ERCP to the techniques used in third-space endoscopy, there is nothing inherent to performing EUS or ERCP that enables one to learn how to perform an ESD or a POEM.
There is a robust training pathway to teach advanced pancreaticobiliary endoscopy, but no formal training pathway exists to teach third-space endoscopy in the United States. Historically, a small number of interested and motivated advanced pancreaticobiliary endoscopists sought out opportunities to learn third-space endoscopy after completion of their advanced endoscopy fellowship, in some cases many years after graduation. For these early adopters in the United States, the only training opportunities required travel to Japan or another Eastern country with arrangements made to observe and participate in third-space endoscopy cases with experts there. With increased recognition of the benefits of ESD and POEM over the past 5-10 years in the United States, there has been greater adoption of third-space endoscopy and with it, more training opportunities. Still, there are very few institutions with formalized training programs in advanced endoscopic resection and third-space endoscopy in the United States to date.
Proof that this model works
In Eastern countries such as Japan, training endoscopists to perform ESD and POEM has been successfully achieved through an apprenticeship model whereby an expert in third-space endoscopy closely supervises a trainee who gains greater autonomy with increasing experience and skill over time. My personal experience is proof that this model works. But, adopting such a model more widely in the United States may prove difficult. We lack a sufficient number of experienced third-space endoscopy operators and, given the challenges to appropriate reimbursement for third-space endoscopy in the United States, there is understandable resistance to accepting the prolonged training period necessary for technical mastery of this skill.
In part, a long training period is needed because of a relative paucity of appropriate target lesions for ESD and the rarity of achalasia in the United States. While there is consensus among experts regarding the benefits of ESD for resection of early gastric cancer (EGC), relatively few EGCs are found in the United States and indications for ESD outside resection of EGC are less well defined with less clear benefits over more widely performed piecemeal EMR. Despite these challenges, it is critical that we continue to develop dedicated training pathways to teach advanced endoscopic resection and third-space endoscopy in the United States. My practice has evolved considerably since completion of fellowship nearly 6 years ago, and I now focus almost exclusively on advanced endoscopic resection and third-space endoscopy. Recently, Dr. Grimm and I began an advanced endoscopic resection elective for the general GI fellows at UNC and we are excited to welcome our first advanced endoscopic resection and third-space endoscopy fellow to UNC this July.
While there are many possible avenues to expertise in advanced endoscopic resection, few will likely follow the same path that I have taken. Trainees who are interested in pursuing this subspecialty should seek out supportive mentors in a setting where there is already a robust case volume of esophageal motility disorders and endoscopic resections. Success requires the persistent motivation to seek out diverse opportunities for self-study, exposure to experts, data on developments in the field, and hands-on exposure to as many ex-vivo and in-vivo cases as possible.
Dr. Kroch is assistant professor of medicine in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. He disclosed having no conflicts of interest.
Advances in endohepatology
Introduction
Historically, the role of endoscopy in hepatology has been limited to intraluminal and bile duct interventions, primarily for the management of varices and biliary strictures. Recently, endoscopic ultrasound (EUS) has broadened the range of endoscopic treatment by enabling transluminal access to the liver parenchyma and associated vasculature. In this review, we will address recent advances in the expanding field of endohepatology.
Endoscopic-ultrasound guided liver biopsy
Liver biopsies are a critical tool in the diagnostic evaluation and management of patients with liver disease. Conventional approaches for obtaining liver tissue have been most commonly through the percutaneous or vascular approaches. In 2007, the first EUS-guided liver biopsy (EUS-LB) was described.1 EUS-LB is performed by advancing a line-array echoendoscope to the duodenal bulb to access the right lobe of the liver or proximal stomach to sample the left lobe. Doppler is first used to identify a pathway with few intervening vessels. Then a 19G or 20G needle is passed and slowly withdrawn to capture tissue (Figure 1). Careful evaluation with Doppler ultrasound to evaluate for bleeding is recommended after EUS-LB and if persistent, a small amount of clot may be reinjected as a blood or “Chang” patch akin to technique to control oozing postlumbar puncture.2
While large prospective studies are needed to compare the methods, it appears that specimen adequacy acquired via EUS-LB are comparable to percutaneous and transjugular approaches.3-5 Utilization of specific needle types and suction may optimize samples. Namely, 19G needles may provide better samples than smaller sizes and contemporary fine-needle biopsy needles with Franseen tips are superior to conventional spring-loaded cutting needles and fork tip needles.6-8 The use of dry suction has been shown to increase the yield of tissue, but at the expense of increased bloodiness. Wet suction, which involves the presence of fluid, rather than air, in the needle lumen to lubricate and improve transmission of negative pressure to the needle tip, is the preferred technique for EUS-LB given improvement in the likelihood of intact liver biopsy cores and increased specimen adequacy.9
There are several advantages to EUS-LB (Table 1). When compared with percutaneous liver biopsy (PC-LB) and transjugular liver biopsy (TJ-LB), EUS-LB is uniquely able to access both liver lobes in a single setting, which minimizes sampling error.3 EUS-LB may also have an advantage in sampling focal liver lesions given the close proximity of the transducer to the liver.10 Another advantage over PC-LB is that EUS-LB can be performed in patients with a large body habitus. Additionally, EUS-LB is better tolerated than PC-LB, with less postprocedure pain and shorter postprocedure monitoring time.4,5
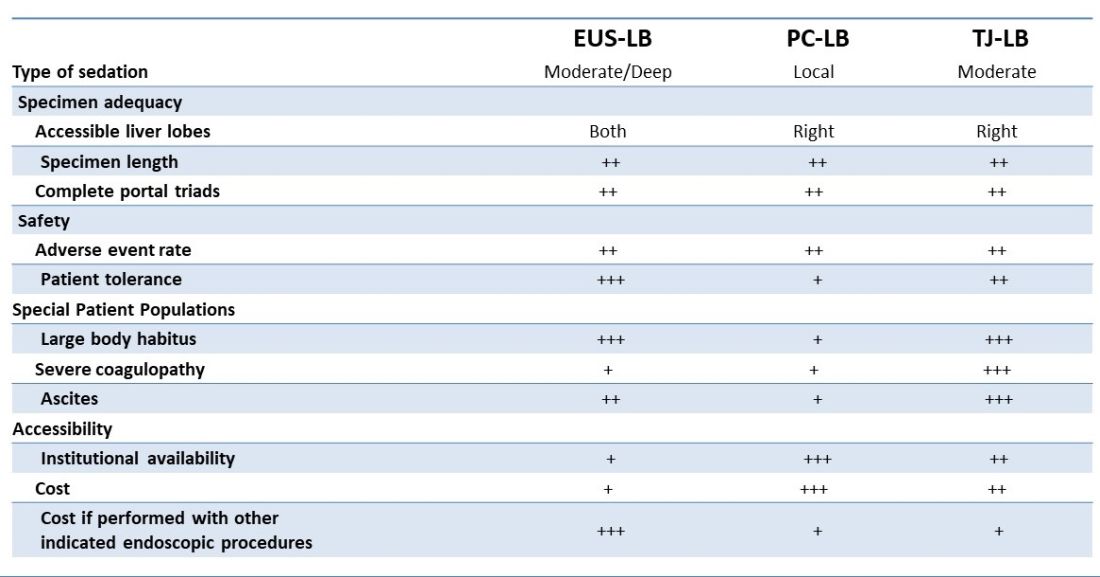
Rates of adverse events appear to be similar between the three methods. Similar to PC-LB, EUS-LB requires capsular puncture, which can lead to intraperitoneal hemorrhage. Therefore, TJ-LB is preferred in patients with significant coagulopathy. While small ascites is not an absolute contraindication for EUS-LB, large ascites can obscure a safe window from the proximal stomach or duodenum to the liver, and thus TJLB is also preferred in these patients.11 Given its relative novelty and logistic challenges, other disadvantages of EUS-LB include limited provider availability and increased cost, especially compared with PC-LB. The most significant limitation is that it requires moderate or deep sedation, as opposed to local anesthetics. However, if there is another indication for endoscopy (that is, variceal screening), then “one-stop shop” procedures including EUS-LB may be more convenient and cost-effective than traditional methods. Nevertheless, rigorous comparative studies are needed.
EUS-guided portal pressure gradient measurement
The presence of clinically significant portal hypertension (CSPH), defined as hepatic venous pressure gradient (HVPG) greater than or equal to 10 is a potent predictor of decompensation. There is growing evidence to support the use of beta-blockers to mitigate this risk.12 Therefore, early identification of patients with CSPH has important diagnostic and therapeutic implications. The current gold standard for diagnosing CSPH is with wedged HVPG measurements performed by interventional radiology.
Since its introduction in 2016, EUS-guided portal pressure gradient measurement (EUS-PPG) has emerged as an alternative to wedged HVPG.13,14 Using a linear echoendoscope, the portal vein is directly accessed with a 25G fine-needle aspiration needle, and three direct measurements are taken using a compact manometer to determine the mean pressure. The hepatic vein, or less commonly the inferior vena cava, pressure is also measured. The direct measurement of portal pressure provides a significant advantage of EUS-PPG over HVPG in patients with presinusoidal and prehepatic portal hypertension. Wedged HVPG, which utilizes the difference between the wedged and free hepatic venous pressure to indirectly estimate the portal venous pressure gradient, yields erroneously low gradients in patients with noncirrhotic portal hypertension.15 An additional advantage of EUS-PPG is that it obviates the need for a central venous line placement, which is associated with thrombosis and, in rare cases, air embolus.16
Observational studies indicate that EUS-PPG has a high degree of consistency with HVPG measurements and a strong correlation between other clinical findings of portal hyper-tension including esophageal varices and thrombocytopenia.13,14 Nevertheless, EUS-PPG is performed under moderate or deep sedation which may impact HVPG measurements.17 In addition, the real-world application of EUS-PPG measurement on clinical care is undefined, but it is the topic of an ongoing clinical trial (ClinicalTrials.gov – NCT05357599).
EUS-guided interventions of gastric varices
Compared with esophageal varices, current approaches to the treatment and prophylaxis of gastric varices are more controversial.18 The most common approach to bleeding gastric varices in the United States is the placement of a transjugular intrahepatic portosystemic shunt (TIPS). Nevertheless, in addition to risks associated with central venous line placement, 5%-35% of individuals develop hepatic encephalopathy after TIPS and ischemic acute liver failure can occur in rare situations.19 Cyanoacrylate (CYA) glue injection is the recommended first-line endoscopic therapy for the treatment of bleeding gastric varices, but use has not been widely adopted in the United States because of a lack of an approved Food and Drug Administration CYA formulation, limited expertise, and risk of serious complications. In particular systemic embolization may result in pulmonary or cerebral infarct.12,18 EUS-guided interventions have been developed to mitigate these safety concerns. EUS-guided coil embolization can be performed, either alone or in combination with CYA injection.20 In the latter approach it acts as a scaffold to prevent migration of the glue bolus. Doppler assessment enables direct visualization of the gastric varix for identification of feeder vessels, more controlled deployment of hemostatic agents, and real-time confirmation of varix obliteration. Fluoroscopy can be used as an adjunct.
EUS-guided interventions in the management of gastric varices appear to be effective and superior to CYA injection under direct endoscopic visualization with improved likelihood of obliteration and lower rebleeding rates, without increase in adverse events.21 Additionally, EUS-guided combination therapy improves technical outcomes and reduces adverse events relative to EUS-guided coil or EUS-guided glue injection therapy alone.21-23 Nevertheless, large-scale prospective trials are needed to determine whether EUS-guided interventions should be considered over TIPS. The role of EUS-guided interventions as primary prophylaxis to prevent bleeding from large gastric varices also requires additional study.24
Future directions
with the goal of optimizing care and increasing efficiency. In addition to new endoscopic procedures to optimize liver biopsy, portal pressure measurement, and gastric variceal treatment, there are a number of emerging technologies including EUS-guided liver elastography, portal venous sampling, liver tumor chemoembolization, and intrahepatic portosystemic shunts.25 However, the practice of endohepatology faces a number of challenges before widespread adoption, including limited provider expertise and institutional availability. Additionally, more robust, multicenter outcomes and cost-effective analyses comparing these novel procedures with traditional approaches are needed to define their clinical impact.
Dr. Bui is a fellow in gastroenterology in the division of gastroenterology and hepatology, University of Southern California, Los Angeles. Dr. Buxbaum is associate professor of medicine (clinical scholar) in the division of gastroenterology and hepatology, University of Southern California. Dr. Buxbaum is a consultant for Cook Medical, Boston Scientific, and Olympus. Dr. Bui has no disclosures.
References
1. Mathew A. Am J Gastroenterol. 2007;102(10):2354-5.
2. Sowa P et al. VideoGIE. 2021;6(11):487-8.
3. Pineda JJ et al. Gastrointest Endosc. 2016;83(2):360-5.
4. Ali AH et al. J Ultrasound. 2020;23(2):157-67.
5. Shuja A et al. Dig Liver Dis. 2019;51(6):826-30.
6. Schulman AR et al. Gastrointest Endosc. 2017;85(2):419-26.
7. DeWitt J et al. Endosc Int Open. 2015;3(5):E471-8.
8. Aggarwal SN et al. Gastrointest Endosc. 2021;93(5):1133-8.
9. Mok SRS et al. Gastrointest Endosc. 2018;88(6):919-25.
10. Lee YN et al. J Gastroenterol Hepatol. 2015;30(7):1161-6.
11. Kalambokis G et al. J Hepatol. 2007;47(2):284-94.
12. de Franchis R et al. J Hepatol. 2022;76(4):959-74.
13. Choi AY et al. J Gastroenterol Hepatol. 2022;37(7):1373-9.
14. Zhang W et al. Gastrointest Endosc. 2021;93(3):565-72.
15. Seijo S et al. Dig Liver Dis. 2012;44(10):855-60.
16. Vesely TM. J Vasc Interv Radiol. 2001;12(11):1291-5.
17. Reverter E et al. Liver Int. 2014;34(1):16-25.
18. Henry Z et al. Clin Gastroenterol Hepatol. 2021;19(6):1098-107.e1091.
19. Ripamonti R et al. Semin Intervent Radiol. 2006;23(2):165-76.
20. Rengstorff DS and Binmoeller KF. Gastrointest Endosc. 2004;59(4):553-8.
21. Mohan BP et al. Endoscopy. 2020;52(4):259-67.
22. Robles-Medranda C et al. Endoscopy. 2020;52(4):268-75.
23. McCarty TR et al. Endosc Ultrasound. 2020;9(1):6-15.
24. Kouanda A et al. Gastrointest Endosc. 2021;94(2):291-6.
25. Bazarbashi AN et al. 2022;24(1):98-107.
Introduction
Historically, the role of endoscopy in hepatology has been limited to intraluminal and bile duct interventions, primarily for the management of varices and biliary strictures. Recently, endoscopic ultrasound (EUS) has broadened the range of endoscopic treatment by enabling transluminal access to the liver parenchyma and associated vasculature. In this review, we will address recent advances in the expanding field of endohepatology.
Endoscopic-ultrasound guided liver biopsy
Liver biopsies are a critical tool in the diagnostic evaluation and management of patients with liver disease. Conventional approaches for obtaining liver tissue have been most commonly through the percutaneous or vascular approaches. In 2007, the first EUS-guided liver biopsy (EUS-LB) was described.1 EUS-LB is performed by advancing a line-array echoendoscope to the duodenal bulb to access the right lobe of the liver or proximal stomach to sample the left lobe. Doppler is first used to identify a pathway with few intervening vessels. Then a 19G or 20G needle is passed and slowly withdrawn to capture tissue (Figure 1). Careful evaluation with Doppler ultrasound to evaluate for bleeding is recommended after EUS-LB and if persistent, a small amount of clot may be reinjected as a blood or “Chang” patch akin to technique to control oozing postlumbar puncture.2
While large prospective studies are needed to compare the methods, it appears that specimen adequacy acquired via EUS-LB are comparable to percutaneous and transjugular approaches.3-5 Utilization of specific needle types and suction may optimize samples. Namely, 19G needles may provide better samples than smaller sizes and contemporary fine-needle biopsy needles with Franseen tips are superior to conventional spring-loaded cutting needles and fork tip needles.6-8 The use of dry suction has been shown to increase the yield of tissue, but at the expense of increased bloodiness. Wet suction, which involves the presence of fluid, rather than air, in the needle lumen to lubricate and improve transmission of negative pressure to the needle tip, is the preferred technique for EUS-LB given improvement in the likelihood of intact liver biopsy cores and increased specimen adequacy.9
There are several advantages to EUS-LB (Table 1). When compared with percutaneous liver biopsy (PC-LB) and transjugular liver biopsy (TJ-LB), EUS-LB is uniquely able to access both liver lobes in a single setting, which minimizes sampling error.3 EUS-LB may also have an advantage in sampling focal liver lesions given the close proximity of the transducer to the liver.10 Another advantage over PC-LB is that EUS-LB can be performed in patients with a large body habitus. Additionally, EUS-LB is better tolerated than PC-LB, with less postprocedure pain and shorter postprocedure monitoring time.4,5
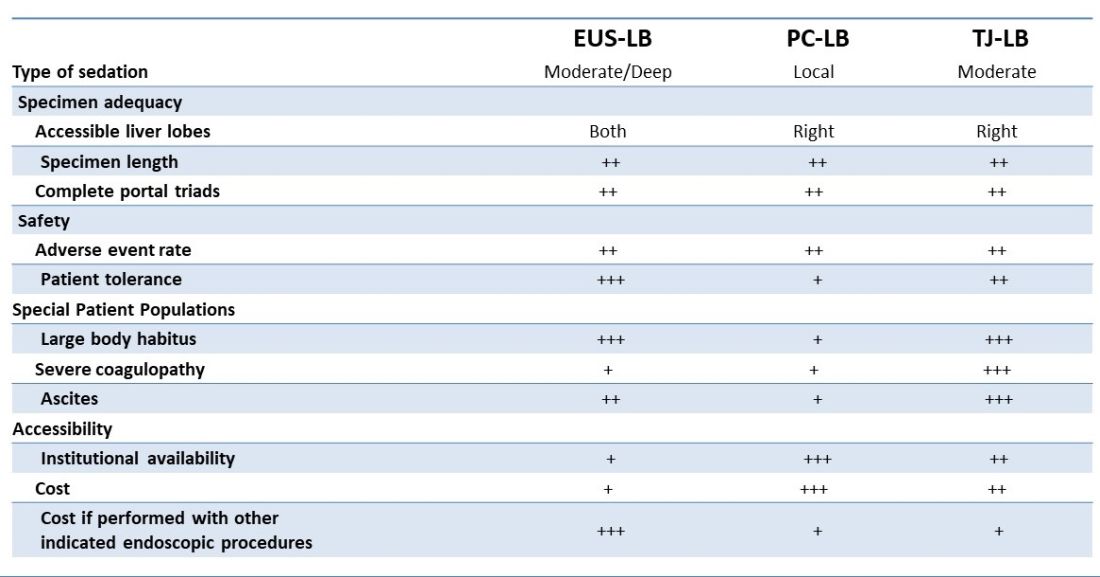
Rates of adverse events appear to be similar between the three methods. Similar to PC-LB, EUS-LB requires capsular puncture, which can lead to intraperitoneal hemorrhage. Therefore, TJ-LB is preferred in patients with significant coagulopathy. While small ascites is not an absolute contraindication for EUS-LB, large ascites can obscure a safe window from the proximal stomach or duodenum to the liver, and thus TJLB is also preferred in these patients.11 Given its relative novelty and logistic challenges, other disadvantages of EUS-LB include limited provider availability and increased cost, especially compared with PC-LB. The most significant limitation is that it requires moderate or deep sedation, as opposed to local anesthetics. However, if there is another indication for endoscopy (that is, variceal screening), then “one-stop shop” procedures including EUS-LB may be more convenient and cost-effective than traditional methods. Nevertheless, rigorous comparative studies are needed.
EUS-guided portal pressure gradient measurement
The presence of clinically significant portal hypertension (CSPH), defined as hepatic venous pressure gradient (HVPG) greater than or equal to 10 is a potent predictor of decompensation. There is growing evidence to support the use of beta-blockers to mitigate this risk.12 Therefore, early identification of patients with CSPH has important diagnostic and therapeutic implications. The current gold standard for diagnosing CSPH is with wedged HVPG measurements performed by interventional radiology.
Since its introduction in 2016, EUS-guided portal pressure gradient measurement (EUS-PPG) has emerged as an alternative to wedged HVPG.13,14 Using a linear echoendoscope, the portal vein is directly accessed with a 25G fine-needle aspiration needle, and three direct measurements are taken using a compact manometer to determine the mean pressure. The hepatic vein, or less commonly the inferior vena cava, pressure is also measured. The direct measurement of portal pressure provides a significant advantage of EUS-PPG over HVPG in patients with presinusoidal and prehepatic portal hypertension. Wedged HVPG, which utilizes the difference between the wedged and free hepatic venous pressure to indirectly estimate the portal venous pressure gradient, yields erroneously low gradients in patients with noncirrhotic portal hypertension.15 An additional advantage of EUS-PPG is that it obviates the need for a central venous line placement, which is associated with thrombosis and, in rare cases, air embolus.16
Observational studies indicate that EUS-PPG has a high degree of consistency with HVPG measurements and a strong correlation between other clinical findings of portal hyper-tension including esophageal varices and thrombocytopenia.13,14 Nevertheless, EUS-PPG is performed under moderate or deep sedation which may impact HVPG measurements.17 In addition, the real-world application of EUS-PPG measurement on clinical care is undefined, but it is the topic of an ongoing clinical trial (ClinicalTrials.gov – NCT05357599).
EUS-guided interventions of gastric varices
Compared with esophageal varices, current approaches to the treatment and prophylaxis of gastric varices are more controversial.18 The most common approach to bleeding gastric varices in the United States is the placement of a transjugular intrahepatic portosystemic shunt (TIPS). Nevertheless, in addition to risks associated with central venous line placement, 5%-35% of individuals develop hepatic encephalopathy after TIPS and ischemic acute liver failure can occur in rare situations.19 Cyanoacrylate (CYA) glue injection is the recommended first-line endoscopic therapy for the treatment of bleeding gastric varices, but use has not been widely adopted in the United States because of a lack of an approved Food and Drug Administration CYA formulation, limited expertise, and risk of serious complications. In particular systemic embolization may result in pulmonary or cerebral infarct.12,18 EUS-guided interventions have been developed to mitigate these safety concerns. EUS-guided coil embolization can be performed, either alone or in combination with CYA injection.20 In the latter approach it acts as a scaffold to prevent migration of the glue bolus. Doppler assessment enables direct visualization of the gastric varix for identification of feeder vessels, more controlled deployment of hemostatic agents, and real-time confirmation of varix obliteration. Fluoroscopy can be used as an adjunct.
EUS-guided interventions in the management of gastric varices appear to be effective and superior to CYA injection under direct endoscopic visualization with improved likelihood of obliteration and lower rebleeding rates, without increase in adverse events.21 Additionally, EUS-guided combination therapy improves technical outcomes and reduces adverse events relative to EUS-guided coil or EUS-guided glue injection therapy alone.21-23 Nevertheless, large-scale prospective trials are needed to determine whether EUS-guided interventions should be considered over TIPS. The role of EUS-guided interventions as primary prophylaxis to prevent bleeding from large gastric varices also requires additional study.24
Future directions
with the goal of optimizing care and increasing efficiency. In addition to new endoscopic procedures to optimize liver biopsy, portal pressure measurement, and gastric variceal treatment, there are a number of emerging technologies including EUS-guided liver elastography, portal venous sampling, liver tumor chemoembolization, and intrahepatic portosystemic shunts.25 However, the practice of endohepatology faces a number of challenges before widespread adoption, including limited provider expertise and institutional availability. Additionally, more robust, multicenter outcomes and cost-effective analyses comparing these novel procedures with traditional approaches are needed to define their clinical impact.
Dr. Bui is a fellow in gastroenterology in the division of gastroenterology and hepatology, University of Southern California, Los Angeles. Dr. Buxbaum is associate professor of medicine (clinical scholar) in the division of gastroenterology and hepatology, University of Southern California. Dr. Buxbaum is a consultant for Cook Medical, Boston Scientific, and Olympus. Dr. Bui has no disclosures.
References
1. Mathew A. Am J Gastroenterol. 2007;102(10):2354-5.
2. Sowa P et al. VideoGIE. 2021;6(11):487-8.
3. Pineda JJ et al. Gastrointest Endosc. 2016;83(2):360-5.
4. Ali AH et al. J Ultrasound. 2020;23(2):157-67.
5. Shuja A et al. Dig Liver Dis. 2019;51(6):826-30.
6. Schulman AR et al. Gastrointest Endosc. 2017;85(2):419-26.
7. DeWitt J et al. Endosc Int Open. 2015;3(5):E471-8.
8. Aggarwal SN et al. Gastrointest Endosc. 2021;93(5):1133-8.
9. Mok SRS et al. Gastrointest Endosc. 2018;88(6):919-25.
10. Lee YN et al. J Gastroenterol Hepatol. 2015;30(7):1161-6.
11. Kalambokis G et al. J Hepatol. 2007;47(2):284-94.
12. de Franchis R et al. J Hepatol. 2022;76(4):959-74.
13. Choi AY et al. J Gastroenterol Hepatol. 2022;37(7):1373-9.
14. Zhang W et al. Gastrointest Endosc. 2021;93(3):565-72.
15. Seijo S et al. Dig Liver Dis. 2012;44(10):855-60.
16. Vesely TM. J Vasc Interv Radiol. 2001;12(11):1291-5.
17. Reverter E et al. Liver Int. 2014;34(1):16-25.
18. Henry Z et al. Clin Gastroenterol Hepatol. 2021;19(6):1098-107.e1091.
19. Ripamonti R et al. Semin Intervent Radiol. 2006;23(2):165-76.
20. Rengstorff DS and Binmoeller KF. Gastrointest Endosc. 2004;59(4):553-8.
21. Mohan BP et al. Endoscopy. 2020;52(4):259-67.
22. Robles-Medranda C et al. Endoscopy. 2020;52(4):268-75.
23. McCarty TR et al. Endosc Ultrasound. 2020;9(1):6-15.
24. Kouanda A et al. Gastrointest Endosc. 2021;94(2):291-6.
25. Bazarbashi AN et al. 2022;24(1):98-107.
Introduction
Historically, the role of endoscopy in hepatology has been limited to intraluminal and bile duct interventions, primarily for the management of varices and biliary strictures. Recently, endoscopic ultrasound (EUS) has broadened the range of endoscopic treatment by enabling transluminal access to the liver parenchyma and associated vasculature. In this review, we will address recent advances in the expanding field of endohepatology.
Endoscopic-ultrasound guided liver biopsy
Liver biopsies are a critical tool in the diagnostic evaluation and management of patients with liver disease. Conventional approaches for obtaining liver tissue have been most commonly through the percutaneous or vascular approaches. In 2007, the first EUS-guided liver biopsy (EUS-LB) was described.1 EUS-LB is performed by advancing a line-array echoendoscope to the duodenal bulb to access the right lobe of the liver or proximal stomach to sample the left lobe. Doppler is first used to identify a pathway with few intervening vessels. Then a 19G or 20G needle is passed and slowly withdrawn to capture tissue (Figure 1). Careful evaluation with Doppler ultrasound to evaluate for bleeding is recommended after EUS-LB and if persistent, a small amount of clot may be reinjected as a blood or “Chang” patch akin to technique to control oozing postlumbar puncture.2
While large prospective studies are needed to compare the methods, it appears that specimen adequacy acquired via EUS-LB are comparable to percutaneous and transjugular approaches.3-5 Utilization of specific needle types and suction may optimize samples. Namely, 19G needles may provide better samples than smaller sizes and contemporary fine-needle biopsy needles with Franseen tips are superior to conventional spring-loaded cutting needles and fork tip needles.6-8 The use of dry suction has been shown to increase the yield of tissue, but at the expense of increased bloodiness. Wet suction, which involves the presence of fluid, rather than air, in the needle lumen to lubricate and improve transmission of negative pressure to the needle tip, is the preferred technique for EUS-LB given improvement in the likelihood of intact liver biopsy cores and increased specimen adequacy.9
There are several advantages to EUS-LB (Table 1). When compared with percutaneous liver biopsy (PC-LB) and transjugular liver biopsy (TJ-LB), EUS-LB is uniquely able to access both liver lobes in a single setting, which minimizes sampling error.3 EUS-LB may also have an advantage in sampling focal liver lesions given the close proximity of the transducer to the liver.10 Another advantage over PC-LB is that EUS-LB can be performed in patients with a large body habitus. Additionally, EUS-LB is better tolerated than PC-LB, with less postprocedure pain and shorter postprocedure monitoring time.4,5
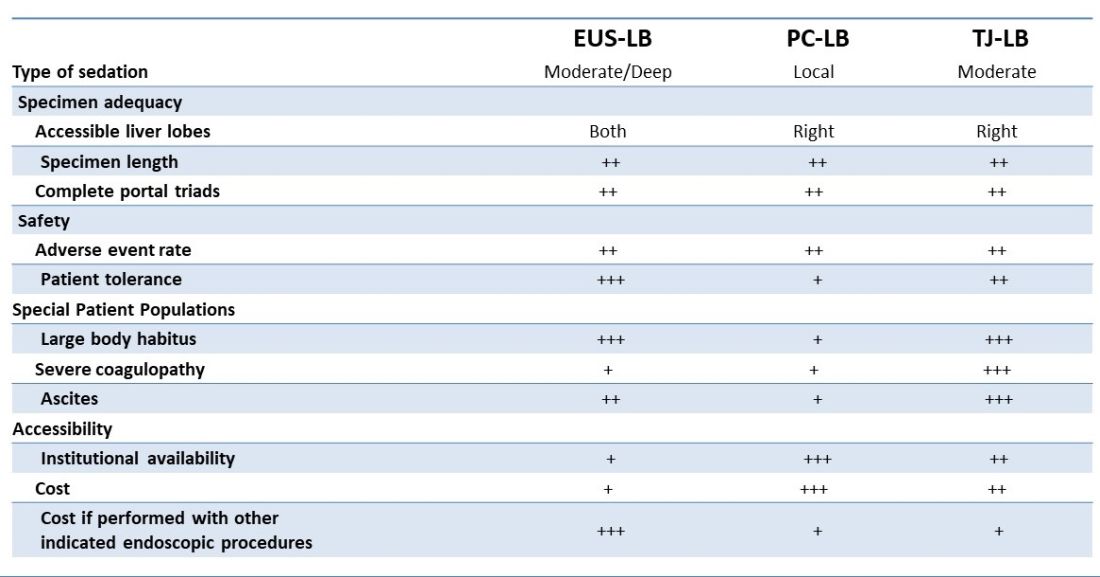
Rates of adverse events appear to be similar between the three methods. Similar to PC-LB, EUS-LB requires capsular puncture, which can lead to intraperitoneal hemorrhage. Therefore, TJ-LB is preferred in patients with significant coagulopathy. While small ascites is not an absolute contraindication for EUS-LB, large ascites can obscure a safe window from the proximal stomach or duodenum to the liver, and thus TJLB is also preferred in these patients.11 Given its relative novelty and logistic challenges, other disadvantages of EUS-LB include limited provider availability and increased cost, especially compared with PC-LB. The most significant limitation is that it requires moderate or deep sedation, as opposed to local anesthetics. However, if there is another indication for endoscopy (that is, variceal screening), then “one-stop shop” procedures including EUS-LB may be more convenient and cost-effective than traditional methods. Nevertheless, rigorous comparative studies are needed.
EUS-guided portal pressure gradient measurement
The presence of clinically significant portal hypertension (CSPH), defined as hepatic venous pressure gradient (HVPG) greater than or equal to 10 is a potent predictor of decompensation. There is growing evidence to support the use of beta-blockers to mitigate this risk.12 Therefore, early identification of patients with CSPH has important diagnostic and therapeutic implications. The current gold standard for diagnosing CSPH is with wedged HVPG measurements performed by interventional radiology.
Since its introduction in 2016, EUS-guided portal pressure gradient measurement (EUS-PPG) has emerged as an alternative to wedged HVPG.13,14 Using a linear echoendoscope, the portal vein is directly accessed with a 25G fine-needle aspiration needle, and three direct measurements are taken using a compact manometer to determine the mean pressure. The hepatic vein, or less commonly the inferior vena cava, pressure is also measured. The direct measurement of portal pressure provides a significant advantage of EUS-PPG over HVPG in patients with presinusoidal and prehepatic portal hypertension. Wedged HVPG, which utilizes the difference between the wedged and free hepatic venous pressure to indirectly estimate the portal venous pressure gradient, yields erroneously low gradients in patients with noncirrhotic portal hypertension.15 An additional advantage of EUS-PPG is that it obviates the need for a central venous line placement, which is associated with thrombosis and, in rare cases, air embolus.16
Observational studies indicate that EUS-PPG has a high degree of consistency with HVPG measurements and a strong correlation between other clinical findings of portal hyper-tension including esophageal varices and thrombocytopenia.13,14 Nevertheless, EUS-PPG is performed under moderate or deep sedation which may impact HVPG measurements.17 In addition, the real-world application of EUS-PPG measurement on clinical care is undefined, but it is the topic of an ongoing clinical trial (ClinicalTrials.gov – NCT05357599).
EUS-guided interventions of gastric varices
Compared with esophageal varices, current approaches to the treatment and prophylaxis of gastric varices are more controversial.18 The most common approach to bleeding gastric varices in the United States is the placement of a transjugular intrahepatic portosystemic shunt (TIPS). Nevertheless, in addition to risks associated with central venous line placement, 5%-35% of individuals develop hepatic encephalopathy after TIPS and ischemic acute liver failure can occur in rare situations.19 Cyanoacrylate (CYA) glue injection is the recommended first-line endoscopic therapy for the treatment of bleeding gastric varices, but use has not been widely adopted in the United States because of a lack of an approved Food and Drug Administration CYA formulation, limited expertise, and risk of serious complications. In particular systemic embolization may result in pulmonary or cerebral infarct.12,18 EUS-guided interventions have been developed to mitigate these safety concerns. EUS-guided coil embolization can be performed, either alone or in combination with CYA injection.20 In the latter approach it acts as a scaffold to prevent migration of the glue bolus. Doppler assessment enables direct visualization of the gastric varix for identification of feeder vessels, more controlled deployment of hemostatic agents, and real-time confirmation of varix obliteration. Fluoroscopy can be used as an adjunct.
EUS-guided interventions in the management of gastric varices appear to be effective and superior to CYA injection under direct endoscopic visualization with improved likelihood of obliteration and lower rebleeding rates, without increase in adverse events.21 Additionally, EUS-guided combination therapy improves technical outcomes and reduces adverse events relative to EUS-guided coil or EUS-guided glue injection therapy alone.21-23 Nevertheless, large-scale prospective trials are needed to determine whether EUS-guided interventions should be considered over TIPS. The role of EUS-guided interventions as primary prophylaxis to prevent bleeding from large gastric varices also requires additional study.24
Future directions
with the goal of optimizing care and increasing efficiency. In addition to new endoscopic procedures to optimize liver biopsy, portal pressure measurement, and gastric variceal treatment, there are a number of emerging technologies including EUS-guided liver elastography, portal venous sampling, liver tumor chemoembolization, and intrahepatic portosystemic shunts.25 However, the practice of endohepatology faces a number of challenges before widespread adoption, including limited provider expertise and institutional availability. Additionally, more robust, multicenter outcomes and cost-effective analyses comparing these novel procedures with traditional approaches are needed to define their clinical impact.
Dr. Bui is a fellow in gastroenterology in the division of gastroenterology and hepatology, University of Southern California, Los Angeles. Dr. Buxbaum is associate professor of medicine (clinical scholar) in the division of gastroenterology and hepatology, University of Southern California. Dr. Buxbaum is a consultant for Cook Medical, Boston Scientific, and Olympus. Dr. Bui has no disclosures.
References
1. Mathew A. Am J Gastroenterol. 2007;102(10):2354-5.
2. Sowa P et al. VideoGIE. 2021;6(11):487-8.
3. Pineda JJ et al. Gastrointest Endosc. 2016;83(2):360-5.
4. Ali AH et al. J Ultrasound. 2020;23(2):157-67.
5. Shuja A et al. Dig Liver Dis. 2019;51(6):826-30.
6. Schulman AR et al. Gastrointest Endosc. 2017;85(2):419-26.
7. DeWitt J et al. Endosc Int Open. 2015;3(5):E471-8.
8. Aggarwal SN et al. Gastrointest Endosc. 2021;93(5):1133-8.
9. Mok SRS et al. Gastrointest Endosc. 2018;88(6):919-25.
10. Lee YN et al. J Gastroenterol Hepatol. 2015;30(7):1161-6.
11. Kalambokis G et al. J Hepatol. 2007;47(2):284-94.
12. de Franchis R et al. J Hepatol. 2022;76(4):959-74.
13. Choi AY et al. J Gastroenterol Hepatol. 2022;37(7):1373-9.
14. Zhang W et al. Gastrointest Endosc. 2021;93(3):565-72.
15. Seijo S et al. Dig Liver Dis. 2012;44(10):855-60.
16. Vesely TM. J Vasc Interv Radiol. 2001;12(11):1291-5.
17. Reverter E et al. Liver Int. 2014;34(1):16-25.
18. Henry Z et al. Clin Gastroenterol Hepatol. 2021;19(6):1098-107.e1091.
19. Ripamonti R et al. Semin Intervent Radiol. 2006;23(2):165-76.
20. Rengstorff DS and Binmoeller KF. Gastrointest Endosc. 2004;59(4):553-8.
21. Mohan BP et al. Endoscopy. 2020;52(4):259-67.
22. Robles-Medranda C et al. Endoscopy. 2020;52(4):268-75.
23. McCarty TR et al. Endosc Ultrasound. 2020;9(1):6-15.
24. Kouanda A et al. Gastrointest Endosc. 2021;94(2):291-6.
25. Bazarbashi AN et al. 2022;24(1):98-107.