User login
50 years of ob.gyn.: Has practice changed for the better?
As a practicing obstetrician-gynecologist for nearly 40 years, Leonard Brabson, MD, has watched his specialty transform in ways both large and small.
For starters, his regular work attire in 1977 – a shirt and tie – is now scrubs. The paper charts that once filled his office shelves have been replaced with electronic records. And the cumbersome machines that once took blurry, still pictures of a fetus have advanced by leaps and bounds and become a staple of prenatal care.
“Back then, we were expected to be generalists. If [a patient] had a cancer, you took care of it. If [she] had a fertility problem or problem with endocrinology, you took care of it. Of course, now if I have a female cancer, we refer them to the gyn-oncologist. But when you go back 40 years and beyond, we did mostly everything.”
The ob.gyns. of today are practicing in a vastly different environment than their predecessors, and while many of the differences have improved patient care and enhanced efficiency, physicians also note that some changes have harmed the doctor-patient relationship and created career dissatisfaction.
“Certainly, the advances of modern medicine have enabled the current physician to provide the patient a level of care unparalleled in history,” said Charles E. Miller, MD, a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.
More volume, less time
Most long-time physicians agree that higher patient volumes and increasing administrative burdens have diminished the time they are able to spend with patients.
Rising clinical documentation and coding are the top administrative tasks taking away from one-on-one patient care, said Kristen Zeligs, MD, chair of the American Congress of Obstetricians and Gynecologists’ Junior Fellow Congress Advisory Council and a gynecologic oncology fellow at Walter Reed National Military Medical Center in Bethesda, Md.
But there are other factors straining the doctor-patient relationship. Decades ago, first-time mothers often stayed with one doctor for a lifetime, Dr. Brabson recalled, having all of her babies delivered by a single ob.gyn. The same can’t be said for today, where insurance changes, job relocations, and a lack of connections often lead patients to switch physicians frequently.
“Now a lot of patients [move on] from one year to the next,” Dr. Brabson said. “There’s not that same loyalty.”
Doctors, too, traditionally stuck with patients over the long haul, he added. In the past, if an ob.gyn treated a patient during pregnancy, that same physician was present during the delivery, even if it meant leaving a vacation early or coming in on a night off.
“Now the younger docs, especially those that have families with small children, when it’s not their night on call and it’s 5 o’clock, they’re checking out,” Dr. Brabson said. “One of my partners right now, she started inducing someone yesterday. Well today’s her day off, so I’m going to do the delivery. That’s been a big change.”
Highs and lows of liability premiums
Another pressure on the specialty over the last couple of decades has been the high cost of liability insurance.
“2003 was really the peak of the liability crisis,” Dr. Montgomery said. “Hospitals were closing. Doctors were giving up practice. It’s a little better now than it was.”
While ob.gyns. still pay higher premiums than many other specialties, the legal climate has improved in recent years, said Paul Greve Jr., executive vice president and senior consultant for the Willis Healthcare Practice, and author of the 2016 Medical Liability Monitor, an annual report that surveys medical liability premiums.
“The best way to characterize the overall environment for medical professional liability is stable,” he said. “In the area of obstetrics, for the first time ever in recent years, we are seeing lower frequency and lower severity [of lawsuits].”
The lower number of filings are largely due to patient safety initiatives among ob.gyn. programs and tort reforms – many of which have been upheld by courts in the last decade, Mr. Greve said.
Of course, the rate of premiums greatly differs depending on location, with ob.gyns. in Eastern New York paying a high of $214,999 and ob.gyns. in Minnesota paying a low of $16,449 in 2016, according to the Medical Liability Monitor.
“The environment is specific to the region,” Mr. Greve said. “New York City is still very problematic. Chicago is still very problematic. There are some pockets around the country where there’s no damage caps, and it’s really tough to defend claims.”
Technology ups and downs
Another fairly new pressure on ob.gyns. is the integration of the electronic health record and the federal reporting requirements that go along with it.
“Most practicing ob.gyns. are really fed up with the computerization of medicine and the tasking and the charting,” Dr. Montgomery said. “For every hour you spend seeing patients, you spend 1 or 2 hours doing computer chart work and paperwork. Most doctors don’t go into medicine so they can type; they go into medicine to take care of patients.”
The Internet age also poses challenges when it comes to patients conducting their own “research,” said Megan Evans, MD, an ob.gyn. at Tufts Medical Center, Boston.
Protecting the security of patients’ medical records in the digital age is another worry, she said.
But for Dr. Evans, who completed her residency training in 2015, having dozens of digital tools at her disposal as she treats patients is definitely an upside to today’s practice environment.
“I can review a practice bulletin, look up the latest treatment regimens, and contact my colleagues with a quick question – all on my iPhone,” she said. “I also believe there is so much potential for electronic medical records and how they communicate with each other.”
Advancements in ultrasound, fetal monitoring, and other medical technologies have also allowed ob.gyns. to intervene earlier and save lives.
Dr. Brabson recalled the helplessness he and other physicians felt in the 1970s when it came to delivering extremely premature babies.
“We didn’t really feel like you could save a baby under 2 pounds,” he said. “When I was a medical student, if you had a baby under 2 pounds, very commonly what they would do is lay the baby up on the table and watch and see how vigorous it was going to be, and if it really did breathe and carry on for awhile, then you might take it to the nursery. The equipment that we have to save babies with today, compared to 40 years ago, that’s a dramatic change.”
A changing focus for the future
If current trends continue, Dr. Brabson’s early experience of being a generalist ob.gyn. won’t be the norm. Instead, more ob.gyns. will choose to subspecialize. Whether this change is positive or negative for the specialty depends on who you ask.
“You could argue the pros and cons for both sides,” Dr. Zeligs said. “For me, it takes away from what drew me to the specialty – the breadth that ob.gyn. offers, both as a primary care specialty and as a surgical subspecialty.”
However, choosing one focus may offer some doctors a way to capture that elusive professional and personal balance, she added.
Despite the changing landscape of clinical duties and business operations, some parts of ob.gyn. practice have remained intact, according to Dr. Brabson. “The most rewarding and enjoyable part of the job is developing a relationship of mutual trust and respect,” he said. “As a result of developing such a relationship, both the patient and the doctor come away with positive feelings. This has not changed.”
agallegos@frontlinemedcom.com
On Twitter @legal_med
As a practicing obstetrician-gynecologist for nearly 40 years, Leonard Brabson, MD, has watched his specialty transform in ways both large and small.
For starters, his regular work attire in 1977 – a shirt and tie – is now scrubs. The paper charts that once filled his office shelves have been replaced with electronic records. And the cumbersome machines that once took blurry, still pictures of a fetus have advanced by leaps and bounds and become a staple of prenatal care.
“Back then, we were expected to be generalists. If [a patient] had a cancer, you took care of it. If [she] had a fertility problem or problem with endocrinology, you took care of it. Of course, now if I have a female cancer, we refer them to the gyn-oncologist. But when you go back 40 years and beyond, we did mostly everything.”
The ob.gyns. of today are practicing in a vastly different environment than their predecessors, and while many of the differences have improved patient care and enhanced efficiency, physicians also note that some changes have harmed the doctor-patient relationship and created career dissatisfaction.
“Certainly, the advances of modern medicine have enabled the current physician to provide the patient a level of care unparalleled in history,” said Charles E. Miller, MD, a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.
More volume, less time
Most long-time physicians agree that higher patient volumes and increasing administrative burdens have diminished the time they are able to spend with patients.
Rising clinical documentation and coding are the top administrative tasks taking away from one-on-one patient care, said Kristen Zeligs, MD, chair of the American Congress of Obstetricians and Gynecologists’ Junior Fellow Congress Advisory Council and a gynecologic oncology fellow at Walter Reed National Military Medical Center in Bethesda, Md.
But there are other factors straining the doctor-patient relationship. Decades ago, first-time mothers often stayed with one doctor for a lifetime, Dr. Brabson recalled, having all of her babies delivered by a single ob.gyn. The same can’t be said for today, where insurance changes, job relocations, and a lack of connections often lead patients to switch physicians frequently.
“Now a lot of patients [move on] from one year to the next,” Dr. Brabson said. “There’s not that same loyalty.”
Doctors, too, traditionally stuck with patients over the long haul, he added. In the past, if an ob.gyn treated a patient during pregnancy, that same physician was present during the delivery, even if it meant leaving a vacation early or coming in on a night off.
“Now the younger docs, especially those that have families with small children, when it’s not their night on call and it’s 5 o’clock, they’re checking out,” Dr. Brabson said. “One of my partners right now, she started inducing someone yesterday. Well today’s her day off, so I’m going to do the delivery. That’s been a big change.”
Highs and lows of liability premiums
Another pressure on the specialty over the last couple of decades has been the high cost of liability insurance.
“2003 was really the peak of the liability crisis,” Dr. Montgomery said. “Hospitals were closing. Doctors were giving up practice. It’s a little better now than it was.”
While ob.gyns. still pay higher premiums than many other specialties, the legal climate has improved in recent years, said Paul Greve Jr., executive vice president and senior consultant for the Willis Healthcare Practice, and author of the 2016 Medical Liability Monitor, an annual report that surveys medical liability premiums.
“The best way to characterize the overall environment for medical professional liability is stable,” he said. “In the area of obstetrics, for the first time ever in recent years, we are seeing lower frequency and lower severity [of lawsuits].”
The lower number of filings are largely due to patient safety initiatives among ob.gyn. programs and tort reforms – many of which have been upheld by courts in the last decade, Mr. Greve said.
Of course, the rate of premiums greatly differs depending on location, with ob.gyns. in Eastern New York paying a high of $214,999 and ob.gyns. in Minnesota paying a low of $16,449 in 2016, according to the Medical Liability Monitor.
“The environment is specific to the region,” Mr. Greve said. “New York City is still very problematic. Chicago is still very problematic. There are some pockets around the country where there’s no damage caps, and it’s really tough to defend claims.”
Technology ups and downs
Another fairly new pressure on ob.gyns. is the integration of the electronic health record and the federal reporting requirements that go along with it.
“Most practicing ob.gyns. are really fed up with the computerization of medicine and the tasking and the charting,” Dr. Montgomery said. “For every hour you spend seeing patients, you spend 1 or 2 hours doing computer chart work and paperwork. Most doctors don’t go into medicine so they can type; they go into medicine to take care of patients.”
The Internet age also poses challenges when it comes to patients conducting their own “research,” said Megan Evans, MD, an ob.gyn. at Tufts Medical Center, Boston.
Protecting the security of patients’ medical records in the digital age is another worry, she said.
But for Dr. Evans, who completed her residency training in 2015, having dozens of digital tools at her disposal as she treats patients is definitely an upside to today’s practice environment.
“I can review a practice bulletin, look up the latest treatment regimens, and contact my colleagues with a quick question – all on my iPhone,” she said. “I also believe there is so much potential for electronic medical records and how they communicate with each other.”
Advancements in ultrasound, fetal monitoring, and other medical technologies have also allowed ob.gyns. to intervene earlier and save lives.
Dr. Brabson recalled the helplessness he and other physicians felt in the 1970s when it came to delivering extremely premature babies.
“We didn’t really feel like you could save a baby under 2 pounds,” he said. “When I was a medical student, if you had a baby under 2 pounds, very commonly what they would do is lay the baby up on the table and watch and see how vigorous it was going to be, and if it really did breathe and carry on for awhile, then you might take it to the nursery. The equipment that we have to save babies with today, compared to 40 years ago, that’s a dramatic change.”
A changing focus for the future
If current trends continue, Dr. Brabson’s early experience of being a generalist ob.gyn. won’t be the norm. Instead, more ob.gyns. will choose to subspecialize. Whether this change is positive or negative for the specialty depends on who you ask.
“You could argue the pros and cons for both sides,” Dr. Zeligs said. “For me, it takes away from what drew me to the specialty – the breadth that ob.gyn. offers, both as a primary care specialty and as a surgical subspecialty.”
However, choosing one focus may offer some doctors a way to capture that elusive professional and personal balance, she added.
Despite the changing landscape of clinical duties and business operations, some parts of ob.gyn. practice have remained intact, according to Dr. Brabson. “The most rewarding and enjoyable part of the job is developing a relationship of mutual trust and respect,” he said. “As a result of developing such a relationship, both the patient and the doctor come away with positive feelings. This has not changed.”
agallegos@frontlinemedcom.com
On Twitter @legal_med
As a practicing obstetrician-gynecologist for nearly 40 years, Leonard Brabson, MD, has watched his specialty transform in ways both large and small.
For starters, his regular work attire in 1977 – a shirt and tie – is now scrubs. The paper charts that once filled his office shelves have been replaced with electronic records. And the cumbersome machines that once took blurry, still pictures of a fetus have advanced by leaps and bounds and become a staple of prenatal care.
“Back then, we were expected to be generalists. If [a patient] had a cancer, you took care of it. If [she] had a fertility problem or problem with endocrinology, you took care of it. Of course, now if I have a female cancer, we refer them to the gyn-oncologist. But when you go back 40 years and beyond, we did mostly everything.”
The ob.gyns. of today are practicing in a vastly different environment than their predecessors, and while many of the differences have improved patient care and enhanced efficiency, physicians also note that some changes have harmed the doctor-patient relationship and created career dissatisfaction.
“Certainly, the advances of modern medicine have enabled the current physician to provide the patient a level of care unparalleled in history,” said Charles E. Miller, MD, a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.
More volume, less time
Most long-time physicians agree that higher patient volumes and increasing administrative burdens have diminished the time they are able to spend with patients.
Rising clinical documentation and coding are the top administrative tasks taking away from one-on-one patient care, said Kristen Zeligs, MD, chair of the American Congress of Obstetricians and Gynecologists’ Junior Fellow Congress Advisory Council and a gynecologic oncology fellow at Walter Reed National Military Medical Center in Bethesda, Md.
But there are other factors straining the doctor-patient relationship. Decades ago, first-time mothers often stayed with one doctor for a lifetime, Dr. Brabson recalled, having all of her babies delivered by a single ob.gyn. The same can’t be said for today, where insurance changes, job relocations, and a lack of connections often lead patients to switch physicians frequently.
“Now a lot of patients [move on] from one year to the next,” Dr. Brabson said. “There’s not that same loyalty.”
Doctors, too, traditionally stuck with patients over the long haul, he added. In the past, if an ob.gyn treated a patient during pregnancy, that same physician was present during the delivery, even if it meant leaving a vacation early or coming in on a night off.
“Now the younger docs, especially those that have families with small children, when it’s not their night on call and it’s 5 o’clock, they’re checking out,” Dr. Brabson said. “One of my partners right now, she started inducing someone yesterday. Well today’s her day off, so I’m going to do the delivery. That’s been a big change.”
Highs and lows of liability premiums
Another pressure on the specialty over the last couple of decades has been the high cost of liability insurance.
“2003 was really the peak of the liability crisis,” Dr. Montgomery said. “Hospitals were closing. Doctors were giving up practice. It’s a little better now than it was.”
While ob.gyns. still pay higher premiums than many other specialties, the legal climate has improved in recent years, said Paul Greve Jr., executive vice president and senior consultant for the Willis Healthcare Practice, and author of the 2016 Medical Liability Monitor, an annual report that surveys medical liability premiums.
“The best way to characterize the overall environment for medical professional liability is stable,” he said. “In the area of obstetrics, for the first time ever in recent years, we are seeing lower frequency and lower severity [of lawsuits].”
The lower number of filings are largely due to patient safety initiatives among ob.gyn. programs and tort reforms – many of which have been upheld by courts in the last decade, Mr. Greve said.
Of course, the rate of premiums greatly differs depending on location, with ob.gyns. in Eastern New York paying a high of $214,999 and ob.gyns. in Minnesota paying a low of $16,449 in 2016, according to the Medical Liability Monitor.
“The environment is specific to the region,” Mr. Greve said. “New York City is still very problematic. Chicago is still very problematic. There are some pockets around the country where there’s no damage caps, and it’s really tough to defend claims.”
Technology ups and downs
Another fairly new pressure on ob.gyns. is the integration of the electronic health record and the federal reporting requirements that go along with it.
“Most practicing ob.gyns. are really fed up with the computerization of medicine and the tasking and the charting,” Dr. Montgomery said. “For every hour you spend seeing patients, you spend 1 or 2 hours doing computer chart work and paperwork. Most doctors don’t go into medicine so they can type; they go into medicine to take care of patients.”
The Internet age also poses challenges when it comes to patients conducting their own “research,” said Megan Evans, MD, an ob.gyn. at Tufts Medical Center, Boston.
Protecting the security of patients’ medical records in the digital age is another worry, she said.
But for Dr. Evans, who completed her residency training in 2015, having dozens of digital tools at her disposal as she treats patients is definitely an upside to today’s practice environment.
“I can review a practice bulletin, look up the latest treatment regimens, and contact my colleagues with a quick question – all on my iPhone,” she said. “I also believe there is so much potential for electronic medical records and how they communicate with each other.”
Advancements in ultrasound, fetal monitoring, and other medical technologies have also allowed ob.gyns. to intervene earlier and save lives.
Dr. Brabson recalled the helplessness he and other physicians felt in the 1970s when it came to delivering extremely premature babies.
“We didn’t really feel like you could save a baby under 2 pounds,” he said. “When I was a medical student, if you had a baby under 2 pounds, very commonly what they would do is lay the baby up on the table and watch and see how vigorous it was going to be, and if it really did breathe and carry on for awhile, then you might take it to the nursery. The equipment that we have to save babies with today, compared to 40 years ago, that’s a dramatic change.”
A changing focus for the future
If current trends continue, Dr. Brabson’s early experience of being a generalist ob.gyn. won’t be the norm. Instead, more ob.gyns. will choose to subspecialize. Whether this change is positive or negative for the specialty depends on who you ask.
“You could argue the pros and cons for both sides,” Dr. Zeligs said. “For me, it takes away from what drew me to the specialty – the breadth that ob.gyn. offers, both as a primary care specialty and as a surgical subspecialty.”
However, choosing one focus may offer some doctors a way to capture that elusive professional and personal balance, she added.
Despite the changing landscape of clinical duties and business operations, some parts of ob.gyn. practice have remained intact, according to Dr. Brabson. “The most rewarding and enjoyable part of the job is developing a relationship of mutual trust and respect,” he said. “As a result of developing such a relationship, both the patient and the doctor come away with positive feelings. This has not changed.”
agallegos@frontlinemedcom.com
On Twitter @legal_med
The 50-year quest for better pregnancy data
Editor’s note: As Ob.Gyn. News celebrates its 50th anniversary, we wanted to know how far the medical community has come in identifying and mitigating drug risks during pregnancy and in the postpartum period. In this article, our four expert columnists share their experiences trying to find and interpret critical pregnancy data, as well as how they weigh the potential risks and benefits for their patients.
The search for information
The biggest advance in the past 50 years is the availability of information, even though limited, relating to the effects of drugs in pregnancy and lactation. In the first few years of this period, it was a daunting task to obtain this information. I can recall spending hours in the hospital’s medical library going through huge volumes of Index Medicus to obtain references that the library could order for me. The appearance of Thomas H. Shepard’s first edition (Catalog of Teratogenic Agents) in 1973 was a step forward and in 1977, O.P. Heinonen and colleagues’ book (Birth Defects and Drugs in Pregnancy) was helpful.
Although all of the above sources were helpful, any book in an evolving field will not have the newest information. Two important services, TERIS and Reprotox, were started to allow clinicians to contact them for up-to-date data. Nevertheless, the biggest change was the availability of current information from the U.S. National Library of Medicine via Toxnet, PubMed, and LactMed, relating to the effects of drugs in pregnancy and lactation.
My method is to ask three questions. First, are there other drugs with a similar mechanism of action that have some human data? In most cases, the answer to this question is no, but even when there are data, it is typically very limited. Second, does the drug cross the human placenta? The answer is typically based on the molecular weight. Any drug with a molecular weight less than 1,000 daltons probably crosses. In the second half of pregnancy, especially in the third trimester, almost every drug crosses. Third, do the animal pregnancy data predict embryo/fetal risk? It was thought that it could if the dose causing harm was less than or equal to 10 times the human dose based on BSA or AUC and there were no signs of maternal toxicity. However, using data from my 10th edition, I and eight coauthors, all of whom are knowledgeable on the effects of drugs in pregnancy, found that the animal data for 311 drugs raised the possibility of human embryo-fetal harm that current data confirmed in only 75 (24%) of the drugs (Am J Obstet Gynecol. 2015 Dec;213[6]:810-5).
The system needs to be fixed. One method is to give the Food and Drug Administration the authority to require manufacturers of drugs likely to be used in pregnancy to gather and publish data on their use in pregnancy. That sounds reasonable, but will it ever occur?
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, and Washington State University, Spokane. He is coauthor of “Drugs in Pregnancy and Lactation,” and coeditor of “Diseases, Complications, and Drug Therapy in Obstetrics.” He has no relevant financial disclosures.
Learning the lessons of the past
During the last 50 years, two of the most potent known human teratogens, thalidomide and isotretinoin, became available for prescription in the United States. Thanks to the efforts of Frances Kelsey, MD, PhD, at the FDA, the initial application for approval of thalidomide in the United States was denied in the early 1960s. Subsequently, based on evidence from other countries where thalidomide was marketed that the drug can cause a pattern of serious birth defects, a very strict pregnancy prevention program was implemented when the drug was finally approved in the United States in 2006.
Over the last 50 years, we have also seen an important evolution in our ability to conduct pregnancy exposure safety studies. Though we still have limited ability to conduct clinical trials in pregnant women, the need for good quality observational studies has become more widely accepted. The Centers for Disease Control and Prevention’s National Birth Defects Prevention Study (now in its most recent iteration known as BD STEPS) has been one very important source of data on the safety of a wide variety of medications. Using a case-control study design, women who have delivered infants with specific birth defects and comparison women who have delivered non-malformed infants are interviewed about their exposures in pregnancy. These data have been extremely helpful in generating new hypotheses, confirming or refuting findings from other studies, and in testing hypotheses regarding the safety of medications widely used in women of reproductive age. These analyses, for example, have contributed to the large body of literature now available on the safety of antidepressant medications in pregnancy.
At the same time, in the last 30 years, we have seen a tremendous increase in the number of pregnancy registries required or recommended upon approval of a new drug in the United States. These registry studies, while challenging to complete in a timely manner, have steadily improved in terms of rigor, and several disease-based pregnancy exposure studies have been implemented, which have allowed us to better understand the comparative risks or safety of anticonvulsants and antiretroviral drugs, to name a few.
It is important to note that with all these advances in the last 50 years, we still have a huge gap in knowledge about medication safety in pregnancy and lactation. Recent reviews suggest that more than 80% of drugs currently marketed have insufficient or no data available. If we include over-the-counter medications, the knowledge gap grows larger. With the 2014 approval of the long-awaited Pregnancy and Lactation Labeling Rule, clinicians are now beginning to experience the elimination of the old A-B-C-D-X category system for pregnancy safety. In its place, data-driven product labels are required. These are expected to provide the clinician with a clear summary of the relevant studies for a given medication, and to place these in the context of the background risks for the underlying maternal disease being treated, as well as the population risks. However, it is painfully clear that we have a long way to go to generate the needed, high-quality data, to populate those labels.
Dr. Chambers is a professor of pediatrics and director of clinical research at Rady Children’s Hospital, San Diego, and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no relevant financial disclosures.
Moving toward personalized medicine
Nowhere is a lack of actionable data more pronounced than in the impact of mental health drugs in pregnancy.
As Dr. Briggs and Dr. Chambers have outlined, the quality of data regarding the reproductive safety of medications across the therapeutic spectrum has historically been fair at best. The methodology and the rigor has been sparse and to a large extent, in psychiatry, we were only able to look for signals of concern. Prior to the late 1980s and early 1990s, there was little to guide clinicians on the safety of even very commonly used psychiatric medications during pregnancy. The health implications for women of reproductive age are extraordinary and yet that urgency was not matched by the level of investigation until more recently.
In psychiatry, we have rapidly improving data informing women about the risk for major congenital malformations. The clinical dilemma of weighing the necessity to stay on a medication to prevent relapse of a psychiatric disorder with the potential risk of malformation in the fetus is a wrenching one for the mother-to-be. Only good information can help patients, together with their physician, make collaborative decisions that make sense for them. Given the same information and the same severity of illness, women will make different decisions, and that’s a good thing. The calculus couples use to make these private decisions is unique to those involved. But they are able to move through the process because they have a platform of high-quality information.
So where do we go in the future? We need to get beyond the question of risk of major malformations and move toward understanding the long-term neurodevelopmental implications of prenatal exposures – whether such exposures confer risk or are even potentially salutary. One needs only look at the vast body of literature regarding fetal exposure to selective serotonin reuptake inhibitors (SSRIs) to observe the realization of this trend. When it comes to SSRIs, a fairly clear picture has emerged that they pose little absolute risk in terms of congenital malformations. What is missing is how SSRIs impact a child’s learning and development at age 3, 5, and 10. There have been a few studies in this area, but not a single, large prospective study that accurately quantifies both exposure to SSRIs and maternal psychiatric illness during pregnancy.
I expect that the future will also bring a greater understanding of the impact of untreated mental illness on the risk for obstetrical, neonatal, and longer-term neurodevelopmental outcomes. Most of the safety concerns have centered around the effect of fetal exposure to medications, but we also need to better understand how untreated psychiatric disorders impact the spectrum of relevant outcomes.
Getting back to the dilemma faced by pregnant women who really need medication to sustain emotional well-being, there simply is no perfect answer. No decision is perfect or risk free. What we can hope is that we’ll have personalized approaches that take into account the best available data and the patient’s individual situation and wishes. We’ve already come a long way toward meeting that goal, and I’m optimistic about where we’re going.
Dr. Cohen is the director of the Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications.
Perception of risk
Every year, numerous new medicines are approved by the FDA without data in pregnancy. Animal studies may show a problem that doesn’t appear in humans, or as was the case with thalidomide, the problem may not be apparent in animals and show up later in humans. There are many drugs that are safe in pregnancy, but women are understandably afraid of the potential impact on fetal development.
While my colleagues have presented the advances we’ve made in understanding the actual risks of medications during the prenatal period, it’s also important to focus on the perception of risk and to recognize that the reality and the perception can be vastly different.
At the same time, we began to ask women, using a visual analog scale, what would be their trend toward continuing or terminating pregnancy? Over several studies, we found that the likelihood of termination was high, and certainly much higher than was supported by the evidence of actual harm to the fetus. Specifically, if a woman received information about the safety of the drug and she still gave more than a 50% probability of terminating the pregnancy when surveyed, there was a good chance that she would terminate the pregnancy.
When you consider that most of the drugs that women are commonly prescribed in pregnancy – from most painkillers to antidepressants – are not known to cause malformations in pregnancy, you begin to see how problematic an inflated perception of risk can become.
But we see different trends in women with serious and chronic health problems, such as lupus or epilepsy. These women are typically under the care of a subspecialist, who in many cases has developed a significant knowledge base and comfort level around prescribing the drugs in this area and is able to communicate more clearly to patients both the risks to the fetus and the consequences of failure to treat their condition.
So clearly, the role of the physician and the ob.gyn. in particular is critical. It’s no secret that physicians face a negative legal climate that encourages defensive medicine and that they are often hesitant to tell women, without reservation, that it is okay to take a drug. But we must all remember that it is very easy to cause a woman not to take a medication in pregnancy and often that’s not what’s best for her health. Many women now postpone the age of starting a family and more have chronic conditions that require treatment. The idea of not treating certain conditions for the length of a pregnancy is not always a viable option. Yet there are quite a few women who would consider termination “just to be on the safe side.” That must be taken very seriously by the medical profession.
Dr. Koren is a professor of physiology/pharmacology at Western University, London, Ont., and a professor of medicine at Tel Aviv University. He is the founder of the Motherisk Program. He reported being a paid consultant for Duchesnay and Novartis.
Editor’s note: As Ob.Gyn. News celebrates its 50th anniversary, we wanted to know how far the medical community has come in identifying and mitigating drug risks during pregnancy and in the postpartum period. In this article, our four expert columnists share their experiences trying to find and interpret critical pregnancy data, as well as how they weigh the potential risks and benefits for their patients.
The search for information
The biggest advance in the past 50 years is the availability of information, even though limited, relating to the effects of drugs in pregnancy and lactation. In the first few years of this period, it was a daunting task to obtain this information. I can recall spending hours in the hospital’s medical library going through huge volumes of Index Medicus to obtain references that the library could order for me. The appearance of Thomas H. Shepard’s first edition (Catalog of Teratogenic Agents) in 1973 was a step forward and in 1977, O.P. Heinonen and colleagues’ book (Birth Defects and Drugs in Pregnancy) was helpful.
Although all of the above sources were helpful, any book in an evolving field will not have the newest information. Two important services, TERIS and Reprotox, were started to allow clinicians to contact them for up-to-date data. Nevertheless, the biggest change was the availability of current information from the U.S. National Library of Medicine via Toxnet, PubMed, and LactMed, relating to the effects of drugs in pregnancy and lactation.
My method is to ask three questions. First, are there other drugs with a similar mechanism of action that have some human data? In most cases, the answer to this question is no, but even when there are data, it is typically very limited. Second, does the drug cross the human placenta? The answer is typically based on the molecular weight. Any drug with a molecular weight less than 1,000 daltons probably crosses. In the second half of pregnancy, especially in the third trimester, almost every drug crosses. Third, do the animal pregnancy data predict embryo/fetal risk? It was thought that it could if the dose causing harm was less than or equal to 10 times the human dose based on BSA or AUC and there were no signs of maternal toxicity. However, using data from my 10th edition, I and eight coauthors, all of whom are knowledgeable on the effects of drugs in pregnancy, found that the animal data for 311 drugs raised the possibility of human embryo-fetal harm that current data confirmed in only 75 (24%) of the drugs (Am J Obstet Gynecol. 2015 Dec;213[6]:810-5).
The system needs to be fixed. One method is to give the Food and Drug Administration the authority to require manufacturers of drugs likely to be used in pregnancy to gather and publish data on their use in pregnancy. That sounds reasonable, but will it ever occur?
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, and Washington State University, Spokane. He is coauthor of “Drugs in Pregnancy and Lactation,” and coeditor of “Diseases, Complications, and Drug Therapy in Obstetrics.” He has no relevant financial disclosures.
Learning the lessons of the past
During the last 50 years, two of the most potent known human teratogens, thalidomide and isotretinoin, became available for prescription in the United States. Thanks to the efforts of Frances Kelsey, MD, PhD, at the FDA, the initial application for approval of thalidomide in the United States was denied in the early 1960s. Subsequently, based on evidence from other countries where thalidomide was marketed that the drug can cause a pattern of serious birth defects, a very strict pregnancy prevention program was implemented when the drug was finally approved in the United States in 2006.
Over the last 50 years, we have also seen an important evolution in our ability to conduct pregnancy exposure safety studies. Though we still have limited ability to conduct clinical trials in pregnant women, the need for good quality observational studies has become more widely accepted. The Centers for Disease Control and Prevention’s National Birth Defects Prevention Study (now in its most recent iteration known as BD STEPS) has been one very important source of data on the safety of a wide variety of medications. Using a case-control study design, women who have delivered infants with specific birth defects and comparison women who have delivered non-malformed infants are interviewed about their exposures in pregnancy. These data have been extremely helpful in generating new hypotheses, confirming or refuting findings from other studies, and in testing hypotheses regarding the safety of medications widely used in women of reproductive age. These analyses, for example, have contributed to the large body of literature now available on the safety of antidepressant medications in pregnancy.
At the same time, in the last 30 years, we have seen a tremendous increase in the number of pregnancy registries required or recommended upon approval of a new drug in the United States. These registry studies, while challenging to complete in a timely manner, have steadily improved in terms of rigor, and several disease-based pregnancy exposure studies have been implemented, which have allowed us to better understand the comparative risks or safety of anticonvulsants and antiretroviral drugs, to name a few.
It is important to note that with all these advances in the last 50 years, we still have a huge gap in knowledge about medication safety in pregnancy and lactation. Recent reviews suggest that more than 80% of drugs currently marketed have insufficient or no data available. If we include over-the-counter medications, the knowledge gap grows larger. With the 2014 approval of the long-awaited Pregnancy and Lactation Labeling Rule, clinicians are now beginning to experience the elimination of the old A-B-C-D-X category system for pregnancy safety. In its place, data-driven product labels are required. These are expected to provide the clinician with a clear summary of the relevant studies for a given medication, and to place these in the context of the background risks for the underlying maternal disease being treated, as well as the population risks. However, it is painfully clear that we have a long way to go to generate the needed, high-quality data, to populate those labels.
Dr. Chambers is a professor of pediatrics and director of clinical research at Rady Children’s Hospital, San Diego, and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no relevant financial disclosures.
Moving toward personalized medicine
Nowhere is a lack of actionable data more pronounced than in the impact of mental health drugs in pregnancy.
As Dr. Briggs and Dr. Chambers have outlined, the quality of data regarding the reproductive safety of medications across the therapeutic spectrum has historically been fair at best. The methodology and the rigor has been sparse and to a large extent, in psychiatry, we were only able to look for signals of concern. Prior to the late 1980s and early 1990s, there was little to guide clinicians on the safety of even very commonly used psychiatric medications during pregnancy. The health implications for women of reproductive age are extraordinary and yet that urgency was not matched by the level of investigation until more recently.
In psychiatry, we have rapidly improving data informing women about the risk for major congenital malformations. The clinical dilemma of weighing the necessity to stay on a medication to prevent relapse of a psychiatric disorder with the potential risk of malformation in the fetus is a wrenching one for the mother-to-be. Only good information can help patients, together with their physician, make collaborative decisions that make sense for them. Given the same information and the same severity of illness, women will make different decisions, and that’s a good thing. The calculus couples use to make these private decisions is unique to those involved. But they are able to move through the process because they have a platform of high-quality information.
So where do we go in the future? We need to get beyond the question of risk of major malformations and move toward understanding the long-term neurodevelopmental implications of prenatal exposures – whether such exposures confer risk or are even potentially salutary. One needs only look at the vast body of literature regarding fetal exposure to selective serotonin reuptake inhibitors (SSRIs) to observe the realization of this trend. When it comes to SSRIs, a fairly clear picture has emerged that they pose little absolute risk in terms of congenital malformations. What is missing is how SSRIs impact a child’s learning and development at age 3, 5, and 10. There have been a few studies in this area, but not a single, large prospective study that accurately quantifies both exposure to SSRIs and maternal psychiatric illness during pregnancy.
I expect that the future will also bring a greater understanding of the impact of untreated mental illness on the risk for obstetrical, neonatal, and longer-term neurodevelopmental outcomes. Most of the safety concerns have centered around the effect of fetal exposure to medications, but we also need to better understand how untreated psychiatric disorders impact the spectrum of relevant outcomes.
Getting back to the dilemma faced by pregnant women who really need medication to sustain emotional well-being, there simply is no perfect answer. No decision is perfect or risk free. What we can hope is that we’ll have personalized approaches that take into account the best available data and the patient’s individual situation and wishes. We’ve already come a long way toward meeting that goal, and I’m optimistic about where we’re going.
Dr. Cohen is the director of the Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications.
Perception of risk
Every year, numerous new medicines are approved by the FDA without data in pregnancy. Animal studies may show a problem that doesn’t appear in humans, or as was the case with thalidomide, the problem may not be apparent in animals and show up later in humans. There are many drugs that are safe in pregnancy, but women are understandably afraid of the potential impact on fetal development.
While my colleagues have presented the advances we’ve made in understanding the actual risks of medications during the prenatal period, it’s also important to focus on the perception of risk and to recognize that the reality and the perception can be vastly different.
At the same time, we began to ask women, using a visual analog scale, what would be their trend toward continuing or terminating pregnancy? Over several studies, we found that the likelihood of termination was high, and certainly much higher than was supported by the evidence of actual harm to the fetus. Specifically, if a woman received information about the safety of the drug and she still gave more than a 50% probability of terminating the pregnancy when surveyed, there was a good chance that she would terminate the pregnancy.
When you consider that most of the drugs that women are commonly prescribed in pregnancy – from most painkillers to antidepressants – are not known to cause malformations in pregnancy, you begin to see how problematic an inflated perception of risk can become.
But we see different trends in women with serious and chronic health problems, such as lupus or epilepsy. These women are typically under the care of a subspecialist, who in many cases has developed a significant knowledge base and comfort level around prescribing the drugs in this area and is able to communicate more clearly to patients both the risks to the fetus and the consequences of failure to treat their condition.
So clearly, the role of the physician and the ob.gyn. in particular is critical. It’s no secret that physicians face a negative legal climate that encourages defensive medicine and that they are often hesitant to tell women, without reservation, that it is okay to take a drug. But we must all remember that it is very easy to cause a woman not to take a medication in pregnancy and often that’s not what’s best for her health. Many women now postpone the age of starting a family and more have chronic conditions that require treatment. The idea of not treating certain conditions for the length of a pregnancy is not always a viable option. Yet there are quite a few women who would consider termination “just to be on the safe side.” That must be taken very seriously by the medical profession.
Dr. Koren is a professor of physiology/pharmacology at Western University, London, Ont., and a professor of medicine at Tel Aviv University. He is the founder of the Motherisk Program. He reported being a paid consultant for Duchesnay and Novartis.
Editor’s note: As Ob.Gyn. News celebrates its 50th anniversary, we wanted to know how far the medical community has come in identifying and mitigating drug risks during pregnancy and in the postpartum period. In this article, our four expert columnists share their experiences trying to find and interpret critical pregnancy data, as well as how they weigh the potential risks and benefits for their patients.
The search for information
The biggest advance in the past 50 years is the availability of information, even though limited, relating to the effects of drugs in pregnancy and lactation. In the first few years of this period, it was a daunting task to obtain this information. I can recall spending hours in the hospital’s medical library going through huge volumes of Index Medicus to obtain references that the library could order for me. The appearance of Thomas H. Shepard’s first edition (Catalog of Teratogenic Agents) in 1973 was a step forward and in 1977, O.P. Heinonen and colleagues’ book (Birth Defects and Drugs in Pregnancy) was helpful.
Although all of the above sources were helpful, any book in an evolving field will not have the newest information. Two important services, TERIS and Reprotox, were started to allow clinicians to contact them for up-to-date data. Nevertheless, the biggest change was the availability of current information from the U.S. National Library of Medicine via Toxnet, PubMed, and LactMed, relating to the effects of drugs in pregnancy and lactation.
My method is to ask three questions. First, are there other drugs with a similar mechanism of action that have some human data? In most cases, the answer to this question is no, but even when there are data, it is typically very limited. Second, does the drug cross the human placenta? The answer is typically based on the molecular weight. Any drug with a molecular weight less than 1,000 daltons probably crosses. In the second half of pregnancy, especially in the third trimester, almost every drug crosses. Third, do the animal pregnancy data predict embryo/fetal risk? It was thought that it could if the dose causing harm was less than or equal to 10 times the human dose based on BSA or AUC and there were no signs of maternal toxicity. However, using data from my 10th edition, I and eight coauthors, all of whom are knowledgeable on the effects of drugs in pregnancy, found that the animal data for 311 drugs raised the possibility of human embryo-fetal harm that current data confirmed in only 75 (24%) of the drugs (Am J Obstet Gynecol. 2015 Dec;213[6]:810-5).
The system needs to be fixed. One method is to give the Food and Drug Administration the authority to require manufacturers of drugs likely to be used in pregnancy to gather and publish data on their use in pregnancy. That sounds reasonable, but will it ever occur?
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, and Washington State University, Spokane. He is coauthor of “Drugs in Pregnancy and Lactation,” and coeditor of “Diseases, Complications, and Drug Therapy in Obstetrics.” He has no relevant financial disclosures.
Learning the lessons of the past
During the last 50 years, two of the most potent known human teratogens, thalidomide and isotretinoin, became available for prescription in the United States. Thanks to the efforts of Frances Kelsey, MD, PhD, at the FDA, the initial application for approval of thalidomide in the United States was denied in the early 1960s. Subsequently, based on evidence from other countries where thalidomide was marketed that the drug can cause a pattern of serious birth defects, a very strict pregnancy prevention program was implemented when the drug was finally approved in the United States in 2006.
Over the last 50 years, we have also seen an important evolution in our ability to conduct pregnancy exposure safety studies. Though we still have limited ability to conduct clinical trials in pregnant women, the need for good quality observational studies has become more widely accepted. The Centers for Disease Control and Prevention’s National Birth Defects Prevention Study (now in its most recent iteration known as BD STEPS) has been one very important source of data on the safety of a wide variety of medications. Using a case-control study design, women who have delivered infants with specific birth defects and comparison women who have delivered non-malformed infants are interviewed about their exposures in pregnancy. These data have been extremely helpful in generating new hypotheses, confirming or refuting findings from other studies, and in testing hypotheses regarding the safety of medications widely used in women of reproductive age. These analyses, for example, have contributed to the large body of literature now available on the safety of antidepressant medications in pregnancy.
At the same time, in the last 30 years, we have seen a tremendous increase in the number of pregnancy registries required or recommended upon approval of a new drug in the United States. These registry studies, while challenging to complete in a timely manner, have steadily improved in terms of rigor, and several disease-based pregnancy exposure studies have been implemented, which have allowed us to better understand the comparative risks or safety of anticonvulsants and antiretroviral drugs, to name a few.
It is important to note that with all these advances in the last 50 years, we still have a huge gap in knowledge about medication safety in pregnancy and lactation. Recent reviews suggest that more than 80% of drugs currently marketed have insufficient or no data available. If we include over-the-counter medications, the knowledge gap grows larger. With the 2014 approval of the long-awaited Pregnancy and Lactation Labeling Rule, clinicians are now beginning to experience the elimination of the old A-B-C-D-X category system for pregnancy safety. In its place, data-driven product labels are required. These are expected to provide the clinician with a clear summary of the relevant studies for a given medication, and to place these in the context of the background risks for the underlying maternal disease being treated, as well as the population risks. However, it is painfully clear that we have a long way to go to generate the needed, high-quality data, to populate those labels.
Dr. Chambers is a professor of pediatrics and director of clinical research at Rady Children’s Hospital, San Diego, and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no relevant financial disclosures.
Moving toward personalized medicine
Nowhere is a lack of actionable data more pronounced than in the impact of mental health drugs in pregnancy.
As Dr. Briggs and Dr. Chambers have outlined, the quality of data regarding the reproductive safety of medications across the therapeutic spectrum has historically been fair at best. The methodology and the rigor has been sparse and to a large extent, in psychiatry, we were only able to look for signals of concern. Prior to the late 1980s and early 1990s, there was little to guide clinicians on the safety of even very commonly used psychiatric medications during pregnancy. The health implications for women of reproductive age are extraordinary and yet that urgency was not matched by the level of investigation until more recently.
In psychiatry, we have rapidly improving data informing women about the risk for major congenital malformations. The clinical dilemma of weighing the necessity to stay on a medication to prevent relapse of a psychiatric disorder with the potential risk of malformation in the fetus is a wrenching one for the mother-to-be. Only good information can help patients, together with their physician, make collaborative decisions that make sense for them. Given the same information and the same severity of illness, women will make different decisions, and that’s a good thing. The calculus couples use to make these private decisions is unique to those involved. But they are able to move through the process because they have a platform of high-quality information.
So where do we go in the future? We need to get beyond the question of risk of major malformations and move toward understanding the long-term neurodevelopmental implications of prenatal exposures – whether such exposures confer risk or are even potentially salutary. One needs only look at the vast body of literature regarding fetal exposure to selective serotonin reuptake inhibitors (SSRIs) to observe the realization of this trend. When it comes to SSRIs, a fairly clear picture has emerged that they pose little absolute risk in terms of congenital malformations. What is missing is how SSRIs impact a child’s learning and development at age 3, 5, and 10. There have been a few studies in this area, but not a single, large prospective study that accurately quantifies both exposure to SSRIs and maternal psychiatric illness during pregnancy.
I expect that the future will also bring a greater understanding of the impact of untreated mental illness on the risk for obstetrical, neonatal, and longer-term neurodevelopmental outcomes. Most of the safety concerns have centered around the effect of fetal exposure to medications, but we also need to better understand how untreated psychiatric disorders impact the spectrum of relevant outcomes.
Getting back to the dilemma faced by pregnant women who really need medication to sustain emotional well-being, there simply is no perfect answer. No decision is perfect or risk free. What we can hope is that we’ll have personalized approaches that take into account the best available data and the patient’s individual situation and wishes. We’ve already come a long way toward meeting that goal, and I’m optimistic about where we’re going.
Dr. Cohen is the director of the Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications.
Perception of risk
Every year, numerous new medicines are approved by the FDA without data in pregnancy. Animal studies may show a problem that doesn’t appear in humans, or as was the case with thalidomide, the problem may not be apparent in animals and show up later in humans. There are many drugs that are safe in pregnancy, but women are understandably afraid of the potential impact on fetal development.
While my colleagues have presented the advances we’ve made in understanding the actual risks of medications during the prenatal period, it’s also important to focus on the perception of risk and to recognize that the reality and the perception can be vastly different.
At the same time, we began to ask women, using a visual analog scale, what would be their trend toward continuing or terminating pregnancy? Over several studies, we found that the likelihood of termination was high, and certainly much higher than was supported by the evidence of actual harm to the fetus. Specifically, if a woman received information about the safety of the drug and she still gave more than a 50% probability of terminating the pregnancy when surveyed, there was a good chance that she would terminate the pregnancy.
When you consider that most of the drugs that women are commonly prescribed in pregnancy – from most painkillers to antidepressants – are not known to cause malformations in pregnancy, you begin to see how problematic an inflated perception of risk can become.
But we see different trends in women with serious and chronic health problems, such as lupus or epilepsy. These women are typically under the care of a subspecialist, who in many cases has developed a significant knowledge base and comfort level around prescribing the drugs in this area and is able to communicate more clearly to patients both the risks to the fetus and the consequences of failure to treat their condition.
So clearly, the role of the physician and the ob.gyn. in particular is critical. It’s no secret that physicians face a negative legal climate that encourages defensive medicine and that they are often hesitant to tell women, without reservation, that it is okay to take a drug. But we must all remember that it is very easy to cause a woman not to take a medication in pregnancy and often that’s not what’s best for her health. Many women now postpone the age of starting a family and more have chronic conditions that require treatment. The idea of not treating certain conditions for the length of a pregnancy is not always a viable option. Yet there are quite a few women who would consider termination “just to be on the safe side.” That must be taken very seriously by the medical profession.
Dr. Koren is a professor of physiology/pharmacology at Western University, London, Ont., and a professor of medicine at Tel Aviv University. He is the founder of the Motherisk Program. He reported being a paid consultant for Duchesnay and Novartis.
Early days of IVF marked by competition, innovation
In 1978, when England’s Louise Brown became the world’s first baby born through in vitro fertilization, physicians at academic centers all over the United States scrambled to figure out how they, too, could provide IVF to the thousands of infertile couples for whom nothing else had worked.
Interest in IVF was strong even before British physiologist Robert Edwards and gynecologist Patrick Steptoe announced their success. “We knew that IVF was being developed, that it had been accomplished in animals, and ultimately we knew it was going to succeed in humans,” said reproductive endocrinologist Zev Rosenwaks, MD, of the Weill Cornell Center for Reproductive Medicine in New York.
In the late 1970s, “we were able to help only about two-thirds of couples with infertility, either with tubal surgery, insemination – often with donor sperm – or ovulation induction. A full third could not be helped. We predicted that IVF would allow us to treat virtually everyone,” Dr. Rosenwaks said.
But even after the first IVF birth, information on the revolutionary procedure remained frustratingly scarce.
“Edwards and Steptoe would talk to nobody,” said Richard Marrs, MD, a reproductive endocrinologist and infertility specialist in Los Angeles.
And federal research support for “test-tube babies,” as IVF was known in the media then, was nil thanks to a ban on government-funded human embryo research that persists to this day.
The U.S. physicians who took part in the rush to achieve an IVF birth – most of them young fellows at the time – recall a period of improvisation, collaboration, shoestring budgets, and surprise findings.
“People who just started 10 or even 20 years ago don’t realize what it took for us to learn how to go about doing IVF,” said Dr. Rosenwaks, who in the first years of IVF worked closely with Dr. Howard Jones and Dr. Georgeanna Jones, the first team in the U.S. to announce an IVF baby.
Labs in closets
In the late 1970s, Dr. Marrs, then a fellow at the University of Southern California, was focused on surgical methods to treat infertility – and demand was sky-high. Intrauterine devices used in the 1970s left many women with severe scarring and inflammation of the fallopian tubes.
“I was very surgically oriented,” Dr. Marrs said. “I thought I could fix any disaster in the pelvis that was put in front of me, especially with microsurgery.”
After the news of IVF success in England, Dr. Marrs threw himself into a side project at a nearby cancer center, working on single-cell cultures. “I thought if I could grow tumor cells, I could one day grow embryos,” he said.
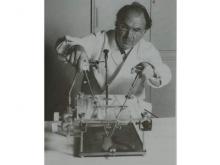
A year later, Dr. Marrs set up the first IVF lab at USC – in a storage closet. “I sterilized the place and that was our first IVF lab, literally a closet with an incubator and a microscope.” Its budget was accordingly thin, as the director at the time felt certain that IVF was a dead end. To fund his work, Dr. Marrs asked IVF candidate patients for research donations in lieu of payment.
But before Dr. Marrs attempted to perform his first IVF, two centers in Australia announced their own IVF babies. “I decided I really needed to go see someone who had had a baby,” he said. He used his vacation time to fly to Melbourne, shuttling between two competing clinics that were “four blocks apart and wouldn’t even talk to each other,” he recalled.
Over 6 weeks, “I learned how to stimulate, how to time ovulation. I watched the PhDs in the lab – how they handled the eggs and the sperm, what the conditions were, the incubator settings,” he said.
The first IVF babies in the United States were born only months apart: The first, in December 1981, was at the Jones Institute for Reproductive Medicine in Norfolk, Va., where Dr. Rosenwaks served as the first director.
The second baby born was at USC. After that, “we had 4,000 women on a waiting list, all under age 35,” Dr. Marrs said. The Jones Institute reportedly had 5,000.
As demand soared and more IVF babies arrived, the cloak of secrecy surrounding the procedure started to lift. British, Australian, and U.S. clinicians started getting together regularly. “We would pick a spot in the world, present our data: what we’d done, how many cycles, what we used for stimulation, when we took the eggs out,” Dr. Marrs said. “I don’t know how many hundreds of thousands of miles I flew in the first years of IVF, because it was the only way I could get information. We would literally stay up all night talking.”
Answering safety questions
Alan H. DeCherney, MD, currently an infertility researcher at the National Institutes of Health, started Yale University’s IVF program at around the same time Dr. Marrs and the Joneses were starting theirs. Yale already had a large infertility practice, and only academic centers had the laboratory resources and skilled staff needed to attempt IVF in those years.
In 1983, when Yale announced the birth of its first IVF baby – the fifth in the United States – Dr. DeCherney was starting to think about measuring outcomes, as there was concern over the potential for congenital anomalies related to IVF. “This was such a change in the way conception occurred, people were afraid that all kinds of crazy things would happen,” he said.
One concern was about ovarian stimulation with fertility drugs or gonadotropins. The earliest efforts – including by Dr. Steptoe and Dr. Edwards – used no drugs, instead trying to pinpoint the moment of natural egg release by measuring a woman’s hormone levels constantly, but these proved disappointing. Use of clomiphene citrate and human menopausal gonadotropin allowed for more control over timing, and for multiple mature eggs to be harvested at once.
But there were still many unanswered questions related to these agents’ safety and dosing, both for women and for babies.
When the NIH refused to fund a study of IVF outcomes, Dr. DeCherney and Dr. Marrs collaborated on a registry funded by a gonadotropin maker. “The drug company didn’t want to be associated with some terrible abnormal outcomes,” Dr. DeCherney recalled, though by then, “there were 10, maybe even 20 babies around the world, and they seemed to be fine,” he said.
The first registry results affirmed no changes in the rate of congenital abnormalities. (Larger, more recent studies have shown a small but significant elevation in birth defect risk associated with IVF.) A few years later, ovarian stimulation was adjusted to correspond with ovarian reserve, reducing the risk of ovarian hyperstimulation syndrome.
But even by the late 1980s, success rates for IVF per attempted cycle were still low overall, leading many critics, even within the profession, to accuse practitioners of misleading couples. Charles E. Miller, MD, an infertility specialist in Chicago, recalled an early investigation by a major newspaper “that looked at all the IVF clinics in Chicago and found the chances of having a baby was under 3%.”
It was true, Dr. Miller acknowledged – “the rates were dismal. But remember that IVF at the time was still considered a procedure of last resort.” Complex diagnostic testing to determine the cause of infertility, surgery, and fertility drugs all came first.
Some important innovations would soon change that and turn IVF into a mainstay of infertility treatment that could help women not only with damaged tubes but also with ovarian failure, low ovarian reserve, or dense pelvic adhesions. Even some types of male factor infertility would find an answer in IVF, by way of intracytoplasmic sperm transfer.
Eggs without surgery
Laparoscopic egg retrieval was the norm in the first decade of IVF. “We went through the belly button, allowing us to directly visualize the ovary and see whether ovulation had already occurred or we had to retrieve it by introducing a needle into the follicle,” Dr. Rosenwaks recalled.
“Some of us were doing 6 or even 10 laparoscopies a day, and it was physically quite challenging,” he said. “There were no video screens in those days. You had to bend over the scope.” And it was worse still for patients, who had to endure multiple surgeries.
Though egg and embryo cryopreservation were already being worked on, it would be years before these techniques were optimized, giving women more chances from a single retrieval of oocytes.
Finding a less invasive means of retrieving eggs was crucial.
Maria Bustillo, MD, an infertility specialist in Miami, recalled being criticized by peers when she and her then-colleagues at the Genetics & IVF Institute in Fairfax, Va., began retrieving eggs via a needle placed in the vagina, using abdominal ultrasound as a guide.
While the technique was far less invasive than laparoscopy, “we were doing it semi-blindly, and were told it was dangerous,” Dr. Bustillo said.
But these freehand ultrasound retrievals paved the way for what would become a revolutionary advance – the vaginal ultrasound probe, which by the end of the 1980s made nonsurgical extraction of eggs the norm.
Dr. Marrs recalled receiving a prototype of a vaginal ultrasound probe, in the mid-1980s, and finding patients unwilling to use it, except one who relented only because she had an empty bladder. Abdominal ultrasonography required a full bladder to work.
“It was as though somebody had removed the cloud cover,” he said. “I couldn’t believe it. I could see everything: her ovaries, tiny follicles, the uterus.”
Later probes were fitted with a needle and aspirator to retrieve eggs. Multiple IVF cycles no longer meant multiple surgeries, and the less-invasive procedure helped in recruiting egg donors, allowing women with ovarian disease or low ovarian reserves, including older women, to receive IVF.
“It didn’t make sense for a volunteer to go through a surgery, especially back in the early ’80s when the results were not all that great,” Dr. Bustillo said.
Improving ‘home brews’
The culture media in which embryos were grown was another strong factor limiting the success rates of early IVF. James Toner, MD, PhD, an IVF specialist in Atlanta, called the early media “home brews.”
“Everyone made them themselves,” said Dr. Toner, who spent 15 years at the Jones Institute. “You had to do a hamster or mouse embryo test on every batch to make sure embryos would grow.” And often they did not.
Poor success rates resulted in the emergence of alternative procedures: GIFT (gamete intrafallopian transfer) and ZIFT (zygote intrafallopian transfer). Both aimed to get embryos back into the patient as soon as possible, with the thought that the natural environment offered a better chance for success.
But advances in culture media allowed more time for embryos to be observed. With longer development, “you could do a better job selecting the ones that had a chance, and de-selecting those with no chance,” Dr. Toner said.
This also meant fewer embryos could be transferred back into patients, lowering the likelihood of multiples. Ultimately, for young women, single-embryo transfer would become the norm. “The problem of multiple pregnancy that we used to have no longer exists for IVF,” Dr. Toner said.
Allowing embryos to reach the blastocyst stage – day 5 or 6 – opened other, previously unthinkable possibilities: placing embryos directly into the uterus, without surgery, and pre-implementation genetic screening for abnormalities.
“As the cell number went up, the idea that you could do a genetic test with minimal impact on the embryo eventually became true,” Dr. Toner said.
A genetic revolution?
While many important IVF innovations were achieved in countries with staunch government support, one of the remarkable things about IVF’s evolution in the United States is that so many occurred with virtually none.
By the mid-1990s, most of the early practitioners had moved from academic settings into private practice, though they continued to publish. “After a while it didn’t help to be in academics. It just sort of slowed you down. Because you weren’t going to get any [government] money anyway, you might as well be in a place that’s a little more nimble,” Dr. Toner said.
At the same time, he said, IVF remains a costly, usually unreimbursed procedure – limiting patients’ willingness to take part in randomized trials. “IVF research is built more on cohort studies.”
Most of the current research focus in IVF is on possibilities for genetic screening. Dr. Miller said that rapid DNA sequencing is allowing specialists to “look at more, pick up more abnormalities. That will continue to improve so that we will be able to see virtually everything.”
But he cautioned there is still much to be done in IVF apart from the genetics – he’s concerned, he said, that the field has moved too far from its surgical origins, and is working with the academic societies to encourage more surgical training.
“We don’t do the same work we did before on fallopian tubes, which is good,” Dr. Miller said, noting that there have been many advances, particularly minimally invasive surgeries in the uterus or ovaries, that have occurred parallel to IVF and can improve success rates. “I think we have a better understanding of what kind of patients require surgical treatments and what kind of surgeries can help enhance fertility, and also what not to do.”
Dr. Bustillo said that “cytogenetics is wonderful, but not everything. You have embryos that are genetically normal and still don’t implant. There’s a lot of work to be done on the interaction between the mother and the embryo.”
Dr. Marrs said that even safety questions related to stimulation have yet to be fully answered. “I’ve always been a big believer that lower is better, but we need to know whether stimulation creates genetic abnormalities and whether less stimulation produces fewer – and we need more data to prove it,” he said. Dr. Marrs is an investigator on a national randomized trial comparing outcomes from IVF with standard-dose and ultra-low dose stimulation.
Access, income, and age
The IVF pioneers agree broadly that access to IVF is nowhere near what it should be in the United States, where only 15 states mandate any insurance coverage for infertility.
“Our limited access to care is a crime,” Dr. Toner said. “People who, through no fault of their own, find themselves infertile are asked to write a check for $15,000 to get pregnant. That’s not fair.”
Dr. DeCherney called access “an ethical issue, because who gets IVF? People with higher incomes. And if IVF allows you to select better embryos – whatever that means – it gives that group another advantage.”
Dr. Toner warned that the push toward genetic testing of embryos, especially in the absence of known hereditary disease, could create new problems for the profession – not unlike in the early days of IVF, when the Jones Institute and other clinics were picketed over the specter of “test tube babies.”
“It’s one thing to say this embryo does not have the right number of chromosomes and couldn’t possibly be a child, so let’s not use it, but what about looking for traits? Sex selection? We have this privileged position in which the government does not really interfere in what we do, but to retain this status we need to stay within the bounds that our society accepts,” Dr. Toner said.
In recent years, IVF uptake has been high among women of advanced reproductive age, which poses its own set of challenges. Outcomes in older women using their own eggs become progressively poorer with age, though donor eggs drastically improve their chances, and egg freezing offers the possibility of preserving quality eggs for later pregnancies.
“We could make this situation better by promoting social freezing, doing more work for women early in their lives to get out their own eggs and store them,” Dr. Miller said. “But again, you still face the issue of access.”
Regardless of what technologies are available or become available in assisted reproduction, doctors and women alike need to be better educated on their options and chances early, with a clearer understanding of what happens as they age, Dr. Bustillo said.
“This is not to pressure them, but just so they understand that when they get to be 42 and are just thinking about reproducing, it’s not a major surprise when I tell them this could be a problem,” she said.
Throughout 2016, Ob.Gyn. News is celebrating its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit.
In 1978, when England’s Louise Brown became the world’s first baby born through in vitro fertilization, physicians at academic centers all over the United States scrambled to figure out how they, too, could provide IVF to the thousands of infertile couples for whom nothing else had worked.
Interest in IVF was strong even before British physiologist Robert Edwards and gynecologist Patrick Steptoe announced their success. “We knew that IVF was being developed, that it had been accomplished in animals, and ultimately we knew it was going to succeed in humans,” said reproductive endocrinologist Zev Rosenwaks, MD, of the Weill Cornell Center for Reproductive Medicine in New York.
In the late 1970s, “we were able to help only about two-thirds of couples with infertility, either with tubal surgery, insemination – often with donor sperm – or ovulation induction. A full third could not be helped. We predicted that IVF would allow us to treat virtually everyone,” Dr. Rosenwaks said.
But even after the first IVF birth, information on the revolutionary procedure remained frustratingly scarce.
“Edwards and Steptoe would talk to nobody,” said Richard Marrs, MD, a reproductive endocrinologist and infertility specialist in Los Angeles.
And federal research support for “test-tube babies,” as IVF was known in the media then, was nil thanks to a ban on government-funded human embryo research that persists to this day.
The U.S. physicians who took part in the rush to achieve an IVF birth – most of them young fellows at the time – recall a period of improvisation, collaboration, shoestring budgets, and surprise findings.
“People who just started 10 or even 20 years ago don’t realize what it took for us to learn how to go about doing IVF,” said Dr. Rosenwaks, who in the first years of IVF worked closely with Dr. Howard Jones and Dr. Georgeanna Jones, the first team in the U.S. to announce an IVF baby.
Labs in closets
In the late 1970s, Dr. Marrs, then a fellow at the University of Southern California, was focused on surgical methods to treat infertility – and demand was sky-high. Intrauterine devices used in the 1970s left many women with severe scarring and inflammation of the fallopian tubes.
“I was very surgically oriented,” Dr. Marrs said. “I thought I could fix any disaster in the pelvis that was put in front of me, especially with microsurgery.”
After the news of IVF success in England, Dr. Marrs threw himself into a side project at a nearby cancer center, working on single-cell cultures. “I thought if I could grow tumor cells, I could one day grow embryos,” he said.
A year later, Dr. Marrs set up the first IVF lab at USC – in a storage closet. “I sterilized the place and that was our first IVF lab, literally a closet with an incubator and a microscope.” Its budget was accordingly thin, as the director at the time felt certain that IVF was a dead end. To fund his work, Dr. Marrs asked IVF candidate patients for research donations in lieu of payment.
But before Dr. Marrs attempted to perform his first IVF, two centers in Australia announced their own IVF babies. “I decided I really needed to go see someone who had had a baby,” he said. He used his vacation time to fly to Melbourne, shuttling between two competing clinics that were “four blocks apart and wouldn’t even talk to each other,” he recalled.
Over 6 weeks, “I learned how to stimulate, how to time ovulation. I watched the PhDs in the lab – how they handled the eggs and the sperm, what the conditions were, the incubator settings,” he said.
The first IVF babies in the United States were born only months apart: The first, in December 1981, was at the Jones Institute for Reproductive Medicine in Norfolk, Va., where Dr. Rosenwaks served as the first director.
The second baby born was at USC. After that, “we had 4,000 women on a waiting list, all under age 35,” Dr. Marrs said. The Jones Institute reportedly had 5,000.
As demand soared and more IVF babies arrived, the cloak of secrecy surrounding the procedure started to lift. British, Australian, and U.S. clinicians started getting together regularly. “We would pick a spot in the world, present our data: what we’d done, how many cycles, what we used for stimulation, when we took the eggs out,” Dr. Marrs said. “I don’t know how many hundreds of thousands of miles I flew in the first years of IVF, because it was the only way I could get information. We would literally stay up all night talking.”
Answering safety questions
Alan H. DeCherney, MD, currently an infertility researcher at the National Institutes of Health, started Yale University’s IVF program at around the same time Dr. Marrs and the Joneses were starting theirs. Yale already had a large infertility practice, and only academic centers had the laboratory resources and skilled staff needed to attempt IVF in those years.
In 1983, when Yale announced the birth of its first IVF baby – the fifth in the United States – Dr. DeCherney was starting to think about measuring outcomes, as there was concern over the potential for congenital anomalies related to IVF. “This was such a change in the way conception occurred, people were afraid that all kinds of crazy things would happen,” he said.
One concern was about ovarian stimulation with fertility drugs or gonadotropins. The earliest efforts – including by Dr. Steptoe and Dr. Edwards – used no drugs, instead trying to pinpoint the moment of natural egg release by measuring a woman’s hormone levels constantly, but these proved disappointing. Use of clomiphene citrate and human menopausal gonadotropin allowed for more control over timing, and for multiple mature eggs to be harvested at once.
But there were still many unanswered questions related to these agents’ safety and dosing, both for women and for babies.
When the NIH refused to fund a study of IVF outcomes, Dr. DeCherney and Dr. Marrs collaborated on a registry funded by a gonadotropin maker. “The drug company didn’t want to be associated with some terrible abnormal outcomes,” Dr. DeCherney recalled, though by then, “there were 10, maybe even 20 babies around the world, and they seemed to be fine,” he said.
The first registry results affirmed no changes in the rate of congenital abnormalities. (Larger, more recent studies have shown a small but significant elevation in birth defect risk associated with IVF.) A few years later, ovarian stimulation was adjusted to correspond with ovarian reserve, reducing the risk of ovarian hyperstimulation syndrome.
But even by the late 1980s, success rates for IVF per attempted cycle were still low overall, leading many critics, even within the profession, to accuse practitioners of misleading couples. Charles E. Miller, MD, an infertility specialist in Chicago, recalled an early investigation by a major newspaper “that looked at all the IVF clinics in Chicago and found the chances of having a baby was under 3%.”
It was true, Dr. Miller acknowledged – “the rates were dismal. But remember that IVF at the time was still considered a procedure of last resort.” Complex diagnostic testing to determine the cause of infertility, surgery, and fertility drugs all came first.
Some important innovations would soon change that and turn IVF into a mainstay of infertility treatment that could help women not only with damaged tubes but also with ovarian failure, low ovarian reserve, or dense pelvic adhesions. Even some types of male factor infertility would find an answer in IVF, by way of intracytoplasmic sperm transfer.
Eggs without surgery
Laparoscopic egg retrieval was the norm in the first decade of IVF. “We went through the belly button, allowing us to directly visualize the ovary and see whether ovulation had already occurred or we had to retrieve it by introducing a needle into the follicle,” Dr. Rosenwaks recalled.
“Some of us were doing 6 or even 10 laparoscopies a day, and it was physically quite challenging,” he said. “There were no video screens in those days. You had to bend over the scope.” And it was worse still for patients, who had to endure multiple surgeries.
Though egg and embryo cryopreservation were already being worked on, it would be years before these techniques were optimized, giving women more chances from a single retrieval of oocytes.
Finding a less invasive means of retrieving eggs was crucial.
Maria Bustillo, MD, an infertility specialist in Miami, recalled being criticized by peers when she and her then-colleagues at the Genetics & IVF Institute in Fairfax, Va., began retrieving eggs via a needle placed in the vagina, using abdominal ultrasound as a guide.
While the technique was far less invasive than laparoscopy, “we were doing it semi-blindly, and were told it was dangerous,” Dr. Bustillo said.
But these freehand ultrasound retrievals paved the way for what would become a revolutionary advance – the vaginal ultrasound probe, which by the end of the 1980s made nonsurgical extraction of eggs the norm.
Dr. Marrs recalled receiving a prototype of a vaginal ultrasound probe, in the mid-1980s, and finding patients unwilling to use it, except one who relented only because she had an empty bladder. Abdominal ultrasonography required a full bladder to work.
“It was as though somebody had removed the cloud cover,” he said. “I couldn’t believe it. I could see everything: her ovaries, tiny follicles, the uterus.”
Later probes were fitted with a needle and aspirator to retrieve eggs. Multiple IVF cycles no longer meant multiple surgeries, and the less-invasive procedure helped in recruiting egg donors, allowing women with ovarian disease or low ovarian reserves, including older women, to receive IVF.
“It didn’t make sense for a volunteer to go through a surgery, especially back in the early ’80s when the results were not all that great,” Dr. Bustillo said.
Improving ‘home brews’
The culture media in which embryos were grown was another strong factor limiting the success rates of early IVF. James Toner, MD, PhD, an IVF specialist in Atlanta, called the early media “home brews.”
“Everyone made them themselves,” said Dr. Toner, who spent 15 years at the Jones Institute. “You had to do a hamster or mouse embryo test on every batch to make sure embryos would grow.” And often they did not.
Poor success rates resulted in the emergence of alternative procedures: GIFT (gamete intrafallopian transfer) and ZIFT (zygote intrafallopian transfer). Both aimed to get embryos back into the patient as soon as possible, with the thought that the natural environment offered a better chance for success.
But advances in culture media allowed more time for embryos to be observed. With longer development, “you could do a better job selecting the ones that had a chance, and de-selecting those with no chance,” Dr. Toner said.
This also meant fewer embryos could be transferred back into patients, lowering the likelihood of multiples. Ultimately, for young women, single-embryo transfer would become the norm. “The problem of multiple pregnancy that we used to have no longer exists for IVF,” Dr. Toner said.
Allowing embryos to reach the blastocyst stage – day 5 or 6 – opened other, previously unthinkable possibilities: placing embryos directly into the uterus, without surgery, and pre-implementation genetic screening for abnormalities.
“As the cell number went up, the idea that you could do a genetic test with minimal impact on the embryo eventually became true,” Dr. Toner said.
A genetic revolution?
While many important IVF innovations were achieved in countries with staunch government support, one of the remarkable things about IVF’s evolution in the United States is that so many occurred with virtually none.
By the mid-1990s, most of the early practitioners had moved from academic settings into private practice, though they continued to publish. “After a while it didn’t help to be in academics. It just sort of slowed you down. Because you weren’t going to get any [government] money anyway, you might as well be in a place that’s a little more nimble,” Dr. Toner said.
At the same time, he said, IVF remains a costly, usually unreimbursed procedure – limiting patients’ willingness to take part in randomized trials. “IVF research is built more on cohort studies.”
Most of the current research focus in IVF is on possibilities for genetic screening. Dr. Miller said that rapid DNA sequencing is allowing specialists to “look at more, pick up more abnormalities. That will continue to improve so that we will be able to see virtually everything.”
But he cautioned there is still much to be done in IVF apart from the genetics – he’s concerned, he said, that the field has moved too far from its surgical origins, and is working with the academic societies to encourage more surgical training.
“We don’t do the same work we did before on fallopian tubes, which is good,” Dr. Miller said, noting that there have been many advances, particularly minimally invasive surgeries in the uterus or ovaries, that have occurred parallel to IVF and can improve success rates. “I think we have a better understanding of what kind of patients require surgical treatments and what kind of surgeries can help enhance fertility, and also what not to do.”
Dr. Bustillo said that “cytogenetics is wonderful, but not everything. You have embryos that are genetically normal and still don’t implant. There’s a lot of work to be done on the interaction between the mother and the embryo.”
Dr. Marrs said that even safety questions related to stimulation have yet to be fully answered. “I’ve always been a big believer that lower is better, but we need to know whether stimulation creates genetic abnormalities and whether less stimulation produces fewer – and we need more data to prove it,” he said. Dr. Marrs is an investigator on a national randomized trial comparing outcomes from IVF with standard-dose and ultra-low dose stimulation.
Access, income, and age
The IVF pioneers agree broadly that access to IVF is nowhere near what it should be in the United States, where only 15 states mandate any insurance coverage for infertility.
“Our limited access to care is a crime,” Dr. Toner said. “People who, through no fault of their own, find themselves infertile are asked to write a check for $15,000 to get pregnant. That’s not fair.”
Dr. DeCherney called access “an ethical issue, because who gets IVF? People with higher incomes. And if IVF allows you to select better embryos – whatever that means – it gives that group another advantage.”
Dr. Toner warned that the push toward genetic testing of embryos, especially in the absence of known hereditary disease, could create new problems for the profession – not unlike in the early days of IVF, when the Jones Institute and other clinics were picketed over the specter of “test tube babies.”
“It’s one thing to say this embryo does not have the right number of chromosomes and couldn’t possibly be a child, so let’s not use it, but what about looking for traits? Sex selection? We have this privileged position in which the government does not really interfere in what we do, but to retain this status we need to stay within the bounds that our society accepts,” Dr. Toner said.
In recent years, IVF uptake has been high among women of advanced reproductive age, which poses its own set of challenges. Outcomes in older women using their own eggs become progressively poorer with age, though donor eggs drastically improve their chances, and egg freezing offers the possibility of preserving quality eggs for later pregnancies.
“We could make this situation better by promoting social freezing, doing more work for women early in their lives to get out their own eggs and store them,” Dr. Miller said. “But again, you still face the issue of access.”
Regardless of what technologies are available or become available in assisted reproduction, doctors and women alike need to be better educated on their options and chances early, with a clearer understanding of what happens as they age, Dr. Bustillo said.
“This is not to pressure them, but just so they understand that when they get to be 42 and are just thinking about reproducing, it’s not a major surprise when I tell them this could be a problem,” she said.
Throughout 2016, Ob.Gyn. News is celebrating its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit.
In 1978, when England’s Louise Brown became the world’s first baby born through in vitro fertilization, physicians at academic centers all over the United States scrambled to figure out how they, too, could provide IVF to the thousands of infertile couples for whom nothing else had worked.
Interest in IVF was strong even before British physiologist Robert Edwards and gynecologist Patrick Steptoe announced their success. “We knew that IVF was being developed, that it had been accomplished in animals, and ultimately we knew it was going to succeed in humans,” said reproductive endocrinologist Zev Rosenwaks, MD, of the Weill Cornell Center for Reproductive Medicine in New York.
In the late 1970s, “we were able to help only about two-thirds of couples with infertility, either with tubal surgery, insemination – often with donor sperm – or ovulation induction. A full third could not be helped. We predicted that IVF would allow us to treat virtually everyone,” Dr. Rosenwaks said.
But even after the first IVF birth, information on the revolutionary procedure remained frustratingly scarce.
“Edwards and Steptoe would talk to nobody,” said Richard Marrs, MD, a reproductive endocrinologist and infertility specialist in Los Angeles.
And federal research support for “test-tube babies,” as IVF was known in the media then, was nil thanks to a ban on government-funded human embryo research that persists to this day.
The U.S. physicians who took part in the rush to achieve an IVF birth – most of them young fellows at the time – recall a period of improvisation, collaboration, shoestring budgets, and surprise findings.
“People who just started 10 or even 20 years ago don’t realize what it took for us to learn how to go about doing IVF,” said Dr. Rosenwaks, who in the first years of IVF worked closely with Dr. Howard Jones and Dr. Georgeanna Jones, the first team in the U.S. to announce an IVF baby.
Labs in closets
In the late 1970s, Dr. Marrs, then a fellow at the University of Southern California, was focused on surgical methods to treat infertility – and demand was sky-high. Intrauterine devices used in the 1970s left many women with severe scarring and inflammation of the fallopian tubes.
“I was very surgically oriented,” Dr. Marrs said. “I thought I could fix any disaster in the pelvis that was put in front of me, especially with microsurgery.”
After the news of IVF success in England, Dr. Marrs threw himself into a side project at a nearby cancer center, working on single-cell cultures. “I thought if I could grow tumor cells, I could one day grow embryos,” he said.
A year later, Dr. Marrs set up the first IVF lab at USC – in a storage closet. “I sterilized the place and that was our first IVF lab, literally a closet with an incubator and a microscope.” Its budget was accordingly thin, as the director at the time felt certain that IVF was a dead end. To fund his work, Dr. Marrs asked IVF candidate patients for research donations in lieu of payment.
But before Dr. Marrs attempted to perform his first IVF, two centers in Australia announced their own IVF babies. “I decided I really needed to go see someone who had had a baby,” he said. He used his vacation time to fly to Melbourne, shuttling between two competing clinics that were “four blocks apart and wouldn’t even talk to each other,” he recalled.
Over 6 weeks, “I learned how to stimulate, how to time ovulation. I watched the PhDs in the lab – how they handled the eggs and the sperm, what the conditions were, the incubator settings,” he said.
The first IVF babies in the United States were born only months apart: The first, in December 1981, was at the Jones Institute for Reproductive Medicine in Norfolk, Va., where Dr. Rosenwaks served as the first director.
The second baby born was at USC. After that, “we had 4,000 women on a waiting list, all under age 35,” Dr. Marrs said. The Jones Institute reportedly had 5,000.
As demand soared and more IVF babies arrived, the cloak of secrecy surrounding the procedure started to lift. British, Australian, and U.S. clinicians started getting together regularly. “We would pick a spot in the world, present our data: what we’d done, how many cycles, what we used for stimulation, when we took the eggs out,” Dr. Marrs said. “I don’t know how many hundreds of thousands of miles I flew in the first years of IVF, because it was the only way I could get information. We would literally stay up all night talking.”
Answering safety questions
Alan H. DeCherney, MD, currently an infertility researcher at the National Institutes of Health, started Yale University’s IVF program at around the same time Dr. Marrs and the Joneses were starting theirs. Yale already had a large infertility practice, and only academic centers had the laboratory resources and skilled staff needed to attempt IVF in those years.
In 1983, when Yale announced the birth of its first IVF baby – the fifth in the United States – Dr. DeCherney was starting to think about measuring outcomes, as there was concern over the potential for congenital anomalies related to IVF. “This was such a change in the way conception occurred, people were afraid that all kinds of crazy things would happen,” he said.
One concern was about ovarian stimulation with fertility drugs or gonadotropins. The earliest efforts – including by Dr. Steptoe and Dr. Edwards – used no drugs, instead trying to pinpoint the moment of natural egg release by measuring a woman’s hormone levels constantly, but these proved disappointing. Use of clomiphene citrate and human menopausal gonadotropin allowed for more control over timing, and for multiple mature eggs to be harvested at once.
But there were still many unanswered questions related to these agents’ safety and dosing, both for women and for babies.
When the NIH refused to fund a study of IVF outcomes, Dr. DeCherney and Dr. Marrs collaborated on a registry funded by a gonadotropin maker. “The drug company didn’t want to be associated with some terrible abnormal outcomes,” Dr. DeCherney recalled, though by then, “there were 10, maybe even 20 babies around the world, and they seemed to be fine,” he said.
The first registry results affirmed no changes in the rate of congenital abnormalities. (Larger, more recent studies have shown a small but significant elevation in birth defect risk associated with IVF.) A few years later, ovarian stimulation was adjusted to correspond with ovarian reserve, reducing the risk of ovarian hyperstimulation syndrome.
But even by the late 1980s, success rates for IVF per attempted cycle were still low overall, leading many critics, even within the profession, to accuse practitioners of misleading couples. Charles E. Miller, MD, an infertility specialist in Chicago, recalled an early investigation by a major newspaper “that looked at all the IVF clinics in Chicago and found the chances of having a baby was under 3%.”
It was true, Dr. Miller acknowledged – “the rates were dismal. But remember that IVF at the time was still considered a procedure of last resort.” Complex diagnostic testing to determine the cause of infertility, surgery, and fertility drugs all came first.
Some important innovations would soon change that and turn IVF into a mainstay of infertility treatment that could help women not only with damaged tubes but also with ovarian failure, low ovarian reserve, or dense pelvic adhesions. Even some types of male factor infertility would find an answer in IVF, by way of intracytoplasmic sperm transfer.
Eggs without surgery
Laparoscopic egg retrieval was the norm in the first decade of IVF. “We went through the belly button, allowing us to directly visualize the ovary and see whether ovulation had already occurred or we had to retrieve it by introducing a needle into the follicle,” Dr. Rosenwaks recalled.
“Some of us were doing 6 or even 10 laparoscopies a day, and it was physically quite challenging,” he said. “There were no video screens in those days. You had to bend over the scope.” And it was worse still for patients, who had to endure multiple surgeries.
Though egg and embryo cryopreservation were already being worked on, it would be years before these techniques were optimized, giving women more chances from a single retrieval of oocytes.
Finding a less invasive means of retrieving eggs was crucial.
Maria Bustillo, MD, an infertility specialist in Miami, recalled being criticized by peers when she and her then-colleagues at the Genetics & IVF Institute in Fairfax, Va., began retrieving eggs via a needle placed in the vagina, using abdominal ultrasound as a guide.
While the technique was far less invasive than laparoscopy, “we were doing it semi-blindly, and were told it was dangerous,” Dr. Bustillo said.
But these freehand ultrasound retrievals paved the way for what would become a revolutionary advance – the vaginal ultrasound probe, which by the end of the 1980s made nonsurgical extraction of eggs the norm.
Dr. Marrs recalled receiving a prototype of a vaginal ultrasound probe, in the mid-1980s, and finding patients unwilling to use it, except one who relented only because she had an empty bladder. Abdominal ultrasonography required a full bladder to work.
“It was as though somebody had removed the cloud cover,” he said. “I couldn’t believe it. I could see everything: her ovaries, tiny follicles, the uterus.”
Later probes were fitted with a needle and aspirator to retrieve eggs. Multiple IVF cycles no longer meant multiple surgeries, and the less-invasive procedure helped in recruiting egg donors, allowing women with ovarian disease or low ovarian reserves, including older women, to receive IVF.
“It didn’t make sense for a volunteer to go through a surgery, especially back in the early ’80s when the results were not all that great,” Dr. Bustillo said.
Improving ‘home brews’
The culture media in which embryos were grown was another strong factor limiting the success rates of early IVF. James Toner, MD, PhD, an IVF specialist in Atlanta, called the early media “home brews.”
“Everyone made them themselves,” said Dr. Toner, who spent 15 years at the Jones Institute. “You had to do a hamster or mouse embryo test on every batch to make sure embryos would grow.” And often they did not.
Poor success rates resulted in the emergence of alternative procedures: GIFT (gamete intrafallopian transfer) and ZIFT (zygote intrafallopian transfer). Both aimed to get embryos back into the patient as soon as possible, with the thought that the natural environment offered a better chance for success.
But advances in culture media allowed more time for embryos to be observed. With longer development, “you could do a better job selecting the ones that had a chance, and de-selecting those with no chance,” Dr. Toner said.
This also meant fewer embryos could be transferred back into patients, lowering the likelihood of multiples. Ultimately, for young women, single-embryo transfer would become the norm. “The problem of multiple pregnancy that we used to have no longer exists for IVF,” Dr. Toner said.
Allowing embryos to reach the blastocyst stage – day 5 or 6 – opened other, previously unthinkable possibilities: placing embryos directly into the uterus, without surgery, and pre-implementation genetic screening for abnormalities.
“As the cell number went up, the idea that you could do a genetic test with minimal impact on the embryo eventually became true,” Dr. Toner said.
A genetic revolution?
While many important IVF innovations were achieved in countries with staunch government support, one of the remarkable things about IVF’s evolution in the United States is that so many occurred with virtually none.
By the mid-1990s, most of the early practitioners had moved from academic settings into private practice, though they continued to publish. “After a while it didn’t help to be in academics. It just sort of slowed you down. Because you weren’t going to get any [government] money anyway, you might as well be in a place that’s a little more nimble,” Dr. Toner said.
At the same time, he said, IVF remains a costly, usually unreimbursed procedure – limiting patients’ willingness to take part in randomized trials. “IVF research is built more on cohort studies.”
Most of the current research focus in IVF is on possibilities for genetic screening. Dr. Miller said that rapid DNA sequencing is allowing specialists to “look at more, pick up more abnormalities. That will continue to improve so that we will be able to see virtually everything.”
But he cautioned there is still much to be done in IVF apart from the genetics – he’s concerned, he said, that the field has moved too far from its surgical origins, and is working with the academic societies to encourage more surgical training.
“We don’t do the same work we did before on fallopian tubes, which is good,” Dr. Miller said, noting that there have been many advances, particularly minimally invasive surgeries in the uterus or ovaries, that have occurred parallel to IVF and can improve success rates. “I think we have a better understanding of what kind of patients require surgical treatments and what kind of surgeries can help enhance fertility, and also what not to do.”
Dr. Bustillo said that “cytogenetics is wonderful, but not everything. You have embryos that are genetically normal and still don’t implant. There’s a lot of work to be done on the interaction between the mother and the embryo.”
Dr. Marrs said that even safety questions related to stimulation have yet to be fully answered. “I’ve always been a big believer that lower is better, but we need to know whether stimulation creates genetic abnormalities and whether less stimulation produces fewer – and we need more data to prove it,” he said. Dr. Marrs is an investigator on a national randomized trial comparing outcomes from IVF with standard-dose and ultra-low dose stimulation.
Access, income, and age
The IVF pioneers agree broadly that access to IVF is nowhere near what it should be in the United States, where only 15 states mandate any insurance coverage for infertility.
“Our limited access to care is a crime,” Dr. Toner said. “People who, through no fault of their own, find themselves infertile are asked to write a check for $15,000 to get pregnant. That’s not fair.”
Dr. DeCherney called access “an ethical issue, because who gets IVF? People with higher incomes. And if IVF allows you to select better embryos – whatever that means – it gives that group another advantage.”
Dr. Toner warned that the push toward genetic testing of embryos, especially in the absence of known hereditary disease, could create new problems for the profession – not unlike in the early days of IVF, when the Jones Institute and other clinics were picketed over the specter of “test tube babies.”
“It’s one thing to say this embryo does not have the right number of chromosomes and couldn’t possibly be a child, so let’s not use it, but what about looking for traits? Sex selection? We have this privileged position in which the government does not really interfere in what we do, but to retain this status we need to stay within the bounds that our society accepts,” Dr. Toner said.
In recent years, IVF uptake has been high among women of advanced reproductive age, which poses its own set of challenges. Outcomes in older women using their own eggs become progressively poorer with age, though donor eggs drastically improve their chances, and egg freezing offers the possibility of preserving quality eggs for later pregnancies.
“We could make this situation better by promoting social freezing, doing more work for women early in their lives to get out their own eggs and store them,” Dr. Miller said. “But again, you still face the issue of access.”
Regardless of what technologies are available or become available in assisted reproduction, doctors and women alike need to be better educated on their options and chances early, with a clearer understanding of what happens as they age, Dr. Bustillo said.
“This is not to pressure them, but just so they understand that when they get to be 42 and are just thinking about reproducing, it’s not a major surprise when I tell them this could be a problem,” she said.
Throughout 2016, Ob.Gyn. News is celebrating its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit.
Obstetrics Moonshots: 50 years of discoveries
In 1961 before Congress, and in 1962 at Rice University, Houston, President John F. Kennedy called on America to land a man on the moon and bring him back safely, and to look beyond the moon as well, and pursue an ambitious space exploration program. He challenged the country to think and act boldly, telling Americans in his speech at Rice that “we choose to go the moon in this decade and do the other things, not because they are easy, but because they are hard.”
When Neil Armstrong and Buzz Aldrin set foot on the moon in 1969 – even before President Kennedy’s 10-year deadline had arrived – the country’s primary moonshot was realized. The President had inspired the nation, teams of engineers and others had collectively met daunting technological challenges, and space consequently was more open to us than ever before.
In looking at the field of obstetrics and how far it has come in the past 50 years, since the 1960s, it is similarly astonishing and inspiring to reflect on what extraordinary advances we have made. Who would have thought that the fetus would become such a visible and intimate patient – one who, like the mother, can be interrogated, monitored, and sometimes treated before birth? Who would have thought we would be utilizing genomic studies in a now well-established field of prenatal diagnosis, or that fetal therapy would become a field in and of itself?
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Our specialty has advanced through a series of moonshots that have been inspired and driven by technological advancement and by our continually bold goals and vision for the health and well-being of women and their offspring. We have taken on ambitious challenges, achieved many goals, and embraced advancements in practice only to then set new targets that previously were unimaginable.
Yet just as our country’s space exploration program has faced disappointments, so has our field. It is sobering, for instance, that we have made only incremental improvements in prematurity and infant mortality, and that the age-old maternal problem of preeclampsia is still with us. We also face new challenges, such as the rising rate of maternal obesity and diabetes, which threaten both maternal and fetal health.
President Kennedy spoke of having “examined where we are strong, and where we are not.” Such self-reflection and assessment is a critical underpinning of advancement in fields across all of science, medicine, and health care, and in our specialty, it is a process that has driven ambitious new research efforts to improve fetal and maternal health.
A step back to more in-depth fundamental research on the biomolecular mechanisms of premature labor and diabetes-associated birth defects, for instance, as well as new efforts to approach fetal surgery less invasively, are positioning us to both conquer our disappointments and achieve ambitious new moonshots.
The fetus as our patient
Fifty years ago, in 1966, a seminal paper in the Lancet reported that amniotic fluid cells could be cultured and were suitable for karyotyping (1[7434]:383-5). The tapping and examination of amniotic fluid had been reported on sporadically for many decades, for various clinical purposes, but by and large the fetal compartment was not invaded or directly examined. The fetus was instead the hopeful beneficiary of pregnancy care that focused on the mother. Fetal outcome was clouded in mystery, known only at birth.
With the Lancet report, prenatal detection of chromosomal disorders began to feel achievable, and the 1960s marked the beginning of a journey first through invasive methods of prenatal diagnosis and then through increasingly non-invasive approaches.
In 1970, just several years after the report on chromosome analysis of amniotic-fluid cells, another landmark paper in the New England Journal of Medicine described 162 amniocenteses performed between the 13th and 18th weeks of gestation and the detection of 10 cases of Down syndrome, as well as a few other cases of metabolic and other disorders (282[11]:596-9). This report provided an impetus for broader use of the procedure to detect neural tube defects, Down syndrome, and other abnormalities.
The adoption of amniocentesis for prenatal diagnosis still took some time, however. The procedure was used primarily early on to determine fetal lung maturity, and to predict the ability of the fetus to survive after delivery.
At the time, it was widely praised as an advanced method for evaluating the fetus. Yet, looking back, the early years of the procedure seem primitive. The procedure was done late in pregnancy and it was performed blindly, with the puncture site located either with external palpation of the uterus or with the assistance of static ultrasound. Patients who had scans would usually visit the radiologist, who would mark on the patient’s abdomen a suggested location for needle insertion. Upon the patient’s return, the obstetrician would then insert a needle into that spot, blindly and likely after the fetus had moved.
The development and adoption of real-time ultrasound was a revolutionary achievement. Ultrasound-guided amniocentesis was first described in 1972, 14 years after Ian Donald’s seminal paper introducing obstetric ultrasound was published in the Lancet (1958 Jun 7;1[7032]:1188-95).
As real-time ultrasound made its way into practice, it marked the true realization of a moonshot for obstetrics.
Not only could we simultaneously visualize the needle tip and place the needle safety, but we could see the real-time movement of the fetus, its activity, and the surrounding pockets of fluid. It was like looking up into the sky and seeing the stars for the first time. We could see fetal arrhythmia – not only hear it. With this window into the fetal compartment, we could visualize the fetal bowel migrating into the chest cavity due to a hole (hernia) in the diaphragm. We could visualize other malformations as well.
Chorionic villus sampling (CVS) was technically more difficult and took longer to evolve. For years, through the early 1980s, it was performed only at select centers throughout the country. Patients traveled for the procedure and faced relatively significant risks of complications.
By the end of the 1980s, however, with successive improvements in equipment and technique (including development of a transabdominal approach in addition to transvaginal) the procedure was deemed safe, effective, and acceptable for routine use. Fetoscopy, pioneered by John Hobbins, MD, and his colleagues at Yale University, New Haven, Conn., had also advanced and was being used to diagnose sickle cell anemia, Tay-Sachs disease, congenital fetal skin diseases, and other disorders.
With these advances and with our newfound ability to obtain and analyze a tissue sample earlier in pregnancy – even before a woman shared the news of her pregnancy, in some cases – it seemed that we had achieved our goals and may have even reached past the moon.
Yet there were other moonshots being pursued, including initiatives to make prenatal diagnosis less invasive. The discovery in 1997 of cell-free fetal DNA in maternal plasma and serum, for instance, was a pivotal development that opened the door for noninvasive prenatal testing.
This, and other advances in areas from biochemistry to ultrasound to genomic analysis, led to an array of prenatal diagnostic tools that today enable women and their physicians to assess the genetic, chromosomal, and biophysical aspects of their fetus considerably before the time of viability, and from both the maternal side and directly in the fetal compartment.
First-trimester screening is a current option, and we now have the ability to more selectively perform amniocentesis and CVS based on probability testing, and not solely on maternal age. Ultrasound technology now encompasses color Doppler, 3D and 4D imaging, and other techniques that can be used to assess the placenta, various structures inside the brain, and the heart, as well as blood flow through the ductus venosus.
Parents have called for and welcomed having the option of assessing the fetus in greater detail, and of having either assurance when anomalies are excluded or the opportunity to plan and make decisions when anomalies are detected.
Fetal surgery has been a natural extension of our unprecedented access to the fetus. Our ability to visualize malformations and their evolution led to animal studies that advanced our interest in arresting, correcting, or reversing fetal anomalies through in-utero interventions. In 1981, surgeons performed the first human open fetal surgery to correct congenital hydronephrosis.
Today, we can employ endoscopic laser ablation or laser coagulation to treat severe twin-to-twin syndrome, for instance, as well as other surgical techniques to repair defects such as congenital diaphragmatic hernia, lower urinary tract obstruction, and myelomeningocele. Such advances were unimaginable decades ago.
Old foes and new threats
Despite these advances in diagnosis and care, obstetrics faces unrealized moonshots – lingering challenges that, 50 years ago, we would have predicted would have been solved. Who would have thought that we would still have as high an infant mortality rate as we do, and that we would not be further along in solving the problem of prematurity? Our progress has been only incremental.
Fifty years ago, we lacked an understanding of the basic biology of preterm labor. Prematurity was viewed simply as term labor occurring too early, and many efforts were made over the years to halt the premature labor process through the use of various drugs and other therapeutics, with variable and minimally impactful levels of success.
In the last 25 years, and especially in the last decade, we have made greater efforts to better understand the biology of premature labor – to elucidate how and why it occurs – and we have come to understand that premature labor is very different physiologically from term labor.
Thanks to the work at the Perinatology Research Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), led by Roberto Romero, MD, attention has consequently shifted toward prediction, identification of women at highest risk, and prevention of the onset of premature labor among those deemed to be at highest risk.
Cervical length in the mid-trimester is now a well-verified predictor of preterm birth, and vaginal progesterone has been shown to benefit women without other known risk factors who are diagnosed with a shortened cervical length.
We have consequently seen the preterm birth rate decline a bit. In 2013, the last year for which we have complete data, the preterm birth rate dropped to 11.4%, down from a high of 12.8% in 2006, according to the Centers for Disease Control and Prevention.
Infant mortality similarly remains unacceptably high, due largely to the high preterm birth rate and to our failure to significantly alter the prevalence of birth defects. In 2010, according to the CDC, the infant mortality rate in the U.S. was 6.1 deaths per 1,000 live births (compared with 6.87 in 2005), and the United States ranked 26th in infant mortality among countries belonging to the Organisation for Economic Co-operation and Development, despite the fact that we spend a significant portion of our gross domestic product (17.5% in 2014) on health care.
Birth defects have taken over as a leading cause of infant mortality after early newborn life, and while we’ve made some advancements in understanding and diagnosing them, the majority of causes of birth defects are still unknown.
On the maternal side of obstetrical care, our progress has similarly been more modest than we have hoped for. Preeclampsia remains a problem, for instance. Despite decades of research into its pathogenesis, our advancements have been only incremental, and the condition – particularly its severe form – continues to be a vexing and high-risk problem.
Added to such age-old foes, moreover, are the growing threats of maternal obesity and diabetes, two closely related and often chronic conditions that affect not only the health of the mother but the in-utero environment and the health of the fetus. Today, more than one-third of all adults in the U.S., and 34% of women aged 20-39 years, are obese, and almost 10% of the U.S. population has diabetes.
Both conditions are on the rise, and obstetrics is confronting an epidemic of “diabesity” that would not necessarily have been predicted 50 years ago. It is particularly alarming given our growing knowledge of how obesity can be programmed in-utero and essentially passed on from generation to generation, of how diabetes can negatively affect perinatal outcomes, and of how the two conditions can have an additive effect on fetal complications.
Achieving new moonshots
Concerted efforts in the past several decades to step back and try to understand the basic biology and physiology of term labor and of premature labor have better positioned our specialty to achieve the moonshot of significantly reducing the incidence of preterm birth.
Establishment in the mid-1980s of the NICHD’s Perinatology Research Branch was a major development in this regard, helping to build and direct research efforts, including basic laboratory science, toward questions about what triggers and propagates labor. There has been notable progress in the past decade, in particular, and our specialty is now on the right path toward development of therapeutic interventions for preventing prematurity.
Additionally, the NICHD’s recently launched Human Placenta Project is building upon the branch-sponsored animal and cell culture model systems of the placenta to allow researchers, for the first time, to monitor human placental health in real time. By more fully understanding the role of the placenta in health and disease, we will be able to better evaluate pregnancy risks and improve pregnancy outcomes.
We also are learning through research in the University of Maryland Birth Defects Research Laboratory, which I am privileged to direct, and at other facilities, that maternal hyperglycemia is a teratogen, creating insults that can trigger a series of developmental fetal defects. By studying the biomolecular mechanisms of hyperglycemia-induced birth defects and developing “molecular maps,” we expect to be able to develop strategies for preventing or mitigating the development of such anomalies. I hope and expect that these future advancements, combined with reductions in prematurity, will significantly impact the infant mortality rate.
Fetal therapy and surgery will also continue to advance, with a much more minimally invasive approach taken in the next 50 years to addressing the fetal condition without putting the mother at increased risk. Just as surgery in other fields has moved from open laparotomy to minimally invasive techniques, I believe we will develop endoscopic or laparoscopic means of correcting the various problems in-utero, such as the repair of neural tube defects and diaphragmatic hernias. It already appears likely that a fetoscopic approach to treating myelomeningocele can reduce maternal morbidity while achieving infant neurological outcomes that are at least as good as outcomes achieved with open fetal surgery.
We’re in a much different position than we were 50 years ago in that we have two patients – the mother and the fetus – with whom we can closely work. We also have a relatively new and urgent obligation to place our attention not only on women’s reproductive health, but on the general gynecologic state. Ob.gyns. often are the only primary care physicians whom women see for routine care, and the quality of our attention to their weight and their diabetes risk factors will have far-reaching consequences, both for them and for their offspring.
As we have since the 1960s, we will continue to set new moonshots and meet new challenges, working with each other and with our patients to evaluate where we are strong and where we must improve. We will persistently harness the power of technology, choosing to do the things that “are hard,” while stepping back as needed to ask and address fundamental questions.
As a result, I can envision the next 50 years as a revolutionary time period for obstetrics – a time in which current problems and disorders are abated or eliminated through a combination of genomics, microbiomics, and other technological advances. Someday in the future, we will look back on some of our many achievements and marvel at how we have transformed the unimaginable to reality.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at obnews@frontlinemedcom.com.
Select advances through the years
1960s
1965: Siemens Corp. introduces first real-time ultrasound scanner.
1966: Lancet paper reports that amniotic fluid cells can be cultured and karyotyped.
1970s
1970: New England Journal of Medicine paper describes mid-trimester amniocenteses and detection of Down syndrome cases.
1972: Ultrasound-guided amniocentesis first described.
1973: Fetoscopy introduced.
1980s
1981: First human open fetal surgery to correct congenital hydronephrosis.
Early 1980s: Chorionic villus sampling introduced at select centers.
1985: Color Doppler incorporated into ultrasound.
1990s
1990: Embryoscopy first described.
Mid-1990s: 3D/4D ultrasound begins to assume major role in ob.gyn. imaging.1997: Discovery of cell-free fetal DNA in maternal plasma.
2000s
2003: MOMS (Management of Myelomeningocele Study) was launched.
2010s
2012: The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine support cell-free DNA screening for women at increased risk of fetal aneuploidy.
2013: Preterm birth rate drops to 11.4%
2014: Diabetes incidence marks a 4-fold increase since 1980.
In 1961 before Congress, and in 1962 at Rice University, Houston, President John F. Kennedy called on America to land a man on the moon and bring him back safely, and to look beyond the moon as well, and pursue an ambitious space exploration program. He challenged the country to think and act boldly, telling Americans in his speech at Rice that “we choose to go the moon in this decade and do the other things, not because they are easy, but because they are hard.”
When Neil Armstrong and Buzz Aldrin set foot on the moon in 1969 – even before President Kennedy’s 10-year deadline had arrived – the country’s primary moonshot was realized. The President had inspired the nation, teams of engineers and others had collectively met daunting technological challenges, and space consequently was more open to us than ever before.
In looking at the field of obstetrics and how far it has come in the past 50 years, since the 1960s, it is similarly astonishing and inspiring to reflect on what extraordinary advances we have made. Who would have thought that the fetus would become such a visible and intimate patient – one who, like the mother, can be interrogated, monitored, and sometimes treated before birth? Who would have thought we would be utilizing genomic studies in a now well-established field of prenatal diagnosis, or that fetal therapy would become a field in and of itself?
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Our specialty has advanced through a series of moonshots that have been inspired and driven by technological advancement and by our continually bold goals and vision for the health and well-being of women and their offspring. We have taken on ambitious challenges, achieved many goals, and embraced advancements in practice only to then set new targets that previously were unimaginable.
Yet just as our country’s space exploration program has faced disappointments, so has our field. It is sobering, for instance, that we have made only incremental improvements in prematurity and infant mortality, and that the age-old maternal problem of preeclampsia is still with us. We also face new challenges, such as the rising rate of maternal obesity and diabetes, which threaten both maternal and fetal health.
President Kennedy spoke of having “examined where we are strong, and where we are not.” Such self-reflection and assessment is a critical underpinning of advancement in fields across all of science, medicine, and health care, and in our specialty, it is a process that has driven ambitious new research efforts to improve fetal and maternal health.
A step back to more in-depth fundamental research on the biomolecular mechanisms of premature labor and diabetes-associated birth defects, for instance, as well as new efforts to approach fetal surgery less invasively, are positioning us to both conquer our disappointments and achieve ambitious new moonshots.
The fetus as our patient
Fifty years ago, in 1966, a seminal paper in the Lancet reported that amniotic fluid cells could be cultured and were suitable for karyotyping (1[7434]:383-5). The tapping and examination of amniotic fluid had been reported on sporadically for many decades, for various clinical purposes, but by and large the fetal compartment was not invaded or directly examined. The fetus was instead the hopeful beneficiary of pregnancy care that focused on the mother. Fetal outcome was clouded in mystery, known only at birth.
With the Lancet report, prenatal detection of chromosomal disorders began to feel achievable, and the 1960s marked the beginning of a journey first through invasive methods of prenatal diagnosis and then through increasingly non-invasive approaches.
In 1970, just several years after the report on chromosome analysis of amniotic-fluid cells, another landmark paper in the New England Journal of Medicine described 162 amniocenteses performed between the 13th and 18th weeks of gestation and the detection of 10 cases of Down syndrome, as well as a few other cases of metabolic and other disorders (282[11]:596-9). This report provided an impetus for broader use of the procedure to detect neural tube defects, Down syndrome, and other abnormalities.
The adoption of amniocentesis for prenatal diagnosis still took some time, however. The procedure was used primarily early on to determine fetal lung maturity, and to predict the ability of the fetus to survive after delivery.
At the time, it was widely praised as an advanced method for evaluating the fetus. Yet, looking back, the early years of the procedure seem primitive. The procedure was done late in pregnancy and it was performed blindly, with the puncture site located either with external palpation of the uterus or with the assistance of static ultrasound. Patients who had scans would usually visit the radiologist, who would mark on the patient’s abdomen a suggested location for needle insertion. Upon the patient’s return, the obstetrician would then insert a needle into that spot, blindly and likely after the fetus had moved.
The development and adoption of real-time ultrasound was a revolutionary achievement. Ultrasound-guided amniocentesis was first described in 1972, 14 years after Ian Donald’s seminal paper introducing obstetric ultrasound was published in the Lancet (1958 Jun 7;1[7032]:1188-95).
As real-time ultrasound made its way into practice, it marked the true realization of a moonshot for obstetrics.
Not only could we simultaneously visualize the needle tip and place the needle safety, but we could see the real-time movement of the fetus, its activity, and the surrounding pockets of fluid. It was like looking up into the sky and seeing the stars for the first time. We could see fetal arrhythmia – not only hear it. With this window into the fetal compartment, we could visualize the fetal bowel migrating into the chest cavity due to a hole (hernia) in the diaphragm. We could visualize other malformations as well.
Chorionic villus sampling (CVS) was technically more difficult and took longer to evolve. For years, through the early 1980s, it was performed only at select centers throughout the country. Patients traveled for the procedure and faced relatively significant risks of complications.
By the end of the 1980s, however, with successive improvements in equipment and technique (including development of a transabdominal approach in addition to transvaginal) the procedure was deemed safe, effective, and acceptable for routine use. Fetoscopy, pioneered by John Hobbins, MD, and his colleagues at Yale University, New Haven, Conn., had also advanced and was being used to diagnose sickle cell anemia, Tay-Sachs disease, congenital fetal skin diseases, and other disorders.
With these advances and with our newfound ability to obtain and analyze a tissue sample earlier in pregnancy – even before a woman shared the news of her pregnancy, in some cases – it seemed that we had achieved our goals and may have even reached past the moon.
Yet there were other moonshots being pursued, including initiatives to make prenatal diagnosis less invasive. The discovery in 1997 of cell-free fetal DNA in maternal plasma and serum, for instance, was a pivotal development that opened the door for noninvasive prenatal testing.
This, and other advances in areas from biochemistry to ultrasound to genomic analysis, led to an array of prenatal diagnostic tools that today enable women and their physicians to assess the genetic, chromosomal, and biophysical aspects of their fetus considerably before the time of viability, and from both the maternal side and directly in the fetal compartment.
First-trimester screening is a current option, and we now have the ability to more selectively perform amniocentesis and CVS based on probability testing, and not solely on maternal age. Ultrasound technology now encompasses color Doppler, 3D and 4D imaging, and other techniques that can be used to assess the placenta, various structures inside the brain, and the heart, as well as blood flow through the ductus venosus.
Parents have called for and welcomed having the option of assessing the fetus in greater detail, and of having either assurance when anomalies are excluded or the opportunity to plan and make decisions when anomalies are detected.
Fetal surgery has been a natural extension of our unprecedented access to the fetus. Our ability to visualize malformations and their evolution led to animal studies that advanced our interest in arresting, correcting, or reversing fetal anomalies through in-utero interventions. In 1981, surgeons performed the first human open fetal surgery to correct congenital hydronephrosis.
Today, we can employ endoscopic laser ablation or laser coagulation to treat severe twin-to-twin syndrome, for instance, as well as other surgical techniques to repair defects such as congenital diaphragmatic hernia, lower urinary tract obstruction, and myelomeningocele. Such advances were unimaginable decades ago.
Old foes and new threats
Despite these advances in diagnosis and care, obstetrics faces unrealized moonshots – lingering challenges that, 50 years ago, we would have predicted would have been solved. Who would have thought that we would still have as high an infant mortality rate as we do, and that we would not be further along in solving the problem of prematurity? Our progress has been only incremental.
Fifty years ago, we lacked an understanding of the basic biology of preterm labor. Prematurity was viewed simply as term labor occurring too early, and many efforts were made over the years to halt the premature labor process through the use of various drugs and other therapeutics, with variable and minimally impactful levels of success.
In the last 25 years, and especially in the last decade, we have made greater efforts to better understand the biology of premature labor – to elucidate how and why it occurs – and we have come to understand that premature labor is very different physiologically from term labor.
Thanks to the work at the Perinatology Research Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), led by Roberto Romero, MD, attention has consequently shifted toward prediction, identification of women at highest risk, and prevention of the onset of premature labor among those deemed to be at highest risk.
Cervical length in the mid-trimester is now a well-verified predictor of preterm birth, and vaginal progesterone has been shown to benefit women without other known risk factors who are diagnosed with a shortened cervical length.
We have consequently seen the preterm birth rate decline a bit. In 2013, the last year for which we have complete data, the preterm birth rate dropped to 11.4%, down from a high of 12.8% in 2006, according to the Centers for Disease Control and Prevention.
Infant mortality similarly remains unacceptably high, due largely to the high preterm birth rate and to our failure to significantly alter the prevalence of birth defects. In 2010, according to the CDC, the infant mortality rate in the U.S. was 6.1 deaths per 1,000 live births (compared with 6.87 in 2005), and the United States ranked 26th in infant mortality among countries belonging to the Organisation for Economic Co-operation and Development, despite the fact that we spend a significant portion of our gross domestic product (17.5% in 2014) on health care.
Birth defects have taken over as a leading cause of infant mortality after early newborn life, and while we’ve made some advancements in understanding and diagnosing them, the majority of causes of birth defects are still unknown.
On the maternal side of obstetrical care, our progress has similarly been more modest than we have hoped for. Preeclampsia remains a problem, for instance. Despite decades of research into its pathogenesis, our advancements have been only incremental, and the condition – particularly its severe form – continues to be a vexing and high-risk problem.
Added to such age-old foes, moreover, are the growing threats of maternal obesity and diabetes, two closely related and often chronic conditions that affect not only the health of the mother but the in-utero environment and the health of the fetus. Today, more than one-third of all adults in the U.S., and 34% of women aged 20-39 years, are obese, and almost 10% of the U.S. population has diabetes.
Both conditions are on the rise, and obstetrics is confronting an epidemic of “diabesity” that would not necessarily have been predicted 50 years ago. It is particularly alarming given our growing knowledge of how obesity can be programmed in-utero and essentially passed on from generation to generation, of how diabetes can negatively affect perinatal outcomes, and of how the two conditions can have an additive effect on fetal complications.
Achieving new moonshots
Concerted efforts in the past several decades to step back and try to understand the basic biology and physiology of term labor and of premature labor have better positioned our specialty to achieve the moonshot of significantly reducing the incidence of preterm birth.
Establishment in the mid-1980s of the NICHD’s Perinatology Research Branch was a major development in this regard, helping to build and direct research efforts, including basic laboratory science, toward questions about what triggers and propagates labor. There has been notable progress in the past decade, in particular, and our specialty is now on the right path toward development of therapeutic interventions for preventing prematurity.
Additionally, the NICHD’s recently launched Human Placenta Project is building upon the branch-sponsored animal and cell culture model systems of the placenta to allow researchers, for the first time, to monitor human placental health in real time. By more fully understanding the role of the placenta in health and disease, we will be able to better evaluate pregnancy risks and improve pregnancy outcomes.
We also are learning through research in the University of Maryland Birth Defects Research Laboratory, which I am privileged to direct, and at other facilities, that maternal hyperglycemia is a teratogen, creating insults that can trigger a series of developmental fetal defects. By studying the biomolecular mechanisms of hyperglycemia-induced birth defects and developing “molecular maps,” we expect to be able to develop strategies for preventing or mitigating the development of such anomalies. I hope and expect that these future advancements, combined with reductions in prematurity, will significantly impact the infant mortality rate.
Fetal therapy and surgery will also continue to advance, with a much more minimally invasive approach taken in the next 50 years to addressing the fetal condition without putting the mother at increased risk. Just as surgery in other fields has moved from open laparotomy to minimally invasive techniques, I believe we will develop endoscopic or laparoscopic means of correcting the various problems in-utero, such as the repair of neural tube defects and diaphragmatic hernias. It already appears likely that a fetoscopic approach to treating myelomeningocele can reduce maternal morbidity while achieving infant neurological outcomes that are at least as good as outcomes achieved with open fetal surgery.
We’re in a much different position than we were 50 years ago in that we have two patients – the mother and the fetus – with whom we can closely work. We also have a relatively new and urgent obligation to place our attention not only on women’s reproductive health, but on the general gynecologic state. Ob.gyns. often are the only primary care physicians whom women see for routine care, and the quality of our attention to their weight and their diabetes risk factors will have far-reaching consequences, both for them and for their offspring.
As we have since the 1960s, we will continue to set new moonshots and meet new challenges, working with each other and with our patients to evaluate where we are strong and where we must improve. We will persistently harness the power of technology, choosing to do the things that “are hard,” while stepping back as needed to ask and address fundamental questions.
As a result, I can envision the next 50 years as a revolutionary time period for obstetrics – a time in which current problems and disorders are abated or eliminated through a combination of genomics, microbiomics, and other technological advances. Someday in the future, we will look back on some of our many achievements and marvel at how we have transformed the unimaginable to reality.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at obnews@frontlinemedcom.com.
Select advances through the years
1960s
1965: Siemens Corp. introduces first real-time ultrasound scanner.
1966: Lancet paper reports that amniotic fluid cells can be cultured and karyotyped.
1970s
1970: New England Journal of Medicine paper describes mid-trimester amniocenteses and detection of Down syndrome cases.
1972: Ultrasound-guided amniocentesis first described.
1973: Fetoscopy introduced.
1980s
1981: First human open fetal surgery to correct congenital hydronephrosis.
Early 1980s: Chorionic villus sampling introduced at select centers.
1985: Color Doppler incorporated into ultrasound.
1990s
1990: Embryoscopy first described.
Mid-1990s: 3D/4D ultrasound begins to assume major role in ob.gyn. imaging.1997: Discovery of cell-free fetal DNA in maternal plasma.
2000s
2003: MOMS (Management of Myelomeningocele Study) was launched.
2010s
2012: The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine support cell-free DNA screening for women at increased risk of fetal aneuploidy.
2013: Preterm birth rate drops to 11.4%
2014: Diabetes incidence marks a 4-fold increase since 1980.
In 1961 before Congress, and in 1962 at Rice University, Houston, President John F. Kennedy called on America to land a man on the moon and bring him back safely, and to look beyond the moon as well, and pursue an ambitious space exploration program. He challenged the country to think and act boldly, telling Americans in his speech at Rice that “we choose to go the moon in this decade and do the other things, not because they are easy, but because they are hard.”
When Neil Armstrong and Buzz Aldrin set foot on the moon in 1969 – even before President Kennedy’s 10-year deadline had arrived – the country’s primary moonshot was realized. The President had inspired the nation, teams of engineers and others had collectively met daunting technological challenges, and space consequently was more open to us than ever before.
In looking at the field of obstetrics and how far it has come in the past 50 years, since the 1960s, it is similarly astonishing and inspiring to reflect on what extraordinary advances we have made. Who would have thought that the fetus would become such a visible and intimate patient – one who, like the mother, can be interrogated, monitored, and sometimes treated before birth? Who would have thought we would be utilizing genomic studies in a now well-established field of prenatal diagnosis, or that fetal therapy would become a field in and of itself?
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Our specialty has advanced through a series of moonshots that have been inspired and driven by technological advancement and by our continually bold goals and vision for the health and well-being of women and their offspring. We have taken on ambitious challenges, achieved many goals, and embraced advancements in practice only to then set new targets that previously were unimaginable.
Yet just as our country’s space exploration program has faced disappointments, so has our field. It is sobering, for instance, that we have made only incremental improvements in prematurity and infant mortality, and that the age-old maternal problem of preeclampsia is still with us. We also face new challenges, such as the rising rate of maternal obesity and diabetes, which threaten both maternal and fetal health.
President Kennedy spoke of having “examined where we are strong, and where we are not.” Such self-reflection and assessment is a critical underpinning of advancement in fields across all of science, medicine, and health care, and in our specialty, it is a process that has driven ambitious new research efforts to improve fetal and maternal health.
A step back to more in-depth fundamental research on the biomolecular mechanisms of premature labor and diabetes-associated birth defects, for instance, as well as new efforts to approach fetal surgery less invasively, are positioning us to both conquer our disappointments and achieve ambitious new moonshots.
The fetus as our patient
Fifty years ago, in 1966, a seminal paper in the Lancet reported that amniotic fluid cells could be cultured and were suitable for karyotyping (1[7434]:383-5). The tapping and examination of amniotic fluid had been reported on sporadically for many decades, for various clinical purposes, but by and large the fetal compartment was not invaded or directly examined. The fetus was instead the hopeful beneficiary of pregnancy care that focused on the mother. Fetal outcome was clouded in mystery, known only at birth.
With the Lancet report, prenatal detection of chromosomal disorders began to feel achievable, and the 1960s marked the beginning of a journey first through invasive methods of prenatal diagnosis and then through increasingly non-invasive approaches.
In 1970, just several years after the report on chromosome analysis of amniotic-fluid cells, another landmark paper in the New England Journal of Medicine described 162 amniocenteses performed between the 13th and 18th weeks of gestation and the detection of 10 cases of Down syndrome, as well as a few other cases of metabolic and other disorders (282[11]:596-9). This report provided an impetus for broader use of the procedure to detect neural tube defects, Down syndrome, and other abnormalities.
The adoption of amniocentesis for prenatal diagnosis still took some time, however. The procedure was used primarily early on to determine fetal lung maturity, and to predict the ability of the fetus to survive after delivery.
At the time, it was widely praised as an advanced method for evaluating the fetus. Yet, looking back, the early years of the procedure seem primitive. The procedure was done late in pregnancy and it was performed blindly, with the puncture site located either with external palpation of the uterus or with the assistance of static ultrasound. Patients who had scans would usually visit the radiologist, who would mark on the patient’s abdomen a suggested location for needle insertion. Upon the patient’s return, the obstetrician would then insert a needle into that spot, blindly and likely after the fetus had moved.
The development and adoption of real-time ultrasound was a revolutionary achievement. Ultrasound-guided amniocentesis was first described in 1972, 14 years after Ian Donald’s seminal paper introducing obstetric ultrasound was published in the Lancet (1958 Jun 7;1[7032]:1188-95).
As real-time ultrasound made its way into practice, it marked the true realization of a moonshot for obstetrics.
Not only could we simultaneously visualize the needle tip and place the needle safety, but we could see the real-time movement of the fetus, its activity, and the surrounding pockets of fluid. It was like looking up into the sky and seeing the stars for the first time. We could see fetal arrhythmia – not only hear it. With this window into the fetal compartment, we could visualize the fetal bowel migrating into the chest cavity due to a hole (hernia) in the diaphragm. We could visualize other malformations as well.
Chorionic villus sampling (CVS) was technically more difficult and took longer to evolve. For years, through the early 1980s, it was performed only at select centers throughout the country. Patients traveled for the procedure and faced relatively significant risks of complications.
By the end of the 1980s, however, with successive improvements in equipment and technique (including development of a transabdominal approach in addition to transvaginal) the procedure was deemed safe, effective, and acceptable for routine use. Fetoscopy, pioneered by John Hobbins, MD, and his colleagues at Yale University, New Haven, Conn., had also advanced and was being used to diagnose sickle cell anemia, Tay-Sachs disease, congenital fetal skin diseases, and other disorders.
With these advances and with our newfound ability to obtain and analyze a tissue sample earlier in pregnancy – even before a woman shared the news of her pregnancy, in some cases – it seemed that we had achieved our goals and may have even reached past the moon.
Yet there were other moonshots being pursued, including initiatives to make prenatal diagnosis less invasive. The discovery in 1997 of cell-free fetal DNA in maternal plasma and serum, for instance, was a pivotal development that opened the door for noninvasive prenatal testing.
This, and other advances in areas from biochemistry to ultrasound to genomic analysis, led to an array of prenatal diagnostic tools that today enable women and their physicians to assess the genetic, chromosomal, and biophysical aspects of their fetus considerably before the time of viability, and from both the maternal side and directly in the fetal compartment.
First-trimester screening is a current option, and we now have the ability to more selectively perform amniocentesis and CVS based on probability testing, and not solely on maternal age. Ultrasound technology now encompasses color Doppler, 3D and 4D imaging, and other techniques that can be used to assess the placenta, various structures inside the brain, and the heart, as well as blood flow through the ductus venosus.
Parents have called for and welcomed having the option of assessing the fetus in greater detail, and of having either assurance when anomalies are excluded or the opportunity to plan and make decisions when anomalies are detected.
Fetal surgery has been a natural extension of our unprecedented access to the fetus. Our ability to visualize malformations and their evolution led to animal studies that advanced our interest in arresting, correcting, or reversing fetal anomalies through in-utero interventions. In 1981, surgeons performed the first human open fetal surgery to correct congenital hydronephrosis.
Today, we can employ endoscopic laser ablation or laser coagulation to treat severe twin-to-twin syndrome, for instance, as well as other surgical techniques to repair defects such as congenital diaphragmatic hernia, lower urinary tract obstruction, and myelomeningocele. Such advances were unimaginable decades ago.
Old foes and new threats
Despite these advances in diagnosis and care, obstetrics faces unrealized moonshots – lingering challenges that, 50 years ago, we would have predicted would have been solved. Who would have thought that we would still have as high an infant mortality rate as we do, and that we would not be further along in solving the problem of prematurity? Our progress has been only incremental.
Fifty years ago, we lacked an understanding of the basic biology of preterm labor. Prematurity was viewed simply as term labor occurring too early, and many efforts were made over the years to halt the premature labor process through the use of various drugs and other therapeutics, with variable and minimally impactful levels of success.
In the last 25 years, and especially in the last decade, we have made greater efforts to better understand the biology of premature labor – to elucidate how and why it occurs – and we have come to understand that premature labor is very different physiologically from term labor.
Thanks to the work at the Perinatology Research Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), led by Roberto Romero, MD, attention has consequently shifted toward prediction, identification of women at highest risk, and prevention of the onset of premature labor among those deemed to be at highest risk.
Cervical length in the mid-trimester is now a well-verified predictor of preterm birth, and vaginal progesterone has been shown to benefit women without other known risk factors who are diagnosed with a shortened cervical length.
We have consequently seen the preterm birth rate decline a bit. In 2013, the last year for which we have complete data, the preterm birth rate dropped to 11.4%, down from a high of 12.8% in 2006, according to the Centers for Disease Control and Prevention.
Infant mortality similarly remains unacceptably high, due largely to the high preterm birth rate and to our failure to significantly alter the prevalence of birth defects. In 2010, according to the CDC, the infant mortality rate in the U.S. was 6.1 deaths per 1,000 live births (compared with 6.87 in 2005), and the United States ranked 26th in infant mortality among countries belonging to the Organisation for Economic Co-operation and Development, despite the fact that we spend a significant portion of our gross domestic product (17.5% in 2014) on health care.
Birth defects have taken over as a leading cause of infant mortality after early newborn life, and while we’ve made some advancements in understanding and diagnosing them, the majority of causes of birth defects are still unknown.
On the maternal side of obstetrical care, our progress has similarly been more modest than we have hoped for. Preeclampsia remains a problem, for instance. Despite decades of research into its pathogenesis, our advancements have been only incremental, and the condition – particularly its severe form – continues to be a vexing and high-risk problem.
Added to such age-old foes, moreover, are the growing threats of maternal obesity and diabetes, two closely related and often chronic conditions that affect not only the health of the mother but the in-utero environment and the health of the fetus. Today, more than one-third of all adults in the U.S., and 34% of women aged 20-39 years, are obese, and almost 10% of the U.S. population has diabetes.
Both conditions are on the rise, and obstetrics is confronting an epidemic of “diabesity” that would not necessarily have been predicted 50 years ago. It is particularly alarming given our growing knowledge of how obesity can be programmed in-utero and essentially passed on from generation to generation, of how diabetes can negatively affect perinatal outcomes, and of how the two conditions can have an additive effect on fetal complications.
Achieving new moonshots
Concerted efforts in the past several decades to step back and try to understand the basic biology and physiology of term labor and of premature labor have better positioned our specialty to achieve the moonshot of significantly reducing the incidence of preterm birth.
Establishment in the mid-1980s of the NICHD’s Perinatology Research Branch was a major development in this regard, helping to build and direct research efforts, including basic laboratory science, toward questions about what triggers and propagates labor. There has been notable progress in the past decade, in particular, and our specialty is now on the right path toward development of therapeutic interventions for preventing prematurity.
Additionally, the NICHD’s recently launched Human Placenta Project is building upon the branch-sponsored animal and cell culture model systems of the placenta to allow researchers, for the first time, to monitor human placental health in real time. By more fully understanding the role of the placenta in health and disease, we will be able to better evaluate pregnancy risks and improve pregnancy outcomes.
We also are learning through research in the University of Maryland Birth Defects Research Laboratory, which I am privileged to direct, and at other facilities, that maternal hyperglycemia is a teratogen, creating insults that can trigger a series of developmental fetal defects. By studying the biomolecular mechanisms of hyperglycemia-induced birth defects and developing “molecular maps,” we expect to be able to develop strategies for preventing or mitigating the development of such anomalies. I hope and expect that these future advancements, combined with reductions in prematurity, will significantly impact the infant mortality rate.
Fetal therapy and surgery will also continue to advance, with a much more minimally invasive approach taken in the next 50 years to addressing the fetal condition without putting the mother at increased risk. Just as surgery in other fields has moved from open laparotomy to minimally invasive techniques, I believe we will develop endoscopic or laparoscopic means of correcting the various problems in-utero, such as the repair of neural tube defects and diaphragmatic hernias. It already appears likely that a fetoscopic approach to treating myelomeningocele can reduce maternal morbidity while achieving infant neurological outcomes that are at least as good as outcomes achieved with open fetal surgery.
We’re in a much different position than we were 50 years ago in that we have two patients – the mother and the fetus – with whom we can closely work. We also have a relatively new and urgent obligation to place our attention not only on women’s reproductive health, but on the general gynecologic state. Ob.gyns. often are the only primary care physicians whom women see for routine care, and the quality of our attention to their weight and their diabetes risk factors will have far-reaching consequences, both for them and for their offspring.
As we have since the 1960s, we will continue to set new moonshots and meet new challenges, working with each other and with our patients to evaluate where we are strong and where we must improve. We will persistently harness the power of technology, choosing to do the things that “are hard,” while stepping back as needed to ask and address fundamental questions.
As a result, I can envision the next 50 years as a revolutionary time period for obstetrics – a time in which current problems and disorders are abated or eliminated through a combination of genomics, microbiomics, and other technological advances. Someday in the future, we will look back on some of our many achievements and marvel at how we have transformed the unimaginable to reality.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at obnews@frontlinemedcom.com.
Select advances through the years
1960s
1965: Siemens Corp. introduces first real-time ultrasound scanner.
1966: Lancet paper reports that amniotic fluid cells can be cultured and karyotyped.
1970s
1970: New England Journal of Medicine paper describes mid-trimester amniocenteses and detection of Down syndrome cases.
1972: Ultrasound-guided amniocentesis first described.
1973: Fetoscopy introduced.
1980s
1981: First human open fetal surgery to correct congenital hydronephrosis.
Early 1980s: Chorionic villus sampling introduced at select centers.
1985: Color Doppler incorporated into ultrasound.
1990s
1990: Embryoscopy first described.
Mid-1990s: 3D/4D ultrasound begins to assume major role in ob.gyn. imaging.1997: Discovery of cell-free fetal DNA in maternal plasma.
2000s
2003: MOMS (Management of Myelomeningocele Study) was launched.
2010s
2012: The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine support cell-free DNA screening for women at increased risk of fetal aneuploidy.
2013: Preterm birth rate drops to 11.4%
2014: Diabetes incidence marks a 4-fold increase since 1980.
VIDEO: Expert roundtable explores 50 years of contraception
WASHINGTON – What has the increased access to contraception over the last 50 years meant for American women?
We asked Ob.Gyn. News editorial advisory board member Dr. Eve Espey, professor and chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque, along with three experts in family planning, to explore how expanded contraception options have affected public health, what barriers still remain, and what new products are in the pipeline.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Perhaps the biggest impact for women has been the ability to participate in the workforce, and that includes women entering medical school.
“Over the last 50 years, we’ve seen a big increase in the number of women who are professionals, who are physicians,” Dr. Espey said during the roundtable. “And during that same period of time, we’ve seen the growth of more focus on family planning.”
“I think that really would not be possible without the ability to control our fertility,” said Dr. Sarah W. Prager, associate professor of obstetrics and gynecology and director of the Ryan Family Planning Program at the University of Washington, Seattle.
And the widespread availability of contraception has translated into a decrease in maternal mortality as a result of fewer unintended pregnancies. “The implications for public health – for women and children in this country – is huge,” Dr. Prager said.
LARCs
One of the big shifts in contraceptive trends has been the slow but increasing uptake of long-acting reversible contraceptives (LARCs), such as IUDs and implants. After a drop-off in the 1970s following safety problems with the Dalkon Shield, there has been a resurgence in interest.
In the last decade, the rate of LARC use has grown from about 2% to 10%, corresponding to a slight drop in rates of unintended pregnancy, said Dr. Nikki B. Zite, professor and residency program director in the department of obstetrics and gynecology at the University of Tennessee, Knoxville.
The Contraceptive CHOICE Project, which enrolled more than 9,000 women who were provided with the no-cost reversible contraceptive method of their choice, found that about three-quarters of the women chose an IUD or an implant, which was associated with significant reductions in unintended and teen pregnancies.
“What we saw was that when we removed barriers to contraception in general, that uptake of IUDs and implants really went up,” said Dr. Tessa Madden, director of the division of family planning and associate professor in the department of obstetrics and gynecology at Washington University, St. Louis.
There is no “best” contraceptive method, Dr. Madden said. “Contraception really needs to be tailored to the individual woman [ensuring] that her values and preferences about contraception are taken into consideration during counseling, to help her choose the method that’s going to be the best fit for her.”
Resources
There are resources available to aid in tailoring contraception methods to the needs of patients.
U.S. Medical Eligibility Criteria for Contraceptive Use, guidance that is available through the Centers for Disease Control and Prevention, allows physicians to tailor the method to a patient’s comorbid medical conditions, Dr. Zite said. Physicians can search by contraceptive method or patient characteristic to determine the risk for a given patient, rated on a scale of 1-4 (where 1 or 2 means generally safe, 3 means that the risks may outweigh the benefits, and 4 means that the risks clearly outweigh the benefits).
“It’s a really easy starting-off point to use with patients and physicians when trying to decide what contraceptive method is safe for their patient,” Dr. Zite said.
Common medical comorbidities, including obesity, diabetes, thyroid disease, and hypertension, are all addressed in the medical eligibility criteria.
Another resource is the U.S. Selected Practice Recommendations for Contraceptive Use, which can help in deciding when it is appropriate to start a contraceptive method, what exams and tests are needed before initiation, what follow-up is needed, and how to handle problems such as missed pills or potential side effects.
Barriers
Over the years, many of the barriers to contraceptive access have been reduced. Some forms of emergency contraception are now available over the counter to women of all ages; more states are considering laws allowing women to access up to a year’s supply of hormonal contraceptives at one time; and a few states have passed laws allowing pharmacists to prescribe hormonal birth control directly. In addition, the Affordable Care Act’s mandate for insurers to cover approved methods of contraception without cost sharing has eliminated some cost barriers.
But other systems barriers still remain, such as making women return for multiple visits for the insertion of an IUD or implant, or limiting LARC use only to women who have already had a child. “There’s not a reason to avoid use of IUDs in women that have not had babies but there are still providers out there who will not insert an IUD, so we need to still do a better job to increase access even more,” Dr. Zite said.
Future trends
What new contraceptive options are in the pipeline? Dr. Prager predicted more development in the area of longer-acting injectables and implants, potentially even biodegradable implants. Also likely is the development of nonsurgical sterilization methods for women that eliminate some of the risk and cost barriers. And male contraceptive methods are in the works, both hormonal and nonhormonal, Dr. Prager said.
There’s an increasing interested in nonhormonal longer-acting methods, beyond just the copper IUD, Dr. Madden said, and there are new products on the horizon in that area. Researchers are exploring new methods to protect against HIV and other sexually transmitted infections, while offering contraception, Dr. Zite said.
Dr. Espey reported having no relevant financial disclosures. Dr. Prager is an unpaid trainer for Nexplanon (Merck). Dr. Zite is an unpaid trainer for Nexplanon and serves on an international IUD advisory board for Bayer. Dr. Madden serves on a scientific advisory board for Bayer and on a data safety monitoring board for phase IV safety studies of Bayer contraceptive products.
Throughout 2016, Ob.Gyn. News is celebrating its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of infertility treatment, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
WASHINGTON – What has the increased access to contraception over the last 50 years meant for American women?
We asked Ob.Gyn. News editorial advisory board member Dr. Eve Espey, professor and chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque, along with three experts in family planning, to explore how expanded contraception options have affected public health, what barriers still remain, and what new products are in the pipeline.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Perhaps the biggest impact for women has been the ability to participate in the workforce, and that includes women entering medical school.
“Over the last 50 years, we’ve seen a big increase in the number of women who are professionals, who are physicians,” Dr. Espey said during the roundtable. “And during that same period of time, we’ve seen the growth of more focus on family planning.”
“I think that really would not be possible without the ability to control our fertility,” said Dr. Sarah W. Prager, associate professor of obstetrics and gynecology and director of the Ryan Family Planning Program at the University of Washington, Seattle.
And the widespread availability of contraception has translated into a decrease in maternal mortality as a result of fewer unintended pregnancies. “The implications for public health – for women and children in this country – is huge,” Dr. Prager said.
LARCs
One of the big shifts in contraceptive trends has been the slow but increasing uptake of long-acting reversible contraceptives (LARCs), such as IUDs and implants. After a drop-off in the 1970s following safety problems with the Dalkon Shield, there has been a resurgence in interest.
In the last decade, the rate of LARC use has grown from about 2% to 10%, corresponding to a slight drop in rates of unintended pregnancy, said Dr. Nikki B. Zite, professor and residency program director in the department of obstetrics and gynecology at the University of Tennessee, Knoxville.
The Contraceptive CHOICE Project, which enrolled more than 9,000 women who were provided with the no-cost reversible contraceptive method of their choice, found that about three-quarters of the women chose an IUD or an implant, which was associated with significant reductions in unintended and teen pregnancies.
“What we saw was that when we removed barriers to contraception in general, that uptake of IUDs and implants really went up,” said Dr. Tessa Madden, director of the division of family planning and associate professor in the department of obstetrics and gynecology at Washington University, St. Louis.
There is no “best” contraceptive method, Dr. Madden said. “Contraception really needs to be tailored to the individual woman [ensuring] that her values and preferences about contraception are taken into consideration during counseling, to help her choose the method that’s going to be the best fit for her.”
Resources
There are resources available to aid in tailoring contraception methods to the needs of patients.
U.S. Medical Eligibility Criteria for Contraceptive Use, guidance that is available through the Centers for Disease Control and Prevention, allows physicians to tailor the method to a patient’s comorbid medical conditions, Dr. Zite said. Physicians can search by contraceptive method or patient characteristic to determine the risk for a given patient, rated on a scale of 1-4 (where 1 or 2 means generally safe, 3 means that the risks may outweigh the benefits, and 4 means that the risks clearly outweigh the benefits).
“It’s a really easy starting-off point to use with patients and physicians when trying to decide what contraceptive method is safe for their patient,” Dr. Zite said.
Common medical comorbidities, including obesity, diabetes, thyroid disease, and hypertension, are all addressed in the medical eligibility criteria.
Another resource is the U.S. Selected Practice Recommendations for Contraceptive Use, which can help in deciding when it is appropriate to start a contraceptive method, what exams and tests are needed before initiation, what follow-up is needed, and how to handle problems such as missed pills or potential side effects.
Barriers
Over the years, many of the barriers to contraceptive access have been reduced. Some forms of emergency contraception are now available over the counter to women of all ages; more states are considering laws allowing women to access up to a year’s supply of hormonal contraceptives at one time; and a few states have passed laws allowing pharmacists to prescribe hormonal birth control directly. In addition, the Affordable Care Act’s mandate for insurers to cover approved methods of contraception without cost sharing has eliminated some cost barriers.
But other systems barriers still remain, such as making women return for multiple visits for the insertion of an IUD or implant, or limiting LARC use only to women who have already had a child. “There’s not a reason to avoid use of IUDs in women that have not had babies but there are still providers out there who will not insert an IUD, so we need to still do a better job to increase access even more,” Dr. Zite said.
Future trends
What new contraceptive options are in the pipeline? Dr. Prager predicted more development in the area of longer-acting injectables and implants, potentially even biodegradable implants. Also likely is the development of nonsurgical sterilization methods for women that eliminate some of the risk and cost barriers. And male contraceptive methods are in the works, both hormonal and nonhormonal, Dr. Prager said.
There’s an increasing interested in nonhormonal longer-acting methods, beyond just the copper IUD, Dr. Madden said, and there are new products on the horizon in that area. Researchers are exploring new methods to protect against HIV and other sexually transmitted infections, while offering contraception, Dr. Zite said.
Dr. Espey reported having no relevant financial disclosures. Dr. Prager is an unpaid trainer for Nexplanon (Merck). Dr. Zite is an unpaid trainer for Nexplanon and serves on an international IUD advisory board for Bayer. Dr. Madden serves on a scientific advisory board for Bayer and on a data safety monitoring board for phase IV safety studies of Bayer contraceptive products.
Throughout 2016, Ob.Gyn. News is celebrating its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of infertility treatment, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
WASHINGTON – What has the increased access to contraception over the last 50 years meant for American women?
We asked Ob.Gyn. News editorial advisory board member Dr. Eve Espey, professor and chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque, along with three experts in family planning, to explore how expanded contraception options have affected public health, what barriers still remain, and what new products are in the pipeline.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Perhaps the biggest impact for women has been the ability to participate in the workforce, and that includes women entering medical school.
“Over the last 50 years, we’ve seen a big increase in the number of women who are professionals, who are physicians,” Dr. Espey said during the roundtable. “And during that same period of time, we’ve seen the growth of more focus on family planning.”
“I think that really would not be possible without the ability to control our fertility,” said Dr. Sarah W. Prager, associate professor of obstetrics and gynecology and director of the Ryan Family Planning Program at the University of Washington, Seattle.
And the widespread availability of contraception has translated into a decrease in maternal mortality as a result of fewer unintended pregnancies. “The implications for public health – for women and children in this country – is huge,” Dr. Prager said.
LARCs
One of the big shifts in contraceptive trends has been the slow but increasing uptake of long-acting reversible contraceptives (LARCs), such as IUDs and implants. After a drop-off in the 1970s following safety problems with the Dalkon Shield, there has been a resurgence in interest.
In the last decade, the rate of LARC use has grown from about 2% to 10%, corresponding to a slight drop in rates of unintended pregnancy, said Dr. Nikki B. Zite, professor and residency program director in the department of obstetrics and gynecology at the University of Tennessee, Knoxville.
The Contraceptive CHOICE Project, which enrolled more than 9,000 women who were provided with the no-cost reversible contraceptive method of their choice, found that about three-quarters of the women chose an IUD or an implant, which was associated with significant reductions in unintended and teen pregnancies.
“What we saw was that when we removed barriers to contraception in general, that uptake of IUDs and implants really went up,” said Dr. Tessa Madden, director of the division of family planning and associate professor in the department of obstetrics and gynecology at Washington University, St. Louis.
There is no “best” contraceptive method, Dr. Madden said. “Contraception really needs to be tailored to the individual woman [ensuring] that her values and preferences about contraception are taken into consideration during counseling, to help her choose the method that’s going to be the best fit for her.”
Resources
There are resources available to aid in tailoring contraception methods to the needs of patients.
U.S. Medical Eligibility Criteria for Contraceptive Use, guidance that is available through the Centers for Disease Control and Prevention, allows physicians to tailor the method to a patient’s comorbid medical conditions, Dr. Zite said. Physicians can search by contraceptive method or patient characteristic to determine the risk for a given patient, rated on a scale of 1-4 (where 1 or 2 means generally safe, 3 means that the risks may outweigh the benefits, and 4 means that the risks clearly outweigh the benefits).
“It’s a really easy starting-off point to use with patients and physicians when trying to decide what contraceptive method is safe for their patient,” Dr. Zite said.
Common medical comorbidities, including obesity, diabetes, thyroid disease, and hypertension, are all addressed in the medical eligibility criteria.
Another resource is the U.S. Selected Practice Recommendations for Contraceptive Use, which can help in deciding when it is appropriate to start a contraceptive method, what exams and tests are needed before initiation, what follow-up is needed, and how to handle problems such as missed pills or potential side effects.
Barriers
Over the years, many of the barriers to contraceptive access have been reduced. Some forms of emergency contraception are now available over the counter to women of all ages; more states are considering laws allowing women to access up to a year’s supply of hormonal contraceptives at one time; and a few states have passed laws allowing pharmacists to prescribe hormonal birth control directly. In addition, the Affordable Care Act’s mandate for insurers to cover approved methods of contraception without cost sharing has eliminated some cost barriers.
But other systems barriers still remain, such as making women return for multiple visits for the insertion of an IUD or implant, or limiting LARC use only to women who have already had a child. “There’s not a reason to avoid use of IUDs in women that have not had babies but there are still providers out there who will not insert an IUD, so we need to still do a better job to increase access even more,” Dr. Zite said.
Future trends
What new contraceptive options are in the pipeline? Dr. Prager predicted more development in the area of longer-acting injectables and implants, potentially even biodegradable implants. Also likely is the development of nonsurgical sterilization methods for women that eliminate some of the risk and cost barriers. And male contraceptive methods are in the works, both hormonal and nonhormonal, Dr. Prager said.
There’s an increasing interested in nonhormonal longer-acting methods, beyond just the copper IUD, Dr. Madden said, and there are new products on the horizon in that area. Researchers are exploring new methods to protect against HIV and other sexually transmitted infections, while offering contraception, Dr. Zite said.
Dr. Espey reported having no relevant financial disclosures. Dr. Prager is an unpaid trainer for Nexplanon (Merck). Dr. Zite is an unpaid trainer for Nexplanon and serves on an international IUD advisory board for Bayer. Dr. Madden serves on a scientific advisory board for Bayer and on a data safety monitoring board for phase IV safety studies of Bayer contraceptive products.
Throughout 2016, Ob.Gyn. News is celebrating its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of infertility treatment, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
50 years of gynecologic surgery: A large dose of ingenuity, a small dose of controversy
Over the past 50 years, there has been explosive change in gynecologic surgery. Ob.Gyn. News has been at the forefront of capturing and chronicling this paradigm shift in the treatment of the female patient.
Our beginnings
From antiquity, physicians and surgeons have struggled with pelvic prolapse, uterine fibroids, ovarian cysts, urinary incontinence, vesicovaginal fistulas, pelvic pain, and abnormal uterine bleeding. At the time of the first edition of Ob.Gyn. News, it had been less than a century since Thomas Edison invented the light bulb; just over 50 years since Hans Christian Jacobaeus first created air pneumoperitoneum using a trocar, followed by the Nitze cystoscope; about 40 years since Richard Zollikofer created a carbon dioxide pneumoperitoneum; 25 years since F.H. Powers and A.C. Barnes had first described laparoscopic tubal sterilization by cautery; and about 20 years since Raoul Palmer, considered the father of modern laparoscopy, had first described the technique – left upper quadrant entry, testing insufflation, Trendelenburg positioning, and simple laparoscopic instrumentation.
In the 1950s, Hans Frangenheim would bring monopolar electrosurgery to laparoscopy and Harold Hopkins would introduce fiber optics. It was not until 1967 that Patrick Steptoe would publish the first textbook on laparoscopy in the English language.
Although usage as a diagnostic tool and a method of sterilization increased popularity of laparoscopy in the 1960s and early 1970s, there were few advances. In fact, a review of early editions of Ob.Gyn. News during that time period shows that the majority of articles involving laparoscopy dealt with sterilization; including the introduction of clips for tubal sterilization by Jaroslav Hulka in 1972. This did not deter the efforts of Jordan Phillips, who along with Jacques Rioux, Louis Keith, Richard Soderstrom – four early laparoscopists – incorporated a new society, the American Association of Gynecologic Laparoscopists (the AAGL) in 1971.
Simultaneously, in 1979, James Daniell in the United States, Maurice Bruhart in France, and Yona Tadir in Israel were promoting efforts to couple the carbon dioxide laser to the laparoscope to treat pelvic adhesions and endometriosis. Later on, fiber lasers, KTP, Nd:YAG, and Argon lasers would be utilized in our field. Still, only a few extirpative procedures were being performed via a laparoscope route. This included linear salpingostomy for the treatment of ectopic pregnancy, championed by Professor Bruhart and H. Manhes in Europe, and Alan DeCherney in the United States.
During the 1980s, laparoscopic surgery was at its innovative best. Through the pioneering efforts of Professor Kurt Semm and his protégée, Liselotte Mettler, the gynecologic laparoscopist was introduced to endoloops, simple suturing techniques, and mechanical morcellation techniques.
Procedures such as salpingo-oophorectomy, appendectomy, and myomectomy could now be performed via the laparoscope. Dr. Camran Nezhat coupled the carbon dioxide laser, the laparoscope, and the television monitor, coining the term laparoscopy. Most importantly, the laparoscopic surgeon was liberated; he or she could remain upright and perform surgery with both hands. Through the 1980s and 1990s, Dr. Nezhat, Dr. Harry Reich, and other innovators pushed the envelope in increasing the ability to extirpate endometriosis, excise severe pelvic adhesions, and perform discoid and segmental bowel resection.
The day the earth stood still
Every gynecologic laparoscopic surgeon should remember Jan. 26, 1988, as that was the date that Dr. Harry Reich performed the first total laparoscopic hysterectomy. Now, little more than 25 years later, in many parts of the country, a laparoscopic approach to hysterectomy is indeed the most common route. Over the years, with the evolution of instrumentation, including new energy systems (ultrasonic, advanced bipolar) and the introduction of barbed sutures, hysterectomy can now be performed via minilaparoscopy, single-site laparoscopy, robot-assisted, and robotic single site, all of which have been featured in the Ob.Gyn. News’ Master Class in Gynecologic Surgery.
But hysteroscopy came first
Abulkasim utilized a mirror to reflect light into the vaginal vault in 1,000 A.D. In 1806, Philipp Bozzini originated the idea of illuminating body cavities by an external light source. Through a system of mirrors and tubes, candlelight could be reflected into the body. In 1869, D.C. Pantaleoni used a cystoscope developed by Antoine Desormeaux – who has been called the father of endoscopy – to treat endometrial polyps with silver nitrate.
Through the 50 years of Ob.Gyn. News and over the past 12 years of the Master Class in Gynecologic Surgery, our community has been consistently updated as to advances in hysteroscopy, not only to enhance treatment efficacy, but safety as well. This has included such advances as the continuous flow hysteroscope, the Hamou contact hysteroscope, and fluid management systems to enhance visualization.
In 1978, Robert Neuwirth introduced loops to perform hysteroscopic myomectomy. The loop resectoscope was quickly followed by the rollerball to perform endometrial ablation. In the late 1990s, hysteroscopic bipolar cutting loops were introduced. This enabled use of ionic distension media saline, instead of nonionic media, thus decreasing risks related to hyponatremia.
In 2003, Mark Emanuel introduced hysteroscopic morcellation systems, which enabled more gynecologists to perform operative hysteroscopy safely. Resected tissue is removed immediately to allow superior visualization. The flexible hysteroscope coupled with vaginoscopy has enabled hysteroscopy to be done with minimal to no anesthesia in an in-office setting.
With advances in hysteroscopy over the past 35 years, hysteroscopic procedures such as polypectomy, myomectomy, lysis of adhesions, transection of endometriosis, evacuation of retained products of conception, and endometrial ablation/resection have become routine.
And now, the controversy
Since its inception, laparoscopic surgery has not been without controversy. In 1933, Karl Fervers described explosion and flashes of light from a combination of high frequency electric current and oxygen distension gas while performing laparoscopic adhesiolysis with the coagulation probe of the ureterocystoscope.
In the early 1970s, Professor Kurt Semm’s pioneering effort was not rewarded by his department, in Kiel, Germany, which instead recommended he schedule a brain scan and psychological testing.
Nearly 20 years later, in a 1992 edition of Current Science, Professor Semm, along with Alan DeCherney, stated that “over 80% of gynecological operations can now be performed by laparoscopy.” Shortly thereafter, however, Dr. Roy Pitkin, who at the time was president of the American College of Obstetricians and Gynecologists, wrote an editorial in the Journal of Obstetrics and Gynecology – “Operative Laparoscopy: Surgical Advance or Technical Gimmick?” (Obstet Gynecol. 1992 Mar;79[3]:441-2).
Fortunately, 18 years later, with the continued advances in laparoscopic surgery making it less expensive, safer, and more accessible, Dr. Pitkin did retract his statement (Obstet Gynecol. 2010 May;115[5]:890-1).
Currently, the gynecologic community is embroiled in controversies involving the use of the robot to assist in the performance of laparoscopic surgery, the incorporation of synthetic mesh to enhance urogynecologic procedures, the placement of Essure micro-inserts to occlude fallopian tubes, and the use of electronic power morcellation at time of laparoscopic or robot-assisted hysterectomy, myomectomy, or sacrocolpopexy.
After reading the 2013 article by Dr. Jason Wright, published in JAMA, comparing laparoscopic hysterectomy to robotic hysterectomy, no one can deny that the rise in a minimally invasive route to hysterectomy has coincided with the advent of the robot (JAMA. 2013 Feb 20;309[7]:689-98). On the other hand, many detractors, including Dr. James Breeden (past ACOG president 2012-2013), find the higher cost of robotic surgery very problematic. In fact, many of these detractors cite the paucity of data showing a significant advantage to use of robotics.
While certainly cost, more than ever, must be a major consideration, remember that during the 1990s, there were multiple articles in Ob.Gyn. News raising concerns about the cost of laparoscopic hysterectomy. Interestingly, studies over the past decade by Warren and Jonsdottir show a cost savings when hysterectomy is done laparoscopically as opposed to its being done by laparotomy. Thus, it certainly can be anticipated that with more physician experience, improved instrumentation, and robotic industry competition, the overall cost will become more comparable to a laparoscopic route.
In 1995, Ulf Ulmsten first described the use of tension-free tape (TVT) to treat stress urinary incontinence. In 1998, the Food and Drug Administration approved the use of the TVT sling in the United States. Since then, transobturator tension-free vaginal tape (TVT-O) and single incision mini-slings have been introduced. All of these techniques have been shown to be successful and have been well adapted into the armamentarium of physicians treating stress urinary incontinence.
With the success of synthetic mesh for the treatment of stress urinary incontinence, its use was extended to pelvic prolapse. In 2002, the first mesh device with indications for the treatment of pelvic organ prolapse was approved by the FDA. While the erosion rate utilizing synthetic mesh for stress urinary incontinence has been noted to be 2%, rates up to 8.3% have been noted in patients treated for pelvic prolapse.
In 2008, the FDA issued a warning regarding the use of mesh for prolapse and incontinence repair secondary to the sequelae of mesh erosion. Subsequently, in 2011, the concern was limited to vaginal mesh to correct pelvic organ prolapse. Finally, on Jan. 4, 2016, the FDA issued an order to reclassify surgical mesh to repair pelvic organ prolapse from class II, which includes moderate-risk devices, to class III, which includes high-risk devices. Moreover, the FDA issued a second order to manufacturers to submit a premarket approval application to support the safety and effectiveness of synthetic mesh for transvaginal repair of pelvic organ prolapse.
Essure micro-inserts for permanent birth control received initial approval from the FDA in November 2002. Despite the fact that Essure can be easily placed, is highly effective, and has seemingly low complication rates, concerns have been raised by the Facebook group “Essure Problems” and Erin Brockovich, the focus of the 2000 biographical film starring Julia Roberts.
After more than 5,000 women filed grievances with the FDA between November 2002 and May 2015, based on unintended pregnancies, miscarriages, stillbirths, severe pain, and bleeding, the FDA announced in 2016 that it would require a boxed warning label for Essure. The FDA also called upon Bayer, which makes and markets Essure, to conduct surveillance to assess “risks of the device in a real-world environment.” The agency stated it will use the results to “determine what, if any, further actions related to Essure are needed to protect public health.”
While Jan. 26, 1988, is a very special date in minimally invasive gynecologic surgery, April 17, 2014, is a day of infamy for the gynecologic laparoscopist. For on this day, the FDA announced a warning regarding electronic power morcellation. Many hospitals and hospital systems throughout the country issued bans on electronic power morcellation, leading to needless open laparotomy procedures and thus, introducing prolonged recovery times and increased risk.
At a time when the recent introduction of barbed suture had made both closure of the vaginal cuff at time of hysterectomy and repair of the hysterotomy at myomectomy easier and faster, the gynecologic laparoscopist was taking a step backward. The FDA based this decision and a subsequent boxed warning – issued in November 2014 – on a small number of studies showing potential upstaging of leiomyosarcoma post electronic power morcellation. Interestingly, many of the morcellation procedures cited did not use power morcellation. Furthermore, a more comprehensive meta-analysis by Elizabeth A. Pritts and colleagues, showed a far lower risk than suggested by the FDA (Gynecol Surg. 2015;12[3]:165-77).
Recently, an article by William Parker and colleagues recommended that the FDA reverse its position (Obstet Gynecol. 2016 Jan;127[1]:18-22). Many believe that ultimately, the solution will be morcellation in a containment bag, which I and my colleagues have been performing in virtually every power morcellation procedure since May 2014. During this current power morcellation controversy, the Master Class in Gynecologic Surgery has continued to update its readers with three different articles related to the subject.
And in conclusion
Without a doubt, the past 50 years of gynecologic surgery has been a time of unparalleled innovation with occasional controversy thrown in. Ob.Gyn. News and more recently, the Master Class in Gynecologic Surgery, has had a major leadership role in bringing this profound ingenuity to the gynecology community by introducing this explosion of surgical creativity to its readers.
And what will the next 50 years bring? I believe we will continue to see tremendous advancements in minimally invasive gynecologic surgery. There will be a definite impact of costs on the marketplace. Thus, many of the minor minimally invasive procedures currently performed in the hospital or surgery center will be brought into office settings. In addition, secondary to reimbursement, the more complex cases will be carried out by fewer gynecologic surgeons who have undergone more intense training in pelvic surgery and who can perform these cases more efficiently and with fewer complications. Our ability to perform surgery and what type of procedures we do will not only be based on randomized, controlled trials, but big data collection as well.
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, and past president of the AAGL and the International Society for Gynecologic Endoscopy (ISGE). He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.; director of minimally invasive gynecologic surgery and the director of the AAGL/Society of Reproductive Surgery fellowship in minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.; and the medical editor of this column, Master Class. Dr. Miller is a consultant and is on the speakers bureau for Ethicon.
Over the past 50 years, there has been explosive change in gynecologic surgery. Ob.Gyn. News has been at the forefront of capturing and chronicling this paradigm shift in the treatment of the female patient.
Our beginnings
From antiquity, physicians and surgeons have struggled with pelvic prolapse, uterine fibroids, ovarian cysts, urinary incontinence, vesicovaginal fistulas, pelvic pain, and abnormal uterine bleeding. At the time of the first edition of Ob.Gyn. News, it had been less than a century since Thomas Edison invented the light bulb; just over 50 years since Hans Christian Jacobaeus first created air pneumoperitoneum using a trocar, followed by the Nitze cystoscope; about 40 years since Richard Zollikofer created a carbon dioxide pneumoperitoneum; 25 years since F.H. Powers and A.C. Barnes had first described laparoscopic tubal sterilization by cautery; and about 20 years since Raoul Palmer, considered the father of modern laparoscopy, had first described the technique – left upper quadrant entry, testing insufflation, Trendelenburg positioning, and simple laparoscopic instrumentation.
In the 1950s, Hans Frangenheim would bring monopolar electrosurgery to laparoscopy and Harold Hopkins would introduce fiber optics. It was not until 1967 that Patrick Steptoe would publish the first textbook on laparoscopy in the English language.
Although usage as a diagnostic tool and a method of sterilization increased popularity of laparoscopy in the 1960s and early 1970s, there were few advances. In fact, a review of early editions of Ob.Gyn. News during that time period shows that the majority of articles involving laparoscopy dealt with sterilization; including the introduction of clips for tubal sterilization by Jaroslav Hulka in 1972. This did not deter the efforts of Jordan Phillips, who along with Jacques Rioux, Louis Keith, Richard Soderstrom – four early laparoscopists – incorporated a new society, the American Association of Gynecologic Laparoscopists (the AAGL) in 1971.
Simultaneously, in 1979, James Daniell in the United States, Maurice Bruhart in France, and Yona Tadir in Israel were promoting efforts to couple the carbon dioxide laser to the laparoscope to treat pelvic adhesions and endometriosis. Later on, fiber lasers, KTP, Nd:YAG, and Argon lasers would be utilized in our field. Still, only a few extirpative procedures were being performed via a laparoscope route. This included linear salpingostomy for the treatment of ectopic pregnancy, championed by Professor Bruhart and H. Manhes in Europe, and Alan DeCherney in the United States.
During the 1980s, laparoscopic surgery was at its innovative best. Through the pioneering efforts of Professor Kurt Semm and his protégée, Liselotte Mettler, the gynecologic laparoscopist was introduced to endoloops, simple suturing techniques, and mechanical morcellation techniques.
Procedures such as salpingo-oophorectomy, appendectomy, and myomectomy could now be performed via the laparoscope. Dr. Camran Nezhat coupled the carbon dioxide laser, the laparoscope, and the television monitor, coining the term laparoscopy. Most importantly, the laparoscopic surgeon was liberated; he or she could remain upright and perform surgery with both hands. Through the 1980s and 1990s, Dr. Nezhat, Dr. Harry Reich, and other innovators pushed the envelope in increasing the ability to extirpate endometriosis, excise severe pelvic adhesions, and perform discoid and segmental bowel resection.
The day the earth stood still
Every gynecologic laparoscopic surgeon should remember Jan. 26, 1988, as that was the date that Dr. Harry Reich performed the first total laparoscopic hysterectomy. Now, little more than 25 years later, in many parts of the country, a laparoscopic approach to hysterectomy is indeed the most common route. Over the years, with the evolution of instrumentation, including new energy systems (ultrasonic, advanced bipolar) and the introduction of barbed sutures, hysterectomy can now be performed via minilaparoscopy, single-site laparoscopy, robot-assisted, and robotic single site, all of which have been featured in the Ob.Gyn. News’ Master Class in Gynecologic Surgery.
But hysteroscopy came first
Abulkasim utilized a mirror to reflect light into the vaginal vault in 1,000 A.D. In 1806, Philipp Bozzini originated the idea of illuminating body cavities by an external light source. Through a system of mirrors and tubes, candlelight could be reflected into the body. In 1869, D.C. Pantaleoni used a cystoscope developed by Antoine Desormeaux – who has been called the father of endoscopy – to treat endometrial polyps with silver nitrate.
Through the 50 years of Ob.Gyn. News and over the past 12 years of the Master Class in Gynecologic Surgery, our community has been consistently updated as to advances in hysteroscopy, not only to enhance treatment efficacy, but safety as well. This has included such advances as the continuous flow hysteroscope, the Hamou contact hysteroscope, and fluid management systems to enhance visualization.
In 1978, Robert Neuwirth introduced loops to perform hysteroscopic myomectomy. The loop resectoscope was quickly followed by the rollerball to perform endometrial ablation. In the late 1990s, hysteroscopic bipolar cutting loops were introduced. This enabled use of ionic distension media saline, instead of nonionic media, thus decreasing risks related to hyponatremia.
In 2003, Mark Emanuel introduced hysteroscopic morcellation systems, which enabled more gynecologists to perform operative hysteroscopy safely. Resected tissue is removed immediately to allow superior visualization. The flexible hysteroscope coupled with vaginoscopy has enabled hysteroscopy to be done with minimal to no anesthesia in an in-office setting.
With advances in hysteroscopy over the past 35 years, hysteroscopic procedures such as polypectomy, myomectomy, lysis of adhesions, transection of endometriosis, evacuation of retained products of conception, and endometrial ablation/resection have become routine.
And now, the controversy
Since its inception, laparoscopic surgery has not been without controversy. In 1933, Karl Fervers described explosion and flashes of light from a combination of high frequency electric current and oxygen distension gas while performing laparoscopic adhesiolysis with the coagulation probe of the ureterocystoscope.
In the early 1970s, Professor Kurt Semm’s pioneering effort was not rewarded by his department, in Kiel, Germany, which instead recommended he schedule a brain scan and psychological testing.
Nearly 20 years later, in a 1992 edition of Current Science, Professor Semm, along with Alan DeCherney, stated that “over 80% of gynecological operations can now be performed by laparoscopy.” Shortly thereafter, however, Dr. Roy Pitkin, who at the time was president of the American College of Obstetricians and Gynecologists, wrote an editorial in the Journal of Obstetrics and Gynecology – “Operative Laparoscopy: Surgical Advance or Technical Gimmick?” (Obstet Gynecol. 1992 Mar;79[3]:441-2).
Fortunately, 18 years later, with the continued advances in laparoscopic surgery making it less expensive, safer, and more accessible, Dr. Pitkin did retract his statement (Obstet Gynecol. 2010 May;115[5]:890-1).
Currently, the gynecologic community is embroiled in controversies involving the use of the robot to assist in the performance of laparoscopic surgery, the incorporation of synthetic mesh to enhance urogynecologic procedures, the placement of Essure micro-inserts to occlude fallopian tubes, and the use of electronic power morcellation at time of laparoscopic or robot-assisted hysterectomy, myomectomy, or sacrocolpopexy.
After reading the 2013 article by Dr. Jason Wright, published in JAMA, comparing laparoscopic hysterectomy to robotic hysterectomy, no one can deny that the rise in a minimally invasive route to hysterectomy has coincided with the advent of the robot (JAMA. 2013 Feb 20;309[7]:689-98). On the other hand, many detractors, including Dr. James Breeden (past ACOG president 2012-2013), find the higher cost of robotic surgery very problematic. In fact, many of these detractors cite the paucity of data showing a significant advantage to use of robotics.
While certainly cost, more than ever, must be a major consideration, remember that during the 1990s, there were multiple articles in Ob.Gyn. News raising concerns about the cost of laparoscopic hysterectomy. Interestingly, studies over the past decade by Warren and Jonsdottir show a cost savings when hysterectomy is done laparoscopically as opposed to its being done by laparotomy. Thus, it certainly can be anticipated that with more physician experience, improved instrumentation, and robotic industry competition, the overall cost will become more comparable to a laparoscopic route.
In 1995, Ulf Ulmsten first described the use of tension-free tape (TVT) to treat stress urinary incontinence. In 1998, the Food and Drug Administration approved the use of the TVT sling in the United States. Since then, transobturator tension-free vaginal tape (TVT-O) and single incision mini-slings have been introduced. All of these techniques have been shown to be successful and have been well adapted into the armamentarium of physicians treating stress urinary incontinence.
With the success of synthetic mesh for the treatment of stress urinary incontinence, its use was extended to pelvic prolapse. In 2002, the first mesh device with indications for the treatment of pelvic organ prolapse was approved by the FDA. While the erosion rate utilizing synthetic mesh for stress urinary incontinence has been noted to be 2%, rates up to 8.3% have been noted in patients treated for pelvic prolapse.
In 2008, the FDA issued a warning regarding the use of mesh for prolapse and incontinence repair secondary to the sequelae of mesh erosion. Subsequently, in 2011, the concern was limited to vaginal mesh to correct pelvic organ prolapse. Finally, on Jan. 4, 2016, the FDA issued an order to reclassify surgical mesh to repair pelvic organ prolapse from class II, which includes moderate-risk devices, to class III, which includes high-risk devices. Moreover, the FDA issued a second order to manufacturers to submit a premarket approval application to support the safety and effectiveness of synthetic mesh for transvaginal repair of pelvic organ prolapse.
Essure micro-inserts for permanent birth control received initial approval from the FDA in November 2002. Despite the fact that Essure can be easily placed, is highly effective, and has seemingly low complication rates, concerns have been raised by the Facebook group “Essure Problems” and Erin Brockovich, the focus of the 2000 biographical film starring Julia Roberts.
After more than 5,000 women filed grievances with the FDA between November 2002 and May 2015, based on unintended pregnancies, miscarriages, stillbirths, severe pain, and bleeding, the FDA announced in 2016 that it would require a boxed warning label for Essure. The FDA also called upon Bayer, which makes and markets Essure, to conduct surveillance to assess “risks of the device in a real-world environment.” The agency stated it will use the results to “determine what, if any, further actions related to Essure are needed to protect public health.”
While Jan. 26, 1988, is a very special date in minimally invasive gynecologic surgery, April 17, 2014, is a day of infamy for the gynecologic laparoscopist. For on this day, the FDA announced a warning regarding electronic power morcellation. Many hospitals and hospital systems throughout the country issued bans on electronic power morcellation, leading to needless open laparotomy procedures and thus, introducing prolonged recovery times and increased risk.
At a time when the recent introduction of barbed suture had made both closure of the vaginal cuff at time of hysterectomy and repair of the hysterotomy at myomectomy easier and faster, the gynecologic laparoscopist was taking a step backward. The FDA based this decision and a subsequent boxed warning – issued in November 2014 – on a small number of studies showing potential upstaging of leiomyosarcoma post electronic power morcellation. Interestingly, many of the morcellation procedures cited did not use power morcellation. Furthermore, a more comprehensive meta-analysis by Elizabeth A. Pritts and colleagues, showed a far lower risk than suggested by the FDA (Gynecol Surg. 2015;12[3]:165-77).
Recently, an article by William Parker and colleagues recommended that the FDA reverse its position (Obstet Gynecol. 2016 Jan;127[1]:18-22). Many believe that ultimately, the solution will be morcellation in a containment bag, which I and my colleagues have been performing in virtually every power morcellation procedure since May 2014. During this current power morcellation controversy, the Master Class in Gynecologic Surgery has continued to update its readers with three different articles related to the subject.
And in conclusion
Without a doubt, the past 50 years of gynecologic surgery has been a time of unparalleled innovation with occasional controversy thrown in. Ob.Gyn. News and more recently, the Master Class in Gynecologic Surgery, has had a major leadership role in bringing this profound ingenuity to the gynecology community by introducing this explosion of surgical creativity to its readers.
And what will the next 50 years bring? I believe we will continue to see tremendous advancements in minimally invasive gynecologic surgery. There will be a definite impact of costs on the marketplace. Thus, many of the minor minimally invasive procedures currently performed in the hospital or surgery center will be brought into office settings. In addition, secondary to reimbursement, the more complex cases will be carried out by fewer gynecologic surgeons who have undergone more intense training in pelvic surgery and who can perform these cases more efficiently and with fewer complications. Our ability to perform surgery and what type of procedures we do will not only be based on randomized, controlled trials, but big data collection as well.
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, and past president of the AAGL and the International Society for Gynecologic Endoscopy (ISGE). He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.; director of minimally invasive gynecologic surgery and the director of the AAGL/Society of Reproductive Surgery fellowship in minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.; and the medical editor of this column, Master Class. Dr. Miller is a consultant and is on the speakers bureau for Ethicon.
Over the past 50 years, there has been explosive change in gynecologic surgery. Ob.Gyn. News has been at the forefront of capturing and chronicling this paradigm shift in the treatment of the female patient.
Our beginnings
From antiquity, physicians and surgeons have struggled with pelvic prolapse, uterine fibroids, ovarian cysts, urinary incontinence, vesicovaginal fistulas, pelvic pain, and abnormal uterine bleeding. At the time of the first edition of Ob.Gyn. News, it had been less than a century since Thomas Edison invented the light bulb; just over 50 years since Hans Christian Jacobaeus first created air pneumoperitoneum using a trocar, followed by the Nitze cystoscope; about 40 years since Richard Zollikofer created a carbon dioxide pneumoperitoneum; 25 years since F.H. Powers and A.C. Barnes had first described laparoscopic tubal sterilization by cautery; and about 20 years since Raoul Palmer, considered the father of modern laparoscopy, had first described the technique – left upper quadrant entry, testing insufflation, Trendelenburg positioning, and simple laparoscopic instrumentation.
In the 1950s, Hans Frangenheim would bring monopolar electrosurgery to laparoscopy and Harold Hopkins would introduce fiber optics. It was not until 1967 that Patrick Steptoe would publish the first textbook on laparoscopy in the English language.
Although usage as a diagnostic tool and a method of sterilization increased popularity of laparoscopy in the 1960s and early 1970s, there were few advances. In fact, a review of early editions of Ob.Gyn. News during that time period shows that the majority of articles involving laparoscopy dealt with sterilization; including the introduction of clips for tubal sterilization by Jaroslav Hulka in 1972. This did not deter the efforts of Jordan Phillips, who along with Jacques Rioux, Louis Keith, Richard Soderstrom – four early laparoscopists – incorporated a new society, the American Association of Gynecologic Laparoscopists (the AAGL) in 1971.
Simultaneously, in 1979, James Daniell in the United States, Maurice Bruhart in France, and Yona Tadir in Israel were promoting efforts to couple the carbon dioxide laser to the laparoscope to treat pelvic adhesions and endometriosis. Later on, fiber lasers, KTP, Nd:YAG, and Argon lasers would be utilized in our field. Still, only a few extirpative procedures were being performed via a laparoscope route. This included linear salpingostomy for the treatment of ectopic pregnancy, championed by Professor Bruhart and H. Manhes in Europe, and Alan DeCherney in the United States.
During the 1980s, laparoscopic surgery was at its innovative best. Through the pioneering efforts of Professor Kurt Semm and his protégée, Liselotte Mettler, the gynecologic laparoscopist was introduced to endoloops, simple suturing techniques, and mechanical morcellation techniques.
Procedures such as salpingo-oophorectomy, appendectomy, and myomectomy could now be performed via the laparoscope. Dr. Camran Nezhat coupled the carbon dioxide laser, the laparoscope, and the television monitor, coining the term laparoscopy. Most importantly, the laparoscopic surgeon was liberated; he or she could remain upright and perform surgery with both hands. Through the 1980s and 1990s, Dr. Nezhat, Dr. Harry Reich, and other innovators pushed the envelope in increasing the ability to extirpate endometriosis, excise severe pelvic adhesions, and perform discoid and segmental bowel resection.
The day the earth stood still
Every gynecologic laparoscopic surgeon should remember Jan. 26, 1988, as that was the date that Dr. Harry Reich performed the first total laparoscopic hysterectomy. Now, little more than 25 years later, in many parts of the country, a laparoscopic approach to hysterectomy is indeed the most common route. Over the years, with the evolution of instrumentation, including new energy systems (ultrasonic, advanced bipolar) and the introduction of barbed sutures, hysterectomy can now be performed via minilaparoscopy, single-site laparoscopy, robot-assisted, and robotic single site, all of which have been featured in the Ob.Gyn. News’ Master Class in Gynecologic Surgery.
But hysteroscopy came first
Abulkasim utilized a mirror to reflect light into the vaginal vault in 1,000 A.D. In 1806, Philipp Bozzini originated the idea of illuminating body cavities by an external light source. Through a system of mirrors and tubes, candlelight could be reflected into the body. In 1869, D.C. Pantaleoni used a cystoscope developed by Antoine Desormeaux – who has been called the father of endoscopy – to treat endometrial polyps with silver nitrate.
Through the 50 years of Ob.Gyn. News and over the past 12 years of the Master Class in Gynecologic Surgery, our community has been consistently updated as to advances in hysteroscopy, not only to enhance treatment efficacy, but safety as well. This has included such advances as the continuous flow hysteroscope, the Hamou contact hysteroscope, and fluid management systems to enhance visualization.
In 1978, Robert Neuwirth introduced loops to perform hysteroscopic myomectomy. The loop resectoscope was quickly followed by the rollerball to perform endometrial ablation. In the late 1990s, hysteroscopic bipolar cutting loops were introduced. This enabled use of ionic distension media saline, instead of nonionic media, thus decreasing risks related to hyponatremia.
In 2003, Mark Emanuel introduced hysteroscopic morcellation systems, which enabled more gynecologists to perform operative hysteroscopy safely. Resected tissue is removed immediately to allow superior visualization. The flexible hysteroscope coupled with vaginoscopy has enabled hysteroscopy to be done with minimal to no anesthesia in an in-office setting.
With advances in hysteroscopy over the past 35 years, hysteroscopic procedures such as polypectomy, myomectomy, lysis of adhesions, transection of endometriosis, evacuation of retained products of conception, and endometrial ablation/resection have become routine.
And now, the controversy
Since its inception, laparoscopic surgery has not been without controversy. In 1933, Karl Fervers described explosion and flashes of light from a combination of high frequency electric current and oxygen distension gas while performing laparoscopic adhesiolysis with the coagulation probe of the ureterocystoscope.
In the early 1970s, Professor Kurt Semm’s pioneering effort was not rewarded by his department, in Kiel, Germany, which instead recommended he schedule a brain scan and psychological testing.
Nearly 20 years later, in a 1992 edition of Current Science, Professor Semm, along with Alan DeCherney, stated that “over 80% of gynecological operations can now be performed by laparoscopy.” Shortly thereafter, however, Dr. Roy Pitkin, who at the time was president of the American College of Obstetricians and Gynecologists, wrote an editorial in the Journal of Obstetrics and Gynecology – “Operative Laparoscopy: Surgical Advance or Technical Gimmick?” (Obstet Gynecol. 1992 Mar;79[3]:441-2).
Fortunately, 18 years later, with the continued advances in laparoscopic surgery making it less expensive, safer, and more accessible, Dr. Pitkin did retract his statement (Obstet Gynecol. 2010 May;115[5]:890-1).
Currently, the gynecologic community is embroiled in controversies involving the use of the robot to assist in the performance of laparoscopic surgery, the incorporation of synthetic mesh to enhance urogynecologic procedures, the placement of Essure micro-inserts to occlude fallopian tubes, and the use of electronic power morcellation at time of laparoscopic or robot-assisted hysterectomy, myomectomy, or sacrocolpopexy.
After reading the 2013 article by Dr. Jason Wright, published in JAMA, comparing laparoscopic hysterectomy to robotic hysterectomy, no one can deny that the rise in a minimally invasive route to hysterectomy has coincided with the advent of the robot (JAMA. 2013 Feb 20;309[7]:689-98). On the other hand, many detractors, including Dr. James Breeden (past ACOG president 2012-2013), find the higher cost of robotic surgery very problematic. In fact, many of these detractors cite the paucity of data showing a significant advantage to use of robotics.
While certainly cost, more than ever, must be a major consideration, remember that during the 1990s, there were multiple articles in Ob.Gyn. News raising concerns about the cost of laparoscopic hysterectomy. Interestingly, studies over the past decade by Warren and Jonsdottir show a cost savings when hysterectomy is done laparoscopically as opposed to its being done by laparotomy. Thus, it certainly can be anticipated that with more physician experience, improved instrumentation, and robotic industry competition, the overall cost will become more comparable to a laparoscopic route.
In 1995, Ulf Ulmsten first described the use of tension-free tape (TVT) to treat stress urinary incontinence. In 1998, the Food and Drug Administration approved the use of the TVT sling in the United States. Since then, transobturator tension-free vaginal tape (TVT-O) and single incision mini-slings have been introduced. All of these techniques have been shown to be successful and have been well adapted into the armamentarium of physicians treating stress urinary incontinence.
With the success of synthetic mesh for the treatment of stress urinary incontinence, its use was extended to pelvic prolapse. In 2002, the first mesh device with indications for the treatment of pelvic organ prolapse was approved by the FDA. While the erosion rate utilizing synthetic mesh for stress urinary incontinence has been noted to be 2%, rates up to 8.3% have been noted in patients treated for pelvic prolapse.
In 2008, the FDA issued a warning regarding the use of mesh for prolapse and incontinence repair secondary to the sequelae of mesh erosion. Subsequently, in 2011, the concern was limited to vaginal mesh to correct pelvic organ prolapse. Finally, on Jan. 4, 2016, the FDA issued an order to reclassify surgical mesh to repair pelvic organ prolapse from class II, which includes moderate-risk devices, to class III, which includes high-risk devices. Moreover, the FDA issued a second order to manufacturers to submit a premarket approval application to support the safety and effectiveness of synthetic mesh for transvaginal repair of pelvic organ prolapse.
Essure micro-inserts for permanent birth control received initial approval from the FDA in November 2002. Despite the fact that Essure can be easily placed, is highly effective, and has seemingly low complication rates, concerns have been raised by the Facebook group “Essure Problems” and Erin Brockovich, the focus of the 2000 biographical film starring Julia Roberts.
After more than 5,000 women filed grievances with the FDA between November 2002 and May 2015, based on unintended pregnancies, miscarriages, stillbirths, severe pain, and bleeding, the FDA announced in 2016 that it would require a boxed warning label for Essure. The FDA also called upon Bayer, which makes and markets Essure, to conduct surveillance to assess “risks of the device in a real-world environment.” The agency stated it will use the results to “determine what, if any, further actions related to Essure are needed to protect public health.”
While Jan. 26, 1988, is a very special date in minimally invasive gynecologic surgery, April 17, 2014, is a day of infamy for the gynecologic laparoscopist. For on this day, the FDA announced a warning regarding electronic power morcellation. Many hospitals and hospital systems throughout the country issued bans on electronic power morcellation, leading to needless open laparotomy procedures and thus, introducing prolonged recovery times and increased risk.
At a time when the recent introduction of barbed suture had made both closure of the vaginal cuff at time of hysterectomy and repair of the hysterotomy at myomectomy easier and faster, the gynecologic laparoscopist was taking a step backward. The FDA based this decision and a subsequent boxed warning – issued in November 2014 – on a small number of studies showing potential upstaging of leiomyosarcoma post electronic power morcellation. Interestingly, many of the morcellation procedures cited did not use power morcellation. Furthermore, a more comprehensive meta-analysis by Elizabeth A. Pritts and colleagues, showed a far lower risk than suggested by the FDA (Gynecol Surg. 2015;12[3]:165-77).
Recently, an article by William Parker and colleagues recommended that the FDA reverse its position (Obstet Gynecol. 2016 Jan;127[1]:18-22). Many believe that ultimately, the solution will be morcellation in a containment bag, which I and my colleagues have been performing in virtually every power morcellation procedure since May 2014. During this current power morcellation controversy, the Master Class in Gynecologic Surgery has continued to update its readers with three different articles related to the subject.
And in conclusion
Without a doubt, the past 50 years of gynecologic surgery has been a time of unparalleled innovation with occasional controversy thrown in. Ob.Gyn. News and more recently, the Master Class in Gynecologic Surgery, has had a major leadership role in bringing this profound ingenuity to the gynecology community by introducing this explosion of surgical creativity to its readers.
And what will the next 50 years bring? I believe we will continue to see tremendous advancements in minimally invasive gynecologic surgery. There will be a definite impact of costs on the marketplace. Thus, many of the minor minimally invasive procedures currently performed in the hospital or surgery center will be brought into office settings. In addition, secondary to reimbursement, the more complex cases will be carried out by fewer gynecologic surgeons who have undergone more intense training in pelvic surgery and who can perform these cases more efficiently and with fewer complications. Our ability to perform surgery and what type of procedures we do will not only be based on randomized, controlled trials, but big data collection as well.
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, and past president of the AAGL and the International Society for Gynecologic Endoscopy (ISGE). He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.; director of minimally invasive gynecologic surgery and the director of the AAGL/Society of Reproductive Surgery fellowship in minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.; and the medical editor of this column, Master Class. Dr. Miller is a consultant and is on the speakers bureau for Ethicon.
Women reach for the top in ob.gyn.
Dr. Gloria E. Sarto was one of just six women in her medical school graduating class of 76 in 1958 – a time when many medical schools, she recalled, had quota systems for women and minorities. Later, she became the first female ob.gyn. resident at the University of Wisconsin–Madison.
“When I was interviewing for a residency position, the department chair told me ‘I’m going to treat you like one of the boys,’” the 86-year-old professor emeritus said. “And I said, ‘If you do that, it will be just fine.’”
Yet she still had to lobby sometimes for equal treatment – convincing the department chief in one instance that sleeping on a delivery table during hospital duty because there weren’t any rooms for women was not being treated “like one of the boys.” And she was often bothered by her observation that, in general, “the women [residents] weren’t noticed... they weren’t being recognized.”
Dr. Sarto has since chaired two ob.gyn. departments and was the first woman president of the American Gynecological and Obstetrical Society. Today, however, as she continues mentoring junior faculty and works to ensure the smooth succession of programs she founded, she sees a much different field – one in which women not only command more respect but where they make up a majority of ob.gyns.
Impact on women’s health
In 2014, 62% of all ob.gyns. were women (Obstet Gynecol. 2016 Jan;127[1]:148-52). The majority has been years in the making; more women than men have been entering the specialty since 1993. And if current trends continue, the percentage of women active in the specialty will only increase further. In 2010, women comprised more than 80% of all ob.gyn. residents/fellows, more than any other specialty, according to data from the Association of American Medical Colleges.
Such numerical strength is significant, but for Dr. Sarto and other leaders in the specialty who spoke about their experiences as female ob.gyns., it’s the impact that women physicians have had on women’s health that’s most important.
Dr. Sarto helped to start Lamaze classes in a hospital basement amidst widespread opposition from the male-dominated leadership and staff who felt that women didn’t need such help with labor. She also takes pride in her collaboration with Dr. Florence Haseltine, Phyllis Greenberger, and several other women to address biases in biomedical research. Their work with Congress led to a federal audit of National Institutes of Health policies and practices.
“We knew that when that report came out [in 1990], it would hit every newspaper in the country,” Dr. Sarto said. It just about did, and soon after that, the NIH Office of Research on Women’s Health was established to ensure that women were included in clinical trials and that gaps in knowledge of women’s health were addressed.
Dr. Barbara Levy, who left a private practice and two medical directorships in 2012 to become Vice President for Health Policy at the American College of Obstetricians and Gynecologists, recalls feeling early in her career that women’s health needed to be approached much more holistically.
“What I was seeing and experiencing didn’t match the textbooks,” she said. “The connection, for instance, between chronic pelvic pain and women who’d been victims of sexual abuse – there wasn’t anything in the literature. I’d see women with the same kinds of physical characteristics on their exams... and patients were willing to share with me things that they wouldn’t have been willing to share with my colleagues.”
Dr. Levy graduated from Princeton University in 1974 with the second class of admitted women, and after a year off, went west for medical school. She graduated in 1979 from the University of California, San Diego, with nine other women in a class of 110.
Her desire to care for the “whole patient” had her leaning toward family medicine until a beloved mentor, Dr. Donna Brooks, “reminded me that there were so few women to take care of women... and that as an ob.gyn. I could follow women through pregnancy, delivery, surgeries, hormone issues, and so many [other facets of their health].”
Dr. Levy, who served as president of the American Association of Gynecologic Laparoscopists in 1995, recalls a world “that was very tolerant of sexual harassment” and remembers the energy she needed to expend to be taken seriously and to correct unconscious bias.
When she applied for fellowship in the American College of Surgeons in the late 1980s, the committee members who conducted an interview “told me right away that I couldn’t expect to be a fellow if I hadn’t done my duty [serving on hospital committees],” Dr. Levy said.
“I told them I had volunteered for more than three committees every single year I’d been on staff, and had never been asked to serve,” she said. “They had no idea. Their assumption was that I had children at home and I wasn’t taking the time.”
Entering leadership
When it comes to leadership, a look at academic medicine suggests that women ob.gyns. have made significant strides. In 2013, compared with other major specialties, obstetrics and gynecology had the highest proportion of department leaders who were women. Yet the picture is mixed. According to an analysis published earlier in 2016, women in ob.gyn. and nine other major specialties “were not represented in the proportions in which they entered their fields” (Obstet Gynecol. 2016 Mar;127[3]:442-7).
Women comprised 57% of all faculty in departments of ob.gyn. in 2013. And, according to the analysis, they comprised 62% of ob.gyn. residency program directors, 30% of division directors, and 24% of department chairs.
The high numbers of women serving as residency program directors raises concern because such positions “do not result in advancement in the same way,” said Dr. Levy, adding that women have excelled in such positions and may desire them, but should be mentored early on about what tracks have the potential for upper-level leadership roles.
Dr. Maureen Phipps, who in 2013 was appointed as chair of ob.gyn. and assistant dean in the Warren Albert Medical School of Brown University in Providence, said she carries with her the fact that women are not yet proportionally represented at the upper levels. “I know that my being in this position and in other positions I’ve held is important for women to see,” she said.
Dr. Phipps graduated from the University of Vermont’s College of Medicine in 1994 as a part of a class in which men and women were fairly evenly represented. In addition to her role as department chair and assistant dean, she is also now chief of ob.gyn. at Women & Infants Hospital of Rhode Island, where she did her residency, and executive chief of ob.gyn for the Care New England Health System.
“I’ve had amazing male leaders and mentors in my career – the people who’ve gone to bat for me have been men,” said Dr. Phipps. Yet, “it’s important to have women in leadership... It’s known that we think differently and approach things differently. Having balance and a variety of different lenses will allow us to [further] grow the field.”
Gender pay gap
Both in academic medicine and in practice, a gender pay gap still reportedly affects women physicians across the board. Various reports and analyses have shown women earning disproportionately less than their male colleagues in similar positions.
Notably, a 2011 analysis in Health Affairs found a nearly $17,000 gap between the starting salaries for men and women physicians. This differential accounted for variables such as patient care hours, practice type, and location. It is possible, the study authors reported, that practices “may now be offering greater flexibility and family-friendly attributes that are more appealing but that come at the price of commensurately lower pay” (Health Aff. 2011:30;193-201).
The American Medical Women’s Association, which promotes advocacy on a gender pay gap, said in a statement about the study, however, that “gender discrimination still exists within the echelons of medicine, and gender stereotyping frequently leads to the devaluation of women physicians.”
From her perspective, Dr. Levy said it’s “complicated” to tease apart and understand all the factors that may be involved.
The challenges of balancing work and family/caregiving and are “still really tough” for women ob.gyns., she said, especially those who want to practice obstetrics. Dr. Levy said she gave up obstetrics when it became apparent that she and her husband would need to hire an additional child care provider.
While the hospitalist-laborist model has been a valuable addition to obstetrics, Dr. Phipps said, “it’s our challenge to continue to think creatively about how we can keep clinicians engaged when they’re in the earlier parts of their careers and challenged by family responsibilities and other commitments.”
Both she and Dr. Levy emphasized their concerns about burnout and their desire to keep career satisfaction high – especially now that women are such a big part of ob.gyn. – and both spoke of the importance of making time for whatever activities help women “recharge.”
“We should be doing what we’re doing because we love it,” Dr. Levy said. “We should focus on that every day. Our patients trust us. We need to remind ourselves of what incredible connections we have.”
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
Dr. Gloria E. Sarto was one of just six women in her medical school graduating class of 76 in 1958 – a time when many medical schools, she recalled, had quota systems for women and minorities. Later, she became the first female ob.gyn. resident at the University of Wisconsin–Madison.
“When I was interviewing for a residency position, the department chair told me ‘I’m going to treat you like one of the boys,’” the 86-year-old professor emeritus said. “And I said, ‘If you do that, it will be just fine.’”
Yet she still had to lobby sometimes for equal treatment – convincing the department chief in one instance that sleeping on a delivery table during hospital duty because there weren’t any rooms for women was not being treated “like one of the boys.” And she was often bothered by her observation that, in general, “the women [residents] weren’t noticed... they weren’t being recognized.”
Dr. Sarto has since chaired two ob.gyn. departments and was the first woman president of the American Gynecological and Obstetrical Society. Today, however, as she continues mentoring junior faculty and works to ensure the smooth succession of programs she founded, she sees a much different field – one in which women not only command more respect but where they make up a majority of ob.gyns.
Impact on women’s health
In 2014, 62% of all ob.gyns. were women (Obstet Gynecol. 2016 Jan;127[1]:148-52). The majority has been years in the making; more women than men have been entering the specialty since 1993. And if current trends continue, the percentage of women active in the specialty will only increase further. In 2010, women comprised more than 80% of all ob.gyn. residents/fellows, more than any other specialty, according to data from the Association of American Medical Colleges.
Such numerical strength is significant, but for Dr. Sarto and other leaders in the specialty who spoke about their experiences as female ob.gyns., it’s the impact that women physicians have had on women’s health that’s most important.
Dr. Sarto helped to start Lamaze classes in a hospital basement amidst widespread opposition from the male-dominated leadership and staff who felt that women didn’t need such help with labor. She also takes pride in her collaboration with Dr. Florence Haseltine, Phyllis Greenberger, and several other women to address biases in biomedical research. Their work with Congress led to a federal audit of National Institutes of Health policies and practices.
“We knew that when that report came out [in 1990], it would hit every newspaper in the country,” Dr. Sarto said. It just about did, and soon after that, the NIH Office of Research on Women’s Health was established to ensure that women were included in clinical trials and that gaps in knowledge of women’s health were addressed.
Dr. Barbara Levy, who left a private practice and two medical directorships in 2012 to become Vice President for Health Policy at the American College of Obstetricians and Gynecologists, recalls feeling early in her career that women’s health needed to be approached much more holistically.
“What I was seeing and experiencing didn’t match the textbooks,” she said. “The connection, for instance, between chronic pelvic pain and women who’d been victims of sexual abuse – there wasn’t anything in the literature. I’d see women with the same kinds of physical characteristics on their exams... and patients were willing to share with me things that they wouldn’t have been willing to share with my colleagues.”
Dr. Levy graduated from Princeton University in 1974 with the second class of admitted women, and after a year off, went west for medical school. She graduated in 1979 from the University of California, San Diego, with nine other women in a class of 110.
Her desire to care for the “whole patient” had her leaning toward family medicine until a beloved mentor, Dr. Donna Brooks, “reminded me that there were so few women to take care of women... and that as an ob.gyn. I could follow women through pregnancy, delivery, surgeries, hormone issues, and so many [other facets of their health].”
Dr. Levy, who served as president of the American Association of Gynecologic Laparoscopists in 1995, recalls a world “that was very tolerant of sexual harassment” and remembers the energy she needed to expend to be taken seriously and to correct unconscious bias.
When she applied for fellowship in the American College of Surgeons in the late 1980s, the committee members who conducted an interview “told me right away that I couldn’t expect to be a fellow if I hadn’t done my duty [serving on hospital committees],” Dr. Levy said.
“I told them I had volunteered for more than three committees every single year I’d been on staff, and had never been asked to serve,” she said. “They had no idea. Their assumption was that I had children at home and I wasn’t taking the time.”
Entering leadership
When it comes to leadership, a look at academic medicine suggests that women ob.gyns. have made significant strides. In 2013, compared with other major specialties, obstetrics and gynecology had the highest proportion of department leaders who were women. Yet the picture is mixed. According to an analysis published earlier in 2016, women in ob.gyn. and nine other major specialties “were not represented in the proportions in which they entered their fields” (Obstet Gynecol. 2016 Mar;127[3]:442-7).
Women comprised 57% of all faculty in departments of ob.gyn. in 2013. And, according to the analysis, they comprised 62% of ob.gyn. residency program directors, 30% of division directors, and 24% of department chairs.
The high numbers of women serving as residency program directors raises concern because such positions “do not result in advancement in the same way,” said Dr. Levy, adding that women have excelled in such positions and may desire them, but should be mentored early on about what tracks have the potential for upper-level leadership roles.
Dr. Maureen Phipps, who in 2013 was appointed as chair of ob.gyn. and assistant dean in the Warren Albert Medical School of Brown University in Providence, said she carries with her the fact that women are not yet proportionally represented at the upper levels. “I know that my being in this position and in other positions I’ve held is important for women to see,” she said.
Dr. Phipps graduated from the University of Vermont’s College of Medicine in 1994 as a part of a class in which men and women were fairly evenly represented. In addition to her role as department chair and assistant dean, she is also now chief of ob.gyn. at Women & Infants Hospital of Rhode Island, where she did her residency, and executive chief of ob.gyn for the Care New England Health System.
“I’ve had amazing male leaders and mentors in my career – the people who’ve gone to bat for me have been men,” said Dr. Phipps. Yet, “it’s important to have women in leadership... It’s known that we think differently and approach things differently. Having balance and a variety of different lenses will allow us to [further] grow the field.”
Gender pay gap
Both in academic medicine and in practice, a gender pay gap still reportedly affects women physicians across the board. Various reports and analyses have shown women earning disproportionately less than their male colleagues in similar positions.
Notably, a 2011 analysis in Health Affairs found a nearly $17,000 gap between the starting salaries for men and women physicians. This differential accounted for variables such as patient care hours, practice type, and location. It is possible, the study authors reported, that practices “may now be offering greater flexibility and family-friendly attributes that are more appealing but that come at the price of commensurately lower pay” (Health Aff. 2011:30;193-201).
The American Medical Women’s Association, which promotes advocacy on a gender pay gap, said in a statement about the study, however, that “gender discrimination still exists within the echelons of medicine, and gender stereotyping frequently leads to the devaluation of women physicians.”
From her perspective, Dr. Levy said it’s “complicated” to tease apart and understand all the factors that may be involved.
The challenges of balancing work and family/caregiving and are “still really tough” for women ob.gyns., she said, especially those who want to practice obstetrics. Dr. Levy said she gave up obstetrics when it became apparent that she and her husband would need to hire an additional child care provider.
While the hospitalist-laborist model has been a valuable addition to obstetrics, Dr. Phipps said, “it’s our challenge to continue to think creatively about how we can keep clinicians engaged when they’re in the earlier parts of their careers and challenged by family responsibilities and other commitments.”
Both she and Dr. Levy emphasized their concerns about burnout and their desire to keep career satisfaction high – especially now that women are such a big part of ob.gyn. – and both spoke of the importance of making time for whatever activities help women “recharge.”
“We should be doing what we’re doing because we love it,” Dr. Levy said. “We should focus on that every day. Our patients trust us. We need to remind ourselves of what incredible connections we have.”
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
Dr. Gloria E. Sarto was one of just six women in her medical school graduating class of 76 in 1958 – a time when many medical schools, she recalled, had quota systems for women and minorities. Later, she became the first female ob.gyn. resident at the University of Wisconsin–Madison.
“When I was interviewing for a residency position, the department chair told me ‘I’m going to treat you like one of the boys,’” the 86-year-old professor emeritus said. “And I said, ‘If you do that, it will be just fine.’”
Yet she still had to lobby sometimes for equal treatment – convincing the department chief in one instance that sleeping on a delivery table during hospital duty because there weren’t any rooms for women was not being treated “like one of the boys.” And she was often bothered by her observation that, in general, “the women [residents] weren’t noticed... they weren’t being recognized.”
Dr. Sarto has since chaired two ob.gyn. departments and was the first woman president of the American Gynecological and Obstetrical Society. Today, however, as she continues mentoring junior faculty and works to ensure the smooth succession of programs she founded, she sees a much different field – one in which women not only command more respect but where they make up a majority of ob.gyns.
Impact on women’s health
In 2014, 62% of all ob.gyns. were women (Obstet Gynecol. 2016 Jan;127[1]:148-52). The majority has been years in the making; more women than men have been entering the specialty since 1993. And if current trends continue, the percentage of women active in the specialty will only increase further. In 2010, women comprised more than 80% of all ob.gyn. residents/fellows, more than any other specialty, according to data from the Association of American Medical Colleges.
Such numerical strength is significant, but for Dr. Sarto and other leaders in the specialty who spoke about their experiences as female ob.gyns., it’s the impact that women physicians have had on women’s health that’s most important.
Dr. Sarto helped to start Lamaze classes in a hospital basement amidst widespread opposition from the male-dominated leadership and staff who felt that women didn’t need such help with labor. She also takes pride in her collaboration with Dr. Florence Haseltine, Phyllis Greenberger, and several other women to address biases in biomedical research. Their work with Congress led to a federal audit of National Institutes of Health policies and practices.
“We knew that when that report came out [in 1990], it would hit every newspaper in the country,” Dr. Sarto said. It just about did, and soon after that, the NIH Office of Research on Women’s Health was established to ensure that women were included in clinical trials and that gaps in knowledge of women’s health were addressed.
Dr. Barbara Levy, who left a private practice and two medical directorships in 2012 to become Vice President for Health Policy at the American College of Obstetricians and Gynecologists, recalls feeling early in her career that women’s health needed to be approached much more holistically.
“What I was seeing and experiencing didn’t match the textbooks,” she said. “The connection, for instance, between chronic pelvic pain and women who’d been victims of sexual abuse – there wasn’t anything in the literature. I’d see women with the same kinds of physical characteristics on their exams... and patients were willing to share with me things that they wouldn’t have been willing to share with my colleagues.”
Dr. Levy graduated from Princeton University in 1974 with the second class of admitted women, and after a year off, went west for medical school. She graduated in 1979 from the University of California, San Diego, with nine other women in a class of 110.
Her desire to care for the “whole patient” had her leaning toward family medicine until a beloved mentor, Dr. Donna Brooks, “reminded me that there were so few women to take care of women... and that as an ob.gyn. I could follow women through pregnancy, delivery, surgeries, hormone issues, and so many [other facets of their health].”
Dr. Levy, who served as president of the American Association of Gynecologic Laparoscopists in 1995, recalls a world “that was very tolerant of sexual harassment” and remembers the energy she needed to expend to be taken seriously and to correct unconscious bias.
When she applied for fellowship in the American College of Surgeons in the late 1980s, the committee members who conducted an interview “told me right away that I couldn’t expect to be a fellow if I hadn’t done my duty [serving on hospital committees],” Dr. Levy said.
“I told them I had volunteered for more than three committees every single year I’d been on staff, and had never been asked to serve,” she said. “They had no idea. Their assumption was that I had children at home and I wasn’t taking the time.”
Entering leadership
When it comes to leadership, a look at academic medicine suggests that women ob.gyns. have made significant strides. In 2013, compared with other major specialties, obstetrics and gynecology had the highest proportion of department leaders who were women. Yet the picture is mixed. According to an analysis published earlier in 2016, women in ob.gyn. and nine other major specialties “were not represented in the proportions in which they entered their fields” (Obstet Gynecol. 2016 Mar;127[3]:442-7).
Women comprised 57% of all faculty in departments of ob.gyn. in 2013. And, according to the analysis, they comprised 62% of ob.gyn. residency program directors, 30% of division directors, and 24% of department chairs.
The high numbers of women serving as residency program directors raises concern because such positions “do not result in advancement in the same way,” said Dr. Levy, adding that women have excelled in such positions and may desire them, but should be mentored early on about what tracks have the potential for upper-level leadership roles.
Dr. Maureen Phipps, who in 2013 was appointed as chair of ob.gyn. and assistant dean in the Warren Albert Medical School of Brown University in Providence, said she carries with her the fact that women are not yet proportionally represented at the upper levels. “I know that my being in this position and in other positions I’ve held is important for women to see,” she said.
Dr. Phipps graduated from the University of Vermont’s College of Medicine in 1994 as a part of a class in which men and women were fairly evenly represented. In addition to her role as department chair and assistant dean, she is also now chief of ob.gyn. at Women & Infants Hospital of Rhode Island, where she did her residency, and executive chief of ob.gyn for the Care New England Health System.
“I’ve had amazing male leaders and mentors in my career – the people who’ve gone to bat for me have been men,” said Dr. Phipps. Yet, “it’s important to have women in leadership... It’s known that we think differently and approach things differently. Having balance and a variety of different lenses will allow us to [further] grow the field.”
Gender pay gap
Both in academic medicine and in practice, a gender pay gap still reportedly affects women physicians across the board. Various reports and analyses have shown women earning disproportionately less than their male colleagues in similar positions.
Notably, a 2011 analysis in Health Affairs found a nearly $17,000 gap between the starting salaries for men and women physicians. This differential accounted for variables such as patient care hours, practice type, and location. It is possible, the study authors reported, that practices “may now be offering greater flexibility and family-friendly attributes that are more appealing but that come at the price of commensurately lower pay” (Health Aff. 2011:30;193-201).
The American Medical Women’s Association, which promotes advocacy on a gender pay gap, said in a statement about the study, however, that “gender discrimination still exists within the echelons of medicine, and gender stereotyping frequently leads to the devaluation of women physicians.”
From her perspective, Dr. Levy said it’s “complicated” to tease apart and understand all the factors that may be involved.
The challenges of balancing work and family/caregiving and are “still really tough” for women ob.gyns., she said, especially those who want to practice obstetrics. Dr. Levy said she gave up obstetrics when it became apparent that she and her husband would need to hire an additional child care provider.
While the hospitalist-laborist model has been a valuable addition to obstetrics, Dr. Phipps said, “it’s our challenge to continue to think creatively about how we can keep clinicians engaged when they’re in the earlier parts of their careers and challenged by family responsibilities and other commitments.”
Both she and Dr. Levy emphasized their concerns about burnout and their desire to keep career satisfaction high – especially now that women are such a big part of ob.gyn. – and both spoke of the importance of making time for whatever activities help women “recharge.”
“We should be doing what we’re doing because we love it,” Dr. Levy said. “We should focus on that every day. Our patients trust us. We need to remind ourselves of what incredible connections we have.”
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
Ob.gyn. residency changes with the times
In 1966, Dr. Charles Hammond was wrapping up a 2-year stint at the National Institutes of Health where he served at the behest of the military draft board. He had graduated from medical school just 5 years prior, and was in the middle of his ob.gyn. residency training at Duke University in Durham, N.C. when he was called to serve.
His experience wasn’t unusual for the time.
“When the draft board called, you went,” he said in an interview.
When he returned, he picked up where he left off. Residencies at that time were an “open-ended thing,” sometimes lasting 5 or 6 years, depending on staffing needs and other considerations.
Dr. Hammond, now an emeritus professor at Duke, regards his public service commission as an opportunity that advanced his academic career – despite the interruption of his residency training.
Such draft-related interruptions ended in the wake of the Vietnam War, of course, but the late 1960s and the 1970s ushered in a whole new era of changes in ob.gyn. residency training programs.
By 1968, residencies lasted 4 years, and fellowships were for 2 years. Ob.gyn. subspecialties hadn’t yet been introduced, explained Dr. Sandra A. Carson, vice president for education at the American College of Obstetricians and Gynecologists.
“That is essentially how things worked for a long time,” she said in an interview.
That’s not to say there weren’t numerous other changes taking place in the specialty. In a series of interviews with physicians and educators who discussed the myriad ways that residency training has evolved over the last 50 years, a number of themes emerged.
Women in medicine
A striking change over the past 5 decades has been the increasing number of women in medicine. Nowhere has that been in greater evidence than in obstetrics and gynecology.
“There were a few – but very few,” Dr. Hammond said of women in medicine in the 1960s.
There was “a philosophy that men did it better,” he said, adding, “That has been nicely shown to be inaccurate.”
Currently, about 80% of first-year ob.gyn. residents are women, compared with 15% in 1975.
“Maybe even 83% now,” Dr. Carson said, noting that even in the early 1980s when she was in training, women were “few and far between.”
According to a 2011 workforce report by Dr. William F. Rayburn, obstetrics and gynecology has the highest percentage of women residents of any medical specialty – 80% in 2009 versus an average of 46% for other specialties combined, and that figure has remained fairly constant.
Dr. Kasandra Scales, a fourth-year resident at the State University of New York, Syracuse, said she is glad to be part of this era of the specialty where women play an integral role in the advancement of women’s health care.
“I believe our voice and unique perspective to relate with common experiences, such as the physical birth of a child or personal choices in contraception... has enhanced our specialty,” she said.
That said, the fact that men are noticeably absent from the pool of ob.gyn. applicants and residents concerns her. “There should be a balance, she said. “I think it is important to have diversity of all types in the healthcare system.”
Dr. Hammond looked back on his days in residency training and recalled pockets of resistance to the increasing number of women in medicine, but the ultimate effect was good for the specialty, he said, explaining that the quality of the resident pool improved steadily, because the number of qualified candidates increased.
“It has been an interesting interval to watch,” he said, specifically mentioning the demands that women faced in terms of family obligations, childbirth, and childrearing.
Restrictions on work hours instituted in residency programs in more recent years may have played an important role in opening the door to more women, he said.
Work hours down, learning curve up
Dr. Carson agreed that work-hour restrictions instituted in 2003 and updated in 2011, which cap the work week at 80 hours and also apply limits on shift hours, likely encouraged more women to enter the field. One constant over the last 50 years is the biological clock, she said, explaining that the pressures and demands of residency before limits were put in place may have steered women away.
Work-hour restrictions provide more flexibility, but they aren’t without controversy.
Dr. Hammond said he sees the value in work hour restrictions, but working long hours as a resident – sometimes as many as 110 hours per week – had its benefits, too.
“I remember one time when I’d been on call for about 2 and a half days, and up and working the whole time,” Dr. Hammond said. “I left the hospital, walked out to a bench, sat down, and fell asleep. I woke up and distinctly remember thinking, ‘Why am I doing this?’ But I did do it, and that fatigue helped me with learning to endure. You learned from it.”
Not only have long hours been viewed as a rite of passage in medicine, he said, but there were concerns initially that the level of education would diminish and that the risk of patient errors would increase as patients were handed off from one shift to the next, he said.
Data on the effects of work-hour rules have been conflicting. In one study, Dr. Roger P. Smith found little overall effect on total technical experience among residents before and after the restrictions were put in place (there was no statistically significant difference in the average of median total cases in the 3 years before and after). Previous studies had documented increased costs and reduced faculty job satisfaction, while still others had shown no significant changes in 30-day readmission rates, in-hospital mortality, patient length of stay, or resident performance, he noted. “What is emerging is that both the great hopes and the great fears surrounding resident work-hour restrictions have not come to pass,” Dr. Smith wrote (Obstet Gynecol. 2010 Jun;115[6]:1166-71).
Dr. Scales, who is currently chair of the Junior Fellow District II Advisory Council for ACOG, comes down on the side of wishing for more hours.
“[The restrictions] do limit the things we can do and the exposure we may otherwise have,” she said, noting that it’s frustrating to have to leave when she’d rather stay and “see a cool case.”
“It’s a nice idea in principle, but the same amount of work has to be done. It’s not real life,” she said of work-hour restrictions. “It’s hard, at least for me, to want to give up my patients. Our job is to take in as much as you can before you leave to go out into the big bad world.”
It may be difficult to determine the actual impact of work hour limits on patient outcomes because the field of obstetrics and gynecology has changed so much over time.
Dr. David Forstein, vice chair of clinical operations in the department of obstetrics and gynecology at the University of South Carolina, Greenville, and a member of the Accreditation Council for Graduate Medical Education’s task force on work hours said that, for one thing, patients are generally sicker now than ever before, due in part to the obesity epidemic.
Further, changing trends mean that residents are getting less exposure to some procedures like operative vaginal deliveries, while also having to learn more ways to perform hysterectomy. Residents aren’t necessarily less prepared. They’re just having to work very hard because of the depth and breadth of the required knowledge has increased, Dr. Forstein said. “There’s a lot more to learn.”
Dr. Carson agreed that the approach to education has changed, and that those changes are largely a reflection of overall shifts in education and technology.
Technology trends
Every physician interviewed for this article cited laparoscopy and robotic surgery as key technological advances. Fifty years ago, the surgical tools were simpler, Dr. Carson said. Now residents must learn four approaches to hysterectomy: vaginal, abdominal, laparoscopic, and robotic-assisted laparoscopic hysterectomy.
From ultrasound and birth control to genetic screening and robotic surgery, the evolution of the field has been astounding during this time period. The effects of the birth control pill on family planning alone forced an expansion of curriculum not only to the physiology of these things, but also to the treatment of women as a whole person and often as part of a family unit, she said.
Many of the technologies have dramatically changed the landscape, both in terms of how learning is accomplished (for example, simulation), and how physicians interact with patients, Dr. Hammond agreed. With ultrasound, for example, there was a sense that part of the physician-patient relationship was lost.
“To a point, some of us old guys felt like they were doing ultrasound assessment of patients rather than the tried-and-true ‘talk to them and examine them’ [approach],” he said. “I guess whichever generation you are in seems to be the right one, but it’s probably somewhere in between.”
Residency in 2016
If Dr. Scales is any indication, concerns about the loss of a personal touch are unfounded. She says that for her, that’s what it’s all about.
“We were exposed to [technology] since we were 5 or 6 – it’s all we know,” she said of herself and her fellow residents. “It’s not a disadvantage. It’s about efficiency.”
“We have to get things done as quickly as possible and technology helps us with that,” said Dr. Scales, the daughter of a teacher and blue collar worker, who spent most of her life “surrounded by the underprivileged.”
She always desired to help lift that population up, and while she didn’t have a draft board directing her toward public service, she had her own calling of sorts. As a premed major in college, she worked with a nonprofit organization, and later she worked with Hurricane Katrina survivors.
“I liked that aspect of medicine. I wanted to be able to identify with people on an individual level,” she said.
Technology, work-hour restrictions, gender distribution – they’re just part of the journey.
“I’m glad I chose ob.gyn.,” she said. “Sometimes you go through ... reflection ... Am I ready? My answer is yes. I’m excited about the next step, I’m comfortable in the skill I learned in my residency program, I’m excited about the work I do every day, and I’m very excited about the next chapters.”
In 1966, Dr. Charles Hammond was wrapping up a 2-year stint at the National Institutes of Health where he served at the behest of the military draft board. He had graduated from medical school just 5 years prior, and was in the middle of his ob.gyn. residency training at Duke University in Durham, N.C. when he was called to serve.
His experience wasn’t unusual for the time.
“When the draft board called, you went,” he said in an interview.
When he returned, he picked up where he left off. Residencies at that time were an “open-ended thing,” sometimes lasting 5 or 6 years, depending on staffing needs and other considerations.
Dr. Hammond, now an emeritus professor at Duke, regards his public service commission as an opportunity that advanced his academic career – despite the interruption of his residency training.
Such draft-related interruptions ended in the wake of the Vietnam War, of course, but the late 1960s and the 1970s ushered in a whole new era of changes in ob.gyn. residency training programs.
By 1968, residencies lasted 4 years, and fellowships were for 2 years. Ob.gyn. subspecialties hadn’t yet been introduced, explained Dr. Sandra A. Carson, vice president for education at the American College of Obstetricians and Gynecologists.
“That is essentially how things worked for a long time,” she said in an interview.
That’s not to say there weren’t numerous other changes taking place in the specialty. In a series of interviews with physicians and educators who discussed the myriad ways that residency training has evolved over the last 50 years, a number of themes emerged.
Women in medicine
A striking change over the past 5 decades has been the increasing number of women in medicine. Nowhere has that been in greater evidence than in obstetrics and gynecology.
“There were a few – but very few,” Dr. Hammond said of women in medicine in the 1960s.
There was “a philosophy that men did it better,” he said, adding, “That has been nicely shown to be inaccurate.”
Currently, about 80% of first-year ob.gyn. residents are women, compared with 15% in 1975.
“Maybe even 83% now,” Dr. Carson said, noting that even in the early 1980s when she was in training, women were “few and far between.”
According to a 2011 workforce report by Dr. William F. Rayburn, obstetrics and gynecology has the highest percentage of women residents of any medical specialty – 80% in 2009 versus an average of 46% for other specialties combined, and that figure has remained fairly constant.
Dr. Kasandra Scales, a fourth-year resident at the State University of New York, Syracuse, said she is glad to be part of this era of the specialty where women play an integral role in the advancement of women’s health care.
“I believe our voice and unique perspective to relate with common experiences, such as the physical birth of a child or personal choices in contraception... has enhanced our specialty,” she said.
That said, the fact that men are noticeably absent from the pool of ob.gyn. applicants and residents concerns her. “There should be a balance, she said. “I think it is important to have diversity of all types in the healthcare system.”
Dr. Hammond looked back on his days in residency training and recalled pockets of resistance to the increasing number of women in medicine, but the ultimate effect was good for the specialty, he said, explaining that the quality of the resident pool improved steadily, because the number of qualified candidates increased.
“It has been an interesting interval to watch,” he said, specifically mentioning the demands that women faced in terms of family obligations, childbirth, and childrearing.
Restrictions on work hours instituted in residency programs in more recent years may have played an important role in opening the door to more women, he said.
Work hours down, learning curve up
Dr. Carson agreed that work-hour restrictions instituted in 2003 and updated in 2011, which cap the work week at 80 hours and also apply limits on shift hours, likely encouraged more women to enter the field. One constant over the last 50 years is the biological clock, she said, explaining that the pressures and demands of residency before limits were put in place may have steered women away.
Work-hour restrictions provide more flexibility, but they aren’t without controversy.
Dr. Hammond said he sees the value in work hour restrictions, but working long hours as a resident – sometimes as many as 110 hours per week – had its benefits, too.
“I remember one time when I’d been on call for about 2 and a half days, and up and working the whole time,” Dr. Hammond said. “I left the hospital, walked out to a bench, sat down, and fell asleep. I woke up and distinctly remember thinking, ‘Why am I doing this?’ But I did do it, and that fatigue helped me with learning to endure. You learned from it.”
Not only have long hours been viewed as a rite of passage in medicine, he said, but there were concerns initially that the level of education would diminish and that the risk of patient errors would increase as patients were handed off from one shift to the next, he said.
Data on the effects of work-hour rules have been conflicting. In one study, Dr. Roger P. Smith found little overall effect on total technical experience among residents before and after the restrictions were put in place (there was no statistically significant difference in the average of median total cases in the 3 years before and after). Previous studies had documented increased costs and reduced faculty job satisfaction, while still others had shown no significant changes in 30-day readmission rates, in-hospital mortality, patient length of stay, or resident performance, he noted. “What is emerging is that both the great hopes and the great fears surrounding resident work-hour restrictions have not come to pass,” Dr. Smith wrote (Obstet Gynecol. 2010 Jun;115[6]:1166-71).
Dr. Scales, who is currently chair of the Junior Fellow District II Advisory Council for ACOG, comes down on the side of wishing for more hours.
“[The restrictions] do limit the things we can do and the exposure we may otherwise have,” she said, noting that it’s frustrating to have to leave when she’d rather stay and “see a cool case.”
“It’s a nice idea in principle, but the same amount of work has to be done. It’s not real life,” she said of work-hour restrictions. “It’s hard, at least for me, to want to give up my patients. Our job is to take in as much as you can before you leave to go out into the big bad world.”
It may be difficult to determine the actual impact of work hour limits on patient outcomes because the field of obstetrics and gynecology has changed so much over time.
Dr. David Forstein, vice chair of clinical operations in the department of obstetrics and gynecology at the University of South Carolina, Greenville, and a member of the Accreditation Council for Graduate Medical Education’s task force on work hours said that, for one thing, patients are generally sicker now than ever before, due in part to the obesity epidemic.
Further, changing trends mean that residents are getting less exposure to some procedures like operative vaginal deliveries, while also having to learn more ways to perform hysterectomy. Residents aren’t necessarily less prepared. They’re just having to work very hard because of the depth and breadth of the required knowledge has increased, Dr. Forstein said. “There’s a lot more to learn.”
Dr. Carson agreed that the approach to education has changed, and that those changes are largely a reflection of overall shifts in education and technology.
Technology trends
Every physician interviewed for this article cited laparoscopy and robotic surgery as key technological advances. Fifty years ago, the surgical tools were simpler, Dr. Carson said. Now residents must learn four approaches to hysterectomy: vaginal, abdominal, laparoscopic, and robotic-assisted laparoscopic hysterectomy.
From ultrasound and birth control to genetic screening and robotic surgery, the evolution of the field has been astounding during this time period. The effects of the birth control pill on family planning alone forced an expansion of curriculum not only to the physiology of these things, but also to the treatment of women as a whole person and often as part of a family unit, she said.
Many of the technologies have dramatically changed the landscape, both in terms of how learning is accomplished (for example, simulation), and how physicians interact with patients, Dr. Hammond agreed. With ultrasound, for example, there was a sense that part of the physician-patient relationship was lost.
“To a point, some of us old guys felt like they were doing ultrasound assessment of patients rather than the tried-and-true ‘talk to them and examine them’ [approach],” he said. “I guess whichever generation you are in seems to be the right one, but it’s probably somewhere in between.”
Residency in 2016
If Dr. Scales is any indication, concerns about the loss of a personal touch are unfounded. She says that for her, that’s what it’s all about.
“We were exposed to [technology] since we were 5 or 6 – it’s all we know,” she said of herself and her fellow residents. “It’s not a disadvantage. It’s about efficiency.”
“We have to get things done as quickly as possible and technology helps us with that,” said Dr. Scales, the daughter of a teacher and blue collar worker, who spent most of her life “surrounded by the underprivileged.”
She always desired to help lift that population up, and while she didn’t have a draft board directing her toward public service, she had her own calling of sorts. As a premed major in college, she worked with a nonprofit organization, and later she worked with Hurricane Katrina survivors.
“I liked that aspect of medicine. I wanted to be able to identify with people on an individual level,” she said.
Technology, work-hour restrictions, gender distribution – they’re just part of the journey.
“I’m glad I chose ob.gyn.,” she said. “Sometimes you go through ... reflection ... Am I ready? My answer is yes. I’m excited about the next step, I’m comfortable in the skill I learned in my residency program, I’m excited about the work I do every day, and I’m very excited about the next chapters.”
In 1966, Dr. Charles Hammond was wrapping up a 2-year stint at the National Institutes of Health where he served at the behest of the military draft board. He had graduated from medical school just 5 years prior, and was in the middle of his ob.gyn. residency training at Duke University in Durham, N.C. when he was called to serve.
His experience wasn’t unusual for the time.
“When the draft board called, you went,” he said in an interview.
When he returned, he picked up where he left off. Residencies at that time were an “open-ended thing,” sometimes lasting 5 or 6 years, depending on staffing needs and other considerations.
Dr. Hammond, now an emeritus professor at Duke, regards his public service commission as an opportunity that advanced his academic career – despite the interruption of his residency training.
Such draft-related interruptions ended in the wake of the Vietnam War, of course, but the late 1960s and the 1970s ushered in a whole new era of changes in ob.gyn. residency training programs.
By 1968, residencies lasted 4 years, and fellowships were for 2 years. Ob.gyn. subspecialties hadn’t yet been introduced, explained Dr. Sandra A. Carson, vice president for education at the American College of Obstetricians and Gynecologists.
“That is essentially how things worked for a long time,” she said in an interview.
That’s not to say there weren’t numerous other changes taking place in the specialty. In a series of interviews with physicians and educators who discussed the myriad ways that residency training has evolved over the last 50 years, a number of themes emerged.
Women in medicine
A striking change over the past 5 decades has been the increasing number of women in medicine. Nowhere has that been in greater evidence than in obstetrics and gynecology.
“There were a few – but very few,” Dr. Hammond said of women in medicine in the 1960s.
There was “a philosophy that men did it better,” he said, adding, “That has been nicely shown to be inaccurate.”
Currently, about 80% of first-year ob.gyn. residents are women, compared with 15% in 1975.
“Maybe even 83% now,” Dr. Carson said, noting that even in the early 1980s when she was in training, women were “few and far between.”
According to a 2011 workforce report by Dr. William F. Rayburn, obstetrics and gynecology has the highest percentage of women residents of any medical specialty – 80% in 2009 versus an average of 46% for other specialties combined, and that figure has remained fairly constant.
Dr. Kasandra Scales, a fourth-year resident at the State University of New York, Syracuse, said she is glad to be part of this era of the specialty where women play an integral role in the advancement of women’s health care.
“I believe our voice and unique perspective to relate with common experiences, such as the physical birth of a child or personal choices in contraception... has enhanced our specialty,” she said.
That said, the fact that men are noticeably absent from the pool of ob.gyn. applicants and residents concerns her. “There should be a balance, she said. “I think it is important to have diversity of all types in the healthcare system.”
Dr. Hammond looked back on his days in residency training and recalled pockets of resistance to the increasing number of women in medicine, but the ultimate effect was good for the specialty, he said, explaining that the quality of the resident pool improved steadily, because the number of qualified candidates increased.
“It has been an interesting interval to watch,” he said, specifically mentioning the demands that women faced in terms of family obligations, childbirth, and childrearing.
Restrictions on work hours instituted in residency programs in more recent years may have played an important role in opening the door to more women, he said.
Work hours down, learning curve up
Dr. Carson agreed that work-hour restrictions instituted in 2003 and updated in 2011, which cap the work week at 80 hours and also apply limits on shift hours, likely encouraged more women to enter the field. One constant over the last 50 years is the biological clock, she said, explaining that the pressures and demands of residency before limits were put in place may have steered women away.
Work-hour restrictions provide more flexibility, but they aren’t without controversy.
Dr. Hammond said he sees the value in work hour restrictions, but working long hours as a resident – sometimes as many as 110 hours per week – had its benefits, too.
“I remember one time when I’d been on call for about 2 and a half days, and up and working the whole time,” Dr. Hammond said. “I left the hospital, walked out to a bench, sat down, and fell asleep. I woke up and distinctly remember thinking, ‘Why am I doing this?’ But I did do it, and that fatigue helped me with learning to endure. You learned from it.”
Not only have long hours been viewed as a rite of passage in medicine, he said, but there were concerns initially that the level of education would diminish and that the risk of patient errors would increase as patients were handed off from one shift to the next, he said.
Data on the effects of work-hour rules have been conflicting. In one study, Dr. Roger P. Smith found little overall effect on total technical experience among residents before and after the restrictions were put in place (there was no statistically significant difference in the average of median total cases in the 3 years before and after). Previous studies had documented increased costs and reduced faculty job satisfaction, while still others had shown no significant changes in 30-day readmission rates, in-hospital mortality, patient length of stay, or resident performance, he noted. “What is emerging is that both the great hopes and the great fears surrounding resident work-hour restrictions have not come to pass,” Dr. Smith wrote (Obstet Gynecol. 2010 Jun;115[6]:1166-71).
Dr. Scales, who is currently chair of the Junior Fellow District II Advisory Council for ACOG, comes down on the side of wishing for more hours.
“[The restrictions] do limit the things we can do and the exposure we may otherwise have,” she said, noting that it’s frustrating to have to leave when she’d rather stay and “see a cool case.”
“It’s a nice idea in principle, but the same amount of work has to be done. It’s not real life,” she said of work-hour restrictions. “It’s hard, at least for me, to want to give up my patients. Our job is to take in as much as you can before you leave to go out into the big bad world.”
It may be difficult to determine the actual impact of work hour limits on patient outcomes because the field of obstetrics and gynecology has changed so much over time.
Dr. David Forstein, vice chair of clinical operations in the department of obstetrics and gynecology at the University of South Carolina, Greenville, and a member of the Accreditation Council for Graduate Medical Education’s task force on work hours said that, for one thing, patients are generally sicker now than ever before, due in part to the obesity epidemic.
Further, changing trends mean that residents are getting less exposure to some procedures like operative vaginal deliveries, while also having to learn more ways to perform hysterectomy. Residents aren’t necessarily less prepared. They’re just having to work very hard because of the depth and breadth of the required knowledge has increased, Dr. Forstein said. “There’s a lot more to learn.”
Dr. Carson agreed that the approach to education has changed, and that those changes are largely a reflection of overall shifts in education and technology.
Technology trends
Every physician interviewed for this article cited laparoscopy and robotic surgery as key technological advances. Fifty years ago, the surgical tools were simpler, Dr. Carson said. Now residents must learn four approaches to hysterectomy: vaginal, abdominal, laparoscopic, and robotic-assisted laparoscopic hysterectomy.
From ultrasound and birth control to genetic screening and robotic surgery, the evolution of the field has been astounding during this time period. The effects of the birth control pill on family planning alone forced an expansion of curriculum not only to the physiology of these things, but also to the treatment of women as a whole person and often as part of a family unit, she said.
Many of the technologies have dramatically changed the landscape, both in terms of how learning is accomplished (for example, simulation), and how physicians interact with patients, Dr. Hammond agreed. With ultrasound, for example, there was a sense that part of the physician-patient relationship was lost.
“To a point, some of us old guys felt like they were doing ultrasound assessment of patients rather than the tried-and-true ‘talk to them and examine them’ [approach],” he said. “I guess whichever generation you are in seems to be the right one, but it’s probably somewhere in between.”
Residency in 2016
If Dr. Scales is any indication, concerns about the loss of a personal touch are unfounded. She says that for her, that’s what it’s all about.
“We were exposed to [technology] since we were 5 or 6 – it’s all we know,” she said of herself and her fellow residents. “It’s not a disadvantage. It’s about efficiency.”
“We have to get things done as quickly as possible and technology helps us with that,” said Dr. Scales, the daughter of a teacher and blue collar worker, who spent most of her life “surrounded by the underprivileged.”
She always desired to help lift that population up, and while she didn’t have a draft board directing her toward public service, she had her own calling of sorts. As a premed major in college, she worked with a nonprofit organization, and later she worked with Hurricane Katrina survivors.
“I liked that aspect of medicine. I wanted to be able to identify with people on an individual level,” she said.
Technology, work-hour restrictions, gender distribution – they’re just part of the journey.
“I’m glad I chose ob.gyn.,” she said. “Sometimes you go through ... reflection ... Am I ready? My answer is yes. I’m excited about the next step, I’m comfortable in the skill I learned in my residency program, I’m excited about the work I do every day, and I’m very excited about the next chapters.”
A trip through the history of gynecologic oncology
The subspecialty of gynecologic oncology was formalized less than 50 years ago with the creation of the Society of Gynecologic Oncology and subspecialty training and board certification. The formation of the Gynecologic Oncology Group (GOG) – and the many clinical trials spearheaded by that group – has further advanced evidence-based treatments, resulting in improved survival outcomes, quality of life, and preventive strategies.
While it is not possible to provide a comprehensive and exhaustive review of all of the advances, we hope to highlight many of the notable advances in this article.Cervical cancer
Cervical cancer is the fourth most common cancer in women worldwide with 528,000 new cases in 2012. The majority of cervical cancer cases are caused by infection with human papillomavirus (HPV). While the standard therapies for cervical cancer have been long established (radical hysterectomy for stage I and radiation therapy for locally advanced disease), one of the most significant advances in the past 50 years was the addition of radiation-sensitizing chemotherapy (cisplatin) administered concurrently with radiation therapy.
In randomized trials in both early and advanced cervical cancer, the risk of death was reduced by 30%-50%. These studies changed the paradigm for the treatment of cervical cancer (N Engl J Med. 1999 Apr 15;340[15]:1137-43; N Engl J Med. 1999 Apr 15;340[15]:1144-53; J Clin Oncol. 2000 Apr;18[8]:1606-13).
Future studies evaluating biologic adjuncts or additional chemotherapy are currently underway or awaiting data maturation.
The American Society of Clinical Oncology (ASCO) highlighted the “Top 5 advances in 50 years of Modern Oncology” in 2014, and second on the list was the approval of the HPV vaccine to prevent cervical cancer. Vaccines have been developed that can protect against types 2, 4 or 9 of HPV. In a 2014 study, depending on vaccination coverage, the relative number of cervical cancer cases avoided was 34% in Africa, 27% for America, 26% for Asia, 21% for Europe, and worldwide was estimated at 27% (Vaccine. 2014 Feb 3;32[6]:733-9).
While the benefit from HPV vaccination has been proven, in the United States, only about a third of eligible girls and women have been vaccinated. Efforts should focus on expanding vaccination penetration to eligible girls, boys, women, and men.
Endometrial cancer
Endometrial cancer is the most common gynecologic malignancy in the United States with an estimated 54,870 cases and 10,170 deaths annually. Notable advances in the management of women with endometrial cancer have arisen because of a better understanding that there are two types of endometrial cancer – type I and type II.
The type I endometrial cancers tend to be associated with lower stage of disease at the time of diagnosis and fewer recurrences, while type II endometrial cancer is associated with worse outcomes.
Tailoring the surgical approaches and adjuvant therapy for women with endometrial cancer has led to improved outcomes. The GOG conducted a large prospective randomized trial of laparotomy versus laparoscopic surgical staging for women with clinical early-stage endometrial cancer (LAP2). Laparoscopy was associated with improved perioperative outcomes and was found to be noninferior to laparotomy with regards to survival outcomes (J Clin Oncol. 2012 Mar 1;30[7]:695-700). Therefore, minimally invasive surgery has become widely accepted for the surgical staging of women with endometrial cancer.
Appropriate surgical staging allows for tailoring of postoperative adjuvant therapy. The current evidence suggests that vaginal brachytherapy should be the adjuvant treatment of choice over whole pelvic radiation in women with early-stage endometrial cancer (Lancet. 2010 Mar 6;375[9717]:816-23). Studies are underway to evaluate the role of both adjuvant radiation and chemotherapy in women with early-stage type II endometrial cancer who are felt to be at high risk for recurrent disease, as well as how to improve on the therapeutic options for women with advanced or recurrent disease.
Ovarian cancer
Epithelial ovarian cancer is the most deadly gynecologic malignancy in the United States with 21,290 cases and 14,180 deaths in 2015. The concept of ovarian tumor debulking was first described by Dr. Joe Meigs in 1934, but did not gain traction until the mid-1970s when Dr. C. Thomas Griffiths published his work (Natl Cancer Inst Monogr. 1975 Oct;42:101-4).
While there are no randomized trials proving that surgical cytoreduction improves overall survival, most retrospective studies support this concept. In 2009, Chi et al. showed improved median survival in women with ovarian cancer based on the increased percentage of women who underwent optimal cytoreduction (Gynecol Oncol. 2009 Jul;114[1]:26-31). This has led to modifications of surgical techniques and surgical goals with an effort to maximally cytoreduce all of the visible disease.
While initial surgical debulking is the goal, there are circumstances when a different approach may be indicated. Vergote et al. conducted a prospective randomized trial of 670 women with advanced ovarian cancer. In this study, neoadjuvant chemotherapy followed by interval debulking was not inferior to primary debulking followed by chemotherapy with regards to progression-free survival and overall survival. However, initial surgery was associated with increased surgical complications and perioperative mortality as compared with interval surgery. Therefore, in women who are not felt to be candidates for optimal cytoreduction, neoadjuvant chemotherapy followed by interval surgery may be an appropriate treatment strategy (N Engl J Med. 2010 Sep 2;363[10]:943-53.).
There have been several notable advances and a series of randomized trials – predominately conducted by the GOG – that have resulted in improved overall survival and progression-free interval in women with ovarian cancer. However, none are as significant as the discovery of paclitaxel and platinum-based chemotherapy (cisplatin and carboplatin).
In 1962, samples of the Pacific Yew’s bark were collected and, 2 years later, the extracts from this bark were found to have cytotoxic activity. There were initial difficulties suspending the drug in solution; however, ultimately a formulation in ethanol, cremophor, and saline was found to be effective. In 1984, the National Cancer Institute began clinical trials of paclitaxel and it was found to be highly effective in ovarian cancer. In 1992, it was approved for the treatment of ovarian cancer.
Cisplatin was approved in 1978. Carboplatin entered clinical trials in 1982 and was approved for women with recurrent ovarian cancer in 1989.
There were a series of trials beginning in the late 1980s that established the role of platinum agents and led us to GOG 111. This trial evaluated cisplatin with either cyclophosphamide or paclitaxel. The paclitaxel combination was superior and in 2003 two trials were published that solidified carboplatin and paclitaxel as the cornerstone in the treatment of women with ovarian cancer (J Clin Oncol. 2003 Sep 1;21[17]:3194-200; J Natl Cancer Inst. 2003 Sep 3;95[17]:1320-9).
What has most recently been debated is the route and schedule for both paclitaxel and the platinum agents. In January 2006, the National Cancer Institute released a Clinical Announcement regarding the role of intraperitoneal (IP) chemotherapy for the treatment of women with optimally debulked ovarian cancer. Of the six trials included in the announcement, four trials showed a benefit for progression-free survival and five studies showed an improvement in overall survival. Armstrong et al (GOG 172) showed a 16-month improvement in overall survival with intravenous (IV) paclitaxel, IP cisplatin, and IP paclitaxel. IP chemotherapy has not been universally embraced by physicians and patients in part because of its toxicity, treatment schedule, and the fact that no IP regimen has been compared with the current standard of IV carboplatin and paclitaxel (N Engl J Med. 2006 Jan 5;354[1]:34-43).
While there have been improvements in 5-year survival over time, most women with advanced ovarian cancer will undergo additional chemotherapy in order to achieve subsequent remissions or maintain stability of disease. Other drugs that have Food and Drug Administration approval in the setting of recurrent ovarian cancer include topotecan, liposomal doxorubicin, gemcitabine, bevacizumab, altretamine, carboplatin, cisplatin, cyclophosphamide, and melphalan. Olaparib was recently approved as monotherapy in women with a germline BRCA-mutation who had received three or more prior lines of chemotherapy.
Minimally invasive surgery
Over the last 30 years, minimally invasive surgery (MIS) in gynecologic oncology, particularly for endometrial cancer, has gone from a niche procedure to the standard of care. The introduction of laparoscopy into gynecologic oncology started in the early 1990s. In a series of 59 women undergoing laparoscopy for endometrial cancer, Childers et al. demonstrated feasibility of the technique and low laparotomy conversion rates (Gynecol Oncol. 1993 Oct;51[1]:33-8.). The GOG trial, LAP2, supported the equivalent oncologic outcomes of MIS versus laparotomy for the treatment of endometrial cancer. While many surgeons and centers offered laparoscopic surgery, there were issues with the learning curve that limited its widespread use.
In 2005, the FDA approval of the robotic platform for gynecologic surgery resulted in at least a doubling of the proportion of endometrial cancer patients treated with MIS (Int J Med Robot. 2009 Dec;5[4]:392-7.). In 2012, the Society of Gynecologic Oncology published a consensus statement regarding robotic-assisted surgery in gynecologic oncology (Gynecol Oncol. 2012 Feb;124[2]:180-4.). This review highlights the advantages of the robotics platform with regards to expanding MIS to women with cervical and ovarian cancer; the improvements in outcomes in the obese woman with endometrial cancer; and that the learning curve for robotic surgery is shorter than for traditional laparoscopy. Issues requiring further research include cost analysis as the cost of the new technology decreases, and opportunities for improvement in patient and physician quality of life.
Sentinel node mapping
The rationale for sentinel node mapping is that if one or more sentinel lymph nodes is/are negative for malignancy, then the other regional lymph nodes will also be negative. This would thereby avoid the need for a complete lymph node dissection and its resultant complications, including chronic lymphedema. Much of the work pioneering this strategy has been in breast cancer and melanoma, but data are rapidly emerging for these techniques in gynecologic malignancies.
Candidates for sentinel lymph node biopsy for vulvar cancer include those with a lesion more than 1mm in depth, a tumor less than 4 cm in size, and no obvious metastatic disease on exam or preoperative imaging. Additionally, recommendations have been made regarding case volume in order to achieve limited numbers of false-negative results and to maintain competency. In the study by Van der Zee et al. of 403 patients (623 groins) who underwent sentinel node procedures, the false-negative rate was 0-2%. The overall survival rate was 97% at 3 years (J Clin Oncol. 2008 Feb 20;26[6]:884-9). However, a more recent data from the Gynecologic Oncology Group (GOG 173) showed a slightly higher false-negative rate of 8% (J Clin Oncol. 2012 Nov 1;30[31]:3786-91). Overall survival data are pending from this study.
While sentinel lymph node mapping for endometrial cancer has been feasible for many years and has been well described, the questioned role of completed lymphadenectomy for early-stage endometrial cancer has led to a resurgence of interest in these techniques. While blue dye and radiolabeled tracer methods have historically been the most popular mapping solutions, the advent of endoscopic near-infrared imaging, with its higher sensitivity and good depth penetration, has added options. Indocyanine green fluorescence can be easily detected during robotic surgery and as experience with these techniques increase, successful mapping and sensitivity will increase.
Genetics
While hereditary cancer syndromes have been recognized for many years, detecting the genetic mutations that may increase an individual’s risk of developing a malignancy were not elucidated until the early 1990s. In gynecologic oncology, the most commonly encountered syndromes involve mutations in BRCA1 and BRCA2 and hereditary non–polyposis colorectal cancer, which causes mutations in DNA mismatch-repair genes and increase the risk of endometrial and ovarian cancer.
The SGO recently published a statement on risk assessment for inherited gynecologic cancer predispositions. In this statement “the evaluation for the presence of a hereditary cancer syndrome enables physicians to provide individualized and quantified assessment of cancer risk, as well as options for tailored screening and preventions strategies that may reduce morbidity associated with the development of malignancy” (Gynecol Oncol. 2015 Jan;136[1]:3-7). Beyond risk-reducing salpingo-oophorectomy, therapeutic strategies targeting patients with germline mutations have been developed (PARP inhibitors in BRCA-mutated women with ovarian cancer).
In August 2015, ASCO released an updated policy statement on genetic and genomic testing for cancer susceptibility and highlighted five key areas: germ-line implications of somatic mutation profiling; multigene panel testing for cancer susceptibility; quality assurance in genetic testing; education for oncology professionals; and access to cancer genetic services.
Antiemetics
Rounding out ASCO’s “Top 5 advances in 50 years of Modern Oncology” was the improvement in patients’ quality of life from supportive therapies, in particular antinausea medications.
Several of the agents commonly used in gynecologic oncology rate high (cisplatin) to moderate (carboplatin, cyclophosphamide, doxorubicin, ifosfamide) with regards to emetogenicity. The advent of 5-HT3 receptor antagonists (for example, ondansetron) has significantly improved the quality of life of patients undergoing cytotoxic chemotherapy. In addition to improving quality of life, the decrease in nausea and vomiting can also decrease life-threatening complications such as dehydration and electrolyte imbalance. Both ASCO and the National Comprehensive Cancer Network both have guidelines for the management of nausea and vomiting in patients undergoing chemotherapy.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina, Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology, and a professor in the division of gynecologic oncology at UNC. They reported having no relevant financial disclosures.
The subspecialty of gynecologic oncology was formalized less than 50 years ago with the creation of the Society of Gynecologic Oncology and subspecialty training and board certification. The formation of the Gynecologic Oncology Group (GOG) – and the many clinical trials spearheaded by that group – has further advanced evidence-based treatments, resulting in improved survival outcomes, quality of life, and preventive strategies.
While it is not possible to provide a comprehensive and exhaustive review of all of the advances, we hope to highlight many of the notable advances in this article.Cervical cancer
Cervical cancer is the fourth most common cancer in women worldwide with 528,000 new cases in 2012. The majority of cervical cancer cases are caused by infection with human papillomavirus (HPV). While the standard therapies for cervical cancer have been long established (radical hysterectomy for stage I and radiation therapy for locally advanced disease), one of the most significant advances in the past 50 years was the addition of radiation-sensitizing chemotherapy (cisplatin) administered concurrently with radiation therapy.
In randomized trials in both early and advanced cervical cancer, the risk of death was reduced by 30%-50%. These studies changed the paradigm for the treatment of cervical cancer (N Engl J Med. 1999 Apr 15;340[15]:1137-43; N Engl J Med. 1999 Apr 15;340[15]:1144-53; J Clin Oncol. 2000 Apr;18[8]:1606-13).
Future studies evaluating biologic adjuncts or additional chemotherapy are currently underway or awaiting data maturation.
The American Society of Clinical Oncology (ASCO) highlighted the “Top 5 advances in 50 years of Modern Oncology” in 2014, and second on the list was the approval of the HPV vaccine to prevent cervical cancer. Vaccines have been developed that can protect against types 2, 4 or 9 of HPV. In a 2014 study, depending on vaccination coverage, the relative number of cervical cancer cases avoided was 34% in Africa, 27% for America, 26% for Asia, 21% for Europe, and worldwide was estimated at 27% (Vaccine. 2014 Feb 3;32[6]:733-9).
While the benefit from HPV vaccination has been proven, in the United States, only about a third of eligible girls and women have been vaccinated. Efforts should focus on expanding vaccination penetration to eligible girls, boys, women, and men.
Endometrial cancer
Endometrial cancer is the most common gynecologic malignancy in the United States with an estimated 54,870 cases and 10,170 deaths annually. Notable advances in the management of women with endometrial cancer have arisen because of a better understanding that there are two types of endometrial cancer – type I and type II.
The type I endometrial cancers tend to be associated with lower stage of disease at the time of diagnosis and fewer recurrences, while type II endometrial cancer is associated with worse outcomes.
Tailoring the surgical approaches and adjuvant therapy for women with endometrial cancer has led to improved outcomes. The GOG conducted a large prospective randomized trial of laparotomy versus laparoscopic surgical staging for women with clinical early-stage endometrial cancer (LAP2). Laparoscopy was associated with improved perioperative outcomes and was found to be noninferior to laparotomy with regards to survival outcomes (J Clin Oncol. 2012 Mar 1;30[7]:695-700). Therefore, minimally invasive surgery has become widely accepted for the surgical staging of women with endometrial cancer.
Appropriate surgical staging allows for tailoring of postoperative adjuvant therapy. The current evidence suggests that vaginal brachytherapy should be the adjuvant treatment of choice over whole pelvic radiation in women with early-stage endometrial cancer (Lancet. 2010 Mar 6;375[9717]:816-23). Studies are underway to evaluate the role of both adjuvant radiation and chemotherapy in women with early-stage type II endometrial cancer who are felt to be at high risk for recurrent disease, as well as how to improve on the therapeutic options for women with advanced or recurrent disease.
Ovarian cancer
Epithelial ovarian cancer is the most deadly gynecologic malignancy in the United States with 21,290 cases and 14,180 deaths in 2015. The concept of ovarian tumor debulking was first described by Dr. Joe Meigs in 1934, but did not gain traction until the mid-1970s when Dr. C. Thomas Griffiths published his work (Natl Cancer Inst Monogr. 1975 Oct;42:101-4).
While there are no randomized trials proving that surgical cytoreduction improves overall survival, most retrospective studies support this concept. In 2009, Chi et al. showed improved median survival in women with ovarian cancer based on the increased percentage of women who underwent optimal cytoreduction (Gynecol Oncol. 2009 Jul;114[1]:26-31). This has led to modifications of surgical techniques and surgical goals with an effort to maximally cytoreduce all of the visible disease.
While initial surgical debulking is the goal, there are circumstances when a different approach may be indicated. Vergote et al. conducted a prospective randomized trial of 670 women with advanced ovarian cancer. In this study, neoadjuvant chemotherapy followed by interval debulking was not inferior to primary debulking followed by chemotherapy with regards to progression-free survival and overall survival. However, initial surgery was associated with increased surgical complications and perioperative mortality as compared with interval surgery. Therefore, in women who are not felt to be candidates for optimal cytoreduction, neoadjuvant chemotherapy followed by interval surgery may be an appropriate treatment strategy (N Engl J Med. 2010 Sep 2;363[10]:943-53.).
There have been several notable advances and a series of randomized trials – predominately conducted by the GOG – that have resulted in improved overall survival and progression-free interval in women with ovarian cancer. However, none are as significant as the discovery of paclitaxel and platinum-based chemotherapy (cisplatin and carboplatin).
In 1962, samples of the Pacific Yew’s bark were collected and, 2 years later, the extracts from this bark were found to have cytotoxic activity. There were initial difficulties suspending the drug in solution; however, ultimately a formulation in ethanol, cremophor, and saline was found to be effective. In 1984, the National Cancer Institute began clinical trials of paclitaxel and it was found to be highly effective in ovarian cancer. In 1992, it was approved for the treatment of ovarian cancer.
Cisplatin was approved in 1978. Carboplatin entered clinical trials in 1982 and was approved for women with recurrent ovarian cancer in 1989.
There were a series of trials beginning in the late 1980s that established the role of platinum agents and led us to GOG 111. This trial evaluated cisplatin with either cyclophosphamide or paclitaxel. The paclitaxel combination was superior and in 2003 two trials were published that solidified carboplatin and paclitaxel as the cornerstone in the treatment of women with ovarian cancer (J Clin Oncol. 2003 Sep 1;21[17]:3194-200; J Natl Cancer Inst. 2003 Sep 3;95[17]:1320-9).
What has most recently been debated is the route and schedule for both paclitaxel and the platinum agents. In January 2006, the National Cancer Institute released a Clinical Announcement regarding the role of intraperitoneal (IP) chemotherapy for the treatment of women with optimally debulked ovarian cancer. Of the six trials included in the announcement, four trials showed a benefit for progression-free survival and five studies showed an improvement in overall survival. Armstrong et al (GOG 172) showed a 16-month improvement in overall survival with intravenous (IV) paclitaxel, IP cisplatin, and IP paclitaxel. IP chemotherapy has not been universally embraced by physicians and patients in part because of its toxicity, treatment schedule, and the fact that no IP regimen has been compared with the current standard of IV carboplatin and paclitaxel (N Engl J Med. 2006 Jan 5;354[1]:34-43).
While there have been improvements in 5-year survival over time, most women with advanced ovarian cancer will undergo additional chemotherapy in order to achieve subsequent remissions or maintain stability of disease. Other drugs that have Food and Drug Administration approval in the setting of recurrent ovarian cancer include topotecan, liposomal doxorubicin, gemcitabine, bevacizumab, altretamine, carboplatin, cisplatin, cyclophosphamide, and melphalan. Olaparib was recently approved as monotherapy in women with a germline BRCA-mutation who had received three or more prior lines of chemotherapy.
Minimally invasive surgery
Over the last 30 years, minimally invasive surgery (MIS) in gynecologic oncology, particularly for endometrial cancer, has gone from a niche procedure to the standard of care. The introduction of laparoscopy into gynecologic oncology started in the early 1990s. In a series of 59 women undergoing laparoscopy for endometrial cancer, Childers et al. demonstrated feasibility of the technique and low laparotomy conversion rates (Gynecol Oncol. 1993 Oct;51[1]:33-8.). The GOG trial, LAP2, supported the equivalent oncologic outcomes of MIS versus laparotomy for the treatment of endometrial cancer. While many surgeons and centers offered laparoscopic surgery, there were issues with the learning curve that limited its widespread use.
In 2005, the FDA approval of the robotic platform for gynecologic surgery resulted in at least a doubling of the proportion of endometrial cancer patients treated with MIS (Int J Med Robot. 2009 Dec;5[4]:392-7.). In 2012, the Society of Gynecologic Oncology published a consensus statement regarding robotic-assisted surgery in gynecologic oncology (Gynecol Oncol. 2012 Feb;124[2]:180-4.). This review highlights the advantages of the robotics platform with regards to expanding MIS to women with cervical and ovarian cancer; the improvements in outcomes in the obese woman with endometrial cancer; and that the learning curve for robotic surgery is shorter than for traditional laparoscopy. Issues requiring further research include cost analysis as the cost of the new technology decreases, and opportunities for improvement in patient and physician quality of life.
Sentinel node mapping
The rationale for sentinel node mapping is that if one or more sentinel lymph nodes is/are negative for malignancy, then the other regional lymph nodes will also be negative. This would thereby avoid the need for a complete lymph node dissection and its resultant complications, including chronic lymphedema. Much of the work pioneering this strategy has been in breast cancer and melanoma, but data are rapidly emerging for these techniques in gynecologic malignancies.
Candidates for sentinel lymph node biopsy for vulvar cancer include those with a lesion more than 1mm in depth, a tumor less than 4 cm in size, and no obvious metastatic disease on exam or preoperative imaging. Additionally, recommendations have been made regarding case volume in order to achieve limited numbers of false-negative results and to maintain competency. In the study by Van der Zee et al. of 403 patients (623 groins) who underwent sentinel node procedures, the false-negative rate was 0-2%. The overall survival rate was 97% at 3 years (J Clin Oncol. 2008 Feb 20;26[6]:884-9). However, a more recent data from the Gynecologic Oncology Group (GOG 173) showed a slightly higher false-negative rate of 8% (J Clin Oncol. 2012 Nov 1;30[31]:3786-91). Overall survival data are pending from this study.
While sentinel lymph node mapping for endometrial cancer has been feasible for many years and has been well described, the questioned role of completed lymphadenectomy for early-stage endometrial cancer has led to a resurgence of interest in these techniques. While blue dye and radiolabeled tracer methods have historically been the most popular mapping solutions, the advent of endoscopic near-infrared imaging, with its higher sensitivity and good depth penetration, has added options. Indocyanine green fluorescence can be easily detected during robotic surgery and as experience with these techniques increase, successful mapping and sensitivity will increase.
Genetics
While hereditary cancer syndromes have been recognized for many years, detecting the genetic mutations that may increase an individual’s risk of developing a malignancy were not elucidated until the early 1990s. In gynecologic oncology, the most commonly encountered syndromes involve mutations in BRCA1 and BRCA2 and hereditary non–polyposis colorectal cancer, which causes mutations in DNA mismatch-repair genes and increase the risk of endometrial and ovarian cancer.
The SGO recently published a statement on risk assessment for inherited gynecologic cancer predispositions. In this statement “the evaluation for the presence of a hereditary cancer syndrome enables physicians to provide individualized and quantified assessment of cancer risk, as well as options for tailored screening and preventions strategies that may reduce morbidity associated with the development of malignancy” (Gynecol Oncol. 2015 Jan;136[1]:3-7). Beyond risk-reducing salpingo-oophorectomy, therapeutic strategies targeting patients with germline mutations have been developed (PARP inhibitors in BRCA-mutated women with ovarian cancer).
In August 2015, ASCO released an updated policy statement on genetic and genomic testing for cancer susceptibility and highlighted five key areas: germ-line implications of somatic mutation profiling; multigene panel testing for cancer susceptibility; quality assurance in genetic testing; education for oncology professionals; and access to cancer genetic services.
Antiemetics
Rounding out ASCO’s “Top 5 advances in 50 years of Modern Oncology” was the improvement in patients’ quality of life from supportive therapies, in particular antinausea medications.
Several of the agents commonly used in gynecologic oncology rate high (cisplatin) to moderate (carboplatin, cyclophosphamide, doxorubicin, ifosfamide) with regards to emetogenicity. The advent of 5-HT3 receptor antagonists (for example, ondansetron) has significantly improved the quality of life of patients undergoing cytotoxic chemotherapy. In addition to improving quality of life, the decrease in nausea and vomiting can also decrease life-threatening complications such as dehydration and electrolyte imbalance. Both ASCO and the National Comprehensive Cancer Network both have guidelines for the management of nausea and vomiting in patients undergoing chemotherapy.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina, Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology, and a professor in the division of gynecologic oncology at UNC. They reported having no relevant financial disclosures.
The subspecialty of gynecologic oncology was formalized less than 50 years ago with the creation of the Society of Gynecologic Oncology and subspecialty training and board certification. The formation of the Gynecologic Oncology Group (GOG) – and the many clinical trials spearheaded by that group – has further advanced evidence-based treatments, resulting in improved survival outcomes, quality of life, and preventive strategies.
While it is not possible to provide a comprehensive and exhaustive review of all of the advances, we hope to highlight many of the notable advances in this article.Cervical cancer
Cervical cancer is the fourth most common cancer in women worldwide with 528,000 new cases in 2012. The majority of cervical cancer cases are caused by infection with human papillomavirus (HPV). While the standard therapies for cervical cancer have been long established (radical hysterectomy for stage I and radiation therapy for locally advanced disease), one of the most significant advances in the past 50 years was the addition of radiation-sensitizing chemotherapy (cisplatin) administered concurrently with radiation therapy.
In randomized trials in both early and advanced cervical cancer, the risk of death was reduced by 30%-50%. These studies changed the paradigm for the treatment of cervical cancer (N Engl J Med. 1999 Apr 15;340[15]:1137-43; N Engl J Med. 1999 Apr 15;340[15]:1144-53; J Clin Oncol. 2000 Apr;18[8]:1606-13).
Future studies evaluating biologic adjuncts or additional chemotherapy are currently underway or awaiting data maturation.
The American Society of Clinical Oncology (ASCO) highlighted the “Top 5 advances in 50 years of Modern Oncology” in 2014, and second on the list was the approval of the HPV vaccine to prevent cervical cancer. Vaccines have been developed that can protect against types 2, 4 or 9 of HPV. In a 2014 study, depending on vaccination coverage, the relative number of cervical cancer cases avoided was 34% in Africa, 27% for America, 26% for Asia, 21% for Europe, and worldwide was estimated at 27% (Vaccine. 2014 Feb 3;32[6]:733-9).
While the benefit from HPV vaccination has been proven, in the United States, only about a third of eligible girls and women have been vaccinated. Efforts should focus on expanding vaccination penetration to eligible girls, boys, women, and men.
Endometrial cancer
Endometrial cancer is the most common gynecologic malignancy in the United States with an estimated 54,870 cases and 10,170 deaths annually. Notable advances in the management of women with endometrial cancer have arisen because of a better understanding that there are two types of endometrial cancer – type I and type II.
The type I endometrial cancers tend to be associated with lower stage of disease at the time of diagnosis and fewer recurrences, while type II endometrial cancer is associated with worse outcomes.
Tailoring the surgical approaches and adjuvant therapy for women with endometrial cancer has led to improved outcomes. The GOG conducted a large prospective randomized trial of laparotomy versus laparoscopic surgical staging for women with clinical early-stage endometrial cancer (LAP2). Laparoscopy was associated with improved perioperative outcomes and was found to be noninferior to laparotomy with regards to survival outcomes (J Clin Oncol. 2012 Mar 1;30[7]:695-700). Therefore, minimally invasive surgery has become widely accepted for the surgical staging of women with endometrial cancer.
Appropriate surgical staging allows for tailoring of postoperative adjuvant therapy. The current evidence suggests that vaginal brachytherapy should be the adjuvant treatment of choice over whole pelvic radiation in women with early-stage endometrial cancer (Lancet. 2010 Mar 6;375[9717]:816-23). Studies are underway to evaluate the role of both adjuvant radiation and chemotherapy in women with early-stage type II endometrial cancer who are felt to be at high risk for recurrent disease, as well as how to improve on the therapeutic options for women with advanced or recurrent disease.
Ovarian cancer
Epithelial ovarian cancer is the most deadly gynecologic malignancy in the United States with 21,290 cases and 14,180 deaths in 2015. The concept of ovarian tumor debulking was first described by Dr. Joe Meigs in 1934, but did not gain traction until the mid-1970s when Dr. C. Thomas Griffiths published his work (Natl Cancer Inst Monogr. 1975 Oct;42:101-4).
While there are no randomized trials proving that surgical cytoreduction improves overall survival, most retrospective studies support this concept. In 2009, Chi et al. showed improved median survival in women with ovarian cancer based on the increased percentage of women who underwent optimal cytoreduction (Gynecol Oncol. 2009 Jul;114[1]:26-31). This has led to modifications of surgical techniques and surgical goals with an effort to maximally cytoreduce all of the visible disease.
While initial surgical debulking is the goal, there are circumstances when a different approach may be indicated. Vergote et al. conducted a prospective randomized trial of 670 women with advanced ovarian cancer. In this study, neoadjuvant chemotherapy followed by interval debulking was not inferior to primary debulking followed by chemotherapy with regards to progression-free survival and overall survival. However, initial surgery was associated with increased surgical complications and perioperative mortality as compared with interval surgery. Therefore, in women who are not felt to be candidates for optimal cytoreduction, neoadjuvant chemotherapy followed by interval surgery may be an appropriate treatment strategy (N Engl J Med. 2010 Sep 2;363[10]:943-53.).
There have been several notable advances and a series of randomized trials – predominately conducted by the GOG – that have resulted in improved overall survival and progression-free interval in women with ovarian cancer. However, none are as significant as the discovery of paclitaxel and platinum-based chemotherapy (cisplatin and carboplatin).
In 1962, samples of the Pacific Yew’s bark were collected and, 2 years later, the extracts from this bark were found to have cytotoxic activity. There were initial difficulties suspending the drug in solution; however, ultimately a formulation in ethanol, cremophor, and saline was found to be effective. In 1984, the National Cancer Institute began clinical trials of paclitaxel and it was found to be highly effective in ovarian cancer. In 1992, it was approved for the treatment of ovarian cancer.
Cisplatin was approved in 1978. Carboplatin entered clinical trials in 1982 and was approved for women with recurrent ovarian cancer in 1989.
There were a series of trials beginning in the late 1980s that established the role of platinum agents and led us to GOG 111. This trial evaluated cisplatin with either cyclophosphamide or paclitaxel. The paclitaxel combination was superior and in 2003 two trials were published that solidified carboplatin and paclitaxel as the cornerstone in the treatment of women with ovarian cancer (J Clin Oncol. 2003 Sep 1;21[17]:3194-200; J Natl Cancer Inst. 2003 Sep 3;95[17]:1320-9).
What has most recently been debated is the route and schedule for both paclitaxel and the platinum agents. In January 2006, the National Cancer Institute released a Clinical Announcement regarding the role of intraperitoneal (IP) chemotherapy for the treatment of women with optimally debulked ovarian cancer. Of the six trials included in the announcement, four trials showed a benefit for progression-free survival and five studies showed an improvement in overall survival. Armstrong et al (GOG 172) showed a 16-month improvement in overall survival with intravenous (IV) paclitaxel, IP cisplatin, and IP paclitaxel. IP chemotherapy has not been universally embraced by physicians and patients in part because of its toxicity, treatment schedule, and the fact that no IP regimen has been compared with the current standard of IV carboplatin and paclitaxel (N Engl J Med. 2006 Jan 5;354[1]:34-43).
While there have been improvements in 5-year survival over time, most women with advanced ovarian cancer will undergo additional chemotherapy in order to achieve subsequent remissions or maintain stability of disease. Other drugs that have Food and Drug Administration approval in the setting of recurrent ovarian cancer include topotecan, liposomal doxorubicin, gemcitabine, bevacizumab, altretamine, carboplatin, cisplatin, cyclophosphamide, and melphalan. Olaparib was recently approved as monotherapy in women with a germline BRCA-mutation who had received three or more prior lines of chemotherapy.
Minimally invasive surgery
Over the last 30 years, minimally invasive surgery (MIS) in gynecologic oncology, particularly for endometrial cancer, has gone from a niche procedure to the standard of care. The introduction of laparoscopy into gynecologic oncology started in the early 1990s. In a series of 59 women undergoing laparoscopy for endometrial cancer, Childers et al. demonstrated feasibility of the technique and low laparotomy conversion rates (Gynecol Oncol. 1993 Oct;51[1]:33-8.). The GOG trial, LAP2, supported the equivalent oncologic outcomes of MIS versus laparotomy for the treatment of endometrial cancer. While many surgeons and centers offered laparoscopic surgery, there were issues with the learning curve that limited its widespread use.
In 2005, the FDA approval of the robotic platform for gynecologic surgery resulted in at least a doubling of the proportion of endometrial cancer patients treated with MIS (Int J Med Robot. 2009 Dec;5[4]:392-7.). In 2012, the Society of Gynecologic Oncology published a consensus statement regarding robotic-assisted surgery in gynecologic oncology (Gynecol Oncol. 2012 Feb;124[2]:180-4.). This review highlights the advantages of the robotics platform with regards to expanding MIS to women with cervical and ovarian cancer; the improvements in outcomes in the obese woman with endometrial cancer; and that the learning curve for robotic surgery is shorter than for traditional laparoscopy. Issues requiring further research include cost analysis as the cost of the new technology decreases, and opportunities for improvement in patient and physician quality of life.
Sentinel node mapping
The rationale for sentinel node mapping is that if one or more sentinel lymph nodes is/are negative for malignancy, then the other regional lymph nodes will also be negative. This would thereby avoid the need for a complete lymph node dissection and its resultant complications, including chronic lymphedema. Much of the work pioneering this strategy has been in breast cancer and melanoma, but data are rapidly emerging for these techniques in gynecologic malignancies.
Candidates for sentinel lymph node biopsy for vulvar cancer include those with a lesion more than 1mm in depth, a tumor less than 4 cm in size, and no obvious metastatic disease on exam or preoperative imaging. Additionally, recommendations have been made regarding case volume in order to achieve limited numbers of false-negative results and to maintain competency. In the study by Van der Zee et al. of 403 patients (623 groins) who underwent sentinel node procedures, the false-negative rate was 0-2%. The overall survival rate was 97% at 3 years (J Clin Oncol. 2008 Feb 20;26[6]:884-9). However, a more recent data from the Gynecologic Oncology Group (GOG 173) showed a slightly higher false-negative rate of 8% (J Clin Oncol. 2012 Nov 1;30[31]:3786-91). Overall survival data are pending from this study.
While sentinel lymph node mapping for endometrial cancer has been feasible for many years and has been well described, the questioned role of completed lymphadenectomy for early-stage endometrial cancer has led to a resurgence of interest in these techniques. While blue dye and radiolabeled tracer methods have historically been the most popular mapping solutions, the advent of endoscopic near-infrared imaging, with its higher sensitivity and good depth penetration, has added options. Indocyanine green fluorescence can be easily detected during robotic surgery and as experience with these techniques increase, successful mapping and sensitivity will increase.
Genetics
While hereditary cancer syndromes have been recognized for many years, detecting the genetic mutations that may increase an individual’s risk of developing a malignancy were not elucidated until the early 1990s. In gynecologic oncology, the most commonly encountered syndromes involve mutations in BRCA1 and BRCA2 and hereditary non–polyposis colorectal cancer, which causes mutations in DNA mismatch-repair genes and increase the risk of endometrial and ovarian cancer.
The SGO recently published a statement on risk assessment for inherited gynecologic cancer predispositions. In this statement “the evaluation for the presence of a hereditary cancer syndrome enables physicians to provide individualized and quantified assessment of cancer risk, as well as options for tailored screening and preventions strategies that may reduce morbidity associated with the development of malignancy” (Gynecol Oncol. 2015 Jan;136[1]:3-7). Beyond risk-reducing salpingo-oophorectomy, therapeutic strategies targeting patients with germline mutations have been developed (PARP inhibitors in BRCA-mutated women with ovarian cancer).
In August 2015, ASCO released an updated policy statement on genetic and genomic testing for cancer susceptibility and highlighted five key areas: germ-line implications of somatic mutation profiling; multigene panel testing for cancer susceptibility; quality assurance in genetic testing; education for oncology professionals; and access to cancer genetic services.
Antiemetics
Rounding out ASCO’s “Top 5 advances in 50 years of Modern Oncology” was the improvement in patients’ quality of life from supportive therapies, in particular antinausea medications.
Several of the agents commonly used in gynecologic oncology rate high (cisplatin) to moderate (carboplatin, cyclophosphamide, doxorubicin, ifosfamide) with regards to emetogenicity. The advent of 5-HT3 receptor antagonists (for example, ondansetron) has significantly improved the quality of life of patients undergoing cytotoxic chemotherapy. In addition to improving quality of life, the decrease in nausea and vomiting can also decrease life-threatening complications such as dehydration and electrolyte imbalance. Both ASCO and the National Comprehensive Cancer Network both have guidelines for the management of nausea and vomiting in patients undergoing chemotherapy.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina, Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology, and a professor in the division of gynecologic oncology at UNC. They reported having no relevant financial disclosures.
More ob.gyns. find their niche as subspecialists
After 12 years as a private practice ob.gyn., Dr. Brigid McCue was beginning to feel overwhelmed. She loved her work, but keeping up with the kaleidoscope of care components and ever-changing clinical developments was daunting.
“I felt like it was hard to stay really good at all the different aspects of care,” Dr. McCue said. “I was doing fine with obstetrics, and I felt like I was managing my office well, but it’s hard to stay on top of the latest developments, especially in surgical areas. The other thing that was really hard to keep up with was the business aspect of medicine and running a private practice.”
So when an opportunity presented itself, Dr. McCue leaped at the chance to narrow her expertise to obstetrical hospital medicine. She helped establish the ob.gyn. hospitalist program at Beth Israel Deaconess Hospital-Plymouth in Massachusetts, and now serves as chief of ob.gyn. and midwifery for the hospital.
“I love the fact that I now have the time to get really good at [what] I really like, [such as] labor and delivery,” said Dr. McCue, who is president of the Society of OB/GYN Hospitalists. “Since I made this change, I feel like I’m so much more on top of things. I do simulations here on my unit over things like shoulder dystocia. When I was in private practice, I would go to one meeting a year and pray that I never had a shoulder dystocia [case]. Now I really understand the whole process and I take the time to run through that with my midwives and my other nurses and doctors.”
Dr. McCue is one of a growing number of ob.gyns. who have chosen to target their expertise to a single subspecialty or concentrated practice area. Data show subspecialization is on the rise in ob.gyn.
From 1985 to 2015, certificates issued by the American Board of Obstetrics and Gynecology (ABOG) for gynecologic oncology nearly tripled, and certificates issued for reproductive endocrinology and infertility more than doubled, according to data provided by the American Board of Medical Specialties (ABMS). Certificates issued for maternal-fetal medicine rose from 35 in 1985 to 100 in 2015.

Opportunities for ob.gyns. to subspecialize have steadily increased over the last 50 years. The subspecialties of maternal-fetal medicine, gynecologic oncology, and reproductive endocrinology and infertility were first approved for certification by ABOG in 1973. In 1983, ABMS approved a certificate of “added qualification” for ob.gyns. who complete fellowships in critical care. In 1995, ABOG and the American Board of Urology started the subspecialty of female pelvic medicine and reconstructive surgery, which was approved for certification by ABMS in 2011.
ABMS also approved a certificate of “added qualification” for ob.gyns. who complete a fellowship in hospice and palliative medicine in 2008. And fellowships now exist for minimally invasive gynecologic surgery and ob.gyn. hospital medicine.
The reasons that ob.gyns. choose to subspecialize are multifold, said Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill., and one of the medical editors of the Ob.Gyn. News column, Master Class.
“Physicians subspecialize so that they can provide more medical and surgical expertise for a given population,” he said. “Secondly, physicians may be driven to subspecialize for lifestyle reasons. Generalists refer to subspecialists when technical expertise is desired to help with a clinical situation and potentially reduce medical legal risk.”
Ultimately, it’s patients who benefit from the increased care provided by subspecialists, noted Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology, and women’s health at Rutgers, the State University of New Jersey, Newark. Generalist ob.gyns. are tremendously knowledgeable and experienced, he said, but there’s no way for them to know every area, he said. It’s the difference between someone who might be doing a complicated surgery one or twice a year versus someone who is doing that surgery once or twice a week, he added.
“That is ultimately helpful for patients,” Dr. Einstein said. “It’s really about outcomes. This is all better for the patient. That’s the most important thing.”
Not every consequence of subspecialization is positive, however.
“As with everything, subspecialization has both positive and negative effects,” said Dr. Sandra Ann Carson, vice president for education at the American College of Obstetricians and Gynecologists. “The more time one has to focus on a small area, the better that area becomes. However, if all you have is a hammer, everything looks like a nail. The larger population may not need the care that someone with a rare disease may need.”
Dr. Miller refers to this challenge as “losing the forest.” He explains that subspecialists sometimes become so focused on their area of expertise, that they may overlook suitable treatment plans with which they are unfamiliar. An infertility specialist, for example, who neglects to consider a minimally invasive surgical procedure that could allow a patient to become pregnant naturally and instead recommends in vitro fertilization treatment.
“The infertility specialist does not have that particular skill and therefore directs that patient to IVF,” Dr. Miller said. “In the process of subspecializing, we have a tendency to lose the forest and look only at the trees.”
Finding a job is another challenge for the growing number of subspecialists. In many cases, fellowship-trained minimally invasive gynecologic surgeons may have to go back to practicing general gynecology because of a lack of positions, Dr. Miller said.
“We have to be careful that we do not “oversubspecialize” so that we are oversaturating the field,” he said.
In the future, the number of ob.gyn subspecialists will likely continue to grow and become more refined, said Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center in Phoenix.
“I think subspecialists will continue to become more and more developed,” Dr. Chase said. “Perhaps, some areas like family planning or minimally invasive surgery may grow further and become board certified.”
Dr. Carson foresees subspecialization becoming more focused on centralized teaching hospitals, with patients who need special care being sent to these hubs.
“Telemedicine and long-distance communication with a local obstetrician-gynecologist managing the whole patient will allow the best of both worlds,” she said.
Regardless of how subspecialist growth evolves, general ob.gyns. and other primary care physicians will always be needed, said Dr. Mary E. Norton, a maternal-fetal medicine specialist and clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“With increasing complexity, experts are needed to interpret advances,” Dr. Norton said. “However, patients also need a ‘medical home’ and primary provider who sees the big picture, and provides ongoing care beyond a single pregnancy or pregnancy complication.”
Why I chose to subspecialize
“I went to medical school with a particular interest in obstetrics. Once there, I was exposed to pediatrics and to high-risk OB, which I found to be fascinating. I particularly enjoyed my exposure to genetics during my pediatrics rotation and cared for a few children with genetic diseases that had a big impact and made a substantial impression on me. I ultimately decided to pursue an ob.gyn. residency and loved the OB part, particularly the prenatal genetics and high-risk OB. I found the balance of maternal and fetal medicine to be an exciting opportunity to care for two patients. I did an elective in prenatal diagnosis during my third year, including a bit of research, and was hooked.”
Dr. Mary E. Norton, a maternal-fetal medicine specialist and a clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“In my second year of residency, I became really interested in [gynecology-oncology] because I was fascinated by the surgery and interested in the chemotherapy practice, which is interesting because there’s always new research and new agents and interesting changes in how you treat the various cancers. It’s a very comprehensive, research-based field and that was fascinating to me. It’s a very busy subspecialty with very complex cases on multiple levels. You do these radical surgeries but then you have to be really involved in the choice for which chemotherapy agent to use, what type of radiation to give, and you also get really involved with the families ... Every case is so different and you treat women who are 16 years old, but you also treat women who are 96 years old. You see women from all walks of life with all sorts of different issues. The ability to really get involved with cancer research is a great part of the field.”
Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center, Phoenix.
“I took the opportunity to come to a new program where they were looking for an ob.gyn. hospitalist. That was exciting for me because I got to help establish the program... I feel like we’re a better department because I’m here monitoring labor, but I’m also writing protocols and making sure everyone is up to date. And I still get to do what I love the most, which is birth and babies.”
Dr. Brigid McCue, an ob.gyn. hospitalist and chief of ob.gyn. and midwifery, Beth Israel Deaconess Hospital-Plymouth, Massachusetts.
“I never considered delivering babies for the rest of my life. I was always focused on treating infertile couples. I completed my fellowship in reproductive endocrinology-infertility at the University of Pennsylvania, Philadelphia, at a time when in vitro fertilization was in its infancy and the laparoscope and hysteroscope were virtually diagnostic tools ... As IVF became more successful, I felt it was essential to add this expertise to my armamentarium ... It is truly gratifying to be part of a subspecialty that has advanced so far that the majority of our patients are able to achieve pregnancy via IVF.”
Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill.
“During medical school, I was very interested in the surgical aspects of patient care. When I rotated in gyn-oncology – now knowing that I rotated with some of the best gyn-oncologists who ever practiced – I found myself drawn to the complexity of surgery, acuity of the patients, and the close relationships gyn-oncologists have with their patients. It hit me like a brick that this was the specialty for me. During my residency and fellowship, I was particularly drawn to the multiple modalities we use to treat cancers. I relished the idea that through clinical trials, gyn-oncologists keep pushing the bar to solve the cancer problem. What we do now is different than what we did 5 years ago. It keeps us professionally challenged all the time.”
Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology and women’s health at Rutgers, the State University of New Jersey, Newark.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
On Twitter @legal_med
After 12 years as a private practice ob.gyn., Dr. Brigid McCue was beginning to feel overwhelmed. She loved her work, but keeping up with the kaleidoscope of care components and ever-changing clinical developments was daunting.
“I felt like it was hard to stay really good at all the different aspects of care,” Dr. McCue said. “I was doing fine with obstetrics, and I felt like I was managing my office well, but it’s hard to stay on top of the latest developments, especially in surgical areas. The other thing that was really hard to keep up with was the business aspect of medicine and running a private practice.”
So when an opportunity presented itself, Dr. McCue leaped at the chance to narrow her expertise to obstetrical hospital medicine. She helped establish the ob.gyn. hospitalist program at Beth Israel Deaconess Hospital-Plymouth in Massachusetts, and now serves as chief of ob.gyn. and midwifery for the hospital.
“I love the fact that I now have the time to get really good at [what] I really like, [such as] labor and delivery,” said Dr. McCue, who is president of the Society of OB/GYN Hospitalists. “Since I made this change, I feel like I’m so much more on top of things. I do simulations here on my unit over things like shoulder dystocia. When I was in private practice, I would go to one meeting a year and pray that I never had a shoulder dystocia [case]. Now I really understand the whole process and I take the time to run through that with my midwives and my other nurses and doctors.”
Dr. McCue is one of a growing number of ob.gyns. who have chosen to target their expertise to a single subspecialty or concentrated practice area. Data show subspecialization is on the rise in ob.gyn.
From 1985 to 2015, certificates issued by the American Board of Obstetrics and Gynecology (ABOG) for gynecologic oncology nearly tripled, and certificates issued for reproductive endocrinology and infertility more than doubled, according to data provided by the American Board of Medical Specialties (ABMS). Certificates issued for maternal-fetal medicine rose from 35 in 1985 to 100 in 2015.

Opportunities for ob.gyns. to subspecialize have steadily increased over the last 50 years. The subspecialties of maternal-fetal medicine, gynecologic oncology, and reproductive endocrinology and infertility were first approved for certification by ABOG in 1973. In 1983, ABMS approved a certificate of “added qualification” for ob.gyns. who complete fellowships in critical care. In 1995, ABOG and the American Board of Urology started the subspecialty of female pelvic medicine and reconstructive surgery, which was approved for certification by ABMS in 2011.
ABMS also approved a certificate of “added qualification” for ob.gyns. who complete a fellowship in hospice and palliative medicine in 2008. And fellowships now exist for minimally invasive gynecologic surgery and ob.gyn. hospital medicine.
The reasons that ob.gyns. choose to subspecialize are multifold, said Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill., and one of the medical editors of the Ob.Gyn. News column, Master Class.
“Physicians subspecialize so that they can provide more medical and surgical expertise for a given population,” he said. “Secondly, physicians may be driven to subspecialize for lifestyle reasons. Generalists refer to subspecialists when technical expertise is desired to help with a clinical situation and potentially reduce medical legal risk.”
Ultimately, it’s patients who benefit from the increased care provided by subspecialists, noted Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology, and women’s health at Rutgers, the State University of New Jersey, Newark. Generalist ob.gyns. are tremendously knowledgeable and experienced, he said, but there’s no way for them to know every area, he said. It’s the difference between someone who might be doing a complicated surgery one or twice a year versus someone who is doing that surgery once or twice a week, he added.
“That is ultimately helpful for patients,” Dr. Einstein said. “It’s really about outcomes. This is all better for the patient. That’s the most important thing.”
Not every consequence of subspecialization is positive, however.
“As with everything, subspecialization has both positive and negative effects,” said Dr. Sandra Ann Carson, vice president for education at the American College of Obstetricians and Gynecologists. “The more time one has to focus on a small area, the better that area becomes. However, if all you have is a hammer, everything looks like a nail. The larger population may not need the care that someone with a rare disease may need.”
Dr. Miller refers to this challenge as “losing the forest.” He explains that subspecialists sometimes become so focused on their area of expertise, that they may overlook suitable treatment plans with which they are unfamiliar. An infertility specialist, for example, who neglects to consider a minimally invasive surgical procedure that could allow a patient to become pregnant naturally and instead recommends in vitro fertilization treatment.
“The infertility specialist does not have that particular skill and therefore directs that patient to IVF,” Dr. Miller said. “In the process of subspecializing, we have a tendency to lose the forest and look only at the trees.”
Finding a job is another challenge for the growing number of subspecialists. In many cases, fellowship-trained minimally invasive gynecologic surgeons may have to go back to practicing general gynecology because of a lack of positions, Dr. Miller said.
“We have to be careful that we do not “oversubspecialize” so that we are oversaturating the field,” he said.
In the future, the number of ob.gyn subspecialists will likely continue to grow and become more refined, said Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center in Phoenix.
“I think subspecialists will continue to become more and more developed,” Dr. Chase said. “Perhaps, some areas like family planning or minimally invasive surgery may grow further and become board certified.”
Dr. Carson foresees subspecialization becoming more focused on centralized teaching hospitals, with patients who need special care being sent to these hubs.
“Telemedicine and long-distance communication with a local obstetrician-gynecologist managing the whole patient will allow the best of both worlds,” she said.
Regardless of how subspecialist growth evolves, general ob.gyns. and other primary care physicians will always be needed, said Dr. Mary E. Norton, a maternal-fetal medicine specialist and clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“With increasing complexity, experts are needed to interpret advances,” Dr. Norton said. “However, patients also need a ‘medical home’ and primary provider who sees the big picture, and provides ongoing care beyond a single pregnancy or pregnancy complication.”
Why I chose to subspecialize
“I went to medical school with a particular interest in obstetrics. Once there, I was exposed to pediatrics and to high-risk OB, which I found to be fascinating. I particularly enjoyed my exposure to genetics during my pediatrics rotation and cared for a few children with genetic diseases that had a big impact and made a substantial impression on me. I ultimately decided to pursue an ob.gyn. residency and loved the OB part, particularly the prenatal genetics and high-risk OB. I found the balance of maternal and fetal medicine to be an exciting opportunity to care for two patients. I did an elective in prenatal diagnosis during my third year, including a bit of research, and was hooked.”
Dr. Mary E. Norton, a maternal-fetal medicine specialist and a clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“In my second year of residency, I became really interested in [gynecology-oncology] because I was fascinated by the surgery and interested in the chemotherapy practice, which is interesting because there’s always new research and new agents and interesting changes in how you treat the various cancers. It’s a very comprehensive, research-based field and that was fascinating to me. It’s a very busy subspecialty with very complex cases on multiple levels. You do these radical surgeries but then you have to be really involved in the choice for which chemotherapy agent to use, what type of radiation to give, and you also get really involved with the families ... Every case is so different and you treat women who are 16 years old, but you also treat women who are 96 years old. You see women from all walks of life with all sorts of different issues. The ability to really get involved with cancer research is a great part of the field.”
Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center, Phoenix.
“I took the opportunity to come to a new program where they were looking for an ob.gyn. hospitalist. That was exciting for me because I got to help establish the program... I feel like we’re a better department because I’m here monitoring labor, but I’m also writing protocols and making sure everyone is up to date. And I still get to do what I love the most, which is birth and babies.”
Dr. Brigid McCue, an ob.gyn. hospitalist and chief of ob.gyn. and midwifery, Beth Israel Deaconess Hospital-Plymouth, Massachusetts.
“I never considered delivering babies for the rest of my life. I was always focused on treating infertile couples. I completed my fellowship in reproductive endocrinology-infertility at the University of Pennsylvania, Philadelphia, at a time when in vitro fertilization was in its infancy and the laparoscope and hysteroscope were virtually diagnostic tools ... As IVF became more successful, I felt it was essential to add this expertise to my armamentarium ... It is truly gratifying to be part of a subspecialty that has advanced so far that the majority of our patients are able to achieve pregnancy via IVF.”
Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill.
“During medical school, I was very interested in the surgical aspects of patient care. When I rotated in gyn-oncology – now knowing that I rotated with some of the best gyn-oncologists who ever practiced – I found myself drawn to the complexity of surgery, acuity of the patients, and the close relationships gyn-oncologists have with their patients. It hit me like a brick that this was the specialty for me. During my residency and fellowship, I was particularly drawn to the multiple modalities we use to treat cancers. I relished the idea that through clinical trials, gyn-oncologists keep pushing the bar to solve the cancer problem. What we do now is different than what we did 5 years ago. It keeps us professionally challenged all the time.”
Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology and women’s health at Rutgers, the State University of New Jersey, Newark.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
On Twitter @legal_med
After 12 years as a private practice ob.gyn., Dr. Brigid McCue was beginning to feel overwhelmed. She loved her work, but keeping up with the kaleidoscope of care components and ever-changing clinical developments was daunting.
“I felt like it was hard to stay really good at all the different aspects of care,” Dr. McCue said. “I was doing fine with obstetrics, and I felt like I was managing my office well, but it’s hard to stay on top of the latest developments, especially in surgical areas. The other thing that was really hard to keep up with was the business aspect of medicine and running a private practice.”
So when an opportunity presented itself, Dr. McCue leaped at the chance to narrow her expertise to obstetrical hospital medicine. She helped establish the ob.gyn. hospitalist program at Beth Israel Deaconess Hospital-Plymouth in Massachusetts, and now serves as chief of ob.gyn. and midwifery for the hospital.
“I love the fact that I now have the time to get really good at [what] I really like, [such as] labor and delivery,” said Dr. McCue, who is president of the Society of OB/GYN Hospitalists. “Since I made this change, I feel like I’m so much more on top of things. I do simulations here on my unit over things like shoulder dystocia. When I was in private practice, I would go to one meeting a year and pray that I never had a shoulder dystocia [case]. Now I really understand the whole process and I take the time to run through that with my midwives and my other nurses and doctors.”
Dr. McCue is one of a growing number of ob.gyns. who have chosen to target their expertise to a single subspecialty or concentrated practice area. Data show subspecialization is on the rise in ob.gyn.
From 1985 to 2015, certificates issued by the American Board of Obstetrics and Gynecology (ABOG) for gynecologic oncology nearly tripled, and certificates issued for reproductive endocrinology and infertility more than doubled, according to data provided by the American Board of Medical Specialties (ABMS). Certificates issued for maternal-fetal medicine rose from 35 in 1985 to 100 in 2015.

Opportunities for ob.gyns. to subspecialize have steadily increased over the last 50 years. The subspecialties of maternal-fetal medicine, gynecologic oncology, and reproductive endocrinology and infertility were first approved for certification by ABOG in 1973. In 1983, ABMS approved a certificate of “added qualification” for ob.gyns. who complete fellowships in critical care. In 1995, ABOG and the American Board of Urology started the subspecialty of female pelvic medicine and reconstructive surgery, which was approved for certification by ABMS in 2011.
ABMS also approved a certificate of “added qualification” for ob.gyns. who complete a fellowship in hospice and palliative medicine in 2008. And fellowships now exist for minimally invasive gynecologic surgery and ob.gyn. hospital medicine.
The reasons that ob.gyns. choose to subspecialize are multifold, said Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill., and one of the medical editors of the Ob.Gyn. News column, Master Class.
“Physicians subspecialize so that they can provide more medical and surgical expertise for a given population,” he said. “Secondly, physicians may be driven to subspecialize for lifestyle reasons. Generalists refer to subspecialists when technical expertise is desired to help with a clinical situation and potentially reduce medical legal risk.”
Ultimately, it’s patients who benefit from the increased care provided by subspecialists, noted Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology, and women’s health at Rutgers, the State University of New Jersey, Newark. Generalist ob.gyns. are tremendously knowledgeable and experienced, he said, but there’s no way for them to know every area, he said. It’s the difference between someone who might be doing a complicated surgery one or twice a year versus someone who is doing that surgery once or twice a week, he added.
“That is ultimately helpful for patients,” Dr. Einstein said. “It’s really about outcomes. This is all better for the patient. That’s the most important thing.”
Not every consequence of subspecialization is positive, however.
“As with everything, subspecialization has both positive and negative effects,” said Dr. Sandra Ann Carson, vice president for education at the American College of Obstetricians and Gynecologists. “The more time one has to focus on a small area, the better that area becomes. However, if all you have is a hammer, everything looks like a nail. The larger population may not need the care that someone with a rare disease may need.”
Dr. Miller refers to this challenge as “losing the forest.” He explains that subspecialists sometimes become so focused on their area of expertise, that they may overlook suitable treatment plans with which they are unfamiliar. An infertility specialist, for example, who neglects to consider a minimally invasive surgical procedure that could allow a patient to become pregnant naturally and instead recommends in vitro fertilization treatment.
“The infertility specialist does not have that particular skill and therefore directs that patient to IVF,” Dr. Miller said. “In the process of subspecializing, we have a tendency to lose the forest and look only at the trees.”
Finding a job is another challenge for the growing number of subspecialists. In many cases, fellowship-trained minimally invasive gynecologic surgeons may have to go back to practicing general gynecology because of a lack of positions, Dr. Miller said.
“We have to be careful that we do not “oversubspecialize” so that we are oversaturating the field,” he said.
In the future, the number of ob.gyn subspecialists will likely continue to grow and become more refined, said Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center in Phoenix.
“I think subspecialists will continue to become more and more developed,” Dr. Chase said. “Perhaps, some areas like family planning or minimally invasive surgery may grow further and become board certified.”
Dr. Carson foresees subspecialization becoming more focused on centralized teaching hospitals, with patients who need special care being sent to these hubs.
“Telemedicine and long-distance communication with a local obstetrician-gynecologist managing the whole patient will allow the best of both worlds,” she said.
Regardless of how subspecialist growth evolves, general ob.gyns. and other primary care physicians will always be needed, said Dr. Mary E. Norton, a maternal-fetal medicine specialist and clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“With increasing complexity, experts are needed to interpret advances,” Dr. Norton said. “However, patients also need a ‘medical home’ and primary provider who sees the big picture, and provides ongoing care beyond a single pregnancy or pregnancy complication.”
Why I chose to subspecialize
“I went to medical school with a particular interest in obstetrics. Once there, I was exposed to pediatrics and to high-risk OB, which I found to be fascinating. I particularly enjoyed my exposure to genetics during my pediatrics rotation and cared for a few children with genetic diseases that had a big impact and made a substantial impression on me. I ultimately decided to pursue an ob.gyn. residency and loved the OB part, particularly the prenatal genetics and high-risk OB. I found the balance of maternal and fetal medicine to be an exciting opportunity to care for two patients. I did an elective in prenatal diagnosis during my third year, including a bit of research, and was hooked.”
Dr. Mary E. Norton, a maternal-fetal medicine specialist and a clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“In my second year of residency, I became really interested in [gynecology-oncology] because I was fascinated by the surgery and interested in the chemotherapy practice, which is interesting because there’s always new research and new agents and interesting changes in how you treat the various cancers. It’s a very comprehensive, research-based field and that was fascinating to me. It’s a very busy subspecialty with very complex cases on multiple levels. You do these radical surgeries but then you have to be really involved in the choice for which chemotherapy agent to use, what type of radiation to give, and you also get really involved with the families ... Every case is so different and you treat women who are 16 years old, but you also treat women who are 96 years old. You see women from all walks of life with all sorts of different issues. The ability to really get involved with cancer research is a great part of the field.”
Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center, Phoenix.
“I took the opportunity to come to a new program where they were looking for an ob.gyn. hospitalist. That was exciting for me because I got to help establish the program... I feel like we’re a better department because I’m here monitoring labor, but I’m also writing protocols and making sure everyone is up to date. And I still get to do what I love the most, which is birth and babies.”
Dr. Brigid McCue, an ob.gyn. hospitalist and chief of ob.gyn. and midwifery, Beth Israel Deaconess Hospital-Plymouth, Massachusetts.
“I never considered delivering babies for the rest of my life. I was always focused on treating infertile couples. I completed my fellowship in reproductive endocrinology-infertility at the University of Pennsylvania, Philadelphia, at a time when in vitro fertilization was in its infancy and the laparoscope and hysteroscope were virtually diagnostic tools ... As IVF became more successful, I felt it was essential to add this expertise to my armamentarium ... It is truly gratifying to be part of a subspecialty that has advanced so far that the majority of our patients are able to achieve pregnancy via IVF.”
Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill.
“During medical school, I was very interested in the surgical aspects of patient care. When I rotated in gyn-oncology – now knowing that I rotated with some of the best gyn-oncologists who ever practiced – I found myself drawn to the complexity of surgery, acuity of the patients, and the close relationships gyn-oncologists have with their patients. It hit me like a brick that this was the specialty for me. During my residency and fellowship, I was particularly drawn to the multiple modalities we use to treat cancers. I relished the idea that through clinical trials, gyn-oncologists keep pushing the bar to solve the cancer problem. What we do now is different than what we did 5 years ago. It keeps us professionally challenged all the time.”
Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology and women’s health at Rutgers, the State University of New Jersey, Newark.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
On Twitter @legal_med