User login
Reflecting on 2021, looking forward to 2022
This month marks the end of my first full calendar year as SHM CEO. Over the years, I have made it a habit to take time to reflect during the month of December, assessing the previous year by reviewing what went well and what could have gone better, and how I can grow and change to meet the needs of future challenges. This reflection sets the stage for my personal and professional “New Year” goals.
This year, 2021, is certainly a year deserving of reflection, and I believe 2022 (and beyond) will need ambitious goals made by dedicated leaders, hospitalists included. Here are my thoughts on what went well in 2021 and what I wish went better – from our greater society to our specialty, to SHM.
Society (as in the larger society)
What went well: Vaccines
There is a lot to be impressed with in 2021, and for me, at the top of that list are the COVID-19 vaccines. I realize the research for mRNA vaccines started more than 20 years ago, and the most successful mRNA vaccine companies have been around for more than a decade, but to roll out a COVID-19 vaccine in less than a year is still just incredible. To take a disease with a 2% mortality rate for someone like myself and effectively reduce that to near zero is something historians will be writing about for years to come.
What I wish went better: Open dialogue
I can’t remember when we stopped listening to each other, and by that, I mean listening to those who do not think exactly like ourselves. As a kid, I was taught to be careful about discussing topics at social events that could go sideways. That usually involved politics, money, or strong beliefs, but wow – now, that list is much longer. Talking about the weather used to be safe, but not anymore. If I were to show pictures of the recent flooding in Annapolis? There would almost certainly be a debate about climate change. At least we can agree on Ted Lasso as a safe topic.
Our specialty
What went well: Hospitalists are vital
There are many, many professions that deserve “hero” status for their part in taming this pandemic: nurses, doctors, emergency medical services, physical therapists, physician assistants, nurse practitioners, administrators, and more. But in the doctor category, hospitalists are at the top. Along with our emergency department and intensivist colleagues, hospitalists are one of the pillars of the inpatient response to COVID. More than 3.2 million COVID-19 hospitalizations have occurred, according to the Centers for Disease Control and Prevention, with numerous state dashboards showing three-quarters of those are cared for on general medical wards, the domain of hospitalists (for example, see my own state of Maryland’s COVID-19 dashboard: https://coronavirus.maryland.gov).
We’ve always had “two patients” – the patient in the bed and the health care system. Many hospitalists have helped their institutions by building COVID care teams, COVID wards, or in the case of Dr. Mindy Kantsiper, building an entire COVID field hospital in a convention center. Without hospitalists, both patients and the system that serves them would have fared much worse in this pandemic. Hospitalists are vital to patients and the health care system. The end. Period. End of story.
What I wish went better: Getting credit
As a profession, we need to be more deliberate about getting credit for the fantastic work we have done to care for COVID-19 patients, as well as inpatients in general. SHM can and must focus more on how to highlight the great work hospitalists have done and will continue to do. A greater understanding by the health care industry – as well as the general public – regarding the important role we play for patient care will help add autonomy in our profession, which in turn adds to resilience during these challenging times.
SHM
What went well: Membership grew
This is the one thing that we at SHM – and I personally – are most proud of. SHM is a membership society; it is the single most important metric for me personally. If physicians aren’t joining, then we are not meeting our core mission to provide value to hospitalists. My sense is the services SHM provides to hospitalists continue to be of value – even during these strenuous times of the pandemic when we had to be physically distant.
Whether it’s our Government Relations Department advocating for hospitalists in Washington, or the Journal of Hospital Medicine, or this very magazine, The Hospitalist, or SHM’s numerous educational offerings, chapter events, and SHM national meetings (Converge, Pediatric Hospital Medicine, Leadership Academies, Academic Hospitalist Academy, and more), SHM continues to provide hospitalists with vital tools to help you in your career.
This is also very much a two-way street. If you are reading this, know that without you, our members, our success would not be possible. Your passion and partnership drive us to innovate to meet your needs and those of the patients you serve every day. Thank you for your continued support and inspiration.
What could have gone better: Seeing more of you, in person
This is a tough one for me. Everything I worried about going wrong for SHM in 2021 never materialized. A year ago, my fears for SHM were that membership would shrink, finances would dry up, and the SHM staff would leave (by furlough or by choice). Thankfully, membership grew, our finances are in very good shape for any year, let alone a pandemic year, and the staff have remained at SHM and are engaged and dedicated! SHM even received a “Best Place to Work” award from the Philadelphia Business Journal.
Maybe the one regret I have is that we could not do more in-person events. But even there, I think we did better than most. We had some chapter meetings in person, and the October 2021 Leadership Academy hosted 110 hospitalist leaders, in person, at Amelia Island, Fla. That Leadership Academy went off without a hitch, and the early reviews are superb. I am very optimistic about 2022 in-person events!
Looking forward: 2022 and beyond
I have no illusions that 2022 is going to be easy. I know that the pandemic will not be gone (even though cases are falling nationwide as of this writing), that our nation will struggle with how to deal with polarization, and the workplace will continue to be redefined. Yet, I can’t help but be optimistic.
The pandemic will end eventually; all pandemics do. My hope is that young leaders will step forward to help our nation work through the divisive challenges, and some of those leaders will even be hospitalists! I also know that our profession is more vital than ever, for both patients and the health care system. We’re even getting ready to celebrate SHM’s 25th anniversary, and we can’t wait to revisit our humble beginnings while looking at the bright future of our society and our field.
I am working on my 2022 “New Year” goals, but you can be pretty sure they will revolve around making the world a better place, investing in people, and being ethical and transparent.
Dr. Howell is the CEO of the Society of Hospital Medicine.
This month marks the end of my first full calendar year as SHM CEO. Over the years, I have made it a habit to take time to reflect during the month of December, assessing the previous year by reviewing what went well and what could have gone better, and how I can grow and change to meet the needs of future challenges. This reflection sets the stage for my personal and professional “New Year” goals.
This year, 2021, is certainly a year deserving of reflection, and I believe 2022 (and beyond) will need ambitious goals made by dedicated leaders, hospitalists included. Here are my thoughts on what went well in 2021 and what I wish went better – from our greater society to our specialty, to SHM.
Society (as in the larger society)
What went well: Vaccines
There is a lot to be impressed with in 2021, and for me, at the top of that list are the COVID-19 vaccines. I realize the research for mRNA vaccines started more than 20 years ago, and the most successful mRNA vaccine companies have been around for more than a decade, but to roll out a COVID-19 vaccine in less than a year is still just incredible. To take a disease with a 2% mortality rate for someone like myself and effectively reduce that to near zero is something historians will be writing about for years to come.
What I wish went better: Open dialogue
I can’t remember when we stopped listening to each other, and by that, I mean listening to those who do not think exactly like ourselves. As a kid, I was taught to be careful about discussing topics at social events that could go sideways. That usually involved politics, money, or strong beliefs, but wow – now, that list is much longer. Talking about the weather used to be safe, but not anymore. If I were to show pictures of the recent flooding in Annapolis? There would almost certainly be a debate about climate change. At least we can agree on Ted Lasso as a safe topic.
Our specialty
What went well: Hospitalists are vital
There are many, many professions that deserve “hero” status for their part in taming this pandemic: nurses, doctors, emergency medical services, physical therapists, physician assistants, nurse practitioners, administrators, and more. But in the doctor category, hospitalists are at the top. Along with our emergency department and intensivist colleagues, hospitalists are one of the pillars of the inpatient response to COVID. More than 3.2 million COVID-19 hospitalizations have occurred, according to the Centers for Disease Control and Prevention, with numerous state dashboards showing three-quarters of those are cared for on general medical wards, the domain of hospitalists (for example, see my own state of Maryland’s COVID-19 dashboard: https://coronavirus.maryland.gov).
We’ve always had “two patients” – the patient in the bed and the health care system. Many hospitalists have helped their institutions by building COVID care teams, COVID wards, or in the case of Dr. Mindy Kantsiper, building an entire COVID field hospital in a convention center. Without hospitalists, both patients and the system that serves them would have fared much worse in this pandemic. Hospitalists are vital to patients and the health care system. The end. Period. End of story.
What I wish went better: Getting credit
As a profession, we need to be more deliberate about getting credit for the fantastic work we have done to care for COVID-19 patients, as well as inpatients in general. SHM can and must focus more on how to highlight the great work hospitalists have done and will continue to do. A greater understanding by the health care industry – as well as the general public – regarding the important role we play for patient care will help add autonomy in our profession, which in turn adds to resilience during these challenging times.
SHM
What went well: Membership grew
This is the one thing that we at SHM – and I personally – are most proud of. SHM is a membership society; it is the single most important metric for me personally. If physicians aren’t joining, then we are not meeting our core mission to provide value to hospitalists. My sense is the services SHM provides to hospitalists continue to be of value – even during these strenuous times of the pandemic when we had to be physically distant.
Whether it’s our Government Relations Department advocating for hospitalists in Washington, or the Journal of Hospital Medicine, or this very magazine, The Hospitalist, or SHM’s numerous educational offerings, chapter events, and SHM national meetings (Converge, Pediatric Hospital Medicine, Leadership Academies, Academic Hospitalist Academy, and more), SHM continues to provide hospitalists with vital tools to help you in your career.
This is also very much a two-way street. If you are reading this, know that without you, our members, our success would not be possible. Your passion and partnership drive us to innovate to meet your needs and those of the patients you serve every day. Thank you for your continued support and inspiration.
What could have gone better: Seeing more of you, in person
This is a tough one for me. Everything I worried about going wrong for SHM in 2021 never materialized. A year ago, my fears for SHM were that membership would shrink, finances would dry up, and the SHM staff would leave (by furlough or by choice). Thankfully, membership grew, our finances are in very good shape for any year, let alone a pandemic year, and the staff have remained at SHM and are engaged and dedicated! SHM even received a “Best Place to Work” award from the Philadelphia Business Journal.
Maybe the one regret I have is that we could not do more in-person events. But even there, I think we did better than most. We had some chapter meetings in person, and the October 2021 Leadership Academy hosted 110 hospitalist leaders, in person, at Amelia Island, Fla. That Leadership Academy went off without a hitch, and the early reviews are superb. I am very optimistic about 2022 in-person events!
Looking forward: 2022 and beyond
I have no illusions that 2022 is going to be easy. I know that the pandemic will not be gone (even though cases are falling nationwide as of this writing), that our nation will struggle with how to deal with polarization, and the workplace will continue to be redefined. Yet, I can’t help but be optimistic.
The pandemic will end eventually; all pandemics do. My hope is that young leaders will step forward to help our nation work through the divisive challenges, and some of those leaders will even be hospitalists! I also know that our profession is more vital than ever, for both patients and the health care system. We’re even getting ready to celebrate SHM’s 25th anniversary, and we can’t wait to revisit our humble beginnings while looking at the bright future of our society and our field.
I am working on my 2022 “New Year” goals, but you can be pretty sure they will revolve around making the world a better place, investing in people, and being ethical and transparent.
Dr. Howell is the CEO of the Society of Hospital Medicine.
This month marks the end of my first full calendar year as SHM CEO. Over the years, I have made it a habit to take time to reflect during the month of December, assessing the previous year by reviewing what went well and what could have gone better, and how I can grow and change to meet the needs of future challenges. This reflection sets the stage for my personal and professional “New Year” goals.
This year, 2021, is certainly a year deserving of reflection, and I believe 2022 (and beyond) will need ambitious goals made by dedicated leaders, hospitalists included. Here are my thoughts on what went well in 2021 and what I wish went better – from our greater society to our specialty, to SHM.
Society (as in the larger society)
What went well: Vaccines
There is a lot to be impressed with in 2021, and for me, at the top of that list are the COVID-19 vaccines. I realize the research for mRNA vaccines started more than 20 years ago, and the most successful mRNA vaccine companies have been around for more than a decade, but to roll out a COVID-19 vaccine in less than a year is still just incredible. To take a disease with a 2% mortality rate for someone like myself and effectively reduce that to near zero is something historians will be writing about for years to come.
What I wish went better: Open dialogue
I can’t remember when we stopped listening to each other, and by that, I mean listening to those who do not think exactly like ourselves. As a kid, I was taught to be careful about discussing topics at social events that could go sideways. That usually involved politics, money, or strong beliefs, but wow – now, that list is much longer. Talking about the weather used to be safe, but not anymore. If I were to show pictures of the recent flooding in Annapolis? There would almost certainly be a debate about climate change. At least we can agree on Ted Lasso as a safe topic.
Our specialty
What went well: Hospitalists are vital
There are many, many professions that deserve “hero” status for their part in taming this pandemic: nurses, doctors, emergency medical services, physical therapists, physician assistants, nurse practitioners, administrators, and more. But in the doctor category, hospitalists are at the top. Along with our emergency department and intensivist colleagues, hospitalists are one of the pillars of the inpatient response to COVID. More than 3.2 million COVID-19 hospitalizations have occurred, according to the Centers for Disease Control and Prevention, with numerous state dashboards showing three-quarters of those are cared for on general medical wards, the domain of hospitalists (for example, see my own state of Maryland’s COVID-19 dashboard: https://coronavirus.maryland.gov).
We’ve always had “two patients” – the patient in the bed and the health care system. Many hospitalists have helped their institutions by building COVID care teams, COVID wards, or in the case of Dr. Mindy Kantsiper, building an entire COVID field hospital in a convention center. Without hospitalists, both patients and the system that serves them would have fared much worse in this pandemic. Hospitalists are vital to patients and the health care system. The end. Period. End of story.
What I wish went better: Getting credit
As a profession, we need to be more deliberate about getting credit for the fantastic work we have done to care for COVID-19 patients, as well as inpatients in general. SHM can and must focus more on how to highlight the great work hospitalists have done and will continue to do. A greater understanding by the health care industry – as well as the general public – regarding the important role we play for patient care will help add autonomy in our profession, which in turn adds to resilience during these challenging times.
SHM
What went well: Membership grew
This is the one thing that we at SHM – and I personally – are most proud of. SHM is a membership society; it is the single most important metric for me personally. If physicians aren’t joining, then we are not meeting our core mission to provide value to hospitalists. My sense is the services SHM provides to hospitalists continue to be of value – even during these strenuous times of the pandemic when we had to be physically distant.
Whether it’s our Government Relations Department advocating for hospitalists in Washington, or the Journal of Hospital Medicine, or this very magazine, The Hospitalist, or SHM’s numerous educational offerings, chapter events, and SHM national meetings (Converge, Pediatric Hospital Medicine, Leadership Academies, Academic Hospitalist Academy, and more), SHM continues to provide hospitalists with vital tools to help you in your career.
This is also very much a two-way street. If you are reading this, know that without you, our members, our success would not be possible. Your passion and partnership drive us to innovate to meet your needs and those of the patients you serve every day. Thank you for your continued support and inspiration.
What could have gone better: Seeing more of you, in person
This is a tough one for me. Everything I worried about going wrong for SHM in 2021 never materialized. A year ago, my fears for SHM were that membership would shrink, finances would dry up, and the SHM staff would leave (by furlough or by choice). Thankfully, membership grew, our finances are in very good shape for any year, let alone a pandemic year, and the staff have remained at SHM and are engaged and dedicated! SHM even received a “Best Place to Work” award from the Philadelphia Business Journal.
Maybe the one regret I have is that we could not do more in-person events. But even there, I think we did better than most. We had some chapter meetings in person, and the October 2021 Leadership Academy hosted 110 hospitalist leaders, in person, at Amelia Island, Fla. That Leadership Academy went off without a hitch, and the early reviews are superb. I am very optimistic about 2022 in-person events!
Looking forward: 2022 and beyond
I have no illusions that 2022 is going to be easy. I know that the pandemic will not be gone (even though cases are falling nationwide as of this writing), that our nation will struggle with how to deal with polarization, and the workplace will continue to be redefined. Yet, I can’t help but be optimistic.
The pandemic will end eventually; all pandemics do. My hope is that young leaders will step forward to help our nation work through the divisive challenges, and some of those leaders will even be hospitalists! I also know that our profession is more vital than ever, for both patients and the health care system. We’re even getting ready to celebrate SHM’s 25th anniversary, and we can’t wait to revisit our humble beginnings while looking at the bright future of our society and our field.
I am working on my 2022 “New Year” goals, but you can be pretty sure they will revolve around making the world a better place, investing in people, and being ethical and transparent.
Dr. Howell is the CEO of the Society of Hospital Medicine.
Mean leadership
The differences between the mean and median of leadership data
Let me apologize for misleading all of you; this is not an article about malignant physician leaders; instead, it goes over the numbers and trends uncovered by the 2020 State of Hospital Medicine report (SoHM).1 The hospital medicine leader ends up doing many tasks like planning, growth, collaboration, finance, recruiting, scheduling, onboarding, coaching, and most near and dear to our hearts, putting out the fires and conflict resolution.
Ratio of leadership FTE to physician hospitalists FTE
If my pun has already put you off, you can avoid reading the rest of the piece and go to the 2020 SoHM to look at pages 52 (Table 3.7c), 121 (Table 4.7c), and 166 (Table 5.7c). It has a newly added table (3.7c), and it is phenomenal; it is the ratio of leadership FTE to physician hospitalists FTE. As an avid user of SoHM, I always ended up doing a makeshift calculation to “guesstimate” this number. Now that we have it calculated for us and the ultimate revelation lies in its narrow range across all groups. We might differ in the region, employment type, academics, teaching, or size, but this range is relatively narrow.
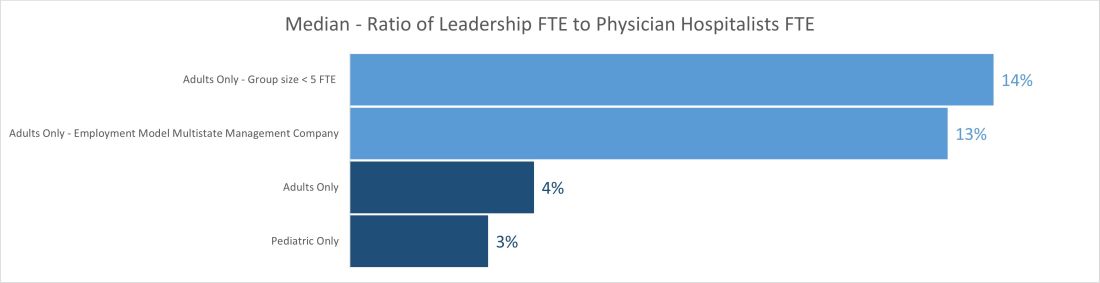
The median ratio of leadership FTE to total FTE lies between 2% and 5% in pediatric groups and between 3% and 6% for most adult groups. The only two outliers are on the adult side, with less than 5 FTE and multistate management companies. The higher median for the less than 5 FTE group size is understandable because of the small number of hospitalist FTEs that the leader’s time must be spread over. Even a small amount of dedicated leadership time will result in a high ratio of leader time to hospitalist clinical time if the group is very small. The multistate management company is probably a result of multiple layers of physician leadership (for example, regional medical directors) and travel-related time adjustments. Still, it raises the question of why the local leadership is not developed to decrease the leadership cost and better access.
Another helpful pattern is the decrease in standard deviation with the increase in group size. The hospital medicine leaders and CEOs of the hospital need to watch this number closely; any extremes on high or low side would be indicators for a deep dive in leadership structure and health.
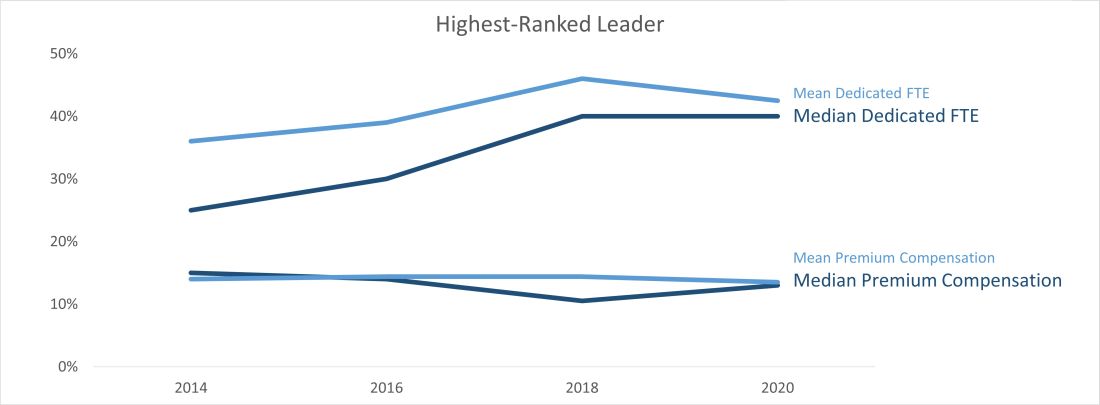
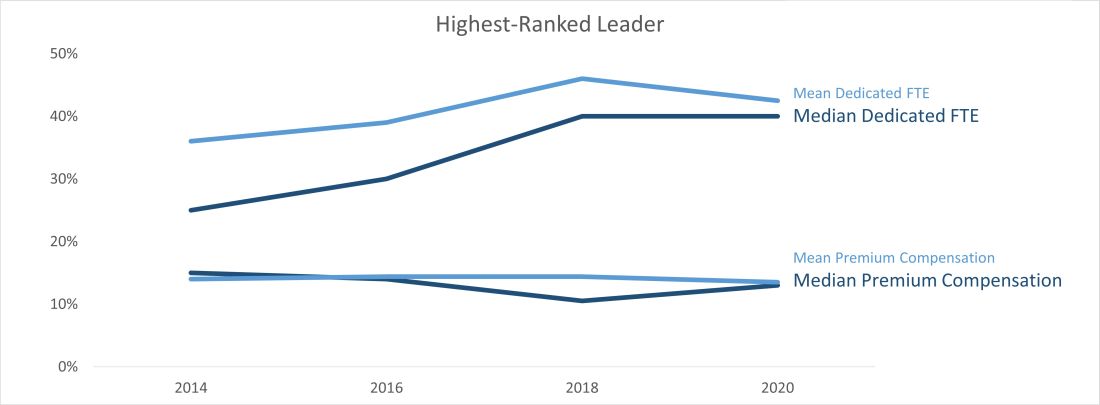
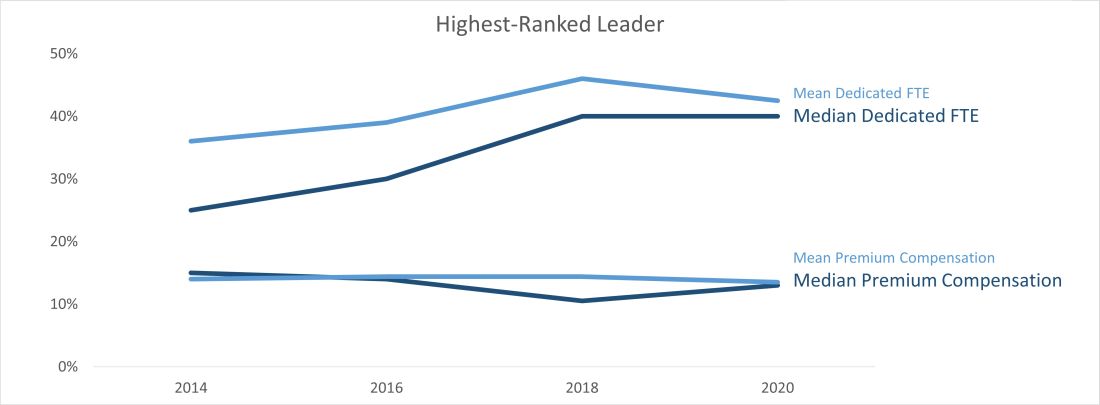
Total number and total dedicated FTE for all physician leaders
Once we start seeing the differences between the mean and median of leadership data, we can see the median is relatively static while the mean has increased year after year and took a big jump in the 2020 SoHM. The chart below shows trends for the number of individuals in leadership positions (“Total No” and total FTEs allocated to leadership (“Total FTE”) over the last several surveys. The data is heavily skewed toward the right (positive); so, it makes sense to use the median in this case rather than mean. A few factors could explain the right skew of data.
- Large groups of 30 or more hospitalists are increasing, and so is their leadership need.
- There is more recognition of the need for dedicated leadership individuals and FTE.
- The leadership is getting less concentrated among just one or a few leaders.
- Outliers on the high side.
- Lower bounds of 0 or 0.1 FTE.
Highest-ranked leader dedicated FTE and premium compensation
Another pleasing trend is an increase in dedicated FTE for the highest-paid leader. Like any skill-set development, leadership requires the investment of deliberate practice, financial acumen, negotiation skills, and increased vulnerability. Time helps way more in developing these skill sets than money. SoHM trends show increase in dedicated FTE for the highest physician leader over the years and static premium compensation.
At last, we can say median leadership is always better than “mean” leadership in skewed data. Pun apart, every group needs leadership, and SoHM offers a nice window to the trends in leadership amongst many practice groups. It is a valuable resource for every group.
Dr. Chadha is chief of the division of hospital medicine at the University of Kentucky Healthcare, Lexington. He actively leads efforts of recruiting, practice analysis, and operation of the group. He is finishing his first tenure in the Practice Analysis Committee. He is often found spending a lot more than required time with spreadsheets and graphs.
Reference
1. 2020 State of Hospital Medicine. www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
The differences between the mean and median of leadership data
The differences between the mean and median of leadership data
Let me apologize for misleading all of you; this is not an article about malignant physician leaders; instead, it goes over the numbers and trends uncovered by the 2020 State of Hospital Medicine report (SoHM).1 The hospital medicine leader ends up doing many tasks like planning, growth, collaboration, finance, recruiting, scheduling, onboarding, coaching, and most near and dear to our hearts, putting out the fires and conflict resolution.
Ratio of leadership FTE to physician hospitalists FTE
If my pun has already put you off, you can avoid reading the rest of the piece and go to the 2020 SoHM to look at pages 52 (Table 3.7c), 121 (Table 4.7c), and 166 (Table 5.7c). It has a newly added table (3.7c), and it is phenomenal; it is the ratio of leadership FTE to physician hospitalists FTE. As an avid user of SoHM, I always ended up doing a makeshift calculation to “guesstimate” this number. Now that we have it calculated for us and the ultimate revelation lies in its narrow range across all groups. We might differ in the region, employment type, academics, teaching, or size, but this range is relatively narrow.
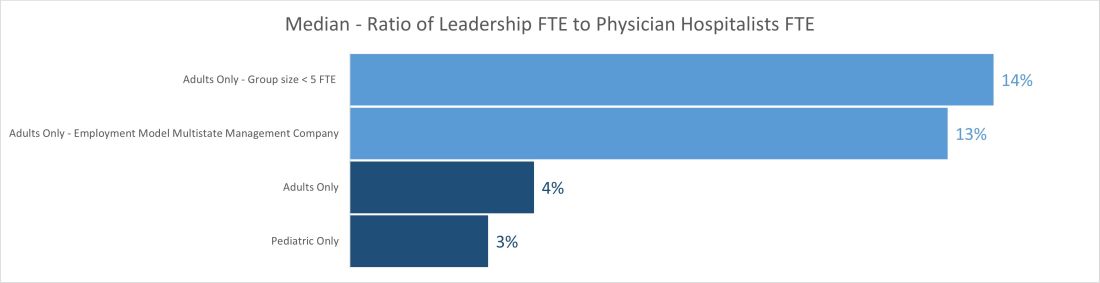
The median ratio of leadership FTE to total FTE lies between 2% and 5% in pediatric groups and between 3% and 6% for most adult groups. The only two outliers are on the adult side, with less than 5 FTE and multistate management companies. The higher median for the less than 5 FTE group size is understandable because of the small number of hospitalist FTEs that the leader’s time must be spread over. Even a small amount of dedicated leadership time will result in a high ratio of leader time to hospitalist clinical time if the group is very small. The multistate management company is probably a result of multiple layers of physician leadership (for example, regional medical directors) and travel-related time adjustments. Still, it raises the question of why the local leadership is not developed to decrease the leadership cost and better access.
Another helpful pattern is the decrease in standard deviation with the increase in group size. The hospital medicine leaders and CEOs of the hospital need to watch this number closely; any extremes on high or low side would be indicators for a deep dive in leadership structure and health.
Total number and total dedicated FTE for all physician leaders
Once we start seeing the differences between the mean and median of leadership data, we can see the median is relatively static while the mean has increased year after year and took a big jump in the 2020 SoHM. The chart below shows trends for the number of individuals in leadership positions (“Total No” and total FTEs allocated to leadership (“Total FTE”) over the last several surveys. The data is heavily skewed toward the right (positive); so, it makes sense to use the median in this case rather than mean. A few factors could explain the right skew of data.
- Large groups of 30 or more hospitalists are increasing, and so is their leadership need.
- There is more recognition of the need for dedicated leadership individuals and FTE.
- The leadership is getting less concentrated among just one or a few leaders.
- Outliers on the high side.
- Lower bounds of 0 or 0.1 FTE.
Highest-ranked leader dedicated FTE and premium compensation
Another pleasing trend is an increase in dedicated FTE for the highest-paid leader. Like any skill-set development, leadership requires the investment of deliberate practice, financial acumen, negotiation skills, and increased vulnerability. Time helps way more in developing these skill sets than money. SoHM trends show increase in dedicated FTE for the highest physician leader over the years and static premium compensation.
At last, we can say median leadership is always better than “mean” leadership in skewed data. Pun apart, every group needs leadership, and SoHM offers a nice window to the trends in leadership amongst many practice groups. It is a valuable resource for every group.
Dr. Chadha is chief of the division of hospital medicine at the University of Kentucky Healthcare, Lexington. He actively leads efforts of recruiting, practice analysis, and operation of the group. He is finishing his first tenure in the Practice Analysis Committee. He is often found spending a lot more than required time with spreadsheets and graphs.
Reference
1. 2020 State of Hospital Medicine. www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
Let me apologize for misleading all of you; this is not an article about malignant physician leaders; instead, it goes over the numbers and trends uncovered by the 2020 State of Hospital Medicine report (SoHM).1 The hospital medicine leader ends up doing many tasks like planning, growth, collaboration, finance, recruiting, scheduling, onboarding, coaching, and most near and dear to our hearts, putting out the fires and conflict resolution.
Ratio of leadership FTE to physician hospitalists FTE
If my pun has already put you off, you can avoid reading the rest of the piece and go to the 2020 SoHM to look at pages 52 (Table 3.7c), 121 (Table 4.7c), and 166 (Table 5.7c). It has a newly added table (3.7c), and it is phenomenal; it is the ratio of leadership FTE to physician hospitalists FTE. As an avid user of SoHM, I always ended up doing a makeshift calculation to “guesstimate” this number. Now that we have it calculated for us and the ultimate revelation lies in its narrow range across all groups. We might differ in the region, employment type, academics, teaching, or size, but this range is relatively narrow.
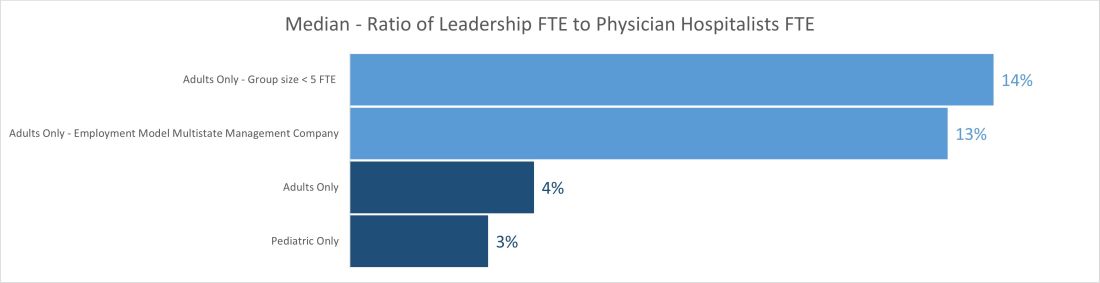
The median ratio of leadership FTE to total FTE lies between 2% and 5% in pediatric groups and between 3% and 6% for most adult groups. The only two outliers are on the adult side, with less than 5 FTE and multistate management companies. The higher median for the less than 5 FTE group size is understandable because of the small number of hospitalist FTEs that the leader’s time must be spread over. Even a small amount of dedicated leadership time will result in a high ratio of leader time to hospitalist clinical time if the group is very small. The multistate management company is probably a result of multiple layers of physician leadership (for example, regional medical directors) and travel-related time adjustments. Still, it raises the question of why the local leadership is not developed to decrease the leadership cost and better access.
Another helpful pattern is the decrease in standard deviation with the increase in group size. The hospital medicine leaders and CEOs of the hospital need to watch this number closely; any extremes on high or low side would be indicators for a deep dive in leadership structure and health.
Total number and total dedicated FTE for all physician leaders
Once we start seeing the differences between the mean and median of leadership data, we can see the median is relatively static while the mean has increased year after year and took a big jump in the 2020 SoHM. The chart below shows trends for the number of individuals in leadership positions (“Total No” and total FTEs allocated to leadership (“Total FTE”) over the last several surveys. The data is heavily skewed toward the right (positive); so, it makes sense to use the median in this case rather than mean. A few factors could explain the right skew of data.
- Large groups of 30 or more hospitalists are increasing, and so is their leadership need.
- There is more recognition of the need for dedicated leadership individuals and FTE.
- The leadership is getting less concentrated among just one or a few leaders.
- Outliers on the high side.
- Lower bounds of 0 or 0.1 FTE.
Highest-ranked leader dedicated FTE and premium compensation
Another pleasing trend is an increase in dedicated FTE for the highest-paid leader. Like any skill-set development, leadership requires the investment of deliberate practice, financial acumen, negotiation skills, and increased vulnerability. Time helps way more in developing these skill sets than money. SoHM trends show increase in dedicated FTE for the highest physician leader over the years and static premium compensation.
At last, we can say median leadership is always better than “mean” leadership in skewed data. Pun apart, every group needs leadership, and SoHM offers a nice window to the trends in leadership amongst many practice groups. It is a valuable resource for every group.
Dr. Chadha is chief of the division of hospital medicine at the University of Kentucky Healthcare, Lexington. He actively leads efforts of recruiting, practice analysis, and operation of the group. He is finishing his first tenure in the Practice Analysis Committee. He is often found spending a lot more than required time with spreadsheets and graphs.
Reference
1. 2020 State of Hospital Medicine. www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
Trio of awardees illustrate excellence in SHM chapters
2020 required resiliency, innovation
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
2020 required resiliency, innovation
2020 required resiliency, innovation
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
SHM’s Center for Quality Improvement to partner on NIH grant
The Society of Hospital Medicine has announced that its award-winning Center for Quality Improvement will partner on the National Institutes of Health National, Heart, Lung, and Blood Institute study, “The SIP Study: Simultaneously Implementing Pathways for Improving Asthma, Pneumonia, and Bronchiolitis Care for Hospitalized Children” (NIH R61HL157804). The core objectives of the planned 5-year study are to identify and test practical, sustainable strategies for implementing a multicondition clinical pathway intervention for children hospitalized with asthma, pneumonia, or bronchiolitis in community hospitals.
Under the leadership of principal investigator Sunitha Kaiser, MD, MSc, a pediatric hospitalist at the University of California, San Francisco, the study will employ rigorous implementation science methods and SHM’s mentored implementation model.
“The lessons learned from this study could inform improved care delivery strategies for the millions of children hospitalized with respiratory illnesses across the U.S. each year,” said Jenna Goldstein, chief of strategic partnerships at SHM and director of SHM’s Center for Quality Improvement.
The team will recruit a diverse group of community hospitals in partnership with SHM, the Value in Inpatient Pediatrics Network (within the American Academy of Pediatrics), the Pediatric Research in Inpatient Settings Network, America’s Hospital Essentials, and the National Improvement Partnership Network. In collaboration with these national organizations and the participating hospitals, the team seeks to realize the following aims:
- Aim 1. (Preimplementation) Identify barriers and facilitators of implementing a multicondition pathway intervention and refine the intervention for community hospitals.
- Aim 2a. Determine the effects of the intervention, compared with control via chart reviews of children hospitalized with asthma, pneumonia, or bronchiolitis.
- Aim 2b. Determine if the core implementation strategies (audit and feedback, electronic order sets, Plan-Do-Study-Act cycles) are associated with clinicians’ guideline adoption.
“SHM’s Center for Quality Improvement is a recognized partner in facilitating process and culture change in the hospital to improve outcomes for patients,” said Eric E. Howell, MD, MHM, chief executive officer of SHM. “SHM is committed to supporting quality-improvement research, and we look forward to contributing to improved care for hospitalized pediatric patients through this study and beyond.”
To learn more about SHM’s Center for Quality Improvement, visit hospitalmedicine.org/qi.
The Society of Hospital Medicine has announced that its award-winning Center for Quality Improvement will partner on the National Institutes of Health National, Heart, Lung, and Blood Institute study, “The SIP Study: Simultaneously Implementing Pathways for Improving Asthma, Pneumonia, and Bronchiolitis Care for Hospitalized Children” (NIH R61HL157804). The core objectives of the planned 5-year study are to identify and test practical, sustainable strategies for implementing a multicondition clinical pathway intervention for children hospitalized with asthma, pneumonia, or bronchiolitis in community hospitals.
Under the leadership of principal investigator Sunitha Kaiser, MD, MSc, a pediatric hospitalist at the University of California, San Francisco, the study will employ rigorous implementation science methods and SHM’s mentored implementation model.
“The lessons learned from this study could inform improved care delivery strategies for the millions of children hospitalized with respiratory illnesses across the U.S. each year,” said Jenna Goldstein, chief of strategic partnerships at SHM and director of SHM’s Center for Quality Improvement.
The team will recruit a diverse group of community hospitals in partnership with SHM, the Value in Inpatient Pediatrics Network (within the American Academy of Pediatrics), the Pediatric Research in Inpatient Settings Network, America’s Hospital Essentials, and the National Improvement Partnership Network. In collaboration with these national organizations and the participating hospitals, the team seeks to realize the following aims:
- Aim 1. (Preimplementation) Identify barriers and facilitators of implementing a multicondition pathway intervention and refine the intervention for community hospitals.
- Aim 2a. Determine the effects of the intervention, compared with control via chart reviews of children hospitalized with asthma, pneumonia, or bronchiolitis.
- Aim 2b. Determine if the core implementation strategies (audit and feedback, electronic order sets, Plan-Do-Study-Act cycles) are associated with clinicians’ guideline adoption.
“SHM’s Center for Quality Improvement is a recognized partner in facilitating process and culture change in the hospital to improve outcomes for patients,” said Eric E. Howell, MD, MHM, chief executive officer of SHM. “SHM is committed to supporting quality-improvement research, and we look forward to contributing to improved care for hospitalized pediatric patients through this study and beyond.”
To learn more about SHM’s Center for Quality Improvement, visit hospitalmedicine.org/qi.
The Society of Hospital Medicine has announced that its award-winning Center for Quality Improvement will partner on the National Institutes of Health National, Heart, Lung, and Blood Institute study, “The SIP Study: Simultaneously Implementing Pathways for Improving Asthma, Pneumonia, and Bronchiolitis Care for Hospitalized Children” (NIH R61HL157804). The core objectives of the planned 5-year study are to identify and test practical, sustainable strategies for implementing a multicondition clinical pathway intervention for children hospitalized with asthma, pneumonia, or bronchiolitis in community hospitals.
Under the leadership of principal investigator Sunitha Kaiser, MD, MSc, a pediatric hospitalist at the University of California, San Francisco, the study will employ rigorous implementation science methods and SHM’s mentored implementation model.
“The lessons learned from this study could inform improved care delivery strategies for the millions of children hospitalized with respiratory illnesses across the U.S. each year,” said Jenna Goldstein, chief of strategic partnerships at SHM and director of SHM’s Center for Quality Improvement.
The team will recruit a diverse group of community hospitals in partnership with SHM, the Value in Inpatient Pediatrics Network (within the American Academy of Pediatrics), the Pediatric Research in Inpatient Settings Network, America’s Hospital Essentials, and the National Improvement Partnership Network. In collaboration with these national organizations and the participating hospitals, the team seeks to realize the following aims:
- Aim 1. (Preimplementation) Identify barriers and facilitators of implementing a multicondition pathway intervention and refine the intervention for community hospitals.
- Aim 2a. Determine the effects of the intervention, compared with control via chart reviews of children hospitalized with asthma, pneumonia, or bronchiolitis.
- Aim 2b. Determine if the core implementation strategies (audit and feedback, electronic order sets, Plan-Do-Study-Act cycles) are associated with clinicians’ guideline adoption.
“SHM’s Center for Quality Improvement is a recognized partner in facilitating process and culture change in the hospital to improve outcomes for patients,” said Eric E. Howell, MD, MHM, chief executive officer of SHM. “SHM is committed to supporting quality-improvement research, and we look forward to contributing to improved care for hospitalized pediatric patients through this study and beyond.”
To learn more about SHM’s Center for Quality Improvement, visit hospitalmedicine.org/qi.
Never prouder to be a hospitalist
I have been a proud hospitalist for more than 20 years, and yet I have never been prouder to be a hospitalist than now. The pandemic has been brutal, killing more than 600,000 Americans as of this writing. It has stretched the health care system, its doctors, nurses, and other providers to the limit. Yet we will get through it, we are getting through it, and hospitalists deserve a huge portion of the credit.
According to the CDC, there have been over 2.3 million COVID-19 hospitalizations. In my home state of Maryland, between two-thirds and three-quarters of hospitalized COVID patients are cared for on general medical floors, the domain of hospitalists. When hospitals needed COVID units, hospitalists stepped up to design and staff them. When our ICU colleagues needed support, especially in those early dark days, hospitalists stepped in. When our outpatient colleagues were called into the hospital, hospitalists were there to help them on board. When the House of Medicine was in chaos due to COVID-19, hospitalists ran towards that fire. Our previous 20+ years of collective experience made us the ideal specialty to manage the inpatient challenges over the last 18 months.
Need a new clinical schedule by Sunday? Check.
Need help with new clinical protocols? Check.
Need to help other colleagues? Check.
Need to reprogram the EMR? Check.
Need a new way to teach residents and students on the wards? Check.
Need a whole new unit – no, wait – a new hospital wing? No, scratch that – a whole new COVID hospital in a few weeks? Check. (I personally did that last one at the Baltimore Convention Center!)
For me and many hospitalists like me, it is as if the last 20 years were prep work for the pandemic.
Here at SHM, we know the pandemic is hard work – exhausting, even. SHM has been actively focused on supporting hospitalists during this crisis so that hospitalists can focus on patients. Early in the pandemic, SHM quickly pivoted to supply hospitalists with COVID-19 resources in their fight against the coronavirus. Numerous COVID-19 webinars, a COVID addendum to the State of Hospital Medicine Report, and a dedicated COVID issue of the Journal of Hospital Medicine were early and successful information dissemination strategies.
As the world – and hospitalists – dug in for a multi-year pandemic, SHM continued to advance the care of patients by opening our library of educational content for free to anyone. Our Public Policy Committee was active around both COVID-19- and hospitalist-related topics: immigration, telehealth, wellbeing, and financial impacts, to name a few.
As the pandemic slogged on, our Wellbeing Task Force came up with innovative support measures, including a check-in guide for hospitalists and fellow health care workers and dedicated wellness sessions complete with a licensed therapist for members. All the while, despite the restrictions and hurdles the pandemic has thrown our way, SHM members keep meeting and collaborating through virtual chapter events, committee work, special interest groups, and our annual conference, SHM Converge. Thank you to the countless members who donated their time to SHM, so that SHM could support hospitalists and their patients.
Now, we are transitioning into a new phase of the pandemic. The medical miracles that are the COVID-19 vaccines have made that possible. Fully vaccinated, I no longer worry that every time someone sneezes, or when I care for patients with a fever, that I am playing a high stakes poker game with my life. Don’t get me wrong; as I write, the Delta variant has a hold on the nation, and I know it’s not over yet. But it does appear as if the medical war on COVID is shifting from national to regional (or even local) responses.
During this new phase, we must rebuild our personal and professional lives. If you haven’t read Retired Lieutenant General Mark Hertling’s perspective piece in the August issue of the Journal of Hospital Medicine, I strongly encourage you to do so. He shares profound lessons on transitioning from active combat that are directly applicable to hospitalists who have been “deployed” battling COVID-19.
SHM will continue to pivot to meet our members’ needs too. We are already gearing up for more in-person education and networking. Chapters are starting to meet in person, and SHM is happy to provide visiting faculty. I will visit members from Florida to Maine and places in between starting this fall! Our Board of Directors and other SHM leaders are also starting to meet with members in person. Our own Leadership Academy will take place at Amelia Island in Florida in October, where we can learn, network, and even decompress. We also can’t wait for SHM Converge 2022 in Nashville, where we hope to reunite with many of you after 2 years of virtual conferences.
Our response to the pandemic, a once in a century crisis where our own safety was at risk, where doing the right thing might mean death or harming loved ones, our response of running into the fire to save lives is truly inspiring. The power of care – for our patients, for our family and friends, and for our hospital medicine community and the community at large – is evident more now than ever.
There have always been good reasons to be proud of being a hospitalist: taking care of the acutely ill, helping hospitals improve, teaching young doctors, and watching my specialty grow by leaps and bounds, to name just a few. But I’ve never been prouder than I am now.
Dr. Howell is the CEO of the Society of Hospital Medicine.
I have been a proud hospitalist for more than 20 years, and yet I have never been prouder to be a hospitalist than now. The pandemic has been brutal, killing more than 600,000 Americans as of this writing. It has stretched the health care system, its doctors, nurses, and other providers to the limit. Yet we will get through it, we are getting through it, and hospitalists deserve a huge portion of the credit.
According to the CDC, there have been over 2.3 million COVID-19 hospitalizations. In my home state of Maryland, between two-thirds and three-quarters of hospitalized COVID patients are cared for on general medical floors, the domain of hospitalists. When hospitals needed COVID units, hospitalists stepped up to design and staff them. When our ICU colleagues needed support, especially in those early dark days, hospitalists stepped in. When our outpatient colleagues were called into the hospital, hospitalists were there to help them on board. When the House of Medicine was in chaos due to COVID-19, hospitalists ran towards that fire. Our previous 20+ years of collective experience made us the ideal specialty to manage the inpatient challenges over the last 18 months.
Need a new clinical schedule by Sunday? Check.
Need help with new clinical protocols? Check.
Need to help other colleagues? Check.
Need to reprogram the EMR? Check.
Need a new way to teach residents and students on the wards? Check.
Need a whole new unit – no, wait – a new hospital wing? No, scratch that – a whole new COVID hospital in a few weeks? Check. (I personally did that last one at the Baltimore Convention Center!)
For me and many hospitalists like me, it is as if the last 20 years were prep work for the pandemic.
Here at SHM, we know the pandemic is hard work – exhausting, even. SHM has been actively focused on supporting hospitalists during this crisis so that hospitalists can focus on patients. Early in the pandemic, SHM quickly pivoted to supply hospitalists with COVID-19 resources in their fight against the coronavirus. Numerous COVID-19 webinars, a COVID addendum to the State of Hospital Medicine Report, and a dedicated COVID issue of the Journal of Hospital Medicine were early and successful information dissemination strategies.
As the world – and hospitalists – dug in for a multi-year pandemic, SHM continued to advance the care of patients by opening our library of educational content for free to anyone. Our Public Policy Committee was active around both COVID-19- and hospitalist-related topics: immigration, telehealth, wellbeing, and financial impacts, to name a few.
As the pandemic slogged on, our Wellbeing Task Force came up with innovative support measures, including a check-in guide for hospitalists and fellow health care workers and dedicated wellness sessions complete with a licensed therapist for members. All the while, despite the restrictions and hurdles the pandemic has thrown our way, SHM members keep meeting and collaborating through virtual chapter events, committee work, special interest groups, and our annual conference, SHM Converge. Thank you to the countless members who donated their time to SHM, so that SHM could support hospitalists and their patients.
Now, we are transitioning into a new phase of the pandemic. The medical miracles that are the COVID-19 vaccines have made that possible. Fully vaccinated, I no longer worry that every time someone sneezes, or when I care for patients with a fever, that I am playing a high stakes poker game with my life. Don’t get me wrong; as I write, the Delta variant has a hold on the nation, and I know it’s not over yet. But it does appear as if the medical war on COVID is shifting from national to regional (or even local) responses.
During this new phase, we must rebuild our personal and professional lives. If you haven’t read Retired Lieutenant General Mark Hertling’s perspective piece in the August issue of the Journal of Hospital Medicine, I strongly encourage you to do so. He shares profound lessons on transitioning from active combat that are directly applicable to hospitalists who have been “deployed” battling COVID-19.
SHM will continue to pivot to meet our members’ needs too. We are already gearing up for more in-person education and networking. Chapters are starting to meet in person, and SHM is happy to provide visiting faculty. I will visit members from Florida to Maine and places in between starting this fall! Our Board of Directors and other SHM leaders are also starting to meet with members in person. Our own Leadership Academy will take place at Amelia Island in Florida in October, where we can learn, network, and even decompress. We also can’t wait for SHM Converge 2022 in Nashville, where we hope to reunite with many of you after 2 years of virtual conferences.
Our response to the pandemic, a once in a century crisis where our own safety was at risk, where doing the right thing might mean death or harming loved ones, our response of running into the fire to save lives is truly inspiring. The power of care – for our patients, for our family and friends, and for our hospital medicine community and the community at large – is evident more now than ever.
There have always been good reasons to be proud of being a hospitalist: taking care of the acutely ill, helping hospitals improve, teaching young doctors, and watching my specialty grow by leaps and bounds, to name just a few. But I’ve never been prouder than I am now.
Dr. Howell is the CEO of the Society of Hospital Medicine.
I have been a proud hospitalist for more than 20 years, and yet I have never been prouder to be a hospitalist than now. The pandemic has been brutal, killing more than 600,000 Americans as of this writing. It has stretched the health care system, its doctors, nurses, and other providers to the limit. Yet we will get through it, we are getting through it, and hospitalists deserve a huge portion of the credit.
According to the CDC, there have been over 2.3 million COVID-19 hospitalizations. In my home state of Maryland, between two-thirds and three-quarters of hospitalized COVID patients are cared for on general medical floors, the domain of hospitalists. When hospitals needed COVID units, hospitalists stepped up to design and staff them. When our ICU colleagues needed support, especially in those early dark days, hospitalists stepped in. When our outpatient colleagues were called into the hospital, hospitalists were there to help them on board. When the House of Medicine was in chaos due to COVID-19, hospitalists ran towards that fire. Our previous 20+ years of collective experience made us the ideal specialty to manage the inpatient challenges over the last 18 months.
Need a new clinical schedule by Sunday? Check.
Need help with new clinical protocols? Check.
Need to help other colleagues? Check.
Need to reprogram the EMR? Check.
Need a new way to teach residents and students on the wards? Check.
Need a whole new unit – no, wait – a new hospital wing? No, scratch that – a whole new COVID hospital in a few weeks? Check. (I personally did that last one at the Baltimore Convention Center!)
For me and many hospitalists like me, it is as if the last 20 years were prep work for the pandemic.
Here at SHM, we know the pandemic is hard work – exhausting, even. SHM has been actively focused on supporting hospitalists during this crisis so that hospitalists can focus on patients. Early in the pandemic, SHM quickly pivoted to supply hospitalists with COVID-19 resources in their fight against the coronavirus. Numerous COVID-19 webinars, a COVID addendum to the State of Hospital Medicine Report, and a dedicated COVID issue of the Journal of Hospital Medicine were early and successful information dissemination strategies.
As the world – and hospitalists – dug in for a multi-year pandemic, SHM continued to advance the care of patients by opening our library of educational content for free to anyone. Our Public Policy Committee was active around both COVID-19- and hospitalist-related topics: immigration, telehealth, wellbeing, and financial impacts, to name a few.
As the pandemic slogged on, our Wellbeing Task Force came up with innovative support measures, including a check-in guide for hospitalists and fellow health care workers and dedicated wellness sessions complete with a licensed therapist for members. All the while, despite the restrictions and hurdles the pandemic has thrown our way, SHM members keep meeting and collaborating through virtual chapter events, committee work, special interest groups, and our annual conference, SHM Converge. Thank you to the countless members who donated their time to SHM, so that SHM could support hospitalists and their patients.
Now, we are transitioning into a new phase of the pandemic. The medical miracles that are the COVID-19 vaccines have made that possible. Fully vaccinated, I no longer worry that every time someone sneezes, or when I care for patients with a fever, that I am playing a high stakes poker game with my life. Don’t get me wrong; as I write, the Delta variant has a hold on the nation, and I know it’s not over yet. But it does appear as if the medical war on COVID is shifting from national to regional (or even local) responses.
During this new phase, we must rebuild our personal and professional lives. If you haven’t read Retired Lieutenant General Mark Hertling’s perspective piece in the August issue of the Journal of Hospital Medicine, I strongly encourage you to do so. He shares profound lessons on transitioning from active combat that are directly applicable to hospitalists who have been “deployed” battling COVID-19.
SHM will continue to pivot to meet our members’ needs too. We are already gearing up for more in-person education and networking. Chapters are starting to meet in person, and SHM is happy to provide visiting faculty. I will visit members from Florida to Maine and places in between starting this fall! Our Board of Directors and other SHM leaders are also starting to meet with members in person. Our own Leadership Academy will take place at Amelia Island in Florida in October, where we can learn, network, and even decompress. We also can’t wait for SHM Converge 2022 in Nashville, where we hope to reunite with many of you after 2 years of virtual conferences.
Our response to the pandemic, a once in a century crisis where our own safety was at risk, where doing the right thing might mean death or harming loved ones, our response of running into the fire to save lives is truly inspiring. The power of care – for our patients, for our family and friends, and for our hospital medicine community and the community at large – is evident more now than ever.
There have always been good reasons to be proud of being a hospitalist: taking care of the acutely ill, helping hospitals improve, teaching young doctors, and watching my specialty grow by leaps and bounds, to name just a few. But I’ve never been prouder than I am now.
Dr. Howell is the CEO of the Society of Hospital Medicine.
Converging to build for tomorrow
Last month we converged virtually for our annual conference, SHM Converge – the second time since the start of the coronavirus pandemic. We are thankful for innovations and advancements in technology that have allowed the world, including SHM, to continue connecting us all together. And yet, 18 months in, having forged new roads, experienced unique and life-changing events, we long for the in-person human connection that allows us to share a common experience. At a time of imperatives in our world – a global pandemic, systemic racism, and deep geopolitical divides – more than ever, we need to converge. Isolation only festers, deepening our divisions and conflicts.
In high school, I read Robert Frost’s poem “The Road Not Taken” and clung to the notion of diverging roads and choosing the road less traveled. Like most young people, my years since reading the poem were filled with attempts at forging new paths and experiencing great things – and yet, always feeling unaccomplished. Was Oscar Wilde right when he wrote: “Life imitates Art far more than Art imitates Life?” After all, these past 18 months, we have shared in the traumas of our times, and still, we remain isolated and alone. Our diverse experiences have been real, both tragic and heroic, from east to west, city to country, black to white, and red to blue.
At SHM, it’s time to converge and face the great challenges of our lifetime. A deadly pandemic continues to rage around the world, bringing unprecedented human suffering and loss of lives. In its wake, this pandemic also laid bare the ugly face of systemic racism, brought our deepest divisions to the surface – all threatening the very fabric of our society. This pandemic has been a stress test for health care systems, revealing our vulnerabilities and expanding the chasm of care between urban and rural communities, all in turn worsening our growing health disparities. This moment needs convergence to rekindle connection and solidarity.
Scholars do not interpret “The Road Not Taken” as a recommendation to take the road less traveled. Instead, it is a suggestion that the diverging roads lead to a common place having been “worn about the same” as they “equally lay.” It is true that our roads are unique and shape our lives, but so, too, does the destination and common place our roads lead us to. At that common place, during these taxing times, SHM enables hospitalists to tackle these great challenges.
For over 2 decades of dynamic changes in health care, SHM has been the workshop where hospitalists converged to sharpen clinical skills, improve quality and safety, develop acute care models inside and outside of hospitals, advocate for better health policy and blaze new trails. Though the issues evolved, and new ones emerge, today is no different.
Indeed, this is an historic time. This weighted moment meets us at the crossroads. A moment that demands synergy, cooperation, and creativity. A dynamic change to health care policy, advances in care innovation, renewed prioritization of public health, and rich national discourse on our social fabric; hospitalists are essential to every one of those conversations. SHM has evolved to meet our growing needs, equipping hospitalists with tools to engage at every level, and most importantly, enabled us to find our common place.
Where do we go now? I suggest we continue to take the roads not taken and at the destination, build the map of tomorrow, together.
Dr. Siy is division medical director, hospital specialties, in the departments of hospital medicine and community senior and palliative care at HealthPartners in Bloomington, Minn. He is the new president of SHM.
Last month we converged virtually for our annual conference, SHM Converge – the second time since the start of the coronavirus pandemic. We are thankful for innovations and advancements in technology that have allowed the world, including SHM, to continue connecting us all together. And yet, 18 months in, having forged new roads, experienced unique and life-changing events, we long for the in-person human connection that allows us to share a common experience. At a time of imperatives in our world – a global pandemic, systemic racism, and deep geopolitical divides – more than ever, we need to converge. Isolation only festers, deepening our divisions and conflicts.
In high school, I read Robert Frost’s poem “The Road Not Taken” and clung to the notion of diverging roads and choosing the road less traveled. Like most young people, my years since reading the poem were filled with attempts at forging new paths and experiencing great things – and yet, always feeling unaccomplished. Was Oscar Wilde right when he wrote: “Life imitates Art far more than Art imitates Life?” After all, these past 18 months, we have shared in the traumas of our times, and still, we remain isolated and alone. Our diverse experiences have been real, both tragic and heroic, from east to west, city to country, black to white, and red to blue.
At SHM, it’s time to converge and face the great challenges of our lifetime. A deadly pandemic continues to rage around the world, bringing unprecedented human suffering and loss of lives. In its wake, this pandemic also laid bare the ugly face of systemic racism, brought our deepest divisions to the surface – all threatening the very fabric of our society. This pandemic has been a stress test for health care systems, revealing our vulnerabilities and expanding the chasm of care between urban and rural communities, all in turn worsening our growing health disparities. This moment needs convergence to rekindle connection and solidarity.
Scholars do not interpret “The Road Not Taken” as a recommendation to take the road less traveled. Instead, it is a suggestion that the diverging roads lead to a common place having been “worn about the same” as they “equally lay.” It is true that our roads are unique and shape our lives, but so, too, does the destination and common place our roads lead us to. At that common place, during these taxing times, SHM enables hospitalists to tackle these great challenges.
For over 2 decades of dynamic changes in health care, SHM has been the workshop where hospitalists converged to sharpen clinical skills, improve quality and safety, develop acute care models inside and outside of hospitals, advocate for better health policy and blaze new trails. Though the issues evolved, and new ones emerge, today is no different.
Indeed, this is an historic time. This weighted moment meets us at the crossroads. A moment that demands synergy, cooperation, and creativity. A dynamic change to health care policy, advances in care innovation, renewed prioritization of public health, and rich national discourse on our social fabric; hospitalists are essential to every one of those conversations. SHM has evolved to meet our growing needs, equipping hospitalists with tools to engage at every level, and most importantly, enabled us to find our common place.
Where do we go now? I suggest we continue to take the roads not taken and at the destination, build the map of tomorrow, together.
Dr. Siy is division medical director, hospital specialties, in the departments of hospital medicine and community senior and palliative care at HealthPartners in Bloomington, Minn. He is the new president of SHM.
Last month we converged virtually for our annual conference, SHM Converge – the second time since the start of the coronavirus pandemic. We are thankful for innovations and advancements in technology that have allowed the world, including SHM, to continue connecting us all together. And yet, 18 months in, having forged new roads, experienced unique and life-changing events, we long for the in-person human connection that allows us to share a common experience. At a time of imperatives in our world – a global pandemic, systemic racism, and deep geopolitical divides – more than ever, we need to converge. Isolation only festers, deepening our divisions and conflicts.
In high school, I read Robert Frost’s poem “The Road Not Taken” and clung to the notion of diverging roads and choosing the road less traveled. Like most young people, my years since reading the poem were filled with attempts at forging new paths and experiencing great things – and yet, always feeling unaccomplished. Was Oscar Wilde right when he wrote: “Life imitates Art far more than Art imitates Life?” After all, these past 18 months, we have shared in the traumas of our times, and still, we remain isolated and alone. Our diverse experiences have been real, both tragic and heroic, from east to west, city to country, black to white, and red to blue.
At SHM, it’s time to converge and face the great challenges of our lifetime. A deadly pandemic continues to rage around the world, bringing unprecedented human suffering and loss of lives. In its wake, this pandemic also laid bare the ugly face of systemic racism, brought our deepest divisions to the surface – all threatening the very fabric of our society. This pandemic has been a stress test for health care systems, revealing our vulnerabilities and expanding the chasm of care between urban and rural communities, all in turn worsening our growing health disparities. This moment needs convergence to rekindle connection and solidarity.
Scholars do not interpret “The Road Not Taken” as a recommendation to take the road less traveled. Instead, it is a suggestion that the diverging roads lead to a common place having been “worn about the same” as they “equally lay.” It is true that our roads are unique and shape our lives, but so, too, does the destination and common place our roads lead us to. At that common place, during these taxing times, SHM enables hospitalists to tackle these great challenges.
For over 2 decades of dynamic changes in health care, SHM has been the workshop where hospitalists converged to sharpen clinical skills, improve quality and safety, develop acute care models inside and outside of hospitals, advocate for better health policy and blaze new trails. Though the issues evolved, and new ones emerge, today is no different.
Indeed, this is an historic time. This weighted moment meets us at the crossroads. A moment that demands synergy, cooperation, and creativity. A dynamic change to health care policy, advances in care innovation, renewed prioritization of public health, and rich national discourse on our social fabric; hospitalists are essential to every one of those conversations. SHM has evolved to meet our growing needs, equipping hospitalists with tools to engage at every level, and most importantly, enabled us to find our common place.
Where do we go now? I suggest we continue to take the roads not taken and at the destination, build the map of tomorrow, together.
Dr. Siy is division medical director, hospital specialties, in the departments of hospital medicine and community senior and palliative care at HealthPartners in Bloomington, Minn. He is the new president of SHM.
A tumultuous and unforgettable year
SHM president bids farewell
As my SHM presidency wraps up, it is a good time to reflect on the past year in hospital medicine. Dominated by COVID-19 preparedness, mitigation, and (now) recovery efforts, the impacts of COVID-19 throughout the medical industry have been profound. For hospital medicine, although we have endured work and home stress unlike anything in recent memory, fortunately a few notably good changes have come about as a result of COVID-19.
Hospitalists have proven that we are extremely capable of adapting to rapidly changing evidence-based practice. The old adage of evidence taking 7 years to become mainstream clinical practice certainly has not been the paradigm during COVID-19. In many cases, clinical care pathways were changing by the week, or even by the day. Usage of SHM’s website, HMX, and educational platforms rose exponentially to keep pace with the changing landscape. Information exchange between and among hospital medicine groups was efficient and effective. This is exactly how it should be, with SHM serving as the catalyst for such information exchange.
Hospitalists were able to shift to telehealth care as the need arose. The use of telehealth is now becoming a core competency for hospitalists around the country, and we are leading the way for other specialists in adoption. COVID-19 enabled not only rapid transformation, but also better payer coverage for the use of all types of telehealth services. SHM will remain a source of training and education in telehealth best practices going forward.
Related, hospitalists also found their programs were being asked to become purveyors for remote monitoring and hospital-at-home programs. Because CMS has allowed some reimbursement for these programs, at least during the public health emergency, hospital medicine programs can more feasibly pursue building and sustaining such programs, and SHM can serve as the hub for best practice exchanges in the field.
The pandemic also created a sizable shift in the mindset of the need and enthusiasm for mainstream maintenance of certification. Although there were already questions about the value of high-stakes exams before the pandemic, both within and outside the medical industry, the pandemic created an immediate need to shift away from such exams. Now, the entire pipeline is questioning the value of these high-stakes exams, such as SATs and ACTs for college admissions, Step 1 exams for medical students, and certification exams for physicians. The pandemic has made us question these milestone exams with more scrutiny and has created a sense of urgency for a change to more adult-learner–focused alternatives. SHM will continue to be at the centerpiece of the discussion, as well as the leader in cultivating educational venues for continuous learning.
So where do we go from here?
I am confident that SHM will continue to pay deep attention to the activities that bring value to hospitalists and support changing practice patterns such as telehealth and hospital-at-home work. Not only will SHM serve as a center for best practices and a conduit for networking and information sharing at the national level – there will be significantly more focus on the support and growth of local chapters. SHM realizes that local chapters are a vital source of networking, education, and pipeline development and will continue to increase the resources to make the chapter programs dynamic and inviting for everyone interested in hospital medicine.
While this presidency year was far different than expected, I have continuously been amazed and delighted with the resiliency and endurance of our hospitalists around the country. We stood out at the front lines of the pandemic, with a mission toward service and a relentless commitment to our patients. Although we still have a long way to go before the pandemic is behind us, I firmly believe we are emerging from the haze stronger and more agile than ever. Thank you for allowing me to serve this incredible organization during such a tumultuous and unforgettable year.
Yours in service.
Dr. Scheurer is a hospitalist and chief quality officer, MUSC Health System, Medical University of South Carolina, Charleston. She is the outgoing president of SHM.
SHM president bids farewell
SHM president bids farewell
As my SHM presidency wraps up, it is a good time to reflect on the past year in hospital medicine. Dominated by COVID-19 preparedness, mitigation, and (now) recovery efforts, the impacts of COVID-19 throughout the medical industry have been profound. For hospital medicine, although we have endured work and home stress unlike anything in recent memory, fortunately a few notably good changes have come about as a result of COVID-19.
Hospitalists have proven that we are extremely capable of adapting to rapidly changing evidence-based practice. The old adage of evidence taking 7 years to become mainstream clinical practice certainly has not been the paradigm during COVID-19. In many cases, clinical care pathways were changing by the week, or even by the day. Usage of SHM’s website, HMX, and educational platforms rose exponentially to keep pace with the changing landscape. Information exchange between and among hospital medicine groups was efficient and effective. This is exactly how it should be, with SHM serving as the catalyst for such information exchange.
Hospitalists were able to shift to telehealth care as the need arose. The use of telehealth is now becoming a core competency for hospitalists around the country, and we are leading the way for other specialists in adoption. COVID-19 enabled not only rapid transformation, but also better payer coverage for the use of all types of telehealth services. SHM will remain a source of training and education in telehealth best practices going forward.
Related, hospitalists also found their programs were being asked to become purveyors for remote monitoring and hospital-at-home programs. Because CMS has allowed some reimbursement for these programs, at least during the public health emergency, hospital medicine programs can more feasibly pursue building and sustaining such programs, and SHM can serve as the hub for best practice exchanges in the field.
The pandemic also created a sizable shift in the mindset of the need and enthusiasm for mainstream maintenance of certification. Although there were already questions about the value of high-stakes exams before the pandemic, both within and outside the medical industry, the pandemic created an immediate need to shift away from such exams. Now, the entire pipeline is questioning the value of these high-stakes exams, such as SATs and ACTs for college admissions, Step 1 exams for medical students, and certification exams for physicians. The pandemic has made us question these milestone exams with more scrutiny and has created a sense of urgency for a change to more adult-learner–focused alternatives. SHM will continue to be at the centerpiece of the discussion, as well as the leader in cultivating educational venues for continuous learning.
So where do we go from here?
I am confident that SHM will continue to pay deep attention to the activities that bring value to hospitalists and support changing practice patterns such as telehealth and hospital-at-home work. Not only will SHM serve as a center for best practices and a conduit for networking and information sharing at the national level – there will be significantly more focus on the support and growth of local chapters. SHM realizes that local chapters are a vital source of networking, education, and pipeline development and will continue to increase the resources to make the chapter programs dynamic and inviting for everyone interested in hospital medicine.
While this presidency year was far different than expected, I have continuously been amazed and delighted with the resiliency and endurance of our hospitalists around the country. We stood out at the front lines of the pandemic, with a mission toward service and a relentless commitment to our patients. Although we still have a long way to go before the pandemic is behind us, I firmly believe we are emerging from the haze stronger and more agile than ever. Thank you for allowing me to serve this incredible organization during such a tumultuous and unforgettable year.
Yours in service.
Dr. Scheurer is a hospitalist and chief quality officer, MUSC Health System, Medical University of South Carolina, Charleston. She is the outgoing president of SHM.
As my SHM presidency wraps up, it is a good time to reflect on the past year in hospital medicine. Dominated by COVID-19 preparedness, mitigation, and (now) recovery efforts, the impacts of COVID-19 throughout the medical industry have been profound. For hospital medicine, although we have endured work and home stress unlike anything in recent memory, fortunately a few notably good changes have come about as a result of COVID-19.
Hospitalists have proven that we are extremely capable of adapting to rapidly changing evidence-based practice. The old adage of evidence taking 7 years to become mainstream clinical practice certainly has not been the paradigm during COVID-19. In many cases, clinical care pathways were changing by the week, or even by the day. Usage of SHM’s website, HMX, and educational platforms rose exponentially to keep pace with the changing landscape. Information exchange between and among hospital medicine groups was efficient and effective. This is exactly how it should be, with SHM serving as the catalyst for such information exchange.
Hospitalists were able to shift to telehealth care as the need arose. The use of telehealth is now becoming a core competency for hospitalists around the country, and we are leading the way for other specialists in adoption. COVID-19 enabled not only rapid transformation, but also better payer coverage for the use of all types of telehealth services. SHM will remain a source of training and education in telehealth best practices going forward.
Related, hospitalists also found their programs were being asked to become purveyors for remote monitoring and hospital-at-home programs. Because CMS has allowed some reimbursement for these programs, at least during the public health emergency, hospital medicine programs can more feasibly pursue building and sustaining such programs, and SHM can serve as the hub for best practice exchanges in the field.
The pandemic also created a sizable shift in the mindset of the need and enthusiasm for mainstream maintenance of certification. Although there were already questions about the value of high-stakes exams before the pandemic, both within and outside the medical industry, the pandemic created an immediate need to shift away from such exams. Now, the entire pipeline is questioning the value of these high-stakes exams, such as SATs and ACTs for college admissions, Step 1 exams for medical students, and certification exams for physicians. The pandemic has made us question these milestone exams with more scrutiny and has created a sense of urgency for a change to more adult-learner–focused alternatives. SHM will continue to be at the centerpiece of the discussion, as well as the leader in cultivating educational venues for continuous learning.
So where do we go from here?
I am confident that SHM will continue to pay deep attention to the activities that bring value to hospitalists and support changing practice patterns such as telehealth and hospital-at-home work. Not only will SHM serve as a center for best practices and a conduit for networking and information sharing at the national level – there will be significantly more focus on the support and growth of local chapters. SHM realizes that local chapters are a vital source of networking, education, and pipeline development and will continue to increase the resources to make the chapter programs dynamic and inviting for everyone interested in hospital medicine.
While this presidency year was far different than expected, I have continuously been amazed and delighted with the resiliency and endurance of our hospitalists around the country. We stood out at the front lines of the pandemic, with a mission toward service and a relentless commitment to our patients. Although we still have a long way to go before the pandemic is behind us, I firmly believe we are emerging from the haze stronger and more agile than ever. Thank you for allowing me to serve this incredible organization during such a tumultuous and unforgettable year.
Yours in service.
Dr. Scheurer is a hospitalist and chief quality officer, MUSC Health System, Medical University of South Carolina, Charleston. She is the outgoing president of SHM.
SHM 2021 Awards of Excellence and Junior Investigator Awards
Clinical Leadership for Physicians
Christopher P. Bruti, MD, MPH
Dr. Christopher P. Bruti is the division chief of hospital medicine at Rush University and the program director of Rush’s combined Internal Medicine–Pediatrics Residency Program. He is an associate professor of internal medicine and pediatrics and practices as a hospitalist in both departments.
Dr. Bruti always rises to any challenge that comes his way with empathetic, organized, and insightful leadership. Dr. Bruti is known for his innovation in patient care and optimization practices in the hospital setting – from expanding and optimizing the nonteaching service and a high-functioning observation unit to geolocalization and reorganization of medical teams. While his reputation as a leader was well established before the pandemic hit, the way he rose to the many challenges over the past year has been truly remarkable. After he identified one of the first cases of COVID-19 in his hospital, Dr. Bruti’s leadership was evident. He ensured that his staff was wearing proper PPE, reorganized hospitalist staffing, coordinated onboarding of subspecialists, developed algorithms around testing, and created safety-driven patient transfer strategies.
He is a member of the Rush University Medical Center Medical Executive Committee and is the chair of its Medical Records Committee. He has been recognized by both Internal Medicine and Pediatrics clerkships multiple times for excellence in teaching.
Dr. Bruti became a member of SHM in 2014 and has been extremely active with the Chicago chapter. He has also served on the Quality Improvement and Pediatric Medicine Special Interest Groups.
Clinical Leadership for NPs & PAs
Krystle D. Apodaca, DNP, FHM
Dr. Krystle D. Apodaca is a nurse practitioner hospitalist at the University of New Mexico Hospital, where she is assistant professor of medicine within the university’s Clinician Education Track.
She was one of the first APPs welcomed into the UNM Hospital Medicine division and has been integral not only in the development of UNM’s APP program, but also its APP Hospital Medicine Fellowship, which she helped to cofound. She is a member of the UNM Hospital Medicine Executive Committee as well as its LGBTQ Collaborative.
She is known for her leadership within Project ECHO at UNM, a worldwide program focused on democratizing medical knowledge. She is the co–medical director of its National Nursing Home COVID-19 Safety and Medicaid Quality Improvement Hospitalization Avoidance efforts, both focused on improving nursing home practices. This program, in partnership with the Agency for Healthcare Research and Quality, UNM’s ECHO Institute, and the Institute for Healthcare Improvement, is now a national initiative dedicated to standardizing COVID-19 best practices at nursing homes across the country. To achieve its goals, more than 15,000 nursing homes have been certified and a community of more than 250 training centers has been built through Project ECHO.
Dr. Apodaca has been a member of SHM since 2015. She has been an active member of SHM’s NP/PA Special Interest Group since she joined and was appointed as the first APP president of SHM’s New Mexico chapter in April 2020. Under her leadership, the chapter achieved Gold and Platinum status as well as the Chapter of the Year Award. She is also a Fellow in Hospital Medicine.
Certificate of Leadership in Hospital Medicine
Mihir Patel, MD, MBA, MPH, CLHM, SFHM
The Certificate of Leadership in Hospital Medicine (CLHM) cultivates leadership skills in the context of specific hospital medicine challenges. This designation informs employers – or potential employers – with confidence that a candidate is equipped and ready to lead teams and grow an organization.
Dr. Mihir Patel serves as medical director of virtual medicine and a full-time hospitalist at Ballad Health in Johnson City, Tenn. He also works part time as a telehospitalist with Sound Physicians, covering multiple hospitals in California and Washington State. He has previously served in a number of administrative roles including medical director of hospitalist program, chief of staff, and director of medical informatics committee, in addition to working as hospitalist in both rural and urban hospitals. He is cofounder and president of the Blue Ridge Chapter of the Society of Hospital Medicine.
Dr. Mihir’s research and clinical interests focus on integration of telemedicine, electronic medical records, and principles of lean healthcare to reduce waste and cost of care while improving overall quality and safety.
Humanitarian Services
Eileen Barrett, MD, MPH, MACP, SFHM
Dr. Eileen Barrett is an internal medicine hospitalist at the University of New Mexico, where she also serves as associate professor of medicine and the director of Continuing Medical Education in the Office of Continuous Professional Learning.
In addition to current clinical and educational roles at UNM, Dr. Barrett has extensive leadership experience as the former director of Graduate Medical Education Wellness Initiatives, the current District 10 Chair of SHM, as chair of a multiorganizational Diversity Equity and Inclusion (DEI) Collaborative Task Force, and as a former regent of the American College of Physicians.
Her tremendous efforts in humanitarian services are reflected in her dedication to supporting communities in need. In 2015, Dr. Barrett traveled to Sierra Leone, where she served as an Ebola response clinician. There, she helped to develop safer care protocols, including initiating morning huddles, standardizing onboarding, and improving medication administration and documentation. These skills were developed while she worked for the Navajo Area Indian Health Service (including as an infection control consultant) for more than 9 years and in volunteering at the Myanmar-Thai border with refugees. Her work abroad helped support her training for directing UNM hospitalist COVID-19 Operations while also providing direct care.
Dr. Barrett has represented the specialty of hospital medicine both nationally and internationally. She has served on national committees and spoken from the perspective of an academic and community hospitalist leader on issues such as performance management, patient engagement, DEI, and professional fulfillment.
She has been a member of SHM since 2014 and has served as cochair of the three most recent Innovations Poster Competitions. Dr. Barrett is a former president of SHM’s New Mexico chapter where under her leadership the chapter received SHM’s Outstanding Chapter Award in 2018. She is a dedicated member of SHM’s Physicians in Training Committee and Chapter Support Committee. Dr. Barrett is an elected member of the Gold Humanism Honor Society, received a 2019 Exemplary Mentor Award from the American Medical Women’s Association, and is a Senior Fellow in Hospital Medicine.
Leadership for Practice Management
Leah Lleras, MS
Leah Lleras is the division administrator for the University of Colorado, Anschutz Medical Campus, and holds a Master of Science Management and Organization degree from the University of Colorado.
Her leadership as a practice manager is exemplified through her efforts in challenges of salary inequity. After joining the Division of Hospital Medicine in 2018, Ms. Lleras was successful in launching and achieving compensation equity and transparency across the department. She has demonstrated an incredible ability to collaborate with clinical leadership to marry the vision of clinical leaders with the administrative support required to turn a vision into a reality. During the COVID-19 pandemic, Ms. Lleras has been instrumental in ensuring that the division was prepared and supported to care for an influx of new patients. She did this by leading emergent onboarding of new practitioners, strategizing financial management of hazard pay for frontline clinicians, and creating a streamlined budget system during rapid change.
Ms. Lleras joined the Society in 2018 and has been an active member of the Rocky Mountain Chapter and the Hospital Medicine Administrator Special Interest Group.
Outstanding Service
Robert Zipper, MD, MMM, SFHM
Dr. Robert Zipper is a physician advisor and senior policy advisor for Sound Physicians, with more than 20 years of clinical experience as a hospital medicine leader.
He has a diverse background in quality and patient safety, hospitalist program design, and performance management. He began working as a hospitalist in 1999, in private practice. In 2006, he launched his career at Sound, where he began as a hospitalist but eventually managed Sound’s West Coast programs. In 2017, he was appointed Sound vice president of innovation technology. He later became Sound’s leader for healthcare policy, and now serves as a senior policy advisor for Sound, and physician advisor within the Advisory Services line.
Dr. Zipper has been a longtime supporter and advocate of SHM and the field of hospital medicine since joining in 2005. He attended his first Leadership Academy in 2006 and went on to serve as facilitator four times. His passion for SHM’s conferences is evident, as he has presented at three Annual Conferences alongside notable SHM leaders. He has been active in a variety of committees, including Quality and Safety, Leadership, and Performance Measurement and Reporting.
He is a member of the Society’s Public Policy Committee, and his insight has elevated hospital medicine both in the eyes of peer specialties and in discussions with the Centers for Medicare and Medicaid Services. Dr. Zipper has joined a number of calls with key Capitol Hill and CMS staff to help advocate for issues affecting hospital medicine. His ability to explain issues clearly and eloquently has helped stakeholders better understand the issues and move them forward on lawmakers’ agendas.
Research
S. Ryan Greysen, MD, MHS, SFHM
Dr. S. Ryan Greysen is chief of the Section of Hospital Medicine and associate professor at the University of Pennsylvania. He is the executive director for the Center for Evidence-based Practice (CEP) which serves all hospitals in the University of Pennsylvania Health System.
Dr. Greysen’s work comprises more than 80 peer-reviewed publications focused on improving outcomes of care for older adults during and after acute illness. Prior to arriving at Penn, he practiced at the University of California, San Francisco, where the impact of his work was extremely visible on the wards. He helped implement care pathways for an Acute Care for Elders (ACE) unit that uses evidence-based protocols and order sets to prevent functional decline and delirium of vulnerable seniors.
At Penn, he has continued to champion care for seniors and has supported other successful programs focused on vulnerable populations: SOAR (Supporting Older Adults at Risk), STEP (Supporting Transitions and Empowering Patients), and MED (Mental health Engagement navigation & Delivery).
During the COVID-19 pandemic, Dr. Greysen helped to accelerate the synthesis of emerging evidence through CEP and the Hospital Medicine Re-engineering Network (HOMERuN) to produce rapid evidence summaries in record speed. These reports have been broadly disseminated across other networks, such as AHRQ and the VA Evidence Synthesis Program.
Since joining the Society 10 years ago, Dr. Greysen has been an engaged member of SHM’s Greater Philadelphia Chapter and has held leadership roles on SHM’s Research Committee and the JHM Editorial Team as an associate editor. He has presented at multiple SHM annual conferences and is an ambassador of the specialty and of the importance of research in hospital medicine.
He is a Senior Fellow in Hospital Medicine.
Teaching
Grace C. Huang, MD
Dr. Grace C. Huang is an educator and hospitalist at Beth Israel Deaconess Medical Center and associate professor of medicine at Harvard Medical School who epitomizes commitment to education and lifelong learning.
Dr. Huang’s nationally recognized hospitalist expertise spans medical education and innovation, administrative management, and editorial leadership. She was among the early hospitalist pioneers who helped to transform how residents were trained to do procedures. Her early work led to the creation of one of the first procedure rotations for residents in the country – an RCT on central line simulation, the validation of a central line placement instrument, and a systematic review on procedural training for nonsurgeons.
Dr. Huang is vice chair for career development and mentoring in the department of medicine and oversees faculty development at the institutional level. She leads a Harvard Medical School–wide medical education fellowship for faculty and codirects the BIDMC Academy. On a broader scale, her efforts in the field have helped to catalyze the growth of computer-based simulation, define new standards for critical thinking education, and influence high-value care and invasive bedside procedure teaching approaches. Finally, she is editor-in-chief of MedEdPORTAL, an innovative journal of the Association of American Medical Colleges that publishes and disseminates educational resources.
Dr. Huang has been awarded the Gordon J. Strewler Mentoring of Resident Research Award in 2018, the Robert Stone Award for Excellence in Teaching Award, and most recently the A. Clifford Barger Excellence in Mentoring Award at Harvard Medical School, among many others. She is an editorial board member of Academic Medicine.
Dr. Huang joined SHM in 2010. Since then, she has been an engaged member of the Boston Chapter and has regularly participated in SHM’s annual conferences. She was also a member of SHM’s Practice Analysis Committee for 7 years.
Teamwork in Quality Improvement
Intermountain Healthcare
Intermountain Healthcare is a not-for-profit health system based in Salt Lake City serving the needs of patients primarily in Utah, Idaho, and Nevada. Intermountain recently reimagined its leadership structure with an integrated approach focused on developing and implementing common goals across its 23-hospital healthcare system, which was previously divided into regions. With key focus areas including communication, best practices, and goal setting, this structure has helped to combat former fragmentation struggles by creating an environment that provides a consistent high-level care experience regardless of the treatment center a patient selects.
With this reorganization came improved structure allowing for a unique team-based approach while still promoting clear communication lines across the 23 hospitals. This innovative Med/Surg Operations Lane allowed for flexible adaptation to the rapidly changing landscape of the COVID-19 pandemic. Intermountain Healthcare utilized its new framework to ensure crisis-ready operations by defining best practices through real-time literature review and teaming with ED, ICU, and Nursing to create COVID-19 workflows, order sets, and dashboards. Capacity issues were addressed with a variety of strategies: (1) daily systemwide huddles to facilitate load leveling between hospitals; (2) the use of telehealth for early discharges; and (3) remote patient monitoring and admission to the “Intermountain at Home” program, which preserved the ability to deliver critical surgical services.
This new value model clearly sets Intermountain apart from its peers.
Diversity
Lilia Cervantes, MD
Dr. Lilia Cervantes is associate professor in the department of medicine at Denver Health Medical Center and the University of Colorado, where she demonstrates an unparalleled commitment to diversity through her patient care, community service efforts, research, and health policy activism.
Following her internal medicine residency at the University of Colorado in 2008, Dr. Cervantes went on to obtain her master of science degree in clinical science, and became associate professor of medicine and a hospitalist at Denver Health Medical Center. In addition to her patient-centric roles at Denver Health, Dr. Cervantes has held a variety of roles in the health equity space. These include founding Denver Health Medical Center’s Health Equity Learning Series and the Healthcare Interest Program, a pre–health pipeline program for undergraduate students interested in a healthcare career.
Dr. Cervantes attributes her passion for becoming a physician to her background as a bilingual Latina who grew up in poverty. She says that her upbringing allows her to use this unique lens to connect with her diverse patient population and to advocate for marginalized communities and eliminate structural inequities.
Her experience with Hilda, an undocumented immigrant with kidney failure, was the catalyst for further research on marginalized patients without access to healthcare, which earned her interviews with NPR and CNN’s Chief Health Correspondent Dr. Sanjay Gupta. Her research and advocacy led to Colorado Medicaid’s expanding access to scheduled dialysis for undocumented immigrants with kidney failure. Upon announcement of the change, Dr. Cervantes was recognized as the driving force whose research informed the decision.
During the COVID-19 pandemic, Dr. Cervantes has worked diligently to launch research projects and create grant-funded programs to reduce the disproportionate burden of COVID-19 cases and deaths in the Latinx community in Denver. One of her studies centers on the Latinx community – through qualitative interviews of Latinx who had survived a COVID-19 hospitalization, Dr. Cervantes learned about the challenges faced during the pandemic. These findings informed local and national interventions to reduce COVID-19 in the Latinx community.
She has received numerous accolades, including the inaugural Outstanding Service to the Community in 2019 by Denver Health, the Florence Rena Sabin Award from the University of Colorado, and awards from the community – Health Equity Champion Award from the Center for Health Progress and the Unsung Heroine Award from the Latina First Foundation. She serves on several boards including two community-based organizations – the Center for Health Progress and Vuela for Health.
Dr. Cervantes has been an active member of SHM since 2009 and served as keynote speaker for the annual “Summit of the Rockies” Rocky Mountain Chapter SHM conference, “The role of advocacy: Moving the needle towards health equity.”
Junior Investigator Award
Matthew Pappas, MD, MPH, FHM
Dr. Matthew Pappas is a staff physician at the Cleveland Clinic, where he serves as assistant professor at the Lerner College of Medicine and Research Investigator at the Center for Value-Based Care Research.
Dr. Pappas completed his residency at the University of Michigan Health System and a postdoctoral fellowship with the VA Ann Arbor Healthcare System in 2016. Currently a hospitalist, he believes in addressing the tension between evidence-based and personal decisions, a fundamental hypothesis of his research career. As a Fellow, he created a model to predict the benefit of bridging anticoagulation for patients with atrial fibrillation. He sees his research mission as addressing the importance of these balanced decisions.
In 2019, Dr. Pappas secured a K08 award from the National Heart, Lung, and Blood Institute, and has turned his attention to preoperative cardiac testing and perioperative outcomes. He has published two manuscripts from this project, with a robust pipeline of others in progress.
He was recognized for his research by the Society of General Internal Medicine in 2018 with the Hamolsky Award for best abstract and had one of his research articles included in the Top 10 Articles of 2019 by the Journal of Hospital Medicine. Dr. Pappas has ongoing research support from the National Heart, Lung and Blood Institute.
He has been a member of SHM since 2015 and currently serves on the Perioperative Special Interest Group and Research Committee.
Clinical Leadership for Physicians
Christopher P. Bruti, MD, MPH
Dr. Christopher P. Bruti is the division chief of hospital medicine at Rush University and the program director of Rush’s combined Internal Medicine–Pediatrics Residency Program. He is an associate professor of internal medicine and pediatrics and practices as a hospitalist in both departments.
Dr. Bruti always rises to any challenge that comes his way with empathetic, organized, and insightful leadership. Dr. Bruti is known for his innovation in patient care and optimization practices in the hospital setting – from expanding and optimizing the nonteaching service and a high-functioning observation unit to geolocalization and reorganization of medical teams. While his reputation as a leader was well established before the pandemic hit, the way he rose to the many challenges over the past year has been truly remarkable. After he identified one of the first cases of COVID-19 in his hospital, Dr. Bruti’s leadership was evident. He ensured that his staff was wearing proper PPE, reorganized hospitalist staffing, coordinated onboarding of subspecialists, developed algorithms around testing, and created safety-driven patient transfer strategies.
He is a member of the Rush University Medical Center Medical Executive Committee and is the chair of its Medical Records Committee. He has been recognized by both Internal Medicine and Pediatrics clerkships multiple times for excellence in teaching.
Dr. Bruti became a member of SHM in 2014 and has been extremely active with the Chicago chapter. He has also served on the Quality Improvement and Pediatric Medicine Special Interest Groups.
Clinical Leadership for NPs & PAs
Krystle D. Apodaca, DNP, FHM
Dr. Krystle D. Apodaca is a nurse practitioner hospitalist at the University of New Mexico Hospital, where she is assistant professor of medicine within the university’s Clinician Education Track.
She was one of the first APPs welcomed into the UNM Hospital Medicine division and has been integral not only in the development of UNM’s APP program, but also its APP Hospital Medicine Fellowship, which she helped to cofound. She is a member of the UNM Hospital Medicine Executive Committee as well as its LGBTQ Collaborative.
She is known for her leadership within Project ECHO at UNM, a worldwide program focused on democratizing medical knowledge. She is the co–medical director of its National Nursing Home COVID-19 Safety and Medicaid Quality Improvement Hospitalization Avoidance efforts, both focused on improving nursing home practices. This program, in partnership with the Agency for Healthcare Research and Quality, UNM’s ECHO Institute, and the Institute for Healthcare Improvement, is now a national initiative dedicated to standardizing COVID-19 best practices at nursing homes across the country. To achieve its goals, more than 15,000 nursing homes have been certified and a community of more than 250 training centers has been built through Project ECHO.
Dr. Apodaca has been a member of SHM since 2015. She has been an active member of SHM’s NP/PA Special Interest Group since she joined and was appointed as the first APP president of SHM’s New Mexico chapter in April 2020. Under her leadership, the chapter achieved Gold and Platinum status as well as the Chapter of the Year Award. She is also a Fellow in Hospital Medicine.
Certificate of Leadership in Hospital Medicine
Mihir Patel, MD, MBA, MPH, CLHM, SFHM
The Certificate of Leadership in Hospital Medicine (CLHM) cultivates leadership skills in the context of specific hospital medicine challenges. This designation informs employers – or potential employers – with confidence that a candidate is equipped and ready to lead teams and grow an organization.
Dr. Mihir Patel serves as medical director of virtual medicine and a full-time hospitalist at Ballad Health in Johnson City, Tenn. He also works part time as a telehospitalist with Sound Physicians, covering multiple hospitals in California and Washington State. He has previously served in a number of administrative roles including medical director of hospitalist program, chief of staff, and director of medical informatics committee, in addition to working as hospitalist in both rural and urban hospitals. He is cofounder and president of the Blue Ridge Chapter of the Society of Hospital Medicine.
Dr. Mihir’s research and clinical interests focus on integration of telemedicine, electronic medical records, and principles of lean healthcare to reduce waste and cost of care while improving overall quality and safety.
Humanitarian Services
Eileen Barrett, MD, MPH, MACP, SFHM
Dr. Eileen Barrett is an internal medicine hospitalist at the University of New Mexico, where she also serves as associate professor of medicine and the director of Continuing Medical Education in the Office of Continuous Professional Learning.
In addition to current clinical and educational roles at UNM, Dr. Barrett has extensive leadership experience as the former director of Graduate Medical Education Wellness Initiatives, the current District 10 Chair of SHM, as chair of a multiorganizational Diversity Equity and Inclusion (DEI) Collaborative Task Force, and as a former regent of the American College of Physicians.
Her tremendous efforts in humanitarian services are reflected in her dedication to supporting communities in need. In 2015, Dr. Barrett traveled to Sierra Leone, where she served as an Ebola response clinician. There, she helped to develop safer care protocols, including initiating morning huddles, standardizing onboarding, and improving medication administration and documentation. These skills were developed while she worked for the Navajo Area Indian Health Service (including as an infection control consultant) for more than 9 years and in volunteering at the Myanmar-Thai border with refugees. Her work abroad helped support her training for directing UNM hospitalist COVID-19 Operations while also providing direct care.
Dr. Barrett has represented the specialty of hospital medicine both nationally and internationally. She has served on national committees and spoken from the perspective of an academic and community hospitalist leader on issues such as performance management, patient engagement, DEI, and professional fulfillment.
She has been a member of SHM since 2014 and has served as cochair of the three most recent Innovations Poster Competitions. Dr. Barrett is a former president of SHM’s New Mexico chapter where under her leadership the chapter received SHM’s Outstanding Chapter Award in 2018. She is a dedicated member of SHM’s Physicians in Training Committee and Chapter Support Committee. Dr. Barrett is an elected member of the Gold Humanism Honor Society, received a 2019 Exemplary Mentor Award from the American Medical Women’s Association, and is a Senior Fellow in Hospital Medicine.
Leadership for Practice Management
Leah Lleras, MS
Leah Lleras is the division administrator for the University of Colorado, Anschutz Medical Campus, and holds a Master of Science Management and Organization degree from the University of Colorado.
Her leadership as a practice manager is exemplified through her efforts in challenges of salary inequity. After joining the Division of Hospital Medicine in 2018, Ms. Lleras was successful in launching and achieving compensation equity and transparency across the department. She has demonstrated an incredible ability to collaborate with clinical leadership to marry the vision of clinical leaders with the administrative support required to turn a vision into a reality. During the COVID-19 pandemic, Ms. Lleras has been instrumental in ensuring that the division was prepared and supported to care for an influx of new patients. She did this by leading emergent onboarding of new practitioners, strategizing financial management of hazard pay for frontline clinicians, and creating a streamlined budget system during rapid change.
Ms. Lleras joined the Society in 2018 and has been an active member of the Rocky Mountain Chapter and the Hospital Medicine Administrator Special Interest Group.
Outstanding Service
Robert Zipper, MD, MMM, SFHM
Dr. Robert Zipper is a physician advisor and senior policy advisor for Sound Physicians, with more than 20 years of clinical experience as a hospital medicine leader.
He has a diverse background in quality and patient safety, hospitalist program design, and performance management. He began working as a hospitalist in 1999, in private practice. In 2006, he launched his career at Sound, where he began as a hospitalist but eventually managed Sound’s West Coast programs. In 2017, he was appointed Sound vice president of innovation technology. He later became Sound’s leader for healthcare policy, and now serves as a senior policy advisor for Sound, and physician advisor within the Advisory Services line.
Dr. Zipper has been a longtime supporter and advocate of SHM and the field of hospital medicine since joining in 2005. He attended his first Leadership Academy in 2006 and went on to serve as facilitator four times. His passion for SHM’s conferences is evident, as he has presented at three Annual Conferences alongside notable SHM leaders. He has been active in a variety of committees, including Quality and Safety, Leadership, and Performance Measurement and Reporting.
He is a member of the Society’s Public Policy Committee, and his insight has elevated hospital medicine both in the eyes of peer specialties and in discussions with the Centers for Medicare and Medicaid Services. Dr. Zipper has joined a number of calls with key Capitol Hill and CMS staff to help advocate for issues affecting hospital medicine. His ability to explain issues clearly and eloquently has helped stakeholders better understand the issues and move them forward on lawmakers’ agendas.
Research
S. Ryan Greysen, MD, MHS, SFHM
Dr. S. Ryan Greysen is chief of the Section of Hospital Medicine and associate professor at the University of Pennsylvania. He is the executive director for the Center for Evidence-based Practice (CEP) which serves all hospitals in the University of Pennsylvania Health System.
Dr. Greysen’s work comprises more than 80 peer-reviewed publications focused on improving outcomes of care for older adults during and after acute illness. Prior to arriving at Penn, he practiced at the University of California, San Francisco, where the impact of his work was extremely visible on the wards. He helped implement care pathways for an Acute Care for Elders (ACE) unit that uses evidence-based protocols and order sets to prevent functional decline and delirium of vulnerable seniors.
At Penn, he has continued to champion care for seniors and has supported other successful programs focused on vulnerable populations: SOAR (Supporting Older Adults at Risk), STEP (Supporting Transitions and Empowering Patients), and MED (Mental health Engagement navigation & Delivery).
During the COVID-19 pandemic, Dr. Greysen helped to accelerate the synthesis of emerging evidence through CEP and the Hospital Medicine Re-engineering Network (HOMERuN) to produce rapid evidence summaries in record speed. These reports have been broadly disseminated across other networks, such as AHRQ and the VA Evidence Synthesis Program.
Since joining the Society 10 years ago, Dr. Greysen has been an engaged member of SHM’s Greater Philadelphia Chapter and has held leadership roles on SHM’s Research Committee and the JHM Editorial Team as an associate editor. He has presented at multiple SHM annual conferences and is an ambassador of the specialty and of the importance of research in hospital medicine.
He is a Senior Fellow in Hospital Medicine.
Teaching
Grace C. Huang, MD
Dr. Grace C. Huang is an educator and hospitalist at Beth Israel Deaconess Medical Center and associate professor of medicine at Harvard Medical School who epitomizes commitment to education and lifelong learning.
Dr. Huang’s nationally recognized hospitalist expertise spans medical education and innovation, administrative management, and editorial leadership. She was among the early hospitalist pioneers who helped to transform how residents were trained to do procedures. Her early work led to the creation of one of the first procedure rotations for residents in the country – an RCT on central line simulation, the validation of a central line placement instrument, and a systematic review on procedural training for nonsurgeons.
Dr. Huang is vice chair for career development and mentoring in the department of medicine and oversees faculty development at the institutional level. She leads a Harvard Medical School–wide medical education fellowship for faculty and codirects the BIDMC Academy. On a broader scale, her efforts in the field have helped to catalyze the growth of computer-based simulation, define new standards for critical thinking education, and influence high-value care and invasive bedside procedure teaching approaches. Finally, she is editor-in-chief of MedEdPORTAL, an innovative journal of the Association of American Medical Colleges that publishes and disseminates educational resources.
Dr. Huang has been awarded the Gordon J. Strewler Mentoring of Resident Research Award in 2018, the Robert Stone Award for Excellence in Teaching Award, and most recently the A. Clifford Barger Excellence in Mentoring Award at Harvard Medical School, among many others. She is an editorial board member of Academic Medicine.
Dr. Huang joined SHM in 2010. Since then, she has been an engaged member of the Boston Chapter and has regularly participated in SHM’s annual conferences. She was also a member of SHM’s Practice Analysis Committee for 7 years.
Teamwork in Quality Improvement
Intermountain Healthcare
Intermountain Healthcare is a not-for-profit health system based in Salt Lake City serving the needs of patients primarily in Utah, Idaho, and Nevada. Intermountain recently reimagined its leadership structure with an integrated approach focused on developing and implementing common goals across its 23-hospital healthcare system, which was previously divided into regions. With key focus areas including communication, best practices, and goal setting, this structure has helped to combat former fragmentation struggles by creating an environment that provides a consistent high-level care experience regardless of the treatment center a patient selects.
With this reorganization came improved structure allowing for a unique team-based approach while still promoting clear communication lines across the 23 hospitals. This innovative Med/Surg Operations Lane allowed for flexible adaptation to the rapidly changing landscape of the COVID-19 pandemic. Intermountain Healthcare utilized its new framework to ensure crisis-ready operations by defining best practices through real-time literature review and teaming with ED, ICU, and Nursing to create COVID-19 workflows, order sets, and dashboards. Capacity issues were addressed with a variety of strategies: (1) daily systemwide huddles to facilitate load leveling between hospitals; (2) the use of telehealth for early discharges; and (3) remote patient monitoring and admission to the “Intermountain at Home” program, which preserved the ability to deliver critical surgical services.
This new value model clearly sets Intermountain apart from its peers.
Diversity
Lilia Cervantes, MD
Dr. Lilia Cervantes is associate professor in the department of medicine at Denver Health Medical Center and the University of Colorado, where she demonstrates an unparalleled commitment to diversity through her patient care, community service efforts, research, and health policy activism.
Following her internal medicine residency at the University of Colorado in 2008, Dr. Cervantes went on to obtain her master of science degree in clinical science, and became associate professor of medicine and a hospitalist at Denver Health Medical Center. In addition to her patient-centric roles at Denver Health, Dr. Cervantes has held a variety of roles in the health equity space. These include founding Denver Health Medical Center’s Health Equity Learning Series and the Healthcare Interest Program, a pre–health pipeline program for undergraduate students interested in a healthcare career.
Dr. Cervantes attributes her passion for becoming a physician to her background as a bilingual Latina who grew up in poverty. She says that her upbringing allows her to use this unique lens to connect with her diverse patient population and to advocate for marginalized communities and eliminate structural inequities.
Her experience with Hilda, an undocumented immigrant with kidney failure, was the catalyst for further research on marginalized patients without access to healthcare, which earned her interviews with NPR and CNN’s Chief Health Correspondent Dr. Sanjay Gupta. Her research and advocacy led to Colorado Medicaid’s expanding access to scheduled dialysis for undocumented immigrants with kidney failure. Upon announcement of the change, Dr. Cervantes was recognized as the driving force whose research informed the decision.
During the COVID-19 pandemic, Dr. Cervantes has worked diligently to launch research projects and create grant-funded programs to reduce the disproportionate burden of COVID-19 cases and deaths in the Latinx community in Denver. One of her studies centers on the Latinx community – through qualitative interviews of Latinx who had survived a COVID-19 hospitalization, Dr. Cervantes learned about the challenges faced during the pandemic. These findings informed local and national interventions to reduce COVID-19 in the Latinx community.
She has received numerous accolades, including the inaugural Outstanding Service to the Community in 2019 by Denver Health, the Florence Rena Sabin Award from the University of Colorado, and awards from the community – Health Equity Champion Award from the Center for Health Progress and the Unsung Heroine Award from the Latina First Foundation. She serves on several boards including two community-based organizations – the Center for Health Progress and Vuela for Health.
Dr. Cervantes has been an active member of SHM since 2009 and served as keynote speaker for the annual “Summit of the Rockies” Rocky Mountain Chapter SHM conference, “The role of advocacy: Moving the needle towards health equity.”
Junior Investigator Award
Matthew Pappas, MD, MPH, FHM
Dr. Matthew Pappas is a staff physician at the Cleveland Clinic, where he serves as assistant professor at the Lerner College of Medicine and Research Investigator at the Center for Value-Based Care Research.
Dr. Pappas completed his residency at the University of Michigan Health System and a postdoctoral fellowship with the VA Ann Arbor Healthcare System in 2016. Currently a hospitalist, he believes in addressing the tension between evidence-based and personal decisions, a fundamental hypothesis of his research career. As a Fellow, he created a model to predict the benefit of bridging anticoagulation for patients with atrial fibrillation. He sees his research mission as addressing the importance of these balanced decisions.
In 2019, Dr. Pappas secured a K08 award from the National Heart, Lung, and Blood Institute, and has turned his attention to preoperative cardiac testing and perioperative outcomes. He has published two manuscripts from this project, with a robust pipeline of others in progress.
He was recognized for his research by the Society of General Internal Medicine in 2018 with the Hamolsky Award for best abstract and had one of his research articles included in the Top 10 Articles of 2019 by the Journal of Hospital Medicine. Dr. Pappas has ongoing research support from the National Heart, Lung and Blood Institute.
He has been a member of SHM since 2015 and currently serves on the Perioperative Special Interest Group and Research Committee.
Clinical Leadership for Physicians
Christopher P. Bruti, MD, MPH
Dr. Christopher P. Bruti is the division chief of hospital medicine at Rush University and the program director of Rush’s combined Internal Medicine–Pediatrics Residency Program. He is an associate professor of internal medicine and pediatrics and practices as a hospitalist in both departments.
Dr. Bruti always rises to any challenge that comes his way with empathetic, organized, and insightful leadership. Dr. Bruti is known for his innovation in patient care and optimization practices in the hospital setting – from expanding and optimizing the nonteaching service and a high-functioning observation unit to geolocalization and reorganization of medical teams. While his reputation as a leader was well established before the pandemic hit, the way he rose to the many challenges over the past year has been truly remarkable. After he identified one of the first cases of COVID-19 in his hospital, Dr. Bruti’s leadership was evident. He ensured that his staff was wearing proper PPE, reorganized hospitalist staffing, coordinated onboarding of subspecialists, developed algorithms around testing, and created safety-driven patient transfer strategies.
He is a member of the Rush University Medical Center Medical Executive Committee and is the chair of its Medical Records Committee. He has been recognized by both Internal Medicine and Pediatrics clerkships multiple times for excellence in teaching.
Dr. Bruti became a member of SHM in 2014 and has been extremely active with the Chicago chapter. He has also served on the Quality Improvement and Pediatric Medicine Special Interest Groups.
Clinical Leadership for NPs & PAs
Krystle D. Apodaca, DNP, FHM
Dr. Krystle D. Apodaca is a nurse practitioner hospitalist at the University of New Mexico Hospital, where she is assistant professor of medicine within the university’s Clinician Education Track.
She was one of the first APPs welcomed into the UNM Hospital Medicine division and has been integral not only in the development of UNM’s APP program, but also its APP Hospital Medicine Fellowship, which she helped to cofound. She is a member of the UNM Hospital Medicine Executive Committee as well as its LGBTQ Collaborative.
She is known for her leadership within Project ECHO at UNM, a worldwide program focused on democratizing medical knowledge. She is the co–medical director of its National Nursing Home COVID-19 Safety and Medicaid Quality Improvement Hospitalization Avoidance efforts, both focused on improving nursing home practices. This program, in partnership with the Agency for Healthcare Research and Quality, UNM’s ECHO Institute, and the Institute for Healthcare Improvement, is now a national initiative dedicated to standardizing COVID-19 best practices at nursing homes across the country. To achieve its goals, more than 15,000 nursing homes have been certified and a community of more than 250 training centers has been built through Project ECHO.
Dr. Apodaca has been a member of SHM since 2015. She has been an active member of SHM’s NP/PA Special Interest Group since she joined and was appointed as the first APP president of SHM’s New Mexico chapter in April 2020. Under her leadership, the chapter achieved Gold and Platinum status as well as the Chapter of the Year Award. She is also a Fellow in Hospital Medicine.
Certificate of Leadership in Hospital Medicine
Mihir Patel, MD, MBA, MPH, CLHM, SFHM
The Certificate of Leadership in Hospital Medicine (CLHM) cultivates leadership skills in the context of specific hospital medicine challenges. This designation informs employers – or potential employers – with confidence that a candidate is equipped and ready to lead teams and grow an organization.
Dr. Mihir Patel serves as medical director of virtual medicine and a full-time hospitalist at Ballad Health in Johnson City, Tenn. He also works part time as a telehospitalist with Sound Physicians, covering multiple hospitals in California and Washington State. He has previously served in a number of administrative roles including medical director of hospitalist program, chief of staff, and director of medical informatics committee, in addition to working as hospitalist in both rural and urban hospitals. He is cofounder and president of the Blue Ridge Chapter of the Society of Hospital Medicine.
Dr. Mihir’s research and clinical interests focus on integration of telemedicine, electronic medical records, and principles of lean healthcare to reduce waste and cost of care while improving overall quality and safety.
Humanitarian Services
Eileen Barrett, MD, MPH, MACP, SFHM
Dr. Eileen Barrett is an internal medicine hospitalist at the University of New Mexico, where she also serves as associate professor of medicine and the director of Continuing Medical Education in the Office of Continuous Professional Learning.
In addition to current clinical and educational roles at UNM, Dr. Barrett has extensive leadership experience as the former director of Graduate Medical Education Wellness Initiatives, the current District 10 Chair of SHM, as chair of a multiorganizational Diversity Equity and Inclusion (DEI) Collaborative Task Force, and as a former regent of the American College of Physicians.
Her tremendous efforts in humanitarian services are reflected in her dedication to supporting communities in need. In 2015, Dr. Barrett traveled to Sierra Leone, where she served as an Ebola response clinician. There, she helped to develop safer care protocols, including initiating morning huddles, standardizing onboarding, and improving medication administration and documentation. These skills were developed while she worked for the Navajo Area Indian Health Service (including as an infection control consultant) for more than 9 years and in volunteering at the Myanmar-Thai border with refugees. Her work abroad helped support her training for directing UNM hospitalist COVID-19 Operations while also providing direct care.
Dr. Barrett has represented the specialty of hospital medicine both nationally and internationally. She has served on national committees and spoken from the perspective of an academic and community hospitalist leader on issues such as performance management, patient engagement, DEI, and professional fulfillment.
She has been a member of SHM since 2014 and has served as cochair of the three most recent Innovations Poster Competitions. Dr. Barrett is a former president of SHM’s New Mexico chapter where under her leadership the chapter received SHM’s Outstanding Chapter Award in 2018. She is a dedicated member of SHM’s Physicians in Training Committee and Chapter Support Committee. Dr. Barrett is an elected member of the Gold Humanism Honor Society, received a 2019 Exemplary Mentor Award from the American Medical Women’s Association, and is a Senior Fellow in Hospital Medicine.
Leadership for Practice Management
Leah Lleras, MS
Leah Lleras is the division administrator for the University of Colorado, Anschutz Medical Campus, and holds a Master of Science Management and Organization degree from the University of Colorado.
Her leadership as a practice manager is exemplified through her efforts in challenges of salary inequity. After joining the Division of Hospital Medicine in 2018, Ms. Lleras was successful in launching and achieving compensation equity and transparency across the department. She has demonstrated an incredible ability to collaborate with clinical leadership to marry the vision of clinical leaders with the administrative support required to turn a vision into a reality. During the COVID-19 pandemic, Ms. Lleras has been instrumental in ensuring that the division was prepared and supported to care for an influx of new patients. She did this by leading emergent onboarding of new practitioners, strategizing financial management of hazard pay for frontline clinicians, and creating a streamlined budget system during rapid change.
Ms. Lleras joined the Society in 2018 and has been an active member of the Rocky Mountain Chapter and the Hospital Medicine Administrator Special Interest Group.
Outstanding Service
Robert Zipper, MD, MMM, SFHM
Dr. Robert Zipper is a physician advisor and senior policy advisor for Sound Physicians, with more than 20 years of clinical experience as a hospital medicine leader.
He has a diverse background in quality and patient safety, hospitalist program design, and performance management. He began working as a hospitalist in 1999, in private practice. In 2006, he launched his career at Sound, where he began as a hospitalist but eventually managed Sound’s West Coast programs. In 2017, he was appointed Sound vice president of innovation technology. He later became Sound’s leader for healthcare policy, and now serves as a senior policy advisor for Sound, and physician advisor within the Advisory Services line.
Dr. Zipper has been a longtime supporter and advocate of SHM and the field of hospital medicine since joining in 2005. He attended his first Leadership Academy in 2006 and went on to serve as facilitator four times. His passion for SHM’s conferences is evident, as he has presented at three Annual Conferences alongside notable SHM leaders. He has been active in a variety of committees, including Quality and Safety, Leadership, and Performance Measurement and Reporting.
He is a member of the Society’s Public Policy Committee, and his insight has elevated hospital medicine both in the eyes of peer specialties and in discussions with the Centers for Medicare and Medicaid Services. Dr. Zipper has joined a number of calls with key Capitol Hill and CMS staff to help advocate for issues affecting hospital medicine. His ability to explain issues clearly and eloquently has helped stakeholders better understand the issues and move them forward on lawmakers’ agendas.
Research
S. Ryan Greysen, MD, MHS, SFHM
Dr. S. Ryan Greysen is chief of the Section of Hospital Medicine and associate professor at the University of Pennsylvania. He is the executive director for the Center for Evidence-based Practice (CEP) which serves all hospitals in the University of Pennsylvania Health System.
Dr. Greysen’s work comprises more than 80 peer-reviewed publications focused on improving outcomes of care for older adults during and after acute illness. Prior to arriving at Penn, he practiced at the University of California, San Francisco, where the impact of his work was extremely visible on the wards. He helped implement care pathways for an Acute Care for Elders (ACE) unit that uses evidence-based protocols and order sets to prevent functional decline and delirium of vulnerable seniors.
At Penn, he has continued to champion care for seniors and has supported other successful programs focused on vulnerable populations: SOAR (Supporting Older Adults at Risk), STEP (Supporting Transitions and Empowering Patients), and MED (Mental health Engagement navigation & Delivery).
During the COVID-19 pandemic, Dr. Greysen helped to accelerate the synthesis of emerging evidence through CEP and the Hospital Medicine Re-engineering Network (HOMERuN) to produce rapid evidence summaries in record speed. These reports have been broadly disseminated across other networks, such as AHRQ and the VA Evidence Synthesis Program.
Since joining the Society 10 years ago, Dr. Greysen has been an engaged member of SHM’s Greater Philadelphia Chapter and has held leadership roles on SHM’s Research Committee and the JHM Editorial Team as an associate editor. He has presented at multiple SHM annual conferences and is an ambassador of the specialty and of the importance of research in hospital medicine.
He is a Senior Fellow in Hospital Medicine.
Teaching
Grace C. Huang, MD
Dr. Grace C. Huang is an educator and hospitalist at Beth Israel Deaconess Medical Center and associate professor of medicine at Harvard Medical School who epitomizes commitment to education and lifelong learning.
Dr. Huang’s nationally recognized hospitalist expertise spans medical education and innovation, administrative management, and editorial leadership. She was among the early hospitalist pioneers who helped to transform how residents were trained to do procedures. Her early work led to the creation of one of the first procedure rotations for residents in the country – an RCT on central line simulation, the validation of a central line placement instrument, and a systematic review on procedural training for nonsurgeons.
Dr. Huang is vice chair for career development and mentoring in the department of medicine and oversees faculty development at the institutional level. She leads a Harvard Medical School–wide medical education fellowship for faculty and codirects the BIDMC Academy. On a broader scale, her efforts in the field have helped to catalyze the growth of computer-based simulation, define new standards for critical thinking education, and influence high-value care and invasive bedside procedure teaching approaches. Finally, she is editor-in-chief of MedEdPORTAL, an innovative journal of the Association of American Medical Colleges that publishes and disseminates educational resources.
Dr. Huang has been awarded the Gordon J. Strewler Mentoring of Resident Research Award in 2018, the Robert Stone Award for Excellence in Teaching Award, and most recently the A. Clifford Barger Excellence in Mentoring Award at Harvard Medical School, among many others. She is an editorial board member of Academic Medicine.
Dr. Huang joined SHM in 2010. Since then, she has been an engaged member of the Boston Chapter and has regularly participated in SHM’s annual conferences. She was also a member of SHM’s Practice Analysis Committee for 7 years.
Teamwork in Quality Improvement
Intermountain Healthcare
Intermountain Healthcare is a not-for-profit health system based in Salt Lake City serving the needs of patients primarily in Utah, Idaho, and Nevada. Intermountain recently reimagined its leadership structure with an integrated approach focused on developing and implementing common goals across its 23-hospital healthcare system, which was previously divided into regions. With key focus areas including communication, best practices, and goal setting, this structure has helped to combat former fragmentation struggles by creating an environment that provides a consistent high-level care experience regardless of the treatment center a patient selects.
With this reorganization came improved structure allowing for a unique team-based approach while still promoting clear communication lines across the 23 hospitals. This innovative Med/Surg Operations Lane allowed for flexible adaptation to the rapidly changing landscape of the COVID-19 pandemic. Intermountain Healthcare utilized its new framework to ensure crisis-ready operations by defining best practices through real-time literature review and teaming with ED, ICU, and Nursing to create COVID-19 workflows, order sets, and dashboards. Capacity issues were addressed with a variety of strategies: (1) daily systemwide huddles to facilitate load leveling between hospitals; (2) the use of telehealth for early discharges; and (3) remote patient monitoring and admission to the “Intermountain at Home” program, which preserved the ability to deliver critical surgical services.
This new value model clearly sets Intermountain apart from its peers.
Diversity
Lilia Cervantes, MD
Dr. Lilia Cervantes is associate professor in the department of medicine at Denver Health Medical Center and the University of Colorado, where she demonstrates an unparalleled commitment to diversity through her patient care, community service efforts, research, and health policy activism.
Following her internal medicine residency at the University of Colorado in 2008, Dr. Cervantes went on to obtain her master of science degree in clinical science, and became associate professor of medicine and a hospitalist at Denver Health Medical Center. In addition to her patient-centric roles at Denver Health, Dr. Cervantes has held a variety of roles in the health equity space. These include founding Denver Health Medical Center’s Health Equity Learning Series and the Healthcare Interest Program, a pre–health pipeline program for undergraduate students interested in a healthcare career.
Dr. Cervantes attributes her passion for becoming a physician to her background as a bilingual Latina who grew up in poverty. She says that her upbringing allows her to use this unique lens to connect with her diverse patient population and to advocate for marginalized communities and eliminate structural inequities.
Her experience with Hilda, an undocumented immigrant with kidney failure, was the catalyst for further research on marginalized patients without access to healthcare, which earned her interviews with NPR and CNN’s Chief Health Correspondent Dr. Sanjay Gupta. Her research and advocacy led to Colorado Medicaid’s expanding access to scheduled dialysis for undocumented immigrants with kidney failure. Upon announcement of the change, Dr. Cervantes was recognized as the driving force whose research informed the decision.
During the COVID-19 pandemic, Dr. Cervantes has worked diligently to launch research projects and create grant-funded programs to reduce the disproportionate burden of COVID-19 cases and deaths in the Latinx community in Denver. One of her studies centers on the Latinx community – through qualitative interviews of Latinx who had survived a COVID-19 hospitalization, Dr. Cervantes learned about the challenges faced during the pandemic. These findings informed local and national interventions to reduce COVID-19 in the Latinx community.
She has received numerous accolades, including the inaugural Outstanding Service to the Community in 2019 by Denver Health, the Florence Rena Sabin Award from the University of Colorado, and awards from the community – Health Equity Champion Award from the Center for Health Progress and the Unsung Heroine Award from the Latina First Foundation. She serves on several boards including two community-based organizations – the Center for Health Progress and Vuela for Health.
Dr. Cervantes has been an active member of SHM since 2009 and served as keynote speaker for the annual “Summit of the Rockies” Rocky Mountain Chapter SHM conference, “The role of advocacy: Moving the needle towards health equity.”
Junior Investigator Award
Matthew Pappas, MD, MPH, FHM
Dr. Matthew Pappas is a staff physician at the Cleveland Clinic, where he serves as assistant professor at the Lerner College of Medicine and Research Investigator at the Center for Value-Based Care Research.
Dr. Pappas completed his residency at the University of Michigan Health System and a postdoctoral fellowship with the VA Ann Arbor Healthcare System in 2016. Currently a hospitalist, he believes in addressing the tension between evidence-based and personal decisions, a fundamental hypothesis of his research career. As a Fellow, he created a model to predict the benefit of bridging anticoagulation for patients with atrial fibrillation. He sees his research mission as addressing the importance of these balanced decisions.
In 2019, Dr. Pappas secured a K08 award from the National Heart, Lung, and Blood Institute, and has turned his attention to preoperative cardiac testing and perioperative outcomes. He has published two manuscripts from this project, with a robust pipeline of others in progress.
He was recognized for his research by the Society of General Internal Medicine in 2018 with the Hamolsky Award for best abstract and had one of his research articles included in the Top 10 Articles of 2019 by the Journal of Hospital Medicine. Dr. Pappas has ongoing research support from the National Heart, Lung and Blood Institute.
He has been a member of SHM since 2015 and currently serves on the Perioperative Special Interest Group and Research Committee.
FROM SHM CONVERGE 2021
SHM names new Masters in Hospital Medicine at Converge 2021
This year, the Society of Hospital Medicine will induct three new Masters in Hospital Medicine (MHM), the society’s highest professional honor.
SHM first introduced the MHM designation in 2010. The honor is reserved for hospitalists who have uniquely distinguished themselves in the specialty through the excellence and significance of their contributions to hospital medicine specifically and healthcare as a whole. SHM members are nominated for MHM consideration, and the SHM Board of Directors rigorously reviews qualifications and selects each year’s MHM class.
The three hospitalists receiving the MHM designation at SHM Converge 2021 are Dr. Nasim Afsar, Dr. Shaun D. Frost, and Dr. Jeffrey L. Schnipper.
Nasim Afsar, MD, MBA, MHM
Dr. Nasim Afsar has been elected a Master in Hospital Medicine, honoring her unwavering dedication to hospital medicine and the Society as an accomplished medical leader.
She is known for her accomplishments in establishing and optimizing complex systems of care in the ambulatory and inpatient settings. Her contributions to hospital medicine can be seen through her extensive leadership experience in health care operations, quality, finance, and management.
Dr. Afsar received her MD from the UC Davis School of Medicine, and went on to complete her residency and internship at UCSD and UCLA, internal medicine programs. She currently serves as the chief operating officer for ambulatory care for UCI Health, with the vision of delivering flawless care for the population of patients in Orange County, Calif.
Over her career, Dr. Afsar has led the development and successful implementation of forward-thinking and ambitious healthcare quality strategies across multiple organizations. Her work in patient safety and quality improvement has earned her numerous accolades and awards, including the 2011 John M. Eisenberg Award.
She served on SHM’s Board of Directors from April 2012 through April 2020, including as president and treasurer. During her time on the board, she was instrumental in defining SHM’s role in population health.
Dr. Afsar has held a variety of positions within the Society, including as chair of SHM’s Hospital Quality & Patient Safety Committee, founder and past copresident of SHM’s Los Angeles Chapter, and as faculty at numerous annual conferences. She was an esteemed mentor within SHM’s Project BOOST, a program within SHM’s Center for Quality Improvement focused on care transitions, and served as an associate editor of the Journal of Hospital Medicine for nearly 13 years.
Dr. Afsar is a hospital medicine leader and true champion for our Society and for our specialty. She epitomizes what it means to be a passionate, driven, and accomplished hospital medicine pioneer.
Shaun D. Frost, MD, MHM
Dr. Shaun D. Frost has been elected a Master in Hospital Medicine, celebrating his enduring commitment to hospital medicine and to the Society for more than 20 years.
After completing his internal medicine residency at the University of Texas, Southwestern Medical School in 1998, he launched his career at the Cleveland Clinic Foundation, where he was a clinical assistant professor of internal medicine at Penn State’s College of Medicine.
His contributions to hospital medicine can be seen through his comprehensive leadership background, commitment to medical education, innovation in hospitalist program operations, and various publications. He is also well known for his mentorship of young hospitalist leaders.
Dr. Frost currently serves as the associate medical director of care delivery systems at HealthPartners Health Insurance Plan. He is a practicing hospitalist at Regions Hospital in St. Paul, Minn., and is assistant professor at the University of Minnesota’s Medical School. Prior to this role, he worked at the Cleveland Clinic as the director of Nonteaching Inpatient Services for 6 years, and also served as the Northeast Region chief medical officer of Cogent Healthcare from 2006 to 2012 where he standardized program operations through structured leadership training according to phased priorities and critical functions.
Dr. Frost is well known for his expansive contributions to the Society of Hospital Medicine, and was recognized by SHM in 2005 with the National Award for Clinical Excellence.
Dr. Frost joined the Society in 1999, and soon thereafter founded and led the Northeast Ohio Chapter. His influence, leadership, and guidance helped to shape the creation of SHM’s Chapter Program, which is an integral part of the Society, connecting hospitalists at the local level.
He served on SHM’s Board of Directors for 6 years, including as president and treasurer. He has spoken at many of SHM’s annual conferences, participated on annual meeting planning committees, and served as course director for the annual meeting’s Perioperative Medicine Precourse. He also has served as a facilitator at SHM’s Leadership Academies.
Dr. Frost has led and actively participated in numerous SHM committees, councils, and workgroups, including service as the chair of SHM’s Membership Committee for 5 years. In fact, the SHM fellow designations, including this very distinction, the Master in Hospital Medicine, originated within this committee under his leadership.
During his tenure as SHM president in 2012-2013, he helped to focus the organization’s work to define hospital medicine’s strengths and benefits to healthcare, culminating in the publication of the “Key Principles and Characteristics of an Effective Hospital Medicine Group.”
Dr. Frost is a specialty vanguard, innovator, and SHM leader. He demonstrates what it means to be a passionate and dedicated hospital medicine professional in his community and within the field at-large.
Jeffrey L. Schnipper, MD, MPH, MHM
Dr. Jeffrey L. Schnipper has been elected a Master in Hospital Medicine, honoring his commitment to hospital medicine as an accomplished hospitalist, researcher, and quality improvement enthusiast.
He graduated from Harvard Medical School in 1996 and went on to receive his master’s degree in public health from the Harvard School of Public Health in 2001. Dr. Schnipper also completed his residency, along with a General Medicine Fellowship, at Massachusetts General Hospital in 2001.
Dr. Schnipper currently serves as the director of clinical research in Brigham and Women’s Hospital’s Hospital Medicine Unit. He also serves as the research director of its General Internal Medicine and Primary Care Division and the fellowship director of the Harvard-Brigham Research Fellowship in Hospital Medicine. He is an associate physician at Brigham and Women’s Hospital and is professor of medicine at Harvard Medical School.
His contributions to hospital medicine are demonstrated through his research efforts focused on improving the quality of healthcare delivery for general medical patients, including inpatient diabetes management, care transitions, medication reconciliation, and hospital at home care. His medication reconciliation research project (known as MARQUIS) was funded through AHRQ and led to a 5+ year partnership with the SHM Center for Quality Improvement. When Dr. Schnipper obtained a second AHRQ grant for the MARQUIS2 study, he also partnered with SHM’s Center for Quality Improvement.
Dr. Schnipper joined the Society in 2005 and remains an engaged member of the Boston Association of Academic Hospital Medicine Chapter. He has been a member of SHM’s Annual Conference Committee and serves on the editorial team of the Journal of Hospital Medicine as an associate editor. He has been invited to speak at numerous SHM annual conferences. His research efforts and impact on the medical field can be found in over 150 peer-reviewed publications including JHM, JAMA Internal Medicine, Annals of Internal Medicine, and the Journal of the American Medical Informatics Association.
Dr. Schnipper has received numerous awards and honors throughout his career, including SHM’s Excellence in Research Award in 2013. He is an established researcher, educator, and physician with a broad spectrum of clinical interests that embody what it means to be a hospitalist leader and a top-notch patient care provider.
This year, the Society of Hospital Medicine will induct three new Masters in Hospital Medicine (MHM), the society’s highest professional honor.
SHM first introduced the MHM designation in 2010. The honor is reserved for hospitalists who have uniquely distinguished themselves in the specialty through the excellence and significance of their contributions to hospital medicine specifically and healthcare as a whole. SHM members are nominated for MHM consideration, and the SHM Board of Directors rigorously reviews qualifications and selects each year’s MHM class.
The three hospitalists receiving the MHM designation at SHM Converge 2021 are Dr. Nasim Afsar, Dr. Shaun D. Frost, and Dr. Jeffrey L. Schnipper.
Nasim Afsar, MD, MBA, MHM
Dr. Nasim Afsar has been elected a Master in Hospital Medicine, honoring her unwavering dedication to hospital medicine and the Society as an accomplished medical leader.
She is known for her accomplishments in establishing and optimizing complex systems of care in the ambulatory and inpatient settings. Her contributions to hospital medicine can be seen through her extensive leadership experience in health care operations, quality, finance, and management.
Dr. Afsar received her MD from the UC Davis School of Medicine, and went on to complete her residency and internship at UCSD and UCLA, internal medicine programs. She currently serves as the chief operating officer for ambulatory care for UCI Health, with the vision of delivering flawless care for the population of patients in Orange County, Calif.
Over her career, Dr. Afsar has led the development and successful implementation of forward-thinking and ambitious healthcare quality strategies across multiple organizations. Her work in patient safety and quality improvement has earned her numerous accolades and awards, including the 2011 John M. Eisenberg Award.
She served on SHM’s Board of Directors from April 2012 through April 2020, including as president and treasurer. During her time on the board, she was instrumental in defining SHM’s role in population health.
Dr. Afsar has held a variety of positions within the Society, including as chair of SHM’s Hospital Quality & Patient Safety Committee, founder and past copresident of SHM’s Los Angeles Chapter, and as faculty at numerous annual conferences. She was an esteemed mentor within SHM’s Project BOOST, a program within SHM’s Center for Quality Improvement focused on care transitions, and served as an associate editor of the Journal of Hospital Medicine for nearly 13 years.
Dr. Afsar is a hospital medicine leader and true champion for our Society and for our specialty. She epitomizes what it means to be a passionate, driven, and accomplished hospital medicine pioneer.
Shaun D. Frost, MD, MHM
Dr. Shaun D. Frost has been elected a Master in Hospital Medicine, celebrating his enduring commitment to hospital medicine and to the Society for more than 20 years.
After completing his internal medicine residency at the University of Texas, Southwestern Medical School in 1998, he launched his career at the Cleveland Clinic Foundation, where he was a clinical assistant professor of internal medicine at Penn State’s College of Medicine.
His contributions to hospital medicine can be seen through his comprehensive leadership background, commitment to medical education, innovation in hospitalist program operations, and various publications. He is also well known for his mentorship of young hospitalist leaders.
Dr. Frost currently serves as the associate medical director of care delivery systems at HealthPartners Health Insurance Plan. He is a practicing hospitalist at Regions Hospital in St. Paul, Minn., and is assistant professor at the University of Minnesota’s Medical School. Prior to this role, he worked at the Cleveland Clinic as the director of Nonteaching Inpatient Services for 6 years, and also served as the Northeast Region chief medical officer of Cogent Healthcare from 2006 to 2012 where he standardized program operations through structured leadership training according to phased priorities and critical functions.
Dr. Frost is well known for his expansive contributions to the Society of Hospital Medicine, and was recognized by SHM in 2005 with the National Award for Clinical Excellence.
Dr. Frost joined the Society in 1999, and soon thereafter founded and led the Northeast Ohio Chapter. His influence, leadership, and guidance helped to shape the creation of SHM’s Chapter Program, which is an integral part of the Society, connecting hospitalists at the local level.
He served on SHM’s Board of Directors for 6 years, including as president and treasurer. He has spoken at many of SHM’s annual conferences, participated on annual meeting planning committees, and served as course director for the annual meeting’s Perioperative Medicine Precourse. He also has served as a facilitator at SHM’s Leadership Academies.
Dr. Frost has led and actively participated in numerous SHM committees, councils, and workgroups, including service as the chair of SHM’s Membership Committee for 5 years. In fact, the SHM fellow designations, including this very distinction, the Master in Hospital Medicine, originated within this committee under his leadership.
During his tenure as SHM president in 2012-2013, he helped to focus the organization’s work to define hospital medicine’s strengths and benefits to healthcare, culminating in the publication of the “Key Principles and Characteristics of an Effective Hospital Medicine Group.”
Dr. Frost is a specialty vanguard, innovator, and SHM leader. He demonstrates what it means to be a passionate and dedicated hospital medicine professional in his community and within the field at-large.
Jeffrey L. Schnipper, MD, MPH, MHM
Dr. Jeffrey L. Schnipper has been elected a Master in Hospital Medicine, honoring his commitment to hospital medicine as an accomplished hospitalist, researcher, and quality improvement enthusiast.
He graduated from Harvard Medical School in 1996 and went on to receive his master’s degree in public health from the Harvard School of Public Health in 2001. Dr. Schnipper also completed his residency, along with a General Medicine Fellowship, at Massachusetts General Hospital in 2001.
Dr. Schnipper currently serves as the director of clinical research in Brigham and Women’s Hospital’s Hospital Medicine Unit. He also serves as the research director of its General Internal Medicine and Primary Care Division and the fellowship director of the Harvard-Brigham Research Fellowship in Hospital Medicine. He is an associate physician at Brigham and Women’s Hospital and is professor of medicine at Harvard Medical School.
His contributions to hospital medicine are demonstrated through his research efforts focused on improving the quality of healthcare delivery for general medical patients, including inpatient diabetes management, care transitions, medication reconciliation, and hospital at home care. His medication reconciliation research project (known as MARQUIS) was funded through AHRQ and led to a 5+ year partnership with the SHM Center for Quality Improvement. When Dr. Schnipper obtained a second AHRQ grant for the MARQUIS2 study, he also partnered with SHM’s Center for Quality Improvement.
Dr. Schnipper joined the Society in 2005 and remains an engaged member of the Boston Association of Academic Hospital Medicine Chapter. He has been a member of SHM’s Annual Conference Committee and serves on the editorial team of the Journal of Hospital Medicine as an associate editor. He has been invited to speak at numerous SHM annual conferences. His research efforts and impact on the medical field can be found in over 150 peer-reviewed publications including JHM, JAMA Internal Medicine, Annals of Internal Medicine, and the Journal of the American Medical Informatics Association.
Dr. Schnipper has received numerous awards and honors throughout his career, including SHM’s Excellence in Research Award in 2013. He is an established researcher, educator, and physician with a broad spectrum of clinical interests that embody what it means to be a hospitalist leader and a top-notch patient care provider.
This year, the Society of Hospital Medicine will induct three new Masters in Hospital Medicine (MHM), the society’s highest professional honor.
SHM first introduced the MHM designation in 2010. The honor is reserved for hospitalists who have uniquely distinguished themselves in the specialty through the excellence and significance of their contributions to hospital medicine specifically and healthcare as a whole. SHM members are nominated for MHM consideration, and the SHM Board of Directors rigorously reviews qualifications and selects each year’s MHM class.
The three hospitalists receiving the MHM designation at SHM Converge 2021 are Dr. Nasim Afsar, Dr. Shaun D. Frost, and Dr. Jeffrey L. Schnipper.
Nasim Afsar, MD, MBA, MHM
Dr. Nasim Afsar has been elected a Master in Hospital Medicine, honoring her unwavering dedication to hospital medicine and the Society as an accomplished medical leader.
She is known for her accomplishments in establishing and optimizing complex systems of care in the ambulatory and inpatient settings. Her contributions to hospital medicine can be seen through her extensive leadership experience in health care operations, quality, finance, and management.
Dr. Afsar received her MD from the UC Davis School of Medicine, and went on to complete her residency and internship at UCSD and UCLA, internal medicine programs. She currently serves as the chief operating officer for ambulatory care for UCI Health, with the vision of delivering flawless care for the population of patients in Orange County, Calif.
Over her career, Dr. Afsar has led the development and successful implementation of forward-thinking and ambitious healthcare quality strategies across multiple organizations. Her work in patient safety and quality improvement has earned her numerous accolades and awards, including the 2011 John M. Eisenberg Award.
She served on SHM’s Board of Directors from April 2012 through April 2020, including as president and treasurer. During her time on the board, she was instrumental in defining SHM’s role in population health.
Dr. Afsar has held a variety of positions within the Society, including as chair of SHM’s Hospital Quality & Patient Safety Committee, founder and past copresident of SHM’s Los Angeles Chapter, and as faculty at numerous annual conferences. She was an esteemed mentor within SHM’s Project BOOST, a program within SHM’s Center for Quality Improvement focused on care transitions, and served as an associate editor of the Journal of Hospital Medicine for nearly 13 years.
Dr. Afsar is a hospital medicine leader and true champion for our Society and for our specialty. She epitomizes what it means to be a passionate, driven, and accomplished hospital medicine pioneer.
Shaun D. Frost, MD, MHM
Dr. Shaun D. Frost has been elected a Master in Hospital Medicine, celebrating his enduring commitment to hospital medicine and to the Society for more than 20 years.
After completing his internal medicine residency at the University of Texas, Southwestern Medical School in 1998, he launched his career at the Cleveland Clinic Foundation, where he was a clinical assistant professor of internal medicine at Penn State’s College of Medicine.
His contributions to hospital medicine can be seen through his comprehensive leadership background, commitment to medical education, innovation in hospitalist program operations, and various publications. He is also well known for his mentorship of young hospitalist leaders.
Dr. Frost currently serves as the associate medical director of care delivery systems at HealthPartners Health Insurance Plan. He is a practicing hospitalist at Regions Hospital in St. Paul, Minn., and is assistant professor at the University of Minnesota’s Medical School. Prior to this role, he worked at the Cleveland Clinic as the director of Nonteaching Inpatient Services for 6 years, and also served as the Northeast Region chief medical officer of Cogent Healthcare from 2006 to 2012 where he standardized program operations through structured leadership training according to phased priorities and critical functions.
Dr. Frost is well known for his expansive contributions to the Society of Hospital Medicine, and was recognized by SHM in 2005 with the National Award for Clinical Excellence.
Dr. Frost joined the Society in 1999, and soon thereafter founded and led the Northeast Ohio Chapter. His influence, leadership, and guidance helped to shape the creation of SHM’s Chapter Program, which is an integral part of the Society, connecting hospitalists at the local level.
He served on SHM’s Board of Directors for 6 years, including as president and treasurer. He has spoken at many of SHM’s annual conferences, participated on annual meeting planning committees, and served as course director for the annual meeting’s Perioperative Medicine Precourse. He also has served as a facilitator at SHM’s Leadership Academies.
Dr. Frost has led and actively participated in numerous SHM committees, councils, and workgroups, including service as the chair of SHM’s Membership Committee for 5 years. In fact, the SHM fellow designations, including this very distinction, the Master in Hospital Medicine, originated within this committee under his leadership.
During his tenure as SHM president in 2012-2013, he helped to focus the organization’s work to define hospital medicine’s strengths and benefits to healthcare, culminating in the publication of the “Key Principles and Characteristics of an Effective Hospital Medicine Group.”
Dr. Frost is a specialty vanguard, innovator, and SHM leader. He demonstrates what it means to be a passionate and dedicated hospital medicine professional in his community and within the field at-large.
Jeffrey L. Schnipper, MD, MPH, MHM
Dr. Jeffrey L. Schnipper has been elected a Master in Hospital Medicine, honoring his commitment to hospital medicine as an accomplished hospitalist, researcher, and quality improvement enthusiast.
He graduated from Harvard Medical School in 1996 and went on to receive his master’s degree in public health from the Harvard School of Public Health in 2001. Dr. Schnipper also completed his residency, along with a General Medicine Fellowship, at Massachusetts General Hospital in 2001.
Dr. Schnipper currently serves as the director of clinical research in Brigham and Women’s Hospital’s Hospital Medicine Unit. He also serves as the research director of its General Internal Medicine and Primary Care Division and the fellowship director of the Harvard-Brigham Research Fellowship in Hospital Medicine. He is an associate physician at Brigham and Women’s Hospital and is professor of medicine at Harvard Medical School.
His contributions to hospital medicine are demonstrated through his research efforts focused on improving the quality of healthcare delivery for general medical patients, including inpatient diabetes management, care transitions, medication reconciliation, and hospital at home care. His medication reconciliation research project (known as MARQUIS) was funded through AHRQ and led to a 5+ year partnership with the SHM Center for Quality Improvement. When Dr. Schnipper obtained a second AHRQ grant for the MARQUIS2 study, he also partnered with SHM’s Center for Quality Improvement.
Dr. Schnipper joined the Society in 2005 and remains an engaged member of the Boston Association of Academic Hospital Medicine Chapter. He has been a member of SHM’s Annual Conference Committee and serves on the editorial team of the Journal of Hospital Medicine as an associate editor. He has been invited to speak at numerous SHM annual conferences. His research efforts and impact on the medical field can be found in over 150 peer-reviewed publications including JHM, JAMA Internal Medicine, Annals of Internal Medicine, and the Journal of the American Medical Informatics Association.
Dr. Schnipper has received numerous awards and honors throughout his career, including SHM’s Excellence in Research Award in 2013. He is an established researcher, educator, and physician with a broad spectrum of clinical interests that embody what it means to be a hospitalist leader and a top-notch patient care provider.
FROM SHM CONVERGE 2021
U.S. Surgeon General Vivek Murthy to Speak at SHM Converge
U.S. Surgeon General, Vice Admiral Vivek H. Murthy, MD, MBA, will be a keynote speaker at SHM Converge, the Society of Hospital Meidicine’s annual conference.
Dr. Murthy will discuss burnout and well-being in health care, key themes of the conference, during a fireside chat with Danielle Scheurer, MD, MSCR, SFHM, president of SHM’s board of directors. The conversation will be held on Thursday, May 6, 2021 from 1:30 to 2:00 p.m. ET.
“It is an honor to welcome Dr. Murthy back to SHM’s annual conference during a time when his leadership is more important than ever,” said Eric E. Howell, MD, MHM, chief executive officer of SHM. “Dr. Murthy is dedicated to the health of the American people and to the well-being of those who care for them. I know his message will resonate with hospitalists who have been on the front lines of the pandemic since day one. They are key to navigating the future of our nation’s health care system.”
Dr. Murthy has devoted himself to improving public health through service, clinical care, research, education, and entrepreneurship. In addition to clinical practice, Dr. Murthy has two decades of experience in improving health in communities around the world and served as the 19th U.S. Surgeon General from 2014 to 2017, prior to being reappointed with an expanded role earlier in 2021. As “America’s Doctor,” the Surgeon General’s role is to provide clear, consistent guidance and healthcare resources for the public, ensuring to reach the nation’s most vulnerable communities.
“As we guide our nation out of the pandemic, hospitalists can look to Dr. Murthy as a leader and innovator who will do what is best for our hospitalist community and the patients they serve,” Dr. Scheurer said. “Dr. Murthy will provide a unique perspective to help hospitalists care for themselves during a time when they have been hyper-focused on caring for others.”
In addition to Dr. Murthy, SHM Converge will feature three keynote speakers who will address pressing topics in hospital medicine:
- Mark Hertling, DBA: Coming Out of Combat: Post-Pandemic Recovery
- Vineet Arora, MD, MAPP, MHM: Hospitalists Healing: Surviving, Salvaging, Sustaining, and Succeeding for a Pandemic World
- Larry Wellikson, MD, MHM: Out of COVID and Into the Light: Hospitalists More Essential Than Ever
SHM Converge is the premier educational experience for hospital medicine professionals. This year’s virtual conference will be held from May 3-7, 2021 and offers 21 educational tracks, more than 250 speakers, advanced learning courses, networking opportunities, a scientific abstract competition, and more. SHM Converge On Demand is also available until 2024, including the opportunity to earn additional continuing medical education credit.
To register for SHM Converge, visit shmconverge.org. If you are a member of the media who would like to obtain a press pass, email media@hospitalmedicine.org.
U.S. Surgeon General, Vice Admiral Vivek H. Murthy, MD, MBA, will be a keynote speaker at SHM Converge, the Society of Hospital Meidicine’s annual conference.
Dr. Murthy will discuss burnout and well-being in health care, key themes of the conference, during a fireside chat with Danielle Scheurer, MD, MSCR, SFHM, president of SHM’s board of directors. The conversation will be held on Thursday, May 6, 2021 from 1:30 to 2:00 p.m. ET.
“It is an honor to welcome Dr. Murthy back to SHM’s annual conference during a time when his leadership is more important than ever,” said Eric E. Howell, MD, MHM, chief executive officer of SHM. “Dr. Murthy is dedicated to the health of the American people and to the well-being of those who care for them. I know his message will resonate with hospitalists who have been on the front lines of the pandemic since day one. They are key to navigating the future of our nation’s health care system.”
Dr. Murthy has devoted himself to improving public health through service, clinical care, research, education, and entrepreneurship. In addition to clinical practice, Dr. Murthy has two decades of experience in improving health in communities around the world and served as the 19th U.S. Surgeon General from 2014 to 2017, prior to being reappointed with an expanded role earlier in 2021. As “America’s Doctor,” the Surgeon General’s role is to provide clear, consistent guidance and healthcare resources for the public, ensuring to reach the nation’s most vulnerable communities.
“As we guide our nation out of the pandemic, hospitalists can look to Dr. Murthy as a leader and innovator who will do what is best for our hospitalist community and the patients they serve,” Dr. Scheurer said. “Dr. Murthy will provide a unique perspective to help hospitalists care for themselves during a time when they have been hyper-focused on caring for others.”
In addition to Dr. Murthy, SHM Converge will feature three keynote speakers who will address pressing topics in hospital medicine:
- Mark Hertling, DBA: Coming Out of Combat: Post-Pandemic Recovery
- Vineet Arora, MD, MAPP, MHM: Hospitalists Healing: Surviving, Salvaging, Sustaining, and Succeeding for a Pandemic World
- Larry Wellikson, MD, MHM: Out of COVID and Into the Light: Hospitalists More Essential Than Ever
SHM Converge is the premier educational experience for hospital medicine professionals. This year’s virtual conference will be held from May 3-7, 2021 and offers 21 educational tracks, more than 250 speakers, advanced learning courses, networking opportunities, a scientific abstract competition, and more. SHM Converge On Demand is also available until 2024, including the opportunity to earn additional continuing medical education credit.
To register for SHM Converge, visit shmconverge.org. If you are a member of the media who would like to obtain a press pass, email media@hospitalmedicine.org.
U.S. Surgeon General, Vice Admiral Vivek H. Murthy, MD, MBA, will be a keynote speaker at SHM Converge, the Society of Hospital Meidicine’s annual conference.
Dr. Murthy will discuss burnout and well-being in health care, key themes of the conference, during a fireside chat with Danielle Scheurer, MD, MSCR, SFHM, president of SHM’s board of directors. The conversation will be held on Thursday, May 6, 2021 from 1:30 to 2:00 p.m. ET.
“It is an honor to welcome Dr. Murthy back to SHM’s annual conference during a time when his leadership is more important than ever,” said Eric E. Howell, MD, MHM, chief executive officer of SHM. “Dr. Murthy is dedicated to the health of the American people and to the well-being of those who care for them. I know his message will resonate with hospitalists who have been on the front lines of the pandemic since day one. They are key to navigating the future of our nation’s health care system.”
Dr. Murthy has devoted himself to improving public health through service, clinical care, research, education, and entrepreneurship. In addition to clinical practice, Dr. Murthy has two decades of experience in improving health in communities around the world and served as the 19th U.S. Surgeon General from 2014 to 2017, prior to being reappointed with an expanded role earlier in 2021. As “America’s Doctor,” the Surgeon General’s role is to provide clear, consistent guidance and healthcare resources for the public, ensuring to reach the nation’s most vulnerable communities.
“As we guide our nation out of the pandemic, hospitalists can look to Dr. Murthy as a leader and innovator who will do what is best for our hospitalist community and the patients they serve,” Dr. Scheurer said. “Dr. Murthy will provide a unique perspective to help hospitalists care for themselves during a time when they have been hyper-focused on caring for others.”
In addition to Dr. Murthy, SHM Converge will feature three keynote speakers who will address pressing topics in hospital medicine:
- Mark Hertling, DBA: Coming Out of Combat: Post-Pandemic Recovery
- Vineet Arora, MD, MAPP, MHM: Hospitalists Healing: Surviving, Salvaging, Sustaining, and Succeeding for a Pandemic World
- Larry Wellikson, MD, MHM: Out of COVID and Into the Light: Hospitalists More Essential Than Ever
SHM Converge is the premier educational experience for hospital medicine professionals. This year’s virtual conference will be held from May 3-7, 2021 and offers 21 educational tracks, more than 250 speakers, advanced learning courses, networking opportunities, a scientific abstract competition, and more. SHM Converge On Demand is also available until 2024, including the opportunity to earn additional continuing medical education credit.
To register for SHM Converge, visit shmconverge.org. If you are a member of the media who would like to obtain a press pass, email media@hospitalmedicine.org.





























