User login
The changing landscape of medical education
A brave new world
It’s Monday morning, and your intern is presenting an overnight admission. Lost in the details of his disorganized introduction, your mind wanders. “Why doesn’t this intern know how to present? When I trained, all those admissions during long sleepless nights really taught me to do this right.” But can we equate hours worked with competency achieved? And if not, what is the alternative? This article introduces some major changes in medical education and their implications for hospitalists.
Most hospitalists trained in an educational system influenced by Sir William Osler. In the early 1900s, he introduced the natural method of teaching, positing that student exposure to patients and experience over time ensured that physicians in training would become competent doctors.1 His influence led to the current structure of medical education, which includes conventional third-year clerkships and time-limited rotations (such as a 2-week nephrology block).
While familiarity may be comforting, there are signs our current model of medical education is inefficient, inadequate, and obsolete.
For one, the traditional system is failing to adequately prepare physicians to provide safe and complex care. Reports, such as the Institute of Medicine’s (IOM) “To Err is Human,”2 describe a high rate of preventable errors, highlighting considerable room for improvement in training the next generation of physicians.3,4
Meanwhile, trainees are still largely being deemed ready for the workforce by length of training completed (for example, completion of four-year medical school) rather than a skill set distinctly achieved. Our system leaves little flexibility to individualize learner goals, which is significant given some students and residents take shorter or longer periods of time to achieve proficiency. In addition, learner outcomes can be quite variable, as we have all experienced.
Even our methods of assessment may not adequately evaluate trainees’ skill sets. For example, most clerkships still rely heavily on the shelf exam5 as a surrogate for medical knowledge. As such, learners may conclude that testing performance trumps development of other professional skills.6 Efforts are being made to revamp evaluation systems to reflect mastery (such as Entrustable Professional Activities, or EPAs) toward competencies.7 Still, many institutions continue to rely on faculty evaluations that often reflect interpersonal dynamics rather than true critical thinking skills.6
Recognizing the above limitations, many educators have called for changing to outcome-based, or competency-based, training (CBME). CBME targets attainment of skills in performing concrete critical clinical activities,8 such as identifying unstable patients, providing initial management, and obtaining help. To be successful, supervisors must directly observe trainees, assess demonstrated skills, and provide feedback about progress.
Unfortunately, this considerable investment of time and effort is often poorly compensated. Additionally, unanswered questions remain. For example, how will residency programs continue to challenge physicians deemed “competent” in a required skill? What happens when a trainee is deficient and not appropriately progressing in a required skill? Is flexible training time part of the future of medical education? While CBME appears to be a more effective method of education, questions like these must be addressed during implementation.
Beyond the fact that hours worked cannot be used as a surrogate for competency, excessive unregulated work hours can be detrimental to learners, their supervisors, and patients. In 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented a major change in medical education: duty hour limitations. The premise that sleep-deprived providers are more prone to error is well established. However, controversy remains as to whether these regulations translate into improved patient care and provider well-being. Studies published following the ACGME change demonstrate increasing burnout among physicians,9-11 which has led some educators to explore the potential relationship between burnout and duty hour restrictions.
The recent “iCOMPARE” trial, which compared internal medicine (IM) residencies with “standard duty-hour” policies to those with “flexible” policies (that is, they did not specify limits on shift length or mandatory time off between shifts), supported a lack of correlation between hours worked and burnout.12 Researchers administered the Maslach Burnout Inventory to all participants.13 While those in the “flexible hours” arm reported greater dissatisfaction with the effect of the program on their personal lives, both groups reported significant burnout, with interns recording high scores in emotional exhaustion (79% in flexible programs vs. 72% in standard), depersonalization (75% vs. 72%), and lack of personal accomplishment (71% vs. 69%).
Disturbingly, these scores were not restricted to interns but were present in all residents. The good news? Limiting duty hours does not cause burnout. On the other hand, it does not protect from burnout. Trainee burnout appears to transcend the issue of hours worked. Clearly, we need to address the systemic flaws in our work environments that contribute to this epidemic. Nationwide, educators and organizations are continuing to define causes of burnout and test interventions to improve wellness.
A final front of change in medical education worth mentioning is the use of the electronic medical record (EMR). While the EMR has improved many aspects of patient care, its implementation is associated with decreased time spent with patients and parallels the rise in burnout. Another unforeseen consequence has been its disruptive impact on medical student documentation. A national survey of clerkship directors found that, while 64% of programs allowed students to use the EMR, only two-thirds of those programs permitted students to document electronically.14
Many institutions limit student access because of either liability concerns or the fact that student notes cannot be used to support medical billing. Concerning workarounds among preceptors, such as logging in students under their own credentials to write notes, have been identified.15 Yet medical students need to learn how to document a clinical encounter and maintain medical records.7,16 Authoring notes engages students, promotes a sense of patient ownership, and empowers them to feel like essential team members. Participating in the EMR also allows for critical feedback and skill development.
In 2016, the Society of Hospital Medicine joined several major internal medicine organizations in asking the federal government to reconsider guidelines prohibiting attendings from referring to medical student notes. In February 2018, the Centers for Medicare & Medicaid Services (CMS) revised its student documentation guidelines (see Box A), allowing teaching physicians to use all student documentation (not just Review of Systems, Family History, and Social History) for billable services.
While the guidelines officially went into effect in March 2018, many institutions are still fine-tuning their implementation, in part because of nonspecific policy language. For instance, if a student composes a note and a resident edits and signs it, can the attending physician simply cosign the resident note? Also, once a student has presented a case, can the attending see the patient and verify findings without the student present?
Despite the above challenges, the revision to CMS guidelines is a significant “win” and can potentially reduce the documentation burden on teaching physicians. With more oversight of their notes, the next generation of students will be encouraged to produce accurate, high-quality documentation.
In summary, these changes in the way we define competency, in duty hours, and in the use of the EMR demonstrate that medical education is continuously improving via robust critique and educator engagement in outcomes. We are fortunate to train in a system that respects the scientific method and utilizes data and critical events to drive important changes in practice. Understanding these changes might help hospitalists relate to the backgrounds and needs of learners. And who knows – maybe next time that intern will do a better job presenting!
Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System (VASDHS) and an associate professor at the University of California, San Diego, in the division of hospital medicine. He is the chair of the SHM Physicians in Training committee. Dr. Sebasky is an associate clinical professor at UCSD in the division of hospital medicine. Dr. Muchmore is a hematologist/oncologist and professor of clinical medicine in the department of medicine at UCSD and associate chief of staff for education at VASDHS.
References
1. Osler W. “The Hospital as a College.” In Aequanimitas. Osler W, Ed. (Philadelphia: P. Blakiston’s Son & Co., 1932).
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health Care System. (Washington: National Academies Press, 1999).
3. Ten Cate O. Competency-based postgraduate medical education: Past, present and future. GMS J Med Educ. 2017 Nov 15. doi: 10.3205/zma001146.
4. Carraccio C, Englander R, Van Melle E, et al. Advancing competency-based medical education: A charter for clinician–educators. Acad Med. 2016;91(5):645-9.
5. 2016 NBME Clinical Clerkship Subject Examination Survey.
6. Mehta NB, Hull AL, Young JB, et al. Just imagine: New paradigms for medical education. Acad Med. 2013;88(10):1418-23.
7. Fazio SB, Ledford CH, Aronowitz PB, et al. Competency-based medical education in the internal medicine clerkship: A report from the Alliance for Academic Internal Medicine Undergraduate Medical Education Task Force. Acad Med. 2018;93(3):421-7.
8. Ten Cate O, Scheele F. Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Acad Med. 2007 Jun;82(6):542-7.
9. Dewa CS, Loong D, Bonato S, et al. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open. 2017. doi: 10.1136/bmjopen-2016-015141.
10. Hall LH, Johnson J, Watt I, et al. Healthcare Staff wellbeing, burnout, and patient safety: A systematic review. PLoS ONE. 2016. doi: 10.1371/journal.pone.0159015.
11. Salyers MP, Bonfils KA, Luther L, et al. The relationship between professional burnout and quality and safety in healthcare: A meta-analysis. Gen Intern Med. 2017 Apr; 32(4):475-82.
12. Desai SV, Asch DA, Bellini LM, et al. Education outcomes in a duty hour flexibility trial in internal medicine. N Engl J Med. 2018 378:1494-508.
13. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. (Palo Alto, CA: Consulting Psychologists Press, 1996).
14. Hammoud MM, Margo K, Christner JG, et al. Opportunities and challenges in integrating electronic health records into undergraduate medical education: A national survey of clerkship directors. Teach Learn Med. 2012;24(3):219-24.
15. White J, Anthony D, WinklerPrins V, et al. Electronic medical records, medical students, and ambulatory family physicians: A multi-institution study. Acad Med. 2017;92(10):1485-90.
16. Pageler NM, Friedman CP, Longhurst CA. Refocusing medical education in the EMR era. JAMA 2013;310(21):2249-50.
Box A
“Students may document services in the medical record. However, the teaching physician must verify in the medical record all student documentation or findings, including history, physical exam, and/or medical decision making. The teaching physician must personally perform (or re-perform) the physical exam and medical decision making activities of the E/M service being billed, but may verify any student documentation of them in the medical record, rather than re-documenting this work.”
A brave new world
A brave new world
It’s Monday morning, and your intern is presenting an overnight admission. Lost in the details of his disorganized introduction, your mind wanders. “Why doesn’t this intern know how to present? When I trained, all those admissions during long sleepless nights really taught me to do this right.” But can we equate hours worked with competency achieved? And if not, what is the alternative? This article introduces some major changes in medical education and their implications for hospitalists.
Most hospitalists trained in an educational system influenced by Sir William Osler. In the early 1900s, he introduced the natural method of teaching, positing that student exposure to patients and experience over time ensured that physicians in training would become competent doctors.1 His influence led to the current structure of medical education, which includes conventional third-year clerkships and time-limited rotations (such as a 2-week nephrology block).
While familiarity may be comforting, there are signs our current model of medical education is inefficient, inadequate, and obsolete.
For one, the traditional system is failing to adequately prepare physicians to provide safe and complex care. Reports, such as the Institute of Medicine’s (IOM) “To Err is Human,”2 describe a high rate of preventable errors, highlighting considerable room for improvement in training the next generation of physicians.3,4
Meanwhile, trainees are still largely being deemed ready for the workforce by length of training completed (for example, completion of four-year medical school) rather than a skill set distinctly achieved. Our system leaves little flexibility to individualize learner goals, which is significant given some students and residents take shorter or longer periods of time to achieve proficiency. In addition, learner outcomes can be quite variable, as we have all experienced.
Even our methods of assessment may not adequately evaluate trainees’ skill sets. For example, most clerkships still rely heavily on the shelf exam5 as a surrogate for medical knowledge. As such, learners may conclude that testing performance trumps development of other professional skills.6 Efforts are being made to revamp evaluation systems to reflect mastery (such as Entrustable Professional Activities, or EPAs) toward competencies.7 Still, many institutions continue to rely on faculty evaluations that often reflect interpersonal dynamics rather than true critical thinking skills.6
Recognizing the above limitations, many educators have called for changing to outcome-based, or competency-based, training (CBME). CBME targets attainment of skills in performing concrete critical clinical activities,8 such as identifying unstable patients, providing initial management, and obtaining help. To be successful, supervisors must directly observe trainees, assess demonstrated skills, and provide feedback about progress.
Unfortunately, this considerable investment of time and effort is often poorly compensated. Additionally, unanswered questions remain. For example, how will residency programs continue to challenge physicians deemed “competent” in a required skill? What happens when a trainee is deficient and not appropriately progressing in a required skill? Is flexible training time part of the future of medical education? While CBME appears to be a more effective method of education, questions like these must be addressed during implementation.
Beyond the fact that hours worked cannot be used as a surrogate for competency, excessive unregulated work hours can be detrimental to learners, their supervisors, and patients. In 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented a major change in medical education: duty hour limitations. The premise that sleep-deprived providers are more prone to error is well established. However, controversy remains as to whether these regulations translate into improved patient care and provider well-being. Studies published following the ACGME change demonstrate increasing burnout among physicians,9-11 which has led some educators to explore the potential relationship between burnout and duty hour restrictions.
The recent “iCOMPARE” trial, which compared internal medicine (IM) residencies with “standard duty-hour” policies to those with “flexible” policies (that is, they did not specify limits on shift length or mandatory time off between shifts), supported a lack of correlation between hours worked and burnout.12 Researchers administered the Maslach Burnout Inventory to all participants.13 While those in the “flexible hours” arm reported greater dissatisfaction with the effect of the program on their personal lives, both groups reported significant burnout, with interns recording high scores in emotional exhaustion (79% in flexible programs vs. 72% in standard), depersonalization (75% vs. 72%), and lack of personal accomplishment (71% vs. 69%).
Disturbingly, these scores were not restricted to interns but were present in all residents. The good news? Limiting duty hours does not cause burnout. On the other hand, it does not protect from burnout. Trainee burnout appears to transcend the issue of hours worked. Clearly, we need to address the systemic flaws in our work environments that contribute to this epidemic. Nationwide, educators and organizations are continuing to define causes of burnout and test interventions to improve wellness.
A final front of change in medical education worth mentioning is the use of the electronic medical record (EMR). While the EMR has improved many aspects of patient care, its implementation is associated with decreased time spent with patients and parallels the rise in burnout. Another unforeseen consequence has been its disruptive impact on medical student documentation. A national survey of clerkship directors found that, while 64% of programs allowed students to use the EMR, only two-thirds of those programs permitted students to document electronically.14
Many institutions limit student access because of either liability concerns or the fact that student notes cannot be used to support medical billing. Concerning workarounds among preceptors, such as logging in students under their own credentials to write notes, have been identified.15 Yet medical students need to learn how to document a clinical encounter and maintain medical records.7,16 Authoring notes engages students, promotes a sense of patient ownership, and empowers them to feel like essential team members. Participating in the EMR also allows for critical feedback and skill development.
In 2016, the Society of Hospital Medicine joined several major internal medicine organizations in asking the federal government to reconsider guidelines prohibiting attendings from referring to medical student notes. In February 2018, the Centers for Medicare & Medicaid Services (CMS) revised its student documentation guidelines (see Box A), allowing teaching physicians to use all student documentation (not just Review of Systems, Family History, and Social History) for billable services.
While the guidelines officially went into effect in March 2018, many institutions are still fine-tuning their implementation, in part because of nonspecific policy language. For instance, if a student composes a note and a resident edits and signs it, can the attending physician simply cosign the resident note? Also, once a student has presented a case, can the attending see the patient and verify findings without the student present?
Despite the above challenges, the revision to CMS guidelines is a significant “win” and can potentially reduce the documentation burden on teaching physicians. With more oversight of their notes, the next generation of students will be encouraged to produce accurate, high-quality documentation.
In summary, these changes in the way we define competency, in duty hours, and in the use of the EMR demonstrate that medical education is continuously improving via robust critique and educator engagement in outcomes. We are fortunate to train in a system that respects the scientific method and utilizes data and critical events to drive important changes in practice. Understanding these changes might help hospitalists relate to the backgrounds and needs of learners. And who knows – maybe next time that intern will do a better job presenting!
Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System (VASDHS) and an associate professor at the University of California, San Diego, in the division of hospital medicine. He is the chair of the SHM Physicians in Training committee. Dr. Sebasky is an associate clinical professor at UCSD in the division of hospital medicine. Dr. Muchmore is a hematologist/oncologist and professor of clinical medicine in the department of medicine at UCSD and associate chief of staff for education at VASDHS.
References
1. Osler W. “The Hospital as a College.” In Aequanimitas. Osler W, Ed. (Philadelphia: P. Blakiston’s Son & Co., 1932).
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health Care System. (Washington: National Academies Press, 1999).
3. Ten Cate O. Competency-based postgraduate medical education: Past, present and future. GMS J Med Educ. 2017 Nov 15. doi: 10.3205/zma001146.
4. Carraccio C, Englander R, Van Melle E, et al. Advancing competency-based medical education: A charter for clinician–educators. Acad Med. 2016;91(5):645-9.
5. 2016 NBME Clinical Clerkship Subject Examination Survey.
6. Mehta NB, Hull AL, Young JB, et al. Just imagine: New paradigms for medical education. Acad Med. 2013;88(10):1418-23.
7. Fazio SB, Ledford CH, Aronowitz PB, et al. Competency-based medical education in the internal medicine clerkship: A report from the Alliance for Academic Internal Medicine Undergraduate Medical Education Task Force. Acad Med. 2018;93(3):421-7.
8. Ten Cate O, Scheele F. Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Acad Med. 2007 Jun;82(6):542-7.
9. Dewa CS, Loong D, Bonato S, et al. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open. 2017. doi: 10.1136/bmjopen-2016-015141.
10. Hall LH, Johnson J, Watt I, et al. Healthcare Staff wellbeing, burnout, and patient safety: A systematic review. PLoS ONE. 2016. doi: 10.1371/journal.pone.0159015.
11. Salyers MP, Bonfils KA, Luther L, et al. The relationship between professional burnout and quality and safety in healthcare: A meta-analysis. Gen Intern Med. 2017 Apr; 32(4):475-82.
12. Desai SV, Asch DA, Bellini LM, et al. Education outcomes in a duty hour flexibility trial in internal medicine. N Engl J Med. 2018 378:1494-508.
13. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. (Palo Alto, CA: Consulting Psychologists Press, 1996).
14. Hammoud MM, Margo K, Christner JG, et al. Opportunities and challenges in integrating electronic health records into undergraduate medical education: A national survey of clerkship directors. Teach Learn Med. 2012;24(3):219-24.
15. White J, Anthony D, WinklerPrins V, et al. Electronic medical records, medical students, and ambulatory family physicians: A multi-institution study. Acad Med. 2017;92(10):1485-90.
16. Pageler NM, Friedman CP, Longhurst CA. Refocusing medical education in the EMR era. JAMA 2013;310(21):2249-50.
Box A
“Students may document services in the medical record. However, the teaching physician must verify in the medical record all student documentation or findings, including history, physical exam, and/or medical decision making. The teaching physician must personally perform (or re-perform) the physical exam and medical decision making activities of the E/M service being billed, but may verify any student documentation of them in the medical record, rather than re-documenting this work.”
It’s Monday morning, and your intern is presenting an overnight admission. Lost in the details of his disorganized introduction, your mind wanders. “Why doesn’t this intern know how to present? When I trained, all those admissions during long sleepless nights really taught me to do this right.” But can we equate hours worked with competency achieved? And if not, what is the alternative? This article introduces some major changes in medical education and their implications for hospitalists.
Most hospitalists trained in an educational system influenced by Sir William Osler. In the early 1900s, he introduced the natural method of teaching, positing that student exposure to patients and experience over time ensured that physicians in training would become competent doctors.1 His influence led to the current structure of medical education, which includes conventional third-year clerkships and time-limited rotations (such as a 2-week nephrology block).
While familiarity may be comforting, there are signs our current model of medical education is inefficient, inadequate, and obsolete.
For one, the traditional system is failing to adequately prepare physicians to provide safe and complex care. Reports, such as the Institute of Medicine’s (IOM) “To Err is Human,”2 describe a high rate of preventable errors, highlighting considerable room for improvement in training the next generation of physicians.3,4
Meanwhile, trainees are still largely being deemed ready for the workforce by length of training completed (for example, completion of four-year medical school) rather than a skill set distinctly achieved. Our system leaves little flexibility to individualize learner goals, which is significant given some students and residents take shorter or longer periods of time to achieve proficiency. In addition, learner outcomes can be quite variable, as we have all experienced.
Even our methods of assessment may not adequately evaluate trainees’ skill sets. For example, most clerkships still rely heavily on the shelf exam5 as a surrogate for medical knowledge. As such, learners may conclude that testing performance trumps development of other professional skills.6 Efforts are being made to revamp evaluation systems to reflect mastery (such as Entrustable Professional Activities, or EPAs) toward competencies.7 Still, many institutions continue to rely on faculty evaluations that often reflect interpersonal dynamics rather than true critical thinking skills.6
Recognizing the above limitations, many educators have called for changing to outcome-based, or competency-based, training (CBME). CBME targets attainment of skills in performing concrete critical clinical activities,8 such as identifying unstable patients, providing initial management, and obtaining help. To be successful, supervisors must directly observe trainees, assess demonstrated skills, and provide feedback about progress.
Unfortunately, this considerable investment of time and effort is often poorly compensated. Additionally, unanswered questions remain. For example, how will residency programs continue to challenge physicians deemed “competent” in a required skill? What happens when a trainee is deficient and not appropriately progressing in a required skill? Is flexible training time part of the future of medical education? While CBME appears to be a more effective method of education, questions like these must be addressed during implementation.
Beyond the fact that hours worked cannot be used as a surrogate for competency, excessive unregulated work hours can be detrimental to learners, their supervisors, and patients. In 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented a major change in medical education: duty hour limitations. The premise that sleep-deprived providers are more prone to error is well established. However, controversy remains as to whether these regulations translate into improved patient care and provider well-being. Studies published following the ACGME change demonstrate increasing burnout among physicians,9-11 which has led some educators to explore the potential relationship between burnout and duty hour restrictions.
The recent “iCOMPARE” trial, which compared internal medicine (IM) residencies with “standard duty-hour” policies to those with “flexible” policies (that is, they did not specify limits on shift length or mandatory time off between shifts), supported a lack of correlation between hours worked and burnout.12 Researchers administered the Maslach Burnout Inventory to all participants.13 While those in the “flexible hours” arm reported greater dissatisfaction with the effect of the program on their personal lives, both groups reported significant burnout, with interns recording high scores in emotional exhaustion (79% in flexible programs vs. 72% in standard), depersonalization (75% vs. 72%), and lack of personal accomplishment (71% vs. 69%).
Disturbingly, these scores were not restricted to interns but were present in all residents. The good news? Limiting duty hours does not cause burnout. On the other hand, it does not protect from burnout. Trainee burnout appears to transcend the issue of hours worked. Clearly, we need to address the systemic flaws in our work environments that contribute to this epidemic. Nationwide, educators and organizations are continuing to define causes of burnout and test interventions to improve wellness.
A final front of change in medical education worth mentioning is the use of the electronic medical record (EMR). While the EMR has improved many aspects of patient care, its implementation is associated with decreased time spent with patients and parallels the rise in burnout. Another unforeseen consequence has been its disruptive impact on medical student documentation. A national survey of clerkship directors found that, while 64% of programs allowed students to use the EMR, only two-thirds of those programs permitted students to document electronically.14
Many institutions limit student access because of either liability concerns or the fact that student notes cannot be used to support medical billing. Concerning workarounds among preceptors, such as logging in students under their own credentials to write notes, have been identified.15 Yet medical students need to learn how to document a clinical encounter and maintain medical records.7,16 Authoring notes engages students, promotes a sense of patient ownership, and empowers them to feel like essential team members. Participating in the EMR also allows for critical feedback and skill development.
In 2016, the Society of Hospital Medicine joined several major internal medicine organizations in asking the federal government to reconsider guidelines prohibiting attendings from referring to medical student notes. In February 2018, the Centers for Medicare & Medicaid Services (CMS) revised its student documentation guidelines (see Box A), allowing teaching physicians to use all student documentation (not just Review of Systems, Family History, and Social History) for billable services.
While the guidelines officially went into effect in March 2018, many institutions are still fine-tuning their implementation, in part because of nonspecific policy language. For instance, if a student composes a note and a resident edits and signs it, can the attending physician simply cosign the resident note? Also, once a student has presented a case, can the attending see the patient and verify findings without the student present?
Despite the above challenges, the revision to CMS guidelines is a significant “win” and can potentially reduce the documentation burden on teaching physicians. With more oversight of their notes, the next generation of students will be encouraged to produce accurate, high-quality documentation.
In summary, these changes in the way we define competency, in duty hours, and in the use of the EMR demonstrate that medical education is continuously improving via robust critique and educator engagement in outcomes. We are fortunate to train in a system that respects the scientific method and utilizes data and critical events to drive important changes in practice. Understanding these changes might help hospitalists relate to the backgrounds and needs of learners. And who knows – maybe next time that intern will do a better job presenting!
Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System (VASDHS) and an associate professor at the University of California, San Diego, in the division of hospital medicine. He is the chair of the SHM Physicians in Training committee. Dr. Sebasky is an associate clinical professor at UCSD in the division of hospital medicine. Dr. Muchmore is a hematologist/oncologist and professor of clinical medicine in the department of medicine at UCSD and associate chief of staff for education at VASDHS.
References
1. Osler W. “The Hospital as a College.” In Aequanimitas. Osler W, Ed. (Philadelphia: P. Blakiston’s Son & Co., 1932).
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health Care System. (Washington: National Academies Press, 1999).
3. Ten Cate O. Competency-based postgraduate medical education: Past, present and future. GMS J Med Educ. 2017 Nov 15. doi: 10.3205/zma001146.
4. Carraccio C, Englander R, Van Melle E, et al. Advancing competency-based medical education: A charter for clinician–educators. Acad Med. 2016;91(5):645-9.
5. 2016 NBME Clinical Clerkship Subject Examination Survey.
6. Mehta NB, Hull AL, Young JB, et al. Just imagine: New paradigms for medical education. Acad Med. 2013;88(10):1418-23.
7. Fazio SB, Ledford CH, Aronowitz PB, et al. Competency-based medical education in the internal medicine clerkship: A report from the Alliance for Academic Internal Medicine Undergraduate Medical Education Task Force. Acad Med. 2018;93(3):421-7.
8. Ten Cate O, Scheele F. Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Acad Med. 2007 Jun;82(6):542-7.
9. Dewa CS, Loong D, Bonato S, et al. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open. 2017. doi: 10.1136/bmjopen-2016-015141.
10. Hall LH, Johnson J, Watt I, et al. Healthcare Staff wellbeing, burnout, and patient safety: A systematic review. PLoS ONE. 2016. doi: 10.1371/journal.pone.0159015.
11. Salyers MP, Bonfils KA, Luther L, et al. The relationship between professional burnout and quality and safety in healthcare: A meta-analysis. Gen Intern Med. 2017 Apr; 32(4):475-82.
12. Desai SV, Asch DA, Bellini LM, et al. Education outcomes in a duty hour flexibility trial in internal medicine. N Engl J Med. 2018 378:1494-508.
13. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. (Palo Alto, CA: Consulting Psychologists Press, 1996).
14. Hammoud MM, Margo K, Christner JG, et al. Opportunities and challenges in integrating electronic health records into undergraduate medical education: A national survey of clerkship directors. Teach Learn Med. 2012;24(3):219-24.
15. White J, Anthony D, WinklerPrins V, et al. Electronic medical records, medical students, and ambulatory family physicians: A multi-institution study. Acad Med. 2017;92(10):1485-90.
16. Pageler NM, Friedman CP, Longhurst CA. Refocusing medical education in the EMR era. JAMA 2013;310(21):2249-50.
Box A
“Students may document services in the medical record. However, the teaching physician must verify in the medical record all student documentation or findings, including history, physical exam, and/or medical decision making. The teaching physician must personally perform (or re-perform) the physical exam and medical decision making activities of the E/M service being billed, but may verify any student documentation of them in the medical record, rather than re-documenting this work.”
Laurence Wellikson, MD, MHM, announces retirement as CEO of Society of Hospital Medicine
Society recognizes Dr. Wellikson’s leadership, retains Spencer Stuart for successor search
Philadelphia – After serving as the first and only chief executive officer of the Society of Hospital Medicine since January of 2000, Laurence Wellikson, MD, MHM, has announced his retirement effective on Dec. 31, 2020. In parallel, the SHM Board of Directors have commenced a search for his successor.
“When I began as CEO 20 years ago, SHM – then known as the National Association of Inpatient Physicians – was a young national organization with approximately 500 members, and there was minimal understanding as to the value that hospitalists could add to their health communities,” Dr. Wellikson said. “I am proud to say that, nearly 20 years later, SHM boasts a growing membership of more than 17,000, and hospitalists are on the front line of innovation as a driving force in improving patient care.”
SHM has not only grown its membership but also its diverse portfolio of offerings for hospital medicine professionals under Dr. Wellikson’s leadership. Its first annual conference welcomed approximately 300 attendees; the most recent conference, Hospital Medicine 2019, saw that number increase more than tenfold to nearly 4,000. Its conferences, publications, online education, chapter program, advocacy efforts, quality improvement programs, and more have evolved significantly to ensure hospitalists at all stages of their careers – and those who support them – have access to resources to keep them up to date and demonstrate their value in America’s health care system.
During Dr. Wellikson’s tenure, SHM launched its peer-reviewed Journal of Hospital Medicine, the premier, ISI-indexed publication for the specialty, successfully advocated for a Focused Practice in Hospital Medicine certification option and C6 hospitalist specialty code, and earned the John M. Eisenberg Patient Safety and Quality Award for its quality improvement programs. These are just a few of the noteworthy accomplishments that have elevated SHM as a key partner for hospitalists and their institutions.
To assist with the search for SHM’s next CEO, the society has retained Spencer Stuart, a leading global executive and leadership advisory firm. The search process is being overseen by a diverse search committee led by the president-elect of SHM’s Board of Directors, Danielle Scheurer, MD, MSCR, SFHM.
“On behalf of the society and its members, I want to extend a sincere thank you to Larry for his years of dedication and service to SHM, its staff, and the hospital medicine professionals we serve,” said Christopher Frost, MD, SFHM, president of SHM’s Board of Directors. “His legacy will allow SHM to continue its growth trajectory through key programs and services supporting members’ needs for years to come. Larry has taken the specialty of hospital medicine and created a movement in SHM, where the entire hospital medicine team can come for education, community, and betterment of the care we provide to our patients. We are indebted to him beyond words.”
Those who are interested in leading SHM into the future as its next CEO are encouraged to contact either Jennifer P. Heenan (jheenan@spencerstuart.com) or Mark Furman, MD (mfurman@spencerstuart.com).
Society recognizes Dr. Wellikson’s leadership, retains Spencer Stuart for successor search
Society recognizes Dr. Wellikson’s leadership, retains Spencer Stuart for successor search
Philadelphia – After serving as the first and only chief executive officer of the Society of Hospital Medicine since January of 2000, Laurence Wellikson, MD, MHM, has announced his retirement effective on Dec. 31, 2020. In parallel, the SHM Board of Directors have commenced a search for his successor.
“When I began as CEO 20 years ago, SHM – then known as the National Association of Inpatient Physicians – was a young national organization with approximately 500 members, and there was minimal understanding as to the value that hospitalists could add to their health communities,” Dr. Wellikson said. “I am proud to say that, nearly 20 years later, SHM boasts a growing membership of more than 17,000, and hospitalists are on the front line of innovation as a driving force in improving patient care.”
SHM has not only grown its membership but also its diverse portfolio of offerings for hospital medicine professionals under Dr. Wellikson’s leadership. Its first annual conference welcomed approximately 300 attendees; the most recent conference, Hospital Medicine 2019, saw that number increase more than tenfold to nearly 4,000. Its conferences, publications, online education, chapter program, advocacy efforts, quality improvement programs, and more have evolved significantly to ensure hospitalists at all stages of their careers – and those who support them – have access to resources to keep them up to date and demonstrate their value in America’s health care system.
During Dr. Wellikson’s tenure, SHM launched its peer-reviewed Journal of Hospital Medicine, the premier, ISI-indexed publication for the specialty, successfully advocated for a Focused Practice in Hospital Medicine certification option and C6 hospitalist specialty code, and earned the John M. Eisenberg Patient Safety and Quality Award for its quality improvement programs. These are just a few of the noteworthy accomplishments that have elevated SHM as a key partner for hospitalists and their institutions.
To assist with the search for SHM’s next CEO, the society has retained Spencer Stuart, a leading global executive and leadership advisory firm. The search process is being overseen by a diverse search committee led by the president-elect of SHM’s Board of Directors, Danielle Scheurer, MD, MSCR, SFHM.
“On behalf of the society and its members, I want to extend a sincere thank you to Larry for his years of dedication and service to SHM, its staff, and the hospital medicine professionals we serve,” said Christopher Frost, MD, SFHM, president of SHM’s Board of Directors. “His legacy will allow SHM to continue its growth trajectory through key programs and services supporting members’ needs for years to come. Larry has taken the specialty of hospital medicine and created a movement in SHM, where the entire hospital medicine team can come for education, community, and betterment of the care we provide to our patients. We are indebted to him beyond words.”
Those who are interested in leading SHM into the future as its next CEO are encouraged to contact either Jennifer P. Heenan (jheenan@spencerstuart.com) or Mark Furman, MD (mfurman@spencerstuart.com).
Philadelphia – After serving as the first and only chief executive officer of the Society of Hospital Medicine since January of 2000, Laurence Wellikson, MD, MHM, has announced his retirement effective on Dec. 31, 2020. In parallel, the SHM Board of Directors have commenced a search for his successor.
“When I began as CEO 20 years ago, SHM – then known as the National Association of Inpatient Physicians – was a young national organization with approximately 500 members, and there was minimal understanding as to the value that hospitalists could add to their health communities,” Dr. Wellikson said. “I am proud to say that, nearly 20 years later, SHM boasts a growing membership of more than 17,000, and hospitalists are on the front line of innovation as a driving force in improving patient care.”
SHM has not only grown its membership but also its diverse portfolio of offerings for hospital medicine professionals under Dr. Wellikson’s leadership. Its first annual conference welcomed approximately 300 attendees; the most recent conference, Hospital Medicine 2019, saw that number increase more than tenfold to nearly 4,000. Its conferences, publications, online education, chapter program, advocacy efforts, quality improvement programs, and more have evolved significantly to ensure hospitalists at all stages of their careers – and those who support them – have access to resources to keep them up to date and demonstrate their value in America’s health care system.
During Dr. Wellikson’s tenure, SHM launched its peer-reviewed Journal of Hospital Medicine, the premier, ISI-indexed publication for the specialty, successfully advocated for a Focused Practice in Hospital Medicine certification option and C6 hospitalist specialty code, and earned the John M. Eisenberg Patient Safety and Quality Award for its quality improvement programs. These are just a few of the noteworthy accomplishments that have elevated SHM as a key partner for hospitalists and their institutions.
To assist with the search for SHM’s next CEO, the society has retained Spencer Stuart, a leading global executive and leadership advisory firm. The search process is being overseen by a diverse search committee led by the president-elect of SHM’s Board of Directors, Danielle Scheurer, MD, MSCR, SFHM.
“On behalf of the society and its members, I want to extend a sincere thank you to Larry for his years of dedication and service to SHM, its staff, and the hospital medicine professionals we serve,” said Christopher Frost, MD, SFHM, president of SHM’s Board of Directors. “His legacy will allow SHM to continue its growth trajectory through key programs and services supporting members’ needs for years to come. Larry has taken the specialty of hospital medicine and created a movement in SHM, where the entire hospital medicine team can come for education, community, and betterment of the care we provide to our patients. We are indebted to him beyond words.”
Those who are interested in leading SHM into the future as its next CEO are encouraged to contact either Jennifer P. Heenan (jheenan@spencerstuart.com) or Mark Furman, MD (mfurman@spencerstuart.com).
Maximize your leadership in academic hospital medicine
AHA Level 2 course now available
Over the past 2 decades, hospital medicine has grown from a nascent collection of hospitalists to one of the fastest growing specialties, with more than 60,000 active practitioners today.
Ten years ago, the need for mentoring and growth of a new generation of young academic faculty led to the development of the first Academic Hospitalist Academy (AHA) through the coordinated efforts of the Society of Hospital Medicine, the Society of General Internal Medicine, and the Association of Clinical Leaders of General Internal Medicine.
As modern medicine moves at an increasing pace, the intersection of patient care, research, and education has opened further opportunities for fostering the expertise of hospital medicine practitioners. The next level of training is now available with the advent of AHA’s Level 2 course.
Ever wonder why the new clinical service you’ve designed to improve physician and patient efficiency isn’t functioning like it did in the beginning? Patients are staying longer in the hospital, and physicians are working harder. The principles of change management, personal leadership styles, and adult learning will be covered in the AHA Level 2 course. How do I get my project funded and then what do I do with the results? Keys to negotiating for time and resources as well as the skills to write and disseminate your work are integrated into the curriculum.
Participants will be engaged in an interactive course designed around the challenges of practicing and leading in an academic environment. AHA Level 2 aims to help attendees – regardless of their areas of interest – identify and acquire the skills necessary to advance their career, describe the business and cultural landscape of academic health systems, and learn how to leverage that knowledge; to list resources and techniques to continue to further build their skills, and identify and pursue their unique scholarly niche.
Based on the success of AHA’s Level 1 course and the feedback from the almost 1,000 participants who have attended, AHA Level 2 is a 2.5-day course that will allow for the exchange of ideas and skills from nationally regarded faculty and fellow attendees. Through plenary sessions, workshops, small groups, and networking opportunities, attendees will be immersed in the realm of modern academic hospital medicine. The new course is offered in parallel with AHA Level 1 at the Inverness Resort, outside of Denver, on Sept. 10-12, 2019.
The course will leave attendees with an individualized career plan and enhance their area of expertise. The lessons learned and shared will allow participants to return to their institutions and continue to lead in the areas of patient care, financial resourcefulness, and the education of current and future generations of hospital medicine specialists.
Dr. O’Dorisio is a Med-Peds hospitalist at the Ohio State University, Columbus.
AHA Level 2 course now available
AHA Level 2 course now available
Over the past 2 decades, hospital medicine has grown from a nascent collection of hospitalists to one of the fastest growing specialties, with more than 60,000 active practitioners today.
Ten years ago, the need for mentoring and growth of a new generation of young academic faculty led to the development of the first Academic Hospitalist Academy (AHA) through the coordinated efforts of the Society of Hospital Medicine, the Society of General Internal Medicine, and the Association of Clinical Leaders of General Internal Medicine.
As modern medicine moves at an increasing pace, the intersection of patient care, research, and education has opened further opportunities for fostering the expertise of hospital medicine practitioners. The next level of training is now available with the advent of AHA’s Level 2 course.
Ever wonder why the new clinical service you’ve designed to improve physician and patient efficiency isn’t functioning like it did in the beginning? Patients are staying longer in the hospital, and physicians are working harder. The principles of change management, personal leadership styles, and adult learning will be covered in the AHA Level 2 course. How do I get my project funded and then what do I do with the results? Keys to negotiating for time and resources as well as the skills to write and disseminate your work are integrated into the curriculum.
Participants will be engaged in an interactive course designed around the challenges of practicing and leading in an academic environment. AHA Level 2 aims to help attendees – regardless of their areas of interest – identify and acquire the skills necessary to advance their career, describe the business and cultural landscape of academic health systems, and learn how to leverage that knowledge; to list resources and techniques to continue to further build their skills, and identify and pursue their unique scholarly niche.
Based on the success of AHA’s Level 1 course and the feedback from the almost 1,000 participants who have attended, AHA Level 2 is a 2.5-day course that will allow for the exchange of ideas and skills from nationally regarded faculty and fellow attendees. Through plenary sessions, workshops, small groups, and networking opportunities, attendees will be immersed in the realm of modern academic hospital medicine. The new course is offered in parallel with AHA Level 1 at the Inverness Resort, outside of Denver, on Sept. 10-12, 2019.
The course will leave attendees with an individualized career plan and enhance their area of expertise. The lessons learned and shared will allow participants to return to their institutions and continue to lead in the areas of patient care, financial resourcefulness, and the education of current and future generations of hospital medicine specialists.
Dr. O’Dorisio is a Med-Peds hospitalist at the Ohio State University, Columbus.
Over the past 2 decades, hospital medicine has grown from a nascent collection of hospitalists to one of the fastest growing specialties, with more than 60,000 active practitioners today.
Ten years ago, the need for mentoring and growth of a new generation of young academic faculty led to the development of the first Academic Hospitalist Academy (AHA) through the coordinated efforts of the Society of Hospital Medicine, the Society of General Internal Medicine, and the Association of Clinical Leaders of General Internal Medicine.
As modern medicine moves at an increasing pace, the intersection of patient care, research, and education has opened further opportunities for fostering the expertise of hospital medicine practitioners. The next level of training is now available with the advent of AHA’s Level 2 course.
Ever wonder why the new clinical service you’ve designed to improve physician and patient efficiency isn’t functioning like it did in the beginning? Patients are staying longer in the hospital, and physicians are working harder. The principles of change management, personal leadership styles, and adult learning will be covered in the AHA Level 2 course. How do I get my project funded and then what do I do with the results? Keys to negotiating for time and resources as well as the skills to write and disseminate your work are integrated into the curriculum.
Participants will be engaged in an interactive course designed around the challenges of practicing and leading in an academic environment. AHA Level 2 aims to help attendees – regardless of their areas of interest – identify and acquire the skills necessary to advance their career, describe the business and cultural landscape of academic health systems, and learn how to leverage that knowledge; to list resources and techniques to continue to further build their skills, and identify and pursue their unique scholarly niche.
Based on the success of AHA’s Level 1 course and the feedback from the almost 1,000 participants who have attended, AHA Level 2 is a 2.5-day course that will allow for the exchange of ideas and skills from nationally regarded faculty and fellow attendees. Through plenary sessions, workshops, small groups, and networking opportunities, attendees will be immersed in the realm of modern academic hospital medicine. The new course is offered in parallel with AHA Level 1 at the Inverness Resort, outside of Denver, on Sept. 10-12, 2019.
The course will leave attendees with an individualized career plan and enhance their area of expertise. The lessons learned and shared will allow participants to return to their institutions and continue to lead in the areas of patient care, financial resourcefulness, and the education of current and future generations of hospital medicine specialists.
Dr. O’Dorisio is a Med-Peds hospitalist at the Ohio State University, Columbus.
Dealing with staffing shortfalls
Five options for covering unfilled positions
Being in stressful situations is part of being a hospitalist. During a hospitalist’s work shift, one of the key determinants of stress is adequate staffing. With use of survey data from 569 hospital medicine groups (HMGs) across the nation, one of the topics examined in the 2018 State of Hospital Medicine Report is how HMGs cope with unfilled hospitalist physician positions.
The survey presented five options for covering unfilled hospitalist physician positions: use of locum tenens, use of moonlighters, use of voluntary extra shifts by the HMG’s existing hospitalists, use of required extra shifts, and leaving some shifts uncovered. Recipients were instructed to select all options that applied, so totals exceeded 100%. The data is organized according to HMGs that serve adults only, children only, and both adults and children.
For all three types of HMGs, the most common tactic to fill coverage gaps is through voluntary extra shifts by existing clinicians, reportedly used by 70.3% of HMGs that cover adults only, 66.7% by those that cover children only, and 76.9% by those that cover both adults and children. Data for adults-only HMGs was further broken down by geographic region, academic status, teaching status, group size, and employment model. Among adults-only HMGs, there is a direct correlation between group size and having members voluntarily work extra shifts, with 91.1% of groups with 30 or more full-time equivalent positions employing this tactic.
For HMGs that cover adults only and those that cover children only, the second most common tactic is to use moonlighters (57.4% and 53.3% respectively), while use of moonlighters is the third most commonly employed surveyed tactic for HMGs that cover both adults and children (53.8%).
HMGs that serve both adults and children were much more likely to utilize locum tenens to cover unfilled positions (69.2%) than were groups that serve adults only (44.0%) or children only (26.7%). The variability in the use of locum tenens is likely because of the willingness and/or ability of the respective groups to afford this option because it is generally the most expensive option of those surveyed.
Requiring that members of the group work extra shifts is the least popular staffing method among adults-only HMGs (10.0%) and HMGs serving both children and adults (7.7%). This strategy is unpopular, especially when there is little advance warning. Surprisingly, 40.0% of HMGs that see children only require members to work extra shifts to cover unfilled slots. This could be because pediatric HMGs are often smaller, and it would be more difficult to absorb the work if the shift is left uncovered. In fact, many pediatric HMGs staff with only one clinician at a time, so there may be no option besides requiring someone else in the group to come in and work.Of the options surveyed, perhaps the most uncomfortable for those hospitalist physicians on duty is to leave some shifts uncovered. The rapid growth and development of the specialty of hospital medicine has made it difficult for HMGs to continuously hire qualified hospitalists fast enough to meet demand. The survey found 46.2% of HMGs that serve both adults and children and 31.4% of groups that serve adults only have employed the staffing model of going short-staffed for at least some shifts. HMGs serving children-only are much less likely to go short-staffed (20.0%).
I work with a large HMG that has more than 70 members, and when it has been short-staffed, it tries to ensure a full complement of evening and night staff as the top priority because these shifts are typically more stressful. Since we have more hospitalist capacity during the day to absorb the loss of a physician, we pull staff from their daytime rounding schedules to execute this strategy. While going short-staffed is not ideal, this option has worked for many groups out of sheer necessity.
Dr. Stephan is a hospitalist at Allina Health’s Abbott Northwestern Hospital in Minneapolis and is a member of the SHM Practice Analysis Committee.
Five options for covering unfilled positions
Five options for covering unfilled positions
Being in stressful situations is part of being a hospitalist. During a hospitalist’s work shift, one of the key determinants of stress is adequate staffing. With use of survey data from 569 hospital medicine groups (HMGs) across the nation, one of the topics examined in the 2018 State of Hospital Medicine Report is how HMGs cope with unfilled hospitalist physician positions.
The survey presented five options for covering unfilled hospitalist physician positions: use of locum tenens, use of moonlighters, use of voluntary extra shifts by the HMG’s existing hospitalists, use of required extra shifts, and leaving some shifts uncovered. Recipients were instructed to select all options that applied, so totals exceeded 100%. The data is organized according to HMGs that serve adults only, children only, and both adults and children.
For all three types of HMGs, the most common tactic to fill coverage gaps is through voluntary extra shifts by existing clinicians, reportedly used by 70.3% of HMGs that cover adults only, 66.7% by those that cover children only, and 76.9% by those that cover both adults and children. Data for adults-only HMGs was further broken down by geographic region, academic status, teaching status, group size, and employment model. Among adults-only HMGs, there is a direct correlation between group size and having members voluntarily work extra shifts, with 91.1% of groups with 30 or more full-time equivalent positions employing this tactic.
For HMGs that cover adults only and those that cover children only, the second most common tactic is to use moonlighters (57.4% and 53.3% respectively), while use of moonlighters is the third most commonly employed surveyed tactic for HMGs that cover both adults and children (53.8%).
HMGs that serve both adults and children were much more likely to utilize locum tenens to cover unfilled positions (69.2%) than were groups that serve adults only (44.0%) or children only (26.7%). The variability in the use of locum tenens is likely because of the willingness and/or ability of the respective groups to afford this option because it is generally the most expensive option of those surveyed.
Requiring that members of the group work extra shifts is the least popular staffing method among adults-only HMGs (10.0%) and HMGs serving both children and adults (7.7%). This strategy is unpopular, especially when there is little advance warning. Surprisingly, 40.0% of HMGs that see children only require members to work extra shifts to cover unfilled slots. This could be because pediatric HMGs are often smaller, and it would be more difficult to absorb the work if the shift is left uncovered. In fact, many pediatric HMGs staff with only one clinician at a time, so there may be no option besides requiring someone else in the group to come in and work.Of the options surveyed, perhaps the most uncomfortable for those hospitalist physicians on duty is to leave some shifts uncovered. The rapid growth and development of the specialty of hospital medicine has made it difficult for HMGs to continuously hire qualified hospitalists fast enough to meet demand. The survey found 46.2% of HMGs that serve both adults and children and 31.4% of groups that serve adults only have employed the staffing model of going short-staffed for at least some shifts. HMGs serving children-only are much less likely to go short-staffed (20.0%).
I work with a large HMG that has more than 70 members, and when it has been short-staffed, it tries to ensure a full complement of evening and night staff as the top priority because these shifts are typically more stressful. Since we have more hospitalist capacity during the day to absorb the loss of a physician, we pull staff from their daytime rounding schedules to execute this strategy. While going short-staffed is not ideal, this option has worked for many groups out of sheer necessity.
Dr. Stephan is a hospitalist at Allina Health’s Abbott Northwestern Hospital in Minneapolis and is a member of the SHM Practice Analysis Committee.
Being in stressful situations is part of being a hospitalist. During a hospitalist’s work shift, one of the key determinants of stress is adequate staffing. With use of survey data from 569 hospital medicine groups (HMGs) across the nation, one of the topics examined in the 2018 State of Hospital Medicine Report is how HMGs cope with unfilled hospitalist physician positions.
The survey presented five options for covering unfilled hospitalist physician positions: use of locum tenens, use of moonlighters, use of voluntary extra shifts by the HMG’s existing hospitalists, use of required extra shifts, and leaving some shifts uncovered. Recipients were instructed to select all options that applied, so totals exceeded 100%. The data is organized according to HMGs that serve adults only, children only, and both adults and children.
For all three types of HMGs, the most common tactic to fill coverage gaps is through voluntary extra shifts by existing clinicians, reportedly used by 70.3% of HMGs that cover adults only, 66.7% by those that cover children only, and 76.9% by those that cover both adults and children. Data for adults-only HMGs was further broken down by geographic region, academic status, teaching status, group size, and employment model. Among adults-only HMGs, there is a direct correlation between group size and having members voluntarily work extra shifts, with 91.1% of groups with 30 or more full-time equivalent positions employing this tactic.
For HMGs that cover adults only and those that cover children only, the second most common tactic is to use moonlighters (57.4% and 53.3% respectively), while use of moonlighters is the third most commonly employed surveyed tactic for HMGs that cover both adults and children (53.8%).
HMGs that serve both adults and children were much more likely to utilize locum tenens to cover unfilled positions (69.2%) than were groups that serve adults only (44.0%) or children only (26.7%). The variability in the use of locum tenens is likely because of the willingness and/or ability of the respective groups to afford this option because it is generally the most expensive option of those surveyed.
Requiring that members of the group work extra shifts is the least popular staffing method among adults-only HMGs (10.0%) and HMGs serving both children and adults (7.7%). This strategy is unpopular, especially when there is little advance warning. Surprisingly, 40.0% of HMGs that see children only require members to work extra shifts to cover unfilled slots. This could be because pediatric HMGs are often smaller, and it would be more difficult to absorb the work if the shift is left uncovered. In fact, many pediatric HMGs staff with only one clinician at a time, so there may be no option besides requiring someone else in the group to come in and work.Of the options surveyed, perhaps the most uncomfortable for those hospitalist physicians on duty is to leave some shifts uncovered. The rapid growth and development of the specialty of hospital medicine has made it difficult for HMGs to continuously hire qualified hospitalists fast enough to meet demand. The survey found 46.2% of HMGs that serve both adults and children and 31.4% of groups that serve adults only have employed the staffing model of going short-staffed for at least some shifts. HMGs serving children-only are much less likely to go short-staffed (20.0%).
I work with a large HMG that has more than 70 members, and when it has been short-staffed, it tries to ensure a full complement of evening and night staff as the top priority because these shifts are typically more stressful. Since we have more hospitalist capacity during the day to absorb the loss of a physician, we pull staff from their daytime rounding schedules to execute this strategy. While going short-staffed is not ideal, this option has worked for many groups out of sheer necessity.
Dr. Stephan is a hospitalist at Allina Health’s Abbott Northwestern Hospital in Minneapolis and is a member of the SHM Practice Analysis Committee.
July: An important month for pediatric hospital medicine
National conferences and grassroots initiatives
Each July, the largest gathering of pediatric hospitalists occurs, and 2019 is no different! This year, hospitalists who care for children will gather at Pediatric Hospital Medicine (PHM) in Seattle from July 25 to 28, with the goal of enhancing participants’ knowledge and competence in the areas of innovation, clinical medicine, education, health services, practice management, quality improvement, and research.
But what makes this year particularly special is the launch of the subspecialty exam for certification in pediatric hospital medicine coming later this fall, solidifying its growth and importance within hospital medicine and the entire health care landscape. The American Board of Pediatrics (ABP) has approved PHM as the newest board subspecialty with a 2-year fellowship accredited by the Accreditation Council for Graduate Medical Education (ACGME). This conference will be a great opportunity to join with others to review competencies for board review, as well as to network with those who are also navigating the road ahead.
During 2019, the Pediatric Hospitalist Special Interest Group (SIG) of SHM has been working tirelessly on several initiatives, including a revision of the Pediatric Hospital Medicine Core Competencies as well as additional work to develop Choosing Wisely 2.0 recommendations. These will help us ensure we are developing the best curricula for the next generation of pediatric hospitalists, while cutting back on unnecessary tests and procedures for those practicing today. Each of these initiatives, as well as the July conference, highlights the opportunities that we have within SHM to work with other like-minded providers who care for children. While we partner with all professionals across many organizations, like the American Academy of Pediatrics and the Academic Pediatric Association to name a few, I wanted to share my reflections on SHM and my appreciation for the “big tent” philosophy that has served us so well thus far.
Having an opportunity to sit on the board of SHM has allowed me a chance to really appreciate the efforts that this organization invests in all who care for patients in the hospital; we have an active group of advanced-practice providers, practice administrators, residents, students, academic hospitalists, and the list goes on and on. We collaborate with a number of spectacular societies dedicated to medical specialties, and we are always open to new ways of improving the methods of delivering care to patients, in hospitals, post-acute care facilities, homes – you name it! As health care delivery models continue to evolve, I believe we are well positioned to be leaders in the delivery of acute care medicine in the hospital and beyond.
I have also learned of happenings at the grassroots level by attending SHM chapter meetings across the United States. For example, the Hampton Roads Chapter led a great Point-of-Care Ultrasound (POCUS) workshop, and influenced by that, I shared an idea at home in Nashville – borrowing my son as a model to demonstrate ultrasound techniques that hospitalists can use to assist in clinical care. I hope you, as pediatric hospitalists, will see if you have a local chapter and attend a meeting; whether you are a member of SHM or not, you can mingle with those who provide acute care treatments to all your communities and share best practices. If you don’t see an SHM chapter close by, let’s get one going! SHM is here to help launch a chapter that can help bring your community together and provide education and networking closer to home.
If you can’t attend PHM in Seattle this year, I hope you will make every effort to be at PHM 2020, where our own SIG leader, Dr. Jeffrey Grill from Louisville, Ky., will be chairing the next rendition of this amazing conference. The SHM Meetings team led by Michelle Kann will be working tirelessly to make it a great event with continued growth in content and attendance.
Dr. Rehm is associate professor, pediatrics, and director, division of pediatric outreach medicine at Vanderbilt University and Monroe Carell Jr. Children’s Hospital at Vanderbilt, both in Nashville, Tenn. She is also a member of the SHM board of directors.
National conferences and grassroots initiatives
National conferences and grassroots initiatives
Each July, the largest gathering of pediatric hospitalists occurs, and 2019 is no different! This year, hospitalists who care for children will gather at Pediatric Hospital Medicine (PHM) in Seattle from July 25 to 28, with the goal of enhancing participants’ knowledge and competence in the areas of innovation, clinical medicine, education, health services, practice management, quality improvement, and research.
But what makes this year particularly special is the launch of the subspecialty exam for certification in pediatric hospital medicine coming later this fall, solidifying its growth and importance within hospital medicine and the entire health care landscape. The American Board of Pediatrics (ABP) has approved PHM as the newest board subspecialty with a 2-year fellowship accredited by the Accreditation Council for Graduate Medical Education (ACGME). This conference will be a great opportunity to join with others to review competencies for board review, as well as to network with those who are also navigating the road ahead.
During 2019, the Pediatric Hospitalist Special Interest Group (SIG) of SHM has been working tirelessly on several initiatives, including a revision of the Pediatric Hospital Medicine Core Competencies as well as additional work to develop Choosing Wisely 2.0 recommendations. These will help us ensure we are developing the best curricula for the next generation of pediatric hospitalists, while cutting back on unnecessary tests and procedures for those practicing today. Each of these initiatives, as well as the July conference, highlights the opportunities that we have within SHM to work with other like-minded providers who care for children. While we partner with all professionals across many organizations, like the American Academy of Pediatrics and the Academic Pediatric Association to name a few, I wanted to share my reflections on SHM and my appreciation for the “big tent” philosophy that has served us so well thus far.
Having an opportunity to sit on the board of SHM has allowed me a chance to really appreciate the efforts that this organization invests in all who care for patients in the hospital; we have an active group of advanced-practice providers, practice administrators, residents, students, academic hospitalists, and the list goes on and on. We collaborate with a number of spectacular societies dedicated to medical specialties, and we are always open to new ways of improving the methods of delivering care to patients, in hospitals, post-acute care facilities, homes – you name it! As health care delivery models continue to evolve, I believe we are well positioned to be leaders in the delivery of acute care medicine in the hospital and beyond.
I have also learned of happenings at the grassroots level by attending SHM chapter meetings across the United States. For example, the Hampton Roads Chapter led a great Point-of-Care Ultrasound (POCUS) workshop, and influenced by that, I shared an idea at home in Nashville – borrowing my son as a model to demonstrate ultrasound techniques that hospitalists can use to assist in clinical care. I hope you, as pediatric hospitalists, will see if you have a local chapter and attend a meeting; whether you are a member of SHM or not, you can mingle with those who provide acute care treatments to all your communities and share best practices. If you don’t see an SHM chapter close by, let’s get one going! SHM is here to help launch a chapter that can help bring your community together and provide education and networking closer to home.
If you can’t attend PHM in Seattle this year, I hope you will make every effort to be at PHM 2020, where our own SIG leader, Dr. Jeffrey Grill from Louisville, Ky., will be chairing the next rendition of this amazing conference. The SHM Meetings team led by Michelle Kann will be working tirelessly to make it a great event with continued growth in content and attendance.
Dr. Rehm is associate professor, pediatrics, and director, division of pediatric outreach medicine at Vanderbilt University and Monroe Carell Jr. Children’s Hospital at Vanderbilt, both in Nashville, Tenn. She is also a member of the SHM board of directors.
Each July, the largest gathering of pediatric hospitalists occurs, and 2019 is no different! This year, hospitalists who care for children will gather at Pediatric Hospital Medicine (PHM) in Seattle from July 25 to 28, with the goal of enhancing participants’ knowledge and competence in the areas of innovation, clinical medicine, education, health services, practice management, quality improvement, and research.
But what makes this year particularly special is the launch of the subspecialty exam for certification in pediatric hospital medicine coming later this fall, solidifying its growth and importance within hospital medicine and the entire health care landscape. The American Board of Pediatrics (ABP) has approved PHM as the newest board subspecialty with a 2-year fellowship accredited by the Accreditation Council for Graduate Medical Education (ACGME). This conference will be a great opportunity to join with others to review competencies for board review, as well as to network with those who are also navigating the road ahead.
During 2019, the Pediatric Hospitalist Special Interest Group (SIG) of SHM has been working tirelessly on several initiatives, including a revision of the Pediatric Hospital Medicine Core Competencies as well as additional work to develop Choosing Wisely 2.0 recommendations. These will help us ensure we are developing the best curricula for the next generation of pediatric hospitalists, while cutting back on unnecessary tests and procedures for those practicing today. Each of these initiatives, as well as the July conference, highlights the opportunities that we have within SHM to work with other like-minded providers who care for children. While we partner with all professionals across many organizations, like the American Academy of Pediatrics and the Academic Pediatric Association to name a few, I wanted to share my reflections on SHM and my appreciation for the “big tent” philosophy that has served us so well thus far.
Having an opportunity to sit on the board of SHM has allowed me a chance to really appreciate the efforts that this organization invests in all who care for patients in the hospital; we have an active group of advanced-practice providers, practice administrators, residents, students, academic hospitalists, and the list goes on and on. We collaborate with a number of spectacular societies dedicated to medical specialties, and we are always open to new ways of improving the methods of delivering care to patients, in hospitals, post-acute care facilities, homes – you name it! As health care delivery models continue to evolve, I believe we are well positioned to be leaders in the delivery of acute care medicine in the hospital and beyond.
I have also learned of happenings at the grassroots level by attending SHM chapter meetings across the United States. For example, the Hampton Roads Chapter led a great Point-of-Care Ultrasound (POCUS) workshop, and influenced by that, I shared an idea at home in Nashville – borrowing my son as a model to demonstrate ultrasound techniques that hospitalists can use to assist in clinical care. I hope you, as pediatric hospitalists, will see if you have a local chapter and attend a meeting; whether you are a member of SHM or not, you can mingle with those who provide acute care treatments to all your communities and share best practices. If you don’t see an SHM chapter close by, let’s get one going! SHM is here to help launch a chapter that can help bring your community together and provide education and networking closer to home.
If you can’t attend PHM in Seattle this year, I hope you will make every effort to be at PHM 2020, where our own SIG leader, Dr. Jeffrey Grill from Louisville, Ky., will be chairing the next rendition of this amazing conference. The SHM Meetings team led by Michelle Kann will be working tirelessly to make it a great event with continued growth in content and attendance.
Dr. Rehm is associate professor, pediatrics, and director, division of pediatric outreach medicine at Vanderbilt University and Monroe Carell Jr. Children’s Hospital at Vanderbilt, both in Nashville, Tenn. She is also a member of the SHM board of directors.
The hospitalist role in treating opioid use disorder
Screen patients at the time of admission
Let’s begin with a brief case. A 25-year-old patient with a history of injection heroin use is in your care. He is admitted for treatment of endocarditis and will remain in the hospital for intravenous antibiotics for several weeks. Over the first few days of hospitalization, he frequently asks for pain medicine, stating that he is in severe pain, withdrawal, and having opioid cravings. On day 3, he leaves the hospital against medical advice. After 2 weeks, he presents to the ED in septic shock and spends several weeks in the ICU. Or, alternatively, he is found down in the community and pronounced dead from a heroin overdose.
These cases occur all too often, and hospitalists across the nation are actively building knowledge and programs to improve care for patients with opioid use disorder (OUD). It is evident that opioid misuse is the public health crisis of our time. In 2017, over 70,000 patients died from an overdose, and over 2 million patients in the United States have a diagnosis of OUD.1,2 Many of these patients interact with the hospital at some point during the course of their illness for management of overdose, withdrawal, and other complications of OUD, including endocarditis, osteomyelitis, and skin and soft tissue infections. Moreover, just 20% of the 580,000 patients hospitalized with OUD in 2015 presented as a direct sequelae of the disease.3 Patients with OUD are often admitted for unrelated reasons, but their addiction goes unaddressed.
Opioid use disorder, like many of the other conditions we see, is a chronic relapsing remitting medical disease and a risk factor for premature mortality. When a patient with diabetes is admitted with cellulitis, we might check an A1C, provide diabetic counseling, and offer evidence-based diabetes treatment, including medications like insulin. We rarely build similar systems of care within the walls of our hospitals to treat OUD like we do for diabetes or other commonly encountered diseases like heart failure and chronic obstructive pulmonary disease.
We should be intentional about separating prevention from treatment. Significant work has gone into reducing the availability of prescription opioids and increasing utilization of prescription drug monitoring programs. As a result, the average morphine milligram equivalent per opioid prescription has decreased since 2010.4 An unintended consequence of restricting legal opioids is potentially pushing patients with opioid addiction towards heroin and fentanyl. Limiting opioid prescriptions alone will only decrease opioid overdose mortality by 5% through 2025.5 Thus, treatment of OUD is critical and something that hospitalists should be trained and engaged in.
Food and Drug Administration–approved OUD treatment includes buprenorphine, methadone, and extended-release naltrexone. Buprenorphine is a partial opioid agonist that treats withdrawal and cravings. Buprenorphine started in the hospital reduces mortality, increases time spent in outpatient treatment after discharge, and reduces opioid-related 30-day readmissions by over 50%.6-8 The number needed to treat with buprenorphine to prevent return to illicit opioid use is two.9 While physicians require an 8-hour “x-waiver” training (physician assistants and nurse practitioners require a 24-hour training) to prescribe buprenorphine for the outpatient treatment of OUD, such certification is not required to order the medication as part of an acute hospitalization.
Hospitalization represents a reachable moment and unique opportunity to start treatment for OUD. Patients are away from triggering environments and surrounded by supportive staff. Unfortunately, up to 30% of these patients leave the hospital against medical advice because of inadequately treated withdrawal, unaddressed cravings, and fear of mistreatment.10 Buprenorphine therapy may help tackle the physiological piece of hospital-based treatment, but we also must work on shifting the culture of our institutions. Importantly, OUD is a medical diagnosis. These patients must receive the same dignity, autonomy, and meaningful care afforded to patients with other medical diagnoses. Patients with OUD are not “addicts,” “abusers,” or “frequent fliers.”
Hospitalists have a clear and compelling role in treating OUD. The National Academy of Medicine recently held a workshop where they compared similarities of the HIV crisis with today’s opioid epidemic. The Academy advocated for the development of hospital-based protocols that empower physicians, physician assistants, and nurse practitioners to integrate the treatment of OUD into their practice.11 Some in our field may feel that treating underlying addiction is a role for behavioral health practitioners. This is akin to having said that HIV specialists should be the only providers to treat patients with HIV during its peak. There are simply not enough psychiatrists or addiction medicine specialists to treat all of the patients who need us during this time of national urgency.
There are several examples of institutions that are laying the groundwork for this important work. The University of California, San Francisco; Oregon Health and Science University, Portland; the University of Colorado at Denver, Aurora; Rush Medical College, Boston; Boston Medical Center; the Icahn School of Medicine at Mount Sinai, New York; and the University of Texas at Austin – to name a few. Offering OUD treatment in the hospital setting must be our new and only acceptable standard of care.
What is next? We can start by screening patients for OUD at the time of admission. This can be accomplished by asking two questions: Does the patient misuse prescription or nonprescription opioids? And if so, does the patient become sick if they abruptly stop? If the patient says yes to both, steps should be taken to provide direct and purposeful care related to OUD. Hospitalists should become familiar with buprenorphine therapy and work to reduce stigma by using people-first language with patients, staff, and in medical documentation.
As a society, we should balance our past focus on optimizing opioid prescribing with current efforts to bolster treatment. To that end, a group of SHM members applied to establish a Substance Use Disorder Special Interest Group, which was recently approved by the SHM board of directors. Details on its rollout will be announced shortly. The intention is that this group will serve as a resource to SHM membership and leadership
As practitioners of hospital medicine, we may not have anticipated playing a direct role in treating patients’ underlying addiction. By empowering hospitalists and wisely using medical hospitalization as a time to treat OUD, we can all have an incredible impact on our patients. Let’s get to work.
Mr. Bottner is a hospitalist at Dell Seton Medical Center, Austin, Texas, and clinical assistant professor at the University of Texas at Austin.
References
1. Katz J. You draw it: Just how bad is the drug overdose epidemic? New York Times. https://www.nytimes.com/interactive/2017/04/14/upshot/drug-overdose-epidemic-you-draw-it.html. Published Oct 26, 2017.
2. National Institute on Drug Abuse. Ohio – Opioid summaries by state. 2018. https://d14rmgtrwzf5a.cloudfront.net/sites/default/files/ohio_2018.pdf.
3. Peterson C et al. U.S. hospital discharges documenting patient opioid use disorder without opioid overdose or treatment services, 2011-2015. J Subst Abuse Treat. 2018;92:35-39. doi: 10.1016/j.jsat.2018.06.008.
4. Guy GP. Vital Signs: Changes in opioid prescribing in the United States, 2006-2015. Morb Mortal Wkly Rep. 2017;66. doi: 10.15585/mmwr.mm6626a4.
5. Chen Q et al. Prevention of prescription opioid misuse and projected overdose deaths in the United States. JAMA Netw Open. doi: 10.1001/jamanetworkopen.2018.7621.
6. Liebschutz J et al. Buprenorphine treatment for hospitalized, opioid-dependent patients: A randomized clinical trial. JAMA Intern Med. 2014;174(8):1369-76.
7. Moreno JL et al. Predictors for 30-day and 90-day hospital readmission among patients with opioid use disorder. J Addict Med. 2019. doi: 10.1097/ADM.0000000000000499.
8. Larochelle MR et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: A cohort study. Ann Intern Med. June 2018. doi: 10.7326/M17-3107.
9. Raleigh MF. Buprenorphine maintenance vs. placebo for opioid dependence. Am Fam Physician. 2017;95(5). https://www.aafp.org/afp/2017/0301/od1.html. Accessed May 12, 2019.
10. Ti L et al. Leaving the hospital against medical advice among people who use illicit drugs: A systematic review. Am J Public Health. 2015;105(12):2587. doi: 10.2105/AJPH.2015.302885a.
11. Springer SAM et al. Integrating treatment at the intersection of opioid use disorder and infectious disease epidemics in medical settings: A call for action after a National Academies of Sciences, Engineering, and Medicine workshop. Ann Intern Med. 2018;169(5):335-6. doi: 10.7326/M18-1203.
Screen patients at the time of admission
Screen patients at the time of admission
Let’s begin with a brief case. A 25-year-old patient with a history of injection heroin use is in your care. He is admitted for treatment of endocarditis and will remain in the hospital for intravenous antibiotics for several weeks. Over the first few days of hospitalization, he frequently asks for pain medicine, stating that he is in severe pain, withdrawal, and having opioid cravings. On day 3, he leaves the hospital against medical advice. After 2 weeks, he presents to the ED in septic shock and spends several weeks in the ICU. Or, alternatively, he is found down in the community and pronounced dead from a heroin overdose.
These cases occur all too often, and hospitalists across the nation are actively building knowledge and programs to improve care for patients with opioid use disorder (OUD). It is evident that opioid misuse is the public health crisis of our time. In 2017, over 70,000 patients died from an overdose, and over 2 million patients in the United States have a diagnosis of OUD.1,2 Many of these patients interact with the hospital at some point during the course of their illness for management of overdose, withdrawal, and other complications of OUD, including endocarditis, osteomyelitis, and skin and soft tissue infections. Moreover, just 20% of the 580,000 patients hospitalized with OUD in 2015 presented as a direct sequelae of the disease.3 Patients with OUD are often admitted for unrelated reasons, but their addiction goes unaddressed.
Opioid use disorder, like many of the other conditions we see, is a chronic relapsing remitting medical disease and a risk factor for premature mortality. When a patient with diabetes is admitted with cellulitis, we might check an A1C, provide diabetic counseling, and offer evidence-based diabetes treatment, including medications like insulin. We rarely build similar systems of care within the walls of our hospitals to treat OUD like we do for diabetes or other commonly encountered diseases like heart failure and chronic obstructive pulmonary disease.
We should be intentional about separating prevention from treatment. Significant work has gone into reducing the availability of prescription opioids and increasing utilization of prescription drug monitoring programs. As a result, the average morphine milligram equivalent per opioid prescription has decreased since 2010.4 An unintended consequence of restricting legal opioids is potentially pushing patients with opioid addiction towards heroin and fentanyl. Limiting opioid prescriptions alone will only decrease opioid overdose mortality by 5% through 2025.5 Thus, treatment of OUD is critical and something that hospitalists should be trained and engaged in.
Food and Drug Administration–approved OUD treatment includes buprenorphine, methadone, and extended-release naltrexone. Buprenorphine is a partial opioid agonist that treats withdrawal and cravings. Buprenorphine started in the hospital reduces mortality, increases time spent in outpatient treatment after discharge, and reduces opioid-related 30-day readmissions by over 50%.6-8 The number needed to treat with buprenorphine to prevent return to illicit opioid use is two.9 While physicians require an 8-hour “x-waiver” training (physician assistants and nurse practitioners require a 24-hour training) to prescribe buprenorphine for the outpatient treatment of OUD, such certification is not required to order the medication as part of an acute hospitalization.
Hospitalization represents a reachable moment and unique opportunity to start treatment for OUD. Patients are away from triggering environments and surrounded by supportive staff. Unfortunately, up to 30% of these patients leave the hospital against medical advice because of inadequately treated withdrawal, unaddressed cravings, and fear of mistreatment.10 Buprenorphine therapy may help tackle the physiological piece of hospital-based treatment, but we also must work on shifting the culture of our institutions. Importantly, OUD is a medical diagnosis. These patients must receive the same dignity, autonomy, and meaningful care afforded to patients with other medical diagnoses. Patients with OUD are not “addicts,” “abusers,” or “frequent fliers.”
Hospitalists have a clear and compelling role in treating OUD. The National Academy of Medicine recently held a workshop where they compared similarities of the HIV crisis with today’s opioid epidemic. The Academy advocated for the development of hospital-based protocols that empower physicians, physician assistants, and nurse practitioners to integrate the treatment of OUD into their practice.11 Some in our field may feel that treating underlying addiction is a role for behavioral health practitioners. This is akin to having said that HIV specialists should be the only providers to treat patients with HIV during its peak. There are simply not enough psychiatrists or addiction medicine specialists to treat all of the patients who need us during this time of national urgency.
There are several examples of institutions that are laying the groundwork for this important work. The University of California, San Francisco; Oregon Health and Science University, Portland; the University of Colorado at Denver, Aurora; Rush Medical College, Boston; Boston Medical Center; the Icahn School of Medicine at Mount Sinai, New York; and the University of Texas at Austin – to name a few. Offering OUD treatment in the hospital setting must be our new and only acceptable standard of care.
What is next? We can start by screening patients for OUD at the time of admission. This can be accomplished by asking two questions: Does the patient misuse prescription or nonprescription opioids? And if so, does the patient become sick if they abruptly stop? If the patient says yes to both, steps should be taken to provide direct and purposeful care related to OUD. Hospitalists should become familiar with buprenorphine therapy and work to reduce stigma by using people-first language with patients, staff, and in medical documentation.
As a society, we should balance our past focus on optimizing opioid prescribing with current efforts to bolster treatment. To that end, a group of SHM members applied to establish a Substance Use Disorder Special Interest Group, which was recently approved by the SHM board of directors. Details on its rollout will be announced shortly. The intention is that this group will serve as a resource to SHM membership and leadership
As practitioners of hospital medicine, we may not have anticipated playing a direct role in treating patients’ underlying addiction. By empowering hospitalists and wisely using medical hospitalization as a time to treat OUD, we can all have an incredible impact on our patients. Let’s get to work.
Mr. Bottner is a hospitalist at Dell Seton Medical Center, Austin, Texas, and clinical assistant professor at the University of Texas at Austin.
References
1. Katz J. You draw it: Just how bad is the drug overdose epidemic? New York Times. https://www.nytimes.com/interactive/2017/04/14/upshot/drug-overdose-epidemic-you-draw-it.html. Published Oct 26, 2017.
2. National Institute on Drug Abuse. Ohio – Opioid summaries by state. 2018. https://d14rmgtrwzf5a.cloudfront.net/sites/default/files/ohio_2018.pdf.
3. Peterson C et al. U.S. hospital discharges documenting patient opioid use disorder without opioid overdose or treatment services, 2011-2015. J Subst Abuse Treat. 2018;92:35-39. doi: 10.1016/j.jsat.2018.06.008.
4. Guy GP. Vital Signs: Changes in opioid prescribing in the United States, 2006-2015. Morb Mortal Wkly Rep. 2017;66. doi: 10.15585/mmwr.mm6626a4.
5. Chen Q et al. Prevention of prescription opioid misuse and projected overdose deaths in the United States. JAMA Netw Open. doi: 10.1001/jamanetworkopen.2018.7621.
6. Liebschutz J et al. Buprenorphine treatment for hospitalized, opioid-dependent patients: A randomized clinical trial. JAMA Intern Med. 2014;174(8):1369-76.
7. Moreno JL et al. Predictors for 30-day and 90-day hospital readmission among patients with opioid use disorder. J Addict Med. 2019. doi: 10.1097/ADM.0000000000000499.
8. Larochelle MR et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: A cohort study. Ann Intern Med. June 2018. doi: 10.7326/M17-3107.
9. Raleigh MF. Buprenorphine maintenance vs. placebo for opioid dependence. Am Fam Physician. 2017;95(5). https://www.aafp.org/afp/2017/0301/od1.html. Accessed May 12, 2019.
10. Ti L et al. Leaving the hospital against medical advice among people who use illicit drugs: A systematic review. Am J Public Health. 2015;105(12):2587. doi: 10.2105/AJPH.2015.302885a.
11. Springer SAM et al. Integrating treatment at the intersection of opioid use disorder and infectious disease epidemics in medical settings: A call for action after a National Academies of Sciences, Engineering, and Medicine workshop. Ann Intern Med. 2018;169(5):335-6. doi: 10.7326/M18-1203.
Let’s begin with a brief case. A 25-year-old patient with a history of injection heroin use is in your care. He is admitted for treatment of endocarditis and will remain in the hospital for intravenous antibiotics for several weeks. Over the first few days of hospitalization, he frequently asks for pain medicine, stating that he is in severe pain, withdrawal, and having opioid cravings. On day 3, he leaves the hospital against medical advice. After 2 weeks, he presents to the ED in septic shock and spends several weeks in the ICU. Or, alternatively, he is found down in the community and pronounced dead from a heroin overdose.
These cases occur all too often, and hospitalists across the nation are actively building knowledge and programs to improve care for patients with opioid use disorder (OUD). It is evident that opioid misuse is the public health crisis of our time. In 2017, over 70,000 patients died from an overdose, and over 2 million patients in the United States have a diagnosis of OUD.1,2 Many of these patients interact with the hospital at some point during the course of their illness for management of overdose, withdrawal, and other complications of OUD, including endocarditis, osteomyelitis, and skin and soft tissue infections. Moreover, just 20% of the 580,000 patients hospitalized with OUD in 2015 presented as a direct sequelae of the disease.3 Patients with OUD are often admitted for unrelated reasons, but their addiction goes unaddressed.
Opioid use disorder, like many of the other conditions we see, is a chronic relapsing remitting medical disease and a risk factor for premature mortality. When a patient with diabetes is admitted with cellulitis, we might check an A1C, provide diabetic counseling, and offer evidence-based diabetes treatment, including medications like insulin. We rarely build similar systems of care within the walls of our hospitals to treat OUD like we do for diabetes or other commonly encountered diseases like heart failure and chronic obstructive pulmonary disease.
We should be intentional about separating prevention from treatment. Significant work has gone into reducing the availability of prescription opioids and increasing utilization of prescription drug monitoring programs. As a result, the average morphine milligram equivalent per opioid prescription has decreased since 2010.4 An unintended consequence of restricting legal opioids is potentially pushing patients with opioid addiction towards heroin and fentanyl. Limiting opioid prescriptions alone will only decrease opioid overdose mortality by 5% through 2025.5 Thus, treatment of OUD is critical and something that hospitalists should be trained and engaged in.
Food and Drug Administration–approved OUD treatment includes buprenorphine, methadone, and extended-release naltrexone. Buprenorphine is a partial opioid agonist that treats withdrawal and cravings. Buprenorphine started in the hospital reduces mortality, increases time spent in outpatient treatment after discharge, and reduces opioid-related 30-day readmissions by over 50%.6-8 The number needed to treat with buprenorphine to prevent return to illicit opioid use is two.9 While physicians require an 8-hour “x-waiver” training (physician assistants and nurse practitioners require a 24-hour training) to prescribe buprenorphine for the outpatient treatment of OUD, such certification is not required to order the medication as part of an acute hospitalization.
Hospitalization represents a reachable moment and unique opportunity to start treatment for OUD. Patients are away from triggering environments and surrounded by supportive staff. Unfortunately, up to 30% of these patients leave the hospital against medical advice because of inadequately treated withdrawal, unaddressed cravings, and fear of mistreatment.10 Buprenorphine therapy may help tackle the physiological piece of hospital-based treatment, but we also must work on shifting the culture of our institutions. Importantly, OUD is a medical diagnosis. These patients must receive the same dignity, autonomy, and meaningful care afforded to patients with other medical diagnoses. Patients with OUD are not “addicts,” “abusers,” or “frequent fliers.”
Hospitalists have a clear and compelling role in treating OUD. The National Academy of Medicine recently held a workshop where they compared similarities of the HIV crisis with today’s opioid epidemic. The Academy advocated for the development of hospital-based protocols that empower physicians, physician assistants, and nurse practitioners to integrate the treatment of OUD into their practice.11 Some in our field may feel that treating underlying addiction is a role for behavioral health practitioners. This is akin to having said that HIV specialists should be the only providers to treat patients with HIV during its peak. There are simply not enough psychiatrists or addiction medicine specialists to treat all of the patients who need us during this time of national urgency.
There are several examples of institutions that are laying the groundwork for this important work. The University of California, San Francisco; Oregon Health and Science University, Portland; the University of Colorado at Denver, Aurora; Rush Medical College, Boston; Boston Medical Center; the Icahn School of Medicine at Mount Sinai, New York; and the University of Texas at Austin – to name a few. Offering OUD treatment in the hospital setting must be our new and only acceptable standard of care.
What is next? We can start by screening patients for OUD at the time of admission. This can be accomplished by asking two questions: Does the patient misuse prescription or nonprescription opioids? And if so, does the patient become sick if they abruptly stop? If the patient says yes to both, steps should be taken to provide direct and purposeful care related to OUD. Hospitalists should become familiar with buprenorphine therapy and work to reduce stigma by using people-first language with patients, staff, and in medical documentation.
As a society, we should balance our past focus on optimizing opioid prescribing with current efforts to bolster treatment. To that end, a group of SHM members applied to establish a Substance Use Disorder Special Interest Group, which was recently approved by the SHM board of directors. Details on its rollout will be announced shortly. The intention is that this group will serve as a resource to SHM membership and leadership
As practitioners of hospital medicine, we may not have anticipated playing a direct role in treating patients’ underlying addiction. By empowering hospitalists and wisely using medical hospitalization as a time to treat OUD, we can all have an incredible impact on our patients. Let’s get to work.
Mr. Bottner is a hospitalist at Dell Seton Medical Center, Austin, Texas, and clinical assistant professor at the University of Texas at Austin.
References
1. Katz J. You draw it: Just how bad is the drug overdose epidemic? New York Times. https://www.nytimes.com/interactive/2017/04/14/upshot/drug-overdose-epidemic-you-draw-it.html. Published Oct 26, 2017.
2. National Institute on Drug Abuse. Ohio – Opioid summaries by state. 2018. https://d14rmgtrwzf5a.cloudfront.net/sites/default/files/ohio_2018.pdf.
3. Peterson C et al. U.S. hospital discharges documenting patient opioid use disorder without opioid overdose or treatment services, 2011-2015. J Subst Abuse Treat. 2018;92:35-39. doi: 10.1016/j.jsat.2018.06.008.
4. Guy GP. Vital Signs: Changes in opioid prescribing in the United States, 2006-2015. Morb Mortal Wkly Rep. 2017;66. doi: 10.15585/mmwr.mm6626a4.
5. Chen Q et al. Prevention of prescription opioid misuse and projected overdose deaths in the United States. JAMA Netw Open. doi: 10.1001/jamanetworkopen.2018.7621.
6. Liebschutz J et al. Buprenorphine treatment for hospitalized, opioid-dependent patients: A randomized clinical trial. JAMA Intern Med. 2014;174(8):1369-76.
7. Moreno JL et al. Predictors for 30-day and 90-day hospital readmission among patients with opioid use disorder. J Addict Med. 2019. doi: 10.1097/ADM.0000000000000499.
8. Larochelle MR et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: A cohort study. Ann Intern Med. June 2018. doi: 10.7326/M17-3107.
9. Raleigh MF. Buprenorphine maintenance vs. placebo for opioid dependence. Am Fam Physician. 2017;95(5). https://www.aafp.org/afp/2017/0301/od1.html. Accessed May 12, 2019.
10. Ti L et al. Leaving the hospital against medical advice among people who use illicit drugs: A systematic review. Am J Public Health. 2015;105(12):2587. doi: 10.2105/AJPH.2015.302885a.
11. Springer SAM et al. Integrating treatment at the intersection of opioid use disorder and infectious disease epidemics in medical settings: A call for action after a National Academies of Sciences, Engineering, and Medicine workshop. Ann Intern Med. 2018;169(5):335-6. doi: 10.7326/M18-1203.
Are hospitalists being more highly valued?
An uptrend in financial support
Since the inception of hospital medicine more than 2 decades ago, the total number of hospitalists has rapidly increased to more than 60,000. The Society of Hospital Medicine’s State of Hospital Medicine Report (SoHM), published biennially, captures new changes in our growing field and sheds light on current practice trends.
Among its findings, the 2018 SoHM Report reassuringly reveals that financial support from hospitals to hospital medicine groups (HMGs) continues to climb, even in the setting of rising health care costs and ongoing budget pressure.
The median amount of financial support per full-time equivalent (FTE) physician for HMGs serving adults was $176,658, according to the 2018 SoHM Report, which is up 12% from the 2016 median of $157,535. While there is no correlation between group sizes and the amount of financial support per FTE physician, there are significant differences across regions, with HMGs in the Midwest garnering the highest median support, at $193,121 per FTE physician.
The report also reveals big differences by employment model. For example, private multispecialty and primary care medical groups receive much less financial support ($58,396 per FTE physician) than HMGs employed by hospitals. This likely signifies that their main source of revenue is from professional service fees. Regardless of the types of employment models, past surveys have reported more than 95% of HMGs receive support from their hospitals to help cover expenses.
The median amount of financial support per FTE provider (including nurse practitioners, physician assistants, and locum tenens) was $134,300, which represents a 3.3% decrease, compared with the 2016 SoHM Report. For the first time, the 2018 SoHM also collected data on financial support per “work relative value unit” (wRVU) in addition to support per FTE physician and support per FTE provider. HMGs and their hospitals can use support per wRVU data to evaluate the support per unit of work, regardless of who (whether it is a physician, an advanced practice provider, and/or others) performed that work.
The median amount of financial support per wRVU for HMGs serving adults in 2018 was $41.92, with academic HMGs reporting a higher amount ($45.81) than nonacademic HMGs ($41.28). It will be interesting to track these numbers over time.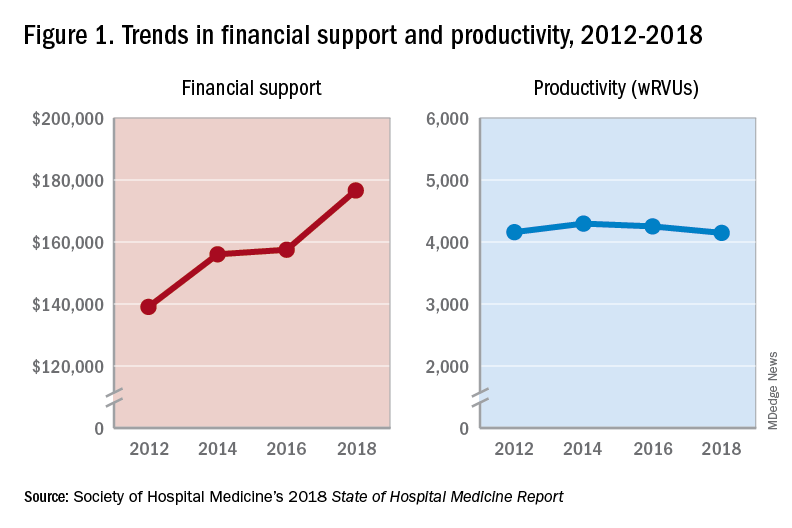
One of the most intriguing findings from the SHM’s 2018 SoHM Report is that financial support has risen despite relatively flat professional fee productivity (see Figure 1). Productivity, calculated as work relative value units (wRVUs) per physician declined slightly from 4,252 in 2016 to 4,147 in 2018.
There may be a few reasons why wRVUs per physician has remained relatively unchanged over the years. Many hospitals emphasize quality of care above provider productivity. The volume-to-value shift in theory serves as a means to reduce hospital-associated complications, length of stay, and readmission rates, thereby avoiding penalties and saving the overall costs for the hospitals in the long run.
Hospitalists involved in quality improvement projects and other essential nonclinical work perform tasks that are rarely captured in the wRVU metric. Improving patient experience, one of the Triple Aim components, necessitates extra time and effort, which also are nonbillable. In addition, increasing productivity can be challenging, a double-edged sword that may further escalate burnout and turnover rates. The static productivity may portend that it has leveled off or hit the ceiling in spite of ongoing efforts to improve efficacy.
In my view, the decision to invest in hospitalists for their contributions and dedications should not be determined based on a single metric such as wRVUs per physician. Hospitalist work on quality improvements; patient safety; efficiency, from direct bedside patient care to nonclinical efforts; teaching; research; involvements in various committees; administrative tasks; and leadership roles in improving health care systems are immeasurable. These are the reasons that most hospitals chose to adopt the hospitalist model and continue to support it. In fact, demand for hospitalists still outstrips supply, as evidenced by more than half of the hospital medicine groups with unfilled positions and an overall high turnover rate per 2018 SoHM data.
Although hospitalists are needed for the value that they provide, they should not take the status quo for granted. Instead, in return for the favorable financial support and in appreciation of being valued, hospitalists have a responsibility to prove that they are the right group chosen to do the work and help achieve their hospital’s mission and goals.
Dr. Vuong is a hospitalist at HealthPartners Medical Group in St Paul, Minn., and an assistant professor of medicine at the University of Minnesota. He is a member of SHM’s Practice Analysis Committee.
References
Afsar N. Looking into the Future and Making History. Hospitalist. 2019;23(1):31.
Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
FitzGerald S. Not a Time for Modesty. Oct. 2009. Retrieved from https://acphospitalist.org/archives/2009/10/value.htm.
Watcher RM et al. Zero to 50,000 – The 20th Anniversary of the Hospitalist. N Eng J Med. 2016. 375(11):1009-11.
An uptrend in financial support
An uptrend in financial support
Since the inception of hospital medicine more than 2 decades ago, the total number of hospitalists has rapidly increased to more than 60,000. The Society of Hospital Medicine’s State of Hospital Medicine Report (SoHM), published biennially, captures new changes in our growing field and sheds light on current practice trends.
Among its findings, the 2018 SoHM Report reassuringly reveals that financial support from hospitals to hospital medicine groups (HMGs) continues to climb, even in the setting of rising health care costs and ongoing budget pressure.
The median amount of financial support per full-time equivalent (FTE) physician for HMGs serving adults was $176,658, according to the 2018 SoHM Report, which is up 12% from the 2016 median of $157,535. While there is no correlation between group sizes and the amount of financial support per FTE physician, there are significant differences across regions, with HMGs in the Midwest garnering the highest median support, at $193,121 per FTE physician.
The report also reveals big differences by employment model. For example, private multispecialty and primary care medical groups receive much less financial support ($58,396 per FTE physician) than HMGs employed by hospitals. This likely signifies that their main source of revenue is from professional service fees. Regardless of the types of employment models, past surveys have reported more than 95% of HMGs receive support from their hospitals to help cover expenses.
The median amount of financial support per FTE provider (including nurse practitioners, physician assistants, and locum tenens) was $134,300, which represents a 3.3% decrease, compared with the 2016 SoHM Report. For the first time, the 2018 SoHM also collected data on financial support per “work relative value unit” (wRVU) in addition to support per FTE physician and support per FTE provider. HMGs and their hospitals can use support per wRVU data to evaluate the support per unit of work, regardless of who (whether it is a physician, an advanced practice provider, and/or others) performed that work.
The median amount of financial support per wRVU for HMGs serving adults in 2018 was $41.92, with academic HMGs reporting a higher amount ($45.81) than nonacademic HMGs ($41.28). It will be interesting to track these numbers over time.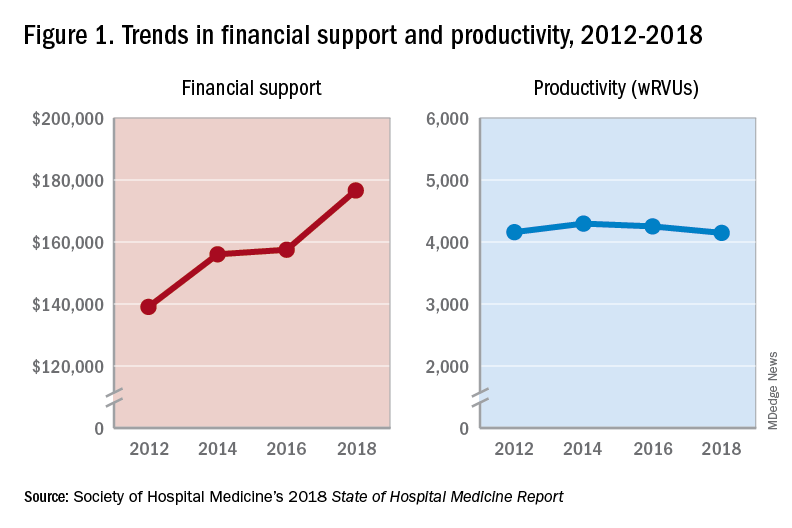
One of the most intriguing findings from the SHM’s 2018 SoHM Report is that financial support has risen despite relatively flat professional fee productivity (see Figure 1). Productivity, calculated as work relative value units (wRVUs) per physician declined slightly from 4,252 in 2016 to 4,147 in 2018.
There may be a few reasons why wRVUs per physician has remained relatively unchanged over the years. Many hospitals emphasize quality of care above provider productivity. The volume-to-value shift in theory serves as a means to reduce hospital-associated complications, length of stay, and readmission rates, thereby avoiding penalties and saving the overall costs for the hospitals in the long run.
Hospitalists involved in quality improvement projects and other essential nonclinical work perform tasks that are rarely captured in the wRVU metric. Improving patient experience, one of the Triple Aim components, necessitates extra time and effort, which also are nonbillable. In addition, increasing productivity can be challenging, a double-edged sword that may further escalate burnout and turnover rates. The static productivity may portend that it has leveled off or hit the ceiling in spite of ongoing efforts to improve efficacy.
In my view, the decision to invest in hospitalists for their contributions and dedications should not be determined based on a single metric such as wRVUs per physician. Hospitalist work on quality improvements; patient safety; efficiency, from direct bedside patient care to nonclinical efforts; teaching; research; involvements in various committees; administrative tasks; and leadership roles in improving health care systems are immeasurable. These are the reasons that most hospitals chose to adopt the hospitalist model and continue to support it. In fact, demand for hospitalists still outstrips supply, as evidenced by more than half of the hospital medicine groups with unfilled positions and an overall high turnover rate per 2018 SoHM data.
Although hospitalists are needed for the value that they provide, they should not take the status quo for granted. Instead, in return for the favorable financial support and in appreciation of being valued, hospitalists have a responsibility to prove that they are the right group chosen to do the work and help achieve their hospital’s mission and goals.
Dr. Vuong is a hospitalist at HealthPartners Medical Group in St Paul, Minn., and an assistant professor of medicine at the University of Minnesota. He is a member of SHM’s Practice Analysis Committee.
References
Afsar N. Looking into the Future and Making History. Hospitalist. 2019;23(1):31.
Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
FitzGerald S. Not a Time for Modesty. Oct. 2009. Retrieved from https://acphospitalist.org/archives/2009/10/value.htm.
Watcher RM et al. Zero to 50,000 – The 20th Anniversary of the Hospitalist. N Eng J Med. 2016. 375(11):1009-11.
Since the inception of hospital medicine more than 2 decades ago, the total number of hospitalists has rapidly increased to more than 60,000. The Society of Hospital Medicine’s State of Hospital Medicine Report (SoHM), published biennially, captures new changes in our growing field and sheds light on current practice trends.
Among its findings, the 2018 SoHM Report reassuringly reveals that financial support from hospitals to hospital medicine groups (HMGs) continues to climb, even in the setting of rising health care costs and ongoing budget pressure.
The median amount of financial support per full-time equivalent (FTE) physician for HMGs serving adults was $176,658, according to the 2018 SoHM Report, which is up 12% from the 2016 median of $157,535. While there is no correlation between group sizes and the amount of financial support per FTE physician, there are significant differences across regions, with HMGs in the Midwest garnering the highest median support, at $193,121 per FTE physician.
The report also reveals big differences by employment model. For example, private multispecialty and primary care medical groups receive much less financial support ($58,396 per FTE physician) than HMGs employed by hospitals. This likely signifies that their main source of revenue is from professional service fees. Regardless of the types of employment models, past surveys have reported more than 95% of HMGs receive support from their hospitals to help cover expenses.
The median amount of financial support per FTE provider (including nurse practitioners, physician assistants, and locum tenens) was $134,300, which represents a 3.3% decrease, compared with the 2016 SoHM Report. For the first time, the 2018 SoHM also collected data on financial support per “work relative value unit” (wRVU) in addition to support per FTE physician and support per FTE provider. HMGs and their hospitals can use support per wRVU data to evaluate the support per unit of work, regardless of who (whether it is a physician, an advanced practice provider, and/or others) performed that work.
The median amount of financial support per wRVU for HMGs serving adults in 2018 was $41.92, with academic HMGs reporting a higher amount ($45.81) than nonacademic HMGs ($41.28). It will be interesting to track these numbers over time.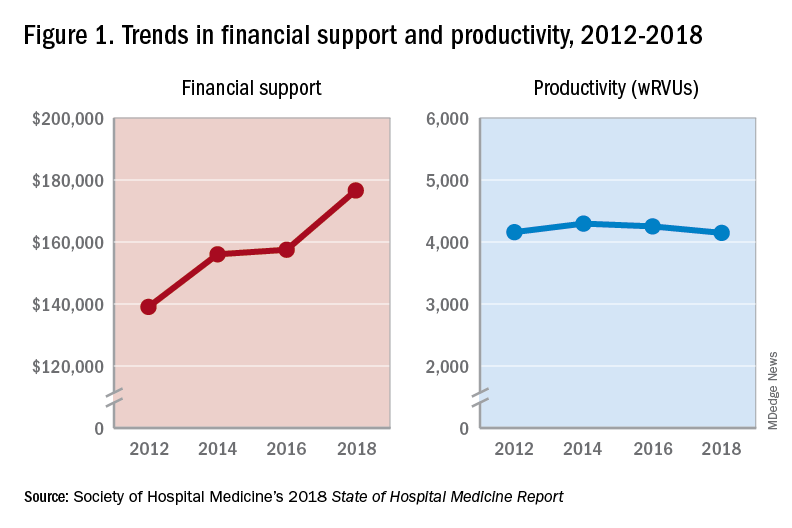
One of the most intriguing findings from the SHM’s 2018 SoHM Report is that financial support has risen despite relatively flat professional fee productivity (see Figure 1). Productivity, calculated as work relative value units (wRVUs) per physician declined slightly from 4,252 in 2016 to 4,147 in 2018.
There may be a few reasons why wRVUs per physician has remained relatively unchanged over the years. Many hospitals emphasize quality of care above provider productivity. The volume-to-value shift in theory serves as a means to reduce hospital-associated complications, length of stay, and readmission rates, thereby avoiding penalties and saving the overall costs for the hospitals in the long run.
Hospitalists involved in quality improvement projects and other essential nonclinical work perform tasks that are rarely captured in the wRVU metric. Improving patient experience, one of the Triple Aim components, necessitates extra time and effort, which also are nonbillable. In addition, increasing productivity can be challenging, a double-edged sword that may further escalate burnout and turnover rates. The static productivity may portend that it has leveled off or hit the ceiling in spite of ongoing efforts to improve efficacy.
In my view, the decision to invest in hospitalists for their contributions and dedications should not be determined based on a single metric such as wRVUs per physician. Hospitalist work on quality improvements; patient safety; efficiency, from direct bedside patient care to nonclinical efforts; teaching; research; involvements in various committees; administrative tasks; and leadership roles in improving health care systems are immeasurable. These are the reasons that most hospitals chose to adopt the hospitalist model and continue to support it. In fact, demand for hospitalists still outstrips supply, as evidenced by more than half of the hospital medicine groups with unfilled positions and an overall high turnover rate per 2018 SoHM data.
Although hospitalists are needed for the value that they provide, they should not take the status quo for granted. Instead, in return for the favorable financial support and in appreciation of being valued, hospitalists have a responsibility to prove that they are the right group chosen to do the work and help achieve their hospital’s mission and goals.
Dr. Vuong is a hospitalist at HealthPartners Medical Group in St Paul, Minn., and an assistant professor of medicine at the University of Minnesota. He is a member of SHM’s Practice Analysis Committee.
References
Afsar N. Looking into the Future and Making History. Hospitalist. 2019;23(1):31.
Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
FitzGerald S. Not a Time for Modesty. Oct. 2009. Retrieved from https://acphospitalist.org/archives/2009/10/value.htm.
Watcher RM et al. Zero to 50,000 – The 20th Anniversary of the Hospitalist. N Eng J Med. 2016. 375(11):1009-11.
Focus on science, not format
How JHM is improving the author experience
“No hassle” new manuscript submission process
Many authors have experienced the frustration of formatting a manuscript for submission to a medical journal. The process is time consuming and each journal has different requirements. This means that if you decide to submit your manuscript to one journal and later decide that another journal is a better fit, you may spend an hour (or several hours) reformatting to meet the new journal’s unique requirements.
To allow authors to spend more time on what matters to them, we’re pleased to introduce our “No Hassle” process for initial original research and brief report manuscript submissions to the Journal of Hospital Medicine. Our goal is to eliminate unnecessary and burdensome steps in the manuscript submission process. Thus, we have relaxed formatting requirements for initial manuscript submissions. Any conventional and readable manuscript format and reference style is acceptable.
Tables and figures can be embedded in the main document file or uploaded individually, depending on your preference. Funding and disclosures should be included on the title page but there is no need to submit completed disclosure or copyright forms unless we request a manuscript revision.
Timely decisions
We have all experienced the agony of waiting months on end for a journal to make a decision about our manuscript. The review process itself can take many months (or even longer). Furthermore, a manuscript may not be published for many more months (or even longer) following acceptance. At the Journal of Hospital Medicine, we commit to making timely decisions and publishing your accepted manuscript as fast as we can.
We currently reject approximately half of all original research and brief report manuscript submissions without formal peer review. We do this for two reasons. First, we want to ensure that we’re not overburdening our peer reviewers so we only ask them to review manuscripts that we are seriously considering for publication. Second, we want to ensure that we’re being respectful of our authors’ time. If we are unlikely to publish a manuscript based on lower priority scores assigned by me, as editor-in-chief, or other journal editors, we don’t want to subject your manuscript to a lengthy peer review, but would rather return the manuscript to you quickly for timely submission elsewhere.
Here are data that support our timely decision making:
- 1.3 days = our average time from manuscript submission to rejection without formal peer review (median, less than one day).
- 23 days = our average time from manuscript submission to first decision for manuscripts sent for peer review.
We also are working to improve our time to publication. Our goal is to publish accepted manuscripts within 120 days from initial submission to publication, and within 60 days from acceptance to publication.
Dissemination
Finally, little public knowledge is gleaned from medical research unless the study is published and widely read. The Journal of Hospital Medicine is at the leading edge of helping authors disseminate their work to a broader audience. Of course, we produce press releases and distribute those to many media outlets in partnership with the Society of Hospital Medicine. We also leverage social media to promote your article through tweets, visual abstracts, and, more recently, comics or graphic medicine abstracts. Some articles are even discussed on #JHMChat, our twitter-based journal club. This work is led by our exceptional Digital Media Editors, Dr. Vineet Arora (@FutureDocs), Dr. Charlie Wray (@WrayCharles), and Dr. Grace Farris (@gracefarris).
In summary, we are committed to making the Journal of Hospital Medicine even more author friendly. To that end, we’re making it easy for authors to submit their work, making timely disposition decisions, and facilitating dissemination of the work we publish.
Dr. Shah is chief metrics officer and director of the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. He is the current editor-in-chief of the Journal of Hospital Medicine.
How JHM is improving the author experience
How JHM is improving the author experience
“No hassle” new manuscript submission process
Many authors have experienced the frustration of formatting a manuscript for submission to a medical journal. The process is time consuming and each journal has different requirements. This means that if you decide to submit your manuscript to one journal and later decide that another journal is a better fit, you may spend an hour (or several hours) reformatting to meet the new journal’s unique requirements.
To allow authors to spend more time on what matters to them, we’re pleased to introduce our “No Hassle” process for initial original research and brief report manuscript submissions to the Journal of Hospital Medicine. Our goal is to eliminate unnecessary and burdensome steps in the manuscript submission process. Thus, we have relaxed formatting requirements for initial manuscript submissions. Any conventional and readable manuscript format and reference style is acceptable.
Tables and figures can be embedded in the main document file or uploaded individually, depending on your preference. Funding and disclosures should be included on the title page but there is no need to submit completed disclosure or copyright forms unless we request a manuscript revision.
Timely decisions
We have all experienced the agony of waiting months on end for a journal to make a decision about our manuscript. The review process itself can take many months (or even longer). Furthermore, a manuscript may not be published for many more months (or even longer) following acceptance. At the Journal of Hospital Medicine, we commit to making timely decisions and publishing your accepted manuscript as fast as we can.
We currently reject approximately half of all original research and brief report manuscript submissions without formal peer review. We do this for two reasons. First, we want to ensure that we’re not overburdening our peer reviewers so we only ask them to review manuscripts that we are seriously considering for publication. Second, we want to ensure that we’re being respectful of our authors’ time. If we are unlikely to publish a manuscript based on lower priority scores assigned by me, as editor-in-chief, or other journal editors, we don’t want to subject your manuscript to a lengthy peer review, but would rather return the manuscript to you quickly for timely submission elsewhere.
Here are data that support our timely decision making:
- 1.3 days = our average time from manuscript submission to rejection without formal peer review (median, less than one day).
- 23 days = our average time from manuscript submission to first decision for manuscripts sent for peer review.
We also are working to improve our time to publication. Our goal is to publish accepted manuscripts within 120 days from initial submission to publication, and within 60 days from acceptance to publication.
Dissemination
Finally, little public knowledge is gleaned from medical research unless the study is published and widely read. The Journal of Hospital Medicine is at the leading edge of helping authors disseminate their work to a broader audience. Of course, we produce press releases and distribute those to many media outlets in partnership with the Society of Hospital Medicine. We also leverage social media to promote your article through tweets, visual abstracts, and, more recently, comics or graphic medicine abstracts. Some articles are even discussed on #JHMChat, our twitter-based journal club. This work is led by our exceptional Digital Media Editors, Dr. Vineet Arora (@FutureDocs), Dr. Charlie Wray (@WrayCharles), and Dr. Grace Farris (@gracefarris).
In summary, we are committed to making the Journal of Hospital Medicine even more author friendly. To that end, we’re making it easy for authors to submit their work, making timely disposition decisions, and facilitating dissemination of the work we publish.
Dr. Shah is chief metrics officer and director of the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. He is the current editor-in-chief of the Journal of Hospital Medicine.
“No hassle” new manuscript submission process
Many authors have experienced the frustration of formatting a manuscript for submission to a medical journal. The process is time consuming and each journal has different requirements. This means that if you decide to submit your manuscript to one journal and later decide that another journal is a better fit, you may spend an hour (or several hours) reformatting to meet the new journal’s unique requirements.
To allow authors to spend more time on what matters to them, we’re pleased to introduce our “No Hassle” process for initial original research and brief report manuscript submissions to the Journal of Hospital Medicine. Our goal is to eliminate unnecessary and burdensome steps in the manuscript submission process. Thus, we have relaxed formatting requirements for initial manuscript submissions. Any conventional and readable manuscript format and reference style is acceptable.
Tables and figures can be embedded in the main document file or uploaded individually, depending on your preference. Funding and disclosures should be included on the title page but there is no need to submit completed disclosure or copyright forms unless we request a manuscript revision.
Timely decisions
We have all experienced the agony of waiting months on end for a journal to make a decision about our manuscript. The review process itself can take many months (or even longer). Furthermore, a manuscript may not be published for many more months (or even longer) following acceptance. At the Journal of Hospital Medicine, we commit to making timely decisions and publishing your accepted manuscript as fast as we can.
We currently reject approximately half of all original research and brief report manuscript submissions without formal peer review. We do this for two reasons. First, we want to ensure that we’re not overburdening our peer reviewers so we only ask them to review manuscripts that we are seriously considering for publication. Second, we want to ensure that we’re being respectful of our authors’ time. If we are unlikely to publish a manuscript based on lower priority scores assigned by me, as editor-in-chief, or other journal editors, we don’t want to subject your manuscript to a lengthy peer review, but would rather return the manuscript to you quickly for timely submission elsewhere.
Here are data that support our timely decision making:
- 1.3 days = our average time from manuscript submission to rejection without formal peer review (median, less than one day).
- 23 days = our average time from manuscript submission to first decision for manuscripts sent for peer review.
We also are working to improve our time to publication. Our goal is to publish accepted manuscripts within 120 days from initial submission to publication, and within 60 days from acceptance to publication.
Dissemination
Finally, little public knowledge is gleaned from medical research unless the study is published and widely read. The Journal of Hospital Medicine is at the leading edge of helping authors disseminate their work to a broader audience. Of course, we produce press releases and distribute those to many media outlets in partnership with the Society of Hospital Medicine. We also leverage social media to promote your article through tweets, visual abstracts, and, more recently, comics or graphic medicine abstracts. Some articles are even discussed on #JHMChat, our twitter-based journal club. This work is led by our exceptional Digital Media Editors, Dr. Vineet Arora (@FutureDocs), Dr. Charlie Wray (@WrayCharles), and Dr. Grace Farris (@gracefarris).
In summary, we are committed to making the Journal of Hospital Medicine even more author friendly. To that end, we’re making it easy for authors to submit their work, making timely disposition decisions, and facilitating dissemination of the work we publish.
Dr. Shah is chief metrics officer and director of the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. He is the current editor-in-chief of the Journal of Hospital Medicine.
Living into your legacy
What I learned from women of impact
The word legacy has been synonymous with death to me. When so and so dies, we discuss their legacy. I had a powerful experience that changed my mind on this word that is befitting for this Legacies column.
Seven years ago, I was sitting in a room of powerful women and I was the youngest one there. I wasn’t sure how I got there, but I was glad I did because it changed my life. At the time, I was panicked. The exercise was called “Craft your legacy statement.”
But, this exercise was different. The ask was to “live into your legacy.” Craft a legacy statement in THREE minutes that summarizes what you want your legacy to be … and then decide the three things you need to do now to get there. So, here is my exact legacy 3-minute statement: I am an innovator pushing teaching hospitals to optimize training and patient care delivery through novel technologies and systems science. Clearly, I did not aim high enough. One of the other attendees stated her legacy simply as “Unleash the impossible!” So clearly, I was not able to think big at that moment, but I trudged on.
Next, I had to write the three things I was going to do to enact my legacy today. Things went from bad to worse quickly since I knew this was not going to be easy. The #1 thing had to be something I was going to stop doing because it did not fit with my legacy; #2 was what I was going to start doing to enact this legacy now; and, #3 was something I was going to do to get me closer to what I wanted to be doing. So, my #1, resign my current leadership role that I had had for 8 years; #2, start joining national committees that bridge education and quality; and #3, meet with senior leadership to pitch this new role as a bridging leader, aligning education and quality.
Like all conferences, I went home and forgot what I had done and learned. I settled back into my old life and routines. A few weeks later, a plain looking envelope with awful penmanship showed up at my doorstep addressed to me. It wasn’t until after I opened it and read what was inside that I realized I was the one with horrible penmanship! I completely forgot that I wrote this letter to myself even though they told me it would come and I would forget I wrote it! So, how did I do? Let’s just say if the letter did not arrive, I am not sure where I would be. Fortunately, it did come, and I followed my own orders. Fast forward to present day and I recently stepped into a new role – associate chief medical officer: clinical learning environment – a bridging leader who aligns education and clinical care missions for our health system. Let’s just say again, had that letter not arrived, I am not sure where I would be now.
I have been fortunate to do many things in hospital medicine – clinician, researcher, educator, and my latest role as a leader. Through it all, I would say that there are some lessons that I have picked up along the way that helped me advance, in ways I did not realize:
- Be bold. Years ago, when I was asked by my chair who they should pick to be chief resident, I thought “This must be a trick question – I should definitely tell him why I should be chosen – and then pick the next best person who I want to work with.” Apparently, I was the only person who did that, and that is why my chair chose me. Everyone else picked two other people. So the take-home point here is do not sell yourself short … ever.
- Look for the hidden gateways. A few years ago, I was asked if I wanted to be an institutional leader by the person who currently had that role. I was kind of thrown for a loop, since of course I would not want to appear like I wanted to take his job. I said everything was fine and I felt pretty good about my current positions. It was only a few weeks later that I realized that he was ascertaining my interest in his job since he was leaving. They gave the job to someone else and the word on the street was I was not interested. I totally missed the gate! While it wasn’t necessarily the job I missed out on, it was the opportunity to consider the job because I was afraid. So, don’t miss the gate. It’s the wormhole to a different life that may be the right one for you, but you need to “see it” to seize it.
- Work hard for the money and for the fun. There are many things Gwyneth Paltrow does that I do not agree with, but I will give her credit for one important lesson: she divides her movie roles into those she does for love (for example, The Royal Tenenbaums) and those she does for money (for example, Shallow Hal). It made me realize that even a Hollywood starlet has to do the stuff she may not want to do for the money. So, as a young person, you have to work hard for the money, but ideally it will help you take on a project you love, whatever it is. You’ve won the game when you’re mostly paid to work for the fun ... but that may take some time.
- Always optimize what is best for you personally AND professionally. While I was on maternity leave, the job of my dreams presented itself – or so I thought it did. It was at the intersection of policy, quality, and education, with a national stage, and I would not need to move. But, I knew I could not accept the travel commitment with a young child. While I wondered if I would have regrets, it turns out the right decision professionally also has to work personally. Likewise, there are professional obligations that I take on because it works personally.
- Figure out who your tea house pals are. A few years ago, I was in San Francisco with two close friends having an epic moment about what to do with our lives as adults. We were all on the cusp of changing our directions. Not surprisingly, we could see what the other needed to do, but we could not see it for ourselves. We still text each other sometimes about the need to go back to the Tea House. Sometimes your “tea house pals” are not necessarily those around you every day. They know you, but not everyone in your work place. This “arm’s length” or distance gives them the rational, unbiased perspective to advise you, that you or your colleagues will never have.
- Look for ways to enjoy the journey. Medicine is a very long road. I routinely think about this working with all the trainees and junior faculty I encounter. You can’t be in this solely for the end of the journey. The key is to find the joy in the journey. For me, that has always come from seeking out like-minded fellow travelers to share my highs and lows. While I tweet for many reasons, a big reason is that I take pleasure in watching others on the journey and also sharing my own journey.
Here’s to your journey and living your legacy!
Dr. Arora is associate chief medical officer, clinical learning environment, at University of Chicago Medicine, and assistant dean for scholarship and discovery at the University of Chicago Pritzker School of Medicine. You can follow her journey on Twitter.
What I learned from women of impact
What I learned from women of impact
The word legacy has been synonymous with death to me. When so and so dies, we discuss their legacy. I had a powerful experience that changed my mind on this word that is befitting for this Legacies column.
Seven years ago, I was sitting in a room of powerful women and I was the youngest one there. I wasn’t sure how I got there, but I was glad I did because it changed my life. At the time, I was panicked. The exercise was called “Craft your legacy statement.”
But, this exercise was different. The ask was to “live into your legacy.” Craft a legacy statement in THREE minutes that summarizes what you want your legacy to be … and then decide the three things you need to do now to get there. So, here is my exact legacy 3-minute statement: I am an innovator pushing teaching hospitals to optimize training and patient care delivery through novel technologies and systems science. Clearly, I did not aim high enough. One of the other attendees stated her legacy simply as “Unleash the impossible!” So clearly, I was not able to think big at that moment, but I trudged on.
Next, I had to write the three things I was going to do to enact my legacy today. Things went from bad to worse quickly since I knew this was not going to be easy. The #1 thing had to be something I was going to stop doing because it did not fit with my legacy; #2 was what I was going to start doing to enact this legacy now; and, #3 was something I was going to do to get me closer to what I wanted to be doing. So, my #1, resign my current leadership role that I had had for 8 years; #2, start joining national committees that bridge education and quality; and #3, meet with senior leadership to pitch this new role as a bridging leader, aligning education and quality.
Like all conferences, I went home and forgot what I had done and learned. I settled back into my old life and routines. A few weeks later, a plain looking envelope with awful penmanship showed up at my doorstep addressed to me. It wasn’t until after I opened it and read what was inside that I realized I was the one with horrible penmanship! I completely forgot that I wrote this letter to myself even though they told me it would come and I would forget I wrote it! So, how did I do? Let’s just say if the letter did not arrive, I am not sure where I would be. Fortunately, it did come, and I followed my own orders. Fast forward to present day and I recently stepped into a new role – associate chief medical officer: clinical learning environment – a bridging leader who aligns education and clinical care missions for our health system. Let’s just say again, had that letter not arrived, I am not sure where I would be now.
I have been fortunate to do many things in hospital medicine – clinician, researcher, educator, and my latest role as a leader. Through it all, I would say that there are some lessons that I have picked up along the way that helped me advance, in ways I did not realize:
- Be bold. Years ago, when I was asked by my chair who they should pick to be chief resident, I thought “This must be a trick question – I should definitely tell him why I should be chosen – and then pick the next best person who I want to work with.” Apparently, I was the only person who did that, and that is why my chair chose me. Everyone else picked two other people. So the take-home point here is do not sell yourself short … ever.
- Look for the hidden gateways. A few years ago, I was asked if I wanted to be an institutional leader by the person who currently had that role. I was kind of thrown for a loop, since of course I would not want to appear like I wanted to take his job. I said everything was fine and I felt pretty good about my current positions. It was only a few weeks later that I realized that he was ascertaining my interest in his job since he was leaving. They gave the job to someone else and the word on the street was I was not interested. I totally missed the gate! While it wasn’t necessarily the job I missed out on, it was the opportunity to consider the job because I was afraid. So, don’t miss the gate. It’s the wormhole to a different life that may be the right one for you, but you need to “see it” to seize it.
- Work hard for the money and for the fun. There are many things Gwyneth Paltrow does that I do not agree with, but I will give her credit for one important lesson: she divides her movie roles into those she does for love (for example, The Royal Tenenbaums) and those she does for money (for example, Shallow Hal). It made me realize that even a Hollywood starlet has to do the stuff she may not want to do for the money. So, as a young person, you have to work hard for the money, but ideally it will help you take on a project you love, whatever it is. You’ve won the game when you’re mostly paid to work for the fun ... but that may take some time.
- Always optimize what is best for you personally AND professionally. While I was on maternity leave, the job of my dreams presented itself – or so I thought it did. It was at the intersection of policy, quality, and education, with a national stage, and I would not need to move. But, I knew I could not accept the travel commitment with a young child. While I wondered if I would have regrets, it turns out the right decision professionally also has to work personally. Likewise, there are professional obligations that I take on because it works personally.
- Figure out who your tea house pals are. A few years ago, I was in San Francisco with two close friends having an epic moment about what to do with our lives as adults. We were all on the cusp of changing our directions. Not surprisingly, we could see what the other needed to do, but we could not see it for ourselves. We still text each other sometimes about the need to go back to the Tea House. Sometimes your “tea house pals” are not necessarily those around you every day. They know you, but not everyone in your work place. This “arm’s length” or distance gives them the rational, unbiased perspective to advise you, that you or your colleagues will never have.
- Look for ways to enjoy the journey. Medicine is a very long road. I routinely think about this working with all the trainees and junior faculty I encounter. You can’t be in this solely for the end of the journey. The key is to find the joy in the journey. For me, that has always come from seeking out like-minded fellow travelers to share my highs and lows. While I tweet for many reasons, a big reason is that I take pleasure in watching others on the journey and also sharing my own journey.
Here’s to your journey and living your legacy!
Dr. Arora is associate chief medical officer, clinical learning environment, at University of Chicago Medicine, and assistant dean for scholarship and discovery at the University of Chicago Pritzker School of Medicine. You can follow her journey on Twitter.
The word legacy has been synonymous with death to me. When so and so dies, we discuss their legacy. I had a powerful experience that changed my mind on this word that is befitting for this Legacies column.
Seven years ago, I was sitting in a room of powerful women and I was the youngest one there. I wasn’t sure how I got there, but I was glad I did because it changed my life. At the time, I was panicked. The exercise was called “Craft your legacy statement.”
But, this exercise was different. The ask was to “live into your legacy.” Craft a legacy statement in THREE minutes that summarizes what you want your legacy to be … and then decide the three things you need to do now to get there. So, here is my exact legacy 3-minute statement: I am an innovator pushing teaching hospitals to optimize training and patient care delivery through novel technologies and systems science. Clearly, I did not aim high enough. One of the other attendees stated her legacy simply as “Unleash the impossible!” So clearly, I was not able to think big at that moment, but I trudged on.
Next, I had to write the three things I was going to do to enact my legacy today. Things went from bad to worse quickly since I knew this was not going to be easy. The #1 thing had to be something I was going to stop doing because it did not fit with my legacy; #2 was what I was going to start doing to enact this legacy now; and, #3 was something I was going to do to get me closer to what I wanted to be doing. So, my #1, resign my current leadership role that I had had for 8 years; #2, start joining national committees that bridge education and quality; and #3, meet with senior leadership to pitch this new role as a bridging leader, aligning education and quality.
Like all conferences, I went home and forgot what I had done and learned. I settled back into my old life and routines. A few weeks later, a plain looking envelope with awful penmanship showed up at my doorstep addressed to me. It wasn’t until after I opened it and read what was inside that I realized I was the one with horrible penmanship! I completely forgot that I wrote this letter to myself even though they told me it would come and I would forget I wrote it! So, how did I do? Let’s just say if the letter did not arrive, I am not sure where I would be. Fortunately, it did come, and I followed my own orders. Fast forward to present day and I recently stepped into a new role – associate chief medical officer: clinical learning environment – a bridging leader who aligns education and clinical care missions for our health system. Let’s just say again, had that letter not arrived, I am not sure where I would be now.
I have been fortunate to do many things in hospital medicine – clinician, researcher, educator, and my latest role as a leader. Through it all, I would say that there are some lessons that I have picked up along the way that helped me advance, in ways I did not realize:
- Be bold. Years ago, when I was asked by my chair who they should pick to be chief resident, I thought “This must be a trick question – I should definitely tell him why I should be chosen – and then pick the next best person who I want to work with.” Apparently, I was the only person who did that, and that is why my chair chose me. Everyone else picked two other people. So the take-home point here is do not sell yourself short … ever.
- Look for the hidden gateways. A few years ago, I was asked if I wanted to be an institutional leader by the person who currently had that role. I was kind of thrown for a loop, since of course I would not want to appear like I wanted to take his job. I said everything was fine and I felt pretty good about my current positions. It was only a few weeks later that I realized that he was ascertaining my interest in his job since he was leaving. They gave the job to someone else and the word on the street was I was not interested. I totally missed the gate! While it wasn’t necessarily the job I missed out on, it was the opportunity to consider the job because I was afraid. So, don’t miss the gate. It’s the wormhole to a different life that may be the right one for you, but you need to “see it” to seize it.
- Work hard for the money and for the fun. There are many things Gwyneth Paltrow does that I do not agree with, but I will give her credit for one important lesson: she divides her movie roles into those she does for love (for example, The Royal Tenenbaums) and those she does for money (for example, Shallow Hal). It made me realize that even a Hollywood starlet has to do the stuff she may not want to do for the money. So, as a young person, you have to work hard for the money, but ideally it will help you take on a project you love, whatever it is. You’ve won the game when you’re mostly paid to work for the fun ... but that may take some time.
- Always optimize what is best for you personally AND professionally. While I was on maternity leave, the job of my dreams presented itself – or so I thought it did. It was at the intersection of policy, quality, and education, with a national stage, and I would not need to move. But, I knew I could not accept the travel commitment with a young child. While I wondered if I would have regrets, it turns out the right decision professionally also has to work personally. Likewise, there are professional obligations that I take on because it works personally.
- Figure out who your tea house pals are. A few years ago, I was in San Francisco with two close friends having an epic moment about what to do with our lives as adults. We were all on the cusp of changing our directions. Not surprisingly, we could see what the other needed to do, but we could not see it for ourselves. We still text each other sometimes about the need to go back to the Tea House. Sometimes your “tea house pals” are not necessarily those around you every day. They know you, but not everyone in your work place. This “arm’s length” or distance gives them the rational, unbiased perspective to advise you, that you or your colleagues will never have.
- Look for ways to enjoy the journey. Medicine is a very long road. I routinely think about this working with all the trainees and junior faculty I encounter. You can’t be in this solely for the end of the journey. The key is to find the joy in the journey. For me, that has always come from seeking out like-minded fellow travelers to share my highs and lows. While I tweet for many reasons, a big reason is that I take pleasure in watching others on the journey and also sharing my own journey.
Here’s to your journey and living your legacy!
Dr. Arora is associate chief medical officer, clinical learning environment, at University of Chicago Medicine, and assistant dean for scholarship and discovery at the University of Chicago Pritzker School of Medicine. You can follow her journey on Twitter.
Just a series of fortunate events?
Building a career in hospital medicine
Residents and junior faculty have frequently asked me how they can attain a position similar to mine, focused on quality and leadership in a health care system. When I was first asked to offer advice on this topic, my response was generally something like, “Heck if I know! I just had a series of lucky accidents to get here!”
Back then, I would recount my career history. I established myself as a clinician educator and associate program director soon after Chief Residency. After that, I would explain, a series of fortunate events and health care trends shaped my career. Evidence-based medicine (EBM), the patient safety movement, a shift to incorporate value (as well as volume) into reimbursement models, and the hospital medicine movement all emerged in interesting and often synergistic ways.
A young SHM organization (then known as NAIP) grew rapidly even while the hospitalist programs I led in Phoenix, then at University of California, San Diego, grew in size and influence. Inevitably, it seemed, I was increasingly involved in quality improvement (QI) efforts, and began to publish and speak about them. Collaborative work with SHM and a number of hospital systems broadened my visibility regionally and nationally. Finally, in 2015, I was recruited away from UC San Diego into a new position, as chief quality officer at UC Davis.
On hearing this history, those seeking my sage advice would look a little confused, and then say something like, “So your advice is that I should get lucky??? Gee, thanks a lot! Really helpful!” (Insert sarcasm here).
The honor of being asked to contribute to the “Legacies” series in The Hospitalist gave me an opportunity to think about this a little differently. No one really wanted to know about how past changes in the health care environment led to my career success. They wanted advice on tools and strategies that will allow them to thrive in an environment of ongoing, disruptive change that is likely only going to accelerate. I now present my upgraded points of advice, intertwined with examples of how SHM positively influenced my career (and could assist yours):
Learn how your hospital works. Hospitalists obviously have an inside track on many aspects of hospital operations, but sometimes remain oblivious to the organizational and committee structure, priorities of hospital leadership, and the mechanism for implementing standardized care. Knowing where to go with new ideas, and the process of implementing protocols, will keep you from hitting political land mines and unintentionally encroaching on someone else’s turf, while aligning your efforts with institutional priorities improves the buy-in and resources available to do the work.
Start small, but think big. Don’t bite off more than you can chew, and make sure your ideas for change work on a small scale before trying to sell the world on them. On the other hand, think big! The care you and others provide is dependent on systems that go far beyond your immediate control. Policies, protocols, standardized order sets, checklists, and an array of other tools can be leveraged to influence care across an entire health system, and in the SHM Mentored Implementation programs, can impact hundreds of hospitals.
Broaden your skills. Commit to learning new skills that can increase your impact and career diversity. Procedural skills; information technology; and EMR, EBM, research, public health, QI, business, leadership, public speaking, advocacy, and telehealth, can all open up a whole world of possibilities when combined with a medical degree. These skills can move you into areas that keep you engaged and excited to go to work.
Engage in mentor/mentee relationships. As an associate program director and clinician-educator, I had a lot of opportunity to mentor residents and fellows. It is so rewarding to watch the mentee grow in experience and skills, and to eventually see many of them assume leadership and mentoring roles themselves. You don’t have to be in a teaching position to act as a mentor (my experience mentoring hospitalists and others in leadership and quality improvement now far surpasses my experience with house staff).
The mentor often benefits as much as the mentee from this relationship. I have been inspired by their passion and dedication, educated by their ideas and innovation, and frequently find I am learning more from them, than they are from me. I have had great experiences in the SHM Mentored Implementation program in the role of mentee and mentor.
Participate in a community. When I first joined NAIP, I was amazed that the giants (Wachter, Nelson, Whitcomb, Holman, Williams, Greeno, Howell, Huddleston, Wellikson, and on and on) were not only approachable, they were warm, friendly, interesting, and extraordinarily welcoming. The ever-expanding and evolving community at SHM continues that tradition and offers a forum to share innovative work, discuss common problems and solutions, contact world experts, or just find an empathetic ear. Working on toolkits and collaborative efforts with this community remains a real highlight of my career, and the source of several lasting friendships. So don’t be shy; step right up; and introduce yourself!
Avoid my past mistakes (this might be a long list). Random things you should try to avoid.
- Tribalism – It is natural to be protective of your hospitalist group, and to focus on the injustices heaped upon you from (insert favorite punching bag here, e.g., ED, orthopedists, cardiologists, nursing staff, evil administration penny pinchers, etc). While some of those injustices might be real, tribalism, defensiveness, and circling the wagons generally only makes things worse. Sit down face to face, learn a little bit about the opposing tribe (both about their work, and about them as people), and see how much more fun and productive work can be.
- Storming out of a meeting with the CMO and CEO, slamming the door, etc. – not productive. Administrative leaders are doing their own juggling act and are generally well intentioned and doing the best they can. Respect that, argue your case, but if things don’t pan out, shake their hand, and live to fight another day.
- Using e-mail (evil-mail) to resolve conflict – And if you’re a young whippersnapper, don’t use Twitter, Facebook, Snapchat, or other social media to address conflict either!
- Forgetting to put patients first – Frame decisions for your group around what best serves your patients, not your doctors. Long term, this gives your group credibility and will serve the hospitalists better as well. SHM does this on a large scale with their advocacy efforts, resulting in more credibility and influence on Capitol Hill.
Make time for friends, family, fitness, fun, and reflection. A sense of humor and an occasional laugh when dealing with ill patients, hospital medicine politics, and the EMR all day provides resilience, as does taking the time to foster self-awareness and insight into your own weaknesses, strengths, and how you react to different stressors. A little bit of exercise and time with family and friends can go a long way towards improving your outlook, work, and life in general, while reducing burnout. Oh yeah, it’s also a good idea to choose a great life partner as well. Thanks Michelle!
Dr. Maynard is chief quality officer, University of California Davis Medical Center, Sacramento, Calif.
Building a career in hospital medicine
Building a career in hospital medicine
Residents and junior faculty have frequently asked me how they can attain a position similar to mine, focused on quality and leadership in a health care system. When I was first asked to offer advice on this topic, my response was generally something like, “Heck if I know! I just had a series of lucky accidents to get here!”
Back then, I would recount my career history. I established myself as a clinician educator and associate program director soon after Chief Residency. After that, I would explain, a series of fortunate events and health care trends shaped my career. Evidence-based medicine (EBM), the patient safety movement, a shift to incorporate value (as well as volume) into reimbursement models, and the hospital medicine movement all emerged in interesting and often synergistic ways.
A young SHM organization (then known as NAIP) grew rapidly even while the hospitalist programs I led in Phoenix, then at University of California, San Diego, grew in size and influence. Inevitably, it seemed, I was increasingly involved in quality improvement (QI) efforts, and began to publish and speak about them. Collaborative work with SHM and a number of hospital systems broadened my visibility regionally and nationally. Finally, in 2015, I was recruited away from UC San Diego into a new position, as chief quality officer at UC Davis.
On hearing this history, those seeking my sage advice would look a little confused, and then say something like, “So your advice is that I should get lucky??? Gee, thanks a lot! Really helpful!” (Insert sarcasm here).
The honor of being asked to contribute to the “Legacies” series in The Hospitalist gave me an opportunity to think about this a little differently. No one really wanted to know about how past changes in the health care environment led to my career success. They wanted advice on tools and strategies that will allow them to thrive in an environment of ongoing, disruptive change that is likely only going to accelerate. I now present my upgraded points of advice, intertwined with examples of how SHM positively influenced my career (and could assist yours):
Learn how your hospital works. Hospitalists obviously have an inside track on many aspects of hospital operations, but sometimes remain oblivious to the organizational and committee structure, priorities of hospital leadership, and the mechanism for implementing standardized care. Knowing where to go with new ideas, and the process of implementing protocols, will keep you from hitting political land mines and unintentionally encroaching on someone else’s turf, while aligning your efforts with institutional priorities improves the buy-in and resources available to do the work.
Start small, but think big. Don’t bite off more than you can chew, and make sure your ideas for change work on a small scale before trying to sell the world on them. On the other hand, think big! The care you and others provide is dependent on systems that go far beyond your immediate control. Policies, protocols, standardized order sets, checklists, and an array of other tools can be leveraged to influence care across an entire health system, and in the SHM Mentored Implementation programs, can impact hundreds of hospitals.
Broaden your skills. Commit to learning new skills that can increase your impact and career diversity. Procedural skills; information technology; and EMR, EBM, research, public health, QI, business, leadership, public speaking, advocacy, and telehealth, can all open up a whole world of possibilities when combined with a medical degree. These skills can move you into areas that keep you engaged and excited to go to work.
Engage in mentor/mentee relationships. As an associate program director and clinician-educator, I had a lot of opportunity to mentor residents and fellows. It is so rewarding to watch the mentee grow in experience and skills, and to eventually see many of them assume leadership and mentoring roles themselves. You don’t have to be in a teaching position to act as a mentor (my experience mentoring hospitalists and others in leadership and quality improvement now far surpasses my experience with house staff).
The mentor often benefits as much as the mentee from this relationship. I have been inspired by their passion and dedication, educated by their ideas and innovation, and frequently find I am learning more from them, than they are from me. I have had great experiences in the SHM Mentored Implementation program in the role of mentee and mentor.
Participate in a community. When I first joined NAIP, I was amazed that the giants (Wachter, Nelson, Whitcomb, Holman, Williams, Greeno, Howell, Huddleston, Wellikson, and on and on) were not only approachable, they were warm, friendly, interesting, and extraordinarily welcoming. The ever-expanding and evolving community at SHM continues that tradition and offers a forum to share innovative work, discuss common problems and solutions, contact world experts, or just find an empathetic ear. Working on toolkits and collaborative efforts with this community remains a real highlight of my career, and the source of several lasting friendships. So don’t be shy; step right up; and introduce yourself!
Avoid my past mistakes (this might be a long list). Random things you should try to avoid.
- Tribalism – It is natural to be protective of your hospitalist group, and to focus on the injustices heaped upon you from (insert favorite punching bag here, e.g., ED, orthopedists, cardiologists, nursing staff, evil administration penny pinchers, etc). While some of those injustices might be real, tribalism, defensiveness, and circling the wagons generally only makes things worse. Sit down face to face, learn a little bit about the opposing tribe (both about their work, and about them as people), and see how much more fun and productive work can be.
- Storming out of a meeting with the CMO and CEO, slamming the door, etc. – not productive. Administrative leaders are doing their own juggling act and are generally well intentioned and doing the best they can. Respect that, argue your case, but if things don’t pan out, shake their hand, and live to fight another day.
- Using e-mail (evil-mail) to resolve conflict – And if you’re a young whippersnapper, don’t use Twitter, Facebook, Snapchat, or other social media to address conflict either!
- Forgetting to put patients first – Frame decisions for your group around what best serves your patients, not your doctors. Long term, this gives your group credibility and will serve the hospitalists better as well. SHM does this on a large scale with their advocacy efforts, resulting in more credibility and influence on Capitol Hill.
Make time for friends, family, fitness, fun, and reflection. A sense of humor and an occasional laugh when dealing with ill patients, hospital medicine politics, and the EMR all day provides resilience, as does taking the time to foster self-awareness and insight into your own weaknesses, strengths, and how you react to different stressors. A little bit of exercise and time with family and friends can go a long way towards improving your outlook, work, and life in general, while reducing burnout. Oh yeah, it’s also a good idea to choose a great life partner as well. Thanks Michelle!
Dr. Maynard is chief quality officer, University of California Davis Medical Center, Sacramento, Calif.
Residents and junior faculty have frequently asked me how they can attain a position similar to mine, focused on quality and leadership in a health care system. When I was first asked to offer advice on this topic, my response was generally something like, “Heck if I know! I just had a series of lucky accidents to get here!”
Back then, I would recount my career history. I established myself as a clinician educator and associate program director soon after Chief Residency. After that, I would explain, a series of fortunate events and health care trends shaped my career. Evidence-based medicine (EBM), the patient safety movement, a shift to incorporate value (as well as volume) into reimbursement models, and the hospital medicine movement all emerged in interesting and often synergistic ways.
A young SHM organization (then known as NAIP) grew rapidly even while the hospitalist programs I led in Phoenix, then at University of California, San Diego, grew in size and influence. Inevitably, it seemed, I was increasingly involved in quality improvement (QI) efforts, and began to publish and speak about them. Collaborative work with SHM and a number of hospital systems broadened my visibility regionally and nationally. Finally, in 2015, I was recruited away from UC San Diego into a new position, as chief quality officer at UC Davis.
On hearing this history, those seeking my sage advice would look a little confused, and then say something like, “So your advice is that I should get lucky??? Gee, thanks a lot! Really helpful!” (Insert sarcasm here).
The honor of being asked to contribute to the “Legacies” series in The Hospitalist gave me an opportunity to think about this a little differently. No one really wanted to know about how past changes in the health care environment led to my career success. They wanted advice on tools and strategies that will allow them to thrive in an environment of ongoing, disruptive change that is likely only going to accelerate. I now present my upgraded points of advice, intertwined with examples of how SHM positively influenced my career (and could assist yours):
Learn how your hospital works. Hospitalists obviously have an inside track on many aspects of hospital operations, but sometimes remain oblivious to the organizational and committee structure, priorities of hospital leadership, and the mechanism for implementing standardized care. Knowing where to go with new ideas, and the process of implementing protocols, will keep you from hitting political land mines and unintentionally encroaching on someone else’s turf, while aligning your efforts with institutional priorities improves the buy-in and resources available to do the work.
Start small, but think big. Don’t bite off more than you can chew, and make sure your ideas for change work on a small scale before trying to sell the world on them. On the other hand, think big! The care you and others provide is dependent on systems that go far beyond your immediate control. Policies, protocols, standardized order sets, checklists, and an array of other tools can be leveraged to influence care across an entire health system, and in the SHM Mentored Implementation programs, can impact hundreds of hospitals.
Broaden your skills. Commit to learning new skills that can increase your impact and career diversity. Procedural skills; information technology; and EMR, EBM, research, public health, QI, business, leadership, public speaking, advocacy, and telehealth, can all open up a whole world of possibilities when combined with a medical degree. These skills can move you into areas that keep you engaged and excited to go to work.
Engage in mentor/mentee relationships. As an associate program director and clinician-educator, I had a lot of opportunity to mentor residents and fellows. It is so rewarding to watch the mentee grow in experience and skills, and to eventually see many of them assume leadership and mentoring roles themselves. You don’t have to be in a teaching position to act as a mentor (my experience mentoring hospitalists and others in leadership and quality improvement now far surpasses my experience with house staff).
The mentor often benefits as much as the mentee from this relationship. I have been inspired by their passion and dedication, educated by their ideas and innovation, and frequently find I am learning more from them, than they are from me. I have had great experiences in the SHM Mentored Implementation program in the role of mentee and mentor.
Participate in a community. When I first joined NAIP, I was amazed that the giants (Wachter, Nelson, Whitcomb, Holman, Williams, Greeno, Howell, Huddleston, Wellikson, and on and on) were not only approachable, they were warm, friendly, interesting, and extraordinarily welcoming. The ever-expanding and evolving community at SHM continues that tradition and offers a forum to share innovative work, discuss common problems and solutions, contact world experts, or just find an empathetic ear. Working on toolkits and collaborative efforts with this community remains a real highlight of my career, and the source of several lasting friendships. So don’t be shy; step right up; and introduce yourself!
Avoid my past mistakes (this might be a long list). Random things you should try to avoid.
- Tribalism – It is natural to be protective of your hospitalist group, and to focus on the injustices heaped upon you from (insert favorite punching bag here, e.g., ED, orthopedists, cardiologists, nursing staff, evil administration penny pinchers, etc). While some of those injustices might be real, tribalism, defensiveness, and circling the wagons generally only makes things worse. Sit down face to face, learn a little bit about the opposing tribe (both about their work, and about them as people), and see how much more fun and productive work can be.
- Storming out of a meeting with the CMO and CEO, slamming the door, etc. – not productive. Administrative leaders are doing their own juggling act and are generally well intentioned and doing the best they can. Respect that, argue your case, but if things don’t pan out, shake their hand, and live to fight another day.
- Using e-mail (evil-mail) to resolve conflict – And if you’re a young whippersnapper, don’t use Twitter, Facebook, Snapchat, or other social media to address conflict either!
- Forgetting to put patients first – Frame decisions for your group around what best serves your patients, not your doctors. Long term, this gives your group credibility and will serve the hospitalists better as well. SHM does this on a large scale with their advocacy efforts, resulting in more credibility and influence on Capitol Hill.
Make time for friends, family, fitness, fun, and reflection. A sense of humor and an occasional laugh when dealing with ill patients, hospital medicine politics, and the EMR all day provides resilience, as does taking the time to foster self-awareness and insight into your own weaknesses, strengths, and how you react to different stressors. A little bit of exercise and time with family and friends can go a long way towards improving your outlook, work, and life in general, while reducing burnout. Oh yeah, it’s also a good idea to choose a great life partner as well. Thanks Michelle!
Dr. Maynard is chief quality officer, University of California Davis Medical Center, Sacramento, Calif.