User login
Discrepancies in dyschromia
Dyschromias are one of the most common skin concerns among women and persons of color. In the April issue of Journal of Drugs in Dermatology, Dr. S.J. Kang and associates conducted an excellent study to determine whether racial or ethnic groups are treated differently for dyschromia.
The investigators searched the National Ambulatory Medical Care Survey (NAMCS) database for visits including the diagnosis of dyschromia (ICD-9 codes 709.00 or 709.09) during an 18-year period (1993-2010). They found 24.7 million visits for dyschromia and 5,531,000 patients with a sole diagnosis of dyschromia. Of those with a sole diagnosis of dyschromia, 76% were seen by a dermatologist, and more than half were female. Seventy-five percent were white, 11% African American, 7% Asian/Pacific Islander, and 9% Hispanic, although Asians demonstrated the highest number of visits per 100,000 persons.
In this review, hydroquinone monotherapy was the most commonly prescribed medication by dermatologists. Combination therapy with hydroquinone plus a retinoid and corticosteroid was utilized for women 10 times more than for men. African American patients were less likely to be prescribed combination therapy or receive procedures (such as cryotherapy, chemical peels or lasers). Additionally, sunscreens were recommended less often to black and Asian patients, compared with white patients.
While the underlying reason for dyschromia plays a role in the type of treatment given, overall combination therapies are often more effective than therapy with hydroquinone alone. This study demonstrates that combination therapy may be under-utilized in patients of color.
In my practice, I find that unless the patient’s skin is completely hydroquinone-naive, combination therapy with hydroquinone, retinoid, and corticosteroid is often a first-line treatment that may achieve faster results. Sun protection is a vital component in the treatment of dyschromia, and it is recommended for every patient, regardless of race or ethnicity. Nonhydroquinone topical agents containing ingredients such as kojic acid, arbutin, licorice, niacinamide, resveratrol, and superficial chemical peels are also used in all ethnic groups. In my Asian, Hispanic, and African American or darker-skinned patients, I do use caution with deeper peels and lasers and often perform a test spot first if this type of therapy is considered.
Dr. Wesley practices dermatology in Beverly Hills, Calif.
Dyschromias are one of the most common skin concerns among women and persons of color. In the April issue of Journal of Drugs in Dermatology, Dr. S.J. Kang and associates conducted an excellent study to determine whether racial or ethnic groups are treated differently for dyschromia.
The investigators searched the National Ambulatory Medical Care Survey (NAMCS) database for visits including the diagnosis of dyschromia (ICD-9 codes 709.00 or 709.09) during an 18-year period (1993-2010). They found 24.7 million visits for dyschromia and 5,531,000 patients with a sole diagnosis of dyschromia. Of those with a sole diagnosis of dyschromia, 76% were seen by a dermatologist, and more than half were female. Seventy-five percent were white, 11% African American, 7% Asian/Pacific Islander, and 9% Hispanic, although Asians demonstrated the highest number of visits per 100,000 persons.
In this review, hydroquinone monotherapy was the most commonly prescribed medication by dermatologists. Combination therapy with hydroquinone plus a retinoid and corticosteroid was utilized for women 10 times more than for men. African American patients were less likely to be prescribed combination therapy or receive procedures (such as cryotherapy, chemical peels or lasers). Additionally, sunscreens were recommended less often to black and Asian patients, compared with white patients.
While the underlying reason for dyschromia plays a role in the type of treatment given, overall combination therapies are often more effective than therapy with hydroquinone alone. This study demonstrates that combination therapy may be under-utilized in patients of color.
In my practice, I find that unless the patient’s skin is completely hydroquinone-naive, combination therapy with hydroquinone, retinoid, and corticosteroid is often a first-line treatment that may achieve faster results. Sun protection is a vital component in the treatment of dyschromia, and it is recommended for every patient, regardless of race or ethnicity. Nonhydroquinone topical agents containing ingredients such as kojic acid, arbutin, licorice, niacinamide, resveratrol, and superficial chemical peels are also used in all ethnic groups. In my Asian, Hispanic, and African American or darker-skinned patients, I do use caution with deeper peels and lasers and often perform a test spot first if this type of therapy is considered.
Dr. Wesley practices dermatology in Beverly Hills, Calif.
Dyschromias are one of the most common skin concerns among women and persons of color. In the April issue of Journal of Drugs in Dermatology, Dr. S.J. Kang and associates conducted an excellent study to determine whether racial or ethnic groups are treated differently for dyschromia.
The investigators searched the National Ambulatory Medical Care Survey (NAMCS) database for visits including the diagnosis of dyschromia (ICD-9 codes 709.00 or 709.09) during an 18-year period (1993-2010). They found 24.7 million visits for dyschromia and 5,531,000 patients with a sole diagnosis of dyschromia. Of those with a sole diagnosis of dyschromia, 76% were seen by a dermatologist, and more than half were female. Seventy-five percent were white, 11% African American, 7% Asian/Pacific Islander, and 9% Hispanic, although Asians demonstrated the highest number of visits per 100,000 persons.
In this review, hydroquinone monotherapy was the most commonly prescribed medication by dermatologists. Combination therapy with hydroquinone plus a retinoid and corticosteroid was utilized for women 10 times more than for men. African American patients were less likely to be prescribed combination therapy or receive procedures (such as cryotherapy, chemical peels or lasers). Additionally, sunscreens were recommended less often to black and Asian patients, compared with white patients.
While the underlying reason for dyschromia plays a role in the type of treatment given, overall combination therapies are often more effective than therapy with hydroquinone alone. This study demonstrates that combination therapy may be under-utilized in patients of color.
In my practice, I find that unless the patient’s skin is completely hydroquinone-naive, combination therapy with hydroquinone, retinoid, and corticosteroid is often a first-line treatment that may achieve faster results. Sun protection is a vital component in the treatment of dyschromia, and it is recommended for every patient, regardless of race or ethnicity. Nonhydroquinone topical agents containing ingredients such as kojic acid, arbutin, licorice, niacinamide, resveratrol, and superficial chemical peels are also used in all ethnic groups. In my Asian, Hispanic, and African American or darker-skinned patients, I do use caution with deeper peels and lasers and often perform a test spot first if this type of therapy is considered.
Dr. Wesley practices dermatology in Beverly Hills, Calif.
CO2 laser works best for hypertrophic scars
PHOENIX – A fractional carbon dioxide laser at 10,600 nm was the only one of three laser treatments for hypertrophic scars that produced significant overall improvements in a comparison of data on 141 scars in 66 patients.
Less successful were treatments using a vascular KTP laser at 532 nm or a 1,550-nm nonablative fractional erbium glass laser.
"The only one that showed significant improvement compared with the control scar, adjusted for the baseline scar, was the fractional CO2 laser," Dr. Sigrid Blome-Eberwein said at the annual meeting of the American Society for Laser Medicine and Surgery.
The data came from three prospective controlled studies at one institution. The patients were burn survivors who had at least two scars of similar appearance and physiologic function in the same body area that were at least 6 months from wound healing. Patients underwent a series of at least three treatments at 4-week intervals on one or more scars, with a similar scar left untreated as the control scar.
Subjective assessments of the scars showed statistically significant improvements in scores on the Vancouver Scar Scale with all three treatments compared with control scars, but fewer changes were seen in objective measurements of scar qualities. "Measurements of these improvements are really difficult to tackle. We tried to add some objective measurement instruments to our evaluations," reported Dr. Blome-Eberwein of Lehigh Valley Regional Burn Center, Allentown, Pa.
None of the treatments produced significant changes in elasticity as measured by the Cutometer device. "It’s really a complete mix of results in this value," she said.
The fractional erbium laser produced one statistically significant improvement, compared with control scars, in thickness as measured by high-resolution ultrasound used to assess scar thickness (so that patients could avoid biopsies). The KTP laser also produced one statistically significant improvement, compared with control scars: improved sensation as assessed by Semmes Weinstein monofilaments.
The CO2 laser, however, produced greater improvements in scar thickness and sensation, as well as significant improvements in erythema and pigment (both measured by spectrometry), compared with control scars. Measurements of pain and pruritus did not differ significantly between treated and control scars in any of the studies; pain levels tended to improve in both the treated and control areas and pruritus tended to remain steady.
The KTP laser caused blisters in some patients. The fractional CO2 and fractional erbium lasers produced minimal damage. Increased power was more likely to produce collateral damage and blisters, Dr. Blome-Eberwein said.
Any results were persistent and additive. Because penetration of these lasers is limited, multiple treatments are needed for thick scars, she noted.
Based on these findings and her experience at the burn center, Dr. Blome-Eberwein recommended treating scars that seem to turn hypertrophic early (within 4 weeks of wound healing) and frequently (every 3 weeks) with a nonablative fractional erbium glass laser or pulsed dye laser. The erbium glass laser does seem to prevent "some degree of hypertrophy early on," she said. Either of these early treatments may decrease hypertrophic activity and prevent hypertrophy with no dermal damage.
Dr. Blome-Eberwein said she treats hypertrophic scars 3-12 months after healing with fractional CO2 laser. Treating scar pigment remains a challenge, she added.
"In the future, there will be handheld devices" to treat scars at home "because a lot of people are affected by this problem," she said.
Most of the scars in the studies were from burns, with a few from trauma.
Dr. Blome-Eberwein reported having no financial disclosures.
On Twitter @sherryboschert
PHOENIX – A fractional carbon dioxide laser at 10,600 nm was the only one of three laser treatments for hypertrophic scars that produced significant overall improvements in a comparison of data on 141 scars in 66 patients.
Less successful were treatments using a vascular KTP laser at 532 nm or a 1,550-nm nonablative fractional erbium glass laser.
"The only one that showed significant improvement compared with the control scar, adjusted for the baseline scar, was the fractional CO2 laser," Dr. Sigrid Blome-Eberwein said at the annual meeting of the American Society for Laser Medicine and Surgery.
The data came from three prospective controlled studies at one institution. The patients were burn survivors who had at least two scars of similar appearance and physiologic function in the same body area that were at least 6 months from wound healing. Patients underwent a series of at least three treatments at 4-week intervals on one or more scars, with a similar scar left untreated as the control scar.
Subjective assessments of the scars showed statistically significant improvements in scores on the Vancouver Scar Scale with all three treatments compared with control scars, but fewer changes were seen in objective measurements of scar qualities. "Measurements of these improvements are really difficult to tackle. We tried to add some objective measurement instruments to our evaluations," reported Dr. Blome-Eberwein of Lehigh Valley Regional Burn Center, Allentown, Pa.
None of the treatments produced significant changes in elasticity as measured by the Cutometer device. "It’s really a complete mix of results in this value," she said.
The fractional erbium laser produced one statistically significant improvement, compared with control scars, in thickness as measured by high-resolution ultrasound used to assess scar thickness (so that patients could avoid biopsies). The KTP laser also produced one statistically significant improvement, compared with control scars: improved sensation as assessed by Semmes Weinstein monofilaments.
The CO2 laser, however, produced greater improvements in scar thickness and sensation, as well as significant improvements in erythema and pigment (both measured by spectrometry), compared with control scars. Measurements of pain and pruritus did not differ significantly between treated and control scars in any of the studies; pain levels tended to improve in both the treated and control areas and pruritus tended to remain steady.
The KTP laser caused blisters in some patients. The fractional CO2 and fractional erbium lasers produced minimal damage. Increased power was more likely to produce collateral damage and blisters, Dr. Blome-Eberwein said.
Any results were persistent and additive. Because penetration of these lasers is limited, multiple treatments are needed for thick scars, she noted.
Based on these findings and her experience at the burn center, Dr. Blome-Eberwein recommended treating scars that seem to turn hypertrophic early (within 4 weeks of wound healing) and frequently (every 3 weeks) with a nonablative fractional erbium glass laser or pulsed dye laser. The erbium glass laser does seem to prevent "some degree of hypertrophy early on," she said. Either of these early treatments may decrease hypertrophic activity and prevent hypertrophy with no dermal damage.
Dr. Blome-Eberwein said she treats hypertrophic scars 3-12 months after healing with fractional CO2 laser. Treating scar pigment remains a challenge, she added.
"In the future, there will be handheld devices" to treat scars at home "because a lot of people are affected by this problem," she said.
Most of the scars in the studies were from burns, with a few from trauma.
Dr. Blome-Eberwein reported having no financial disclosures.
On Twitter @sherryboschert
PHOENIX – A fractional carbon dioxide laser at 10,600 nm was the only one of three laser treatments for hypertrophic scars that produced significant overall improvements in a comparison of data on 141 scars in 66 patients.
Less successful were treatments using a vascular KTP laser at 532 nm or a 1,550-nm nonablative fractional erbium glass laser.
"The only one that showed significant improvement compared with the control scar, adjusted for the baseline scar, was the fractional CO2 laser," Dr. Sigrid Blome-Eberwein said at the annual meeting of the American Society for Laser Medicine and Surgery.
The data came from three prospective controlled studies at one institution. The patients were burn survivors who had at least two scars of similar appearance and physiologic function in the same body area that were at least 6 months from wound healing. Patients underwent a series of at least three treatments at 4-week intervals on one or more scars, with a similar scar left untreated as the control scar.
Subjective assessments of the scars showed statistically significant improvements in scores on the Vancouver Scar Scale with all three treatments compared with control scars, but fewer changes were seen in objective measurements of scar qualities. "Measurements of these improvements are really difficult to tackle. We tried to add some objective measurement instruments to our evaluations," reported Dr. Blome-Eberwein of Lehigh Valley Regional Burn Center, Allentown, Pa.
None of the treatments produced significant changes in elasticity as measured by the Cutometer device. "It’s really a complete mix of results in this value," she said.
The fractional erbium laser produced one statistically significant improvement, compared with control scars, in thickness as measured by high-resolution ultrasound used to assess scar thickness (so that patients could avoid biopsies). The KTP laser also produced one statistically significant improvement, compared with control scars: improved sensation as assessed by Semmes Weinstein monofilaments.
The CO2 laser, however, produced greater improvements in scar thickness and sensation, as well as significant improvements in erythema and pigment (both measured by spectrometry), compared with control scars. Measurements of pain and pruritus did not differ significantly between treated and control scars in any of the studies; pain levels tended to improve in both the treated and control areas and pruritus tended to remain steady.
The KTP laser caused blisters in some patients. The fractional CO2 and fractional erbium lasers produced minimal damage. Increased power was more likely to produce collateral damage and blisters, Dr. Blome-Eberwein said.
Any results were persistent and additive. Because penetration of these lasers is limited, multiple treatments are needed for thick scars, she noted.
Based on these findings and her experience at the burn center, Dr. Blome-Eberwein recommended treating scars that seem to turn hypertrophic early (within 4 weeks of wound healing) and frequently (every 3 weeks) with a nonablative fractional erbium glass laser or pulsed dye laser. The erbium glass laser does seem to prevent "some degree of hypertrophy early on," she said. Either of these early treatments may decrease hypertrophic activity and prevent hypertrophy with no dermal damage.
Dr. Blome-Eberwein said she treats hypertrophic scars 3-12 months after healing with fractional CO2 laser. Treating scar pigment remains a challenge, she added.
"In the future, there will be handheld devices" to treat scars at home "because a lot of people are affected by this problem," she said.
Most of the scars in the studies were from burns, with a few from trauma.
Dr. Blome-Eberwein reported having no financial disclosures.
On Twitter @sherryboschert
AT LASER 2014
Major finding: The fractional CO2 laser significantly improved scar thickness, sensation, erythema, and pigment, compared with untreated scars. The KTP laser improved sensation and the erbium glass laser improved thickness in treated scars, compared with control scars.
Data source: An analysis of data from three prospective controlled studies of laser treatments in 66 patients with 141 scars.
Disclosures: Dr. Blome-Eberwein reported having no financial disclosures.
VIDEO: Concise guide to lasers: cellulite, tattoo removal, and skin tightening
DENVER – In 15 minutes, Dr. M. Christine Lee brings you a definitive guide to lasers for various patient needs, including tattoo removal, treatment of cellulite, skin tightening, and skin resurfacing. Learn more about lasers that you might want to add to your practice and get ideas on how to make the most of devices you already have.
Dr. Lee is with the department of dermatologic surgery at the University of California, San Francisco, and director of East Bay Laser & Skin Care Center in Walnut Creek, Calif. In this video, she also shares clinical pearls about different types of laser procedures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
DENVER – In 15 minutes, Dr. M. Christine Lee brings you a definitive guide to lasers for various patient needs, including tattoo removal, treatment of cellulite, skin tightening, and skin resurfacing. Learn more about lasers that you might want to add to your practice and get ideas on how to make the most of devices you already have.
Dr. Lee is with the department of dermatologic surgery at the University of California, San Francisco, and director of East Bay Laser & Skin Care Center in Walnut Creek, Calif. In this video, she also shares clinical pearls about different types of laser procedures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
DENVER – In 15 minutes, Dr. M. Christine Lee brings you a definitive guide to lasers for various patient needs, including tattoo removal, treatment of cellulite, skin tightening, and skin resurfacing. Learn more about lasers that you might want to add to your practice and get ideas on how to make the most of devices you already have.
Dr. Lee is with the department of dermatologic surgery at the University of California, San Francisco, and director of East Bay Laser & Skin Care Center in Walnut Creek, Calif. In this video, she also shares clinical pearls about different types of laser procedures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
EXPERT ANALYSIS FROM THE AAD ANNUAL MEETING
Cosmetic Corner: Dermatologists Weigh in on OTC Hair Restoration
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top OTC hair restoration products. Consideration must be given to:
- Glytone by Ducray
- Rogaine Unscented Foam 5% and Rogaine Extra Strength Solution
- Toppik
- Triple Moisture Deep Recovery Hair Mask
- Viviscal
Cutis invites readers to send us their recommendations. Antiperspirants, stretch mark therapies, exfoliators, and hair removal products will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to the Editorial Office.
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc. and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc. endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top OTC hair restoration products. Consideration must be given to:
- Glytone by Ducray
- Rogaine Unscented Foam 5% and Rogaine Extra Strength Solution
- Toppik
- Triple Moisture Deep Recovery Hair Mask
- Viviscal
Cutis invites readers to send us their recommendations. Antiperspirants, stretch mark therapies, exfoliators, and hair removal products will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to the Editorial Office.
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc. and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc. endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top OTC hair restoration products. Consideration must be given to:
- Glytone by Ducray
- Rogaine Unscented Foam 5% and Rogaine Extra Strength Solution
- Toppik
- Triple Moisture Deep Recovery Hair Mask
- Viviscal
Cutis invites readers to send us their recommendations. Antiperspirants, stretch mark therapies, exfoliators, and hair removal products will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to the Editorial Office.
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc. and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc. endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
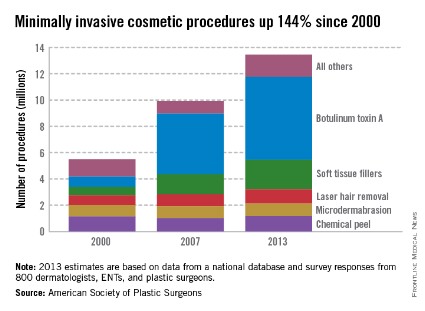
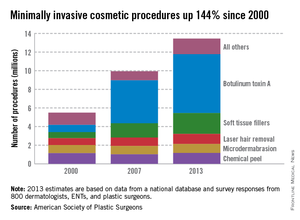
Botulinum toxin A tops list of nonsurgical cosmetic procedures in 2013
Injection of botulinum toxin type A continues to be the most popular form of minimally invasive cosmetic surgery, with a total of more than 6.3 million procedures performed in 2013, the American Society of Plastic Surgeons reported.
Overall, botulinum toxins such as Botox and Dysport accounted for 47% of the market for minimally invasive procedures, which totaled 13.4 million procedures in 2013, according to the ASPS.
The second most popular surgery was injection of soft tissue fillers, with 2.2 million procedures performed, followed by chemical peels (1.2 million procedures), laser hair removal (1.1 million), and microdermabrasion (970,000), the ASPS said.
The total number of minimally invasive procedures increased by 3% from 2012, as did the number of botulinum injections. The largest increase for a single type of procedure was seen for the soft tissue fillers, with hyaluronic acid injections up 18% from 2012 to 2013, the ASPS noted.
The estimates for 2013 are based on data from a national database and survey responses from 800 dermatologists, ENTs, and plastic surgeons.
Injection of botulinum toxin type A continues to be the most popular form of minimally invasive cosmetic surgery, with a total of more than 6.3 million procedures performed in 2013, the American Society of Plastic Surgeons reported.
Overall, botulinum toxins such as Botox and Dysport accounted for 47% of the market for minimally invasive procedures, which totaled 13.4 million procedures in 2013, according to the ASPS.
The second most popular surgery was injection of soft tissue fillers, with 2.2 million procedures performed, followed by chemical peels (1.2 million procedures), laser hair removal (1.1 million), and microdermabrasion (970,000), the ASPS said.
The total number of minimally invasive procedures increased by 3% from 2012, as did the number of botulinum injections. The largest increase for a single type of procedure was seen for the soft tissue fillers, with hyaluronic acid injections up 18% from 2012 to 2013, the ASPS noted.
The estimates for 2013 are based on data from a national database and survey responses from 800 dermatologists, ENTs, and plastic surgeons.
Injection of botulinum toxin type A continues to be the most popular form of minimally invasive cosmetic surgery, with a total of more than 6.3 million procedures performed in 2013, the American Society of Plastic Surgeons reported.
Overall, botulinum toxins such as Botox and Dysport accounted for 47% of the market for minimally invasive procedures, which totaled 13.4 million procedures in 2013, according to the ASPS.
The second most popular surgery was injection of soft tissue fillers, with 2.2 million procedures performed, followed by chemical peels (1.2 million procedures), laser hair removal (1.1 million), and microdermabrasion (970,000), the ASPS said.
The total number of minimally invasive procedures increased by 3% from 2012, as did the number of botulinum injections. The largest increase for a single type of procedure was seen for the soft tissue fillers, with hyaluronic acid injections up 18% from 2012 to 2013, the ASPS noted.
The estimates for 2013 are based on data from a national database and survey responses from 800 dermatologists, ENTs, and plastic surgeons.
Doctors reconstruct noses, create vaginas using engineered human tissue
Researchers have successfully engineered human tissue from autologous tissue for the reconstruction of nasal alar lobules in one first-in-human trial while investigators in separate study were able to engineer and implant vaginas in young women with congenital aplagia.
The results move human tissue engineering closer to one day becoming mainstream health care, according to an editorial accompanying the two studies published in the Lancet.
"Progression from first-in-human experiences in only a few patients ... to a full integration into health systems involves many steps, and is often an uphill struggle," according to Dr. Martin A. Birchall, professor of laryngology at University College London, and Alexander M. Seifalian, Ph.D., professor of nanotechnology and regenerative medicine at the same institution, in an editorial on both studies (Lancet 2014 April 11 [doi: 10.1016/S0140-6736(14)60533-X]). However, because the human tissue engineering field is not unique in its need for larger trials and long-term follow-up to show efficacy in larger patient cohorts, further progress might be facilitated by the fact that "many countries now have large translational income streams, engaged biotech companies, and streamlined regulatory processes that might lower these barriers."
The two studies achieve three important milestones in the field of human tissue engineering, according to Dr. Birchall and Dr. Seifalian. They provide evidence that when biological scaffolds with or without cells are placed in the body, native tissue will grow in its place rather than scar tissue. And this can be achieved in pediatric populations.
The third – and possibly most important – milestone is that implanting large-scale engineered tissue is possible, since in situ angiogenesis was found to be adequate in the vaginal vaults constructed and implanted in the second study, wrote Dr. Birchall and Dr. Seifalian. The findings help to "edge tissue engineering towards the mainstream of organ and tissue replacement needs," they said.
For the nasal reconstruction study, researchers used nasal septum cartilage cells from each of the five study participants to grow and shape cartilage grafts, which were then implanted in the respective patients whose alar lobule had been badly damaged by treatment for nonmelanoma skin cancer, according to Dr. Ilario Fulco and his associates in the departments of surgery and regenerative medicine at the University of Basel in Switzerland (Lancet 2014 April 11 [doi: 10.1016/S0140-6736(14)60544-4]).
Growth factor was used to expand the cells over the course of 2 weeks before they were seeded onto collagen membranes and cultured for another 2 weeks, until they grew into cartilage that was 40 times larger than the original biopsy. The cartilage was then shaped to fit the defect and was implanted.
At 1-year follow-up, all five reconstruction recipients reported they were satisfied with their ability to breathe, were happy with the look of their nose, and had not experienced any relevant adverse events.
"The engineered cartilage had clinical results comparable to the gold standard cartilage graft surgery," said Dr. Fulco. "This new technique could help the body accept the new tissue more easily, and improve the stability and functionality of the nostril."
Currently, for this kind of reconstruction, grafts are made using cartilage excised from the nasal septum, ear, or rib, which is painful and requires additional surgery, often fraught with complications.
The second study dealt with four female patients, who had congenital vaginal aplagia. The investigators fashioned vaginal vaults from smooth muscle and vaginal epithelial cells taken from the patients’ own vulvar tissues and grown on vagina-shaped biodegradable scaffolds. The engineered vaults then were transplanted into each of the young women, who were aged 13-18 years at the time of surgery, according to Dr. Atlántida M. Raya-Rivera, a professor of bioengineering at the Metropolitan Autonomous University, Mexico City, and her associates.
At 8 years’ follow-up, all the vaginas were determined to be structurally and functionally normal. At that time, all four women reported that they were sexually active; were satisfied with their desire, arousal, lubrication, and orgasm; and did not experience pain during intercourse.
"Yearly tissue biopsy samples show that the reconstructed tissue is histologically and functionally similar to normal vaginal tissue," noted Dr. Raya-Rivera. The results mean that this method is a "viable" alternative to current vaginal reconstructive techniques because it requires only a small tissue sample and can help avoid the complications inherent when using nonvaginal tissue such as from the large intestine or skin; the complications include infections or grafts that shrink, she noted (Lancet 2014 April 11 [doi: 10.1016/S0140-6736(14)60542-0]).
"With the syndrome these women have, both the uterus and vagina can be missing or malformed. In this study, two of the patients were born with uteri, and there is potential for them to have children," Dr. Raya-Rivera said in an interview.
In both studies, the authors wrote respectively that further "fundamental studies" and "clinical experience" are warranted. Dr. Birchall and Dr. Seifalian concluded that the two studies show that "disruptive innovation might be nigh."
Funding for the study led by Dr. Fulco was provided by the department of surgery, University Hospital Basel, and Krebsliga bedier Basel; funding for the study led by Dr. Raya-Rivera was provided by Wake Forest University and Hospital Infantil de Mexico Federico Gomez. None of the researchers associated with the studies or the commentary reported having any relevant disclosures.
On Twitter @whitneymcknight
Researchers have successfully engineered human tissue from autologous tissue for the reconstruction of nasal alar lobules in one first-in-human trial while investigators in separate study were able to engineer and implant vaginas in young women with congenital aplagia.
The results move human tissue engineering closer to one day becoming mainstream health care, according to an editorial accompanying the two studies published in the Lancet.
"Progression from first-in-human experiences in only a few patients ... to a full integration into health systems involves many steps, and is often an uphill struggle," according to Dr. Martin A. Birchall, professor of laryngology at University College London, and Alexander M. Seifalian, Ph.D., professor of nanotechnology and regenerative medicine at the same institution, in an editorial on both studies (Lancet 2014 April 11 [doi: 10.1016/S0140-6736(14)60533-X]). However, because the human tissue engineering field is not unique in its need for larger trials and long-term follow-up to show efficacy in larger patient cohorts, further progress might be facilitated by the fact that "many countries now have large translational income streams, engaged biotech companies, and streamlined regulatory processes that might lower these barriers."
The two studies achieve three important milestones in the field of human tissue engineering, according to Dr. Birchall and Dr. Seifalian. They provide evidence that when biological scaffolds with or without cells are placed in the body, native tissue will grow in its place rather than scar tissue. And this can be achieved in pediatric populations.
The third – and possibly most important – milestone is that implanting large-scale engineered tissue is possible, since in situ angiogenesis was found to be adequate in the vaginal vaults constructed and implanted in the second study, wrote Dr. Birchall and Dr. Seifalian. The findings help to "edge tissue engineering towards the mainstream of organ and tissue replacement needs," they said.
For the nasal reconstruction study, researchers used nasal septum cartilage cells from each of the five study participants to grow and shape cartilage grafts, which were then implanted in the respective patients whose alar lobule had been badly damaged by treatment for nonmelanoma skin cancer, according to Dr. Ilario Fulco and his associates in the departments of surgery and regenerative medicine at the University of Basel in Switzerland (Lancet 2014 April 11 [doi: 10.1016/S0140-6736(14)60544-4]).
Growth factor was used to expand the cells over the course of 2 weeks before they were seeded onto collagen membranes and cultured for another 2 weeks, until they grew into cartilage that was 40 times larger than the original biopsy. The cartilage was then shaped to fit the defect and was implanted.
At 1-year follow-up, all five reconstruction recipients reported they were satisfied with their ability to breathe, were happy with the look of their nose, and had not experienced any relevant adverse events.
"The engineered cartilage had clinical results comparable to the gold standard cartilage graft surgery," said Dr. Fulco. "This new technique could help the body accept the new tissue more easily, and improve the stability and functionality of the nostril."
Currently, for this kind of reconstruction, grafts are made using cartilage excised from the nasal septum, ear, or rib, which is painful and requires additional surgery, often fraught with complications.
The second study dealt with four female patients, who had congenital vaginal aplagia. The investigators fashioned vaginal vaults from smooth muscle and vaginal epithelial cells taken from the patients’ own vulvar tissues and grown on vagina-shaped biodegradable scaffolds. The engineered vaults then were transplanted into each of the young women, who were aged 13-18 years at the time of surgery, according to Dr. Atlántida M. Raya-Rivera, a professor of bioengineering at the Metropolitan Autonomous University, Mexico City, and her associates.
At 8 years’ follow-up, all the vaginas were determined to be structurally and functionally normal. At that time, all four women reported that they were sexually active; were satisfied with their desire, arousal, lubrication, and orgasm; and did not experience pain during intercourse.
"Yearly tissue biopsy samples show that the reconstructed tissue is histologically and functionally similar to normal vaginal tissue," noted Dr. Raya-Rivera. The results mean that this method is a "viable" alternative to current vaginal reconstructive techniques because it requires only a small tissue sample and can help avoid the complications inherent when using nonvaginal tissue such as from the large intestine or skin; the complications include infections or grafts that shrink, she noted (Lancet 2014 April 11 [doi: 10.1016/S0140-6736(14)60542-0]).
"With the syndrome these women have, both the uterus and vagina can be missing or malformed. In this study, two of the patients were born with uteri, and there is potential for them to have children," Dr. Raya-Rivera said in an interview.
In both studies, the authors wrote respectively that further "fundamental studies" and "clinical experience" are warranted. Dr. Birchall and Dr. Seifalian concluded that the two studies show that "disruptive innovation might be nigh."
Funding for the study led by Dr. Fulco was provided by the department of surgery, University Hospital Basel, and Krebsliga bedier Basel; funding for the study led by Dr. Raya-Rivera was provided by Wake Forest University and Hospital Infantil de Mexico Federico Gomez. None of the researchers associated with the studies or the commentary reported having any relevant disclosures.
On Twitter @whitneymcknight
Researchers have successfully engineered human tissue from autologous tissue for the reconstruction of nasal alar lobules in one first-in-human trial while investigators in separate study were able to engineer and implant vaginas in young women with congenital aplagia.
The results move human tissue engineering closer to one day becoming mainstream health care, according to an editorial accompanying the two studies published in the Lancet.
"Progression from first-in-human experiences in only a few patients ... to a full integration into health systems involves many steps, and is often an uphill struggle," according to Dr. Martin A. Birchall, professor of laryngology at University College London, and Alexander M. Seifalian, Ph.D., professor of nanotechnology and regenerative medicine at the same institution, in an editorial on both studies (Lancet 2014 April 11 [doi: 10.1016/S0140-6736(14)60533-X]). However, because the human tissue engineering field is not unique in its need for larger trials and long-term follow-up to show efficacy in larger patient cohorts, further progress might be facilitated by the fact that "many countries now have large translational income streams, engaged biotech companies, and streamlined regulatory processes that might lower these barriers."
The two studies achieve three important milestones in the field of human tissue engineering, according to Dr. Birchall and Dr. Seifalian. They provide evidence that when biological scaffolds with or without cells are placed in the body, native tissue will grow in its place rather than scar tissue. And this can be achieved in pediatric populations.
The third – and possibly most important – milestone is that implanting large-scale engineered tissue is possible, since in situ angiogenesis was found to be adequate in the vaginal vaults constructed and implanted in the second study, wrote Dr. Birchall and Dr. Seifalian. The findings help to "edge tissue engineering towards the mainstream of organ and tissue replacement needs," they said.
For the nasal reconstruction study, researchers used nasal septum cartilage cells from each of the five study participants to grow and shape cartilage grafts, which were then implanted in the respective patients whose alar lobule had been badly damaged by treatment for nonmelanoma skin cancer, according to Dr. Ilario Fulco and his associates in the departments of surgery and regenerative medicine at the University of Basel in Switzerland (Lancet 2014 April 11 [doi: 10.1016/S0140-6736(14)60544-4]).
Growth factor was used to expand the cells over the course of 2 weeks before they were seeded onto collagen membranes and cultured for another 2 weeks, until they grew into cartilage that was 40 times larger than the original biopsy. The cartilage was then shaped to fit the defect and was implanted.
At 1-year follow-up, all five reconstruction recipients reported they were satisfied with their ability to breathe, were happy with the look of their nose, and had not experienced any relevant adverse events.
"The engineered cartilage had clinical results comparable to the gold standard cartilage graft surgery," said Dr. Fulco. "This new technique could help the body accept the new tissue more easily, and improve the stability and functionality of the nostril."
Currently, for this kind of reconstruction, grafts are made using cartilage excised from the nasal septum, ear, or rib, which is painful and requires additional surgery, often fraught with complications.
The second study dealt with four female patients, who had congenital vaginal aplagia. The investigators fashioned vaginal vaults from smooth muscle and vaginal epithelial cells taken from the patients’ own vulvar tissues and grown on vagina-shaped biodegradable scaffolds. The engineered vaults then were transplanted into each of the young women, who were aged 13-18 years at the time of surgery, according to Dr. Atlántida M. Raya-Rivera, a professor of bioengineering at the Metropolitan Autonomous University, Mexico City, and her associates.
At 8 years’ follow-up, all the vaginas were determined to be structurally and functionally normal. At that time, all four women reported that they were sexually active; were satisfied with their desire, arousal, lubrication, and orgasm; and did not experience pain during intercourse.
"Yearly tissue biopsy samples show that the reconstructed tissue is histologically and functionally similar to normal vaginal tissue," noted Dr. Raya-Rivera. The results mean that this method is a "viable" alternative to current vaginal reconstructive techniques because it requires only a small tissue sample and can help avoid the complications inherent when using nonvaginal tissue such as from the large intestine or skin; the complications include infections or grafts that shrink, she noted (Lancet 2014 April 11 [doi: 10.1016/S0140-6736(14)60542-0]).
"With the syndrome these women have, both the uterus and vagina can be missing or malformed. In this study, two of the patients were born with uteri, and there is potential for them to have children," Dr. Raya-Rivera said in an interview.
In both studies, the authors wrote respectively that further "fundamental studies" and "clinical experience" are warranted. Dr. Birchall and Dr. Seifalian concluded that the two studies show that "disruptive innovation might be nigh."
Funding for the study led by Dr. Fulco was provided by the department of surgery, University Hospital Basel, and Krebsliga bedier Basel; funding for the study led by Dr. Raya-Rivera was provided by Wake Forest University and Hospital Infantil de Mexico Federico Gomez. None of the researchers associated with the studies or the commentary reported having any relevant disclosures.
On Twitter @whitneymcknight
FROM THE LANCET
Major finding: Nasal septum cartilage cells and vaginal epithelial cells were used to grow human tissue for implantation.
Data source: An observational first-in-human trial of nasal reconstruction post skin cancer in five patients, and a pilot cohort study of vaginal implantation in four patients who had congenital vaginal aplagia.
Disclosures: Funding for the study led by Dr. Fulco was provided by the department of surgery, University Hospital Basel, and Krebsliga bedier Basel; funding for the study led by Dr. Raya-Rivera was provided by Wake Forest University and Hospital Infantil de Mexico Federico Gomez. None of the researchers associated with the studies or the commentary reported having any relevant disclosures.
Simplifying Sun Safety: A Guide to the New FDA Sunscreen Monograph
Cutaneous Metastasis From Primary Gastric Cancer: A Case Report and Review of the Literature
More ways to make the most of lasers in clinical practice
PHOENIX – What’s the latest in lasers? The most stubborn tattoos – those with blue or green ink – are now the easiest to remove with new laser technology and techniques. Microwave treatment for armpit hair is a real option, even on difficult-to-remove blond hair. Cutaneous laser expert Dr. Roy Geronemus, director of the Laser and Skin Surgery Center of New York, describes what dermatologists need to know about these and other innovative cosmetic treatments in an interview at the annual meeting of the American Society for Laser Medicine and Surgery.
But that’s not all. More data support the use of lasers for common medical conditions, says Dr. Geronemus. Hear his description of how the same new laser used for tattoo removal can be a noninvasive treatment to reduce either hypertrophic or atrophic scarring in any skin type, with practically no downtime. He also explains several new approaches that show promise as acne therapy.
On Twitter @sherryboschert
PHOENIX – What’s the latest in lasers? The most stubborn tattoos – those with blue or green ink – are now the easiest to remove with new laser technology and techniques. Microwave treatment for armpit hair is a real option, even on difficult-to-remove blond hair. Cutaneous laser expert Dr. Roy Geronemus, director of the Laser and Skin Surgery Center of New York, describes what dermatologists need to know about these and other innovative cosmetic treatments in an interview at the annual meeting of the American Society for Laser Medicine and Surgery.
But that’s not all. More data support the use of lasers for common medical conditions, says Dr. Geronemus. Hear his description of how the same new laser used for tattoo removal can be a noninvasive treatment to reduce either hypertrophic or atrophic scarring in any skin type, with practically no downtime. He also explains several new approaches that show promise as acne therapy.
On Twitter @sherryboschert
PHOENIX – What’s the latest in lasers? The most stubborn tattoos – those with blue or green ink – are now the easiest to remove with new laser technology and techniques. Microwave treatment for armpit hair is a real option, even on difficult-to-remove blond hair. Cutaneous laser expert Dr. Roy Geronemus, director of the Laser and Skin Surgery Center of New York, describes what dermatologists need to know about these and other innovative cosmetic treatments in an interview at the annual meeting of the American Society for Laser Medicine and Surgery.
But that’s not all. More data support the use of lasers for common medical conditions, says Dr. Geronemus. Hear his description of how the same new laser used for tattoo removal can be a noninvasive treatment to reduce either hypertrophic or atrophic scarring in any skin type, with practically no downtime. He also explains several new approaches that show promise as acne therapy.
On Twitter @sherryboschert
AT LASER 2014
Acne scar improvements maintained after laser treatment
PHOENIX – Improvements in acne scarring were maintained 3 months after six laser treatments with a diffractive lens array and a picosecond 755-nm alexandrite laser. Changes seen on histology suggest the improvements stem from more than collagen remodeling alone.
Twenty adults with facial acne scars and Fitzpatrick skin types I-V underwent six laser treatments performed every 4-8 weeks at a single center using a 755-nm wavelength, diffractive lens array, pulse duration of 750-850 picoseconds, and repetition rate of 5 Hz, with a fixed spot size of 6 mm and fluence of 0.71 J/cm2.
Three physicians who were blinded to the results evaluated two- and three-dimensional images taken at baseline and at follow-up visits. Analysis of two-dimensional photos produced acne scar improvement scores averaging 1.5 at the 1-month follow-up visit and 1.4 at the 3-month visit on a 4-point scale (with 0 indicating 0-25% improvement and 3 indicating greater than 75% improvement), Dr. Jeremy Brauer and his associates reported.
Scar volume decreased by an average of 24% by 1 month post treatment and 27% by 3 months post treatment, according to analyses of the three-dimensional images, Dr. Brauer said at the annual meeting of the American Society for Laser Medicine and Surgery.
Histology of biopsy specimens taken at baseline and at 3 months after the last treatment showed elongation and increased density of elastic fibers, increased dermal collagen, and increased dermal mucin after treatment. These findings suggest that the improvements in scarring are caused by dermal changes beyond remodeling of collagen alone, said Dr. Brauer of the Laser & Skin Surgery Center in New York.
Dr. Brauer and his associates previously reported that the picosecond laser and diffractive lens array can improve acne scarring with minimal preparation and down time, "in many cases with no anesthesia at all," he said. The investigators offered topical anesthesia and antiviral prophylaxis to patients, but most declined.
The diffractive lens array delivers varying levels of heat at a fixed spot size and fluence. High-energy pulses that are 500 mcm apart deliver 70% of the fluence, with a lower level of heating surrounding these higher-level pulses. In total, approximately 10% of the tissue is exposed to the high-fluence regions.
The 15 women and 5 men in the study ranged in age from 27 to 62 years.
Previous methods of treating acne scarring with lasers, intense pulsed light, or other energy devices typically cause thermal injury that produces collagen synthesis and remodeling. Those procedures usually require anesthesia and can cause collateral damage that may take a long time to heal, he said.
The investigators chose the picosecond 755-nm alexandrite laser because it has been used successfully to remove tattoos or treat pigmented lesions while causing fewer side effects and coupled it with the specialized diffractive lens array.
The study excluded patients with hypersensitivity to light; localized or systemic infection, prior laser treatment in the past 3 months; and a history of skin cancer, keloidal scarring, immunosuppression, or immune deficiency disorder. Also excluded were patients who used isotretinoin in the past year and women who were pregnant, breastfeeding, or contemplating pregnancy.
Dr. Brauer and a coinvestigator reported financial associations with Cynosure, which also loaned equipment for the study.
On Twitter @sherryboschert
PHOENIX – Improvements in acne scarring were maintained 3 months after six laser treatments with a diffractive lens array and a picosecond 755-nm alexandrite laser. Changes seen on histology suggest the improvements stem from more than collagen remodeling alone.
Twenty adults with facial acne scars and Fitzpatrick skin types I-V underwent six laser treatments performed every 4-8 weeks at a single center using a 755-nm wavelength, diffractive lens array, pulse duration of 750-850 picoseconds, and repetition rate of 5 Hz, with a fixed spot size of 6 mm and fluence of 0.71 J/cm2.
Three physicians who were blinded to the results evaluated two- and three-dimensional images taken at baseline and at follow-up visits. Analysis of two-dimensional photos produced acne scar improvement scores averaging 1.5 at the 1-month follow-up visit and 1.4 at the 3-month visit on a 4-point scale (with 0 indicating 0-25% improvement and 3 indicating greater than 75% improvement), Dr. Jeremy Brauer and his associates reported.
Scar volume decreased by an average of 24% by 1 month post treatment and 27% by 3 months post treatment, according to analyses of the three-dimensional images, Dr. Brauer said at the annual meeting of the American Society for Laser Medicine and Surgery.
Histology of biopsy specimens taken at baseline and at 3 months after the last treatment showed elongation and increased density of elastic fibers, increased dermal collagen, and increased dermal mucin after treatment. These findings suggest that the improvements in scarring are caused by dermal changes beyond remodeling of collagen alone, said Dr. Brauer of the Laser & Skin Surgery Center in New York.
Dr. Brauer and his associates previously reported that the picosecond laser and diffractive lens array can improve acne scarring with minimal preparation and down time, "in many cases with no anesthesia at all," he said. The investigators offered topical anesthesia and antiviral prophylaxis to patients, but most declined.
The diffractive lens array delivers varying levels of heat at a fixed spot size and fluence. High-energy pulses that are 500 mcm apart deliver 70% of the fluence, with a lower level of heating surrounding these higher-level pulses. In total, approximately 10% of the tissue is exposed to the high-fluence regions.
The 15 women and 5 men in the study ranged in age from 27 to 62 years.
Previous methods of treating acne scarring with lasers, intense pulsed light, or other energy devices typically cause thermal injury that produces collagen synthesis and remodeling. Those procedures usually require anesthesia and can cause collateral damage that may take a long time to heal, he said.
The investigators chose the picosecond 755-nm alexandrite laser because it has been used successfully to remove tattoos or treat pigmented lesions while causing fewer side effects and coupled it with the specialized diffractive lens array.
The study excluded patients with hypersensitivity to light; localized or systemic infection, prior laser treatment in the past 3 months; and a history of skin cancer, keloidal scarring, immunosuppression, or immune deficiency disorder. Also excluded were patients who used isotretinoin in the past year and women who were pregnant, breastfeeding, or contemplating pregnancy.
Dr. Brauer and a coinvestigator reported financial associations with Cynosure, which also loaned equipment for the study.
On Twitter @sherryboschert
PHOENIX – Improvements in acne scarring were maintained 3 months after six laser treatments with a diffractive lens array and a picosecond 755-nm alexandrite laser. Changes seen on histology suggest the improvements stem from more than collagen remodeling alone.
Twenty adults with facial acne scars and Fitzpatrick skin types I-V underwent six laser treatments performed every 4-8 weeks at a single center using a 755-nm wavelength, diffractive lens array, pulse duration of 750-850 picoseconds, and repetition rate of 5 Hz, with a fixed spot size of 6 mm and fluence of 0.71 J/cm2.
Three physicians who were blinded to the results evaluated two- and three-dimensional images taken at baseline and at follow-up visits. Analysis of two-dimensional photos produced acne scar improvement scores averaging 1.5 at the 1-month follow-up visit and 1.4 at the 3-month visit on a 4-point scale (with 0 indicating 0-25% improvement and 3 indicating greater than 75% improvement), Dr. Jeremy Brauer and his associates reported.
Scar volume decreased by an average of 24% by 1 month post treatment and 27% by 3 months post treatment, according to analyses of the three-dimensional images, Dr. Brauer said at the annual meeting of the American Society for Laser Medicine and Surgery.
Histology of biopsy specimens taken at baseline and at 3 months after the last treatment showed elongation and increased density of elastic fibers, increased dermal collagen, and increased dermal mucin after treatment. These findings suggest that the improvements in scarring are caused by dermal changes beyond remodeling of collagen alone, said Dr. Brauer of the Laser & Skin Surgery Center in New York.
Dr. Brauer and his associates previously reported that the picosecond laser and diffractive lens array can improve acne scarring with minimal preparation and down time, "in many cases with no anesthesia at all," he said. The investigators offered topical anesthesia and antiviral prophylaxis to patients, but most declined.
The diffractive lens array delivers varying levels of heat at a fixed spot size and fluence. High-energy pulses that are 500 mcm apart deliver 70% of the fluence, with a lower level of heating surrounding these higher-level pulses. In total, approximately 10% of the tissue is exposed to the high-fluence regions.
The 15 women and 5 men in the study ranged in age from 27 to 62 years.
Previous methods of treating acne scarring with lasers, intense pulsed light, or other energy devices typically cause thermal injury that produces collagen synthesis and remodeling. Those procedures usually require anesthesia and can cause collateral damage that may take a long time to heal, he said.
The investigators chose the picosecond 755-nm alexandrite laser because it has been used successfully to remove tattoos or treat pigmented lesions while causing fewer side effects and coupled it with the specialized diffractive lens array.
The study excluded patients with hypersensitivity to light; localized or systemic infection, prior laser treatment in the past 3 months; and a history of skin cancer, keloidal scarring, immunosuppression, or immune deficiency disorder. Also excluded were patients who used isotretinoin in the past year and women who were pregnant, breastfeeding, or contemplating pregnancy.
Dr. Brauer and a coinvestigator reported financial associations with Cynosure, which also loaned equipment for the study.
On Twitter @sherryboschert
AT LASER 2014
Major finding: Acne scar volume decreased 24% by 1 month after treatment ended and 27% by 3 months post treatment, compared with baseline.
Key clinical point: Histologic data suggest that using a diffractive lens array and a picosecond 755-nm laser to treat acne scars caused dermal changes beyond skin remodeling alone.
Data source: Single-center study of 20 adults and photographic assessments by three physicians who were blinded to the results.
Disclosures: Dr. Brauer and a coinvestigator reported financial associations with Cynosure, which also loaned equipment for the study.