User login
B-cell energy levels linked to leukemic transformation

Photo from Business Wire
A pair of transcription factors protect B cells from malignant transformation by keeping the cells’ glucose and energy levels low, according to research published in Nature.
“While transformation to cancer and childhood leukemia takes large amounts of energy, we discovered that low energy levels in B cells protects from malignant transformation toward leukemia and cancer,” said study author Markus Müschen, MD, PhD, of City of Hope Comprehensive Cancer Center in Duarte, California.
“The low energy levels in normal B cells are simply too low to allow transformation to leukemia.”
Dr Müschen and his colleagues found that PAX5 and IKZF1, transcription factors that are critical for early B-cell development, “enforce a state of chronic energy deprivation” that results in constitutive activation of the energy-stress sensor AMPK.
However, dominant-negative mutants of PAX5 and IKZF1 reverse this effect.
Past research has suggested that mutations and deletions in the PAX5 and IKZF1 genes occur in more than 80% of cases of pre-B-cell acute lymphoblastic leukemia (ALL).
In the current study, Dr Müschen and his colleagues found that heterozygous deletion of Pax5 in a mouse model of pre-B ALL greatly increased glucose uptake and ATP levels.
Similarly, when they reconstituted PAX5 and IKZF1 in samples from patients with pre-B ALL, the investigators observed “an energy crisis” that prompted leukemic cell death.
Dr Müschen and his colleagues also performed a CRISPR/Cas9-based screen of PAX5 and IKZF1 transcriptional targets. They said this revealed that NR3C1, TXNIP, and CNR2 are central effectors of B-lymphoid restriction of glucose and energy.
To build upon this finding, the investigators tested TXNIP and CNR2 agonists as well as a small-molecule AMPK inhibitor. They found these compounds synergized with glucocorticoids in patient-derived pre-B ALL cells.
The team therefore concluded that TXNIP, CNR2, and AMPK are potential therapeutic targets for pre-B ALL.
The investigators also said the results of this study support a previous finding that obese children with high blood sugar levels are much more likely to develop drug-resistant leukemia than children who are not overweight. So dieting could be an important consideration for children who have survived leukemia.
“Avoiding obesity and excessive energy supply may help to decrease the risk of leukemia relapse,” said study author Lai Chan, PhD, also of City of Hope.
To test that theory, Drs Chan and Müschen and their colleagues plan to perform experiments in animal models to evaluate the efficacy of dietary restriction on patient-derived childhood leukemia cells, and to assess the activity of drugs that reduce leukemia cells’ glucose and energy supply.
“Based on the outcome of these studies, we plan to introduce dietary restriction and/or glucose-restricting drugs into a clinical trial for children who are at risk to develop leukemia relapse,” Dr Müschen said. ![]()

Photo from Business Wire
A pair of transcription factors protect B cells from malignant transformation by keeping the cells’ glucose and energy levels low, according to research published in Nature.
“While transformation to cancer and childhood leukemia takes large amounts of energy, we discovered that low energy levels in B cells protects from malignant transformation toward leukemia and cancer,” said study author Markus Müschen, MD, PhD, of City of Hope Comprehensive Cancer Center in Duarte, California.
“The low energy levels in normal B cells are simply too low to allow transformation to leukemia.”
Dr Müschen and his colleagues found that PAX5 and IKZF1, transcription factors that are critical for early B-cell development, “enforce a state of chronic energy deprivation” that results in constitutive activation of the energy-stress sensor AMPK.
However, dominant-negative mutants of PAX5 and IKZF1 reverse this effect.
Past research has suggested that mutations and deletions in the PAX5 and IKZF1 genes occur in more than 80% of cases of pre-B-cell acute lymphoblastic leukemia (ALL).
In the current study, Dr Müschen and his colleagues found that heterozygous deletion of Pax5 in a mouse model of pre-B ALL greatly increased glucose uptake and ATP levels.
Similarly, when they reconstituted PAX5 and IKZF1 in samples from patients with pre-B ALL, the investigators observed “an energy crisis” that prompted leukemic cell death.
Dr Müschen and his colleagues also performed a CRISPR/Cas9-based screen of PAX5 and IKZF1 transcriptional targets. They said this revealed that NR3C1, TXNIP, and CNR2 are central effectors of B-lymphoid restriction of glucose and energy.
To build upon this finding, the investigators tested TXNIP and CNR2 agonists as well as a small-molecule AMPK inhibitor. They found these compounds synergized with glucocorticoids in patient-derived pre-B ALL cells.
The team therefore concluded that TXNIP, CNR2, and AMPK are potential therapeutic targets for pre-B ALL.
The investigators also said the results of this study support a previous finding that obese children with high blood sugar levels are much more likely to develop drug-resistant leukemia than children who are not overweight. So dieting could be an important consideration for children who have survived leukemia.
“Avoiding obesity and excessive energy supply may help to decrease the risk of leukemia relapse,” said study author Lai Chan, PhD, also of City of Hope.
To test that theory, Drs Chan and Müschen and their colleagues plan to perform experiments in animal models to evaluate the efficacy of dietary restriction on patient-derived childhood leukemia cells, and to assess the activity of drugs that reduce leukemia cells’ glucose and energy supply.
“Based on the outcome of these studies, we plan to introduce dietary restriction and/or glucose-restricting drugs into a clinical trial for children who are at risk to develop leukemia relapse,” Dr Müschen said. ![]()

Photo from Business Wire
A pair of transcription factors protect B cells from malignant transformation by keeping the cells’ glucose and energy levels low, according to research published in Nature.
“While transformation to cancer and childhood leukemia takes large amounts of energy, we discovered that low energy levels in B cells protects from malignant transformation toward leukemia and cancer,” said study author Markus Müschen, MD, PhD, of City of Hope Comprehensive Cancer Center in Duarte, California.
“The low energy levels in normal B cells are simply too low to allow transformation to leukemia.”
Dr Müschen and his colleagues found that PAX5 and IKZF1, transcription factors that are critical for early B-cell development, “enforce a state of chronic energy deprivation” that results in constitutive activation of the energy-stress sensor AMPK.
However, dominant-negative mutants of PAX5 and IKZF1 reverse this effect.
Past research has suggested that mutations and deletions in the PAX5 and IKZF1 genes occur in more than 80% of cases of pre-B-cell acute lymphoblastic leukemia (ALL).
In the current study, Dr Müschen and his colleagues found that heterozygous deletion of Pax5 in a mouse model of pre-B ALL greatly increased glucose uptake and ATP levels.
Similarly, when they reconstituted PAX5 and IKZF1 in samples from patients with pre-B ALL, the investigators observed “an energy crisis” that prompted leukemic cell death.
Dr Müschen and his colleagues also performed a CRISPR/Cas9-based screen of PAX5 and IKZF1 transcriptional targets. They said this revealed that NR3C1, TXNIP, and CNR2 are central effectors of B-lymphoid restriction of glucose and energy.
To build upon this finding, the investigators tested TXNIP and CNR2 agonists as well as a small-molecule AMPK inhibitor. They found these compounds synergized with glucocorticoids in patient-derived pre-B ALL cells.
The team therefore concluded that TXNIP, CNR2, and AMPK are potential therapeutic targets for pre-B ALL.
The investigators also said the results of this study support a previous finding that obese children with high blood sugar levels are much more likely to develop drug-resistant leukemia than children who are not overweight. So dieting could be an important consideration for children who have survived leukemia.
“Avoiding obesity and excessive energy supply may help to decrease the risk of leukemia relapse,” said study author Lai Chan, PhD, also of City of Hope.
To test that theory, Drs Chan and Müschen and their colleagues plan to perform experiments in animal models to evaluate the efficacy of dietary restriction on patient-derived childhood leukemia cells, and to assess the activity of drugs that reduce leukemia cells’ glucose and energy supply.
“Based on the outcome of these studies, we plan to introduce dietary restriction and/or glucose-restricting drugs into a clinical trial for children who are at risk to develop leukemia relapse,” Dr Müschen said. ![]()
Kids, parents over-report ALL treatment adherence

New research published in Blood suggests young patients with acute lymphoblastic leukemia (ALL)—and their parents—are likely to over-report treatment adherence.
In a study of 416 pediatric ALL patients, 84% of patients or their parents said the patients took more 6-mercaptopurine (6MP) than they actually did.
6MP is prescribed for 2 years after chemotherapy with the goal of producing durable remissions, but studies show that over 95% of the prescribed doses must be taken for the medication to be effective.
“Because this therapy is administered orally every day, we cannot supervise our patients to make sure they are taking their pills,” said study author Smita Bhatia, MD, of the University of Alabama at Birmingham.
“Findings from this study suggest that we need better ways to monitor intake of medications as prescribed.”
This study included 416 pediatric ALL patients followed over 4 months. Patients received prescription pill bottles for their 6MP that contained a microprocessor chip in the cap to log the date and time the bottle was opened.
The logs were compared to self-report questionnaires completed by patients or their parents and provided to physicians at monthly check-ups.
Patients were classified as:
- Perfect reporters—self-report corresponded to data from the Medication Event Monitoring System (MEMS)
- Over-reporters—self-report was greater than MEMS data by more than 5 days per month for more than 50% of the study months
- Others—all patients not meeting criteria for perfect- or over-reporter.
Twelve percent of patients were classified as perfect reporters, 23.6% were over-reporters, 0.5% were under-reporters, and 63.9% were classified as “others.”
Self-reported 6MP intake exceeded MEMS data at least some of the time in 84% of patients.
“We observed that there was an inverse relationship between over-reporting and the extent of non-adherence,” Dr Bhatia noted.
Of the patients who adhered to their regimens (defined as taking their prescribed dose 95% of the time), a small percentage (8%) over-reported their intake.
However, among those found to be non-adherent, a substantially larger percent (47%) over-reported.
In order to find out why patients were not taking their prescribed medication, study author Wendy Landier, PhD, RN, also of the University of Alabama at Birmingham, organized interviews with patients and their parents.
In these interviews, Dr Landier noted that forgetfulness was the primary reason for non-adherence.
“We found that partnering with a parent was very conducive to our patients’ adherence, playing a key role in combatting forgetfulness,” she said.
Recognizing the importance of parental involvement in patient adherence, the researchers were inspired to conduct further research to make parents more involved.
In a trial that builds on this study, physicians send personalized text messages to both patients and their parents at a prescribed time reminding them to take their medicine. Both patient and parent then report back, via text, that the indicated dose was taken.
“Our first study showed that non-adherence was prevalent, increasing the risk of relapse,” Dr Bhatia said. “We then found that parental vigilance was an important facilitator to adherence, while forgetting to take the medication was the most commonly reported barrier.”
“We used these findings to inform the intervention trial to help families improve adherence to treatment. We hope that this will be a real step in improving outcomes in children with leukemia.” ![]()

New research published in Blood suggests young patients with acute lymphoblastic leukemia (ALL)—and their parents—are likely to over-report treatment adherence.
In a study of 416 pediatric ALL patients, 84% of patients or their parents said the patients took more 6-mercaptopurine (6MP) than they actually did.
6MP is prescribed for 2 years after chemotherapy with the goal of producing durable remissions, but studies show that over 95% of the prescribed doses must be taken for the medication to be effective.
“Because this therapy is administered orally every day, we cannot supervise our patients to make sure they are taking their pills,” said study author Smita Bhatia, MD, of the University of Alabama at Birmingham.
“Findings from this study suggest that we need better ways to monitor intake of medications as prescribed.”
This study included 416 pediatric ALL patients followed over 4 months. Patients received prescription pill bottles for their 6MP that contained a microprocessor chip in the cap to log the date and time the bottle was opened.
The logs were compared to self-report questionnaires completed by patients or their parents and provided to physicians at monthly check-ups.
Patients were classified as:
- Perfect reporters—self-report corresponded to data from the Medication Event Monitoring System (MEMS)
- Over-reporters—self-report was greater than MEMS data by more than 5 days per month for more than 50% of the study months
- Others—all patients not meeting criteria for perfect- or over-reporter.
Twelve percent of patients were classified as perfect reporters, 23.6% were over-reporters, 0.5% were under-reporters, and 63.9% were classified as “others.”
Self-reported 6MP intake exceeded MEMS data at least some of the time in 84% of patients.
“We observed that there was an inverse relationship between over-reporting and the extent of non-adherence,” Dr Bhatia noted.
Of the patients who adhered to their regimens (defined as taking their prescribed dose 95% of the time), a small percentage (8%) over-reported their intake.
However, among those found to be non-adherent, a substantially larger percent (47%) over-reported.
In order to find out why patients were not taking their prescribed medication, study author Wendy Landier, PhD, RN, also of the University of Alabama at Birmingham, organized interviews with patients and their parents.
In these interviews, Dr Landier noted that forgetfulness was the primary reason for non-adherence.
“We found that partnering with a parent was very conducive to our patients’ adherence, playing a key role in combatting forgetfulness,” she said.
Recognizing the importance of parental involvement in patient adherence, the researchers were inspired to conduct further research to make parents more involved.
In a trial that builds on this study, physicians send personalized text messages to both patients and their parents at a prescribed time reminding them to take their medicine. Both patient and parent then report back, via text, that the indicated dose was taken.
“Our first study showed that non-adherence was prevalent, increasing the risk of relapse,” Dr Bhatia said. “We then found that parental vigilance was an important facilitator to adherence, while forgetting to take the medication was the most commonly reported barrier.”
“We used these findings to inform the intervention trial to help families improve adherence to treatment. We hope that this will be a real step in improving outcomes in children with leukemia.” ![]()

New research published in Blood suggests young patients with acute lymphoblastic leukemia (ALL)—and their parents—are likely to over-report treatment adherence.
In a study of 416 pediatric ALL patients, 84% of patients or their parents said the patients took more 6-mercaptopurine (6MP) than they actually did.
6MP is prescribed for 2 years after chemotherapy with the goal of producing durable remissions, but studies show that over 95% of the prescribed doses must be taken for the medication to be effective.
“Because this therapy is administered orally every day, we cannot supervise our patients to make sure they are taking their pills,” said study author Smita Bhatia, MD, of the University of Alabama at Birmingham.
“Findings from this study suggest that we need better ways to monitor intake of medications as prescribed.”
This study included 416 pediatric ALL patients followed over 4 months. Patients received prescription pill bottles for their 6MP that contained a microprocessor chip in the cap to log the date and time the bottle was opened.
The logs were compared to self-report questionnaires completed by patients or their parents and provided to physicians at monthly check-ups.
Patients were classified as:
- Perfect reporters—self-report corresponded to data from the Medication Event Monitoring System (MEMS)
- Over-reporters—self-report was greater than MEMS data by more than 5 days per month for more than 50% of the study months
- Others—all patients not meeting criteria for perfect- or over-reporter.
Twelve percent of patients were classified as perfect reporters, 23.6% were over-reporters, 0.5% were under-reporters, and 63.9% were classified as “others.”
Self-reported 6MP intake exceeded MEMS data at least some of the time in 84% of patients.
“We observed that there was an inverse relationship between over-reporting and the extent of non-adherence,” Dr Bhatia noted.
Of the patients who adhered to their regimens (defined as taking their prescribed dose 95% of the time), a small percentage (8%) over-reported their intake.
However, among those found to be non-adherent, a substantially larger percent (47%) over-reported.
In order to find out why patients were not taking their prescribed medication, study author Wendy Landier, PhD, RN, also of the University of Alabama at Birmingham, organized interviews with patients and their parents.
In these interviews, Dr Landier noted that forgetfulness was the primary reason for non-adherence.
“We found that partnering with a parent was very conducive to our patients’ adherence, playing a key role in combatting forgetfulness,” she said.
Recognizing the importance of parental involvement in patient adherence, the researchers were inspired to conduct further research to make parents more involved.
In a trial that builds on this study, physicians send personalized text messages to both patients and their parents at a prescribed time reminding them to take their medicine. Both patient and parent then report back, via text, that the indicated dose was taken.
“Our first study showed that non-adherence was prevalent, increasing the risk of relapse,” Dr Bhatia said. “We then found that parental vigilance was an important facilitator to adherence, while forgetting to take the medication was the most commonly reported barrier.”
“We used these findings to inform the intervention trial to help families improve adherence to treatment. We hope that this will be a real step in improving outcomes in children with leukemia.” ![]()
CHMP recommends hybrid drug for ALL, other disorders

The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for an oral formulation of methotrexate (Jylamvo) as a treatment for acute lymphoblastic leukemia (ALL) and other disorders.
Jylamvo is a hybrid medicine of Methotrexat “Lederle” 25 mg-Stechampulle and Methotrexate “Lederle” 2.5 mg tablets, which have been authorized in the European Union since 1984 and 1959, respectively.
Jylamvo contains the same active substance as these reference medicines—the antineoplastic and immunomodulating agent methotrexate—but is given by mouth as a solution (2 mg/mL).
Jylamvo is intended for use as maintenance treatment in ALL patients age 3 and older.
The drug is also intended to treat:
- Active rheumatoid arthritis in adults
- Polyarthritic forms of active, severe juvenile idiopathic arthritis in adolescents and children age 3 and older when the response to non-steroidal anti-inflammatory drugs has been inadequate
- Severe, treatment-refractory, disabling psoriasis that does not respond sufficiently to other forms of treatment (such as phototherapy, retinoids, and psoralen and ultraviolet A radiation therapy) and severe psoriatic arthritis in adults.
The applicant for Jylamvo is Therakind Limited. Applications for hybrid medicines rely, in part, on the results of preclinical tests and clinical trials for a reference product and, in part, on new data.
The CHMP said studies have demonstrated the satisfactory quality of Jylamvo and its bioequivalence to Methotrexate “Lederle” 2.5 mg tablets and a third product, Ebetrexat 10 mg tablets, which is authorized for similar indications.
The CHMP has proposed that Jylamvo be prescribed by physicians with experience of the various properties of the medicinal product and its mode of action.
Detailed recommendations for the use of Jylamvo will be described in the summary of product characteristics, which will be published in the European public assessment report and made available in all official European Union languages if the European Commission grants marketing authorization for Jylamvo.
The European Commission typically makes a decision on a product within 67 days of the time the CHMP adopts its opinion. ![]()

The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for an oral formulation of methotrexate (Jylamvo) as a treatment for acute lymphoblastic leukemia (ALL) and other disorders.
Jylamvo is a hybrid medicine of Methotrexat “Lederle” 25 mg-Stechampulle and Methotrexate “Lederle” 2.5 mg tablets, which have been authorized in the European Union since 1984 and 1959, respectively.
Jylamvo contains the same active substance as these reference medicines—the antineoplastic and immunomodulating agent methotrexate—but is given by mouth as a solution (2 mg/mL).
Jylamvo is intended for use as maintenance treatment in ALL patients age 3 and older.
The drug is also intended to treat:
- Active rheumatoid arthritis in adults
- Polyarthritic forms of active, severe juvenile idiopathic arthritis in adolescents and children age 3 and older when the response to non-steroidal anti-inflammatory drugs has been inadequate
- Severe, treatment-refractory, disabling psoriasis that does not respond sufficiently to other forms of treatment (such as phototherapy, retinoids, and psoralen and ultraviolet A radiation therapy) and severe psoriatic arthritis in adults.
The applicant for Jylamvo is Therakind Limited. Applications for hybrid medicines rely, in part, on the results of preclinical tests and clinical trials for a reference product and, in part, on new data.
The CHMP said studies have demonstrated the satisfactory quality of Jylamvo and its bioequivalence to Methotrexate “Lederle” 2.5 mg tablets and a third product, Ebetrexat 10 mg tablets, which is authorized for similar indications.
The CHMP has proposed that Jylamvo be prescribed by physicians with experience of the various properties of the medicinal product and its mode of action.
Detailed recommendations for the use of Jylamvo will be described in the summary of product characteristics, which will be published in the European public assessment report and made available in all official European Union languages if the European Commission grants marketing authorization for Jylamvo.
The European Commission typically makes a decision on a product within 67 days of the time the CHMP adopts its opinion. ![]()

The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for an oral formulation of methotrexate (Jylamvo) as a treatment for acute lymphoblastic leukemia (ALL) and other disorders.
Jylamvo is a hybrid medicine of Methotrexat “Lederle” 25 mg-Stechampulle and Methotrexate “Lederle” 2.5 mg tablets, which have been authorized in the European Union since 1984 and 1959, respectively.
Jylamvo contains the same active substance as these reference medicines—the antineoplastic and immunomodulating agent methotrexate—but is given by mouth as a solution (2 mg/mL).
Jylamvo is intended for use as maintenance treatment in ALL patients age 3 and older.
The drug is also intended to treat:
- Active rheumatoid arthritis in adults
- Polyarthritic forms of active, severe juvenile idiopathic arthritis in adolescents and children age 3 and older when the response to non-steroidal anti-inflammatory drugs has been inadequate
- Severe, treatment-refractory, disabling psoriasis that does not respond sufficiently to other forms of treatment (such as phototherapy, retinoids, and psoralen and ultraviolet A radiation therapy) and severe psoriatic arthritis in adults.
The applicant for Jylamvo is Therakind Limited. Applications for hybrid medicines rely, in part, on the results of preclinical tests and clinical trials for a reference product and, in part, on new data.
The CHMP said studies have demonstrated the satisfactory quality of Jylamvo and its bioequivalence to Methotrexate “Lederle” 2.5 mg tablets and a third product, Ebetrexat 10 mg tablets, which is authorized for similar indications.
The CHMP has proposed that Jylamvo be prescribed by physicians with experience of the various properties of the medicinal product and its mode of action.
Detailed recommendations for the use of Jylamvo will be described in the summary of product characteristics, which will be published in the European public assessment report and made available in all official European Union languages if the European Commission grants marketing authorization for Jylamvo.
The European Commission typically makes a decision on a product within 67 days of the time the CHMP adopts its opinion. ![]()
AML leads percent gains in 5-year survival among leukemias
Over the 60-year span from the early 1950s to 2013, the 5-year survival rate for all leukemias increased by 500%, according to data from the Surveillance, Epidemiology, and End Results Program.
For 2008-2013, the 5-year relative survival rate for all leukemias was 60.1%, compared with 10% during 1950-1954, said Ali H. Mokdad, PhD, and his associates at the Institute for Health Metrics and Evaluation at the University of Washington, Seattle (JAMA 2017;317[4]:388-406).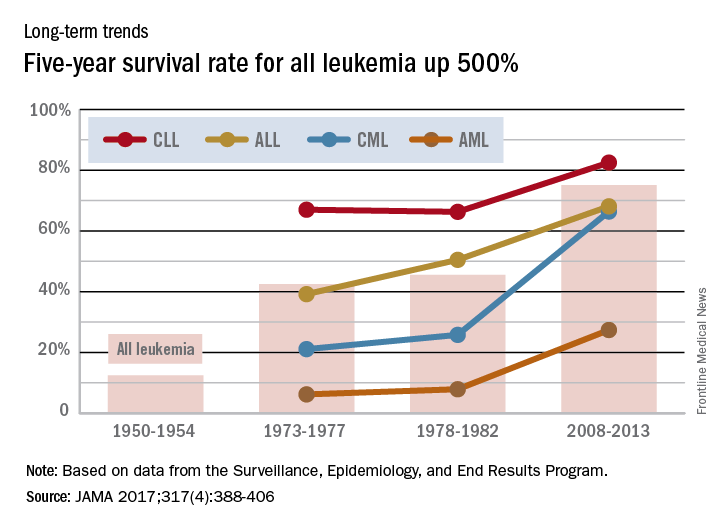
Over the 60-year span from the early 1950s to 2013, the 5-year survival rate for all leukemias increased by 500%, according to data from the Surveillance, Epidemiology, and End Results Program.
For 2008-2013, the 5-year relative survival rate for all leukemias was 60.1%, compared with 10% during 1950-1954, said Ali H. Mokdad, PhD, and his associates at the Institute for Health Metrics and Evaluation at the University of Washington, Seattle (JAMA 2017;317[4]:388-406).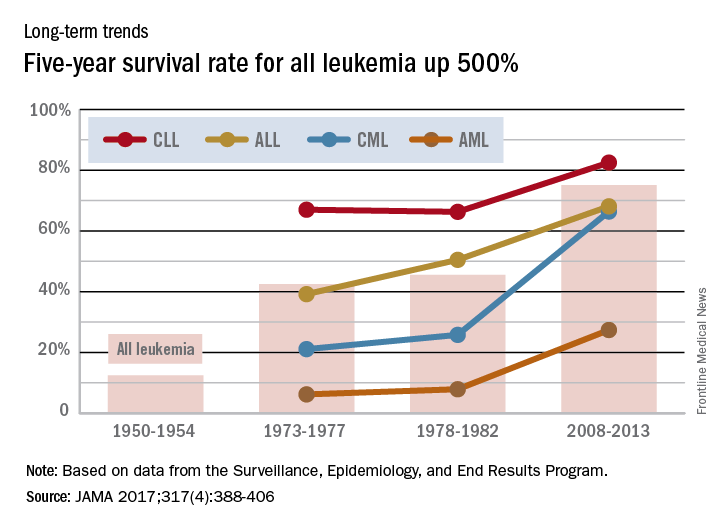
Over the 60-year span from the early 1950s to 2013, the 5-year survival rate for all leukemias increased by 500%, according to data from the Surveillance, Epidemiology, and End Results Program.
For 2008-2013, the 5-year relative survival rate for all leukemias was 60.1%, compared with 10% during 1950-1954, said Ali H. Mokdad, PhD, and his associates at the Institute for Health Metrics and Evaluation at the University of Washington, Seattle (JAMA 2017;317[4]:388-406).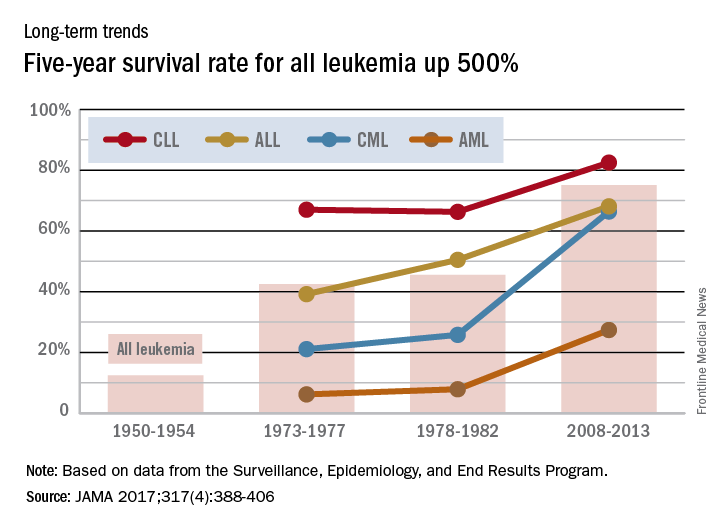
Donor CAR T cells bridge to HSCT in infants with ALL

treated with UCART19
Photo courtesy of GOSH
New research suggests that “universal,” donor-derived, chimeric antigen receptor (CAR) T cells may be a viable treatment option for very young children who do not have sufficient healthy T cells for autologous CAR T-cell therapy.
The universal CAR T-cell therapy, known as UCART19, was given to 2 infants with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) who had previously
exhausted all other treatment options.
Both infants achieved remission after UCART19 and were able to proceed to transplant.
Both were still alive and leukemia-free at last follow-up—12 months and 18 months after UCART19, respectively.
Waseem Qasim, MBBS, PhD, of University College London’s Institute of Child Health and Great Ormond Street Hospital (GOSH) in London, UK, and his colleagues reported these results in Science Translational Medicine.
About the therapy
UCART19 consists of donor T cells modified using transcription activator-like effector nucleases. The cells are programmed to target CD19 and be insensitive to alemtuzumab. That way, a patient can receive alemtuzumab to prevent rejection of HLA-mismatched cells.
UCART19 was under development by Cellectis but is now being developed by Servier and Pfizer Inc. Pfizer has exclusive rights to develop and commercialize UCART19 in the US, while Servier retains exclusive rights for all other countries.
In Science Translational Medicine, Dr Qasim and his colleagues reported results in the first patients ever treated with UCART19. That research was funded, in part, by Cellectis.
Subject 1
The first patient was an 11-month-old, mixed-race infant with high-risk, t(11;19), CD19+ B-ALL. She had already failed chemotherapy, an allogeneic hematopoietic stem cell transplant (HSCT), and blinatumomab.
Prior to UCART19, she received a dose of vincristine and asparaginase and 7 days of dexamethasone, followed by cytoreduction with fludarabine, cyclophosphamide, and alemtuzumab. She then received a single dose of UCART19 (4.6 × 106/kg).
The patient had neutrophil recovery by day 30, although this was dependent on granulocyte colony-stimulating factor. After that, she developed multilineage cytopenia that persisted until she underwent a second allogeneic HSCT.
Prior to the second HSCT, the patient achieved cytogenetic and molecular remission but also developed grade 2 skin graft-vs-host disease. This was managed with systemic steroids.
The child received rituximab and conditioning with antithymocyte globulin, fludarabine, cyclophosphamide, thiotepa, and total body irradiation, followed by an HSCT from the original mismatched, unrelated donor.
The child achieved a complete remission and has remained minimal residual disease-negative, with full donor chimerism and normalized lymphocyte profiles, at 18 months after UCART19.
Results with this patient were previously reported by GOSH in November 2015 and at the 2015 ASH Annual Meeting.
Subject 2
The second patient was a 16-month-old Caucasian infant who had been diagnosed at 4 weeks of age with high-risk, congenital, mixed lineage leukemia–rearranged B-ALL.
She had already undergone HSCT from a matched, unrelated donor but relapsed. She did not respond to subsequent blinatumomab.
After these failed treatments, the patient received fludarabine, cyclophosphamide, and alemtuzumab, followed by a single infusion of UCART19 (4.0 × 106/kg).
She developed an erythematous rash after treatment, but this was immediately responsive to topical steroids.
The child achieved donor-derived neutrophil recovery and went on to receive a transplant from the same matched, unrelated donor as her previous HSCT.
The child received the transplant within 10 weeks of UCART19 therapy, after receiving rituximab and conditioning with antithymocyte globulin, fludarabine, cyclophosphamide, and total body irradiation.
At 12 months after UCART19, the child remains minimal residual disease-negative and “clinically well.”
“Both infants who have had this treatment have been at home for some time and are doing well,” Dr Qasim said. “We continue to monitor them closely, and, while we have reduced the frequency of their hospital visits and checks, we will still need to keep an eye on them for some time.”
Dr Qasim added that there are phase 1 trials of UCART19 underway for children and adults with chronic lymphocytic leukemia and acute lymphoblastic leukemia. ![]()

treated with UCART19
Photo courtesy of GOSH
New research suggests that “universal,” donor-derived, chimeric antigen receptor (CAR) T cells may be a viable treatment option for very young children who do not have sufficient healthy T cells for autologous CAR T-cell therapy.
The universal CAR T-cell therapy, known as UCART19, was given to 2 infants with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) who had previously
exhausted all other treatment options.
Both infants achieved remission after UCART19 and were able to proceed to transplant.
Both were still alive and leukemia-free at last follow-up—12 months and 18 months after UCART19, respectively.
Waseem Qasim, MBBS, PhD, of University College London’s Institute of Child Health and Great Ormond Street Hospital (GOSH) in London, UK, and his colleagues reported these results in Science Translational Medicine.
About the therapy
UCART19 consists of donor T cells modified using transcription activator-like effector nucleases. The cells are programmed to target CD19 and be insensitive to alemtuzumab. That way, a patient can receive alemtuzumab to prevent rejection of HLA-mismatched cells.
UCART19 was under development by Cellectis but is now being developed by Servier and Pfizer Inc. Pfizer has exclusive rights to develop and commercialize UCART19 in the US, while Servier retains exclusive rights for all other countries.
In Science Translational Medicine, Dr Qasim and his colleagues reported results in the first patients ever treated with UCART19. That research was funded, in part, by Cellectis.
Subject 1
The first patient was an 11-month-old, mixed-race infant with high-risk, t(11;19), CD19+ B-ALL. She had already failed chemotherapy, an allogeneic hematopoietic stem cell transplant (HSCT), and blinatumomab.
Prior to UCART19, she received a dose of vincristine and asparaginase and 7 days of dexamethasone, followed by cytoreduction with fludarabine, cyclophosphamide, and alemtuzumab. She then received a single dose of UCART19 (4.6 × 106/kg).
The patient had neutrophil recovery by day 30, although this was dependent on granulocyte colony-stimulating factor. After that, she developed multilineage cytopenia that persisted until she underwent a second allogeneic HSCT.
Prior to the second HSCT, the patient achieved cytogenetic and molecular remission but also developed grade 2 skin graft-vs-host disease. This was managed with systemic steroids.
The child received rituximab and conditioning with antithymocyte globulin, fludarabine, cyclophosphamide, thiotepa, and total body irradiation, followed by an HSCT from the original mismatched, unrelated donor.
The child achieved a complete remission and has remained minimal residual disease-negative, with full donor chimerism and normalized lymphocyte profiles, at 18 months after UCART19.
Results with this patient were previously reported by GOSH in November 2015 and at the 2015 ASH Annual Meeting.
Subject 2
The second patient was a 16-month-old Caucasian infant who had been diagnosed at 4 weeks of age with high-risk, congenital, mixed lineage leukemia–rearranged B-ALL.
She had already undergone HSCT from a matched, unrelated donor but relapsed. She did not respond to subsequent blinatumomab.
After these failed treatments, the patient received fludarabine, cyclophosphamide, and alemtuzumab, followed by a single infusion of UCART19 (4.0 × 106/kg).
She developed an erythematous rash after treatment, but this was immediately responsive to topical steroids.
The child achieved donor-derived neutrophil recovery and went on to receive a transplant from the same matched, unrelated donor as her previous HSCT.
The child received the transplant within 10 weeks of UCART19 therapy, after receiving rituximab and conditioning with antithymocyte globulin, fludarabine, cyclophosphamide, and total body irradiation.
At 12 months after UCART19, the child remains minimal residual disease-negative and “clinically well.”
“Both infants who have had this treatment have been at home for some time and are doing well,” Dr Qasim said. “We continue to monitor them closely, and, while we have reduced the frequency of their hospital visits and checks, we will still need to keep an eye on them for some time.”
Dr Qasim added that there are phase 1 trials of UCART19 underway for children and adults with chronic lymphocytic leukemia and acute lymphoblastic leukemia. ![]()

treated with UCART19
Photo courtesy of GOSH
New research suggests that “universal,” donor-derived, chimeric antigen receptor (CAR) T cells may be a viable treatment option for very young children who do not have sufficient healthy T cells for autologous CAR T-cell therapy.
The universal CAR T-cell therapy, known as UCART19, was given to 2 infants with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) who had previously
exhausted all other treatment options.
Both infants achieved remission after UCART19 and were able to proceed to transplant.
Both were still alive and leukemia-free at last follow-up—12 months and 18 months after UCART19, respectively.
Waseem Qasim, MBBS, PhD, of University College London’s Institute of Child Health and Great Ormond Street Hospital (GOSH) in London, UK, and his colleagues reported these results in Science Translational Medicine.
About the therapy
UCART19 consists of donor T cells modified using transcription activator-like effector nucleases. The cells are programmed to target CD19 and be insensitive to alemtuzumab. That way, a patient can receive alemtuzumab to prevent rejection of HLA-mismatched cells.
UCART19 was under development by Cellectis but is now being developed by Servier and Pfizer Inc. Pfizer has exclusive rights to develop and commercialize UCART19 in the US, while Servier retains exclusive rights for all other countries.
In Science Translational Medicine, Dr Qasim and his colleagues reported results in the first patients ever treated with UCART19. That research was funded, in part, by Cellectis.
Subject 1
The first patient was an 11-month-old, mixed-race infant with high-risk, t(11;19), CD19+ B-ALL. She had already failed chemotherapy, an allogeneic hematopoietic stem cell transplant (HSCT), and blinatumomab.
Prior to UCART19, she received a dose of vincristine and asparaginase and 7 days of dexamethasone, followed by cytoreduction with fludarabine, cyclophosphamide, and alemtuzumab. She then received a single dose of UCART19 (4.6 × 106/kg).
The patient had neutrophil recovery by day 30, although this was dependent on granulocyte colony-stimulating factor. After that, she developed multilineage cytopenia that persisted until she underwent a second allogeneic HSCT.
Prior to the second HSCT, the patient achieved cytogenetic and molecular remission but also developed grade 2 skin graft-vs-host disease. This was managed with systemic steroids.
The child received rituximab and conditioning with antithymocyte globulin, fludarabine, cyclophosphamide, thiotepa, and total body irradiation, followed by an HSCT from the original mismatched, unrelated donor.
The child achieved a complete remission and has remained minimal residual disease-negative, with full donor chimerism and normalized lymphocyte profiles, at 18 months after UCART19.
Results with this patient were previously reported by GOSH in November 2015 and at the 2015 ASH Annual Meeting.
Subject 2
The second patient was a 16-month-old Caucasian infant who had been diagnosed at 4 weeks of age with high-risk, congenital, mixed lineage leukemia–rearranged B-ALL.
She had already undergone HSCT from a matched, unrelated donor but relapsed. She did not respond to subsequent blinatumomab.
After these failed treatments, the patient received fludarabine, cyclophosphamide, and alemtuzumab, followed by a single infusion of UCART19 (4.0 × 106/kg).
She developed an erythematous rash after treatment, but this was immediately responsive to topical steroids.
The child achieved donor-derived neutrophil recovery and went on to receive a transplant from the same matched, unrelated donor as her previous HSCT.
The child received the transplant within 10 weeks of UCART19 therapy, after receiving rituximab and conditioning with antithymocyte globulin, fludarabine, cyclophosphamide, and total body irradiation.
At 12 months after UCART19, the child remains minimal residual disease-negative and “clinically well.”
“Both infants who have had this treatment have been at home for some time and are doing well,” Dr Qasim said. “We continue to monitor them closely, and, while we have reduced the frequency of their hospital visits and checks, we will still need to keep an eye on them for some time.”
Dr Qasim added that there are phase 1 trials of UCART19 underway for children and adults with chronic lymphocytic leukemia and acute lymphoblastic leukemia. ![]()
Study quantifies 5-year survival rates for blood cancers

chemotherapy
Photo by Rhoda Baer
A new study shows that 5-year survival rates for US patients with hematologic malignancies have increased greatly since the 1950s, but there is still room for improvement, particularly for patients with acute myeloid leukemia (AML).
Researchers found the absolute difference in improvement for 5-year survival from 1950-1954 to 2008-2013 ranged from 38.2% for non-Hodgkin lymphoma (NHL) to 56.6% for Hodgkin lymphoma.
And although the 5-year survival rate for Hodgkin lymphoma patients reached 86.6% for 2008-2013, the 5-year survival rate for patients with AML only reached 27.4%.
This study also revealed large disparities in overall cancer mortality rates between different counties across the country.
Ali H. Mokdad, PhD, of the Institute for Health Metrics and Evaluation in Seattle, Washington, and his colleagues reported these findings in JAMA.
Overall cancer deaths
The researchers found there were 19,511,910 cancer deaths recorded in the US between 1980 and 2014. Cancer mortality decreased by 20.1% between 1980 and 2014, from 240.2 deaths per 100,000 people to 192.0 deaths per 100,000 people.
In 1980, cancer mortality ranged from 130.6 per 100,000 in Summit County, Colorado, to 386.9 per 100,000 in North Slope Borough, Alaska.
In 2014, cancer mortality ranged from 70.7 per 100,000 in Summit County, Colorado, to 503.1 per 100,000 in Union County, Florida.
“Such significant disparities among US counties is unacceptable,” Dr Mokdad said. “Every person should have access to early screenings for cancer, as well as adequate treatment.”
Mortality rates for hematologic malignancies
In 2014, the mortality rates, per 100,000 people, for hematologic malignancies were:
- 0.4 for Hodgkin lymphoma (rank out of all cancers, 27)
- 8.3 for NHL (rank, 7)
- 3.9 for multiple myeloma (rank, 16)
- 9.0 for all leukemias (rank, 6)
- 0.7 for acute lymphoid leukemia (ALL)
- 2.6 for chronic lymphoid leukemia (CLL)
- 5.1 for AML
- 0.6 for chronic myeloid leukemia (CML).
The leukemia subtypes were not assigned a rank.
5-year survival rates for hematologic malignancies
Hodgkin lymphoma
- 30% for 1950-54
- 68.6% for 1973-77
- 72.1% for 1978-82
- 86.6% for 2008-2013
- Absolute difference (between the first and latest year of data), 56.6%.
NHL
- 33% for 1950-54
- 45.3% for 1973-77
- 48.7% for 1978-82
- 71.2% for 2008-2013
- Absolute difference, 38.2%.
Multiple myeloma
- 6% for 1950-54
- 23.4% for 1973-77
- 26.6% for 1978-82
- 49.8% for 2008-2013
- Absolute difference, 43.8%.
Leukemia
- 10% for 1950-54
- 34% for 1973-77
- 36.3% for 1978-82
- 60.1% for 2008-2013
- Absolute difference, 50.1%.
ALL
- 39.2% for 1973-77
- 50.5% for 1978-82
- 68.1% for 2008-2013
- Absolute difference, 28.9%.
CLL
- 67% for 1973-77
- 66.3% for 1978-82
- 82.5% for 2008-2013
- Absolute difference, 15.5%.
AML
- 6.2% for 1973-77
- 7.9% for 1978-82
- 27.4% for 2008-2013
- Absolute difference, 21.2%.
CML
- 21.1% for 1973-77
- 25.8% for 1978-82
- 66.4% for 2008-2013
- Absolute difference, 45.3%.
For the leukemia subtypes, there was no data for 1950 to 1954. ![]()

chemotherapy
Photo by Rhoda Baer
A new study shows that 5-year survival rates for US patients with hematologic malignancies have increased greatly since the 1950s, but there is still room for improvement, particularly for patients with acute myeloid leukemia (AML).
Researchers found the absolute difference in improvement for 5-year survival from 1950-1954 to 2008-2013 ranged from 38.2% for non-Hodgkin lymphoma (NHL) to 56.6% for Hodgkin lymphoma.
And although the 5-year survival rate for Hodgkin lymphoma patients reached 86.6% for 2008-2013, the 5-year survival rate for patients with AML only reached 27.4%.
This study also revealed large disparities in overall cancer mortality rates between different counties across the country.
Ali H. Mokdad, PhD, of the Institute for Health Metrics and Evaluation in Seattle, Washington, and his colleagues reported these findings in JAMA.
Overall cancer deaths
The researchers found there were 19,511,910 cancer deaths recorded in the US between 1980 and 2014. Cancer mortality decreased by 20.1% between 1980 and 2014, from 240.2 deaths per 100,000 people to 192.0 deaths per 100,000 people.
In 1980, cancer mortality ranged from 130.6 per 100,000 in Summit County, Colorado, to 386.9 per 100,000 in North Slope Borough, Alaska.
In 2014, cancer mortality ranged from 70.7 per 100,000 in Summit County, Colorado, to 503.1 per 100,000 in Union County, Florida.
“Such significant disparities among US counties is unacceptable,” Dr Mokdad said. “Every person should have access to early screenings for cancer, as well as adequate treatment.”
Mortality rates for hematologic malignancies
In 2014, the mortality rates, per 100,000 people, for hematologic malignancies were:
- 0.4 for Hodgkin lymphoma (rank out of all cancers, 27)
- 8.3 for NHL (rank, 7)
- 3.9 for multiple myeloma (rank, 16)
- 9.0 for all leukemias (rank, 6)
- 0.7 for acute lymphoid leukemia (ALL)
- 2.6 for chronic lymphoid leukemia (CLL)
- 5.1 for AML
- 0.6 for chronic myeloid leukemia (CML).
The leukemia subtypes were not assigned a rank.
5-year survival rates for hematologic malignancies
Hodgkin lymphoma
- 30% for 1950-54
- 68.6% for 1973-77
- 72.1% for 1978-82
- 86.6% for 2008-2013
- Absolute difference (between the first and latest year of data), 56.6%.
NHL
- 33% for 1950-54
- 45.3% for 1973-77
- 48.7% for 1978-82
- 71.2% for 2008-2013
- Absolute difference, 38.2%.
Multiple myeloma
- 6% for 1950-54
- 23.4% for 1973-77
- 26.6% for 1978-82
- 49.8% for 2008-2013
- Absolute difference, 43.8%.
Leukemia
- 10% for 1950-54
- 34% for 1973-77
- 36.3% for 1978-82
- 60.1% for 2008-2013
- Absolute difference, 50.1%.
ALL
- 39.2% for 1973-77
- 50.5% for 1978-82
- 68.1% for 2008-2013
- Absolute difference, 28.9%.
CLL
- 67% for 1973-77
- 66.3% for 1978-82
- 82.5% for 2008-2013
- Absolute difference, 15.5%.
AML
- 6.2% for 1973-77
- 7.9% for 1978-82
- 27.4% for 2008-2013
- Absolute difference, 21.2%.
CML
- 21.1% for 1973-77
- 25.8% for 1978-82
- 66.4% for 2008-2013
- Absolute difference, 45.3%.
For the leukemia subtypes, there was no data for 1950 to 1954. ![]()

chemotherapy
Photo by Rhoda Baer
A new study shows that 5-year survival rates for US patients with hematologic malignancies have increased greatly since the 1950s, but there is still room for improvement, particularly for patients with acute myeloid leukemia (AML).
Researchers found the absolute difference in improvement for 5-year survival from 1950-1954 to 2008-2013 ranged from 38.2% for non-Hodgkin lymphoma (NHL) to 56.6% for Hodgkin lymphoma.
And although the 5-year survival rate for Hodgkin lymphoma patients reached 86.6% for 2008-2013, the 5-year survival rate for patients with AML only reached 27.4%.
This study also revealed large disparities in overall cancer mortality rates between different counties across the country.
Ali H. Mokdad, PhD, of the Institute for Health Metrics and Evaluation in Seattle, Washington, and his colleagues reported these findings in JAMA.
Overall cancer deaths
The researchers found there were 19,511,910 cancer deaths recorded in the US between 1980 and 2014. Cancer mortality decreased by 20.1% between 1980 and 2014, from 240.2 deaths per 100,000 people to 192.0 deaths per 100,000 people.
In 1980, cancer mortality ranged from 130.6 per 100,000 in Summit County, Colorado, to 386.9 per 100,000 in North Slope Borough, Alaska.
In 2014, cancer mortality ranged from 70.7 per 100,000 in Summit County, Colorado, to 503.1 per 100,000 in Union County, Florida.
“Such significant disparities among US counties is unacceptable,” Dr Mokdad said. “Every person should have access to early screenings for cancer, as well as adequate treatment.”
Mortality rates for hematologic malignancies
In 2014, the mortality rates, per 100,000 people, for hematologic malignancies were:
- 0.4 for Hodgkin lymphoma (rank out of all cancers, 27)
- 8.3 for NHL (rank, 7)
- 3.9 for multiple myeloma (rank, 16)
- 9.0 for all leukemias (rank, 6)
- 0.7 for acute lymphoid leukemia (ALL)
- 2.6 for chronic lymphoid leukemia (CLL)
- 5.1 for AML
- 0.6 for chronic myeloid leukemia (CML).
The leukemia subtypes were not assigned a rank.
5-year survival rates for hematologic malignancies
Hodgkin lymphoma
- 30% for 1950-54
- 68.6% for 1973-77
- 72.1% for 1978-82
- 86.6% for 2008-2013
- Absolute difference (between the first and latest year of data), 56.6%.
NHL
- 33% for 1950-54
- 45.3% for 1973-77
- 48.7% for 1978-82
- 71.2% for 2008-2013
- Absolute difference, 38.2%.
Multiple myeloma
- 6% for 1950-54
- 23.4% for 1973-77
- 26.6% for 1978-82
- 49.8% for 2008-2013
- Absolute difference, 43.8%.
Leukemia
- 10% for 1950-54
- 34% for 1973-77
- 36.3% for 1978-82
- 60.1% for 2008-2013
- Absolute difference, 50.1%.
ALL
- 39.2% for 1973-77
- 50.5% for 1978-82
- 68.1% for 2008-2013
- Absolute difference, 28.9%.
CLL
- 67% for 1973-77
- 66.3% for 1978-82
- 82.5% for 2008-2013
- Absolute difference, 15.5%.
AML
- 6.2% for 1973-77
- 7.9% for 1978-82
- 27.4% for 2008-2013
- Absolute difference, 21.2%.
CML
- 21.1% for 1973-77
- 25.8% for 1978-82
- 66.4% for 2008-2013
- Absolute difference, 45.3%.
For the leukemia subtypes, there was no data for 1950 to 1954. ![]()
Enzyme derived from yeast kills ALL cells

as it buds before dividing
Image by Carolyn Larabell
L-asparaginase derived from baker’s yeast has shown early promise for treating acute lymphoblastic leukemia (ALL), according to researchers.
The team isolated L-asparaginase from Saccharomyces cerevisiae and found the enzyme could kill ALL cells in vitro, while largely sparing healthy control cells.
Gisele Monteiro de Souza, PhD, of the University of São Paulo in São Paulo, Brazil, and her colleagues detailed these findings in Scientific Reports.
“In this study, we characterized the enzyme L-asparaginase from S cerevisiae,” Dr Souza said. “The results show this protein can efficiently annihilate leukemia cells with low cytotoxicity to healthy cells.”
She and her colleagues conducted this study in search of alternatives to L-asparaginase extracted from bacteria (Escherichia coli and Erwinia chrysanthemi).
“Our goal in this project wasn’t to produce the enzyme, but rather to find a new source of the biodrug in microorganisms for use in patients who develop resistance to the bacterial enzyme,” said study author Marcos Antonio de Oliveira, of São Paulo State University in São Vicente, Brazil.
To this end, the researchers isolated fungi from several different Brazilian environments as well as marine and land environments in Antarctica. According to Oliveira, these organisms often secrete asparaginase into the extracellular medium in response to a shortage of nitrogen.
“This lowers the cost of purifying the molecule for drug production, an important factor from an industrial standpoint,” he said.
The group also used bioinformatics tools to mine information on the genomes of several microorganisms from international databases.
In this way, they identified a gene responsible for producing an enzyme that closely resembles the enzymes found in E coli and E chrysanthemi, but with a number of advantages, in the genome of S cerevisiae.
The gene of interest from L-asparaginase was cloned, and the researchers used genetic engineering to make E coli express large amounts of the enzyme originally found in yeast.
“We were able to obtain the recombinant protein,” said study author Iris Munhoz Costa, of the University of São Paulo.
“We then performed studies to characterize its secondary structure and identify important regions called catalytic sites. Finally, we evaluated its efficacy in vitro.”
The enzyme was tested in 3 different cell lines: ALL cells incapable of producing asparagine at normal levels (MOLT4), another ALL cell line capable of producing asparagine at normal levels (REH), and non-malignant control cells (HUVECs).
These 3 cell lines were subdivided into 2 groups. One was treated with L-asparaginase derived from E coli enzyme, and the other was treated with L-asparaginase from yeast.
“The bacterial enzyme killed about 90% of the MOLT4 human leukemia cells and displayed low toxicity to the healthy HUVEC cells, killing only 10%,” Dr Souza said.
“The yeast enzyme killed between 70% and 80% of the MOLT4 cells and displayed less than 10% toxicity for HUVEC cells. Neither was significantly effective against REH cells.”
In her view, the results are encouraging, in contrast with those of studies performed with the same enzyme in the 1970s. At that time, the tests involved a version of the protein extracted directly from yeast and containing many impurities.
The group’s next step is to perform new in vitro trials with different cell types to evaluate the immune response and toxicity. If the results are positive, the first tests in animals may be next.
The researchers are also studying possible modifications that could be made to the molecule’s structure to increase antitumor activity and extend the enzyme’s half-life. ![]()

as it buds before dividing
Image by Carolyn Larabell
L-asparaginase derived from baker’s yeast has shown early promise for treating acute lymphoblastic leukemia (ALL), according to researchers.
The team isolated L-asparaginase from Saccharomyces cerevisiae and found the enzyme could kill ALL cells in vitro, while largely sparing healthy control cells.
Gisele Monteiro de Souza, PhD, of the University of São Paulo in São Paulo, Brazil, and her colleagues detailed these findings in Scientific Reports.
“In this study, we characterized the enzyme L-asparaginase from S cerevisiae,” Dr Souza said. “The results show this protein can efficiently annihilate leukemia cells with low cytotoxicity to healthy cells.”
She and her colleagues conducted this study in search of alternatives to L-asparaginase extracted from bacteria (Escherichia coli and Erwinia chrysanthemi).
“Our goal in this project wasn’t to produce the enzyme, but rather to find a new source of the biodrug in microorganisms for use in patients who develop resistance to the bacterial enzyme,” said study author Marcos Antonio de Oliveira, of São Paulo State University in São Vicente, Brazil.
To this end, the researchers isolated fungi from several different Brazilian environments as well as marine and land environments in Antarctica. According to Oliveira, these organisms often secrete asparaginase into the extracellular medium in response to a shortage of nitrogen.
“This lowers the cost of purifying the molecule for drug production, an important factor from an industrial standpoint,” he said.
The group also used bioinformatics tools to mine information on the genomes of several microorganisms from international databases.
In this way, they identified a gene responsible for producing an enzyme that closely resembles the enzymes found in E coli and E chrysanthemi, but with a number of advantages, in the genome of S cerevisiae.
The gene of interest from L-asparaginase was cloned, and the researchers used genetic engineering to make E coli express large amounts of the enzyme originally found in yeast.
“We were able to obtain the recombinant protein,” said study author Iris Munhoz Costa, of the University of São Paulo.
“We then performed studies to characterize its secondary structure and identify important regions called catalytic sites. Finally, we evaluated its efficacy in vitro.”
The enzyme was tested in 3 different cell lines: ALL cells incapable of producing asparagine at normal levels (MOLT4), another ALL cell line capable of producing asparagine at normal levels (REH), and non-malignant control cells (HUVECs).
These 3 cell lines were subdivided into 2 groups. One was treated with L-asparaginase derived from E coli enzyme, and the other was treated with L-asparaginase from yeast.
“The bacterial enzyme killed about 90% of the MOLT4 human leukemia cells and displayed low toxicity to the healthy HUVEC cells, killing only 10%,” Dr Souza said.
“The yeast enzyme killed between 70% and 80% of the MOLT4 cells and displayed less than 10% toxicity for HUVEC cells. Neither was significantly effective against REH cells.”
In her view, the results are encouraging, in contrast with those of studies performed with the same enzyme in the 1970s. At that time, the tests involved a version of the protein extracted directly from yeast and containing many impurities.
The group’s next step is to perform new in vitro trials with different cell types to evaluate the immune response and toxicity. If the results are positive, the first tests in animals may be next.
The researchers are also studying possible modifications that could be made to the molecule’s structure to increase antitumor activity and extend the enzyme’s half-life. ![]()

as it buds before dividing
Image by Carolyn Larabell
L-asparaginase derived from baker’s yeast has shown early promise for treating acute lymphoblastic leukemia (ALL), according to researchers.
The team isolated L-asparaginase from Saccharomyces cerevisiae and found the enzyme could kill ALL cells in vitro, while largely sparing healthy control cells.
Gisele Monteiro de Souza, PhD, of the University of São Paulo in São Paulo, Brazil, and her colleagues detailed these findings in Scientific Reports.
“In this study, we characterized the enzyme L-asparaginase from S cerevisiae,” Dr Souza said. “The results show this protein can efficiently annihilate leukemia cells with low cytotoxicity to healthy cells.”
She and her colleagues conducted this study in search of alternatives to L-asparaginase extracted from bacteria (Escherichia coli and Erwinia chrysanthemi).
“Our goal in this project wasn’t to produce the enzyme, but rather to find a new source of the biodrug in microorganisms for use in patients who develop resistance to the bacterial enzyme,” said study author Marcos Antonio de Oliveira, of São Paulo State University in São Vicente, Brazil.
To this end, the researchers isolated fungi from several different Brazilian environments as well as marine and land environments in Antarctica. According to Oliveira, these organisms often secrete asparaginase into the extracellular medium in response to a shortage of nitrogen.
“This lowers the cost of purifying the molecule for drug production, an important factor from an industrial standpoint,” he said.
The group also used bioinformatics tools to mine information on the genomes of several microorganisms from international databases.
In this way, they identified a gene responsible for producing an enzyme that closely resembles the enzymes found in E coli and E chrysanthemi, but with a number of advantages, in the genome of S cerevisiae.
The gene of interest from L-asparaginase was cloned, and the researchers used genetic engineering to make E coli express large amounts of the enzyme originally found in yeast.
“We were able to obtain the recombinant protein,” said study author Iris Munhoz Costa, of the University of São Paulo.
“We then performed studies to characterize its secondary structure and identify important regions called catalytic sites. Finally, we evaluated its efficacy in vitro.”
The enzyme was tested in 3 different cell lines: ALL cells incapable of producing asparagine at normal levels (MOLT4), another ALL cell line capable of producing asparagine at normal levels (REH), and non-malignant control cells (HUVECs).
These 3 cell lines were subdivided into 2 groups. One was treated with L-asparaginase derived from E coli enzyme, and the other was treated with L-asparaginase from yeast.
“The bacterial enzyme killed about 90% of the MOLT4 human leukemia cells and displayed low toxicity to the healthy HUVEC cells, killing only 10%,” Dr Souza said.
“The yeast enzyme killed between 70% and 80% of the MOLT4 cells and displayed less than 10% toxicity for HUVEC cells. Neither was significantly effective against REH cells.”
In her view, the results are encouraging, in contrast with those of studies performed with the same enzyme in the 1970s. At that time, the tests involved a version of the protein extracted directly from yeast and containing many impurities.
The group’s next step is to perform new in vitro trials with different cell types to evaluate the immune response and toxicity. If the results are positive, the first tests in animals may be next.
The researchers are also studying possible modifications that could be made to the molecule’s structure to increase antitumor activity and extend the enzyme’s half-life. ![]()
Team characterizes therapy-resistant ALL cells

Image by Vashi Donsk
Researchers say they have characterized a subpopulation of leukemia cells that are responsible for relapse in acute lymphoblastic leukemia (ALL).
The team identified these dormant, therapy-resistant cells in mouse models of ALL and found that removing the cells from their environment makes them sensitive to treatment.
The researchers believe these findings could pave the way to better relapse prevention in patients with ALL.
“Previously, the biological principles responsible for a relapse in leukemia were not fully understood,” said study author Irmela Jeremias, MD, PhD, of Helmholtz Zentrum München in Munich, Germany.
“Our new approach is to isolate dormant cells, which gives us the first possibility of developing therapies that switch off these cells.”
Dr Jeremias and colleagues described this approach in Cancer Cell.
First, the researchers created mouse models recapitulating minimal residual disease (MRD) and relapse in ALL patients.
The team then used genetic engineering and proliferation-sensitive dyes to isolate and characterize relapse-inducing cells.
This revealed a subpopulation of leukemia cells that exhibited long-term dormancy, treatment resistance, and stemness. These cells were similar to primary ALL cells isolated from pediatric and adult patients with MRD.
However, the dormant leukemia cells found in the mice changed once they were removed from the in vivo environment. They began to proliferate and became sensitive to ex vivo treatment with chemotherapy drugs.
“[T]hese cells, once they have been dissolved out of their surroundings, are indeed susceptible to therapy and react well to therapeutics,” said study author Erbey Özdemir, a doctoral candidate at Helmholtz Zentrum München.
The researchers therefore believe that therapeutic strategies aimed at dissociating dormant leukemia cells from their protective niche might prevent relapse in ALL patients.
“This has brought us a small step closer to the global goal of preventing disease relapse in patients suffering from leukemia,” Dr Jeremias said. “It might serve as basis for new therapies that destroy resistant leukemia cells before they induce relapse.” ![]()

Image by Vashi Donsk
Researchers say they have characterized a subpopulation of leukemia cells that are responsible for relapse in acute lymphoblastic leukemia (ALL).
The team identified these dormant, therapy-resistant cells in mouse models of ALL and found that removing the cells from their environment makes them sensitive to treatment.
The researchers believe these findings could pave the way to better relapse prevention in patients with ALL.
“Previously, the biological principles responsible for a relapse in leukemia were not fully understood,” said study author Irmela Jeremias, MD, PhD, of Helmholtz Zentrum München in Munich, Germany.
“Our new approach is to isolate dormant cells, which gives us the first possibility of developing therapies that switch off these cells.”
Dr Jeremias and colleagues described this approach in Cancer Cell.
First, the researchers created mouse models recapitulating minimal residual disease (MRD) and relapse in ALL patients.
The team then used genetic engineering and proliferation-sensitive dyes to isolate and characterize relapse-inducing cells.
This revealed a subpopulation of leukemia cells that exhibited long-term dormancy, treatment resistance, and stemness. These cells were similar to primary ALL cells isolated from pediatric and adult patients with MRD.
However, the dormant leukemia cells found in the mice changed once they were removed from the in vivo environment. They began to proliferate and became sensitive to ex vivo treatment with chemotherapy drugs.
“[T]hese cells, once they have been dissolved out of their surroundings, are indeed susceptible to therapy and react well to therapeutics,” said study author Erbey Özdemir, a doctoral candidate at Helmholtz Zentrum München.
The researchers therefore believe that therapeutic strategies aimed at dissociating dormant leukemia cells from their protective niche might prevent relapse in ALL patients.
“This has brought us a small step closer to the global goal of preventing disease relapse in patients suffering from leukemia,” Dr Jeremias said. “It might serve as basis for new therapies that destroy resistant leukemia cells before they induce relapse.” ![]()

Image by Vashi Donsk
Researchers say they have characterized a subpopulation of leukemia cells that are responsible for relapse in acute lymphoblastic leukemia (ALL).
The team identified these dormant, therapy-resistant cells in mouse models of ALL and found that removing the cells from their environment makes them sensitive to treatment.
The researchers believe these findings could pave the way to better relapse prevention in patients with ALL.
“Previously, the biological principles responsible for a relapse in leukemia were not fully understood,” said study author Irmela Jeremias, MD, PhD, of Helmholtz Zentrum München in Munich, Germany.
“Our new approach is to isolate dormant cells, which gives us the first possibility of developing therapies that switch off these cells.”
Dr Jeremias and colleagues described this approach in Cancer Cell.
First, the researchers created mouse models recapitulating minimal residual disease (MRD) and relapse in ALL patients.
The team then used genetic engineering and proliferation-sensitive dyes to isolate and characterize relapse-inducing cells.
This revealed a subpopulation of leukemia cells that exhibited long-term dormancy, treatment resistance, and stemness. These cells were similar to primary ALL cells isolated from pediatric and adult patients with MRD.
However, the dormant leukemia cells found in the mice changed once they were removed from the in vivo environment. They began to proliferate and became sensitive to ex vivo treatment with chemotherapy drugs.
“[T]hese cells, once they have been dissolved out of their surroundings, are indeed susceptible to therapy and react well to therapeutics,” said study author Erbey Özdemir, a doctoral candidate at Helmholtz Zentrum München.
The researchers therefore believe that therapeutic strategies aimed at dissociating dormant leukemia cells from their protective niche might prevent relapse in ALL patients.
“This has brought us a small step closer to the global goal of preventing disease relapse in patients suffering from leukemia,” Dr Jeremias said. “It might serve as basis for new therapies that destroy resistant leukemia cells before they induce relapse.”
All cases of CRS are not created equal

2016 ASH Annual Meeting
SAN DIEGO—Investigators have found that life-threatening cytokine release syndrome (CRS) and its symptoms are due to the release of macrophage activation syndrome (MAS) cytokines, such as IL-6, IL-8, and IL2RA.
MAS cytokines, at least in vitro, are not made by chimeric antigen receptor (CAR) T cells and are not necessary for CAR T-cell efficacy, the team says.
The cytokines are produced by antigen-presenting cells (APCs) in response to CAR-mediated killing of leukemia.
What’s more, they say, is that this is likely to be different for each CAR structure and possibly even tumor type.
“Understanding these mechanisms, as it relates to our treatment, will be critical to understanding how best to take care of patients and maintain efficacy without toxicity,” said David Barrett, MD, PhD, of the University of Pennsylvania in Philadelphia.
Dr Barrett discussed the relationship between IL-6, CRS, and CAR T-cell therapy at the 2016 ASH Annual Meeting (abstract 654).
“Every CAR system is slightly different,” he explained, “and it’s very important to understand that when we’re talking about efficacy and toxicity.”
Dr Barrett focused on CTL019 (also known as CART19), the CD19-directed 4-1BB CD3ζ CAR used at the Children’s Hospital of Philadelphia (CHOP).
In pediatric acute lymphoblastic leukemia (ALL), CTL019 produced a 93% response rate at 1 month and an overall survival rate of 79% at 12 months in 59 patients.
“Some relapses take place,” Dr Barrett noted. “This is not a perfect therapy, although it has been transformative in the care of patients.”
Eighty-eight percent of the patients experienced CRS of any grade, and 2 died from it. CRS causes high fever and myalgias, and severe CRS causes unstable hypotension that can require mechanical ventilation.
Tocilizumab, the IL-6R blocking antibody, was used in 27% of the patients, generally for grade 4 CRS.
CRS with CTL019
Dr Barrett described CRS in the first patient treated with CTL019 at CHOP in April 2012. The CRS was quite severe, with high fevers and unstable hypotension requiring multiple vasopressors and the need for mechanical ventilation.
“[W]e had no idea what was happening,” he said. “We didn’t understand what the source of the illness was.”
The patient did not respond to steroids or to etanercept, which Dr Barrett indicated is known to help in acute respiratory distress in transplant patients.
“And it was only through some incredible clinical acumen of the treating physicians as well as incredible critical care that was delivered by our ICU that kept this patient alive long enough for us to try tocilizumab,” Dr Barrett continued, “which, thankfully, worked by blocking the most severe side effects in this patient and allowed her to survive.”
Dr Barrett described the course of another patient who developed grade 4 CRS that continued to get worse even after he received tocilizumab, siltuximab, and steroids.
The patient required vasoactive drugs, had seizures, required milrinone, and was placed on a ventilator. One year after receiving CAR T-cell therapy, he recovered.
“This is an incredibly terrifying syndrome to take care of when we don’t understand what’s triggering it or how to stop it,” Dr Barrett emphasized.
Studying CRS
IL-6 is clearly a critical cytokine in the toxicity of CAR T-cell therapy, Dr Barrett said, but IFNγ and other cytokines are also important.
He and his colleagues performed a comprehensive cytokine analysis of pediatric patients treated with CTL019—specifically, engineered T cells composed of an anti-CD19 single-chain variable fragment, CD3ζ activation domain, a 4-1BB costimulatory domain, and transduced with a lentivirus grown on CD3/CD28 beads with a little bit of IL-2.
With that specific CAR, Dr Barrett said they observed a MAS pattern—IFNγ, IL-10, IL-6, and IL-8, which are most elevated in grades 4 and 5 CRS.
“[S]o this pattern, and this clinical syndrome [CRS] was what we believe was driving toxicity in this model,” he said.
To figure out why this was happening, the investigators created 4-1BB CAR-mediated CRS in a mouse model.
The team took leukemia cells from the first patient treated and clinical T cells from her CAR product and put them in an NSG mouse model that they had used for preclinical development.
The investigators then measured cytokine production in the serum of animals 3 and 7 days post-treatment with CTL019.
“And nothing happened,” Dr Barrett said. “The mice didn’t get sick, they cleared their leukemia, and when you looked for cytokines, you found IFNγ, IL-2, and GM-CSF, but you did not find IL-6.”
The team had also included etanercept and tocilizumab in this model, but since the mice didn’t make the toxic cytokines, the antibodies didn’t do anything.
“So why did she get so sick but yet her cancer and her CAR T cells did not make these mice sick and not generate these cytokines?” Dr Barrett asked.
The investigators hypothesized that APCs—not the CAR T cells—were responsible for the toxic cytokines secreted.
“[I]t would be the CAR T-cell-mediated killing of leukemia which would induce this cytokine release from the antigen-presenting cell lineages,” Dr Barrett explained.
To test this theory, the investigators co-cultured CTL019 and Nalm-6 leukemia, with or without cells derived from peripheral blood monocytes.
The team found that IL-6 levels were elevated several logs when CAR T cells killed leukemia in the presence of the APCs.
On the other hand, co-culture of only CTL019 and Nalm-6 produced high levels of GM-CSF, IFNγ, IL-2, and IL-10 but no detectable IL-6 or IL-8.
Transwell in vitro experiments separating CTL019 and Nalm-6 from the APCs showed the same pattern.
The investigators thus confirmed that IL-6 is made by APCs in response to CAR-mediated killing of leukemia.
Nanostring profiling
The team then performed nanostring RNA analysis of separated cell populations recovered from that experiment.
They found that IL-6 and IL-8 are produced by APCs but not by CTL019. IL-2 and IFNγ are produced by CTL019 and not by APCs, and GM-CSF was produced from CTL019.
“There was a clear separation in cytokine production in this model,” Dr Barrett said.
The investigators also observed that the CTL019 nanostring profile was unaffected by proximity to the APCs and all the IL-6 they make.
“CART19 T cells did not seem to care, on a transcriptional level, that all this IL-6 was floating around,” Dr Barrett said.
In contrast, the APCs do change, he said, when CAR T cells are killing leukemia nearby.
“There are dozens and dozens of changes,” he said, “including many in chemokines and IL-6 and IL-8.”
The investigators performed multiple in vitro killing assays and found no difference in CAR T-cell killing potential in the presence or absence of the MAS cytokines.
They also performed peripheral blood analysis of patients experiencing CRS of grades 2 to 5. The team observed that clinical CRS may be divided into MAS and not-MAS patterns. In addition, they detected no IL-6 transcript in any of the CAR T cells isolated from these patients.
“I think we’re going to discover that cytokine release syndrome is a clinical entity that has multiple mechanisms,” Dr Barrett said. “And so it’s very important, when we are talking about our models and talking about our results, to be sure that we’re all speaking the same language.”

2016 ASH Annual Meeting
SAN DIEGO—Investigators have found that life-threatening cytokine release syndrome (CRS) and its symptoms are due to the release of macrophage activation syndrome (MAS) cytokines, such as IL-6, IL-8, and IL2RA.
MAS cytokines, at least in vitro, are not made by chimeric antigen receptor (CAR) T cells and are not necessary for CAR T-cell efficacy, the team says.
The cytokines are produced by antigen-presenting cells (APCs) in response to CAR-mediated killing of leukemia.
What’s more, they say, is that this is likely to be different for each CAR structure and possibly even tumor type.
“Understanding these mechanisms, as it relates to our treatment, will be critical to understanding how best to take care of patients and maintain efficacy without toxicity,” said David Barrett, MD, PhD, of the University of Pennsylvania in Philadelphia.
Dr Barrett discussed the relationship between IL-6, CRS, and CAR T-cell therapy at the 2016 ASH Annual Meeting (abstract 654).
“Every CAR system is slightly different,” he explained, “and it’s very important to understand that when we’re talking about efficacy and toxicity.”
Dr Barrett focused on CTL019 (also known as CART19), the CD19-directed 4-1BB CD3ζ CAR used at the Children’s Hospital of Philadelphia (CHOP).
In pediatric acute lymphoblastic leukemia (ALL), CTL019 produced a 93% response rate at 1 month and an overall survival rate of 79% at 12 months in 59 patients.
“Some relapses take place,” Dr Barrett noted. “This is not a perfect therapy, although it has been transformative in the care of patients.”
Eighty-eight percent of the patients experienced CRS of any grade, and 2 died from it. CRS causes high fever and myalgias, and severe CRS causes unstable hypotension that can require mechanical ventilation.
Tocilizumab, the IL-6R blocking antibody, was used in 27% of the patients, generally for grade 4 CRS.
CRS with CTL019
Dr Barrett described CRS in the first patient treated with CTL019 at CHOP in April 2012. The CRS was quite severe, with high fevers and unstable hypotension requiring multiple vasopressors and the need for mechanical ventilation.
“[W]e had no idea what was happening,” he said. “We didn’t understand what the source of the illness was.”
The patient did not respond to steroids or to etanercept, which Dr Barrett indicated is known to help in acute respiratory distress in transplant patients.
“And it was only through some incredible clinical acumen of the treating physicians as well as incredible critical care that was delivered by our ICU that kept this patient alive long enough for us to try tocilizumab,” Dr Barrett continued, “which, thankfully, worked by blocking the most severe side effects in this patient and allowed her to survive.”
Dr Barrett described the course of another patient who developed grade 4 CRS that continued to get worse even after he received tocilizumab, siltuximab, and steroids.
The patient required vasoactive drugs, had seizures, required milrinone, and was placed on a ventilator. One year after receiving CAR T-cell therapy, he recovered.
“This is an incredibly terrifying syndrome to take care of when we don’t understand what’s triggering it or how to stop it,” Dr Barrett emphasized.
Studying CRS
IL-6 is clearly a critical cytokine in the toxicity of CAR T-cell therapy, Dr Barrett said, but IFNγ and other cytokines are also important.
He and his colleagues performed a comprehensive cytokine analysis of pediatric patients treated with CTL019—specifically, engineered T cells composed of an anti-CD19 single-chain variable fragment, CD3ζ activation domain, a 4-1BB costimulatory domain, and transduced with a lentivirus grown on CD3/CD28 beads with a little bit of IL-2.
With that specific CAR, Dr Barrett said they observed a MAS pattern—IFNγ, IL-10, IL-6, and IL-8, which are most elevated in grades 4 and 5 CRS.
“[S]o this pattern, and this clinical syndrome [CRS] was what we believe was driving toxicity in this model,” he said.
To figure out why this was happening, the investigators created 4-1BB CAR-mediated CRS in a mouse model.
The team took leukemia cells from the first patient treated and clinical T cells from her CAR product and put them in an NSG mouse model that they had used for preclinical development.
The investigators then measured cytokine production in the serum of animals 3 and 7 days post-treatment with CTL019.
“And nothing happened,” Dr Barrett said. “The mice didn’t get sick, they cleared their leukemia, and when you looked for cytokines, you found IFNγ, IL-2, and GM-CSF, but you did not find IL-6.”
The team had also included etanercept and tocilizumab in this model, but since the mice didn’t make the toxic cytokines, the antibodies didn’t do anything.
“So why did she get so sick but yet her cancer and her CAR T cells did not make these mice sick and not generate these cytokines?” Dr Barrett asked.
The investigators hypothesized that APCs—not the CAR T cells—were responsible for the toxic cytokines secreted.
“[I]t would be the CAR T-cell-mediated killing of leukemia which would induce this cytokine release from the antigen-presenting cell lineages,” Dr Barrett explained.
To test this theory, the investigators co-cultured CTL019 and Nalm-6 leukemia, with or without cells derived from peripheral blood monocytes.
The team found that IL-6 levels were elevated several logs when CAR T cells killed leukemia in the presence of the APCs.
On the other hand, co-culture of only CTL019 and Nalm-6 produced high levels of GM-CSF, IFNγ, IL-2, and IL-10 but no detectable IL-6 or IL-8.
Transwell in vitro experiments separating CTL019 and Nalm-6 from the APCs showed the same pattern.
The investigators thus confirmed that IL-6 is made by APCs in response to CAR-mediated killing of leukemia.
Nanostring profiling
The team then performed nanostring RNA analysis of separated cell populations recovered from that experiment.
They found that IL-6 and IL-8 are produced by APCs but not by CTL019. IL-2 and IFNγ are produced by CTL019 and not by APCs, and GM-CSF was produced from CTL019.
“There was a clear separation in cytokine production in this model,” Dr Barrett said.
The investigators also observed that the CTL019 nanostring profile was unaffected by proximity to the APCs and all the IL-6 they make.
“CART19 T cells did not seem to care, on a transcriptional level, that all this IL-6 was floating around,” Dr Barrett said.
In contrast, the APCs do change, he said, when CAR T cells are killing leukemia nearby.
“There are dozens and dozens of changes,” he said, “including many in chemokines and IL-6 and IL-8.”
The investigators performed multiple in vitro killing assays and found no difference in CAR T-cell killing potential in the presence or absence of the MAS cytokines.
They also performed peripheral blood analysis of patients experiencing CRS of grades 2 to 5. The team observed that clinical CRS may be divided into MAS and not-MAS patterns. In addition, they detected no IL-6 transcript in any of the CAR T cells isolated from these patients.
“I think we’re going to discover that cytokine release syndrome is a clinical entity that has multiple mechanisms,” Dr Barrett said. “And so it’s very important, when we are talking about our models and talking about our results, to be sure that we’re all speaking the same language.”

2016 ASH Annual Meeting
SAN DIEGO—Investigators have found that life-threatening cytokine release syndrome (CRS) and its symptoms are due to the release of macrophage activation syndrome (MAS) cytokines, such as IL-6, IL-8, and IL2RA.
MAS cytokines, at least in vitro, are not made by chimeric antigen receptor (CAR) T cells and are not necessary for CAR T-cell efficacy, the team says.
The cytokines are produced by antigen-presenting cells (APCs) in response to CAR-mediated killing of leukemia.
What’s more, they say, is that this is likely to be different for each CAR structure and possibly even tumor type.
“Understanding these mechanisms, as it relates to our treatment, will be critical to understanding how best to take care of patients and maintain efficacy without toxicity,” said David Barrett, MD, PhD, of the University of Pennsylvania in Philadelphia.
Dr Barrett discussed the relationship between IL-6, CRS, and CAR T-cell therapy at the 2016 ASH Annual Meeting (abstract 654).
“Every CAR system is slightly different,” he explained, “and it’s very important to understand that when we’re talking about efficacy and toxicity.”
Dr Barrett focused on CTL019 (also known as CART19), the CD19-directed 4-1BB CD3ζ CAR used at the Children’s Hospital of Philadelphia (CHOP).
In pediatric acute lymphoblastic leukemia (ALL), CTL019 produced a 93% response rate at 1 month and an overall survival rate of 79% at 12 months in 59 patients.
“Some relapses take place,” Dr Barrett noted. “This is not a perfect therapy, although it has been transformative in the care of patients.”
Eighty-eight percent of the patients experienced CRS of any grade, and 2 died from it. CRS causes high fever and myalgias, and severe CRS causes unstable hypotension that can require mechanical ventilation.
Tocilizumab, the IL-6R blocking antibody, was used in 27% of the patients, generally for grade 4 CRS.
CRS with CTL019
Dr Barrett described CRS in the first patient treated with CTL019 at CHOP in April 2012. The CRS was quite severe, with high fevers and unstable hypotension requiring multiple vasopressors and the need for mechanical ventilation.
“[W]e had no idea what was happening,” he said. “We didn’t understand what the source of the illness was.”
The patient did not respond to steroids or to etanercept, which Dr Barrett indicated is known to help in acute respiratory distress in transplant patients.
“And it was only through some incredible clinical acumen of the treating physicians as well as incredible critical care that was delivered by our ICU that kept this patient alive long enough for us to try tocilizumab,” Dr Barrett continued, “which, thankfully, worked by blocking the most severe side effects in this patient and allowed her to survive.”
Dr Barrett described the course of another patient who developed grade 4 CRS that continued to get worse even after he received tocilizumab, siltuximab, and steroids.
The patient required vasoactive drugs, had seizures, required milrinone, and was placed on a ventilator. One year after receiving CAR T-cell therapy, he recovered.
“This is an incredibly terrifying syndrome to take care of when we don’t understand what’s triggering it or how to stop it,” Dr Barrett emphasized.
Studying CRS
IL-6 is clearly a critical cytokine in the toxicity of CAR T-cell therapy, Dr Barrett said, but IFNγ and other cytokines are also important.
He and his colleagues performed a comprehensive cytokine analysis of pediatric patients treated with CTL019—specifically, engineered T cells composed of an anti-CD19 single-chain variable fragment, CD3ζ activation domain, a 4-1BB costimulatory domain, and transduced with a lentivirus grown on CD3/CD28 beads with a little bit of IL-2.
With that specific CAR, Dr Barrett said they observed a MAS pattern—IFNγ, IL-10, IL-6, and IL-8, which are most elevated in grades 4 and 5 CRS.
“[S]o this pattern, and this clinical syndrome [CRS] was what we believe was driving toxicity in this model,” he said.
To figure out why this was happening, the investigators created 4-1BB CAR-mediated CRS in a mouse model.
The team took leukemia cells from the first patient treated and clinical T cells from her CAR product and put them in an NSG mouse model that they had used for preclinical development.
The investigators then measured cytokine production in the serum of animals 3 and 7 days post-treatment with CTL019.
“And nothing happened,” Dr Barrett said. “The mice didn’t get sick, they cleared their leukemia, and when you looked for cytokines, you found IFNγ, IL-2, and GM-CSF, but you did not find IL-6.”
The team had also included etanercept and tocilizumab in this model, but since the mice didn’t make the toxic cytokines, the antibodies didn’t do anything.
“So why did she get so sick but yet her cancer and her CAR T cells did not make these mice sick and not generate these cytokines?” Dr Barrett asked.
The investigators hypothesized that APCs—not the CAR T cells—were responsible for the toxic cytokines secreted.
“[I]t would be the CAR T-cell-mediated killing of leukemia which would induce this cytokine release from the antigen-presenting cell lineages,” Dr Barrett explained.
To test this theory, the investigators co-cultured CTL019 and Nalm-6 leukemia, with or without cells derived from peripheral blood monocytes.
The team found that IL-6 levels were elevated several logs when CAR T cells killed leukemia in the presence of the APCs.
On the other hand, co-culture of only CTL019 and Nalm-6 produced high levels of GM-CSF, IFNγ, IL-2, and IL-10 but no detectable IL-6 or IL-8.
Transwell in vitro experiments separating CTL019 and Nalm-6 from the APCs showed the same pattern.
The investigators thus confirmed that IL-6 is made by APCs in response to CAR-mediated killing of leukemia.
Nanostring profiling
The team then performed nanostring RNA analysis of separated cell populations recovered from that experiment.
They found that IL-6 and IL-8 are produced by APCs but not by CTL019. IL-2 and IFNγ are produced by CTL019 and not by APCs, and GM-CSF was produced from CTL019.
“There was a clear separation in cytokine production in this model,” Dr Barrett said.
The investigators also observed that the CTL019 nanostring profile was unaffected by proximity to the APCs and all the IL-6 they make.
“CART19 T cells did not seem to care, on a transcriptional level, that all this IL-6 was floating around,” Dr Barrett said.
In contrast, the APCs do change, he said, when CAR T cells are killing leukemia nearby.
“There are dozens and dozens of changes,” he said, “including many in chemokines and IL-6 and IL-8.”
The investigators performed multiple in vitro killing assays and found no difference in CAR T-cell killing potential in the presence or absence of the MAS cytokines.
They also performed peripheral blood analysis of patients experiencing CRS of grades 2 to 5. The team observed that clinical CRS may be divided into MAS and not-MAS patterns. In addition, they detected no IL-6 transcript in any of the CAR T cells isolated from these patients.
“I think we’re going to discover that cytokine release syndrome is a clinical entity that has multiple mechanisms,” Dr Barrett said. “And so it’s very important, when we are talking about our models and talking about our results, to be sure that we’re all speaking the same language.”
KTE-C19 feasible in most young, high-risk ALL patients, study suggests

Photo by Bill Branson
SAN DIEGO—Trial results suggest treatment with the chimeric antigen receptor (CAR) T-cell therapy KTE-C19 is feasible for most young patients with high-risk B-cell acute lymphoblastic leukemia (ALL).
Nearly all ALL patients in this trial were able to receive their assigned dose of KTE-C19 after a preparative chemotherapy regimen.
The complete response (CR) rate in these patients was 62%, and the rate of severe cytokine release syndrome (CRS) was low.
Daniel W. Lee III, MD, of the University of Virginia in Charlottesville, presented these results at the 2016 ASH Annual Meeting (abstract 218).
Dr Lee noted that CAR T cells have shown promise in early studies, but morbidity related to high-grade CRS and/or neurotoxicity could limit wide applicability of this treatment in patients with high disease burden. Among those who achieve CR to CD19 CAR T-cell therapy, nearly half of patients relapse in the first year.
At ASH, Dr Lee reported results of a non-randomized clinical trial of KTE-C19, a CD19 CAR T-cell therapy under development by Kite Pharmaceuticals. The company did not sponsor this study, although investigators reported relationships with Kite and other companies. The trial was sponsored by the National Cancer Institute.
The trial included 53 children and young adults with relapsed/refractory ALL (n=51) or diffuse large B-cell lymphoma (n=2). The patients’ median age was 13 (range, 4-30), and most were male (n=41).
Of the ALL patients, 11 had primary refractory disease, 5 had Ph-positive ALL, 3 had Down syndrome, 6 had central nervous system (CNS) disease (2 with CNS3, 4 with CNS2), and 2 had MLL-rearranged ALL. The median ALL disease burden was 27%.
The first 21 patients received a low-dose fludarabine/cyclophosphamide preparative regimen, and the subsequent 32 patients received an alternative intensified preparative regimen in an attempt to mitigate severe CRS risk and improve response.
Possible intensive preparative regimens included higher-dose fludarabine/cyclophosphamide, fludarabine/high-dose cytarabine/G-CSF, and ifosfamide/etoposide.
All 53 patients had peripheral blood cells collected, and 52 were infused with CAR T cells. One patient did not receive an infusion due to progressive fungal pneumonia, and 2 patients received less than their assigned dose.
Therefore, Dr Lee said KTE-C19 was feasible in 94% of patients.
Efficacy
The median follow-up was 18.7 months.
Dr Lee said KTE-C19 “produced robust responses in very high-risk ALL patients.” He noted, however, that the CR rate was lower among patients with high disease burden.
The CR rate among the ALL patients was 62%. Of the 31 patients who achieved a CR, 28 had a minimal residual disease (MRD)-negative remission.
The rate of MRD-negative CR was 100% among the 11 patients with primary refractory ALL, 100% among the 6 patients with CNS disease, 60% among the 5 patients with Ph+ ALL, and 67% among the 3 with Down syndrome. Neither of the 2 patients with MLL-rearranged ALL responded.
“Attempts to increase response rate by modifying the preparative regimen have not yet been successful,” Dr Lee pointed out.
However, he noted superior response and overall survival rates among patients who received a fludarabine/cyclophosphamide preparative regimen.
“Median overall survival in all enrolled patients is 13.3 months with fludarabine/cyclophosphamide prep versus 5.5 months with other regimens,” he said.
The overall survival rate for the ALL patients was 28%, and the median overall survival was 11.2 months.
For patients who achieved an MRD-negative remission, the leukemia-free survival (LFS) rate was 56%. The median LFS was not reached.
Dr Lee noted that hematopoietic stem cell transplant (HSCT) after KTE-C19 correlated with decreased relapse rates and led to superior LFS.
Of the 28 patients who achieved MRD-negative CR, 21 went on to HSCT after KTE-C19. The median time to HSCT after CAR T-cell dose was 54 days. (Ten of the 28 patients had HSCT before receiving KTE-C19.)
Nineteen (91%) of the patients who proceeded to HSCT after KTE-C19 did not relapse, compared to 1 (14%) of the patients who did not have a post-CAR T transplant.
The median LFS was 4.9 months among the MRD responders who did not proceed to HSCT and undefined among MRD responders with a transplant after KTE-C19.
The probability of survival was 65% beginning at 18 months among patients who underwent HSCT and 14% beginning at 9.8 months among patients without a post-KTE-C19 transplant.
CD19 escape remains a challenge, Dr Lee said. The risk may be diminished, but not eradicated, with HSCT.
Toxicity
“There was a low rate of CRS, which was successfully managed with a grade-driven algorithm,” Dr Lee noted.
Five patients (10%) had grade 3 CRS, and 2 (4%) had grade 4 CRS.
Other grade 3/4 adverse events that were considered at least possibly related to therapy included fever (38% grade 3), febrile neutropenia (23% grade
3), hypotension (9% grade 3, 4% grade 4), LV systolic dysfunction (9% grade 3), prolonged QTc (2% grade 3), dysphasia (2% grade 3), cardiac arrest (2% grade 4), multi-organ failure (2% grade 3), hypoxia (2% grade 3, 2% grade 4), and pulmonary embolism (2% grade 3).
“There were no severe or permanent neurologic toxicities,” Dr Lee said. “Intensive neuropsychological testing in 13 patients revealed no consistent treatment-related neurocognitive decline, and several patients improved following therapy.”
In all, there were 46 cases of neurotoxicity, including visual hallucination (8 grade 1, 17%), headache (1 grade 3 [2%], 3 grade 2 [6%]), confusion (2 grade 1, 4%),
dysphasia (1 grade 3, 2%), delirium (1 grade 3, 2%), seizure (1 grade 2, 1 grade 1 [2% each]), ataxia (1 grade 2, 2%), tremor (1 grade 2, 2%), dysesthesia (1 grade 2, 2%), and dysarthria (1 grade 1, 2%).

Photo by Bill Branson
SAN DIEGO—Trial results suggest treatment with the chimeric antigen receptor (CAR) T-cell therapy KTE-C19 is feasible for most young patients with high-risk B-cell acute lymphoblastic leukemia (ALL).
Nearly all ALL patients in this trial were able to receive their assigned dose of KTE-C19 after a preparative chemotherapy regimen.
The complete response (CR) rate in these patients was 62%, and the rate of severe cytokine release syndrome (CRS) was low.
Daniel W. Lee III, MD, of the University of Virginia in Charlottesville, presented these results at the 2016 ASH Annual Meeting (abstract 218).
Dr Lee noted that CAR T cells have shown promise in early studies, but morbidity related to high-grade CRS and/or neurotoxicity could limit wide applicability of this treatment in patients with high disease burden. Among those who achieve CR to CD19 CAR T-cell therapy, nearly half of patients relapse in the first year.
At ASH, Dr Lee reported results of a non-randomized clinical trial of KTE-C19, a CD19 CAR T-cell therapy under development by Kite Pharmaceuticals. The company did not sponsor this study, although investigators reported relationships with Kite and other companies. The trial was sponsored by the National Cancer Institute.
The trial included 53 children and young adults with relapsed/refractory ALL (n=51) or diffuse large B-cell lymphoma (n=2). The patients’ median age was 13 (range, 4-30), and most were male (n=41).
Of the ALL patients, 11 had primary refractory disease, 5 had Ph-positive ALL, 3 had Down syndrome, 6 had central nervous system (CNS) disease (2 with CNS3, 4 with CNS2), and 2 had MLL-rearranged ALL. The median ALL disease burden was 27%.
The first 21 patients received a low-dose fludarabine/cyclophosphamide preparative regimen, and the subsequent 32 patients received an alternative intensified preparative regimen in an attempt to mitigate severe CRS risk and improve response.
Possible intensive preparative regimens included higher-dose fludarabine/cyclophosphamide, fludarabine/high-dose cytarabine/G-CSF, and ifosfamide/etoposide.
All 53 patients had peripheral blood cells collected, and 52 were infused with CAR T cells. One patient did not receive an infusion due to progressive fungal pneumonia, and 2 patients received less than their assigned dose.
Therefore, Dr Lee said KTE-C19 was feasible in 94% of patients.
Efficacy
The median follow-up was 18.7 months.
Dr Lee said KTE-C19 “produced robust responses in very high-risk ALL patients.” He noted, however, that the CR rate was lower among patients with high disease burden.
The CR rate among the ALL patients was 62%. Of the 31 patients who achieved a CR, 28 had a minimal residual disease (MRD)-negative remission.
The rate of MRD-negative CR was 100% among the 11 patients with primary refractory ALL, 100% among the 6 patients with CNS disease, 60% among the 5 patients with Ph+ ALL, and 67% among the 3 with Down syndrome. Neither of the 2 patients with MLL-rearranged ALL responded.
“Attempts to increase response rate by modifying the preparative regimen have not yet been successful,” Dr Lee pointed out.
However, he noted superior response and overall survival rates among patients who received a fludarabine/cyclophosphamide preparative regimen.
“Median overall survival in all enrolled patients is 13.3 months with fludarabine/cyclophosphamide prep versus 5.5 months with other regimens,” he said.
The overall survival rate for the ALL patients was 28%, and the median overall survival was 11.2 months.
For patients who achieved an MRD-negative remission, the leukemia-free survival (LFS) rate was 56%. The median LFS was not reached.
Dr Lee noted that hematopoietic stem cell transplant (HSCT) after KTE-C19 correlated with decreased relapse rates and led to superior LFS.
Of the 28 patients who achieved MRD-negative CR, 21 went on to HSCT after KTE-C19. The median time to HSCT after CAR T-cell dose was 54 days. (Ten of the 28 patients had HSCT before receiving KTE-C19.)
Nineteen (91%) of the patients who proceeded to HSCT after KTE-C19 did not relapse, compared to 1 (14%) of the patients who did not have a post-CAR T transplant.
The median LFS was 4.9 months among the MRD responders who did not proceed to HSCT and undefined among MRD responders with a transplant after KTE-C19.
The probability of survival was 65% beginning at 18 months among patients who underwent HSCT and 14% beginning at 9.8 months among patients without a post-KTE-C19 transplant.
CD19 escape remains a challenge, Dr Lee said. The risk may be diminished, but not eradicated, with HSCT.
Toxicity
“There was a low rate of CRS, which was successfully managed with a grade-driven algorithm,” Dr Lee noted.
Five patients (10%) had grade 3 CRS, and 2 (4%) had grade 4 CRS.
Other grade 3/4 adverse events that were considered at least possibly related to therapy included fever (38% grade 3), febrile neutropenia (23% grade
3), hypotension (9% grade 3, 4% grade 4), LV systolic dysfunction (9% grade 3), prolonged QTc (2% grade 3), dysphasia (2% grade 3), cardiac arrest (2% grade 4), multi-organ failure (2% grade 3), hypoxia (2% grade 3, 2% grade 4), and pulmonary embolism (2% grade 3).
“There were no severe or permanent neurologic toxicities,” Dr Lee said. “Intensive neuropsychological testing in 13 patients revealed no consistent treatment-related neurocognitive decline, and several patients improved following therapy.”
In all, there were 46 cases of neurotoxicity, including visual hallucination (8 grade 1, 17%), headache (1 grade 3 [2%], 3 grade 2 [6%]), confusion (2 grade 1, 4%),
dysphasia (1 grade 3, 2%), delirium (1 grade 3, 2%), seizure (1 grade 2, 1 grade 1 [2% each]), ataxia (1 grade 2, 2%), tremor (1 grade 2, 2%), dysesthesia (1 grade 2, 2%), and dysarthria (1 grade 1, 2%).

Photo by Bill Branson
SAN DIEGO—Trial results suggest treatment with the chimeric antigen receptor (CAR) T-cell therapy KTE-C19 is feasible for most young patients with high-risk B-cell acute lymphoblastic leukemia (ALL).
Nearly all ALL patients in this trial were able to receive their assigned dose of KTE-C19 after a preparative chemotherapy regimen.
The complete response (CR) rate in these patients was 62%, and the rate of severe cytokine release syndrome (CRS) was low.
Daniel W. Lee III, MD, of the University of Virginia in Charlottesville, presented these results at the 2016 ASH Annual Meeting (abstract 218).
Dr Lee noted that CAR T cells have shown promise in early studies, but morbidity related to high-grade CRS and/or neurotoxicity could limit wide applicability of this treatment in patients with high disease burden. Among those who achieve CR to CD19 CAR T-cell therapy, nearly half of patients relapse in the first year.
At ASH, Dr Lee reported results of a non-randomized clinical trial of KTE-C19, a CD19 CAR T-cell therapy under development by Kite Pharmaceuticals. The company did not sponsor this study, although investigators reported relationships with Kite and other companies. The trial was sponsored by the National Cancer Institute.
The trial included 53 children and young adults with relapsed/refractory ALL (n=51) or diffuse large B-cell lymphoma (n=2). The patients’ median age was 13 (range, 4-30), and most were male (n=41).
Of the ALL patients, 11 had primary refractory disease, 5 had Ph-positive ALL, 3 had Down syndrome, 6 had central nervous system (CNS) disease (2 with CNS3, 4 with CNS2), and 2 had MLL-rearranged ALL. The median ALL disease burden was 27%.
The first 21 patients received a low-dose fludarabine/cyclophosphamide preparative regimen, and the subsequent 32 patients received an alternative intensified preparative regimen in an attempt to mitigate severe CRS risk and improve response.
Possible intensive preparative regimens included higher-dose fludarabine/cyclophosphamide, fludarabine/high-dose cytarabine/G-CSF, and ifosfamide/etoposide.
All 53 patients had peripheral blood cells collected, and 52 were infused with CAR T cells. One patient did not receive an infusion due to progressive fungal pneumonia, and 2 patients received less than their assigned dose.
Therefore, Dr Lee said KTE-C19 was feasible in 94% of patients.
Efficacy
The median follow-up was 18.7 months.
Dr Lee said KTE-C19 “produced robust responses in very high-risk ALL patients.” He noted, however, that the CR rate was lower among patients with high disease burden.
The CR rate among the ALL patients was 62%. Of the 31 patients who achieved a CR, 28 had a minimal residual disease (MRD)-negative remission.
The rate of MRD-negative CR was 100% among the 11 patients with primary refractory ALL, 100% among the 6 patients with CNS disease, 60% among the 5 patients with Ph+ ALL, and 67% among the 3 with Down syndrome. Neither of the 2 patients with MLL-rearranged ALL responded.
“Attempts to increase response rate by modifying the preparative regimen have not yet been successful,” Dr Lee pointed out.
However, he noted superior response and overall survival rates among patients who received a fludarabine/cyclophosphamide preparative regimen.
“Median overall survival in all enrolled patients is 13.3 months with fludarabine/cyclophosphamide prep versus 5.5 months with other regimens,” he said.
The overall survival rate for the ALL patients was 28%, and the median overall survival was 11.2 months.
For patients who achieved an MRD-negative remission, the leukemia-free survival (LFS) rate was 56%. The median LFS was not reached.
Dr Lee noted that hematopoietic stem cell transplant (HSCT) after KTE-C19 correlated with decreased relapse rates and led to superior LFS.
Of the 28 patients who achieved MRD-negative CR, 21 went on to HSCT after KTE-C19. The median time to HSCT after CAR T-cell dose was 54 days. (Ten of the 28 patients had HSCT before receiving KTE-C19.)
Nineteen (91%) of the patients who proceeded to HSCT after KTE-C19 did not relapse, compared to 1 (14%) of the patients who did not have a post-CAR T transplant.
The median LFS was 4.9 months among the MRD responders who did not proceed to HSCT and undefined among MRD responders with a transplant after KTE-C19.
The probability of survival was 65% beginning at 18 months among patients who underwent HSCT and 14% beginning at 9.8 months among patients without a post-KTE-C19 transplant.
CD19 escape remains a challenge, Dr Lee said. The risk may be diminished, but not eradicated, with HSCT.
Toxicity
“There was a low rate of CRS, which was successfully managed with a grade-driven algorithm,” Dr Lee noted.
Five patients (10%) had grade 3 CRS, and 2 (4%) had grade 4 CRS.
Other grade 3/4 adverse events that were considered at least possibly related to therapy included fever (38% grade 3), febrile neutropenia (23% grade
3), hypotension (9% grade 3, 4% grade 4), LV systolic dysfunction (9% grade 3), prolonged QTc (2% grade 3), dysphasia (2% grade 3), cardiac arrest (2% grade 4), multi-organ failure (2% grade 3), hypoxia (2% grade 3, 2% grade 4), and pulmonary embolism (2% grade 3).
“There were no severe or permanent neurologic toxicities,” Dr Lee said. “Intensive neuropsychological testing in 13 patients revealed no consistent treatment-related neurocognitive decline, and several patients improved following therapy.”
In all, there were 46 cases of neurotoxicity, including visual hallucination (8 grade 1, 17%), headache (1 grade 3 [2%], 3 grade 2 [6%]), confusion (2 grade 1, 4%),
dysphasia (1 grade 3, 2%), delirium (1 grade 3, 2%), seizure (1 grade 2, 1 grade 1 [2% each]), ataxia (1 grade 2, 2%), tremor (1 grade 2, 2%), dysesthesia (1 grade 2, 2%), and dysarthria (1 grade 1, 2%).