User login
Inhibitor outperforms rivals in leukemia, lymphoma
CHICAGO—Preclinical research suggests the pan-FLT3/pan-BTK inhibitor CG’806 is more effective than other kinase inhibitors in fighting certain hematologic malignancies.
In one study, CG’806 proved more potent than comparator drugs in primary samples of acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL).
In another study, CG’806 demonstrated greater cytotoxicity than comparators in a range of malignant B cell lines.
Data from both studies were presented at the AACR Annual Meeting 2018 (abstracts 791 and 794).
The research was supported by Aptose Biosciences, Inc., the company developing CG’806.
CG’806 is a small molecule that inhibits wild-type (WT) FLT3, as well as FLT3 housing the ITD mutation or with point mutations in the tyrosine kinase domain (TKD, including D835G, D835Y, D835H) or in the gatekeeper region (F691L). CG’806 also inhibits BTK-WT and BTK-C481S.
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented results with CG’806 in primary patient samples.
The team found that CG’806 demonstrated greater potency against AML samples relative to other FLT3 inhibitors.
Median IC50 values in 188 AML patient samples were 0.0765 µM for CG’806, 0.125 µM for gilteritinib, 0.199 µM for quizartinib, 0.551 µM for dovitinib, 2.25 µM for midostaurin, 2.93 µM for sorafenib, and 5.01 µM for crenolanib.
The researchers said CG’806 sensitivity was enhanced in FLT3-ITD and FLT3-TKD positive cases.
In CLL patient samples, CG’806 exhibited greater potency and a greater range of activity than the BTK inhibitor ibrutinib. Across 95 CLL samples, the median IC50 values were 0.114 µM for CG’806 and 4.09 µM for ibrutinib.
The researchers said this greater potency of CG’806 may be due to the activity of CG’806 on CSF1R, which has been identified as a therapeutic target in CLL.
“The clinical benefit of current FLT3 inhibitors in AML is transient, as resistance develops after several months of treatment,” Dr Kurtz noted. “Similarly, ibrutinib . . . is limited by acquired resistance as well as refractory disease and tolerance challenges. As a pan-FLT3/pan-BTK inhibitor . . ., CG’806 offers important potential to address these limitations.”
Hongying Zhang, MD, PhD, of Aptose Biosciences, and her colleagues presented results with CG’806 in malignant B-cell and AML cell lines.
The researchers found that CG’806 inhibited FLT3-ITD signaling and induced apoptosis more effectively than quizartinib in FLT3-ITD AML cells (MV4-11). The team noted that CG’806 caused G0/G1 cell-cycle arrest in the cells.
CG’806 also exhibited greater cytotoxic activity than quizartinib in FLT3-WT AML cell lines (KG-1 and NOMO-1).
In addition, CG’806 was more potent than quizartinib, gilteritinib, and crenolanib in Ba/F3 cells transfected with FLT3-WT, ITD, D835Y, and ITD-F691. CG’806 was more potent than quizartinib and crenolanib—but not gilteritinib—in Ba/F3 cells transfected with FLT3-ITD-D835Y.
The researchers said they found that CG’806 inhibits BTK, AURK, and downstream signals in FLT3-WT AML cells.
The team also found that CG’806 decreased BTK phosphorylation in all tested cell lines of B-cell malignancies. This included acute lymphoblastic leukemia, mantle cell lymphoma, Burkitt lymphoma, diffuse large B-cell lymphoma, and follicular lymphoma cell lines.
Across all cell lines, CG’806 killed malignant B cells more effectively than ibrutinib. And CG’806 was “equally potent” against WT and C481S-mutant BTK, according to the researchers.
The team also said CG’806 inhibited AURK and induced polyploidy in B-cell malignancies.
“[C]G’806 has demonstrated the ability to kill a broad range of AML and B-cell malignancies through inhibition of multiple oncogenic pathways,” said William G. Rice, PhD, chairman and chief executive officer of Aptose.
“These studies are critical for understanding how to develop and position CG’806 as we prepare for clinical development in these challenging hematologic malignancies.”
CHICAGO—Preclinical research suggests the pan-FLT3/pan-BTK inhibitor CG’806 is more effective than other kinase inhibitors in fighting certain hematologic malignancies.
In one study, CG’806 proved more potent than comparator drugs in primary samples of acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL).
In another study, CG’806 demonstrated greater cytotoxicity than comparators in a range of malignant B cell lines.
Data from both studies were presented at the AACR Annual Meeting 2018 (abstracts 791 and 794).
The research was supported by Aptose Biosciences, Inc., the company developing CG’806.
CG’806 is a small molecule that inhibits wild-type (WT) FLT3, as well as FLT3 housing the ITD mutation or with point mutations in the tyrosine kinase domain (TKD, including D835G, D835Y, D835H) or in the gatekeeper region (F691L). CG’806 also inhibits BTK-WT and BTK-C481S.
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented results with CG’806 in primary patient samples.
The team found that CG’806 demonstrated greater potency against AML samples relative to other FLT3 inhibitors.
Median IC50 values in 188 AML patient samples were 0.0765 µM for CG’806, 0.125 µM for gilteritinib, 0.199 µM for quizartinib, 0.551 µM for dovitinib, 2.25 µM for midostaurin, 2.93 µM for sorafenib, and 5.01 µM for crenolanib.
The researchers said CG’806 sensitivity was enhanced in FLT3-ITD and FLT3-TKD positive cases.
In CLL patient samples, CG’806 exhibited greater potency and a greater range of activity than the BTK inhibitor ibrutinib. Across 95 CLL samples, the median IC50 values were 0.114 µM for CG’806 and 4.09 µM for ibrutinib.
The researchers said this greater potency of CG’806 may be due to the activity of CG’806 on CSF1R, which has been identified as a therapeutic target in CLL.
“The clinical benefit of current FLT3 inhibitors in AML is transient, as resistance develops after several months of treatment,” Dr Kurtz noted. “Similarly, ibrutinib . . . is limited by acquired resistance as well as refractory disease and tolerance challenges. As a pan-FLT3/pan-BTK inhibitor . . ., CG’806 offers important potential to address these limitations.”
Hongying Zhang, MD, PhD, of Aptose Biosciences, and her colleagues presented results with CG’806 in malignant B-cell and AML cell lines.
The researchers found that CG’806 inhibited FLT3-ITD signaling and induced apoptosis more effectively than quizartinib in FLT3-ITD AML cells (MV4-11). The team noted that CG’806 caused G0/G1 cell-cycle arrest in the cells.
CG’806 also exhibited greater cytotoxic activity than quizartinib in FLT3-WT AML cell lines (KG-1 and NOMO-1).
In addition, CG’806 was more potent than quizartinib, gilteritinib, and crenolanib in Ba/F3 cells transfected with FLT3-WT, ITD, D835Y, and ITD-F691. CG’806 was more potent than quizartinib and crenolanib—but not gilteritinib—in Ba/F3 cells transfected with FLT3-ITD-D835Y.
The researchers said they found that CG’806 inhibits BTK, AURK, and downstream signals in FLT3-WT AML cells.
The team also found that CG’806 decreased BTK phosphorylation in all tested cell lines of B-cell malignancies. This included acute lymphoblastic leukemia, mantle cell lymphoma, Burkitt lymphoma, diffuse large B-cell lymphoma, and follicular lymphoma cell lines.
Across all cell lines, CG’806 killed malignant B cells more effectively than ibrutinib. And CG’806 was “equally potent” against WT and C481S-mutant BTK, according to the researchers.
The team also said CG’806 inhibited AURK and induced polyploidy in B-cell malignancies.
“[C]G’806 has demonstrated the ability to kill a broad range of AML and B-cell malignancies through inhibition of multiple oncogenic pathways,” said William G. Rice, PhD, chairman and chief executive officer of Aptose.
“These studies are critical for understanding how to develop and position CG’806 as we prepare for clinical development in these challenging hematologic malignancies.”
CHICAGO—Preclinical research suggests the pan-FLT3/pan-BTK inhibitor CG’806 is more effective than other kinase inhibitors in fighting certain hematologic malignancies.
In one study, CG’806 proved more potent than comparator drugs in primary samples of acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL).
In another study, CG’806 demonstrated greater cytotoxicity than comparators in a range of malignant B cell lines.
Data from both studies were presented at the AACR Annual Meeting 2018 (abstracts 791 and 794).
The research was supported by Aptose Biosciences, Inc., the company developing CG’806.
CG’806 is a small molecule that inhibits wild-type (WT) FLT3, as well as FLT3 housing the ITD mutation or with point mutations in the tyrosine kinase domain (TKD, including D835G, D835Y, D835H) or in the gatekeeper region (F691L). CG’806 also inhibits BTK-WT and BTK-C481S.
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented results with CG’806 in primary patient samples.
The team found that CG’806 demonstrated greater potency against AML samples relative to other FLT3 inhibitors.
Median IC50 values in 188 AML patient samples were 0.0765 µM for CG’806, 0.125 µM for gilteritinib, 0.199 µM for quizartinib, 0.551 µM for dovitinib, 2.25 µM for midostaurin, 2.93 µM for sorafenib, and 5.01 µM for crenolanib.
The researchers said CG’806 sensitivity was enhanced in FLT3-ITD and FLT3-TKD positive cases.
In CLL patient samples, CG’806 exhibited greater potency and a greater range of activity than the BTK inhibitor ibrutinib. Across 95 CLL samples, the median IC50 values were 0.114 µM for CG’806 and 4.09 µM for ibrutinib.
The researchers said this greater potency of CG’806 may be due to the activity of CG’806 on CSF1R, which has been identified as a therapeutic target in CLL.
“The clinical benefit of current FLT3 inhibitors in AML is transient, as resistance develops after several months of treatment,” Dr Kurtz noted. “Similarly, ibrutinib . . . is limited by acquired resistance as well as refractory disease and tolerance challenges. As a pan-FLT3/pan-BTK inhibitor . . ., CG’806 offers important potential to address these limitations.”
Hongying Zhang, MD, PhD, of Aptose Biosciences, and her colleagues presented results with CG’806 in malignant B-cell and AML cell lines.
The researchers found that CG’806 inhibited FLT3-ITD signaling and induced apoptosis more effectively than quizartinib in FLT3-ITD AML cells (MV4-11). The team noted that CG’806 caused G0/G1 cell-cycle arrest in the cells.
CG’806 also exhibited greater cytotoxic activity than quizartinib in FLT3-WT AML cell lines (KG-1 and NOMO-1).
In addition, CG’806 was more potent than quizartinib, gilteritinib, and crenolanib in Ba/F3 cells transfected with FLT3-WT, ITD, D835Y, and ITD-F691. CG’806 was more potent than quizartinib and crenolanib—but not gilteritinib—in Ba/F3 cells transfected with FLT3-ITD-D835Y.
The researchers said they found that CG’806 inhibits BTK, AURK, and downstream signals in FLT3-WT AML cells.
The team also found that CG’806 decreased BTK phosphorylation in all tested cell lines of B-cell malignancies. This included acute lymphoblastic leukemia, mantle cell lymphoma, Burkitt lymphoma, diffuse large B-cell lymphoma, and follicular lymphoma cell lines.
Across all cell lines, CG’806 killed malignant B cells more effectively than ibrutinib. And CG’806 was “equally potent” against WT and C481S-mutant BTK, according to the researchers.
The team also said CG’806 inhibited AURK and induced polyploidy in B-cell malignancies.
“[C]G’806 has demonstrated the ability to kill a broad range of AML and B-cell malignancies through inhibition of multiple oncogenic pathways,” said William G. Rice, PhD, chairman and chief executive officer of Aptose.
“These studies are critical for understanding how to develop and position CG’806 as we prepare for clinical development in these challenging hematologic malignancies.”
Antibody has ‘potent’ effects against AML
CHICAGO—The bispecific antibody APVO436 has demonstrated robust T-cell activation with limited cytokine release in acute myeloid leukemia (AML), according to researchers.
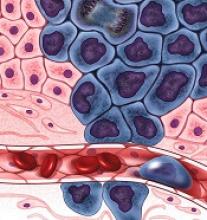
APVO436 binds CD123 and CD3 to redirect T-cell cytotoxicity against CD123-expressing tumor cells.
Researchers found that APVO436 induced T-cell cytotoxicity in AML cells in vitro and in mouse models.
In addition, levels of several cytokines were lower in experiments with APVO436 than in experiments with a comparator antibody.
These findings were presented in a poster at the AACR Annual Meeting 2018 (abstract 1786).
The research was conducted by employees of Aptevo Therapeutics Inc., the company developing APVO436.
“We are especially excited about these latest data for APVO436, which continue to show robust T-cell engagement and cytotoxic activity with reduced levels of cytokine release,” said Jane Gross, PhD, senior vice president and chief scientific officer for Aptevo.
Dr Gross and her colleagues found that APVO436 binds human CD123 and CD3-expressing cells and has “potent” target-specific activity against CD123-expressing AML cell lines (Molm-13 and KG-1a).
In addition, APVO436 induced endogenous T-cell activation and proliferation, accompanied by depletion of CD123-expressing cells, in samples from AML patients and healthy donors.
T cells from these cultures (both AML and non-AML) were expanded and co-cultured with Molm-13 cells and APVO436 or a control antibody. Again, the researchers observed “potent” cytotoxic activity in the presence of APVO436.
Dr Gross and her colleagues also tested APVO436, co-administered with human T cells, in mice with established disseminated Molm-13 tumors. The treatment resulted in a “rapid and significant” reduction in skeletal tumor burden.
Finally, the team compared APVO436 with an Aptevo-generated version of MGD006, a CD123 x CD3 dual-affinity re-targeting molecule being developed by Macrogenics, Inc.
The researchers took purified T cells from healthy donors and cultured them with Molm-13 cells, as well as APVO436, Aptevo’s version of MGD006, and a control antibody.
Both APVO436 and Aptevo’s version of MGD006 were effective at stimulating a tumor-directed immune response, inducing comparable levels of T-cell activation, proliferation, and cytotoxicity.
However, APVO436 induced lower levels of several cytokines—including IFNγ, IL-2, IL-6, and TNFα.
“Importantly, IFNγ, IL-6, and TNFα are considered to be the most relevant cytokines responsible for dosing toxicities observed in clinical studies with T-cell engaging molecules, which suggests that APVO436 could offer the potential for reduced toxicities compared to other CD123 x CD3 T-cell engagers at comparable or higher doses,” Dr Gross said.
She added that Aptevo is planning to launch a phase 1 trial of APVO436 in patients with AML and myelodysplastic syndromes later this year.
CHICAGO—The bispecific antibody APVO436 has demonstrated robust T-cell activation with limited cytokine release in acute myeloid leukemia (AML), according to researchers.
APVO436 binds CD123 and CD3 to redirect T-cell cytotoxicity against CD123-expressing tumor cells.
Researchers found that APVO436 induced T-cell cytotoxicity in AML cells in vitro and in mouse models.
In addition, levels of several cytokines were lower in experiments with APVO436 than in experiments with a comparator antibody.
These findings were presented in a poster at the AACR Annual Meeting 2018 (abstract 1786).
The research was conducted by employees of Aptevo Therapeutics Inc., the company developing APVO436.
“We are especially excited about these latest data for APVO436, which continue to show robust T-cell engagement and cytotoxic activity with reduced levels of cytokine release,” said Jane Gross, PhD, senior vice president and chief scientific officer for Aptevo.
Dr Gross and her colleagues found that APVO436 binds human CD123 and CD3-expressing cells and has “potent” target-specific activity against CD123-expressing AML cell lines (Molm-13 and KG-1a).
In addition, APVO436 induced endogenous T-cell activation and proliferation, accompanied by depletion of CD123-expressing cells, in samples from AML patients and healthy donors.
T cells from these cultures (both AML and non-AML) were expanded and co-cultured with Molm-13 cells and APVO436 or a control antibody. Again, the researchers observed “potent” cytotoxic activity in the presence of APVO436.
Dr Gross and her colleagues also tested APVO436, co-administered with human T cells, in mice with established disseminated Molm-13 tumors. The treatment resulted in a “rapid and significant” reduction in skeletal tumor burden.
Finally, the team compared APVO436 with an Aptevo-generated version of MGD006, a CD123 x CD3 dual-affinity re-targeting molecule being developed by Macrogenics, Inc.
The researchers took purified T cells from healthy donors and cultured them with Molm-13 cells, as well as APVO436, Aptevo’s version of MGD006, and a control antibody.
Both APVO436 and Aptevo’s version of MGD006 were effective at stimulating a tumor-directed immune response, inducing comparable levels of T-cell activation, proliferation, and cytotoxicity.
However, APVO436 induced lower levels of several cytokines—including IFNγ, IL-2, IL-6, and TNFα.
“Importantly, IFNγ, IL-6, and TNFα are considered to be the most relevant cytokines responsible for dosing toxicities observed in clinical studies with T-cell engaging molecules, which suggests that APVO436 could offer the potential for reduced toxicities compared to other CD123 x CD3 T-cell engagers at comparable or higher doses,” Dr Gross said.
She added that Aptevo is planning to launch a phase 1 trial of APVO436 in patients with AML and myelodysplastic syndromes later this year.
CHICAGO—The bispecific antibody APVO436 has demonstrated robust T-cell activation with limited cytokine release in acute myeloid leukemia (AML), according to researchers.
APVO436 binds CD123 and CD3 to redirect T-cell cytotoxicity against CD123-expressing tumor cells.
Researchers found that APVO436 induced T-cell cytotoxicity in AML cells in vitro and in mouse models.
In addition, levels of several cytokines were lower in experiments with APVO436 than in experiments with a comparator antibody.
These findings were presented in a poster at the AACR Annual Meeting 2018 (abstract 1786).
The research was conducted by employees of Aptevo Therapeutics Inc., the company developing APVO436.
“We are especially excited about these latest data for APVO436, which continue to show robust T-cell engagement and cytotoxic activity with reduced levels of cytokine release,” said Jane Gross, PhD, senior vice president and chief scientific officer for Aptevo.
Dr Gross and her colleagues found that APVO436 binds human CD123 and CD3-expressing cells and has “potent” target-specific activity against CD123-expressing AML cell lines (Molm-13 and KG-1a).
In addition, APVO436 induced endogenous T-cell activation and proliferation, accompanied by depletion of CD123-expressing cells, in samples from AML patients and healthy donors.
T cells from these cultures (both AML and non-AML) were expanded and co-cultured with Molm-13 cells and APVO436 or a control antibody. Again, the researchers observed “potent” cytotoxic activity in the presence of APVO436.
Dr Gross and her colleagues also tested APVO436, co-administered with human T cells, in mice with established disseminated Molm-13 tumors. The treatment resulted in a “rapid and significant” reduction in skeletal tumor burden.
Finally, the team compared APVO436 with an Aptevo-generated version of MGD006, a CD123 x CD3 dual-affinity re-targeting molecule being developed by Macrogenics, Inc.
The researchers took purified T cells from healthy donors and cultured them with Molm-13 cells, as well as APVO436, Aptevo’s version of MGD006, and a control antibody.
Both APVO436 and Aptevo’s version of MGD006 were effective at stimulating a tumor-directed immune response, inducing comparable levels of T-cell activation, proliferation, and cytotoxicity.
However, APVO436 induced lower levels of several cytokines—including IFNγ, IL-2, IL-6, and TNFα.
“Importantly, IFNγ, IL-6, and TNFα are considered to be the most relevant cytokines responsible for dosing toxicities observed in clinical studies with T-cell engaging molecules, which suggests that APVO436 could offer the potential for reduced toxicities compared to other CD123 x CD3 T-cell engagers at comparable or higher doses,” Dr Gross said.
She added that Aptevo is planning to launch a phase 1 trial of APVO436 in patients with AML and myelodysplastic syndromes later this year.
Checkpoint inhibition after HiDAC shows promise in AML
NEWPORT BEACH, CALIF. – Adding pembrolizumab after high-dose cytarabine in patients with relapsed or refractory acute myeloid leukemia (AML) appears safe and feasible and shows promising efficacy, according to early results from a multicenter phase 2 study.
The overall response rate to this novel treatment approach in 19 evaluable patients (of 20 enrolled to date) was 42%, with 7 patients (37%) achieving a complete response or complete response with incomplete blood count recovery, and 1 (5%) achieving a partial response, reported Joshua Zeidner, MD, in a poster at the Acute Leukemia Forum of Hemedicus.
Those who went on to allogeneic stem cell transplant included three patients in complete response and one of the five who received pembrolizumab maintenance. That patient on pembrolizumab maintenance went to transplant after two cycles, three others on it relapsed after a median duration of 2.8 months in complete response, and one initially achieved a partial response and had stable disease for a “pretty remarkable” 12 cycles before progressing, he said.
Preliminary analyses in the first six patients, including three with complete response and three nonresponders, showed increased posttreatment diversity of the T-cell receptor repertoire versus baseline in peripheral blood CD8+ T cells in the complete response patients, compared with nonresponders. This suggests that T-cell diversity at baseline is a promising biomarker for programmed death-1 (PD-1) blockade response, Dr. Zeidner noted.
PD-1 suppresses immune activation, and the PD-1 pathway is exploited by AML cells to evade immune surveillance, Dr. Zeidner explained. PD-1 blockade has been shown to have antileukemic effects in vivo, there is expression of multiple coinhibitory receptors in AML patients at the time of diagnosis (that persists in refractory AML), and the ligand for PD-1 is up-regulated on AML blasts, particularly in relapsed/refractory disease, he added.
He and his colleagues hypothesized that targeting PD-1 with pembrolizumab after high-dose cytarabine (HiDAC) salvage chemotherapy would stimulate a T cell–mediated antileukemic immune response and lead to improved efficacy in patients with relapsed or refractory AML.
The ongoing study, with planned enrollment of 37 patients, includes patients aged 18-70 years with relapsed/refractory AML (median age of first 20 enrolled is 54 years). Those under age 60 years receive 2 g/m2 of intravenous HiDAC every 12 hours on days 1-5, and those over age 60 years receive 1.5 g/m2 every 12 hours on days 1-5. In both age groups, this is followed by intravenous pembrolizumab given at 200 mg on day 14.
Overall responders receive maintenance phase intravenous pembrolizumab at 200 mg every 3 weeks for up to 2 years until relapse or progression. Patients are allowed to proceed to stem cell transplant before or after the maintenance phase.
A number of correlative studies, including serial peripheral blood and bone marrow flow cytometry and T-cell receptor clonality studies, also are being conducted to look for predictive biomarkers of response, Dr. Zeidner said.
The study population to date is a relatively young, very-high-risk subgroup of AML patients; European LeukemiaNet-2017 genetic risk status was favorable in only 3 of the first 20 patients (15%), intermediate in 7 (35%), and adverse in 10 (50%). Treatment has been well tolerated; toxicities have been rare and manageable. “Overall, there have been no unexpected toxicities,” he said.
The most common overall toxicities included febrile neutropenia in 70% of patients; transaminitis (including one grade 3 case) in 50%, hyperbilirubinemia in 35%, and fatigue, increased alkaline phosphatase, and rash in 25% each.
Novel therapies for relapsed/refractory AML are urgently needed, and these early results demonstrated the safety and feasibility of adding pembrolizumab after HiDAC chemotherapy in relapsed/refractory AML patients. The preliminary finding that broadening of the immune repertoire, which may occur via increasing T-cell responses beyond endogenous viral responses, was associated with complete response was particularly encouraging, Dr. Zeidner said. The investigators hope to determine predictors of response to immune checkpoint blockade in AML through a comprehensive immune biomarker discovery approach, he added.
This study was funded by Merck. Dr. Zeidner reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Zeidner J et al. ALF 2018, Poster Session.
NEWPORT BEACH, CALIF. – Adding pembrolizumab after high-dose cytarabine in patients with relapsed or refractory acute myeloid leukemia (AML) appears safe and feasible and shows promising efficacy, according to early results from a multicenter phase 2 study.
The overall response rate to this novel treatment approach in 19 evaluable patients (of 20 enrolled to date) was 42%, with 7 patients (37%) achieving a complete response or complete response with incomplete blood count recovery, and 1 (5%) achieving a partial response, reported Joshua Zeidner, MD, in a poster at the Acute Leukemia Forum of Hemedicus.
Those who went on to allogeneic stem cell transplant included three patients in complete response and one of the five who received pembrolizumab maintenance. That patient on pembrolizumab maintenance went to transplant after two cycles, three others on it relapsed after a median duration of 2.8 months in complete response, and one initially achieved a partial response and had stable disease for a “pretty remarkable” 12 cycles before progressing, he said.
Preliminary analyses in the first six patients, including three with complete response and three nonresponders, showed increased posttreatment diversity of the T-cell receptor repertoire versus baseline in peripheral blood CD8+ T cells in the complete response patients, compared with nonresponders. This suggests that T-cell diversity at baseline is a promising biomarker for programmed death-1 (PD-1) blockade response, Dr. Zeidner noted.
PD-1 suppresses immune activation, and the PD-1 pathway is exploited by AML cells to evade immune surveillance, Dr. Zeidner explained. PD-1 blockade has been shown to have antileukemic effects in vivo, there is expression of multiple coinhibitory receptors in AML patients at the time of diagnosis (that persists in refractory AML), and the ligand for PD-1 is up-regulated on AML blasts, particularly in relapsed/refractory disease, he added.
He and his colleagues hypothesized that targeting PD-1 with pembrolizumab after high-dose cytarabine (HiDAC) salvage chemotherapy would stimulate a T cell–mediated antileukemic immune response and lead to improved efficacy in patients with relapsed or refractory AML.
The ongoing study, with planned enrollment of 37 patients, includes patients aged 18-70 years with relapsed/refractory AML (median age of first 20 enrolled is 54 years). Those under age 60 years receive 2 g/m2 of intravenous HiDAC every 12 hours on days 1-5, and those over age 60 years receive 1.5 g/m2 every 12 hours on days 1-5. In both age groups, this is followed by intravenous pembrolizumab given at 200 mg on day 14.
Overall responders receive maintenance phase intravenous pembrolizumab at 200 mg every 3 weeks for up to 2 years until relapse or progression. Patients are allowed to proceed to stem cell transplant before or after the maintenance phase.
A number of correlative studies, including serial peripheral blood and bone marrow flow cytometry and T-cell receptor clonality studies, also are being conducted to look for predictive biomarkers of response, Dr. Zeidner said.
The study population to date is a relatively young, very-high-risk subgroup of AML patients; European LeukemiaNet-2017 genetic risk status was favorable in only 3 of the first 20 patients (15%), intermediate in 7 (35%), and adverse in 10 (50%). Treatment has been well tolerated; toxicities have been rare and manageable. “Overall, there have been no unexpected toxicities,” he said.
The most common overall toxicities included febrile neutropenia in 70% of patients; transaminitis (including one grade 3 case) in 50%, hyperbilirubinemia in 35%, and fatigue, increased alkaline phosphatase, and rash in 25% each.
Novel therapies for relapsed/refractory AML are urgently needed, and these early results demonstrated the safety and feasibility of adding pembrolizumab after HiDAC chemotherapy in relapsed/refractory AML patients. The preliminary finding that broadening of the immune repertoire, which may occur via increasing T-cell responses beyond endogenous viral responses, was associated with complete response was particularly encouraging, Dr. Zeidner said. The investigators hope to determine predictors of response to immune checkpoint blockade in AML through a comprehensive immune biomarker discovery approach, he added.
This study was funded by Merck. Dr. Zeidner reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Zeidner J et al. ALF 2018, Poster Session.
NEWPORT BEACH, CALIF. – Adding pembrolizumab after high-dose cytarabine in patients with relapsed or refractory acute myeloid leukemia (AML) appears safe and feasible and shows promising efficacy, according to early results from a multicenter phase 2 study.
The overall response rate to this novel treatment approach in 19 evaluable patients (of 20 enrolled to date) was 42%, with 7 patients (37%) achieving a complete response or complete response with incomplete blood count recovery, and 1 (5%) achieving a partial response, reported Joshua Zeidner, MD, in a poster at the Acute Leukemia Forum of Hemedicus.
Those who went on to allogeneic stem cell transplant included three patients in complete response and one of the five who received pembrolizumab maintenance. That patient on pembrolizumab maintenance went to transplant after two cycles, three others on it relapsed after a median duration of 2.8 months in complete response, and one initially achieved a partial response and had stable disease for a “pretty remarkable” 12 cycles before progressing, he said.
Preliminary analyses in the first six patients, including three with complete response and three nonresponders, showed increased posttreatment diversity of the T-cell receptor repertoire versus baseline in peripheral blood CD8+ T cells in the complete response patients, compared with nonresponders. This suggests that T-cell diversity at baseline is a promising biomarker for programmed death-1 (PD-1) blockade response, Dr. Zeidner noted.
PD-1 suppresses immune activation, and the PD-1 pathway is exploited by AML cells to evade immune surveillance, Dr. Zeidner explained. PD-1 blockade has been shown to have antileukemic effects in vivo, there is expression of multiple coinhibitory receptors in AML patients at the time of diagnosis (that persists in refractory AML), and the ligand for PD-1 is up-regulated on AML blasts, particularly in relapsed/refractory disease, he added.
He and his colleagues hypothesized that targeting PD-1 with pembrolizumab after high-dose cytarabine (HiDAC) salvage chemotherapy would stimulate a T cell–mediated antileukemic immune response and lead to improved efficacy in patients with relapsed or refractory AML.
The ongoing study, with planned enrollment of 37 patients, includes patients aged 18-70 years with relapsed/refractory AML (median age of first 20 enrolled is 54 years). Those under age 60 years receive 2 g/m2 of intravenous HiDAC every 12 hours on days 1-5, and those over age 60 years receive 1.5 g/m2 every 12 hours on days 1-5. In both age groups, this is followed by intravenous pembrolizumab given at 200 mg on day 14.
Overall responders receive maintenance phase intravenous pembrolizumab at 200 mg every 3 weeks for up to 2 years until relapse or progression. Patients are allowed to proceed to stem cell transplant before or after the maintenance phase.
A number of correlative studies, including serial peripheral blood and bone marrow flow cytometry and T-cell receptor clonality studies, also are being conducted to look for predictive biomarkers of response, Dr. Zeidner said.
The study population to date is a relatively young, very-high-risk subgroup of AML patients; European LeukemiaNet-2017 genetic risk status was favorable in only 3 of the first 20 patients (15%), intermediate in 7 (35%), and adverse in 10 (50%). Treatment has been well tolerated; toxicities have been rare and manageable. “Overall, there have been no unexpected toxicities,” he said.
The most common overall toxicities included febrile neutropenia in 70% of patients; transaminitis (including one grade 3 case) in 50%, hyperbilirubinemia in 35%, and fatigue, increased alkaline phosphatase, and rash in 25% each.
Novel therapies for relapsed/refractory AML are urgently needed, and these early results demonstrated the safety and feasibility of adding pembrolizumab after HiDAC chemotherapy in relapsed/refractory AML patients. The preliminary finding that broadening of the immune repertoire, which may occur via increasing T-cell responses beyond endogenous viral responses, was associated with complete response was particularly encouraging, Dr. Zeidner said. The investigators hope to determine predictors of response to immune checkpoint blockade in AML through a comprehensive immune biomarker discovery approach, he added.
This study was funded by Merck. Dr. Zeidner reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Zeidner J et al. ALF 2018, Poster Session.
REPORTING FROM ALF 2018
Key clinical point:
Major finding: The overall response rate was 42%; 37% of patients achieved complete response or CR with incomplete blood count recovery, and 5% achieved partial response.
Study details: A multicenter, phase 2 study with early results from the first 20 patients enrolled.
Disclosures: This study was funded by Merck. Dr. Zeidner reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
Source: Zeidner J et al. ALF 2018, Poster Session.
5- and 10-day decitabine go head-to-head in poor-risk AML
NEWPORT BEACH, CALIF. – Response and survival rates are similar with 5- and 10-day dosing of decitabine in poor-risk older adults with previously untreated acute myeloid leukemia, according to findings from a randomized phase 2 trial.
The overall response rates in 25 patients randomized to receive 5 days of decitabine and 40 patients randomized to receive 10 days of decitabine were 44% and 38%, respectively. Complete response rates were 28% and 30%, respectively, and the median number of cycles to best response was two in both arms, Nicholas J. Short, MD, reported in a poster at the Acute Leukemia Forum of Hemedicus.
Patients were followed for a median of 38 months. Median remission duration was 9.4 months in 11 responders who received 5 days of decitabine, and 6.4 months in 15 responders in the 10-day treatment arm. The 1-year continued remission rates were 25% and 30%, respectively (P = .85). Median overall survival was 4.9 and 7.1 months, respectively, and 1-year overall survival rates were 27% and 25%, respectively, he said, adding that none of the differences in the groups were statistically significant.
Further, no differences in survival were seen when patients in the two treatment arms were stratified by cytogenetics, de novo versus secondary or treatment-related disease, or TP53 mutations; however, these subgroups were small, he noted.
Study subjects were adults aged 60 years or older (median, 77 and 78 years) with newly diagnosed and untreated acute myeloid leukemia (AML), and adults under age 60 years who were not suitable candidates for intensive chemotherapy. They were enrolled between February 2013 and July 2017. About 30% of patients had performance status scores of 2-3, and 45% of patients had secondary AML.
“About 40% of patients in the 5-day arm had poor-risk cytogenetics, and about half in the 10-day arm had poor-risk cytogenetics,” Dr. Short said in an interview, adding that 6 of 21 tested patients in the 5-day arm and 16 of 38 tested patients in the 10-day arm had a TP53 mutation.
Patients received intravenous decitabine at a dose of 20 mg/m2 for the assigned duration of either 5 or 10 consecutive days for the first three cycles of induction, and those who responded to treatment received additional consolidation cycles every 4-8 weeks for up to 24 total cycles. Patients in the 10-day arm were switched to 5-day dosing after achieving complete response or complete response with incomplete blood count recovery.
The groups were well balanced with respect to baseline characteristics and the imbalance in patient numbers in the arms was mainly because of adaptive randomization; the 10-day patients had better responses during the early part of the study, Dr. Short explained.
None of the patients underwent allogeneic stem cell transplantation, he added.
Older patients with acute AML often have poor tolerance for intensive chemotherapy, but decitabine has been shown to improve survival when compared with supportive care or low-dose cytarabine in these patients. However, while some single-arm studies have suggested that 5- and 10-day dosing may result in similar outcomes, and another suggested that 10-day dosing may be superior in TP53-mutated AML, no studies have directly compared 5- and 10-day dosing, he said.
“In this relatively poor-risk cohort of older adults with newly diagnosed AML, decitabine for 5 and 10 days resulted in similar response rates, survival, and early mortality,” he concluded.
This study was funded by a University of Texas MD Anderson Cancer Center support grant. Dr. Short reported having no financial disclosures.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Short NJ et al. ALF 2018, Poster Session.
NEWPORT BEACH, CALIF. – Response and survival rates are similar with 5- and 10-day dosing of decitabine in poor-risk older adults with previously untreated acute myeloid leukemia, according to findings from a randomized phase 2 trial.
The overall response rates in 25 patients randomized to receive 5 days of decitabine and 40 patients randomized to receive 10 days of decitabine were 44% and 38%, respectively. Complete response rates were 28% and 30%, respectively, and the median number of cycles to best response was two in both arms, Nicholas J. Short, MD, reported in a poster at the Acute Leukemia Forum of Hemedicus.
Patients were followed for a median of 38 months. Median remission duration was 9.4 months in 11 responders who received 5 days of decitabine, and 6.4 months in 15 responders in the 10-day treatment arm. The 1-year continued remission rates were 25% and 30%, respectively (P = .85). Median overall survival was 4.9 and 7.1 months, respectively, and 1-year overall survival rates were 27% and 25%, respectively, he said, adding that none of the differences in the groups were statistically significant.
Further, no differences in survival were seen when patients in the two treatment arms were stratified by cytogenetics, de novo versus secondary or treatment-related disease, or TP53 mutations; however, these subgroups were small, he noted.
Study subjects were adults aged 60 years or older (median, 77 and 78 years) with newly diagnosed and untreated acute myeloid leukemia (AML), and adults under age 60 years who were not suitable candidates for intensive chemotherapy. They were enrolled between February 2013 and July 2017. About 30% of patients had performance status scores of 2-3, and 45% of patients had secondary AML.
“About 40% of patients in the 5-day arm had poor-risk cytogenetics, and about half in the 10-day arm had poor-risk cytogenetics,” Dr. Short said in an interview, adding that 6 of 21 tested patients in the 5-day arm and 16 of 38 tested patients in the 10-day arm had a TP53 mutation.
Patients received intravenous decitabine at a dose of 20 mg/m2 for the assigned duration of either 5 or 10 consecutive days for the first three cycles of induction, and those who responded to treatment received additional consolidation cycles every 4-8 weeks for up to 24 total cycles. Patients in the 10-day arm were switched to 5-day dosing after achieving complete response or complete response with incomplete blood count recovery.
The groups were well balanced with respect to baseline characteristics and the imbalance in patient numbers in the arms was mainly because of adaptive randomization; the 10-day patients had better responses during the early part of the study, Dr. Short explained.
None of the patients underwent allogeneic stem cell transplantation, he added.
Older patients with acute AML often have poor tolerance for intensive chemotherapy, but decitabine has been shown to improve survival when compared with supportive care or low-dose cytarabine in these patients. However, while some single-arm studies have suggested that 5- and 10-day dosing may result in similar outcomes, and another suggested that 10-day dosing may be superior in TP53-mutated AML, no studies have directly compared 5- and 10-day dosing, he said.
“In this relatively poor-risk cohort of older adults with newly diagnosed AML, decitabine for 5 and 10 days resulted in similar response rates, survival, and early mortality,” he concluded.
This study was funded by a University of Texas MD Anderson Cancer Center support grant. Dr. Short reported having no financial disclosures.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Short NJ et al. ALF 2018, Poster Session.
NEWPORT BEACH, CALIF. – Response and survival rates are similar with 5- and 10-day dosing of decitabine in poor-risk older adults with previously untreated acute myeloid leukemia, according to findings from a randomized phase 2 trial.
The overall response rates in 25 patients randomized to receive 5 days of decitabine and 40 patients randomized to receive 10 days of decitabine were 44% and 38%, respectively. Complete response rates were 28% and 30%, respectively, and the median number of cycles to best response was two in both arms, Nicholas J. Short, MD, reported in a poster at the Acute Leukemia Forum of Hemedicus.
Patients were followed for a median of 38 months. Median remission duration was 9.4 months in 11 responders who received 5 days of decitabine, and 6.4 months in 15 responders in the 10-day treatment arm. The 1-year continued remission rates were 25% and 30%, respectively (P = .85). Median overall survival was 4.9 and 7.1 months, respectively, and 1-year overall survival rates were 27% and 25%, respectively, he said, adding that none of the differences in the groups were statistically significant.
Further, no differences in survival were seen when patients in the two treatment arms were stratified by cytogenetics, de novo versus secondary or treatment-related disease, or TP53 mutations; however, these subgroups were small, he noted.
Study subjects were adults aged 60 years or older (median, 77 and 78 years) with newly diagnosed and untreated acute myeloid leukemia (AML), and adults under age 60 years who were not suitable candidates for intensive chemotherapy. They were enrolled between February 2013 and July 2017. About 30% of patients had performance status scores of 2-3, and 45% of patients had secondary AML.
“About 40% of patients in the 5-day arm had poor-risk cytogenetics, and about half in the 10-day arm had poor-risk cytogenetics,” Dr. Short said in an interview, adding that 6 of 21 tested patients in the 5-day arm and 16 of 38 tested patients in the 10-day arm had a TP53 mutation.
Patients received intravenous decitabine at a dose of 20 mg/m2 for the assigned duration of either 5 or 10 consecutive days for the first three cycles of induction, and those who responded to treatment received additional consolidation cycles every 4-8 weeks for up to 24 total cycles. Patients in the 10-day arm were switched to 5-day dosing after achieving complete response or complete response with incomplete blood count recovery.
The groups were well balanced with respect to baseline characteristics and the imbalance in patient numbers in the arms was mainly because of adaptive randomization; the 10-day patients had better responses during the early part of the study, Dr. Short explained.
None of the patients underwent allogeneic stem cell transplantation, he added.
Older patients with acute AML often have poor tolerance for intensive chemotherapy, but decitabine has been shown to improve survival when compared with supportive care or low-dose cytarabine in these patients. However, while some single-arm studies have suggested that 5- and 10-day dosing may result in similar outcomes, and another suggested that 10-day dosing may be superior in TP53-mutated AML, no studies have directly compared 5- and 10-day dosing, he said.
“In this relatively poor-risk cohort of older adults with newly diagnosed AML, decitabine for 5 and 10 days resulted in similar response rates, survival, and early mortality,” he concluded.
This study was funded by a University of Texas MD Anderson Cancer Center support grant. Dr. Short reported having no financial disclosures.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Short NJ et al. ALF 2018, Poster Session.
REPORTING FROM ALF 2018
Key clinical point:
Major finding: Overall response rates were 44% with 5-day dosing and 38% with 10-day dosing.
Study details: A randomized phase 2 study of 65 patients.
Disclosures: This study was funded by an University of Texas MD Anderson Cancer Center support grant. Dr. Short reported having no financial disclosures.
Source: Short NJ et al. ALF 2018, Poster Session.
Statin plus chemo yields encouraging results in poor-risk AML
Patients with poor-risk acute myelogenous leukemia (AML) had promising rates of response and survival following treatment with a statin added to standard chemotherapy, researchers reported.
Pravastatin in combination with idarubicin and cytarabine had a 30% response rate in poor-risk AML patients, according to Anjali S. Advani, MD, of the Taussig Cancer Institute at the Cleveland Clinic, and her coauthors.
Although that response rate did not meet a prespecified threshold for statistical significance, results of the phase 2 study were nevertheless “encouraging” for a group of patients with unfavorable cytogenetics and poor-risk molecular mutations, the researchers wrote. The study was published in Leukemia Research.
The estimated median overall survival was 4.1 months in the phase 2 trial, known as SWOG S0919. About one-quarter of the patients were able to proceed to allogeneic hematopoietic stem cell transplant, and for that group, median overall survival was 27.1 months.
These findings appear to provide further support for the hypothesis that targeting the cholesterol pathway may be a promising approach in patients with AML.
Some previous investigations suggested that AML blasts overexpress genes for lipoprotein receptors and regulatory enzymes, while others showed that these cells import and synthesize cholesterol at levels higher than what is seen in normal progenitor cells. In addition, some AML patients have hypocholesterolemia that usually resolves when they achieve a complete remission.
“These observations suggest that AML cells may require high levels of cholesterol for their survival and that abnormalities in cholesterol homeostasis are necessary for AML cell survival,” the researchers wrote.
This led to a phase 1 trial of pravastatin plus idarubicin/cytarabine, followed by the phase 2 SWOG S0919 trial, which demonstrated a 75% rate of complete response (CR) or complete response with incomplete count recovery (CRi) for the regimen.
The SWOG S0919 study was amended to include the poor-risk AML patients described in the present study. That cohort of 46 patients had a CR/CRi of less than 6 months after their last induction regimen or refractory disease. Many had poor-risk cytogenetics (43%) or one of a number of poor-risk mutations, according to the study report.
Pravastatin, in addition to working on the cholesterol pathway in AML, may also have a therapeutic advantage in patients with FLT3 mutations. Three out of six patients with FLT3 mutations achieved CR/CRi, corroborating earlier preclinical studies and suggesting further study of this specific patient population would be worthwhile, the researchers noted.
The study was supported in part by the National Institutes of Health and Bristol-Myers Squibb. Dr. Advani reported having no financial disclosures but other study authors reported relationships with various pharmaceutical companies.
SOURCE: Advani AS et al. Leuk Res. 2018 Apr;67:17-20.
Patients with poor-risk acute myelogenous leukemia (AML) had promising rates of response and survival following treatment with a statin added to standard chemotherapy, researchers reported.
Pravastatin in combination with idarubicin and cytarabine had a 30% response rate in poor-risk AML patients, according to Anjali S. Advani, MD, of the Taussig Cancer Institute at the Cleveland Clinic, and her coauthors.
Although that response rate did not meet a prespecified threshold for statistical significance, results of the phase 2 study were nevertheless “encouraging” for a group of patients with unfavorable cytogenetics and poor-risk molecular mutations, the researchers wrote. The study was published in Leukemia Research.
The estimated median overall survival was 4.1 months in the phase 2 trial, known as SWOG S0919. About one-quarter of the patients were able to proceed to allogeneic hematopoietic stem cell transplant, and for that group, median overall survival was 27.1 months.
These findings appear to provide further support for the hypothesis that targeting the cholesterol pathway may be a promising approach in patients with AML.
Some previous investigations suggested that AML blasts overexpress genes for lipoprotein receptors and regulatory enzymes, while others showed that these cells import and synthesize cholesterol at levels higher than what is seen in normal progenitor cells. In addition, some AML patients have hypocholesterolemia that usually resolves when they achieve a complete remission.
“These observations suggest that AML cells may require high levels of cholesterol for their survival and that abnormalities in cholesterol homeostasis are necessary for AML cell survival,” the researchers wrote.
This led to a phase 1 trial of pravastatin plus idarubicin/cytarabine, followed by the phase 2 SWOG S0919 trial, which demonstrated a 75% rate of complete response (CR) or complete response with incomplete count recovery (CRi) for the regimen.
The SWOG S0919 study was amended to include the poor-risk AML patients described in the present study. That cohort of 46 patients had a CR/CRi of less than 6 months after their last induction regimen or refractory disease. Many had poor-risk cytogenetics (43%) or one of a number of poor-risk mutations, according to the study report.
Pravastatin, in addition to working on the cholesterol pathway in AML, may also have a therapeutic advantage in patients with FLT3 mutations. Three out of six patients with FLT3 mutations achieved CR/CRi, corroborating earlier preclinical studies and suggesting further study of this specific patient population would be worthwhile, the researchers noted.
The study was supported in part by the National Institutes of Health and Bristol-Myers Squibb. Dr. Advani reported having no financial disclosures but other study authors reported relationships with various pharmaceutical companies.
SOURCE: Advani AS et al. Leuk Res. 2018 Apr;67:17-20.
Patients with poor-risk acute myelogenous leukemia (AML) had promising rates of response and survival following treatment with a statin added to standard chemotherapy, researchers reported.
Pravastatin in combination with idarubicin and cytarabine had a 30% response rate in poor-risk AML patients, according to Anjali S. Advani, MD, of the Taussig Cancer Institute at the Cleveland Clinic, and her coauthors.
Although that response rate did not meet a prespecified threshold for statistical significance, results of the phase 2 study were nevertheless “encouraging” for a group of patients with unfavorable cytogenetics and poor-risk molecular mutations, the researchers wrote. The study was published in Leukemia Research.
The estimated median overall survival was 4.1 months in the phase 2 trial, known as SWOG S0919. About one-quarter of the patients were able to proceed to allogeneic hematopoietic stem cell transplant, and for that group, median overall survival was 27.1 months.
These findings appear to provide further support for the hypothesis that targeting the cholesterol pathway may be a promising approach in patients with AML.
Some previous investigations suggested that AML blasts overexpress genes for lipoprotein receptors and regulatory enzymes, while others showed that these cells import and synthesize cholesterol at levels higher than what is seen in normal progenitor cells. In addition, some AML patients have hypocholesterolemia that usually resolves when they achieve a complete remission.
“These observations suggest that AML cells may require high levels of cholesterol for their survival and that abnormalities in cholesterol homeostasis are necessary for AML cell survival,” the researchers wrote.
This led to a phase 1 trial of pravastatin plus idarubicin/cytarabine, followed by the phase 2 SWOG S0919 trial, which demonstrated a 75% rate of complete response (CR) or complete response with incomplete count recovery (CRi) for the regimen.
The SWOG S0919 study was amended to include the poor-risk AML patients described in the present study. That cohort of 46 patients had a CR/CRi of less than 6 months after their last induction regimen or refractory disease. Many had poor-risk cytogenetics (43%) or one of a number of poor-risk mutations, according to the study report.
Pravastatin, in addition to working on the cholesterol pathway in AML, may also have a therapeutic advantage in patients with FLT3 mutations. Three out of six patients with FLT3 mutations achieved CR/CRi, corroborating earlier preclinical studies and suggesting further study of this specific patient population would be worthwhile, the researchers noted.
The study was supported in part by the National Institutes of Health and Bristol-Myers Squibb. Dr. Advani reported having no financial disclosures but other study authors reported relationships with various pharmaceutical companies.
SOURCE: Advani AS et al. Leuk Res. 2018 Apr;67:17-20.
FROM LEUKEMIA RESEARCH
Key clinical point:
Major finding: Pravastatin in combination with idarubicin and cytarabine had a 30% response rate in poor risk AML patients.
Study details: Results from the poor-risk cohort (n = 46) in SWOG S0919, a phase 2 study.
Disclosures: The research was supported in part by the National Institutes of Health and Bristol-Myers Squibb. Dr. Advani reported having no financial disclosures but other study authors reported relationships with various pharmaceutical companies.
Source: Advani AS et al. Leuk Res. 2018 Apr;67:17-20.
Drug appears to aid chemo in AML
Adding an experimental compound to chemotherapy is a “promising” treatment approach for certain patients with acute myeloid leukemia (AML), according to researchers.
They tested the compound, CPI-613, in combination with high-dose cytarabine and mitoxantrone in a phase 1 trial of patients with relapsed or refractory AML.
The combination produced similar response rates in the overall patient population (50%), patients age 60 and older (47%), and those with poor-risk cytogenetics (46%).
The most common grade 3/4 adverse events (AEs) were hematologic toxicities, and there was 1 fatal AE—hypotension.
Mortality rates in this trial were similar to those observed in historical controls treated with high-dose cytarabine, mitoxantrone, and asparaginase.
“These data are very encouraging, especially for patients 60 years of age or older who have historically done very poorly with this disease,” said Timothy Pardee, MD, PhD, a professor at Wake Forest Baptist Health in Winston-Salem, North Carolina, and chief medical officer of Rafael Pharmaceuticals, Inc., the company developing CPI-613.
Dr Pardee and his colleagues reported these results in Clinical Cancer Research.
The researchers noted that CPI-613 is designed to target mitochondrial metabolism in cancer cells, and preclinical research showed that CPI-613 sensitized AML cells to chemotherapy.
To investigate this further, the team tested CPI-613 in combination with high-dose cytarabine and mitoxantrone in the phase 1 trial. The study included 66 patients with relapsed or refractory AML, as well as a patient with advanced-phase chronic myeloid leukemia (CML) who was mistakenly enrolled.
The patients’ median age was 60 (range, 21-79), and 54% were age 60 and older. Their median percentage of marrow blasts was 43%. Forty percent of patients had poor-risk cytogenetics, and 49% had intermediate-risk cytogenetics.
Most patients (72%) had no prior salvage therapy, 13% had 1 prior line of salvage, 10% had 2 prior lines, and 4% had more than 2. Thirty-one percent of patients had refractory disease.
Seven percent of patients had previously received high-dose cytarabine and mitoxantrone, and 25% had previous salvage including high-dose or intermediate-dose cytarabine.
Treatment
Patients received CPI-613, given over 2 hours, on days 1 to 5 of cycle 1. Doses ranged from 500 mg/m2 to 2750 mg/m2.
Starting on day 3, patients received 5 doses of cytarabine at 3 gm/m2 (for patients younger than 60) or 1.5 gm/m2 (for older patients) in 500 mL normal saline, over 3 hours, every 12 hours.
Patients also received 3 daily doses of mitoxantrone at 6 mg/m2 in 50 mL normal saline, given over 15 minutes, after the first, third, and fifth doses of cytarabine.
Patients were initially assigned to receive 1 cycle of treatment. Those with at least 5% blasts after the first cycle could receive a second course—either a full course or a 3-day course. And patients who responded to the first course could receive up to 2 cycles of the 3-day course.
Safety
There were 2 dose-limiting toxicities when CPI-613 was given at the 2750 mg/m2 dose. One of these toxicities was grade 3 diarrhea that didn’t respond to anti-diarrheals, and the other was grade 3 nausea that didn’t respond to antiemetics.
Because of these events, 2500 mg/m2 was deemed the maximum-tolerated dose. However, the recommended phase 2 dose is 2000 mg/m2.
The most common AEs—occurring in at least 50% of all patients who received CPI-613 (n=67)—included hemoglobin decrease (67%), hyperglycemia (67%), neutropenia (67%), thrombocytopenia (67%), hypomagnesemia (66%), leukopenia (66%), lymphopenia (66%), hypoalbuminemia (65%), hypokalemia (60%), hypocalcemia (57%), and diarrhea (55%).
All cases of neutropenia, thrombocytopenia, leukopenia, and lymphopenia were grade 3/4. Other common grade 3/4 AEs (occurring in at least 20% of patients) included hemoglobin decrease (62%), febrile neutropenia (28%), hypophosphatemia (24%), and hypokalemia (23%).
The only grade 5 AE was hypotension.
The mortality rate was 12% (n=8) at 30 days and 19% (n=13) at 60 days. The researchers said this was similar to the historical experience with high-dose cytarabine, mitoxantrone, and asparaginase. Mortality rates with this regimen were 13% at 30 days and 22% at 60 days.
Efficacy
Sixty-two patients were evaluable for response. Of the 5 patients who were not evaluable, 1 didn’t complete the first cycle of treatment, 1 was the CML patient, and 3 died before assessment.
The overall response rate was 50% (31/62). This included 26 patients with a complete response (CR) and 5 patients who had a CR with incomplete count recovery (CRi).
The rate of CR/CRi was 47% (15/32) in patients older than 60 years of age, 46% (11/24) in patients who had poor-risk cytogenetics, and 53% (8/15) when CPI-613 was given at the recommended phase 2 dose—2000 mg/m2.
The median overall survival (OS) was 6.7 months for all evaluable patients and 13.2 months for patients who achieved a CR/CRi.
The median OS was 6.9 months for patients age 60 and older, which was not significantly different from the median OS in younger patients (P=0.9642).
This study was sponsored by Wake Forest University Health Sciences and the National Cancer Institute.
Adding an experimental compound to chemotherapy is a “promising” treatment approach for certain patients with acute myeloid leukemia (AML), according to researchers.
They tested the compound, CPI-613, in combination with high-dose cytarabine and mitoxantrone in a phase 1 trial of patients with relapsed or refractory AML.
The combination produced similar response rates in the overall patient population (50%), patients age 60 and older (47%), and those with poor-risk cytogenetics (46%).
The most common grade 3/4 adverse events (AEs) were hematologic toxicities, and there was 1 fatal AE—hypotension.
Mortality rates in this trial were similar to those observed in historical controls treated with high-dose cytarabine, mitoxantrone, and asparaginase.
“These data are very encouraging, especially for patients 60 years of age or older who have historically done very poorly with this disease,” said Timothy Pardee, MD, PhD, a professor at Wake Forest Baptist Health in Winston-Salem, North Carolina, and chief medical officer of Rafael Pharmaceuticals, Inc., the company developing CPI-613.
Dr Pardee and his colleagues reported these results in Clinical Cancer Research.
The researchers noted that CPI-613 is designed to target mitochondrial metabolism in cancer cells, and preclinical research showed that CPI-613 sensitized AML cells to chemotherapy.
To investigate this further, the team tested CPI-613 in combination with high-dose cytarabine and mitoxantrone in the phase 1 trial. The study included 66 patients with relapsed or refractory AML, as well as a patient with advanced-phase chronic myeloid leukemia (CML) who was mistakenly enrolled.
The patients’ median age was 60 (range, 21-79), and 54% were age 60 and older. Their median percentage of marrow blasts was 43%. Forty percent of patients had poor-risk cytogenetics, and 49% had intermediate-risk cytogenetics.
Most patients (72%) had no prior salvage therapy, 13% had 1 prior line of salvage, 10% had 2 prior lines, and 4% had more than 2. Thirty-one percent of patients had refractory disease.
Seven percent of patients had previously received high-dose cytarabine and mitoxantrone, and 25% had previous salvage including high-dose or intermediate-dose cytarabine.
Treatment
Patients received CPI-613, given over 2 hours, on days 1 to 5 of cycle 1. Doses ranged from 500 mg/m2 to 2750 mg/m2.
Starting on day 3, patients received 5 doses of cytarabine at 3 gm/m2 (for patients younger than 60) or 1.5 gm/m2 (for older patients) in 500 mL normal saline, over 3 hours, every 12 hours.
Patients also received 3 daily doses of mitoxantrone at 6 mg/m2 in 50 mL normal saline, given over 15 minutes, after the first, third, and fifth doses of cytarabine.
Patients were initially assigned to receive 1 cycle of treatment. Those with at least 5% blasts after the first cycle could receive a second course—either a full course or a 3-day course. And patients who responded to the first course could receive up to 2 cycles of the 3-day course.
Safety
There were 2 dose-limiting toxicities when CPI-613 was given at the 2750 mg/m2 dose. One of these toxicities was grade 3 diarrhea that didn’t respond to anti-diarrheals, and the other was grade 3 nausea that didn’t respond to antiemetics.
Because of these events, 2500 mg/m2 was deemed the maximum-tolerated dose. However, the recommended phase 2 dose is 2000 mg/m2.
The most common AEs—occurring in at least 50% of all patients who received CPI-613 (n=67)—included hemoglobin decrease (67%), hyperglycemia (67%), neutropenia (67%), thrombocytopenia (67%), hypomagnesemia (66%), leukopenia (66%), lymphopenia (66%), hypoalbuminemia (65%), hypokalemia (60%), hypocalcemia (57%), and diarrhea (55%).
All cases of neutropenia, thrombocytopenia, leukopenia, and lymphopenia were grade 3/4. Other common grade 3/4 AEs (occurring in at least 20% of patients) included hemoglobin decrease (62%), febrile neutropenia (28%), hypophosphatemia (24%), and hypokalemia (23%).
The only grade 5 AE was hypotension.
The mortality rate was 12% (n=8) at 30 days and 19% (n=13) at 60 days. The researchers said this was similar to the historical experience with high-dose cytarabine, mitoxantrone, and asparaginase. Mortality rates with this regimen were 13% at 30 days and 22% at 60 days.
Efficacy
Sixty-two patients were evaluable for response. Of the 5 patients who were not evaluable, 1 didn’t complete the first cycle of treatment, 1 was the CML patient, and 3 died before assessment.
The overall response rate was 50% (31/62). This included 26 patients with a complete response (CR) and 5 patients who had a CR with incomplete count recovery (CRi).
The rate of CR/CRi was 47% (15/32) in patients older than 60 years of age, 46% (11/24) in patients who had poor-risk cytogenetics, and 53% (8/15) when CPI-613 was given at the recommended phase 2 dose—2000 mg/m2.
The median overall survival (OS) was 6.7 months for all evaluable patients and 13.2 months for patients who achieved a CR/CRi.
The median OS was 6.9 months for patients age 60 and older, which was not significantly different from the median OS in younger patients (P=0.9642).
This study was sponsored by Wake Forest University Health Sciences and the National Cancer Institute.
Adding an experimental compound to chemotherapy is a “promising” treatment approach for certain patients with acute myeloid leukemia (AML), according to researchers.
They tested the compound, CPI-613, in combination with high-dose cytarabine and mitoxantrone in a phase 1 trial of patients with relapsed or refractory AML.
The combination produced similar response rates in the overall patient population (50%), patients age 60 and older (47%), and those with poor-risk cytogenetics (46%).
The most common grade 3/4 adverse events (AEs) were hematologic toxicities, and there was 1 fatal AE—hypotension.
Mortality rates in this trial were similar to those observed in historical controls treated with high-dose cytarabine, mitoxantrone, and asparaginase.
“These data are very encouraging, especially for patients 60 years of age or older who have historically done very poorly with this disease,” said Timothy Pardee, MD, PhD, a professor at Wake Forest Baptist Health in Winston-Salem, North Carolina, and chief medical officer of Rafael Pharmaceuticals, Inc., the company developing CPI-613.
Dr Pardee and his colleagues reported these results in Clinical Cancer Research.
The researchers noted that CPI-613 is designed to target mitochondrial metabolism in cancer cells, and preclinical research showed that CPI-613 sensitized AML cells to chemotherapy.
To investigate this further, the team tested CPI-613 in combination with high-dose cytarabine and mitoxantrone in the phase 1 trial. The study included 66 patients with relapsed or refractory AML, as well as a patient with advanced-phase chronic myeloid leukemia (CML) who was mistakenly enrolled.
The patients’ median age was 60 (range, 21-79), and 54% were age 60 and older. Their median percentage of marrow blasts was 43%. Forty percent of patients had poor-risk cytogenetics, and 49% had intermediate-risk cytogenetics.
Most patients (72%) had no prior salvage therapy, 13% had 1 prior line of salvage, 10% had 2 prior lines, and 4% had more than 2. Thirty-one percent of patients had refractory disease.
Seven percent of patients had previously received high-dose cytarabine and mitoxantrone, and 25% had previous salvage including high-dose or intermediate-dose cytarabine.
Treatment
Patients received CPI-613, given over 2 hours, on days 1 to 5 of cycle 1. Doses ranged from 500 mg/m2 to 2750 mg/m2.
Starting on day 3, patients received 5 doses of cytarabine at 3 gm/m2 (for patients younger than 60) or 1.5 gm/m2 (for older patients) in 500 mL normal saline, over 3 hours, every 12 hours.
Patients also received 3 daily doses of mitoxantrone at 6 mg/m2 in 50 mL normal saline, given over 15 minutes, after the first, third, and fifth doses of cytarabine.
Patients were initially assigned to receive 1 cycle of treatment. Those with at least 5% blasts after the first cycle could receive a second course—either a full course or a 3-day course. And patients who responded to the first course could receive up to 2 cycles of the 3-day course.
Safety
There were 2 dose-limiting toxicities when CPI-613 was given at the 2750 mg/m2 dose. One of these toxicities was grade 3 diarrhea that didn’t respond to anti-diarrheals, and the other was grade 3 nausea that didn’t respond to antiemetics.
Because of these events, 2500 mg/m2 was deemed the maximum-tolerated dose. However, the recommended phase 2 dose is 2000 mg/m2.
The most common AEs—occurring in at least 50% of all patients who received CPI-613 (n=67)—included hemoglobin decrease (67%), hyperglycemia (67%), neutropenia (67%), thrombocytopenia (67%), hypomagnesemia (66%), leukopenia (66%), lymphopenia (66%), hypoalbuminemia (65%), hypokalemia (60%), hypocalcemia (57%), and diarrhea (55%).
All cases of neutropenia, thrombocytopenia, leukopenia, and lymphopenia were grade 3/4. Other common grade 3/4 AEs (occurring in at least 20% of patients) included hemoglobin decrease (62%), febrile neutropenia (28%), hypophosphatemia (24%), and hypokalemia (23%).
The only grade 5 AE was hypotension.
The mortality rate was 12% (n=8) at 30 days and 19% (n=13) at 60 days. The researchers said this was similar to the historical experience with high-dose cytarabine, mitoxantrone, and asparaginase. Mortality rates with this regimen were 13% at 30 days and 22% at 60 days.
Efficacy
Sixty-two patients were evaluable for response. Of the 5 patients who were not evaluable, 1 didn’t complete the first cycle of treatment, 1 was the CML patient, and 3 died before assessment.
The overall response rate was 50% (31/62). This included 26 patients with a complete response (CR) and 5 patients who had a CR with incomplete count recovery (CRi).
The rate of CR/CRi was 47% (15/32) in patients older than 60 years of age, 46% (11/24) in patients who had poor-risk cytogenetics, and 53% (8/15) when CPI-613 was given at the recommended phase 2 dose—2000 mg/m2.
The median overall survival (OS) was 6.7 months for all evaluable patients and 13.2 months for patients who achieved a CR/CRi.
The median OS was 6.9 months for patients age 60 and older, which was not significantly different from the median OS in younger patients (P=0.9642).
This study was sponsored by Wake Forest University Health Sciences and the National Cancer Institute.
Drug shows promise for treating AML, MDS
Preclinical results support clinical testing of an experimental agent in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to researchers.
The agent, ALRN-6924, was shown to combat AML and MDS by restoring activity of the tumor-suppressing protein p53.
ALRN-6924 exhibited antileukemic activity in AML cells and mouse models of the disease, as well as in a patient with MDS and excess leukemic blasts who received the drug on a compassionate-use basis.
These results, published in Science Translational Medicine, have led to a phase 1 trial of ALRN-6924 in patients with AML or MDS.
ALRN-6924 was developed by Aileron Therapeutics Inc., to target p53 by inhibiting 2 naturally occurring proteins, MDMX and MDM2. Overexpression of these proteins inactivates p53, allowing cancer cells to multiply unchecked.
In the current study, researchers set out to confirm ALRN-6924’s mechanism of action and determine the efficacy of the drug in AML/MDS. This work was supported, in part, by grants from Aileron Therapeutics Inc., and the National Institutes of Health.
The researchers did find that ALRN-6924 targets both MDMX and MDM2, blocking their interaction with p53 in AML cells.
The team said ALRN-6924 inhibited proliferation by inducing cell-cycle arrest and apoptosis in AML cell lines and AML patient cells, including leukemic stem cell-enriched populations.
“This is important because AML is driven by stem cells, and, if you don’t target stem cells, the disease will come back very quickly,” said study author Ulrich Steidl, MD, PhD, of Albert Einstein College of Medicine in Bronx, New York.
The researchers also found that ALRN-6924 greatly increased survival in a mouse model of AML. The median survival was 34 days in vehicle-treated control mice, 83 days in mice that received ALRN-6924 at 20 mg/kg twice a week, and 151 days in mice that received ALRN-6924 at 20 mg/kg three times a week.
“This is a very striking response,” Dr Steidl said. “Most experimental drugs for leukemia achieve an increase in survival of only a few days in these preclinical models. Even more importantly, ALRN-6924 effectively cured about 40% of the treated mice, meaning they were disease-free more than 1 year after treatment, essentially a lifetime for a mouse.”
Finally, the researchers assessed the effects of ALRN-6924 in a patient who had high-risk MDS with excess leukemic blasts.
The team found the p53 protein “was rapidly induced” in CD34+ leukemic blasts but not in healthy lymphocytes. And ALRN-6924 reduced the number of malignant cells circulating in the blood.
“This test was not designed to assess the efficacy of the drug in humans,” Dr Steidl noted. “That has to be done in a proper clinical trial. Our goal was to determine whether it can hit the desired target in human cells in a clinical setting, which it did in this individual.”
ALRN-6924 is a stapled alpha-helical peptide, a class of drugs whose helical structure is stabilized using hydrocarbon “staples.” The stapling prevents the peptides from being degraded by enzymes before reaching their intended target. ALRN-6924 is the first stapled peptide therapeutic to be tested in patients.
In the phase 1 trial (NCT02909972), researchers are testing ALRN-6924 in patients with relapsed/refractory AML or advanced MDS.
Preclinical results support clinical testing of an experimental agent in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to researchers.
The agent, ALRN-6924, was shown to combat AML and MDS by restoring activity of the tumor-suppressing protein p53.
ALRN-6924 exhibited antileukemic activity in AML cells and mouse models of the disease, as well as in a patient with MDS and excess leukemic blasts who received the drug on a compassionate-use basis.
These results, published in Science Translational Medicine, have led to a phase 1 trial of ALRN-6924 in patients with AML or MDS.
ALRN-6924 was developed by Aileron Therapeutics Inc., to target p53 by inhibiting 2 naturally occurring proteins, MDMX and MDM2. Overexpression of these proteins inactivates p53, allowing cancer cells to multiply unchecked.
In the current study, researchers set out to confirm ALRN-6924’s mechanism of action and determine the efficacy of the drug in AML/MDS. This work was supported, in part, by grants from Aileron Therapeutics Inc., and the National Institutes of Health.
The researchers did find that ALRN-6924 targets both MDMX and MDM2, blocking their interaction with p53 in AML cells.
The team said ALRN-6924 inhibited proliferation by inducing cell-cycle arrest and apoptosis in AML cell lines and AML patient cells, including leukemic stem cell-enriched populations.
“This is important because AML is driven by stem cells, and, if you don’t target stem cells, the disease will come back very quickly,” said study author Ulrich Steidl, MD, PhD, of Albert Einstein College of Medicine in Bronx, New York.
The researchers also found that ALRN-6924 greatly increased survival in a mouse model of AML. The median survival was 34 days in vehicle-treated control mice, 83 days in mice that received ALRN-6924 at 20 mg/kg twice a week, and 151 days in mice that received ALRN-6924 at 20 mg/kg three times a week.
“This is a very striking response,” Dr Steidl said. “Most experimental drugs for leukemia achieve an increase in survival of only a few days in these preclinical models. Even more importantly, ALRN-6924 effectively cured about 40% of the treated mice, meaning they were disease-free more than 1 year after treatment, essentially a lifetime for a mouse.”
Finally, the researchers assessed the effects of ALRN-6924 in a patient who had high-risk MDS with excess leukemic blasts.
The team found the p53 protein “was rapidly induced” in CD34+ leukemic blasts but not in healthy lymphocytes. And ALRN-6924 reduced the number of malignant cells circulating in the blood.
“This test was not designed to assess the efficacy of the drug in humans,” Dr Steidl noted. “That has to be done in a proper clinical trial. Our goal was to determine whether it can hit the desired target in human cells in a clinical setting, which it did in this individual.”
ALRN-6924 is a stapled alpha-helical peptide, a class of drugs whose helical structure is stabilized using hydrocarbon “staples.” The stapling prevents the peptides from being degraded by enzymes before reaching their intended target. ALRN-6924 is the first stapled peptide therapeutic to be tested in patients.
In the phase 1 trial (NCT02909972), researchers are testing ALRN-6924 in patients with relapsed/refractory AML or advanced MDS.
Preclinical results support clinical testing of an experimental agent in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to researchers.
The agent, ALRN-6924, was shown to combat AML and MDS by restoring activity of the tumor-suppressing protein p53.
ALRN-6924 exhibited antileukemic activity in AML cells and mouse models of the disease, as well as in a patient with MDS and excess leukemic blasts who received the drug on a compassionate-use basis.
These results, published in Science Translational Medicine, have led to a phase 1 trial of ALRN-6924 in patients with AML or MDS.
ALRN-6924 was developed by Aileron Therapeutics Inc., to target p53 by inhibiting 2 naturally occurring proteins, MDMX and MDM2. Overexpression of these proteins inactivates p53, allowing cancer cells to multiply unchecked.
In the current study, researchers set out to confirm ALRN-6924’s mechanism of action and determine the efficacy of the drug in AML/MDS. This work was supported, in part, by grants from Aileron Therapeutics Inc., and the National Institutes of Health.
The researchers did find that ALRN-6924 targets both MDMX and MDM2, blocking their interaction with p53 in AML cells.
The team said ALRN-6924 inhibited proliferation by inducing cell-cycle arrest and apoptosis in AML cell lines and AML patient cells, including leukemic stem cell-enriched populations.
“This is important because AML is driven by stem cells, and, if you don’t target stem cells, the disease will come back very quickly,” said study author Ulrich Steidl, MD, PhD, of Albert Einstein College of Medicine in Bronx, New York.
The researchers also found that ALRN-6924 greatly increased survival in a mouse model of AML. The median survival was 34 days in vehicle-treated control mice, 83 days in mice that received ALRN-6924 at 20 mg/kg twice a week, and 151 days in mice that received ALRN-6924 at 20 mg/kg three times a week.
“This is a very striking response,” Dr Steidl said. “Most experimental drugs for leukemia achieve an increase in survival of only a few days in these preclinical models. Even more importantly, ALRN-6924 effectively cured about 40% of the treated mice, meaning they were disease-free more than 1 year after treatment, essentially a lifetime for a mouse.”
Finally, the researchers assessed the effects of ALRN-6924 in a patient who had high-risk MDS with excess leukemic blasts.
The team found the p53 protein “was rapidly induced” in CD34+ leukemic blasts but not in healthy lymphocytes. And ALRN-6924 reduced the number of malignant cells circulating in the blood.
“This test was not designed to assess the efficacy of the drug in humans,” Dr Steidl noted. “That has to be done in a proper clinical trial. Our goal was to determine whether it can hit the desired target in human cells in a clinical setting, which it did in this individual.”
ALRN-6924 is a stapled alpha-helical peptide, a class of drugs whose helical structure is stabilized using hydrocarbon “staples.” The stapling prevents the peptides from being degraded by enzymes before reaching their intended target. ALRN-6924 is the first stapled peptide therapeutic to be tested in patients.
In the phase 1 trial (NCT02909972), researchers are testing ALRN-6924 in patients with relapsed/refractory AML or advanced MDS.
Gene variants linked to survival after HSCT
New research has revealed a link between rare gene variants and survival after hematopoietic stem cell transplant (HSCT).
Researchers performed exome sequencing in nearly 2500 HSCT recipients and their matched, unrelated donors.
The sequencing revealed several gene variants—in both donors and recipients—that were significantly associated with overall survival (OS), transplant-related mortality (TRM), and disease-related mortality (DRM) after HSCT.
Qianqian Zhu, PhD, of Roswell Park Comprehensive Cancer Center in Buffalo, New York, and her colleagues described these findings in Blood.
The team performed exome sequencing—using the Illumina HumanExome BeadChip—in patients who participated in the DISCOVeRY-BMT study.
This included 2473 HSCT recipients who had acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic syndromes. It also included 2221 donors who were a 10/10 human leukocyte antigen match for each recipient.
The researchers looked at genetic variants in donors and recipients and assessed the variants’ associations with OS, TRM, and DRM.
Variants in recipients
Analyses revealed an increased risk of TRM when there was a mismatch between donors and recipients for a variant in TEX38—rs200092801. The increased risk was even more pronounced when either the recipient or the donor was female.
Among the recipients mismatched with their donors at rs200092801, every female recipient and every recipient with a female donor died from TRM. In comparison, 44% of the male recipients with male donors died from TRM.
The researchers said the rs200092801 variant may prompt the production of a mutant peptide that can be presented by MHC-I molecules to immune cells to trigger downstream immune response and TRM.
Dr Zhu and her colleagues also identified variants that appeared to have a positive impact on TRM and OS.
Recipients who had any of 6 variants in the gene OR51D1 had a decreased risk of TRM and improved OS.
The variants (rs138224979, rs148606808, rs141786655, rs61745314, rs200394876, and rs149135276) were not associated with DRM, so the researchers concluded that the improvement in OS was driven by protection against TRM.
Donor variants linked to OS
Donors had variants in 4 genes—ALPP, EMID1, SLC44A5, and LRP1—that were associated with OS but not TRM or DRM.
The 3 variants identified in ALPP (rs144454460, rs140078460, and rs142493383) were associated with improved OS.
And the 2 variants in SLC44A5 (rs143004355 and rs149696907) were associated with worse OS.
There were 2 variants in EMID1. One was associated with improved OS (rs34772704), and the other was associated with decreased OS (rs139996840).
And there were 27 variants in LRP1. Some had a positive association with OS, and others had a negative association.
Donor variants linked to TRM and DRM
Six variants in the HHAT gene were associated with TRM. Five of the variants appeared to have a protective effect against TRM (rs145455128, rs146916002, rs61744143, rs149597734, and rs145943928). For the other variant (rs141591165), the apparent effect was inconsistent between patient cohorts.
There were 3 variants in LYZL4 associated with DRM. Two were associated with an increased risk of DRM (rs147770623 and rs76947105), and 1 appeared to have a protective effect (rs181886204).
Six variants in NT5E appeared to have a protective effect against DRM (rs200250022, rs200369370, rs41271617, rs200648774, rs144719925, and rs145505137).
The researchers said the variants in NT5E probably reduce the enzyme activity of the gene. This supports preclinical findings showing that targeted blockade of NT5E can slow tumor growth.
“We have just started to uncover the biological relevance of these new and unexpected genes to a patient’s survival after [HSCT],” Dr Zhu said.
“Our findings shed light on new areas that were not considered before, but we need to further replicate and test our findings. We’re hoping that additional studies of this type will continue to discover novel genes leading to improved outcomes for patients.”
New research has revealed a link between rare gene variants and survival after hematopoietic stem cell transplant (HSCT).
Researchers performed exome sequencing in nearly 2500 HSCT recipients and their matched, unrelated donors.
The sequencing revealed several gene variants—in both donors and recipients—that were significantly associated with overall survival (OS), transplant-related mortality (TRM), and disease-related mortality (DRM) after HSCT.
Qianqian Zhu, PhD, of Roswell Park Comprehensive Cancer Center in Buffalo, New York, and her colleagues described these findings in Blood.
The team performed exome sequencing—using the Illumina HumanExome BeadChip—in patients who participated in the DISCOVeRY-BMT study.
This included 2473 HSCT recipients who had acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic syndromes. It also included 2221 donors who were a 10/10 human leukocyte antigen match for each recipient.
The researchers looked at genetic variants in donors and recipients and assessed the variants’ associations with OS, TRM, and DRM.
Variants in recipients
Analyses revealed an increased risk of TRM when there was a mismatch between donors and recipients for a variant in TEX38—rs200092801. The increased risk was even more pronounced when either the recipient or the donor was female.
Among the recipients mismatched with their donors at rs200092801, every female recipient and every recipient with a female donor died from TRM. In comparison, 44% of the male recipients with male donors died from TRM.
The researchers said the rs200092801 variant may prompt the production of a mutant peptide that can be presented by MHC-I molecules to immune cells to trigger downstream immune response and TRM.
Dr Zhu and her colleagues also identified variants that appeared to have a positive impact on TRM and OS.
Recipients who had any of 6 variants in the gene OR51D1 had a decreased risk of TRM and improved OS.
The variants (rs138224979, rs148606808, rs141786655, rs61745314, rs200394876, and rs149135276) were not associated with DRM, so the researchers concluded that the improvement in OS was driven by protection against TRM.
Donor variants linked to OS
Donors had variants in 4 genes—ALPP, EMID1, SLC44A5, and LRP1—that were associated with OS but not TRM or DRM.
The 3 variants identified in ALPP (rs144454460, rs140078460, and rs142493383) were associated with improved OS.
And the 2 variants in SLC44A5 (rs143004355 and rs149696907) were associated with worse OS.
There were 2 variants in EMID1. One was associated with improved OS (rs34772704), and the other was associated with decreased OS (rs139996840).
And there were 27 variants in LRP1. Some had a positive association with OS, and others had a negative association.
Donor variants linked to TRM and DRM
Six variants in the HHAT gene were associated with TRM. Five of the variants appeared to have a protective effect against TRM (rs145455128, rs146916002, rs61744143, rs149597734, and rs145943928). For the other variant (rs141591165), the apparent effect was inconsistent between patient cohorts.
There were 3 variants in LYZL4 associated with DRM. Two were associated with an increased risk of DRM (rs147770623 and rs76947105), and 1 appeared to have a protective effect (rs181886204).
Six variants in NT5E appeared to have a protective effect against DRM (rs200250022, rs200369370, rs41271617, rs200648774, rs144719925, and rs145505137).
The researchers said the variants in NT5E probably reduce the enzyme activity of the gene. This supports preclinical findings showing that targeted blockade of NT5E can slow tumor growth.
“We have just started to uncover the biological relevance of these new and unexpected genes to a patient’s survival after [HSCT],” Dr Zhu said.
“Our findings shed light on new areas that were not considered before, but we need to further replicate and test our findings. We’re hoping that additional studies of this type will continue to discover novel genes leading to improved outcomes for patients.”
New research has revealed a link between rare gene variants and survival after hematopoietic stem cell transplant (HSCT).
Researchers performed exome sequencing in nearly 2500 HSCT recipients and their matched, unrelated donors.
The sequencing revealed several gene variants—in both donors and recipients—that were significantly associated with overall survival (OS), transplant-related mortality (TRM), and disease-related mortality (DRM) after HSCT.
Qianqian Zhu, PhD, of Roswell Park Comprehensive Cancer Center in Buffalo, New York, and her colleagues described these findings in Blood.
The team performed exome sequencing—using the Illumina HumanExome BeadChip—in patients who participated in the DISCOVeRY-BMT study.
This included 2473 HSCT recipients who had acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic syndromes. It also included 2221 donors who were a 10/10 human leukocyte antigen match for each recipient.
The researchers looked at genetic variants in donors and recipients and assessed the variants’ associations with OS, TRM, and DRM.
Variants in recipients
Analyses revealed an increased risk of TRM when there was a mismatch between donors and recipients for a variant in TEX38—rs200092801. The increased risk was even more pronounced when either the recipient or the donor was female.
Among the recipients mismatched with their donors at rs200092801, every female recipient and every recipient with a female donor died from TRM. In comparison, 44% of the male recipients with male donors died from TRM.
The researchers said the rs200092801 variant may prompt the production of a mutant peptide that can be presented by MHC-I molecules to immune cells to trigger downstream immune response and TRM.
Dr Zhu and her colleagues also identified variants that appeared to have a positive impact on TRM and OS.
Recipients who had any of 6 variants in the gene OR51D1 had a decreased risk of TRM and improved OS.
The variants (rs138224979, rs148606808, rs141786655, rs61745314, rs200394876, and rs149135276) were not associated with DRM, so the researchers concluded that the improvement in OS was driven by protection against TRM.
Donor variants linked to OS
Donors had variants in 4 genes—ALPP, EMID1, SLC44A5, and LRP1—that were associated with OS but not TRM or DRM.
The 3 variants identified in ALPP (rs144454460, rs140078460, and rs142493383) were associated with improved OS.
And the 2 variants in SLC44A5 (rs143004355 and rs149696907) were associated with worse OS.
There were 2 variants in EMID1. One was associated with improved OS (rs34772704), and the other was associated with decreased OS (rs139996840).
And there were 27 variants in LRP1. Some had a positive association with OS, and others had a negative association.
Donor variants linked to TRM and DRM
Six variants in the HHAT gene were associated with TRM. Five of the variants appeared to have a protective effect against TRM (rs145455128, rs146916002, rs61744143, rs149597734, and rs145943928). For the other variant (rs141591165), the apparent effect was inconsistent between patient cohorts.
There were 3 variants in LYZL4 associated with DRM. Two were associated with an increased risk of DRM (rs147770623 and rs76947105), and 1 appeared to have a protective effect (rs181886204).
Six variants in NT5E appeared to have a protective effect against DRM (rs200250022, rs200369370, rs41271617, rs200648774, rs144719925, and rs145505137).
The researchers said the variants in NT5E probably reduce the enzyme activity of the gene. This supports preclinical findings showing that targeted blockade of NT5E can slow tumor growth.
“We have just started to uncover the biological relevance of these new and unexpected genes to a patient’s survival after [HSCT],” Dr Zhu said.
“Our findings shed light on new areas that were not considered before, but we need to further replicate and test our findings. We’re hoping that additional studies of this type will continue to discover novel genes leading to improved outcomes for patients.”
Project provides ‘unprecedented understanding’ of cancers
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
Agent exhibits activity in leukemias, MDS
The experimental agent prexigebersen (formerly BP1001) was considered well-tolerated and demonstrated early evidence of activity against relapsed/refractory hematologic disorders in a phase 1/1b trial.
The drug reduced blasts in the bone marrow and peripheral blood for patients with acute myeloid leukemia (AML), chronic myeloid leukemia (CML), and myelodysplastic syndrome (MDS).
When given in combination with low-dose cytarabine, prexigebersen produced complete responses (CRs) in patients with AML.
Researchers said that, overall, the toxic effects of prexigebersen were manageable.
There was 1 patient who had dose-limiting toxicities, 1 who discontinued treatment due to possible drug-related toxic effects, and 1 treatment-related death.
Still, the maximum tolerated dose of prexigebersen was not established.
These results were published in The Lancet Haematology. The study was sponsored by Bio-Path Holdings, Inc., the company developing prexigebersen.
Prexigebersen is an anti-sense oligodeoxynucleotide developed to block Grb2 expression and function. Researchers tested the drug in a single-center, dose-escalation, phase 1/1b trial that enrolled and treated 39 patients.
In the phase 1 portion of the trial, patients received prexigebersen monotherapy. In the phase 1b portion, they received the drug in combination with low-dose cytarabine.
There were 32 patients in the phase 1 portion of the trial. Most (n=23) had AML, 5 had CML in blast phase, and 4 had MDS. The patients’ median age was 63 (range, 56-73), and they had received a median of 4 prior therapies.
All 7 patients in the phase 1b portion had AML. They had a median age of 72 (range, 70-76) and had all received 1 prior therapy.
For phase 1, prexigebersen was administered intravenously, twice weekly for 28 days at doses of 5 mg/m² in cohort 1 (n=13), 10 mg/m² in cohort 2 (n=6), 20 mg/m² in cohort 3 (n=3), 40 mg/m² in cohort 4 (n=3), 60 mg/m² in cohort 5 (n=3), and 90 mg/m² in cohort 6 (n=4).
In the phase 1b portion, patients received prexigebersen at 60 mg/m² (n=4) or 90 mg/m² (n=3) in combination with 20 mg of cytarabine (twice-daily subcutaneous injections).
Safety
Twenty-seven patients were evaluable for dose-limiting toxicity—21 from phase 1 and 6 from 1b.
One patient in cohort 1 developed mucositis and hand-foot syndrome, which were considered possibly related to prexigebersen and deemed dose-limiting toxicities. The patient was also receiving hydroxyurea (3 g/day) for CML and had a history of hydroxyurea-induced mucositis.
There were no other dose-limiting toxicities, and the researchers did not identify a maximum tolerated dose of prexigebersen.
The most common grade 3-4 adverse events (AEs) were cardiopulmonary disorders and fevers (including neutropenic fevers and infections).
In the monotherapy group, 17% of patients had grade 3-4 cardiopulmonary AEs, and 11% had fevers. In the prexigebersen-cytarabine combination group, 8% had grade 3-4 cardiopulmonary AEs, and 6% had fevers.
There were 5 grade 5 AEs in 4 patients, all of whom received monotherapy. These included cardiopulmonary disorders (n=2), fevers (n=2), and multi-organ failure (n=1). One patient had both fever (sepsis) and multi-organ failure.
Efficacy
According to the researchers’ assessments, 22% of phase 1 patients (7/32) benefited from prexigebersen monotherapy and therefore received more than 1 cycle of treatment. Five of these patients had AML, and 2 had MDS.
Single-agent activity was observed in other patients as well.
Thirty-three percent (9/27) of patients who had peripheral blood blasts at baseline saw their blasts reduced by 50% or more while receiving monotherapy. One of these patients had CML, and the rest had AML.
Ten percent (3/29) of patients with bone marrow blasts at baseline had a reduction in blasts of 50% or more while receiving monotherapy. Two of these patients had AML, and 1 had MDS.
Of the 7 patients receiving prexigebersen with cytarabine, 2 achieved a CR, and 1 had a CR with incomplete hematological recovery.
Two of the patients had stable disease, and the remaining 2 patients progressed. One of the patients with progressive disease withdrew from the study, and the other died.
Deaths
There were a total of 8 deaths.
One death was considered treatment-related. This patient had progressive CML in blast phase and died of multiple organ failure. This was the first patient treated on the trial, who also had the only dose-limiting toxicities.
Two patients with AML and 1 with MDS died of disease progression. Three AML patients died of sepsis, pneumonia, and cardiac arrest. And a CML patient died of respiratory distress.
The experimental agent prexigebersen (formerly BP1001) was considered well-tolerated and demonstrated early evidence of activity against relapsed/refractory hematologic disorders in a phase 1/1b trial.
The drug reduced blasts in the bone marrow and peripheral blood for patients with acute myeloid leukemia (AML), chronic myeloid leukemia (CML), and myelodysplastic syndrome (MDS).
When given in combination with low-dose cytarabine, prexigebersen produced complete responses (CRs) in patients with AML.
Researchers said that, overall, the toxic effects of prexigebersen were manageable.
There was 1 patient who had dose-limiting toxicities, 1 who discontinued treatment due to possible drug-related toxic effects, and 1 treatment-related death.
Still, the maximum tolerated dose of prexigebersen was not established.
These results were published in The Lancet Haematology. The study was sponsored by Bio-Path Holdings, Inc., the company developing prexigebersen.
Prexigebersen is an anti-sense oligodeoxynucleotide developed to block Grb2 expression and function. Researchers tested the drug in a single-center, dose-escalation, phase 1/1b trial that enrolled and treated 39 patients.
In the phase 1 portion of the trial, patients received prexigebersen monotherapy. In the phase 1b portion, they received the drug in combination with low-dose cytarabine.
There were 32 patients in the phase 1 portion of the trial. Most (n=23) had AML, 5 had CML in blast phase, and 4 had MDS. The patients’ median age was 63 (range, 56-73), and they had received a median of 4 prior therapies.
All 7 patients in the phase 1b portion had AML. They had a median age of 72 (range, 70-76) and had all received 1 prior therapy.
For phase 1, prexigebersen was administered intravenously, twice weekly for 28 days at doses of 5 mg/m² in cohort 1 (n=13), 10 mg/m² in cohort 2 (n=6), 20 mg/m² in cohort 3 (n=3), 40 mg/m² in cohort 4 (n=3), 60 mg/m² in cohort 5 (n=3), and 90 mg/m² in cohort 6 (n=4).
In the phase 1b portion, patients received prexigebersen at 60 mg/m² (n=4) or 90 mg/m² (n=3) in combination with 20 mg of cytarabine (twice-daily subcutaneous injections).
Safety
Twenty-seven patients were evaluable for dose-limiting toxicity—21 from phase 1 and 6 from 1b.
One patient in cohort 1 developed mucositis and hand-foot syndrome, which were considered possibly related to prexigebersen and deemed dose-limiting toxicities. The patient was also receiving hydroxyurea (3 g/day) for CML and had a history of hydroxyurea-induced mucositis.
There were no other dose-limiting toxicities, and the researchers did not identify a maximum tolerated dose of prexigebersen.
The most common grade 3-4 adverse events (AEs) were cardiopulmonary disorders and fevers (including neutropenic fevers and infections).
In the monotherapy group, 17% of patients had grade 3-4 cardiopulmonary AEs, and 11% had fevers. In the prexigebersen-cytarabine combination group, 8% had grade 3-4 cardiopulmonary AEs, and 6% had fevers.
There were 5 grade 5 AEs in 4 patients, all of whom received monotherapy. These included cardiopulmonary disorders (n=2), fevers (n=2), and multi-organ failure (n=1). One patient had both fever (sepsis) and multi-organ failure.
Efficacy
According to the researchers’ assessments, 22% of phase 1 patients (7/32) benefited from prexigebersen monotherapy and therefore received more than 1 cycle of treatment. Five of these patients had AML, and 2 had MDS.
Single-agent activity was observed in other patients as well.
Thirty-three percent (9/27) of patients who had peripheral blood blasts at baseline saw their blasts reduced by 50% or more while receiving monotherapy. One of these patients had CML, and the rest had AML.
Ten percent (3/29) of patients with bone marrow blasts at baseline had a reduction in blasts of 50% or more while receiving monotherapy. Two of these patients had AML, and 1 had MDS.
Of the 7 patients receiving prexigebersen with cytarabine, 2 achieved a CR, and 1 had a CR with incomplete hematological recovery.
Two of the patients had stable disease, and the remaining 2 patients progressed. One of the patients with progressive disease withdrew from the study, and the other died.
Deaths
There were a total of 8 deaths.
One death was considered treatment-related. This patient had progressive CML in blast phase and died of multiple organ failure. This was the first patient treated on the trial, who also had the only dose-limiting toxicities.
Two patients with AML and 1 with MDS died of disease progression. Three AML patients died of sepsis, pneumonia, and cardiac arrest. And a CML patient died of respiratory distress.
The experimental agent prexigebersen (formerly BP1001) was considered well-tolerated and demonstrated early evidence of activity against relapsed/refractory hematologic disorders in a phase 1/1b trial.
The drug reduced blasts in the bone marrow and peripheral blood for patients with acute myeloid leukemia (AML), chronic myeloid leukemia (CML), and myelodysplastic syndrome (MDS).
When given in combination with low-dose cytarabine, prexigebersen produced complete responses (CRs) in patients with AML.
Researchers said that, overall, the toxic effects of prexigebersen were manageable.
There was 1 patient who had dose-limiting toxicities, 1 who discontinued treatment due to possible drug-related toxic effects, and 1 treatment-related death.
Still, the maximum tolerated dose of prexigebersen was not established.
These results were published in The Lancet Haematology. The study was sponsored by Bio-Path Holdings, Inc., the company developing prexigebersen.
Prexigebersen is an anti-sense oligodeoxynucleotide developed to block Grb2 expression and function. Researchers tested the drug in a single-center, dose-escalation, phase 1/1b trial that enrolled and treated 39 patients.
In the phase 1 portion of the trial, patients received prexigebersen monotherapy. In the phase 1b portion, they received the drug in combination with low-dose cytarabine.
There were 32 patients in the phase 1 portion of the trial. Most (n=23) had AML, 5 had CML in blast phase, and 4 had MDS. The patients’ median age was 63 (range, 56-73), and they had received a median of 4 prior therapies.
All 7 patients in the phase 1b portion had AML. They had a median age of 72 (range, 70-76) and had all received 1 prior therapy.
For phase 1, prexigebersen was administered intravenously, twice weekly for 28 days at doses of 5 mg/m² in cohort 1 (n=13), 10 mg/m² in cohort 2 (n=6), 20 mg/m² in cohort 3 (n=3), 40 mg/m² in cohort 4 (n=3), 60 mg/m² in cohort 5 (n=3), and 90 mg/m² in cohort 6 (n=4).
In the phase 1b portion, patients received prexigebersen at 60 mg/m² (n=4) or 90 mg/m² (n=3) in combination with 20 mg of cytarabine (twice-daily subcutaneous injections).
Safety
Twenty-seven patients were evaluable for dose-limiting toxicity—21 from phase 1 and 6 from 1b.
One patient in cohort 1 developed mucositis and hand-foot syndrome, which were considered possibly related to prexigebersen and deemed dose-limiting toxicities. The patient was also receiving hydroxyurea (3 g/day) for CML and had a history of hydroxyurea-induced mucositis.
There were no other dose-limiting toxicities, and the researchers did not identify a maximum tolerated dose of prexigebersen.
The most common grade 3-4 adverse events (AEs) were cardiopulmonary disorders and fevers (including neutropenic fevers and infections).
In the monotherapy group, 17% of patients had grade 3-4 cardiopulmonary AEs, and 11% had fevers. In the prexigebersen-cytarabine combination group, 8% had grade 3-4 cardiopulmonary AEs, and 6% had fevers.
There were 5 grade 5 AEs in 4 patients, all of whom received monotherapy. These included cardiopulmonary disorders (n=2), fevers (n=2), and multi-organ failure (n=1). One patient had both fever (sepsis) and multi-organ failure.
Efficacy
According to the researchers’ assessments, 22% of phase 1 patients (7/32) benefited from prexigebersen monotherapy and therefore received more than 1 cycle of treatment. Five of these patients had AML, and 2 had MDS.
Single-agent activity was observed in other patients as well.
Thirty-three percent (9/27) of patients who had peripheral blood blasts at baseline saw their blasts reduced by 50% or more while receiving monotherapy. One of these patients had CML, and the rest had AML.
Ten percent (3/29) of patients with bone marrow blasts at baseline had a reduction in blasts of 50% or more while receiving monotherapy. Two of these patients had AML, and 1 had MDS.
Of the 7 patients receiving prexigebersen with cytarabine, 2 achieved a CR, and 1 had a CR with incomplete hematological recovery.
Two of the patients had stable disease, and the remaining 2 patients progressed. One of the patients with progressive disease withdrew from the study, and the other died.
Deaths
There were a total of 8 deaths.
One death was considered treatment-related. This patient had progressive CML in blast phase and died of multiple organ failure. This was the first patient treated on the trial, who also had the only dose-limiting toxicities.
Two patients with AML and 1 with MDS died of disease progression. Three AML patients died of sepsis, pneumonia, and cardiac arrest. And a CML patient died of respiratory distress.