User login
Site of care may impact survival for AYAs with ALL, AML
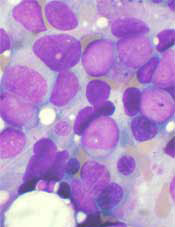
Receiving treatment at specialized cancer centers may improve survival for adolescents and young adults (AYAs) with acute leukemia, according to a study published in Cancer Epidemiology, Biomarkers & Prevention.
The study showed that, when patients were treated at specialized cancer centers, survival rates were similar for younger AYAs and children with acute lymphoblastic leukemia (ALL) or acute myeloid leukemia (AML).
However, older AYAs did not appear to reap the same survival benefit from receiving treatment at a specialized cancer center.
And AYAs of all ages had significantly worse survival than children if they were not treated at specialized cancer centers.
AYAs (patients ages 15 to 39) with ALL and AML have significantly worse survival outcomes than children ages 14 and under, according to study author Julie Wolfson, MD, of the University of Alabama at Birmingham.
“A much smaller percentage of AYAs with cancer are treated at specialized cancer centers than children with cancer,” she added. “We wanted to understand whether this difference in the site of cancer care is associated with the difference in survival outcomes.”
Dr Wolfson and her colleagues used data from the Los Angeles County Cancer Surveillance Program to identify patients diagnosed with ALL or AML from ages 1 to 39.
Patients were said to have been treated at a specialized cancer center if, at any age, they were cared for at any of the National Cancer Institute-designated Comprehensive Cancer Centers (CCC) in Los Angeles County or if, at the age of 21 or younger, they were cared for at any of the Children’s Oncology Group (COG) sites not designated a Comprehensive Cancer Center.
Included in the analysis were 978 patients diagnosed with ALL as a child (ages 1 to 14), 402 patients diagnosed with ALL as an AYA (ages 15 to 39), 131 patients diagnosed with AML as a child, and 359 patients diagnosed with AML as an AYA.
Seventy percent of the children with ALL and 30% of the AYAs with ALL were treated at CCC/COG sites. Seventy-four percent of the children with AML and 22% of the AYAs with AML were treated at CCC/COG sites.
Results in ALL
AYAs diagnosed with ALL at ages 15 to 21 and 22 to 29 who were treated at CCC/COG sites had comparable survival to children who were diagnosed with ALL from ages 10 to 14 and treated at CCC/COG sites. The hazard ratios (HRs) were 1.3 for the 15-21 age group (P=0.3) and 1.2 for the 22-29 age group (P=0.8).
The reference group for this analysis was 10- to 14-year-olds treated at CCC/COG sites because the researchers excluded data from children with ALL ages 1 to 9. These patients were excluded because they have significantly better survival than the other groups, potentially as a result of different disease biology.
The researchers also found that treatment at CCC/COG sites did not improve survival for 30- to 39-year-olds with ALL. The HR for them was 3.4 (P<0.001).
Likewise, all AYAs with ALL who were not treated at CCC/COG sites had worse survival than 10- to 14-year-olds treated at CCC/COG sites. The HRs were 1.9 for the 15-21 age group (P=0.005), 2.6 for the 22-29 age group (P<0.001), and 3.0 for the 30-39 age group (P<0.001).
Results in AML
For AML patients, the reference group was 1- to 14-year-olds treated at CCC/COG sites. Compared to these patients, 15- to 21-year-olds not treated at CCC/COG sites had an increased hazard of death (HR=1.7, P=0.02), whereas 15- to 21-year-olds treated at CCC/COG sites did not (HR=1.3; P=0.4).
All 22- to 39-year-olds, regardless of the site of care, had an increased hazard of death compared to the children treated at CCC/COG sites. The HR was 3.4 (P<0.001) for 22- to 39-year-olds treated at CCC/COG sites, and the HR was 3.0 (P<0.001) for 22- to 39-year-olds not treated at CCC/COG sites.
“The fact that the older AYAs did not appear to benefit from treatment at a specialized cancer center suggests to us that the biology of the disease in these patients differs from that in younger individuals,” Dr Wolfson said.
“The most important thing we can do to help these patients is to enroll them on clinical trials so that we can better understand the biology of the disease and its response to therapy. ![]()
Receiving treatment at specialized cancer centers may improve survival for adolescents and young adults (AYAs) with acute leukemia, according to a study published in Cancer Epidemiology, Biomarkers & Prevention.
The study showed that, when patients were treated at specialized cancer centers, survival rates were similar for younger AYAs and children with acute lymphoblastic leukemia (ALL) or acute myeloid leukemia (AML).
However, older AYAs did not appear to reap the same survival benefit from receiving treatment at a specialized cancer center.
And AYAs of all ages had significantly worse survival than children if they were not treated at specialized cancer centers.
AYAs (patients ages 15 to 39) with ALL and AML have significantly worse survival outcomes than children ages 14 and under, according to study author Julie Wolfson, MD, of the University of Alabama at Birmingham.
“A much smaller percentage of AYAs with cancer are treated at specialized cancer centers than children with cancer,” she added. “We wanted to understand whether this difference in the site of cancer care is associated with the difference in survival outcomes.”
Dr Wolfson and her colleagues used data from the Los Angeles County Cancer Surveillance Program to identify patients diagnosed with ALL or AML from ages 1 to 39.
Patients were said to have been treated at a specialized cancer center if, at any age, they were cared for at any of the National Cancer Institute-designated Comprehensive Cancer Centers (CCC) in Los Angeles County or if, at the age of 21 or younger, they were cared for at any of the Children’s Oncology Group (COG) sites not designated a Comprehensive Cancer Center.
Included in the analysis were 978 patients diagnosed with ALL as a child (ages 1 to 14), 402 patients diagnosed with ALL as an AYA (ages 15 to 39), 131 patients diagnosed with AML as a child, and 359 patients diagnosed with AML as an AYA.
Seventy percent of the children with ALL and 30% of the AYAs with ALL were treated at CCC/COG sites. Seventy-four percent of the children with AML and 22% of the AYAs with AML were treated at CCC/COG sites.
Results in ALL
AYAs diagnosed with ALL at ages 15 to 21 and 22 to 29 who were treated at CCC/COG sites had comparable survival to children who were diagnosed with ALL from ages 10 to 14 and treated at CCC/COG sites. The hazard ratios (HRs) were 1.3 for the 15-21 age group (P=0.3) and 1.2 for the 22-29 age group (P=0.8).
The reference group for this analysis was 10- to 14-year-olds treated at CCC/COG sites because the researchers excluded data from children with ALL ages 1 to 9. These patients were excluded because they have significantly better survival than the other groups, potentially as a result of different disease biology.
The researchers also found that treatment at CCC/COG sites did not improve survival for 30- to 39-year-olds with ALL. The HR for them was 3.4 (P<0.001).
Likewise, all AYAs with ALL who were not treated at CCC/COG sites had worse survival than 10- to 14-year-olds treated at CCC/COG sites. The HRs were 1.9 for the 15-21 age group (P=0.005), 2.6 for the 22-29 age group (P<0.001), and 3.0 for the 30-39 age group (P<0.001).
Results in AML
For AML patients, the reference group was 1- to 14-year-olds treated at CCC/COG sites. Compared to these patients, 15- to 21-year-olds not treated at CCC/COG sites had an increased hazard of death (HR=1.7, P=0.02), whereas 15- to 21-year-olds treated at CCC/COG sites did not (HR=1.3; P=0.4).
All 22- to 39-year-olds, regardless of the site of care, had an increased hazard of death compared to the children treated at CCC/COG sites. The HR was 3.4 (P<0.001) for 22- to 39-year-olds treated at CCC/COG sites, and the HR was 3.0 (P<0.001) for 22- to 39-year-olds not treated at CCC/COG sites.
“The fact that the older AYAs did not appear to benefit from treatment at a specialized cancer center suggests to us that the biology of the disease in these patients differs from that in younger individuals,” Dr Wolfson said.
“The most important thing we can do to help these patients is to enroll them on clinical trials so that we can better understand the biology of the disease and its response to therapy. ![]()
Receiving treatment at specialized cancer centers may improve survival for adolescents and young adults (AYAs) with acute leukemia, according to a study published in Cancer Epidemiology, Biomarkers & Prevention.
The study showed that, when patients were treated at specialized cancer centers, survival rates were similar for younger AYAs and children with acute lymphoblastic leukemia (ALL) or acute myeloid leukemia (AML).
However, older AYAs did not appear to reap the same survival benefit from receiving treatment at a specialized cancer center.
And AYAs of all ages had significantly worse survival than children if they were not treated at specialized cancer centers.
AYAs (patients ages 15 to 39) with ALL and AML have significantly worse survival outcomes than children ages 14 and under, according to study author Julie Wolfson, MD, of the University of Alabama at Birmingham.
“A much smaller percentage of AYAs with cancer are treated at specialized cancer centers than children with cancer,” she added. “We wanted to understand whether this difference in the site of cancer care is associated with the difference in survival outcomes.”
Dr Wolfson and her colleagues used data from the Los Angeles County Cancer Surveillance Program to identify patients diagnosed with ALL or AML from ages 1 to 39.
Patients were said to have been treated at a specialized cancer center if, at any age, they were cared for at any of the National Cancer Institute-designated Comprehensive Cancer Centers (CCC) in Los Angeles County or if, at the age of 21 or younger, they were cared for at any of the Children’s Oncology Group (COG) sites not designated a Comprehensive Cancer Center.
Included in the analysis were 978 patients diagnosed with ALL as a child (ages 1 to 14), 402 patients diagnosed with ALL as an AYA (ages 15 to 39), 131 patients diagnosed with AML as a child, and 359 patients diagnosed with AML as an AYA.
Seventy percent of the children with ALL and 30% of the AYAs with ALL were treated at CCC/COG sites. Seventy-four percent of the children with AML and 22% of the AYAs with AML were treated at CCC/COG sites.
Results in ALL
AYAs diagnosed with ALL at ages 15 to 21 and 22 to 29 who were treated at CCC/COG sites had comparable survival to children who were diagnosed with ALL from ages 10 to 14 and treated at CCC/COG sites. The hazard ratios (HRs) were 1.3 for the 15-21 age group (P=0.3) and 1.2 for the 22-29 age group (P=0.8).
The reference group for this analysis was 10- to 14-year-olds treated at CCC/COG sites because the researchers excluded data from children with ALL ages 1 to 9. These patients were excluded because they have significantly better survival than the other groups, potentially as a result of different disease biology.
The researchers also found that treatment at CCC/COG sites did not improve survival for 30- to 39-year-olds with ALL. The HR for them was 3.4 (P<0.001).
Likewise, all AYAs with ALL who were not treated at CCC/COG sites had worse survival than 10- to 14-year-olds treated at CCC/COG sites. The HRs were 1.9 for the 15-21 age group (P=0.005), 2.6 for the 22-29 age group (P<0.001), and 3.0 for the 30-39 age group (P<0.001).
Results in AML
For AML patients, the reference group was 1- to 14-year-olds treated at CCC/COG sites. Compared to these patients, 15- to 21-year-olds not treated at CCC/COG sites had an increased hazard of death (HR=1.7, P=0.02), whereas 15- to 21-year-olds treated at CCC/COG sites did not (HR=1.3; P=0.4).
All 22- to 39-year-olds, regardless of the site of care, had an increased hazard of death compared to the children treated at CCC/COG sites. The HR was 3.4 (P<0.001) for 22- to 39-year-olds treated at CCC/COG sites, and the HR was 3.0 (P<0.001) for 22- to 39-year-olds not treated at CCC/COG sites.
“The fact that the older AYAs did not appear to benefit from treatment at a specialized cancer center suggests to us that the biology of the disease in these patients differs from that in younger individuals,” Dr Wolfson said.
“The most important thing we can do to help these patients is to enroll them on clinical trials so that we can better understand the biology of the disease and its response to therapy. ![]()
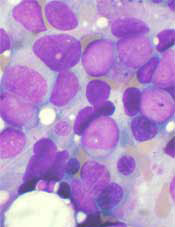
Styrene exposure linked to myeloid leukemia, HL
A new study links styrene—a chemical used in the manufacture of plastics, rubber, and resins—to certain cancers.
The research showed that, contrary to previous suggestions, employees who have worked with styrene do not have an increased incidence of esophageal, pancreatic, lung, kidney, or bladder cancer.
On the other hand, they may have an increased risk of nasal and paranasal cancer, as well as myeloid leukemia and Hodgkin lymphoma (HL).
The research was published in Epidemiology.
“It is important to know for present and former workers exposed to styrene that they are unlikely to have become ill by doing their job if they have developed cancer of the esophagus, pancreas, lungs, kidneys, bladder, or a wide range of other types of cancer,” said study author Henrik A. Kolstad, MD, PhD, of Aarhus University in Denmark.
“This is also new and important knowledge in the USA, where styrene was added to the list of carcinogenic substances in 2011.”
In relation to the cancers for which the study shows a possible increased risk, Dr Kolstad emphasized that additional research is needed to determine if styrene is the actual cause of the employees’ disease.
For the current study, Dr Kolstad and his colleagues analyzed data on 72,292 employees who worked for 1 of 443 small and medium-sized companies in Denmark that used styrene for the production of wind turbines, pleasure boats, and other products from 1964 to 2007.
There were 8961 incident cases of cancer in this cohort from 1968 to 2012. The standardized incidence rate ratio (SIR) for all cancers was 1.04. When the researchers included a 10-year lag period, the SIR for all cancers was still 1.04.
As for hematologic malignancies, the researchers said they observed increased rate ratios associated with increased duration of employment for HL and myeloid leukemia.
For HL, the SIRs were 1.21 with no lag and 1.22 with a 10-year lag. For myeloid leukemia, the SIRs were 1.06 and 1.13, respectively.
The SIRs for non-Hodgkin lymphoma were 0.97 with no lag and 0.94 with a 10-year lag. The SIRs for multiple myeloma were 0.79 and 0.77, respectively.
For cancers of lymphatic and hematopoietic tissue, the SIRs were 0.97 with no lag and 0.96 with a 10-year lag. For lymphatic leukemia, the SIR was 0.96 for both time points.
The SIRs for monocytic leukemia were 0.77 with no lag and 0.56 with a 10-year lag. The SIRs for other and unspecified leukemias were 1.05 and 1.26, respectively.
The researchers noted that workers first employed in the 1960s had a higher risk of HL than workers first employed in subsequent years.
The SIRs were 2.12 for those first employed in 1964-1969, 0.82 for 1970-1979, 1.07 for 1980-1989, 1.52 for 1990-1999, and 1.10 for those first employed in 2000-2007.
There were no such associations for other cancer sites. ![]()
A new study links styrene—a chemical used in the manufacture of plastics, rubber, and resins—to certain cancers.
The research showed that, contrary to previous suggestions, employees who have worked with styrene do not have an increased incidence of esophageal, pancreatic, lung, kidney, or bladder cancer.
On the other hand, they may have an increased risk of nasal and paranasal cancer, as well as myeloid leukemia and Hodgkin lymphoma (HL).
The research was published in Epidemiology.
“It is important to know for present and former workers exposed to styrene that they are unlikely to have become ill by doing their job if they have developed cancer of the esophagus, pancreas, lungs, kidneys, bladder, or a wide range of other types of cancer,” said study author Henrik A. Kolstad, MD, PhD, of Aarhus University in Denmark.
“This is also new and important knowledge in the USA, where styrene was added to the list of carcinogenic substances in 2011.”
In relation to the cancers for which the study shows a possible increased risk, Dr Kolstad emphasized that additional research is needed to determine if styrene is the actual cause of the employees’ disease.
For the current study, Dr Kolstad and his colleagues analyzed data on 72,292 employees who worked for 1 of 443 small and medium-sized companies in Denmark that used styrene for the production of wind turbines, pleasure boats, and other products from 1964 to 2007.
There were 8961 incident cases of cancer in this cohort from 1968 to 2012. The standardized incidence rate ratio (SIR) for all cancers was 1.04. When the researchers included a 10-year lag period, the SIR for all cancers was still 1.04.
As for hematologic malignancies, the researchers said they observed increased rate ratios associated with increased duration of employment for HL and myeloid leukemia.
For HL, the SIRs were 1.21 with no lag and 1.22 with a 10-year lag. For myeloid leukemia, the SIRs were 1.06 and 1.13, respectively.
The SIRs for non-Hodgkin lymphoma were 0.97 with no lag and 0.94 with a 10-year lag. The SIRs for multiple myeloma were 0.79 and 0.77, respectively.
For cancers of lymphatic and hematopoietic tissue, the SIRs were 0.97 with no lag and 0.96 with a 10-year lag. For lymphatic leukemia, the SIR was 0.96 for both time points.
The SIRs for monocytic leukemia were 0.77 with no lag and 0.56 with a 10-year lag. The SIRs for other and unspecified leukemias were 1.05 and 1.26, respectively.
The researchers noted that workers first employed in the 1960s had a higher risk of HL than workers first employed in subsequent years.
The SIRs were 2.12 for those first employed in 1964-1969, 0.82 for 1970-1979, 1.07 for 1980-1989, 1.52 for 1990-1999, and 1.10 for those first employed in 2000-2007.
There were no such associations for other cancer sites. ![]()
A new study links styrene—a chemical used in the manufacture of plastics, rubber, and resins—to certain cancers.
The research showed that, contrary to previous suggestions, employees who have worked with styrene do not have an increased incidence of esophageal, pancreatic, lung, kidney, or bladder cancer.
On the other hand, they may have an increased risk of nasal and paranasal cancer, as well as myeloid leukemia and Hodgkin lymphoma (HL).
The research was published in Epidemiology.
“It is important to know for present and former workers exposed to styrene that they are unlikely to have become ill by doing their job if they have developed cancer of the esophagus, pancreas, lungs, kidneys, bladder, or a wide range of other types of cancer,” said study author Henrik A. Kolstad, MD, PhD, of Aarhus University in Denmark.
“This is also new and important knowledge in the USA, where styrene was added to the list of carcinogenic substances in 2011.”
In relation to the cancers for which the study shows a possible increased risk, Dr Kolstad emphasized that additional research is needed to determine if styrene is the actual cause of the employees’ disease.
For the current study, Dr Kolstad and his colleagues analyzed data on 72,292 employees who worked for 1 of 443 small and medium-sized companies in Denmark that used styrene for the production of wind turbines, pleasure boats, and other products from 1964 to 2007.
There were 8961 incident cases of cancer in this cohort from 1968 to 2012. The standardized incidence rate ratio (SIR) for all cancers was 1.04. When the researchers included a 10-year lag period, the SIR for all cancers was still 1.04.
As for hematologic malignancies, the researchers said they observed increased rate ratios associated with increased duration of employment for HL and myeloid leukemia.
For HL, the SIRs were 1.21 with no lag and 1.22 with a 10-year lag. For myeloid leukemia, the SIRs were 1.06 and 1.13, respectively.
The SIRs for non-Hodgkin lymphoma were 0.97 with no lag and 0.94 with a 10-year lag. The SIRs for multiple myeloma were 0.79 and 0.77, respectively.
For cancers of lymphatic and hematopoietic tissue, the SIRs were 0.97 with no lag and 0.96 with a 10-year lag. For lymphatic leukemia, the SIR was 0.96 for both time points.
The SIRs for monocytic leukemia were 0.77 with no lag and 0.56 with a 10-year lag. The SIRs for other and unspecified leukemias were 1.05 and 1.26, respectively.
The researchers noted that workers first employed in the 1960s had a higher risk of HL than workers first employed in subsequent years.
The SIRs were 2.12 for those first employed in 1964-1969, 0.82 for 1970-1979, 1.07 for 1980-1989, 1.52 for 1990-1999, and 1.10 for those first employed in 2000-2007.
There were no such associations for other cancer sites. ![]()
Group identifies ‘essential’ genes in AML
CRISPR-based genetic screens have revealed essential genes—those required for cellular proliferation and survival—in 14 acute myeloid leukemia (AML) cell lines, according to investigators.
By combining this information with the existing genomic information on these cell lines, the investigators believe they have identified vulnerabilities that could potentially be exploited with new therapies.
The group described their research in Cell.
A major aspect of their study focused on the genes and protein pathways connected to the Ras oncogene, which is the most commonly mutated oncogene in human cancers and plays a role in AML.
“For the most part, the mutant Ras protein itself has been considered to be ‘undruggable,’” said study author Tim Wang, a doctoral student at the Massachusetts Institute of Technology in Cambridge.
“An alternative approach has been to find other genes that Ras-mutant cancers rely on with the hope that one of them may be druggable. Unfortunately, such ‘Ras-synthetic-lethal’ genes have been difficult to identify.”
Using CRISPR-based screens, the investigators were able to gauge the impact of individually knocking out each of the 18,000 protein-coding genes in the human genome.
“This process rapidly enabled us to identify the short list of genes that were selectively required in only the Ras-mutant cells,” explained study author David Sabatini, MD, PhD, of the Massachusetts Institute of Technology.
He and his colleagues found that the enzymes catalyzing the latter steps of the Ras processing pathway, Rce1 and Icmt, displayed synthetic lethality with oncogenic Ras, which suggests they might be therapeutic targets in AML and other cancers driven by oncogenic Ras.
The investigators also said their findings provide further support for the central role of MAPK signaling in Ras-driven cancers, suggest PREX1 and the Rac pathway are critical regulators of MAPK pathway activation, and indicate that c-Raf could be a therapeutic target in cancers driven by oncogenic Ras.
In addition to defining the Ras-specific gene essentiality network, the investigators said they were able to determine the function of previously unstudied genes.
The team started by focusing on genes that were essential in some of the AML cell lines but dispensable for others. For each of these genes, the investigators sifted through their data to find others that showed a matching pattern of essentiality, with the idea that all of them had similar functions.
Indeed, this analysis revealed gene groups that were already known to act together and uncovered novel associations between genes that were not known to be related or had been previously unstudied.
“What’s particularly exciting about this work is that we have just begun to scratch the surface with our method,” Wang concluded. “By applying it broadly, we could reveal a huge amount of information about the functional organization of human genes and their roles in many diseases.” ![]()
CRISPR-based genetic screens have revealed essential genes—those required for cellular proliferation and survival—in 14 acute myeloid leukemia (AML) cell lines, according to investigators.
By combining this information with the existing genomic information on these cell lines, the investigators believe they have identified vulnerabilities that could potentially be exploited with new therapies.
The group described their research in Cell.
A major aspect of their study focused on the genes and protein pathways connected to the Ras oncogene, which is the most commonly mutated oncogene in human cancers and plays a role in AML.
“For the most part, the mutant Ras protein itself has been considered to be ‘undruggable,’” said study author Tim Wang, a doctoral student at the Massachusetts Institute of Technology in Cambridge.
“An alternative approach has been to find other genes that Ras-mutant cancers rely on with the hope that one of them may be druggable. Unfortunately, such ‘Ras-synthetic-lethal’ genes have been difficult to identify.”
Using CRISPR-based screens, the investigators were able to gauge the impact of individually knocking out each of the 18,000 protein-coding genes in the human genome.
“This process rapidly enabled us to identify the short list of genes that were selectively required in only the Ras-mutant cells,” explained study author David Sabatini, MD, PhD, of the Massachusetts Institute of Technology.
He and his colleagues found that the enzymes catalyzing the latter steps of the Ras processing pathway, Rce1 and Icmt, displayed synthetic lethality with oncogenic Ras, which suggests they might be therapeutic targets in AML and other cancers driven by oncogenic Ras.
The investigators also said their findings provide further support for the central role of MAPK signaling in Ras-driven cancers, suggest PREX1 and the Rac pathway are critical regulators of MAPK pathway activation, and indicate that c-Raf could be a therapeutic target in cancers driven by oncogenic Ras.
In addition to defining the Ras-specific gene essentiality network, the investigators said they were able to determine the function of previously unstudied genes.
The team started by focusing on genes that were essential in some of the AML cell lines but dispensable for others. For each of these genes, the investigators sifted through their data to find others that showed a matching pattern of essentiality, with the idea that all of them had similar functions.
Indeed, this analysis revealed gene groups that were already known to act together and uncovered novel associations between genes that were not known to be related or had been previously unstudied.
“What’s particularly exciting about this work is that we have just begun to scratch the surface with our method,” Wang concluded. “By applying it broadly, we could reveal a huge amount of information about the functional organization of human genes and their roles in many diseases.” ![]()
CRISPR-based genetic screens have revealed essential genes—those required for cellular proliferation and survival—in 14 acute myeloid leukemia (AML) cell lines, according to investigators.
By combining this information with the existing genomic information on these cell lines, the investigators believe they have identified vulnerabilities that could potentially be exploited with new therapies.
The group described their research in Cell.
A major aspect of their study focused on the genes and protein pathways connected to the Ras oncogene, which is the most commonly mutated oncogene in human cancers and plays a role in AML.
“For the most part, the mutant Ras protein itself has been considered to be ‘undruggable,’” said study author Tim Wang, a doctoral student at the Massachusetts Institute of Technology in Cambridge.
“An alternative approach has been to find other genes that Ras-mutant cancers rely on with the hope that one of them may be druggable. Unfortunately, such ‘Ras-synthetic-lethal’ genes have been difficult to identify.”
Using CRISPR-based screens, the investigators were able to gauge the impact of individually knocking out each of the 18,000 protein-coding genes in the human genome.
“This process rapidly enabled us to identify the short list of genes that were selectively required in only the Ras-mutant cells,” explained study author David Sabatini, MD, PhD, of the Massachusetts Institute of Technology.
He and his colleagues found that the enzymes catalyzing the latter steps of the Ras processing pathway, Rce1 and Icmt, displayed synthetic lethality with oncogenic Ras, which suggests they might be therapeutic targets in AML and other cancers driven by oncogenic Ras.
The investigators also said their findings provide further support for the central role of MAPK signaling in Ras-driven cancers, suggest PREX1 and the Rac pathway are critical regulators of MAPK pathway activation, and indicate that c-Raf could be a therapeutic target in cancers driven by oncogenic Ras.
In addition to defining the Ras-specific gene essentiality network, the investigators said they were able to determine the function of previously unstudied genes.
The team started by focusing on genes that were essential in some of the AML cell lines but dispensable for others. For each of these genes, the investigators sifted through their data to find others that showed a matching pattern of essentiality, with the idea that all of them had similar functions.
Indeed, this analysis revealed gene groups that were already known to act together and uncovered novel associations between genes that were not known to be related or had been previously unstudied.
“What’s particularly exciting about this work is that we have just begun to scratch the surface with our method,” Wang concluded. “By applying it broadly, we could reveal a huge amount of information about the functional organization of human genes and their roles in many diseases.” ![]()
Computer predicts remission, relapse in AML

Photo by Darren Baker
Researchers say they have developed the first computer machine-learning model to accurately predict which patients diagnosed with acute
myeloid leukemia (AML) will go into remission after treatment and which will relapse.
“It’s pretty straightforward to teach a computer to recognize AML, once you develop a robust algorithm, and, in previous work, we did it with almost 100% accuracy,” said study author Murat Dundar, PhD of Indiana University-Purdue University Indianapolis.
“What was challenging was to go beyond that work and teach the computer to accurately predict the direction of change in disease progression in AML patients, interpreting new data to predict the unknown: which new AML patients will go into remission and which will relapse.”
Dr Dundar and his colleagues described this work in IEEE Transactions on Biomedical Engineering.
The researchers said they modeled data from multiple flow cytometry samples to identify functionally distinct cell populations and their local realizations. Each sample was characterized by the proportions of recovered cell populations, which were used to predict the direction of change in disease progression for each AML patient.
“As the input, our computational system employs data from flow cytometry, a widely utilized technology that can rapidly provide detailed characteristics of single cells in samples such as blood or bone marrow,” explained study author Bartek Rajwa, PhD, of Purdue University in Lafayette, Indiana.
“Traditionally, the results of flow cytometry analyses are evaluated by highly trained human experts rather than by machine-learning algorithms. But computers are often better at extracting knowledge from complex data than humans are.”
The researchers used 200 diseased and non-diseased immunophenotypic panels for training and tested
the computational system with samples collected at multiple time points from 36 additional AML patients.
The system was able to predict remission with 100% accuracy (26 of 26 cases) and relapse with 90% accuracy (9 of 10 cases).
“Machine learning is not about modeling data,” Dr Dundar noted. “It’s about extracting knowledge from the data you have so you can build a powerful, intuitive tool that can make predictions about future data that the computer has not previously seen. The machine is learning, not memorizing, and that’s what we did.” ![]()

Photo by Darren Baker
Researchers say they have developed the first computer machine-learning model to accurately predict which patients diagnosed with acute
myeloid leukemia (AML) will go into remission after treatment and which will relapse.
“It’s pretty straightforward to teach a computer to recognize AML, once you develop a robust algorithm, and, in previous work, we did it with almost 100% accuracy,” said study author Murat Dundar, PhD of Indiana University-Purdue University Indianapolis.
“What was challenging was to go beyond that work and teach the computer to accurately predict the direction of change in disease progression in AML patients, interpreting new data to predict the unknown: which new AML patients will go into remission and which will relapse.”
Dr Dundar and his colleagues described this work in IEEE Transactions on Biomedical Engineering.
The researchers said they modeled data from multiple flow cytometry samples to identify functionally distinct cell populations and their local realizations. Each sample was characterized by the proportions of recovered cell populations, which were used to predict the direction of change in disease progression for each AML patient.
“As the input, our computational system employs data from flow cytometry, a widely utilized technology that can rapidly provide detailed characteristics of single cells in samples such as blood or bone marrow,” explained study author Bartek Rajwa, PhD, of Purdue University in Lafayette, Indiana.
“Traditionally, the results of flow cytometry analyses are evaluated by highly trained human experts rather than by machine-learning algorithms. But computers are often better at extracting knowledge from complex data than humans are.”
The researchers used 200 diseased and non-diseased immunophenotypic panels for training and tested
the computational system with samples collected at multiple time points from 36 additional AML patients.
The system was able to predict remission with 100% accuracy (26 of 26 cases) and relapse with 90% accuracy (9 of 10 cases).
“Machine learning is not about modeling data,” Dr Dundar noted. “It’s about extracting knowledge from the data you have so you can build a powerful, intuitive tool that can make predictions about future data that the computer has not previously seen. The machine is learning, not memorizing, and that’s what we did.” ![]()

Photo by Darren Baker
Researchers say they have developed the first computer machine-learning model to accurately predict which patients diagnosed with acute
myeloid leukemia (AML) will go into remission after treatment and which will relapse.
“It’s pretty straightforward to teach a computer to recognize AML, once you develop a robust algorithm, and, in previous work, we did it with almost 100% accuracy,” said study author Murat Dundar, PhD of Indiana University-Purdue University Indianapolis.
“What was challenging was to go beyond that work and teach the computer to accurately predict the direction of change in disease progression in AML patients, interpreting new data to predict the unknown: which new AML patients will go into remission and which will relapse.”
Dr Dundar and his colleagues described this work in IEEE Transactions on Biomedical Engineering.
The researchers said they modeled data from multiple flow cytometry samples to identify functionally distinct cell populations and their local realizations. Each sample was characterized by the proportions of recovered cell populations, which were used to predict the direction of change in disease progression for each AML patient.
“As the input, our computational system employs data from flow cytometry, a widely utilized technology that can rapidly provide detailed characteristics of single cells in samples such as blood or bone marrow,” explained study author Bartek Rajwa, PhD, of Purdue University in Lafayette, Indiana.
“Traditionally, the results of flow cytometry analyses are evaluated by highly trained human experts rather than by machine-learning algorithms. But computers are often better at extracting knowledge from complex data than humans are.”
The researchers used 200 diseased and non-diseased immunophenotypic panels for training and tested
the computational system with samples collected at multiple time points from 36 additional AML patients.
The system was able to predict remission with 100% accuracy (26 of 26 cases) and relapse with 90% accuracy (9 of 10 cases).
“Machine learning is not about modeling data,” Dr Dundar noted. “It’s about extracting knowledge from the data you have so you can build a powerful, intuitive tool that can make predictions about future data that the computer has not previously seen. The machine is learning, not memorizing, and that’s what we did.” ![]()
Azathioprine may increase risk of MDS, AML
Results of a large, retrospective study suggest that taking azathioprine, a drug commonly used to treat autoimmune disease, may increase a person’s risk of developing myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML).
Researchers analyzed data on more than 40,000 patients with 27 common autoimmune diseases and found that azathioprine use was significantly associated with an increased risk of MDS and AML.
“Similar associations were already documented in case reports and case series but have never been evaluated in a broad spectrum of autoimmune diseases in that many patients and in context of individual medications,” said study author Raoul Tibes, MD, PhD, of the Mayo Clinic in Phoenix, Arizona.
“Interestingly, there was no association with length of time on therapy and resulting myeloid neoplasm.”
Dr Tibes and his colleagues reported these findings in JAMA Oncology.
The researchers reviewed data on 40,011 patients with primary autoimmune disorders, such as lupus and rheumatoid arthritis, who were seen at 2 centers from January 1, 2004, to December 31, 2014.
There were 311 patients with MDS or AML, but only 86 met strict inclusion criteria. Fifty-five patients had MDS, 21 had de novo AML, and 10 had AML and a history of MDS.
The researchers collected detailed data on each patient’s drug exposures, treatment duration, and disease characteristics and compared this information to data from patients with autoimmune disorders who did not have MDS or AML.
This revealed that use of azathioprine sodium was more frequent in cases than controls, and azathioprine was significantly associated with an increased risk of MDS and AML. The odds ratio was 7.05 (P<0.001).
Other agents used showed a similar trend, but the results were not statistically significant. The odds ratios were 3.58 for cyclophosphamide and 2.73 for mitoxantrone hydrochloride.
The researchers said that, while these results are intriguing, they should not change or replace the clinical judgments, monitoring, and current standard treatments for patients with autoimmune diseases.
Despite its large size, this study had limitations, including its retrospective nature, the fact that many different autoimmune diseases were analyzed, and that the researchers only looked at cases of MDS and AML.
No definitive causal association was made between taking a particular drug and MDS or AML. The number of patients with autoimmune disease developing MDS or AML is still low overall, and no prediction for individual patients can be concluded from the study.
The researchers plan to perform molecular investigations into the genetic susceptibility for therapy-related myeloid neoplasms as the next phase of this research. ![]()
Results of a large, retrospective study suggest that taking azathioprine, a drug commonly used to treat autoimmune disease, may increase a person’s risk of developing myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML).
Researchers analyzed data on more than 40,000 patients with 27 common autoimmune diseases and found that azathioprine use was significantly associated with an increased risk of MDS and AML.
“Similar associations were already documented in case reports and case series but have never been evaluated in a broad spectrum of autoimmune diseases in that many patients and in context of individual medications,” said study author Raoul Tibes, MD, PhD, of the Mayo Clinic in Phoenix, Arizona.
“Interestingly, there was no association with length of time on therapy and resulting myeloid neoplasm.”
Dr Tibes and his colleagues reported these findings in JAMA Oncology.
The researchers reviewed data on 40,011 patients with primary autoimmune disorders, such as lupus and rheumatoid arthritis, who were seen at 2 centers from January 1, 2004, to December 31, 2014.
There were 311 patients with MDS or AML, but only 86 met strict inclusion criteria. Fifty-five patients had MDS, 21 had de novo AML, and 10 had AML and a history of MDS.
The researchers collected detailed data on each patient’s drug exposures, treatment duration, and disease characteristics and compared this information to data from patients with autoimmune disorders who did not have MDS or AML.
This revealed that use of azathioprine sodium was more frequent in cases than controls, and azathioprine was significantly associated with an increased risk of MDS and AML. The odds ratio was 7.05 (P<0.001).
Other agents used showed a similar trend, but the results were not statistically significant. The odds ratios were 3.58 for cyclophosphamide and 2.73 for mitoxantrone hydrochloride.
The researchers said that, while these results are intriguing, they should not change or replace the clinical judgments, monitoring, and current standard treatments for patients with autoimmune diseases.
Despite its large size, this study had limitations, including its retrospective nature, the fact that many different autoimmune diseases were analyzed, and that the researchers only looked at cases of MDS and AML.
No definitive causal association was made between taking a particular drug and MDS or AML. The number of patients with autoimmune disease developing MDS or AML is still low overall, and no prediction for individual patients can be concluded from the study.
The researchers plan to perform molecular investigations into the genetic susceptibility for therapy-related myeloid neoplasms as the next phase of this research. ![]()
Results of a large, retrospective study suggest that taking azathioprine, a drug commonly used to treat autoimmune disease, may increase a person’s risk of developing myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML).
Researchers analyzed data on more than 40,000 patients with 27 common autoimmune diseases and found that azathioprine use was significantly associated with an increased risk of MDS and AML.
“Similar associations were already documented in case reports and case series but have never been evaluated in a broad spectrum of autoimmune diseases in that many patients and in context of individual medications,” said study author Raoul Tibes, MD, PhD, of the Mayo Clinic in Phoenix, Arizona.
“Interestingly, there was no association with length of time on therapy and resulting myeloid neoplasm.”
Dr Tibes and his colleagues reported these findings in JAMA Oncology.
The researchers reviewed data on 40,011 patients with primary autoimmune disorders, such as lupus and rheumatoid arthritis, who were seen at 2 centers from January 1, 2004, to December 31, 2014.
There were 311 patients with MDS or AML, but only 86 met strict inclusion criteria. Fifty-five patients had MDS, 21 had de novo AML, and 10 had AML and a history of MDS.
The researchers collected detailed data on each patient’s drug exposures, treatment duration, and disease characteristics and compared this information to data from patients with autoimmune disorders who did not have MDS or AML.
This revealed that use of azathioprine sodium was more frequent in cases than controls, and azathioprine was significantly associated with an increased risk of MDS and AML. The odds ratio was 7.05 (P<0.001).
Other agents used showed a similar trend, but the results were not statistically significant. The odds ratios were 3.58 for cyclophosphamide and 2.73 for mitoxantrone hydrochloride.
The researchers said that, while these results are intriguing, they should not change or replace the clinical judgments, monitoring, and current standard treatments for patients with autoimmune diseases.
Despite its large size, this study had limitations, including its retrospective nature, the fact that many different autoimmune diseases were analyzed, and that the researchers only looked at cases of MDS and AML.
No definitive causal association was made between taking a particular drug and MDS or AML. The number of patients with autoimmune disease developing MDS or AML is still low overall, and no prediction for individual patients can be concluded from the study.
The researchers plan to perform molecular investigations into the genetic susceptibility for therapy-related myeloid neoplasms as the next phase of this research. ![]()
Company reports third death in SL-401 trial
Stemline Therapeutics, Inc. has announced another patient death in its ongoing phase 2 trial of SL-401 in patients with blastic plasmacytoid dendritic cell neoplasm (BPDCN) and acute myeloid leukemia (AML).
The company became aware of this death, in a patient with BPDCN, on January 18.
The cause of death has not been determined, but the patient had developed capillary leak syndrome (CLS), a sometimes fatal and well-documented side effect of SL-401.
There have been 2 other deaths reported in patients with CLS in this trial. One of these deaths occurred in a patient with BPDCN and the other in a patient with AML.
Stemline said this study is ongoing, patient enrollment is ahead of schedule, and patients continue to receive SL-401 in the trial. Timelines for study completion and biologics licensing application submission remain on track.
The fact that CLS is an expected complication of SL-401 administration has been noted in filings with the Securities and Exchange Commission and US Food and Drug Administration (FDA), as well as in the study’s informed consent forms and other information provided to investigators.
Stemline said it has and will continue to report data to the FDA in accordance with the study protocol and applicable regulations. The company plans to provide a clinical and safety update on this cohort when the cohort and data are complete.
SL-410 in BPDCN
SL-401 is a targeted therapy directed to the interleukin-3 receptor (IL-3R), which is present in BPDCN and other hematologic malignancies. SL-401 is composed of human IL-3 coupled to a truncated diphtheria toxin payload that inhibits protein synthesis.
SL-401 is being tested in several clinical trials. Results from the phase 2 trial in BPDCN and AML patients were presented at the 2016 ASH Annual Meeting (abstract 342). However, the presentation only included data on the patients with BPDCN.
The trial consists of a lead-in dose-escalation stage (stage 1) and subsequent expansion stage (stage 2). In stage 1, patients received SL-401 as a daily intravenous infusion for up to 5 days (7, 9, 12, or 16 μg/kg/day) every 21 days. In stage 2, patients received SL-401 at the optimal stage 1 dose—12 μg/kg.
As of October 7, 2016, 32 BPDCN patients had been treated—9 in stage 1 and 23 in stage 2. Nineteen patients received SL-401 as first-line treatment, and 13 had relapsed/refractory disease. (Fourteen patients with relapsed/refractory AML were treated in stage 1.)
Efficacy
Of the 19 first-line BPDCN patients, 16 received the optimal dose (12 μg/kg). The overall response rate was 95% among all first-line patients (18/19) and 100% among those who received the optimal dose (16/16).
The complete response rates were 74% (14/19) and 81% (13/16), respectively. Six patients (all who received the optimal dose) proceeded to transplant (autologous and allogeneic).
All 13 relapsed/refractory BPDCN patients received the optimal dose. The overall response rate was 69% (9/13), and the complete response rate was 31% (4/13). One patient proceeded to allogeneic transplant.
Eleven first-line patients, including the 6 who went on to transplant, have ongoing responses. Six relapsed/refractory patients, including the patient who went on to transplant, have ongoing responses.
Among first-line patients treated at the optimal dose, the median progression-free and overall survival have not been reached. Among relapsed/refractory patients (all of whom were treated at the optimal dose), the median progression-free and overall survival are 8.5 months.
Safety
The most common treatment-related adverse events were transaminase elevation (52%), hypoalbuminemia (39%), chills (31%), pyrexia (27%), nausea (23%), fatigue (23%), peripheral edema (23%), thrombocytopenia (19%), hypotension (19%), weight increase (19%), anemia (19%), decreased appetite (19%), and CLS (19%).
In stage 1, two BPDCN patients had CLS—one grade 5 (7 μg/kg) and one grade 4 (12 μg/kg). After this, safety precautions were implemented to minimize the risk of severe CLS.
A second CLS-related death occurred in stage 1 in a patient with relapsed/refractory AML (16 μg/kg).
The other death in a BPDCN patient with CLS was reported after the ASH presentation. Stemline became aware of the death on January 18 and disclosed it to the public on February 2. ![]()
Stemline Therapeutics, Inc. has announced another patient death in its ongoing phase 2 trial of SL-401 in patients with blastic plasmacytoid dendritic cell neoplasm (BPDCN) and acute myeloid leukemia (AML).
The company became aware of this death, in a patient with BPDCN, on January 18.
The cause of death has not been determined, but the patient had developed capillary leak syndrome (CLS), a sometimes fatal and well-documented side effect of SL-401.
There have been 2 other deaths reported in patients with CLS in this trial. One of these deaths occurred in a patient with BPDCN and the other in a patient with AML.
Stemline said this study is ongoing, patient enrollment is ahead of schedule, and patients continue to receive SL-401 in the trial. Timelines for study completion and biologics licensing application submission remain on track.
The fact that CLS is an expected complication of SL-401 administration has been noted in filings with the Securities and Exchange Commission and US Food and Drug Administration (FDA), as well as in the study’s informed consent forms and other information provided to investigators.
Stemline said it has and will continue to report data to the FDA in accordance with the study protocol and applicable regulations. The company plans to provide a clinical and safety update on this cohort when the cohort and data are complete.
SL-410 in BPDCN
SL-401 is a targeted therapy directed to the interleukin-3 receptor (IL-3R), which is present in BPDCN and other hematologic malignancies. SL-401 is composed of human IL-3 coupled to a truncated diphtheria toxin payload that inhibits protein synthesis.
SL-401 is being tested in several clinical trials. Results from the phase 2 trial in BPDCN and AML patients were presented at the 2016 ASH Annual Meeting (abstract 342). However, the presentation only included data on the patients with BPDCN.
The trial consists of a lead-in dose-escalation stage (stage 1) and subsequent expansion stage (stage 2). In stage 1, patients received SL-401 as a daily intravenous infusion for up to 5 days (7, 9, 12, or 16 μg/kg/day) every 21 days. In stage 2, patients received SL-401 at the optimal stage 1 dose—12 μg/kg.
As of October 7, 2016, 32 BPDCN patients had been treated—9 in stage 1 and 23 in stage 2. Nineteen patients received SL-401 as first-line treatment, and 13 had relapsed/refractory disease. (Fourteen patients with relapsed/refractory AML were treated in stage 1.)
Efficacy
Of the 19 first-line BPDCN patients, 16 received the optimal dose (12 μg/kg). The overall response rate was 95% among all first-line patients (18/19) and 100% among those who received the optimal dose (16/16).
The complete response rates were 74% (14/19) and 81% (13/16), respectively. Six patients (all who received the optimal dose) proceeded to transplant (autologous and allogeneic).
All 13 relapsed/refractory BPDCN patients received the optimal dose. The overall response rate was 69% (9/13), and the complete response rate was 31% (4/13). One patient proceeded to allogeneic transplant.
Eleven first-line patients, including the 6 who went on to transplant, have ongoing responses. Six relapsed/refractory patients, including the patient who went on to transplant, have ongoing responses.
Among first-line patients treated at the optimal dose, the median progression-free and overall survival have not been reached. Among relapsed/refractory patients (all of whom were treated at the optimal dose), the median progression-free and overall survival are 8.5 months.
Safety
The most common treatment-related adverse events were transaminase elevation (52%), hypoalbuminemia (39%), chills (31%), pyrexia (27%), nausea (23%), fatigue (23%), peripheral edema (23%), thrombocytopenia (19%), hypotension (19%), weight increase (19%), anemia (19%), decreased appetite (19%), and CLS (19%).
In stage 1, two BPDCN patients had CLS—one grade 5 (7 μg/kg) and one grade 4 (12 μg/kg). After this, safety precautions were implemented to minimize the risk of severe CLS.
A second CLS-related death occurred in stage 1 in a patient with relapsed/refractory AML (16 μg/kg).
The other death in a BPDCN patient with CLS was reported after the ASH presentation. Stemline became aware of the death on January 18 and disclosed it to the public on February 2. ![]()
Stemline Therapeutics, Inc. has announced another patient death in its ongoing phase 2 trial of SL-401 in patients with blastic plasmacytoid dendritic cell neoplasm (BPDCN) and acute myeloid leukemia (AML).
The company became aware of this death, in a patient with BPDCN, on January 18.
The cause of death has not been determined, but the patient had developed capillary leak syndrome (CLS), a sometimes fatal and well-documented side effect of SL-401.
There have been 2 other deaths reported in patients with CLS in this trial. One of these deaths occurred in a patient with BPDCN and the other in a patient with AML.
Stemline said this study is ongoing, patient enrollment is ahead of schedule, and patients continue to receive SL-401 in the trial. Timelines for study completion and biologics licensing application submission remain on track.
The fact that CLS is an expected complication of SL-401 administration has been noted in filings with the Securities and Exchange Commission and US Food and Drug Administration (FDA), as well as in the study’s informed consent forms and other information provided to investigators.
Stemline said it has and will continue to report data to the FDA in accordance with the study protocol and applicable regulations. The company plans to provide a clinical and safety update on this cohort when the cohort and data are complete.
SL-410 in BPDCN
SL-401 is a targeted therapy directed to the interleukin-3 receptor (IL-3R), which is present in BPDCN and other hematologic malignancies. SL-401 is composed of human IL-3 coupled to a truncated diphtheria toxin payload that inhibits protein synthesis.
SL-401 is being tested in several clinical trials. Results from the phase 2 trial in BPDCN and AML patients were presented at the 2016 ASH Annual Meeting (abstract 342). However, the presentation only included data on the patients with BPDCN.
The trial consists of a lead-in dose-escalation stage (stage 1) and subsequent expansion stage (stage 2). In stage 1, patients received SL-401 as a daily intravenous infusion for up to 5 days (7, 9, 12, or 16 μg/kg/day) every 21 days. In stage 2, patients received SL-401 at the optimal stage 1 dose—12 μg/kg.
As of October 7, 2016, 32 BPDCN patients had been treated—9 in stage 1 and 23 in stage 2. Nineteen patients received SL-401 as first-line treatment, and 13 had relapsed/refractory disease. (Fourteen patients with relapsed/refractory AML were treated in stage 1.)
Efficacy
Of the 19 first-line BPDCN patients, 16 received the optimal dose (12 μg/kg). The overall response rate was 95% among all first-line patients (18/19) and 100% among those who received the optimal dose (16/16).
The complete response rates were 74% (14/19) and 81% (13/16), respectively. Six patients (all who received the optimal dose) proceeded to transplant (autologous and allogeneic).
All 13 relapsed/refractory BPDCN patients received the optimal dose. The overall response rate was 69% (9/13), and the complete response rate was 31% (4/13). One patient proceeded to allogeneic transplant.
Eleven first-line patients, including the 6 who went on to transplant, have ongoing responses. Six relapsed/refractory patients, including the patient who went on to transplant, have ongoing responses.
Among first-line patients treated at the optimal dose, the median progression-free and overall survival have not been reached. Among relapsed/refractory patients (all of whom were treated at the optimal dose), the median progression-free and overall survival are 8.5 months.
Safety
The most common treatment-related adverse events were transaminase elevation (52%), hypoalbuminemia (39%), chills (31%), pyrexia (27%), nausea (23%), fatigue (23%), peripheral edema (23%), thrombocytopenia (19%), hypotension (19%), weight increase (19%), anemia (19%), decreased appetite (19%), and CLS (19%).
In stage 1, two BPDCN patients had CLS—one grade 5 (7 μg/kg) and one grade 4 (12 μg/kg). After this, safety precautions were implemented to minimize the risk of severe CLS.
A second CLS-related death occurred in stage 1 in a patient with relapsed/refractory AML (16 μg/kg).
The other death in a BPDCN patient with CLS was reported after the ASH presentation. Stemline became aware of the death on January 18 and disclosed it to the public on February 2. ![]()
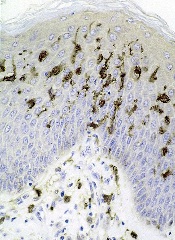
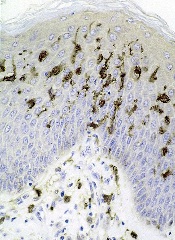
Targeting disease stem cells in AML, MDS
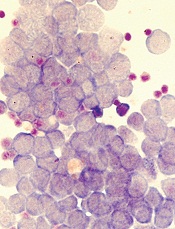
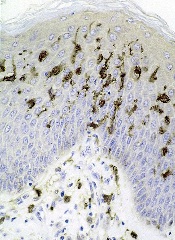
Image by Robert Paulson
The cell surface molecule CD99 occurs more frequently than normal on stem cells responsible for acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to research published in Science Translational Medicine.
Building on this discovery, researchers designed anti-CD99 monoclonal antibodies (mAbs).
In vitro and in vivo experiments
showed that these mAbs can recognize
and destroy AML and MDS stem/progenitor cells.
“Our findings not only identify a new molecule expressed on stem cells that drive these human malignancies, but we show that antibodies against this target can directly kill human AML stem cells,” said study author Christopher Y. Park, MD, PhD, of NYU Langone Medical Center in New York, New York.
“While we still have important details to work out, CD99 is likely to be an exploitable therapeutic target for most AML and MDS patients, and we are working urgently to finalize a therapy for human testing.”
Dr Park and his colleagues first examined stem cell populations from 79 patients with AML and 24 with MDS. More than 80% of stem cells in both groups expressed high levels of CD99.
The levels were so high that leukemia stem cells could be cleanly separated from normal hematopoietic stem cells in AML samples.
Upon confirming that CD99 was abundant on AML and MDS stem cells, the researchers made several anti-CD99 mAbs and tested them in vitro and in mouse models.
The mAbs destroyed AML and MDS stem cells by causing a sudden spike in the activity of SRC family kinases—a group of proteins that are implicated in invasion, tumor progression, and metastasis in a variety of cancers.
However, the mAbs had minimal effects on normal hematopoietic stem cells.
“With the appropriate support, we believe we can rapidly determine the best antibodies for use in patients, produce them at the quality needed to verify our results, and apply for permission to begin clinical trials,” Dr Park said. ![]()
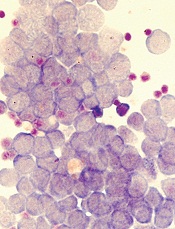
Image by Robert Paulson
The cell surface molecule CD99 occurs more frequently than normal on stem cells responsible for acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to research published in Science Translational Medicine.
Building on this discovery, researchers designed anti-CD99 monoclonal antibodies (mAbs).
In vitro and in vivo experiments
showed that these mAbs can recognize
and destroy AML and MDS stem/progenitor cells.
“Our findings not only identify a new molecule expressed on stem cells that drive these human malignancies, but we show that antibodies against this target can directly kill human AML stem cells,” said study author Christopher Y. Park, MD, PhD, of NYU Langone Medical Center in New York, New York.
“While we still have important details to work out, CD99 is likely to be an exploitable therapeutic target for most AML and MDS patients, and we are working urgently to finalize a therapy for human testing.”
Dr Park and his colleagues first examined stem cell populations from 79 patients with AML and 24 with MDS. More than 80% of stem cells in both groups expressed high levels of CD99.
The levels were so high that leukemia stem cells could be cleanly separated from normal hematopoietic stem cells in AML samples.
Upon confirming that CD99 was abundant on AML and MDS stem cells, the researchers made several anti-CD99 mAbs and tested them in vitro and in mouse models.
The mAbs destroyed AML and MDS stem cells by causing a sudden spike in the activity of SRC family kinases—a group of proteins that are implicated in invasion, tumor progression, and metastasis in a variety of cancers.
However, the mAbs had minimal effects on normal hematopoietic stem cells.
“With the appropriate support, we believe we can rapidly determine the best antibodies for use in patients, produce them at the quality needed to verify our results, and apply for permission to begin clinical trials,” Dr Park said. ![]()
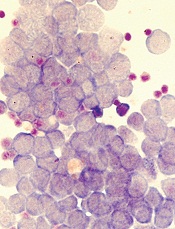
Image by Robert Paulson
The cell surface molecule CD99 occurs more frequently than normal on stem cells responsible for acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to research published in Science Translational Medicine.
Building on this discovery, researchers designed anti-CD99 monoclonal antibodies (mAbs).
In vitro and in vivo experiments
showed that these mAbs can recognize
and destroy AML and MDS stem/progenitor cells.
“Our findings not only identify a new molecule expressed on stem cells that drive these human malignancies, but we show that antibodies against this target can directly kill human AML stem cells,” said study author Christopher Y. Park, MD, PhD, of NYU Langone Medical Center in New York, New York.
“While we still have important details to work out, CD99 is likely to be an exploitable therapeutic target for most AML and MDS patients, and we are working urgently to finalize a therapy for human testing.”
Dr Park and his colleagues first examined stem cell populations from 79 patients with AML and 24 with MDS. More than 80% of stem cells in both groups expressed high levels of CD99.
The levels were so high that leukemia stem cells could be cleanly separated from normal hematopoietic stem cells in AML samples.
Upon confirming that CD99 was abundant on AML and MDS stem cells, the researchers made several anti-CD99 mAbs and tested them in vitro and in mouse models.
The mAbs destroyed AML and MDS stem cells by causing a sudden spike in the activity of SRC family kinases—a group of proteins that are implicated in invasion, tumor progression, and metastasis in a variety of cancers.
However, the mAbs had minimal effects on normal hematopoietic stem cells.
“With the appropriate support, we believe we can rapidly determine the best antibodies for use in patients, produce them at the quality needed to verify our results, and apply for permission to begin clinical trials,” Dr Park said.
AML leads percent gains in 5-year survival among leukemias
Over the 60-year span from the early 1950s to 2013, the 5-year survival rate for all leukemias increased by 500%, according to data from the Surveillance, Epidemiology, and End Results Program.
For 2008-2013, the 5-year relative survival rate for all leukemias was 60.1%, compared with 10% during 1950-1954, said Ali H. Mokdad, PhD, and his associates at the Institute for Health Metrics and Evaluation at the University of Washington, Seattle (JAMA 2017;317[4]:388-406).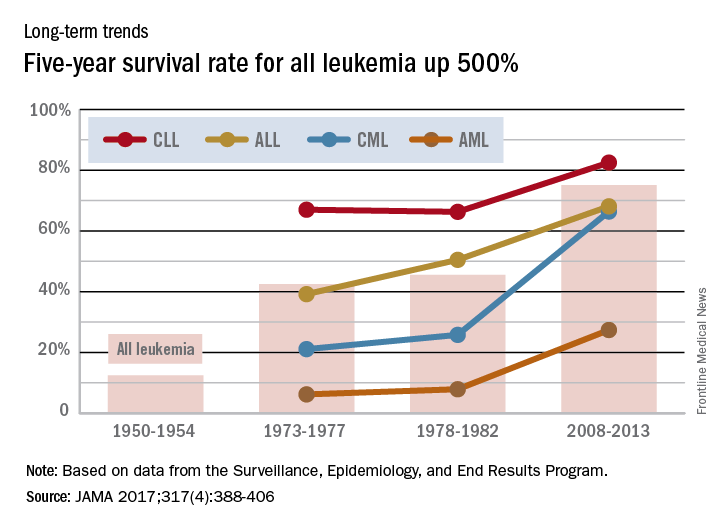
Over the 60-year span from the early 1950s to 2013, the 5-year survival rate for all leukemias increased by 500%, according to data from the Surveillance, Epidemiology, and End Results Program.
For 2008-2013, the 5-year relative survival rate for all leukemias was 60.1%, compared with 10% during 1950-1954, said Ali H. Mokdad, PhD, and his associates at the Institute for Health Metrics and Evaluation at the University of Washington, Seattle (JAMA 2017;317[4]:388-406).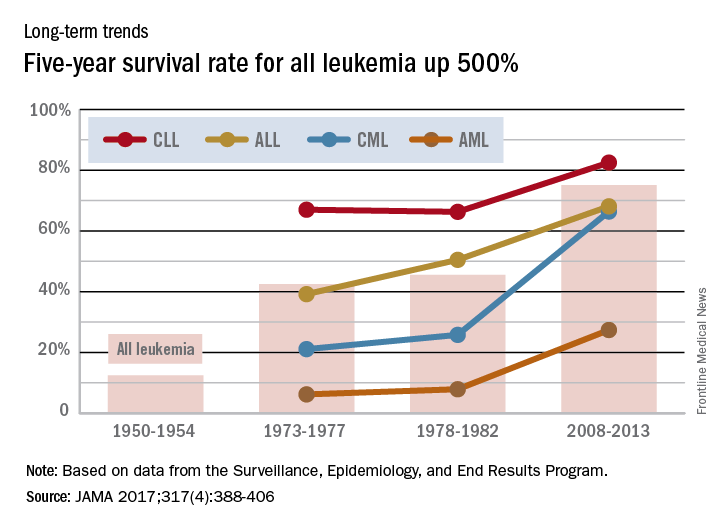
Over the 60-year span from the early 1950s to 2013, the 5-year survival rate for all leukemias increased by 500%, according to data from the Surveillance, Epidemiology, and End Results Program.
For 2008-2013, the 5-year relative survival rate for all leukemias was 60.1%, compared with 10% during 1950-1954, said Ali H. Mokdad, PhD, and his associates at the Institute for Health Metrics and Evaluation at the University of Washington, Seattle (JAMA 2017;317[4]:388-406).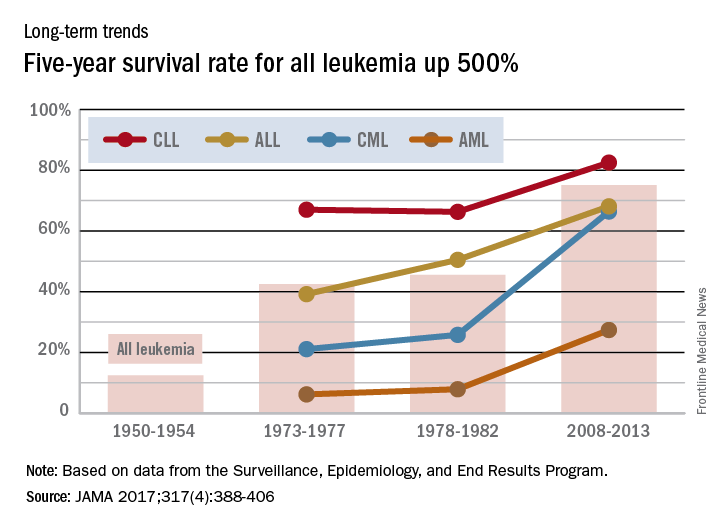
New recommendations for managing adult AML

Photo courtesy of CDC
The European LeukemiaNet (ELN) has released updated recommendations for the diagnosis and treatment of acute myeloid leukemia (AML) in adults.
The recommendations include revised ELN genetic categories, a proposed response category based on minimal residual disease status, and a proposed category for progressive disease for clinical trials.
They also include the updated World Health Organization classification of myeloid neoplasms and acute leukemia.
The recommendations are published in Blood.
“These guidelines are an important update of the current and widely used recommendations for managing AML, for constructing clinical trials, and for predicting outcomes of AML patients,” said Clara D. Bloomfield, MD, of The Ohio State University Comprehensive Cancer Center in Columbus.
“They will be the new standard of care and will replace the 2010 ELN recommendations for managing AML patients and designing clinical trials.”
Dr Bloomfield said updating the ELN recommendations was prompted by new insights into the molecular and genomic causes of AML, by the development of new genetic tests and tests for detecting minimal residual disease, and by the development of novel anti-leukemic agents.
Changes of note, according to Dr Bloomfield, are that there are now 3 genetic risk categories rather than 4, and the FLT3-ITD mutation has been added as a marker of risk.
In addition, “complete remission with no evidence of minimal residual disease” is a new proposed response category. This criterion requires that genetic markers present at diagnosis are no longer detectable.
“It is no longer good enough to examine bone marrow samples and say the leukemia is gone,” Dr Bloomfield said. “We must also see the loss of genetic markers.”
Another change is that “progressive disease” is a new provisional response category to be used in clinical trials only. The purpose of the category is to harmonize the various definitions of progressive disease that are used in different clinical trials.

Photo courtesy of CDC
The European LeukemiaNet (ELN) has released updated recommendations for the diagnosis and treatment of acute myeloid leukemia (AML) in adults.
The recommendations include revised ELN genetic categories, a proposed response category based on minimal residual disease status, and a proposed category for progressive disease for clinical trials.
They also include the updated World Health Organization classification of myeloid neoplasms and acute leukemia.
The recommendations are published in Blood.
“These guidelines are an important update of the current and widely used recommendations for managing AML, for constructing clinical trials, and for predicting outcomes of AML patients,” said Clara D. Bloomfield, MD, of The Ohio State University Comprehensive Cancer Center in Columbus.
“They will be the new standard of care and will replace the 2010 ELN recommendations for managing AML patients and designing clinical trials.”
Dr Bloomfield said updating the ELN recommendations was prompted by new insights into the molecular and genomic causes of AML, by the development of new genetic tests and tests for detecting minimal residual disease, and by the development of novel anti-leukemic agents.
Changes of note, according to Dr Bloomfield, are that there are now 3 genetic risk categories rather than 4, and the FLT3-ITD mutation has been added as a marker of risk.
In addition, “complete remission with no evidence of minimal residual disease” is a new proposed response category. This criterion requires that genetic markers present at diagnosis are no longer detectable.
“It is no longer good enough to examine bone marrow samples and say the leukemia is gone,” Dr Bloomfield said. “We must also see the loss of genetic markers.”
Another change is that “progressive disease” is a new provisional response category to be used in clinical trials only. The purpose of the category is to harmonize the various definitions of progressive disease that are used in different clinical trials.

Photo courtesy of CDC
The European LeukemiaNet (ELN) has released updated recommendations for the diagnosis and treatment of acute myeloid leukemia (AML) in adults.
The recommendations include revised ELN genetic categories, a proposed response category based on minimal residual disease status, and a proposed category for progressive disease for clinical trials.
They also include the updated World Health Organization classification of myeloid neoplasms and acute leukemia.
The recommendations are published in Blood.
“These guidelines are an important update of the current and widely used recommendations for managing AML, for constructing clinical trials, and for predicting outcomes of AML patients,” said Clara D. Bloomfield, MD, of The Ohio State University Comprehensive Cancer Center in Columbus.
“They will be the new standard of care and will replace the 2010 ELN recommendations for managing AML patients and designing clinical trials.”
Dr Bloomfield said updating the ELN recommendations was prompted by new insights into the molecular and genomic causes of AML, by the development of new genetic tests and tests for detecting minimal residual disease, and by the development of novel anti-leukemic agents.
Changes of note, according to Dr Bloomfield, are that there are now 3 genetic risk categories rather than 4, and the FLT3-ITD mutation has been added as a marker of risk.
In addition, “complete remission with no evidence of minimal residual disease” is a new proposed response category. This criterion requires that genetic markers present at diagnosis are no longer detectable.
“It is no longer good enough to examine bone marrow samples and say the leukemia is gone,” Dr Bloomfield said. “We must also see the loss of genetic markers.”
Another change is that “progressive disease” is a new provisional response category to be used in clinical trials only. The purpose of the category is to harmonize the various definitions of progressive disease that are used in different clinical trials.
Study quantifies 5-year survival rates for blood cancers

chemotherapy
Photo by Rhoda Baer
A new study shows that 5-year survival rates for US patients with hematologic malignancies have increased greatly since the 1950s, but there is still room for improvement, particularly for patients with acute myeloid leukemia (AML).
Researchers found the absolute difference in improvement for 5-year survival from 1950-1954 to 2008-2013 ranged from 38.2% for non-Hodgkin lymphoma (NHL) to 56.6% for Hodgkin lymphoma.
And although the 5-year survival rate for Hodgkin lymphoma patients reached 86.6% for 2008-2013, the 5-year survival rate for patients with AML only reached 27.4%.
This study also revealed large disparities in overall cancer mortality rates between different counties across the country.
Ali H. Mokdad, PhD, of the Institute for Health Metrics and Evaluation in Seattle, Washington, and his colleagues reported these findings in JAMA.
Overall cancer deaths
The researchers found there were 19,511,910 cancer deaths recorded in the US between 1980 and 2014. Cancer mortality decreased by 20.1% between 1980 and 2014, from 240.2 deaths per 100,000 people to 192.0 deaths per 100,000 people.
In 1980, cancer mortality ranged from 130.6 per 100,000 in Summit County, Colorado, to 386.9 per 100,000 in North Slope Borough, Alaska.
In 2014, cancer mortality ranged from 70.7 per 100,000 in Summit County, Colorado, to 503.1 per 100,000 in Union County, Florida.
“Such significant disparities among US counties is unacceptable,” Dr Mokdad said. “Every person should have access to early screenings for cancer, as well as adequate treatment.”
Mortality rates for hematologic malignancies
In 2014, the mortality rates, per 100,000 people, for hematologic malignancies were:
- 0.4 for Hodgkin lymphoma (rank out of all cancers, 27)
- 8.3 for NHL (rank, 7)
- 3.9 for multiple myeloma (rank, 16)
- 9.0 for all leukemias (rank, 6)
- 0.7 for acute lymphoid leukemia (ALL)
- 2.6 for chronic lymphoid leukemia (CLL)
- 5.1 for AML
- 0.6 for chronic myeloid leukemia (CML).
The leukemia subtypes were not assigned a rank.
5-year survival rates for hematologic malignancies
Hodgkin lymphoma
- 30% for 1950-54
- 68.6% for 1973-77
- 72.1% for 1978-82
- 86.6% for 2008-2013
- Absolute difference (between the first and latest year of data), 56.6%.
NHL
- 33% for 1950-54
- 45.3% for 1973-77
- 48.7% for 1978-82
- 71.2% for 2008-2013
- Absolute difference, 38.2%.
Multiple myeloma
- 6% for 1950-54
- 23.4% for 1973-77
- 26.6% for 1978-82
- 49.8% for 2008-2013
- Absolute difference, 43.8%.
Leukemia
- 10% for 1950-54
- 34% for 1973-77
- 36.3% for 1978-82
- 60.1% for 2008-2013
- Absolute difference, 50.1%.
ALL
- 39.2% for 1973-77
- 50.5% for 1978-82
- 68.1% for 2008-2013
- Absolute difference, 28.9%.
CLL
- 67% for 1973-77
- 66.3% for 1978-82
- 82.5% for 2008-2013
- Absolute difference, 15.5%.
AML
- 6.2% for 1973-77
- 7.9% for 1978-82
- 27.4% for 2008-2013
- Absolute difference, 21.2%.
CML
- 21.1% for 1973-77
- 25.8% for 1978-82
- 66.4% for 2008-2013
- Absolute difference, 45.3%.
For the leukemia subtypes, there was no data for 1950 to 1954.

chemotherapy
Photo by Rhoda Baer
A new study shows that 5-year survival rates for US patients with hematologic malignancies have increased greatly since the 1950s, but there is still room for improvement, particularly for patients with acute myeloid leukemia (AML).
Researchers found the absolute difference in improvement for 5-year survival from 1950-1954 to 2008-2013 ranged from 38.2% for non-Hodgkin lymphoma (NHL) to 56.6% for Hodgkin lymphoma.
And although the 5-year survival rate for Hodgkin lymphoma patients reached 86.6% for 2008-2013, the 5-year survival rate for patients with AML only reached 27.4%.
This study also revealed large disparities in overall cancer mortality rates between different counties across the country.
Ali H. Mokdad, PhD, of the Institute for Health Metrics and Evaluation in Seattle, Washington, and his colleagues reported these findings in JAMA.
Overall cancer deaths
The researchers found there were 19,511,910 cancer deaths recorded in the US between 1980 and 2014. Cancer mortality decreased by 20.1% between 1980 and 2014, from 240.2 deaths per 100,000 people to 192.0 deaths per 100,000 people.
In 1980, cancer mortality ranged from 130.6 per 100,000 in Summit County, Colorado, to 386.9 per 100,000 in North Slope Borough, Alaska.
In 2014, cancer mortality ranged from 70.7 per 100,000 in Summit County, Colorado, to 503.1 per 100,000 in Union County, Florida.
“Such significant disparities among US counties is unacceptable,” Dr Mokdad said. “Every person should have access to early screenings for cancer, as well as adequate treatment.”
Mortality rates for hematologic malignancies
In 2014, the mortality rates, per 100,000 people, for hematologic malignancies were:
- 0.4 for Hodgkin lymphoma (rank out of all cancers, 27)
- 8.3 for NHL (rank, 7)
- 3.9 for multiple myeloma (rank, 16)
- 9.0 for all leukemias (rank, 6)
- 0.7 for acute lymphoid leukemia (ALL)
- 2.6 for chronic lymphoid leukemia (CLL)
- 5.1 for AML
- 0.6 for chronic myeloid leukemia (CML).
The leukemia subtypes were not assigned a rank.
5-year survival rates for hematologic malignancies
Hodgkin lymphoma
- 30% for 1950-54
- 68.6% for 1973-77
- 72.1% for 1978-82
- 86.6% for 2008-2013
- Absolute difference (between the first and latest year of data), 56.6%.
NHL
- 33% for 1950-54
- 45.3% for 1973-77
- 48.7% for 1978-82
- 71.2% for 2008-2013
- Absolute difference, 38.2%.
Multiple myeloma
- 6% for 1950-54
- 23.4% for 1973-77
- 26.6% for 1978-82
- 49.8% for 2008-2013
- Absolute difference, 43.8%.
Leukemia
- 10% for 1950-54
- 34% for 1973-77
- 36.3% for 1978-82
- 60.1% for 2008-2013
- Absolute difference, 50.1%.
ALL
- 39.2% for 1973-77
- 50.5% for 1978-82
- 68.1% for 2008-2013
- Absolute difference, 28.9%.
CLL
- 67% for 1973-77
- 66.3% for 1978-82
- 82.5% for 2008-2013
- Absolute difference, 15.5%.
AML
- 6.2% for 1973-77
- 7.9% for 1978-82
- 27.4% for 2008-2013
- Absolute difference, 21.2%.
CML
- 21.1% for 1973-77
- 25.8% for 1978-82
- 66.4% for 2008-2013
- Absolute difference, 45.3%.
For the leukemia subtypes, there was no data for 1950 to 1954.

chemotherapy
Photo by Rhoda Baer
A new study shows that 5-year survival rates for US patients with hematologic malignancies have increased greatly since the 1950s, but there is still room for improvement, particularly for patients with acute myeloid leukemia (AML).
Researchers found the absolute difference in improvement for 5-year survival from 1950-1954 to 2008-2013 ranged from 38.2% for non-Hodgkin lymphoma (NHL) to 56.6% for Hodgkin lymphoma.
And although the 5-year survival rate for Hodgkin lymphoma patients reached 86.6% for 2008-2013, the 5-year survival rate for patients with AML only reached 27.4%.
This study also revealed large disparities in overall cancer mortality rates between different counties across the country.
Ali H. Mokdad, PhD, of the Institute for Health Metrics and Evaluation in Seattle, Washington, and his colleagues reported these findings in JAMA.
Overall cancer deaths
The researchers found there were 19,511,910 cancer deaths recorded in the US between 1980 and 2014. Cancer mortality decreased by 20.1% between 1980 and 2014, from 240.2 deaths per 100,000 people to 192.0 deaths per 100,000 people.
In 1980, cancer mortality ranged from 130.6 per 100,000 in Summit County, Colorado, to 386.9 per 100,000 in North Slope Borough, Alaska.
In 2014, cancer mortality ranged from 70.7 per 100,000 in Summit County, Colorado, to 503.1 per 100,000 in Union County, Florida.
“Such significant disparities among US counties is unacceptable,” Dr Mokdad said. “Every person should have access to early screenings for cancer, as well as adequate treatment.”
Mortality rates for hematologic malignancies
In 2014, the mortality rates, per 100,000 people, for hematologic malignancies were:
- 0.4 for Hodgkin lymphoma (rank out of all cancers, 27)
- 8.3 for NHL (rank, 7)
- 3.9 for multiple myeloma (rank, 16)
- 9.0 for all leukemias (rank, 6)
- 0.7 for acute lymphoid leukemia (ALL)
- 2.6 for chronic lymphoid leukemia (CLL)
- 5.1 for AML
- 0.6 for chronic myeloid leukemia (CML).
The leukemia subtypes were not assigned a rank.
5-year survival rates for hematologic malignancies
Hodgkin lymphoma
- 30% for 1950-54
- 68.6% for 1973-77
- 72.1% for 1978-82
- 86.6% for 2008-2013
- Absolute difference (between the first and latest year of data), 56.6%.
NHL
- 33% for 1950-54
- 45.3% for 1973-77
- 48.7% for 1978-82
- 71.2% for 2008-2013
- Absolute difference, 38.2%.
Multiple myeloma
- 6% for 1950-54
- 23.4% for 1973-77
- 26.6% for 1978-82
- 49.8% for 2008-2013
- Absolute difference, 43.8%.
Leukemia
- 10% for 1950-54
- 34% for 1973-77
- 36.3% for 1978-82
- 60.1% for 2008-2013
- Absolute difference, 50.1%.
ALL
- 39.2% for 1973-77
- 50.5% for 1978-82
- 68.1% for 2008-2013
- Absolute difference, 28.9%.
CLL
- 67% for 1973-77
- 66.3% for 1978-82
- 82.5% for 2008-2013
- Absolute difference, 15.5%.
AML
- 6.2% for 1973-77
- 7.9% for 1978-82
- 27.4% for 2008-2013
- Absolute difference, 21.2%.
CML
- 21.1% for 1973-77
- 25.8% for 1978-82
- 66.4% for 2008-2013
- Absolute difference, 45.3%.
For the leukemia subtypes, there was no data for 1950 to 1954.


