User login
Childhood cancer risk linked to mother’s birthplace

Photo by Nina Matthews
New research suggests a mother’s birthplace may affect the risk of certain cancers for Hispanic children.
The study showed that children of Hispanic mothers who were not born in the US had lower risks of brain cancers, neuroblastoma, and Wilms tumor, when compared to children of US-born Hispanic mothers and non-Hispanic white mothers born in the US.
However, all Hispanic children, regardless of where their mothers were born, had higher risks of acute leukemias and Hodgkin lymphoma but a lower risk of non-Hodgkin lymphoma (NHL).
Julia E. Heck, PhD, of the University of California, Los Angeles, and her colleagues reported these findings in JAMA Pediatrics.
The researchers used California birth records to identify children born from 1983 through 2011. Information on cancer cases came from California Cancer Registry records from 1988 to 2012.
The team restricted their analysis to children of US-born white, US-born Hispanic, and non-US-born Hispanic mothers. The study included 13,666 cases of children diagnosed with cancer before the age of 6 and 15,513,718 children who served as control subjects.
To assess the hazard ratios (HRs) for various cancers, the researchers used children of non-Hispanic white mothers as a reference (HR=1.00) and compared them to the children of non-US-born Hispanic mothers and US-born Hispanic mothers.
For children of non-US-born Hispanic mothers, the HR was 0.50 for glioma, 0.43 for astrocytoma, 0.47 for neuroblastoma, and 0.70 for Wilms tumor. For children of US-born Hispanic mothers, the HR was 0.71 for glioma, 0.62 for astrocytoma, 0.66 for neuroblastoma, and 0.88 for Wilms tumor.
When compared to non-Hispanic white children, Hispanic children had an increased risk of acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), and Hodgkin lymphoma but lower risks of NHL and Burkitt lymphoma.
For children of US-born Hispanic mothers, the HR was 1.20 for ALL, 1.28 for AML, 2.49 for Hodgkin lymphoma, 0.79 for NHL, and 0.69 for Burkitt lymphoma.
For children of non-US-born Hispanic mothers, the HR was 1.06 for ALL, 1.05 for AML, 2.35 for Hodgkin lymphoma, 0.76 for NHL, and 0.73 for Burkitt lymphoma.
The researchers said the differences observed between children of US-born and non-US-born Hispanic mothers may be explained by lifestyle differences and varying environmental exposures.
These factors may explain the differences in cancer incidence between Hispanic children and white children as well, but the differences may also be a result of genetic variation and infection exposures early in life. ![]()

Photo by Nina Matthews
New research suggests a mother’s birthplace may affect the risk of certain cancers for Hispanic children.
The study showed that children of Hispanic mothers who were not born in the US had lower risks of brain cancers, neuroblastoma, and Wilms tumor, when compared to children of US-born Hispanic mothers and non-Hispanic white mothers born in the US.
However, all Hispanic children, regardless of where their mothers were born, had higher risks of acute leukemias and Hodgkin lymphoma but a lower risk of non-Hodgkin lymphoma (NHL).
Julia E. Heck, PhD, of the University of California, Los Angeles, and her colleagues reported these findings in JAMA Pediatrics.
The researchers used California birth records to identify children born from 1983 through 2011. Information on cancer cases came from California Cancer Registry records from 1988 to 2012.
The team restricted their analysis to children of US-born white, US-born Hispanic, and non-US-born Hispanic mothers. The study included 13,666 cases of children diagnosed with cancer before the age of 6 and 15,513,718 children who served as control subjects.
To assess the hazard ratios (HRs) for various cancers, the researchers used children of non-Hispanic white mothers as a reference (HR=1.00) and compared them to the children of non-US-born Hispanic mothers and US-born Hispanic mothers.
For children of non-US-born Hispanic mothers, the HR was 0.50 for glioma, 0.43 for astrocytoma, 0.47 for neuroblastoma, and 0.70 for Wilms tumor. For children of US-born Hispanic mothers, the HR was 0.71 for glioma, 0.62 for astrocytoma, 0.66 for neuroblastoma, and 0.88 for Wilms tumor.
When compared to non-Hispanic white children, Hispanic children had an increased risk of acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), and Hodgkin lymphoma but lower risks of NHL and Burkitt lymphoma.
For children of US-born Hispanic mothers, the HR was 1.20 for ALL, 1.28 for AML, 2.49 for Hodgkin lymphoma, 0.79 for NHL, and 0.69 for Burkitt lymphoma.
For children of non-US-born Hispanic mothers, the HR was 1.06 for ALL, 1.05 for AML, 2.35 for Hodgkin lymphoma, 0.76 for NHL, and 0.73 for Burkitt lymphoma.
The researchers said the differences observed between children of US-born and non-US-born Hispanic mothers may be explained by lifestyle differences and varying environmental exposures.
These factors may explain the differences in cancer incidence between Hispanic children and white children as well, but the differences may also be a result of genetic variation and infection exposures early in life. ![]()

Photo by Nina Matthews
New research suggests a mother’s birthplace may affect the risk of certain cancers for Hispanic children.
The study showed that children of Hispanic mothers who were not born in the US had lower risks of brain cancers, neuroblastoma, and Wilms tumor, when compared to children of US-born Hispanic mothers and non-Hispanic white mothers born in the US.
However, all Hispanic children, regardless of where their mothers were born, had higher risks of acute leukemias and Hodgkin lymphoma but a lower risk of non-Hodgkin lymphoma (NHL).
Julia E. Heck, PhD, of the University of California, Los Angeles, and her colleagues reported these findings in JAMA Pediatrics.
The researchers used California birth records to identify children born from 1983 through 2011. Information on cancer cases came from California Cancer Registry records from 1988 to 2012.
The team restricted their analysis to children of US-born white, US-born Hispanic, and non-US-born Hispanic mothers. The study included 13,666 cases of children diagnosed with cancer before the age of 6 and 15,513,718 children who served as control subjects.
To assess the hazard ratios (HRs) for various cancers, the researchers used children of non-Hispanic white mothers as a reference (HR=1.00) and compared them to the children of non-US-born Hispanic mothers and US-born Hispanic mothers.
For children of non-US-born Hispanic mothers, the HR was 0.50 for glioma, 0.43 for astrocytoma, 0.47 for neuroblastoma, and 0.70 for Wilms tumor. For children of US-born Hispanic mothers, the HR was 0.71 for glioma, 0.62 for astrocytoma, 0.66 for neuroblastoma, and 0.88 for Wilms tumor.
When compared to non-Hispanic white children, Hispanic children had an increased risk of acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), and Hodgkin lymphoma but lower risks of NHL and Burkitt lymphoma.
For children of US-born Hispanic mothers, the HR was 1.20 for ALL, 1.28 for AML, 2.49 for Hodgkin lymphoma, 0.79 for NHL, and 0.69 for Burkitt lymphoma.
For children of non-US-born Hispanic mothers, the HR was 1.06 for ALL, 1.05 for AML, 2.35 for Hodgkin lymphoma, 0.76 for NHL, and 0.73 for Burkitt lymphoma.
The researchers said the differences observed between children of US-born and non-US-born Hispanic mothers may be explained by lifestyle differences and varying environmental exposures.
These factors may explain the differences in cancer incidence between Hispanic children and white children as well, but the differences may also be a result of genetic variation and infection exposures early in life. ![]()
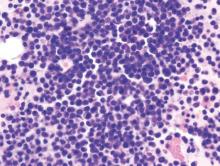
High-dose MTX improves EFS in high-risk B-ALL

Photo by Bill Branson
High-dose methotrexate (MTX) is more effective than escalating doses of MTX for young patients with high-risk B-cell acute lymphoblastic leukemia (B-ALL), according to a study published in the Journal of Clinical Oncology.
Patients who received high-dose MTX during interim maintenance 1 had significantly better event-free survival (EFS) than those who received escalating MTX.
In addition, the study showed that substituting dexamethasone for prednisone during induction was beneficial for younger—but not older—patients.
The high-dose MTX protocol outlined in this study, and the use of dexamethasone in younger patients, has become the standard practice for the treatment of high-risk ALL patients in North America.
Prior to the release of the initial study results, which were first presented last year at the ASCO Annual Meeting, the standard of care for high-risk ALL patients in North America was escalating MTX.
“One of the improvements in outcome for ALL overall has been using methotrexate in a more intense fashion, by giving higher doses,” said study investigator William L. Carroll, MD, of NYU Langone Medical Center in New York, New York.
“We designed this study to compare high-dose and escalating methotrexate to determine the best way to use this drug to increase the survival of high-risk ALL patients.”
Treatment
Between January 2004 and January 2011, Dr Carroll and his colleagues enrolled 3154 patients, ages 1 to 30, with newly diagnosed, high-risk B-ALL. After exclusions, 2914 patients were randomized to treatment.
Using a 2 × 2 factorial design, the patients were randomized to receive dexamethasone for 14 days or prednisone for 28 days during induction and high-dose MTX or Capizzi escalating-dose MTX plus pegaspargase during interim maintenance 1.
So the treatment groups were as follows:
- Prednisone and escalating MTX (n=926)
- Prednisone and high-dose MTX (n=926)
- Dexamethasone and escalating MTX (n=535)
- Dexamethasone and high-dose MTX (n=527).
MTX results
At the planned interim analysis, the 5-year EFS was 82% among patients who received high-dose MTX and 75.4% among those who received escalating MTX (P=0.006).
The final data showed 5-year EFS rates of 79.6% and 75.2%, respectively (P=0.008) and 5-year overall survival rates of 88.9% and 86.1%, respectively (P=0.025).
There was a higher rate of febrile neutropenia during interim maintenance 1 among patients who received escalating MTX than among those who received high-dose MTX—8.3% and 5.1%, respectively (P=0.003).
There were 5 cases of ischemic cerebrovascular toxicity among patients who received high-dose MTX and none among the patients who received escalating MTX (P=0.03).
But there were no other significant differences in adverse events between the high-dose and escalating-dose MTX groups.
Corticosteroid results
Patients age 10 and older saw no benefit from dexamethasone, and, in fact, were at much higher risk of developing osteonecrosis. Because of this risk, the corticosteroid induction arm of this study was closed early, in 2008.
However, the investigators found that patients younger than age 10 did benefit from dexamethasone exposure.
Specifically, patients under 10 who received dexamethasone and high-dose MTX had significantly better EFS than patients who received the other 3 treatment regimens.
The 5-year EFS rate was 91.2% in the dexamethasone and high-dose MTX arm, 83.2% in the dexamethasone and escalating MTX arm, 80.8% in the prednisone and high-dose MTX arm, and 82.1% in the prednisone and escalating MTX arm (P=0.015).
For patients of all ages, there was a higher rate of febrile neutropenia during induction among patients who received dexamethasone than among those who received prednisone—18.2% and 11.0%, respectively (P<0.001).
Patients who received dexamethasone also had a higher rate of infections/infestations—29.4% and 20.3%, respectively (P<0.001).
However, there was no significant difference in induction death rate—1.9% and 1.8%, respectively (P=0.87). The same was true when the investigators looked only at patients younger than 10 (P=0.71) or at patients 10 and older (P=0.69).
Among patients ages 10 and older who participated in the induction corticosteroid randomization before it was closed, the 5-year cumulative incidence of osteonecrosis was 24.3% for patients who received dexamethasone and 15.9% for those who received prednisone (P=0.001).
There were no other significant differences in adverse events between the 2 corticosteroid regimens. ![]()

Photo by Bill Branson
High-dose methotrexate (MTX) is more effective than escalating doses of MTX for young patients with high-risk B-cell acute lymphoblastic leukemia (B-ALL), according to a study published in the Journal of Clinical Oncology.
Patients who received high-dose MTX during interim maintenance 1 had significantly better event-free survival (EFS) than those who received escalating MTX.
In addition, the study showed that substituting dexamethasone for prednisone during induction was beneficial for younger—but not older—patients.
The high-dose MTX protocol outlined in this study, and the use of dexamethasone in younger patients, has become the standard practice for the treatment of high-risk ALL patients in North America.
Prior to the release of the initial study results, which were first presented last year at the ASCO Annual Meeting, the standard of care for high-risk ALL patients in North America was escalating MTX.
“One of the improvements in outcome for ALL overall has been using methotrexate in a more intense fashion, by giving higher doses,” said study investigator William L. Carroll, MD, of NYU Langone Medical Center in New York, New York.
“We designed this study to compare high-dose and escalating methotrexate to determine the best way to use this drug to increase the survival of high-risk ALL patients.”
Treatment
Between January 2004 and January 2011, Dr Carroll and his colleagues enrolled 3154 patients, ages 1 to 30, with newly diagnosed, high-risk B-ALL. After exclusions, 2914 patients were randomized to treatment.
Using a 2 × 2 factorial design, the patients were randomized to receive dexamethasone for 14 days or prednisone for 28 days during induction and high-dose MTX or Capizzi escalating-dose MTX plus pegaspargase during interim maintenance 1.
So the treatment groups were as follows:
- Prednisone and escalating MTX (n=926)
- Prednisone and high-dose MTX (n=926)
- Dexamethasone and escalating MTX (n=535)
- Dexamethasone and high-dose MTX (n=527).
MTX results
At the planned interim analysis, the 5-year EFS was 82% among patients who received high-dose MTX and 75.4% among those who received escalating MTX (P=0.006).
The final data showed 5-year EFS rates of 79.6% and 75.2%, respectively (P=0.008) and 5-year overall survival rates of 88.9% and 86.1%, respectively (P=0.025).
There was a higher rate of febrile neutropenia during interim maintenance 1 among patients who received escalating MTX than among those who received high-dose MTX—8.3% and 5.1%, respectively (P=0.003).
There were 5 cases of ischemic cerebrovascular toxicity among patients who received high-dose MTX and none among the patients who received escalating MTX (P=0.03).
But there were no other significant differences in adverse events between the high-dose and escalating-dose MTX groups.
Corticosteroid results
Patients age 10 and older saw no benefit from dexamethasone, and, in fact, were at much higher risk of developing osteonecrosis. Because of this risk, the corticosteroid induction arm of this study was closed early, in 2008.
However, the investigators found that patients younger than age 10 did benefit from dexamethasone exposure.
Specifically, patients under 10 who received dexamethasone and high-dose MTX had significantly better EFS than patients who received the other 3 treatment regimens.
The 5-year EFS rate was 91.2% in the dexamethasone and high-dose MTX arm, 83.2% in the dexamethasone and escalating MTX arm, 80.8% in the prednisone and high-dose MTX arm, and 82.1% in the prednisone and escalating MTX arm (P=0.015).
For patients of all ages, there was a higher rate of febrile neutropenia during induction among patients who received dexamethasone than among those who received prednisone—18.2% and 11.0%, respectively (P<0.001).
Patients who received dexamethasone also had a higher rate of infections/infestations—29.4% and 20.3%, respectively (P<0.001).
However, there was no significant difference in induction death rate—1.9% and 1.8%, respectively (P=0.87). The same was true when the investigators looked only at patients younger than 10 (P=0.71) or at patients 10 and older (P=0.69).
Among patients ages 10 and older who participated in the induction corticosteroid randomization before it was closed, the 5-year cumulative incidence of osteonecrosis was 24.3% for patients who received dexamethasone and 15.9% for those who received prednisone (P=0.001).
There were no other significant differences in adverse events between the 2 corticosteroid regimens. ![]()

Photo by Bill Branson
High-dose methotrexate (MTX) is more effective than escalating doses of MTX for young patients with high-risk B-cell acute lymphoblastic leukemia (B-ALL), according to a study published in the Journal of Clinical Oncology.
Patients who received high-dose MTX during interim maintenance 1 had significantly better event-free survival (EFS) than those who received escalating MTX.
In addition, the study showed that substituting dexamethasone for prednisone during induction was beneficial for younger—but not older—patients.
The high-dose MTX protocol outlined in this study, and the use of dexamethasone in younger patients, has become the standard practice for the treatment of high-risk ALL patients in North America.
Prior to the release of the initial study results, which were first presented last year at the ASCO Annual Meeting, the standard of care for high-risk ALL patients in North America was escalating MTX.
“One of the improvements in outcome for ALL overall has been using methotrexate in a more intense fashion, by giving higher doses,” said study investigator William L. Carroll, MD, of NYU Langone Medical Center in New York, New York.
“We designed this study to compare high-dose and escalating methotrexate to determine the best way to use this drug to increase the survival of high-risk ALL patients.”
Treatment
Between January 2004 and January 2011, Dr Carroll and his colleagues enrolled 3154 patients, ages 1 to 30, with newly diagnosed, high-risk B-ALL. After exclusions, 2914 patients were randomized to treatment.
Using a 2 × 2 factorial design, the patients were randomized to receive dexamethasone for 14 days or prednisone for 28 days during induction and high-dose MTX or Capizzi escalating-dose MTX plus pegaspargase during interim maintenance 1.
So the treatment groups were as follows:
- Prednisone and escalating MTX (n=926)
- Prednisone and high-dose MTX (n=926)
- Dexamethasone and escalating MTX (n=535)
- Dexamethasone and high-dose MTX (n=527).
MTX results
At the planned interim analysis, the 5-year EFS was 82% among patients who received high-dose MTX and 75.4% among those who received escalating MTX (P=0.006).
The final data showed 5-year EFS rates of 79.6% and 75.2%, respectively (P=0.008) and 5-year overall survival rates of 88.9% and 86.1%, respectively (P=0.025).
There was a higher rate of febrile neutropenia during interim maintenance 1 among patients who received escalating MTX than among those who received high-dose MTX—8.3% and 5.1%, respectively (P=0.003).
There were 5 cases of ischemic cerebrovascular toxicity among patients who received high-dose MTX and none among the patients who received escalating MTX (P=0.03).
But there were no other significant differences in adverse events between the high-dose and escalating-dose MTX groups.
Corticosteroid results
Patients age 10 and older saw no benefit from dexamethasone, and, in fact, were at much higher risk of developing osteonecrosis. Because of this risk, the corticosteroid induction arm of this study was closed early, in 2008.
However, the investigators found that patients younger than age 10 did benefit from dexamethasone exposure.
Specifically, patients under 10 who received dexamethasone and high-dose MTX had significantly better EFS than patients who received the other 3 treatment regimens.
The 5-year EFS rate was 91.2% in the dexamethasone and high-dose MTX arm, 83.2% in the dexamethasone and escalating MTX arm, 80.8% in the prednisone and high-dose MTX arm, and 82.1% in the prednisone and escalating MTX arm (P=0.015).
For patients of all ages, there was a higher rate of febrile neutropenia during induction among patients who received dexamethasone than among those who received prednisone—18.2% and 11.0%, respectively (P<0.001).
Patients who received dexamethasone also had a higher rate of infections/infestations—29.4% and 20.3%, respectively (P<0.001).
However, there was no significant difference in induction death rate—1.9% and 1.8%, respectively (P=0.87). The same was true when the investigators looked only at patients younger than 10 (P=0.71) or at patients 10 and older (P=0.69).
Among patients ages 10 and older who participated in the induction corticosteroid randomization before it was closed, the 5-year cumulative incidence of osteonecrosis was 24.3% for patients who received dexamethasone and 15.9% for those who received prednisone (P=0.001).
There were no other significant differences in adverse events between the 2 corticosteroid regimens. ![]()
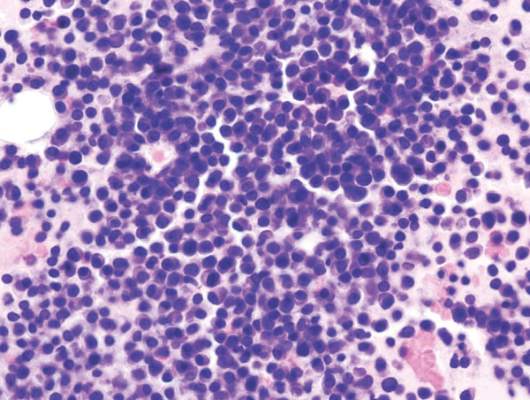
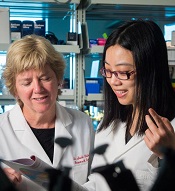
Factors may increase risk of asparaginase-induced pancreatitis in ALL
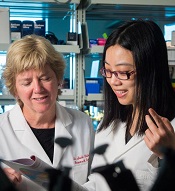
(left) and Chengcheng Liu
Photo courtesy of St. Jude
Children’s Research Hospital
and Peter Barta
Researchers have identified several factors that may increase the risk of asparaginase-induced pancreatitis in patients with acute lymphoblastic leukemia (ALL).
The team found that 16 variants in the CPA2 gene—and 1 rare variant in particular—were associated with a higher risk of asparaginase-induced pancreatitis.
Patients also had a higher risk if they had genetically defined Native American ancestry, were older, and received higher doses of asparaginase.
The researchers reported these findings in the Journal of Clinical Oncology.
“In this study, we identified several independent risk factors for asparaginase-induced pancreatitis and also gained insight into the mechanism responsible for this serious treatment complication,” said study author Mary Relling, PharmD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“Understanding the risk factors for acute pancreatitis is important because, in patients who can tolerate the drug, asparaginase reduces the likelihood that ALL patients will relapse.”
The research included 5398 ALL patients (ages 0 to 30) who were treated in clinical trials organized by St. Jude or the Children’s Oncology Group. In all, 188 patients developed pancreatitis at least once during ALL therapy.
To search for risk factors associated with asparaginase-induced pancreatitis, the researchers checked patient DNA for more than 920,000 gene variants.
The team also sequenced 283 genes, including genes associated with ALL risk and treatment outcome and genes linked to an elevated risk of pancreatitis in patients with different health problems.
The results revealed a rare nonsense variant in CPA2 (rs199695765) that yields a truncated version of the pancreatic enzyme proCPA2. The researchers said this variant was “highly associated” with pancreatitis, with a hazard ratio (HR) of 587 (P=9.0×10−9).
Two study participants each carried 1 copy of the variant, and both patients developed severe pancreatitis within weeks of receiving their first dose of asparaginase.
“That suggests patients with this rare variant cannot tolerate the drug long enough to benefit from treatment,” Dr Relling said. “For these patients, ALL treatment regimens that do not depend on asparaginase may be preferable.”
The researchers estimated that about 9 in 100,000 individuals carry the suspected high-risk CPA2 variant.
The team also found an excess of additional CPA2 variants in patients who developed pancreatitis compared to those who did not (P=0.001).
In all, the researchers identified 380 variants in CPA2. Sixteen of them were significantly associated (P<0.05) with pancreatitis, and 54% (13/24) of patients who carried at least 1 of these variants developed pancreatitis.
The researchers also found links between clinical factors and asparaginase-induced pancreatitis. A multivariate analysis suggested the following were associated with pancreatitis:
- Older age (HR=1.1 per year; P<0.001)
- Genetically defined Native American ancestry (HR=1.2 for every 10% increase in Native American ancestry; P<0.001)
- High-dose (≥240,000 U/m2) asparaginase regimens (HR=3.2; P<0.001).

(left) and Chengcheng Liu
Photo courtesy of St. Jude
Children’s Research Hospital
and Peter Barta
Researchers have identified several factors that may increase the risk of asparaginase-induced pancreatitis in patients with acute lymphoblastic leukemia (ALL).
The team found that 16 variants in the CPA2 gene—and 1 rare variant in particular—were associated with a higher risk of asparaginase-induced pancreatitis.
Patients also had a higher risk if they had genetically defined Native American ancestry, were older, and received higher doses of asparaginase.
The researchers reported these findings in the Journal of Clinical Oncology.
“In this study, we identified several independent risk factors for asparaginase-induced pancreatitis and also gained insight into the mechanism responsible for this serious treatment complication,” said study author Mary Relling, PharmD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“Understanding the risk factors for acute pancreatitis is important because, in patients who can tolerate the drug, asparaginase reduces the likelihood that ALL patients will relapse.”
The research included 5398 ALL patients (ages 0 to 30) who were treated in clinical trials organized by St. Jude or the Children’s Oncology Group. In all, 188 patients developed pancreatitis at least once during ALL therapy.
To search for risk factors associated with asparaginase-induced pancreatitis, the researchers checked patient DNA for more than 920,000 gene variants.
The team also sequenced 283 genes, including genes associated with ALL risk and treatment outcome and genes linked to an elevated risk of pancreatitis in patients with different health problems.
The results revealed a rare nonsense variant in CPA2 (rs199695765) that yields a truncated version of the pancreatic enzyme proCPA2. The researchers said this variant was “highly associated” with pancreatitis, with a hazard ratio (HR) of 587 (P=9.0×10−9).
Two study participants each carried 1 copy of the variant, and both patients developed severe pancreatitis within weeks of receiving their first dose of asparaginase.
“That suggests patients with this rare variant cannot tolerate the drug long enough to benefit from treatment,” Dr Relling said. “For these patients, ALL treatment regimens that do not depend on asparaginase may be preferable.”
The researchers estimated that about 9 in 100,000 individuals carry the suspected high-risk CPA2 variant.
The team also found an excess of additional CPA2 variants in patients who developed pancreatitis compared to those who did not (P=0.001).
In all, the researchers identified 380 variants in CPA2. Sixteen of them were significantly associated (P<0.05) with pancreatitis, and 54% (13/24) of patients who carried at least 1 of these variants developed pancreatitis.
The researchers also found links between clinical factors and asparaginase-induced pancreatitis. A multivariate analysis suggested the following were associated with pancreatitis:
- Older age (HR=1.1 per year; P<0.001)
- Genetically defined Native American ancestry (HR=1.2 for every 10% increase in Native American ancestry; P<0.001)
- High-dose (≥240,000 U/m2) asparaginase regimens (HR=3.2; P<0.001).

(left) and Chengcheng Liu
Photo courtesy of St. Jude
Children’s Research Hospital
and Peter Barta
Researchers have identified several factors that may increase the risk of asparaginase-induced pancreatitis in patients with acute lymphoblastic leukemia (ALL).
The team found that 16 variants in the CPA2 gene—and 1 rare variant in particular—were associated with a higher risk of asparaginase-induced pancreatitis.
Patients also had a higher risk if they had genetically defined Native American ancestry, were older, and received higher doses of asparaginase.
The researchers reported these findings in the Journal of Clinical Oncology.
“In this study, we identified several independent risk factors for asparaginase-induced pancreatitis and also gained insight into the mechanism responsible for this serious treatment complication,” said study author Mary Relling, PharmD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“Understanding the risk factors for acute pancreatitis is important because, in patients who can tolerate the drug, asparaginase reduces the likelihood that ALL patients will relapse.”
The research included 5398 ALL patients (ages 0 to 30) who were treated in clinical trials organized by St. Jude or the Children’s Oncology Group. In all, 188 patients developed pancreatitis at least once during ALL therapy.
To search for risk factors associated with asparaginase-induced pancreatitis, the researchers checked patient DNA for more than 920,000 gene variants.
The team also sequenced 283 genes, including genes associated with ALL risk and treatment outcome and genes linked to an elevated risk of pancreatitis in patients with different health problems.
The results revealed a rare nonsense variant in CPA2 (rs199695765) that yields a truncated version of the pancreatic enzyme proCPA2. The researchers said this variant was “highly associated” with pancreatitis, with a hazard ratio (HR) of 587 (P=9.0×10−9).
Two study participants each carried 1 copy of the variant, and both patients developed severe pancreatitis within weeks of receiving their first dose of asparaginase.
“That suggests patients with this rare variant cannot tolerate the drug long enough to benefit from treatment,” Dr Relling said. “For these patients, ALL treatment regimens that do not depend on asparaginase may be preferable.”
The researchers estimated that about 9 in 100,000 individuals carry the suspected high-risk CPA2 variant.
The team also found an excess of additional CPA2 variants in patients who developed pancreatitis compared to those who did not (P=0.001).
In all, the researchers identified 380 variants in CPA2. Sixteen of them were significantly associated (P<0.05) with pancreatitis, and 54% (13/24) of patients who carried at least 1 of these variants developed pancreatitis.
The researchers also found links between clinical factors and asparaginase-induced pancreatitis. A multivariate analysis suggested the following were associated with pancreatitis:
- Older age (HR=1.1 per year; P<0.001)
- Genetically defined Native American ancestry (HR=1.2 for every 10% increase in Native American ancestry; P<0.001)
- High-dose (≥240,000 U/m2) asparaginase regimens (HR=3.2; P<0.001).

NIH stops production at 2 facilities

Photo by Daniel Sone
The National Institutes of Health (NIH) has suspended production in 2 of its facilities—a National Cancer Institute (NCI) laboratory engaged in the production of cell therapies and a National Institute of Mental Health facility producing positron emission tomography (PET) materials.
Last year, an inspection by the US Food and Drug Administration revealed problems with facilities, equipment, procedures, and training in the NIH Clinical Center Pharmaceutical Development Section (PDS), which is responsible for managing investigational drugs.
So the NIH closed the sterile production unit of the PDS and hired 2 companies specializing in quality assurance for manufacturing and compounding—Working Buildings and Clinical IQ—to evaluate all NIH facilities producing sterile or infused products for administration to research participants.
This review is still underway, and preliminary findings have identified facilities not in compliance with quality and safety standards, and not suitable for the production of sterile or infused products.
As a result, the NIH suspended production in the aforementioned facilities manufacturing cell therapy and PET materials.
The NIH said there is no evidence that any patients have been harmed, but a rigorous clinical review will be conducted. And the NIH will not enroll new patients in affected trials until the issues are resolved.
The NCI facility produces cell therapies in cooperation with Kite Pharma, Inc. The company and the NCI are advancing multiple clinical trials under Cooperative Research and Development Agreements for the treatment of hematologic malignancies and solid tumors.
Patients currently enrolled in ongoing NCI trials of cell therapy will continue to receive treatment, but no new patients will be enrolled until the review is complete.
And Kite Pharma said its 4 trials of the chimeric antigen receptor T-cell therapy KTE-C19 will continue. This includes:
ZUMA-1—KTE-C19 in patients with refractory, aggressive non-Hodgkin lymphoma
ZUMA-2—KTE-C19 in patients with relapsed/refractory mantle cell lymphoma
ZUMA-3—KTE-C19 in adults with relapsed/refractory B-precursor acute lymphoblastic leukemia
ZUMA-4—KTE-C19 in pediatric and adolescent patients with relapsed/refractory B-precursor acute lymphoblastic leukemia.
The company stressed that the review of the NCI’s manufacturing facilities is not related to KTE-C19 or Kite’s manufacturing capabilities. ![]()

Photo by Daniel Sone
The National Institutes of Health (NIH) has suspended production in 2 of its facilities—a National Cancer Institute (NCI) laboratory engaged in the production of cell therapies and a National Institute of Mental Health facility producing positron emission tomography (PET) materials.
Last year, an inspection by the US Food and Drug Administration revealed problems with facilities, equipment, procedures, and training in the NIH Clinical Center Pharmaceutical Development Section (PDS), which is responsible for managing investigational drugs.
So the NIH closed the sterile production unit of the PDS and hired 2 companies specializing in quality assurance for manufacturing and compounding—Working Buildings and Clinical IQ—to evaluate all NIH facilities producing sterile or infused products for administration to research participants.
This review is still underway, and preliminary findings have identified facilities not in compliance with quality and safety standards, and not suitable for the production of sterile or infused products.
As a result, the NIH suspended production in the aforementioned facilities manufacturing cell therapy and PET materials.
The NIH said there is no evidence that any patients have been harmed, but a rigorous clinical review will be conducted. And the NIH will not enroll new patients in affected trials until the issues are resolved.
The NCI facility produces cell therapies in cooperation with Kite Pharma, Inc. The company and the NCI are advancing multiple clinical trials under Cooperative Research and Development Agreements for the treatment of hematologic malignancies and solid tumors.
Patients currently enrolled in ongoing NCI trials of cell therapy will continue to receive treatment, but no new patients will be enrolled until the review is complete.
And Kite Pharma said its 4 trials of the chimeric antigen receptor T-cell therapy KTE-C19 will continue. This includes:
ZUMA-1—KTE-C19 in patients with refractory, aggressive non-Hodgkin lymphoma
ZUMA-2—KTE-C19 in patients with relapsed/refractory mantle cell lymphoma
ZUMA-3—KTE-C19 in adults with relapsed/refractory B-precursor acute lymphoblastic leukemia
ZUMA-4—KTE-C19 in pediatric and adolescent patients with relapsed/refractory B-precursor acute lymphoblastic leukemia.
The company stressed that the review of the NCI’s manufacturing facilities is not related to KTE-C19 or Kite’s manufacturing capabilities. ![]()

Photo by Daniel Sone
The National Institutes of Health (NIH) has suspended production in 2 of its facilities—a National Cancer Institute (NCI) laboratory engaged in the production of cell therapies and a National Institute of Mental Health facility producing positron emission tomography (PET) materials.
Last year, an inspection by the US Food and Drug Administration revealed problems with facilities, equipment, procedures, and training in the NIH Clinical Center Pharmaceutical Development Section (PDS), which is responsible for managing investigational drugs.
So the NIH closed the sterile production unit of the PDS and hired 2 companies specializing in quality assurance for manufacturing and compounding—Working Buildings and Clinical IQ—to evaluate all NIH facilities producing sterile or infused products for administration to research participants.
This review is still underway, and preliminary findings have identified facilities not in compliance with quality and safety standards, and not suitable for the production of sterile or infused products.
As a result, the NIH suspended production in the aforementioned facilities manufacturing cell therapy and PET materials.
The NIH said there is no evidence that any patients have been harmed, but a rigorous clinical review will be conducted. And the NIH will not enroll new patients in affected trials until the issues are resolved.
The NCI facility produces cell therapies in cooperation with Kite Pharma, Inc. The company and the NCI are advancing multiple clinical trials under Cooperative Research and Development Agreements for the treatment of hematologic malignancies and solid tumors.
Patients currently enrolled in ongoing NCI trials of cell therapy will continue to receive treatment, but no new patients will be enrolled until the review is complete.
And Kite Pharma said its 4 trials of the chimeric antigen receptor T-cell therapy KTE-C19 will continue. This includes:
ZUMA-1—KTE-C19 in patients with refractory, aggressive non-Hodgkin lymphoma
ZUMA-2—KTE-C19 in patients with relapsed/refractory mantle cell lymphoma
ZUMA-3—KTE-C19 in adults with relapsed/refractory B-precursor acute lymphoblastic leukemia
ZUMA-4—KTE-C19 in pediatric and adolescent patients with relapsed/refractory B-precursor acute lymphoblastic leukemia.
The company stressed that the review of the NCI’s manufacturing facilities is not related to KTE-C19 or Kite’s manufacturing capabilities. ![]()
CML: T3151 plus additional mutations predicts poor response to ponatinib
Depending on the number and type of BCR-ABL1 mutations, certain patients with chronic myeloid leukemia may have a better response to ponatinib than to other tyrosine kinase inhibitors, according to a report published in Blood.
For patients with CML treated with first- or second-generation tyrosine kinase inhibitors such as imatinib, nilotinib, and dasatinib, the most common cause of treatment failure is the acquisition of mutations in the BCR-ABL1 gene, particularly the T315I mutation, which interfere with drug binding and eventually confer drug resistance. Some of these cancers have proved susceptible to ponatinib, but treatment response varies among patients, said Dr. Wendy T. Parker of the Australian Cancer Research Foundation (ACRF) Cancer Genomics Facility, the Center for Cancer Biology, and the University of Adelaide (Australia) and her associates.
They retrospectively assessed peripheral blood samples from 363 CML patients who had taken part in a phase II study of ponatinib therapy, using their newly developed mass spectrometry–based mutation detection assay to determine which mutations correlated with which treatment outcomes. These study participants contributed blood samples before, during, and after ponatinib treatment. The mass spectrometry–based assay can detect BCR-ABL1 KD mutations present at levels between 10- and 100-fold below those detectable using conventional Sanger sequencing, the researchers said (Blood. 2016;127[15]:1870-80).
Patients who had the T315I mutation plus additional mutations at baseline (32% of the study population) had significantly worse treatment responses and significantly worse outcomes than those who had only the T315I mutation at baseline. “Consequently, these patients may benefit from close monitoring, experimental approaches, or stem-cell transplantation to reduce the risk of tyrosine kinase inhibitor failure,” Dr. Parker and her associates said.
In addition, patients who didn’t have the T315I mutation but had multiple other mutations at baseline responded well to ponatinib. Historically, such patients have not responded well to first- or second-generation tyrosine kinase inhibitors, but ponatinib may prove to be a particularly effective option for this patient population, the investigators said (Blood. 2016;127[15]:1870-80).
These findings demonstrate that mutation analysis, such as that provided by their mass spectrometry–based assay, can be used to guide therapy even after patients have failed on some tyrosine kinase inhibitors, they added.
The study was supported by the maker of ponatinib (Iclusig) Ariad Pharmaceuticals, the Leukemia Foundation of Australia, and the A.R. Clarkson Foundation. Dr. Parker reported having no relevant financial disclosures; some of her associates were employed by Ariad.
Depending on the number and type of BCR-ABL1 mutations, certain patients with chronic myeloid leukemia may have a better response to ponatinib than to other tyrosine kinase inhibitors, according to a report published in Blood.
For patients with CML treated with first- or second-generation tyrosine kinase inhibitors such as imatinib, nilotinib, and dasatinib, the most common cause of treatment failure is the acquisition of mutations in the BCR-ABL1 gene, particularly the T315I mutation, which interfere with drug binding and eventually confer drug resistance. Some of these cancers have proved susceptible to ponatinib, but treatment response varies among patients, said Dr. Wendy T. Parker of the Australian Cancer Research Foundation (ACRF) Cancer Genomics Facility, the Center for Cancer Biology, and the University of Adelaide (Australia) and her associates.
They retrospectively assessed peripheral blood samples from 363 CML patients who had taken part in a phase II study of ponatinib therapy, using their newly developed mass spectrometry–based mutation detection assay to determine which mutations correlated with which treatment outcomes. These study participants contributed blood samples before, during, and after ponatinib treatment. The mass spectrometry–based assay can detect BCR-ABL1 KD mutations present at levels between 10- and 100-fold below those detectable using conventional Sanger sequencing, the researchers said (Blood. 2016;127[15]:1870-80).
Patients who had the T315I mutation plus additional mutations at baseline (32% of the study population) had significantly worse treatment responses and significantly worse outcomes than those who had only the T315I mutation at baseline. “Consequently, these patients may benefit from close monitoring, experimental approaches, or stem-cell transplantation to reduce the risk of tyrosine kinase inhibitor failure,” Dr. Parker and her associates said.
In addition, patients who didn’t have the T315I mutation but had multiple other mutations at baseline responded well to ponatinib. Historically, such patients have not responded well to first- or second-generation tyrosine kinase inhibitors, but ponatinib may prove to be a particularly effective option for this patient population, the investigators said (Blood. 2016;127[15]:1870-80).
These findings demonstrate that mutation analysis, such as that provided by their mass spectrometry–based assay, can be used to guide therapy even after patients have failed on some tyrosine kinase inhibitors, they added.
The study was supported by the maker of ponatinib (Iclusig) Ariad Pharmaceuticals, the Leukemia Foundation of Australia, and the A.R. Clarkson Foundation. Dr. Parker reported having no relevant financial disclosures; some of her associates were employed by Ariad.
Depending on the number and type of BCR-ABL1 mutations, certain patients with chronic myeloid leukemia may have a better response to ponatinib than to other tyrosine kinase inhibitors, according to a report published in Blood.
For patients with CML treated with first- or second-generation tyrosine kinase inhibitors such as imatinib, nilotinib, and dasatinib, the most common cause of treatment failure is the acquisition of mutations in the BCR-ABL1 gene, particularly the T315I mutation, which interfere with drug binding and eventually confer drug resistance. Some of these cancers have proved susceptible to ponatinib, but treatment response varies among patients, said Dr. Wendy T. Parker of the Australian Cancer Research Foundation (ACRF) Cancer Genomics Facility, the Center for Cancer Biology, and the University of Adelaide (Australia) and her associates.
They retrospectively assessed peripheral blood samples from 363 CML patients who had taken part in a phase II study of ponatinib therapy, using their newly developed mass spectrometry–based mutation detection assay to determine which mutations correlated with which treatment outcomes. These study participants contributed blood samples before, during, and after ponatinib treatment. The mass spectrometry–based assay can detect BCR-ABL1 KD mutations present at levels between 10- and 100-fold below those detectable using conventional Sanger sequencing, the researchers said (Blood. 2016;127[15]:1870-80).
Patients who had the T315I mutation plus additional mutations at baseline (32% of the study population) had significantly worse treatment responses and significantly worse outcomes than those who had only the T315I mutation at baseline. “Consequently, these patients may benefit from close monitoring, experimental approaches, or stem-cell transplantation to reduce the risk of tyrosine kinase inhibitor failure,” Dr. Parker and her associates said.
In addition, patients who didn’t have the T315I mutation but had multiple other mutations at baseline responded well to ponatinib. Historically, such patients have not responded well to first- or second-generation tyrosine kinase inhibitors, but ponatinib may prove to be a particularly effective option for this patient population, the investigators said (Blood. 2016;127[15]:1870-80).
These findings demonstrate that mutation analysis, such as that provided by their mass spectrometry–based assay, can be used to guide therapy even after patients have failed on some tyrosine kinase inhibitors, they added.
The study was supported by the maker of ponatinib (Iclusig) Ariad Pharmaceuticals, the Leukemia Foundation of Australia, and the A.R. Clarkson Foundation. Dr. Parker reported having no relevant financial disclosures; some of her associates were employed by Ariad.
FROM BLOOD
Key clinical point: The third-generation tyrosine kinase inhibitor ponatinib appears to be more effective than its predecessors against certain cases of chronic myeloid leukemia defined by the number and type of BCR-ABL1 mutations that patients have.
Major finding: Patients who had the T315I mutation plus additional mutations at baseline (32% of the study population) had significantly worse treatment responses and outcomes than those who had only the T315I mutation and those who had multiple other mutations.
Data source: A retrospective secondary analysis of data from a phase II clinical trial involving 363 patients with CML.
Disclosures: This study was supported by the maker of ponatinib (Iclusig) Ariad Pharmaceuticals, the Leukemia Foundation of Australia, and the A.R. Clarkson Foundation. Dr. Parker reported having no relevant financial disclosures; some of her associates were employed by Ariad.
Daratumumab well tolerated, effective in heavily treated multiple myeloma
Daratumumab monotherapy was associated with an overall response rate of 29.2% and was well tolerated in 106 heavily treated patients with multiple myeloma, based on results from the SIRIUS trial.
Of 106 patients who received daratumumab at 16 mg/kg, 3% achieved a stringent complete response, 9% had a very good partial response, and 17% had a partial response. The median progression-free survival was 3.7 months and median duration of response was 7.4 months. The 12-month overall survival was 64·8%, and, at a subsequent cutoff, median overall survival was 17.5 months.
All of the study patients had been treated with proteasome inhibitors and immunomodulatory drugs, with a median of five previous therapies. Most patients (80%) had received autologous stem cell transplantation, and 97% were refractory to the last line of therapy before study enrollment.
“Resistance to any previous therapy had no effect on the activity of daratumumab, lending support to a novel mechanism of action, but these findings need to be confirmed in larger studies,” wrote Dr. Sagar Lonial of Emory University, Atlanta, and colleagues (Lancet 2016;387:1551-60). Response rates were similar for patients with moderate renal impairment, those over age 75, and those with extramedullary disease or high-risk baseline cytogenetic characteristics.
Daratumumab was well tolerated, and none of the patients discontinued treatment because of treatment-related adverse events. The most common adverse events of any grade were anemia (33%), thrombocytopenia (25%), and neutropenia (23%). Additional supportive care in the form of red blood cell transfusions was received by 38% of patients, platelet transfusions by 13%, and granulocyte colony-stimulating factor by 8%. Fatigue (40%) and nausea (29%) were the most common nonhematologic adverse events. Serious adverse events were observed in 30% of patients.
Daratumumab compares favorably with other regimens such as pomalidomide alone or with dexamethasone or carfilzomib monotherapy, according to the investigators.
The favorable safety profile of daratumumab makes it an attractive candidate for combination regimens, the authors noted, and daratumumab combined with other backbone agents are currently under investigation.
This study was sponsored by Janssen, maker of daratumumab (Darzalex). Dr. Lonial reported consulting or advisory roles with Janssen and several other drug companies.
With its novel mechanism of action, single-agent activity, absence of crossresistance, and tolerability, daratumumab may prove to be a transformative new treatment for multiple myeloma.
 |
| Patrice Wendling/Frontline Medical News Dr. S. Vincent Rajkumar |
The single-agent activity of daratumumab (29%) exceeds that of bortezomib (27%), lenalidomide (26%), carfilzomib (24%), or pomalidomide (18%), even in a heavily pretreated population.
The safety profile is outstanding, and therein lies the reason for enthusiasm: Daratumumab can probably be combined with currently used triplet combinations in multiple myeloma, and can potentially take these highly active regimens to new heights.
Similar to rituximab, daratumumab will probably be added to many active triplet combinations. Daratumumab will likely move rapidly to a front-line setting in clinical trials for treatment of newly diagnosed multiple myeloma, maintenance therapy, and even smoldering multiple myeloma.
However, the data are insufficient to determine the cytogenetic subtypes that respond best to daratumumab. That information will be necessary in order to best sequence drugs according to the subtype of myeloma.
It will be important also to understand how daratumumab, an anti-CD38 drug, can work optimally with elotuzumab, another newly approved monoclonal antibody that targets SLAMF7.
Dr. S. Vincent Rajkumar is with the Mayo Clinic, Rochester, Minn. These remarks were part of an editorial (Lancet 2016; 387:1490-91) accompanying the study in the Lancet.
With its novel mechanism of action, single-agent activity, absence of crossresistance, and tolerability, daratumumab may prove to be a transformative new treatment for multiple myeloma.
 |
| Patrice Wendling/Frontline Medical News Dr. S. Vincent Rajkumar |
The single-agent activity of daratumumab (29%) exceeds that of bortezomib (27%), lenalidomide (26%), carfilzomib (24%), or pomalidomide (18%), even in a heavily pretreated population.
The safety profile is outstanding, and therein lies the reason for enthusiasm: Daratumumab can probably be combined with currently used triplet combinations in multiple myeloma, and can potentially take these highly active regimens to new heights.
Similar to rituximab, daratumumab will probably be added to many active triplet combinations. Daratumumab will likely move rapidly to a front-line setting in clinical trials for treatment of newly diagnosed multiple myeloma, maintenance therapy, and even smoldering multiple myeloma.
However, the data are insufficient to determine the cytogenetic subtypes that respond best to daratumumab. That information will be necessary in order to best sequence drugs according to the subtype of myeloma.
It will be important also to understand how daratumumab, an anti-CD38 drug, can work optimally with elotuzumab, another newly approved monoclonal antibody that targets SLAMF7.
Dr. S. Vincent Rajkumar is with the Mayo Clinic, Rochester, Minn. These remarks were part of an editorial (Lancet 2016; 387:1490-91) accompanying the study in the Lancet.
With its novel mechanism of action, single-agent activity, absence of crossresistance, and tolerability, daratumumab may prove to be a transformative new treatment for multiple myeloma.
 |
| Patrice Wendling/Frontline Medical News Dr. S. Vincent Rajkumar |
The single-agent activity of daratumumab (29%) exceeds that of bortezomib (27%), lenalidomide (26%), carfilzomib (24%), or pomalidomide (18%), even in a heavily pretreated population.
The safety profile is outstanding, and therein lies the reason for enthusiasm: Daratumumab can probably be combined with currently used triplet combinations in multiple myeloma, and can potentially take these highly active regimens to new heights.
Similar to rituximab, daratumumab will probably be added to many active triplet combinations. Daratumumab will likely move rapidly to a front-line setting in clinical trials for treatment of newly diagnosed multiple myeloma, maintenance therapy, and even smoldering multiple myeloma.
However, the data are insufficient to determine the cytogenetic subtypes that respond best to daratumumab. That information will be necessary in order to best sequence drugs according to the subtype of myeloma.
It will be important also to understand how daratumumab, an anti-CD38 drug, can work optimally with elotuzumab, another newly approved monoclonal antibody that targets SLAMF7.
Dr. S. Vincent Rajkumar is with the Mayo Clinic, Rochester, Minn. These remarks were part of an editorial (Lancet 2016; 387:1490-91) accompanying the study in the Lancet.
Daratumumab monotherapy was associated with an overall response rate of 29.2% and was well tolerated in 106 heavily treated patients with multiple myeloma, based on results from the SIRIUS trial.
Of 106 patients who received daratumumab at 16 mg/kg, 3% achieved a stringent complete response, 9% had a very good partial response, and 17% had a partial response. The median progression-free survival was 3.7 months and median duration of response was 7.4 months. The 12-month overall survival was 64·8%, and, at a subsequent cutoff, median overall survival was 17.5 months.
All of the study patients had been treated with proteasome inhibitors and immunomodulatory drugs, with a median of five previous therapies. Most patients (80%) had received autologous stem cell transplantation, and 97% were refractory to the last line of therapy before study enrollment.
“Resistance to any previous therapy had no effect on the activity of daratumumab, lending support to a novel mechanism of action, but these findings need to be confirmed in larger studies,” wrote Dr. Sagar Lonial of Emory University, Atlanta, and colleagues (Lancet 2016;387:1551-60). Response rates were similar for patients with moderate renal impairment, those over age 75, and those with extramedullary disease or high-risk baseline cytogenetic characteristics.
Daratumumab was well tolerated, and none of the patients discontinued treatment because of treatment-related adverse events. The most common adverse events of any grade were anemia (33%), thrombocytopenia (25%), and neutropenia (23%). Additional supportive care in the form of red blood cell transfusions was received by 38% of patients, platelet transfusions by 13%, and granulocyte colony-stimulating factor by 8%. Fatigue (40%) and nausea (29%) were the most common nonhematologic adverse events. Serious adverse events were observed in 30% of patients.
Daratumumab compares favorably with other regimens such as pomalidomide alone or with dexamethasone or carfilzomib monotherapy, according to the investigators.
The favorable safety profile of daratumumab makes it an attractive candidate for combination regimens, the authors noted, and daratumumab combined with other backbone agents are currently under investigation.
This study was sponsored by Janssen, maker of daratumumab (Darzalex). Dr. Lonial reported consulting or advisory roles with Janssen and several other drug companies.
Daratumumab monotherapy was associated with an overall response rate of 29.2% and was well tolerated in 106 heavily treated patients with multiple myeloma, based on results from the SIRIUS trial.
Of 106 patients who received daratumumab at 16 mg/kg, 3% achieved a stringent complete response, 9% had a very good partial response, and 17% had a partial response. The median progression-free survival was 3.7 months and median duration of response was 7.4 months. The 12-month overall survival was 64·8%, and, at a subsequent cutoff, median overall survival was 17.5 months.
All of the study patients had been treated with proteasome inhibitors and immunomodulatory drugs, with a median of five previous therapies. Most patients (80%) had received autologous stem cell transplantation, and 97% were refractory to the last line of therapy before study enrollment.
“Resistance to any previous therapy had no effect on the activity of daratumumab, lending support to a novel mechanism of action, but these findings need to be confirmed in larger studies,” wrote Dr. Sagar Lonial of Emory University, Atlanta, and colleagues (Lancet 2016;387:1551-60). Response rates were similar for patients with moderate renal impairment, those over age 75, and those with extramedullary disease or high-risk baseline cytogenetic characteristics.
Daratumumab was well tolerated, and none of the patients discontinued treatment because of treatment-related adverse events. The most common adverse events of any grade were anemia (33%), thrombocytopenia (25%), and neutropenia (23%). Additional supportive care in the form of red blood cell transfusions was received by 38% of patients, platelet transfusions by 13%, and granulocyte colony-stimulating factor by 8%. Fatigue (40%) and nausea (29%) were the most common nonhematologic adverse events. Serious adverse events were observed in 30% of patients.
Daratumumab compares favorably with other regimens such as pomalidomide alone or with dexamethasone or carfilzomib monotherapy, according to the investigators.
The favorable safety profile of daratumumab makes it an attractive candidate for combination regimens, the authors noted, and daratumumab combined with other backbone agents are currently under investigation.
This study was sponsored by Janssen, maker of daratumumab (Darzalex). Dr. Lonial reported consulting or advisory roles with Janssen and several other drug companies.
FROM THE LANCET
Key clinical point: Daratumumab was well tolerated and showed encouraging activity in heavily treated patients with multiple myeloma.
Major finding: In 106 patients previously treated with a median of five lines of therapy, the overall response rate to daratumumab at 16 mg/kg was 29.2%; 3% achieved a stringent complete response, 9% a very good partial response, and 17% a partial response.
Data sources: Data from the SIRIUS trial for 106 patients in the 16-mg/kg group.
Disclosures: This study was sponsored by Janssen, maker of daratumumab (Darzalex). Dr. Lonial reported consulting or advisory roles with Janssen and several other drug companies.
Chronic conditions decrease HRQOL in CCSs

Photo from Dana-Farber/
Boston Children’s Cancer
and Blood Disorders Center
Young adult survivors of childhood cancer tend to have inferior health-related quality of life (HRQOL) when compared to the general population, according to research published in the Journal of the National Cancer Institute.
Childhood cancer survivors (CCSs) ages 18 to 29 reported overall HRQOL similar to that of people from the general population who were in their 40s.
However, CCSs fared better if they did not have chronic health conditions.
“Our findings indicate survivors’ accelerated aging and also help us understand the health-related risks associated with having had cancer as a child,” said study author Lisa Diller, MD, of Dana-Farber/Boston Children’s Cancer and Blood Disorders Center and Harvard Medical School in Boston, Massachusetts.
“What’s encouraging is that the lower quality of life scores are associated with chronic disease after treatment, not with a history of pediatric cancer itself. If we can prevent treatment-related conditions by changes in the therapy we use for the cancer, then childhood cancer will become an acute, rather than a chronic, illness.”
Dr Diller and her colleagues used information from the Childhood Cancer Survivor Study to compare CCSs (n=7105) and their siblings (n=372) and information from the Medical Expenditures Panel Survey to make comparisons to the general population (n=12,803).
The researchers estimated health utility, a summary measure of quality of life, in these subjects using the Short Form-6D (SF-6D). A score of “1” indicated perfect health, and a score of “0” indicated death.
Results showed that CCSs had significantly lower SF-6D scores than the general population. The mean scores were 0.77 and 0.81, respectively (P<0.001).
But there were no clinically meaningful differences between the CCSs’ siblings and the general population. Their mean SF-6D scores were 0.80 and 0.81, respectively.
Young adult CCSs ages 18 to 29 had a mean score of 0.78, which was roughly equivalent to that reported for 40-to-49-year-old adults in the general population.
However, the presence or absence of chronic health conditions played a role in HRQOL. CCSs who reported no chronic conditions had SF-6D scores similar to the general population, with a mean score of 0.81.
But CCSs with chronic conditions had scores that matched the scores of chronically ill members of the general population. CCSs with 2 chronic conditions had a mean score of 0.77. Those with 3 or more disabling, severe, or life-threatening conditions had a mean score of 0.70.
“By enabling comparisons to the general population, our findings provide context to better understand how the cancer experience may influence the long-term well-being of survivors,” said study author Jennifer Yeh, PhD, of the Harvard T.H. Chan School of Public Health in Boston.
“This is another way to understand the health challenges survivors face and where to focus efforts to improve the long-term health and quality of life of survivors.” ![]()

Photo from Dana-Farber/
Boston Children’s Cancer
and Blood Disorders Center
Young adult survivors of childhood cancer tend to have inferior health-related quality of life (HRQOL) when compared to the general population, according to research published in the Journal of the National Cancer Institute.
Childhood cancer survivors (CCSs) ages 18 to 29 reported overall HRQOL similar to that of people from the general population who were in their 40s.
However, CCSs fared better if they did not have chronic health conditions.
“Our findings indicate survivors’ accelerated aging and also help us understand the health-related risks associated with having had cancer as a child,” said study author Lisa Diller, MD, of Dana-Farber/Boston Children’s Cancer and Blood Disorders Center and Harvard Medical School in Boston, Massachusetts.
“What’s encouraging is that the lower quality of life scores are associated with chronic disease after treatment, not with a history of pediatric cancer itself. If we can prevent treatment-related conditions by changes in the therapy we use for the cancer, then childhood cancer will become an acute, rather than a chronic, illness.”
Dr Diller and her colleagues used information from the Childhood Cancer Survivor Study to compare CCSs (n=7105) and their siblings (n=372) and information from the Medical Expenditures Panel Survey to make comparisons to the general population (n=12,803).
The researchers estimated health utility, a summary measure of quality of life, in these subjects using the Short Form-6D (SF-6D). A score of “1” indicated perfect health, and a score of “0” indicated death.
Results showed that CCSs had significantly lower SF-6D scores than the general population. The mean scores were 0.77 and 0.81, respectively (P<0.001).
But there were no clinically meaningful differences between the CCSs’ siblings and the general population. Their mean SF-6D scores were 0.80 and 0.81, respectively.
Young adult CCSs ages 18 to 29 had a mean score of 0.78, which was roughly equivalent to that reported for 40-to-49-year-old adults in the general population.
However, the presence or absence of chronic health conditions played a role in HRQOL. CCSs who reported no chronic conditions had SF-6D scores similar to the general population, with a mean score of 0.81.
But CCSs with chronic conditions had scores that matched the scores of chronically ill members of the general population. CCSs with 2 chronic conditions had a mean score of 0.77. Those with 3 or more disabling, severe, or life-threatening conditions had a mean score of 0.70.
“By enabling comparisons to the general population, our findings provide context to better understand how the cancer experience may influence the long-term well-being of survivors,” said study author Jennifer Yeh, PhD, of the Harvard T.H. Chan School of Public Health in Boston.
“This is another way to understand the health challenges survivors face and where to focus efforts to improve the long-term health and quality of life of survivors.” ![]()

Photo from Dana-Farber/
Boston Children’s Cancer
and Blood Disorders Center
Young adult survivors of childhood cancer tend to have inferior health-related quality of life (HRQOL) when compared to the general population, according to research published in the Journal of the National Cancer Institute.
Childhood cancer survivors (CCSs) ages 18 to 29 reported overall HRQOL similar to that of people from the general population who were in their 40s.
However, CCSs fared better if they did not have chronic health conditions.
“Our findings indicate survivors’ accelerated aging and also help us understand the health-related risks associated with having had cancer as a child,” said study author Lisa Diller, MD, of Dana-Farber/Boston Children’s Cancer and Blood Disorders Center and Harvard Medical School in Boston, Massachusetts.
“What’s encouraging is that the lower quality of life scores are associated with chronic disease after treatment, not with a history of pediatric cancer itself. If we can prevent treatment-related conditions by changes in the therapy we use for the cancer, then childhood cancer will become an acute, rather than a chronic, illness.”
Dr Diller and her colleagues used information from the Childhood Cancer Survivor Study to compare CCSs (n=7105) and their siblings (n=372) and information from the Medical Expenditures Panel Survey to make comparisons to the general population (n=12,803).
The researchers estimated health utility, a summary measure of quality of life, in these subjects using the Short Form-6D (SF-6D). A score of “1” indicated perfect health, and a score of “0” indicated death.
Results showed that CCSs had significantly lower SF-6D scores than the general population. The mean scores were 0.77 and 0.81, respectively (P<0.001).
But there were no clinically meaningful differences between the CCSs’ siblings and the general population. Their mean SF-6D scores were 0.80 and 0.81, respectively.
Young adult CCSs ages 18 to 29 had a mean score of 0.78, which was roughly equivalent to that reported for 40-to-49-year-old adults in the general population.
However, the presence or absence of chronic health conditions played a role in HRQOL. CCSs who reported no chronic conditions had SF-6D scores similar to the general population, with a mean score of 0.81.
But CCSs with chronic conditions had scores that matched the scores of chronically ill members of the general population. CCSs with 2 chronic conditions had a mean score of 0.77. Those with 3 or more disabling, severe, or life-threatening conditions had a mean score of 0.70.
“By enabling comparisons to the general population, our findings provide context to better understand how the cancer experience may influence the long-term well-being of survivors,” said study author Jennifer Yeh, PhD, of the Harvard T.H. Chan School of Public Health in Boston.
“This is another way to understand the health challenges survivors face and where to focus efforts to improve the long-term health and quality of life of survivors.” ![]()
Change in T-cell distribution predicts LFS, OS in AML

NEW ORLEANS—A phase 4 study has revealed biomarkers that appear to predict the efficacy of treatment with histamine dihydrochloride (HDC) and interleukin-2 (IL-2) in patients with acute myeloid leukemia (AML).
Researchers found that patients who remained in complete remission after 1 cycle of HDC/IL-2 experienced a significant reduction in effector memory T cells (TEM) and a concomitant increase in effector T cells (Teff) during therapy.
This “TEM to Teff transition” was associated with favorable leukemia-free survival (LFS) and overall survival (OS), especially among patients older than 60.
Frida Ewald Sander, PhD, of University of Gothenburg in Sweden, and her colleagues presented this research at the 2016 AACR Annual Meeting (abstract CT116*).
The study was supported by The Swedish Research Council, The Swedish Cancer Society, The Swedish Society for Medical Research, Meda Pharma, and Immune Pharmaceuticals, which markets HDC as Ceplene®.
The combination of HDC and IL-2 is currently approved in more than 30 countries to prevent relapse in AML patients. In this phase 4 study (Re:MISSION), the researchers set out to assess the immunomodulatory properties of this treatment and correlate potential biomarkers with clinical outcomes.
The study included 84 non-transplanted AML patients (ages 18 to 79) in first complete remission. The patients received HDC (0.5 mg SC BID) and human recombinant IL-2 (1MIU SC BID) in 3-week cycles for 18 months. The patients were followed for at least 2 years from the start of immunotherapy to evaluate survival.
The researchers collected blood from the patients before they began HDC/IL-2 therapy and at the end of the first treatment cycle. From these samples, the team assessed the frequency of CD8+ T cells, including naïve T cells (CD45RA+CCR7+), central memory T cells (CD45RO+CCR7+), TEM cells (CD45RO+CCR7-), and Teff cells (CD45RA+CCR7-).
The researchers found that non-relapsing patients experienced a significant reduction in TEM cells (P=0.001) and a significant increase in Teff cells (P=0.007) during cycle 1. However, this effect was not observed in patients who did relapse.
Further analysis revealed that the reduction in TEM cells was significantly associated with favorable LFS and OS in the entire cohort (P=0.0007 and P=0.005, respectively) and among patients over 60 (P<0.0001 and P=0.002, respectively).
Likewise, the increase in Teff cells was associated with favorable LFS and OS in the entire cohort (P=0.07 and P=0.04, respectively) and among patients over 60 (P=0.004 and P=0.0001, respectively).
The concomitant reduction of TEM cells and induction of Teff cells—the TEM to Teff transition—was associated with superior LFS and OS in the overall cohort (P=0.0002 and P=0.002, respectively) and in the over-60 population (P<0.0001 for LFS and OS).
The researchers said these predictors of outcome remained significant when they adjusted for potential confounders (age, risk group classification, number of induction courses required to achieve complete response, and number of consolidation courses).
Therefore, the team concluded that the altered distribution of cytotoxic T cells during treatment with HDC/IL-2 can prognosticate LFS and OS in AML patients, particularly those over 60.
“We believe that the new data may allow a personalized approach to selection of patients who are most likely to benefit from Ceplene/IL-2 treatment in AML—in particular, the older patient population, who have demonstrated almost 100% survival when positive for the T-cell transition biomarkers,” said Miri Ben-Ami, MD, executive vice president of oncology at Immune Pharmaceuticals.
“In addition, current research is revealing the potential synergy between immune checkpoint inhibitors and Ceplene, which could open the possibility of additional therapeutic indications for this combination.” ![]()
*Information in the abstract differs from that presented at the meeting.

NEW ORLEANS—A phase 4 study has revealed biomarkers that appear to predict the efficacy of treatment with histamine dihydrochloride (HDC) and interleukin-2 (IL-2) in patients with acute myeloid leukemia (AML).
Researchers found that patients who remained in complete remission after 1 cycle of HDC/IL-2 experienced a significant reduction in effector memory T cells (TEM) and a concomitant increase in effector T cells (Teff) during therapy.
This “TEM to Teff transition” was associated with favorable leukemia-free survival (LFS) and overall survival (OS), especially among patients older than 60.
Frida Ewald Sander, PhD, of University of Gothenburg in Sweden, and her colleagues presented this research at the 2016 AACR Annual Meeting (abstract CT116*).
The study was supported by The Swedish Research Council, The Swedish Cancer Society, The Swedish Society for Medical Research, Meda Pharma, and Immune Pharmaceuticals, which markets HDC as Ceplene®.
The combination of HDC and IL-2 is currently approved in more than 30 countries to prevent relapse in AML patients. In this phase 4 study (Re:MISSION), the researchers set out to assess the immunomodulatory properties of this treatment and correlate potential biomarkers with clinical outcomes.
The study included 84 non-transplanted AML patients (ages 18 to 79) in first complete remission. The patients received HDC (0.5 mg SC BID) and human recombinant IL-2 (1MIU SC BID) in 3-week cycles for 18 months. The patients were followed for at least 2 years from the start of immunotherapy to evaluate survival.
The researchers collected blood from the patients before they began HDC/IL-2 therapy and at the end of the first treatment cycle. From these samples, the team assessed the frequency of CD8+ T cells, including naïve T cells (CD45RA+CCR7+), central memory T cells (CD45RO+CCR7+), TEM cells (CD45RO+CCR7-), and Teff cells (CD45RA+CCR7-).
The researchers found that non-relapsing patients experienced a significant reduction in TEM cells (P=0.001) and a significant increase in Teff cells (P=0.007) during cycle 1. However, this effect was not observed in patients who did relapse.
Further analysis revealed that the reduction in TEM cells was significantly associated with favorable LFS and OS in the entire cohort (P=0.0007 and P=0.005, respectively) and among patients over 60 (P<0.0001 and P=0.002, respectively).
Likewise, the increase in Teff cells was associated with favorable LFS and OS in the entire cohort (P=0.07 and P=0.04, respectively) and among patients over 60 (P=0.004 and P=0.0001, respectively).
The concomitant reduction of TEM cells and induction of Teff cells—the TEM to Teff transition—was associated with superior LFS and OS in the overall cohort (P=0.0002 and P=0.002, respectively) and in the over-60 population (P<0.0001 for LFS and OS).
The researchers said these predictors of outcome remained significant when they adjusted for potential confounders (age, risk group classification, number of induction courses required to achieve complete response, and number of consolidation courses).
Therefore, the team concluded that the altered distribution of cytotoxic T cells during treatment with HDC/IL-2 can prognosticate LFS and OS in AML patients, particularly those over 60.
“We believe that the new data may allow a personalized approach to selection of patients who are most likely to benefit from Ceplene/IL-2 treatment in AML—in particular, the older patient population, who have demonstrated almost 100% survival when positive for the T-cell transition biomarkers,” said Miri Ben-Ami, MD, executive vice president of oncology at Immune Pharmaceuticals.
“In addition, current research is revealing the potential synergy between immune checkpoint inhibitors and Ceplene, which could open the possibility of additional therapeutic indications for this combination.” ![]()
*Information in the abstract differs from that presented at the meeting.

NEW ORLEANS—A phase 4 study has revealed biomarkers that appear to predict the efficacy of treatment with histamine dihydrochloride (HDC) and interleukin-2 (IL-2) in patients with acute myeloid leukemia (AML).
Researchers found that patients who remained in complete remission after 1 cycle of HDC/IL-2 experienced a significant reduction in effector memory T cells (TEM) and a concomitant increase in effector T cells (Teff) during therapy.
This “TEM to Teff transition” was associated with favorable leukemia-free survival (LFS) and overall survival (OS), especially among patients older than 60.
Frida Ewald Sander, PhD, of University of Gothenburg in Sweden, and her colleagues presented this research at the 2016 AACR Annual Meeting (abstract CT116*).
The study was supported by The Swedish Research Council, The Swedish Cancer Society, The Swedish Society for Medical Research, Meda Pharma, and Immune Pharmaceuticals, which markets HDC as Ceplene®.
The combination of HDC and IL-2 is currently approved in more than 30 countries to prevent relapse in AML patients. In this phase 4 study (Re:MISSION), the researchers set out to assess the immunomodulatory properties of this treatment and correlate potential biomarkers with clinical outcomes.
The study included 84 non-transplanted AML patients (ages 18 to 79) in first complete remission. The patients received HDC (0.5 mg SC BID) and human recombinant IL-2 (1MIU SC BID) in 3-week cycles for 18 months. The patients were followed for at least 2 years from the start of immunotherapy to evaluate survival.
The researchers collected blood from the patients before they began HDC/IL-2 therapy and at the end of the first treatment cycle. From these samples, the team assessed the frequency of CD8+ T cells, including naïve T cells (CD45RA+CCR7+), central memory T cells (CD45RO+CCR7+), TEM cells (CD45RO+CCR7-), and Teff cells (CD45RA+CCR7-).
The researchers found that non-relapsing patients experienced a significant reduction in TEM cells (P=0.001) and a significant increase in Teff cells (P=0.007) during cycle 1. However, this effect was not observed in patients who did relapse.
Further analysis revealed that the reduction in TEM cells was significantly associated with favorable LFS and OS in the entire cohort (P=0.0007 and P=0.005, respectively) and among patients over 60 (P<0.0001 and P=0.002, respectively).
Likewise, the increase in Teff cells was associated with favorable LFS and OS in the entire cohort (P=0.07 and P=0.04, respectively) and among patients over 60 (P=0.004 and P=0.0001, respectively).
The concomitant reduction of TEM cells and induction of Teff cells—the TEM to Teff transition—was associated with superior LFS and OS in the overall cohort (P=0.0002 and P=0.002, respectively) and in the over-60 population (P<0.0001 for LFS and OS).
The researchers said these predictors of outcome remained significant when they adjusted for potential confounders (age, risk group classification, number of induction courses required to achieve complete response, and number of consolidation courses).
Therefore, the team concluded that the altered distribution of cytotoxic T cells during treatment with HDC/IL-2 can prognosticate LFS and OS in AML patients, particularly those over 60.
“We believe that the new data may allow a personalized approach to selection of patients who are most likely to benefit from Ceplene/IL-2 treatment in AML—in particular, the older patient population, who have demonstrated almost 100% survival when positive for the T-cell transition biomarkers,” said Miri Ben-Ami, MD, executive vice president of oncology at Immune Pharmaceuticals.
“In addition, current research is revealing the potential synergy between immune checkpoint inhibitors and Ceplene, which could open the possibility of additional therapeutic indications for this combination.” ![]()
*Information in the abstract differs from that presented at the meeting.
Method detects SNVs better, group says

Researchers have developed a new method for detecting single-nucleotide variants (SNVs) in a single cell, and they believe it could have applications for cancer diagnosis and treatment.
The team said the method, known as Monovar, improves upon current single-cell sequencing (SCS) by more accurately detecting SNVs.
During testing, Monovar identified 28 new somatic SNVs in cells from a patient with acute lymphoblastic leukemia (ALL).
The researchers described Monovar in Nature Methods.
“To improve the SNVs in SCS datasets, we developed Monovar,” said study author Nicholas Navin, PhD, of the University of Texas MD Anderson Cancer Center in Houston.
“Monovar is a novel statistical method able to leverage data from multiple single cells to discover SNVs and provides highly detailed genetic data.”
Dr Navin and his colleagues found Monovar superior to standard algorithms for analyzing cells from previously studied patients with 3 different cancer types.
The team analyzed single cells from a patient with triple-negative breast cancer, a patient with muscle-invasive bladder cancer, and a child with ALL.
In cells from the ALL patient, Monovar discovered 57 somatic mutations, including 28 new somatic SNVs.
The researchers said Monovar identified significant mutations in OR4C3 and GPR107 (all subclones); LRFN5, PKD2L1, and ZNF781 (in subs 2, 4 and 5); DNAH7 (sub 1); LYAR and FMNL1 (sub 2); RGS3 (subs 4 and 5); and ADAMTS13, PRSS3, and PKD2L1 (subs 2-5).
The clonal mutations in OR4C3 and GPR107 and the subclonal mutations in PKD2L1, ADAMTS13, PRSS3, and RGS3 were not identified in the original study of the ALL patient (C Gawad et al. PNAS 2014).
Dr Navin and his colleagues said Monovar could have significant translational applications in cancer diagnosis and treatment, personalized medicine, and prenatal genetic diagnosis, where the accurate detection of SNVs is critical for patient care.
The researchers also believe Monovar could be used for studies in a range of biomedical fields.
“With the recent innovations in SCS methods to analyze thousands of single cells in parallel with RNA analysis, which will soon be extended to DNA analysis, the need for accurate DNA variant detection will continue to grow,” said Ken Chen, PhD, also of MD Anderson Cancer Center.
“Monovar is capable of analyzing large-scale datasets and handling different whole-genome protocols. Therefore, it is well-suited for many types of studies.” ![]()

Researchers have developed a new method for detecting single-nucleotide variants (SNVs) in a single cell, and they believe it could have applications for cancer diagnosis and treatment.
The team said the method, known as Monovar, improves upon current single-cell sequencing (SCS) by more accurately detecting SNVs.
During testing, Monovar identified 28 new somatic SNVs in cells from a patient with acute lymphoblastic leukemia (ALL).
The researchers described Monovar in Nature Methods.
“To improve the SNVs in SCS datasets, we developed Monovar,” said study author Nicholas Navin, PhD, of the University of Texas MD Anderson Cancer Center in Houston.
“Monovar is a novel statistical method able to leverage data from multiple single cells to discover SNVs and provides highly detailed genetic data.”
Dr Navin and his colleagues found Monovar superior to standard algorithms for analyzing cells from previously studied patients with 3 different cancer types.
The team analyzed single cells from a patient with triple-negative breast cancer, a patient with muscle-invasive bladder cancer, and a child with ALL.
In cells from the ALL patient, Monovar discovered 57 somatic mutations, including 28 new somatic SNVs.
The researchers said Monovar identified significant mutations in OR4C3 and GPR107 (all subclones); LRFN5, PKD2L1, and ZNF781 (in subs 2, 4 and 5); DNAH7 (sub 1); LYAR and FMNL1 (sub 2); RGS3 (subs 4 and 5); and ADAMTS13, PRSS3, and PKD2L1 (subs 2-5).
The clonal mutations in OR4C3 and GPR107 and the subclonal mutations in PKD2L1, ADAMTS13, PRSS3, and RGS3 were not identified in the original study of the ALL patient (C Gawad et al. PNAS 2014).
Dr Navin and his colleagues said Monovar could have significant translational applications in cancer diagnosis and treatment, personalized medicine, and prenatal genetic diagnosis, where the accurate detection of SNVs is critical for patient care.
The researchers also believe Monovar could be used for studies in a range of biomedical fields.
“With the recent innovations in SCS methods to analyze thousands of single cells in parallel with RNA analysis, which will soon be extended to DNA analysis, the need for accurate DNA variant detection will continue to grow,” said Ken Chen, PhD, also of MD Anderson Cancer Center.
“Monovar is capable of analyzing large-scale datasets and handling different whole-genome protocols. Therefore, it is well-suited for many types of studies.” ![]()

Researchers have developed a new method for detecting single-nucleotide variants (SNVs) in a single cell, and they believe it could have applications for cancer diagnosis and treatment.
The team said the method, known as Monovar, improves upon current single-cell sequencing (SCS) by more accurately detecting SNVs.
During testing, Monovar identified 28 new somatic SNVs in cells from a patient with acute lymphoblastic leukemia (ALL).
The researchers described Monovar in Nature Methods.
“To improve the SNVs in SCS datasets, we developed Monovar,” said study author Nicholas Navin, PhD, of the University of Texas MD Anderson Cancer Center in Houston.
“Monovar is a novel statistical method able to leverage data from multiple single cells to discover SNVs and provides highly detailed genetic data.”
Dr Navin and his colleagues found Monovar superior to standard algorithms for analyzing cells from previously studied patients with 3 different cancer types.
The team analyzed single cells from a patient with triple-negative breast cancer, a patient with muscle-invasive bladder cancer, and a child with ALL.
In cells from the ALL patient, Monovar discovered 57 somatic mutations, including 28 new somatic SNVs.
The researchers said Monovar identified significant mutations in OR4C3 and GPR107 (all subclones); LRFN5, PKD2L1, and ZNF781 (in subs 2, 4 and 5); DNAH7 (sub 1); LYAR and FMNL1 (sub 2); RGS3 (subs 4 and 5); and ADAMTS13, PRSS3, and PKD2L1 (subs 2-5).
The clonal mutations in OR4C3 and GPR107 and the subclonal mutations in PKD2L1, ADAMTS13, PRSS3, and RGS3 were not identified in the original study of the ALL patient (C Gawad et al. PNAS 2014).
Dr Navin and his colleagues said Monovar could have significant translational applications in cancer diagnosis and treatment, personalized medicine, and prenatal genetic diagnosis, where the accurate detection of SNVs is critical for patient care.
The researchers also believe Monovar could be used for studies in a range of biomedical fields.
“With the recent innovations in SCS methods to analyze thousands of single cells in parallel with RNA analysis, which will soon be extended to DNA analysis, the need for accurate DNA variant detection will continue to grow,” said Ken Chen, PhD, also of MD Anderson Cancer Center.
“Monovar is capable of analyzing large-scale datasets and handling different whole-genome protocols. Therefore, it is well-suited for many types of studies.”
Drug shows early promise for low-grade lymphoma

follicular lymphoma
NEW ORLEANS—The TLR9 agonist SD-101 has produced encouraging early results in patients with low-grade B-cell lymphoma, according to researchers.
In an ongoing phase 1/2 study, patients received low-dose radiation, followed by an injection of SD-101 into one of their tumors.
This prompted changes in the tumor microenvironment that potentially induced a systemic antitumor response and decreased the volume of both treated and untreated tumors.
In addition, SD-101 was considered well tolerated, with no dose-limiting toxicities or maximum-tolerated dose.
“We are pleased to have already demonstrated a safety profile, pharmacodynamics, and preliminary efficacy in this study,” said Ronald Levy, MD, of Stanford University in California.
Dr Levy and his colleagues presented these results at the 2016 AACR Annual Meeting (abstract CT047). The study is sponsored by Dynavax Technologies Corporation, the company developing SD-101.
The researchers reported data for 13 patients with untreated, low-grade B-cell lymphoma. They had a mean age of 63.2, and 53.8% were male.
Patients had follicular lymphoma (n=9), small lymphocytic lymphoma (n=2), chronic lymphocytic leukemia (n=1), and nodal marginal zone lymphoma (n=1).
At least 2 sites of measurable disease were required for participation in this study. One site was treated with low-dose radiation (2 Gy) and injected with SD-101 on days 1, 8, 15, 22, and 29. Other lesions received no treatment.
In Part 1—the dose-escalation portion of the study—patients received SD-101 at 1 mg (n=3), 2 mg (n=3), 4 mg (n=3), or 8 mg (n=4). The phase 2 expansion portion of the study is ongoing, with enrollment in 2 dose cohorts (1 mg and 8 mg).
“This clinical trial design is unique and takes advantage of the fact that lymphoma patients have easily injectable sites of disease,” Dr Levy said. “The local injections are conveniently added to low-dose radiotherapy, a standard treatment for low-grade lymphoma.”
Safety
All 13 patients experienced at least 1 adverse event (AEs), although nearly all were grade 1 or 2.
The most common treatment-related AEs were local injection-site reactions and flu-like symptoms, including fever, chills, and myalgia (n=11 for all 3). However, the researchers said these AEs were primarily short-lived and controlled by over-the-counter acetaminophen in most cases.
In the 8 mg dosing cohort, 1 patient had grade 3 neutropenia and 2 had grade 3 malaise, all of which were considered treatment-related. In addition, there was a case of grade 3 asymptomatic pulmonary embolism in the 4 mg dose cohort, which was deemed serious but unrelated to treatment.
Efficacy
The researchers observed induction of interferon-responsive genes at all dose levels 24 hours after the second dose of SD-101 was given (Day 9).
In addition, T-cell numbers increased at the treated site by Day 8. The total T cells increased in 7 of 10 evaluable patients by Day 8 (range, >300% to 18%).
CD4+ and CD8+ T cells increased simultaneously in 5 of 7 evaluable patients, regulatory T cells decreased in 8 of 10 evaluable patients by Day 8, and follicular T helper cells decreased in 9 of 9 evaluable patients by Day 8.
Furthermore, treated and untreated tumors decreased in volume across all dose groups.
At Day 90, 12 patients had a reduction of the product of diameters in treated tumors (median -45.3%; range, -87 to +100), and 11 patients had a reduction in untreated tumors (median -8.1%; range, -48 to +45).
In 9 patients, these abscopal effects were sustained for at least 180 to 360 days.
However, 6 patients discontinued from the study due to progression. Three had radiographic progression—1 at Day 92 (in the 4 mg cohort) and 2 at 1 year (1 in the 1 mg cohort and 1 in the 2 mg cohort).
Two patients had clinical progression—1 at Day 197 (4 mg) and 1 at Day 273 (2 mg). And 1 patient discontinued at Day 203 due to a combination of clinical and radiographic progression (8 mg).
The researchers pointed out that there was no evidence of a dose response with SD-101, but the study included a limited number of patients.

follicular lymphoma
NEW ORLEANS—The TLR9 agonist SD-101 has produced encouraging early results in patients with low-grade B-cell lymphoma, according to researchers.
In an ongoing phase 1/2 study, patients received low-dose radiation, followed by an injection of SD-101 into one of their tumors.
This prompted changes in the tumor microenvironment that potentially induced a systemic antitumor response and decreased the volume of both treated and untreated tumors.
In addition, SD-101 was considered well tolerated, with no dose-limiting toxicities or maximum-tolerated dose.
“We are pleased to have already demonstrated a safety profile, pharmacodynamics, and preliminary efficacy in this study,” said Ronald Levy, MD, of Stanford University in California.
Dr Levy and his colleagues presented these results at the 2016 AACR Annual Meeting (abstract CT047). The study is sponsored by Dynavax Technologies Corporation, the company developing SD-101.
The researchers reported data for 13 patients with untreated, low-grade B-cell lymphoma. They had a mean age of 63.2, and 53.8% were male.
Patients had follicular lymphoma (n=9), small lymphocytic lymphoma (n=2), chronic lymphocytic leukemia (n=1), and nodal marginal zone lymphoma (n=1).
At least 2 sites of measurable disease were required for participation in this study. One site was treated with low-dose radiation (2 Gy) and injected with SD-101 on days 1, 8, 15, 22, and 29. Other lesions received no treatment.
In Part 1—the dose-escalation portion of the study—patients received SD-101 at 1 mg (n=3), 2 mg (n=3), 4 mg (n=3), or 8 mg (n=4). The phase 2 expansion portion of the study is ongoing, with enrollment in 2 dose cohorts (1 mg and 8 mg).
“This clinical trial design is unique and takes advantage of the fact that lymphoma patients have easily injectable sites of disease,” Dr Levy said. “The local injections are conveniently added to low-dose radiotherapy, a standard treatment for low-grade lymphoma.”
Safety
All 13 patients experienced at least 1 adverse event (AEs), although nearly all were grade 1 or 2.
The most common treatment-related AEs were local injection-site reactions and flu-like symptoms, including fever, chills, and myalgia (n=11 for all 3). However, the researchers said these AEs were primarily short-lived and controlled by over-the-counter acetaminophen in most cases.
In the 8 mg dosing cohort, 1 patient had grade 3 neutropenia and 2 had grade 3 malaise, all of which were considered treatment-related. In addition, there was a case of grade 3 asymptomatic pulmonary embolism in the 4 mg dose cohort, which was deemed serious but unrelated to treatment.
Efficacy
The researchers observed induction of interferon-responsive genes at all dose levels 24 hours after the second dose of SD-101 was given (Day 9).
In addition, T-cell numbers increased at the treated site by Day 8. The total T cells increased in 7 of 10 evaluable patients by Day 8 (range, >300% to 18%).
CD4+ and CD8+ T cells increased simultaneously in 5 of 7 evaluable patients, regulatory T cells decreased in 8 of 10 evaluable patients by Day 8, and follicular T helper cells decreased in 9 of 9 evaluable patients by Day 8.
Furthermore, treated and untreated tumors decreased in volume across all dose groups.
At Day 90, 12 patients had a reduction of the product of diameters in treated tumors (median -45.3%; range, -87 to +100), and 11 patients had a reduction in untreated tumors (median -8.1%; range, -48 to +45).
In 9 patients, these abscopal effects were sustained for at least 180 to 360 days.
However, 6 patients discontinued from the study due to progression. Three had radiographic progression—1 at Day 92 (in the 4 mg cohort) and 2 at 1 year (1 in the 1 mg cohort and 1 in the 2 mg cohort).
Two patients had clinical progression—1 at Day 197 (4 mg) and 1 at Day 273 (2 mg). And 1 patient discontinued at Day 203 due to a combination of clinical and radiographic progression (8 mg).
The researchers pointed out that there was no evidence of a dose response with SD-101, but the study included a limited number of patients.

follicular lymphoma
NEW ORLEANS—The TLR9 agonist SD-101 has produced encouraging early results in patients with low-grade B-cell lymphoma, according to researchers.
In an ongoing phase 1/2 study, patients received low-dose radiation, followed by an injection of SD-101 into one of their tumors.
This prompted changes in the tumor microenvironment that potentially induced a systemic antitumor response and decreased the volume of both treated and untreated tumors.
In addition, SD-101 was considered well tolerated, with no dose-limiting toxicities or maximum-tolerated dose.
“We are pleased to have already demonstrated a safety profile, pharmacodynamics, and preliminary efficacy in this study,” said Ronald Levy, MD, of Stanford University in California.
Dr Levy and his colleagues presented these results at the 2016 AACR Annual Meeting (abstract CT047). The study is sponsored by Dynavax Technologies Corporation, the company developing SD-101.
The researchers reported data for 13 patients with untreated, low-grade B-cell lymphoma. They had a mean age of 63.2, and 53.8% were male.
Patients had follicular lymphoma (n=9), small lymphocytic lymphoma (n=2), chronic lymphocytic leukemia (n=1), and nodal marginal zone lymphoma (n=1).
At least 2 sites of measurable disease were required for participation in this study. One site was treated with low-dose radiation (2 Gy) and injected with SD-101 on days 1, 8, 15, 22, and 29. Other lesions received no treatment.
In Part 1—the dose-escalation portion of the study—patients received SD-101 at 1 mg (n=3), 2 mg (n=3), 4 mg (n=3), or 8 mg (n=4). The phase 2 expansion portion of the study is ongoing, with enrollment in 2 dose cohorts (1 mg and 8 mg).
“This clinical trial design is unique and takes advantage of the fact that lymphoma patients have easily injectable sites of disease,” Dr Levy said. “The local injections are conveniently added to low-dose radiotherapy, a standard treatment for low-grade lymphoma.”
Safety
All 13 patients experienced at least 1 adverse event (AEs), although nearly all were grade 1 or 2.
The most common treatment-related AEs were local injection-site reactions and flu-like symptoms, including fever, chills, and myalgia (n=11 for all 3). However, the researchers said these AEs were primarily short-lived and controlled by over-the-counter acetaminophen in most cases.
In the 8 mg dosing cohort, 1 patient had grade 3 neutropenia and 2 had grade 3 malaise, all of which were considered treatment-related. In addition, there was a case of grade 3 asymptomatic pulmonary embolism in the 4 mg dose cohort, which was deemed serious but unrelated to treatment.
Efficacy
The researchers observed induction of interferon-responsive genes at all dose levels 24 hours after the second dose of SD-101 was given (Day 9).
In addition, T-cell numbers increased at the treated site by Day 8. The total T cells increased in 7 of 10 evaluable patients by Day 8 (range, >300% to 18%).
CD4+ and CD8+ T cells increased simultaneously in 5 of 7 evaluable patients, regulatory T cells decreased in 8 of 10 evaluable patients by Day 8, and follicular T helper cells decreased in 9 of 9 evaluable patients by Day 8.
Furthermore, treated and untreated tumors decreased in volume across all dose groups.
At Day 90, 12 patients had a reduction of the product of diameters in treated tumors (median -45.3%; range, -87 to +100), and 11 patients had a reduction in untreated tumors (median -8.1%; range, -48 to +45).
In 9 patients, these abscopal effects were sustained for at least 180 to 360 days.
However, 6 patients discontinued from the study due to progression. Three had radiographic progression—1 at Day 92 (in the 4 mg cohort) and 2 at 1 year (1 in the 1 mg cohort and 1 in the 2 mg cohort).
Two patients had clinical progression—1 at Day 197 (4 mg) and 1 at Day 273 (2 mg). And 1 patient discontinued at Day 203 due to a combination of clinical and radiographic progression (8 mg).
The researchers pointed out that there was no evidence of a dose response with SD-101, but the study included a limited number of patients.