User login
Antibody shows activity against ALL, CLL

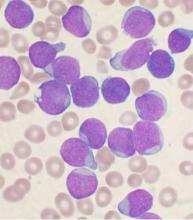
Photo by Aaron Logan
NEW ORLEANS—Preclinical data suggest IMMU-114, a humanized anti-HLA-DR IgG4 antibody, is active against acute and chronic leukemias.
In a mouse model of chronic lymphocytic leukemia (CLL), IMMU-114 significantly prolonged survival when compared to rituximab.
IMMU-114 also produced a significant survival benefit in a mouse model of acute lymphoblastic leukemia (ALL) that is refractory to doxorubicin.
These results were presented at the 2016 AACR Annual Meeting (abstract 587). The research was carried out by employees of Immunomedics, Inc., the company developing IMMU-114.
The researchers generated a mouse model of human CLL by growing the cell line JVM-3 in SCID mice. The team noted that this model has similar HLA-DR and CD20 expression.
So they compared the efficacy of IMMU-114 and the anti-CD20 antibody rituximab in these mice and found that, at all doses tested, IMMU-114 significantly improved the median survival time (MST).
When both drugs were given at 50 µg, the MST was 42 days with IMMU-114 and 19 days with rituximab (P<0.0001).
When both drugs were given at 100 µg, the MSTs were 54 days and 18 days, respectively (P=0.017). And when both drugs were given at 200 µg, the MSTs were 46 days and 18 days, respectively (P<0.0001).
In control mice that received only saline, the MST was 14 days.
In in vitro experiments with the cell line JVM-3, IMMU-114 and the BTK inhibitor ibrutinib exhibited synergy fighting against the CLL cells. When given with the PI3K inhibitor idelalisib, IMMU-114 produced an additive effect.
In a doxorubicin-refractory mouse model of ALL (MN 60), IMMU-114 provided a significant survival benefit over doxorubicin and saline controls.
The MSTs were 21 days with saline, 23 days with doxorubicin, 39 days with IMMU-114 at 25 µg (P<0.0001), and 42.5 days with IMMU-114 at 50 µg (P<0.0001).
The researchers said IMMU-114 was well tolerated in these experiments, as evidenced by no significant weight loss in the mice. ![]()

Photo by Aaron Logan
NEW ORLEANS—Preclinical data suggest IMMU-114, a humanized anti-HLA-DR IgG4 antibody, is active against acute and chronic leukemias.
In a mouse model of chronic lymphocytic leukemia (CLL), IMMU-114 significantly prolonged survival when compared to rituximab.
IMMU-114 also produced a significant survival benefit in a mouse model of acute lymphoblastic leukemia (ALL) that is refractory to doxorubicin.
These results were presented at the 2016 AACR Annual Meeting (abstract 587). The research was carried out by employees of Immunomedics, Inc., the company developing IMMU-114.
The researchers generated a mouse model of human CLL by growing the cell line JVM-3 in SCID mice. The team noted that this model has similar HLA-DR and CD20 expression.
So they compared the efficacy of IMMU-114 and the anti-CD20 antibody rituximab in these mice and found that, at all doses tested, IMMU-114 significantly improved the median survival time (MST).
When both drugs were given at 50 µg, the MST was 42 days with IMMU-114 and 19 days with rituximab (P<0.0001).
When both drugs were given at 100 µg, the MSTs were 54 days and 18 days, respectively (P=0.017). And when both drugs were given at 200 µg, the MSTs were 46 days and 18 days, respectively (P<0.0001).
In control mice that received only saline, the MST was 14 days.
In in vitro experiments with the cell line JVM-3, IMMU-114 and the BTK inhibitor ibrutinib exhibited synergy fighting against the CLL cells. When given with the PI3K inhibitor idelalisib, IMMU-114 produced an additive effect.
In a doxorubicin-refractory mouse model of ALL (MN 60), IMMU-114 provided a significant survival benefit over doxorubicin and saline controls.
The MSTs were 21 days with saline, 23 days with doxorubicin, 39 days with IMMU-114 at 25 µg (P<0.0001), and 42.5 days with IMMU-114 at 50 µg (P<0.0001).
The researchers said IMMU-114 was well tolerated in these experiments, as evidenced by no significant weight loss in the mice. ![]()

Photo by Aaron Logan
NEW ORLEANS—Preclinical data suggest IMMU-114, a humanized anti-HLA-DR IgG4 antibody, is active against acute and chronic leukemias.
In a mouse model of chronic lymphocytic leukemia (CLL), IMMU-114 significantly prolonged survival when compared to rituximab.
IMMU-114 also produced a significant survival benefit in a mouse model of acute lymphoblastic leukemia (ALL) that is refractory to doxorubicin.
These results were presented at the 2016 AACR Annual Meeting (abstract 587). The research was carried out by employees of Immunomedics, Inc., the company developing IMMU-114.
The researchers generated a mouse model of human CLL by growing the cell line JVM-3 in SCID mice. The team noted that this model has similar HLA-DR and CD20 expression.
So they compared the efficacy of IMMU-114 and the anti-CD20 antibody rituximab in these mice and found that, at all doses tested, IMMU-114 significantly improved the median survival time (MST).
When both drugs were given at 50 µg, the MST was 42 days with IMMU-114 and 19 days with rituximab (P<0.0001).
When both drugs were given at 100 µg, the MSTs were 54 days and 18 days, respectively (P=0.017). And when both drugs were given at 200 µg, the MSTs were 46 days and 18 days, respectively (P<0.0001).
In control mice that received only saline, the MST was 14 days.
In in vitro experiments with the cell line JVM-3, IMMU-114 and the BTK inhibitor ibrutinib exhibited synergy fighting against the CLL cells. When given with the PI3K inhibitor idelalisib, IMMU-114 produced an additive effect.
In a doxorubicin-refractory mouse model of ALL (MN 60), IMMU-114 provided a significant survival benefit over doxorubicin and saline controls.
The MSTs were 21 days with saline, 23 days with doxorubicin, 39 days with IMMU-114 at 25 µg (P<0.0001), and 42.5 days with IMMU-114 at 50 µg (P<0.0001).
The researchers said IMMU-114 was well tolerated in these experiments, as evidenced by no significant weight loss in the mice. ![]()
Model used to estimate CSCs in CML

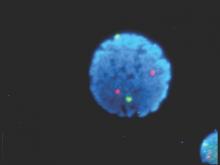
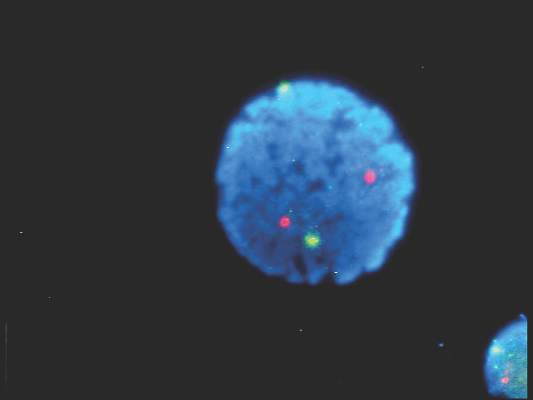
Image from UC San Diego
Scientists say they have developed a model that can be used to calculate the proportion of cancer stem cells (CSCs) present over the course of treatment.
The model is designed to enable estimation of CSC fractions from longitudinal measurements of tumor burden.
The scientists tested the model in patients with chronic myeloid leukemia (CML) and found evidence to suggest the proportion of CSCs increases
substantially during extended treatment.
The team believes the model could eventually be used to help doctors predict tumor development and help them select suitable treatments for cancer patients.
“Cancer stem cells not only promote the growth of a tumor, they can also be resistant to radiotherapy and chemotherapy,” said Philipp Altrock, PhD, of the Dana Farber Cancer Institute in Boston, Massachusetts.
“If we can estimate the number of cancer stem cells at diagnosis and over the course of treatment, the treatment can be tailored accordingly.”
Dr Altrock and his colleagues discussed this possibility in Cancer Research.
The team first explained that their model incorporates tumor dynamics and tumor burden information. They said tumor expansion and regression curves can be leveraged to estimate the proportion of CSCs in individual patients at baseline and during therapy.
To test their model, the scientists used 2 independent cohorts of CML patients. The team evaluated the growth and decline of CML over the course of treatment with the tyrosine kinase inhibitor imatinib.
Based on the change of disease burden during treatment, the model calculated the proportion of CSCs.
Results suggested the proportion of CSCs in CML patients increases 100-fold after a year of treatment with imatinib. And that proportion continues to increase up to 1000-fold after 5 years of treatment.
The scientists noted that this model is parameter-free, so it can be applied to different types of cancer. However, they said further development is required before the model can be used in clinical practice. ![]()

Image from UC San Diego
Scientists say they have developed a model that can be used to calculate the proportion of cancer stem cells (CSCs) present over the course of treatment.
The model is designed to enable estimation of CSC fractions from longitudinal measurements of tumor burden.
The scientists tested the model in patients with chronic myeloid leukemia (CML) and found evidence to suggest the proportion of CSCs increases
substantially during extended treatment.
The team believes the model could eventually be used to help doctors predict tumor development and help them select suitable treatments for cancer patients.
“Cancer stem cells not only promote the growth of a tumor, they can also be resistant to radiotherapy and chemotherapy,” said Philipp Altrock, PhD, of the Dana Farber Cancer Institute in Boston, Massachusetts.
“If we can estimate the number of cancer stem cells at diagnosis and over the course of treatment, the treatment can be tailored accordingly.”
Dr Altrock and his colleagues discussed this possibility in Cancer Research.
The team first explained that their model incorporates tumor dynamics and tumor burden information. They said tumor expansion and regression curves can be leveraged to estimate the proportion of CSCs in individual patients at baseline and during therapy.
To test their model, the scientists used 2 independent cohorts of CML patients. The team evaluated the growth and decline of CML over the course of treatment with the tyrosine kinase inhibitor imatinib.
Based on the change of disease burden during treatment, the model calculated the proportion of CSCs.
Results suggested the proportion of CSCs in CML patients increases 100-fold after a year of treatment with imatinib. And that proportion continues to increase up to 1000-fold after 5 years of treatment.
The scientists noted that this model is parameter-free, so it can be applied to different types of cancer. However, they said further development is required before the model can be used in clinical practice. ![]()

Image from UC San Diego
Scientists say they have developed a model that can be used to calculate the proportion of cancer stem cells (CSCs) present over the course of treatment.
The model is designed to enable estimation of CSC fractions from longitudinal measurements of tumor burden.
The scientists tested the model in patients with chronic myeloid leukemia (CML) and found evidence to suggest the proportion of CSCs increases
substantially during extended treatment.
The team believes the model could eventually be used to help doctors predict tumor development and help them select suitable treatments for cancer patients.
“Cancer stem cells not only promote the growth of a tumor, they can also be resistant to radiotherapy and chemotherapy,” said Philipp Altrock, PhD, of the Dana Farber Cancer Institute in Boston, Massachusetts.
“If we can estimate the number of cancer stem cells at diagnosis and over the course of treatment, the treatment can be tailored accordingly.”
Dr Altrock and his colleagues discussed this possibility in Cancer Research.
The team first explained that their model incorporates tumor dynamics and tumor burden information. They said tumor expansion and regression curves can be leveraged to estimate the proportion of CSCs in individual patients at baseline and during therapy.
To test their model, the scientists used 2 independent cohorts of CML patients. The team evaluated the growth and decline of CML over the course of treatment with the tyrosine kinase inhibitor imatinib.
Based on the change of disease burden during treatment, the model calculated the proportion of CSCs.
Results suggested the proportion of CSCs in CML patients increases 100-fold after a year of treatment with imatinib. And that proportion continues to increase up to 1000-fold after 5 years of treatment.
The scientists noted that this model is parameter-free, so it can be applied to different types of cancer. However, they said further development is required before the model can be used in clinical practice. ![]()
Targeted corticosteroids cut GVHD incidence
Short-term low-dose corticosteroid prophylaxis reduces the incidence of graft-vs.-host disease in patients who undergo allogeneic haploidentical stem-cell transplantation to treat hematologic neoplasms, according to a report published online April 18 in the Journal of Clinical Oncology.
The key to selecting patients most likely to benefit from the corticosteroid therapy is to identify those at high risk for graft-vs.-host disease (GVHD) using two biomarkers: high levels of CD56bright natural killer cells in allogeneic grafts or high CD4:CD8 ratios in bone marrow grafts, according to Dr. Ying-Jun Chang of Peking University People’s Hospital, Beijing, and associates.
The investigators performed an open-label trial involving 228 patients aged 15-60 years treated at a single medical center during an 18-month period for acute myeloid leukemia, acute lymphoblastic leukemia, chronic myeloid leukemia, myelodysplastic syndrome, or other hematologic neoplasms. Using the two biomarkers, the patients were categorized as either high or low risk for developing GVHD. They were randomly assigned to three study groups: 72 high-risk patients who received short-term low-dose corticosteroids, 73 high-risk patients who received usual care, and 83 low-risk patients who received usual care.
The cumulative 100-day incidence of acute grade-II to grade-IV GVHD was significantly lower in the high-risk patients who received prophylaxis (21%) than in the high-risk patients who did not receive prophylaxis (48%). In fact, corticosteroids decreased the rate of GVHD so that it was comparable with that in the low-risk patients (26%), Dr. Chang and associates said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.63l.8817).
Moreover, in the high-risk patients the median interval until GVHD developed was 25 days for those who took corticosteroids, compared with only 15 days for those who did not. Median times to myeloid recovery and platelet recovery were significantly shorter for high-risk patients who received corticosteroids than for either of the other study groups. However, 3-year overall survival and leukemia-free survival were comparable among the three study groups.
The short-term low-dose regimen of corticosteroids did not raise the rate of adverse events, including infection, which suggests that it is preferable to standard corticosteroid regimens in this patient population. The incidences of cytomegalovirus or Epstein-Barr virus reactivation, post-transplantation lymphoproliferative disorder, hemorrhagic cystitis, bacteremia, and invasive fungal infections were comparable among the three study groups. Of note, the incidences of osteonecrosis of the femoral head and secondary hypertension were significantly lower among high-risk patients who received corticosteroid prophylaxis than among those who did not.
“These results provide the first test, to our knowledge, of a novel risk-stratification-directed prophylaxis strategy that effectively prevented acute GVHD among patients who were at high risk for GVHD, without unnecessarily exposing patients who were at low risk to excessive toxicity from additional immunosuppressive agents,” Dr. Chang and associates said.
Despite the encouraging results of Chang et al, it would be premature to routinely use corticosteroid prophylaxis to prevent GVHD until further studies are completed.
This study wasn’t sufficiently powered to determine whether corticosteroids reduced treatment-specific mortality or improved overall survival. Future studies must examine these end points, as well as relapse rates, before this method of prophylaxis is widely adopted.
Dr. Edwin P. Alyea is at Dana-Farber Cancer Institute, Boston. He reported having no relevant financial disclosures. Dr. Alyea made these remarks in an editorial accompanying Dr. Chang’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.66.0902).
Despite the encouraging results of Chang et al, it would be premature to routinely use corticosteroid prophylaxis to prevent GVHD until further studies are completed.
This study wasn’t sufficiently powered to determine whether corticosteroids reduced treatment-specific mortality or improved overall survival. Future studies must examine these end points, as well as relapse rates, before this method of prophylaxis is widely adopted.
Dr. Edwin P. Alyea is at Dana-Farber Cancer Institute, Boston. He reported having no relevant financial disclosures. Dr. Alyea made these remarks in an editorial accompanying Dr. Chang’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.66.0902).
Despite the encouraging results of Chang et al, it would be premature to routinely use corticosteroid prophylaxis to prevent GVHD until further studies are completed.
This study wasn’t sufficiently powered to determine whether corticosteroids reduced treatment-specific mortality or improved overall survival. Future studies must examine these end points, as well as relapse rates, before this method of prophylaxis is widely adopted.
Dr. Edwin P. Alyea is at Dana-Farber Cancer Institute, Boston. He reported having no relevant financial disclosures. Dr. Alyea made these remarks in an editorial accompanying Dr. Chang’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.66.0902).
Short-term low-dose corticosteroid prophylaxis reduces the incidence of graft-vs.-host disease in patients who undergo allogeneic haploidentical stem-cell transplantation to treat hematologic neoplasms, according to a report published online April 18 in the Journal of Clinical Oncology.
The key to selecting patients most likely to benefit from the corticosteroid therapy is to identify those at high risk for graft-vs.-host disease (GVHD) using two biomarkers: high levels of CD56bright natural killer cells in allogeneic grafts or high CD4:CD8 ratios in bone marrow grafts, according to Dr. Ying-Jun Chang of Peking University People’s Hospital, Beijing, and associates.
The investigators performed an open-label trial involving 228 patients aged 15-60 years treated at a single medical center during an 18-month period for acute myeloid leukemia, acute lymphoblastic leukemia, chronic myeloid leukemia, myelodysplastic syndrome, or other hematologic neoplasms. Using the two biomarkers, the patients were categorized as either high or low risk for developing GVHD. They were randomly assigned to three study groups: 72 high-risk patients who received short-term low-dose corticosteroids, 73 high-risk patients who received usual care, and 83 low-risk patients who received usual care.
The cumulative 100-day incidence of acute grade-II to grade-IV GVHD was significantly lower in the high-risk patients who received prophylaxis (21%) than in the high-risk patients who did not receive prophylaxis (48%). In fact, corticosteroids decreased the rate of GVHD so that it was comparable with that in the low-risk patients (26%), Dr. Chang and associates said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.63l.8817).
Moreover, in the high-risk patients the median interval until GVHD developed was 25 days for those who took corticosteroids, compared with only 15 days for those who did not. Median times to myeloid recovery and platelet recovery were significantly shorter for high-risk patients who received corticosteroids than for either of the other study groups. However, 3-year overall survival and leukemia-free survival were comparable among the three study groups.
The short-term low-dose regimen of corticosteroids did not raise the rate of adverse events, including infection, which suggests that it is preferable to standard corticosteroid regimens in this patient population. The incidences of cytomegalovirus or Epstein-Barr virus reactivation, post-transplantation lymphoproliferative disorder, hemorrhagic cystitis, bacteremia, and invasive fungal infections were comparable among the three study groups. Of note, the incidences of osteonecrosis of the femoral head and secondary hypertension were significantly lower among high-risk patients who received corticosteroid prophylaxis than among those who did not.
“These results provide the first test, to our knowledge, of a novel risk-stratification-directed prophylaxis strategy that effectively prevented acute GVHD among patients who were at high risk for GVHD, without unnecessarily exposing patients who were at low risk to excessive toxicity from additional immunosuppressive agents,” Dr. Chang and associates said.
Short-term low-dose corticosteroid prophylaxis reduces the incidence of graft-vs.-host disease in patients who undergo allogeneic haploidentical stem-cell transplantation to treat hematologic neoplasms, according to a report published online April 18 in the Journal of Clinical Oncology.
The key to selecting patients most likely to benefit from the corticosteroid therapy is to identify those at high risk for graft-vs.-host disease (GVHD) using two biomarkers: high levels of CD56bright natural killer cells in allogeneic grafts or high CD4:CD8 ratios in bone marrow grafts, according to Dr. Ying-Jun Chang of Peking University People’s Hospital, Beijing, and associates.
The investigators performed an open-label trial involving 228 patients aged 15-60 years treated at a single medical center during an 18-month period for acute myeloid leukemia, acute lymphoblastic leukemia, chronic myeloid leukemia, myelodysplastic syndrome, or other hematologic neoplasms. Using the two biomarkers, the patients were categorized as either high or low risk for developing GVHD. They were randomly assigned to three study groups: 72 high-risk patients who received short-term low-dose corticosteroids, 73 high-risk patients who received usual care, and 83 low-risk patients who received usual care.
The cumulative 100-day incidence of acute grade-II to grade-IV GVHD was significantly lower in the high-risk patients who received prophylaxis (21%) than in the high-risk patients who did not receive prophylaxis (48%). In fact, corticosteroids decreased the rate of GVHD so that it was comparable with that in the low-risk patients (26%), Dr. Chang and associates said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.63l.8817).
Moreover, in the high-risk patients the median interval until GVHD developed was 25 days for those who took corticosteroids, compared with only 15 days for those who did not. Median times to myeloid recovery and platelet recovery were significantly shorter for high-risk patients who received corticosteroids than for either of the other study groups. However, 3-year overall survival and leukemia-free survival were comparable among the three study groups.
The short-term low-dose regimen of corticosteroids did not raise the rate of adverse events, including infection, which suggests that it is preferable to standard corticosteroid regimens in this patient population. The incidences of cytomegalovirus or Epstein-Barr virus reactivation, post-transplantation lymphoproliferative disorder, hemorrhagic cystitis, bacteremia, and invasive fungal infections were comparable among the three study groups. Of note, the incidences of osteonecrosis of the femoral head and secondary hypertension were significantly lower among high-risk patients who received corticosteroid prophylaxis than among those who did not.
“These results provide the first test, to our knowledge, of a novel risk-stratification-directed prophylaxis strategy that effectively prevented acute GVHD among patients who were at high risk for GVHD, without unnecessarily exposing patients who were at low risk to excessive toxicity from additional immunosuppressive agents,” Dr. Chang and associates said.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Short-term low-dose corticosteroid prophylaxis reduces the incidence of the GVHD in patients who undergo haploidentical stem-cell transplantation to treat hematologic neoplasms.
Major finding: The 100-day incidence of acute GVHD was significantly lower in the high-risk patients who received corticosteroid prophylaxis (21%) than in the high-risk patients who did not (48%).
Data source: An open-label randomized controlled trial involving 228 Chinese patients who underwent stem-cell transplantation.
Disclosures: This study was supported by the Beijing Committee of Science and Technology, the National High Technology Research and Development Program of China, and the National Natural Science Foundation of China. Dr. Chang and associates reported having no relevant financial disclosures.
Donor EBV status affects recipient graft-vs-host disease risk
In allogeneic hematopoietic stem-cell transplantation, the donor’s status regarding Epstein-Barr virus affects the recipient’s risk of developing graft-vs-host disease – a “completely new and striking” finding, according to a report published online April 18 in the Journal of Clinical Oncology.
Approximately 80% of the general population has been infected with EBV and carries persistent virus in memory B cells. When viral material is transmitted to stem-cell recipients, it is known to cause posttransplantation lymphoproliferative disorder. Until now, however, no data were available to examine EBV serology’s effect on other posttransplantation outcomes, said Dr. Jan Styczynski of the department of pediatric hematology and oncology at Nicolaus Copernicus University, Bydgoszcz, Poland, and his associates.
They analyzed information in the European Society of Blood and Marrow Transplantation database for 11,364 patients with acute lymphoblastic leukemia or acute myeloblastic leukemia who underwent stem-cell transplantation between 1997 and 2012 and who were followed for approximately 5 years. Most of the donors (82%) were seropositive for EBV. Acute graft-vs-host disease (GVHD) developed in 32% and chronic GVHD developed in 40% of these stem cell–transplant recipients.
The incidence of chronic GVHD was significantly higher when the donor was EBV-seropositive (41%) than when the donor was EBV-seronegative (31%). Similarly, the incidence of acute GVHD was significantly higher when the donor was EBV-seropositive (32% vs 30%), but the magnitude of the difference between the two groups was smaller. The risk for GVHD increased even though patients receiving transplants from EBV-seropositive donors underwent more intensive GVHD prophylaxis than did those who had seronegative donors, the investigators said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.64.2405).
In contrast, the transplant recipients’ EBV status did not affect their risk of developing GVHD.
“Despite the effect of donor EBV serostatus on GVHD, we did not observe a corresponding GVHD-related death rate, and as a result, there was no effect on overall survival, relapse-free survival, relapse incidence, and nonrelapse mortality. However, it should be kept in mind that many other pre- and posttransplantation factors play a role in contributing to final transplantation outcomes,” Dr. Styczynski and his associates noted.
The current recommendation to monitor transplantation recipients for EBV and to give them “preemptive” rituximab to stave off the development of posttransplantation lymphoproliferative disorder might prove useful in also preventing GVHD, they added.
The findings of Dr. Styczynski and his associates raise the possibility that we may be able to prevent or treat GVHD in transplant recipients by controlling EBV infection.
Selecting only EBV-negative donors would be one way to accomplish this, but that would be impractical given the high seroprevalence of EBV in the general population. Depleting memory B cells, the reservoir of EBV infection, using monoclonal antibodies may prove helpful, and these agents might provide additional therapeutic effects. And novel antivirals such as retroviral integrase inhibitors may be more specific at targeting EBV than acyclovir and related agents, which have limited activity against latently infected B cells. These novel drugs, however, are not without risks and adverse effects.
A promising alternative might be to boost immunity to EBV using vaccination or adoptive transfer of ex vivo expanded EBV-specific cytotoxic T cells.
Dr. Katayoun Rezvani and Dr. Richard E. Champlin are with the University of Texas MD Andersen Cancer Center, Houston. Their financial disclosures are available at www.jco.org. They made these remarks in an editorial accompanying Dr. Styczynski’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2016.66.6099).
The findings of Dr. Styczynski and his associates raise the possibility that we may be able to prevent or treat GVHD in transplant recipients by controlling EBV infection.
Selecting only EBV-negative donors would be one way to accomplish this, but that would be impractical given the high seroprevalence of EBV in the general population. Depleting memory B cells, the reservoir of EBV infection, using monoclonal antibodies may prove helpful, and these agents might provide additional therapeutic effects. And novel antivirals such as retroviral integrase inhibitors may be more specific at targeting EBV than acyclovir and related agents, which have limited activity against latently infected B cells. These novel drugs, however, are not without risks and adverse effects.
A promising alternative might be to boost immunity to EBV using vaccination or adoptive transfer of ex vivo expanded EBV-specific cytotoxic T cells.
Dr. Katayoun Rezvani and Dr. Richard E. Champlin are with the University of Texas MD Andersen Cancer Center, Houston. Their financial disclosures are available at www.jco.org. They made these remarks in an editorial accompanying Dr. Styczynski’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2016.66.6099).
The findings of Dr. Styczynski and his associates raise the possibility that we may be able to prevent or treat GVHD in transplant recipients by controlling EBV infection.
Selecting only EBV-negative donors would be one way to accomplish this, but that would be impractical given the high seroprevalence of EBV in the general population. Depleting memory B cells, the reservoir of EBV infection, using monoclonal antibodies may prove helpful, and these agents might provide additional therapeutic effects. And novel antivirals such as retroviral integrase inhibitors may be more specific at targeting EBV than acyclovir and related agents, which have limited activity against latently infected B cells. These novel drugs, however, are not without risks and adverse effects.
A promising alternative might be to boost immunity to EBV using vaccination or adoptive transfer of ex vivo expanded EBV-specific cytotoxic T cells.
Dr. Katayoun Rezvani and Dr. Richard E. Champlin are with the University of Texas MD Andersen Cancer Center, Houston. Their financial disclosures are available at www.jco.org. They made these remarks in an editorial accompanying Dr. Styczynski’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2016.66.6099).
In allogeneic hematopoietic stem-cell transplantation, the donor’s status regarding Epstein-Barr virus affects the recipient’s risk of developing graft-vs-host disease – a “completely new and striking” finding, according to a report published online April 18 in the Journal of Clinical Oncology.
Approximately 80% of the general population has been infected with EBV and carries persistent virus in memory B cells. When viral material is transmitted to stem-cell recipients, it is known to cause posttransplantation lymphoproliferative disorder. Until now, however, no data were available to examine EBV serology’s effect on other posttransplantation outcomes, said Dr. Jan Styczynski of the department of pediatric hematology and oncology at Nicolaus Copernicus University, Bydgoszcz, Poland, and his associates.
They analyzed information in the European Society of Blood and Marrow Transplantation database for 11,364 patients with acute lymphoblastic leukemia or acute myeloblastic leukemia who underwent stem-cell transplantation between 1997 and 2012 and who were followed for approximately 5 years. Most of the donors (82%) were seropositive for EBV. Acute graft-vs-host disease (GVHD) developed in 32% and chronic GVHD developed in 40% of these stem cell–transplant recipients.
The incidence of chronic GVHD was significantly higher when the donor was EBV-seropositive (41%) than when the donor was EBV-seronegative (31%). Similarly, the incidence of acute GVHD was significantly higher when the donor was EBV-seropositive (32% vs 30%), but the magnitude of the difference between the two groups was smaller. The risk for GVHD increased even though patients receiving transplants from EBV-seropositive donors underwent more intensive GVHD prophylaxis than did those who had seronegative donors, the investigators said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.64.2405).
In contrast, the transplant recipients’ EBV status did not affect their risk of developing GVHD.
“Despite the effect of donor EBV serostatus on GVHD, we did not observe a corresponding GVHD-related death rate, and as a result, there was no effect on overall survival, relapse-free survival, relapse incidence, and nonrelapse mortality. However, it should be kept in mind that many other pre- and posttransplantation factors play a role in contributing to final transplantation outcomes,” Dr. Styczynski and his associates noted.
The current recommendation to monitor transplantation recipients for EBV and to give them “preemptive” rituximab to stave off the development of posttransplantation lymphoproliferative disorder might prove useful in also preventing GVHD, they added.
In allogeneic hematopoietic stem-cell transplantation, the donor’s status regarding Epstein-Barr virus affects the recipient’s risk of developing graft-vs-host disease – a “completely new and striking” finding, according to a report published online April 18 in the Journal of Clinical Oncology.
Approximately 80% of the general population has been infected with EBV and carries persistent virus in memory B cells. When viral material is transmitted to stem-cell recipients, it is known to cause posttransplantation lymphoproliferative disorder. Until now, however, no data were available to examine EBV serology’s effect on other posttransplantation outcomes, said Dr. Jan Styczynski of the department of pediatric hematology and oncology at Nicolaus Copernicus University, Bydgoszcz, Poland, and his associates.
They analyzed information in the European Society of Blood and Marrow Transplantation database for 11,364 patients with acute lymphoblastic leukemia or acute myeloblastic leukemia who underwent stem-cell transplantation between 1997 and 2012 and who were followed for approximately 5 years. Most of the donors (82%) were seropositive for EBV. Acute graft-vs-host disease (GVHD) developed in 32% and chronic GVHD developed in 40% of these stem cell–transplant recipients.
The incidence of chronic GVHD was significantly higher when the donor was EBV-seropositive (41%) than when the donor was EBV-seronegative (31%). Similarly, the incidence of acute GVHD was significantly higher when the donor was EBV-seropositive (32% vs 30%), but the magnitude of the difference between the two groups was smaller. The risk for GVHD increased even though patients receiving transplants from EBV-seropositive donors underwent more intensive GVHD prophylaxis than did those who had seronegative donors, the investigators said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.64.2405).
In contrast, the transplant recipients’ EBV status did not affect their risk of developing GVHD.
“Despite the effect of donor EBV serostatus on GVHD, we did not observe a corresponding GVHD-related death rate, and as a result, there was no effect on overall survival, relapse-free survival, relapse incidence, and nonrelapse mortality. However, it should be kept in mind that many other pre- and posttransplantation factors play a role in contributing to final transplantation outcomes,” Dr. Styczynski and his associates noted.
The current recommendation to monitor transplantation recipients for EBV and to give them “preemptive” rituximab to stave off the development of posttransplantation lymphoproliferative disorder might prove useful in also preventing GVHD, they added.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: In allogeneic hematopoietic stem-cell transplantation, the donor’s EBV status affects the recipient’s risk of developing GVHD.
Major finding: Chronic GVHD was significantly more likely to develop when the donor was EBV-seropositive (41%) than EBV-seronegative (31%).
Data source: A retrospective analysis of data regarding 11,364 European patients with acute leukemia who underwent stem-cell transplantation and were followed for 5 years.
Disclosures: No study sponsor was identified. Dr. Styczynski reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Patients with ASD may have lower cancer risk

Photo by Darren Baker
New research suggests that patients diagnosed with an autism spectrum disorder (ASD) have a higher burden of mutations in oncogenes but lower rates of cancer than the rest of the population.
Investigators analyzed large, publicly available genomic databases of patients with ASD and found that, compared to a set of control subjects, ASD patients had significantly higher rates of DNA variation in oncogenes.
The team followed up this result with an analysis of the University of Iowa Hospitals and Clinics’ electronic medical record and discovered that ASD patients were also significantly less likely to have a co-occurring diagnosis of cancer.
“It’s a very provocative result that makes sense on one level and is extremely perplexing on another,” said Benjamin Darbro, MD, PhD, of the University of Iowa Carver College of Medicine in Iowa City.
Dr Darbro and his colleagues discussed the result, and the research that led to it, in a paper published in PLOS ONE.
The investigators used exome sequencing data from the ARRA Autism Sequencing Collaboration and compared that data to a control cohort from the Exome Variant Server database.
This revealed that rare, coding variants within oncogenes were greatly enriched in the ARRA ASD cohort. By comparison, variants were not significantly enriched in tumor suppressor genes.
To ensure the genetic differences were not technical artifacts but actually bona fide differences in genetic architecture in ASD, the investigators ran numerous controls.
As expected, they found that individuals with ASD had many more DNA variations in genes previously associated with autism, epilepsy, and intellectual disability compared to control individuals.
However, there was no difference between the ASD and control groups when it came to genes involved in other, unrelated conditions such as skeletal dysplasia, retinitis pigmentosa, dilated cardiomyopathy, and non-syndromic hearing loss.
The investigators then turned their attention to the electronic medical record at the University of Iowa Hospitals and Clinics and conducted a retrospective case-control analysis comparing 1837 patients with ASD to 9336 patients with any other diagnosis, and determined what proportion of each group carried a cancer diagnosis.
The team found that, for children and adults with ASD, there appeared to be a protective effect against cancer. The cancer incidence was 1.3% for patients with ASD and 3.9% for controls.
The protective effect was evident in both males and females with ASD, but it was strongest for the youngest group of patients and decreased with age. For ASD patients who were under 14 years of age, the odds of having cancer were reduced by 94% compared to controls.
When the investigators determined the rates of other systemic diseases—such as high blood pressure and diabetes—in the ASD population, they found no relationship.
Furthermore, the team found no relationship with cancer when they examined the rates of other common conditions such as esophageal reflux, allergic rhinitis, atopic dermatitis, and short stature. They said this demonstrated that the inverse relationship observed between ASD and cancer is not due to a technical artifact. ![]()

Photo by Darren Baker
New research suggests that patients diagnosed with an autism spectrum disorder (ASD) have a higher burden of mutations in oncogenes but lower rates of cancer than the rest of the population.
Investigators analyzed large, publicly available genomic databases of patients with ASD and found that, compared to a set of control subjects, ASD patients had significantly higher rates of DNA variation in oncogenes.
The team followed up this result with an analysis of the University of Iowa Hospitals and Clinics’ electronic medical record and discovered that ASD patients were also significantly less likely to have a co-occurring diagnosis of cancer.
“It’s a very provocative result that makes sense on one level and is extremely perplexing on another,” said Benjamin Darbro, MD, PhD, of the University of Iowa Carver College of Medicine in Iowa City.
Dr Darbro and his colleagues discussed the result, and the research that led to it, in a paper published in PLOS ONE.
The investigators used exome sequencing data from the ARRA Autism Sequencing Collaboration and compared that data to a control cohort from the Exome Variant Server database.
This revealed that rare, coding variants within oncogenes were greatly enriched in the ARRA ASD cohort. By comparison, variants were not significantly enriched in tumor suppressor genes.
To ensure the genetic differences were not technical artifacts but actually bona fide differences in genetic architecture in ASD, the investigators ran numerous controls.
As expected, they found that individuals with ASD had many more DNA variations in genes previously associated with autism, epilepsy, and intellectual disability compared to control individuals.
However, there was no difference between the ASD and control groups when it came to genes involved in other, unrelated conditions such as skeletal dysplasia, retinitis pigmentosa, dilated cardiomyopathy, and non-syndromic hearing loss.
The investigators then turned their attention to the electronic medical record at the University of Iowa Hospitals and Clinics and conducted a retrospective case-control analysis comparing 1837 patients with ASD to 9336 patients with any other diagnosis, and determined what proportion of each group carried a cancer diagnosis.
The team found that, for children and adults with ASD, there appeared to be a protective effect against cancer. The cancer incidence was 1.3% for patients with ASD and 3.9% for controls.
The protective effect was evident in both males and females with ASD, but it was strongest for the youngest group of patients and decreased with age. For ASD patients who were under 14 years of age, the odds of having cancer were reduced by 94% compared to controls.
When the investigators determined the rates of other systemic diseases—such as high blood pressure and diabetes—in the ASD population, they found no relationship.
Furthermore, the team found no relationship with cancer when they examined the rates of other common conditions such as esophageal reflux, allergic rhinitis, atopic dermatitis, and short stature. They said this demonstrated that the inverse relationship observed between ASD and cancer is not due to a technical artifact. ![]()

Photo by Darren Baker
New research suggests that patients diagnosed with an autism spectrum disorder (ASD) have a higher burden of mutations in oncogenes but lower rates of cancer than the rest of the population.
Investigators analyzed large, publicly available genomic databases of patients with ASD and found that, compared to a set of control subjects, ASD patients had significantly higher rates of DNA variation in oncogenes.
The team followed up this result with an analysis of the University of Iowa Hospitals and Clinics’ electronic medical record and discovered that ASD patients were also significantly less likely to have a co-occurring diagnosis of cancer.
“It’s a very provocative result that makes sense on one level and is extremely perplexing on another,” said Benjamin Darbro, MD, PhD, of the University of Iowa Carver College of Medicine in Iowa City.
Dr Darbro and his colleagues discussed the result, and the research that led to it, in a paper published in PLOS ONE.
The investigators used exome sequencing data from the ARRA Autism Sequencing Collaboration and compared that data to a control cohort from the Exome Variant Server database.
This revealed that rare, coding variants within oncogenes were greatly enriched in the ARRA ASD cohort. By comparison, variants were not significantly enriched in tumor suppressor genes.
To ensure the genetic differences were not technical artifacts but actually bona fide differences in genetic architecture in ASD, the investigators ran numerous controls.
As expected, they found that individuals with ASD had many more DNA variations in genes previously associated with autism, epilepsy, and intellectual disability compared to control individuals.
However, there was no difference between the ASD and control groups when it came to genes involved in other, unrelated conditions such as skeletal dysplasia, retinitis pigmentosa, dilated cardiomyopathy, and non-syndromic hearing loss.
The investigators then turned their attention to the electronic medical record at the University of Iowa Hospitals and Clinics and conducted a retrospective case-control analysis comparing 1837 patients with ASD to 9336 patients with any other diagnosis, and determined what proportion of each group carried a cancer diagnosis.
The team found that, for children and adults with ASD, there appeared to be a protective effect against cancer. The cancer incidence was 1.3% for patients with ASD and 3.9% for controls.
The protective effect was evident in both males and females with ASD, but it was strongest for the youngest group of patients and decreased with age. For ASD patients who were under 14 years of age, the odds of having cancer were reduced by 94% compared to controls.
When the investigators determined the rates of other systemic diseases—such as high blood pressure and diabetes—in the ASD population, they found no relationship.
Furthermore, the team found no relationship with cancer when they examined the rates of other common conditions such as esophageal reflux, allergic rhinitis, atopic dermatitis, and short stature. They said this demonstrated that the inverse relationship observed between ASD and cancer is not due to a technical artifact. ![]()
Prelabor cesarean delivery linked to increased risk of childhood ALL
An increased risk of acute lymphoblastic leukemia (ALL) was seen in young children born by prelabor cesarean delivery, in a pooled analysis of 13 case-control studies from nine countries.
The odds ratio was significant at 1.23 for an association between prelabor cesarean delivery and ALL (P = .018); there was not a significant association between ALL and all indications of cesarean delivery nor was there an association with emergency cesarean delivery. Further, the risk for childhood AML was not associated with cesarean delivery, prelabor cesarean delivery, or emergency cesarean delivery, reported Erin L. Marcotte, Ph.D., of the University of Minnesota, Minneapolis, and her associates.
The association between ALL and prelabor cesarean delivery is based on 13 case-control studies from the Childhood Leukemia International Consortium. Birth delivery method was known for 97%-99% of 8,780 ALL cases, 1,332 AML cases, and 23,459 controls in those studies. In four of the studies, the indications for cesarean delivery were known for 1,061 of 4,313 ALL cases, 138 of 664 AML cases, and 1,401 of 5,884 controls. The multivariable logistic regression models used for the analysis were adjusted for birth weight, sex, age, ethnic origin, parental education, maternal age, and study.
If the association proves to be causal, “maladaptive immune activation due to an absence of stress response before birth in children born by prelabor caesarean delivery could be considered as a potential mechanism,” the researchers wrote (Lancet Haematol. 2016;3[4]:e176–e185).
ALL involves genetic and developmental aberrations that are probably modified by exposure and response to infectious agents. Early exposure to a variety of infections seems to decrease risk, and a vigorous response to infections (quantified by physician visits for infections) increases risk. During vaginal birth, the newborn is exposed to commensal bacteria that modulate immune development, Joseph Weimels, Ph.D., of the University of California at San Francisco, and Xiaomei Ma, Ph.D., of the Yale School of Public Health, New Haven, Conn., wrote in an editorial published in the same issue of The Lancet Haematology. Children delivered vaginally have different gut microbiomes and T-cell reactivity persisting up to age 2 years compared with children born by cesarean, they wrote.
The National Cancer Institute funded the study. The researchers had no relevant disclosures.
On Twitter @maryjodales
An increased risk of acute lymphoblastic leukemia (ALL) was seen in young children born by prelabor cesarean delivery, in a pooled analysis of 13 case-control studies from nine countries.
The odds ratio was significant at 1.23 for an association between prelabor cesarean delivery and ALL (P = .018); there was not a significant association between ALL and all indications of cesarean delivery nor was there an association with emergency cesarean delivery. Further, the risk for childhood AML was not associated with cesarean delivery, prelabor cesarean delivery, or emergency cesarean delivery, reported Erin L. Marcotte, Ph.D., of the University of Minnesota, Minneapolis, and her associates.
The association between ALL and prelabor cesarean delivery is based on 13 case-control studies from the Childhood Leukemia International Consortium. Birth delivery method was known for 97%-99% of 8,780 ALL cases, 1,332 AML cases, and 23,459 controls in those studies. In four of the studies, the indications for cesarean delivery were known for 1,061 of 4,313 ALL cases, 138 of 664 AML cases, and 1,401 of 5,884 controls. The multivariable logistic regression models used for the analysis were adjusted for birth weight, sex, age, ethnic origin, parental education, maternal age, and study.
If the association proves to be causal, “maladaptive immune activation due to an absence of stress response before birth in children born by prelabor caesarean delivery could be considered as a potential mechanism,” the researchers wrote (Lancet Haematol. 2016;3[4]:e176–e185).
ALL involves genetic and developmental aberrations that are probably modified by exposure and response to infectious agents. Early exposure to a variety of infections seems to decrease risk, and a vigorous response to infections (quantified by physician visits for infections) increases risk. During vaginal birth, the newborn is exposed to commensal bacteria that modulate immune development, Joseph Weimels, Ph.D., of the University of California at San Francisco, and Xiaomei Ma, Ph.D., of the Yale School of Public Health, New Haven, Conn., wrote in an editorial published in the same issue of The Lancet Haematology. Children delivered vaginally have different gut microbiomes and T-cell reactivity persisting up to age 2 years compared with children born by cesarean, they wrote.
The National Cancer Institute funded the study. The researchers had no relevant disclosures.
On Twitter @maryjodales
An increased risk of acute lymphoblastic leukemia (ALL) was seen in young children born by prelabor cesarean delivery, in a pooled analysis of 13 case-control studies from nine countries.
The odds ratio was significant at 1.23 for an association between prelabor cesarean delivery and ALL (P = .018); there was not a significant association between ALL and all indications of cesarean delivery nor was there an association with emergency cesarean delivery. Further, the risk for childhood AML was not associated with cesarean delivery, prelabor cesarean delivery, or emergency cesarean delivery, reported Erin L. Marcotte, Ph.D., of the University of Minnesota, Minneapolis, and her associates.
The association between ALL and prelabor cesarean delivery is based on 13 case-control studies from the Childhood Leukemia International Consortium. Birth delivery method was known for 97%-99% of 8,780 ALL cases, 1,332 AML cases, and 23,459 controls in those studies. In four of the studies, the indications for cesarean delivery were known for 1,061 of 4,313 ALL cases, 138 of 664 AML cases, and 1,401 of 5,884 controls. The multivariable logistic regression models used for the analysis were adjusted for birth weight, sex, age, ethnic origin, parental education, maternal age, and study.
If the association proves to be causal, “maladaptive immune activation due to an absence of stress response before birth in children born by prelabor caesarean delivery could be considered as a potential mechanism,” the researchers wrote (Lancet Haematol. 2016;3[4]:e176–e185).
ALL involves genetic and developmental aberrations that are probably modified by exposure and response to infectious agents. Early exposure to a variety of infections seems to decrease risk, and a vigorous response to infections (quantified by physician visits for infections) increases risk. During vaginal birth, the newborn is exposed to commensal bacteria that modulate immune development, Joseph Weimels, Ph.D., of the University of California at San Francisco, and Xiaomei Ma, Ph.D., of the Yale School of Public Health, New Haven, Conn., wrote in an editorial published in the same issue of The Lancet Haematology. Children delivered vaginally have different gut microbiomes and T-cell reactivity persisting up to age 2 years compared with children born by cesarean, they wrote.
The National Cancer Institute funded the study. The researchers had no relevant disclosures.
On Twitter @maryjodales
THE LANCET HAEMATOLOGY
Key clinical point: Prelabor cesarean delivery was associated with an increased risk of childhood ALL, but not AML.
Major finding: The odds ratio was significant at 1.23 for an association between prelabor cesarean delivery and ALL (P = .018).
Data source: Thirteen case-control studies from the Childhood Leukemia International Consortium.
Disclosures: The National Cancer Institute funded the study. The researchers had no relevant disclosures.
TKI trial leaves questions unanswered

Image by Difu Wu
The phase 3 EPIC trial, a comparison of tyrosine kinase inhibitors (TKIs), has left some questions unanswered.
The trial did not determine whether the third-generation TKI ponatinib is more effective than the first-generation TKI imatinib for patients with previously untreated chronic myeloid leukemia (CML).
The study was terminated early due to safety concerns associated with ponatinib, so the primary endpoint could only be analyzed in a small number of patients.
Results in these patients showed no significant difference in that endpoint—major molecular response (MMR) at 12 months—between the imatinib and ponatinib arms.
Results in the entire study cohort suggested that, overall, ponatinib was more toxic than imatinib. In particular, ponatinib produced more arterial occlusive events.
However, the trial’s investigators have questioned whether reducing the dose of ponatinib might change that.
Jeffrey H. Lipton, MD, of Princess Margaret Cancer Centre in Toronto, Ontario, Canada, and his colleagues reported results from the EPIC trial in The Lancet Oncology. The trial was supported by Ariad Pharmaceuticals.
Problems with ponatinib
Ponatinib was approved by the US Food and Drug Administration (FDA) in December 2012 to treat adults with CML or Philadelphia chromosome-positive acute lymphoblastic leukemia that is resistant to or intolerant of other TKIs.
In October 2013, follow-up results from the phase 2 PACE trial suggested ponatinib can increase a patient’s risk of arterial and venous thrombotic events. So all trials of the drug were placed on partial clinical hold, with the exception of the EPIC trial, which was terminated.
That November, the FDA suspended sales and marketing of ponatinib, pending results of a safety evaluation. In December, the agency decided ponatinib could return to the market if new safety measures were implemented. In January 2014, ponatinib was put back on the market in the US.
EPIC trial
The trial enrolled 307 patients with newly diagnosed, chronic-phase CML. Patients were randomized to receive ponatinib at 45 mg (n=155) or imatinib at 400 mg (n=152) once daily until progression, unacceptable toxicity, or other criteria for withdrawal were met.
The median age was 55 (range, 18-89) in the ponatinib arm and 52 (range, 18-86) in the imatinib arm. Most patients were male—63% and 61%, respectively—and most had an ECOG performance status of 0—75% and 78%, respectively.
Patients were randomized between August 14, 2012, and October 9, 2013, and the trial was terminated on October 17, 2013.
Because of the early termination, only 10 patients in the ponatinib arm and 13 in the imatinib arm were evaluable for the primary endpoint—MMR at 12 months. Eighty percent (8/10) of the evaluable patients in the ponatinib arm and 38% (5/13) of those in the imatinib arm achieved an MMR at 12 months (P=0.074).
The investigators also evaluated the incidence of MMR at any time in patients with any post-baseline molecular response assessment. This time, the incidence of MMR was significantly higher in the ponatinib arm than the imatinib arm—41% (61/149) and 18% (25/142), respectively (P<0.0001).
All of the patients were evaluable for safety—154 in the ponatinib arm and 152 in the imatinib arm.
Arterial occlusive events occurred in 7% (n=11) of patients in the ponatinib arm and 2% (n=3) in the imatinib arm (P=0.052). These events were considered serious in 6% (n=10) and 1% (n=1), respectively (P=0.010).
Common grade 3/4 adverse events—in the ponatinib and imatinib arms, respectively—were increased lipase (14% vs 2%), thrombocytopenia (12% vs 7%), rash (6% vs 1%), and neutropenia (3% vs 8%).
Serious adverse events that occurred in 3 or more patients in the ponatinib arm were pancreatitis (n=5), atrial fibrillation (n=3), and thrombocytopenia (n=3). There were no serious adverse events that occurred in 3 or more patients in the imatinib arm.
Dr Lipton and his colleagues said the premature termination of the EPIC trial restricts the interpretation of its results, but the available data provide some insight into the activity and safety of ponatinib in previously untreated CML.
The investigators also noted that data from this trial and the clinical development program for ponatinib suggest that lowering doses of the drug could improve its vascular safety profile and, therefore, the benefit-risk balance.
Two ongoing trials (NCT02467270 and NCT02627677) may provide more insight. Both are investigating starting doses of ponatinib at 15 mg or 30 mg. ![]()

Image by Difu Wu
The phase 3 EPIC trial, a comparison of tyrosine kinase inhibitors (TKIs), has left some questions unanswered.
The trial did not determine whether the third-generation TKI ponatinib is more effective than the first-generation TKI imatinib for patients with previously untreated chronic myeloid leukemia (CML).
The study was terminated early due to safety concerns associated with ponatinib, so the primary endpoint could only be analyzed in a small number of patients.
Results in these patients showed no significant difference in that endpoint—major molecular response (MMR) at 12 months—between the imatinib and ponatinib arms.
Results in the entire study cohort suggested that, overall, ponatinib was more toxic than imatinib. In particular, ponatinib produced more arterial occlusive events.
However, the trial’s investigators have questioned whether reducing the dose of ponatinib might change that.
Jeffrey H. Lipton, MD, of Princess Margaret Cancer Centre in Toronto, Ontario, Canada, and his colleagues reported results from the EPIC trial in The Lancet Oncology. The trial was supported by Ariad Pharmaceuticals.
Problems with ponatinib
Ponatinib was approved by the US Food and Drug Administration (FDA) in December 2012 to treat adults with CML or Philadelphia chromosome-positive acute lymphoblastic leukemia that is resistant to or intolerant of other TKIs.
In October 2013, follow-up results from the phase 2 PACE trial suggested ponatinib can increase a patient’s risk of arterial and venous thrombotic events. So all trials of the drug were placed on partial clinical hold, with the exception of the EPIC trial, which was terminated.
That November, the FDA suspended sales and marketing of ponatinib, pending results of a safety evaluation. In December, the agency decided ponatinib could return to the market if new safety measures were implemented. In January 2014, ponatinib was put back on the market in the US.
EPIC trial
The trial enrolled 307 patients with newly diagnosed, chronic-phase CML. Patients were randomized to receive ponatinib at 45 mg (n=155) or imatinib at 400 mg (n=152) once daily until progression, unacceptable toxicity, or other criteria for withdrawal were met.
The median age was 55 (range, 18-89) in the ponatinib arm and 52 (range, 18-86) in the imatinib arm. Most patients were male—63% and 61%, respectively—and most had an ECOG performance status of 0—75% and 78%, respectively.
Patients were randomized between August 14, 2012, and October 9, 2013, and the trial was terminated on October 17, 2013.
Because of the early termination, only 10 patients in the ponatinib arm and 13 in the imatinib arm were evaluable for the primary endpoint—MMR at 12 months. Eighty percent (8/10) of the evaluable patients in the ponatinib arm and 38% (5/13) of those in the imatinib arm achieved an MMR at 12 months (P=0.074).
The investigators also evaluated the incidence of MMR at any time in patients with any post-baseline molecular response assessment. This time, the incidence of MMR was significantly higher in the ponatinib arm than the imatinib arm—41% (61/149) and 18% (25/142), respectively (P<0.0001).
All of the patients were evaluable for safety—154 in the ponatinib arm and 152 in the imatinib arm.
Arterial occlusive events occurred in 7% (n=11) of patients in the ponatinib arm and 2% (n=3) in the imatinib arm (P=0.052). These events were considered serious in 6% (n=10) and 1% (n=1), respectively (P=0.010).
Common grade 3/4 adverse events—in the ponatinib and imatinib arms, respectively—were increased lipase (14% vs 2%), thrombocytopenia (12% vs 7%), rash (6% vs 1%), and neutropenia (3% vs 8%).
Serious adverse events that occurred in 3 or more patients in the ponatinib arm were pancreatitis (n=5), atrial fibrillation (n=3), and thrombocytopenia (n=3). There were no serious adverse events that occurred in 3 or more patients in the imatinib arm.
Dr Lipton and his colleagues said the premature termination of the EPIC trial restricts the interpretation of its results, but the available data provide some insight into the activity and safety of ponatinib in previously untreated CML.
The investigators also noted that data from this trial and the clinical development program for ponatinib suggest that lowering doses of the drug could improve its vascular safety profile and, therefore, the benefit-risk balance.
Two ongoing trials (NCT02467270 and NCT02627677) may provide more insight. Both are investigating starting doses of ponatinib at 15 mg or 30 mg. ![]()

Image by Difu Wu
The phase 3 EPIC trial, a comparison of tyrosine kinase inhibitors (TKIs), has left some questions unanswered.
The trial did not determine whether the third-generation TKI ponatinib is more effective than the first-generation TKI imatinib for patients with previously untreated chronic myeloid leukemia (CML).
The study was terminated early due to safety concerns associated with ponatinib, so the primary endpoint could only be analyzed in a small number of patients.
Results in these patients showed no significant difference in that endpoint—major molecular response (MMR) at 12 months—between the imatinib and ponatinib arms.
Results in the entire study cohort suggested that, overall, ponatinib was more toxic than imatinib. In particular, ponatinib produced more arterial occlusive events.
However, the trial’s investigators have questioned whether reducing the dose of ponatinib might change that.
Jeffrey H. Lipton, MD, of Princess Margaret Cancer Centre in Toronto, Ontario, Canada, and his colleagues reported results from the EPIC trial in The Lancet Oncology. The trial was supported by Ariad Pharmaceuticals.
Problems with ponatinib
Ponatinib was approved by the US Food and Drug Administration (FDA) in December 2012 to treat adults with CML or Philadelphia chromosome-positive acute lymphoblastic leukemia that is resistant to or intolerant of other TKIs.
In October 2013, follow-up results from the phase 2 PACE trial suggested ponatinib can increase a patient’s risk of arterial and venous thrombotic events. So all trials of the drug were placed on partial clinical hold, with the exception of the EPIC trial, which was terminated.
That November, the FDA suspended sales and marketing of ponatinib, pending results of a safety evaluation. In December, the agency decided ponatinib could return to the market if new safety measures were implemented. In January 2014, ponatinib was put back on the market in the US.
EPIC trial
The trial enrolled 307 patients with newly diagnosed, chronic-phase CML. Patients were randomized to receive ponatinib at 45 mg (n=155) or imatinib at 400 mg (n=152) once daily until progression, unacceptable toxicity, or other criteria for withdrawal were met.
The median age was 55 (range, 18-89) in the ponatinib arm and 52 (range, 18-86) in the imatinib arm. Most patients were male—63% and 61%, respectively—and most had an ECOG performance status of 0—75% and 78%, respectively.
Patients were randomized between August 14, 2012, and October 9, 2013, and the trial was terminated on October 17, 2013.
Because of the early termination, only 10 patients in the ponatinib arm and 13 in the imatinib arm were evaluable for the primary endpoint—MMR at 12 months. Eighty percent (8/10) of the evaluable patients in the ponatinib arm and 38% (5/13) of those in the imatinib arm achieved an MMR at 12 months (P=0.074).
The investigators also evaluated the incidence of MMR at any time in patients with any post-baseline molecular response assessment. This time, the incidence of MMR was significantly higher in the ponatinib arm than the imatinib arm—41% (61/149) and 18% (25/142), respectively (P<0.0001).
All of the patients were evaluable for safety—154 in the ponatinib arm and 152 in the imatinib arm.
Arterial occlusive events occurred in 7% (n=11) of patients in the ponatinib arm and 2% (n=3) in the imatinib arm (P=0.052). These events were considered serious in 6% (n=10) and 1% (n=1), respectively (P=0.010).
Common grade 3/4 adverse events—in the ponatinib and imatinib arms, respectively—were increased lipase (14% vs 2%), thrombocytopenia (12% vs 7%), rash (6% vs 1%), and neutropenia (3% vs 8%).
Serious adverse events that occurred in 3 or more patients in the ponatinib arm were pancreatitis (n=5), atrial fibrillation (n=3), and thrombocytopenia (n=3). There were no serious adverse events that occurred in 3 or more patients in the imatinib arm.
Dr Lipton and his colleagues said the premature termination of the EPIC trial restricts the interpretation of its results, but the available data provide some insight into the activity and safety of ponatinib in previously untreated CML.
The investigators also noted that data from this trial and the clinical development program for ponatinib suggest that lowering doses of the drug could improve its vascular safety profile and, therefore, the benefit-risk balance.
Two ongoing trials (NCT02467270 and NCT02627677) may provide more insight. Both are investigating starting doses of ponatinib at 15 mg or 30 mg. ![]()
In newly diagnosed CLL, mutation tests are advised
Patients with newly diagnosed chronic lymphocytic leukemia should standardly undergo immunoglobulin heavy-chain variable region gene (IGHV) mutation status and interphase fluorescence in situ hybridization (FISH) tests, based on the results of a meta-analysis published in Blood.
“This change will help define the minimal standard initial prognostic evaluation for patients with CLL and help facilitate use of the powerful, recently developed, integrated prognostic indices, all of which are dependent on these 2 variables,” wrote Dr. Sameer A. Parikh of Mayo Clinic, Rochester, Minn., and associates.
IGHV and FISH have prognostic value independent of clinical stage in patients with newly diagnosed and previously untreated CLL, they said (Blood. 2016;127[14]:1752-60). Better understanding of the patient’s risk of disease progression at diagnosis can guide counseling and follow-up intervals, and could potentially influence the decision to treat high-risk patients on early intervention protocols.
IGHV and FISH also appear to provide additional information on progression-free and overall survival.
The researchers cautioned, however, that the results of these tests should not be used to initiate CLL-specific therapy. Only patients who meet indications for therapy based on the 2008 International Workshop on Chronic Lymphocytic Leukemia guidelines should receive treatment.
Further, they noted, the median age of patients included in studies that they analyzed was 64 years; the median age of patients with CLL is 72 years. The prognostic abilities of IGHV mutation and FISH may differ in these older individuals with CLL.
The researchers analyzed 31 studies that met the criteria for inclusion – full-length publications that included at least 200 patients and reported on the prognostic value of IGHV and/or FISH for predicting progression-free or overall survival in patients with newly diagnosed CLL.
They found that the median progression-free survival (range, about 1-5 years) was significantly shorter for patients with unmutated IGHV genes, than was the median progression-free survival (range, about 9-19 years) for those with mutated IGHV genes. Similarly, the median overall survival was significantly shorter for patients with unmutated IGHV (range, about 3-10 years) than for those with mutated IGHV (range, about 18-26 years).
For patients with high-risk FISH (including del17p13 and del11q23), the median progression-free survival was significantly shorter (range, about 0.1-5 years) than for those with low/intermediate-risk FISH (including del13q, normal, and trisomy 12; range, about 1.5-22 years). Median overall survival also significantly differed, ranging from about 3-10 years for patients with high-risk FISH and from about 7.5-20.5 years for those with low/intermediate-risk FISH.
In multivariable analyses, the hazard ratio for high-risk FISH ranged from 1.3 to 4.7 for progression-free survival and from 0.9 to 8.2 for overall survival. In studies reporting the results of multivariable analysis, high-risk FISH remained an independent predictor of progression-free survival in 8 of 17 studies and of overall survival in 10 of 14 studies, including in 10 of 13 studies adjusting for the prognostic impact of IGHV.
In multivariable analyses, IGHV remained an independent predictor of progression-free survival in 15 of 18 studies, including 12 of 15 studies adjusting for the prognostic impact of FISH. IGHV remained an independent predictor of overall survival in 11 of 15 studies reporting the results of multivariable analysis, including 10 of 14 studies adjusting for the prognostic impact of FISH.
Patients with newly diagnosed chronic lymphocytic leukemia should standardly undergo immunoglobulin heavy-chain variable region gene (IGHV) mutation status and interphase fluorescence in situ hybridization (FISH) tests, based on the results of a meta-analysis published in Blood.
“This change will help define the minimal standard initial prognostic evaluation for patients with CLL and help facilitate use of the powerful, recently developed, integrated prognostic indices, all of which are dependent on these 2 variables,” wrote Dr. Sameer A. Parikh of Mayo Clinic, Rochester, Minn., and associates.
IGHV and FISH have prognostic value independent of clinical stage in patients with newly diagnosed and previously untreated CLL, they said (Blood. 2016;127[14]:1752-60). Better understanding of the patient’s risk of disease progression at diagnosis can guide counseling and follow-up intervals, and could potentially influence the decision to treat high-risk patients on early intervention protocols.
IGHV and FISH also appear to provide additional information on progression-free and overall survival.
The researchers cautioned, however, that the results of these tests should not be used to initiate CLL-specific therapy. Only patients who meet indications for therapy based on the 2008 International Workshop on Chronic Lymphocytic Leukemia guidelines should receive treatment.
Further, they noted, the median age of patients included in studies that they analyzed was 64 years; the median age of patients with CLL is 72 years. The prognostic abilities of IGHV mutation and FISH may differ in these older individuals with CLL.
The researchers analyzed 31 studies that met the criteria for inclusion – full-length publications that included at least 200 patients and reported on the prognostic value of IGHV and/or FISH for predicting progression-free or overall survival in patients with newly diagnosed CLL.
They found that the median progression-free survival (range, about 1-5 years) was significantly shorter for patients with unmutated IGHV genes, than was the median progression-free survival (range, about 9-19 years) for those with mutated IGHV genes. Similarly, the median overall survival was significantly shorter for patients with unmutated IGHV (range, about 3-10 years) than for those with mutated IGHV (range, about 18-26 years).
For patients with high-risk FISH (including del17p13 and del11q23), the median progression-free survival was significantly shorter (range, about 0.1-5 years) than for those with low/intermediate-risk FISH (including del13q, normal, and trisomy 12; range, about 1.5-22 years). Median overall survival also significantly differed, ranging from about 3-10 years for patients with high-risk FISH and from about 7.5-20.5 years for those with low/intermediate-risk FISH.
In multivariable analyses, the hazard ratio for high-risk FISH ranged from 1.3 to 4.7 for progression-free survival and from 0.9 to 8.2 for overall survival. In studies reporting the results of multivariable analysis, high-risk FISH remained an independent predictor of progression-free survival in 8 of 17 studies and of overall survival in 10 of 14 studies, including in 10 of 13 studies adjusting for the prognostic impact of IGHV.
In multivariable analyses, IGHV remained an independent predictor of progression-free survival in 15 of 18 studies, including 12 of 15 studies adjusting for the prognostic impact of FISH. IGHV remained an independent predictor of overall survival in 11 of 15 studies reporting the results of multivariable analysis, including 10 of 14 studies adjusting for the prognostic impact of FISH.
Patients with newly diagnosed chronic lymphocytic leukemia should standardly undergo immunoglobulin heavy-chain variable region gene (IGHV) mutation status and interphase fluorescence in situ hybridization (FISH) tests, based on the results of a meta-analysis published in Blood.
“This change will help define the minimal standard initial prognostic evaluation for patients with CLL and help facilitate use of the powerful, recently developed, integrated prognostic indices, all of which are dependent on these 2 variables,” wrote Dr. Sameer A. Parikh of Mayo Clinic, Rochester, Minn., and associates.
IGHV and FISH have prognostic value independent of clinical stage in patients with newly diagnosed and previously untreated CLL, they said (Blood. 2016;127[14]:1752-60). Better understanding of the patient’s risk of disease progression at diagnosis can guide counseling and follow-up intervals, and could potentially influence the decision to treat high-risk patients on early intervention protocols.
IGHV and FISH also appear to provide additional information on progression-free and overall survival.
The researchers cautioned, however, that the results of these tests should not be used to initiate CLL-specific therapy. Only patients who meet indications for therapy based on the 2008 International Workshop on Chronic Lymphocytic Leukemia guidelines should receive treatment.
Further, they noted, the median age of patients included in studies that they analyzed was 64 years; the median age of patients with CLL is 72 years. The prognostic abilities of IGHV mutation and FISH may differ in these older individuals with CLL.
The researchers analyzed 31 studies that met the criteria for inclusion – full-length publications that included at least 200 patients and reported on the prognostic value of IGHV and/or FISH for predicting progression-free or overall survival in patients with newly diagnosed CLL.
They found that the median progression-free survival (range, about 1-5 years) was significantly shorter for patients with unmutated IGHV genes, than was the median progression-free survival (range, about 9-19 years) for those with mutated IGHV genes. Similarly, the median overall survival was significantly shorter for patients with unmutated IGHV (range, about 3-10 years) than for those with mutated IGHV (range, about 18-26 years).
For patients with high-risk FISH (including del17p13 and del11q23), the median progression-free survival was significantly shorter (range, about 0.1-5 years) than for those with low/intermediate-risk FISH (including del13q, normal, and trisomy 12; range, about 1.5-22 years). Median overall survival also significantly differed, ranging from about 3-10 years for patients with high-risk FISH and from about 7.5-20.5 years for those with low/intermediate-risk FISH.
In multivariable analyses, the hazard ratio for high-risk FISH ranged from 1.3 to 4.7 for progression-free survival and from 0.9 to 8.2 for overall survival. In studies reporting the results of multivariable analysis, high-risk FISH remained an independent predictor of progression-free survival in 8 of 17 studies and of overall survival in 10 of 14 studies, including in 10 of 13 studies adjusting for the prognostic impact of IGHV.
In multivariable analyses, IGHV remained an independent predictor of progression-free survival in 15 of 18 studies, including 12 of 15 studies adjusting for the prognostic impact of FISH. IGHV remained an independent predictor of overall survival in 11 of 15 studies reporting the results of multivariable analysis, including 10 of 14 studies adjusting for the prognostic impact of FISH.
FROM BLOOD
Rigosertib falls short for high-risk myelodysplastic syndromes after failure on azacitidine or decitabine
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
THE LANCET ONCOLOGY
Key clinical point: Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
Major finding: Median overall survival was 8.2 months (95% CI, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group.
Data source: An open-label, randomized controlled trial involving 299 patients at 74 medical centers.
Disclosures: The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society..
Rigosertib falls short for high-risk myelodysplastic syndromes after failure on azacitidine or decitabine
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
THE LANCET ONCOLOGY
Key clinical point: Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
Major finding: Median overall survival was 8.2 months (95% CI, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group.
Data source: An open-label, randomized controlled trial involving 299 patients at 74 medical centers.
Disclosures: The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society..