User login
FIRST trial analysis shows more benefit for lenalidomide
Lenalidomide with low-dose dexamethasone showed a significant overall survival benefit, compared with melphalan with prednisone and thalidomide, for patients with transplant-ineligible newly diagnosed multiple myeloma, according to the final analysis of the phase 3 FIRST trial.
The prespecified final analysis evaluated overall survival (OS) at a follow-up of 60 months or longer, according to the study, which was published in Blood. The FIRST study included 1,623 patients randomized to receive lenalidomide with low-dose dexamethasone continuously until disease progression (Rd continuous), lenalidomide plus low-dose dexamethasone for 18 cycles instead of continuously (Rd18), or melphalan plus prednisone and thalidomide (MPT). Patients with high-risk cytogenetics were distributed evenly across the three treatment arms.
The Rd continuous cohort also experienced significantly longer PFS, compared with the MPT arm (HR, 0.69, 95% CI, 0.59-0.79, P less than .00001).
“Taken together, these findings suggest that Rd affords a clinical advantage in subsequent lines of therapy and highlight the importance of using Rd continuous and not MPT as first-line treatment of transplant-ineligible patients with [newly-diagnosed multiple myeloma],” the researchers wrote.
The OS benefit was similar for patients who received Rd continuous (59.1 months) and Rd18 (62.3 months). The researchers suggested that the similar survival could be due to a combination of factors, including the impact of subsequent lines of treatment and the older age of the patient population.
However, the benefit for Rd18 was not seen in the PFS analysis. Patients in the Rd18 group had a median PFS similar to that of patients in the MPT group (21 months vs. 21.9 months), both of which were shorter than the Rd continuous group (26 months).
The 4-year PFS more than doubled among patients in the Rd continuous arm (32.6%), compared with patients in both the Rd18 group (14.3%) and the MPT group (13.6%).
Patients in the Rd continuous group also experienced a decreased risk for progression or death, compared with patients in the Rd18 group (HR, 0.70, 95% CI, 0.60-0.81).
The researchers noted that no new safety concerns were observed in the final analysis. Second primary malignancies, including hematologic and solid tumors, were found in 36% of patients in the Rd continuous group, 38% of patients in the Rd18 group, and 46% of patients in the MPT group.
Celgene Corporation sponsored the study. Dr. Facon and his coauthors reported financial ties to various pharmaceutical companies, including Celgene.
SOURCE: Facon T et al. Blood. 2018 Jan 18;131(3):301-10.
Lenalidomide with low-dose dexamethasone showed a significant overall survival benefit, compared with melphalan with prednisone and thalidomide, for patients with transplant-ineligible newly diagnosed multiple myeloma, according to the final analysis of the phase 3 FIRST trial.
The prespecified final analysis evaluated overall survival (OS) at a follow-up of 60 months or longer, according to the study, which was published in Blood. The FIRST study included 1,623 patients randomized to receive lenalidomide with low-dose dexamethasone continuously until disease progression (Rd continuous), lenalidomide plus low-dose dexamethasone for 18 cycles instead of continuously (Rd18), or melphalan plus prednisone and thalidomide (MPT). Patients with high-risk cytogenetics were distributed evenly across the three treatment arms.
The Rd continuous cohort also experienced significantly longer PFS, compared with the MPT arm (HR, 0.69, 95% CI, 0.59-0.79, P less than .00001).
“Taken together, these findings suggest that Rd affords a clinical advantage in subsequent lines of therapy and highlight the importance of using Rd continuous and not MPT as first-line treatment of transplant-ineligible patients with [newly-diagnosed multiple myeloma],” the researchers wrote.
The OS benefit was similar for patients who received Rd continuous (59.1 months) and Rd18 (62.3 months). The researchers suggested that the similar survival could be due to a combination of factors, including the impact of subsequent lines of treatment and the older age of the patient population.
However, the benefit for Rd18 was not seen in the PFS analysis. Patients in the Rd18 group had a median PFS similar to that of patients in the MPT group (21 months vs. 21.9 months), both of which were shorter than the Rd continuous group (26 months).
The 4-year PFS more than doubled among patients in the Rd continuous arm (32.6%), compared with patients in both the Rd18 group (14.3%) and the MPT group (13.6%).
Patients in the Rd continuous group also experienced a decreased risk for progression or death, compared with patients in the Rd18 group (HR, 0.70, 95% CI, 0.60-0.81).
The researchers noted that no new safety concerns were observed in the final analysis. Second primary malignancies, including hematologic and solid tumors, were found in 36% of patients in the Rd continuous group, 38% of patients in the Rd18 group, and 46% of patients in the MPT group.
Celgene Corporation sponsored the study. Dr. Facon and his coauthors reported financial ties to various pharmaceutical companies, including Celgene.
SOURCE: Facon T et al. Blood. 2018 Jan 18;131(3):301-10.
Lenalidomide with low-dose dexamethasone showed a significant overall survival benefit, compared with melphalan with prednisone and thalidomide, for patients with transplant-ineligible newly diagnosed multiple myeloma, according to the final analysis of the phase 3 FIRST trial.
The prespecified final analysis evaluated overall survival (OS) at a follow-up of 60 months or longer, according to the study, which was published in Blood. The FIRST study included 1,623 patients randomized to receive lenalidomide with low-dose dexamethasone continuously until disease progression (Rd continuous), lenalidomide plus low-dose dexamethasone for 18 cycles instead of continuously (Rd18), or melphalan plus prednisone and thalidomide (MPT). Patients with high-risk cytogenetics were distributed evenly across the three treatment arms.
The Rd continuous cohort also experienced significantly longer PFS, compared with the MPT arm (HR, 0.69, 95% CI, 0.59-0.79, P less than .00001).
“Taken together, these findings suggest that Rd affords a clinical advantage in subsequent lines of therapy and highlight the importance of using Rd continuous and not MPT as first-line treatment of transplant-ineligible patients with [newly-diagnosed multiple myeloma],” the researchers wrote.
The OS benefit was similar for patients who received Rd continuous (59.1 months) and Rd18 (62.3 months). The researchers suggested that the similar survival could be due to a combination of factors, including the impact of subsequent lines of treatment and the older age of the patient population.
However, the benefit for Rd18 was not seen in the PFS analysis. Patients in the Rd18 group had a median PFS similar to that of patients in the MPT group (21 months vs. 21.9 months), both of which were shorter than the Rd continuous group (26 months).
The 4-year PFS more than doubled among patients in the Rd continuous arm (32.6%), compared with patients in both the Rd18 group (14.3%) and the MPT group (13.6%).
Patients in the Rd continuous group also experienced a decreased risk for progression or death, compared with patients in the Rd18 group (HR, 0.70, 95% CI, 0.60-0.81).
The researchers noted that no new safety concerns were observed in the final analysis. Second primary malignancies, including hematologic and solid tumors, were found in 36% of patients in the Rd continuous group, 38% of patients in the Rd18 group, and 46% of patients in the MPT group.
Celgene Corporation sponsored the study. Dr. Facon and his coauthors reported financial ties to various pharmaceutical companies, including Celgene.
SOURCE: Facon T et al. Blood. 2018 Jan 18;131(3):301-10.
FROM BLOOD
Key clinical point:
Major finding: Continuously administered lenalidomide with dexamethasone regimen improved PFS (HR, 0.69) and OS (HR, 0.78), compared with melphalan, prednisone, and thalidomide.
Study details: Final analysis of the phase 3 FIRST trial.
Disclosures: Celgene Corporation sponsored the study. Dr. Facon and his coauthors reported financial ties to various pharmaceutical companies, including Celgene.
Source: Facon T et al. Blood. 2018 Jan 18;131(3):301-10.
FDG PET can’t replace BM biopsy, study suggests
LA JOLLA, CA—Fluorodeoxyglucose positron emission tomography (FDG PET) cannot replace bone marrow (BM) biopsy in T-cell lymphomas, according to a speaker at the 10th Annual T-cell Lymphoma Forum.
Researchers found that FDG PET results did not exactly correlate with BM biopsy results relating to tumor involvement in patients with T-cell lymphomas.
However, results from FDG PET were found to be an independent prognostic factor for progression-free survival (PFS) and overall survival (OS).
Youngil Koh, MD, of Seoul National University Hospital in Seoul, South Korea, presented this research in a poster and oral presentation at this year’s T-cell Lymphoma Forum.
He and his colleagues set out to investigate the clinical value of FDG PET for evaluating BM tumor involvement and prognosis in T-cell lymphoma patients.
The team analyzed 109 patients who underwent staging with FDG PET and BM biopsy. Most patients had extranodal natural killer/T-cell lymphoma, nasal type (NKTCL, n=46), or angioimmunoblastic T-cell lymphoma (AITL, n=41).
Patients also had peripheral T-cell lymphoma not otherwise specified (n=12), anaplastic large-cell lymphoma (n=4), enteropathy-associated T-cell lymphoma (n=4), and subcutaneous panniculitis-like T-cell lymphoma (n=2).
Most patients (87.2%) received chemotherapy as first-line treatment. Fifty percent were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) or CHOP-like regimens, 48.1% were IMEP (ifosphamide, methotrexate, etoposide, and prednisolone) or IMEP-like regimens, and 1.9% were “other” regimens.
Other first-line treatments included radiotherapy followed by chemotherapy (10.1%), excision (0.9%), and no treatment (1.8%).
The patients’ median OS was 60.03 months, and the median PFS was 15.7 months.
BM involvement
The researchers analyzed PET BM uptake both visually and quantitatively using the marrow-to-liver ratio (MLR), and they compared these results to BM biopsy results.
According to BM biopsy, 35.8% of patients had tumor involvement.
By visual analysis, the sensitivity of PET for diagnosing positive BM biopsy was 58.5%, and the specificity was 77.9%. By MLR, the sensitivity was 64.1%, and the specificity was 72.9%.
The diagnostic performance of PET for BM involvement was not different across the lymphoma subtypes, Dr Koh said.
Prognosis
“Although FDG PET did not correlate very well with bone marrow biopsy, it had prognostic value, especially MLR,” Dr Koh noted. “And most importantly, in bone marrow biopsy-negative patients, it [MLR] had prognostic value.”
MLR was a significant prognostic factor for PFS (P=0.005) and OS (P<0.001). The same was true for BM biopsy (P=0.009 for PFS and P<0.001 for OS), while visual PET analysis was a significant prognostic factor for OS (P=0.015) but not PFS (P=0.476).
In patients negative by BM biopsy, MLR was a significant prognostic factor for PFS (P=0.001) and OS (P=0.005).
Dr Koh and his colleagues also analyzed the prognostic value of PET and BM biopsy specifically in patients with NKTCL and AITL.
In AITL patients, BM biopsy was a significant prognostic factor for OS (P=0.002) but not PFS (P=0.246). Visual PET analysis was not significant for PFS (P=0.910) or OS (P=0.581), and neither was MLR (P=0.053 for PFS and P=0.156 for OS).
In patients with NKTCL, BM biopsy was a significant prognostic factor for PFS (P=0.008) and OS (P<0.001). Visual PET analysis was not significant for PFS (P=0.469) or OS (P=0.092). And MLR was significant for PFS (P=0.004) and OS (P=0.012).
“Bone marrow findings of FDG PET are an independent prognostic factor in these tumors,” Dr Koh said, “suggesting the biologic relevance of FDG PET findings for aggressiveness or covert bone marrow involvement of tumor cells.” ![]()
LA JOLLA, CA—Fluorodeoxyglucose positron emission tomography (FDG PET) cannot replace bone marrow (BM) biopsy in T-cell lymphomas, according to a speaker at the 10th Annual T-cell Lymphoma Forum.
Researchers found that FDG PET results did not exactly correlate with BM biopsy results relating to tumor involvement in patients with T-cell lymphomas.
However, results from FDG PET were found to be an independent prognostic factor for progression-free survival (PFS) and overall survival (OS).
Youngil Koh, MD, of Seoul National University Hospital in Seoul, South Korea, presented this research in a poster and oral presentation at this year’s T-cell Lymphoma Forum.
He and his colleagues set out to investigate the clinical value of FDG PET for evaluating BM tumor involvement and prognosis in T-cell lymphoma patients.
The team analyzed 109 patients who underwent staging with FDG PET and BM biopsy. Most patients had extranodal natural killer/T-cell lymphoma, nasal type (NKTCL, n=46), or angioimmunoblastic T-cell lymphoma (AITL, n=41).
Patients also had peripheral T-cell lymphoma not otherwise specified (n=12), anaplastic large-cell lymphoma (n=4), enteropathy-associated T-cell lymphoma (n=4), and subcutaneous panniculitis-like T-cell lymphoma (n=2).
Most patients (87.2%) received chemotherapy as first-line treatment. Fifty percent were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) or CHOP-like regimens, 48.1% were IMEP (ifosphamide, methotrexate, etoposide, and prednisolone) or IMEP-like regimens, and 1.9% were “other” regimens.
Other first-line treatments included radiotherapy followed by chemotherapy (10.1%), excision (0.9%), and no treatment (1.8%).
The patients’ median OS was 60.03 months, and the median PFS was 15.7 months.
BM involvement
The researchers analyzed PET BM uptake both visually and quantitatively using the marrow-to-liver ratio (MLR), and they compared these results to BM biopsy results.
According to BM biopsy, 35.8% of patients had tumor involvement.
By visual analysis, the sensitivity of PET for diagnosing positive BM biopsy was 58.5%, and the specificity was 77.9%. By MLR, the sensitivity was 64.1%, and the specificity was 72.9%.
The diagnostic performance of PET for BM involvement was not different across the lymphoma subtypes, Dr Koh said.
Prognosis
“Although FDG PET did not correlate very well with bone marrow biopsy, it had prognostic value, especially MLR,” Dr Koh noted. “And most importantly, in bone marrow biopsy-negative patients, it [MLR] had prognostic value.”
MLR was a significant prognostic factor for PFS (P=0.005) and OS (P<0.001). The same was true for BM biopsy (P=0.009 for PFS and P<0.001 for OS), while visual PET analysis was a significant prognostic factor for OS (P=0.015) but not PFS (P=0.476).
In patients negative by BM biopsy, MLR was a significant prognostic factor for PFS (P=0.001) and OS (P=0.005).
Dr Koh and his colleagues also analyzed the prognostic value of PET and BM biopsy specifically in patients with NKTCL and AITL.
In AITL patients, BM biopsy was a significant prognostic factor for OS (P=0.002) but not PFS (P=0.246). Visual PET analysis was not significant for PFS (P=0.910) or OS (P=0.581), and neither was MLR (P=0.053 for PFS and P=0.156 for OS).
In patients with NKTCL, BM biopsy was a significant prognostic factor for PFS (P=0.008) and OS (P<0.001). Visual PET analysis was not significant for PFS (P=0.469) or OS (P=0.092). And MLR was significant for PFS (P=0.004) and OS (P=0.012).
“Bone marrow findings of FDG PET are an independent prognostic factor in these tumors,” Dr Koh said, “suggesting the biologic relevance of FDG PET findings for aggressiveness or covert bone marrow involvement of tumor cells.” ![]()
LA JOLLA, CA—Fluorodeoxyglucose positron emission tomography (FDG PET) cannot replace bone marrow (BM) biopsy in T-cell lymphomas, according to a speaker at the 10th Annual T-cell Lymphoma Forum.
Researchers found that FDG PET results did not exactly correlate with BM biopsy results relating to tumor involvement in patients with T-cell lymphomas.
However, results from FDG PET were found to be an independent prognostic factor for progression-free survival (PFS) and overall survival (OS).
Youngil Koh, MD, of Seoul National University Hospital in Seoul, South Korea, presented this research in a poster and oral presentation at this year’s T-cell Lymphoma Forum.
He and his colleagues set out to investigate the clinical value of FDG PET for evaluating BM tumor involvement and prognosis in T-cell lymphoma patients.
The team analyzed 109 patients who underwent staging with FDG PET and BM biopsy. Most patients had extranodal natural killer/T-cell lymphoma, nasal type (NKTCL, n=46), or angioimmunoblastic T-cell lymphoma (AITL, n=41).
Patients also had peripheral T-cell lymphoma not otherwise specified (n=12), anaplastic large-cell lymphoma (n=4), enteropathy-associated T-cell lymphoma (n=4), and subcutaneous panniculitis-like T-cell lymphoma (n=2).
Most patients (87.2%) received chemotherapy as first-line treatment. Fifty percent were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) or CHOP-like regimens, 48.1% were IMEP (ifosphamide, methotrexate, etoposide, and prednisolone) or IMEP-like regimens, and 1.9% were “other” regimens.
Other first-line treatments included radiotherapy followed by chemotherapy (10.1%), excision (0.9%), and no treatment (1.8%).
The patients’ median OS was 60.03 months, and the median PFS was 15.7 months.
BM involvement
The researchers analyzed PET BM uptake both visually and quantitatively using the marrow-to-liver ratio (MLR), and they compared these results to BM biopsy results.
According to BM biopsy, 35.8% of patients had tumor involvement.
By visual analysis, the sensitivity of PET for diagnosing positive BM biopsy was 58.5%, and the specificity was 77.9%. By MLR, the sensitivity was 64.1%, and the specificity was 72.9%.
The diagnostic performance of PET for BM involvement was not different across the lymphoma subtypes, Dr Koh said.
Prognosis
“Although FDG PET did not correlate very well with bone marrow biopsy, it had prognostic value, especially MLR,” Dr Koh noted. “And most importantly, in bone marrow biopsy-negative patients, it [MLR] had prognostic value.”
MLR was a significant prognostic factor for PFS (P=0.005) and OS (P<0.001). The same was true for BM biopsy (P=0.009 for PFS and P<0.001 for OS), while visual PET analysis was a significant prognostic factor for OS (P=0.015) but not PFS (P=0.476).
In patients negative by BM biopsy, MLR was a significant prognostic factor for PFS (P=0.001) and OS (P=0.005).
Dr Koh and his colleagues also analyzed the prognostic value of PET and BM biopsy specifically in patients with NKTCL and AITL.
In AITL patients, BM biopsy was a significant prognostic factor for OS (P=0.002) but not PFS (P=0.246). Visual PET analysis was not significant for PFS (P=0.910) or OS (P=0.581), and neither was MLR (P=0.053 for PFS and P=0.156 for OS).
In patients with NKTCL, BM biopsy was a significant prognostic factor for PFS (P=0.008) and OS (P<0.001). Visual PET analysis was not significant for PFS (P=0.469) or OS (P=0.092). And MLR was significant for PFS (P=0.004) and OS (P=0.012).
“Bone marrow findings of FDG PET are an independent prognostic factor in these tumors,” Dr Koh said, “suggesting the biologic relevance of FDG PET findings for aggressiveness or covert bone marrow involvement of tumor cells.” ![]()
Inhibitor provides clinical improvement in MF
LA JOLLA, CA—Results of a phase 1 trial suggest MRG-106 can provide clinical improvement in patients with mycosis fungoides (MF), whether the drug is given alone or in conjunction with other therapies.
MRG-106 is an inhibitor of microRNA-155, which is upregulated in MF.
In this ongoing trial, 90% of patients who received MRG-106 have experienced an improvement in mSWAT score, and 59% of patients who received the drug for at least 1 month had a partial response.
The most common adverse events (AEs) attributed to MRG-106 were neutropenia, injection site pain, and fatigue.
Christiane Querfeld, MD, PhD, of the City of Hope in Duarte, California, presented these results at the 10th Annual T-cell Lymphoma Forum. The research is sponsored by miRagen Therapeutics, Inc., the company developing MRG-106.
The trial has enrolled 36 MF patients, 69% of whom are male. Their median age at enrollment was 63 (range, 21-85).
Patients had received a median of 4 prior systemic therapies (range, 1-13) and a median of 3 prior skin-directed therapies (range, 1-8).
At baseline, patients had a median mSWAT score of 43 (range, 2-180). The modified Severity Weighted Assessment Tool (mSWAT) measures the severity of skin disease over a patient’s body.
Part A
In part A of the study, 6 patients received MRG-106 via intralesional injection. A 75 mg dose of the drug was found to be well-tolerated, producing generally minor injection site reactions.
In addition, intralesional injection of MRG-106 produced improvements in CAILS score. The Composite Assessment of Index Lesion Severity (CAILS) score is obtained by adding the severity score of erythema, scaling, plaque elevation, and surface area for up to 5 index lesions.
Part B
In part B, 30 patients received MRG-106 via subcutaneous (SQ) injection, intravenous (IV) infusion, or IV bolus injection.
Patients who received SQ injection or IV infusion received doses of 300 mg, 600 mg, or 900 mg. Those who received an IV bolus only received the 300 mg dose.
Twenty-nine of the 30 patients in part B were evaluable for efficacy. Twenty-six of these patients—90%—had an improvement in mSWAT score from baseline.
“Twenty-six patients had at least stable disease to partial response,” Dr Querfeld noted. “No complete responses yet, but we’re close.”
Twelve patients were still receiving MRG-106 at last follow-up.
Ten of the 17 patients (59%) who had received MRG-106 for more than 1 month had at least a 50% improvement in mSWAT score, or a partial response. Once this was achieved, responses were durable.
One patient was still in response at roughly 470 days of follow-up.
Concomitant therapies
Dr Querfeld and her colleagues looked at patient outcomes in the context of concomitant therapies as well. They analyzed data from 26 patients who had received at least 6 doses of MRG-106.
Half of these patients were receiving MRG-106 alone, and the other half were receiving concomitant therapies, including bexarotene (n=7), interferon-alfa (n=2), methotrexate (n=1), vorinostat (n=1), and “other” treatments (n=2). Patients had been receiving these therapies for anywhere from 4 months to 45 months.
Outcomes were similar in the monotherapy and combination treatment groups. Seven patients in each group had at least a 50% improvement in mSWAT score.
Dosing and administration
“It appears the infusion is superior to the subcutaneous administration,” Dr Querfeld said.
She noted that durable partial responses have been achieved at all dose levels, but the 300 mg and 600 mg IV infusions had the best efficacy and tolerability profiles.
With the 300 mg IV bolus, fewer patients remained on treatment for more than 1 cycle, as compared to the other dosing cohorts. Dr Querfeld said this may be a result of lower total exposure or tolerability due to higher plasma Cmax.
She also noted that patients who received MRG-106 SQ at 600 mg or higher had a higher incidence of injection site reactions.
Safety
AEs of any grade that were attributed to MRG-106 include neutropenia (16%), injection site pain (16%), fatigue (14%), nausea (5%), pruritus (5%), and headache (5%).
Grade 3/4 AEs attributed to MRG-106 were neutropenia (5%) and pruritus (5%).
There were no serious AEs attributed to MRG-106, but there were 2 dose-limiting toxicities. One was a grade 3 tumor flare in a patient receiving the 300 mg IV bolus.
The other dose-limiting toxicity was grade 3 worsening pruritus and possible tumor flare, which occurred twice in 1 patient—with the 900 mg SQ dose and with the 300 mg IV infusion.
The 300 mg IV infusion is the anticipated phase 2 dose. ![]()
LA JOLLA, CA—Results of a phase 1 trial suggest MRG-106 can provide clinical improvement in patients with mycosis fungoides (MF), whether the drug is given alone or in conjunction with other therapies.
MRG-106 is an inhibitor of microRNA-155, which is upregulated in MF.
In this ongoing trial, 90% of patients who received MRG-106 have experienced an improvement in mSWAT score, and 59% of patients who received the drug for at least 1 month had a partial response.
The most common adverse events (AEs) attributed to MRG-106 were neutropenia, injection site pain, and fatigue.
Christiane Querfeld, MD, PhD, of the City of Hope in Duarte, California, presented these results at the 10th Annual T-cell Lymphoma Forum. The research is sponsored by miRagen Therapeutics, Inc., the company developing MRG-106.
The trial has enrolled 36 MF patients, 69% of whom are male. Their median age at enrollment was 63 (range, 21-85).
Patients had received a median of 4 prior systemic therapies (range, 1-13) and a median of 3 prior skin-directed therapies (range, 1-8).
At baseline, patients had a median mSWAT score of 43 (range, 2-180). The modified Severity Weighted Assessment Tool (mSWAT) measures the severity of skin disease over a patient’s body.
Part A
In part A of the study, 6 patients received MRG-106 via intralesional injection. A 75 mg dose of the drug was found to be well-tolerated, producing generally minor injection site reactions.
In addition, intralesional injection of MRG-106 produced improvements in CAILS score. The Composite Assessment of Index Lesion Severity (CAILS) score is obtained by adding the severity score of erythema, scaling, plaque elevation, and surface area for up to 5 index lesions.
Part B
In part B, 30 patients received MRG-106 via subcutaneous (SQ) injection, intravenous (IV) infusion, or IV bolus injection.
Patients who received SQ injection or IV infusion received doses of 300 mg, 600 mg, or 900 mg. Those who received an IV bolus only received the 300 mg dose.
Twenty-nine of the 30 patients in part B were evaluable for efficacy. Twenty-six of these patients—90%—had an improvement in mSWAT score from baseline.
“Twenty-six patients had at least stable disease to partial response,” Dr Querfeld noted. “No complete responses yet, but we’re close.”
Twelve patients were still receiving MRG-106 at last follow-up.
Ten of the 17 patients (59%) who had received MRG-106 for more than 1 month had at least a 50% improvement in mSWAT score, or a partial response. Once this was achieved, responses were durable.
One patient was still in response at roughly 470 days of follow-up.
Concomitant therapies
Dr Querfeld and her colleagues looked at patient outcomes in the context of concomitant therapies as well. They analyzed data from 26 patients who had received at least 6 doses of MRG-106.
Half of these patients were receiving MRG-106 alone, and the other half were receiving concomitant therapies, including bexarotene (n=7), interferon-alfa (n=2), methotrexate (n=1), vorinostat (n=1), and “other” treatments (n=2). Patients had been receiving these therapies for anywhere from 4 months to 45 months.
Outcomes were similar in the monotherapy and combination treatment groups. Seven patients in each group had at least a 50% improvement in mSWAT score.
Dosing and administration
“It appears the infusion is superior to the subcutaneous administration,” Dr Querfeld said.
She noted that durable partial responses have been achieved at all dose levels, but the 300 mg and 600 mg IV infusions had the best efficacy and tolerability profiles.
With the 300 mg IV bolus, fewer patients remained on treatment for more than 1 cycle, as compared to the other dosing cohorts. Dr Querfeld said this may be a result of lower total exposure or tolerability due to higher plasma Cmax.
She also noted that patients who received MRG-106 SQ at 600 mg or higher had a higher incidence of injection site reactions.
Safety
AEs of any grade that were attributed to MRG-106 include neutropenia (16%), injection site pain (16%), fatigue (14%), nausea (5%), pruritus (5%), and headache (5%).
Grade 3/4 AEs attributed to MRG-106 were neutropenia (5%) and pruritus (5%).
There were no serious AEs attributed to MRG-106, but there were 2 dose-limiting toxicities. One was a grade 3 tumor flare in a patient receiving the 300 mg IV bolus.
The other dose-limiting toxicity was grade 3 worsening pruritus and possible tumor flare, which occurred twice in 1 patient—with the 900 mg SQ dose and with the 300 mg IV infusion.
The 300 mg IV infusion is the anticipated phase 2 dose. ![]()
LA JOLLA, CA—Results of a phase 1 trial suggest MRG-106 can provide clinical improvement in patients with mycosis fungoides (MF), whether the drug is given alone or in conjunction with other therapies.
MRG-106 is an inhibitor of microRNA-155, which is upregulated in MF.
In this ongoing trial, 90% of patients who received MRG-106 have experienced an improvement in mSWAT score, and 59% of patients who received the drug for at least 1 month had a partial response.
The most common adverse events (AEs) attributed to MRG-106 were neutropenia, injection site pain, and fatigue.
Christiane Querfeld, MD, PhD, of the City of Hope in Duarte, California, presented these results at the 10th Annual T-cell Lymphoma Forum. The research is sponsored by miRagen Therapeutics, Inc., the company developing MRG-106.
The trial has enrolled 36 MF patients, 69% of whom are male. Their median age at enrollment was 63 (range, 21-85).
Patients had received a median of 4 prior systemic therapies (range, 1-13) and a median of 3 prior skin-directed therapies (range, 1-8).
At baseline, patients had a median mSWAT score of 43 (range, 2-180). The modified Severity Weighted Assessment Tool (mSWAT) measures the severity of skin disease over a patient’s body.
Part A
In part A of the study, 6 patients received MRG-106 via intralesional injection. A 75 mg dose of the drug was found to be well-tolerated, producing generally minor injection site reactions.
In addition, intralesional injection of MRG-106 produced improvements in CAILS score. The Composite Assessment of Index Lesion Severity (CAILS) score is obtained by adding the severity score of erythema, scaling, plaque elevation, and surface area for up to 5 index lesions.
Part B
In part B, 30 patients received MRG-106 via subcutaneous (SQ) injection, intravenous (IV) infusion, or IV bolus injection.
Patients who received SQ injection or IV infusion received doses of 300 mg, 600 mg, or 900 mg. Those who received an IV bolus only received the 300 mg dose.
Twenty-nine of the 30 patients in part B were evaluable for efficacy. Twenty-six of these patients—90%—had an improvement in mSWAT score from baseline.
“Twenty-six patients had at least stable disease to partial response,” Dr Querfeld noted. “No complete responses yet, but we’re close.”
Twelve patients were still receiving MRG-106 at last follow-up.
Ten of the 17 patients (59%) who had received MRG-106 for more than 1 month had at least a 50% improvement in mSWAT score, or a partial response. Once this was achieved, responses were durable.
One patient was still in response at roughly 470 days of follow-up.
Concomitant therapies
Dr Querfeld and her colleagues looked at patient outcomes in the context of concomitant therapies as well. They analyzed data from 26 patients who had received at least 6 doses of MRG-106.
Half of these patients were receiving MRG-106 alone, and the other half were receiving concomitant therapies, including bexarotene (n=7), interferon-alfa (n=2), methotrexate (n=1), vorinostat (n=1), and “other” treatments (n=2). Patients had been receiving these therapies for anywhere from 4 months to 45 months.
Outcomes were similar in the monotherapy and combination treatment groups. Seven patients in each group had at least a 50% improvement in mSWAT score.
Dosing and administration
“It appears the infusion is superior to the subcutaneous administration,” Dr Querfeld said.
She noted that durable partial responses have been achieved at all dose levels, but the 300 mg and 600 mg IV infusions had the best efficacy and tolerability profiles.
With the 300 mg IV bolus, fewer patients remained on treatment for more than 1 cycle, as compared to the other dosing cohorts. Dr Querfeld said this may be a result of lower total exposure or tolerability due to higher plasma Cmax.
She also noted that patients who received MRG-106 SQ at 600 mg or higher had a higher incidence of injection site reactions.
Safety
AEs of any grade that were attributed to MRG-106 include neutropenia (16%), injection site pain (16%), fatigue (14%), nausea (5%), pruritus (5%), and headache (5%).
Grade 3/4 AEs attributed to MRG-106 were neutropenia (5%) and pruritus (5%).
There were no serious AEs attributed to MRG-106, but there were 2 dose-limiting toxicities. One was a grade 3 tumor flare in a patient receiving the 300 mg IV bolus.
The other dose-limiting toxicity was grade 3 worsening pruritus and possible tumor flare, which occurred twice in 1 patient—with the 900 mg SQ dose and with the 300 mg IV infusion.
The 300 mg IV infusion is the anticipated phase 2 dose. ![]()
T-cell lymphoma therapies on the horizon
LA JOLLA, CALIF. – There are several biologic compounds in early clinical development for treatment of patients with T-cell lymphomas, including an antibody-drug conjugate, novel immune checkpoint inhibitor, and bi-specific antibody.
These investigational agents show promising single-agent activity and have the potential to improve clinical responses when combined with combination chemotherapy regimens or other treatments, Ahmed Sawas, MD, of the Center for Lymphoid Malignancies at Columbia University, New York, said at the annual T-cell Lymphoma Forum.
AGS67E: Antibody-drug conjugate
AGS67E is an antibody-drug conjugate targeted against CD37, a transmembrane protein preferentially expressed on malignant B cells, T cells, and acute myeloid leukemia cells. In a study published in 2015 in Molecular Cancer Therapeutics, investigators from Agensys (an affiliate of Astellas Pharma) reported that this compound bound to more than 80% of patient-derived T cells in vitro (Mol Cancer Ther. 2015;14[7]:1650-60).
In a phase 1 dose-escalation study reported at the 2017 International Conference on Malignant Lymphoma in Lugano, Switzerland, Dr. Sawas and his colleagues found that patients with B-cell and T-cell malignancies, including cutaneous T-cell lymphoma and peripheral T-cell lymphoma, tolerated the drug well when it was delivered both with or without growth factor. Neutropenia was the most frequent adverse event and dose-limiting toxicity.
The drug showed single-agent activity in 16 of 53 patients with heavily pretreated non-Hodgkin lymphoma, including a partial response in one of two patients with cutaneous T-cell lymphoma, and partial responses in two of four patients with peripheral T-cell lymphoma. There were no complete responses at any of three dose levels of the drug, with or without growth factor.
One patient, a 75-year-old man with stage IVB mycosis fungoides who had disease progression on prior therapy with methotrexate, romidepsin, bendamustine, whole-body irradiation, liposomal doxorubicin, pralatrexate, and pembrolizumab experienced significant reduction in tumor burden and resolution of lymph node involvement after three 3-week cycles of therapy with AGS67E. The patient had a deepening of the response with additional cycles, and remained on therapy for 30 cycles until he experienced disease progression.
TTI-621: Tuck in, macrophages
TT1-621 is a molecule with two functions: It acts as an immune checkpoint inhibitor by blocking CD47, which binds to signal-regulatory protein alpha to produce an antiphagocytic or “do not eat” signal. TTI-621 does not, however, bind to CD47-positive erythrocytes.
In addition to blocking CD47 and the do-not-eat signal, TTI-621 delivers an activating signal to macrophages through Fc gamma receptors, telling them, in effect, “bon appétit.”
In a study presented at the 2017 annual meeting of the American Society of Hematology (Abstract 4076), investigators from City of Hope in Duarte, Calif., and other centers reported that a single direct intratumoral injection of TTI-621 was associated with significant antitumor activity in patients with relapsed or refractory mycosis fungoides and Sézary syndrome, with one of nine patients having a complete response in the injected lesion, and five having decreases in tumor size and/or circulating Sézary cells.
Patients appeared to tolerate this agent very well, with 1 of 18 having a grade 3 increase in white blood cell count. The most commonly reported side effects were fatigue, chills, decreased appetite, headache, injection site pain, and generalized pruritus, each occurring in 3 of the 18 patients.
TTI-621 injection was associated with rapid declines in Composite Assessment of Index Lesion Severity scores in dose-finding studies in patients with heavily pretreated cutaneous T-cell lymphoma, Dr. Sawas said.
AFM13: Two for the price of one
AFM13 is a bi-specific antibody that binds to CD30, which is expressed on anaplastic large cell lymphoma cells, as well as Reed-Sternberg cells of classical Hodgkin lymphoma. This antibody also engages CD16A-positive cells, resulting in lysis of CD30-positive tumor cells. It is a specific recruiter of natural killer cells, and does not bind to neutrophils.
In an early biologic effects study of this agent in CD30-positive lymphoid malignancies with cutaneous presentation, Dr. Sawas and his colleagues observed an early response and regression of cutaneous anaplastic large cell lymphoma lesions in a heavily pretreated patient, with progression occurring when the patient went off therapy, and tumors that diminished on reinitiation of therapy that sustained beyond a second discontinuation of therapy. This patient had measurable reductions in lymphoma burden on PET CT scans and improvements in cutaneous lesions. Dr. Sawas did not present safety data for this agent.
AGS67E studies are supported by Agensys. TTI-621 studies are supported by Trillium Therapeutics. The AFM13 study is supported by Columbia University, with Dr. Sawas listed as the sponsor. He did not report potential conflicts of interests. The T-Cell Lymphoma Forum is held by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. – There are several biologic compounds in early clinical development for treatment of patients with T-cell lymphomas, including an antibody-drug conjugate, novel immune checkpoint inhibitor, and bi-specific antibody.
These investigational agents show promising single-agent activity and have the potential to improve clinical responses when combined with combination chemotherapy regimens or other treatments, Ahmed Sawas, MD, of the Center for Lymphoid Malignancies at Columbia University, New York, said at the annual T-cell Lymphoma Forum.
AGS67E: Antibody-drug conjugate
AGS67E is an antibody-drug conjugate targeted against CD37, a transmembrane protein preferentially expressed on malignant B cells, T cells, and acute myeloid leukemia cells. In a study published in 2015 in Molecular Cancer Therapeutics, investigators from Agensys (an affiliate of Astellas Pharma) reported that this compound bound to more than 80% of patient-derived T cells in vitro (Mol Cancer Ther. 2015;14[7]:1650-60).
In a phase 1 dose-escalation study reported at the 2017 International Conference on Malignant Lymphoma in Lugano, Switzerland, Dr. Sawas and his colleagues found that patients with B-cell and T-cell malignancies, including cutaneous T-cell lymphoma and peripheral T-cell lymphoma, tolerated the drug well when it was delivered both with or without growth factor. Neutropenia was the most frequent adverse event and dose-limiting toxicity.
The drug showed single-agent activity in 16 of 53 patients with heavily pretreated non-Hodgkin lymphoma, including a partial response in one of two patients with cutaneous T-cell lymphoma, and partial responses in two of four patients with peripheral T-cell lymphoma. There were no complete responses at any of three dose levels of the drug, with or without growth factor.
One patient, a 75-year-old man with stage IVB mycosis fungoides who had disease progression on prior therapy with methotrexate, romidepsin, bendamustine, whole-body irradiation, liposomal doxorubicin, pralatrexate, and pembrolizumab experienced significant reduction in tumor burden and resolution of lymph node involvement after three 3-week cycles of therapy with AGS67E. The patient had a deepening of the response with additional cycles, and remained on therapy for 30 cycles until he experienced disease progression.
TTI-621: Tuck in, macrophages
TT1-621 is a molecule with two functions: It acts as an immune checkpoint inhibitor by blocking CD47, which binds to signal-regulatory protein alpha to produce an antiphagocytic or “do not eat” signal. TTI-621 does not, however, bind to CD47-positive erythrocytes.
In addition to blocking CD47 and the do-not-eat signal, TTI-621 delivers an activating signal to macrophages through Fc gamma receptors, telling them, in effect, “bon appétit.”
In a study presented at the 2017 annual meeting of the American Society of Hematology (Abstract 4076), investigators from City of Hope in Duarte, Calif., and other centers reported that a single direct intratumoral injection of TTI-621 was associated with significant antitumor activity in patients with relapsed or refractory mycosis fungoides and Sézary syndrome, with one of nine patients having a complete response in the injected lesion, and five having decreases in tumor size and/or circulating Sézary cells.
Patients appeared to tolerate this agent very well, with 1 of 18 having a grade 3 increase in white blood cell count. The most commonly reported side effects were fatigue, chills, decreased appetite, headache, injection site pain, and generalized pruritus, each occurring in 3 of the 18 patients.
TTI-621 injection was associated with rapid declines in Composite Assessment of Index Lesion Severity scores in dose-finding studies in patients with heavily pretreated cutaneous T-cell lymphoma, Dr. Sawas said.
AFM13: Two for the price of one
AFM13 is a bi-specific antibody that binds to CD30, which is expressed on anaplastic large cell lymphoma cells, as well as Reed-Sternberg cells of classical Hodgkin lymphoma. This antibody also engages CD16A-positive cells, resulting in lysis of CD30-positive tumor cells. It is a specific recruiter of natural killer cells, and does not bind to neutrophils.
In an early biologic effects study of this agent in CD30-positive lymphoid malignancies with cutaneous presentation, Dr. Sawas and his colleagues observed an early response and regression of cutaneous anaplastic large cell lymphoma lesions in a heavily pretreated patient, with progression occurring when the patient went off therapy, and tumors that diminished on reinitiation of therapy that sustained beyond a second discontinuation of therapy. This patient had measurable reductions in lymphoma burden on PET CT scans and improvements in cutaneous lesions. Dr. Sawas did not present safety data for this agent.
AGS67E studies are supported by Agensys. TTI-621 studies are supported by Trillium Therapeutics. The AFM13 study is supported by Columbia University, with Dr. Sawas listed as the sponsor. He did not report potential conflicts of interests. The T-Cell Lymphoma Forum is held by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. – There are several biologic compounds in early clinical development for treatment of patients with T-cell lymphomas, including an antibody-drug conjugate, novel immune checkpoint inhibitor, and bi-specific antibody.
These investigational agents show promising single-agent activity and have the potential to improve clinical responses when combined with combination chemotherapy regimens or other treatments, Ahmed Sawas, MD, of the Center for Lymphoid Malignancies at Columbia University, New York, said at the annual T-cell Lymphoma Forum.
AGS67E: Antibody-drug conjugate
AGS67E is an antibody-drug conjugate targeted against CD37, a transmembrane protein preferentially expressed on malignant B cells, T cells, and acute myeloid leukemia cells. In a study published in 2015 in Molecular Cancer Therapeutics, investigators from Agensys (an affiliate of Astellas Pharma) reported that this compound bound to more than 80% of patient-derived T cells in vitro (Mol Cancer Ther. 2015;14[7]:1650-60).
In a phase 1 dose-escalation study reported at the 2017 International Conference on Malignant Lymphoma in Lugano, Switzerland, Dr. Sawas and his colleagues found that patients with B-cell and T-cell malignancies, including cutaneous T-cell lymphoma and peripheral T-cell lymphoma, tolerated the drug well when it was delivered both with or without growth factor. Neutropenia was the most frequent adverse event and dose-limiting toxicity.
The drug showed single-agent activity in 16 of 53 patients with heavily pretreated non-Hodgkin lymphoma, including a partial response in one of two patients with cutaneous T-cell lymphoma, and partial responses in two of four patients with peripheral T-cell lymphoma. There were no complete responses at any of three dose levels of the drug, with or without growth factor.
One patient, a 75-year-old man with stage IVB mycosis fungoides who had disease progression on prior therapy with methotrexate, romidepsin, bendamustine, whole-body irradiation, liposomal doxorubicin, pralatrexate, and pembrolizumab experienced significant reduction in tumor burden and resolution of lymph node involvement after three 3-week cycles of therapy with AGS67E. The patient had a deepening of the response with additional cycles, and remained on therapy for 30 cycles until he experienced disease progression.
TTI-621: Tuck in, macrophages
TT1-621 is a molecule with two functions: It acts as an immune checkpoint inhibitor by blocking CD47, which binds to signal-regulatory protein alpha to produce an antiphagocytic or “do not eat” signal. TTI-621 does not, however, bind to CD47-positive erythrocytes.
In addition to blocking CD47 and the do-not-eat signal, TTI-621 delivers an activating signal to macrophages through Fc gamma receptors, telling them, in effect, “bon appétit.”
In a study presented at the 2017 annual meeting of the American Society of Hematology (Abstract 4076), investigators from City of Hope in Duarte, Calif., and other centers reported that a single direct intratumoral injection of TTI-621 was associated with significant antitumor activity in patients with relapsed or refractory mycosis fungoides and Sézary syndrome, with one of nine patients having a complete response in the injected lesion, and five having decreases in tumor size and/or circulating Sézary cells.
Patients appeared to tolerate this agent very well, with 1 of 18 having a grade 3 increase in white blood cell count. The most commonly reported side effects were fatigue, chills, decreased appetite, headache, injection site pain, and generalized pruritus, each occurring in 3 of the 18 patients.
TTI-621 injection was associated with rapid declines in Composite Assessment of Index Lesion Severity scores in dose-finding studies in patients with heavily pretreated cutaneous T-cell lymphoma, Dr. Sawas said.
AFM13: Two for the price of one
AFM13 is a bi-specific antibody that binds to CD30, which is expressed on anaplastic large cell lymphoma cells, as well as Reed-Sternberg cells of classical Hodgkin lymphoma. This antibody also engages CD16A-positive cells, resulting in lysis of CD30-positive tumor cells. It is a specific recruiter of natural killer cells, and does not bind to neutrophils.
In an early biologic effects study of this agent in CD30-positive lymphoid malignancies with cutaneous presentation, Dr. Sawas and his colleagues observed an early response and regression of cutaneous anaplastic large cell lymphoma lesions in a heavily pretreated patient, with progression occurring when the patient went off therapy, and tumors that diminished on reinitiation of therapy that sustained beyond a second discontinuation of therapy. This patient had measurable reductions in lymphoma burden on PET CT scans and improvements in cutaneous lesions. Dr. Sawas did not present safety data for this agent.
AGS67E studies are supported by Agensys. TTI-621 studies are supported by Trillium Therapeutics. The AFM13 study is supported by Columbia University, with Dr. Sawas listed as the sponsor. He did not report potential conflicts of interests. The T-Cell Lymphoma Forum is held by Jonathan Wood & Associates, which is owned by the same company as this news organization.
EXPERT ANALYSIS FROM TCLF 2018
Drug may be option for B- and T-cell lymphomas
LA JOLLA, CA—The EZH1/2 inhibitor DS-3201b could be a novel therapeutic option for non-Hodgkin lymphoma (NHL), according to a speaker at the 10th Annual T-cell Lymphoma Forum.
DS-3201b was considered well tolerated in a phase 1 study of Japanese patients with relapsed/refractory NHL.
In addition, DS-3201b demonstrated activity against B- and T-cell lymphomas, producing an overall response rate of 59%.
Kunihiro Tsukasaki, MD, PhD, of Saitama Medical University in Moroyama, Saitama, Japan, presented these results at the meeting.
The trial was sponsored by Daiichi Sankyo Co., Ltd.
Dr Tsukasaki presented data on 18 patients with relapsed/refractory NHL.
The 12 B-cell lymphoma patients had follicular lymphoma (n=5), diffuse large B-cell lymphoma (n=3), MALT lymphoma (n=2), nodal marginal zone lymphoma (n=1), and lymphoplasmacytic lymphoma (n=1).
The 6 patients with T-cell lymphoma had peripheral T-cell lymphoma not otherwise specified (n=2), angioimmunoblastic T-cell lymphoma (n=2), and adult T-cell leukemia/lymphoma (n=2).
The patients’ median age was 67 (range, 44-75), and 10 were female. All patients had an ECOG performance status of 0 (72%) or 1 (28%).
Patients had a median of 2 prior chemotherapy regimens (range, 1-8).
For this study, they received DS-3201b at 150 mg (n=7), 200 mg (n=9), or 300 mg (n=2). They received the drug once daily in 28-day cycles until they progressed or experienced unacceptable toxicity.
DLTs and AEs
Dose-limiting toxicities (DLTs) were evaluated in cycle 1. All 18 patients were evaluable for DLT assessment.
There were 4 treatment-emergent adverse events (AEs) that met the definition of DLTs:
- 3 cases of grade 4 platelet count decrease (n=1 at 200 mg, n=2 at 300 mg)
- 1 case of grade 3 anemia requiring blood transfusion (at 300 mg).
All 4 DLTs led to treatment interruption.
There were 5 serious AEs reported in 3 patients. Only one of these—pneumocystis jiroveci pneumonia—was considered related to DS-3201b.
Hematologic AEs included decreases in platelets (grade 1-4), lymphocytes (grade 1-4), neutrophils (grade 2-4), and white blood cells (grade 2-3), as well as anemia (grade 1-3).
Other AEs (all grade 1/2) included dysgeusia, alopecia, diarrhea, decreased appetite, alanine aminotransferase increase, aspartate aminotransferase increase, nasopharyngitis, rash, and dry skin.
No deaths had been reported as of the data cutoff last November.
Responses
Seventeen patients were evaluable for response.
The overall response rate was 59%, with 1 patient achieving a complete response (CR) and 9 achieving a partial response (PR). Four patients had stable disease (SD), and 3 progressed.
Among the T-cell lymphoma patients, 1 had a CR, 4 had PRs, and 1 progressed. The complete responder had angioimmunoblastic T-cell lymphoma, and the patient who progressed had adult T-cell leukemia/lymphoma.
Among the B-cell lymphoma patients, 5 had PRs, 4 had SD, and 2 progressed.
Dr Tsukasaki said DS-3201b has demonstrated early clinical activity and therefore has the potential to be a novel therapeutic option for B-cell and T-cell lymphomas. However, further evaluation is warranted to determine the optimal dosing regimen and target diseases. ![]()
LA JOLLA, CA—The EZH1/2 inhibitor DS-3201b could be a novel therapeutic option for non-Hodgkin lymphoma (NHL), according to a speaker at the 10th Annual T-cell Lymphoma Forum.
DS-3201b was considered well tolerated in a phase 1 study of Japanese patients with relapsed/refractory NHL.
In addition, DS-3201b demonstrated activity against B- and T-cell lymphomas, producing an overall response rate of 59%.
Kunihiro Tsukasaki, MD, PhD, of Saitama Medical University in Moroyama, Saitama, Japan, presented these results at the meeting.
The trial was sponsored by Daiichi Sankyo Co., Ltd.
Dr Tsukasaki presented data on 18 patients with relapsed/refractory NHL.
The 12 B-cell lymphoma patients had follicular lymphoma (n=5), diffuse large B-cell lymphoma (n=3), MALT lymphoma (n=2), nodal marginal zone lymphoma (n=1), and lymphoplasmacytic lymphoma (n=1).
The 6 patients with T-cell lymphoma had peripheral T-cell lymphoma not otherwise specified (n=2), angioimmunoblastic T-cell lymphoma (n=2), and adult T-cell leukemia/lymphoma (n=2).
The patients’ median age was 67 (range, 44-75), and 10 were female. All patients had an ECOG performance status of 0 (72%) or 1 (28%).
Patients had a median of 2 prior chemotherapy regimens (range, 1-8).
For this study, they received DS-3201b at 150 mg (n=7), 200 mg (n=9), or 300 mg (n=2). They received the drug once daily in 28-day cycles until they progressed or experienced unacceptable toxicity.
DLTs and AEs
Dose-limiting toxicities (DLTs) were evaluated in cycle 1. All 18 patients were evaluable for DLT assessment.
There were 4 treatment-emergent adverse events (AEs) that met the definition of DLTs:
- 3 cases of grade 4 platelet count decrease (n=1 at 200 mg, n=2 at 300 mg)
- 1 case of grade 3 anemia requiring blood transfusion (at 300 mg).
All 4 DLTs led to treatment interruption.
There were 5 serious AEs reported in 3 patients. Only one of these—pneumocystis jiroveci pneumonia—was considered related to DS-3201b.
Hematologic AEs included decreases in platelets (grade 1-4), lymphocytes (grade 1-4), neutrophils (grade 2-4), and white blood cells (grade 2-3), as well as anemia (grade 1-3).
Other AEs (all grade 1/2) included dysgeusia, alopecia, diarrhea, decreased appetite, alanine aminotransferase increase, aspartate aminotransferase increase, nasopharyngitis, rash, and dry skin.
No deaths had been reported as of the data cutoff last November.
Responses
Seventeen patients were evaluable for response.
The overall response rate was 59%, with 1 patient achieving a complete response (CR) and 9 achieving a partial response (PR). Four patients had stable disease (SD), and 3 progressed.
Among the T-cell lymphoma patients, 1 had a CR, 4 had PRs, and 1 progressed. The complete responder had angioimmunoblastic T-cell lymphoma, and the patient who progressed had adult T-cell leukemia/lymphoma.
Among the B-cell lymphoma patients, 5 had PRs, 4 had SD, and 2 progressed.
Dr Tsukasaki said DS-3201b has demonstrated early clinical activity and therefore has the potential to be a novel therapeutic option for B-cell and T-cell lymphomas. However, further evaluation is warranted to determine the optimal dosing regimen and target diseases. ![]()
LA JOLLA, CA—The EZH1/2 inhibitor DS-3201b could be a novel therapeutic option for non-Hodgkin lymphoma (NHL), according to a speaker at the 10th Annual T-cell Lymphoma Forum.
DS-3201b was considered well tolerated in a phase 1 study of Japanese patients with relapsed/refractory NHL.
In addition, DS-3201b demonstrated activity against B- and T-cell lymphomas, producing an overall response rate of 59%.
Kunihiro Tsukasaki, MD, PhD, of Saitama Medical University in Moroyama, Saitama, Japan, presented these results at the meeting.
The trial was sponsored by Daiichi Sankyo Co., Ltd.
Dr Tsukasaki presented data on 18 patients with relapsed/refractory NHL.
The 12 B-cell lymphoma patients had follicular lymphoma (n=5), diffuse large B-cell lymphoma (n=3), MALT lymphoma (n=2), nodal marginal zone lymphoma (n=1), and lymphoplasmacytic lymphoma (n=1).
The 6 patients with T-cell lymphoma had peripheral T-cell lymphoma not otherwise specified (n=2), angioimmunoblastic T-cell lymphoma (n=2), and adult T-cell leukemia/lymphoma (n=2).
The patients’ median age was 67 (range, 44-75), and 10 were female. All patients had an ECOG performance status of 0 (72%) or 1 (28%).
Patients had a median of 2 prior chemotherapy regimens (range, 1-8).
For this study, they received DS-3201b at 150 mg (n=7), 200 mg (n=9), or 300 mg (n=2). They received the drug once daily in 28-day cycles until they progressed or experienced unacceptable toxicity.
DLTs and AEs
Dose-limiting toxicities (DLTs) were evaluated in cycle 1. All 18 patients were evaluable for DLT assessment.
There were 4 treatment-emergent adverse events (AEs) that met the definition of DLTs:
- 3 cases of grade 4 platelet count decrease (n=1 at 200 mg, n=2 at 300 mg)
- 1 case of grade 3 anemia requiring blood transfusion (at 300 mg).
All 4 DLTs led to treatment interruption.
There were 5 serious AEs reported in 3 patients. Only one of these—pneumocystis jiroveci pneumonia—was considered related to DS-3201b.
Hematologic AEs included decreases in platelets (grade 1-4), lymphocytes (grade 1-4), neutrophils (grade 2-4), and white blood cells (grade 2-3), as well as anemia (grade 1-3).
Other AEs (all grade 1/2) included dysgeusia, alopecia, diarrhea, decreased appetite, alanine aminotransferase increase, aspartate aminotransferase increase, nasopharyngitis, rash, and dry skin.
No deaths had been reported as of the data cutoff last November.
Responses
Seventeen patients were evaluable for response.
The overall response rate was 59%, with 1 patient achieving a complete response (CR) and 9 achieving a partial response (PR). Four patients had stable disease (SD), and 3 progressed.
Among the T-cell lymphoma patients, 1 had a CR, 4 had PRs, and 1 progressed. The complete responder had angioimmunoblastic T-cell lymphoma, and the patient who progressed had adult T-cell leukemia/lymphoma.
Among the B-cell lymphoma patients, 5 had PRs, 4 had SD, and 2 progressed.
Dr Tsukasaki said DS-3201b has demonstrated early clinical activity and therefore has the potential to be a novel therapeutic option for B-cell and T-cell lymphomas. However, further evaluation is warranted to determine the optimal dosing regimen and target diseases. ![]()
Assay identifies actionable mutations in lymphoid malignancies
Researchers say hybrid capture sequencing is an accurate and sensitive method for identifying actionable gene mutations in lymphoid malignancies.
This method revealed potentially actionable mutations in 91% of patients studied, who had diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL), or chronic lymphocytic leukemia (CLL).
The researchers therefore believe hybrid capture sequencing will bring the benefits of precision diagnosis and individualized therapy to patients with lymphoid malignancies.
“To realize the benefits of the most recent progress in cancer genomics, clinical implementation of precision medicine approaches is needed in the form of novel biomarker assays,” said study author Christian Steidl, MD, of the University of British Columbia in Vancouver, Canada.
“Fully implemented targeted sequencing-based assays in routine diagnostic pathology laboratories are currently lacking in lymphoid cancer care. Our findings demonstrate the feasibility and outline the clinical utility of integrating a lymphoma-specific pipeline into personalized cancer care.”
Dr Steidl and his colleagues reported these findings in The Journal of Molecular Diagnostics.
The researchers first compared capture hybridization and amplicon sequencing using samples from 8 patients with lymphoma. Fresh-frozen and formalin-fixed, paraffin-embedded tumor samples were sequenced using a panel of 20 lymphoma-specific genes.
The team found that capture hybridization provided “deep, more uniform coverage” and yielded “higher sensitivity for variant calling” than amplicon sequencing.
The researchers then developed a targeted sequencing pipeline using a 32-gene panel. The panel was developed with input from a group of 6 specialists who kept updating it based on the latest available information.
“This allows for continuous integration of additional gene features as our knowledge base improves,” Dr Steidl noted.
He and his colleagues then applied the hybrid capture sequencing assay and 32-gene panel to tissues from 219 patients—114 with FL, 76 with DLBCL, and 29 with CLL—who were treated in British Columbia between 2013 and 2016.
Results revealed at least one actionable mutation in 91% of the tumors. And the assay uncovered subtype-specific mutational profiles that were highly similar to published mutational profiles for FL, DLBCL, and CLL.
Furthermore, the assay had 93% concordance with whole-genome sequencing.
“Our developed assay harnesses the power of modern sequencing for clinical diagnostics purposes and potentially better deployment of novel treatments in lymphoid cancers,” Dr Steidl said. “We believe our study will help establish evidence-based approaches to decision making in lymphoid cancer care.”
“The next steps are to implement sequencing-based biomarker assays, such as reported in our study, in accredited pathology laboratories. Toward the goal of biomarker-driven clinical decision making, testing of potentially predictive biomarker assays is needed alongside clinical trials investigating novel cancer therapeutics.” ![]()
Researchers say hybrid capture sequencing is an accurate and sensitive method for identifying actionable gene mutations in lymphoid malignancies.
This method revealed potentially actionable mutations in 91% of patients studied, who had diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL), or chronic lymphocytic leukemia (CLL).
The researchers therefore believe hybrid capture sequencing will bring the benefits of precision diagnosis and individualized therapy to patients with lymphoid malignancies.
“To realize the benefits of the most recent progress in cancer genomics, clinical implementation of precision medicine approaches is needed in the form of novel biomarker assays,” said study author Christian Steidl, MD, of the University of British Columbia in Vancouver, Canada.
“Fully implemented targeted sequencing-based assays in routine diagnostic pathology laboratories are currently lacking in lymphoid cancer care. Our findings demonstrate the feasibility and outline the clinical utility of integrating a lymphoma-specific pipeline into personalized cancer care.”
Dr Steidl and his colleagues reported these findings in The Journal of Molecular Diagnostics.
The researchers first compared capture hybridization and amplicon sequencing using samples from 8 patients with lymphoma. Fresh-frozen and formalin-fixed, paraffin-embedded tumor samples were sequenced using a panel of 20 lymphoma-specific genes.
The team found that capture hybridization provided “deep, more uniform coverage” and yielded “higher sensitivity for variant calling” than amplicon sequencing.
The researchers then developed a targeted sequencing pipeline using a 32-gene panel. The panel was developed with input from a group of 6 specialists who kept updating it based on the latest available information.
“This allows for continuous integration of additional gene features as our knowledge base improves,” Dr Steidl noted.
He and his colleagues then applied the hybrid capture sequencing assay and 32-gene panel to tissues from 219 patients—114 with FL, 76 with DLBCL, and 29 with CLL—who were treated in British Columbia between 2013 and 2016.
Results revealed at least one actionable mutation in 91% of the tumors. And the assay uncovered subtype-specific mutational profiles that were highly similar to published mutational profiles for FL, DLBCL, and CLL.
Furthermore, the assay had 93% concordance with whole-genome sequencing.
“Our developed assay harnesses the power of modern sequencing for clinical diagnostics purposes and potentially better deployment of novel treatments in lymphoid cancers,” Dr Steidl said. “We believe our study will help establish evidence-based approaches to decision making in lymphoid cancer care.”
“The next steps are to implement sequencing-based biomarker assays, such as reported in our study, in accredited pathology laboratories. Toward the goal of biomarker-driven clinical decision making, testing of potentially predictive biomarker assays is needed alongside clinical trials investigating novel cancer therapeutics.” ![]()
Researchers say hybrid capture sequencing is an accurate and sensitive method for identifying actionable gene mutations in lymphoid malignancies.
This method revealed potentially actionable mutations in 91% of patients studied, who had diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL), or chronic lymphocytic leukemia (CLL).
The researchers therefore believe hybrid capture sequencing will bring the benefits of precision diagnosis and individualized therapy to patients with lymphoid malignancies.
“To realize the benefits of the most recent progress in cancer genomics, clinical implementation of precision medicine approaches is needed in the form of novel biomarker assays,” said study author Christian Steidl, MD, of the University of British Columbia in Vancouver, Canada.
“Fully implemented targeted sequencing-based assays in routine diagnostic pathology laboratories are currently lacking in lymphoid cancer care. Our findings demonstrate the feasibility and outline the clinical utility of integrating a lymphoma-specific pipeline into personalized cancer care.”
Dr Steidl and his colleagues reported these findings in The Journal of Molecular Diagnostics.
The researchers first compared capture hybridization and amplicon sequencing using samples from 8 patients with lymphoma. Fresh-frozen and formalin-fixed, paraffin-embedded tumor samples were sequenced using a panel of 20 lymphoma-specific genes.
The team found that capture hybridization provided “deep, more uniform coverage” and yielded “higher sensitivity for variant calling” than amplicon sequencing.
The researchers then developed a targeted sequencing pipeline using a 32-gene panel. The panel was developed with input from a group of 6 specialists who kept updating it based on the latest available information.
“This allows for continuous integration of additional gene features as our knowledge base improves,” Dr Steidl noted.
He and his colleagues then applied the hybrid capture sequencing assay and 32-gene panel to tissues from 219 patients—114 with FL, 76 with DLBCL, and 29 with CLL—who were treated in British Columbia between 2013 and 2016.
Results revealed at least one actionable mutation in 91% of the tumors. And the assay uncovered subtype-specific mutational profiles that were highly similar to published mutational profiles for FL, DLBCL, and CLL.
Furthermore, the assay had 93% concordance with whole-genome sequencing.
“Our developed assay harnesses the power of modern sequencing for clinical diagnostics purposes and potentially better deployment of novel treatments in lymphoid cancers,” Dr Steidl said. “We believe our study will help establish evidence-based approaches to decision making in lymphoid cancer care.”
“The next steps are to implement sequencing-based biomarker assays, such as reported in our study, in accredited pathology laboratories. Toward the goal of biomarker-driven clinical decision making, testing of potentially predictive biomarker assays is needed alongside clinical trials investigating novel cancer therapeutics.” ![]()
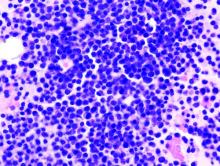
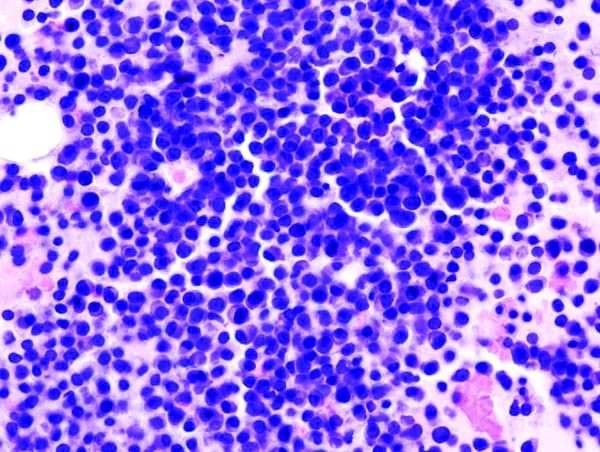
Meningococcal Arthritis Masking as Possible Myeloma
For a group of clinicians in Australia, the diagnosis of meningococcal arthritis was “straightforward” except for abnormal serum total protein, anemia, and immunoglobulin results, which suggested their patient might have a hematological disorder such as myeloma.
The patient came to the hospital after 4 days of worsening knee and arm pain so severe he could not stand. His knees and both wrists showed swelling but no palpable lymphadenopathy or hepatosplenomegaly. The patient’s medical history showed he was taking no regular medications.
Joint aspiration grew Neisseria meningitidis. The patient’s blood tests showed hemoglobin 126 g/dL, white blood cell count 15.3 x 109/L, an unusually high total protein level (100 g/L), and an IgM kappa paraprotein band of 45 g/L on protein electrophoresis. A computed tomography scan showed widespread lymphadenopathy, hepatosplenomegaly, and multilevel thoracic vertebral collapse. A bone marrow biopsy showed evidence of a lymphocytic infiltrate, with lymphoplasmacytoid differentiation.
The histology best fitted a diagnosis of nodal marginal zone lymphoma with plasmacytic differentiation, the clinicians say. Having ruled out other possibilities, they settled on non-Hodgkin lymphoma.
Initially, the suspicion was that the patient had septic arthritis due to Staphylococcus aureus (the most common organism isolated in septic arthritis), and he was given piperacillin/tazobactam. That was changed to flucloxacillin and then to ceftriaxone after the result of N meningitidis. The patient also was treated with rituximab and bendamustine for the lymphoma with a complete remission.
Meningococcal infection presenting as septic arthritis in the case of invasive meningococcemia is rare, the clinicians say, but primary meningococcal arthritis is even rarer. The case highlights the important aspect that “diagnosis of one condition can lead to diagnosis of another”—in this case, the lymphoma-weakened immune system led to the symptoms of polyarthropathy and the diagnosis of primary meningococcal arthritis. The clinicians also cited a case of a patient who presented with meningococcal meningitis and arthritis who was found to have an underlying Waldenström disease, and a patient whose HIV was diagnosed again after the patient presented with meningococcal arthritis symptoms.
The clinicans say such cases underscore the importance of screening for an underlying impaired immune response in patients presenting with rare conditions such as meningococcal arthritis.
For a group of clinicians in Australia, the diagnosis of meningococcal arthritis was “straightforward” except for abnormal serum total protein, anemia, and immunoglobulin results, which suggested their patient might have a hematological disorder such as myeloma.
The patient came to the hospital after 4 days of worsening knee and arm pain so severe he could not stand. His knees and both wrists showed swelling but no palpable lymphadenopathy or hepatosplenomegaly. The patient’s medical history showed he was taking no regular medications.
Joint aspiration grew Neisseria meningitidis. The patient’s blood tests showed hemoglobin 126 g/dL, white blood cell count 15.3 x 109/L, an unusually high total protein level (100 g/L), and an IgM kappa paraprotein band of 45 g/L on protein electrophoresis. A computed tomography scan showed widespread lymphadenopathy, hepatosplenomegaly, and multilevel thoracic vertebral collapse. A bone marrow biopsy showed evidence of a lymphocytic infiltrate, with lymphoplasmacytoid differentiation.
The histology best fitted a diagnosis of nodal marginal zone lymphoma with plasmacytic differentiation, the clinicians say. Having ruled out other possibilities, they settled on non-Hodgkin lymphoma.
Initially, the suspicion was that the patient had septic arthritis due to Staphylococcus aureus (the most common organism isolated in septic arthritis), and he was given piperacillin/tazobactam. That was changed to flucloxacillin and then to ceftriaxone after the result of N meningitidis. The patient also was treated with rituximab and bendamustine for the lymphoma with a complete remission.
Meningococcal infection presenting as septic arthritis in the case of invasive meningococcemia is rare, the clinicians say, but primary meningococcal arthritis is even rarer. The case highlights the important aspect that “diagnosis of one condition can lead to diagnosis of another”—in this case, the lymphoma-weakened immune system led to the symptoms of polyarthropathy and the diagnosis of primary meningococcal arthritis. The clinicians also cited a case of a patient who presented with meningococcal meningitis and arthritis who was found to have an underlying Waldenström disease, and a patient whose HIV was diagnosed again after the patient presented with meningococcal arthritis symptoms.
The clinicans say such cases underscore the importance of screening for an underlying impaired immune response in patients presenting with rare conditions such as meningococcal arthritis.
For a group of clinicians in Australia, the diagnosis of meningococcal arthritis was “straightforward” except for abnormal serum total protein, anemia, and immunoglobulin results, which suggested their patient might have a hematological disorder such as myeloma.
The patient came to the hospital after 4 days of worsening knee and arm pain so severe he could not stand. His knees and both wrists showed swelling but no palpable lymphadenopathy or hepatosplenomegaly. The patient’s medical history showed he was taking no regular medications.
Joint aspiration grew Neisseria meningitidis. The patient’s blood tests showed hemoglobin 126 g/dL, white blood cell count 15.3 x 109/L, an unusually high total protein level (100 g/L), and an IgM kappa paraprotein band of 45 g/L on protein electrophoresis. A computed tomography scan showed widespread lymphadenopathy, hepatosplenomegaly, and multilevel thoracic vertebral collapse. A bone marrow biopsy showed evidence of a lymphocytic infiltrate, with lymphoplasmacytoid differentiation.
The histology best fitted a diagnosis of nodal marginal zone lymphoma with plasmacytic differentiation, the clinicians say. Having ruled out other possibilities, they settled on non-Hodgkin lymphoma.
Initially, the suspicion was that the patient had septic arthritis due to Staphylococcus aureus (the most common organism isolated in septic arthritis), and he was given piperacillin/tazobactam. That was changed to flucloxacillin and then to ceftriaxone after the result of N meningitidis. The patient also was treated with rituximab and bendamustine for the lymphoma with a complete remission.
Meningococcal infection presenting as septic arthritis in the case of invasive meningococcemia is rare, the clinicians say, but primary meningococcal arthritis is even rarer. The case highlights the important aspect that “diagnosis of one condition can lead to diagnosis of another”—in this case, the lymphoma-weakened immune system led to the symptoms of polyarthropathy and the diagnosis of primary meningococcal arthritis. The clinicians also cited a case of a patient who presented with meningococcal meningitis and arthritis who was found to have an underlying Waldenström disease, and a patient whose HIV was diagnosed again after the patient presented with meningococcal arthritis symptoms.
The clinicans say such cases underscore the importance of screening for an underlying impaired immune response in patients presenting with rare conditions such as meningococcal arthritis.
Favorable results with chidamide in rel/ref NKTCL
LA JOLLA, CA—Results of a phase 2 study suggest chidamide can produce durable responses in patients with relapsed/refractory natural killer/T-cell lymphoma (NKTCL).
The overall response rate was 57.2% in these patients, and the complete response (CR) rate was 28.6%.
Seven of 14 evaluable patients were still receiving chidamide and still in response at last follow-up. For one patient, this was 50 weeks from initiating treatment with chidamide.
“The response is quite promising and encouraging,” said study investigator Huiqiang Huang, MD, PhD, of Sun Yat-sen University Cancer Center in Guangzhou, China.
“In terms of safety, the toxicity is mild to moderate.”
Dr Huang presented these results at the 10th Annual T-cell Lymphoma Forum.
This investigator-sponsored trial enrolled patients with relapsed/refractory non-Hodgkin lymphoma, but Dr Huang presented results in NKTCL patients only.
There were 15 NKTCL patients, most of whom were male (n=12). Their median age was 41 (range, 17-65). All 15 had an ECOG status of 0 or 1, 9 had stage I/II disease, and 6 had B symptoms.
Nine patients had Epstein-Barr virus (EBV) DNA levels of at least 1000 copy/mL at baseline, and 5 patients had lactate dehydrogenase levels of at least 245 U/L.
The patients had a median of 2 prior systemic therapies (range, 1-3), and 2 patients had undergone a transplant.
Efficacy
Patients received chidamide at 2 doses—10 mg daily or 30 mg twice a week. Dr Huang said both doses were effective against the lymphoma types studied, but the 30 mg twice-weekly dose appeared to be more effective for patients with NKTCL.
Fourteen NKTCL patients were evaluable for efficacy, and the median follow-up was 17.6 weeks (range, 2.6-50).
The overall response rate was 68.2% (6/14), and the CR rate was 28.6% (4/14). The disease control rate was 71.4%, meaning 10 of 14 patients had a CR, partial response (PR), or stable disease (SD).
Dr Huang noted that response was associated with elevated H3 acetylation level.
The median time to response was 5.25 weeks (range, 1.1-6.6).
As for duration of response, the 4 complete responders were still on treatment and in CR at last follow-up, which was 22.7 weeks, 38.1 weeks, 41.3 weeks, and 50 weeks, respectively, from treatment initiation.
Three of the 4 partial responders were still on treatment and in PR at 14.1 weeks, 26.9 weeks, and 32 weeks, respectively. Two patients with SD were still on treatment and in SD at 15.3 weeks and 15.9 weeks, respectively.
Three patients progressed while on treatment and died. A fourth patient died 2.6 weeks after treatment initiation.
Safety
Dr Huang noted that adverse events (AEs) were similar with the 2 dose groups. However, patients who received 30 mg biweekly had a higher incidence of gastrointestinal AEs.
Overall, the most common AEs were hematologic—anemia, thrombocytopenia, etc.—but dose reductions allowed for quick resolution of these AEs, according to Dr Huang.
AEs included:
- Lymphopenia—10 grade 1/2 and 1 grade 3/4
- Anemia—9 grade 1/2 and 3 grade 3/4
- Thrombocytopenia—7 grade 1/2 and grade 3/4
- Leukopenia—7 grade 1/2 and 6 grade 3/4
- Increased alanine aminotransferase—7 grade 1/2
- Neutropenia—6 grade 1/2 and 7 grade 3/4
- Increased aspartate aminotransferase—5 grade 1/2
- Hypoalbuminemia—4 grade 1/2
- Nausea—4 grade 1/2 and 1 grade 3/4
- Vomiting—3 grade 1/2
- Mucositis—2 grade 1/2
- Fatigue—2 grade 1/2
- Epistaxis—2 grade 1/2
- Abdominal distension—1 grade 1/2
- Loss of appetite—1 grade 1/2
- Diarrhea—1 grade 1/2
- Hyperbilirubinemia—1 grade 1/2
- Fever—1 grade 1/2 and grade 3/4
- Pain—1 grade 1/2
- Cough—1 grade 1/2
- Constipation—1 grade 1/2.
Dr Huang said EBV reactivation was not confirmed in this study. An elevated EBV DNA load was only observed in 2 patients with progressive disease. ![]()
LA JOLLA, CA—Results of a phase 2 study suggest chidamide can produce durable responses in patients with relapsed/refractory natural killer/T-cell lymphoma (NKTCL).
The overall response rate was 57.2% in these patients, and the complete response (CR) rate was 28.6%.
Seven of 14 evaluable patients were still receiving chidamide and still in response at last follow-up. For one patient, this was 50 weeks from initiating treatment with chidamide.
“The response is quite promising and encouraging,” said study investigator Huiqiang Huang, MD, PhD, of Sun Yat-sen University Cancer Center in Guangzhou, China.
“In terms of safety, the toxicity is mild to moderate.”
Dr Huang presented these results at the 10th Annual T-cell Lymphoma Forum.
This investigator-sponsored trial enrolled patients with relapsed/refractory non-Hodgkin lymphoma, but Dr Huang presented results in NKTCL patients only.
There were 15 NKTCL patients, most of whom were male (n=12). Their median age was 41 (range, 17-65). All 15 had an ECOG status of 0 or 1, 9 had stage I/II disease, and 6 had B symptoms.
Nine patients had Epstein-Barr virus (EBV) DNA levels of at least 1000 copy/mL at baseline, and 5 patients had lactate dehydrogenase levels of at least 245 U/L.
The patients had a median of 2 prior systemic therapies (range, 1-3), and 2 patients had undergone a transplant.
Efficacy
Patients received chidamide at 2 doses—10 mg daily or 30 mg twice a week. Dr Huang said both doses were effective against the lymphoma types studied, but the 30 mg twice-weekly dose appeared to be more effective for patients with NKTCL.
Fourteen NKTCL patients were evaluable for efficacy, and the median follow-up was 17.6 weeks (range, 2.6-50).
The overall response rate was 68.2% (6/14), and the CR rate was 28.6% (4/14). The disease control rate was 71.4%, meaning 10 of 14 patients had a CR, partial response (PR), or stable disease (SD).
Dr Huang noted that response was associated with elevated H3 acetylation level.
The median time to response was 5.25 weeks (range, 1.1-6.6).
As for duration of response, the 4 complete responders were still on treatment and in CR at last follow-up, which was 22.7 weeks, 38.1 weeks, 41.3 weeks, and 50 weeks, respectively, from treatment initiation.
Three of the 4 partial responders were still on treatment and in PR at 14.1 weeks, 26.9 weeks, and 32 weeks, respectively. Two patients with SD were still on treatment and in SD at 15.3 weeks and 15.9 weeks, respectively.
Three patients progressed while on treatment and died. A fourth patient died 2.6 weeks after treatment initiation.
Safety
Dr Huang noted that adverse events (AEs) were similar with the 2 dose groups. However, patients who received 30 mg biweekly had a higher incidence of gastrointestinal AEs.
Overall, the most common AEs were hematologic—anemia, thrombocytopenia, etc.—but dose reductions allowed for quick resolution of these AEs, according to Dr Huang.
AEs included:
- Lymphopenia—10 grade 1/2 and 1 grade 3/4
- Anemia—9 grade 1/2 and 3 grade 3/4
- Thrombocytopenia—7 grade 1/2 and grade 3/4
- Leukopenia—7 grade 1/2 and 6 grade 3/4
- Increased alanine aminotransferase—7 grade 1/2
- Neutropenia—6 grade 1/2 and 7 grade 3/4
- Increased aspartate aminotransferase—5 grade 1/2
- Hypoalbuminemia—4 grade 1/2
- Nausea—4 grade 1/2 and 1 grade 3/4
- Vomiting—3 grade 1/2
- Mucositis—2 grade 1/2
- Fatigue—2 grade 1/2
- Epistaxis—2 grade 1/2
- Abdominal distension—1 grade 1/2
- Loss of appetite—1 grade 1/2
- Diarrhea—1 grade 1/2
- Hyperbilirubinemia—1 grade 1/2
- Fever—1 grade 1/2 and grade 3/4
- Pain—1 grade 1/2
- Cough—1 grade 1/2
- Constipation—1 grade 1/2.
Dr Huang said EBV reactivation was not confirmed in this study. An elevated EBV DNA load was only observed in 2 patients with progressive disease. ![]()
LA JOLLA, CA—Results of a phase 2 study suggest chidamide can produce durable responses in patients with relapsed/refractory natural killer/T-cell lymphoma (NKTCL).
The overall response rate was 57.2% in these patients, and the complete response (CR) rate was 28.6%.
Seven of 14 evaluable patients were still receiving chidamide and still in response at last follow-up. For one patient, this was 50 weeks from initiating treatment with chidamide.
“The response is quite promising and encouraging,” said study investigator Huiqiang Huang, MD, PhD, of Sun Yat-sen University Cancer Center in Guangzhou, China.
“In terms of safety, the toxicity is mild to moderate.”
Dr Huang presented these results at the 10th Annual T-cell Lymphoma Forum.
This investigator-sponsored trial enrolled patients with relapsed/refractory non-Hodgkin lymphoma, but Dr Huang presented results in NKTCL patients only.
There were 15 NKTCL patients, most of whom were male (n=12). Their median age was 41 (range, 17-65). All 15 had an ECOG status of 0 or 1, 9 had stage I/II disease, and 6 had B symptoms.
Nine patients had Epstein-Barr virus (EBV) DNA levels of at least 1000 copy/mL at baseline, and 5 patients had lactate dehydrogenase levels of at least 245 U/L.
The patients had a median of 2 prior systemic therapies (range, 1-3), and 2 patients had undergone a transplant.
Efficacy
Patients received chidamide at 2 doses—10 mg daily or 30 mg twice a week. Dr Huang said both doses were effective against the lymphoma types studied, but the 30 mg twice-weekly dose appeared to be more effective for patients with NKTCL.
Fourteen NKTCL patients were evaluable for efficacy, and the median follow-up was 17.6 weeks (range, 2.6-50).
The overall response rate was 68.2% (6/14), and the CR rate was 28.6% (4/14). The disease control rate was 71.4%, meaning 10 of 14 patients had a CR, partial response (PR), or stable disease (SD).
Dr Huang noted that response was associated with elevated H3 acetylation level.
The median time to response was 5.25 weeks (range, 1.1-6.6).
As for duration of response, the 4 complete responders were still on treatment and in CR at last follow-up, which was 22.7 weeks, 38.1 weeks, 41.3 weeks, and 50 weeks, respectively, from treatment initiation.
Three of the 4 partial responders were still on treatment and in PR at 14.1 weeks, 26.9 weeks, and 32 weeks, respectively. Two patients with SD were still on treatment and in SD at 15.3 weeks and 15.9 weeks, respectively.
Three patients progressed while on treatment and died. A fourth patient died 2.6 weeks after treatment initiation.
Safety
Dr Huang noted that adverse events (AEs) were similar with the 2 dose groups. However, patients who received 30 mg biweekly had a higher incidence of gastrointestinal AEs.
Overall, the most common AEs were hematologic—anemia, thrombocytopenia, etc.—but dose reductions allowed for quick resolution of these AEs, according to Dr Huang.
AEs included:
- Lymphopenia—10 grade 1/2 and 1 grade 3/4
- Anemia—9 grade 1/2 and 3 grade 3/4
- Thrombocytopenia—7 grade 1/2 and grade 3/4
- Leukopenia—7 grade 1/2 and 6 grade 3/4
- Increased alanine aminotransferase—7 grade 1/2
- Neutropenia—6 grade 1/2 and 7 grade 3/4
- Increased aspartate aminotransferase—5 grade 1/2
- Hypoalbuminemia—4 grade 1/2
- Nausea—4 grade 1/2 and 1 grade 3/4
- Vomiting—3 grade 1/2
- Mucositis—2 grade 1/2
- Fatigue—2 grade 1/2
- Epistaxis—2 grade 1/2
- Abdominal distension—1 grade 1/2
- Loss of appetite—1 grade 1/2
- Diarrhea—1 grade 1/2
- Hyperbilirubinemia—1 grade 1/2
- Fever—1 grade 1/2 and grade 3/4
- Pain—1 grade 1/2
- Cough—1 grade 1/2
- Constipation—1 grade 1/2.
Dr Huang said EBV reactivation was not confirmed in this study. An elevated EBV DNA load was only observed in 2 patients with progressive disease. ![]()
Combo is preferentially active in T-cell lymphomas
LA JOLLA, CA—A 2-drug combination has demonstrated preferential activity in T-cell lymphomas over B-cell lymphomas, according to researchers.
In a small, phase 1/2 study, treatment with oral 5-azacitidine and romidepsin produced a higher overall response rate (ORR) and prolonged progression-free survival (PFS) in patients with T-cell lymphomas.
“In a very limited sample, we’ve definitely observed exquisite activity of the combination in patients with T-cell lymphoma compared to all other subtypes,” said Lorenzo Falchi, MD, of Columbia University Medical Center in New York, New York.
Dr Falchi presented these results at the 10th Annual T-cell Lymphoma Forum.
The research was funded by the Leukemia and Lymphoma Society, the Lymphoma Research Fund at Columbia University, and Celgene.
The phase 1 portion of this study included patients with previously treated non-Hodgkin lymphoma (NHL) or Hodgkin lymphoma. The phase 2 portion included only patients with T-cell lymphomas, newly diagnosed or previously treated.
Thirty-three patients were enrolled—12 with Hodgkin lymphoma, 8 with B-cell NHL, and 13 with T-cell NHL.
The patients’ median age was 54 (range, 23-79). Fifty-seven percent (n=19) were male. Sixty-one percent of patients were non-Hispanic white (n=20), 24% (n=8) were black, and 12% (n=4) were Asian.
“This was a very heavily pretreated patient population,” Dr Falchi noted. “I’d like to emphasize that the median number of prior treatments is 5 [range, 0-15].”
“Over half of patients had had stem cell transplantation [17 autologous and 5 allogeneic]. And, if you look at the subtypes by histology, all patients, pretty much, at some point, received all the standard chemotherapy or treatment approaches that are typically used for that subtype.”
Treatment
Patients were divided into 7 dosing cohorts. Azacitidine doses ranged from 100 mg to 300 mg on days 1-14 or days 1-21 per cycle.
Romidepsin doses ranged from 10 mg/m2 to 14 mg/m2. The drug was given on days 8 and 15 every 21 or 28 days, or it was given on days 8, 15, and 22 every 35 days.
There were 2 dose-limiting toxicities (DLTs) in cohort 2—grade 3 thrombocytopenia and grade 3 pleural effusion. In this cohort, 3 patients received azacitidine at 200 mg on days 1-14 plus romidepsin at 10 mg/m2 on days 8 and 15 every 21 days.
There were 3 DLTs in cohort 7—2 cases of grade 4 neutropenia and 1 case of grade 3 thrombocytopenia. In this cohort, 5 patients received azacitidine at 300 mg on days 1 to 21 plus romidepsin at 14 mg/m2 on days 8, 15, and 22 every 35 days.
Because of the DLTs in cohort 7, cohort 6 was chosen as the maximum tolerated dose. In cohort 6, 3 patients received azacitidine at 300 mg on days 1-14 plus romidepsin at 14 mg/m2 on days 8, 15, and 22 every 35 days.
Patients in the expansion cohort received treatment at the maximum tolerated dose. This cohort included 7 patients with T-cell lymphoma.
Safety
Treatment-emergent adverse events occurring in at least 5% of patients included:
- Anemia—3% grade 3
- Anorexia—9% grade 1
- Back pain—6% grade 2
- Constipation—6% grade 1
- Cough—9% grade 1
- Depression—3% grade 1 and 2
- Diarrhea—15% grade 1 and 6% grade 2
- Dyspnea—3% grade 1 and 2
- Fatigue—21% grade 1, 9% grade 2, and 3% grade 3
- Febrile neutropenia—3% grade 3 and 4
- Fever—6% grade 1 and 3% grade 2
- General disorders and administration site conditions—15% grade 1
- Hyperglycemia—3% grade 3
- Hypokalemia—6% grade 1
- Hypotension—3% grade 3
- Insomnia—6% grade 1
- Oral mucositis—9% grade 1 and 3% grade 2
- Nausea—18% grade 1, 27% grade 2, and 3% grade 3
- Neutrophil count decrease—3% grade 3 and 4
- Pain—3% grade 1 and 6% grade 2
- Pain of skin—3% grade 1 and 2
- Platelet count decrease—6% grade 2, 9% grade 3, and 6% grade 4
- Urinary tract infection—3% grade 3
- Vomiting—18% grade 1 and 21% grade 2.
Efficacy
Twenty-eight patients were evaluable for efficacy. The ORR for these patients was 36% (n=10).
The complete response (CR) rate was 22% (n=6), and the partial response (PR) rate was 14% (n=4). Twenty-five percent of patients (n=7) had stable disease, and 39% (n=11) progressed.
Dr Falchi noted that the ORR was “much higher” in patients with T-cell lymphoma than in those with B-cell lymphoma—80% (n=8) and 11% (n=2), respectively.
The CR rates were 50% (n=5) in T-cell lymphoma patients and 5.5% (n=1) in B-cell patients. PR rates were 30% (n=3) and 5.5% (n=1), respectively. Thirty-nine percent (n=7) of B-cell patients had stable disease, but none of the T-cell patients did.
“Patients with non-T-cell lymphoma were much more likely to progress on treatment,” Dr Falchi noted. “Half of them did so [n=9].”
This is in comparison to the 20% of T-cell lymphoma patients who progressed on treatment (n=2).
Disease subtypes for complete responders included transformed follicular lymphoma (n=1), T-lymphoblastic lymphoma (n=1), adult T-cell leukemia/lymphoma (n=1), extranodal NK/T-cell lymphoma (n=1), and angioimmunoblastic T-cell lymphoma (n=2).
Partial responders had follicular lymphoma (n=1), cutaneous peripheral T-cell lymphoma (n=1), cutaneous anaplastic large-cell lymphoma (n=1), and angioimmunoblastic T-cell lymphoma (n=1).
The 2 responders with B-cell lymphoma (1 CR and 1 PR) ultimately progressed and died.
Of the 8 responders with T-cell lymphoma, 3 have an ongoing CR, and 2 of these patients proceeded to transplant.
One T-cell patient who achieved a CR and proceeded to transplant was lost to follow-up. Another died after transplant.
Two T-cell patients who achieved a PR progressed and died. And 1 patient has an ongoing PR.
In total, 75% of patients (n=21) progressed. The median PFS for the entire study cohort was 3.6 months (range, 1.5-5.7).
The median PFS was 2.2 months (range, 1.1-3.2) for patients with B-cell lymphomas and was not reached for the T-cell lymphoma patients.
Eighty-nine percent of B-cell patients progressed (n=16), as did 40% of T-cell patients (n=4).
Dr Falchi and his colleagues are now conducting studies to correlate the pharmacokinetics of azacitidine-romidepsin with genome-wide methylation and correlate TET2, IDH2, and DNMT3A mutation status with clinical response. ![]()
LA JOLLA, CA—A 2-drug combination has demonstrated preferential activity in T-cell lymphomas over B-cell lymphomas, according to researchers.
In a small, phase 1/2 study, treatment with oral 5-azacitidine and romidepsin produced a higher overall response rate (ORR) and prolonged progression-free survival (PFS) in patients with T-cell lymphomas.
“In a very limited sample, we’ve definitely observed exquisite activity of the combination in patients with T-cell lymphoma compared to all other subtypes,” said Lorenzo Falchi, MD, of Columbia University Medical Center in New York, New York.
Dr Falchi presented these results at the 10th Annual T-cell Lymphoma Forum.
The research was funded by the Leukemia and Lymphoma Society, the Lymphoma Research Fund at Columbia University, and Celgene.
The phase 1 portion of this study included patients with previously treated non-Hodgkin lymphoma (NHL) or Hodgkin lymphoma. The phase 2 portion included only patients with T-cell lymphomas, newly diagnosed or previously treated.
Thirty-three patients were enrolled—12 with Hodgkin lymphoma, 8 with B-cell NHL, and 13 with T-cell NHL.
The patients’ median age was 54 (range, 23-79). Fifty-seven percent (n=19) were male. Sixty-one percent of patients were non-Hispanic white (n=20), 24% (n=8) were black, and 12% (n=4) were Asian.
“This was a very heavily pretreated patient population,” Dr Falchi noted. “I’d like to emphasize that the median number of prior treatments is 5 [range, 0-15].”
“Over half of patients had had stem cell transplantation [17 autologous and 5 allogeneic]. And, if you look at the subtypes by histology, all patients, pretty much, at some point, received all the standard chemotherapy or treatment approaches that are typically used for that subtype.”
Treatment
Patients were divided into 7 dosing cohorts. Azacitidine doses ranged from 100 mg to 300 mg on days 1-14 or days 1-21 per cycle.
Romidepsin doses ranged from 10 mg/m2 to 14 mg/m2. The drug was given on days 8 and 15 every 21 or 28 days, or it was given on days 8, 15, and 22 every 35 days.
There were 2 dose-limiting toxicities (DLTs) in cohort 2—grade 3 thrombocytopenia and grade 3 pleural effusion. In this cohort, 3 patients received azacitidine at 200 mg on days 1-14 plus romidepsin at 10 mg/m2 on days 8 and 15 every 21 days.
There were 3 DLTs in cohort 7—2 cases of grade 4 neutropenia and 1 case of grade 3 thrombocytopenia. In this cohort, 5 patients received azacitidine at 300 mg on days 1 to 21 plus romidepsin at 14 mg/m2 on days 8, 15, and 22 every 35 days.
Because of the DLTs in cohort 7, cohort 6 was chosen as the maximum tolerated dose. In cohort 6, 3 patients received azacitidine at 300 mg on days 1-14 plus romidepsin at 14 mg/m2 on days 8, 15, and 22 every 35 days.
Patients in the expansion cohort received treatment at the maximum tolerated dose. This cohort included 7 patients with T-cell lymphoma.
Safety
Treatment-emergent adverse events occurring in at least 5% of patients included:
- Anemia—3% grade 3
- Anorexia—9% grade 1
- Back pain—6% grade 2
- Constipation—6% grade 1
- Cough—9% grade 1
- Depression—3% grade 1 and 2
- Diarrhea—15% grade 1 and 6% grade 2
- Dyspnea—3% grade 1 and 2
- Fatigue—21% grade 1, 9% grade 2, and 3% grade 3
- Febrile neutropenia—3% grade 3 and 4
- Fever—6% grade 1 and 3% grade 2
- General disorders and administration site conditions—15% grade 1
- Hyperglycemia—3% grade 3
- Hypokalemia—6% grade 1
- Hypotension—3% grade 3
- Insomnia—6% grade 1
- Oral mucositis—9% grade 1 and 3% grade 2
- Nausea—18% grade 1, 27% grade 2, and 3% grade 3
- Neutrophil count decrease—3% grade 3 and 4
- Pain—3% grade 1 and 6% grade 2
- Pain of skin—3% grade 1 and 2
- Platelet count decrease—6% grade 2, 9% grade 3, and 6% grade 4
- Urinary tract infection—3% grade 3
- Vomiting—18% grade 1 and 21% grade 2.
Efficacy
Twenty-eight patients were evaluable for efficacy. The ORR for these patients was 36% (n=10).
The complete response (CR) rate was 22% (n=6), and the partial response (PR) rate was 14% (n=4). Twenty-five percent of patients (n=7) had stable disease, and 39% (n=11) progressed.
Dr Falchi noted that the ORR was “much higher” in patients with T-cell lymphoma than in those with B-cell lymphoma—80% (n=8) and 11% (n=2), respectively.
The CR rates were 50% (n=5) in T-cell lymphoma patients and 5.5% (n=1) in B-cell patients. PR rates were 30% (n=3) and 5.5% (n=1), respectively. Thirty-nine percent (n=7) of B-cell patients had stable disease, but none of the T-cell patients did.
“Patients with non-T-cell lymphoma were much more likely to progress on treatment,” Dr Falchi noted. “Half of them did so [n=9].”
This is in comparison to the 20% of T-cell lymphoma patients who progressed on treatment (n=2).
Disease subtypes for complete responders included transformed follicular lymphoma (n=1), T-lymphoblastic lymphoma (n=1), adult T-cell leukemia/lymphoma (n=1), extranodal NK/T-cell lymphoma (n=1), and angioimmunoblastic T-cell lymphoma (n=2).
Partial responders had follicular lymphoma (n=1), cutaneous peripheral T-cell lymphoma (n=1), cutaneous anaplastic large-cell lymphoma (n=1), and angioimmunoblastic T-cell lymphoma (n=1).
The 2 responders with B-cell lymphoma (1 CR and 1 PR) ultimately progressed and died.
Of the 8 responders with T-cell lymphoma, 3 have an ongoing CR, and 2 of these patients proceeded to transplant.
One T-cell patient who achieved a CR and proceeded to transplant was lost to follow-up. Another died after transplant.
Two T-cell patients who achieved a PR progressed and died. And 1 patient has an ongoing PR.
In total, 75% of patients (n=21) progressed. The median PFS for the entire study cohort was 3.6 months (range, 1.5-5.7).
The median PFS was 2.2 months (range, 1.1-3.2) for patients with B-cell lymphomas and was not reached for the T-cell lymphoma patients.
Eighty-nine percent of B-cell patients progressed (n=16), as did 40% of T-cell patients (n=4).
Dr Falchi and his colleagues are now conducting studies to correlate the pharmacokinetics of azacitidine-romidepsin with genome-wide methylation and correlate TET2, IDH2, and DNMT3A mutation status with clinical response. ![]()
LA JOLLA, CA—A 2-drug combination has demonstrated preferential activity in T-cell lymphomas over B-cell lymphomas, according to researchers.
In a small, phase 1/2 study, treatment with oral 5-azacitidine and romidepsin produced a higher overall response rate (ORR) and prolonged progression-free survival (PFS) in patients with T-cell lymphomas.
“In a very limited sample, we’ve definitely observed exquisite activity of the combination in patients with T-cell lymphoma compared to all other subtypes,” said Lorenzo Falchi, MD, of Columbia University Medical Center in New York, New York.
Dr Falchi presented these results at the 10th Annual T-cell Lymphoma Forum.
The research was funded by the Leukemia and Lymphoma Society, the Lymphoma Research Fund at Columbia University, and Celgene.
The phase 1 portion of this study included patients with previously treated non-Hodgkin lymphoma (NHL) or Hodgkin lymphoma. The phase 2 portion included only patients with T-cell lymphomas, newly diagnosed or previously treated.
Thirty-three patients were enrolled—12 with Hodgkin lymphoma, 8 with B-cell NHL, and 13 with T-cell NHL.
The patients’ median age was 54 (range, 23-79). Fifty-seven percent (n=19) were male. Sixty-one percent of patients were non-Hispanic white (n=20), 24% (n=8) were black, and 12% (n=4) were Asian.
“This was a very heavily pretreated patient population,” Dr Falchi noted. “I’d like to emphasize that the median number of prior treatments is 5 [range, 0-15].”
“Over half of patients had had stem cell transplantation [17 autologous and 5 allogeneic]. And, if you look at the subtypes by histology, all patients, pretty much, at some point, received all the standard chemotherapy or treatment approaches that are typically used for that subtype.”
Treatment
Patients were divided into 7 dosing cohorts. Azacitidine doses ranged from 100 mg to 300 mg on days 1-14 or days 1-21 per cycle.
Romidepsin doses ranged from 10 mg/m2 to 14 mg/m2. The drug was given on days 8 and 15 every 21 or 28 days, or it was given on days 8, 15, and 22 every 35 days.
There were 2 dose-limiting toxicities (DLTs) in cohort 2—grade 3 thrombocytopenia and grade 3 pleural effusion. In this cohort, 3 patients received azacitidine at 200 mg on days 1-14 plus romidepsin at 10 mg/m2 on days 8 and 15 every 21 days.
There were 3 DLTs in cohort 7—2 cases of grade 4 neutropenia and 1 case of grade 3 thrombocytopenia. In this cohort, 5 patients received azacitidine at 300 mg on days 1 to 21 plus romidepsin at 14 mg/m2 on days 8, 15, and 22 every 35 days.
Because of the DLTs in cohort 7, cohort 6 was chosen as the maximum tolerated dose. In cohort 6, 3 patients received azacitidine at 300 mg on days 1-14 plus romidepsin at 14 mg/m2 on days 8, 15, and 22 every 35 days.
Patients in the expansion cohort received treatment at the maximum tolerated dose. This cohort included 7 patients with T-cell lymphoma.
Safety
Treatment-emergent adverse events occurring in at least 5% of patients included:
- Anemia—3% grade 3
- Anorexia—9% grade 1
- Back pain—6% grade 2
- Constipation—6% grade 1
- Cough—9% grade 1
- Depression—3% grade 1 and 2
- Diarrhea—15% grade 1 and 6% grade 2
- Dyspnea—3% grade 1 and 2
- Fatigue—21% grade 1, 9% grade 2, and 3% grade 3
- Febrile neutropenia—3% grade 3 and 4
- Fever—6% grade 1 and 3% grade 2
- General disorders and administration site conditions—15% grade 1
- Hyperglycemia—3% grade 3
- Hypokalemia—6% grade 1
- Hypotension—3% grade 3
- Insomnia—6% grade 1
- Oral mucositis—9% grade 1 and 3% grade 2
- Nausea—18% grade 1, 27% grade 2, and 3% grade 3
- Neutrophil count decrease—3% grade 3 and 4
- Pain—3% grade 1 and 6% grade 2
- Pain of skin—3% grade 1 and 2
- Platelet count decrease—6% grade 2, 9% grade 3, and 6% grade 4
- Urinary tract infection—3% grade 3
- Vomiting—18% grade 1 and 21% grade 2.
Efficacy
Twenty-eight patients were evaluable for efficacy. The ORR for these patients was 36% (n=10).
The complete response (CR) rate was 22% (n=6), and the partial response (PR) rate was 14% (n=4). Twenty-five percent of patients (n=7) had stable disease, and 39% (n=11) progressed.
Dr Falchi noted that the ORR was “much higher” in patients with T-cell lymphoma than in those with B-cell lymphoma—80% (n=8) and 11% (n=2), respectively.
The CR rates were 50% (n=5) in T-cell lymphoma patients and 5.5% (n=1) in B-cell patients. PR rates were 30% (n=3) and 5.5% (n=1), respectively. Thirty-nine percent (n=7) of B-cell patients had stable disease, but none of the T-cell patients did.
“Patients with non-T-cell lymphoma were much more likely to progress on treatment,” Dr Falchi noted. “Half of them did so [n=9].”
This is in comparison to the 20% of T-cell lymphoma patients who progressed on treatment (n=2).
Disease subtypes for complete responders included transformed follicular lymphoma (n=1), T-lymphoblastic lymphoma (n=1), adult T-cell leukemia/lymphoma (n=1), extranodal NK/T-cell lymphoma (n=1), and angioimmunoblastic T-cell lymphoma (n=2).
Partial responders had follicular lymphoma (n=1), cutaneous peripheral T-cell lymphoma (n=1), cutaneous anaplastic large-cell lymphoma (n=1), and angioimmunoblastic T-cell lymphoma (n=1).
The 2 responders with B-cell lymphoma (1 CR and 1 PR) ultimately progressed and died.
Of the 8 responders with T-cell lymphoma, 3 have an ongoing CR, and 2 of these patients proceeded to transplant.
One T-cell patient who achieved a CR and proceeded to transplant was lost to follow-up. Another died after transplant.
Two T-cell patients who achieved a PR progressed and died. And 1 patient has an ongoing PR.
In total, 75% of patients (n=21) progressed. The median PFS for the entire study cohort was 3.6 months (range, 1.5-5.7).
The median PFS was 2.2 months (range, 1.1-3.2) for patients with B-cell lymphomas and was not reached for the T-cell lymphoma patients.
Eighty-nine percent of B-cell patients progressed (n=16), as did 40% of T-cell patients (n=4).
Dr Falchi and his colleagues are now conducting studies to correlate the pharmacokinetics of azacitidine-romidepsin with genome-wide methylation and correlate TET2, IDH2, and DNMT3A mutation status with clinical response. ![]()
Duvelisib combos show promise for PTCL, CTCL
LA JOLLA, CA—Phase 1 results suggest duvelisib combination therapies can be active and well-tolerated in patients with relapsed/refractory T-cell lymphomas.
Researchers said duvelisib had an acceptable safety profile when given in combination with romidepsin or bortezomib to patients with relapsed/refractory peripheral T-cell lymphoma (PTCL) or cutaneous T-cell lymphoma (CTCL).
Duvelisib plus romidepsin produced a 60% overall response rate (ORR) in these patients, and duvelisib plus bortezomib produced a 35% ORR.
Response rates were higher in PTCL patients than CTCL patients.
Neha Mehta-Shah, MD, of Washington University in St. Louis, Missouri, and her colleagues presented these results in a poster at the 10th Annual T-cell Lymphoma Forum.
The research was supported by the Leukemia & Lymphoma Society, Infinity Pharmaceuticals, and Verastem Inc.
This phase 1 trial consists of parallel arms evaluating duvelisib in combination with romidepsin (arm A) or bortezomib (arm B). The trial enrolled patients with PTCL or CTCL that had progressed after at least 1 prior therapy.
All patients received duvelisib at 25 mg, 50 mg, or 75 mg twice daily for 28-day cycles.
Patients in arm A received romidepsin at 10 mg/m2 on days 1, 8, and 15 of each cycle.
Patients in arm B received bortezomib at 1 mg/m2 on days 1, 4, 8, and 11 of each cycle.
Romidepsin combination
Sixteen patients received duvelisib plus romidepsin, and 15 of them were evaluable for efficacy. Eleven patients had PTCL, and 4 had CTCL.
The ORR was 60% (9/16), and the complete response (CR) rate was 27% (n=4). The median time to response was 51 days (range, 49-54).
The ORR was 64% in the PTCL patients and 50% in the CTCL patients. All 4 CRs occurred in PTCL patients, 2 in patients with PTCL not otherwise specified (NOS) and 2 in patients with angioimmunoblastic T-cell lymphoma (AITL).
There were 5 responses among patients who received the 75 mg dose of duvelisib (n=8) and 2 responses each in the 50 mg dose group (n=3) and 25 mg dose group (n=4).
There were no dose-limiting toxicities, so the 75 mg dose of duvelisib was considered the maximum tolerated dose.
All 16 patients were evaluable for safety. There were 2 serious adverse events (AEs) considered possibly related to treatment—grade 3 fatigue and grade 2 aspartate aminotransferase (AST) increase.
There were 2 deaths considered unrelated to treatment—diffuse alveolar hemorrhage after allogeneic transplant and sepsis in the setting of disease progression.
Treatment-related AEs (occurring in at least 2 patients) were fatigue (56%), nausea (50%), altered taste (50%), diarrhea (38%), neutropenia (38%), rash (31%), thrombocytopenia (25%), dysphagia (25%), and anorexia (25%).
Grade 3/4 treatment-related AEs included neutropenia (38%) and thrombocytopenia (6%).
One patient discontinued duvelisib-romidepsin due to toxicity, and 7 discontinued due to progressive disease.
Three patients proceeded to bone marrow transplant/donor lymphocyte infusion, and 4 patients are still receiving study treatment.
Bortezomib combination
There were 17 patients who received duvelisib plus bortezomib—10 with PTCL and 7 with CTCL.
The ORR was 35% (6/17), and the CR rate was 18% (n=3). The median time to response was 52 days (range, 47-57).
The ORR was 50% in PTCL patients and 14% among CTCL patients.
All 3 CRs occurred in the PTCL patients—1 in a patient with AITL, 1 in a patient with PTCL-NOS, and 1 in a patient who had intestinal T-cell lymphoma with B-cell lymphoproliferative disorder.
There were 3 responses among patients who received the 25 mg dose of duvelisib (n=8), 2 responses in the 50 mg dose group (n=3), and 1 response in the 75 mg dose group (n=6).
There was 1 dose-limiting toxicity—pneumonia—in a patient treated at the 25 mg dose.
The 25 mg dose was deemed optimal due to grade 3 alanine transaminase (ALT)/AST elevations observed after cycle 1 with the 50 mg dose (n=3) and the 75 mg dose (n=2).
There were 6 serious AEs considered possibly related to treatment:
- Grade 3 pneumonia (n=2)
- Grade 3 infectious colitis (n=1)
- Grade 3 colitis (n=1)
- Grade 4 ALT/AST elevation (n=1)
- Grade 5 Stevens-Johnson syndrome (n=1).
The fatal case of Stevens-Johnson syndrome was considered possibly related to bortezomib, duvelisib, and trimethoprim-sulfamethoxazole, a medication that was started at the beginning of the study.
Treatment-related AEs (occurring in at least 2 patients) included diarrhea/colitis (71%), ALT/AST increase (41%), rash (24%), neutropenia (24%), nausea/vomiting (24%), chills (24%), fatigue (24%), and alkaline phosphatase increase (12%).
Grade 3/4 AEs included ALT/AST increase (35%), rash (12%), neutropenia (12%), diarrhea/colitis (6%), and alkaline phosphatase increase (6%).
Seven patients discontinued duvelisib-bortezomib due to toxicity, and 8 discontinued due to disease progression. Two patients are still on study treatment. ![]()
LA JOLLA, CA—Phase 1 results suggest duvelisib combination therapies can be active and well-tolerated in patients with relapsed/refractory T-cell lymphomas.
Researchers said duvelisib had an acceptable safety profile when given in combination with romidepsin or bortezomib to patients with relapsed/refractory peripheral T-cell lymphoma (PTCL) or cutaneous T-cell lymphoma (CTCL).
Duvelisib plus romidepsin produced a 60% overall response rate (ORR) in these patients, and duvelisib plus bortezomib produced a 35% ORR.
Response rates were higher in PTCL patients than CTCL patients.
Neha Mehta-Shah, MD, of Washington University in St. Louis, Missouri, and her colleagues presented these results in a poster at the 10th Annual T-cell Lymphoma Forum.
The research was supported by the Leukemia & Lymphoma Society, Infinity Pharmaceuticals, and Verastem Inc.
This phase 1 trial consists of parallel arms evaluating duvelisib in combination with romidepsin (arm A) or bortezomib (arm B). The trial enrolled patients with PTCL or CTCL that had progressed after at least 1 prior therapy.
All patients received duvelisib at 25 mg, 50 mg, or 75 mg twice daily for 28-day cycles.
Patients in arm A received romidepsin at 10 mg/m2 on days 1, 8, and 15 of each cycle.
Patients in arm B received bortezomib at 1 mg/m2 on days 1, 4, 8, and 11 of each cycle.
Romidepsin combination
Sixteen patients received duvelisib plus romidepsin, and 15 of them were evaluable for efficacy. Eleven patients had PTCL, and 4 had CTCL.
The ORR was 60% (9/16), and the complete response (CR) rate was 27% (n=4). The median time to response was 51 days (range, 49-54).
The ORR was 64% in the PTCL patients and 50% in the CTCL patients. All 4 CRs occurred in PTCL patients, 2 in patients with PTCL not otherwise specified (NOS) and 2 in patients with angioimmunoblastic T-cell lymphoma (AITL).
There were 5 responses among patients who received the 75 mg dose of duvelisib (n=8) and 2 responses each in the 50 mg dose group (n=3) and 25 mg dose group (n=4).
There were no dose-limiting toxicities, so the 75 mg dose of duvelisib was considered the maximum tolerated dose.
All 16 patients were evaluable for safety. There were 2 serious adverse events (AEs) considered possibly related to treatment—grade 3 fatigue and grade 2 aspartate aminotransferase (AST) increase.
There were 2 deaths considered unrelated to treatment—diffuse alveolar hemorrhage after allogeneic transplant and sepsis in the setting of disease progression.
Treatment-related AEs (occurring in at least 2 patients) were fatigue (56%), nausea (50%), altered taste (50%), diarrhea (38%), neutropenia (38%), rash (31%), thrombocytopenia (25%), dysphagia (25%), and anorexia (25%).
Grade 3/4 treatment-related AEs included neutropenia (38%) and thrombocytopenia (6%).
One patient discontinued duvelisib-romidepsin due to toxicity, and 7 discontinued due to progressive disease.
Three patients proceeded to bone marrow transplant/donor lymphocyte infusion, and 4 patients are still receiving study treatment.
Bortezomib combination
There were 17 patients who received duvelisib plus bortezomib—10 with PTCL and 7 with CTCL.
The ORR was 35% (6/17), and the CR rate was 18% (n=3). The median time to response was 52 days (range, 47-57).
The ORR was 50% in PTCL patients and 14% among CTCL patients.
All 3 CRs occurred in the PTCL patients—1 in a patient with AITL, 1 in a patient with PTCL-NOS, and 1 in a patient who had intestinal T-cell lymphoma with B-cell lymphoproliferative disorder.
There were 3 responses among patients who received the 25 mg dose of duvelisib (n=8), 2 responses in the 50 mg dose group (n=3), and 1 response in the 75 mg dose group (n=6).
There was 1 dose-limiting toxicity—pneumonia—in a patient treated at the 25 mg dose.
The 25 mg dose was deemed optimal due to grade 3 alanine transaminase (ALT)/AST elevations observed after cycle 1 with the 50 mg dose (n=3) and the 75 mg dose (n=2).
There were 6 serious AEs considered possibly related to treatment:
- Grade 3 pneumonia (n=2)
- Grade 3 infectious colitis (n=1)
- Grade 3 colitis (n=1)
- Grade 4 ALT/AST elevation (n=1)
- Grade 5 Stevens-Johnson syndrome (n=1).
The fatal case of Stevens-Johnson syndrome was considered possibly related to bortezomib, duvelisib, and trimethoprim-sulfamethoxazole, a medication that was started at the beginning of the study.
Treatment-related AEs (occurring in at least 2 patients) included diarrhea/colitis (71%), ALT/AST increase (41%), rash (24%), neutropenia (24%), nausea/vomiting (24%), chills (24%), fatigue (24%), and alkaline phosphatase increase (12%).
Grade 3/4 AEs included ALT/AST increase (35%), rash (12%), neutropenia (12%), diarrhea/colitis (6%), and alkaline phosphatase increase (6%).
Seven patients discontinued duvelisib-bortezomib due to toxicity, and 8 discontinued due to disease progression. Two patients are still on study treatment. ![]()
LA JOLLA, CA—Phase 1 results suggest duvelisib combination therapies can be active and well-tolerated in patients with relapsed/refractory T-cell lymphomas.
Researchers said duvelisib had an acceptable safety profile when given in combination with romidepsin or bortezomib to patients with relapsed/refractory peripheral T-cell lymphoma (PTCL) or cutaneous T-cell lymphoma (CTCL).
Duvelisib plus romidepsin produced a 60% overall response rate (ORR) in these patients, and duvelisib plus bortezomib produced a 35% ORR.
Response rates were higher in PTCL patients than CTCL patients.
Neha Mehta-Shah, MD, of Washington University in St. Louis, Missouri, and her colleagues presented these results in a poster at the 10th Annual T-cell Lymphoma Forum.
The research was supported by the Leukemia & Lymphoma Society, Infinity Pharmaceuticals, and Verastem Inc.
This phase 1 trial consists of parallel arms evaluating duvelisib in combination with romidepsin (arm A) or bortezomib (arm B). The trial enrolled patients with PTCL or CTCL that had progressed after at least 1 prior therapy.
All patients received duvelisib at 25 mg, 50 mg, or 75 mg twice daily for 28-day cycles.
Patients in arm A received romidepsin at 10 mg/m2 on days 1, 8, and 15 of each cycle.
Patients in arm B received bortezomib at 1 mg/m2 on days 1, 4, 8, and 11 of each cycle.
Romidepsin combination
Sixteen patients received duvelisib plus romidepsin, and 15 of them were evaluable for efficacy. Eleven patients had PTCL, and 4 had CTCL.
The ORR was 60% (9/16), and the complete response (CR) rate was 27% (n=4). The median time to response was 51 days (range, 49-54).
The ORR was 64% in the PTCL patients and 50% in the CTCL patients. All 4 CRs occurred in PTCL patients, 2 in patients with PTCL not otherwise specified (NOS) and 2 in patients with angioimmunoblastic T-cell lymphoma (AITL).
There were 5 responses among patients who received the 75 mg dose of duvelisib (n=8) and 2 responses each in the 50 mg dose group (n=3) and 25 mg dose group (n=4).
There were no dose-limiting toxicities, so the 75 mg dose of duvelisib was considered the maximum tolerated dose.
All 16 patients were evaluable for safety. There were 2 serious adverse events (AEs) considered possibly related to treatment—grade 3 fatigue and grade 2 aspartate aminotransferase (AST) increase.
There were 2 deaths considered unrelated to treatment—diffuse alveolar hemorrhage after allogeneic transplant and sepsis in the setting of disease progression.
Treatment-related AEs (occurring in at least 2 patients) were fatigue (56%), nausea (50%), altered taste (50%), diarrhea (38%), neutropenia (38%), rash (31%), thrombocytopenia (25%), dysphagia (25%), and anorexia (25%).
Grade 3/4 treatment-related AEs included neutropenia (38%) and thrombocytopenia (6%).
One patient discontinued duvelisib-romidepsin due to toxicity, and 7 discontinued due to progressive disease.
Three patients proceeded to bone marrow transplant/donor lymphocyte infusion, and 4 patients are still receiving study treatment.
Bortezomib combination
There were 17 patients who received duvelisib plus bortezomib—10 with PTCL and 7 with CTCL.
The ORR was 35% (6/17), and the CR rate was 18% (n=3). The median time to response was 52 days (range, 47-57).
The ORR was 50% in PTCL patients and 14% among CTCL patients.
All 3 CRs occurred in the PTCL patients—1 in a patient with AITL, 1 in a patient with PTCL-NOS, and 1 in a patient who had intestinal T-cell lymphoma with B-cell lymphoproliferative disorder.
There were 3 responses among patients who received the 25 mg dose of duvelisib (n=8), 2 responses in the 50 mg dose group (n=3), and 1 response in the 75 mg dose group (n=6).
There was 1 dose-limiting toxicity—pneumonia—in a patient treated at the 25 mg dose.
The 25 mg dose was deemed optimal due to grade 3 alanine transaminase (ALT)/AST elevations observed after cycle 1 with the 50 mg dose (n=3) and the 75 mg dose (n=2).
There were 6 serious AEs considered possibly related to treatment:
- Grade 3 pneumonia (n=2)
- Grade 3 infectious colitis (n=1)
- Grade 3 colitis (n=1)
- Grade 4 ALT/AST elevation (n=1)
- Grade 5 Stevens-Johnson syndrome (n=1).
The fatal case of Stevens-Johnson syndrome was considered possibly related to bortezomib, duvelisib, and trimethoprim-sulfamethoxazole, a medication that was started at the beginning of the study.
Treatment-related AEs (occurring in at least 2 patients) included diarrhea/colitis (71%), ALT/AST increase (41%), rash (24%), neutropenia (24%), nausea/vomiting (24%), chills (24%), fatigue (24%), and alkaline phosphatase increase (12%).
Grade 3/4 AEs included ALT/AST increase (35%), rash (12%), neutropenia (12%), diarrhea/colitis (6%), and alkaline phosphatase increase (6%).
Seven patients discontinued duvelisib-bortezomib due to toxicity, and 8 discontinued due to disease progression. Two patients are still on study treatment.