User login
Three-drug combo delivers PFS for myeloma in OPTIMISMM trial
The addition of pomalidomide to bortezomib and low-dose dexamethasone showed a statistically significant improvement in progression-free survival for patients with relapsed/refractory multiple myeloma, compared with just the two agents, according to Celgene.
Celgene, which markets pomalidomide, announced the results from the phase 3 OPTIMISMM trial (NCT01734928) on Feb. 6. The company expects the results to be presented at future medical meetings, they said.
OPTIMISMM is the first phase 3 trial to examine a triple-drug combination for multiple myeloma patients who have all received prior lenalidomide, Celgene noted.
The pomalidomide/bortezomib/low-dose dexamethasone combination is not currently approved, but pomalidomide plus dexamethasone is approved for multiple myeloma patients who have received at least two prior therapies, including lenalidomide and a proteasome inhibitor, and have shown disease progression within 60 days of last therapy.
The addition of pomalidomide to bortezomib and low-dose dexamethasone showed a statistically significant improvement in progression-free survival for patients with relapsed/refractory multiple myeloma, compared with just the two agents, according to Celgene.
Celgene, which markets pomalidomide, announced the results from the phase 3 OPTIMISMM trial (NCT01734928) on Feb. 6. The company expects the results to be presented at future medical meetings, they said.
OPTIMISMM is the first phase 3 trial to examine a triple-drug combination for multiple myeloma patients who have all received prior lenalidomide, Celgene noted.
The pomalidomide/bortezomib/low-dose dexamethasone combination is not currently approved, but pomalidomide plus dexamethasone is approved for multiple myeloma patients who have received at least two prior therapies, including lenalidomide and a proteasome inhibitor, and have shown disease progression within 60 days of last therapy.
The addition of pomalidomide to bortezomib and low-dose dexamethasone showed a statistically significant improvement in progression-free survival for patients with relapsed/refractory multiple myeloma, compared with just the two agents, according to Celgene.
Celgene, which markets pomalidomide, announced the results from the phase 3 OPTIMISMM trial (NCT01734928) on Feb. 6. The company expects the results to be presented at future medical meetings, they said.
OPTIMISMM is the first phase 3 trial to examine a triple-drug combination for multiple myeloma patients who have all received prior lenalidomide, Celgene noted.
The pomalidomide/bortezomib/low-dose dexamethasone combination is not currently approved, but pomalidomide plus dexamethasone is approved for multiple myeloma patients who have received at least two prior therapies, including lenalidomide and a proteasome inhibitor, and have shown disease progression within 60 days of last therapy.
TRANSCEND NHL trial identifies window for CAR T expansion
for CAR T expansion
SAN FRANCISCO – The CD19-directed 4-1BB chimeric antigen receptor (CAR) T-cell product JCAR017 demonstrated increased CAR T-cell expansion and persistence, and higher durability of response at higher dose levels – with manageable toxicities – in a pivotal phase 1 trial of relapsed/refractory B-cell non-Hodgkin lymphoma.
However, preliminary modeling data suggest that a therapeutic window exists for the CAR T-cell expansion, which means that development of strategies for pushing patients into that window could enhance efficacy and limit toxicity associated with JCAR017, Tanya Siddiqi, MD, of City of Hope Comprehensive Cancer Center, Duarte, Calif., reported at the ASCO-SITC Clinical Immuno-Oncology Symposium.
TRANSCEND NHL 001 is a multicenter, seamless design, pivotal trial, which started as a phase 1 first-in-human study of JCAR017, a defined composition CAR T-cell product also known as lisocabtagene maraleucel and administered at precise doses of CD4+ and CD8+ CAR T cells. Dose-finding and dose-expansion cohorts have been investigated, and currently the pivotal diffuse large B-cell lymphoma (DLBCL) cohort is enrolling, Dr. Saddiqi said, noting that dose level 2 (1 x 108 cells given as a single dose) was selected for that cohort.
The current findings are based on the TRANSCEND core population – a set of patients selected from the dose-finding and dose-expansion cohorts. This population includes patients with DLBCL not otherwise specified, transformed follicular lymphoma, or high-grade double- or triple-hit lymphomas, she said, explaining that she and her colleagues looked at prelymphodepletion baseline patient characteristics and biomarkers to assess how they related to outcomes and toxicities. This precise dosing of JCAR017 reduces variability, enabling the identification of potential patient factors associated with clinical outcomes, she said.
Response rates among 27 patients who received dose level 2 were high, with an 81% overall response rate and a 63% complete response rate.
“Patients with complete remission seemed to have more of a durable response,” she said. “In the core population at dose level 2, 50% with 6 months of follow-up seemed to remain in complete response, so there’s a dose-response effect in these patients.”
It doesn’t appear that the dose affects development of cytokine release syndrome (CRS) or neurotoxicity (NT), as the rates of these (30% and 20%, respectively) did not differ by dose level or schedule, but certain baseline features, such as a lactate dehydrogenase (LDH) level above 500 U/L and tumor burden measured as the sum of the product of diameters of 50 cm or greater, do appear to affect the development of these toxicities.
For example, 10 of 13 (77%) of patients with both of those baseline characteristics developed CRS, and 7 of 13 (54%) developed NT; for those without these characteristics, the odds of developing CRS and NT were significantly lower, she said.
Of note, higher Cmax, or peak expansion of CAR T cells in vivo, was seen at dose level 2, and exposure (area under the curve) was also higher, as was expected at that dose level, Dr. Siddiqi said.
“It also appears that there is a trend of patients with higher tumor burden to have higher expansion of their CAR T cells in vivo,” she said, noting that some of those patients were “superexpanders” with very high expansion of CAR T cells. “Similarly there were certain cytokines at the prelymphodepletion time point that seem to be higher … in patients who also go on to have higher expansion of their CAR T cells.”
These included interleukin-7, IL-15, MIP (macrophage inflammatory protein)–1alpha, and tumor necrosis factor (TNF)–alpha.
“Patients with certain higher inflammatory cytokines and biomarkers of inflammation also were noted to have higher events of CRS and neurotoxicity, so not just higher tumor burden, but also higher inflammatory state at baseline seems to affect patients in terms of getting any grade CRS or any grade neurotoxicity,” she said.
Those associated with CRS included ferritin, C-reactive protein (CRP), IL-10, IL-15, IL-16, TNF-alpha, and MIP-1beta levels, and those associated with NT included ferritin, CRP, d-dimer, IL-6, IL-15, TNF-alpha, and MIP-1alpha levels.
“Interestingly, there’s an inverse relationship between the expression of some of these biomarkers and inflammatory markers and the durability of response at 3 months,” she said.
Patients with higher tumor burden, LDH, and other markers either had no response at 3 months, or they had a very rapid response at the 1-month mark and then lost their response by 3 months, she noted.
“One of the theories could be that these patients with higher tumor burden, higher inflammatory state – they have such a high peak expansion rapidly after receiving their CAR T cells that potentially those CAR T cells may be getting exhausted or dying off very quickly, and therefore patients can lose their response,” she said.
When these data are considered together and modeled, there seems to be a therapeutic window where patients who have optimal expansion of CAR T cells in vivo may have lesser toxicity, higher overall response rates, and better durability of response, she said.
That is, on one end of the spectrum, there are patients with lower CAR T-cell expansion who have lower toxicities, but who also have lower overall response rates and lower durability of response, and on the other end, there are patients with superhigh expansion of CAR T cells, who have higher response rates, but also higher rates of toxicity, and who lose their response quickly.
“So if we can identify patients who would be in this window of optimal target expansion of CAR T cells, and if we could find strategies or mechanisms to move patients who are on either end of that spectrum into this window, we may be able to get patients with better efficacy and lower toxicities, and there could be combination strategies that could help get us there,” she said.
TRANSCEND NHL 001 is sponsored by Juno Therapeutics. Dr. Siddiqi reported serving as a consultant or adviser for Juno Therapeutics, and as a member of the speakers bureau for Pharmacyclics/Janssen and Seattle Genetics. Research funding was provided to her institution by Juno Therapeutics and several other companies.
sworcester@frontlinemedcom.com
SOURCE: Siddiqi T et al. ASCO-SITC, abstract 122.
SAN FRANCISCO – The CD19-directed 4-1BB chimeric antigen receptor (CAR) T-cell product JCAR017 demonstrated increased CAR T-cell expansion and persistence, and higher durability of response at higher dose levels – with manageable toxicities – in a pivotal phase 1 trial of relapsed/refractory B-cell non-Hodgkin lymphoma.
However, preliminary modeling data suggest that a therapeutic window exists for the CAR T-cell expansion, which means that development of strategies for pushing patients into that window could enhance efficacy and limit toxicity associated with JCAR017, Tanya Siddiqi, MD, of City of Hope Comprehensive Cancer Center, Duarte, Calif., reported at the ASCO-SITC Clinical Immuno-Oncology Symposium.
TRANSCEND NHL 001 is a multicenter, seamless design, pivotal trial, which started as a phase 1 first-in-human study of JCAR017, a defined composition CAR T-cell product also known as lisocabtagene maraleucel and administered at precise doses of CD4+ and CD8+ CAR T cells. Dose-finding and dose-expansion cohorts have been investigated, and currently the pivotal diffuse large B-cell lymphoma (DLBCL) cohort is enrolling, Dr. Saddiqi said, noting that dose level 2 (1 x 108 cells given as a single dose) was selected for that cohort.
The current findings are based on the TRANSCEND core population – a set of patients selected from the dose-finding and dose-expansion cohorts. This population includes patients with DLBCL not otherwise specified, transformed follicular lymphoma, or high-grade double- or triple-hit lymphomas, she said, explaining that she and her colleagues looked at prelymphodepletion baseline patient characteristics and biomarkers to assess how they related to outcomes and toxicities. This precise dosing of JCAR017 reduces variability, enabling the identification of potential patient factors associated with clinical outcomes, she said.
Response rates among 27 patients who received dose level 2 were high, with an 81% overall response rate and a 63% complete response rate.
“Patients with complete remission seemed to have more of a durable response,” she said. “In the core population at dose level 2, 50% with 6 months of follow-up seemed to remain in complete response, so there’s a dose-response effect in these patients.”
It doesn’t appear that the dose affects development of cytokine release syndrome (CRS) or neurotoxicity (NT), as the rates of these (30% and 20%, respectively) did not differ by dose level or schedule, but certain baseline features, such as a lactate dehydrogenase (LDH) level above 500 U/L and tumor burden measured as the sum of the product of diameters of 50 cm or greater, do appear to affect the development of these toxicities.
For example, 10 of 13 (77%) of patients with both of those baseline characteristics developed CRS, and 7 of 13 (54%) developed NT; for those without these characteristics, the odds of developing CRS and NT were significantly lower, she said.
Of note, higher Cmax, or peak expansion of CAR T cells in vivo, was seen at dose level 2, and exposure (area under the curve) was also higher, as was expected at that dose level, Dr. Siddiqi said.
“It also appears that there is a trend of patients with higher tumor burden to have higher expansion of their CAR T cells in vivo,” she said, noting that some of those patients were “superexpanders” with very high expansion of CAR T cells. “Similarly there were certain cytokines at the prelymphodepletion time point that seem to be higher … in patients who also go on to have higher expansion of their CAR T cells.”
These included interleukin-7, IL-15, MIP (macrophage inflammatory protein)–1alpha, and tumor necrosis factor (TNF)–alpha.
“Patients with certain higher inflammatory cytokines and biomarkers of inflammation also were noted to have higher events of CRS and neurotoxicity, so not just higher tumor burden, but also higher inflammatory state at baseline seems to affect patients in terms of getting any grade CRS or any grade neurotoxicity,” she said.
Those associated with CRS included ferritin, C-reactive protein (CRP), IL-10, IL-15, IL-16, TNF-alpha, and MIP-1beta levels, and those associated with NT included ferritin, CRP, d-dimer, IL-6, IL-15, TNF-alpha, and MIP-1alpha levels.
“Interestingly, there’s an inverse relationship between the expression of some of these biomarkers and inflammatory markers and the durability of response at 3 months,” she said.
Patients with higher tumor burden, LDH, and other markers either had no response at 3 months, or they had a very rapid response at the 1-month mark and then lost their response by 3 months, she noted.
“One of the theories could be that these patients with higher tumor burden, higher inflammatory state – they have such a high peak expansion rapidly after receiving their CAR T cells that potentially those CAR T cells may be getting exhausted or dying off very quickly, and therefore patients can lose their response,” she said.
When these data are considered together and modeled, there seems to be a therapeutic window where patients who have optimal expansion of CAR T cells in vivo may have lesser toxicity, higher overall response rates, and better durability of response, she said.
That is, on one end of the spectrum, there are patients with lower CAR T-cell expansion who have lower toxicities, but who also have lower overall response rates and lower durability of response, and on the other end, there are patients with superhigh expansion of CAR T cells, who have higher response rates, but also higher rates of toxicity, and who lose their response quickly.
“So if we can identify patients who would be in this window of optimal target expansion of CAR T cells, and if we could find strategies or mechanisms to move patients who are on either end of that spectrum into this window, we may be able to get patients with better efficacy and lower toxicities, and there could be combination strategies that could help get us there,” she said.
TRANSCEND NHL 001 is sponsored by Juno Therapeutics. Dr. Siddiqi reported serving as a consultant or adviser for Juno Therapeutics, and as a member of the speakers bureau for Pharmacyclics/Janssen and Seattle Genetics. Research funding was provided to her institution by Juno Therapeutics and several other companies.
sworcester@frontlinemedcom.com
SOURCE: Siddiqi T et al. ASCO-SITC, abstract 122.
SAN FRANCISCO – The CD19-directed 4-1BB chimeric antigen receptor (CAR) T-cell product JCAR017 demonstrated increased CAR T-cell expansion and persistence, and higher durability of response at higher dose levels – with manageable toxicities – in a pivotal phase 1 trial of relapsed/refractory B-cell non-Hodgkin lymphoma.
However, preliminary modeling data suggest that a therapeutic window exists for the CAR T-cell expansion, which means that development of strategies for pushing patients into that window could enhance efficacy and limit toxicity associated with JCAR017, Tanya Siddiqi, MD, of City of Hope Comprehensive Cancer Center, Duarte, Calif., reported at the ASCO-SITC Clinical Immuno-Oncology Symposium.
TRANSCEND NHL 001 is a multicenter, seamless design, pivotal trial, which started as a phase 1 first-in-human study of JCAR017, a defined composition CAR T-cell product also known as lisocabtagene maraleucel and administered at precise doses of CD4+ and CD8+ CAR T cells. Dose-finding and dose-expansion cohorts have been investigated, and currently the pivotal diffuse large B-cell lymphoma (DLBCL) cohort is enrolling, Dr. Saddiqi said, noting that dose level 2 (1 x 108 cells given as a single dose) was selected for that cohort.
The current findings are based on the TRANSCEND core population – a set of patients selected from the dose-finding and dose-expansion cohorts. This population includes patients with DLBCL not otherwise specified, transformed follicular lymphoma, or high-grade double- or triple-hit lymphomas, she said, explaining that she and her colleagues looked at prelymphodepletion baseline patient characteristics and biomarkers to assess how they related to outcomes and toxicities. This precise dosing of JCAR017 reduces variability, enabling the identification of potential patient factors associated with clinical outcomes, she said.
Response rates among 27 patients who received dose level 2 were high, with an 81% overall response rate and a 63% complete response rate.
“Patients with complete remission seemed to have more of a durable response,” she said. “In the core population at dose level 2, 50% with 6 months of follow-up seemed to remain in complete response, so there’s a dose-response effect in these patients.”
It doesn’t appear that the dose affects development of cytokine release syndrome (CRS) or neurotoxicity (NT), as the rates of these (30% and 20%, respectively) did not differ by dose level or schedule, but certain baseline features, such as a lactate dehydrogenase (LDH) level above 500 U/L and tumor burden measured as the sum of the product of diameters of 50 cm or greater, do appear to affect the development of these toxicities.
For example, 10 of 13 (77%) of patients with both of those baseline characteristics developed CRS, and 7 of 13 (54%) developed NT; for those without these characteristics, the odds of developing CRS and NT were significantly lower, she said.
Of note, higher Cmax, or peak expansion of CAR T cells in vivo, was seen at dose level 2, and exposure (area under the curve) was also higher, as was expected at that dose level, Dr. Siddiqi said.
“It also appears that there is a trend of patients with higher tumor burden to have higher expansion of their CAR T cells in vivo,” she said, noting that some of those patients were “superexpanders” with very high expansion of CAR T cells. “Similarly there were certain cytokines at the prelymphodepletion time point that seem to be higher … in patients who also go on to have higher expansion of their CAR T cells.”
These included interleukin-7, IL-15, MIP (macrophage inflammatory protein)–1alpha, and tumor necrosis factor (TNF)–alpha.
“Patients with certain higher inflammatory cytokines and biomarkers of inflammation also were noted to have higher events of CRS and neurotoxicity, so not just higher tumor burden, but also higher inflammatory state at baseline seems to affect patients in terms of getting any grade CRS or any grade neurotoxicity,” she said.
Those associated with CRS included ferritin, C-reactive protein (CRP), IL-10, IL-15, IL-16, TNF-alpha, and MIP-1beta levels, and those associated with NT included ferritin, CRP, d-dimer, IL-6, IL-15, TNF-alpha, and MIP-1alpha levels.
“Interestingly, there’s an inverse relationship between the expression of some of these biomarkers and inflammatory markers and the durability of response at 3 months,” she said.
Patients with higher tumor burden, LDH, and other markers either had no response at 3 months, or they had a very rapid response at the 1-month mark and then lost their response by 3 months, she noted.
“One of the theories could be that these patients with higher tumor burden, higher inflammatory state – they have such a high peak expansion rapidly after receiving their CAR T cells that potentially those CAR T cells may be getting exhausted or dying off very quickly, and therefore patients can lose their response,” she said.
When these data are considered together and modeled, there seems to be a therapeutic window where patients who have optimal expansion of CAR T cells in vivo may have lesser toxicity, higher overall response rates, and better durability of response, she said.
That is, on one end of the spectrum, there are patients with lower CAR T-cell expansion who have lower toxicities, but who also have lower overall response rates and lower durability of response, and on the other end, there are patients with superhigh expansion of CAR T cells, who have higher response rates, but also higher rates of toxicity, and who lose their response quickly.
“So if we can identify patients who would be in this window of optimal target expansion of CAR T cells, and if we could find strategies or mechanisms to move patients who are on either end of that spectrum into this window, we may be able to get patients with better efficacy and lower toxicities, and there could be combination strategies that could help get us there,” she said.
TRANSCEND NHL 001 is sponsored by Juno Therapeutics. Dr. Siddiqi reported serving as a consultant or adviser for Juno Therapeutics, and as a member of the speakers bureau for Pharmacyclics/Janssen and Seattle Genetics. Research funding was provided to her institution by Juno Therapeutics and several other companies.
sworcester@frontlinemedcom.com
SOURCE: Siddiqi T et al. ASCO-SITC, abstract 122.
for CAR T expansion
for CAR T expansion
REPORTING FROM THE CLINICAL IMMUNO-ONCOLOGY SYNDROME
Key clinical point:
Major finding: In all, 77% of patients with a lactate dehydrogenase level greater than 500 U/L and a sum of the product of diameters of 50 cm or greater developed cytokine release syndrome, and 54% of patients with those characteristics developed neurotoxicity.
Study details: A cohort of 27 patients from the pivotal phase 1 TRANSCEND NHL 001 trial.
Disclosures: TRANSCEND NHL 001 is sponsored by Juno Therapeutics. Dr. Siddiqi reported serving as a consultant or adviser for Juno Therapeutics, and as a member of the speakers bureau for Pharmacyclics/Janssen and Seattle Genetics. Research funding was provided to her institution by Juno Therapeutics and several other companies.
Source: Siddiqi T et al. ASCO-SITC, abstract 122.
FDA investigating VTEs related to ECP
The US Food and Drug Administration (FDA) says it is evaluating reports of venous thromboembolism (VTE) in patients treated with the CELLEX Photopheresis System by Therakos, Inc.
This extracorporeal photopheresis (ECP) device system is FDA-approved for use in patients with cutaneous T-cell lymphoma (CTCL).
The system is used to perform ultraviolet-A irradiation of a patient’s own leukocyte-enriched blood that is then used as palliative treatment for skin manifestations of CTCL that are unresponsive to other forms of treatment.
The CELLEX Photopheresis System is also used to treat graft-vs-host disease (GVHD) that is resistant to standard immunosuppressive therapy and acute cardiac allograft rejection that is resistant to standard immunosuppressive therapy.
The CELLEX Photopheresis System uses methoxsalen as a photosensitizing agent and heparin as an anticoagulant.
Since 2012, the FDA has received 7 reports of pulmonary embolism (PE) and 2 reports of deep vein thrombosis (DVT) occurring during or soon after treatment with the CELLEX Photopheresis System.
Two of the patients who developed a PE died, although it’s not clear whether PE was the cause of death.
Four of the 7 PEs occurred in patients undergoing treatment for GVHD, including the 2 patients who died. Both DVTs occurred in patients undergoing treatment for GVHD as well.
The FDA is recommending that healthcare providers inform patients, clinical staff, and technicians that PE and DVT can occur during or after an ECP procedure.
The agency also recommends that healthcare providers consult device labeling regarding anticoagulation and use clinical judgment in adjusting a patient’s heparin dosage.
Finally, providers should report VTEs related to ECP procedures to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program.
If possible, reports should include the following:
- The indication for ECP therapy
- Comorbidities that may predispose a patient to increased coagulation and history of DVT or PE
- The anticoagulation regimen used
- The number of ECP sessions the patient underwent prior to VTE onset, including the date of the first treatment session, frequency of treatment sessions, and timing of the final treatment
- Timing of the VTE in relation to the most recent treatment session
- Interventions required to manage the VTE.

The US Food and Drug Administration (FDA) says it is evaluating reports of venous thromboembolism (VTE) in patients treated with the CELLEX Photopheresis System by Therakos, Inc.
This extracorporeal photopheresis (ECP) device system is FDA-approved for use in patients with cutaneous T-cell lymphoma (CTCL).
The system is used to perform ultraviolet-A irradiation of a patient’s own leukocyte-enriched blood that is then used as palliative treatment for skin manifestations of CTCL that are unresponsive to other forms of treatment.
The CELLEX Photopheresis System is also used to treat graft-vs-host disease (GVHD) that is resistant to standard immunosuppressive therapy and acute cardiac allograft rejection that is resistant to standard immunosuppressive therapy.
The CELLEX Photopheresis System uses methoxsalen as a photosensitizing agent and heparin as an anticoagulant.
Since 2012, the FDA has received 7 reports of pulmonary embolism (PE) and 2 reports of deep vein thrombosis (DVT) occurring during or soon after treatment with the CELLEX Photopheresis System.
Two of the patients who developed a PE died, although it’s not clear whether PE was the cause of death.
Four of the 7 PEs occurred in patients undergoing treatment for GVHD, including the 2 patients who died. Both DVTs occurred in patients undergoing treatment for GVHD as well.
The FDA is recommending that healthcare providers inform patients, clinical staff, and technicians that PE and DVT can occur during or after an ECP procedure.
The agency also recommends that healthcare providers consult device labeling regarding anticoagulation and use clinical judgment in adjusting a patient’s heparin dosage.
Finally, providers should report VTEs related to ECP procedures to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program.
If possible, reports should include the following:
- The indication for ECP therapy
- Comorbidities that may predispose a patient to increased coagulation and history of DVT or PE
- The anticoagulation regimen used
- The number of ECP sessions the patient underwent prior to VTE onset, including the date of the first treatment session, frequency of treatment sessions, and timing of the final treatment
- Timing of the VTE in relation to the most recent treatment session
- Interventions required to manage the VTE.

The US Food and Drug Administration (FDA) says it is evaluating reports of venous thromboembolism (VTE) in patients treated with the CELLEX Photopheresis System by Therakos, Inc.
This extracorporeal photopheresis (ECP) device system is FDA-approved for use in patients with cutaneous T-cell lymphoma (CTCL).
The system is used to perform ultraviolet-A irradiation of a patient’s own leukocyte-enriched blood that is then used as palliative treatment for skin manifestations of CTCL that are unresponsive to other forms of treatment.
The CELLEX Photopheresis System is also used to treat graft-vs-host disease (GVHD) that is resistant to standard immunosuppressive therapy and acute cardiac allograft rejection that is resistant to standard immunosuppressive therapy.
The CELLEX Photopheresis System uses methoxsalen as a photosensitizing agent and heparin as an anticoagulant.
Since 2012, the FDA has received 7 reports of pulmonary embolism (PE) and 2 reports of deep vein thrombosis (DVT) occurring during or soon after treatment with the CELLEX Photopheresis System.
Two of the patients who developed a PE died, although it’s not clear whether PE was the cause of death.
Four of the 7 PEs occurred in patients undergoing treatment for GVHD, including the 2 patients who died. Both DVTs occurred in patients undergoing treatment for GVHD as well.
The FDA is recommending that healthcare providers inform patients, clinical staff, and technicians that PE and DVT can occur during or after an ECP procedure.
The agency also recommends that healthcare providers consult device labeling regarding anticoagulation and use clinical judgment in adjusting a patient’s heparin dosage.
Finally, providers should report VTEs related to ECP procedures to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program.
If possible, reports should include the following:
- The indication for ECP therapy
- Comorbidities that may predispose a patient to increased coagulation and history of DVT or PE
- The anticoagulation regimen used
- The number of ECP sessions the patient underwent prior to VTE onset, including the date of the first treatment session, frequency of treatment sessions, and timing of the final treatment
- Timing of the VTE in relation to the most recent treatment session
- Interventions required to manage the VTE.

CLL Index proves accurate in predicting survival, time to treat
An international prognostic index for patients with chronic lymphocytic leukemia (CLL), known as CLL-IPI, was predictive of time from diagnosis to first treatment (TTFT) and 5-year median overall survival in patients across different risk categories treated with chemoimmunotherapy, according to a systematic review and meta-analysis published in Blood (2018 Jan 18;131[3]:365-8).
But limited data were available for patients treated with targeted therapies that are likely to have a profound effect on overall survival; thereby restricting the use of CLL-IPI in current clinical practice.
Novel therapies such as ibrutinib, idelalisib, and venetoclax have changed the treatment landscape for CLL, Stefano Molica, MD, of Azienda Ospedaliera Pugliese-Ciaccio, Catanzaro, Italy, and his colleagues wrote. “Because observation remains the standard of care for asymptomatic early-stage patients, the introduction of these agents does not impact the utility of the CLL-IPI for predicting time from diagnosis to first treatment, but it likely has a profound impact on the survival of patients of all risk categories once treatment is indicated.”
The CLL-IPI tool, first published in 2016 to predict clinical outcomes in CLL patients, combines five parameters: age, clinical stage, TP53 status [normal vs. del(17p) and/or TP53 mutation], immunoglobulin heavy chain–variable mutational status, and serum b2-microglobulin. The prognostic tool was validated across several studies conducted in different countries with diverse practice settings, including academic hospitals, national population-based cohorts, and clinical trials.
The researchers conducted a systematic review and meta-analysis to understand the utility of CLL-IPI tool in predicting OS and TTFT across each risk category of CLL patients.
They included nine studies with 7,843 patients to assess the impact of the CLL-IPI on overall survival. The patient distribution into the CLL-IPI risk categories was low risk (median 45.9%), intermediate risk (median 30%), high risk (median 16.5%), and very high risk (median 3.6%).
The researchers relied on 11 series comprising 7,383 patients to assess 5-year survival probability, which was 92% for low risk, 81% for intermediate risk, 60% for high risk, and 34% for very high risk. They used seven studies comprising 5,206 patients to assess TTFT and found that the probability of remaining treatment free at 5 years was 82% in the low-risk group, 45% in the intermediate-risk group, 30% in the high-risk group, and 16% in the very-high-risk group.
Although a significant step toward harmonizing international prognostication for CLL, additional studies validating the utility of the CLL-IPI for predicting OS in patients treated with targeted therapy are needed, they wrote.
The researchers reported having no financial disclosures.
An international prognostic index for patients with chronic lymphocytic leukemia (CLL), known as CLL-IPI, was predictive of time from diagnosis to first treatment (TTFT) and 5-year median overall survival in patients across different risk categories treated with chemoimmunotherapy, according to a systematic review and meta-analysis published in Blood (2018 Jan 18;131[3]:365-8).
But limited data were available for patients treated with targeted therapies that are likely to have a profound effect on overall survival; thereby restricting the use of CLL-IPI in current clinical practice.
Novel therapies such as ibrutinib, idelalisib, and venetoclax have changed the treatment landscape for CLL, Stefano Molica, MD, of Azienda Ospedaliera Pugliese-Ciaccio, Catanzaro, Italy, and his colleagues wrote. “Because observation remains the standard of care for asymptomatic early-stage patients, the introduction of these agents does not impact the utility of the CLL-IPI for predicting time from diagnosis to first treatment, but it likely has a profound impact on the survival of patients of all risk categories once treatment is indicated.”
The CLL-IPI tool, first published in 2016 to predict clinical outcomes in CLL patients, combines five parameters: age, clinical stage, TP53 status [normal vs. del(17p) and/or TP53 mutation], immunoglobulin heavy chain–variable mutational status, and serum b2-microglobulin. The prognostic tool was validated across several studies conducted in different countries with diverse practice settings, including academic hospitals, national population-based cohorts, and clinical trials.
The researchers conducted a systematic review and meta-analysis to understand the utility of CLL-IPI tool in predicting OS and TTFT across each risk category of CLL patients.
They included nine studies with 7,843 patients to assess the impact of the CLL-IPI on overall survival. The patient distribution into the CLL-IPI risk categories was low risk (median 45.9%), intermediate risk (median 30%), high risk (median 16.5%), and very high risk (median 3.6%).
The researchers relied on 11 series comprising 7,383 patients to assess 5-year survival probability, which was 92% for low risk, 81% for intermediate risk, 60% for high risk, and 34% for very high risk. They used seven studies comprising 5,206 patients to assess TTFT and found that the probability of remaining treatment free at 5 years was 82% in the low-risk group, 45% in the intermediate-risk group, 30% in the high-risk group, and 16% in the very-high-risk group.
Although a significant step toward harmonizing international prognostication for CLL, additional studies validating the utility of the CLL-IPI for predicting OS in patients treated with targeted therapy are needed, they wrote.
The researchers reported having no financial disclosures.
An international prognostic index for patients with chronic lymphocytic leukemia (CLL), known as CLL-IPI, was predictive of time from diagnosis to first treatment (TTFT) and 5-year median overall survival in patients across different risk categories treated with chemoimmunotherapy, according to a systematic review and meta-analysis published in Blood (2018 Jan 18;131[3]:365-8).
But limited data were available for patients treated with targeted therapies that are likely to have a profound effect on overall survival; thereby restricting the use of CLL-IPI in current clinical practice.
Novel therapies such as ibrutinib, idelalisib, and venetoclax have changed the treatment landscape for CLL, Stefano Molica, MD, of Azienda Ospedaliera Pugliese-Ciaccio, Catanzaro, Italy, and his colleagues wrote. “Because observation remains the standard of care for asymptomatic early-stage patients, the introduction of these agents does not impact the utility of the CLL-IPI for predicting time from diagnosis to first treatment, but it likely has a profound impact on the survival of patients of all risk categories once treatment is indicated.”
The CLL-IPI tool, first published in 2016 to predict clinical outcomes in CLL patients, combines five parameters: age, clinical stage, TP53 status [normal vs. del(17p) and/or TP53 mutation], immunoglobulin heavy chain–variable mutational status, and serum b2-microglobulin. The prognostic tool was validated across several studies conducted in different countries with diverse practice settings, including academic hospitals, national population-based cohorts, and clinical trials.
The researchers conducted a systematic review and meta-analysis to understand the utility of CLL-IPI tool in predicting OS and TTFT across each risk category of CLL patients.
They included nine studies with 7,843 patients to assess the impact of the CLL-IPI on overall survival. The patient distribution into the CLL-IPI risk categories was low risk (median 45.9%), intermediate risk (median 30%), high risk (median 16.5%), and very high risk (median 3.6%).
The researchers relied on 11 series comprising 7,383 patients to assess 5-year survival probability, which was 92% for low risk, 81% for intermediate risk, 60% for high risk, and 34% for very high risk. They used seven studies comprising 5,206 patients to assess TTFT and found that the probability of remaining treatment free at 5 years was 82% in the low-risk group, 45% in the intermediate-risk group, 30% in the high-risk group, and 16% in the very-high-risk group.
Although a significant step toward harmonizing international prognostication for CLL, additional studies validating the utility of the CLL-IPI for predicting OS in patients treated with targeted therapy are needed, they wrote.
The researchers reported having no financial disclosures.
FROM BLOOD
Mogamulizumab is ‘valuable’ option for CTCL
LA JOLLA, CA—Mogamulizumab is a valuable new therapeutic option for patients with cutaneous T-cell lymphoma (CTCL), according to researchers.
Results of the phase 3 MAVORIC study indicated that mogamulizumab is more effective than vorinostat in previously treated patients with CTCL.
Mogamulizumab produced a better overall response rate (ORR) and prolonged progression-free survival (PFS) in these patients.
Infusion-related reactions and drug eruptions were more common in patients who received mogamulizumab.
Youn H. Kim, MD, of the Stanford Cancer Institute in Palo Alto, California, and her colleagues presented these results in a poster at the 10th Annual T-cell Lymphoma Forum. The study was funded by Kyowa Kirin Pharmaceutical Development, Inc.
MAVORIC enrolled 372 adults with histologically confirmed mycosis fungoides (MF) or Sézary syndrome (SS) who had failed at least 1 systemic therapy. They were randomized to receive mogamulizumab at 1.0 mg/kg (weekly for the first 4-week cycle and then every 2 weeks) or vorinostat at 400 mg daily.
Patients were treated until disease progression or unacceptable toxicity. Those receiving vorinostat could crossover to mogamulizumab if they progressed or experienced intolerable toxicity.
Baseline characteristics were similar between the treatment arms. The median age was 64 (range, 54-73) in the mogamulizumab arm and 65 (range, 56-72) in the vorinostat arm. Ninety-nine percent and 100% of patients, respectively, had an ECOG performance status of 0 to 1.
A little more than half of patients in each arm had MF—57% in the mogamulizumab arm and 53% in the vorinostat arm.
The median number of prior systemic therapies was 3 in both arms (range, 1-18 in the mogamulizumab arm and 0-14 in the vorinostat arm).
Efficacy
The primary endpoint was PFS, and mogamulizumab provided a significant improvement there. The median PFS was 7.7 months with mogamulizumab and 3.1 months with vorinostat (hazard ratio=0.53, P<0.0001).
The researchers also observed a significant improvement in global ORR with mogamulizumab. It was 28% (52/189) in that arm and 5% (9/186) in the vorinostat arm (P<0.0001).
For patients with MF, the ORR was 21% with mogamulizumab and 7% with vorinostat. For SS patients, the ORR was 37% and 2%, respectively.
Responses by disease compartment were superior with mogamulizumab as well.
“Especially in the blood compartment, mogamulizumab had very striking activity over vorinostat,” Dr Kim said.
The blood ORR was 68% with mogamulizumab and 19% with vorinostat. The skin ORR was 42% and 16%, respectively. The lymph node ORR was 17% and 4%, respectively. The viscera ORR was 0% in both arms.
After crossover, the ORR in the mogamulizumab arm was 30% (41/136).
The median duration of response (DOR) was 14 months in the mogamulizumab arm and 9 months in the vorinostat arm.
For MF patients, the median DOR was 13 months with mogamulizumab and 9 months with vorinostat. For SS patients, the median DOR was 17 months and 7 months, respectively.
Safety
“Side effects [of mogamulizumab] were very well tolerable,” Dr Kim said. “Most significant is rash and infusion reactions, but, in terms of severe adverse events, [they] were very minimal.”
The most common treatment-emergent adverse events (AEs), occurring in at least 20% of patients in either arm (mogamulizumab and vorinostat, respectively), were:
- Infusion-related reactions (33.2% vs 0.5%)
- Drug eruptions (23.9% vs 0.5%)
- Diarrhea (23.4% vs 61.8%)
- Nausea (15.2% vs 42.5%)
- Thrombocytopenia (11.4% vs 30.6%)
- Dysgeusia (3.3% vs 28.0%)
- Increased blood creatinine (3.3% vs 28.0%)
- Decreased appetite (7.6% vs 24.7%).
There were no grade 4 AEs in the mogamulizumab arm and 2 cases of grade 4 thrombocytopenia in the vorinostat arm.
Grade 3 AEs in the mogamulizumab arm included drug eruptions (n=8), infusion-related reactions (n=3), fatigue (n=3), decreased appetite (n=2), nausea (n=1), pyrexia (n=1), and diarrhea (n=1).
Grade 3 AEs in the vorinostat arm included thrombocytopenia (n=11), fatigue (n=11), diarrhea (n=9), nausea (n=3), decreased appetite (n=2), and dysgeusia (n=1).
“So the results are, overall, positive,” Dr Kim said. “The data is submitted to the [US Food and Drug Administration]. We are really hoping that [mogamulizumab] will be approved so that we would have a new, exciting treatment for our patients with mycosis fungoides and Sézary syndrome.” ![]()
LA JOLLA, CA—Mogamulizumab is a valuable new therapeutic option for patients with cutaneous T-cell lymphoma (CTCL), according to researchers.
Results of the phase 3 MAVORIC study indicated that mogamulizumab is more effective than vorinostat in previously treated patients with CTCL.
Mogamulizumab produced a better overall response rate (ORR) and prolonged progression-free survival (PFS) in these patients.
Infusion-related reactions and drug eruptions were more common in patients who received mogamulizumab.
Youn H. Kim, MD, of the Stanford Cancer Institute in Palo Alto, California, and her colleagues presented these results in a poster at the 10th Annual T-cell Lymphoma Forum. The study was funded by Kyowa Kirin Pharmaceutical Development, Inc.
MAVORIC enrolled 372 adults with histologically confirmed mycosis fungoides (MF) or Sézary syndrome (SS) who had failed at least 1 systemic therapy. They were randomized to receive mogamulizumab at 1.0 mg/kg (weekly for the first 4-week cycle and then every 2 weeks) or vorinostat at 400 mg daily.
Patients were treated until disease progression or unacceptable toxicity. Those receiving vorinostat could crossover to mogamulizumab if they progressed or experienced intolerable toxicity.
Baseline characteristics were similar between the treatment arms. The median age was 64 (range, 54-73) in the mogamulizumab arm and 65 (range, 56-72) in the vorinostat arm. Ninety-nine percent and 100% of patients, respectively, had an ECOG performance status of 0 to 1.
A little more than half of patients in each arm had MF—57% in the mogamulizumab arm and 53% in the vorinostat arm.
The median number of prior systemic therapies was 3 in both arms (range, 1-18 in the mogamulizumab arm and 0-14 in the vorinostat arm).
Efficacy
The primary endpoint was PFS, and mogamulizumab provided a significant improvement there. The median PFS was 7.7 months with mogamulizumab and 3.1 months with vorinostat (hazard ratio=0.53, P<0.0001).
The researchers also observed a significant improvement in global ORR with mogamulizumab. It was 28% (52/189) in that arm and 5% (9/186) in the vorinostat arm (P<0.0001).
For patients with MF, the ORR was 21% with mogamulizumab and 7% with vorinostat. For SS patients, the ORR was 37% and 2%, respectively.
Responses by disease compartment were superior with mogamulizumab as well.
“Especially in the blood compartment, mogamulizumab had very striking activity over vorinostat,” Dr Kim said.
The blood ORR was 68% with mogamulizumab and 19% with vorinostat. The skin ORR was 42% and 16%, respectively. The lymph node ORR was 17% and 4%, respectively. The viscera ORR was 0% in both arms.
After crossover, the ORR in the mogamulizumab arm was 30% (41/136).
The median duration of response (DOR) was 14 months in the mogamulizumab arm and 9 months in the vorinostat arm.
For MF patients, the median DOR was 13 months with mogamulizumab and 9 months with vorinostat. For SS patients, the median DOR was 17 months and 7 months, respectively.
Safety
“Side effects [of mogamulizumab] were very well tolerable,” Dr Kim said. “Most significant is rash and infusion reactions, but, in terms of severe adverse events, [they] were very minimal.”
The most common treatment-emergent adverse events (AEs), occurring in at least 20% of patients in either arm (mogamulizumab and vorinostat, respectively), were:
- Infusion-related reactions (33.2% vs 0.5%)
- Drug eruptions (23.9% vs 0.5%)
- Diarrhea (23.4% vs 61.8%)
- Nausea (15.2% vs 42.5%)
- Thrombocytopenia (11.4% vs 30.6%)
- Dysgeusia (3.3% vs 28.0%)
- Increased blood creatinine (3.3% vs 28.0%)
- Decreased appetite (7.6% vs 24.7%).
There were no grade 4 AEs in the mogamulizumab arm and 2 cases of grade 4 thrombocytopenia in the vorinostat arm.
Grade 3 AEs in the mogamulizumab arm included drug eruptions (n=8), infusion-related reactions (n=3), fatigue (n=3), decreased appetite (n=2), nausea (n=1), pyrexia (n=1), and diarrhea (n=1).
Grade 3 AEs in the vorinostat arm included thrombocytopenia (n=11), fatigue (n=11), diarrhea (n=9), nausea (n=3), decreased appetite (n=2), and dysgeusia (n=1).
“So the results are, overall, positive,” Dr Kim said. “The data is submitted to the [US Food and Drug Administration]. We are really hoping that [mogamulizumab] will be approved so that we would have a new, exciting treatment for our patients with mycosis fungoides and Sézary syndrome.” ![]()
LA JOLLA, CA—Mogamulizumab is a valuable new therapeutic option for patients with cutaneous T-cell lymphoma (CTCL), according to researchers.
Results of the phase 3 MAVORIC study indicated that mogamulizumab is more effective than vorinostat in previously treated patients with CTCL.
Mogamulizumab produced a better overall response rate (ORR) and prolonged progression-free survival (PFS) in these patients.
Infusion-related reactions and drug eruptions were more common in patients who received mogamulizumab.
Youn H. Kim, MD, of the Stanford Cancer Institute in Palo Alto, California, and her colleagues presented these results in a poster at the 10th Annual T-cell Lymphoma Forum. The study was funded by Kyowa Kirin Pharmaceutical Development, Inc.
MAVORIC enrolled 372 adults with histologically confirmed mycosis fungoides (MF) or Sézary syndrome (SS) who had failed at least 1 systemic therapy. They were randomized to receive mogamulizumab at 1.0 mg/kg (weekly for the first 4-week cycle and then every 2 weeks) or vorinostat at 400 mg daily.
Patients were treated until disease progression or unacceptable toxicity. Those receiving vorinostat could crossover to mogamulizumab if they progressed or experienced intolerable toxicity.
Baseline characteristics were similar between the treatment arms. The median age was 64 (range, 54-73) in the mogamulizumab arm and 65 (range, 56-72) in the vorinostat arm. Ninety-nine percent and 100% of patients, respectively, had an ECOG performance status of 0 to 1.
A little more than half of patients in each arm had MF—57% in the mogamulizumab arm and 53% in the vorinostat arm.
The median number of prior systemic therapies was 3 in both arms (range, 1-18 in the mogamulizumab arm and 0-14 in the vorinostat arm).
Efficacy
The primary endpoint was PFS, and mogamulizumab provided a significant improvement there. The median PFS was 7.7 months with mogamulizumab and 3.1 months with vorinostat (hazard ratio=0.53, P<0.0001).
The researchers also observed a significant improvement in global ORR with mogamulizumab. It was 28% (52/189) in that arm and 5% (9/186) in the vorinostat arm (P<0.0001).
For patients with MF, the ORR was 21% with mogamulizumab and 7% with vorinostat. For SS patients, the ORR was 37% and 2%, respectively.
Responses by disease compartment were superior with mogamulizumab as well.
“Especially in the blood compartment, mogamulizumab had very striking activity over vorinostat,” Dr Kim said.
The blood ORR was 68% with mogamulizumab and 19% with vorinostat. The skin ORR was 42% and 16%, respectively. The lymph node ORR was 17% and 4%, respectively. The viscera ORR was 0% in both arms.
After crossover, the ORR in the mogamulizumab arm was 30% (41/136).
The median duration of response (DOR) was 14 months in the mogamulizumab arm and 9 months in the vorinostat arm.
For MF patients, the median DOR was 13 months with mogamulizumab and 9 months with vorinostat. For SS patients, the median DOR was 17 months and 7 months, respectively.
Safety
“Side effects [of mogamulizumab] were very well tolerable,” Dr Kim said. “Most significant is rash and infusion reactions, but, in terms of severe adverse events, [they] were very minimal.”
The most common treatment-emergent adverse events (AEs), occurring in at least 20% of patients in either arm (mogamulizumab and vorinostat, respectively), were:
- Infusion-related reactions (33.2% vs 0.5%)
- Drug eruptions (23.9% vs 0.5%)
- Diarrhea (23.4% vs 61.8%)
- Nausea (15.2% vs 42.5%)
- Thrombocytopenia (11.4% vs 30.6%)
- Dysgeusia (3.3% vs 28.0%)
- Increased blood creatinine (3.3% vs 28.0%)
- Decreased appetite (7.6% vs 24.7%).
There were no grade 4 AEs in the mogamulizumab arm and 2 cases of grade 4 thrombocytopenia in the vorinostat arm.
Grade 3 AEs in the mogamulizumab arm included drug eruptions (n=8), infusion-related reactions (n=3), fatigue (n=3), decreased appetite (n=2), nausea (n=1), pyrexia (n=1), and diarrhea (n=1).
Grade 3 AEs in the vorinostat arm included thrombocytopenia (n=11), fatigue (n=11), diarrhea (n=9), nausea (n=3), decreased appetite (n=2), and dysgeusia (n=1).
“So the results are, overall, positive,” Dr Kim said. “The data is submitted to the [US Food and Drug Administration]. We are really hoping that [mogamulizumab] will be approved so that we would have a new, exciting treatment for our patients with mycosis fungoides and Sézary syndrome.” ![]()
Triple therapy ups response in refractory mantle cell lymphoma
A combination of ibrutinib, lenalidomide, and rituximab produced an overall response rate of 76% at 17.8 months median follow-up among 50 adults with relapsed or refractory mantle cell lymphoma, according to an open-label, single-arm, phase 2 trial.
There were complete responses in 28 patients (56%) and partial responses in 10 (20%). Median progression-free survival was 16 months and median overall survival was 22 months. Similar proportions of patients, with and without TP53 mutations, had overall and complete responses, suggesting that triple therapy might be particularly useful in patients with high-risk genetic features.
“Our results provide preliminary evidence that the triplet combination of ibrutinib, lenalidomide, and rituximab is an active regimen in patients with relapsed or refractory mantle cell lymphoma, and should be evaluated in a prospective randomized controlled trial,” wrote Mats Jerkeman, MD, of Lund University, Sweden, and colleagues. The report was published in The Lancet Haematology.
“Addition of lenalidomide to ibrutinib and rituximab might increase the proportion of patients who have complete remission ... Previous studies reported complete responses in 44% of patients on ibrutinib and rituximab, in 36% of patients on rituximab and lenalidomide, and in 19% of patients on ibrutinib alone,” they wrote.
Treatment was divided into an induction phase of 12 cycles of 28 days with all three drugs and a maintenance phase with ibrutinib and rituximab only, given until disease progression or unacceptable toxicity. All the patients had previously been treated with at least one rituximab-containing regimen.
Janssen and Celgene funded the work. Dr. Jerkeman reported ties to Janssen and Celgene, as well as AbbVie and Gilead.
SOURCE: Jerkeman M et al. Lancet Haematol. 2018 Jan 29. doi: 10.1016/S2352-3026(18)30018-8.
A combination of ibrutinib, lenalidomide, and rituximab produced an overall response rate of 76% at 17.8 months median follow-up among 50 adults with relapsed or refractory mantle cell lymphoma, according to an open-label, single-arm, phase 2 trial.
There were complete responses in 28 patients (56%) and partial responses in 10 (20%). Median progression-free survival was 16 months and median overall survival was 22 months. Similar proportions of patients, with and without TP53 mutations, had overall and complete responses, suggesting that triple therapy might be particularly useful in patients with high-risk genetic features.
“Our results provide preliminary evidence that the triplet combination of ibrutinib, lenalidomide, and rituximab is an active regimen in patients with relapsed or refractory mantle cell lymphoma, and should be evaluated in a prospective randomized controlled trial,” wrote Mats Jerkeman, MD, of Lund University, Sweden, and colleagues. The report was published in The Lancet Haematology.
“Addition of lenalidomide to ibrutinib and rituximab might increase the proportion of patients who have complete remission ... Previous studies reported complete responses in 44% of patients on ibrutinib and rituximab, in 36% of patients on rituximab and lenalidomide, and in 19% of patients on ibrutinib alone,” they wrote.
Treatment was divided into an induction phase of 12 cycles of 28 days with all three drugs and a maintenance phase with ibrutinib and rituximab only, given until disease progression or unacceptable toxicity. All the patients had previously been treated with at least one rituximab-containing regimen.
Janssen and Celgene funded the work. Dr. Jerkeman reported ties to Janssen and Celgene, as well as AbbVie and Gilead.
SOURCE: Jerkeman M et al. Lancet Haematol. 2018 Jan 29. doi: 10.1016/S2352-3026(18)30018-8.
A combination of ibrutinib, lenalidomide, and rituximab produced an overall response rate of 76% at 17.8 months median follow-up among 50 adults with relapsed or refractory mantle cell lymphoma, according to an open-label, single-arm, phase 2 trial.
There were complete responses in 28 patients (56%) and partial responses in 10 (20%). Median progression-free survival was 16 months and median overall survival was 22 months. Similar proportions of patients, with and without TP53 mutations, had overall and complete responses, suggesting that triple therapy might be particularly useful in patients with high-risk genetic features.
“Our results provide preliminary evidence that the triplet combination of ibrutinib, lenalidomide, and rituximab is an active regimen in patients with relapsed or refractory mantle cell lymphoma, and should be evaluated in a prospective randomized controlled trial,” wrote Mats Jerkeman, MD, of Lund University, Sweden, and colleagues. The report was published in The Lancet Haematology.
“Addition of lenalidomide to ibrutinib and rituximab might increase the proportion of patients who have complete remission ... Previous studies reported complete responses in 44% of patients on ibrutinib and rituximab, in 36% of patients on rituximab and lenalidomide, and in 19% of patients on ibrutinib alone,” they wrote.
Treatment was divided into an induction phase of 12 cycles of 28 days with all three drugs and a maintenance phase with ibrutinib and rituximab only, given until disease progression or unacceptable toxicity. All the patients had previously been treated with at least one rituximab-containing regimen.
Janssen and Celgene funded the work. Dr. Jerkeman reported ties to Janssen and Celgene, as well as AbbVie and Gilead.
SOURCE: Jerkeman M et al. Lancet Haematol. 2018 Jan 29. doi: 10.1016/S2352-3026(18)30018-8.
FROM THE LANCET HAEMATOLOGY
Key clinical point:
Major finding: The overall response from for the combination of the three drugs was 76% at 17.8 months median follow-up.
Study details: An open-label, single-arm, phase 2 trial of 50 adults with relapsed/refractory MCL.
Disclosures: Janssen and Celgene funded the work. Dr. Jerkeman reported ties to Janssen and Celgene, as well as AbbVie and Gilead.
Source: Jerkeman M et al. Lancet Haematol. 2018 Jan 29. doi: 10.1016/S2352-3026(18)30018-8.
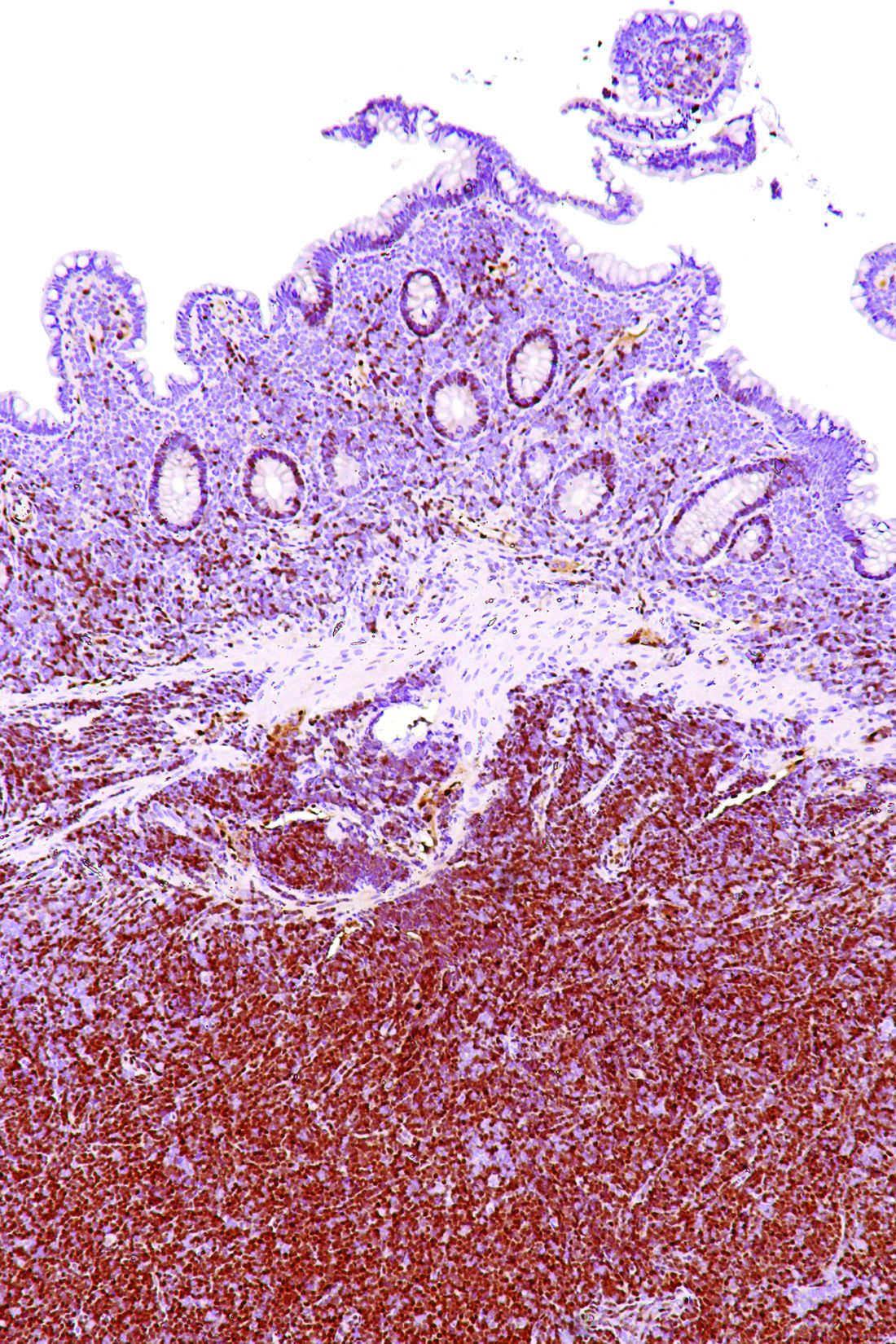
In situ vaccination eradicates lymphoma, other cancers
Experiments in mice have shown that injecting immune-stimulating agents directly into a tumor can help the immune system eradicate tumors in other areas of the body.
The approach worked for several cancers, including lymphomas.
The researchers believe the local application of the agents could serve as a rapid and relatively inexpensive cancer therapy that is unlikely to cause the adverse effects often seen with more widespread immune stimulation.
“Our approach uses a one-time application of very small amounts of two agents to stimulate the immune cells only within the tumor itself,” said Ronald Levy, MD, of Stanford University Medical Center in California.
“In the mice, we saw amazing, body-wide effects, including the elimination of tumors all over the animal. This approach bypasses the need to identify tumor-specific immune targets and doesn’t require wholesale activation of the immune system or customization of a patient’s immune cells.”
Dr Levy and his colleagues described this approach in Science Translational Medicine.
The method involves reactivating cancer-specific T cells by injecting microgram amounts of two agents directly into the tumor site.
One of the agents is an unmethylated CG–enriched oligodeoxynucleotide (CpG)—a Toll-like receptor 9 (TLR9) ligand. It works with nearby immune cells to amplify the expression of OX40 on the surface of T cells.
The other agent is an antibody that binds to OX40. It activates the T cells to lead the charge against the cancer cells.
Because the agents are injected directly into the tumor, only T cells that have infiltrated it are activated. In effect, these T cells are “prescreened” by the body to recognize only cancer-specific proteins.
Some of these tumor-specific, activated T cells then leave the original tumor to find and destroy other identical tumors throughout the body.
The researchers found this approach worked well in mice with A20 B-cell lymphoma tumors transplanted in two sites on their bodies.
Injecting one tumor site with the agents caused regression of the untreated tumor as well as the treated one. In this way, 87 of 90 mice were cured.
Although lymphoma recurred in 3 of the mice, the tumors again regressed after a second treatment with CpG and anti-OX40.
The researchers saw similar results in mice with melanoma as well as breast and colon cancer.
Mice genetically engineered to spontaneously develop breast cancers in all 10 of their mammary pads also responded to the treatment. Treating the first tumor that arose often prevented the occurrence of future tumors and significantly increased the animals’ life span, the researchers found.
Finally, the team explored the specificity of the T cells by transplanting two types of tumors into mice.
They transplanted A20 lymphoma cells in two locations and a colon cancer cell line in a third location. Treatment of one of the lymphoma sites caused the regression of both lymphoma tumors but did not affect the colon cancer cells.
“This is a very targeted approach,” Dr Levy said. “Only the tumor that shares the protein targets displayed by the treated site is affected. We’re attacking specific targets without having to identify exactly what proteins the T cells are recognizing.”
Dr Levy and his colleagues have launched a clinical trial (NCT03410901) to test this treatment approach. The researchers hope to determine the adverse effects and optimal dose of the TLR9 agonist SD-101, the anti-OX40 antibody BMS 986178, and radiation therapy in patients with low-grade B-cell non-Hodgkin lymphomas.
If the trial is successful, Dr Levy believes the treatment could be useful for many tumor types.
“I don’t think there’s a limit to the type of tumor we could potentially treat,” he said, “as long as it has been infiltrated by the immune system.” ![]()
Experiments in mice have shown that injecting immune-stimulating agents directly into a tumor can help the immune system eradicate tumors in other areas of the body.
The approach worked for several cancers, including lymphomas.
The researchers believe the local application of the agents could serve as a rapid and relatively inexpensive cancer therapy that is unlikely to cause the adverse effects often seen with more widespread immune stimulation.
“Our approach uses a one-time application of very small amounts of two agents to stimulate the immune cells only within the tumor itself,” said Ronald Levy, MD, of Stanford University Medical Center in California.
“In the mice, we saw amazing, body-wide effects, including the elimination of tumors all over the animal. This approach bypasses the need to identify tumor-specific immune targets and doesn’t require wholesale activation of the immune system or customization of a patient’s immune cells.”
Dr Levy and his colleagues described this approach in Science Translational Medicine.
The method involves reactivating cancer-specific T cells by injecting microgram amounts of two agents directly into the tumor site.
One of the agents is an unmethylated CG–enriched oligodeoxynucleotide (CpG)—a Toll-like receptor 9 (TLR9) ligand. It works with nearby immune cells to amplify the expression of OX40 on the surface of T cells.
The other agent is an antibody that binds to OX40. It activates the T cells to lead the charge against the cancer cells.
Because the agents are injected directly into the tumor, only T cells that have infiltrated it are activated. In effect, these T cells are “prescreened” by the body to recognize only cancer-specific proteins.
Some of these tumor-specific, activated T cells then leave the original tumor to find and destroy other identical tumors throughout the body.
The researchers found this approach worked well in mice with A20 B-cell lymphoma tumors transplanted in two sites on their bodies.
Injecting one tumor site with the agents caused regression of the untreated tumor as well as the treated one. In this way, 87 of 90 mice were cured.
Although lymphoma recurred in 3 of the mice, the tumors again regressed after a second treatment with CpG and anti-OX40.
The researchers saw similar results in mice with melanoma as well as breast and colon cancer.
Mice genetically engineered to spontaneously develop breast cancers in all 10 of their mammary pads also responded to the treatment. Treating the first tumor that arose often prevented the occurrence of future tumors and significantly increased the animals’ life span, the researchers found.
Finally, the team explored the specificity of the T cells by transplanting two types of tumors into mice.
They transplanted A20 lymphoma cells in two locations and a colon cancer cell line in a third location. Treatment of one of the lymphoma sites caused the regression of both lymphoma tumors but did not affect the colon cancer cells.
“This is a very targeted approach,” Dr Levy said. “Only the tumor that shares the protein targets displayed by the treated site is affected. We’re attacking specific targets without having to identify exactly what proteins the T cells are recognizing.”
Dr Levy and his colleagues have launched a clinical trial (NCT03410901) to test this treatment approach. The researchers hope to determine the adverse effects and optimal dose of the TLR9 agonist SD-101, the anti-OX40 antibody BMS 986178, and radiation therapy in patients with low-grade B-cell non-Hodgkin lymphomas.
If the trial is successful, Dr Levy believes the treatment could be useful for many tumor types.
“I don’t think there’s a limit to the type of tumor we could potentially treat,” he said, “as long as it has been infiltrated by the immune system.” ![]()
Experiments in mice have shown that injecting immune-stimulating agents directly into a tumor can help the immune system eradicate tumors in other areas of the body.
The approach worked for several cancers, including lymphomas.
The researchers believe the local application of the agents could serve as a rapid and relatively inexpensive cancer therapy that is unlikely to cause the adverse effects often seen with more widespread immune stimulation.
“Our approach uses a one-time application of very small amounts of two agents to stimulate the immune cells only within the tumor itself,” said Ronald Levy, MD, of Stanford University Medical Center in California.
“In the mice, we saw amazing, body-wide effects, including the elimination of tumors all over the animal. This approach bypasses the need to identify tumor-specific immune targets and doesn’t require wholesale activation of the immune system or customization of a patient’s immune cells.”
Dr Levy and his colleagues described this approach in Science Translational Medicine.
The method involves reactivating cancer-specific T cells by injecting microgram amounts of two agents directly into the tumor site.
One of the agents is an unmethylated CG–enriched oligodeoxynucleotide (CpG)—a Toll-like receptor 9 (TLR9) ligand. It works with nearby immune cells to amplify the expression of OX40 on the surface of T cells.
The other agent is an antibody that binds to OX40. It activates the T cells to lead the charge against the cancer cells.
Because the agents are injected directly into the tumor, only T cells that have infiltrated it are activated. In effect, these T cells are “prescreened” by the body to recognize only cancer-specific proteins.
Some of these tumor-specific, activated T cells then leave the original tumor to find and destroy other identical tumors throughout the body.
The researchers found this approach worked well in mice with A20 B-cell lymphoma tumors transplanted in two sites on their bodies.
Injecting one tumor site with the agents caused regression of the untreated tumor as well as the treated one. In this way, 87 of 90 mice were cured.
Although lymphoma recurred in 3 of the mice, the tumors again regressed after a second treatment with CpG and anti-OX40.
The researchers saw similar results in mice with melanoma as well as breast and colon cancer.
Mice genetically engineered to spontaneously develop breast cancers in all 10 of their mammary pads also responded to the treatment. Treating the first tumor that arose often prevented the occurrence of future tumors and significantly increased the animals’ life span, the researchers found.
Finally, the team explored the specificity of the T cells by transplanting two types of tumors into mice.
They transplanted A20 lymphoma cells in two locations and a colon cancer cell line in a third location. Treatment of one of the lymphoma sites caused the regression of both lymphoma tumors but did not affect the colon cancer cells.
“This is a very targeted approach,” Dr Levy said. “Only the tumor that shares the protein targets displayed by the treated site is affected. We’re attacking specific targets without having to identify exactly what proteins the T cells are recognizing.”
Dr Levy and his colleagues have launched a clinical trial (NCT03410901) to test this treatment approach. The researchers hope to determine the adverse effects and optimal dose of the TLR9 agonist SD-101, the anti-OX40 antibody BMS 986178, and radiation therapy in patients with low-grade B-cell non-Hodgkin lymphomas.
If the trial is successful, Dr Levy believes the treatment could be useful for many tumor types.
“I don’t think there’s a limit to the type of tumor we could potentially treat,” he said, “as long as it has been infiltrated by the immune system.” ![]()
Combo could treat double-hit lymphoma
Existing drugs could be combined to treat double-hit lymphoma (DHL), according to preclinical research published in Science Translational Medicine.
The drugs are tigecycline, an antibiotic, and venetoclax, a BCL2 inhibitor.
Researchers observed promising activity with these drugs in combination, both in cell lines and mouse models of DHL.
The team therefore believes the drugs could be repurposed to treat DHL, which currently has a dismal prognosis.
Study author Micol Ravà, PhD, of the European Institute of Oncology in Milan, Italy, and her colleagues noted that DHL is driven by the abnormal activation of MYC and BCL2. However, selective BCL2 inhibitors like venetoclax have failed to halt disease progression in DHL patients.
Seeking a way to sensitize DHL to BCL2 inhibitors, the researchers turned to tigecycline, which interferes with mitochondria to trigger a MYC-dependent cell death pathway.
The team found that tigecycline and venetoclax demonstrated synergy in 5 DHL cell lines. The drugs were synergistic in 3 cell lines—Karpas-422, SU-DHL-6, and DOHH-2—in which neither drug alone showed significant pro-apoptotic activity.
In 2 other cell lines—SU-DHL-4 and OCI-LY8—venetoclax was active when given alone, but its activity was enhanced by the addition of tigecycline.
In mouse models of DHL (using the human cell lines SU-DHL-6, DOHH-2, and OCI-LY8), each of the drugs alone were able to slow tumor progression somewhat.
However, combination tigecycline and venetoclax exhibited “strong antitumoral activity,” according to the researchers. In fact, the combination caused full disease regression in all 8 SU-DHL-6 mice and 3 of 9 OCI-LY8 mice.
Dr Ravà and her colleagues also found the combination produced “rapid and marked tumor regression” in mice with a patient-derived xenograft.
The researchers observed no toxicity when tigecycline and venetoclax were given at low doses. However, mice receiving more aggressive treatment had some inflammation in the liver and spleen. And some mice treated with high doses of tigecycline and venetoclax died within 1 week of treatment initiation.
Finally, Dr Ravà and her colleagues found that tigecycline and venetoclax each synergized with rituximab. The team therefore concluded that tigecycline and venetoclax “have the potential to reinforce rituximab-containing therapies in the clinic.” ![]()
Existing drugs could be combined to treat double-hit lymphoma (DHL), according to preclinical research published in Science Translational Medicine.
The drugs are tigecycline, an antibiotic, and venetoclax, a BCL2 inhibitor.
Researchers observed promising activity with these drugs in combination, both in cell lines and mouse models of DHL.
The team therefore believes the drugs could be repurposed to treat DHL, which currently has a dismal prognosis.
Study author Micol Ravà, PhD, of the European Institute of Oncology in Milan, Italy, and her colleagues noted that DHL is driven by the abnormal activation of MYC and BCL2. However, selective BCL2 inhibitors like venetoclax have failed to halt disease progression in DHL patients.
Seeking a way to sensitize DHL to BCL2 inhibitors, the researchers turned to tigecycline, which interferes with mitochondria to trigger a MYC-dependent cell death pathway.
The team found that tigecycline and venetoclax demonstrated synergy in 5 DHL cell lines. The drugs were synergistic in 3 cell lines—Karpas-422, SU-DHL-6, and DOHH-2—in which neither drug alone showed significant pro-apoptotic activity.
In 2 other cell lines—SU-DHL-4 and OCI-LY8—venetoclax was active when given alone, but its activity was enhanced by the addition of tigecycline.
In mouse models of DHL (using the human cell lines SU-DHL-6, DOHH-2, and OCI-LY8), each of the drugs alone were able to slow tumor progression somewhat.
However, combination tigecycline and venetoclax exhibited “strong antitumoral activity,” according to the researchers. In fact, the combination caused full disease regression in all 8 SU-DHL-6 mice and 3 of 9 OCI-LY8 mice.
Dr Ravà and her colleagues also found the combination produced “rapid and marked tumor regression” in mice with a patient-derived xenograft.
The researchers observed no toxicity when tigecycline and venetoclax were given at low doses. However, mice receiving more aggressive treatment had some inflammation in the liver and spleen. And some mice treated with high doses of tigecycline and venetoclax died within 1 week of treatment initiation.
Finally, Dr Ravà and her colleagues found that tigecycline and venetoclax each synergized with rituximab. The team therefore concluded that tigecycline and venetoclax “have the potential to reinforce rituximab-containing therapies in the clinic.” ![]()
Existing drugs could be combined to treat double-hit lymphoma (DHL), according to preclinical research published in Science Translational Medicine.
The drugs are tigecycline, an antibiotic, and venetoclax, a BCL2 inhibitor.
Researchers observed promising activity with these drugs in combination, both in cell lines and mouse models of DHL.
The team therefore believes the drugs could be repurposed to treat DHL, which currently has a dismal prognosis.
Study author Micol Ravà, PhD, of the European Institute of Oncology in Milan, Italy, and her colleagues noted that DHL is driven by the abnormal activation of MYC and BCL2. However, selective BCL2 inhibitors like venetoclax have failed to halt disease progression in DHL patients.
Seeking a way to sensitize DHL to BCL2 inhibitors, the researchers turned to tigecycline, which interferes with mitochondria to trigger a MYC-dependent cell death pathway.
The team found that tigecycline and venetoclax demonstrated synergy in 5 DHL cell lines. The drugs were synergistic in 3 cell lines—Karpas-422, SU-DHL-6, and DOHH-2—in which neither drug alone showed significant pro-apoptotic activity.
In 2 other cell lines—SU-DHL-4 and OCI-LY8—venetoclax was active when given alone, but its activity was enhanced by the addition of tigecycline.
In mouse models of DHL (using the human cell lines SU-DHL-6, DOHH-2, and OCI-LY8), each of the drugs alone were able to slow tumor progression somewhat.
However, combination tigecycline and venetoclax exhibited “strong antitumoral activity,” according to the researchers. In fact, the combination caused full disease regression in all 8 SU-DHL-6 mice and 3 of 9 OCI-LY8 mice.
Dr Ravà and her colleagues also found the combination produced “rapid and marked tumor regression” in mice with a patient-derived xenograft.
The researchers observed no toxicity when tigecycline and venetoclax were given at low doses. However, mice receiving more aggressive treatment had some inflammation in the liver and spleen. And some mice treated with high doses of tigecycline and venetoclax died within 1 week of treatment initiation.
Finally, Dr Ravà and her colleagues found that tigecycline and venetoclax each synergized with rituximab. The team therefore concluded that tigecycline and venetoclax “have the potential to reinforce rituximab-containing therapies in the clinic.” ![]()
Rituximab Still Proves Safe Long Term
Rituximab, a B-cell–depleting agent, has been found safe and effective in clinical trials of patients with multiple sclerosis and patients with rheumatoid arthritis, among others. However, progressive multifocal leukoencephalopathy (PML) and malignancies have been reported in patients with lymphoma, rheumatoid arthritis, and lupus who also received multiple immunosuppressive therapies, say researchers from Wayne State University in Michigan and University of Chicago in Illinois. In studies with ocrelizumab, which also depletes B-cells, adverse effects (AEs) have included infections, such as, herpes virus-associated infection, and neoplasms.
Although most research has found rituximab and ocrelizumab safe and effective, there is a “paucity of literature” on the safety of continuous B-cell depletion over a long period, the researchers say. They conducted a retrospective study involving 29 patients with immune-mediated neurologic disorders who received continuous cycles of rituximab infusions every 6 to 9 months for up to 7 years. Although small, the study was longer than the trials with ocrelizumab in multiple sclerosis . The mean duration of treatment was 51 months; with a mean of 9 treatment cycles.
The researchers found a low incidence of adverse events and prolonged rituximab-induced B-cell depletion did not lead to any life-threatening AEs, including malignancy. Overall, 32 AEs were reported. Four were serious; 3 were noted after 9 cycles (48 months), and 1 after 11 cycles (60 months). There were no cases of PML or malignancies. Repeated rituximab infusions were well tolerated The rate of AEs remained low over the 7-year observation period.
Source:
Memon AB, Javed A, Caon C, et al. PLoS ONE. 2018;13(1):e0190425.
doi: 10.1371/journal.pone.0190425.
Rituximab, a B-cell–depleting agent, has been found safe and effective in clinical trials of patients with multiple sclerosis and patients with rheumatoid arthritis, among others. However, progressive multifocal leukoencephalopathy (PML) and malignancies have been reported in patients with lymphoma, rheumatoid arthritis, and lupus who also received multiple immunosuppressive therapies, say researchers from Wayne State University in Michigan and University of Chicago in Illinois. In studies with ocrelizumab, which also depletes B-cells, adverse effects (AEs) have included infections, such as, herpes virus-associated infection, and neoplasms.
Although most research has found rituximab and ocrelizumab safe and effective, there is a “paucity of literature” on the safety of continuous B-cell depletion over a long period, the researchers say. They conducted a retrospective study involving 29 patients with immune-mediated neurologic disorders who received continuous cycles of rituximab infusions every 6 to 9 months for up to 7 years. Although small, the study was longer than the trials with ocrelizumab in multiple sclerosis . The mean duration of treatment was 51 months; with a mean of 9 treatment cycles.
The researchers found a low incidence of adverse events and prolonged rituximab-induced B-cell depletion did not lead to any life-threatening AEs, including malignancy. Overall, 32 AEs were reported. Four were serious; 3 were noted after 9 cycles (48 months), and 1 after 11 cycles (60 months). There were no cases of PML or malignancies. Repeated rituximab infusions were well tolerated The rate of AEs remained low over the 7-year observation period.
Source:
Memon AB, Javed A, Caon C, et al. PLoS ONE. 2018;13(1):e0190425.
doi: 10.1371/journal.pone.0190425.
Rituximab, a B-cell–depleting agent, has been found safe and effective in clinical trials of patients with multiple sclerosis and patients with rheumatoid arthritis, among others. However, progressive multifocal leukoencephalopathy (PML) and malignancies have been reported in patients with lymphoma, rheumatoid arthritis, and lupus who also received multiple immunosuppressive therapies, say researchers from Wayne State University in Michigan and University of Chicago in Illinois. In studies with ocrelizumab, which also depletes B-cells, adverse effects (AEs) have included infections, such as, herpes virus-associated infection, and neoplasms.
Although most research has found rituximab and ocrelizumab safe and effective, there is a “paucity of literature” on the safety of continuous B-cell depletion over a long period, the researchers say. They conducted a retrospective study involving 29 patients with immune-mediated neurologic disorders who received continuous cycles of rituximab infusions every 6 to 9 months for up to 7 years. Although small, the study was longer than the trials with ocrelizumab in multiple sclerosis . The mean duration of treatment was 51 months; with a mean of 9 treatment cycles.
The researchers found a low incidence of adverse events and prolonged rituximab-induced B-cell depletion did not lead to any life-threatening AEs, including malignancy. Overall, 32 AEs were reported. Four were serious; 3 were noted after 9 cycles (48 months), and 1 after 11 cycles (60 months). There were no cases of PML or malignancies. Repeated rituximab infusions were well tolerated The rate of AEs remained low over the 7-year observation period.
Source:
Memon AB, Javed A, Caon C, et al. PLoS ONE. 2018;13(1):e0190425.
doi: 10.1371/journal.pone.0190425.
Background color a dermoscopic clue to cutaneous B-cell lymphoma
A salmon-colored background and prominent serpentine blood vessels are two characteristic features of primary cutaneous B-cell lymphoma (PCBCL) that can be identified dermoscopically and may aid diagnosis, researchers say.
In the January issue of the Journal of the European Academy of Dermatology and Venereology, researchers reported the results of a retrospective observational study using the dermoscopic images of 58 biopsy-confirmed primary cutaneous B-cell lymphoma lesions in 51 patients.
While all the lesions were nonpigmented, 46 (79.3%) of them showed salmon- or yellow- to orange- colored background areas. More than three-quarters of the lesions also featured prominent blood vessels (77.6%), the majority of which were serpentine in nature.
, while only 8.6% of the lesions showed neither feature.
Of the 58 lesions, the authors selected 17 to be evaluated by two dermoscopy experts who were blinded to the diagnosis. In 70.6% of these cases they included cutaneous B-cell lymphoma in the differential diagnosis, while other diagnoses included spider bite (58.8%), basal cell carcinoma (52.9%), amelanotic melanoma (47.1%), and scar/keloid (47.1%). Overall, the two experts did not agree on almost 30% of the suggested differential diagnoses.
“The presentation of cutaneous lymphomas in general and of PCBCLs in particular can be nonspecific, and a biopsy is essential for a definitive diagnosis,” wrote Shamir Geller, MD, of the dermatology service at Memorial Sloan Kettering Cancer Center, New York, and his coauthors.
The 58 PCBCLs analyzed were among 172 biopsy-proven PCBCL lesions in the study, which were newly diagnosed and whose pathology reports included the clinical differential diagnosis in the pathology requisition slip, in patients referred to the cancer center between 1992 and 2016. In only 16.3% of these cases, the clinician suspected cutaneous lymphoma. Skin malignancies were suspected in 54.7% of cases, with the leading diagnosis being basal cell carcinoma in 17.4% of cases. Basal cell carcinoma was considered in nearly one-third of lesions, particularly those on the head and neck.
Nonneoplastic conditions suspected by clinicians included cyst in 21.5% of cases, granulomatous processes in 15.7%, and infectious disease in 4.7%.
The authors commented that a low index of suspicion for skin lymphoma was seen regardless of the subtype or site.
“While dermoscopy offers a bridge between the naked eye examination and the histopathological appearance, cutaneous lymphoma is diagnosed on a cellular level using histopathology, immunohistochemistry and molecular studies,” they wrote. “Therefore, dermoscopy may serve as an ancillary tool in PCBCL; however, it cannot be diagnostic.”
The study was supported in part by the National Institutes of Health/National Cancer Institute Cancer Center. Dr. Geller is a recipient of a grant from the American Physicians and Friends For Medicine in Israel. No conflicts of interest were declared.
SOURCE: Geller S et al. J Eur Acad Dermatol Venereol. 2018 Jan;32(1):53-6.
A salmon-colored background and prominent serpentine blood vessels are two characteristic features of primary cutaneous B-cell lymphoma (PCBCL) that can be identified dermoscopically and may aid diagnosis, researchers say.
In the January issue of the Journal of the European Academy of Dermatology and Venereology, researchers reported the results of a retrospective observational study using the dermoscopic images of 58 biopsy-confirmed primary cutaneous B-cell lymphoma lesions in 51 patients.
While all the lesions were nonpigmented, 46 (79.3%) of them showed salmon- or yellow- to orange- colored background areas. More than three-quarters of the lesions also featured prominent blood vessels (77.6%), the majority of which were serpentine in nature.
, while only 8.6% of the lesions showed neither feature.
Of the 58 lesions, the authors selected 17 to be evaluated by two dermoscopy experts who were blinded to the diagnosis. In 70.6% of these cases they included cutaneous B-cell lymphoma in the differential diagnosis, while other diagnoses included spider bite (58.8%), basal cell carcinoma (52.9%), amelanotic melanoma (47.1%), and scar/keloid (47.1%). Overall, the two experts did not agree on almost 30% of the suggested differential diagnoses.
“The presentation of cutaneous lymphomas in general and of PCBCLs in particular can be nonspecific, and a biopsy is essential for a definitive diagnosis,” wrote Shamir Geller, MD, of the dermatology service at Memorial Sloan Kettering Cancer Center, New York, and his coauthors.
The 58 PCBCLs analyzed were among 172 biopsy-proven PCBCL lesions in the study, which were newly diagnosed and whose pathology reports included the clinical differential diagnosis in the pathology requisition slip, in patients referred to the cancer center between 1992 and 2016. In only 16.3% of these cases, the clinician suspected cutaneous lymphoma. Skin malignancies were suspected in 54.7% of cases, with the leading diagnosis being basal cell carcinoma in 17.4% of cases. Basal cell carcinoma was considered in nearly one-third of lesions, particularly those on the head and neck.
Nonneoplastic conditions suspected by clinicians included cyst in 21.5% of cases, granulomatous processes in 15.7%, and infectious disease in 4.7%.
The authors commented that a low index of suspicion for skin lymphoma was seen regardless of the subtype or site.
“While dermoscopy offers a bridge between the naked eye examination and the histopathological appearance, cutaneous lymphoma is diagnosed on a cellular level using histopathology, immunohistochemistry and molecular studies,” they wrote. “Therefore, dermoscopy may serve as an ancillary tool in PCBCL; however, it cannot be diagnostic.”
The study was supported in part by the National Institutes of Health/National Cancer Institute Cancer Center. Dr. Geller is a recipient of a grant from the American Physicians and Friends For Medicine in Israel. No conflicts of interest were declared.
SOURCE: Geller S et al. J Eur Acad Dermatol Venereol. 2018 Jan;32(1):53-6.
A salmon-colored background and prominent serpentine blood vessels are two characteristic features of primary cutaneous B-cell lymphoma (PCBCL) that can be identified dermoscopically and may aid diagnosis, researchers say.
In the January issue of the Journal of the European Academy of Dermatology and Venereology, researchers reported the results of a retrospective observational study using the dermoscopic images of 58 biopsy-confirmed primary cutaneous B-cell lymphoma lesions in 51 patients.
While all the lesions were nonpigmented, 46 (79.3%) of them showed salmon- or yellow- to orange- colored background areas. More than three-quarters of the lesions also featured prominent blood vessels (77.6%), the majority of which were serpentine in nature.
, while only 8.6% of the lesions showed neither feature.
Of the 58 lesions, the authors selected 17 to be evaluated by two dermoscopy experts who were blinded to the diagnosis. In 70.6% of these cases they included cutaneous B-cell lymphoma in the differential diagnosis, while other diagnoses included spider bite (58.8%), basal cell carcinoma (52.9%), amelanotic melanoma (47.1%), and scar/keloid (47.1%). Overall, the two experts did not agree on almost 30% of the suggested differential diagnoses.
“The presentation of cutaneous lymphomas in general and of PCBCLs in particular can be nonspecific, and a biopsy is essential for a definitive diagnosis,” wrote Shamir Geller, MD, of the dermatology service at Memorial Sloan Kettering Cancer Center, New York, and his coauthors.
The 58 PCBCLs analyzed were among 172 biopsy-proven PCBCL lesions in the study, which were newly diagnosed and whose pathology reports included the clinical differential diagnosis in the pathology requisition slip, in patients referred to the cancer center between 1992 and 2016. In only 16.3% of these cases, the clinician suspected cutaneous lymphoma. Skin malignancies were suspected in 54.7% of cases, with the leading diagnosis being basal cell carcinoma in 17.4% of cases. Basal cell carcinoma was considered in nearly one-third of lesions, particularly those on the head and neck.
Nonneoplastic conditions suspected by clinicians included cyst in 21.5% of cases, granulomatous processes in 15.7%, and infectious disease in 4.7%.
The authors commented that a low index of suspicion for skin lymphoma was seen regardless of the subtype or site.
“While dermoscopy offers a bridge between the naked eye examination and the histopathological appearance, cutaneous lymphoma is diagnosed on a cellular level using histopathology, immunohistochemistry and molecular studies,” they wrote. “Therefore, dermoscopy may serve as an ancillary tool in PCBCL; however, it cannot be diagnostic.”
The study was supported in part by the National Institutes of Health/National Cancer Institute Cancer Center. Dr. Geller is a recipient of a grant from the American Physicians and Friends For Medicine in Israel. No conflicts of interest were declared.
SOURCE: Geller S et al. J Eur Acad Dermatol Venereol. 2018 Jan;32(1):53-6.
FROM THE JOURNAL OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Key clinical point: A salmon-colored background and prominent serpentine blood vessels are two characteristic dermoscopic features of primary cutaneous B-cell lymphoma (PCBCL).
Major finding: Nearly 80% of PCBCLs had a salmon-colored background on dermoscopy.
Data source: A retrospective observational study that analyzed 172 biopsy-proven PCBCLs, including 58 PCBCL dermoscopic images.
Disclosures: The study was supported by the NIH/NCI Cancer Center. The lead author received a grant from the American Physicians and Friends for Medicine in Israel. No conflicts of interest were declared.
Source: Geller S et al. J Eur Acad Dermatol Venereol. 2018 Jan;32(1):53-6.