User login
For smokers, prenatal vitamin C improves infants’ lung function
Daily vitamin C during smokers’ pregnancies significantly improved the lung function of their infants at birth and reduced the incidence of wheezing during the first year of life, compared with infants of smokers who weren’t exposed to the vitamin.
Those infants had significantly poorer respiratory outcomes, both at birth and 1 year, according to Dr. Cindy McEvoy and colleagues. The study was presented at an international conference of the American Thoracic Society and simultaneously published in the May 18 issue ofthe Journal of the American Medical Association.
While it’s not entirely clear how vitamin C influences prenatal lung development, there are tantalizing hints, wrote Dr. McEvoy of the Oregon Health and Science University, Portland, and her coinvestigators. "Supplemental vitamin C may act by blocking formation of reactive oxygen species, which stimulate abnormal patterns of airway cell proliferation, resulting in narrowed airways and abnormal airway geometry," they said.
Dr. McEvoy and her team randomized 179 pregnant smokers to either placebo or 500 mg vitamin C daily from week 16 of pregnancy. At birth, they examined two respiratory function measures: the ratio of time to peak expiratory flow/expiratory time (TPTEF:TE) and passive respiratory compliance per kg (Crs/kg). They also compared the incidences of wheezing during the first year. A control group of 76 infants from nonsmokers provided a comparator (JAMA 2014 May 18 [doi:10.1001/jama.2014.5217]).
The women were a mean age of 26 years at baseline. Most were white (about 85%), and 20% had at least some college education. In the placebo group, 36% smoked at least 10 cigarettes a day; in the active group, 41% smoked that many. All smoking mothers were offered the chance to participate in a smoking cessation program; 10% were able to stop.
At birth, infants exposed to vitamin C had significantly better lung function than nonexposed infants on both measures. The TPTEF:TE was 10% better in the exposed group (0.383 vs. 0.345) – similar to the ratio in the comparator group of infants from nonsmoking mothers. The Crs/kg was also significantly better (11%) in the vitamin C group (1.32 vs. 1.20 mL/cmH20/kg).
Almost all of the babies had 1-year follow-up (92%). At that time, the incidence of wheezing during the first year was 21% in the treated group and 40% in the placebo group (adjusted relative risk, 0.56). However, the authors noted, there was no between-group difference in the other lung function measures at 1 year.
A subgroup of 173 mothers was genotyped for two polymorphisms that are strongly associated with a lifelong risk of nicotine addiction, lung cancer, and chronic obstructive pulmonary disease.
The infants of mothers who were heterozygous for one of those (rs16969968), experienced the largest benefit from vitamin C exposure. The incidence of wheezing through 1 year in these infants was 14%, compared with 48% among those randomized to placebo.
The National Heart, Lung, and Blood Institute sponsored the study. Neither Dr. McEvoy nor any of her coauthors had any financial disclosures.
Quitting is the best way for smokers to protect their unborn babies against the harms of tobacco.
But unfortunately, quitting doesn’t always happen. Thus, the finding that vitamin C may offer babies some protection against the harms of tobacco is heartening news. Although the improvement over placebo was rather small (10%), it could have a profound effect.
"Small population-level changes in lung function may lead to significant public health benefits, and the improvements in lung function reported here could be associated with future benefit."
The study was well designed and well executed, and the 1-year endpoints intriguing. However, there is no evidence that vitamin C fully prevents or reverses the effects of maternal smoking during gestation. Thus, prenatal treatment should never be seen as a panacea.
"Achieving smoking cessation should be the primary goal for women who smoke and who intend to become pregnant. By preventing her developing fetus and newborn infant from becoming exposed to tobacco smoke, a pregnant woman can do more for the respiratory health and overall health of her child than any amount of vitamin C may be able to accomplish."
Graham L. Hall, Ph.D., is head of pediatric respiratory physiology and research at the Telethon Kids Institute, University of Western Australia, West Perth. These remarks were taken from his accompanying editorial (JAMA 2014 May 18 [doi:10.1001/jama.2014.5218]).
Quitting is the best way for smokers to protect their unborn babies against the harms of tobacco.
But unfortunately, quitting doesn’t always happen. Thus, the finding that vitamin C may offer babies some protection against the harms of tobacco is heartening news. Although the improvement over placebo was rather small (10%), it could have a profound effect.
"Small population-level changes in lung function may lead to significant public health benefits, and the improvements in lung function reported here could be associated with future benefit."
The study was well designed and well executed, and the 1-year endpoints intriguing. However, there is no evidence that vitamin C fully prevents or reverses the effects of maternal smoking during gestation. Thus, prenatal treatment should never be seen as a panacea.
"Achieving smoking cessation should be the primary goal for women who smoke and who intend to become pregnant. By preventing her developing fetus and newborn infant from becoming exposed to tobacco smoke, a pregnant woman can do more for the respiratory health and overall health of her child than any amount of vitamin C may be able to accomplish."
Graham L. Hall, Ph.D., is head of pediatric respiratory physiology and research at the Telethon Kids Institute, University of Western Australia, West Perth. These remarks were taken from his accompanying editorial (JAMA 2014 May 18 [doi:10.1001/jama.2014.5218]).
Quitting is the best way for smokers to protect their unborn babies against the harms of tobacco.
But unfortunately, quitting doesn’t always happen. Thus, the finding that vitamin C may offer babies some protection against the harms of tobacco is heartening news. Although the improvement over placebo was rather small (10%), it could have a profound effect.
"Small population-level changes in lung function may lead to significant public health benefits, and the improvements in lung function reported here could be associated with future benefit."
The study was well designed and well executed, and the 1-year endpoints intriguing. However, there is no evidence that vitamin C fully prevents or reverses the effects of maternal smoking during gestation. Thus, prenatal treatment should never be seen as a panacea.
"Achieving smoking cessation should be the primary goal for women who smoke and who intend to become pregnant. By preventing her developing fetus and newborn infant from becoming exposed to tobacco smoke, a pregnant woman can do more for the respiratory health and overall health of her child than any amount of vitamin C may be able to accomplish."
Graham L. Hall, Ph.D., is head of pediatric respiratory physiology and research at the Telethon Kids Institute, University of Western Australia, West Perth. These remarks were taken from his accompanying editorial (JAMA 2014 May 18 [doi:10.1001/jama.2014.5218]).
Daily vitamin C during smokers’ pregnancies significantly improved the lung function of their infants at birth and reduced the incidence of wheezing during the first year of life, compared with infants of smokers who weren’t exposed to the vitamin.
Those infants had significantly poorer respiratory outcomes, both at birth and 1 year, according to Dr. Cindy McEvoy and colleagues. The study was presented at an international conference of the American Thoracic Society and simultaneously published in the May 18 issue ofthe Journal of the American Medical Association.
While it’s not entirely clear how vitamin C influences prenatal lung development, there are tantalizing hints, wrote Dr. McEvoy of the Oregon Health and Science University, Portland, and her coinvestigators. "Supplemental vitamin C may act by blocking formation of reactive oxygen species, which stimulate abnormal patterns of airway cell proliferation, resulting in narrowed airways and abnormal airway geometry," they said.
Dr. McEvoy and her team randomized 179 pregnant smokers to either placebo or 500 mg vitamin C daily from week 16 of pregnancy. At birth, they examined two respiratory function measures: the ratio of time to peak expiratory flow/expiratory time (TPTEF:TE) and passive respiratory compliance per kg (Crs/kg). They also compared the incidences of wheezing during the first year. A control group of 76 infants from nonsmokers provided a comparator (JAMA 2014 May 18 [doi:10.1001/jama.2014.5217]).
The women were a mean age of 26 years at baseline. Most were white (about 85%), and 20% had at least some college education. In the placebo group, 36% smoked at least 10 cigarettes a day; in the active group, 41% smoked that many. All smoking mothers were offered the chance to participate in a smoking cessation program; 10% were able to stop.
At birth, infants exposed to vitamin C had significantly better lung function than nonexposed infants on both measures. The TPTEF:TE was 10% better in the exposed group (0.383 vs. 0.345) – similar to the ratio in the comparator group of infants from nonsmoking mothers. The Crs/kg was also significantly better (11%) in the vitamin C group (1.32 vs. 1.20 mL/cmH20/kg).
Almost all of the babies had 1-year follow-up (92%). At that time, the incidence of wheezing during the first year was 21% in the treated group and 40% in the placebo group (adjusted relative risk, 0.56). However, the authors noted, there was no between-group difference in the other lung function measures at 1 year.
A subgroup of 173 mothers was genotyped for two polymorphisms that are strongly associated with a lifelong risk of nicotine addiction, lung cancer, and chronic obstructive pulmonary disease.
The infants of mothers who were heterozygous for one of those (rs16969968), experienced the largest benefit from vitamin C exposure. The incidence of wheezing through 1 year in these infants was 14%, compared with 48% among those randomized to placebo.
The National Heart, Lung, and Blood Institute sponsored the study. Neither Dr. McEvoy nor any of her coauthors had any financial disclosures.
Daily vitamin C during smokers’ pregnancies significantly improved the lung function of their infants at birth and reduced the incidence of wheezing during the first year of life, compared with infants of smokers who weren’t exposed to the vitamin.
Those infants had significantly poorer respiratory outcomes, both at birth and 1 year, according to Dr. Cindy McEvoy and colleagues. The study was presented at an international conference of the American Thoracic Society and simultaneously published in the May 18 issue ofthe Journal of the American Medical Association.
While it’s not entirely clear how vitamin C influences prenatal lung development, there are tantalizing hints, wrote Dr. McEvoy of the Oregon Health and Science University, Portland, and her coinvestigators. "Supplemental vitamin C may act by blocking formation of reactive oxygen species, which stimulate abnormal patterns of airway cell proliferation, resulting in narrowed airways and abnormal airway geometry," they said.
Dr. McEvoy and her team randomized 179 pregnant smokers to either placebo or 500 mg vitamin C daily from week 16 of pregnancy. At birth, they examined two respiratory function measures: the ratio of time to peak expiratory flow/expiratory time (TPTEF:TE) and passive respiratory compliance per kg (Crs/kg). They also compared the incidences of wheezing during the first year. A control group of 76 infants from nonsmokers provided a comparator (JAMA 2014 May 18 [doi:10.1001/jama.2014.5217]).
The women were a mean age of 26 years at baseline. Most were white (about 85%), and 20% had at least some college education. In the placebo group, 36% smoked at least 10 cigarettes a day; in the active group, 41% smoked that many. All smoking mothers were offered the chance to participate in a smoking cessation program; 10% were able to stop.
At birth, infants exposed to vitamin C had significantly better lung function than nonexposed infants on both measures. The TPTEF:TE was 10% better in the exposed group (0.383 vs. 0.345) – similar to the ratio in the comparator group of infants from nonsmoking mothers. The Crs/kg was also significantly better (11%) in the vitamin C group (1.32 vs. 1.20 mL/cmH20/kg).
Almost all of the babies had 1-year follow-up (92%). At that time, the incidence of wheezing during the first year was 21% in the treated group and 40% in the placebo group (adjusted relative risk, 0.56). However, the authors noted, there was no between-group difference in the other lung function measures at 1 year.
A subgroup of 173 mothers was genotyped for two polymorphisms that are strongly associated with a lifelong risk of nicotine addiction, lung cancer, and chronic obstructive pulmonary disease.
The infants of mothers who were heterozygous for one of those (rs16969968), experienced the largest benefit from vitamin C exposure. The incidence of wheezing through 1 year in these infants was 14%, compared with 48% among those randomized to placebo.
The National Heart, Lung, and Blood Institute sponsored the study. Neither Dr. McEvoy nor any of her coauthors had any financial disclosures.
FROM ATS 2014
Key clinical point: Giving Vitamin C to pregnant smokers may improve newborns’ lung health.
Major finding: Lung function at birth was about 10% better in infants’ of smokers 500 mg vitamin C daily during pregnancy, compared to those who did not. The incidence of wheezing during the first year was 21% in the treated group vs. 40% in the placebo group.
Data source: A randomized, placebo-controlled study of 179 pregnant smokers.
Disclosures: The National Heart, Lung, and Blood Institute funded the study. None of the authors had financial disclosures.
Hydroxychloroquine safe to continue for SLE during pregnancy
LIVERPOOL, ENGLAND – Hydroxychloroquine was not associated with any adverse long-term complications in the children of women with systemic lupus erythematosus who used the drug during pregnancy or while breastfeeding in a multicenter, cross-sectional survey.
In fact the research, recently reported at the British Society for Rheumatology annual conference, showed that the disease-modifying antirheumatic drug (DMARD) reduced exposed children’s risk of admission to hospital for infection (14% vs. 24.8% for nonexposed children; P = .03) and the need for outpatient visits (12.6% vs. 23.1%; P = .0.03).
There was no significant increased risk for congenital anomalies (2.1% vs. 2.2%), including congenital heart block (2.0% vs. 2.9%), or developmental problems such as attention-deficit hyperactivity disorder (0% vs. 2.9% for ADHD). Mothers who used the DMARD were also no more at risk of developing eclampsia during their pregnancy than those who did not (11% vs. 9%; P = .75).
"Hydroxychloroquine should be continued during pregnancy and breastfeeding," advised study investigator Dr. Mary Gayed of the department of rheumatology at the University of Birmingham (England).
Dr. Gayed, who presented the study findings on behalf of the British Isles Lupus Assessment Group (BILAG), said that these were hopefully reassuring findings. "We know that immunosuppressive agents, including hydroxychloroquine, are used in SLE [systemic lupus erythematosus] during pregnancy to prevent disease flare and to ensure optimum outcomes for both mother and child," she said, explaining the rationale behind the research, "but there are few published data regarding the long-term outcome of these children."
Randomized, controlled study data have shown that women who continue treatment with hydroxychloroquine during their pregnancy exhibit no disease activity and require only low doses of steroids by the end of their pregnancy, Dr. Gayed observed. This has been corroborated by other studies that have shown that discontinuing the DMARD leads to higher disease activity and the need for higher steroid doses.
Lack of good disease control during pregnancy is linked to maternal complications such as high blood pressure, proteinuria, thrombocytopenia, and secondary antiphospholipid syndrome. "We also know that women who have active lupus during pregnancy have a reduced rate of live births, earlier deliveries, increased pregnancy losses, and increased small-for-gestational-age babies, which makes it key to control disease activity throughout pregnancy," said Dr. Gayed.
Dr. Gayed and associates have previously reported their findings on the long-term out comes of all DMARDs used to treat SLE in pregnancy and will release further data from their survey on the safety of azathioprine at the upcoming European League Against Rheumatism Congress next month in Paris. The current research question was to look at their data specifically with regard to hydroxychloroquine and how this affected maternal, neonatal, and childhood outcomes.
Their retrospective survey involved 200 women with SLE, defined using American College of Rheumatology criteria, who gave birth to a total of 287 children. Of these, 118 women used the DMARD during their pregnancy or while breastfeeding, with 149 children exposed to hydroxychloroquine during the neonatal or postnatal periods. The majority of women (n = 76) used the drug during pregnancy and breastfeeding, 42 during pregnancy only, and 4 only while they were breastfeeding. There were 102 women who did not use the drug during pregnancy or breastfeeding and who gave birth to 138 nonexposed children.
At the birth of their children, the mean age of mothers was 32 years, and they had a mean disease duration of 7.5 years overall, with a mean maternal disease duration of 6.5 years versus 8.6 years comparing the hydroxychloroquine-exposed with the nonexposed children. The majority (66%) of the women were white, 15% were South Asian, 10% Afro-Caribbean, 1% Chinese, 1% Hispanic, and the remainder of other or unstated ethnicity. There was no significant difference in the use of azathioprine, aspirin, or heparin, but mothers who used hydroxychloroquine were significantly more likely to use steroids than women who did not use the DMARD (66% vs. 51%; P = .02).
The median gestational age at delivery was 38 weeks in both hydroxychloroquine-exposed and nonexposed children. There was no statistical difference in birth weight between the groups, which was a mean of 2.8 kg in both exposed and nonexposed children. The median age of children exposed to hydroxychloroquine at enrollment was 2.1 years versus 4.6 years for nonexposed children.
The findings are limited by the fact that these are self-reported data, and it was not always possible to check medical records, Dr. Gayed said. Data on disease activity and prednisolone dose were also not available. That said, "this U.K. cross-sectional survey highlights that hydroxychloroquine is compatible with pregnancy," Dr. Gayed concluded.
Dr. Gayed and coauthors reported no conflicts of interest.
LIVERPOOL, ENGLAND – Hydroxychloroquine was not associated with any adverse long-term complications in the children of women with systemic lupus erythematosus who used the drug during pregnancy or while breastfeeding in a multicenter, cross-sectional survey.
In fact the research, recently reported at the British Society for Rheumatology annual conference, showed that the disease-modifying antirheumatic drug (DMARD) reduced exposed children’s risk of admission to hospital for infection (14% vs. 24.8% for nonexposed children; P = .03) and the need for outpatient visits (12.6% vs. 23.1%; P = .0.03).
There was no significant increased risk for congenital anomalies (2.1% vs. 2.2%), including congenital heart block (2.0% vs. 2.9%), or developmental problems such as attention-deficit hyperactivity disorder (0% vs. 2.9% for ADHD). Mothers who used the DMARD were also no more at risk of developing eclampsia during their pregnancy than those who did not (11% vs. 9%; P = .75).
"Hydroxychloroquine should be continued during pregnancy and breastfeeding," advised study investigator Dr. Mary Gayed of the department of rheumatology at the University of Birmingham (England).
Dr. Gayed, who presented the study findings on behalf of the British Isles Lupus Assessment Group (BILAG), said that these were hopefully reassuring findings. "We know that immunosuppressive agents, including hydroxychloroquine, are used in SLE [systemic lupus erythematosus] during pregnancy to prevent disease flare and to ensure optimum outcomes for both mother and child," she said, explaining the rationale behind the research, "but there are few published data regarding the long-term outcome of these children."
Randomized, controlled study data have shown that women who continue treatment with hydroxychloroquine during their pregnancy exhibit no disease activity and require only low doses of steroids by the end of their pregnancy, Dr. Gayed observed. This has been corroborated by other studies that have shown that discontinuing the DMARD leads to higher disease activity and the need for higher steroid doses.
Lack of good disease control during pregnancy is linked to maternal complications such as high blood pressure, proteinuria, thrombocytopenia, and secondary antiphospholipid syndrome. "We also know that women who have active lupus during pregnancy have a reduced rate of live births, earlier deliveries, increased pregnancy losses, and increased small-for-gestational-age babies, which makes it key to control disease activity throughout pregnancy," said Dr. Gayed.
Dr. Gayed and associates have previously reported their findings on the long-term out comes of all DMARDs used to treat SLE in pregnancy and will release further data from their survey on the safety of azathioprine at the upcoming European League Against Rheumatism Congress next month in Paris. The current research question was to look at their data specifically with regard to hydroxychloroquine and how this affected maternal, neonatal, and childhood outcomes.
Their retrospective survey involved 200 women with SLE, defined using American College of Rheumatology criteria, who gave birth to a total of 287 children. Of these, 118 women used the DMARD during their pregnancy or while breastfeeding, with 149 children exposed to hydroxychloroquine during the neonatal or postnatal periods. The majority of women (n = 76) used the drug during pregnancy and breastfeeding, 42 during pregnancy only, and 4 only while they were breastfeeding. There were 102 women who did not use the drug during pregnancy or breastfeeding and who gave birth to 138 nonexposed children.
At the birth of their children, the mean age of mothers was 32 years, and they had a mean disease duration of 7.5 years overall, with a mean maternal disease duration of 6.5 years versus 8.6 years comparing the hydroxychloroquine-exposed with the nonexposed children. The majority (66%) of the women were white, 15% were South Asian, 10% Afro-Caribbean, 1% Chinese, 1% Hispanic, and the remainder of other or unstated ethnicity. There was no significant difference in the use of azathioprine, aspirin, or heparin, but mothers who used hydroxychloroquine were significantly more likely to use steroids than women who did not use the DMARD (66% vs. 51%; P = .02).
The median gestational age at delivery was 38 weeks in both hydroxychloroquine-exposed and nonexposed children. There was no statistical difference in birth weight between the groups, which was a mean of 2.8 kg in both exposed and nonexposed children. The median age of children exposed to hydroxychloroquine at enrollment was 2.1 years versus 4.6 years for nonexposed children.
The findings are limited by the fact that these are self-reported data, and it was not always possible to check medical records, Dr. Gayed said. Data on disease activity and prednisolone dose were also not available. That said, "this U.K. cross-sectional survey highlights that hydroxychloroquine is compatible with pregnancy," Dr. Gayed concluded.
Dr. Gayed and coauthors reported no conflicts of interest.
LIVERPOOL, ENGLAND – Hydroxychloroquine was not associated with any adverse long-term complications in the children of women with systemic lupus erythematosus who used the drug during pregnancy or while breastfeeding in a multicenter, cross-sectional survey.
In fact the research, recently reported at the British Society for Rheumatology annual conference, showed that the disease-modifying antirheumatic drug (DMARD) reduced exposed children’s risk of admission to hospital for infection (14% vs. 24.8% for nonexposed children; P = .03) and the need for outpatient visits (12.6% vs. 23.1%; P = .0.03).
There was no significant increased risk for congenital anomalies (2.1% vs. 2.2%), including congenital heart block (2.0% vs. 2.9%), or developmental problems such as attention-deficit hyperactivity disorder (0% vs. 2.9% for ADHD). Mothers who used the DMARD were also no more at risk of developing eclampsia during their pregnancy than those who did not (11% vs. 9%; P = .75).
"Hydroxychloroquine should be continued during pregnancy and breastfeeding," advised study investigator Dr. Mary Gayed of the department of rheumatology at the University of Birmingham (England).
Dr. Gayed, who presented the study findings on behalf of the British Isles Lupus Assessment Group (BILAG), said that these were hopefully reassuring findings. "We know that immunosuppressive agents, including hydroxychloroquine, are used in SLE [systemic lupus erythematosus] during pregnancy to prevent disease flare and to ensure optimum outcomes for both mother and child," she said, explaining the rationale behind the research, "but there are few published data regarding the long-term outcome of these children."
Randomized, controlled study data have shown that women who continue treatment with hydroxychloroquine during their pregnancy exhibit no disease activity and require only low doses of steroids by the end of their pregnancy, Dr. Gayed observed. This has been corroborated by other studies that have shown that discontinuing the DMARD leads to higher disease activity and the need for higher steroid doses.
Lack of good disease control during pregnancy is linked to maternal complications such as high blood pressure, proteinuria, thrombocytopenia, and secondary antiphospholipid syndrome. "We also know that women who have active lupus during pregnancy have a reduced rate of live births, earlier deliveries, increased pregnancy losses, and increased small-for-gestational-age babies, which makes it key to control disease activity throughout pregnancy," said Dr. Gayed.
Dr. Gayed and associates have previously reported their findings on the long-term out comes of all DMARDs used to treat SLE in pregnancy and will release further data from their survey on the safety of azathioprine at the upcoming European League Against Rheumatism Congress next month in Paris. The current research question was to look at their data specifically with regard to hydroxychloroquine and how this affected maternal, neonatal, and childhood outcomes.
Their retrospective survey involved 200 women with SLE, defined using American College of Rheumatology criteria, who gave birth to a total of 287 children. Of these, 118 women used the DMARD during their pregnancy or while breastfeeding, with 149 children exposed to hydroxychloroquine during the neonatal or postnatal periods. The majority of women (n = 76) used the drug during pregnancy and breastfeeding, 42 during pregnancy only, and 4 only while they were breastfeeding. There were 102 women who did not use the drug during pregnancy or breastfeeding and who gave birth to 138 nonexposed children.
At the birth of their children, the mean age of mothers was 32 years, and they had a mean disease duration of 7.5 years overall, with a mean maternal disease duration of 6.5 years versus 8.6 years comparing the hydroxychloroquine-exposed with the nonexposed children. The majority (66%) of the women were white, 15% were South Asian, 10% Afro-Caribbean, 1% Chinese, 1% Hispanic, and the remainder of other or unstated ethnicity. There was no significant difference in the use of azathioprine, aspirin, or heparin, but mothers who used hydroxychloroquine were significantly more likely to use steroids than women who did not use the DMARD (66% vs. 51%; P = .02).
The median gestational age at delivery was 38 weeks in both hydroxychloroquine-exposed and nonexposed children. There was no statistical difference in birth weight between the groups, which was a mean of 2.8 kg in both exposed and nonexposed children. The median age of children exposed to hydroxychloroquine at enrollment was 2.1 years versus 4.6 years for nonexposed children.
The findings are limited by the fact that these are self-reported data, and it was not always possible to check medical records, Dr. Gayed said. Data on disease activity and prednisolone dose were also not available. That said, "this U.K. cross-sectional survey highlights that hydroxychloroquine is compatible with pregnancy," Dr. Gayed concluded.
Dr. Gayed and coauthors reported no conflicts of interest.
AT RHEUMATOLOGY 2014
Key clinical point: Women with SLE should not stop hydroxychloroquine during pregnancy and breastfeeding.
Major finding: Fewer children exposed to hydroxychloroquine than those who were not needed hospital admission for infection (14% vs. 24.8%; P = .03) or outpatient visits (12.6% vs. 23.1%; P = .0.03).
Data source: Multicenter, cross-sectional, retrospective survey of 200 women with SLE who gave birth to 287 children who were (n = 149) or were not (n = 138) exposed to hydroxychloroquine while their mother was pregnant or breastfeeding.
Disclosures: The researchers reported no conflicts of interest.
Newborn screening spots most cases of early CMV-related hearing loss
VANCOUVER, B.C. – A targeted cytomegalovirus screening approach that tests only newborns who do not pass their hearing test would identify the majority of those who have CMV-related sensorineural hearing loss at birth, according to data from the CMV and Hearing Multicenter Screening Study.
All of 99,778 newborns born during 2007-2012 in seven states studied had both auditory testing and virologic testing of saliva for CMV infection shortly after birth.
Overall, 461 (0.5%) tested positive for CMV infection, lead investigator Karen B. Fowler, Dr.P.H., a professor at the University of Alabama, Birmingham, reported at the annual meeting of the Pediatric Academic Societies.
The proportion of newborns who did not pass their hearing test and were therefore referred for further evaluation was higher in the CMV-positive group than in the CMV-negative group (7.1% vs. 0.9%; P less than .0001). Findings were similar whether the newborn was in the well-baby nursery or in the neonatal intensive care unit.
Hearing screening identified 21 (60%) of the 35 newborns with CMV-related sensorineural hearing loss. However, this amounted to only 4.5% of all CMV-positive infants in the cohort.
"Our study found that infants who are CMV positive will refer or not pass their newborn hearing screening at a significantly higher rate than infants without CMV infection, suggesting that newborns who refer on their hearing screen and have no other known etiology for their possible hearing loss should be screened for CMV infection," Dr. Fowler said in an interview.
This targeted approach "does not identify all infants with congenital CMV infection or all CMV-related hearing loss. However, our study found that 60% of the CMV-related hearing loss that occurs in the newborn period was identified using this approach," she added.
As for clinical implications, "infants who are CMV positive with sensorineural hearing loss will need continued monitoring of their hearing loss for further deterioration, as well as possible antiviral treatment. Those infants who are CMV positive, even if further evaluation indicates that hearing loss is not present, will need continued monitoring for possible late-onset hearing loss. Although appropriate early intervention should occur for any infant with hearing loss, monitoring for late-onset and progressive hearing losses might not occur for CMV-positive infants if the etiology of the hearing loss was unknown," noted Dr. Fowler.
The investigators plan "to continue to explore possible mechanisms of CMV-related hearing loss and whether there are predictors or indicators of which children with CMV infection will go on to have hearing loss or further deterioration of their hearing loss. Currently, no such indicators exist," she concluded.
Dr. Fowler disclosed no relevant conflicts of interest.
VANCOUVER, B.C. – A targeted cytomegalovirus screening approach that tests only newborns who do not pass their hearing test would identify the majority of those who have CMV-related sensorineural hearing loss at birth, according to data from the CMV and Hearing Multicenter Screening Study.
All of 99,778 newborns born during 2007-2012 in seven states studied had both auditory testing and virologic testing of saliva for CMV infection shortly after birth.
Overall, 461 (0.5%) tested positive for CMV infection, lead investigator Karen B. Fowler, Dr.P.H., a professor at the University of Alabama, Birmingham, reported at the annual meeting of the Pediatric Academic Societies.
The proportion of newborns who did not pass their hearing test and were therefore referred for further evaluation was higher in the CMV-positive group than in the CMV-negative group (7.1% vs. 0.9%; P less than .0001). Findings were similar whether the newborn was in the well-baby nursery or in the neonatal intensive care unit.
Hearing screening identified 21 (60%) of the 35 newborns with CMV-related sensorineural hearing loss. However, this amounted to only 4.5% of all CMV-positive infants in the cohort.
"Our study found that infants who are CMV positive will refer or not pass their newborn hearing screening at a significantly higher rate than infants without CMV infection, suggesting that newborns who refer on their hearing screen and have no other known etiology for their possible hearing loss should be screened for CMV infection," Dr. Fowler said in an interview.
This targeted approach "does not identify all infants with congenital CMV infection or all CMV-related hearing loss. However, our study found that 60% of the CMV-related hearing loss that occurs in the newborn period was identified using this approach," she added.
As for clinical implications, "infants who are CMV positive with sensorineural hearing loss will need continued monitoring of their hearing loss for further deterioration, as well as possible antiviral treatment. Those infants who are CMV positive, even if further evaluation indicates that hearing loss is not present, will need continued monitoring for possible late-onset hearing loss. Although appropriate early intervention should occur for any infant with hearing loss, monitoring for late-onset and progressive hearing losses might not occur for CMV-positive infants if the etiology of the hearing loss was unknown," noted Dr. Fowler.
The investigators plan "to continue to explore possible mechanisms of CMV-related hearing loss and whether there are predictors or indicators of which children with CMV infection will go on to have hearing loss or further deterioration of their hearing loss. Currently, no such indicators exist," she concluded.
Dr. Fowler disclosed no relevant conflicts of interest.
VANCOUVER, B.C. – A targeted cytomegalovirus screening approach that tests only newborns who do not pass their hearing test would identify the majority of those who have CMV-related sensorineural hearing loss at birth, according to data from the CMV and Hearing Multicenter Screening Study.
All of 99,778 newborns born during 2007-2012 in seven states studied had both auditory testing and virologic testing of saliva for CMV infection shortly after birth.
Overall, 461 (0.5%) tested positive for CMV infection, lead investigator Karen B. Fowler, Dr.P.H., a professor at the University of Alabama, Birmingham, reported at the annual meeting of the Pediatric Academic Societies.
The proportion of newborns who did not pass their hearing test and were therefore referred for further evaluation was higher in the CMV-positive group than in the CMV-negative group (7.1% vs. 0.9%; P less than .0001). Findings were similar whether the newborn was in the well-baby nursery or in the neonatal intensive care unit.
Hearing screening identified 21 (60%) of the 35 newborns with CMV-related sensorineural hearing loss. However, this amounted to only 4.5% of all CMV-positive infants in the cohort.
"Our study found that infants who are CMV positive will refer or not pass their newborn hearing screening at a significantly higher rate than infants without CMV infection, suggesting that newborns who refer on their hearing screen and have no other known etiology for their possible hearing loss should be screened for CMV infection," Dr. Fowler said in an interview.
This targeted approach "does not identify all infants with congenital CMV infection or all CMV-related hearing loss. However, our study found that 60% of the CMV-related hearing loss that occurs in the newborn period was identified using this approach," she added.
As for clinical implications, "infants who are CMV positive with sensorineural hearing loss will need continued monitoring of their hearing loss for further deterioration, as well as possible antiviral treatment. Those infants who are CMV positive, even if further evaluation indicates that hearing loss is not present, will need continued monitoring for possible late-onset hearing loss. Although appropriate early intervention should occur for any infant with hearing loss, monitoring for late-onset and progressive hearing losses might not occur for CMV-positive infants if the etiology of the hearing loss was unknown," noted Dr. Fowler.
The investigators plan "to continue to explore possible mechanisms of CMV-related hearing loss and whether there are predictors or indicators of which children with CMV infection will go on to have hearing loss or further deterioration of their hearing loss. Currently, no such indicators exist," she concluded.
Dr. Fowler disclosed no relevant conflicts of interest.
AT THE PAS ANNUAL MEETING
Top clinical point: CMV screening of newborns is useful to identify hearing loss.
Major finding: Hearing screening identified 60% of newborns who had CMV-related sensorineural hearing loss.
Data source: A cohort study of 99,778 newborns who had both hearing screening and CMV testing at birth.
Disclosures: Dr. Fowler disclosed no relevant conflicts of interest.
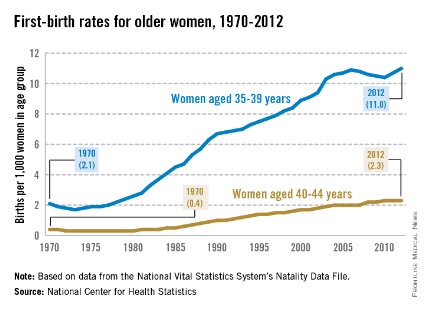
First-birth rates in older women up more than 400% since 1970
The rate of first births among women aged 35-39 years went up 424% from 1970 to 2012, while the first-birth rate for women aged 40-44 years rose 475%, the National Center for Health Statistics reported.
The first-birth rate for women aged 35-39 years was 11.0 per 1,000 women in that age group in 2012, compared with 2.1 per 1,000 in 1970. For women aged 40-49 years, the rate of first births was 2.3 per 1,000 in 2012, compared with 0.4 in 1970, according to the NCHS.
The investigators noted that first-birth rates for women aged 30-34 years "have increased but not as steadily since the early 2000s," and that rates for women under 30 years old "have declined in the past decade."
From 1990 to 2012, first-birth rates in both age groups increased for all races/ethnicities. Among 35- to 39-year-old women, non-Hispanic blacks had the largest increase, while Asian/Pacific Islanders had the largest increase for those aged 40-44 years. American Indian/Alaska native women had the smallest increases in both age groups, the report showed.
The NCHS analysis was based on data from the National Vital Statistics System’s Natality Data File, which includes information for all births in the United States.

The rate of first births among women aged 35-39 years went up 424% from 1970 to 2012, while the first-birth rate for women aged 40-44 years rose 475%, the National Center for Health Statistics reported.
The first-birth rate for women aged 35-39 years was 11.0 per 1,000 women in that age group in 2012, compared with 2.1 per 1,000 in 1970. For women aged 40-49 years, the rate of first births was 2.3 per 1,000 in 2012, compared with 0.4 in 1970, according to the NCHS.
The investigators noted that first-birth rates for women aged 30-34 years "have increased but not as steadily since the early 2000s," and that rates for women under 30 years old "have declined in the past decade."
From 1990 to 2012, first-birth rates in both age groups increased for all races/ethnicities. Among 35- to 39-year-old women, non-Hispanic blacks had the largest increase, while Asian/Pacific Islanders had the largest increase for those aged 40-44 years. American Indian/Alaska native women had the smallest increases in both age groups, the report showed.
The NCHS analysis was based on data from the National Vital Statistics System’s Natality Data File, which includes information for all births in the United States.

The rate of first births among women aged 35-39 years went up 424% from 1970 to 2012, while the first-birth rate for women aged 40-44 years rose 475%, the National Center for Health Statistics reported.
The first-birth rate for women aged 35-39 years was 11.0 per 1,000 women in that age group in 2012, compared with 2.1 per 1,000 in 1970. For women aged 40-49 years, the rate of first births was 2.3 per 1,000 in 2012, compared with 0.4 in 1970, according to the NCHS.
The investigators noted that first-birth rates for women aged 30-34 years "have increased but not as steadily since the early 2000s," and that rates for women under 30 years old "have declined in the past decade."
From 1990 to 2012, first-birth rates in both age groups increased for all races/ethnicities. Among 35- to 39-year-old women, non-Hispanic blacks had the largest increase, while Asian/Pacific Islanders had the largest increase for those aged 40-44 years. American Indian/Alaska native women had the smallest increases in both age groups, the report showed.
The NCHS analysis was based on data from the National Vital Statistics System’s Natality Data File, which includes information for all births in the United States.

Circumcision-related adverse events increase after infancy
The incidence of adverse events related to circumcision varies according to the age of the patient, increasing substantially in boys and adolescent males, compared with infants, according to a report published online May 12 in JAMA Pediatrics.
In the largest study by far of circumcisions in the United States, the rate of associated adverse events was 20-fold higher among boys who underwent the procedure between 1 and 9 years of age, and 10-fold higher among boys who had it after 10 years of age, than among boys who were circumcised during infancy, said Charbel El Bcheraoui, Ph.D., of the office of surveillance epidemiology and laboratory services at the Centers for Disease Control & Prevention, and associates.
Until now, studies of circumcision-related adverse events "were based on small samples, a single clinical site or state, cross-sectional data, or nonrepresentative cohorts," the investigators said. Their study, which included approximately 1.4 million circumcisions across the country, is the first to compare rates of adverse events across all age groups from neonates to adults, said Dr. El Bcheraoui, who is also of the Institute for Health Metrics and Evaluation at the University of Washington, Seattle, and colleagues.
To determine the risks associated with circumcision, the investigators analyzed information in a database representing 120 million inpatient hospitalizations at urban and rural, academic and nonacademic, medical centers of all sizes in every region of the country, as well as representing 870,000 outpatient medical providers. They reviewed 1,400,920 reimbursement claims for circumcisions to males of all ages during a 10-year period.
Of these, 95.3% procedures were done during infancy, 2.0% were done at ages 1-9 years, and 2.7% were done at ages 10 years and older.
The researchers identified ICD codes for adverse events that were likely related to circumcision, namely, partial or complete amputation of the penis; open wound on the penis; suturing of a penile laceration; reconstruction of the penis; replantation of the penis; division of penile adhesions; lysis or excision of postcircumcision penile adhesions; repair of incomplete circumcision; vascular disorder of the penis, including death or decay of tissue caused by insufficient blood supply; penile inflammation or edema; urethral or other penile strictures; and suturing of an incised penile artery.
The incidence of adverse events was 0.4% among boys circumcised during infancy, 9.06% among those circumcised at ages 1-9 years, and 5.31% among boys, adolescents, and adults circumcised at age 10 years or older, the investigators reported (JAMA Ped. 2014 May 12 [doi:10.1001/jamapediatrics.2013.5414]).
The most common adverse events were related to correctional procedures and bleeding.
The incidence of the most severe adverse event – penile amputation – was highest, at 0.17%, in the 10-and-older group. The total number of amputations was 71. The database doesn’t distinguish between partial and complete amputations, so the exact number of each type is not known.
It is possible that this analysis was affected by some confounding by indication, because older males in the United States are more likely to undergo circumcision for medical indications (infections or adhesions) than for cultural or religious reasons. "Future studies will need to carefully adjust for this potential source of confounding," Dr. El Bcheraoui and associates noted.
Dr. El Bcheraoui and associates reported no financial conflicts of interest.
The incidence of adverse events related to circumcision varies according to the age of the patient, increasing substantially in boys and adolescent males, compared with infants, according to a report published online May 12 in JAMA Pediatrics.
In the largest study by far of circumcisions in the United States, the rate of associated adverse events was 20-fold higher among boys who underwent the procedure between 1 and 9 years of age, and 10-fold higher among boys who had it after 10 years of age, than among boys who were circumcised during infancy, said Charbel El Bcheraoui, Ph.D., of the office of surveillance epidemiology and laboratory services at the Centers for Disease Control & Prevention, and associates.
Until now, studies of circumcision-related adverse events "were based on small samples, a single clinical site or state, cross-sectional data, or nonrepresentative cohorts," the investigators said. Their study, which included approximately 1.4 million circumcisions across the country, is the first to compare rates of adverse events across all age groups from neonates to adults, said Dr. El Bcheraoui, who is also of the Institute for Health Metrics and Evaluation at the University of Washington, Seattle, and colleagues.
To determine the risks associated with circumcision, the investigators analyzed information in a database representing 120 million inpatient hospitalizations at urban and rural, academic and nonacademic, medical centers of all sizes in every region of the country, as well as representing 870,000 outpatient medical providers. They reviewed 1,400,920 reimbursement claims for circumcisions to males of all ages during a 10-year period.
Of these, 95.3% procedures were done during infancy, 2.0% were done at ages 1-9 years, and 2.7% were done at ages 10 years and older.
The researchers identified ICD codes for adverse events that were likely related to circumcision, namely, partial or complete amputation of the penis; open wound on the penis; suturing of a penile laceration; reconstruction of the penis; replantation of the penis; division of penile adhesions; lysis or excision of postcircumcision penile adhesions; repair of incomplete circumcision; vascular disorder of the penis, including death or decay of tissue caused by insufficient blood supply; penile inflammation or edema; urethral or other penile strictures; and suturing of an incised penile artery.
The incidence of adverse events was 0.4% among boys circumcised during infancy, 9.06% among those circumcised at ages 1-9 years, and 5.31% among boys, adolescents, and adults circumcised at age 10 years or older, the investigators reported (JAMA Ped. 2014 May 12 [doi:10.1001/jamapediatrics.2013.5414]).
The most common adverse events were related to correctional procedures and bleeding.
The incidence of the most severe adverse event – penile amputation – was highest, at 0.17%, in the 10-and-older group. The total number of amputations was 71. The database doesn’t distinguish between partial and complete amputations, so the exact number of each type is not known.
It is possible that this analysis was affected by some confounding by indication, because older males in the United States are more likely to undergo circumcision for medical indications (infections or adhesions) than for cultural or religious reasons. "Future studies will need to carefully adjust for this potential source of confounding," Dr. El Bcheraoui and associates noted.
Dr. El Bcheraoui and associates reported no financial conflicts of interest.
The incidence of adverse events related to circumcision varies according to the age of the patient, increasing substantially in boys and adolescent males, compared with infants, according to a report published online May 12 in JAMA Pediatrics.
In the largest study by far of circumcisions in the United States, the rate of associated adverse events was 20-fold higher among boys who underwent the procedure between 1 and 9 years of age, and 10-fold higher among boys who had it after 10 years of age, than among boys who were circumcised during infancy, said Charbel El Bcheraoui, Ph.D., of the office of surveillance epidemiology and laboratory services at the Centers for Disease Control & Prevention, and associates.
Until now, studies of circumcision-related adverse events "were based on small samples, a single clinical site or state, cross-sectional data, or nonrepresentative cohorts," the investigators said. Their study, which included approximately 1.4 million circumcisions across the country, is the first to compare rates of adverse events across all age groups from neonates to adults, said Dr. El Bcheraoui, who is also of the Institute for Health Metrics and Evaluation at the University of Washington, Seattle, and colleagues.
To determine the risks associated with circumcision, the investigators analyzed information in a database representing 120 million inpatient hospitalizations at urban and rural, academic and nonacademic, medical centers of all sizes in every region of the country, as well as representing 870,000 outpatient medical providers. They reviewed 1,400,920 reimbursement claims for circumcisions to males of all ages during a 10-year period.
Of these, 95.3% procedures were done during infancy, 2.0% were done at ages 1-9 years, and 2.7% were done at ages 10 years and older.
The researchers identified ICD codes for adverse events that were likely related to circumcision, namely, partial or complete amputation of the penis; open wound on the penis; suturing of a penile laceration; reconstruction of the penis; replantation of the penis; division of penile adhesions; lysis or excision of postcircumcision penile adhesions; repair of incomplete circumcision; vascular disorder of the penis, including death or decay of tissue caused by insufficient blood supply; penile inflammation or edema; urethral or other penile strictures; and suturing of an incised penile artery.
The incidence of adverse events was 0.4% among boys circumcised during infancy, 9.06% among those circumcised at ages 1-9 years, and 5.31% among boys, adolescents, and adults circumcised at age 10 years or older, the investigators reported (JAMA Ped. 2014 May 12 [doi:10.1001/jamapediatrics.2013.5414]).
The most common adverse events were related to correctional procedures and bleeding.
The incidence of the most severe adverse event – penile amputation – was highest, at 0.17%, in the 10-and-older group. The total number of amputations was 71. The database doesn’t distinguish between partial and complete amputations, so the exact number of each type is not known.
It is possible that this analysis was affected by some confounding by indication, because older males in the United States are more likely to undergo circumcision for medical indications (infections or adhesions) than for cultural or religious reasons. "Future studies will need to carefully adjust for this potential source of confounding," Dr. El Bcheraoui and associates noted.
Dr. El Bcheraoui and associates reported no financial conflicts of interest.
FROM JAMA PEDIATRICS
Key clinical point: It is safer to perform circumcision during infancy.
Major finding: The incidence of circumcision-related adverse events was 0.4% among boys circumcised during infancy, 9.06% among those circumcised at ages 1-9 years, and 5.31% among males circumcised at age 10 years or older.
Data source: A retrospective cohort study of 1,400,920 circumcisions during a 10-year period among infants (95.3%), boys aged 1-9 years (2.0%), or males aged 10 years or older (2.7%) at all types of hospitals across the United States.
Disclosures: Dr. El Bcheraoui and associates reported no financial conflicts of interest.
One prenatal steroid dose is better than none
VANCOUVER, B.C. – When there isn’t time for a full course of prenatal steroids before early preterm birth, a partial course is better than nothing, according to investigators at the National Institute of Child Health and Human Development’s Neonatal Research Network.
In a study of 5,248 infants born between 24 and 27 weeks’ gestational age who were alive at 18-22 months, 17.6% (120/683) whose mothers got no prenatal steroids (PNS) before delivery had cerebral palsy, a statistically significant difference from the 13% (178/1,369) whose mothers got one dose of PNS – betamethasone in almost all cases – and the 10.5% (336/3,196) whose mothers got the full course of two betamethasone doses, 24 hours apart.
Similarly, intact survival at follow-up – survival free of hearing loss, blindness, and cerebral palsy, plus scores greater than 85 points on the Bayley Scales of Infant and Toddler Development III – was 55% in the no-PNS infants, 65% in the partial-PNS infants, and 69% in the PNS infants who got a full course, all statistically significant differences.
Compared with full-course PNS infants, those who got no PNS (odds ratio, 1.4; 95% confidence interval, 1.2-1.7) or partial PNS (OR, 1.2; 95% CI, 1.1-1.4) were more likely to have died or have neurodevelopmental impairment at 18-22 months.
Earlier results of the study, at discharge, were largely the same, with greater survival and fewer neurodevelopmental impairments when mothers got at least one dose of PNS before delivery.
The reason was that even one dose before delivery helped prevent both brain hemorrhages and cystic periventricular leucomalacia, the investigators found.
Prenatal steroids have long been known to help prevent both problems. What’s new in the findings is confirmation that even one dose helps.
"The intention is always to give a complete course," but when imminent delivery makes that impossible, even "one dose is better than no dose. The results help us counsel parents when we know" what dose children got before delivery. Also, "for research, the question shouldn’t be [prenatal] steroids, yes or no," but the completeness of the course, said lead investigator and neonatologist Sanjay Chawla of the department of pediatrics at the Children’s Hospital of Michigan, Detroit.
"Some people say, ‘She’s going to C-section in an hour, so it doesn’t matter’" That’s wrong. "One shot [of betamethasone] is still better than nothing. It makes a difference," said Dr. Nathalie Maitre, a neonatologist at Vanderbilt University in Nashville, Tenn., who helped moderate Dr. Chawla’s presentation at the Pediatric Academic Societies annual meeting.
There were some significant differences between the groups. No-PNS infants were born a bit earlier, at a mean of 24 weeks instead of about 25 weeks, and were a bit lighter at birth, 690 g instead of almost 800 g in the partial and full PNS groups. They were also a bit more likely to be black and on Medicaid.
Also, partial and full PNS infants were a bit more likely to be born by C-section. Boys and girls were split 50-50 in all three groups.
Dr. Chawla and Dr. Maitre said they had no relevant financial disclosures. The National Institutes of Health funded the work.
The findings of this study are not surprising, but confirm what physicians have intuitively believed to be true: that a partial dose of antenatal steroids is better than no steroids for infants delivered preterm, commented Dr. James Cummings.
Two small retrospective studies done about 10 years ago suggested a dose-dependent effect of antenatal steroids on several neonatal outcomes, including intracranial hemorrhage and death, but neither study reported long-term follow-up data, as the current study does.
"We don't really know how much antenatal steroid to give the mother, because we have limited knowledge regarding the optimal fetal levels to improve outcome. But the data are irrefutable that maternal administration of steroids does reduce the risk of respiratory distress syndrome and intracranial hemorrhage. This study is reassuring and consistent with what we know," he said.
What is missing, and the researchers may have this information, is whether the proximity of steroid dosing to delivery affected outcomes. This is important, since we know that the physiologic effects of steroids generally accrue over several hours. This suggests that when threatened with a preterm delivery, the obstetrician shouldn't hesitate about giving steroids, but should administer them as soon as possible, Dr. Cummings said.
Dr. Cummings is vice chair of pediatrics at Albany (N.Y.) Medical College and a member of the American Academy of Pediatrics Committee on the Fetus and Newborn. Dr. Cummings, who was asked to comment on the study, said he had no relevant financial disclosures.
The findings of this study are not surprising, but confirm what physicians have intuitively believed to be true: that a partial dose of antenatal steroids is better than no steroids for infants delivered preterm, commented Dr. James Cummings.
Two small retrospective studies done about 10 years ago suggested a dose-dependent effect of antenatal steroids on several neonatal outcomes, including intracranial hemorrhage and death, but neither study reported long-term follow-up data, as the current study does.
"We don't really know how much antenatal steroid to give the mother, because we have limited knowledge regarding the optimal fetal levels to improve outcome. But the data are irrefutable that maternal administration of steroids does reduce the risk of respiratory distress syndrome and intracranial hemorrhage. This study is reassuring and consistent with what we know," he said.
What is missing, and the researchers may have this information, is whether the proximity of steroid dosing to delivery affected outcomes. This is important, since we know that the physiologic effects of steroids generally accrue over several hours. This suggests that when threatened with a preterm delivery, the obstetrician shouldn't hesitate about giving steroids, but should administer them as soon as possible, Dr. Cummings said.
Dr. Cummings is vice chair of pediatrics at Albany (N.Y.) Medical College and a member of the American Academy of Pediatrics Committee on the Fetus and Newborn. Dr. Cummings, who was asked to comment on the study, said he had no relevant financial disclosures.
The findings of this study are not surprising, but confirm what physicians have intuitively believed to be true: that a partial dose of antenatal steroids is better than no steroids for infants delivered preterm, commented Dr. James Cummings.
Two small retrospective studies done about 10 years ago suggested a dose-dependent effect of antenatal steroids on several neonatal outcomes, including intracranial hemorrhage and death, but neither study reported long-term follow-up data, as the current study does.
"We don't really know how much antenatal steroid to give the mother, because we have limited knowledge regarding the optimal fetal levels to improve outcome. But the data are irrefutable that maternal administration of steroids does reduce the risk of respiratory distress syndrome and intracranial hemorrhage. This study is reassuring and consistent with what we know," he said.
What is missing, and the researchers may have this information, is whether the proximity of steroid dosing to delivery affected outcomes. This is important, since we know that the physiologic effects of steroids generally accrue over several hours. This suggests that when threatened with a preterm delivery, the obstetrician shouldn't hesitate about giving steroids, but should administer them as soon as possible, Dr. Cummings said.
Dr. Cummings is vice chair of pediatrics at Albany (N.Y.) Medical College and a member of the American Academy of Pediatrics Committee on the Fetus and Newborn. Dr. Cummings, who was asked to comment on the study, said he had no relevant financial disclosures.
VANCOUVER, B.C. – When there isn’t time for a full course of prenatal steroids before early preterm birth, a partial course is better than nothing, according to investigators at the National Institute of Child Health and Human Development’s Neonatal Research Network.
In a study of 5,248 infants born between 24 and 27 weeks’ gestational age who were alive at 18-22 months, 17.6% (120/683) whose mothers got no prenatal steroids (PNS) before delivery had cerebral palsy, a statistically significant difference from the 13% (178/1,369) whose mothers got one dose of PNS – betamethasone in almost all cases – and the 10.5% (336/3,196) whose mothers got the full course of two betamethasone doses, 24 hours apart.
Similarly, intact survival at follow-up – survival free of hearing loss, blindness, and cerebral palsy, plus scores greater than 85 points on the Bayley Scales of Infant and Toddler Development III – was 55% in the no-PNS infants, 65% in the partial-PNS infants, and 69% in the PNS infants who got a full course, all statistically significant differences.
Compared with full-course PNS infants, those who got no PNS (odds ratio, 1.4; 95% confidence interval, 1.2-1.7) or partial PNS (OR, 1.2; 95% CI, 1.1-1.4) were more likely to have died or have neurodevelopmental impairment at 18-22 months.
Earlier results of the study, at discharge, were largely the same, with greater survival and fewer neurodevelopmental impairments when mothers got at least one dose of PNS before delivery.
The reason was that even one dose before delivery helped prevent both brain hemorrhages and cystic periventricular leucomalacia, the investigators found.
Prenatal steroids have long been known to help prevent both problems. What’s new in the findings is confirmation that even one dose helps.
"The intention is always to give a complete course," but when imminent delivery makes that impossible, even "one dose is better than no dose. The results help us counsel parents when we know" what dose children got before delivery. Also, "for research, the question shouldn’t be [prenatal] steroids, yes or no," but the completeness of the course, said lead investigator and neonatologist Sanjay Chawla of the department of pediatrics at the Children’s Hospital of Michigan, Detroit.
"Some people say, ‘She’s going to C-section in an hour, so it doesn’t matter’" That’s wrong. "One shot [of betamethasone] is still better than nothing. It makes a difference," said Dr. Nathalie Maitre, a neonatologist at Vanderbilt University in Nashville, Tenn., who helped moderate Dr. Chawla’s presentation at the Pediatric Academic Societies annual meeting.
There were some significant differences between the groups. No-PNS infants were born a bit earlier, at a mean of 24 weeks instead of about 25 weeks, and were a bit lighter at birth, 690 g instead of almost 800 g in the partial and full PNS groups. They were also a bit more likely to be black and on Medicaid.
Also, partial and full PNS infants were a bit more likely to be born by C-section. Boys and girls were split 50-50 in all three groups.
Dr. Chawla and Dr. Maitre said they had no relevant financial disclosures. The National Institutes of Health funded the work.
VANCOUVER, B.C. – When there isn’t time for a full course of prenatal steroids before early preterm birth, a partial course is better than nothing, according to investigators at the National Institute of Child Health and Human Development’s Neonatal Research Network.
In a study of 5,248 infants born between 24 and 27 weeks’ gestational age who were alive at 18-22 months, 17.6% (120/683) whose mothers got no prenatal steroids (PNS) before delivery had cerebral palsy, a statistically significant difference from the 13% (178/1,369) whose mothers got one dose of PNS – betamethasone in almost all cases – and the 10.5% (336/3,196) whose mothers got the full course of two betamethasone doses, 24 hours apart.
Similarly, intact survival at follow-up – survival free of hearing loss, blindness, and cerebral palsy, plus scores greater than 85 points on the Bayley Scales of Infant and Toddler Development III – was 55% in the no-PNS infants, 65% in the partial-PNS infants, and 69% in the PNS infants who got a full course, all statistically significant differences.
Compared with full-course PNS infants, those who got no PNS (odds ratio, 1.4; 95% confidence interval, 1.2-1.7) or partial PNS (OR, 1.2; 95% CI, 1.1-1.4) were more likely to have died or have neurodevelopmental impairment at 18-22 months.
Earlier results of the study, at discharge, were largely the same, with greater survival and fewer neurodevelopmental impairments when mothers got at least one dose of PNS before delivery.
The reason was that even one dose before delivery helped prevent both brain hemorrhages and cystic periventricular leucomalacia, the investigators found.
Prenatal steroids have long been known to help prevent both problems. What’s new in the findings is confirmation that even one dose helps.
"The intention is always to give a complete course," but when imminent delivery makes that impossible, even "one dose is better than no dose. The results help us counsel parents when we know" what dose children got before delivery. Also, "for research, the question shouldn’t be [prenatal] steroids, yes or no," but the completeness of the course, said lead investigator and neonatologist Sanjay Chawla of the department of pediatrics at the Children’s Hospital of Michigan, Detroit.
"Some people say, ‘She’s going to C-section in an hour, so it doesn’t matter’" That’s wrong. "One shot [of betamethasone] is still better than nothing. It makes a difference," said Dr. Nathalie Maitre, a neonatologist at Vanderbilt University in Nashville, Tenn., who helped moderate Dr. Chawla’s presentation at the Pediatric Academic Societies annual meeting.
There were some significant differences between the groups. No-PNS infants were born a bit earlier, at a mean of 24 weeks instead of about 25 weeks, and were a bit lighter at birth, 690 g instead of almost 800 g in the partial and full PNS groups. They were also a bit more likely to be black and on Medicaid.
Also, partial and full PNS infants were a bit more likely to be born by C-section. Boys and girls were split 50-50 in all three groups.
Dr. Chawla and Dr. Maitre said they had no relevant financial disclosures. The National Institutes of Health funded the work.
AT THE PAS ANNUAL MEETING
Key clinical point: It is important to give at least a partial course of prenatal steroids before early preterm delivery.
Major finding: Compared with complete prenatal steroid courses, no PNS (OR, 1.4; 95% CI, 1.2-1.7) and partial PNS (OR, 1.2; 95% CI, 1.1-1.4) are both associated with neurodevelopmental impairment and mortality at 18-22 months.
Data source: A Neonatal Research Network study of infants born from 24 to 27 weeks’ gestational age
Disclosures: The lead investigator had no disclosures. The National Institutes of Health funded the work.
Vertical incision at C-section in morbidly obese women led to lower infection rates
NEW ORLEANS – Vertical incisions in morbidly obese women undergoing a primary cesarean delivery are associated with fewer wound complications, compared with transverse incisions.
The findings were "contrary to expectations," presenter Dr. Caroline C. Marrs told an audience at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
The registry study of morbidly obese women who had had a primary C-section showed that those with a vertical incision were found to have higher rates of all adverse maternal outcomes, except for transfusions, but had lower incision-to-delivery times (9.2 plus or minus 5.5 vs. 11.1 plus or minus 6.1, P less than .001). "However, there was significant confounder bias, because after adjusting for significant baseline and clinical characteristics such as race, smoking status, and body mass index, vertical incisions were not associated with higher rates of composite maternal morbidity," said Dr. Marrs of the University of Texas Health Science Center in Houston.
Using data collected between 1999 and 2002 for the cesarean registry of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network from 19 academic medical centers, Dr. Marrs and her colleagues identified 3,200 women with a body mass index of 40 kg/m2 at the time of their delivery by primary C-section whose incision type was known
The transverse skin incision cohort numbered 2,603 (81%), and the vertical incision group was 597 (19%).
An analysis of patient characteristics indicated the type of incision a woman had positively correlated with her race, smoking status, and insurance type, as well as whether the woman had gestational diabetes, chorioamnionitis, non–lower-segment hysterotomy, and an emergency C-section.
Logistical regression showed that vertical skin incisions were associated with parity (1.16, adjusted odds ratio 1.09-1.25); black race (1.24, AOR 1.03-1.51), maternal body mass index (1.06, AOR 1.04-1.08), low transverse hysterotomy (4.46, AOR 3.21-6.20), and nonemergent cesarean delivery (0.49, AOR 0.39-0.62).
A univariate analysis of composite wound complications such as seroma or hematoma indicated that vertical wounds were more associated with higher complication rates (4.2% of the vertical group vs. 1.7% of the transverse group, P less than .001).
Multivariate progression analysis indicated that the adjusted odds ratio for a vertical incision being a risk factor for wound complications was 0.32 (0.17-62). Other risk factors noted were: nonwhite race (0.48, AOR 0.25 to 0.94), maternal BMI (1.05, AOR 1.00 to 1.09), and ASA score (2.10, AOR 1.21-3.65).
"We suspect selection bias played a role," said Dr. Marrs. "Given the differences in baseline clinical characteristics of women who had vertical incisions, surgeons may have chosen this route based on selected factors such as BMI or need for emergency delivery."
Dr. Marrs did not have any relevant disclosures.
NEW ORLEANS – Vertical incisions in morbidly obese women undergoing a primary cesarean delivery are associated with fewer wound complications, compared with transverse incisions.
The findings were "contrary to expectations," presenter Dr. Caroline C. Marrs told an audience at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
The registry study of morbidly obese women who had had a primary C-section showed that those with a vertical incision were found to have higher rates of all adverse maternal outcomes, except for transfusions, but had lower incision-to-delivery times (9.2 plus or minus 5.5 vs. 11.1 plus or minus 6.1, P less than .001). "However, there was significant confounder bias, because after adjusting for significant baseline and clinical characteristics such as race, smoking status, and body mass index, vertical incisions were not associated with higher rates of composite maternal morbidity," said Dr. Marrs of the University of Texas Health Science Center in Houston.
Using data collected between 1999 and 2002 for the cesarean registry of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network from 19 academic medical centers, Dr. Marrs and her colleagues identified 3,200 women with a body mass index of 40 kg/m2 at the time of their delivery by primary C-section whose incision type was known
The transverse skin incision cohort numbered 2,603 (81%), and the vertical incision group was 597 (19%).
An analysis of patient characteristics indicated the type of incision a woman had positively correlated with her race, smoking status, and insurance type, as well as whether the woman had gestational diabetes, chorioamnionitis, non–lower-segment hysterotomy, and an emergency C-section.
Logistical regression showed that vertical skin incisions were associated with parity (1.16, adjusted odds ratio 1.09-1.25); black race (1.24, AOR 1.03-1.51), maternal body mass index (1.06, AOR 1.04-1.08), low transverse hysterotomy (4.46, AOR 3.21-6.20), and nonemergent cesarean delivery (0.49, AOR 0.39-0.62).
A univariate analysis of composite wound complications such as seroma or hematoma indicated that vertical wounds were more associated with higher complication rates (4.2% of the vertical group vs. 1.7% of the transverse group, P less than .001).
Multivariate progression analysis indicated that the adjusted odds ratio for a vertical incision being a risk factor for wound complications was 0.32 (0.17-62). Other risk factors noted were: nonwhite race (0.48, AOR 0.25 to 0.94), maternal BMI (1.05, AOR 1.00 to 1.09), and ASA score (2.10, AOR 1.21-3.65).
"We suspect selection bias played a role," said Dr. Marrs. "Given the differences in baseline clinical characteristics of women who had vertical incisions, surgeons may have chosen this route based on selected factors such as BMI or need for emergency delivery."
Dr. Marrs did not have any relevant disclosures.
NEW ORLEANS – Vertical incisions in morbidly obese women undergoing a primary cesarean delivery are associated with fewer wound complications, compared with transverse incisions.
The findings were "contrary to expectations," presenter Dr. Caroline C. Marrs told an audience at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
The registry study of morbidly obese women who had had a primary C-section showed that those with a vertical incision were found to have higher rates of all adverse maternal outcomes, except for transfusions, but had lower incision-to-delivery times (9.2 plus or minus 5.5 vs. 11.1 plus or minus 6.1, P less than .001). "However, there was significant confounder bias, because after adjusting for significant baseline and clinical characteristics such as race, smoking status, and body mass index, vertical incisions were not associated with higher rates of composite maternal morbidity," said Dr. Marrs of the University of Texas Health Science Center in Houston.
Using data collected between 1999 and 2002 for the cesarean registry of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network from 19 academic medical centers, Dr. Marrs and her colleagues identified 3,200 women with a body mass index of 40 kg/m2 at the time of their delivery by primary C-section whose incision type was known
The transverse skin incision cohort numbered 2,603 (81%), and the vertical incision group was 597 (19%).
An analysis of patient characteristics indicated the type of incision a woman had positively correlated with her race, smoking status, and insurance type, as well as whether the woman had gestational diabetes, chorioamnionitis, non–lower-segment hysterotomy, and an emergency C-section.
Logistical regression showed that vertical skin incisions were associated with parity (1.16, adjusted odds ratio 1.09-1.25); black race (1.24, AOR 1.03-1.51), maternal body mass index (1.06, AOR 1.04-1.08), low transverse hysterotomy (4.46, AOR 3.21-6.20), and nonemergent cesarean delivery (0.49, AOR 0.39-0.62).
A univariate analysis of composite wound complications such as seroma or hematoma indicated that vertical wounds were more associated with higher complication rates (4.2% of the vertical group vs. 1.7% of the transverse group, P less than .001).
Multivariate progression analysis indicated that the adjusted odds ratio for a vertical incision being a risk factor for wound complications was 0.32 (0.17-62). Other risk factors noted were: nonwhite race (0.48, AOR 0.25 to 0.94), maternal BMI (1.05, AOR 1.00 to 1.09), and ASA score (2.10, AOR 1.21-3.65).
"We suspect selection bias played a role," said Dr. Marrs. "Given the differences in baseline clinical characteristics of women who had vertical incisions, surgeons may have chosen this route based on selected factors such as BMI or need for emergency delivery."
Dr. Marrs did not have any relevant disclosures.
AT THE PREGNANCY MEETING
Key clinical point: Vertical incisions at primary C-section appear to be a better choice for morbidly obese women, at least in terms of infection rate.
Major finding: Vertical incisions are associated with lower wound complication rates compared with transverse incisions in morbidly obese pregnant women.
Data source: Registry cohort study with multivariate analysis of 3,200 morbidly obese women who underwent primary cesarean delivery: 2,603 with a transverse incision and 597 with a vertical one.
Disclosures: Dr. Marrs did not have any relevant disclosures.
Data support suture vs. staple skin closure after cesarean delivery
CHICAGO – Suture closure of the skin incision after cesarean delivery was associated with significantly improved patient satisfaction, compared with staple closure, according to findings in a prospective, randomized, multicenter study of 746 women.
Suture closure also was associated with improved patient and physician assessments of cosmesis, compared with staple closure, Dr. Jonah Fleisher reported at the annual meeting of the American Congress of Obstetricians and Gynecologists.
The median interquartile range of overall "satisfaction with method of closure" scores on the validated Patient and Observer Scar Assessment Scale (POSAS) differed significantly for 299 suture patients and 307 staple patients for whom the data were available (scores of 10 vs. 9, respectively), as did median "satisfaction with appearance of skin incision" scores (also 10 vs. 9, respectively), said Dr. Fleisher of Geisinger Health System, Danville, Pa.
The cosmetic-specific question was included to help adjust for the multifactorial nature of the overall satisfaction score, which could be affected by the patient’s degree of pain, healing time, need for extra office visits, and frequency of complications, among other factors.
The two measures correlated positively, and both subjective and objective components of the POSAS favored suture closure, he noted.
Study participants were women undergoing cesarean delivery via low-transverse skin incisions at any of three participating centers. After fascia closure, the women were allocated to either the suture (type was surgeon’s choice) or metal staple closure group. Staples were removed between postoperative days 4 and 10.
About 1.3 million cesarean deliveries are performed each year in the United States, Dr. Fleisher said.
"Those scars that are formed as a result are very important to patients, both as far as cosmetic and general satisfaction ... and it turns out they are important to obstetricians, too," he added, noting that data to guide decision making are lacking.
In the current study, the differences between the suture and staple groups were significant, but patients in both groups had high rates of satisfaction.
"Given these considerations, I would suggest that we ought to incorporate wound complications rates into the decision of which method to use," he said.
An article that addresses the wound complication rates in this study is currently in press and scheduled for publication in the American Journal of Obstetrics & Gynecology in June. The data show a 57% lower complication rate with suture closure vs. staple closure, Dr. Fleisher said.
"The bottom line is, for all these reasons, we have moved to recommending suture closure in all transverse C-sections," he said.
As for whether the findings apply to other types of surgical operations, such as abdominal hysterectomy, Dr. Fleisher said there are many changes in pregnancy, including immunologic changes, that don’t necessarily apply to nonobstetric situations.
"There is some literature in the general surgery area about this, and some literature in gynecologic surgery, but given the immunologic changes – I think we’re seeing that even the adhesion data is not necessarily the same in those two contexts. ... I wouldn’t want to generalize from this to nonobstetric indications," he said.
This study was supported by Ethicon. Dr. Fleisher reported having no disclosures.
CHICAGO – Suture closure of the skin incision after cesarean delivery was associated with significantly improved patient satisfaction, compared with staple closure, according to findings in a prospective, randomized, multicenter study of 746 women.
Suture closure also was associated with improved patient and physician assessments of cosmesis, compared with staple closure, Dr. Jonah Fleisher reported at the annual meeting of the American Congress of Obstetricians and Gynecologists.
The median interquartile range of overall "satisfaction with method of closure" scores on the validated Patient and Observer Scar Assessment Scale (POSAS) differed significantly for 299 suture patients and 307 staple patients for whom the data were available (scores of 10 vs. 9, respectively), as did median "satisfaction with appearance of skin incision" scores (also 10 vs. 9, respectively), said Dr. Fleisher of Geisinger Health System, Danville, Pa.
The cosmetic-specific question was included to help adjust for the multifactorial nature of the overall satisfaction score, which could be affected by the patient’s degree of pain, healing time, need for extra office visits, and frequency of complications, among other factors.
The two measures correlated positively, and both subjective and objective components of the POSAS favored suture closure, he noted.
Study participants were women undergoing cesarean delivery via low-transverse skin incisions at any of three participating centers. After fascia closure, the women were allocated to either the suture (type was surgeon’s choice) or metal staple closure group. Staples were removed between postoperative days 4 and 10.
About 1.3 million cesarean deliveries are performed each year in the United States, Dr. Fleisher said.
"Those scars that are formed as a result are very important to patients, both as far as cosmetic and general satisfaction ... and it turns out they are important to obstetricians, too," he added, noting that data to guide decision making are lacking.
In the current study, the differences between the suture and staple groups were significant, but patients in both groups had high rates of satisfaction.
"Given these considerations, I would suggest that we ought to incorporate wound complications rates into the decision of which method to use," he said.
An article that addresses the wound complication rates in this study is currently in press and scheduled for publication in the American Journal of Obstetrics & Gynecology in June. The data show a 57% lower complication rate with suture closure vs. staple closure, Dr. Fleisher said.
"The bottom line is, for all these reasons, we have moved to recommending suture closure in all transverse C-sections," he said.
As for whether the findings apply to other types of surgical operations, such as abdominal hysterectomy, Dr. Fleisher said there are many changes in pregnancy, including immunologic changes, that don’t necessarily apply to nonobstetric situations.
"There is some literature in the general surgery area about this, and some literature in gynecologic surgery, but given the immunologic changes – I think we’re seeing that even the adhesion data is not necessarily the same in those two contexts. ... I wouldn’t want to generalize from this to nonobstetric indications," he said.
This study was supported by Ethicon. Dr. Fleisher reported having no disclosures.
CHICAGO – Suture closure of the skin incision after cesarean delivery was associated with significantly improved patient satisfaction, compared with staple closure, according to findings in a prospective, randomized, multicenter study of 746 women.
Suture closure also was associated with improved patient and physician assessments of cosmesis, compared with staple closure, Dr. Jonah Fleisher reported at the annual meeting of the American Congress of Obstetricians and Gynecologists.
The median interquartile range of overall "satisfaction with method of closure" scores on the validated Patient and Observer Scar Assessment Scale (POSAS) differed significantly for 299 suture patients and 307 staple patients for whom the data were available (scores of 10 vs. 9, respectively), as did median "satisfaction with appearance of skin incision" scores (also 10 vs. 9, respectively), said Dr. Fleisher of Geisinger Health System, Danville, Pa.
The cosmetic-specific question was included to help adjust for the multifactorial nature of the overall satisfaction score, which could be affected by the patient’s degree of pain, healing time, need for extra office visits, and frequency of complications, among other factors.
The two measures correlated positively, and both subjective and objective components of the POSAS favored suture closure, he noted.
Study participants were women undergoing cesarean delivery via low-transverse skin incisions at any of three participating centers. After fascia closure, the women were allocated to either the suture (type was surgeon’s choice) or metal staple closure group. Staples were removed between postoperative days 4 and 10.
About 1.3 million cesarean deliveries are performed each year in the United States, Dr. Fleisher said.
"Those scars that are formed as a result are very important to patients, both as far as cosmetic and general satisfaction ... and it turns out they are important to obstetricians, too," he added, noting that data to guide decision making are lacking.
In the current study, the differences between the suture and staple groups were significant, but patients in both groups had high rates of satisfaction.
"Given these considerations, I would suggest that we ought to incorporate wound complications rates into the decision of which method to use," he said.
An article that addresses the wound complication rates in this study is currently in press and scheduled for publication in the American Journal of Obstetrics & Gynecology in June. The data show a 57% lower complication rate with suture closure vs. staple closure, Dr. Fleisher said.
"The bottom line is, for all these reasons, we have moved to recommending suture closure in all transverse C-sections," he said.
As for whether the findings apply to other types of surgical operations, such as abdominal hysterectomy, Dr. Fleisher said there are many changes in pregnancy, including immunologic changes, that don’t necessarily apply to nonobstetric situations.
"There is some literature in the general surgery area about this, and some literature in gynecologic surgery, but given the immunologic changes – I think we’re seeing that even the adhesion data is not necessarily the same in those two contexts. ... I wouldn’t want to generalize from this to nonobstetric indications," he said.
This study was supported by Ethicon. Dr. Fleisher reported having no disclosures.
AT THE ACOG ANNUAL CLINICAL MEETING
Key clinical point: Patients and physicians preferred sutures over staples for skin closure after cesarean section.
Major finding: Satisfaction scores were 10 and 9 (interquartile range) for sutures vs. staples.
Data source: A prospective, multicenter, randomized trial involving 746 women.
Disclosures: This study was supported by Ethicon. Dr. Fleisher reported having no disclosures.
Doubt cast on benefit of endotracheal suctioning for meconium
VANCOUVER – The long-standing practice of endotracheal suctioning in nonvigorous neonates born with meconium-stained amniotic fluid does not reduce adverse outcomes, finds an open-label, randomized trial conducted among 175 term singleton neonates at a tertiary care hospital in India.
Although this practice has been used since the 1970s, it has not been rigorously tested in randomized trials, noted lead investigator Dr. Sushma Nangia, a neonatologist and professor of pediatrics at Lady Hardinge Medical College in New Delhi.
In a statement addressing neonatal resuscitation, the American Academy of Pediatrics and American Heart Association found "insufficient evidence to recommend a change in the current practice" (Pediatrics. 2010;126:e1400-13).
Trial results showed that 26% of the neonates who were not intubated and suctioned developed meconium aspiration syndrome, compared with 32% of their intubated and suctioned counterparts, a nonsignificant difference, researchers reported at the annual meeting of the Pediatric Academic Societies. The distribution of syndrome severity was also statistically indistinguishable.
Additionally, 5% of the neonates in the nonsuctioned group and 10% in the suctioned group died, another nonsignificant difference.
Rates of other adverse outcomes also were essentially the same, except that the nonsuctioned neonates actually had significantly shorter durations of respiratory distress (19 vs. 43 hours) and mechanical ventilation (25 vs. 43 hours).
"In nonvigorous full-term neonates born to mothers with meconium-stained amniotic fluid, our study demonstrated that not performing endotracheal suction to clear the airway during neonatal resuscitation did not increase the incidence of meconium aspiration syndrome or predispose to death," Dr. Nangia commented.
Session attendee Dr. Martin Keszler of Brown University, Providence, R.I., said, "Congratulations for having the courage to do this important study. All of us have been wondering about it, but it’s a practice so deeply ingrained that at least in our litigious environment, it would be very difficult to do. ... I think that this is a very important study because it can reassure future investigators to get the courage up to do this very important work."
"Certainly, it was encouraging that [no endotracheal suctioning] was no worse than control. It even seems that it was better. ... I wonder if you could speculate ..., is the intervention truly harmful and are we really better off leaving them alone?" he asked.
"We really don’t have the numbers that are required to do kind of an equivalence study," Dr. Nangia replied. "So this is just the pilot where we have 175 babies."
Another attendee asked, "With these results, can you give us an idea of the sample size you need to prove [the findings] particularly in the babies with thick meconium? How many babies will you need to test the hypothesis?"
Given the incidence of meconium aspiration syndrome, "from a national perinatal database, we think we would require about 480 babies to study the difference," said Dr. Nangia.
Dr. Nangia disclosed no relevant conflicts of interest.
VANCOUVER – The long-standing practice of endotracheal suctioning in nonvigorous neonates born with meconium-stained amniotic fluid does not reduce adverse outcomes, finds an open-label, randomized trial conducted among 175 term singleton neonates at a tertiary care hospital in India.
Although this practice has been used since the 1970s, it has not been rigorously tested in randomized trials, noted lead investigator Dr. Sushma Nangia, a neonatologist and professor of pediatrics at Lady Hardinge Medical College in New Delhi.
In a statement addressing neonatal resuscitation, the American Academy of Pediatrics and American Heart Association found "insufficient evidence to recommend a change in the current practice" (Pediatrics. 2010;126:e1400-13).
Trial results showed that 26% of the neonates who were not intubated and suctioned developed meconium aspiration syndrome, compared with 32% of their intubated and suctioned counterparts, a nonsignificant difference, researchers reported at the annual meeting of the Pediatric Academic Societies. The distribution of syndrome severity was also statistically indistinguishable.
Additionally, 5% of the neonates in the nonsuctioned group and 10% in the suctioned group died, another nonsignificant difference.
Rates of other adverse outcomes also were essentially the same, except that the nonsuctioned neonates actually had significantly shorter durations of respiratory distress (19 vs. 43 hours) and mechanical ventilation (25 vs. 43 hours).
"In nonvigorous full-term neonates born to mothers with meconium-stained amniotic fluid, our study demonstrated that not performing endotracheal suction to clear the airway during neonatal resuscitation did not increase the incidence of meconium aspiration syndrome or predispose to death," Dr. Nangia commented.
Session attendee Dr. Martin Keszler of Brown University, Providence, R.I., said, "Congratulations for having the courage to do this important study. All of us have been wondering about it, but it’s a practice so deeply ingrained that at least in our litigious environment, it would be very difficult to do. ... I think that this is a very important study because it can reassure future investigators to get the courage up to do this very important work."
"Certainly, it was encouraging that [no endotracheal suctioning] was no worse than control. It even seems that it was better. ... I wonder if you could speculate ..., is the intervention truly harmful and are we really better off leaving them alone?" he asked.
"We really don’t have the numbers that are required to do kind of an equivalence study," Dr. Nangia replied. "So this is just the pilot where we have 175 babies."
Another attendee asked, "With these results, can you give us an idea of the sample size you need to prove [the findings] particularly in the babies with thick meconium? How many babies will you need to test the hypothesis?"
Given the incidence of meconium aspiration syndrome, "from a national perinatal database, we think we would require about 480 babies to study the difference," said Dr. Nangia.
Dr. Nangia disclosed no relevant conflicts of interest.
VANCOUVER – The long-standing practice of endotracheal suctioning in nonvigorous neonates born with meconium-stained amniotic fluid does not reduce adverse outcomes, finds an open-label, randomized trial conducted among 175 term singleton neonates at a tertiary care hospital in India.
Although this practice has been used since the 1970s, it has not been rigorously tested in randomized trials, noted lead investigator Dr. Sushma Nangia, a neonatologist and professor of pediatrics at Lady Hardinge Medical College in New Delhi.
In a statement addressing neonatal resuscitation, the American Academy of Pediatrics and American Heart Association found "insufficient evidence to recommend a change in the current practice" (Pediatrics. 2010;126:e1400-13).
Trial results showed that 26% of the neonates who were not intubated and suctioned developed meconium aspiration syndrome, compared with 32% of their intubated and suctioned counterparts, a nonsignificant difference, researchers reported at the annual meeting of the Pediatric Academic Societies. The distribution of syndrome severity was also statistically indistinguishable.
Additionally, 5% of the neonates in the nonsuctioned group and 10% in the suctioned group died, another nonsignificant difference.
Rates of other adverse outcomes also were essentially the same, except that the nonsuctioned neonates actually had significantly shorter durations of respiratory distress (19 vs. 43 hours) and mechanical ventilation (25 vs. 43 hours).
"In nonvigorous full-term neonates born to mothers with meconium-stained amniotic fluid, our study demonstrated that not performing endotracheal suction to clear the airway during neonatal resuscitation did not increase the incidence of meconium aspiration syndrome or predispose to death," Dr. Nangia commented.
Session attendee Dr. Martin Keszler of Brown University, Providence, R.I., said, "Congratulations for having the courage to do this important study. All of us have been wondering about it, but it’s a practice so deeply ingrained that at least in our litigious environment, it would be very difficult to do. ... I think that this is a very important study because it can reassure future investigators to get the courage up to do this very important work."
"Certainly, it was encouraging that [no endotracheal suctioning] was no worse than control. It even seems that it was better. ... I wonder if you could speculate ..., is the intervention truly harmful and are we really better off leaving them alone?" he asked.
"We really don’t have the numbers that are required to do kind of an equivalence study," Dr. Nangia replied. "So this is just the pilot where we have 175 babies."
Another attendee asked, "With these results, can you give us an idea of the sample size you need to prove [the findings] particularly in the babies with thick meconium? How many babies will you need to test the hypothesis?"
Given the incidence of meconium aspiration syndrome, "from a national perinatal database, we think we would require about 480 babies to study the difference," said Dr. Nangia.
Dr. Nangia disclosed no relevant conflicts of interest.
AT THE PAS ANNUAL MEETING
Top clinical point: It may be better to not perform endotracheal suctioning in nonvigorous neonates born with meconium-stained amniotic fluid.
Major finding: The incidences of meconium aspiration syndrome and death did not differ significantly between infants who did and did not receive endotracheal suctioning.
Data source: A randomized trial among 175 nonvigorous neonates born with meconium-stained amniotic fluid.
Disclosures: Dr. Nangia disclosed no relevant conflicts of interest.
Perineal body stretch during labor does not predict adverse outcomes
SCOTTSDALE, ARIZ. – The extent of stretching of the perineal body during the second stage of labor is not helpful in predicting which women will experience adverse obstetric and postpartum outcomes, new data show.
Short perineal body length is known to increase the risk of severe perineal laceration at the time of delivery as well as postpartum functional disorders, noted presenting author Dr. Jill Alldredge. Maternal expulsive efforts during the second stage of labor that stretch the pelvic floor may also damage the pelvic floor muscles.
She and her colleagues performed a planned secondary analysis of the APPLE cohort (Alterations in the Pelvic Floor in Pregnancy, Labor and Ensuing Years), analyzing data from 448 nulliparous women who had a vaginal birth attended by a certified nurse-midwife, had repeated perineal measurements over time, and were followed prospectively to 12 months post partum.
On average, perineal body length increased by about 2.4 cm in the cohort between the antepartum period and the maximal length during the second stage of labor, according to data reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
However, neither perineal body length nor change in this length at any time point was associated with perineal lacerations, or with urinary or anal incontinence or not being sexually active at 6 months post partum.
"We can see that the perineum is dynamic and does stretch during labor. However, measurement of the perineal body length and change in perineal body length between the antepartum, intrapartum, and post partum time periods does not predict perineal trauma or postpartum pelvic floor dysfunction," commented Dr. Alldredge, an obstetrics-gynecology resident at the University of New Mexico in Albuquerque.
APPLE participants had measurement of the perineal body length during the antepartum period, at the onset of labor, at the onset of and every 10 minutes during the second stage, and at 6 and 12 months post partum. The anal opening and the genital hiatus also were measured during the second stage of labor.
At 6 months, the women completed a set of questionnaires assessing pelvic floor function: the Incontinence Severity Index, the Wexner Fecal Incontinence Scale, and the Female Sexual Function Index.
The mean perineal body length was 3.7 cm during the antepartum period, and the mean maximal perineal body length during the second stage of labor was 6.1 cm, she said at the meeting, jointly sponsored by the American College of Surgeons.
During the second stage of labor, the maximal anal opening was 2.0 cm on average. The genital hiatus had an anterior-posterior maximal diameter of 7.5 cm, a maximal transverse diameter of 4.7 cm, and a maximal introital area of 119.4 cm2.
Overall, 35% of women experienced a second-degree or worse perineal tear. And at 6 months post partum, 72% had at least mild urinary incontinence, 68% had at least mild anal incontinence, and 13% were not sexually active.
However, analyses showed that neither perineal body length nor stretch at any of the time points assessed was significantly associated with any of these outcomes.
Dr. Alldredge disclosed no relevant conflicts of interest.
SCOTTSDALE, ARIZ. – The extent of stretching of the perineal body during the second stage of labor is not helpful in predicting which women will experience adverse obstetric and postpartum outcomes, new data show.
Short perineal body length is known to increase the risk of severe perineal laceration at the time of delivery as well as postpartum functional disorders, noted presenting author Dr. Jill Alldredge. Maternal expulsive efforts during the second stage of labor that stretch the pelvic floor may also damage the pelvic floor muscles.
She and her colleagues performed a planned secondary analysis of the APPLE cohort (Alterations in the Pelvic Floor in Pregnancy, Labor and Ensuing Years), analyzing data from 448 nulliparous women who had a vaginal birth attended by a certified nurse-midwife, had repeated perineal measurements over time, and were followed prospectively to 12 months post partum.
On average, perineal body length increased by about 2.4 cm in the cohort between the antepartum period and the maximal length during the second stage of labor, according to data reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
However, neither perineal body length nor change in this length at any time point was associated with perineal lacerations, or with urinary or anal incontinence or not being sexually active at 6 months post partum.
"We can see that the perineum is dynamic and does stretch during labor. However, measurement of the perineal body length and change in perineal body length between the antepartum, intrapartum, and post partum time periods does not predict perineal trauma or postpartum pelvic floor dysfunction," commented Dr. Alldredge, an obstetrics-gynecology resident at the University of New Mexico in Albuquerque.
APPLE participants had measurement of the perineal body length during the antepartum period, at the onset of labor, at the onset of and every 10 minutes during the second stage, and at 6 and 12 months post partum. The anal opening and the genital hiatus also were measured during the second stage of labor.
At 6 months, the women completed a set of questionnaires assessing pelvic floor function: the Incontinence Severity Index, the Wexner Fecal Incontinence Scale, and the Female Sexual Function Index.
The mean perineal body length was 3.7 cm during the antepartum period, and the mean maximal perineal body length during the second stage of labor was 6.1 cm, she said at the meeting, jointly sponsored by the American College of Surgeons.
During the second stage of labor, the maximal anal opening was 2.0 cm on average. The genital hiatus had an anterior-posterior maximal diameter of 7.5 cm, a maximal transverse diameter of 4.7 cm, and a maximal introital area of 119.4 cm2.
Overall, 35% of women experienced a second-degree or worse perineal tear. And at 6 months post partum, 72% had at least mild urinary incontinence, 68% had at least mild anal incontinence, and 13% were not sexually active.
However, analyses showed that neither perineal body length nor stretch at any of the time points assessed was significantly associated with any of these outcomes.
Dr. Alldredge disclosed no relevant conflicts of interest.
SCOTTSDALE, ARIZ. – The extent of stretching of the perineal body during the second stage of labor is not helpful in predicting which women will experience adverse obstetric and postpartum outcomes, new data show.
Short perineal body length is known to increase the risk of severe perineal laceration at the time of delivery as well as postpartum functional disorders, noted presenting author Dr. Jill Alldredge. Maternal expulsive efforts during the second stage of labor that stretch the pelvic floor may also damage the pelvic floor muscles.
She and her colleagues performed a planned secondary analysis of the APPLE cohort (Alterations in the Pelvic Floor in Pregnancy, Labor and Ensuing Years), analyzing data from 448 nulliparous women who had a vaginal birth attended by a certified nurse-midwife, had repeated perineal measurements over time, and were followed prospectively to 12 months post partum.
On average, perineal body length increased by about 2.4 cm in the cohort between the antepartum period and the maximal length during the second stage of labor, according to data reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
However, neither perineal body length nor change in this length at any time point was associated with perineal lacerations, or with urinary or anal incontinence or not being sexually active at 6 months post partum.
"We can see that the perineum is dynamic and does stretch during labor. However, measurement of the perineal body length and change in perineal body length between the antepartum, intrapartum, and post partum time periods does not predict perineal trauma or postpartum pelvic floor dysfunction," commented Dr. Alldredge, an obstetrics-gynecology resident at the University of New Mexico in Albuquerque.
APPLE participants had measurement of the perineal body length during the antepartum period, at the onset of labor, at the onset of and every 10 minutes during the second stage, and at 6 and 12 months post partum. The anal opening and the genital hiatus also were measured during the second stage of labor.
At 6 months, the women completed a set of questionnaires assessing pelvic floor function: the Incontinence Severity Index, the Wexner Fecal Incontinence Scale, and the Female Sexual Function Index.
The mean perineal body length was 3.7 cm during the antepartum period, and the mean maximal perineal body length during the second stage of labor was 6.1 cm, she said at the meeting, jointly sponsored by the American College of Surgeons.
During the second stage of labor, the maximal anal opening was 2.0 cm on average. The genital hiatus had an anterior-posterior maximal diameter of 7.5 cm, a maximal transverse diameter of 4.7 cm, and a maximal introital area of 119.4 cm2.
Overall, 35% of women experienced a second-degree or worse perineal tear. And at 6 months post partum, 72% had at least mild urinary incontinence, 68% had at least mild anal incontinence, and 13% were not sexually active.
However, analyses showed that neither perineal body length nor stretch at any of the time points assessed was significantly associated with any of these outcomes.
Dr. Alldredge disclosed no relevant conflicts of interest.
AT SGS 2014