User login
Are Knee and Hip Replacements Bad For the Heart?
Researchers found that patients with osteoarthritis who had total knee or hip joint arthroplasty were at increased risk of myocardial infarction in the early post-operative period, according to a study published online ahead of print August 31 in Arthritis & Rheumatology. However, findings indicate that long-term risk of heart attack did not persist, while the risk for venous thromboembolism remained years after the procedure was performed.
The cohort study included 13,849 patients who underwent total knee replacement surgery and 13,849 matched controls that did not have surgery. Patients were ages 50 or older and were diagnosed with knee or hip osteoarthritis between January 2000 and December 2012.
Findings indicate that 306 patients in the arthroplasty group and 286 in the non-surgical group developed myocardial infarction during the follow-up period.
Risk of heart attack was significantly higher during the first postoperative month in those who had knee replacement surgery compared with those in the non-surgical group (hazard ratio 8.75), and gradually declined over time. Venous thromboembolism was a significant risk during the first month and over time for those who had total knee or total hip arthroplasty.
“Our findings provide the first general population-based evidence that osteoarthritis patients who have total knee or total hip replacement surgery are at increased risk of heart attack in the immediate postoperative period,” said Yuqing Zhang, DSc, Professor of Medicine and Epidemiology at Boston University School of Medicine. “The long-term risk of heart attack was insignificant, but risk of blood clots in the lung remained for years after surgery to replace a hip or knee damaged by osteoarthritis,” said Dr. Zhang.
Suggested Reading
Lu N, Misra D, Neogi T, et al. Total joint arthroplasty and the risk of myocardial infarction - a general population, propensity score-matched cohort study. Arthritis Rheumatol. 2015 Aug 31 [Epub ahead of print].
Researchers found that patients with osteoarthritis who had total knee or hip joint arthroplasty were at increased risk of myocardial infarction in the early post-operative period, according to a study published online ahead of print August 31 in Arthritis & Rheumatology. However, findings indicate that long-term risk of heart attack did not persist, while the risk for venous thromboembolism remained years after the procedure was performed.
The cohort study included 13,849 patients who underwent total knee replacement surgery and 13,849 matched controls that did not have surgery. Patients were ages 50 or older and were diagnosed with knee or hip osteoarthritis between January 2000 and December 2012.
Findings indicate that 306 patients in the arthroplasty group and 286 in the non-surgical group developed myocardial infarction during the follow-up period.
Risk of heart attack was significantly higher during the first postoperative month in those who had knee replacement surgery compared with those in the non-surgical group (hazard ratio 8.75), and gradually declined over time. Venous thromboembolism was a significant risk during the first month and over time for those who had total knee or total hip arthroplasty.
“Our findings provide the first general population-based evidence that osteoarthritis patients who have total knee or total hip replacement surgery are at increased risk of heart attack in the immediate postoperative period,” said Yuqing Zhang, DSc, Professor of Medicine and Epidemiology at Boston University School of Medicine. “The long-term risk of heart attack was insignificant, but risk of blood clots in the lung remained for years after surgery to replace a hip or knee damaged by osteoarthritis,” said Dr. Zhang.
Researchers found that patients with osteoarthritis who had total knee or hip joint arthroplasty were at increased risk of myocardial infarction in the early post-operative period, according to a study published online ahead of print August 31 in Arthritis & Rheumatology. However, findings indicate that long-term risk of heart attack did not persist, while the risk for venous thromboembolism remained years after the procedure was performed.
The cohort study included 13,849 patients who underwent total knee replacement surgery and 13,849 matched controls that did not have surgery. Patients were ages 50 or older and were diagnosed with knee or hip osteoarthritis between January 2000 and December 2012.
Findings indicate that 306 patients in the arthroplasty group and 286 in the non-surgical group developed myocardial infarction during the follow-up period.
Risk of heart attack was significantly higher during the first postoperative month in those who had knee replacement surgery compared with those in the non-surgical group (hazard ratio 8.75), and gradually declined over time. Venous thromboembolism was a significant risk during the first month and over time for those who had total knee or total hip arthroplasty.
“Our findings provide the first general population-based evidence that osteoarthritis patients who have total knee or total hip replacement surgery are at increased risk of heart attack in the immediate postoperative period,” said Yuqing Zhang, DSc, Professor of Medicine and Epidemiology at Boston University School of Medicine. “The long-term risk of heart attack was insignificant, but risk of blood clots in the lung remained for years after surgery to replace a hip or knee damaged by osteoarthritis,” said Dr. Zhang.
Suggested Reading
Lu N, Misra D, Neogi T, et al. Total joint arthroplasty and the risk of myocardial infarction - a general population, propensity score-matched cohort study. Arthritis Rheumatol. 2015 Aug 31 [Epub ahead of print].
Suggested Reading
Lu N, Misra D, Neogi T, et al. Total joint arthroplasty and the risk of myocardial infarction - a general population, propensity score-matched cohort study. Arthritis Rheumatol. 2015 Aug 31 [Epub ahead of print].
Commentary to "Measurement of Resource Utilization for Total and Reverse Shoulder Arthroplasty"
In this month’s issue of The American Journal of Orthopedics, Tannenbaum and colleagues present a “5 Points” article on “Measurement of Resource Utilization for Total and Reverse Shoulder Arthroplasty.” This is an excellent article that summarizes the authors’ methodology of determining not only the overall cost of hospital care for shoulder replacement but a detailed analysis of many components contributing to that cost.
The steps are fairly straightforward: identify the various components of the cost, gather the data contributing to those costs, and then analyze what are the major expenditures that contribute to the overall cost. Sounds simple, but, in practice, it is anything but!
As health care expenditures in the United States continue to increase and approach 20% of the gross domestic product, every sector of the health care industry is searching for ways to curtail and eventually decrease the cost of health care. However, one cannot control costs without accurate data that defines those costs. In this article, Tannenbaum and colleagues have provided a methodology to help both hospital administrators and surgeons determine the overall cost of shoulder arthroplasty, but their principles of analysis can be applied to all aspects of hospital care.
Such efforts are gaining the attention of many leaders of the health care industry. For example, in the September 8, 2015, edition of The New York Times, I was very interested to read the article “What are a Hospital’s Costs? Utah System Is Trying to Learn.”1 The article reviewed the efforts of Dr. Vivian Lee, chief executive at University of Utah Health Care, to determine the actual cost of all care provided by the university hospital, the same goal as the present 5 Points article on shoulder arthroplasty but on a vastly greater scale. Analyzing those costs guided Dr. Lee and her colleagues to alter clinical programs, which led to a decrease of 30% in hospital expenditures and fewer complications.1
We are all indebted to Mr. Tannenbaum and his coauthors for providing the journal’s readers with a clear map that we can use to both understand and navigate the current maze of hospital costs. Using such a guide, we will be able to gather information that not only saves money, but will improve care by directing resources to services that actually benefit our patients.
Reference
1. Kolata G. What are a hospital’s costs? Utah system is trying to learn. New York Times. September 8, 2015:A1. http://www.nytimes.com/2015/09/08/health/what-are-a-hospitals-costs-utah-system-is-trying-to-learn.html. Accessed September 17, 2015.
In this month’s issue of The American Journal of Orthopedics, Tannenbaum and colleagues present a “5 Points” article on “Measurement of Resource Utilization for Total and Reverse Shoulder Arthroplasty.” This is an excellent article that summarizes the authors’ methodology of determining not only the overall cost of hospital care for shoulder replacement but a detailed analysis of many components contributing to that cost.
The steps are fairly straightforward: identify the various components of the cost, gather the data contributing to those costs, and then analyze what are the major expenditures that contribute to the overall cost. Sounds simple, but, in practice, it is anything but!
As health care expenditures in the United States continue to increase and approach 20% of the gross domestic product, every sector of the health care industry is searching for ways to curtail and eventually decrease the cost of health care. However, one cannot control costs without accurate data that defines those costs. In this article, Tannenbaum and colleagues have provided a methodology to help both hospital administrators and surgeons determine the overall cost of shoulder arthroplasty, but their principles of analysis can be applied to all aspects of hospital care.
Such efforts are gaining the attention of many leaders of the health care industry. For example, in the September 8, 2015, edition of The New York Times, I was very interested to read the article “What are a Hospital’s Costs? Utah System Is Trying to Learn.”1 The article reviewed the efforts of Dr. Vivian Lee, chief executive at University of Utah Health Care, to determine the actual cost of all care provided by the university hospital, the same goal as the present 5 Points article on shoulder arthroplasty but on a vastly greater scale. Analyzing those costs guided Dr. Lee and her colleagues to alter clinical programs, which led to a decrease of 30% in hospital expenditures and fewer complications.1
We are all indebted to Mr. Tannenbaum and his coauthors for providing the journal’s readers with a clear map that we can use to both understand and navigate the current maze of hospital costs. Using such a guide, we will be able to gather information that not only saves money, but will improve care by directing resources to services that actually benefit our patients.
In this month’s issue of The American Journal of Orthopedics, Tannenbaum and colleagues present a “5 Points” article on “Measurement of Resource Utilization for Total and Reverse Shoulder Arthroplasty.” This is an excellent article that summarizes the authors’ methodology of determining not only the overall cost of hospital care for shoulder replacement but a detailed analysis of many components contributing to that cost.
The steps are fairly straightforward: identify the various components of the cost, gather the data contributing to those costs, and then analyze what are the major expenditures that contribute to the overall cost. Sounds simple, but, in practice, it is anything but!
As health care expenditures in the United States continue to increase and approach 20% of the gross domestic product, every sector of the health care industry is searching for ways to curtail and eventually decrease the cost of health care. However, one cannot control costs without accurate data that defines those costs. In this article, Tannenbaum and colleagues have provided a methodology to help both hospital administrators and surgeons determine the overall cost of shoulder arthroplasty, but their principles of analysis can be applied to all aspects of hospital care.
Such efforts are gaining the attention of many leaders of the health care industry. For example, in the September 8, 2015, edition of The New York Times, I was very interested to read the article “What are a Hospital’s Costs? Utah System Is Trying to Learn.”1 The article reviewed the efforts of Dr. Vivian Lee, chief executive at University of Utah Health Care, to determine the actual cost of all care provided by the university hospital, the same goal as the present 5 Points article on shoulder arthroplasty but on a vastly greater scale. Analyzing those costs guided Dr. Lee and her colleagues to alter clinical programs, which led to a decrease of 30% in hospital expenditures and fewer complications.1
We are all indebted to Mr. Tannenbaum and his coauthors for providing the journal’s readers with a clear map that we can use to both understand and navigate the current maze of hospital costs. Using such a guide, we will be able to gather information that not only saves money, but will improve care by directing resources to services that actually benefit our patients.
Reference
1. Kolata G. What are a hospital’s costs? Utah system is trying to learn. New York Times. September 8, 2015:A1. http://www.nytimes.com/2015/09/08/health/what-are-a-hospitals-costs-utah-system-is-trying-to-learn.html. Accessed September 17, 2015.
Reference
1. Kolata G. What are a hospital’s costs? Utah system is trying to learn. New York Times. September 8, 2015:A1. http://www.nytimes.com/2015/09/08/health/what-are-a-hospitals-costs-utah-system-is-trying-to-learn.html. Accessed September 17, 2015.
Imaging Evaluation of Superior Labral Anteroposterior (SLAP) Tears
Superior labral anteroposterior (SLAP) tears are common labral injuries. They occur at the attachment of the long head of the biceps tendon on the superior glenoid and extend anterior and/or posterior to the biceps anchor. The mechanism of action for SLAP tears is traction on the superior labrum by the long head of the biceps tendon, resulting in “peeling” of the labrum off the glenoid. Such forces may result from repetitive overhead arm motion (pitching) or from direct trauma.
Clinical diagnosis is challenging with SLAP tears, as they often present with nonspecific shoulder pain and may not be associated with an acute injury. A further complication is that they are often associated with other shoulder pathology, such as rotator cuff tears.1 As physical examination is typically nonspecific, proper diagnostic imaging is essential for diagnosis.
We prefer to assess potential SLAP tears with magnetic resonance arthrography (MRA).2 Dilute (1:200) gadolinium contrast material (12-15 mL) is introduced into the glenohumeral joint under sonographic or fluoroscopic guidance. Capsular distention by dilute intra-articular contrast enables superior imaging resolution of the labroligamentous complex. We think the increase in diagnostic confidence enabled by direct arthrography outweighs the additional invasiveness and cost associated with MRA relative to noncontrast magnetic resonance imaging (MRI).
The MRA protocol differs from our routine noncontrast shoulder imaging. We perform a fat-saturated coronal oblique T1 sequence that maximizes the conspicuity of intra-articular contrast in the plane that optimally visualizes the superior labrum. Three planes of intermediate-weighted fast spin echo not only contrast the high-signal intra-articular fluid with the low-signal fibrocartilaginous labrum and the stratified intermediate signal of glenoid articular cartilage, but they also allow optimal assessment of the rotator cuff. In addition, we perform a fat-saturated coronal T2 sequence that highlights all fluid signal structures as well as edema.
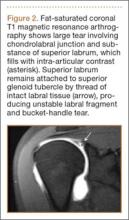
SLAP tears appear on MRA as the insinuation of intra-articular contrast between the articular cartilage and the attachment of the superior labrum,3 within the substance of the labrum, or as detachment of the labrum from the glenoid rim4 (Figure 1). Findings can range from labral fraying to complete detachment with displacement. Tears can extend into other quadrants of the labrum, extend from a Bankart lesion, or involve the biceps tendon and/or the glenohumeral ligaments (Figures 2–4). Up to 10 types of SLAP tears have been described on arthroscopy. This classification scheme, however, is seldom helpful in the interpretation of SLAP tears on MRI. More important in guiding treatment is having a detailed description of the tear, including location, extent, and morphology, along with associated abnormalities.
Several findings can aid in the diagnosis of SLAP tears. Normal anatomical variants of the anterior-superior labrum do not extend posterior to the biceps anchor—an important finding for discerning normal morphologic variants from tears. Therefore, high signal within the posterior third of the superior labrum or extension of high signal laterally within the labrum and away from the glenoid suggests a SLAP tear.5 A paralabral cyst is almost always associated with a labral tear,1 so signal abnormality of the superior labrum with a paralabral cyst suggests a SLAP tear (Figure 5).
MRA is not the only method for diagnosing SLAP tears. Standard 3-Tesla MRI had 83% sensitivity and 99% specificity for diagnosing SLAP tears in a recent study, though MRA had 98% sensitivity and 99% specificity—a statistically significant sensitivity difference.6 In another study, computed tomography arthrography (CTA) had 95% sensitivity and 88% specificity for diagnosing recurrent SLAP tears after surgery.7 CTA is associated with ionizing radiation and is limited in its assessment of other structures that may show concomitant abnormalities, such as the articular cartilage and the rotator cuff. Indirect MRA, wherein magnetic resonance sequences are obtained after intravenous injection of gadolinium contrast and exercise of the affected shoulder, had a high sensitivity of detection of labral tears of all types.8
MRA is most sensitive and specific for diagnosing SLAP tears; 3-Tesla MRI, indirect MRA, and CTA are useful alternative modalities for cases in which MRA cannot be performed.
1. Chang D, Mohana-Borges A, Borso M, Chung CB. SLAP lesions: anatomy, clinical presentation, MR imaging diagnosis and characterization. Eur J Radiol. 2008;68(1):72-87.
2. Jee WH, McCauley TR, Katz LD, Matheny JM, Ruwe PA, Daigneault JP. Superior labral anterior posterior (SLAP) lesions of the glenoid labrum: reliability and accuracy of MR arthrography for diagnosis. Radiology. 2001;218(1):127-132.
3. Fitzpatrick D, Walz DM. Shoulder MR imaging normal variants and imaging artifacts. Magn Reson Imaging Clin N Am. 2010;18(4):615-632.
4. Bencardino JT, Beltran J, Rosenberg ZS, et al. Superior labrum anterior-posterior lesions: diagnosis with MR arthrography of the shoulder. Radiology. 2000;214(1):267-271.
5. Tuite MJ, Cirillo RL, De Smet AA, Orwin JF. Superior labrum anterior-posterior (SLAP) tears: evaluation of three MR signs on T2-weighted images. Radiology. 2000;215(3):841-845.
6. Magee T. 3-T MRI of the shoulder: is MR arthrography necessary? AJR Am J Roentgenol. 2009;192(1):86-92.
7. De Filippo M, Araoz PA, Pogliacomi F, et al. Recurrent superior labral anterior-to-posterior tears after surgery: detection and grading with CT arthrography. Radiology. 2009;252(3):781-788.
8. Fallahi F, Green N, Gadde S, Jeavons L, Armstrong P, Jonker L. Indirect magnetic resonance arthrography of the shoulder; a reliable diagnostic tool for investigation of suspected labral pathology. Skeletal Radiol. 2013;42(9):1225-1233.
Superior labral anteroposterior (SLAP) tears are common labral injuries. They occur at the attachment of the long head of the biceps tendon on the superior glenoid and extend anterior and/or posterior to the biceps anchor. The mechanism of action for SLAP tears is traction on the superior labrum by the long head of the biceps tendon, resulting in “peeling” of the labrum off the glenoid. Such forces may result from repetitive overhead arm motion (pitching) or from direct trauma.
Clinical diagnosis is challenging with SLAP tears, as they often present with nonspecific shoulder pain and may not be associated with an acute injury. A further complication is that they are often associated with other shoulder pathology, such as rotator cuff tears.1 As physical examination is typically nonspecific, proper diagnostic imaging is essential for diagnosis.
We prefer to assess potential SLAP tears with magnetic resonance arthrography (MRA).2 Dilute (1:200) gadolinium contrast material (12-15 mL) is introduced into the glenohumeral joint under sonographic or fluoroscopic guidance. Capsular distention by dilute intra-articular contrast enables superior imaging resolution of the labroligamentous complex. We think the increase in diagnostic confidence enabled by direct arthrography outweighs the additional invasiveness and cost associated with MRA relative to noncontrast magnetic resonance imaging (MRI).
The MRA protocol differs from our routine noncontrast shoulder imaging. We perform a fat-saturated coronal oblique T1 sequence that maximizes the conspicuity of intra-articular contrast in the plane that optimally visualizes the superior labrum. Three planes of intermediate-weighted fast spin echo not only contrast the high-signal intra-articular fluid with the low-signal fibrocartilaginous labrum and the stratified intermediate signal of glenoid articular cartilage, but they also allow optimal assessment of the rotator cuff. In addition, we perform a fat-saturated coronal T2 sequence that highlights all fluid signal structures as well as edema.
SLAP tears appear on MRA as the insinuation of intra-articular contrast between the articular cartilage and the attachment of the superior labrum,3 within the substance of the labrum, or as detachment of the labrum from the glenoid rim4 (Figure 1). Findings can range from labral fraying to complete detachment with displacement. Tears can extend into other quadrants of the labrum, extend from a Bankart lesion, or involve the biceps tendon and/or the glenohumeral ligaments (Figures 2–4). Up to 10 types of SLAP tears have been described on arthroscopy. This classification scheme, however, is seldom helpful in the interpretation of SLAP tears on MRI. More important in guiding treatment is having a detailed description of the tear, including location, extent, and morphology, along with associated abnormalities.
Several findings can aid in the diagnosis of SLAP tears. Normal anatomical variants of the anterior-superior labrum do not extend posterior to the biceps anchor—an important finding for discerning normal morphologic variants from tears. Therefore, high signal within the posterior third of the superior labrum or extension of high signal laterally within the labrum and away from the glenoid suggests a SLAP tear.5 A paralabral cyst is almost always associated with a labral tear,1 so signal abnormality of the superior labrum with a paralabral cyst suggests a SLAP tear (Figure 5).
MRA is not the only method for diagnosing SLAP tears. Standard 3-Tesla MRI had 83% sensitivity and 99% specificity for diagnosing SLAP tears in a recent study, though MRA had 98% sensitivity and 99% specificity—a statistically significant sensitivity difference.6 In another study, computed tomography arthrography (CTA) had 95% sensitivity and 88% specificity for diagnosing recurrent SLAP tears after surgery.7 CTA is associated with ionizing radiation and is limited in its assessment of other structures that may show concomitant abnormalities, such as the articular cartilage and the rotator cuff. Indirect MRA, wherein magnetic resonance sequences are obtained after intravenous injection of gadolinium contrast and exercise of the affected shoulder, had a high sensitivity of detection of labral tears of all types.8
MRA is most sensitive and specific for diagnosing SLAP tears; 3-Tesla MRI, indirect MRA, and CTA are useful alternative modalities for cases in which MRA cannot be performed.
Superior labral anteroposterior (SLAP) tears are common labral injuries. They occur at the attachment of the long head of the biceps tendon on the superior glenoid and extend anterior and/or posterior to the biceps anchor. The mechanism of action for SLAP tears is traction on the superior labrum by the long head of the biceps tendon, resulting in “peeling” of the labrum off the glenoid. Such forces may result from repetitive overhead arm motion (pitching) or from direct trauma.
Clinical diagnosis is challenging with SLAP tears, as they often present with nonspecific shoulder pain and may not be associated with an acute injury. A further complication is that they are often associated with other shoulder pathology, such as rotator cuff tears.1 As physical examination is typically nonspecific, proper diagnostic imaging is essential for diagnosis.
We prefer to assess potential SLAP tears with magnetic resonance arthrography (MRA).2 Dilute (1:200) gadolinium contrast material (12-15 mL) is introduced into the glenohumeral joint under sonographic or fluoroscopic guidance. Capsular distention by dilute intra-articular contrast enables superior imaging resolution of the labroligamentous complex. We think the increase in diagnostic confidence enabled by direct arthrography outweighs the additional invasiveness and cost associated with MRA relative to noncontrast magnetic resonance imaging (MRI).
The MRA protocol differs from our routine noncontrast shoulder imaging. We perform a fat-saturated coronal oblique T1 sequence that maximizes the conspicuity of intra-articular contrast in the plane that optimally visualizes the superior labrum. Three planes of intermediate-weighted fast spin echo not only contrast the high-signal intra-articular fluid with the low-signal fibrocartilaginous labrum and the stratified intermediate signal of glenoid articular cartilage, but they also allow optimal assessment of the rotator cuff. In addition, we perform a fat-saturated coronal T2 sequence that highlights all fluid signal structures as well as edema.
SLAP tears appear on MRA as the insinuation of intra-articular contrast between the articular cartilage and the attachment of the superior labrum,3 within the substance of the labrum, or as detachment of the labrum from the glenoid rim4 (Figure 1). Findings can range from labral fraying to complete detachment with displacement. Tears can extend into other quadrants of the labrum, extend from a Bankart lesion, or involve the biceps tendon and/or the glenohumeral ligaments (Figures 2–4). Up to 10 types of SLAP tears have been described on arthroscopy. This classification scheme, however, is seldom helpful in the interpretation of SLAP tears on MRI. More important in guiding treatment is having a detailed description of the tear, including location, extent, and morphology, along with associated abnormalities.
Several findings can aid in the diagnosis of SLAP tears. Normal anatomical variants of the anterior-superior labrum do not extend posterior to the biceps anchor—an important finding for discerning normal morphologic variants from tears. Therefore, high signal within the posterior third of the superior labrum or extension of high signal laterally within the labrum and away from the glenoid suggests a SLAP tear.5 A paralabral cyst is almost always associated with a labral tear,1 so signal abnormality of the superior labrum with a paralabral cyst suggests a SLAP tear (Figure 5).
MRA is not the only method for diagnosing SLAP tears. Standard 3-Tesla MRI had 83% sensitivity and 99% specificity for diagnosing SLAP tears in a recent study, though MRA had 98% sensitivity and 99% specificity—a statistically significant sensitivity difference.6 In another study, computed tomography arthrography (CTA) had 95% sensitivity and 88% specificity for diagnosing recurrent SLAP tears after surgery.7 CTA is associated with ionizing radiation and is limited in its assessment of other structures that may show concomitant abnormalities, such as the articular cartilage and the rotator cuff. Indirect MRA, wherein magnetic resonance sequences are obtained after intravenous injection of gadolinium contrast and exercise of the affected shoulder, had a high sensitivity of detection of labral tears of all types.8
MRA is most sensitive and specific for diagnosing SLAP tears; 3-Tesla MRI, indirect MRA, and CTA are useful alternative modalities for cases in which MRA cannot be performed.
1. Chang D, Mohana-Borges A, Borso M, Chung CB. SLAP lesions: anatomy, clinical presentation, MR imaging diagnosis and characterization. Eur J Radiol. 2008;68(1):72-87.
2. Jee WH, McCauley TR, Katz LD, Matheny JM, Ruwe PA, Daigneault JP. Superior labral anterior posterior (SLAP) lesions of the glenoid labrum: reliability and accuracy of MR arthrography for diagnosis. Radiology. 2001;218(1):127-132.
3. Fitzpatrick D, Walz DM. Shoulder MR imaging normal variants and imaging artifacts. Magn Reson Imaging Clin N Am. 2010;18(4):615-632.
4. Bencardino JT, Beltran J, Rosenberg ZS, et al. Superior labrum anterior-posterior lesions: diagnosis with MR arthrography of the shoulder. Radiology. 2000;214(1):267-271.
5. Tuite MJ, Cirillo RL, De Smet AA, Orwin JF. Superior labrum anterior-posterior (SLAP) tears: evaluation of three MR signs on T2-weighted images. Radiology. 2000;215(3):841-845.
6. Magee T. 3-T MRI of the shoulder: is MR arthrography necessary? AJR Am J Roentgenol. 2009;192(1):86-92.
7. De Filippo M, Araoz PA, Pogliacomi F, et al. Recurrent superior labral anterior-to-posterior tears after surgery: detection and grading with CT arthrography. Radiology. 2009;252(3):781-788.
8. Fallahi F, Green N, Gadde S, Jeavons L, Armstrong P, Jonker L. Indirect magnetic resonance arthrography of the shoulder; a reliable diagnostic tool for investigation of suspected labral pathology. Skeletal Radiol. 2013;42(9):1225-1233.
1. Chang D, Mohana-Borges A, Borso M, Chung CB. SLAP lesions: anatomy, clinical presentation, MR imaging diagnosis and characterization. Eur J Radiol. 2008;68(1):72-87.
2. Jee WH, McCauley TR, Katz LD, Matheny JM, Ruwe PA, Daigneault JP. Superior labral anterior posterior (SLAP) lesions of the glenoid labrum: reliability and accuracy of MR arthrography for diagnosis. Radiology. 2001;218(1):127-132.
3. Fitzpatrick D, Walz DM. Shoulder MR imaging normal variants and imaging artifacts. Magn Reson Imaging Clin N Am. 2010;18(4):615-632.
4. Bencardino JT, Beltran J, Rosenberg ZS, et al. Superior labrum anterior-posterior lesions: diagnosis with MR arthrography of the shoulder. Radiology. 2000;214(1):267-271.
5. Tuite MJ, Cirillo RL, De Smet AA, Orwin JF. Superior labrum anterior-posterior (SLAP) tears: evaluation of three MR signs on T2-weighted images. Radiology. 2000;215(3):841-845.
6. Magee T. 3-T MRI of the shoulder: is MR arthrography necessary? AJR Am J Roentgenol. 2009;192(1):86-92.
7. De Filippo M, Araoz PA, Pogliacomi F, et al. Recurrent superior labral anterior-to-posterior tears after surgery: detection and grading with CT arthrography. Radiology. 2009;252(3):781-788.
8. Fallahi F, Green N, Gadde S, Jeavons L, Armstrong P, Jonker L. Indirect magnetic resonance arthrography of the shoulder; a reliable diagnostic tool for investigation of suspected labral pathology. Skeletal Radiol. 2013;42(9):1225-1233.
Measurement of Resource Utilization for Total and Reverse Shoulder Arthroplasty
As total health care costs reach almost $3 trillion per year—capturing more than 17% of the total US gross domestic product—payers are searching for more effective ways to limit health care spending.1,2 One increasingly discussed plan is payment bundling.3 This one-lump-sum payment model arose as a result of rapid year-on-year increases in total reimbursements under the current, fee-for-service model. The Centers for Medicare & Medicaid Services hypothesized that a single all-inclusive payment for a procedure or set of services would incentivize improvements in patient-centered care and disincentivize cost-shifting behaviors.4 Bundled reimbursement is becoming increasingly common in orthopedic practice. With the recent introduction of the Bundled Payment for Care Improvement Initiative, several orthopedic practices around the United States are already actively engaged in creating models for bundled payment for common elective procedures and for associated services provided up to 90 days after surgery.3,5
Bundled payment increases the burden on the provider to understand the cost of care provided during a care cycle. However, not only has the current system blinded physicians to the cost of care, but current antitrust legislation has made discussions of pricing with colleagues (so-called price collusion) illegal and subject to fines of up to $1 million per person and $100 million per organization,6 therefore limiting orthopedic physician involvement.
Given these legal constraints, instead of measuring direct costs of goods, we developed a “grocery list” approach in which direct comparisons are made of resources (goods and services) used and delivered during the entire 90-day cycle of care for patients who undergo anatomical total shoulder arthroplasty (TSA) or reverse shoulder arthroplasty (RSA). We used one surgeon’s practice experience as a model for measuring other orthopedic surgeons’ resource utilization, based on their electronic medical records (EMR) system data. By capturing the costs of the components of resource utilization rather than just the final cost of care, we can assess, compare, understand, endorse, and address these driving factors.
1. The significance of resource utilization
To maximize the efficiency of their practices, high-volume shoulder surgeons have introduced standardization to health care delivery.7 Identifying specific efficiencies makes uniform acceptance of beneficial practice patterns possible.
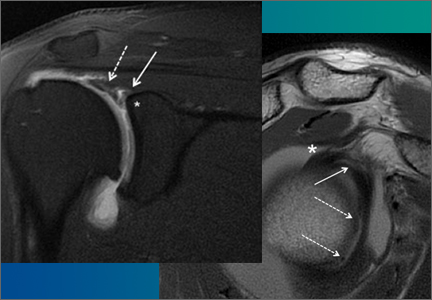
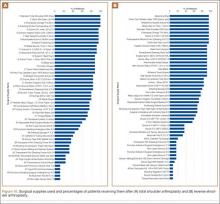
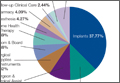
To facilitate comparison of goods and services used during an episode of surgical care, Virani and colleagues8,9 studied the costs of TSA and RSA and calculated the top 10 driving cost factors for these procedures (Figure 1). Their systematic analysis provided a framework for a common method of communication, allowing an orthopedic surgeon to gain a more complete understanding of the resources used during a particular operative procedure in his or her practice, and allowing several physicians to compare and contrast the resources collectively used for a single procedure, facilitating an understanding of different practice patterns within a local community. At a societal level, these data can be collected to help guide overall recommendations.
2. How we defined utilization
To define the resources used, we had to decide which procedure components cost the most. Virani and colleagues8,9 found that the top 10 cost drivers accounted for 93.11% and 94.77% of the total cost of the TSA and RSA care cycles, respectively (Figure 1). For each cost driver, information on resources used (goods, services, overhead) was collected on 2 forms, the Hospital Utilization Form (7 hospital-based items) and the Clinical Utilization Form (3 non-hospital-based items). To make hospital data easy to compile, we piloted use of a “smart form” in the EpicCare EMR system to isolate and auto-populate specific data fields.
3. EMR data collection
With EMR becoming mandatory for all public and private health care providers starting in 2014, utilization data are now included in a single unified system. Working with our in-house information technology department, we developed an algorithm to populate this information in a separate, easy-to-follow hospital utilization form. This form can be adopted by other institutions. Although EpicCare EMR is used by 52% of hospitals and at our institution, the data points required to make the same measurements are generalizable and exist in other EMRs.
Smartlinks, a tool in this EMR, allows utilization data to be quickly retrieved from different locations in a medical record and allows a form to be electronically completed in seconds. Data can be retrieved for any patient in the EMR system, regardless of when that patient’s hospital stay occurred. We populated data from surgeries performed 2 years before the start of this project.
4. What we can learn from these data
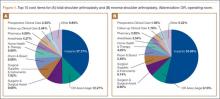
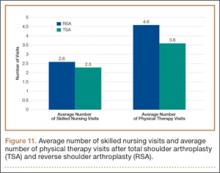
Data from a pilot study of 25 patients who underwent primary anatomical TSA for osteoarthritis and 25 patients who underwent primary RSA for massive rotator cuff tear allowed us to generate graphical representations of a single surgeon’s practice patterns that most affected the cost of care. Time in holding, time in the operating room, time in the postanesthesia care unit, and percentage of patients receiving different medications were recorded for each procedure (Figures 2–11). The study did not capture the wide variances in practice patterns in shoulder arthroplasty, and therefore other surgeons’ resource utilization may differ from ours. However, replicating this methodology at other institutions will produce a more robust data set from which conclusions about resource utilization and, indirectly, cost of care can be made.
5. Future possibilities
By using existing EMR tools to better understand resource utilization, orthopedic surgeons can play a constructive role in the dialogue on health care costs and new reimbursement models. The data presented here are not meant to be interpreted as hard and fast numbers on global resource utilization, but instead we intend to establish a model for collecting data on resource utilization. Resource utilization begins the dialogue that allows orthopedic surgeons and specialty societies to speak a common language without discussing actual cost numbers, which is discouraged under antitrust regulation. The data presented will allow comparisons to be made between surgeons in all practice settings to highlight areas of inconsistency in order to further improve patient care. Although this work involved only 50 patients undergoing only 2 types of surgeries, the resource-capturing methodology can be expanded to include more procedures and orthopedic practices. As all hospitals are now required to have EMRs, the metrics tracked in this work can be found on any patient medical record and auto-populated using our open-source utilization forms. Starting this data collection at your hospital may require no more than a conversation with the informatics department, as the metrics can for the most part be populated into a database on surgeon request.
As orthopedic surgeons return to the economic health care discussion, this information could prove essential in helping the individual surgeon and the orthopedic community justify the cost of care as well as fully understand the cost drivers for musculoskeletal care.
Click here to read the commentary on this article by Peter D. McCann, MD
1. National health expenditures 2013 highlights. Centers for Medicare & Medicaid Services website. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/highlights.pdf. Accessed September 14, 2015.
2. Wilson KB. Health care costs 101: slow growth persists. California HealthCare Foundation website. http://www.chcf.org/publications/2014/07/health-care-costs-101. Published July 2014. Accessed August 24, 2015.
3. Froimson MI, Rana A, White RE Jr, et al. Bundled Payments for Care Improvement Initiative: the next evolution of payment formulations: AAHKS Bundled Payment Task Force. J Arthroplasty. 2013;28(8 suppl):157-165.
4. Morley M, Bogasky S, Gage B, Flood S, Ingber MJ. Medicare post-acute care episodes and payment bundling. Medicare Medicaid Res Rev. 2014;4(1).
5. Teusink MJ, Virani NA, Polikandriotis JA, Frankle MA. Cost analysis in shoulder arthroplasty surgery. Adv Orthop. 2012;2012:692869.
6. Fassbender E, Pandya S. Legislation focuses on AAOS priorities. American Academy of Orthopaedic Surgeons website. http://www.aaos.org/news/aaosnow/may14/advocacy2.asp. AAOS Now. Published May 2014. Accessed August 24, 2015.
7. Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. Boston, MA: Harvard Business School Press; 2006.
8. Virani NA, Williams CD, Clark R, Polikandriotis J, Downes KL, Frankle MA. Preparing for the bundled-payment initiative: the cost and clinical outcomes of reverse shoulder arthroplasty for the surgical treatment of advanced rotator cuff deficiency at an average 4-year follow-up. J Shoulder Elbow Surg. 2013;22(12):1612-1622.
9. Virani NA, Williams CD, Clark R, Polikandriotis J, Downes KL, Frankle MA. Preparing for the bundled-payment initiative: the cost and clinical outcomes of total shoulder arthroplasty for the surgical treatment of glenohumeral arthritis at an average 4-year follow-up. J Shoulder Elbow Surg. 2013;22(12):1601-1611.
As total health care costs reach almost $3 trillion per year—capturing more than 17% of the total US gross domestic product—payers are searching for more effective ways to limit health care spending.1,2 One increasingly discussed plan is payment bundling.3 This one-lump-sum payment model arose as a result of rapid year-on-year increases in total reimbursements under the current, fee-for-service model. The Centers for Medicare & Medicaid Services hypothesized that a single all-inclusive payment for a procedure or set of services would incentivize improvements in patient-centered care and disincentivize cost-shifting behaviors.4 Bundled reimbursement is becoming increasingly common in orthopedic practice. With the recent introduction of the Bundled Payment for Care Improvement Initiative, several orthopedic practices around the United States are already actively engaged in creating models for bundled payment for common elective procedures and for associated services provided up to 90 days after surgery.3,5
Bundled payment increases the burden on the provider to understand the cost of care provided during a care cycle. However, not only has the current system blinded physicians to the cost of care, but current antitrust legislation has made discussions of pricing with colleagues (so-called price collusion) illegal and subject to fines of up to $1 million per person and $100 million per organization,6 therefore limiting orthopedic physician involvement.
Given these legal constraints, instead of measuring direct costs of goods, we developed a “grocery list” approach in which direct comparisons are made of resources (goods and services) used and delivered during the entire 90-day cycle of care for patients who undergo anatomical total shoulder arthroplasty (TSA) or reverse shoulder arthroplasty (RSA). We used one surgeon’s practice experience as a model for measuring other orthopedic surgeons’ resource utilization, based on their electronic medical records (EMR) system data. By capturing the costs of the components of resource utilization rather than just the final cost of care, we can assess, compare, understand, endorse, and address these driving factors.
1. The significance of resource utilization
To maximize the efficiency of their practices, high-volume shoulder surgeons have introduced standardization to health care delivery.7 Identifying specific efficiencies makes uniform acceptance of beneficial practice patterns possible.
To facilitate comparison of goods and services used during an episode of surgical care, Virani and colleagues8,9 studied the costs of TSA and RSA and calculated the top 10 driving cost factors for these procedures (Figure 1). Their systematic analysis provided a framework for a common method of communication, allowing an orthopedic surgeon to gain a more complete understanding of the resources used during a particular operative procedure in his or her practice, and allowing several physicians to compare and contrast the resources collectively used for a single procedure, facilitating an understanding of different practice patterns within a local community. At a societal level, these data can be collected to help guide overall recommendations.
2. How we defined utilization
To define the resources used, we had to decide which procedure components cost the most. Virani and colleagues8,9 found that the top 10 cost drivers accounted for 93.11% and 94.77% of the total cost of the TSA and RSA care cycles, respectively (Figure 1). For each cost driver, information on resources used (goods, services, overhead) was collected on 2 forms, the Hospital Utilization Form (7 hospital-based items) and the Clinical Utilization Form (3 non-hospital-based items). To make hospital data easy to compile, we piloted use of a “smart form” in the EpicCare EMR system to isolate and auto-populate specific data fields.
3. EMR data collection
With EMR becoming mandatory for all public and private health care providers starting in 2014, utilization data are now included in a single unified system. Working with our in-house information technology department, we developed an algorithm to populate this information in a separate, easy-to-follow hospital utilization form. This form can be adopted by other institutions. Although EpicCare EMR is used by 52% of hospitals and at our institution, the data points required to make the same measurements are generalizable and exist in other EMRs.
Smartlinks, a tool in this EMR, allows utilization data to be quickly retrieved from different locations in a medical record and allows a form to be electronically completed in seconds. Data can be retrieved for any patient in the EMR system, regardless of when that patient’s hospital stay occurred. We populated data from surgeries performed 2 years before the start of this project.
4. What we can learn from these data
Data from a pilot study of 25 patients who underwent primary anatomical TSA for osteoarthritis and 25 patients who underwent primary RSA for massive rotator cuff tear allowed us to generate graphical representations of a single surgeon’s practice patterns that most affected the cost of care. Time in holding, time in the operating room, time in the postanesthesia care unit, and percentage of patients receiving different medications were recorded for each procedure (Figures 2–11). The study did not capture the wide variances in practice patterns in shoulder arthroplasty, and therefore other surgeons’ resource utilization may differ from ours. However, replicating this methodology at other institutions will produce a more robust data set from which conclusions about resource utilization and, indirectly, cost of care can be made.
5. Future possibilities
By using existing EMR tools to better understand resource utilization, orthopedic surgeons can play a constructive role in the dialogue on health care costs and new reimbursement models. The data presented here are not meant to be interpreted as hard and fast numbers on global resource utilization, but instead we intend to establish a model for collecting data on resource utilization. Resource utilization begins the dialogue that allows orthopedic surgeons and specialty societies to speak a common language without discussing actual cost numbers, which is discouraged under antitrust regulation. The data presented will allow comparisons to be made between surgeons in all practice settings to highlight areas of inconsistency in order to further improve patient care. Although this work involved only 50 patients undergoing only 2 types of surgeries, the resource-capturing methodology can be expanded to include more procedures and orthopedic practices. As all hospitals are now required to have EMRs, the metrics tracked in this work can be found on any patient medical record and auto-populated using our open-source utilization forms. Starting this data collection at your hospital may require no more than a conversation with the informatics department, as the metrics can for the most part be populated into a database on surgeon request.
As orthopedic surgeons return to the economic health care discussion, this information could prove essential in helping the individual surgeon and the orthopedic community justify the cost of care as well as fully understand the cost drivers for musculoskeletal care.
Click here to read the commentary on this article by Peter D. McCann, MD
As total health care costs reach almost $3 trillion per year—capturing more than 17% of the total US gross domestic product—payers are searching for more effective ways to limit health care spending.1,2 One increasingly discussed plan is payment bundling.3 This one-lump-sum payment model arose as a result of rapid year-on-year increases in total reimbursements under the current, fee-for-service model. The Centers for Medicare & Medicaid Services hypothesized that a single all-inclusive payment for a procedure or set of services would incentivize improvements in patient-centered care and disincentivize cost-shifting behaviors.4 Bundled reimbursement is becoming increasingly common in orthopedic practice. With the recent introduction of the Bundled Payment for Care Improvement Initiative, several orthopedic practices around the United States are already actively engaged in creating models for bundled payment for common elective procedures and for associated services provided up to 90 days after surgery.3,5
Bundled payment increases the burden on the provider to understand the cost of care provided during a care cycle. However, not only has the current system blinded physicians to the cost of care, but current antitrust legislation has made discussions of pricing with colleagues (so-called price collusion) illegal and subject to fines of up to $1 million per person and $100 million per organization,6 therefore limiting orthopedic physician involvement.
Given these legal constraints, instead of measuring direct costs of goods, we developed a “grocery list” approach in which direct comparisons are made of resources (goods and services) used and delivered during the entire 90-day cycle of care for patients who undergo anatomical total shoulder arthroplasty (TSA) or reverse shoulder arthroplasty (RSA). We used one surgeon’s practice experience as a model for measuring other orthopedic surgeons’ resource utilization, based on their electronic medical records (EMR) system data. By capturing the costs of the components of resource utilization rather than just the final cost of care, we can assess, compare, understand, endorse, and address these driving factors.
1. The significance of resource utilization
To maximize the efficiency of their practices, high-volume shoulder surgeons have introduced standardization to health care delivery.7 Identifying specific efficiencies makes uniform acceptance of beneficial practice patterns possible.
To facilitate comparison of goods and services used during an episode of surgical care, Virani and colleagues8,9 studied the costs of TSA and RSA and calculated the top 10 driving cost factors for these procedures (Figure 1). Their systematic analysis provided a framework for a common method of communication, allowing an orthopedic surgeon to gain a more complete understanding of the resources used during a particular operative procedure in his or her practice, and allowing several physicians to compare and contrast the resources collectively used for a single procedure, facilitating an understanding of different practice patterns within a local community. At a societal level, these data can be collected to help guide overall recommendations.
2. How we defined utilization
To define the resources used, we had to decide which procedure components cost the most. Virani and colleagues8,9 found that the top 10 cost drivers accounted for 93.11% and 94.77% of the total cost of the TSA and RSA care cycles, respectively (Figure 1). For each cost driver, information on resources used (goods, services, overhead) was collected on 2 forms, the Hospital Utilization Form (7 hospital-based items) and the Clinical Utilization Form (3 non-hospital-based items). To make hospital data easy to compile, we piloted use of a “smart form” in the EpicCare EMR system to isolate and auto-populate specific data fields.
3. EMR data collection
With EMR becoming mandatory for all public and private health care providers starting in 2014, utilization data are now included in a single unified system. Working with our in-house information technology department, we developed an algorithm to populate this information in a separate, easy-to-follow hospital utilization form. This form can be adopted by other institutions. Although EpicCare EMR is used by 52% of hospitals and at our institution, the data points required to make the same measurements are generalizable and exist in other EMRs.
Smartlinks, a tool in this EMR, allows utilization data to be quickly retrieved from different locations in a medical record and allows a form to be electronically completed in seconds. Data can be retrieved for any patient in the EMR system, regardless of when that patient’s hospital stay occurred. We populated data from surgeries performed 2 years before the start of this project.
4. What we can learn from these data
Data from a pilot study of 25 patients who underwent primary anatomical TSA for osteoarthritis and 25 patients who underwent primary RSA for massive rotator cuff tear allowed us to generate graphical representations of a single surgeon’s practice patterns that most affected the cost of care. Time in holding, time in the operating room, time in the postanesthesia care unit, and percentage of patients receiving different medications were recorded for each procedure (Figures 2–11). The study did not capture the wide variances in practice patterns in shoulder arthroplasty, and therefore other surgeons’ resource utilization may differ from ours. However, replicating this methodology at other institutions will produce a more robust data set from which conclusions about resource utilization and, indirectly, cost of care can be made.
5. Future possibilities
By using existing EMR tools to better understand resource utilization, orthopedic surgeons can play a constructive role in the dialogue on health care costs and new reimbursement models. The data presented here are not meant to be interpreted as hard and fast numbers on global resource utilization, but instead we intend to establish a model for collecting data on resource utilization. Resource utilization begins the dialogue that allows orthopedic surgeons and specialty societies to speak a common language without discussing actual cost numbers, which is discouraged under antitrust regulation. The data presented will allow comparisons to be made between surgeons in all practice settings to highlight areas of inconsistency in order to further improve patient care. Although this work involved only 50 patients undergoing only 2 types of surgeries, the resource-capturing methodology can be expanded to include more procedures and orthopedic practices. As all hospitals are now required to have EMRs, the metrics tracked in this work can be found on any patient medical record and auto-populated using our open-source utilization forms. Starting this data collection at your hospital may require no more than a conversation with the informatics department, as the metrics can for the most part be populated into a database on surgeon request.
As orthopedic surgeons return to the economic health care discussion, this information could prove essential in helping the individual surgeon and the orthopedic community justify the cost of care as well as fully understand the cost drivers for musculoskeletal care.
Click here to read the commentary on this article by Peter D. McCann, MD
1. National health expenditures 2013 highlights. Centers for Medicare & Medicaid Services website. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/highlights.pdf. Accessed September 14, 2015.
2. Wilson KB. Health care costs 101: slow growth persists. California HealthCare Foundation website. http://www.chcf.org/publications/2014/07/health-care-costs-101. Published July 2014. Accessed August 24, 2015.
3. Froimson MI, Rana A, White RE Jr, et al. Bundled Payments for Care Improvement Initiative: the next evolution of payment formulations: AAHKS Bundled Payment Task Force. J Arthroplasty. 2013;28(8 suppl):157-165.
4. Morley M, Bogasky S, Gage B, Flood S, Ingber MJ. Medicare post-acute care episodes and payment bundling. Medicare Medicaid Res Rev. 2014;4(1).
5. Teusink MJ, Virani NA, Polikandriotis JA, Frankle MA. Cost analysis in shoulder arthroplasty surgery. Adv Orthop. 2012;2012:692869.
6. Fassbender E, Pandya S. Legislation focuses on AAOS priorities. American Academy of Orthopaedic Surgeons website. http://www.aaos.org/news/aaosnow/may14/advocacy2.asp. AAOS Now. Published May 2014. Accessed August 24, 2015.
7. Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. Boston, MA: Harvard Business School Press; 2006.
8. Virani NA, Williams CD, Clark R, Polikandriotis J, Downes KL, Frankle MA. Preparing for the bundled-payment initiative: the cost and clinical outcomes of reverse shoulder arthroplasty for the surgical treatment of advanced rotator cuff deficiency at an average 4-year follow-up. J Shoulder Elbow Surg. 2013;22(12):1612-1622.
9. Virani NA, Williams CD, Clark R, Polikandriotis J, Downes KL, Frankle MA. Preparing for the bundled-payment initiative: the cost and clinical outcomes of total shoulder arthroplasty for the surgical treatment of glenohumeral arthritis at an average 4-year follow-up. J Shoulder Elbow Surg. 2013;22(12):1601-1611.
1. National health expenditures 2013 highlights. Centers for Medicare & Medicaid Services website. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/highlights.pdf. Accessed September 14, 2015.
2. Wilson KB. Health care costs 101: slow growth persists. California HealthCare Foundation website. http://www.chcf.org/publications/2014/07/health-care-costs-101. Published July 2014. Accessed August 24, 2015.
3. Froimson MI, Rana A, White RE Jr, et al. Bundled Payments for Care Improvement Initiative: the next evolution of payment formulations: AAHKS Bundled Payment Task Force. J Arthroplasty. 2013;28(8 suppl):157-165.
4. Morley M, Bogasky S, Gage B, Flood S, Ingber MJ. Medicare post-acute care episodes and payment bundling. Medicare Medicaid Res Rev. 2014;4(1).
5. Teusink MJ, Virani NA, Polikandriotis JA, Frankle MA. Cost analysis in shoulder arthroplasty surgery. Adv Orthop. 2012;2012:692869.
6. Fassbender E, Pandya S. Legislation focuses on AAOS priorities. American Academy of Orthopaedic Surgeons website. http://www.aaos.org/news/aaosnow/may14/advocacy2.asp. AAOS Now. Published May 2014. Accessed August 24, 2015.
7. Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. Boston, MA: Harvard Business School Press; 2006.
8. Virani NA, Williams CD, Clark R, Polikandriotis J, Downes KL, Frankle MA. Preparing for the bundled-payment initiative: the cost and clinical outcomes of reverse shoulder arthroplasty for the surgical treatment of advanced rotator cuff deficiency at an average 4-year follow-up. J Shoulder Elbow Surg. 2013;22(12):1612-1622.
9. Virani NA, Williams CD, Clark R, Polikandriotis J, Downes KL, Frankle MA. Preparing for the bundled-payment initiative: the cost and clinical outcomes of total shoulder arthroplasty for the surgical treatment of glenohumeral arthritis at an average 4-year follow-up. J Shoulder Elbow Surg. 2013;22(12):1601-1611.
Technique of Open Reduction and Internal Fixation of Comminuted Proximal Humerus Fractures With Allograft Femoral Head Metaphyseal Reconstruction
Proximal humerus fractures are exceedingly common and account for almost 5% of all fractures. As osteoporosis is a risk factor for these fractures, their incidence rises with patient age.1
In 1970, Neer2 described these type of fractures and classified them as having 2, 3, or 4 parts based on the amount of angulation and displacement of the humeral head and the greater and lesser tuberosities with respect to the shaft.
Three- and 4-part proximal humerus fractures can be treated either nonoperatively, or surgically with closed reduction and percutaneous fixation, intramedullary fixation, open reduction and internal fixation (ORIF), or arthroplasty. There remains controversy over the best treatment, but a key component of any surgical treatment is anatomical reduction, stable fixation, and then healing of the tuberosities. A current common form of treatment is augmentation with an allograft fibula placed in the medullary canal. Although not formally reported, anecdotal evidence demonstrates that revision to arthroplasty is very difficult in the setting of an ingrown graft in the medullary canal of the humerus.
In this article, we present a novel technique of using allograft femoral head to reconstruct the metaphysis in ORIF of comminuted proximal humerus fractures.
Technique
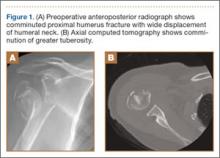
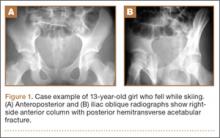
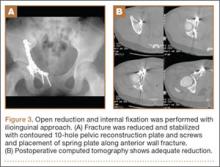
Presented in Figure 1 are preoperative images of a representative displaced 4-part proximal humerus fracture treated surgically using the technique described here. General anesthesia is used. After intubation on the operating table, the patient is placed in the beach-chair position with about 75° of hip flexion. All bony prominences are padded, and the head and trunk are well secured. A pneumatic arm positioner is used to alleviate the need for an assistant to manipulate the arm. An image intensifier is used before preparing to verify that appropriate images of the proximal humerus can be obtained. Once adequate images are confirmed, the floor can be marked at the position of the fluoroscopic unit’s wheels to allow easy reproduction of images once the arm is prepared and draped. The intensifier is then removed from the field, the shoulder is prepared and draped in usual fashion, and prophylactic antibiotics are administered.
A deltopectoral incision is used, and sharp dissection is made through the subcutaneous tissue to raise full-thickness subcutaneous flaps on each side. The deltopectoral interval is sharply dissected while protecting the cephalic vein. Subdeltoid adhesions are then released. Palpation of the axillary nerve in the quadrilateral space to identify its location is helpful to avoid injury during the procedure.
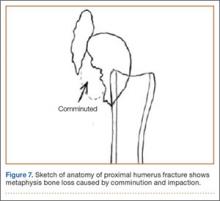
The fracture is then identified, and No. 5 permanent suture is placed through the posterior and superior rotator cuff and through the subscapularis insertion (Figure 2). The tuberosities are freed from the humeral head sharply. A blunt elevator is then used to gently elevate the humeral head upward, with care taken to avoid comminuting the metaphyseal bone while levering. Reduction is achieved by manipulating the sutures and levering the head with the elevator while placing the arm in extension and posterior translation. Fluoroscopic images are used to verify correct anatomical alignment. Generally, the metaphysis demonstrates comminution and impaction, with poor bone quality necessitating use of bone graft.
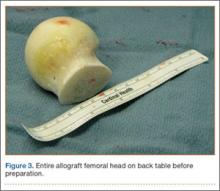
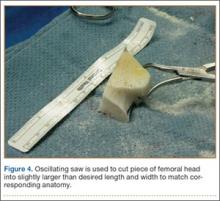
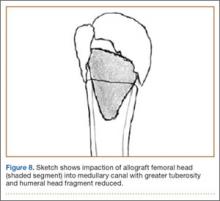
A frozen allograft femoral head is then obtained and split into 2 equal pieces using a saw (Figures 3–5). One piece is fashioned with a saw and a burr into a trapezoid such that the proximal portion is wider, and the distal, tapered portion is sized to fit the canal. The broad, proximal portion of the graft will serve as a pedestal to reduce the head to the shaft. Measuring the internal diameter of the humeral canal can be useful in estimating the necessary dimensions of the distal portion of the allograft. The graft often needs several small adjustments that necessitate attempting to place it in the intramedullary canal and then trimming as necessary to ensure proper fit distally within the shaft. For this reason, it is beneficial to perform the graft preparation near the surgical field. Once completed, the distal portion is then impacted into the humeral canal (Figure 6). Because of this impaction, there is no possibility for subsidence or pistoning of the graft within the canal, which can occur with a fibular graft. The humeral head is reduced onto the shaft with the already placed sutures; this is achieved by abducting the shoulder. The image intensifier is then used to confirm appropriate alignment and positioning of the fragments, making sure that both neck–shaft angle and medial calcar alignment have been restored (Figures 7, 8).
An appropriately sized proximal humerus plate is then selected based on the location of the fracture line. We have used standard lateral proximal humerus locking plates as well as laterality-specific anterolateral proximal humerus plates and found that both are suitable for incorporation of the screws through the graft and into the head. The plate is positioned on the humerus, and a guide pin is placed by hand through the proximal-most hole so that the appropriate height of the plate can be verified on fluoroscopy. The first screw is then a nonlocking bicortical screw placed through the oval hole in the shaft of the plate to allow further fine manipulation of the plate more proximally or distally as needed. The final height is confirmed, and the screw is firmly tightened (Figure 9). The locking-screw guide is fixed to the proximal portion of the plate, and 2 locking screws are then placed into the head. The arm is then rotated to an anteroposterior view by placing the arm in external rotation and neutral flexion and is then abducted and internally rotated to recreate a lateral view to perform final verification of the position of the plate on orthogonal images. If the surgeon is satisfied with the position of the plate, another nonlocking screw is placed distally, and then the proximal holes are used to place locking screws as needed. If the surgeon is not satisfied, the 2 proximal screws can be removed and the plate repositioned.
After each screw is placed, fluoroscopy is used to ensure there has been no breach of the articular surface. The number of proximal screws placed depends on fracture configuration and surgeon preference.
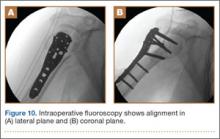
The sutures through the rotator cuff are then fixed to the plate, securing the tuberosities. Final intraoperative radiographs are used to confirm reduction, alignment, and final position of hardware (Figure 10). After copious irrigation, a surgical drain is placed as needed, and the wound is closed in layered fashion. Three years after surgery, follow-up examination revealed no radiographic change in alignment, no necrosis, and no varus collapse (Figure 11), and the patient was pain-free during activities.
Discussion
Surgical treatment of comminuted proximal humerus fractures usually consists of some type of plate fixation with screw fixation of the shaft, screws or smooth pegs to support the chondral surfaces, and screw fixation or suture cerclage of the tuberosities.
Fixed-angle locking-plate-and-screw constructs increased the biomechanical stability and pullout strength of proximal humerus plates.3,4 Nevertheless, avascular necrosis, malunion, and nonunion are still known complications of proximal humerus fractures, especially those with comminution, with up to 14% of patients still experiencing loss of fixation.5
For this reason, several authors have proposed using allograft bone and/or augmentation with calcium-containing cement to supplement fixation and provide an endosteal form of support for the head and tuberosities to decrease the risk for varus collapse. Osteobiologics (eg, calcium phosphate or sulfate cement) have been shown to decrease the risk for loss of reduction of proximal humerus fractures and decrease the risk for intra-articular screw penetration.6,7 Many calcium phosphate cements are commercially available. Cost and availability are 2 reasons that these supplements are not more widely used. Cancellous chips have also been used to aid in the reduction of proximal humerus fractures.8 No randomized study has been conducted to show a clinical advantage of this technique, though retrospective studies have shown that it is not as advantageous as using calcium phosphate cement with respect to loss of reduction or screw penetration.6 Certainly, cancellous chips are easily available in most hospitals and are less expensive than some alternatives. A recent review of these techniques in osteoporotic proximal humerus fractures found no clear indication for using one of these supplements over another.9
However, some fracture patterns require a structural graft to reduce the tuberosities and head component. Although described more than 30 years ago as a treatment for nonunions with an intramedullary “peg” of iliac crest graft,10 the graft most commonly reported today is allograft fibula.11-15 This technique consists of preparing the humeral shaft and often the fractured head segment with reaming to create a channel to receive the graft. Even with use of a small fibula, it is often time-consuming to use a saw, rasp, or burr to size the fibular segment to fit the medullary canal of the humerus. Once in place, the graft provides a strut on which the head fragment can be reduced and around which the tuberosities can be reduced. Although this technique is successful clinically and is biomechanically superior to plate-only constructs,16,17 concerns remain.
One such concern is keeping this graft in routine supply at most hospitals. Supply and pricing from vendors can differ significantly between hospitals, and a surgeon may need to request grafts in advance, which makes their use nonviable in a trauma case. Certain grafts are often kept in routine supply based on their overall utilization. At our institution, allograft femoral heads meet this criterion and are routinely stocked.
Of more importance are the ramifications of these procedures for future revision surgeries. The need for arthroplasty revision is common after ORIF of a proximal humerus fracture.18
Arthroplasty revision is an already challenging procedure that becomes more complex with the need to remove 6 to 8 cm of ingrown endosteal bone from a shell of outer osteoporotic cortical bone. Our experience with these complex revisions provided the impetus to search for an alternate graft type that still provides a strut for reducing the head and tuberosities but limits the amount of endosteal bone that would need to be removed in arthroplasty revision in order to place a stemmed component into the humeral canal.
Some currently available arthroplasty fracture systems modify the previous anatomy of the stem to provide a more anatomical platform to reduce the tuberosities to a broader metaphyseal construct that incorporates bone grafting to assist with healing.
Because of these concerns and factors, we adapted our technique to create an individual-specific pedestal with allograft femoral head that can be anatomically matched to each patient. This provides a strut to reduce the head and tuberosity fragments but still limits the amount of allograft bone needed to seat into the existing canal. The geometry of the allograft can also be customized to the fracture, with most 3- and 4-part fractures needing a trapezoidal strut that resembles the metaphyseal portion of a fracture-specific shoulder arthroplasty implant.
We have used this technique for comminuted 3- and 4-part fractures of the proximal humerus in 14 cases with at least 2-year follow-up and in several more cases that have not reached 2-year follow-up. All cases have gone on to radiographic union; none have had to be revised either with revision ORIF or to an arthroplasty. Formal measurements of final postoperative range of motion have not been tabulated in all cases, as some cases have been lost to follow-up after radiographic union was achieved. Medium- and long-term results are not yet available, but no short-term complications have been noted.
Disadvantages of this technique are that, while an individualized graft is created, proper shaping still takes time, and a moderate amount of the femoral head is not used. However, we have found that, if a graft is inadvertently undersized, there is still ample femoral head remaining to create another sized graft. Other disadvantages are the added cost and the (rare) risk of disease transmission, which come with use of any allograft, but the technique is used instead of another type of allograft, so these disadvantages are largely equivalent. At our hospital, differences in cost and availability between femoral head or fibular allografts are negligible.
This procedure, which is easily performed in a short amount of time, allows a stable base of bone graft to be used as an aid in the anatomical reduction of proximal humerus fractures, without the need for reaming and preparation of the medullary canal and without further increasing the difficulty associated with a future revision procedure.
1. Barrett JA, Baron JA, Karagas MR, Beach ML. Fracture risk in the U.S. Medicare population. J Clin Epidemiol. 1999;52(3):243-249.
2. Neer CS 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077-1089.
3. Liew AS, Johnson JA, Patterson SD, King GJ, Chess DG. Effect of screw placement on fixation in the humeral head. J Shoulder Elbow Surg. 2000;9(5):423-426.
4. Weinstein DM, Bratton DR, Ciccone WJ 2nd, Elias JJ. Locking plates improve torsional resistance in the stabilization of three-part proximal humeral fractures. J Shoulder Elbow Surg. 2006;15(2):239-243.
5. Agudelo J, Schurmann M, Stahel P, et al. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2007;21(10):676-681.
6. Egol KA, Sugi MT, Ong CC, Montero N, Davidovitch R, Zuckerman JD. Fracture site augmentation with calcium phosphate cement reduces screw penetration after open reduction-internal fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2012;21(6):741-748.
7. Gradl G, Knobe M, Stoffel M, Prescher A, Dirrichs T, Pape HC. Biomechanical evaluation of locking plate fixation of proximal humeral fractures augmented with calcium phosphate cement. J Orthop Trauma. 2013;27(7):399-404.
8. Ong CC, Kwon YW, Walsh M, Davidovitch R, Zuckerman JD, Egol KA. Outcomes of open reduction and internal fixation of proximal humerus fractures managed with locking plates. Am J Orthop. 2012;41(9):407-412.
9. Namdari S, Voleti PB, Mehta S. Evaluation of the osteoporotic proximal humeral fracture and strategies for structural augmentation during surgical treatment. J Shoulder Elbow Surg. 2012;21(12):1787-1795.
10. Scheck M. Surgical treatment of nonunions of the surgical neck of the humerus. Clin Orthop Relat Res. 1982;(167):255-259.
11. Hettrich CM, Neviaser A, Beamer BS, Paul O, Helfet DL, Lorich DG. Locked plating of the proximal humerus using an endosteal implant. J Orthop Trauma. 2012;26(4):212-215.
12. Neviaser AS, Hettrich CM, Beamer BS, Dines JS, Lorich DG. Endosteal strut augment reduces complications associated with proximal humeral locking plates. Clin Orthop Relat Res. 2011;469(12):3300-3306.
13. Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant. J Orthop Trauma. 2008;22(3):195-200.
14. Matassi F, Angeloni R, Carulli C, et al. Locking plate and fibular allograft augmentation in unstable fractures of proximal humerus. Injury. 2012;43(11):1939-1942.
15. Little MT, Berkes MB, Schottel PC, et al. The impact of preoperative coronal plane deformity on proximal humerus fixation with endosteal augmentation. J Orthop Trauma. 2014;28(6):338-347.
16. Mathison C, Chaudhary R, Beaupre L, Reynolds M, Adeeb S, Bouliane M. Biomechanical analysis of proximal humeral fixation using locking plate fixation with an intramedullary fibular allograft. Clin Biomech. 2010;25(7):642-646.
17. Chow RM, Begum F, Beaupre LA, Carey JP, Adeeb S, Bouliane MJ. Proximal humeral fracture fixation: locking plate construct +/- intramedullary fibular allograft. J Shoulder Elbow Surg. 2012;21(7):894-901.
18. Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2013;22(4):542-549.
Proximal humerus fractures are exceedingly common and account for almost 5% of all fractures. As osteoporosis is a risk factor for these fractures, their incidence rises with patient age.1
In 1970, Neer2 described these type of fractures and classified them as having 2, 3, or 4 parts based on the amount of angulation and displacement of the humeral head and the greater and lesser tuberosities with respect to the shaft.
Three- and 4-part proximal humerus fractures can be treated either nonoperatively, or surgically with closed reduction and percutaneous fixation, intramedullary fixation, open reduction and internal fixation (ORIF), or arthroplasty. There remains controversy over the best treatment, but a key component of any surgical treatment is anatomical reduction, stable fixation, and then healing of the tuberosities. A current common form of treatment is augmentation with an allograft fibula placed in the medullary canal. Although not formally reported, anecdotal evidence demonstrates that revision to arthroplasty is very difficult in the setting of an ingrown graft in the medullary canal of the humerus.
In this article, we present a novel technique of using allograft femoral head to reconstruct the metaphysis in ORIF of comminuted proximal humerus fractures.
Technique
Presented in Figure 1 are preoperative images of a representative displaced 4-part proximal humerus fracture treated surgically using the technique described here. General anesthesia is used. After intubation on the operating table, the patient is placed in the beach-chair position with about 75° of hip flexion. All bony prominences are padded, and the head and trunk are well secured. A pneumatic arm positioner is used to alleviate the need for an assistant to manipulate the arm. An image intensifier is used before preparing to verify that appropriate images of the proximal humerus can be obtained. Once adequate images are confirmed, the floor can be marked at the position of the fluoroscopic unit’s wheels to allow easy reproduction of images once the arm is prepared and draped. The intensifier is then removed from the field, the shoulder is prepared and draped in usual fashion, and prophylactic antibiotics are administered.
A deltopectoral incision is used, and sharp dissection is made through the subcutaneous tissue to raise full-thickness subcutaneous flaps on each side. The deltopectoral interval is sharply dissected while protecting the cephalic vein. Subdeltoid adhesions are then released. Palpation of the axillary nerve in the quadrilateral space to identify its location is helpful to avoid injury during the procedure.
The fracture is then identified, and No. 5 permanent suture is placed through the posterior and superior rotator cuff and through the subscapularis insertion (Figure 2). The tuberosities are freed from the humeral head sharply. A blunt elevator is then used to gently elevate the humeral head upward, with care taken to avoid comminuting the metaphyseal bone while levering. Reduction is achieved by manipulating the sutures and levering the head with the elevator while placing the arm in extension and posterior translation. Fluoroscopic images are used to verify correct anatomical alignment. Generally, the metaphysis demonstrates comminution and impaction, with poor bone quality necessitating use of bone graft.
A frozen allograft femoral head is then obtained and split into 2 equal pieces using a saw (Figures 3–5). One piece is fashioned with a saw and a burr into a trapezoid such that the proximal portion is wider, and the distal, tapered portion is sized to fit the canal. The broad, proximal portion of the graft will serve as a pedestal to reduce the head to the shaft. Measuring the internal diameter of the humeral canal can be useful in estimating the necessary dimensions of the distal portion of the allograft. The graft often needs several small adjustments that necessitate attempting to place it in the intramedullary canal and then trimming as necessary to ensure proper fit distally within the shaft. For this reason, it is beneficial to perform the graft preparation near the surgical field. Once completed, the distal portion is then impacted into the humeral canal (Figure 6). Because of this impaction, there is no possibility for subsidence or pistoning of the graft within the canal, which can occur with a fibular graft. The humeral head is reduced onto the shaft with the already placed sutures; this is achieved by abducting the shoulder. The image intensifier is then used to confirm appropriate alignment and positioning of the fragments, making sure that both neck–shaft angle and medial calcar alignment have been restored (Figures 7, 8).
An appropriately sized proximal humerus plate is then selected based on the location of the fracture line. We have used standard lateral proximal humerus locking plates as well as laterality-specific anterolateral proximal humerus plates and found that both are suitable for incorporation of the screws through the graft and into the head. The plate is positioned on the humerus, and a guide pin is placed by hand through the proximal-most hole so that the appropriate height of the plate can be verified on fluoroscopy. The first screw is then a nonlocking bicortical screw placed through the oval hole in the shaft of the plate to allow further fine manipulation of the plate more proximally or distally as needed. The final height is confirmed, and the screw is firmly tightened (Figure 9). The locking-screw guide is fixed to the proximal portion of the plate, and 2 locking screws are then placed into the head. The arm is then rotated to an anteroposterior view by placing the arm in external rotation and neutral flexion and is then abducted and internally rotated to recreate a lateral view to perform final verification of the position of the plate on orthogonal images. If the surgeon is satisfied with the position of the plate, another nonlocking screw is placed distally, and then the proximal holes are used to place locking screws as needed. If the surgeon is not satisfied, the 2 proximal screws can be removed and the plate repositioned.
After each screw is placed, fluoroscopy is used to ensure there has been no breach of the articular surface. The number of proximal screws placed depends on fracture configuration and surgeon preference.
The sutures through the rotator cuff are then fixed to the plate, securing the tuberosities. Final intraoperative radiographs are used to confirm reduction, alignment, and final position of hardware (Figure 10). After copious irrigation, a surgical drain is placed as needed, and the wound is closed in layered fashion. Three years after surgery, follow-up examination revealed no radiographic change in alignment, no necrosis, and no varus collapse (Figure 11), and the patient was pain-free during activities.
Discussion
Surgical treatment of comminuted proximal humerus fractures usually consists of some type of plate fixation with screw fixation of the shaft, screws or smooth pegs to support the chondral surfaces, and screw fixation or suture cerclage of the tuberosities.
Fixed-angle locking-plate-and-screw constructs increased the biomechanical stability and pullout strength of proximal humerus plates.3,4 Nevertheless, avascular necrosis, malunion, and nonunion are still known complications of proximal humerus fractures, especially those with comminution, with up to 14% of patients still experiencing loss of fixation.5
For this reason, several authors have proposed using allograft bone and/or augmentation with calcium-containing cement to supplement fixation and provide an endosteal form of support for the head and tuberosities to decrease the risk for varus collapse. Osteobiologics (eg, calcium phosphate or sulfate cement) have been shown to decrease the risk for loss of reduction of proximal humerus fractures and decrease the risk for intra-articular screw penetration.6,7 Many calcium phosphate cements are commercially available. Cost and availability are 2 reasons that these supplements are not more widely used. Cancellous chips have also been used to aid in the reduction of proximal humerus fractures.8 No randomized study has been conducted to show a clinical advantage of this technique, though retrospective studies have shown that it is not as advantageous as using calcium phosphate cement with respect to loss of reduction or screw penetration.6 Certainly, cancellous chips are easily available in most hospitals and are less expensive than some alternatives. A recent review of these techniques in osteoporotic proximal humerus fractures found no clear indication for using one of these supplements over another.9
However, some fracture patterns require a structural graft to reduce the tuberosities and head component. Although described more than 30 years ago as a treatment for nonunions with an intramedullary “peg” of iliac crest graft,10 the graft most commonly reported today is allograft fibula.11-15 This technique consists of preparing the humeral shaft and often the fractured head segment with reaming to create a channel to receive the graft. Even with use of a small fibula, it is often time-consuming to use a saw, rasp, or burr to size the fibular segment to fit the medullary canal of the humerus. Once in place, the graft provides a strut on which the head fragment can be reduced and around which the tuberosities can be reduced. Although this technique is successful clinically and is biomechanically superior to plate-only constructs,16,17 concerns remain.
One such concern is keeping this graft in routine supply at most hospitals. Supply and pricing from vendors can differ significantly between hospitals, and a surgeon may need to request grafts in advance, which makes their use nonviable in a trauma case. Certain grafts are often kept in routine supply based on their overall utilization. At our institution, allograft femoral heads meet this criterion and are routinely stocked.
Of more importance are the ramifications of these procedures for future revision surgeries. The need for arthroplasty revision is common after ORIF of a proximal humerus fracture.18
Arthroplasty revision is an already challenging procedure that becomes more complex with the need to remove 6 to 8 cm of ingrown endosteal bone from a shell of outer osteoporotic cortical bone. Our experience with these complex revisions provided the impetus to search for an alternate graft type that still provides a strut for reducing the head and tuberosities but limits the amount of endosteal bone that would need to be removed in arthroplasty revision in order to place a stemmed component into the humeral canal.
Some currently available arthroplasty fracture systems modify the previous anatomy of the stem to provide a more anatomical platform to reduce the tuberosities to a broader metaphyseal construct that incorporates bone grafting to assist with healing.
Because of these concerns and factors, we adapted our technique to create an individual-specific pedestal with allograft femoral head that can be anatomically matched to each patient. This provides a strut to reduce the head and tuberosity fragments but still limits the amount of allograft bone needed to seat into the existing canal. The geometry of the allograft can also be customized to the fracture, with most 3- and 4-part fractures needing a trapezoidal strut that resembles the metaphyseal portion of a fracture-specific shoulder arthroplasty implant.
We have used this technique for comminuted 3- and 4-part fractures of the proximal humerus in 14 cases with at least 2-year follow-up and in several more cases that have not reached 2-year follow-up. All cases have gone on to radiographic union; none have had to be revised either with revision ORIF or to an arthroplasty. Formal measurements of final postoperative range of motion have not been tabulated in all cases, as some cases have been lost to follow-up after radiographic union was achieved. Medium- and long-term results are not yet available, but no short-term complications have been noted.
Disadvantages of this technique are that, while an individualized graft is created, proper shaping still takes time, and a moderate amount of the femoral head is not used. However, we have found that, if a graft is inadvertently undersized, there is still ample femoral head remaining to create another sized graft. Other disadvantages are the added cost and the (rare) risk of disease transmission, which come with use of any allograft, but the technique is used instead of another type of allograft, so these disadvantages are largely equivalent. At our hospital, differences in cost and availability between femoral head or fibular allografts are negligible.
This procedure, which is easily performed in a short amount of time, allows a stable base of bone graft to be used as an aid in the anatomical reduction of proximal humerus fractures, without the need for reaming and preparation of the medullary canal and without further increasing the difficulty associated with a future revision procedure.
Proximal humerus fractures are exceedingly common and account for almost 5% of all fractures. As osteoporosis is a risk factor for these fractures, their incidence rises with patient age.1
In 1970, Neer2 described these type of fractures and classified them as having 2, 3, or 4 parts based on the amount of angulation and displacement of the humeral head and the greater and lesser tuberosities with respect to the shaft.
Three- and 4-part proximal humerus fractures can be treated either nonoperatively, or surgically with closed reduction and percutaneous fixation, intramedullary fixation, open reduction and internal fixation (ORIF), or arthroplasty. There remains controversy over the best treatment, but a key component of any surgical treatment is anatomical reduction, stable fixation, and then healing of the tuberosities. A current common form of treatment is augmentation with an allograft fibula placed in the medullary canal. Although not formally reported, anecdotal evidence demonstrates that revision to arthroplasty is very difficult in the setting of an ingrown graft in the medullary canal of the humerus.
In this article, we present a novel technique of using allograft femoral head to reconstruct the metaphysis in ORIF of comminuted proximal humerus fractures.
Technique
Presented in Figure 1 are preoperative images of a representative displaced 4-part proximal humerus fracture treated surgically using the technique described here. General anesthesia is used. After intubation on the operating table, the patient is placed in the beach-chair position with about 75° of hip flexion. All bony prominences are padded, and the head and trunk are well secured. A pneumatic arm positioner is used to alleviate the need for an assistant to manipulate the arm. An image intensifier is used before preparing to verify that appropriate images of the proximal humerus can be obtained. Once adequate images are confirmed, the floor can be marked at the position of the fluoroscopic unit’s wheels to allow easy reproduction of images once the arm is prepared and draped. The intensifier is then removed from the field, the shoulder is prepared and draped in usual fashion, and prophylactic antibiotics are administered.
A deltopectoral incision is used, and sharp dissection is made through the subcutaneous tissue to raise full-thickness subcutaneous flaps on each side. The deltopectoral interval is sharply dissected while protecting the cephalic vein. Subdeltoid adhesions are then released. Palpation of the axillary nerve in the quadrilateral space to identify its location is helpful to avoid injury during the procedure.
The fracture is then identified, and No. 5 permanent suture is placed through the posterior and superior rotator cuff and through the subscapularis insertion (Figure 2). The tuberosities are freed from the humeral head sharply. A blunt elevator is then used to gently elevate the humeral head upward, with care taken to avoid comminuting the metaphyseal bone while levering. Reduction is achieved by manipulating the sutures and levering the head with the elevator while placing the arm in extension and posterior translation. Fluoroscopic images are used to verify correct anatomical alignment. Generally, the metaphysis demonstrates comminution and impaction, with poor bone quality necessitating use of bone graft.
A frozen allograft femoral head is then obtained and split into 2 equal pieces using a saw (Figures 3–5). One piece is fashioned with a saw and a burr into a trapezoid such that the proximal portion is wider, and the distal, tapered portion is sized to fit the canal. The broad, proximal portion of the graft will serve as a pedestal to reduce the head to the shaft. Measuring the internal diameter of the humeral canal can be useful in estimating the necessary dimensions of the distal portion of the allograft. The graft often needs several small adjustments that necessitate attempting to place it in the intramedullary canal and then trimming as necessary to ensure proper fit distally within the shaft. For this reason, it is beneficial to perform the graft preparation near the surgical field. Once completed, the distal portion is then impacted into the humeral canal (Figure 6). Because of this impaction, there is no possibility for subsidence or pistoning of the graft within the canal, which can occur with a fibular graft. The humeral head is reduced onto the shaft with the already placed sutures; this is achieved by abducting the shoulder. The image intensifier is then used to confirm appropriate alignment and positioning of the fragments, making sure that both neck–shaft angle and medial calcar alignment have been restored (Figures 7, 8).
An appropriately sized proximal humerus plate is then selected based on the location of the fracture line. We have used standard lateral proximal humerus locking plates as well as laterality-specific anterolateral proximal humerus plates and found that both are suitable for incorporation of the screws through the graft and into the head. The plate is positioned on the humerus, and a guide pin is placed by hand through the proximal-most hole so that the appropriate height of the plate can be verified on fluoroscopy. The first screw is then a nonlocking bicortical screw placed through the oval hole in the shaft of the plate to allow further fine manipulation of the plate more proximally or distally as needed. The final height is confirmed, and the screw is firmly tightened (Figure 9). The locking-screw guide is fixed to the proximal portion of the plate, and 2 locking screws are then placed into the head. The arm is then rotated to an anteroposterior view by placing the arm in external rotation and neutral flexion and is then abducted and internally rotated to recreate a lateral view to perform final verification of the position of the plate on orthogonal images. If the surgeon is satisfied with the position of the plate, another nonlocking screw is placed distally, and then the proximal holes are used to place locking screws as needed. If the surgeon is not satisfied, the 2 proximal screws can be removed and the plate repositioned.
After each screw is placed, fluoroscopy is used to ensure there has been no breach of the articular surface. The number of proximal screws placed depends on fracture configuration and surgeon preference.
The sutures through the rotator cuff are then fixed to the plate, securing the tuberosities. Final intraoperative radiographs are used to confirm reduction, alignment, and final position of hardware (Figure 10). After copious irrigation, a surgical drain is placed as needed, and the wound is closed in layered fashion. Three years after surgery, follow-up examination revealed no radiographic change in alignment, no necrosis, and no varus collapse (Figure 11), and the patient was pain-free during activities.
Discussion
Surgical treatment of comminuted proximal humerus fractures usually consists of some type of plate fixation with screw fixation of the shaft, screws or smooth pegs to support the chondral surfaces, and screw fixation or suture cerclage of the tuberosities.
Fixed-angle locking-plate-and-screw constructs increased the biomechanical stability and pullout strength of proximal humerus plates.3,4 Nevertheless, avascular necrosis, malunion, and nonunion are still known complications of proximal humerus fractures, especially those with comminution, with up to 14% of patients still experiencing loss of fixation.5
For this reason, several authors have proposed using allograft bone and/or augmentation with calcium-containing cement to supplement fixation and provide an endosteal form of support for the head and tuberosities to decrease the risk for varus collapse. Osteobiologics (eg, calcium phosphate or sulfate cement) have been shown to decrease the risk for loss of reduction of proximal humerus fractures and decrease the risk for intra-articular screw penetration.6,7 Many calcium phosphate cements are commercially available. Cost and availability are 2 reasons that these supplements are not more widely used. Cancellous chips have also been used to aid in the reduction of proximal humerus fractures.8 No randomized study has been conducted to show a clinical advantage of this technique, though retrospective studies have shown that it is not as advantageous as using calcium phosphate cement with respect to loss of reduction or screw penetration.6 Certainly, cancellous chips are easily available in most hospitals and are less expensive than some alternatives. A recent review of these techniques in osteoporotic proximal humerus fractures found no clear indication for using one of these supplements over another.9
However, some fracture patterns require a structural graft to reduce the tuberosities and head component. Although described more than 30 years ago as a treatment for nonunions with an intramedullary “peg” of iliac crest graft,10 the graft most commonly reported today is allograft fibula.11-15 This technique consists of preparing the humeral shaft and often the fractured head segment with reaming to create a channel to receive the graft. Even with use of a small fibula, it is often time-consuming to use a saw, rasp, or burr to size the fibular segment to fit the medullary canal of the humerus. Once in place, the graft provides a strut on which the head fragment can be reduced and around which the tuberosities can be reduced. Although this technique is successful clinically and is biomechanically superior to plate-only constructs,16,17 concerns remain.
One such concern is keeping this graft in routine supply at most hospitals. Supply and pricing from vendors can differ significantly between hospitals, and a surgeon may need to request grafts in advance, which makes their use nonviable in a trauma case. Certain grafts are often kept in routine supply based on their overall utilization. At our institution, allograft femoral heads meet this criterion and are routinely stocked.
Of more importance are the ramifications of these procedures for future revision surgeries. The need for arthroplasty revision is common after ORIF of a proximal humerus fracture.18
Arthroplasty revision is an already challenging procedure that becomes more complex with the need to remove 6 to 8 cm of ingrown endosteal bone from a shell of outer osteoporotic cortical bone. Our experience with these complex revisions provided the impetus to search for an alternate graft type that still provides a strut for reducing the head and tuberosities but limits the amount of endosteal bone that would need to be removed in arthroplasty revision in order to place a stemmed component into the humeral canal.
Some currently available arthroplasty fracture systems modify the previous anatomy of the stem to provide a more anatomical platform to reduce the tuberosities to a broader metaphyseal construct that incorporates bone grafting to assist with healing.
Because of these concerns and factors, we adapted our technique to create an individual-specific pedestal with allograft femoral head that can be anatomically matched to each patient. This provides a strut to reduce the head and tuberosity fragments but still limits the amount of allograft bone needed to seat into the existing canal. The geometry of the allograft can also be customized to the fracture, with most 3- and 4-part fractures needing a trapezoidal strut that resembles the metaphyseal portion of a fracture-specific shoulder arthroplasty implant.
We have used this technique for comminuted 3- and 4-part fractures of the proximal humerus in 14 cases with at least 2-year follow-up and in several more cases that have not reached 2-year follow-up. All cases have gone on to radiographic union; none have had to be revised either with revision ORIF or to an arthroplasty. Formal measurements of final postoperative range of motion have not been tabulated in all cases, as some cases have been lost to follow-up after radiographic union was achieved. Medium- and long-term results are not yet available, but no short-term complications have been noted.
Disadvantages of this technique are that, while an individualized graft is created, proper shaping still takes time, and a moderate amount of the femoral head is not used. However, we have found that, if a graft is inadvertently undersized, there is still ample femoral head remaining to create another sized graft. Other disadvantages are the added cost and the (rare) risk of disease transmission, which come with use of any allograft, but the technique is used instead of another type of allograft, so these disadvantages are largely equivalent. At our hospital, differences in cost and availability between femoral head or fibular allografts are negligible.
This procedure, which is easily performed in a short amount of time, allows a stable base of bone graft to be used as an aid in the anatomical reduction of proximal humerus fractures, without the need for reaming and preparation of the medullary canal and without further increasing the difficulty associated with a future revision procedure.
1. Barrett JA, Baron JA, Karagas MR, Beach ML. Fracture risk in the U.S. Medicare population. J Clin Epidemiol. 1999;52(3):243-249.
2. Neer CS 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077-1089.
3. Liew AS, Johnson JA, Patterson SD, King GJ, Chess DG. Effect of screw placement on fixation in the humeral head. J Shoulder Elbow Surg. 2000;9(5):423-426.
4. Weinstein DM, Bratton DR, Ciccone WJ 2nd, Elias JJ. Locking plates improve torsional resistance in the stabilization of three-part proximal humeral fractures. J Shoulder Elbow Surg. 2006;15(2):239-243.
5. Agudelo J, Schurmann M, Stahel P, et al. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2007;21(10):676-681.
6. Egol KA, Sugi MT, Ong CC, Montero N, Davidovitch R, Zuckerman JD. Fracture site augmentation with calcium phosphate cement reduces screw penetration after open reduction-internal fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2012;21(6):741-748.
7. Gradl G, Knobe M, Stoffel M, Prescher A, Dirrichs T, Pape HC. Biomechanical evaluation of locking plate fixation of proximal humeral fractures augmented with calcium phosphate cement. J Orthop Trauma. 2013;27(7):399-404.
8. Ong CC, Kwon YW, Walsh M, Davidovitch R, Zuckerman JD, Egol KA. Outcomes of open reduction and internal fixation of proximal humerus fractures managed with locking plates. Am J Orthop. 2012;41(9):407-412.
9. Namdari S, Voleti PB, Mehta S. Evaluation of the osteoporotic proximal humeral fracture and strategies for structural augmentation during surgical treatment. J Shoulder Elbow Surg. 2012;21(12):1787-1795.
10. Scheck M. Surgical treatment of nonunions of the surgical neck of the humerus. Clin Orthop Relat Res. 1982;(167):255-259.
11. Hettrich CM, Neviaser A, Beamer BS, Paul O, Helfet DL, Lorich DG. Locked plating of the proximal humerus using an endosteal implant. J Orthop Trauma. 2012;26(4):212-215.
12. Neviaser AS, Hettrich CM, Beamer BS, Dines JS, Lorich DG. Endosteal strut augment reduces complications associated with proximal humeral locking plates. Clin Orthop Relat Res. 2011;469(12):3300-3306.
13. Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant. J Orthop Trauma. 2008;22(3):195-200.
14. Matassi F, Angeloni R, Carulli C, et al. Locking plate and fibular allograft augmentation in unstable fractures of proximal humerus. Injury. 2012;43(11):1939-1942.
15. Little MT, Berkes MB, Schottel PC, et al. The impact of preoperative coronal plane deformity on proximal humerus fixation with endosteal augmentation. J Orthop Trauma. 2014;28(6):338-347.
16. Mathison C, Chaudhary R, Beaupre L, Reynolds M, Adeeb S, Bouliane M. Biomechanical analysis of proximal humeral fixation using locking plate fixation with an intramedullary fibular allograft. Clin Biomech. 2010;25(7):642-646.
17. Chow RM, Begum F, Beaupre LA, Carey JP, Adeeb S, Bouliane MJ. Proximal humeral fracture fixation: locking plate construct +/- intramedullary fibular allograft. J Shoulder Elbow Surg. 2012;21(7):894-901.
18. Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2013;22(4):542-549.
1. Barrett JA, Baron JA, Karagas MR, Beach ML. Fracture risk in the U.S. Medicare population. J Clin Epidemiol. 1999;52(3):243-249.
2. Neer CS 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077-1089.
3. Liew AS, Johnson JA, Patterson SD, King GJ, Chess DG. Effect of screw placement on fixation in the humeral head. J Shoulder Elbow Surg. 2000;9(5):423-426.
4. Weinstein DM, Bratton DR, Ciccone WJ 2nd, Elias JJ. Locking plates improve torsional resistance in the stabilization of three-part proximal humeral fractures. J Shoulder Elbow Surg. 2006;15(2):239-243.
5. Agudelo J, Schurmann M, Stahel P, et al. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2007;21(10):676-681.
6. Egol KA, Sugi MT, Ong CC, Montero N, Davidovitch R, Zuckerman JD. Fracture site augmentation with calcium phosphate cement reduces screw penetration after open reduction-internal fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2012;21(6):741-748.
7. Gradl G, Knobe M, Stoffel M, Prescher A, Dirrichs T, Pape HC. Biomechanical evaluation of locking plate fixation of proximal humeral fractures augmented with calcium phosphate cement. J Orthop Trauma. 2013;27(7):399-404.
8. Ong CC, Kwon YW, Walsh M, Davidovitch R, Zuckerman JD, Egol KA. Outcomes of open reduction and internal fixation of proximal humerus fractures managed with locking plates. Am J Orthop. 2012;41(9):407-412.
9. Namdari S, Voleti PB, Mehta S. Evaluation of the osteoporotic proximal humeral fracture and strategies for structural augmentation during surgical treatment. J Shoulder Elbow Surg. 2012;21(12):1787-1795.
10. Scheck M. Surgical treatment of nonunions of the surgical neck of the humerus. Clin Orthop Relat Res. 1982;(167):255-259.
11. Hettrich CM, Neviaser A, Beamer BS, Paul O, Helfet DL, Lorich DG. Locked plating of the proximal humerus using an endosteal implant. J Orthop Trauma. 2012;26(4):212-215.
12. Neviaser AS, Hettrich CM, Beamer BS, Dines JS, Lorich DG. Endosteal strut augment reduces complications associated with proximal humeral locking plates. Clin Orthop Relat Res. 2011;469(12):3300-3306.
13. Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant. J Orthop Trauma. 2008;22(3):195-200.
14. Matassi F, Angeloni R, Carulli C, et al. Locking plate and fibular allograft augmentation in unstable fractures of proximal humerus. Injury. 2012;43(11):1939-1942.
15. Little MT, Berkes MB, Schottel PC, et al. The impact of preoperative coronal plane deformity on proximal humerus fixation with endosteal augmentation. J Orthop Trauma. 2014;28(6):338-347.
16. Mathison C, Chaudhary R, Beaupre L, Reynolds M, Adeeb S, Bouliane M. Biomechanical analysis of proximal humeral fixation using locking plate fixation with an intramedullary fibular allograft. Clin Biomech. 2010;25(7):642-646.
17. Chow RM, Begum F, Beaupre LA, Carey JP, Adeeb S, Bouliane MJ. Proximal humeral fracture fixation: locking plate construct +/- intramedullary fibular allograft. J Shoulder Elbow Surg. 2012;21(7):894-901.
18. Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2013;22(4):542-549.
Treatment of Acetabular Fractures in Adolescents
In children, pelvic fractures are uncommon, with an incidence ranging from 1% to 4.6% of all pediatric fractures,1-4 and acetabular fractures make up only 0.8% to 15% of pelvic fractures.1,3,5,6 Acetabular fractures are so uncommon in children partly because of the cartilaginous nature of the immature acetabulum. The increased cartilage volume relative to adults provides greater capacity for energy absorption, resulting in greater elastic and plastic deformation before fracture occurrence. More force is therefore required to cause a fracture, and associated visceral injuries, head injuries, and long-bone fractures are common.3,7,8
The impact of acetabular fractures on adolescents warrants special attention because any resulting disability will affect them during their most productive years. Both avascular necrosis (AVN) and degenerative arthritis are particularly devastating complications in this age group. Complications such as premature physeal closure9-15 are unique to adolescents, and there is little information available on how injury in older children affects growth in this area.
There have been very few studies of the outcomes of these injuries in children. Mostly, there have been case reports and small series primarily dealing with nonoperative management of acetabular fractures in adolescents.3,10,11,16-20 By contrast, operative treatment of acetabular fractures in adults has been well described, and outcomes widely reported. As a result, much of our knowledge about managing these injuries is extrapolated from the adult literature. Although treatment of acetabular fractures in adults has evolved substantially, treatment of these injuries in adolescents remains primarily nonoperative. We conducted a study to evaluate outcomes of treatment of adolescent acetabular fractures.
Patients and Methods
After obtaining institutional review board approval for this study, we retrospectively reviewed the cases of all adolescent patients admitted with a diagnosis of acetabular fracture to 2 academic institutions between 1991 and 2003. Thirty-eight patients (28 males, 10 females) were identified. Mean age at time of injury was 15 years (range, 11-18 years). Mean follow-up was 3.2 years (range, 5-180 months).
Data on fracture types, treatment methods, associated injuries, complications, union rates, pain, and return to normal activities were collected. Acetabular fractures were classified according to the system of Letournel and Judet.21 There were 20 elementary and 18 associated fractures.
Of the 38 patients, 30 sustained high-energy trauma in motor vehicle accidents (25) or in falls from significant heights (5). The other 8 patients injured themselves playing sports (4 had severe traumatic brain injury, 2 had labial wounds, and 2 had injuries involving the abdominal viscera). Twelve patients had associated pelvic ring injuries, 18 had femoral head dislocations, 2 had femoral head fractures, and 13 had evidence of impaction injury to the femoral head articular cartilage. Twelve patients had marginal impaction of the acetabular wall. Fifteen patients had open triradiate physes at time of injury (Table 1).
Thirty-seven of the 38 patients were treated with open reduction and internal fixation (ORIF) by an experienced orthopedic trauma surgeon; 1 patient with a stable posterior wall fracture was treated nonoperatively. Surgical indications were articular displacement of more than 1 mm, hip joint instability, irreducible hip dislocation, and intra-articular fracture fragments. In the 37 surgically treated cases, the approaches used were Kocher-Langenbeck (22), ilioinguinal (8), combined Kocher-Langenbeck/ilioinguinal (5), and triradiate (2).
Immediate postoperative radiographs were evaluated by 3 orthopedic surgeons blinded to the patients’ clinical outcomes. Displacement was evaluated on anteroposterior (AP) and Judet views of the pelvis, as described by Matta,22 and reductions were classified as anatomical (0-1 mm of displacement), imperfect (>1 to 3 mm), poor (>3 mm), or surgical secondary congruence (Table 2).
Results
Thirty-seven patients underwent acetabular fracture ORIF. Immediate postoperative radiographs showed 30 anatomical reductions and 7 imperfect reductions. One patient had surgical secondary congruence and developed AVN of the hip. We could not identify an association between the quality of the reduction and the outcome with respect to pain or return to activity. However, no patient had a poor reduction. An illustrative case is presented in Figures 1 to 4.
All acetabular fractures united within 4.5 months (range, 3.0-8.0 months) after the index procedure. Early postoperative complications included 3 cases of meralgia paresthetica and 13 cases of abductor weakness. Meralgia paresthetica resolved spontaneously in all 3 patients. Of the 13 patients with abductor weakness, 11 improved with physical therapy, 1 was limited by the head injury, and 1 subsequently underwent hip fusion. One patient had a deep vein thrombosis (DVT) that was identified before surgery and managed with warfarin.
Other complications included 1 case of deep infection of the surgical wound. This infection presented 4 months after surgery and was treated with débridement, hardware removal, and a 3-month course of antibiotics. Two patients who sustained hip dislocations at time of injury developed AVN of the femoral head. Both developed osteoarthritis, and 1 underwent hip fusion. Eight patients developed heterotopic ossification on the side of the acetabular fracture; 4 of them underwent surgical excision. Four patients required a separate operation for hardware removal. Four patients with triradiate cartilage involvement went on to premature closure. No patient had any leg-length discrepancy or dysplasia at time of follow-up.
Thirty-four of the 38 patients returned to their regular activities. For these patients, mean time to return to full activity was 7.0 months (range, 3-30 months); there was no difference in mean time to return to full activity between skeletally mature and skeletally immature patients (6.6 vs 7.4 months; P = .57). Of the other 4 patients, 1 had permanent cognitive and physical disability with an ataxic gait as a result of a traumatic brain injury, 2 were limited by AVN (1 underwent hip fusion), and 1 was limited by an ipsilateral knee injury.
Of the 38 patients, 29 were pain-free; 6 had occasional, intermittent mild pain that did not limit their activities; and 3 had severe, activity-limiting pain. Of the 6 patients with mild pain, 2 had femoral impaction injuries, and 4 had marginal impaction injuries. Of the 3 patients with severe pain, 2 developed femoral head AVN, and 1 had multiple ipsilateral extremity injuries involving the femur, knee, and tibia.
Discussion
The traditional treatment for acetabular fractures in children has been nonoperative,8,10 and there are few specific treatment guidelines.13 Recent recommendations are nonoperative treatment for minimally displaced fractures (<1 mm) and acetabular fracture ORIF for fractures displaced more than 2 mm.11 No clear consensus exists on management for fractures displaced 1 to 2 mm. Few studies have investigated the outcomes of operative management of these fractures in the pediatric or adolescent population.
In our series of adolescent acetabular fractures, we examined unions, complications, and return to activity. Of 38 patients with acetabular fractures, 37 were treated with ORIF. Anatomical reduction was achieved in the majority of patients. Posterior wall fractures were by far the most common fracture type, which is consistent with previous reports.10,11 All acetabular fractures united, and most patients were pain-free at latest follow-up. There was a low incidence of major complications in our patient population. One major complication was a DVT in a 14-year-old boy who was in a motor vehicle accident and sustained a T-type fracture of the right acetabulum with contralateral femoral shaft and ankle fractures. The DVT was in the right internal iliac and common femoral veins and was diagnosed on magnetic resonance venography. The patient was treated with warfarin for 3 months without incident.
Two patients developed AVN of the femoral head. One of these patients was an 11-year-old girl who was in a motor vehicle accident and sustained a T-type fracture with marginal impaction of the posterior wall, posterior hip dislocation, and a pelvic ring injury. She was treated with ORIF through combined Kocher-Langenbeck/ilioinguinal approaches. By 4 months after surgery, the acetabular fracture was united. Nine months after surgery, she still had pain (activity-limiting) and a 35° flexion contracture of the hip, and she was ambulating with a cane. The diagnosis was AVN of the hip. The patient underwent hip fusion 1 year after surgery.
The second patient with femoral head AVN was a 12-year-old boy who fell while skiing and sustained a fracture of the posterior wall and a hip dislocation with impaction of the femoral head. Initial treatment at an outside institution consisted of open reduction of the hip and excision of a “loose body” from the joint. Eight weeks after surgery, the patient continued to have pain and was referred to our institution. A second operation was performed. Findings included a defect involving 40% of the posterior wall, and signs that the posterior wall had been excised during the initial operation. The patient eventually developed AVN of the hip. This patient was also diagnosed with a deep wound infection 4 months after surgery. He presented with pain and a fluid collection around the hip. The infection was not confirmed through fluid culture, and, as he eventually developed AVN of the hip, his symptoms may have been the result of chondrolysis or AVN rather than infection.
There were no cases of nonunion or malunion, leg-length discrepancy, or permanent sciatic nerve palsy. Although there were a few cases of premature closure of the triradiate cartilage, no acetabular dysplasia was seen at latest follow-up, likely because of the relative maturity of our pediatric group (age range, 11-18 years). Age at time of injury is thought to be the most important factor influencing growth and development of the acetabulum.9,13 In addition, previous studies have demonstrated a tendency toward acetabular fractures in patients with mature triradiate cartilage—versus pelvic ring injuries in patients with immature triradiate cartilage.8,11 This may also account for the older age of our study group.
Minor complications (eg, meralgia paresthetica) resolved spontaneously. The most common complications were abductor weakness and heterotopic ossification. In only 4 cases was a secondary procedure for excision of the heterotopic bone required. Abductor weakness, more commonly associated with a Kocher-Langenbeck approach to the hip, resolved with therapy in almost all cases. Only 4 of our patients required removal of hardware from the acetabulum.
Although the majority of acetabular fractures resulted from high-energy trauma, 8 cases were sports-related. Six of these involved posterior wall fractures, suggesting the injury resulted from a fall on flexed knee and hip. This was not known to be a common mechanism of injury in this age group.3,7 An additional concern was how to size the posterior wall fragment when not ossified. At one center, preoperative magnetic resonance imaging (MRI) was effectively used to size the osteochondral posterior wall fragment as standard protocol for patients with posterior wall fractures in this age group—resulting in better decisions regarding the need for ORIF. At the other institution, preoperative MRI was not performed routinely for this subset of patients.
Thirty-four of our 38 patients returned to their normal activities. Of the other 4 patients, 1 was permanently disabled secondary to traumatic brain injury, 1 had other ipsilateral extremity injuries that limited his mobility, and 2 developed AVN of the femoral head. Both patients with AVN had hip dislocations. Four of the 6 patients who were symptomatic during activity sustained impaction injuries of the femoral head or posterior wall. This suggests that poorer outcomes may be associated with dislocation or with articular injuries—similar to what has been reported in the adult literature.
This study had several limitations. First, it was a retrospective case series, so there was no control group for comparison. Second, the relatively short follow-up did not allow evaluation of the incidence of degenerative arthritis secondary to articular injury, the symptoms of which may develop 1 to 2 decades after injury.13 This phenomenon was well described by Letournel and Judet21 in the adult population, and there is no reason to presume the adolescent population is any different. Third, our sample was small and unlikely to represent a uniform sampling of the general pediatric population. Fourth, it was not possible to draw detailed conclusions about the outcome of ORIF for a particular type of acetabular fracture. Fifth, we did not see as many of the associated visceral injuries that are so prevalent in the literature. This may reflect improvement in safety specifications for automobiles, or our group may not have had the most severe or high-energy injuries. Here our population sample may have skewed our results, leading to better than expected outcomes.
One last study limitation, a major one, was the age of our population, 11 to 18 years, which makes it difficult to extrapolate results to the entire pediatric population. On one hand, a more immature skeleton has a higher chance of remodeling and is more forgiving of deformities and small amounts of displacement. On the other hand, injury and premature triradiate cartilage fusion in a younger patient can lead to significant deformity and acetabular dysplasia.9 Whether ORIF of these fractures would alter the outcome of an injury to the triradiate cartilage is yet to be determined.
Conclusion
In agreement with earlier studies,10,11,15,18 the good outcomes in our series correlated with congruence of reduction. Outcome predictors such as dislocation, femoral head injury, and marginal impaction are similar to those described in the adult literature. Although our study did not have a nonoperative group for comparison, the favorable outcomes of ORIF of acetabular fractures suggest that a more aggressive approach to treatment should be considered. Given the added benefits of early, pain-free mobilization, we think that only stable, undisplaced fractures (<1 mm) should be managed nonoperatively. In the adolescent population, we recommend ORIF for optimal management of unstable acetabular fractures, fractures with any hip subluxation, and fractures displaced more than 1 mm.
1. Canale ST, Beaty JH. Fractures of the pelvis. In: Beaty JH, Kassler JR, eds. Rockwood and Wilkin’s Fractures in Children. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:883-991.
2. Demetriades D, Karaiskakis M, Velmahos GC, Alo K, Murray J, Chan L. Pelvic fractures in pediatric and adult trauma patients: are they different injuries? J Trauma. 2003;54(6):1146-1151.
3. Grisoni N, Connor S, Marsh E, Thompson GH, Cooperman DR, Blakemore LC. Pelvic fractures in a pediatric level I trauma center. J Orthop Trauma. 2002;16(7):458-463.
4. Ismail N, Bellemare JF, Mollitt DL, Di Scala C, Koeppel B, Tepas JJ. Death from pelvic fracture: children are different. J Pediatr Surg. 1996;31(1):82-85.
5. Schlickwei W, Keck T. Pelvic and acetabular fractures in childhood. Injury. 2005;36(suppl 1):A57-A63.
6. Swiontkowski MF. Fractures and dislocations about the hip and pelvis. In: Green NE, Swiontkowski MF, eds. Skeletal Trauma in Children. Philadelphia, PA: Saunders; 2003:371-406.
7. Silber JS, Flynn JM, Koffler KM, Dormans JP, Drummond DS. Analysis of the cause, classification, and associated injuries of 166 consecutive pediatric pelvic fractures. J Pediatr Orthop. 2001;21(4):446-450.
8. Silber JS, Flynn JM. Changing patterns of pediatric pelvic fractures with skeletal maturation: implications for classification and management. J Pediatr Orthop. 2002;22(1):22-26.
9. Bucholz RW, Ezaki M, Ogden JA. Injury to the acetabular triradiate physeal cartilage. J Bone Joint Surg Am. 1982;64(4):600-609.
10. Heeg M, Klasen HJ, Visser JD. Acetabular fractures in children and adolescents. J Bone Joint Surg Br. 1989;71(3):418-421.
11. Heeg M, de Ridder VA, Tornetta P, de Lange S, Klasen HJ. Acetabular fractures in children and adolescents. Clin Orthop Relat Res. 2000;(376):80-86.
12. Heeg M, Visser JD, Oostvogel HJ. Injuries of the acetabular triradiate cartilage and sacroiliac joint. J Bone Joint Surg Br. 1988;70(1):34-37.
13. Liporace FA, Ong B, Mohaideen A, Ong A, Koval KJ. Development and injury of the triradiate cartilage with its effects on acetabular development: review of the literature. J Trauma. 2003;54(6):1245-1249.
14. Rodrigues KF. Injury of the acetabular epiphysis. Injury. 1973;4(3):258-260.
15. Trousdale RT, Ganz R. Posttraumatic acetabular dysplasia. Clin Orthop Relat Res. 1994;(305):124-132.
16. Brooks E, Rosman M. Central fracture-dislocation of the hip in a child. J Trauma. 1988;28(11):1590-1592.
17. Habacker TA, Heinrich SD, Dehne R. Fracture of the superior pelvic quadrant in a child. J Pediatr Orthop. 1995;15(1):69-72.
18. Karunakar MA, Goulet JA, Mueller KL, Bedi A, Le TT. Operative treatment of unstable pediatric pelvis and acetabular fractures. J Pediatr Orthop. 2005;25(1):34-38.
19. Rieger H, Brug E. Fractures of the pelvis in children. Clin Orthop Relat Res. 1997;(336);226-239.
20. Torode I, Zieg D. Pelvic fractures in children. J Pediatr Orthop. 1985;5(1):76-84.
21. Letournel E, Judet R. Fractures of the Acetabulum. 2nd ed. New York, NY: Springer-Verlag; 1993.
22. Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks of the injury. J Bone Joint Surg Am. 1996;78(11):1632-1645.
In children, pelvic fractures are uncommon, with an incidence ranging from 1% to 4.6% of all pediatric fractures,1-4 and acetabular fractures make up only 0.8% to 15% of pelvic fractures.1,3,5,6 Acetabular fractures are so uncommon in children partly because of the cartilaginous nature of the immature acetabulum. The increased cartilage volume relative to adults provides greater capacity for energy absorption, resulting in greater elastic and plastic deformation before fracture occurrence. More force is therefore required to cause a fracture, and associated visceral injuries, head injuries, and long-bone fractures are common.3,7,8
The impact of acetabular fractures on adolescents warrants special attention because any resulting disability will affect them during their most productive years. Both avascular necrosis (AVN) and degenerative arthritis are particularly devastating complications in this age group. Complications such as premature physeal closure9-15 are unique to adolescents, and there is little information available on how injury in older children affects growth in this area.
There have been very few studies of the outcomes of these injuries in children. Mostly, there have been case reports and small series primarily dealing with nonoperative management of acetabular fractures in adolescents.3,10,11,16-20 By contrast, operative treatment of acetabular fractures in adults has been well described, and outcomes widely reported. As a result, much of our knowledge about managing these injuries is extrapolated from the adult literature. Although treatment of acetabular fractures in adults has evolved substantially, treatment of these injuries in adolescents remains primarily nonoperative. We conducted a study to evaluate outcomes of treatment of adolescent acetabular fractures.
Patients and Methods
After obtaining institutional review board approval for this study, we retrospectively reviewed the cases of all adolescent patients admitted with a diagnosis of acetabular fracture to 2 academic institutions between 1991 and 2003. Thirty-eight patients (28 males, 10 females) were identified. Mean age at time of injury was 15 years (range, 11-18 years). Mean follow-up was 3.2 years (range, 5-180 months).
Data on fracture types, treatment methods, associated injuries, complications, union rates, pain, and return to normal activities were collected. Acetabular fractures were classified according to the system of Letournel and Judet.21 There were 20 elementary and 18 associated fractures.
Of the 38 patients, 30 sustained high-energy trauma in motor vehicle accidents (25) or in falls from significant heights (5). The other 8 patients injured themselves playing sports (4 had severe traumatic brain injury, 2 had labial wounds, and 2 had injuries involving the abdominal viscera). Twelve patients had associated pelvic ring injuries, 18 had femoral head dislocations, 2 had femoral head fractures, and 13 had evidence of impaction injury to the femoral head articular cartilage. Twelve patients had marginal impaction of the acetabular wall. Fifteen patients had open triradiate physes at time of injury (Table 1).
Thirty-seven of the 38 patients were treated with open reduction and internal fixation (ORIF) by an experienced orthopedic trauma surgeon; 1 patient with a stable posterior wall fracture was treated nonoperatively. Surgical indications were articular displacement of more than 1 mm, hip joint instability, irreducible hip dislocation, and intra-articular fracture fragments. In the 37 surgically treated cases, the approaches used were Kocher-Langenbeck (22), ilioinguinal (8), combined Kocher-Langenbeck/ilioinguinal (5), and triradiate (2).
Immediate postoperative radiographs were evaluated by 3 orthopedic surgeons blinded to the patients’ clinical outcomes. Displacement was evaluated on anteroposterior (AP) and Judet views of the pelvis, as described by Matta,22 and reductions were classified as anatomical (0-1 mm of displacement), imperfect (>1 to 3 mm), poor (>3 mm), or surgical secondary congruence (Table 2).
Results
Thirty-seven patients underwent acetabular fracture ORIF. Immediate postoperative radiographs showed 30 anatomical reductions and 7 imperfect reductions. One patient had surgical secondary congruence and developed AVN of the hip. We could not identify an association between the quality of the reduction and the outcome with respect to pain or return to activity. However, no patient had a poor reduction. An illustrative case is presented in Figures 1 to 4.
All acetabular fractures united within 4.5 months (range, 3.0-8.0 months) after the index procedure. Early postoperative complications included 3 cases of meralgia paresthetica and 13 cases of abductor weakness. Meralgia paresthetica resolved spontaneously in all 3 patients. Of the 13 patients with abductor weakness, 11 improved with physical therapy, 1 was limited by the head injury, and 1 subsequently underwent hip fusion. One patient had a deep vein thrombosis (DVT) that was identified before surgery and managed with warfarin.
Other complications included 1 case of deep infection of the surgical wound. This infection presented 4 months after surgery and was treated with débridement, hardware removal, and a 3-month course of antibiotics. Two patients who sustained hip dislocations at time of injury developed AVN of the femoral head. Both developed osteoarthritis, and 1 underwent hip fusion. Eight patients developed heterotopic ossification on the side of the acetabular fracture; 4 of them underwent surgical excision. Four patients required a separate operation for hardware removal. Four patients with triradiate cartilage involvement went on to premature closure. No patient had any leg-length discrepancy or dysplasia at time of follow-up.
Thirty-four of the 38 patients returned to their regular activities. For these patients, mean time to return to full activity was 7.0 months (range, 3-30 months); there was no difference in mean time to return to full activity between skeletally mature and skeletally immature patients (6.6 vs 7.4 months; P = .57). Of the other 4 patients, 1 had permanent cognitive and physical disability with an ataxic gait as a result of a traumatic brain injury, 2 were limited by AVN (1 underwent hip fusion), and 1 was limited by an ipsilateral knee injury.
Of the 38 patients, 29 were pain-free; 6 had occasional, intermittent mild pain that did not limit their activities; and 3 had severe, activity-limiting pain. Of the 6 patients with mild pain, 2 had femoral impaction injuries, and 4 had marginal impaction injuries. Of the 3 patients with severe pain, 2 developed femoral head AVN, and 1 had multiple ipsilateral extremity injuries involving the femur, knee, and tibia.
Discussion
The traditional treatment for acetabular fractures in children has been nonoperative,8,10 and there are few specific treatment guidelines.13 Recent recommendations are nonoperative treatment for minimally displaced fractures (<1 mm) and acetabular fracture ORIF for fractures displaced more than 2 mm.11 No clear consensus exists on management for fractures displaced 1 to 2 mm. Few studies have investigated the outcomes of operative management of these fractures in the pediatric or adolescent population.
In our series of adolescent acetabular fractures, we examined unions, complications, and return to activity. Of 38 patients with acetabular fractures, 37 were treated with ORIF. Anatomical reduction was achieved in the majority of patients. Posterior wall fractures were by far the most common fracture type, which is consistent with previous reports.10,11 All acetabular fractures united, and most patients were pain-free at latest follow-up. There was a low incidence of major complications in our patient population. One major complication was a DVT in a 14-year-old boy who was in a motor vehicle accident and sustained a T-type fracture of the right acetabulum with contralateral femoral shaft and ankle fractures. The DVT was in the right internal iliac and common femoral veins and was diagnosed on magnetic resonance venography. The patient was treated with warfarin for 3 months without incident.
Two patients developed AVN of the femoral head. One of these patients was an 11-year-old girl who was in a motor vehicle accident and sustained a T-type fracture with marginal impaction of the posterior wall, posterior hip dislocation, and a pelvic ring injury. She was treated with ORIF through combined Kocher-Langenbeck/ilioinguinal approaches. By 4 months after surgery, the acetabular fracture was united. Nine months after surgery, she still had pain (activity-limiting) and a 35° flexion contracture of the hip, and she was ambulating with a cane. The diagnosis was AVN of the hip. The patient underwent hip fusion 1 year after surgery.
The second patient with femoral head AVN was a 12-year-old boy who fell while skiing and sustained a fracture of the posterior wall and a hip dislocation with impaction of the femoral head. Initial treatment at an outside institution consisted of open reduction of the hip and excision of a “loose body” from the joint. Eight weeks after surgery, the patient continued to have pain and was referred to our institution. A second operation was performed. Findings included a defect involving 40% of the posterior wall, and signs that the posterior wall had been excised during the initial operation. The patient eventually developed AVN of the hip. This patient was also diagnosed with a deep wound infection 4 months after surgery. He presented with pain and a fluid collection around the hip. The infection was not confirmed through fluid culture, and, as he eventually developed AVN of the hip, his symptoms may have been the result of chondrolysis or AVN rather than infection.
There were no cases of nonunion or malunion, leg-length discrepancy, or permanent sciatic nerve palsy. Although there were a few cases of premature closure of the triradiate cartilage, no acetabular dysplasia was seen at latest follow-up, likely because of the relative maturity of our pediatric group (age range, 11-18 years). Age at time of injury is thought to be the most important factor influencing growth and development of the acetabulum.9,13 In addition, previous studies have demonstrated a tendency toward acetabular fractures in patients with mature triradiate cartilage—versus pelvic ring injuries in patients with immature triradiate cartilage.8,11 This may also account for the older age of our study group.
Minor complications (eg, meralgia paresthetica) resolved spontaneously. The most common complications were abductor weakness and heterotopic ossification. In only 4 cases was a secondary procedure for excision of the heterotopic bone required. Abductor weakness, more commonly associated with a Kocher-Langenbeck approach to the hip, resolved with therapy in almost all cases. Only 4 of our patients required removal of hardware from the acetabulum.
Although the majority of acetabular fractures resulted from high-energy trauma, 8 cases were sports-related. Six of these involved posterior wall fractures, suggesting the injury resulted from a fall on flexed knee and hip. This was not known to be a common mechanism of injury in this age group.3,7 An additional concern was how to size the posterior wall fragment when not ossified. At one center, preoperative magnetic resonance imaging (MRI) was effectively used to size the osteochondral posterior wall fragment as standard protocol for patients with posterior wall fractures in this age group—resulting in better decisions regarding the need for ORIF. At the other institution, preoperative MRI was not performed routinely for this subset of patients.
Thirty-four of our 38 patients returned to their normal activities. Of the other 4 patients, 1 was permanently disabled secondary to traumatic brain injury, 1 had other ipsilateral extremity injuries that limited his mobility, and 2 developed AVN of the femoral head. Both patients with AVN had hip dislocations. Four of the 6 patients who were symptomatic during activity sustained impaction injuries of the femoral head or posterior wall. This suggests that poorer outcomes may be associated with dislocation or with articular injuries—similar to what has been reported in the adult literature.
This study had several limitations. First, it was a retrospective case series, so there was no control group for comparison. Second, the relatively short follow-up did not allow evaluation of the incidence of degenerative arthritis secondary to articular injury, the symptoms of which may develop 1 to 2 decades after injury.13 This phenomenon was well described by Letournel and Judet21 in the adult population, and there is no reason to presume the adolescent population is any different. Third, our sample was small and unlikely to represent a uniform sampling of the general pediatric population. Fourth, it was not possible to draw detailed conclusions about the outcome of ORIF for a particular type of acetabular fracture. Fifth, we did not see as many of the associated visceral injuries that are so prevalent in the literature. This may reflect improvement in safety specifications for automobiles, or our group may not have had the most severe or high-energy injuries. Here our population sample may have skewed our results, leading to better than expected outcomes.
One last study limitation, a major one, was the age of our population, 11 to 18 years, which makes it difficult to extrapolate results to the entire pediatric population. On one hand, a more immature skeleton has a higher chance of remodeling and is more forgiving of deformities and small amounts of displacement. On the other hand, injury and premature triradiate cartilage fusion in a younger patient can lead to significant deformity and acetabular dysplasia.9 Whether ORIF of these fractures would alter the outcome of an injury to the triradiate cartilage is yet to be determined.
Conclusion
In agreement with earlier studies,10,11,15,18 the good outcomes in our series correlated with congruence of reduction. Outcome predictors such as dislocation, femoral head injury, and marginal impaction are similar to those described in the adult literature. Although our study did not have a nonoperative group for comparison, the favorable outcomes of ORIF of acetabular fractures suggest that a more aggressive approach to treatment should be considered. Given the added benefits of early, pain-free mobilization, we think that only stable, undisplaced fractures (<1 mm) should be managed nonoperatively. In the adolescent population, we recommend ORIF for optimal management of unstable acetabular fractures, fractures with any hip subluxation, and fractures displaced more than 1 mm.
In children, pelvic fractures are uncommon, with an incidence ranging from 1% to 4.6% of all pediatric fractures,1-4 and acetabular fractures make up only 0.8% to 15% of pelvic fractures.1,3,5,6 Acetabular fractures are so uncommon in children partly because of the cartilaginous nature of the immature acetabulum. The increased cartilage volume relative to adults provides greater capacity for energy absorption, resulting in greater elastic and plastic deformation before fracture occurrence. More force is therefore required to cause a fracture, and associated visceral injuries, head injuries, and long-bone fractures are common.3,7,8
The impact of acetabular fractures on adolescents warrants special attention because any resulting disability will affect them during their most productive years. Both avascular necrosis (AVN) and degenerative arthritis are particularly devastating complications in this age group. Complications such as premature physeal closure9-15 are unique to adolescents, and there is little information available on how injury in older children affects growth in this area.
There have been very few studies of the outcomes of these injuries in children. Mostly, there have been case reports and small series primarily dealing with nonoperative management of acetabular fractures in adolescents.3,10,11,16-20 By contrast, operative treatment of acetabular fractures in adults has been well described, and outcomes widely reported. As a result, much of our knowledge about managing these injuries is extrapolated from the adult literature. Although treatment of acetabular fractures in adults has evolved substantially, treatment of these injuries in adolescents remains primarily nonoperative. We conducted a study to evaluate outcomes of treatment of adolescent acetabular fractures.
Patients and Methods
After obtaining institutional review board approval for this study, we retrospectively reviewed the cases of all adolescent patients admitted with a diagnosis of acetabular fracture to 2 academic institutions between 1991 and 2003. Thirty-eight patients (28 males, 10 females) were identified. Mean age at time of injury was 15 years (range, 11-18 years). Mean follow-up was 3.2 years (range, 5-180 months).
Data on fracture types, treatment methods, associated injuries, complications, union rates, pain, and return to normal activities were collected. Acetabular fractures were classified according to the system of Letournel and Judet.21 There were 20 elementary and 18 associated fractures.
Of the 38 patients, 30 sustained high-energy trauma in motor vehicle accidents (25) or in falls from significant heights (5). The other 8 patients injured themselves playing sports (4 had severe traumatic brain injury, 2 had labial wounds, and 2 had injuries involving the abdominal viscera). Twelve patients had associated pelvic ring injuries, 18 had femoral head dislocations, 2 had femoral head fractures, and 13 had evidence of impaction injury to the femoral head articular cartilage. Twelve patients had marginal impaction of the acetabular wall. Fifteen patients had open triradiate physes at time of injury (Table 1).
Thirty-seven of the 38 patients were treated with open reduction and internal fixation (ORIF) by an experienced orthopedic trauma surgeon; 1 patient with a stable posterior wall fracture was treated nonoperatively. Surgical indications were articular displacement of more than 1 mm, hip joint instability, irreducible hip dislocation, and intra-articular fracture fragments. In the 37 surgically treated cases, the approaches used were Kocher-Langenbeck (22), ilioinguinal (8), combined Kocher-Langenbeck/ilioinguinal (5), and triradiate (2).
Immediate postoperative radiographs were evaluated by 3 orthopedic surgeons blinded to the patients’ clinical outcomes. Displacement was evaluated on anteroposterior (AP) and Judet views of the pelvis, as described by Matta,22 and reductions were classified as anatomical (0-1 mm of displacement), imperfect (>1 to 3 mm), poor (>3 mm), or surgical secondary congruence (Table 2).
Results
Thirty-seven patients underwent acetabular fracture ORIF. Immediate postoperative radiographs showed 30 anatomical reductions and 7 imperfect reductions. One patient had surgical secondary congruence and developed AVN of the hip. We could not identify an association between the quality of the reduction and the outcome with respect to pain or return to activity. However, no patient had a poor reduction. An illustrative case is presented in Figures 1 to 4.
All acetabular fractures united within 4.5 months (range, 3.0-8.0 months) after the index procedure. Early postoperative complications included 3 cases of meralgia paresthetica and 13 cases of abductor weakness. Meralgia paresthetica resolved spontaneously in all 3 patients. Of the 13 patients with abductor weakness, 11 improved with physical therapy, 1 was limited by the head injury, and 1 subsequently underwent hip fusion. One patient had a deep vein thrombosis (DVT) that was identified before surgery and managed with warfarin.
Other complications included 1 case of deep infection of the surgical wound. This infection presented 4 months after surgery and was treated with débridement, hardware removal, and a 3-month course of antibiotics. Two patients who sustained hip dislocations at time of injury developed AVN of the femoral head. Both developed osteoarthritis, and 1 underwent hip fusion. Eight patients developed heterotopic ossification on the side of the acetabular fracture; 4 of them underwent surgical excision. Four patients required a separate operation for hardware removal. Four patients with triradiate cartilage involvement went on to premature closure. No patient had any leg-length discrepancy or dysplasia at time of follow-up.
Thirty-four of the 38 patients returned to their regular activities. For these patients, mean time to return to full activity was 7.0 months (range, 3-30 months); there was no difference in mean time to return to full activity between skeletally mature and skeletally immature patients (6.6 vs 7.4 months; P = .57). Of the other 4 patients, 1 had permanent cognitive and physical disability with an ataxic gait as a result of a traumatic brain injury, 2 were limited by AVN (1 underwent hip fusion), and 1 was limited by an ipsilateral knee injury.
Of the 38 patients, 29 were pain-free; 6 had occasional, intermittent mild pain that did not limit their activities; and 3 had severe, activity-limiting pain. Of the 6 patients with mild pain, 2 had femoral impaction injuries, and 4 had marginal impaction injuries. Of the 3 patients with severe pain, 2 developed femoral head AVN, and 1 had multiple ipsilateral extremity injuries involving the femur, knee, and tibia.
Discussion
The traditional treatment for acetabular fractures in children has been nonoperative,8,10 and there are few specific treatment guidelines.13 Recent recommendations are nonoperative treatment for minimally displaced fractures (<1 mm) and acetabular fracture ORIF for fractures displaced more than 2 mm.11 No clear consensus exists on management for fractures displaced 1 to 2 mm. Few studies have investigated the outcomes of operative management of these fractures in the pediatric or adolescent population.
In our series of adolescent acetabular fractures, we examined unions, complications, and return to activity. Of 38 patients with acetabular fractures, 37 were treated with ORIF. Anatomical reduction was achieved in the majority of patients. Posterior wall fractures were by far the most common fracture type, which is consistent with previous reports.10,11 All acetabular fractures united, and most patients were pain-free at latest follow-up. There was a low incidence of major complications in our patient population. One major complication was a DVT in a 14-year-old boy who was in a motor vehicle accident and sustained a T-type fracture of the right acetabulum with contralateral femoral shaft and ankle fractures. The DVT was in the right internal iliac and common femoral veins and was diagnosed on magnetic resonance venography. The patient was treated with warfarin for 3 months without incident.
Two patients developed AVN of the femoral head. One of these patients was an 11-year-old girl who was in a motor vehicle accident and sustained a T-type fracture with marginal impaction of the posterior wall, posterior hip dislocation, and a pelvic ring injury. She was treated with ORIF through combined Kocher-Langenbeck/ilioinguinal approaches. By 4 months after surgery, the acetabular fracture was united. Nine months after surgery, she still had pain (activity-limiting) and a 35° flexion contracture of the hip, and she was ambulating with a cane. The diagnosis was AVN of the hip. The patient underwent hip fusion 1 year after surgery.
The second patient with femoral head AVN was a 12-year-old boy who fell while skiing and sustained a fracture of the posterior wall and a hip dislocation with impaction of the femoral head. Initial treatment at an outside institution consisted of open reduction of the hip and excision of a “loose body” from the joint. Eight weeks after surgery, the patient continued to have pain and was referred to our institution. A second operation was performed. Findings included a defect involving 40% of the posterior wall, and signs that the posterior wall had been excised during the initial operation. The patient eventually developed AVN of the hip. This patient was also diagnosed with a deep wound infection 4 months after surgery. He presented with pain and a fluid collection around the hip. The infection was not confirmed through fluid culture, and, as he eventually developed AVN of the hip, his symptoms may have been the result of chondrolysis or AVN rather than infection.
There were no cases of nonunion or malunion, leg-length discrepancy, or permanent sciatic nerve palsy. Although there were a few cases of premature closure of the triradiate cartilage, no acetabular dysplasia was seen at latest follow-up, likely because of the relative maturity of our pediatric group (age range, 11-18 years). Age at time of injury is thought to be the most important factor influencing growth and development of the acetabulum.9,13 In addition, previous studies have demonstrated a tendency toward acetabular fractures in patients with mature triradiate cartilage—versus pelvic ring injuries in patients with immature triradiate cartilage.8,11 This may also account for the older age of our study group.
Minor complications (eg, meralgia paresthetica) resolved spontaneously. The most common complications were abductor weakness and heterotopic ossification. In only 4 cases was a secondary procedure for excision of the heterotopic bone required. Abductor weakness, more commonly associated with a Kocher-Langenbeck approach to the hip, resolved with therapy in almost all cases. Only 4 of our patients required removal of hardware from the acetabulum.
Although the majority of acetabular fractures resulted from high-energy trauma, 8 cases were sports-related. Six of these involved posterior wall fractures, suggesting the injury resulted from a fall on flexed knee and hip. This was not known to be a common mechanism of injury in this age group.3,7 An additional concern was how to size the posterior wall fragment when not ossified. At one center, preoperative magnetic resonance imaging (MRI) was effectively used to size the osteochondral posterior wall fragment as standard protocol for patients with posterior wall fractures in this age group—resulting in better decisions regarding the need for ORIF. At the other institution, preoperative MRI was not performed routinely for this subset of patients.
Thirty-four of our 38 patients returned to their normal activities. Of the other 4 patients, 1 was permanently disabled secondary to traumatic brain injury, 1 had other ipsilateral extremity injuries that limited his mobility, and 2 developed AVN of the femoral head. Both patients with AVN had hip dislocations. Four of the 6 patients who were symptomatic during activity sustained impaction injuries of the femoral head or posterior wall. This suggests that poorer outcomes may be associated with dislocation or with articular injuries—similar to what has been reported in the adult literature.
This study had several limitations. First, it was a retrospective case series, so there was no control group for comparison. Second, the relatively short follow-up did not allow evaluation of the incidence of degenerative arthritis secondary to articular injury, the symptoms of which may develop 1 to 2 decades after injury.13 This phenomenon was well described by Letournel and Judet21 in the adult population, and there is no reason to presume the adolescent population is any different. Third, our sample was small and unlikely to represent a uniform sampling of the general pediatric population. Fourth, it was not possible to draw detailed conclusions about the outcome of ORIF for a particular type of acetabular fracture. Fifth, we did not see as many of the associated visceral injuries that are so prevalent in the literature. This may reflect improvement in safety specifications for automobiles, or our group may not have had the most severe or high-energy injuries. Here our population sample may have skewed our results, leading to better than expected outcomes.
One last study limitation, a major one, was the age of our population, 11 to 18 years, which makes it difficult to extrapolate results to the entire pediatric population. On one hand, a more immature skeleton has a higher chance of remodeling and is more forgiving of deformities and small amounts of displacement. On the other hand, injury and premature triradiate cartilage fusion in a younger patient can lead to significant deformity and acetabular dysplasia.9 Whether ORIF of these fractures would alter the outcome of an injury to the triradiate cartilage is yet to be determined.
Conclusion
In agreement with earlier studies,10,11,15,18 the good outcomes in our series correlated with congruence of reduction. Outcome predictors such as dislocation, femoral head injury, and marginal impaction are similar to those described in the adult literature. Although our study did not have a nonoperative group for comparison, the favorable outcomes of ORIF of acetabular fractures suggest that a more aggressive approach to treatment should be considered. Given the added benefits of early, pain-free mobilization, we think that only stable, undisplaced fractures (<1 mm) should be managed nonoperatively. In the adolescent population, we recommend ORIF for optimal management of unstable acetabular fractures, fractures with any hip subluxation, and fractures displaced more than 1 mm.
1. Canale ST, Beaty JH. Fractures of the pelvis. In: Beaty JH, Kassler JR, eds. Rockwood and Wilkin’s Fractures in Children. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:883-991.
2. Demetriades D, Karaiskakis M, Velmahos GC, Alo K, Murray J, Chan L. Pelvic fractures in pediatric and adult trauma patients: are they different injuries? J Trauma. 2003;54(6):1146-1151.
3. Grisoni N, Connor S, Marsh E, Thompson GH, Cooperman DR, Blakemore LC. Pelvic fractures in a pediatric level I trauma center. J Orthop Trauma. 2002;16(7):458-463.
4. Ismail N, Bellemare JF, Mollitt DL, Di Scala C, Koeppel B, Tepas JJ. Death from pelvic fracture: children are different. J Pediatr Surg. 1996;31(1):82-85.
5. Schlickwei W, Keck T. Pelvic and acetabular fractures in childhood. Injury. 2005;36(suppl 1):A57-A63.
6. Swiontkowski MF. Fractures and dislocations about the hip and pelvis. In: Green NE, Swiontkowski MF, eds. Skeletal Trauma in Children. Philadelphia, PA: Saunders; 2003:371-406.
7. Silber JS, Flynn JM, Koffler KM, Dormans JP, Drummond DS. Analysis of the cause, classification, and associated injuries of 166 consecutive pediatric pelvic fractures. J Pediatr Orthop. 2001;21(4):446-450.
8. Silber JS, Flynn JM. Changing patterns of pediatric pelvic fractures with skeletal maturation: implications for classification and management. J Pediatr Orthop. 2002;22(1):22-26.
9. Bucholz RW, Ezaki M, Ogden JA. Injury to the acetabular triradiate physeal cartilage. J Bone Joint Surg Am. 1982;64(4):600-609.
10. Heeg M, Klasen HJ, Visser JD. Acetabular fractures in children and adolescents. J Bone Joint Surg Br. 1989;71(3):418-421.
11. Heeg M, de Ridder VA, Tornetta P, de Lange S, Klasen HJ. Acetabular fractures in children and adolescents. Clin Orthop Relat Res. 2000;(376):80-86.
12. Heeg M, Visser JD, Oostvogel HJ. Injuries of the acetabular triradiate cartilage and sacroiliac joint. J Bone Joint Surg Br. 1988;70(1):34-37.
13. Liporace FA, Ong B, Mohaideen A, Ong A, Koval KJ. Development and injury of the triradiate cartilage with its effects on acetabular development: review of the literature. J Trauma. 2003;54(6):1245-1249.
14. Rodrigues KF. Injury of the acetabular epiphysis. Injury. 1973;4(3):258-260.
15. Trousdale RT, Ganz R. Posttraumatic acetabular dysplasia. Clin Orthop Relat Res. 1994;(305):124-132.
16. Brooks E, Rosman M. Central fracture-dislocation of the hip in a child. J Trauma. 1988;28(11):1590-1592.
17. Habacker TA, Heinrich SD, Dehne R. Fracture of the superior pelvic quadrant in a child. J Pediatr Orthop. 1995;15(1):69-72.
18. Karunakar MA, Goulet JA, Mueller KL, Bedi A, Le TT. Operative treatment of unstable pediatric pelvis and acetabular fractures. J Pediatr Orthop. 2005;25(1):34-38.
19. Rieger H, Brug E. Fractures of the pelvis in children. Clin Orthop Relat Res. 1997;(336);226-239.
20. Torode I, Zieg D. Pelvic fractures in children. J Pediatr Orthop. 1985;5(1):76-84.
21. Letournel E, Judet R. Fractures of the Acetabulum. 2nd ed. New York, NY: Springer-Verlag; 1993.
22. Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks of the injury. J Bone Joint Surg Am. 1996;78(11):1632-1645.
1. Canale ST, Beaty JH. Fractures of the pelvis. In: Beaty JH, Kassler JR, eds. Rockwood and Wilkin’s Fractures in Children. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:883-991.
2. Demetriades D, Karaiskakis M, Velmahos GC, Alo K, Murray J, Chan L. Pelvic fractures in pediatric and adult trauma patients: are they different injuries? J Trauma. 2003;54(6):1146-1151.
3. Grisoni N, Connor S, Marsh E, Thompson GH, Cooperman DR, Blakemore LC. Pelvic fractures in a pediatric level I trauma center. J Orthop Trauma. 2002;16(7):458-463.
4. Ismail N, Bellemare JF, Mollitt DL, Di Scala C, Koeppel B, Tepas JJ. Death from pelvic fracture: children are different. J Pediatr Surg. 1996;31(1):82-85.
5. Schlickwei W, Keck T. Pelvic and acetabular fractures in childhood. Injury. 2005;36(suppl 1):A57-A63.
6. Swiontkowski MF. Fractures and dislocations about the hip and pelvis. In: Green NE, Swiontkowski MF, eds. Skeletal Trauma in Children. Philadelphia, PA: Saunders; 2003:371-406.
7. Silber JS, Flynn JM, Koffler KM, Dormans JP, Drummond DS. Analysis of the cause, classification, and associated injuries of 166 consecutive pediatric pelvic fractures. J Pediatr Orthop. 2001;21(4):446-450.
8. Silber JS, Flynn JM. Changing patterns of pediatric pelvic fractures with skeletal maturation: implications for classification and management. J Pediatr Orthop. 2002;22(1):22-26.
9. Bucholz RW, Ezaki M, Ogden JA. Injury to the acetabular triradiate physeal cartilage. J Bone Joint Surg Am. 1982;64(4):600-609.
10. Heeg M, Klasen HJ, Visser JD. Acetabular fractures in children and adolescents. J Bone Joint Surg Br. 1989;71(3):418-421.
11. Heeg M, de Ridder VA, Tornetta P, de Lange S, Klasen HJ. Acetabular fractures in children and adolescents. Clin Orthop Relat Res. 2000;(376):80-86.
12. Heeg M, Visser JD, Oostvogel HJ. Injuries of the acetabular triradiate cartilage and sacroiliac joint. J Bone Joint Surg Br. 1988;70(1):34-37.
13. Liporace FA, Ong B, Mohaideen A, Ong A, Koval KJ. Development and injury of the triradiate cartilage with its effects on acetabular development: review of the literature. J Trauma. 2003;54(6):1245-1249.
14. Rodrigues KF. Injury of the acetabular epiphysis. Injury. 1973;4(3):258-260.
15. Trousdale RT, Ganz R. Posttraumatic acetabular dysplasia. Clin Orthop Relat Res. 1994;(305):124-132.
16. Brooks E, Rosman M. Central fracture-dislocation of the hip in a child. J Trauma. 1988;28(11):1590-1592.
17. Habacker TA, Heinrich SD, Dehne R. Fracture of the superior pelvic quadrant in a child. J Pediatr Orthop. 1995;15(1):69-72.
18. Karunakar MA, Goulet JA, Mueller KL, Bedi A, Le TT. Operative treatment of unstable pediatric pelvis and acetabular fractures. J Pediatr Orthop. 2005;25(1):34-38.
19. Rieger H, Brug E. Fractures of the pelvis in children. Clin Orthop Relat Res. 1997;(336);226-239.
20. Torode I, Zieg D. Pelvic fractures in children. J Pediatr Orthop. 1985;5(1):76-84.
21. Letournel E, Judet R. Fractures of the Acetabulum. 2nd ed. New York, NY: Springer-Verlag; 1993.
22. Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks of the injury. J Bone Joint Surg Am. 1996;78(11):1632-1645.
Hip Fracture and the Weekend Effect: Does Weekend Admission Affect Patient Outcomes?
Weekend admission has been hypothesized to be a risk factor for increased patient mortality and complications during hospital stays—commonly referred to as the weekend effect.1 Reduced hospital staffing on weekends, particularly of senior-level physicians and ancillary nursing services, may affect the quality of diagnosis and management for patients admitted for traumatic and emergent conditions. Investigators have found increased mortality in weekend admissions for stroke,2 subdural hematoma,3 gastrointestinal bleeding,4,5 atrial fibrillation,6 and pulmonary embolism.7 Investigators have not found increased mortality in weekend admissions for hip fracture, though the majority of the data was derived from European patient populations, which may be subject to management and staffing strategies different from those for US patients.8-10 Furthermore, data on this topic in US patients are limited to a multispecialty study of 50 different admission diagnoses, which used 1 year of data from a single US state.1
We conducted a study to comprehensively assess the effect of weekend admission on adverse outcomes during hospital stays. The literature suggests that surgery for hip fracture can be delayed up to 48 hours without significant additional risk of death,11-13 allowing orthopedic departments to stabilize routine hip fracture admissions on weekends and operate whenever limited surgical teams become available. Surgical delay has not been thoroughly analyzed by day of admission among US patients,14 but the combined potential of more conservative preoperative management and the availability of fewer senior physicians and ancillary providers may result in worse outcomes for weekend versus weekday admissions.
Materials and Methods
Study Population
Part of the Healthcare Cost and Utilization Project, the Nationwide Inpatient Sample (NIS) provides a 20% representative sample of annual US hospital admissions.15 For these admissions, the NIS includes data related to demographic and clinical variables, such as International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes, as well as descriptive variables for the hospitals where the patients were admitted. The NIS is publicly available to researchers. As its health information is deidentified, we did not have to obtain institutional review board approval for this study.
Ascertainment of Cases
Our initial study population, drawn from the period 1998–2010, consisted of 821,531 patients with a principal ICD-9-CM diagnosis of femoral neck fracture (820.0-820.9). To best capture the typical presentation of hip fracture, we excluded:
- Patients with open femoral neck fractures (820.1, 820.3, 820.9).
- Patients who did not have open reduction and internal fixation (ORIF) (79.35), hemiarthroplasty (81.52), closed reduction and internal fixation (CRIF) (79.15), internal fixation (78.55), or total hip arthroplasty (THA) (81.51) as their primary surgical procedure.
- Patients admitted from sources other than the emergency department.
- Patients who underwent surgery before admission.
- Patients whose admission type was not classified as emergency or urgent.
Ascertainment of Covariates
For all patients, we extracted data on exposure of interest, day of admission (weekend or weekday), and demographic variables including age, sex, race (white, black, Hispanic, other, missing), and insurance (Medicare, Medicaid, private, other). We used the Elixhauser method to determine 30 different comorbidities from ICD-9-CM diagnosis coding16 and sorted patients by total number of comorbidities (0, 1, 2, 3 or 4, ≥5). As has been done before,17 we excluded blood loss anemia, coagulopathy, and fluid and electrolyte disorders from this comorbidity calculation, as these conditions can be secondary to trauma. We also extracted data on the admission itself, including hospital region (Northeast, Midwest, South, West), hospital bed size (small, medium, large), hospital teaching status (nonteaching, teaching), and hospital location (rural, urban). We used diagnosis codes to categorize fracture location as “not otherwise specified” (820.8), intracapsular (820.0), or extracapsular (820.2).
Because of low frequencies, we collapsed 2 race designations (Native American, Asian or Pacific Islander) into the “other race” category and 2 insurance designations (self-pay, no charge) into the “other insurance” category. For a substantial number of patients, race information was missing, so we included “missing” as its own category in analyses. Patients who were missing data on day of admission, age, sex, insurance, or hospital characteristics were excluded from our final cohort, as missing frequencies for each variable were small.
Ascertainment of Outcomes
For all patients, we extracted data on death status at discharge and length of hospital stay. We log-transformed length of stay because of its right skew, assigning the value of 12 hours to patients admitted and discharged the same day. Perioperative complications were calculated using ICD-9-CM codes as defined by a recent study of orthopedics-related complications by Lin and colleagues.18 There were 14 possible complications, including acute renal failure (584.5-9), tachycardia (427), wound hemorrhage (719.15, 998.31-2), wound disruption (998.3, 998.31-2), wound infection (682.6, 686.9, 891, 891.1-2, 894, 894.1-2, 998.5, 998.51, 998.6, 998.83, 998.59), deep vein thrombosis (453.4, 453.41-2, 453.9), acute myocardial infarction (410, 410.01, 410.11, 410.2, 410.21, 410.3, 410.31, 410.4, 410.41, 410.5, 410.51, 410.6, 410.9, 410.91, 997.1), pneumonia (480-480.9, 481, 482-482.9, 483, 483.1, 483.8, 484, 484.1, 484.3, 484.5-8, 485, 486, 487, 507), pulmonary embolism (415.11, 415.19), sepsis (995.91-2), stroke (997.02), urinary tract infection (599, 997.5), implant infection (996.66-7, 996.69), and incision and débridement (86.04, 86.09, 86.22, 86.28, 86.3). In our statistical analyses, we examined both the risk of having a complicated admission (≥1 perioperative complication) and the risk of having each specific complication.
Statistical Analysis
To assess similarity between weekend and weekday admissions, we used the Fisher exact test and χ2P values. Logistic regression was used to calculate the odds ratios (ORs) of mortality and perioperative complications for weekend versus weekday admissions. Linear regression was used to calculate parameter estimates for length of hospital stay for weekend versus weekday admissions. We interpreted parameter estimates as percentage differences using the formula 100(eb–1), where b is the estimated standardized regression coefficient of a log-transformed outcome variable.19 All regression models were controlled for age, sex, race, insurance, number of comorbidities, fracture location, hospital region, hospital bed size, hospital teaching status, and hospital location. We also stratified our study population by surgical delay in hours (<24, 24-48, 49-72, 73-120, ≥121) and by surgery performed (ORIF, hemiarthroplasty, CRIF, internal fixation only, THA, multiple procedures) to examine the effect of weekend admission on mortality, perioperative complications, and length of stay within each stratum. We did not control for these variables in our regression models because they were potential mediators of mortality, complications, and length of stay. All statistical analyses in this study were performed using SAS Version 9.1 (SAS Institute), and P < .05 was interpreted as statistically significant.
Results
After exclusions, our study population consisted of 96,892 weekend admissions and 248,097 weekday admissions. Among all admissions, mean age was 79.3 years (range, 0-113 years), with patients primarily being female and white, paying with Medicare, and having 1 to 4 comorbidities. Admissions were primarily for extracapsular femoral neck fractures and occurred most often in the South region, in hospitals with large beds, in nonteaching hospitals, and in urban locations. Table 1 lists details of baseline characteristics for weekend and weekday admissions.
Hospital stay details, including surgical delay and procedure performed, were examined for weekend and weekday admissions. Mean delay to surgery was 31.0 hours for weekend admissions and 30.2 hours for weekday admissions (P < .0001). The difference was driven by a higher proportion of weekend admissions in which surgery was performed 24 to 120 hours after admission. Patients admitted on the weekend also underwent more ORIF procedures and fewer hemiarthroplasties. Table 2 is a full list of hospital stay characteristics.
In regression analyses, weekend OR of mortality was 0.94 (95% CI, 0.89-0.99), weekend OR of having at least 1 complication was 1.00 (95% CI, 0.98-1.02), and weekend mean hospital stay was 3.74% shorter (95% CI, 3.40-4.08) in comparison with weekday figures. Within our models, risk of mortality and complications and mean length of stay increased as the number of patient comorbidities increased. Table 3 lists selected results from our regression models. Comprehensive tables for each outcome’s model are presented in Appendices 1 to 3.
In our analyses of specific complications, there were no significant associations between weekend admissions and risk of acute renal failure, wound hemorrhage, wound disruption, wound infection, deep vein thrombosis, myocardial infarction, pneumonia, pulmonary embolism, sepsis, urinary tract infection, implant infection, or incision and débridement. In addition, we found a lower risk of tachycardia (OR, 0.90; 95% CI, 0.82-1.00) and a higher risk (P < .10) of stroke (OR, 1.16; 95% CI, 0.99-1.35). Table 4 is a full list of the specific complications and their risks for weekend versus weekday admissions.
According to stratified analyses involving surgical delay, weekend admissions in which patients had surgery the same day as admission had decreased risk of mortality (OR, 0.81; 95% CI, 0.72-0.91) and perioperative complications (OR, 0.96; 95% CI, 0.92-0.99). In addition, hospital stay was shorter for weekend admissions with surgical delay of less than 24 hours (4.89% shorter; 95% CI, 4.22-5.55), 24 to 48 hours (5.93% shorter; 95% CI, 5.51-6.35), and 49 to 72 hours (3.50% shorter; 95% CI, 2.80-4.20). When admissions were stratified by procedure performed, patients who were admitted on the weekend and underwent ORIF, hemiarthroplasty, CRIF, internal fixation only, and THA had shorter stays than patients admitted on weekdays. For all surgeries performed, the risk of both mortality and complications did not significantly differ by day of admission. Table 5 lists the comprehensive results of all our stratified analyses.
Discussion
In this large, multiyear analysis of patients admitted for hip fracture in the United States, risk of mortality was slightly lower for weekend versus weekday admissions, hospital stay was significantly shorter, and risk of perioperative complications was not significantly different between admission types. In secondary analyses, shorter hospital stay was limited to patients who were admitted on weekends and underwent surgery within 48 hours. Our results therefore suggest that the weekend effect does not apply to hip fracture patients in the United States.
Our results are largely consistent with the literature on the topic.11-14 An Australian study of 4183 patients with acute hip fracture found no significant difference in 2- or 30-day mortality among weekend and weekday admissions.11 Similarly, 2 Danish studies did not find a difference in hospital-stay or 30-day mortality between weekend and weekday admissions among samples of 600 and 38,020 patients with hip fracture, respectively.12,13 In US patients, a cross-specialty study that included hip fractures did not find a difference in hospital-stay mortality among 22,001 admissions in the state of California in 1998.14 Our analysis significantly extended the findings of these studies by using comprehensive admission data from 46 US states over a 13-year period (1998–2010) and by examining outcomes other than mortality, including perioperative complications and length of hospital stay.
Our study had several limitations. First, the clinical data on fracture diagnoses and surgical procedures were based on ICD-9-CM codes, limiting our ability to account for the full details of fracture severity and subsequent management. Second, our analyses were limited to outcomes during the hospital stay, and we could not examine the effect of weekend admission on readmission and long-term mortality. Third, because of the dichotomization of admission day in the NIS database, we could not selectively examine the effect of Friday, Saturday, or Sunday admission on our outcomes. Fourth, we excluded admissions that were missing demographic and clinical data, potentially creating a complete-case bias. However, these exclusions were needed to accurately capture the common presentation of acute hip fracture, and there is no reason to believe that differences in record coding were nonrandom. Last, our study was observational, and we cannot rule out the effect of residual confounding on our results.
Our results failed to show a weekend effect on mortality, perioperative complications, or length of hospital stay in US patients with hip fracture. The reason for this, as suggested before,12 may be that hip fractures are becoming easier to diagnose. Furthermore, the observation that hospital stay was shorter for weekend admissions suggests that, despite decreased staffing of nursing and rehabilitation services, the lower volume of elective surgeries on weekends may actually increase staff availability to hip fracture patients.
1. Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117(3):151-157.
2. Saposnik G, Baibergenova A, Bayer N, Hachinski V. Weekends: a dangerous time for having a stroke? Stroke. 2007;38(4):1211-1215.
3. Busl KM, Prabhakaran S. Predictors of mortality in nontraumatic subdural hematoma. J Neurosurg. 2013;119(5):1296-1301.
4. Ananthakrishnan AN, McGinley EL, Saeian K. Outcomes of weekend admissions for upper gastrointestinal hemorrhage: a nationwide analysis. Clin Gastroenterol Hepatol. 2009;7(3):296e1-302e1.
5. Shaheen AA, Kaplan GG, Myers RP. Weekend versus weekday admission and mortality from gastrointestinal hemorrhage caused by peptic ulcer disease. Clin Gastroenterol Hepatol. 2009;7(3):303-310.
6. Deshmukh A, Pant S, Kumar G, Bursac Z, Paydak H, Mehta JL. Comparison of outcomes of weekend versus weekday admissions for atrial fibrillation. Am J Cardiol. 2012;110(2):208-211.
7. Aujesky D, Jiménez D, Mor MK, Geng M, Fine MJ, Ibrahim SA. Weekend versus weekday admission and mortality after acute pulmonary embolism. Circulation. 2009;119(7):962-968.
8. Clarke MS, Wills RA, Bowman RV, et al. Exploratory study of the ‘weekend effect’ for acute medical admissions to public hospitals in Queensland, Australia. Intern Med J. 2010;40(11):777-783.
9. Daugaard CL, Jørgensen HL, Riis T, Lauritzen JB, Duus BR, Van der mark S. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38,020 patients. Acta Orthop. 2012;83(6):609-613.
10. Foss NB, Kehlet H. Short-term mortality in hip fracture patients admitted during weekends and holidays. Br J Anaesth. 2006;96(4):450-4514.
11. Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis and meta-regression. Can J Anaesth. 2008;55(3):146-154.
12. Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1995;77(10):1551-1556.
13. Lefaivre KA, Macadam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br. 2009;91(7):922-927.
14. Ho V, Hamilton BH, Roos LL. Multiple approaches to assessing the effects of delays for hip fracture patients in the United States and Canada. Health Serv Res. 2000;34(7):1499-1518.
15. Steiner C, Elixhauser A, Schnaier J. The Healthcare Cost and Utilization Project: an overview. Eff Clin Pract. 2002;5(3):143-151.
16. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27.
17. Brasel KJ, Guse CE, Layde P, Weigelt JA. Rib fractures: relationship with pneumonia and mortality. Crit Care Med. 2006;34(6):1642-1646.
18. Lin CA, Kuo AC, Takemoto S. Comorbidities and perioperative complications in HIV-positive patients undergoing primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2013;95(11):1028-1036.
19. Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. 2nd ed. New York, NY: Springer-Verlag; 2012. Statistics for Biology and Health.
Weekend admission has been hypothesized to be a risk factor for increased patient mortality and complications during hospital stays—commonly referred to as the weekend effect.1 Reduced hospital staffing on weekends, particularly of senior-level physicians and ancillary nursing services, may affect the quality of diagnosis and management for patients admitted for traumatic and emergent conditions. Investigators have found increased mortality in weekend admissions for stroke,2 subdural hematoma,3 gastrointestinal bleeding,4,5 atrial fibrillation,6 and pulmonary embolism.7 Investigators have not found increased mortality in weekend admissions for hip fracture, though the majority of the data was derived from European patient populations, which may be subject to management and staffing strategies different from those for US patients.8-10 Furthermore, data on this topic in US patients are limited to a multispecialty study of 50 different admission diagnoses, which used 1 year of data from a single US state.1
We conducted a study to comprehensively assess the effect of weekend admission on adverse outcomes during hospital stays. The literature suggests that surgery for hip fracture can be delayed up to 48 hours without significant additional risk of death,11-13 allowing orthopedic departments to stabilize routine hip fracture admissions on weekends and operate whenever limited surgical teams become available. Surgical delay has not been thoroughly analyzed by day of admission among US patients,14 but the combined potential of more conservative preoperative management and the availability of fewer senior physicians and ancillary providers may result in worse outcomes for weekend versus weekday admissions.
Materials and Methods
Study Population
Part of the Healthcare Cost and Utilization Project, the Nationwide Inpatient Sample (NIS) provides a 20% representative sample of annual US hospital admissions.15 For these admissions, the NIS includes data related to demographic and clinical variables, such as International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes, as well as descriptive variables for the hospitals where the patients were admitted. The NIS is publicly available to researchers. As its health information is deidentified, we did not have to obtain institutional review board approval for this study.
Ascertainment of Cases
Our initial study population, drawn from the period 1998–2010, consisted of 821,531 patients with a principal ICD-9-CM diagnosis of femoral neck fracture (820.0-820.9). To best capture the typical presentation of hip fracture, we excluded:
- Patients with open femoral neck fractures (820.1, 820.3, 820.9).
- Patients who did not have open reduction and internal fixation (ORIF) (79.35), hemiarthroplasty (81.52), closed reduction and internal fixation (CRIF) (79.15), internal fixation (78.55), or total hip arthroplasty (THA) (81.51) as their primary surgical procedure.
- Patients admitted from sources other than the emergency department.
- Patients who underwent surgery before admission.
- Patients whose admission type was not classified as emergency or urgent.
Ascertainment of Covariates
For all patients, we extracted data on exposure of interest, day of admission (weekend or weekday), and demographic variables including age, sex, race (white, black, Hispanic, other, missing), and insurance (Medicare, Medicaid, private, other). We used the Elixhauser method to determine 30 different comorbidities from ICD-9-CM diagnosis coding16 and sorted patients by total number of comorbidities (0, 1, 2, 3 or 4, ≥5). As has been done before,17 we excluded blood loss anemia, coagulopathy, and fluid and electrolyte disorders from this comorbidity calculation, as these conditions can be secondary to trauma. We also extracted data on the admission itself, including hospital region (Northeast, Midwest, South, West), hospital bed size (small, medium, large), hospital teaching status (nonteaching, teaching), and hospital location (rural, urban). We used diagnosis codes to categorize fracture location as “not otherwise specified” (820.8), intracapsular (820.0), or extracapsular (820.2).
Because of low frequencies, we collapsed 2 race designations (Native American, Asian or Pacific Islander) into the “other race” category and 2 insurance designations (self-pay, no charge) into the “other insurance” category. For a substantial number of patients, race information was missing, so we included “missing” as its own category in analyses. Patients who were missing data on day of admission, age, sex, insurance, or hospital characteristics were excluded from our final cohort, as missing frequencies for each variable were small.
Ascertainment of Outcomes
For all patients, we extracted data on death status at discharge and length of hospital stay. We log-transformed length of stay because of its right skew, assigning the value of 12 hours to patients admitted and discharged the same day. Perioperative complications were calculated using ICD-9-CM codes as defined by a recent study of orthopedics-related complications by Lin and colleagues.18 There were 14 possible complications, including acute renal failure (584.5-9), tachycardia (427), wound hemorrhage (719.15, 998.31-2), wound disruption (998.3, 998.31-2), wound infection (682.6, 686.9, 891, 891.1-2, 894, 894.1-2, 998.5, 998.51, 998.6, 998.83, 998.59), deep vein thrombosis (453.4, 453.41-2, 453.9), acute myocardial infarction (410, 410.01, 410.11, 410.2, 410.21, 410.3, 410.31, 410.4, 410.41, 410.5, 410.51, 410.6, 410.9, 410.91, 997.1), pneumonia (480-480.9, 481, 482-482.9, 483, 483.1, 483.8, 484, 484.1, 484.3, 484.5-8, 485, 486, 487, 507), pulmonary embolism (415.11, 415.19), sepsis (995.91-2), stroke (997.02), urinary tract infection (599, 997.5), implant infection (996.66-7, 996.69), and incision and débridement (86.04, 86.09, 86.22, 86.28, 86.3). In our statistical analyses, we examined both the risk of having a complicated admission (≥1 perioperative complication) and the risk of having each specific complication.
Statistical Analysis
To assess similarity between weekend and weekday admissions, we used the Fisher exact test and χ2P values. Logistic regression was used to calculate the odds ratios (ORs) of mortality and perioperative complications for weekend versus weekday admissions. Linear regression was used to calculate parameter estimates for length of hospital stay for weekend versus weekday admissions. We interpreted parameter estimates as percentage differences using the formula 100(eb–1), where b is the estimated standardized regression coefficient of a log-transformed outcome variable.19 All regression models were controlled for age, sex, race, insurance, number of comorbidities, fracture location, hospital region, hospital bed size, hospital teaching status, and hospital location. We also stratified our study population by surgical delay in hours (<24, 24-48, 49-72, 73-120, ≥121) and by surgery performed (ORIF, hemiarthroplasty, CRIF, internal fixation only, THA, multiple procedures) to examine the effect of weekend admission on mortality, perioperative complications, and length of stay within each stratum. We did not control for these variables in our regression models because they were potential mediators of mortality, complications, and length of stay. All statistical analyses in this study were performed using SAS Version 9.1 (SAS Institute), and P < .05 was interpreted as statistically significant.
Results
After exclusions, our study population consisted of 96,892 weekend admissions and 248,097 weekday admissions. Among all admissions, mean age was 79.3 years (range, 0-113 years), with patients primarily being female and white, paying with Medicare, and having 1 to 4 comorbidities. Admissions were primarily for extracapsular femoral neck fractures and occurred most often in the South region, in hospitals with large beds, in nonteaching hospitals, and in urban locations. Table 1 lists details of baseline characteristics for weekend and weekday admissions.
Hospital stay details, including surgical delay and procedure performed, were examined for weekend and weekday admissions. Mean delay to surgery was 31.0 hours for weekend admissions and 30.2 hours for weekday admissions (P < .0001). The difference was driven by a higher proportion of weekend admissions in which surgery was performed 24 to 120 hours after admission. Patients admitted on the weekend also underwent more ORIF procedures and fewer hemiarthroplasties. Table 2 is a full list of hospital stay characteristics.
In regression analyses, weekend OR of mortality was 0.94 (95% CI, 0.89-0.99), weekend OR of having at least 1 complication was 1.00 (95% CI, 0.98-1.02), and weekend mean hospital stay was 3.74% shorter (95% CI, 3.40-4.08) in comparison with weekday figures. Within our models, risk of mortality and complications and mean length of stay increased as the number of patient comorbidities increased. Table 3 lists selected results from our regression models. Comprehensive tables for each outcome’s model are presented in Appendices 1 to 3.
In our analyses of specific complications, there were no significant associations between weekend admissions and risk of acute renal failure, wound hemorrhage, wound disruption, wound infection, deep vein thrombosis, myocardial infarction, pneumonia, pulmonary embolism, sepsis, urinary tract infection, implant infection, or incision and débridement. In addition, we found a lower risk of tachycardia (OR, 0.90; 95% CI, 0.82-1.00) and a higher risk (P < .10) of stroke (OR, 1.16; 95% CI, 0.99-1.35). Table 4 is a full list of the specific complications and their risks for weekend versus weekday admissions.
According to stratified analyses involving surgical delay, weekend admissions in which patients had surgery the same day as admission had decreased risk of mortality (OR, 0.81; 95% CI, 0.72-0.91) and perioperative complications (OR, 0.96; 95% CI, 0.92-0.99). In addition, hospital stay was shorter for weekend admissions with surgical delay of less than 24 hours (4.89% shorter; 95% CI, 4.22-5.55), 24 to 48 hours (5.93% shorter; 95% CI, 5.51-6.35), and 49 to 72 hours (3.50% shorter; 95% CI, 2.80-4.20). When admissions were stratified by procedure performed, patients who were admitted on the weekend and underwent ORIF, hemiarthroplasty, CRIF, internal fixation only, and THA had shorter stays than patients admitted on weekdays. For all surgeries performed, the risk of both mortality and complications did not significantly differ by day of admission. Table 5 lists the comprehensive results of all our stratified analyses.
Discussion
In this large, multiyear analysis of patients admitted for hip fracture in the United States, risk of mortality was slightly lower for weekend versus weekday admissions, hospital stay was significantly shorter, and risk of perioperative complications was not significantly different between admission types. In secondary analyses, shorter hospital stay was limited to patients who were admitted on weekends and underwent surgery within 48 hours. Our results therefore suggest that the weekend effect does not apply to hip fracture patients in the United States.
Our results are largely consistent with the literature on the topic.11-14 An Australian study of 4183 patients with acute hip fracture found no significant difference in 2- or 30-day mortality among weekend and weekday admissions.11 Similarly, 2 Danish studies did not find a difference in hospital-stay or 30-day mortality between weekend and weekday admissions among samples of 600 and 38,020 patients with hip fracture, respectively.12,13 In US patients, a cross-specialty study that included hip fractures did not find a difference in hospital-stay mortality among 22,001 admissions in the state of California in 1998.14 Our analysis significantly extended the findings of these studies by using comprehensive admission data from 46 US states over a 13-year period (1998–2010) and by examining outcomes other than mortality, including perioperative complications and length of hospital stay.
Our study had several limitations. First, the clinical data on fracture diagnoses and surgical procedures were based on ICD-9-CM codes, limiting our ability to account for the full details of fracture severity and subsequent management. Second, our analyses were limited to outcomes during the hospital stay, and we could not examine the effect of weekend admission on readmission and long-term mortality. Third, because of the dichotomization of admission day in the NIS database, we could not selectively examine the effect of Friday, Saturday, or Sunday admission on our outcomes. Fourth, we excluded admissions that were missing demographic and clinical data, potentially creating a complete-case bias. However, these exclusions were needed to accurately capture the common presentation of acute hip fracture, and there is no reason to believe that differences in record coding were nonrandom. Last, our study was observational, and we cannot rule out the effect of residual confounding on our results.
Our results failed to show a weekend effect on mortality, perioperative complications, or length of hospital stay in US patients with hip fracture. The reason for this, as suggested before,12 may be that hip fractures are becoming easier to diagnose. Furthermore, the observation that hospital stay was shorter for weekend admissions suggests that, despite decreased staffing of nursing and rehabilitation services, the lower volume of elective surgeries on weekends may actually increase staff availability to hip fracture patients.
Weekend admission has been hypothesized to be a risk factor for increased patient mortality and complications during hospital stays—commonly referred to as the weekend effect.1 Reduced hospital staffing on weekends, particularly of senior-level physicians and ancillary nursing services, may affect the quality of diagnosis and management for patients admitted for traumatic and emergent conditions. Investigators have found increased mortality in weekend admissions for stroke,2 subdural hematoma,3 gastrointestinal bleeding,4,5 atrial fibrillation,6 and pulmonary embolism.7 Investigators have not found increased mortality in weekend admissions for hip fracture, though the majority of the data was derived from European patient populations, which may be subject to management and staffing strategies different from those for US patients.8-10 Furthermore, data on this topic in US patients are limited to a multispecialty study of 50 different admission diagnoses, which used 1 year of data from a single US state.1
We conducted a study to comprehensively assess the effect of weekend admission on adverse outcomes during hospital stays. The literature suggests that surgery for hip fracture can be delayed up to 48 hours without significant additional risk of death,11-13 allowing orthopedic departments to stabilize routine hip fracture admissions on weekends and operate whenever limited surgical teams become available. Surgical delay has not been thoroughly analyzed by day of admission among US patients,14 but the combined potential of more conservative preoperative management and the availability of fewer senior physicians and ancillary providers may result in worse outcomes for weekend versus weekday admissions.
Materials and Methods
Study Population
Part of the Healthcare Cost and Utilization Project, the Nationwide Inpatient Sample (NIS) provides a 20% representative sample of annual US hospital admissions.15 For these admissions, the NIS includes data related to demographic and clinical variables, such as International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes, as well as descriptive variables for the hospitals where the patients were admitted. The NIS is publicly available to researchers. As its health information is deidentified, we did not have to obtain institutional review board approval for this study.
Ascertainment of Cases
Our initial study population, drawn from the period 1998–2010, consisted of 821,531 patients with a principal ICD-9-CM diagnosis of femoral neck fracture (820.0-820.9). To best capture the typical presentation of hip fracture, we excluded:
- Patients with open femoral neck fractures (820.1, 820.3, 820.9).
- Patients who did not have open reduction and internal fixation (ORIF) (79.35), hemiarthroplasty (81.52), closed reduction and internal fixation (CRIF) (79.15), internal fixation (78.55), or total hip arthroplasty (THA) (81.51) as their primary surgical procedure.
- Patients admitted from sources other than the emergency department.
- Patients who underwent surgery before admission.
- Patients whose admission type was not classified as emergency or urgent.
Ascertainment of Covariates
For all patients, we extracted data on exposure of interest, day of admission (weekend or weekday), and demographic variables including age, sex, race (white, black, Hispanic, other, missing), and insurance (Medicare, Medicaid, private, other). We used the Elixhauser method to determine 30 different comorbidities from ICD-9-CM diagnosis coding16 and sorted patients by total number of comorbidities (0, 1, 2, 3 or 4, ≥5). As has been done before,17 we excluded blood loss anemia, coagulopathy, and fluid and electrolyte disorders from this comorbidity calculation, as these conditions can be secondary to trauma. We also extracted data on the admission itself, including hospital region (Northeast, Midwest, South, West), hospital bed size (small, medium, large), hospital teaching status (nonteaching, teaching), and hospital location (rural, urban). We used diagnosis codes to categorize fracture location as “not otherwise specified” (820.8), intracapsular (820.0), or extracapsular (820.2).
Because of low frequencies, we collapsed 2 race designations (Native American, Asian or Pacific Islander) into the “other race” category and 2 insurance designations (self-pay, no charge) into the “other insurance” category. For a substantial number of patients, race information was missing, so we included “missing” as its own category in analyses. Patients who were missing data on day of admission, age, sex, insurance, or hospital characteristics were excluded from our final cohort, as missing frequencies for each variable were small.
Ascertainment of Outcomes
For all patients, we extracted data on death status at discharge and length of hospital stay. We log-transformed length of stay because of its right skew, assigning the value of 12 hours to patients admitted and discharged the same day. Perioperative complications were calculated using ICD-9-CM codes as defined by a recent study of orthopedics-related complications by Lin and colleagues.18 There were 14 possible complications, including acute renal failure (584.5-9), tachycardia (427), wound hemorrhage (719.15, 998.31-2), wound disruption (998.3, 998.31-2), wound infection (682.6, 686.9, 891, 891.1-2, 894, 894.1-2, 998.5, 998.51, 998.6, 998.83, 998.59), deep vein thrombosis (453.4, 453.41-2, 453.9), acute myocardial infarction (410, 410.01, 410.11, 410.2, 410.21, 410.3, 410.31, 410.4, 410.41, 410.5, 410.51, 410.6, 410.9, 410.91, 997.1), pneumonia (480-480.9, 481, 482-482.9, 483, 483.1, 483.8, 484, 484.1, 484.3, 484.5-8, 485, 486, 487, 507), pulmonary embolism (415.11, 415.19), sepsis (995.91-2), stroke (997.02), urinary tract infection (599, 997.5), implant infection (996.66-7, 996.69), and incision and débridement (86.04, 86.09, 86.22, 86.28, 86.3). In our statistical analyses, we examined both the risk of having a complicated admission (≥1 perioperative complication) and the risk of having each specific complication.
Statistical Analysis
To assess similarity between weekend and weekday admissions, we used the Fisher exact test and χ2P values. Logistic regression was used to calculate the odds ratios (ORs) of mortality and perioperative complications for weekend versus weekday admissions. Linear regression was used to calculate parameter estimates for length of hospital stay for weekend versus weekday admissions. We interpreted parameter estimates as percentage differences using the formula 100(eb–1), where b is the estimated standardized regression coefficient of a log-transformed outcome variable.19 All regression models were controlled for age, sex, race, insurance, number of comorbidities, fracture location, hospital region, hospital bed size, hospital teaching status, and hospital location. We also stratified our study population by surgical delay in hours (<24, 24-48, 49-72, 73-120, ≥121) and by surgery performed (ORIF, hemiarthroplasty, CRIF, internal fixation only, THA, multiple procedures) to examine the effect of weekend admission on mortality, perioperative complications, and length of stay within each stratum. We did not control for these variables in our regression models because they were potential mediators of mortality, complications, and length of stay. All statistical analyses in this study were performed using SAS Version 9.1 (SAS Institute), and P < .05 was interpreted as statistically significant.
Results
After exclusions, our study population consisted of 96,892 weekend admissions and 248,097 weekday admissions. Among all admissions, mean age was 79.3 years (range, 0-113 years), with patients primarily being female and white, paying with Medicare, and having 1 to 4 comorbidities. Admissions were primarily for extracapsular femoral neck fractures and occurred most often in the South region, in hospitals with large beds, in nonteaching hospitals, and in urban locations. Table 1 lists details of baseline characteristics for weekend and weekday admissions.
Hospital stay details, including surgical delay and procedure performed, were examined for weekend and weekday admissions. Mean delay to surgery was 31.0 hours for weekend admissions and 30.2 hours for weekday admissions (P < .0001). The difference was driven by a higher proportion of weekend admissions in which surgery was performed 24 to 120 hours after admission. Patients admitted on the weekend also underwent more ORIF procedures and fewer hemiarthroplasties. Table 2 is a full list of hospital stay characteristics.
In regression analyses, weekend OR of mortality was 0.94 (95% CI, 0.89-0.99), weekend OR of having at least 1 complication was 1.00 (95% CI, 0.98-1.02), and weekend mean hospital stay was 3.74% shorter (95% CI, 3.40-4.08) in comparison with weekday figures. Within our models, risk of mortality and complications and mean length of stay increased as the number of patient comorbidities increased. Table 3 lists selected results from our regression models. Comprehensive tables for each outcome’s model are presented in Appendices 1 to 3.
In our analyses of specific complications, there were no significant associations between weekend admissions and risk of acute renal failure, wound hemorrhage, wound disruption, wound infection, deep vein thrombosis, myocardial infarction, pneumonia, pulmonary embolism, sepsis, urinary tract infection, implant infection, or incision and débridement. In addition, we found a lower risk of tachycardia (OR, 0.90; 95% CI, 0.82-1.00) and a higher risk (P < .10) of stroke (OR, 1.16; 95% CI, 0.99-1.35). Table 4 is a full list of the specific complications and their risks for weekend versus weekday admissions.
According to stratified analyses involving surgical delay, weekend admissions in which patients had surgery the same day as admission had decreased risk of mortality (OR, 0.81; 95% CI, 0.72-0.91) and perioperative complications (OR, 0.96; 95% CI, 0.92-0.99). In addition, hospital stay was shorter for weekend admissions with surgical delay of less than 24 hours (4.89% shorter; 95% CI, 4.22-5.55), 24 to 48 hours (5.93% shorter; 95% CI, 5.51-6.35), and 49 to 72 hours (3.50% shorter; 95% CI, 2.80-4.20). When admissions were stratified by procedure performed, patients who were admitted on the weekend and underwent ORIF, hemiarthroplasty, CRIF, internal fixation only, and THA had shorter stays than patients admitted on weekdays. For all surgeries performed, the risk of both mortality and complications did not significantly differ by day of admission. Table 5 lists the comprehensive results of all our stratified analyses.
Discussion
In this large, multiyear analysis of patients admitted for hip fracture in the United States, risk of mortality was slightly lower for weekend versus weekday admissions, hospital stay was significantly shorter, and risk of perioperative complications was not significantly different between admission types. In secondary analyses, shorter hospital stay was limited to patients who were admitted on weekends and underwent surgery within 48 hours. Our results therefore suggest that the weekend effect does not apply to hip fracture patients in the United States.
Our results are largely consistent with the literature on the topic.11-14 An Australian study of 4183 patients with acute hip fracture found no significant difference in 2- or 30-day mortality among weekend and weekday admissions.11 Similarly, 2 Danish studies did not find a difference in hospital-stay or 30-day mortality between weekend and weekday admissions among samples of 600 and 38,020 patients with hip fracture, respectively.12,13 In US patients, a cross-specialty study that included hip fractures did not find a difference in hospital-stay mortality among 22,001 admissions in the state of California in 1998.14 Our analysis significantly extended the findings of these studies by using comprehensive admission data from 46 US states over a 13-year period (1998–2010) and by examining outcomes other than mortality, including perioperative complications and length of hospital stay.
Our study had several limitations. First, the clinical data on fracture diagnoses and surgical procedures were based on ICD-9-CM codes, limiting our ability to account for the full details of fracture severity and subsequent management. Second, our analyses were limited to outcomes during the hospital stay, and we could not examine the effect of weekend admission on readmission and long-term mortality. Third, because of the dichotomization of admission day in the NIS database, we could not selectively examine the effect of Friday, Saturday, or Sunday admission on our outcomes. Fourth, we excluded admissions that were missing demographic and clinical data, potentially creating a complete-case bias. However, these exclusions were needed to accurately capture the common presentation of acute hip fracture, and there is no reason to believe that differences in record coding were nonrandom. Last, our study was observational, and we cannot rule out the effect of residual confounding on our results.
Our results failed to show a weekend effect on mortality, perioperative complications, or length of hospital stay in US patients with hip fracture. The reason for this, as suggested before,12 may be that hip fractures are becoming easier to diagnose. Furthermore, the observation that hospital stay was shorter for weekend admissions suggests that, despite decreased staffing of nursing and rehabilitation services, the lower volume of elective surgeries on weekends may actually increase staff availability to hip fracture patients.
1. Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117(3):151-157.
2. Saposnik G, Baibergenova A, Bayer N, Hachinski V. Weekends: a dangerous time for having a stroke? Stroke. 2007;38(4):1211-1215.
3. Busl KM, Prabhakaran S. Predictors of mortality in nontraumatic subdural hematoma. J Neurosurg. 2013;119(5):1296-1301.
4. Ananthakrishnan AN, McGinley EL, Saeian K. Outcomes of weekend admissions for upper gastrointestinal hemorrhage: a nationwide analysis. Clin Gastroenterol Hepatol. 2009;7(3):296e1-302e1.
5. Shaheen AA, Kaplan GG, Myers RP. Weekend versus weekday admission and mortality from gastrointestinal hemorrhage caused by peptic ulcer disease. Clin Gastroenterol Hepatol. 2009;7(3):303-310.
6. Deshmukh A, Pant S, Kumar G, Bursac Z, Paydak H, Mehta JL. Comparison of outcomes of weekend versus weekday admissions for atrial fibrillation. Am J Cardiol. 2012;110(2):208-211.
7. Aujesky D, Jiménez D, Mor MK, Geng M, Fine MJ, Ibrahim SA. Weekend versus weekday admission and mortality after acute pulmonary embolism. Circulation. 2009;119(7):962-968.
8. Clarke MS, Wills RA, Bowman RV, et al. Exploratory study of the ‘weekend effect’ for acute medical admissions to public hospitals in Queensland, Australia. Intern Med J. 2010;40(11):777-783.
9. Daugaard CL, Jørgensen HL, Riis T, Lauritzen JB, Duus BR, Van der mark S. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38,020 patients. Acta Orthop. 2012;83(6):609-613.
10. Foss NB, Kehlet H. Short-term mortality in hip fracture patients admitted during weekends and holidays. Br J Anaesth. 2006;96(4):450-4514.
11. Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis and meta-regression. Can J Anaesth. 2008;55(3):146-154.
12. Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1995;77(10):1551-1556.
13. Lefaivre KA, Macadam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br. 2009;91(7):922-927.
14. Ho V, Hamilton BH, Roos LL. Multiple approaches to assessing the effects of delays for hip fracture patients in the United States and Canada. Health Serv Res. 2000;34(7):1499-1518.
15. Steiner C, Elixhauser A, Schnaier J. The Healthcare Cost and Utilization Project: an overview. Eff Clin Pract. 2002;5(3):143-151.
16. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27.
17. Brasel KJ, Guse CE, Layde P, Weigelt JA. Rib fractures: relationship with pneumonia and mortality. Crit Care Med. 2006;34(6):1642-1646.
18. Lin CA, Kuo AC, Takemoto S. Comorbidities and perioperative complications in HIV-positive patients undergoing primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2013;95(11):1028-1036.
19. Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. 2nd ed. New York, NY: Springer-Verlag; 2012. Statistics for Biology and Health.
1. Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117(3):151-157.
2. Saposnik G, Baibergenova A, Bayer N, Hachinski V. Weekends: a dangerous time for having a stroke? Stroke. 2007;38(4):1211-1215.
3. Busl KM, Prabhakaran S. Predictors of mortality in nontraumatic subdural hematoma. J Neurosurg. 2013;119(5):1296-1301.
4. Ananthakrishnan AN, McGinley EL, Saeian K. Outcomes of weekend admissions for upper gastrointestinal hemorrhage: a nationwide analysis. Clin Gastroenterol Hepatol. 2009;7(3):296e1-302e1.
5. Shaheen AA, Kaplan GG, Myers RP. Weekend versus weekday admission and mortality from gastrointestinal hemorrhage caused by peptic ulcer disease. Clin Gastroenterol Hepatol. 2009;7(3):303-310.
6. Deshmukh A, Pant S, Kumar G, Bursac Z, Paydak H, Mehta JL. Comparison of outcomes of weekend versus weekday admissions for atrial fibrillation. Am J Cardiol. 2012;110(2):208-211.
7. Aujesky D, Jiménez D, Mor MK, Geng M, Fine MJ, Ibrahim SA. Weekend versus weekday admission and mortality after acute pulmonary embolism. Circulation. 2009;119(7):962-968.
8. Clarke MS, Wills RA, Bowman RV, et al. Exploratory study of the ‘weekend effect’ for acute medical admissions to public hospitals in Queensland, Australia. Intern Med J. 2010;40(11):777-783.
9. Daugaard CL, Jørgensen HL, Riis T, Lauritzen JB, Duus BR, Van der mark S. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38,020 patients. Acta Orthop. 2012;83(6):609-613.
10. Foss NB, Kehlet H. Short-term mortality in hip fracture patients admitted during weekends and holidays. Br J Anaesth. 2006;96(4):450-4514.
11. Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis and meta-regression. Can J Anaesth. 2008;55(3):146-154.
12. Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1995;77(10):1551-1556.
13. Lefaivre KA, Macadam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br. 2009;91(7):922-927.
14. Ho V, Hamilton BH, Roos LL. Multiple approaches to assessing the effects of delays for hip fracture patients in the United States and Canada. Health Serv Res. 2000;34(7):1499-1518.
15. Steiner C, Elixhauser A, Schnaier J. The Healthcare Cost and Utilization Project: an overview. Eff Clin Pract. 2002;5(3):143-151.
16. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27.
17. Brasel KJ, Guse CE, Layde P, Weigelt JA. Rib fractures: relationship with pneumonia and mortality. Crit Care Med. 2006;34(6):1642-1646.
18. Lin CA, Kuo AC, Takemoto S. Comorbidities and perioperative complications in HIV-positive patients undergoing primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2013;95(11):1028-1036.
19. Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. 2nd ed. New York, NY: Springer-Verlag; 2012. Statistics for Biology and Health.
The Pathobiology of Diabetes Mellitus in Bone Metabolism, Fracture Healing, and Complications
Diabetes mellitus (DM) affects a significant portion of the world’s people, and the problem is increasing in magnitude as the population ages and becomes more obese.1 An estimated 347 million people have diabetes.1 In the United States, 26 million (roughly 8% of the population) are affected, making DM a major health issue.2 Given the prevalence of diabetes in the general population, it is not surprising that increasing numbers of fracture patients have DM. Unfortunately, for these patients, many relatively simple fractures can have disastrous outcomes. Infections and wound complications occur in disproportionate numbers, healing time is delayed, and risk for nonunion or malunion is substantially higher.3
It is imperative to understand the pathophysiology of DM to appreciate potential interventions and strategies aimed at decreasing complications and improving outcomes of fractures in patients with the disease. In type 1 DM (T1DM), autoimmune destruction of the insulin-secreting β cells in the pancreas results in a complete absence of insulin. Patients with T1DM are dependent on exogenous insulin, and, despite hyperglycemia, most cells in the body are starved for energy. This leads to a catabolic condition, high lipid and protein metabolism, and, in many cases, ketoacidosis. When insulin resistance develops, the β cells are forced to secrete large amounts of insulin; when they fail to keep up, type 2 DM (T2DM) develops. T2DM is often associated with obesity, as excess adipose tissue leads to insulin resistance. Although exogenous insulin may be necessary to treat advanced T2DM, other medications are commonly used to effectively lower blood glucose: Secretagogues (eg, sulfonylureas) facilitate insulin release from β cells, and sensitizers (eg, metformin) increase insulin sensitivity.4,5
The potential morbidity of fractures in patients with DM can be appreciated with the example of ankle fractures. These typically uncomplicated fractures can have very poor outcomes in the setting of DM. In a prospective study of approximately 1500 patients with ankle fractures treated with open reduction and internal fixation, Wukich and colleagues6 found that 9.5% of patients with DM (vs 2.4% of patients without DM) developed surgical site infections. As defined by Jones and colleagues,7 major complications of treating ankle fractures in patients with DM include infection, malunion, nonunion, Charcot arthropathy, and amputation. The authors reported major complications in 31% and 17% of patients with and without DM, respectively. Highlighting the importance of glycemic control, Wukich and colleagues6 found relative risks of 3.8 for infection, 3.4 for noninfectious complications, and 5.0 for revision in complicated (vs uncomplicated) fractures in patients with DM.
Given the magnitude of problems in the treatment of fractures in patients with DM, we focus our review on the pathobiology of diabetes in terms of bone metabolism and fracture healing, wound healing and vasculopathy, infection, and potential new treatment modalities.
Bone Metabolism and Fracture Healing in Diabetes
Insulin appears to play a role in bone metabolism and fracture healing. Therefore, absence of insulin in T1DM and elevated insulin levels associated with T2DM likely influence these metabolic and fracture-healing processes. Insulin has been hypothesized to have an anabolic effect on bone, and in both human and animal models bone mineral density (BMD) is significantly lower in T1DM. Furthermore, BMD in T2DM has been shown to be normal or even elevated.8 Other metabolic effects of insulin on bone metabolism and growth include slower growth rates and lower BMD in pediatric patients with T1DM versus patients without diabetes, and some animal models show bone microarchitecture altered in the absence of insulin (and reversible with insulin supplementation).9 These factors seem to contradict the markedly elevated risk for osteoporotic fracture in patients with T2DM, but the mechanisms responsible for this have not been elucidated.8
In terms of fracture healing, resorption of cartilage during transition to hard callus appears to be influenced by diabetes. It has been hypothesized that the smaller callus observed in diabetic mice may be secondary to upregulation of osteoclasts. Initial callus size appears not to differ between mice with streptozotocin-induced diabetes, which exhibit a complete absence of insulin, and control mice, but levels of osteoclast and osteoclastogenesis mediators were significantly higher in the diabetic mice.10 Some investigators think that the reduction in cartilage callus size in diabetic mice is caused by altered mRNA expression and collagen production.11 Diabetic mice, in addition to showing increased resorption by osteoclasts, demonstrate increased chondrocyte apoptosis, which is thought to activate cartilage resorption events. Exogenous insulin effectively reverses this cartilage loss to baseline levels.12
Osteoblasts are a crucial component of the fracture-healing cascade, and acute and chronic hyperglycemia, the hallmark of diabetes, has a variety of effects on osteoblasts.13 Genes for cell-signal proteins such as osteocalcin, MMP-13, and vascular endothelial growth factor are downregulated in the presence of chronic hyperglycemia, whereas genes for alkaline phosphate are upregulated. Acute hyperglycemia by way of hyperosmolarity is associated with MMP-13 downregulation. Thus, osteoblasts appear to respond to hyperglycemia through 2 different processes: Hyperosmolarity, through osteoblast cell shrinkage, influences the acute response, and hyperglycemia itself, through pathways such as nonenzymatic glycosylation, protein kinase C (PKC) signaling, and the polyol pathway, is the force behind the chronic response.14 The lineage of osteoblasts from mesenchymal stem cells also can be affected by hyperglycemia, with lower growth rates for mesenchymal stem cells and preferential development toward the adipocyte lineage, while the osteoblast and chondrocyte lineages are downregulated.15
Increased osteoblast apoptosis has been associated with diabetes through advanced glycation end-products (AGEs), which modify the structure and function of bioactive compounds through AGE receptors that cross-link and bond to amino groups on bioactive molecules.16 It has been reported that AGEs interfere with osteoblast development and collagen and osteocalcin production.17 A common AGE, carboxymethyl lysine-modified collagen, has been associated with a significant increase in apoptosis through the mitogen-activated protein kinase (MAPK) pathway. Although most of the literature suggests that osteoblast apoptosis is activated by hypoxia, nitric oxide, or integrins, these factors all have the MAPK pathway in common.18
Osteoclasts are also influenced by diabetes. Recent work in T1DM demonstrated that osteoclasts are hyperactive and more sensitive to receptor activator of nuclear factor kB ligand (RANKL) compared with osteoclasts from the population without diabetes. It is also known that osteoclasts are under the control of immunologic mediators like lipopolysaccharide (LPS), a surface component of gram-negative bacteria, and various other proinflammatory cytokines. In patients with diabetes, osteoclasts react differently to LPS and other proinflammatory cytokines, at times with opposing effects, including secretion of RANKL to stimulate resorption by the osteoclast, and precursors preventing progression into osteoclasts. In healthy people, high LPS levels not only prevent precursors from producing more osteoclasts, but promote them to mature into immune-like cells that actually phagocytose bacteria. So, in a state of infection, precursors shift from bone-resorbing osteoclasts to protective immune cells. This phenomenon does not occur in patients with diabetes, in whom the osteoclasts instead resorb more bone and stimulate inflammation by releasing cytokines.19
Interestingly, osteoblasts and osteoclasts are also affected by medications commonly used to treat diabetes. Thiazolidinediones are a class of sensitizers often used to treat patients with T2DM. Thiazolidinediones, particularly rosiglitazone, have been associated with increased bone loss primarily caused by increased bone resorption by osteoclasts.20 In addition, some investigators think that thiazolidinediones induce osteocyte apoptosis, contributing to impaired bone growth.8 Metformin, an insulin sensitizer, appears to have a positive effect on bone growth and fracture risk by enhancing osteoblastogenesis and inhibiting osteoclastogenesis, leading to a protective effect on bone.8
Peripheral neuropathy, which is often associated with diabetes, appears to play a major role in fracture-healing complications, even more so than hyperglycemia does. A recent clinical paper found that patients with diabetic neuropathy had a 44% risk of foot and ankle fracture-healing complications.21 Regardless of the risk, the pathogenesis of diabetic neuropathy can be caused by several mechanisms. Neural tissue does not require insulin for glucose uptake; therefore, in a state of hyperglycemia, aldose reductase shunts glucose to sorbitol while using protective glutathione and generating reactive oxygen species. This oxidative stress results in nerve damage or neuropathy. Microangiopathy, which we discuss in more detail later, also contributes to the development of neuropathy, through compromised flow of blood to neural tissue.22 Another mechanism contributing to diabetic neuropathy involves PKC, which is activated by 1,2-diacylglycerol in the presence of glucose, leading to vascular changes that restrict the flow of blood to peripheral nerves.23 Finally, AGEs may also participate by altering nerve function after binding to neural tissue.
Charcot neuroarthropathy is a complication associated with diabetes, particularly after injury in which chronic inflammation results in damage to the joint through fracture, dislocation, and osteolytic bony destruction. The pathophysiology is attributed to repeated microtrauma caused by loss of protective sensibility and hyperemia caused by dysregulation.24 Sympathetic and sensory nerve fibers are associated with bone, but a few serve as mechanoreceptors and nociceptors, which can activate substance P, calcitonin gene-related peptide, and vasoactive intestinal peptide—neuropeptides all thought to be involved in the inflammatory process, and in the activation of osteoblasts and osteoclasts. In diabetic neuropathy, many of these neuropeptides show a reduced regulation response, which can lead to impaired fracture healing. In particular, osteoclast activity is upregulated, and consequently bone resorption is increased. In addition to the neuropeptides mentioned, RANKL is one mechanism by which this upregulation occurs.25
It is clear that bone metabolism and fracture healing are complex processes. In the patient with diabetes, many factors are affected, including BMD, bone microarchitecture and bone growth, cartilage resorption during callus formation, osteoblast and osteoclast activation through both altered responses to cell signals and pharmacologic interactions, and, finally, peripheral neuropathy. Given the complex interactions described, it is likely that these factors in combination, as well as those yet undiscovered, negatively affect fracture healing.
Wound Healing and Vasculopathy in Diabetes
Bone healing and soft-tissue healing depend on many of the same factors. Therefore, interactions between neuropathy and vasculopathy can have a tremendous influence on wound healing in patients with diabetes. The vascular pathology that occurs in diabetes depends in part on the fact that endothelial cells do not require insulin for glucose uptake and therefore are more susceptible to damage by hyperglycemia. As already discussed, shunting of glucose through the polyol pathway with the resultant oxidative stress is partly responsible for angiopathy in diabetes.
Also as already discussed, AGEs affect intracellular processes by protein binding and gene regulation and by disrupting the communication between cells and the surrounding matrix. From an extracellular standpoint, AGEs bind to circulating proteins, promoting inflammation and upregulation/downregulation of growth factors, including endothelial nitric oxide synthase, a critical vasodilator. Endothelin 1, on the other hand, is a potent vasoconstrictor. It is upregulated while transforming growth factor b and plasminogen activator inhibitor 1 are upregulated, resulting in further vascular damage.26 The common mechanism for this vasculopathy appears to be superoxide production in the mitochondria, caused by excess glucose oxidation forcing coenzyme Q to donate electrons to oxygen, producing the superoxides. Superoxides in turn inhibit glyceraldehyde 3-phosphate dehydrogenase, which activates the polyol pathway, AGE formation, PKC, and the hexosamine pathway.26 In addition to coenzyme Q, several other enzymes generate reactive oxygen species, including nicotinamide adenine dinucleotide phosphate oxidase, aldehyde oxidase, xanthine oxidase, and glucose oxidase.27 These reactive oxygen species exacerbate oxidative stress, leading to further endothelial cell damage, and cause vascular smooth muscle injury.28
Further influencing the wound-healing environment are the effects of diabetes on blood vessel maintenance and repair as well as angiogenesis in response to local-tissue hypoxia. Vessel-repair mechanisms require endothelial progenitor cells (EPCs), which are released in response to cytokines and neural impulses.29 Bone marrow–derived EPCs have inadequate proliferative and migratory ability in patients with diabetes.28,30 In a diabetic mouse model, EPCs appear in the bone marrow at normal levels, but levels in circulation are lower than anticipated, because of poor proliferation and mobilization, it is thought. In terms of local-tissue hypoxia, hypoxia-inducible factor 1 (HIF-1) is an important transcription factor that promotes the expression of genes that in turn induce angiogenesis. The mechanism of this response is complex, and hyperglycemia has the potential to interfere in various steps of the cycle. In response to local-tissue hypoxia, the HIF-1a subunit must localize to the target site, where it combines with HIF-1b to create the active dimer, HIF-1.31 This active dimer is regulated through degradation of the a subunit in the presence of normal oxygen levels. However, in a state of hypoxia, the molecule is stabilized, promoting angiogenesis and fibroblast migration.32 Recent evidence suggests that hyperglycemia interferes with the dimerization process and that there is a failure of HIF-1a to locate into the nucleus, which is crucial for gene upregulation.31-33
Infection in Diabetes
Throughout the literature, the risk for infection after fracture is consistently higher in patients with diabetes than without diabetes. There likely are many contributing factors, including diminished blood flow and vasculopathy as well as a dampened immune response as a result of defective granulocytic, phagocytic, and chemotactic functions and defective macrophagic activity. Typically, polymorphonuclear leukocytes (PMNs) migrate to bacteria and initiate bacteriocidal activity, and then macrophages phagocytize PMNs and other damaged cells. PMNs demonstrate impaired function in patients with diabetes—reduced phagocytic response and respiratory burst as well as chemotaxis impairment. The diminished phagocytic potential is substantial, with experiments showing an almost 50% reduction in ingestion of Staphylococcus aureus in a patient with diabetes than in one without diabetes.34 Expression of surface integrins, which mediate PMN adhesion to the basement membrane of the tissue, appears to be negatively altered in both T1DM and T2DM, furthering diminishing the chemotactic response of PMNs.35 Impaired leukocyte function may also be a downstream effect of vasculopathy and associated hypoxia/hypoxemia as PMNs use superoxide radicals and other oxidizing agents to create a bacteriocidal environment that is negatively impacted in a low oxygen state.3 In addition, macrophages are disabled in patients with diabetes. (In rats with streptozotocin-induced diabetes, there is inadequate activation of macrophages in the early stages of healing.36) Furthermore, AGEs similar to those mentioned earlier have a significant negative impact on macrophagic function.37 Thus, both the activation and the activity of macrophages appear to be impeded in the setting of diabetes.
Potential New Treatment Modalities
There is tremendous potential for clinical intervention to prevent pathologic outcomes in patients with diabetes, given the complex tissue, cellular, and molecular interactions, particularly those caused by hyperglycemia. At the bone tissue level, increased osteoclastic activity in patients with diabetes has been associated with many complications, including Charcot arthropathy. RANKL modulates differentiation and activation of osteoclasts; thus, RANKL inhibition is a possible therapeutic target.38 Elevated AGE levels have also been observed in patients with Charcot arthropathy, and RAGE, the receptor for AGE, has been seen at lower than expected levels in patients with diabetes. RAGE appears to provide a protective effect against excessive bone resorption; therefore, treatment that increases RAGE levels—such as angiotensin-converting-enzyme inhibitors, statins, and glitazones—may be capable of mitigating the osteoclastic effects in Charcot arthropathy.39
AGE formation appears to be central to many pathologic processes in diabetes, so it is a logical therapeutic target, particularly for pathologic processes at the vascular tissue level. Aminoguanidine is an anti-AGE agent that was initially used to prevent diabetic retinopathy, but it has also been shown to prevent general vascular complications in diabetic animal models. The terminal amino residue in the compound specifically binds glucose-derived reactive intermediates and prevents cross-linking, which renders them inactive. Disrupting those cross-links is another treatment strategy. N-phenacylthiazolium bromide and 3-phenacyl-4,5-dimethylthiazolium chloride (ALT-711 or alagebrium) are compounds that have been shown to break cross-links in a diabetic rat model.16
Another tactic for reducing vascular pathology involves mitigating superoxide radicals, as these radicals are generated from the glycolytic intermediates in hyperglycemic states. It has been reasoned that, if the concentration of these intermediates can be decreased, there would be less substrate available for the pathways that lead to radical formation. One approach is to use transketolase, an enzyme that shunts intermediates to pathways that do not produce superoxide radicals. In the treatment of patients with diabetic retinopathy, early data appear promising with benfotiamine, a thiamine derivative, which upregulates transketolase 250%. An additional tactic involves catalytic antioxidants—namely, superoxide dismutase/catalase mimetic, which has been shown to reduce hyperglycemia-induced superoxides. These interventions are appealing because of their nonstoichiometric reactions, which render them potentially more potent antioxidants.26
Potential neurologic interventions include recombinant human nerve growth factor, neurotrophic factors, and gene therapy, all directed toward preventing or regenerating neuropathic tissues in patients with diabetes. Most of these interventions, however, remain theoretical. Few trials have demonstrated clinically significant improvement. In patients with T1DM, however, the absence of circulating C-peptide is thought to contribute to diabetic neuropathy. Results of trials with subcutaneous C-peptide treatment suggest improvement in both sural sensory and vibration perception after only 12 weeks.40 These novel treatments further emphasize the potential for intervention at the tissue, cellular, and molecular levels.
Conclusion
Whereas most fractures are uncomplicated in healthy patients, they can have devastating consequences in patients with diabetes. In this review, we have highlighted many of the pathologic processes that can influence outcomes of fractures in patients with diabetes. These problems will become more common as the population ages, age-related risks for osteoporosis and fragility fracture increase, and diabetes becomes nearly epidemic in our increasingly obese, sedentary society. Although some progress has been made, a more thorough intervention strategy is needed to improve both bone and soft-tissue outcomes of fractures in patients with diabetes.
1. Danaei G, Finucane MM, Lu Y, et al; Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose). National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378(9785):31-40.
2. Centers for Disease Control and Prevention. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2011.
3. Wukich DK, Joseph A, Ryan M, Ramirez C, Irrgang JJ. Outcomes of ankle fractures in patients with uncomplicated versus complicated diabetes. Foot Ankle Int. 2011;32(2):120-130.
4. Kumar V, Abbas AK, Fausto N, Robbins SL, Cotran RS. Pathologic Basis of Disease. 8th ed. Philadelphia, PA: Elsevier Saunders; 2010.
5. Diabetes basics. Centers for Disease Control and Prevention website. http://www.cdc.gov/diabetes/basics/index.html. Updated October 25, 2014. Accessed August 24, 2015.
6. Wukich DK, McMillen RL, Lowery NJ, Frykberg RG. Surgical site infections after foot and ankle surgery. Diabetes Care. 2001;34(10):2211-2213.
7. Jones KB, Maiers-Yelden KA, Marsh JL, et al. Ankle fractures in patients with diabetes mellitus. J Bone Joint Surg Br. 2005;87(4):489-495.
8. Yan W, Li X. Impact of diabetes and its treatments on skeletal diseases. Front Med. 2013;7(1):81-90.
9. Thrailkill K, Lumpkin C Jr, Bunn R, Kemp S, Fowlkes J. Is insulin an anabolic agent in bone? Dissecting the diabetic bone for clues. Am J Physiol Endocrinol Metab. 2005;289(5):E735-E745.
10. Kayal RA, Tsatsas D, Bauer MA, et al. Diminished bone formation during diabetic fracture healing is related to the premature resorption of cartilage associated with increased osteoclast activity. J Bone Miner Res. 2007;22(4):560-568.
11. Gooch HL, Hale JE, Fujioka H, Balian G, Hurwitz SR. Alterations of cartilage and collagen expression during fracture healing in experimental diabetes. Connect Tissue Res. 2000;41(2):81-91.
12. Kayal RA, Alblowi J, McKenzie E, et al. Diabetes causes the accelerated loss of cartilage during fracture repair which is reversed by insulin treatment. Bone. 2009;44(2):357-363.
13. Motyl K, Botolin S, Irwin R, et al. Bone inflammation and altered gene expression with type I diabetes early onset. J Cell Physiol. 2009;218(3):575-583.
14. Botolin S, McCabe LR. Chronic hyperglycemia modulates osteoblast gene expression through osmotic and non-osmotic pathways. J Cell Biochem. 2006;99(2):411-424.
15. Keats E, Khanz ZA. Unique responses of stem cell-derived vascular endothelial and mesenchymal cells to high levels of glucose. PLoS One. 2012;7(6):e38752.
16. Vlassara H, Palace MR. Diabetes and advanced glycation endproducts. J Intern Med. 2002;251(2):87-101.
17. Fong Y, Edelstein D, Wang E, Brownlee M. Inhibition of matrix-induced bone differentiation by advanced glycation end-products in rats. Diabetologia. 1993;36(9):802-807.
18. Alikhani M, Alikhani Z, Boyd C, et al. Advanced glycation endproducts stimulate osteoblast apoptosis via the MAP kinase and cytosolic apoptotic pathways. Bone. 2007;40(2):345-353.
19. Catalfamo DL, Calderon NL, Harden SW, Sorenson HL, Neiva KG, Wallet SM. Augmented LPS responsiveness in type 1 diabetes-derived osteoclasts. J Cell Physiol. 2013;228(2):349-361.
20. Kahn SE, Lachin JM, Zinman B, et al; ADOPT Study Group. Effects of rosiglitazone, glyburide, and metformin on β-cell function and insulin sensitivity in ADOPT. Diabetes. 2011;60(5):1552-1560.
21. Shibuya N, Humphers JM, Fluhman BL, Jupiter DC. Factors associated with nonunion, delayed union, and malunion in foot and ankle surgery in diabetic patients. J Foot Ankle Surg. 2013;52(2):207-211.
22. Shami SK, Chittenden SJ. Microangiopathy in diabetes mellitus: II. Features, complications and investigation. Diabetes Res. 1991;17(4):157-168.
23. Nishikawa T, Edelstein D, Du XL, et al. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycemic damage. Nature. 2000;404(6779):787-790.
24. Jeffcoate WJ. Theories concerning the pathogenesis of the acute Charcot foot suggest future therapy. Curr Diab Rep. 2005;5(6):430-435.
25. Lerner UH, Persson E. Osteotropic effects by the neuropeptides calcitonin gene-related peptide, substance P and vasoactive intestinal peptide. J Musculoskelet Neuronal Interact. 2008;8(2):154-165.
26. Brownlee M. The pathobiology of diabetic complications—a unifying mechanism. Diabetes. 2005;54(6):1615-1625.
27. Tsuji S, Taniuchi S, Hasui M, Yamamoto A, Kobayashi Y. Increased nitric oxide production by neutrophils from patients with chronic granulomatous disease on trimethoprim-sulfamethoxazole. Nitric Oxide. 2002;7(4):283-288.
28. Kolluru GK, Bir SC, Kevil CG. Endothelial dysfunction and diabetes: effects on angiogenesis, vascular remodeling, and wound healing. Int J Vasc Med. 2012;2012:918267.
29. Westerweel PE. Impaired endothelial progenitor cell mobilization and dysfunctional bone marrow stroma in diabetes mellitus. PLoS One. 2013;8(3):e60357.
30. Fadini GP, Avogaro A. It is all in the blood: the multifaceted contribution of circulating progenitor cells in diabetic complications. Exp Diabetes Res. 2012;2012:742976.
31. Gadad PC, Matthews KH, Knott RM. Role of HIF1α and PKCβ in mediating the effect of oxygen and glucose in a novel wound assay. Microvasc Res. 2013;88:61-69.
32. Botusan IR, Sunkari VG, Savu O, et al. Stabilization of HIF-1alpha is critical to improve wound healing in diabetic mice. Proc Natl Acad Sci U S A. 2008;105(49):19426-19431.
33. Catrina SB, Okamoto K, Pereira T, Brismar K, Poellinger L. Hyperglycemia regulates hypoxia-inducible factor-1alpha protein stability and function. Diabetes. 2004;53(12):3226-3232.
34. Marhoffer W, Stein M, Maeser E, Federlin K. Impairment of polymorphonuclear leukocyte function and metabolic control of diabetes. Diabetes Care. 1992;15(2):256-260.
35. Calmi G, Montana M, Citarella R, Porretto F, Catania A, Lo Presti R. Polymorphonuclear leukocyte integrin profile in diabetes mellitus. Clin Hemorheol Microcirc. 2002;27(2):83-89.
36. Miao M, Niu Y, Xie T, Yuan B, Qing C, Lu S. Diabetes-impaired wound healing and altered macrophage activation: a possible pathophysiologic correlation. Wound Repair Regen. 2012;20(2):203-213.
37. Liu BF, Miyata S, Kojima H, et al. Low phagocytic activity of resident peritoneal macrophages in diabetic mice: relevance to the formation of advanced glycation end products. Diabetes. 1999;48(10):2074-2082.
38. Mabilleau G, Petrova NL, Edmonds ME, Sabokbar A. Increased osteoclastic activity in acute Charcot’s osteoarthropathy: the role of receptor activator of nuclear factor-kappaB ligand. Diabetologia. 2008;51(6):1035-1040.
39. Witzke KA, Vinik AI, Grant LM, et al. Loss of RAGE defense: a cause of Charcot neuroarthropathy? Diabetes Care. 2011;34(7):1617-1621.
40. Pittenger G, Vinik A. Nerve growth factor and diabetic neuropathy. Exp Diabesity Res. 2003;4(4):271-285.
Diabetes mellitus (DM) affects a significant portion of the world’s people, and the problem is increasing in magnitude as the population ages and becomes more obese.1 An estimated 347 million people have diabetes.1 In the United States, 26 million (roughly 8% of the population) are affected, making DM a major health issue.2 Given the prevalence of diabetes in the general population, it is not surprising that increasing numbers of fracture patients have DM. Unfortunately, for these patients, many relatively simple fractures can have disastrous outcomes. Infections and wound complications occur in disproportionate numbers, healing time is delayed, and risk for nonunion or malunion is substantially higher.3
It is imperative to understand the pathophysiology of DM to appreciate potential interventions and strategies aimed at decreasing complications and improving outcomes of fractures in patients with the disease. In type 1 DM (T1DM), autoimmune destruction of the insulin-secreting β cells in the pancreas results in a complete absence of insulin. Patients with T1DM are dependent on exogenous insulin, and, despite hyperglycemia, most cells in the body are starved for energy. This leads to a catabolic condition, high lipid and protein metabolism, and, in many cases, ketoacidosis. When insulin resistance develops, the β cells are forced to secrete large amounts of insulin; when they fail to keep up, type 2 DM (T2DM) develops. T2DM is often associated with obesity, as excess adipose tissue leads to insulin resistance. Although exogenous insulin may be necessary to treat advanced T2DM, other medications are commonly used to effectively lower blood glucose: Secretagogues (eg, sulfonylureas) facilitate insulin release from β cells, and sensitizers (eg, metformin) increase insulin sensitivity.4,5
The potential morbidity of fractures in patients with DM can be appreciated with the example of ankle fractures. These typically uncomplicated fractures can have very poor outcomes in the setting of DM. In a prospective study of approximately 1500 patients with ankle fractures treated with open reduction and internal fixation, Wukich and colleagues6 found that 9.5% of patients with DM (vs 2.4% of patients without DM) developed surgical site infections. As defined by Jones and colleagues,7 major complications of treating ankle fractures in patients with DM include infection, malunion, nonunion, Charcot arthropathy, and amputation. The authors reported major complications in 31% and 17% of patients with and without DM, respectively. Highlighting the importance of glycemic control, Wukich and colleagues6 found relative risks of 3.8 for infection, 3.4 for noninfectious complications, and 5.0 for revision in complicated (vs uncomplicated) fractures in patients with DM.
Given the magnitude of problems in the treatment of fractures in patients with DM, we focus our review on the pathobiology of diabetes in terms of bone metabolism and fracture healing, wound healing and vasculopathy, infection, and potential new treatment modalities.
Bone Metabolism and Fracture Healing in Diabetes
Insulin appears to play a role in bone metabolism and fracture healing. Therefore, absence of insulin in T1DM and elevated insulin levels associated with T2DM likely influence these metabolic and fracture-healing processes. Insulin has been hypothesized to have an anabolic effect on bone, and in both human and animal models bone mineral density (BMD) is significantly lower in T1DM. Furthermore, BMD in T2DM has been shown to be normal or even elevated.8 Other metabolic effects of insulin on bone metabolism and growth include slower growth rates and lower BMD in pediatric patients with T1DM versus patients without diabetes, and some animal models show bone microarchitecture altered in the absence of insulin (and reversible with insulin supplementation).9 These factors seem to contradict the markedly elevated risk for osteoporotic fracture in patients with T2DM, but the mechanisms responsible for this have not been elucidated.8
In terms of fracture healing, resorption of cartilage during transition to hard callus appears to be influenced by diabetes. It has been hypothesized that the smaller callus observed in diabetic mice may be secondary to upregulation of osteoclasts. Initial callus size appears not to differ between mice with streptozotocin-induced diabetes, which exhibit a complete absence of insulin, and control mice, but levels of osteoclast and osteoclastogenesis mediators were significantly higher in the diabetic mice.10 Some investigators think that the reduction in cartilage callus size in diabetic mice is caused by altered mRNA expression and collagen production.11 Diabetic mice, in addition to showing increased resorption by osteoclasts, demonstrate increased chondrocyte apoptosis, which is thought to activate cartilage resorption events. Exogenous insulin effectively reverses this cartilage loss to baseline levels.12
Osteoblasts are a crucial component of the fracture-healing cascade, and acute and chronic hyperglycemia, the hallmark of diabetes, has a variety of effects on osteoblasts.13 Genes for cell-signal proteins such as osteocalcin, MMP-13, and vascular endothelial growth factor are downregulated in the presence of chronic hyperglycemia, whereas genes for alkaline phosphate are upregulated. Acute hyperglycemia by way of hyperosmolarity is associated with MMP-13 downregulation. Thus, osteoblasts appear to respond to hyperglycemia through 2 different processes: Hyperosmolarity, through osteoblast cell shrinkage, influences the acute response, and hyperglycemia itself, through pathways such as nonenzymatic glycosylation, protein kinase C (PKC) signaling, and the polyol pathway, is the force behind the chronic response.14 The lineage of osteoblasts from mesenchymal stem cells also can be affected by hyperglycemia, with lower growth rates for mesenchymal stem cells and preferential development toward the adipocyte lineage, while the osteoblast and chondrocyte lineages are downregulated.15
Increased osteoblast apoptosis has been associated with diabetes through advanced glycation end-products (AGEs), which modify the structure and function of bioactive compounds through AGE receptors that cross-link and bond to amino groups on bioactive molecules.16 It has been reported that AGEs interfere with osteoblast development and collagen and osteocalcin production.17 A common AGE, carboxymethyl lysine-modified collagen, has been associated with a significant increase in apoptosis through the mitogen-activated protein kinase (MAPK) pathway. Although most of the literature suggests that osteoblast apoptosis is activated by hypoxia, nitric oxide, or integrins, these factors all have the MAPK pathway in common.18
Osteoclasts are also influenced by diabetes. Recent work in T1DM demonstrated that osteoclasts are hyperactive and more sensitive to receptor activator of nuclear factor kB ligand (RANKL) compared with osteoclasts from the population without diabetes. It is also known that osteoclasts are under the control of immunologic mediators like lipopolysaccharide (LPS), a surface component of gram-negative bacteria, and various other proinflammatory cytokines. In patients with diabetes, osteoclasts react differently to LPS and other proinflammatory cytokines, at times with opposing effects, including secretion of RANKL to stimulate resorption by the osteoclast, and precursors preventing progression into osteoclasts. In healthy people, high LPS levels not only prevent precursors from producing more osteoclasts, but promote them to mature into immune-like cells that actually phagocytose bacteria. So, in a state of infection, precursors shift from bone-resorbing osteoclasts to protective immune cells. This phenomenon does not occur in patients with diabetes, in whom the osteoclasts instead resorb more bone and stimulate inflammation by releasing cytokines.19
Interestingly, osteoblasts and osteoclasts are also affected by medications commonly used to treat diabetes. Thiazolidinediones are a class of sensitizers often used to treat patients with T2DM. Thiazolidinediones, particularly rosiglitazone, have been associated with increased bone loss primarily caused by increased bone resorption by osteoclasts.20 In addition, some investigators think that thiazolidinediones induce osteocyte apoptosis, contributing to impaired bone growth.8 Metformin, an insulin sensitizer, appears to have a positive effect on bone growth and fracture risk by enhancing osteoblastogenesis and inhibiting osteoclastogenesis, leading to a protective effect on bone.8
Peripheral neuropathy, which is often associated with diabetes, appears to play a major role in fracture-healing complications, even more so than hyperglycemia does. A recent clinical paper found that patients with diabetic neuropathy had a 44% risk of foot and ankle fracture-healing complications.21 Regardless of the risk, the pathogenesis of diabetic neuropathy can be caused by several mechanisms. Neural tissue does not require insulin for glucose uptake; therefore, in a state of hyperglycemia, aldose reductase shunts glucose to sorbitol while using protective glutathione and generating reactive oxygen species. This oxidative stress results in nerve damage or neuropathy. Microangiopathy, which we discuss in more detail later, also contributes to the development of neuropathy, through compromised flow of blood to neural tissue.22 Another mechanism contributing to diabetic neuropathy involves PKC, which is activated by 1,2-diacylglycerol in the presence of glucose, leading to vascular changes that restrict the flow of blood to peripheral nerves.23 Finally, AGEs may also participate by altering nerve function after binding to neural tissue.
Charcot neuroarthropathy is a complication associated with diabetes, particularly after injury in which chronic inflammation results in damage to the joint through fracture, dislocation, and osteolytic bony destruction. The pathophysiology is attributed to repeated microtrauma caused by loss of protective sensibility and hyperemia caused by dysregulation.24 Sympathetic and sensory nerve fibers are associated with bone, but a few serve as mechanoreceptors and nociceptors, which can activate substance P, calcitonin gene-related peptide, and vasoactive intestinal peptide—neuropeptides all thought to be involved in the inflammatory process, and in the activation of osteoblasts and osteoclasts. In diabetic neuropathy, many of these neuropeptides show a reduced regulation response, which can lead to impaired fracture healing. In particular, osteoclast activity is upregulated, and consequently bone resorption is increased. In addition to the neuropeptides mentioned, RANKL is one mechanism by which this upregulation occurs.25
It is clear that bone metabolism and fracture healing are complex processes. In the patient with diabetes, many factors are affected, including BMD, bone microarchitecture and bone growth, cartilage resorption during callus formation, osteoblast and osteoclast activation through both altered responses to cell signals and pharmacologic interactions, and, finally, peripheral neuropathy. Given the complex interactions described, it is likely that these factors in combination, as well as those yet undiscovered, negatively affect fracture healing.
Wound Healing and Vasculopathy in Diabetes
Bone healing and soft-tissue healing depend on many of the same factors. Therefore, interactions between neuropathy and vasculopathy can have a tremendous influence on wound healing in patients with diabetes. The vascular pathology that occurs in diabetes depends in part on the fact that endothelial cells do not require insulin for glucose uptake and therefore are more susceptible to damage by hyperglycemia. As already discussed, shunting of glucose through the polyol pathway with the resultant oxidative stress is partly responsible for angiopathy in diabetes.
Also as already discussed, AGEs affect intracellular processes by protein binding and gene regulation and by disrupting the communication between cells and the surrounding matrix. From an extracellular standpoint, AGEs bind to circulating proteins, promoting inflammation and upregulation/downregulation of growth factors, including endothelial nitric oxide synthase, a critical vasodilator. Endothelin 1, on the other hand, is a potent vasoconstrictor. It is upregulated while transforming growth factor b and plasminogen activator inhibitor 1 are upregulated, resulting in further vascular damage.26 The common mechanism for this vasculopathy appears to be superoxide production in the mitochondria, caused by excess glucose oxidation forcing coenzyme Q to donate electrons to oxygen, producing the superoxides. Superoxides in turn inhibit glyceraldehyde 3-phosphate dehydrogenase, which activates the polyol pathway, AGE formation, PKC, and the hexosamine pathway.26 In addition to coenzyme Q, several other enzymes generate reactive oxygen species, including nicotinamide adenine dinucleotide phosphate oxidase, aldehyde oxidase, xanthine oxidase, and glucose oxidase.27 These reactive oxygen species exacerbate oxidative stress, leading to further endothelial cell damage, and cause vascular smooth muscle injury.28
Further influencing the wound-healing environment are the effects of diabetes on blood vessel maintenance and repair as well as angiogenesis in response to local-tissue hypoxia. Vessel-repair mechanisms require endothelial progenitor cells (EPCs), which are released in response to cytokines and neural impulses.29 Bone marrow–derived EPCs have inadequate proliferative and migratory ability in patients with diabetes.28,30 In a diabetic mouse model, EPCs appear in the bone marrow at normal levels, but levels in circulation are lower than anticipated, because of poor proliferation and mobilization, it is thought. In terms of local-tissue hypoxia, hypoxia-inducible factor 1 (HIF-1) is an important transcription factor that promotes the expression of genes that in turn induce angiogenesis. The mechanism of this response is complex, and hyperglycemia has the potential to interfere in various steps of the cycle. In response to local-tissue hypoxia, the HIF-1a subunit must localize to the target site, where it combines with HIF-1b to create the active dimer, HIF-1.31 This active dimer is regulated through degradation of the a subunit in the presence of normal oxygen levels. However, in a state of hypoxia, the molecule is stabilized, promoting angiogenesis and fibroblast migration.32 Recent evidence suggests that hyperglycemia interferes with the dimerization process and that there is a failure of HIF-1a to locate into the nucleus, which is crucial for gene upregulation.31-33
Infection in Diabetes
Throughout the literature, the risk for infection after fracture is consistently higher in patients with diabetes than without diabetes. There likely are many contributing factors, including diminished blood flow and vasculopathy as well as a dampened immune response as a result of defective granulocytic, phagocytic, and chemotactic functions and defective macrophagic activity. Typically, polymorphonuclear leukocytes (PMNs) migrate to bacteria and initiate bacteriocidal activity, and then macrophages phagocytize PMNs and other damaged cells. PMNs demonstrate impaired function in patients with diabetes—reduced phagocytic response and respiratory burst as well as chemotaxis impairment. The diminished phagocytic potential is substantial, with experiments showing an almost 50% reduction in ingestion of Staphylococcus aureus in a patient with diabetes than in one without diabetes.34 Expression of surface integrins, which mediate PMN adhesion to the basement membrane of the tissue, appears to be negatively altered in both T1DM and T2DM, furthering diminishing the chemotactic response of PMNs.35 Impaired leukocyte function may also be a downstream effect of vasculopathy and associated hypoxia/hypoxemia as PMNs use superoxide radicals and other oxidizing agents to create a bacteriocidal environment that is negatively impacted in a low oxygen state.3 In addition, macrophages are disabled in patients with diabetes. (In rats with streptozotocin-induced diabetes, there is inadequate activation of macrophages in the early stages of healing.36) Furthermore, AGEs similar to those mentioned earlier have a significant negative impact on macrophagic function.37 Thus, both the activation and the activity of macrophages appear to be impeded in the setting of diabetes.
Potential New Treatment Modalities
There is tremendous potential for clinical intervention to prevent pathologic outcomes in patients with diabetes, given the complex tissue, cellular, and molecular interactions, particularly those caused by hyperglycemia. At the bone tissue level, increased osteoclastic activity in patients with diabetes has been associated with many complications, including Charcot arthropathy. RANKL modulates differentiation and activation of osteoclasts; thus, RANKL inhibition is a possible therapeutic target.38 Elevated AGE levels have also been observed in patients with Charcot arthropathy, and RAGE, the receptor for AGE, has been seen at lower than expected levels in patients with diabetes. RAGE appears to provide a protective effect against excessive bone resorption; therefore, treatment that increases RAGE levels—such as angiotensin-converting-enzyme inhibitors, statins, and glitazones—may be capable of mitigating the osteoclastic effects in Charcot arthropathy.39
AGE formation appears to be central to many pathologic processes in diabetes, so it is a logical therapeutic target, particularly for pathologic processes at the vascular tissue level. Aminoguanidine is an anti-AGE agent that was initially used to prevent diabetic retinopathy, but it has also been shown to prevent general vascular complications in diabetic animal models. The terminal amino residue in the compound specifically binds glucose-derived reactive intermediates and prevents cross-linking, which renders them inactive. Disrupting those cross-links is another treatment strategy. N-phenacylthiazolium bromide and 3-phenacyl-4,5-dimethylthiazolium chloride (ALT-711 or alagebrium) are compounds that have been shown to break cross-links in a diabetic rat model.16
Another tactic for reducing vascular pathology involves mitigating superoxide radicals, as these radicals are generated from the glycolytic intermediates in hyperglycemic states. It has been reasoned that, if the concentration of these intermediates can be decreased, there would be less substrate available for the pathways that lead to radical formation. One approach is to use transketolase, an enzyme that shunts intermediates to pathways that do not produce superoxide radicals. In the treatment of patients with diabetic retinopathy, early data appear promising with benfotiamine, a thiamine derivative, which upregulates transketolase 250%. An additional tactic involves catalytic antioxidants—namely, superoxide dismutase/catalase mimetic, which has been shown to reduce hyperglycemia-induced superoxides. These interventions are appealing because of their nonstoichiometric reactions, which render them potentially more potent antioxidants.26
Potential neurologic interventions include recombinant human nerve growth factor, neurotrophic factors, and gene therapy, all directed toward preventing or regenerating neuropathic tissues in patients with diabetes. Most of these interventions, however, remain theoretical. Few trials have demonstrated clinically significant improvement. In patients with T1DM, however, the absence of circulating C-peptide is thought to contribute to diabetic neuropathy. Results of trials with subcutaneous C-peptide treatment suggest improvement in both sural sensory and vibration perception after only 12 weeks.40 These novel treatments further emphasize the potential for intervention at the tissue, cellular, and molecular levels.
Conclusion
Whereas most fractures are uncomplicated in healthy patients, they can have devastating consequences in patients with diabetes. In this review, we have highlighted many of the pathologic processes that can influence outcomes of fractures in patients with diabetes. These problems will become more common as the population ages, age-related risks for osteoporosis and fragility fracture increase, and diabetes becomes nearly epidemic in our increasingly obese, sedentary society. Although some progress has been made, a more thorough intervention strategy is needed to improve both bone and soft-tissue outcomes of fractures in patients with diabetes.
Diabetes mellitus (DM) affects a significant portion of the world’s people, and the problem is increasing in magnitude as the population ages and becomes more obese.1 An estimated 347 million people have diabetes.1 In the United States, 26 million (roughly 8% of the population) are affected, making DM a major health issue.2 Given the prevalence of diabetes in the general population, it is not surprising that increasing numbers of fracture patients have DM. Unfortunately, for these patients, many relatively simple fractures can have disastrous outcomes. Infections and wound complications occur in disproportionate numbers, healing time is delayed, and risk for nonunion or malunion is substantially higher.3
It is imperative to understand the pathophysiology of DM to appreciate potential interventions and strategies aimed at decreasing complications and improving outcomes of fractures in patients with the disease. In type 1 DM (T1DM), autoimmune destruction of the insulin-secreting β cells in the pancreas results in a complete absence of insulin. Patients with T1DM are dependent on exogenous insulin, and, despite hyperglycemia, most cells in the body are starved for energy. This leads to a catabolic condition, high lipid and protein metabolism, and, in many cases, ketoacidosis. When insulin resistance develops, the β cells are forced to secrete large amounts of insulin; when they fail to keep up, type 2 DM (T2DM) develops. T2DM is often associated with obesity, as excess adipose tissue leads to insulin resistance. Although exogenous insulin may be necessary to treat advanced T2DM, other medications are commonly used to effectively lower blood glucose: Secretagogues (eg, sulfonylureas) facilitate insulin release from β cells, and sensitizers (eg, metformin) increase insulin sensitivity.4,5
The potential morbidity of fractures in patients with DM can be appreciated with the example of ankle fractures. These typically uncomplicated fractures can have very poor outcomes in the setting of DM. In a prospective study of approximately 1500 patients with ankle fractures treated with open reduction and internal fixation, Wukich and colleagues6 found that 9.5% of patients with DM (vs 2.4% of patients without DM) developed surgical site infections. As defined by Jones and colleagues,7 major complications of treating ankle fractures in patients with DM include infection, malunion, nonunion, Charcot arthropathy, and amputation. The authors reported major complications in 31% and 17% of patients with and without DM, respectively. Highlighting the importance of glycemic control, Wukich and colleagues6 found relative risks of 3.8 for infection, 3.4 for noninfectious complications, and 5.0 for revision in complicated (vs uncomplicated) fractures in patients with DM.
Given the magnitude of problems in the treatment of fractures in patients with DM, we focus our review on the pathobiology of diabetes in terms of bone metabolism and fracture healing, wound healing and vasculopathy, infection, and potential new treatment modalities.
Bone Metabolism and Fracture Healing in Diabetes
Insulin appears to play a role in bone metabolism and fracture healing. Therefore, absence of insulin in T1DM and elevated insulin levels associated with T2DM likely influence these metabolic and fracture-healing processes. Insulin has been hypothesized to have an anabolic effect on bone, and in both human and animal models bone mineral density (BMD) is significantly lower in T1DM. Furthermore, BMD in T2DM has been shown to be normal or even elevated.8 Other metabolic effects of insulin on bone metabolism and growth include slower growth rates and lower BMD in pediatric patients with T1DM versus patients without diabetes, and some animal models show bone microarchitecture altered in the absence of insulin (and reversible with insulin supplementation).9 These factors seem to contradict the markedly elevated risk for osteoporotic fracture in patients with T2DM, but the mechanisms responsible for this have not been elucidated.8
In terms of fracture healing, resorption of cartilage during transition to hard callus appears to be influenced by diabetes. It has been hypothesized that the smaller callus observed in diabetic mice may be secondary to upregulation of osteoclasts. Initial callus size appears not to differ between mice with streptozotocin-induced diabetes, which exhibit a complete absence of insulin, and control mice, but levels of osteoclast and osteoclastogenesis mediators were significantly higher in the diabetic mice.10 Some investigators think that the reduction in cartilage callus size in diabetic mice is caused by altered mRNA expression and collagen production.11 Diabetic mice, in addition to showing increased resorption by osteoclasts, demonstrate increased chondrocyte apoptosis, which is thought to activate cartilage resorption events. Exogenous insulin effectively reverses this cartilage loss to baseline levels.12
Osteoblasts are a crucial component of the fracture-healing cascade, and acute and chronic hyperglycemia, the hallmark of diabetes, has a variety of effects on osteoblasts.13 Genes for cell-signal proteins such as osteocalcin, MMP-13, and vascular endothelial growth factor are downregulated in the presence of chronic hyperglycemia, whereas genes for alkaline phosphate are upregulated. Acute hyperglycemia by way of hyperosmolarity is associated with MMP-13 downregulation. Thus, osteoblasts appear to respond to hyperglycemia through 2 different processes: Hyperosmolarity, through osteoblast cell shrinkage, influences the acute response, and hyperglycemia itself, through pathways such as nonenzymatic glycosylation, protein kinase C (PKC) signaling, and the polyol pathway, is the force behind the chronic response.14 The lineage of osteoblasts from mesenchymal stem cells also can be affected by hyperglycemia, with lower growth rates for mesenchymal stem cells and preferential development toward the adipocyte lineage, while the osteoblast and chondrocyte lineages are downregulated.15
Increased osteoblast apoptosis has been associated with diabetes through advanced glycation end-products (AGEs), which modify the structure and function of bioactive compounds through AGE receptors that cross-link and bond to amino groups on bioactive molecules.16 It has been reported that AGEs interfere with osteoblast development and collagen and osteocalcin production.17 A common AGE, carboxymethyl lysine-modified collagen, has been associated with a significant increase in apoptosis through the mitogen-activated protein kinase (MAPK) pathway. Although most of the literature suggests that osteoblast apoptosis is activated by hypoxia, nitric oxide, or integrins, these factors all have the MAPK pathway in common.18
Osteoclasts are also influenced by diabetes. Recent work in T1DM demonstrated that osteoclasts are hyperactive and more sensitive to receptor activator of nuclear factor kB ligand (RANKL) compared with osteoclasts from the population without diabetes. It is also known that osteoclasts are under the control of immunologic mediators like lipopolysaccharide (LPS), a surface component of gram-negative bacteria, and various other proinflammatory cytokines. In patients with diabetes, osteoclasts react differently to LPS and other proinflammatory cytokines, at times with opposing effects, including secretion of RANKL to stimulate resorption by the osteoclast, and precursors preventing progression into osteoclasts. In healthy people, high LPS levels not only prevent precursors from producing more osteoclasts, but promote them to mature into immune-like cells that actually phagocytose bacteria. So, in a state of infection, precursors shift from bone-resorbing osteoclasts to protective immune cells. This phenomenon does not occur in patients with diabetes, in whom the osteoclasts instead resorb more bone and stimulate inflammation by releasing cytokines.19
Interestingly, osteoblasts and osteoclasts are also affected by medications commonly used to treat diabetes. Thiazolidinediones are a class of sensitizers often used to treat patients with T2DM. Thiazolidinediones, particularly rosiglitazone, have been associated with increased bone loss primarily caused by increased bone resorption by osteoclasts.20 In addition, some investigators think that thiazolidinediones induce osteocyte apoptosis, contributing to impaired bone growth.8 Metformin, an insulin sensitizer, appears to have a positive effect on bone growth and fracture risk by enhancing osteoblastogenesis and inhibiting osteoclastogenesis, leading to a protective effect on bone.8
Peripheral neuropathy, which is often associated with diabetes, appears to play a major role in fracture-healing complications, even more so than hyperglycemia does. A recent clinical paper found that patients with diabetic neuropathy had a 44% risk of foot and ankle fracture-healing complications.21 Regardless of the risk, the pathogenesis of diabetic neuropathy can be caused by several mechanisms. Neural tissue does not require insulin for glucose uptake; therefore, in a state of hyperglycemia, aldose reductase shunts glucose to sorbitol while using protective glutathione and generating reactive oxygen species. This oxidative stress results in nerve damage or neuropathy. Microangiopathy, which we discuss in more detail later, also contributes to the development of neuropathy, through compromised flow of blood to neural tissue.22 Another mechanism contributing to diabetic neuropathy involves PKC, which is activated by 1,2-diacylglycerol in the presence of glucose, leading to vascular changes that restrict the flow of blood to peripheral nerves.23 Finally, AGEs may also participate by altering nerve function after binding to neural tissue.
Charcot neuroarthropathy is a complication associated with diabetes, particularly after injury in which chronic inflammation results in damage to the joint through fracture, dislocation, and osteolytic bony destruction. The pathophysiology is attributed to repeated microtrauma caused by loss of protective sensibility and hyperemia caused by dysregulation.24 Sympathetic and sensory nerve fibers are associated with bone, but a few serve as mechanoreceptors and nociceptors, which can activate substance P, calcitonin gene-related peptide, and vasoactive intestinal peptide—neuropeptides all thought to be involved in the inflammatory process, and in the activation of osteoblasts and osteoclasts. In diabetic neuropathy, many of these neuropeptides show a reduced regulation response, which can lead to impaired fracture healing. In particular, osteoclast activity is upregulated, and consequently bone resorption is increased. In addition to the neuropeptides mentioned, RANKL is one mechanism by which this upregulation occurs.25
It is clear that bone metabolism and fracture healing are complex processes. In the patient with diabetes, many factors are affected, including BMD, bone microarchitecture and bone growth, cartilage resorption during callus formation, osteoblast and osteoclast activation through both altered responses to cell signals and pharmacologic interactions, and, finally, peripheral neuropathy. Given the complex interactions described, it is likely that these factors in combination, as well as those yet undiscovered, negatively affect fracture healing.
Wound Healing and Vasculopathy in Diabetes
Bone healing and soft-tissue healing depend on many of the same factors. Therefore, interactions between neuropathy and vasculopathy can have a tremendous influence on wound healing in patients with diabetes. The vascular pathology that occurs in diabetes depends in part on the fact that endothelial cells do not require insulin for glucose uptake and therefore are more susceptible to damage by hyperglycemia. As already discussed, shunting of glucose through the polyol pathway with the resultant oxidative stress is partly responsible for angiopathy in diabetes.
Also as already discussed, AGEs affect intracellular processes by protein binding and gene regulation and by disrupting the communication between cells and the surrounding matrix. From an extracellular standpoint, AGEs bind to circulating proteins, promoting inflammation and upregulation/downregulation of growth factors, including endothelial nitric oxide synthase, a critical vasodilator. Endothelin 1, on the other hand, is a potent vasoconstrictor. It is upregulated while transforming growth factor b and plasminogen activator inhibitor 1 are upregulated, resulting in further vascular damage.26 The common mechanism for this vasculopathy appears to be superoxide production in the mitochondria, caused by excess glucose oxidation forcing coenzyme Q to donate electrons to oxygen, producing the superoxides. Superoxides in turn inhibit glyceraldehyde 3-phosphate dehydrogenase, which activates the polyol pathway, AGE formation, PKC, and the hexosamine pathway.26 In addition to coenzyme Q, several other enzymes generate reactive oxygen species, including nicotinamide adenine dinucleotide phosphate oxidase, aldehyde oxidase, xanthine oxidase, and glucose oxidase.27 These reactive oxygen species exacerbate oxidative stress, leading to further endothelial cell damage, and cause vascular smooth muscle injury.28
Further influencing the wound-healing environment are the effects of diabetes on blood vessel maintenance and repair as well as angiogenesis in response to local-tissue hypoxia. Vessel-repair mechanisms require endothelial progenitor cells (EPCs), which are released in response to cytokines and neural impulses.29 Bone marrow–derived EPCs have inadequate proliferative and migratory ability in patients with diabetes.28,30 In a diabetic mouse model, EPCs appear in the bone marrow at normal levels, but levels in circulation are lower than anticipated, because of poor proliferation and mobilization, it is thought. In terms of local-tissue hypoxia, hypoxia-inducible factor 1 (HIF-1) is an important transcription factor that promotes the expression of genes that in turn induce angiogenesis. The mechanism of this response is complex, and hyperglycemia has the potential to interfere in various steps of the cycle. In response to local-tissue hypoxia, the HIF-1a subunit must localize to the target site, where it combines with HIF-1b to create the active dimer, HIF-1.31 This active dimer is regulated through degradation of the a subunit in the presence of normal oxygen levels. However, in a state of hypoxia, the molecule is stabilized, promoting angiogenesis and fibroblast migration.32 Recent evidence suggests that hyperglycemia interferes with the dimerization process and that there is a failure of HIF-1a to locate into the nucleus, which is crucial for gene upregulation.31-33
Infection in Diabetes
Throughout the literature, the risk for infection after fracture is consistently higher in patients with diabetes than without diabetes. There likely are many contributing factors, including diminished blood flow and vasculopathy as well as a dampened immune response as a result of defective granulocytic, phagocytic, and chemotactic functions and defective macrophagic activity. Typically, polymorphonuclear leukocytes (PMNs) migrate to bacteria and initiate bacteriocidal activity, and then macrophages phagocytize PMNs and other damaged cells. PMNs demonstrate impaired function in patients with diabetes—reduced phagocytic response and respiratory burst as well as chemotaxis impairment. The diminished phagocytic potential is substantial, with experiments showing an almost 50% reduction in ingestion of Staphylococcus aureus in a patient with diabetes than in one without diabetes.34 Expression of surface integrins, which mediate PMN adhesion to the basement membrane of the tissue, appears to be negatively altered in both T1DM and T2DM, furthering diminishing the chemotactic response of PMNs.35 Impaired leukocyte function may also be a downstream effect of vasculopathy and associated hypoxia/hypoxemia as PMNs use superoxide radicals and other oxidizing agents to create a bacteriocidal environment that is negatively impacted in a low oxygen state.3 In addition, macrophages are disabled in patients with diabetes. (In rats with streptozotocin-induced diabetes, there is inadequate activation of macrophages in the early stages of healing.36) Furthermore, AGEs similar to those mentioned earlier have a significant negative impact on macrophagic function.37 Thus, both the activation and the activity of macrophages appear to be impeded in the setting of diabetes.
Potential New Treatment Modalities
There is tremendous potential for clinical intervention to prevent pathologic outcomes in patients with diabetes, given the complex tissue, cellular, and molecular interactions, particularly those caused by hyperglycemia. At the bone tissue level, increased osteoclastic activity in patients with diabetes has been associated with many complications, including Charcot arthropathy. RANKL modulates differentiation and activation of osteoclasts; thus, RANKL inhibition is a possible therapeutic target.38 Elevated AGE levels have also been observed in patients with Charcot arthropathy, and RAGE, the receptor for AGE, has been seen at lower than expected levels in patients with diabetes. RAGE appears to provide a protective effect against excessive bone resorption; therefore, treatment that increases RAGE levels—such as angiotensin-converting-enzyme inhibitors, statins, and glitazones—may be capable of mitigating the osteoclastic effects in Charcot arthropathy.39
AGE formation appears to be central to many pathologic processes in diabetes, so it is a logical therapeutic target, particularly for pathologic processes at the vascular tissue level. Aminoguanidine is an anti-AGE agent that was initially used to prevent diabetic retinopathy, but it has also been shown to prevent general vascular complications in diabetic animal models. The terminal amino residue in the compound specifically binds glucose-derived reactive intermediates and prevents cross-linking, which renders them inactive. Disrupting those cross-links is another treatment strategy. N-phenacylthiazolium bromide and 3-phenacyl-4,5-dimethylthiazolium chloride (ALT-711 or alagebrium) are compounds that have been shown to break cross-links in a diabetic rat model.16
Another tactic for reducing vascular pathology involves mitigating superoxide radicals, as these radicals are generated from the glycolytic intermediates in hyperglycemic states. It has been reasoned that, if the concentration of these intermediates can be decreased, there would be less substrate available for the pathways that lead to radical formation. One approach is to use transketolase, an enzyme that shunts intermediates to pathways that do not produce superoxide radicals. In the treatment of patients with diabetic retinopathy, early data appear promising with benfotiamine, a thiamine derivative, which upregulates transketolase 250%. An additional tactic involves catalytic antioxidants—namely, superoxide dismutase/catalase mimetic, which has been shown to reduce hyperglycemia-induced superoxides. These interventions are appealing because of their nonstoichiometric reactions, which render them potentially more potent antioxidants.26
Potential neurologic interventions include recombinant human nerve growth factor, neurotrophic factors, and gene therapy, all directed toward preventing or regenerating neuropathic tissues in patients with diabetes. Most of these interventions, however, remain theoretical. Few trials have demonstrated clinically significant improvement. In patients with T1DM, however, the absence of circulating C-peptide is thought to contribute to diabetic neuropathy. Results of trials with subcutaneous C-peptide treatment suggest improvement in both sural sensory and vibration perception after only 12 weeks.40 These novel treatments further emphasize the potential for intervention at the tissue, cellular, and molecular levels.
Conclusion
Whereas most fractures are uncomplicated in healthy patients, they can have devastating consequences in patients with diabetes. In this review, we have highlighted many of the pathologic processes that can influence outcomes of fractures in patients with diabetes. These problems will become more common as the population ages, age-related risks for osteoporosis and fragility fracture increase, and diabetes becomes nearly epidemic in our increasingly obese, sedentary society. Although some progress has been made, a more thorough intervention strategy is needed to improve both bone and soft-tissue outcomes of fractures in patients with diabetes.
1. Danaei G, Finucane MM, Lu Y, et al; Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose). National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378(9785):31-40.
2. Centers for Disease Control and Prevention. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2011.
3. Wukich DK, Joseph A, Ryan M, Ramirez C, Irrgang JJ. Outcomes of ankle fractures in patients with uncomplicated versus complicated diabetes. Foot Ankle Int. 2011;32(2):120-130.
4. Kumar V, Abbas AK, Fausto N, Robbins SL, Cotran RS. Pathologic Basis of Disease. 8th ed. Philadelphia, PA: Elsevier Saunders; 2010.
5. Diabetes basics. Centers for Disease Control and Prevention website. http://www.cdc.gov/diabetes/basics/index.html. Updated October 25, 2014. Accessed August 24, 2015.
6. Wukich DK, McMillen RL, Lowery NJ, Frykberg RG. Surgical site infections after foot and ankle surgery. Diabetes Care. 2001;34(10):2211-2213.
7. Jones KB, Maiers-Yelden KA, Marsh JL, et al. Ankle fractures in patients with diabetes mellitus. J Bone Joint Surg Br. 2005;87(4):489-495.
8. Yan W, Li X. Impact of diabetes and its treatments on skeletal diseases. Front Med. 2013;7(1):81-90.
9. Thrailkill K, Lumpkin C Jr, Bunn R, Kemp S, Fowlkes J. Is insulin an anabolic agent in bone? Dissecting the diabetic bone for clues. Am J Physiol Endocrinol Metab. 2005;289(5):E735-E745.
10. Kayal RA, Tsatsas D, Bauer MA, et al. Diminished bone formation during diabetic fracture healing is related to the premature resorption of cartilage associated with increased osteoclast activity. J Bone Miner Res. 2007;22(4):560-568.
11. Gooch HL, Hale JE, Fujioka H, Balian G, Hurwitz SR. Alterations of cartilage and collagen expression during fracture healing in experimental diabetes. Connect Tissue Res. 2000;41(2):81-91.
12. Kayal RA, Alblowi J, McKenzie E, et al. Diabetes causes the accelerated loss of cartilage during fracture repair which is reversed by insulin treatment. Bone. 2009;44(2):357-363.
13. Motyl K, Botolin S, Irwin R, et al. Bone inflammation and altered gene expression with type I diabetes early onset. J Cell Physiol. 2009;218(3):575-583.
14. Botolin S, McCabe LR. Chronic hyperglycemia modulates osteoblast gene expression through osmotic and non-osmotic pathways. J Cell Biochem. 2006;99(2):411-424.
15. Keats E, Khanz ZA. Unique responses of stem cell-derived vascular endothelial and mesenchymal cells to high levels of glucose. PLoS One. 2012;7(6):e38752.
16. Vlassara H, Palace MR. Diabetes and advanced glycation endproducts. J Intern Med. 2002;251(2):87-101.
17. Fong Y, Edelstein D, Wang E, Brownlee M. Inhibition of matrix-induced bone differentiation by advanced glycation end-products in rats. Diabetologia. 1993;36(9):802-807.
18. Alikhani M, Alikhani Z, Boyd C, et al. Advanced glycation endproducts stimulate osteoblast apoptosis via the MAP kinase and cytosolic apoptotic pathways. Bone. 2007;40(2):345-353.
19. Catalfamo DL, Calderon NL, Harden SW, Sorenson HL, Neiva KG, Wallet SM. Augmented LPS responsiveness in type 1 diabetes-derived osteoclasts. J Cell Physiol. 2013;228(2):349-361.
20. Kahn SE, Lachin JM, Zinman B, et al; ADOPT Study Group. Effects of rosiglitazone, glyburide, and metformin on β-cell function and insulin sensitivity in ADOPT. Diabetes. 2011;60(5):1552-1560.
21. Shibuya N, Humphers JM, Fluhman BL, Jupiter DC. Factors associated with nonunion, delayed union, and malunion in foot and ankle surgery in diabetic patients. J Foot Ankle Surg. 2013;52(2):207-211.
22. Shami SK, Chittenden SJ. Microangiopathy in diabetes mellitus: II. Features, complications and investigation. Diabetes Res. 1991;17(4):157-168.
23. Nishikawa T, Edelstein D, Du XL, et al. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycemic damage. Nature. 2000;404(6779):787-790.
24. Jeffcoate WJ. Theories concerning the pathogenesis of the acute Charcot foot suggest future therapy. Curr Diab Rep. 2005;5(6):430-435.
25. Lerner UH, Persson E. Osteotropic effects by the neuropeptides calcitonin gene-related peptide, substance P and vasoactive intestinal peptide. J Musculoskelet Neuronal Interact. 2008;8(2):154-165.
26. Brownlee M. The pathobiology of diabetic complications—a unifying mechanism. Diabetes. 2005;54(6):1615-1625.
27. Tsuji S, Taniuchi S, Hasui M, Yamamoto A, Kobayashi Y. Increased nitric oxide production by neutrophils from patients with chronic granulomatous disease on trimethoprim-sulfamethoxazole. Nitric Oxide. 2002;7(4):283-288.
28. Kolluru GK, Bir SC, Kevil CG. Endothelial dysfunction and diabetes: effects on angiogenesis, vascular remodeling, and wound healing. Int J Vasc Med. 2012;2012:918267.
29. Westerweel PE. Impaired endothelial progenitor cell mobilization and dysfunctional bone marrow stroma in diabetes mellitus. PLoS One. 2013;8(3):e60357.
30. Fadini GP, Avogaro A. It is all in the blood: the multifaceted contribution of circulating progenitor cells in diabetic complications. Exp Diabetes Res. 2012;2012:742976.
31. Gadad PC, Matthews KH, Knott RM. Role of HIF1α and PKCβ in mediating the effect of oxygen and glucose in a novel wound assay. Microvasc Res. 2013;88:61-69.
32. Botusan IR, Sunkari VG, Savu O, et al. Stabilization of HIF-1alpha is critical to improve wound healing in diabetic mice. Proc Natl Acad Sci U S A. 2008;105(49):19426-19431.
33. Catrina SB, Okamoto K, Pereira T, Brismar K, Poellinger L. Hyperglycemia regulates hypoxia-inducible factor-1alpha protein stability and function. Diabetes. 2004;53(12):3226-3232.
34. Marhoffer W, Stein M, Maeser E, Federlin K. Impairment of polymorphonuclear leukocyte function and metabolic control of diabetes. Diabetes Care. 1992;15(2):256-260.
35. Calmi G, Montana M, Citarella R, Porretto F, Catania A, Lo Presti R. Polymorphonuclear leukocyte integrin profile in diabetes mellitus. Clin Hemorheol Microcirc. 2002;27(2):83-89.
36. Miao M, Niu Y, Xie T, Yuan B, Qing C, Lu S. Diabetes-impaired wound healing and altered macrophage activation: a possible pathophysiologic correlation. Wound Repair Regen. 2012;20(2):203-213.
37. Liu BF, Miyata S, Kojima H, et al. Low phagocytic activity of resident peritoneal macrophages in diabetic mice: relevance to the formation of advanced glycation end products. Diabetes. 1999;48(10):2074-2082.
38. Mabilleau G, Petrova NL, Edmonds ME, Sabokbar A. Increased osteoclastic activity in acute Charcot’s osteoarthropathy: the role of receptor activator of nuclear factor-kappaB ligand. Diabetologia. 2008;51(6):1035-1040.
39. Witzke KA, Vinik AI, Grant LM, et al. Loss of RAGE defense: a cause of Charcot neuroarthropathy? Diabetes Care. 2011;34(7):1617-1621.
40. Pittenger G, Vinik A. Nerve growth factor and diabetic neuropathy. Exp Diabesity Res. 2003;4(4):271-285.
1. Danaei G, Finucane MM, Lu Y, et al; Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose). National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378(9785):31-40.
2. Centers for Disease Control and Prevention. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2011.
3. Wukich DK, Joseph A, Ryan M, Ramirez C, Irrgang JJ. Outcomes of ankle fractures in patients with uncomplicated versus complicated diabetes. Foot Ankle Int. 2011;32(2):120-130.
4. Kumar V, Abbas AK, Fausto N, Robbins SL, Cotran RS. Pathologic Basis of Disease. 8th ed. Philadelphia, PA: Elsevier Saunders; 2010.
5. Diabetes basics. Centers for Disease Control and Prevention website. http://www.cdc.gov/diabetes/basics/index.html. Updated October 25, 2014. Accessed August 24, 2015.
6. Wukich DK, McMillen RL, Lowery NJ, Frykberg RG. Surgical site infections after foot and ankle surgery. Diabetes Care. 2001;34(10):2211-2213.
7. Jones KB, Maiers-Yelden KA, Marsh JL, et al. Ankle fractures in patients with diabetes mellitus. J Bone Joint Surg Br. 2005;87(4):489-495.
8. Yan W, Li X. Impact of diabetes and its treatments on skeletal diseases. Front Med. 2013;7(1):81-90.
9. Thrailkill K, Lumpkin C Jr, Bunn R, Kemp S, Fowlkes J. Is insulin an anabolic agent in bone? Dissecting the diabetic bone for clues. Am J Physiol Endocrinol Metab. 2005;289(5):E735-E745.
10. Kayal RA, Tsatsas D, Bauer MA, et al. Diminished bone formation during diabetic fracture healing is related to the premature resorption of cartilage associated with increased osteoclast activity. J Bone Miner Res. 2007;22(4):560-568.
11. Gooch HL, Hale JE, Fujioka H, Balian G, Hurwitz SR. Alterations of cartilage and collagen expression during fracture healing in experimental diabetes. Connect Tissue Res. 2000;41(2):81-91.
12. Kayal RA, Alblowi J, McKenzie E, et al. Diabetes causes the accelerated loss of cartilage during fracture repair which is reversed by insulin treatment. Bone. 2009;44(2):357-363.
13. Motyl K, Botolin S, Irwin R, et al. Bone inflammation and altered gene expression with type I diabetes early onset. J Cell Physiol. 2009;218(3):575-583.
14. Botolin S, McCabe LR. Chronic hyperglycemia modulates osteoblast gene expression through osmotic and non-osmotic pathways. J Cell Biochem. 2006;99(2):411-424.
15. Keats E, Khanz ZA. Unique responses of stem cell-derived vascular endothelial and mesenchymal cells to high levels of glucose. PLoS One. 2012;7(6):e38752.
16. Vlassara H, Palace MR. Diabetes and advanced glycation endproducts. J Intern Med. 2002;251(2):87-101.
17. Fong Y, Edelstein D, Wang E, Brownlee M. Inhibition of matrix-induced bone differentiation by advanced glycation end-products in rats. Diabetologia. 1993;36(9):802-807.
18. Alikhani M, Alikhani Z, Boyd C, et al. Advanced glycation endproducts stimulate osteoblast apoptosis via the MAP kinase and cytosolic apoptotic pathways. Bone. 2007;40(2):345-353.
19. Catalfamo DL, Calderon NL, Harden SW, Sorenson HL, Neiva KG, Wallet SM. Augmented LPS responsiveness in type 1 diabetes-derived osteoclasts. J Cell Physiol. 2013;228(2):349-361.
20. Kahn SE, Lachin JM, Zinman B, et al; ADOPT Study Group. Effects of rosiglitazone, glyburide, and metformin on β-cell function and insulin sensitivity in ADOPT. Diabetes. 2011;60(5):1552-1560.
21. Shibuya N, Humphers JM, Fluhman BL, Jupiter DC. Factors associated with nonunion, delayed union, and malunion in foot and ankle surgery in diabetic patients. J Foot Ankle Surg. 2013;52(2):207-211.
22. Shami SK, Chittenden SJ. Microangiopathy in diabetes mellitus: II. Features, complications and investigation. Diabetes Res. 1991;17(4):157-168.
23. Nishikawa T, Edelstein D, Du XL, et al. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycemic damage. Nature. 2000;404(6779):787-790.
24. Jeffcoate WJ. Theories concerning the pathogenesis of the acute Charcot foot suggest future therapy. Curr Diab Rep. 2005;5(6):430-435.
25. Lerner UH, Persson E. Osteotropic effects by the neuropeptides calcitonin gene-related peptide, substance P and vasoactive intestinal peptide. J Musculoskelet Neuronal Interact. 2008;8(2):154-165.
26. Brownlee M. The pathobiology of diabetic complications—a unifying mechanism. Diabetes. 2005;54(6):1615-1625.
27. Tsuji S, Taniuchi S, Hasui M, Yamamoto A, Kobayashi Y. Increased nitric oxide production by neutrophils from patients with chronic granulomatous disease on trimethoprim-sulfamethoxazole. Nitric Oxide. 2002;7(4):283-288.
28. Kolluru GK, Bir SC, Kevil CG. Endothelial dysfunction and diabetes: effects on angiogenesis, vascular remodeling, and wound healing. Int J Vasc Med. 2012;2012:918267.
29. Westerweel PE. Impaired endothelial progenitor cell mobilization and dysfunctional bone marrow stroma in diabetes mellitus. PLoS One. 2013;8(3):e60357.
30. Fadini GP, Avogaro A. It is all in the blood: the multifaceted contribution of circulating progenitor cells in diabetic complications. Exp Diabetes Res. 2012;2012:742976.
31. Gadad PC, Matthews KH, Knott RM. Role of HIF1α and PKCβ in mediating the effect of oxygen and glucose in a novel wound assay. Microvasc Res. 2013;88:61-69.
32. Botusan IR, Sunkari VG, Savu O, et al. Stabilization of HIF-1alpha is critical to improve wound healing in diabetic mice. Proc Natl Acad Sci U S A. 2008;105(49):19426-19431.
33. Catrina SB, Okamoto K, Pereira T, Brismar K, Poellinger L. Hyperglycemia regulates hypoxia-inducible factor-1alpha protein stability and function. Diabetes. 2004;53(12):3226-3232.
34. Marhoffer W, Stein M, Maeser E, Federlin K. Impairment of polymorphonuclear leukocyte function and metabolic control of diabetes. Diabetes Care. 1992;15(2):256-260.
35. Calmi G, Montana M, Citarella R, Porretto F, Catania A, Lo Presti R. Polymorphonuclear leukocyte integrin profile in diabetes mellitus. Clin Hemorheol Microcirc. 2002;27(2):83-89.
36. Miao M, Niu Y, Xie T, Yuan B, Qing C, Lu S. Diabetes-impaired wound healing and altered macrophage activation: a possible pathophysiologic correlation. Wound Repair Regen. 2012;20(2):203-213.
37. Liu BF, Miyata S, Kojima H, et al. Low phagocytic activity of resident peritoneal macrophages in diabetic mice: relevance to the formation of advanced glycation end products. Diabetes. 1999;48(10):2074-2082.
38. Mabilleau G, Petrova NL, Edmonds ME, Sabokbar A. Increased osteoclastic activity in acute Charcot’s osteoarthropathy: the role of receptor activator of nuclear factor-kappaB ligand. Diabetologia. 2008;51(6):1035-1040.
39. Witzke KA, Vinik AI, Grant LM, et al. Loss of RAGE defense: a cause of Charcot neuroarthropathy? Diabetes Care. 2011;34(7):1617-1621.
40. Pittenger G, Vinik A. Nerve growth factor and diabetic neuropathy. Exp Diabesity Res. 2003;4(4):271-285.
Nothing Is Sacred: The Need for Unceasing Questioning in Scientific Research
As we look at the trauma articles lined up in this issue of The American Journal of Orthopedics, we are reminded of one of the principle missions of our academic journals, the evaluation and dissemination of new knowledge. All 4 trauma articles offer an improvement in treatment or new perspective in the evaluation of musculoskeletal injury. As an Associate Editor of the journal, I often hear comments from reviewers like “nothing new here,” “retrospective study,” or “has been done before.” But I’m continually reminded that we can never get enough quality information in our quest to provide truth and knowledge to our readership.
Things are not always as they seem. Nothing reminds us of this as much as the revelations seen in the recent work showcased on the front page of The New York Times on August 27, 2015.1 A research group at the Center for Open Science in Charlottesville, Virginia, attempted to reproduce 100 studies published in leading psychology journals and discovered that only 35% could be verified.1 No fraud was inferred, just the “conclusion” that the results were not as definitive as originally felt to be. Interesting, shocking, or stimulating? I would contend it’s the latter. Though many things written in major and respected journals are held as sacred tenets of our craft, all should be challenged. Clinical science particularly needs to be continually refined, as one study is rarely powerful enough to be definitive.
There is nothing so true that it should not be retested. For centuries great academicians accepted and repeatedly published on the “fact” that the earth was the center of our universe. Phlebotomy was an accepted and practiced treatment for febrile illness for centuries. It is alleged to have played a significant role in the death of our country’s first president, George Washington, who succumbed to suppurative pharyngitis.2 Needless to say, we no longer hold these truths to be valid.
Even in our own recent literature, clinical solutions held to be advances, such as metal-on-metal arthroplasty, bone morphogenetic proteins (BMPs), and the aggressive arthroscopic treatment of superior labrum, anterior to posterior (SLAP) lesions, have been properly and helpfully challenged, clarifying their role in our armamentarium. Consider this issue of the journal to be a salute to the investigators and authors who honestly report their findings to us in hopes of better understanding.
But we should never be dissuaded from taking a second look, or even a third, at a clinical principle or basic science belief. In his comments to The New York Times, Brian Nosek, psychology professor at the University of Virginia and director of the Center for Open Science stated, “We see this is a call to action…to the research community to do more replication.”1 I could not agree more. Continued curiosity and constructive criticism should be encouraged. We should never be cowed into complacency because something “has already been done.” We encourage investigators to unceasingly question and work to test their hypotheses. They help us add to our fund of knowledge. Without their continued diligence we will have nothing to fill these pages. We thank them.
1. Carey B. Many psychology findings not as strong as claimed, study says. New York Times. August 27, 2015:A1. http://www.nytimes.com/2015/08/28/science/many-social-science-findings-not-as-strong-as-claimed-study-says.html?_r=0. Accessed September 11, 2015.
2. Wallenborn WM. George Washington’s terminal illness: a modern medical analysis of the last illness and death of George Washington. Papers of George Washington website. http://gwpapers.virginia.edu/history/articles/illness. Published November 5, 1997. Accessed September 11, 2015.
As we look at the trauma articles lined up in this issue of The American Journal of Orthopedics, we are reminded of one of the principle missions of our academic journals, the evaluation and dissemination of new knowledge. All 4 trauma articles offer an improvement in treatment or new perspective in the evaluation of musculoskeletal injury. As an Associate Editor of the journal, I often hear comments from reviewers like “nothing new here,” “retrospective study,” or “has been done before.” But I’m continually reminded that we can never get enough quality information in our quest to provide truth and knowledge to our readership.
Things are not always as they seem. Nothing reminds us of this as much as the revelations seen in the recent work showcased on the front page of The New York Times on August 27, 2015.1 A research group at the Center for Open Science in Charlottesville, Virginia, attempted to reproduce 100 studies published in leading psychology journals and discovered that only 35% could be verified.1 No fraud was inferred, just the “conclusion” that the results were not as definitive as originally felt to be. Interesting, shocking, or stimulating? I would contend it’s the latter. Though many things written in major and respected journals are held as sacred tenets of our craft, all should be challenged. Clinical science particularly needs to be continually refined, as one study is rarely powerful enough to be definitive.
There is nothing so true that it should not be retested. For centuries great academicians accepted and repeatedly published on the “fact” that the earth was the center of our universe. Phlebotomy was an accepted and practiced treatment for febrile illness for centuries. It is alleged to have played a significant role in the death of our country’s first president, George Washington, who succumbed to suppurative pharyngitis.2 Needless to say, we no longer hold these truths to be valid.
Even in our own recent literature, clinical solutions held to be advances, such as metal-on-metal arthroplasty, bone morphogenetic proteins (BMPs), and the aggressive arthroscopic treatment of superior labrum, anterior to posterior (SLAP) lesions, have been properly and helpfully challenged, clarifying their role in our armamentarium. Consider this issue of the journal to be a salute to the investigators and authors who honestly report their findings to us in hopes of better understanding.
But we should never be dissuaded from taking a second look, or even a third, at a clinical principle or basic science belief. In his comments to The New York Times, Brian Nosek, psychology professor at the University of Virginia and director of the Center for Open Science stated, “We see this is a call to action…to the research community to do more replication.”1 I could not agree more. Continued curiosity and constructive criticism should be encouraged. We should never be cowed into complacency because something “has already been done.” We encourage investigators to unceasingly question and work to test their hypotheses. They help us add to our fund of knowledge. Without their continued diligence we will have nothing to fill these pages. We thank them.
As we look at the trauma articles lined up in this issue of The American Journal of Orthopedics, we are reminded of one of the principle missions of our academic journals, the evaluation and dissemination of new knowledge. All 4 trauma articles offer an improvement in treatment or new perspective in the evaluation of musculoskeletal injury. As an Associate Editor of the journal, I often hear comments from reviewers like “nothing new here,” “retrospective study,” or “has been done before.” But I’m continually reminded that we can never get enough quality information in our quest to provide truth and knowledge to our readership.
Things are not always as they seem. Nothing reminds us of this as much as the revelations seen in the recent work showcased on the front page of The New York Times on August 27, 2015.1 A research group at the Center for Open Science in Charlottesville, Virginia, attempted to reproduce 100 studies published in leading psychology journals and discovered that only 35% could be verified.1 No fraud was inferred, just the “conclusion” that the results were not as definitive as originally felt to be. Interesting, shocking, or stimulating? I would contend it’s the latter. Though many things written in major and respected journals are held as sacred tenets of our craft, all should be challenged. Clinical science particularly needs to be continually refined, as one study is rarely powerful enough to be definitive.
There is nothing so true that it should not be retested. For centuries great academicians accepted and repeatedly published on the “fact” that the earth was the center of our universe. Phlebotomy was an accepted and practiced treatment for febrile illness for centuries. It is alleged to have played a significant role in the death of our country’s first president, George Washington, who succumbed to suppurative pharyngitis.2 Needless to say, we no longer hold these truths to be valid.
Even in our own recent literature, clinical solutions held to be advances, such as metal-on-metal arthroplasty, bone morphogenetic proteins (BMPs), and the aggressive arthroscopic treatment of superior labrum, anterior to posterior (SLAP) lesions, have been properly and helpfully challenged, clarifying their role in our armamentarium. Consider this issue of the journal to be a salute to the investigators and authors who honestly report their findings to us in hopes of better understanding.
But we should never be dissuaded from taking a second look, or even a third, at a clinical principle or basic science belief. In his comments to The New York Times, Brian Nosek, psychology professor at the University of Virginia and director of the Center for Open Science stated, “We see this is a call to action…to the research community to do more replication.”1 I could not agree more. Continued curiosity and constructive criticism should be encouraged. We should never be cowed into complacency because something “has already been done.” We encourage investigators to unceasingly question and work to test their hypotheses. They help us add to our fund of knowledge. Without their continued diligence we will have nothing to fill these pages. We thank them.
1. Carey B. Many psychology findings not as strong as claimed, study says. New York Times. August 27, 2015:A1. http://www.nytimes.com/2015/08/28/science/many-social-science-findings-not-as-strong-as-claimed-study-says.html?_r=0. Accessed September 11, 2015.
2. Wallenborn WM. George Washington’s terminal illness: a modern medical analysis of the last illness and death of George Washington. Papers of George Washington website. http://gwpapers.virginia.edu/history/articles/illness. Published November 5, 1997. Accessed September 11, 2015.
1. Carey B. Many psychology findings not as strong as claimed, study says. New York Times. August 27, 2015:A1. http://www.nytimes.com/2015/08/28/science/many-social-science-findings-not-as-strong-as-claimed-study-says.html?_r=0. Accessed September 11, 2015.
2. Wallenborn WM. George Washington’s terminal illness: a modern medical analysis of the last illness and death of George Washington. Papers of George Washington website. http://gwpapers.virginia.edu/history/articles/illness. Published November 5, 1997. Accessed September 11, 2015.
PsA, PsC do not affect total hip replacement outcomes
Neither psoriatic arthritis (PsA) nor cutaneous psoriasis (PsC) is an independent predictor of poor postoperative pain or function following a total hip arthroplasty, according to the results of a case-control study by Dr. Lisa A. Mandl and her colleagues.
The study’s participants underwent surgery between May 1, 2007, and Dec. 31, 2010, in a center that performs more than 4,300 THAs annually. All subjects lived for at least 2 years after their operations. The researchers compared pre- and postoperative data from patients in the following three categories: those with PsA, those with PsC without evidence of inflammatory arthritis, and those with osteoarthritis (OA). Patients with OA comprised the control group, which excluded any patient who self-reported a history of PsA, rheumatoid arthritis, lupus erythematosus, or any other systematic rheumatic disease, or who had documentation of skin psoriasis. The researchers acquired postoperative self-report data from 47 PsA patients, 106 PsC patients, and 864 OA patients. Seventeen percent of patients submitted information on their status at 1 year, 69% at 2 years, and 14% at 3-5 years.
The primary outcomes of interest were postoperative pain and function, which were assessed via the Hip Osteoarthritis Outcome Score (HOOS), from which the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was derived.
There were no statistically significant differences in postoperative WOMAC pain or function scores between the three groups of patients (P = .78 and .96, respectively). The mean pain scores were 14.9, 6.1, and 15.8 for patients with PsA, PsC, and OA, respectively. These patients’ mean function scores were 16.3, 19.6, and 18.8 for the PsA, PsC and OA groups, respectively.
Overall levels of satisfaction with the surgery were similar among the three groups (P = .54). Ninety-three percent of the PsA patients, 79% of the PsC patients, and 84% of the OA patients were “very satisfied” with their total hip arthroplasty. Between 1% and 3% of each group reported being “very dissatisfied” with their surgery. The researchers found that extent of skin disease was not associated with worse postoperative pain or function.
“Further work needs to be done to better understand the interplay of disease activity and quality of life on the outcomes of [total hip arthroplasty] in PsA and PsC,” they wrote.
Read the report in Arthritis & Rheumatology (doi: 10.1002/art.39431).
Neither psoriatic arthritis (PsA) nor cutaneous psoriasis (PsC) is an independent predictor of poor postoperative pain or function following a total hip arthroplasty, according to the results of a case-control study by Dr. Lisa A. Mandl and her colleagues.
The study’s participants underwent surgery between May 1, 2007, and Dec. 31, 2010, in a center that performs more than 4,300 THAs annually. All subjects lived for at least 2 years after their operations. The researchers compared pre- and postoperative data from patients in the following three categories: those with PsA, those with PsC without evidence of inflammatory arthritis, and those with osteoarthritis (OA). Patients with OA comprised the control group, which excluded any patient who self-reported a history of PsA, rheumatoid arthritis, lupus erythematosus, or any other systematic rheumatic disease, or who had documentation of skin psoriasis. The researchers acquired postoperative self-report data from 47 PsA patients, 106 PsC patients, and 864 OA patients. Seventeen percent of patients submitted information on their status at 1 year, 69% at 2 years, and 14% at 3-5 years.
The primary outcomes of interest were postoperative pain and function, which were assessed via the Hip Osteoarthritis Outcome Score (HOOS), from which the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was derived.
There were no statistically significant differences in postoperative WOMAC pain or function scores between the three groups of patients (P = .78 and .96, respectively). The mean pain scores were 14.9, 6.1, and 15.8 for patients with PsA, PsC, and OA, respectively. These patients’ mean function scores were 16.3, 19.6, and 18.8 for the PsA, PsC and OA groups, respectively.
Overall levels of satisfaction with the surgery were similar among the three groups (P = .54). Ninety-three percent of the PsA patients, 79% of the PsC patients, and 84% of the OA patients were “very satisfied” with their total hip arthroplasty. Between 1% and 3% of each group reported being “very dissatisfied” with their surgery. The researchers found that extent of skin disease was not associated with worse postoperative pain or function.
“Further work needs to be done to better understand the interplay of disease activity and quality of life on the outcomes of [total hip arthroplasty] in PsA and PsC,” they wrote.
Read the report in Arthritis & Rheumatology (doi: 10.1002/art.39431).
Neither psoriatic arthritis (PsA) nor cutaneous psoriasis (PsC) is an independent predictor of poor postoperative pain or function following a total hip arthroplasty, according to the results of a case-control study by Dr. Lisa A. Mandl and her colleagues.
The study’s participants underwent surgery between May 1, 2007, and Dec. 31, 2010, in a center that performs more than 4,300 THAs annually. All subjects lived for at least 2 years after their operations. The researchers compared pre- and postoperative data from patients in the following three categories: those with PsA, those with PsC without evidence of inflammatory arthritis, and those with osteoarthritis (OA). Patients with OA comprised the control group, which excluded any patient who self-reported a history of PsA, rheumatoid arthritis, lupus erythematosus, or any other systematic rheumatic disease, or who had documentation of skin psoriasis. The researchers acquired postoperative self-report data from 47 PsA patients, 106 PsC patients, and 864 OA patients. Seventeen percent of patients submitted information on their status at 1 year, 69% at 2 years, and 14% at 3-5 years.
The primary outcomes of interest were postoperative pain and function, which were assessed via the Hip Osteoarthritis Outcome Score (HOOS), from which the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was derived.
There were no statistically significant differences in postoperative WOMAC pain or function scores between the three groups of patients (P = .78 and .96, respectively). The mean pain scores were 14.9, 6.1, and 15.8 for patients with PsA, PsC, and OA, respectively. These patients’ mean function scores were 16.3, 19.6, and 18.8 for the PsA, PsC and OA groups, respectively.
Overall levels of satisfaction with the surgery were similar among the three groups (P = .54). Ninety-three percent of the PsA patients, 79% of the PsC patients, and 84% of the OA patients were “very satisfied” with their total hip arthroplasty. Between 1% and 3% of each group reported being “very dissatisfied” with their surgery. The researchers found that extent of skin disease was not associated with worse postoperative pain or function.
“Further work needs to be done to better understand the interplay of disease activity and quality of life on the outcomes of [total hip arthroplasty] in PsA and PsC,” they wrote.
Read the report in Arthritis & Rheumatology (doi: 10.1002/art.39431).
FROM ARTHRITIS & RHEUMATOLOGY