User login
Brodalumab achieved primary endpoints for moderate to severe psoriasis at 52 weeks
SAN FRANCISCO– Significantly more psoriasis patients who received the investigational biologic agent brodalumab achieved a PASI 100 response compared with those who received ustekinumab, and clinical responses persisted through 52 weeks, according to data from the pivotal phase III AMAGINE-2 trial.
Brodalumab also met its co-primary endpoints (PASI 75 and sPGA 0 or 1) compared with placebo at week 12 when given at doses of either 210 or 140 mg every two weeks, Dr. Mark Lebwohl said at the annual meeting of the American Academy of Dermatology.
But patients maintained the best responses at the higher brodalumab dose, Dr. Lebwohl, professor and chair of dermatology at the Icahn School of Medicine at Mount Sinai, New York, reported. “Nearly 44% of patients in this group had not a dot of psoriasis left,” he said.
The interleukin-17 (IL-17) receptor and cytokine family play a key role in the pathogenesis of plaque psoriasis. Brodalumab works by binding the IL-17 receptor, thereby blocking binding by the A, F, and A/F IL-17 cytokines. The AMAGINE-2 trial is the last of a trio of phase III studies to assess brodalumab’s safety and efficacy in patients with moderate to severe plaque psoriasis, Dr. Lebwohl and his associates noted. The findings are consistent with those from earlier trials, they said.
For the study, the researchers enrolled 1,831 patients with moderate to severe plaque psoriasis, of whom 1,776 completed the 12-week induction phase. During induction, patients received either 210 or 140 mg brodalumab, 45 mg of ustekinumab (or 90 mg if they weighed more than 100 kg), or placebo. At week 12, patients were re-randomized to one of the brodalumab or ustekinumab arms.
Fully 44% of patients who received 210 mg brodalumab achieved total clearance of skin disease, or Psoriasis Area Severity Index (PASI) 100 – twice the proportion of the ustekinumab group (22%; P < .001), Dr. Lebwohl said. The 210-mg brodalumab dose also achieved the highest PASI 75 response rate (86%, compared with 70% for ustekinumab, 67% for 140 mg brodalumab, and 8% for placebo), although the adjusted p-value comparing 210 mg brodalumab and ustekinumab did not reach statistical significance (P = .078), he noted. Finally, 79% of patients who received 210 mg brodalumab and 58% of those who received 140 mg brodalumab achieved clear or almost clear skin at week 12 according to the static Physician Global Assessment (sPGA), compared with only 4% of the placebo group (P < .001), he reported.
Brodalumab’s safety profile during the 12-week induction phase resembled that for previous trials, said Dr. Lebwohl. The most common adverse events were nasopharyngitis, upper respiratory tract infection, headache, and arthralgia. “But the punch line was Candida,” he said. Candidiasis affected 0.6% of patients in the placebo arm, compared with 1.4% for brodalumab-treated patients at week 12. By week 52, about 4% to 6.5% of treated patients had developed Candida infections.
Similarly small proportions of patients across all arms experienced serious side effects (1% to 2.6%) during the placebo-controlled period, noted Dr. Lebwohl. After adjusting for exposure time, rates of adverse events were similar for all groups, he said. “However, due to disparity in patient-years of exposure between treatment groups, we cannot draw conclusions about potential dose effects,” he added.
Dr. Lebwohl reported receiving research support from Amgen, which is developing brodalumab together with AstraZeneca/MedImmune.
SAN FRANCISCO– Significantly more psoriasis patients who received the investigational biologic agent brodalumab achieved a PASI 100 response compared with those who received ustekinumab, and clinical responses persisted through 52 weeks, according to data from the pivotal phase III AMAGINE-2 trial.
Brodalumab also met its co-primary endpoints (PASI 75 and sPGA 0 or 1) compared with placebo at week 12 when given at doses of either 210 or 140 mg every two weeks, Dr. Mark Lebwohl said at the annual meeting of the American Academy of Dermatology.
But patients maintained the best responses at the higher brodalumab dose, Dr. Lebwohl, professor and chair of dermatology at the Icahn School of Medicine at Mount Sinai, New York, reported. “Nearly 44% of patients in this group had not a dot of psoriasis left,” he said.
The interleukin-17 (IL-17) receptor and cytokine family play a key role in the pathogenesis of plaque psoriasis. Brodalumab works by binding the IL-17 receptor, thereby blocking binding by the A, F, and A/F IL-17 cytokines. The AMAGINE-2 trial is the last of a trio of phase III studies to assess brodalumab’s safety and efficacy in patients with moderate to severe plaque psoriasis, Dr. Lebwohl and his associates noted. The findings are consistent with those from earlier trials, they said.
For the study, the researchers enrolled 1,831 patients with moderate to severe plaque psoriasis, of whom 1,776 completed the 12-week induction phase. During induction, patients received either 210 or 140 mg brodalumab, 45 mg of ustekinumab (or 90 mg if they weighed more than 100 kg), or placebo. At week 12, patients were re-randomized to one of the brodalumab or ustekinumab arms.
Fully 44% of patients who received 210 mg brodalumab achieved total clearance of skin disease, or Psoriasis Area Severity Index (PASI) 100 – twice the proportion of the ustekinumab group (22%; P < .001), Dr. Lebwohl said. The 210-mg brodalumab dose also achieved the highest PASI 75 response rate (86%, compared with 70% for ustekinumab, 67% for 140 mg brodalumab, and 8% for placebo), although the adjusted p-value comparing 210 mg brodalumab and ustekinumab did not reach statistical significance (P = .078), he noted. Finally, 79% of patients who received 210 mg brodalumab and 58% of those who received 140 mg brodalumab achieved clear or almost clear skin at week 12 according to the static Physician Global Assessment (sPGA), compared with only 4% of the placebo group (P < .001), he reported.
Brodalumab’s safety profile during the 12-week induction phase resembled that for previous trials, said Dr. Lebwohl. The most common adverse events were nasopharyngitis, upper respiratory tract infection, headache, and arthralgia. “But the punch line was Candida,” he said. Candidiasis affected 0.6% of patients in the placebo arm, compared with 1.4% for brodalumab-treated patients at week 12. By week 52, about 4% to 6.5% of treated patients had developed Candida infections.
Similarly small proportions of patients across all arms experienced serious side effects (1% to 2.6%) during the placebo-controlled period, noted Dr. Lebwohl. After adjusting for exposure time, rates of adverse events were similar for all groups, he said. “However, due to disparity in patient-years of exposure between treatment groups, we cannot draw conclusions about potential dose effects,” he added.
Dr. Lebwohl reported receiving research support from Amgen, which is developing brodalumab together with AstraZeneca/MedImmune.
SAN FRANCISCO– Significantly more psoriasis patients who received the investigational biologic agent brodalumab achieved a PASI 100 response compared with those who received ustekinumab, and clinical responses persisted through 52 weeks, according to data from the pivotal phase III AMAGINE-2 trial.
Brodalumab also met its co-primary endpoints (PASI 75 and sPGA 0 or 1) compared with placebo at week 12 when given at doses of either 210 or 140 mg every two weeks, Dr. Mark Lebwohl said at the annual meeting of the American Academy of Dermatology.
But patients maintained the best responses at the higher brodalumab dose, Dr. Lebwohl, professor and chair of dermatology at the Icahn School of Medicine at Mount Sinai, New York, reported. “Nearly 44% of patients in this group had not a dot of psoriasis left,” he said.
The interleukin-17 (IL-17) receptor and cytokine family play a key role in the pathogenesis of plaque psoriasis. Brodalumab works by binding the IL-17 receptor, thereby blocking binding by the A, F, and A/F IL-17 cytokines. The AMAGINE-2 trial is the last of a trio of phase III studies to assess brodalumab’s safety and efficacy in patients with moderate to severe plaque psoriasis, Dr. Lebwohl and his associates noted. The findings are consistent with those from earlier trials, they said.
For the study, the researchers enrolled 1,831 patients with moderate to severe plaque psoriasis, of whom 1,776 completed the 12-week induction phase. During induction, patients received either 210 or 140 mg brodalumab, 45 mg of ustekinumab (or 90 mg if they weighed more than 100 kg), or placebo. At week 12, patients were re-randomized to one of the brodalumab or ustekinumab arms.
Fully 44% of patients who received 210 mg brodalumab achieved total clearance of skin disease, or Psoriasis Area Severity Index (PASI) 100 – twice the proportion of the ustekinumab group (22%; P < .001), Dr. Lebwohl said. The 210-mg brodalumab dose also achieved the highest PASI 75 response rate (86%, compared with 70% for ustekinumab, 67% for 140 mg brodalumab, and 8% for placebo), although the adjusted p-value comparing 210 mg brodalumab and ustekinumab did not reach statistical significance (P = .078), he noted. Finally, 79% of patients who received 210 mg brodalumab and 58% of those who received 140 mg brodalumab achieved clear or almost clear skin at week 12 according to the static Physician Global Assessment (sPGA), compared with only 4% of the placebo group (P < .001), he reported.
Brodalumab’s safety profile during the 12-week induction phase resembled that for previous trials, said Dr. Lebwohl. The most common adverse events were nasopharyngitis, upper respiratory tract infection, headache, and arthralgia. “But the punch line was Candida,” he said. Candidiasis affected 0.6% of patients in the placebo arm, compared with 1.4% for brodalumab-treated patients at week 12. By week 52, about 4% to 6.5% of treated patients had developed Candida infections.
Similarly small proportions of patients across all arms experienced serious side effects (1% to 2.6%) during the placebo-controlled period, noted Dr. Lebwohl. After adjusting for exposure time, rates of adverse events were similar for all groups, he said. “However, due to disparity in patient-years of exposure between treatment groups, we cannot draw conclusions about potential dose effects,” he added.
Dr. Lebwohl reported receiving research support from Amgen, which is developing brodalumab together with AstraZeneca/MedImmune.
Key clinical point: At 52 weeks, brodalumab met its PASI 100 endpoint compared with ustekinumab in the pivotal phase III AMAGINE-2 trial.
Major finding: Forty-four percent of patients who received 210 mg brodalumab achieved PASI 100 compared with 22% of the ustekinumab group (P < .001).
Data source: Randomized, placebo-controlled phase III trial of brodalumab, ustekinumab, and placebo in 1,831 patients with moderate to severe plaque psoriasis.
Disclosures: Dr. Lebwohl reported receiving research support from Amgen, which is developing brodalumab together with AstraZeneca/MedImmune.
Halting biologics before surgery tied to flares in psoriasis, psoriatic arthritis
Interrupting biologic therapy before surgery led to flares in psoriasis and psoriatic arthritis and did not appear to prevent postoperative complications in a small, retrospective cohort study.
“Our findings are in keeping with most of the existing literature on this topic,” said Dr. Waseem Bakkour and his associates at the University of Manchester (England). “However, it is important to acknowledge the deficiencies of our data, in particular the small data set and retrospective study design with numerous complexities associated with interpreting it” (J. Eur. Acad. Dermatol. Venereol. 2015 Mar. 2 [doi:10.1111/jdv.12997]).
The British Association of Dermatologists and the British Society for Rheumatology recommend stopping biologics for at least four half-lives before surgery, but the guideline is based mostly on retrospective studies of rheumatoid arthritis and inflammatory bowel disease, the researchers said. For their study, they reviewed electronic health records from 42 patients with psoriasis and psoriatic arthritis who underwent 77 major and minor surgical procedures during a 6-year period. Discontinuing biologic therapy before surgery was linked to a significant risk of flare of psoriasis or psoriatic arthritis (40% with stoppage vs. 8.7% with continuation; P = .003). For three-quarters of procedures, patients continued biologic therapy (usually etanercept, but also adalimumab and infliximab), with no apparent effect on rates of postoperative infections or delayed wound healing. About 48% of procedures required general anesthesia, and most of the rest were skin surgeries.
The findings contradict those from a larger retrospective study (Arthritis Care Res. 2006;55:333-7) that linked biologic therapy before orthopedic surgery to a fourfold rise in the odds of postoperative infections, the investigators noted. “Whilst the current evidence, not surprisingly, suggests a link between stopping treatment and disease flare, it remains equivocal regarding the question of whether continuing biologic therapy perioperatively increases the risk of postsurgical complications,” they wrote.
The authors reported no funding sources. They disclosed financial and advisory relationships with many companies that manufacture biologic therapies.
Interrupting biologic therapy before surgery led to flares in psoriasis and psoriatic arthritis and did not appear to prevent postoperative complications in a small, retrospective cohort study.
“Our findings are in keeping with most of the existing literature on this topic,” said Dr. Waseem Bakkour and his associates at the University of Manchester (England). “However, it is important to acknowledge the deficiencies of our data, in particular the small data set and retrospective study design with numerous complexities associated with interpreting it” (J. Eur. Acad. Dermatol. Venereol. 2015 Mar. 2 [doi:10.1111/jdv.12997]).
The British Association of Dermatologists and the British Society for Rheumatology recommend stopping biologics for at least four half-lives before surgery, but the guideline is based mostly on retrospective studies of rheumatoid arthritis and inflammatory bowel disease, the researchers said. For their study, they reviewed electronic health records from 42 patients with psoriasis and psoriatic arthritis who underwent 77 major and minor surgical procedures during a 6-year period. Discontinuing biologic therapy before surgery was linked to a significant risk of flare of psoriasis or psoriatic arthritis (40% with stoppage vs. 8.7% with continuation; P = .003). For three-quarters of procedures, patients continued biologic therapy (usually etanercept, but also adalimumab and infliximab), with no apparent effect on rates of postoperative infections or delayed wound healing. About 48% of procedures required general anesthesia, and most of the rest were skin surgeries.
The findings contradict those from a larger retrospective study (Arthritis Care Res. 2006;55:333-7) that linked biologic therapy before orthopedic surgery to a fourfold rise in the odds of postoperative infections, the investigators noted. “Whilst the current evidence, not surprisingly, suggests a link between stopping treatment and disease flare, it remains equivocal regarding the question of whether continuing biologic therapy perioperatively increases the risk of postsurgical complications,” they wrote.
The authors reported no funding sources. They disclosed financial and advisory relationships with many companies that manufacture biologic therapies.
Interrupting biologic therapy before surgery led to flares in psoriasis and psoriatic arthritis and did not appear to prevent postoperative complications in a small, retrospective cohort study.
“Our findings are in keeping with most of the existing literature on this topic,” said Dr. Waseem Bakkour and his associates at the University of Manchester (England). “However, it is important to acknowledge the deficiencies of our data, in particular the small data set and retrospective study design with numerous complexities associated with interpreting it” (J. Eur. Acad. Dermatol. Venereol. 2015 Mar. 2 [doi:10.1111/jdv.12997]).
The British Association of Dermatologists and the British Society for Rheumatology recommend stopping biologics for at least four half-lives before surgery, but the guideline is based mostly on retrospective studies of rheumatoid arthritis and inflammatory bowel disease, the researchers said. For their study, they reviewed electronic health records from 42 patients with psoriasis and psoriatic arthritis who underwent 77 major and minor surgical procedures during a 6-year period. Discontinuing biologic therapy before surgery was linked to a significant risk of flare of psoriasis or psoriatic arthritis (40% with stoppage vs. 8.7% with continuation; P = .003). For three-quarters of procedures, patients continued biologic therapy (usually etanercept, but also adalimumab and infliximab), with no apparent effect on rates of postoperative infections or delayed wound healing. About 48% of procedures required general anesthesia, and most of the rest were skin surgeries.
The findings contradict those from a larger retrospective study (Arthritis Care Res. 2006;55:333-7) that linked biologic therapy before orthopedic surgery to a fourfold rise in the odds of postoperative infections, the investigators noted. “Whilst the current evidence, not surprisingly, suggests a link between stopping treatment and disease flare, it remains equivocal regarding the question of whether continuing biologic therapy perioperatively increases the risk of postsurgical complications,” they wrote.
The authors reported no funding sources. They disclosed financial and advisory relationships with many companies that manufacture biologic therapies.
FROM THE JOURNAL OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Key clinical point: Interrupting biologic therapy before surgery led to flares in psoriasis and psoriatic arthritis.
Major finding: Discontinuing biologic therapy before surgery was associated with a significant risk of flare (40% with stoppage vs. 8.7% with continuation; P = .003).
Data source: A retrospective cohort study of 42 patients with psoriasis and/or psoriatic arthritis who underwent 77 surgical procedures.
Disclosures: The authors reported no funding sources. They disclosed financial and advisory relationships with many companies that manufacture biologic therapies.
Novel Psoriasis Therapies and Patient Outcomes, Part 1: Topical Medications
Topical therapies are a mainstay in the management of patients with mild to moderate psoriasis (Figure). Presently, US Food and Drug Administration–approved topical medications that are commercially available for use in patients with psoriasis include corticosteroids, vitamin D3 analogues, calcineurin inhibitors, retinoids, anthralin, and tar-based formulations.1 In recent years, research has furthered our understanding of the molecular mechanisms underlying the pathogenesis of psoriasis and has afforded the development of more targeted therapies. Novel topical medications currently in phase 2 and phase 3 clinical trials are discussed in this article, and a summary is provided in the Table.
AN2728 (Phosphodiesterase 4 Inhibitor)
AN2728 (Anacor Pharmaceuticals, Inc) is a phosphodiesterase 4 inhibitor that blocks the inactivation of cyclic adenosine monophosphate, resulting in decreased production of inflammatory cytokines (eg, IL-6, IL-12, IL-23, tumor necrosis factor α [TNF-α]).2,3 In a randomized, double-blind, phase 2 clinical trial (N=35), 40% of patients treated with AN2728 ointment 5% reported improvement of more than 2 points in overall target plaque severity score versus 6% of patients treated with vehicle. In another randomized, double-blind, dose-response trial of 145 patients, those treated with AN2728 ointment 2% twice daily reported a 60% improvement versus 40% improvement in those treated with AN2728 ointment 0.5% once daily.3 In total, 3 phase 1 trials (registered at www.clinicaltrials.gov with the identifiers NCT01258088, NCT00762658, NCT00763204) and 4 phase 2 trials (NCT01029405, NCT00755196, NCT00759161, NCT01300052) have been completed; results were not available at the time of publication.
AS101 (Integrin Inhibitor)
AS101 (BioMAS Ltd), or ammonium trichloro (dioxoethylene-o,o') tellurate, acts as stimulator of regulatory T cells and a redox modulator inhibiting the leukocyte integrins α4β1 and α4β7 that enable CD4+ T-cell and macrophage extravasation; it also limits expression of the inflammatory cytokines IL-6 and IL-17.4 A randomized, placebo-controlled, double-blind, phase 2 study evaluating the efficacy of AS101 cream 4% twice daily for 12 weeks was withdrawn prior to enrollment (NCT00788424).
Tofacitinib (Janus Kinase 1 and 3 Inhibitor)
Tofacitinib (formerly known as CP-690,550)(Pfizer Inc) is a selective Janus kinase (Jak) 1 and Jak3 inhibitor that limits expression of cytokines that promote inflammation (eg, IFN-γ) and inhibits helper T cells (TH17) by downregulating expression of the IL-23 receptor. Epidermal keratinocyte proliferation in psoriasis is activated by TH17 cells that release IL-17 as well as TH1 cells that release IFN-γ and tumor necrosis factor. A phase 2a trial showed statistically significant improvement from baseline in the target plaque severity score for tofacitinib ointment 2% (least squares mean, −54.4%) versus vehicle (least squares mean, −41.5%).5 Two other phase 2 trials (NCT01246583, NCT00678561) assessing the efficacy, safety, tolerability, and pharmacokinetics of tofacitinib ointment in patients with mild to moderate psoriasis have been completed; results were not available at the time of publication. A phase 2b study that compared 2 dose strengths of tofacitinib ointment—10 mg/g and 20 mg/g—versus placebo over a 12-week period also was completed (NCT01831466); results were not available at the time of publication.
CT327 (Tyrosine Kinase Inhibitor)
CT327 (Creabilis SA) is a tyrosine kinase A (TrkA) inhibitor that affords a novel perspective in the treatment of pruritus by shifting the focus to sensory neurons. In a phase 2b study of 160 patients, a 60% change in the visual analog scale was noted at 8 weeks in the treatment group versus 21% in the placebo group.6 Two other phase 2 studies have been completed, one with a cream formulation of pegylated K252a (NCT00995969) and another with an ointment formulation (NCT01465282); results were not available at the time of publication.
DPS-101 (Vitamin D Analogue)
DPS-101 (Dermipsor Ltd) is a combination of calcipotriol and niacinamide. Calcipotriol is a vitamin D3 analogue that increases IL-10 expression while decreasing IL-8 expression.7 It curbs epidermal keratinocyte proliferation by limiting the expression of polo-like kinase 2 and early growth response-1.8 It also may induce keratinocyte apoptosis.9 Niacinamide is the amide of vitamin B3 and inhibits proinflammatory cytokines such as TNF-α, IL-1β, IL-6, and IL-8.10 In a dose-response phase 2b trial of 168 patients, DPS-101 demonstrated better results than either calcipotriol or niacinamide alone.11
IDP-118 (Proprietary Steroid and Retinoid Combination)
IDP-118 (Valeant Pharmaceuticals International, Inc) is a combination of halobetasol propionate (HP) 0.01% (a topical corticosteroid) and tazar-otene 0.045% (a selective topical retinoid) in a lotion formulation. In isolation, tazarotene is as effective as a mid to highly potent corticosteroid, but irritation may limit its tolerability. The use of combination treatments of mid to highly potent corticosteroids and tazarotene has shown enhanced tolerability and therapeutic efficacy.12 Ongoing studies include a phase 1 trial and a phase 2 trial to evaluate low- and high-strength preparations of IDP-118, respectively (NCT01670513). Another phase 2 trial evaluating the efficacy and safety of IDP-118 lotion (HP 0.01% and tazarotene 0.045%) versus IDP-118 monad HP 0.01% lotion, IDP-118 monad tazar-otene 0.045% lotion, and placebo has been completed (NCT02045277); results were not available at the time of publication.
Ruxolitinib (Jak1 and Jak2 Inhibitor)
Ruxolitinib (formerly known as INCB18424)(Incyte Corporation) is a selective Jak1 and Jak2 inhibitor. A phase 2 trial of ruxolitinib showed a 53% decline in the score for mean total lesions in patients treated with ruxolitinib phosphate cream 1% (P=.033) versus 54% in those treated with ruxolitinib phosphate cream 1.5% (P=.056) and 32% in those treated with placebo.13 Three other phase 2 studies (NCT00617994, NCT00820950, NCT00778700) have been completed; results were not available at the time of publication.
LAS41004 (Proprietary Steroid and Retinoid Combination)
LAS41004 (Almirall, SA) is an ointment containing the corticosteroid betamethasone dipropionate and the retinoid bexarotene that is being evaluated for treatment of mild to moderate psoriasis. Five phase 2 studies (NCT01119339, NCT01283698, NCT01360944, NCT02111499, NCT01462643) have been completed; results were not available at the time of publication. A randomized, double-blind, phase 2a study (NCT02180464) with a left-right design assessing clinical response to LAS41004 versus control in patients with mild to moderate psoriasis was actively recruiting at the time of publication.
LEO 80190 (Vitamin D3 Analogue and Steroid Combination)
LEO 80190 (LEO Pharma) is a combination of the vitamin D3 analogue calcipotriol and the corticosteroid hydrocortisone. It was developed as a treatment for sensitive areas such as the face and intertriginous regions. A randomized, investigator-blind, phase 3 trial (NCT00640822) of LEO 80190 ointment versus tacalcitol ointment and placebo once daily for 8 weeks demonstrated controlled disease of the face in 56.8% (183/322) of patients in the LEO 80190 group, 46.4% (147/317) in the tacalcitol group, and 36.3% (37/102) in the placebo group.14 Another phase 2 study (NCT00704262) and 2 phase 3 studies (NCT00691002, NCT01007591) have been completed; results were not available at the time of publication.
LEO 90100 (Vitamin D Analogue and Steroid Combination)
LEO 90100 (LEO Pharma) contains the vitamin D3 analogue calcipotriol and the corticosteroid betamethasone. Three phase 2 studies (NCT01347255, NCT01536886, NCT01536938) and a phase 3 study (NCT01866163) examining the efficacy and safety of various vehicles and formulations of LEO 90100 have been completed; results were not available at the time of publication. Another phase 3 study (NCT02132936) is ongoing but not recruiting participants. Other completed studies whose results were not yet available include a phase 1 pharmacodynamic study (NCT01946386), a phase 1 study that used patch testing to assess the degree of skin irritation and sensitization associated with LEO 90100 (NCT01935869), and a phase 2 study examining the impact of LEO 90100 on calcium metabolism and the hypothalamic-pituitary-adrenal axis (NCT01600222).
M518101 (Vitamin D Analogue)
M518101 (Maruho Co, Ltd) is a novel topical vitamin D3 analogue. Phase 1 (NCT01844973) and phase 2 (NCT01301157, NCT00884169) trials evaluating the safety, pharmacokinetics, and efficacy of M518101 have been completed; results were not available at the time of publication. A phase 3 study (NCT01989429) assessing the safety and therapeutic efficacy of M518101 according to changes in the modified psoriasis area and severity index over an 8-week treatment period also has been completed; results were not yet available. Three phase 3 studies assessing the safety and therapeutic efficacy of M518101 are ongoing: one is currently closed to recruitment (NCT01908595) and 2 are actively recruiting participants at the time of publication (NCT01878461, NCT01873677).
MOL4239 and MOL4249 (Phosphorylated Signal Transducer and Activator of Transcription 3 Inhibitors)
MOL4239 (Moleculin, LLC) is a novel topical agent for use in mild to moderate psoriasis that acts via phosphorylated signal transducer and activator of transcription 3 (p-STAT3) inhibition.15 The p-STAT3 protein has increased expression in psoriasis.16 A phase 2 trial of MOL4239 ointment (NCT01826201) has been completed, showing a greater mean (standard deviation) change in the psoriasis severity score in lesions treated at 28 days with MOL4239 ointment 10% (−1.9 [1.45]) versus lesions treated with placebo ointment (−1.5 [1.87]).17
MOL4249 (Moleculin, LLC) is more potent than MOL4239 with better lipid solubility. In the MOL4249 subset of a placebo-controlled, double-blind, phase 2a study of 16 patients with mild to moderate psoriasis, 10% (1/10) of patients experienced complete clearance of psoriatic plaques, 30% (3/10) of patients experienced 75% or greater improvement, and 50% (5/10) of patients experienced 50% or greater improvement compared to 17% (1/6) in the placebo group. Currently, a phase 2a contralateral study, a phase 2b psoriasis area and severity index trial, and a phase 3 pivotal trial are planned, according to the manufacturer.18
MQX-5902 (Dihydrofolate Reductase Inhibitor)
MQX-5902 (MediQuest Therapeutics) is a topical preparation of methotrexate for the treatment of fingernail psoriasis. Methotrexate is a dihydrofolate reductase inhibitor and antimetabolite that inhibits folic acid metabolism, thereby disrupting DNA synthesis.19 A phase 2b dose-ranging trial (NCT00666354) was designed to assess the therapeutic efficacy and safety of MQX-5902 delivered via a proprietary drug delivery formulation in fingernail psoriasis; the outcome of this trial was not available at the time of publication.
PH-10 (Xanthine Dye)
PH-10 (Provectus Biopharmaceuticals, Inc) is a topical aqueous hydrogel derived from rose bengal disodium that may be beneficial in treating skin conditions such as atopic dermatitis and mild to moderate psoriasis. Rose bengal disodium is a hydrophilic xanthine dye with diagnostic utility in ophthalmology and gastroenterology as well as projected use as a melanoma treatment as demonstrated in phase 1 and phase 2 clinical trials of PV-10 (Provectus Biopharmaceuticals, Inc).20 Two phase 2 studies assessing the safety and therapeutic efficacy of PH-10 in psoriasis (NCT01247818, NCT00941278) have been completed; results were not available at the time of publication.
STF115469 (Vitamin D Analogue)
STF115469 (GlaxoSmithKline) is a calcipotriene foam. At the time of publication, a randomized, placebo-controlled, double-blind, phase 3 trial (NCT01582932) of this vitamin D3 analogue with a projected enrollment of 180 participants was actively recruiting patients aged 2 to 11 years with mild to moderate plaque psoriasis to study the efficacy, safety, and tolerability of STF115469, as well as its pharmacokinetics and pharmacodynamics.
WBI-1001 (Proprietary Product)
WBI-1001 (Welichem Biotech Inc), or 2-isopropyl-5-[(E)-2-phenylethenyl] benzene-1, 3-diol, is a novel proprietary agent that inhibits proinflammatory cytokines (eg, IFN-γ, TNF-α). A randomized, placebo-controlled, double-blind, phase 1 trial (NCT00830817) assessing the efficacy, safety, tolerability, and pharmacokinetics of WBI-1001 has been completed; results were not available at the time of publication. Another randomized, placebo-controlled, double-blind, phase 2 trial (NCT01098721) evaluating its efficacy and safety according to the physician’s global assessment demonstrated a therapeutic benefit of 62.8% in patients treated with WBI-1001 cream 1% versus 13.0% in those treated with a placebo after a 12-week treatment period (P<.0001).21 WBI-1001 may offer a novel approach in the treatment of mild to moderate psoriasis.
Conclusion
Enhanced knowledge of the underlying pathogeneses of psoriasis and psoriatic arthritis has identified new therapeutic targets and enabled the development of exciting novel treatments for these conditions. The topical agents currently in phase 2 and phase 3 clinical trials show promise in enhancing the way physicians treat psoriasis. There is hope for more individualized treatment regimens with improved tolerability and better safety profiles with increased therapeutic efficacy. As our understanding of the molecular underpinnings of psoriasis continues to deepen, it will afford the development of even more innovative therapeutics for use in the management of psoriasis.
1. Mason A, Mason J, Cork M, et al. Topical treatments for chronic plaque psoriasis: an abridged Cochrane systematic review. J Am Acad Dermatol. 2013;69:799-807.
2. Nazarian R, Weinberg JM. AN-2728, a PDE4 inhibitor for the potential topical treatment of psoriasis and atopic dermatitis. Curr Opin Investig Drugs. 2009;10:1236-1242.
3. Moustafa F, Feldman SR. A review of phosphodiesterase-inhibition and the potential role for phosphodiesterase 4-inhibitors in clinical dermatology. Dermatol Online J. 2014;20:22608.
4. Halpert G, Sredni B. The effect of the novel tellurium compound AS101 on autoimmune diseases. Autoimmun Rev. 2014;13:1230-1235.
5. Ports WC, Khan S, Lan S, et al. A randomized phase 2a efficacy and safety trial of the topical Janus kinase inhibitor tofacitinib in the treatment of chronic plaque psoriasis. Br J Dermatol. 2013;169:137-145.
6. Yosipovitch G, Roblin D, Traversa S, et al. A novel topical targeted anti-pruritic treatment in phase 2b development for chronic pruritus. Paper presented at: 72nd Annual Meeting of the American Academy of Dermatology; March 21-25, 2014; Denver, CO.
7. Kang S, Yi S, Griffiths CE, et al. Calcipotriene-induced improvement in psoriasis is associated with reduced interleukin-8 and increased interleukin-10 levels within lesions. Br J Dermatol. 1998;138:77-83.
8. Kristl J, Slanc P, Krasna M, et al. Calcipotriol affects keratinocyte proliferation by decreasing expression of early growth response-1 and polo-like kinase-2. Pharm Res. 2008;25:521-529.
9. Tiberio R, Bozzo C, Pertusi G, et al. Calcipotriol induces apoptosis in psoriatic keratinocytes. Clin Exp Dermatol. 2009;34:e972-e974.
10. Luger T, Seite S, Humbert P, et al. Recommendations for adjunctive basic skin care in patients with psoriasis. Eur J Dermatol. 2014;24:194-200.
11. Dermipsor reports good results in DPS-101 Phase IIb study for plaque psoriasis [press release]. Evaluate Web site. http://www.evaluategroup.com/Universal/View.aspx?type=Story&id=250042. Published October 15, 2007. Accessed February 13, 2015.
12. Rivera AM, Hsu S. Topical halobetasol propionate in the treatment of plaque psoriasis: a review. Am J Clin Dermatol. 2005;6:311-316.
13. Punwani N, Scherle P, Flores R, et al. Preliminary clinical activity of a topical JAK1/2 inhibitor in the treatment of psoriasis. J Am Acad Dermatol. 2012;67:658-664.
14. Efficacy and safety of calcipotriol plus hydrocortisone ointment compared with tacalcitol ointment in patients with psoriasis on the face and skin folds (NCT00640822). https://clinicaltrials.gov/ct2/show/results/NCT00640822?term=NCT00640822&rank=1. Updated October 21, 2013. Accessed May 30, 2014.
15. Product candidates: targeting p-STAT3 for improved psoriasis treatment. Moleculin Web site. http://moleculin.com/product-candidates/mol4239. Accessed February 13, 2015.
16. Chowdhari S, Saini N. hsa-miR-4516 mediated downregulation of STAT3/CDK6/UBE2N plays a role in PUVA induced apoptosis in keratinocytes. J Cell Physiol. 2014;229:1630-1638.
17. Paired psoriasis lesion, comparative, study to evaluate MOL4239 in psoriasis (NCT01826201). https://clinicaltrials.gov/ct2/show/results/NCT01826201?term=NCT01826201&rank=1§=X01256#all. Updated December 22, 2014. Accessed February 25, 2015.
18. Clinical development pipeline. Moleculin Web site. http://moleculin.com/clinical-trials/psoriasis-trials. Accessed February 13, 2015.
19. de la Brassinne M, Nikkels A. Psoriasis: state of the art 2013. Acta Clin Belg. 2013;68:433-441.
20. Ross MI. Intralesional therapy with PV-10 (Rose Bengal) for in-transit melanoma. J Surg Oncol. 2014;109:314-319.
21. Bissonnette R, Bolduc C, Maari C, et al. Efficacy and safety of topical WBI-1001 in patients with mild to moderate psoriasis: results from a randomized, double-blind placebo-controlled, phase II trial. J Eur Acad Dermatol Venereol. 2012;26:1516-1521.
Topical therapies are a mainstay in the management of patients with mild to moderate psoriasis (Figure). Presently, US Food and Drug Administration–approved topical medications that are commercially available for use in patients with psoriasis include corticosteroids, vitamin D3 analogues, calcineurin inhibitors, retinoids, anthralin, and tar-based formulations.1 In recent years, research has furthered our understanding of the molecular mechanisms underlying the pathogenesis of psoriasis and has afforded the development of more targeted therapies. Novel topical medications currently in phase 2 and phase 3 clinical trials are discussed in this article, and a summary is provided in the Table.
AN2728 (Phosphodiesterase 4 Inhibitor)
AN2728 (Anacor Pharmaceuticals, Inc) is a phosphodiesterase 4 inhibitor that blocks the inactivation of cyclic adenosine monophosphate, resulting in decreased production of inflammatory cytokines (eg, IL-6, IL-12, IL-23, tumor necrosis factor α [TNF-α]).2,3 In a randomized, double-blind, phase 2 clinical trial (N=35), 40% of patients treated with AN2728 ointment 5% reported improvement of more than 2 points in overall target plaque severity score versus 6% of patients treated with vehicle. In another randomized, double-blind, dose-response trial of 145 patients, those treated with AN2728 ointment 2% twice daily reported a 60% improvement versus 40% improvement in those treated with AN2728 ointment 0.5% once daily.3 In total, 3 phase 1 trials (registered at www.clinicaltrials.gov with the identifiers NCT01258088, NCT00762658, NCT00763204) and 4 phase 2 trials (NCT01029405, NCT00755196, NCT00759161, NCT01300052) have been completed; results were not available at the time of publication.
AS101 (Integrin Inhibitor)
AS101 (BioMAS Ltd), or ammonium trichloro (dioxoethylene-o,o') tellurate, acts as stimulator of regulatory T cells and a redox modulator inhibiting the leukocyte integrins α4β1 and α4β7 that enable CD4+ T-cell and macrophage extravasation; it also limits expression of the inflammatory cytokines IL-6 and IL-17.4 A randomized, placebo-controlled, double-blind, phase 2 study evaluating the efficacy of AS101 cream 4% twice daily for 12 weeks was withdrawn prior to enrollment (NCT00788424).
Tofacitinib (Janus Kinase 1 and 3 Inhibitor)
Tofacitinib (formerly known as CP-690,550)(Pfizer Inc) is a selective Janus kinase (Jak) 1 and Jak3 inhibitor that limits expression of cytokines that promote inflammation (eg, IFN-γ) and inhibits helper T cells (TH17) by downregulating expression of the IL-23 receptor. Epidermal keratinocyte proliferation in psoriasis is activated by TH17 cells that release IL-17 as well as TH1 cells that release IFN-γ and tumor necrosis factor. A phase 2a trial showed statistically significant improvement from baseline in the target plaque severity score for tofacitinib ointment 2% (least squares mean, −54.4%) versus vehicle (least squares mean, −41.5%).5 Two other phase 2 trials (NCT01246583, NCT00678561) assessing the efficacy, safety, tolerability, and pharmacokinetics of tofacitinib ointment in patients with mild to moderate psoriasis have been completed; results were not available at the time of publication. A phase 2b study that compared 2 dose strengths of tofacitinib ointment—10 mg/g and 20 mg/g—versus placebo over a 12-week period also was completed (NCT01831466); results were not available at the time of publication.
CT327 (Tyrosine Kinase Inhibitor)
CT327 (Creabilis SA) is a tyrosine kinase A (TrkA) inhibitor that affords a novel perspective in the treatment of pruritus by shifting the focus to sensory neurons. In a phase 2b study of 160 patients, a 60% change in the visual analog scale was noted at 8 weeks in the treatment group versus 21% in the placebo group.6 Two other phase 2 studies have been completed, one with a cream formulation of pegylated K252a (NCT00995969) and another with an ointment formulation (NCT01465282); results were not available at the time of publication.
DPS-101 (Vitamin D Analogue)
DPS-101 (Dermipsor Ltd) is a combination of calcipotriol and niacinamide. Calcipotriol is a vitamin D3 analogue that increases IL-10 expression while decreasing IL-8 expression.7 It curbs epidermal keratinocyte proliferation by limiting the expression of polo-like kinase 2 and early growth response-1.8 It also may induce keratinocyte apoptosis.9 Niacinamide is the amide of vitamin B3 and inhibits proinflammatory cytokines such as TNF-α, IL-1β, IL-6, and IL-8.10 In a dose-response phase 2b trial of 168 patients, DPS-101 demonstrated better results than either calcipotriol or niacinamide alone.11
IDP-118 (Proprietary Steroid and Retinoid Combination)
IDP-118 (Valeant Pharmaceuticals International, Inc) is a combination of halobetasol propionate (HP) 0.01% (a topical corticosteroid) and tazar-otene 0.045% (a selective topical retinoid) in a lotion formulation. In isolation, tazarotene is as effective as a mid to highly potent corticosteroid, but irritation may limit its tolerability. The use of combination treatments of mid to highly potent corticosteroids and tazarotene has shown enhanced tolerability and therapeutic efficacy.12 Ongoing studies include a phase 1 trial and a phase 2 trial to evaluate low- and high-strength preparations of IDP-118, respectively (NCT01670513). Another phase 2 trial evaluating the efficacy and safety of IDP-118 lotion (HP 0.01% and tazarotene 0.045%) versus IDP-118 monad HP 0.01% lotion, IDP-118 monad tazar-otene 0.045% lotion, and placebo has been completed (NCT02045277); results were not available at the time of publication.
Ruxolitinib (Jak1 and Jak2 Inhibitor)
Ruxolitinib (formerly known as INCB18424)(Incyte Corporation) is a selective Jak1 and Jak2 inhibitor. A phase 2 trial of ruxolitinib showed a 53% decline in the score for mean total lesions in patients treated with ruxolitinib phosphate cream 1% (P=.033) versus 54% in those treated with ruxolitinib phosphate cream 1.5% (P=.056) and 32% in those treated with placebo.13 Three other phase 2 studies (NCT00617994, NCT00820950, NCT00778700) have been completed; results were not available at the time of publication.
LAS41004 (Proprietary Steroid and Retinoid Combination)
LAS41004 (Almirall, SA) is an ointment containing the corticosteroid betamethasone dipropionate and the retinoid bexarotene that is being evaluated for treatment of mild to moderate psoriasis. Five phase 2 studies (NCT01119339, NCT01283698, NCT01360944, NCT02111499, NCT01462643) have been completed; results were not available at the time of publication. A randomized, double-blind, phase 2a study (NCT02180464) with a left-right design assessing clinical response to LAS41004 versus control in patients with mild to moderate psoriasis was actively recruiting at the time of publication.
LEO 80190 (Vitamin D3 Analogue and Steroid Combination)
LEO 80190 (LEO Pharma) is a combination of the vitamin D3 analogue calcipotriol and the corticosteroid hydrocortisone. It was developed as a treatment for sensitive areas such as the face and intertriginous regions. A randomized, investigator-blind, phase 3 trial (NCT00640822) of LEO 80190 ointment versus tacalcitol ointment and placebo once daily for 8 weeks demonstrated controlled disease of the face in 56.8% (183/322) of patients in the LEO 80190 group, 46.4% (147/317) in the tacalcitol group, and 36.3% (37/102) in the placebo group.14 Another phase 2 study (NCT00704262) and 2 phase 3 studies (NCT00691002, NCT01007591) have been completed; results were not available at the time of publication.
LEO 90100 (Vitamin D Analogue and Steroid Combination)
LEO 90100 (LEO Pharma) contains the vitamin D3 analogue calcipotriol and the corticosteroid betamethasone. Three phase 2 studies (NCT01347255, NCT01536886, NCT01536938) and a phase 3 study (NCT01866163) examining the efficacy and safety of various vehicles and formulations of LEO 90100 have been completed; results were not available at the time of publication. Another phase 3 study (NCT02132936) is ongoing but not recruiting participants. Other completed studies whose results were not yet available include a phase 1 pharmacodynamic study (NCT01946386), a phase 1 study that used patch testing to assess the degree of skin irritation and sensitization associated with LEO 90100 (NCT01935869), and a phase 2 study examining the impact of LEO 90100 on calcium metabolism and the hypothalamic-pituitary-adrenal axis (NCT01600222).
M518101 (Vitamin D Analogue)
M518101 (Maruho Co, Ltd) is a novel topical vitamin D3 analogue. Phase 1 (NCT01844973) and phase 2 (NCT01301157, NCT00884169) trials evaluating the safety, pharmacokinetics, and efficacy of M518101 have been completed; results were not available at the time of publication. A phase 3 study (NCT01989429) assessing the safety and therapeutic efficacy of M518101 according to changes in the modified psoriasis area and severity index over an 8-week treatment period also has been completed; results were not yet available. Three phase 3 studies assessing the safety and therapeutic efficacy of M518101 are ongoing: one is currently closed to recruitment (NCT01908595) and 2 are actively recruiting participants at the time of publication (NCT01878461, NCT01873677).
MOL4239 and MOL4249 (Phosphorylated Signal Transducer and Activator of Transcription 3 Inhibitors)
MOL4239 (Moleculin, LLC) is a novel topical agent for use in mild to moderate psoriasis that acts via phosphorylated signal transducer and activator of transcription 3 (p-STAT3) inhibition.15 The p-STAT3 protein has increased expression in psoriasis.16 A phase 2 trial of MOL4239 ointment (NCT01826201) has been completed, showing a greater mean (standard deviation) change in the psoriasis severity score in lesions treated at 28 days with MOL4239 ointment 10% (−1.9 [1.45]) versus lesions treated with placebo ointment (−1.5 [1.87]).17
MOL4249 (Moleculin, LLC) is more potent than MOL4239 with better lipid solubility. In the MOL4249 subset of a placebo-controlled, double-blind, phase 2a study of 16 patients with mild to moderate psoriasis, 10% (1/10) of patients experienced complete clearance of psoriatic plaques, 30% (3/10) of patients experienced 75% or greater improvement, and 50% (5/10) of patients experienced 50% or greater improvement compared to 17% (1/6) in the placebo group. Currently, a phase 2a contralateral study, a phase 2b psoriasis area and severity index trial, and a phase 3 pivotal trial are planned, according to the manufacturer.18
MQX-5902 (Dihydrofolate Reductase Inhibitor)
MQX-5902 (MediQuest Therapeutics) is a topical preparation of methotrexate for the treatment of fingernail psoriasis. Methotrexate is a dihydrofolate reductase inhibitor and antimetabolite that inhibits folic acid metabolism, thereby disrupting DNA synthesis.19 A phase 2b dose-ranging trial (NCT00666354) was designed to assess the therapeutic efficacy and safety of MQX-5902 delivered via a proprietary drug delivery formulation in fingernail psoriasis; the outcome of this trial was not available at the time of publication.
PH-10 (Xanthine Dye)
PH-10 (Provectus Biopharmaceuticals, Inc) is a topical aqueous hydrogel derived from rose bengal disodium that may be beneficial in treating skin conditions such as atopic dermatitis and mild to moderate psoriasis. Rose bengal disodium is a hydrophilic xanthine dye with diagnostic utility in ophthalmology and gastroenterology as well as projected use as a melanoma treatment as demonstrated in phase 1 and phase 2 clinical trials of PV-10 (Provectus Biopharmaceuticals, Inc).20 Two phase 2 studies assessing the safety and therapeutic efficacy of PH-10 in psoriasis (NCT01247818, NCT00941278) have been completed; results were not available at the time of publication.
STF115469 (Vitamin D Analogue)
STF115469 (GlaxoSmithKline) is a calcipotriene foam. At the time of publication, a randomized, placebo-controlled, double-blind, phase 3 trial (NCT01582932) of this vitamin D3 analogue with a projected enrollment of 180 participants was actively recruiting patients aged 2 to 11 years with mild to moderate plaque psoriasis to study the efficacy, safety, and tolerability of STF115469, as well as its pharmacokinetics and pharmacodynamics.
WBI-1001 (Proprietary Product)
WBI-1001 (Welichem Biotech Inc), or 2-isopropyl-5-[(E)-2-phenylethenyl] benzene-1, 3-diol, is a novel proprietary agent that inhibits proinflammatory cytokines (eg, IFN-γ, TNF-α). A randomized, placebo-controlled, double-blind, phase 1 trial (NCT00830817) assessing the efficacy, safety, tolerability, and pharmacokinetics of WBI-1001 has been completed; results were not available at the time of publication. Another randomized, placebo-controlled, double-blind, phase 2 trial (NCT01098721) evaluating its efficacy and safety according to the physician’s global assessment demonstrated a therapeutic benefit of 62.8% in patients treated with WBI-1001 cream 1% versus 13.0% in those treated with a placebo after a 12-week treatment period (P<.0001).21 WBI-1001 may offer a novel approach in the treatment of mild to moderate psoriasis.
Conclusion
Enhanced knowledge of the underlying pathogeneses of psoriasis and psoriatic arthritis has identified new therapeutic targets and enabled the development of exciting novel treatments for these conditions. The topical agents currently in phase 2 and phase 3 clinical trials show promise in enhancing the way physicians treat psoriasis. There is hope for more individualized treatment regimens with improved tolerability and better safety profiles with increased therapeutic efficacy. As our understanding of the molecular underpinnings of psoriasis continues to deepen, it will afford the development of even more innovative therapeutics for use in the management of psoriasis.
Topical therapies are a mainstay in the management of patients with mild to moderate psoriasis (Figure). Presently, US Food and Drug Administration–approved topical medications that are commercially available for use in patients with psoriasis include corticosteroids, vitamin D3 analogues, calcineurin inhibitors, retinoids, anthralin, and tar-based formulations.1 In recent years, research has furthered our understanding of the molecular mechanisms underlying the pathogenesis of psoriasis and has afforded the development of more targeted therapies. Novel topical medications currently in phase 2 and phase 3 clinical trials are discussed in this article, and a summary is provided in the Table.
AN2728 (Phosphodiesterase 4 Inhibitor)
AN2728 (Anacor Pharmaceuticals, Inc) is a phosphodiesterase 4 inhibitor that blocks the inactivation of cyclic adenosine monophosphate, resulting in decreased production of inflammatory cytokines (eg, IL-6, IL-12, IL-23, tumor necrosis factor α [TNF-α]).2,3 In a randomized, double-blind, phase 2 clinical trial (N=35), 40% of patients treated with AN2728 ointment 5% reported improvement of more than 2 points in overall target plaque severity score versus 6% of patients treated with vehicle. In another randomized, double-blind, dose-response trial of 145 patients, those treated with AN2728 ointment 2% twice daily reported a 60% improvement versus 40% improvement in those treated with AN2728 ointment 0.5% once daily.3 In total, 3 phase 1 trials (registered at www.clinicaltrials.gov with the identifiers NCT01258088, NCT00762658, NCT00763204) and 4 phase 2 trials (NCT01029405, NCT00755196, NCT00759161, NCT01300052) have been completed; results were not available at the time of publication.
AS101 (Integrin Inhibitor)
AS101 (BioMAS Ltd), or ammonium trichloro (dioxoethylene-o,o') tellurate, acts as stimulator of regulatory T cells and a redox modulator inhibiting the leukocyte integrins α4β1 and α4β7 that enable CD4+ T-cell and macrophage extravasation; it also limits expression of the inflammatory cytokines IL-6 and IL-17.4 A randomized, placebo-controlled, double-blind, phase 2 study evaluating the efficacy of AS101 cream 4% twice daily for 12 weeks was withdrawn prior to enrollment (NCT00788424).
Tofacitinib (Janus Kinase 1 and 3 Inhibitor)
Tofacitinib (formerly known as CP-690,550)(Pfizer Inc) is a selective Janus kinase (Jak) 1 and Jak3 inhibitor that limits expression of cytokines that promote inflammation (eg, IFN-γ) and inhibits helper T cells (TH17) by downregulating expression of the IL-23 receptor. Epidermal keratinocyte proliferation in psoriasis is activated by TH17 cells that release IL-17 as well as TH1 cells that release IFN-γ and tumor necrosis factor. A phase 2a trial showed statistically significant improvement from baseline in the target plaque severity score for tofacitinib ointment 2% (least squares mean, −54.4%) versus vehicle (least squares mean, −41.5%).5 Two other phase 2 trials (NCT01246583, NCT00678561) assessing the efficacy, safety, tolerability, and pharmacokinetics of tofacitinib ointment in patients with mild to moderate psoriasis have been completed; results were not available at the time of publication. A phase 2b study that compared 2 dose strengths of tofacitinib ointment—10 mg/g and 20 mg/g—versus placebo over a 12-week period also was completed (NCT01831466); results were not available at the time of publication.
CT327 (Tyrosine Kinase Inhibitor)
CT327 (Creabilis SA) is a tyrosine kinase A (TrkA) inhibitor that affords a novel perspective in the treatment of pruritus by shifting the focus to sensory neurons. In a phase 2b study of 160 patients, a 60% change in the visual analog scale was noted at 8 weeks in the treatment group versus 21% in the placebo group.6 Two other phase 2 studies have been completed, one with a cream formulation of pegylated K252a (NCT00995969) and another with an ointment formulation (NCT01465282); results were not available at the time of publication.
DPS-101 (Vitamin D Analogue)
DPS-101 (Dermipsor Ltd) is a combination of calcipotriol and niacinamide. Calcipotriol is a vitamin D3 analogue that increases IL-10 expression while decreasing IL-8 expression.7 It curbs epidermal keratinocyte proliferation by limiting the expression of polo-like kinase 2 and early growth response-1.8 It also may induce keratinocyte apoptosis.9 Niacinamide is the amide of vitamin B3 and inhibits proinflammatory cytokines such as TNF-α, IL-1β, IL-6, and IL-8.10 In a dose-response phase 2b trial of 168 patients, DPS-101 demonstrated better results than either calcipotriol or niacinamide alone.11
IDP-118 (Proprietary Steroid and Retinoid Combination)
IDP-118 (Valeant Pharmaceuticals International, Inc) is a combination of halobetasol propionate (HP) 0.01% (a topical corticosteroid) and tazar-otene 0.045% (a selective topical retinoid) in a lotion formulation. In isolation, tazarotene is as effective as a mid to highly potent corticosteroid, but irritation may limit its tolerability. The use of combination treatments of mid to highly potent corticosteroids and tazarotene has shown enhanced tolerability and therapeutic efficacy.12 Ongoing studies include a phase 1 trial and a phase 2 trial to evaluate low- and high-strength preparations of IDP-118, respectively (NCT01670513). Another phase 2 trial evaluating the efficacy and safety of IDP-118 lotion (HP 0.01% and tazarotene 0.045%) versus IDP-118 monad HP 0.01% lotion, IDP-118 monad tazar-otene 0.045% lotion, and placebo has been completed (NCT02045277); results were not available at the time of publication.
Ruxolitinib (Jak1 and Jak2 Inhibitor)
Ruxolitinib (formerly known as INCB18424)(Incyte Corporation) is a selective Jak1 and Jak2 inhibitor. A phase 2 trial of ruxolitinib showed a 53% decline in the score for mean total lesions in patients treated with ruxolitinib phosphate cream 1% (P=.033) versus 54% in those treated with ruxolitinib phosphate cream 1.5% (P=.056) and 32% in those treated with placebo.13 Three other phase 2 studies (NCT00617994, NCT00820950, NCT00778700) have been completed; results were not available at the time of publication.
LAS41004 (Proprietary Steroid and Retinoid Combination)
LAS41004 (Almirall, SA) is an ointment containing the corticosteroid betamethasone dipropionate and the retinoid bexarotene that is being evaluated for treatment of mild to moderate psoriasis. Five phase 2 studies (NCT01119339, NCT01283698, NCT01360944, NCT02111499, NCT01462643) have been completed; results were not available at the time of publication. A randomized, double-blind, phase 2a study (NCT02180464) with a left-right design assessing clinical response to LAS41004 versus control in patients with mild to moderate psoriasis was actively recruiting at the time of publication.
LEO 80190 (Vitamin D3 Analogue and Steroid Combination)
LEO 80190 (LEO Pharma) is a combination of the vitamin D3 analogue calcipotriol and the corticosteroid hydrocortisone. It was developed as a treatment for sensitive areas such as the face and intertriginous regions. A randomized, investigator-blind, phase 3 trial (NCT00640822) of LEO 80190 ointment versus tacalcitol ointment and placebo once daily for 8 weeks demonstrated controlled disease of the face in 56.8% (183/322) of patients in the LEO 80190 group, 46.4% (147/317) in the tacalcitol group, and 36.3% (37/102) in the placebo group.14 Another phase 2 study (NCT00704262) and 2 phase 3 studies (NCT00691002, NCT01007591) have been completed; results were not available at the time of publication.
LEO 90100 (Vitamin D Analogue and Steroid Combination)
LEO 90100 (LEO Pharma) contains the vitamin D3 analogue calcipotriol and the corticosteroid betamethasone. Three phase 2 studies (NCT01347255, NCT01536886, NCT01536938) and a phase 3 study (NCT01866163) examining the efficacy and safety of various vehicles and formulations of LEO 90100 have been completed; results were not available at the time of publication. Another phase 3 study (NCT02132936) is ongoing but not recruiting participants. Other completed studies whose results were not yet available include a phase 1 pharmacodynamic study (NCT01946386), a phase 1 study that used patch testing to assess the degree of skin irritation and sensitization associated with LEO 90100 (NCT01935869), and a phase 2 study examining the impact of LEO 90100 on calcium metabolism and the hypothalamic-pituitary-adrenal axis (NCT01600222).
M518101 (Vitamin D Analogue)
M518101 (Maruho Co, Ltd) is a novel topical vitamin D3 analogue. Phase 1 (NCT01844973) and phase 2 (NCT01301157, NCT00884169) trials evaluating the safety, pharmacokinetics, and efficacy of M518101 have been completed; results were not available at the time of publication. A phase 3 study (NCT01989429) assessing the safety and therapeutic efficacy of M518101 according to changes in the modified psoriasis area and severity index over an 8-week treatment period also has been completed; results were not yet available. Three phase 3 studies assessing the safety and therapeutic efficacy of M518101 are ongoing: one is currently closed to recruitment (NCT01908595) and 2 are actively recruiting participants at the time of publication (NCT01878461, NCT01873677).
MOL4239 and MOL4249 (Phosphorylated Signal Transducer and Activator of Transcription 3 Inhibitors)
MOL4239 (Moleculin, LLC) is a novel topical agent for use in mild to moderate psoriasis that acts via phosphorylated signal transducer and activator of transcription 3 (p-STAT3) inhibition.15 The p-STAT3 protein has increased expression in psoriasis.16 A phase 2 trial of MOL4239 ointment (NCT01826201) has been completed, showing a greater mean (standard deviation) change in the psoriasis severity score in lesions treated at 28 days with MOL4239 ointment 10% (−1.9 [1.45]) versus lesions treated with placebo ointment (−1.5 [1.87]).17
MOL4249 (Moleculin, LLC) is more potent than MOL4239 with better lipid solubility. In the MOL4249 subset of a placebo-controlled, double-blind, phase 2a study of 16 patients with mild to moderate psoriasis, 10% (1/10) of patients experienced complete clearance of psoriatic plaques, 30% (3/10) of patients experienced 75% or greater improvement, and 50% (5/10) of patients experienced 50% or greater improvement compared to 17% (1/6) in the placebo group. Currently, a phase 2a contralateral study, a phase 2b psoriasis area and severity index trial, and a phase 3 pivotal trial are planned, according to the manufacturer.18
MQX-5902 (Dihydrofolate Reductase Inhibitor)
MQX-5902 (MediQuest Therapeutics) is a topical preparation of methotrexate for the treatment of fingernail psoriasis. Methotrexate is a dihydrofolate reductase inhibitor and antimetabolite that inhibits folic acid metabolism, thereby disrupting DNA synthesis.19 A phase 2b dose-ranging trial (NCT00666354) was designed to assess the therapeutic efficacy and safety of MQX-5902 delivered via a proprietary drug delivery formulation in fingernail psoriasis; the outcome of this trial was not available at the time of publication.
PH-10 (Xanthine Dye)
PH-10 (Provectus Biopharmaceuticals, Inc) is a topical aqueous hydrogel derived from rose bengal disodium that may be beneficial in treating skin conditions such as atopic dermatitis and mild to moderate psoriasis. Rose bengal disodium is a hydrophilic xanthine dye with diagnostic utility in ophthalmology and gastroenterology as well as projected use as a melanoma treatment as demonstrated in phase 1 and phase 2 clinical trials of PV-10 (Provectus Biopharmaceuticals, Inc).20 Two phase 2 studies assessing the safety and therapeutic efficacy of PH-10 in psoriasis (NCT01247818, NCT00941278) have been completed; results were not available at the time of publication.
STF115469 (Vitamin D Analogue)
STF115469 (GlaxoSmithKline) is a calcipotriene foam. At the time of publication, a randomized, placebo-controlled, double-blind, phase 3 trial (NCT01582932) of this vitamin D3 analogue with a projected enrollment of 180 participants was actively recruiting patients aged 2 to 11 years with mild to moderate plaque psoriasis to study the efficacy, safety, and tolerability of STF115469, as well as its pharmacokinetics and pharmacodynamics.
WBI-1001 (Proprietary Product)
WBI-1001 (Welichem Biotech Inc), or 2-isopropyl-5-[(E)-2-phenylethenyl] benzene-1, 3-diol, is a novel proprietary agent that inhibits proinflammatory cytokines (eg, IFN-γ, TNF-α). A randomized, placebo-controlled, double-blind, phase 1 trial (NCT00830817) assessing the efficacy, safety, tolerability, and pharmacokinetics of WBI-1001 has been completed; results were not available at the time of publication. Another randomized, placebo-controlled, double-blind, phase 2 trial (NCT01098721) evaluating its efficacy and safety according to the physician’s global assessment demonstrated a therapeutic benefit of 62.8% in patients treated with WBI-1001 cream 1% versus 13.0% in those treated with a placebo after a 12-week treatment period (P<.0001).21 WBI-1001 may offer a novel approach in the treatment of mild to moderate psoriasis.
Conclusion
Enhanced knowledge of the underlying pathogeneses of psoriasis and psoriatic arthritis has identified new therapeutic targets and enabled the development of exciting novel treatments for these conditions. The topical agents currently in phase 2 and phase 3 clinical trials show promise in enhancing the way physicians treat psoriasis. There is hope for more individualized treatment regimens with improved tolerability and better safety profiles with increased therapeutic efficacy. As our understanding of the molecular underpinnings of psoriasis continues to deepen, it will afford the development of even more innovative therapeutics for use in the management of psoriasis.
1. Mason A, Mason J, Cork M, et al. Topical treatments for chronic plaque psoriasis: an abridged Cochrane systematic review. J Am Acad Dermatol. 2013;69:799-807.
2. Nazarian R, Weinberg JM. AN-2728, a PDE4 inhibitor for the potential topical treatment of psoriasis and atopic dermatitis. Curr Opin Investig Drugs. 2009;10:1236-1242.
3. Moustafa F, Feldman SR. A review of phosphodiesterase-inhibition and the potential role for phosphodiesterase 4-inhibitors in clinical dermatology. Dermatol Online J. 2014;20:22608.
4. Halpert G, Sredni B. The effect of the novel tellurium compound AS101 on autoimmune diseases. Autoimmun Rev. 2014;13:1230-1235.
5. Ports WC, Khan S, Lan S, et al. A randomized phase 2a efficacy and safety trial of the topical Janus kinase inhibitor tofacitinib in the treatment of chronic plaque psoriasis. Br J Dermatol. 2013;169:137-145.
6. Yosipovitch G, Roblin D, Traversa S, et al. A novel topical targeted anti-pruritic treatment in phase 2b development for chronic pruritus. Paper presented at: 72nd Annual Meeting of the American Academy of Dermatology; March 21-25, 2014; Denver, CO.
7. Kang S, Yi S, Griffiths CE, et al. Calcipotriene-induced improvement in psoriasis is associated with reduced interleukin-8 and increased interleukin-10 levels within lesions. Br J Dermatol. 1998;138:77-83.
8. Kristl J, Slanc P, Krasna M, et al. Calcipotriol affects keratinocyte proliferation by decreasing expression of early growth response-1 and polo-like kinase-2. Pharm Res. 2008;25:521-529.
9. Tiberio R, Bozzo C, Pertusi G, et al. Calcipotriol induces apoptosis in psoriatic keratinocytes. Clin Exp Dermatol. 2009;34:e972-e974.
10. Luger T, Seite S, Humbert P, et al. Recommendations for adjunctive basic skin care in patients with psoriasis. Eur J Dermatol. 2014;24:194-200.
11. Dermipsor reports good results in DPS-101 Phase IIb study for plaque psoriasis [press release]. Evaluate Web site. http://www.evaluategroup.com/Universal/View.aspx?type=Story&id=250042. Published October 15, 2007. Accessed February 13, 2015.
12. Rivera AM, Hsu S. Topical halobetasol propionate in the treatment of plaque psoriasis: a review. Am J Clin Dermatol. 2005;6:311-316.
13. Punwani N, Scherle P, Flores R, et al. Preliminary clinical activity of a topical JAK1/2 inhibitor in the treatment of psoriasis. J Am Acad Dermatol. 2012;67:658-664.
14. Efficacy and safety of calcipotriol plus hydrocortisone ointment compared with tacalcitol ointment in patients with psoriasis on the face and skin folds (NCT00640822). https://clinicaltrials.gov/ct2/show/results/NCT00640822?term=NCT00640822&rank=1. Updated October 21, 2013. Accessed May 30, 2014.
15. Product candidates: targeting p-STAT3 for improved psoriasis treatment. Moleculin Web site. http://moleculin.com/product-candidates/mol4239. Accessed February 13, 2015.
16. Chowdhari S, Saini N. hsa-miR-4516 mediated downregulation of STAT3/CDK6/UBE2N plays a role in PUVA induced apoptosis in keratinocytes. J Cell Physiol. 2014;229:1630-1638.
17. Paired psoriasis lesion, comparative, study to evaluate MOL4239 in psoriasis (NCT01826201). https://clinicaltrials.gov/ct2/show/results/NCT01826201?term=NCT01826201&rank=1§=X01256#all. Updated December 22, 2014. Accessed February 25, 2015.
18. Clinical development pipeline. Moleculin Web site. http://moleculin.com/clinical-trials/psoriasis-trials. Accessed February 13, 2015.
19. de la Brassinne M, Nikkels A. Psoriasis: state of the art 2013. Acta Clin Belg. 2013;68:433-441.
20. Ross MI. Intralesional therapy with PV-10 (Rose Bengal) for in-transit melanoma. J Surg Oncol. 2014;109:314-319.
21. Bissonnette R, Bolduc C, Maari C, et al. Efficacy and safety of topical WBI-1001 in patients with mild to moderate psoriasis: results from a randomized, double-blind placebo-controlled, phase II trial. J Eur Acad Dermatol Venereol. 2012;26:1516-1521.
1. Mason A, Mason J, Cork M, et al. Topical treatments for chronic plaque psoriasis: an abridged Cochrane systematic review. J Am Acad Dermatol. 2013;69:799-807.
2. Nazarian R, Weinberg JM. AN-2728, a PDE4 inhibitor for the potential topical treatment of psoriasis and atopic dermatitis. Curr Opin Investig Drugs. 2009;10:1236-1242.
3. Moustafa F, Feldman SR. A review of phosphodiesterase-inhibition and the potential role for phosphodiesterase 4-inhibitors in clinical dermatology. Dermatol Online J. 2014;20:22608.
4. Halpert G, Sredni B. The effect of the novel tellurium compound AS101 on autoimmune diseases. Autoimmun Rev. 2014;13:1230-1235.
5. Ports WC, Khan S, Lan S, et al. A randomized phase 2a efficacy and safety trial of the topical Janus kinase inhibitor tofacitinib in the treatment of chronic plaque psoriasis. Br J Dermatol. 2013;169:137-145.
6. Yosipovitch G, Roblin D, Traversa S, et al. A novel topical targeted anti-pruritic treatment in phase 2b development for chronic pruritus. Paper presented at: 72nd Annual Meeting of the American Academy of Dermatology; March 21-25, 2014; Denver, CO.
7. Kang S, Yi S, Griffiths CE, et al. Calcipotriene-induced improvement in psoriasis is associated with reduced interleukin-8 and increased interleukin-10 levels within lesions. Br J Dermatol. 1998;138:77-83.
8. Kristl J, Slanc P, Krasna M, et al. Calcipotriol affects keratinocyte proliferation by decreasing expression of early growth response-1 and polo-like kinase-2. Pharm Res. 2008;25:521-529.
9. Tiberio R, Bozzo C, Pertusi G, et al. Calcipotriol induces apoptosis in psoriatic keratinocytes. Clin Exp Dermatol. 2009;34:e972-e974.
10. Luger T, Seite S, Humbert P, et al. Recommendations for adjunctive basic skin care in patients with psoriasis. Eur J Dermatol. 2014;24:194-200.
11. Dermipsor reports good results in DPS-101 Phase IIb study for plaque psoriasis [press release]. Evaluate Web site. http://www.evaluategroup.com/Universal/View.aspx?type=Story&id=250042. Published October 15, 2007. Accessed February 13, 2015.
12. Rivera AM, Hsu S. Topical halobetasol propionate in the treatment of plaque psoriasis: a review. Am J Clin Dermatol. 2005;6:311-316.
13. Punwani N, Scherle P, Flores R, et al. Preliminary clinical activity of a topical JAK1/2 inhibitor in the treatment of psoriasis. J Am Acad Dermatol. 2012;67:658-664.
14. Efficacy and safety of calcipotriol plus hydrocortisone ointment compared with tacalcitol ointment in patients with psoriasis on the face and skin folds (NCT00640822). https://clinicaltrials.gov/ct2/show/results/NCT00640822?term=NCT00640822&rank=1. Updated October 21, 2013. Accessed May 30, 2014.
15. Product candidates: targeting p-STAT3 for improved psoriasis treatment. Moleculin Web site. http://moleculin.com/product-candidates/mol4239. Accessed February 13, 2015.
16. Chowdhari S, Saini N. hsa-miR-4516 mediated downregulation of STAT3/CDK6/UBE2N plays a role in PUVA induced apoptosis in keratinocytes. J Cell Physiol. 2014;229:1630-1638.
17. Paired psoriasis lesion, comparative, study to evaluate MOL4239 in psoriasis (NCT01826201). https://clinicaltrials.gov/ct2/show/results/NCT01826201?term=NCT01826201&rank=1§=X01256#all. Updated December 22, 2014. Accessed February 25, 2015.
18. Clinical development pipeline. Moleculin Web site. http://moleculin.com/clinical-trials/psoriasis-trials. Accessed February 13, 2015.
19. de la Brassinne M, Nikkels A. Psoriasis: state of the art 2013. Acta Clin Belg. 2013;68:433-441.
20. Ross MI. Intralesional therapy with PV-10 (Rose Bengal) for in-transit melanoma. J Surg Oncol. 2014;109:314-319.
21. Bissonnette R, Bolduc C, Maari C, et al. Efficacy and safety of topical WBI-1001 in patients with mild to moderate psoriasis: results from a randomized, double-blind placebo-controlled, phase II trial. J Eur Acad Dermatol Venereol. 2012;26:1516-1521.
Practice Points
- Topical therapies are the cornerstone of treating patients with mild to moderate psoriasis. Commercially available medications approved by the US Food and Drug Administration for use in patients with psoriasis include corticosteroids, vitamin D3 analogues, calcineurin inhibitors, retinoids, anthralin, and tar-based formulations.
- Recent developments in our understanding of inflammatory mediators and the underlying pathogenesis of psoriasis have revealed new potential therapeutic targets, leading to the discovery of many promising treatments.
- Novel topical therapies currently in phase 2 and phase 3 clinical trials for patients with mild to moderate psoriasis may offer hope to patients who have reported a suboptimal therapeutic response to conventional treatments.
New Systemic Therapies for Psoriasis
Psoriasis is a common chronic inflammatory skin disease affecting 1% to 8% of the world population, depending on the country.1 Psoriasis can greatly impact quality of life in affected individuals, even in those with limited body surface involvement.2 Studies have demonstrated a high degree of psychological distress associated with psoriasis, leading to depression and poor self-esteem.3
Over the last decade, our improved understanding of the autoimmune inflammatory pathways and the associated changing concepts in psoriasis pathogenesis have led to the development of biological drugs targeting specific components of effector immune mechanisms, and these biological drugs have revolutionized the treatment of psoriasis.4 Although response rates of these biological agents are greater compared to those of conventional systemic drugs,5 current biological drugs fail to demonstrate efficacy in some patients or lose their efficacy over time. In addition to the high costs associated with these drugs, these limitations have driven a continued search for alternative therapies.
Helper T cells (TH17) and the proinflammatory cytokine IL-17 have been shown to play a key role in the pathophysiology of psoriasis, bridging innate and adaptive immune responses. IL-17 is involved in the modulation of proinflammatory cytokines, hematopoietic growth factors, antimicrobial peptides, and chemokines. Increased TH17 activity and high levels of IL-17 have been found in psoriatic plaques, and increased levels of TH17 are found in the plasma of psoriasis patients.6 Increased IL-17 induces neutrophilia, inflammation, and angiogenesis.7 Other cytokines that are highly upregulated in involved skin are tumor necrosis factor a (TNF-α), IL-23, IL-22, and IL-21.8 IL-23 is involved in regulating TH17 cells and is a potent activator of keratinocyte proliferation.9 Blockade of IL-12/23 causes downregulation of TH17 and TH22 cell responses.10 As IL-17 has a key role in protecting skin and mucous membranes from bacterial and fungal infections, IL-17 inhibition can potentially interfere with the inflammatory cascade. However, available data suggest that sufficient residual IL-17 activity remains to maintain immunity against infections.11
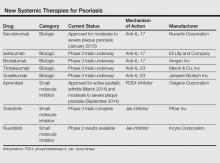
Currently approved biological agents for psoriasis target proinflammatory cytokines such as TNF-α, or the p40 subunit of IL-12 and IL-23. A number of novel targeted therapies including biologics as well as small molecule inhibitors targeting various cytokines and molecules involved in the pathogenesis of psoriasis are currently in different stages of development (Table). These drugs include 3 IL-17 inhibitors (secukinumab, ixekizumab, and brodalumab); 2 IL-23 blockers (tildrakizumab and guselkumab); and small molecule inhibitors that target the kinase pathway including apremilast (a phosphodiesterase 4 [PDE4] inhibitor), as well as tofacitinib, baricitinib, and ruxolitinib (Janus kinase [Jak] inhibitors). Small molecule inhibitors can be administered orally and are less expensive to produce than biological agents. This article reviews available data on these new systemic agents in the pipeline.
Novel Biologics
Secukinumab
Secukinumab is a fully human monoclonal IgG1k antibody that selectively binds and neutralizes IL-17A.12 It is the first of the IL-17 antibodies to receive approval for the treatment of moderate to severe psoriasis. In 2 phase 3, double-blind, 52-week trials—ERASURE (Efficacy of Response and Safety of Two Fixed Secukinumab Regimens in Psoriasis) and FIXTURE (Full Year Investigative Examination of Secukinumab vs Etanercept Using Two Dosing Regimens to Determine Efficacy in Psoriasis)—participants were randomly assigned to receive subcutaneous secukinumab at doses of 300 mg (n=245 and n=327, respectively) or 150 mg (n=245 and n=327, respectively) once weekly for 5 weeks then every 4 weeks, or placebo (n=248 and n=326, respectively); in the FIXTURE study only, an etanercept group (n=326) was given a 50-mg dose twice weekly for 12 weeks then once weekly.13
In the ERASURE study, the proportion of participants showing a reduction of 75% or more in psoriasis area and severity index (PASI) score from baseline to week 12 was 81.6% with secukinumab 300 mg, 71.6% with secukinumab 150 mg, and 4.5% with placebo.13 Secondary end point results demonstrated the proportion of participants showing a 90% reduction in PASI score was 59.2% with secukinumab 300 mg and 39.1% with secukinumab 150 mg, which were both superior to placebo (1.2%). The proportion of participants who met the criteria for 100% reduction in PASI score at week 12 also was greater with each secukinumab dose than with placebo.13
In the FIXTURE study, the proportion of participants showing a reduction of 75% or more from baseline in PASI score at week 12 was 77.1% with secukinumab 300 mg, 67.0% with secukinumab 150 mg, 44.0% with etanercept, and 4.9% with placebo.13 Secondary end point results demonstrated the proportion of participants showing a 90% reduction in PASI score was 54.2% with secukinumab 300 mg, 41.9% with secukinumab 150 mg, 20.7% with etanercept, and 1.5% with placebo. The speed of response, which was assessed as the median time to a 50% reduction in mean PASI score from baseline, was significantly shorter with both doses of secukinumab (3.0 weeks and 3.9 weeks, respectively) than with etanercept (7.0 weeks)(P<.001 for both).13
In the FIXTURE study, incidences of adverse events (AEs) were similar in the secukinumab and etanercept groups during both the induction period and the entire treatment period.13 The most common AEs in the secukinumab groups were nasopharyngitis, headache, and diarrhea. The rates of infections or infestations during the induction period were 26.7% with secukinumab 300 mg, 30.9% with secukinumab 150 mg, 24.5% with etanercept, and 19.3% with placebo. Candidal infections were more common with secukinumab than with etanercept during the entire treatment period (4.7% and 2.3% of participants in the secukinumab 300 mg and 150 mg groups, respectively, reported mild or moderate candidal infections). None of these infections resulted in chronic mucocutaneous candidiasis or discontinuation of the study drug and all resolved on their own or with standard therapy. Candidal infection was reported in 1.2% of participants in the etanercept group. Responses at week 12 were sustained in the majority of participants through week 52 with continued secukinumab therapy every 4 weeks. Grade 3 neutropenia occurred in 1.0% of secukinumab-treated participants and in none of the participants in the etanercept group. There were no apparent dose-related differences between the secukinumab groups with respect to AEs, with the exception of mild and moderate candidal infections.13
These efficacy data are impressive and no specific serious safety concerns have been identified to date. However, IL-17A plays a key role in host defense, particularly in mucocutaneous immunity against Candida albicans,14 as well as in hematopoiesis through stimulation of granulopoiesis and neutrophil trafficking,15 and thus we need to remain watchful with regards to Candida albicans infections and neutropenia.
Ixekizumab
Ixekizumab is a humanized IgG4 anti–IL-17A monoclonal antibody. In a phase 2, double-blind, placebo-controlled trial, 142 participants with chronic moderate to severe plaque psoriasis were randomly assigned to receive 150-mg (n=28), 75-mg (n=29), 25-mg (n=30), or 10-mg (n=28) subcutaneous injections of ixekizumab or placebo (n=27) at weeks 0, 2, 4, 8, 12, and 16.16 At 12 weeks, the percentage of participants who achieved a 75% reduction in PASI score from baseline was significantly greater with ixekizumab (82.1% with 150-mg dose, 82.8% with 75-mg dose, 76.7% with 25-mg dose) than with placebo (7.7%)(P<.001 for each comparison), except with the 10-mg dose. Similarly, a greater percentage of participants in the same ixekizumab groups achieved a 90% reduction (71.4% with 150-mg dose, 58.6% with 75-mg dose, 50.0% with 25-mg dose) and a 100% reduction (39.3% with 150-mg dose, 37.9% with 75-mg dose) in PASI score compared to placebo (0%)(P<.001 for each comparison). Significant reductions in PASI scores were evident as early as week 1 in the 150-mg and 75-mg groups, and these reductions were sustained for 20 weeks (P<.05).16 Phase 3 studies of ixekizumab currently are underway.
Brodalumab
The third IL-17 blocker in the pipeline is brodalumab, a human monoclonal antibody against IL-17RA, which blocks signaling of IL-17A and IL-17F as well as the IL-17A/F heterodimer, all of which are involved in the inflammatory process of psoriasis. Brodalumab was evaluated in a phase 2, double-blind, placebo-controlled, dose-ranging study of 198 participants who were randomized to receive 70 mg (n=39), 140 mg (n=39), 210 mg (n=40), or 280 mg (n=42) of brodalumab or placebo (n=38).17 At week 12, improvements of at least 75% and at least 90% in PASI score were achieved by 77% and 72%, respectively, in the 140-mg group, and 82% and 75%, respectively, in the 210-mg group compared to 0% of the placebo group (P<.001 for all comparisons). One hundred percent improvement in PASI was achieved by 38% of participants in the 140-mg group and 62% in the 210-mg group. No participants in the placebo group demonstrated improvement of 75% or higher. The most common AEs were nasopharyngitis, upper respiratory tract infection, arthralgia, and injection-site erythema. Serious AEs reported during the study included renal colic (1 participant), ec-topic pregnancy (1 participant), and grade 3 asymptomatic neutropenia (2 participants). Both cases of neutropenia were noted at the first assessment after brodalumab initiation (week 2) and resolved when the study drug was withheld.17
Results for this new IL-17 blocker are encouraging, but phase 3 data of brodalumab will need to be awaited.
Tildrakizumab
Tildrakizumab is a humanized IgG1 monoclonal antibody that blocks the p19 subunit of IL-23. In a randomized, double-blind, phase 2b trial, 355 adults with moderate to severe psoriasis were randomized to receive subcutaneous injections of tildrakizumab (5 mg, 25 mg, 100 mg, or 200 mg) or placebo.18 In part 1 of the study, injections were administered at weeks 0 and 4. Part 2 of the study started at week 16. In part 2, responders with a 75% improvement in PASI score in the 5- and 25-mg groups continued their dose, while responders in the 100- or 200-mg groups were randomized again to continue the same dose or a reduced dose (100 mg to 25 mg; 200 mg to 100 mg) every 12 weeks from weeks 16 to 52. Those in the placebo group received tildrakizumab 25 mg every 12 weeks in part 2. The primary end point was the mean change in PASI score from baseline to week 16, which was significantly greater in all tildrakizumab groups than in the placebo group (P<.001 for all comparisons). Improvements of 75% in PASI score were achieved by 74% in the 200-mg group, 66% in the 100-mg group, 64% in the 25-mg group, and 33% in the 5-mg group. In contrast, 4.9% in the placebo group achieved an improvement of 75%. At week 52, no loss of efficacy was seen in those participants who had achieved 75% improvement in PASI score at week 16 and had continued their prior doses. The rates of AEs seen in the tildrakizumab groups were 60% to 71% compared to 69% in the placebo group. The most common AE was nasopharyngitis, occurring in 12% to 20% of participants in each group. Serious AEs were uncommon.18 Phase 3 studies are currently underway.19
Guselkumab
Guselkumab is a human IgG1 monoclonal antibody in clinical development that specifically blocks the p19 subunit of IL-23. In a double-blind, placebo-controlled, phase 1 study, 24 participants with moderate to severe plaque psoriasis were randomized to receive a single 10-mg (n=5), 30-mg (n=5), 100-mg (n=5), or 300-mg (n=5) dose of guselkumab or placebo (n=4).20 At week 12, 50% in the 10-mg group, 60% in both the 30- and 100-mg groups, and 100% in the 300-mg group showed 75% improvement in PASI score versus 0% in the placebo group. Improvements in PASI scores were generally maintained through week 24. The rates of AEs were 65% (13/20) in the combined guselkumab group and 50% (2/4) in the placebo group.20
Small Molecule Inhibitors
In contrast to biologics, which mainly target soluble cytokine or cellular receptors, small molecule inhibitors target enzymes within signaling pathways. Small molecule inhibitors have some advantages over biologics in that they are relatively inexpensive to produce and can be administered orally; thus, they may be preferred by some patients over injectable drugs. There are several agents that are undergoing clinical trials in psoriasis, including PDE4 inhibitors and Jak inhibitors.
Apremilast
Apremilast is an oral small molecule PDE4 inhibitor that was approved by the US Food and Drug Administration in March 2014 for the treatment of adult patients with active psoriatic arthritis; an indication for moderate to severe plaque psoriasis was approved in September 2014.21 Phosphodiesterase 4 is a cyclic adenosine monophosphate–specific phosphodiesterase inhibitor, which is dominant in inflammatory cells. Inhibition of PDE4 increases intracellular cyclic adenosine monophosphate levels, thus downregulating proinflammatory cytokines such as TNF-α, IFN-γ, IL-2, IL-12, and IL-23, and increasing the production of anti-inflammatory cytokines such as IL-10.22
Phase 2 and phase 3 studies have demonstrated the clinical efficacy of apremilast in the treatment of patients with moderate to severe plaque psoriasis. In a 16-week randomized, placebo-controlled, phase 3 trial (ESTEEM 2), 408 participants were randomized to receive oral apremilast 30 mg twice daily (n=275) or placebo (n=138).23 Improvement of 75% in PASI score was achieved by 29% of participants in the apremilast group at week 16. The most common AEs were diarrhea (16%) and nausea (18%), which were predominantly mild, occurring most commonly in the first week and resolving within 1 month. No cases of severe diarrhea or severe nausea were reported. Apremilast had no apparent effect on the results of hematological or serum chemistry tests.23 Although the US Food and Drug Administration warns of a possible link between apremilast and depression,24 data are mostly related to roflumilast, another PDE4 inhibitor. Studies in patients with chronic obstructive pulmonary disease have noted increased cases of depression (1.21% vs 0.82%) and suicidal ideation/attempt (0.03% vs 0.02%) in patients treated with roflumilast versus placebo.25
Jak Inhibitors
Janus kinases are a family of intracellular tyrosine kinases that connect several cytokine receptors to the signal transducer and activator of transcription pathways.26 There are 4 Jak family members: Jak1, Jak2, Jak3, and tyrosine kinase 2. Janus kinases 1 and 2 have roles in interferon signaling, while Jak3 transduces signals from IL-2, IL-7, IL-15, and IL-21, which are T-cell growth and survival factors.
Tofacitinib is a novel oral signal transduction molecule that blocks the Jak3 pathway. A phase 2b, 12-week, dose-ranging study was conducted to assess the efficacy and safety of 3 twice-daily regimens of tofacitinib versus placebo in patients with moderate to severe chronic plaque psoriasis.27 One hundred and ninety-seven participants were randomized to receive oral tofacitinib (2 mg, 5 mg, or 15 mg; n=49 each) or placebo (n=50) twice daily for 12 weeks with a 4-week follow-up period. The primary end point was the proportion of participants achieving at least a 75% reduction in PASI score at week 12 (25.0% with 2 mg, 40.8% with 5 mg, 66.7% with 15 mg, 2.0% with placebo). Similarly, a higher proportion of participants achieving 90% reduction in PASI score was seen at weeks 8 and 12 in all tofacitinib-treated participants versus placebo. The most common AEs were upper respiratory tract infection, sinusitis, nasopharyngitis, and headache. A number of changes in laboratory parameters occurred in the tofacitinib groups. Mild dose-related decreases in hemoglobin were noted at week 12 for all tofacitinib groups, and a small increase (mean, 0.04 mg/dL) in serum creatinine levels was observed in the 15-mg group. Decreases in neutrophil counts were observed with higher doses of tofacitinib, with the maximum mean decrease of 0.9×103/mm3 from baseline observed in the 15-mg group at week 4. After weeks 4 through 8, mean neutrophil counts began to return to baseline levels. Dose-related increases in total cholesterol, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol were observed by week 2 and remained at this level through week 12; mean lipid levels decreased to baseline levels after cessation of active treatment. One participant in the 15-mg group developed an elevated alanine aminotransferase level that was more than 2.5 times the highest normal limit. Three participants experienced 5 serious AEs.27 These early results show that tofacitinib can be a safe and effective treatment in patients with psoriasis, but further data from phase 3 studies will need to be awaited.
Another Jak inhibitor under investigationfor the treatment of psoriasis is ruxolitinib, an inhibitor of Jak1 and Jak2, which has been primarily studied as a topical agent for milder cases of the disease.28
Conclusion
Many new drugs are currently on the horizon and will increase our armamentarium for treating psoriasis. Some of these agents promise greater levels of efficacy than currently used therapies. Although this review focuses on systemic agents, there also are a number of topical formulations in the pipeline. These new agents will certainly increase our options when choosing the most suitable treatment for a patient with psoriasis, but safety will remain a primary concern, and time and experience will tell whether efficacy outweighs any potential side effects.
1. Parisi R, Symmons DP, Griffiths CE, et al. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013;133:377-385.
2. Rapp SR, Feldman SR, Exum ML, et al. Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol. 1999;41(3 pt 1):401-407.
3. Shah R, Bewley A. Psoriasis: ‘the badge of shame.’ a case report of a psychological intervention to reduce and potentially clear chronic skin disease. Clin Exp Dermatol. 2014;39:600-603.
4. Vincent FB, Morand EF, Murphy K, et al. Antidrug antibodies (ADAb) to tumour necrosis factor (TNF)-specific neutralising agents in chronic inflammatory diseases: a real issue, a clinical perspective. Ann Rheum Dis. 2013;72:165-178.
5. Chi CC, Wang SH. Efficacy and cost-efficacy of biologic therapies for moderate to severe psoriasis: a meta-analysis and cost-efficacy analysis using the intention-to-treat principle. Biomed Res Int. 2014;2014:862851.
6. Kagami S, Rizzo HL, Lee JJ, et al. Circulating Th17, Th22, and Th1 cells are increased in psoriasis. J Invest Dermatol. 2010;130:1373-1383.
7. Leonardi CL, Gordon KB. New and emerging therapies in psoriasis. Semin Cutan Med Surg. 2014;33(2, suppl 2):S37-S41.
8. Lowes MA, Kikuchi T, Fuentes-Duculan J, et al. Psoriasis vulgaris lesions contain discrete populations of Th1 and Th17 T cells. J Invest Dermatol. 2008;128:1207-1211.
9. Nickoloff BJ, Qin JZ, Nestle FO. Immunopathogenesis of psoriasis. Clin Rev Allergy Immunol. 2007;33:45-56.
10. Fitch E, Harper E, Skorcheva I, et al. Pathophysiology of psoriasis: recent advances on IL-23 and Th17 cytokines. Curr Rheumatol Rep. 2007;9:461-467.
11. Adami S, Cavani A, Rossi F, et al. The role of interleukin-17A in psoriatic disease. BioDrugs. 2014;28:487-497.
12. Hueber W, Patel DD, Dryja T, et al. Effects of AIN457, a fully human antibody to interleukin-17A, on psoriasis, rheumatoid arthritis, and uveitis. Sci Transl Med. 2010;2:52ra72.
13. Langley RG, Elewski BE, Lebwohl M, et al. Secukinumab in plaque psoriasis—results of two phase 3 trials. N Engl J Med. 2014;371:326-338.
14. Puel A, Cypowyj S, Bustamante J, et al. Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity. Science. 2011;332:65-68.
15. Krstic A, Mojsilovic S, Jovcic G, et al. The potential of interleukin-17 to mediate hematopoietic response. Immunol Res. 2012;52:34-41.
16. Leonardi C, Matheson R, Zachariae C, et al. Anti-interleukin-17 monoclonal antibody ixekizumab in chronic plaque psoriasis. N Engl J Med. 2012;366:1190-1199.
17. Papp KA, Leonardi C, Menter A, et al. Brodalumab, an anti-interleukin-17-receptor antibody for psoriasis. N Engl J Med. 2012;366:1181-1189.
18. Langley RGB, Thaci D, Papp KA, et al. MK-3222, an anti–IL-23p19 humanized monoclonal antibody, provides significant improvement in psoriasis over 52 weeks of treatment that is maintained after discontinuation of dosing. Poster presented at: 73rd Annual Meeting of the American Academy of Dermatology; March 21-25, 2014; Denver, CO. Poster 8056.
19. Tausend W, Downing C, Tyring S. Systematic review of interleukin-12, interleukin-17, and interleukin-23 pathway inhibitors for the treatment of moderate-to-severe chronic plaque psoriasis: ustekinumab, briakinumab, tildrakizumab, guselkumab, secukinumab, ixekizumab, and brodalumab. J Cutan Med Surg. 2014;18:156-169.
20. Sofen H, Smith S, Matheson RT, et al. Guselkumab (an IL-23-specific mAb) demonstrates clinical and molecular response in patients with moderate-to-severe psoriasis. J Allergy Clin Immunol. 2014;133:1032-1040.
21. Schafer PH, Parton A, Capone L, et al. Apremilast is a selective PDE4 inhibitor with regulatory effects on innate immunity. Cell Signal. 2014;26:2016-2029.
22. van de Kerkhof PC. Apremilast: a step forward in the treatment of psoriasis? Lancet. 2012;380:708-709.
23. Paul C, Crowley J, Cather J, et al. Apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate to severe psoriasis: 16-week results of a phase 3, randomized, controlled trial (ESTEEM 2). Poster presented at: 73rd Annual Meeting of the American Academy of Dermatology; March 21-25, 2014; Denver, CO. Poster 8412.
24. Otezla [product insert]. Summit, NJ: Celgene Corporation; 2014.
25. Rabe KF. Update on roflumilast, a phosphodiesterase 4 inhibitor for the treatment of chronic obstructive pulmonary disease. Br J Pharmacol. 2011;163:53-67.
26. Palanivel JA, Macbeth AE, Chetty NC, et al. An insight into JAK-STAT signalling in dermatology. Clin Exp Dermatol. 2014;39:513-518.
27. Papp KA, Menter A, Strober B, et al. Efficacy and safety of tofacitinib, an oral Janus kinase inhibitor, in the treatment of psoriasis: a phase 2b randomized placebo-controlled dose-ranging study. Br J Dermatol. 2012;167:668-677.
28. Hsu L, Armstrong AW. JAK inhibitors: treatment efficacy and safety profile in patients with psoriasis. J Immunol Res. 2014;2014:283617.
Psoriasis is a common chronic inflammatory skin disease affecting 1% to 8% of the world population, depending on the country.1 Psoriasis can greatly impact quality of life in affected individuals, even in those with limited body surface involvement.2 Studies have demonstrated a high degree of psychological distress associated with psoriasis, leading to depression and poor self-esteem.3
Over the last decade, our improved understanding of the autoimmune inflammatory pathways and the associated changing concepts in psoriasis pathogenesis have led to the development of biological drugs targeting specific components of effector immune mechanisms, and these biological drugs have revolutionized the treatment of psoriasis.4 Although response rates of these biological agents are greater compared to those of conventional systemic drugs,5 current biological drugs fail to demonstrate efficacy in some patients or lose their efficacy over time. In addition to the high costs associated with these drugs, these limitations have driven a continued search for alternative therapies.
Helper T cells (TH17) and the proinflammatory cytokine IL-17 have been shown to play a key role in the pathophysiology of psoriasis, bridging innate and adaptive immune responses. IL-17 is involved in the modulation of proinflammatory cytokines, hematopoietic growth factors, antimicrobial peptides, and chemokines. Increased TH17 activity and high levels of IL-17 have been found in psoriatic plaques, and increased levels of TH17 are found in the plasma of psoriasis patients.6 Increased IL-17 induces neutrophilia, inflammation, and angiogenesis.7 Other cytokines that are highly upregulated in involved skin are tumor necrosis factor a (TNF-α), IL-23, IL-22, and IL-21.8 IL-23 is involved in regulating TH17 cells and is a potent activator of keratinocyte proliferation.9 Blockade of IL-12/23 causes downregulation of TH17 and TH22 cell responses.10 As IL-17 has a key role in protecting skin and mucous membranes from bacterial and fungal infections, IL-17 inhibition can potentially interfere with the inflammatory cascade. However, available data suggest that sufficient residual IL-17 activity remains to maintain immunity against infections.11
Currently approved biological agents for psoriasis target proinflammatory cytokines such as TNF-α, or the p40 subunit of IL-12 and IL-23. A number of novel targeted therapies including biologics as well as small molecule inhibitors targeting various cytokines and molecules involved in the pathogenesis of psoriasis are currently in different stages of development (Table). These drugs include 3 IL-17 inhibitors (secukinumab, ixekizumab, and brodalumab); 2 IL-23 blockers (tildrakizumab and guselkumab); and small molecule inhibitors that target the kinase pathway including apremilast (a phosphodiesterase 4 [PDE4] inhibitor), as well as tofacitinib, baricitinib, and ruxolitinib (Janus kinase [Jak] inhibitors). Small molecule inhibitors can be administered orally and are less expensive to produce than biological agents. This article reviews available data on these new systemic agents in the pipeline.
Novel Biologics
Secukinumab
Secukinumab is a fully human monoclonal IgG1k antibody that selectively binds and neutralizes IL-17A.12 It is the first of the IL-17 antibodies to receive approval for the treatment of moderate to severe psoriasis. In 2 phase 3, double-blind, 52-week trials—ERASURE (Efficacy of Response and Safety of Two Fixed Secukinumab Regimens in Psoriasis) and FIXTURE (Full Year Investigative Examination of Secukinumab vs Etanercept Using Two Dosing Regimens to Determine Efficacy in Psoriasis)—participants were randomly assigned to receive subcutaneous secukinumab at doses of 300 mg (n=245 and n=327, respectively) or 150 mg (n=245 and n=327, respectively) once weekly for 5 weeks then every 4 weeks, or placebo (n=248 and n=326, respectively); in the FIXTURE study only, an etanercept group (n=326) was given a 50-mg dose twice weekly for 12 weeks then once weekly.13
In the ERASURE study, the proportion of participants showing a reduction of 75% or more in psoriasis area and severity index (PASI) score from baseline to week 12 was 81.6% with secukinumab 300 mg, 71.6% with secukinumab 150 mg, and 4.5% with placebo.13 Secondary end point results demonstrated the proportion of participants showing a 90% reduction in PASI score was 59.2% with secukinumab 300 mg and 39.1% with secukinumab 150 mg, which were both superior to placebo (1.2%). The proportion of participants who met the criteria for 100% reduction in PASI score at week 12 also was greater with each secukinumab dose than with placebo.13
In the FIXTURE study, the proportion of participants showing a reduction of 75% or more from baseline in PASI score at week 12 was 77.1% with secukinumab 300 mg, 67.0% with secukinumab 150 mg, 44.0% with etanercept, and 4.9% with placebo.13 Secondary end point results demonstrated the proportion of participants showing a 90% reduction in PASI score was 54.2% with secukinumab 300 mg, 41.9% with secukinumab 150 mg, 20.7% with etanercept, and 1.5% with placebo. The speed of response, which was assessed as the median time to a 50% reduction in mean PASI score from baseline, was significantly shorter with both doses of secukinumab (3.0 weeks and 3.9 weeks, respectively) than with etanercept (7.0 weeks)(P<.001 for both).13
In the FIXTURE study, incidences of adverse events (AEs) were similar in the secukinumab and etanercept groups during both the induction period and the entire treatment period.13 The most common AEs in the secukinumab groups were nasopharyngitis, headache, and diarrhea. The rates of infections or infestations during the induction period were 26.7% with secukinumab 300 mg, 30.9% with secukinumab 150 mg, 24.5% with etanercept, and 19.3% with placebo. Candidal infections were more common with secukinumab than with etanercept during the entire treatment period (4.7% and 2.3% of participants in the secukinumab 300 mg and 150 mg groups, respectively, reported mild or moderate candidal infections). None of these infections resulted in chronic mucocutaneous candidiasis or discontinuation of the study drug and all resolved on their own or with standard therapy. Candidal infection was reported in 1.2% of participants in the etanercept group. Responses at week 12 were sustained in the majority of participants through week 52 with continued secukinumab therapy every 4 weeks. Grade 3 neutropenia occurred in 1.0% of secukinumab-treated participants and in none of the participants in the etanercept group. There were no apparent dose-related differences between the secukinumab groups with respect to AEs, with the exception of mild and moderate candidal infections.13
These efficacy data are impressive and no specific serious safety concerns have been identified to date. However, IL-17A plays a key role in host defense, particularly in mucocutaneous immunity against Candida albicans,14 as well as in hematopoiesis through stimulation of granulopoiesis and neutrophil trafficking,15 and thus we need to remain watchful with regards to Candida albicans infections and neutropenia.
Ixekizumab
Ixekizumab is a humanized IgG4 anti–IL-17A monoclonal antibody. In a phase 2, double-blind, placebo-controlled trial, 142 participants with chronic moderate to severe plaque psoriasis were randomly assigned to receive 150-mg (n=28), 75-mg (n=29), 25-mg (n=30), or 10-mg (n=28) subcutaneous injections of ixekizumab or placebo (n=27) at weeks 0, 2, 4, 8, 12, and 16.16 At 12 weeks, the percentage of participants who achieved a 75% reduction in PASI score from baseline was significantly greater with ixekizumab (82.1% with 150-mg dose, 82.8% with 75-mg dose, 76.7% with 25-mg dose) than with placebo (7.7%)(P<.001 for each comparison), except with the 10-mg dose. Similarly, a greater percentage of participants in the same ixekizumab groups achieved a 90% reduction (71.4% with 150-mg dose, 58.6% with 75-mg dose, 50.0% with 25-mg dose) and a 100% reduction (39.3% with 150-mg dose, 37.9% with 75-mg dose) in PASI score compared to placebo (0%)(P<.001 for each comparison). Significant reductions in PASI scores were evident as early as week 1 in the 150-mg and 75-mg groups, and these reductions were sustained for 20 weeks (P<.05).16 Phase 3 studies of ixekizumab currently are underway.
Brodalumab
The third IL-17 blocker in the pipeline is brodalumab, a human monoclonal antibody against IL-17RA, which blocks signaling of IL-17A and IL-17F as well as the IL-17A/F heterodimer, all of which are involved in the inflammatory process of psoriasis. Brodalumab was evaluated in a phase 2, double-blind, placebo-controlled, dose-ranging study of 198 participants who were randomized to receive 70 mg (n=39), 140 mg (n=39), 210 mg (n=40), or 280 mg (n=42) of brodalumab or placebo (n=38).17 At week 12, improvements of at least 75% and at least 90% in PASI score were achieved by 77% and 72%, respectively, in the 140-mg group, and 82% and 75%, respectively, in the 210-mg group compared to 0% of the placebo group (P<.001 for all comparisons). One hundred percent improvement in PASI was achieved by 38% of participants in the 140-mg group and 62% in the 210-mg group. No participants in the placebo group demonstrated improvement of 75% or higher. The most common AEs were nasopharyngitis, upper respiratory tract infection, arthralgia, and injection-site erythema. Serious AEs reported during the study included renal colic (1 participant), ec-topic pregnancy (1 participant), and grade 3 asymptomatic neutropenia (2 participants). Both cases of neutropenia were noted at the first assessment after brodalumab initiation (week 2) and resolved when the study drug was withheld.17
Results for this new IL-17 blocker are encouraging, but phase 3 data of brodalumab will need to be awaited.
Tildrakizumab
Tildrakizumab is a humanized IgG1 monoclonal antibody that blocks the p19 subunit of IL-23. In a randomized, double-blind, phase 2b trial, 355 adults with moderate to severe psoriasis were randomized to receive subcutaneous injections of tildrakizumab (5 mg, 25 mg, 100 mg, or 200 mg) or placebo.18 In part 1 of the study, injections were administered at weeks 0 and 4. Part 2 of the study started at week 16. In part 2, responders with a 75% improvement in PASI score in the 5- and 25-mg groups continued their dose, while responders in the 100- or 200-mg groups were randomized again to continue the same dose or a reduced dose (100 mg to 25 mg; 200 mg to 100 mg) every 12 weeks from weeks 16 to 52. Those in the placebo group received tildrakizumab 25 mg every 12 weeks in part 2. The primary end point was the mean change in PASI score from baseline to week 16, which was significantly greater in all tildrakizumab groups than in the placebo group (P<.001 for all comparisons). Improvements of 75% in PASI score were achieved by 74% in the 200-mg group, 66% in the 100-mg group, 64% in the 25-mg group, and 33% in the 5-mg group. In contrast, 4.9% in the placebo group achieved an improvement of 75%. At week 52, no loss of efficacy was seen in those participants who had achieved 75% improvement in PASI score at week 16 and had continued their prior doses. The rates of AEs seen in the tildrakizumab groups were 60% to 71% compared to 69% in the placebo group. The most common AE was nasopharyngitis, occurring in 12% to 20% of participants in each group. Serious AEs were uncommon.18 Phase 3 studies are currently underway.19
Guselkumab
Guselkumab is a human IgG1 monoclonal antibody in clinical development that specifically blocks the p19 subunit of IL-23. In a double-blind, placebo-controlled, phase 1 study, 24 participants with moderate to severe plaque psoriasis were randomized to receive a single 10-mg (n=5), 30-mg (n=5), 100-mg (n=5), or 300-mg (n=5) dose of guselkumab or placebo (n=4).20 At week 12, 50% in the 10-mg group, 60% in both the 30- and 100-mg groups, and 100% in the 300-mg group showed 75% improvement in PASI score versus 0% in the placebo group. Improvements in PASI scores were generally maintained through week 24. The rates of AEs were 65% (13/20) in the combined guselkumab group and 50% (2/4) in the placebo group.20
Small Molecule Inhibitors
In contrast to biologics, which mainly target soluble cytokine or cellular receptors, small molecule inhibitors target enzymes within signaling pathways. Small molecule inhibitors have some advantages over biologics in that they are relatively inexpensive to produce and can be administered orally; thus, they may be preferred by some patients over injectable drugs. There are several agents that are undergoing clinical trials in psoriasis, including PDE4 inhibitors and Jak inhibitors.
Apremilast
Apremilast is an oral small molecule PDE4 inhibitor that was approved by the US Food and Drug Administration in March 2014 for the treatment of adult patients with active psoriatic arthritis; an indication for moderate to severe plaque psoriasis was approved in September 2014.21 Phosphodiesterase 4 is a cyclic adenosine monophosphate–specific phosphodiesterase inhibitor, which is dominant in inflammatory cells. Inhibition of PDE4 increases intracellular cyclic adenosine monophosphate levels, thus downregulating proinflammatory cytokines such as TNF-α, IFN-γ, IL-2, IL-12, and IL-23, and increasing the production of anti-inflammatory cytokines such as IL-10.22
Phase 2 and phase 3 studies have demonstrated the clinical efficacy of apremilast in the treatment of patients with moderate to severe plaque psoriasis. In a 16-week randomized, placebo-controlled, phase 3 trial (ESTEEM 2), 408 participants were randomized to receive oral apremilast 30 mg twice daily (n=275) or placebo (n=138).23 Improvement of 75% in PASI score was achieved by 29% of participants in the apremilast group at week 16. The most common AEs were diarrhea (16%) and nausea (18%), which were predominantly mild, occurring most commonly in the first week and resolving within 1 month. No cases of severe diarrhea or severe nausea were reported. Apremilast had no apparent effect on the results of hematological or serum chemistry tests.23 Although the US Food and Drug Administration warns of a possible link between apremilast and depression,24 data are mostly related to roflumilast, another PDE4 inhibitor. Studies in patients with chronic obstructive pulmonary disease have noted increased cases of depression (1.21% vs 0.82%) and suicidal ideation/attempt (0.03% vs 0.02%) in patients treated with roflumilast versus placebo.25
Jak Inhibitors
Janus kinases are a family of intracellular tyrosine kinases that connect several cytokine receptors to the signal transducer and activator of transcription pathways.26 There are 4 Jak family members: Jak1, Jak2, Jak3, and tyrosine kinase 2. Janus kinases 1 and 2 have roles in interferon signaling, while Jak3 transduces signals from IL-2, IL-7, IL-15, and IL-21, which are T-cell growth and survival factors.
Tofacitinib is a novel oral signal transduction molecule that blocks the Jak3 pathway. A phase 2b, 12-week, dose-ranging study was conducted to assess the efficacy and safety of 3 twice-daily regimens of tofacitinib versus placebo in patients with moderate to severe chronic plaque psoriasis.27 One hundred and ninety-seven participants were randomized to receive oral tofacitinib (2 mg, 5 mg, or 15 mg; n=49 each) or placebo (n=50) twice daily for 12 weeks with a 4-week follow-up period. The primary end point was the proportion of participants achieving at least a 75% reduction in PASI score at week 12 (25.0% with 2 mg, 40.8% with 5 mg, 66.7% with 15 mg, 2.0% with placebo). Similarly, a higher proportion of participants achieving 90% reduction in PASI score was seen at weeks 8 and 12 in all tofacitinib-treated participants versus placebo. The most common AEs were upper respiratory tract infection, sinusitis, nasopharyngitis, and headache. A number of changes in laboratory parameters occurred in the tofacitinib groups. Mild dose-related decreases in hemoglobin were noted at week 12 for all tofacitinib groups, and a small increase (mean, 0.04 mg/dL) in serum creatinine levels was observed in the 15-mg group. Decreases in neutrophil counts were observed with higher doses of tofacitinib, with the maximum mean decrease of 0.9×103/mm3 from baseline observed in the 15-mg group at week 4. After weeks 4 through 8, mean neutrophil counts began to return to baseline levels. Dose-related increases in total cholesterol, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol were observed by week 2 and remained at this level through week 12; mean lipid levels decreased to baseline levels after cessation of active treatment. One participant in the 15-mg group developed an elevated alanine aminotransferase level that was more than 2.5 times the highest normal limit. Three participants experienced 5 serious AEs.27 These early results show that tofacitinib can be a safe and effective treatment in patients with psoriasis, but further data from phase 3 studies will need to be awaited.
Another Jak inhibitor under investigationfor the treatment of psoriasis is ruxolitinib, an inhibitor of Jak1 and Jak2, which has been primarily studied as a topical agent for milder cases of the disease.28
Conclusion
Many new drugs are currently on the horizon and will increase our armamentarium for treating psoriasis. Some of these agents promise greater levels of efficacy than currently used therapies. Although this review focuses on systemic agents, there also are a number of topical formulations in the pipeline. These new agents will certainly increase our options when choosing the most suitable treatment for a patient with psoriasis, but safety will remain a primary concern, and time and experience will tell whether efficacy outweighs any potential side effects.
Psoriasis is a common chronic inflammatory skin disease affecting 1% to 8% of the world population, depending on the country.1 Psoriasis can greatly impact quality of life in affected individuals, even in those with limited body surface involvement.2 Studies have demonstrated a high degree of psychological distress associated with psoriasis, leading to depression and poor self-esteem.3
Over the last decade, our improved understanding of the autoimmune inflammatory pathways and the associated changing concepts in psoriasis pathogenesis have led to the development of biological drugs targeting specific components of effector immune mechanisms, and these biological drugs have revolutionized the treatment of psoriasis.4 Although response rates of these biological agents are greater compared to those of conventional systemic drugs,5 current biological drugs fail to demonstrate efficacy in some patients or lose their efficacy over time. In addition to the high costs associated with these drugs, these limitations have driven a continued search for alternative therapies.
Helper T cells (TH17) and the proinflammatory cytokine IL-17 have been shown to play a key role in the pathophysiology of psoriasis, bridging innate and adaptive immune responses. IL-17 is involved in the modulation of proinflammatory cytokines, hematopoietic growth factors, antimicrobial peptides, and chemokines. Increased TH17 activity and high levels of IL-17 have been found in psoriatic plaques, and increased levels of TH17 are found in the plasma of psoriasis patients.6 Increased IL-17 induces neutrophilia, inflammation, and angiogenesis.7 Other cytokines that are highly upregulated in involved skin are tumor necrosis factor a (TNF-α), IL-23, IL-22, and IL-21.8 IL-23 is involved in regulating TH17 cells and is a potent activator of keratinocyte proliferation.9 Blockade of IL-12/23 causes downregulation of TH17 and TH22 cell responses.10 As IL-17 has a key role in protecting skin and mucous membranes from bacterial and fungal infections, IL-17 inhibition can potentially interfere with the inflammatory cascade. However, available data suggest that sufficient residual IL-17 activity remains to maintain immunity against infections.11
Currently approved biological agents for psoriasis target proinflammatory cytokines such as TNF-α, or the p40 subunit of IL-12 and IL-23. A number of novel targeted therapies including biologics as well as small molecule inhibitors targeting various cytokines and molecules involved in the pathogenesis of psoriasis are currently in different stages of development (Table). These drugs include 3 IL-17 inhibitors (secukinumab, ixekizumab, and brodalumab); 2 IL-23 blockers (tildrakizumab and guselkumab); and small molecule inhibitors that target the kinase pathway including apremilast (a phosphodiesterase 4 [PDE4] inhibitor), as well as tofacitinib, baricitinib, and ruxolitinib (Janus kinase [Jak] inhibitors). Small molecule inhibitors can be administered orally and are less expensive to produce than biological agents. This article reviews available data on these new systemic agents in the pipeline.
Novel Biologics
Secukinumab
Secukinumab is a fully human monoclonal IgG1k antibody that selectively binds and neutralizes IL-17A.12 It is the first of the IL-17 antibodies to receive approval for the treatment of moderate to severe psoriasis. In 2 phase 3, double-blind, 52-week trials—ERASURE (Efficacy of Response and Safety of Two Fixed Secukinumab Regimens in Psoriasis) and FIXTURE (Full Year Investigative Examination of Secukinumab vs Etanercept Using Two Dosing Regimens to Determine Efficacy in Psoriasis)—participants were randomly assigned to receive subcutaneous secukinumab at doses of 300 mg (n=245 and n=327, respectively) or 150 mg (n=245 and n=327, respectively) once weekly for 5 weeks then every 4 weeks, or placebo (n=248 and n=326, respectively); in the FIXTURE study only, an etanercept group (n=326) was given a 50-mg dose twice weekly for 12 weeks then once weekly.13
In the ERASURE study, the proportion of participants showing a reduction of 75% or more in psoriasis area and severity index (PASI) score from baseline to week 12 was 81.6% with secukinumab 300 mg, 71.6% with secukinumab 150 mg, and 4.5% with placebo.13 Secondary end point results demonstrated the proportion of participants showing a 90% reduction in PASI score was 59.2% with secukinumab 300 mg and 39.1% with secukinumab 150 mg, which were both superior to placebo (1.2%). The proportion of participants who met the criteria for 100% reduction in PASI score at week 12 also was greater with each secukinumab dose than with placebo.13
In the FIXTURE study, the proportion of participants showing a reduction of 75% or more from baseline in PASI score at week 12 was 77.1% with secukinumab 300 mg, 67.0% with secukinumab 150 mg, 44.0% with etanercept, and 4.9% with placebo.13 Secondary end point results demonstrated the proportion of participants showing a 90% reduction in PASI score was 54.2% with secukinumab 300 mg, 41.9% with secukinumab 150 mg, 20.7% with etanercept, and 1.5% with placebo. The speed of response, which was assessed as the median time to a 50% reduction in mean PASI score from baseline, was significantly shorter with both doses of secukinumab (3.0 weeks and 3.9 weeks, respectively) than with etanercept (7.0 weeks)(P<.001 for both).13
In the FIXTURE study, incidences of adverse events (AEs) were similar in the secukinumab and etanercept groups during both the induction period and the entire treatment period.13 The most common AEs in the secukinumab groups were nasopharyngitis, headache, and diarrhea. The rates of infections or infestations during the induction period were 26.7% with secukinumab 300 mg, 30.9% with secukinumab 150 mg, 24.5% with etanercept, and 19.3% with placebo. Candidal infections were more common with secukinumab than with etanercept during the entire treatment period (4.7% and 2.3% of participants in the secukinumab 300 mg and 150 mg groups, respectively, reported mild or moderate candidal infections). None of these infections resulted in chronic mucocutaneous candidiasis or discontinuation of the study drug and all resolved on their own or with standard therapy. Candidal infection was reported in 1.2% of participants in the etanercept group. Responses at week 12 were sustained in the majority of participants through week 52 with continued secukinumab therapy every 4 weeks. Grade 3 neutropenia occurred in 1.0% of secukinumab-treated participants and in none of the participants in the etanercept group. There were no apparent dose-related differences between the secukinumab groups with respect to AEs, with the exception of mild and moderate candidal infections.13
These efficacy data are impressive and no specific serious safety concerns have been identified to date. However, IL-17A plays a key role in host defense, particularly in mucocutaneous immunity against Candida albicans,14 as well as in hematopoiesis through stimulation of granulopoiesis and neutrophil trafficking,15 and thus we need to remain watchful with regards to Candida albicans infections and neutropenia.
Ixekizumab
Ixekizumab is a humanized IgG4 anti–IL-17A monoclonal antibody. In a phase 2, double-blind, placebo-controlled trial, 142 participants with chronic moderate to severe plaque psoriasis were randomly assigned to receive 150-mg (n=28), 75-mg (n=29), 25-mg (n=30), or 10-mg (n=28) subcutaneous injections of ixekizumab or placebo (n=27) at weeks 0, 2, 4, 8, 12, and 16.16 At 12 weeks, the percentage of participants who achieved a 75% reduction in PASI score from baseline was significantly greater with ixekizumab (82.1% with 150-mg dose, 82.8% with 75-mg dose, 76.7% with 25-mg dose) than with placebo (7.7%)(P<.001 for each comparison), except with the 10-mg dose. Similarly, a greater percentage of participants in the same ixekizumab groups achieved a 90% reduction (71.4% with 150-mg dose, 58.6% with 75-mg dose, 50.0% with 25-mg dose) and a 100% reduction (39.3% with 150-mg dose, 37.9% with 75-mg dose) in PASI score compared to placebo (0%)(P<.001 for each comparison). Significant reductions in PASI scores were evident as early as week 1 in the 150-mg and 75-mg groups, and these reductions were sustained for 20 weeks (P<.05).16 Phase 3 studies of ixekizumab currently are underway.
Brodalumab
The third IL-17 blocker in the pipeline is brodalumab, a human monoclonal antibody against IL-17RA, which blocks signaling of IL-17A and IL-17F as well as the IL-17A/F heterodimer, all of which are involved in the inflammatory process of psoriasis. Brodalumab was evaluated in a phase 2, double-blind, placebo-controlled, dose-ranging study of 198 participants who were randomized to receive 70 mg (n=39), 140 mg (n=39), 210 mg (n=40), or 280 mg (n=42) of brodalumab or placebo (n=38).17 At week 12, improvements of at least 75% and at least 90% in PASI score were achieved by 77% and 72%, respectively, in the 140-mg group, and 82% and 75%, respectively, in the 210-mg group compared to 0% of the placebo group (P<.001 for all comparisons). One hundred percent improvement in PASI was achieved by 38% of participants in the 140-mg group and 62% in the 210-mg group. No participants in the placebo group demonstrated improvement of 75% or higher. The most common AEs were nasopharyngitis, upper respiratory tract infection, arthralgia, and injection-site erythema. Serious AEs reported during the study included renal colic (1 participant), ec-topic pregnancy (1 participant), and grade 3 asymptomatic neutropenia (2 participants). Both cases of neutropenia were noted at the first assessment after brodalumab initiation (week 2) and resolved when the study drug was withheld.17
Results for this new IL-17 blocker are encouraging, but phase 3 data of brodalumab will need to be awaited.
Tildrakizumab
Tildrakizumab is a humanized IgG1 monoclonal antibody that blocks the p19 subunit of IL-23. In a randomized, double-blind, phase 2b trial, 355 adults with moderate to severe psoriasis were randomized to receive subcutaneous injections of tildrakizumab (5 mg, 25 mg, 100 mg, or 200 mg) or placebo.18 In part 1 of the study, injections were administered at weeks 0 and 4. Part 2 of the study started at week 16. In part 2, responders with a 75% improvement in PASI score in the 5- and 25-mg groups continued their dose, while responders in the 100- or 200-mg groups were randomized again to continue the same dose or a reduced dose (100 mg to 25 mg; 200 mg to 100 mg) every 12 weeks from weeks 16 to 52. Those in the placebo group received tildrakizumab 25 mg every 12 weeks in part 2. The primary end point was the mean change in PASI score from baseline to week 16, which was significantly greater in all tildrakizumab groups than in the placebo group (P<.001 for all comparisons). Improvements of 75% in PASI score were achieved by 74% in the 200-mg group, 66% in the 100-mg group, 64% in the 25-mg group, and 33% in the 5-mg group. In contrast, 4.9% in the placebo group achieved an improvement of 75%. At week 52, no loss of efficacy was seen in those participants who had achieved 75% improvement in PASI score at week 16 and had continued their prior doses. The rates of AEs seen in the tildrakizumab groups were 60% to 71% compared to 69% in the placebo group. The most common AE was nasopharyngitis, occurring in 12% to 20% of participants in each group. Serious AEs were uncommon.18 Phase 3 studies are currently underway.19
Guselkumab
Guselkumab is a human IgG1 monoclonal antibody in clinical development that specifically blocks the p19 subunit of IL-23. In a double-blind, placebo-controlled, phase 1 study, 24 participants with moderate to severe plaque psoriasis were randomized to receive a single 10-mg (n=5), 30-mg (n=5), 100-mg (n=5), or 300-mg (n=5) dose of guselkumab or placebo (n=4).20 At week 12, 50% in the 10-mg group, 60% in both the 30- and 100-mg groups, and 100% in the 300-mg group showed 75% improvement in PASI score versus 0% in the placebo group. Improvements in PASI scores were generally maintained through week 24. The rates of AEs were 65% (13/20) in the combined guselkumab group and 50% (2/4) in the placebo group.20
Small Molecule Inhibitors
In contrast to biologics, which mainly target soluble cytokine or cellular receptors, small molecule inhibitors target enzymes within signaling pathways. Small molecule inhibitors have some advantages over biologics in that they are relatively inexpensive to produce and can be administered orally; thus, they may be preferred by some patients over injectable drugs. There are several agents that are undergoing clinical trials in psoriasis, including PDE4 inhibitors and Jak inhibitors.
Apremilast
Apremilast is an oral small molecule PDE4 inhibitor that was approved by the US Food and Drug Administration in March 2014 for the treatment of adult patients with active psoriatic arthritis; an indication for moderate to severe plaque psoriasis was approved in September 2014.21 Phosphodiesterase 4 is a cyclic adenosine monophosphate–specific phosphodiesterase inhibitor, which is dominant in inflammatory cells. Inhibition of PDE4 increases intracellular cyclic adenosine monophosphate levels, thus downregulating proinflammatory cytokines such as TNF-α, IFN-γ, IL-2, IL-12, and IL-23, and increasing the production of anti-inflammatory cytokines such as IL-10.22
Phase 2 and phase 3 studies have demonstrated the clinical efficacy of apremilast in the treatment of patients with moderate to severe plaque psoriasis. In a 16-week randomized, placebo-controlled, phase 3 trial (ESTEEM 2), 408 participants were randomized to receive oral apremilast 30 mg twice daily (n=275) or placebo (n=138).23 Improvement of 75% in PASI score was achieved by 29% of participants in the apremilast group at week 16. The most common AEs were diarrhea (16%) and nausea (18%), which were predominantly mild, occurring most commonly in the first week and resolving within 1 month. No cases of severe diarrhea or severe nausea were reported. Apremilast had no apparent effect on the results of hematological or serum chemistry tests.23 Although the US Food and Drug Administration warns of a possible link between apremilast and depression,24 data are mostly related to roflumilast, another PDE4 inhibitor. Studies in patients with chronic obstructive pulmonary disease have noted increased cases of depression (1.21% vs 0.82%) and suicidal ideation/attempt (0.03% vs 0.02%) in patients treated with roflumilast versus placebo.25
Jak Inhibitors
Janus kinases are a family of intracellular tyrosine kinases that connect several cytokine receptors to the signal transducer and activator of transcription pathways.26 There are 4 Jak family members: Jak1, Jak2, Jak3, and tyrosine kinase 2. Janus kinases 1 and 2 have roles in interferon signaling, while Jak3 transduces signals from IL-2, IL-7, IL-15, and IL-21, which are T-cell growth and survival factors.
Tofacitinib is a novel oral signal transduction molecule that blocks the Jak3 pathway. A phase 2b, 12-week, dose-ranging study was conducted to assess the efficacy and safety of 3 twice-daily regimens of tofacitinib versus placebo in patients with moderate to severe chronic plaque psoriasis.27 One hundred and ninety-seven participants were randomized to receive oral tofacitinib (2 mg, 5 mg, or 15 mg; n=49 each) or placebo (n=50) twice daily for 12 weeks with a 4-week follow-up period. The primary end point was the proportion of participants achieving at least a 75% reduction in PASI score at week 12 (25.0% with 2 mg, 40.8% with 5 mg, 66.7% with 15 mg, 2.0% with placebo). Similarly, a higher proportion of participants achieving 90% reduction in PASI score was seen at weeks 8 and 12 in all tofacitinib-treated participants versus placebo. The most common AEs were upper respiratory tract infection, sinusitis, nasopharyngitis, and headache. A number of changes in laboratory parameters occurred in the tofacitinib groups. Mild dose-related decreases in hemoglobin were noted at week 12 for all tofacitinib groups, and a small increase (mean, 0.04 mg/dL) in serum creatinine levels was observed in the 15-mg group. Decreases in neutrophil counts were observed with higher doses of tofacitinib, with the maximum mean decrease of 0.9×103/mm3 from baseline observed in the 15-mg group at week 4. After weeks 4 through 8, mean neutrophil counts began to return to baseline levels. Dose-related increases in total cholesterol, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol were observed by week 2 and remained at this level through week 12; mean lipid levels decreased to baseline levels after cessation of active treatment. One participant in the 15-mg group developed an elevated alanine aminotransferase level that was more than 2.5 times the highest normal limit. Three participants experienced 5 serious AEs.27 These early results show that tofacitinib can be a safe and effective treatment in patients with psoriasis, but further data from phase 3 studies will need to be awaited.
Another Jak inhibitor under investigationfor the treatment of psoriasis is ruxolitinib, an inhibitor of Jak1 and Jak2, which has been primarily studied as a topical agent for milder cases of the disease.28
Conclusion
Many new drugs are currently on the horizon and will increase our armamentarium for treating psoriasis. Some of these agents promise greater levels of efficacy than currently used therapies. Although this review focuses on systemic agents, there also are a number of topical formulations in the pipeline. These new agents will certainly increase our options when choosing the most suitable treatment for a patient with psoriasis, but safety will remain a primary concern, and time and experience will tell whether efficacy outweighs any potential side effects.
1. Parisi R, Symmons DP, Griffiths CE, et al. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013;133:377-385.
2. Rapp SR, Feldman SR, Exum ML, et al. Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol. 1999;41(3 pt 1):401-407.
3. Shah R, Bewley A. Psoriasis: ‘the badge of shame.’ a case report of a psychological intervention to reduce and potentially clear chronic skin disease. Clin Exp Dermatol. 2014;39:600-603.
4. Vincent FB, Morand EF, Murphy K, et al. Antidrug antibodies (ADAb) to tumour necrosis factor (TNF)-specific neutralising agents in chronic inflammatory diseases: a real issue, a clinical perspective. Ann Rheum Dis. 2013;72:165-178.
5. Chi CC, Wang SH. Efficacy and cost-efficacy of biologic therapies for moderate to severe psoriasis: a meta-analysis and cost-efficacy analysis using the intention-to-treat principle. Biomed Res Int. 2014;2014:862851.
6. Kagami S, Rizzo HL, Lee JJ, et al. Circulating Th17, Th22, and Th1 cells are increased in psoriasis. J Invest Dermatol. 2010;130:1373-1383.
7. Leonardi CL, Gordon KB. New and emerging therapies in psoriasis. Semin Cutan Med Surg. 2014;33(2, suppl 2):S37-S41.
8. Lowes MA, Kikuchi T, Fuentes-Duculan J, et al. Psoriasis vulgaris lesions contain discrete populations of Th1 and Th17 T cells. J Invest Dermatol. 2008;128:1207-1211.
9. Nickoloff BJ, Qin JZ, Nestle FO. Immunopathogenesis of psoriasis. Clin Rev Allergy Immunol. 2007;33:45-56.
10. Fitch E, Harper E, Skorcheva I, et al. Pathophysiology of psoriasis: recent advances on IL-23 and Th17 cytokines. Curr Rheumatol Rep. 2007;9:461-467.
11. Adami S, Cavani A, Rossi F, et al. The role of interleukin-17A in psoriatic disease. BioDrugs. 2014;28:487-497.
12. Hueber W, Patel DD, Dryja T, et al. Effects of AIN457, a fully human antibody to interleukin-17A, on psoriasis, rheumatoid arthritis, and uveitis. Sci Transl Med. 2010;2:52ra72.
13. Langley RG, Elewski BE, Lebwohl M, et al. Secukinumab in plaque psoriasis—results of two phase 3 trials. N Engl J Med. 2014;371:326-338.
14. Puel A, Cypowyj S, Bustamante J, et al. Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity. Science. 2011;332:65-68.
15. Krstic A, Mojsilovic S, Jovcic G, et al. The potential of interleukin-17 to mediate hematopoietic response. Immunol Res. 2012;52:34-41.
16. Leonardi C, Matheson R, Zachariae C, et al. Anti-interleukin-17 monoclonal antibody ixekizumab in chronic plaque psoriasis. N Engl J Med. 2012;366:1190-1199.
17. Papp KA, Leonardi C, Menter A, et al. Brodalumab, an anti-interleukin-17-receptor antibody for psoriasis. N Engl J Med. 2012;366:1181-1189.
18. Langley RGB, Thaci D, Papp KA, et al. MK-3222, an anti–IL-23p19 humanized monoclonal antibody, provides significant improvement in psoriasis over 52 weeks of treatment that is maintained after discontinuation of dosing. Poster presented at: 73rd Annual Meeting of the American Academy of Dermatology; March 21-25, 2014; Denver, CO. Poster 8056.
19. Tausend W, Downing C, Tyring S. Systematic review of interleukin-12, interleukin-17, and interleukin-23 pathway inhibitors for the treatment of moderate-to-severe chronic plaque psoriasis: ustekinumab, briakinumab, tildrakizumab, guselkumab, secukinumab, ixekizumab, and brodalumab. J Cutan Med Surg. 2014;18:156-169.
20. Sofen H, Smith S, Matheson RT, et al. Guselkumab (an IL-23-specific mAb) demonstrates clinical and molecular response in patients with moderate-to-severe psoriasis. J Allergy Clin Immunol. 2014;133:1032-1040.
21. Schafer PH, Parton A, Capone L, et al. Apremilast is a selective PDE4 inhibitor with regulatory effects on innate immunity. Cell Signal. 2014;26:2016-2029.
22. van de Kerkhof PC. Apremilast: a step forward in the treatment of psoriasis? Lancet. 2012;380:708-709.
23. Paul C, Crowley J, Cather J, et al. Apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate to severe psoriasis: 16-week results of a phase 3, randomized, controlled trial (ESTEEM 2). Poster presented at: 73rd Annual Meeting of the American Academy of Dermatology; March 21-25, 2014; Denver, CO. Poster 8412.
24. Otezla [product insert]. Summit, NJ: Celgene Corporation; 2014.
25. Rabe KF. Update on roflumilast, a phosphodiesterase 4 inhibitor for the treatment of chronic obstructive pulmonary disease. Br J Pharmacol. 2011;163:53-67.
26. Palanivel JA, Macbeth AE, Chetty NC, et al. An insight into JAK-STAT signalling in dermatology. Clin Exp Dermatol. 2014;39:513-518.
27. Papp KA, Menter A, Strober B, et al. Efficacy and safety of tofacitinib, an oral Janus kinase inhibitor, in the treatment of psoriasis: a phase 2b randomized placebo-controlled dose-ranging study. Br J Dermatol. 2012;167:668-677.
28. Hsu L, Armstrong AW. JAK inhibitors: treatment efficacy and safety profile in patients with psoriasis. J Immunol Res. 2014;2014:283617.
1. Parisi R, Symmons DP, Griffiths CE, et al. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013;133:377-385.
2. Rapp SR, Feldman SR, Exum ML, et al. Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol. 1999;41(3 pt 1):401-407.
3. Shah R, Bewley A. Psoriasis: ‘the badge of shame.’ a case report of a psychological intervention to reduce and potentially clear chronic skin disease. Clin Exp Dermatol. 2014;39:600-603.
4. Vincent FB, Morand EF, Murphy K, et al. Antidrug antibodies (ADAb) to tumour necrosis factor (TNF)-specific neutralising agents in chronic inflammatory diseases: a real issue, a clinical perspective. Ann Rheum Dis. 2013;72:165-178.
5. Chi CC, Wang SH. Efficacy and cost-efficacy of biologic therapies for moderate to severe psoriasis: a meta-analysis and cost-efficacy analysis using the intention-to-treat principle. Biomed Res Int. 2014;2014:862851.
6. Kagami S, Rizzo HL, Lee JJ, et al. Circulating Th17, Th22, and Th1 cells are increased in psoriasis. J Invest Dermatol. 2010;130:1373-1383.
7. Leonardi CL, Gordon KB. New and emerging therapies in psoriasis. Semin Cutan Med Surg. 2014;33(2, suppl 2):S37-S41.
8. Lowes MA, Kikuchi T, Fuentes-Duculan J, et al. Psoriasis vulgaris lesions contain discrete populations of Th1 and Th17 T cells. J Invest Dermatol. 2008;128:1207-1211.
9. Nickoloff BJ, Qin JZ, Nestle FO. Immunopathogenesis of psoriasis. Clin Rev Allergy Immunol. 2007;33:45-56.
10. Fitch E, Harper E, Skorcheva I, et al. Pathophysiology of psoriasis: recent advances on IL-23 and Th17 cytokines. Curr Rheumatol Rep. 2007;9:461-467.
11. Adami S, Cavani A, Rossi F, et al. The role of interleukin-17A in psoriatic disease. BioDrugs. 2014;28:487-497.
12. Hueber W, Patel DD, Dryja T, et al. Effects of AIN457, a fully human antibody to interleukin-17A, on psoriasis, rheumatoid arthritis, and uveitis. Sci Transl Med. 2010;2:52ra72.
13. Langley RG, Elewski BE, Lebwohl M, et al. Secukinumab in plaque psoriasis—results of two phase 3 trials. N Engl J Med. 2014;371:326-338.
14. Puel A, Cypowyj S, Bustamante J, et al. Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity. Science. 2011;332:65-68.
15. Krstic A, Mojsilovic S, Jovcic G, et al. The potential of interleukin-17 to mediate hematopoietic response. Immunol Res. 2012;52:34-41.
16. Leonardi C, Matheson R, Zachariae C, et al. Anti-interleukin-17 monoclonal antibody ixekizumab in chronic plaque psoriasis. N Engl J Med. 2012;366:1190-1199.
17. Papp KA, Leonardi C, Menter A, et al. Brodalumab, an anti-interleukin-17-receptor antibody for psoriasis. N Engl J Med. 2012;366:1181-1189.
18. Langley RGB, Thaci D, Papp KA, et al. MK-3222, an anti–IL-23p19 humanized monoclonal antibody, provides significant improvement in psoriasis over 52 weeks of treatment that is maintained after discontinuation of dosing. Poster presented at: 73rd Annual Meeting of the American Academy of Dermatology; March 21-25, 2014; Denver, CO. Poster 8056.
19. Tausend W, Downing C, Tyring S. Systematic review of interleukin-12, interleukin-17, and interleukin-23 pathway inhibitors for the treatment of moderate-to-severe chronic plaque psoriasis: ustekinumab, briakinumab, tildrakizumab, guselkumab, secukinumab, ixekizumab, and brodalumab. J Cutan Med Surg. 2014;18:156-169.
20. Sofen H, Smith S, Matheson RT, et al. Guselkumab (an IL-23-specific mAb) demonstrates clinical and molecular response in patients with moderate-to-severe psoriasis. J Allergy Clin Immunol. 2014;133:1032-1040.
21. Schafer PH, Parton A, Capone L, et al. Apremilast is a selective PDE4 inhibitor with regulatory effects on innate immunity. Cell Signal. 2014;26:2016-2029.
22. van de Kerkhof PC. Apremilast: a step forward in the treatment of psoriasis? Lancet. 2012;380:708-709.
23. Paul C, Crowley J, Cather J, et al. Apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate to severe psoriasis: 16-week results of a phase 3, randomized, controlled trial (ESTEEM 2). Poster presented at: 73rd Annual Meeting of the American Academy of Dermatology; March 21-25, 2014; Denver, CO. Poster 8412.
24. Otezla [product insert]. Summit, NJ: Celgene Corporation; 2014.
25. Rabe KF. Update on roflumilast, a phosphodiesterase 4 inhibitor for the treatment of chronic obstructive pulmonary disease. Br J Pharmacol. 2011;163:53-67.
26. Palanivel JA, Macbeth AE, Chetty NC, et al. An insight into JAK-STAT signalling in dermatology. Clin Exp Dermatol. 2014;39:513-518.
27. Papp KA, Menter A, Strober B, et al. Efficacy and safety of tofacitinib, an oral Janus kinase inhibitor, in the treatment of psoriasis: a phase 2b randomized placebo-controlled dose-ranging study. Br J Dermatol. 2012;167:668-677.
28. Hsu L, Armstrong AW. JAK inhibitors: treatment efficacy and safety profile in patients with psoriasis. J Immunol Res. 2014;2014:283617.
Practice Points
- Secukinumab is an anti–IL-17 antibody approved for the treatment of psoriasis. It is indicated for the treatment of moderate to severe plaque psoriasis in adult patients who are candidates for systemic therapy or phototherapy.
- The new biological agents have shown promising results with some patients achieving psoriasis area and severity index scores of 90 and 100.
- A number of small molecule inhibitors also are in the pipeline, with apremilast the first one to have reached approval for psoriasis.
Disease Burden and Quality of Life in Psoriasis Patients With and Without Comorbid Psoriatic Arthritis: Results From National Psoriasis Foundation Panel Surveys
Approximately 3% of the US adult population, or roughly 5 million Americans, have been diagnosed with psoriasis.1 Psoriasis has a high disease burden, with one review of 817 quality-of-life (QOL) studies concluding that the degree to which psoriasis negatively affects patients’ QOL is comparable with major diseases such as diabetes mellitus or cancer.2
Psoriatic arthritis (PsA) is a chronic, often progressive, inflammatory arthropathy that can lead to permanent joint damage and severe disability.3,4 Psoriatic arthritis is a common comorbidity among patients with psoriasis, affecting 6% to 10% of psoriasis patients overall5 and 20% to 40% of psoriasis patients with more extensive skin involvement.5-7
The comorbidity profile and overall disease impact are not well understood in psoriasis patients with and without comorbid PsA. The primary objective of this study was to compare disease characteristics, comorbidities, and psoriasis-related QOL in patients with moderate to severe psoriasis with and without comorbid PsA.
Methods
Study Design and Participants
Since 2003 the National Psoriasis Foundation (NPF) has conducted semiannual survey panels to collect patient-reported data on topics including disease characteristics, treatment utilization, and psoriasis-related QOL impact. Responses from approximately 5604 individuals have been collected and analyzed from a total of 13 survey panels conducted from 2003-2009 and 2011. No data were available for 2010. In each survey panel, responses from approximately 400 randomly selected respondents were collected, with approximately 300 respondents having moderate to severe psoriasis and 200 respondents being NPF members. Respondents were surveyed via telephone and the Internet.
This study examined 2 main patient groups: (1) adults (>18 years of age) with psoriasis alone and (2) those with comorbid PsA. The 2 study groups were subdivided according to percentage of body surface area (BSA) affected; specifically, patients with psoriasis alone were classified as having mild psoriasis (<3% BSA) or moderate to severe psoriasis (>3% BSA) and patients with PsA were classified as having mild to no psoriasis (<3% BSA) or moderate to severe psoriasis (≥3% BSA).8
Assessments
Comparisons of patient demographics, disease characteristics, comorbidities, psoriasis-related QOL, and symptom impact were made for patients with moderate to severe psoriasis and PsA versus those with moderate to severe psoriasis alone. The overall impact of psoriasis on patients’ physical and emotional QOL was assessed via a 12-item survey with each item rated on an 11-point scale (0=not at all; 5=somewhat; 10=very much). Total QOL scores ranged from 0 to 120. Higher scores indicated greater (ie, worse) impact of psoriasis on the patient’s QOL. To evaluate symptom impact (ie, to what degree a patient felt affected by individual symptoms), ratings from 3 symptoms—itching, irritation, and pain—that were included in the overall QOL assessment also were analyzed individually. Results also were compared for patients with mild psoriasis alone versus those with moderate to severe psoriasis alone as well as for patients with PsA and mild to no psoriasis versus those with PsA and moderate to severe psoriasis.
Statistical Analysis
Adult survey respondents who answered survey questions relevant to the analysis were included. For patient demographics and comorbidities, t tests were used for continuous variables and Χ2 tests were used for categorical variables. For overall psoriasis-related QOL and symptom impact scores, differences among the study groups were compared using analyses of covariance, which adjusted for age, gender, and race. All analyses were conducted using SAS version 9.2.
Results
Patient Demographics
Of 5467 total respondents, 3532 reported moderate to severe psoriasis of which 1280 (36.2%) had comorbid PsA (Table 1). Compared to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA were older, less commonly male, less likely to be employed, had a longer duration of psoriasis, were more likely to be white, and were more likely to have health insurance coverage. Among the psoriasis alone group, those patients reporting moderate to severe psoriasis were younger, less likely to have health insurance coverage, and were less likely to be treated by a dermatologist only than those with mild psoriasis. Among the group with PsA, patients with moderate to severe psoriasis were more likely to be treated by a dermatologist only versus those with mild or no psoriasis (Table 1).
Patient Comorbidities
Patients with moderate to severe psoriasis and comorbid PsA reported significantly higher rates of diabetes mellitus, lupus, rheumatoid arthritis, other arthritis, ankylosing spondylitis, and high blood pressure than patients with moderate to severe psoriasis alone (P<.05)(Table 2). In the group with psoriasis alone, patients with moderate to severe psoriasis had significantly lower rates of lupus compared to those with mild psoriasis (P<.05). In the group with PsA, patients with moderate to severe psoriasis were significantly more likely to report diagnoses of colitis, diabetes mellitus, heart disease, and high blood pressure compared to those with mild to no psoriasis (P<.05).
Psoriasis-Related QOL
The psoriasis-related QOL analyses are shown in Table 3. Patients with moderate to severe psoriasis and comorbid PsA reported a greater impact on overall QOL compared to their counterparts with moderate to severe psoriasis alone. Similarly, patients with moderate to severe psoriasis and comorbid PsA reported a greater impact of itching, physical irritation/soreness, and pain symptoms.
Disease severity was associated with psoriasis-related QOL. Compared to patients with mild psoriasis alone, those with moderate to severe psoriasis alone had significantly higher (ie, worse) scores in the categories of itching, irritation, pain, and overall QOL (P<.05). In the PsA group, patients with moderate to severe psoriasis also reported significantly worse itching, irritation, pain, and overall QOL compared to their counterparts with mild to no psoriasis (P<.05).
Comment
The results of this study showed that patient demographics, comorbidities, and psoriasis-related QOL in psoriasis patients varied significantly depending on presence or absence of comorbid PsA as well as disease severity. Patients with more severe cutaneous psoriasis with and without PsA were associated with worse QOL scores and higher rates of self-reported heart disease and hypertension. Among patients with moderate to severe psoriasis, those with comorbid PsA were associated with greater rates of self-reported diabetes mellitus and high blood pressure and worse QOL scores including worse itching, irritation, and pain than those with moderate to severe psoriasis alone.
The present study is one of the first to compare psoriasis-related QOL in patients with and without PsA. A prior study demonstrated patients with PsA had worse physical impairment, fatigue severity, and health status relative to patients with psoriasis alone but no differences in dermatology-specific QOL measures.9 Our analysis revealed that patients with moderate to severe psoriasis and comorbid PsA experienced a greater impact on overall QOL as well as symptoms of itching, irritation, and pain relative to patients with moderate to severe psoriasis alone. Among both treatment groups, reports of overall QOL and itching, irritation, and pain became worse as the disease severity increased. These findings are consistent with prior studies that have shown greater impairment of QOL among patients with severe psoriasis compared to mild psoriasis.10-12
Relative to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA reported a greater prevalence of comorbid diagnoses overall, with notably higher rates of type 2 diabetes mellitus, hypertension, and rheumatoid arthritis. These findings are consistent with an earlier report by Husted et al.13
Limitations
The results of this study should be interpreted in light of several important limitations associated with survey data (ie, patient-reported data, no details on length of therapy or comorbid disease, multiple surveys taken over time, respondents aged >18 years only).
Conclusion
This study provides evidence that patients with moderate to severe psoriasis and comorbid PsA have a higher psoriasis-related disease burden compared to those with moderate to severe psoriasis alone, which suggests that physicians may wish to consider this comorbidity when designing patient treatment plans. Our findings also confirm that disease severity is associated with comorbid conditions and psoriasis-related QOL impact in psoriasis patients. These findings highlight the importance of screening for PsA in patients with psoriasis and effective treatment of skin disease in patients with PsA.
Acknowledgment
The authors thank Maureen Lage, PhD, Healthmetrics, Bonita Springs, Florida, for her work in drafting the manuscript.
1. Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003-2004. J Am Acad Dermatol. 2009;60:218-224.
2. Raho G, Koleva DM, Garattini L, et al. The burden of moderate to severe psoriasis: an overview. Pharmacoeconomics. 2012;30:1005-1013.
3. Gladman DD, Antoni C, Mease P, et al. Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Ann Rheum Dis. 2005;64(suppl 2):14-17.
4. Ogdie A, Langan S, Love T, et al. Prevalence and treatment patterns of psoriatic arthritis in the UK. Rheumatology (Oxford). 2013;52:568-575.
5. Ogdie A, Gelfand JM. Identification of risk factors for psoriatic arthritis: scientific opportunity meets clinical need. Arch Dermatol. 2010;146:785-788.
6. Gelfand JM, Gladman DD, Mease PJ, et al. Epidemiology of psoriatic arthritis in the population of the United States. J Am Acad Dermatol. 2005;53:573.
7. Richardson SK, Gelfand JM. Update on the natural history and systemic treatment of psoriasis. Adv Dermatol. 2008;24:171-196.
8. Armstrong AW, Robertson AD, Wu J, et al. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003-2011. JAMA Dermatol. 2013;149:1180-1185.
9. Rosen CF, Mussani F, Chandran V, et al. Patients with psoriatic arthritis have worse quality of life than those with psoriasis alone. Rheumatology (Oxford). 2012;51:571-576.
10. Armstrong AW, Schupp C, Wu J, et al. Quality of life and work productivity impairment among psoriasis patients: findings from the National Psoriasis Foundation survey data 2003-2011. PLoS ONE. 2012;7:e52935.
11. Colombo G, Altomare G, Peris K, et al. Moderate and severe plaque psoriasis: cost-of-illness study in Italy. Ther Clin Risk Manag. 2008;4:559-568.
12. Gelfand JM, Feldman SR, Stern RS, et al. Determinants of quality of life in patients with psoriasis: a study from the US population. J Am Acad Dermatol. 2004;51:704-708.
13. Husted JA, Thavaneswaran A, Chandran V, et al. Cardiovascular and other comorbidities in patients with psoriatic arthritis: a comparison with patients with psoriasis. Arthritis Care Res (Hoboken). 2011;63:1729-1735.
Approximately 3% of the US adult population, or roughly 5 million Americans, have been diagnosed with psoriasis.1 Psoriasis has a high disease burden, with one review of 817 quality-of-life (QOL) studies concluding that the degree to which psoriasis negatively affects patients’ QOL is comparable with major diseases such as diabetes mellitus or cancer.2
Psoriatic arthritis (PsA) is a chronic, often progressive, inflammatory arthropathy that can lead to permanent joint damage and severe disability.3,4 Psoriatic arthritis is a common comorbidity among patients with psoriasis, affecting 6% to 10% of psoriasis patients overall5 and 20% to 40% of psoriasis patients with more extensive skin involvement.5-7
The comorbidity profile and overall disease impact are not well understood in psoriasis patients with and without comorbid PsA. The primary objective of this study was to compare disease characteristics, comorbidities, and psoriasis-related QOL in patients with moderate to severe psoriasis with and without comorbid PsA.
Methods
Study Design and Participants
Since 2003 the National Psoriasis Foundation (NPF) has conducted semiannual survey panels to collect patient-reported data on topics including disease characteristics, treatment utilization, and psoriasis-related QOL impact. Responses from approximately 5604 individuals have been collected and analyzed from a total of 13 survey panels conducted from 2003-2009 and 2011. No data were available for 2010. In each survey panel, responses from approximately 400 randomly selected respondents were collected, with approximately 300 respondents having moderate to severe psoriasis and 200 respondents being NPF members. Respondents were surveyed via telephone and the Internet.
This study examined 2 main patient groups: (1) adults (>18 years of age) with psoriasis alone and (2) those with comorbid PsA. The 2 study groups were subdivided according to percentage of body surface area (BSA) affected; specifically, patients with psoriasis alone were classified as having mild psoriasis (<3% BSA) or moderate to severe psoriasis (>3% BSA) and patients with PsA were classified as having mild to no psoriasis (<3% BSA) or moderate to severe psoriasis (≥3% BSA).8
Assessments
Comparisons of patient demographics, disease characteristics, comorbidities, psoriasis-related QOL, and symptom impact were made for patients with moderate to severe psoriasis and PsA versus those with moderate to severe psoriasis alone. The overall impact of psoriasis on patients’ physical and emotional QOL was assessed via a 12-item survey with each item rated on an 11-point scale (0=not at all; 5=somewhat; 10=very much). Total QOL scores ranged from 0 to 120. Higher scores indicated greater (ie, worse) impact of psoriasis on the patient’s QOL. To evaluate symptom impact (ie, to what degree a patient felt affected by individual symptoms), ratings from 3 symptoms—itching, irritation, and pain—that were included in the overall QOL assessment also were analyzed individually. Results also were compared for patients with mild psoriasis alone versus those with moderate to severe psoriasis alone as well as for patients with PsA and mild to no psoriasis versus those with PsA and moderate to severe psoriasis.
Statistical Analysis
Adult survey respondents who answered survey questions relevant to the analysis were included. For patient demographics and comorbidities, t tests were used for continuous variables and Χ2 tests were used for categorical variables. For overall psoriasis-related QOL and symptom impact scores, differences among the study groups were compared using analyses of covariance, which adjusted for age, gender, and race. All analyses were conducted using SAS version 9.2.
Results
Patient Demographics
Of 5467 total respondents, 3532 reported moderate to severe psoriasis of which 1280 (36.2%) had comorbid PsA (Table 1). Compared to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA were older, less commonly male, less likely to be employed, had a longer duration of psoriasis, were more likely to be white, and were more likely to have health insurance coverage. Among the psoriasis alone group, those patients reporting moderate to severe psoriasis were younger, less likely to have health insurance coverage, and were less likely to be treated by a dermatologist only than those with mild psoriasis. Among the group with PsA, patients with moderate to severe psoriasis were more likely to be treated by a dermatologist only versus those with mild or no psoriasis (Table 1).
Patient Comorbidities
Patients with moderate to severe psoriasis and comorbid PsA reported significantly higher rates of diabetes mellitus, lupus, rheumatoid arthritis, other arthritis, ankylosing spondylitis, and high blood pressure than patients with moderate to severe psoriasis alone (P<.05)(Table 2). In the group with psoriasis alone, patients with moderate to severe psoriasis had significantly lower rates of lupus compared to those with mild psoriasis (P<.05). In the group with PsA, patients with moderate to severe psoriasis were significantly more likely to report diagnoses of colitis, diabetes mellitus, heart disease, and high blood pressure compared to those with mild to no psoriasis (P<.05).
Psoriasis-Related QOL
The psoriasis-related QOL analyses are shown in Table 3. Patients with moderate to severe psoriasis and comorbid PsA reported a greater impact on overall QOL compared to their counterparts with moderate to severe psoriasis alone. Similarly, patients with moderate to severe psoriasis and comorbid PsA reported a greater impact of itching, physical irritation/soreness, and pain symptoms.
Disease severity was associated with psoriasis-related QOL. Compared to patients with mild psoriasis alone, those with moderate to severe psoriasis alone had significantly higher (ie, worse) scores in the categories of itching, irritation, pain, and overall QOL (P<.05). In the PsA group, patients with moderate to severe psoriasis also reported significantly worse itching, irritation, pain, and overall QOL compared to their counterparts with mild to no psoriasis (P<.05).
Comment
The results of this study showed that patient demographics, comorbidities, and psoriasis-related QOL in psoriasis patients varied significantly depending on presence or absence of comorbid PsA as well as disease severity. Patients with more severe cutaneous psoriasis with and without PsA were associated with worse QOL scores and higher rates of self-reported heart disease and hypertension. Among patients with moderate to severe psoriasis, those with comorbid PsA were associated with greater rates of self-reported diabetes mellitus and high blood pressure and worse QOL scores including worse itching, irritation, and pain than those with moderate to severe psoriasis alone.
The present study is one of the first to compare psoriasis-related QOL in patients with and without PsA. A prior study demonstrated patients with PsA had worse physical impairment, fatigue severity, and health status relative to patients with psoriasis alone but no differences in dermatology-specific QOL measures.9 Our analysis revealed that patients with moderate to severe psoriasis and comorbid PsA experienced a greater impact on overall QOL as well as symptoms of itching, irritation, and pain relative to patients with moderate to severe psoriasis alone. Among both treatment groups, reports of overall QOL and itching, irritation, and pain became worse as the disease severity increased. These findings are consistent with prior studies that have shown greater impairment of QOL among patients with severe psoriasis compared to mild psoriasis.10-12
Relative to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA reported a greater prevalence of comorbid diagnoses overall, with notably higher rates of type 2 diabetes mellitus, hypertension, and rheumatoid arthritis. These findings are consistent with an earlier report by Husted et al.13
Limitations
The results of this study should be interpreted in light of several important limitations associated with survey data (ie, patient-reported data, no details on length of therapy or comorbid disease, multiple surveys taken over time, respondents aged >18 years only).
Conclusion
This study provides evidence that patients with moderate to severe psoriasis and comorbid PsA have a higher psoriasis-related disease burden compared to those with moderate to severe psoriasis alone, which suggests that physicians may wish to consider this comorbidity when designing patient treatment plans. Our findings also confirm that disease severity is associated with comorbid conditions and psoriasis-related QOL impact in psoriasis patients. These findings highlight the importance of screening for PsA in patients with psoriasis and effective treatment of skin disease in patients with PsA.
Acknowledgment
The authors thank Maureen Lage, PhD, Healthmetrics, Bonita Springs, Florida, for her work in drafting the manuscript.
Approximately 3% of the US adult population, or roughly 5 million Americans, have been diagnosed with psoriasis.1 Psoriasis has a high disease burden, with one review of 817 quality-of-life (QOL) studies concluding that the degree to which psoriasis negatively affects patients’ QOL is comparable with major diseases such as diabetes mellitus or cancer.2
Psoriatic arthritis (PsA) is a chronic, often progressive, inflammatory arthropathy that can lead to permanent joint damage and severe disability.3,4 Psoriatic arthritis is a common comorbidity among patients with psoriasis, affecting 6% to 10% of psoriasis patients overall5 and 20% to 40% of psoriasis patients with more extensive skin involvement.5-7
The comorbidity profile and overall disease impact are not well understood in psoriasis patients with and without comorbid PsA. The primary objective of this study was to compare disease characteristics, comorbidities, and psoriasis-related QOL in patients with moderate to severe psoriasis with and without comorbid PsA.
Methods
Study Design and Participants
Since 2003 the National Psoriasis Foundation (NPF) has conducted semiannual survey panels to collect patient-reported data on topics including disease characteristics, treatment utilization, and psoriasis-related QOL impact. Responses from approximately 5604 individuals have been collected and analyzed from a total of 13 survey panels conducted from 2003-2009 and 2011. No data were available for 2010. In each survey panel, responses from approximately 400 randomly selected respondents were collected, with approximately 300 respondents having moderate to severe psoriasis and 200 respondents being NPF members. Respondents were surveyed via telephone and the Internet.
This study examined 2 main patient groups: (1) adults (>18 years of age) with psoriasis alone and (2) those with comorbid PsA. The 2 study groups were subdivided according to percentage of body surface area (BSA) affected; specifically, patients with psoriasis alone were classified as having mild psoriasis (<3% BSA) or moderate to severe psoriasis (>3% BSA) and patients with PsA were classified as having mild to no psoriasis (<3% BSA) or moderate to severe psoriasis (≥3% BSA).8
Assessments
Comparisons of patient demographics, disease characteristics, comorbidities, psoriasis-related QOL, and symptom impact were made for patients with moderate to severe psoriasis and PsA versus those with moderate to severe psoriasis alone. The overall impact of psoriasis on patients’ physical and emotional QOL was assessed via a 12-item survey with each item rated on an 11-point scale (0=not at all; 5=somewhat; 10=very much). Total QOL scores ranged from 0 to 120. Higher scores indicated greater (ie, worse) impact of psoriasis on the patient’s QOL. To evaluate symptom impact (ie, to what degree a patient felt affected by individual symptoms), ratings from 3 symptoms—itching, irritation, and pain—that were included in the overall QOL assessment also were analyzed individually. Results also were compared for patients with mild psoriasis alone versus those with moderate to severe psoriasis alone as well as for patients with PsA and mild to no psoriasis versus those with PsA and moderate to severe psoriasis.
Statistical Analysis
Adult survey respondents who answered survey questions relevant to the analysis were included. For patient demographics and comorbidities, t tests were used for continuous variables and Χ2 tests were used for categorical variables. For overall psoriasis-related QOL and symptom impact scores, differences among the study groups were compared using analyses of covariance, which adjusted for age, gender, and race. All analyses were conducted using SAS version 9.2.
Results
Patient Demographics
Of 5467 total respondents, 3532 reported moderate to severe psoriasis of which 1280 (36.2%) had comorbid PsA (Table 1). Compared to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA were older, less commonly male, less likely to be employed, had a longer duration of psoriasis, were more likely to be white, and were more likely to have health insurance coverage. Among the psoriasis alone group, those patients reporting moderate to severe psoriasis were younger, less likely to have health insurance coverage, and were less likely to be treated by a dermatologist only than those with mild psoriasis. Among the group with PsA, patients with moderate to severe psoriasis were more likely to be treated by a dermatologist only versus those with mild or no psoriasis (Table 1).
Patient Comorbidities
Patients with moderate to severe psoriasis and comorbid PsA reported significantly higher rates of diabetes mellitus, lupus, rheumatoid arthritis, other arthritis, ankylosing spondylitis, and high blood pressure than patients with moderate to severe psoriasis alone (P<.05)(Table 2). In the group with psoriasis alone, patients with moderate to severe psoriasis had significantly lower rates of lupus compared to those with mild psoriasis (P<.05). In the group with PsA, patients with moderate to severe psoriasis were significantly more likely to report diagnoses of colitis, diabetes mellitus, heart disease, and high blood pressure compared to those with mild to no psoriasis (P<.05).
Psoriasis-Related QOL
The psoriasis-related QOL analyses are shown in Table 3. Patients with moderate to severe psoriasis and comorbid PsA reported a greater impact on overall QOL compared to their counterparts with moderate to severe psoriasis alone. Similarly, patients with moderate to severe psoriasis and comorbid PsA reported a greater impact of itching, physical irritation/soreness, and pain symptoms.
Disease severity was associated with psoriasis-related QOL. Compared to patients with mild psoriasis alone, those with moderate to severe psoriasis alone had significantly higher (ie, worse) scores in the categories of itching, irritation, pain, and overall QOL (P<.05). In the PsA group, patients with moderate to severe psoriasis also reported significantly worse itching, irritation, pain, and overall QOL compared to their counterparts with mild to no psoriasis (P<.05).
Comment
The results of this study showed that patient demographics, comorbidities, and psoriasis-related QOL in psoriasis patients varied significantly depending on presence or absence of comorbid PsA as well as disease severity. Patients with more severe cutaneous psoriasis with and without PsA were associated with worse QOL scores and higher rates of self-reported heart disease and hypertension. Among patients with moderate to severe psoriasis, those with comorbid PsA were associated with greater rates of self-reported diabetes mellitus and high blood pressure and worse QOL scores including worse itching, irritation, and pain than those with moderate to severe psoriasis alone.
The present study is one of the first to compare psoriasis-related QOL in patients with and without PsA. A prior study demonstrated patients with PsA had worse physical impairment, fatigue severity, and health status relative to patients with psoriasis alone but no differences in dermatology-specific QOL measures.9 Our analysis revealed that patients with moderate to severe psoriasis and comorbid PsA experienced a greater impact on overall QOL as well as symptoms of itching, irritation, and pain relative to patients with moderate to severe psoriasis alone. Among both treatment groups, reports of overall QOL and itching, irritation, and pain became worse as the disease severity increased. These findings are consistent with prior studies that have shown greater impairment of QOL among patients with severe psoriasis compared to mild psoriasis.10-12
Relative to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA reported a greater prevalence of comorbid diagnoses overall, with notably higher rates of type 2 diabetes mellitus, hypertension, and rheumatoid arthritis. These findings are consistent with an earlier report by Husted et al.13
Limitations
The results of this study should be interpreted in light of several important limitations associated with survey data (ie, patient-reported data, no details on length of therapy or comorbid disease, multiple surveys taken over time, respondents aged >18 years only).
Conclusion
This study provides evidence that patients with moderate to severe psoriasis and comorbid PsA have a higher psoriasis-related disease burden compared to those with moderate to severe psoriasis alone, which suggests that physicians may wish to consider this comorbidity when designing patient treatment plans. Our findings also confirm that disease severity is associated with comorbid conditions and psoriasis-related QOL impact in psoriasis patients. These findings highlight the importance of screening for PsA in patients with psoriasis and effective treatment of skin disease in patients with PsA.
Acknowledgment
The authors thank Maureen Lage, PhD, Healthmetrics, Bonita Springs, Florida, for her work in drafting the manuscript.
1. Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003-2004. J Am Acad Dermatol. 2009;60:218-224.
2. Raho G, Koleva DM, Garattini L, et al. The burden of moderate to severe psoriasis: an overview. Pharmacoeconomics. 2012;30:1005-1013.
3. Gladman DD, Antoni C, Mease P, et al. Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Ann Rheum Dis. 2005;64(suppl 2):14-17.
4. Ogdie A, Langan S, Love T, et al. Prevalence and treatment patterns of psoriatic arthritis in the UK. Rheumatology (Oxford). 2013;52:568-575.
5. Ogdie A, Gelfand JM. Identification of risk factors for psoriatic arthritis: scientific opportunity meets clinical need. Arch Dermatol. 2010;146:785-788.
6. Gelfand JM, Gladman DD, Mease PJ, et al. Epidemiology of psoriatic arthritis in the population of the United States. J Am Acad Dermatol. 2005;53:573.
7. Richardson SK, Gelfand JM. Update on the natural history and systemic treatment of psoriasis. Adv Dermatol. 2008;24:171-196.
8. Armstrong AW, Robertson AD, Wu J, et al. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003-2011. JAMA Dermatol. 2013;149:1180-1185.
9. Rosen CF, Mussani F, Chandran V, et al. Patients with psoriatic arthritis have worse quality of life than those with psoriasis alone. Rheumatology (Oxford). 2012;51:571-576.
10. Armstrong AW, Schupp C, Wu J, et al. Quality of life and work productivity impairment among psoriasis patients: findings from the National Psoriasis Foundation survey data 2003-2011. PLoS ONE. 2012;7:e52935.
11. Colombo G, Altomare G, Peris K, et al. Moderate and severe plaque psoriasis: cost-of-illness study in Italy. Ther Clin Risk Manag. 2008;4:559-568.
12. Gelfand JM, Feldman SR, Stern RS, et al. Determinants of quality of life in patients with psoriasis: a study from the US population. J Am Acad Dermatol. 2004;51:704-708.
13. Husted JA, Thavaneswaran A, Chandran V, et al. Cardiovascular and other comorbidities in patients with psoriatic arthritis: a comparison with patients with psoriasis. Arthritis Care Res (Hoboken). 2011;63:1729-1735.
1. Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003-2004. J Am Acad Dermatol. 2009;60:218-224.
2. Raho G, Koleva DM, Garattini L, et al. The burden of moderate to severe psoriasis: an overview. Pharmacoeconomics. 2012;30:1005-1013.
3. Gladman DD, Antoni C, Mease P, et al. Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Ann Rheum Dis. 2005;64(suppl 2):14-17.
4. Ogdie A, Langan S, Love T, et al. Prevalence and treatment patterns of psoriatic arthritis in the UK. Rheumatology (Oxford). 2013;52:568-575.
5. Ogdie A, Gelfand JM. Identification of risk factors for psoriatic arthritis: scientific opportunity meets clinical need. Arch Dermatol. 2010;146:785-788.
6. Gelfand JM, Gladman DD, Mease PJ, et al. Epidemiology of psoriatic arthritis in the population of the United States. J Am Acad Dermatol. 2005;53:573.
7. Richardson SK, Gelfand JM. Update on the natural history and systemic treatment of psoriasis. Adv Dermatol. 2008;24:171-196.
8. Armstrong AW, Robertson AD, Wu J, et al. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003-2011. JAMA Dermatol. 2013;149:1180-1185.
9. Rosen CF, Mussani F, Chandran V, et al. Patients with psoriatic arthritis have worse quality of life than those with psoriasis alone. Rheumatology (Oxford). 2012;51:571-576.
10. Armstrong AW, Schupp C, Wu J, et al. Quality of life and work productivity impairment among psoriasis patients: findings from the National Psoriasis Foundation survey data 2003-2011. PLoS ONE. 2012;7:e52935.
11. Colombo G, Altomare G, Peris K, et al. Moderate and severe plaque psoriasis: cost-of-illness study in Italy. Ther Clin Risk Manag. 2008;4:559-568.
12. Gelfand JM, Feldman SR, Stern RS, et al. Determinants of quality of life in patients with psoriasis: a study from the US population. J Am Acad Dermatol. 2004;51:704-708.
13. Husted JA, Thavaneswaran A, Chandran V, et al. Cardiovascular and other comorbidities in patients with psoriatic arthritis: a comparison with patients with psoriasis. Arthritis Care Res (Hoboken). 2011;63:1729-1735.
Practice Points
- Patients with psoriatic arthritis (PsA) often have severe cutaneous psoriasis. These patients may be at higher risk for comorbid conditions and impaired quality of life (QOL) compared to patients with psoriasis alone.
- The severity of cutaneous psoriasis, both in patients with psoriasis alone and those with comorbid PsA, is remarkable and is associated with worse QOL scores.
Update on Pediatric Psoriasis
Psoriasis affects 2% to 4% of the US population, with approximately one-third of cases beginning in childhood. The understanding of pediatric psoriasis has developed at a far slower pace than adult disease, with limitations in care including few medications that are approved by the US Food and Drug Administration for pediatric and adolescent use. Recently, a stable fixed-combination dose of calcipo-triene 0.005%–betamethasone dipropionate 0.064% topical suspension was approved for treatment of plaque psoriasis of the scalp in patients aged 12 to 17 years, which hopefully will lead a trend in psoriasis medication approval for children and teenagers.1 Based on a PubMed search of articles indexed for MEDLINE using the search terms pediatric psoriasis, psoriasis, and strep that were published from April 2012 to April 2014, this article reviews newer data to address the issues that surround pediatric psoriasis and to provide an update on prior review articles on pediatric psoriasis.2-5 This article reviews some of the newer literature on clinical presentation and comorbidities in pediatric psoriasis.5 Based on these recent findings, additional screenings including review of obesity parameters are recommended for pediatric patients with psoriasis (Table 1).
Update on Disease Manifestations, Associations, and Comorbidities
Disease Manifestations
A 2013 multicenter study delineated the clinical features of pediatric psoriasis.6 The study was conducted at 8 geographically diverse dermatology clinics in the United States to delineate the clinical manifestations of pediatric psoriasis. In an assessment of 181 participants aged 5 to 17 years, the investigators sought to determine the frequency of disease sites, severity, and guttate disease. Over a period of approximately 2 years, 43.1% of participants were determined to have mild disease and 56.9% had severe disease. Family history of psoriasis was present in 51.4% of participants, with first-degree relatives affected in 59.8% of cases. Scalp involvement at some time was noted in 79.0% of participants, and nail disease was noted in 55% of boys and 29% of girls. Guttate psoriasis was noted in 30% of participants, with more cases in the severe range (35.9%) versus the mild range (21.8%). Additionally, 22.1% of participants had a precipitating streptococcal infection, with the association being more common in pediatric patients with guttate psoriasis than plaque psoriasis.6 This study highlighted that pediatric psoriasis has a genetic basis, is frequently guttate in nature, commonly affects the nails, shows a trend toward being classified as severe, and may be triggered by streptococcal infections.
Streptococcal Infection
Pediatric psoriasis may be triggered or flared by Streptococcus pyogenes (group A β-hemolytic streptococci) infections, specifically β-hemolytic streptococci groups A, C, and G that have streptococcal M protein,2,3,7 and this tendency can be associated with HLA-Cw6 or guttate psoriasis. Newer data have elucidated the role of streptococcal throat infections in psoriasis. Given that streptococcal throat infections are most common in school-aged children, these studies suggest a putative mechanism in pediatric psoriasis for triggering streptococcal infections, which would need to be confirmed in future studies, specifically in pediatric psoriasis patients.
It has been shown that T cells in psoriasis patients recognize common streptococcal M proteins and keratin determinants.7 Ferran et al8 recently demonstrated activation of circulating cutaneous lymphocyte–associated antigen (CLA)+ T cells but not CLA- memory T cells in 27 psoriasis patients (ages not specified) when mixed with streptococcal throat extracts, causing production of IL-17, IP-10, IL-22, and IFN-γ; activation was not found in 6 healthy control patients. Antistreptolysin O levels were correlated with the messenger RNA up- regulation for IL-17, IP-10, IL-22, and IFN-γ, and also correlated with psoriasis area and severity index score in psoriasis patients. In this same study, injection of the activated culture supernatant into mouse skin caused epidermal hyperkeratosis and activation of nonlesional epidermal cells from psoriatic patients. This study thereby delineated some of the potential pathways of the streptococcal induction of psoriasis and psoriatic flares in childhood8; however, confirmation is needed through further study of pediatric psoriatic lymphocyte activity.
Differential Diagnosis
Additions to the extensive differential list have been cited in the recent literature. The differential diagnosis of pediatric psoriasis now includes sodium valproate–induced psoriasiform drug eruption9 and allergic contact dermatitis to methylchloroisothiazolinone and methylisothiazolinone, which are present in many sanitizing hand and diaper wipes and has been reported to cause psoriasiform dermatitis in a periorificial or perineal distribution.10 Clinicians should inquire about the use of these wipes, as caregivers rarely suspect this agent to be causative of the eruption.
Psoriatic Arthritis
Previously, psoriasis and psoriatic arthritis have been linked to autoimmune thyroid disease in adults.11 A study of the Childhood Arthritis & Rheumatology Research Alliance (CARRA) registry showed that family history of psoriasis, autoimmune thyroiditis, Crohn disease, and ankylosing spondylitis in a first-degree relative has been linked to juvenile idiopathic arthritis, highlighting that pediatric psoriasis can be genetically linked or associated with multiple autoimmune conditions and vice versa.12
Obesity, Metabolic Syndrome, and Cardiovascular Risks
Obesity is associated with pediatric psoriasis as highlighted in a growing body of recent literature.13 Excess adiposity as manifested by body mass index in the 85th percentile or greater (37.9% of 155 pediatric psoriasis patients vs 20.5% of 42 controls) and excess central adiposity as manifested by excess waist circumference and increased waist-to-height ratios are more common in pediatric patients with psoriasis than in controls.14
Obesity may be a trigger or associated with increased disease activity in pediatric psoriasis patients. Excess overall adiposity correlates with more severe disease. Obesity parameters may correlate with the onset of psoriasis and with disease severity. In fact, the odds of obesity may be higher in childhood than in adults.14,15 A 2011 report of pediatric psoriasis patients aged 10 to 17 years (n=12) and wart controls (n=6)(mean age, 13.2 and 13.5 years, respectively) demonstrated that 4 of 12 patients with psoriasis and 0 of 6 patients with warts met criteria for metabolic syndrome as defined by 3 of the following: (1) triglycerides greater than or equal to 100 mg/dL; (2) high-density lipoprotein cholesterol less than 50 mg/dL in females and less than 5 mg/dL in males; (3) fasting blood glucose levels greater than or equal to 110 mg/dL, (4) waist circumference greater than the 75th percentile for age and sex; and (5) systolic or diastolic blood pressure greater than the 90th percentile for age, sex, and height.16 These studies highlight that obesity and metabolic syndrome are of concern in pediatric psoriasis patients; however, the best management approach using diet and weight interventions has yet to be identified.
Adiposity may precede the onset of psoriasis. A recent cohort of 27 pediatric psoriasis patients reported that the average age at onset of psoriasis was 8.7 years and the average age at onset of obesity was 4.1 years.15 In this study, 93% (25/27) of patients had adiposity preceding their psoriasis by 2 or more years. It is unclear if this is nature or nurture, as 48% (13/27) of patients had a family history of obesity, 41% (11/27) had a family history of psoriasis, and 48% (13/27) had a family history of hyperlipidemia.15 Therefore, obesity may be cultivated in some psoriatic families. The issue of household influences on diet and obesity needs to be addressed if successful weight management is to be achieved in future studies of pediatric psoriasis.
Cardiovascular risks in the pediatric psoriasis population are the subject of ongoing assessment but will likely mimic studies of adult psoriasis patients when reviewed longitudinally.16 Weight loss and healthy lifestyle interventions likely are beneficial to long-term health, but there is a lack of published data addressing dietary modification as a disease modifier for long-term care of pediatric psoriasis.
Anxiety and Depression
Anxiety and depression have been noted in adults with chronic skin diseases. A recent study assessed 118 patients and caregivers of pediatric patients with atopic dermatitis (n=50), psoriasis (n=25), or vitiligo (n=43) using the Children’s Dermatology Life Quality Index, the Hamilton Anxiety Scale, and the Beck Depression Inventory.17 Anxiety and depression were found in 36% of caregivers of pediatric psoriasis patients and depression was found in 36% of pediatric psoriasis patients, highlighting the need for interventions on a personal and family level to improve quality of life. As a comparator, anxiety was more prevalent in vitiligo caregivers (42%), but depression was only found in 26% of caregivers in the same group. Extent of disease (25%–75% body surface area affected) correlated with both depression and anxiety in the caregivers of pediatric patients with psoriasis as well as with anxiety in caregivers of pediatric patients with increased visible surface area of vitiligo.17 Parental anxiety has been reported at times to be linked to corticosteroid phobia, or corticophobia, which may interfere with disease therapy, as topical corticosteroids are considered the mainstay of therapy in childhood disease.18 Coordinating care with caregivers and addressing their concerns about the safety of medications should be integral to the pediatric psoriasis visit.
Pustular Psoriasis
Pustular psoriasis can be seen in any age group. Researchers recently have attempted to delineate the features and successful management of this severe subset of pediatric psoriasis patients. Twenty-four pediatric pustular psoriasis cases reviewed by Posso-De Los Rios et al19 revealed that 92% (22/24) had generalized and 8% (2/24) had limited acral disease. The mean (standard deviation) age at onset of pediatric pustular psoriasis was 6.3 (4.9) years. Half of the reported cases required more than one intervention. Treatment with acitretin, cyclosporine, and methotrexate was effective, but the investigators identified that there is a true dearth of evidence-based therapeutics in pediatric pustular psoriasis and much rebound with discontinuation.19 Although the subset of pediatric pustular psoriasis is rare, study of evidence-based intervention is needed.
Therapy
Recent reviews of pediatric and adolescent psoriasis highlight the paucity of therapeutic information for these patient populations. Investigators typically focus on topical therapies as the basis of treatment,20 as well as the addition of phototherapy in mild to moderate plaque or guttate psoriasis and biologic or systemic agents in moderate to severe flares of plaque, erythrodermic, or pustular psoriasis.21 Further studies are needed to identify evidence-based therapeutic paradigms for pediatric psoriasis and to pinpoint therapies associated with the best quality of life in patients and their caregivers.
Tumor Necrosis Factor α Inhibitors
Safety and efficacy of etanercept for juvenile idiopathic arthritis including oligoarthritis, enthesitis-related arthritis, and psoriatic arthritis recently was reviewed by Windschall et al22 using data from the German pediatric Biologika in der Kinderrheumatologie registry. Juvenile Arthritis Disease Activity Score 10 improved from baseline for 127 pediatric patients with psoriatic arthritis in 3 to 24 months (mean [standard deviation], 14.7 [6.4], 5.0 [4.6], 5.3 [6.4] at baseline, 3 months, and 24 months, respectively). Overall side effects were relatively higher in the psoriatic arthritis group; the rate of serious (relative risk, 1.39 [0.95-2.03; P=.08]) and nonserious (relative risk, 1.18 [1.02-1.35; P=.03]) adverse events also was elevated. Uveitis risk was greatest in the psoriatic arthritis group and the number of associated cases of inflammatory bowel disease outnumbered those seen in other forms of arthritis. The investigators concluded that monitoring for extra-articular immunopathies should be conducted in pediatric patients with psoriatic arthritis who are undergoing etanercept therapy.22
Tumor necrosis factor α (TNF-α) inhibitors have been associated with triggering psoriasiform dermatitis in pediatric patients treated for inflammatory bowel disease. A Finnish study of infliximab side effects in pediatric patients with inflammatory bowel disease (n=84; Crohn disease: n=64) demonstrated that almost half (47.6% [40/84]) of the participants presented with chronic skin reactions, 23% of which were severe in nature.23 Psoriasiform lesions of the scalp and ears were most common, followed by the periorificial area, genitals, trunk, and extremities. Rare association with HLA-Cw*0602 genotype was noted. Skin manifestations did not correlate with gut inflammation (as determined by fecal calprotectin levels). Discontinuation of therapy rarely was required.23 Other studies also have highlighted this side effect, suggesting an incidence of 2.7% in adults with colitis treated with TNF-α inhibitors24 and 10.5% in pediatric patients with Crohn disease.25 In a study by Sherlock et al,25 pediatric patients with Crohn disease developing psoriasis following infliximab therapy were more likely to be homozygous for specific polymorphisms in the IL-23R gene (rs10489628, rs10789229, and rs1343151).
Methotrexate
For pediatric patients who are being treated with methotrexate, the polyglutamate assay recently has been reported to be helpful in identifying patients needing a dose escalation.26 Higher numbers on the polyglutamate assay are associated with superior response to methotrexate therapy. Doses can be increased after 12 weeks in patients with low assays.26
IL-23
The safety of IL-23 blockade in pediatric psoriasis patients has not yet been established, but data from adult cases have implicated the IL-17 and IL-23 pathways in psoriasis/psoriatic arthritis, including an association with IL-23R polymorphisms27 and increases in soluble IL-20 and IL-22 associated with disease severity and an association of IL-17 levels with activity on the psoriasis area and severity index scores.28 The data are more limited for pediatric cases. Pediatric patients with inflammatory bowel disease who have an IL-23R polymorphism appear to be susceptible to psoriatic flares while on TNF-α inhibitor therapy,25 which suggests that the IL-23 blockade may be of benefit for some pediatric patients with psoriasis or psoriatic arthritis.
Conclusion
Pediatric psoriasis and psoriatic arthritis have now been identified as being part of the autoimmune spectrum and are associated with metabolic syndrome, including obesity and excess central adiposity, similar to their adult variants. An overview of potential unmet needs in pediatric psoriasis is included in Table 2. These unmet needs include further delineation of diet and weight modification in the care and prevention of psoriasis; expansion of therapeutic trials and US Food and Drug Administration–approved medications for children with psoriasis, especially severe variants such as extensive plaque and pustular disease; and development of guidelines for ongoing monitoring of children with psoriasis. The role of therapeutic interventions and weight management on long-term disease course remains to be shown in extended clinical trials. Despite the great advancements in psoriatic care, knowledge gaps remain in pediatric psoriasis that will need to be addressed in the future.
1. Taclonex Expanded Indication. OptumRx Web site. https://www.optumrx.com/vgnpreview/HCP/Assets/RxNews/Clinical%20Updates_Taclonex_2014-1003.pdf. Published August 29, 2014. Accessed January 28, 2015.
2. Silverberg NB. Update on pediatric psoriasis, part 1: clinical features and demographics. Cutis. 2010;86:118-124.
3. Silverberg NB. Update on pediatric psoriasis, part 2: therapeutic management. Cutis. 2010;86:172-176.
4. Cather JC. Psoriasis in children and women: addressing some special needs. Semin Cutan Med Surg. 2014;33(2 suppl 2):S42-S44.
5. Khorsand K, Sidbury R. Recent advances in pediatric dermatology. Arch Dis Child. 2014;99:944-948.
6. Mercy K, Kwasny M, Cordoro KM, et al. Clinical manifestations of pediatric psoriasis: results of a multicenter study in the United States. Pediatr Dermatol. 2013;30:424-428.
7. Gudjonsson JE, Thorarinsson AM, Sigurgeirsson B, et al. Streptococcal throat infections and exacerbation of chronic plaque psoriasis: a prospective study. Br J Dermatol. 2003;149:530-534.
8. Ferran M, Galván AB, Rincón C, et al. Streptococcus induces circulating CLA(+) memory T-cell-dependent epidermal cell activation in psoriasis. J Invest Dermatol. 2013;133:999-1007.
9. Gul Mert G, Incecik F, Gunasti S, et al. Psoriasiform drug eruption associated with sodium valproate [published online ahead of print November 13, 2013]. Case Rep Pediatr. 2013;2013:823469.
10. Chang MW, Nakrani R. Six children with allergic contact dermatitis to methylisothiazolinone in wet wipes (baby wipes). Pediatrics. 2014;133:e434-e438.
11. Gul U, Gonul M, Kaya I, et al. Autoimmune thyroid disorders in patients with psoriasis. Eur J Dermatol. 2009;19:221-223.
12. Prahalad S, McCracken C, Ponder L, et al. A120: Familial autoimmunity in the CARRA registry. Arthritis Rheumatol. 2014;66(suppl 11):S157.
13. Mercy KM, Paller AS. The relationship between obesity and psoriasis in the pediatric population: implications and future directions. Cutis. 2013;92:107-109.
14. Paller AS, Mercy K, Kwasny MJ, et al. Association of pediatric psoriasis severity with excess and central adiposity: an international cross-sectional study. JAMA Dermatol. 2013;149:166-176.
15. Becker L, Tom WL, Eshagh K, et al. Excess adiposity preceding pediatric psoriasis. JAMA Dermatol. 2014;150:573-574.
16. Volf EM, Levine DE, Michelon MA, et al. Assessor-blinded study of the metabolic syndrome and surrogate markers of increased cardiovascular risk in children with moderate-to-severe psoriasis compared with age-matched population of children with warts. J Drugs Dermatol. 2011;10:900-901.
17. Manzoni AP, Weber MB, Nagatomi AR, et al. Assessing depression and anxiety in the caregivers of pediatric patients with chronic skin disorders. An Bras Dermatol. 2013;88:894-899.
18. Belloni Fortina A, Neri L. Topical steroids and corticophobia. G Ital Dermatol Venereol. 2013;148:651-654.
19. Posso-De Los Rios CJ, Pope E, Lara-Corrales I. A systematic review of systemic medications for pustular psoriasis in pediatrics. Pediatr Dermatol. 2014;31:430-439.
20. Tollefson MM. Diagnosis and management of psoriasis in children. Pediatr Clin North Am. 2014;61:261-277.
21. Fotiadou C, Lazaridou E, Ioannides D. Management of psoriasis in adolescence. Adolesc Health Med Ther. 2014;5:25-34.
22. Windschall D, Müller T, Becker I, et al. Safety and efficacy of etanercept in children with the JIA categories extended oligoarthritis, enthesitis-related arthritis and psoriasis arthritis [published online ahead of print July 18, 2014]. Clin Rheumatol. 2015;34:61-69.
23. Mälkönen T, Wikström A, Heiskanen K, et al. Skin reactions during anti-TNFa therapy for pediatric inflammatory bowel disease: a 2-year prospective study. Inflamm Bowel Dis. 2014;20:1309-1315.
24. Afzali A, Wheat CL, Hu JK, et al. The association of psoriasiform rash with anti-tumor necrosis factor (anti-TNF) therapy in inflammatory bowel disease: a single academic center case series. J Crohns Colitis. 2014;8:480-488.
25. Sherlock ME, Walters T, Tabbers MM, et al. Infliximab-induced psoriasis and psoriasiform skin lesions in pediatric Crohn disease and a potential association with IL-23 receptor polymorphisms. J Pediatr Gastroenterol Nutr. 2013;56:512-518.
26. Rahman SI, Siegfried E, Flanagan KH, et al. The methotrexate polyglutamate assay supports the efficacy of methotrexate for severe inflammatory skin disease in children. J Am Acad Dermatol. 2014;70:252-256.
27. Suzuki E, Mellins ED, Gershwin ME, et al. The IL-23/IL-17 axis in psoriatic arthritis. Autoimmun Rev. 2014;13:496-502.
28. Michalak-Stoma A, Bartosi´nska J, Kowal M, et al. Serum levels of selected Th17 and Th22 cytokines in psoriatic patients. Dis Markers. 2013;35:625-631.
Psoriasis affects 2% to 4% of the US population, with approximately one-third of cases beginning in childhood. The understanding of pediatric psoriasis has developed at a far slower pace than adult disease, with limitations in care including few medications that are approved by the US Food and Drug Administration for pediatric and adolescent use. Recently, a stable fixed-combination dose of calcipo-triene 0.005%–betamethasone dipropionate 0.064% topical suspension was approved for treatment of plaque psoriasis of the scalp in patients aged 12 to 17 years, which hopefully will lead a trend in psoriasis medication approval for children and teenagers.1 Based on a PubMed search of articles indexed for MEDLINE using the search terms pediatric psoriasis, psoriasis, and strep that were published from April 2012 to April 2014, this article reviews newer data to address the issues that surround pediatric psoriasis and to provide an update on prior review articles on pediatric psoriasis.2-5 This article reviews some of the newer literature on clinical presentation and comorbidities in pediatric psoriasis.5 Based on these recent findings, additional screenings including review of obesity parameters are recommended for pediatric patients with psoriasis (Table 1).
Update on Disease Manifestations, Associations, and Comorbidities
Disease Manifestations
A 2013 multicenter study delineated the clinical features of pediatric psoriasis.6 The study was conducted at 8 geographically diverse dermatology clinics in the United States to delineate the clinical manifestations of pediatric psoriasis. In an assessment of 181 participants aged 5 to 17 years, the investigators sought to determine the frequency of disease sites, severity, and guttate disease. Over a period of approximately 2 years, 43.1% of participants were determined to have mild disease and 56.9% had severe disease. Family history of psoriasis was present in 51.4% of participants, with first-degree relatives affected in 59.8% of cases. Scalp involvement at some time was noted in 79.0% of participants, and nail disease was noted in 55% of boys and 29% of girls. Guttate psoriasis was noted in 30% of participants, with more cases in the severe range (35.9%) versus the mild range (21.8%). Additionally, 22.1% of participants had a precipitating streptococcal infection, with the association being more common in pediatric patients with guttate psoriasis than plaque psoriasis.6 This study highlighted that pediatric psoriasis has a genetic basis, is frequently guttate in nature, commonly affects the nails, shows a trend toward being classified as severe, and may be triggered by streptococcal infections.
Streptococcal Infection
Pediatric psoriasis may be triggered or flared by Streptococcus pyogenes (group A β-hemolytic streptococci) infections, specifically β-hemolytic streptococci groups A, C, and G that have streptococcal M protein,2,3,7 and this tendency can be associated with HLA-Cw6 or guttate psoriasis. Newer data have elucidated the role of streptococcal throat infections in psoriasis. Given that streptococcal throat infections are most common in school-aged children, these studies suggest a putative mechanism in pediatric psoriasis for triggering streptococcal infections, which would need to be confirmed in future studies, specifically in pediatric psoriasis patients.
It has been shown that T cells in psoriasis patients recognize common streptococcal M proteins and keratin determinants.7 Ferran et al8 recently demonstrated activation of circulating cutaneous lymphocyte–associated antigen (CLA)+ T cells but not CLA- memory T cells in 27 psoriasis patients (ages not specified) when mixed with streptococcal throat extracts, causing production of IL-17, IP-10, IL-22, and IFN-γ; activation was not found in 6 healthy control patients. Antistreptolysin O levels were correlated with the messenger RNA up- regulation for IL-17, IP-10, IL-22, and IFN-γ, and also correlated with psoriasis area and severity index score in psoriasis patients. In this same study, injection of the activated culture supernatant into mouse skin caused epidermal hyperkeratosis and activation of nonlesional epidermal cells from psoriatic patients. This study thereby delineated some of the potential pathways of the streptococcal induction of psoriasis and psoriatic flares in childhood8; however, confirmation is needed through further study of pediatric psoriatic lymphocyte activity.
Differential Diagnosis
Additions to the extensive differential list have been cited in the recent literature. The differential diagnosis of pediatric psoriasis now includes sodium valproate–induced psoriasiform drug eruption9 and allergic contact dermatitis to methylchloroisothiazolinone and methylisothiazolinone, which are present in many sanitizing hand and diaper wipes and has been reported to cause psoriasiform dermatitis in a periorificial or perineal distribution.10 Clinicians should inquire about the use of these wipes, as caregivers rarely suspect this agent to be causative of the eruption.
Psoriatic Arthritis
Previously, psoriasis and psoriatic arthritis have been linked to autoimmune thyroid disease in adults.11 A study of the Childhood Arthritis & Rheumatology Research Alliance (CARRA) registry showed that family history of psoriasis, autoimmune thyroiditis, Crohn disease, and ankylosing spondylitis in a first-degree relative has been linked to juvenile idiopathic arthritis, highlighting that pediatric psoriasis can be genetically linked or associated with multiple autoimmune conditions and vice versa.12
Obesity, Metabolic Syndrome, and Cardiovascular Risks
Obesity is associated with pediatric psoriasis as highlighted in a growing body of recent literature.13 Excess adiposity as manifested by body mass index in the 85th percentile or greater (37.9% of 155 pediatric psoriasis patients vs 20.5% of 42 controls) and excess central adiposity as manifested by excess waist circumference and increased waist-to-height ratios are more common in pediatric patients with psoriasis than in controls.14
Obesity may be a trigger or associated with increased disease activity in pediatric psoriasis patients. Excess overall adiposity correlates with more severe disease. Obesity parameters may correlate with the onset of psoriasis and with disease severity. In fact, the odds of obesity may be higher in childhood than in adults.14,15 A 2011 report of pediatric psoriasis patients aged 10 to 17 years (n=12) and wart controls (n=6)(mean age, 13.2 and 13.5 years, respectively) demonstrated that 4 of 12 patients with psoriasis and 0 of 6 patients with warts met criteria for metabolic syndrome as defined by 3 of the following: (1) triglycerides greater than or equal to 100 mg/dL; (2) high-density lipoprotein cholesterol less than 50 mg/dL in females and less than 5 mg/dL in males; (3) fasting blood glucose levels greater than or equal to 110 mg/dL, (4) waist circumference greater than the 75th percentile for age and sex; and (5) systolic or diastolic blood pressure greater than the 90th percentile for age, sex, and height.16 These studies highlight that obesity and metabolic syndrome are of concern in pediatric psoriasis patients; however, the best management approach using diet and weight interventions has yet to be identified.
Adiposity may precede the onset of psoriasis. A recent cohort of 27 pediatric psoriasis patients reported that the average age at onset of psoriasis was 8.7 years and the average age at onset of obesity was 4.1 years.15 In this study, 93% (25/27) of patients had adiposity preceding their psoriasis by 2 or more years. It is unclear if this is nature or nurture, as 48% (13/27) of patients had a family history of obesity, 41% (11/27) had a family history of psoriasis, and 48% (13/27) had a family history of hyperlipidemia.15 Therefore, obesity may be cultivated in some psoriatic families. The issue of household influences on diet and obesity needs to be addressed if successful weight management is to be achieved in future studies of pediatric psoriasis.
Cardiovascular risks in the pediatric psoriasis population are the subject of ongoing assessment but will likely mimic studies of adult psoriasis patients when reviewed longitudinally.16 Weight loss and healthy lifestyle interventions likely are beneficial to long-term health, but there is a lack of published data addressing dietary modification as a disease modifier for long-term care of pediatric psoriasis.
Anxiety and Depression
Anxiety and depression have been noted in adults with chronic skin diseases. A recent study assessed 118 patients and caregivers of pediatric patients with atopic dermatitis (n=50), psoriasis (n=25), or vitiligo (n=43) using the Children’s Dermatology Life Quality Index, the Hamilton Anxiety Scale, and the Beck Depression Inventory.17 Anxiety and depression were found in 36% of caregivers of pediatric psoriasis patients and depression was found in 36% of pediatric psoriasis patients, highlighting the need for interventions on a personal and family level to improve quality of life. As a comparator, anxiety was more prevalent in vitiligo caregivers (42%), but depression was only found in 26% of caregivers in the same group. Extent of disease (25%–75% body surface area affected) correlated with both depression and anxiety in the caregivers of pediatric patients with psoriasis as well as with anxiety in caregivers of pediatric patients with increased visible surface area of vitiligo.17 Parental anxiety has been reported at times to be linked to corticosteroid phobia, or corticophobia, which may interfere with disease therapy, as topical corticosteroids are considered the mainstay of therapy in childhood disease.18 Coordinating care with caregivers and addressing their concerns about the safety of medications should be integral to the pediatric psoriasis visit.
Pustular Psoriasis
Pustular psoriasis can be seen in any age group. Researchers recently have attempted to delineate the features and successful management of this severe subset of pediatric psoriasis patients. Twenty-four pediatric pustular psoriasis cases reviewed by Posso-De Los Rios et al19 revealed that 92% (22/24) had generalized and 8% (2/24) had limited acral disease. The mean (standard deviation) age at onset of pediatric pustular psoriasis was 6.3 (4.9) years. Half of the reported cases required more than one intervention. Treatment with acitretin, cyclosporine, and methotrexate was effective, but the investigators identified that there is a true dearth of evidence-based therapeutics in pediatric pustular psoriasis and much rebound with discontinuation.19 Although the subset of pediatric pustular psoriasis is rare, study of evidence-based intervention is needed.
Therapy
Recent reviews of pediatric and adolescent psoriasis highlight the paucity of therapeutic information for these patient populations. Investigators typically focus on topical therapies as the basis of treatment,20 as well as the addition of phototherapy in mild to moderate plaque or guttate psoriasis and biologic or systemic agents in moderate to severe flares of plaque, erythrodermic, or pustular psoriasis.21 Further studies are needed to identify evidence-based therapeutic paradigms for pediatric psoriasis and to pinpoint therapies associated with the best quality of life in patients and their caregivers.
Tumor Necrosis Factor α Inhibitors
Safety and efficacy of etanercept for juvenile idiopathic arthritis including oligoarthritis, enthesitis-related arthritis, and psoriatic arthritis recently was reviewed by Windschall et al22 using data from the German pediatric Biologika in der Kinderrheumatologie registry. Juvenile Arthritis Disease Activity Score 10 improved from baseline for 127 pediatric patients with psoriatic arthritis in 3 to 24 months (mean [standard deviation], 14.7 [6.4], 5.0 [4.6], 5.3 [6.4] at baseline, 3 months, and 24 months, respectively). Overall side effects were relatively higher in the psoriatic arthritis group; the rate of serious (relative risk, 1.39 [0.95-2.03; P=.08]) and nonserious (relative risk, 1.18 [1.02-1.35; P=.03]) adverse events also was elevated. Uveitis risk was greatest in the psoriatic arthritis group and the number of associated cases of inflammatory bowel disease outnumbered those seen in other forms of arthritis. The investigators concluded that monitoring for extra-articular immunopathies should be conducted in pediatric patients with psoriatic arthritis who are undergoing etanercept therapy.22
Tumor necrosis factor α (TNF-α) inhibitors have been associated with triggering psoriasiform dermatitis in pediatric patients treated for inflammatory bowel disease. A Finnish study of infliximab side effects in pediatric patients with inflammatory bowel disease (n=84; Crohn disease: n=64) demonstrated that almost half (47.6% [40/84]) of the participants presented with chronic skin reactions, 23% of which were severe in nature.23 Psoriasiform lesions of the scalp and ears were most common, followed by the periorificial area, genitals, trunk, and extremities. Rare association with HLA-Cw*0602 genotype was noted. Skin manifestations did not correlate with gut inflammation (as determined by fecal calprotectin levels). Discontinuation of therapy rarely was required.23 Other studies also have highlighted this side effect, suggesting an incidence of 2.7% in adults with colitis treated with TNF-α inhibitors24 and 10.5% in pediatric patients with Crohn disease.25 In a study by Sherlock et al,25 pediatric patients with Crohn disease developing psoriasis following infliximab therapy were more likely to be homozygous for specific polymorphisms in the IL-23R gene (rs10489628, rs10789229, and rs1343151).
Methotrexate
For pediatric patients who are being treated with methotrexate, the polyglutamate assay recently has been reported to be helpful in identifying patients needing a dose escalation.26 Higher numbers on the polyglutamate assay are associated with superior response to methotrexate therapy. Doses can be increased after 12 weeks in patients with low assays.26
IL-23
The safety of IL-23 blockade in pediatric psoriasis patients has not yet been established, but data from adult cases have implicated the IL-17 and IL-23 pathways in psoriasis/psoriatic arthritis, including an association with IL-23R polymorphisms27 and increases in soluble IL-20 and IL-22 associated with disease severity and an association of IL-17 levels with activity on the psoriasis area and severity index scores.28 The data are more limited for pediatric cases. Pediatric patients with inflammatory bowel disease who have an IL-23R polymorphism appear to be susceptible to psoriatic flares while on TNF-α inhibitor therapy,25 which suggests that the IL-23 blockade may be of benefit for some pediatric patients with psoriasis or psoriatic arthritis.
Conclusion
Pediatric psoriasis and psoriatic arthritis have now been identified as being part of the autoimmune spectrum and are associated with metabolic syndrome, including obesity and excess central adiposity, similar to their adult variants. An overview of potential unmet needs in pediatric psoriasis is included in Table 2. These unmet needs include further delineation of diet and weight modification in the care and prevention of psoriasis; expansion of therapeutic trials and US Food and Drug Administration–approved medications for children with psoriasis, especially severe variants such as extensive plaque and pustular disease; and development of guidelines for ongoing monitoring of children with psoriasis. The role of therapeutic interventions and weight management on long-term disease course remains to be shown in extended clinical trials. Despite the great advancements in psoriatic care, knowledge gaps remain in pediatric psoriasis that will need to be addressed in the future.
Psoriasis affects 2% to 4% of the US population, with approximately one-third of cases beginning in childhood. The understanding of pediatric psoriasis has developed at a far slower pace than adult disease, with limitations in care including few medications that are approved by the US Food and Drug Administration for pediatric and adolescent use. Recently, a stable fixed-combination dose of calcipo-triene 0.005%–betamethasone dipropionate 0.064% topical suspension was approved for treatment of plaque psoriasis of the scalp in patients aged 12 to 17 years, which hopefully will lead a trend in psoriasis medication approval for children and teenagers.1 Based on a PubMed search of articles indexed for MEDLINE using the search terms pediatric psoriasis, psoriasis, and strep that were published from April 2012 to April 2014, this article reviews newer data to address the issues that surround pediatric psoriasis and to provide an update on prior review articles on pediatric psoriasis.2-5 This article reviews some of the newer literature on clinical presentation and comorbidities in pediatric psoriasis.5 Based on these recent findings, additional screenings including review of obesity parameters are recommended for pediatric patients with psoriasis (Table 1).
Update on Disease Manifestations, Associations, and Comorbidities
Disease Manifestations
A 2013 multicenter study delineated the clinical features of pediatric psoriasis.6 The study was conducted at 8 geographically diverse dermatology clinics in the United States to delineate the clinical manifestations of pediatric psoriasis. In an assessment of 181 participants aged 5 to 17 years, the investigators sought to determine the frequency of disease sites, severity, and guttate disease. Over a period of approximately 2 years, 43.1% of participants were determined to have mild disease and 56.9% had severe disease. Family history of psoriasis was present in 51.4% of participants, with first-degree relatives affected in 59.8% of cases. Scalp involvement at some time was noted in 79.0% of participants, and nail disease was noted in 55% of boys and 29% of girls. Guttate psoriasis was noted in 30% of participants, with more cases in the severe range (35.9%) versus the mild range (21.8%). Additionally, 22.1% of participants had a precipitating streptococcal infection, with the association being more common in pediatric patients with guttate psoriasis than plaque psoriasis.6 This study highlighted that pediatric psoriasis has a genetic basis, is frequently guttate in nature, commonly affects the nails, shows a trend toward being classified as severe, and may be triggered by streptococcal infections.
Streptococcal Infection
Pediatric psoriasis may be triggered or flared by Streptococcus pyogenes (group A β-hemolytic streptococci) infections, specifically β-hemolytic streptococci groups A, C, and G that have streptococcal M protein,2,3,7 and this tendency can be associated with HLA-Cw6 or guttate psoriasis. Newer data have elucidated the role of streptococcal throat infections in psoriasis. Given that streptococcal throat infections are most common in school-aged children, these studies suggest a putative mechanism in pediatric psoriasis for triggering streptococcal infections, which would need to be confirmed in future studies, specifically in pediatric psoriasis patients.
It has been shown that T cells in psoriasis patients recognize common streptococcal M proteins and keratin determinants.7 Ferran et al8 recently demonstrated activation of circulating cutaneous lymphocyte–associated antigen (CLA)+ T cells but not CLA- memory T cells in 27 psoriasis patients (ages not specified) when mixed with streptococcal throat extracts, causing production of IL-17, IP-10, IL-22, and IFN-γ; activation was not found in 6 healthy control patients. Antistreptolysin O levels were correlated with the messenger RNA up- regulation for IL-17, IP-10, IL-22, and IFN-γ, and also correlated with psoriasis area and severity index score in psoriasis patients. In this same study, injection of the activated culture supernatant into mouse skin caused epidermal hyperkeratosis and activation of nonlesional epidermal cells from psoriatic patients. This study thereby delineated some of the potential pathways of the streptococcal induction of psoriasis and psoriatic flares in childhood8; however, confirmation is needed through further study of pediatric psoriatic lymphocyte activity.
Differential Diagnosis
Additions to the extensive differential list have been cited in the recent literature. The differential diagnosis of pediatric psoriasis now includes sodium valproate–induced psoriasiform drug eruption9 and allergic contact dermatitis to methylchloroisothiazolinone and methylisothiazolinone, which are present in many sanitizing hand and diaper wipes and has been reported to cause psoriasiform dermatitis in a periorificial or perineal distribution.10 Clinicians should inquire about the use of these wipes, as caregivers rarely suspect this agent to be causative of the eruption.
Psoriatic Arthritis
Previously, psoriasis and psoriatic arthritis have been linked to autoimmune thyroid disease in adults.11 A study of the Childhood Arthritis & Rheumatology Research Alliance (CARRA) registry showed that family history of psoriasis, autoimmune thyroiditis, Crohn disease, and ankylosing spondylitis in a first-degree relative has been linked to juvenile idiopathic arthritis, highlighting that pediatric psoriasis can be genetically linked or associated with multiple autoimmune conditions and vice versa.12
Obesity, Metabolic Syndrome, and Cardiovascular Risks
Obesity is associated with pediatric psoriasis as highlighted in a growing body of recent literature.13 Excess adiposity as manifested by body mass index in the 85th percentile or greater (37.9% of 155 pediatric psoriasis patients vs 20.5% of 42 controls) and excess central adiposity as manifested by excess waist circumference and increased waist-to-height ratios are more common in pediatric patients with psoriasis than in controls.14
Obesity may be a trigger or associated with increased disease activity in pediatric psoriasis patients. Excess overall adiposity correlates with more severe disease. Obesity parameters may correlate with the onset of psoriasis and with disease severity. In fact, the odds of obesity may be higher in childhood than in adults.14,15 A 2011 report of pediatric psoriasis patients aged 10 to 17 years (n=12) and wart controls (n=6)(mean age, 13.2 and 13.5 years, respectively) demonstrated that 4 of 12 patients with psoriasis and 0 of 6 patients with warts met criteria for metabolic syndrome as defined by 3 of the following: (1) triglycerides greater than or equal to 100 mg/dL; (2) high-density lipoprotein cholesterol less than 50 mg/dL in females and less than 5 mg/dL in males; (3) fasting blood glucose levels greater than or equal to 110 mg/dL, (4) waist circumference greater than the 75th percentile for age and sex; and (5) systolic or diastolic blood pressure greater than the 90th percentile for age, sex, and height.16 These studies highlight that obesity and metabolic syndrome are of concern in pediatric psoriasis patients; however, the best management approach using diet and weight interventions has yet to be identified.
Adiposity may precede the onset of psoriasis. A recent cohort of 27 pediatric psoriasis patients reported that the average age at onset of psoriasis was 8.7 years and the average age at onset of obesity was 4.1 years.15 In this study, 93% (25/27) of patients had adiposity preceding their psoriasis by 2 or more years. It is unclear if this is nature or nurture, as 48% (13/27) of patients had a family history of obesity, 41% (11/27) had a family history of psoriasis, and 48% (13/27) had a family history of hyperlipidemia.15 Therefore, obesity may be cultivated in some psoriatic families. The issue of household influences on diet and obesity needs to be addressed if successful weight management is to be achieved in future studies of pediatric psoriasis.
Cardiovascular risks in the pediatric psoriasis population are the subject of ongoing assessment but will likely mimic studies of adult psoriasis patients when reviewed longitudinally.16 Weight loss and healthy lifestyle interventions likely are beneficial to long-term health, but there is a lack of published data addressing dietary modification as a disease modifier for long-term care of pediatric psoriasis.
Anxiety and Depression
Anxiety and depression have been noted in adults with chronic skin diseases. A recent study assessed 118 patients and caregivers of pediatric patients with atopic dermatitis (n=50), psoriasis (n=25), or vitiligo (n=43) using the Children’s Dermatology Life Quality Index, the Hamilton Anxiety Scale, and the Beck Depression Inventory.17 Anxiety and depression were found in 36% of caregivers of pediatric psoriasis patients and depression was found in 36% of pediatric psoriasis patients, highlighting the need for interventions on a personal and family level to improve quality of life. As a comparator, anxiety was more prevalent in vitiligo caregivers (42%), but depression was only found in 26% of caregivers in the same group. Extent of disease (25%–75% body surface area affected) correlated with both depression and anxiety in the caregivers of pediatric patients with psoriasis as well as with anxiety in caregivers of pediatric patients with increased visible surface area of vitiligo.17 Parental anxiety has been reported at times to be linked to corticosteroid phobia, or corticophobia, which may interfere with disease therapy, as topical corticosteroids are considered the mainstay of therapy in childhood disease.18 Coordinating care with caregivers and addressing their concerns about the safety of medications should be integral to the pediatric psoriasis visit.
Pustular Psoriasis
Pustular psoriasis can be seen in any age group. Researchers recently have attempted to delineate the features and successful management of this severe subset of pediatric psoriasis patients. Twenty-four pediatric pustular psoriasis cases reviewed by Posso-De Los Rios et al19 revealed that 92% (22/24) had generalized and 8% (2/24) had limited acral disease. The mean (standard deviation) age at onset of pediatric pustular psoriasis was 6.3 (4.9) years. Half of the reported cases required more than one intervention. Treatment with acitretin, cyclosporine, and methotrexate was effective, but the investigators identified that there is a true dearth of evidence-based therapeutics in pediatric pustular psoriasis and much rebound with discontinuation.19 Although the subset of pediatric pustular psoriasis is rare, study of evidence-based intervention is needed.
Therapy
Recent reviews of pediatric and adolescent psoriasis highlight the paucity of therapeutic information for these patient populations. Investigators typically focus on topical therapies as the basis of treatment,20 as well as the addition of phototherapy in mild to moderate plaque or guttate psoriasis and biologic or systemic agents in moderate to severe flares of plaque, erythrodermic, or pustular psoriasis.21 Further studies are needed to identify evidence-based therapeutic paradigms for pediatric psoriasis and to pinpoint therapies associated with the best quality of life in patients and their caregivers.
Tumor Necrosis Factor α Inhibitors
Safety and efficacy of etanercept for juvenile idiopathic arthritis including oligoarthritis, enthesitis-related arthritis, and psoriatic arthritis recently was reviewed by Windschall et al22 using data from the German pediatric Biologika in der Kinderrheumatologie registry. Juvenile Arthritis Disease Activity Score 10 improved from baseline for 127 pediatric patients with psoriatic arthritis in 3 to 24 months (mean [standard deviation], 14.7 [6.4], 5.0 [4.6], 5.3 [6.4] at baseline, 3 months, and 24 months, respectively). Overall side effects were relatively higher in the psoriatic arthritis group; the rate of serious (relative risk, 1.39 [0.95-2.03; P=.08]) and nonserious (relative risk, 1.18 [1.02-1.35; P=.03]) adverse events also was elevated. Uveitis risk was greatest in the psoriatic arthritis group and the number of associated cases of inflammatory bowel disease outnumbered those seen in other forms of arthritis. The investigators concluded that monitoring for extra-articular immunopathies should be conducted in pediatric patients with psoriatic arthritis who are undergoing etanercept therapy.22
Tumor necrosis factor α (TNF-α) inhibitors have been associated with triggering psoriasiform dermatitis in pediatric patients treated for inflammatory bowel disease. A Finnish study of infliximab side effects in pediatric patients with inflammatory bowel disease (n=84; Crohn disease: n=64) demonstrated that almost half (47.6% [40/84]) of the participants presented with chronic skin reactions, 23% of which were severe in nature.23 Psoriasiform lesions of the scalp and ears were most common, followed by the periorificial area, genitals, trunk, and extremities. Rare association with HLA-Cw*0602 genotype was noted. Skin manifestations did not correlate with gut inflammation (as determined by fecal calprotectin levels). Discontinuation of therapy rarely was required.23 Other studies also have highlighted this side effect, suggesting an incidence of 2.7% in adults with colitis treated with TNF-α inhibitors24 and 10.5% in pediatric patients with Crohn disease.25 In a study by Sherlock et al,25 pediatric patients with Crohn disease developing psoriasis following infliximab therapy were more likely to be homozygous for specific polymorphisms in the IL-23R gene (rs10489628, rs10789229, and rs1343151).
Methotrexate
For pediatric patients who are being treated with methotrexate, the polyglutamate assay recently has been reported to be helpful in identifying patients needing a dose escalation.26 Higher numbers on the polyglutamate assay are associated with superior response to methotrexate therapy. Doses can be increased after 12 weeks in patients with low assays.26
IL-23
The safety of IL-23 blockade in pediatric psoriasis patients has not yet been established, but data from adult cases have implicated the IL-17 and IL-23 pathways in psoriasis/psoriatic arthritis, including an association with IL-23R polymorphisms27 and increases in soluble IL-20 and IL-22 associated with disease severity and an association of IL-17 levels with activity on the psoriasis area and severity index scores.28 The data are more limited for pediatric cases. Pediatric patients with inflammatory bowel disease who have an IL-23R polymorphism appear to be susceptible to psoriatic flares while on TNF-α inhibitor therapy,25 which suggests that the IL-23 blockade may be of benefit for some pediatric patients with psoriasis or psoriatic arthritis.
Conclusion
Pediatric psoriasis and psoriatic arthritis have now been identified as being part of the autoimmune spectrum and are associated with metabolic syndrome, including obesity and excess central adiposity, similar to their adult variants. An overview of potential unmet needs in pediatric psoriasis is included in Table 2. These unmet needs include further delineation of diet and weight modification in the care and prevention of psoriasis; expansion of therapeutic trials and US Food and Drug Administration–approved medications for children with psoriasis, especially severe variants such as extensive plaque and pustular disease; and development of guidelines for ongoing monitoring of children with psoriasis. The role of therapeutic interventions and weight management on long-term disease course remains to be shown in extended clinical trials. Despite the great advancements in psoriatic care, knowledge gaps remain in pediatric psoriasis that will need to be addressed in the future.
1. Taclonex Expanded Indication. OptumRx Web site. https://www.optumrx.com/vgnpreview/HCP/Assets/RxNews/Clinical%20Updates_Taclonex_2014-1003.pdf. Published August 29, 2014. Accessed January 28, 2015.
2. Silverberg NB. Update on pediatric psoriasis, part 1: clinical features and demographics. Cutis. 2010;86:118-124.
3. Silverberg NB. Update on pediatric psoriasis, part 2: therapeutic management. Cutis. 2010;86:172-176.
4. Cather JC. Psoriasis in children and women: addressing some special needs. Semin Cutan Med Surg. 2014;33(2 suppl 2):S42-S44.
5. Khorsand K, Sidbury R. Recent advances in pediatric dermatology. Arch Dis Child. 2014;99:944-948.
6. Mercy K, Kwasny M, Cordoro KM, et al. Clinical manifestations of pediatric psoriasis: results of a multicenter study in the United States. Pediatr Dermatol. 2013;30:424-428.
7. Gudjonsson JE, Thorarinsson AM, Sigurgeirsson B, et al. Streptococcal throat infections and exacerbation of chronic plaque psoriasis: a prospective study. Br J Dermatol. 2003;149:530-534.
8. Ferran M, Galván AB, Rincón C, et al. Streptococcus induces circulating CLA(+) memory T-cell-dependent epidermal cell activation in psoriasis. J Invest Dermatol. 2013;133:999-1007.
9. Gul Mert G, Incecik F, Gunasti S, et al. Psoriasiform drug eruption associated with sodium valproate [published online ahead of print November 13, 2013]. Case Rep Pediatr. 2013;2013:823469.
10. Chang MW, Nakrani R. Six children with allergic contact dermatitis to methylisothiazolinone in wet wipes (baby wipes). Pediatrics. 2014;133:e434-e438.
11. Gul U, Gonul M, Kaya I, et al. Autoimmune thyroid disorders in patients with psoriasis. Eur J Dermatol. 2009;19:221-223.
12. Prahalad S, McCracken C, Ponder L, et al. A120: Familial autoimmunity in the CARRA registry. Arthritis Rheumatol. 2014;66(suppl 11):S157.
13. Mercy KM, Paller AS. The relationship between obesity and psoriasis in the pediatric population: implications and future directions. Cutis. 2013;92:107-109.
14. Paller AS, Mercy K, Kwasny MJ, et al. Association of pediatric psoriasis severity with excess and central adiposity: an international cross-sectional study. JAMA Dermatol. 2013;149:166-176.
15. Becker L, Tom WL, Eshagh K, et al. Excess adiposity preceding pediatric psoriasis. JAMA Dermatol. 2014;150:573-574.
16. Volf EM, Levine DE, Michelon MA, et al. Assessor-blinded study of the metabolic syndrome and surrogate markers of increased cardiovascular risk in children with moderate-to-severe psoriasis compared with age-matched population of children with warts. J Drugs Dermatol. 2011;10:900-901.
17. Manzoni AP, Weber MB, Nagatomi AR, et al. Assessing depression and anxiety in the caregivers of pediatric patients with chronic skin disorders. An Bras Dermatol. 2013;88:894-899.
18. Belloni Fortina A, Neri L. Topical steroids and corticophobia. G Ital Dermatol Venereol. 2013;148:651-654.
19. Posso-De Los Rios CJ, Pope E, Lara-Corrales I. A systematic review of systemic medications for pustular psoriasis in pediatrics. Pediatr Dermatol. 2014;31:430-439.
20. Tollefson MM. Diagnosis and management of psoriasis in children. Pediatr Clin North Am. 2014;61:261-277.
21. Fotiadou C, Lazaridou E, Ioannides D. Management of psoriasis in adolescence. Adolesc Health Med Ther. 2014;5:25-34.
22. Windschall D, Müller T, Becker I, et al. Safety and efficacy of etanercept in children with the JIA categories extended oligoarthritis, enthesitis-related arthritis and psoriasis arthritis [published online ahead of print July 18, 2014]. Clin Rheumatol. 2015;34:61-69.
23. Mälkönen T, Wikström A, Heiskanen K, et al. Skin reactions during anti-TNFa therapy for pediatric inflammatory bowel disease: a 2-year prospective study. Inflamm Bowel Dis. 2014;20:1309-1315.
24. Afzali A, Wheat CL, Hu JK, et al. The association of psoriasiform rash with anti-tumor necrosis factor (anti-TNF) therapy in inflammatory bowel disease: a single academic center case series. J Crohns Colitis. 2014;8:480-488.
25. Sherlock ME, Walters T, Tabbers MM, et al. Infliximab-induced psoriasis and psoriasiform skin lesions in pediatric Crohn disease and a potential association with IL-23 receptor polymorphisms. J Pediatr Gastroenterol Nutr. 2013;56:512-518.
26. Rahman SI, Siegfried E, Flanagan KH, et al. The methotrexate polyglutamate assay supports the efficacy of methotrexate for severe inflammatory skin disease in children. J Am Acad Dermatol. 2014;70:252-256.
27. Suzuki E, Mellins ED, Gershwin ME, et al. The IL-23/IL-17 axis in psoriatic arthritis. Autoimmun Rev. 2014;13:496-502.
28. Michalak-Stoma A, Bartosi´nska J, Kowal M, et al. Serum levels of selected Th17 and Th22 cytokines in psoriatic patients. Dis Markers. 2013;35:625-631.
1. Taclonex Expanded Indication. OptumRx Web site. https://www.optumrx.com/vgnpreview/HCP/Assets/RxNews/Clinical%20Updates_Taclonex_2014-1003.pdf. Published August 29, 2014. Accessed January 28, 2015.
2. Silverberg NB. Update on pediatric psoriasis, part 1: clinical features and demographics. Cutis. 2010;86:118-124.
3. Silverberg NB. Update on pediatric psoriasis, part 2: therapeutic management. Cutis. 2010;86:172-176.
4. Cather JC. Psoriasis in children and women: addressing some special needs. Semin Cutan Med Surg. 2014;33(2 suppl 2):S42-S44.
5. Khorsand K, Sidbury R. Recent advances in pediatric dermatology. Arch Dis Child. 2014;99:944-948.
6. Mercy K, Kwasny M, Cordoro KM, et al. Clinical manifestations of pediatric psoriasis: results of a multicenter study in the United States. Pediatr Dermatol. 2013;30:424-428.
7. Gudjonsson JE, Thorarinsson AM, Sigurgeirsson B, et al. Streptococcal throat infections and exacerbation of chronic plaque psoriasis: a prospective study. Br J Dermatol. 2003;149:530-534.
8. Ferran M, Galván AB, Rincón C, et al. Streptococcus induces circulating CLA(+) memory T-cell-dependent epidermal cell activation in psoriasis. J Invest Dermatol. 2013;133:999-1007.
9. Gul Mert G, Incecik F, Gunasti S, et al. Psoriasiform drug eruption associated with sodium valproate [published online ahead of print November 13, 2013]. Case Rep Pediatr. 2013;2013:823469.
10. Chang MW, Nakrani R. Six children with allergic contact dermatitis to methylisothiazolinone in wet wipes (baby wipes). Pediatrics. 2014;133:e434-e438.
11. Gul U, Gonul M, Kaya I, et al. Autoimmune thyroid disorders in patients with psoriasis. Eur J Dermatol. 2009;19:221-223.
12. Prahalad S, McCracken C, Ponder L, et al. A120: Familial autoimmunity in the CARRA registry. Arthritis Rheumatol. 2014;66(suppl 11):S157.
13. Mercy KM, Paller AS. The relationship between obesity and psoriasis in the pediatric population: implications and future directions. Cutis. 2013;92:107-109.
14. Paller AS, Mercy K, Kwasny MJ, et al. Association of pediatric psoriasis severity with excess and central adiposity: an international cross-sectional study. JAMA Dermatol. 2013;149:166-176.
15. Becker L, Tom WL, Eshagh K, et al. Excess adiposity preceding pediatric psoriasis. JAMA Dermatol. 2014;150:573-574.
16. Volf EM, Levine DE, Michelon MA, et al. Assessor-blinded study of the metabolic syndrome and surrogate markers of increased cardiovascular risk in children with moderate-to-severe psoriasis compared with age-matched population of children with warts. J Drugs Dermatol. 2011;10:900-901.
17. Manzoni AP, Weber MB, Nagatomi AR, et al. Assessing depression and anxiety in the caregivers of pediatric patients with chronic skin disorders. An Bras Dermatol. 2013;88:894-899.
18. Belloni Fortina A, Neri L. Topical steroids and corticophobia. G Ital Dermatol Venereol. 2013;148:651-654.
19. Posso-De Los Rios CJ, Pope E, Lara-Corrales I. A systematic review of systemic medications for pustular psoriasis in pediatrics. Pediatr Dermatol. 2014;31:430-439.
20. Tollefson MM. Diagnosis and management of psoriasis in children. Pediatr Clin North Am. 2014;61:261-277.
21. Fotiadou C, Lazaridou E, Ioannides D. Management of psoriasis in adolescence. Adolesc Health Med Ther. 2014;5:25-34.
22. Windschall D, Müller T, Becker I, et al. Safety and efficacy of etanercept in children with the JIA categories extended oligoarthritis, enthesitis-related arthritis and psoriasis arthritis [published online ahead of print July 18, 2014]. Clin Rheumatol. 2015;34:61-69.
23. Mälkönen T, Wikström A, Heiskanen K, et al. Skin reactions during anti-TNFa therapy for pediatric inflammatory bowel disease: a 2-year prospective study. Inflamm Bowel Dis. 2014;20:1309-1315.
24. Afzali A, Wheat CL, Hu JK, et al. The association of psoriasiform rash with anti-tumor necrosis factor (anti-TNF) therapy in inflammatory bowel disease: a single academic center case series. J Crohns Colitis. 2014;8:480-488.
25. Sherlock ME, Walters T, Tabbers MM, et al. Infliximab-induced psoriasis and psoriasiform skin lesions in pediatric Crohn disease and a potential association with IL-23 receptor polymorphisms. J Pediatr Gastroenterol Nutr. 2013;56:512-518.
26. Rahman SI, Siegfried E, Flanagan KH, et al. The methotrexate polyglutamate assay supports the efficacy of methotrexate for severe inflammatory skin disease in children. J Am Acad Dermatol. 2014;70:252-256.
27. Suzuki E, Mellins ED, Gershwin ME, et al. The IL-23/IL-17 axis in psoriatic arthritis. Autoimmun Rev. 2014;13:496-502.
28. Michalak-Stoma A, Bartosi´nska J, Kowal M, et al. Serum levels of selected Th17 and Th22 cytokines in psoriatic patients. Dis Markers. 2013;35:625-631.
Practice Points
- The majority of children with psoriasis have severe disease, scalp involvement, and a family history.
- Pediatric psoriasis is associated with metabolic syndrome, especially obesity.
- Anxiety and depression may be noted in children with psoriasis as well as their caregivers.
First Refusal
Treatment success in psoriasis, as in any dermatologic condition, is dependent on many factors. The willingness of patients to follow our suggested therapeutic plans certainly is one of the most important components of this process.
Halioua et al1 analyzed the issue of treatment refusal, which they defined as “a patient actively refusing to take treatment despite physician recommendations,” among psoriasis patients. Treatment refusal is a more complex phenomenon than nonadherence, as it requires an affirmative act that goes beyond more passive acts of not filling prescriptions, taking a medication sporadically, or forgetting to take a medication. Their objective was to investigate refusal of topical treatments by patients living with psoriasis in France as well as the factors that influence such refusal.1
The authors evaluated responses to an Internet study.1 Responses from participants who refused topical therapy (n=50) were compared to individuals who successfully applied topical treatment (n=205). Individuals receiving phototherapy, biologic therapy, and oral treatment were not included in the analysis. Spearman rank correlations completed by Fisher exact tests and Student t tests were performed.1
The researchers found that objective aspects of psoriasis, including comorbidities, localization of lesions, and symptoms associated with psoriasis, were not significant predictors of treatment refusal. The factors that did appear to influence refusal related more to patient perception of disease and its treatment.1
First, treatment refusal was defined by patient attitude toward treatment. In the treatment refusal group, significantly fewer participants reported believing that psoriasis can be managed (20.0% vs 38.5%; P<.01), and significantly more participants in the treatment refusal group reported believing that topical psoriasis treatments never work (58.0% vs 27.5%; odds ratio, 2.09; P<.0001). Additionally, significantly fewer participants in the treatment refusal group were willing to stay on prescription medications long-term (30.0% vs 77.6%; P<.001), and significantly more patients in the treatment refusal group believed that all creams (prescription or over-the-counter) work the same (54.0% vs 31.7%; odds ratio, 1.07; P=.003).1
The physician-patient relationship also influenced refusal. In the treatment refusal group, 60% of participants reported no longer consulting physicians for psoriasis treatment. The main reasons for cessation of medical care were lack of improvement of psoriasis (40%) and feeling that the physician did not take psoriasis seriously (20%). In the treatment acceptance group, only 10% of participants no longer consulted physicians.1 Among participants who continued to consult their physician (40% for the treatment refusal group and 90.2% for the treatment acceptance group), significantly fewer participants in the treatment refusal group reported that they were substantially helped by their physician (50.0% vs 73.0%; P=.03) and that they always followed physician recommendations (65.0% vs 85.4%; P=.02). Additionally, significantly fewer participants in the treatment refusal group considered that their physician took the time to listen to what he/she had to say (65.0% vs 85.9%; P=.02) and that their physician had provided clear instructions on how to utilize the treatment (65.0% vs 83.2%; P=.046).1
Therefore, treatment refusal is an important factor to be considered in the management of psoriasis. The findings of this study indicate possible strategies to reduce patient refusal. For example, enhanced education about the therapeutic options for psoriasis and their benefits could counter negative perceptions about these therapies. It also appears that increased focus on the physician-patient relationship may have a positive impact in this area.
Reference
1. Halioua B, Maury Le Breton A, de Fontaubert A, et al. Treatment refusal among patients with psoriasis [published online ahead of print]. J Dermatolog Treat. 2015;2:1-5.
Treatment success in psoriasis, as in any dermatologic condition, is dependent on many factors. The willingness of patients to follow our suggested therapeutic plans certainly is one of the most important components of this process.
Halioua et al1 analyzed the issue of treatment refusal, which they defined as “a patient actively refusing to take treatment despite physician recommendations,” among psoriasis patients. Treatment refusal is a more complex phenomenon than nonadherence, as it requires an affirmative act that goes beyond more passive acts of not filling prescriptions, taking a medication sporadically, or forgetting to take a medication. Their objective was to investigate refusal of topical treatments by patients living with psoriasis in France as well as the factors that influence such refusal.1
The authors evaluated responses to an Internet study.1 Responses from participants who refused topical therapy (n=50) were compared to individuals who successfully applied topical treatment (n=205). Individuals receiving phototherapy, biologic therapy, and oral treatment were not included in the analysis. Spearman rank correlations completed by Fisher exact tests and Student t tests were performed.1
The researchers found that objective aspects of psoriasis, including comorbidities, localization of lesions, and symptoms associated with psoriasis, were not significant predictors of treatment refusal. The factors that did appear to influence refusal related more to patient perception of disease and its treatment.1
First, treatment refusal was defined by patient attitude toward treatment. In the treatment refusal group, significantly fewer participants reported believing that psoriasis can be managed (20.0% vs 38.5%; P<.01), and significantly more participants in the treatment refusal group reported believing that topical psoriasis treatments never work (58.0% vs 27.5%; odds ratio, 2.09; P<.0001). Additionally, significantly fewer participants in the treatment refusal group were willing to stay on prescription medications long-term (30.0% vs 77.6%; P<.001), and significantly more patients in the treatment refusal group believed that all creams (prescription or over-the-counter) work the same (54.0% vs 31.7%; odds ratio, 1.07; P=.003).1
The physician-patient relationship also influenced refusal. In the treatment refusal group, 60% of participants reported no longer consulting physicians for psoriasis treatment. The main reasons for cessation of medical care were lack of improvement of psoriasis (40%) and feeling that the physician did not take psoriasis seriously (20%). In the treatment acceptance group, only 10% of participants no longer consulted physicians.1 Among participants who continued to consult their physician (40% for the treatment refusal group and 90.2% for the treatment acceptance group), significantly fewer participants in the treatment refusal group reported that they were substantially helped by their physician (50.0% vs 73.0%; P=.03) and that they always followed physician recommendations (65.0% vs 85.4%; P=.02). Additionally, significantly fewer participants in the treatment refusal group considered that their physician took the time to listen to what he/she had to say (65.0% vs 85.9%; P=.02) and that their physician had provided clear instructions on how to utilize the treatment (65.0% vs 83.2%; P=.046).1
Therefore, treatment refusal is an important factor to be considered in the management of psoriasis. The findings of this study indicate possible strategies to reduce patient refusal. For example, enhanced education about the therapeutic options for psoriasis and their benefits could counter negative perceptions about these therapies. It also appears that increased focus on the physician-patient relationship may have a positive impact in this area.
Treatment success in psoriasis, as in any dermatologic condition, is dependent on many factors. The willingness of patients to follow our suggested therapeutic plans certainly is one of the most important components of this process.
Halioua et al1 analyzed the issue of treatment refusal, which they defined as “a patient actively refusing to take treatment despite physician recommendations,” among psoriasis patients. Treatment refusal is a more complex phenomenon than nonadherence, as it requires an affirmative act that goes beyond more passive acts of not filling prescriptions, taking a medication sporadically, or forgetting to take a medication. Their objective was to investigate refusal of topical treatments by patients living with psoriasis in France as well as the factors that influence such refusal.1
The authors evaluated responses to an Internet study.1 Responses from participants who refused topical therapy (n=50) were compared to individuals who successfully applied topical treatment (n=205). Individuals receiving phototherapy, biologic therapy, and oral treatment were not included in the analysis. Spearman rank correlations completed by Fisher exact tests and Student t tests were performed.1
The researchers found that objective aspects of psoriasis, including comorbidities, localization of lesions, and symptoms associated with psoriasis, were not significant predictors of treatment refusal. The factors that did appear to influence refusal related more to patient perception of disease and its treatment.1
First, treatment refusal was defined by patient attitude toward treatment. In the treatment refusal group, significantly fewer participants reported believing that psoriasis can be managed (20.0% vs 38.5%; P<.01), and significantly more participants in the treatment refusal group reported believing that topical psoriasis treatments never work (58.0% vs 27.5%; odds ratio, 2.09; P<.0001). Additionally, significantly fewer participants in the treatment refusal group were willing to stay on prescription medications long-term (30.0% vs 77.6%; P<.001), and significantly more patients in the treatment refusal group believed that all creams (prescription or over-the-counter) work the same (54.0% vs 31.7%; odds ratio, 1.07; P=.003).1
The physician-patient relationship also influenced refusal. In the treatment refusal group, 60% of participants reported no longer consulting physicians for psoriasis treatment. The main reasons for cessation of medical care were lack of improvement of psoriasis (40%) and feeling that the physician did not take psoriasis seriously (20%). In the treatment acceptance group, only 10% of participants no longer consulted physicians.1 Among participants who continued to consult their physician (40% for the treatment refusal group and 90.2% for the treatment acceptance group), significantly fewer participants in the treatment refusal group reported that they were substantially helped by their physician (50.0% vs 73.0%; P=.03) and that they always followed physician recommendations (65.0% vs 85.4%; P=.02). Additionally, significantly fewer participants in the treatment refusal group considered that their physician took the time to listen to what he/she had to say (65.0% vs 85.9%; P=.02) and that their physician had provided clear instructions on how to utilize the treatment (65.0% vs 83.2%; P=.046).1
Therefore, treatment refusal is an important factor to be considered in the management of psoriasis. The findings of this study indicate possible strategies to reduce patient refusal. For example, enhanced education about the therapeutic options for psoriasis and their benefits could counter negative perceptions about these therapies. It also appears that increased focus on the physician-patient relationship may have a positive impact in this area.
Reference
1. Halioua B, Maury Le Breton A, de Fontaubert A, et al. Treatment refusal among patients with psoriasis [published online ahead of print]. J Dermatolog Treat. 2015;2:1-5.
Reference
1. Halioua B, Maury Le Breton A, de Fontaubert A, et al. Treatment refusal among patients with psoriasis [published online ahead of print]. J Dermatolog Treat. 2015;2:1-5.
Interleukin-23 inhibition with tildrakizumab achieves significant psoriasis improvements
A monoclonal antibody targeting an interleukin-23 subunit has shown a significant reduction in psoriasis area and disease severity in 77 psoriasis patients, according to data from a randomized, placebo-controlled phase I trial.
Three doses of intravenous tildrakizumab (0.05–10 mg/kg1) – given 1-2 months apart – were associated with 50%-80% reductions in mean placebo-corrected psoriasis area and severity index (PASI) scores at 112 days after commencing treatment, and was well tolerated with minor adverse events.
Researchers observed 50% reductions in PASI score 308 days after the last administered dose, and all subjects given 3 or 10 mg/kg achieved a 75% reduction in PASI score by day 196, according to a paper published online March 9 in Nature (doi: 10.1038/nature14175).
“Further development of tildrakizumab is warranted based on these results to determine whether selective targeting of IL-23 can provide similar or better efficacy while reducing safety concerns that are associated with other biologic agents currently approved for the treatment of psoriasis,” wrote Dr. Tamara Kopp, from the Juvenis Medical Center, Vienna, and coauthors.
The study was funded by tildrakizumab-developer Merck & Co. Inc, and several authors were employees of Merck & Co. Inc.
A monoclonal antibody targeting an interleukin-23 subunit has shown a significant reduction in psoriasis area and disease severity in 77 psoriasis patients, according to data from a randomized, placebo-controlled phase I trial.
Three doses of intravenous tildrakizumab (0.05–10 mg/kg1) – given 1-2 months apart – were associated with 50%-80% reductions in mean placebo-corrected psoriasis area and severity index (PASI) scores at 112 days after commencing treatment, and was well tolerated with minor adverse events.
Researchers observed 50% reductions in PASI score 308 days after the last administered dose, and all subjects given 3 or 10 mg/kg achieved a 75% reduction in PASI score by day 196, according to a paper published online March 9 in Nature (doi: 10.1038/nature14175).
“Further development of tildrakizumab is warranted based on these results to determine whether selective targeting of IL-23 can provide similar or better efficacy while reducing safety concerns that are associated with other biologic agents currently approved for the treatment of psoriasis,” wrote Dr. Tamara Kopp, from the Juvenis Medical Center, Vienna, and coauthors.
The study was funded by tildrakizumab-developer Merck & Co. Inc, and several authors were employees of Merck & Co. Inc.
A monoclonal antibody targeting an interleukin-23 subunit has shown a significant reduction in psoriasis area and disease severity in 77 psoriasis patients, according to data from a randomized, placebo-controlled phase I trial.
Three doses of intravenous tildrakizumab (0.05–10 mg/kg1) – given 1-2 months apart – were associated with 50%-80% reductions in mean placebo-corrected psoriasis area and severity index (PASI) scores at 112 days after commencing treatment, and was well tolerated with minor adverse events.
Researchers observed 50% reductions in PASI score 308 days after the last administered dose, and all subjects given 3 or 10 mg/kg achieved a 75% reduction in PASI score by day 196, according to a paper published online March 9 in Nature (doi: 10.1038/nature14175).
“Further development of tildrakizumab is warranted based on these results to determine whether selective targeting of IL-23 can provide similar or better efficacy while reducing safety concerns that are associated with other biologic agents currently approved for the treatment of psoriasis,” wrote Dr. Tamara Kopp, from the Juvenis Medical Center, Vienna, and coauthors.
The study was funded by tildrakizumab-developer Merck & Co. Inc, and several authors were employees of Merck & Co. Inc.
VIDEO: Secukinumab ‘exciting’ new agent for psoriasis
KAUAI, HAWAII – The Food and Drug administration recently approved a new class of drug for psoriasis. Secukinumab, indicated for the treatment of mild to severe psoriasis, targets IL-17, a cytokine highly implicated in the disease.
“I’m very excited to try this drug in my patients,” Dr. Kristina Callis Duffin said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
In this report, Dr. Duffin of the University of Utah explains the drug’s mechanism of action, describes how it differs from other biologic agents used to treat psoriasis, and shares promising data showing improved scores on the Psoriasis Area and Severity Index (PASI).
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
KAUAI, HAWAII – The Food and Drug administration recently approved a new class of drug for psoriasis. Secukinumab, indicated for the treatment of mild to severe psoriasis, targets IL-17, a cytokine highly implicated in the disease.
“I’m very excited to try this drug in my patients,” Dr. Kristina Callis Duffin said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
In this report, Dr. Duffin of the University of Utah explains the drug’s mechanism of action, describes how it differs from other biologic agents used to treat psoriasis, and shares promising data showing improved scores on the Psoriasis Area and Severity Index (PASI).
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
KAUAI, HAWAII – The Food and Drug administration recently approved a new class of drug for psoriasis. Secukinumab, indicated for the treatment of mild to severe psoriasis, targets IL-17, a cytokine highly implicated in the disease.
“I’m very excited to try this drug in my patients,” Dr. Kristina Callis Duffin said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
In this report, Dr. Duffin of the University of Utah explains the drug’s mechanism of action, describes how it differs from other biologic agents used to treat psoriasis, and shares promising data showing improved scores on the Psoriasis Area and Severity Index (PASI).
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
AT SDEF HAWAII DERMATOLOGY SEMINAR
Infliximab most common cause of drug-induced liver injury
Infliximab caused liver injury in 8.3% of treated patients in a prospective study, exceeding rates for other tumor necrosis factor-alpha antagonists, investigators reported online in Clinical Gastroenterology and Hepatology.
The findings show that “liver injury associated with the use of TNF-alpha antagonists is more common than previously reported, occurring in 1 in 120 of those exposed to infliximab,” said Dr. Einar S. Björnsson at the University of Iceland in Reykjavik and his associates. Furthermore, neither anti-TNF treatment dose nor baseline antinuclear acid antibody (ANA) status predicted which patients would develop drug-induced liver injury (DILI), the researchers said.
Since emerging in the 1990s, anti-TNF agents have dramatically altered the treatment landscape for autoimmune diseases such as rheumatoid arthritis, psoriasis, and inflammatory bowel disease. Although they are known to cause liver damage in some patients, data on the topic mainly come from single case reports, the researchers said (Clin. Gastroenterol. Hepatol. 2014 [doi: http://dx.doi.org/10.1016/j.cgh.2014.07.062]) To better understand the association, the researchers prospectively studied patients who received anti-TNF agents between 2009 and 2013 at the University Hospital in Iceland. They defined liver injury as aspartate aminotransferase or alanine aminotransferase (ALT) levels that were at least triple the normal upper limit, or alkaline phosphatase levels of at least double the upper limit.
A total of 1,776 patients were treated with anti-TNF agents during the 5-year study period, the researchers reported. In all, 11 developed drug-induced liver injury (DILI), of which nine cases were caused by infliximab, they said. Liver injury developed in 8.3% of patients treated with infliximab, compared with only 3.7% of those who received adalimumab and 2.3% of those given etanercept, they added. In a past analysis, the researchers calculated that one in every 148 patients would develop DILI during 2 years of treatment with infliximab (Gastroenterology 2014;144:1419-25). Patients who developed DILI on one anti-TNF agent were able to switch therapies without DILI recurring, the investigators said. Seven patients were switched from infliximab to adalimumab, etanercept, or both, and one was switched to infliximab after developing DILI on adalimumab, they added.
The researchers also compared the 11 cases to 22 randomized controls matched by age, sex, underlying condition, and treatment. Notably, among the 11 patients diagnosed with DILI, just 1 (9%) was receiving methotrexate at the time of diagnosis, compared with 59% of the controls (P = .009), they reported. “The reason for this is not clear,” they added. “Methotrexate has been shown to lead to a decrease in circulating autoantibodies in cutaneous lupus erythematosus, but the influence of methotrexate could not be confirmed during infliximab treatment.”
Five of the 11 patients with DILI had liver biopsies, of which three showed severe acute hepatitis, two indicated mild unspecified chronic hepatitis, and one showed pure canalicular cholestasis, the researchers reported. About half the patients needed steroids acutely, but “the vast majority” did not need long-term steroid treatment, they said. Exactly how anti-TNF agents cause liver injury remains unclear, they added. Future studies might evaluate whether these drugs trigger CD4 T cells to react against liver cells, as is the case in classic autoimmune hepatitis, they said.
The researchers reported no funding sources and declared having no conflicts of interest.
Infliximab caused liver injury in 8.3% of treated patients in a prospective study, exceeding rates for other tumor necrosis factor-alpha antagonists, investigators reported online in Clinical Gastroenterology and Hepatology.
The findings show that “liver injury associated with the use of TNF-alpha antagonists is more common than previously reported, occurring in 1 in 120 of those exposed to infliximab,” said Dr. Einar S. Björnsson at the University of Iceland in Reykjavik and his associates. Furthermore, neither anti-TNF treatment dose nor baseline antinuclear acid antibody (ANA) status predicted which patients would develop drug-induced liver injury (DILI), the researchers said.
Since emerging in the 1990s, anti-TNF agents have dramatically altered the treatment landscape for autoimmune diseases such as rheumatoid arthritis, psoriasis, and inflammatory bowel disease. Although they are known to cause liver damage in some patients, data on the topic mainly come from single case reports, the researchers said (Clin. Gastroenterol. Hepatol. 2014 [doi: http://dx.doi.org/10.1016/j.cgh.2014.07.062]) To better understand the association, the researchers prospectively studied patients who received anti-TNF agents between 2009 and 2013 at the University Hospital in Iceland. They defined liver injury as aspartate aminotransferase or alanine aminotransferase (ALT) levels that were at least triple the normal upper limit, or alkaline phosphatase levels of at least double the upper limit.
A total of 1,776 patients were treated with anti-TNF agents during the 5-year study period, the researchers reported. In all, 11 developed drug-induced liver injury (DILI), of which nine cases were caused by infliximab, they said. Liver injury developed in 8.3% of patients treated with infliximab, compared with only 3.7% of those who received adalimumab and 2.3% of those given etanercept, they added. In a past analysis, the researchers calculated that one in every 148 patients would develop DILI during 2 years of treatment with infliximab (Gastroenterology 2014;144:1419-25). Patients who developed DILI on one anti-TNF agent were able to switch therapies without DILI recurring, the investigators said. Seven patients were switched from infliximab to adalimumab, etanercept, or both, and one was switched to infliximab after developing DILI on adalimumab, they added.
The researchers also compared the 11 cases to 22 randomized controls matched by age, sex, underlying condition, and treatment. Notably, among the 11 patients diagnosed with DILI, just 1 (9%) was receiving methotrexate at the time of diagnosis, compared with 59% of the controls (P = .009), they reported. “The reason for this is not clear,” they added. “Methotrexate has been shown to lead to a decrease in circulating autoantibodies in cutaneous lupus erythematosus, but the influence of methotrexate could not be confirmed during infliximab treatment.”
Five of the 11 patients with DILI had liver biopsies, of which three showed severe acute hepatitis, two indicated mild unspecified chronic hepatitis, and one showed pure canalicular cholestasis, the researchers reported. About half the patients needed steroids acutely, but “the vast majority” did not need long-term steroid treatment, they said. Exactly how anti-TNF agents cause liver injury remains unclear, they added. Future studies might evaluate whether these drugs trigger CD4 T cells to react against liver cells, as is the case in classic autoimmune hepatitis, they said.
The researchers reported no funding sources and declared having no conflicts of interest.
Infliximab caused liver injury in 8.3% of treated patients in a prospective study, exceeding rates for other tumor necrosis factor-alpha antagonists, investigators reported online in Clinical Gastroenterology and Hepatology.
The findings show that “liver injury associated with the use of TNF-alpha antagonists is more common than previously reported, occurring in 1 in 120 of those exposed to infliximab,” said Dr. Einar S. Björnsson at the University of Iceland in Reykjavik and his associates. Furthermore, neither anti-TNF treatment dose nor baseline antinuclear acid antibody (ANA) status predicted which patients would develop drug-induced liver injury (DILI), the researchers said.
Since emerging in the 1990s, anti-TNF agents have dramatically altered the treatment landscape for autoimmune diseases such as rheumatoid arthritis, psoriasis, and inflammatory bowel disease. Although they are known to cause liver damage in some patients, data on the topic mainly come from single case reports, the researchers said (Clin. Gastroenterol. Hepatol. 2014 [doi: http://dx.doi.org/10.1016/j.cgh.2014.07.062]) To better understand the association, the researchers prospectively studied patients who received anti-TNF agents between 2009 and 2013 at the University Hospital in Iceland. They defined liver injury as aspartate aminotransferase or alanine aminotransferase (ALT) levels that were at least triple the normal upper limit, or alkaline phosphatase levels of at least double the upper limit.
A total of 1,776 patients were treated with anti-TNF agents during the 5-year study period, the researchers reported. In all, 11 developed drug-induced liver injury (DILI), of which nine cases were caused by infliximab, they said. Liver injury developed in 8.3% of patients treated with infliximab, compared with only 3.7% of those who received adalimumab and 2.3% of those given etanercept, they added. In a past analysis, the researchers calculated that one in every 148 patients would develop DILI during 2 years of treatment with infliximab (Gastroenterology 2014;144:1419-25). Patients who developed DILI on one anti-TNF agent were able to switch therapies without DILI recurring, the investigators said. Seven patients were switched from infliximab to adalimumab, etanercept, or both, and one was switched to infliximab after developing DILI on adalimumab, they added.
The researchers also compared the 11 cases to 22 randomized controls matched by age, sex, underlying condition, and treatment. Notably, among the 11 patients diagnosed with DILI, just 1 (9%) was receiving methotrexate at the time of diagnosis, compared with 59% of the controls (P = .009), they reported. “The reason for this is not clear,” they added. “Methotrexate has been shown to lead to a decrease in circulating autoantibodies in cutaneous lupus erythematosus, but the influence of methotrexate could not be confirmed during infliximab treatment.”
Five of the 11 patients with DILI had liver biopsies, of which three showed severe acute hepatitis, two indicated mild unspecified chronic hepatitis, and one showed pure canalicular cholestasis, the researchers reported. About half the patients needed steroids acutely, but “the vast majority” did not need long-term steroid treatment, they said. Exactly how anti-TNF agents cause liver injury remains unclear, they added. Future studies might evaluate whether these drugs trigger CD4 T cells to react against liver cells, as is the case in classic autoimmune hepatitis, they said.
The researchers reported no funding sources and declared having no conflicts of interest.
Key clinical point: Infliximab was the most common anti–tumor necrosis factor-alpha agent linked to liver injury.
Major finding: Rates of drug-induced liver injury were highest among patients treated with infliximab (8.3%), compared with 3.7% for adalimumab and 2.3% for etanercept.
Data source: Prospective study of 11 cases of drug-induced liver injury and 22 controls.
Disclosures: The researchers declared no funding sources or conflicts of interest.