User login
Enhancing Molecular Testing Documentation in Prostate Cancer
Background
Prostate cancer is the most common non-cutaneous malignancy at the Veterans Health Administration (VHA) and every year approximately 15,000 Veterans are diagnosed and treated. Many advanced prostate cancer cases harbor genetic mutations that significantly impact prognosis, treatment decisions, and familial screening. In February 2021, the Prostate Cancer Molecular Testing Pathway (PCMTP) flow map was developed to increase appropriate genetic testing.
Methods
VHA initiated the Oncology Clinical Pathways (OCP) program to standardize cancer care for Veterans. The PCMTP was developed by a multidisciplinary team that created interactive templates within the Computerized Patient Record System (CPRS), to facilitate identification of eligible Veterans for germline and comprehensive genomic profiling (CGP). Clinical decision-making for these tests is documented as Health Factors (HF), in CPRS, allowing for assessment of pathway adherence and overall uptake.
Results
The PCMTP has achieved success, as there is over 90% compliance to molecular testing among participating Veterans which exceeds the pathway benchmark of 80%. PCMTP has been utilized at 88 VA sites, by over 700 distinct VA providers, with over 7,000 Veterans participating. This implementation has yielded over 19,200 Health Factors within CPRS.
Conclusions
The PCMTP has markedly improved the documentation and application of germline and CGP testing among Veterans diagnosed with prostate cancer. By facilitating genomic testing in appropriate patients, the PCMTP aims to enhance patient outcomes and optimize the quality of care. Prior to PCMTP establishment, assessing the prevalence of germline and CGP testing in eligible Veterans posed significant challenges. Future work will concentrate on increasing PCMTP utilization, evaluating downstream outcomes from genomic testing, including the identification of pathogenic variants, utilization of genetic counseling services, referrals to clinical trials, and the genomic impact on treatment strategies.
Background
Prostate cancer is the most common non-cutaneous malignancy at the Veterans Health Administration (VHA) and every year approximately 15,000 Veterans are diagnosed and treated. Many advanced prostate cancer cases harbor genetic mutations that significantly impact prognosis, treatment decisions, and familial screening. In February 2021, the Prostate Cancer Molecular Testing Pathway (PCMTP) flow map was developed to increase appropriate genetic testing.
Methods
VHA initiated the Oncology Clinical Pathways (OCP) program to standardize cancer care for Veterans. The PCMTP was developed by a multidisciplinary team that created interactive templates within the Computerized Patient Record System (CPRS), to facilitate identification of eligible Veterans for germline and comprehensive genomic profiling (CGP). Clinical decision-making for these tests is documented as Health Factors (HF), in CPRS, allowing for assessment of pathway adherence and overall uptake.
Results
The PCMTP has achieved success, as there is over 90% compliance to molecular testing among participating Veterans which exceeds the pathway benchmark of 80%. PCMTP has been utilized at 88 VA sites, by over 700 distinct VA providers, with over 7,000 Veterans participating. This implementation has yielded over 19,200 Health Factors within CPRS.
Conclusions
The PCMTP has markedly improved the documentation and application of germline and CGP testing among Veterans diagnosed with prostate cancer. By facilitating genomic testing in appropriate patients, the PCMTP aims to enhance patient outcomes and optimize the quality of care. Prior to PCMTP establishment, assessing the prevalence of germline and CGP testing in eligible Veterans posed significant challenges. Future work will concentrate on increasing PCMTP utilization, evaluating downstream outcomes from genomic testing, including the identification of pathogenic variants, utilization of genetic counseling services, referrals to clinical trials, and the genomic impact on treatment strategies.
Background
Prostate cancer is the most common non-cutaneous malignancy at the Veterans Health Administration (VHA) and every year approximately 15,000 Veterans are diagnosed and treated. Many advanced prostate cancer cases harbor genetic mutations that significantly impact prognosis, treatment decisions, and familial screening. In February 2021, the Prostate Cancer Molecular Testing Pathway (PCMTP) flow map was developed to increase appropriate genetic testing.
Methods
VHA initiated the Oncology Clinical Pathways (OCP) program to standardize cancer care for Veterans. The PCMTP was developed by a multidisciplinary team that created interactive templates within the Computerized Patient Record System (CPRS), to facilitate identification of eligible Veterans for germline and comprehensive genomic profiling (CGP). Clinical decision-making for these tests is documented as Health Factors (HF), in CPRS, allowing for assessment of pathway adherence and overall uptake.
Results
The PCMTP has achieved success, as there is over 90% compliance to molecular testing among participating Veterans which exceeds the pathway benchmark of 80%. PCMTP has been utilized at 88 VA sites, by over 700 distinct VA providers, with over 7,000 Veterans participating. This implementation has yielded over 19,200 Health Factors within CPRS.
Conclusions
The PCMTP has markedly improved the documentation and application of germline and CGP testing among Veterans diagnosed with prostate cancer. By facilitating genomic testing in appropriate patients, the PCMTP aims to enhance patient outcomes and optimize the quality of care. Prior to PCMTP establishment, assessing the prevalence of germline and CGP testing in eligible Veterans posed significant challenges. Future work will concentrate on increasing PCMTP utilization, evaluating downstream outcomes from genomic testing, including the identification of pathogenic variants, utilization of genetic counseling services, referrals to clinical trials, and the genomic impact on treatment strategies.
Enhancing Veteran Health Research: A Quality Improvement Initiative to Optimize Biorepository Efficiency
Purpose
Biorepositories are critical to scientific research within the VA. They offer high-quality, well-characterized biospecimens linked to clinical, demographic, and molecular data. Biorepositories support studies on disease mechanisms, personalized therapies, and emerging infectious diseases by systematically collecting, processing, storing, and distributing biological materials, including tissue, blood, and DNA samples. Within the Department of Veterans Affairs (VA), biorepositories provide essential support to clinical and translational research on service- related conditions such as PTSD, traumatic brain injury, cancers, and toxic exposures. While the need for harmonized quality processes and resource allocation has long been acknowledged within the biorepository community (Siwek, 2015), each biorepository operates independently, limiting scalability and standardization. This quality improvement project describes a collaboration between two VA biorepository sites supporting a national genomic study investigating disease risk and treatment outcomes. The project aimed to expand capacity, improve processing times, and enhance quality control. Each site mirrors the other’s functions, including receiving, accessioning, processing, storing, and shipping biospecimens, and serves as a contingency site to strengthen operational resilience.
Methods
To address space limitations and improve processing efficiency, one site implemented a custom rack design, expanding storage capacity per freezer. Robotic workflows were optimized, reducing biospecimen processing time. An in-process quality control step was introduced to identify data discrepancies earlier in the workflow, reducing investigation time and supporting overall data integrity. Efficiency was measured by the increase in storage capacity and decreased processing time. Descriptive statistics were used to evaluate changes in performance. Metrics were monitored over twelve months and compared against baseline data.
Results
Following implementation, storage capacity per freezer increased by 20%, and specimen processing time decreased by 30%. The new quality control checkpoint reduced investigation times by 98%, resulting in a more streamlined workflow. These improvements enhanced coordination between sites and improved support for ongoing studies.
Conclusions
This effort demonstrates that collaboration between biorepositories can significantly enhance efficiency, reduce turnaround times, and support high-quality research. Strengthening infrastructure through joint initiatives enables more effective support of large-scale clinical studies and contributes to improved outcomes for Veterans. These findings may also inform process improvements at other VA research facilities.
Purpose
Biorepositories are critical to scientific research within the VA. They offer high-quality, well-characterized biospecimens linked to clinical, demographic, and molecular data. Biorepositories support studies on disease mechanisms, personalized therapies, and emerging infectious diseases by systematically collecting, processing, storing, and distributing biological materials, including tissue, blood, and DNA samples. Within the Department of Veterans Affairs (VA), biorepositories provide essential support to clinical and translational research on service- related conditions such as PTSD, traumatic brain injury, cancers, and toxic exposures. While the need for harmonized quality processes and resource allocation has long been acknowledged within the biorepository community (Siwek, 2015), each biorepository operates independently, limiting scalability and standardization. This quality improvement project describes a collaboration between two VA biorepository sites supporting a national genomic study investigating disease risk and treatment outcomes. The project aimed to expand capacity, improve processing times, and enhance quality control. Each site mirrors the other’s functions, including receiving, accessioning, processing, storing, and shipping biospecimens, and serves as a contingency site to strengthen operational resilience.
Methods
To address space limitations and improve processing efficiency, one site implemented a custom rack design, expanding storage capacity per freezer. Robotic workflows were optimized, reducing biospecimen processing time. An in-process quality control step was introduced to identify data discrepancies earlier in the workflow, reducing investigation time and supporting overall data integrity. Efficiency was measured by the increase in storage capacity and decreased processing time. Descriptive statistics were used to evaluate changes in performance. Metrics were monitored over twelve months and compared against baseline data.
Results
Following implementation, storage capacity per freezer increased by 20%, and specimen processing time decreased by 30%. The new quality control checkpoint reduced investigation times by 98%, resulting in a more streamlined workflow. These improvements enhanced coordination between sites and improved support for ongoing studies.
Conclusions
This effort demonstrates that collaboration between biorepositories can significantly enhance efficiency, reduce turnaround times, and support high-quality research. Strengthening infrastructure through joint initiatives enables more effective support of large-scale clinical studies and contributes to improved outcomes for Veterans. These findings may also inform process improvements at other VA research facilities.
Purpose
Biorepositories are critical to scientific research within the VA. They offer high-quality, well-characterized biospecimens linked to clinical, demographic, and molecular data. Biorepositories support studies on disease mechanisms, personalized therapies, and emerging infectious diseases by systematically collecting, processing, storing, and distributing biological materials, including tissue, blood, and DNA samples. Within the Department of Veterans Affairs (VA), biorepositories provide essential support to clinical and translational research on service- related conditions such as PTSD, traumatic brain injury, cancers, and toxic exposures. While the need for harmonized quality processes and resource allocation has long been acknowledged within the biorepository community (Siwek, 2015), each biorepository operates independently, limiting scalability and standardization. This quality improvement project describes a collaboration between two VA biorepository sites supporting a national genomic study investigating disease risk and treatment outcomes. The project aimed to expand capacity, improve processing times, and enhance quality control. Each site mirrors the other’s functions, including receiving, accessioning, processing, storing, and shipping biospecimens, and serves as a contingency site to strengthen operational resilience.
Methods
To address space limitations and improve processing efficiency, one site implemented a custom rack design, expanding storage capacity per freezer. Robotic workflows were optimized, reducing biospecimen processing time. An in-process quality control step was introduced to identify data discrepancies earlier in the workflow, reducing investigation time and supporting overall data integrity. Efficiency was measured by the increase in storage capacity and decreased processing time. Descriptive statistics were used to evaluate changes in performance. Metrics were monitored over twelve months and compared against baseline data.
Results
Following implementation, storage capacity per freezer increased by 20%, and specimen processing time decreased by 30%. The new quality control checkpoint reduced investigation times by 98%, resulting in a more streamlined workflow. These improvements enhanced coordination between sites and improved support for ongoing studies.
Conclusions
This effort demonstrates that collaboration between biorepositories can significantly enhance efficiency, reduce turnaround times, and support high-quality research. Strengthening infrastructure through joint initiatives enables more effective support of large-scale clinical studies and contributes to improved outcomes for Veterans. These findings may also inform process improvements at other VA research facilities.
Trending at SHM
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Do 30-day readmissions mean anything?
Hospitalists have been paying close attention to 30-day readmission figures since public reporting and payment programs embraced that number as an indicator of the quality of hospital care. But there is limited evidence to demonstrate 30-day readmission is really a meaningful interval of time, according to a recent study, “Rethinking Thirty-Day Hospital Readmissions: Shorter Intervals Might Be Better Indicators of Quality of Care.”
“I began to dig through the literature to find some sort of evidence to support this figure – I couldn’t find anything. In talking with quality experts, they all, more or less, believe that things that happen outside of 7 or 10 days are really out of the control of the clinician,” says lead author David L. Chin, PhD, of the Center for Healthcare Policy and Research at the University of California, Davis.
Dr. Chin and his team examined the 30-day risk of unplanned inpatient readmission at the hospital level for Medicare patients aged 65 and older in four states and for three conditions: acute myocardial infarction, heart failure, and pneumonia. Across states and diagnoses, the hospital-level quality signal captured in readmission risk was highest on the first day after discharge, and it declined quickly to its lowest level at day 7.
“The rapid decay in the quality signal suggests that most readmissions after the seventh-day postdischarge were explained by community- and household-level factors beyond hospitals’ control,” the authors concluded.
Dr. Chin said the study results show the 30-day measure is “a blunt instrument.”
“It isn’t really measuring anything that we’re supposed to be measuring,” he explains. “Essentially, 97% of the reasons a person comes back to the hospital is due to some other, non-hospital thing.”
He does not advocate for 7 days as the new standard, however.
“This is more intended to be a message that this is really not the right way of approaching [readmissions] to begin with,” he says. “I think we convincingly showed that it shouldn’t be 30 days, but we don’t really have a very good picture of what is driving readmission. Hospitals are getting dinged on these things that have happened that, really, they don’t have direct influence on.”
Reference
1. Chin DL, Bang H, Manickam RN, Romano PS. Rethinking thirty-day hospital readmissions: shorter intervals might be better indicators of quality of care. Health Aff (Millwood). 2016;35(10):1867-75.
Quality Improvement: Overuse as medical error
Hospitalists may recognize a culture of overuse at their hospitals, but how can they address it? That’s the question behind an HM16 abstract, “Occam’s Conference: Overuse as a Medical Error.”
“We wanted to change the culture of overuse here among the hospitalists and the house staff,” said lead author Hyung Cho, MD, director of quality and patient safety at the Icahn School of Medicine at Mount Sinai in New York City. “We wanted to frame it in a way that people can recognize and feel free to talk about and also give it the weight that it deserves. It’s a common thing that we all do: the chest x-ray or the EKG before a surgery, things like that.”
Seeing overuse as a medical error is a place to start.
“A framework in which overuse is considered a medical error would facilitate understanding of the drivers of overuse and systems factors that lead to it,” the authors wrote.
Dr. Cho and colleagues chose a monthly inpatient conference format, with all the relevant players gathered together.
“We also wanted to use the formula that Brandon Combs had with the ‘Do No Harm’ project, which is taking cases of overuse that actually lead to harm or a near miss. I think people respond to that as opposed to just talking about the cost, which people have a hard time actually figuring out,” Dr. Cho said.
The resulting Occam’s Conference provides a process to identify and discuss overuse as a medical error. It uses a fish-bone diagram to help analyze each case.
“That conversation needs to happen,” Dr. Cho said. “You realize that people are all on the same page, and if they’re not, they need to get on the same page and have an open dialogue.”
Reference
1. Cho HJ, Lutz C, Truong TTN, et al. Occam’s Conference: overuse as a medical error [abstract]. J Hosp Med. 2016;11(suppl1).
Practice Management: There’s an app for … end-of-life communications
Hospitalists wanting to help patients navigate end-of-life decisions or assist bereaved families in dealing with the death of a loved one have some new tools, according to The New York Times article, “Start-Ups for the End of Life.”
A start-up called Grace is intended to help its users deal with the myriad issues family members face after a death; it connects users with estate lawyers, financial planners, funeral homes, and caterers. Grace customers receive a list of tasks to complete before and after a death, and it includes relevant paperwork. The app also has staff ready to assist customers.
Currently, there’s little guidance available in this area, Alex Kruger, Grace’s cofounder and chief executive, and a licensed funeral director, told the New York Times: “At Grace we say, ‘Here are the 17 things you need to do this week’ and you can check them off as you do them. Here’s what you do the week before someone dies, when they die and then two weeks later.”
Another start-up mentioned in the article that could be relevant to hospitalists and their patients is called Parting. It provides an online directory of funeral homes searchable by ZIP code so users can quickly compare prices, services, and locations.
Reference
1. Zimmerman E. “Start-ups for the end of life,” New York Times, Nov. 22, 2016.
Quality Improvement: How to create a high-value culture
Hospitalists today are overseeing the health system’s movement toward an emphasis on value over volume.
“As leaders begin to strategize the best ways to spur transformation, our team realized that checklists and algorithms alone would likely not be enough to create sustained change in divisions and practices across the country,” said Reshma Gupta, MD, MSHPM, of the Robert Wood Johnson Clinical Scholars Program in the department of medicine at the University of California, Los Angeles. She’s the lead author of the recent study, “Development of a High-Value Care Culture Survey: A Modified Delphi Process and Psychometric Evaluation.”“Patient safety culture surveys have previously been used to drive care improvements, but no comparable survey of high-value care culture currently exists,” the authors wrote. “We aimed to develop a High-Value Care Culture Survey (HVCCS) for use by health care leaders and training programs to target future improvements in value-based care.”
Researchers conducted a two-phase, national modified Delphi process among 28 physicians and nurse experts with diverse backgrounds. They then administered a cross-sectional survey at two large academic medical centers among 162 internal medicine residents and 91 hospitalists for psychometric evaluation.
Four factors emerged with strong reliability:
• Leadership and health system messaging.
• Data transparency and access.
• Comfort with cost conversations.
• Blame-free environment.
The HVCCS can assist hospitalists and administrators in identifying tangible areas to target, Dr. Gupta said. The instrument was found to have good reliability and appears to correlate with an important patient outcome metric: the Centers for Medicare & Medicaid Services value-based purchasing score that has determined hospital reimbursement in recent years.
Now that this instrument has been created, the next step is for hospitals to begin using it. Dr. Gupta recognizes hospital medicine already has been a national leader in efforts to promote value-based care.
“With hospitalists leading many operational or research efforts in this area,” she says, “it will be vital to measure and address culture change. We believe this tool can aid them in their efforts to shape the story of value promotion at their institutions.”
Reference
Gupta R, Moriates C, Harrison JD, et al. Development of a high-value care culture survey: a modified Delphi process and psychometric evaluation [published online ahead of print Oct. 26, 2016]. BMJ Qual Saf. doi: 10.1136/bmjqs-2016-005612.
Quick Byte: Cleaning robotic surgical instruments
Robotic surgical instruments can retain some contamination even after cleaning, a new study suggests. Over 21 months, the researchers assessed protein residue on robotic and standard surgical instruments that were cleaned according to manufacturers’ instructions. The cleanings were 99.1% effective on the standard instruments but 97.6% effective on the robotic instruments, suggesting complete eradication of surface contaminants from robotic surgical instruments may not be possible with the current cleaning procedures.
Reference
1. Preidt R. “Robotic surgical tools tough to keep clean,” HealthDay News, Nov. 1, 2016.
Suzanne Bopp is a freelance writer in New Jersey.
Hospitalists have been paying close attention to 30-day readmission figures since public reporting and payment programs embraced that number as an indicator of the quality of hospital care. But there is limited evidence to demonstrate 30-day readmission is really a meaningful interval of time, according to a recent study, “Rethinking Thirty-Day Hospital Readmissions: Shorter Intervals Might Be Better Indicators of Quality of Care.”
“I began to dig through the literature to find some sort of evidence to support this figure – I couldn’t find anything. In talking with quality experts, they all, more or less, believe that things that happen outside of 7 or 10 days are really out of the control of the clinician,” says lead author David L. Chin, PhD, of the Center for Healthcare Policy and Research at the University of California, Davis.
Dr. Chin and his team examined the 30-day risk of unplanned inpatient readmission at the hospital level for Medicare patients aged 65 and older in four states and for three conditions: acute myocardial infarction, heart failure, and pneumonia. Across states and diagnoses, the hospital-level quality signal captured in readmission risk was highest on the first day after discharge, and it declined quickly to its lowest level at day 7.
“The rapid decay in the quality signal suggests that most readmissions after the seventh-day postdischarge were explained by community- and household-level factors beyond hospitals’ control,” the authors concluded.
Dr. Chin said the study results show the 30-day measure is “a blunt instrument.”
“It isn’t really measuring anything that we’re supposed to be measuring,” he explains. “Essentially, 97% of the reasons a person comes back to the hospital is due to some other, non-hospital thing.”
He does not advocate for 7 days as the new standard, however.
“This is more intended to be a message that this is really not the right way of approaching [readmissions] to begin with,” he says. “I think we convincingly showed that it shouldn’t be 30 days, but we don’t really have a very good picture of what is driving readmission. Hospitals are getting dinged on these things that have happened that, really, they don’t have direct influence on.”
Reference
1. Chin DL, Bang H, Manickam RN, Romano PS. Rethinking thirty-day hospital readmissions: shorter intervals might be better indicators of quality of care. Health Aff (Millwood). 2016;35(10):1867-75.
Quality Improvement: Overuse as medical error
Hospitalists may recognize a culture of overuse at their hospitals, but how can they address it? That’s the question behind an HM16 abstract, “Occam’s Conference: Overuse as a Medical Error.”
“We wanted to change the culture of overuse here among the hospitalists and the house staff,” said lead author Hyung Cho, MD, director of quality and patient safety at the Icahn School of Medicine at Mount Sinai in New York City. “We wanted to frame it in a way that people can recognize and feel free to talk about and also give it the weight that it deserves. It’s a common thing that we all do: the chest x-ray or the EKG before a surgery, things like that.”
Seeing overuse as a medical error is a place to start.
“A framework in which overuse is considered a medical error would facilitate understanding of the drivers of overuse and systems factors that lead to it,” the authors wrote.
Dr. Cho and colleagues chose a monthly inpatient conference format, with all the relevant players gathered together.
“We also wanted to use the formula that Brandon Combs had with the ‘Do No Harm’ project, which is taking cases of overuse that actually lead to harm or a near miss. I think people respond to that as opposed to just talking about the cost, which people have a hard time actually figuring out,” Dr. Cho said.
The resulting Occam’s Conference provides a process to identify and discuss overuse as a medical error. It uses a fish-bone diagram to help analyze each case.
“That conversation needs to happen,” Dr. Cho said. “You realize that people are all on the same page, and if they’re not, they need to get on the same page and have an open dialogue.”
Reference
1. Cho HJ, Lutz C, Truong TTN, et al. Occam’s Conference: overuse as a medical error [abstract]. J Hosp Med. 2016;11(suppl1).
Practice Management: There’s an app for … end-of-life communications
Hospitalists wanting to help patients navigate end-of-life decisions or assist bereaved families in dealing with the death of a loved one have some new tools, according to The New York Times article, “Start-Ups for the End of Life.”
A start-up called Grace is intended to help its users deal with the myriad issues family members face after a death; it connects users with estate lawyers, financial planners, funeral homes, and caterers. Grace customers receive a list of tasks to complete before and after a death, and it includes relevant paperwork. The app also has staff ready to assist customers.
Currently, there’s little guidance available in this area, Alex Kruger, Grace’s cofounder and chief executive, and a licensed funeral director, told the New York Times: “At Grace we say, ‘Here are the 17 things you need to do this week’ and you can check them off as you do them. Here’s what you do the week before someone dies, when they die and then two weeks later.”
Another start-up mentioned in the article that could be relevant to hospitalists and their patients is called Parting. It provides an online directory of funeral homes searchable by ZIP code so users can quickly compare prices, services, and locations.
Reference
1. Zimmerman E. “Start-ups for the end of life,” New York Times, Nov. 22, 2016.
Quality Improvement: How to create a high-value culture
Hospitalists today are overseeing the health system’s movement toward an emphasis on value over volume.
“As leaders begin to strategize the best ways to spur transformation, our team realized that checklists and algorithms alone would likely not be enough to create sustained change in divisions and practices across the country,” said Reshma Gupta, MD, MSHPM, of the Robert Wood Johnson Clinical Scholars Program in the department of medicine at the University of California, Los Angeles. She’s the lead author of the recent study, “Development of a High-Value Care Culture Survey: A Modified Delphi Process and Psychometric Evaluation.”“Patient safety culture surveys have previously been used to drive care improvements, but no comparable survey of high-value care culture currently exists,” the authors wrote. “We aimed to develop a High-Value Care Culture Survey (HVCCS) for use by health care leaders and training programs to target future improvements in value-based care.”
Researchers conducted a two-phase, national modified Delphi process among 28 physicians and nurse experts with diverse backgrounds. They then administered a cross-sectional survey at two large academic medical centers among 162 internal medicine residents and 91 hospitalists for psychometric evaluation.
Four factors emerged with strong reliability:
• Leadership and health system messaging.
• Data transparency and access.
• Comfort with cost conversations.
• Blame-free environment.
The HVCCS can assist hospitalists and administrators in identifying tangible areas to target, Dr. Gupta said. The instrument was found to have good reliability and appears to correlate with an important patient outcome metric: the Centers for Medicare & Medicaid Services value-based purchasing score that has determined hospital reimbursement in recent years.
Now that this instrument has been created, the next step is for hospitals to begin using it. Dr. Gupta recognizes hospital medicine already has been a national leader in efforts to promote value-based care.
“With hospitalists leading many operational or research efforts in this area,” she says, “it will be vital to measure and address culture change. We believe this tool can aid them in their efforts to shape the story of value promotion at their institutions.”
Reference
Gupta R, Moriates C, Harrison JD, et al. Development of a high-value care culture survey: a modified Delphi process and psychometric evaluation [published online ahead of print Oct. 26, 2016]. BMJ Qual Saf. doi: 10.1136/bmjqs-2016-005612.
Quick Byte: Cleaning robotic surgical instruments
Robotic surgical instruments can retain some contamination even after cleaning, a new study suggests. Over 21 months, the researchers assessed protein residue on robotic and standard surgical instruments that were cleaned according to manufacturers’ instructions. The cleanings were 99.1% effective on the standard instruments but 97.6% effective on the robotic instruments, suggesting complete eradication of surface contaminants from robotic surgical instruments may not be possible with the current cleaning procedures.
Reference
1. Preidt R. “Robotic surgical tools tough to keep clean,” HealthDay News, Nov. 1, 2016.
Suzanne Bopp is a freelance writer in New Jersey.
Hospitalists have been paying close attention to 30-day readmission figures since public reporting and payment programs embraced that number as an indicator of the quality of hospital care. But there is limited evidence to demonstrate 30-day readmission is really a meaningful interval of time, according to a recent study, “Rethinking Thirty-Day Hospital Readmissions: Shorter Intervals Might Be Better Indicators of Quality of Care.”
“I began to dig through the literature to find some sort of evidence to support this figure – I couldn’t find anything. In talking with quality experts, they all, more or less, believe that things that happen outside of 7 or 10 days are really out of the control of the clinician,” says lead author David L. Chin, PhD, of the Center for Healthcare Policy and Research at the University of California, Davis.
Dr. Chin and his team examined the 30-day risk of unplanned inpatient readmission at the hospital level for Medicare patients aged 65 and older in four states and for three conditions: acute myocardial infarction, heart failure, and pneumonia. Across states and diagnoses, the hospital-level quality signal captured in readmission risk was highest on the first day after discharge, and it declined quickly to its lowest level at day 7.
“The rapid decay in the quality signal suggests that most readmissions after the seventh-day postdischarge were explained by community- and household-level factors beyond hospitals’ control,” the authors concluded.
Dr. Chin said the study results show the 30-day measure is “a blunt instrument.”
“It isn’t really measuring anything that we’re supposed to be measuring,” he explains. “Essentially, 97% of the reasons a person comes back to the hospital is due to some other, non-hospital thing.”
He does not advocate for 7 days as the new standard, however.
“This is more intended to be a message that this is really not the right way of approaching [readmissions] to begin with,” he says. “I think we convincingly showed that it shouldn’t be 30 days, but we don’t really have a very good picture of what is driving readmission. Hospitals are getting dinged on these things that have happened that, really, they don’t have direct influence on.”
Reference
1. Chin DL, Bang H, Manickam RN, Romano PS. Rethinking thirty-day hospital readmissions: shorter intervals might be better indicators of quality of care. Health Aff (Millwood). 2016;35(10):1867-75.
Quality Improvement: Overuse as medical error
Hospitalists may recognize a culture of overuse at their hospitals, but how can they address it? That’s the question behind an HM16 abstract, “Occam’s Conference: Overuse as a Medical Error.”
“We wanted to change the culture of overuse here among the hospitalists and the house staff,” said lead author Hyung Cho, MD, director of quality and patient safety at the Icahn School of Medicine at Mount Sinai in New York City. “We wanted to frame it in a way that people can recognize and feel free to talk about and also give it the weight that it deserves. It’s a common thing that we all do: the chest x-ray or the EKG before a surgery, things like that.”
Seeing overuse as a medical error is a place to start.
“A framework in which overuse is considered a medical error would facilitate understanding of the drivers of overuse and systems factors that lead to it,” the authors wrote.
Dr. Cho and colleagues chose a monthly inpatient conference format, with all the relevant players gathered together.
“We also wanted to use the formula that Brandon Combs had with the ‘Do No Harm’ project, which is taking cases of overuse that actually lead to harm or a near miss. I think people respond to that as opposed to just talking about the cost, which people have a hard time actually figuring out,” Dr. Cho said.
The resulting Occam’s Conference provides a process to identify and discuss overuse as a medical error. It uses a fish-bone diagram to help analyze each case.
“That conversation needs to happen,” Dr. Cho said. “You realize that people are all on the same page, and if they’re not, they need to get on the same page and have an open dialogue.”
Reference
1. Cho HJ, Lutz C, Truong TTN, et al. Occam’s Conference: overuse as a medical error [abstract]. J Hosp Med. 2016;11(suppl1).
Practice Management: There’s an app for … end-of-life communications
Hospitalists wanting to help patients navigate end-of-life decisions or assist bereaved families in dealing with the death of a loved one have some new tools, according to The New York Times article, “Start-Ups for the End of Life.”
A start-up called Grace is intended to help its users deal with the myriad issues family members face after a death; it connects users with estate lawyers, financial planners, funeral homes, and caterers. Grace customers receive a list of tasks to complete before and after a death, and it includes relevant paperwork. The app also has staff ready to assist customers.
Currently, there’s little guidance available in this area, Alex Kruger, Grace’s cofounder and chief executive, and a licensed funeral director, told the New York Times: “At Grace we say, ‘Here are the 17 things you need to do this week’ and you can check them off as you do them. Here’s what you do the week before someone dies, when they die and then two weeks later.”
Another start-up mentioned in the article that could be relevant to hospitalists and their patients is called Parting. It provides an online directory of funeral homes searchable by ZIP code so users can quickly compare prices, services, and locations.
Reference
1. Zimmerman E. “Start-ups for the end of life,” New York Times, Nov. 22, 2016.
Quality Improvement: How to create a high-value culture
Hospitalists today are overseeing the health system’s movement toward an emphasis on value over volume.
“As leaders begin to strategize the best ways to spur transformation, our team realized that checklists and algorithms alone would likely not be enough to create sustained change in divisions and practices across the country,” said Reshma Gupta, MD, MSHPM, of the Robert Wood Johnson Clinical Scholars Program in the department of medicine at the University of California, Los Angeles. She’s the lead author of the recent study, “Development of a High-Value Care Culture Survey: A Modified Delphi Process and Psychometric Evaluation.”“Patient safety culture surveys have previously been used to drive care improvements, but no comparable survey of high-value care culture currently exists,” the authors wrote. “We aimed to develop a High-Value Care Culture Survey (HVCCS) for use by health care leaders and training programs to target future improvements in value-based care.”
Researchers conducted a two-phase, national modified Delphi process among 28 physicians and nurse experts with diverse backgrounds. They then administered a cross-sectional survey at two large academic medical centers among 162 internal medicine residents and 91 hospitalists for psychometric evaluation.
Four factors emerged with strong reliability:
• Leadership and health system messaging.
• Data transparency and access.
• Comfort with cost conversations.
• Blame-free environment.
The HVCCS can assist hospitalists and administrators in identifying tangible areas to target, Dr. Gupta said. The instrument was found to have good reliability and appears to correlate with an important patient outcome metric: the Centers for Medicare & Medicaid Services value-based purchasing score that has determined hospital reimbursement in recent years.
Now that this instrument has been created, the next step is for hospitals to begin using it. Dr. Gupta recognizes hospital medicine already has been a national leader in efforts to promote value-based care.
“With hospitalists leading many operational or research efforts in this area,” she says, “it will be vital to measure and address culture change. We believe this tool can aid them in their efforts to shape the story of value promotion at their institutions.”
Reference
Gupta R, Moriates C, Harrison JD, et al. Development of a high-value care culture survey: a modified Delphi process and psychometric evaluation [published online ahead of print Oct. 26, 2016]. BMJ Qual Saf. doi: 10.1136/bmjqs-2016-005612.
Quick Byte: Cleaning robotic surgical instruments
Robotic surgical instruments can retain some contamination even after cleaning, a new study suggests. Over 21 months, the researchers assessed protein residue on robotic and standard surgical instruments that were cleaned according to manufacturers’ instructions. The cleanings were 99.1% effective on the standard instruments but 97.6% effective on the robotic instruments, suggesting complete eradication of surface contaminants from robotic surgical instruments may not be possible with the current cleaning procedures.
Reference
1. Preidt R. “Robotic surgical tools tough to keep clean,” HealthDay News, Nov. 1, 2016.
Suzanne Bopp is a freelance writer in New Jersey.
Sneak Peek: The Hospital Leader blog
Editor’s note: First published on The Hospital Leader blog under the title, “How I Realized QI Could Be a Dirty Word.”
With the recent election, there has been a new recognition of the various “bubbles” we all seem to be living in. It reminds me of the parable I like to often mention, popularized by the late great writer David Foster Wallace: Two fish were swimming along when an older fish swam by, nodded his head at them and said, “Mornin’ boys, how’s the water?” The two young fish nod back and swim for a bit, then one turns to the other and says, “What the hell is water?”
Imagine the hard reality that hit me when I read this quote from a resident: “Truly, the first thing I think of when I hear [QI] is going to make more work for residents.”
Wait – is QI actually a dirty word for other residents and physicians?
The quote comes from an Academic Medicine study titled “ ‘It Feels Like a Lot of Extra Work’: Resident Attitudes About Quality Improvement and Implications for an Effective Learning Health Care System.” I read on, and it got worse.
“This hasn’t really made any difference to the patients. Like this checklist we do on rounds, like I don’t know. Maybe it has.”
And, by far, most concerning: “There’s like the central line protocols … If you suspect that anybody has any type of bacteremia, you don’t do a blood culture; you just do a urine culture and pull the lines … we just don’t even test for it because the quality improvement then like marks you off.”
Wow.
That is some harsh truth about unintended consequences right there. (Also, apparently us kids of the 1990s still say “like” a lot, which is, like, not very professional and also like kinda grating.)
The residents in this study were from the University of Utah, Salt Lake City – an institution I frequently– and publicly – admire for their incredible progress on systematically introducing value improvement into their practice.
What can we do?
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
- THIS Is What Teamwork Looks Like, by Danielle Scheurer, MD, MSCR, SFHM
- The Medicaid Overhaul and How Hospitals and Their Providers Could Be Hardest Hit, by Brad Flansbaum, DO, MPH, MHM
- Count Me – and My Intuition – In, by Tracy Cardin, ACNP-BC, SFHM
Editor’s note: First published on The Hospital Leader blog under the title, “How I Realized QI Could Be a Dirty Word.”
With the recent election, there has been a new recognition of the various “bubbles” we all seem to be living in. It reminds me of the parable I like to often mention, popularized by the late great writer David Foster Wallace: Two fish were swimming along when an older fish swam by, nodded his head at them and said, “Mornin’ boys, how’s the water?” The two young fish nod back and swim for a bit, then one turns to the other and says, “What the hell is water?”
Imagine the hard reality that hit me when I read this quote from a resident: “Truly, the first thing I think of when I hear [QI] is going to make more work for residents.”
Wait – is QI actually a dirty word for other residents and physicians?
The quote comes from an Academic Medicine study titled “ ‘It Feels Like a Lot of Extra Work’: Resident Attitudes About Quality Improvement and Implications for an Effective Learning Health Care System.” I read on, and it got worse.
“This hasn’t really made any difference to the patients. Like this checklist we do on rounds, like I don’t know. Maybe it has.”
And, by far, most concerning: “There’s like the central line protocols … If you suspect that anybody has any type of bacteremia, you don’t do a blood culture; you just do a urine culture and pull the lines … we just don’t even test for it because the quality improvement then like marks you off.”
Wow.
That is some harsh truth about unintended consequences right there. (Also, apparently us kids of the 1990s still say “like” a lot, which is, like, not very professional and also like kinda grating.)
The residents in this study were from the University of Utah, Salt Lake City – an institution I frequently– and publicly – admire for their incredible progress on systematically introducing value improvement into their practice.
What can we do?
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
- THIS Is What Teamwork Looks Like, by Danielle Scheurer, MD, MSCR, SFHM
- The Medicaid Overhaul and How Hospitals and Their Providers Could Be Hardest Hit, by Brad Flansbaum, DO, MPH, MHM
- Count Me – and My Intuition – In, by Tracy Cardin, ACNP-BC, SFHM
Editor’s note: First published on The Hospital Leader blog under the title, “How I Realized QI Could Be a Dirty Word.”
With the recent election, there has been a new recognition of the various “bubbles” we all seem to be living in. It reminds me of the parable I like to often mention, popularized by the late great writer David Foster Wallace: Two fish were swimming along when an older fish swam by, nodded his head at them and said, “Mornin’ boys, how’s the water?” The two young fish nod back and swim for a bit, then one turns to the other and says, “What the hell is water?”
Imagine the hard reality that hit me when I read this quote from a resident: “Truly, the first thing I think of when I hear [QI] is going to make more work for residents.”
Wait – is QI actually a dirty word for other residents and physicians?
The quote comes from an Academic Medicine study titled “ ‘It Feels Like a Lot of Extra Work’: Resident Attitudes About Quality Improvement and Implications for an Effective Learning Health Care System.” I read on, and it got worse.
“This hasn’t really made any difference to the patients. Like this checklist we do on rounds, like I don’t know. Maybe it has.”
And, by far, most concerning: “There’s like the central line protocols … If you suspect that anybody has any type of bacteremia, you don’t do a blood culture; you just do a urine culture and pull the lines … we just don’t even test for it because the quality improvement then like marks you off.”
Wow.
That is some harsh truth about unintended consequences right there. (Also, apparently us kids of the 1990s still say “like” a lot, which is, like, not very professional and also like kinda grating.)
The residents in this study were from the University of Utah, Salt Lake City – an institution I frequently– and publicly – admire for their incredible progress on systematically introducing value improvement into their practice.
What can we do?
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
- THIS Is What Teamwork Looks Like, by Danielle Scheurer, MD, MSCR, SFHM
- The Medicaid Overhaul and How Hospitals and Their Providers Could Be Hardest Hit, by Brad Flansbaum, DO, MPH, MHM
- Count Me – and My Intuition – In, by Tracy Cardin, ACNP-BC, SFHM
‘I can handle it’– The state of hospitalist group backup systems
It took my hospital medicine group (HMG) 20 years to implement a formal backup system. Of all the reasons we resisted creating a backup system, foremost was that we did not want to mandate additional work. Because our compensation model did not have a mechanism to financially reward hospitalists for unexpectedly having to come in on unscheduled work days (other than the work relative value units generated by seeing patients), there was not enough motivational energy to get a system started.
It turns out our group is not unlike many other HMGs across the nation. According to the 2016 State of Hospital Medicine report (SoHM), 58.3% of adult-only HMGs, 72.2% of pediatric-only HMGs, and 52.6% of HMGs serving both adults and children did not have staffing backup systems. Interestingly, the report also showed that for groups serving adults only, academic HMGs were more likely to have formal backup systems in place (62.6%, compared with 37.3% in nonacademic HMGs).
The reason most HMGs create backup systems is to have a consistent and fair approach for dealing with unanticipated absences and/or high-volume census. In addition to creating a safety net, implementing a backup system addresses the common problem of the same hospitalists disproportionately filling in during times of crisis.
Although our group created a formal backup system starting January 2015, it is not comprehensive and deals only with high patient volumes occurring during the late evening and night hours. Hospitalists rotate through a schedule, taking a week of backup call for which no additional compensation is offered. Then, if they are actually called to come in, an hourly stipend is paid in addition to work RVUs generated. Implementing a backup system was not necessarily a popular idea. Nevertheless, the system has successfully remained in place. Triggering the system infrequently, having a clear set of criteria for when to activate backup, and providing additional compensation for the additional work are key factors in our system’s success.

When data from the 2016 SoHM report are compared with the 2014 SoHM report, the proportion of groups with formal backup systems actually decreases for both adults-only HMGs and HMGs serving both adults and children. For adult-only HMGs, there was a decline to 41.8% from 57.6%. For adult/pediatric HMGs, there was a decline to 47.4% from 58.8%. It also is notable that pediatric HMGs in particular are much less likely to have formal backup systems, only 27.8%, which has changed little since the last survey (28.8 % in 2014).
All in all, the reasons for the decline in backup systems are unclear. Possibly, the decrease is because of issues surrounding compensation, as approximately one-third of survey respondents with backup systems received no additional compensation. But in my view, it’s more likely that the reason for the decreased percentage of groups with backup systems has to do with differences in the particular set of HMGs that responded to the survey this year.
Dr. Stephan is a hospitalist at Abbott Northwestern Hospital in Minneapolis and a member of SHM’s Practice Analysis Committee.
It took my hospital medicine group (HMG) 20 years to implement a formal backup system. Of all the reasons we resisted creating a backup system, foremost was that we did not want to mandate additional work. Because our compensation model did not have a mechanism to financially reward hospitalists for unexpectedly having to come in on unscheduled work days (other than the work relative value units generated by seeing patients), there was not enough motivational energy to get a system started.
It turns out our group is not unlike many other HMGs across the nation. According to the 2016 State of Hospital Medicine report (SoHM), 58.3% of adult-only HMGs, 72.2% of pediatric-only HMGs, and 52.6% of HMGs serving both adults and children did not have staffing backup systems. Interestingly, the report also showed that for groups serving adults only, academic HMGs were more likely to have formal backup systems in place (62.6%, compared with 37.3% in nonacademic HMGs).
The reason most HMGs create backup systems is to have a consistent and fair approach for dealing with unanticipated absences and/or high-volume census. In addition to creating a safety net, implementing a backup system addresses the common problem of the same hospitalists disproportionately filling in during times of crisis.
Although our group created a formal backup system starting January 2015, it is not comprehensive and deals only with high patient volumes occurring during the late evening and night hours. Hospitalists rotate through a schedule, taking a week of backup call for which no additional compensation is offered. Then, if they are actually called to come in, an hourly stipend is paid in addition to work RVUs generated. Implementing a backup system was not necessarily a popular idea. Nevertheless, the system has successfully remained in place. Triggering the system infrequently, having a clear set of criteria for when to activate backup, and providing additional compensation for the additional work are key factors in our system’s success.

When data from the 2016 SoHM report are compared with the 2014 SoHM report, the proportion of groups with formal backup systems actually decreases for both adults-only HMGs and HMGs serving both adults and children. For adult-only HMGs, there was a decline to 41.8% from 57.6%. For adult/pediatric HMGs, there was a decline to 47.4% from 58.8%. It also is notable that pediatric HMGs in particular are much less likely to have formal backup systems, only 27.8%, which has changed little since the last survey (28.8 % in 2014).
All in all, the reasons for the decline in backup systems are unclear. Possibly, the decrease is because of issues surrounding compensation, as approximately one-third of survey respondents with backup systems received no additional compensation. But in my view, it’s more likely that the reason for the decreased percentage of groups with backup systems has to do with differences in the particular set of HMGs that responded to the survey this year.
Dr. Stephan is a hospitalist at Abbott Northwestern Hospital in Minneapolis and a member of SHM’s Practice Analysis Committee.
It took my hospital medicine group (HMG) 20 years to implement a formal backup system. Of all the reasons we resisted creating a backup system, foremost was that we did not want to mandate additional work. Because our compensation model did not have a mechanism to financially reward hospitalists for unexpectedly having to come in on unscheduled work days (other than the work relative value units generated by seeing patients), there was not enough motivational energy to get a system started.
It turns out our group is not unlike many other HMGs across the nation. According to the 2016 State of Hospital Medicine report (SoHM), 58.3% of adult-only HMGs, 72.2% of pediatric-only HMGs, and 52.6% of HMGs serving both adults and children did not have staffing backup systems. Interestingly, the report also showed that for groups serving adults only, academic HMGs were more likely to have formal backup systems in place (62.6%, compared with 37.3% in nonacademic HMGs).
The reason most HMGs create backup systems is to have a consistent and fair approach for dealing with unanticipated absences and/or high-volume census. In addition to creating a safety net, implementing a backup system addresses the common problem of the same hospitalists disproportionately filling in during times of crisis.
Although our group created a formal backup system starting January 2015, it is not comprehensive and deals only with high patient volumes occurring during the late evening and night hours. Hospitalists rotate through a schedule, taking a week of backup call for which no additional compensation is offered. Then, if they are actually called to come in, an hourly stipend is paid in addition to work RVUs generated. Implementing a backup system was not necessarily a popular idea. Nevertheless, the system has successfully remained in place. Triggering the system infrequently, having a clear set of criteria for when to activate backup, and providing additional compensation for the additional work are key factors in our system’s success.

When data from the 2016 SoHM report are compared with the 2014 SoHM report, the proportion of groups with formal backup systems actually decreases for both adults-only HMGs and HMGs serving both adults and children. For adult-only HMGs, there was a decline to 41.8% from 57.6%. For adult/pediatric HMGs, there was a decline to 47.4% from 58.8%. It also is notable that pediatric HMGs in particular are much less likely to have formal backup systems, only 27.8%, which has changed little since the last survey (28.8 % in 2014).
All in all, the reasons for the decline in backup systems are unclear. Possibly, the decrease is because of issues surrounding compensation, as approximately one-third of survey respondents with backup systems received no additional compensation. But in my view, it’s more likely that the reason for the decreased percentage of groups with backup systems has to do with differences in the particular set of HMGs that responded to the survey this year.
Dr. Stephan is a hospitalist at Abbott Northwestern Hospital in Minneapolis and a member of SHM’s Practice Analysis Committee.
Eight things hospitalists need to know about post-acute care
Whether you’re a hospitalist who works only in a hospital, a hospitalist who works only in a post-acute care (PAC) setting, or a hospitalist who works in both types of facilities, knowing about current trends at PAC facilities and what the future may hold can help you excel in your current capacity and, ultimately, improve patient care.
The Hospitalist tapped experts in the post-acute space to tell us what they thought HM should know about working in PAC – which, in many ways, is quite different from the hospital setting. Here’s a compilation of their top eight must-knows.
1. PAC settings rely more on mid-level medical staff than hospitals do.
PAC facilities employ more mid-level providers, such as nurse practitioners and physician assistants, because they can support the level of medical complexity and decision making 95% of the time, says James D. Tollman, MD, FHM, president of Essex Inpatient Physicians in Boxford, Mass. Further, they are more heavily staffed by licensed practical nurses than are acute-care settings.
Usually, there is no physician or nurse practitioner presence at night. Clinicians rely on nursing staff’s assessment to make decisions regarding changes in patient status during off-hours, says Virginia Cummings, MD, director of long-term care, gerontology division, at Boston-based Beth Israel Deaconess Medical Center.
2. Testing takes longer, and options are limited.
Access to some acute urgent resources such as laboratory testing, imaging tests, and pharmacy products is more challenging at PAC facilities because most of these resources are not on-site. Consequently, there is a time lag between ordering tests and new medications and implementing these orders.
“If a patient needs something performed diagnostically immediately, they usually have to be transported to the emergency room or a facility with the necessary testing equipment,” Dr. Tollman says.
However, Paul T. Liistro, managing partner, Arbors of Hop Brook Limited Partnership in Manchester, Conn., and Vernon Manor Health Care Center in Vernon, Conn., and administrator, Manchester Manor Health Care Center, notes that it’s possible for a laboratory service or mobile diagnostic unit to provide laboratory testing or certain imaging at a PAC facility. More-involved diagnostics, such as an MRI or a PET scan, typically require testing at a remote location.
3. Patient populations mainly include rehab and terminally ill patients.
Patients are typically sent to a PAC facility either to recover from an illness or injury or because they are chronically ill and have exhausted treatment options. Regarding the latter, “They are mostly there for palliation; we don’t perform daily tests or prescribe aggressive medications on these patients,” Dr. Nazir says.
Dr. Cummings explains that PAC clinicians go through “the dying process with the patient.”
“They may or may not have assistance from hospice organizations,” she says, “and when they don’t, [hospitalists] take on the role of palliative-care providers.”
Dr. Cummings has seen an increase in psychiatric patients entering PAC facilities.
“Many patients with chronic psychological problems are aging, and there are fewer inpatient psychiatric beds available to those with concurrent medical and psychiatric problems,” she says. Much of this work is now being done in PAC settings. 
4. You can build a relationship with your patient.
Because the pace of a PAC facility is slower and a patient typically stays in a PAC facility longer than at a hospital, there’s time for a hospitalist to have more in-depth conversations with patients and their families.
“Building a deeper relationship with a patient may give the hospitalist an opportunity to discover the cause of an acute problem,” Dr. Nazir says. “They can go in-depth into the psychosocial aspect of medicine and may be able to find out what led to the initial problem and the real root cause, which can help prevent future recurrences, such as repeat falls or forgetting to take a medication.”
5. Using EHRs can improve transitions.
Care transitions between a hospital and PAC facility can be compromised by a lack of information sharing, and they can affect the quality and safety of patient care, says Dori Cross, a doctoral candidate in health services organization and policy at the University of Michigan School of Public Health in Ann Arbor. Handoffs between providers require information continuity – information that is complete, timely, and in a usable format – to ensure appropriate medical decisions and to provide high-quality care during and after transition.
Electronic health records (EHRs) as well as health information exchanges (HIEs) allow providers to communicate and share patient information. For example, hospitals can send information electronically to PAC facilities (“push” exchange) or make information available online securely for PAC providers to log in and access (“pull” exchange). According to a 2014 survey data by the American Hospital Association, more than 50% of hospitals report sending structured summary-of-care records electronically to long-term care settings; a little less than half of those hospitals (23% of the total sample of hospitals) were also receiving information electronically from long-term care sites.1
“This bidirectional exchange, in particular, can make it easier to share information across provider organizations electronically and, in turn, improve care delivery,” says Ms. Cross, who authored an accepted paper on the subject in the Journal of Post-Acute and Long-Term Medicine.
6. Hospitalists can work with providers in PAC settings to improve transitions.
Despite improvements in the electronic transfer of medical information, gaps still exist and can cause problems. One chasm when discharging patients to a PAC facility, is when a hospital IT system is incapable of communicating with the PAC facility system. In this instance, Dr. Nazir says, the hospitalist “can help bridge the gap.”
“[We] can verbally relay relevant information to physicians at PAC facilities so they understand the patient’s status, needs, and expectations,” he says. “Furthermore, hospitalists and a PAC facility’s administration can brainstorm methods to improve the systems of care so the patient receives more effective and timely care.”
7. Hospitalists switching to the PAC setting should have formal training.
The two main obstacles for hospitalists who change from working in a hospital to a PAC facility are the lack of exposure to PAC work in training and the assumption that it requires the same skills sets of a typical hospitalist, according to Manoj K. Mathew, MD, SFHM, national medical director of Los Angeles–based Agilon Health. The PAC setting has quite a number of differences compared with a hospital setting. For example, some regulations apply specifically to PAC facilities. In addition to formal training, hospitalists can benefit from using SHM’s Post-Acute Care Transitions Toolkit, having a mentor, or using resources from other organizations that function in this space such as The Society for Post-Acute and Long-Term Care Medicine, Dr. Nazir says.
8. A variety of payors and payment models are in play.
Commercial insurers continue to be major payors for PAC, especially for individuals younger than 65 years. Medicare and Medicaid, administered by the Centers for Medicare & Medicaid Services, are the primary payors for patients aged 65 years and older.
“These scorecards are using a variety of criteria to rank providers, such as length of stay, cost, readmissions to hospitals, and quality.”
Because Medicare Part A covers many patients discharged to a PAC setting, any changes in payment incentives or benefit structures by the Medicare program will drive changes in PAC.
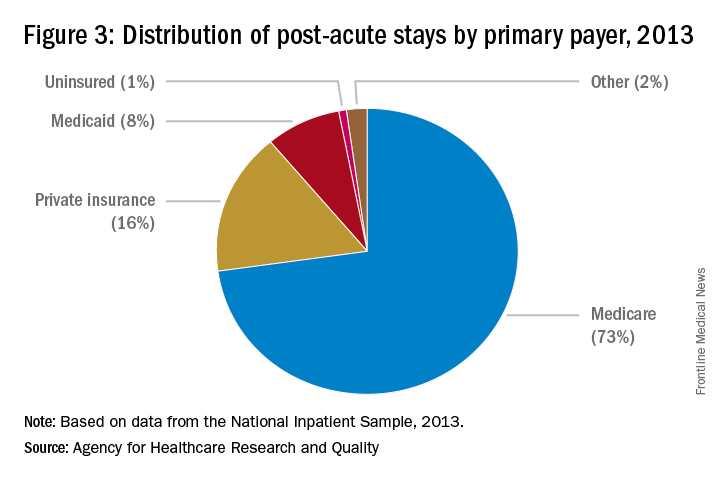
“For example, as Medicare implements payment adjustments for hospitals that have high rates of readmissions, hospitals have a new incentive to work closely with SNFs and other providers of PAC to ensure patients can avoid unnecessary readmissions,” says Tiffany A. Radcliff, PhD, a health economist and associate professor in the department of health policy and management at Texas A&M University School of Public Health in College Station.
Providers must follow the billing rules for each payor. The rules for Medicare payments are outlined on CMS’ website. Bundled payments for PAC under the Medicare Part A program are scheduled to be implemented by 2018.
Reference
Cross DA, Adler-Milstein J. Investing in post-acute care transitions: electronic information exchange between hospitals and long-term care facilities [published online ahead of print Sept. 14, 2016]. JAMDA. doi: http://dx.doi.org/10.1016/j.jamda.2016.07.024.
Whether you’re a hospitalist who works only in a hospital, a hospitalist who works only in a post-acute care (PAC) setting, or a hospitalist who works in both types of facilities, knowing about current trends at PAC facilities and what the future may hold can help you excel in your current capacity and, ultimately, improve patient care.
The Hospitalist tapped experts in the post-acute space to tell us what they thought HM should know about working in PAC – which, in many ways, is quite different from the hospital setting. Here’s a compilation of their top eight must-knows.
1. PAC settings rely more on mid-level medical staff than hospitals do.
PAC facilities employ more mid-level providers, such as nurse practitioners and physician assistants, because they can support the level of medical complexity and decision making 95% of the time, says James D. Tollman, MD, FHM, president of Essex Inpatient Physicians in Boxford, Mass. Further, they are more heavily staffed by licensed practical nurses than are acute-care settings.
Usually, there is no physician or nurse practitioner presence at night. Clinicians rely on nursing staff’s assessment to make decisions regarding changes in patient status during off-hours, says Virginia Cummings, MD, director of long-term care, gerontology division, at Boston-based Beth Israel Deaconess Medical Center.
2. Testing takes longer, and options are limited.
Access to some acute urgent resources such as laboratory testing, imaging tests, and pharmacy products is more challenging at PAC facilities because most of these resources are not on-site. Consequently, there is a time lag between ordering tests and new medications and implementing these orders.
“If a patient needs something performed diagnostically immediately, they usually have to be transported to the emergency room or a facility with the necessary testing equipment,” Dr. Tollman says.
However, Paul T. Liistro, managing partner, Arbors of Hop Brook Limited Partnership in Manchester, Conn., and Vernon Manor Health Care Center in Vernon, Conn., and administrator, Manchester Manor Health Care Center, notes that it’s possible for a laboratory service or mobile diagnostic unit to provide laboratory testing or certain imaging at a PAC facility. More-involved diagnostics, such as an MRI or a PET scan, typically require testing at a remote location.
3. Patient populations mainly include rehab and terminally ill patients.
Patients are typically sent to a PAC facility either to recover from an illness or injury or because they are chronically ill and have exhausted treatment options. Regarding the latter, “They are mostly there for palliation; we don’t perform daily tests or prescribe aggressive medications on these patients,” Dr. Nazir says.
Dr. Cummings explains that PAC clinicians go through “the dying process with the patient.”
“They may or may not have assistance from hospice organizations,” she says, “and when they don’t, [hospitalists] take on the role of palliative-care providers.”
Dr. Cummings has seen an increase in psychiatric patients entering PAC facilities.
“Many patients with chronic psychological problems are aging, and there are fewer inpatient psychiatric beds available to those with concurrent medical and psychiatric problems,” she says. Much of this work is now being done in PAC settings. 
4. You can build a relationship with your patient.
Because the pace of a PAC facility is slower and a patient typically stays in a PAC facility longer than at a hospital, there’s time for a hospitalist to have more in-depth conversations with patients and their families.
“Building a deeper relationship with a patient may give the hospitalist an opportunity to discover the cause of an acute problem,” Dr. Nazir says. “They can go in-depth into the psychosocial aspect of medicine and may be able to find out what led to the initial problem and the real root cause, which can help prevent future recurrences, such as repeat falls or forgetting to take a medication.”
5. Using EHRs can improve transitions.
Care transitions between a hospital and PAC facility can be compromised by a lack of information sharing, and they can affect the quality and safety of patient care, says Dori Cross, a doctoral candidate in health services organization and policy at the University of Michigan School of Public Health in Ann Arbor. Handoffs between providers require information continuity – information that is complete, timely, and in a usable format – to ensure appropriate medical decisions and to provide high-quality care during and after transition.
Electronic health records (EHRs) as well as health information exchanges (HIEs) allow providers to communicate and share patient information. For example, hospitals can send information electronically to PAC facilities (“push” exchange) or make information available online securely for PAC providers to log in and access (“pull” exchange). According to a 2014 survey data by the American Hospital Association, more than 50% of hospitals report sending structured summary-of-care records electronically to long-term care settings; a little less than half of those hospitals (23% of the total sample of hospitals) were also receiving information electronically from long-term care sites.1
“This bidirectional exchange, in particular, can make it easier to share information across provider organizations electronically and, in turn, improve care delivery,” says Ms. Cross, who authored an accepted paper on the subject in the Journal of Post-Acute and Long-Term Medicine.
6. Hospitalists can work with providers in PAC settings to improve transitions.
Despite improvements in the electronic transfer of medical information, gaps still exist and can cause problems. One chasm when discharging patients to a PAC facility, is when a hospital IT system is incapable of communicating with the PAC facility system. In this instance, Dr. Nazir says, the hospitalist “can help bridge the gap.”
“[We] can verbally relay relevant information to physicians at PAC facilities so they understand the patient’s status, needs, and expectations,” he says. “Furthermore, hospitalists and a PAC facility’s administration can brainstorm methods to improve the systems of care so the patient receives more effective and timely care.”
7. Hospitalists switching to the PAC setting should have formal training.
The two main obstacles for hospitalists who change from working in a hospital to a PAC facility are the lack of exposure to PAC work in training and the assumption that it requires the same skills sets of a typical hospitalist, according to Manoj K. Mathew, MD, SFHM, national medical director of Los Angeles–based Agilon Health. The PAC setting has quite a number of differences compared with a hospital setting. For example, some regulations apply specifically to PAC facilities. In addition to formal training, hospitalists can benefit from using SHM’s Post-Acute Care Transitions Toolkit, having a mentor, or using resources from other organizations that function in this space such as The Society for Post-Acute and Long-Term Care Medicine, Dr. Nazir says.
8. A variety of payors and payment models are in play.
Commercial insurers continue to be major payors for PAC, especially for individuals younger than 65 years. Medicare and Medicaid, administered by the Centers for Medicare & Medicaid Services, are the primary payors for patients aged 65 years and older.
“These scorecards are using a variety of criteria to rank providers, such as length of stay, cost, readmissions to hospitals, and quality.”
Because Medicare Part A covers many patients discharged to a PAC setting, any changes in payment incentives or benefit structures by the Medicare program will drive changes in PAC.
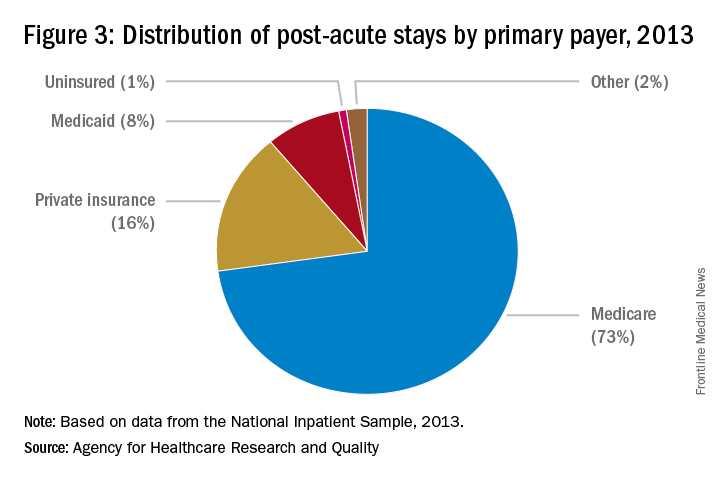
“For example, as Medicare implements payment adjustments for hospitals that have high rates of readmissions, hospitals have a new incentive to work closely with SNFs and other providers of PAC to ensure patients can avoid unnecessary readmissions,” says Tiffany A. Radcliff, PhD, a health economist and associate professor in the department of health policy and management at Texas A&M University School of Public Health in College Station.
Providers must follow the billing rules for each payor. The rules for Medicare payments are outlined on CMS’ website. Bundled payments for PAC under the Medicare Part A program are scheduled to be implemented by 2018.
Reference
Cross DA, Adler-Milstein J. Investing in post-acute care transitions: electronic information exchange between hospitals and long-term care facilities [published online ahead of print Sept. 14, 2016]. JAMDA. doi: http://dx.doi.org/10.1016/j.jamda.2016.07.024.
Whether you’re a hospitalist who works only in a hospital, a hospitalist who works only in a post-acute care (PAC) setting, or a hospitalist who works in both types of facilities, knowing about current trends at PAC facilities and what the future may hold can help you excel in your current capacity and, ultimately, improve patient care.
The Hospitalist tapped experts in the post-acute space to tell us what they thought HM should know about working in PAC – which, in many ways, is quite different from the hospital setting. Here’s a compilation of their top eight must-knows.
1. PAC settings rely more on mid-level medical staff than hospitals do.
PAC facilities employ more mid-level providers, such as nurse practitioners and physician assistants, because they can support the level of medical complexity and decision making 95% of the time, says James D. Tollman, MD, FHM, president of Essex Inpatient Physicians in Boxford, Mass. Further, they are more heavily staffed by licensed practical nurses than are acute-care settings.
Usually, there is no physician or nurse practitioner presence at night. Clinicians rely on nursing staff’s assessment to make decisions regarding changes in patient status during off-hours, says Virginia Cummings, MD, director of long-term care, gerontology division, at Boston-based Beth Israel Deaconess Medical Center.
2. Testing takes longer, and options are limited.
Access to some acute urgent resources such as laboratory testing, imaging tests, and pharmacy products is more challenging at PAC facilities because most of these resources are not on-site. Consequently, there is a time lag between ordering tests and new medications and implementing these orders.
“If a patient needs something performed diagnostically immediately, they usually have to be transported to the emergency room or a facility with the necessary testing equipment,” Dr. Tollman says.
However, Paul T. Liistro, managing partner, Arbors of Hop Brook Limited Partnership in Manchester, Conn., and Vernon Manor Health Care Center in Vernon, Conn., and administrator, Manchester Manor Health Care Center, notes that it’s possible for a laboratory service or mobile diagnostic unit to provide laboratory testing or certain imaging at a PAC facility. More-involved diagnostics, such as an MRI or a PET scan, typically require testing at a remote location.
3. Patient populations mainly include rehab and terminally ill patients.
Patients are typically sent to a PAC facility either to recover from an illness or injury or because they are chronically ill and have exhausted treatment options. Regarding the latter, “They are mostly there for palliation; we don’t perform daily tests or prescribe aggressive medications on these patients,” Dr. Nazir says.
Dr. Cummings explains that PAC clinicians go through “the dying process with the patient.”
“They may or may not have assistance from hospice organizations,” she says, “and when they don’t, [hospitalists] take on the role of palliative-care providers.”
Dr. Cummings has seen an increase in psychiatric patients entering PAC facilities.
“Many patients with chronic psychological problems are aging, and there are fewer inpatient psychiatric beds available to those with concurrent medical and psychiatric problems,” she says. Much of this work is now being done in PAC settings. 
4. You can build a relationship with your patient.
Because the pace of a PAC facility is slower and a patient typically stays in a PAC facility longer than at a hospital, there’s time for a hospitalist to have more in-depth conversations with patients and their families.
“Building a deeper relationship with a patient may give the hospitalist an opportunity to discover the cause of an acute problem,” Dr. Nazir says. “They can go in-depth into the psychosocial aspect of medicine and may be able to find out what led to the initial problem and the real root cause, which can help prevent future recurrences, such as repeat falls or forgetting to take a medication.”
5. Using EHRs can improve transitions.
Care transitions between a hospital and PAC facility can be compromised by a lack of information sharing, and they can affect the quality and safety of patient care, says Dori Cross, a doctoral candidate in health services organization and policy at the University of Michigan School of Public Health in Ann Arbor. Handoffs between providers require information continuity – information that is complete, timely, and in a usable format – to ensure appropriate medical decisions and to provide high-quality care during and after transition.
Electronic health records (EHRs) as well as health information exchanges (HIEs) allow providers to communicate and share patient information. For example, hospitals can send information electronically to PAC facilities (“push” exchange) or make information available online securely for PAC providers to log in and access (“pull” exchange). According to a 2014 survey data by the American Hospital Association, more than 50% of hospitals report sending structured summary-of-care records electronically to long-term care settings; a little less than half of those hospitals (23% of the total sample of hospitals) were also receiving information electronically from long-term care sites.1
“This bidirectional exchange, in particular, can make it easier to share information across provider organizations electronically and, in turn, improve care delivery,” says Ms. Cross, who authored an accepted paper on the subject in the Journal of Post-Acute and Long-Term Medicine.
6. Hospitalists can work with providers in PAC settings to improve transitions.
Despite improvements in the electronic transfer of medical information, gaps still exist and can cause problems. One chasm when discharging patients to a PAC facility, is when a hospital IT system is incapable of communicating with the PAC facility system. In this instance, Dr. Nazir says, the hospitalist “can help bridge the gap.”
“[We] can verbally relay relevant information to physicians at PAC facilities so they understand the patient’s status, needs, and expectations,” he says. “Furthermore, hospitalists and a PAC facility’s administration can brainstorm methods to improve the systems of care so the patient receives more effective and timely care.”
7. Hospitalists switching to the PAC setting should have formal training.
The two main obstacles for hospitalists who change from working in a hospital to a PAC facility are the lack of exposure to PAC work in training and the assumption that it requires the same skills sets of a typical hospitalist, according to Manoj K. Mathew, MD, SFHM, national medical director of Los Angeles–based Agilon Health. The PAC setting has quite a number of differences compared with a hospital setting. For example, some regulations apply specifically to PAC facilities. In addition to formal training, hospitalists can benefit from using SHM’s Post-Acute Care Transitions Toolkit, having a mentor, or using resources from other organizations that function in this space such as The Society for Post-Acute and Long-Term Care Medicine, Dr. Nazir says.
8. A variety of payors and payment models are in play.
Commercial insurers continue to be major payors for PAC, especially for individuals younger than 65 years. Medicare and Medicaid, administered by the Centers for Medicare & Medicaid Services, are the primary payors for patients aged 65 years and older.
“These scorecards are using a variety of criteria to rank providers, such as length of stay, cost, readmissions to hospitals, and quality.”
Because Medicare Part A covers many patients discharged to a PAC setting, any changes in payment incentives or benefit structures by the Medicare program will drive changes in PAC.
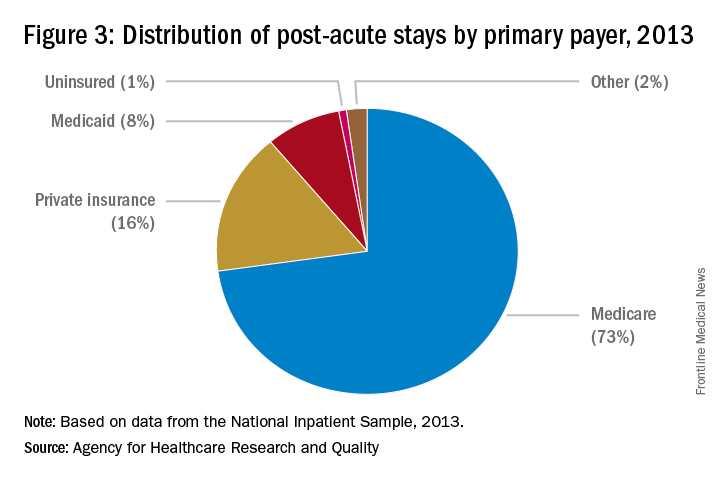
“For example, as Medicare implements payment adjustments for hospitals that have high rates of readmissions, hospitals have a new incentive to work closely with SNFs and other providers of PAC to ensure patients can avoid unnecessary readmissions,” says Tiffany A. Radcliff, PhD, a health economist and associate professor in the department of health policy and management at Texas A&M University School of Public Health in College Station.
Providers must follow the billing rules for each payor. The rules for Medicare payments are outlined on CMS’ website. Bundled payments for PAC under the Medicare Part A program are scheduled to be implemented by 2018.
Reference
Cross DA, Adler-Milstein J. Investing in post-acute care transitions: electronic information exchange between hospitals and long-term care facilities [published online ahead of print Sept. 14, 2016]. JAMDA. doi: http://dx.doi.org/10.1016/j.jamda.2016.07.024.
Female physicians, lower mortality, lower readmissions: A case study
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.
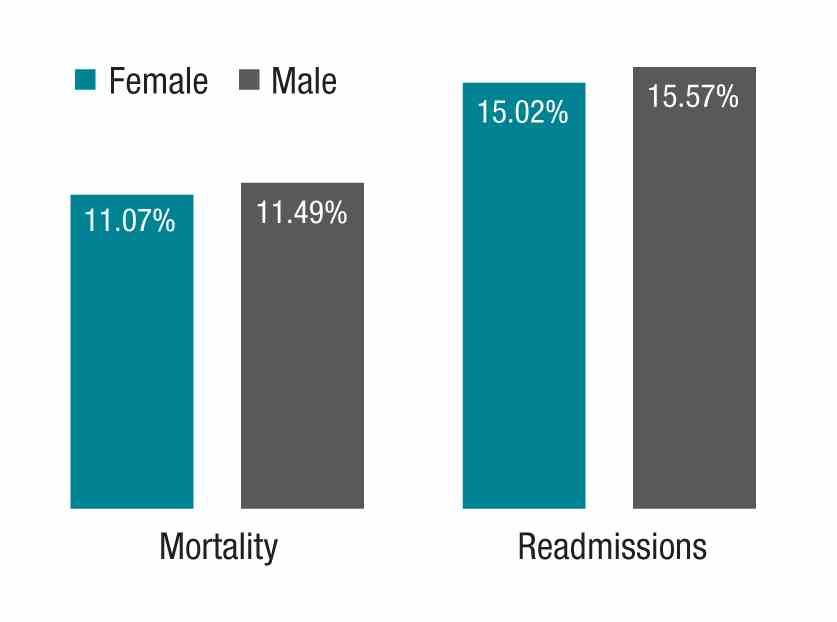
My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at wfwhit@comcast.net.
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.
My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at wfwhit@comcast.net.
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.
My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at wfwhit@comcast.net.
Sneak Peek: Journal of Hospital Medicine
Background: Frailty, history of dementia (HoD), and acute confusional states (ACS) are common in older patients admitted to hospital.
Objective: To study the association of frailty (≥six points in the Clinical Frailty Scale [CFS]), HoD, and ACS with hospital outcomes, controlling for age, gender, acute illness severity (measured by a Modified Early Warning Score in the emergency department), comorbidity (Charlson Comorbidity Index), and discharging specialty (general medicine, geriatric medicine, surgery).
Design: Retrospective, observational study.
Setting: Large university hospital in England.
Patients: We analyzed 8,202 first nonelective inpatient episodes of people ages 75 years and older between October 2014 and October 2015.
Measurements: The outcomes studied were prolonged length of stay (LOS 10 days), inpatient mortality, delayed discharge, institutionalization, and 30-day readmission. Statistical analyses were based on multivariate regression models.
Results: Independently of controlling variables, prolonged LOS was predicted by CFS greater than or equal to 6: odds ratio (OR) = 1.55; 95% confidence interval (CI), 1.36-1.77; P less than .001; HOD: OR = 2.16; 95% CI, 1.79-2.61; P less than .001; and ACS: OR = 3.31; 95% CI, 2.64-4.15; P less than .001. Inpatient mortality was predicted by CFS greater than or equal to 6: OR = 2.29; 95% CI, 1.79-2.94, P less than .001. Delayed discharge was predicted by CFS greater than or equal to 6: OR = 1.46; 95% CI, 1.27-1.67; P less than .001; HOD: OR = 2.17; 95% CI, 1.80-2.62; P less than .001, and ACS: OR = 2.29; 95% CI: 1.83-2.85; P less than .001. Institutionalization was predicted by CFS greater than or equal to 6: OR=2.56; 95% CI, 2.09-3.14; P less than .001; HOD: OR = 2.51; 95% CI, 2.00-3.14; P less than .001; and ACS: OR = 1.93; 95% CI, 1.46-2.56; P less than .001. Readmission was predicted by ACS: OR = 1.36; 95% CI, 1.09-1.71; P = .006.
Conclusion: Routine screening for frailty, HoD, and ACS in hospitals may aid the development of acute care pathways for older adults.
Read the full article at journalofhospitalmedicine.com.
Also in JHM this month…
- Screening for Depression in Hospitalized Medical Patients
AUTHORS: Waguih William IsHak, MD, FAPA, Katherine Collison, Itai Danovitch, MD, MBA, Lili Shek, MD, Payam Kharazi, Tae Kim, DO Candidate, Karim Y. Jaffer, MD Candidate, Lancer Naghdechi, DO Candidate, Enrique Lopez, PsyD, Teryl Nuckols, MD, MSHS, FHM
- Patient-Level Exclusions from mHealth in a Safety-Net Health System
AUTHORS: Keiki Hinami, MD, MS, Bhrandon A. Harris, MD, Ricardo Uriostegui, MD, Wilnise Jasmin, MD, MBA, Mario Lopez, MD, William E. Trick, MD
- Medical and Economic Burden of Heparin-Induced Thrombocytopenia: A Retrospective Nationwide Inpatient Sample (NIS) Study
AUTHORS: Ranjan Pathak, MD, Vijaya Raj Bhatt, MD, Paras Karmacharya, MD, Madan Raj Aryal, MD, Anthony A. Donato, MD, MHPE
- Assessment of the Readability, Understandability and Completeness of Pediatric Hospital Medicine Discharge Instructions
AUTHORS: Ndidi I. Unaka, MD, Med, Angela Statile, MD, Med, Julianne Haney, Andrew F. Beck, MD, MPH, Patrick W. Brady, MD, MSc, Karen E. Jerardi, MD, MEd
- Impact of Patient-Centered Discharge Tools: A Systematic Review
AUTHORS: Karen Okrainec, MD, MSc, Davina Lau, BSc, Howard B Abrams, MD, Shoshanna Hahn-Goldberg, PhD, Ronak Brahmbhatt, MBBS, MPH, Tai Huynh, MBA, Kenneth Lam, MD, Chaim M Bell, MD, PhD
Background: Frailty, history of dementia (HoD), and acute confusional states (ACS) are common in older patients admitted to hospital.
Objective: To study the association of frailty (≥six points in the Clinical Frailty Scale [CFS]), HoD, and ACS with hospital outcomes, controlling for age, gender, acute illness severity (measured by a Modified Early Warning Score in the emergency department), comorbidity (Charlson Comorbidity Index), and discharging specialty (general medicine, geriatric medicine, surgery).
Design: Retrospective, observational study.
Setting: Large university hospital in England.
Patients: We analyzed 8,202 first nonelective inpatient episodes of people ages 75 years and older between October 2014 and October 2015.
Measurements: The outcomes studied were prolonged length of stay (LOS 10 days), inpatient mortality, delayed discharge, institutionalization, and 30-day readmission. Statistical analyses were based on multivariate regression models.
Results: Independently of controlling variables, prolonged LOS was predicted by CFS greater than or equal to 6: odds ratio (OR) = 1.55; 95% confidence interval (CI), 1.36-1.77; P less than .001; HOD: OR = 2.16; 95% CI, 1.79-2.61; P less than .001; and ACS: OR = 3.31; 95% CI, 2.64-4.15; P less than .001. Inpatient mortality was predicted by CFS greater than or equal to 6: OR = 2.29; 95% CI, 1.79-2.94, P less than .001. Delayed discharge was predicted by CFS greater than or equal to 6: OR = 1.46; 95% CI, 1.27-1.67; P less than .001; HOD: OR = 2.17; 95% CI, 1.80-2.62; P less than .001, and ACS: OR = 2.29; 95% CI: 1.83-2.85; P less than .001. Institutionalization was predicted by CFS greater than or equal to 6: OR=2.56; 95% CI, 2.09-3.14; P less than .001; HOD: OR = 2.51; 95% CI, 2.00-3.14; P less than .001; and ACS: OR = 1.93; 95% CI, 1.46-2.56; P less than .001. Readmission was predicted by ACS: OR = 1.36; 95% CI, 1.09-1.71; P = .006.
Conclusion: Routine screening for frailty, HoD, and ACS in hospitals may aid the development of acute care pathways for older adults.
Read the full article at journalofhospitalmedicine.com.
Also in JHM this month…
- Screening for Depression in Hospitalized Medical Patients
AUTHORS: Waguih William IsHak, MD, FAPA, Katherine Collison, Itai Danovitch, MD, MBA, Lili Shek, MD, Payam Kharazi, Tae Kim, DO Candidate, Karim Y. Jaffer, MD Candidate, Lancer Naghdechi, DO Candidate, Enrique Lopez, PsyD, Teryl Nuckols, MD, MSHS, FHM
- Patient-Level Exclusions from mHealth in a Safety-Net Health System
AUTHORS: Keiki Hinami, MD, MS, Bhrandon A. Harris, MD, Ricardo Uriostegui, MD, Wilnise Jasmin, MD, MBA, Mario Lopez, MD, William E. Trick, MD
- Medical and Economic Burden of Heparin-Induced Thrombocytopenia: A Retrospective Nationwide Inpatient Sample (NIS) Study
AUTHORS: Ranjan Pathak, MD, Vijaya Raj Bhatt, MD, Paras Karmacharya, MD, Madan Raj Aryal, MD, Anthony A. Donato, MD, MHPE
- Assessment of the Readability, Understandability and Completeness of Pediatric Hospital Medicine Discharge Instructions
AUTHORS: Ndidi I. Unaka, MD, Med, Angela Statile, MD, Med, Julianne Haney, Andrew F. Beck, MD, MPH, Patrick W. Brady, MD, MSc, Karen E. Jerardi, MD, MEd
- Impact of Patient-Centered Discharge Tools: A Systematic Review
AUTHORS: Karen Okrainec, MD, MSc, Davina Lau, BSc, Howard B Abrams, MD, Shoshanna Hahn-Goldberg, PhD, Ronak Brahmbhatt, MBBS, MPH, Tai Huynh, MBA, Kenneth Lam, MD, Chaim M Bell, MD, PhD
Background: Frailty, history of dementia (HoD), and acute confusional states (ACS) are common in older patients admitted to hospital.
Objective: To study the association of frailty (≥six points in the Clinical Frailty Scale [CFS]), HoD, and ACS with hospital outcomes, controlling for age, gender, acute illness severity (measured by a Modified Early Warning Score in the emergency department), comorbidity (Charlson Comorbidity Index), and discharging specialty (general medicine, geriatric medicine, surgery).
Design: Retrospective, observational study.
Setting: Large university hospital in England.
Patients: We analyzed 8,202 first nonelective inpatient episodes of people ages 75 years and older between October 2014 and October 2015.
Measurements: The outcomes studied were prolonged length of stay (LOS 10 days), inpatient mortality, delayed discharge, institutionalization, and 30-day readmission. Statistical analyses were based on multivariate regression models.
Results: Independently of controlling variables, prolonged LOS was predicted by CFS greater than or equal to 6: odds ratio (OR) = 1.55; 95% confidence interval (CI), 1.36-1.77; P less than .001; HOD: OR = 2.16; 95% CI, 1.79-2.61; P less than .001; and ACS: OR = 3.31; 95% CI, 2.64-4.15; P less than .001. Inpatient mortality was predicted by CFS greater than or equal to 6: OR = 2.29; 95% CI, 1.79-2.94, P less than .001. Delayed discharge was predicted by CFS greater than or equal to 6: OR = 1.46; 95% CI, 1.27-1.67; P less than .001; HOD: OR = 2.17; 95% CI, 1.80-2.62; P less than .001, and ACS: OR = 2.29; 95% CI: 1.83-2.85; P less than .001. Institutionalization was predicted by CFS greater than or equal to 6: OR=2.56; 95% CI, 2.09-3.14; P less than .001; HOD: OR = 2.51; 95% CI, 2.00-3.14; P less than .001; and ACS: OR = 1.93; 95% CI, 1.46-2.56; P less than .001. Readmission was predicted by ACS: OR = 1.36; 95% CI, 1.09-1.71; P = .006.
Conclusion: Routine screening for frailty, HoD, and ACS in hospitals may aid the development of acute care pathways for older adults.
Read the full article at journalofhospitalmedicine.com.
Also in JHM this month…
- Screening for Depression in Hospitalized Medical Patients
AUTHORS: Waguih William IsHak, MD, FAPA, Katherine Collison, Itai Danovitch, MD, MBA, Lili Shek, MD, Payam Kharazi, Tae Kim, DO Candidate, Karim Y. Jaffer, MD Candidate, Lancer Naghdechi, DO Candidate, Enrique Lopez, PsyD, Teryl Nuckols, MD, MSHS, FHM
- Patient-Level Exclusions from mHealth in a Safety-Net Health System
AUTHORS: Keiki Hinami, MD, MS, Bhrandon A. Harris, MD, Ricardo Uriostegui, MD, Wilnise Jasmin, MD, MBA, Mario Lopez, MD, William E. Trick, MD
- Medical and Economic Burden of Heparin-Induced Thrombocytopenia: A Retrospective Nationwide Inpatient Sample (NIS) Study
AUTHORS: Ranjan Pathak, MD, Vijaya Raj Bhatt, MD, Paras Karmacharya, MD, Madan Raj Aryal, MD, Anthony A. Donato, MD, MHPE
- Assessment of the Readability, Understandability and Completeness of Pediatric Hospital Medicine Discharge Instructions
AUTHORS: Ndidi I. Unaka, MD, Med, Angela Statile, MD, Med, Julianne Haney, Andrew F. Beck, MD, MPH, Patrick W. Brady, MD, MSc, Karen E. Jerardi, MD, MEd
- Impact of Patient-Centered Discharge Tools: A Systematic Review
AUTHORS: Karen Okrainec, MD, MSc, Davina Lau, BSc, Howard B Abrams, MD, Shoshanna Hahn-Goldberg, PhD, Ronak Brahmbhatt, MBBS, MPH, Tai Huynh, MBA, Kenneth Lam, MD, Chaim M Bell, MD, PhD
Have you Googled yourself lately?
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.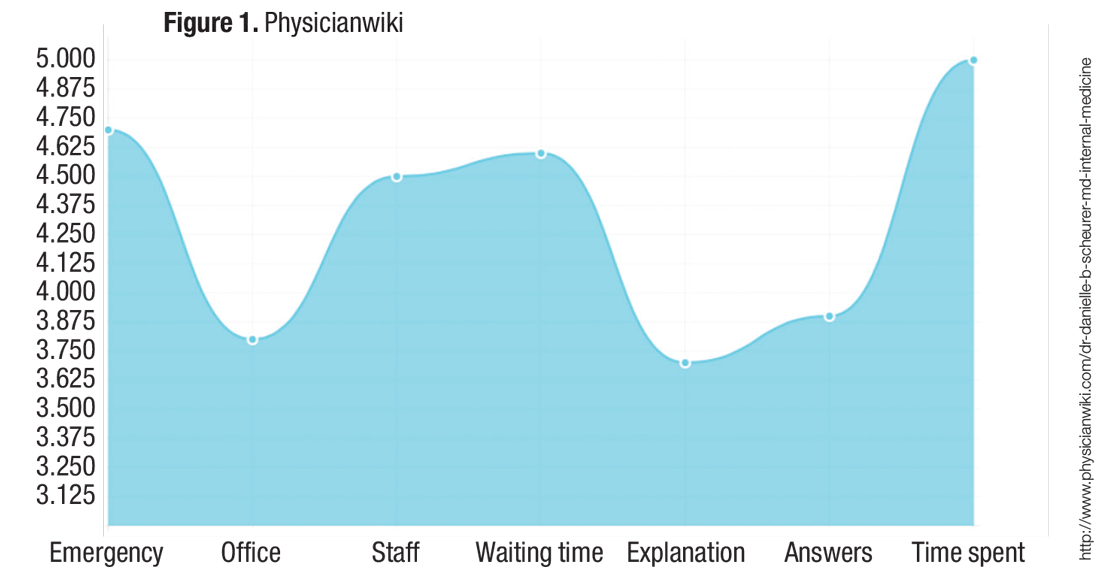
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.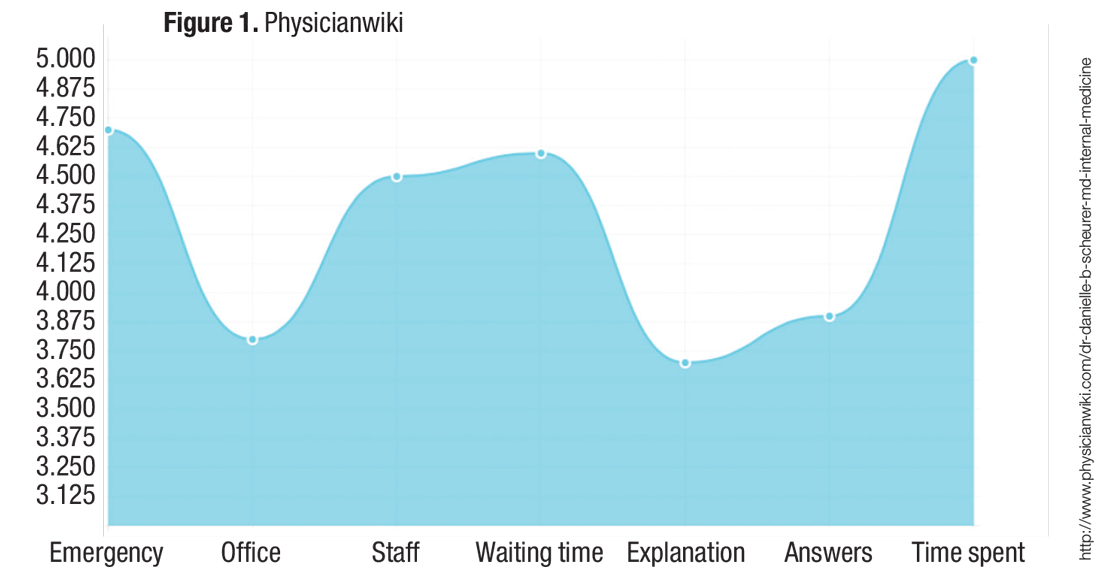
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.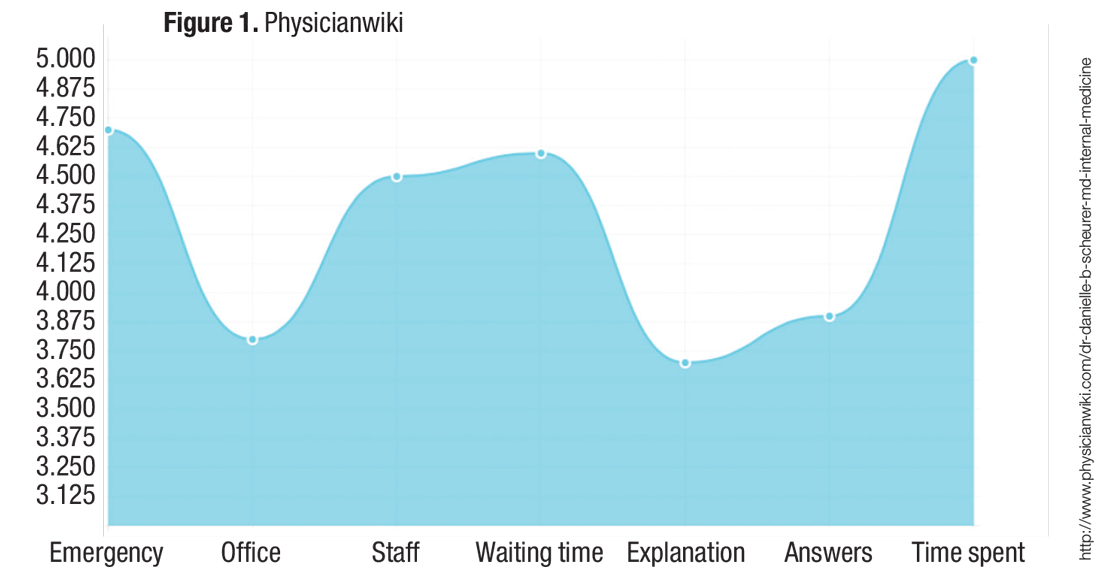
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.