User login
Hospitalists Can Address Causes of Skyrocketing Health Care Costs
Alarms about our nation’s health-care costs have been sounding for well over a decade. According to the Centers for Medicare & Medicaid Services (CMS), spending on U.S. health care doubled between 1999 and 2011, climbing to $2.7 trillion from $1.3 trillion, and now represents 17.9% of the United States’ GDP.1
“The medical care system is bankrupting the country,” Paul B. Ginsburg, PhD, president of the Center for Studying Health System Change (HSC), based in Washington, D.C., says bluntly. A four-decade-long upward spending trend is “unsustainable,” he wrote in the New England Journal of Medicine with Chapin White, PhD, a senior health researcher at HSC.2
Recent reports suggest that rising premiums and out-of-pocket costs are rendering the price of health care untenable for the average consumer. A 2011 RAND Corp. study found that, for the average American family, the rate of increased costs for health care had outpaced growth in earnings from 1999 to 2009.3 And last year, for the first time, the cost of health care for a typical American family of four surpassed $20,000, the annual Milliman Medical Index reported.4
Should hospitalists be concerned, professionally and personally, about these trends? Absolutely, say hospitalist leaders who spoke with The Hospitalist. HM clinicians have much to contribute at both the macro level (addressing systemic causes of overutilization through quality improvement and other initiatives) and at the micro level, by understanding their personal contributions and by engaging patients and their families in shared decision-making.
But getting at and addressing the root causes of rising health-care costs, according to health-care policy analysts and veteran hospitalists, will require major shifts in thinking and processes.
Contributors to Rising Costs
It’s difficult to pinpoint the root causes of the recent surge in health-care costs. Victor Fuchs, emeritus professor of economics and health research and policy at Stanford University, points to the U.S.’ high administrative costs and complicated billing systems.5 A fragmented, nontransparent system for negotiating fees between insurers and providers also plays a role, as demonstrated in a Consumer Reports investigation into geographic variations in costs for common tests and procedures. A complete blood count might be as low as $15 or as high as $105; a colonoscopy ranges from $800 to $3,160.6
Bradley Flansbaum, DO, MPH, SFHM, an SHM Public Policy Committee member and AMA delegate, says rising costs are a provider-specific issue. He challenges colleagues to take an honest look at their own practice patterns to assess whether they’re contributing to overuse of resources (see “A Lesson in Change,”).
“The culture of practice has developed so that this is not going to change overnight,” says Dr. Flansbaum, director of hospitalist services at Lenox Hill Hospital in New York City. That’s because many physicians fail to view their own decisions as a problem. For example, says Dr. Flansbaum, “an oncologist may not identify a third round of chemotherapy as an embodiment of the problem, or a gastroenterologist might not embody the colonoscopy at Year Four instead of Year Five as the problem. We must come to grips with the usual mindset, look in the mirror, and admit, ‘Maybe we are part of the problem.’”

—Bradley Flansbaum, DO, MPH, SFHM
Potential Solutions
Hospitalists, intensivists, and ED clinicians are tasked with finding a balance between being prudent stewards of resources and staying within a comfort zone that promotes patient safety. SHM supports the goals of the ABIM Foundation’s Choosing Wisely campaign, which aims to reduce waste by curtailing duplicative and unnecessary care (see “Better Choices, Better Care,” March 2013). Also included in the campaign (www.ChoosingWisely.org) are the American College of Physicians’ recommendations against low-value testing (e.g. obtaining imaging studies in patients with nonspecific low back pain).
“Those recommendations are not going to solve our health spending problem,” says White, “but they are part of a broader move to give permission to clinicians, based on evidence, to follow more conservative practice patterns.”
Still, counters David I. Auerbach, PhD, a health economist at RAND in Boston and author of the RAND study, “there’s another value to these tests that the cost-effectiveness equations do not always consider, which is, they can bring peace of mind. We’re trying to nudge patients down the pathway that we think is best for them without rationing care. That’s a delicate balance.”
Dr. Flansbaum says SHM’s Public Policy Committee has discussed a variety of issues related to rising costs, although the group has not directly tackled advice in the form of a white paper. He suggests some ways that hospitalists can address cost savings:
- Involve patients in shared decision-making, and discuss the evidence against unnecessary testing;
- Utilize generic medications on discharge, when available, especially if patients are uninsured or have limited drug coverage with their insurance plans;
- Use palliative care whenever appropriate; and
- Adhere to transitional-care standards.
On the macro level, HM has “always been the specialty invited to champion the important discussion relating to resource utilization, and the evidence-based medicine driving that resource utilization,” says Christopher Frost, MD, FHM, medical director of hospital medicine at the Hospital Corporation of America (HCA) in Nashville, Tenn. He points to SHM’s leadership with Project BOOST (www.hospitalmedicine.org/boost) as one example of addressing the utilization of resources in caring for older adults (see “Resources for Improving Transitions in Care,”).
What else can hospitalists do? Going forward, says Dan Fuller, president and co-founder of IN Compass Health in Alpharetta, Ga., it might be a good idea for the SHM Practice Analysis Committee, of which he’s a member, to look at its possible role in the issue.

—Dr. Frederickson
Embrace Reality
Whatever the downstream developments around the Affordable Care Act, Dr. Ginsburg is “confident” that Medicare policies will continue in a direction of reduced reimbursements. Thomas Frederickson, MD, FACP, FHM, MBA, medical director of the hospital medicine service at Alegent Health in Omaha, Neb., agrees with such an assessment. He also believes that hospitalists are in a prime position to improve care delivery at less cost. To do so, though, requires deliberate partnership-building with outpatient providers to better bridge the transitions of care.
At his institution, Dr. Frederickson says, hospitalists invite themselves to primary-care physicians’ (PCP) meetings. This facilitates rapport so that calls to PCPs at discharge not only communicate essential clinical information, but also build confidence in the hospitalists’ care of their patients. As hospitalists demonstrate value, they must intentionally put metrics in place so that administrators appreciate the need to keep the census at a certain level, Dr. Frederickson says.
“We need the time to make these calls, to sit down with families,” he says. “This adds value to our health system and to society at large.”
SHM does a good job, says Dr. Frost, of being part of the conversation as the hospital C-suite focuses more on episodes of care.
“The intensity of that discussion is getting dialed up and will be driven more by government and the payors,” he adds. The challenge going forward will be to bridge those arenas just outside the acute episode of care, where hospitalists have ownership of processes, to those where they do not have as much control. If payors apply broader definitions to the episode of care, Dr. Frost says, hospitalists might be “invited to play an increasing role, that of ‘transitionist.’”
And in that context, he says, hospitalists need to look at length of stay with a new lens.
Partnership-building will become more important as the definition of “episode of care” expands beyond the hospital stay to the post-acute setting.
“Including post-acute care in the episode of care is a core aspect of the whole” value-based purchasing approach, Dr. Ginsburg says. “Hospitals [and hospitalists] will be wise to opt for the model with the greatest potential to reduce costs, particularly costs incurred by other providers.”
Gretchen Henkel is a freelance writer in California.
References
- Centers for Medicare & Medicaid Services. National health expenditures 2011 highlights. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/highlights.pdf. Accessed May 6, 2013. costs how much? Consumer Reports website. Available at: http://www.consumerreports.org/cro/magazine/ 2012/07/that-ct-scan-costs-how-much/index.htm. Accessed Aug. 2, 2012.
- White C, Ginsburg PB. Slower growth in Medicare spending—is this the new normal? N Engl J Med. 2012;366(12):1073-1075.
- Auerbach DI, Kellermann AL. A decade of health care cost growth has wiped out real income gains for an average US family. Health Aff (Millwood). 2011;30(9):1630-1636.
- Milliman Inc. 2012 Milliman Medical Index. Milliman Inc. website. Available at: http://publications.milliman.com/periodicals/mmi/pdfs/milliman-medical-index-2012.pdf. Accessed Aug. 1, 2012.
- Kolata G. Knotty challenges in health care costs. The New York Times website. Available at: http://www.nytimes.com/2012/03/06/health/policy/an-interview-with-victor-fuchs-on-health-care-costs.html. Accessed March 8, 2012.
- Consumer Reports. That CT scan costs how much? Consumer Reports website. Available at: http://www.consumerreports.org/cro/magazine/ 2012/07/that-ct-scan-costs-how-much/index.htm.
Alarms about our nation’s health-care costs have been sounding for well over a decade. According to the Centers for Medicare & Medicaid Services (CMS), spending on U.S. health care doubled between 1999 and 2011, climbing to $2.7 trillion from $1.3 trillion, and now represents 17.9% of the United States’ GDP.1
“The medical care system is bankrupting the country,” Paul B. Ginsburg, PhD, president of the Center for Studying Health System Change (HSC), based in Washington, D.C., says bluntly. A four-decade-long upward spending trend is “unsustainable,” he wrote in the New England Journal of Medicine with Chapin White, PhD, a senior health researcher at HSC.2
Recent reports suggest that rising premiums and out-of-pocket costs are rendering the price of health care untenable for the average consumer. A 2011 RAND Corp. study found that, for the average American family, the rate of increased costs for health care had outpaced growth in earnings from 1999 to 2009.3 And last year, for the first time, the cost of health care for a typical American family of four surpassed $20,000, the annual Milliman Medical Index reported.4
Should hospitalists be concerned, professionally and personally, about these trends? Absolutely, say hospitalist leaders who spoke with The Hospitalist. HM clinicians have much to contribute at both the macro level (addressing systemic causes of overutilization through quality improvement and other initiatives) and at the micro level, by understanding their personal contributions and by engaging patients and their families in shared decision-making.
But getting at and addressing the root causes of rising health-care costs, according to health-care policy analysts and veteran hospitalists, will require major shifts in thinking and processes.
Contributors to Rising Costs
It’s difficult to pinpoint the root causes of the recent surge in health-care costs. Victor Fuchs, emeritus professor of economics and health research and policy at Stanford University, points to the U.S.’ high administrative costs and complicated billing systems.5 A fragmented, nontransparent system for negotiating fees between insurers and providers also plays a role, as demonstrated in a Consumer Reports investigation into geographic variations in costs for common tests and procedures. A complete blood count might be as low as $15 or as high as $105; a colonoscopy ranges from $800 to $3,160.6
Bradley Flansbaum, DO, MPH, SFHM, an SHM Public Policy Committee member and AMA delegate, says rising costs are a provider-specific issue. He challenges colleagues to take an honest look at their own practice patterns to assess whether they’re contributing to overuse of resources (see “A Lesson in Change,”).
“The culture of practice has developed so that this is not going to change overnight,” says Dr. Flansbaum, director of hospitalist services at Lenox Hill Hospital in New York City. That’s because many physicians fail to view their own decisions as a problem. For example, says Dr. Flansbaum, “an oncologist may not identify a third round of chemotherapy as an embodiment of the problem, or a gastroenterologist might not embody the colonoscopy at Year Four instead of Year Five as the problem. We must come to grips with the usual mindset, look in the mirror, and admit, ‘Maybe we are part of the problem.’”

—Bradley Flansbaum, DO, MPH, SFHM
Potential Solutions
Hospitalists, intensivists, and ED clinicians are tasked with finding a balance between being prudent stewards of resources and staying within a comfort zone that promotes patient safety. SHM supports the goals of the ABIM Foundation’s Choosing Wisely campaign, which aims to reduce waste by curtailing duplicative and unnecessary care (see “Better Choices, Better Care,” March 2013). Also included in the campaign (www.ChoosingWisely.org) are the American College of Physicians’ recommendations against low-value testing (e.g. obtaining imaging studies in patients with nonspecific low back pain).
“Those recommendations are not going to solve our health spending problem,” says White, “but they are part of a broader move to give permission to clinicians, based on evidence, to follow more conservative practice patterns.”
Still, counters David I. Auerbach, PhD, a health economist at RAND in Boston and author of the RAND study, “there’s another value to these tests that the cost-effectiveness equations do not always consider, which is, they can bring peace of mind. We’re trying to nudge patients down the pathway that we think is best for them without rationing care. That’s a delicate balance.”
Dr. Flansbaum says SHM’s Public Policy Committee has discussed a variety of issues related to rising costs, although the group has not directly tackled advice in the form of a white paper. He suggests some ways that hospitalists can address cost savings:
- Involve patients in shared decision-making, and discuss the evidence against unnecessary testing;
- Utilize generic medications on discharge, when available, especially if patients are uninsured or have limited drug coverage with their insurance plans;
- Use palliative care whenever appropriate; and
- Adhere to transitional-care standards.
On the macro level, HM has “always been the specialty invited to champion the important discussion relating to resource utilization, and the evidence-based medicine driving that resource utilization,” says Christopher Frost, MD, FHM, medical director of hospital medicine at the Hospital Corporation of America (HCA) in Nashville, Tenn. He points to SHM’s leadership with Project BOOST (www.hospitalmedicine.org/boost) as one example of addressing the utilization of resources in caring for older adults (see “Resources for Improving Transitions in Care,”).
What else can hospitalists do? Going forward, says Dan Fuller, president and co-founder of IN Compass Health in Alpharetta, Ga., it might be a good idea for the SHM Practice Analysis Committee, of which he’s a member, to look at its possible role in the issue.

—Dr. Frederickson
Embrace Reality
Whatever the downstream developments around the Affordable Care Act, Dr. Ginsburg is “confident” that Medicare policies will continue in a direction of reduced reimbursements. Thomas Frederickson, MD, FACP, FHM, MBA, medical director of the hospital medicine service at Alegent Health in Omaha, Neb., agrees with such an assessment. He also believes that hospitalists are in a prime position to improve care delivery at less cost. To do so, though, requires deliberate partnership-building with outpatient providers to better bridge the transitions of care.
At his institution, Dr. Frederickson says, hospitalists invite themselves to primary-care physicians’ (PCP) meetings. This facilitates rapport so that calls to PCPs at discharge not only communicate essential clinical information, but also build confidence in the hospitalists’ care of their patients. As hospitalists demonstrate value, they must intentionally put metrics in place so that administrators appreciate the need to keep the census at a certain level, Dr. Frederickson says.
“We need the time to make these calls, to sit down with families,” he says. “This adds value to our health system and to society at large.”
SHM does a good job, says Dr. Frost, of being part of the conversation as the hospital C-suite focuses more on episodes of care.
“The intensity of that discussion is getting dialed up and will be driven more by government and the payors,” he adds. The challenge going forward will be to bridge those arenas just outside the acute episode of care, where hospitalists have ownership of processes, to those where they do not have as much control. If payors apply broader definitions to the episode of care, Dr. Frost says, hospitalists might be “invited to play an increasing role, that of ‘transitionist.’”
And in that context, he says, hospitalists need to look at length of stay with a new lens.
Partnership-building will become more important as the definition of “episode of care” expands beyond the hospital stay to the post-acute setting.
“Including post-acute care in the episode of care is a core aspect of the whole” value-based purchasing approach, Dr. Ginsburg says. “Hospitals [and hospitalists] will be wise to opt for the model with the greatest potential to reduce costs, particularly costs incurred by other providers.”
Gretchen Henkel is a freelance writer in California.
References
- Centers for Medicare & Medicaid Services. National health expenditures 2011 highlights. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/highlights.pdf. Accessed May 6, 2013. costs how much? Consumer Reports website. Available at: http://www.consumerreports.org/cro/magazine/ 2012/07/that-ct-scan-costs-how-much/index.htm. Accessed Aug. 2, 2012.
- White C, Ginsburg PB. Slower growth in Medicare spending—is this the new normal? N Engl J Med. 2012;366(12):1073-1075.
- Auerbach DI, Kellermann AL. A decade of health care cost growth has wiped out real income gains for an average US family. Health Aff (Millwood). 2011;30(9):1630-1636.
- Milliman Inc. 2012 Milliman Medical Index. Milliman Inc. website. Available at: http://publications.milliman.com/periodicals/mmi/pdfs/milliman-medical-index-2012.pdf. Accessed Aug. 1, 2012.
- Kolata G. Knotty challenges in health care costs. The New York Times website. Available at: http://www.nytimes.com/2012/03/06/health/policy/an-interview-with-victor-fuchs-on-health-care-costs.html. Accessed March 8, 2012.
- Consumer Reports. That CT scan costs how much? Consumer Reports website. Available at: http://www.consumerreports.org/cro/magazine/ 2012/07/that-ct-scan-costs-how-much/index.htm.
Alarms about our nation’s health-care costs have been sounding for well over a decade. According to the Centers for Medicare & Medicaid Services (CMS), spending on U.S. health care doubled between 1999 and 2011, climbing to $2.7 trillion from $1.3 trillion, and now represents 17.9% of the United States’ GDP.1
“The medical care system is bankrupting the country,” Paul B. Ginsburg, PhD, president of the Center for Studying Health System Change (HSC), based in Washington, D.C., says bluntly. A four-decade-long upward spending trend is “unsustainable,” he wrote in the New England Journal of Medicine with Chapin White, PhD, a senior health researcher at HSC.2
Recent reports suggest that rising premiums and out-of-pocket costs are rendering the price of health care untenable for the average consumer. A 2011 RAND Corp. study found that, for the average American family, the rate of increased costs for health care had outpaced growth in earnings from 1999 to 2009.3 And last year, for the first time, the cost of health care for a typical American family of four surpassed $20,000, the annual Milliman Medical Index reported.4
Should hospitalists be concerned, professionally and personally, about these trends? Absolutely, say hospitalist leaders who spoke with The Hospitalist. HM clinicians have much to contribute at both the macro level (addressing systemic causes of overutilization through quality improvement and other initiatives) and at the micro level, by understanding their personal contributions and by engaging patients and their families in shared decision-making.
But getting at and addressing the root causes of rising health-care costs, according to health-care policy analysts and veteran hospitalists, will require major shifts in thinking and processes.
Contributors to Rising Costs
It’s difficult to pinpoint the root causes of the recent surge in health-care costs. Victor Fuchs, emeritus professor of economics and health research and policy at Stanford University, points to the U.S.’ high administrative costs and complicated billing systems.5 A fragmented, nontransparent system for negotiating fees between insurers and providers also plays a role, as demonstrated in a Consumer Reports investigation into geographic variations in costs for common tests and procedures. A complete blood count might be as low as $15 or as high as $105; a colonoscopy ranges from $800 to $3,160.6
Bradley Flansbaum, DO, MPH, SFHM, an SHM Public Policy Committee member and AMA delegate, says rising costs are a provider-specific issue. He challenges colleagues to take an honest look at their own practice patterns to assess whether they’re contributing to overuse of resources (see “A Lesson in Change,”).
“The culture of practice has developed so that this is not going to change overnight,” says Dr. Flansbaum, director of hospitalist services at Lenox Hill Hospital in New York City. That’s because many physicians fail to view their own decisions as a problem. For example, says Dr. Flansbaum, “an oncologist may not identify a third round of chemotherapy as an embodiment of the problem, or a gastroenterologist might not embody the colonoscopy at Year Four instead of Year Five as the problem. We must come to grips with the usual mindset, look in the mirror, and admit, ‘Maybe we are part of the problem.’”

—Bradley Flansbaum, DO, MPH, SFHM
Potential Solutions
Hospitalists, intensivists, and ED clinicians are tasked with finding a balance between being prudent stewards of resources and staying within a comfort zone that promotes patient safety. SHM supports the goals of the ABIM Foundation’s Choosing Wisely campaign, which aims to reduce waste by curtailing duplicative and unnecessary care (see “Better Choices, Better Care,” March 2013). Also included in the campaign (www.ChoosingWisely.org) are the American College of Physicians’ recommendations against low-value testing (e.g. obtaining imaging studies in patients with nonspecific low back pain).
“Those recommendations are not going to solve our health spending problem,” says White, “but they are part of a broader move to give permission to clinicians, based on evidence, to follow more conservative practice patterns.”
Still, counters David I. Auerbach, PhD, a health economist at RAND in Boston and author of the RAND study, “there’s another value to these tests that the cost-effectiveness equations do not always consider, which is, they can bring peace of mind. We’re trying to nudge patients down the pathway that we think is best for them without rationing care. That’s a delicate balance.”
Dr. Flansbaum says SHM’s Public Policy Committee has discussed a variety of issues related to rising costs, although the group has not directly tackled advice in the form of a white paper. He suggests some ways that hospitalists can address cost savings:
- Involve patients in shared decision-making, and discuss the evidence against unnecessary testing;
- Utilize generic medications on discharge, when available, especially if patients are uninsured or have limited drug coverage with their insurance plans;
- Use palliative care whenever appropriate; and
- Adhere to transitional-care standards.
On the macro level, HM has “always been the specialty invited to champion the important discussion relating to resource utilization, and the evidence-based medicine driving that resource utilization,” says Christopher Frost, MD, FHM, medical director of hospital medicine at the Hospital Corporation of America (HCA) in Nashville, Tenn. He points to SHM’s leadership with Project BOOST (www.hospitalmedicine.org/boost) as one example of addressing the utilization of resources in caring for older adults (see “Resources for Improving Transitions in Care,”).
What else can hospitalists do? Going forward, says Dan Fuller, president and co-founder of IN Compass Health in Alpharetta, Ga., it might be a good idea for the SHM Practice Analysis Committee, of which he’s a member, to look at its possible role in the issue.

—Dr. Frederickson
Embrace Reality
Whatever the downstream developments around the Affordable Care Act, Dr. Ginsburg is “confident” that Medicare policies will continue in a direction of reduced reimbursements. Thomas Frederickson, MD, FACP, FHM, MBA, medical director of the hospital medicine service at Alegent Health in Omaha, Neb., agrees with such an assessment. He also believes that hospitalists are in a prime position to improve care delivery at less cost. To do so, though, requires deliberate partnership-building with outpatient providers to better bridge the transitions of care.
At his institution, Dr. Frederickson says, hospitalists invite themselves to primary-care physicians’ (PCP) meetings. This facilitates rapport so that calls to PCPs at discharge not only communicate essential clinical information, but also build confidence in the hospitalists’ care of their patients. As hospitalists demonstrate value, they must intentionally put metrics in place so that administrators appreciate the need to keep the census at a certain level, Dr. Frederickson says.
“We need the time to make these calls, to sit down with families,” he says. “This adds value to our health system and to society at large.”
SHM does a good job, says Dr. Frost, of being part of the conversation as the hospital C-suite focuses more on episodes of care.
“The intensity of that discussion is getting dialed up and will be driven more by government and the payors,” he adds. The challenge going forward will be to bridge those arenas just outside the acute episode of care, where hospitalists have ownership of processes, to those where they do not have as much control. If payors apply broader definitions to the episode of care, Dr. Frost says, hospitalists might be “invited to play an increasing role, that of ‘transitionist.’”
And in that context, he says, hospitalists need to look at length of stay with a new lens.
Partnership-building will become more important as the definition of “episode of care” expands beyond the hospital stay to the post-acute setting.
“Including post-acute care in the episode of care is a core aspect of the whole” value-based purchasing approach, Dr. Ginsburg says. “Hospitals [and hospitalists] will be wise to opt for the model with the greatest potential to reduce costs, particularly costs incurred by other providers.”
Gretchen Henkel is a freelance writer in California.
References
- Centers for Medicare & Medicaid Services. National health expenditures 2011 highlights. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/highlights.pdf. Accessed May 6, 2013. costs how much? Consumer Reports website. Available at: http://www.consumerreports.org/cro/magazine/ 2012/07/that-ct-scan-costs-how-much/index.htm. Accessed Aug. 2, 2012.
- White C, Ginsburg PB. Slower growth in Medicare spending—is this the new normal? N Engl J Med. 2012;366(12):1073-1075.
- Auerbach DI, Kellermann AL. A decade of health care cost growth has wiped out real income gains for an average US family. Health Aff (Millwood). 2011;30(9):1630-1636.
- Milliman Inc. 2012 Milliman Medical Index. Milliman Inc. website. Available at: http://publications.milliman.com/periodicals/mmi/pdfs/milliman-medical-index-2012.pdf. Accessed Aug. 1, 2012.
- Kolata G. Knotty challenges in health care costs. The New York Times website. Available at: http://www.nytimes.com/2012/03/06/health/policy/an-interview-with-victor-fuchs-on-health-care-costs.html. Accessed March 8, 2012.
- Consumer Reports. That CT scan costs how much? Consumer Reports website. Available at: http://www.consumerreports.org/cro/magazine/ 2012/07/that-ct-scan-costs-how-much/index.htm.
Letters: Medicare Official Says 'Physician Compare' Website Does Not Provide Performance Data on Individual Doctors
I read the article “Call for Transparency in Health-Care Performance Results to Impact Hospitalists” (January 2013, p. 47) by Shaun Frost, MD, SFHM, president of the Society of Hospital Medicine, with interest. I’d like to clarify a key point about Physician Compare. In the article, the statement that the Physician Compare website (www.medicare.gov/find-a-doctor) provides performance information on individual doctors is inaccurate.
The Affordable Care Act (ACA) states that the Centers for Medicare & Medicaid Services (CMS) must have a plan in place by Jan. 1, 2013, to include quality-of-care information on the site. To meet that requirement, CMS has established a plan that initiates a phased approach to public reporting. The 2012 Physician Fee Schedule (PFS) Final Rule was the first step in that phased approach. This rule established that the first measures to be reported on the site would be group-level measures for data collected no sooner than program year 2012. A second critical step is the 2013 PFS Proposed Rule, which outlines a longer-term public reporting plan. According to this plan, we expect the first set of group-level quality measure data to be included on the site in calendar year 2014. We are targeting publishing individual-level quality measures no sooner than 2015 reflecting data collected in program year 2014, if technically feasible.
As you may be aware, Physician Compare is undergoing a redesign to significantly improve the underlying database and thus the information on Physician Compare, as well as the ease of use and functionality of the site. We’ll be unveiling the redesigned site soon. We welcome your feedback and look forward to maintaining a dialogue with you as Physician Compare continues to evolve.
Rashaan Byers, MPH, social science research analyst, Centers forMedicare & Medicaid Services, Center for Clinical Standards & Quality, Quality Measurement & Health Assessment Group
Dr. Frost responds:
I thank Mr. Byers for his clarification regarding the current content on the CMS Physician Compare website, and agree that at the present time the website does not report individual physician clinical performance data.
Physician Compare, however, does currently report if an individual physician participated in the CMS Physician Quality Reporting System (PQRS) by stating “this professional chose to take part in Medicare’s PQRS, and reported quality information satisfactorily for the year 2010.” For those physicians who did not participate in PQRS, their personal website pages do not make reference to the PQRS program.
As the intent of transparency is to educate consumers to make informed choices about where to seek health care, care providers should know that their participation in PQRS is currently publically reported. It is, therefore, possible that patient decisions about whom to seek care from may be influenced by this.
As acknowledged in my January 2013 column in The Hospitalist, Physician Compare currently reports very little information. We should expect this to change, however, as Medicare moves forward with developing a plan to publically report valid and reliable individual physician performance metrics. CMS’ clarification of the timeline by which we can expect to see more detailed information is thus greatly appreciated.
The take-home message for hospitalists is that public reporting of care provider performance will become increasingly comprehensive and transparent in the future. As pointed out, CMS’ present plan targets the publication of individual, physician-level quality measures as soon as 2015, which will reflect actual performance during program year 2014. The measurement period is thus less than one year away, so it behooves us all to focus ever more intently on delivering high-value healthcare.
Shaun Frost, MD, SFHM, past president, SHM
I read the article “Call for Transparency in Health-Care Performance Results to Impact Hospitalists” (January 2013, p. 47) by Shaun Frost, MD, SFHM, president of the Society of Hospital Medicine, with interest. I’d like to clarify a key point about Physician Compare. In the article, the statement that the Physician Compare website (www.medicare.gov/find-a-doctor) provides performance information on individual doctors is inaccurate.
The Affordable Care Act (ACA) states that the Centers for Medicare & Medicaid Services (CMS) must have a plan in place by Jan. 1, 2013, to include quality-of-care information on the site. To meet that requirement, CMS has established a plan that initiates a phased approach to public reporting. The 2012 Physician Fee Schedule (PFS) Final Rule was the first step in that phased approach. This rule established that the first measures to be reported on the site would be group-level measures for data collected no sooner than program year 2012. A second critical step is the 2013 PFS Proposed Rule, which outlines a longer-term public reporting plan. According to this plan, we expect the first set of group-level quality measure data to be included on the site in calendar year 2014. We are targeting publishing individual-level quality measures no sooner than 2015 reflecting data collected in program year 2014, if technically feasible.
As you may be aware, Physician Compare is undergoing a redesign to significantly improve the underlying database and thus the information on Physician Compare, as well as the ease of use and functionality of the site. We’ll be unveiling the redesigned site soon. We welcome your feedback and look forward to maintaining a dialogue with you as Physician Compare continues to evolve.
Rashaan Byers, MPH, social science research analyst, Centers forMedicare & Medicaid Services, Center for Clinical Standards & Quality, Quality Measurement & Health Assessment Group
Dr. Frost responds:
I thank Mr. Byers for his clarification regarding the current content on the CMS Physician Compare website, and agree that at the present time the website does not report individual physician clinical performance data.
Physician Compare, however, does currently report if an individual physician participated in the CMS Physician Quality Reporting System (PQRS) by stating “this professional chose to take part in Medicare’s PQRS, and reported quality information satisfactorily for the year 2010.” For those physicians who did not participate in PQRS, their personal website pages do not make reference to the PQRS program.
As the intent of transparency is to educate consumers to make informed choices about where to seek health care, care providers should know that their participation in PQRS is currently publically reported. It is, therefore, possible that patient decisions about whom to seek care from may be influenced by this.
As acknowledged in my January 2013 column in The Hospitalist, Physician Compare currently reports very little information. We should expect this to change, however, as Medicare moves forward with developing a plan to publically report valid and reliable individual physician performance metrics. CMS’ clarification of the timeline by which we can expect to see more detailed information is thus greatly appreciated.
The take-home message for hospitalists is that public reporting of care provider performance will become increasingly comprehensive and transparent in the future. As pointed out, CMS’ present plan targets the publication of individual, physician-level quality measures as soon as 2015, which will reflect actual performance during program year 2014. The measurement period is thus less than one year away, so it behooves us all to focus ever more intently on delivering high-value healthcare.
Shaun Frost, MD, SFHM, past president, SHM
I read the article “Call for Transparency in Health-Care Performance Results to Impact Hospitalists” (January 2013, p. 47) by Shaun Frost, MD, SFHM, president of the Society of Hospital Medicine, with interest. I’d like to clarify a key point about Physician Compare. In the article, the statement that the Physician Compare website (www.medicare.gov/find-a-doctor) provides performance information on individual doctors is inaccurate.
The Affordable Care Act (ACA) states that the Centers for Medicare & Medicaid Services (CMS) must have a plan in place by Jan. 1, 2013, to include quality-of-care information on the site. To meet that requirement, CMS has established a plan that initiates a phased approach to public reporting. The 2012 Physician Fee Schedule (PFS) Final Rule was the first step in that phased approach. This rule established that the first measures to be reported on the site would be group-level measures for data collected no sooner than program year 2012. A second critical step is the 2013 PFS Proposed Rule, which outlines a longer-term public reporting plan. According to this plan, we expect the first set of group-level quality measure data to be included on the site in calendar year 2014. We are targeting publishing individual-level quality measures no sooner than 2015 reflecting data collected in program year 2014, if technically feasible.
As you may be aware, Physician Compare is undergoing a redesign to significantly improve the underlying database and thus the information on Physician Compare, as well as the ease of use and functionality of the site. We’ll be unveiling the redesigned site soon. We welcome your feedback and look forward to maintaining a dialogue with you as Physician Compare continues to evolve.
Rashaan Byers, MPH, social science research analyst, Centers forMedicare & Medicaid Services, Center for Clinical Standards & Quality, Quality Measurement & Health Assessment Group
Dr. Frost responds:
I thank Mr. Byers for his clarification regarding the current content on the CMS Physician Compare website, and agree that at the present time the website does not report individual physician clinical performance data.
Physician Compare, however, does currently report if an individual physician participated in the CMS Physician Quality Reporting System (PQRS) by stating “this professional chose to take part in Medicare’s PQRS, and reported quality information satisfactorily for the year 2010.” For those physicians who did not participate in PQRS, their personal website pages do not make reference to the PQRS program.
As the intent of transparency is to educate consumers to make informed choices about where to seek health care, care providers should know that their participation in PQRS is currently publically reported. It is, therefore, possible that patient decisions about whom to seek care from may be influenced by this.
As acknowledged in my January 2013 column in The Hospitalist, Physician Compare currently reports very little information. We should expect this to change, however, as Medicare moves forward with developing a plan to publically report valid and reliable individual physician performance metrics. CMS’ clarification of the timeline by which we can expect to see more detailed information is thus greatly appreciated.
The take-home message for hospitalists is that public reporting of care provider performance will become increasingly comprehensive and transparent in the future. As pointed out, CMS’ present plan targets the publication of individual, physician-level quality measures as soon as 2015, which will reflect actual performance during program year 2014. The measurement period is thus less than one year away, so it behooves us all to focus ever more intently on delivering high-value healthcare.
Shaun Frost, MD, SFHM, past president, SHM
Hospitalists Poised to Advance Health Care Through Teamwork
The problems that ail the American health-care system are numerous, complex, and interrelated. In writing about how to fix our chronically dysfunctional system, Hoffman and Emanuel recently cautioned that single solutions will not be effective.1 In their estimation, “individually implemented changes are divisive rather than unifying,” and “the cure … to this complex problem … will require a multimodal approach with a focus on re-engineering the entire care delivery process.”
If single solutions are insufficient (or even counterproductive and divisive), health care’s key stakeholders must figure out how to work more effectively together. In a nutshell, effective collaboration is critical. Those who collaborate well will thrive in the future, while those who are unable to break down silos to innovatively engage their patients, colleagues, and communities will fail.
Our Tradition of Teamwork
Hospitalists understand the importance of collaboration, as teamwork has been a fundamental value of our specialty since its inception. We have a rich tradition of creating novel, collaborative working relationships with a diverse group of key stakeholders that includes primary-care providers (PCPs), nurses, subspecialists, surgeons, case managers, social workers, nursing homes, transitional-care units, home health agencies, hospice programs, and hospital administrators. We have created innovative, collaborative strategies to effectively and safely comanage patients with other physicians, navigate care transitions, and integrate the input of the many people required to manage day-to-day hospital care.
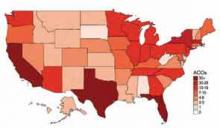
These experiences will serve us well in a future in which collaboration is essential. We should plan to share our expertise in creating effective teams by assuming leadership roles within our institutions as they implement collaborative initiatives on a larger scale through such concepts as the accountable-care organization (ACO).
We should furthermore plan to seek out new, collaborative opportunities by identifying novel agendas to champion. Two critically important, novel agendas for hospitalists to advance are:
- Enhanced physician-patient collaboration; and
- Collaboration to share and propagate new innovation among hospitalists and HM programs across the country.
True Collaboration with Patients
In my last column, I wrote about how enhancing the patient experience of care will have far-reaching, positive effects on health-care reform.2 Attending to the patient experience has been proven to enhance patient satisfaction, care quality, and care affordability. Initiatives to enhance care experience thus hold promise as global, Triple Aim (better health and better care at lower cost) effectors.
The key to improving patient experience is patient engagement, and the key to patient engagement is incorporating patient expectations into the care planning process. The question thus becomes, “How do physicians identify and appropriately act on patient expectations?” The answer is by collaborating with patients to arrive at care decisions that respect their interests. Care providers must work together with patients to create care plans that respect patient preferences, values, and goals. This will require shared decision-making characterized by collaborative discussions that help patients decide between multiple acceptable health-care choices in accordance with their expectations.
SHM is commissioning a Patient Experience Advisory Board to identify how the society can support its members to effectively collaborate with patients and their loved ones. Expect in the near future to learn more from SHM about how to truly engage your patients to enhance the value of the care you deliver.
The Commodification of Health-Care Quality and Affordability
I recently learned of a subspecialty group that had created a new clinical protocol that promised to deliver higher-quality, more affordable care to their patients. When asked if they would share this with physicians outside of their own group, they flat-out refused. What would motivate a physician group to refuse to collaborate with their community to propagate a new innovation that promises to enhance the value of health care? The answer may lie with an economic concept known as commodification.
Commodification is the process by which an item that possesses no economic interest is assigned monetary worth, and hence how economic values can replace social values that previously governed how the item was treated. Commodification describes a transformation of relationships formerly untainted by commerce into commercial relationships that are influenced by monetary interests.
As payors move away from reimbursing providers simply for performing services (volume-based purchasing) to paying them for the value they deliver (value-based purchasing), we must acknowledge that we are “commodifying” health-care quality and affordability. By doing so, the economic viability of medical practices and health-care institutions will depend on delivering value, and to the extent that this determines a competitive advantage in the marketplace, providers might be reluctant to share innovations in quality and affordability.
We must not let this happen to health care. Competing on the ability to effectively deploy and manage new innovations to enhance quality and affordability is acceptable. Competing, however, on the access to these innovations is ethically unacceptable for an industry that is indispensable to the health and well-being of its consumers.
Coke and Pepsi do not provide indispensable products to society. It is thus fine for soft-drink makers to keep their recipes top secret and fight vigorously to prevent others from gaining access to their innovations. Health-care providers, however, cannot morally defend refusing to share new products and processes that decrease costs, improve patient experience, decrease morbidity, prolong life, or otherwise enhance quality.
We must, therefore, strive to continuously collaborate with our hospitalist colleagues and HM programs across the country to propagate new innovation. When someone builds a better mouse trap, it should be shared freely so that all patients have the opportunity to benefit. We must not let the pursuit of economic competitive advantage prevent us from collaborating and sharing ideas on how to make our health-care system better.
Conclusion
Fixing health care is complicated, and employing collaboration in order to do so will be required. Hospitalists have vast experience in working effectively with others, and should leverage this experience to lead the charge on efforts to enhance physician-patient collaboration. Hospitalists should strive to continuously collaborate with their colleagues to ensure open access to new discoveries that improve health-care quality and affordability. Those interested in learning more about how to be successful collaborators might find it helpful to seek out additional resources on the subject. Collaboration, by Morten T. Hansen, is a good source on how to turn this concept into action.3
References
- Hoffman A, Emanuel E. Reengineering US health care. JAMA. 2013;309(7):661-662.
- Frost, S. A matter of perspective: deconstructing satisfaction measurements by focusing on patient goals. The Hospitalist. 2013:17(3):59.
- Hansen M. Collaboration: how leaders avoid the traps, create unity, and reap big results. Boston: Harvard Business Press; 2009.
The problems that ail the American health-care system are numerous, complex, and interrelated. In writing about how to fix our chronically dysfunctional system, Hoffman and Emanuel recently cautioned that single solutions will not be effective.1 In their estimation, “individually implemented changes are divisive rather than unifying,” and “the cure … to this complex problem … will require a multimodal approach with a focus on re-engineering the entire care delivery process.”
If single solutions are insufficient (or even counterproductive and divisive), health care’s key stakeholders must figure out how to work more effectively together. In a nutshell, effective collaboration is critical. Those who collaborate well will thrive in the future, while those who are unable to break down silos to innovatively engage their patients, colleagues, and communities will fail.
Our Tradition of Teamwork
Hospitalists understand the importance of collaboration, as teamwork has been a fundamental value of our specialty since its inception. We have a rich tradition of creating novel, collaborative working relationships with a diverse group of key stakeholders that includes primary-care providers (PCPs), nurses, subspecialists, surgeons, case managers, social workers, nursing homes, transitional-care units, home health agencies, hospice programs, and hospital administrators. We have created innovative, collaborative strategies to effectively and safely comanage patients with other physicians, navigate care transitions, and integrate the input of the many people required to manage day-to-day hospital care.
These experiences will serve us well in a future in which collaboration is essential. We should plan to share our expertise in creating effective teams by assuming leadership roles within our institutions as they implement collaborative initiatives on a larger scale through such concepts as the accountable-care organization (ACO).
We should furthermore plan to seek out new, collaborative opportunities by identifying novel agendas to champion. Two critically important, novel agendas for hospitalists to advance are:
- Enhanced physician-patient collaboration; and
- Collaboration to share and propagate new innovation among hospitalists and HM programs across the country.
True Collaboration with Patients
In my last column, I wrote about how enhancing the patient experience of care will have far-reaching, positive effects on health-care reform.2 Attending to the patient experience has been proven to enhance patient satisfaction, care quality, and care affordability. Initiatives to enhance care experience thus hold promise as global, Triple Aim (better health and better care at lower cost) effectors.
The key to improving patient experience is patient engagement, and the key to patient engagement is incorporating patient expectations into the care planning process. The question thus becomes, “How do physicians identify and appropriately act on patient expectations?” The answer is by collaborating with patients to arrive at care decisions that respect their interests. Care providers must work together with patients to create care plans that respect patient preferences, values, and goals. This will require shared decision-making characterized by collaborative discussions that help patients decide between multiple acceptable health-care choices in accordance with their expectations.
SHM is commissioning a Patient Experience Advisory Board to identify how the society can support its members to effectively collaborate with patients and their loved ones. Expect in the near future to learn more from SHM about how to truly engage your patients to enhance the value of the care you deliver.
The Commodification of Health-Care Quality and Affordability
I recently learned of a subspecialty group that had created a new clinical protocol that promised to deliver higher-quality, more affordable care to their patients. When asked if they would share this with physicians outside of their own group, they flat-out refused. What would motivate a physician group to refuse to collaborate with their community to propagate a new innovation that promises to enhance the value of health care? The answer may lie with an economic concept known as commodification.
Commodification is the process by which an item that possesses no economic interest is assigned monetary worth, and hence how economic values can replace social values that previously governed how the item was treated. Commodification describes a transformation of relationships formerly untainted by commerce into commercial relationships that are influenced by monetary interests.
As payors move away from reimbursing providers simply for performing services (volume-based purchasing) to paying them for the value they deliver (value-based purchasing), we must acknowledge that we are “commodifying” health-care quality and affordability. By doing so, the economic viability of medical practices and health-care institutions will depend on delivering value, and to the extent that this determines a competitive advantage in the marketplace, providers might be reluctant to share innovations in quality and affordability.
We must not let this happen to health care. Competing on the ability to effectively deploy and manage new innovations to enhance quality and affordability is acceptable. Competing, however, on the access to these innovations is ethically unacceptable for an industry that is indispensable to the health and well-being of its consumers.
Coke and Pepsi do not provide indispensable products to society. It is thus fine for soft-drink makers to keep their recipes top secret and fight vigorously to prevent others from gaining access to their innovations. Health-care providers, however, cannot morally defend refusing to share new products and processes that decrease costs, improve patient experience, decrease morbidity, prolong life, or otherwise enhance quality.
We must, therefore, strive to continuously collaborate with our hospitalist colleagues and HM programs across the country to propagate new innovation. When someone builds a better mouse trap, it should be shared freely so that all patients have the opportunity to benefit. We must not let the pursuit of economic competitive advantage prevent us from collaborating and sharing ideas on how to make our health-care system better.
Conclusion
Fixing health care is complicated, and employing collaboration in order to do so will be required. Hospitalists have vast experience in working effectively with others, and should leverage this experience to lead the charge on efforts to enhance physician-patient collaboration. Hospitalists should strive to continuously collaborate with their colleagues to ensure open access to new discoveries that improve health-care quality and affordability. Those interested in learning more about how to be successful collaborators might find it helpful to seek out additional resources on the subject. Collaboration, by Morten T. Hansen, is a good source on how to turn this concept into action.3
References
- Hoffman A, Emanuel E. Reengineering US health care. JAMA. 2013;309(7):661-662.
- Frost, S. A matter of perspective: deconstructing satisfaction measurements by focusing on patient goals. The Hospitalist. 2013:17(3):59.
- Hansen M. Collaboration: how leaders avoid the traps, create unity, and reap big results. Boston: Harvard Business Press; 2009.
The problems that ail the American health-care system are numerous, complex, and interrelated. In writing about how to fix our chronically dysfunctional system, Hoffman and Emanuel recently cautioned that single solutions will not be effective.1 In their estimation, “individually implemented changes are divisive rather than unifying,” and “the cure … to this complex problem … will require a multimodal approach with a focus on re-engineering the entire care delivery process.”
If single solutions are insufficient (or even counterproductive and divisive), health care’s key stakeholders must figure out how to work more effectively together. In a nutshell, effective collaboration is critical. Those who collaborate well will thrive in the future, while those who are unable to break down silos to innovatively engage their patients, colleagues, and communities will fail.
Our Tradition of Teamwork
Hospitalists understand the importance of collaboration, as teamwork has been a fundamental value of our specialty since its inception. We have a rich tradition of creating novel, collaborative working relationships with a diverse group of key stakeholders that includes primary-care providers (PCPs), nurses, subspecialists, surgeons, case managers, social workers, nursing homes, transitional-care units, home health agencies, hospice programs, and hospital administrators. We have created innovative, collaborative strategies to effectively and safely comanage patients with other physicians, navigate care transitions, and integrate the input of the many people required to manage day-to-day hospital care.
These experiences will serve us well in a future in which collaboration is essential. We should plan to share our expertise in creating effective teams by assuming leadership roles within our institutions as they implement collaborative initiatives on a larger scale through such concepts as the accountable-care organization (ACO).
We should furthermore plan to seek out new, collaborative opportunities by identifying novel agendas to champion. Two critically important, novel agendas for hospitalists to advance are:
- Enhanced physician-patient collaboration; and
- Collaboration to share and propagate new innovation among hospitalists and HM programs across the country.
True Collaboration with Patients
In my last column, I wrote about how enhancing the patient experience of care will have far-reaching, positive effects on health-care reform.2 Attending to the patient experience has been proven to enhance patient satisfaction, care quality, and care affordability. Initiatives to enhance care experience thus hold promise as global, Triple Aim (better health and better care at lower cost) effectors.
The key to improving patient experience is patient engagement, and the key to patient engagement is incorporating patient expectations into the care planning process. The question thus becomes, “How do physicians identify and appropriately act on patient expectations?” The answer is by collaborating with patients to arrive at care decisions that respect their interests. Care providers must work together with patients to create care plans that respect patient preferences, values, and goals. This will require shared decision-making characterized by collaborative discussions that help patients decide between multiple acceptable health-care choices in accordance with their expectations.
SHM is commissioning a Patient Experience Advisory Board to identify how the society can support its members to effectively collaborate with patients and their loved ones. Expect in the near future to learn more from SHM about how to truly engage your patients to enhance the value of the care you deliver.
The Commodification of Health-Care Quality and Affordability
I recently learned of a subspecialty group that had created a new clinical protocol that promised to deliver higher-quality, more affordable care to their patients. When asked if they would share this with physicians outside of their own group, they flat-out refused. What would motivate a physician group to refuse to collaborate with their community to propagate a new innovation that promises to enhance the value of health care? The answer may lie with an economic concept known as commodification.
Commodification is the process by which an item that possesses no economic interest is assigned monetary worth, and hence how economic values can replace social values that previously governed how the item was treated. Commodification describes a transformation of relationships formerly untainted by commerce into commercial relationships that are influenced by monetary interests.
As payors move away from reimbursing providers simply for performing services (volume-based purchasing) to paying them for the value they deliver (value-based purchasing), we must acknowledge that we are “commodifying” health-care quality and affordability. By doing so, the economic viability of medical practices and health-care institutions will depend on delivering value, and to the extent that this determines a competitive advantage in the marketplace, providers might be reluctant to share innovations in quality and affordability.
We must not let this happen to health care. Competing on the ability to effectively deploy and manage new innovations to enhance quality and affordability is acceptable. Competing, however, on the access to these innovations is ethically unacceptable for an industry that is indispensable to the health and well-being of its consumers.
Coke and Pepsi do not provide indispensable products to society. It is thus fine for soft-drink makers to keep their recipes top secret and fight vigorously to prevent others from gaining access to their innovations. Health-care providers, however, cannot morally defend refusing to share new products and processes that decrease costs, improve patient experience, decrease morbidity, prolong life, or otherwise enhance quality.
We must, therefore, strive to continuously collaborate with our hospitalist colleagues and HM programs across the country to propagate new innovation. When someone builds a better mouse trap, it should be shared freely so that all patients have the opportunity to benefit. We must not let the pursuit of economic competitive advantage prevent us from collaborating and sharing ideas on how to make our health-care system better.
Conclusion
Fixing health care is complicated, and employing collaboration in order to do so will be required. Hospitalists have vast experience in working effectively with others, and should leverage this experience to lead the charge on efforts to enhance physician-patient collaboration. Hospitalists should strive to continuously collaborate with their colleagues to ensure open access to new discoveries that improve health-care quality and affordability. Those interested in learning more about how to be successful collaborators might find it helpful to seek out additional resources on the subject. Collaboration, by Morten T. Hansen, is a good source on how to turn this concept into action.3
References
- Hoffman A, Emanuel E. Reengineering US health care. JAMA. 2013;309(7):661-662.
- Frost, S. A matter of perspective: deconstructing satisfaction measurements by focusing on patient goals. The Hospitalist. 2013:17(3):59.
- Hansen M. Collaboration: how leaders avoid the traps, create unity, and reap big results. Boston: Harvard Business Press; 2009.
AMA Report Offers Nine Steps to Help PCPs Prevent Readmissions
The American Medical Association recently released a report developed by a 21-member expert panel proposing a nine-step plan for primary-care-physician (PCP) practices to play an integral role in improving care transitions and preventing avoidable rehospitalizations.2 The report recommends focusing on more than just the hospital-admitting diagnosis, conducting a thorough patient health assessment, clarifying the patient’s short- and long-term goals, and coordinating care with other care settings.
With simultaneous research in JAMA concluding that the vast majority of readmissions are for reasons unrelated to the previous hospital stay, coordination between the inpatient and outpatient teams is crucial to successful transitions of care.3 Moreover, a recent survey showed that nearly 30% of PCPs say they miss alerts about patients’ test results from an electronic health record (EHR) notification system.4 According to the survey by Hardeep Singh, MD, MPH, and colleagues from the Michael E. DeBakey VA Medical Center in Houston, the doctors received on average 63 such alerts per day. Seventy percent reported that they cannot effectively manage the alerts, and more than half said that the current EHR notification system makes it possible to miss test results.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
The American Medical Association recently released a report developed by a 21-member expert panel proposing a nine-step plan for primary-care-physician (PCP) practices to play an integral role in improving care transitions and preventing avoidable rehospitalizations.2 The report recommends focusing on more than just the hospital-admitting diagnosis, conducting a thorough patient health assessment, clarifying the patient’s short- and long-term goals, and coordinating care with other care settings.
With simultaneous research in JAMA concluding that the vast majority of readmissions are for reasons unrelated to the previous hospital stay, coordination between the inpatient and outpatient teams is crucial to successful transitions of care.3 Moreover, a recent survey showed that nearly 30% of PCPs say they miss alerts about patients’ test results from an electronic health record (EHR) notification system.4 According to the survey by Hardeep Singh, MD, MPH, and colleagues from the Michael E. DeBakey VA Medical Center in Houston, the doctors received on average 63 such alerts per day. Seventy percent reported that they cannot effectively manage the alerts, and more than half said that the current EHR notification system makes it possible to miss test results.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
The American Medical Association recently released a report developed by a 21-member expert panel proposing a nine-step plan for primary-care-physician (PCP) practices to play an integral role in improving care transitions and preventing avoidable rehospitalizations.2 The report recommends focusing on more than just the hospital-admitting diagnosis, conducting a thorough patient health assessment, clarifying the patient’s short- and long-term goals, and coordinating care with other care settings.
With simultaneous research in JAMA concluding that the vast majority of readmissions are for reasons unrelated to the previous hospital stay, coordination between the inpatient and outpatient teams is crucial to successful transitions of care.3 Moreover, a recent survey showed that nearly 30% of PCPs say they miss alerts about patients’ test results from an electronic health record (EHR) notification system.4 According to the survey by Hardeep Singh, MD, MPH, and colleagues from the Michael E. DeBakey VA Medical Center in Houston, the doctors received on average 63 such alerts per day. Seventy percent reported that they cannot effectively manage the alerts, and more than half said that the current EHR notification system makes it possible to miss test results.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
UCSF Engages Hospitalists to Improve Patient Communication
In a poster presented at HM12, Kathryn Quinn, MPH, CPPS, FACHE, described how her quality team at the University of California at San Francisco (UCSF) developed a checklist to improve physician communication with patients, then taught it to the attending hospitalist faculty.1 The project began with a list of 29 best practices for patient-physician interaction, as identified in medical literature. Hospitalists then voted for the elements they felt were most important to their practice, as well as those best able to be measured, and a top-10 list was created.
Quinn, the program manager for quality and safety in the division of hospital medicine at UCSF, says the communication best practices were “chosen by the people whose practices we are trying to change.”
The quality team presented the best practices in one-hour training sessions that included small-group role plays, explains co-investigator and UCSF hospitalist Diane Sliwka, MD. The training extended to outpatient physicians, medical specialists, and chief residents. Participants also were provided a laminated pocket card listing the interventions. They also received feedback from structured observations with patients on service.
Quinn says UCSF hospitalists have improved at knocking and asking permission to enter patient rooms, introducing themselves by name and role, and encouraging questions at the end of the interaction. They have been less successful at inquiring about the patient’s concerns early in the interview and at discussing duration of treatment and next steps.
“We learned that it takes more than just talk,” Quinn says. “Just telling physicians how to improve communication doesn’t mean it’s easy to do.”
Still to be determined is the project’s impact on patient satisfaction scores, although the hospitalists reported that they found the training and feedback helpful.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
In a poster presented at HM12, Kathryn Quinn, MPH, CPPS, FACHE, described how her quality team at the University of California at San Francisco (UCSF) developed a checklist to improve physician communication with patients, then taught it to the attending hospitalist faculty.1 The project began with a list of 29 best practices for patient-physician interaction, as identified in medical literature. Hospitalists then voted for the elements they felt were most important to their practice, as well as those best able to be measured, and a top-10 list was created.
Quinn, the program manager for quality and safety in the division of hospital medicine at UCSF, says the communication best practices were “chosen by the people whose practices we are trying to change.”
The quality team presented the best practices in one-hour training sessions that included small-group role plays, explains co-investigator and UCSF hospitalist Diane Sliwka, MD. The training extended to outpatient physicians, medical specialists, and chief residents. Participants also were provided a laminated pocket card listing the interventions. They also received feedback from structured observations with patients on service.
Quinn says UCSF hospitalists have improved at knocking and asking permission to enter patient rooms, introducing themselves by name and role, and encouraging questions at the end of the interaction. They have been less successful at inquiring about the patient’s concerns early in the interview and at discussing duration of treatment and next steps.
“We learned that it takes more than just talk,” Quinn says. “Just telling physicians how to improve communication doesn’t mean it’s easy to do.”
Still to be determined is the project’s impact on patient satisfaction scores, although the hospitalists reported that they found the training and feedback helpful.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
In a poster presented at HM12, Kathryn Quinn, MPH, CPPS, FACHE, described how her quality team at the University of California at San Francisco (UCSF) developed a checklist to improve physician communication with patients, then taught it to the attending hospitalist faculty.1 The project began with a list of 29 best practices for patient-physician interaction, as identified in medical literature. Hospitalists then voted for the elements they felt were most important to their practice, as well as those best able to be measured, and a top-10 list was created.
Quinn, the program manager for quality and safety in the division of hospital medicine at UCSF, says the communication best practices were “chosen by the people whose practices we are trying to change.”
The quality team presented the best practices in one-hour training sessions that included small-group role plays, explains co-investigator and UCSF hospitalist Diane Sliwka, MD. The training extended to outpatient physicians, medical specialists, and chief residents. Participants also were provided a laminated pocket card listing the interventions. They also received feedback from structured observations with patients on service.
Quinn says UCSF hospitalists have improved at knocking and asking permission to enter patient rooms, introducing themselves by name and role, and encouraging questions at the end of the interaction. They have been less successful at inquiring about the patient’s concerns early in the interview and at discussing duration of treatment and next steps.
“We learned that it takes more than just talk,” Quinn says. “Just telling physicians how to improve communication doesn’t mean it’s easy to do.”
Still to be determined is the project’s impact on patient satisfaction scores, although the hospitalists reported that they found the training and feedback helpful.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
Hospitalists Can Get Ahead Through Quality and Patient Safety Initiatives
Are you a hospitalist who, on daily rounds, often thinks, “There’s got to be a better way to do this”? You might be just the type of person who can carve a niche for yourself in hospital quality and patient safety—and advance your career in the process.
Successful navigation of the quality-improvement (QI) and patient-safety domains, according to three veteran hospitalists, requires an initial passion and an incremental approach. Now is an especially good time, they agree, for young hospitalists to engage in these types of initiatives.
Why Do It?
In her capacity as president of the Mid-Atlantic Business Unit for Brentwood, Tenn.-based CogentHMG, Julia Wright, MD, SFHM, FACP, often encourages young recruits to consider participation in QI and patient-safety initiatives. She admits that the transition from residency to a busy HM practice, with its higher patient volumes and a faster pace, can be daunting at first. Still, she tries to cultivate interest in initiatives and establish a realistic timeframe for involvement.
There are many reasons to consider this as a career step. Dr. Wright says that quality and patient safety dovetail with hospitalists’ initial reasons for choosing medicine: to improve patients’ lives.
Janet Nagamine, RN, MD, SFHM, former patient safety officer and assistant chief of quality at Kaiser Permanente in Santa Clara, Calif., describes the fit this way: “I might be a good doctor, but as a hospitalist, I rely on many others within the system to deliver, so my patients can’t get good care until the entire system is running well,” she says. “There are all kinds of opportunities to fix our [hospital] system, and I really believe that hospitalists cannot separate themselves from that engagement.”
Elizabeth Gundersen, MD, FHM, of Fort Lauderdale, Fla., agrees that it’s a natural step to think about the ways to make a difference on a larger level. At her former institution, the University of Massachusetts (UMass) Medical School in Worcester, she parlayed her interest in QI to work her way up from ground-level hospitalist to associate chief of her division and quality officer for the hospital. “Physicians get a lot of satisfaction from helping individual patients,” she says. “One thing I really liked about getting involved with quality improvement was being able to make a difference for patients on a systems level.”
An Incremental Path
The path to her current position began with a very specific issue for Dr. Nagamine, an SHM board member who also serves as a Project BOOST co-investigator. “Although I have been doing patient safety since before they had a name for it, I didn’t start out saying that I wanted a career in quality and safety,” she says. “I was trying to take better care of my patients with diabetes, but controlling their glucose was extremely challenging because all the related variables—timing and amount of their insulin dosage, when and how much they had eaten—were charted in different places. This made it hard to adjust their insulin appropriately.”
It quickly became clear to Dr. Nagamine that the solution had to be systemic. She realized that something as basic as taking care of her patients with diabetes required multiple departments (i.e. dietary, nursing, and pharmacy) to furnish information in an integrated manner. So she joined the diabetes committee and went to work on the issue. She helped devise a flow chart that could be used by all relevant departments. A further evolution on the path emanated from one of her patients receiving the wrong medication. She joined the medication safety committee, became chair, “and the next thing you know, I’m in charge of patient safety, and an assistant chief of quality.”
Training Is Necessary
QI and patient-safety methodologies have become sophisticated disciplines in the past two decades, Dr. Wright says. Access to training in QI basics now is readily available to early-career hospitalists. For example, CogentHMG offers program support for QI so that anyone interested “doesn’t have to start from scratch anymore; we can help show them the way and support them in doing it.”
This month, HM13 (www.hospital medicine2013.org)—just outside Washington, D.C.—will offer multiple sessions on quality, as well as the “Initiating Quality Improvement Projects with Built-In Sustainment” workshop, led by Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) core investigator Peter Kaboli, MD, MS, who will address sustainability.
Beyond methodological tools, success in quality and patient safety requires the ability to motivate people, often across multiple disciplines, Dr. Nagamine says. “If you want things to work better, you must invite the right people to the table. For example, we often forget to include key nonclinical stakeholders,” she adds.
When working with hospitals across the country to implement rapid-response tTeams, Dr. Nagamine often reminds them to invite the operators, or “key people,” in the process.
“If you put patient safety at the core of your initiative and create the context for that, most people will agree that it’s the right thing to do and will get on board, even if it’s an extra step for them,” she says. “Know your audience, listen to their perspective, and learn what matters to them. And to most people, it matters that they give good patient care.”
Gretchen Henkel is a freelance writer in California.
Are you a hospitalist who, on daily rounds, often thinks, “There’s got to be a better way to do this”? You might be just the type of person who can carve a niche for yourself in hospital quality and patient safety—and advance your career in the process.
Successful navigation of the quality-improvement (QI) and patient-safety domains, according to three veteran hospitalists, requires an initial passion and an incremental approach. Now is an especially good time, they agree, for young hospitalists to engage in these types of initiatives.
Why Do It?
In her capacity as president of the Mid-Atlantic Business Unit for Brentwood, Tenn.-based CogentHMG, Julia Wright, MD, SFHM, FACP, often encourages young recruits to consider participation in QI and patient-safety initiatives. She admits that the transition from residency to a busy HM practice, with its higher patient volumes and a faster pace, can be daunting at first. Still, she tries to cultivate interest in initiatives and establish a realistic timeframe for involvement.
There are many reasons to consider this as a career step. Dr. Wright says that quality and patient safety dovetail with hospitalists’ initial reasons for choosing medicine: to improve patients’ lives.
Janet Nagamine, RN, MD, SFHM, former patient safety officer and assistant chief of quality at Kaiser Permanente in Santa Clara, Calif., describes the fit this way: “I might be a good doctor, but as a hospitalist, I rely on many others within the system to deliver, so my patients can’t get good care until the entire system is running well,” she says. “There are all kinds of opportunities to fix our [hospital] system, and I really believe that hospitalists cannot separate themselves from that engagement.”
Elizabeth Gundersen, MD, FHM, of Fort Lauderdale, Fla., agrees that it’s a natural step to think about the ways to make a difference on a larger level. At her former institution, the University of Massachusetts (UMass) Medical School in Worcester, she parlayed her interest in QI to work her way up from ground-level hospitalist to associate chief of her division and quality officer for the hospital. “Physicians get a lot of satisfaction from helping individual patients,” she says. “One thing I really liked about getting involved with quality improvement was being able to make a difference for patients on a systems level.”
An Incremental Path
The path to her current position began with a very specific issue for Dr. Nagamine, an SHM board member who also serves as a Project BOOST co-investigator. “Although I have been doing patient safety since before they had a name for it, I didn’t start out saying that I wanted a career in quality and safety,” she says. “I was trying to take better care of my patients with diabetes, but controlling their glucose was extremely challenging because all the related variables—timing and amount of their insulin dosage, when and how much they had eaten—were charted in different places. This made it hard to adjust their insulin appropriately.”
It quickly became clear to Dr. Nagamine that the solution had to be systemic. She realized that something as basic as taking care of her patients with diabetes required multiple departments (i.e. dietary, nursing, and pharmacy) to furnish information in an integrated manner. So she joined the diabetes committee and went to work on the issue. She helped devise a flow chart that could be used by all relevant departments. A further evolution on the path emanated from one of her patients receiving the wrong medication. She joined the medication safety committee, became chair, “and the next thing you know, I’m in charge of patient safety, and an assistant chief of quality.”
Training Is Necessary
QI and patient-safety methodologies have become sophisticated disciplines in the past two decades, Dr. Wright says. Access to training in QI basics now is readily available to early-career hospitalists. For example, CogentHMG offers program support for QI so that anyone interested “doesn’t have to start from scratch anymore; we can help show them the way and support them in doing it.”
This month, HM13 (www.hospital medicine2013.org)—just outside Washington, D.C.—will offer multiple sessions on quality, as well as the “Initiating Quality Improvement Projects with Built-In Sustainment” workshop, led by Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) core investigator Peter Kaboli, MD, MS, who will address sustainability.
Beyond methodological tools, success in quality and patient safety requires the ability to motivate people, often across multiple disciplines, Dr. Nagamine says. “If you want things to work better, you must invite the right people to the table. For example, we often forget to include key nonclinical stakeholders,” she adds.
When working with hospitals across the country to implement rapid-response tTeams, Dr. Nagamine often reminds them to invite the operators, or “key people,” in the process.
“If you put patient safety at the core of your initiative and create the context for that, most people will agree that it’s the right thing to do and will get on board, even if it’s an extra step for them,” she says. “Know your audience, listen to their perspective, and learn what matters to them. And to most people, it matters that they give good patient care.”
Gretchen Henkel is a freelance writer in California.
Are you a hospitalist who, on daily rounds, often thinks, “There’s got to be a better way to do this”? You might be just the type of person who can carve a niche for yourself in hospital quality and patient safety—and advance your career in the process.
Successful navigation of the quality-improvement (QI) and patient-safety domains, according to three veteran hospitalists, requires an initial passion and an incremental approach. Now is an especially good time, they agree, for young hospitalists to engage in these types of initiatives.
Why Do It?
In her capacity as president of the Mid-Atlantic Business Unit for Brentwood, Tenn.-based CogentHMG, Julia Wright, MD, SFHM, FACP, often encourages young recruits to consider participation in QI and patient-safety initiatives. She admits that the transition from residency to a busy HM practice, with its higher patient volumes and a faster pace, can be daunting at first. Still, she tries to cultivate interest in initiatives and establish a realistic timeframe for involvement.
There are many reasons to consider this as a career step. Dr. Wright says that quality and patient safety dovetail with hospitalists’ initial reasons for choosing medicine: to improve patients’ lives.
Janet Nagamine, RN, MD, SFHM, former patient safety officer and assistant chief of quality at Kaiser Permanente in Santa Clara, Calif., describes the fit this way: “I might be a good doctor, but as a hospitalist, I rely on many others within the system to deliver, so my patients can’t get good care until the entire system is running well,” she says. “There are all kinds of opportunities to fix our [hospital] system, and I really believe that hospitalists cannot separate themselves from that engagement.”
Elizabeth Gundersen, MD, FHM, of Fort Lauderdale, Fla., agrees that it’s a natural step to think about the ways to make a difference on a larger level. At her former institution, the University of Massachusetts (UMass) Medical School in Worcester, she parlayed her interest in QI to work her way up from ground-level hospitalist to associate chief of her division and quality officer for the hospital. “Physicians get a lot of satisfaction from helping individual patients,” she says. “One thing I really liked about getting involved with quality improvement was being able to make a difference for patients on a systems level.”
An Incremental Path
The path to her current position began with a very specific issue for Dr. Nagamine, an SHM board member who also serves as a Project BOOST co-investigator. “Although I have been doing patient safety since before they had a name for it, I didn’t start out saying that I wanted a career in quality and safety,” she says. “I was trying to take better care of my patients with diabetes, but controlling their glucose was extremely challenging because all the related variables—timing and amount of their insulin dosage, when and how much they had eaten—were charted in different places. This made it hard to adjust their insulin appropriately.”
It quickly became clear to Dr. Nagamine that the solution had to be systemic. She realized that something as basic as taking care of her patients with diabetes required multiple departments (i.e. dietary, nursing, and pharmacy) to furnish information in an integrated manner. So she joined the diabetes committee and went to work on the issue. She helped devise a flow chart that could be used by all relevant departments. A further evolution on the path emanated from one of her patients receiving the wrong medication. She joined the medication safety committee, became chair, “and the next thing you know, I’m in charge of patient safety, and an assistant chief of quality.”
Training Is Necessary
QI and patient-safety methodologies have become sophisticated disciplines in the past two decades, Dr. Wright says. Access to training in QI basics now is readily available to early-career hospitalists. For example, CogentHMG offers program support for QI so that anyone interested “doesn’t have to start from scratch anymore; we can help show them the way and support them in doing it.”
This month, HM13 (www.hospital medicine2013.org)—just outside Washington, D.C.—will offer multiple sessions on quality, as well as the “Initiating Quality Improvement Projects with Built-In Sustainment” workshop, led by Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) core investigator Peter Kaboli, MD, MS, who will address sustainability.
Beyond methodological tools, success in quality and patient safety requires the ability to motivate people, often across multiple disciplines, Dr. Nagamine says. “If you want things to work better, you must invite the right people to the table. For example, we often forget to include key nonclinical stakeholders,” she adds.
When working with hospitals across the country to implement rapid-response tTeams, Dr. Nagamine often reminds them to invite the operators, or “key people,” in the process.
“If you put patient safety at the core of your initiative and create the context for that, most people will agree that it’s the right thing to do and will get on board, even if it’s an extra step for them,” she says. “Know your audience, listen to their perspective, and learn what matters to them. And to most people, it matters that they give good patient care.”
Gretchen Henkel is a freelance writer in California.
Drive Change in an ACO
From informal polls I’ve recently conducted of hospitalists, many are not even aware they are part of an accountable-care organization (ACO). And if they are aware, they might not be engaging in meaningful dialogue with ACO leaders about their role in these organizations. But, in the long term, ACOs will need to bring hospitalists to the table in order to be successful.
Are You Part of an ACO?
David Muhlestein, who blogs for Health Affairs, tracks the growth of ACOs around the country. He states that, as of Jan. 31, there were 428 ACOs in the U.S. (see Figure 1).1 In terms of numbers, Florida, Texas, and California lead the nation with 42, 33, and 46 ACOs, respectively. So it is likely that you are part of an ACO. If you are unsure, ask your chief medical officer or president of the medical staff.
How ACOs Work
All ACOs seek to manage a group, or population, of patients as efficiently as possible while maintaining or improving quality of care. For Medicare ACOs, the goal is to bring together hospitals and physicians in order to share savings derived from efficiencies in care. But before any savings can be shared, the Medicare ACO must demonstrate that it achieved high-quality care across four domains, totaling 33 individual quality measures. (see Table 1)
Main Flavors of ACOs
There are two types of ACOs: private ACOs and Medicare ACOs. Prior to Medicare ACOs, which were launched in January 2012, there were 150 private-sector ACOs, and this number continues to grow. Private ACOs represent a heterogeneous group in terms of reimbursement model. Some operate under shared savings programs; others use full or partial capitation, bundled payments, and/or other types of arrangements. But nearly all ACOs operate under the premise that the incentives used to make care more efficient and less costly can only be applied if measurable quality is maintained or improved. ACOs do not pay doctors or hospitals more unless high quality is demonstrated.
ACO Quality Measures and Hospitalists
Most of the 33 quality measures required by Medicare ACOs are based in ambulatory practice. These include measures related to blood pressure, immunizations, cancer, and fall-risk screening, and measures for diabetics, such as lipids and hemoglobin A1C. However, there are a few measures for which hospitalists should share in accountability, including:
- All-cause hospital readmission rate—risk-standardized;
- Ambulatory sensitive condition hospital admission rates (CHF, COPD); and
- Medication reconciliation after discharge from an inpatient facility.
Four Key Actions for Hospitalists
Hospitalists make a significant contribution to the quality and the financial performance of ACOs. In addition to the quality metrics cited above, hospitalists impact the inpatient portion of the overall population’s cost of care. Furthermore, hospitalists are vital partners in the care coordination required for an ACO to be successful.
Here are four actions I suggest taking in order for your hospitalist group to be effective as participants in an ACO:
- Have a representative from your group participate in ACO committees that address hospital utilization and related matters, such as care coordination impacting pre- and post-hospital care.
- Learn how to work with ACO case managers on care transitions, including post-discharge follow-up and information transfer.
- Understand an ACO’s approach to engagement of and coordination with post-acute-care facilities. The ability of a post-acute facility, such a skilled nursing facility, to accept patients who have complex care needs, to manage changes in condition in the facility when appropriate, and to send complete information upon transfer to the hospital are important strategies for an ACO’s success.
- Understand how an ACO reports quality and cost performance and how savings will be shared among participants.
Mindset Change
If hospitalists are part of the chain of ACO physicians and providers held accountable for the health of a population of patients, we must work more closely with the medical home/neighborhood, post-acute-care facilities, and home-care providers. The change in mindset will occur only if we have a set of tools to get the job done, such as case managers and information technology, and the appropriate incentives to support better care coordination. I encourage my fellow hospitalists to make things happen, instead of taking a passive role in this monumental transformation.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at wfwhit@comcast.net.
From informal polls I’ve recently conducted of hospitalists, many are not even aware they are part of an accountable-care organization (ACO). And if they are aware, they might not be engaging in meaningful dialogue with ACO leaders about their role in these organizations. But, in the long term, ACOs will need to bring hospitalists to the table in order to be successful.
Are You Part of an ACO?
David Muhlestein, who blogs for Health Affairs, tracks the growth of ACOs around the country. He states that, as of Jan. 31, there were 428 ACOs in the U.S. (see Figure 1).1 In terms of numbers, Florida, Texas, and California lead the nation with 42, 33, and 46 ACOs, respectively. So it is likely that you are part of an ACO. If you are unsure, ask your chief medical officer or president of the medical staff.
How ACOs Work
All ACOs seek to manage a group, or population, of patients as efficiently as possible while maintaining or improving quality of care. For Medicare ACOs, the goal is to bring together hospitals and physicians in order to share savings derived from efficiencies in care. But before any savings can be shared, the Medicare ACO must demonstrate that it achieved high-quality care across four domains, totaling 33 individual quality measures. (see Table 1)
Main Flavors of ACOs
There are two types of ACOs: private ACOs and Medicare ACOs. Prior to Medicare ACOs, which were launched in January 2012, there were 150 private-sector ACOs, and this number continues to grow. Private ACOs represent a heterogeneous group in terms of reimbursement model. Some operate under shared savings programs; others use full or partial capitation, bundled payments, and/or other types of arrangements. But nearly all ACOs operate under the premise that the incentives used to make care more efficient and less costly can only be applied if measurable quality is maintained or improved. ACOs do not pay doctors or hospitals more unless high quality is demonstrated.
ACO Quality Measures and Hospitalists
Most of the 33 quality measures required by Medicare ACOs are based in ambulatory practice. These include measures related to blood pressure, immunizations, cancer, and fall-risk screening, and measures for diabetics, such as lipids and hemoglobin A1C. However, there are a few measures for which hospitalists should share in accountability, including:
- All-cause hospital readmission rate—risk-standardized;
- Ambulatory sensitive condition hospital admission rates (CHF, COPD); and
- Medication reconciliation after discharge from an inpatient facility.
Four Key Actions for Hospitalists
Hospitalists make a significant contribution to the quality and the financial performance of ACOs. In addition to the quality metrics cited above, hospitalists impact the inpatient portion of the overall population’s cost of care. Furthermore, hospitalists are vital partners in the care coordination required for an ACO to be successful.
Here are four actions I suggest taking in order for your hospitalist group to be effective as participants in an ACO:
- Have a representative from your group participate in ACO committees that address hospital utilization and related matters, such as care coordination impacting pre- and post-hospital care.
- Learn how to work with ACO case managers on care transitions, including post-discharge follow-up and information transfer.
- Understand an ACO’s approach to engagement of and coordination with post-acute-care facilities. The ability of a post-acute facility, such a skilled nursing facility, to accept patients who have complex care needs, to manage changes in condition in the facility when appropriate, and to send complete information upon transfer to the hospital are important strategies for an ACO’s success.
- Understand how an ACO reports quality and cost performance and how savings will be shared among participants.
Mindset Change
If hospitalists are part of the chain of ACO physicians and providers held accountable for the health of a population of patients, we must work more closely with the medical home/neighborhood, post-acute-care facilities, and home-care providers. The change in mindset will occur only if we have a set of tools to get the job done, such as case managers and information technology, and the appropriate incentives to support better care coordination. I encourage my fellow hospitalists to make things happen, instead of taking a passive role in this monumental transformation.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at wfwhit@comcast.net.
From informal polls I’ve recently conducted of hospitalists, many are not even aware they are part of an accountable-care organization (ACO). And if they are aware, they might not be engaging in meaningful dialogue with ACO leaders about their role in these organizations. But, in the long term, ACOs will need to bring hospitalists to the table in order to be successful.
Are You Part of an ACO?
David Muhlestein, who blogs for Health Affairs, tracks the growth of ACOs around the country. He states that, as of Jan. 31, there were 428 ACOs in the U.S. (see Figure 1).1 In terms of numbers, Florida, Texas, and California lead the nation with 42, 33, and 46 ACOs, respectively. So it is likely that you are part of an ACO. If you are unsure, ask your chief medical officer or president of the medical staff.
How ACOs Work
All ACOs seek to manage a group, or population, of patients as efficiently as possible while maintaining or improving quality of care. For Medicare ACOs, the goal is to bring together hospitals and physicians in order to share savings derived from efficiencies in care. But before any savings can be shared, the Medicare ACO must demonstrate that it achieved high-quality care across four domains, totaling 33 individual quality measures. (see Table 1)
Main Flavors of ACOs
There are two types of ACOs: private ACOs and Medicare ACOs. Prior to Medicare ACOs, which were launched in January 2012, there were 150 private-sector ACOs, and this number continues to grow. Private ACOs represent a heterogeneous group in terms of reimbursement model. Some operate under shared savings programs; others use full or partial capitation, bundled payments, and/or other types of arrangements. But nearly all ACOs operate under the premise that the incentives used to make care more efficient and less costly can only be applied if measurable quality is maintained or improved. ACOs do not pay doctors or hospitals more unless high quality is demonstrated.
ACO Quality Measures and Hospitalists
Most of the 33 quality measures required by Medicare ACOs are based in ambulatory practice. These include measures related to blood pressure, immunizations, cancer, and fall-risk screening, and measures for diabetics, such as lipids and hemoglobin A1C. However, there are a few measures for which hospitalists should share in accountability, including:
- All-cause hospital readmission rate—risk-standardized;
- Ambulatory sensitive condition hospital admission rates (CHF, COPD); and
- Medication reconciliation after discharge from an inpatient facility.
Four Key Actions for Hospitalists
Hospitalists make a significant contribution to the quality and the financial performance of ACOs. In addition to the quality metrics cited above, hospitalists impact the inpatient portion of the overall population’s cost of care. Furthermore, hospitalists are vital partners in the care coordination required for an ACO to be successful.
Here are four actions I suggest taking in order for your hospitalist group to be effective as participants in an ACO:
- Have a representative from your group participate in ACO committees that address hospital utilization and related matters, such as care coordination impacting pre- and post-hospital care.
- Learn how to work with ACO case managers on care transitions, including post-discharge follow-up and information transfer.
- Understand an ACO’s approach to engagement of and coordination with post-acute-care facilities. The ability of a post-acute facility, such a skilled nursing facility, to accept patients who have complex care needs, to manage changes in condition in the facility when appropriate, and to send complete information upon transfer to the hospital are important strategies for an ACO’s success.
- Understand how an ACO reports quality and cost performance and how savings will be shared among participants.
Mindset Change
If hospitalists are part of the chain of ACO physicians and providers held accountable for the health of a population of patients, we must work more closely with the medical home/neighborhood, post-acute-care facilities, and home-care providers. The change in mindset will occur only if we have a set of tools to get the job done, such as case managers and information technology, and the appropriate incentives to support better care coordination. I encourage my fellow hospitalists to make things happen, instead of taking a passive role in this monumental transformation.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at wfwhit@comcast.net.
UCLA Exec: Patient-Centered Approach Essential to Quality of Hospital Care

–David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles
Patient satisfaction is a buzzword in HM circles, as compensation is increasingly tied to performance in keeping inpatients happy. David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles, could be called a guru of patient satisfaction.
Just don’t tell him that.
“I hope I’m not seen as ‘patient satisfaction,’” he says. “I hope I’m seen as ‘patient centeredness.’ And patient satisfaction is a key piece of patient centeredness.”
Dr. Feinberg, who assumed his current role UCLA Health System in 2011, is a national voice for pushing a patient-centric model of care delivery. To wit, he will be one of the keynote speakers at HM13 next month at the Gaylord National Resort & Convention Center in National Harbor, Md. His address is fittingly titled “Healing Humankind One Patient at a Time.”
The Hospitalist spoke to Dr. Feinberg about his message to hospitalists.
Question: What do you think is the evolution of patient centeredness, as that becomes more of a focus for others?
Answer: Patient centeredness to me is the true north, and I think everything else that we’ve done that isn’t patient-centered has been a distraction. … It’s why we signed up to get into healthcare. It’s what we should be doing today and tonight, and it should guide our future tomorrow. It would be like me saying to the restaurateur, “How important is the food?”
Q: Is it something that hasn’t always been done?
A: It’s pathetic. You’re totally right. We’ve lost our way.
Q: If it’s so common-sense, how did we lose our way?
A: It really became, to me, the coin of the realm in medicine was how much the doctor made, how great their reputation was. It even got to the point of: You were a good doctor if your waiting room was packed. … I keep saying the waiting room should be for the doctors. The patient shouldn’t have to wait. You should be back in the exam room and the doctor should be waiting to see you. So we’ve got to completely change the paradigm. … It’s really the patient who’s at the top of the pyramid. And I just think we’ve lost that completely.
Q: How does a hospitalist engage quickly to ensure that they’re trying to accomplish patient centeredness and manage outcomes properly?
A: Hospitalists have a unique opportunity there, because everybody remembers when they got put in the hospital. It is a big deal when you’re hospitalized. Your family is in a vulnerable state, everybody is in a heightened sense of alertness and focus. Think about how important those four days are around education, around myths and demystifying, around beliefs and disbelief.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Q: So what is the one thing you want hospitalists to take away from your address?
A: That they should join with all of us who want to heal humankind; that they are healers, above all.
Q: How do you translate “I want to be a healer” to the grind of daily work?
A: Well, I don’t think this is a grind. I think that when you’re in this healing profession, that you come here with a purpose. I think if we asked them to look at their personal statements of why they went into med school, every single one of them has something to do with, “I was sick as a kid, my grandmother got sick, I had had this doctor who was a role model, I like to help people, I was a volunteer and I met this patient.” Everyone says that. So this is different than trying to inspire the workers at Costco. These are people that, by definition, have gone and chosen this. We know they’re all smart. They could have all become investment bankers, they could have all become schoolteachers, but what they chose was to go into this field that’s about healing others, and that’s what I think we need to and what I would want them to do, is to get back in touch with themselves because I know it’s there. By definition, it’s there.
Q: Then why don’t more people just make that connection? What is the hurdle?
A: There are a lot of distractions. There are a lot of things coming your way. Worrying about your own life; doctors have lives at home. Worrying about the pressures of making a living. Some of this stuff is really, really hard. There are a million things going on. I believe, and I hope at UCLA, that we believe the strategy to make all of that stuff work is to get it right with the patient. And if you get it right with the patient, then all of that other stuff seems to fall into place and starts to make sense. The finances work out. The market share works out. The healthcare reform works out. I think it is the answer.
Richard Quinn is a freelance writer in New Jersey.

–David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles
Patient satisfaction is a buzzword in HM circles, as compensation is increasingly tied to performance in keeping inpatients happy. David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles, could be called a guru of patient satisfaction.
Just don’t tell him that.
“I hope I’m not seen as ‘patient satisfaction,’” he says. “I hope I’m seen as ‘patient centeredness.’ And patient satisfaction is a key piece of patient centeredness.”
Dr. Feinberg, who assumed his current role UCLA Health System in 2011, is a national voice for pushing a patient-centric model of care delivery. To wit, he will be one of the keynote speakers at HM13 next month at the Gaylord National Resort & Convention Center in National Harbor, Md. His address is fittingly titled “Healing Humankind One Patient at a Time.”
The Hospitalist spoke to Dr. Feinberg about his message to hospitalists.
Question: What do you think is the evolution of patient centeredness, as that becomes more of a focus for others?
Answer: Patient centeredness to me is the true north, and I think everything else that we’ve done that isn’t patient-centered has been a distraction. … It’s why we signed up to get into healthcare. It’s what we should be doing today and tonight, and it should guide our future tomorrow. It would be like me saying to the restaurateur, “How important is the food?”
Q: Is it something that hasn’t always been done?
A: It’s pathetic. You’re totally right. We’ve lost our way.
Q: If it’s so common-sense, how did we lose our way?
A: It really became, to me, the coin of the realm in medicine was how much the doctor made, how great their reputation was. It even got to the point of: You were a good doctor if your waiting room was packed. … I keep saying the waiting room should be for the doctors. The patient shouldn’t have to wait. You should be back in the exam room and the doctor should be waiting to see you. So we’ve got to completely change the paradigm. … It’s really the patient who’s at the top of the pyramid. And I just think we’ve lost that completely.
Q: How does a hospitalist engage quickly to ensure that they’re trying to accomplish patient centeredness and manage outcomes properly?
A: Hospitalists have a unique opportunity there, because everybody remembers when they got put in the hospital. It is a big deal when you’re hospitalized. Your family is in a vulnerable state, everybody is in a heightened sense of alertness and focus. Think about how important those four days are around education, around myths and demystifying, around beliefs and disbelief.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Q: So what is the one thing you want hospitalists to take away from your address?
A: That they should join with all of us who want to heal humankind; that they are healers, above all.
Q: How do you translate “I want to be a healer” to the grind of daily work?
A: Well, I don’t think this is a grind. I think that when you’re in this healing profession, that you come here with a purpose. I think if we asked them to look at their personal statements of why they went into med school, every single one of them has something to do with, “I was sick as a kid, my grandmother got sick, I had had this doctor who was a role model, I like to help people, I was a volunteer and I met this patient.” Everyone says that. So this is different than trying to inspire the workers at Costco. These are people that, by definition, have gone and chosen this. We know they’re all smart. They could have all become investment bankers, they could have all become schoolteachers, but what they chose was to go into this field that’s about healing others, and that’s what I think we need to and what I would want them to do, is to get back in touch with themselves because I know it’s there. By definition, it’s there.
Q: Then why don’t more people just make that connection? What is the hurdle?
A: There are a lot of distractions. There are a lot of things coming your way. Worrying about your own life; doctors have lives at home. Worrying about the pressures of making a living. Some of this stuff is really, really hard. There are a million things going on. I believe, and I hope at UCLA, that we believe the strategy to make all of that stuff work is to get it right with the patient. And if you get it right with the patient, then all of that other stuff seems to fall into place and starts to make sense. The finances work out. The market share works out. The healthcare reform works out. I think it is the answer.
Richard Quinn is a freelance writer in New Jersey.

–David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles
Patient satisfaction is a buzzword in HM circles, as compensation is increasingly tied to performance in keeping inpatients happy. David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles, could be called a guru of patient satisfaction.
Just don’t tell him that.
“I hope I’m not seen as ‘patient satisfaction,’” he says. “I hope I’m seen as ‘patient centeredness.’ And patient satisfaction is a key piece of patient centeredness.”
Dr. Feinberg, who assumed his current role UCLA Health System in 2011, is a national voice for pushing a patient-centric model of care delivery. To wit, he will be one of the keynote speakers at HM13 next month at the Gaylord National Resort & Convention Center in National Harbor, Md. His address is fittingly titled “Healing Humankind One Patient at a Time.”
The Hospitalist spoke to Dr. Feinberg about his message to hospitalists.
Question: What do you think is the evolution of patient centeredness, as that becomes more of a focus for others?
Answer: Patient centeredness to me is the true north, and I think everything else that we’ve done that isn’t patient-centered has been a distraction. … It’s why we signed up to get into healthcare. It’s what we should be doing today and tonight, and it should guide our future tomorrow. It would be like me saying to the restaurateur, “How important is the food?”
Q: Is it something that hasn’t always been done?
A: It’s pathetic. You’re totally right. We’ve lost our way.
Q: If it’s so common-sense, how did we lose our way?
A: It really became, to me, the coin of the realm in medicine was how much the doctor made, how great their reputation was. It even got to the point of: You were a good doctor if your waiting room was packed. … I keep saying the waiting room should be for the doctors. The patient shouldn’t have to wait. You should be back in the exam room and the doctor should be waiting to see you. So we’ve got to completely change the paradigm. … It’s really the patient who’s at the top of the pyramid. And I just think we’ve lost that completely.
Q: How does a hospitalist engage quickly to ensure that they’re trying to accomplish patient centeredness and manage outcomes properly?
A: Hospitalists have a unique opportunity there, because everybody remembers when they got put in the hospital. It is a big deal when you’re hospitalized. Your family is in a vulnerable state, everybody is in a heightened sense of alertness and focus. Think about how important those four days are around education, around myths and demystifying, around beliefs and disbelief.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Q: So what is the one thing you want hospitalists to take away from your address?
A: That they should join with all of us who want to heal humankind; that they are healers, above all.
Q: How do you translate “I want to be a healer” to the grind of daily work?
A: Well, I don’t think this is a grind. I think that when you’re in this healing profession, that you come here with a purpose. I think if we asked them to look at their personal statements of why they went into med school, every single one of them has something to do with, “I was sick as a kid, my grandmother got sick, I had had this doctor who was a role model, I like to help people, I was a volunteer and I met this patient.” Everyone says that. So this is different than trying to inspire the workers at Costco. These are people that, by definition, have gone and chosen this. We know they’re all smart. They could have all become investment bankers, they could have all become schoolteachers, but what they chose was to go into this field that’s about healing others, and that’s what I think we need to and what I would want them to do, is to get back in touch with themselves because I know it’s there. By definition, it’s there.
Q: Then why don’t more people just make that connection? What is the hurdle?
A: There are a lot of distractions. There are a lot of things coming your way. Worrying about your own life; doctors have lives at home. Worrying about the pressures of making a living. Some of this stuff is really, really hard. There are a million things going on. I believe, and I hope at UCLA, that we believe the strategy to make all of that stuff work is to get it right with the patient. And if you get it right with the patient, then all of that other stuff seems to fall into place and starts to make sense. The finances work out. The market share works out. The healthcare reform works out. I think it is the answer.
Richard Quinn is a freelance writer in New Jersey.
Medicare CMO Encourages Hospitalists to Become Experts in Managing Quality Patient Care

–Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer, Centers for Medicaid & Medicare Service
Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer of the Centers for Medicaid & Medicare Services (CMS), often says that physicians need to come to the proverbial table to tell CMS what they think is best. So it’s fitting that at HM13 at the Gaylord National Resort & Convention Center in National Harbor, Md., Dr. Conway will be a keynote speaker who can deliver his message of quality through teamwork to more than 2,500 hospitalists.
A pediatric hospitalist who also serves as director of the Office of Clinical Standards and Quality at the U.S. Department of Health and Human Services in Washington, D.C., Dr. Conway will paint a picture of what hospitalists can do to become the quality-improvement (QI) leaders healthcare needs in the coming years in a presentation titled “The Ideal Hospitalist in 2014 and Beyond: Active Change Agent.”
“Are hospitalists going to accept that challenge?” he asks. “I hope they are.”
This is the second year in a row that Dr. Conway will be a plenary speaker. Last year in San Diego, he told a packed room that CMS had to move from a “passive payor to an active facilitator and catalyst for quality improvement,” says Danielle Scheurer, MD, MSCR, SFHM, physician editor of The Hospitalist. Or, in his own words: “better health, better care, and lower cost.”
But many of the issues in his 2012 commentary were in flux. The Affordable Care Act (ACA), now moving through the slow process of implementation, was then still a law very much in doubt. It wasn’t until last summer that the law was upheld by a bitterly divided U.S. Supreme Court and it became clear much of the proposed reforms would move forward.
This year, he will urge hospitalists to step up their focus on patient-centered outcomes and stop questioning whether that should be the way the HM and other physicians should be judged.
“Given the changing context of payment, hospitalists are going to have to become true experts in managing the quality of care,” Dr. Conway says. “The days of you just graduating residency, seeing as many patients as you can, and you go home at the end of the day—that’s gone for hospital medicine.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Hospitalists can take charge of quality initiatives via involvement with accountable-care organizations (ACOs), health exchanges, and CMS’ value-based purchasing modifier (VBPM). In part, HM is perfectly positioned to assume leadership roles over the next few years because hospitalists already work across multiple departments.
“Hospital medicine is already ahead of a lot of specialties,” Dr. Conway says. “Hospital medicine physicians are already taking on much larger roles in their systems. I think you’re going to see an increasing trend.”
Richard Quinn is a freelance writer in New Jersey.

–Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer, Centers for Medicaid & Medicare Service
Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer of the Centers for Medicaid & Medicare Services (CMS), often says that physicians need to come to the proverbial table to tell CMS what they think is best. So it’s fitting that at HM13 at the Gaylord National Resort & Convention Center in National Harbor, Md., Dr. Conway will be a keynote speaker who can deliver his message of quality through teamwork to more than 2,500 hospitalists.
A pediatric hospitalist who also serves as director of the Office of Clinical Standards and Quality at the U.S. Department of Health and Human Services in Washington, D.C., Dr. Conway will paint a picture of what hospitalists can do to become the quality-improvement (QI) leaders healthcare needs in the coming years in a presentation titled “The Ideal Hospitalist in 2014 and Beyond: Active Change Agent.”
“Are hospitalists going to accept that challenge?” he asks. “I hope they are.”
This is the second year in a row that Dr. Conway will be a plenary speaker. Last year in San Diego, he told a packed room that CMS had to move from a “passive payor to an active facilitator and catalyst for quality improvement,” says Danielle Scheurer, MD, MSCR, SFHM, physician editor of The Hospitalist. Or, in his own words: “better health, better care, and lower cost.”
But many of the issues in his 2012 commentary were in flux. The Affordable Care Act (ACA), now moving through the slow process of implementation, was then still a law very much in doubt. It wasn’t until last summer that the law was upheld by a bitterly divided U.S. Supreme Court and it became clear much of the proposed reforms would move forward.
This year, he will urge hospitalists to step up their focus on patient-centered outcomes and stop questioning whether that should be the way the HM and other physicians should be judged.
“Given the changing context of payment, hospitalists are going to have to become true experts in managing the quality of care,” Dr. Conway says. “The days of you just graduating residency, seeing as many patients as you can, and you go home at the end of the day—that’s gone for hospital medicine.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Hospitalists can take charge of quality initiatives via involvement with accountable-care organizations (ACOs), health exchanges, and CMS’ value-based purchasing modifier (VBPM). In part, HM is perfectly positioned to assume leadership roles over the next few years because hospitalists already work across multiple departments.
“Hospital medicine is already ahead of a lot of specialties,” Dr. Conway says. “Hospital medicine physicians are already taking on much larger roles in their systems. I think you’re going to see an increasing trend.”
Richard Quinn is a freelance writer in New Jersey.

–Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer, Centers for Medicaid & Medicare Service
Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer of the Centers for Medicaid & Medicare Services (CMS), often says that physicians need to come to the proverbial table to tell CMS what they think is best. So it’s fitting that at HM13 at the Gaylord National Resort & Convention Center in National Harbor, Md., Dr. Conway will be a keynote speaker who can deliver his message of quality through teamwork to more than 2,500 hospitalists.
A pediatric hospitalist who also serves as director of the Office of Clinical Standards and Quality at the U.S. Department of Health and Human Services in Washington, D.C., Dr. Conway will paint a picture of what hospitalists can do to become the quality-improvement (QI) leaders healthcare needs in the coming years in a presentation titled “The Ideal Hospitalist in 2014 and Beyond: Active Change Agent.”
“Are hospitalists going to accept that challenge?” he asks. “I hope they are.”
This is the second year in a row that Dr. Conway will be a plenary speaker. Last year in San Diego, he told a packed room that CMS had to move from a “passive payor to an active facilitator and catalyst for quality improvement,” says Danielle Scheurer, MD, MSCR, SFHM, physician editor of The Hospitalist. Or, in his own words: “better health, better care, and lower cost.”
But many of the issues in his 2012 commentary were in flux. The Affordable Care Act (ACA), now moving through the slow process of implementation, was then still a law very much in doubt. It wasn’t until last summer that the law was upheld by a bitterly divided U.S. Supreme Court and it became clear much of the proposed reforms would move forward.
This year, he will urge hospitalists to step up their focus on patient-centered outcomes and stop questioning whether that should be the way the HM and other physicians should be judged.
“Given the changing context of payment, hospitalists are going to have to become true experts in managing the quality of care,” Dr. Conway says. “The days of you just graduating residency, seeing as many patients as you can, and you go home at the end of the day—that’s gone for hospital medicine.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Hospitalists can take charge of quality initiatives via involvement with accountable-care organizations (ACOs), health exchanges, and CMS’ value-based purchasing modifier (VBPM). In part, HM is perfectly positioned to assume leadership roles over the next few years because hospitalists already work across multiple departments.
“Hospital medicine is already ahead of a lot of specialties,” Dr. Conway says. “Hospital medicine physicians are already taking on much larger roles in their systems. I think you’re going to see an increasing trend.”
Richard Quinn is a freelance writer in New Jersey.
Team Hospitalist Recommends Nine Don’t-Miss Sessions at HM13
Eight educational tracks, an equal number of credit bearing pre-courses, a score of small-group forums, three plenaries, and an SHM Town Hall meeting offers a lot of professional development in a four-day span. But that’s just a sampling of what HM13 has slated May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md., just outside Washington, D.C.
So how does one get the most value out of the conference?
“The highest-yield content is going to depend on what your background is and how to spend that time in a way that augments your knowledge, your perspective, or your exposure to like-minded colleagues in a very individual way,” says HM13 course director Daniel Brotman, MD, FACP, SFHM, director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “One of the things that’s so cool about hospital medicine is its diversity.”
But don’t take Dr. Brotman’s well-educated word for it. Here’s a list of recommendations from Team Hospitalist, the only reader-involvement group of its kind in HM, on events they would not miss this year.
The New Anticoagulants: When Should We Be Using Them?
2:45 p.m., May 17
Dr. Ma: “I’m very interested about the new anticoagulants talk. What I’m curious to see is what the speaker thinks about the survivability of these medications in our society, with so many lawyers. Pradaxa already has fallen out of favor. Let’s see what happens to Xarelto.”
How do CFOs Value Their Hospitalist Programs?
2:50 p.m., May 18
Dr. Ma: “The problem today is CFOs have to valuate their hospitalists in the setting of other specialists who also receive subsidies. There is less money to be spent on hospitalists, as other specialists vie for this allotment of savings from hospital-based value purchasing.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Mentoring/Coaching an Improvement Team: Lessons from SHM’s Mentored Implementation Programs
2:45 p.m., May 17
Dr. Perumalswami: “As a Project BOOST physician mentor in Illinois, I would highly recommend the session because the discussion will involve an inside look into valuable experience-based observations and analysis for the success of any process improvement team. The nature of teams and the culture of improvement at various sites will also be discussed. There will be a mentee side of the presentation, too, which will help other mentors of implementation programs better understand what the issues are ‘from the other side.’”
Strategies to Improve Communication with Patients and Families to Improve Care
2:45 p.m., May 17
Dr. Hale: “It is well known in pediatrics that you are treating two patients: both the child and the parents. If the family has a shared understanding of the child’s illness and there is collaboration for the care plan, there will be improved care.”
Neonatal HSV: When to Consider It, How to Evaluate for It, and How to Treat It
11 a.m., May 18
Dr. Hale: “Neonatal HSV is a devastating disease. It is essential to recognize high-risk patients to decrease morbidity and mortality for this illness. There have been recent updates in the understanding of epidemiology of this disease that can assist the provider in recognizing high-risk patients.”
Supporting Transition for Youth with Special Healthcare Needs: Coordinating Care and Preparing to Pass the Baton
4:15 p.m., May 18
Dr. Hale: “The transition of adolescents and young adults from pediatric-care teams to adult-medicine-care teams should be seamless for the sake of the patient, but often it is a blurry transition over the course of years. This session is high-yield for both pediatric and adult hospitalists.”
Getting Ready for Physician Value-Based Purchasing
9:50 a.m., May 19
Dr. Simone: “Dr. [Pat] Torcson’s presentation last year was one of the best at HM12, and I expect this year to be the same. He chairs SHM’s Performance Measurement and Reporting Committee and is well versed in these matters. He speaks in terms that will capture all audiences, whether they are experienced or new to the business aspects of medicine. Highly recommended.”
BOOSTing the Hospital Discharge Process: What Works and What Doesn’t
10:35 a.m., May 17
Dr. Simone: “Both panelists are excellent presenters as well as leading authorities when it comes to discharge processes. This presentation is very timely with the new CMS payment system, which penalizes unnecessary and unexpected readmissions.”
Success Stories: How to Integrate NPs and PAs into a Hospitalist Practice
4:15 p.m., May 18
Cardin: “This is an important session because, as every hard-working hospitalist knows, there simply aren’t enough physicians to fill the needs of our medically complex hospitalized patients. It is simply a reality that there will be an increased need in the future for mid-level providers, and it is valuable to maximize the success of a program by learning how to assimilate them into hospitalized practice.”
Diagnostic Errors and the Hospitalist: Why They Happen and How to Avoid Them
12:45 p.m., May 17
Cardin: “Half of practicing medicine is pattern recognition, and if there are patterns to making diagnostic errors, it would be so valuable to be aware of them. We have tremendous responsibility when caring for patients, and I think it is always beneficial to learn from mistakes.”
Richard Quinn is a freelance writer in New Jersey.
Eight educational tracks, an equal number of credit bearing pre-courses, a score of small-group forums, three plenaries, and an SHM Town Hall meeting offers a lot of professional development in a four-day span. But that’s just a sampling of what HM13 has slated May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md., just outside Washington, D.C.
So how does one get the most value out of the conference?
“The highest-yield content is going to depend on what your background is and how to spend that time in a way that augments your knowledge, your perspective, or your exposure to like-minded colleagues in a very individual way,” says HM13 course director Daniel Brotman, MD, FACP, SFHM, director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “One of the things that’s so cool about hospital medicine is its diversity.”
But don’t take Dr. Brotman’s well-educated word for it. Here’s a list of recommendations from Team Hospitalist, the only reader-involvement group of its kind in HM, on events they would not miss this year.
The New Anticoagulants: When Should We Be Using Them?
2:45 p.m., May 17
Dr. Ma: “I’m very interested about the new anticoagulants talk. What I’m curious to see is what the speaker thinks about the survivability of these medications in our society, with so many lawyers. Pradaxa already has fallen out of favor. Let’s see what happens to Xarelto.”
How do CFOs Value Their Hospitalist Programs?
2:50 p.m., May 18
Dr. Ma: “The problem today is CFOs have to valuate their hospitalists in the setting of other specialists who also receive subsidies. There is less money to be spent on hospitalists, as other specialists vie for this allotment of savings from hospital-based value purchasing.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Mentoring/Coaching an Improvement Team: Lessons from SHM’s Mentored Implementation Programs
2:45 p.m., May 17
Dr. Perumalswami: “As a Project BOOST physician mentor in Illinois, I would highly recommend the session because the discussion will involve an inside look into valuable experience-based observations and analysis for the success of any process improvement team. The nature of teams and the culture of improvement at various sites will also be discussed. There will be a mentee side of the presentation, too, which will help other mentors of implementation programs better understand what the issues are ‘from the other side.’”
Strategies to Improve Communication with Patients and Families to Improve Care
2:45 p.m., May 17
Dr. Hale: “It is well known in pediatrics that you are treating two patients: both the child and the parents. If the family has a shared understanding of the child’s illness and there is collaboration for the care plan, there will be improved care.”
Neonatal HSV: When to Consider It, How to Evaluate for It, and How to Treat It
11 a.m., May 18
Dr. Hale: “Neonatal HSV is a devastating disease. It is essential to recognize high-risk patients to decrease morbidity and mortality for this illness. There have been recent updates in the understanding of epidemiology of this disease that can assist the provider in recognizing high-risk patients.”
Supporting Transition for Youth with Special Healthcare Needs: Coordinating Care and Preparing to Pass the Baton
4:15 p.m., May 18
Dr. Hale: “The transition of adolescents and young adults from pediatric-care teams to adult-medicine-care teams should be seamless for the sake of the patient, but often it is a blurry transition over the course of years. This session is high-yield for both pediatric and adult hospitalists.”
Getting Ready for Physician Value-Based Purchasing
9:50 a.m., May 19
Dr. Simone: “Dr. [Pat] Torcson’s presentation last year was one of the best at HM12, and I expect this year to be the same. He chairs SHM’s Performance Measurement and Reporting Committee and is well versed in these matters. He speaks in terms that will capture all audiences, whether they are experienced or new to the business aspects of medicine. Highly recommended.”
BOOSTing the Hospital Discharge Process: What Works and What Doesn’t
10:35 a.m., May 17
Dr. Simone: “Both panelists are excellent presenters as well as leading authorities when it comes to discharge processes. This presentation is very timely with the new CMS payment system, which penalizes unnecessary and unexpected readmissions.”
Success Stories: How to Integrate NPs and PAs into a Hospitalist Practice
4:15 p.m., May 18
Cardin: “This is an important session because, as every hard-working hospitalist knows, there simply aren’t enough physicians to fill the needs of our medically complex hospitalized patients. It is simply a reality that there will be an increased need in the future for mid-level providers, and it is valuable to maximize the success of a program by learning how to assimilate them into hospitalized practice.”
Diagnostic Errors and the Hospitalist: Why They Happen and How to Avoid Them
12:45 p.m., May 17
Cardin: “Half of practicing medicine is pattern recognition, and if there are patterns to making diagnostic errors, it would be so valuable to be aware of them. We have tremendous responsibility when caring for patients, and I think it is always beneficial to learn from mistakes.”
Richard Quinn is a freelance writer in New Jersey.
Eight educational tracks, an equal number of credit bearing pre-courses, a score of small-group forums, three plenaries, and an SHM Town Hall meeting offers a lot of professional development in a four-day span. But that’s just a sampling of what HM13 has slated May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md., just outside Washington, D.C.
So how does one get the most value out of the conference?
“The highest-yield content is going to depend on what your background is and how to spend that time in a way that augments your knowledge, your perspective, or your exposure to like-minded colleagues in a very individual way,” says HM13 course director Daniel Brotman, MD, FACP, SFHM, director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “One of the things that’s so cool about hospital medicine is its diversity.”
But don’t take Dr. Brotman’s well-educated word for it. Here’s a list of recommendations from Team Hospitalist, the only reader-involvement group of its kind in HM, on events they would not miss this year.
The New Anticoagulants: When Should We Be Using Them?
2:45 p.m., May 17
Dr. Ma: “I’m very interested about the new anticoagulants talk. What I’m curious to see is what the speaker thinks about the survivability of these medications in our society, with so many lawyers. Pradaxa already has fallen out of favor. Let’s see what happens to Xarelto.”
How do CFOs Value Their Hospitalist Programs?
2:50 p.m., May 18
Dr. Ma: “The problem today is CFOs have to valuate their hospitalists in the setting of other specialists who also receive subsidies. There is less money to be spent on hospitalists, as other specialists vie for this allotment of savings from hospital-based value purchasing.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Mentoring/Coaching an Improvement Team: Lessons from SHM’s Mentored Implementation Programs
2:45 p.m., May 17
Dr. Perumalswami: “As a Project BOOST physician mentor in Illinois, I would highly recommend the session because the discussion will involve an inside look into valuable experience-based observations and analysis for the success of any process improvement team. The nature of teams and the culture of improvement at various sites will also be discussed. There will be a mentee side of the presentation, too, which will help other mentors of implementation programs better understand what the issues are ‘from the other side.’”
Strategies to Improve Communication with Patients and Families to Improve Care
2:45 p.m., May 17
Dr. Hale: “It is well known in pediatrics that you are treating two patients: both the child and the parents. If the family has a shared understanding of the child’s illness and there is collaboration for the care plan, there will be improved care.”
Neonatal HSV: When to Consider It, How to Evaluate for It, and How to Treat It
11 a.m., May 18
Dr. Hale: “Neonatal HSV is a devastating disease. It is essential to recognize high-risk patients to decrease morbidity and mortality for this illness. There have been recent updates in the understanding of epidemiology of this disease that can assist the provider in recognizing high-risk patients.”
Supporting Transition for Youth with Special Healthcare Needs: Coordinating Care and Preparing to Pass the Baton
4:15 p.m., May 18
Dr. Hale: “The transition of adolescents and young adults from pediatric-care teams to adult-medicine-care teams should be seamless for the sake of the patient, but often it is a blurry transition over the course of years. This session is high-yield for both pediatric and adult hospitalists.”
Getting Ready for Physician Value-Based Purchasing
9:50 a.m., May 19
Dr. Simone: “Dr. [Pat] Torcson’s presentation last year was one of the best at HM12, and I expect this year to be the same. He chairs SHM’s Performance Measurement and Reporting Committee and is well versed in these matters. He speaks in terms that will capture all audiences, whether they are experienced or new to the business aspects of medicine. Highly recommended.”
BOOSTing the Hospital Discharge Process: What Works and What Doesn’t
10:35 a.m., May 17
Dr. Simone: “Both panelists are excellent presenters as well as leading authorities when it comes to discharge processes. This presentation is very timely with the new CMS payment system, which penalizes unnecessary and unexpected readmissions.”
Success Stories: How to Integrate NPs and PAs into a Hospitalist Practice
4:15 p.m., May 18
Cardin: “This is an important session because, as every hard-working hospitalist knows, there simply aren’t enough physicians to fill the needs of our medically complex hospitalized patients. It is simply a reality that there will be an increased need in the future for mid-level providers, and it is valuable to maximize the success of a program by learning how to assimilate them into hospitalized practice.”
Diagnostic Errors and the Hospitalist: Why They Happen and How to Avoid Them
12:45 p.m., May 17
Cardin: “Half of practicing medicine is pattern recognition, and if there are patterns to making diagnostic errors, it would be so valuable to be aware of them. We have tremendous responsibility when caring for patients, and I think it is always beneficial to learn from mistakes.”
Richard Quinn is a freelance writer in New Jersey.