User login
Long-Term Βeta-Blocker Use May Cause More Harm in Patients Undergoing Surgery
Clinical question: What is the harm associated with long-term beta-blocker therapy in patients with uncomplicated hypertension undergoing non-cardiac surgery?
Background: Given the recent concerns over the validity of prior studies, there is uncertainty about which patients benefit most from perioperative beta-blockade. Current guidelines suggest continuing beta-blockers in the perioperative period. More data are needed to delineate which patients maximally benefit from perioperative beta-blockade.
Study design: Association study.
Setting: Danish nationwide cohort of patients.
Synopsis: Study investigators included 55,320 uncomplicated hypertension (no cardiovascular, renal, or liver disease) patients >19 years of age on ≥2 antihypertensive drugs undergoing non-cardiac surgery. In the 14,664 patients who received beta-blockers, the rates of 30-day major adverse cardiovascular events (MACE; cardiovascular death, nonfatal ischemic stroke, and nonfatal myocardial infarction) and 30-day all-cause mortality were 1.32% and 1.93%, respectively. However, in the 40,676 patients who did not receive beta-blockers, 30-day MACEs and 30-day all-cause mortality rates were 0.84% and 1.32%, respectively (P<0.001). When looking at the individual MACEs, cardiovascular death was the only statistically significant event with higher incidence (0.9% versus 0.45%, P<0.001).
Combination therapy with beta-blocker and RAS inhibitor, calcium channel blockers, or thiazide was associated with statistically significant higher risks of MACEs and all-cause mortality when compared to the combination of RAS inhibitor plus thiazide. Men >70 years of age or undergoing urgent surgery had the highest risk of harm. This study was not a randomized control trial, so caution must be used when attributing causality to beta-blockers, MACEs, and all-cause mortality.
Bottom line: Antihypertensive regimens containing beta-blockers may increase risk of perioperative MACEs and all-cause mortality in patients with uncomplicated hypertension.
Citation: Jorgensen ME, Hlatky MA, Kober L, et al. β-blocker-associated risks in patients with uncomplicated hypertension undergoing noncardiac surgery. JAMA Intern Med. 2015;175(12):1923-1931.
Clinical question: What is the harm associated with long-term beta-blocker therapy in patients with uncomplicated hypertension undergoing non-cardiac surgery?
Background: Given the recent concerns over the validity of prior studies, there is uncertainty about which patients benefit most from perioperative beta-blockade. Current guidelines suggest continuing beta-blockers in the perioperative period. More data are needed to delineate which patients maximally benefit from perioperative beta-blockade.
Study design: Association study.
Setting: Danish nationwide cohort of patients.
Synopsis: Study investigators included 55,320 uncomplicated hypertension (no cardiovascular, renal, or liver disease) patients >19 years of age on ≥2 antihypertensive drugs undergoing non-cardiac surgery. In the 14,664 patients who received beta-blockers, the rates of 30-day major adverse cardiovascular events (MACE; cardiovascular death, nonfatal ischemic stroke, and nonfatal myocardial infarction) and 30-day all-cause mortality were 1.32% and 1.93%, respectively. However, in the 40,676 patients who did not receive beta-blockers, 30-day MACEs and 30-day all-cause mortality rates were 0.84% and 1.32%, respectively (P<0.001). When looking at the individual MACEs, cardiovascular death was the only statistically significant event with higher incidence (0.9% versus 0.45%, P<0.001).
Combination therapy with beta-blocker and RAS inhibitor, calcium channel blockers, or thiazide was associated with statistically significant higher risks of MACEs and all-cause mortality when compared to the combination of RAS inhibitor plus thiazide. Men >70 years of age or undergoing urgent surgery had the highest risk of harm. This study was not a randomized control trial, so caution must be used when attributing causality to beta-blockers, MACEs, and all-cause mortality.
Bottom line: Antihypertensive regimens containing beta-blockers may increase risk of perioperative MACEs and all-cause mortality in patients with uncomplicated hypertension.
Citation: Jorgensen ME, Hlatky MA, Kober L, et al. β-blocker-associated risks in patients with uncomplicated hypertension undergoing noncardiac surgery. JAMA Intern Med. 2015;175(12):1923-1931.
Clinical question: What is the harm associated with long-term beta-blocker therapy in patients with uncomplicated hypertension undergoing non-cardiac surgery?
Background: Given the recent concerns over the validity of prior studies, there is uncertainty about which patients benefit most from perioperative beta-blockade. Current guidelines suggest continuing beta-blockers in the perioperative period. More data are needed to delineate which patients maximally benefit from perioperative beta-blockade.
Study design: Association study.
Setting: Danish nationwide cohort of patients.
Synopsis: Study investigators included 55,320 uncomplicated hypertension (no cardiovascular, renal, or liver disease) patients >19 years of age on ≥2 antihypertensive drugs undergoing non-cardiac surgery. In the 14,664 patients who received beta-blockers, the rates of 30-day major adverse cardiovascular events (MACE; cardiovascular death, nonfatal ischemic stroke, and nonfatal myocardial infarction) and 30-day all-cause mortality were 1.32% and 1.93%, respectively. However, in the 40,676 patients who did not receive beta-blockers, 30-day MACEs and 30-day all-cause mortality rates were 0.84% and 1.32%, respectively (P<0.001). When looking at the individual MACEs, cardiovascular death was the only statistically significant event with higher incidence (0.9% versus 0.45%, P<0.001).
Combination therapy with beta-blocker and RAS inhibitor, calcium channel blockers, or thiazide was associated with statistically significant higher risks of MACEs and all-cause mortality when compared to the combination of RAS inhibitor plus thiazide. Men >70 years of age or undergoing urgent surgery had the highest risk of harm. This study was not a randomized control trial, so caution must be used when attributing causality to beta-blockers, MACEs, and all-cause mortality.
Bottom line: Antihypertensive regimens containing beta-blockers may increase risk of perioperative MACEs and all-cause mortality in patients with uncomplicated hypertension.
Citation: Jorgensen ME, Hlatky MA, Kober L, et al. β-blocker-associated risks in patients with uncomplicated hypertension undergoing noncardiac surgery. JAMA Intern Med. 2015;175(12):1923-1931.
Hybrid option ‘reasonable’ for HLHS?
Although the classic Norwood palliation for infants with hypoplastic left heart syndrome (HLHS) has been well established, the procedure has had its drawbacks, namely the need for cardiopulmonary bypass with hypothermia and a because it rules out biventricular correction months later. A hybrid procedure avoids the need for bypass and accommodates short-term biventricular correction, but it has lacked strong evidence.
Researchers from Justus-Liebig University Giessen, Germany, reported on 182 patients with HLHS who had the three-stage Giessen hybrid procedure, noting 10-year survival of almost 80% with almost a third of patients requiring no artery intervention in that time (J Thorac Cardiovasc Surg. 2016 April;151:1112-23).
“In view of the early results and long-term outcome after Giessen hybrid palliation, the hybrid approach has become a reasonable alternative to the conventional strategy to treat neonates with HLHS and variants,” wrote Dr. Can Yerebakan and colleagues. “Further refinements are warranted to decrease patient morbidity.”
The Giessen hybrid procedure uses a technique to control pulmonary blood flow that is different from the Norwood procedure. The hybrid approach involves stenting of the arterial duct or prostaglandin therapy to maintain systemic perfusion combined with off-pump bilateral banding of the pulmonary arteries (bPAB) in the neonatal period. The Giessen hybrid operation defers the Norwood-type palliation using cardiopulmonary bypass that involves an aortic arch reconstruction, including a superior cavopulmonary connection or a biventricular correction, if indicated, until the infant is 4-8 months of age.
“In recent years, hybrid treatment has moved from a myth to an alternative modality in a growing number of institutions globally,” Dr. Yerebakan and colleagues said. The hybrid procedure has been used in high-risk patients. One report claimed higher morbidity in the hybrid procedure due to bPAB (Ann Thorac Surg. 2013;96:1382-8). Another study raised concerns about an adequate pulmonary artery rehabilitation at the time of the Fontan operation, the third stage in the hybrid strategy (J Thorac Cardiovasc Surg. 2014;147:706-12).
But with the hybrid approach, patients retain the potential to receive a biventricular correction up to 8 months later without compromising survival, “postponing an immediate definitive decision in the newborn period in comparison with the classic Norwood palliation,” Dr. Yerebakan and coauthors noted.
The doctors at the Pediatric Heart Center Giessen treat all types and variants of HLHS with the modified Giessen hybrid strategy. Between 1998 and 2015, 182 patients with HLHS had the Giessen hybrid stage I operation, including 126 patients who received univentricular palliation or a heart transplant. The median age of stage I recipients was 6 days, and median weight 3.2 kg. The stage II operation was performed at 4.5 months, with a range of 2.9 to 39.5 months, and Fontan completion was established at 33.7 months, with a range of 21 to 108 months.
Median follow-up after the stage I procedure was 4.6 years, and the death rate was 2.5%. After stage II, mortality was 4.9%; no deaths were reported after Fontan completion. Body weight less than 2.5 kg and aortic atresia had no significant effect on survival. Mortality rates were 8.9% between stages I and II and 5.3% between stage II and Fontan completion. “Cumulative interstage mortality was 14.2%,” Dr. Yerebakan and colleagues noted. “At 10 years, the probability of survival is 77.8%.”
Also at 10 years, 32.2% of patients were free from further pulmonary artery intervention, and 16.7% needed aortic arch reconstruction. Two patients required reoperations for aortic arch reconstruction.
Dr. Yerebakan and colleagues suggested several steps to improve outcomes with the hybrid approach: “intense collaboration” with anesthesiology and pediatric cardiology during and after the procedure to risk stratify individual patients; implementation of standards for management of all stages, including out-of-hospital care, in all departments that participate in a case; and liberalized indications for use of MRI before the stage II and Fontan completion.
Among the limitations of the study the authors noted were its retrospective nature and a median follow-up of only 5 years when the center has some cases with up to 15 years of follow-up. But Dr. Yerebakan and coauthors said they could not determine if the patients benefit from the hybrid treatment in the long-term.
The researchers had no disclosures.
The study by Dr. Yerebakan and colleagues is one of the largest single-center series of patients with HLHS who routinely undergo a hybrid palliation to date, and while the study is open to criticisms, “the authors should be applauded,” Dr. Ralph S. Mosca of New York University said in his invited commentary (J Thorac Cardiovasc Surg. 2016;151:1123-25).
Among the criticisms Dr. Mosca mentioned are that the hybrid approach requires a more extensive stage II reconstruction, “often further complicated by the presence of significant branch PA stenosis and a difficult aortic arch reconstruction”; that there is “appreciable” interstage mortality at 12.2%; and that there is an absence of data on renal or respiratory insufficiency, infection rates, and neurologic outcomes.
Dr. Mosca cited the cause for applause, however: “Through their persistence and collective experience, [the authors] have achieved commendable results in this difficult patient population.”
Yet, Dr. Mosca also noted a number of “potential problems” with the hybrid approach: bilateral banding of the pulmonary artery is a “crude procedure”; arterial duct stenting can lead to retrograde aortic arch reduction; and the interstage mortality “remains significant.”
Results of the hybrid and Norwood procedures are “strikingly similar,” Dr. Mosca said. While the hybrid approach may lower neonatal mortality, it may also carry longer-term consequences “predicated upon the need to closely observe and intervene,” he said. Clinicians need more information on hybrid outcomes, but in time it will likely take its place as an option for HLHS alongside the Norwood procedure, Dr. Mosca said.
The study by Dr. Yerebakan and colleagues is one of the largest single-center series of patients with HLHS who routinely undergo a hybrid palliation to date, and while the study is open to criticisms, “the authors should be applauded,” Dr. Ralph S. Mosca of New York University said in his invited commentary (J Thorac Cardiovasc Surg. 2016;151:1123-25).
Among the criticisms Dr. Mosca mentioned are that the hybrid approach requires a more extensive stage II reconstruction, “often further complicated by the presence of significant branch PA stenosis and a difficult aortic arch reconstruction”; that there is “appreciable” interstage mortality at 12.2%; and that there is an absence of data on renal or respiratory insufficiency, infection rates, and neurologic outcomes.
Dr. Mosca cited the cause for applause, however: “Through their persistence and collective experience, [the authors] have achieved commendable results in this difficult patient population.”
Yet, Dr. Mosca also noted a number of “potential problems” with the hybrid approach: bilateral banding of the pulmonary artery is a “crude procedure”; arterial duct stenting can lead to retrograde aortic arch reduction; and the interstage mortality “remains significant.”
Results of the hybrid and Norwood procedures are “strikingly similar,” Dr. Mosca said. While the hybrid approach may lower neonatal mortality, it may also carry longer-term consequences “predicated upon the need to closely observe and intervene,” he said. Clinicians need more information on hybrid outcomes, but in time it will likely take its place as an option for HLHS alongside the Norwood procedure, Dr. Mosca said.
The study by Dr. Yerebakan and colleagues is one of the largest single-center series of patients with HLHS who routinely undergo a hybrid palliation to date, and while the study is open to criticisms, “the authors should be applauded,” Dr. Ralph S. Mosca of New York University said in his invited commentary (J Thorac Cardiovasc Surg. 2016;151:1123-25).
Among the criticisms Dr. Mosca mentioned are that the hybrid approach requires a more extensive stage II reconstruction, “often further complicated by the presence of significant branch PA stenosis and a difficult aortic arch reconstruction”; that there is “appreciable” interstage mortality at 12.2%; and that there is an absence of data on renal or respiratory insufficiency, infection rates, and neurologic outcomes.
Dr. Mosca cited the cause for applause, however: “Through their persistence and collective experience, [the authors] have achieved commendable results in this difficult patient population.”
Yet, Dr. Mosca also noted a number of “potential problems” with the hybrid approach: bilateral banding of the pulmonary artery is a “crude procedure”; arterial duct stenting can lead to retrograde aortic arch reduction; and the interstage mortality “remains significant.”
Results of the hybrid and Norwood procedures are “strikingly similar,” Dr. Mosca said. While the hybrid approach may lower neonatal mortality, it may also carry longer-term consequences “predicated upon the need to closely observe and intervene,” he said. Clinicians need more information on hybrid outcomes, but in time it will likely take its place as an option for HLHS alongside the Norwood procedure, Dr. Mosca said.
Although the classic Norwood palliation for infants with hypoplastic left heart syndrome (HLHS) has been well established, the procedure has had its drawbacks, namely the need for cardiopulmonary bypass with hypothermia and a because it rules out biventricular correction months later. A hybrid procedure avoids the need for bypass and accommodates short-term biventricular correction, but it has lacked strong evidence.
Researchers from Justus-Liebig University Giessen, Germany, reported on 182 patients with HLHS who had the three-stage Giessen hybrid procedure, noting 10-year survival of almost 80% with almost a third of patients requiring no artery intervention in that time (J Thorac Cardiovasc Surg. 2016 April;151:1112-23).
“In view of the early results and long-term outcome after Giessen hybrid palliation, the hybrid approach has become a reasonable alternative to the conventional strategy to treat neonates with HLHS and variants,” wrote Dr. Can Yerebakan and colleagues. “Further refinements are warranted to decrease patient morbidity.”
The Giessen hybrid procedure uses a technique to control pulmonary blood flow that is different from the Norwood procedure. The hybrid approach involves stenting of the arterial duct or prostaglandin therapy to maintain systemic perfusion combined with off-pump bilateral banding of the pulmonary arteries (bPAB) in the neonatal period. The Giessen hybrid operation defers the Norwood-type palliation using cardiopulmonary bypass that involves an aortic arch reconstruction, including a superior cavopulmonary connection or a biventricular correction, if indicated, until the infant is 4-8 months of age.
“In recent years, hybrid treatment has moved from a myth to an alternative modality in a growing number of institutions globally,” Dr. Yerebakan and colleagues said. The hybrid procedure has been used in high-risk patients. One report claimed higher morbidity in the hybrid procedure due to bPAB (Ann Thorac Surg. 2013;96:1382-8). Another study raised concerns about an adequate pulmonary artery rehabilitation at the time of the Fontan operation, the third stage in the hybrid strategy (J Thorac Cardiovasc Surg. 2014;147:706-12).
But with the hybrid approach, patients retain the potential to receive a biventricular correction up to 8 months later without compromising survival, “postponing an immediate definitive decision in the newborn period in comparison with the classic Norwood palliation,” Dr. Yerebakan and coauthors noted.
The doctors at the Pediatric Heart Center Giessen treat all types and variants of HLHS with the modified Giessen hybrid strategy. Between 1998 and 2015, 182 patients with HLHS had the Giessen hybrid stage I operation, including 126 patients who received univentricular palliation or a heart transplant. The median age of stage I recipients was 6 days, and median weight 3.2 kg. The stage II operation was performed at 4.5 months, with a range of 2.9 to 39.5 months, and Fontan completion was established at 33.7 months, with a range of 21 to 108 months.
Median follow-up after the stage I procedure was 4.6 years, and the death rate was 2.5%. After stage II, mortality was 4.9%; no deaths were reported after Fontan completion. Body weight less than 2.5 kg and aortic atresia had no significant effect on survival. Mortality rates were 8.9% between stages I and II and 5.3% between stage II and Fontan completion. “Cumulative interstage mortality was 14.2%,” Dr. Yerebakan and colleagues noted. “At 10 years, the probability of survival is 77.8%.”
Also at 10 years, 32.2% of patients were free from further pulmonary artery intervention, and 16.7% needed aortic arch reconstruction. Two patients required reoperations for aortic arch reconstruction.
Dr. Yerebakan and colleagues suggested several steps to improve outcomes with the hybrid approach: “intense collaboration” with anesthesiology and pediatric cardiology during and after the procedure to risk stratify individual patients; implementation of standards for management of all stages, including out-of-hospital care, in all departments that participate in a case; and liberalized indications for use of MRI before the stage II and Fontan completion.
Among the limitations of the study the authors noted were its retrospective nature and a median follow-up of only 5 years when the center has some cases with up to 15 years of follow-up. But Dr. Yerebakan and coauthors said they could not determine if the patients benefit from the hybrid treatment in the long-term.
The researchers had no disclosures.
Although the classic Norwood palliation for infants with hypoplastic left heart syndrome (HLHS) has been well established, the procedure has had its drawbacks, namely the need for cardiopulmonary bypass with hypothermia and a because it rules out biventricular correction months later. A hybrid procedure avoids the need for bypass and accommodates short-term biventricular correction, but it has lacked strong evidence.
Researchers from Justus-Liebig University Giessen, Germany, reported on 182 patients with HLHS who had the three-stage Giessen hybrid procedure, noting 10-year survival of almost 80% with almost a third of patients requiring no artery intervention in that time (J Thorac Cardiovasc Surg. 2016 April;151:1112-23).
“In view of the early results and long-term outcome after Giessen hybrid palliation, the hybrid approach has become a reasonable alternative to the conventional strategy to treat neonates with HLHS and variants,” wrote Dr. Can Yerebakan and colleagues. “Further refinements are warranted to decrease patient morbidity.”
The Giessen hybrid procedure uses a technique to control pulmonary blood flow that is different from the Norwood procedure. The hybrid approach involves stenting of the arterial duct or prostaglandin therapy to maintain systemic perfusion combined with off-pump bilateral banding of the pulmonary arteries (bPAB) in the neonatal period. The Giessen hybrid operation defers the Norwood-type palliation using cardiopulmonary bypass that involves an aortic arch reconstruction, including a superior cavopulmonary connection or a biventricular correction, if indicated, until the infant is 4-8 months of age.
“In recent years, hybrid treatment has moved from a myth to an alternative modality in a growing number of institutions globally,” Dr. Yerebakan and colleagues said. The hybrid procedure has been used in high-risk patients. One report claimed higher morbidity in the hybrid procedure due to bPAB (Ann Thorac Surg. 2013;96:1382-8). Another study raised concerns about an adequate pulmonary artery rehabilitation at the time of the Fontan operation, the third stage in the hybrid strategy (J Thorac Cardiovasc Surg. 2014;147:706-12).
But with the hybrid approach, patients retain the potential to receive a biventricular correction up to 8 months later without compromising survival, “postponing an immediate definitive decision in the newborn period in comparison with the classic Norwood palliation,” Dr. Yerebakan and coauthors noted.
The doctors at the Pediatric Heart Center Giessen treat all types and variants of HLHS with the modified Giessen hybrid strategy. Between 1998 and 2015, 182 patients with HLHS had the Giessen hybrid stage I operation, including 126 patients who received univentricular palliation or a heart transplant. The median age of stage I recipients was 6 days, and median weight 3.2 kg. The stage II operation was performed at 4.5 months, with a range of 2.9 to 39.5 months, and Fontan completion was established at 33.7 months, with a range of 21 to 108 months.
Median follow-up after the stage I procedure was 4.6 years, and the death rate was 2.5%. After stage II, mortality was 4.9%; no deaths were reported after Fontan completion. Body weight less than 2.5 kg and aortic atresia had no significant effect on survival. Mortality rates were 8.9% between stages I and II and 5.3% between stage II and Fontan completion. “Cumulative interstage mortality was 14.2%,” Dr. Yerebakan and colleagues noted. “At 10 years, the probability of survival is 77.8%.”
Also at 10 years, 32.2% of patients were free from further pulmonary artery intervention, and 16.7% needed aortic arch reconstruction. Two patients required reoperations for aortic arch reconstruction.
Dr. Yerebakan and colleagues suggested several steps to improve outcomes with the hybrid approach: “intense collaboration” with anesthesiology and pediatric cardiology during and after the procedure to risk stratify individual patients; implementation of standards for management of all stages, including out-of-hospital care, in all departments that participate in a case; and liberalized indications for use of MRI before the stage II and Fontan completion.
Among the limitations of the study the authors noted were its retrospective nature and a median follow-up of only 5 years when the center has some cases with up to 15 years of follow-up. But Dr. Yerebakan and coauthors said they could not determine if the patients benefit from the hybrid treatment in the long-term.
The researchers had no disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: A hybrid operation for hypoplastic left heart syndrome (HLHS) and variants in neonates is emerging as an alternative to the Norwood palliation.
Major finding: At 10 years, the probability of survival with the hybrid procedure was 77.8%. Low body weight (less than 2.5 kg) and aortic atresia had no significant impact on survival.
Data source: Retrospective study of 182 patients who had the hybrid procedure at a single center between June 1998 and February 2015.
Disclosures: The study investigators had no relationships to disclose.
Study finds inappropriate oophorectomy at time of hysterectomy
Among premenopausal California women undergoing nonradical hysterectomies over a 7-year period, more than one-third underwent concurrent oophorectomies for no apparent reason.
“Regardless of what our national guidelines are telling us to do, we’re still not doing a good enough job of educating our patients and providing guideline-driven care,” Dr. Amandeep S. Mahal said in an interview prior to the annual scientific meeting of the Society of Gynecologic Surgeons.
Emerging evidence suggests that premenopausal oophorectomy is associated with worsened long-term health outcomes, including increased mortality and risk of cardiovascular events, said Dr. Mahal, a second-year fellow in the department of obstetrics and gynecology at Stanford (Calif.) University Hospital. The current recommendation by the American College of Obstetricians and Gynecologists (ACOG) is that “strong consideration should be given to retaining normal ovaries in premenopausal women who are not at increased genetic risk of ovarian cancer. However, given the risk of ovarian cancer in postmenopausal women, ovarian removal at the time of hysterectomy should be considered for these women” (Obstet. Gynecol. 2008;111[1]:231-41).
In an effort to determine the rate of potentially unnecessary oophorectomies being performed in premenopausal women for benign indications, the researchers reviewed 259,294 inpatient, nonradical hysterectomies performed in California hospitals between 2005 and 2011. Women younger than age 50 were categorized as premenopausal. The records were obtained from California’s Office of Statewide Health Planning patient discharge database, which includes all non–federal hospital discharges. Each discharge contains a primary diagnosis as well as up to 19 secondary procedure codes and 24 secondary diagnosis codes. Dr. Mahal and his associates considered oophorectomies as appropriate if a supporting ICD-9 code such as “ovarian cyst” or “endometriosis” was linked to it, and inappropriate if no such codes were linked.
Of the 259,294 benign hysterectomies performed during the study period, 37% included concomitant removal of all ovaries, and 53% of the oophorectomies were performed in premenopausal women. Of the oophorectomies in premenopausal women, 37% were deemed to be “inappropriate” based on the documented reason for removal. The researchers observed that the total number of premenopausal hysterectomies with oophorectomy decreased from 10,166 per year in 2004 to 4,672 per year in 2011, but the percentage of oophorectomies deemed to be inappropriate remained stable, in the range of 36%-38%.
“We were very diligent and went through every possible diagnosis we could think of that would give you a reason to remove ovaries,” Dr. Mahal said. “Even being exhaustive in that manner, we could not find a reason why for more than one in three women who underwent oophorectomy prior to natural menopause.”
Logistic regression analysis revealed Hispanic and black race as the only demographic factors associated with an increased odds of inappropriate oophorectomy at the time of hysterectomy (P less than .001). Hospital characteristics and type of insurance did not account for any observed differences.
Even if premenopausal women have no risk factors for ovarian cancer in the future, undergoing an oophorectomy “is a decision they should make with their physician,” Dr. Mahal said. “One of the things we don’t know [about this study] is how many patients had a conversation with their doctor, understood the risks, and decided ‘it’s worth it for me to go ahead and remove the ovaries at the time of the hysterectomy.’ ”
The meeting was jointly sponsored by the American College of Surgeons.
Dr. Mahal reported having no financial disclosures.
Among premenopausal California women undergoing nonradical hysterectomies over a 7-year period, more than one-third underwent concurrent oophorectomies for no apparent reason.
“Regardless of what our national guidelines are telling us to do, we’re still not doing a good enough job of educating our patients and providing guideline-driven care,” Dr. Amandeep S. Mahal said in an interview prior to the annual scientific meeting of the Society of Gynecologic Surgeons.
Emerging evidence suggests that premenopausal oophorectomy is associated with worsened long-term health outcomes, including increased mortality and risk of cardiovascular events, said Dr. Mahal, a second-year fellow in the department of obstetrics and gynecology at Stanford (Calif.) University Hospital. The current recommendation by the American College of Obstetricians and Gynecologists (ACOG) is that “strong consideration should be given to retaining normal ovaries in premenopausal women who are not at increased genetic risk of ovarian cancer. However, given the risk of ovarian cancer in postmenopausal women, ovarian removal at the time of hysterectomy should be considered for these women” (Obstet. Gynecol. 2008;111[1]:231-41).
In an effort to determine the rate of potentially unnecessary oophorectomies being performed in premenopausal women for benign indications, the researchers reviewed 259,294 inpatient, nonradical hysterectomies performed in California hospitals between 2005 and 2011. Women younger than age 50 were categorized as premenopausal. The records were obtained from California’s Office of Statewide Health Planning patient discharge database, which includes all non–federal hospital discharges. Each discharge contains a primary diagnosis as well as up to 19 secondary procedure codes and 24 secondary diagnosis codes. Dr. Mahal and his associates considered oophorectomies as appropriate if a supporting ICD-9 code such as “ovarian cyst” or “endometriosis” was linked to it, and inappropriate if no such codes were linked.
Of the 259,294 benign hysterectomies performed during the study period, 37% included concomitant removal of all ovaries, and 53% of the oophorectomies were performed in premenopausal women. Of the oophorectomies in premenopausal women, 37% were deemed to be “inappropriate” based on the documented reason for removal. The researchers observed that the total number of premenopausal hysterectomies with oophorectomy decreased from 10,166 per year in 2004 to 4,672 per year in 2011, but the percentage of oophorectomies deemed to be inappropriate remained stable, in the range of 36%-38%.
“We were very diligent and went through every possible diagnosis we could think of that would give you a reason to remove ovaries,” Dr. Mahal said. “Even being exhaustive in that manner, we could not find a reason why for more than one in three women who underwent oophorectomy prior to natural menopause.”
Logistic regression analysis revealed Hispanic and black race as the only demographic factors associated with an increased odds of inappropriate oophorectomy at the time of hysterectomy (P less than .001). Hospital characteristics and type of insurance did not account for any observed differences.
Even if premenopausal women have no risk factors for ovarian cancer in the future, undergoing an oophorectomy “is a decision they should make with their physician,” Dr. Mahal said. “One of the things we don’t know [about this study] is how many patients had a conversation with their doctor, understood the risks, and decided ‘it’s worth it for me to go ahead and remove the ovaries at the time of the hysterectomy.’ ”
The meeting was jointly sponsored by the American College of Surgeons.
Dr. Mahal reported having no financial disclosures.
Among premenopausal California women undergoing nonradical hysterectomies over a 7-year period, more than one-third underwent concurrent oophorectomies for no apparent reason.
“Regardless of what our national guidelines are telling us to do, we’re still not doing a good enough job of educating our patients and providing guideline-driven care,” Dr. Amandeep S. Mahal said in an interview prior to the annual scientific meeting of the Society of Gynecologic Surgeons.
Emerging evidence suggests that premenopausal oophorectomy is associated with worsened long-term health outcomes, including increased mortality and risk of cardiovascular events, said Dr. Mahal, a second-year fellow in the department of obstetrics and gynecology at Stanford (Calif.) University Hospital. The current recommendation by the American College of Obstetricians and Gynecologists (ACOG) is that “strong consideration should be given to retaining normal ovaries in premenopausal women who are not at increased genetic risk of ovarian cancer. However, given the risk of ovarian cancer in postmenopausal women, ovarian removal at the time of hysterectomy should be considered for these women” (Obstet. Gynecol. 2008;111[1]:231-41).
In an effort to determine the rate of potentially unnecessary oophorectomies being performed in premenopausal women for benign indications, the researchers reviewed 259,294 inpatient, nonradical hysterectomies performed in California hospitals between 2005 and 2011. Women younger than age 50 were categorized as premenopausal. The records were obtained from California’s Office of Statewide Health Planning patient discharge database, which includes all non–federal hospital discharges. Each discharge contains a primary diagnosis as well as up to 19 secondary procedure codes and 24 secondary diagnosis codes. Dr. Mahal and his associates considered oophorectomies as appropriate if a supporting ICD-9 code such as “ovarian cyst” or “endometriosis” was linked to it, and inappropriate if no such codes were linked.
Of the 259,294 benign hysterectomies performed during the study period, 37% included concomitant removal of all ovaries, and 53% of the oophorectomies were performed in premenopausal women. Of the oophorectomies in premenopausal women, 37% were deemed to be “inappropriate” based on the documented reason for removal. The researchers observed that the total number of premenopausal hysterectomies with oophorectomy decreased from 10,166 per year in 2004 to 4,672 per year in 2011, but the percentage of oophorectomies deemed to be inappropriate remained stable, in the range of 36%-38%.
“We were very diligent and went through every possible diagnosis we could think of that would give you a reason to remove ovaries,” Dr. Mahal said. “Even being exhaustive in that manner, we could not find a reason why for more than one in three women who underwent oophorectomy prior to natural menopause.”
Logistic regression analysis revealed Hispanic and black race as the only demographic factors associated with an increased odds of inappropriate oophorectomy at the time of hysterectomy (P less than .001). Hospital characteristics and type of insurance did not account for any observed differences.
Even if premenopausal women have no risk factors for ovarian cancer in the future, undergoing an oophorectomy “is a decision they should make with their physician,” Dr. Mahal said. “One of the things we don’t know [about this study] is how many patients had a conversation with their doctor, understood the risks, and decided ‘it’s worth it for me to go ahead and remove the ovaries at the time of the hysterectomy.’ ”
The meeting was jointly sponsored by the American College of Surgeons.
Dr. Mahal reported having no financial disclosures.
FROM SGS 2016
Key clinical point: More than one in three women underwent oophorectomy prior to natural menopause for no apparent reason.
Major finding: Of the oophorectomies in premenopausal women, 37% were deemed to be “inappropriate” based on the documented reason for removal.
Data source: A review of 259,294 inpatient, nonradical hysterectomies performed in California hospitals between 2005 and 2011.
Disclosures: Dr. Mahal reported having no financial disclosures.
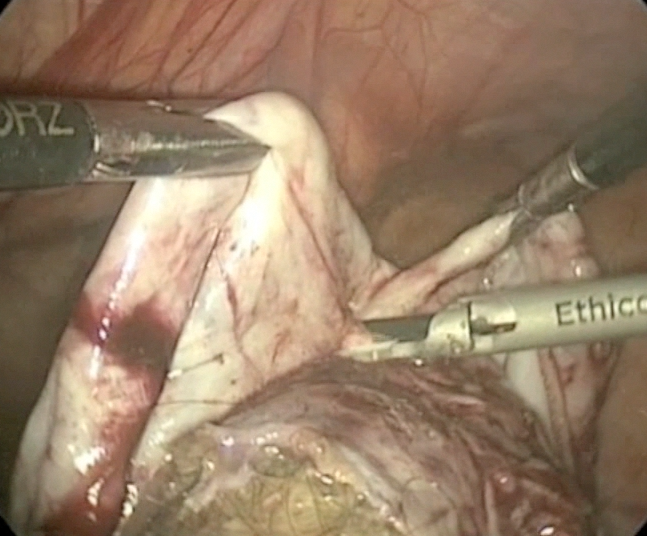
Laparoscopic cystectomy for large, bilateral ovarian dermoids
For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org
For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org
For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org
This video is brought to you by 
Surgical issues top reasons for readmissions after hysterectomy
INDIAN WELLS, CALIF. – Unplanned, 30-day readmissions after hysterectomy for benign indications mainly occur because of surgical complications, regardless of approach, with the most common issue being surgical site infections.
Additionally, there is an increased vulnerability to readmission shortly after discharge, especially within the first 15 days.
Those are the key findings from an analysis of the American College of Surgeons National Surgical Quality Improvement Project (ACS NSQIP) database participant user file for 2012 and 2013, presented by Dr. Courtney Penn at the annual scientific meeting of the Society of Gynecologic Surgeons.
“A seminal article in 2009 found that one in five Medicare patients are readmitted within 30 days, and unplanned readmissions account for 17% of total hospital payments from Medicare, or $17.4 billion annually,” said Dr. Penn, the lead study author and a resident in the department of obstetrics and gynecology at the University of Michigan, Ann Arbor. “Thus, addressing the problem of hospital readmissions is viewed as a golden opportunity to reduce healthcare costs and improve patient care quality. Despite this national focus on hospital readmissions, little is known about readmissions after hysterectomy.”
In an effort to characterize the most common reasons for unplanned 30-day readmissions following hysterectomy, and to characterize the timing of readmissions, the researchers retrospectively evaluated data from the ACS NSQIP database participant user file for 2012 and 2013. After using the International Classification of Diseases, Ninth Revision, Clinical Modification to identify common readmission diagnoses, they divided reasons for readmission into several categories: surgical site infection, surgical injury, non-infectious wound complications, gastrointestinal, genitourinary, venous thromboembolic, pain, medical, and “other” reasons. Results were stratified based on surgical approach.
Dr. Penn reported results from 40,580 patients who underwent hysterectomies at hospitals that participated in the ACS NSQIP. The overall, unadjusted readmission rate following hysterectomy was 2.8%, and was highest among those who underwent the procedure by abdominal approach (3.7%), followed by those who underwent the procedure by laparoscopic and vaginal approaches (2.6% vs. 2.1%, respectively).
After adjusting for potential confounding factors such as age, race, BMI, and operative time, readmissions were not significantly more likely when performed laparoscopically than with the vaginal approach. However, readmissions were significantly more likely when hysterectomy was performed via the open abdominal route, compared with the vaginal approach.
When categorizing reasons for reasons for readmission, traditional surgical complications, including surgical site infection, visceral entities, and non-infectious wound complications, were more common reasons for readmission than traditional medical complications, such as venous thromboembolism, myocardial infarction, and pulmonary edema. Slightly more than half of all readmissions (52%) were surgical in nature, compared with 9% that were attributable to traditional medical complications.
“This trend held true regardless of surgical approach, whether vaginal, laparoscopic, or abdominal,” Dr. Penn said.
Surgical site infections were the most common primary readmission diagnosis overall. “It was the underlying reason for readmission in approximately one-third of total readmissions,” she said. It was also the most common reason for readmission diagnosis for each surgical approach: 37% of abdominal, 28% of laparoscopic, and 33% of vaginal hysterectomy readmissions had a surgical site infection as the primary readmission diagnosis.
The researchers observed a few differences on reasons for readmission based on surgical approach. For example, surgical injury – such as hematoma and visceral injury – was higher after laparoscopic and vaginal hysterectomy, compared with that observed for abdominal cases (odds ratio, 2.4 and 2.8, respectively). Additionally, the proportion of readmissions related to gastrointestinal complications was higher after abdominal hysterectomies, compared with that observed among laparoscopic and vaginal cases (OR, 2.4 and 2.8, respectively).
For all surgical approaches, there was an increased likelihood of unplanned readmission within the first 15 days of discharge. In fact, 82% of all readmissions occurred within the first 15 days after discharge.
“We found that all major readmissions categories had a median time to readmission within the first 10 days after discharge, and the median time to readmission varied based on readmission diagnosis,” Dr. Penn said at the meeting, which was jointly sponsored by the American College of Surgeons. “Pain-related reasons for readmission had the shortest time to readmission, with a median of 3 days, and non-infectious wound complications had the longest time to readmission, with a median of 10 days.”
She acknowledged certain limitations of the study including the retrospective design, the database’s over-representation of urban and academic medical centers, as well the study’s reliance on one readmission diagnosis to capture the principal cause of readmission, “when the true reason for readmission may be multifactorial.”
Dr. Penn reported having no financial disclosures.
INDIAN WELLS, CALIF. – Unplanned, 30-day readmissions after hysterectomy for benign indications mainly occur because of surgical complications, regardless of approach, with the most common issue being surgical site infections.
Additionally, there is an increased vulnerability to readmission shortly after discharge, especially within the first 15 days.
Those are the key findings from an analysis of the American College of Surgeons National Surgical Quality Improvement Project (ACS NSQIP) database participant user file for 2012 and 2013, presented by Dr. Courtney Penn at the annual scientific meeting of the Society of Gynecologic Surgeons.
“A seminal article in 2009 found that one in five Medicare patients are readmitted within 30 days, and unplanned readmissions account for 17% of total hospital payments from Medicare, or $17.4 billion annually,” said Dr. Penn, the lead study author and a resident in the department of obstetrics and gynecology at the University of Michigan, Ann Arbor. “Thus, addressing the problem of hospital readmissions is viewed as a golden opportunity to reduce healthcare costs and improve patient care quality. Despite this national focus on hospital readmissions, little is known about readmissions after hysterectomy.”
In an effort to characterize the most common reasons for unplanned 30-day readmissions following hysterectomy, and to characterize the timing of readmissions, the researchers retrospectively evaluated data from the ACS NSQIP database participant user file for 2012 and 2013. After using the International Classification of Diseases, Ninth Revision, Clinical Modification to identify common readmission diagnoses, they divided reasons for readmission into several categories: surgical site infection, surgical injury, non-infectious wound complications, gastrointestinal, genitourinary, venous thromboembolic, pain, medical, and “other” reasons. Results were stratified based on surgical approach.
Dr. Penn reported results from 40,580 patients who underwent hysterectomies at hospitals that participated in the ACS NSQIP. The overall, unadjusted readmission rate following hysterectomy was 2.8%, and was highest among those who underwent the procedure by abdominal approach (3.7%), followed by those who underwent the procedure by laparoscopic and vaginal approaches (2.6% vs. 2.1%, respectively).
After adjusting for potential confounding factors such as age, race, BMI, and operative time, readmissions were not significantly more likely when performed laparoscopically than with the vaginal approach. However, readmissions were significantly more likely when hysterectomy was performed via the open abdominal route, compared with the vaginal approach.
When categorizing reasons for reasons for readmission, traditional surgical complications, including surgical site infection, visceral entities, and non-infectious wound complications, were more common reasons for readmission than traditional medical complications, such as venous thromboembolism, myocardial infarction, and pulmonary edema. Slightly more than half of all readmissions (52%) were surgical in nature, compared with 9% that were attributable to traditional medical complications.
“This trend held true regardless of surgical approach, whether vaginal, laparoscopic, or abdominal,” Dr. Penn said.
Surgical site infections were the most common primary readmission diagnosis overall. “It was the underlying reason for readmission in approximately one-third of total readmissions,” she said. It was also the most common reason for readmission diagnosis for each surgical approach: 37% of abdominal, 28% of laparoscopic, and 33% of vaginal hysterectomy readmissions had a surgical site infection as the primary readmission diagnosis.
The researchers observed a few differences on reasons for readmission based on surgical approach. For example, surgical injury – such as hematoma and visceral injury – was higher after laparoscopic and vaginal hysterectomy, compared with that observed for abdominal cases (odds ratio, 2.4 and 2.8, respectively). Additionally, the proportion of readmissions related to gastrointestinal complications was higher after abdominal hysterectomies, compared with that observed among laparoscopic and vaginal cases (OR, 2.4 and 2.8, respectively).
For all surgical approaches, there was an increased likelihood of unplanned readmission within the first 15 days of discharge. In fact, 82% of all readmissions occurred within the first 15 days after discharge.
“We found that all major readmissions categories had a median time to readmission within the first 10 days after discharge, and the median time to readmission varied based on readmission diagnosis,” Dr. Penn said at the meeting, which was jointly sponsored by the American College of Surgeons. “Pain-related reasons for readmission had the shortest time to readmission, with a median of 3 days, and non-infectious wound complications had the longest time to readmission, with a median of 10 days.”
She acknowledged certain limitations of the study including the retrospective design, the database’s over-representation of urban and academic medical centers, as well the study’s reliance on one readmission diagnosis to capture the principal cause of readmission, “when the true reason for readmission may be multifactorial.”
Dr. Penn reported having no financial disclosures.
INDIAN WELLS, CALIF. – Unplanned, 30-day readmissions after hysterectomy for benign indications mainly occur because of surgical complications, regardless of approach, with the most common issue being surgical site infections.
Additionally, there is an increased vulnerability to readmission shortly after discharge, especially within the first 15 days.
Those are the key findings from an analysis of the American College of Surgeons National Surgical Quality Improvement Project (ACS NSQIP) database participant user file for 2012 and 2013, presented by Dr. Courtney Penn at the annual scientific meeting of the Society of Gynecologic Surgeons.
“A seminal article in 2009 found that one in five Medicare patients are readmitted within 30 days, and unplanned readmissions account for 17% of total hospital payments from Medicare, or $17.4 billion annually,” said Dr. Penn, the lead study author and a resident in the department of obstetrics and gynecology at the University of Michigan, Ann Arbor. “Thus, addressing the problem of hospital readmissions is viewed as a golden opportunity to reduce healthcare costs and improve patient care quality. Despite this national focus on hospital readmissions, little is known about readmissions after hysterectomy.”
In an effort to characterize the most common reasons for unplanned 30-day readmissions following hysterectomy, and to characterize the timing of readmissions, the researchers retrospectively evaluated data from the ACS NSQIP database participant user file for 2012 and 2013. After using the International Classification of Diseases, Ninth Revision, Clinical Modification to identify common readmission diagnoses, they divided reasons for readmission into several categories: surgical site infection, surgical injury, non-infectious wound complications, gastrointestinal, genitourinary, venous thromboembolic, pain, medical, and “other” reasons. Results were stratified based on surgical approach.
Dr. Penn reported results from 40,580 patients who underwent hysterectomies at hospitals that participated in the ACS NSQIP. The overall, unadjusted readmission rate following hysterectomy was 2.8%, and was highest among those who underwent the procedure by abdominal approach (3.7%), followed by those who underwent the procedure by laparoscopic and vaginal approaches (2.6% vs. 2.1%, respectively).
After adjusting for potential confounding factors such as age, race, BMI, and operative time, readmissions were not significantly more likely when performed laparoscopically than with the vaginal approach. However, readmissions were significantly more likely when hysterectomy was performed via the open abdominal route, compared with the vaginal approach.
When categorizing reasons for reasons for readmission, traditional surgical complications, including surgical site infection, visceral entities, and non-infectious wound complications, were more common reasons for readmission than traditional medical complications, such as venous thromboembolism, myocardial infarction, and pulmonary edema. Slightly more than half of all readmissions (52%) were surgical in nature, compared with 9% that were attributable to traditional medical complications.
“This trend held true regardless of surgical approach, whether vaginal, laparoscopic, or abdominal,” Dr. Penn said.
Surgical site infections were the most common primary readmission diagnosis overall. “It was the underlying reason for readmission in approximately one-third of total readmissions,” she said. It was also the most common reason for readmission diagnosis for each surgical approach: 37% of abdominal, 28% of laparoscopic, and 33% of vaginal hysterectomy readmissions had a surgical site infection as the primary readmission diagnosis.
The researchers observed a few differences on reasons for readmission based on surgical approach. For example, surgical injury – such as hematoma and visceral injury – was higher after laparoscopic and vaginal hysterectomy, compared with that observed for abdominal cases (odds ratio, 2.4 and 2.8, respectively). Additionally, the proportion of readmissions related to gastrointestinal complications was higher after abdominal hysterectomies, compared with that observed among laparoscopic and vaginal cases (OR, 2.4 and 2.8, respectively).
For all surgical approaches, there was an increased likelihood of unplanned readmission within the first 15 days of discharge. In fact, 82% of all readmissions occurred within the first 15 days after discharge.
“We found that all major readmissions categories had a median time to readmission within the first 10 days after discharge, and the median time to readmission varied based on readmission diagnosis,” Dr. Penn said at the meeting, which was jointly sponsored by the American College of Surgeons. “Pain-related reasons for readmission had the shortest time to readmission, with a median of 3 days, and non-infectious wound complications had the longest time to readmission, with a median of 10 days.”
She acknowledged certain limitations of the study including the retrospective design, the database’s over-representation of urban and academic medical centers, as well the study’s reliance on one readmission diagnosis to capture the principal cause of readmission, “when the true reason for readmission may be multifactorial.”
Dr. Penn reported having no financial disclosures.
AT SGS 2016
Key clinical point: More than half of readmissions following hysterectomy were for surgical reasons.
Major finding: Slightly more than half of all readmissions (52%) were attributed to surgical complications, compared with 9% for medical complications.
Data source: A retrospective review of 40,580 patients who underwent hysterectomies at hospitals nationwide.
Disclosures: Dr. Penn reported having no financial disclosures.
On-site reporting from the Society of Gynecologic Surgeons 2016 annual meeting
4/13/16. DAY 4 AT SGS
A jam-packed day of sessions, posters, awards, and clinical updates
Our last educational day was kicked off by a fascinating lecture by Dr. Amy Park on the “Genetic Determinants of Pelvic Organ Prolapse in Women of European American Descent: The Women’s Health Initiative.” Dr. Park and her colleagues found that there is evidence of phenotypic and genotypic heterogeneity in patients with pelvic organ prolapse, and there were 4 genetic loci identified that correlated with prolapse. Any uterine prolapse was associated with a genome-wide significant intergenic variant on chromosome 13, cystocele was associated with LOXL2, and all prolapse was associated with BMP.
Surmounting surgical site infection
Dr. Sarah Andiman then gave a lecture on the effects of a perioperative bundle and offered timely feedback for surgical site infection (SSI) prevention in hysterectomy. We all know that wound infections are a major morbidity associated with surgery, and Dr. Andiman’s group at Yale found that, by implementing this prevention program, the surgical site infection decreased 52.8%. Another suggestion from the audience was to have all patients use chlorhexidine wipes the night before and morning of a surgery to decrease wound infection. Similarly, Dr. Ali Bazzi gave a lecture on “Chlorhexidine-Alcohol Compared with Povidone-Iodine for Surgical-Site Antisepsis after Abdominal Hysterectomy.” The chlorhexidine was associated with 30% lower odds of SSI compared with povidone-iodine, even though this group had several medical comorbidities and risk factors known for SSIs.
Oral poster presenters make several interesting points
Dr. Christopher Ripperda from UT Southwestern Medical Center in Dallas, Texas, found that medical comorbidities and the presence of detrusor overactivity and PVR are predictors of early postoperative voiding dysfunction following a midurethral sling placement. Dr. Nabila Noor then described a fabulous surgical alternative to the use of morcellation to remove the uterus after a supracervical hysterectomy. She described the technique for performing a posterior colpotomy and stated that patients who had a surgery performed at her institution using this technique did not experience increased postoperative pain or longer postoperative stay.
Dr. Jennifer Thompson then shed some light on a very important question related to the Sunshine Act: Are physicians including all of their disclosures when they submit articles to a conference? When the physicians who submitted an abstract to the Society of Gynecologic Surgeons (SGS) in 2015 were searched on the Centers for Medicare and Medicaid Services (CMS) website, 62% of them had incomplete disclosures, with a total of nondisclosed CMS transactions equaling $1.3 million. We can do better!
Status update: The FPRN and passing of the torch
Congratulations to Dr. Kristin Jacobs, the new Fellows’ Pelvic Research Network (FPRN) Chair! The morning session ended with an innovative video from Dr. Janet Li and colleagues on the “Use of Suprapubic Carter-Thomason Needle to Assist in Cystoscopic Excision of Intravesical Foreign Object.”
The winner of the Distinguished Surgeon Award was given to Dr. Javier Magrina, and the SGS gavel was passed on to Dr. Vivian Sung! Congratulations!
Dr. Stephanie Pickett kicked off the eighth scientific session with a study entitled, “Comparing Methods of NSAID Delivery for Postoperative Pain.” When she and her colleagues compared IV toradol to IV ibuprofen for postoperative pain control after urogynecologic surgery, they found that patients experienced similar rates of pain control and satisfaction regardless of the type of analgesia.
Why are patients being readmitted after gynecologic oncology surgery?
The answer to this question is important as readmission rates are being considered for physician and hospital reimbursement. Dr. MaryAnn Wilbur and colleagues looked at the rates of unplanned 30-day readmission in gyn oncology patients. The patients who were readmitted had the following characteristics: ovarian cancer, creation of ostomy, Charleston score >5, language barrier, and positive discharge screen. Gastrointestinal disturbance and SSI were the most common reasons for readmission, and the total readmission-related costs for these patients was about $4.5 million.
Considering tissue extraction, surgical complications, and cognitive impairment
We then had 3 fabulous oral poster presentations. Dr. Emily Von Bargen and colleagues presented a study entitled, “Prevalence of Occult Pre-malignant or Malignant Pathology at the time of Uterine Morcellation for Benign Disease.” They performed a multicenter retrospective cohort study and found that 1.2% of women had a premalignant or malignant uterine pathology after surgery, with a prevalence of 0.66% of occult malignancy. She was unable to identify risk factors for those patients who had a premalignant or malignant pathology. Overall she found a low prevalence of premalignant or malignant uterine pathology when uterine morcellation was performed for benign disease.
Dr. Alix Leader-Cramer from Northwestern University pointed out “risk factors for a 30-day perioperative complications for total vaginal hysterectomy,” including chronic steroid use, higher ASA classification, current smoking status, diabetes, and lower preoperative serum albumin and sodium levels. Adnexectomy and resident participation were also associated with increased perioperative complications. About 9.5% of patients had a perioperative complication in the study population studied.
Finally, Dr. Elisa Trowbridge pointed out in her talk, on “Cognitive Impairment among Elderly Urogynecologic Patients,” that cognitive impairment is very prevalent among such women aged older than 75 years, and the Mini-Cog is a feasible screening tool.
What a way to end an AMAZING conference!
The conference ended with a fabulous video presentation by Dr. Andrea Benton, entitled “Surgical Approaches to the Management of Bladder and Ureteral Endometriosis.” Overall, the themes of this year’s SGS conference were to:
- emphasize the importance of performing a vaginal hysterectomy when feasible
- continue to strive to balance innovation with experimentation
- ensure that patients are being operated on by surgeons who are competent and frequently performing the indicated procedure.
Thank you to everyone who shared their research to educate the attendees at the conference! I can’t wait until next year!
4/12/16. DAY 3 AT SGS
Vaginal hysterectomy, fecal incontinence, transgender surgery amid tackled topics in Palm Springs
I could get used to sipping my coffee with the sunny background here in Palm Springs! It was a beautiful morning to learn.
We started the day with breakfast and a fabulous lecture on the inferior gluteal neurovascular anatomy in female cadavers, and an insightful lecture by Dr. Bhumy Dave, who brought up concerns about tracking for obstetrics and gynecology residency programs. She specifically highlighted the need for more experience with vaginal hysterectomies for residents who are going to be in a subspecialty that performs vaginal surgery. As the number of hysterectomies, specifically vaginal hysterectomies, declines every year, we need to make sure we are adequately training the physicians who will be performing this procedure in the future. One solution is to have residents join a track their 4th year of residency, after their future career path has been established. Another possible solution would be to increase use of a simulation model for vaginal hysterectomy, as described by Dr. Douglas Miyazaki.
Indigo carmine replacement? A recent issue in gynecologic surgery resulted when there was a national shortage of indigo carmine, which is commonly used to identify UO efflux at the time of cystoscopy. Dr. Katie Propst provided a solution: In the setting of planned cystoscopy, she found that preoperative phenazopyridine is an acceptable alternative and its use led to similar UO identification as with indigo carmine without an increase in complications.
Who should have a vaginal hysterectomy? Dr. Jennifer Schmitt from the Mayo Clinic gave another wonderful lecture describing a decision-tree algorithm for determining the ideal route of hysterectomy. According to a retrospective review of patients at their institution, vaginal hysterectomy was associated with lower infection rates, operative times, and costs.
The highlight of the morning was a very insightful Presidential Address by Dr. Andrew Walter! Not only is a he a very entertaining speaker but he also shed some light on 2 challenges that we currently face in the field. He eloquently stated that, “every woman who is a candidate for a vaginal hysterectomy should be able to get one and have it performed competently, and every woman who needs surgery should have one performed by someone who performs enough surgeries every year to competently perform the surgery.” He frequently alluded to the wise Dr. Mayo, who stated, “The best interest of the patient is the only interest to be considered…” Let’s never forget this as physicians!
Do you find removing the adnexa challenging when performing vaginal surgery? Check out the amazing idea from the Cleveland Clinic shown in video presentation 05! They clearly demonstrate using a single-site gel port or surgical glove placed in the vaginal incision to perform laparoscopy through the vagina. What a novel idea to avoid any abdominal incisions when there is a difficult vaginal adnexal surgery!
After the morning break, we watched a master vaginal surgeon perform a sacral colpopexy through the vaginal route. For details on this method, please reference video presentation 06.
An increase in health care costs is a huge problem in this country. Dr. Mary Van Meter suggested that one area in which we can improve is in the operating room (OR), specifically through decreasing the number of instruments sterilized. She found that only approximately 20% of the instruments on the operating field were actually used by the OR physician. It costs about $3 per instrument on the tray at Vanderbilt University, she said. When you think of the few number of instruments actually used, if we work to limit the number of instruments on the trays, we could cut significant costs. As reimbursement is getting increasingly linked to cost reduction, we all should be thinking about innovative ways to cut costs.
The oral posters were all excellent!
Dr. Ann Peters showed that, at a high-volume tertiary-care center, multimodal preoperative testing failed to definitively identify leiomyosarcoma (LMS), and the factors associated with increased LMS risk included older age, menopause, and presence of fibroids with concurrent pelvic, uterine, or adnexal mass.
Dr. Kevin Kremer found that preoperative antibiotics were used in 23% of cases in which they were not indicated, and the increased use rate was associated with entrance into the abdomen during surgery, the individual surgeon, and time under anesthesia.
Dr. Jessica Heft then stated that the incontinence rate after midurethral sling revision for vaginal exposure or pain was significantly higher with a partial as opposed to complete mesh excision.
Fecal incontinence treatment options
Dr. Peter Rosenblatt tackled the issue of “Innovation or experimentation: Where do we draw the line?” in the TeLinde lecture. He started by describing a condition for which he feels we do not have an acceptable amount of treatment options for patients: fecal incontinence. He described how he observed that the puborectalis muscle, not the external anal sphincter, was critical for fecal continence. He then devised a surgery that created a sling that would act as a synthetic puborectalis muscle. He had amazing success until one patient had a serious complication. Should you abandon a successful, innovative surgery due to one very severe complication, was the question. Where do we draw the line? I don’t have an answer…but I do know that we all need to thank our puborectalis muscle for our daily fecal continence!
This is not a new issue in medicine, explained Dr. Rosenblatt. From the beginning of medicine, there has been a balance between innovation and experimentation. So, what is innovation? It is when someone improves upon a device or process. In medicine, is it innovation or just variation? We frequently use medications and devices “off label,” and these techniques often improve our surgeries and outcomes for our patients. Innovation comes about through careful planning, a necessity created by an emergency, advances in technology, and through evolution of a procedure. Who are the innovators? YOU are! We are the ones who understand the unmet needs and the potential opportunities for improving medicine. Let’s all work together to innovate NOT experiment and make medicine better so our patients have the best care possible!
“New Frontiers in Gynecologic Surgery: Transgender Surgery and Functional Clitoroplasty after Female Genital Mutilation”
The final talk for the day was by the groundbreaking Dr. Marci Bowers, whose lecture started by reminding everyone that there is a difference between gender identity and gender expression. Once a person knows his or her gender identity they use gender expression to express this to the world, she pointed out. Dr. Bowers is a true innovator and is performing gender reassignment surgeries as well as female genital mutilation corrective surgeries. She has perfected a one-stage vaginoplasty, and she showed a video of the procedure, which results in a 90% chance of orgasm. She also noted that she is able to restore clitoral function in 100% of the cases of genital mutilation, and she performs these procedures free of charge.
She reminded us that all ObGyns need to be trained in treating transgender patients, and given the high rate of suicide among adolescent transgender individuals, we all need to work together to provide a supportive medical environment to help these patients. What a fascinating end to the day!
Some relaxation, and entertainment, amid the sun and outdoors
We then had the afternoon to compete in a golf tournament, explore the area on mountain bikes, or lounge by the pool. Regardless of the daytime activities, we all came back together for the great lip-synch competition! All 4 teams gave an impressive performance, but the team from Brown University went home with the win! Such an entertaining event! (Thanks to incoming SGS President Vivian Sung @wih_sung for the pic!)
4/11/16. DAY 2 AT SGS
Experts talk surgical innovations, complementary therapies, value-based payment, and much more at SGS day 2
Wake up and learn! The second day of the 42nd Annual Scientific Meeting of the Society of Gynecologic Surgeons began with a review of research posters at the Poster Session as the sun rose over the Palm Springs mountains. We then moved indoors for the scientific sessions.
In the first lecture, "Reasons for Unplanned 30-Day Readmission After Hysterectomy for Benign Disease," Dr. Courtney Penn and colleagues reiterated that the postsurgical readmission rate is higher for patients undergoing abdominal hysterectomy compared with those who have a laparoscopic or vaginal hysterectomy. Similarly, Dr. Jennifer Schmitt and colleagues suggested that in a patient with a relative contraindication for vaginal hysterectomy, when this procedure is performed by an experienced surgeon there may not be increased complications. However, keep in mind that the study described—"A Comparison of Vaginal and Robotic Hysterectomy for Commonly Cited Relative Contraindications to Vaginal Hysterectomy"—was performed at the Mayo Clinic by expert, highly trained surgeons, and this fact may limit the generalizability of the study. As one audience member eloquently stated, it is important to remember that: "Just because it is feasible does not mean it is the correct procedure."
That yoga or barre class may be doing more good than you think! Lunge, bridge, and cat-into-cow movements may provide a greater degree of pelvic floor muscle unit recruitment than traditional Kegel exercises, according to a presentation by Dr. Bruce Crawford on Kegels versus specialized movement.
Perhaps those exercises should be recommended for surgeons as well. As Dr. Ruchira Singh pointed out, surgeons experience a high amount of musculoskeletal strain when performing vaginal procedures while sitting, regardless of the type of chair used during surgery. Dr. Singh and colleagues’ study, "Effect of Different Chairs on Work-Related Musculoskeletal Discomfort During Vaginal Surgery," found that while the round stool with a backrest and the Capisco chair were more comfortable, they did not eliminate the high risk for musculoskeletal strain, particularly in the head and neck.
Dr. Ann Peters and colleagues, from Magee-Womens Hospital of the University of Pittsburgh Medical Center, gave a fabulous video presentation on "Anatomic and Vascular Considerations in Laparoscopic Uterine Artery Ligation During Hysterectomy."
Need a novel treatment for interstitial cystitis/bladder pain syndrome? Consider mindfulness-based stress reduction. A randomized controlled study performed by Dr. Gregg Kanter and colleagues describes how this technique may help patients and could be considered a first-line therapy.
What is value-based payment and this new trend in reimbursement? And how does it apply to vaginal hysterectomy? Dr. Tina Groat addressed these issues in her keynote lecture. According to the American Congress of Obstetricians and Gynecologists, “Evidence demonstrates that, in general, vaginal hysterectomy is associated with better outcomes and fewer complications than laparoscopic or abdominal hysterectomy.” This is in opposition to what is actually being performed clinically. Dr. Groat explained that United Healthcare decided to incentivize physicians by requiring a prior authorization for all hysterectomies for benign disease. There is both a quality and cost benefit to performing a vaginal hysterectomy. Most insurance companies are moving away from a “fee for service” structure to performance-based payment. Change is always scary and, while I think the overall goal of moving toward the best care for our patients is a positive, this approach may create new challenges for the medical field. What do you think? Is performance-based payment beneficial? Or does it limit physicians and potentially force them to perform a procedure they do not feel as comfortable performing? Will this result in physicians rejecting certain patient populations? [Note from OBG MANAGEMENT: Let Dr. Collins know your thoughts through social media, or email OBG MANAGEMENT with a Letter to the Editor (rbarbieri@frontlinemedcom.com).]
The debate on the best route for hysterectomy continues: According to Dr. Carolyn Swenson and colleagues in their presentation, "Comparison of Robotic and Other Minimally Invasive Routes of Hysterectomy for Benign Indications," while there may be lower complications associated with robotic hysterectomy, the cost of performing a robotic hysterectomy is significantly higher than the cost of laparoscopic or vaginal hysterectomy, thus limiting its utility.
How can we teach a rare surgical procedure to learners? We channel our inner Martha Stewart and make a model out of a beef tongue and chicken. For about $8 a challenging and rare surgery can be taught to residents and medical students, according to the video presentation by Dr. Jana Illston and colleagues, titled "Modified Beef Tongue Model for Fourth-Degree Laceration Repair Simulation."
After the Day 2 lunch break, there was a rousing debate surrounding "Surgeons as Innovators—What Is the Patient Expecting?" Where do we draw the line between using an older more proven therapy as opposed to trying an innovative technology that may actually offer a potential benefit? Dr. Dennis Miller made a good point regarding innovation and pharmaceutical and device companies: If we ignore industry, we lose the ability to help with innovation and shape the future of medical treatments. Perhaps we should use the golden rule: If we would perform the surgery or use the device on ourselves, then we should perform it on our patient. Patients have a greater burden now, because there are more treatment options that they must choose among. Our job as physicians is to educate our patients and to guide them to innovative and evidence-based treatments.
Highlights from the afternoon oral poster session included a presentation by Dr. Caryn Russman that noted the high risk for recurrent urinary tract infection (UTI) after a mid-urethral sling procedure, which seems to be related to specific preoperative risk factors (such as a history of recurrent UTI). Dr. Tanya Hoke suggested that residents and attending physicians have inaccurate estimates of uterine weight, and an educational program may be necessary to improve these estimates. Finally, a study from Massachusetts General Hospital showed that a shorter stay in the hospital, ideally same-day surgery, resulted in a lower complication risk, lower number of emergency department visits, and a decreased readmission rate for patients undergoing urogynecology procedures.
The following recommendations were then suggested regarding vaginal hysterectomy:
- Preoperative prep with 4% chlorhexidine or povidine iodine
- Intracervical vasopressin injection to decrease blood loss
- Use of a pedicle-sealing device for pedicle ligation
- Vertical cuff closure is preferred to maximize vaginal length
Another important point made was that a prior cesarean delivery is not a contraindication to performing a vaginal hysterectomy.
Recommendations regarding recurrent UTI were also made, which include the recommendation for preoperative use of antibiotics to decrease the rate of UTI, with no benefit for a longer course of antibiotics.
News from the Fellows’ Pelvic Research Network
So much exciting research currently is ongoing with the FPRN! New project ideas include comparison of trimethoprim with methenamie for treatment of recurrent UTI; comparison of laparoscopic/robotic sacrocolpopexy with vaginal USLS for management of apical prolapse; a survey study examining surgeon preferences for timing of midurethral sling placement when performed at the time of pelvic organ prolapse (POP) repair; an assessment of the effect of a midurethal sling on overactive bladder in surgical repair in POP; and a study evaluating female pelvic reconstructive surgery in the setting of human immunodeficiency virus infection. It is so great to see the fellows working together to provide groundbreaking research!
Fun with stats
Learning statistics at the end of the day is never easy, but Dr. Matthew Barber did a fabulous job explaining this often-confusing topic. He reminded attendees that the key to learning statistics is repetition. One new recommendation he offered to enhance understanding is to use common language instead of numbers for P values. For example, instead of saying P <.001, use “is superior,” and instead of saying P = .3, use “seems not superior” or “inconclusive.”
A night to remember
The night ended with a wonderful awards ceremony and the president’s reception. Overall, day 2 was a very educational—and fun—day!
4/10/16. DAY 1 AT SGS
Postgrad courses address pain management and social media education
Mastering pelvic pain
With the beautiful Palm Springs, California, backdrop of mountains and palm trees, the 2016 meeting of the Society of Gynecologic Surgeons kicked off with 4 postgraduate courses. At the “Mastering Pelvic Pain: Strategies and Techniques for a Multimodal Approach” course, directed by Dr. Cara King, Dr. Matt Siedhoff explained the key components of the history and physical examination: Keep in mind that this generally is a multifactorial issue and may require a multidisciplinary approach, he told attendees. It is also important to make sure that the patient is fully prepared to combat the chronic pelvic pain (CPP) symptoms by focusing on the fundamentals, he said, including smoking, diet, exercise, weight loss, sleep, and relationship stress.
How is your posture? It turns out that something as simple as altering your posture can significantly affect pelvic floor control. Carol Sobeck, PT, demonstrated this importance with a simple group exercise that proved how the ability to contract the pelvic floor changes significantly with posture. Get to know your pelvic floor physical therapist—they are critical in helping with the treatment of CPP.
But what to do when physical therapy fails? Dr. Jennifer Gunter shed some light on this very difficult medical situation. One suggestion, she said, is to consider the possibility of a local presentation of a systemic issue and screen for the following: fibromyalgia, Ehlers-Danlos syndrome, statin use, and diabetes mellitus. Other treatment ideas include trigger point injections and onabotulinumtoxin A (Botox) therapy. A trigger point is a hypercontracted focus of muscle. To treat a trigger point, a needle must mechanically disrupt the trigger point to reduce the pelvic pain, and injection of local anesthetic is only used to help with postprocedure discomfort. Botox in my pelvis, you ask? Yes! The goal is to block presynaptic release of acetylcholine, which is very effective at reducing muscle spasm.
Tackling endometriosis. Dr. King then described surgical techniques for endometriosis. She recommended that, for mild disease not in close proximity to vital structures, ablation is likely equivalent to excision. For deeply infiltrating endometriosis, or lesions in close proximity to vital structures, excision is more beneficial. Excision is always beneficial for pathologic diagnosis, she said. And she offered this tip for bladder endometriosis: place a stitch in the nodule to allow for counter traction. Here is another tip, for ovarian cystectomy: inject vasopressin (20 U in 60 mL) to help dissect the plane between the ovary and cyst wall, and consider presacral neurectomy for midline pain.
Dr. Frank Tu then explained that we should not think of it as the “terrible triad: endometriosis, irritable bowel syndrome, and interstitial cystsis,” but rather as a system out of balance. Both peripheral and central mechanisms are involved in the generation and maintenance of cross-organ sensitization, he pointed out, which may explain why patients receive multiple diagnoses that describe a myriad of complaints due to a lack of overall homeostasis.
While Dr. Alaa Abd-Elsayed described innovative nerve blocks for CPP, he emphasized that no one specific treatment will result in a complete resolution of symptoms.
Vaginal mesh placement and pain. Dr. Mario Castellanos gave a fabulous lecture describing the pain issues that surround vaginal mesh placement. Interestingly, he noted that many patients had pelvic pain prior to placement of vaginal mesh, and that pain likely only will worsen with mesh placement. Mesh may cause pain by causing inflammation, visceral injury, muscle injury, and nerve injury. While there are guidelines for where mesh should be placed for bladder slings (TVT and TOT) and for prolapse repair, studies show, he pointed out, that the mesh placement often disrupts several muscle groups and may directly injure a nerve.
Alternatives to the typical diagnoses for CPP. The morning ended with a lecture by Dr. Suzie As-Sanie, in which she reminded everyone to start with “gold standard” therapy but, if those fail, consider alternative diagnoses or a central pain disorder. She also suggested cognitive behavioral therapy for treatment of CPP. For patients who cannot afford cognitive behavioral therapy, there is a free online source at fibroguide.med.umich.edu. Other alternative treatment options include exercise, patient education, instruction on sleep hygiene, and neurostimulatory therapies.
Overall, all the speakers this morning agreed that CPP is rarely treated with one modality, and it is best treated with a multidisciplinary approach.
Let’s get social!
The afternoon was spent learning about ways to use social networking sites to educate our patients, in another postgraduate course on “Making Media Social,” presented by the SGS Social Media Committee. Given that a recent survey demonstrated that 74.1% of women have some type of social networking account, it can be a very useful source for medical information for patients. If you have any questions about what is appropriate on social media, check out ACOG committee opinion 622.
Here are some tips that I learned:
Facebook:
- Keep your private Facebook page private and create a separate professional Facebook page
- Adjust your login setting so only administrators can post on your professional page
- Adjust settings so your professional profile cannot be “tagged”
- If a patient contacts your personal page, direct them to your professional page
- Do not give medical advice since Facebook is not digitally encrypted
Twitter:
- “Short bursts of inconsequential information”
- Follow societies, medical centers, and medical journals
LinkedIn:
- It provides a great way to find jobs, people, and business opportunities that are recommended by someone in your contact group
- It is specifically there to help you grow your business and show people who you are and where you have come from
Doximity:
Before we get to tips, first, what is it? Well, Doximity is basically a “LinkedIn” for physicians. It is “a way to find relevant specialists for patients; a rolodex; an email and text service; and a virtual lounge.” It is currently transforming from social network into a ‘platform.’ Now more than 1,000 hospitals and health systems are part of Doximity. Tips:
- There is a secure message option, which is HIPAA compliant
- Provides a way for residents and fellows to understand possible future places of employment
- It is a great way to find someone to refer patients to in an unfamiliar location
Vimeo:
- A benefit over YouTube is the lack of advertisements
- Check out the SGS video archives!
- You also can set privacy settings and embedding stats
Fifty-nine percent of US adults have looked online for health information in the past year. Therefore, it is important for physicians to get good information out for people to see!
A relaxing day’s end
The night ended with a beautiful poolside reception! I can’t wait to see what day 2 will bring!
4/13/16. DAY 4 AT SGS
A jam-packed day of sessions, posters, awards, and clinical updates
Our last educational day was kicked off by a fascinating lecture by Dr. Amy Park on the “Genetic Determinants of Pelvic Organ Prolapse in Women of European American Descent: The Women’s Health Initiative.” Dr. Park and her colleagues found that there is evidence of phenotypic and genotypic heterogeneity in patients with pelvic organ prolapse, and there were 4 genetic loci identified that correlated with prolapse. Any uterine prolapse was associated with a genome-wide significant intergenic variant on chromosome 13, cystocele was associated with LOXL2, and all prolapse was associated with BMP.
Surmounting surgical site infection
Dr. Sarah Andiman then gave a lecture on the effects of a perioperative bundle and offered timely feedback for surgical site infection (SSI) prevention in hysterectomy. We all know that wound infections are a major morbidity associated with surgery, and Dr. Andiman’s group at Yale found that, by implementing this prevention program, the surgical site infection decreased 52.8%. Another suggestion from the audience was to have all patients use chlorhexidine wipes the night before and morning of a surgery to decrease wound infection. Similarly, Dr. Ali Bazzi gave a lecture on “Chlorhexidine-Alcohol Compared with Povidone-Iodine for Surgical-Site Antisepsis after Abdominal Hysterectomy.” The chlorhexidine was associated with 30% lower odds of SSI compared with povidone-iodine, even though this group had several medical comorbidities and risk factors known for SSIs.
Oral poster presenters make several interesting points
Dr. Christopher Ripperda from UT Southwestern Medical Center in Dallas, Texas, found that medical comorbidities and the presence of detrusor overactivity and PVR are predictors of early postoperative voiding dysfunction following a midurethral sling placement. Dr. Nabila Noor then described a fabulous surgical alternative to the use of morcellation to remove the uterus after a supracervical hysterectomy. She described the technique for performing a posterior colpotomy and stated that patients who had a surgery performed at her institution using this technique did not experience increased postoperative pain or longer postoperative stay.
Dr. Jennifer Thompson then shed some light on a very important question related to the Sunshine Act: Are physicians including all of their disclosures when they submit articles to a conference? When the physicians who submitted an abstract to the Society of Gynecologic Surgeons (SGS) in 2015 were searched on the Centers for Medicare and Medicaid Services (CMS) website, 62% of them had incomplete disclosures, with a total of nondisclosed CMS transactions equaling $1.3 million. We can do better!
Status update: The FPRN and passing of the torch
Congratulations to Dr. Kristin Jacobs, the new Fellows’ Pelvic Research Network (FPRN) Chair! The morning session ended with an innovative video from Dr. Janet Li and colleagues on the “Use of Suprapubic Carter-Thomason Needle to Assist in Cystoscopic Excision of Intravesical Foreign Object.”
The winner of the Distinguished Surgeon Award was given to Dr. Javier Magrina, and the SGS gavel was passed on to Dr. Vivian Sung! Congratulations!
Dr. Stephanie Pickett kicked off the eighth scientific session with a study entitled, “Comparing Methods of NSAID Delivery for Postoperative Pain.” When she and her colleagues compared IV toradol to IV ibuprofen for postoperative pain control after urogynecologic surgery, they found that patients experienced similar rates of pain control and satisfaction regardless of the type of analgesia.
Why are patients being readmitted after gynecologic oncology surgery?
The answer to this question is important as readmission rates are being considered for physician and hospital reimbursement. Dr. MaryAnn Wilbur and colleagues looked at the rates of unplanned 30-day readmission in gyn oncology patients. The patients who were readmitted had the following characteristics: ovarian cancer, creation of ostomy, Charleston score >5, language barrier, and positive discharge screen. Gastrointestinal disturbance and SSI were the most common reasons for readmission, and the total readmission-related costs for these patients was about $4.5 million.
Considering tissue extraction, surgical complications, and cognitive impairment
We then had 3 fabulous oral poster presentations. Dr. Emily Von Bargen and colleagues presented a study entitled, “Prevalence of Occult Pre-malignant or Malignant Pathology at the time of Uterine Morcellation for Benign Disease.” They performed a multicenter retrospective cohort study and found that 1.2% of women had a premalignant or malignant uterine pathology after surgery, with a prevalence of 0.66% of occult malignancy. She was unable to identify risk factors for those patients who had a premalignant or malignant pathology. Overall she found a low prevalence of premalignant or malignant uterine pathology when uterine morcellation was performed for benign disease.
Dr. Alix Leader-Cramer from Northwestern University pointed out “risk factors for a 30-day perioperative complications for total vaginal hysterectomy,” including chronic steroid use, higher ASA classification, current smoking status, diabetes, and lower preoperative serum albumin and sodium levels. Adnexectomy and resident participation were also associated with increased perioperative complications. About 9.5% of patients had a perioperative complication in the study population studied.
Finally, Dr. Elisa Trowbridge pointed out in her talk, on “Cognitive Impairment among Elderly Urogynecologic Patients,” that cognitive impairment is very prevalent among such women aged older than 75 years, and the Mini-Cog is a feasible screening tool.
What a way to end an AMAZING conference!
The conference ended with a fabulous video presentation by Dr. Andrea Benton, entitled “Surgical Approaches to the Management of Bladder and Ureteral Endometriosis.” Overall, the themes of this year’s SGS conference were to:
- emphasize the importance of performing a vaginal hysterectomy when feasible
- continue to strive to balance innovation with experimentation
- ensure that patients are being operated on by surgeons who are competent and frequently performing the indicated procedure.
Thank you to everyone who shared their research to educate the attendees at the conference! I can’t wait until next year!
4/12/16. DAY 3 AT SGS
Vaginal hysterectomy, fecal incontinence, transgender surgery amid tackled topics in Palm Springs
I could get used to sipping my coffee with the sunny background here in Palm Springs! It was a beautiful morning to learn.
We started the day with breakfast and a fabulous lecture on the inferior gluteal neurovascular anatomy in female cadavers, and an insightful lecture by Dr. Bhumy Dave, who brought up concerns about tracking for obstetrics and gynecology residency programs. She specifically highlighted the need for more experience with vaginal hysterectomies for residents who are going to be in a subspecialty that performs vaginal surgery. As the number of hysterectomies, specifically vaginal hysterectomies, declines every year, we need to make sure we are adequately training the physicians who will be performing this procedure in the future. One solution is to have residents join a track their 4th year of residency, after their future career path has been established. Another possible solution would be to increase use of a simulation model for vaginal hysterectomy, as described by Dr. Douglas Miyazaki.
Indigo carmine replacement? A recent issue in gynecologic surgery resulted when there was a national shortage of indigo carmine, which is commonly used to identify UO efflux at the time of cystoscopy. Dr. Katie Propst provided a solution: In the setting of planned cystoscopy, she found that preoperative phenazopyridine is an acceptable alternative and its use led to similar UO identification as with indigo carmine without an increase in complications.
Who should have a vaginal hysterectomy? Dr. Jennifer Schmitt from the Mayo Clinic gave another wonderful lecture describing a decision-tree algorithm for determining the ideal route of hysterectomy. According to a retrospective review of patients at their institution, vaginal hysterectomy was associated with lower infection rates, operative times, and costs.
The highlight of the morning was a very insightful Presidential Address by Dr. Andrew Walter! Not only is a he a very entertaining speaker but he also shed some light on 2 challenges that we currently face in the field. He eloquently stated that, “every woman who is a candidate for a vaginal hysterectomy should be able to get one and have it performed competently, and every woman who needs surgery should have one performed by someone who performs enough surgeries every year to competently perform the surgery.” He frequently alluded to the wise Dr. Mayo, who stated, “The best interest of the patient is the only interest to be considered…” Let’s never forget this as physicians!
Do you find removing the adnexa challenging when performing vaginal surgery? Check out the amazing idea from the Cleveland Clinic shown in video presentation 05! They clearly demonstrate using a single-site gel port or surgical glove placed in the vaginal incision to perform laparoscopy through the vagina. What a novel idea to avoid any abdominal incisions when there is a difficult vaginal adnexal surgery!
After the morning break, we watched a master vaginal surgeon perform a sacral colpopexy through the vaginal route. For details on this method, please reference video presentation 06.
An increase in health care costs is a huge problem in this country. Dr. Mary Van Meter suggested that one area in which we can improve is in the operating room (OR), specifically through decreasing the number of instruments sterilized. She found that only approximately 20% of the instruments on the operating field were actually used by the OR physician. It costs about $3 per instrument on the tray at Vanderbilt University, she said. When you think of the few number of instruments actually used, if we work to limit the number of instruments on the trays, we could cut significant costs. As reimbursement is getting increasingly linked to cost reduction, we all should be thinking about innovative ways to cut costs.
The oral posters were all excellent!
Dr. Ann Peters showed that, at a high-volume tertiary-care center, multimodal preoperative testing failed to definitively identify leiomyosarcoma (LMS), and the factors associated with increased LMS risk included older age, menopause, and presence of fibroids with concurrent pelvic, uterine, or adnexal mass.
Dr. Kevin Kremer found that preoperative antibiotics were used in 23% of cases in which they were not indicated, and the increased use rate was associated with entrance into the abdomen during surgery, the individual surgeon, and time under anesthesia.
Dr. Jessica Heft then stated that the incontinence rate after midurethral sling revision for vaginal exposure or pain was significantly higher with a partial as opposed to complete mesh excision.
Fecal incontinence treatment options
Dr. Peter Rosenblatt tackled the issue of “Innovation or experimentation: Where do we draw the line?” in the TeLinde lecture. He started by describing a condition for which he feels we do not have an acceptable amount of treatment options for patients: fecal incontinence. He described how he observed that the puborectalis muscle, not the external anal sphincter, was critical for fecal continence. He then devised a surgery that created a sling that would act as a synthetic puborectalis muscle. He had amazing success until one patient had a serious complication. Should you abandon a successful, innovative surgery due to one very severe complication, was the question. Where do we draw the line? I don’t have an answer…but I do know that we all need to thank our puborectalis muscle for our daily fecal continence!
This is not a new issue in medicine, explained Dr. Rosenblatt. From the beginning of medicine, there has been a balance between innovation and experimentation. So, what is innovation? It is when someone improves upon a device or process. In medicine, is it innovation or just variation? We frequently use medications and devices “off label,” and these techniques often improve our surgeries and outcomes for our patients. Innovation comes about through careful planning, a necessity created by an emergency, advances in technology, and through evolution of a procedure. Who are the innovators? YOU are! We are the ones who understand the unmet needs and the potential opportunities for improving medicine. Let’s all work together to innovate NOT experiment and make medicine better so our patients have the best care possible!
“New Frontiers in Gynecologic Surgery: Transgender Surgery and Functional Clitoroplasty after Female Genital Mutilation”
The final talk for the day was by the groundbreaking Dr. Marci Bowers, whose lecture started by reminding everyone that there is a difference between gender identity and gender expression. Once a person knows his or her gender identity they use gender expression to express this to the world, she pointed out. Dr. Bowers is a true innovator and is performing gender reassignment surgeries as well as female genital mutilation corrective surgeries. She has perfected a one-stage vaginoplasty, and she showed a video of the procedure, which results in a 90% chance of orgasm. She also noted that she is able to restore clitoral function in 100% of the cases of genital mutilation, and she performs these procedures free of charge.
She reminded us that all ObGyns need to be trained in treating transgender patients, and given the high rate of suicide among adolescent transgender individuals, we all need to work together to provide a supportive medical environment to help these patients. What a fascinating end to the day!
Some relaxation, and entertainment, amid the sun and outdoors
We then had the afternoon to compete in a golf tournament, explore the area on mountain bikes, or lounge by the pool. Regardless of the daytime activities, we all came back together for the great lip-synch competition! All 4 teams gave an impressive performance, but the team from Brown University went home with the win! Such an entertaining event! (Thanks to incoming SGS President Vivian Sung @wih_sung for the pic!)
4/11/16. DAY 2 AT SGS
Experts talk surgical innovations, complementary therapies, value-based payment, and much more at SGS day 2
Wake up and learn! The second day of the 42nd Annual Scientific Meeting of the Society of Gynecologic Surgeons began with a review of research posters at the Poster Session as the sun rose over the Palm Springs mountains. We then moved indoors for the scientific sessions.
In the first lecture, "Reasons for Unplanned 30-Day Readmission After Hysterectomy for Benign Disease," Dr. Courtney Penn and colleagues reiterated that the postsurgical readmission rate is higher for patients undergoing abdominal hysterectomy compared with those who have a laparoscopic or vaginal hysterectomy. Similarly, Dr. Jennifer Schmitt and colleagues suggested that in a patient with a relative contraindication for vaginal hysterectomy, when this procedure is performed by an experienced surgeon there may not be increased complications. However, keep in mind that the study described—"A Comparison of Vaginal and Robotic Hysterectomy for Commonly Cited Relative Contraindications to Vaginal Hysterectomy"—was performed at the Mayo Clinic by expert, highly trained surgeons, and this fact may limit the generalizability of the study. As one audience member eloquently stated, it is important to remember that: "Just because it is feasible does not mean it is the correct procedure."
That yoga or barre class may be doing more good than you think! Lunge, bridge, and cat-into-cow movements may provide a greater degree of pelvic floor muscle unit recruitment than traditional Kegel exercises, according to a presentation by Dr. Bruce Crawford on Kegels versus specialized movement.
Perhaps those exercises should be recommended for surgeons as well. As Dr. Ruchira Singh pointed out, surgeons experience a high amount of musculoskeletal strain when performing vaginal procedures while sitting, regardless of the type of chair used during surgery. Dr. Singh and colleagues’ study, "Effect of Different Chairs on Work-Related Musculoskeletal Discomfort During Vaginal Surgery," found that while the round stool with a backrest and the Capisco chair were more comfortable, they did not eliminate the high risk for musculoskeletal strain, particularly in the head and neck.
Dr. Ann Peters and colleagues, from Magee-Womens Hospital of the University of Pittsburgh Medical Center, gave a fabulous video presentation on "Anatomic and Vascular Considerations in Laparoscopic Uterine Artery Ligation During Hysterectomy."
Need a novel treatment for interstitial cystitis/bladder pain syndrome? Consider mindfulness-based stress reduction. A randomized controlled study performed by Dr. Gregg Kanter and colleagues describes how this technique may help patients and could be considered a first-line therapy.
What is value-based payment and this new trend in reimbursement? And how does it apply to vaginal hysterectomy? Dr. Tina Groat addressed these issues in her keynote lecture. According to the American Congress of Obstetricians and Gynecologists, “Evidence demonstrates that, in general, vaginal hysterectomy is associated with better outcomes and fewer complications than laparoscopic or abdominal hysterectomy.” This is in opposition to what is actually being performed clinically. Dr. Groat explained that United Healthcare decided to incentivize physicians by requiring a prior authorization for all hysterectomies for benign disease. There is both a quality and cost benefit to performing a vaginal hysterectomy. Most insurance companies are moving away from a “fee for service” structure to performance-based payment. Change is always scary and, while I think the overall goal of moving toward the best care for our patients is a positive, this approach may create new challenges for the medical field. What do you think? Is performance-based payment beneficial? Or does it limit physicians and potentially force them to perform a procedure they do not feel as comfortable performing? Will this result in physicians rejecting certain patient populations? [Note from OBG MANAGEMENT: Let Dr. Collins know your thoughts through social media, or email OBG MANAGEMENT with a Letter to the Editor (rbarbieri@frontlinemedcom.com).]
The debate on the best route for hysterectomy continues: According to Dr. Carolyn Swenson and colleagues in their presentation, "Comparison of Robotic and Other Minimally Invasive Routes of Hysterectomy for Benign Indications," while there may be lower complications associated with robotic hysterectomy, the cost of performing a robotic hysterectomy is significantly higher than the cost of laparoscopic or vaginal hysterectomy, thus limiting its utility.
How can we teach a rare surgical procedure to learners? We channel our inner Martha Stewart and make a model out of a beef tongue and chicken. For about $8 a challenging and rare surgery can be taught to residents and medical students, according to the video presentation by Dr. Jana Illston and colleagues, titled "Modified Beef Tongue Model for Fourth-Degree Laceration Repair Simulation."
After the Day 2 lunch break, there was a rousing debate surrounding "Surgeons as Innovators—What Is the Patient Expecting?" Where do we draw the line between using an older more proven therapy as opposed to trying an innovative technology that may actually offer a potential benefit? Dr. Dennis Miller made a good point regarding innovation and pharmaceutical and device companies: If we ignore industry, we lose the ability to help with innovation and shape the future of medical treatments. Perhaps we should use the golden rule: If we would perform the surgery or use the device on ourselves, then we should perform it on our patient. Patients have a greater burden now, because there are more treatment options that they must choose among. Our job as physicians is to educate our patients and to guide them to innovative and evidence-based treatments.
Highlights from the afternoon oral poster session included a presentation by Dr. Caryn Russman that noted the high risk for recurrent urinary tract infection (UTI) after a mid-urethral sling procedure, which seems to be related to specific preoperative risk factors (such as a history of recurrent UTI). Dr. Tanya Hoke suggested that residents and attending physicians have inaccurate estimates of uterine weight, and an educational program may be necessary to improve these estimates. Finally, a study from Massachusetts General Hospital showed that a shorter stay in the hospital, ideally same-day surgery, resulted in a lower complication risk, lower number of emergency department visits, and a decreased readmission rate for patients undergoing urogynecology procedures.
The following recommendations were then suggested regarding vaginal hysterectomy:
- Preoperative prep with 4% chlorhexidine or povidine iodine
- Intracervical vasopressin injection to decrease blood loss
- Use of a pedicle-sealing device for pedicle ligation
- Vertical cuff closure is preferred to maximize vaginal length
Another important point made was that a prior cesarean delivery is not a contraindication to performing a vaginal hysterectomy.
Recommendations regarding recurrent UTI were also made, which include the recommendation for preoperative use of antibiotics to decrease the rate of UTI, with no benefit for a longer course of antibiotics.
News from the Fellows’ Pelvic Research Network
So much exciting research currently is ongoing with the FPRN! New project ideas include comparison of trimethoprim with methenamie for treatment of recurrent UTI; comparison of laparoscopic/robotic sacrocolpopexy with vaginal USLS for management of apical prolapse; a survey study examining surgeon preferences for timing of midurethral sling placement when performed at the time of pelvic organ prolapse (POP) repair; an assessment of the effect of a midurethal sling on overactive bladder in surgical repair in POP; and a study evaluating female pelvic reconstructive surgery in the setting of human immunodeficiency virus infection. It is so great to see the fellows working together to provide groundbreaking research!
Fun with stats
Learning statistics at the end of the day is never easy, but Dr. Matthew Barber did a fabulous job explaining this often-confusing topic. He reminded attendees that the key to learning statistics is repetition. One new recommendation he offered to enhance understanding is to use common language instead of numbers for P values. For example, instead of saying P <.001, use “is superior,” and instead of saying P = .3, use “seems not superior” or “inconclusive.”
A night to remember
The night ended with a wonderful awards ceremony and the president’s reception. Overall, day 2 was a very educational—and fun—day!
4/10/16. DAY 1 AT SGS
Postgrad courses address pain management and social media education
Mastering pelvic pain
With the beautiful Palm Springs, California, backdrop of mountains and palm trees, the 2016 meeting of the Society of Gynecologic Surgeons kicked off with 4 postgraduate courses. At the “Mastering Pelvic Pain: Strategies and Techniques for a Multimodal Approach” course, directed by Dr. Cara King, Dr. Matt Siedhoff explained the key components of the history and physical examination: Keep in mind that this generally is a multifactorial issue and may require a multidisciplinary approach, he told attendees. It is also important to make sure that the patient is fully prepared to combat the chronic pelvic pain (CPP) symptoms by focusing on the fundamentals, he said, including smoking, diet, exercise, weight loss, sleep, and relationship stress.
How is your posture? It turns out that something as simple as altering your posture can significantly affect pelvic floor control. Carol Sobeck, PT, demonstrated this importance with a simple group exercise that proved how the ability to contract the pelvic floor changes significantly with posture. Get to know your pelvic floor physical therapist—they are critical in helping with the treatment of CPP.
But what to do when physical therapy fails? Dr. Jennifer Gunter shed some light on this very difficult medical situation. One suggestion, she said, is to consider the possibility of a local presentation of a systemic issue and screen for the following: fibromyalgia, Ehlers-Danlos syndrome, statin use, and diabetes mellitus. Other treatment ideas include trigger point injections and onabotulinumtoxin A (Botox) therapy. A trigger point is a hypercontracted focus of muscle. To treat a trigger point, a needle must mechanically disrupt the trigger point to reduce the pelvic pain, and injection of local anesthetic is only used to help with postprocedure discomfort. Botox in my pelvis, you ask? Yes! The goal is to block presynaptic release of acetylcholine, which is very effective at reducing muscle spasm.
Tackling endometriosis. Dr. King then described surgical techniques for endometriosis. She recommended that, for mild disease not in close proximity to vital structures, ablation is likely equivalent to excision. For deeply infiltrating endometriosis, or lesions in close proximity to vital structures, excision is more beneficial. Excision is always beneficial for pathologic diagnosis, she said. And she offered this tip for bladder endometriosis: place a stitch in the nodule to allow for counter traction. Here is another tip, for ovarian cystectomy: inject vasopressin (20 U in 60 mL) to help dissect the plane between the ovary and cyst wall, and consider presacral neurectomy for midline pain.
Dr. Frank Tu then explained that we should not think of it as the “terrible triad: endometriosis, irritable bowel syndrome, and interstitial cystsis,” but rather as a system out of balance. Both peripheral and central mechanisms are involved in the generation and maintenance of cross-organ sensitization, he pointed out, which may explain why patients receive multiple diagnoses that describe a myriad of complaints due to a lack of overall homeostasis.
While Dr. Alaa Abd-Elsayed described innovative nerve blocks for CPP, he emphasized that no one specific treatment will result in a complete resolution of symptoms.
Vaginal mesh placement and pain. Dr. Mario Castellanos gave a fabulous lecture describing the pain issues that surround vaginal mesh placement. Interestingly, he noted that many patients had pelvic pain prior to placement of vaginal mesh, and that pain likely only will worsen with mesh placement. Mesh may cause pain by causing inflammation, visceral injury, muscle injury, and nerve injury. While there are guidelines for where mesh should be placed for bladder slings (TVT and TOT) and for prolapse repair, studies show, he pointed out, that the mesh placement often disrupts several muscle groups and may directly injure a nerve.
Alternatives to the typical diagnoses for CPP. The morning ended with a lecture by Dr. Suzie As-Sanie, in which she reminded everyone to start with “gold standard” therapy but, if those fail, consider alternative diagnoses or a central pain disorder. She also suggested cognitive behavioral therapy for treatment of CPP. For patients who cannot afford cognitive behavioral therapy, there is a free online source at fibroguide.med.umich.edu. Other alternative treatment options include exercise, patient education, instruction on sleep hygiene, and neurostimulatory therapies.
Overall, all the speakers this morning agreed that CPP is rarely treated with one modality, and it is best treated with a multidisciplinary approach.
Let’s get social!
The afternoon was spent learning about ways to use social networking sites to educate our patients, in another postgraduate course on “Making Media Social,” presented by the SGS Social Media Committee. Given that a recent survey demonstrated that 74.1% of women have some type of social networking account, it can be a very useful source for medical information for patients. If you have any questions about what is appropriate on social media, check out ACOG committee opinion 622.
Here are some tips that I learned:
Facebook:
- Keep your private Facebook page private and create a separate professional Facebook page
- Adjust your login setting so only administrators can post on your professional page
- Adjust settings so your professional profile cannot be “tagged”
- If a patient contacts your personal page, direct them to your professional page
- Do not give medical advice since Facebook is not digitally encrypted
Twitter:
- “Short bursts of inconsequential information”
- Follow societies, medical centers, and medical journals
LinkedIn:
- It provides a great way to find jobs, people, and business opportunities that are recommended by someone in your contact group
- It is specifically there to help you grow your business and show people who you are and where you have come from
Doximity:
Before we get to tips, first, what is it? Well, Doximity is basically a “LinkedIn” for physicians. It is “a way to find relevant specialists for patients; a rolodex; an email and text service; and a virtual lounge.” It is currently transforming from social network into a ‘platform.’ Now more than 1,000 hospitals and health systems are part of Doximity. Tips:
- There is a secure message option, which is HIPAA compliant
- Provides a way for residents and fellows to understand possible future places of employment
- It is a great way to find someone to refer patients to in an unfamiliar location
Vimeo:
- A benefit over YouTube is the lack of advertisements
- Check out the SGS video archives!
- You also can set privacy settings and embedding stats
Fifty-nine percent of US adults have looked online for health information in the past year. Therefore, it is important for physicians to get good information out for people to see!
A relaxing day’s end
The night ended with a beautiful poolside reception! I can’t wait to see what day 2 will bring!
4/13/16. DAY 4 AT SGS
A jam-packed day of sessions, posters, awards, and clinical updates
Our last educational day was kicked off by a fascinating lecture by Dr. Amy Park on the “Genetic Determinants of Pelvic Organ Prolapse in Women of European American Descent: The Women’s Health Initiative.” Dr. Park and her colleagues found that there is evidence of phenotypic and genotypic heterogeneity in patients with pelvic organ prolapse, and there were 4 genetic loci identified that correlated with prolapse. Any uterine prolapse was associated with a genome-wide significant intergenic variant on chromosome 13, cystocele was associated with LOXL2, and all prolapse was associated with BMP.
Surmounting surgical site infection
Dr. Sarah Andiman then gave a lecture on the effects of a perioperative bundle and offered timely feedback for surgical site infection (SSI) prevention in hysterectomy. We all know that wound infections are a major morbidity associated with surgery, and Dr. Andiman’s group at Yale found that, by implementing this prevention program, the surgical site infection decreased 52.8%. Another suggestion from the audience was to have all patients use chlorhexidine wipes the night before and morning of a surgery to decrease wound infection. Similarly, Dr. Ali Bazzi gave a lecture on “Chlorhexidine-Alcohol Compared with Povidone-Iodine for Surgical-Site Antisepsis after Abdominal Hysterectomy.” The chlorhexidine was associated with 30% lower odds of SSI compared with povidone-iodine, even though this group had several medical comorbidities and risk factors known for SSIs.
Oral poster presenters make several interesting points
Dr. Christopher Ripperda from UT Southwestern Medical Center in Dallas, Texas, found that medical comorbidities and the presence of detrusor overactivity and PVR are predictors of early postoperative voiding dysfunction following a midurethral sling placement. Dr. Nabila Noor then described a fabulous surgical alternative to the use of morcellation to remove the uterus after a supracervical hysterectomy. She described the technique for performing a posterior colpotomy and stated that patients who had a surgery performed at her institution using this technique did not experience increased postoperative pain or longer postoperative stay.
Dr. Jennifer Thompson then shed some light on a very important question related to the Sunshine Act: Are physicians including all of their disclosures when they submit articles to a conference? When the physicians who submitted an abstract to the Society of Gynecologic Surgeons (SGS) in 2015 were searched on the Centers for Medicare and Medicaid Services (CMS) website, 62% of them had incomplete disclosures, with a total of nondisclosed CMS transactions equaling $1.3 million. We can do better!
Status update: The FPRN and passing of the torch
Congratulations to Dr. Kristin Jacobs, the new Fellows’ Pelvic Research Network (FPRN) Chair! The morning session ended with an innovative video from Dr. Janet Li and colleagues on the “Use of Suprapubic Carter-Thomason Needle to Assist in Cystoscopic Excision of Intravesical Foreign Object.”
The winner of the Distinguished Surgeon Award was given to Dr. Javier Magrina, and the SGS gavel was passed on to Dr. Vivian Sung! Congratulations!
Dr. Stephanie Pickett kicked off the eighth scientific session with a study entitled, “Comparing Methods of NSAID Delivery for Postoperative Pain.” When she and her colleagues compared IV toradol to IV ibuprofen for postoperative pain control after urogynecologic surgery, they found that patients experienced similar rates of pain control and satisfaction regardless of the type of analgesia.
Why are patients being readmitted after gynecologic oncology surgery?
The answer to this question is important as readmission rates are being considered for physician and hospital reimbursement. Dr. MaryAnn Wilbur and colleagues looked at the rates of unplanned 30-day readmission in gyn oncology patients. The patients who were readmitted had the following characteristics: ovarian cancer, creation of ostomy, Charleston score >5, language barrier, and positive discharge screen. Gastrointestinal disturbance and SSI were the most common reasons for readmission, and the total readmission-related costs for these patients was about $4.5 million.
Considering tissue extraction, surgical complications, and cognitive impairment
We then had 3 fabulous oral poster presentations. Dr. Emily Von Bargen and colleagues presented a study entitled, “Prevalence of Occult Pre-malignant or Malignant Pathology at the time of Uterine Morcellation for Benign Disease.” They performed a multicenter retrospective cohort study and found that 1.2% of women had a premalignant or malignant uterine pathology after surgery, with a prevalence of 0.66% of occult malignancy. She was unable to identify risk factors for those patients who had a premalignant or malignant pathology. Overall she found a low prevalence of premalignant or malignant uterine pathology when uterine morcellation was performed for benign disease.
Dr. Alix Leader-Cramer from Northwestern University pointed out “risk factors for a 30-day perioperative complications for total vaginal hysterectomy,” including chronic steroid use, higher ASA classification, current smoking status, diabetes, and lower preoperative serum albumin and sodium levels. Adnexectomy and resident participation were also associated with increased perioperative complications. About 9.5% of patients had a perioperative complication in the study population studied.
Finally, Dr. Elisa Trowbridge pointed out in her talk, on “Cognitive Impairment among Elderly Urogynecologic Patients,” that cognitive impairment is very prevalent among such women aged older than 75 years, and the Mini-Cog is a feasible screening tool.
What a way to end an AMAZING conference!
The conference ended with a fabulous video presentation by Dr. Andrea Benton, entitled “Surgical Approaches to the Management of Bladder and Ureteral Endometriosis.” Overall, the themes of this year’s SGS conference were to:
- emphasize the importance of performing a vaginal hysterectomy when feasible
- continue to strive to balance innovation with experimentation
- ensure that patients are being operated on by surgeons who are competent and frequently performing the indicated procedure.
Thank you to everyone who shared their research to educate the attendees at the conference! I can’t wait until next year!
4/12/16. DAY 3 AT SGS
Vaginal hysterectomy, fecal incontinence, transgender surgery amid tackled topics in Palm Springs
I could get used to sipping my coffee with the sunny background here in Palm Springs! It was a beautiful morning to learn.
We started the day with breakfast and a fabulous lecture on the inferior gluteal neurovascular anatomy in female cadavers, and an insightful lecture by Dr. Bhumy Dave, who brought up concerns about tracking for obstetrics and gynecology residency programs. She specifically highlighted the need for more experience with vaginal hysterectomies for residents who are going to be in a subspecialty that performs vaginal surgery. As the number of hysterectomies, specifically vaginal hysterectomies, declines every year, we need to make sure we are adequately training the physicians who will be performing this procedure in the future. One solution is to have residents join a track their 4th year of residency, after their future career path has been established. Another possible solution would be to increase use of a simulation model for vaginal hysterectomy, as described by Dr. Douglas Miyazaki.
Indigo carmine replacement? A recent issue in gynecologic surgery resulted when there was a national shortage of indigo carmine, which is commonly used to identify UO efflux at the time of cystoscopy. Dr. Katie Propst provided a solution: In the setting of planned cystoscopy, she found that preoperative phenazopyridine is an acceptable alternative and its use led to similar UO identification as with indigo carmine without an increase in complications.
Who should have a vaginal hysterectomy? Dr. Jennifer Schmitt from the Mayo Clinic gave another wonderful lecture describing a decision-tree algorithm for determining the ideal route of hysterectomy. According to a retrospective review of patients at their institution, vaginal hysterectomy was associated with lower infection rates, operative times, and costs.
The highlight of the morning was a very insightful Presidential Address by Dr. Andrew Walter! Not only is a he a very entertaining speaker but he also shed some light on 2 challenges that we currently face in the field. He eloquently stated that, “every woman who is a candidate for a vaginal hysterectomy should be able to get one and have it performed competently, and every woman who needs surgery should have one performed by someone who performs enough surgeries every year to competently perform the surgery.” He frequently alluded to the wise Dr. Mayo, who stated, “The best interest of the patient is the only interest to be considered…” Let’s never forget this as physicians!
Do you find removing the adnexa challenging when performing vaginal surgery? Check out the amazing idea from the Cleveland Clinic shown in video presentation 05! They clearly demonstrate using a single-site gel port or surgical glove placed in the vaginal incision to perform laparoscopy through the vagina. What a novel idea to avoid any abdominal incisions when there is a difficult vaginal adnexal surgery!
After the morning break, we watched a master vaginal surgeon perform a sacral colpopexy through the vaginal route. For details on this method, please reference video presentation 06.
An increase in health care costs is a huge problem in this country. Dr. Mary Van Meter suggested that one area in which we can improve is in the operating room (OR), specifically through decreasing the number of instruments sterilized. She found that only approximately 20% of the instruments on the operating field were actually used by the OR physician. It costs about $3 per instrument on the tray at Vanderbilt University, she said. When you think of the few number of instruments actually used, if we work to limit the number of instruments on the trays, we could cut significant costs. As reimbursement is getting increasingly linked to cost reduction, we all should be thinking about innovative ways to cut costs.
The oral posters were all excellent!
Dr. Ann Peters showed that, at a high-volume tertiary-care center, multimodal preoperative testing failed to definitively identify leiomyosarcoma (LMS), and the factors associated with increased LMS risk included older age, menopause, and presence of fibroids with concurrent pelvic, uterine, or adnexal mass.
Dr. Kevin Kremer found that preoperative antibiotics were used in 23% of cases in which they were not indicated, and the increased use rate was associated with entrance into the abdomen during surgery, the individual surgeon, and time under anesthesia.
Dr. Jessica Heft then stated that the incontinence rate after midurethral sling revision for vaginal exposure or pain was significantly higher with a partial as opposed to complete mesh excision.
Fecal incontinence treatment options
Dr. Peter Rosenblatt tackled the issue of “Innovation or experimentation: Where do we draw the line?” in the TeLinde lecture. He started by describing a condition for which he feels we do not have an acceptable amount of treatment options for patients: fecal incontinence. He described how he observed that the puborectalis muscle, not the external anal sphincter, was critical for fecal continence. He then devised a surgery that created a sling that would act as a synthetic puborectalis muscle. He had amazing success until one patient had a serious complication. Should you abandon a successful, innovative surgery due to one very severe complication, was the question. Where do we draw the line? I don’t have an answer…but I do know that we all need to thank our puborectalis muscle for our daily fecal continence!
This is not a new issue in medicine, explained Dr. Rosenblatt. From the beginning of medicine, there has been a balance between innovation and experimentation. So, what is innovation? It is when someone improves upon a device or process. In medicine, is it innovation or just variation? We frequently use medications and devices “off label,” and these techniques often improve our surgeries and outcomes for our patients. Innovation comes about through careful planning, a necessity created by an emergency, advances in technology, and through evolution of a procedure. Who are the innovators? YOU are! We are the ones who understand the unmet needs and the potential opportunities for improving medicine. Let’s all work together to innovate NOT experiment and make medicine better so our patients have the best care possible!
“New Frontiers in Gynecologic Surgery: Transgender Surgery and Functional Clitoroplasty after Female Genital Mutilation”
The final talk for the day was by the groundbreaking Dr. Marci Bowers, whose lecture started by reminding everyone that there is a difference between gender identity and gender expression. Once a person knows his or her gender identity they use gender expression to express this to the world, she pointed out. Dr. Bowers is a true innovator and is performing gender reassignment surgeries as well as female genital mutilation corrective surgeries. She has perfected a one-stage vaginoplasty, and she showed a video of the procedure, which results in a 90% chance of orgasm. She also noted that she is able to restore clitoral function in 100% of the cases of genital mutilation, and she performs these procedures free of charge.
She reminded us that all ObGyns need to be trained in treating transgender patients, and given the high rate of suicide among adolescent transgender individuals, we all need to work together to provide a supportive medical environment to help these patients. What a fascinating end to the day!
Some relaxation, and entertainment, amid the sun and outdoors
We then had the afternoon to compete in a golf tournament, explore the area on mountain bikes, or lounge by the pool. Regardless of the daytime activities, we all came back together for the great lip-synch competition! All 4 teams gave an impressive performance, but the team from Brown University went home with the win! Such an entertaining event! (Thanks to incoming SGS President Vivian Sung @wih_sung for the pic!)
4/11/16. DAY 2 AT SGS
Experts talk surgical innovations, complementary therapies, value-based payment, and much more at SGS day 2
Wake up and learn! The second day of the 42nd Annual Scientific Meeting of the Society of Gynecologic Surgeons began with a review of research posters at the Poster Session as the sun rose over the Palm Springs mountains. We then moved indoors for the scientific sessions.
In the first lecture, "Reasons for Unplanned 30-Day Readmission After Hysterectomy for Benign Disease," Dr. Courtney Penn and colleagues reiterated that the postsurgical readmission rate is higher for patients undergoing abdominal hysterectomy compared with those who have a laparoscopic or vaginal hysterectomy. Similarly, Dr. Jennifer Schmitt and colleagues suggested that in a patient with a relative contraindication for vaginal hysterectomy, when this procedure is performed by an experienced surgeon there may not be increased complications. However, keep in mind that the study described—"A Comparison of Vaginal and Robotic Hysterectomy for Commonly Cited Relative Contraindications to Vaginal Hysterectomy"—was performed at the Mayo Clinic by expert, highly trained surgeons, and this fact may limit the generalizability of the study. As one audience member eloquently stated, it is important to remember that: "Just because it is feasible does not mean it is the correct procedure."
That yoga or barre class may be doing more good than you think! Lunge, bridge, and cat-into-cow movements may provide a greater degree of pelvic floor muscle unit recruitment than traditional Kegel exercises, according to a presentation by Dr. Bruce Crawford on Kegels versus specialized movement.
Perhaps those exercises should be recommended for surgeons as well. As Dr. Ruchira Singh pointed out, surgeons experience a high amount of musculoskeletal strain when performing vaginal procedures while sitting, regardless of the type of chair used during surgery. Dr. Singh and colleagues’ study, "Effect of Different Chairs on Work-Related Musculoskeletal Discomfort During Vaginal Surgery," found that while the round stool with a backrest and the Capisco chair were more comfortable, they did not eliminate the high risk for musculoskeletal strain, particularly in the head and neck.
Dr. Ann Peters and colleagues, from Magee-Womens Hospital of the University of Pittsburgh Medical Center, gave a fabulous video presentation on "Anatomic and Vascular Considerations in Laparoscopic Uterine Artery Ligation During Hysterectomy."
Need a novel treatment for interstitial cystitis/bladder pain syndrome? Consider mindfulness-based stress reduction. A randomized controlled study performed by Dr. Gregg Kanter and colleagues describes how this technique may help patients and could be considered a first-line therapy.
What is value-based payment and this new trend in reimbursement? And how does it apply to vaginal hysterectomy? Dr. Tina Groat addressed these issues in her keynote lecture. According to the American Congress of Obstetricians and Gynecologists, “Evidence demonstrates that, in general, vaginal hysterectomy is associated with better outcomes and fewer complications than laparoscopic or abdominal hysterectomy.” This is in opposition to what is actually being performed clinically. Dr. Groat explained that United Healthcare decided to incentivize physicians by requiring a prior authorization for all hysterectomies for benign disease. There is both a quality and cost benefit to performing a vaginal hysterectomy. Most insurance companies are moving away from a “fee for service” structure to performance-based payment. Change is always scary and, while I think the overall goal of moving toward the best care for our patients is a positive, this approach may create new challenges for the medical field. What do you think? Is performance-based payment beneficial? Or does it limit physicians and potentially force them to perform a procedure they do not feel as comfortable performing? Will this result in physicians rejecting certain patient populations? [Note from OBG MANAGEMENT: Let Dr. Collins know your thoughts through social media, or email OBG MANAGEMENT with a Letter to the Editor (rbarbieri@frontlinemedcom.com).]
The debate on the best route for hysterectomy continues: According to Dr. Carolyn Swenson and colleagues in their presentation, "Comparison of Robotic and Other Minimally Invasive Routes of Hysterectomy for Benign Indications," while there may be lower complications associated with robotic hysterectomy, the cost of performing a robotic hysterectomy is significantly higher than the cost of laparoscopic or vaginal hysterectomy, thus limiting its utility.
How can we teach a rare surgical procedure to learners? We channel our inner Martha Stewart and make a model out of a beef tongue and chicken. For about $8 a challenging and rare surgery can be taught to residents and medical students, according to the video presentation by Dr. Jana Illston and colleagues, titled "Modified Beef Tongue Model for Fourth-Degree Laceration Repair Simulation."
After the Day 2 lunch break, there was a rousing debate surrounding "Surgeons as Innovators—What Is the Patient Expecting?" Where do we draw the line between using an older more proven therapy as opposed to trying an innovative technology that may actually offer a potential benefit? Dr. Dennis Miller made a good point regarding innovation and pharmaceutical and device companies: If we ignore industry, we lose the ability to help with innovation and shape the future of medical treatments. Perhaps we should use the golden rule: If we would perform the surgery or use the device on ourselves, then we should perform it on our patient. Patients have a greater burden now, because there are more treatment options that they must choose among. Our job as physicians is to educate our patients and to guide them to innovative and evidence-based treatments.
Highlights from the afternoon oral poster session included a presentation by Dr. Caryn Russman that noted the high risk for recurrent urinary tract infection (UTI) after a mid-urethral sling procedure, which seems to be related to specific preoperative risk factors (such as a history of recurrent UTI). Dr. Tanya Hoke suggested that residents and attending physicians have inaccurate estimates of uterine weight, and an educational program may be necessary to improve these estimates. Finally, a study from Massachusetts General Hospital showed that a shorter stay in the hospital, ideally same-day surgery, resulted in a lower complication risk, lower number of emergency department visits, and a decreased readmission rate for patients undergoing urogynecology procedures.
The following recommendations were then suggested regarding vaginal hysterectomy:
- Preoperative prep with 4% chlorhexidine or povidine iodine
- Intracervical vasopressin injection to decrease blood loss
- Use of a pedicle-sealing device for pedicle ligation
- Vertical cuff closure is preferred to maximize vaginal length
Another important point made was that a prior cesarean delivery is not a contraindication to performing a vaginal hysterectomy.
Recommendations regarding recurrent UTI were also made, which include the recommendation for preoperative use of antibiotics to decrease the rate of UTI, with no benefit for a longer course of antibiotics.
News from the Fellows’ Pelvic Research Network
So much exciting research currently is ongoing with the FPRN! New project ideas include comparison of trimethoprim with methenamie for treatment of recurrent UTI; comparison of laparoscopic/robotic sacrocolpopexy with vaginal USLS for management of apical prolapse; a survey study examining surgeon preferences for timing of midurethral sling placement when performed at the time of pelvic organ prolapse (POP) repair; an assessment of the effect of a midurethal sling on overactive bladder in surgical repair in POP; and a study evaluating female pelvic reconstructive surgery in the setting of human immunodeficiency virus infection. It is so great to see the fellows working together to provide groundbreaking research!
Fun with stats
Learning statistics at the end of the day is never easy, but Dr. Matthew Barber did a fabulous job explaining this often-confusing topic. He reminded attendees that the key to learning statistics is repetition. One new recommendation he offered to enhance understanding is to use common language instead of numbers for P values. For example, instead of saying P <.001, use “is superior,” and instead of saying P = .3, use “seems not superior” or “inconclusive.”
A night to remember
The night ended with a wonderful awards ceremony and the president’s reception. Overall, day 2 was a very educational—and fun—day!
4/10/16. DAY 1 AT SGS
Postgrad courses address pain management and social media education
Mastering pelvic pain
With the beautiful Palm Springs, California, backdrop of mountains and palm trees, the 2016 meeting of the Society of Gynecologic Surgeons kicked off with 4 postgraduate courses. At the “Mastering Pelvic Pain: Strategies and Techniques for a Multimodal Approach” course, directed by Dr. Cara King, Dr. Matt Siedhoff explained the key components of the history and physical examination: Keep in mind that this generally is a multifactorial issue and may require a multidisciplinary approach, he told attendees. It is also important to make sure that the patient is fully prepared to combat the chronic pelvic pain (CPP) symptoms by focusing on the fundamentals, he said, including smoking, diet, exercise, weight loss, sleep, and relationship stress.
How is your posture? It turns out that something as simple as altering your posture can significantly affect pelvic floor control. Carol Sobeck, PT, demonstrated this importance with a simple group exercise that proved how the ability to contract the pelvic floor changes significantly with posture. Get to know your pelvic floor physical therapist—they are critical in helping with the treatment of CPP.
But what to do when physical therapy fails? Dr. Jennifer Gunter shed some light on this very difficult medical situation. One suggestion, she said, is to consider the possibility of a local presentation of a systemic issue and screen for the following: fibromyalgia, Ehlers-Danlos syndrome, statin use, and diabetes mellitus. Other treatment ideas include trigger point injections and onabotulinumtoxin A (Botox) therapy. A trigger point is a hypercontracted focus of muscle. To treat a trigger point, a needle must mechanically disrupt the trigger point to reduce the pelvic pain, and injection of local anesthetic is only used to help with postprocedure discomfort. Botox in my pelvis, you ask? Yes! The goal is to block presynaptic release of acetylcholine, which is very effective at reducing muscle spasm.
Tackling endometriosis. Dr. King then described surgical techniques for endometriosis. She recommended that, for mild disease not in close proximity to vital structures, ablation is likely equivalent to excision. For deeply infiltrating endometriosis, or lesions in close proximity to vital structures, excision is more beneficial. Excision is always beneficial for pathologic diagnosis, she said. And she offered this tip for bladder endometriosis: place a stitch in the nodule to allow for counter traction. Here is another tip, for ovarian cystectomy: inject vasopressin (20 U in 60 mL) to help dissect the plane between the ovary and cyst wall, and consider presacral neurectomy for midline pain.
Dr. Frank Tu then explained that we should not think of it as the “terrible triad: endometriosis, irritable bowel syndrome, and interstitial cystsis,” but rather as a system out of balance. Both peripheral and central mechanisms are involved in the generation and maintenance of cross-organ sensitization, he pointed out, which may explain why patients receive multiple diagnoses that describe a myriad of complaints due to a lack of overall homeostasis.
While Dr. Alaa Abd-Elsayed described innovative nerve blocks for CPP, he emphasized that no one specific treatment will result in a complete resolution of symptoms.
Vaginal mesh placement and pain. Dr. Mario Castellanos gave a fabulous lecture describing the pain issues that surround vaginal mesh placement. Interestingly, he noted that many patients had pelvic pain prior to placement of vaginal mesh, and that pain likely only will worsen with mesh placement. Mesh may cause pain by causing inflammation, visceral injury, muscle injury, and nerve injury. While there are guidelines for where mesh should be placed for bladder slings (TVT and TOT) and for prolapse repair, studies show, he pointed out, that the mesh placement often disrupts several muscle groups and may directly injure a nerve.
Alternatives to the typical diagnoses for CPP. The morning ended with a lecture by Dr. Suzie As-Sanie, in which she reminded everyone to start with “gold standard” therapy but, if those fail, consider alternative diagnoses or a central pain disorder. She also suggested cognitive behavioral therapy for treatment of CPP. For patients who cannot afford cognitive behavioral therapy, there is a free online source at fibroguide.med.umich.edu. Other alternative treatment options include exercise, patient education, instruction on sleep hygiene, and neurostimulatory therapies.
Overall, all the speakers this morning agreed that CPP is rarely treated with one modality, and it is best treated with a multidisciplinary approach.
Let’s get social!
The afternoon was spent learning about ways to use social networking sites to educate our patients, in another postgraduate course on “Making Media Social,” presented by the SGS Social Media Committee. Given that a recent survey demonstrated that 74.1% of women have some type of social networking account, it can be a very useful source for medical information for patients. If you have any questions about what is appropriate on social media, check out ACOG committee opinion 622.
Here are some tips that I learned:
Facebook:
- Keep your private Facebook page private and create a separate professional Facebook page
- Adjust your login setting so only administrators can post on your professional page
- Adjust settings so your professional profile cannot be “tagged”
- If a patient contacts your personal page, direct them to your professional page
- Do not give medical advice since Facebook is not digitally encrypted
Twitter:
- “Short bursts of inconsequential information”
- Follow societies, medical centers, and medical journals
LinkedIn:
- It provides a great way to find jobs, people, and business opportunities that are recommended by someone in your contact group
- It is specifically there to help you grow your business and show people who you are and where you have come from
Doximity:
Before we get to tips, first, what is it? Well, Doximity is basically a “LinkedIn” for physicians. It is “a way to find relevant specialists for patients; a rolodex; an email and text service; and a virtual lounge.” It is currently transforming from social network into a ‘platform.’ Now more than 1,000 hospitals and health systems are part of Doximity. Tips:
- There is a secure message option, which is HIPAA compliant
- Provides a way for residents and fellows to understand possible future places of employment
- It is a great way to find someone to refer patients to in an unfamiliar location
Vimeo:
- A benefit over YouTube is the lack of advertisements
- Check out the SGS video archives!
- You also can set privacy settings and embedding stats
Fifty-nine percent of US adults have looked online for health information in the past year. Therefore, it is important for physicians to get good information out for people to see!
A relaxing day’s end
The night ended with a beautiful poolside reception! I can’t wait to see what day 2 will bring!
Study raises questions about cost effectiveness of robot-assisted hysterectomy
With few exceptions, the rates of complications, readmissions, and reoperations were similar among patients who underwent robotic hysterectomy for benign indications, compared with those who underwent the procedure by other minimally invasive routes, results from a large analysis demonstrated.
Yet the price tag for nonrobotic, minimally invasive approaches to hysterectomy was 24% lower overall per case.
“In general, people tend to favor newer technologies over older ones because the assumption is that because it’s new, it’s better,” Dr. Carolyn W. Swenson, lead study author, said in an interview before the annual scientific meeting of the Society of Gynecologic Surgeons. “Physicians are not immune to this kind of thinking. But in medicine, we have an obligation to use evidence-based practices to try and optimize outcomes for our patients. If study after study is concluding that, for benign hysterectomy, the additional cost of the robot doesn’t produce better outcomes, then we should be seriously evaluating why and how we choose to use this tool.”
In the past 10 years, use of the robot for benign hysterectomy has increased by more than 25-fold in the Unites States, while other routes of minimally invasive hysterectomy (vaginal and conventional laparoscopic) have decreased, according to Dr. Swenson, a specialist in female pelvic medicine and reconstructive surgery at the University of Michigan, Ann Arbor.
“We know that robot-assisted technology adds, on average, $2,000 to $3,000 per hysterectomy, but that major complications are no different when compared to conventional laparoscopy,” she said. “Vaginal hysterectomy is actually the most minimally invasive and most cost-effective route and it’s also associated with lower complications compared to abdominal and conventional laparoscopic routes. But vaginal hysterectomy is often left out of comparative studies with robotic hysterectomy. So what we’ve been missing up to this point is a study comparing outcomes between robot-assisted laparoscopy and all other routes of minimally invasive hysterectomy, including vaginal and vaginal-assisted laparoscopic routes in addition to conventional laparoscopy.”
In an effort to compare the clinical outcomes and the estimated cost of robot-assisted hysterectomy to all other routes of minimally invasive hysterectomy for benign indications, the researchers analyzed records from a statewide database in Michigan for all such procedures performed from July 1, 2012, to July 1, 2014. They used propensity-matched scoring to control for demographic, clinical, and hospital factors and went on to perform a one-to-one match between women who had a hysterectomy with robotic assistance, and those had a hysterectomy by other minimally invasive routes (laparoscopic and vaginal, with or without laparoscopy). Next, they compared the two cohorts for perioperative outcomes, intraoperative bowel and bladder injury, 30-day postoperative complications, readmission, and reoperation.
Dr. Swenson reported results from 11,004 hysterectomy cases. Of these, 6,222 were performed with robotic assistance, while the remaining 4,782 were performed via other minimally-invasive surgical routes. Over the study period, the proportion of hysterectomies performed with robotic assistance ranged from 43% to 45%, while rates of laparoscopy were 10%-13%, and rates of vaginal hysterectomy (with or without laparoscopy) were 19%-24%.
“I was surprised at how many robotic hysterectomies are being done in the state of Michigan for benign indications,” she said. “The rate is over three times the national average.”
After the propensity score analysis was done, 1,338 hysterectomies from each group were successfully matched and the researchers found that compared with the other minimally invasive routes, hysterectomy cases done with robotic assistance had lower estimated blood loss (94.2 vs. 175.3 mL, respectively; P less than .0001); longer surgical time (2.3 vs. 2 hours; P less .0001), and larger specimen weights (178.9 vs. 160.6 grams; P less than .0001). Intraoperative and bladder complications were similar between the two groups.
Compared with the other minimally invasive hysterectomy routes, the rate of any postoperative complication was lower among cases performed with robotic assistance (3.5% vs. 5.6%; P = .01) and was driven by lower rates of superficial surgical site infections (SSIs) (.07% vs. .7%; P = .01) and blood transfusion (.8% vs. 1.9%; P = .02). However, rates of major complications including deep/organ space SSI, thromboembolic events, MI/stroke, pneumonia, sepsis or death, and readmission and reoperation rates did not differ between the two groups.
After applying hospital cost estimates drawn from published data to results from the hysterectomies included in the propensity match, Dr. Swenson and her associates estimated that the nonrobotic minimally invasive hysterectomy routes led to a 24% lower overall cost per case ($10,160, compared with $13,429 per case performed with robotic assistance), even when considering the cost of additional cases of superficial SSI and blood transfusion. This calculation excluded maintenance costs of the robot.
“Because utilization of robotic hysterectomy for benign indications in Michigan is so much higher than the national average, the generalizability our findings might be limited,” she said. “Also, our cost data were based on estimates from the literature and were not linked to cases in our database, which would have been ideal.”
The meeting was jointly sponsored by the American College of Surgeons.
Dr. Swenson reported having no financial disclosures.
With few exceptions, the rates of complications, readmissions, and reoperations were similar among patients who underwent robotic hysterectomy for benign indications, compared with those who underwent the procedure by other minimally invasive routes, results from a large analysis demonstrated.
Yet the price tag for nonrobotic, minimally invasive approaches to hysterectomy was 24% lower overall per case.
“In general, people tend to favor newer technologies over older ones because the assumption is that because it’s new, it’s better,” Dr. Carolyn W. Swenson, lead study author, said in an interview before the annual scientific meeting of the Society of Gynecologic Surgeons. “Physicians are not immune to this kind of thinking. But in medicine, we have an obligation to use evidence-based practices to try and optimize outcomes for our patients. If study after study is concluding that, for benign hysterectomy, the additional cost of the robot doesn’t produce better outcomes, then we should be seriously evaluating why and how we choose to use this tool.”
In the past 10 years, use of the robot for benign hysterectomy has increased by more than 25-fold in the Unites States, while other routes of minimally invasive hysterectomy (vaginal and conventional laparoscopic) have decreased, according to Dr. Swenson, a specialist in female pelvic medicine and reconstructive surgery at the University of Michigan, Ann Arbor.
“We know that robot-assisted technology adds, on average, $2,000 to $3,000 per hysterectomy, but that major complications are no different when compared to conventional laparoscopy,” she said. “Vaginal hysterectomy is actually the most minimally invasive and most cost-effective route and it’s also associated with lower complications compared to abdominal and conventional laparoscopic routes. But vaginal hysterectomy is often left out of comparative studies with robotic hysterectomy. So what we’ve been missing up to this point is a study comparing outcomes between robot-assisted laparoscopy and all other routes of minimally invasive hysterectomy, including vaginal and vaginal-assisted laparoscopic routes in addition to conventional laparoscopy.”
In an effort to compare the clinical outcomes and the estimated cost of robot-assisted hysterectomy to all other routes of minimally invasive hysterectomy for benign indications, the researchers analyzed records from a statewide database in Michigan for all such procedures performed from July 1, 2012, to July 1, 2014. They used propensity-matched scoring to control for demographic, clinical, and hospital factors and went on to perform a one-to-one match between women who had a hysterectomy with robotic assistance, and those had a hysterectomy by other minimally invasive routes (laparoscopic and vaginal, with or without laparoscopy). Next, they compared the two cohorts for perioperative outcomes, intraoperative bowel and bladder injury, 30-day postoperative complications, readmission, and reoperation.
Dr. Swenson reported results from 11,004 hysterectomy cases. Of these, 6,222 were performed with robotic assistance, while the remaining 4,782 were performed via other minimally-invasive surgical routes. Over the study period, the proportion of hysterectomies performed with robotic assistance ranged from 43% to 45%, while rates of laparoscopy were 10%-13%, and rates of vaginal hysterectomy (with or without laparoscopy) were 19%-24%.
“I was surprised at how many robotic hysterectomies are being done in the state of Michigan for benign indications,” she said. “The rate is over three times the national average.”
After the propensity score analysis was done, 1,338 hysterectomies from each group were successfully matched and the researchers found that compared with the other minimally invasive routes, hysterectomy cases done with robotic assistance had lower estimated blood loss (94.2 vs. 175.3 mL, respectively; P less than .0001); longer surgical time (2.3 vs. 2 hours; P less .0001), and larger specimen weights (178.9 vs. 160.6 grams; P less than .0001). Intraoperative and bladder complications were similar between the two groups.
Compared with the other minimally invasive hysterectomy routes, the rate of any postoperative complication was lower among cases performed with robotic assistance (3.5% vs. 5.6%; P = .01) and was driven by lower rates of superficial surgical site infections (SSIs) (.07% vs. .7%; P = .01) and blood transfusion (.8% vs. 1.9%; P = .02). However, rates of major complications including deep/organ space SSI, thromboembolic events, MI/stroke, pneumonia, sepsis or death, and readmission and reoperation rates did not differ between the two groups.
After applying hospital cost estimates drawn from published data to results from the hysterectomies included in the propensity match, Dr. Swenson and her associates estimated that the nonrobotic minimally invasive hysterectomy routes led to a 24% lower overall cost per case ($10,160, compared with $13,429 per case performed with robotic assistance), even when considering the cost of additional cases of superficial SSI and blood transfusion. This calculation excluded maintenance costs of the robot.
“Because utilization of robotic hysterectomy for benign indications in Michigan is so much higher than the national average, the generalizability our findings might be limited,” she said. “Also, our cost data were based on estimates from the literature and were not linked to cases in our database, which would have been ideal.”
The meeting was jointly sponsored by the American College of Surgeons.
Dr. Swenson reported having no financial disclosures.
With few exceptions, the rates of complications, readmissions, and reoperations were similar among patients who underwent robotic hysterectomy for benign indications, compared with those who underwent the procedure by other minimally invasive routes, results from a large analysis demonstrated.
Yet the price tag for nonrobotic, minimally invasive approaches to hysterectomy was 24% lower overall per case.
“In general, people tend to favor newer technologies over older ones because the assumption is that because it’s new, it’s better,” Dr. Carolyn W. Swenson, lead study author, said in an interview before the annual scientific meeting of the Society of Gynecologic Surgeons. “Physicians are not immune to this kind of thinking. But in medicine, we have an obligation to use evidence-based practices to try and optimize outcomes for our patients. If study after study is concluding that, for benign hysterectomy, the additional cost of the robot doesn’t produce better outcomes, then we should be seriously evaluating why and how we choose to use this tool.”
In the past 10 years, use of the robot for benign hysterectomy has increased by more than 25-fold in the Unites States, while other routes of minimally invasive hysterectomy (vaginal and conventional laparoscopic) have decreased, according to Dr. Swenson, a specialist in female pelvic medicine and reconstructive surgery at the University of Michigan, Ann Arbor.
“We know that robot-assisted technology adds, on average, $2,000 to $3,000 per hysterectomy, but that major complications are no different when compared to conventional laparoscopy,” she said. “Vaginal hysterectomy is actually the most minimally invasive and most cost-effective route and it’s also associated with lower complications compared to abdominal and conventional laparoscopic routes. But vaginal hysterectomy is often left out of comparative studies with robotic hysterectomy. So what we’ve been missing up to this point is a study comparing outcomes between robot-assisted laparoscopy and all other routes of minimally invasive hysterectomy, including vaginal and vaginal-assisted laparoscopic routes in addition to conventional laparoscopy.”
In an effort to compare the clinical outcomes and the estimated cost of robot-assisted hysterectomy to all other routes of minimally invasive hysterectomy for benign indications, the researchers analyzed records from a statewide database in Michigan for all such procedures performed from July 1, 2012, to July 1, 2014. They used propensity-matched scoring to control for demographic, clinical, and hospital factors and went on to perform a one-to-one match between women who had a hysterectomy with robotic assistance, and those had a hysterectomy by other minimally invasive routes (laparoscopic and vaginal, with or without laparoscopy). Next, they compared the two cohorts for perioperative outcomes, intraoperative bowel and bladder injury, 30-day postoperative complications, readmission, and reoperation.
Dr. Swenson reported results from 11,004 hysterectomy cases. Of these, 6,222 were performed with robotic assistance, while the remaining 4,782 were performed via other minimally-invasive surgical routes. Over the study period, the proportion of hysterectomies performed with robotic assistance ranged from 43% to 45%, while rates of laparoscopy were 10%-13%, and rates of vaginal hysterectomy (with or without laparoscopy) were 19%-24%.
“I was surprised at how many robotic hysterectomies are being done in the state of Michigan for benign indications,” she said. “The rate is over three times the national average.”
After the propensity score analysis was done, 1,338 hysterectomies from each group were successfully matched and the researchers found that compared with the other minimally invasive routes, hysterectomy cases done with robotic assistance had lower estimated blood loss (94.2 vs. 175.3 mL, respectively; P less than .0001); longer surgical time (2.3 vs. 2 hours; P less .0001), and larger specimen weights (178.9 vs. 160.6 grams; P less than .0001). Intraoperative and bladder complications were similar between the two groups.
Compared with the other minimally invasive hysterectomy routes, the rate of any postoperative complication was lower among cases performed with robotic assistance (3.5% vs. 5.6%; P = .01) and was driven by lower rates of superficial surgical site infections (SSIs) (.07% vs. .7%; P = .01) and blood transfusion (.8% vs. 1.9%; P = .02). However, rates of major complications including deep/organ space SSI, thromboembolic events, MI/stroke, pneumonia, sepsis or death, and readmission and reoperation rates did not differ between the two groups.
After applying hospital cost estimates drawn from published data to results from the hysterectomies included in the propensity match, Dr. Swenson and her associates estimated that the nonrobotic minimally invasive hysterectomy routes led to a 24% lower overall cost per case ($10,160, compared with $13,429 per case performed with robotic assistance), even when considering the cost of additional cases of superficial SSI and blood transfusion. This calculation excluded maintenance costs of the robot.
“Because utilization of robotic hysterectomy for benign indications in Michigan is so much higher than the national average, the generalizability our findings might be limited,” she said. “Also, our cost data were based on estimates from the literature and were not linked to cases in our database, which would have been ideal.”
The meeting was jointly sponsored by the American College of Surgeons.
Dr. Swenson reported having no financial disclosures.
FROM SGS 2016
Key clinical point: Major complication rates were similar for hysterectomies performed for benign indications using robotic assistance, compared with those performed via other MIS routes, but the robotic costs were higher.
Major finding: Compared with the other minimally invasive hysterectomy routes, the rate of any postoperative complication was lower among cases performed with robotic assistance (3.5% vs. 5.6%; P = .01), but rates for major complications did not differ between the groups.
Data source: An analysis of state records from 11,004 hysterectomies performed in Michigan from July 1, 2012, to July 1, 2014.
Disclosures: Dr. Swenson reported having no financial disclosures.
Surgeons commonly off the mark in estimating blood loss
MONTREAL – Surgeons, nurses, and anesthesia providers were all pretty bad at estimating surgical blood loss in a small study. And more experience doesn’t improve accuracy, though experienced providers were more confident in their estimates.
These were the findings from a study that simulated operating room scenarios and asked providers to estimate blood loss. “Estimation of blood loss is inaccurate and unreliable,” Dr. Luke Rothermel said at the Central Surgical Association’s annual meeting.
Dr. Rothermel, a resident at Case Western Reserve University, Cleveland, noted that although the Joint Commission requires operative notes to contain estimated blood loss, “no study in the United States has compared the characteristics of operating room personnel or conditions associated with improved accuracy or reliability of blood loss estimation.”
Beyond the required reporting, estimating blood loss (EBL) also provides important guidance in perioperative care. Still, said Dr. Rothermel, previous studies have shown that EBL is typically inaccurate.
To assess providers’ ability to be accurate and reliable in estimating blood loss, Dr. Rothermel and his collaborator, Dr. Jeremy Lipman, assistant residency director at MetroHealth, Cleveland, designed a study to simulate three different operating room scenarios, involving high, medium, and low blood loss volumes. The materials used, such as blood-soaked sponges and suction canisters, were identical to what’s actually used in the operating room (porcine blood was used in the simulations).
Before the study, Dr. Rothermel said that he and Dr. Lipman hypothesized that those providers who had more experience and those who were working at the operating field would be more accurate in estimating blood loss. They also hypothesized that estimations in procedures with lower volumes of blood loss would be more accurate.
The study recruited providers from the surgery, anesthesia, and nursing services at an urban level 1 trauma center. Each scenario included a written description of the procedure performed and the course of surgery, and participants could handle study materials for each scenario under the supervision of study staff.
A total of 60 participants (22 from surgery, 17 from anesthesia, and 21 from nursing) participated; they had an average of 12.8 years of experience. The surgical participants included surgical scrub techs, trainees, and attending physicians. Anesthesia participants included anesthesia assistants, CRNAs, trainees, and attending physicians. Nursing participants were all RNs.
The findings? All over the board: “There was no association between specialty, years of experience, or confidence in ability with the consistency or accuracy of estimated blood loss,” said Dr. Rothermel.
Most participants were far shy of the mark, with just 5% of study participants overall able to come within 25% accuracy in judging EBL in all scenarios. Just over a quarter were consistent in over- or underestimating blood loss.
These findings held true across scenarios, across disciplines, and regardless of the number of years of experience. “Increased years of experience trended toward increased error,” said Dr. Rothermel, though the difference was not statistically significant. However, those with more years of experience tended to be more confident of their judgments.
Dr. Rothermel noted the small study size and single institution studied as limitations. Also, “this model was not a high fidelity representation of the OR experience, “ he said, explaining that during surgery, caregivers continually assess intraoperative blood loss and may form an estimate in a different – and potentially more accurate – manner than occurs when presented with the contrived presentation of a scenario.
The study calls into question the validity of using EBL as a quality indicator in assessing physician performance and patient outcomes, said Dr. Rothermel, who had no financial disclosures.
On Twitter @karioakes
MONTREAL – Surgeons, nurses, and anesthesia providers were all pretty bad at estimating surgical blood loss in a small study. And more experience doesn’t improve accuracy, though experienced providers were more confident in their estimates.
These were the findings from a study that simulated operating room scenarios and asked providers to estimate blood loss. “Estimation of blood loss is inaccurate and unreliable,” Dr. Luke Rothermel said at the Central Surgical Association’s annual meeting.
Dr. Rothermel, a resident at Case Western Reserve University, Cleveland, noted that although the Joint Commission requires operative notes to contain estimated blood loss, “no study in the United States has compared the characteristics of operating room personnel or conditions associated with improved accuracy or reliability of blood loss estimation.”
Beyond the required reporting, estimating blood loss (EBL) also provides important guidance in perioperative care. Still, said Dr. Rothermel, previous studies have shown that EBL is typically inaccurate.
To assess providers’ ability to be accurate and reliable in estimating blood loss, Dr. Rothermel and his collaborator, Dr. Jeremy Lipman, assistant residency director at MetroHealth, Cleveland, designed a study to simulate three different operating room scenarios, involving high, medium, and low blood loss volumes. The materials used, such as blood-soaked sponges and suction canisters, were identical to what’s actually used in the operating room (porcine blood was used in the simulations).
Before the study, Dr. Rothermel said that he and Dr. Lipman hypothesized that those providers who had more experience and those who were working at the operating field would be more accurate in estimating blood loss. They also hypothesized that estimations in procedures with lower volumes of blood loss would be more accurate.
The study recruited providers from the surgery, anesthesia, and nursing services at an urban level 1 trauma center. Each scenario included a written description of the procedure performed and the course of surgery, and participants could handle study materials for each scenario under the supervision of study staff.
A total of 60 participants (22 from surgery, 17 from anesthesia, and 21 from nursing) participated; they had an average of 12.8 years of experience. The surgical participants included surgical scrub techs, trainees, and attending physicians. Anesthesia participants included anesthesia assistants, CRNAs, trainees, and attending physicians. Nursing participants were all RNs.
The findings? All over the board: “There was no association between specialty, years of experience, or confidence in ability with the consistency or accuracy of estimated blood loss,” said Dr. Rothermel.
Most participants were far shy of the mark, with just 5% of study participants overall able to come within 25% accuracy in judging EBL in all scenarios. Just over a quarter were consistent in over- or underestimating blood loss.
These findings held true across scenarios, across disciplines, and regardless of the number of years of experience. “Increased years of experience trended toward increased error,” said Dr. Rothermel, though the difference was not statistically significant. However, those with more years of experience tended to be more confident of their judgments.
Dr. Rothermel noted the small study size and single institution studied as limitations. Also, “this model was not a high fidelity representation of the OR experience, “ he said, explaining that during surgery, caregivers continually assess intraoperative blood loss and may form an estimate in a different – and potentially more accurate – manner than occurs when presented with the contrived presentation of a scenario.
The study calls into question the validity of using EBL as a quality indicator in assessing physician performance and patient outcomes, said Dr. Rothermel, who had no financial disclosures.
On Twitter @karioakes
MONTREAL – Surgeons, nurses, and anesthesia providers were all pretty bad at estimating surgical blood loss in a small study. And more experience doesn’t improve accuracy, though experienced providers were more confident in their estimates.
These were the findings from a study that simulated operating room scenarios and asked providers to estimate blood loss. “Estimation of blood loss is inaccurate and unreliable,” Dr. Luke Rothermel said at the Central Surgical Association’s annual meeting.
Dr. Rothermel, a resident at Case Western Reserve University, Cleveland, noted that although the Joint Commission requires operative notes to contain estimated blood loss, “no study in the United States has compared the characteristics of operating room personnel or conditions associated with improved accuracy or reliability of blood loss estimation.”
Beyond the required reporting, estimating blood loss (EBL) also provides important guidance in perioperative care. Still, said Dr. Rothermel, previous studies have shown that EBL is typically inaccurate.
To assess providers’ ability to be accurate and reliable in estimating blood loss, Dr. Rothermel and his collaborator, Dr. Jeremy Lipman, assistant residency director at MetroHealth, Cleveland, designed a study to simulate three different operating room scenarios, involving high, medium, and low blood loss volumes. The materials used, such as blood-soaked sponges and suction canisters, were identical to what’s actually used in the operating room (porcine blood was used in the simulations).
Before the study, Dr. Rothermel said that he and Dr. Lipman hypothesized that those providers who had more experience and those who were working at the operating field would be more accurate in estimating blood loss. They also hypothesized that estimations in procedures with lower volumes of blood loss would be more accurate.
The study recruited providers from the surgery, anesthesia, and nursing services at an urban level 1 trauma center. Each scenario included a written description of the procedure performed and the course of surgery, and participants could handle study materials for each scenario under the supervision of study staff.
A total of 60 participants (22 from surgery, 17 from anesthesia, and 21 from nursing) participated; they had an average of 12.8 years of experience. The surgical participants included surgical scrub techs, trainees, and attending physicians. Anesthesia participants included anesthesia assistants, CRNAs, trainees, and attending physicians. Nursing participants were all RNs.
The findings? All over the board: “There was no association between specialty, years of experience, or confidence in ability with the consistency or accuracy of estimated blood loss,” said Dr. Rothermel.
Most participants were far shy of the mark, with just 5% of study participants overall able to come within 25% accuracy in judging EBL in all scenarios. Just over a quarter were consistent in over- or underestimating blood loss.
These findings held true across scenarios, across disciplines, and regardless of the number of years of experience. “Increased years of experience trended toward increased error,” said Dr. Rothermel, though the difference was not statistically significant. However, those with more years of experience tended to be more confident of their judgments.
Dr. Rothermel noted the small study size and single institution studied as limitations. Also, “this model was not a high fidelity representation of the OR experience, “ he said, explaining that during surgery, caregivers continually assess intraoperative blood loss and may form an estimate in a different – and potentially more accurate – manner than occurs when presented with the contrived presentation of a scenario.
The study calls into question the validity of using EBL as a quality indicator in assessing physician performance and patient outcomes, said Dr. Rothermel, who had no financial disclosures.
On Twitter @karioakes
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: Surgery, anesthesia, and nursing providers were inaccurate and unreliable in estimating surgical blood loss.
Major finding: Only 5% of providers could come within 25% accuracy of simulated surgical blood loss.
Data source: Simulations of surgical scenarios depicting varying amounts of blood loss using porcine blood, presented to 60 providers.
Disclosures: The study authors reported no relevant disclosures.
Uterus transplant update: Fungal infection may have caused complication
The failure of the first U.S. uterus transplant may have been due a complication triggered by an infection of Candida, according to the Cleveland Clinic.
“Preliminary results suggest that the complication was due to an infection caused by an organism that is commonly found in a woman’s reproductive system,” officials at the Cleveland Clinic said in an April 8 statement. “The infection appears to have compromised the blood supply to the uterus, causing the need for its removal. There is an ongoing review of all the data and the team is modifying the protocol to reduce the chances of this complication occurring again in the future. The health of our patient is and has always been our primary concern.”
A team of surgeons at the Cleveland Clinic performed the first U.S. uterus transplant on a 26-year-old woman with uterine factor infertility on Feb. 24, but had to remove the transplanted uterus several days later following a sudden complication. The transplant is part of a study aimed at achieving pregnancy in women with uterine factor infertility. The study is still ongoing.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
The failure of the first U.S. uterus transplant may have been due a complication triggered by an infection of Candida, according to the Cleveland Clinic.
“Preliminary results suggest that the complication was due to an infection caused by an organism that is commonly found in a woman’s reproductive system,” officials at the Cleveland Clinic said in an April 8 statement. “The infection appears to have compromised the blood supply to the uterus, causing the need for its removal. There is an ongoing review of all the data and the team is modifying the protocol to reduce the chances of this complication occurring again in the future. The health of our patient is and has always been our primary concern.”
A team of surgeons at the Cleveland Clinic performed the first U.S. uterus transplant on a 26-year-old woman with uterine factor infertility on Feb. 24, but had to remove the transplanted uterus several days later following a sudden complication. The transplant is part of a study aimed at achieving pregnancy in women with uterine factor infertility. The study is still ongoing.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
The failure of the first U.S. uterus transplant may have been due a complication triggered by an infection of Candida, according to the Cleveland Clinic.
“Preliminary results suggest that the complication was due to an infection caused by an organism that is commonly found in a woman’s reproductive system,” officials at the Cleveland Clinic said in an April 8 statement. “The infection appears to have compromised the blood supply to the uterus, causing the need for its removal. There is an ongoing review of all the data and the team is modifying the protocol to reduce the chances of this complication occurring again in the future. The health of our patient is and has always been our primary concern.”
A team of surgeons at the Cleveland Clinic performed the first U.S. uterus transplant on a 26-year-old woman with uterine factor infertility on Feb. 24, but had to remove the transplanted uterus several days later following a sudden complication. The transplant is part of a study aimed at achieving pregnancy in women with uterine factor infertility. The study is still ongoing.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Postoperative Clostridium Difficile Infection Associated with Number of Antibiotics, Surgical Procedure Complexity
Clinical question: What are the factors that increase risk of Clostridium difficile infection (CDI) in postoperative patients?
Background: CDI has become an important infectious etiology for morbidity, lengthy and costly hospital admissions, and mortality. This study focused on the risks for postoperative patients to be infected with C. diff. Awareness of the risk factors for CDI allows for processes to be implemented that can decrease the rate of infection.
Study design: Retrospective, observational study.
Setting: Multiple Veterans Health Administration surgery programs.
Synopsis: The study investigated 468,386 surgical procedures in 134 surgical programs in 12 subspecialties over a four-year period. Overall, the postoperative CDI rate was 0.4% per year. Rates were higher in emergency or complex procedures, older patients, patients with longer preoperative hospital stays, and those who received three or more classes of antibiotics. CDI in postoperative patients was associated with five times higher risk of mortality, a 12 times higher risk of morbidity, and longer hospital stays (17.9 versus 3.6 days) compared with those without CDI. Further studies with a larger population size will confirm the findings of this study.
The study was conducted on middle-aged to elderly male veterans, and it can only be assumed that these results will translate to other populations. Nevertheless, CDI can lead to significant morbidity and mortality, and the study reinforces the importance of infection control and prevention to reduce CDI incidence and disease severity.
Bottom line: Postoperative CDI is significantly associated with the number of postoperative antibiotics, surgical procedure complexity, preoperative length of stay, and patient comorbidities.
Citation: Li X, Wilson M, Nylander W, Smith T, Lynn M, Gunnar W. Analysis of morbidity and mortality outcomes in postoperative Clostridium difficile infection in the Veterans Health Administration. JAMA Surg. 2015;25:1-9.
Clinical question: What are the factors that increase risk of Clostridium difficile infection (CDI) in postoperative patients?
Background: CDI has become an important infectious etiology for morbidity, lengthy and costly hospital admissions, and mortality. This study focused on the risks for postoperative patients to be infected with C. diff. Awareness of the risk factors for CDI allows for processes to be implemented that can decrease the rate of infection.
Study design: Retrospective, observational study.
Setting: Multiple Veterans Health Administration surgery programs.
Synopsis: The study investigated 468,386 surgical procedures in 134 surgical programs in 12 subspecialties over a four-year period. Overall, the postoperative CDI rate was 0.4% per year. Rates were higher in emergency or complex procedures, older patients, patients with longer preoperative hospital stays, and those who received three or more classes of antibiotics. CDI in postoperative patients was associated with five times higher risk of mortality, a 12 times higher risk of morbidity, and longer hospital stays (17.9 versus 3.6 days) compared with those without CDI. Further studies with a larger population size will confirm the findings of this study.
The study was conducted on middle-aged to elderly male veterans, and it can only be assumed that these results will translate to other populations. Nevertheless, CDI can lead to significant morbidity and mortality, and the study reinforces the importance of infection control and prevention to reduce CDI incidence and disease severity.
Bottom line: Postoperative CDI is significantly associated with the number of postoperative antibiotics, surgical procedure complexity, preoperative length of stay, and patient comorbidities.
Citation: Li X, Wilson M, Nylander W, Smith T, Lynn M, Gunnar W. Analysis of morbidity and mortality outcomes in postoperative Clostridium difficile infection in the Veterans Health Administration. JAMA Surg. 2015;25:1-9.
Clinical question: What are the factors that increase risk of Clostridium difficile infection (CDI) in postoperative patients?
Background: CDI has become an important infectious etiology for morbidity, lengthy and costly hospital admissions, and mortality. This study focused on the risks for postoperative patients to be infected with C. diff. Awareness of the risk factors for CDI allows for processes to be implemented that can decrease the rate of infection.
Study design: Retrospective, observational study.
Setting: Multiple Veterans Health Administration surgery programs.
Synopsis: The study investigated 468,386 surgical procedures in 134 surgical programs in 12 subspecialties over a four-year period. Overall, the postoperative CDI rate was 0.4% per year. Rates were higher in emergency or complex procedures, older patients, patients with longer preoperative hospital stays, and those who received three or more classes of antibiotics. CDI in postoperative patients was associated with five times higher risk of mortality, a 12 times higher risk of morbidity, and longer hospital stays (17.9 versus 3.6 days) compared with those without CDI. Further studies with a larger population size will confirm the findings of this study.
The study was conducted on middle-aged to elderly male veterans, and it can only be assumed that these results will translate to other populations. Nevertheless, CDI can lead to significant morbidity and mortality, and the study reinforces the importance of infection control and prevention to reduce CDI incidence and disease severity.
Bottom line: Postoperative CDI is significantly associated with the number of postoperative antibiotics, surgical procedure complexity, preoperative length of stay, and patient comorbidities.
Citation: Li X, Wilson M, Nylander W, Smith T, Lynn M, Gunnar W. Analysis of morbidity and mortality outcomes in postoperative Clostridium difficile infection in the Veterans Health Administration. JAMA Surg. 2015;25:1-9.