User login
VIDEO: Treating opioid addiction in emerging adults
BALTIMORE – The treatment of opioid addiction in adults aged 18-25 years is fraught with challenging issues for clinicians, Dr. Marc J. Fishman said the annual conference of the American Society of Addiction Medicine.
“It’s very hard to reach them. They don’t necessarily want to be in ‘lame group or in rehab.’ They want to be out doing their thing, and so how can we be more engaging is part of the question,” said Dr. Fishman of the department of psychiatry and behavioral sciences at Johns Hopkins University in Baltimore.
In general, the standard of care for young adults with opioid addiction should include integrating relapse-prevention medications such as buprenorphine, extended-release naltrexone, “and perhaps to a lesser extent, methadone – the same tools we use for adults,” he said in a video interview. “But these tools should be adapted in a “developmentally specific, youth-friendly sort of way.”
He also discussed what parents and other caring adults can do to help young adult patients stick with treatment. “Full abstinence, full recovery is the gold standard, but it won’t happen overnight,” he said. “The good news: Young adults do respond to treatment.”
Dr. Fishman did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BALTIMORE – The treatment of opioid addiction in adults aged 18-25 years is fraught with challenging issues for clinicians, Dr. Marc J. Fishman said the annual conference of the American Society of Addiction Medicine.
“It’s very hard to reach them. They don’t necessarily want to be in ‘lame group or in rehab.’ They want to be out doing their thing, and so how can we be more engaging is part of the question,” said Dr. Fishman of the department of psychiatry and behavioral sciences at Johns Hopkins University in Baltimore.
In general, the standard of care for young adults with opioid addiction should include integrating relapse-prevention medications such as buprenorphine, extended-release naltrexone, “and perhaps to a lesser extent, methadone – the same tools we use for adults,” he said in a video interview. “But these tools should be adapted in a “developmentally specific, youth-friendly sort of way.”
He also discussed what parents and other caring adults can do to help young adult patients stick with treatment. “Full abstinence, full recovery is the gold standard, but it won’t happen overnight,” he said. “The good news: Young adults do respond to treatment.”
Dr. Fishman did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BALTIMORE – The treatment of opioid addiction in adults aged 18-25 years is fraught with challenging issues for clinicians, Dr. Marc J. Fishman said the annual conference of the American Society of Addiction Medicine.
“It’s very hard to reach them. They don’t necessarily want to be in ‘lame group or in rehab.’ They want to be out doing their thing, and so how can we be more engaging is part of the question,” said Dr. Fishman of the department of psychiatry and behavioral sciences at Johns Hopkins University in Baltimore.
In general, the standard of care for young adults with opioid addiction should include integrating relapse-prevention medications such as buprenorphine, extended-release naltrexone, “and perhaps to a lesser extent, methadone – the same tools we use for adults,” he said in a video interview. “But these tools should be adapted in a “developmentally specific, youth-friendly sort of way.”
He also discussed what parents and other caring adults can do to help young adult patients stick with treatment. “Full abstinence, full recovery is the gold standard, but it won’t happen overnight,” he said. “The good news: Young adults do respond to treatment.”
Dr. Fishman did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE ASAM ANNUAL CONFERENCE
VIDEO: Stenting to improve quality of life in esophageal cancer
PHILADELPHIA – An esophageal stent can improve quality of life for patients with advanced esophageal cancer, according to Dr. Sushil Ahlawat, director of endoscopy at Rutgers University, New Brunswick, N.J.
“An esophageal stent can be an important modality for palliating patients’ dysphagia, [which] can happen because the tumor is obstructing the esophagus,” says Dr. Ahlawat in this video. He also discusses how this minimally invasive procedure can support those undergoing chemoradiation therapy or surgery for esophageal cancer.
The video was recorded at this year’s meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy for Medical Education and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – An esophageal stent can improve quality of life for patients with advanced esophageal cancer, according to Dr. Sushil Ahlawat, director of endoscopy at Rutgers University, New Brunswick, N.J.
“An esophageal stent can be an important modality for palliating patients’ dysphagia, [which] can happen because the tumor is obstructing the esophagus,” says Dr. Ahlawat in this video. He also discusses how this minimally invasive procedure can support those undergoing chemoradiation therapy or surgery for esophageal cancer.
The video was recorded at this year’s meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy for Medical Education and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – An esophageal stent can improve quality of life for patients with advanced esophageal cancer, according to Dr. Sushil Ahlawat, director of endoscopy at Rutgers University, New Brunswick, N.J.
“An esophageal stent can be an important modality for palliating patients’ dysphagia, [which] can happen because the tumor is obstructing the esophagus,” says Dr. Ahlawat in this video. He also discusses how this minimally invasive procedure can support those undergoing chemoradiation therapy or surgery for esophageal cancer.
The video was recorded at this year’s meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy for Medical Education and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM DIGESTIVE DISEASES: NEW ADVANCES
Lars Edvinsson, MD
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: Serial lung fluid measurement improved heart failure outcomes
CHICAGO – Regular assessment of a heart failure patient’s lung fluid volume using a device that measures electrical conduction through the chest – lung impedance – helped guide clinicians to make timely adjustments in a patient’s medications and thereby significantly reduce mortality and hospitalizations during an average 4 years of follow-up in a randomized, controlled study with 256 patients.
Monthly measurement of lung impedance and medication adjustments based on the information led to a 58% reduction in hospitalizations for acute heart failure during the first year of the study, compared with control patients, and a 56% reduction in heart failure hospitalizations, compared with controls, during the entire course of the study, the study’s two primary endpoints, Dr. Michael K. Shochat reported at the annual meeting of the American College of Cardiology.
The results also showed that performing regular lung impedance measurements and using the results to guide treatment led to a 43% reduction in all-cause mortality and a 62% drop in heart failure mortality during the average 4-year course of the study, said Dr. Shochat, a cardiologist at the Heart Institute of Hillel Yaffe Medical Center in Hadera, Israel. Concurrent with Dr. Shochat’s report at the meeting the results also appeared in an article published online (J Card Failure. 2016;doi:10.1016/j.cardfail.2016.03.015).
A key aspect of the study was that the clinicians who treated the enrolled patients who underwent lung impedance monitoring used this information to adjust medications the patients received. Overall, patients who underwent monitoring had more than twice the number of medication dose adjustments, compared with the control patients. These adjustments particularly focused on diuretic dosages, which changed three times as often in the monitored patients, compared with controls, Dr. Shochat reported. Changes in the dosages of beta-blockers and ACE inhibitors also showed marked increases in the monitored patients, compared with the controls.
The Non-Invasive Lung IMPEDANCE-Guided Preemptive Treatment in Chronic Heart Failure Patients (IMPEDANCE-HF) trial enrolled 256 patients at two centers in Israel during 2005-2014. Patients had New York Heart Association class II-IV heart failure and a left ventricular ejection fraction of 35% or less. The enrolled patients averaged 67 years of age, and 80% were men.
Clinicians measured lung impedance using a proprietary device that places external electrodes on opposite sides of the patient’s chest. Calculation of impedance used a formula that eliminated the noise from chest wall impedance and focused exclusively on lung impedance. Once the electrodes are placed collection of the impedance data takes about 1 minute, Dr. Shochat said. The study protocol called for impedance data to be collected monthly, and in practice it occurred about 11 times a year during the study.
The investigators calculated for each patient in the active arm of the study a “basal” lung impedance level that reflected their level of lung conductivity when their lungs were clear of excess fluid. Participating clinicians were instructed to intervene by altering medications when the impedance level dropped more than 18% below the basal level. Their goal was to prevent impedance from dropping to more than 24% below the basal level, which correlated with when heart failure patients usually required hospitalization for acute decompensation. The specifics of how to adjust medications to manage patients who showed these signs of fluid overload were left to the discretion of each attending physician.
MPEDANCE-HF was sponsored by the RSMM Company, which is developing the lung impedance measurement device used in the study. Dr. Shochat is a cofounder of RSMM and is a member of the company’s board of directors.
On Twitter @mitchelzoler
The very exciting results reported by Dr. Shochat came from a small, positive trial that showed impedance monitoring was an effective way to detect an increased amount of fluid in a heart failure patient’s lungs. This resulted in improved outcomes, compared with patients managed using usual care, including fewer hospitalizations and reduced mortality.
These results suggest that when physicians had lung impedance information, they identified episodes of acute heart failure decompensation sooner and that they used this alert to change treatment and prevent patient worsening. Heart failure exacerbations and decompensation events are a recurring problem for heart failure patients, and the earlier they are identified and addressed with altered treatment, the better it is for the patient’s well being. The next step is to see if these positive results can be confirmed by other research groups and in larger numbers of patients.
These results contrast with the findings from a German study reported in 2015 that used lung impedance information collected by implantable cardioverter defibrillators in heart failure patients to identify episodes of fluid buildup and decompensation. That study failed to show a statistically significant impact on patient outcomes. The researchers speculated that this may have been because patients often did not go online to allow their information to get transmitted to their physician, and physicians often did not act on the information because the patients reported no coincident change in symptoms.
This problem with the German study highlights that collecting lung impedance information will only improve outcomes if physicians then act on the information and modify a patient’s treatment. In the new study reported by Dr. Shochat, patients consistently underwent evaluation for their lung impedance status every month, and when the results suggested a growing problem of fluid overload the physicians consistently acted on the information by adjusting medication dosages.
Use of lung impedance measurement is similar to another approach for monitoring patients with heart failure that recently entered routine U.S. practice, an implanted device to monitor pulmonary artery pressure and identify episodes of fluid overload and acute decompensation. In the future, it will be interesting to compare the efficacy and ease of use of managing heart failure patients with pulmonary artery pressure monitoring with an implanted device and monitoring fluid build up in the lungs with lung impedance.
Dr. John A. Jarcho is a cardiologist at Brigham and Women’s Hospital, Boston. He had no disclosures. He made these comments as a discussant of Dr. Shochat’s report and in an interview.
The very exciting results reported by Dr. Shochat came from a small, positive trial that showed impedance monitoring was an effective way to detect an increased amount of fluid in a heart failure patient’s lungs. This resulted in improved outcomes, compared with patients managed using usual care, including fewer hospitalizations and reduced mortality.
These results suggest that when physicians had lung impedance information, they identified episodes of acute heart failure decompensation sooner and that they used this alert to change treatment and prevent patient worsening. Heart failure exacerbations and decompensation events are a recurring problem for heart failure patients, and the earlier they are identified and addressed with altered treatment, the better it is for the patient’s well being. The next step is to see if these positive results can be confirmed by other research groups and in larger numbers of patients.
These results contrast with the findings from a German study reported in 2015 that used lung impedance information collected by implantable cardioverter defibrillators in heart failure patients to identify episodes of fluid buildup and decompensation. That study failed to show a statistically significant impact on patient outcomes. The researchers speculated that this may have been because patients often did not go online to allow their information to get transmitted to their physician, and physicians often did not act on the information because the patients reported no coincident change in symptoms.
This problem with the German study highlights that collecting lung impedance information will only improve outcomes if physicians then act on the information and modify a patient’s treatment. In the new study reported by Dr. Shochat, patients consistently underwent evaluation for their lung impedance status every month, and when the results suggested a growing problem of fluid overload the physicians consistently acted on the information by adjusting medication dosages.
Use of lung impedance measurement is similar to another approach for monitoring patients with heart failure that recently entered routine U.S. practice, an implanted device to monitor pulmonary artery pressure and identify episodes of fluid overload and acute decompensation. In the future, it will be interesting to compare the efficacy and ease of use of managing heart failure patients with pulmonary artery pressure monitoring with an implanted device and monitoring fluid build up in the lungs with lung impedance.
Dr. John A. Jarcho is a cardiologist at Brigham and Women’s Hospital, Boston. He had no disclosures. He made these comments as a discussant of Dr. Shochat’s report and in an interview.
The very exciting results reported by Dr. Shochat came from a small, positive trial that showed impedance monitoring was an effective way to detect an increased amount of fluid in a heart failure patient’s lungs. This resulted in improved outcomes, compared with patients managed using usual care, including fewer hospitalizations and reduced mortality.
These results suggest that when physicians had lung impedance information, they identified episodes of acute heart failure decompensation sooner and that they used this alert to change treatment and prevent patient worsening. Heart failure exacerbations and decompensation events are a recurring problem for heart failure patients, and the earlier they are identified and addressed with altered treatment, the better it is for the patient’s well being. The next step is to see if these positive results can be confirmed by other research groups and in larger numbers of patients.
These results contrast with the findings from a German study reported in 2015 that used lung impedance information collected by implantable cardioverter defibrillators in heart failure patients to identify episodes of fluid buildup and decompensation. That study failed to show a statistically significant impact on patient outcomes. The researchers speculated that this may have been because patients often did not go online to allow their information to get transmitted to their physician, and physicians often did not act on the information because the patients reported no coincident change in symptoms.
This problem with the German study highlights that collecting lung impedance information will only improve outcomes if physicians then act on the information and modify a patient’s treatment. In the new study reported by Dr. Shochat, patients consistently underwent evaluation for their lung impedance status every month, and when the results suggested a growing problem of fluid overload the physicians consistently acted on the information by adjusting medication dosages.
Use of lung impedance measurement is similar to another approach for monitoring patients with heart failure that recently entered routine U.S. practice, an implanted device to monitor pulmonary artery pressure and identify episodes of fluid overload and acute decompensation. In the future, it will be interesting to compare the efficacy and ease of use of managing heart failure patients with pulmonary artery pressure monitoring with an implanted device and monitoring fluid build up in the lungs with lung impedance.
Dr. John A. Jarcho is a cardiologist at Brigham and Women’s Hospital, Boston. He had no disclosures. He made these comments as a discussant of Dr. Shochat’s report and in an interview.
CHICAGO – Regular assessment of a heart failure patient’s lung fluid volume using a device that measures electrical conduction through the chest – lung impedance – helped guide clinicians to make timely adjustments in a patient’s medications and thereby significantly reduce mortality and hospitalizations during an average 4 years of follow-up in a randomized, controlled study with 256 patients.
Monthly measurement of lung impedance and medication adjustments based on the information led to a 58% reduction in hospitalizations for acute heart failure during the first year of the study, compared with control patients, and a 56% reduction in heart failure hospitalizations, compared with controls, during the entire course of the study, the study’s two primary endpoints, Dr. Michael K. Shochat reported at the annual meeting of the American College of Cardiology.
The results also showed that performing regular lung impedance measurements and using the results to guide treatment led to a 43% reduction in all-cause mortality and a 62% drop in heart failure mortality during the average 4-year course of the study, said Dr. Shochat, a cardiologist at the Heart Institute of Hillel Yaffe Medical Center in Hadera, Israel. Concurrent with Dr. Shochat’s report at the meeting the results also appeared in an article published online (J Card Failure. 2016;doi:10.1016/j.cardfail.2016.03.015).
A key aspect of the study was that the clinicians who treated the enrolled patients who underwent lung impedance monitoring used this information to adjust medications the patients received. Overall, patients who underwent monitoring had more than twice the number of medication dose adjustments, compared with the control patients. These adjustments particularly focused on diuretic dosages, which changed three times as often in the monitored patients, compared with controls, Dr. Shochat reported. Changes in the dosages of beta-blockers and ACE inhibitors also showed marked increases in the monitored patients, compared with the controls.
The Non-Invasive Lung IMPEDANCE-Guided Preemptive Treatment in Chronic Heart Failure Patients (IMPEDANCE-HF) trial enrolled 256 patients at two centers in Israel during 2005-2014. Patients had New York Heart Association class II-IV heart failure and a left ventricular ejection fraction of 35% or less. The enrolled patients averaged 67 years of age, and 80% were men.
Clinicians measured lung impedance using a proprietary device that places external electrodes on opposite sides of the patient’s chest. Calculation of impedance used a formula that eliminated the noise from chest wall impedance and focused exclusively on lung impedance. Once the electrodes are placed collection of the impedance data takes about 1 minute, Dr. Shochat said. The study protocol called for impedance data to be collected monthly, and in practice it occurred about 11 times a year during the study.
The investigators calculated for each patient in the active arm of the study a “basal” lung impedance level that reflected their level of lung conductivity when their lungs were clear of excess fluid. Participating clinicians were instructed to intervene by altering medications when the impedance level dropped more than 18% below the basal level. Their goal was to prevent impedance from dropping to more than 24% below the basal level, which correlated with when heart failure patients usually required hospitalization for acute decompensation. The specifics of how to adjust medications to manage patients who showed these signs of fluid overload were left to the discretion of each attending physician.
MPEDANCE-HF was sponsored by the RSMM Company, which is developing the lung impedance measurement device used in the study. Dr. Shochat is a cofounder of RSMM and is a member of the company’s board of directors.
On Twitter @mitchelzoler
CHICAGO – Regular assessment of a heart failure patient’s lung fluid volume using a device that measures electrical conduction through the chest – lung impedance – helped guide clinicians to make timely adjustments in a patient’s medications and thereby significantly reduce mortality and hospitalizations during an average 4 years of follow-up in a randomized, controlled study with 256 patients.
Monthly measurement of lung impedance and medication adjustments based on the information led to a 58% reduction in hospitalizations for acute heart failure during the first year of the study, compared with control patients, and a 56% reduction in heart failure hospitalizations, compared with controls, during the entire course of the study, the study’s two primary endpoints, Dr. Michael K. Shochat reported at the annual meeting of the American College of Cardiology.
The results also showed that performing regular lung impedance measurements and using the results to guide treatment led to a 43% reduction in all-cause mortality and a 62% drop in heart failure mortality during the average 4-year course of the study, said Dr. Shochat, a cardiologist at the Heart Institute of Hillel Yaffe Medical Center in Hadera, Israel. Concurrent with Dr. Shochat’s report at the meeting the results also appeared in an article published online (J Card Failure. 2016;doi:10.1016/j.cardfail.2016.03.015).
A key aspect of the study was that the clinicians who treated the enrolled patients who underwent lung impedance monitoring used this information to adjust medications the patients received. Overall, patients who underwent monitoring had more than twice the number of medication dose adjustments, compared with the control patients. These adjustments particularly focused on diuretic dosages, which changed three times as often in the monitored patients, compared with controls, Dr. Shochat reported. Changes in the dosages of beta-blockers and ACE inhibitors also showed marked increases in the monitored patients, compared with the controls.
The Non-Invasive Lung IMPEDANCE-Guided Preemptive Treatment in Chronic Heart Failure Patients (IMPEDANCE-HF) trial enrolled 256 patients at two centers in Israel during 2005-2014. Patients had New York Heart Association class II-IV heart failure and a left ventricular ejection fraction of 35% or less. The enrolled patients averaged 67 years of age, and 80% were men.
Clinicians measured lung impedance using a proprietary device that places external electrodes on opposite sides of the patient’s chest. Calculation of impedance used a formula that eliminated the noise from chest wall impedance and focused exclusively on lung impedance. Once the electrodes are placed collection of the impedance data takes about 1 minute, Dr. Shochat said. The study protocol called for impedance data to be collected monthly, and in practice it occurred about 11 times a year during the study.
The investigators calculated for each patient in the active arm of the study a “basal” lung impedance level that reflected their level of lung conductivity when their lungs were clear of excess fluid. Participating clinicians were instructed to intervene by altering medications when the impedance level dropped more than 18% below the basal level. Their goal was to prevent impedance from dropping to more than 24% below the basal level, which correlated with when heart failure patients usually required hospitalization for acute decompensation. The specifics of how to adjust medications to manage patients who showed these signs of fluid overload were left to the discretion of each attending physician.
MPEDANCE-HF was sponsored by the RSMM Company, which is developing the lung impedance measurement device used in the study. Dr. Shochat is a cofounder of RSMM and is a member of the company’s board of directors.
On Twitter @mitchelzoler
AT ACC 2016
Key clinical point: Monthly, noninvasive measurement of lung fluid levels using lung impedance produced better fluid control in heart failure patients and significantly fewer deaths and heart failure hospitalizations.
Major finding: Lung impedance–based management produced a 56% cut in heart failure hospitalizations, compared with standard care.
Data source: IMPEDANCE-HF, a randomized study with 256 heart failure patients at two Israeli centers.
Disclosures: IMPEDANCE-HF was sponsored by the RSMM Company, which is developing the lung impedance measurement device used in the study. Dr. Shochat is a cofounder of RSMM and is a member of the company’s board of directors.
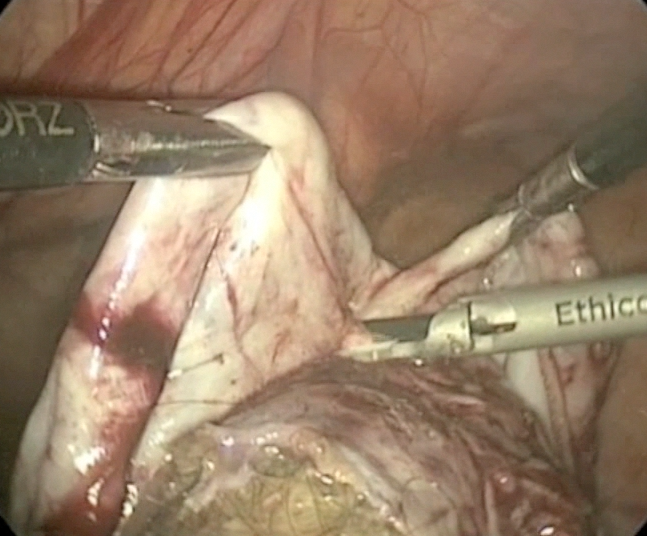
Laparoscopic cystectomy for large, bilateral ovarian dermoids
For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org
For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org
For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org
This video is brought to you by 
Suicidal ideation: Team-based care requires knowledge, resources
Continuity of care for the 18-year-old male who told Dr. Lillian M. Beard about his depression requires collaboration with colleagues, but coordinating that care takes resources. Who is in charge of ensuring care?
“This is where teams come in,” says Dr. April Barbour, associate professor of medicine and chief of general internal medicine George Washington University, Washington. “Because it doesn’t necessarily need to be the psychiatrist. A discharge coordinator could serve that role and send that information back.”
“I agree. And then we come back to the next thing: Who’s going to pay for the team? Who’s going to manage the team? Also, the other thing – with any team, someone’s got to be the quarterback – someone has to make sure or verify that it happened,” says Dr. Lorenzo Norris, cohost of Mental Health Consult, and assistant professor of psychiatry and behavioral sciences at George Washington University.
“When you are treating mental illness, you need a team-based approach so that you can look at everything that is going on. If you are strictly algorithmic based, there are going to be fatal errors,” Dr. Norris says. “It doesn’t reduce down to that level.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Continuity of care for the 18-year-old male who told Dr. Lillian M. Beard about his depression requires collaboration with colleagues, but coordinating that care takes resources. Who is in charge of ensuring care?
“This is where teams come in,” says Dr. April Barbour, associate professor of medicine and chief of general internal medicine George Washington University, Washington. “Because it doesn’t necessarily need to be the psychiatrist. A discharge coordinator could serve that role and send that information back.”
“I agree. And then we come back to the next thing: Who’s going to pay for the team? Who’s going to manage the team? Also, the other thing – with any team, someone’s got to be the quarterback – someone has to make sure or verify that it happened,” says Dr. Lorenzo Norris, cohost of Mental Health Consult, and assistant professor of psychiatry and behavioral sciences at George Washington University.
“When you are treating mental illness, you need a team-based approach so that you can look at everything that is going on. If you are strictly algorithmic based, there are going to be fatal errors,” Dr. Norris says. “It doesn’t reduce down to that level.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Continuity of care for the 18-year-old male who told Dr. Lillian M. Beard about his depression requires collaboration with colleagues, but coordinating that care takes resources. Who is in charge of ensuring care?
“This is where teams come in,” says Dr. April Barbour, associate professor of medicine and chief of general internal medicine George Washington University, Washington. “Because it doesn’t necessarily need to be the psychiatrist. A discharge coordinator could serve that role and send that information back.”
“I agree. And then we come back to the next thing: Who’s going to pay for the team? Who’s going to manage the team? Also, the other thing – with any team, someone’s got to be the quarterback – someone has to make sure or verify that it happened,” says Dr. Lorenzo Norris, cohost of Mental Health Consult, and assistant professor of psychiatry and behavioral sciences at George Washington University.
“When you are treating mental illness, you need a team-based approach so that you can look at everything that is going on. If you are strictly algorithmic based, there are going to be fatal errors,” Dr. Norris says. “It doesn’t reduce down to that level.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Suicidal ideation: An 18-year-old male presents in crisis
When a patient presents with depression, how is it possible to determine whether serious mental illnesses such as first-episode psychosis are unfolding? In this video, Dr. Lillian M. Beard, who practices pediatrics in Silver Spring, Md., discusses the case of an 18-year-old male with thoughts of suicide whose situation was exacerbated by poor continuity of care.
“From the crisis center, [the patient] was admitted to a hospital, but there wasn’t a follow-up,” Dr. Beard says.
This discussion between Dr. Beard; Dr. Lorenzo Norris, cohost of Mental Health Consult and medical director of psychiatric and behavioral services at George Washington University Hospital, Washington; and Dr. David Pickar, adjunct professor of psychiatry at Johns Hopkins University, Baltimore, explores how these kinds of circumstances might affect the patient’s case, as well as other clinical considerations that should help guide referral.
When a patient presents with depression, how is it possible to determine whether serious mental illnesses such as first-episode psychosis are unfolding? In this video, Dr. Lillian M. Beard, who practices pediatrics in Silver Spring, Md., discusses the case of an 18-year-old male with thoughts of suicide whose situation was exacerbated by poor continuity of care.
“From the crisis center, [the patient] was admitted to a hospital, but there wasn’t a follow-up,” Dr. Beard says.
This discussion between Dr. Beard; Dr. Lorenzo Norris, cohost of Mental Health Consult and medical director of psychiatric and behavioral services at George Washington University Hospital, Washington; and Dr. David Pickar, adjunct professor of psychiatry at Johns Hopkins University, Baltimore, explores how these kinds of circumstances might affect the patient’s case, as well as other clinical considerations that should help guide referral.
When a patient presents with depression, how is it possible to determine whether serious mental illnesses such as first-episode psychosis are unfolding? In this video, Dr. Lillian M. Beard, who practices pediatrics in Silver Spring, Md., discusses the case of an 18-year-old male with thoughts of suicide whose situation was exacerbated by poor continuity of care.
“From the crisis center, [the patient] was admitted to a hospital, but there wasn’t a follow-up,” Dr. Beard says.
This discussion between Dr. Beard; Dr. Lorenzo Norris, cohost of Mental Health Consult and medical director of psychiatric and behavioral services at George Washington University Hospital, Washington; and Dr. David Pickar, adjunct professor of psychiatry at Johns Hopkins University, Baltimore, explores how these kinds of circumstances might affect the patient’s case, as well as other clinical considerations that should help guide referral.
VIDEO: Proposed revision of medullary thyroid cancer staging improves risk-stratification analysis
BOSTON – An analysis of data from medullary thyroid cancer patients that partitioned the patients into groups with similar overall survival has spurred a rethink of the current American Joint Committee on Cancer (AJCC) staging system.
The results from researchers at Duke University, Durham, N.C., presented at the annual meeting of the Endocrine Society by Dr. Mohamed Abdelgadir Adam, are timely, as the AJCC has embarked on a reconsideration of the staging of cancers, including medullary thyroid cancer (MTC), as part revisions for the eighth edition of the staging system.
“The existing AJCC staging system for MTC appears to be less than optimal in discriminating the risk of mortality among disease stage groups,” said Dr. Adam, who discussed the findings in a video interview.
MTC, a neuroendocrine tumor that affects C cells of the thyroid, comprises 3%-5% of all cases of thyroid cancer and it can be a more aggressive disease than differentiated thyroid cancer. Yet the current AJCC MTC staging system has been extrapolated from differentiated thyroid cancer data.
“We sought to evaluate how well the current AJCC seventh edition stage groupings predict survival for patients with MTC, to suggest a possible staging revision to sharpen estimates of prognosis,” said Dr. Adam.
The researchers utilized the National Cancer Data Base, representing over 70% of incident cancer cases in the United States.
MTC patients who underwent thyroid surgery from 1998 to 2012 were identified. Patients with missing values for pathologic T, N, or M were excluded. The primary outcome in the 3,315 patients was survival.
The researchers used a form of decision-tree analysis called recursive partitioning. In general, recursive partitioning is able to classify a population by splitting subjects into subgroups, each of which is homogeneous based on the particular outcome. In this study, the subgroup allocations were based on T, N, and M stages, with the outcome being overall survival. Kaplan-Meier and adjusted survival analyses enabled survival differences among the four subgroups (groups I, II, III and IV) to be explored.
The four groups were distinct in terms of survival time and allowed more accurate risk stratification. In particular, groups I and II were markedly better distinguished from one another than is the case with the current staging system. Survival differences across the stages were more distinct with the newly created T, N, and M groupings, compared with the current AJCC staging system.
After adjustment, survival differences across TNM groups were more distinct with the newly created TNM groupings (compared to subgroup I, hazard ratio of 3.06 for subgroup II; HR, 6.79 for III; and HR, 17.03 for IV), compared with the current AJCC staging (compared to stage I, HR, 1.45 for stage II; HR, 2.17 for III; and HR, 5.33 for IV).
“The AJCC is reevaluating all staging schemas, including MTC. The current AJCC staging system could be improved with the newly identified TNM groupings suggested here for more accurate patient risk stratification and possibly treatment selection,” said Dr. Adam.
Dr. Adam had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – An analysis of data from medullary thyroid cancer patients that partitioned the patients into groups with similar overall survival has spurred a rethink of the current American Joint Committee on Cancer (AJCC) staging system.
The results from researchers at Duke University, Durham, N.C., presented at the annual meeting of the Endocrine Society by Dr. Mohamed Abdelgadir Adam, are timely, as the AJCC has embarked on a reconsideration of the staging of cancers, including medullary thyroid cancer (MTC), as part revisions for the eighth edition of the staging system.
“The existing AJCC staging system for MTC appears to be less than optimal in discriminating the risk of mortality among disease stage groups,” said Dr. Adam, who discussed the findings in a video interview.
MTC, a neuroendocrine tumor that affects C cells of the thyroid, comprises 3%-5% of all cases of thyroid cancer and it can be a more aggressive disease than differentiated thyroid cancer. Yet the current AJCC MTC staging system has been extrapolated from differentiated thyroid cancer data.
“We sought to evaluate how well the current AJCC seventh edition stage groupings predict survival for patients with MTC, to suggest a possible staging revision to sharpen estimates of prognosis,” said Dr. Adam.
The researchers utilized the National Cancer Data Base, representing over 70% of incident cancer cases in the United States.
MTC patients who underwent thyroid surgery from 1998 to 2012 were identified. Patients with missing values for pathologic T, N, or M were excluded. The primary outcome in the 3,315 patients was survival.
The researchers used a form of decision-tree analysis called recursive partitioning. In general, recursive partitioning is able to classify a population by splitting subjects into subgroups, each of which is homogeneous based on the particular outcome. In this study, the subgroup allocations were based on T, N, and M stages, with the outcome being overall survival. Kaplan-Meier and adjusted survival analyses enabled survival differences among the four subgroups (groups I, II, III and IV) to be explored.
The four groups were distinct in terms of survival time and allowed more accurate risk stratification. In particular, groups I and II were markedly better distinguished from one another than is the case with the current staging system. Survival differences across the stages were more distinct with the newly created T, N, and M groupings, compared with the current AJCC staging system.
After adjustment, survival differences across TNM groups were more distinct with the newly created TNM groupings (compared to subgroup I, hazard ratio of 3.06 for subgroup II; HR, 6.79 for III; and HR, 17.03 for IV), compared with the current AJCC staging (compared to stage I, HR, 1.45 for stage II; HR, 2.17 for III; and HR, 5.33 for IV).
“The AJCC is reevaluating all staging schemas, including MTC. The current AJCC staging system could be improved with the newly identified TNM groupings suggested here for more accurate patient risk stratification and possibly treatment selection,” said Dr. Adam.
Dr. Adam had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – An analysis of data from medullary thyroid cancer patients that partitioned the patients into groups with similar overall survival has spurred a rethink of the current American Joint Committee on Cancer (AJCC) staging system.
The results from researchers at Duke University, Durham, N.C., presented at the annual meeting of the Endocrine Society by Dr. Mohamed Abdelgadir Adam, are timely, as the AJCC has embarked on a reconsideration of the staging of cancers, including medullary thyroid cancer (MTC), as part revisions for the eighth edition of the staging system.
“The existing AJCC staging system for MTC appears to be less than optimal in discriminating the risk of mortality among disease stage groups,” said Dr. Adam, who discussed the findings in a video interview.
MTC, a neuroendocrine tumor that affects C cells of the thyroid, comprises 3%-5% of all cases of thyroid cancer and it can be a more aggressive disease than differentiated thyroid cancer. Yet the current AJCC MTC staging system has been extrapolated from differentiated thyroid cancer data.
“We sought to evaluate how well the current AJCC seventh edition stage groupings predict survival for patients with MTC, to suggest a possible staging revision to sharpen estimates of prognosis,” said Dr. Adam.
The researchers utilized the National Cancer Data Base, representing over 70% of incident cancer cases in the United States.
MTC patients who underwent thyroid surgery from 1998 to 2012 were identified. Patients with missing values for pathologic T, N, or M were excluded. The primary outcome in the 3,315 patients was survival.
The researchers used a form of decision-tree analysis called recursive partitioning. In general, recursive partitioning is able to classify a population by splitting subjects into subgroups, each of which is homogeneous based on the particular outcome. In this study, the subgroup allocations were based on T, N, and M stages, with the outcome being overall survival. Kaplan-Meier and adjusted survival analyses enabled survival differences among the four subgroups (groups I, II, III and IV) to be explored.
The four groups were distinct in terms of survival time and allowed more accurate risk stratification. In particular, groups I and II were markedly better distinguished from one another than is the case with the current staging system. Survival differences across the stages were more distinct with the newly created T, N, and M groupings, compared with the current AJCC staging system.
After adjustment, survival differences across TNM groups were more distinct with the newly created TNM groupings (compared to subgroup I, hazard ratio of 3.06 for subgroup II; HR, 6.79 for III; and HR, 17.03 for IV), compared with the current AJCC staging (compared to stage I, HR, 1.45 for stage II; HR, 2.17 for III; and HR, 5.33 for IV).
“The AJCC is reevaluating all staging schemas, including MTC. The current AJCC staging system could be improved with the newly identified TNM groupings suggested here for more accurate patient risk stratification and possibly treatment selection,” said Dr. Adam.
Dr. Adam had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Key clinical point: A proposed revision of the AJCC thyroid cancer staging system improves risk stratification analysis.
Major finding: In the proposed staging system, compared to subgroup I, hazard ratio for survival was 3.06 for subgroup II; HR, 6.79 for III; and HR, 17.03 for IV, compared with the current AJCC staging of HR, 1.45 for stage II; HR, 2.17 for III; and HR, 5.33 for IV.
Data source: Data from 3,315 patients with medullary thyroid cancer was drawn from the National Cancer Database.
Disclosures: Dr. Adam had no disclosures.
VIDEO: Beyond amyloid, the complexity of Alzheimer’s deepens
BETHESDA, MD. – Dr. John Hardy first theorized the amyloid cascade hypothesis in 1992. Since then, amyloid-beta has remained the prime focus of Alzheimer’s disease research and therapy. But as the understanding of Alzheimer’s pathogenesis deepens, critical genetic and environmental interactions with amyloid become ever more important in untangling the disorder’s mysteries.
In this interview at the National Institutes of Health’s Alzheimer’s Disease–Related Dementias 2016 Summit, Dr. Hardy of University College London Institute of Neurology discusses some of the issues behind treating and studying clinical differences in Alzheimer’s disease and other types of dementia.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
BETHESDA, MD. – Dr. John Hardy first theorized the amyloid cascade hypothesis in 1992. Since then, amyloid-beta has remained the prime focus of Alzheimer’s disease research and therapy. But as the understanding of Alzheimer’s pathogenesis deepens, critical genetic and environmental interactions with amyloid become ever more important in untangling the disorder’s mysteries.
In this interview at the National Institutes of Health’s Alzheimer’s Disease–Related Dementias 2016 Summit, Dr. Hardy of University College London Institute of Neurology discusses some of the issues behind treating and studying clinical differences in Alzheimer’s disease and other types of dementia.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
BETHESDA, MD. – Dr. John Hardy first theorized the amyloid cascade hypothesis in 1992. Since then, amyloid-beta has remained the prime focus of Alzheimer’s disease research and therapy. But as the understanding of Alzheimer’s pathogenesis deepens, critical genetic and environmental interactions with amyloid become ever more important in untangling the disorder’s mysteries.
In this interview at the National Institutes of Health’s Alzheimer’s Disease–Related Dementias 2016 Summit, Dr. Hardy of University College London Institute of Neurology discusses some of the issues behind treating and studying clinical differences in Alzheimer’s disease and other types of dementia.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
EXPERT ANALYSIS FROM THE ADRD SUMMIT 2016
VIDEO: Weight cycling common following weight loss in obese individuals
BOSTON – Examination of weight-loss patterns in over 177,000 people has revealed that, regardless of the initial 6-month weight loss, after 2 years the majority of patients become “cyclers,” with periods of weight gain and loss rather than maintenance of the initial weight loss.
“One-third of American adults are obese. In 2010, the cost of obesity and obesity-related comorbidities in the United States was estimated to be $315.8 billion. Achieving and maintaining weight loss has proven to be difficult,” said Joanna Huang, PharmD, senior manager of health economics and outcomes research at Novo Nordisk, Plainsboro, N.J., and lead investigator of the study presented at the annual meeting of the Endocrine Society.
The study examined the electronic records of about 178,000 obese patients whose weight loss had been by deliberate intent and not due to illness. The subjects were allocated into four groups based on the extent of weight loss in terms of body mass index (BMI) over 6 months: Those who remained stable and lost less than 5% (n = 151,902), those who lost 5%-10% (modest loss; n = 16,637), those who lost 10%-15% (moderate loss; n = 4,035), and those who lost in excess of 15% (high loss; n = 5,945).
The subjects who were at least 18 years of age at baseline (mean age 54-58 years), had at least one BMI measurement that was indicative of obesity (greater than or equal to 30 kg/m2), with at least four BMI determinations done over at least 5 years. Subjects were mostly white (about 66% in all four groups) and mostly from the southern United States.
Regardless of the amount that the participants lost in the first 6 months, regain of 50% of more of body weight was common in the modest weight-loss group (40%) and moderate weight-loss group (36%), while only 19% of those in the high weight-loss group cycled back up in weight, reported study presenter Maral DerSarkissian, PhD, of the Analysis Group in Boston.
More than 73% and about 70% of those in the moderate and modest weight-loss group, respectively, experienced weight cycling within 2 years. In the stable and high weight-loss groups, the situation was somewhat more optimistic, with about 60% of participants cycling in weight within 2 years. Total regain of lost weight occurred in about 23%, 16%, and 7% of the modest, moderate, and high weight-loss group, respectively.
“Weight loss maintenance, even in the moderate and high weight-loss groups, is very difficult to achieve,” said Dr. Huang.
Interventions that seek to maintain the weight conventionally are directed at dietary changes. But, according to Dr. DerSarkissian, “these modifications alone might not be enough to achieve and maintain weight loss.”
Pharmacotherapy is another weight-loss option. The data indicated that only 2% of the participants were receiving weight-loss pharmacotherapy. Whether this figure is accurate is an open question, according to Dr. Huang, since a lot of the data were compiled from physicians’ notes. Since clinicians may not record weight-loss advice offered to their patients, the data base may well not reflect lifestyle interventions, including pharmacotherapy.
In addition, since the data captured only primary outpatient care, whether or not a patient ever had bariatric surgery was unknown. Other unrecorded factors that can influence weight over time included comorbidities, use of medications, diet changes, and changes in physical activity.
The data points to a multifactor approach to weight loss that includes counseling, positive reinforcement, dietary advice, pharmacotherapy where appropriate, and, in some cases, bariatric surgery.
“Successful and sustained clinically meaningful weight loss requires chronic and effective weight management strategies,” said Dr. Huang.
Dr. Huang is an employee of Novo Nordisk and Dr. DerSarkissian is a researcher for Novo Nordisk.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Examination of weight-loss patterns in over 177,000 people has revealed that, regardless of the initial 6-month weight loss, after 2 years the majority of patients become “cyclers,” with periods of weight gain and loss rather than maintenance of the initial weight loss.
“One-third of American adults are obese. In 2010, the cost of obesity and obesity-related comorbidities in the United States was estimated to be $315.8 billion. Achieving and maintaining weight loss has proven to be difficult,” said Joanna Huang, PharmD, senior manager of health economics and outcomes research at Novo Nordisk, Plainsboro, N.J., and lead investigator of the study presented at the annual meeting of the Endocrine Society.
The study examined the electronic records of about 178,000 obese patients whose weight loss had been by deliberate intent and not due to illness. The subjects were allocated into four groups based on the extent of weight loss in terms of body mass index (BMI) over 6 months: Those who remained stable and lost less than 5% (n = 151,902), those who lost 5%-10% (modest loss; n = 16,637), those who lost 10%-15% (moderate loss; n = 4,035), and those who lost in excess of 15% (high loss; n = 5,945).
The subjects who were at least 18 years of age at baseline (mean age 54-58 years), had at least one BMI measurement that was indicative of obesity (greater than or equal to 30 kg/m2), with at least four BMI determinations done over at least 5 years. Subjects were mostly white (about 66% in all four groups) and mostly from the southern United States.
Regardless of the amount that the participants lost in the first 6 months, regain of 50% of more of body weight was common in the modest weight-loss group (40%) and moderate weight-loss group (36%), while only 19% of those in the high weight-loss group cycled back up in weight, reported study presenter Maral DerSarkissian, PhD, of the Analysis Group in Boston.
More than 73% and about 70% of those in the moderate and modest weight-loss group, respectively, experienced weight cycling within 2 years. In the stable and high weight-loss groups, the situation was somewhat more optimistic, with about 60% of participants cycling in weight within 2 years. Total regain of lost weight occurred in about 23%, 16%, and 7% of the modest, moderate, and high weight-loss group, respectively.
“Weight loss maintenance, even in the moderate and high weight-loss groups, is very difficult to achieve,” said Dr. Huang.
Interventions that seek to maintain the weight conventionally are directed at dietary changes. But, according to Dr. DerSarkissian, “these modifications alone might not be enough to achieve and maintain weight loss.”
Pharmacotherapy is another weight-loss option. The data indicated that only 2% of the participants were receiving weight-loss pharmacotherapy. Whether this figure is accurate is an open question, according to Dr. Huang, since a lot of the data were compiled from physicians’ notes. Since clinicians may not record weight-loss advice offered to their patients, the data base may well not reflect lifestyle interventions, including pharmacotherapy.
In addition, since the data captured only primary outpatient care, whether or not a patient ever had bariatric surgery was unknown. Other unrecorded factors that can influence weight over time included comorbidities, use of medications, diet changes, and changes in physical activity.
The data points to a multifactor approach to weight loss that includes counseling, positive reinforcement, dietary advice, pharmacotherapy where appropriate, and, in some cases, bariatric surgery.
“Successful and sustained clinically meaningful weight loss requires chronic and effective weight management strategies,” said Dr. Huang.
Dr. Huang is an employee of Novo Nordisk and Dr. DerSarkissian is a researcher for Novo Nordisk.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Examination of weight-loss patterns in over 177,000 people has revealed that, regardless of the initial 6-month weight loss, after 2 years the majority of patients become “cyclers,” with periods of weight gain and loss rather than maintenance of the initial weight loss.
“One-third of American adults are obese. In 2010, the cost of obesity and obesity-related comorbidities in the United States was estimated to be $315.8 billion. Achieving and maintaining weight loss has proven to be difficult,” said Joanna Huang, PharmD, senior manager of health economics and outcomes research at Novo Nordisk, Plainsboro, N.J., and lead investigator of the study presented at the annual meeting of the Endocrine Society.
The study examined the electronic records of about 178,000 obese patients whose weight loss had been by deliberate intent and not due to illness. The subjects were allocated into four groups based on the extent of weight loss in terms of body mass index (BMI) over 6 months: Those who remained stable and lost less than 5% (n = 151,902), those who lost 5%-10% (modest loss; n = 16,637), those who lost 10%-15% (moderate loss; n = 4,035), and those who lost in excess of 15% (high loss; n = 5,945).
The subjects who were at least 18 years of age at baseline (mean age 54-58 years), had at least one BMI measurement that was indicative of obesity (greater than or equal to 30 kg/m2), with at least four BMI determinations done over at least 5 years. Subjects were mostly white (about 66% in all four groups) and mostly from the southern United States.
Regardless of the amount that the participants lost in the first 6 months, regain of 50% of more of body weight was common in the modest weight-loss group (40%) and moderate weight-loss group (36%), while only 19% of those in the high weight-loss group cycled back up in weight, reported study presenter Maral DerSarkissian, PhD, of the Analysis Group in Boston.
More than 73% and about 70% of those in the moderate and modest weight-loss group, respectively, experienced weight cycling within 2 years. In the stable and high weight-loss groups, the situation was somewhat more optimistic, with about 60% of participants cycling in weight within 2 years. Total regain of lost weight occurred in about 23%, 16%, and 7% of the modest, moderate, and high weight-loss group, respectively.
“Weight loss maintenance, even in the moderate and high weight-loss groups, is very difficult to achieve,” said Dr. Huang.
Interventions that seek to maintain the weight conventionally are directed at dietary changes. But, according to Dr. DerSarkissian, “these modifications alone might not be enough to achieve and maintain weight loss.”
Pharmacotherapy is another weight-loss option. The data indicated that only 2% of the participants were receiving weight-loss pharmacotherapy. Whether this figure is accurate is an open question, according to Dr. Huang, since a lot of the data were compiled from physicians’ notes. Since clinicians may not record weight-loss advice offered to their patients, the data base may well not reflect lifestyle interventions, including pharmacotherapy.
In addition, since the data captured only primary outpatient care, whether or not a patient ever had bariatric surgery was unknown. Other unrecorded factors that can influence weight over time included comorbidities, use of medications, diet changes, and changes in physical activity.
The data points to a multifactor approach to weight loss that includes counseling, positive reinforcement, dietary advice, pharmacotherapy where appropriate, and, in some cases, bariatric surgery.
“Successful and sustained clinically meaningful weight loss requires chronic and effective weight management strategies,” said Dr. Huang.
Dr. Huang is an employee of Novo Nordisk and Dr. DerSarkissian is a researcher for Novo Nordisk.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ENDO 2016
Key clinical point: Most patients who lose modest or moderate amounts of weight experience periods of both gain and loss within 2 years.
Major finding: More than 73% and about 70% of those in the moderate and modest weight-loss group, respectively, experienced weight cycling within 2 years. Total regain of lost weight occurred in about 23%, 16%, and 7% of the modest, moderate, and high weight-loss group, respectively.
Data source: Electronic records of 177,743 obese patients whose weight loss had been by deliberate intent and not due to illness.
Disclosures: Dr. Huang is an employee of Novo Nordisk and Dr. DerSarkissian is a researcher for Novo Nordisk.