User login
You, Me, and Your A1C
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
VIDEO: Painful skin conditions need pain management by dermatologists
Patients with painful skin conditions need pain management that is provided by their dermatologists, Robert G. Micheletti, MD, contended in a presentation at the annual meeting of the American Academy of Dermatology.
Dermatologists are the experts when it comes to treating painful skin conditions like pyoderma gangrenosum, hidradenitis suppurativa, calciphylaxis, and vasculopathies. “We should be willing to treat the pain that goes with (these conditions), at least within our scope of practice,” said Dr. Micheletti, co-director of the Inpatient Dermatology Consult Service at the University of Pennsylvania, Philadelphia. “At the same time, we know opioids should be prescribed only when necessary, at the lowest effective dose, and for the shortest possible duration.”
In our exclusive video interview, Dr. Micheletti outlined the keys to successful care of patients with painful skin disease. He described patient characteristics that influence prescribing choices and tips for accurately assessing pain needs with a preference for a conservative regimen that utilizes non-opioids and avoids over-reliance on narcotics.
Source: Micheletti, R., Session F013
Patients with painful skin conditions need pain management that is provided by their dermatologists, Robert G. Micheletti, MD, contended in a presentation at the annual meeting of the American Academy of Dermatology.
Dermatologists are the experts when it comes to treating painful skin conditions like pyoderma gangrenosum, hidradenitis suppurativa, calciphylaxis, and vasculopathies. “We should be willing to treat the pain that goes with (these conditions), at least within our scope of practice,” said Dr. Micheletti, co-director of the Inpatient Dermatology Consult Service at the University of Pennsylvania, Philadelphia. “At the same time, we know opioids should be prescribed only when necessary, at the lowest effective dose, and for the shortest possible duration.”
In our exclusive video interview, Dr. Micheletti outlined the keys to successful care of patients with painful skin disease. He described patient characteristics that influence prescribing choices and tips for accurately assessing pain needs with a preference for a conservative regimen that utilizes non-opioids and avoids over-reliance on narcotics.
Source: Micheletti, R., Session F013
Patients with painful skin conditions need pain management that is provided by their dermatologists, Robert G. Micheletti, MD, contended in a presentation at the annual meeting of the American Academy of Dermatology.
Dermatologists are the experts when it comes to treating painful skin conditions like pyoderma gangrenosum, hidradenitis suppurativa, calciphylaxis, and vasculopathies. “We should be willing to treat the pain that goes with (these conditions), at least within our scope of practice,” said Dr. Micheletti, co-director of the Inpatient Dermatology Consult Service at the University of Pennsylvania, Philadelphia. “At the same time, we know opioids should be prescribed only when necessary, at the lowest effective dose, and for the shortest possible duration.”
In our exclusive video interview, Dr. Micheletti outlined the keys to successful care of patients with painful skin disease. He described patient characteristics that influence prescribing choices and tips for accurately assessing pain needs with a preference for a conservative regimen that utilizes non-opioids and avoids over-reliance on narcotics.
Source: Micheletti, R., Session F013
VIDEO: Delusional parasitosis? Try these real solutions
SAN DIEGO – The path to successful treatment of patients with imagined skin disorders is paved with compassion, according to John Koo, MD, a dermatologist and psychiatrist with the University of California at San Francisco.
When a patient presents with delusional parasitosis -- horror stories about imagined infestations of parasites or bugs – the key to successful treatment is a positive attitude and validation, not denial, Dr. Koo said in a presentation at the annual meeting of the American Academy of Dermatology.
"I cannot afford to go in (the exam room) with a long face," he said. "If I go in and I’m not looking happy, things can deteriorate quickly. So I make sure I go in with the biggest smile on my face like I'm meeting my favorite Hollywood star."
"When I say something like 'It's like a living hell, isn't it,' patients are really touched, he said. The patient’s response is typically 'You're the first dermatologist to understand what I'm going through.' You cannot endorse their delusion, but you can endorse their suffering."
In our video interview, Dr. Koo delved into techniques for the successful work-up and evaluation of patients with delusional parasitosis, the varying degrees of the condition, medications used for treatment, and the prospects for eventual drug-free relief.
Dr. Koo reports no relevant financial disclosures.
SAN DIEGO – The path to successful treatment of patients with imagined skin disorders is paved with compassion, according to John Koo, MD, a dermatologist and psychiatrist with the University of California at San Francisco.
When a patient presents with delusional parasitosis -- horror stories about imagined infestations of parasites or bugs – the key to successful treatment is a positive attitude and validation, not denial, Dr. Koo said in a presentation at the annual meeting of the American Academy of Dermatology.
"I cannot afford to go in (the exam room) with a long face," he said. "If I go in and I’m not looking happy, things can deteriorate quickly. So I make sure I go in with the biggest smile on my face like I'm meeting my favorite Hollywood star."
"When I say something like 'It's like a living hell, isn't it,' patients are really touched, he said. The patient’s response is typically 'You're the first dermatologist to understand what I'm going through.' You cannot endorse their delusion, but you can endorse their suffering."
In our video interview, Dr. Koo delved into techniques for the successful work-up and evaluation of patients with delusional parasitosis, the varying degrees of the condition, medications used for treatment, and the prospects for eventual drug-free relief.
Dr. Koo reports no relevant financial disclosures.
SAN DIEGO – The path to successful treatment of patients with imagined skin disorders is paved with compassion, according to John Koo, MD, a dermatologist and psychiatrist with the University of California at San Francisco.
When a patient presents with delusional parasitosis -- horror stories about imagined infestations of parasites or bugs – the key to successful treatment is a positive attitude and validation, not denial, Dr. Koo said in a presentation at the annual meeting of the American Academy of Dermatology.
"I cannot afford to go in (the exam room) with a long face," he said. "If I go in and I’m not looking happy, things can deteriorate quickly. So I make sure I go in with the biggest smile on my face like I'm meeting my favorite Hollywood star."
"When I say something like 'It's like a living hell, isn't it,' patients are really touched, he said. The patient’s response is typically 'You're the first dermatologist to understand what I'm going through.' You cannot endorse their delusion, but you can endorse their suffering."
In our video interview, Dr. Koo delved into techniques for the successful work-up and evaluation of patients with delusional parasitosis, the varying degrees of the condition, medications used for treatment, and the prospects for eventual drug-free relief.
Dr. Koo reports no relevant financial disclosures.
REPORTING FROM AAD 18
VIDEO: Gene test guides need for sentinel node biopsy in elderly melanoma patients
SAN DIEGO – The results of a gene expression test, along with tumor thickness and patient age, can guide the need for sentinel lymph node biopsy, based on results from more than1,400 consecutively tested patients from 26 U.S. surgical oncology, medical oncology and dermatologic practices.
The findings, presented by John Vetto, MD, at the annual meeting of the American Academy of Dermatology, indicate the DecisionDx test correctly identified patients aged 65 and older with T1-T2 tumors whose risk of sentinel node metastasis was lower than 5%. The most recent melanoma guidelines from the National Comprehensive Cancer Network recommend that clinicians “discuss and offer” sentinel node biopsy if a patient has a greater than 10% likelihood of a positive node. If the likelihood is 5%-10%, the recommendation is to “discuss and consider” the procedure. But if the likelihood of a positive node is less than 5%, the guidelines recommend against a biopsy.
“Sentinel node biopsy (has) risks, especially in medically compromised older patients,” Dr. Vetto, professor of surgery at the Oregon Health and Sciences University, Portland, said in an interview, in which he discussed clinical use of the test. “This test offers us a good way to assess the risk/benefit ratio so we can better care for patients, and follow the newest guidelines about sentinel node biopsy.”
The DecisionDx Melanoma, developed by Castle Biosciences, tests for the expression of 28 genes know to play a role in melanoma metastasis, and three control genes. Tumors are stratified either as Class 1, with a 3% chance of spreading within 5 years, or Class 2, with a 69% risk of metastasis. There are two subclasses: 1A, which has an extremely low risk of progression, and 2b, which has an extremely high risk of progression.
For patients with T1-T2 tumors who had a Class 1A test result (lowest risk of recurrence), SLN positivity was 4.6% for all ages, 2.8% in patients 55 years and older, and 1.6% in patients 65 years and older. For patients with T1-T2 tumors who had a Class 2B test result (highest risk of recurrence), SLN positivity was 18.8% for all ages, 16.4% in patients 55 years and older and 11.9% in patients 65 years and older.
Dr. Vetto is a paid speaker for Castle Biosciences.
SOURCE: Vetto et al. AAD 2018 late-breaking research, Abstract 6805
SAN DIEGO – The results of a gene expression test, along with tumor thickness and patient age, can guide the need for sentinel lymph node biopsy, based on results from more than1,400 consecutively tested patients from 26 U.S. surgical oncology, medical oncology and dermatologic practices.
The findings, presented by John Vetto, MD, at the annual meeting of the American Academy of Dermatology, indicate the DecisionDx test correctly identified patients aged 65 and older with T1-T2 tumors whose risk of sentinel node metastasis was lower than 5%. The most recent melanoma guidelines from the National Comprehensive Cancer Network recommend that clinicians “discuss and offer” sentinel node biopsy if a patient has a greater than 10% likelihood of a positive node. If the likelihood is 5%-10%, the recommendation is to “discuss and consider” the procedure. But if the likelihood of a positive node is less than 5%, the guidelines recommend against a biopsy.
“Sentinel node biopsy (has) risks, especially in medically compromised older patients,” Dr. Vetto, professor of surgery at the Oregon Health and Sciences University, Portland, said in an interview, in which he discussed clinical use of the test. “This test offers us a good way to assess the risk/benefit ratio so we can better care for patients, and follow the newest guidelines about sentinel node biopsy.”
The DecisionDx Melanoma, developed by Castle Biosciences, tests for the expression of 28 genes know to play a role in melanoma metastasis, and three control genes. Tumors are stratified either as Class 1, with a 3% chance of spreading within 5 years, or Class 2, with a 69% risk of metastasis. There are two subclasses: 1A, which has an extremely low risk of progression, and 2b, which has an extremely high risk of progression.
For patients with T1-T2 tumors who had a Class 1A test result (lowest risk of recurrence), SLN positivity was 4.6% for all ages, 2.8% in patients 55 years and older, and 1.6% in patients 65 years and older. For patients with T1-T2 tumors who had a Class 2B test result (highest risk of recurrence), SLN positivity was 18.8% for all ages, 16.4% in patients 55 years and older and 11.9% in patients 65 years and older.
Dr. Vetto is a paid speaker for Castle Biosciences.
SOURCE: Vetto et al. AAD 2018 late-breaking research, Abstract 6805
SAN DIEGO – The results of a gene expression test, along with tumor thickness and patient age, can guide the need for sentinel lymph node biopsy, based on results from more than1,400 consecutively tested patients from 26 U.S. surgical oncology, medical oncology and dermatologic practices.
The findings, presented by John Vetto, MD, at the annual meeting of the American Academy of Dermatology, indicate the DecisionDx test correctly identified patients aged 65 and older with T1-T2 tumors whose risk of sentinel node metastasis was lower than 5%. The most recent melanoma guidelines from the National Comprehensive Cancer Network recommend that clinicians “discuss and offer” sentinel node biopsy if a patient has a greater than 10% likelihood of a positive node. If the likelihood is 5%-10%, the recommendation is to “discuss and consider” the procedure. But if the likelihood of a positive node is less than 5%, the guidelines recommend against a biopsy.
“Sentinel node biopsy (has) risks, especially in medically compromised older patients,” Dr. Vetto, professor of surgery at the Oregon Health and Sciences University, Portland, said in an interview, in which he discussed clinical use of the test. “This test offers us a good way to assess the risk/benefit ratio so we can better care for patients, and follow the newest guidelines about sentinel node biopsy.”
The DecisionDx Melanoma, developed by Castle Biosciences, tests for the expression of 28 genes know to play a role in melanoma metastasis, and three control genes. Tumors are stratified either as Class 1, with a 3% chance of spreading within 5 years, or Class 2, with a 69% risk of metastasis. There are two subclasses: 1A, which has an extremely low risk of progression, and 2b, which has an extremely high risk of progression.
For patients with T1-T2 tumors who had a Class 1A test result (lowest risk of recurrence), SLN positivity was 4.6% for all ages, 2.8% in patients 55 years and older, and 1.6% in patients 65 years and older. For patients with T1-T2 tumors who had a Class 2B test result (highest risk of recurrence), SLN positivity was 18.8% for all ages, 16.4% in patients 55 years and older and 11.9% in patients 65 years and older.
Dr. Vetto is a paid speaker for Castle Biosciences.
SOURCE: Vetto et al. AAD 2018 late-breaking research, Abstract 6805
REPORTING FROM AAD 18
VIDEO: Parabens named ‘nonallergen’ of the year
SAN DIEGO – With propylene glycol already declared 2018 Allergen of the Year in a published journal article, the news at the Allergen of the Year session of the American Contact Dermatitis Society was announcement of the 2019 pick, parabens.
From a skin perspective, parabens are “perhaps the safest” preservative, but despite that they have a bad public reputation Donald V. Belsito, MD, said in his Allergen of the Year talk during the Society’s annual meeting held the day before the annual meeting of the American Academy of Dermatology.
There is an unfounded public perception that parabens cause endocrine disruption. Naming parabens the “nonallergen” of the year for 2019 is an effort to dispel this myth, Dr. Belsito said in a video interview.
The public prejudice against parabens, exacerbated by many products that tout being paraben free, has helped cause a crisis because preservative systems in general have been under attack and facing restrictions. Dr. Belsito cited European limitations on the preservative methylisothiazolinone (Allergen of the Year in 2013) and withdrawal of formaldehyde (2015 Allergen of the Year) from many products.
Dr. Belsito also highlighted why propylene glycol received the nod as 2018’s Allergen of the Year (Dermatitis. 2018 Jan/Feb;29[1]:3-5). Propylene glycol is a very ubiquitous emulsifier found in cosmetics, foods, and both topical and oral medications. Caution is needed when running a patch test on the agent to distinguish an irritation reaction from an allergic reaction. Interpreting the test result correctly is very important, said Dr. Belsito, professor of dermatology at Columbia University in New York.
Parabens is the 20th Allergen of the Year named by the Society, an annual event since 2000.
Dr. Belsito has participated in the program since its start.
SAN DIEGO – With propylene glycol already declared 2018 Allergen of the Year in a published journal article, the news at the Allergen of the Year session of the American Contact Dermatitis Society was announcement of the 2019 pick, parabens.
From a skin perspective, parabens are “perhaps the safest” preservative, but despite that they have a bad public reputation Donald V. Belsito, MD, said in his Allergen of the Year talk during the Society’s annual meeting held the day before the annual meeting of the American Academy of Dermatology.
There is an unfounded public perception that parabens cause endocrine disruption. Naming parabens the “nonallergen” of the year for 2019 is an effort to dispel this myth, Dr. Belsito said in a video interview.
The public prejudice against parabens, exacerbated by many products that tout being paraben free, has helped cause a crisis because preservative systems in general have been under attack and facing restrictions. Dr. Belsito cited European limitations on the preservative methylisothiazolinone (Allergen of the Year in 2013) and withdrawal of formaldehyde (2015 Allergen of the Year) from many products.
Dr. Belsito also highlighted why propylene glycol received the nod as 2018’s Allergen of the Year (Dermatitis. 2018 Jan/Feb;29[1]:3-5). Propylene glycol is a very ubiquitous emulsifier found in cosmetics, foods, and both topical and oral medications. Caution is needed when running a patch test on the agent to distinguish an irritation reaction from an allergic reaction. Interpreting the test result correctly is very important, said Dr. Belsito, professor of dermatology at Columbia University in New York.
Parabens is the 20th Allergen of the Year named by the Society, an annual event since 2000.
Dr. Belsito has participated in the program since its start.
SAN DIEGO – With propylene glycol already declared 2018 Allergen of the Year in a published journal article, the news at the Allergen of the Year session of the American Contact Dermatitis Society was announcement of the 2019 pick, parabens.
From a skin perspective, parabens are “perhaps the safest” preservative, but despite that they have a bad public reputation Donald V. Belsito, MD, said in his Allergen of the Year talk during the Society’s annual meeting held the day before the annual meeting of the American Academy of Dermatology.
There is an unfounded public perception that parabens cause endocrine disruption. Naming parabens the “nonallergen” of the year for 2019 is an effort to dispel this myth, Dr. Belsito said in a video interview.
The public prejudice against parabens, exacerbated by many products that tout being paraben free, has helped cause a crisis because preservative systems in general have been under attack and facing restrictions. Dr. Belsito cited European limitations on the preservative methylisothiazolinone (Allergen of the Year in 2013) and withdrawal of formaldehyde (2015 Allergen of the Year) from many products.
Dr. Belsito also highlighted why propylene glycol received the nod as 2018’s Allergen of the Year (Dermatitis. 2018 Jan/Feb;29[1]:3-5). Propylene glycol is a very ubiquitous emulsifier found in cosmetics, foods, and both topical and oral medications. Caution is needed when running a patch test on the agent to distinguish an irritation reaction from an allergic reaction. Interpreting the test result correctly is very important, said Dr. Belsito, professor of dermatology at Columbia University in New York.
Parabens is the 20th Allergen of the Year named by the Society, an annual event since 2000.
Dr. Belsito has participated in the program since its start.
FROM ACDS 18
VIDEO: Stroke benefits from stem cells maintained for 2 years
LOS ANGELES – , Gary K. Steinberg, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
Seeing sustained benefit out to 2 years was “quite surprising. We thought we’d lose the benefit,” Dr. Steinberg said in a video interview.
The findings “change our notion of what happens after a stroke. The damaged circuits can be resurrected,” said Dr. Steinberg, professor and chair of neurosurgery at Stanford (Calif.) University.
He reported long-term follow-up data for 18 chronic stroke patients who had received transplantation of allogeneic bone marrow–derived stem cells. The study’s primary efficacy endpoint, at 6 months after treatment, showed clinically meaningful improvements in several measures of stroke disability and function in 13 of the 18 patients (72%), including a rise of at least 10 points in the Fugl-Meyer total motor function score.
His new report on 2-year follow-up showed that these 6-month improvements continued. The average increase in Fugl-Meyer score over baseline was about 18 points at 6, 12, and 24 months of follow-up.
Based on the promise shown in this pilot study, Dr. Steinberg and his associates are running a randomized study with 156 patients. Enrollment recently completed, and the results should be available during the second half of 2019, Dr. Steinberg said.
SanBio funded the study. Dr. Steinberg has been a consultant or advisor to Qool Therapeutics, Peter Lazic US, and NeuroSave.
SOURCE: Steinberg K et al. International Stroke Conference 2018, Abstract LB14.
LOS ANGELES – , Gary K. Steinberg, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
Seeing sustained benefit out to 2 years was “quite surprising. We thought we’d lose the benefit,” Dr. Steinberg said in a video interview.
The findings “change our notion of what happens after a stroke. The damaged circuits can be resurrected,” said Dr. Steinberg, professor and chair of neurosurgery at Stanford (Calif.) University.
He reported long-term follow-up data for 18 chronic stroke patients who had received transplantation of allogeneic bone marrow–derived stem cells. The study’s primary efficacy endpoint, at 6 months after treatment, showed clinically meaningful improvements in several measures of stroke disability and function in 13 of the 18 patients (72%), including a rise of at least 10 points in the Fugl-Meyer total motor function score.
His new report on 2-year follow-up showed that these 6-month improvements continued. The average increase in Fugl-Meyer score over baseline was about 18 points at 6, 12, and 24 months of follow-up.
Based on the promise shown in this pilot study, Dr. Steinberg and his associates are running a randomized study with 156 patients. Enrollment recently completed, and the results should be available during the second half of 2019, Dr. Steinberg said.
SanBio funded the study. Dr. Steinberg has been a consultant or advisor to Qool Therapeutics, Peter Lazic US, and NeuroSave.
SOURCE: Steinberg K et al. International Stroke Conference 2018, Abstract LB14.
LOS ANGELES – , Gary K. Steinberg, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
Seeing sustained benefit out to 2 years was “quite surprising. We thought we’d lose the benefit,” Dr. Steinberg said in a video interview.
The findings “change our notion of what happens after a stroke. The damaged circuits can be resurrected,” said Dr. Steinberg, professor and chair of neurosurgery at Stanford (Calif.) University.
He reported long-term follow-up data for 18 chronic stroke patients who had received transplantation of allogeneic bone marrow–derived stem cells. The study’s primary efficacy endpoint, at 6 months after treatment, showed clinically meaningful improvements in several measures of stroke disability and function in 13 of the 18 patients (72%), including a rise of at least 10 points in the Fugl-Meyer total motor function score.
His new report on 2-year follow-up showed that these 6-month improvements continued. The average increase in Fugl-Meyer score over baseline was about 18 points at 6, 12, and 24 months of follow-up.
Based on the promise shown in this pilot study, Dr. Steinberg and his associates are running a randomized study with 156 patients. Enrollment recently completed, and the results should be available during the second half of 2019, Dr. Steinberg said.
SanBio funded the study. Dr. Steinberg has been a consultant or advisor to Qool Therapeutics, Peter Lazic US, and NeuroSave.
SOURCE: Steinberg K et al. International Stroke Conference 2018, Abstract LB14.
REPORTING FROM ISC 2018
Key clinical point: The stroke benefits from cell transplantation continued during 2-year follow-up.
Major finding: Among 18 treated patients, 13 (72%) had a sustained, clinically meaningful rise in their total motor function score.
Study details: Review of 18 patients who received intracranial cell transplantations at two U.S. sites.
Disclosures: SanBio funded the study. Dr. Steinberg has been a consultant or adviser to Qool Therapeutics, Peter Lazic US, and NeuroSave.
Source: Steinberg K et al. International Stroke Conference 2018, Abstract LB14.
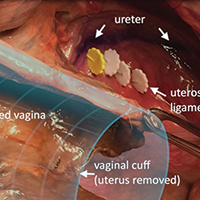
Surgical anatomy and steps of the uterosacral ligament colpopexy

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
This video is brought to you by
Video roundtable–Endometriosis: Expert perspectives on medical and surgical management

Read the article: Endometriosis: Expert perspectives on medical and surgical management

Read the article: Endometriosis: Expert perspectives on medical and surgical management

Read the article: Endometriosis: Expert perspectives on medical and surgical management
How to avoid and manage complications when placing ports and docking



A Peek at Our February 2018 Issue
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel