User login
AHA: Broadening evidence for CABG over PCI in diabetics
ORLANDO – New evidence further strengthens the case for coronary artery bypass grafting over percutaneous coronary intervention as the preferred revascularization strategy in diabetic patients with multivessel coronary artery disease.
An analysis of 4,819 such patients in a British Columbia province-wide registry who underwent revascularization during 2007-2014 led to the conclusion that the 30-day adjusted risk of the primary composite endpoint of death, MI, or stroke was 39% lower in those who underwent coronary artery bypass grafting (CABG), Dr. Krishnan Ramanathan reported at the American Heart Association scientific sessions.
From day 31 through 5 years of follow-up, the relative risk reduction was 36% in favor of CABG, again after adjustment for age, sex, presentation with stable ischemic heart disease or stabilized acute coronary syndrome (ACS), urgency, renal insufficiency, liver disease, peripheral arterial disease, and left ventricular ejection fraction, added Dr. Ramanathan of the University of British Columbia in Vancouver.
These results in a broad patient population in real-world clinical practice, albeit in an observational, nonrandomized setting, mirror those in the earlier randomized FREEDOM trial sponsored by the National Heart, Lung, and Blood Institute. The 5-year rate of the composite of death, MI, or stroke in FREEDOM was 18.7% in the CABG group and 26.6% with percutaneous coronary intervention (PCI). The number needed to treat with CABG instead of PCI in FREEDOM in order to avoid one case of the composite endpoint was 12.6 (N Engl J Med. 2012 Dec 20;367[25]:2375-84).
An important difference between the British Columbia and the FREEDOM trial is that the registry contained a much higher proportion of diabetic patients with multivessel disease who presented with acute coronary syndrome. Indeed, the ratio of stabilized ACS to stable ischemic heart disease patients in the registry was 62% to 38% as compared with 36% to 64% in FREEDOM. The registry patients underwent a median of 7.8 days of stabilization from the time of initial catheterization to CABG.
The registry data really shore up the advantages of CABG over PCI in diabetics with multivessel disease and ACS, Dr. Ramanathan noted. In the registry, the 30-day composite endpoint occurred in 4.4% of CABG-treated ACS patients, compared with 8.3% with PCI. For 31 days through 5 years, the rates were 21.4% versus 34.7%. The differences favoring CABG were highly significant at both time points.
FREEDOM led to two important revisions in the 2014 guidelines on coronary revascularization, issued by the American College of Cardiology, American Heart Association, American Academy of Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiac Angiography and Interventions, and Society of Thoracic Surgeons. In a focused update issued earlier this year, a new class I recommendation was issued calling for a heart team approach to revascularization in patients with diabetes mellitus and complex multivessel coronary artery disease (CAD). And a recommendation for CABG over PCI for improving survival in diabetic patients with multivessel CAD was upgraded from class IIa to class I.
Even though FREEDOM was a major randomized trial that might be expected to be practice changing, that hasn’t happened. A report from the ACC’s National Cardiovascular Data ACTION Registry presented earlier this year at the ACC annual scientific session documented that the most common revascularization strategy for diabetic patients with multivessel CAD following a non–ST elevation ACS remains PCI, as has been the case since the registry was created. In fact, following the 2012 publication of FREEDOM, the proportion of such patients treated by PCI took a sharp uptick in 2013-2014, according to Dr. Ramanathan.
In the British Columbia registry, 64% of diabetic patients with multivessel disease and an ACS were treated by PCI, 36% by CABG.
“Overall, CABG in stabilized ACS patients is underutilized,” he said.
Discussant Dr. Marc Ruel declared, “The salient finding about the British Columbia study is not so much about the stable ischemic heart disease patients, but about the high proportion of ACS patients in the study. CABG was better than PCI for all major adverse cardiovascular events and each component of the endpoint.”
Dr. Ruel, professor and chair of cardiac surgery at the University of Ottawa Heart Institute, coauthored a meta-analysis of randomized controlled trials comparing CABG to PCI in diabetic patients. Half of the trials used later-generation drug-eluting stents. At 5 years of follow-up, the relative risk of all-cause mortality in diabetic patients allocated to CABG was 0.67 (Lancet Diabetes Endocrinol. 2013 Dec;1[4]:317-28).
“Remember that 0.67 because it’s a recurring number in our literature,” he advised.
For example, in the British Columbia study the relative risk of death, MI, or stroke from 31 days to 5 years was 0.64 in the CABG as compared with the PCI group. And in a patient-level meta-analysis of the FREEDOM, BARI-2D, and COURAGE trials presented by Dr. John Mancini earlier at the AHA scientific sessions in Orlando, CABG plus optimal medical therapy was associated with a 0.65 relative risk of death, MI, or stroke, compared with PCI plus optimal medical therapy, which in turn wasn’t significantly better than optimal medical therapy alone, Dr. Ruel noted.
The 2015 European Society of Cardiology guidelines on management of ACS state that a heart team discussion involving a cardiologist and cardiac surgeon does not need to take place for every patient presenting with multivessel disease and a non–ST elevation ACS. The British Columbia study, coupled with the other evidence, “gives new credence” to a call for revision of that recommendation in diabetic patients, he said.
The British Columbia study was supported by the British Columbia Provincial Health Services Authority. Dr. Ramanathan reported having no financial conflicts.
ORLANDO – New evidence further strengthens the case for coronary artery bypass grafting over percutaneous coronary intervention as the preferred revascularization strategy in diabetic patients with multivessel coronary artery disease.
An analysis of 4,819 such patients in a British Columbia province-wide registry who underwent revascularization during 2007-2014 led to the conclusion that the 30-day adjusted risk of the primary composite endpoint of death, MI, or stroke was 39% lower in those who underwent coronary artery bypass grafting (CABG), Dr. Krishnan Ramanathan reported at the American Heart Association scientific sessions.
From day 31 through 5 years of follow-up, the relative risk reduction was 36% in favor of CABG, again after adjustment for age, sex, presentation with stable ischemic heart disease or stabilized acute coronary syndrome (ACS), urgency, renal insufficiency, liver disease, peripheral arterial disease, and left ventricular ejection fraction, added Dr. Ramanathan of the University of British Columbia in Vancouver.
These results in a broad patient population in real-world clinical practice, albeit in an observational, nonrandomized setting, mirror those in the earlier randomized FREEDOM trial sponsored by the National Heart, Lung, and Blood Institute. The 5-year rate of the composite of death, MI, or stroke in FREEDOM was 18.7% in the CABG group and 26.6% with percutaneous coronary intervention (PCI). The number needed to treat with CABG instead of PCI in FREEDOM in order to avoid one case of the composite endpoint was 12.6 (N Engl J Med. 2012 Dec 20;367[25]:2375-84).
An important difference between the British Columbia and the FREEDOM trial is that the registry contained a much higher proportion of diabetic patients with multivessel disease who presented with acute coronary syndrome. Indeed, the ratio of stabilized ACS to stable ischemic heart disease patients in the registry was 62% to 38% as compared with 36% to 64% in FREEDOM. The registry patients underwent a median of 7.8 days of stabilization from the time of initial catheterization to CABG.
The registry data really shore up the advantages of CABG over PCI in diabetics with multivessel disease and ACS, Dr. Ramanathan noted. In the registry, the 30-day composite endpoint occurred in 4.4% of CABG-treated ACS patients, compared with 8.3% with PCI. For 31 days through 5 years, the rates were 21.4% versus 34.7%. The differences favoring CABG were highly significant at both time points.
FREEDOM led to two important revisions in the 2014 guidelines on coronary revascularization, issued by the American College of Cardiology, American Heart Association, American Academy of Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiac Angiography and Interventions, and Society of Thoracic Surgeons. In a focused update issued earlier this year, a new class I recommendation was issued calling for a heart team approach to revascularization in patients with diabetes mellitus and complex multivessel coronary artery disease (CAD). And a recommendation for CABG over PCI for improving survival in diabetic patients with multivessel CAD was upgraded from class IIa to class I.
Even though FREEDOM was a major randomized trial that might be expected to be practice changing, that hasn’t happened. A report from the ACC’s National Cardiovascular Data ACTION Registry presented earlier this year at the ACC annual scientific session documented that the most common revascularization strategy for diabetic patients with multivessel CAD following a non–ST elevation ACS remains PCI, as has been the case since the registry was created. In fact, following the 2012 publication of FREEDOM, the proportion of such patients treated by PCI took a sharp uptick in 2013-2014, according to Dr. Ramanathan.
In the British Columbia registry, 64% of diabetic patients with multivessel disease and an ACS were treated by PCI, 36% by CABG.
“Overall, CABG in stabilized ACS patients is underutilized,” he said.
Discussant Dr. Marc Ruel declared, “The salient finding about the British Columbia study is not so much about the stable ischemic heart disease patients, but about the high proportion of ACS patients in the study. CABG was better than PCI for all major adverse cardiovascular events and each component of the endpoint.”
Dr. Ruel, professor and chair of cardiac surgery at the University of Ottawa Heart Institute, coauthored a meta-analysis of randomized controlled trials comparing CABG to PCI in diabetic patients. Half of the trials used later-generation drug-eluting stents. At 5 years of follow-up, the relative risk of all-cause mortality in diabetic patients allocated to CABG was 0.67 (Lancet Diabetes Endocrinol. 2013 Dec;1[4]:317-28).
“Remember that 0.67 because it’s a recurring number in our literature,” he advised.
For example, in the British Columbia study the relative risk of death, MI, or stroke from 31 days to 5 years was 0.64 in the CABG as compared with the PCI group. And in a patient-level meta-analysis of the FREEDOM, BARI-2D, and COURAGE trials presented by Dr. John Mancini earlier at the AHA scientific sessions in Orlando, CABG plus optimal medical therapy was associated with a 0.65 relative risk of death, MI, or stroke, compared with PCI plus optimal medical therapy, which in turn wasn’t significantly better than optimal medical therapy alone, Dr. Ruel noted.
The 2015 European Society of Cardiology guidelines on management of ACS state that a heart team discussion involving a cardiologist and cardiac surgeon does not need to take place for every patient presenting with multivessel disease and a non–ST elevation ACS. The British Columbia study, coupled with the other evidence, “gives new credence” to a call for revision of that recommendation in diabetic patients, he said.
The British Columbia study was supported by the British Columbia Provincial Health Services Authority. Dr. Ramanathan reported having no financial conflicts.
ORLANDO – New evidence further strengthens the case for coronary artery bypass grafting over percutaneous coronary intervention as the preferred revascularization strategy in diabetic patients with multivessel coronary artery disease.
An analysis of 4,819 such patients in a British Columbia province-wide registry who underwent revascularization during 2007-2014 led to the conclusion that the 30-day adjusted risk of the primary composite endpoint of death, MI, or stroke was 39% lower in those who underwent coronary artery bypass grafting (CABG), Dr. Krishnan Ramanathan reported at the American Heart Association scientific sessions.
From day 31 through 5 years of follow-up, the relative risk reduction was 36% in favor of CABG, again after adjustment for age, sex, presentation with stable ischemic heart disease or stabilized acute coronary syndrome (ACS), urgency, renal insufficiency, liver disease, peripheral arterial disease, and left ventricular ejection fraction, added Dr. Ramanathan of the University of British Columbia in Vancouver.
These results in a broad patient population in real-world clinical practice, albeit in an observational, nonrandomized setting, mirror those in the earlier randomized FREEDOM trial sponsored by the National Heart, Lung, and Blood Institute. The 5-year rate of the composite of death, MI, or stroke in FREEDOM was 18.7% in the CABG group and 26.6% with percutaneous coronary intervention (PCI). The number needed to treat with CABG instead of PCI in FREEDOM in order to avoid one case of the composite endpoint was 12.6 (N Engl J Med. 2012 Dec 20;367[25]:2375-84).
An important difference between the British Columbia and the FREEDOM trial is that the registry contained a much higher proportion of diabetic patients with multivessel disease who presented with acute coronary syndrome. Indeed, the ratio of stabilized ACS to stable ischemic heart disease patients in the registry was 62% to 38% as compared with 36% to 64% in FREEDOM. The registry patients underwent a median of 7.8 days of stabilization from the time of initial catheterization to CABG.
The registry data really shore up the advantages of CABG over PCI in diabetics with multivessel disease and ACS, Dr. Ramanathan noted. In the registry, the 30-day composite endpoint occurred in 4.4% of CABG-treated ACS patients, compared with 8.3% with PCI. For 31 days through 5 years, the rates were 21.4% versus 34.7%. The differences favoring CABG were highly significant at both time points.
FREEDOM led to two important revisions in the 2014 guidelines on coronary revascularization, issued by the American College of Cardiology, American Heart Association, American Academy of Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiac Angiography and Interventions, and Society of Thoracic Surgeons. In a focused update issued earlier this year, a new class I recommendation was issued calling for a heart team approach to revascularization in patients with diabetes mellitus and complex multivessel coronary artery disease (CAD). And a recommendation for CABG over PCI for improving survival in diabetic patients with multivessel CAD was upgraded from class IIa to class I.
Even though FREEDOM was a major randomized trial that might be expected to be practice changing, that hasn’t happened. A report from the ACC’s National Cardiovascular Data ACTION Registry presented earlier this year at the ACC annual scientific session documented that the most common revascularization strategy for diabetic patients with multivessel CAD following a non–ST elevation ACS remains PCI, as has been the case since the registry was created. In fact, following the 2012 publication of FREEDOM, the proportion of such patients treated by PCI took a sharp uptick in 2013-2014, according to Dr. Ramanathan.
In the British Columbia registry, 64% of diabetic patients with multivessel disease and an ACS were treated by PCI, 36% by CABG.
“Overall, CABG in stabilized ACS patients is underutilized,” he said.
Discussant Dr. Marc Ruel declared, “The salient finding about the British Columbia study is not so much about the stable ischemic heart disease patients, but about the high proportion of ACS patients in the study. CABG was better than PCI for all major adverse cardiovascular events and each component of the endpoint.”
Dr. Ruel, professor and chair of cardiac surgery at the University of Ottawa Heart Institute, coauthored a meta-analysis of randomized controlled trials comparing CABG to PCI in diabetic patients. Half of the trials used later-generation drug-eluting stents. At 5 years of follow-up, the relative risk of all-cause mortality in diabetic patients allocated to CABG was 0.67 (Lancet Diabetes Endocrinol. 2013 Dec;1[4]:317-28).
“Remember that 0.67 because it’s a recurring number in our literature,” he advised.
For example, in the British Columbia study the relative risk of death, MI, or stroke from 31 days to 5 years was 0.64 in the CABG as compared with the PCI group. And in a patient-level meta-analysis of the FREEDOM, BARI-2D, and COURAGE trials presented by Dr. John Mancini earlier at the AHA scientific sessions in Orlando, CABG plus optimal medical therapy was associated with a 0.65 relative risk of death, MI, or stroke, compared with PCI plus optimal medical therapy, which in turn wasn’t significantly better than optimal medical therapy alone, Dr. Ruel noted.
The 2015 European Society of Cardiology guidelines on management of ACS state that a heart team discussion involving a cardiologist and cardiac surgeon does not need to take place for every patient presenting with multivessel disease and a non–ST elevation ACS. The British Columbia study, coupled with the other evidence, “gives new credence” to a call for revision of that recommendation in diabetic patients, he said.
The British Columbia study was supported by the British Columbia Provincial Health Services Authority. Dr. Ramanathan reported having no financial conflicts.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: New evidence reinforces CABG as preferred over PCI for revascularization in diabetic patients with multivessel CAD.
Major finding: Diabetic patients with multivessel CAD were 36% less likely to experience death, MI, or stroke within the next 5 years if they underwent revascularization with CABG than PCI.
Data source: This observational registry study included 4,819 diabetic patients with multivessel CAD who underwent CABG or isolated PCI for stable ischemic heart disease or stabilized acute coronary syndrome.
Disclosures: The study was supported by the British Columbia Provincial Health Services Authority. The presenter reported having no financial conflicts of interest.
AHA: New emphasis on percent LDL reduction on-treatment
ORLANDO – The individual variability in percent reduction in LDL cholesterol levels in response to high-intensity statin therapy is far greater than generally appreciated, and this has important implications for clinical practice, Dr. Paul M. Ridker said at the American Heart Association scientific sessions.
A new secondary analysis from the landmark JUPITER trial highlighted this substantial variability in percent reduction in LDL cholesterol on 20 mg/day of rosuvastatin (Crestor). Moreover, it showed that the size of this reduction was directly related to the magnitude of reduction in cardiovascular events.
“These data provide general support for the concept of introducing percent reduction in LDL cholesterol into broader clinical practice,” said Dr. Ridker, director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, Boston.
The concept of percent LDL reduction as a treatment target is already widely embedded in the ACC/AHA, European Society of Cardiology, and Canadian Cardiovascular Society cholesterol management guidelines, he noted.
For example, the 2013 ACC/AHA guidelines state that lower-risk individuals who qualify for statin therapy should receive a moderate-intensity statin regimen capable of reducing LDL by 30%-50% from baseline, while higher-risk patients should be placed on a high-intensity statin, described as an agent that gives a 50% or greater reduction in LDL. The new JUPITER analysis makes the case for featuring percent LDL reduction more prominently as an explicit personalized treatment target in the guidelines, Dr. Ridker continued.
In JUPITER, 17,802 apparently healthy subjects with an LDL cholesterol level below 130 mg/dL were randomized to rosuvastatin or placebo. The trial was halted early, after a median of 1.9 years, because the rosuvastatin group showed a compelling 44% reduction in the composite endpoint of MI, stroke, unstable angina treated by revascularization, or cardiovascular death (N Engl J Med. 2008 Nov 20;359[21]:2195-320).
In JUPITER, rosuvastatin reduced LDL cholesterol by an average of 50% in the 7,856 treated patients. But as the new analysis demonstrates, individual variability in response was huge, ranging from no LDL reduction at all to a greater than 85% reduction. And cardiovascular event rates varied accordingly: from 11.2 events per 1,000 person-years with placebo to 9.2 in rosuvastatin-treated patients with no LDL reduction, 6.7 in those with less than a 50% drop in LDL, and 4.8 events per 1,000 person-years in subjects with a greater than 50% reduction in LDL on rosuvastatin. Thus, the one-half of rosuvastatin-treated patients who had more than a 50% decrease in LDL had an adjusted 59% reduction in major cardiovascular events, compared with placebo, while those with a drop of less than 50% in LDL had a 39% risk reduction.
The same exceptionally wide individual variability was seen in on-treatment reductions in apolipoprotein B cholesterol and non–HDL cholesterol levels, and once again, the magnitude of the percent reduction in these lipids tracked with the size of the reduction in cardiovascular events.
This new analysis from JUPITER essentially confirms the findings of an earlier meta-analysis of eight randomized controlled trials with more than 38,000 patients assigned to statin therapy. The meta-analysis showed very large interindividual variations in reductions in LDL, non–HDL cholesterol, and apolipoprotein B in response to high-dose statin therapy. Moreover, patients who achieved very low LDL levels on-treatment had a lower risk of cardiovascular events than those who achieved more moderate LDL reductions (J Am Coll Cardiol. 2014 Aug 5;64[5]:485-94).
Dr. Ridker said the new findings from JUPITER and the meta-analysis, in addition to their implications for clinical practice, could also be relevant in the future with regard to treatment decisions regarding when to prescribe proprotein convertase subtilisin–kexin type 9 (PCSK9) inhibitors, assuming ongoing clinical trials ultimately show that this novel and expensive class of superpotent LDL-lowering agents reduces the risk of cardiovascular events.
He noted that 20% of rosuvastatin-treated JUPITER participants had a greater than 60% reduction in LDL. In theory, he explained, this might be the group where the PCSK9 inhibitors would have the least benefit because those patients already have a 70%-80% reduction in LDL on a high-intensity statin.
On the other hand, the 35% of JUPITER participants with an on-treatment LDL reduction ranging from zero to less than 40% would have the greatest theoretic benefit from a PCSK9 inhibitor, while patients who obtained a 40%-60% LDL reduction on rosuvastatin would be expected to derive an intermediate benefit from the new drugs.
Discussant Michael J. Pencina, Ph.D., said the current U.S. cholesterol management guidelines focus heavily on cardiovascular risk as determined by the risk calculator equation. This needs to be balanced by a more explicit focus on assessment of the anticipated benefit of therapy, he added. For this reason, he agreed with Dr. Ridker’s call to incorporate measurement of percent reduction in lipid levels into individualized assessment of therapeutic benefit.
It will be important for the ongoing randomized trials of PCSK9 inhibitors to report results stratified by the percent reduction in LDL cholesterol achieved by background statin therapy. This will be useful, as Dr. Ridker said, in figuring out how best to allocate this new class of lipid-lowering medications, added Dr. Pencina, professor of biostatistics and bioinformatics at Duke University, Durham, N.C.
Dr. Ridker reported receiving research grants from AstraZeneca, Pfizer, Amgen, and the National Institutes of Health.
ORLANDO – The individual variability in percent reduction in LDL cholesterol levels in response to high-intensity statin therapy is far greater than generally appreciated, and this has important implications for clinical practice, Dr. Paul M. Ridker said at the American Heart Association scientific sessions.
A new secondary analysis from the landmark JUPITER trial highlighted this substantial variability in percent reduction in LDL cholesterol on 20 mg/day of rosuvastatin (Crestor). Moreover, it showed that the size of this reduction was directly related to the magnitude of reduction in cardiovascular events.
“These data provide general support for the concept of introducing percent reduction in LDL cholesterol into broader clinical practice,” said Dr. Ridker, director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, Boston.
The concept of percent LDL reduction as a treatment target is already widely embedded in the ACC/AHA, European Society of Cardiology, and Canadian Cardiovascular Society cholesterol management guidelines, he noted.
For example, the 2013 ACC/AHA guidelines state that lower-risk individuals who qualify for statin therapy should receive a moderate-intensity statin regimen capable of reducing LDL by 30%-50% from baseline, while higher-risk patients should be placed on a high-intensity statin, described as an agent that gives a 50% or greater reduction in LDL. The new JUPITER analysis makes the case for featuring percent LDL reduction more prominently as an explicit personalized treatment target in the guidelines, Dr. Ridker continued.
In JUPITER, 17,802 apparently healthy subjects with an LDL cholesterol level below 130 mg/dL were randomized to rosuvastatin or placebo. The trial was halted early, after a median of 1.9 years, because the rosuvastatin group showed a compelling 44% reduction in the composite endpoint of MI, stroke, unstable angina treated by revascularization, or cardiovascular death (N Engl J Med. 2008 Nov 20;359[21]:2195-320).
In JUPITER, rosuvastatin reduced LDL cholesterol by an average of 50% in the 7,856 treated patients. But as the new analysis demonstrates, individual variability in response was huge, ranging from no LDL reduction at all to a greater than 85% reduction. And cardiovascular event rates varied accordingly: from 11.2 events per 1,000 person-years with placebo to 9.2 in rosuvastatin-treated patients with no LDL reduction, 6.7 in those with less than a 50% drop in LDL, and 4.8 events per 1,000 person-years in subjects with a greater than 50% reduction in LDL on rosuvastatin. Thus, the one-half of rosuvastatin-treated patients who had more than a 50% decrease in LDL had an adjusted 59% reduction in major cardiovascular events, compared with placebo, while those with a drop of less than 50% in LDL had a 39% risk reduction.
The same exceptionally wide individual variability was seen in on-treatment reductions in apolipoprotein B cholesterol and non–HDL cholesterol levels, and once again, the magnitude of the percent reduction in these lipids tracked with the size of the reduction in cardiovascular events.
This new analysis from JUPITER essentially confirms the findings of an earlier meta-analysis of eight randomized controlled trials with more than 38,000 patients assigned to statin therapy. The meta-analysis showed very large interindividual variations in reductions in LDL, non–HDL cholesterol, and apolipoprotein B in response to high-dose statin therapy. Moreover, patients who achieved very low LDL levels on-treatment had a lower risk of cardiovascular events than those who achieved more moderate LDL reductions (J Am Coll Cardiol. 2014 Aug 5;64[5]:485-94).
Dr. Ridker said the new findings from JUPITER and the meta-analysis, in addition to their implications for clinical practice, could also be relevant in the future with regard to treatment decisions regarding when to prescribe proprotein convertase subtilisin–kexin type 9 (PCSK9) inhibitors, assuming ongoing clinical trials ultimately show that this novel and expensive class of superpotent LDL-lowering agents reduces the risk of cardiovascular events.
He noted that 20% of rosuvastatin-treated JUPITER participants had a greater than 60% reduction in LDL. In theory, he explained, this might be the group where the PCSK9 inhibitors would have the least benefit because those patients already have a 70%-80% reduction in LDL on a high-intensity statin.
On the other hand, the 35% of JUPITER participants with an on-treatment LDL reduction ranging from zero to less than 40% would have the greatest theoretic benefit from a PCSK9 inhibitor, while patients who obtained a 40%-60% LDL reduction on rosuvastatin would be expected to derive an intermediate benefit from the new drugs.
Discussant Michael J. Pencina, Ph.D., said the current U.S. cholesterol management guidelines focus heavily on cardiovascular risk as determined by the risk calculator equation. This needs to be balanced by a more explicit focus on assessment of the anticipated benefit of therapy, he added. For this reason, he agreed with Dr. Ridker’s call to incorporate measurement of percent reduction in lipid levels into individualized assessment of therapeutic benefit.
It will be important for the ongoing randomized trials of PCSK9 inhibitors to report results stratified by the percent reduction in LDL cholesterol achieved by background statin therapy. This will be useful, as Dr. Ridker said, in figuring out how best to allocate this new class of lipid-lowering medications, added Dr. Pencina, professor of biostatistics and bioinformatics at Duke University, Durham, N.C.
Dr. Ridker reported receiving research grants from AstraZeneca, Pfizer, Amgen, and the National Institutes of Health.
ORLANDO – The individual variability in percent reduction in LDL cholesterol levels in response to high-intensity statin therapy is far greater than generally appreciated, and this has important implications for clinical practice, Dr. Paul M. Ridker said at the American Heart Association scientific sessions.
A new secondary analysis from the landmark JUPITER trial highlighted this substantial variability in percent reduction in LDL cholesterol on 20 mg/day of rosuvastatin (Crestor). Moreover, it showed that the size of this reduction was directly related to the magnitude of reduction in cardiovascular events.
“These data provide general support for the concept of introducing percent reduction in LDL cholesterol into broader clinical practice,” said Dr. Ridker, director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, Boston.
The concept of percent LDL reduction as a treatment target is already widely embedded in the ACC/AHA, European Society of Cardiology, and Canadian Cardiovascular Society cholesterol management guidelines, he noted.
For example, the 2013 ACC/AHA guidelines state that lower-risk individuals who qualify for statin therapy should receive a moderate-intensity statin regimen capable of reducing LDL by 30%-50% from baseline, while higher-risk patients should be placed on a high-intensity statin, described as an agent that gives a 50% or greater reduction in LDL. The new JUPITER analysis makes the case for featuring percent LDL reduction more prominently as an explicit personalized treatment target in the guidelines, Dr. Ridker continued.
In JUPITER, 17,802 apparently healthy subjects with an LDL cholesterol level below 130 mg/dL were randomized to rosuvastatin or placebo. The trial was halted early, after a median of 1.9 years, because the rosuvastatin group showed a compelling 44% reduction in the composite endpoint of MI, stroke, unstable angina treated by revascularization, or cardiovascular death (N Engl J Med. 2008 Nov 20;359[21]:2195-320).
In JUPITER, rosuvastatin reduced LDL cholesterol by an average of 50% in the 7,856 treated patients. But as the new analysis demonstrates, individual variability in response was huge, ranging from no LDL reduction at all to a greater than 85% reduction. And cardiovascular event rates varied accordingly: from 11.2 events per 1,000 person-years with placebo to 9.2 in rosuvastatin-treated patients with no LDL reduction, 6.7 in those with less than a 50% drop in LDL, and 4.8 events per 1,000 person-years in subjects with a greater than 50% reduction in LDL on rosuvastatin. Thus, the one-half of rosuvastatin-treated patients who had more than a 50% decrease in LDL had an adjusted 59% reduction in major cardiovascular events, compared with placebo, while those with a drop of less than 50% in LDL had a 39% risk reduction.
The same exceptionally wide individual variability was seen in on-treatment reductions in apolipoprotein B cholesterol and non–HDL cholesterol levels, and once again, the magnitude of the percent reduction in these lipids tracked with the size of the reduction in cardiovascular events.
This new analysis from JUPITER essentially confirms the findings of an earlier meta-analysis of eight randomized controlled trials with more than 38,000 patients assigned to statin therapy. The meta-analysis showed very large interindividual variations in reductions in LDL, non–HDL cholesterol, and apolipoprotein B in response to high-dose statin therapy. Moreover, patients who achieved very low LDL levels on-treatment had a lower risk of cardiovascular events than those who achieved more moderate LDL reductions (J Am Coll Cardiol. 2014 Aug 5;64[5]:485-94).
Dr. Ridker said the new findings from JUPITER and the meta-analysis, in addition to their implications for clinical practice, could also be relevant in the future with regard to treatment decisions regarding when to prescribe proprotein convertase subtilisin–kexin type 9 (PCSK9) inhibitors, assuming ongoing clinical trials ultimately show that this novel and expensive class of superpotent LDL-lowering agents reduces the risk of cardiovascular events.
He noted that 20% of rosuvastatin-treated JUPITER participants had a greater than 60% reduction in LDL. In theory, he explained, this might be the group where the PCSK9 inhibitors would have the least benefit because those patients already have a 70%-80% reduction in LDL on a high-intensity statin.
On the other hand, the 35% of JUPITER participants with an on-treatment LDL reduction ranging from zero to less than 40% would have the greatest theoretic benefit from a PCSK9 inhibitor, while patients who obtained a 40%-60% LDL reduction on rosuvastatin would be expected to derive an intermediate benefit from the new drugs.
Discussant Michael J. Pencina, Ph.D., said the current U.S. cholesterol management guidelines focus heavily on cardiovascular risk as determined by the risk calculator equation. This needs to be balanced by a more explicit focus on assessment of the anticipated benefit of therapy, he added. For this reason, he agreed with Dr. Ridker’s call to incorporate measurement of percent reduction in lipid levels into individualized assessment of therapeutic benefit.
It will be important for the ongoing randomized trials of PCSK9 inhibitors to report results stratified by the percent reduction in LDL cholesterol achieved by background statin therapy. This will be useful, as Dr. Ridker said, in figuring out how best to allocate this new class of lipid-lowering medications, added Dr. Pencina, professor of biostatistics and bioinformatics at Duke University, Durham, N.C.
Dr. Ridker reported receiving research grants from AstraZeneca, Pfizer, Amgen, and the National Institutes of Health.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: An individual’s percent reduction in LDL cholesterol achieved on statin therapy is a clinically important measurement.
Major finding: The percent LDL cholesterol lowering achieved with high-intensity statin therapy varies widely between individuals and tracks closely with the magnitude of cardiovascular risk reduction.
Data source: A secondary analysis of the JUPITER trial, in which more than 17,000 apparently healthy subjects were randomized to 20 mg/day of rosuvastatin or placebo.
Disclosures: The presenter reported receiving research grants from AstraZeneca, Pfizer, Amgen, and the National Institutes of Health.
AHA: Older Breast Cancer Patients More Likely to Die of Heart Disease Than Malignancy
ORLANDO – Women diagnosed with localized breast cancer while in their 70s have a higher mortality from cardiovascular disease than from their breast cancer, according to new data from the Women’s Health Initiative.
“Identification and treatment of cardiovascular disease risk factors among older women with breast cancer will likely improve survivorship and should be a high priority, especially for older women with incident localized breast cancer,” Na-Jin Park, Ph.D., said at the American Heart Association scientific sessions.
She presented an analysis that included 101,916 women who were free of cardiovascular disease and breast cancer upon enrollment in the Women’s Health Initiative (WHI) at age 50-79 years during 1993-1998. During follow-up in this prospective cohort study, 4,340 of them developed invasive breast cancer. The diagnosis occurred an average of 5 years into the study, and patients were followed for 10 years afterwards. “Forty-one percent of women with breast cancer already had cardiovascular risk factors at baseline, way before their breast cancer diagnosis,” noted Dr. Park of the University of Pittsburgh.
Among women diagnosed with breast cancer in their 50s, 40% of all deaths were from breast cancer and 15% were caused by cardiovascular disease. In contrast, the cumulative impact of atherosclerosis was far more prominent in women diagnosed with breast cancer at a more advanced age. Indeed, among women diagnosed with breast cancer in their 70s, about 15% of deaths were caused by breast cancer, while 25% resulted from cardiovascular disease.
The number of baseline cardiovascular risk factors present at enrollment in the WHI turned out to be a powerful determinant of the likelihood of acute MI or death as a result of coronary heart disease in participants who developed breast cancer.
Of the 4,340 women who later developed invasive breast cancer, 2,562 were free of hypertension, diabetes, and hypercholesterolemia and were nonsmokers upon enrollment. In an age-adjusted analysis in which this risk factor–free group served as the reference population, the risk of MI after breast cancer diagnosis was increased 1.65-fold in those with a single baseline risk factor, 3.2-fold in those with two, and 5.8-fold in women with three cardiovascular risk factors. Similarly, the breast cancer patients’ risk of CHD death climbed stepwise by 1.78-, 2.28-, and 3.6-fold as the number of baseline cardiovascular risk factors increased from one to three.
The greatest risk was seen in breast cancer patients who at WHI enrollment were current smokers with an additional cardiovascular risk factor. They had a 9.6-fold greater risk of an acute MI after developing breast cancer, compared with breast cancer patients with none of the baseline cardiovascular risk factors. They also had a 7.7-fold increased risk of CHD death.
The WHI was funded by the National Heart, Lung, and Blood Institute. Dr. Park reported having no financial conflicts of interest.
ORLANDO – Women diagnosed with localized breast cancer while in their 70s have a higher mortality from cardiovascular disease than from their breast cancer, according to new data from the Women’s Health Initiative.
“Identification and treatment of cardiovascular disease risk factors among older women with breast cancer will likely improve survivorship and should be a high priority, especially for older women with incident localized breast cancer,” Na-Jin Park, Ph.D., said at the American Heart Association scientific sessions.
She presented an analysis that included 101,916 women who were free of cardiovascular disease and breast cancer upon enrollment in the Women’s Health Initiative (WHI) at age 50-79 years during 1993-1998. During follow-up in this prospective cohort study, 4,340 of them developed invasive breast cancer. The diagnosis occurred an average of 5 years into the study, and patients were followed for 10 years afterwards. “Forty-one percent of women with breast cancer already had cardiovascular risk factors at baseline, way before their breast cancer diagnosis,” noted Dr. Park of the University of Pittsburgh.
Among women diagnosed with breast cancer in their 50s, 40% of all deaths were from breast cancer and 15% were caused by cardiovascular disease. In contrast, the cumulative impact of atherosclerosis was far more prominent in women diagnosed with breast cancer at a more advanced age. Indeed, among women diagnosed with breast cancer in their 70s, about 15% of deaths were caused by breast cancer, while 25% resulted from cardiovascular disease.
The number of baseline cardiovascular risk factors present at enrollment in the WHI turned out to be a powerful determinant of the likelihood of acute MI or death as a result of coronary heart disease in participants who developed breast cancer.
Of the 4,340 women who later developed invasive breast cancer, 2,562 were free of hypertension, diabetes, and hypercholesterolemia and were nonsmokers upon enrollment. In an age-adjusted analysis in which this risk factor–free group served as the reference population, the risk of MI after breast cancer diagnosis was increased 1.65-fold in those with a single baseline risk factor, 3.2-fold in those with two, and 5.8-fold in women with three cardiovascular risk factors. Similarly, the breast cancer patients’ risk of CHD death climbed stepwise by 1.78-, 2.28-, and 3.6-fold as the number of baseline cardiovascular risk factors increased from one to three.
The greatest risk was seen in breast cancer patients who at WHI enrollment were current smokers with an additional cardiovascular risk factor. They had a 9.6-fold greater risk of an acute MI after developing breast cancer, compared with breast cancer patients with none of the baseline cardiovascular risk factors. They also had a 7.7-fold increased risk of CHD death.
The WHI was funded by the National Heart, Lung, and Blood Institute. Dr. Park reported having no financial conflicts of interest.
ORLANDO – Women diagnosed with localized breast cancer while in their 70s have a higher mortality from cardiovascular disease than from their breast cancer, according to new data from the Women’s Health Initiative.
“Identification and treatment of cardiovascular disease risk factors among older women with breast cancer will likely improve survivorship and should be a high priority, especially for older women with incident localized breast cancer,” Na-Jin Park, Ph.D., said at the American Heart Association scientific sessions.
She presented an analysis that included 101,916 women who were free of cardiovascular disease and breast cancer upon enrollment in the Women’s Health Initiative (WHI) at age 50-79 years during 1993-1998. During follow-up in this prospective cohort study, 4,340 of them developed invasive breast cancer. The diagnosis occurred an average of 5 years into the study, and patients were followed for 10 years afterwards. “Forty-one percent of women with breast cancer already had cardiovascular risk factors at baseline, way before their breast cancer diagnosis,” noted Dr. Park of the University of Pittsburgh.
Among women diagnosed with breast cancer in their 50s, 40% of all deaths were from breast cancer and 15% were caused by cardiovascular disease. In contrast, the cumulative impact of atherosclerosis was far more prominent in women diagnosed with breast cancer at a more advanced age. Indeed, among women diagnosed with breast cancer in their 70s, about 15% of deaths were caused by breast cancer, while 25% resulted from cardiovascular disease.
The number of baseline cardiovascular risk factors present at enrollment in the WHI turned out to be a powerful determinant of the likelihood of acute MI or death as a result of coronary heart disease in participants who developed breast cancer.
Of the 4,340 women who later developed invasive breast cancer, 2,562 were free of hypertension, diabetes, and hypercholesterolemia and were nonsmokers upon enrollment. In an age-adjusted analysis in which this risk factor–free group served as the reference population, the risk of MI after breast cancer diagnosis was increased 1.65-fold in those with a single baseline risk factor, 3.2-fold in those with two, and 5.8-fold in women with three cardiovascular risk factors. Similarly, the breast cancer patients’ risk of CHD death climbed stepwise by 1.78-, 2.28-, and 3.6-fold as the number of baseline cardiovascular risk factors increased from one to three.
The greatest risk was seen in breast cancer patients who at WHI enrollment were current smokers with an additional cardiovascular risk factor. They had a 9.6-fold greater risk of an acute MI after developing breast cancer, compared with breast cancer patients with none of the baseline cardiovascular risk factors. They also had a 7.7-fold increased risk of CHD death.
The WHI was funded by the National Heart, Lung, and Blood Institute. Dr. Park reported having no financial conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
AHA: Older breast cancer patients more likely to die of heart disease than malignancy
ORLANDO – Women diagnosed with localized breast cancer while in their 70s have a higher mortality from cardiovascular disease than from their breast cancer, according to new data from the Women’s Health Initiative.
“Identification and treatment of cardiovascular disease risk factors among older women with breast cancer will likely improve survivorship and should be a high priority, especially for older women with incident localized breast cancer,” Na-Jin Park, Ph.D., said at the American Heart Association scientific sessions.
She presented an analysis that included 101,916 women who were free of cardiovascular disease and breast cancer upon enrollment in the Women’s Health Initiative (WHI) at age 50-79 years during 1993-1998. During follow-up in this prospective cohort study, 4,340 of them developed invasive breast cancer. The diagnosis occurred an average of 5 years into the study, and patients were followed for 10 years afterwards. “Forty-one percent of women with breast cancer already had cardiovascular risk factors at baseline, way before their breast cancer diagnosis,” noted Dr. Park of the University of Pittsburgh.
Among women diagnosed with breast cancer in their 50s, 40% of all deaths were from breast cancer and 15% were caused by cardiovascular disease. In contrast, the cumulative impact of atherosclerosis was far more prominent in women diagnosed with breast cancer at a more advanced age. Indeed, among women diagnosed with breast cancer in their 70s, about 15% of deaths were caused by breast cancer, while 25% resulted from cardiovascular disease.
The number of baseline cardiovascular risk factors present at enrollment in the WHI turned out to be a powerful determinant of the likelihood of acute MI or death as a result of coronary heart disease in participants who developed breast cancer.
Of the 4,340 women who later developed invasive breast cancer, 2,562 were free of hypertension, diabetes, and hypercholesterolemia and were nonsmokers upon enrollment. In an age-adjusted analysis in which this risk factor–free group served as the reference population, the risk of MI after breast cancer diagnosis was increased 1.65-fold in those with a single baseline risk factor, 3.2-fold in those with two, and 5.8-fold in women with three cardiovascular risk factors. Similarly, the breast cancer patients’ risk of CHD death climbed stepwise by 1.78-, 2.28-, and 3.6-fold as the number of baseline cardiovascular risk factors increased from one to three.
The greatest risk was seen in breast cancer patients who at WHI enrollment were current smokers with an additional cardiovascular risk factor. They had a 9.6-fold greater risk of an acute MI after developing breast cancer, compared with breast cancer patients with none of the baseline cardiovascular risk factors. They also had a 7.7-fold increased risk of CHD death.
The WHI was funded by the National Heart, Lung, and Blood Institute. Dr. Park reported having no financial conflicts of interest.
ORLANDO – Women diagnosed with localized breast cancer while in their 70s have a higher mortality from cardiovascular disease than from their breast cancer, according to new data from the Women’s Health Initiative.
“Identification and treatment of cardiovascular disease risk factors among older women with breast cancer will likely improve survivorship and should be a high priority, especially for older women with incident localized breast cancer,” Na-Jin Park, Ph.D., said at the American Heart Association scientific sessions.
She presented an analysis that included 101,916 women who were free of cardiovascular disease and breast cancer upon enrollment in the Women’s Health Initiative (WHI) at age 50-79 years during 1993-1998. During follow-up in this prospective cohort study, 4,340 of them developed invasive breast cancer. The diagnosis occurred an average of 5 years into the study, and patients were followed for 10 years afterwards. “Forty-one percent of women with breast cancer already had cardiovascular risk factors at baseline, way before their breast cancer diagnosis,” noted Dr. Park of the University of Pittsburgh.
Among women diagnosed with breast cancer in their 50s, 40% of all deaths were from breast cancer and 15% were caused by cardiovascular disease. In contrast, the cumulative impact of atherosclerosis was far more prominent in women diagnosed with breast cancer at a more advanced age. Indeed, among women diagnosed with breast cancer in their 70s, about 15% of deaths were caused by breast cancer, while 25% resulted from cardiovascular disease.
The number of baseline cardiovascular risk factors present at enrollment in the WHI turned out to be a powerful determinant of the likelihood of acute MI or death as a result of coronary heart disease in participants who developed breast cancer.
Of the 4,340 women who later developed invasive breast cancer, 2,562 were free of hypertension, diabetes, and hypercholesterolemia and were nonsmokers upon enrollment. In an age-adjusted analysis in which this risk factor–free group served as the reference population, the risk of MI after breast cancer diagnosis was increased 1.65-fold in those with a single baseline risk factor, 3.2-fold in those with two, and 5.8-fold in women with three cardiovascular risk factors. Similarly, the breast cancer patients’ risk of CHD death climbed stepwise by 1.78-, 2.28-, and 3.6-fold as the number of baseline cardiovascular risk factors increased from one to three.
The greatest risk was seen in breast cancer patients who at WHI enrollment were current smokers with an additional cardiovascular risk factor. They had a 9.6-fold greater risk of an acute MI after developing breast cancer, compared with breast cancer patients with none of the baseline cardiovascular risk factors. They also had a 7.7-fold increased risk of CHD death.
The WHI was funded by the National Heart, Lung, and Blood Institute. Dr. Park reported having no financial conflicts of interest.
ORLANDO – Women diagnosed with localized breast cancer while in their 70s have a higher mortality from cardiovascular disease than from their breast cancer, according to new data from the Women’s Health Initiative.
“Identification and treatment of cardiovascular disease risk factors among older women with breast cancer will likely improve survivorship and should be a high priority, especially for older women with incident localized breast cancer,” Na-Jin Park, Ph.D., said at the American Heart Association scientific sessions.
She presented an analysis that included 101,916 women who were free of cardiovascular disease and breast cancer upon enrollment in the Women’s Health Initiative (WHI) at age 50-79 years during 1993-1998. During follow-up in this prospective cohort study, 4,340 of them developed invasive breast cancer. The diagnosis occurred an average of 5 years into the study, and patients were followed for 10 years afterwards. “Forty-one percent of women with breast cancer already had cardiovascular risk factors at baseline, way before their breast cancer diagnosis,” noted Dr. Park of the University of Pittsburgh.
Among women diagnosed with breast cancer in their 50s, 40% of all deaths were from breast cancer and 15% were caused by cardiovascular disease. In contrast, the cumulative impact of atherosclerosis was far more prominent in women diagnosed with breast cancer at a more advanced age. Indeed, among women diagnosed with breast cancer in their 70s, about 15% of deaths were caused by breast cancer, while 25% resulted from cardiovascular disease.
The number of baseline cardiovascular risk factors present at enrollment in the WHI turned out to be a powerful determinant of the likelihood of acute MI or death as a result of coronary heart disease in participants who developed breast cancer.
Of the 4,340 women who later developed invasive breast cancer, 2,562 were free of hypertension, diabetes, and hypercholesterolemia and were nonsmokers upon enrollment. In an age-adjusted analysis in which this risk factor–free group served as the reference population, the risk of MI after breast cancer diagnosis was increased 1.65-fold in those with a single baseline risk factor, 3.2-fold in those with two, and 5.8-fold in women with three cardiovascular risk factors. Similarly, the breast cancer patients’ risk of CHD death climbed stepwise by 1.78-, 2.28-, and 3.6-fold as the number of baseline cardiovascular risk factors increased from one to three.
The greatest risk was seen in breast cancer patients who at WHI enrollment were current smokers with an additional cardiovascular risk factor. They had a 9.6-fold greater risk of an acute MI after developing breast cancer, compared with breast cancer patients with none of the baseline cardiovascular risk factors. They also had a 7.7-fold increased risk of CHD death.
The WHI was funded by the National Heart, Lung, and Blood Institute. Dr. Park reported having no financial conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Among women diagnosed with breast cancer in their 70s, more will die from cardiovascular disease than from their malignancy.
Major finding: Among women diagnosed with breast cancer in their 70s, only about 15% of deaths were caused by breast cancer, while 25% resulted from cardiovascular disease.
Data source: This prospective cohort analysis from the Women’s Health Initiative included 101,916 women free of cardiovascular disease and breast cancer upon enrollment, of whom 4,340 later developed invasive breast cancer.
Disclosures: The Women’s Health Initiative was funded by the National Heart, Lung, and Blood Institute. The presenter reported having no financial conflicts of interest.
AHA: Low-dose beta-blockers may provide equivalent cardioprotection
ORLANDO – Low-dose beta-blockade appears to be at least as effective as standard full-dose beta-blocker therapy for cardioprotection in patients who’ve had an acute coronary syndrome, Dr. Jason E. Allen reported at the American Heart Association scientific sessions.
“This is an important observation, because in clinical practice patients often don’t tolerate high-dose beta-blockers. They prefer not to be on them. They experience hemodynamic issues like orthostatic hypotension and bradycardia. Plus, at times it’s important to have blood pressure room for other things – comorbid conditions like diabetes, where ACE inhibitors might also have an important role,” said Dr. Allen of Intermountain Medical Center in Salt Lake City.
While beta-blockade is a cornerstone of optimal medical management for reducing cardiovascular events in patients with symptomatic coronary artery disease, the high doses recommended today are based on decades-old randomized trials, which may not be entirely applicable in the current era of advanced medical and interventional therapies. That’s why he and his coinvestigators conducted a retrospective observational study using the Intermountain Healthcare database for the years 1993-2013.
They identified 7,158 patients with angiographically documented CAD who were discharged on beta-blocker therapy following an ACS. Eighty-five percent were discharged on a low-dose beta-blocker, defined by investigators as 25% or less of standard-dose metoprolol tartrate at 200 mg/day or its equivalent. Only 15% were discharged on high-dose therapy, defined as at least 100 mg/day of metoprolol or its equivalent.
The study endpoint was the incidence of the composite endpoint of all-cause mortality, MI, or stroke during follow-up. Because the group on high-dose beta-blockers typically had higher baseline rates of hypertension and hyperlipidemia, and a higher body mass index, propensity scores were utilized to adjust for these differences in a Cox proportional hazards analysis.
The incidence of the composite major adverse cardiovascular event (MACE) outcome from discharge through 6 months of follow-up was 4.3% among patients on a low-dose beta-blocker, which was equivalent to but not statistically superior to the 4.6% rate in those on high-dose therapy.
Among patients who didn’t have a MACE event in the first 6 months of follow-up, the incidence during months 7-24 was 4.8% in the low-dose group and 5.7% in the high-dose group, which once again was not a statistically significant difference. Of note, rates of all three components of the composite endpoint were numerically lower in the low-dose group.
A third analysis was restricted to the 6,844 patients who never switched between low- and high-dose therapy during the entire 24-month follow-up period. The composite MACE rate was 8.9% in the low-dose group, which was statistically equivalent to the 9.7% rate in patients on high-dose beta-blocker therapy throughout.
Dr. Allen was quick to point out that an observational study such as this can’t provide definitive proof. That would have to come from a randomized, controlled trial of high- versus low-dose beta-blocker therapy for secondary prevention. Such a trial also would be helpful in determining the mechanism of the putative equivalence seen in the Intermountain Healthcare study.
Dr. Allen’s study was conducted with institutional funds. He reported having no financial conflicts.
ORLANDO – Low-dose beta-blockade appears to be at least as effective as standard full-dose beta-blocker therapy for cardioprotection in patients who’ve had an acute coronary syndrome, Dr. Jason E. Allen reported at the American Heart Association scientific sessions.
“This is an important observation, because in clinical practice patients often don’t tolerate high-dose beta-blockers. They prefer not to be on them. They experience hemodynamic issues like orthostatic hypotension and bradycardia. Plus, at times it’s important to have blood pressure room for other things – comorbid conditions like diabetes, where ACE inhibitors might also have an important role,” said Dr. Allen of Intermountain Medical Center in Salt Lake City.
While beta-blockade is a cornerstone of optimal medical management for reducing cardiovascular events in patients with symptomatic coronary artery disease, the high doses recommended today are based on decades-old randomized trials, which may not be entirely applicable in the current era of advanced medical and interventional therapies. That’s why he and his coinvestigators conducted a retrospective observational study using the Intermountain Healthcare database for the years 1993-2013.
They identified 7,158 patients with angiographically documented CAD who were discharged on beta-blocker therapy following an ACS. Eighty-five percent were discharged on a low-dose beta-blocker, defined by investigators as 25% or less of standard-dose metoprolol tartrate at 200 mg/day or its equivalent. Only 15% were discharged on high-dose therapy, defined as at least 100 mg/day of metoprolol or its equivalent.
The study endpoint was the incidence of the composite endpoint of all-cause mortality, MI, or stroke during follow-up. Because the group on high-dose beta-blockers typically had higher baseline rates of hypertension and hyperlipidemia, and a higher body mass index, propensity scores were utilized to adjust for these differences in a Cox proportional hazards analysis.
The incidence of the composite major adverse cardiovascular event (MACE) outcome from discharge through 6 months of follow-up was 4.3% among patients on a low-dose beta-blocker, which was equivalent to but not statistically superior to the 4.6% rate in those on high-dose therapy.
Among patients who didn’t have a MACE event in the first 6 months of follow-up, the incidence during months 7-24 was 4.8% in the low-dose group and 5.7% in the high-dose group, which once again was not a statistically significant difference. Of note, rates of all three components of the composite endpoint were numerically lower in the low-dose group.
A third analysis was restricted to the 6,844 patients who never switched between low- and high-dose therapy during the entire 24-month follow-up period. The composite MACE rate was 8.9% in the low-dose group, which was statistically equivalent to the 9.7% rate in patients on high-dose beta-blocker therapy throughout.
Dr. Allen was quick to point out that an observational study such as this can’t provide definitive proof. That would have to come from a randomized, controlled trial of high- versus low-dose beta-blocker therapy for secondary prevention. Such a trial also would be helpful in determining the mechanism of the putative equivalence seen in the Intermountain Healthcare study.
Dr. Allen’s study was conducted with institutional funds. He reported having no financial conflicts.
ORLANDO – Low-dose beta-blockade appears to be at least as effective as standard full-dose beta-blocker therapy for cardioprotection in patients who’ve had an acute coronary syndrome, Dr. Jason E. Allen reported at the American Heart Association scientific sessions.
“This is an important observation, because in clinical practice patients often don’t tolerate high-dose beta-blockers. They prefer not to be on them. They experience hemodynamic issues like orthostatic hypotension and bradycardia. Plus, at times it’s important to have blood pressure room for other things – comorbid conditions like diabetes, where ACE inhibitors might also have an important role,” said Dr. Allen of Intermountain Medical Center in Salt Lake City.
While beta-blockade is a cornerstone of optimal medical management for reducing cardiovascular events in patients with symptomatic coronary artery disease, the high doses recommended today are based on decades-old randomized trials, which may not be entirely applicable in the current era of advanced medical and interventional therapies. That’s why he and his coinvestigators conducted a retrospective observational study using the Intermountain Healthcare database for the years 1993-2013.
They identified 7,158 patients with angiographically documented CAD who were discharged on beta-blocker therapy following an ACS. Eighty-five percent were discharged on a low-dose beta-blocker, defined by investigators as 25% or less of standard-dose metoprolol tartrate at 200 mg/day or its equivalent. Only 15% were discharged on high-dose therapy, defined as at least 100 mg/day of metoprolol or its equivalent.
The study endpoint was the incidence of the composite endpoint of all-cause mortality, MI, or stroke during follow-up. Because the group on high-dose beta-blockers typically had higher baseline rates of hypertension and hyperlipidemia, and a higher body mass index, propensity scores were utilized to adjust for these differences in a Cox proportional hazards analysis.
The incidence of the composite major adverse cardiovascular event (MACE) outcome from discharge through 6 months of follow-up was 4.3% among patients on a low-dose beta-blocker, which was equivalent to but not statistically superior to the 4.6% rate in those on high-dose therapy.
Among patients who didn’t have a MACE event in the first 6 months of follow-up, the incidence during months 7-24 was 4.8% in the low-dose group and 5.7% in the high-dose group, which once again was not a statistically significant difference. Of note, rates of all three components of the composite endpoint were numerically lower in the low-dose group.
A third analysis was restricted to the 6,844 patients who never switched between low- and high-dose therapy during the entire 24-month follow-up period. The composite MACE rate was 8.9% in the low-dose group, which was statistically equivalent to the 9.7% rate in patients on high-dose beta-blocker therapy throughout.
Dr. Allen was quick to point out that an observational study such as this can’t provide definitive proof. That would have to come from a randomized, controlled trial of high- versus low-dose beta-blocker therapy for secondary prevention. Such a trial also would be helpful in determining the mechanism of the putative equivalence seen in the Intermountain Healthcare study.
Dr. Allen’s study was conducted with institutional funds. He reported having no financial conflicts.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: When it comes to secondary cardiovascular prevention following an acute coronary syndrome, low-dose beta-blockade may be as effective as high-dose.
Major finding: The rate of all-cause mortality, MI, or stroke during 24 months after discharge following an acute coronary syndrome was 8.9% in patients on a low-dose beta-blocker throughout, equivalent to the 9.7% rate in those on high-dose therapy throughout.
Data source: This retrospective observational study included 7,158 patients discharged on beta-blocker therapy after an acute coronary syndrome and followed for 24 months.
Disclosures: This study was conducted with institutional funds. The presenter reported having no financial conflicts.
AHA: Asthma History Boosts Heart Disease Risk in Postmenopausal Women
ORLANDO – A history of asthma was independently associated with a 24% increase in the risk of new-onset coronary heart disease among postmenopausal women in an analysis from the Women’s Health Initiative.
The study cohort included 90,168 women aged 50-79 years who were free of cardiovascular disease at enrollment in the Women’s Health Initiative (WHI), of whom 6,921 reported a history of physician-diagnosed asthma at baseline. During follow-up in the prospective study, the incidence of a CHD event was 8.6% in subjects with a history of asthma and 6.97% in the no-asthma group, Dr. Fady Y. Marmoush reported at the American Heart Association scientific sessions.
Moreover, the incidence of a first cardiovascular event was 11.6% in the asthma group, compared with 9.7% in the no-asthma controls, added Dr. Marmoush of Memorial Hospital of Rhode Island, Pawtucket.
The asthma group had an absolute 1%-2% greater baseline prevalence of hypertension, diabetes, and family history of CHD. Those with asthma also were more likely to be obese. On the other hand, they were less likely to have ever smoked.
In a multivariate analysis adjusted for these and other potential confounders, including age, dyslipidemia, and waist-hip ratio, the women with a history of asthma had a 24% greater risk of CHD during prospective follow-up in the WHI, as well as a 21% increased rate of cardiovascular events, including stroke, compared with the no-asthma group.
Thus, a history of asthma could be a useful consideration – a tie breaker of sorts – in older women whose calculated 10-year atherosclerotic cardiovascular disease risk based on the standard risk factors places them on the borderline as candidates for statin therapy. The most likely mechanism for the observed association between asthma history and increased risk of cardiovascular disease is the chronic inflammatory state that’s a hallmark of asthma accelerating the atherosclerotic process, which also is inflammatory, she said.
The WHI is funded by the National Heart, Lung, and Blood Institute. Dr. Marmoush reported having no financial conflicts.
ORLANDO – A history of asthma was independently associated with a 24% increase in the risk of new-onset coronary heart disease among postmenopausal women in an analysis from the Women’s Health Initiative.
The study cohort included 90,168 women aged 50-79 years who were free of cardiovascular disease at enrollment in the Women’s Health Initiative (WHI), of whom 6,921 reported a history of physician-diagnosed asthma at baseline. During follow-up in the prospective study, the incidence of a CHD event was 8.6% in subjects with a history of asthma and 6.97% in the no-asthma group, Dr. Fady Y. Marmoush reported at the American Heart Association scientific sessions.
Moreover, the incidence of a first cardiovascular event was 11.6% in the asthma group, compared with 9.7% in the no-asthma controls, added Dr. Marmoush of Memorial Hospital of Rhode Island, Pawtucket.
The asthma group had an absolute 1%-2% greater baseline prevalence of hypertension, diabetes, and family history of CHD. Those with asthma also were more likely to be obese. On the other hand, they were less likely to have ever smoked.
In a multivariate analysis adjusted for these and other potential confounders, including age, dyslipidemia, and waist-hip ratio, the women with a history of asthma had a 24% greater risk of CHD during prospective follow-up in the WHI, as well as a 21% increased rate of cardiovascular events, including stroke, compared with the no-asthma group.
Thus, a history of asthma could be a useful consideration – a tie breaker of sorts – in older women whose calculated 10-year atherosclerotic cardiovascular disease risk based on the standard risk factors places them on the borderline as candidates for statin therapy. The most likely mechanism for the observed association between asthma history and increased risk of cardiovascular disease is the chronic inflammatory state that’s a hallmark of asthma accelerating the atherosclerotic process, which also is inflammatory, she said.
The WHI is funded by the National Heart, Lung, and Blood Institute. Dr. Marmoush reported having no financial conflicts.
ORLANDO – A history of asthma was independently associated with a 24% increase in the risk of new-onset coronary heart disease among postmenopausal women in an analysis from the Women’s Health Initiative.
The study cohort included 90,168 women aged 50-79 years who were free of cardiovascular disease at enrollment in the Women’s Health Initiative (WHI), of whom 6,921 reported a history of physician-diagnosed asthma at baseline. During follow-up in the prospective study, the incidence of a CHD event was 8.6% in subjects with a history of asthma and 6.97% in the no-asthma group, Dr. Fady Y. Marmoush reported at the American Heart Association scientific sessions.
Moreover, the incidence of a first cardiovascular event was 11.6% in the asthma group, compared with 9.7% in the no-asthma controls, added Dr. Marmoush of Memorial Hospital of Rhode Island, Pawtucket.
The asthma group had an absolute 1%-2% greater baseline prevalence of hypertension, diabetes, and family history of CHD. Those with asthma also were more likely to be obese. On the other hand, they were less likely to have ever smoked.
In a multivariate analysis adjusted for these and other potential confounders, including age, dyslipidemia, and waist-hip ratio, the women with a history of asthma had a 24% greater risk of CHD during prospective follow-up in the WHI, as well as a 21% increased rate of cardiovascular events, including stroke, compared with the no-asthma group.
Thus, a history of asthma could be a useful consideration – a tie breaker of sorts – in older women whose calculated 10-year atherosclerotic cardiovascular disease risk based on the standard risk factors places them on the borderline as candidates for statin therapy. The most likely mechanism for the observed association between asthma history and increased risk of cardiovascular disease is the chronic inflammatory state that’s a hallmark of asthma accelerating the atherosclerotic process, which also is inflammatory, she said.
The WHI is funded by the National Heart, Lung, and Blood Institute. Dr. Marmoush reported having no financial conflicts.
AT THE AHA SCIENTIFIC SESSIONS
AHA: Asthma history boosts heart disease risk in postmenopausal women
ORLANDO – A history of asthma was independently associated with a 24% increase in the risk of new-onset coronary heart disease among postmenopausal women in an analysis from the Women’s Health Initiative.
The study cohort included 90,168 women aged 50-79 years who were free of cardiovascular disease at enrollment in the Women’s Health Initiative (WHI), of whom 6,921 reported a history of physician-diagnosed asthma at baseline. During follow-up in the prospective study, the incidence of a CHD event was 8.6% in subjects with a history of asthma and 6.97% in the no-asthma group, Dr. Fady Y. Marmoush reported at the American Heart Association scientific sessions.
Moreover, the incidence of a first cardiovascular event was 11.6% in the asthma group, compared with 9.7% in the no-asthma controls, added Dr. Marmoush of Memorial Hospital of Rhode Island, Pawtucket.
The asthma group had an absolute 1%-2% greater baseline prevalence of hypertension, diabetes, and family history of CHD. Those with asthma also were more likely to be obese. On the other hand, they were less likely to have ever smoked.
In a multivariate analysis adjusted for these and other potential confounders, including age, dyslipidemia, and waist-hip ratio, the women with a history of asthma had a 24% greater risk of CHD during prospective follow-up in the WHI, as well as a 21% increased rate of cardiovascular events, including stroke, compared with the no-asthma group.
Thus, a history of asthma could be a useful consideration – a tie breaker of sorts – in older women whose calculated 10-year atherosclerotic cardiovascular disease risk based on the standard risk factors places them on the borderline as candidates for statin therapy. The most likely mechanism for the observed association between asthma history and increased risk of cardiovascular disease is the chronic inflammatory state that’s a hallmark of asthma accelerating the atherosclerotic process, which also is inflammatory, she said.
The WHI is funded by the National Heart, Lung, and Blood Institute. Dr. Marmoush reported having no financial conflicts.
ORLANDO – A history of asthma was independently associated with a 24% increase in the risk of new-onset coronary heart disease among postmenopausal women in an analysis from the Women’s Health Initiative.
The study cohort included 90,168 women aged 50-79 years who were free of cardiovascular disease at enrollment in the Women’s Health Initiative (WHI), of whom 6,921 reported a history of physician-diagnosed asthma at baseline. During follow-up in the prospective study, the incidence of a CHD event was 8.6% in subjects with a history of asthma and 6.97% in the no-asthma group, Dr. Fady Y. Marmoush reported at the American Heart Association scientific sessions.
Moreover, the incidence of a first cardiovascular event was 11.6% in the asthma group, compared with 9.7% in the no-asthma controls, added Dr. Marmoush of Memorial Hospital of Rhode Island, Pawtucket.
The asthma group had an absolute 1%-2% greater baseline prevalence of hypertension, diabetes, and family history of CHD. Those with asthma also were more likely to be obese. On the other hand, they were less likely to have ever smoked.
In a multivariate analysis adjusted for these and other potential confounders, including age, dyslipidemia, and waist-hip ratio, the women with a history of asthma had a 24% greater risk of CHD during prospective follow-up in the WHI, as well as a 21% increased rate of cardiovascular events, including stroke, compared with the no-asthma group.
Thus, a history of asthma could be a useful consideration – a tie breaker of sorts – in older women whose calculated 10-year atherosclerotic cardiovascular disease risk based on the standard risk factors places them on the borderline as candidates for statin therapy. The most likely mechanism for the observed association between asthma history and increased risk of cardiovascular disease is the chronic inflammatory state that’s a hallmark of asthma accelerating the atherosclerotic process, which also is inflammatory, she said.
The WHI is funded by the National Heart, Lung, and Blood Institute. Dr. Marmoush reported having no financial conflicts.
ORLANDO – A history of asthma was independently associated with a 24% increase in the risk of new-onset coronary heart disease among postmenopausal women in an analysis from the Women’s Health Initiative.
The study cohort included 90,168 women aged 50-79 years who were free of cardiovascular disease at enrollment in the Women’s Health Initiative (WHI), of whom 6,921 reported a history of physician-diagnosed asthma at baseline. During follow-up in the prospective study, the incidence of a CHD event was 8.6% in subjects with a history of asthma and 6.97% in the no-asthma group, Dr. Fady Y. Marmoush reported at the American Heart Association scientific sessions.
Moreover, the incidence of a first cardiovascular event was 11.6% in the asthma group, compared with 9.7% in the no-asthma controls, added Dr. Marmoush of Memorial Hospital of Rhode Island, Pawtucket.
The asthma group had an absolute 1%-2% greater baseline prevalence of hypertension, diabetes, and family history of CHD. Those with asthma also were more likely to be obese. On the other hand, they were less likely to have ever smoked.
In a multivariate analysis adjusted for these and other potential confounders, including age, dyslipidemia, and waist-hip ratio, the women with a history of asthma had a 24% greater risk of CHD during prospective follow-up in the WHI, as well as a 21% increased rate of cardiovascular events, including stroke, compared with the no-asthma group.
Thus, a history of asthma could be a useful consideration – a tie breaker of sorts – in older women whose calculated 10-year atherosclerotic cardiovascular disease risk based on the standard risk factors places them on the borderline as candidates for statin therapy. The most likely mechanism for the observed association between asthma history and increased risk of cardiovascular disease is the chronic inflammatory state that’s a hallmark of asthma accelerating the atherosclerotic process, which also is inflammatory, she said.
The WHI is funded by the National Heart, Lung, and Blood Institute. Dr. Marmoush reported having no financial conflicts.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: A history of asthma appears to substantially increase the risk of a first cardiovascular event in postmenopausal women.
Major finding: In a multivariate analysis adjusted for conventional cardiovascular risk factors, older women with a history of asthma had a 24% higher risk for a first coronary heart disease event and 21% greater risk of a cardiovascular event than those without such a history.
Data source: The Women’s Health Initiative is a prospective cohort study. This analysis included 90,168 women aged 50-79 at enrollment, of whom 6,921 reported a history of physician-diagnosed asthma.
Disclosures: The study is supported by the National Heart, Lung, and Blood Institute. The presenter reported having no financial conflicts.
AHA: Coronary calcium personalizes ACC/AHA risk calculator
ORLANDO – Combining the coronary artery calcium score with the ACC/AHA cardiovascular risk calculator tool enables physicians to refine their decision making about who to recommend for statin therapy, Dr. Salman Waheed reported at the American Heart Association scientific sessions.
He presented an analysis of 1,225 asymptomatic adults followed for a median of 3.9 years in the observational arm of the St. Francis Health Study, an early landmark prospective study of the relationship between electron beam CT coronary artery calcium (CAC) score and cardiovascular event risk.
The 217 subjects who today would not be recommended for statin therapy on the basis of a 10-year atherosclerotic cardiovascular disease risk of 5%-7.4% as determined by the risk calculator included in the 2013 ACC/AHA cholesterol management guidelines (Circulation. 2014 Jun 24;129[25 Suppl 2]:S1-45) would be reclassified as warranting statin therapy if they had a CAC greater than 0, as was the case for 169 of the 217 (78%). Indeed, the presence of a CAC of 1 or more boosted their estimated 10-year risk to 10.8%.
On the other hand, there were 510 patients who would be classified as high risk by the ACC/AHA clinical risk calculator, with a 10-year risk of 7.5%-20%. Taking their CAC score into account would result in 73 being reclassified as low risk and becoming no longer statin candidates because their CAC of 0 was associated with a 10-year event risk of less than 1%. In contrast, for the 447 remaining subjects with a CAC greater than 0, the 10-year risk climbed to 21.9%, according to Dr. Waheed of the University of Kansas, Kansas City.
The composite outcome utilized in this analysis from the St. Francis Heart Study was comprised of nonfatal MI, coronary death, stroke, peripheral arterial revascularization, or coronary revascularization. Of note, heart failure wasn’t included.
Among the 545 subjects deemed at low cardiovascular risk because they weren’t eligible for statin therapy according to the 2013 ACC/AHA guidelines, 209 would be recategorized as high risk on the basis of a CAC score at or above the 80th percentile adjusted for age and gender. The adjusted risk of a cardiovascular event in the high CAC/low clinical risk group was 24.9-fold greater than in the low CAC/low clinical risk group.
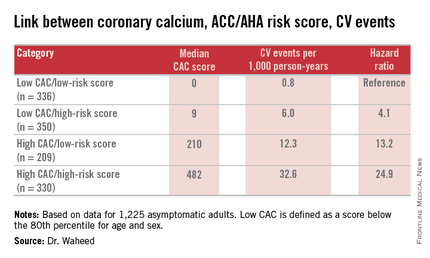
“Among those eligible for statin therapy based upon current guidelines, high CAC portends a sixfold higher outcome risk than low CAC,” Dr. Waheed added.
The magnitude of CAC progression over the course of 4 years was similar across the baseline risk categories; however, the absolute CAC progression was greater among those with a high CAC at baseline.
Audience member Dr. Daniel S. Berman observed that the results of Dr. Waheed’s study are highly concordant with an earlier report from the Multi-Ethnic Study of Atherosclerosis in which a CAC of 0 was quite common in patients for whom statins would be recommended under the current ACC/AHA guidelines.
“Your data support the idea that stratification based upon CAC could more personalize the statin recommendations,” said Dr. Berman, chief of cardiac imaging and nuclear cardiology at Cedars-Sinai Medical Center and professor of medicine at the University of California, Los Angeles.
Another audience member, Dr. Donald M. Lloyd-Jones, one of the architects of the current guidelines, commented that the analyses from the St. Francis Heart Study and the Multi-Ethnic Study of Atherosclerosis suggest CAC screening coupled with the ACC/AHA risk score provides added value in a select group of patients.
“Your analysis continues to reinforce the point that we probably shouldn’t be doing universal CAC screening because in the people with a 10-year risk of less than 5% the yield is low and the CAC didn’t change anything, while in the people with a 10-year risk of 20% or higher the yield is incredibly high and the CAC didn’t change anything,” observed Dr. Lloyd-Jones, professor and chair of the department of preventive medicine at Northwestern University, Chicago.
“So CAC really is for those intermediate-risk folks where we’re on the bubble, where we might consider withholding therapy. And I’d love to see a trial to show that’s safe, by the way, but maybe that day will come. But we certainly would be comfortable up-classifying somebody if more CAC is present than there should be,” he added.
Dr. Waheed reported having no financial conflicts regarding his study.
ORLANDO – Combining the coronary artery calcium score with the ACC/AHA cardiovascular risk calculator tool enables physicians to refine their decision making about who to recommend for statin therapy, Dr. Salman Waheed reported at the American Heart Association scientific sessions.
He presented an analysis of 1,225 asymptomatic adults followed for a median of 3.9 years in the observational arm of the St. Francis Health Study, an early landmark prospective study of the relationship between electron beam CT coronary artery calcium (CAC) score and cardiovascular event risk.
The 217 subjects who today would not be recommended for statin therapy on the basis of a 10-year atherosclerotic cardiovascular disease risk of 5%-7.4% as determined by the risk calculator included in the 2013 ACC/AHA cholesterol management guidelines (Circulation. 2014 Jun 24;129[25 Suppl 2]:S1-45) would be reclassified as warranting statin therapy if they had a CAC greater than 0, as was the case for 169 of the 217 (78%). Indeed, the presence of a CAC of 1 or more boosted their estimated 10-year risk to 10.8%.
On the other hand, there were 510 patients who would be classified as high risk by the ACC/AHA clinical risk calculator, with a 10-year risk of 7.5%-20%. Taking their CAC score into account would result in 73 being reclassified as low risk and becoming no longer statin candidates because their CAC of 0 was associated with a 10-year event risk of less than 1%. In contrast, for the 447 remaining subjects with a CAC greater than 0, the 10-year risk climbed to 21.9%, according to Dr. Waheed of the University of Kansas, Kansas City.
The composite outcome utilized in this analysis from the St. Francis Heart Study was comprised of nonfatal MI, coronary death, stroke, peripheral arterial revascularization, or coronary revascularization. Of note, heart failure wasn’t included.
Among the 545 subjects deemed at low cardiovascular risk because they weren’t eligible for statin therapy according to the 2013 ACC/AHA guidelines, 209 would be recategorized as high risk on the basis of a CAC score at or above the 80th percentile adjusted for age and gender. The adjusted risk of a cardiovascular event in the high CAC/low clinical risk group was 24.9-fold greater than in the low CAC/low clinical risk group.
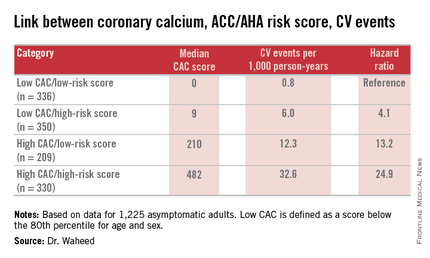
“Among those eligible for statin therapy based upon current guidelines, high CAC portends a sixfold higher outcome risk than low CAC,” Dr. Waheed added.
The magnitude of CAC progression over the course of 4 years was similar across the baseline risk categories; however, the absolute CAC progression was greater among those with a high CAC at baseline.
Audience member Dr. Daniel S. Berman observed that the results of Dr. Waheed’s study are highly concordant with an earlier report from the Multi-Ethnic Study of Atherosclerosis in which a CAC of 0 was quite common in patients for whom statins would be recommended under the current ACC/AHA guidelines.
“Your data support the idea that stratification based upon CAC could more personalize the statin recommendations,” said Dr. Berman, chief of cardiac imaging and nuclear cardiology at Cedars-Sinai Medical Center and professor of medicine at the University of California, Los Angeles.
Another audience member, Dr. Donald M. Lloyd-Jones, one of the architects of the current guidelines, commented that the analyses from the St. Francis Heart Study and the Multi-Ethnic Study of Atherosclerosis suggest CAC screening coupled with the ACC/AHA risk score provides added value in a select group of patients.
“Your analysis continues to reinforce the point that we probably shouldn’t be doing universal CAC screening because in the people with a 10-year risk of less than 5% the yield is low and the CAC didn’t change anything, while in the people with a 10-year risk of 20% or higher the yield is incredibly high and the CAC didn’t change anything,” observed Dr. Lloyd-Jones, professor and chair of the department of preventive medicine at Northwestern University, Chicago.
“So CAC really is for those intermediate-risk folks where we’re on the bubble, where we might consider withholding therapy. And I’d love to see a trial to show that’s safe, by the way, but maybe that day will come. But we certainly would be comfortable up-classifying somebody if more CAC is present than there should be,” he added.
Dr. Waheed reported having no financial conflicts regarding his study.
ORLANDO – Combining the coronary artery calcium score with the ACC/AHA cardiovascular risk calculator tool enables physicians to refine their decision making about who to recommend for statin therapy, Dr. Salman Waheed reported at the American Heart Association scientific sessions.
He presented an analysis of 1,225 asymptomatic adults followed for a median of 3.9 years in the observational arm of the St. Francis Health Study, an early landmark prospective study of the relationship between electron beam CT coronary artery calcium (CAC) score and cardiovascular event risk.
The 217 subjects who today would not be recommended for statin therapy on the basis of a 10-year atherosclerotic cardiovascular disease risk of 5%-7.4% as determined by the risk calculator included in the 2013 ACC/AHA cholesterol management guidelines (Circulation. 2014 Jun 24;129[25 Suppl 2]:S1-45) would be reclassified as warranting statin therapy if they had a CAC greater than 0, as was the case for 169 of the 217 (78%). Indeed, the presence of a CAC of 1 or more boosted their estimated 10-year risk to 10.8%.
On the other hand, there were 510 patients who would be classified as high risk by the ACC/AHA clinical risk calculator, with a 10-year risk of 7.5%-20%. Taking their CAC score into account would result in 73 being reclassified as low risk and becoming no longer statin candidates because their CAC of 0 was associated with a 10-year event risk of less than 1%. In contrast, for the 447 remaining subjects with a CAC greater than 0, the 10-year risk climbed to 21.9%, according to Dr. Waheed of the University of Kansas, Kansas City.
The composite outcome utilized in this analysis from the St. Francis Heart Study was comprised of nonfatal MI, coronary death, stroke, peripheral arterial revascularization, or coronary revascularization. Of note, heart failure wasn’t included.
Among the 545 subjects deemed at low cardiovascular risk because they weren’t eligible for statin therapy according to the 2013 ACC/AHA guidelines, 209 would be recategorized as high risk on the basis of a CAC score at or above the 80th percentile adjusted for age and gender. The adjusted risk of a cardiovascular event in the high CAC/low clinical risk group was 24.9-fold greater than in the low CAC/low clinical risk group.
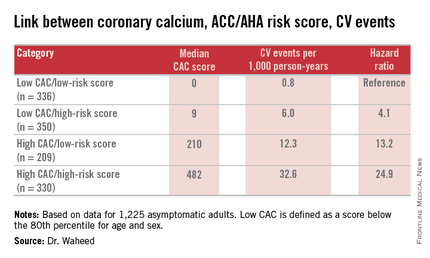
“Among those eligible for statin therapy based upon current guidelines, high CAC portends a sixfold higher outcome risk than low CAC,” Dr. Waheed added.
The magnitude of CAC progression over the course of 4 years was similar across the baseline risk categories; however, the absolute CAC progression was greater among those with a high CAC at baseline.
Audience member Dr. Daniel S. Berman observed that the results of Dr. Waheed’s study are highly concordant with an earlier report from the Multi-Ethnic Study of Atherosclerosis in which a CAC of 0 was quite common in patients for whom statins would be recommended under the current ACC/AHA guidelines.
“Your data support the idea that stratification based upon CAC could more personalize the statin recommendations,” said Dr. Berman, chief of cardiac imaging and nuclear cardiology at Cedars-Sinai Medical Center and professor of medicine at the University of California, Los Angeles.
Another audience member, Dr. Donald M. Lloyd-Jones, one of the architects of the current guidelines, commented that the analyses from the St. Francis Heart Study and the Multi-Ethnic Study of Atherosclerosis suggest CAC screening coupled with the ACC/AHA risk score provides added value in a select group of patients.
“Your analysis continues to reinforce the point that we probably shouldn’t be doing universal CAC screening because in the people with a 10-year risk of less than 5% the yield is low and the CAC didn’t change anything, while in the people with a 10-year risk of 20% or higher the yield is incredibly high and the CAC didn’t change anything,” observed Dr. Lloyd-Jones, professor and chair of the department of preventive medicine at Northwestern University, Chicago.
“So CAC really is for those intermediate-risk folks where we’re on the bubble, where we might consider withholding therapy. And I’d love to see a trial to show that’s safe, by the way, but maybe that day will come. But we certainly would be comfortable up-classifying somebody if more CAC is present than there should be,” he added.
Dr. Waheed reported having no financial conflicts regarding his study.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Measuring coronary artery calcium provides added value in refining the 10-year atherosclerotic cardiovascular disease risk, especially in patients with an intermediate-risk score on the ACC/AHA risk calculator.
Major finding: Seventy-eight percent of a group of patients for whom statin therapy wouldn’t be recommended under the current ACC/AHA guidelines because their estimated 10-year event risk was 5%-7.5% would be reclassified as warranting statin therapy because their coronary artery calcium score was greater than 0, pushing their estimated risk to 10.8%.
Data source: A retrospective analysis of data on 1,225 asymptomatic adults followed prospectively with coronary artery calcium measurements in the St. Francis Health Study.
Disclosures: The study presenter reported having no financial conflicts of interest.
AHA: HDL – the waters grow muddier
ORLANDO – For years, HDL cholesterol was known as “the good cholesterol.” A low level was associated with increased cardiovascular risk. More HDL cholesterol was thought to be cardioprotective, perhaps even capable of offsetting at least some of the risk conferred by a high LDL cholesterol level.
But it turns out that when it comes to HDL cholesterol, more isn’t always better.
A new study utilizing the increasingly popular “big data” analytic approach indicates that the relationship between HDL cholesterol level and mortality isn’t linear. Instead, it’s U-shaped, with both low and high HDL cholesterol levels being associated with significantly increased mortality risk, Dr. Dennis T. Ko reported at the American Heart Association scientific sessions.
This is the latest in a string of bad news regarding the former “good cholesterol.” Large, multicenter, randomized trials of niacin and cholesterol ester transfer protein (CETP) inhibitors aimed at boosting HDL cholesterol levels in patients with low HDL cholesterol as a means of reducing cardiovascular risk succeeded in raising HDL cholesterol, but with no impact on major cardiovascular endpoints, noted Dr. Ko of the Institute for Clinical Evaluative Sciences and the University of Toronto.
He presented a population-based study of 631,762 Ontario residents who were free of prior cardiovascular disease and at least 40 years old in 2008. This study group, known as the CANHEART cohort, was formed by combining 17 large regional databases. The advantage of working with such a large study population is that it provides new and statistically powerful insights into the impact of the full range of HDL cholesterol values, not just in terms of cardiovascular events but the full spectrum of disease, Dr. Ko explained. Up until now, the conventional knowledge about HDL cholesterol has been based largely upon relatively small observational studies, such as the Framingham Heart Study; most of those studies didn’t look at noncardiovascular events.
During a mean 4.9 years of follow-up of the CANHEART cohort, 9,339 deaths occurred in men and 8,613 in women. In an analysis adjusted for age, non–HDL cholesterol levels, cardiac risk factors, sex, comorbid conditions, and income, HDL cholesterol levels below the reference range of 41-50 mg/dL in women and 51-60 mg/dL in men were associated with increased risks of mortality from all three causes: cardiovascular, cancer, and other. The lower the HDL cholesterol level, the greater the risks.
As HDL cholesterol groupings moved decile by decile above the reference ranges there was no protective effect seen against cardiovascular or noncardiovascular deaths. Instead, the risk of death due to causes other than heart disease or cancer took a turn upward as HDL cholesterol levels approached the outer end of the bell curve, achieving significance in men with an HDL cholesterol of 71-80 mg/dL and peaking in those with a level greater than 90 mg/dL. In women, the U-shaped curve was shallower, with an increased mortality risk – again, as in men, restricted to causes other than cancer or heart disease – becoming statistically significant only in women with an HDL cholesterol level greater than 90 mg/dL, Dr. Ko continued.
It’s worth noting that men with an HDL cholesterol level of 81 mg/dL or above also showed a trend for increased risks of both cardiovascular and cancer deaths, although this didn’t reach statistical significance.
Patients at the low end of the HDL cholesterol spectrum had an increased prevalence of unhealthy lifestyle, COPD and other comorbid conditions, cardiac risk factors, and low income. In contrast, those with high HDL cholesterol levels were more likely to have a body mass index below 25 kg/m2, engage in 30 minutes or more of brisk walking or other moderate exercise daily, and consume five or more servings of fruits and vegetables daily. So they were, overall, healthier. On the other hand, they were also more likely to be heavy alcohol users as defined by consuming five or more drinks per occasion at least once monthly during the year prior to study enrollment. Alcohol, like physical exercise, is known to boost HDL cholesterol levels.
These CANHEART data and other evidence warrant a reappraisal of HDL cholesterol as a cardiovascular risk/protective factor, according to Dr. Ko.
“HDL is unlikely to represent a cardiovascular-specific risk factor, given similarities in its association with noncardiovascular outcomes,” he observed.
Discussant Jacques Genest concurred.
“Maybe HDL cholesterol mass is the wrong biomarker for HDL function,” opined Dr. Genest, professor of medicine at McGill University in Montreal.
He noted that a causal relationship between HDL cholesterol and cardiovascular risk has been cast into doubt not only by the negative randomized trials of niacin and the CETP inhibitors and the U-shaped mortality curve described by Dr. Ko, but also by randomized Mendelian genetic studies suggesting that genes causing HDL deficiency aren’t linked to increased cardiovascular risk.
It’s likely true that what’s important is not HDL cholesterol levels as measured in conventional lipid panels, but rather HDL function. HDL particles have many beneficial effects: antioxidative, anti-inflammatory, vasodilatory, antiapoptotic, and antithrombotic. A better biomarker – one that reflects these functional benefits – may be cholesterol efflux capacity, as was shown in a recent study by investigators in the Dallas Heart Study (N Engl J Med. 2014; Dec 18;371[25]:2383-93), according to Dr. Genest.
Session cochair Dr. Christie Ballantyne was particularly interested in the 2.8% of CANHEART participants with an HDL cholesterol level greater than 90 mg/dL and their associated increased mortality from causes other than cancer and cardiovascular disease.
“I’ve seen similar data once before, in a Russian cohort. Cold weather and alcohol – I wonder if that’s a factor here. The alcohol exposure we saw in the Russian cohort with the 90 HDL levels was really rather striking. And it wasn’t cardiovascular or cancer mortality that they faced, it was other mortality. So I wonder if it’s not an alcohol-related thing, especially in places where you have long, cold winters,” commented Dr. Ballantyne, professor of medicine and of molecular and human genetics at Baylor College of Medicine and director of the Center for Cardiovascular Disease Prevention at the Methodist Debakey Heart Center in Houston.
Dr. Genest was skeptical.
“I think clinicians would argue that seeing an HDL of 90 would be very unusual in a male even if he drinks like an American at a football game,” the Canadian quipped. “ It’s probable that a genetic predisposition plus heavy alcohol is involved.”
Dr. Ko said he and his coinvestigators are scrutinizing the “other deaths” in the very-high HDL cholesterol subgroup, looking for an increase in deaths due to liver cirrhosis, trauma, and other obvious alcohol-related causes. “We haven’t really found a specific pattern,” according to the physician.
Dr. Ballantyne was undeterred. “It may end up being that the person who drinks heavily has some general health issues where trouble occurs because of alcohol in combination with medications rather than a specifically alcohol-related death,” he advised.
The CANHEART study is sponsored by the Canadian Institutes of Health Research. Dr. Ko reported having no financial conflicts of interest.
ORLANDO – For years, HDL cholesterol was known as “the good cholesterol.” A low level was associated with increased cardiovascular risk. More HDL cholesterol was thought to be cardioprotective, perhaps even capable of offsetting at least some of the risk conferred by a high LDL cholesterol level.
But it turns out that when it comes to HDL cholesterol, more isn’t always better.
A new study utilizing the increasingly popular “big data” analytic approach indicates that the relationship between HDL cholesterol level and mortality isn’t linear. Instead, it’s U-shaped, with both low and high HDL cholesterol levels being associated with significantly increased mortality risk, Dr. Dennis T. Ko reported at the American Heart Association scientific sessions.
This is the latest in a string of bad news regarding the former “good cholesterol.” Large, multicenter, randomized trials of niacin and cholesterol ester transfer protein (CETP) inhibitors aimed at boosting HDL cholesterol levels in patients with low HDL cholesterol as a means of reducing cardiovascular risk succeeded in raising HDL cholesterol, but with no impact on major cardiovascular endpoints, noted Dr. Ko of the Institute for Clinical Evaluative Sciences and the University of Toronto.
He presented a population-based study of 631,762 Ontario residents who were free of prior cardiovascular disease and at least 40 years old in 2008. This study group, known as the CANHEART cohort, was formed by combining 17 large regional databases. The advantage of working with such a large study population is that it provides new and statistically powerful insights into the impact of the full range of HDL cholesterol values, not just in terms of cardiovascular events but the full spectrum of disease, Dr. Ko explained. Up until now, the conventional knowledge about HDL cholesterol has been based largely upon relatively small observational studies, such as the Framingham Heart Study; most of those studies didn’t look at noncardiovascular events.
During a mean 4.9 years of follow-up of the CANHEART cohort, 9,339 deaths occurred in men and 8,613 in women. In an analysis adjusted for age, non–HDL cholesterol levels, cardiac risk factors, sex, comorbid conditions, and income, HDL cholesterol levels below the reference range of 41-50 mg/dL in women and 51-60 mg/dL in men were associated with increased risks of mortality from all three causes: cardiovascular, cancer, and other. The lower the HDL cholesterol level, the greater the risks.
As HDL cholesterol groupings moved decile by decile above the reference ranges there was no protective effect seen against cardiovascular or noncardiovascular deaths. Instead, the risk of death due to causes other than heart disease or cancer took a turn upward as HDL cholesterol levels approached the outer end of the bell curve, achieving significance in men with an HDL cholesterol of 71-80 mg/dL and peaking in those with a level greater than 90 mg/dL. In women, the U-shaped curve was shallower, with an increased mortality risk – again, as in men, restricted to causes other than cancer or heart disease – becoming statistically significant only in women with an HDL cholesterol level greater than 90 mg/dL, Dr. Ko continued.
It’s worth noting that men with an HDL cholesterol level of 81 mg/dL or above also showed a trend for increased risks of both cardiovascular and cancer deaths, although this didn’t reach statistical significance.
Patients at the low end of the HDL cholesterol spectrum had an increased prevalence of unhealthy lifestyle, COPD and other comorbid conditions, cardiac risk factors, and low income. In contrast, those with high HDL cholesterol levels were more likely to have a body mass index below 25 kg/m2, engage in 30 minutes or more of brisk walking or other moderate exercise daily, and consume five or more servings of fruits and vegetables daily. So they were, overall, healthier. On the other hand, they were also more likely to be heavy alcohol users as defined by consuming five or more drinks per occasion at least once monthly during the year prior to study enrollment. Alcohol, like physical exercise, is known to boost HDL cholesterol levels.
These CANHEART data and other evidence warrant a reappraisal of HDL cholesterol as a cardiovascular risk/protective factor, according to Dr. Ko.
“HDL is unlikely to represent a cardiovascular-specific risk factor, given similarities in its association with noncardiovascular outcomes,” he observed.
Discussant Jacques Genest concurred.
“Maybe HDL cholesterol mass is the wrong biomarker for HDL function,” opined Dr. Genest, professor of medicine at McGill University in Montreal.
He noted that a causal relationship between HDL cholesterol and cardiovascular risk has been cast into doubt not only by the negative randomized trials of niacin and the CETP inhibitors and the U-shaped mortality curve described by Dr. Ko, but also by randomized Mendelian genetic studies suggesting that genes causing HDL deficiency aren’t linked to increased cardiovascular risk.
It’s likely true that what’s important is not HDL cholesterol levels as measured in conventional lipid panels, but rather HDL function. HDL particles have many beneficial effects: antioxidative, anti-inflammatory, vasodilatory, antiapoptotic, and antithrombotic. A better biomarker – one that reflects these functional benefits – may be cholesterol efflux capacity, as was shown in a recent study by investigators in the Dallas Heart Study (N Engl J Med. 2014; Dec 18;371[25]:2383-93), according to Dr. Genest.
Session cochair Dr. Christie Ballantyne was particularly interested in the 2.8% of CANHEART participants with an HDL cholesterol level greater than 90 mg/dL and their associated increased mortality from causes other than cancer and cardiovascular disease.
“I’ve seen similar data once before, in a Russian cohort. Cold weather and alcohol – I wonder if that’s a factor here. The alcohol exposure we saw in the Russian cohort with the 90 HDL levels was really rather striking. And it wasn’t cardiovascular or cancer mortality that they faced, it was other mortality. So I wonder if it’s not an alcohol-related thing, especially in places where you have long, cold winters,” commented Dr. Ballantyne, professor of medicine and of molecular and human genetics at Baylor College of Medicine and director of the Center for Cardiovascular Disease Prevention at the Methodist Debakey Heart Center in Houston.
Dr. Genest was skeptical.
“I think clinicians would argue that seeing an HDL of 90 would be very unusual in a male even if he drinks like an American at a football game,” the Canadian quipped. “ It’s probable that a genetic predisposition plus heavy alcohol is involved.”
Dr. Ko said he and his coinvestigators are scrutinizing the “other deaths” in the very-high HDL cholesterol subgroup, looking for an increase in deaths due to liver cirrhosis, trauma, and other obvious alcohol-related causes. “We haven’t really found a specific pattern,” according to the physician.
Dr. Ballantyne was undeterred. “It may end up being that the person who drinks heavily has some general health issues where trouble occurs because of alcohol in combination with medications rather than a specifically alcohol-related death,” he advised.
The CANHEART study is sponsored by the Canadian Institutes of Health Research. Dr. Ko reported having no financial conflicts of interest.
ORLANDO – For years, HDL cholesterol was known as “the good cholesterol.” A low level was associated with increased cardiovascular risk. More HDL cholesterol was thought to be cardioprotective, perhaps even capable of offsetting at least some of the risk conferred by a high LDL cholesterol level.
But it turns out that when it comes to HDL cholesterol, more isn’t always better.
A new study utilizing the increasingly popular “big data” analytic approach indicates that the relationship between HDL cholesterol level and mortality isn’t linear. Instead, it’s U-shaped, with both low and high HDL cholesterol levels being associated with significantly increased mortality risk, Dr. Dennis T. Ko reported at the American Heart Association scientific sessions.
This is the latest in a string of bad news regarding the former “good cholesterol.” Large, multicenter, randomized trials of niacin and cholesterol ester transfer protein (CETP) inhibitors aimed at boosting HDL cholesterol levels in patients with low HDL cholesterol as a means of reducing cardiovascular risk succeeded in raising HDL cholesterol, but with no impact on major cardiovascular endpoints, noted Dr. Ko of the Institute for Clinical Evaluative Sciences and the University of Toronto.
He presented a population-based study of 631,762 Ontario residents who were free of prior cardiovascular disease and at least 40 years old in 2008. This study group, known as the CANHEART cohort, was formed by combining 17 large regional databases. The advantage of working with such a large study population is that it provides new and statistically powerful insights into the impact of the full range of HDL cholesterol values, not just in terms of cardiovascular events but the full spectrum of disease, Dr. Ko explained. Up until now, the conventional knowledge about HDL cholesterol has been based largely upon relatively small observational studies, such as the Framingham Heart Study; most of those studies didn’t look at noncardiovascular events.
During a mean 4.9 years of follow-up of the CANHEART cohort, 9,339 deaths occurred in men and 8,613 in women. In an analysis adjusted for age, non–HDL cholesterol levels, cardiac risk factors, sex, comorbid conditions, and income, HDL cholesterol levels below the reference range of 41-50 mg/dL in women and 51-60 mg/dL in men were associated with increased risks of mortality from all three causes: cardiovascular, cancer, and other. The lower the HDL cholesterol level, the greater the risks.
As HDL cholesterol groupings moved decile by decile above the reference ranges there was no protective effect seen against cardiovascular or noncardiovascular deaths. Instead, the risk of death due to causes other than heart disease or cancer took a turn upward as HDL cholesterol levels approached the outer end of the bell curve, achieving significance in men with an HDL cholesterol of 71-80 mg/dL and peaking in those with a level greater than 90 mg/dL. In women, the U-shaped curve was shallower, with an increased mortality risk – again, as in men, restricted to causes other than cancer or heart disease – becoming statistically significant only in women with an HDL cholesterol level greater than 90 mg/dL, Dr. Ko continued.
It’s worth noting that men with an HDL cholesterol level of 81 mg/dL or above also showed a trend for increased risks of both cardiovascular and cancer deaths, although this didn’t reach statistical significance.
Patients at the low end of the HDL cholesterol spectrum had an increased prevalence of unhealthy lifestyle, COPD and other comorbid conditions, cardiac risk factors, and low income. In contrast, those with high HDL cholesterol levels were more likely to have a body mass index below 25 kg/m2, engage in 30 minutes or more of brisk walking or other moderate exercise daily, and consume five or more servings of fruits and vegetables daily. So they were, overall, healthier. On the other hand, they were also more likely to be heavy alcohol users as defined by consuming five or more drinks per occasion at least once monthly during the year prior to study enrollment. Alcohol, like physical exercise, is known to boost HDL cholesterol levels.
These CANHEART data and other evidence warrant a reappraisal of HDL cholesterol as a cardiovascular risk/protective factor, according to Dr. Ko.
“HDL is unlikely to represent a cardiovascular-specific risk factor, given similarities in its association with noncardiovascular outcomes,” he observed.
Discussant Jacques Genest concurred.
“Maybe HDL cholesterol mass is the wrong biomarker for HDL function,” opined Dr. Genest, professor of medicine at McGill University in Montreal.
He noted that a causal relationship between HDL cholesterol and cardiovascular risk has been cast into doubt not only by the negative randomized trials of niacin and the CETP inhibitors and the U-shaped mortality curve described by Dr. Ko, but also by randomized Mendelian genetic studies suggesting that genes causing HDL deficiency aren’t linked to increased cardiovascular risk.
It’s likely true that what’s important is not HDL cholesterol levels as measured in conventional lipid panels, but rather HDL function. HDL particles have many beneficial effects: antioxidative, anti-inflammatory, vasodilatory, antiapoptotic, and antithrombotic. A better biomarker – one that reflects these functional benefits – may be cholesterol efflux capacity, as was shown in a recent study by investigators in the Dallas Heart Study (N Engl J Med. 2014; Dec 18;371[25]:2383-93), according to Dr. Genest.
Session cochair Dr. Christie Ballantyne was particularly interested in the 2.8% of CANHEART participants with an HDL cholesterol level greater than 90 mg/dL and their associated increased mortality from causes other than cancer and cardiovascular disease.
“I’ve seen similar data once before, in a Russian cohort. Cold weather and alcohol – I wonder if that’s a factor here. The alcohol exposure we saw in the Russian cohort with the 90 HDL levels was really rather striking. And it wasn’t cardiovascular or cancer mortality that they faced, it was other mortality. So I wonder if it’s not an alcohol-related thing, especially in places where you have long, cold winters,” commented Dr. Ballantyne, professor of medicine and of molecular and human genetics at Baylor College of Medicine and director of the Center for Cardiovascular Disease Prevention at the Methodist Debakey Heart Center in Houston.
Dr. Genest was skeptical.
“I think clinicians would argue that seeing an HDL of 90 would be very unusual in a male even if he drinks like an American at a football game,” the Canadian quipped. “ It’s probable that a genetic predisposition plus heavy alcohol is involved.”
Dr. Ko said he and his coinvestigators are scrutinizing the “other deaths” in the very-high HDL cholesterol subgroup, looking for an increase in deaths due to liver cirrhosis, trauma, and other obvious alcohol-related causes. “We haven’t really found a specific pattern,” according to the physician.
Dr. Ballantyne was undeterred. “It may end up being that the person who drinks heavily has some general health issues where trouble occurs because of alcohol in combination with medications rather than a specifically alcohol-related death,” he advised.
The CANHEART study is sponsored by the Canadian Institutes of Health Research. Dr. Ko reported having no financial conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Doubt has emerged about the validity of HDL cholesterol as a straightforward cardiovascular risk factor.
Major finding: The relationship between HDL cholesterol and mortality isn’t linear, it’s U-shaped, with increased risk seen at both low and high levels.
Data source: This registry study included 631,762 Ontario adults free of cardiovascular disease at baseline and followed for a mean of 4.9 years.
Disclosures: The study is sponsored by the Canadian Institutes of Health Research. The presenter reported having no financial conflicts of interest.
AHA: Physician awareness of women’s heart risk due for upgrade
ORLANDO – Heart disease in women is not a top-level concern for most primary care physicians or cardiologists, according to a national survey.
Less than two in five (39%) of the surveyed primary care physicians rated heart disease as their top concern in female patients. It ranked third, behind overweight/obesity followed by breast health, even though cardiovascular disease is the No. 1 cause of death for women in the United States, Dr. Holly S. Andersen reported at the American Heart Association scientific sessions.
“Cardiovascular disease is the leading health care threat for women, yet public awareness and physician action have stalled, particularly in younger women and among ethnic minorities. Women are less likely to receive evidence-based preventive, diagnostic, and therapeutic strategies for cardiovascular disease,” declared Dr. Andersen, a cardiologist at New York-Presbyterian Hospital.
She presented the results of a survey of 200 primary care physicians and 100 cardiologists, all in practice for 3 or more years. The survey of a nationally representative sample was commissioned by the Women’s Heart Alliance, for which Dr. Andersen serves as scientific adviser.
Primary care physicians’ emphasis on reducing overweight/obesity as a top priority in female patients is actually counterproductive from a cardiovascular risk perspective, Dr. Andersen said. Since sustained weight loss is often a losing battle, she explained, many women who’ve failed to reduce their body weight in response to their physicians’ encouragement simply put off further office visits, and so their other cardiovascular risk factors go unaddressed.
The survey results demonstrate that awareness about heart disease in women is low among both primary care physicians and cardiologists, she observed. Among the key survey findings:
• Under a quarter (22%) of primary care physicians and 42% of cardiologists feel “extremely well prepared” to assess heart disease risk in female patients, while another 42% of primary care physicians and 40% of cardiologists consider themselves “very well prepared.”
• Less than half (44%) of primary care physicians and 53% of cardiologists use the atherosclerotic cardiovascular disease (ASCVD) risk assessment calculator introduced in the latest cholesterol management guidelines from the American College of Cardiology and the American Heart Association (Circulation. 2013 November. doi: 10.1161/01.cir.0000437738.63853.7a). Moreover, 31% of primary care physicians and 15% of cardiologists said they’ve never used it. The tool is used to calculate a patient’s estimated 10-year and lifetime risks of ASCVD. Experts consider it a cornerstone of the current guidelines.
• Less than half (49%) of primary care physicians and 59% of cardiologists say they feel their medical school training prepared them to assess female patients’ risk of heart disease.
The survey was done in conjunction with a campaign by the Women’s Heart Alliance to increase physician awareness of women’s cardiovascular risk and to prepare to take action to improve it. The upcoming campaign will promote efforts to educate women about the importance of going to their physicians to find out their personal risk levels.
Most (87%) of the surveyed primary care physicians and 82% of the cardiologists were favorably disposed to the campaign and the notion of physician education programs to address practice gaps in women’s heart risk assessment.
“What’s different about this new effort is that it will give women a single, meaningful action they can take: a routine heart check with a health care professional,” Dr. Andersen said. A key part of this heart check will include use of the ASCVD risk assessment calculator.
“By uniting with health care professionals to encourage women to not only know their numbers but understand what they mean for their heart health, the effort will help women personalize their risk so they can take the steps they need to keep their hearts healthy,” she continued.
The portion of the campaign aimed at exhorting women to visit physicians for a discussion of personal cardiovascular risk will employ as a catchphrase “#getHeartChecked.”
Support for the physician survey was provided by the National Institutes of Health, Cedars-Sinai Medical Center in Los Angeles, and several foundations. Dr. Andersen reported having no financial conflicts of interest.
ORLANDO – Heart disease in women is not a top-level concern for most primary care physicians or cardiologists, according to a national survey.
Less than two in five (39%) of the surveyed primary care physicians rated heart disease as their top concern in female patients. It ranked third, behind overweight/obesity followed by breast health, even though cardiovascular disease is the No. 1 cause of death for women in the United States, Dr. Holly S. Andersen reported at the American Heart Association scientific sessions.
“Cardiovascular disease is the leading health care threat for women, yet public awareness and physician action have stalled, particularly in younger women and among ethnic minorities. Women are less likely to receive evidence-based preventive, diagnostic, and therapeutic strategies for cardiovascular disease,” declared Dr. Andersen, a cardiologist at New York-Presbyterian Hospital.
She presented the results of a survey of 200 primary care physicians and 100 cardiologists, all in practice for 3 or more years. The survey of a nationally representative sample was commissioned by the Women’s Heart Alliance, for which Dr. Andersen serves as scientific adviser.
Primary care physicians’ emphasis on reducing overweight/obesity as a top priority in female patients is actually counterproductive from a cardiovascular risk perspective, Dr. Andersen said. Since sustained weight loss is often a losing battle, she explained, many women who’ve failed to reduce their body weight in response to their physicians’ encouragement simply put off further office visits, and so their other cardiovascular risk factors go unaddressed.
The survey results demonstrate that awareness about heart disease in women is low among both primary care physicians and cardiologists, she observed. Among the key survey findings:
• Under a quarter (22%) of primary care physicians and 42% of cardiologists feel “extremely well prepared” to assess heart disease risk in female patients, while another 42% of primary care physicians and 40% of cardiologists consider themselves “very well prepared.”
• Less than half (44%) of primary care physicians and 53% of cardiologists use the atherosclerotic cardiovascular disease (ASCVD) risk assessment calculator introduced in the latest cholesterol management guidelines from the American College of Cardiology and the American Heart Association (Circulation. 2013 November. doi: 10.1161/01.cir.0000437738.63853.7a). Moreover, 31% of primary care physicians and 15% of cardiologists said they’ve never used it. The tool is used to calculate a patient’s estimated 10-year and lifetime risks of ASCVD. Experts consider it a cornerstone of the current guidelines.
• Less than half (49%) of primary care physicians and 59% of cardiologists say they feel their medical school training prepared them to assess female patients’ risk of heart disease.
The survey was done in conjunction with a campaign by the Women’s Heart Alliance to increase physician awareness of women’s cardiovascular risk and to prepare to take action to improve it. The upcoming campaign will promote efforts to educate women about the importance of going to their physicians to find out their personal risk levels.
Most (87%) of the surveyed primary care physicians and 82% of the cardiologists were favorably disposed to the campaign and the notion of physician education programs to address practice gaps in women’s heart risk assessment.
“What’s different about this new effort is that it will give women a single, meaningful action they can take: a routine heart check with a health care professional,” Dr. Andersen said. A key part of this heart check will include use of the ASCVD risk assessment calculator.
“By uniting with health care professionals to encourage women to not only know their numbers but understand what they mean for their heart health, the effort will help women personalize their risk so they can take the steps they need to keep their hearts healthy,” she continued.
The portion of the campaign aimed at exhorting women to visit physicians for a discussion of personal cardiovascular risk will employ as a catchphrase “#getHeartChecked.”
Support for the physician survey was provided by the National Institutes of Health, Cedars-Sinai Medical Center in Los Angeles, and several foundations. Dr. Andersen reported having no financial conflicts of interest.
ORLANDO – Heart disease in women is not a top-level concern for most primary care physicians or cardiologists, according to a national survey.
Less than two in five (39%) of the surveyed primary care physicians rated heart disease as their top concern in female patients. It ranked third, behind overweight/obesity followed by breast health, even though cardiovascular disease is the No. 1 cause of death for women in the United States, Dr. Holly S. Andersen reported at the American Heart Association scientific sessions.
“Cardiovascular disease is the leading health care threat for women, yet public awareness and physician action have stalled, particularly in younger women and among ethnic minorities. Women are less likely to receive evidence-based preventive, diagnostic, and therapeutic strategies for cardiovascular disease,” declared Dr. Andersen, a cardiologist at New York-Presbyterian Hospital.
She presented the results of a survey of 200 primary care physicians and 100 cardiologists, all in practice for 3 or more years. The survey of a nationally representative sample was commissioned by the Women’s Heart Alliance, for which Dr. Andersen serves as scientific adviser.
Primary care physicians’ emphasis on reducing overweight/obesity as a top priority in female patients is actually counterproductive from a cardiovascular risk perspective, Dr. Andersen said. Since sustained weight loss is often a losing battle, she explained, many women who’ve failed to reduce their body weight in response to their physicians’ encouragement simply put off further office visits, and so their other cardiovascular risk factors go unaddressed.
The survey results demonstrate that awareness about heart disease in women is low among both primary care physicians and cardiologists, she observed. Among the key survey findings:
• Under a quarter (22%) of primary care physicians and 42% of cardiologists feel “extremely well prepared” to assess heart disease risk in female patients, while another 42% of primary care physicians and 40% of cardiologists consider themselves “very well prepared.”
• Less than half (44%) of primary care physicians and 53% of cardiologists use the atherosclerotic cardiovascular disease (ASCVD) risk assessment calculator introduced in the latest cholesterol management guidelines from the American College of Cardiology and the American Heart Association (Circulation. 2013 November. doi: 10.1161/01.cir.0000437738.63853.7a). Moreover, 31% of primary care physicians and 15% of cardiologists said they’ve never used it. The tool is used to calculate a patient’s estimated 10-year and lifetime risks of ASCVD. Experts consider it a cornerstone of the current guidelines.
• Less than half (49%) of primary care physicians and 59% of cardiologists say they feel their medical school training prepared them to assess female patients’ risk of heart disease.
The survey was done in conjunction with a campaign by the Women’s Heart Alliance to increase physician awareness of women’s cardiovascular risk and to prepare to take action to improve it. The upcoming campaign will promote efforts to educate women about the importance of going to their physicians to find out their personal risk levels.
Most (87%) of the surveyed primary care physicians and 82% of the cardiologists were favorably disposed to the campaign and the notion of physician education programs to address practice gaps in women’s heart risk assessment.
“What’s different about this new effort is that it will give women a single, meaningful action they can take: a routine heart check with a health care professional,” Dr. Andersen said. A key part of this heart check will include use of the ASCVD risk assessment calculator.
“By uniting with health care professionals to encourage women to not only know their numbers but understand what they mean for their heart health, the effort will help women personalize their risk so they can take the steps they need to keep their hearts healthy,” she continued.
The portion of the campaign aimed at exhorting women to visit physicians for a discussion of personal cardiovascular risk will employ as a catchphrase “#getHeartChecked.”
Support for the physician survey was provided by the National Institutes of Health, Cedars-Sinai Medical Center in Los Angeles, and several foundations. Dr. Andersen reported having no financial conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Systematic assessment of heart disease risk in women is underutilized by physicians and will be the focus of a national consumer/physician educational campaign.
Major finding: Forty-four percent of primary care physicians and 53% of cardiologists surveyed used the atherosclerotic cardiovascular disease risk assessment calculator introduced in the current ACC/AHA cholesterol management guidelines.
Data source: Survey of a nationally representative panel of 200 primary care physicians and 100 cardiologists.
Disclosures: The National Institutes of Health, Cedars-Sinai Medical Center in Los Angeles, and several foundations supported the survey. Dr. Anderson reported having no financial conflicts of interest.