User login
AHA: It’s best to have a cardiac arrest in Midwest
ORLANDO – Considerable regional variation exists across the United States in outcomes, including survival and hospital charges following out-of-hospital cardiac arrest, Dr. Aiham Albaeni reported at the American Heart Association scientific sessions.
He presented an analysis of 155,592 adults who survived at least until hospital admission following non–trauma-related out-of-hospital cardiac arrest (OHCA) during 2002-2012. The data came from the Agency for Healthcare Research and Quality’s Nationwide Inpatient Sample, the largest all-payer U.S. inpatient database.
Mortality was lowest among patients whose OHCA occurred in the Midwest. Indeed, taking the Northeast region as the reference point in a multivariate analysis, the adjusted mortality risk was 14% lower in the Midwest and 9% lower in the South. There was no difference in survival rates between the West and Northeast in this analysis adjusted for age, gender, race, primary diagnosis, income, Charlson Comorbidity Index, primary payer, and hospital size and teaching status, reported Dr. Albaeni of Johns Hopkins University, Baltimore.
Total hospital charges for patients admitted following OHCA were far and away highest in the West, and this increased expenditure didn’t pay off in terms of a survival advantage. The Consumer Price Index–adjusted mean total hospital charges averaged $85,592 per patient in the West, $66,290 in the Northeast, $55,257 in the Midwest, and $54,878 in the South.
Outliers in terms of cost of care – that is, patients admitted with OHCA whose total hospital charges exceeded $109,000 per admission – were 85% more common in the West than the other three regions, he noted.
Hospital length of stay greater than 8 days occurred most often in the Northeast. These lengthier stays were 10%-12% less common in the other regions.
The explanation for the marked regional differences observed in this study remains unknown.
“These findings call for more efforts to identify a high-quality model of excellence that standardizes health care delivery and improves quality of care in low-performing regions,” said Dr. Albaeni.
He reported having no financial conflicts of interest regarding his study.
ORLANDO – Considerable regional variation exists across the United States in outcomes, including survival and hospital charges following out-of-hospital cardiac arrest, Dr. Aiham Albaeni reported at the American Heart Association scientific sessions.
He presented an analysis of 155,592 adults who survived at least until hospital admission following non–trauma-related out-of-hospital cardiac arrest (OHCA) during 2002-2012. The data came from the Agency for Healthcare Research and Quality’s Nationwide Inpatient Sample, the largest all-payer U.S. inpatient database.
Mortality was lowest among patients whose OHCA occurred in the Midwest. Indeed, taking the Northeast region as the reference point in a multivariate analysis, the adjusted mortality risk was 14% lower in the Midwest and 9% lower in the South. There was no difference in survival rates between the West and Northeast in this analysis adjusted for age, gender, race, primary diagnosis, income, Charlson Comorbidity Index, primary payer, and hospital size and teaching status, reported Dr. Albaeni of Johns Hopkins University, Baltimore.
Total hospital charges for patients admitted following OHCA were far and away highest in the West, and this increased expenditure didn’t pay off in terms of a survival advantage. The Consumer Price Index–adjusted mean total hospital charges averaged $85,592 per patient in the West, $66,290 in the Northeast, $55,257 in the Midwest, and $54,878 in the South.
Outliers in terms of cost of care – that is, patients admitted with OHCA whose total hospital charges exceeded $109,000 per admission – were 85% more common in the West than the other three regions, he noted.
Hospital length of stay greater than 8 days occurred most often in the Northeast. These lengthier stays were 10%-12% less common in the other regions.
The explanation for the marked regional differences observed in this study remains unknown.
“These findings call for more efforts to identify a high-quality model of excellence that standardizes health care delivery and improves quality of care in low-performing regions,” said Dr. Albaeni.
He reported having no financial conflicts of interest regarding his study.
ORLANDO – Considerable regional variation exists across the United States in outcomes, including survival and hospital charges following out-of-hospital cardiac arrest, Dr. Aiham Albaeni reported at the American Heart Association scientific sessions.
He presented an analysis of 155,592 adults who survived at least until hospital admission following non–trauma-related out-of-hospital cardiac arrest (OHCA) during 2002-2012. The data came from the Agency for Healthcare Research and Quality’s Nationwide Inpatient Sample, the largest all-payer U.S. inpatient database.
Mortality was lowest among patients whose OHCA occurred in the Midwest. Indeed, taking the Northeast region as the reference point in a multivariate analysis, the adjusted mortality risk was 14% lower in the Midwest and 9% lower in the South. There was no difference in survival rates between the West and Northeast in this analysis adjusted for age, gender, race, primary diagnosis, income, Charlson Comorbidity Index, primary payer, and hospital size and teaching status, reported Dr. Albaeni of Johns Hopkins University, Baltimore.
Total hospital charges for patients admitted following OHCA were far and away highest in the West, and this increased expenditure didn’t pay off in terms of a survival advantage. The Consumer Price Index–adjusted mean total hospital charges averaged $85,592 per patient in the West, $66,290 in the Northeast, $55,257 in the Midwest, and $54,878 in the South.
Outliers in terms of cost of care – that is, patients admitted with OHCA whose total hospital charges exceeded $109,000 per admission – were 85% more common in the West than the other three regions, he noted.
Hospital length of stay greater than 8 days occurred most often in the Northeast. These lengthier stays were 10%-12% less common in the other regions.
The explanation for the marked regional differences observed in this study remains unknown.
“These findings call for more efforts to identify a high-quality model of excellence that standardizes health care delivery and improves quality of care in low-performing regions,” said Dr. Albaeni.
He reported having no financial conflicts of interest regarding his study.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Substantial and as-yet unexplained regional differences in survival and total hospital charges following out-of-hospital cardiac arrest exist across the United States.
Major finding: Mortality among adults hospitalized after experiencing out-of-hospital cardiac arrest was 14% lower in the Midwest than in the Northeast.
Data source: A retrospective analysis of data from the Nationwide Inpatient Sample for 2002-2012 that included 155,592 adults with out-of-hospital cardiac arrest who survived to hospital admission.
Disclosures: The presenter reported having no financial conflicts of interest.
AHA: PCI renal complications keep climbing
ORLANDO – Cases of contrast-induced nephropathy increased dramatically among Medicare patients undergoing percutaneous coronary intervention (PCI) during a recent 5-year period, despite the increased attention that has been drawn to the problem.
“These findings suggest that despite a longstanding focus on preventing CIN [contrast-induced nephropathy], the complication is increasing steadily and new efforts to reduce PCI-related CIN are warranted,” Dr. Phillip P. Brown said at the American Heart Association scientific sessions.
A fresh approach is a priority for Medicare, in part because new-onset renal failure requiring hemodialysis as a result of CIN increases health care costs substantially for the remainder of the patient’s life, noted Dr. Brown of Cardiac Data Solutions in Atlanta.
He presented a retrospective analysis of Medicare data files for 2009-2013. Among 1,552,960 Medicare beneficiaries who underwent PCI without valve surgery or coronary artery bypass graft surgery, 275,471 were admitted for nonelective PCI.
The rate of new hemodialysis as a complication of nonelective PCI increased by 24.8% annually during the study period, climbing to an incidence of 1.15% in 2013. Among patients admitted for elective PCI, the rate of new-onset renal failure requiring hemodialysis essentially doubled from 1% to 2% during the 5-year period.
The rate of new-onset acute renal failure as a complication of nonelective PCI increased by an average of 6.9% annually, reaching 7.67% in 2013. The increase in acute renal failure as a complication of elective PCI was even steeper: an average of 10.6% per year.
In addition to the rising rates of acute renal failure and need for dialysis as a complication of PCI, the proportion of patients who presented with prior dialysis or acute renal failure at admission for the procedure also rose year by year. In 2013, acute renal failure was present at admission in 6.12% of patients undergoing elective and 7.02% having nonelective PCI. Prior dialysis at admission was present in 2.61% and 0.94%, respectively.
Dr. Brown reported having no financial conflicts regarding this descriptive study.
ORLANDO – Cases of contrast-induced nephropathy increased dramatically among Medicare patients undergoing percutaneous coronary intervention (PCI) during a recent 5-year period, despite the increased attention that has been drawn to the problem.
“These findings suggest that despite a longstanding focus on preventing CIN [contrast-induced nephropathy], the complication is increasing steadily and new efforts to reduce PCI-related CIN are warranted,” Dr. Phillip P. Brown said at the American Heart Association scientific sessions.
A fresh approach is a priority for Medicare, in part because new-onset renal failure requiring hemodialysis as a result of CIN increases health care costs substantially for the remainder of the patient’s life, noted Dr. Brown of Cardiac Data Solutions in Atlanta.
He presented a retrospective analysis of Medicare data files for 2009-2013. Among 1,552,960 Medicare beneficiaries who underwent PCI without valve surgery or coronary artery bypass graft surgery, 275,471 were admitted for nonelective PCI.
The rate of new hemodialysis as a complication of nonelective PCI increased by 24.8% annually during the study period, climbing to an incidence of 1.15% in 2013. Among patients admitted for elective PCI, the rate of new-onset renal failure requiring hemodialysis essentially doubled from 1% to 2% during the 5-year period.
The rate of new-onset acute renal failure as a complication of nonelective PCI increased by an average of 6.9% annually, reaching 7.67% in 2013. The increase in acute renal failure as a complication of elective PCI was even steeper: an average of 10.6% per year.
In addition to the rising rates of acute renal failure and need for dialysis as a complication of PCI, the proportion of patients who presented with prior dialysis or acute renal failure at admission for the procedure also rose year by year. In 2013, acute renal failure was present at admission in 6.12% of patients undergoing elective and 7.02% having nonelective PCI. Prior dialysis at admission was present in 2.61% and 0.94%, respectively.
Dr. Brown reported having no financial conflicts regarding this descriptive study.
ORLANDO – Cases of contrast-induced nephropathy increased dramatically among Medicare patients undergoing percutaneous coronary intervention (PCI) during a recent 5-year period, despite the increased attention that has been drawn to the problem.
“These findings suggest that despite a longstanding focus on preventing CIN [contrast-induced nephropathy], the complication is increasing steadily and new efforts to reduce PCI-related CIN are warranted,” Dr. Phillip P. Brown said at the American Heart Association scientific sessions.
A fresh approach is a priority for Medicare, in part because new-onset renal failure requiring hemodialysis as a result of CIN increases health care costs substantially for the remainder of the patient’s life, noted Dr. Brown of Cardiac Data Solutions in Atlanta.
He presented a retrospective analysis of Medicare data files for 2009-2013. Among 1,552,960 Medicare beneficiaries who underwent PCI without valve surgery or coronary artery bypass graft surgery, 275,471 were admitted for nonelective PCI.
The rate of new hemodialysis as a complication of nonelective PCI increased by 24.8% annually during the study period, climbing to an incidence of 1.15% in 2013. Among patients admitted for elective PCI, the rate of new-onset renal failure requiring hemodialysis essentially doubled from 1% to 2% during the 5-year period.
The rate of new-onset acute renal failure as a complication of nonelective PCI increased by an average of 6.9% annually, reaching 7.67% in 2013. The increase in acute renal failure as a complication of elective PCI was even steeper: an average of 10.6% per year.
In addition to the rising rates of acute renal failure and need for dialysis as a complication of PCI, the proportion of patients who presented with prior dialysis or acute renal failure at admission for the procedure also rose year by year. In 2013, acute renal failure was present at admission in 6.12% of patients undergoing elective and 7.02% having nonelective PCI. Prior dialysis at admission was present in 2.61% and 0.94%, respectively.
Dr. Brown reported having no financial conflicts regarding this descriptive study.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Renal complication rates in Medicare patients undergoing PCI continue to rise dramatically.
Major finding: The combined rate of acute renal failure and need for hemodialysis as a complication of elective PCI in Medicare patients climbed by 18% per year during a recent 5-year period and by nearly 32% annually in those undergoing nonelective PCI.
Data source: A retrospective study of 1.5 million Medicare beneficiaries who underwent elective or nonelective PCI during 2009-2013.
Disclosures: The presenter of this study reported having no financial conflicts.
Diabetic foot ulcer: Early closure optimal
SAN DIEGO – Early wound closure prior to hospital discharge after surgical debridement of infected diabetic foot ulcers yields higher ulcer healing rates and a shorter time to healing, compared with various nonclosure wound management methods, according to a propensity-matched study.
How best to manage the open wound following nonamputative surgery of infected diabetic foot ulcers has been controversial. But early wound closure during the index hospitalization was the clear winner in this comparative study, according to Dr. Shey-Ying Chen who presented the research at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
He presented a retrospective comparison between 179 diabetic foot ulcer (DFU) patients with early wound closure after surgical debridement and an equal number of matched controls treated with various nonclosure techniques, including negative pressure wound therapy and the repeated application of moist dressings.
The two study groups were matched first on the basis of DFU location – toe, forefoot, midfoot, or rear foot – and then further propensity matched based on demographics, comorbid conditions, the presence of neuropathy, ulcer status by Wagner classification, infection severity, revascularization procedures, and other variables.
During 1 year of follow-up post discharge, ulcer healing occurred in 75% of the early wound closure group, compared with 66% of the nonclosure patients. Readmission for further treatment of the index ulcer occurred in 33% of the early closure group and 53% of the nonclosure group.
Other outcomes were also superior in the early wound closure group, noted Dr. Chen of Beth Israel Deaconess Medical Center, Boston.
Two independent predictors of DFU healing during the follow-up period emerged from a Cox regression analysis: early wound closure, with an adjusted odds ratio of 1.63, and acute as opposed to chronic DFU, with an OR of 1.35.
Ulcer healing was significantly less likely in those patients who had peripheral vascular disease, with an OR of 0.62; or neuropathy, with an OR of 0.53; and methicillin-resistant Staphylococcus aureus wound infection, with an OR of 0.59, Dr. Chen continued.
Underscoring the longer-term difficulties faced by patients with DFUs, it’s noteworthy that 11.5% of patients in both study arms underwent new amputations during the year of follow-up.
Moreover, a new diagnosis of osteomyelitis was made in 20% of the early wound closure group and 26% of the nonclosure group, a nonsignificant difference.
Dr. Adolf W. Karchmer, Dr. Chen’s senior coinvestigator, said the outcome data are too new to be able to gauge how vascular, orthopedic, and podiatric surgeons will react.
The investigators reported that they had no financial conflicts with regard to this study, which was conducted without commercial sponsorship.
With increasing prevalence of diabetes in the population, diabetic foot ulcers and infections present a significant clinical problem. Infected diabetic foot ulcers usually require an initial debridement of infected and necrotic tissue but there are many options for subsequent wound management.These included secondary wound closure, if possible, or use of adjunctive techniques for wound care, including negative pressure wound therapy, hyperbaric oxygen and a variety of wound care products designed for optimal healing.
Dr. Chen and his colleagues report their retrospective experience in 179 patients treated with early wound closure and compare outcomes with an equal number of matched controls treated with various nonclosure techniques such as negative pressure wound therapy and repeated applications of moist dressings. They found improved outcomes with the early closure group when analyzed for ulcer healing, readmission, and other outcome assessments. Specific times for healing after surgical debridement were an average of 105 days in the early wound closure group versus 136 days in those wounds managed with nonclosure techniques. As would be predicted, peripheral vascular disease and methicillin-resistant Staphylococcus aureus wound infections were found to adversely affect wound healing in both groups.
It is unclear in this report how many of the wounds were not amenable to early closure or what specific wound care regimen was used in the patients treated with continued wound care only. In addition, although it is stated that peripheral vascular disease adversely affected wound healing, it is not clear if these patients underwent revascularization as part of their comprehensive management.
Finally, Dr. Adolf W. Karchmer, the senior co-investigator in the trial, states that these data are too new to assess how other specialists will react. Clearly wound care and diabetic foot care should involve a multidisciplinary approach including wound care specialists as well as vascular surgeons, podiatrists, orthopedic surgeons, infectious disease specialists, and others. Observations and studies such as this are important to advance the science and specialty of wound care and continued data collection will help to optimize patient outcomes.
Dr. Larry Scher is a professor of clinical surgery and attending vascular surgeon at Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, N.Y. He is also an associate medical editor for Vascular Specialist.
With increasing prevalence of diabetes in the population, diabetic foot ulcers and infections present a significant clinical problem. Infected diabetic foot ulcers usually require an initial debridement of infected and necrotic tissue but there are many options for subsequent wound management.These included secondary wound closure, if possible, or use of adjunctive techniques for wound care, including negative pressure wound therapy, hyperbaric oxygen and a variety of wound care products designed for optimal healing.
Dr. Chen and his colleagues report their retrospective experience in 179 patients treated with early wound closure and compare outcomes with an equal number of matched controls treated with various nonclosure techniques such as negative pressure wound therapy and repeated applications of moist dressings. They found improved outcomes with the early closure group when analyzed for ulcer healing, readmission, and other outcome assessments. Specific times for healing after surgical debridement were an average of 105 days in the early wound closure group versus 136 days in those wounds managed with nonclosure techniques. As would be predicted, peripheral vascular disease and methicillin-resistant Staphylococcus aureus wound infections were found to adversely affect wound healing in both groups.
It is unclear in this report how many of the wounds were not amenable to early closure or what specific wound care regimen was used in the patients treated with continued wound care only. In addition, although it is stated that peripheral vascular disease adversely affected wound healing, it is not clear if these patients underwent revascularization as part of their comprehensive management.
Finally, Dr. Adolf W. Karchmer, the senior co-investigator in the trial, states that these data are too new to assess how other specialists will react. Clearly wound care and diabetic foot care should involve a multidisciplinary approach including wound care specialists as well as vascular surgeons, podiatrists, orthopedic surgeons, infectious disease specialists, and others. Observations and studies such as this are important to advance the science and specialty of wound care and continued data collection will help to optimize patient outcomes.
Dr. Larry Scher is a professor of clinical surgery and attending vascular surgeon at Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, N.Y. He is also an associate medical editor for Vascular Specialist.
With increasing prevalence of diabetes in the population, diabetic foot ulcers and infections present a significant clinical problem. Infected diabetic foot ulcers usually require an initial debridement of infected and necrotic tissue but there are many options for subsequent wound management.These included secondary wound closure, if possible, or use of adjunctive techniques for wound care, including negative pressure wound therapy, hyperbaric oxygen and a variety of wound care products designed for optimal healing.
Dr. Chen and his colleagues report their retrospective experience in 179 patients treated with early wound closure and compare outcomes with an equal number of matched controls treated with various nonclosure techniques such as negative pressure wound therapy and repeated applications of moist dressings. They found improved outcomes with the early closure group when analyzed for ulcer healing, readmission, and other outcome assessments. Specific times for healing after surgical debridement were an average of 105 days in the early wound closure group versus 136 days in those wounds managed with nonclosure techniques. As would be predicted, peripheral vascular disease and methicillin-resistant Staphylococcus aureus wound infections were found to adversely affect wound healing in both groups.
It is unclear in this report how many of the wounds were not amenable to early closure or what specific wound care regimen was used in the patients treated with continued wound care only. In addition, although it is stated that peripheral vascular disease adversely affected wound healing, it is not clear if these patients underwent revascularization as part of their comprehensive management.
Finally, Dr. Adolf W. Karchmer, the senior co-investigator in the trial, states that these data are too new to assess how other specialists will react. Clearly wound care and diabetic foot care should involve a multidisciplinary approach including wound care specialists as well as vascular surgeons, podiatrists, orthopedic surgeons, infectious disease specialists, and others. Observations and studies such as this are important to advance the science and specialty of wound care and continued data collection will help to optimize patient outcomes.
Dr. Larry Scher is a professor of clinical surgery and attending vascular surgeon at Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, N.Y. He is also an associate medical editor for Vascular Specialist.
SAN DIEGO – Early wound closure prior to hospital discharge after surgical debridement of infected diabetic foot ulcers yields higher ulcer healing rates and a shorter time to healing, compared with various nonclosure wound management methods, according to a propensity-matched study.
How best to manage the open wound following nonamputative surgery of infected diabetic foot ulcers has been controversial. But early wound closure during the index hospitalization was the clear winner in this comparative study, according to Dr. Shey-Ying Chen who presented the research at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
He presented a retrospective comparison between 179 diabetic foot ulcer (DFU) patients with early wound closure after surgical debridement and an equal number of matched controls treated with various nonclosure techniques, including negative pressure wound therapy and the repeated application of moist dressings.
The two study groups were matched first on the basis of DFU location – toe, forefoot, midfoot, or rear foot – and then further propensity matched based on demographics, comorbid conditions, the presence of neuropathy, ulcer status by Wagner classification, infection severity, revascularization procedures, and other variables.
During 1 year of follow-up post discharge, ulcer healing occurred in 75% of the early wound closure group, compared with 66% of the nonclosure patients. Readmission for further treatment of the index ulcer occurred in 33% of the early closure group and 53% of the nonclosure group.
Other outcomes were also superior in the early wound closure group, noted Dr. Chen of Beth Israel Deaconess Medical Center, Boston.
Two independent predictors of DFU healing during the follow-up period emerged from a Cox regression analysis: early wound closure, with an adjusted odds ratio of 1.63, and acute as opposed to chronic DFU, with an OR of 1.35.
Ulcer healing was significantly less likely in those patients who had peripheral vascular disease, with an OR of 0.62; or neuropathy, with an OR of 0.53; and methicillin-resistant Staphylococcus aureus wound infection, with an OR of 0.59, Dr. Chen continued.
Underscoring the longer-term difficulties faced by patients with DFUs, it’s noteworthy that 11.5% of patients in both study arms underwent new amputations during the year of follow-up.
Moreover, a new diagnosis of osteomyelitis was made in 20% of the early wound closure group and 26% of the nonclosure group, a nonsignificant difference.
Dr. Adolf W. Karchmer, Dr. Chen’s senior coinvestigator, said the outcome data are too new to be able to gauge how vascular, orthopedic, and podiatric surgeons will react.
The investigators reported that they had no financial conflicts with regard to this study, which was conducted without commercial sponsorship.
SAN DIEGO – Early wound closure prior to hospital discharge after surgical debridement of infected diabetic foot ulcers yields higher ulcer healing rates and a shorter time to healing, compared with various nonclosure wound management methods, according to a propensity-matched study.
How best to manage the open wound following nonamputative surgery of infected diabetic foot ulcers has been controversial. But early wound closure during the index hospitalization was the clear winner in this comparative study, according to Dr. Shey-Ying Chen who presented the research at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
He presented a retrospective comparison between 179 diabetic foot ulcer (DFU) patients with early wound closure after surgical debridement and an equal number of matched controls treated with various nonclosure techniques, including negative pressure wound therapy and the repeated application of moist dressings.
The two study groups were matched first on the basis of DFU location – toe, forefoot, midfoot, or rear foot – and then further propensity matched based on demographics, comorbid conditions, the presence of neuropathy, ulcer status by Wagner classification, infection severity, revascularization procedures, and other variables.
During 1 year of follow-up post discharge, ulcer healing occurred in 75% of the early wound closure group, compared with 66% of the nonclosure patients. Readmission for further treatment of the index ulcer occurred in 33% of the early closure group and 53% of the nonclosure group.
Other outcomes were also superior in the early wound closure group, noted Dr. Chen of Beth Israel Deaconess Medical Center, Boston.
Two independent predictors of DFU healing during the follow-up period emerged from a Cox regression analysis: early wound closure, with an adjusted odds ratio of 1.63, and acute as opposed to chronic DFU, with an OR of 1.35.
Ulcer healing was significantly less likely in those patients who had peripheral vascular disease, with an OR of 0.62; or neuropathy, with an OR of 0.53; and methicillin-resistant Staphylococcus aureus wound infection, with an OR of 0.59, Dr. Chen continued.
Underscoring the longer-term difficulties faced by patients with DFUs, it’s noteworthy that 11.5% of patients in both study arms underwent new amputations during the year of follow-up.
Moreover, a new diagnosis of osteomyelitis was made in 20% of the early wound closure group and 26% of the nonclosure group, a nonsignificant difference.
Dr. Adolf W. Karchmer, Dr. Chen’s senior coinvestigator, said the outcome data are too new to be able to gauge how vascular, orthopedic, and podiatric surgeons will react.
The investigators reported that they had no financial conflicts with regard to this study, which was conducted without commercial sponsorship.
Resistant gonorrhea rates high in China, raise concerns in U.S.
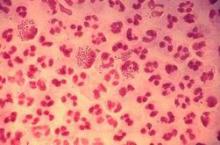
SAN DIEGO – Experts in the field of Neisseria gonorrhoeae antimicrobial resistance are warily watching developments in China, where rates of nonsusceptibility to ceftriaxone are reportedly shooting through the roof.
In the United States at present, gonococcal resistance to ceftriaxone is exceedingly rare: well under 1% of isolates have elevated minimum inhibitory concentrations (MICs) to this cornerstone of empiric therapy. In Europe, the rate is about 3%. What’s really disturbing is that recent data from the World Health Organization Gonococcal Antimicrobial Surveillance Program indicate ceftriaxone nonsusceptibility rates in China are in the 20%-30%-plus range, Dr. Joseph Duncan said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is very concerning for the potential spread of this type of resistance across the world at some point. It’s just ready to explode,” observed Dr. Duncan of the University of North Carolina, Chapel Hill.
Anytime gonococcal resistance rates to a drug reach about 5%, it spells trouble.
“Gonorrhea treatment is often syndromic. An isolated swab is taken, identified by Gram stain, you give them empiric therapy, and the patients walk out of the clinic and never come back. So you don’t want to have a 5% failure rate for your initial therapy,” he explained.
Neisseria gonorrhoeae has acquired resistance to virtually every antibiotic ever used to treat the infection. Treatment options are running out, which is why the Centers for Disease Control and Prevention has designated gonorrhea as an immediate public health threat requiring urgent and aggressive action.
The 2015 CDC Sexually Transmitted Disease Treatment Guidelines recommend only one front-line treatment for gonorrhea: dual therapy with ceftriaxone at 250 mg IM in a single dose plus azithromycin 1 g orally, also in a single dose. Given N. gonorrhoeae’s adaptability, experts believe that’s not a long-term solution.
After all, 5%-10% of gonococcal isolates in Europe and China are azithromycin-resistant, and while CDC surveillance data showed less than 1% of strains in the United States were azithromycin-resistant through 2013, preliminary data for 2014 show a concerning jump to 2.5%, according to Dr. Duncan’s fellow panelist Dr. Kimberly Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 CDC STD guidelines.
Dr. Duncan described the state of the ongoing aggressive multipronged attempts to combat antimicrobial resistance in N. gonorrhoeae. This effort includes new antibiotics in the developmental pipeline, attempts to repurpose existing antibiotics, rapid point-of-care antibiotic susceptibility tests, and vaccine development.
He also highlighted the factors that have led to the bug’s capacity to acquire resistance to so many antibiotics having different mechanisms of action. One key factor is the organism’s sheer competence as expressed in genetic lability.
“This bacteria is continually sampling DNA from the environment. The organisms are constantly swapping genes and DNA segments with commensal Neisseria species. In fact, even human DNA sequences have been found inside the gonococcal genome,” Dr. Duncan said.
While high-level antibiotic resistance can be acquired in a single dramatic step, it can also come about through multiple smaller steps, each one yielding only low-level resistance. “This allows for the sort of creeping [minimum inhibitory concentration] that we’ve seen with the gonococcus, particularly with the extended-spectrum cephalosporin antibiotics,” Dr. Duncan continued.
Also, it’s apparent that even in the absence of antibiotics, other pressures can select for antibiotic-resistant strains. Dr. Duncan credited one of his mentors, William M. Shafer, Ph.D., of Emory University, with developing the hypothesis that fecal lipids might be an important driver of increased resistance rates. Supporting this hypothesis, he noted, is the finding in multiple studies that rectal gonococcal isolates consistently have a somewhat higher prevalence of resistance than those obtained from other sites.
Turning to the effort to curb antibiotic resistance, Dr. Duncan said the drug farthest along in the pipeline is solithromycin, a novel macrolide being developed by Cempra Pharmaceuticals in both oral and IV formulations. Solithromycin, a first-in-class fluoroketolide, is active against a broad range of Gram-positive organisms, among them Legionella, Chlamydia, Mycoplasma, and Ureaplasma, including macrolide-resistant strains. Its ability to bind to three ribosomal sites is thought to minimize development of resistance.
Two positive phase 3 clinical trials of solithromycin have been completed in patients with community-acquired bacterial pneumonia. A phase 3 trial in gonorrhea is ongoing after a positive phase 2 study.
Two bacterial topoisomerase inhibitors are in soon-to-be-completed phase 2 studies.
Delafloxacin, a new fluoroquinolone, was in a phase 3 clinical trial for gonorrhea that was terminated early due to ineffectiveness.
There is considerable interest in bringing back single-dose IM gentamicin (Garamycin) for the treatment of gonorrhea. A systematic review of five studies (Syst Rev. 2014 Sep 19;3:104. doi: 10.1186/2046-4053-3-104) reported cure rates that were mostly in the 90% range, but “not quite high enough to say you’d want to go to gentamicin as your front-line therapy,” in Dr. Duncan’s opinion.
Dr. Workowski noted that the National Institutes of Health is interested in trying to resurrect cefixime (Suprax) for gonorrhea after the CDC guidelines demoted it several years ago. An ongoing clinical trial is examining the impact of increasing the dose and duration of therapy.
Public health officials are also interested in spectinomycin, an antibiotic not currently available in the United States, which has achieved high cure rates as single-dose therapy in several foreign studies.
Dr. Duncan noted that a randomized trial of gentamicin plus azithromycin or gemifloxacin (Factive) plus azithromycin reported cure rates of 100% and 99.5%, respectively (Clin Infect Dis. 2014 Oct 15;59(8):1083-91). He found the study less than convincing, however: “These strains were almost all susceptibile to azithromycin, so you can’t actually say that gentamicin or gemifloxacin added a lot,” he said.
A number of researchers are working on rapid tests for susceptibility of a particular gonococcal strain so physicians could choose an effective antimicrobial for an individual patient right from the start.
“These are all in the developmental phase. It’s going to be difficult, because there are so many different mechanisms for resistance,” he said.
Similarly, vaccine development in the gonococcal field is a great challenge. The microorganism’s multiple mechanisms of immune evasion make it tough to identify correlates of protection, Dr. Duncan continued.
“Epidemiologic studies suggest there is not efficient development of natural immunity. Folks who get gonorrhea and then come back with reinfection often have the exact same strain,” he noted.
Dr. Duncan’s research is funded by the National Institutes of Health and the Burroughs Wellcome Fund. He reported having no financial conflicts of interest.
SAN DIEGO – Experts in the field of Neisseria gonorrhoeae antimicrobial resistance are warily watching developments in China, where rates of nonsusceptibility to ceftriaxone are reportedly shooting through the roof.
In the United States at present, gonococcal resistance to ceftriaxone is exceedingly rare: well under 1% of isolates have elevated minimum inhibitory concentrations (MICs) to this cornerstone of empiric therapy. In Europe, the rate is about 3%. What’s really disturbing is that recent data from the World Health Organization Gonococcal Antimicrobial Surveillance Program indicate ceftriaxone nonsusceptibility rates in China are in the 20%-30%-plus range, Dr. Joseph Duncan said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is very concerning for the potential spread of this type of resistance across the world at some point. It’s just ready to explode,” observed Dr. Duncan of the University of North Carolina, Chapel Hill.
Anytime gonococcal resistance rates to a drug reach about 5%, it spells trouble.
“Gonorrhea treatment is often syndromic. An isolated swab is taken, identified by Gram stain, you give them empiric therapy, and the patients walk out of the clinic and never come back. So you don’t want to have a 5% failure rate for your initial therapy,” he explained.
Neisseria gonorrhoeae has acquired resistance to virtually every antibiotic ever used to treat the infection. Treatment options are running out, which is why the Centers for Disease Control and Prevention has designated gonorrhea as an immediate public health threat requiring urgent and aggressive action.
The 2015 CDC Sexually Transmitted Disease Treatment Guidelines recommend only one front-line treatment for gonorrhea: dual therapy with ceftriaxone at 250 mg IM in a single dose plus azithromycin 1 g orally, also in a single dose. Given N. gonorrhoeae’s adaptability, experts believe that’s not a long-term solution.
After all, 5%-10% of gonococcal isolates in Europe and China are azithromycin-resistant, and while CDC surveillance data showed less than 1% of strains in the United States were azithromycin-resistant through 2013, preliminary data for 2014 show a concerning jump to 2.5%, according to Dr. Duncan’s fellow panelist Dr. Kimberly Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 CDC STD guidelines.
Dr. Duncan described the state of the ongoing aggressive multipronged attempts to combat antimicrobial resistance in N. gonorrhoeae. This effort includes new antibiotics in the developmental pipeline, attempts to repurpose existing antibiotics, rapid point-of-care antibiotic susceptibility tests, and vaccine development.
He also highlighted the factors that have led to the bug’s capacity to acquire resistance to so many antibiotics having different mechanisms of action. One key factor is the organism’s sheer competence as expressed in genetic lability.
“This bacteria is continually sampling DNA from the environment. The organisms are constantly swapping genes and DNA segments with commensal Neisseria species. In fact, even human DNA sequences have been found inside the gonococcal genome,” Dr. Duncan said.
While high-level antibiotic resistance can be acquired in a single dramatic step, it can also come about through multiple smaller steps, each one yielding only low-level resistance. “This allows for the sort of creeping [minimum inhibitory concentration] that we’ve seen with the gonococcus, particularly with the extended-spectrum cephalosporin antibiotics,” Dr. Duncan continued.
Also, it’s apparent that even in the absence of antibiotics, other pressures can select for antibiotic-resistant strains. Dr. Duncan credited one of his mentors, William M. Shafer, Ph.D., of Emory University, with developing the hypothesis that fecal lipids might be an important driver of increased resistance rates. Supporting this hypothesis, he noted, is the finding in multiple studies that rectal gonococcal isolates consistently have a somewhat higher prevalence of resistance than those obtained from other sites.
Turning to the effort to curb antibiotic resistance, Dr. Duncan said the drug farthest along in the pipeline is solithromycin, a novel macrolide being developed by Cempra Pharmaceuticals in both oral and IV formulations. Solithromycin, a first-in-class fluoroketolide, is active against a broad range of Gram-positive organisms, among them Legionella, Chlamydia, Mycoplasma, and Ureaplasma, including macrolide-resistant strains. Its ability to bind to three ribosomal sites is thought to minimize development of resistance.
Two positive phase 3 clinical trials of solithromycin have been completed in patients with community-acquired bacterial pneumonia. A phase 3 trial in gonorrhea is ongoing after a positive phase 2 study.
Two bacterial topoisomerase inhibitors are in soon-to-be-completed phase 2 studies.
Delafloxacin, a new fluoroquinolone, was in a phase 3 clinical trial for gonorrhea that was terminated early due to ineffectiveness.
There is considerable interest in bringing back single-dose IM gentamicin (Garamycin) for the treatment of gonorrhea. A systematic review of five studies (Syst Rev. 2014 Sep 19;3:104. doi: 10.1186/2046-4053-3-104) reported cure rates that were mostly in the 90% range, but “not quite high enough to say you’d want to go to gentamicin as your front-line therapy,” in Dr. Duncan’s opinion.
Dr. Workowski noted that the National Institutes of Health is interested in trying to resurrect cefixime (Suprax) for gonorrhea after the CDC guidelines demoted it several years ago. An ongoing clinical trial is examining the impact of increasing the dose and duration of therapy.
Public health officials are also interested in spectinomycin, an antibiotic not currently available in the United States, which has achieved high cure rates as single-dose therapy in several foreign studies.
Dr. Duncan noted that a randomized trial of gentamicin plus azithromycin or gemifloxacin (Factive) plus azithromycin reported cure rates of 100% and 99.5%, respectively (Clin Infect Dis. 2014 Oct 15;59(8):1083-91). He found the study less than convincing, however: “These strains were almost all susceptibile to azithromycin, so you can’t actually say that gentamicin or gemifloxacin added a lot,” he said.
A number of researchers are working on rapid tests for susceptibility of a particular gonococcal strain so physicians could choose an effective antimicrobial for an individual patient right from the start.
“These are all in the developmental phase. It’s going to be difficult, because there are so many different mechanisms for resistance,” he said.
Similarly, vaccine development in the gonococcal field is a great challenge. The microorganism’s multiple mechanisms of immune evasion make it tough to identify correlates of protection, Dr. Duncan continued.
“Epidemiologic studies suggest there is not efficient development of natural immunity. Folks who get gonorrhea and then come back with reinfection often have the exact same strain,” he noted.
Dr. Duncan’s research is funded by the National Institutes of Health and the Burroughs Wellcome Fund. He reported having no financial conflicts of interest.
SAN DIEGO – Experts in the field of Neisseria gonorrhoeae antimicrobial resistance are warily watching developments in China, where rates of nonsusceptibility to ceftriaxone are reportedly shooting through the roof.
In the United States at present, gonococcal resistance to ceftriaxone is exceedingly rare: well under 1% of isolates have elevated minimum inhibitory concentrations (MICs) to this cornerstone of empiric therapy. In Europe, the rate is about 3%. What’s really disturbing is that recent data from the World Health Organization Gonococcal Antimicrobial Surveillance Program indicate ceftriaxone nonsusceptibility rates in China are in the 20%-30%-plus range, Dr. Joseph Duncan said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is very concerning for the potential spread of this type of resistance across the world at some point. It’s just ready to explode,” observed Dr. Duncan of the University of North Carolina, Chapel Hill.
Anytime gonococcal resistance rates to a drug reach about 5%, it spells trouble.
“Gonorrhea treatment is often syndromic. An isolated swab is taken, identified by Gram stain, you give them empiric therapy, and the patients walk out of the clinic and never come back. So you don’t want to have a 5% failure rate for your initial therapy,” he explained.
Neisseria gonorrhoeae has acquired resistance to virtually every antibiotic ever used to treat the infection. Treatment options are running out, which is why the Centers for Disease Control and Prevention has designated gonorrhea as an immediate public health threat requiring urgent and aggressive action.
The 2015 CDC Sexually Transmitted Disease Treatment Guidelines recommend only one front-line treatment for gonorrhea: dual therapy with ceftriaxone at 250 mg IM in a single dose plus azithromycin 1 g orally, also in a single dose. Given N. gonorrhoeae’s adaptability, experts believe that’s not a long-term solution.
After all, 5%-10% of gonococcal isolates in Europe and China are azithromycin-resistant, and while CDC surveillance data showed less than 1% of strains in the United States were azithromycin-resistant through 2013, preliminary data for 2014 show a concerning jump to 2.5%, according to Dr. Duncan’s fellow panelist Dr. Kimberly Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 CDC STD guidelines.
Dr. Duncan described the state of the ongoing aggressive multipronged attempts to combat antimicrobial resistance in N. gonorrhoeae. This effort includes new antibiotics in the developmental pipeline, attempts to repurpose existing antibiotics, rapid point-of-care antibiotic susceptibility tests, and vaccine development.
He also highlighted the factors that have led to the bug’s capacity to acquire resistance to so many antibiotics having different mechanisms of action. One key factor is the organism’s sheer competence as expressed in genetic lability.
“This bacteria is continually sampling DNA from the environment. The organisms are constantly swapping genes and DNA segments with commensal Neisseria species. In fact, even human DNA sequences have been found inside the gonococcal genome,” Dr. Duncan said.
While high-level antibiotic resistance can be acquired in a single dramatic step, it can also come about through multiple smaller steps, each one yielding only low-level resistance. “This allows for the sort of creeping [minimum inhibitory concentration] that we’ve seen with the gonococcus, particularly with the extended-spectrum cephalosporin antibiotics,” Dr. Duncan continued.
Also, it’s apparent that even in the absence of antibiotics, other pressures can select for antibiotic-resistant strains. Dr. Duncan credited one of his mentors, William M. Shafer, Ph.D., of Emory University, with developing the hypothesis that fecal lipids might be an important driver of increased resistance rates. Supporting this hypothesis, he noted, is the finding in multiple studies that rectal gonococcal isolates consistently have a somewhat higher prevalence of resistance than those obtained from other sites.
Turning to the effort to curb antibiotic resistance, Dr. Duncan said the drug farthest along in the pipeline is solithromycin, a novel macrolide being developed by Cempra Pharmaceuticals in both oral and IV formulations. Solithromycin, a first-in-class fluoroketolide, is active against a broad range of Gram-positive organisms, among them Legionella, Chlamydia, Mycoplasma, and Ureaplasma, including macrolide-resistant strains. Its ability to bind to three ribosomal sites is thought to minimize development of resistance.
Two positive phase 3 clinical trials of solithromycin have been completed in patients with community-acquired bacterial pneumonia. A phase 3 trial in gonorrhea is ongoing after a positive phase 2 study.
Two bacterial topoisomerase inhibitors are in soon-to-be-completed phase 2 studies.
Delafloxacin, a new fluoroquinolone, was in a phase 3 clinical trial for gonorrhea that was terminated early due to ineffectiveness.
There is considerable interest in bringing back single-dose IM gentamicin (Garamycin) for the treatment of gonorrhea. A systematic review of five studies (Syst Rev. 2014 Sep 19;3:104. doi: 10.1186/2046-4053-3-104) reported cure rates that were mostly in the 90% range, but “not quite high enough to say you’d want to go to gentamicin as your front-line therapy,” in Dr. Duncan’s opinion.
Dr. Workowski noted that the National Institutes of Health is interested in trying to resurrect cefixime (Suprax) for gonorrhea after the CDC guidelines demoted it several years ago. An ongoing clinical trial is examining the impact of increasing the dose and duration of therapy.
Public health officials are also interested in spectinomycin, an antibiotic not currently available in the United States, which has achieved high cure rates as single-dose therapy in several foreign studies.
Dr. Duncan noted that a randomized trial of gentamicin plus azithromycin or gemifloxacin (Factive) plus azithromycin reported cure rates of 100% and 99.5%, respectively (Clin Infect Dis. 2014 Oct 15;59(8):1083-91). He found the study less than convincing, however: “These strains were almost all susceptibile to azithromycin, so you can’t actually say that gentamicin or gemifloxacin added a lot,” he said.
A number of researchers are working on rapid tests for susceptibility of a particular gonococcal strain so physicians could choose an effective antimicrobial for an individual patient right from the start.
“These are all in the developmental phase. It’s going to be difficult, because there are so many different mechanisms for resistance,” he said.
Similarly, vaccine development in the gonococcal field is a great challenge. The microorganism’s multiple mechanisms of immune evasion make it tough to identify correlates of protection, Dr. Duncan continued.
“Epidemiologic studies suggest there is not efficient development of natural immunity. Folks who get gonorrhea and then come back with reinfection often have the exact same strain,” he noted.
Dr. Duncan’s research is funded by the National Institutes of Health and the Burroughs Wellcome Fund. He reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM ICAAC 2015
Case series supports oral itraconazole for infantile hemangiomas
COPENHAGEN – Ever since Dr. Yuping Ran published his initial report of successful treatment of infantile hemangiomas using oral itraconazole, dermatologists from around the world have been bombarding him with the same three questions: Does it really work? Is the treatment safe? What’s the mechanism for the response?
His research has continued at a brisk clip since that preliminary publication (J Dermatol. 2015 Feb;42(2):202-6), so he was able to provide updated answers to those three key questions at the annual congress of the European Academy of Dermatology and Venereology.
Efficacy: His case series is now up to 17 treated patients, average age 3.6 months, with disfiguring or functionally significant infantile hemangiomas. Twelve of the 17 (71%) were successfully treated as defined by 80%-100% improvement that met with the approval of parents and physicians, said Dr. Ran, professor of dermatology at Sichuan University in Chengdu, China.
Treatment was given for an average of 8.8 weeks with oral itraconazole at 5 mg/kg/day. Dr. Ran’s initial serendipitous observation of a therapeutic effect on infantile hemangioma came from a baby he was treating with itraconazole capsules for a Candida albicans infection. He now uses only the oral solution, however, because it’s so much easier for parents to administer.
Safety: “We’ve monitored liver function before, during, and after treatment. It has always been within normal range,” Dr. Ran reported. Roughly 30% of infants have developed mild diarrhea on treatment. This has been readily manageable and hasn’t led to any halt in treatment.
Mechanism of benefit: In vitro studies conducted in Dr. Ran’s laboratory have shown that itraconazole inhibits growth and migration of proliferating human hemangioma epithelial cells, while ketoconazole does not. Moreover, when Dr. Ran and coworkers compared itraconazole to propranolol – a first-line medical treatment for infantile hemangiomas – itraconazole inhibited hemangioma epithelial cells far more efficiently than propranolol. Indeed, in order for propranolol to match itraconazole’s apoptotic effect, the cells had to be exposed to the beta blocker at a concentration that was 10-fold greater than that of itraconazole.
In further studies, Dr. Ran and coworkers have shown that itraconazole downregulates two key pathways in hemangioma cell growth: the hedgehog pathway and the P13K/AKT/mTOR signaling pathway. This is the likely mechanism of therapeutic effect, he said.
Dr. Ran’s studies are supported by the National Natural Science Foundation of China. He reported having no financial conflicts of interest.
COPENHAGEN – Ever since Dr. Yuping Ran published his initial report of successful treatment of infantile hemangiomas using oral itraconazole, dermatologists from around the world have been bombarding him with the same three questions: Does it really work? Is the treatment safe? What’s the mechanism for the response?
His research has continued at a brisk clip since that preliminary publication (J Dermatol. 2015 Feb;42(2):202-6), so he was able to provide updated answers to those three key questions at the annual congress of the European Academy of Dermatology and Venereology.
Efficacy: His case series is now up to 17 treated patients, average age 3.6 months, with disfiguring or functionally significant infantile hemangiomas. Twelve of the 17 (71%) were successfully treated as defined by 80%-100% improvement that met with the approval of parents and physicians, said Dr. Ran, professor of dermatology at Sichuan University in Chengdu, China.
Treatment was given for an average of 8.8 weeks with oral itraconazole at 5 mg/kg/day. Dr. Ran’s initial serendipitous observation of a therapeutic effect on infantile hemangioma came from a baby he was treating with itraconazole capsules for a Candida albicans infection. He now uses only the oral solution, however, because it’s so much easier for parents to administer.
Safety: “We’ve monitored liver function before, during, and after treatment. It has always been within normal range,” Dr. Ran reported. Roughly 30% of infants have developed mild diarrhea on treatment. This has been readily manageable and hasn’t led to any halt in treatment.
Mechanism of benefit: In vitro studies conducted in Dr. Ran’s laboratory have shown that itraconazole inhibits growth and migration of proliferating human hemangioma epithelial cells, while ketoconazole does not. Moreover, when Dr. Ran and coworkers compared itraconazole to propranolol – a first-line medical treatment for infantile hemangiomas – itraconazole inhibited hemangioma epithelial cells far more efficiently than propranolol. Indeed, in order for propranolol to match itraconazole’s apoptotic effect, the cells had to be exposed to the beta blocker at a concentration that was 10-fold greater than that of itraconazole.
In further studies, Dr. Ran and coworkers have shown that itraconazole downregulates two key pathways in hemangioma cell growth: the hedgehog pathway and the P13K/AKT/mTOR signaling pathway. This is the likely mechanism of therapeutic effect, he said.
Dr. Ran’s studies are supported by the National Natural Science Foundation of China. He reported having no financial conflicts of interest.
COPENHAGEN – Ever since Dr. Yuping Ran published his initial report of successful treatment of infantile hemangiomas using oral itraconazole, dermatologists from around the world have been bombarding him with the same three questions: Does it really work? Is the treatment safe? What’s the mechanism for the response?
His research has continued at a brisk clip since that preliminary publication (J Dermatol. 2015 Feb;42(2):202-6), so he was able to provide updated answers to those three key questions at the annual congress of the European Academy of Dermatology and Venereology.
Efficacy: His case series is now up to 17 treated patients, average age 3.6 months, with disfiguring or functionally significant infantile hemangiomas. Twelve of the 17 (71%) were successfully treated as defined by 80%-100% improvement that met with the approval of parents and physicians, said Dr. Ran, professor of dermatology at Sichuan University in Chengdu, China.
Treatment was given for an average of 8.8 weeks with oral itraconazole at 5 mg/kg/day. Dr. Ran’s initial serendipitous observation of a therapeutic effect on infantile hemangioma came from a baby he was treating with itraconazole capsules for a Candida albicans infection. He now uses only the oral solution, however, because it’s so much easier for parents to administer.
Safety: “We’ve monitored liver function before, during, and after treatment. It has always been within normal range,” Dr. Ran reported. Roughly 30% of infants have developed mild diarrhea on treatment. This has been readily manageable and hasn’t led to any halt in treatment.
Mechanism of benefit: In vitro studies conducted in Dr. Ran’s laboratory have shown that itraconazole inhibits growth and migration of proliferating human hemangioma epithelial cells, while ketoconazole does not. Moreover, when Dr. Ran and coworkers compared itraconazole to propranolol – a first-line medical treatment for infantile hemangiomas – itraconazole inhibited hemangioma epithelial cells far more efficiently than propranolol. Indeed, in order for propranolol to match itraconazole’s apoptotic effect, the cells had to be exposed to the beta blocker at a concentration that was 10-fold greater than that of itraconazole.
In further studies, Dr. Ran and coworkers have shown that itraconazole downregulates two key pathways in hemangioma cell growth: the hedgehog pathway and the P13K/AKT/mTOR signaling pathway. This is the likely mechanism of therapeutic effect, he said.
Dr. Ran’s studies are supported by the National Natural Science Foundation of China. He reported having no financial conflicts of interest.
AT THE EADV CONGRESS
Key clinical point: Oral itraconazole appears to be an effective alternative to propranolol for treatment of infantile hemangiomas.
Major finding: Twelve of 17 infants with painful, disruptive hemangiomas experienced 80%-100% improvement in response to oral itraconazole for an average of 8.8 weeks at 5 mg/kg/day.
Data source: This is an ongoing open-label case series supported by translational studies aimed at uncovering the mechanism of benefit.
Disclosures: This study was supported by the National Natural Science Foundation of China. The presenter reported having no financial conflicts of interest.
AHA: Candesartan protects against cardiotoxicity in breast cancer patients in PRADA
ORLANDO – Concomitant treatment with candesartan protects against the early decline in left ventricular ejection fraction associated with adjunct therapy for early breast cancer.
That was the key finding in the PRADA trial (PRevention of cArdiac Dysfunction during Adjuvant breast cancer therapy), the largest study to date looking at prevention of cardiac dysfunction in a breast cancer population.
Another important finding in PRADA was that unlike the angiotensin receptor blocker candesartan (Atacand), metoprolol, a beta blocker, didn’t prevent the early drop in LVEF commonly seen in breast cancer patients treated with anthracyclines and trastuzumab (Herceptin), even though both classes of heart medications are cornerstones of the treatment of ischemic and hypertensive cardiomyopathy, Dr. Geeta Gulati reported at the American Heart Association scientific sessions.
Although the cardiotoxicity of certain breast cancer treatments is widely recognized and has spawned the emerging field of cardio-oncology, the literature in this area is weak. Indeed, a recent meta-analysis identified only four published randomized studies evaluating the possible cardioprotective role for beta blockers and angiotensin antagonists in patients undergoing anthracycline-based chemotherapy (Postgrad Med J doi:10.1136/ postgradmedj-2015-133535). None of the studies was double-blind, all relied upon echocardiographic assessment of changes in LVEF rather than gold-standard cardiac MRI, and the study sizes were small -- just 18-45 breast cancer patients.
Most problematic of all, the studies employed a variety of different definitions of cardiotoxicity, noted Dr. Gulati of Akershus University Hospital in Lorenskog, Norway.
In contrast, PRADA was a double-blind, placebo-controlled, 2 by 2 factorial design, single-center trial, which included 120 patients with early breast cancer. Participants were randomized to candesartan at a starting dose of 8 mg and target dose of 32 mg/day, metoprolol starting at 25 mg with a target of 100 mg/day, or placebo after breast cancer surgery but before the start of anthracycline-containing chemotherapy.
The primary endpoint was change in LVEF from baseline to completion of adjuvant therapy, a period as short as 10 weeks and as long as 64 weeks depending upon whether a woman also underwent courses of trastuzumab, taxanes, and/or radiation therapy.
The overall decline in LVEF was 2.6% in the placebo group and 0.6% in the candesartan group, a significant difference. Metoprolol didn’t put a dent in the LVEF decline.
“Observational studies show early reduction in LVEF is associated with increased risk of developing heart failure later. So if a sustained, long-term effect of angiotensin inhibition can be confirmed in larger multicenter trials, preventive therapy may be indicated as standard care for breast cancer patients,” Dr. Gulati said.
Discussant Dr. Bonnie Ky of the University of Pennsylvania, Philadelphia, called PRADA an important study that moves the field of cardio-oncology forward, yet it’s also a trial that raises more questions than it answers.
PRADA certainly addresses a major problem: “The incidence of heart failure and cardiomyopathy increases over time in breast cancer patients exposed to anthracyclines and trastuzumab. Because patients are living longer because of cancer chemotherapy, their risk of dying of cardiovascular disease actually exceeds that of recurrent cancer in the long term,” she observed.
The study has three major limitations that prevent its findings being implemented in routine clinical practice at this time, Dr. Ky said. One is its relatively small size, even though it’s far bigger than any previous study. Another limitation is that this was an extremely low-cardiovascular-risk patient cohort: the baseline prevalence of diabetes was only 1.5%, fewer than 7% of patients had hypertension, and the baseline LVEF was 63%. That may be why no one developed a substantial decrement in LVEF or actual heart failure.
And since the incidence of cardiomyopathy following breast cancer therapy is known to climb over time, reaching a cumulative 12% at 6 years followup in trastuzumab-treated patients and 20% in those who receive both anthracyclines and trastuzumab (J Natl Cancer Inst. 2012 Sep 5;104(17):1293-305), the lack of extended followup time in PRADA is a significant shortcoming, she added.
The important questions raised by PRADA, Dr. Ky continued, include whether carvedilol or another beta blocker would have generated a positive result where metoprolol failed. Also, should the target population for prevention of cardiotoxicity be more narrowly focused on those at higher baseline cardiovascular risk? And bearing in mind that change in LVEF is a surrogate endpoint, what might be a more clinically meaningful and valid outcome measure? What’s the effect of carvedilol and other cardioprotective medications on cardiac biomarkers in breast cancer patients? And the most important questions of all, she said: What would be the effects of longer followup time and extended therapy?
“This study highlights for us in the field of cardio-oncology the critical need to develop a robust consensus definition of cardiotoxicity and a methodology to identify high cardiovascular risk patients,” she concluded.
PRADA was funded primarily by the University of Oslo and the Norwegian Cancer Society. Dr. Gulati reported having no financial conflicts of interest. Dr. Ky reported receiving a research grant from Pfizer and serving as a consultant to Bristol Myers Squibb.
ORLANDO – Concomitant treatment with candesartan protects against the early decline in left ventricular ejection fraction associated with adjunct therapy for early breast cancer.
That was the key finding in the PRADA trial (PRevention of cArdiac Dysfunction during Adjuvant breast cancer therapy), the largest study to date looking at prevention of cardiac dysfunction in a breast cancer population.
Another important finding in PRADA was that unlike the angiotensin receptor blocker candesartan (Atacand), metoprolol, a beta blocker, didn’t prevent the early drop in LVEF commonly seen in breast cancer patients treated with anthracyclines and trastuzumab (Herceptin), even though both classes of heart medications are cornerstones of the treatment of ischemic and hypertensive cardiomyopathy, Dr. Geeta Gulati reported at the American Heart Association scientific sessions.
Although the cardiotoxicity of certain breast cancer treatments is widely recognized and has spawned the emerging field of cardio-oncology, the literature in this area is weak. Indeed, a recent meta-analysis identified only four published randomized studies evaluating the possible cardioprotective role for beta blockers and angiotensin antagonists in patients undergoing anthracycline-based chemotherapy (Postgrad Med J doi:10.1136/ postgradmedj-2015-133535). None of the studies was double-blind, all relied upon echocardiographic assessment of changes in LVEF rather than gold-standard cardiac MRI, and the study sizes were small -- just 18-45 breast cancer patients.
Most problematic of all, the studies employed a variety of different definitions of cardiotoxicity, noted Dr. Gulati of Akershus University Hospital in Lorenskog, Norway.
In contrast, PRADA was a double-blind, placebo-controlled, 2 by 2 factorial design, single-center trial, which included 120 patients with early breast cancer. Participants were randomized to candesartan at a starting dose of 8 mg and target dose of 32 mg/day, metoprolol starting at 25 mg with a target of 100 mg/day, or placebo after breast cancer surgery but before the start of anthracycline-containing chemotherapy.
The primary endpoint was change in LVEF from baseline to completion of adjuvant therapy, a period as short as 10 weeks and as long as 64 weeks depending upon whether a woman also underwent courses of trastuzumab, taxanes, and/or radiation therapy.
The overall decline in LVEF was 2.6% in the placebo group and 0.6% in the candesartan group, a significant difference. Metoprolol didn’t put a dent in the LVEF decline.
“Observational studies show early reduction in LVEF is associated with increased risk of developing heart failure later. So if a sustained, long-term effect of angiotensin inhibition can be confirmed in larger multicenter trials, preventive therapy may be indicated as standard care for breast cancer patients,” Dr. Gulati said.
Discussant Dr. Bonnie Ky of the University of Pennsylvania, Philadelphia, called PRADA an important study that moves the field of cardio-oncology forward, yet it’s also a trial that raises more questions than it answers.
PRADA certainly addresses a major problem: “The incidence of heart failure and cardiomyopathy increases over time in breast cancer patients exposed to anthracyclines and trastuzumab. Because patients are living longer because of cancer chemotherapy, their risk of dying of cardiovascular disease actually exceeds that of recurrent cancer in the long term,” she observed.
The study has three major limitations that prevent its findings being implemented in routine clinical practice at this time, Dr. Ky said. One is its relatively small size, even though it’s far bigger than any previous study. Another limitation is that this was an extremely low-cardiovascular-risk patient cohort: the baseline prevalence of diabetes was only 1.5%, fewer than 7% of patients had hypertension, and the baseline LVEF was 63%. That may be why no one developed a substantial decrement in LVEF or actual heart failure.
And since the incidence of cardiomyopathy following breast cancer therapy is known to climb over time, reaching a cumulative 12% at 6 years followup in trastuzumab-treated patients and 20% in those who receive both anthracyclines and trastuzumab (J Natl Cancer Inst. 2012 Sep 5;104(17):1293-305), the lack of extended followup time in PRADA is a significant shortcoming, she added.
The important questions raised by PRADA, Dr. Ky continued, include whether carvedilol or another beta blocker would have generated a positive result where metoprolol failed. Also, should the target population for prevention of cardiotoxicity be more narrowly focused on those at higher baseline cardiovascular risk? And bearing in mind that change in LVEF is a surrogate endpoint, what might be a more clinically meaningful and valid outcome measure? What’s the effect of carvedilol and other cardioprotective medications on cardiac biomarkers in breast cancer patients? And the most important questions of all, she said: What would be the effects of longer followup time and extended therapy?
“This study highlights for us in the field of cardio-oncology the critical need to develop a robust consensus definition of cardiotoxicity and a methodology to identify high cardiovascular risk patients,” she concluded.
PRADA was funded primarily by the University of Oslo and the Norwegian Cancer Society. Dr. Gulati reported having no financial conflicts of interest. Dr. Ky reported receiving a research grant from Pfizer and serving as a consultant to Bristol Myers Squibb.
ORLANDO – Concomitant treatment with candesartan protects against the early decline in left ventricular ejection fraction associated with adjunct therapy for early breast cancer.
That was the key finding in the PRADA trial (PRevention of cArdiac Dysfunction during Adjuvant breast cancer therapy), the largest study to date looking at prevention of cardiac dysfunction in a breast cancer population.
Another important finding in PRADA was that unlike the angiotensin receptor blocker candesartan (Atacand), metoprolol, a beta blocker, didn’t prevent the early drop in LVEF commonly seen in breast cancer patients treated with anthracyclines and trastuzumab (Herceptin), even though both classes of heart medications are cornerstones of the treatment of ischemic and hypertensive cardiomyopathy, Dr. Geeta Gulati reported at the American Heart Association scientific sessions.
Although the cardiotoxicity of certain breast cancer treatments is widely recognized and has spawned the emerging field of cardio-oncology, the literature in this area is weak. Indeed, a recent meta-analysis identified only four published randomized studies evaluating the possible cardioprotective role for beta blockers and angiotensin antagonists in patients undergoing anthracycline-based chemotherapy (Postgrad Med J doi:10.1136/ postgradmedj-2015-133535). None of the studies was double-blind, all relied upon echocardiographic assessment of changes in LVEF rather than gold-standard cardiac MRI, and the study sizes were small -- just 18-45 breast cancer patients.
Most problematic of all, the studies employed a variety of different definitions of cardiotoxicity, noted Dr. Gulati of Akershus University Hospital in Lorenskog, Norway.
In contrast, PRADA was a double-blind, placebo-controlled, 2 by 2 factorial design, single-center trial, which included 120 patients with early breast cancer. Participants were randomized to candesartan at a starting dose of 8 mg and target dose of 32 mg/day, metoprolol starting at 25 mg with a target of 100 mg/day, or placebo after breast cancer surgery but before the start of anthracycline-containing chemotherapy.
The primary endpoint was change in LVEF from baseline to completion of adjuvant therapy, a period as short as 10 weeks and as long as 64 weeks depending upon whether a woman also underwent courses of trastuzumab, taxanes, and/or radiation therapy.
The overall decline in LVEF was 2.6% in the placebo group and 0.6% in the candesartan group, a significant difference. Metoprolol didn’t put a dent in the LVEF decline.
“Observational studies show early reduction in LVEF is associated with increased risk of developing heart failure later. So if a sustained, long-term effect of angiotensin inhibition can be confirmed in larger multicenter trials, preventive therapy may be indicated as standard care for breast cancer patients,” Dr. Gulati said.
Discussant Dr. Bonnie Ky of the University of Pennsylvania, Philadelphia, called PRADA an important study that moves the field of cardio-oncology forward, yet it’s also a trial that raises more questions than it answers.
PRADA certainly addresses a major problem: “The incidence of heart failure and cardiomyopathy increases over time in breast cancer patients exposed to anthracyclines and trastuzumab. Because patients are living longer because of cancer chemotherapy, their risk of dying of cardiovascular disease actually exceeds that of recurrent cancer in the long term,” she observed.
The study has three major limitations that prevent its findings being implemented in routine clinical practice at this time, Dr. Ky said. One is its relatively small size, even though it’s far bigger than any previous study. Another limitation is that this was an extremely low-cardiovascular-risk patient cohort: the baseline prevalence of diabetes was only 1.5%, fewer than 7% of patients had hypertension, and the baseline LVEF was 63%. That may be why no one developed a substantial decrement in LVEF or actual heart failure.
And since the incidence of cardiomyopathy following breast cancer therapy is known to climb over time, reaching a cumulative 12% at 6 years followup in trastuzumab-treated patients and 20% in those who receive both anthracyclines and trastuzumab (J Natl Cancer Inst. 2012 Sep 5;104(17):1293-305), the lack of extended followup time in PRADA is a significant shortcoming, she added.
The important questions raised by PRADA, Dr. Ky continued, include whether carvedilol or another beta blocker would have generated a positive result where metoprolol failed. Also, should the target population for prevention of cardiotoxicity be more narrowly focused on those at higher baseline cardiovascular risk? And bearing in mind that change in LVEF is a surrogate endpoint, what might be a more clinically meaningful and valid outcome measure? What’s the effect of carvedilol and other cardioprotective medications on cardiac biomarkers in breast cancer patients? And the most important questions of all, she said: What would be the effects of longer followup time and extended therapy?
“This study highlights for us in the field of cardio-oncology the critical need to develop a robust consensus definition of cardiotoxicity and a methodology to identify high cardiovascular risk patients,” she concluded.
PRADA was funded primarily by the University of Oslo and the Norwegian Cancer Society. Dr. Gulati reported having no financial conflicts of interest. Dr. Ky reported receiving a research grant from Pfizer and serving as a consultant to Bristol Myers Squibb.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Inroads are being made in the growing problem of breast cancer treatment-associated cardiomyopathy.
Major finding: The average 2.6% decline from baseline in breast cancer patients during adjuvant therapy with anthracyclines with or without trastuzumab was negated by concomitant candesartan but not by metoprolol.
Data source: The PRADA trial was a randomized, double-blind, placebo-controlled, 2 by 2 factorial design study involving 120 patients undergoing adjuvant therapy for early breast cancer.
Disclosures: The primary sponsors of the study were the University of Oslo and the Norwegian Cancer Society. Additional support was provided by Abbott Diagnostic and AstraZeneca. The presenter reported no financial conflicts of interest.
Starting ACS patients on varenicline in the hospital boosted smoking quit rates
ORLANDO – Starting varenicline in smokers while hospitalized for an acute coronary syndrome resulted in substantially higher smoking abstinence rates than with placebo at all time points through 6 months of follow-up in the double-blind, randomized EVITA trial.
“The ACS population is typically older, they’re long-term smokers, and they come into the hospital with a life-threatening condition. Their family is all around them. They’ve had angioplasty or CABG [coronary artery bypass graft] surgery. So they have pressure on them to stop smoking. This is a teachable moment, a window of opportunity. The public health benefit for smoking cessation in this population is huge. You can cut their risk of death and significant morbidity in half if you can get them to stop,” Dr. Mark J. Eisenberg said in presenting the EVITA results at the American Heart Association scientific sessions.
“To our knowledge, this is the highest-risk population that’s been exposed to varenicline,” said Dr. Eisenberg, professor of medicine at McGill University and director of the cardiovascular health services research program at Jewish General Hospital in Montreal.
The primary study endpoint was continuous self-reported abstinence since baseline backed by biochemical confirmation in the form of an exhaled carbon monoxide level of 10 ppm or less at week 24 as well as at all the earlier follow-up visits. The rate was 47.3% in the varenicline group, compared with 32.5% in placebo-treated controls. That placebo response rate is in line with numerous prior studies that have shown that less than one-third of smokers with ACS remain abstinent after leaving the hospital.
“Most cardiologists would say, ‘All my patients stop smoking.’ But in the clinic if you look in the patients’ pockets, you find a pack of cigarettes. They stop smoking while in hospital, but as soon as they’re discharged, the relapse rate is almost immediate. Most patients are smoking the day they get out of hospital,” according to Dr. Eisenberg.
In EVITA, the number-needed-to-treat with varenicline for 12 weeks in order to produce 1 extra nonsmoker at 6 months was 6.8 patients.
The secondary endpoint of at least a 50% reduction in the number of cigarettes per day from baseline to 6 months was met by 67.4% of the varenicline group and 55.6% of controls, with a number-needed-to-treat of 8.5, he continued.
No safety issues emerged in the study, although as Dr. Eisenberg noted, EVITA wasn’t sufficiently powered to look at safety. The only side effect more common in varenicline-treated patients was abnormal dreams, with a 12-week incidence of 15%, threefold higher than in controls, a phenomenon seen in other, larger varenicline studies as well.
The EVITA investigators plan to follow participants out to 12 months. “If we see someone who at 1 year post MI is still smoking, maybe it’s time to go after them again, perhaps with another medication or behavioral therapy,” he said.
There are no randomized clinical trials demonstrating that starting nicotine patches or bupropion in the hospital is effective for smoking cessation in the ACS population, according to the cardiologist.
Dr. Eisenberg predicted this study will change clinical practice. In much the same way physicians now routinely start ACS patients on a statin, beta-blocker, and aspirin before they leave the hospital, physicians will capitalize on this opportunity to help ACS patients quit smoking as well, he said.
“The use of varenicline in ACS patients before they leave the hospital is a very important step forward. Cardiologists are increasingly comfortable with the idea of starting secondary prevention medications in the hospital, and there’s very little more important for a person with heart disease who smokes cigarettes than to help them quit smoking. It’s probably the No. 1 priority. So evidence that we can start a medication in the hospital and get more people who smoke cigarettes to quit smoking is definitely game changing, I think,” said Dr. Goff, professor of epidemiology and dean of the Colorado School of Public Health in Aurora.
Dr. Eisenberg reported receiving funding from Pfizer to perform the EVITA trial. He has also gotten honoraria from the company for providing continuing medical education talks on smoking cessation.
ORLANDO – Starting varenicline in smokers while hospitalized for an acute coronary syndrome resulted in substantially higher smoking abstinence rates than with placebo at all time points through 6 months of follow-up in the double-blind, randomized EVITA trial.
“The ACS population is typically older, they’re long-term smokers, and they come into the hospital with a life-threatening condition. Their family is all around them. They’ve had angioplasty or CABG [coronary artery bypass graft] surgery. So they have pressure on them to stop smoking. This is a teachable moment, a window of opportunity. The public health benefit for smoking cessation in this population is huge. You can cut their risk of death and significant morbidity in half if you can get them to stop,” Dr. Mark J. Eisenberg said in presenting the EVITA results at the American Heart Association scientific sessions.
“To our knowledge, this is the highest-risk population that’s been exposed to varenicline,” said Dr. Eisenberg, professor of medicine at McGill University and director of the cardiovascular health services research program at Jewish General Hospital in Montreal.
The primary study endpoint was continuous self-reported abstinence since baseline backed by biochemical confirmation in the form of an exhaled carbon monoxide level of 10 ppm or less at week 24 as well as at all the earlier follow-up visits. The rate was 47.3% in the varenicline group, compared with 32.5% in placebo-treated controls. That placebo response rate is in line with numerous prior studies that have shown that less than one-third of smokers with ACS remain abstinent after leaving the hospital.
“Most cardiologists would say, ‘All my patients stop smoking.’ But in the clinic if you look in the patients’ pockets, you find a pack of cigarettes. They stop smoking while in hospital, but as soon as they’re discharged, the relapse rate is almost immediate. Most patients are smoking the day they get out of hospital,” according to Dr. Eisenberg.
In EVITA, the number-needed-to-treat with varenicline for 12 weeks in order to produce 1 extra nonsmoker at 6 months was 6.8 patients.
The secondary endpoint of at least a 50% reduction in the number of cigarettes per day from baseline to 6 months was met by 67.4% of the varenicline group and 55.6% of controls, with a number-needed-to-treat of 8.5, he continued.
No safety issues emerged in the study, although as Dr. Eisenberg noted, EVITA wasn’t sufficiently powered to look at safety. The only side effect more common in varenicline-treated patients was abnormal dreams, with a 12-week incidence of 15%, threefold higher than in controls, a phenomenon seen in other, larger varenicline studies as well.
The EVITA investigators plan to follow participants out to 12 months. “If we see someone who at 1 year post MI is still smoking, maybe it’s time to go after them again, perhaps with another medication or behavioral therapy,” he said.
There are no randomized clinical trials demonstrating that starting nicotine patches or bupropion in the hospital is effective for smoking cessation in the ACS population, according to the cardiologist.
Dr. Eisenberg predicted this study will change clinical practice. In much the same way physicians now routinely start ACS patients on a statin, beta-blocker, and aspirin before they leave the hospital, physicians will capitalize on this opportunity to help ACS patients quit smoking as well, he said.
“The use of varenicline in ACS patients before they leave the hospital is a very important step forward. Cardiologists are increasingly comfortable with the idea of starting secondary prevention medications in the hospital, and there’s very little more important for a person with heart disease who smokes cigarettes than to help them quit smoking. It’s probably the No. 1 priority. So evidence that we can start a medication in the hospital and get more people who smoke cigarettes to quit smoking is definitely game changing, I think,” said Dr. Goff, professor of epidemiology and dean of the Colorado School of Public Health in Aurora.
Dr. Eisenberg reported receiving funding from Pfizer to perform the EVITA trial. He has also gotten honoraria from the company for providing continuing medical education talks on smoking cessation.
ORLANDO – Starting varenicline in smokers while hospitalized for an acute coronary syndrome resulted in substantially higher smoking abstinence rates than with placebo at all time points through 6 months of follow-up in the double-blind, randomized EVITA trial.
“The ACS population is typically older, they’re long-term smokers, and they come into the hospital with a life-threatening condition. Their family is all around them. They’ve had angioplasty or CABG [coronary artery bypass graft] surgery. So they have pressure on them to stop smoking. This is a teachable moment, a window of opportunity. The public health benefit for smoking cessation in this population is huge. You can cut their risk of death and significant morbidity in half if you can get them to stop,” Dr. Mark J. Eisenberg said in presenting the EVITA results at the American Heart Association scientific sessions.
“To our knowledge, this is the highest-risk population that’s been exposed to varenicline,” said Dr. Eisenberg, professor of medicine at McGill University and director of the cardiovascular health services research program at Jewish General Hospital in Montreal.
The primary study endpoint was continuous self-reported abstinence since baseline backed by biochemical confirmation in the form of an exhaled carbon monoxide level of 10 ppm or less at week 24 as well as at all the earlier follow-up visits. The rate was 47.3% in the varenicline group, compared with 32.5% in placebo-treated controls. That placebo response rate is in line with numerous prior studies that have shown that less than one-third of smokers with ACS remain abstinent after leaving the hospital.
“Most cardiologists would say, ‘All my patients stop smoking.’ But in the clinic if you look in the patients’ pockets, you find a pack of cigarettes. They stop smoking while in hospital, but as soon as they’re discharged, the relapse rate is almost immediate. Most patients are smoking the day they get out of hospital,” according to Dr. Eisenberg.
In EVITA, the number-needed-to-treat with varenicline for 12 weeks in order to produce 1 extra nonsmoker at 6 months was 6.8 patients.
The secondary endpoint of at least a 50% reduction in the number of cigarettes per day from baseline to 6 months was met by 67.4% of the varenicline group and 55.6% of controls, with a number-needed-to-treat of 8.5, he continued.
No safety issues emerged in the study, although as Dr. Eisenberg noted, EVITA wasn’t sufficiently powered to look at safety. The only side effect more common in varenicline-treated patients was abnormal dreams, with a 12-week incidence of 15%, threefold higher than in controls, a phenomenon seen in other, larger varenicline studies as well.
The EVITA investigators plan to follow participants out to 12 months. “If we see someone who at 1 year post MI is still smoking, maybe it’s time to go after them again, perhaps with another medication or behavioral therapy,” he said.
There are no randomized clinical trials demonstrating that starting nicotine patches or bupropion in the hospital is effective for smoking cessation in the ACS population, according to the cardiologist.
Dr. Eisenberg predicted this study will change clinical practice. In much the same way physicians now routinely start ACS patients on a statin, beta-blocker, and aspirin before they leave the hospital, physicians will capitalize on this opportunity to help ACS patients quit smoking as well, he said.
“The use of varenicline in ACS patients before they leave the hospital is a very important step forward. Cardiologists are increasingly comfortable with the idea of starting secondary prevention medications in the hospital, and there’s very little more important for a person with heart disease who smokes cigarettes than to help them quit smoking. It’s probably the No. 1 priority. So evidence that we can start a medication in the hospital and get more people who smoke cigarettes to quit smoking is definitely game changing, I think,” said Dr. Goff, professor of epidemiology and dean of the Colorado School of Public Health in Aurora.
Dr. Eisenberg reported receiving funding from Pfizer to perform the EVITA trial. He has also gotten honoraria from the company for providing continuing medical education talks on smoking cessation.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: The number of smokers who need to be started on varenicline while hospitalized for an acute coronary syndrome in order to produce one extra nonsmoker at 6 months is 6.8.
Data source: EVITA, a double-blind, randomized multicenter trial in 302 smokers hospitalized for ACS who were prospectively followed for 6 months.
Disclosures: The EVITA study was funded by Pfizer. The presenter reported receiving a grant from the company to conduct the trial, as well as honoraria for giving continuing medical education talks on smoking cessation.
VIDEO: Study shows how to stand up to the ‘sitting disease’
ORLANDO – Interrupting prolonged sitting with brief bouts of light-intensity activity throughout the workday resulted in an impressive drop in blood pressure in overweight sedentary men and women with type 2 diabetes, Bronwyn Kingwell, Ph.D., said in a video interview at the American Heart Association scientific sessions.
A total of 24 such individuals were randomized in crossover fashion to a 3-day study conducted under controlled conditions in a physiology lab. On one day participants did what they usually do: They sat at their desks for an 8-hour workday. On another day they rose from their desks every 30 minutes for 3 minutes of walking down the hall at a 2-mph pace. And on yet another day they stood up every 30 minutes and did 3 minutes of simple resistance activities at their desks: half squats, knee raises, calf stretches.
Blood pressure was measured eight times per day, and plasma norepinephrine as a measure of sympathetic activity was measured nine times. At the end of the light walking day, subjects’ blood pressure was on average 14/8 mm Hg lower than on the uninterrupted sitting day. On the simple resistance activity day, it was 16/10 mm Hg lower.
“This is quite an impressive reduction, and more than we might have anticipated. It’s similar to the type of reduction you might see with single-drug antihypertensive therapy. And I thought it was interesting that two-thirds of subjects were already taking antihypertensive drugs,” observed Dr. Kingwell, head of metabolic and vascular physiology at the Baker IDI Heart and Diabetes Institute in Melbourne.
“I think the new thing here is that even with these very small bouts of activity – just 3 minutes – we’re getting this reduction that’s sustained throughout the day, provided you break it up every 30 minutes,” she said. “We’ve seen an increase in sitting behavior in most industrialized countries, particularly over the last 10 years, and we also see low adherence to structured exercise programs. The approach examined in this simple study may represent a practical strategy which could contribute to blood pressure reduction in a group that is at high risk.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Interrupting prolonged sitting with brief bouts of light-intensity activity throughout the workday resulted in an impressive drop in blood pressure in overweight sedentary men and women with type 2 diabetes, Bronwyn Kingwell, Ph.D., said in a video interview at the American Heart Association scientific sessions.
A total of 24 such individuals were randomized in crossover fashion to a 3-day study conducted under controlled conditions in a physiology lab. On one day participants did what they usually do: They sat at their desks for an 8-hour workday. On another day they rose from their desks every 30 minutes for 3 minutes of walking down the hall at a 2-mph pace. And on yet another day they stood up every 30 minutes and did 3 minutes of simple resistance activities at their desks: half squats, knee raises, calf stretches.
Blood pressure was measured eight times per day, and plasma norepinephrine as a measure of sympathetic activity was measured nine times. At the end of the light walking day, subjects’ blood pressure was on average 14/8 mm Hg lower than on the uninterrupted sitting day. On the simple resistance activity day, it was 16/10 mm Hg lower.
“This is quite an impressive reduction, and more than we might have anticipated. It’s similar to the type of reduction you might see with single-drug antihypertensive therapy. And I thought it was interesting that two-thirds of subjects were already taking antihypertensive drugs,” observed Dr. Kingwell, head of metabolic and vascular physiology at the Baker IDI Heart and Diabetes Institute in Melbourne.
“I think the new thing here is that even with these very small bouts of activity – just 3 minutes – we’re getting this reduction that’s sustained throughout the day, provided you break it up every 30 minutes,” she said. “We’ve seen an increase in sitting behavior in most industrialized countries, particularly over the last 10 years, and we also see low adherence to structured exercise programs. The approach examined in this simple study may represent a practical strategy which could contribute to blood pressure reduction in a group that is at high risk.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Interrupting prolonged sitting with brief bouts of light-intensity activity throughout the workday resulted in an impressive drop in blood pressure in overweight sedentary men and women with type 2 diabetes, Bronwyn Kingwell, Ph.D., said in a video interview at the American Heart Association scientific sessions.
A total of 24 such individuals were randomized in crossover fashion to a 3-day study conducted under controlled conditions in a physiology lab. On one day participants did what they usually do: They sat at their desks for an 8-hour workday. On another day they rose from their desks every 30 minutes for 3 minutes of walking down the hall at a 2-mph pace. And on yet another day they stood up every 30 minutes and did 3 minutes of simple resistance activities at their desks: half squats, knee raises, calf stretches.
Blood pressure was measured eight times per day, and plasma norepinephrine as a measure of sympathetic activity was measured nine times. At the end of the light walking day, subjects’ blood pressure was on average 14/8 mm Hg lower than on the uninterrupted sitting day. On the simple resistance activity day, it was 16/10 mm Hg lower.
“This is quite an impressive reduction, and more than we might have anticipated. It’s similar to the type of reduction you might see with single-drug antihypertensive therapy. And I thought it was interesting that two-thirds of subjects were already taking antihypertensive drugs,” observed Dr. Kingwell, head of metabolic and vascular physiology at the Baker IDI Heart and Diabetes Institute in Melbourne.
“I think the new thing here is that even with these very small bouts of activity – just 3 minutes – we’re getting this reduction that’s sustained throughout the day, provided you break it up every 30 minutes,” she said. “We’ve seen an increase in sitting behavior in most industrialized countries, particularly over the last 10 years, and we also see low adherence to structured exercise programs. The approach examined in this simple study may represent a practical strategy which could contribute to blood pressure reduction in a group that is at high risk.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AHA SCIENTIFIC SESSIONS
VIDEO: College football linemen develop unwelcome cardiac changes
ORLANDO – College football linemen develop adverse cardiac structural and functional changes over the course of their freshman season that are not seen in teammates who play at other positions, Dr. Jeffrey Lin said in an interview at the American Heart Association scientific sessions.
He followed 30 Harvard University linemen and 57 players at other football positions through their 3-month fall freshman season by means of serial blood pressure measurements and 2-D echocardiography, including speckle tracking. During the course of that season, 90% of the linemen developed prehypertension or hypertension, 30% showed clear echocardiographic evidence of concentric left ventricular hypertrophy, and as a group they also developed a relative decrease in systolic function, with a reduction from baseline in global longitudinal strain by speckle tracking.
It’s concerning because these 18-year-old linemen are going to expose themselves to another 3 years of the stresses of year-round intensive training along with three more seasons of university-level football, noted Dr. Lin, a cardiac imaging fellow at Columbia University in New York.
These cardiac changes were not seen in non-linemen. They developed adaptive cardiac structural remodeling with eccentric hypertrophy and an increase in global longitudinal strain, which is characteristic of what’s been called the “athlete’s heart,” according to Dr. Lin.
Watch the video to learn what he thinks may be going on.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – College football linemen develop adverse cardiac structural and functional changes over the course of their freshman season that are not seen in teammates who play at other positions, Dr. Jeffrey Lin said in an interview at the American Heart Association scientific sessions.
He followed 30 Harvard University linemen and 57 players at other football positions through their 3-month fall freshman season by means of serial blood pressure measurements and 2-D echocardiography, including speckle tracking. During the course of that season, 90% of the linemen developed prehypertension or hypertension, 30% showed clear echocardiographic evidence of concentric left ventricular hypertrophy, and as a group they also developed a relative decrease in systolic function, with a reduction from baseline in global longitudinal strain by speckle tracking.
It’s concerning because these 18-year-old linemen are going to expose themselves to another 3 years of the stresses of year-round intensive training along with three more seasons of university-level football, noted Dr. Lin, a cardiac imaging fellow at Columbia University in New York.
These cardiac changes were not seen in non-linemen. They developed adaptive cardiac structural remodeling with eccentric hypertrophy and an increase in global longitudinal strain, which is characteristic of what’s been called the “athlete’s heart,” according to Dr. Lin.
Watch the video to learn what he thinks may be going on.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – College football linemen develop adverse cardiac structural and functional changes over the course of their freshman season that are not seen in teammates who play at other positions, Dr. Jeffrey Lin said in an interview at the American Heart Association scientific sessions.
He followed 30 Harvard University linemen and 57 players at other football positions through their 3-month fall freshman season by means of serial blood pressure measurements and 2-D echocardiography, including speckle tracking. During the course of that season, 90% of the linemen developed prehypertension or hypertension, 30% showed clear echocardiographic evidence of concentric left ventricular hypertrophy, and as a group they also developed a relative decrease in systolic function, with a reduction from baseline in global longitudinal strain by speckle tracking.
It’s concerning because these 18-year-old linemen are going to expose themselves to another 3 years of the stresses of year-round intensive training along with three more seasons of university-level football, noted Dr. Lin, a cardiac imaging fellow at Columbia University in New York.
These cardiac changes were not seen in non-linemen. They developed adaptive cardiac structural remodeling with eccentric hypertrophy and an increase in global longitudinal strain, which is characteristic of what’s been called the “athlete’s heart,” according to Dr. Lin.
Watch the video to learn what he thinks may be going on.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AHA SCIENTIFIC SESSIONS
AHA: Homemade meals cut type 2 diabetes risk by 13%
ORLANDO – The more homemade meals a middle-aged person eats, the lower the risk of developing type 2 diabetes.
That’s the key take-away from a long-term prospective observational study of nearly 100,000 health care professionals. In an analysis adjusted for demographics and lifestyle factors, the participants who ate an average of 11-14 home-prepared lunches and dinners per week had a 13% lower risk of developing type 2 diabetes than those consuming 6 or fewer, Geng Zong, Ph.D., reported at the American Heart Association scientific sessions.
He scrutinized the eating habits of 57,994 women in the Nurses’ Health Study and 41,679 men in the Health Professionals Follow-Up Study, all of whom were free of cardiovascular disease, diabetes, and cancer at enrollment. During 26 years of biannual prospective follow-up, or 2.3 million person-years, 8,959 subjects were diagnosed with type 2 diabetes.
A dose-response relationship was evident. Looking at homemade meals as a continuous variable, each home-prepared lunch or dinner eaten per week decreased the long-term risk of developing type 2 diabetes by 1%-2%, according to Dr. Zong of Harvard School of Public Health, Boston.
He noted that, since this was an observational study, it can’t prove causality. Nonetheless, he offered several possible explanations to help explain the observed association. For one, health care professionals who ate 11-14 homemade lunches and dinners per week had a 15% lower risk of developing obesity during the first 8 years of follow-up, compared with those who ate 0-6. Men who ate in that fashion gained about 1 kg less body weight in the first 8 years of follow-up and women gained about 0.5 kg less than those who ate fewer home-prepared meals – that’s probably because eating out often means consuming high-fat, high-salt, processed fast foods.
Participants who frequently ate home-prepared meals also consumed fewer sugar-sweetened beverages. Dr. Zong’s coinvestigators have previously shown that drinking sugar-sweetened beverages is associated with increased risk of metabolic syndrome and type 2 diabetes (Diabetes Care. 2010;33[11]:2477-83).
Breakfast eating patterns weren’t included in the study because there were insufficient data. The study was funded by the National Institutes of Health. Dr. Zong reported having no financial conflicts of interest.
ORLANDO – The more homemade meals a middle-aged person eats, the lower the risk of developing type 2 diabetes.
That’s the key take-away from a long-term prospective observational study of nearly 100,000 health care professionals. In an analysis adjusted for demographics and lifestyle factors, the participants who ate an average of 11-14 home-prepared lunches and dinners per week had a 13% lower risk of developing type 2 diabetes than those consuming 6 or fewer, Geng Zong, Ph.D., reported at the American Heart Association scientific sessions.
He scrutinized the eating habits of 57,994 women in the Nurses’ Health Study and 41,679 men in the Health Professionals Follow-Up Study, all of whom were free of cardiovascular disease, diabetes, and cancer at enrollment. During 26 years of biannual prospective follow-up, or 2.3 million person-years, 8,959 subjects were diagnosed with type 2 diabetes.
A dose-response relationship was evident. Looking at homemade meals as a continuous variable, each home-prepared lunch or dinner eaten per week decreased the long-term risk of developing type 2 diabetes by 1%-2%, according to Dr. Zong of Harvard School of Public Health, Boston.
He noted that, since this was an observational study, it can’t prove causality. Nonetheless, he offered several possible explanations to help explain the observed association. For one, health care professionals who ate 11-14 homemade lunches and dinners per week had a 15% lower risk of developing obesity during the first 8 years of follow-up, compared with those who ate 0-6. Men who ate in that fashion gained about 1 kg less body weight in the first 8 years of follow-up and women gained about 0.5 kg less than those who ate fewer home-prepared meals – that’s probably because eating out often means consuming high-fat, high-salt, processed fast foods.
Participants who frequently ate home-prepared meals also consumed fewer sugar-sweetened beverages. Dr. Zong’s coinvestigators have previously shown that drinking sugar-sweetened beverages is associated with increased risk of metabolic syndrome and type 2 diabetes (Diabetes Care. 2010;33[11]:2477-83).
Breakfast eating patterns weren’t included in the study because there were insufficient data. The study was funded by the National Institutes of Health. Dr. Zong reported having no financial conflicts of interest.
ORLANDO – The more homemade meals a middle-aged person eats, the lower the risk of developing type 2 diabetes.
That’s the key take-away from a long-term prospective observational study of nearly 100,000 health care professionals. In an analysis adjusted for demographics and lifestyle factors, the participants who ate an average of 11-14 home-prepared lunches and dinners per week had a 13% lower risk of developing type 2 diabetes than those consuming 6 or fewer, Geng Zong, Ph.D., reported at the American Heart Association scientific sessions.
He scrutinized the eating habits of 57,994 women in the Nurses’ Health Study and 41,679 men in the Health Professionals Follow-Up Study, all of whom were free of cardiovascular disease, diabetes, and cancer at enrollment. During 26 years of biannual prospective follow-up, or 2.3 million person-years, 8,959 subjects were diagnosed with type 2 diabetes.
A dose-response relationship was evident. Looking at homemade meals as a continuous variable, each home-prepared lunch or dinner eaten per week decreased the long-term risk of developing type 2 diabetes by 1%-2%, according to Dr. Zong of Harvard School of Public Health, Boston.
He noted that, since this was an observational study, it can’t prove causality. Nonetheless, he offered several possible explanations to help explain the observed association. For one, health care professionals who ate 11-14 homemade lunches and dinners per week had a 15% lower risk of developing obesity during the first 8 years of follow-up, compared with those who ate 0-6. Men who ate in that fashion gained about 1 kg less body weight in the first 8 years of follow-up and women gained about 0.5 kg less than those who ate fewer home-prepared meals – that’s probably because eating out often means consuming high-fat, high-salt, processed fast foods.
Participants who frequently ate home-prepared meals also consumed fewer sugar-sweetened beverages. Dr. Zong’s coinvestigators have previously shown that drinking sugar-sweetened beverages is associated with increased risk of metabolic syndrome and type 2 diabetes (Diabetes Care. 2010;33[11]:2477-83).
Breakfast eating patterns weren’t included in the study because there were insufficient data. The study was funded by the National Institutes of Health. Dr. Zong reported having no financial conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Eating more home-prepared lunches and dinners is associated in dose-dependent fashion with lower risk of developing type 2 diabetes.
Major finding: Middle-aged subjects who ate 11-14 home-prepared meals per week had an adjusted 13% lower risk of developing type 2 diabetes than did those consuming 6 or fewer.
Data Source: This prospective observational study featured 26 years of biannual follow-up of nearly 100,000 male and female health care professionals in the Nurses’ Health Study and the Health Professionals Follow-Up Study.
Disclosures: The study was funded by the National Institutes of Health. The presenter reported having no financial conflicts.