User login
Suicide Prevention Grant Program Reauthorized
Suicide Prevention Grant Program Reauthorized
Community-based organizations that provide suicide-prevention services can now access about $52.5 million in US Department of Veterans Affairs (VA) grants. The grant is part of the 3-year Staff Sergeant Fox Suicide Prevention Grant Program, which honors Parker Gordon Fox, a sniper instructor at the U.S. Army Infantry School at Fort Benning, Georgia, who died by suicide in 2020. In consecutive Congressional hearings, lawmakers called for the reauthorization of the program to address gaps in VA care.
“It has been a game-changer for so many veterans,” Sen. Richard Blumenthal (D-CT) said.
The money provides or coordinates primarily nonclinical suicide prevention services, including outreach and linkage to VA and community resources. Services also may include baseline mental health screenings, case management and peer support, education on suicide risk, VA benefits assistance, and emergency clinical services.
Since its inception in 2022, the program has awarded $157.5 million to 95 organizations in 43 states, US territories, and tribal lands. Speaking before the House Committee on Veterans’ Affairs on May 15, VA Secretary Doug Collins praised the Fox program for bringing “different voices into the conversation,” but added it wasn’t enough. He noted that the veteran suicide rate has not changed since 2008, despite the VA annually spending $588 million on suicide prevention over the past few years.
In an op-ed, Russell Lemle, a senior policy analyst at the Veterans Healthcare Policy Institute, disputed Collins' characterization of veteran suicides. Between 2008 and 2022 (the last year for which complete data is available), US deaths by suicide increased 37% while the number of veteran deaths by suicide fell 2%. “This data collection was the single best part of the program,” he argued, calling for reauthorization to continue requiring data-targeted solutions.
According to a 2024 VA interim report on the Fox grant program, grantees had completed > 16,590 outreach contacts and engaged 3204 participants as of September 30, 2023. An additional 864 individuals were onboarding at the time of the report.
The current version of the grant program requires grantees to use validated tools, including the VA Data Collection Tool, and other assessments furnished by VA to determine the effectiveness of the suicide prevention services. They must also provide each participant with a satisfaction survey and submit periodic and annual financial and performance reports.
Despite the Trump administration’s cuts and cancellations to the federal workforce and federal programs, Collins told the Senate committee he is firmly on the side of working with community-based organizations like the Fox grant program to broaden the VA’s reach: “I want to use grants and programs like [the Fox grant program] to reach out beyond the scope of where we’re currently reaching, to say how can we actually touch the veteran that’s not being touched right now by these programs,” Collins said. “We’ve got to do better at using the grants, using our programs to go outside the normal bubble and use others to help get the word out.”
Grant applications are due in July and VA will choose awardees in September. Organizations can apply for grants worth up to $750,000 and may apply to renew awards from year to year throughout the length of the program.
Community-based organizations that provide suicide-prevention services can now access about $52.5 million in US Department of Veterans Affairs (VA) grants. The grant is part of the 3-year Staff Sergeant Fox Suicide Prevention Grant Program, which honors Parker Gordon Fox, a sniper instructor at the U.S. Army Infantry School at Fort Benning, Georgia, who died by suicide in 2020. In consecutive Congressional hearings, lawmakers called for the reauthorization of the program to address gaps in VA care.
“It has been a game-changer for so many veterans,” Sen. Richard Blumenthal (D-CT) said.
The money provides or coordinates primarily nonclinical suicide prevention services, including outreach and linkage to VA and community resources. Services also may include baseline mental health screenings, case management and peer support, education on suicide risk, VA benefits assistance, and emergency clinical services.
Since its inception in 2022, the program has awarded $157.5 million to 95 organizations in 43 states, US territories, and tribal lands. Speaking before the House Committee on Veterans’ Affairs on May 15, VA Secretary Doug Collins praised the Fox program for bringing “different voices into the conversation,” but added it wasn’t enough. He noted that the veteran suicide rate has not changed since 2008, despite the VA annually spending $588 million on suicide prevention over the past few years.
In an op-ed, Russell Lemle, a senior policy analyst at the Veterans Healthcare Policy Institute, disputed Collins' characterization of veteran suicides. Between 2008 and 2022 (the last year for which complete data is available), US deaths by suicide increased 37% while the number of veteran deaths by suicide fell 2%. “This data collection was the single best part of the program,” he argued, calling for reauthorization to continue requiring data-targeted solutions.
According to a 2024 VA interim report on the Fox grant program, grantees had completed > 16,590 outreach contacts and engaged 3204 participants as of September 30, 2023. An additional 864 individuals were onboarding at the time of the report.
The current version of the grant program requires grantees to use validated tools, including the VA Data Collection Tool, and other assessments furnished by VA to determine the effectiveness of the suicide prevention services. They must also provide each participant with a satisfaction survey and submit periodic and annual financial and performance reports.
Despite the Trump administration’s cuts and cancellations to the federal workforce and federal programs, Collins told the Senate committee he is firmly on the side of working with community-based organizations like the Fox grant program to broaden the VA’s reach: “I want to use grants and programs like [the Fox grant program] to reach out beyond the scope of where we’re currently reaching, to say how can we actually touch the veteran that’s not being touched right now by these programs,” Collins said. “We’ve got to do better at using the grants, using our programs to go outside the normal bubble and use others to help get the word out.”
Grant applications are due in July and VA will choose awardees in September. Organizations can apply for grants worth up to $750,000 and may apply to renew awards from year to year throughout the length of the program.
Community-based organizations that provide suicide-prevention services can now access about $52.5 million in US Department of Veterans Affairs (VA) grants. The grant is part of the 3-year Staff Sergeant Fox Suicide Prevention Grant Program, which honors Parker Gordon Fox, a sniper instructor at the U.S. Army Infantry School at Fort Benning, Georgia, who died by suicide in 2020. In consecutive Congressional hearings, lawmakers called for the reauthorization of the program to address gaps in VA care.
“It has been a game-changer for so many veterans,” Sen. Richard Blumenthal (D-CT) said.
The money provides or coordinates primarily nonclinical suicide prevention services, including outreach and linkage to VA and community resources. Services also may include baseline mental health screenings, case management and peer support, education on suicide risk, VA benefits assistance, and emergency clinical services.
Since its inception in 2022, the program has awarded $157.5 million to 95 organizations in 43 states, US territories, and tribal lands. Speaking before the House Committee on Veterans’ Affairs on May 15, VA Secretary Doug Collins praised the Fox program for bringing “different voices into the conversation,” but added it wasn’t enough. He noted that the veteran suicide rate has not changed since 2008, despite the VA annually spending $588 million on suicide prevention over the past few years.
In an op-ed, Russell Lemle, a senior policy analyst at the Veterans Healthcare Policy Institute, disputed Collins' characterization of veteran suicides. Between 2008 and 2022 (the last year for which complete data is available), US deaths by suicide increased 37% while the number of veteran deaths by suicide fell 2%. “This data collection was the single best part of the program,” he argued, calling for reauthorization to continue requiring data-targeted solutions.
According to a 2024 VA interim report on the Fox grant program, grantees had completed > 16,590 outreach contacts and engaged 3204 participants as of September 30, 2023. An additional 864 individuals were onboarding at the time of the report.
The current version of the grant program requires grantees to use validated tools, including the VA Data Collection Tool, and other assessments furnished by VA to determine the effectiveness of the suicide prevention services. They must also provide each participant with a satisfaction survey and submit periodic and annual financial and performance reports.
Despite the Trump administration’s cuts and cancellations to the federal workforce and federal programs, Collins told the Senate committee he is firmly on the side of working with community-based organizations like the Fox grant program to broaden the VA’s reach: “I want to use grants and programs like [the Fox grant program] to reach out beyond the scope of where we’re currently reaching, to say how can we actually touch the veteran that’s not being touched right now by these programs,” Collins said. “We’ve got to do better at using the grants, using our programs to go outside the normal bubble and use others to help get the word out.”
Grant applications are due in July and VA will choose awardees in September. Organizations can apply for grants worth up to $750,000 and may apply to renew awards from year to year throughout the length of the program.
Suicide Prevention Grant Program Reauthorized
Suicide Prevention Grant Program Reauthorized
Collins Lays Out Plans to Reduce VA by 15% in Congressional Hearings
Collins Lays Out Plans to Reduce VA by 15% in Senate Hearing
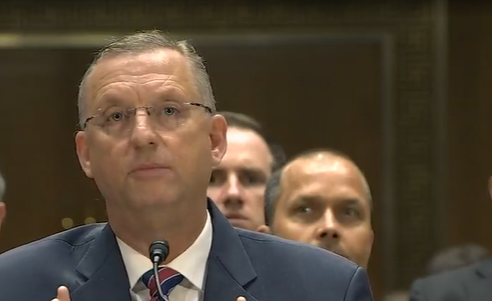
US Department of Veterans Affairs (VA) Secretary Doug Collins testified in US House of Representatives and US Senate committees hearings that bringing staff numbers down to fiscal year 2019 figures was simply a goal: “Our goal, as we look at it, as everything goes forward, is a 15% decrease,” he told the senators. “It’s a goal. You have to start somewhere.”
“It’s a process we’re going through and I’m not going to work out a process in front of a committee or anywhere else,” Collins testified in the Senate on May 6, adding that it would be “incompetence” or “malpractice” to do so before time. “[When] we’re doing something as large as we are in an organization as sensitive on this Hill, it would not be right for us to do that in public. It would not be right for us to just come out and say here’s everything that we got and then have everybody scared because in the end it may not be the final decision.”
“We’re going to come to the best possible decision we can for the veterans in this country so they can have a VA system that actually works,” Collins argued in the Senate. “The VA’s been an issue for a long time. We’re trying to not make it an issue anymore.”
Collins later told a House committee on May 15 that VA was conducting a thorough review of department structure and staffing across the enterpise. "Our goal is to increase productivity and efficiency and to eliminate waste and bureaucracy improving health care delivery and benefits to our veterans. We are going to maintain VA essential jobs like doctors and nurses and claims processors" but eliminate positions it deemed "nonmission-critical" and consolidating areas of "overlap and waste."
Senate ranking member Richard Blumenthal (D-CT) and Chairman Jerry Moran (R-KS) both placed an emphasis on accountability for responsible resizing at the hearing.
“The department is at a critical juncture,” Moran said. “Perhaps that’s always true, and I want to hear from you that the changes under way at the VA are backed by data, informed by veteran demand, focused on improving outcomes for men and women the VA serves, and will be carried out in close coordination with this committee, as well as with veterans, VA staff, and veteran organizations.” Moran stressed that cutting should be about right-sizing, done carefully, and while treating people “with gratitude and respect.”
Blumenthal was more direct in his criticism of the approach: “You cannot slash and trash the VA without eliminating those essential positions which provide access and availability of health care. It simply cannot be done,” he told Collins.
In response, Collins replied, “You have stated on several occasions already that I am saying we are going to fire 83,000 employees. That is wrong.” Collins insisted that the VA was “looking at a goal of how many employees we have and how many employees that are actually working in the front line taking care. I have doctors and nurses right now that do not see patients. Is that helping veteran health care?”
Collins defended the actions of the VA and spoke about challenges he was “constantly fighting” in the early weeks of his tenure. “We’ve been hit by a barrage of false rumors, innuendo, disinformation, speculation implying firing doctors and nurses, and forcing staff to work in closets and showers and that there’s chaos in the department, none of which have been backed up. Why? Because we canceled some contracts that worked for the VA that we should be doing in-house and we let go of less than one half of one percent of nonmission critical employees.”
The Trump Administration offered federal employees the option of resigning, which purportedly will go toward meeting the 15% target. NPR reported that VA employees have since shared data showing that 11,273 agency employees nationwide have applied for deferred resignation. Most of those employees are nurses (about 1300), medical support assistants (about 800), and social workers (about 300).
Collins stressed that the aim of restructuring was to protect veterans’ health care. By getting rid of DEI initiatives, the VA saved $14 million, which he said was redirected to veterans with disabilities who need prosthetics.
Sen. Bernie Sanders (D-VT) addressed concerns about the existing shortage of clinicians at the VA, asking Collins what he was doing to bring in more doctors, nurses, and social workers. In addition to moving doctors and nurses from nonpatient care to patient care, Collins said, he planned to work with Congress to make salaries more competitive.
But money and adding more employees are not always the solution, Collins said. For example, he said, the VA has been spending $588 million a year veteran suicide research, its top clinical priority. Yet, he said there has not been a significant decrease in veteran suicide rates since 2008.
The most recent VA suicide report, released in 2024, indicates suicide rates have remained steady since 2001. However, in 2022, the number of suicides among veterans (6407) was actually lower than in 12 of the previous 14 years.
According to media reports, congressional lawmakers, and union officials, Veteran Crisis Line (VCL) staff were among the 2400 probationary employees fired in February. In a Feb. 20 video, Collins accused Democrats of spreading lies and insisted no one who answered the phone was fired.
Later, in a letter to senators, Collins admitted that 24 VCL support staff were “erroneously” sent termination notices. The firings were later reversed, Collins said, and all VCL employees had been reinstated at the same position they previously held. “Ensuring the VCL is always accessible 24/7 is one of the department’s top priorities,” Collins insisted.
Collins shared his approval of keeping and expanding VA programs and studies on psychedelic treatments for patients with posttraumatic stress disorder and traumatic brain injury. He also spoke to the proposed 2026 budget calling for a $5.4 billion increase for the VA. If approved, that money would be targeted for medical care and homelessness.
US Department of Veterans Affairs (VA) Secretary Doug Collins testified in US House of Representatives and US Senate committees hearings that bringing staff numbers down to fiscal year 2019 figures was simply a goal: “Our goal, as we look at it, as everything goes forward, is a 15% decrease,” he told the senators. “It’s a goal. You have to start somewhere.”
“It’s a process we’re going through and I’m not going to work out a process in front of a committee or anywhere else,” Collins testified in the Senate on May 6, adding that it would be “incompetence” or “malpractice” to do so before time. “[When] we’re doing something as large as we are in an organization as sensitive on this Hill, it would not be right for us to do that in public. It would not be right for us to just come out and say here’s everything that we got and then have everybody scared because in the end it may not be the final decision.”
“We’re going to come to the best possible decision we can for the veterans in this country so they can have a VA system that actually works,” Collins argued in the Senate. “The VA’s been an issue for a long time. We’re trying to not make it an issue anymore.”
Collins later told a House committee on May 15 that VA was conducting a thorough review of department structure and staffing across the enterpise. "Our goal is to increase productivity and efficiency and to eliminate waste and bureaucracy improving health care delivery and benefits to our veterans. We are going to maintain VA essential jobs like doctors and nurses and claims processors" but eliminate positions it deemed "nonmission-critical" and consolidating areas of "overlap and waste."
Senate ranking member Richard Blumenthal (D-CT) and Chairman Jerry Moran (R-KS) both placed an emphasis on accountability for responsible resizing at the hearing.
“The department is at a critical juncture,” Moran said. “Perhaps that’s always true, and I want to hear from you that the changes under way at the VA are backed by data, informed by veteran demand, focused on improving outcomes for men and women the VA serves, and will be carried out in close coordination with this committee, as well as with veterans, VA staff, and veteran organizations.” Moran stressed that cutting should be about right-sizing, done carefully, and while treating people “with gratitude and respect.”
Blumenthal was more direct in his criticism of the approach: “You cannot slash and trash the VA without eliminating those essential positions which provide access and availability of health care. It simply cannot be done,” he told Collins.
In response, Collins replied, “You have stated on several occasions already that I am saying we are going to fire 83,000 employees. That is wrong.” Collins insisted that the VA was “looking at a goal of how many employees we have and how many employees that are actually working in the front line taking care. I have doctors and nurses right now that do not see patients. Is that helping veteran health care?”
Collins defended the actions of the VA and spoke about challenges he was “constantly fighting” in the early weeks of his tenure. “We’ve been hit by a barrage of false rumors, innuendo, disinformation, speculation implying firing doctors and nurses, and forcing staff to work in closets and showers and that there’s chaos in the department, none of which have been backed up. Why? Because we canceled some contracts that worked for the VA that we should be doing in-house and we let go of less than one half of one percent of nonmission critical employees.”
The Trump Administration offered federal employees the option of resigning, which purportedly will go toward meeting the 15% target. NPR reported that VA employees have since shared data showing that 11,273 agency employees nationwide have applied for deferred resignation. Most of those employees are nurses (about 1300), medical support assistants (about 800), and social workers (about 300).
Collins stressed that the aim of restructuring was to protect veterans’ health care. By getting rid of DEI initiatives, the VA saved $14 million, which he said was redirected to veterans with disabilities who need prosthetics.
Sen. Bernie Sanders (D-VT) addressed concerns about the existing shortage of clinicians at the VA, asking Collins what he was doing to bring in more doctors, nurses, and social workers. In addition to moving doctors and nurses from nonpatient care to patient care, Collins said, he planned to work with Congress to make salaries more competitive.
But money and adding more employees are not always the solution, Collins said. For example, he said, the VA has been spending $588 million a year veteran suicide research, its top clinical priority. Yet, he said there has not been a significant decrease in veteran suicide rates since 2008.
The most recent VA suicide report, released in 2024, indicates suicide rates have remained steady since 2001. However, in 2022, the number of suicides among veterans (6407) was actually lower than in 12 of the previous 14 years.
According to media reports, congressional lawmakers, and union officials, Veteran Crisis Line (VCL) staff were among the 2400 probationary employees fired in February. In a Feb. 20 video, Collins accused Democrats of spreading lies and insisted no one who answered the phone was fired.
Later, in a letter to senators, Collins admitted that 24 VCL support staff were “erroneously” sent termination notices. The firings were later reversed, Collins said, and all VCL employees had been reinstated at the same position they previously held. “Ensuring the VCL is always accessible 24/7 is one of the department’s top priorities,” Collins insisted.
Collins shared his approval of keeping and expanding VA programs and studies on psychedelic treatments for patients with posttraumatic stress disorder and traumatic brain injury. He also spoke to the proposed 2026 budget calling for a $5.4 billion increase for the VA. If approved, that money would be targeted for medical care and homelessness.
US Department of Veterans Affairs (VA) Secretary Doug Collins testified in US House of Representatives and US Senate committees hearings that bringing staff numbers down to fiscal year 2019 figures was simply a goal: “Our goal, as we look at it, as everything goes forward, is a 15% decrease,” he told the senators. “It’s a goal. You have to start somewhere.”
“It’s a process we’re going through and I’m not going to work out a process in front of a committee or anywhere else,” Collins testified in the Senate on May 6, adding that it would be “incompetence” or “malpractice” to do so before time. “[When] we’re doing something as large as we are in an organization as sensitive on this Hill, it would not be right for us to do that in public. It would not be right for us to just come out and say here’s everything that we got and then have everybody scared because in the end it may not be the final decision.”
“We’re going to come to the best possible decision we can for the veterans in this country so they can have a VA system that actually works,” Collins argued in the Senate. “The VA’s been an issue for a long time. We’re trying to not make it an issue anymore.”
Collins later told a House committee on May 15 that VA was conducting a thorough review of department structure and staffing across the enterpise. "Our goal is to increase productivity and efficiency and to eliminate waste and bureaucracy improving health care delivery and benefits to our veterans. We are going to maintain VA essential jobs like doctors and nurses and claims processors" but eliminate positions it deemed "nonmission-critical" and consolidating areas of "overlap and waste."
Senate ranking member Richard Blumenthal (D-CT) and Chairman Jerry Moran (R-KS) both placed an emphasis on accountability for responsible resizing at the hearing.
“The department is at a critical juncture,” Moran said. “Perhaps that’s always true, and I want to hear from you that the changes under way at the VA are backed by data, informed by veteran demand, focused on improving outcomes for men and women the VA serves, and will be carried out in close coordination with this committee, as well as with veterans, VA staff, and veteran organizations.” Moran stressed that cutting should be about right-sizing, done carefully, and while treating people “with gratitude and respect.”
Blumenthal was more direct in his criticism of the approach: “You cannot slash and trash the VA without eliminating those essential positions which provide access and availability of health care. It simply cannot be done,” he told Collins.
In response, Collins replied, “You have stated on several occasions already that I am saying we are going to fire 83,000 employees. That is wrong.” Collins insisted that the VA was “looking at a goal of how many employees we have and how many employees that are actually working in the front line taking care. I have doctors and nurses right now that do not see patients. Is that helping veteran health care?”
Collins defended the actions of the VA and spoke about challenges he was “constantly fighting” in the early weeks of his tenure. “We’ve been hit by a barrage of false rumors, innuendo, disinformation, speculation implying firing doctors and nurses, and forcing staff to work in closets and showers and that there’s chaos in the department, none of which have been backed up. Why? Because we canceled some contracts that worked for the VA that we should be doing in-house and we let go of less than one half of one percent of nonmission critical employees.”
The Trump Administration offered federal employees the option of resigning, which purportedly will go toward meeting the 15% target. NPR reported that VA employees have since shared data showing that 11,273 agency employees nationwide have applied for deferred resignation. Most of those employees are nurses (about 1300), medical support assistants (about 800), and social workers (about 300).
Collins stressed that the aim of restructuring was to protect veterans’ health care. By getting rid of DEI initiatives, the VA saved $14 million, which he said was redirected to veterans with disabilities who need prosthetics.
Sen. Bernie Sanders (D-VT) addressed concerns about the existing shortage of clinicians at the VA, asking Collins what he was doing to bring in more doctors, nurses, and social workers. In addition to moving doctors and nurses from nonpatient care to patient care, Collins said, he planned to work with Congress to make salaries more competitive.
But money and adding more employees are not always the solution, Collins said. For example, he said, the VA has been spending $588 million a year veteran suicide research, its top clinical priority. Yet, he said there has not been a significant decrease in veteran suicide rates since 2008.
The most recent VA suicide report, released in 2024, indicates suicide rates have remained steady since 2001. However, in 2022, the number of suicides among veterans (6407) was actually lower than in 12 of the previous 14 years.
According to media reports, congressional lawmakers, and union officials, Veteran Crisis Line (VCL) staff were among the 2400 probationary employees fired in February. In a Feb. 20 video, Collins accused Democrats of spreading lies and insisted no one who answered the phone was fired.
Later, in a letter to senators, Collins admitted that 24 VCL support staff were “erroneously” sent termination notices. The firings were later reversed, Collins said, and all VCL employees had been reinstated at the same position they previously held. “Ensuring the VCL is always accessible 24/7 is one of the department’s top priorities,” Collins insisted.
Collins shared his approval of keeping and expanding VA programs and studies on psychedelic treatments for patients with posttraumatic stress disorder and traumatic brain injury. He also spoke to the proposed 2026 budget calling for a $5.4 billion increase for the VA. If approved, that money would be targeted for medical care and homelessness.
Collins Lays Out Plans to Reduce VA by 15% in Senate Hearing
Collins Lays Out Plans to Reduce VA by 15% in Senate Hearing
Study Investigates Non-Hodgkin Lymphoma in Air Force Missileers
Individuals working near intercontinental ballistic missiles (ICBMs), may be at higher risk of developing non-Hodgkin lymphoma (NHL) according to a preprint analysis conducted on missileers at Malmstrom Air Force Base in Montana. The study, which has not undergone peer review, found higher rates of NHL diagnosis at younger ages compared with the general population. The study also found a statistically significant increase in NHL diagnoses among older missileers, with such rates surpassing expected benchmarks.
The findings build on anecdotal and evidentiary data gathered in the last 50-plus years, including from the Torchlight Initiative, established in 2023 to collect self-reported cancer diagnoses and related fatalities from personnel and family members associated with the ICBM community.
The report shows patterns that “warranted a detailed statistical analysis,” leading to a granular examination of the registry and categorization of the data by cancer type, geographical location, and specific demographics. This narrowed the focus to 18 missileers who served at Malmstrom and were diagnosed with NHL.
In 2001, the Air Force Institute for Operational Health did a site evaluation and sampled for potential chemical and biological contaminants at Malmstrom following various reports of cancers from missileers, including 2 who died after being diagnosed with NHL. In a 2005 review, the Air Force said, “there is not sufficient evidence to consider the possibility of a cancer clustering to justify further investigation.”
In 2022, Lt. Col. Daniel Sebeck, a vice commander of Space Delta 8 in Colorado who served at Malmstrom and a close friend and fellow missileer were diagnosed with NHL. Sebeck discovered 36 cancer cases among missileers who had been stationed at Malmstrom. Ten developed NHL, 2 developed Hodgkin lymphoma, and 24 developed another form of cancer. The Air Force has acknowledged the concerns.
In 2023, US Air Force School of Aerospace Medicine (USAFSAM) approved the Missile Community Cancer Study (MCCS) to assess “specific cancer concerns raised by missile community members across related career fields and also examines the possibility of clusters of non-Hodgkin’s lymphoma at intercontinental ballistic missile bases.” The study compares 14 common cancers in the general population with that of missile-related career fields. The USAFSAM is reviewing records from former and current Missile Community members on active duty from 1976-2010, as well as state and national cancer data from multiple registries.
Early results from the MCCS suggested elevated rates of some cancers—mainly breast and prostate cancer—among missileers, maintainers, and other ICMB-related job positions, which aligns with other national cancer data.
At a June 2024 AFGSC town hall, officials announced that missileers would now have their information submitted to the Defense Occupational and Environmental Health Readiness System (DOEHRS), a Pentagon database for reporting occupational and exposure hazards.
"This info from DOEHRS flows into the recently developed Individual Longitudinal Exposure Record, a system that compiles occupational and environmental health data throughout a person's career," Lt. Col. John Severns, a spokesperson for Air Force Global Strike Command, said. DOEHRS, which has tracked Air Force records since 2010, allows US Department of Defense and US Department of Veterans Affairs clinical staff to access the information.
MCCS considers potential PCB exposures an occupational hazard. The Air Force says researchers are working with the System Program Offices and leadership to determine the timeframe of PCB removal from bases.
The lack of incontrovertible evidence connecting workplace toxins to NHL has often stymied patients and their family members from receiving appropriate benefits. An “informal talk” in April led by Rep. Mark Takano (D-CA) and Sen. Richard Blumenthal (D-CT) focused on exposures to hazardous materials at US military bases. Participants included various advocacy groups like the Torchlight Initiative, the Invisible Enemy, and Burn Pits 360.
More than a dozen veterans spoke about serving at military bases where they were exposed to a variety of harmful substances, and issues they faced in receiving coverage. David Crete, a veteran and chairman of The Invisible Enemy, said, “I am asking Congress to please allow us to get the benefits every other veteran earned. We are not asking to be special but to be treated equal.”
Rep. Takano called for greater focus on toxic exposures at US military bases: “We must push back against the idea that service members are only in harm’s way in war zones.”
Individuals working near intercontinental ballistic missiles (ICBMs), may be at higher risk of developing non-Hodgkin lymphoma (NHL) according to a preprint analysis conducted on missileers at Malmstrom Air Force Base in Montana. The study, which has not undergone peer review, found higher rates of NHL diagnosis at younger ages compared with the general population. The study also found a statistically significant increase in NHL diagnoses among older missileers, with such rates surpassing expected benchmarks.
The findings build on anecdotal and evidentiary data gathered in the last 50-plus years, including from the Torchlight Initiative, established in 2023 to collect self-reported cancer diagnoses and related fatalities from personnel and family members associated with the ICBM community.
The report shows patterns that “warranted a detailed statistical analysis,” leading to a granular examination of the registry and categorization of the data by cancer type, geographical location, and specific demographics. This narrowed the focus to 18 missileers who served at Malmstrom and were diagnosed with NHL.
In 2001, the Air Force Institute for Operational Health did a site evaluation and sampled for potential chemical and biological contaminants at Malmstrom following various reports of cancers from missileers, including 2 who died after being diagnosed with NHL. In a 2005 review, the Air Force said, “there is not sufficient evidence to consider the possibility of a cancer clustering to justify further investigation.”
In 2022, Lt. Col. Daniel Sebeck, a vice commander of Space Delta 8 in Colorado who served at Malmstrom and a close friend and fellow missileer were diagnosed with NHL. Sebeck discovered 36 cancer cases among missileers who had been stationed at Malmstrom. Ten developed NHL, 2 developed Hodgkin lymphoma, and 24 developed another form of cancer. The Air Force has acknowledged the concerns.
In 2023, US Air Force School of Aerospace Medicine (USAFSAM) approved the Missile Community Cancer Study (MCCS) to assess “specific cancer concerns raised by missile community members across related career fields and also examines the possibility of clusters of non-Hodgkin’s lymphoma at intercontinental ballistic missile bases.” The study compares 14 common cancers in the general population with that of missile-related career fields. The USAFSAM is reviewing records from former and current Missile Community members on active duty from 1976-2010, as well as state and national cancer data from multiple registries.
Early results from the MCCS suggested elevated rates of some cancers—mainly breast and prostate cancer—among missileers, maintainers, and other ICMB-related job positions, which aligns with other national cancer data.
At a June 2024 AFGSC town hall, officials announced that missileers would now have their information submitted to the Defense Occupational and Environmental Health Readiness System (DOEHRS), a Pentagon database for reporting occupational and exposure hazards.
"This info from DOEHRS flows into the recently developed Individual Longitudinal Exposure Record, a system that compiles occupational and environmental health data throughout a person's career," Lt. Col. John Severns, a spokesperson for Air Force Global Strike Command, said. DOEHRS, which has tracked Air Force records since 2010, allows US Department of Defense and US Department of Veterans Affairs clinical staff to access the information.
MCCS considers potential PCB exposures an occupational hazard. The Air Force says researchers are working with the System Program Offices and leadership to determine the timeframe of PCB removal from bases.
The lack of incontrovertible evidence connecting workplace toxins to NHL has often stymied patients and their family members from receiving appropriate benefits. An “informal talk” in April led by Rep. Mark Takano (D-CA) and Sen. Richard Blumenthal (D-CT) focused on exposures to hazardous materials at US military bases. Participants included various advocacy groups like the Torchlight Initiative, the Invisible Enemy, and Burn Pits 360.
More than a dozen veterans spoke about serving at military bases where they were exposed to a variety of harmful substances, and issues they faced in receiving coverage. David Crete, a veteran and chairman of The Invisible Enemy, said, “I am asking Congress to please allow us to get the benefits every other veteran earned. We are not asking to be special but to be treated equal.”
Rep. Takano called for greater focus on toxic exposures at US military bases: “We must push back against the idea that service members are only in harm’s way in war zones.”
Individuals working near intercontinental ballistic missiles (ICBMs), may be at higher risk of developing non-Hodgkin lymphoma (NHL) according to a preprint analysis conducted on missileers at Malmstrom Air Force Base in Montana. The study, which has not undergone peer review, found higher rates of NHL diagnosis at younger ages compared with the general population. The study also found a statistically significant increase in NHL diagnoses among older missileers, with such rates surpassing expected benchmarks.
The findings build on anecdotal and evidentiary data gathered in the last 50-plus years, including from the Torchlight Initiative, established in 2023 to collect self-reported cancer diagnoses and related fatalities from personnel and family members associated with the ICBM community.
The report shows patterns that “warranted a detailed statistical analysis,” leading to a granular examination of the registry and categorization of the data by cancer type, geographical location, and specific demographics. This narrowed the focus to 18 missileers who served at Malmstrom and were diagnosed with NHL.
In 2001, the Air Force Institute for Operational Health did a site evaluation and sampled for potential chemical and biological contaminants at Malmstrom following various reports of cancers from missileers, including 2 who died after being diagnosed with NHL. In a 2005 review, the Air Force said, “there is not sufficient evidence to consider the possibility of a cancer clustering to justify further investigation.”
In 2022, Lt. Col. Daniel Sebeck, a vice commander of Space Delta 8 in Colorado who served at Malmstrom and a close friend and fellow missileer were diagnosed with NHL. Sebeck discovered 36 cancer cases among missileers who had been stationed at Malmstrom. Ten developed NHL, 2 developed Hodgkin lymphoma, and 24 developed another form of cancer. The Air Force has acknowledged the concerns.
In 2023, US Air Force School of Aerospace Medicine (USAFSAM) approved the Missile Community Cancer Study (MCCS) to assess “specific cancer concerns raised by missile community members across related career fields and also examines the possibility of clusters of non-Hodgkin’s lymphoma at intercontinental ballistic missile bases.” The study compares 14 common cancers in the general population with that of missile-related career fields. The USAFSAM is reviewing records from former and current Missile Community members on active duty from 1976-2010, as well as state and national cancer data from multiple registries.
Early results from the MCCS suggested elevated rates of some cancers—mainly breast and prostate cancer—among missileers, maintainers, and other ICMB-related job positions, which aligns with other national cancer data.
At a June 2024 AFGSC town hall, officials announced that missileers would now have their information submitted to the Defense Occupational and Environmental Health Readiness System (DOEHRS), a Pentagon database for reporting occupational and exposure hazards.
"This info from DOEHRS flows into the recently developed Individual Longitudinal Exposure Record, a system that compiles occupational and environmental health data throughout a person's career," Lt. Col. John Severns, a spokesperson for Air Force Global Strike Command, said. DOEHRS, which has tracked Air Force records since 2010, allows US Department of Defense and US Department of Veterans Affairs clinical staff to access the information.
MCCS considers potential PCB exposures an occupational hazard. The Air Force says researchers are working with the System Program Offices and leadership to determine the timeframe of PCB removal from bases.
The lack of incontrovertible evidence connecting workplace toxins to NHL has often stymied patients and their family members from receiving appropriate benefits. An “informal talk” in April led by Rep. Mark Takano (D-CA) and Sen. Richard Blumenthal (D-CT) focused on exposures to hazardous materials at US military bases. Participants included various advocacy groups like the Torchlight Initiative, the Invisible Enemy, and Burn Pits 360.
More than a dozen veterans spoke about serving at military bases where they were exposed to a variety of harmful substances, and issues they faced in receiving coverage. David Crete, a veteran and chairman of The Invisible Enemy, said, “I am asking Congress to please allow us to get the benefits every other veteran earned. We are not asking to be special but to be treated equal.”
Rep. Takano called for greater focus on toxic exposures at US military bases: “We must push back against the idea that service members are only in harm’s way in war zones.”
Clinicians Should Have Private Spaces for Telehealth According to VA Memo
US Department of Veterans Affairs (VA) officials are insisting that when remote telehealth clinicians return to an office setting, they must have private workspaces “that foster trusted, confidential, and therapeutic relationships with veterans,” according to an April internal memo reported on by NPR.
The return-to-office mandate followed a Trump Administration executive order in February indicated that mental health clinicians at the US Department of Veterans Affairs (VA) must physically return to their workplace by May 5. For some, the deadline came as early as April 14; however, that order, like many others, may now be being revised or reconsidered due to concerns that have been raised. Many mental health clinicians were hired specifically to work remotely. They worried there would simply not be enough space for them, particularly to provide confidential counseling.
Millions of veterans use telehealth to access VA care. More than 98% of VA mental health clinicians have conducted ≥ 1 video visit to screen and treat patients for anxiety, depression, posttraumatic stress disorder, and more. Telehealth has been particularly important for veterans living in rural communities.
The April VA memo stipulated that “spaces used to deliver synchronous telehealth services should offer the same level of privacy and therapeutic environment applicable to an in-person visit in the same space.”
Therapists, patients, advocacy groups, and lawmakers have expressed concern about the potential impacts the policy change could have on patient care for veterans and, above all, about what it could mean for privacy. On Mar. 27, the American Psychological Association issued a statement noting that the change “resulted in providers being asked to conduct sensitive therapy sessions in open office environments, cubicles, or shared spaces that fail to meet basic confidentiality and privacy requirements for the delivery of mental health care services.”
Twenty Democrats in the House of Representatives sent a letter to VA Secretary Doug Collins expressing concern with the return to office policy. According to the letter a VA social worker supervisor reported managing their caseload while sharing a 100 ft2 shower space with another supervisor. It also reported that Clinical Resource Hub employees were being told to report to buildings where federal employees from other agencies work. “We have heard from countless stakeholders, veterans, and Department of Veterans Affairs (VA) employees that by carrying out President Trump’s blanket return-to-office policy your administration is damaging veteran and employee trust in VA, disrupting and impeding veterans’ access to care, and creating untenable and inefficient conditions for both veterans and the VA workforce,” the letter stated.
“This is a clear violation of veterans’ privacy and VA’s obligation to protect veterans’ private health information, and risks violation of the Health Insurance Portability and Accountability Act (HIPAA),” the letter added.
The lawmakers noted that, as of March 10, the VA was exempting Veterans Crisis Line workers, most of whom had been working remotely for the past 5 years, responding to more than 10 million calls, texts, and chats. That move, they said, indicated “that you understand there will be negative impacts to veterans’ care due to the return-to-office order and that these must be mitigated.”
VA spokesperson Peter Kasperowicz called the privacy concerns “nonsensical” and blamed “fear mongering from the media.” The VA, he said, “is no longer a place where the status quo for employees is to simply phone it in from home.” He also claimed that “the small number of employees who are desperate to avoid returning to the office will do more to drive away staff and patients than VA’s commonsense return-to-office policy ever will.”
VA care, he said, would continue uninterrupted and the “VA will ensure that employees have a workspace that is appropriate for the work they do.”
US Department of Veterans Affairs (VA) officials are insisting that when remote telehealth clinicians return to an office setting, they must have private workspaces “that foster trusted, confidential, and therapeutic relationships with veterans,” according to an April internal memo reported on by NPR.
The return-to-office mandate followed a Trump Administration executive order in February indicated that mental health clinicians at the US Department of Veterans Affairs (VA) must physically return to their workplace by May 5. For some, the deadline came as early as April 14; however, that order, like many others, may now be being revised or reconsidered due to concerns that have been raised. Many mental health clinicians were hired specifically to work remotely. They worried there would simply not be enough space for them, particularly to provide confidential counseling.
Millions of veterans use telehealth to access VA care. More than 98% of VA mental health clinicians have conducted ≥ 1 video visit to screen and treat patients for anxiety, depression, posttraumatic stress disorder, and more. Telehealth has been particularly important for veterans living in rural communities.
The April VA memo stipulated that “spaces used to deliver synchronous telehealth services should offer the same level of privacy and therapeutic environment applicable to an in-person visit in the same space.”
Therapists, patients, advocacy groups, and lawmakers have expressed concern about the potential impacts the policy change could have on patient care for veterans and, above all, about what it could mean for privacy. On Mar. 27, the American Psychological Association issued a statement noting that the change “resulted in providers being asked to conduct sensitive therapy sessions in open office environments, cubicles, or shared spaces that fail to meet basic confidentiality and privacy requirements for the delivery of mental health care services.”
Twenty Democrats in the House of Representatives sent a letter to VA Secretary Doug Collins expressing concern with the return to office policy. According to the letter a VA social worker supervisor reported managing their caseload while sharing a 100 ft2 shower space with another supervisor. It also reported that Clinical Resource Hub employees were being told to report to buildings where federal employees from other agencies work. “We have heard from countless stakeholders, veterans, and Department of Veterans Affairs (VA) employees that by carrying out President Trump’s blanket return-to-office policy your administration is damaging veteran and employee trust in VA, disrupting and impeding veterans’ access to care, and creating untenable and inefficient conditions for both veterans and the VA workforce,” the letter stated.
“This is a clear violation of veterans’ privacy and VA’s obligation to protect veterans’ private health information, and risks violation of the Health Insurance Portability and Accountability Act (HIPAA),” the letter added.
The lawmakers noted that, as of March 10, the VA was exempting Veterans Crisis Line workers, most of whom had been working remotely for the past 5 years, responding to more than 10 million calls, texts, and chats. That move, they said, indicated “that you understand there will be negative impacts to veterans’ care due to the return-to-office order and that these must be mitigated.”
VA spokesperson Peter Kasperowicz called the privacy concerns “nonsensical” and blamed “fear mongering from the media.” The VA, he said, “is no longer a place where the status quo for employees is to simply phone it in from home.” He also claimed that “the small number of employees who are desperate to avoid returning to the office will do more to drive away staff and patients than VA’s commonsense return-to-office policy ever will.”
VA care, he said, would continue uninterrupted and the “VA will ensure that employees have a workspace that is appropriate for the work they do.”
US Department of Veterans Affairs (VA) officials are insisting that when remote telehealth clinicians return to an office setting, they must have private workspaces “that foster trusted, confidential, and therapeutic relationships with veterans,” according to an April internal memo reported on by NPR.
The return-to-office mandate followed a Trump Administration executive order in February indicated that mental health clinicians at the US Department of Veterans Affairs (VA) must physically return to their workplace by May 5. For some, the deadline came as early as April 14; however, that order, like many others, may now be being revised or reconsidered due to concerns that have been raised. Many mental health clinicians were hired specifically to work remotely. They worried there would simply not be enough space for them, particularly to provide confidential counseling.
Millions of veterans use telehealth to access VA care. More than 98% of VA mental health clinicians have conducted ≥ 1 video visit to screen and treat patients for anxiety, depression, posttraumatic stress disorder, and more. Telehealth has been particularly important for veterans living in rural communities.
The April VA memo stipulated that “spaces used to deliver synchronous telehealth services should offer the same level of privacy and therapeutic environment applicable to an in-person visit in the same space.”
Therapists, patients, advocacy groups, and lawmakers have expressed concern about the potential impacts the policy change could have on patient care for veterans and, above all, about what it could mean for privacy. On Mar. 27, the American Psychological Association issued a statement noting that the change “resulted in providers being asked to conduct sensitive therapy sessions in open office environments, cubicles, or shared spaces that fail to meet basic confidentiality and privacy requirements for the delivery of mental health care services.”
Twenty Democrats in the House of Representatives sent a letter to VA Secretary Doug Collins expressing concern with the return to office policy. According to the letter a VA social worker supervisor reported managing their caseload while sharing a 100 ft2 shower space with another supervisor. It also reported that Clinical Resource Hub employees were being told to report to buildings where federal employees from other agencies work. “We have heard from countless stakeholders, veterans, and Department of Veterans Affairs (VA) employees that by carrying out President Trump’s blanket return-to-office policy your administration is damaging veteran and employee trust in VA, disrupting and impeding veterans’ access to care, and creating untenable and inefficient conditions for both veterans and the VA workforce,” the letter stated.
“This is a clear violation of veterans’ privacy and VA’s obligation to protect veterans’ private health information, and risks violation of the Health Insurance Portability and Accountability Act (HIPAA),” the letter added.
The lawmakers noted that, as of March 10, the VA was exempting Veterans Crisis Line workers, most of whom had been working remotely for the past 5 years, responding to more than 10 million calls, texts, and chats. That move, they said, indicated “that you understand there will be negative impacts to veterans’ care due to the return-to-office order and that these must be mitigated.”
VA spokesperson Peter Kasperowicz called the privacy concerns “nonsensical” and blamed “fear mongering from the media.” The VA, he said, “is no longer a place where the status quo for employees is to simply phone it in from home.” He also claimed that “the small number of employees who are desperate to avoid returning to the office will do more to drive away staff and patients than VA’s commonsense return-to-office policy ever will.”
VA care, he said, would continue uninterrupted and the “VA will ensure that employees have a workspace that is appropriate for the work they do.”
HHS Cuts Thousands of Jobs, Eliminates Entire Services
On March 27, Health and Human Services (HHS) Secretary Robert F. Kennedy Jr. said he planned to cut about 10,000 full-time jobs from the department in a sweeping “reorganization.” Less than a week later, the reduction in force (RIF) notifications were sent out, and in the very early hours of April 1, hundreds of employees found themselves locked out from their offices, often so abruptly their belongings were left behind.
Most affected employees were told they would be placed on administrative leave; some were told to continue working until they can hand off their duties but they would be formally separated on June 2. Many of the email RIF notifications used the recommended wording provided by the US Office of Personnel Management: “This RIF action does not reflect directly on your service, performance, or conduct.”
"The Trump Administration has launched an unprecedented attack on the federal health workforce," said House Energy and Commerce Committee Ranking Member Frank Pallone, Jr. (D-NJ), during an oversight and investigations hearing on medical device technology and cybersecurity.
The cuts in personnel and programs are broad and deep, and touch every aspect of public health. Alzheimer’s disease programs are being eliminated, measles vaccine clinics are being shuttered, and tuberculosis, HIV prevention, and cancer research are being stalled. A Reddit thread for RIF notices from HHS employees had nearly 750 postings, suggesting a broad cross-section of individuals and departments had received them.
Secretary Kennedy stated the layoffs and restructuring will save $1.8 billion a year. “We aren’t just reducing bureaucratic sprawl," he said in a statement. "We are realigning the organization with its core mission and our new priorities in reversing the chronic disease epidemic.” On the social platform X, Kennedy acknowledged, “This will be a painful period for HHS.”
Entire offices devoted to Freedom of Information Act-related requests, communications, and human resources were also shut down, according to multiple reports.
The agency's 28 divisions will be reformatted into a “new, unified entity” of 15 divisions—the Administration for a Healthy America, or AHA, aimed at carrying out Kennedy's “Make America Healthy Again” agenda. The AHA will include the Substance Abuse and Mental Health Services Administration (SAMHSA), the Agency for Toxic Substances and Disease Registry, and the National Institute for Occupational Safety and Health. The Administration for Community Living's functions will shift into the Centers for Medicare and Medicaid Services, the Administration for Children and Families, and the Assistant Secretary for Planning and Evaluation (ASPE). ASPE will be combined with the Agency for Health Research and Quality into the Office of Strategy
“This centralization,” HHS says, “will improve coordination of health resources for low-income Americans and will focus on areas including, Primary Care, Maternal and Child Health, Mental Health, Environmental Health, HIV/AIDS, and Workforce development.”
US Food and Drug Administration
An estimated 3500 full-time FDA employees are expected to receive RIF notices. The agency said reductions will not affect drug, medical device, or food reviewers or inspectors.
Politico spoke with fired employees on condition of anonymity. According to them, Dr. Peter Stein, director of the FDA Office of New Drugs (OND), was let go. The policy office inside of OND was also eliminated. Another top FDA regulator, Dr. Brian King, the director of the Center for Tobacco Products (CTP), was placed on administrative leave, according to an email sent to his staff and obtained by Politico. “I encourage you to hold your heads high and never compromise the guiding tenets that CTP has held dear since its inception,” King wrote in the email to his staff. “We obeyed the law. We followed the science. We told the truth.”
Julie Tierney, who was recently elevated to acting director of the FDA Center for Biologics Evaluation and Research, according to an agency website, was also placed on administrative leave, according to 2 people familiar with the decision. The FDA Office of Strategic Programs, including its director, Sridhar Mantha, has been completely shuttered. Mantha cochaired the Artificial Intelligence (AI) Council at the Center for Drug Evaluation and Research (CDER), which helped develop policy around AI use in drug development and assisted the FDA in using AI internally.
Centers for Disease Control and Prevention
About 2400 CDC employees are expected to receive RIF notices. According to Government Executive, the National Institute for Occupational Safety and Health (NIOSH) sustained more than one-third of the cuts at CDC. About 80% of the 1100 employees at the institute were laid off, including its director and deputy director. An HHS letter to a labor union said about 185 NIOSH employees would be let go in just the Morgantown, W. Va., location. However, NIOSH is apparently slated to be part of the newly created AHA.
Other layoffs hit the National Center for Chronic Disease Prevention and Health Promotion; National Center for Injury Prevention and Control; the National Center for HIV, Viral Hepatitis, STD, and Tuberculosis Prevention; the Global Health Center; the National Center on Birth Defects and Developmental Disabilities; and the National Center for Environmental Health. Two sources familiar with the firings said the Office on Smoking and Health was eliminated. The Administration for Strategic Preparedness and Response, currently part of the US Public Health Service, will move to the CDC.
A compensation program for employees who developed cancer due to radiation exposure while working for the federal government was also eliminated. Similarly, a national registry that tracks rates of cancer among firefighters was cut. One employee said NIOSH laid off veterinarians despite the bureau having laboratory animals that need care.
National Institutes of Health
NIH will lose 1200 employees, due to "centralizing” procurement, human resources, and communications across its 27 institutes and centers. According to the employees who spoke with Politico, scientists were also targeted, including National Institute of Nursing Research Director Shannon Zenk; National Institute of Child Health and Human Development Director Diana Bianchi; Emily Erbelding, who leads the Division of Microbiology and Infectious Diseases at National Institutes of Allergy and Infectious Diseases; and National Institute on Minority Health and Health Disparities Director Eliseo Pérez-Stable. National Institute of Allergy and Infectious Diseases Director Jeanne Marrazzo, who replaced Anthony Fauci, was also put on leave.
In his “welcome” email to staff, the new NIH director, Dr. Jay Bhattacharya, wrote: “I recognize that I am joining NIH at a time of tremendous change. Every inch of the federal government is under scrutiny—and NIH is not exempt. These reductions in the workforce will have a profound impact on key NIH administrative functions, including communications, legislative affairs, procurement, and human resources, and will require an entirely new approach to how we carry them out.”
Deep Cuts at Other HHS Agencies
As many as 500 to 600 people were let go at the Health Resource and Services Administration (HRSA). Its Bureau of Primary Health Care, which oversees the national network of health care centers that collectively provide care to 31 million people, was “severely impacted,” and the agency lost much of its regional staff, according to an article in Government Executive. “This will have an enormous impact on the program and viability of health centers,” an HRSA employee said.
About 50% of the nearly 900 SAMHSA employees were laid off and its 10 regional offices were closed. SAMHSA will be “hamstrung for data,” according to an agency employee, who added contracts may be cut en masse due the departure of the contract management staff. They added that even if funding remains for the agency, the support systems for grantees were being decimated.
More than 800 people lost their jobs at the CDER, according to an official who was laid off; this part of the agency had around 6,000 employees before the cuts.
Indian Health Service
The IHS offers a rare bright spot. Although it was also in line for massive cuts, it has been spared, for now. According to a statement emailed to Native News Online, Secretary Kennedy said the Trump administration intends to prioritize the IHS.
“The Indian Health Service has always been treated as the redheaded stepchild at HHS,” Secretary Kennedy wrote. “My father often complained that IHS was chronically understaffed and underfunded. President Trump wants me to rectify this sad history. Indians suffer at the highest level of chronic disease of any demographic. IHS will be a priority over the next 4 years. President Trump wants me to end the chronic disease epidemic beginning in Indian country.”
March layoffs that had been announced for 1000 IHS employees were rescinded.
“We can confirm the layoffs were rescinded thanks at least in part to advocacy by the many Tribal organizations,” a spokesperson for the National Indian Health Board told Native News Online.
In fact, top career executives across the department are now being offered reassignments to the IHS, which employees must accept to keep their jobs. One executive who received the offer told Native News Online that no details on positions or location were provided, and they doubted that everyone who got such a notice would ultimately be matched to a suitable position.
"Streamline the Agency"
The dramatic actions at HHS were not unexpected. In fact, employees had been in an unsettling limbo since Kennedy was appointed Secretary, not knowing when the axe would fall, or where, or on whom. Kennedy, when describing the restructuring plans, said, “We're going to streamline our agency and eliminate the redundancies and invite everyone to align behind a simple, bold mission. I want every HHS employee to wake up every morning asking themselves, ‘What can I do to restore American Health?’ I want to empower everyone in the HHS family to have a sense of purpose and pride and a sense of personal agency and responsibility to this larger goal.”
“The FDA as we've known it is finished,” Dr. Robert M. Califf, who served as FDA commissioner twice, wrote on LinkedIn. In an interview with CNN, Califf said he was dismayed to see how federal workers were being treated.
“This is a sad and inhumane way to treat people,” he said. “It’s different when you’re a company and you’re out of money and you can’t pay people, but the federal government can pay people and do things in an orderly, respectful fashion—and not have them end up in line trying to get to work and have their badges not work as a way to fire them.”
But the fired HHS employees aren’t the only ones who will bear the brunt of the cuts. “Today’s announcement is not just a restructuring of the Department of Health and Human Services. It is a catastrophe for the health care of every American,” Senator Ed Markey (D-MA) said in a press briefing.
Calling the cuts “a recipe for disaster,” former CDC director Tom Frieden said, “[Secretary] Kennedy claims that health care services will not be harmed by the dramatic downsizing, but he is wrong, and everyone who is paying any attention knows it.”
Senators Bill Cassidy (R-LA) and Bernie Sanders (I-VT), of the Senate Health, Education, Labor, and Pensions Committee, announced Tuesday that they were inviting Kennedy to a hearing April 10 about the restructuring of HHS. “This will be a good opportunity,” Cassidy said in a statement, “for him to set the record straight and speak to the goals, structure and benefits of the proposed reorganization.”
On March 27, Health and Human Services (HHS) Secretary Robert F. Kennedy Jr. said he planned to cut about 10,000 full-time jobs from the department in a sweeping “reorganization.” Less than a week later, the reduction in force (RIF) notifications were sent out, and in the very early hours of April 1, hundreds of employees found themselves locked out from their offices, often so abruptly their belongings were left behind.
Most affected employees were told they would be placed on administrative leave; some were told to continue working until they can hand off their duties but they would be formally separated on June 2. Many of the email RIF notifications used the recommended wording provided by the US Office of Personnel Management: “This RIF action does not reflect directly on your service, performance, or conduct.”
"The Trump Administration has launched an unprecedented attack on the federal health workforce," said House Energy and Commerce Committee Ranking Member Frank Pallone, Jr. (D-NJ), during an oversight and investigations hearing on medical device technology and cybersecurity.
The cuts in personnel and programs are broad and deep, and touch every aspect of public health. Alzheimer’s disease programs are being eliminated, measles vaccine clinics are being shuttered, and tuberculosis, HIV prevention, and cancer research are being stalled. A Reddit thread for RIF notices from HHS employees had nearly 750 postings, suggesting a broad cross-section of individuals and departments had received them.
Secretary Kennedy stated the layoffs and restructuring will save $1.8 billion a year. “We aren’t just reducing bureaucratic sprawl," he said in a statement. "We are realigning the organization with its core mission and our new priorities in reversing the chronic disease epidemic.” On the social platform X, Kennedy acknowledged, “This will be a painful period for HHS.”
Entire offices devoted to Freedom of Information Act-related requests, communications, and human resources were also shut down, according to multiple reports.
The agency's 28 divisions will be reformatted into a “new, unified entity” of 15 divisions—the Administration for a Healthy America, or AHA, aimed at carrying out Kennedy's “Make America Healthy Again” agenda. The AHA will include the Substance Abuse and Mental Health Services Administration (SAMHSA), the Agency for Toxic Substances and Disease Registry, and the National Institute for Occupational Safety and Health. The Administration for Community Living's functions will shift into the Centers for Medicare and Medicaid Services, the Administration for Children and Families, and the Assistant Secretary for Planning and Evaluation (ASPE). ASPE will be combined with the Agency for Health Research and Quality into the Office of Strategy
“This centralization,” HHS says, “will improve coordination of health resources for low-income Americans and will focus on areas including, Primary Care, Maternal and Child Health, Mental Health, Environmental Health, HIV/AIDS, and Workforce development.”
US Food and Drug Administration
An estimated 3500 full-time FDA employees are expected to receive RIF notices. The agency said reductions will not affect drug, medical device, or food reviewers or inspectors.
Politico spoke with fired employees on condition of anonymity. According to them, Dr. Peter Stein, director of the FDA Office of New Drugs (OND), was let go. The policy office inside of OND was also eliminated. Another top FDA regulator, Dr. Brian King, the director of the Center for Tobacco Products (CTP), was placed on administrative leave, according to an email sent to his staff and obtained by Politico. “I encourage you to hold your heads high and never compromise the guiding tenets that CTP has held dear since its inception,” King wrote in the email to his staff. “We obeyed the law. We followed the science. We told the truth.”
Julie Tierney, who was recently elevated to acting director of the FDA Center for Biologics Evaluation and Research, according to an agency website, was also placed on administrative leave, according to 2 people familiar with the decision. The FDA Office of Strategic Programs, including its director, Sridhar Mantha, has been completely shuttered. Mantha cochaired the Artificial Intelligence (AI) Council at the Center for Drug Evaluation and Research (CDER), which helped develop policy around AI use in drug development and assisted the FDA in using AI internally.
Centers for Disease Control and Prevention
About 2400 CDC employees are expected to receive RIF notices. According to Government Executive, the National Institute for Occupational Safety and Health (NIOSH) sustained more than one-third of the cuts at CDC. About 80% of the 1100 employees at the institute were laid off, including its director and deputy director. An HHS letter to a labor union said about 185 NIOSH employees would be let go in just the Morgantown, W. Va., location. However, NIOSH is apparently slated to be part of the newly created AHA.
Other layoffs hit the National Center for Chronic Disease Prevention and Health Promotion; National Center for Injury Prevention and Control; the National Center for HIV, Viral Hepatitis, STD, and Tuberculosis Prevention; the Global Health Center; the National Center on Birth Defects and Developmental Disabilities; and the National Center for Environmental Health. Two sources familiar with the firings said the Office on Smoking and Health was eliminated. The Administration for Strategic Preparedness and Response, currently part of the US Public Health Service, will move to the CDC.
A compensation program for employees who developed cancer due to radiation exposure while working for the federal government was also eliminated. Similarly, a national registry that tracks rates of cancer among firefighters was cut. One employee said NIOSH laid off veterinarians despite the bureau having laboratory animals that need care.
National Institutes of Health
NIH will lose 1200 employees, due to "centralizing” procurement, human resources, and communications across its 27 institutes and centers. According to the employees who spoke with Politico, scientists were also targeted, including National Institute of Nursing Research Director Shannon Zenk; National Institute of Child Health and Human Development Director Diana Bianchi; Emily Erbelding, who leads the Division of Microbiology and Infectious Diseases at National Institutes of Allergy and Infectious Diseases; and National Institute on Minority Health and Health Disparities Director Eliseo Pérez-Stable. National Institute of Allergy and Infectious Diseases Director Jeanne Marrazzo, who replaced Anthony Fauci, was also put on leave.
In his “welcome” email to staff, the new NIH director, Dr. Jay Bhattacharya, wrote: “I recognize that I am joining NIH at a time of tremendous change. Every inch of the federal government is under scrutiny—and NIH is not exempt. These reductions in the workforce will have a profound impact on key NIH administrative functions, including communications, legislative affairs, procurement, and human resources, and will require an entirely new approach to how we carry them out.”
Deep Cuts at Other HHS Agencies
As many as 500 to 600 people were let go at the Health Resource and Services Administration (HRSA). Its Bureau of Primary Health Care, which oversees the national network of health care centers that collectively provide care to 31 million people, was “severely impacted,” and the agency lost much of its regional staff, according to an article in Government Executive. “This will have an enormous impact on the program and viability of health centers,” an HRSA employee said.
About 50% of the nearly 900 SAMHSA employees were laid off and its 10 regional offices were closed. SAMHSA will be “hamstrung for data,” according to an agency employee, who added contracts may be cut en masse due the departure of the contract management staff. They added that even if funding remains for the agency, the support systems for grantees were being decimated.
More than 800 people lost their jobs at the CDER, according to an official who was laid off; this part of the agency had around 6,000 employees before the cuts.
Indian Health Service
The IHS offers a rare bright spot. Although it was also in line for massive cuts, it has been spared, for now. According to a statement emailed to Native News Online, Secretary Kennedy said the Trump administration intends to prioritize the IHS.
“The Indian Health Service has always been treated as the redheaded stepchild at HHS,” Secretary Kennedy wrote. “My father often complained that IHS was chronically understaffed and underfunded. President Trump wants me to rectify this sad history. Indians suffer at the highest level of chronic disease of any demographic. IHS will be a priority over the next 4 years. President Trump wants me to end the chronic disease epidemic beginning in Indian country.”
March layoffs that had been announced for 1000 IHS employees were rescinded.
“We can confirm the layoffs were rescinded thanks at least in part to advocacy by the many Tribal organizations,” a spokesperson for the National Indian Health Board told Native News Online.
In fact, top career executives across the department are now being offered reassignments to the IHS, which employees must accept to keep their jobs. One executive who received the offer told Native News Online that no details on positions or location were provided, and they doubted that everyone who got such a notice would ultimately be matched to a suitable position.
"Streamline the Agency"
The dramatic actions at HHS were not unexpected. In fact, employees had been in an unsettling limbo since Kennedy was appointed Secretary, not knowing when the axe would fall, or where, or on whom. Kennedy, when describing the restructuring plans, said, “We're going to streamline our agency and eliminate the redundancies and invite everyone to align behind a simple, bold mission. I want every HHS employee to wake up every morning asking themselves, ‘What can I do to restore American Health?’ I want to empower everyone in the HHS family to have a sense of purpose and pride and a sense of personal agency and responsibility to this larger goal.”
“The FDA as we've known it is finished,” Dr. Robert M. Califf, who served as FDA commissioner twice, wrote on LinkedIn. In an interview with CNN, Califf said he was dismayed to see how federal workers were being treated.
“This is a sad and inhumane way to treat people,” he said. “It’s different when you’re a company and you’re out of money and you can’t pay people, but the federal government can pay people and do things in an orderly, respectful fashion—and not have them end up in line trying to get to work and have their badges not work as a way to fire them.”
But the fired HHS employees aren’t the only ones who will bear the brunt of the cuts. “Today’s announcement is not just a restructuring of the Department of Health and Human Services. It is a catastrophe for the health care of every American,” Senator Ed Markey (D-MA) said in a press briefing.
Calling the cuts “a recipe for disaster,” former CDC director Tom Frieden said, “[Secretary] Kennedy claims that health care services will not be harmed by the dramatic downsizing, but he is wrong, and everyone who is paying any attention knows it.”
Senators Bill Cassidy (R-LA) and Bernie Sanders (I-VT), of the Senate Health, Education, Labor, and Pensions Committee, announced Tuesday that they were inviting Kennedy to a hearing April 10 about the restructuring of HHS. “This will be a good opportunity,” Cassidy said in a statement, “for him to set the record straight and speak to the goals, structure and benefits of the proposed reorganization.”
On March 27, Health and Human Services (HHS) Secretary Robert F. Kennedy Jr. said he planned to cut about 10,000 full-time jobs from the department in a sweeping “reorganization.” Less than a week later, the reduction in force (RIF) notifications were sent out, and in the very early hours of April 1, hundreds of employees found themselves locked out from their offices, often so abruptly their belongings were left behind.
Most affected employees were told they would be placed on administrative leave; some were told to continue working until they can hand off their duties but they would be formally separated on June 2. Many of the email RIF notifications used the recommended wording provided by the US Office of Personnel Management: “This RIF action does not reflect directly on your service, performance, or conduct.”
"The Trump Administration has launched an unprecedented attack on the federal health workforce," said House Energy and Commerce Committee Ranking Member Frank Pallone, Jr. (D-NJ), during an oversight and investigations hearing on medical device technology and cybersecurity.
The cuts in personnel and programs are broad and deep, and touch every aspect of public health. Alzheimer’s disease programs are being eliminated, measles vaccine clinics are being shuttered, and tuberculosis, HIV prevention, and cancer research are being stalled. A Reddit thread for RIF notices from HHS employees had nearly 750 postings, suggesting a broad cross-section of individuals and departments had received them.
Secretary Kennedy stated the layoffs and restructuring will save $1.8 billion a year. “We aren’t just reducing bureaucratic sprawl," he said in a statement. "We are realigning the organization with its core mission and our new priorities in reversing the chronic disease epidemic.” On the social platform X, Kennedy acknowledged, “This will be a painful period for HHS.”
Entire offices devoted to Freedom of Information Act-related requests, communications, and human resources were also shut down, according to multiple reports.
The agency's 28 divisions will be reformatted into a “new, unified entity” of 15 divisions—the Administration for a Healthy America, or AHA, aimed at carrying out Kennedy's “Make America Healthy Again” agenda. The AHA will include the Substance Abuse and Mental Health Services Administration (SAMHSA), the Agency for Toxic Substances and Disease Registry, and the National Institute for Occupational Safety and Health. The Administration for Community Living's functions will shift into the Centers for Medicare and Medicaid Services, the Administration for Children and Families, and the Assistant Secretary for Planning and Evaluation (ASPE). ASPE will be combined with the Agency for Health Research and Quality into the Office of Strategy
“This centralization,” HHS says, “will improve coordination of health resources for low-income Americans and will focus on areas including, Primary Care, Maternal and Child Health, Mental Health, Environmental Health, HIV/AIDS, and Workforce development.”
US Food and Drug Administration
An estimated 3500 full-time FDA employees are expected to receive RIF notices. The agency said reductions will not affect drug, medical device, or food reviewers or inspectors.
Politico spoke with fired employees on condition of anonymity. According to them, Dr. Peter Stein, director of the FDA Office of New Drugs (OND), was let go. The policy office inside of OND was also eliminated. Another top FDA regulator, Dr. Brian King, the director of the Center for Tobacco Products (CTP), was placed on administrative leave, according to an email sent to his staff and obtained by Politico. “I encourage you to hold your heads high and never compromise the guiding tenets that CTP has held dear since its inception,” King wrote in the email to his staff. “We obeyed the law. We followed the science. We told the truth.”
Julie Tierney, who was recently elevated to acting director of the FDA Center for Biologics Evaluation and Research, according to an agency website, was also placed on administrative leave, according to 2 people familiar with the decision. The FDA Office of Strategic Programs, including its director, Sridhar Mantha, has been completely shuttered. Mantha cochaired the Artificial Intelligence (AI) Council at the Center for Drug Evaluation and Research (CDER), which helped develop policy around AI use in drug development and assisted the FDA in using AI internally.
Centers for Disease Control and Prevention
About 2400 CDC employees are expected to receive RIF notices. According to Government Executive, the National Institute for Occupational Safety and Health (NIOSH) sustained more than one-third of the cuts at CDC. About 80% of the 1100 employees at the institute were laid off, including its director and deputy director. An HHS letter to a labor union said about 185 NIOSH employees would be let go in just the Morgantown, W. Va., location. However, NIOSH is apparently slated to be part of the newly created AHA.
Other layoffs hit the National Center for Chronic Disease Prevention and Health Promotion; National Center for Injury Prevention and Control; the National Center for HIV, Viral Hepatitis, STD, and Tuberculosis Prevention; the Global Health Center; the National Center on Birth Defects and Developmental Disabilities; and the National Center for Environmental Health. Two sources familiar with the firings said the Office on Smoking and Health was eliminated. The Administration for Strategic Preparedness and Response, currently part of the US Public Health Service, will move to the CDC.
A compensation program for employees who developed cancer due to radiation exposure while working for the federal government was also eliminated. Similarly, a national registry that tracks rates of cancer among firefighters was cut. One employee said NIOSH laid off veterinarians despite the bureau having laboratory animals that need care.
National Institutes of Health
NIH will lose 1200 employees, due to "centralizing” procurement, human resources, and communications across its 27 institutes and centers. According to the employees who spoke with Politico, scientists were also targeted, including National Institute of Nursing Research Director Shannon Zenk; National Institute of Child Health and Human Development Director Diana Bianchi; Emily Erbelding, who leads the Division of Microbiology and Infectious Diseases at National Institutes of Allergy and Infectious Diseases; and National Institute on Minority Health and Health Disparities Director Eliseo Pérez-Stable. National Institute of Allergy and Infectious Diseases Director Jeanne Marrazzo, who replaced Anthony Fauci, was also put on leave.
In his “welcome” email to staff, the new NIH director, Dr. Jay Bhattacharya, wrote: “I recognize that I am joining NIH at a time of tremendous change. Every inch of the federal government is under scrutiny—and NIH is not exempt. These reductions in the workforce will have a profound impact on key NIH administrative functions, including communications, legislative affairs, procurement, and human resources, and will require an entirely new approach to how we carry them out.”
Deep Cuts at Other HHS Agencies
As many as 500 to 600 people were let go at the Health Resource and Services Administration (HRSA). Its Bureau of Primary Health Care, which oversees the national network of health care centers that collectively provide care to 31 million people, was “severely impacted,” and the agency lost much of its regional staff, according to an article in Government Executive. “This will have an enormous impact on the program and viability of health centers,” an HRSA employee said.
About 50% of the nearly 900 SAMHSA employees were laid off and its 10 regional offices were closed. SAMHSA will be “hamstrung for data,” according to an agency employee, who added contracts may be cut en masse due the departure of the contract management staff. They added that even if funding remains for the agency, the support systems for grantees were being decimated.
More than 800 people lost their jobs at the CDER, according to an official who was laid off; this part of the agency had around 6,000 employees before the cuts.
Indian Health Service
The IHS offers a rare bright spot. Although it was also in line for massive cuts, it has been spared, for now. According to a statement emailed to Native News Online, Secretary Kennedy said the Trump administration intends to prioritize the IHS.
“The Indian Health Service has always been treated as the redheaded stepchild at HHS,” Secretary Kennedy wrote. “My father often complained that IHS was chronically understaffed and underfunded. President Trump wants me to rectify this sad history. Indians suffer at the highest level of chronic disease of any demographic. IHS will be a priority over the next 4 years. President Trump wants me to end the chronic disease epidemic beginning in Indian country.”
March layoffs that had been announced for 1000 IHS employees were rescinded.
“We can confirm the layoffs were rescinded thanks at least in part to advocacy by the many Tribal organizations,” a spokesperson for the National Indian Health Board told Native News Online.
In fact, top career executives across the department are now being offered reassignments to the IHS, which employees must accept to keep their jobs. One executive who received the offer told Native News Online that no details on positions or location were provided, and they doubted that everyone who got such a notice would ultimately be matched to a suitable position.
"Streamline the Agency"
The dramatic actions at HHS were not unexpected. In fact, employees had been in an unsettling limbo since Kennedy was appointed Secretary, not knowing when the axe would fall, or where, or on whom. Kennedy, when describing the restructuring plans, said, “We're going to streamline our agency and eliminate the redundancies and invite everyone to align behind a simple, bold mission. I want every HHS employee to wake up every morning asking themselves, ‘What can I do to restore American Health?’ I want to empower everyone in the HHS family to have a sense of purpose and pride and a sense of personal agency and responsibility to this larger goal.”
“The FDA as we've known it is finished,” Dr. Robert M. Califf, who served as FDA commissioner twice, wrote on LinkedIn. In an interview with CNN, Califf said he was dismayed to see how federal workers were being treated.
“This is a sad and inhumane way to treat people,” he said. “It’s different when you’re a company and you’re out of money and you can’t pay people, but the federal government can pay people and do things in an orderly, respectful fashion—and not have them end up in line trying to get to work and have their badges not work as a way to fire them.”
But the fired HHS employees aren’t the only ones who will bear the brunt of the cuts. “Today’s announcement is not just a restructuring of the Department of Health and Human Services. It is a catastrophe for the health care of every American,” Senator Ed Markey (D-MA) said in a press briefing.
Calling the cuts “a recipe for disaster,” former CDC director Tom Frieden said, “[Secretary] Kennedy claims that health care services will not be harmed by the dramatic downsizing, but he is wrong, and everyone who is paying any attention knows it.”
Senators Bill Cassidy (R-LA) and Bernie Sanders (I-VT), of the Senate Health, Education, Labor, and Pensions Committee, announced Tuesday that they were inviting Kennedy to a hearing April 10 about the restructuring of HHS. “This will be a good opportunity,” Cassidy said in a statement, “for him to set the record straight and speak to the goals, structure and benefits of the proposed reorganization.”
VA Restarts Contract Cancellation Process
The US Department of Veterans Affairs (VA) has begun canceling 585 “non-mission–critical or duplicative” contracts, valued at about $1.8 billion. After accounting for the money already spent on the contracts, the VA expects to be able to redirect > $900 million back toward health care, benefits and services for VA beneficiaries.
This new directive, announced March 3, differs from the an earlier February contract cancellation plan. In late February, VA Secretary Doug Collins posted a video message on X outlining the cancellation of up to 875 contracts that was then relayed in an email to agency staff. In the post, Collins claimed to find “nearly $2 billion in VA contracts that we’ll be canceling so we can redirect the funds back to Veterans health care and benefits. No more paying consultants to do things like make Power Point slides and write meeting minutes!”
In a Feb. 25 statement Senate Veterans’ Affairs Committee Ranking Member Richard Blumenthal (D-CT) worried that the cancelled programs provided "critical services to veterans and their families, and allow VA to conduct oversight operations to identify waste, fraud, and abuse.” Blumenthal cited contracts to help process disability compensation benefits, modernize the VA Home Loan Program, cover medical services, provide cancer care, recruit doctors and other medical staff, and provide burial services to veterans.
This time, the VA insists the contract cancellations “were identified through a deliberative, multi-level review that involved the career subject-matter expert employees responsible for the contracts as well as VA senior leaders and contracting officials.” During the review, VA says it found many duplicative contracts that were providing the same services, such as third-party certifications for items like enhanced-use leases. The duplicative contracts were eliminated, while others remain to provide those services to ensure operational continuity.
The canceled contracts will be phased out over the next few days and represent < 1% of the roughly 90,000 current contracts worth > $67 billion, the VA said. According to the VA, contracts that directly support veterans and beneficiaries or provide services that VA cannot do itself, such as a nurse who sees patients or an organization that provides third-party certification services, respectively, were not canceled.
The US Department of Veterans Affairs (VA) has begun canceling 585 “non-mission–critical or duplicative” contracts, valued at about $1.8 billion. After accounting for the money already spent on the contracts, the VA expects to be able to redirect > $900 million back toward health care, benefits and services for VA beneficiaries.
This new directive, announced March 3, differs from the an earlier February contract cancellation plan. In late February, VA Secretary Doug Collins posted a video message on X outlining the cancellation of up to 875 contracts that was then relayed in an email to agency staff. In the post, Collins claimed to find “nearly $2 billion in VA contracts that we’ll be canceling so we can redirect the funds back to Veterans health care and benefits. No more paying consultants to do things like make Power Point slides and write meeting minutes!”
In a Feb. 25 statement Senate Veterans’ Affairs Committee Ranking Member Richard Blumenthal (D-CT) worried that the cancelled programs provided "critical services to veterans and their families, and allow VA to conduct oversight operations to identify waste, fraud, and abuse.” Blumenthal cited contracts to help process disability compensation benefits, modernize the VA Home Loan Program, cover medical services, provide cancer care, recruit doctors and other medical staff, and provide burial services to veterans.
This time, the VA insists the contract cancellations “were identified through a deliberative, multi-level review that involved the career subject-matter expert employees responsible for the contracts as well as VA senior leaders and contracting officials.” During the review, VA says it found many duplicative contracts that were providing the same services, such as third-party certifications for items like enhanced-use leases. The duplicative contracts were eliminated, while others remain to provide those services to ensure operational continuity.
The canceled contracts will be phased out over the next few days and represent < 1% of the roughly 90,000 current contracts worth > $67 billion, the VA said. According to the VA, contracts that directly support veterans and beneficiaries or provide services that VA cannot do itself, such as a nurse who sees patients or an organization that provides third-party certification services, respectively, were not canceled.
The US Department of Veterans Affairs (VA) has begun canceling 585 “non-mission–critical or duplicative” contracts, valued at about $1.8 billion. After accounting for the money already spent on the contracts, the VA expects to be able to redirect > $900 million back toward health care, benefits and services for VA beneficiaries.
This new directive, announced March 3, differs from the an earlier February contract cancellation plan. In late February, VA Secretary Doug Collins posted a video message on X outlining the cancellation of up to 875 contracts that was then relayed in an email to agency staff. In the post, Collins claimed to find “nearly $2 billion in VA contracts that we’ll be canceling so we can redirect the funds back to Veterans health care and benefits. No more paying consultants to do things like make Power Point slides and write meeting minutes!”
In a Feb. 25 statement Senate Veterans’ Affairs Committee Ranking Member Richard Blumenthal (D-CT) worried that the cancelled programs provided "critical services to veterans and their families, and allow VA to conduct oversight operations to identify waste, fraud, and abuse.” Blumenthal cited contracts to help process disability compensation benefits, modernize the VA Home Loan Program, cover medical services, provide cancer care, recruit doctors and other medical staff, and provide burial services to veterans.
This time, the VA insists the contract cancellations “were identified through a deliberative, multi-level review that involved the career subject-matter expert employees responsible for the contracts as well as VA senior leaders and contracting officials.” During the review, VA says it found many duplicative contracts that were providing the same services, such as third-party certifications for items like enhanced-use leases. The duplicative contracts were eliminated, while others remain to provide those services to ensure operational continuity.
The canceled contracts will be phased out over the next few days and represent < 1% of the roughly 90,000 current contracts worth > $67 billion, the VA said. According to the VA, contracts that directly support veterans and beneficiaries or provide services that VA cannot do itself, such as a nurse who sees patients or an organization that provides third-party certification services, respectively, were not canceled.
Head of Defense Health Agency Abruptly Retires
Army Lt. Gen. Telita Crosland, MD, MPH, MS, fourth director of the Defense Health Agency (DHA) and first Black woman to hold the position, has retired, bringing an abrupt end to an illustrious 32-year military career.
Acting Assistant Secretary of Defense for Health Affairs Stephen Ferrara, MD, said Crosland was “beginning her retirement” effective Feb. 28. According to Reuters, the statement offered no reasoning for Crosland’s quick departure, but 2 officials said she was informed that she must retire and was not given a reason why.
When she was promoted to director in January 2023, Lt. Gen. Crosland made history as the first Black woman to lead the DHA. Her former boss, Army Surgeon General Lt. Gen. R. Scott Dingle, called Crosland a “wonder woman” and “the baddest woman in the Army.” Her awards and decorations include the Legion of Merit with 2 oak leaf clusters, Meritorious Service Medal with 4 oak leaf clusters, Army Commendation Medal with 3 oak leaf clusters, Joint Service Achievement Medal, Army Staff Badge, and the Parachutist’s Badge. Lt. Gen. Crosland is also a member of the Order of Military Medical Merit. In addition to her medical and public health degrees, she has an master’s of science in national resource strategy.
Crosland entered the Army as a Medical Corps officer in 1993. Before becoming Director, she served as the Army’s Deputy Surgeon General, during which she oversaw response to a plethora of challenges: the COVID-19 pandemic, reformation of medical structures of the Army and other branches of services, and the Afghanistan withdrawal brought hundreds of evacuees with health needs.
“It was a sporty 3 years,” Crosland said in an interview with Military Times and other media, shortly before her promotion ceremony. But the pandemic and the Afghanistan mission helped her clarify how the services can work together as a team, she said.
Then, following a congressional mandate in 2024, > 700 military medical, dental, and veterinary facilities from the Army, Navy, and Air Force were being shifted over to the DHA. “The transition was tough. It was tough,” Crosland said. “First of all, it’s change, arguably the largest change in the Department of Defense since the Air Force moved from the Army. We’re talking about bringing all the military health care systems into one entity. Change is difficult.”
But the essence of the services’ military health care has never changed, she said in the press conference. A family health physician, Crosland emphasized the importance of caring for all the 9.6 million beneficiaries in the Military Health System. “The pandemic showed what we’re for,” she said. “We’re still a military health care system that has to take care of the force, and the beneficiaries we’re privileged to serve.”
Family medicine is about the holistic person, Crosland said. “That will come out as I look at our health care system to make sure that ultimately that’s what we’re about … improving the health of an individual, whether you wear a uniform, you wore a uniform, or you served side-by-side with someone who wore a uniform.”
Crosland’s departure came just days before she was scheduled to speak at the AMSUS - Society of Federal Health Professionals’ annual military and federal health care conference. It also comes days after the Trump administration fired multiple top military leaders, including Joint Chiefs of Staff Chairman Gen. CQ Brown, Chief of Naval Operations Adm. Lisa Franchetti, Air Force Vice Chief of Staff Gen. James C. Slife and several top military lawyers.
Ferrara thanked Crosland “for her dedication to the nation, to the Military Health System, and to Army Medicine for the past 32 years.”
David Smith, MD, acting principal deputy assistant secretary of defense for health affairs, will serve as acting director of DHA while the US Department of Defense conducts a nomination process to replace Crosland.
Army Lt. Gen. Telita Crosland, MD, MPH, MS, fourth director of the Defense Health Agency (DHA) and first Black woman to hold the position, has retired, bringing an abrupt end to an illustrious 32-year military career.
Acting Assistant Secretary of Defense for Health Affairs Stephen Ferrara, MD, said Crosland was “beginning her retirement” effective Feb. 28. According to Reuters, the statement offered no reasoning for Crosland’s quick departure, but 2 officials said she was informed that she must retire and was not given a reason why.
When she was promoted to director in January 2023, Lt. Gen. Crosland made history as the first Black woman to lead the DHA. Her former boss, Army Surgeon General Lt. Gen. R. Scott Dingle, called Crosland a “wonder woman” and “the baddest woman in the Army.” Her awards and decorations include the Legion of Merit with 2 oak leaf clusters, Meritorious Service Medal with 4 oak leaf clusters, Army Commendation Medal with 3 oak leaf clusters, Joint Service Achievement Medal, Army Staff Badge, and the Parachutist’s Badge. Lt. Gen. Crosland is also a member of the Order of Military Medical Merit. In addition to her medical and public health degrees, she has an master’s of science in national resource strategy.
Crosland entered the Army as a Medical Corps officer in 1993. Before becoming Director, she served as the Army’s Deputy Surgeon General, during which she oversaw response to a plethora of challenges: the COVID-19 pandemic, reformation of medical structures of the Army and other branches of services, and the Afghanistan withdrawal brought hundreds of evacuees with health needs.
“It was a sporty 3 years,” Crosland said in an interview with Military Times and other media, shortly before her promotion ceremony. But the pandemic and the Afghanistan mission helped her clarify how the services can work together as a team, she said.
Then, following a congressional mandate in 2024, > 700 military medical, dental, and veterinary facilities from the Army, Navy, and Air Force were being shifted over to the DHA. “The transition was tough. It was tough,” Crosland said. “First of all, it’s change, arguably the largest change in the Department of Defense since the Air Force moved from the Army. We’re talking about bringing all the military health care systems into one entity. Change is difficult.”
But the essence of the services’ military health care has never changed, she said in the press conference. A family health physician, Crosland emphasized the importance of caring for all the 9.6 million beneficiaries in the Military Health System. “The pandemic showed what we’re for,” she said. “We’re still a military health care system that has to take care of the force, and the beneficiaries we’re privileged to serve.”
Family medicine is about the holistic person, Crosland said. “That will come out as I look at our health care system to make sure that ultimately that’s what we’re about … improving the health of an individual, whether you wear a uniform, you wore a uniform, or you served side-by-side with someone who wore a uniform.”
Crosland’s departure came just days before she was scheduled to speak at the AMSUS - Society of Federal Health Professionals’ annual military and federal health care conference. It also comes days after the Trump administration fired multiple top military leaders, including Joint Chiefs of Staff Chairman Gen. CQ Brown, Chief of Naval Operations Adm. Lisa Franchetti, Air Force Vice Chief of Staff Gen. James C. Slife and several top military lawyers.
Ferrara thanked Crosland “for her dedication to the nation, to the Military Health System, and to Army Medicine for the past 32 years.”
David Smith, MD, acting principal deputy assistant secretary of defense for health affairs, will serve as acting director of DHA while the US Department of Defense conducts a nomination process to replace Crosland.
Army Lt. Gen. Telita Crosland, MD, MPH, MS, fourth director of the Defense Health Agency (DHA) and first Black woman to hold the position, has retired, bringing an abrupt end to an illustrious 32-year military career.
Acting Assistant Secretary of Defense for Health Affairs Stephen Ferrara, MD, said Crosland was “beginning her retirement” effective Feb. 28. According to Reuters, the statement offered no reasoning for Crosland’s quick departure, but 2 officials said she was informed that she must retire and was not given a reason why.
When she was promoted to director in January 2023, Lt. Gen. Crosland made history as the first Black woman to lead the DHA. Her former boss, Army Surgeon General Lt. Gen. R. Scott Dingle, called Crosland a “wonder woman” and “the baddest woman in the Army.” Her awards and decorations include the Legion of Merit with 2 oak leaf clusters, Meritorious Service Medal with 4 oak leaf clusters, Army Commendation Medal with 3 oak leaf clusters, Joint Service Achievement Medal, Army Staff Badge, and the Parachutist’s Badge. Lt. Gen. Crosland is also a member of the Order of Military Medical Merit. In addition to her medical and public health degrees, she has an master’s of science in national resource strategy.
Crosland entered the Army as a Medical Corps officer in 1993. Before becoming Director, she served as the Army’s Deputy Surgeon General, during which she oversaw response to a plethora of challenges: the COVID-19 pandemic, reformation of medical structures of the Army and other branches of services, and the Afghanistan withdrawal brought hundreds of evacuees with health needs.
“It was a sporty 3 years,” Crosland said in an interview with Military Times and other media, shortly before her promotion ceremony. But the pandemic and the Afghanistan mission helped her clarify how the services can work together as a team, she said.
Then, following a congressional mandate in 2024, > 700 military medical, dental, and veterinary facilities from the Army, Navy, and Air Force were being shifted over to the DHA. “The transition was tough. It was tough,” Crosland said. “First of all, it’s change, arguably the largest change in the Department of Defense since the Air Force moved from the Army. We’re talking about bringing all the military health care systems into one entity. Change is difficult.”
But the essence of the services’ military health care has never changed, she said in the press conference. A family health physician, Crosland emphasized the importance of caring for all the 9.6 million beneficiaries in the Military Health System. “The pandemic showed what we’re for,” she said. “We’re still a military health care system that has to take care of the force, and the beneficiaries we’re privileged to serve.”
Family medicine is about the holistic person, Crosland said. “That will come out as I look at our health care system to make sure that ultimately that’s what we’re about … improving the health of an individual, whether you wear a uniform, you wore a uniform, or you served side-by-side with someone who wore a uniform.”
Crosland’s departure came just days before she was scheduled to speak at the AMSUS - Society of Federal Health Professionals’ annual military and federal health care conference. It also comes days after the Trump administration fired multiple top military leaders, including Joint Chiefs of Staff Chairman Gen. CQ Brown, Chief of Naval Operations Adm. Lisa Franchetti, Air Force Vice Chief of Staff Gen. James C. Slife and several top military lawyers.
Ferrara thanked Crosland “for her dedication to the nation, to the Military Health System, and to Army Medicine for the past 32 years.”
David Smith, MD, acting principal deputy assistant secretary of defense for health affairs, will serve as acting director of DHA while the US Department of Defense conducts a nomination process to replace Crosland.
More Layoffs at VA and Other Health Agencies
The large-scale layoffs in the federal government that began in January continue, as the US Department of Veterans Affairs (VA) announced the dismissal of > 1400 employees in “non-mission critical roles,” including those “related to DEI” (diversity, equity, inclusion) on Feb. 24. According to VA, those fired are bargaining-unit probationary employees who have served > 1 year in a competitive service appointment or who have served > 2 years in an excepted service appointment.
The agency says the “personnel moves” will save > $83 million annually, which will be redirected back toward health care, benefits and services for VA beneficiaries.
Of the nearly 40,000 probationary employees in the department, the majority were exempt, the VA says, because they serve in mission-critical positions—primarily those supporting benefits and services for VA beneficiaries, such as Veterans Crisis Line responders. VA employees who elected to participate in the Office of Personnel Management’s (OPM) deferred resignation program are also exempt. As an “additional safeguard,” the VA says the first Senior Executive Service (SES) or SES-equivalent leader in a dismissed employee’s chain of command can request the employee be exempted from removal.
The latest cuts follow the dismissal of > 1000 employees announced Feb. 13. In that case, the VA expected to save > $98 million annually, also to be “redirected back” toward health care, benefits, and services. VA insists it continues to hire for mission-critical positions that are exempt from the federal hiring freeze.
Layoffs are also impacting other federal public health agencies. Although the White House has not released figures, a ProPublica investigation details the impact of the layoffs on organ transplant and maternal mortality programs. Other layoffs that have been reported include :
- About 750 workers at the Centers for Disease Control and Prevention
- More than 1000 staffers at the National Institutes of Health
- “Dozens” at the Centers for Medicare and Medicaid Services
- “Scores” at the US Food and Drug Administration
- Downsizing at the VA EHR Modernization Integration Office
“By gutting essential health staff, hiding vital public health data, and silencing health experts, these actions have left every American family more vulnerable to deadly disease outbreaks, unsafe food and water, and preventable deaths,” the American Public Health Association said in a press release. “This is also not just an attack on federal institutions – it's a direct attack on every parent trying to protect their child from disease, every worker relying on public health safeguards and every family depending on rapid responses to outbreaks and emergencies.” American Public Health Association also announced that is suing the Department of Government Efficiency for violating federal transparency laws. “It is unfathomable that anybody thinks these cuts have value and are doing anything other than being performative.”
In 2024, the VA had planned to trim its 458,000-member workforce by about 2%, or 10,000 employees, through attrition (with most of the reduction coming from VHA). VHA Chief Financial Officer Laura Duke told reporters in March 2024 that the reduction was needed because the agency had far exceeded its hiring goals last year, and was also seeing higher-than-expected retention rates.
“These and other recent personnel decisions are extraordinarily difficult, but VA is focused on allocating its resources to help as many veterans, families, caregivers, and survivors as possible,” VA Secretary Doug Collins said. “These moves will not hurt VA health care, benefits or beneficiaries. In fact, veterans are going to notice a change for the better. In the coming weeks and months, VA will be announcing plans to put these resources to work helping the department fulfill its core mission: providing the best possible care and benefits to veterans, their families, caregivers and survivors.”
Senate Veterans’ Affairs Committee Ranking Member Richard Blumenthal (D-CT) and a group of 35 Democratic senators signed a letter earlier in February calling for Sec. Collins to immediately reinstate the terminated VA employees. “[W]e were outraged,” the letter said, “by the Administration’s abrupt and indiscriminate termination of tens of thousands of workers across almost every government agency, including more than 1000 Department of Veterans Affairs (VA) employees. We were further disturbed by the manner in which you publicly celebrated this reprehensible announcement—a clear departure from the assurances provided throughout your confirmation process to never ‘balance budgets on the back of veterans’ benefits’ and to always ‘put the veteran first.’”
Blumenthal also notes that the “continued mass terminations” come at a time when the VA faces critical staffing shortages and increased demand for its services. The senators detailed the effects the cuts were having, including how openings for new clinics were delayed because the VA cannot hire the necessary staff to open their doors; service lines at VA hospitals and clinics halted; beds and operating rooms at VA facilities suspended; support lines for caregivers reduced; Veterans Crisis Line employees fired; and suicide prevention training sessions postponed or canceled.
The large-scale layoffs in the federal government that began in January continue, as the US Department of Veterans Affairs (VA) announced the dismissal of > 1400 employees in “non-mission critical roles,” including those “related to DEI” (diversity, equity, inclusion) on Feb. 24. According to VA, those fired are bargaining-unit probationary employees who have served > 1 year in a competitive service appointment or who have served > 2 years in an excepted service appointment.
The agency says the “personnel moves” will save > $83 million annually, which will be redirected back toward health care, benefits and services for VA beneficiaries.
Of the nearly 40,000 probationary employees in the department, the majority were exempt, the VA says, because they serve in mission-critical positions—primarily those supporting benefits and services for VA beneficiaries, such as Veterans Crisis Line responders. VA employees who elected to participate in the Office of Personnel Management’s (OPM) deferred resignation program are also exempt. As an “additional safeguard,” the VA says the first Senior Executive Service (SES) or SES-equivalent leader in a dismissed employee’s chain of command can request the employee be exempted from removal.
The latest cuts follow the dismissal of > 1000 employees announced Feb. 13. In that case, the VA expected to save > $98 million annually, also to be “redirected back” toward health care, benefits, and services. VA insists it continues to hire for mission-critical positions that are exempt from the federal hiring freeze.
Layoffs are also impacting other federal public health agencies. Although the White House has not released figures, a ProPublica investigation details the impact of the layoffs on organ transplant and maternal mortality programs. Other layoffs that have been reported include :
- About 750 workers at the Centers for Disease Control and Prevention
- More than 1000 staffers at the National Institutes of Health
- “Dozens” at the Centers for Medicare and Medicaid Services
- “Scores” at the US Food and Drug Administration
- Downsizing at the VA EHR Modernization Integration Office
“By gutting essential health staff, hiding vital public health data, and silencing health experts, these actions have left every American family more vulnerable to deadly disease outbreaks, unsafe food and water, and preventable deaths,” the American Public Health Association said in a press release. “This is also not just an attack on federal institutions – it's a direct attack on every parent trying to protect their child from disease, every worker relying on public health safeguards and every family depending on rapid responses to outbreaks and emergencies.” American Public Health Association also announced that is suing the Department of Government Efficiency for violating federal transparency laws. “It is unfathomable that anybody thinks these cuts have value and are doing anything other than being performative.”
In 2024, the VA had planned to trim its 458,000-member workforce by about 2%, or 10,000 employees, through attrition (with most of the reduction coming from VHA). VHA Chief Financial Officer Laura Duke told reporters in March 2024 that the reduction was needed because the agency had far exceeded its hiring goals last year, and was also seeing higher-than-expected retention rates.
“These and other recent personnel decisions are extraordinarily difficult, but VA is focused on allocating its resources to help as many veterans, families, caregivers, and survivors as possible,” VA Secretary Doug Collins said. “These moves will not hurt VA health care, benefits or beneficiaries. In fact, veterans are going to notice a change for the better. In the coming weeks and months, VA will be announcing plans to put these resources to work helping the department fulfill its core mission: providing the best possible care and benefits to veterans, their families, caregivers and survivors.”
Senate Veterans’ Affairs Committee Ranking Member Richard Blumenthal (D-CT) and a group of 35 Democratic senators signed a letter earlier in February calling for Sec. Collins to immediately reinstate the terminated VA employees. “[W]e were outraged,” the letter said, “by the Administration’s abrupt and indiscriminate termination of tens of thousands of workers across almost every government agency, including more than 1000 Department of Veterans Affairs (VA) employees. We were further disturbed by the manner in which you publicly celebrated this reprehensible announcement—a clear departure from the assurances provided throughout your confirmation process to never ‘balance budgets on the back of veterans’ benefits’ and to always ‘put the veteran first.’”
Blumenthal also notes that the “continued mass terminations” come at a time when the VA faces critical staffing shortages and increased demand for its services. The senators detailed the effects the cuts were having, including how openings for new clinics were delayed because the VA cannot hire the necessary staff to open their doors; service lines at VA hospitals and clinics halted; beds and operating rooms at VA facilities suspended; support lines for caregivers reduced; Veterans Crisis Line employees fired; and suicide prevention training sessions postponed or canceled.
The large-scale layoffs in the federal government that began in January continue, as the US Department of Veterans Affairs (VA) announced the dismissal of > 1400 employees in “non-mission critical roles,” including those “related to DEI” (diversity, equity, inclusion) on Feb. 24. According to VA, those fired are bargaining-unit probationary employees who have served > 1 year in a competitive service appointment or who have served > 2 years in an excepted service appointment.
The agency says the “personnel moves” will save > $83 million annually, which will be redirected back toward health care, benefits and services for VA beneficiaries.
Of the nearly 40,000 probationary employees in the department, the majority were exempt, the VA says, because they serve in mission-critical positions—primarily those supporting benefits and services for VA beneficiaries, such as Veterans Crisis Line responders. VA employees who elected to participate in the Office of Personnel Management’s (OPM) deferred resignation program are also exempt. As an “additional safeguard,” the VA says the first Senior Executive Service (SES) or SES-equivalent leader in a dismissed employee’s chain of command can request the employee be exempted from removal.
The latest cuts follow the dismissal of > 1000 employees announced Feb. 13. In that case, the VA expected to save > $98 million annually, also to be “redirected back” toward health care, benefits, and services. VA insists it continues to hire for mission-critical positions that are exempt from the federal hiring freeze.
Layoffs are also impacting other federal public health agencies. Although the White House has not released figures, a ProPublica investigation details the impact of the layoffs on organ transplant and maternal mortality programs. Other layoffs that have been reported include :
- About 750 workers at the Centers for Disease Control and Prevention
- More than 1000 staffers at the National Institutes of Health
- “Dozens” at the Centers for Medicare and Medicaid Services
- “Scores” at the US Food and Drug Administration
- Downsizing at the VA EHR Modernization Integration Office
“By gutting essential health staff, hiding vital public health data, and silencing health experts, these actions have left every American family more vulnerable to deadly disease outbreaks, unsafe food and water, and preventable deaths,” the American Public Health Association said in a press release. “This is also not just an attack on federal institutions – it's a direct attack on every parent trying to protect their child from disease, every worker relying on public health safeguards and every family depending on rapid responses to outbreaks and emergencies.” American Public Health Association also announced that is suing the Department of Government Efficiency for violating federal transparency laws. “It is unfathomable that anybody thinks these cuts have value and are doing anything other than being performative.”
In 2024, the VA had planned to trim its 458,000-member workforce by about 2%, or 10,000 employees, through attrition (with most of the reduction coming from VHA). VHA Chief Financial Officer Laura Duke told reporters in March 2024 that the reduction was needed because the agency had far exceeded its hiring goals last year, and was also seeing higher-than-expected retention rates.
“These and other recent personnel decisions are extraordinarily difficult, but VA is focused on allocating its resources to help as many veterans, families, caregivers, and survivors as possible,” VA Secretary Doug Collins said. “These moves will not hurt VA health care, benefits or beneficiaries. In fact, veterans are going to notice a change for the better. In the coming weeks and months, VA will be announcing plans to put these resources to work helping the department fulfill its core mission: providing the best possible care and benefits to veterans, their families, caregivers and survivors.”
Senate Veterans’ Affairs Committee Ranking Member Richard Blumenthal (D-CT) and a group of 35 Democratic senators signed a letter earlier in February calling for Sec. Collins to immediately reinstate the terminated VA employees. “[W]e were outraged,” the letter said, “by the Administration’s abrupt and indiscriminate termination of tens of thousands of workers across almost every government agency, including more than 1000 Department of Veterans Affairs (VA) employees. We were further disturbed by the manner in which you publicly celebrated this reprehensible announcement—a clear departure from the assurances provided throughout your confirmation process to never ‘balance budgets on the back of veterans’ benefits’ and to always ‘put the veteran first.’”
Blumenthal also notes that the “continued mass terminations” come at a time when the VA faces critical staffing shortages and increased demand for its services. The senators detailed the effects the cuts were having, including how openings for new clinics were delayed because the VA cannot hire the necessary staff to open their doors; service lines at VA hospitals and clinics halted; beds and operating rooms at VA facilities suspended; support lines for caregivers reduced; Veterans Crisis Line employees fired; and suicide prevention training sessions postponed or canceled.
Landmark VA Study Uncovers Gene Variant Linked to Prostate Cancer
Only about 5% of hereditary prostate cancer (HPC) cases can be explained by known genetic variants, but a groundbreaking US Department of Veterans Affairs (VA) study could revolutionize the diagnosis, prevention, and treatment of HPC in a similar fashion that the discovery of the BRAC2 gene did in breast cancer.
The study, conducted at the VA Tennessee Valley Healthcare System in accordance with Vanderbilt University Medical Center and the VA Million Veteran Program (MVP), linked variants of the WNT9B gene with a greater risk of prostate cancer.
About 15,000 veterans are diagnosed with prostate cancer and treated at the VA annually, and > 200,000 veterans are prostate cancer survivors. According to Bruce Montgomery, MD, an oncologist with VA Puget Sound Health Care System, “Veterans are unique in that those men exposed to Agent Orange during the Vietnam War are at elevated risk for prostate cancer.” Montgomery added that germline pathogenic variants in genes such as BRCA2 and HOXB13 are other risk factors.
This genome-wide study searched for recurrently observed variants that carried the most risk. The study gathered data from a familial case-control population in the Nashville Familial Prostate Cancer Study (NFPCS) and International Consortium for Prostate Cancer Genetics (ICPCG). For evidence of replication, the study turned to 4 biobanks: the MVP, All of Us, the UK Biobank, and FinnGen.
The NFPCS is a case-control study based on family history. Patients included those undergoing treatment for prostate cancer and controls undergoing routine screening at Vanderbilt University Medical Center and the Nashville VA Medical Center between 2003 and 2009. Patients were included in the analysis if they had also had a first- or second-degree relative with prostate cancer.
The ICPCG dataset encompasses unrelated HPC cases aggregated from 12 study sites across Finland, France, Germany, the UK, and the US. The MVP is the nation’s largest biorepository of veteran data and has one of the world’s most diverse cohorts of any genetic research program. More than 1 million veterans are enrolled, and 800-plus researchers are working on > 100 projects.
Pathogenic variants of only 2 genes met the replication requirement with genome-wide significance: HOXB13 and WNT9B. HOXB13 has been reported on in the literature, but this is the first study to investigate WNT9B.
Researchers identified 2 variants of the WNT9B gene: WNT9B E152K carried 2.5-fold risk and reached genome-wide significance under meta-analysis, collectively encompassing one-half million patients. The association of WNT9B E152K with prostate cancer was supported by the familial study populations and each biobank, with genome-wide significance. Variant WNT9B Q47R reached genome-wide significance in the Finnish study. The Q47R founder haplotype was also carried by familial prostate cancer cases in the US and UK.
Autosomal dominant WNT9B pathogenic variants are already known to cause embryonic developmental sequence defects, leading later to prostatic cysts, enlarged prostate, and seminal vesicle cysts. Seminal vesicle adenocarcinoma (or squamous cell carcinoma) and clear cell carcinoma of the prostate have also been reported.
The study found that HOXB13 and WNT9B “share an unexpected commonality.” Both genes function in embryonic genitourinary development. WNT9B pathogenic variants cause the autosomal dominant Mayer-Rokitansky-Küster-Hauser syndrome, featuring genitourinary developmental defects. The study concluded: “Collectively, our observations implicate inherited variation in pathways guiding embryonic genitourinary development in the development of prostate cancer.”
“Significant investments” in VA-specific clinical trials recently have been pursued through a joint agreement between the VA and the Prostate Cancer Foundation, Montgomery said: “The Prostate Cancer Foundation is supporting tumor and germline sequencing of prostate cancer for veterans with advanced disease and providing resources to set up research infrastructure at 10 centers nationwide.”
The VA has also published a prostate cancer clinical pathway and is in the process of creating a national prostate cancer registry. Such a database, as well as the MVP are both unique to the VA and key to research such as the Predicting Metastatic Progression of High Risk Localized Prostate Cancer study, which began in 2023. Five VA medical centers are collaborating on an artificial intelligence algorithm that will detect patterns indicative of aggressive prostate cancer.
“A digital repository for data will allow for development, testing, and validation of prognostic classifiers that could positively impact clinical management of veterans with high-risk prostate cancer,” said Matthew Rettig, MD, chief of oncology and hematology at the Greater Los Angeles VA Medical Center who was coprincipal investigator for the study. “The infrastructure developed by this research will serve as a valuable hub for future discovery.”
About 12% of men with metastatic prostate cancer carry a pathogenic germline alteration that could warrant the use of PARP (poly [ADP-ribose] polymerase) inhibitors or platinum chemotherapy, neither of which is part of standard care. National Comprehensive Cancer Network guidelines recommend germline testing in men with metastatic prostate cancer. In addition, “the family members of veterans who carry these alterations could benefit from undergoing testing and taking advantage of potentially life-saving interventions and surveillance strategies if they are also carriers,” Montgomery wrote.
The VA is committed to improving access to germline testing for men with metastatic prostate cancer in several ways. Montgomery pointed to the system-wide VA genetic counseling and testing resource, the Genomic Medicine Service, and said somatic testing is available across the VA through the National Precision Oncology Program. Both programs can be extremely important to veterans because they provide access to precision oncology studies, along with off-label use of effective treatments.
Precision oncology is the most rapidly moving area in prostate cancer, according to Montgomery. “In the VA, this has been embraced as a very specific need to find these therapeutic options for all veterans as quickly as possible. I am most excited by how the enthusiasm for these approaches is supported at all levels, both nationally and locally, because it makes implementing very significant changes to research and treatment possible.”
Only about 5% of hereditary prostate cancer (HPC) cases can be explained by known genetic variants, but a groundbreaking US Department of Veterans Affairs (VA) study could revolutionize the diagnosis, prevention, and treatment of HPC in a similar fashion that the discovery of the BRAC2 gene did in breast cancer.
The study, conducted at the VA Tennessee Valley Healthcare System in accordance with Vanderbilt University Medical Center and the VA Million Veteran Program (MVP), linked variants of the WNT9B gene with a greater risk of prostate cancer.
About 15,000 veterans are diagnosed with prostate cancer and treated at the VA annually, and > 200,000 veterans are prostate cancer survivors. According to Bruce Montgomery, MD, an oncologist with VA Puget Sound Health Care System, “Veterans are unique in that those men exposed to Agent Orange during the Vietnam War are at elevated risk for prostate cancer.” Montgomery added that germline pathogenic variants in genes such as BRCA2 and HOXB13 are other risk factors.
This genome-wide study searched for recurrently observed variants that carried the most risk. The study gathered data from a familial case-control population in the Nashville Familial Prostate Cancer Study (NFPCS) and International Consortium for Prostate Cancer Genetics (ICPCG). For evidence of replication, the study turned to 4 biobanks: the MVP, All of Us, the UK Biobank, and FinnGen.
The NFPCS is a case-control study based on family history. Patients included those undergoing treatment for prostate cancer and controls undergoing routine screening at Vanderbilt University Medical Center and the Nashville VA Medical Center between 2003 and 2009. Patients were included in the analysis if they had also had a first- or second-degree relative with prostate cancer.
The ICPCG dataset encompasses unrelated HPC cases aggregated from 12 study sites across Finland, France, Germany, the UK, and the US. The MVP is the nation’s largest biorepository of veteran data and has one of the world’s most diverse cohorts of any genetic research program. More than 1 million veterans are enrolled, and 800-plus researchers are working on > 100 projects.
Pathogenic variants of only 2 genes met the replication requirement with genome-wide significance: HOXB13 and WNT9B. HOXB13 has been reported on in the literature, but this is the first study to investigate WNT9B.
Researchers identified 2 variants of the WNT9B gene: WNT9B E152K carried 2.5-fold risk and reached genome-wide significance under meta-analysis, collectively encompassing one-half million patients. The association of WNT9B E152K with prostate cancer was supported by the familial study populations and each biobank, with genome-wide significance. Variant WNT9B Q47R reached genome-wide significance in the Finnish study. The Q47R founder haplotype was also carried by familial prostate cancer cases in the US and UK.
Autosomal dominant WNT9B pathogenic variants are already known to cause embryonic developmental sequence defects, leading later to prostatic cysts, enlarged prostate, and seminal vesicle cysts. Seminal vesicle adenocarcinoma (or squamous cell carcinoma) and clear cell carcinoma of the prostate have also been reported.
The study found that HOXB13 and WNT9B “share an unexpected commonality.” Both genes function in embryonic genitourinary development. WNT9B pathogenic variants cause the autosomal dominant Mayer-Rokitansky-Küster-Hauser syndrome, featuring genitourinary developmental defects. The study concluded: “Collectively, our observations implicate inherited variation in pathways guiding embryonic genitourinary development in the development of prostate cancer.”
“Significant investments” in VA-specific clinical trials recently have been pursued through a joint agreement between the VA and the Prostate Cancer Foundation, Montgomery said: “The Prostate Cancer Foundation is supporting tumor and germline sequencing of prostate cancer for veterans with advanced disease and providing resources to set up research infrastructure at 10 centers nationwide.”
The VA has also published a prostate cancer clinical pathway and is in the process of creating a national prostate cancer registry. Such a database, as well as the MVP are both unique to the VA and key to research such as the Predicting Metastatic Progression of High Risk Localized Prostate Cancer study, which began in 2023. Five VA medical centers are collaborating on an artificial intelligence algorithm that will detect patterns indicative of aggressive prostate cancer.
“A digital repository for data will allow for development, testing, and validation of prognostic classifiers that could positively impact clinical management of veterans with high-risk prostate cancer,” said Matthew Rettig, MD, chief of oncology and hematology at the Greater Los Angeles VA Medical Center who was coprincipal investigator for the study. “The infrastructure developed by this research will serve as a valuable hub for future discovery.”
About 12% of men with metastatic prostate cancer carry a pathogenic germline alteration that could warrant the use of PARP (poly [ADP-ribose] polymerase) inhibitors or platinum chemotherapy, neither of which is part of standard care. National Comprehensive Cancer Network guidelines recommend germline testing in men with metastatic prostate cancer. In addition, “the family members of veterans who carry these alterations could benefit from undergoing testing and taking advantage of potentially life-saving interventions and surveillance strategies if they are also carriers,” Montgomery wrote.
The VA is committed to improving access to germline testing for men with metastatic prostate cancer in several ways. Montgomery pointed to the system-wide VA genetic counseling and testing resource, the Genomic Medicine Service, and said somatic testing is available across the VA through the National Precision Oncology Program. Both programs can be extremely important to veterans because they provide access to precision oncology studies, along with off-label use of effective treatments.
Precision oncology is the most rapidly moving area in prostate cancer, according to Montgomery. “In the VA, this has been embraced as a very specific need to find these therapeutic options for all veterans as quickly as possible. I am most excited by how the enthusiasm for these approaches is supported at all levels, both nationally and locally, because it makes implementing very significant changes to research and treatment possible.”
Only about 5% of hereditary prostate cancer (HPC) cases can be explained by known genetic variants, but a groundbreaking US Department of Veterans Affairs (VA) study could revolutionize the diagnosis, prevention, and treatment of HPC in a similar fashion that the discovery of the BRAC2 gene did in breast cancer.
The study, conducted at the VA Tennessee Valley Healthcare System in accordance with Vanderbilt University Medical Center and the VA Million Veteran Program (MVP), linked variants of the WNT9B gene with a greater risk of prostate cancer.
About 15,000 veterans are diagnosed with prostate cancer and treated at the VA annually, and > 200,000 veterans are prostate cancer survivors. According to Bruce Montgomery, MD, an oncologist with VA Puget Sound Health Care System, “Veterans are unique in that those men exposed to Agent Orange during the Vietnam War are at elevated risk for prostate cancer.” Montgomery added that germline pathogenic variants in genes such as BRCA2 and HOXB13 are other risk factors.
This genome-wide study searched for recurrently observed variants that carried the most risk. The study gathered data from a familial case-control population in the Nashville Familial Prostate Cancer Study (NFPCS) and International Consortium for Prostate Cancer Genetics (ICPCG). For evidence of replication, the study turned to 4 biobanks: the MVP, All of Us, the UK Biobank, and FinnGen.
The NFPCS is a case-control study based on family history. Patients included those undergoing treatment for prostate cancer and controls undergoing routine screening at Vanderbilt University Medical Center and the Nashville VA Medical Center between 2003 and 2009. Patients were included in the analysis if they had also had a first- or second-degree relative with prostate cancer.
The ICPCG dataset encompasses unrelated HPC cases aggregated from 12 study sites across Finland, France, Germany, the UK, and the US. The MVP is the nation’s largest biorepository of veteran data and has one of the world’s most diverse cohorts of any genetic research program. More than 1 million veterans are enrolled, and 800-plus researchers are working on > 100 projects.
Pathogenic variants of only 2 genes met the replication requirement with genome-wide significance: HOXB13 and WNT9B. HOXB13 has been reported on in the literature, but this is the first study to investigate WNT9B.
Researchers identified 2 variants of the WNT9B gene: WNT9B E152K carried 2.5-fold risk and reached genome-wide significance under meta-analysis, collectively encompassing one-half million patients. The association of WNT9B E152K with prostate cancer was supported by the familial study populations and each biobank, with genome-wide significance. Variant WNT9B Q47R reached genome-wide significance in the Finnish study. The Q47R founder haplotype was also carried by familial prostate cancer cases in the US and UK.
Autosomal dominant WNT9B pathogenic variants are already known to cause embryonic developmental sequence defects, leading later to prostatic cysts, enlarged prostate, and seminal vesicle cysts. Seminal vesicle adenocarcinoma (or squamous cell carcinoma) and clear cell carcinoma of the prostate have also been reported.
The study found that HOXB13 and WNT9B “share an unexpected commonality.” Both genes function in embryonic genitourinary development. WNT9B pathogenic variants cause the autosomal dominant Mayer-Rokitansky-Küster-Hauser syndrome, featuring genitourinary developmental defects. The study concluded: “Collectively, our observations implicate inherited variation in pathways guiding embryonic genitourinary development in the development of prostate cancer.”
“Significant investments” in VA-specific clinical trials recently have been pursued through a joint agreement between the VA and the Prostate Cancer Foundation, Montgomery said: “The Prostate Cancer Foundation is supporting tumor and germline sequencing of prostate cancer for veterans with advanced disease and providing resources to set up research infrastructure at 10 centers nationwide.”
The VA has also published a prostate cancer clinical pathway and is in the process of creating a national prostate cancer registry. Such a database, as well as the MVP are both unique to the VA and key to research such as the Predicting Metastatic Progression of High Risk Localized Prostate Cancer study, which began in 2023. Five VA medical centers are collaborating on an artificial intelligence algorithm that will detect patterns indicative of aggressive prostate cancer.
“A digital repository for data will allow for development, testing, and validation of prognostic classifiers that could positively impact clinical management of veterans with high-risk prostate cancer,” said Matthew Rettig, MD, chief of oncology and hematology at the Greater Los Angeles VA Medical Center who was coprincipal investigator for the study. “The infrastructure developed by this research will serve as a valuable hub for future discovery.”
About 12% of men with metastatic prostate cancer carry a pathogenic germline alteration that could warrant the use of PARP (poly [ADP-ribose] polymerase) inhibitors or platinum chemotherapy, neither of which is part of standard care. National Comprehensive Cancer Network guidelines recommend germline testing in men with metastatic prostate cancer. In addition, “the family members of veterans who carry these alterations could benefit from undergoing testing and taking advantage of potentially life-saving interventions and surveillance strategies if they are also carriers,” Montgomery wrote.
The VA is committed to improving access to germline testing for men with metastatic prostate cancer in several ways. Montgomery pointed to the system-wide VA genetic counseling and testing resource, the Genomic Medicine Service, and said somatic testing is available across the VA through the National Precision Oncology Program. Both programs can be extremely important to veterans because they provide access to precision oncology studies, along with off-label use of effective treatments.
Precision oncology is the most rapidly moving area in prostate cancer, according to Montgomery. “In the VA, this has been embraced as a very specific need to find these therapeutic options for all veterans as quickly as possible. I am most excited by how the enthusiasm for these approaches is supported at all levels, both nationally and locally, because it makes implementing very significant changes to research and treatment possible.”
VA Exempts Clinical Staff From OPM Deferred Resignation Program
The US Department of Veterans Affairs (VA) announced on Feb. 7, 2025, that 116 Veterans Health Administration job classifications will not be eligible for the deferred resignation plan emailed by the Office of Personnel Management (OPM). The exemptions include Title 38 and Hybrid Title 38 positions, including doctors, nurses, and most medical staff.
The original OPM email offer had a Feb. 6, 2025, deadline for accepting the offer and a resignation date of no later than Sept. 30, 2025. However, the offer has been put on hold following a limited temporary restraining order from a Federal District Court in Massachusetts. Judge George O’Toole enjoined the OPM from “taking any further action to implement the so-called Fork Directive.” Arguments on the program’s legal merits began at a separate hearing on Monday.
The 116 roles exempted include physicians, nurses, pharmacists and pharmacy technicians, therapists, data scientists, dieticians, health and medical instrument technicians, among other roles.
OPM also included Voluntary Early Retirement Authority (VERA) in the deferred resignation offer. In a Feb. 6 email, the VA’s Office of the Chief Human Capital Officer (OCHCO) said: “The Department of Veterans Affairs established a list of occupations that are excluded from participating in DRP and VERA. If your occupation is on this list, you are not eligible to participate in the DRP.”
The US Department of Veterans Affairs (VA) announced on Feb. 7, 2025, that 116 Veterans Health Administration job classifications will not be eligible for the deferred resignation plan emailed by the Office of Personnel Management (OPM). The exemptions include Title 38 and Hybrid Title 38 positions, including doctors, nurses, and most medical staff.
The original OPM email offer had a Feb. 6, 2025, deadline for accepting the offer and a resignation date of no later than Sept. 30, 2025. However, the offer has been put on hold following a limited temporary restraining order from a Federal District Court in Massachusetts. Judge George O’Toole enjoined the OPM from “taking any further action to implement the so-called Fork Directive.” Arguments on the program’s legal merits began at a separate hearing on Monday.
The 116 roles exempted include physicians, nurses, pharmacists and pharmacy technicians, therapists, data scientists, dieticians, health and medical instrument technicians, among other roles.
OPM also included Voluntary Early Retirement Authority (VERA) in the deferred resignation offer. In a Feb. 6 email, the VA’s Office of the Chief Human Capital Officer (OCHCO) said: “The Department of Veterans Affairs established a list of occupations that are excluded from participating in DRP and VERA. If your occupation is on this list, you are not eligible to participate in the DRP.”
The US Department of Veterans Affairs (VA) announced on Feb. 7, 2025, that 116 Veterans Health Administration job classifications will not be eligible for the deferred resignation plan emailed by the Office of Personnel Management (OPM). The exemptions include Title 38 and Hybrid Title 38 positions, including doctors, nurses, and most medical staff.
The original OPM email offer had a Feb. 6, 2025, deadline for accepting the offer and a resignation date of no later than Sept. 30, 2025. However, the offer has been put on hold following a limited temporary restraining order from a Federal District Court in Massachusetts. Judge George O’Toole enjoined the OPM from “taking any further action to implement the so-called Fork Directive.” Arguments on the program’s legal merits began at a separate hearing on Monday.
The 116 roles exempted include physicians, nurses, pharmacists and pharmacy technicians, therapists, data scientists, dieticians, health and medical instrument technicians, among other roles.
OPM also included Voluntary Early Retirement Authority (VERA) in the deferred resignation offer. In a Feb. 6 email, the VA’s Office of the Chief Human Capital Officer (OCHCO) said: “The Department of Veterans Affairs established a list of occupations that are excluded from participating in DRP and VERA. If your occupation is on this list, you are not eligible to participate in the DRP.”