User login
Three popular IBS diets found equivalent
Three widely followed diets for nonconstipated irritable bowel syndrome (IBS) produce similar results, but traditional dietary advice (TDA) is easier to follow, researchers say.
“We recommend TDA as the first-choice dietary option due to its widespread availability and patient friendliness,” Anupam Rej, MBChB, from Teaching Hospitals NHS Foundation Trust in Sheffield, England, and colleagues write.
According to their study, about half the people following each of three diets – TDA; gluten-free; and low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAP) – reported at least a 50% reduction in their symptoms.
They noted, however, that the low-FODMAP diet produced the most improvement in depression and dysphoria.
The study was published online in Clinical Gastroenterology and Hepatology.
What the dietary options entailed
The three diets have different origins and methodologies, but all are designed to reduce the abdominal pain, bloating, and altered bowel habits that characterize IBS.
TDA is based on recommendations of the UK National Institute for Health and Care Excellence and the British Dietetic Association. It includes “sensible eating patterns,” such as regular meals, never having too much or too little, and sufficient hydration. It calls for a reduction in alcoholic, caffeinated, and “fizzy” drinks; spicy, fatty, and processed foods; fresh fruit (a maximum of three per day); and fiber and other gas-producing foods, such as beans, bread, and sweeteners. It also asks people to address any perceived food intolerance, such as dairy.
In North America, the low-FODMAP diet is prescribed as first-line therapy, and the American College of Gastroenterology has given it a conditional recommendation.
FODMAPs are short-chain fermentable carbohydrates found in many fruits, vegetables, dairy products, artificial sweeteners, and wheat. They increase small intestinal water volume and colonic gas production that can induce gastrointestinal symptoms in people with visceral hypersensitivity.
People following the low-FODMAP diet start by eliminating all FODMAPs for 4-6 weeks, then gradually reintroducing them to determine which are most likely to trigger symptoms.
A gluten-free diet, inspired by what is prescribed to treat celiac disease, has gained popularity in recent years. Although researchers debate the mechanism by which this diet improves symptoms, one leading theory is a reduction in fructans that accompany gluten in foods such as bread.
A rare head-to-head comparison trial
The low-FODMAP diet has proved itself in more clinical trials than the other two approaches, but few, if any, trials have compared them head-to-head in a pragmatic randomized trial, Dr. Rej and colleagues found after reviewing the literature.
They set about filling this gap by recruiting 114 people with IBS and randomly assigning each of them to one of the diets. Ninety-nine people finished the trial, with 33 following each of the diets. People with IBS-constipation were excluded.
Participants were a mean age of 37 years. Seventy-one percent were female, and 88% were White. Their mean IBS symptom severity score was 301, with 9% rating their symptoms as mild, 47% as moderate, and 45% as severe.
The proportion who reported at least a 50% reduction in their symptoms was 58% for the gluten-free diet, 55% for the low-FODMAP diet, and 42% for the TDA. The differences in these proportions were not significant (P = .43).
The diets worked about as well regardless of whether the patients had IBS with diarrhea or IBS with mixed diarrhea and constipation.
More of the people on the low-FODMAP diet reported significant improvement in their depression and dysphoria than people on the other two diets.
Changes in anxiety, somatization, and other aspects of IBS quality of life didn’t differ significantly with diet.
Where the diets differ: cost and ease
Fewer people following the TDA rated it as expensive, difficult, or socially awkward, compared with the people following the other two diets.
More of those following the TDA and gluten-free diet found them easy to incorporate into their lives than those following the low-FODMAP diet. About two-thirds of the people in each of these groups said they would consider continuing their diets after the end of the study.
The proportion of people consuming the recommended dietary reference values for macronutrients did not change with any of the diets. However, those in the TDA group reduced their intake of potassium and iron. In the other groups, the researchers noted a reduction in thiamine and magnesium.
Because of COVID-19 restrictions, the researchers were able to collect stool samples from only half of participants. What they did collect showed no difference among the groups in dysbiosis index or functional bacterial profiles.
Baseline factors such as age, gender, IBS subtype, dysbiosis index, somatization, and mood did not predict response to the three diets.
Participants improved as much whether they received dietary instructions face-to-face or through a live virtual consultation.
Applications and limitations
At least one previous study showed that the low-FODMAP diet produced better results than the standard diets patients had been following, said Brian E. Lacy, MD, PhD, a professor of medicine at the Mayo Clinic in Jacksonville, Fla., who was not involved in the current study.
He agreed with the study’s conclusion that the TDA could be a good place for people with IBS to start.
“Based on their research, and the findings that patients thought the diet was less expensive, easier to follow, and easier to shop for, this is a reasonable approach,” he told this news organization. “However, if there’s no benefit with the traditional diet, then moving on to the more rigorous low-FODMAP diet makes sense to me.”
Study limitations include a short duration, lack of information about how patients can add foods back into their diet (particularly with the low-FODMAP diet), and insufficient sample size and lack of a placebo group contributing to an inability to detect all clinically significant differences among the diets, he said.
“Although this study is not definitive and doesn’t answer all key questions about which diet is best and how each performs in the long run, it does provide important information for patients and providers,” said Dr. Lacy.
The study was funded by Schaer. One of the study authors has reported receiving an educational grant from Schaer. Dr. Lacy has reported being on scientific advisory boards for Ironwood, Salix, and Allakos.
A version of this article first appeared on Medscape.com.
Three widely followed diets for nonconstipated irritable bowel syndrome (IBS) produce similar results, but traditional dietary advice (TDA) is easier to follow, researchers say.
“We recommend TDA as the first-choice dietary option due to its widespread availability and patient friendliness,” Anupam Rej, MBChB, from Teaching Hospitals NHS Foundation Trust in Sheffield, England, and colleagues write.
According to their study, about half the people following each of three diets – TDA; gluten-free; and low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAP) – reported at least a 50% reduction in their symptoms.
They noted, however, that the low-FODMAP diet produced the most improvement in depression and dysphoria.
The study was published online in Clinical Gastroenterology and Hepatology.
What the dietary options entailed
The three diets have different origins and methodologies, but all are designed to reduce the abdominal pain, bloating, and altered bowel habits that characterize IBS.
TDA is based on recommendations of the UK National Institute for Health and Care Excellence and the British Dietetic Association. It includes “sensible eating patterns,” such as regular meals, never having too much or too little, and sufficient hydration. It calls for a reduction in alcoholic, caffeinated, and “fizzy” drinks; spicy, fatty, and processed foods; fresh fruit (a maximum of three per day); and fiber and other gas-producing foods, such as beans, bread, and sweeteners. It also asks people to address any perceived food intolerance, such as dairy.
In North America, the low-FODMAP diet is prescribed as first-line therapy, and the American College of Gastroenterology has given it a conditional recommendation.
FODMAPs are short-chain fermentable carbohydrates found in many fruits, vegetables, dairy products, artificial sweeteners, and wheat. They increase small intestinal water volume and colonic gas production that can induce gastrointestinal symptoms in people with visceral hypersensitivity.
People following the low-FODMAP diet start by eliminating all FODMAPs for 4-6 weeks, then gradually reintroducing them to determine which are most likely to trigger symptoms.
A gluten-free diet, inspired by what is prescribed to treat celiac disease, has gained popularity in recent years. Although researchers debate the mechanism by which this diet improves symptoms, one leading theory is a reduction in fructans that accompany gluten in foods such as bread.
A rare head-to-head comparison trial
The low-FODMAP diet has proved itself in more clinical trials than the other two approaches, but few, if any, trials have compared them head-to-head in a pragmatic randomized trial, Dr. Rej and colleagues found after reviewing the literature.
They set about filling this gap by recruiting 114 people with IBS and randomly assigning each of them to one of the diets. Ninety-nine people finished the trial, with 33 following each of the diets. People with IBS-constipation were excluded.
Participants were a mean age of 37 years. Seventy-one percent were female, and 88% were White. Their mean IBS symptom severity score was 301, with 9% rating their symptoms as mild, 47% as moderate, and 45% as severe.
The proportion who reported at least a 50% reduction in their symptoms was 58% for the gluten-free diet, 55% for the low-FODMAP diet, and 42% for the TDA. The differences in these proportions were not significant (P = .43).
The diets worked about as well regardless of whether the patients had IBS with diarrhea or IBS with mixed diarrhea and constipation.
More of the people on the low-FODMAP diet reported significant improvement in their depression and dysphoria than people on the other two diets.
Changes in anxiety, somatization, and other aspects of IBS quality of life didn’t differ significantly with diet.
Where the diets differ: cost and ease
Fewer people following the TDA rated it as expensive, difficult, or socially awkward, compared with the people following the other two diets.
More of those following the TDA and gluten-free diet found them easy to incorporate into their lives than those following the low-FODMAP diet. About two-thirds of the people in each of these groups said they would consider continuing their diets after the end of the study.
The proportion of people consuming the recommended dietary reference values for macronutrients did not change with any of the diets. However, those in the TDA group reduced their intake of potassium and iron. In the other groups, the researchers noted a reduction in thiamine and magnesium.
Because of COVID-19 restrictions, the researchers were able to collect stool samples from only half of participants. What they did collect showed no difference among the groups in dysbiosis index or functional bacterial profiles.
Baseline factors such as age, gender, IBS subtype, dysbiosis index, somatization, and mood did not predict response to the three diets.
Participants improved as much whether they received dietary instructions face-to-face or through a live virtual consultation.
Applications and limitations
At least one previous study showed that the low-FODMAP diet produced better results than the standard diets patients had been following, said Brian E. Lacy, MD, PhD, a professor of medicine at the Mayo Clinic in Jacksonville, Fla., who was not involved in the current study.
He agreed with the study’s conclusion that the TDA could be a good place for people with IBS to start.
“Based on their research, and the findings that patients thought the diet was less expensive, easier to follow, and easier to shop for, this is a reasonable approach,” he told this news organization. “However, if there’s no benefit with the traditional diet, then moving on to the more rigorous low-FODMAP diet makes sense to me.”
Study limitations include a short duration, lack of information about how patients can add foods back into their diet (particularly with the low-FODMAP diet), and insufficient sample size and lack of a placebo group contributing to an inability to detect all clinically significant differences among the diets, he said.
“Although this study is not definitive and doesn’t answer all key questions about which diet is best and how each performs in the long run, it does provide important information for patients and providers,” said Dr. Lacy.
The study was funded by Schaer. One of the study authors has reported receiving an educational grant from Schaer. Dr. Lacy has reported being on scientific advisory boards for Ironwood, Salix, and Allakos.
A version of this article first appeared on Medscape.com.
Three widely followed diets for nonconstipated irritable bowel syndrome (IBS) produce similar results, but traditional dietary advice (TDA) is easier to follow, researchers say.
“We recommend TDA as the first-choice dietary option due to its widespread availability and patient friendliness,” Anupam Rej, MBChB, from Teaching Hospitals NHS Foundation Trust in Sheffield, England, and colleagues write.
According to their study, about half the people following each of three diets – TDA; gluten-free; and low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAP) – reported at least a 50% reduction in their symptoms.
They noted, however, that the low-FODMAP diet produced the most improvement in depression and dysphoria.
The study was published online in Clinical Gastroenterology and Hepatology.
What the dietary options entailed
The three diets have different origins and methodologies, but all are designed to reduce the abdominal pain, bloating, and altered bowel habits that characterize IBS.
TDA is based on recommendations of the UK National Institute for Health and Care Excellence and the British Dietetic Association. It includes “sensible eating patterns,” such as regular meals, never having too much or too little, and sufficient hydration. It calls for a reduction in alcoholic, caffeinated, and “fizzy” drinks; spicy, fatty, and processed foods; fresh fruit (a maximum of three per day); and fiber and other gas-producing foods, such as beans, bread, and sweeteners. It also asks people to address any perceived food intolerance, such as dairy.
In North America, the low-FODMAP diet is prescribed as first-line therapy, and the American College of Gastroenterology has given it a conditional recommendation.
FODMAPs are short-chain fermentable carbohydrates found in many fruits, vegetables, dairy products, artificial sweeteners, and wheat. They increase small intestinal water volume and colonic gas production that can induce gastrointestinal symptoms in people with visceral hypersensitivity.
People following the low-FODMAP diet start by eliminating all FODMAPs for 4-6 weeks, then gradually reintroducing them to determine which are most likely to trigger symptoms.
A gluten-free diet, inspired by what is prescribed to treat celiac disease, has gained popularity in recent years. Although researchers debate the mechanism by which this diet improves symptoms, one leading theory is a reduction in fructans that accompany gluten in foods such as bread.
A rare head-to-head comparison trial
The low-FODMAP diet has proved itself in more clinical trials than the other two approaches, but few, if any, trials have compared them head-to-head in a pragmatic randomized trial, Dr. Rej and colleagues found after reviewing the literature.
They set about filling this gap by recruiting 114 people with IBS and randomly assigning each of them to one of the diets. Ninety-nine people finished the trial, with 33 following each of the diets. People with IBS-constipation were excluded.
Participants were a mean age of 37 years. Seventy-one percent were female, and 88% were White. Their mean IBS symptom severity score was 301, with 9% rating their symptoms as mild, 47% as moderate, and 45% as severe.
The proportion who reported at least a 50% reduction in their symptoms was 58% for the gluten-free diet, 55% for the low-FODMAP diet, and 42% for the TDA. The differences in these proportions were not significant (P = .43).
The diets worked about as well regardless of whether the patients had IBS with diarrhea or IBS with mixed diarrhea and constipation.
More of the people on the low-FODMAP diet reported significant improvement in their depression and dysphoria than people on the other two diets.
Changes in anxiety, somatization, and other aspects of IBS quality of life didn’t differ significantly with diet.
Where the diets differ: cost and ease
Fewer people following the TDA rated it as expensive, difficult, or socially awkward, compared with the people following the other two diets.
More of those following the TDA and gluten-free diet found them easy to incorporate into their lives than those following the low-FODMAP diet. About two-thirds of the people in each of these groups said they would consider continuing their diets after the end of the study.
The proportion of people consuming the recommended dietary reference values for macronutrients did not change with any of the diets. However, those in the TDA group reduced their intake of potassium and iron. In the other groups, the researchers noted a reduction in thiamine and magnesium.
Because of COVID-19 restrictions, the researchers were able to collect stool samples from only half of participants. What they did collect showed no difference among the groups in dysbiosis index or functional bacterial profiles.
Baseline factors such as age, gender, IBS subtype, dysbiosis index, somatization, and mood did not predict response to the three diets.
Participants improved as much whether they received dietary instructions face-to-face or through a live virtual consultation.
Applications and limitations
At least one previous study showed that the low-FODMAP diet produced better results than the standard diets patients had been following, said Brian E. Lacy, MD, PhD, a professor of medicine at the Mayo Clinic in Jacksonville, Fla., who was not involved in the current study.
He agreed with the study’s conclusion that the TDA could be a good place for people with IBS to start.
“Based on their research, and the findings that patients thought the diet was less expensive, easier to follow, and easier to shop for, this is a reasonable approach,” he told this news organization. “However, if there’s no benefit with the traditional diet, then moving on to the more rigorous low-FODMAP diet makes sense to me.”
Study limitations include a short duration, lack of information about how patients can add foods back into their diet (particularly with the low-FODMAP diet), and insufficient sample size and lack of a placebo group contributing to an inability to detect all clinically significant differences among the diets, he said.
“Although this study is not definitive and doesn’t answer all key questions about which diet is best and how each performs in the long run, it does provide important information for patients and providers,” said Dr. Lacy.
The study was funded by Schaer. One of the study authors has reported receiving an educational grant from Schaer. Dr. Lacy has reported being on scientific advisory boards for Ironwood, Salix, and Allakos.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Weekend catch-up sleep may help fatty liver
People who don’t get enough sleep during the week may be able to reduce their risk for nonalcoholic fatty liver disease (NAFLD) by catching up on the weekends, researchers say.
“Our study revealed that people who get enough sleep have a lower risk of developing NAFLD than those who get insufficient sleep,” Sangheun Lee, MD, PhD, from Catholic Kwandong University, Incheon, South Korea, and colleagues wrote in Annals of Hepatology.
However, they cautioned that further research is needed to verify their finding.
Previous studies have associated insufficient sleep with obesity, hypertension, diabetes mellitus, and cardiovascular disease, as well as liver fibrosis.
A busy weekday schedule can make it harder to get enough sleep, and some people try to compensate by sleeping longer on weekends. Studies so far have produced mixed findings on this strategy, with some showing that more sleep on the weekend reduces the risk for obesity, hypertension, and metabolic syndrome, and others showing no effect on metabolic dysregulation or energy balance.
Accessing a nation’s sleep data
To explore the relationship between sleep patterns and NAFLD, Dr. Lee and colleagues analyzed data from Korea National Health and Nutrition Examination Surveys collected from 2008 to 2019. They excluded people aged less than 20 years, those with hepatitis B or C infections, liver cirrhosis or liver cancer, shift workers and others who “slept irregularly,” and those who consumed alcohol excessively, leaving a cohort of 101,138 participants.
The survey didn’t distinguish between sleep on weekdays and weekends until 2016, so the researchers divided their findings into two: 68,759 people surveyed from 2008 to 2015 (set 1) and 32,379 surveyed from 2016 to 2019 (set 2).
Set 1 was further divided into those who averaged more than 7 hours of sleep per day and those who slept less than that. Set 2 was divided into three groups: one that averaged less than 7 hours of sleep per day and did not catch up on weekends, one that averaged less than 7 hours of sleep per day and did catch up on weekends, and one that averaged more than 7 hours of sleep throughout the week.
The researchers used the hepatic steatosis index (HSI) to determine the presence of a fatty liver, calculated as 8 x (ratio of serum ALT to serum AST) + body mass index (+ 2 for female, + 2 in case of diabetes). An HSI of at least36 was considered an indicator of fatty liver.
Less sleep, more risk
Participants in set 1 slept for a mean of 6.8 hours, with 58.6% sleeping more than 7 hours a day. Those in set 2 slept a mean of 6.9 hours during weekdays, with 59.9% sleeping more than 7 hours. They also slept a mean of 7.7 hours on weekends.
In set 1, sleeping at least7 hours was associated with a 16% lower risk for NAFLD (odds ratio, 0.84; 95% confidence interval, 0.79-0.89).
In set 2, sleeping at least 7 hours on weekdays was associated with a 19% reduced risk for NAFLD (OR, 0.81; 95% CI, 0.74-0.89). Sleeping at least 7 hours on the weekend was associated with a 22% reduced risk for NAFLD (OR, 0.78; 95% CI, 0.70-0.87). Compared with those who slept less than 7 hours throughout the week, those who slept less than 7 hours on weekdays and more than 7 hours on weekends had a 20% lower rate of NAFLD (OR, 0.80; 95% CI, 0.70-0.92).
All these associations held true for both men and women.
Why getting your Z’s may have hepatic advantages
One explanation for the link between sleep patterns and NAFLD is that dysregulation of cortisol, inflammatory cytokines, and norepinephrine are associated with both variations in sleep and NAFLD onset, Dr. Lee and colleagues wrote.
They also pointed out that a lack of sleep can reduce the secretion of two hormones that promote satiety: leptin and glucagonlike peptide–1. As a result, people who sleep less may eat more and gain weight, which increases the risk for NAFLD.
Ashwani K. Singal, MD, MS, a professor of medicine at the University of South Dakota, Vermillion, who was not involved in the study, noted that it was based on comparing a cross section of a population instead of following the participants over time.
“So, I think it’s an association rather than a cause and effect,” he said in an interview.
The authors don’t report a multivariate analysis to determine whether comorbidities or other characteristics of the patients could explain the association, he pointed out, noting that obesity, for example, can increase the risk for both NAFLD and sleep apnea.
Still, Dr. Singal said, the paper will influence him to mention sleep in the context of lifestyle factors that can affect fatty liver disease. “I’m going to tell my patients, and tell the community physicians to tell their patients, to follow a good sleep hygiene and make sure that they sleep at least 5-7 hours.”
Dr. Singal and the study authors all reported no relevant financial relationships. The study was supported by the National Research Foundation of Korea.
A version of this article first appeared on Medscape.com.
People who don’t get enough sleep during the week may be able to reduce their risk for nonalcoholic fatty liver disease (NAFLD) by catching up on the weekends, researchers say.
“Our study revealed that people who get enough sleep have a lower risk of developing NAFLD than those who get insufficient sleep,” Sangheun Lee, MD, PhD, from Catholic Kwandong University, Incheon, South Korea, and colleagues wrote in Annals of Hepatology.
However, they cautioned that further research is needed to verify their finding.
Previous studies have associated insufficient sleep with obesity, hypertension, diabetes mellitus, and cardiovascular disease, as well as liver fibrosis.
A busy weekday schedule can make it harder to get enough sleep, and some people try to compensate by sleeping longer on weekends. Studies so far have produced mixed findings on this strategy, with some showing that more sleep on the weekend reduces the risk for obesity, hypertension, and metabolic syndrome, and others showing no effect on metabolic dysregulation or energy balance.
Accessing a nation’s sleep data
To explore the relationship between sleep patterns and NAFLD, Dr. Lee and colleagues analyzed data from Korea National Health and Nutrition Examination Surveys collected from 2008 to 2019. They excluded people aged less than 20 years, those with hepatitis B or C infections, liver cirrhosis or liver cancer, shift workers and others who “slept irregularly,” and those who consumed alcohol excessively, leaving a cohort of 101,138 participants.
The survey didn’t distinguish between sleep on weekdays and weekends until 2016, so the researchers divided their findings into two: 68,759 people surveyed from 2008 to 2015 (set 1) and 32,379 surveyed from 2016 to 2019 (set 2).
Set 1 was further divided into those who averaged more than 7 hours of sleep per day and those who slept less than that. Set 2 was divided into three groups: one that averaged less than 7 hours of sleep per day and did not catch up on weekends, one that averaged less than 7 hours of sleep per day and did catch up on weekends, and one that averaged more than 7 hours of sleep throughout the week.
The researchers used the hepatic steatosis index (HSI) to determine the presence of a fatty liver, calculated as 8 x (ratio of serum ALT to serum AST) + body mass index (+ 2 for female, + 2 in case of diabetes). An HSI of at least36 was considered an indicator of fatty liver.
Less sleep, more risk
Participants in set 1 slept for a mean of 6.8 hours, with 58.6% sleeping more than 7 hours a day. Those in set 2 slept a mean of 6.9 hours during weekdays, with 59.9% sleeping more than 7 hours. They also slept a mean of 7.7 hours on weekends.
In set 1, sleeping at least7 hours was associated with a 16% lower risk for NAFLD (odds ratio, 0.84; 95% confidence interval, 0.79-0.89).
In set 2, sleeping at least 7 hours on weekdays was associated with a 19% reduced risk for NAFLD (OR, 0.81; 95% CI, 0.74-0.89). Sleeping at least 7 hours on the weekend was associated with a 22% reduced risk for NAFLD (OR, 0.78; 95% CI, 0.70-0.87). Compared with those who slept less than 7 hours throughout the week, those who slept less than 7 hours on weekdays and more than 7 hours on weekends had a 20% lower rate of NAFLD (OR, 0.80; 95% CI, 0.70-0.92).
All these associations held true for both men and women.
Why getting your Z’s may have hepatic advantages
One explanation for the link between sleep patterns and NAFLD is that dysregulation of cortisol, inflammatory cytokines, and norepinephrine are associated with both variations in sleep and NAFLD onset, Dr. Lee and colleagues wrote.
They also pointed out that a lack of sleep can reduce the secretion of two hormones that promote satiety: leptin and glucagonlike peptide–1. As a result, people who sleep less may eat more and gain weight, which increases the risk for NAFLD.
Ashwani K. Singal, MD, MS, a professor of medicine at the University of South Dakota, Vermillion, who was not involved in the study, noted that it was based on comparing a cross section of a population instead of following the participants over time.
“So, I think it’s an association rather than a cause and effect,” he said in an interview.
The authors don’t report a multivariate analysis to determine whether comorbidities or other characteristics of the patients could explain the association, he pointed out, noting that obesity, for example, can increase the risk for both NAFLD and sleep apnea.
Still, Dr. Singal said, the paper will influence him to mention sleep in the context of lifestyle factors that can affect fatty liver disease. “I’m going to tell my patients, and tell the community physicians to tell their patients, to follow a good sleep hygiene and make sure that they sleep at least 5-7 hours.”
Dr. Singal and the study authors all reported no relevant financial relationships. The study was supported by the National Research Foundation of Korea.
A version of this article first appeared on Medscape.com.
People who don’t get enough sleep during the week may be able to reduce their risk for nonalcoholic fatty liver disease (NAFLD) by catching up on the weekends, researchers say.
“Our study revealed that people who get enough sleep have a lower risk of developing NAFLD than those who get insufficient sleep,” Sangheun Lee, MD, PhD, from Catholic Kwandong University, Incheon, South Korea, and colleagues wrote in Annals of Hepatology.
However, they cautioned that further research is needed to verify their finding.
Previous studies have associated insufficient sleep with obesity, hypertension, diabetes mellitus, and cardiovascular disease, as well as liver fibrosis.
A busy weekday schedule can make it harder to get enough sleep, and some people try to compensate by sleeping longer on weekends. Studies so far have produced mixed findings on this strategy, with some showing that more sleep on the weekend reduces the risk for obesity, hypertension, and metabolic syndrome, and others showing no effect on metabolic dysregulation or energy balance.
Accessing a nation’s sleep data
To explore the relationship between sleep patterns and NAFLD, Dr. Lee and colleagues analyzed data from Korea National Health and Nutrition Examination Surveys collected from 2008 to 2019. They excluded people aged less than 20 years, those with hepatitis B or C infections, liver cirrhosis or liver cancer, shift workers and others who “slept irregularly,” and those who consumed alcohol excessively, leaving a cohort of 101,138 participants.
The survey didn’t distinguish between sleep on weekdays and weekends until 2016, so the researchers divided their findings into two: 68,759 people surveyed from 2008 to 2015 (set 1) and 32,379 surveyed from 2016 to 2019 (set 2).
Set 1 was further divided into those who averaged more than 7 hours of sleep per day and those who slept less than that. Set 2 was divided into three groups: one that averaged less than 7 hours of sleep per day and did not catch up on weekends, one that averaged less than 7 hours of sleep per day and did catch up on weekends, and one that averaged more than 7 hours of sleep throughout the week.
The researchers used the hepatic steatosis index (HSI) to determine the presence of a fatty liver, calculated as 8 x (ratio of serum ALT to serum AST) + body mass index (+ 2 for female, + 2 in case of diabetes). An HSI of at least36 was considered an indicator of fatty liver.
Less sleep, more risk
Participants in set 1 slept for a mean of 6.8 hours, with 58.6% sleeping more than 7 hours a day. Those in set 2 slept a mean of 6.9 hours during weekdays, with 59.9% sleeping more than 7 hours. They also slept a mean of 7.7 hours on weekends.
In set 1, sleeping at least7 hours was associated with a 16% lower risk for NAFLD (odds ratio, 0.84; 95% confidence interval, 0.79-0.89).
In set 2, sleeping at least 7 hours on weekdays was associated with a 19% reduced risk for NAFLD (OR, 0.81; 95% CI, 0.74-0.89). Sleeping at least 7 hours on the weekend was associated with a 22% reduced risk for NAFLD (OR, 0.78; 95% CI, 0.70-0.87). Compared with those who slept less than 7 hours throughout the week, those who slept less than 7 hours on weekdays and more than 7 hours on weekends had a 20% lower rate of NAFLD (OR, 0.80; 95% CI, 0.70-0.92).
All these associations held true for both men and women.
Why getting your Z’s may have hepatic advantages
One explanation for the link between sleep patterns and NAFLD is that dysregulation of cortisol, inflammatory cytokines, and norepinephrine are associated with both variations in sleep and NAFLD onset, Dr. Lee and colleagues wrote.
They also pointed out that a lack of sleep can reduce the secretion of two hormones that promote satiety: leptin and glucagonlike peptide–1. As a result, people who sleep less may eat more and gain weight, which increases the risk for NAFLD.
Ashwani K. Singal, MD, MS, a professor of medicine at the University of South Dakota, Vermillion, who was not involved in the study, noted that it was based on comparing a cross section of a population instead of following the participants over time.
“So, I think it’s an association rather than a cause and effect,” he said in an interview.
The authors don’t report a multivariate analysis to determine whether comorbidities or other characteristics of the patients could explain the association, he pointed out, noting that obesity, for example, can increase the risk for both NAFLD and sleep apnea.
Still, Dr. Singal said, the paper will influence him to mention sleep in the context of lifestyle factors that can affect fatty liver disease. “I’m going to tell my patients, and tell the community physicians to tell their patients, to follow a good sleep hygiene and make sure that they sleep at least 5-7 hours.”
Dr. Singal and the study authors all reported no relevant financial relationships. The study was supported by the National Research Foundation of Korea.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF HEPATOLOGY
Freiburg index accurately predicts survival in liver procedure
A new prognostic score is more accurate than the commonly used Model for End-Stage Liver Disease (MELD) in predicting post–transjugular intrahepatic portosystemic shunt (TIPS) survival, researchers say.
The Freiburg Index of Post-TIPS Survival (FIPS) could help patients and doctors weigh the benefits and risks of the procedure, said Chongtu Yang, MD, a postgraduate fellow at the Huazhong University of Science and Technology, Wuhan, China.
“For patients defined as high risk, the TIPS procedure may not be the optimal choice, and transplantation may be better,” Dr. Yang told this news organization. He cautioned that FIPS needs further validation before being applied in clinical practice.
The study by Dr. Yang and his colleagues was published online Feb. 9 in the American Journal of Roentgenology. To their knowledge, this is the first study to validate FIPS in a cohort of Asian patients.
Decompensated cirrhosis can cause variceal bleeding and refractory ascites and may be life threatening. TIPS can manage these complications but comes with its own risks.
To determine which patients can best benefit from the procedure, researchers have proposed a variety of prognostic scoring systems. Some were developed for other purposes, such as predicting survival following hospitalization, rather than specifically for TIPS. Additionally, few studies have compared these approaches to each other.
A four-way comparison
To fill that gap, Dr. Yang and his colleagues compared four predictive models: the MELD, the sodium MELD (MELD-Na), the Chronic Liver Failure–Consortium Acute Decompensation (CLIF-CAD), and FIPS.
The MELD score uses serum bilirubin, serum creatinine, and the international normalized ratio (INR) of prothrombin time. MELD-Na adds sodium to this algorithm. The CLIF-CAD score is calculated using age, serum creatinine, INR, white blood count, and sodium level. FIPS, which was recently devised to predict results with TIPS, uses age, bilirubin, albumin, and creatinine.
To see which yielded more accurate predictions, Dr. Yang and his colleagues followed 383 patients with cirrhosis (mean age, 55 years; 341 with variceal bleeding and 42 with refractory ascites) who underwent TIPS placement at Wuhan Union Hospital between January 2016 and August 2021.
The most common cause of cirrhosis was hepatitis B infection (58.2% of patients), followed by hepatitis C infection (11.7%) and alcohol use (13.6%).
The researchers followed the patients for a median of 23.4 months. They lost track of 31 patients over that time, and another 72 died. The survival rate after TIPS placement was 92.3% at 6 months, 87.8% at 12 months, and 81.2% at 24 months. Thirty-seven patients received a TIPS revision.
In their first measure of the models’ accuracy, the researchers used a concordance index, which compares actual results with predicted results. The number of concordant pairs are divided by the total number of possible evaluation pairs. A score of 1 represents 100% accuracy.
By this measure, the prediction of survival at 6 months was highest for FIPS followed by CLIF-CAD, MELD, and MELD-Na. However, the confidence intervals overlapped.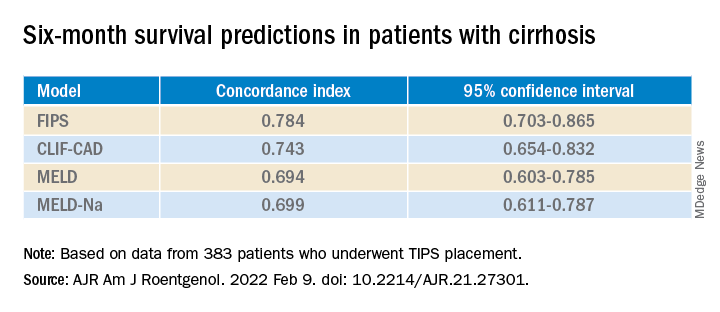
FIPS also scored highest in the concordance index at 12 and 24 months.
In a second measure of the models’ accuracy, the researchers used Brier scores, which calculate the mean squared error between predicted probabilities and actual values. Like the concordance index, Brier scores range from 0.0 to 1.0 but differ in that the lowest Brier score number represents the highest accuracy.
At 6 months, the CLIF-CAD score was the best, at 0.074. MELD and FIPS were equivalent at 0.075, with MELD-Na coming in at 0.077. However, FIPS attained slightly better scores than the other systems at 12 and 24 months.
Is FIPS worth implementing?
With scores this close, it may not be worth changing the predictive model clinicians use for choosing TIPS candidates, said Nancy Reau, MD, chief of hepatology at Rush University Medical Center, Chicago, who was not involved in the study.
MELD scores are already programmed into many electronic medical record systems in the United States, and clinicians are familiar with using that system to aid in further decisions, such as decisions regarding other kinds of surgery, she told this news organization.
“If you’re going to try to advocate for a new system, you really have to show that the performance of the predictive score is monumentally better than the tried and true,” she said.
Dr. Yang and Dr. Reau report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new prognostic score is more accurate than the commonly used Model for End-Stage Liver Disease (MELD) in predicting post–transjugular intrahepatic portosystemic shunt (TIPS) survival, researchers say.
The Freiburg Index of Post-TIPS Survival (FIPS) could help patients and doctors weigh the benefits and risks of the procedure, said Chongtu Yang, MD, a postgraduate fellow at the Huazhong University of Science and Technology, Wuhan, China.
“For patients defined as high risk, the TIPS procedure may not be the optimal choice, and transplantation may be better,” Dr. Yang told this news organization. He cautioned that FIPS needs further validation before being applied in clinical practice.
The study by Dr. Yang and his colleagues was published online Feb. 9 in the American Journal of Roentgenology. To their knowledge, this is the first study to validate FIPS in a cohort of Asian patients.
Decompensated cirrhosis can cause variceal bleeding and refractory ascites and may be life threatening. TIPS can manage these complications but comes with its own risks.
To determine which patients can best benefit from the procedure, researchers have proposed a variety of prognostic scoring systems. Some were developed for other purposes, such as predicting survival following hospitalization, rather than specifically for TIPS. Additionally, few studies have compared these approaches to each other.
A four-way comparison
To fill that gap, Dr. Yang and his colleagues compared four predictive models: the MELD, the sodium MELD (MELD-Na), the Chronic Liver Failure–Consortium Acute Decompensation (CLIF-CAD), and FIPS.
The MELD score uses serum bilirubin, serum creatinine, and the international normalized ratio (INR) of prothrombin time. MELD-Na adds sodium to this algorithm. The CLIF-CAD score is calculated using age, serum creatinine, INR, white blood count, and sodium level. FIPS, which was recently devised to predict results with TIPS, uses age, bilirubin, albumin, and creatinine.
To see which yielded more accurate predictions, Dr. Yang and his colleagues followed 383 patients with cirrhosis (mean age, 55 years; 341 with variceal bleeding and 42 with refractory ascites) who underwent TIPS placement at Wuhan Union Hospital between January 2016 and August 2021.
The most common cause of cirrhosis was hepatitis B infection (58.2% of patients), followed by hepatitis C infection (11.7%) and alcohol use (13.6%).
The researchers followed the patients for a median of 23.4 months. They lost track of 31 patients over that time, and another 72 died. The survival rate after TIPS placement was 92.3% at 6 months, 87.8% at 12 months, and 81.2% at 24 months. Thirty-seven patients received a TIPS revision.
In their first measure of the models’ accuracy, the researchers used a concordance index, which compares actual results with predicted results. The number of concordant pairs are divided by the total number of possible evaluation pairs. A score of 1 represents 100% accuracy.
By this measure, the prediction of survival at 6 months was highest for FIPS followed by CLIF-CAD, MELD, and MELD-Na. However, the confidence intervals overlapped.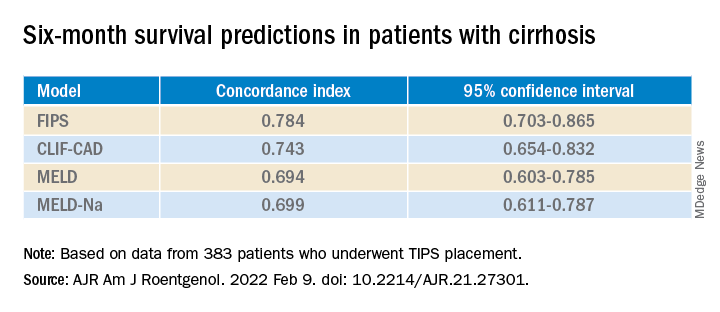
FIPS also scored highest in the concordance index at 12 and 24 months.
In a second measure of the models’ accuracy, the researchers used Brier scores, which calculate the mean squared error between predicted probabilities and actual values. Like the concordance index, Brier scores range from 0.0 to 1.0 but differ in that the lowest Brier score number represents the highest accuracy.
At 6 months, the CLIF-CAD score was the best, at 0.074. MELD and FIPS were equivalent at 0.075, with MELD-Na coming in at 0.077. However, FIPS attained slightly better scores than the other systems at 12 and 24 months.
Is FIPS worth implementing?
With scores this close, it may not be worth changing the predictive model clinicians use for choosing TIPS candidates, said Nancy Reau, MD, chief of hepatology at Rush University Medical Center, Chicago, who was not involved in the study.
MELD scores are already programmed into many electronic medical record systems in the United States, and clinicians are familiar with using that system to aid in further decisions, such as decisions regarding other kinds of surgery, she told this news organization.
“If you’re going to try to advocate for a new system, you really have to show that the performance of the predictive score is monumentally better than the tried and true,” she said.
Dr. Yang and Dr. Reau report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new prognostic score is more accurate than the commonly used Model for End-Stage Liver Disease (MELD) in predicting post–transjugular intrahepatic portosystemic shunt (TIPS) survival, researchers say.
The Freiburg Index of Post-TIPS Survival (FIPS) could help patients and doctors weigh the benefits and risks of the procedure, said Chongtu Yang, MD, a postgraduate fellow at the Huazhong University of Science and Technology, Wuhan, China.
“For patients defined as high risk, the TIPS procedure may not be the optimal choice, and transplantation may be better,” Dr. Yang told this news organization. He cautioned that FIPS needs further validation before being applied in clinical practice.
The study by Dr. Yang and his colleagues was published online Feb. 9 in the American Journal of Roentgenology. To their knowledge, this is the first study to validate FIPS in a cohort of Asian patients.
Decompensated cirrhosis can cause variceal bleeding and refractory ascites and may be life threatening. TIPS can manage these complications but comes with its own risks.
To determine which patients can best benefit from the procedure, researchers have proposed a variety of prognostic scoring systems. Some were developed for other purposes, such as predicting survival following hospitalization, rather than specifically for TIPS. Additionally, few studies have compared these approaches to each other.
A four-way comparison
To fill that gap, Dr. Yang and his colleagues compared four predictive models: the MELD, the sodium MELD (MELD-Na), the Chronic Liver Failure–Consortium Acute Decompensation (CLIF-CAD), and FIPS.
The MELD score uses serum bilirubin, serum creatinine, and the international normalized ratio (INR) of prothrombin time. MELD-Na adds sodium to this algorithm. The CLIF-CAD score is calculated using age, serum creatinine, INR, white blood count, and sodium level. FIPS, which was recently devised to predict results with TIPS, uses age, bilirubin, albumin, and creatinine.
To see which yielded more accurate predictions, Dr. Yang and his colleagues followed 383 patients with cirrhosis (mean age, 55 years; 341 with variceal bleeding and 42 with refractory ascites) who underwent TIPS placement at Wuhan Union Hospital between January 2016 and August 2021.
The most common cause of cirrhosis was hepatitis B infection (58.2% of patients), followed by hepatitis C infection (11.7%) and alcohol use (13.6%).
The researchers followed the patients for a median of 23.4 months. They lost track of 31 patients over that time, and another 72 died. The survival rate after TIPS placement was 92.3% at 6 months, 87.8% at 12 months, and 81.2% at 24 months. Thirty-seven patients received a TIPS revision.
In their first measure of the models’ accuracy, the researchers used a concordance index, which compares actual results with predicted results. The number of concordant pairs are divided by the total number of possible evaluation pairs. A score of 1 represents 100% accuracy.
By this measure, the prediction of survival at 6 months was highest for FIPS followed by CLIF-CAD, MELD, and MELD-Na. However, the confidence intervals overlapped.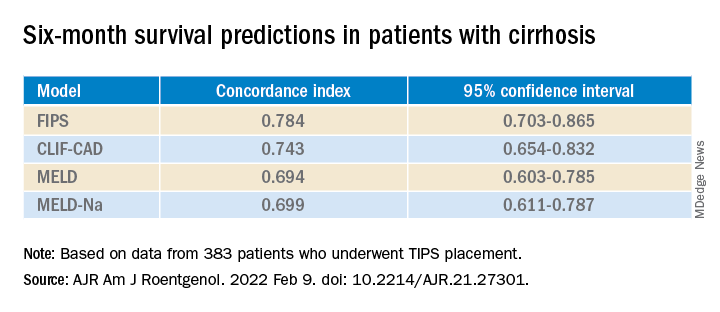
FIPS also scored highest in the concordance index at 12 and 24 months.
In a second measure of the models’ accuracy, the researchers used Brier scores, which calculate the mean squared error between predicted probabilities and actual values. Like the concordance index, Brier scores range from 0.0 to 1.0 but differ in that the lowest Brier score number represents the highest accuracy.
At 6 months, the CLIF-CAD score was the best, at 0.074. MELD and FIPS were equivalent at 0.075, with MELD-Na coming in at 0.077. However, FIPS attained slightly better scores than the other systems at 12 and 24 months.
Is FIPS worth implementing?
With scores this close, it may not be worth changing the predictive model clinicians use for choosing TIPS candidates, said Nancy Reau, MD, chief of hepatology at Rush University Medical Center, Chicago, who was not involved in the study.
MELD scores are already programmed into many electronic medical record systems in the United States, and clinicians are familiar with using that system to aid in further decisions, such as decisions regarding other kinds of surgery, she told this news organization.
“If you’re going to try to advocate for a new system, you really have to show that the performance of the predictive score is monumentally better than the tried and true,” she said.
Dr. Yang and Dr. Reau report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF ROENTGENOLOGY
Anesthesia care team may be quicker for GI endoscopy
Gastrointestinal endoscopy takes less time when an anesthesiologist oversees the sedation, researchers say.
“We have increased patient access to our GI unit by making these modifications,” said Adeel Faruki, MD, a senior instructor of anesthesiology and fellow in operations at the University of Colorado at Denver, Aurora.
The finding was presented at the American Society of Anesthesiologists’ ADVANCE 2022, the Anesthesiology Business Event.
Sedation for endoscopy in the United States generally follows one of two models, Dr. Faruki told this news organization: nurse-administered sedation (NAS) or monitored anesthesia care (MAC). During NAS, a GI proceduralist monitors a registered nurse who sedates patients using medications such as fentanyl, midazolam, and diphenhydramine. This was the approach at the researchers’ GI unit until July 1, 2021.
After that date, the GI unit switched to the MAC model, in which an anesthesiologist supervises a certified registered nurse anesthesiologist or an anesthesiology assistant who administers propofol. Propofol is faster acting than the drug combination the GI unit previously used and causes deeper sedation. But it can also cause respiratory or cardiovascular depression or low blood pressure, Dr. Faruki said, so most institutions require an anesthesiologist to oversee its use.
NAS versus MAC: Seeking the superior model
To see which approach was faster, Dr. Faruki and colleagues recorded times for endoscopic procedures from Aug. 1, 2021, to Oct. 31, 2021, and compared them with the data they had logged in electronic medical records from Jan. 1, 2021, to June 30, 2021. They excluded the month of July to allow for a transition period between the two approaches.
After comparing results from 4,606 patients undergoing endoscopy with NAS to 1,034 undergoing it with MAC, they observed that switching to the latter model reduced the time from sedation start to scope-in by 2-2.5 minutes.
Because recovery is faster with propofol, the patients also spent 7 minutes less in the postanesthesia care unit for upper GI endoscopies and 2 minutes less for lower GI endoscopies. Patients also told the researchers they felt less groggy.
At the same time the unit was transitioning from NAS to MAC, they also began requiring patients to sign consent forms for both the anesthesia and GI procedures in the preoperative room rather than in the procedure room. That saved about 19 minutes.
Putting all these changes together, the researchers calculated that they increased the capacity of their GI unit by 25%.
“With a pandemic raging and capacity crises continuing, it becomes very relevant to the care we can provide patients,” Dr. Faruki said. “That’s something we’re actually really proud of.”
The university is now instituting similar procedures at its other ambulatory surgical centers, he added.
How efficient is your endoscopy center?
“Other factors can also affect the efficiency of endoscopy,” said Joseph Vicari, MD, MBA, a partner at Rockford (Ill.) Gastroenterology Associates, who was not involved in this study.
For example, the unit has to have enough endoscopes and enough techs to clean them so they’re always available, he said in an interview. There have to be enough nurses and other staff to turn the rooms over efficiently. There also have to be enough pre- and postoperative beds, so that no one is waiting for either one.
Dr. Vicari recommended that GI endoscopy centers compare their times with those of benchmarks provided by professional societies and in published papers.
Having sorted out these factors, the MAC and NAS approaches both have their pros and cons, said Dr. Vicari.
“I think it’s a good idea for units that are struggling with efficiency, especially hospital-based units, to consider new ways to upload patient information and maybe have a dedicated anesthesia team to improve efficiency,” he said. “Procedure time can be reduced because you generally have a much steadier state of sedation with MAC, and then the recovery is much faster with propofol. Your patients wake up faster.”
But Rockford Gastroenterology continues to use the NAS approach in at least 90% of its endoscopies, because it is already so efficient that it doesn’t believe that MAC would make a significant difference.
“Academic centers tend to be less efficient,” he said. “Units like ours, an ambulatory endoscopy center, are different.”
NAS is also less expensive, Dr. Vicari said. “We have leveraged our lower-cost ambulatory endoscopy center by providing fentanyl and Versed [midazolam], turning it into an advantage in developing bundled contracts. Payers can significantly reduce expenses.”
The involvement of an anesthesiologist could increase the cost, Dr. Faruki acknowledged, and he said the researchers are analyzing that question. But he added that anesthesiologists can also oversee four rooms at once.
Dr. Faruki and Dr. Vicari reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Gastrointestinal endoscopy takes less time when an anesthesiologist oversees the sedation, researchers say.
“We have increased patient access to our GI unit by making these modifications,” said Adeel Faruki, MD, a senior instructor of anesthesiology and fellow in operations at the University of Colorado at Denver, Aurora.
The finding was presented at the American Society of Anesthesiologists’ ADVANCE 2022, the Anesthesiology Business Event.
Sedation for endoscopy in the United States generally follows one of two models, Dr. Faruki told this news organization: nurse-administered sedation (NAS) or monitored anesthesia care (MAC). During NAS, a GI proceduralist monitors a registered nurse who sedates patients using medications such as fentanyl, midazolam, and diphenhydramine. This was the approach at the researchers’ GI unit until July 1, 2021.
After that date, the GI unit switched to the MAC model, in which an anesthesiologist supervises a certified registered nurse anesthesiologist or an anesthesiology assistant who administers propofol. Propofol is faster acting than the drug combination the GI unit previously used and causes deeper sedation. But it can also cause respiratory or cardiovascular depression or low blood pressure, Dr. Faruki said, so most institutions require an anesthesiologist to oversee its use.
NAS versus MAC: Seeking the superior model
To see which approach was faster, Dr. Faruki and colleagues recorded times for endoscopic procedures from Aug. 1, 2021, to Oct. 31, 2021, and compared them with the data they had logged in electronic medical records from Jan. 1, 2021, to June 30, 2021. They excluded the month of July to allow for a transition period between the two approaches.
After comparing results from 4,606 patients undergoing endoscopy with NAS to 1,034 undergoing it with MAC, they observed that switching to the latter model reduced the time from sedation start to scope-in by 2-2.5 minutes.
Because recovery is faster with propofol, the patients also spent 7 minutes less in the postanesthesia care unit for upper GI endoscopies and 2 minutes less for lower GI endoscopies. Patients also told the researchers they felt less groggy.
At the same time the unit was transitioning from NAS to MAC, they also began requiring patients to sign consent forms for both the anesthesia and GI procedures in the preoperative room rather than in the procedure room. That saved about 19 minutes.
Putting all these changes together, the researchers calculated that they increased the capacity of their GI unit by 25%.
“With a pandemic raging and capacity crises continuing, it becomes very relevant to the care we can provide patients,” Dr. Faruki said. “That’s something we’re actually really proud of.”
The university is now instituting similar procedures at its other ambulatory surgical centers, he added.
How efficient is your endoscopy center?
“Other factors can also affect the efficiency of endoscopy,” said Joseph Vicari, MD, MBA, a partner at Rockford (Ill.) Gastroenterology Associates, who was not involved in this study.
For example, the unit has to have enough endoscopes and enough techs to clean them so they’re always available, he said in an interview. There have to be enough nurses and other staff to turn the rooms over efficiently. There also have to be enough pre- and postoperative beds, so that no one is waiting for either one.
Dr. Vicari recommended that GI endoscopy centers compare their times with those of benchmarks provided by professional societies and in published papers.
Having sorted out these factors, the MAC and NAS approaches both have their pros and cons, said Dr. Vicari.
“I think it’s a good idea for units that are struggling with efficiency, especially hospital-based units, to consider new ways to upload patient information and maybe have a dedicated anesthesia team to improve efficiency,” he said. “Procedure time can be reduced because you generally have a much steadier state of sedation with MAC, and then the recovery is much faster with propofol. Your patients wake up faster.”
But Rockford Gastroenterology continues to use the NAS approach in at least 90% of its endoscopies, because it is already so efficient that it doesn’t believe that MAC would make a significant difference.
“Academic centers tend to be less efficient,” he said. “Units like ours, an ambulatory endoscopy center, are different.”
NAS is also less expensive, Dr. Vicari said. “We have leveraged our lower-cost ambulatory endoscopy center by providing fentanyl and Versed [midazolam], turning it into an advantage in developing bundled contracts. Payers can significantly reduce expenses.”
The involvement of an anesthesiologist could increase the cost, Dr. Faruki acknowledged, and he said the researchers are analyzing that question. But he added that anesthesiologists can also oversee four rooms at once.
Dr. Faruki and Dr. Vicari reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Gastrointestinal endoscopy takes less time when an anesthesiologist oversees the sedation, researchers say.
“We have increased patient access to our GI unit by making these modifications,” said Adeel Faruki, MD, a senior instructor of anesthesiology and fellow in operations at the University of Colorado at Denver, Aurora.
The finding was presented at the American Society of Anesthesiologists’ ADVANCE 2022, the Anesthesiology Business Event.
Sedation for endoscopy in the United States generally follows one of two models, Dr. Faruki told this news organization: nurse-administered sedation (NAS) or monitored anesthesia care (MAC). During NAS, a GI proceduralist monitors a registered nurse who sedates patients using medications such as fentanyl, midazolam, and diphenhydramine. This was the approach at the researchers’ GI unit until July 1, 2021.
After that date, the GI unit switched to the MAC model, in which an anesthesiologist supervises a certified registered nurse anesthesiologist or an anesthesiology assistant who administers propofol. Propofol is faster acting than the drug combination the GI unit previously used and causes deeper sedation. But it can also cause respiratory or cardiovascular depression or low blood pressure, Dr. Faruki said, so most institutions require an anesthesiologist to oversee its use.
NAS versus MAC: Seeking the superior model
To see which approach was faster, Dr. Faruki and colleagues recorded times for endoscopic procedures from Aug. 1, 2021, to Oct. 31, 2021, and compared them with the data they had logged in electronic medical records from Jan. 1, 2021, to June 30, 2021. They excluded the month of July to allow for a transition period between the two approaches.
After comparing results from 4,606 patients undergoing endoscopy with NAS to 1,034 undergoing it with MAC, they observed that switching to the latter model reduced the time from sedation start to scope-in by 2-2.5 minutes.
Because recovery is faster with propofol, the patients also spent 7 minutes less in the postanesthesia care unit for upper GI endoscopies and 2 minutes less for lower GI endoscopies. Patients also told the researchers they felt less groggy.
At the same time the unit was transitioning from NAS to MAC, they also began requiring patients to sign consent forms for both the anesthesia and GI procedures in the preoperative room rather than in the procedure room. That saved about 19 minutes.
Putting all these changes together, the researchers calculated that they increased the capacity of their GI unit by 25%.
“With a pandemic raging and capacity crises continuing, it becomes very relevant to the care we can provide patients,” Dr. Faruki said. “That’s something we’re actually really proud of.”
The university is now instituting similar procedures at its other ambulatory surgical centers, he added.
How efficient is your endoscopy center?
“Other factors can also affect the efficiency of endoscopy,” said Joseph Vicari, MD, MBA, a partner at Rockford (Ill.) Gastroenterology Associates, who was not involved in this study.
For example, the unit has to have enough endoscopes and enough techs to clean them so they’re always available, he said in an interview. There have to be enough nurses and other staff to turn the rooms over efficiently. There also have to be enough pre- and postoperative beds, so that no one is waiting for either one.
Dr. Vicari recommended that GI endoscopy centers compare their times with those of benchmarks provided by professional societies and in published papers.
Having sorted out these factors, the MAC and NAS approaches both have their pros and cons, said Dr. Vicari.
“I think it’s a good idea for units that are struggling with efficiency, especially hospital-based units, to consider new ways to upload patient information and maybe have a dedicated anesthesia team to improve efficiency,” he said. “Procedure time can be reduced because you generally have a much steadier state of sedation with MAC, and then the recovery is much faster with propofol. Your patients wake up faster.”
But Rockford Gastroenterology continues to use the NAS approach in at least 90% of its endoscopies, because it is already so efficient that it doesn’t believe that MAC would make a significant difference.
“Academic centers tend to be less efficient,” he said. “Units like ours, an ambulatory endoscopy center, are different.”
NAS is also less expensive, Dr. Vicari said. “We have leveraged our lower-cost ambulatory endoscopy center by providing fentanyl and Versed [midazolam], turning it into an advantage in developing bundled contracts. Payers can significantly reduce expenses.”
The involvement of an anesthesiologist could increase the cost, Dr. Faruki acknowledged, and he said the researchers are analyzing that question. But he added that anesthesiologists can also oversee four rooms at once.
Dr. Faruki and Dr. Vicari reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ADVANCE 2022
Endoscopic mucosal resection valuable for cancer diagnosis
said a physician presenting at the 2022 Gastrointestinal Cancers Symposium.
Vani Konda, MD, a gastroenterologist with Baylor Scott and White Center for Esophageal Diseases, Dallas, participated in an educational session on approaches for treating localized gastroesophageal cancer. In her presentation, she addressed the advantages and disadvantages of EMR and endoscopic submucosal dissection (ESD) for esophageal neoplasia for both diagnosis and treatment.
Esophageal neoplasia therapy includes tissue-acquiring (lesion removal and histopathologic samples) and non–tissue-acquiring therapies (which include radiofrequency ablation, cryotherapy and hybrid-argon plasma coagulation.
The optimal therapy may vary with the esophageal cancer, and the cancer may vary with geography. Worldwide, squamous cell carcinoma is predominant, while in Western countries, esophageal adenocarcinoma is most prevalent. The incidence and mortality of esophageal adenocarcinoma has been rising for several decades, Dr. Konda said.
Considering risk factors
Barrett’s esophagus is a known risk factor for esophageal adenocarcinoma. It can be seen endoscopically as salmon-colored lining, and histologically as specialized intestinal metaplasia.
A lesion extending beyond the basement membrane into the lamina propria is an intramucosal carcinoma, or T1a lesion. A lesion extending beyond the muscularis mucosa into the submucosa is a submucosal carcinoma, or T1b tumor, Dr. Konda said.
“The difference between T1a and T1b is important in the selection of treatment approaches due to the risk of [lymph node] metastasis,” she said. She equated a T1a lesion with a 2% or smaller risk of lymph node metastasis, and a T1b tumor with a 20% risk.*
Endoscopic therapy is more reasonable for a T1a lesion, especially since the alternative, esophagectomy, may have a mortality rate of 2% or higher, she said, while for T1b tumors, surgical or systemic treatments are warranted.
A diagnosis of high-grade dysplasia by biopsy is associated with a 40% risk of prevalent cancer, mostly intramucosal carcinoma. On the other hand, submucosal carcinoma is rare in the absence of endoscopically visible lesions. “This risk of prevalent cancer, especially in visible lesions, is the reason that we should address all visible lesions with endoscopic resection, especially in the setting of dysplasia,” Dr. Konda said.
EMR is more accurate than biopsies; diagnoses change up to half the time when EMR is done after a preresection biopsy, and there’s a higher interobserver agreement among pathologists with EMR, she said.
The goal of therapy in Barrett’s esophagus is total Barrett’s eradication to treat not only the known neoplasia, but also the rest of the at-risk epithelium.
Piecemeal EMR for the entire Barrett’s epithelium can bring about a 96% or greater neoplasia eradication rate. But the stricture rate may reach 37%, and bleeding and perforation are also common.
Combining endoscopic mucosal resection for visible lesions with ablation for the rest of the at-risk lining can achieve an eradication rate of 93% with a more favorable complication profile.
Weighing the benefits of ESD
In contrast to EMR, ESD has been practiced more frequently in Asia. It provides an en bloc specimen.
A 2014 systematic review of 380 EMR procedures and 333 ESD procedures for Barret’s associated neoplasia indicated that ESD takes longer. The recurrence rate was 0.7% for ESD versus 2.6% for EMR, but this difference fell just short of statistical significance (P = .06). Bleeding and perforation rates were similar, but stricture rates reached 22.3% with wide-field EMR, 3.4% with ESD and 0.7% with focal EMR.
In a 2016 head-to-head trial, researchers assigned 20 patients each to EMR or ESD. They found the procedure longer, but the en bloc resection was higher in ESD. Complete remission of the neoplasia was not statistically different between the two groups, with 15 of 16 patients achieving this goal with ESD and 16 of 17 with EMR. All the patients had complete remission after one retreatment of residual neoplasia. There were two severe adverse events in the ESD group, and none in the EMR group.
Weighing the pros and cons, Dr. Konda concluded that EMR is technically easier and adequate in most cases of Barrett’s esophagus, while ESD may be preferred in select cases with concern for submucosal carcinoma or nonlifting lesions.
She advocated taking patient characteristics, disease characteristics, and available expertise into account.
Dr. Konda reported financial relationships with Ambu, Cernostics, Exact Sciences, Medtronic, and Lucid Sciences. The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
*Correction, 1/28/22: An earlier version of this article mischaracterized lymph node metastasis.
said a physician presenting at the 2022 Gastrointestinal Cancers Symposium.
Vani Konda, MD, a gastroenterologist with Baylor Scott and White Center for Esophageal Diseases, Dallas, participated in an educational session on approaches for treating localized gastroesophageal cancer. In her presentation, she addressed the advantages and disadvantages of EMR and endoscopic submucosal dissection (ESD) for esophageal neoplasia for both diagnosis and treatment.
Esophageal neoplasia therapy includes tissue-acquiring (lesion removal and histopathologic samples) and non–tissue-acquiring therapies (which include radiofrequency ablation, cryotherapy and hybrid-argon plasma coagulation.
The optimal therapy may vary with the esophageal cancer, and the cancer may vary with geography. Worldwide, squamous cell carcinoma is predominant, while in Western countries, esophageal adenocarcinoma is most prevalent. The incidence and mortality of esophageal adenocarcinoma has been rising for several decades, Dr. Konda said.
Considering risk factors
Barrett’s esophagus is a known risk factor for esophageal adenocarcinoma. It can be seen endoscopically as salmon-colored lining, and histologically as specialized intestinal metaplasia.
A lesion extending beyond the basement membrane into the lamina propria is an intramucosal carcinoma, or T1a lesion. A lesion extending beyond the muscularis mucosa into the submucosa is a submucosal carcinoma, or T1b tumor, Dr. Konda said.
“The difference between T1a and T1b is important in the selection of treatment approaches due to the risk of [lymph node] metastasis,” she said. She equated a T1a lesion with a 2% or smaller risk of lymph node metastasis, and a T1b tumor with a 20% risk.*
Endoscopic therapy is more reasonable for a T1a lesion, especially since the alternative, esophagectomy, may have a mortality rate of 2% or higher, she said, while for T1b tumors, surgical or systemic treatments are warranted.
A diagnosis of high-grade dysplasia by biopsy is associated with a 40% risk of prevalent cancer, mostly intramucosal carcinoma. On the other hand, submucosal carcinoma is rare in the absence of endoscopically visible lesions. “This risk of prevalent cancer, especially in visible lesions, is the reason that we should address all visible lesions with endoscopic resection, especially in the setting of dysplasia,” Dr. Konda said.
EMR is more accurate than biopsies; diagnoses change up to half the time when EMR is done after a preresection biopsy, and there’s a higher interobserver agreement among pathologists with EMR, she said.
The goal of therapy in Barrett’s esophagus is total Barrett’s eradication to treat not only the known neoplasia, but also the rest of the at-risk epithelium.
Piecemeal EMR for the entire Barrett’s epithelium can bring about a 96% or greater neoplasia eradication rate. But the stricture rate may reach 37%, and bleeding and perforation are also common.
Combining endoscopic mucosal resection for visible lesions with ablation for the rest of the at-risk lining can achieve an eradication rate of 93% with a more favorable complication profile.
Weighing the benefits of ESD
In contrast to EMR, ESD has been practiced more frequently in Asia. It provides an en bloc specimen.
A 2014 systematic review of 380 EMR procedures and 333 ESD procedures for Barret’s associated neoplasia indicated that ESD takes longer. The recurrence rate was 0.7% for ESD versus 2.6% for EMR, but this difference fell just short of statistical significance (P = .06). Bleeding and perforation rates were similar, but stricture rates reached 22.3% with wide-field EMR, 3.4% with ESD and 0.7% with focal EMR.
In a 2016 head-to-head trial, researchers assigned 20 patients each to EMR or ESD. They found the procedure longer, but the en bloc resection was higher in ESD. Complete remission of the neoplasia was not statistically different between the two groups, with 15 of 16 patients achieving this goal with ESD and 16 of 17 with EMR. All the patients had complete remission after one retreatment of residual neoplasia. There were two severe adverse events in the ESD group, and none in the EMR group.
Weighing the pros and cons, Dr. Konda concluded that EMR is technically easier and adequate in most cases of Barrett’s esophagus, while ESD may be preferred in select cases with concern for submucosal carcinoma or nonlifting lesions.
She advocated taking patient characteristics, disease characteristics, and available expertise into account.
Dr. Konda reported financial relationships with Ambu, Cernostics, Exact Sciences, Medtronic, and Lucid Sciences. The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
*Correction, 1/28/22: An earlier version of this article mischaracterized lymph node metastasis.
said a physician presenting at the 2022 Gastrointestinal Cancers Symposium.
Vani Konda, MD, a gastroenterologist with Baylor Scott and White Center for Esophageal Diseases, Dallas, participated in an educational session on approaches for treating localized gastroesophageal cancer. In her presentation, she addressed the advantages and disadvantages of EMR and endoscopic submucosal dissection (ESD) for esophageal neoplasia for both diagnosis and treatment.
Esophageal neoplasia therapy includes tissue-acquiring (lesion removal and histopathologic samples) and non–tissue-acquiring therapies (which include radiofrequency ablation, cryotherapy and hybrid-argon plasma coagulation.
The optimal therapy may vary with the esophageal cancer, and the cancer may vary with geography. Worldwide, squamous cell carcinoma is predominant, while in Western countries, esophageal adenocarcinoma is most prevalent. The incidence and mortality of esophageal adenocarcinoma has been rising for several decades, Dr. Konda said.
Considering risk factors
Barrett’s esophagus is a known risk factor for esophageal adenocarcinoma. It can be seen endoscopically as salmon-colored lining, and histologically as specialized intestinal metaplasia.
A lesion extending beyond the basement membrane into the lamina propria is an intramucosal carcinoma, or T1a lesion. A lesion extending beyond the muscularis mucosa into the submucosa is a submucosal carcinoma, or T1b tumor, Dr. Konda said.
“The difference between T1a and T1b is important in the selection of treatment approaches due to the risk of [lymph node] metastasis,” she said. She equated a T1a lesion with a 2% or smaller risk of lymph node metastasis, and a T1b tumor with a 20% risk.*
Endoscopic therapy is more reasonable for a T1a lesion, especially since the alternative, esophagectomy, may have a mortality rate of 2% or higher, she said, while for T1b tumors, surgical or systemic treatments are warranted.
A diagnosis of high-grade dysplasia by biopsy is associated with a 40% risk of prevalent cancer, mostly intramucosal carcinoma. On the other hand, submucosal carcinoma is rare in the absence of endoscopically visible lesions. “This risk of prevalent cancer, especially in visible lesions, is the reason that we should address all visible lesions with endoscopic resection, especially in the setting of dysplasia,” Dr. Konda said.
EMR is more accurate than biopsies; diagnoses change up to half the time when EMR is done after a preresection biopsy, and there’s a higher interobserver agreement among pathologists with EMR, she said.
The goal of therapy in Barrett’s esophagus is total Barrett’s eradication to treat not only the known neoplasia, but also the rest of the at-risk epithelium.
Piecemeal EMR for the entire Barrett’s epithelium can bring about a 96% or greater neoplasia eradication rate. But the stricture rate may reach 37%, and bleeding and perforation are also common.
Combining endoscopic mucosal resection for visible lesions with ablation for the rest of the at-risk lining can achieve an eradication rate of 93% with a more favorable complication profile.
Weighing the benefits of ESD
In contrast to EMR, ESD has been practiced more frequently in Asia. It provides an en bloc specimen.
A 2014 systematic review of 380 EMR procedures and 333 ESD procedures for Barret’s associated neoplasia indicated that ESD takes longer. The recurrence rate was 0.7% for ESD versus 2.6% for EMR, but this difference fell just short of statistical significance (P = .06). Bleeding and perforation rates were similar, but stricture rates reached 22.3% with wide-field EMR, 3.4% with ESD and 0.7% with focal EMR.
In a 2016 head-to-head trial, researchers assigned 20 patients each to EMR or ESD. They found the procedure longer, but the en bloc resection was higher in ESD. Complete remission of the neoplasia was not statistically different between the two groups, with 15 of 16 patients achieving this goal with ESD and 16 of 17 with EMR. All the patients had complete remission after one retreatment of residual neoplasia. There were two severe adverse events in the ESD group, and none in the EMR group.
Weighing the pros and cons, Dr. Konda concluded that EMR is technically easier and adequate in most cases of Barrett’s esophagus, while ESD may be preferred in select cases with concern for submucosal carcinoma or nonlifting lesions.
She advocated taking patient characteristics, disease characteristics, and available expertise into account.
Dr. Konda reported financial relationships with Ambu, Cernostics, Exact Sciences, Medtronic, and Lucid Sciences. The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
*Correction, 1/28/22: An earlier version of this article mischaracterized lymph node metastasis.
FROM GI CANCERS SYMPOSIUM 2022
Decades of research fail to resolve disparities in gastrointestinal cancer care
Men and White people receive better treatment for gastroesophageal cancer than women, Blacks, and Latinos despite years of studies highlighting disparities in care, researchers say.
The problem is complex because it stems from both biological and socioeconomic factors, but some signs of improvement are beginning to show, said Nathaniel R. Evans III, MD, a professor of surgery at Thomas Jefferson University in Philadelphia.
“Repeatedly, we see that, although we know how patients should be treated, there are oftentimes subsets of patients who don’t receive that same level of care,” said Dr. Evans in a general session talk at the American Society of Clinical Oncology Gastrointestinal Cancers Symposium.
Black patients with esophageal cancer are 38% more likely to die from the condition than White patients, he said, citing a 2013 study (Ann Surg Oncol. 2013 doi: 10.1245/s10434-012-2807-3). For Latino patients, mortality is 20% higher than for White patients.
The difference can mostly be explained by the rate of esophagectomy, which is 52% lower for Black patients and 29% lower for Latino patients, compared with White patients, the study found.
Besides race and gender, insurance status also influences who gets surgery, Dr. Evans said, citing data from the National Cancer Database. Black patients are less likely to get surgery and more likely to die at all stages and histologies, he said. They wait longer for treatment and are more likely to receive no treatment at all.
Women also suffer from disparities, said Anna Dorothea Wagner, MD, head of the gastrointestinal cancer clinic at Lausanne University Hospital in Lausanne (Switzerland), who spoke at the symposium with Dr Evans.
Seventy-five percent of men with esophageal and gastric adenocarcinoma get curative treatments, compared with only 60% of women, Dr. Wagner said, citing a 2020 study on which she is an author. Women are more likely to get palliative care. As a result, only 30% of women survive the condition for 5 years or more compared to 34% of men, she said. “At the moment we don’t know whether this is due to either patient preferences or cognitive or bias of physicians.”
Disparities in treatment outcomes because of biological differences
For women, some disparities also arise out of clear biological differences, Dr. Wagner said. Sex hormone signaling affects cancer susceptibility, and sex-biased gene expression signatures have been detected in multiple cancer types.
Women with poorly differentiated and signet-cell pathology are less likely to survive their cancer than men with the same histology, she said.
Many studies have shown that chemotherapy is more toxic to women than men without being more efficacious, she added. This suggests that the optimal doses might be different for women and men.
Responding to a question from the audience, Dr. Wagner said more research is needed on transgender patients to understand how these factors affect them.
Dr. Evans attributed the racial and ethnic disparities to some combination of differential histology, stage at diagnosis, access to care, socioeconomics, and inherent bias.
“The problem is not new,” Dr. Evans said. He described studies that found disparities in the 1970s. “But the good news is that things do seem to be getting better.”
Between 2000 and 2011, the number of esophagectomies being performed at high-volume hospitals increased, he said. The overall mortality after esophagectomy has consequently decreased over this time, and the gap in this rate between White and Black people has closed, he said. “Specialization and centralization clearly improve outcomes for certain surgical procedures.”
To address the problem everyone should acknowledge the disparities, particularly in the access to surgery. “I think one of the best tools we have to try to address the disparity is education, both for patients and providers,” Dr. Evans said.
Care teams must become more diverse and culturally competent to combat longstanding distrust and improve communication, he said.
In December, ASCO announced an “action plan” to address equity, diversity and inclusion in cancer care. The organization promised to improve clinical trial eligibility, and train researchers about inherent bias in order to make the trials more representative of the cancer population.
It vowed to increase participation of underrepresented groups in its professional development programs and leadership roles, and educate its members about equity. And, it resolved to provide resources to providers so they could advocate for better quality of care, especially in rural and disadvantaged settings.
Dr. Wagner disclosed relationships with Alligator Bioscience, BMS, Dragonfly Therapeutics, Lilly, Merck KGaA, MSD Oncology, Servier/Pfizer, and Abbvie. Dr. Evans disclosed relationships with Bristol Myers Squibb Foundation and Intuitive Surgical.
This article was updated 1/28/22.
Men and White people receive better treatment for gastroesophageal cancer than women, Blacks, and Latinos despite years of studies highlighting disparities in care, researchers say.
The problem is complex because it stems from both biological and socioeconomic factors, but some signs of improvement are beginning to show, said Nathaniel R. Evans III, MD, a professor of surgery at Thomas Jefferson University in Philadelphia.
“Repeatedly, we see that, although we know how patients should be treated, there are oftentimes subsets of patients who don’t receive that same level of care,” said Dr. Evans in a general session talk at the American Society of Clinical Oncology Gastrointestinal Cancers Symposium.
Black patients with esophageal cancer are 38% more likely to die from the condition than White patients, he said, citing a 2013 study (Ann Surg Oncol. 2013 doi: 10.1245/s10434-012-2807-3). For Latino patients, mortality is 20% higher than for White patients.
The difference can mostly be explained by the rate of esophagectomy, which is 52% lower for Black patients and 29% lower for Latino patients, compared with White patients, the study found.
Besides race and gender, insurance status also influences who gets surgery, Dr. Evans said, citing data from the National Cancer Database. Black patients are less likely to get surgery and more likely to die at all stages and histologies, he said. They wait longer for treatment and are more likely to receive no treatment at all.
Women also suffer from disparities, said Anna Dorothea Wagner, MD, head of the gastrointestinal cancer clinic at Lausanne University Hospital in Lausanne (Switzerland), who spoke at the symposium with Dr Evans.
Seventy-five percent of men with esophageal and gastric adenocarcinoma get curative treatments, compared with only 60% of women, Dr. Wagner said, citing a 2020 study on which she is an author. Women are more likely to get palliative care. As a result, only 30% of women survive the condition for 5 years or more compared to 34% of men, she said. “At the moment we don’t know whether this is due to either patient preferences or cognitive or bias of physicians.”
Disparities in treatment outcomes because of biological differences
For women, some disparities also arise out of clear biological differences, Dr. Wagner said. Sex hormone signaling affects cancer susceptibility, and sex-biased gene expression signatures have been detected in multiple cancer types.
Women with poorly differentiated and signet-cell pathology are less likely to survive their cancer than men with the same histology, she said.
Many studies have shown that chemotherapy is more toxic to women than men without being more efficacious, she added. This suggests that the optimal doses might be different for women and men.
Responding to a question from the audience, Dr. Wagner said more research is needed on transgender patients to understand how these factors affect them.
Dr. Evans attributed the racial and ethnic disparities to some combination of differential histology, stage at diagnosis, access to care, socioeconomics, and inherent bias.
“The problem is not new,” Dr. Evans said. He described studies that found disparities in the 1970s. “But the good news is that things do seem to be getting better.”
Between 2000 and 2011, the number of esophagectomies being performed at high-volume hospitals increased, he said. The overall mortality after esophagectomy has consequently decreased over this time, and the gap in this rate between White and Black people has closed, he said. “Specialization and centralization clearly improve outcomes for certain surgical procedures.”
To address the problem everyone should acknowledge the disparities, particularly in the access to surgery. “I think one of the best tools we have to try to address the disparity is education, both for patients and providers,” Dr. Evans said.
Care teams must become more diverse and culturally competent to combat longstanding distrust and improve communication, he said.
In December, ASCO announced an “action plan” to address equity, diversity and inclusion in cancer care. The organization promised to improve clinical trial eligibility, and train researchers about inherent bias in order to make the trials more representative of the cancer population.
It vowed to increase participation of underrepresented groups in its professional development programs and leadership roles, and educate its members about equity. And, it resolved to provide resources to providers so they could advocate for better quality of care, especially in rural and disadvantaged settings.
Dr. Wagner disclosed relationships with Alligator Bioscience, BMS, Dragonfly Therapeutics, Lilly, Merck KGaA, MSD Oncology, Servier/Pfizer, and Abbvie. Dr. Evans disclosed relationships with Bristol Myers Squibb Foundation and Intuitive Surgical.
This article was updated 1/28/22.
Men and White people receive better treatment for gastroesophageal cancer than women, Blacks, and Latinos despite years of studies highlighting disparities in care, researchers say.
The problem is complex because it stems from both biological and socioeconomic factors, but some signs of improvement are beginning to show, said Nathaniel R. Evans III, MD, a professor of surgery at Thomas Jefferson University in Philadelphia.
“Repeatedly, we see that, although we know how patients should be treated, there are oftentimes subsets of patients who don’t receive that same level of care,” said Dr. Evans in a general session talk at the American Society of Clinical Oncology Gastrointestinal Cancers Symposium.
Black patients with esophageal cancer are 38% more likely to die from the condition than White patients, he said, citing a 2013 study (Ann Surg Oncol. 2013 doi: 10.1245/s10434-012-2807-3). For Latino patients, mortality is 20% higher than for White patients.
The difference can mostly be explained by the rate of esophagectomy, which is 52% lower for Black patients and 29% lower for Latino patients, compared with White patients, the study found.
Besides race and gender, insurance status also influences who gets surgery, Dr. Evans said, citing data from the National Cancer Database. Black patients are less likely to get surgery and more likely to die at all stages and histologies, he said. They wait longer for treatment and are more likely to receive no treatment at all.
Women also suffer from disparities, said Anna Dorothea Wagner, MD, head of the gastrointestinal cancer clinic at Lausanne University Hospital in Lausanne (Switzerland), who spoke at the symposium with Dr Evans.
Seventy-five percent of men with esophageal and gastric adenocarcinoma get curative treatments, compared with only 60% of women, Dr. Wagner said, citing a 2020 study on which she is an author. Women are more likely to get palliative care. As a result, only 30% of women survive the condition for 5 years or more compared to 34% of men, she said. “At the moment we don’t know whether this is due to either patient preferences or cognitive or bias of physicians.”
Disparities in treatment outcomes because of biological differences
For women, some disparities also arise out of clear biological differences, Dr. Wagner said. Sex hormone signaling affects cancer susceptibility, and sex-biased gene expression signatures have been detected in multiple cancer types.
Women with poorly differentiated and signet-cell pathology are less likely to survive their cancer than men with the same histology, she said.
Many studies have shown that chemotherapy is more toxic to women than men without being more efficacious, she added. This suggests that the optimal doses might be different for women and men.
Responding to a question from the audience, Dr. Wagner said more research is needed on transgender patients to understand how these factors affect them.
Dr. Evans attributed the racial and ethnic disparities to some combination of differential histology, stage at diagnosis, access to care, socioeconomics, and inherent bias.
“The problem is not new,” Dr. Evans said. He described studies that found disparities in the 1970s. “But the good news is that things do seem to be getting better.”
Between 2000 and 2011, the number of esophagectomies being performed at high-volume hospitals increased, he said. The overall mortality after esophagectomy has consequently decreased over this time, and the gap in this rate between White and Black people has closed, he said. “Specialization and centralization clearly improve outcomes for certain surgical procedures.”
To address the problem everyone should acknowledge the disparities, particularly in the access to surgery. “I think one of the best tools we have to try to address the disparity is education, both for patients and providers,” Dr. Evans said.
Care teams must become more diverse and culturally competent to combat longstanding distrust and improve communication, he said.
In December, ASCO announced an “action plan” to address equity, diversity and inclusion in cancer care. The organization promised to improve clinical trial eligibility, and train researchers about inherent bias in order to make the trials more representative of the cancer population.
It vowed to increase participation of underrepresented groups in its professional development programs and leadership roles, and educate its members about equity. And, it resolved to provide resources to providers so they could advocate for better quality of care, especially in rural and disadvantaged settings.
Dr. Wagner disclosed relationships with Alligator Bioscience, BMS, Dragonfly Therapeutics, Lilly, Merck KGaA, MSD Oncology, Servier/Pfizer, and Abbvie. Dr. Evans disclosed relationships with Bristol Myers Squibb Foundation and Intuitive Surgical.
This article was updated 1/28/22.
FROM GI CANCERS SYMPOSIUM 2022
Virtual reality making progress as depression treatment
Virtual reality (VR) has been taking positive steps in a variety of treatment areas for some time. Now a Japanese company is asking the question: Can people with depression benefit from watching VR scenarios in which actors portray characters coping with the condition?
That’s the assertion of the Tokyo-based company Jolly Good, a VR start-up that introduced the U.S. version of its VRDTx program at the annual meeting of the Consumer Electronics Show.
“Using this as an adjunct for psychotherapy to help someone see an example of someone who’s struggling with depression can be a helpful tool,” said Katharine Larsson, PhD, RN, clinical director of Boston Behavioral Medicine in Brookline. Larsson and her BBM colleague, Amaro J. Laria, PhD, are helping Jolly Good to adapt the program for use in the United States.
VRDTx uses techniques from cognitive-behavioral therapy (CBT). Donning goggles, viewers watch people acting out situations common to depression.
One technique frequently used in CBT is to make a detailed plan, Dr. Laria said. For example, VRDTx users might watch a character with depression struggling to get out of bed but resolving to get up for at least 10 minutes one day, to go for a walk the next day, etc. “The virtual reality allows you to watch a person actually going through the process of applying the intervention,” he said.
In this way, the program could work like hypnotherapy or imaginal therapy where patients picture themselves in a situation that might trigger their depression and then picture themselves coping with that situation.
Dr. Larsson advised using the program primarily as a sort of homework. “ she said. “Using it to substitute or replace the time with a therapist, I don’t think it could begin to have any kind of real efficacy.”
Deploying virtual reality to treat mood disorders is not new, said Preethi Premkumar, PhD, a senior lecturer in psychology at London South Bank University, who has no relationship to Jolly Good.
Dr. Premkumar is first author of a study of a VR program used to treat people who have anxiety about speaking in public. The program depicts the user speaking before an audience and allows the user to vary the number of people in the audience and the audience’s reactions. The users gave it high marks, Dr. Premkumar said. “They felt that it encouraged them to take on public speaking more in reality.”
VR could work in a similar way for depressed people because they tend to catastrophize about specific situations. “Virtual reality can recreate those scenes and then make people confront it without overexposing them,” Dr. Premkumar said.
One recent review article found several studies on VR as a treatment for anxiety. While only a handful focused on depression, they had mostly favorable results.
Jolly Good sponsored one such study, presented Sept. 17, 2021, at the European Association for Behavioural and Cognitive Therapies. “Results indicate improvement in the scores of the targeted patients with depression,” according to an abstract the company published online. “Use of VR caused no adverse events, demonstrating that VR can be used safely in the CBT for of depression.” The company did not respond to a request for more details.
After viewing scenarios created for Japanese patients, Dr. Larsson and Dr. Laria offered Jolly Good several tips about making the transition to the United States. The actors should be more emotionally expressive. They should portray a more diverse cast of characters, including some female bosses. And not all scenes should be set in the workplace.
“In the U.S., at least in our experience, a lot of what depressed patients talk about is just their personal lives, their intimate relationship with a significant other, family relations, friends,” Dr. Laria said. “We gave them a whole list of topics that we felt would be more relevant for a U.S. audience.”
Dr. Larsson and Dr. Laria are consultants to Jolly Good. Dr. Premkumar reported no relevant financial interests.
A version of this article first appeared on Medscape.com.
Virtual reality (VR) has been taking positive steps in a variety of treatment areas for some time. Now a Japanese company is asking the question: Can people with depression benefit from watching VR scenarios in which actors portray characters coping with the condition?
That’s the assertion of the Tokyo-based company Jolly Good, a VR start-up that introduced the U.S. version of its VRDTx program at the annual meeting of the Consumer Electronics Show.
“Using this as an adjunct for psychotherapy to help someone see an example of someone who’s struggling with depression can be a helpful tool,” said Katharine Larsson, PhD, RN, clinical director of Boston Behavioral Medicine in Brookline. Larsson and her BBM colleague, Amaro J. Laria, PhD, are helping Jolly Good to adapt the program for use in the United States.
VRDTx uses techniques from cognitive-behavioral therapy (CBT). Donning goggles, viewers watch people acting out situations common to depression.
One technique frequently used in CBT is to make a detailed plan, Dr. Laria said. For example, VRDTx users might watch a character with depression struggling to get out of bed but resolving to get up for at least 10 minutes one day, to go for a walk the next day, etc. “The virtual reality allows you to watch a person actually going through the process of applying the intervention,” he said.
In this way, the program could work like hypnotherapy or imaginal therapy where patients picture themselves in a situation that might trigger their depression and then picture themselves coping with that situation.
Dr. Larsson advised using the program primarily as a sort of homework. “ she said. “Using it to substitute or replace the time with a therapist, I don’t think it could begin to have any kind of real efficacy.”
Deploying virtual reality to treat mood disorders is not new, said Preethi Premkumar, PhD, a senior lecturer in psychology at London South Bank University, who has no relationship to Jolly Good.
Dr. Premkumar is first author of a study of a VR program used to treat people who have anxiety about speaking in public. The program depicts the user speaking before an audience and allows the user to vary the number of people in the audience and the audience’s reactions. The users gave it high marks, Dr. Premkumar said. “They felt that it encouraged them to take on public speaking more in reality.”
VR could work in a similar way for depressed people because they tend to catastrophize about specific situations. “Virtual reality can recreate those scenes and then make people confront it without overexposing them,” Dr. Premkumar said.
One recent review article found several studies on VR as a treatment for anxiety. While only a handful focused on depression, they had mostly favorable results.
Jolly Good sponsored one such study, presented Sept. 17, 2021, at the European Association for Behavioural and Cognitive Therapies. “Results indicate improvement in the scores of the targeted patients with depression,” according to an abstract the company published online. “Use of VR caused no adverse events, demonstrating that VR can be used safely in the CBT for of depression.” The company did not respond to a request for more details.
After viewing scenarios created for Japanese patients, Dr. Larsson and Dr. Laria offered Jolly Good several tips about making the transition to the United States. The actors should be more emotionally expressive. They should portray a more diverse cast of characters, including some female bosses. And not all scenes should be set in the workplace.
“In the U.S., at least in our experience, a lot of what depressed patients talk about is just their personal lives, their intimate relationship with a significant other, family relations, friends,” Dr. Laria said. “We gave them a whole list of topics that we felt would be more relevant for a U.S. audience.”
Dr. Larsson and Dr. Laria are consultants to Jolly Good. Dr. Premkumar reported no relevant financial interests.
A version of this article first appeared on Medscape.com.
Virtual reality (VR) has been taking positive steps in a variety of treatment areas for some time. Now a Japanese company is asking the question: Can people with depression benefit from watching VR scenarios in which actors portray characters coping with the condition?
That’s the assertion of the Tokyo-based company Jolly Good, a VR start-up that introduced the U.S. version of its VRDTx program at the annual meeting of the Consumer Electronics Show.
“Using this as an adjunct for psychotherapy to help someone see an example of someone who’s struggling with depression can be a helpful tool,” said Katharine Larsson, PhD, RN, clinical director of Boston Behavioral Medicine in Brookline. Larsson and her BBM colleague, Amaro J. Laria, PhD, are helping Jolly Good to adapt the program for use in the United States.
VRDTx uses techniques from cognitive-behavioral therapy (CBT). Donning goggles, viewers watch people acting out situations common to depression.
One technique frequently used in CBT is to make a detailed plan, Dr. Laria said. For example, VRDTx users might watch a character with depression struggling to get out of bed but resolving to get up for at least 10 minutes one day, to go for a walk the next day, etc. “The virtual reality allows you to watch a person actually going through the process of applying the intervention,” he said.
In this way, the program could work like hypnotherapy or imaginal therapy where patients picture themselves in a situation that might trigger their depression and then picture themselves coping with that situation.
Dr. Larsson advised using the program primarily as a sort of homework. “ she said. “Using it to substitute or replace the time with a therapist, I don’t think it could begin to have any kind of real efficacy.”
Deploying virtual reality to treat mood disorders is not new, said Preethi Premkumar, PhD, a senior lecturer in psychology at London South Bank University, who has no relationship to Jolly Good.
Dr. Premkumar is first author of a study of a VR program used to treat people who have anxiety about speaking in public. The program depicts the user speaking before an audience and allows the user to vary the number of people in the audience and the audience’s reactions. The users gave it high marks, Dr. Premkumar said. “They felt that it encouraged them to take on public speaking more in reality.”
VR could work in a similar way for depressed people because they tend to catastrophize about specific situations. “Virtual reality can recreate those scenes and then make people confront it without overexposing them,” Dr. Premkumar said.
One recent review article found several studies on VR as a treatment for anxiety. While only a handful focused on depression, they had mostly favorable results.
Jolly Good sponsored one such study, presented Sept. 17, 2021, at the European Association for Behavioural and Cognitive Therapies. “Results indicate improvement in the scores of the targeted patients with depression,” according to an abstract the company published online. “Use of VR caused no adverse events, demonstrating that VR can be used safely in the CBT for of depression.” The company did not respond to a request for more details.
After viewing scenarios created for Japanese patients, Dr. Larsson and Dr. Laria offered Jolly Good several tips about making the transition to the United States. The actors should be more emotionally expressive. They should portray a more diverse cast of characters, including some female bosses. And not all scenes should be set in the workplace.
“In the U.S., at least in our experience, a lot of what depressed patients talk about is just their personal lives, their intimate relationship with a significant other, family relations, friends,” Dr. Laria said. “We gave them a whole list of topics that we felt would be more relevant for a U.S. audience.”
Dr. Larsson and Dr. Laria are consultants to Jolly Good. Dr. Premkumar reported no relevant financial interests.
A version of this article first appeared on Medscape.com.
Doctors as trusted messengers
On a recent Friday, oncologist Christine Berg, MD, devoted 3 hours to a webinar about electrification of heavy- and medium-duty trucks in Maryland.
It’s not the way most cancer specialists choose to spend their time. But Dr. Berg, who is board certified in medical oncology, radiation oncology, and internal medicine, has made air pollution her current focus. Through organizations such as the Public Employees for Environmental Responsibility, she is working to raise awareness of the huge impact it can have on cancer.
“I think oncologists can make a difference,” she said.
That’s why Dr. Berg took a keen interest in a recent study by ProPublica, the nonprofit journalism organization, that identified previously ignored “hot spots of cancer-causing air.” While the ProPublica report gives an incomplete picture of airborne carcinogens, it puts an important spotlight on industrial air pollution, Dr. Berg and other experts say.
Relying on data from the Environmental Protection Agency’s Risk-Screening Environmental Indicators (RSEI), ProPublica researchers estimated the effects of industrial air pollution around the country and found problems the EPA overlooked, they reported. “The EPA collects data on each individual facility, but it doesn’t consider the excess cancer risk from all of the facilities’ combined emissions,” reporter Lylla Younes and colleagues wrote. “ProPublica did.”
The ProPublica team produced a map of cancer-causing industrial air pollution hot spots. They estimated that 256,000 people in the United States live in areas where incidences of cancer caused by air pollution exceed the EPA’s upper limit of acceptable risk.
While some of the spots are scattered around the country, they are concentrated along the Gulf Coast of Texas and Louisiana. For example, near the Equistar Chemicals Bayport Chemical Plant in Pasadena, Texas, ProPublica calculated the increased risk of cancer at 1 in 220, “46 times the EPA’s acceptable risk.” (The agency defines an acceptable risk as less than a 1 in 10,000 chance of developing cancer.)
Almost all the hot spots with the highest level of risk are in southern United States “known for having weaker environmental regulations,” the report said.
The researchers also identified race as a risk factor. In predominantly Black census tracts, they estimated the risk from toxic air pollution is more than double the risk in predominantly White census tracts. It attributed this pattern to deliberate policies of redlining that segregated neighborhoods and to zoning ordinances that encouraged industry in communities of color.
Measuring risk not straightforward
In response to a query from this news organization, an EPA spokesperson provided a statement saying the RSEI data are not intended for the purpose used by ProPublica. “RSEI does not provide a risk assessment (e.g., excess cancer case estimates),” the statement said. The RSEI data are poorly suited to this purpose because they use “worst-case assumptions about toxicity and potential exposure where data are lacking, and also use simplifying assumptions to reduce the complexity of the calculations,” the statement said.
Instead, the data are meant as a kind of index to compare one place to another, or show changes over time, the agency said. In this way, it can prompt regulators to investigate further. “A more refined assessment is required before any conclusions about health impacts can be drawn.” The agency is working on just such a refined approach, per the EPA statement.
That’s not just bureaucratic stonewalling, said Stan Meiberg, PhD, MA, a former EPA official and director of graduate studies in sustainability at Wake Forest University in Winston-Salem, N.C. “To say that you can speak with great precision, that the risk of individuals getting cancer is 1 in 100, may be a little overstating the date on which that statement is based.”
Risk estimates are improving as citizens gain access to more sophisticated monitoring devices, he said. And the primary point of the ProPublica report, that the EPA has underestimated risk by looking at individual sources of pollution rather than combining them, is not an original one, Dr. Meiberg said. “This is an issue that’s been kicking around for quite some time.”
Still, it’s one that demands attention. EPA regulations have succeeded in reducing the overall risk from industrial air pollution over the past few decades. “But there remain areas of particular geographic concentrations,” he said. “And the ProPublica article hit two of them, which have been the subject of discussion for many years, the Houston Ship Channel area and the Baton Rouge to New Orleans industrial corridor where you have a significant proportion of all the chemical petrochemical industry in the United States.”
Improvements in containment of the pollutants, and changes to the industrial processes that produce them, can also help reduce exposure. These changes should occur in the context of dialogue within the communities exposed to the pollution, Dr. Meiberg said.
The role of cancer-causing airborne particulate matter
But even if measures are perfectly implemented, Joan Schiller, MD, will not breathe easy. An adjunct professor of oncology at the University of Virginia in Charlottesville, Dr. Schiller has researched the role of airborne particulate matter in causing cancer, a correlation barely mentioned in the ProPublica analysis, she pointed out.
Particulate matter contains a wide range of toxic substances, she said. Researchers have focused on particles 2.5 microns in diameter, or PM 2.5. Some studies have indicated that it’s responsible for one in seven deaths from lung cancer, Dr. Schiller said. “Air pollution also causes lung cancer in never smokers, people who’ve never smoked, not just in smokers.”
Power plants and automobile traffic may be more significant sources of PM 2.5 than industry, and wildfires have recently emerged as increasingly important source, a result of climate change and poor forest management, she said.
PM 2.5 doesn’t affect just lung cancer, said Alexandra White, PhD, an investigator at the National Institute of Environmental Health Sciences in Research Triangle Park, N.C. “My work, as well as work of others, is increasingly suggesting that air pollution is also related to breast cancer risk, in particular, air pollution that is arising from traffic related forces.” And more research is needed on other cancers, she said. “I think that the lack of findings of other cancer sites reflects a lack of study.”
Other pollutants not analyzed in the ProPublica report are also correlated to cancer risk. In a recent meta-analysis, researcher Stephan Gabet, PhD, PharmD, and colleagues at the University of Grenoble, France, estimated that 3.15% of new breast cancer cases in that country could be attributed to nitrogen dioxide and 2.15% to PM 10.
Sources of nitrogen dioxide, PM 2.5, and PM 10 in France include automobile traffic, inefficient wood-burning stoves, and coal-burning power plants in neighboring countries, Dr. Gabet said.
A good approach to reducing pollution from road traffic is the implementation of low-emission zones that prohibit the most polluting vehicles, he said. But a 2019 United Kingdom government study found that brake wear, tire wear, and road surface wear account for 72% of the PM 10 and 60% of the PM 2.5 pollution from road traffic, suggesting that a transition to electric vehicles won’t fix the problem. Better yet, is “the promotion of active modes like walking, cycling, etc., because like this, you can bring additional health gains due to the increase in physical activity,” he said.
Oncologists can help their patients reduce their exposure to air pollution, Dr. Schiller said. “If you have lung cancer, air pollution will hasten your demise. It makes you sicker. Oncologists should be telling their patients about this and advising them to move away from air pollution if possible, and also making sure they know to monitor the health of the air.”
On days when air pollution is high, patients may want to avoid exercising outdoors, or stay indoors altogether, Dr. Berg said. Air purifiers and N95 masks may also help.
And physicians can make a difference by speaking out in their communities, Dr. Schiller said. She is inviting oncologists to join a new group, Oncologists Understanding for Climate and Health. Through this group or on their own, oncologists can speak to their local legislatures or city councils in support of measures to reduce pollution, she said. “Doctors are trusted messengers.”
Dr. Berg disclosed affiliations with Grail, Mercy BioAnalytics and Lucid Diagnostics.
On a recent Friday, oncologist Christine Berg, MD, devoted 3 hours to a webinar about electrification of heavy- and medium-duty trucks in Maryland.
It’s not the way most cancer specialists choose to spend their time. But Dr. Berg, who is board certified in medical oncology, radiation oncology, and internal medicine, has made air pollution her current focus. Through organizations such as the Public Employees for Environmental Responsibility, she is working to raise awareness of the huge impact it can have on cancer.
“I think oncologists can make a difference,” she said.
That’s why Dr. Berg took a keen interest in a recent study by ProPublica, the nonprofit journalism organization, that identified previously ignored “hot spots of cancer-causing air.” While the ProPublica report gives an incomplete picture of airborne carcinogens, it puts an important spotlight on industrial air pollution, Dr. Berg and other experts say.
Relying on data from the Environmental Protection Agency’s Risk-Screening Environmental Indicators (RSEI), ProPublica researchers estimated the effects of industrial air pollution around the country and found problems the EPA overlooked, they reported. “The EPA collects data on each individual facility, but it doesn’t consider the excess cancer risk from all of the facilities’ combined emissions,” reporter Lylla Younes and colleagues wrote. “ProPublica did.”
The ProPublica team produced a map of cancer-causing industrial air pollution hot spots. They estimated that 256,000 people in the United States live in areas where incidences of cancer caused by air pollution exceed the EPA’s upper limit of acceptable risk.
While some of the spots are scattered around the country, they are concentrated along the Gulf Coast of Texas and Louisiana. For example, near the Equistar Chemicals Bayport Chemical Plant in Pasadena, Texas, ProPublica calculated the increased risk of cancer at 1 in 220, “46 times the EPA’s acceptable risk.” (The agency defines an acceptable risk as less than a 1 in 10,000 chance of developing cancer.)
Almost all the hot spots with the highest level of risk are in southern United States “known for having weaker environmental regulations,” the report said.
The researchers also identified race as a risk factor. In predominantly Black census tracts, they estimated the risk from toxic air pollution is more than double the risk in predominantly White census tracts. It attributed this pattern to deliberate policies of redlining that segregated neighborhoods and to zoning ordinances that encouraged industry in communities of color.
Measuring risk not straightforward
In response to a query from this news organization, an EPA spokesperson provided a statement saying the RSEI data are not intended for the purpose used by ProPublica. “RSEI does not provide a risk assessment (e.g., excess cancer case estimates),” the statement said. The RSEI data are poorly suited to this purpose because they use “worst-case assumptions about toxicity and potential exposure where data are lacking, and also use simplifying assumptions to reduce the complexity of the calculations,” the statement said.
Instead, the data are meant as a kind of index to compare one place to another, or show changes over time, the agency said. In this way, it can prompt regulators to investigate further. “A more refined assessment is required before any conclusions about health impacts can be drawn.” The agency is working on just such a refined approach, per the EPA statement.
That’s not just bureaucratic stonewalling, said Stan Meiberg, PhD, MA, a former EPA official and director of graduate studies in sustainability at Wake Forest University in Winston-Salem, N.C. “To say that you can speak with great precision, that the risk of individuals getting cancer is 1 in 100, may be a little overstating the date on which that statement is based.”
Risk estimates are improving as citizens gain access to more sophisticated monitoring devices, he said. And the primary point of the ProPublica report, that the EPA has underestimated risk by looking at individual sources of pollution rather than combining them, is not an original one, Dr. Meiberg said. “This is an issue that’s been kicking around for quite some time.”
Still, it’s one that demands attention. EPA regulations have succeeded in reducing the overall risk from industrial air pollution over the past few decades. “But there remain areas of particular geographic concentrations,” he said. “And the ProPublica article hit two of them, which have been the subject of discussion for many years, the Houston Ship Channel area and the Baton Rouge to New Orleans industrial corridor where you have a significant proportion of all the chemical petrochemical industry in the United States.”
Improvements in containment of the pollutants, and changes to the industrial processes that produce them, can also help reduce exposure. These changes should occur in the context of dialogue within the communities exposed to the pollution, Dr. Meiberg said.
The role of cancer-causing airborne particulate matter
But even if measures are perfectly implemented, Joan Schiller, MD, will not breathe easy. An adjunct professor of oncology at the University of Virginia in Charlottesville, Dr. Schiller has researched the role of airborne particulate matter in causing cancer, a correlation barely mentioned in the ProPublica analysis, she pointed out.
Particulate matter contains a wide range of toxic substances, she said. Researchers have focused on particles 2.5 microns in diameter, or PM 2.5. Some studies have indicated that it’s responsible for one in seven deaths from lung cancer, Dr. Schiller said. “Air pollution also causes lung cancer in never smokers, people who’ve never smoked, not just in smokers.”
Power plants and automobile traffic may be more significant sources of PM 2.5 than industry, and wildfires have recently emerged as increasingly important source, a result of climate change and poor forest management, she said.
PM 2.5 doesn’t affect just lung cancer, said Alexandra White, PhD, an investigator at the National Institute of Environmental Health Sciences in Research Triangle Park, N.C. “My work, as well as work of others, is increasingly suggesting that air pollution is also related to breast cancer risk, in particular, air pollution that is arising from traffic related forces.” And more research is needed on other cancers, she said. “I think that the lack of findings of other cancer sites reflects a lack of study.”
Other pollutants not analyzed in the ProPublica report are also correlated to cancer risk. In a recent meta-analysis, researcher Stephan Gabet, PhD, PharmD, and colleagues at the University of Grenoble, France, estimated that 3.15% of new breast cancer cases in that country could be attributed to nitrogen dioxide and 2.15% to PM 10.
Sources of nitrogen dioxide, PM 2.5, and PM 10 in France include automobile traffic, inefficient wood-burning stoves, and coal-burning power plants in neighboring countries, Dr. Gabet said.
A good approach to reducing pollution from road traffic is the implementation of low-emission zones that prohibit the most polluting vehicles, he said. But a 2019 United Kingdom government study found that brake wear, tire wear, and road surface wear account for 72% of the PM 10 and 60% of the PM 2.5 pollution from road traffic, suggesting that a transition to electric vehicles won’t fix the problem. Better yet, is “the promotion of active modes like walking, cycling, etc., because like this, you can bring additional health gains due to the increase in physical activity,” he said.
Oncologists can help their patients reduce their exposure to air pollution, Dr. Schiller said. “If you have lung cancer, air pollution will hasten your demise. It makes you sicker. Oncologists should be telling their patients about this and advising them to move away from air pollution if possible, and also making sure they know to monitor the health of the air.”
On days when air pollution is high, patients may want to avoid exercising outdoors, or stay indoors altogether, Dr. Berg said. Air purifiers and N95 masks may also help.
And physicians can make a difference by speaking out in their communities, Dr. Schiller said. She is inviting oncologists to join a new group, Oncologists Understanding for Climate and Health. Through this group or on their own, oncologists can speak to their local legislatures or city councils in support of measures to reduce pollution, she said. “Doctors are trusted messengers.”
Dr. Berg disclosed affiliations with Grail, Mercy BioAnalytics and Lucid Diagnostics.
On a recent Friday, oncologist Christine Berg, MD, devoted 3 hours to a webinar about electrification of heavy- and medium-duty trucks in Maryland.
It’s not the way most cancer specialists choose to spend their time. But Dr. Berg, who is board certified in medical oncology, radiation oncology, and internal medicine, has made air pollution her current focus. Through organizations such as the Public Employees for Environmental Responsibility, she is working to raise awareness of the huge impact it can have on cancer.
“I think oncologists can make a difference,” she said.
That’s why Dr. Berg took a keen interest in a recent study by ProPublica, the nonprofit journalism organization, that identified previously ignored “hot spots of cancer-causing air.” While the ProPublica report gives an incomplete picture of airborne carcinogens, it puts an important spotlight on industrial air pollution, Dr. Berg and other experts say.
Relying on data from the Environmental Protection Agency’s Risk-Screening Environmental Indicators (RSEI), ProPublica researchers estimated the effects of industrial air pollution around the country and found problems the EPA overlooked, they reported. “The EPA collects data on each individual facility, but it doesn’t consider the excess cancer risk from all of the facilities’ combined emissions,” reporter Lylla Younes and colleagues wrote. “ProPublica did.”
The ProPublica team produced a map of cancer-causing industrial air pollution hot spots. They estimated that 256,000 people in the United States live in areas where incidences of cancer caused by air pollution exceed the EPA’s upper limit of acceptable risk.
While some of the spots are scattered around the country, they are concentrated along the Gulf Coast of Texas and Louisiana. For example, near the Equistar Chemicals Bayport Chemical Plant in Pasadena, Texas, ProPublica calculated the increased risk of cancer at 1 in 220, “46 times the EPA’s acceptable risk.” (The agency defines an acceptable risk as less than a 1 in 10,000 chance of developing cancer.)
Almost all the hot spots with the highest level of risk are in southern United States “known for having weaker environmental regulations,” the report said.
The researchers also identified race as a risk factor. In predominantly Black census tracts, they estimated the risk from toxic air pollution is more than double the risk in predominantly White census tracts. It attributed this pattern to deliberate policies of redlining that segregated neighborhoods and to zoning ordinances that encouraged industry in communities of color.
Measuring risk not straightforward
In response to a query from this news organization, an EPA spokesperson provided a statement saying the RSEI data are not intended for the purpose used by ProPublica. “RSEI does not provide a risk assessment (e.g., excess cancer case estimates),” the statement said. The RSEI data are poorly suited to this purpose because they use “worst-case assumptions about toxicity and potential exposure where data are lacking, and also use simplifying assumptions to reduce the complexity of the calculations,” the statement said.
Instead, the data are meant as a kind of index to compare one place to another, or show changes over time, the agency said. In this way, it can prompt regulators to investigate further. “A more refined assessment is required before any conclusions about health impacts can be drawn.” The agency is working on just such a refined approach, per the EPA statement.
That’s not just bureaucratic stonewalling, said Stan Meiberg, PhD, MA, a former EPA official and director of graduate studies in sustainability at Wake Forest University in Winston-Salem, N.C. “To say that you can speak with great precision, that the risk of individuals getting cancer is 1 in 100, may be a little overstating the date on which that statement is based.”
Risk estimates are improving as citizens gain access to more sophisticated monitoring devices, he said. And the primary point of the ProPublica report, that the EPA has underestimated risk by looking at individual sources of pollution rather than combining them, is not an original one, Dr. Meiberg said. “This is an issue that’s been kicking around for quite some time.”
Still, it’s one that demands attention. EPA regulations have succeeded in reducing the overall risk from industrial air pollution over the past few decades. “But there remain areas of particular geographic concentrations,” he said. “And the ProPublica article hit two of them, which have been the subject of discussion for many years, the Houston Ship Channel area and the Baton Rouge to New Orleans industrial corridor where you have a significant proportion of all the chemical petrochemical industry in the United States.”
Improvements in containment of the pollutants, and changes to the industrial processes that produce them, can also help reduce exposure. These changes should occur in the context of dialogue within the communities exposed to the pollution, Dr. Meiberg said.
The role of cancer-causing airborne particulate matter
But even if measures are perfectly implemented, Joan Schiller, MD, will not breathe easy. An adjunct professor of oncology at the University of Virginia in Charlottesville, Dr. Schiller has researched the role of airborne particulate matter in causing cancer, a correlation barely mentioned in the ProPublica analysis, she pointed out.
Particulate matter contains a wide range of toxic substances, she said. Researchers have focused on particles 2.5 microns in diameter, or PM 2.5. Some studies have indicated that it’s responsible for one in seven deaths from lung cancer, Dr. Schiller said. “Air pollution also causes lung cancer in never smokers, people who’ve never smoked, not just in smokers.”
Power plants and automobile traffic may be more significant sources of PM 2.5 than industry, and wildfires have recently emerged as increasingly important source, a result of climate change and poor forest management, she said.
PM 2.5 doesn’t affect just lung cancer, said Alexandra White, PhD, an investigator at the National Institute of Environmental Health Sciences in Research Triangle Park, N.C. “My work, as well as work of others, is increasingly suggesting that air pollution is also related to breast cancer risk, in particular, air pollution that is arising from traffic related forces.” And more research is needed on other cancers, she said. “I think that the lack of findings of other cancer sites reflects a lack of study.”
Other pollutants not analyzed in the ProPublica report are also correlated to cancer risk. In a recent meta-analysis, researcher Stephan Gabet, PhD, PharmD, and colleagues at the University of Grenoble, France, estimated that 3.15% of new breast cancer cases in that country could be attributed to nitrogen dioxide and 2.15% to PM 10.
Sources of nitrogen dioxide, PM 2.5, and PM 10 in France include automobile traffic, inefficient wood-burning stoves, and coal-burning power plants in neighboring countries, Dr. Gabet said.
A good approach to reducing pollution from road traffic is the implementation of low-emission zones that prohibit the most polluting vehicles, he said. But a 2019 United Kingdom government study found that brake wear, tire wear, and road surface wear account for 72% of the PM 10 and 60% of the PM 2.5 pollution from road traffic, suggesting that a transition to electric vehicles won’t fix the problem. Better yet, is “the promotion of active modes like walking, cycling, etc., because like this, you can bring additional health gains due to the increase in physical activity,” he said.
Oncologists can help their patients reduce their exposure to air pollution, Dr. Schiller said. “If you have lung cancer, air pollution will hasten your demise. It makes you sicker. Oncologists should be telling their patients about this and advising them to move away from air pollution if possible, and also making sure they know to monitor the health of the air.”
On days when air pollution is high, patients may want to avoid exercising outdoors, or stay indoors altogether, Dr. Berg said. Air purifiers and N95 masks may also help.
And physicians can make a difference by speaking out in their communities, Dr. Schiller said. She is inviting oncologists to join a new group, Oncologists Understanding for Climate and Health. Through this group or on their own, oncologists can speak to their local legislatures or city councils in support of measures to reduce pollution, she said. “Doctors are trusted messengers.”
Dr. Berg disclosed affiliations with Grail, Mercy BioAnalytics and Lucid Diagnostics.
People of color missing in inflammatory bowel disease trials
LAS VEGAS – Clinical trials of treatments for inflammatory bowel disease (IBD) have disproportionately enrolled White people, researchers say.
These skewed demographics could result in researchers overlooking differences in how the disease and its treatments might affect other racial and ethnic groups, said Jellyana Peraza, MD, a chief resident at Albert Einstein College of Medicine, New York.
“The only way we can determine that therapies work differently in different populations is by including those populations in these clinical trials,” she said in an interview. “We think that diversity should be present, and that will answer some questions about the pathogenesis of the disease in general.”
Dr. Peraza presented the findings at the annual meeting of the American College of Gastroenterology.
Previous studies have found that, in trials of other conditions, such as cancer and cardiovascular disease, White people have been disproportionately represented. However, little research has been conducted regarding race and ethnicity in IBD trials.
To fill that gap, Dr. Peraza and colleagues analyzed data from completed trials through the U.S. National Library of Medicine’s registry, ClinicalTrials.gov, for the period from 2000 to 2020.
They found 22 trials conducted exclusively in the United States and 56 conducted in other countries that reported the race or ethnicity of participants; 54 trials did not include this information.
With regard to the prevalence of IBD in White people and Asian people, these populations were overrepresented in U.S. clinical trials. All other groups were underrepresented.
The researchers calculated the odds ratio of being included in an IBD clinical trial for each group. Compared with White people, all the other groups were less likely to be included except for Asian people, who were 85% more likely to be included. These ORs were all statistically significant (P < .03) except for Hispanic people (OR, 0.81; 95% confidence interval, 0.65-1.01; P = .06).
It’s not clear why Asian people are overrepresented, Dr. Peraza said. “Honestly, that was kind of surprising for us. We initially thought that could be related to where these studies were conducted, for example, if some of them were conducted on the West Coast, where maybe more Asian communities are located. However, we didn’t find any specific association between location and Asian representation.”
IBD is more prevalent among White people, although its prevalence is increasing among other groups, Dr. Peraza said. However, that is not reflected in the trials. In an analysis of data in 5-year increments, the researchers found that the participation of White and Hispanic people in IBD trials had not changed much, whereas the participation of Black people had declined, and the participation of Asian and Native American people had increased.
On the basis of work of other researchers, Dr. Peraza said that people of color are as willing to participate in trials as White people. “There is not so much a mistrust as a lack of education and a lack of access to the tertiary centers or the centers where these studies are conducted,” she said.
Clinical trial investigators should recruit more participants from community centers, and health care practitioners should talk about the trials with people in underrepresented groups, she said. “They should have the conversation with their patients about how these clinical trials can benefit the evolution of their diseases.”
One research center that is working hard to diversify its IBD trials is the Ohio State University IBD Center, Columbus, said Anita Afzali, MD, its medical director.
“We have a great team that works actively on the recruitment of all patients,” she said in an interview. “Oftentimes, it just takes a little bit of education and spending time with the patient on discussing what the options are for them.”
Some research indicates that Black people with IBD are more likely to have fistulizing disease, Dr. Afzali said. “However, it doesn’t come so much of their differences in phenotype that we’re seeing but more so the differences in access to care and getting the appropriate therapy in a timely way.”
Dr. Peraza and Dr. Afzali disclosed no relevant financial relationships.
AGA applauds researchers who are working to raise our awareness of health disparities in digestive diseases. AGA is committed to addressing this important societal issue head on. Learn more about AGA’s commitment through the AGA Equity Project.
A version of this article first appeared on Medscape.com.
LAS VEGAS – Clinical trials of treatments for inflammatory bowel disease (IBD) have disproportionately enrolled White people, researchers say.
These skewed demographics could result in researchers overlooking differences in how the disease and its treatments might affect other racial and ethnic groups, said Jellyana Peraza, MD, a chief resident at Albert Einstein College of Medicine, New York.
“The only way we can determine that therapies work differently in different populations is by including those populations in these clinical trials,” she said in an interview. “We think that diversity should be present, and that will answer some questions about the pathogenesis of the disease in general.”
Dr. Peraza presented the findings at the annual meeting of the American College of Gastroenterology.
Previous studies have found that, in trials of other conditions, such as cancer and cardiovascular disease, White people have been disproportionately represented. However, little research has been conducted regarding race and ethnicity in IBD trials.
To fill that gap, Dr. Peraza and colleagues analyzed data from completed trials through the U.S. National Library of Medicine’s registry, ClinicalTrials.gov, for the period from 2000 to 2020.
They found 22 trials conducted exclusively in the United States and 56 conducted in other countries that reported the race or ethnicity of participants; 54 trials did not include this information.
With regard to the prevalence of IBD in White people and Asian people, these populations were overrepresented in U.S. clinical trials. All other groups were underrepresented.
The researchers calculated the odds ratio of being included in an IBD clinical trial for each group. Compared with White people, all the other groups were less likely to be included except for Asian people, who were 85% more likely to be included. These ORs were all statistically significant (P < .03) except for Hispanic people (OR, 0.81; 95% confidence interval, 0.65-1.01; P = .06).
It’s not clear why Asian people are overrepresented, Dr. Peraza said. “Honestly, that was kind of surprising for us. We initially thought that could be related to where these studies were conducted, for example, if some of them were conducted on the West Coast, where maybe more Asian communities are located. However, we didn’t find any specific association between location and Asian representation.”
IBD is more prevalent among White people, although its prevalence is increasing among other groups, Dr. Peraza said. However, that is not reflected in the trials. In an analysis of data in 5-year increments, the researchers found that the participation of White and Hispanic people in IBD trials had not changed much, whereas the participation of Black people had declined, and the participation of Asian and Native American people had increased.
On the basis of work of other researchers, Dr. Peraza said that people of color are as willing to participate in trials as White people. “There is not so much a mistrust as a lack of education and a lack of access to the tertiary centers or the centers where these studies are conducted,” she said.
Clinical trial investigators should recruit more participants from community centers, and health care practitioners should talk about the trials with people in underrepresented groups, she said. “They should have the conversation with their patients about how these clinical trials can benefit the evolution of their diseases.”
One research center that is working hard to diversify its IBD trials is the Ohio State University IBD Center, Columbus, said Anita Afzali, MD, its medical director.
“We have a great team that works actively on the recruitment of all patients,” she said in an interview. “Oftentimes, it just takes a little bit of education and spending time with the patient on discussing what the options are for them.”
Some research indicates that Black people with IBD are more likely to have fistulizing disease, Dr. Afzali said. “However, it doesn’t come so much of their differences in phenotype that we’re seeing but more so the differences in access to care and getting the appropriate therapy in a timely way.”
Dr. Peraza and Dr. Afzali disclosed no relevant financial relationships.
AGA applauds researchers who are working to raise our awareness of health disparities in digestive diseases. AGA is committed to addressing this important societal issue head on. Learn more about AGA’s commitment through the AGA Equity Project.
A version of this article first appeared on Medscape.com.
LAS VEGAS – Clinical trials of treatments for inflammatory bowel disease (IBD) have disproportionately enrolled White people, researchers say.
These skewed demographics could result in researchers overlooking differences in how the disease and its treatments might affect other racial and ethnic groups, said Jellyana Peraza, MD, a chief resident at Albert Einstein College of Medicine, New York.
“The only way we can determine that therapies work differently in different populations is by including those populations in these clinical trials,” she said in an interview. “We think that diversity should be present, and that will answer some questions about the pathogenesis of the disease in general.”
Dr. Peraza presented the findings at the annual meeting of the American College of Gastroenterology.
Previous studies have found that, in trials of other conditions, such as cancer and cardiovascular disease, White people have been disproportionately represented. However, little research has been conducted regarding race and ethnicity in IBD trials.
To fill that gap, Dr. Peraza and colleagues analyzed data from completed trials through the U.S. National Library of Medicine’s registry, ClinicalTrials.gov, for the period from 2000 to 2020.
They found 22 trials conducted exclusively in the United States and 56 conducted in other countries that reported the race or ethnicity of participants; 54 trials did not include this information.
With regard to the prevalence of IBD in White people and Asian people, these populations were overrepresented in U.S. clinical trials. All other groups were underrepresented.
The researchers calculated the odds ratio of being included in an IBD clinical trial for each group. Compared with White people, all the other groups were less likely to be included except for Asian people, who were 85% more likely to be included. These ORs were all statistically significant (P < .03) except for Hispanic people (OR, 0.81; 95% confidence interval, 0.65-1.01; P = .06).
It’s not clear why Asian people are overrepresented, Dr. Peraza said. “Honestly, that was kind of surprising for us. We initially thought that could be related to where these studies were conducted, for example, if some of them were conducted on the West Coast, where maybe more Asian communities are located. However, we didn’t find any specific association between location and Asian representation.”
IBD is more prevalent among White people, although its prevalence is increasing among other groups, Dr. Peraza said. However, that is not reflected in the trials. In an analysis of data in 5-year increments, the researchers found that the participation of White and Hispanic people in IBD trials had not changed much, whereas the participation of Black people had declined, and the participation of Asian and Native American people had increased.
On the basis of work of other researchers, Dr. Peraza said that people of color are as willing to participate in trials as White people. “There is not so much a mistrust as a lack of education and a lack of access to the tertiary centers or the centers where these studies are conducted,” she said.
Clinical trial investigators should recruit more participants from community centers, and health care practitioners should talk about the trials with people in underrepresented groups, she said. “They should have the conversation with their patients about how these clinical trials can benefit the evolution of their diseases.”
One research center that is working hard to diversify its IBD trials is the Ohio State University IBD Center, Columbus, said Anita Afzali, MD, its medical director.
“We have a great team that works actively on the recruitment of all patients,” she said in an interview. “Oftentimes, it just takes a little bit of education and spending time with the patient on discussing what the options are for them.”
Some research indicates that Black people with IBD are more likely to have fistulizing disease, Dr. Afzali said. “However, it doesn’t come so much of their differences in phenotype that we’re seeing but more so the differences in access to care and getting the appropriate therapy in a timely way.”
Dr. Peraza and Dr. Afzali disclosed no relevant financial relationships.
AGA applauds researchers who are working to raise our awareness of health disparities in digestive diseases. AGA is committed to addressing this important societal issue head on. Learn more about AGA’s commitment through the AGA Equity Project.
A version of this article first appeared on Medscape.com.
AT ACG 2021
Ulcerative colitis study: Ozanimod tops adalimumab, equals vedolizumab
LAS VEGAS – In a comparison of data from clinical trials for ulcerative colitis, ozanimod (Zeposia) appeared to be more useful than adalimumab (Humira) and as useful as vedolizumab (Entyvio).
The U.S. Food and Drug Administration approved ozanimod for ulcerative colitis in May of this year, and clinicians are trying to figure out where it fits into the armamentarium, said Marla Dubinsky, MD, professor of pediatrics and medicine in the Division of Pediatric Gastroenterology at Icahn School of Medicine at Mount Sinai, New York.
“It’s an extremely heterogeneous disease,” Dr. Dubinsky told this news organization. “A lot of these indirect comparisons are being done, because these therapies are coming out so quickly.”
No clinical trials have compared either ozanimod to adalimumab or ozanimod to vedolizumab head to head, so Dr. Dubinsky and colleagues pitted the drugs against each other by matching data from individual patients from the True North trial of ozanimod to published data from the ULTRA 1 and 2 trials of adalimumab and the GEMINI 1 trial of vedolizumab.
She presented the findings here at the American College of Gastroenterology (ACG) 2021 Annual Scientific Meeting.
From the 1990s until 2014, physicians relied heavily on tumor necrosis factor (TNF) inhibitors, such as adalimumab, to treat ulcerative colitis, Dr. Dubinsky said. Although often effective, these drugs can increase patients’ vulnerability to infections and malignancies.
Approved by the FDA in 2014, vedolizumab works differently: it blocks α4β7 integrin. “The safety profile was extremely favorable,” Dr. Dubinsky said. “That was a revolution, in my opinion.” Still, vedolizumab isn’t always effective, especially for patients who have already received TNF inhibitors without success.
As reported by this news organization, ozanimod works by yet another mechanism: sphingosine l-phosphate receptor modulation.
How does ozanimod measure up?
To see how ozanimod stacks up to the two older drugs, Dr. Dubinsky and colleagues weighted the data from True North to match the patient populations in the other trials by age, sex, baseline total Mayo score, disease extent, and prior anti-TNF treatment.
They calculated the odds that ozanimod would produce better clinical and endoscopic responses or be associated with more serious or infectious adverse events in comparison with each of the other drugs. The comparisons included both the induction and maintenance phases of the trials.
The researchers compared ozanimod to adalimumab for patients who were anti-TNF naive. They found that the patients who took ozanimod were more likely to experience a clinical response than those who took adalimumab (odds ratio, 1.68; 95% CI, 1.03-2.74). The patients who took ozanimod were also more likely to have endoscopic improvement (OR, 2.73; 95% CI, 1.44-5.17).
They found that the patients who had received a TNF inhibitor were also more likely to experience a clinical response with ozanimod than with adalimumab (OR, 2.53; 95% CI, 1.13-5.67).
In both the induction and the maintenance phases, the other differences in efficacy between ozanimod and adalimumab did not reach statistical significance.
As for safety, in the induction phases of the trials, the researchers found that 11.3% of patients who received ozanimod had infections, compared to 20.2% of those taking adalimumab, which was statistically significant (P < .01). Other differences in safety were not statistically significant.
With regard to vedolizumab, Dr. Dubinsky and colleagues found no statistically significant differences between it and ozanimod in the induction phases.
In the maintenance phases, among patients who were anti-TNF naive, the odds of clinical response were lower with ozanimod than with vedolizumab (OR, 0.40; 95% CI, 0.21-0.76). The odds of endoscopic improvement were very nearly lower (OR, 0.52; 95% CI, 0.27-1.01). The researchers attributed these findings to a higher placebo response in the True North trial (the ozanimod trial) than in GEMINI 1 (the vedolizumab trial).
There were no other significant differences in efficacy between ozanimod and vedolizumab, either in the cohort that had received a TNF inhibitor or in the cohort that had not.
As for safety, there were also no statistically significant differences between vedolizumab and ozanimod in the induction phases. During the maintenance phases, 71.3% of patients who received vedolizumab had infections, compared to 25.0% in the matched cohort of patients who received ozanimod, which was a statistically significant difference (P < .001). The other differences in this phase were not significant.
Dr. Dubinsky acknowledged that the results were not as reliable as would have been the case in a prospective, head-to-head comparison, because the researchers could not be sure that they had fully adjusted for the differences in the populations and the designs of the studies.
“In TNF-inhibitor–naive patients, I could use vedolizumab or ozanimod,” Dr. Dubinsky said. But these are not the only options, she said. She said that “in TNF failure, I would use ustekinumab or even tofacitinib.” Ustekinumab (Stelara) is a human interleukin-12 and -23 antagonist; tofacitinib (Xeljanz) is a Janus kinase inhibitor.
The study’s limitations are significant, said session moderator Jonathan Leighton, MD, a professor of medicine at the Mayo Clinic in Phoenix, Arizona, “but it certainly shows that ozanimod had a positive profile compared to adalimumab and has overall comparable benefits with vedolizumab,” he said in an interview.
Dr. Leighton added that someday researchers may find biomarkers that will identify the best drug for each patient. In the meantime, clinicians are often left choosing therapies on the basis of such factors as which route of administration the patients prefer, he said. Vedolizumab is given by intravenous infusion, ozanimod is taken orally, and adalimumab is given by subcutaneous injection.
The study was funded by Bristol-Myers Squibb. Dr. Leighton has financial relationships with Olympus and Pfizer. Dr. Dubinsky has relationships with all or most of the companies that make drugs for inflammatory bowel disease.
A version of this article first appeared on Medscape.com.
LAS VEGAS – In a comparison of data from clinical trials for ulcerative colitis, ozanimod (Zeposia) appeared to be more useful than adalimumab (Humira) and as useful as vedolizumab (Entyvio).
The U.S. Food and Drug Administration approved ozanimod for ulcerative colitis in May of this year, and clinicians are trying to figure out where it fits into the armamentarium, said Marla Dubinsky, MD, professor of pediatrics and medicine in the Division of Pediatric Gastroenterology at Icahn School of Medicine at Mount Sinai, New York.
“It’s an extremely heterogeneous disease,” Dr. Dubinsky told this news organization. “A lot of these indirect comparisons are being done, because these therapies are coming out so quickly.”
No clinical trials have compared either ozanimod to adalimumab or ozanimod to vedolizumab head to head, so Dr. Dubinsky and colleagues pitted the drugs against each other by matching data from individual patients from the True North trial of ozanimod to published data from the ULTRA 1 and 2 trials of adalimumab and the GEMINI 1 trial of vedolizumab.
She presented the findings here at the American College of Gastroenterology (ACG) 2021 Annual Scientific Meeting.
From the 1990s until 2014, physicians relied heavily on tumor necrosis factor (TNF) inhibitors, such as adalimumab, to treat ulcerative colitis, Dr. Dubinsky said. Although often effective, these drugs can increase patients’ vulnerability to infections and malignancies.
Approved by the FDA in 2014, vedolizumab works differently: it blocks α4β7 integrin. “The safety profile was extremely favorable,” Dr. Dubinsky said. “That was a revolution, in my opinion.” Still, vedolizumab isn’t always effective, especially for patients who have already received TNF inhibitors without success.
As reported by this news organization, ozanimod works by yet another mechanism: sphingosine l-phosphate receptor modulation.
How does ozanimod measure up?
To see how ozanimod stacks up to the two older drugs, Dr. Dubinsky and colleagues weighted the data from True North to match the patient populations in the other trials by age, sex, baseline total Mayo score, disease extent, and prior anti-TNF treatment.
They calculated the odds that ozanimod would produce better clinical and endoscopic responses or be associated with more serious or infectious adverse events in comparison with each of the other drugs. The comparisons included both the induction and maintenance phases of the trials.
The researchers compared ozanimod to adalimumab for patients who were anti-TNF naive. They found that the patients who took ozanimod were more likely to experience a clinical response than those who took adalimumab (odds ratio, 1.68; 95% CI, 1.03-2.74). The patients who took ozanimod were also more likely to have endoscopic improvement (OR, 2.73; 95% CI, 1.44-5.17).
They found that the patients who had received a TNF inhibitor were also more likely to experience a clinical response with ozanimod than with adalimumab (OR, 2.53; 95% CI, 1.13-5.67).
In both the induction and the maintenance phases, the other differences in efficacy between ozanimod and adalimumab did not reach statistical significance.
As for safety, in the induction phases of the trials, the researchers found that 11.3% of patients who received ozanimod had infections, compared to 20.2% of those taking adalimumab, which was statistically significant (P < .01). Other differences in safety were not statistically significant.
With regard to vedolizumab, Dr. Dubinsky and colleagues found no statistically significant differences between it and ozanimod in the induction phases.
In the maintenance phases, among patients who were anti-TNF naive, the odds of clinical response were lower with ozanimod than with vedolizumab (OR, 0.40; 95% CI, 0.21-0.76). The odds of endoscopic improvement were very nearly lower (OR, 0.52; 95% CI, 0.27-1.01). The researchers attributed these findings to a higher placebo response in the True North trial (the ozanimod trial) than in GEMINI 1 (the vedolizumab trial).
There were no other significant differences in efficacy between ozanimod and vedolizumab, either in the cohort that had received a TNF inhibitor or in the cohort that had not.
As for safety, there were also no statistically significant differences between vedolizumab and ozanimod in the induction phases. During the maintenance phases, 71.3% of patients who received vedolizumab had infections, compared to 25.0% in the matched cohort of patients who received ozanimod, which was a statistically significant difference (P < .001). The other differences in this phase were not significant.
Dr. Dubinsky acknowledged that the results were not as reliable as would have been the case in a prospective, head-to-head comparison, because the researchers could not be sure that they had fully adjusted for the differences in the populations and the designs of the studies.
“In TNF-inhibitor–naive patients, I could use vedolizumab or ozanimod,” Dr. Dubinsky said. But these are not the only options, she said. She said that “in TNF failure, I would use ustekinumab or even tofacitinib.” Ustekinumab (Stelara) is a human interleukin-12 and -23 antagonist; tofacitinib (Xeljanz) is a Janus kinase inhibitor.
The study’s limitations are significant, said session moderator Jonathan Leighton, MD, a professor of medicine at the Mayo Clinic in Phoenix, Arizona, “but it certainly shows that ozanimod had a positive profile compared to adalimumab and has overall comparable benefits with vedolizumab,” he said in an interview.
Dr. Leighton added that someday researchers may find biomarkers that will identify the best drug for each patient. In the meantime, clinicians are often left choosing therapies on the basis of such factors as which route of administration the patients prefer, he said. Vedolizumab is given by intravenous infusion, ozanimod is taken orally, and adalimumab is given by subcutaneous injection.
The study was funded by Bristol-Myers Squibb. Dr. Leighton has financial relationships with Olympus and Pfizer. Dr. Dubinsky has relationships with all or most of the companies that make drugs for inflammatory bowel disease.
A version of this article first appeared on Medscape.com.
LAS VEGAS – In a comparison of data from clinical trials for ulcerative colitis, ozanimod (Zeposia) appeared to be more useful than adalimumab (Humira) and as useful as vedolizumab (Entyvio).
The U.S. Food and Drug Administration approved ozanimod for ulcerative colitis in May of this year, and clinicians are trying to figure out where it fits into the armamentarium, said Marla Dubinsky, MD, professor of pediatrics and medicine in the Division of Pediatric Gastroenterology at Icahn School of Medicine at Mount Sinai, New York.
“It’s an extremely heterogeneous disease,” Dr. Dubinsky told this news organization. “A lot of these indirect comparisons are being done, because these therapies are coming out so quickly.”
No clinical trials have compared either ozanimod to adalimumab or ozanimod to vedolizumab head to head, so Dr. Dubinsky and colleagues pitted the drugs against each other by matching data from individual patients from the True North trial of ozanimod to published data from the ULTRA 1 and 2 trials of adalimumab and the GEMINI 1 trial of vedolizumab.
She presented the findings here at the American College of Gastroenterology (ACG) 2021 Annual Scientific Meeting.
From the 1990s until 2014, physicians relied heavily on tumor necrosis factor (TNF) inhibitors, such as adalimumab, to treat ulcerative colitis, Dr. Dubinsky said. Although often effective, these drugs can increase patients’ vulnerability to infections and malignancies.
Approved by the FDA in 2014, vedolizumab works differently: it blocks α4β7 integrin. “The safety profile was extremely favorable,” Dr. Dubinsky said. “That was a revolution, in my opinion.” Still, vedolizumab isn’t always effective, especially for patients who have already received TNF inhibitors without success.
As reported by this news organization, ozanimod works by yet another mechanism: sphingosine l-phosphate receptor modulation.
How does ozanimod measure up?
To see how ozanimod stacks up to the two older drugs, Dr. Dubinsky and colleagues weighted the data from True North to match the patient populations in the other trials by age, sex, baseline total Mayo score, disease extent, and prior anti-TNF treatment.
They calculated the odds that ozanimod would produce better clinical and endoscopic responses or be associated with more serious or infectious adverse events in comparison with each of the other drugs. The comparisons included both the induction and maintenance phases of the trials.
The researchers compared ozanimod to adalimumab for patients who were anti-TNF naive. They found that the patients who took ozanimod were more likely to experience a clinical response than those who took adalimumab (odds ratio, 1.68; 95% CI, 1.03-2.74). The patients who took ozanimod were also more likely to have endoscopic improvement (OR, 2.73; 95% CI, 1.44-5.17).
They found that the patients who had received a TNF inhibitor were also more likely to experience a clinical response with ozanimod than with adalimumab (OR, 2.53; 95% CI, 1.13-5.67).
In both the induction and the maintenance phases, the other differences in efficacy between ozanimod and adalimumab did not reach statistical significance.
As for safety, in the induction phases of the trials, the researchers found that 11.3% of patients who received ozanimod had infections, compared to 20.2% of those taking adalimumab, which was statistically significant (P < .01). Other differences in safety were not statistically significant.
With regard to vedolizumab, Dr. Dubinsky and colleagues found no statistically significant differences between it and ozanimod in the induction phases.
In the maintenance phases, among patients who were anti-TNF naive, the odds of clinical response were lower with ozanimod than with vedolizumab (OR, 0.40; 95% CI, 0.21-0.76). The odds of endoscopic improvement were very nearly lower (OR, 0.52; 95% CI, 0.27-1.01). The researchers attributed these findings to a higher placebo response in the True North trial (the ozanimod trial) than in GEMINI 1 (the vedolizumab trial).
There were no other significant differences in efficacy between ozanimod and vedolizumab, either in the cohort that had received a TNF inhibitor or in the cohort that had not.
As for safety, there were also no statistically significant differences between vedolizumab and ozanimod in the induction phases. During the maintenance phases, 71.3% of patients who received vedolizumab had infections, compared to 25.0% in the matched cohort of patients who received ozanimod, which was a statistically significant difference (P < .001). The other differences in this phase were not significant.
Dr. Dubinsky acknowledged that the results were not as reliable as would have been the case in a prospective, head-to-head comparison, because the researchers could not be sure that they had fully adjusted for the differences in the populations and the designs of the studies.
“In TNF-inhibitor–naive patients, I could use vedolizumab or ozanimod,” Dr. Dubinsky said. But these are not the only options, she said. She said that “in TNF failure, I would use ustekinumab or even tofacitinib.” Ustekinumab (Stelara) is a human interleukin-12 and -23 antagonist; tofacitinib (Xeljanz) is a Janus kinase inhibitor.
The study’s limitations are significant, said session moderator Jonathan Leighton, MD, a professor of medicine at the Mayo Clinic in Phoenix, Arizona, “but it certainly shows that ozanimod had a positive profile compared to adalimumab and has overall comparable benefits with vedolizumab,” he said in an interview.
Dr. Leighton added that someday researchers may find biomarkers that will identify the best drug for each patient. In the meantime, clinicians are often left choosing therapies on the basis of such factors as which route of administration the patients prefer, he said. Vedolizumab is given by intravenous infusion, ozanimod is taken orally, and adalimumab is given by subcutaneous injection.
The study was funded by Bristol-Myers Squibb. Dr. Leighton has financial relationships with Olympus and Pfizer. Dr. Dubinsky has relationships with all or most of the companies that make drugs for inflammatory bowel disease.
A version of this article first appeared on Medscape.com.