User login
Gastroenterology groups map a return to elective endoscopy
Gastroenterologists can safely return to elective procedures when adequate personal protective equipment (PPE) is available, professional societies say.
Noting that some states have already lifted restrictions imposed to guard against COVID-19, the American Gastroenterological Association (AGA) and the Digestive Health Physicians Association (DHPA) on April 27 announced guidelines for resuming procedures delayed by the pandemic.
“Gastroenterologists are looking for some framework, however fluid it might be, to guide them in the next 2 to 4 weeks,” Paul Berggreen, MD, secretary of the DHPA, told Medscape Medical News.
The AGA and DHPA guidelines envision a return to elective procedures in areas where COVID-19 cases have been declining for at least 2 weeks and where they are permitted by government directives.
Decisions hinge on the availability of testing, Berggreen said. The guidelines recommend polymerase chain reaction (PCR) tests for COVID-19 infections prior to elective endoscopy. When these tests are not available, a daily temperature log for 10 days prior to the procedure may substitute, they say.
However, if no PCR test is done, the guidelines call on all procedure room personnel to use N95 masks or the equivalent. If these masks aren’t available, “consider delaying resumption of endoscopic procedures,” the guidelines say. The procedure should also be postponed or moved to an inpatient setting in the event of a positive test, according to the guidelines.
Only if the patient has a negative test result should the procedure go forward with the use of standard surgical masks rather than N95 masks or the equivalent, the guidelines say.
The mask recommendations differ slightly from a decision tree put forward during an American College of Gastroenterology (ACG) webinar on April 27, ACG President Mark Pochapin, MD, told Medscape Medical News.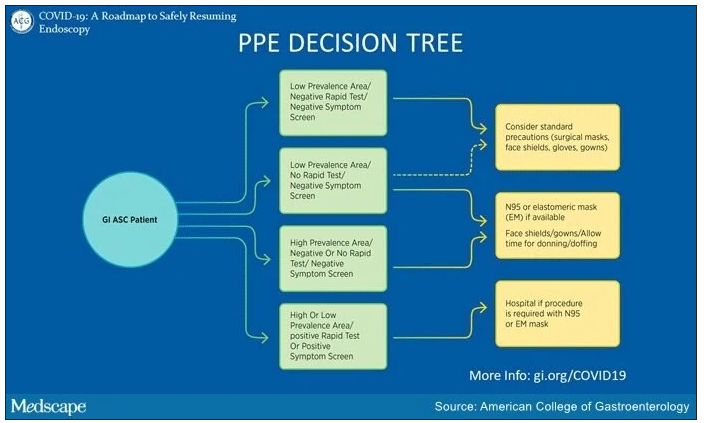
The ACG decision tree takes into consideration local prevalence of COVID-19. “In a low prevalence area if you have a negative test you can wear a regular surgical mask if the patient wears a surgical mask,” Pochapin said.
The ACG decision tree also envisions the possibility of endoscopy with surgical masks along with face shields in areas with low prevalence of COVID-19, even in the absence of testing, if a patient doesn’t have symptoms.
In contrast, the ACG decision tree calls for N95 or elastomeric masks in areas of high prevalence even with a negative test and a negative symptom screen. And it calls for a hospital procedure with an N95 or elastomeric mask in patients with either a positive symptom screen or a positive test.
In addition to masks, the AGA and DHPA guidelines recommend use of other PPE, such as water-resistant gowns, shoe covers, scrubs, double-gloving, and surgical head coverings.
They recommend daily screening of endoscopy center staff with temperature checks and surveys of COVID-19 symptoms and exposure.
Moreover, they call for social distancing of patients, visitors, and staff, and high-level disinfection of endoscopes. They recommend against endotracheal intubation of patients undergoing elective upper endoscopy.
The number of states allowing elective procedures is changing by the day, Berggreen said. In Arizona, where he practices, Gov. Doug Ducey removed all restrictions on elective procedures starting May 1. But other states, where caseloads have been higher, including New York and Massachusetts, have yet to follow suit.
“We are still in kind of a holding pattern,” Richard Hodin, MD, AGAF, chief of gastrointestinal surgery at Massachusetts General Hospital in Boston, told Medscape Medical News. Currently his facility is only doing procedures when a patient’s life is in danger.
The availability of testing also ranges widely from one practice to another. New York University, where Pochapin is director of gastroenterology, is able to do its own tests. Berggreen’s practice, Arizona Digestive Health in Phoenix, has assigned staff to swab patients in its parking lot and then send the samples to a lab by courier for analysis.
Berggreen said his practice has been essentially closed for the past month. In May, he expects his team will do about 30% of its normal volume. They will not start with purely elective procedures, such as following up on a polyp, but with semi-urgent cases, said Berggreen.
“Elective procedures can still be delayed a little bit longer,” he said. “But we’re trying to take care of our patients that are not purely elective: somebody with abdominal pain that you think is very likely a stomach ulcer, somebody with rectal bleeding or persistent diarrhea that›s really impacting their life and you›re thinking this could be an inflammatory condition of the colon.»
Berggreen said he is reassured by a recent survey of 968 healthcare workers in Northern Italy who conducted gastrointestinal endoscopy there during the COVID-19 outbreak. Only 4.3% of respondents tested positive for COVID-19, and 85.7% of these infections occurred before the introduction of PPE and measures to reduce cases. Results were similarly encouraging for patients.
Providing more endoscopy will relieve many patients, Berggreen said. “We all understand the need to limit the spread of the coronavirus but we also have patients who are going to start to have more struggles and potentially worse outcomes by sitting on a condition that requires endoscopy to diagnose and appropriately manage.”
Neither Berggreen, Pochapin, nor Hodin reported any relevant financial interests. The authors of the survey did not report a source of funding or any relevant financial interests.
This article first appeared on Medscape.com.
Gastroenterologists can safely return to elective procedures when adequate personal protective equipment (PPE) is available, professional societies say.
Noting that some states have already lifted restrictions imposed to guard against COVID-19, the American Gastroenterological Association (AGA) and the Digestive Health Physicians Association (DHPA) on April 27 announced guidelines for resuming procedures delayed by the pandemic.
“Gastroenterologists are looking for some framework, however fluid it might be, to guide them in the next 2 to 4 weeks,” Paul Berggreen, MD, secretary of the DHPA, told Medscape Medical News.
The AGA and DHPA guidelines envision a return to elective procedures in areas where COVID-19 cases have been declining for at least 2 weeks and where they are permitted by government directives.
Decisions hinge on the availability of testing, Berggreen said. The guidelines recommend polymerase chain reaction (PCR) tests for COVID-19 infections prior to elective endoscopy. When these tests are not available, a daily temperature log for 10 days prior to the procedure may substitute, they say.
However, if no PCR test is done, the guidelines call on all procedure room personnel to use N95 masks or the equivalent. If these masks aren’t available, “consider delaying resumption of endoscopic procedures,” the guidelines say. The procedure should also be postponed or moved to an inpatient setting in the event of a positive test, according to the guidelines.
Only if the patient has a negative test result should the procedure go forward with the use of standard surgical masks rather than N95 masks or the equivalent, the guidelines say.
The mask recommendations differ slightly from a decision tree put forward during an American College of Gastroenterology (ACG) webinar on April 27, ACG President Mark Pochapin, MD, told Medscape Medical News.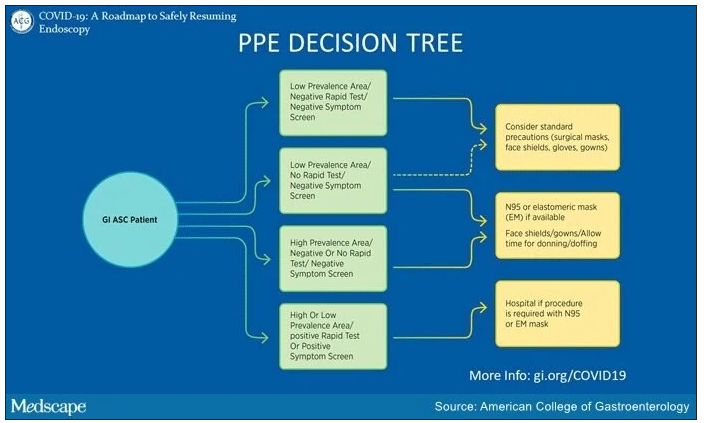
The ACG decision tree takes into consideration local prevalence of COVID-19. “In a low prevalence area if you have a negative test you can wear a regular surgical mask if the patient wears a surgical mask,” Pochapin said.
The ACG decision tree also envisions the possibility of endoscopy with surgical masks along with face shields in areas with low prevalence of COVID-19, even in the absence of testing, if a patient doesn’t have symptoms.
In contrast, the ACG decision tree calls for N95 or elastomeric masks in areas of high prevalence even with a negative test and a negative symptom screen. And it calls for a hospital procedure with an N95 or elastomeric mask in patients with either a positive symptom screen or a positive test.
In addition to masks, the AGA and DHPA guidelines recommend use of other PPE, such as water-resistant gowns, shoe covers, scrubs, double-gloving, and surgical head coverings.
They recommend daily screening of endoscopy center staff with temperature checks and surveys of COVID-19 symptoms and exposure.
Moreover, they call for social distancing of patients, visitors, and staff, and high-level disinfection of endoscopes. They recommend against endotracheal intubation of patients undergoing elective upper endoscopy.
The number of states allowing elective procedures is changing by the day, Berggreen said. In Arizona, where he practices, Gov. Doug Ducey removed all restrictions on elective procedures starting May 1. But other states, where caseloads have been higher, including New York and Massachusetts, have yet to follow suit.
“We are still in kind of a holding pattern,” Richard Hodin, MD, AGAF, chief of gastrointestinal surgery at Massachusetts General Hospital in Boston, told Medscape Medical News. Currently his facility is only doing procedures when a patient’s life is in danger.
The availability of testing also ranges widely from one practice to another. New York University, where Pochapin is director of gastroenterology, is able to do its own tests. Berggreen’s practice, Arizona Digestive Health in Phoenix, has assigned staff to swab patients in its parking lot and then send the samples to a lab by courier for analysis.
Berggreen said his practice has been essentially closed for the past month. In May, he expects his team will do about 30% of its normal volume. They will not start with purely elective procedures, such as following up on a polyp, but with semi-urgent cases, said Berggreen.
“Elective procedures can still be delayed a little bit longer,” he said. “But we’re trying to take care of our patients that are not purely elective: somebody with abdominal pain that you think is very likely a stomach ulcer, somebody with rectal bleeding or persistent diarrhea that›s really impacting their life and you›re thinking this could be an inflammatory condition of the colon.»
Berggreen said he is reassured by a recent survey of 968 healthcare workers in Northern Italy who conducted gastrointestinal endoscopy there during the COVID-19 outbreak. Only 4.3% of respondents tested positive for COVID-19, and 85.7% of these infections occurred before the introduction of PPE and measures to reduce cases. Results were similarly encouraging for patients.
Providing more endoscopy will relieve many patients, Berggreen said. “We all understand the need to limit the spread of the coronavirus but we also have patients who are going to start to have more struggles and potentially worse outcomes by sitting on a condition that requires endoscopy to diagnose and appropriately manage.”
Neither Berggreen, Pochapin, nor Hodin reported any relevant financial interests. The authors of the survey did not report a source of funding or any relevant financial interests.
This article first appeared on Medscape.com.
Gastroenterologists can safely return to elective procedures when adequate personal protective equipment (PPE) is available, professional societies say.
Noting that some states have already lifted restrictions imposed to guard against COVID-19, the American Gastroenterological Association (AGA) and the Digestive Health Physicians Association (DHPA) on April 27 announced guidelines for resuming procedures delayed by the pandemic.
“Gastroenterologists are looking for some framework, however fluid it might be, to guide them in the next 2 to 4 weeks,” Paul Berggreen, MD, secretary of the DHPA, told Medscape Medical News.
The AGA and DHPA guidelines envision a return to elective procedures in areas where COVID-19 cases have been declining for at least 2 weeks and where they are permitted by government directives.
Decisions hinge on the availability of testing, Berggreen said. The guidelines recommend polymerase chain reaction (PCR) tests for COVID-19 infections prior to elective endoscopy. When these tests are not available, a daily temperature log for 10 days prior to the procedure may substitute, they say.
However, if no PCR test is done, the guidelines call on all procedure room personnel to use N95 masks or the equivalent. If these masks aren’t available, “consider delaying resumption of endoscopic procedures,” the guidelines say. The procedure should also be postponed or moved to an inpatient setting in the event of a positive test, according to the guidelines.
Only if the patient has a negative test result should the procedure go forward with the use of standard surgical masks rather than N95 masks or the equivalent, the guidelines say.
The mask recommendations differ slightly from a decision tree put forward during an American College of Gastroenterology (ACG) webinar on April 27, ACG President Mark Pochapin, MD, told Medscape Medical News.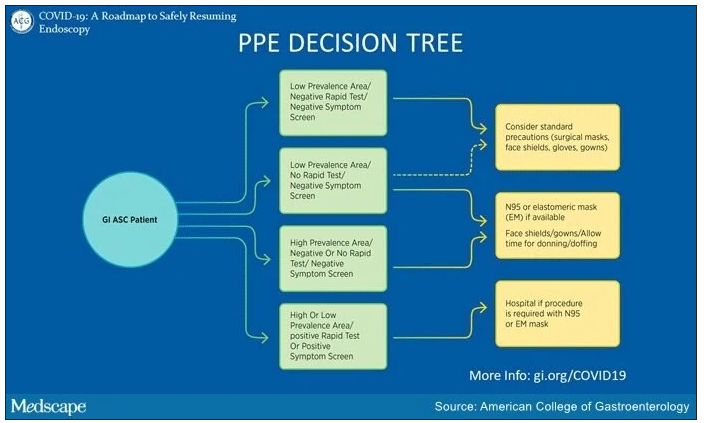
The ACG decision tree takes into consideration local prevalence of COVID-19. “In a low prevalence area if you have a negative test you can wear a regular surgical mask if the patient wears a surgical mask,” Pochapin said.
The ACG decision tree also envisions the possibility of endoscopy with surgical masks along with face shields in areas with low prevalence of COVID-19, even in the absence of testing, if a patient doesn’t have symptoms.
In contrast, the ACG decision tree calls for N95 or elastomeric masks in areas of high prevalence even with a negative test and a negative symptom screen. And it calls for a hospital procedure with an N95 or elastomeric mask in patients with either a positive symptom screen or a positive test.
In addition to masks, the AGA and DHPA guidelines recommend use of other PPE, such as water-resistant gowns, shoe covers, scrubs, double-gloving, and surgical head coverings.
They recommend daily screening of endoscopy center staff with temperature checks and surveys of COVID-19 symptoms and exposure.
Moreover, they call for social distancing of patients, visitors, and staff, and high-level disinfection of endoscopes. They recommend against endotracheal intubation of patients undergoing elective upper endoscopy.
The number of states allowing elective procedures is changing by the day, Berggreen said. In Arizona, where he practices, Gov. Doug Ducey removed all restrictions on elective procedures starting May 1. But other states, where caseloads have been higher, including New York and Massachusetts, have yet to follow suit.
“We are still in kind of a holding pattern,” Richard Hodin, MD, AGAF, chief of gastrointestinal surgery at Massachusetts General Hospital in Boston, told Medscape Medical News. Currently his facility is only doing procedures when a patient’s life is in danger.
The availability of testing also ranges widely from one practice to another. New York University, where Pochapin is director of gastroenterology, is able to do its own tests. Berggreen’s practice, Arizona Digestive Health in Phoenix, has assigned staff to swab patients in its parking lot and then send the samples to a lab by courier for analysis.
Berggreen said his practice has been essentially closed for the past month. In May, he expects his team will do about 30% of its normal volume. They will not start with purely elective procedures, such as following up on a polyp, but with semi-urgent cases, said Berggreen.
“Elective procedures can still be delayed a little bit longer,” he said. “But we’re trying to take care of our patients that are not purely elective: somebody with abdominal pain that you think is very likely a stomach ulcer, somebody with rectal bleeding or persistent diarrhea that›s really impacting their life and you›re thinking this could be an inflammatory condition of the colon.»
Berggreen said he is reassured by a recent survey of 968 healthcare workers in Northern Italy who conducted gastrointestinal endoscopy there during the COVID-19 outbreak. Only 4.3% of respondents tested positive for COVID-19, and 85.7% of these infections occurred before the introduction of PPE and measures to reduce cases. Results were similarly encouraging for patients.
Providing more endoscopy will relieve many patients, Berggreen said. “We all understand the need to limit the spread of the coronavirus but we also have patients who are going to start to have more struggles and potentially worse outcomes by sitting on a condition that requires endoscopy to diagnose and appropriately manage.”
Neither Berggreen, Pochapin, nor Hodin reported any relevant financial interests. The authors of the survey did not report a source of funding or any relevant financial interests.
This article first appeared on Medscape.com.
Anastomotic Leak After Colectomy: Preop Hyperglycemia Ups Death Risk
VANCOUVER, B.C. – Anastomotic leaks after colectomy are more likely to be fatal in patients with preoperative hyperglycemia, based on the results of a database analysis.
Patients with diabetes were not at increased risk of an anastomotic leak. When leaks occurred, however, the associated mortality rate was 25% among those with diabetes and 3.6% among those without diabetes, Dr. Matthew Ziegler reported at the annual meeting of the American Society of Colon and Rectal Surgeons.
Dr. Ziegler, of the William Beaumont Hospital, Royal Oak, Mich., and his colleagues drew their findings from the database of the Michigan Surgical Quality Collaborative. The database included 3,977 patients who had a colectomy from February 2008 to March 2010. Of these, 700 were known to have diabetes. The researchers used a fasting blood glucose value greater than 140 mg/dL as the definition of hyperglycemia.
Fasting glucose values were tested preoperatively in 85% of the patients; 14% had hyperglycemia, and just over half of those patients had diabetes.
At 30 days after surgery, overall mortality was 5.5% for those with diabetes and 2.9% in those without diabetes. Mortality was 8%, which was significantly higher, in the nondiabetic patients with preoperative fasting hyperglycemia.
Parsing the data further, Dr. Ziegler and his colleagues found two risk factors – preoperative steroid use and emergent surgery – that were associated with anastomotic leaks in patients with diabetes. "This may be important, especially in colectomy patients, because of the high morbidity," he said. Dr. Ziegler added that he would hesitate to perform a colectomy on a patient with diabetes who is on preoperative steroids.
Many Americans have diabetes or are on the road to acquiring that disease, said Dr. Ziegler. In addition to the 18 million diagnosed with diabetes in the United States, an estimated 7 million have not yet been diagnosed and 79 million have prediabetes, with elevated fasting glucose or hemoglobin A1c levels.
"Certainly [the findings] merit more study, and improved preoperative screening is needed to better identify and treat this complicated patient population," he said.
Dr. Ziegler said that his hospital has stepped up screening efforts to include preoperative fasting glucose levels and HbA1c levels. "We also have just instituted a so-called ‘sugar nurse’ who is a nurse specialist who meets with patients preoperatively and works on their glycemic management perioperatively with hopefully better outcomes."
VANCOUVER, B.C. – Anastomotic leaks after colectomy are more likely to be fatal in patients with preoperative hyperglycemia, based on the results of a database analysis.
Patients with diabetes were not at increased risk of an anastomotic leak. When leaks occurred, however, the associated mortality rate was 25% among those with diabetes and 3.6% among those without diabetes, Dr. Matthew Ziegler reported at the annual meeting of the American Society of Colon and Rectal Surgeons.
Dr. Ziegler, of the William Beaumont Hospital, Royal Oak, Mich., and his colleagues drew their findings from the database of the Michigan Surgical Quality Collaborative. The database included 3,977 patients who had a colectomy from February 2008 to March 2010. Of these, 700 were known to have diabetes. The researchers used a fasting blood glucose value greater than 140 mg/dL as the definition of hyperglycemia.
Fasting glucose values were tested preoperatively in 85% of the patients; 14% had hyperglycemia, and just over half of those patients had diabetes.
At 30 days after surgery, overall mortality was 5.5% for those with diabetes and 2.9% in those without diabetes. Mortality was 8%, which was significantly higher, in the nondiabetic patients with preoperative fasting hyperglycemia.
Parsing the data further, Dr. Ziegler and his colleagues found two risk factors – preoperative steroid use and emergent surgery – that were associated with anastomotic leaks in patients with diabetes. "This may be important, especially in colectomy patients, because of the high morbidity," he said. Dr. Ziegler added that he would hesitate to perform a colectomy on a patient with diabetes who is on preoperative steroids.
Many Americans have diabetes or are on the road to acquiring that disease, said Dr. Ziegler. In addition to the 18 million diagnosed with diabetes in the United States, an estimated 7 million have not yet been diagnosed and 79 million have prediabetes, with elevated fasting glucose or hemoglobin A1c levels.
"Certainly [the findings] merit more study, and improved preoperative screening is needed to better identify and treat this complicated patient population," he said.
Dr. Ziegler said that his hospital has stepped up screening efforts to include preoperative fasting glucose levels and HbA1c levels. "We also have just instituted a so-called ‘sugar nurse’ who is a nurse specialist who meets with patients preoperatively and works on their glycemic management perioperatively with hopefully better outcomes."
VANCOUVER, B.C. – Anastomotic leaks after colectomy are more likely to be fatal in patients with preoperative hyperglycemia, based on the results of a database analysis.
Patients with diabetes were not at increased risk of an anastomotic leak. When leaks occurred, however, the associated mortality rate was 25% among those with diabetes and 3.6% among those without diabetes, Dr. Matthew Ziegler reported at the annual meeting of the American Society of Colon and Rectal Surgeons.
Dr. Ziegler, of the William Beaumont Hospital, Royal Oak, Mich., and his colleagues drew their findings from the database of the Michigan Surgical Quality Collaborative. The database included 3,977 patients who had a colectomy from February 2008 to March 2010. Of these, 700 were known to have diabetes. The researchers used a fasting blood glucose value greater than 140 mg/dL as the definition of hyperglycemia.
Fasting glucose values were tested preoperatively in 85% of the patients; 14% had hyperglycemia, and just over half of those patients had diabetes.
At 30 days after surgery, overall mortality was 5.5% for those with diabetes and 2.9% in those without diabetes. Mortality was 8%, which was significantly higher, in the nondiabetic patients with preoperative fasting hyperglycemia.
Parsing the data further, Dr. Ziegler and his colleagues found two risk factors – preoperative steroid use and emergent surgery – that were associated with anastomotic leaks in patients with diabetes. "This may be important, especially in colectomy patients, because of the high morbidity," he said. Dr. Ziegler added that he would hesitate to perform a colectomy on a patient with diabetes who is on preoperative steroids.
Many Americans have diabetes or are on the road to acquiring that disease, said Dr. Ziegler. In addition to the 18 million diagnosed with diabetes in the United States, an estimated 7 million have not yet been diagnosed and 79 million have prediabetes, with elevated fasting glucose or hemoglobin A1c levels.
"Certainly [the findings] merit more study, and improved preoperative screening is needed to better identify and treat this complicated patient population," he said.
Dr. Ziegler said that his hospital has stepped up screening efforts to include preoperative fasting glucose levels and HbA1c levels. "We also have just instituted a so-called ‘sugar nurse’ who is a nurse specialist who meets with patients preoperatively and works on their glycemic management perioperatively with hopefully better outcomes."
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF COLON AND RECTAL SURGEONS
Major Finding: Anastomotic leaks after colectomy are associated with a 25% mortality rate in patients with diabetes and a 3.6% mortality rate in those without diabetes.
Data Source: Michigan Surgical Quality Collaborative data on 3,977 patients who had a colectomy from February 2008 to March 2010.
Disclosures: Dr. Ziegler had no relevant financial disclosures.
Anastomotic Leak After Colectomy: Preop Hyperglycemia Ups Death Risk
VANCOUVER, B.C. – Anastomotic leaks after colectomy are more likely to be fatal in patients with preoperative hyperglycemia, based on the results of a database analysis.
Patients with diabetes were not at increased risk of an anastomotic leak. When leaks occurred, however, the associated mortality rate was 25% among those with diabetes and 3.6% among those without diabetes, Dr. Matthew Ziegler reported at the annual meeting of the American Society of Colon and Rectal Surgeons.
Dr. Ziegler, of the William Beaumont Hospital, Royal Oak, Mich., and his colleagues drew their findings from the database of the Michigan Surgical Quality Collaborative. The database included 3,977 patients who had a colectomy from February 2008 to March 2010. Of these, 700 were known to have diabetes. The researchers used a fasting blood glucose value greater than 140 mg/dL as the definition of hyperglycemia.
Fasting glucose values were tested preoperatively in 85% of the patients; 14% had hyperglycemia, and just over half of those patients had diabetes.
At 30 days after surgery, overall mortality was 5.5% for those with diabetes and 2.9% in those without diabetes. Mortality was 8%, which was significantly higher, in the nondiabetic patients with preoperative fasting hyperglycemia.
Parsing the data further, Dr. Ziegler and his colleagues found two risk factors – preoperative steroid use and emergent surgery – that were associated with anastomotic leaks in patients with diabetes. "This may be important, especially in colectomy patients, because of the high morbidity," he said. Dr. Ziegler added that he would hesitate to perform a colectomy on a patient with diabetes who is on preoperative steroids.
Many Americans have diabetes or are on the road to acquiring that disease, said Dr. Ziegler. In addition to the 18 million diagnosed with diabetes in the United States, an estimated 7 million have not yet been diagnosed and 79 million have prediabetes, with elevated fasting glucose or hemoglobin A1c levels.
"Certainly [the findings] merit more study, and improved preoperative screening is needed to better identify and treat this complicated patient population," he said.
Dr. Ziegler said that his hospital has stepped up screening efforts to include preoperative fasting glucose levels and HbA1c levels. "We also have just instituted a so-called ‘sugar nurse’ who is a nurse specialist who meets with patients preoperatively and works on their glycemic management perioperatively with hopefully better outcomes."
VANCOUVER, B.C. – Anastomotic leaks after colectomy are more likely to be fatal in patients with preoperative hyperglycemia, based on the results of a database analysis.
Patients with diabetes were not at increased risk of an anastomotic leak. When leaks occurred, however, the associated mortality rate was 25% among those with diabetes and 3.6% among those without diabetes, Dr. Matthew Ziegler reported at the annual meeting of the American Society of Colon and Rectal Surgeons.
Dr. Ziegler, of the William Beaumont Hospital, Royal Oak, Mich., and his colleagues drew their findings from the database of the Michigan Surgical Quality Collaborative. The database included 3,977 patients who had a colectomy from February 2008 to March 2010. Of these, 700 were known to have diabetes. The researchers used a fasting blood glucose value greater than 140 mg/dL as the definition of hyperglycemia.
Fasting glucose values were tested preoperatively in 85% of the patients; 14% had hyperglycemia, and just over half of those patients had diabetes.
At 30 days after surgery, overall mortality was 5.5% for those with diabetes and 2.9% in those without diabetes. Mortality was 8%, which was significantly higher, in the nondiabetic patients with preoperative fasting hyperglycemia.
Parsing the data further, Dr. Ziegler and his colleagues found two risk factors – preoperative steroid use and emergent surgery – that were associated with anastomotic leaks in patients with diabetes. "This may be important, especially in colectomy patients, because of the high morbidity," he said. Dr. Ziegler added that he would hesitate to perform a colectomy on a patient with diabetes who is on preoperative steroids.
Many Americans have diabetes or are on the road to acquiring that disease, said Dr. Ziegler. In addition to the 18 million diagnosed with diabetes in the United States, an estimated 7 million have not yet been diagnosed and 79 million have prediabetes, with elevated fasting glucose or hemoglobin A1c levels.
"Certainly [the findings] merit more study, and improved preoperative screening is needed to better identify and treat this complicated patient population," he said.
Dr. Ziegler said that his hospital has stepped up screening efforts to include preoperative fasting glucose levels and HbA1c levels. "We also have just instituted a so-called ‘sugar nurse’ who is a nurse specialist who meets with patients preoperatively and works on their glycemic management perioperatively with hopefully better outcomes."
VANCOUVER, B.C. – Anastomotic leaks after colectomy are more likely to be fatal in patients with preoperative hyperglycemia, based on the results of a database analysis.
Patients with diabetes were not at increased risk of an anastomotic leak. When leaks occurred, however, the associated mortality rate was 25% among those with diabetes and 3.6% among those without diabetes, Dr. Matthew Ziegler reported at the annual meeting of the American Society of Colon and Rectal Surgeons.
Dr. Ziegler, of the William Beaumont Hospital, Royal Oak, Mich., and his colleagues drew their findings from the database of the Michigan Surgical Quality Collaborative. The database included 3,977 patients who had a colectomy from February 2008 to March 2010. Of these, 700 were known to have diabetes. The researchers used a fasting blood glucose value greater than 140 mg/dL as the definition of hyperglycemia.
Fasting glucose values were tested preoperatively in 85% of the patients; 14% had hyperglycemia, and just over half of those patients had diabetes.
At 30 days after surgery, overall mortality was 5.5% for those with diabetes and 2.9% in those without diabetes. Mortality was 8%, which was significantly higher, in the nondiabetic patients with preoperative fasting hyperglycemia.
Parsing the data further, Dr. Ziegler and his colleagues found two risk factors – preoperative steroid use and emergent surgery – that were associated with anastomotic leaks in patients with diabetes. "This may be important, especially in colectomy patients, because of the high morbidity," he said. Dr. Ziegler added that he would hesitate to perform a colectomy on a patient with diabetes who is on preoperative steroids.
Many Americans have diabetes or are on the road to acquiring that disease, said Dr. Ziegler. In addition to the 18 million diagnosed with diabetes in the United States, an estimated 7 million have not yet been diagnosed and 79 million have prediabetes, with elevated fasting glucose or hemoglobin A1c levels.
"Certainly [the findings] merit more study, and improved preoperative screening is needed to better identify and treat this complicated patient population," he said.
Dr. Ziegler said that his hospital has stepped up screening efforts to include preoperative fasting glucose levels and HbA1c levels. "We also have just instituted a so-called ‘sugar nurse’ who is a nurse specialist who meets with patients preoperatively and works on their glycemic management perioperatively with hopefully better outcomes."
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF COLON AND RECTAL SURGEONS
Major Finding: Anastomotic leaks after colectomy are associated with a 25% mortality rate in patients with diabetes and a 3.6% mortality rate in those without diabetes.
Data Source: Michigan Surgical Quality Collaborative data on 3,977 patients who had a colectomy from February 2008 to March 2010.
Disclosures: Dr. Ziegler had no relevant financial disclosures.
Anastomotic Leak After Colectomy: Preop Hyperglycemia Ups Death Risk
VANCOUVER, B.C. – Anastomotic leaks after colectomy are more likely to be fatal in patients with preoperative hyperglycemia, based on the results of a database analysis.
Patients with diabetes were not at increased risk of an anastomotic leak. When leaks occurred, however, the associated mortality rate was 25% among those with diabetes and 3.6% among those without diabetes, Dr. Matthew Ziegler reported at the annual meeting of the American Society of Colon and Rectal Surgeons.
Dr. Ziegler, of the William Beaumont Hospital, Royal Oak, Mich., and his colleagues drew their findings from the database of the Michigan Surgical Quality Collaborative. The database included 3,977 patients who had a colectomy from February 2008 to March 2010. Of these, 700 were known to have diabetes. The researchers used a fasting blood glucose value greater than 140 mg/dL as the definition of hyperglycemia.
Fasting glucose values were tested preoperatively in 85% of the patients; 14% had hyperglycemia, and just over half of those patients had diabetes.
At 30 days after surgery, overall mortality was 5.5% for those with diabetes and 2.9% in those without diabetes. Mortality was 8%, which was significantly higher, in the nondiabetic patients with preoperative fasting hyperglycemia.
Parsing the data further, Dr. Ziegler and his colleagues found two risk factors – preoperative steroid use and emergent surgery – that were associated with anastomotic leaks in patients with diabetes. "This may be important, especially in colectomy patients, because of the high morbidity," he said. Dr. Ziegler added that he would hesitate to perform a colectomy on a patient with diabetes who is on preoperative steroids.
Many Americans have diabetes or are on the road to acquiring that disease, said Dr. Ziegler. In addition to the 18 million diagnosed with diabetes in the United States, an estimated 7 million have not yet been diagnosed and 79 million have prediabetes, with elevated fasting glucose or hemoglobin A1c levels.
"Certainly [the findings] merit more study, and improved preoperative screening is needed to better identify and treat this complicated patient population," he said.
Dr. Ziegler said that his hospital has stepped up screening efforts to include preoperative fasting glucose levels and HbA1c levels. "We also have just instituted a so-called ‘sugar nurse’ who is a nurse specialist who meets with patients preoperatively and works on their glycemic management perioperatively with hopefully better outcomes."
VANCOUVER, B.C. – Anastomotic leaks after colectomy are more likely to be fatal in patients with preoperative hyperglycemia, based on the results of a database analysis.
Patients with diabetes were not at increased risk of an anastomotic leak. When leaks occurred, however, the associated mortality rate was 25% among those with diabetes and 3.6% among those without diabetes, Dr. Matthew Ziegler reported at the annual meeting of the American Society of Colon and Rectal Surgeons.
Dr. Ziegler, of the William Beaumont Hospital, Royal Oak, Mich., and his colleagues drew their findings from the database of the Michigan Surgical Quality Collaborative. The database included 3,977 patients who had a colectomy from February 2008 to March 2010. Of these, 700 were known to have diabetes. The researchers used a fasting blood glucose value greater than 140 mg/dL as the definition of hyperglycemia.
Fasting glucose values were tested preoperatively in 85% of the patients; 14% had hyperglycemia, and just over half of those patients had diabetes.
At 30 days after surgery, overall mortality was 5.5% for those with diabetes and 2.9% in those without diabetes. Mortality was 8%, which was significantly higher, in the nondiabetic patients with preoperative fasting hyperglycemia.
Parsing the data further, Dr. Ziegler and his colleagues found two risk factors – preoperative steroid use and emergent surgery – that were associated with anastomotic leaks in patients with diabetes. "This may be important, especially in colectomy patients, because of the high morbidity," he said. Dr. Ziegler added that he would hesitate to perform a colectomy on a patient with diabetes who is on preoperative steroids.
Many Americans have diabetes or are on the road to acquiring that disease, said Dr. Ziegler. In addition to the 18 million diagnosed with diabetes in the United States, an estimated 7 million have not yet been diagnosed and 79 million have prediabetes, with elevated fasting glucose or hemoglobin A1c levels.
"Certainly [the findings] merit more study, and improved preoperative screening is needed to better identify and treat this complicated patient population," he said.
Dr. Ziegler said that his hospital has stepped up screening efforts to include preoperative fasting glucose levels and HbA1c levels. "We also have just instituted a so-called ‘sugar nurse’ who is a nurse specialist who meets with patients preoperatively and works on their glycemic management perioperatively with hopefully better outcomes."
VANCOUVER, B.C. – Anastomotic leaks after colectomy are more likely to be fatal in patients with preoperative hyperglycemia, based on the results of a database analysis.
Patients with diabetes were not at increased risk of an anastomotic leak. When leaks occurred, however, the associated mortality rate was 25% among those with diabetes and 3.6% among those without diabetes, Dr. Matthew Ziegler reported at the annual meeting of the American Society of Colon and Rectal Surgeons.
Dr. Ziegler, of the William Beaumont Hospital, Royal Oak, Mich., and his colleagues drew their findings from the database of the Michigan Surgical Quality Collaborative. The database included 3,977 patients who had a colectomy from February 2008 to March 2010. Of these, 700 were known to have diabetes. The researchers used a fasting blood glucose value greater than 140 mg/dL as the definition of hyperglycemia.
Fasting glucose values were tested preoperatively in 85% of the patients; 14% had hyperglycemia, and just over half of those patients had diabetes.
At 30 days after surgery, overall mortality was 5.5% for those with diabetes and 2.9% in those without diabetes. Mortality was 8%, which was significantly higher, in the nondiabetic patients with preoperative fasting hyperglycemia.
Parsing the data further, Dr. Ziegler and his colleagues found two risk factors – preoperative steroid use and emergent surgery – that were associated with anastomotic leaks in patients with diabetes. "This may be important, especially in colectomy patients, because of the high morbidity," he said. Dr. Ziegler added that he would hesitate to perform a colectomy on a patient with diabetes who is on preoperative steroids.
Many Americans have diabetes or are on the road to acquiring that disease, said Dr. Ziegler. In addition to the 18 million diagnosed with diabetes in the United States, an estimated 7 million have not yet been diagnosed and 79 million have prediabetes, with elevated fasting glucose or hemoglobin A1c levels.
"Certainly [the findings] merit more study, and improved preoperative screening is needed to better identify and treat this complicated patient population," he said.
Dr. Ziegler said that his hospital has stepped up screening efforts to include preoperative fasting glucose levels and HbA1c levels. "We also have just instituted a so-called ‘sugar nurse’ who is a nurse specialist who meets with patients preoperatively and works on their glycemic management perioperatively with hopefully better outcomes."
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF COLON AND RECTAL SURGEONS
Major Finding: Anastomotic leaks after colectomy are associated with a 25% mortality rate in patients with diabetes and a 3.6% mortality rate in those without diabetes.
Data Source: Michigan Surgical Quality Collaborative data on 3,977 patients who had a colectomy from February 2008 to March 2010.
Disclosures: Dr. Ziegler had no relevant financial disclosures.
Alternative Procedure Shows Promise for Benign Colon Polyps
VANCOUVER – Combined endolaparoscopic surgery may offer a good option for patients with difficult but benign polyps, judging by results of a retrospective study.
Difficult benign colonic lesions are typically treated with bowel resection, but even when this is performed laparoscopically, significant morbidity is seen, according to Dr. Sang W. Lee of the department of surgery at New York–Presbyterian Hospital and Cornell University, New York. He suggested that combined endolaparoscopic surgery (CELS) is a safe and effective alternative.
Dr. Lee and his colleagues looked at the records of 66 patients who were taken to the operating room for CELS at New York–Presbyterian. The patients had been referred after failure to clear polyps, mostly because the polyps were large or in difficult locations based on biopsy or endoscopic photographs. Only those patients with at least a year of follow-up including a colonoscopy were included, and those with successful colonoscopic polypectomies were excluded.
The surgeons used CO2 colonoscopy to avoid bowel distention.
"The idea is that if you have a difficult polyp, or a polyp that is located at difficult location, or a very large polyp, then you can laparoscopically help get exposure of that polyp so you can take it out endoscopically," said Dr. Lee at the annual meeting of the American Society of Colon and Rectal Surgeons. "And if you [damage] the bowel wall, you can recognize and repair it laparoscopically."
Once in the operating room, 10 patients were converted to laparoscopic colectomy before CELS was attempted because of suspicion of cancer.
Of the 56 patients in whom the procedure was attempted, 13 were converted to colectomy because of technical difficulty. Two were converted because of suspicion of cancer after the combination procedure was completed.
Of the 12 patients in whom cancer was suspected (10 before the procedure and 2 after), 4 patients had confirmed cancer, giving the team a 33% successful prediction rate. Conversely, of 54 patients thought to have benign polyps, only 1 patient (1.9%) was later found to have cancer.
The largest polyps were the most likely to contain cancer, but even among those greater than 4 cm in diameter, only 13 (7.6%) contained cancer, suggesting that size alone is not an absolute contraindication to performing CELS, said Dr. Lee.
Almost half of the patients went home the day after the procedure. The median time in the operating room was 150 minutes, and the complication rate was 4.4%, said Dr. Lee. Of 41 patients for whom CELS was successful, 5 had limited recurrence. And of those five, four had repeat colonoscopy to repeat the removal of polyps; one had a delayed laparoscopic colectomy, but in this patient the final pathology was benign, he said.
The presentation drew one question from the audience: "Of those patients that you suspected had cancer and who were converted to colectomy, the majority of them were benign. Is there a way to avoid those colectomies that weren’t needed?"
"I would rather be on the safe side," said Dr. Lee. "Unless you take the polyp out completely, you’re not going to know if there’s a cancer there. It’s a little bit of a conundrum, but if you suspect cancer based on the morphology, go ahead and perform a laparoscopic colectomy."
Dr. Lee disclosed that he has served as a speaker and consultant for Covidien, as a course faculty member for Olympus America and Applied Medical, and as a principal investigator for Applied Medical.
VANCOUVER – Combined endolaparoscopic surgery may offer a good option for patients with difficult but benign polyps, judging by results of a retrospective study.
Difficult benign colonic lesions are typically treated with bowel resection, but even when this is performed laparoscopically, significant morbidity is seen, according to Dr. Sang W. Lee of the department of surgery at New York–Presbyterian Hospital and Cornell University, New York. He suggested that combined endolaparoscopic surgery (CELS) is a safe and effective alternative.
Dr. Lee and his colleagues looked at the records of 66 patients who were taken to the operating room for CELS at New York–Presbyterian. The patients had been referred after failure to clear polyps, mostly because the polyps were large or in difficult locations based on biopsy or endoscopic photographs. Only those patients with at least a year of follow-up including a colonoscopy were included, and those with successful colonoscopic polypectomies were excluded.
The surgeons used CO2 colonoscopy to avoid bowel distention.
"The idea is that if you have a difficult polyp, or a polyp that is located at difficult location, or a very large polyp, then you can laparoscopically help get exposure of that polyp so you can take it out endoscopically," said Dr. Lee at the annual meeting of the American Society of Colon and Rectal Surgeons. "And if you [damage] the bowel wall, you can recognize and repair it laparoscopically."
Once in the operating room, 10 patients were converted to laparoscopic colectomy before CELS was attempted because of suspicion of cancer.
Of the 56 patients in whom the procedure was attempted, 13 were converted to colectomy because of technical difficulty. Two were converted because of suspicion of cancer after the combination procedure was completed.
Of the 12 patients in whom cancer was suspected (10 before the procedure and 2 after), 4 patients had confirmed cancer, giving the team a 33% successful prediction rate. Conversely, of 54 patients thought to have benign polyps, only 1 patient (1.9%) was later found to have cancer.
The largest polyps were the most likely to contain cancer, but even among those greater than 4 cm in diameter, only 13 (7.6%) contained cancer, suggesting that size alone is not an absolute contraindication to performing CELS, said Dr. Lee.
Almost half of the patients went home the day after the procedure. The median time in the operating room was 150 minutes, and the complication rate was 4.4%, said Dr. Lee. Of 41 patients for whom CELS was successful, 5 had limited recurrence. And of those five, four had repeat colonoscopy to repeat the removal of polyps; one had a delayed laparoscopic colectomy, but in this patient the final pathology was benign, he said.
The presentation drew one question from the audience: "Of those patients that you suspected had cancer and who were converted to colectomy, the majority of them were benign. Is there a way to avoid those colectomies that weren’t needed?"
"I would rather be on the safe side," said Dr. Lee. "Unless you take the polyp out completely, you’re not going to know if there’s a cancer there. It’s a little bit of a conundrum, but if you suspect cancer based on the morphology, go ahead and perform a laparoscopic colectomy."
Dr. Lee disclosed that he has served as a speaker and consultant for Covidien, as a course faculty member for Olympus America and Applied Medical, and as a principal investigator for Applied Medical.
VANCOUVER – Combined endolaparoscopic surgery may offer a good option for patients with difficult but benign polyps, judging by results of a retrospective study.
Difficult benign colonic lesions are typically treated with bowel resection, but even when this is performed laparoscopically, significant morbidity is seen, according to Dr. Sang W. Lee of the department of surgery at New York–Presbyterian Hospital and Cornell University, New York. He suggested that combined endolaparoscopic surgery (CELS) is a safe and effective alternative.
Dr. Lee and his colleagues looked at the records of 66 patients who were taken to the operating room for CELS at New York–Presbyterian. The patients had been referred after failure to clear polyps, mostly because the polyps were large or in difficult locations based on biopsy or endoscopic photographs. Only those patients with at least a year of follow-up including a colonoscopy were included, and those with successful colonoscopic polypectomies were excluded.
The surgeons used CO2 colonoscopy to avoid bowel distention.
"The idea is that if you have a difficult polyp, or a polyp that is located at difficult location, or a very large polyp, then you can laparoscopically help get exposure of that polyp so you can take it out endoscopically," said Dr. Lee at the annual meeting of the American Society of Colon and Rectal Surgeons. "And if you [damage] the bowel wall, you can recognize and repair it laparoscopically."
Once in the operating room, 10 patients were converted to laparoscopic colectomy before CELS was attempted because of suspicion of cancer.
Of the 56 patients in whom the procedure was attempted, 13 were converted to colectomy because of technical difficulty. Two were converted because of suspicion of cancer after the combination procedure was completed.
Of the 12 patients in whom cancer was suspected (10 before the procedure and 2 after), 4 patients had confirmed cancer, giving the team a 33% successful prediction rate. Conversely, of 54 patients thought to have benign polyps, only 1 patient (1.9%) was later found to have cancer.
The largest polyps were the most likely to contain cancer, but even among those greater than 4 cm in diameter, only 13 (7.6%) contained cancer, suggesting that size alone is not an absolute contraindication to performing CELS, said Dr. Lee.
Almost half of the patients went home the day after the procedure. The median time in the operating room was 150 minutes, and the complication rate was 4.4%, said Dr. Lee. Of 41 patients for whom CELS was successful, 5 had limited recurrence. And of those five, four had repeat colonoscopy to repeat the removal of polyps; one had a delayed laparoscopic colectomy, but in this patient the final pathology was benign, he said.
The presentation drew one question from the audience: "Of those patients that you suspected had cancer and who were converted to colectomy, the majority of them were benign. Is there a way to avoid those colectomies that weren’t needed?"
"I would rather be on the safe side," said Dr. Lee. "Unless you take the polyp out completely, you’re not going to know if there’s a cancer there. It’s a little bit of a conundrum, but if you suspect cancer based on the morphology, go ahead and perform a laparoscopic colectomy."
Dr. Lee disclosed that he has served as a speaker and consultant for Covidien, as a course faculty member for Olympus America and Applied Medical, and as a principal investigator for Applied Medical.
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF COLON AND RECTAL SURGEONS
Major Finding: Combined endolaparoscopic surgery was completed successfully in 41 of 56 patients in which it was attempted.
Data Source: A retrospective study at a single institution.
Disclosures: Dr. Lee disclosed that he has served as a speaker and consultant for Covidien, as a course faculty member for Olympus America and Applied Medical, and as a principal investigator for Applied Medical.
Norovirus Teaches Hard Lessons to a Retirement Community
SAN FRANCISCO – Retirement community staff should prepare themselves for norovirus outbreaks, which can shut down dining halls, damage public relations, and strain residents’ physical and mental health, according to staff members of a Portland, Ore., facility who learned the hard way last year.
"Knowing what we know now, there are a lot of things we would have done differently," said Mjere Simantel, director of social services at Willamette View, a continuing care residential community in Portland, at the annual conference of the American Society on Aging.
Norovirus, which causes diarrhea, vomiting, and fever, is seldom deadly and most patients recover in 48 hours, but it can spread quickly in the tight quarters of a retirement community. And victims can continue shedding the virus for weeks after symptoms fade.
The virus had visited Willamette View before, but without doing much harm. "Previous outbursts were taken care of very quickly," said Rikki Schoenthal, community counselor for the 500-bed facility.
She first became aware of last year’s outbreak in March of 2010 when some residents complained of food poisoning. That was on a Friday, and the local health department was closed because of furloughs. Over the weekend, the number of residents with symptoms began mushrooming. The health department ordered the community to close the dining room and stop cross-traffic between the community’s buildings.
"Our dining service had to figure out how to feed our residents," recalled Ms. Schoenthal. "How were we going to deal with the hair salon, the computer lab, the laundry room, the health center, the pool, the bank, the cleaning room, the library?" Eventually, almost all social activities were canceled.
And the staff found themselves on a sharp learning curve. One hard lesson was that the virus can live on ordinary surfaces indefinitely. "We actually had staff wiping down books," said Ms. Schoenthal.
Another lesson: Hand sanitizers don’t kill the virus. It has to be physically removed from skin with soap, water, and scrubbing. Likewise, vacuuming carpets can send the virus airborne. The community invested in a large stock of chlorine wipes, only to find them ineffective. Some chemicals that were used to sterilize surfaces proved so potent they took the paint off walls, corroded doorknobs, and damaged elevator buttons.
With such confusion, communication proved very important. The management slipped newsletters under each resident’s door every day. Still, residents felt isolated; the only human contact for some was the staff who delivered their meals.
"Some of the residents felt like it was room service," said Ms. Schoenthal. "Others reacted with dismay. They felt like they were being ‘quarantined.’ That word started to be used and we did not want it to be used."
Staff was strained to the breaking point. Those whose work was involved with social activities had to be reassigned. Dining hall staff had to work extra hours. Even the CEO began delivering meals.
The meal deliveries became the community’s main means of checking on the daily health of each resident. The management created a database to track who had fallen sick and who had recovered. Eventually, 96 residents got sick and 2 were hospitalized with dehydration.
Some 50 staff members fell ill as well. "Some of the older adults had accidents, and the environmental staff had to go in there and clean up, and most of them got sick," said Ms. Schoenthal.
She saluted their sacrifice. "The way the staff protected the dignity of the residents in an undignified situation was just stellar," she said. Although the management recognized this effort with a $50 bill for each staff member, many staff members suffered financially because they were forced to take time off after falling ill with the virus. Those who didn’t have enough paid days in their account had to take the time off unpaid. "That was something we still want to explore," said Ms. Schoenthal.
As the outbreak stretched on, the strains increased. The health department insisted that the dining hall be kept closed for 4 weeks, and no visitors or social activities were allowed.
"We had residents who didn’t leave their rooms for 4 weeks," said Ms. Simantel. "Our residents were used to being extremely social. They went from all to nothing. It felt to them like a lockdown, and we still have residents report that they have not recovered."
The staff piped brain teasers into the residents’ rooms through closed-circuit television and began making phone calls to them, but many residents suffered from the isolation. One man had to be referred to hospice care when the restrictions were ended.
The Willamette presenters recommended the following issues for similar communities to consider before they’re hit by norovirus:
• When to activate an emergency plan.
• How to collect data.
• With whom to share the data.
• What role state agencies will play.
• Whether staff has to use paid time off if they get sick from their work.
• What your business insurance will cover.
• How to clean infected rooms.
• How to communicate with state agencies and the news media.
• Whether to use the "Q word" (quarantine).
The presenters also listed the following measures that they would do differently:
• Broadcast a closed-circuit television program of physical exercises.
• Ask health department experts to visit and make recommendations tailored to the community’s circumstances.
• Allow visitors to go to residents’ rooms while wearing gowns, masks, and gloves, which they would discard after each visit.
And audience members who have experienced norovirus outbreaks offered the following additional suggestions:
• Keep a box of supplies on hand for such an emergency.
• Put magnets on the doors of sick residents so that staff can tell which is which.
• Create a system of phone friends to help break the isolation.
Whatever else they do, staff members should be prepared for a longer haul than they expect, said Ms. Schoenthal. "We just kept thinking it would end tomorrow."
SAN FRANCISCO – Retirement community staff should prepare themselves for norovirus outbreaks, which can shut down dining halls, damage public relations, and strain residents’ physical and mental health, according to staff members of a Portland, Ore., facility who learned the hard way last year.
"Knowing what we know now, there are a lot of things we would have done differently," said Mjere Simantel, director of social services at Willamette View, a continuing care residential community in Portland, at the annual conference of the American Society on Aging.
Norovirus, which causes diarrhea, vomiting, and fever, is seldom deadly and most patients recover in 48 hours, but it can spread quickly in the tight quarters of a retirement community. And victims can continue shedding the virus for weeks after symptoms fade.
The virus had visited Willamette View before, but without doing much harm. "Previous outbursts were taken care of very quickly," said Rikki Schoenthal, community counselor for the 500-bed facility.
She first became aware of last year’s outbreak in March of 2010 when some residents complained of food poisoning. That was on a Friday, and the local health department was closed because of furloughs. Over the weekend, the number of residents with symptoms began mushrooming. The health department ordered the community to close the dining room and stop cross-traffic between the community’s buildings.
"Our dining service had to figure out how to feed our residents," recalled Ms. Schoenthal. "How were we going to deal with the hair salon, the computer lab, the laundry room, the health center, the pool, the bank, the cleaning room, the library?" Eventually, almost all social activities were canceled.
And the staff found themselves on a sharp learning curve. One hard lesson was that the virus can live on ordinary surfaces indefinitely. "We actually had staff wiping down books," said Ms. Schoenthal.
Another lesson: Hand sanitizers don’t kill the virus. It has to be physically removed from skin with soap, water, and scrubbing. Likewise, vacuuming carpets can send the virus airborne. The community invested in a large stock of chlorine wipes, only to find them ineffective. Some chemicals that were used to sterilize surfaces proved so potent they took the paint off walls, corroded doorknobs, and damaged elevator buttons.
With such confusion, communication proved very important. The management slipped newsletters under each resident’s door every day. Still, residents felt isolated; the only human contact for some was the staff who delivered their meals.
"Some of the residents felt like it was room service," said Ms. Schoenthal. "Others reacted with dismay. They felt like they were being ‘quarantined.’ That word started to be used and we did not want it to be used."
Staff was strained to the breaking point. Those whose work was involved with social activities had to be reassigned. Dining hall staff had to work extra hours. Even the CEO began delivering meals.
The meal deliveries became the community’s main means of checking on the daily health of each resident. The management created a database to track who had fallen sick and who had recovered. Eventually, 96 residents got sick and 2 were hospitalized with dehydration.
Some 50 staff members fell ill as well. "Some of the older adults had accidents, and the environmental staff had to go in there and clean up, and most of them got sick," said Ms. Schoenthal.
She saluted their sacrifice. "The way the staff protected the dignity of the residents in an undignified situation was just stellar," she said. Although the management recognized this effort with a $50 bill for each staff member, many staff members suffered financially because they were forced to take time off after falling ill with the virus. Those who didn’t have enough paid days in their account had to take the time off unpaid. "That was something we still want to explore," said Ms. Schoenthal.
As the outbreak stretched on, the strains increased. The health department insisted that the dining hall be kept closed for 4 weeks, and no visitors or social activities were allowed.
"We had residents who didn’t leave their rooms for 4 weeks," said Ms. Simantel. "Our residents were used to being extremely social. They went from all to nothing. It felt to them like a lockdown, and we still have residents report that they have not recovered."
The staff piped brain teasers into the residents’ rooms through closed-circuit television and began making phone calls to them, but many residents suffered from the isolation. One man had to be referred to hospice care when the restrictions were ended.
The Willamette presenters recommended the following issues for similar communities to consider before they’re hit by norovirus:
• When to activate an emergency plan.
• How to collect data.
• With whom to share the data.
• What role state agencies will play.
• Whether staff has to use paid time off if they get sick from their work.
• What your business insurance will cover.
• How to clean infected rooms.
• How to communicate with state agencies and the news media.
• Whether to use the "Q word" (quarantine).
The presenters also listed the following measures that they would do differently:
• Broadcast a closed-circuit television program of physical exercises.
• Ask health department experts to visit and make recommendations tailored to the community’s circumstances.
• Allow visitors to go to residents’ rooms while wearing gowns, masks, and gloves, which they would discard after each visit.
And audience members who have experienced norovirus outbreaks offered the following additional suggestions:
• Keep a box of supplies on hand for such an emergency.
• Put magnets on the doors of sick residents so that staff can tell which is which.
• Create a system of phone friends to help break the isolation.
Whatever else they do, staff members should be prepared for a longer haul than they expect, said Ms. Schoenthal. "We just kept thinking it would end tomorrow."
SAN FRANCISCO – Retirement community staff should prepare themselves for norovirus outbreaks, which can shut down dining halls, damage public relations, and strain residents’ physical and mental health, according to staff members of a Portland, Ore., facility who learned the hard way last year.
"Knowing what we know now, there are a lot of things we would have done differently," said Mjere Simantel, director of social services at Willamette View, a continuing care residential community in Portland, at the annual conference of the American Society on Aging.
Norovirus, which causes diarrhea, vomiting, and fever, is seldom deadly and most patients recover in 48 hours, but it can spread quickly in the tight quarters of a retirement community. And victims can continue shedding the virus for weeks after symptoms fade.
The virus had visited Willamette View before, but without doing much harm. "Previous outbursts were taken care of very quickly," said Rikki Schoenthal, community counselor for the 500-bed facility.
She first became aware of last year’s outbreak in March of 2010 when some residents complained of food poisoning. That was on a Friday, and the local health department was closed because of furloughs. Over the weekend, the number of residents with symptoms began mushrooming. The health department ordered the community to close the dining room and stop cross-traffic between the community’s buildings.
"Our dining service had to figure out how to feed our residents," recalled Ms. Schoenthal. "How were we going to deal with the hair salon, the computer lab, the laundry room, the health center, the pool, the bank, the cleaning room, the library?" Eventually, almost all social activities were canceled.
And the staff found themselves on a sharp learning curve. One hard lesson was that the virus can live on ordinary surfaces indefinitely. "We actually had staff wiping down books," said Ms. Schoenthal.
Another lesson: Hand sanitizers don’t kill the virus. It has to be physically removed from skin with soap, water, and scrubbing. Likewise, vacuuming carpets can send the virus airborne. The community invested in a large stock of chlorine wipes, only to find them ineffective. Some chemicals that were used to sterilize surfaces proved so potent they took the paint off walls, corroded doorknobs, and damaged elevator buttons.
With such confusion, communication proved very important. The management slipped newsletters under each resident’s door every day. Still, residents felt isolated; the only human contact for some was the staff who delivered their meals.
"Some of the residents felt like it was room service," said Ms. Schoenthal. "Others reacted with dismay. They felt like they were being ‘quarantined.’ That word started to be used and we did not want it to be used."
Staff was strained to the breaking point. Those whose work was involved with social activities had to be reassigned. Dining hall staff had to work extra hours. Even the CEO began delivering meals.
The meal deliveries became the community’s main means of checking on the daily health of each resident. The management created a database to track who had fallen sick and who had recovered. Eventually, 96 residents got sick and 2 were hospitalized with dehydration.
Some 50 staff members fell ill as well. "Some of the older adults had accidents, and the environmental staff had to go in there and clean up, and most of them got sick," said Ms. Schoenthal.
She saluted their sacrifice. "The way the staff protected the dignity of the residents in an undignified situation was just stellar," she said. Although the management recognized this effort with a $50 bill for each staff member, many staff members suffered financially because they were forced to take time off after falling ill with the virus. Those who didn’t have enough paid days in their account had to take the time off unpaid. "That was something we still want to explore," said Ms. Schoenthal.
As the outbreak stretched on, the strains increased. The health department insisted that the dining hall be kept closed for 4 weeks, and no visitors or social activities were allowed.
"We had residents who didn’t leave their rooms for 4 weeks," said Ms. Simantel. "Our residents were used to being extremely social. They went from all to nothing. It felt to them like a lockdown, and we still have residents report that they have not recovered."
The staff piped brain teasers into the residents’ rooms through closed-circuit television and began making phone calls to them, but many residents suffered from the isolation. One man had to be referred to hospice care when the restrictions were ended.
The Willamette presenters recommended the following issues for similar communities to consider before they’re hit by norovirus:
• When to activate an emergency plan.
• How to collect data.
• With whom to share the data.
• What role state agencies will play.
• Whether staff has to use paid time off if they get sick from their work.
• What your business insurance will cover.
• How to clean infected rooms.
• How to communicate with state agencies and the news media.
• Whether to use the "Q word" (quarantine).
The presenters also listed the following measures that they would do differently:
• Broadcast a closed-circuit television program of physical exercises.
• Ask health department experts to visit and make recommendations tailored to the community’s circumstances.
• Allow visitors to go to residents’ rooms while wearing gowns, masks, and gloves, which they would discard after each visit.
And audience members who have experienced norovirus outbreaks offered the following additional suggestions:
• Keep a box of supplies on hand for such an emergency.
• Put magnets on the doors of sick residents so that staff can tell which is which.
• Create a system of phone friends to help break the isolation.
Whatever else they do, staff members should be prepared for a longer haul than they expect, said Ms. Schoenthal. "We just kept thinking it would end tomorrow."
FROM THE ANNUAL CONFERENCE OF THE AMERICAN SOCIETY OF AGING
Tibial Nerve Stimulation Found Promising for Fecal Incontinence
VANCOUVER, B.C. – Stimulation of the sacral nerve can be an effective treatment for fecal incontinence, lasting for at least a decade, but percutaneous stimulation of the posterior tibial nerve may be a better alternative, according to results of two recent studies.
Although sacral nerve stimulation is considered a first-line procedure for fecal incontinence, the long-term effects are not well known, said Dr. Anil George at the annual meeting of the American Society of Colon and Rectal Surgeons. Nonetheless, in England, sacral nerve stimulation is the standard treatment for patients who have failed conservative treatment and biofeedback, said Dr. George of St. Mark’s Hospital, Harrow.
Previous research suggests that it works in about 30%-80% of patients (Colorectal Dis. 2010 [doi:10.1111/j.1463-1318.2010.02383.x]), but these studies have obtained only short- to medium-term results, according to Dr. George.
He and his colleagues followed 25 patients who underwent sacral nerve stimulation between January 1996 and January 2002 at St. Mark’s. The patients had two or more episodes of fecal incontinence per week, and had failed conservative treatment and biofeedback. Nine of the patients had had previous sphincter surgery.
Of the 25 patients, 23 improved during the trial phase and proceeded to permanent implant. At follow-up last year (88-150 months after the procedure), the researchers found that the treatment was still effective in 21 of the 23 patients.
From a baseline mean of 20 (standard deviation, 3.8), their St. Mark’s incontinence score (SMIS) declined to 7 (3.4) at 3 months, then stayed more or less steady at 8 (3.7) for the latest follow-up.
Similarly, their ability to defer defecation increased from a mean of less than 1 minute (0.9) to 12 minutes (4.7) after 3 months of treatment, and dropped only slightly to 9 minutes (6) at the most recent follow-up. Incontinence episodes dropped from a mean of 27 (3.4) per 2 weeks at baseline to 2 (4.8) at 3 months, and rose slightly to 4 (12.2) at the latest follow-up.
Only two patients lost efficacy, said Dr. George, for unknown reasons. "Our studies show that sacral nerve stimulation can provide a sustained improvement for up to 10 years," he concluded.
As good as these results seemed, Dr. George said that posterior tibial nerve stimulation may prove even better. He noted that it is effective in 60%-80% of patients, but so far the research has been limited to case series (Colorectal Dis. 2010;12:1236-41).
To further examine the possibilities, Dr. George and his colleagues administered the posterior tibial nerve stimulation to two groups of 11 patients twice a week for 30 minutes at a time over the course of 6 consecutive weeks. One group got percutaneous treatment, and the other got transcutaneous treatment.
The researchers used a fixed pulse width of 200 microseconds and a frequency of 20 Hz. A third group of eight patients received a sham transcutaneous treatment with adhesive pads attached and stimulation switched on for less than 10 seconds, then switched off. (The researchers couldn’t think of a sham percutaneous procedure.)
All patients had had two or more episodes of incontinence per week and had failed conservative treatment and biofeedback. Some had sphincter defects.
Of the 11 percutaneous patients, 9 (82%) achieved greater than a 50% reduction in episodes of incontinence. By comparison, 5 of the 11 transcutaneous patients (45%) achieved this response. Only one of the eight sham transcutaneous patients had this good a response.
The percutaneous patients’ ability to defer defecation increased from a mean 1.9 minutes (standard deviation, 0.9) to 6.7 (SD, 4.8), a statistically significant result (P = .009), whereas the transcutaneous patients went from 2.5 minutes (SD, 2.7) to 4.5 (SD, 4.8), a result that approached statistical significance (P = .06). The change in the placebo group was not statistically significant (P = .17), but the difference among the groups was significant (P = .01).
Only the percutaneous group had a statistically significant improvement in SMIS. There were no differences in threshold, urge, and maximal volumes; rectal and anal sensitivity; or resting, endurance squeeze, and involuntary squeeze pressures among the groups.
Although there were no major complications, the patients reported two episodes of mild, self-limiting abdominal pain.
"So what is your belief of why percutaneous is better?" asked an audience member.
"In percutaneous [therapy], we put the needle closer to the nerve," responded Dr. George. "That could be a reason." But he added that previous studies had not found a difference between the transcutaneous and percutaneous approaches.
And transcutaneous posterior tibial nerve stimulation may have at least one advantage, he said. At St. Mark’s, the cost per patient for percutaneous stimulation was £400 ($711), whereas transcutaneous was only £2 ($3) per patient. By comparison, sacral nerve stimulation was £1,500 ($2,423) per patient just for the kit.
"Our results were quite dramatic," said Dr. George. "Tibial nerve stimulation could represent a simple, cheap, and safe option."
Dr. George said he had no disclosures.
VANCOUVER, B.C. – Stimulation of the sacral nerve can be an effective treatment for fecal incontinence, lasting for at least a decade, but percutaneous stimulation of the posterior tibial nerve may be a better alternative, according to results of two recent studies.
Although sacral nerve stimulation is considered a first-line procedure for fecal incontinence, the long-term effects are not well known, said Dr. Anil George at the annual meeting of the American Society of Colon and Rectal Surgeons. Nonetheless, in England, sacral nerve stimulation is the standard treatment for patients who have failed conservative treatment and biofeedback, said Dr. George of St. Mark’s Hospital, Harrow.
Previous research suggests that it works in about 30%-80% of patients (Colorectal Dis. 2010 [doi:10.1111/j.1463-1318.2010.02383.x]), but these studies have obtained only short- to medium-term results, according to Dr. George.
He and his colleagues followed 25 patients who underwent sacral nerve stimulation between January 1996 and January 2002 at St. Mark’s. The patients had two or more episodes of fecal incontinence per week, and had failed conservative treatment and biofeedback. Nine of the patients had had previous sphincter surgery.
Of the 25 patients, 23 improved during the trial phase and proceeded to permanent implant. At follow-up last year (88-150 months after the procedure), the researchers found that the treatment was still effective in 21 of the 23 patients.
From a baseline mean of 20 (standard deviation, 3.8), their St. Mark’s incontinence score (SMIS) declined to 7 (3.4) at 3 months, then stayed more or less steady at 8 (3.7) for the latest follow-up.
Similarly, their ability to defer defecation increased from a mean of less than 1 minute (0.9) to 12 minutes (4.7) after 3 months of treatment, and dropped only slightly to 9 minutes (6) at the most recent follow-up. Incontinence episodes dropped from a mean of 27 (3.4) per 2 weeks at baseline to 2 (4.8) at 3 months, and rose slightly to 4 (12.2) at the latest follow-up.
Only two patients lost efficacy, said Dr. George, for unknown reasons. "Our studies show that sacral nerve stimulation can provide a sustained improvement for up to 10 years," he concluded.
As good as these results seemed, Dr. George said that posterior tibial nerve stimulation may prove even better. He noted that it is effective in 60%-80% of patients, but so far the research has been limited to case series (Colorectal Dis. 2010;12:1236-41).
To further examine the possibilities, Dr. George and his colleagues administered the posterior tibial nerve stimulation to two groups of 11 patients twice a week for 30 minutes at a time over the course of 6 consecutive weeks. One group got percutaneous treatment, and the other got transcutaneous treatment.
The researchers used a fixed pulse width of 200 microseconds and a frequency of 20 Hz. A third group of eight patients received a sham transcutaneous treatment with adhesive pads attached and stimulation switched on for less than 10 seconds, then switched off. (The researchers couldn’t think of a sham percutaneous procedure.)
All patients had had two or more episodes of incontinence per week and had failed conservative treatment and biofeedback. Some had sphincter defects.
Of the 11 percutaneous patients, 9 (82%) achieved greater than a 50% reduction in episodes of incontinence. By comparison, 5 of the 11 transcutaneous patients (45%) achieved this response. Only one of the eight sham transcutaneous patients had this good a response.
The percutaneous patients’ ability to defer defecation increased from a mean 1.9 minutes (standard deviation, 0.9) to 6.7 (SD, 4.8), a statistically significant result (P = .009), whereas the transcutaneous patients went from 2.5 minutes (SD, 2.7) to 4.5 (SD, 4.8), a result that approached statistical significance (P = .06). The change in the placebo group was not statistically significant (P = .17), but the difference among the groups was significant (P = .01).
Only the percutaneous group had a statistically significant improvement in SMIS. There were no differences in threshold, urge, and maximal volumes; rectal and anal sensitivity; or resting, endurance squeeze, and involuntary squeeze pressures among the groups.
Although there were no major complications, the patients reported two episodes of mild, self-limiting abdominal pain.
"So what is your belief of why percutaneous is better?" asked an audience member.
"In percutaneous [therapy], we put the needle closer to the nerve," responded Dr. George. "That could be a reason." But he added that previous studies had not found a difference between the transcutaneous and percutaneous approaches.
And transcutaneous posterior tibial nerve stimulation may have at least one advantage, he said. At St. Mark’s, the cost per patient for percutaneous stimulation was £400 ($711), whereas transcutaneous was only £2 ($3) per patient. By comparison, sacral nerve stimulation was £1,500 ($2,423) per patient just for the kit.
"Our results were quite dramatic," said Dr. George. "Tibial nerve stimulation could represent a simple, cheap, and safe option."
Dr. George said he had no disclosures.
VANCOUVER, B.C. – Stimulation of the sacral nerve can be an effective treatment for fecal incontinence, lasting for at least a decade, but percutaneous stimulation of the posterior tibial nerve may be a better alternative, according to results of two recent studies.
Although sacral nerve stimulation is considered a first-line procedure for fecal incontinence, the long-term effects are not well known, said Dr. Anil George at the annual meeting of the American Society of Colon and Rectal Surgeons. Nonetheless, in England, sacral nerve stimulation is the standard treatment for patients who have failed conservative treatment and biofeedback, said Dr. George of St. Mark’s Hospital, Harrow.
Previous research suggests that it works in about 30%-80% of patients (Colorectal Dis. 2010 [doi:10.1111/j.1463-1318.2010.02383.x]), but these studies have obtained only short- to medium-term results, according to Dr. George.
He and his colleagues followed 25 patients who underwent sacral nerve stimulation between January 1996 and January 2002 at St. Mark’s. The patients had two or more episodes of fecal incontinence per week, and had failed conservative treatment and biofeedback. Nine of the patients had had previous sphincter surgery.
Of the 25 patients, 23 improved during the trial phase and proceeded to permanent implant. At follow-up last year (88-150 months after the procedure), the researchers found that the treatment was still effective in 21 of the 23 patients.
From a baseline mean of 20 (standard deviation, 3.8), their St. Mark’s incontinence score (SMIS) declined to 7 (3.4) at 3 months, then stayed more or less steady at 8 (3.7) for the latest follow-up.
Similarly, their ability to defer defecation increased from a mean of less than 1 minute (0.9) to 12 minutes (4.7) after 3 months of treatment, and dropped only slightly to 9 minutes (6) at the most recent follow-up. Incontinence episodes dropped from a mean of 27 (3.4) per 2 weeks at baseline to 2 (4.8) at 3 months, and rose slightly to 4 (12.2) at the latest follow-up.
Only two patients lost efficacy, said Dr. George, for unknown reasons. "Our studies show that sacral nerve stimulation can provide a sustained improvement for up to 10 years," he concluded.
As good as these results seemed, Dr. George said that posterior tibial nerve stimulation may prove even better. He noted that it is effective in 60%-80% of patients, but so far the research has been limited to case series (Colorectal Dis. 2010;12:1236-41).
To further examine the possibilities, Dr. George and his colleagues administered the posterior tibial nerve stimulation to two groups of 11 patients twice a week for 30 minutes at a time over the course of 6 consecutive weeks. One group got percutaneous treatment, and the other got transcutaneous treatment.
The researchers used a fixed pulse width of 200 microseconds and a frequency of 20 Hz. A third group of eight patients received a sham transcutaneous treatment with adhesive pads attached and stimulation switched on for less than 10 seconds, then switched off. (The researchers couldn’t think of a sham percutaneous procedure.)
All patients had had two or more episodes of incontinence per week and had failed conservative treatment and biofeedback. Some had sphincter defects.
Of the 11 percutaneous patients, 9 (82%) achieved greater than a 50% reduction in episodes of incontinence. By comparison, 5 of the 11 transcutaneous patients (45%) achieved this response. Only one of the eight sham transcutaneous patients had this good a response.
The percutaneous patients’ ability to defer defecation increased from a mean 1.9 minutes (standard deviation, 0.9) to 6.7 (SD, 4.8), a statistically significant result (P = .009), whereas the transcutaneous patients went from 2.5 minutes (SD, 2.7) to 4.5 (SD, 4.8), a result that approached statistical significance (P = .06). The change in the placebo group was not statistically significant (P = .17), but the difference among the groups was significant (P = .01).
Only the percutaneous group had a statistically significant improvement in SMIS. There were no differences in threshold, urge, and maximal volumes; rectal and anal sensitivity; or resting, endurance squeeze, and involuntary squeeze pressures among the groups.
Although there were no major complications, the patients reported two episodes of mild, self-limiting abdominal pain.
"So what is your belief of why percutaneous is better?" asked an audience member.
"In percutaneous [therapy], we put the needle closer to the nerve," responded Dr. George. "That could be a reason." But he added that previous studies had not found a difference between the transcutaneous and percutaneous approaches.
And transcutaneous posterior tibial nerve stimulation may have at least one advantage, he said. At St. Mark’s, the cost per patient for percutaneous stimulation was £400 ($711), whereas transcutaneous was only £2 ($3) per patient. By comparison, sacral nerve stimulation was £1,500 ($2,423) per patient just for the kit.
"Our results were quite dramatic," said Dr. George. "Tibial nerve stimulation could represent a simple, cheap, and safe option."
Dr. George said he had no disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF COLON AND RECTAL SURGEONS
Major Finding: Some 82% of patients achieved greater than a 50% reduction in episodes of fecal incontinence through percutaneous stimulation of their posterior tibial nerves.
Data Source: Dr. Anil George, St. Mark’s Hospital, London.
Disclosures: Dr. George said he had no disclosures.
Tibial Nerve Stimulation Found Promising for Fecal Incontinence
VANCOUVER, B.C. – Stimulation of the sacral nerve can be an effective treatment for fecal incontinence, lasting for at least a decade, but percutaneous stimulation of the posterior tibial nerve may be a better alternative, according to results of two recent studies.
Although sacral nerve stimulation is considered a first-line procedure for fecal incontinence, the long-term effects are not well known, said Dr. Anil George at the annual meeting of the American Society of Colon and Rectal Surgeons. Nonetheless, in England, sacral nerve stimulation is the standard treatment for patients who have failed conservative treatment and biofeedback, said Dr. George of St. Mark’s Hospital, Harrow.
Previous research suggests that it works in about 30%-80% of patients (Colorectal Dis. 2010 [doi:10.1111/j.1463-1318.2010.02383.x]), but these studies have obtained only short- to medium-term results, according to Dr. George.
He and his colleagues followed 25 patients who underwent sacral nerve stimulation between January 1996 and January 2002 at St. Mark’s. The patients had two or more episodes of fecal incontinence per week, and had failed conservative treatment and biofeedback. Nine of the patients had had previous sphincter surgery.
Of the 25 patients, 23 improved during the trial phase and proceeded to permanent implant. At follow-up last year (88-150 months after the procedure), the researchers found that the treatment was still effective in 21 of the 23 patients.
From a baseline mean of 20 (standard deviation, 3.8), their St. Mark’s incontinence score (SMIS) declined to 7 (3.4) at 3 months, then stayed more or less steady at 8 (3.7) for the latest follow-up.
Similarly, their ability to defer defecation increased from a mean of less than 1 minute (0.9) to 12 minutes (4.7) after 3 months of treatment, and dropped only slightly to 9 minutes (6) at the most recent follow-up. Incontinence episodes dropped from a mean of 27 (3.4) per 2 weeks at baseline to 2 (4.8) at 3 months, and rose slightly to 4 (12.2) at the latest follow-up.
Only two patients lost efficacy, said Dr. George, for unknown reasons. "Our studies show that sacral nerve stimulation can provide a sustained improvement for up to 10 years," he concluded.
As good as these results seemed, Dr. George said that posterior tibial nerve stimulation may prove even better. He noted that it is effective in 60%-80% of patients, but so far the research has been limited to case series (Colorectal Dis. 2010;12:1236-41).
To further examine the possibilities, Dr. George and his colleagues administered the posterior tibial nerve stimulation to two groups of 11 patients twice a week for 30 minutes at a time over the course of 6 consecutive weeks. One group got percutaneous treatment, and the other got transcutaneous treatment.
The researchers used a fixed pulse width of 200 microseconds and a frequency of 20 Hz. A third group of eight patients received a sham transcutaneous treatment with adhesive pads attached and stimulation switched on for less than 10 seconds, then switched off. (The researchers couldn’t think of a sham percutaneous procedure.)
All patients had had two or more episodes of incontinence per week and had failed conservative treatment and biofeedback. Some had sphincter defects.
Of the 11 percutaneous patients, 9 (82%) achieved greater than a 50% reduction in episodes of incontinence. By comparison, 5 of the 11 transcutaneous patients (45%) achieved this response. Only one of the eight sham transcutaneous patients had this good a response.
The percutaneous patients’ ability to defer defecation increased from a mean 1.9 minutes (standard deviation, 0.9) to 6.7 (SD, 4.8), a statistically significant result (P = .009), whereas the transcutaneous patients went from 2.5 minutes (SD, 2.7) to 4.5 (SD, 4.8), a result that approached statistical significance (P = .06). The change in the placebo group was not statistically significant (P = .17), but the difference among the groups was significant (P = .01).
Only the percutaneous group had a statistically significant improvement in SMIS. There were no differences in threshold, urge, and maximal volumes; rectal and anal sensitivity; or resting, endurance squeeze, and involuntary squeeze pressures among the groups.
Although there were no major complications, the patients reported two episodes of mild, self-limiting abdominal pain.
"So what is your belief of why percutaneous is better?" asked an audience member.
"In percutaneous [therapy], we put the needle closer to the nerve," responded Dr. George. "That could be a reason." But he added that previous studies had not found a difference between the transcutaneous and percutaneous approaches.
And transcutaneous posterior tibial nerve stimulation may have at least one advantage, he said. At St. Mark’s, the cost per patient for percutaneous stimulation was £400 ($711), whereas transcutaneous was only £2 ($3) per patient. By comparison, sacral nerve stimulation was £1,500 ($2,423) per patient just for the kit.
"Our results were quite dramatic," said Dr. George. "Tibial nerve stimulation could represent a simple, cheap, and safe option."
Dr. George said he had no disclosures.
VANCOUVER, B.C. – Stimulation of the sacral nerve can be an effective treatment for fecal incontinence, lasting for at least a decade, but percutaneous stimulation of the posterior tibial nerve may be a better alternative, according to results of two recent studies.
Although sacral nerve stimulation is considered a first-line procedure for fecal incontinence, the long-term effects are not well known, said Dr. Anil George at the annual meeting of the American Society of Colon and Rectal Surgeons. Nonetheless, in England, sacral nerve stimulation is the standard treatment for patients who have failed conservative treatment and biofeedback, said Dr. George of St. Mark’s Hospital, Harrow.
Previous research suggests that it works in about 30%-80% of patients (Colorectal Dis. 2010 [doi:10.1111/j.1463-1318.2010.02383.x]), but these studies have obtained only short- to medium-term results, according to Dr. George.
He and his colleagues followed 25 patients who underwent sacral nerve stimulation between January 1996 and January 2002 at St. Mark’s. The patients had two or more episodes of fecal incontinence per week, and had failed conservative treatment and biofeedback. Nine of the patients had had previous sphincter surgery.
Of the 25 patients, 23 improved during the trial phase and proceeded to permanent implant. At follow-up last year (88-150 months after the procedure), the researchers found that the treatment was still effective in 21 of the 23 patients.
From a baseline mean of 20 (standard deviation, 3.8), their St. Mark’s incontinence score (SMIS) declined to 7 (3.4) at 3 months, then stayed more or less steady at 8 (3.7) for the latest follow-up.
Similarly, their ability to defer defecation increased from a mean of less than 1 minute (0.9) to 12 minutes (4.7) after 3 months of treatment, and dropped only slightly to 9 minutes (6) at the most recent follow-up. Incontinence episodes dropped from a mean of 27 (3.4) per 2 weeks at baseline to 2 (4.8) at 3 months, and rose slightly to 4 (12.2) at the latest follow-up.
Only two patients lost efficacy, said Dr. George, for unknown reasons. "Our studies show that sacral nerve stimulation can provide a sustained improvement for up to 10 years," he concluded.
As good as these results seemed, Dr. George said that posterior tibial nerve stimulation may prove even better. He noted that it is effective in 60%-80% of patients, but so far the research has been limited to case series (Colorectal Dis. 2010;12:1236-41).
To further examine the possibilities, Dr. George and his colleagues administered the posterior tibial nerve stimulation to two groups of 11 patients twice a week for 30 minutes at a time over the course of 6 consecutive weeks. One group got percutaneous treatment, and the other got transcutaneous treatment.
The researchers used a fixed pulse width of 200 microseconds and a frequency of 20 Hz. A third group of eight patients received a sham transcutaneous treatment with adhesive pads attached and stimulation switched on for less than 10 seconds, then switched off. (The researchers couldn’t think of a sham percutaneous procedure.)
All patients had had two or more episodes of incontinence per week and had failed conservative treatment and biofeedback. Some had sphincter defects.
Of the 11 percutaneous patients, 9 (82%) achieved greater than a 50% reduction in episodes of incontinence. By comparison, 5 of the 11 transcutaneous patients (45%) achieved this response. Only one of the eight sham transcutaneous patients had this good a response.
The percutaneous patients’ ability to defer defecation increased from a mean 1.9 minutes (standard deviation, 0.9) to 6.7 (SD, 4.8), a statistically significant result (P = .009), whereas the transcutaneous patients went from 2.5 minutes (SD, 2.7) to 4.5 (SD, 4.8), a result that approached statistical significance (P = .06). The change in the placebo group was not statistically significant (P = .17), but the difference among the groups was significant (P = .01).
Only the percutaneous group had a statistically significant improvement in SMIS. There were no differences in threshold, urge, and maximal volumes; rectal and anal sensitivity; or resting, endurance squeeze, and involuntary squeeze pressures among the groups.
Although there were no major complications, the patients reported two episodes of mild, self-limiting abdominal pain.
"So what is your belief of why percutaneous is better?" asked an audience member.
"In percutaneous [therapy], we put the needle closer to the nerve," responded Dr. George. "That could be a reason." But he added that previous studies had not found a difference between the transcutaneous and percutaneous approaches.
And transcutaneous posterior tibial nerve stimulation may have at least one advantage, he said. At St. Mark’s, the cost per patient for percutaneous stimulation was £400 ($711), whereas transcutaneous was only £2 ($3) per patient. By comparison, sacral nerve stimulation was £1,500 ($2,423) per patient just for the kit.
"Our results were quite dramatic," said Dr. George. "Tibial nerve stimulation could represent a simple, cheap, and safe option."
Dr. George said he had no disclosures.
VANCOUVER, B.C. – Stimulation of the sacral nerve can be an effective treatment for fecal incontinence, lasting for at least a decade, but percutaneous stimulation of the posterior tibial nerve may be a better alternative, according to results of two recent studies.
Although sacral nerve stimulation is considered a first-line procedure for fecal incontinence, the long-term effects are not well known, said Dr. Anil George at the annual meeting of the American Society of Colon and Rectal Surgeons. Nonetheless, in England, sacral nerve stimulation is the standard treatment for patients who have failed conservative treatment and biofeedback, said Dr. George of St. Mark’s Hospital, Harrow.
Previous research suggests that it works in about 30%-80% of patients (Colorectal Dis. 2010 [doi:10.1111/j.1463-1318.2010.02383.x]), but these studies have obtained only short- to medium-term results, according to Dr. George.
He and his colleagues followed 25 patients who underwent sacral nerve stimulation between January 1996 and January 2002 at St. Mark’s. The patients had two or more episodes of fecal incontinence per week, and had failed conservative treatment and biofeedback. Nine of the patients had had previous sphincter surgery.
Of the 25 patients, 23 improved during the trial phase and proceeded to permanent implant. At follow-up last year (88-150 months after the procedure), the researchers found that the treatment was still effective in 21 of the 23 patients.
From a baseline mean of 20 (standard deviation, 3.8), their St. Mark’s incontinence score (SMIS) declined to 7 (3.4) at 3 months, then stayed more or less steady at 8 (3.7) for the latest follow-up.
Similarly, their ability to defer defecation increased from a mean of less than 1 minute (0.9) to 12 minutes (4.7) after 3 months of treatment, and dropped only slightly to 9 minutes (6) at the most recent follow-up. Incontinence episodes dropped from a mean of 27 (3.4) per 2 weeks at baseline to 2 (4.8) at 3 months, and rose slightly to 4 (12.2) at the latest follow-up.
Only two patients lost efficacy, said Dr. George, for unknown reasons. "Our studies show that sacral nerve stimulation can provide a sustained improvement for up to 10 years," he concluded.
As good as these results seemed, Dr. George said that posterior tibial nerve stimulation may prove even better. He noted that it is effective in 60%-80% of patients, but so far the research has been limited to case series (Colorectal Dis. 2010;12:1236-41).
To further examine the possibilities, Dr. George and his colleagues administered the posterior tibial nerve stimulation to two groups of 11 patients twice a week for 30 minutes at a time over the course of 6 consecutive weeks. One group got percutaneous treatment, and the other got transcutaneous treatment.
The researchers used a fixed pulse width of 200 microseconds and a frequency of 20 Hz. A third group of eight patients received a sham transcutaneous treatment with adhesive pads attached and stimulation switched on for less than 10 seconds, then switched off. (The researchers couldn’t think of a sham percutaneous procedure.)
All patients had had two or more episodes of incontinence per week and had failed conservative treatment and biofeedback. Some had sphincter defects.
Of the 11 percutaneous patients, 9 (82%) achieved greater than a 50% reduction in episodes of incontinence. By comparison, 5 of the 11 transcutaneous patients (45%) achieved this response. Only one of the eight sham transcutaneous patients had this good a response.
The percutaneous patients’ ability to defer defecation increased from a mean 1.9 minutes (standard deviation, 0.9) to 6.7 (SD, 4.8), a statistically significant result (P = .009), whereas the transcutaneous patients went from 2.5 minutes (SD, 2.7) to 4.5 (SD, 4.8), a result that approached statistical significance (P = .06). The change in the placebo group was not statistically significant (P = .17), but the difference among the groups was significant (P = .01).
Only the percutaneous group had a statistically significant improvement in SMIS. There were no differences in threshold, urge, and maximal volumes; rectal and anal sensitivity; or resting, endurance squeeze, and involuntary squeeze pressures among the groups.
Although there were no major complications, the patients reported two episodes of mild, self-limiting abdominal pain.
"So what is your belief of why percutaneous is better?" asked an audience member.
"In percutaneous [therapy], we put the needle closer to the nerve," responded Dr. George. "That could be a reason." But he added that previous studies had not found a difference between the transcutaneous and percutaneous approaches.
And transcutaneous posterior tibial nerve stimulation may have at least one advantage, he said. At St. Mark’s, the cost per patient for percutaneous stimulation was £400 ($711), whereas transcutaneous was only £2 ($3) per patient. By comparison, sacral nerve stimulation was £1,500 ($2,423) per patient just for the kit.
"Our results were quite dramatic," said Dr. George. "Tibial nerve stimulation could represent a simple, cheap, and safe option."
Dr. George said he had no disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF COLON AND RECTAL SURGEONS
Major Finding: Some 82% of patients achieved greater than a 50% reduction in episodes of fecal incontinence through percutaneous stimulation of their posterior tibial nerves.
Data Source: Dr. Anil George, St. Mark’s Hospital, London.
Disclosures: Dr. George said he had no disclosures.
Nursing Homes Grapple With Safety vs. Patient Rights
SAN FRANCISCO – Balancing residents’ autonomy with their safety poses constant challenges for nursing homes, particularly when it comes to topics such as sex and administration of antipsychotic drugs, according to several studies in recent years.
"It’s very difficult," said Dr. Melissa L. Martin, medical director of Margaret Tietz Nursing Home and is in the department of medicine at Cornell University, both in New York.
Dr. Martin and two colleagues presented findings from their research on nursing home resident autonomy in the areas of smoking, dysphagia treatments, sexuality, and antipsychotic drugs at the annual conference of the American Society on Aging. They also gave their listeners advice on how to address autonomy vs. safety in these areas.
Smoking
Between 2% and 10% of nursing home residents smoke, Dr. Martin said. She pointed out that, besides its familiar health implications, smoking can accelerate residents’ cognitive decline and risk fires and personal burns.
Quoting from a study by her copresenters – Dr. Paula E. Lester and Dr. Izchak Kohen – Dr. Martin said that 72% of fire-related deaths in nursing homes result from smoking materials (J. Am. Med. Dir. Assoc. 2008;9[3]:201-3).
One way to evaluate a nursing home resident’s ability to smoke safely is to test whether the person can extinguish a cigarette or hot ashes. Both the capacity to recognize the danger and the physical ability to respond are necessary, Dr. Martin said.
A tangle of regulations complicates the issue. Dr. Martin cited the Omnibus Budget Reconciliation Act (OBRA) of 1987, which defined nursing homes as residences where people have the right to smoke. In effect, nursing homes can’t ban smoking for existing residents without losing their eligibility for Medicare and Medicaid funding, she said.
On the other hand, the Centers for Medicare and Medicaid Services says in its regulations that residents may not smoke in their bedrooms unless supervised by staff, and nursing homes must restrict nursing home smoking in compliance with the National Fire Protection Association’s Life Safety Code . Meanwhile, the Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations) has mandated since 1994 that nursing homes discourage smoking and limit it to designated locations, she said.
Under the CMS’s rules, nursing homes can refuse to admit new residents who smoke. "There are a lot of issues with this, too, because it’s very difficult to identify if someone is a nonsmoker," said Dr. Martin. "If they stopped and start again, do they have the right to smoke?"
In an anonymous survey of 248 directors of nursing by Dr. Lester, Dr. Kohen, and their colleagues, 80% of the nurses agreed that residents have the right to smoke. In 86% of the facilities represented in the survey, nursing staff distributed cigarettes. In 68%, smokers had to wear fire-resistant aprons, and in 69% of the homes, there had to be a fire extinguisher in the smoking area. About a third of the nursing homes required a physician’s order to allow a resident to smoke, the nurses reported (Director 2008 Summer;16[3]:37-9,41,43).
Dr. Martin concluded that nursing homes are inconsistent in what they require, but she noted that more and more facilities are becoming smoke free, presumably by admitting only nonsmokers.
Dysphagia
In his presentation, Dr. Lester, associate medical director for palliative care at Highfield Gardens Care Center in Great Neck, N.Y., offered specific recommendations on how balance safety and autonomy in people with dysphagia.
Dr. Lester, who is also an assistant professor at Stony Brook (N.Y.) University, said that while nursing staff may recognize that these residents are better off not eating normal food, family members often don’t. And many visitors bring food that a dysphagic person might choke on.
In a nationwide survey of nursing directors of skilled nursing facilities through the National Association Directors of Nursing Administration/Long-Term Care, Dr. Lester and her associates found that most survey responders thought they had both a right and a responsibility to restrict residents’ access to over-the-counter medications, cigarettes, and alcoholic beverages (J. Am. Med. Dir. Assoc. 2009;10[6]:419-22). But only 17% thought that facilities had a responsibility to restrict access to food, and 24% thought they had a right to do so.
In fact, while only 10% of residents smoke, 97% of nursing homes have smoking policies. By contrast, 40%-60% of residents in nursing homes have dysphagia, but only 37% of facilities have policies on food brought in by visitors, said Dr. Lester.
One solution is to carefully inform family members of the risks posed by food items, then get the family to sign statements of informed consent. "As long as you can document that all the risks have been discussed, I think that’s probably fine," she said. "Maybe this food is dangerous, but for this favorite food, we can make an exception. Or we will say, ‘OK, she can have this food, but only if someone is in the room watching, so if there is aspiration, we will know right away.’ Sometimes we can minimize risk while maximizing quality of life by making little compromises."
Antipsychotics
Dr. Kohenof the department of clinical psychology at Albert Einstein College of Medicine and an attending faculty member at Zucker Hillside Hospital, both in New York, said that about two-thirds of patients in skilled nursing facilities have diagnosable mental disorders, mostly cognitive impairment. Up to 25% have clinically significant depression, 6%-12% have delirium, and 2% have schizophrenia.
In 1986, a study indicated that nursing homes used sedatives and physical restraints on up to 85% of residents, leading to the passage of OBRA 1987, said Dr. Kohen.
Turning to his own research, Dr. Kohen said that the prevalence of antipsychotic use in nursing homes declined after that event and now is 15%-27% (J. Am. Med. Dir. Assoc. 2010 Sept. 30 [Epub ahead of print]).
However, he said other researchers have reported increasing use of antipsychotics since 1999 because of the advent of new medicines with reduced side effects. The Food and Drug Administration reacted against this trend in 2005 with a "black box" warning that elderly patients with dementia are at increased risk of death when they are prescribed antipsychotics.
Citing the NADONA/LTC study, Dr. Kohen said that 64% of nursing homes give antipsychotics only when family members sign consent forms. The study found that 65% of the facilities were using lower doses of antipsychotics since the FDA warning, but only 39% reported a reduced use of antipsychotics overall. Just over half had increased their use of nonpharmacologic interventions, and a similar proportion was using other types of medications, such as anticonvulsants and benzodiazepines.
Other researchers have found that facilities with higher staff-to-resident ratios use less antipsychotic medication, and the same is true of those that educate staff about these issues, said Dr. Kohen. But one or two staff training sessions won’t do the trick, he said. "My concern is that you have a lot of turnover in nursing homes. You have to keep [training] consistently."
Sexuality
The sexuality of nursing home residents presents a different set of challenges, said Dr. Lester. "There is a myth that the elderly are asexual beings." Citing unpublished data from the NADONA/LTC survey, she said that 71% of directors of nursing reported "issues regarding residents’ sexual activities."
Of these, 58% involved residents having sex with other residents, while 22% involved residents having sex with visitors and 60% involved residents masturbating.
The directors were divided on whether nursing homes should allow residents with moderate-to-severe dementia to have sexual relationships. Forty-five percent said yes, 28% said no, and 27% weren’t sure.
A clear majority (83%) said residents’ responsible parties should be notified if a resident with dementia wanted to have sex with another person, while 5% said no, and 12% were unsure.
Only 37% of the facilities had a policy regarding sexual activity, and a similar 35% had a designated space for trysts. Of the facilities with policies, 52% applied these policies to all residents, regardless of mental condition.
Dr. Lester finished by calling on nursing homes to confront the sexuality of their residents more directly. "Sexuality and intimacy needs of nursing home residents are frequently taboo and ignored," she said.
Dr. Kohen, Dr. Lester, and Dr. Martin all reported that they had no financial interests or affiliations that affected their presentations.
Dr. Melissa L. Martin, resident autonomy, dysphagia treatments, the American Society on Aging, safety,
SAN FRANCISCO – Balancing residents’ autonomy with their safety poses constant challenges for nursing homes, particularly when it comes to topics such as sex and administration of antipsychotic drugs, according to several studies in recent years.
"It’s very difficult," said Dr. Melissa L. Martin, medical director of Margaret Tietz Nursing Home and is in the department of medicine at Cornell University, both in New York.
Dr. Martin and two colleagues presented findings from their research on nursing home resident autonomy in the areas of smoking, dysphagia treatments, sexuality, and antipsychotic drugs at the annual conference of the American Society on Aging. They also gave their listeners advice on how to address autonomy vs. safety in these areas.
Smoking
Between 2% and 10% of nursing home residents smoke, Dr. Martin said. She pointed out that, besides its familiar health implications, smoking can accelerate residents’ cognitive decline and risk fires and personal burns.
Quoting from a study by her copresenters – Dr. Paula E. Lester and Dr. Izchak Kohen – Dr. Martin said that 72% of fire-related deaths in nursing homes result from smoking materials (J. Am. Med. Dir. Assoc. 2008;9[3]:201-3).
One way to evaluate a nursing home resident’s ability to smoke safely is to test whether the person can extinguish a cigarette or hot ashes. Both the capacity to recognize the danger and the physical ability to respond are necessary, Dr. Martin said.
A tangle of regulations complicates the issue. Dr. Martin cited the Omnibus Budget Reconciliation Act (OBRA) of 1987, which defined nursing homes as residences where people have the right to smoke. In effect, nursing homes can’t ban smoking for existing residents without losing their eligibility for Medicare and Medicaid funding, she said.
On the other hand, the Centers for Medicare and Medicaid Services says in its regulations that residents may not smoke in their bedrooms unless supervised by staff, and nursing homes must restrict nursing home smoking in compliance with the National Fire Protection Association’s Life Safety Code . Meanwhile, the Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations) has mandated since 1994 that nursing homes discourage smoking and limit it to designated locations, she said.
Under the CMS’s rules, nursing homes can refuse to admit new residents who smoke. "There are a lot of issues with this, too, because it’s very difficult to identify if someone is a nonsmoker," said Dr. Martin. "If they stopped and start again, do they have the right to smoke?"
In an anonymous survey of 248 directors of nursing by Dr. Lester, Dr. Kohen, and their colleagues, 80% of the nurses agreed that residents have the right to smoke. In 86% of the facilities represented in the survey, nursing staff distributed cigarettes. In 68%, smokers had to wear fire-resistant aprons, and in 69% of the homes, there had to be a fire extinguisher in the smoking area. About a third of the nursing homes required a physician’s order to allow a resident to smoke, the nurses reported (Director 2008 Summer;16[3]:37-9,41,43).
Dr. Martin concluded that nursing homes are inconsistent in what they require, but she noted that more and more facilities are becoming smoke free, presumably by admitting only nonsmokers.
Dysphagia
In his presentation, Dr. Lester, associate medical director for palliative care at Highfield Gardens Care Center in Great Neck, N.Y., offered specific recommendations on how balance safety and autonomy in people with dysphagia.
Dr. Lester, who is also an assistant professor at Stony Brook (N.Y.) University, said that while nursing staff may recognize that these residents are better off not eating normal food, family members often don’t. And many visitors bring food that a dysphagic person might choke on.
In a nationwide survey of nursing directors of skilled nursing facilities through the National Association Directors of Nursing Administration/Long-Term Care, Dr. Lester and her associates found that most survey responders thought they had both a right and a responsibility to restrict residents’ access to over-the-counter medications, cigarettes, and alcoholic beverages (J. Am. Med. Dir. Assoc. 2009;10[6]:419-22). But only 17% thought that facilities had a responsibility to restrict access to food, and 24% thought they had a right to do so.
In fact, while only 10% of residents smoke, 97% of nursing homes have smoking policies. By contrast, 40%-60% of residents in nursing homes have dysphagia, but only 37% of facilities have policies on food brought in by visitors, said Dr. Lester.
One solution is to carefully inform family members of the risks posed by food items, then get the family to sign statements of informed consent. "As long as you can document that all the risks have been discussed, I think that’s probably fine," she said. "Maybe this food is dangerous, but for this favorite food, we can make an exception. Or we will say, ‘OK, she can have this food, but only if someone is in the room watching, so if there is aspiration, we will know right away.’ Sometimes we can minimize risk while maximizing quality of life by making little compromises."
Antipsychotics
Dr. Kohenof the department of clinical psychology at Albert Einstein College of Medicine and an attending faculty member at Zucker Hillside Hospital, both in New York, said that about two-thirds of patients in skilled nursing facilities have diagnosable mental disorders, mostly cognitive impairment. Up to 25% have clinically significant depression, 6%-12% have delirium, and 2% have schizophrenia.
In 1986, a study indicated that nursing homes used sedatives and physical restraints on up to 85% of residents, leading to the passage of OBRA 1987, said Dr. Kohen.
Turning to his own research, Dr. Kohen said that the prevalence of antipsychotic use in nursing homes declined after that event and now is 15%-27% (J. Am. Med. Dir. Assoc. 2010 Sept. 30 [Epub ahead of print]).
However, he said other researchers have reported increasing use of antipsychotics since 1999 because of the advent of new medicines with reduced side effects. The Food and Drug Administration reacted against this trend in 2005 with a "black box" warning that elderly patients with dementia are at increased risk of death when they are prescribed antipsychotics.
Citing the NADONA/LTC study, Dr. Kohen said that 64% of nursing homes give antipsychotics only when family members sign consent forms. The study found that 65% of the facilities were using lower doses of antipsychotics since the FDA warning, but only 39% reported a reduced use of antipsychotics overall. Just over half had increased their use of nonpharmacologic interventions, and a similar proportion was using other types of medications, such as anticonvulsants and benzodiazepines.
Other researchers have found that facilities with higher staff-to-resident ratios use less antipsychotic medication, and the same is true of those that educate staff about these issues, said Dr. Kohen. But one or two staff training sessions won’t do the trick, he said. "My concern is that you have a lot of turnover in nursing homes. You have to keep [training] consistently."
Sexuality
The sexuality of nursing home residents presents a different set of challenges, said Dr. Lester. "There is a myth that the elderly are asexual beings." Citing unpublished data from the NADONA/LTC survey, she said that 71% of directors of nursing reported "issues regarding residents’ sexual activities."
Of these, 58% involved residents having sex with other residents, while 22% involved residents having sex with visitors and 60% involved residents masturbating.
The directors were divided on whether nursing homes should allow residents with moderate-to-severe dementia to have sexual relationships. Forty-five percent said yes, 28% said no, and 27% weren’t sure.
A clear majority (83%) said residents’ responsible parties should be notified if a resident with dementia wanted to have sex with another person, while 5% said no, and 12% were unsure.
Only 37% of the facilities had a policy regarding sexual activity, and a similar 35% had a designated space for trysts. Of the facilities with policies, 52% applied these policies to all residents, regardless of mental condition.
Dr. Lester finished by calling on nursing homes to confront the sexuality of their residents more directly. "Sexuality and intimacy needs of nursing home residents are frequently taboo and ignored," she said.
Dr. Kohen, Dr. Lester, and Dr. Martin all reported that they had no financial interests or affiliations that affected their presentations.
SAN FRANCISCO – Balancing residents’ autonomy with their safety poses constant challenges for nursing homes, particularly when it comes to topics such as sex and administration of antipsychotic drugs, according to several studies in recent years.
"It’s very difficult," said Dr. Melissa L. Martin, medical director of Margaret Tietz Nursing Home and is in the department of medicine at Cornell University, both in New York.
Dr. Martin and two colleagues presented findings from their research on nursing home resident autonomy in the areas of smoking, dysphagia treatments, sexuality, and antipsychotic drugs at the annual conference of the American Society on Aging. They also gave their listeners advice on how to address autonomy vs. safety in these areas.
Smoking
Between 2% and 10% of nursing home residents smoke, Dr. Martin said. She pointed out that, besides its familiar health implications, smoking can accelerate residents’ cognitive decline and risk fires and personal burns.
Quoting from a study by her copresenters – Dr. Paula E. Lester and Dr. Izchak Kohen – Dr. Martin said that 72% of fire-related deaths in nursing homes result from smoking materials (J. Am. Med. Dir. Assoc. 2008;9[3]:201-3).
One way to evaluate a nursing home resident’s ability to smoke safely is to test whether the person can extinguish a cigarette or hot ashes. Both the capacity to recognize the danger and the physical ability to respond are necessary, Dr. Martin said.
A tangle of regulations complicates the issue. Dr. Martin cited the Omnibus Budget Reconciliation Act (OBRA) of 1987, which defined nursing homes as residences where people have the right to smoke. In effect, nursing homes can’t ban smoking for existing residents without losing their eligibility for Medicare and Medicaid funding, she said.
On the other hand, the Centers for Medicare and Medicaid Services says in its regulations that residents may not smoke in their bedrooms unless supervised by staff, and nursing homes must restrict nursing home smoking in compliance with the National Fire Protection Association’s Life Safety Code . Meanwhile, the Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations) has mandated since 1994 that nursing homes discourage smoking and limit it to designated locations, she said.
Under the CMS’s rules, nursing homes can refuse to admit new residents who smoke. "There are a lot of issues with this, too, because it’s very difficult to identify if someone is a nonsmoker," said Dr. Martin. "If they stopped and start again, do they have the right to smoke?"
In an anonymous survey of 248 directors of nursing by Dr. Lester, Dr. Kohen, and their colleagues, 80% of the nurses agreed that residents have the right to smoke. In 86% of the facilities represented in the survey, nursing staff distributed cigarettes. In 68%, smokers had to wear fire-resistant aprons, and in 69% of the homes, there had to be a fire extinguisher in the smoking area. About a third of the nursing homes required a physician’s order to allow a resident to smoke, the nurses reported (Director 2008 Summer;16[3]:37-9,41,43).
Dr. Martin concluded that nursing homes are inconsistent in what they require, but she noted that more and more facilities are becoming smoke free, presumably by admitting only nonsmokers.
Dysphagia
In his presentation, Dr. Lester, associate medical director for palliative care at Highfield Gardens Care Center in Great Neck, N.Y., offered specific recommendations on how balance safety and autonomy in people with dysphagia.
Dr. Lester, who is also an assistant professor at Stony Brook (N.Y.) University, said that while nursing staff may recognize that these residents are better off not eating normal food, family members often don’t. And many visitors bring food that a dysphagic person might choke on.
In a nationwide survey of nursing directors of skilled nursing facilities through the National Association Directors of Nursing Administration/Long-Term Care, Dr. Lester and her associates found that most survey responders thought they had both a right and a responsibility to restrict residents’ access to over-the-counter medications, cigarettes, and alcoholic beverages (J. Am. Med. Dir. Assoc. 2009;10[6]:419-22). But only 17% thought that facilities had a responsibility to restrict access to food, and 24% thought they had a right to do so.
In fact, while only 10% of residents smoke, 97% of nursing homes have smoking policies. By contrast, 40%-60% of residents in nursing homes have dysphagia, but only 37% of facilities have policies on food brought in by visitors, said Dr. Lester.
One solution is to carefully inform family members of the risks posed by food items, then get the family to sign statements of informed consent. "As long as you can document that all the risks have been discussed, I think that’s probably fine," she said. "Maybe this food is dangerous, but for this favorite food, we can make an exception. Or we will say, ‘OK, she can have this food, but only if someone is in the room watching, so if there is aspiration, we will know right away.’ Sometimes we can minimize risk while maximizing quality of life by making little compromises."
Antipsychotics
Dr. Kohenof the department of clinical psychology at Albert Einstein College of Medicine and an attending faculty member at Zucker Hillside Hospital, both in New York, said that about two-thirds of patients in skilled nursing facilities have diagnosable mental disorders, mostly cognitive impairment. Up to 25% have clinically significant depression, 6%-12% have delirium, and 2% have schizophrenia.
In 1986, a study indicated that nursing homes used sedatives and physical restraints on up to 85% of residents, leading to the passage of OBRA 1987, said Dr. Kohen.
Turning to his own research, Dr. Kohen said that the prevalence of antipsychotic use in nursing homes declined after that event and now is 15%-27% (J. Am. Med. Dir. Assoc. 2010 Sept. 30 [Epub ahead of print]).
However, he said other researchers have reported increasing use of antipsychotics since 1999 because of the advent of new medicines with reduced side effects. The Food and Drug Administration reacted against this trend in 2005 with a "black box" warning that elderly patients with dementia are at increased risk of death when they are prescribed antipsychotics.
Citing the NADONA/LTC study, Dr. Kohen said that 64% of nursing homes give antipsychotics only when family members sign consent forms. The study found that 65% of the facilities were using lower doses of antipsychotics since the FDA warning, but only 39% reported a reduced use of antipsychotics overall. Just over half had increased their use of nonpharmacologic interventions, and a similar proportion was using other types of medications, such as anticonvulsants and benzodiazepines.
Other researchers have found that facilities with higher staff-to-resident ratios use less antipsychotic medication, and the same is true of those that educate staff about these issues, said Dr. Kohen. But one or two staff training sessions won’t do the trick, he said. "My concern is that you have a lot of turnover in nursing homes. You have to keep [training] consistently."
Sexuality
The sexuality of nursing home residents presents a different set of challenges, said Dr. Lester. "There is a myth that the elderly are asexual beings." Citing unpublished data from the NADONA/LTC survey, she said that 71% of directors of nursing reported "issues regarding residents’ sexual activities."
Of these, 58% involved residents having sex with other residents, while 22% involved residents having sex with visitors and 60% involved residents masturbating.
The directors were divided on whether nursing homes should allow residents with moderate-to-severe dementia to have sexual relationships. Forty-five percent said yes, 28% said no, and 27% weren’t sure.
A clear majority (83%) said residents’ responsible parties should be notified if a resident with dementia wanted to have sex with another person, while 5% said no, and 12% were unsure.
Only 37% of the facilities had a policy regarding sexual activity, and a similar 35% had a designated space for trysts. Of the facilities with policies, 52% applied these policies to all residents, regardless of mental condition.
Dr. Lester finished by calling on nursing homes to confront the sexuality of their residents more directly. "Sexuality and intimacy needs of nursing home residents are frequently taboo and ignored," she said.
Dr. Kohen, Dr. Lester, and Dr. Martin all reported that they had no financial interests or affiliations that affected their presentations.
Dr. Melissa L. Martin, resident autonomy, dysphagia treatments, the American Society on Aging, safety,
Dr. Melissa L. Martin, resident autonomy, dysphagia treatments, the American Society on Aging, safety,
EXPERT ANALYSIS FROM THE ANNUAL CONFERENCE OF THE AMERICAN SOCIETY ON AGING
Nursing Homes Grapple With Safety vs. Patient Rights
SAN FRANCISCO – Balancing residents’ autonomy with their safety poses constant challenges for nursing homes, particularly when it comes to topics such as sex and administration of antipsychotic drugs, according to several studies in recent years.
"It’s very difficult," said Dr. Melissa L. Martin, medical director of Margaret Tietz Nursing Home and is in the department of medicine at Cornell University, both in New York.
Dr. Martin and two colleagues presented findings from their research on nursing home resident autonomy in the areas of smoking, dysphagia treatments, sexuality, and antipsychotic drugs at the annual conference of the American Society on Aging. They also gave their listeners advice on how to address autonomy vs. safety in these areas.
Smoking
Between 2% and 10% of nursing home residents smoke, Dr. Martin said. She pointed out that, besides its familiar health implications, smoking can accelerate residents’ cognitive decline and risk fires and personal burns.
Quoting from a study by her copresenters – Dr. Paula E. Lester and Dr. Izchak Kohen – Dr. Martin said that 72% of fire-related deaths in nursing homes result from smoking materials (J. Am. Med. Dir. Assoc. 2008;9[3]:201-3).
One way to evaluate a nursing home resident’s ability to smoke safely is to test whether the person can extinguish a cigarette or hot ashes. Both the capacity to recognize the danger and the physical ability to respond are necessary, Dr. Martin said.
A tangle of regulations complicates the issue. Dr. Martin cited the Omnibus Budget Reconciliation Act (OBRA) of 1987, which defined nursing homes as residences where people have the right to smoke. In effect, nursing homes can’t ban smoking for existing residents without losing their eligibility for Medicare and Medicaid funding, she said.
On the other hand, the Centers for Medicare and Medicaid Services says in its regulations that residents may not smoke in their bedrooms unless supervised by staff, and nursing homes must restrict nursing home smoking in compliance with the National Fire Protection Association’s Life Safety Code . Meanwhile, the Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations) has mandated since 1994 that nursing homes discourage smoking and limit it to designated locations, she said.
Under the CMS’s rules, nursing homes can refuse to admit new residents who smoke. "There are a lot of issues with this, too, because it’s very difficult to identify if someone is a nonsmoker," said Dr. Martin. "If they stopped and start again, do they have the right to smoke?"
In an anonymous survey of 248 directors of nursing by Dr. Lester, Dr. Kohen, and their colleagues, 80% of the nurses agreed that residents have the right to smoke. In 86% of the facilities represented in the survey, nursing staff distributed cigarettes. In 68%, smokers had to wear fire-resistant aprons, and in 69% of the homes, there had to be a fire extinguisher in the smoking area. About a third of the nursing homes required a physician’s order to allow a resident to smoke, the nurses reported (Director 2008 Summer;16[3]:37-9,41,43).
Dr. Martin concluded that nursing homes are inconsistent in what they require, but she noted that more and more facilities are becoming smoke free, presumably by admitting only nonsmokers.
Dysphagia
In his presentation, Dr. Lester, associate medical director for palliative care at Highfield Gardens Care Center in Great Neck, N.Y., offered specific recommendations on how balance safety and autonomy in people with dysphagia.
Dr. Lester, who is also an assistant professor at Stony Brook (N.Y.) University, said that while nursing staff may recognize that these residents are better off not eating normal food, family members often don’t. And many visitors bring food that a dysphagic person might choke on.
In a nationwide survey of nursing directors of skilled nursing facilities through the National Association Directors of Nursing Administration/Long-Term Care, Dr. Lester and her associates found that most survey responders thought they had both a right and a responsibility to restrict residents’ access to over-the-counter medications, cigarettes, and alcoholic beverages (J. Am. Med. Dir. Assoc. 2009;10[6]:419-22). But only 17% thought that facilities had a responsibility to restrict access to food, and 24% thought they had a right to do so.
In fact, while only 10% of residents smoke, 97% of nursing homes have smoking policies. By contrast, 40%-60% of residents in nursing homes have dysphagia, but only 37% of facilities have policies on food brought in by visitors, said Dr. Lester.
One solution is to carefully inform family members of the risks posed by food items, then get the family to sign statements of informed consent. "As long as you can document that all the risks have been discussed, I think that’s probably fine," she said. "Maybe this food is dangerous, but for this favorite food, we can make an exception. Or we will say, ‘OK, she can have this food, but only if someone is in the room watching, so if there is aspiration, we will know right away.’ Sometimes we can minimize risk while maximizing quality of life by making little compromises."
Antipsychotics
Dr. Kohenof the department of clinical psychology at Albert Einstein College of Medicine and an attending faculty member at Zucker Hillside Hospital, both in New York, said that about two-thirds of patients in skilled nursing facilities have diagnosable mental disorders, mostly cognitive impairment. Up to 25% have clinically significant depression, 6%-12% have delirium, and 2% have schizophrenia.
In 1986, a study indicated that nursing homes used sedatives and physical restraints on up to 85% of residents, leading to the passage of OBRA 1987, said Dr. Kohen.
Turning to his own research, Dr. Kohen said that the prevalence of antipsychotic use in nursing homes declined after that event and now is 15%-27% (J. Am. Med. Dir. Assoc. 2010 Sept. 30 [Epub ahead of print]).
However, he said other researchers have reported increasing use of antipsychotics since 1999 because of the advent of new medicines with reduced side effects. The Food and Drug Administration reacted against this trend in 2005 with a "black box" warning that elderly patients with dementia are at increased risk of death when they are prescribed antipsychotics.
Citing the NADONA/LTC study, Dr. Kohen said that 64% of nursing homes give antipsychotics only when family members sign consent forms. The study found that 65% of the facilities were using lower doses of antipsychotics since the FDA warning, but only 39% reported a reduced use of antipsychotics overall. Just over half had increased their use of nonpharmacologic interventions, and a similar proportion was using other types of medications, such as anticonvulsants and benzodiazepines.
Other researchers have found that facilities with higher staff-to-resident ratios use less antipsychotic medication, and the same is true of those that educate staff about these issues, said Dr. Kohen. But one or two staff training sessions won’t do the trick, he said. "My concern is that you have a lot of turnover in nursing homes. You have to keep [training] consistently."
Sexuality
The sexuality of nursing home residents presents a different set of challenges, said Dr. Lester. "There is a myth that the elderly are asexual beings." Citing unpublished data from the NADONA/LTC survey, she said that 71% of directors of nursing reported "issues regarding residents’ sexual activities."
Of these, 58% involved residents having sex with other residents, while 22% involved residents having sex with visitors and 60% involved residents masturbating.
The directors were divided on whether nursing homes should allow residents with moderate-to-severe dementia to have sexual relationships. Forty-five percent said yes, 28% said no, and 27% weren’t sure.
A clear majority (83%) said residents’ responsible parties should be notified if a resident with dementia wanted to have sex with another person, while 5% said no, and 12% were unsure.
Only 37% of the facilities had a policy regarding sexual activity, and a similar 35% had a designated space for trysts. Of the facilities with policies, 52% applied these policies to all residents, regardless of mental condition.
Dr. Lester finished by calling on nursing homes to confront the sexuality of their residents more directly. "Sexuality and intimacy needs of nursing home residents are frequently taboo and ignored," she said.
Dr. Kohen, Dr. Lester, and Dr. Martin all reported that they had no financial interests or affiliations that affected their presentations.
Dr. Melissa L. Martin, resident autonomy, dysphagia treatments, the American Society on Aging, safety,
SAN FRANCISCO – Balancing residents’ autonomy with their safety poses constant challenges for nursing homes, particularly when it comes to topics such as sex and administration of antipsychotic drugs, according to several studies in recent years.
"It’s very difficult," said Dr. Melissa L. Martin, medical director of Margaret Tietz Nursing Home and is in the department of medicine at Cornell University, both in New York.
Dr. Martin and two colleagues presented findings from their research on nursing home resident autonomy in the areas of smoking, dysphagia treatments, sexuality, and antipsychotic drugs at the annual conference of the American Society on Aging. They also gave their listeners advice on how to address autonomy vs. safety in these areas.
Smoking
Between 2% and 10% of nursing home residents smoke, Dr. Martin said. She pointed out that, besides its familiar health implications, smoking can accelerate residents’ cognitive decline and risk fires and personal burns.
Quoting from a study by her copresenters – Dr. Paula E. Lester and Dr. Izchak Kohen – Dr. Martin said that 72% of fire-related deaths in nursing homes result from smoking materials (J. Am. Med. Dir. Assoc. 2008;9[3]:201-3).
One way to evaluate a nursing home resident’s ability to smoke safely is to test whether the person can extinguish a cigarette or hot ashes. Both the capacity to recognize the danger and the physical ability to respond are necessary, Dr. Martin said.
A tangle of regulations complicates the issue. Dr. Martin cited the Omnibus Budget Reconciliation Act (OBRA) of 1987, which defined nursing homes as residences where people have the right to smoke. In effect, nursing homes can’t ban smoking for existing residents without losing their eligibility for Medicare and Medicaid funding, she said.
On the other hand, the Centers for Medicare and Medicaid Services says in its regulations that residents may not smoke in their bedrooms unless supervised by staff, and nursing homes must restrict nursing home smoking in compliance with the National Fire Protection Association’s Life Safety Code . Meanwhile, the Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations) has mandated since 1994 that nursing homes discourage smoking and limit it to designated locations, she said.
Under the CMS’s rules, nursing homes can refuse to admit new residents who smoke. "There are a lot of issues with this, too, because it’s very difficult to identify if someone is a nonsmoker," said Dr. Martin. "If they stopped and start again, do they have the right to smoke?"
In an anonymous survey of 248 directors of nursing by Dr. Lester, Dr. Kohen, and their colleagues, 80% of the nurses agreed that residents have the right to smoke. In 86% of the facilities represented in the survey, nursing staff distributed cigarettes. In 68%, smokers had to wear fire-resistant aprons, and in 69% of the homes, there had to be a fire extinguisher in the smoking area. About a third of the nursing homes required a physician’s order to allow a resident to smoke, the nurses reported (Director 2008 Summer;16[3]:37-9,41,43).
Dr. Martin concluded that nursing homes are inconsistent in what they require, but she noted that more and more facilities are becoming smoke free, presumably by admitting only nonsmokers.
Dysphagia
In his presentation, Dr. Lester, associate medical director for palliative care at Highfield Gardens Care Center in Great Neck, N.Y., offered specific recommendations on how balance safety and autonomy in people with dysphagia.
Dr. Lester, who is also an assistant professor at Stony Brook (N.Y.) University, said that while nursing staff may recognize that these residents are better off not eating normal food, family members often don’t. And many visitors bring food that a dysphagic person might choke on.
In a nationwide survey of nursing directors of skilled nursing facilities through the National Association Directors of Nursing Administration/Long-Term Care, Dr. Lester and her associates found that most survey responders thought they had both a right and a responsibility to restrict residents’ access to over-the-counter medications, cigarettes, and alcoholic beverages (J. Am. Med. Dir. Assoc. 2009;10[6]:419-22). But only 17% thought that facilities had a responsibility to restrict access to food, and 24% thought they had a right to do so.
In fact, while only 10% of residents smoke, 97% of nursing homes have smoking policies. By contrast, 40%-60% of residents in nursing homes have dysphagia, but only 37% of facilities have policies on food brought in by visitors, said Dr. Lester.
One solution is to carefully inform family members of the risks posed by food items, then get the family to sign statements of informed consent. "As long as you can document that all the risks have been discussed, I think that’s probably fine," she said. "Maybe this food is dangerous, but for this favorite food, we can make an exception. Or we will say, ‘OK, she can have this food, but only if someone is in the room watching, so if there is aspiration, we will know right away.’ Sometimes we can minimize risk while maximizing quality of life by making little compromises."
Antipsychotics
Dr. Kohenof the department of clinical psychology at Albert Einstein College of Medicine and an attending faculty member at Zucker Hillside Hospital, both in New York, said that about two-thirds of patients in skilled nursing facilities have diagnosable mental disorders, mostly cognitive impairment. Up to 25% have clinically significant depression, 6%-12% have delirium, and 2% have schizophrenia.
In 1986, a study indicated that nursing homes used sedatives and physical restraints on up to 85% of residents, leading to the passage of OBRA 1987, said Dr. Kohen.
Turning to his own research, Dr. Kohen said that the prevalence of antipsychotic use in nursing homes declined after that event and now is 15%-27% (J. Am. Med. Dir. Assoc. 2010 Sept. 30 [Epub ahead of print]).
However, he said other researchers have reported increasing use of antipsychotics since 1999 because of the advent of new medicines with reduced side effects. The Food and Drug Administration reacted against this trend in 2005 with a "black box" warning that elderly patients with dementia are at increased risk of death when they are prescribed antipsychotics.
Citing the NADONA/LTC study, Dr. Kohen said that 64% of nursing homes give antipsychotics only when family members sign consent forms. The study found that 65% of the facilities were using lower doses of antipsychotics since the FDA warning, but only 39% reported a reduced use of antipsychotics overall. Just over half had increased their use of nonpharmacologic interventions, and a similar proportion was using other types of medications, such as anticonvulsants and benzodiazepines.
Other researchers have found that facilities with higher staff-to-resident ratios use less antipsychotic medication, and the same is true of those that educate staff about these issues, said Dr. Kohen. But one or two staff training sessions won’t do the trick, he said. "My concern is that you have a lot of turnover in nursing homes. You have to keep [training] consistently."
Sexuality
The sexuality of nursing home residents presents a different set of challenges, said Dr. Lester. "There is a myth that the elderly are asexual beings." Citing unpublished data from the NADONA/LTC survey, she said that 71% of directors of nursing reported "issues regarding residents’ sexual activities."
Of these, 58% involved residents having sex with other residents, while 22% involved residents having sex with visitors and 60% involved residents masturbating.
The directors were divided on whether nursing homes should allow residents with moderate-to-severe dementia to have sexual relationships. Forty-five percent said yes, 28% said no, and 27% weren’t sure.
A clear majority (83%) said residents’ responsible parties should be notified if a resident with dementia wanted to have sex with another person, while 5% said no, and 12% were unsure.
Only 37% of the facilities had a policy regarding sexual activity, and a similar 35% had a designated space for trysts. Of the facilities with policies, 52% applied these policies to all residents, regardless of mental condition.
Dr. Lester finished by calling on nursing homes to confront the sexuality of their residents more directly. "Sexuality and intimacy needs of nursing home residents are frequently taboo and ignored," she said.
Dr. Kohen, Dr. Lester, and Dr. Martin all reported that they had no financial interests or affiliations that affected their presentations.
SAN FRANCISCO – Balancing residents’ autonomy with their safety poses constant challenges for nursing homes, particularly when it comes to topics such as sex and administration of antipsychotic drugs, according to several studies in recent years.
"It’s very difficult," said Dr. Melissa L. Martin, medical director of Margaret Tietz Nursing Home and is in the department of medicine at Cornell University, both in New York.
Dr. Martin and two colleagues presented findings from their research on nursing home resident autonomy in the areas of smoking, dysphagia treatments, sexuality, and antipsychotic drugs at the annual conference of the American Society on Aging. They also gave their listeners advice on how to address autonomy vs. safety in these areas.
Smoking
Between 2% and 10% of nursing home residents smoke, Dr. Martin said. She pointed out that, besides its familiar health implications, smoking can accelerate residents’ cognitive decline and risk fires and personal burns.
Quoting from a study by her copresenters – Dr. Paula E. Lester and Dr. Izchak Kohen – Dr. Martin said that 72% of fire-related deaths in nursing homes result from smoking materials (J. Am. Med. Dir. Assoc. 2008;9[3]:201-3).
One way to evaluate a nursing home resident’s ability to smoke safely is to test whether the person can extinguish a cigarette or hot ashes. Both the capacity to recognize the danger and the physical ability to respond are necessary, Dr. Martin said.
A tangle of regulations complicates the issue. Dr. Martin cited the Omnibus Budget Reconciliation Act (OBRA) of 1987, which defined nursing homes as residences where people have the right to smoke. In effect, nursing homes can’t ban smoking for existing residents without losing their eligibility for Medicare and Medicaid funding, she said.
On the other hand, the Centers for Medicare and Medicaid Services says in its regulations that residents may not smoke in their bedrooms unless supervised by staff, and nursing homes must restrict nursing home smoking in compliance with the National Fire Protection Association’s Life Safety Code . Meanwhile, the Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations) has mandated since 1994 that nursing homes discourage smoking and limit it to designated locations, she said.
Under the CMS’s rules, nursing homes can refuse to admit new residents who smoke. "There are a lot of issues with this, too, because it’s very difficult to identify if someone is a nonsmoker," said Dr. Martin. "If they stopped and start again, do they have the right to smoke?"
In an anonymous survey of 248 directors of nursing by Dr. Lester, Dr. Kohen, and their colleagues, 80% of the nurses agreed that residents have the right to smoke. In 86% of the facilities represented in the survey, nursing staff distributed cigarettes. In 68%, smokers had to wear fire-resistant aprons, and in 69% of the homes, there had to be a fire extinguisher in the smoking area. About a third of the nursing homes required a physician’s order to allow a resident to smoke, the nurses reported (Director 2008 Summer;16[3]:37-9,41,43).
Dr. Martin concluded that nursing homes are inconsistent in what they require, but she noted that more and more facilities are becoming smoke free, presumably by admitting only nonsmokers.
Dysphagia
In his presentation, Dr. Lester, associate medical director for palliative care at Highfield Gardens Care Center in Great Neck, N.Y., offered specific recommendations on how balance safety and autonomy in people with dysphagia.
Dr. Lester, who is also an assistant professor at Stony Brook (N.Y.) University, said that while nursing staff may recognize that these residents are better off not eating normal food, family members often don’t. And many visitors bring food that a dysphagic person might choke on.
In a nationwide survey of nursing directors of skilled nursing facilities through the National Association Directors of Nursing Administration/Long-Term Care, Dr. Lester and her associates found that most survey responders thought they had both a right and a responsibility to restrict residents’ access to over-the-counter medications, cigarettes, and alcoholic beverages (J. Am. Med. Dir. Assoc. 2009;10[6]:419-22). But only 17% thought that facilities had a responsibility to restrict access to food, and 24% thought they had a right to do so.
In fact, while only 10% of residents smoke, 97% of nursing homes have smoking policies. By contrast, 40%-60% of residents in nursing homes have dysphagia, but only 37% of facilities have policies on food brought in by visitors, said Dr. Lester.
One solution is to carefully inform family members of the risks posed by food items, then get the family to sign statements of informed consent. "As long as you can document that all the risks have been discussed, I think that’s probably fine," she said. "Maybe this food is dangerous, but for this favorite food, we can make an exception. Or we will say, ‘OK, she can have this food, but only if someone is in the room watching, so if there is aspiration, we will know right away.’ Sometimes we can minimize risk while maximizing quality of life by making little compromises."
Antipsychotics
Dr. Kohenof the department of clinical psychology at Albert Einstein College of Medicine and an attending faculty member at Zucker Hillside Hospital, both in New York, said that about two-thirds of patients in skilled nursing facilities have diagnosable mental disorders, mostly cognitive impairment. Up to 25% have clinically significant depression, 6%-12% have delirium, and 2% have schizophrenia.
In 1986, a study indicated that nursing homes used sedatives and physical restraints on up to 85% of residents, leading to the passage of OBRA 1987, said Dr. Kohen.
Turning to his own research, Dr. Kohen said that the prevalence of antipsychotic use in nursing homes declined after that event and now is 15%-27% (J. Am. Med. Dir. Assoc. 2010 Sept. 30 [Epub ahead of print]).
However, he said other researchers have reported increasing use of antipsychotics since 1999 because of the advent of new medicines with reduced side effects. The Food and Drug Administration reacted against this trend in 2005 with a "black box" warning that elderly patients with dementia are at increased risk of death when they are prescribed antipsychotics.
Citing the NADONA/LTC study, Dr. Kohen said that 64% of nursing homes give antipsychotics only when family members sign consent forms. The study found that 65% of the facilities were using lower doses of antipsychotics since the FDA warning, but only 39% reported a reduced use of antipsychotics overall. Just over half had increased their use of nonpharmacologic interventions, and a similar proportion was using other types of medications, such as anticonvulsants and benzodiazepines.
Other researchers have found that facilities with higher staff-to-resident ratios use less antipsychotic medication, and the same is true of those that educate staff about these issues, said Dr. Kohen. But one or two staff training sessions won’t do the trick, he said. "My concern is that you have a lot of turnover in nursing homes. You have to keep [training] consistently."
Sexuality
The sexuality of nursing home residents presents a different set of challenges, said Dr. Lester. "There is a myth that the elderly are asexual beings." Citing unpublished data from the NADONA/LTC survey, she said that 71% of directors of nursing reported "issues regarding residents’ sexual activities."
Of these, 58% involved residents having sex with other residents, while 22% involved residents having sex with visitors and 60% involved residents masturbating.
The directors were divided on whether nursing homes should allow residents with moderate-to-severe dementia to have sexual relationships. Forty-five percent said yes, 28% said no, and 27% weren’t sure.
A clear majority (83%) said residents’ responsible parties should be notified if a resident with dementia wanted to have sex with another person, while 5% said no, and 12% were unsure.
Only 37% of the facilities had a policy regarding sexual activity, and a similar 35% had a designated space for trysts. Of the facilities with policies, 52% applied these policies to all residents, regardless of mental condition.
Dr. Lester finished by calling on nursing homes to confront the sexuality of their residents more directly. "Sexuality and intimacy needs of nursing home residents are frequently taboo and ignored," she said.
Dr. Kohen, Dr. Lester, and Dr. Martin all reported that they had no financial interests or affiliations that affected their presentations.
Dr. Melissa L. Martin, resident autonomy, dysphagia treatments, the American Society on Aging, safety,
Dr. Melissa L. Martin, resident autonomy, dysphagia treatments, the American Society on Aging, safety,
EXPERT ANALYSIS FROM THE ANNUAL CONFERENCE OF THE AMERICAN SOCIETY ON AGING
