User login
Mitchel is a reporter for MDedge based in the Philadelphia area. He started with the company in 1992, when it was International Medical News Group (IMNG), and has since covered a range of medical specialties. Mitchel trained as a virologist at Roswell Park Memorial Institute in Buffalo, and then worked briefly as a researcher at Boston Children's Hospital before pivoting to journalism as a AAAS Mass Media Fellow in 1980. His first reporting job was with Science Digest magazine, and from the mid-1980s to early-1990s he was a reporter with Medical World News. @mitchelzoler
Ticagrelor cuts post-MI events in diabetes patients
CHICAGO – The benefit from dual-antiplatelet therapy in high-risk patients following a myocardial infarction was especially apparent in post-MI patients with diabetes in a prespecified secondary analysis from a multicenter trial of ticagrelor with more than 21,000 patients.
Among post-MI patients with diabetes, treatment with ticagrelor plus aspirin led to an absolute 1.5% reduction in the rate of cardiovascular death, MI, or stroke during a median 33-month follow-up, compared with an absolute 1.1% cut in patients without diabetes, Dr. Deepak L. Bhatt said at the annual meeting of the American College of Cardiology. The relative risk reduction, compared with placebo was 16% in both the diabetes and no diabetes subgroups, statistically significant differences in both subgroups.
“Long-term treatment with ticagrelor reduced the composite of cardiovascular death, MI, or stroke in diabetic patients with a greater absolute risk reduction than in nondiabetic patients,” said Dr. Bhatt, professor of medicine at Harvard Medical School and executive director of Interventional Cardiovascular Programs at Brigham and Women’s Hospital in Boston. Treatment with ticagrelor plus aspirin in post-MI patients with diabetes also led to an increased number of major bleeding episodes, compared with patients on aspirin alone, but no excess of intracerebral hemorrhages or fatal bleeds, he noted.
This finding of a significant benefit from ticagrelor in post-MI patients with diabetes confirms similar, prior findings with other antiplatelet drugs (including clopidogrel, prasugrel, and vorapaxar) and prior findings with ticagrelor, Dr. Bhatt noted.
The new analysis used data collected in the Prevention of Cardiovascular Events in Patients With Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin–Thrombolysis in Myocardial Infarction 54 (PEGASUS-TIMI 54) trial. The primary results from PEGASUS-TIMI 54 had shown that adding ticagrelor to aspirin treatment of high-risk post-MI patients, including those who both had or did not have diabetes, significantly cut the composite rate of cardiovascular death, MI, and stroke, compared with aspirin alone (N Engl J Med. 2015 May 7;372[19]:1791-800). The study group included 6,806 patients with diabetes (type 2 diabetes in 99% of these patients), and 14,355 without diabetes. All patients had their MI 1-3 years before entering the study.
Dr. Bhatt and his associates examined the incidence of the various clinical endpoints measured in the study among only the patients with diabetes divided into those who received any dosage of ticagrelor (60 mg b.i.d. or 90 mg b.i.d.) or placebo, and also among the patients without diabetes. In addition to the primary endpoint, the new analysis showed that the rate of cardiovascular death during follow-up was 3.9% in the diabetes patients on dual therapy and 5.0% among the diabetes patients on aspirin only, a 22% relative risk reduction with ticagrelor added that was statistically significant. In contrast, among patients without diabetes the rates of cardiovascular death between those on and not on ticagrelor only differed by 0.2%, a 9% relative risk reduction that was not statistically significant. The same pattern occurred for the endpoint of death from coronary artery disease.
Concurrent with Dr. Bhatt’s report, the results appeared in an article published online (J Am Coll Cardiol. 2016 Apr; doi: 10.1016/S0735-1097[16]30023-7).
A new study, THEMIS, is examining the safety and efficacy of combined ticagrelor and aspirin treatment in a lower-risk group of patients with diabetes, those with coronary artery disease who have not had a prior MI. Those results may be available in 2018.
PEGASUS-TIMI 54 was sponsored by AstraZeneca, the company that markets ticagrelor (Brilinta). Dr. Bhatt has been an advisor to Cardax and Regado Biosciences and has received research support from AstraZeneca and several other companies.
On Twitter @mitchelzoler
CHICAGO – The benefit from dual-antiplatelet therapy in high-risk patients following a myocardial infarction was especially apparent in post-MI patients with diabetes in a prespecified secondary analysis from a multicenter trial of ticagrelor with more than 21,000 patients.
Among post-MI patients with diabetes, treatment with ticagrelor plus aspirin led to an absolute 1.5% reduction in the rate of cardiovascular death, MI, or stroke during a median 33-month follow-up, compared with an absolute 1.1% cut in patients without diabetes, Dr. Deepak L. Bhatt said at the annual meeting of the American College of Cardiology. The relative risk reduction, compared with placebo was 16% in both the diabetes and no diabetes subgroups, statistically significant differences in both subgroups.
“Long-term treatment with ticagrelor reduced the composite of cardiovascular death, MI, or stroke in diabetic patients with a greater absolute risk reduction than in nondiabetic patients,” said Dr. Bhatt, professor of medicine at Harvard Medical School and executive director of Interventional Cardiovascular Programs at Brigham and Women’s Hospital in Boston. Treatment with ticagrelor plus aspirin in post-MI patients with diabetes also led to an increased number of major bleeding episodes, compared with patients on aspirin alone, but no excess of intracerebral hemorrhages or fatal bleeds, he noted.
This finding of a significant benefit from ticagrelor in post-MI patients with diabetes confirms similar, prior findings with other antiplatelet drugs (including clopidogrel, prasugrel, and vorapaxar) and prior findings with ticagrelor, Dr. Bhatt noted.
The new analysis used data collected in the Prevention of Cardiovascular Events in Patients With Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin–Thrombolysis in Myocardial Infarction 54 (PEGASUS-TIMI 54) trial. The primary results from PEGASUS-TIMI 54 had shown that adding ticagrelor to aspirin treatment of high-risk post-MI patients, including those who both had or did not have diabetes, significantly cut the composite rate of cardiovascular death, MI, and stroke, compared with aspirin alone (N Engl J Med. 2015 May 7;372[19]:1791-800). The study group included 6,806 patients with diabetes (type 2 diabetes in 99% of these patients), and 14,355 without diabetes. All patients had their MI 1-3 years before entering the study.
Dr. Bhatt and his associates examined the incidence of the various clinical endpoints measured in the study among only the patients with diabetes divided into those who received any dosage of ticagrelor (60 mg b.i.d. or 90 mg b.i.d.) or placebo, and also among the patients without diabetes. In addition to the primary endpoint, the new analysis showed that the rate of cardiovascular death during follow-up was 3.9% in the diabetes patients on dual therapy and 5.0% among the diabetes patients on aspirin only, a 22% relative risk reduction with ticagrelor added that was statistically significant. In contrast, among patients without diabetes the rates of cardiovascular death between those on and not on ticagrelor only differed by 0.2%, a 9% relative risk reduction that was not statistically significant. The same pattern occurred for the endpoint of death from coronary artery disease.
Concurrent with Dr. Bhatt’s report, the results appeared in an article published online (J Am Coll Cardiol. 2016 Apr; doi: 10.1016/S0735-1097[16]30023-7).
A new study, THEMIS, is examining the safety and efficacy of combined ticagrelor and aspirin treatment in a lower-risk group of patients with diabetes, those with coronary artery disease who have not had a prior MI. Those results may be available in 2018.
PEGASUS-TIMI 54 was sponsored by AstraZeneca, the company that markets ticagrelor (Brilinta). Dr. Bhatt has been an advisor to Cardax and Regado Biosciences and has received research support from AstraZeneca and several other companies.
On Twitter @mitchelzoler
CHICAGO – The benefit from dual-antiplatelet therapy in high-risk patients following a myocardial infarction was especially apparent in post-MI patients with diabetes in a prespecified secondary analysis from a multicenter trial of ticagrelor with more than 21,000 patients.
Among post-MI patients with diabetes, treatment with ticagrelor plus aspirin led to an absolute 1.5% reduction in the rate of cardiovascular death, MI, or stroke during a median 33-month follow-up, compared with an absolute 1.1% cut in patients without diabetes, Dr. Deepak L. Bhatt said at the annual meeting of the American College of Cardiology. The relative risk reduction, compared with placebo was 16% in both the diabetes and no diabetes subgroups, statistically significant differences in both subgroups.
“Long-term treatment with ticagrelor reduced the composite of cardiovascular death, MI, or stroke in diabetic patients with a greater absolute risk reduction than in nondiabetic patients,” said Dr. Bhatt, professor of medicine at Harvard Medical School and executive director of Interventional Cardiovascular Programs at Brigham and Women’s Hospital in Boston. Treatment with ticagrelor plus aspirin in post-MI patients with diabetes also led to an increased number of major bleeding episodes, compared with patients on aspirin alone, but no excess of intracerebral hemorrhages or fatal bleeds, he noted.
This finding of a significant benefit from ticagrelor in post-MI patients with diabetes confirms similar, prior findings with other antiplatelet drugs (including clopidogrel, prasugrel, and vorapaxar) and prior findings with ticagrelor, Dr. Bhatt noted.
The new analysis used data collected in the Prevention of Cardiovascular Events in Patients With Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin–Thrombolysis in Myocardial Infarction 54 (PEGASUS-TIMI 54) trial. The primary results from PEGASUS-TIMI 54 had shown that adding ticagrelor to aspirin treatment of high-risk post-MI patients, including those who both had or did not have diabetes, significantly cut the composite rate of cardiovascular death, MI, and stroke, compared with aspirin alone (N Engl J Med. 2015 May 7;372[19]:1791-800). The study group included 6,806 patients with diabetes (type 2 diabetes in 99% of these patients), and 14,355 without diabetes. All patients had their MI 1-3 years before entering the study.
Dr. Bhatt and his associates examined the incidence of the various clinical endpoints measured in the study among only the patients with diabetes divided into those who received any dosage of ticagrelor (60 mg b.i.d. or 90 mg b.i.d.) or placebo, and also among the patients without diabetes. In addition to the primary endpoint, the new analysis showed that the rate of cardiovascular death during follow-up was 3.9% in the diabetes patients on dual therapy and 5.0% among the diabetes patients on aspirin only, a 22% relative risk reduction with ticagrelor added that was statistically significant. In contrast, among patients without diabetes the rates of cardiovascular death between those on and not on ticagrelor only differed by 0.2%, a 9% relative risk reduction that was not statistically significant. The same pattern occurred for the endpoint of death from coronary artery disease.
Concurrent with Dr. Bhatt’s report, the results appeared in an article published online (J Am Coll Cardiol. 2016 Apr; doi: 10.1016/S0735-1097[16]30023-7).
A new study, THEMIS, is examining the safety and efficacy of combined ticagrelor and aspirin treatment in a lower-risk group of patients with diabetes, those with coronary artery disease who have not had a prior MI. Those results may be available in 2018.
PEGASUS-TIMI 54 was sponsored by AstraZeneca, the company that markets ticagrelor (Brilinta). Dr. Bhatt has been an advisor to Cardax and Regado Biosciences and has received research support from AstraZeneca and several other companies.
On Twitter @mitchelzoler
AT ACC 2016
Key clinical point: Among post-MI patients with diabetes, dual-antiplatelet therapy with aspirin and ticagrelor produced a significant drop in the rate of cardiovascular death and other ischemic events.
Major finding: Post-MI patients with diabetes had a 10.1% combined endpoint rate on ticagrelor and a 11.6% rate on placebo.
Data source: Prespecified secondary analysis of data from PEGASUS-TIMI 54, a multicenter randomized trial with 21,162 patients.
Disclosures: PEGASUS-TIMI 54 was sponsored by AstraZeneca, the company that markets ticagrelor (Brilinta). Dr. Bhatt has been an advisor to Cardax and Regado Biosciences and has received research support from AstraZeneca and several other companies.
VIDEO: Serial lung fluid measurement improved heart failure outcomes
CHICAGO – Regular assessment of a heart failure patient’s lung fluid volume using a device that measures electrical conduction through the chest – lung impedance – helped guide clinicians to make timely adjustments in a patient’s medications and thereby significantly reduce mortality and hospitalizations during an average 4 years of follow-up in a randomized, controlled study with 256 patients.
Monthly measurement of lung impedance and medication adjustments based on the information led to a 58% reduction in hospitalizations for acute heart failure during the first year of the study, compared with control patients, and a 56% reduction in heart failure hospitalizations, compared with controls, during the entire course of the study, the study’s two primary endpoints, Dr. Michael K. Shochat reported at the annual meeting of the American College of Cardiology.
The results also showed that performing regular lung impedance measurements and using the results to guide treatment led to a 43% reduction in all-cause mortality and a 62% drop in heart failure mortality during the average 4-year course of the study, said Dr. Shochat, a cardiologist at the Heart Institute of Hillel Yaffe Medical Center in Hadera, Israel. Concurrent with Dr. Shochat’s report at the meeting the results also appeared in an article published online (J Card Failure. 2016;doi:10.1016/j.cardfail.2016.03.015).
A key aspect of the study was that the clinicians who treated the enrolled patients who underwent lung impedance monitoring used this information to adjust medications the patients received. Overall, patients who underwent monitoring had more than twice the number of medication dose adjustments, compared with the control patients. These adjustments particularly focused on diuretic dosages, which changed three times as often in the monitored patients, compared with controls, Dr. Shochat reported. Changes in the dosages of beta-blockers and ACE inhibitors also showed marked increases in the monitored patients, compared with the controls.
The Non-Invasive Lung IMPEDANCE-Guided Preemptive Treatment in Chronic Heart Failure Patients (IMPEDANCE-HF) trial enrolled 256 patients at two centers in Israel during 2005-2014. Patients had New York Heart Association class II-IV heart failure and a left ventricular ejection fraction of 35% or less. The enrolled patients averaged 67 years of age, and 80% were men.
Clinicians measured lung impedance using a proprietary device that places external electrodes on opposite sides of the patient’s chest. Calculation of impedance used a formula that eliminated the noise from chest wall impedance and focused exclusively on lung impedance. Once the electrodes are placed collection of the impedance data takes about 1 minute, Dr. Shochat said. The study protocol called for impedance data to be collected monthly, and in practice it occurred about 11 times a year during the study.
The investigators calculated for each patient in the active arm of the study a “basal” lung impedance level that reflected their level of lung conductivity when their lungs were clear of excess fluid. Participating clinicians were instructed to intervene by altering medications when the impedance level dropped more than 18% below the basal level. Their goal was to prevent impedance from dropping to more than 24% below the basal level, which correlated with when heart failure patients usually required hospitalization for acute decompensation. The specifics of how to adjust medications to manage patients who showed these signs of fluid overload were left to the discretion of each attending physician.
MPEDANCE-HF was sponsored by the RSMM Company, which is developing the lung impedance measurement device used in the study. Dr. Shochat is a cofounder of RSMM and is a member of the company’s board of directors.
On Twitter @mitchelzoler
The very exciting results reported by Dr. Shochat came from a small, positive trial that showed impedance monitoring was an effective way to detect an increased amount of fluid in a heart failure patient’s lungs. This resulted in improved outcomes, compared with patients managed using usual care, including fewer hospitalizations and reduced mortality.
These results suggest that when physicians had lung impedance information, they identified episodes of acute heart failure decompensation sooner and that they used this alert to change treatment and prevent patient worsening. Heart failure exacerbations and decompensation events are a recurring problem for heart failure patients, and the earlier they are identified and addressed with altered treatment, the better it is for the patient’s well being. The next step is to see if these positive results can be confirmed by other research groups and in larger numbers of patients.
These results contrast with the findings from a German study reported in 2015 that used lung impedance information collected by implantable cardioverter defibrillators in heart failure patients to identify episodes of fluid buildup and decompensation. That study failed to show a statistically significant impact on patient outcomes. The researchers speculated that this may have been because patients often did not go online to allow their information to get transmitted to their physician, and physicians often did not act on the information because the patients reported no coincident change in symptoms.
This problem with the German study highlights that collecting lung impedance information will only improve outcomes if physicians then act on the information and modify a patient’s treatment. In the new study reported by Dr. Shochat, patients consistently underwent evaluation for their lung impedance status every month, and when the results suggested a growing problem of fluid overload the physicians consistently acted on the information by adjusting medication dosages.
Use of lung impedance measurement is similar to another approach for monitoring patients with heart failure that recently entered routine U.S. practice, an implanted device to monitor pulmonary artery pressure and identify episodes of fluid overload and acute decompensation. In the future, it will be interesting to compare the efficacy and ease of use of managing heart failure patients with pulmonary artery pressure monitoring with an implanted device and monitoring fluid build up in the lungs with lung impedance.
Dr. John A. Jarcho is a cardiologist at Brigham and Women’s Hospital, Boston. He had no disclosures. He made these comments as a discussant of Dr. Shochat’s report and in an interview.
The very exciting results reported by Dr. Shochat came from a small, positive trial that showed impedance monitoring was an effective way to detect an increased amount of fluid in a heart failure patient’s lungs. This resulted in improved outcomes, compared with patients managed using usual care, including fewer hospitalizations and reduced mortality.
These results suggest that when physicians had lung impedance information, they identified episodes of acute heart failure decompensation sooner and that they used this alert to change treatment and prevent patient worsening. Heart failure exacerbations and decompensation events are a recurring problem for heart failure patients, and the earlier they are identified and addressed with altered treatment, the better it is for the patient’s well being. The next step is to see if these positive results can be confirmed by other research groups and in larger numbers of patients.
These results contrast with the findings from a German study reported in 2015 that used lung impedance information collected by implantable cardioverter defibrillators in heart failure patients to identify episodes of fluid buildup and decompensation. That study failed to show a statistically significant impact on patient outcomes. The researchers speculated that this may have been because patients often did not go online to allow their information to get transmitted to their physician, and physicians often did not act on the information because the patients reported no coincident change in symptoms.
This problem with the German study highlights that collecting lung impedance information will only improve outcomes if physicians then act on the information and modify a patient’s treatment. In the new study reported by Dr. Shochat, patients consistently underwent evaluation for their lung impedance status every month, and when the results suggested a growing problem of fluid overload the physicians consistently acted on the information by adjusting medication dosages.
Use of lung impedance measurement is similar to another approach for monitoring patients with heart failure that recently entered routine U.S. practice, an implanted device to monitor pulmonary artery pressure and identify episodes of fluid overload and acute decompensation. In the future, it will be interesting to compare the efficacy and ease of use of managing heart failure patients with pulmonary artery pressure monitoring with an implanted device and monitoring fluid build up in the lungs with lung impedance.
Dr. John A. Jarcho is a cardiologist at Brigham and Women’s Hospital, Boston. He had no disclosures. He made these comments as a discussant of Dr. Shochat’s report and in an interview.
The very exciting results reported by Dr. Shochat came from a small, positive trial that showed impedance monitoring was an effective way to detect an increased amount of fluid in a heart failure patient’s lungs. This resulted in improved outcomes, compared with patients managed using usual care, including fewer hospitalizations and reduced mortality.
These results suggest that when physicians had lung impedance information, they identified episodes of acute heart failure decompensation sooner and that they used this alert to change treatment and prevent patient worsening. Heart failure exacerbations and decompensation events are a recurring problem for heart failure patients, and the earlier they are identified and addressed with altered treatment, the better it is for the patient’s well being. The next step is to see if these positive results can be confirmed by other research groups and in larger numbers of patients.
These results contrast with the findings from a German study reported in 2015 that used lung impedance information collected by implantable cardioverter defibrillators in heart failure patients to identify episodes of fluid buildup and decompensation. That study failed to show a statistically significant impact on patient outcomes. The researchers speculated that this may have been because patients often did not go online to allow their information to get transmitted to their physician, and physicians often did not act on the information because the patients reported no coincident change in symptoms.
This problem with the German study highlights that collecting lung impedance information will only improve outcomes if physicians then act on the information and modify a patient’s treatment. In the new study reported by Dr. Shochat, patients consistently underwent evaluation for their lung impedance status every month, and when the results suggested a growing problem of fluid overload the physicians consistently acted on the information by adjusting medication dosages.
Use of lung impedance measurement is similar to another approach for monitoring patients with heart failure that recently entered routine U.S. practice, an implanted device to monitor pulmonary artery pressure and identify episodes of fluid overload and acute decompensation. In the future, it will be interesting to compare the efficacy and ease of use of managing heart failure patients with pulmonary artery pressure monitoring with an implanted device and monitoring fluid build up in the lungs with lung impedance.
Dr. John A. Jarcho is a cardiologist at Brigham and Women’s Hospital, Boston. He had no disclosures. He made these comments as a discussant of Dr. Shochat’s report and in an interview.
CHICAGO – Regular assessment of a heart failure patient’s lung fluid volume using a device that measures electrical conduction through the chest – lung impedance – helped guide clinicians to make timely adjustments in a patient’s medications and thereby significantly reduce mortality and hospitalizations during an average 4 years of follow-up in a randomized, controlled study with 256 patients.
Monthly measurement of lung impedance and medication adjustments based on the information led to a 58% reduction in hospitalizations for acute heart failure during the first year of the study, compared with control patients, and a 56% reduction in heart failure hospitalizations, compared with controls, during the entire course of the study, the study’s two primary endpoints, Dr. Michael K. Shochat reported at the annual meeting of the American College of Cardiology.
The results also showed that performing regular lung impedance measurements and using the results to guide treatment led to a 43% reduction in all-cause mortality and a 62% drop in heart failure mortality during the average 4-year course of the study, said Dr. Shochat, a cardiologist at the Heart Institute of Hillel Yaffe Medical Center in Hadera, Israel. Concurrent with Dr. Shochat’s report at the meeting the results also appeared in an article published online (J Card Failure. 2016;doi:10.1016/j.cardfail.2016.03.015).
A key aspect of the study was that the clinicians who treated the enrolled patients who underwent lung impedance monitoring used this information to adjust medications the patients received. Overall, patients who underwent monitoring had more than twice the number of medication dose adjustments, compared with the control patients. These adjustments particularly focused on diuretic dosages, which changed three times as often in the monitored patients, compared with controls, Dr. Shochat reported. Changes in the dosages of beta-blockers and ACE inhibitors also showed marked increases in the monitored patients, compared with the controls.
The Non-Invasive Lung IMPEDANCE-Guided Preemptive Treatment in Chronic Heart Failure Patients (IMPEDANCE-HF) trial enrolled 256 patients at two centers in Israel during 2005-2014. Patients had New York Heart Association class II-IV heart failure and a left ventricular ejection fraction of 35% or less. The enrolled patients averaged 67 years of age, and 80% were men.
Clinicians measured lung impedance using a proprietary device that places external electrodes on opposite sides of the patient’s chest. Calculation of impedance used a formula that eliminated the noise from chest wall impedance and focused exclusively on lung impedance. Once the electrodes are placed collection of the impedance data takes about 1 minute, Dr. Shochat said. The study protocol called for impedance data to be collected monthly, and in practice it occurred about 11 times a year during the study.
The investigators calculated for each patient in the active arm of the study a “basal” lung impedance level that reflected their level of lung conductivity when their lungs were clear of excess fluid. Participating clinicians were instructed to intervene by altering medications when the impedance level dropped more than 18% below the basal level. Their goal was to prevent impedance from dropping to more than 24% below the basal level, which correlated with when heart failure patients usually required hospitalization for acute decompensation. The specifics of how to adjust medications to manage patients who showed these signs of fluid overload were left to the discretion of each attending physician.
MPEDANCE-HF was sponsored by the RSMM Company, which is developing the lung impedance measurement device used in the study. Dr. Shochat is a cofounder of RSMM and is a member of the company’s board of directors.
On Twitter @mitchelzoler
CHICAGO – Regular assessment of a heart failure patient’s lung fluid volume using a device that measures electrical conduction through the chest – lung impedance – helped guide clinicians to make timely adjustments in a patient’s medications and thereby significantly reduce mortality and hospitalizations during an average 4 years of follow-up in a randomized, controlled study with 256 patients.
Monthly measurement of lung impedance and medication adjustments based on the information led to a 58% reduction in hospitalizations for acute heart failure during the first year of the study, compared with control patients, and a 56% reduction in heart failure hospitalizations, compared with controls, during the entire course of the study, the study’s two primary endpoints, Dr. Michael K. Shochat reported at the annual meeting of the American College of Cardiology.
The results also showed that performing regular lung impedance measurements and using the results to guide treatment led to a 43% reduction in all-cause mortality and a 62% drop in heart failure mortality during the average 4-year course of the study, said Dr. Shochat, a cardiologist at the Heart Institute of Hillel Yaffe Medical Center in Hadera, Israel. Concurrent with Dr. Shochat’s report at the meeting the results also appeared in an article published online (J Card Failure. 2016;doi:10.1016/j.cardfail.2016.03.015).
A key aspect of the study was that the clinicians who treated the enrolled patients who underwent lung impedance monitoring used this information to adjust medications the patients received. Overall, patients who underwent monitoring had more than twice the number of medication dose adjustments, compared with the control patients. These adjustments particularly focused on diuretic dosages, which changed three times as often in the monitored patients, compared with controls, Dr. Shochat reported. Changes in the dosages of beta-blockers and ACE inhibitors also showed marked increases in the monitored patients, compared with the controls.
The Non-Invasive Lung IMPEDANCE-Guided Preemptive Treatment in Chronic Heart Failure Patients (IMPEDANCE-HF) trial enrolled 256 patients at two centers in Israel during 2005-2014. Patients had New York Heart Association class II-IV heart failure and a left ventricular ejection fraction of 35% or less. The enrolled patients averaged 67 years of age, and 80% were men.
Clinicians measured lung impedance using a proprietary device that places external electrodes on opposite sides of the patient’s chest. Calculation of impedance used a formula that eliminated the noise from chest wall impedance and focused exclusively on lung impedance. Once the electrodes are placed collection of the impedance data takes about 1 minute, Dr. Shochat said. The study protocol called for impedance data to be collected monthly, and in practice it occurred about 11 times a year during the study.
The investigators calculated for each patient in the active arm of the study a “basal” lung impedance level that reflected their level of lung conductivity when their lungs were clear of excess fluid. Participating clinicians were instructed to intervene by altering medications when the impedance level dropped more than 18% below the basal level. Their goal was to prevent impedance from dropping to more than 24% below the basal level, which correlated with when heart failure patients usually required hospitalization for acute decompensation. The specifics of how to adjust medications to manage patients who showed these signs of fluid overload were left to the discretion of each attending physician.
MPEDANCE-HF was sponsored by the RSMM Company, which is developing the lung impedance measurement device used in the study. Dr. Shochat is a cofounder of RSMM and is a member of the company’s board of directors.
On Twitter @mitchelzoler
AT ACC 2016
Key clinical point: Monthly, noninvasive measurement of lung fluid levels using lung impedance produced better fluid control in heart failure patients and significantly fewer deaths and heart failure hospitalizations.
Major finding: Lung impedance–based management produced a 56% cut in heart failure hospitalizations, compared with standard care.
Data source: IMPEDANCE-HF, a randomized study with 256 heart failure patients at two Israeli centers.
Disclosures: IMPEDANCE-HF was sponsored by the RSMM Company, which is developing the lung impedance measurement device used in the study. Dr. Shochat is a cofounder of RSMM and is a member of the company’s board of directors.
Stem cells show heart failure benefits in phase II trial
CHICAGO – After rattling around in early-stage clinical studies for more than a decade, stem cell therapy for heart failure may have finally gained the efficacy evidence to send it to the next level: large-scale, phase III trials.
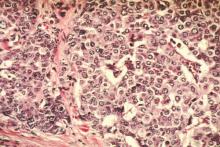
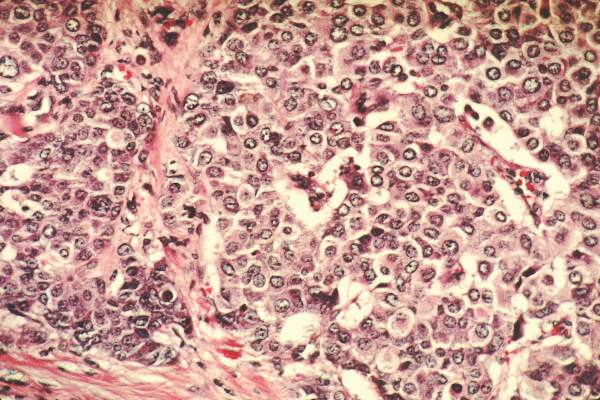
Patients with ischemic cardiomyopathy and severe heart failure showed a statistically significant 37% relative reduction in their combined rate of death and cardiovascular hospitalization during 1 year of follow-up after autologous stem cell injections to their left ventricular myocardium in a multicenter, fully blinded control, phase II trial with 109 North American patients.
The treatment used a technique in commercial development by Vericel that selectively expands ex vivo bone marrow cells taken from the heart failure patient. Clinicians inject 0.4 mL aliquots of the expanded cells – enriched for mesenchymal stem cells and M2 macrophages – via a transcatheter approach into the left ventricular myocardium using 12-17 injections per patient. The bone marrow preparation during ex vivo expansion is called ixmyelocel-T.
This treatment now needs testing in more patients, Dr. Timothy D. Henry said at the annual meeting of the American College of Cardiology. “We need a new generation of cell trials in larger studies with completely double-blind, placebo controls using a more uniform preparation of cells,” said Dr. Henry.
“To the best of our knowledge, ixCELL-DCM is the largest randomized, double-blind clinical trial to date for cell therapy use in congestive heart failure,” said Dr. Henry and his associates in their report. The concept of stem cell therapy to replace damaged myocardium “has been very attractive, but most clinical trials to date have been small and unblinded, and used unselected bone marrow cells,” explained Dr. Henry, director of cardiology at the Cedars-Sinai Heart Institute in Los Angeles.
The ixCELL-DCM study ran at 31 sites in the United States and Canada. About 90% of patients had New York Heart Association class III disease, the average left ventricular ejection fraction was about 25%, patients on average would cover about 310 m during a 6-minute walk test, and the average serum level of NT-ProBNP was about 1,900 pg/L. Patients in the control arm all underwent the same bone marrow retrieval and transcatheter injection into the left ventricle, but the injections only contained carrier material without active cells.
The primary endpoint of death or a cardiovascular event, primarily hospitalization, occurred at a rate of 110 events per 100 patient years during 1-year follow-up of 51 patients in the sham-treatment group. In the active-treatment arm, the endpoint occurred at a rate of 70 events per 100 patient years among 58 patients. The difference was primarily driven by a 3% death rate with cell therapy, compared with a 14% rate in the controls, and a 38% hospitalization rate, compared with a 47% rate among controls.
The study results appeared online concurrent with Dr. Henry’s report (Lancet. 2016 Apr 5. doi: 10.1016/S0140-6736[16]30137-4).
The results showed no significant differences between the active and sham groups for changes in left ventricular size, ejection fraction, and 6-minute walk distance.
“This trial was designed to look at events. It is not a cause for concern that we did not see effects on heart function,” Dr. Henry said. The current results were also generally consistent with results from two earlier, controlled, phase II studies with a total of 61 patients (Circ Res. 2014 Sep 26;115[8]:730-7).
In the safety analysis, done in 114 patients, the rates of all adverse events and major adverse cardiovascular events were similar in the two arms. The rate of serious adverse events was significantly reduced in the patients treated with expanded bone marrow cells, compared with the controls.
The high rate of death and hospitalization of patients with severe heart failure “is a very large, unmet need, so it’s a natural to go to a larger trial,” Dr. Henry said. “The cell preparation was very safe and easy to do.”
Another pressing research issue is to try to understand the mechanism by which the cell treatment improves clinical outcomes, with improved heart function or improved exercise capacity apparently excluded as mechanisms.
The trial was sponsored by Vericel, the company developing the ex vivo protocol for selective marrow cell expansion. Dr. Henry has been a consultant to or received honoraria from Abbott Vascular, Baxter, Capricor, Cytori, Eli Lilly, and the Medicines Company, and he has received research grants from Aastrom, Baxter International, Mesoblast, and Vericel.
On Twitter @mitchelzoler
The results reported by Dr. Henry come from one of the first trials of stem cell or bone marrow treatment of failing hearts that used clinical outcomes as the primary endpoint. In contrast, prior studies focused on changes in functional characteristics of patients, such as 6-minute walk distance or left ventricular ejection fraction or size. What makes Dr. Henry’s study distinctive is that it showed benefit for a clinical outcome: the rate of death or cardiovascular hospitalization.
Another distinct difference, compared with the vast majority of earlier trials, was the way the bone marrow was handled prior to placement in a heart. The bone marrow cells underwent a 12-day period of ex vivo treatment designed to expand the content of certain mesenchymal stem cells and macrophages.
The current study was also larger than most prior reported studies, with 114 randomized patients available for the safety analysis and 109 for the efficacy analysis. But by no means was this a large study; in fact, it is relatively small. Although it produced a statistically significant result for the primary endpoint, the efficacy needs expanded testing in larger numbers.
It’s currently unclear how the expanded bone marrow cell injections improve clinical status and lead to reduced deaths and hospitalization. The results show essentially no impact from the treatment on ejection fraction or 6-minute walk distance, raising the question of what alternative mechanisms link this treatment to improved clinical outcomes.
Until now, it has not been possible to move beyond early-stage trial designs for cell therapy of failing hearts. Now, for the first time, we have study results that suggest a phase III trial is indicated.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. John A. Jarcho is a deputy editor of the New England Journal of Medicine and a cardiologist at Brigham and Women’s Hospital, both in Boston. He had no disclosures. He made these comments as a discussant of Dr. Henry’s report and in an interview.
The results reported by Dr. Henry come from one of the first trials of stem cell or bone marrow treatment of failing hearts that used clinical outcomes as the primary endpoint. In contrast, prior studies focused on changes in functional characteristics of patients, such as 6-minute walk distance or left ventricular ejection fraction or size. What makes Dr. Henry’s study distinctive is that it showed benefit for a clinical outcome: the rate of death or cardiovascular hospitalization.
Another distinct difference, compared with the vast majority of earlier trials, was the way the bone marrow was handled prior to placement in a heart. The bone marrow cells underwent a 12-day period of ex vivo treatment designed to expand the content of certain mesenchymal stem cells and macrophages.
The current study was also larger than most prior reported studies, with 114 randomized patients available for the safety analysis and 109 for the efficacy analysis. But by no means was this a large study; in fact, it is relatively small. Although it produced a statistically significant result for the primary endpoint, the efficacy needs expanded testing in larger numbers.
It’s currently unclear how the expanded bone marrow cell injections improve clinical status and lead to reduced deaths and hospitalization. The results show essentially no impact from the treatment on ejection fraction or 6-minute walk distance, raising the question of what alternative mechanisms link this treatment to improved clinical outcomes.
Until now, it has not been possible to move beyond early-stage trial designs for cell therapy of failing hearts. Now, for the first time, we have study results that suggest a phase III trial is indicated.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. John A. Jarcho is a deputy editor of the New England Journal of Medicine and a cardiologist at Brigham and Women’s Hospital, both in Boston. He had no disclosures. He made these comments as a discussant of Dr. Henry’s report and in an interview.
The results reported by Dr. Henry come from one of the first trials of stem cell or bone marrow treatment of failing hearts that used clinical outcomes as the primary endpoint. In contrast, prior studies focused on changes in functional characteristics of patients, such as 6-minute walk distance or left ventricular ejection fraction or size. What makes Dr. Henry’s study distinctive is that it showed benefit for a clinical outcome: the rate of death or cardiovascular hospitalization.
Another distinct difference, compared with the vast majority of earlier trials, was the way the bone marrow was handled prior to placement in a heart. The bone marrow cells underwent a 12-day period of ex vivo treatment designed to expand the content of certain mesenchymal stem cells and macrophages.
The current study was also larger than most prior reported studies, with 114 randomized patients available for the safety analysis and 109 for the efficacy analysis. But by no means was this a large study; in fact, it is relatively small. Although it produced a statistically significant result for the primary endpoint, the efficacy needs expanded testing in larger numbers.
It’s currently unclear how the expanded bone marrow cell injections improve clinical status and lead to reduced deaths and hospitalization. The results show essentially no impact from the treatment on ejection fraction or 6-minute walk distance, raising the question of what alternative mechanisms link this treatment to improved clinical outcomes.
Until now, it has not been possible to move beyond early-stage trial designs for cell therapy of failing hearts. Now, for the first time, we have study results that suggest a phase III trial is indicated.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. John A. Jarcho is a deputy editor of the New England Journal of Medicine and a cardiologist at Brigham and Women’s Hospital, both in Boston. He had no disclosures. He made these comments as a discussant of Dr. Henry’s report and in an interview.
CHICAGO – After rattling around in early-stage clinical studies for more than a decade, stem cell therapy for heart failure may have finally gained the efficacy evidence to send it to the next level: large-scale, phase III trials.
Patients with ischemic cardiomyopathy and severe heart failure showed a statistically significant 37% relative reduction in their combined rate of death and cardiovascular hospitalization during 1 year of follow-up after autologous stem cell injections to their left ventricular myocardium in a multicenter, fully blinded control, phase II trial with 109 North American patients.
The treatment used a technique in commercial development by Vericel that selectively expands ex vivo bone marrow cells taken from the heart failure patient. Clinicians inject 0.4 mL aliquots of the expanded cells – enriched for mesenchymal stem cells and M2 macrophages – via a transcatheter approach into the left ventricular myocardium using 12-17 injections per patient. The bone marrow preparation during ex vivo expansion is called ixmyelocel-T.
This treatment now needs testing in more patients, Dr. Timothy D. Henry said at the annual meeting of the American College of Cardiology. “We need a new generation of cell trials in larger studies with completely double-blind, placebo controls using a more uniform preparation of cells,” said Dr. Henry.
“To the best of our knowledge, ixCELL-DCM is the largest randomized, double-blind clinical trial to date for cell therapy use in congestive heart failure,” said Dr. Henry and his associates in their report. The concept of stem cell therapy to replace damaged myocardium “has been very attractive, but most clinical trials to date have been small and unblinded, and used unselected bone marrow cells,” explained Dr. Henry, director of cardiology at the Cedars-Sinai Heart Institute in Los Angeles.
The ixCELL-DCM study ran at 31 sites in the United States and Canada. About 90% of patients had New York Heart Association class III disease, the average left ventricular ejection fraction was about 25%, patients on average would cover about 310 m during a 6-minute walk test, and the average serum level of NT-ProBNP was about 1,900 pg/L. Patients in the control arm all underwent the same bone marrow retrieval and transcatheter injection into the left ventricle, but the injections only contained carrier material without active cells.
The primary endpoint of death or a cardiovascular event, primarily hospitalization, occurred at a rate of 110 events per 100 patient years during 1-year follow-up of 51 patients in the sham-treatment group. In the active-treatment arm, the endpoint occurred at a rate of 70 events per 100 patient years among 58 patients. The difference was primarily driven by a 3% death rate with cell therapy, compared with a 14% rate in the controls, and a 38% hospitalization rate, compared with a 47% rate among controls.
The study results appeared online concurrent with Dr. Henry’s report (Lancet. 2016 Apr 5. doi: 10.1016/S0140-6736[16]30137-4).
The results showed no significant differences between the active and sham groups for changes in left ventricular size, ejection fraction, and 6-minute walk distance.
“This trial was designed to look at events. It is not a cause for concern that we did not see effects on heart function,” Dr. Henry said. The current results were also generally consistent with results from two earlier, controlled, phase II studies with a total of 61 patients (Circ Res. 2014 Sep 26;115[8]:730-7).
In the safety analysis, done in 114 patients, the rates of all adverse events and major adverse cardiovascular events were similar in the two arms. The rate of serious adverse events was significantly reduced in the patients treated with expanded bone marrow cells, compared with the controls.
The high rate of death and hospitalization of patients with severe heart failure “is a very large, unmet need, so it’s a natural to go to a larger trial,” Dr. Henry said. “The cell preparation was very safe and easy to do.”
Another pressing research issue is to try to understand the mechanism by which the cell treatment improves clinical outcomes, with improved heart function or improved exercise capacity apparently excluded as mechanisms.
The trial was sponsored by Vericel, the company developing the ex vivo protocol for selective marrow cell expansion. Dr. Henry has been a consultant to or received honoraria from Abbott Vascular, Baxter, Capricor, Cytori, Eli Lilly, and the Medicines Company, and he has received research grants from Aastrom, Baxter International, Mesoblast, and Vericel.
On Twitter @mitchelzoler
CHICAGO – After rattling around in early-stage clinical studies for more than a decade, stem cell therapy for heart failure may have finally gained the efficacy evidence to send it to the next level: large-scale, phase III trials.
Patients with ischemic cardiomyopathy and severe heart failure showed a statistically significant 37% relative reduction in their combined rate of death and cardiovascular hospitalization during 1 year of follow-up after autologous stem cell injections to their left ventricular myocardium in a multicenter, fully blinded control, phase II trial with 109 North American patients.
The treatment used a technique in commercial development by Vericel that selectively expands ex vivo bone marrow cells taken from the heart failure patient. Clinicians inject 0.4 mL aliquots of the expanded cells – enriched for mesenchymal stem cells and M2 macrophages – via a transcatheter approach into the left ventricular myocardium using 12-17 injections per patient. The bone marrow preparation during ex vivo expansion is called ixmyelocel-T.
This treatment now needs testing in more patients, Dr. Timothy D. Henry said at the annual meeting of the American College of Cardiology. “We need a new generation of cell trials in larger studies with completely double-blind, placebo controls using a more uniform preparation of cells,” said Dr. Henry.
“To the best of our knowledge, ixCELL-DCM is the largest randomized, double-blind clinical trial to date for cell therapy use in congestive heart failure,” said Dr. Henry and his associates in their report. The concept of stem cell therapy to replace damaged myocardium “has been very attractive, but most clinical trials to date have been small and unblinded, and used unselected bone marrow cells,” explained Dr. Henry, director of cardiology at the Cedars-Sinai Heart Institute in Los Angeles.
The ixCELL-DCM study ran at 31 sites in the United States and Canada. About 90% of patients had New York Heart Association class III disease, the average left ventricular ejection fraction was about 25%, patients on average would cover about 310 m during a 6-minute walk test, and the average serum level of NT-ProBNP was about 1,900 pg/L. Patients in the control arm all underwent the same bone marrow retrieval and transcatheter injection into the left ventricle, but the injections only contained carrier material without active cells.
The primary endpoint of death or a cardiovascular event, primarily hospitalization, occurred at a rate of 110 events per 100 patient years during 1-year follow-up of 51 patients in the sham-treatment group. In the active-treatment arm, the endpoint occurred at a rate of 70 events per 100 patient years among 58 patients. The difference was primarily driven by a 3% death rate with cell therapy, compared with a 14% rate in the controls, and a 38% hospitalization rate, compared with a 47% rate among controls.
The study results appeared online concurrent with Dr. Henry’s report (Lancet. 2016 Apr 5. doi: 10.1016/S0140-6736[16]30137-4).
The results showed no significant differences between the active and sham groups for changes in left ventricular size, ejection fraction, and 6-minute walk distance.
“This trial was designed to look at events. It is not a cause for concern that we did not see effects on heart function,” Dr. Henry said. The current results were also generally consistent with results from two earlier, controlled, phase II studies with a total of 61 patients (Circ Res. 2014 Sep 26;115[8]:730-7).
In the safety analysis, done in 114 patients, the rates of all adverse events and major adverse cardiovascular events were similar in the two arms. The rate of serious adverse events was significantly reduced in the patients treated with expanded bone marrow cells, compared with the controls.
The high rate of death and hospitalization of patients with severe heart failure “is a very large, unmet need, so it’s a natural to go to a larger trial,” Dr. Henry said. “The cell preparation was very safe and easy to do.”
Another pressing research issue is to try to understand the mechanism by which the cell treatment improves clinical outcomes, with improved heart function or improved exercise capacity apparently excluded as mechanisms.
The trial was sponsored by Vericel, the company developing the ex vivo protocol for selective marrow cell expansion. Dr. Henry has been a consultant to or received honoraria from Abbott Vascular, Baxter, Capricor, Cytori, Eli Lilly, and the Medicines Company, and he has received research grants from Aastrom, Baxter International, Mesoblast, and Vericel.
On Twitter @mitchelzoler
AT ACC 16
Key clinical point: Severe, ischemic heart failure patients had a significant cut in death and cardiovascular hospitalizations 1 year after endovascular myocardial injection with selectively expanded autologous bone marrow cells in a fully blinded, placebo-controlled phase II study.
Major finding: Cell-treated patients had a 37% drop in death and cardiovascular hospitalization relative to controls in 1-year follow-up.
Data source: A multicenter, fully blinded study with 109 patients for the per protocol efficacy analysis, and 114 patients for the safety analysis.
Disclosures: The trial was sponsored by Vericel, the company developing the ex vivo protocol for selective marrow cell expansion. Dr. Henry has been a consultant to or received honoraria from Abbott Vascular, Baxter, Capricor, Cytori, Eli Lilly, and the Medicines Company, and he has received research grants from Aastrom, Baxter International, Mesoblast, and Vericel.
PCSK9 inhibitor overcomes muscle-related statin intolerance
CHICAGO – Statin-associated muscle symptoms are real for roughly 40% of patients with a history of this adverse effect, and for such patients who are truly unable to tolerate a statin treatment, a PCSK9 inhibitor provided an effective and well-tolerated alternative in a randomized trial with more than 500 patients.
“Controversy has surrounded the issue of statin-associated muscle symptoms because of large differences in the incidence of this disorder in randomized trials and observational studies. The GAUSS-3 study results demonstrate that muscle-related intolerance is reproducible during blinded statin rechallenge in a substantial fraction, about 40%, of patients with a history of symptoms,” Dr. Steven E. Nissen said at the annual meeting of the American College of Cardiology. “Alternative approaches to reducing low-density lipoprotein cholesterol in these patients represents an important medical priority.”
Statin intolerance has been a challenging diagnosis for physicians to confirm because no biomarker exists to definitively document it, which led to this study to test a more systematic and objective approach to confirm the diagnosis, explained Dr. Nissen, chairman of the department of cardiology at the Cleveland Clinic. GAUSS-3 (Goal Achievement After Utilizing an Anti-PCSK9 Antibody in Statin Intolerant Subjects 3), run at 53 centers worldwide, included two distinct phases.
In the first phase, researchers enrolled 511 patients with elevated LDL cholesterol levels who had a history of an inability to tolerate treatment with atorvastatin plus at least one other statin or at least three statins of any type. Following a 4-week washout period with no lipid-lowering treatments, they randomized patients to 10 weeks of 20 mg atorvastatin daily or placebo, followed by crossover to the alternative treatment for an additional 10 weeks. The patients averaged 61 years old, with an average LDL cholesterol level of 212 mg/dL.
During this phase, 43% of the patients reported having intolerable muscle symptoms while on atorvastatin, but not on placebo. In addition, 27% reported intolerable muscle symptoms while on placebo but not on atorvastatin, demonstrating the high incidence of psychosomatic muscle symptoms experienced by many patients with this history, Dr. Nissen noted. This placebo-controlled statin rechallenge provides a model for how clinicians can reliably confirm which patients experience statin-specific muscle symptoms.
“This gives physicians a strategy for managing these patients. This was the best strategy we could use to find out who really has intolerance,” Dr. Nissen said.
The second phase included 218 patients who had their muscle symptoms confirmed in the first phase plus a small number of patients with a history of muscle-related statin intolerance who skipped the first phase because their serum creatinine kinase level was greater than 10-times above the upper limit of normal. The researchers randomized these patients to treatment with either a monthly subcutaneous injection with 420 mg of evolocumab (Repatha) or 10 mg of oral ezetimibe (Zetia) given daily. To maintain blinding, all patients received simultaneous placebo treatment that mimicked the drug they were not assigned to receive. The patients enrolled in the second phase had an average entry LDL cholesterol level of about 220 mg/dL.
After 24 weeks on treatment, patients on ezetimibe had an average 17% reduction in their LDL cholesterol level, while those on evolocumab had an average reduction of 53%. An LDL cholesterol level of less than 100 mg/dL was achieved in 2% of the ezetimibe patients and in 64% of those on evolocumab. Muscle-related symptoms occurred in 29% of the ezetimibe patients and in 21% of those on evolocumab, but discontinuations because of muscle symptoms were limited to 1 patient on evolocumab and 5 patients on ezetimibe, Dr. Nissen reported. Concurrent with his report at the meeting, an article with the results appeared online (JAMA. 2016 Apr 3. doi: 10.1001/jama.2016.3608).
“These findings show that it pays to be patient” when dealing with patients who report statin-associated muscle symptoms as more than half of them were able to tolerate the daily 20 mg atorvastatin challenge for 10 weeks, commented Dr. Frederick A. Masoudi, a cardiologist and professor of medicine at the University of Colorado at Denver, Aurora. The report also “gives us a better approach for dealing with patients who have this nonspecific reaction to statin treatment, which remains the mainstay of cholesterol-lowering treatment.”
Dr. Nissen stressed that in his opinion, it is appropriate to use a PCSK9 inhibitor in this off-label way despite the controversial high cost for these drugs. “We have to do something for these patients who say that they cannot take a statin, but have multiple coronary disease risk factors and LDL cholesterol levels above 200 mg/dL. They are an accident waiting to happen. I am unwilling to leave patients with an LDL cholesterol of 200 mg/dL who can’t take statins and just walk away.”
GAUSS-3 was sponsored by Amgen, which markets evolocumab. Dr. Nissen has received research grants from Amgen and several other drug companies. Dr. Masoudi had no disclosures.
On Twitter @mitchelzoler
Dr. Nissen and his associates did a great job in this study of bringing much more clarity to the issue of muscle-related statin intolerance. Results from observational studies have suggested that this occurs in roughly 10%-20% of patients who start treatment on a statin. The rate has often been much lower in randomized statin trials because statin-intolerant patients are often identified and excluded from participation during a run-in phase before the randomized phase begins.
The first phase of GAUSS-3 showed that significant and treatment-limiting myalgia in response to statin treatment is real, and affects about 40% of patients who have a history of reporting muscle pain while taking statins. This part of the study provides clinicians with an important message about how to determine whether a patient really has muscle-related statin intolerance, and also showed that controlled rechallenge with a statin can identify many patients who can tolerate a statin despite a history of intolerance.
 |
Dr. Roger Blumenthal |
The second phase of GAUSS-3 showed that most patients with a history of muscle-related statin intolerance could nicely tolerate treatment with an effective regimen of either ezetimibe or the PCSK9 inhibitor evolocumab. Evolocumab was especially effective, reducing patient levels of LDL cholesterol by more than 50%.
Currently, the Food and Drug Administration–approved indications for treatment with PCSK9 inhibitors are limited to patients with familial hypercholesterolemia or with poorly-controlled LDL cholesterol levels and clinical atherosclerotic cardiovascular disease. That’s because we still await reports of longer-term follow-up of studies designed to confirm the clinical benefits of lowering LDL cholesterol using a PCSK9 inhibitor. Results from these studies should be available within the next year.
Dr. Roger Blumenthal is professor of medicine and director of the Ciccarone Center for the Prevention of Heart Disease at Johns Hopkins University in Baltimore. He had no disclosures. He made these comments in an interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Nissen and his associates did a great job in this study of bringing much more clarity to the issue of muscle-related statin intolerance. Results from observational studies have suggested that this occurs in roughly 10%-20% of patients who start treatment on a statin. The rate has often been much lower in randomized statin trials because statin-intolerant patients are often identified and excluded from participation during a run-in phase before the randomized phase begins.
The first phase of GAUSS-3 showed that significant and treatment-limiting myalgia in response to statin treatment is real, and affects about 40% of patients who have a history of reporting muscle pain while taking statins. This part of the study provides clinicians with an important message about how to determine whether a patient really has muscle-related statin intolerance, and also showed that controlled rechallenge with a statin can identify many patients who can tolerate a statin despite a history of intolerance.
 |
Dr. Roger Blumenthal |
The second phase of GAUSS-3 showed that most patients with a history of muscle-related statin intolerance could nicely tolerate treatment with an effective regimen of either ezetimibe or the PCSK9 inhibitor evolocumab. Evolocumab was especially effective, reducing patient levels of LDL cholesterol by more than 50%.
Currently, the Food and Drug Administration–approved indications for treatment with PCSK9 inhibitors are limited to patients with familial hypercholesterolemia or with poorly-controlled LDL cholesterol levels and clinical atherosclerotic cardiovascular disease. That’s because we still await reports of longer-term follow-up of studies designed to confirm the clinical benefits of lowering LDL cholesterol using a PCSK9 inhibitor. Results from these studies should be available within the next year.
Dr. Roger Blumenthal is professor of medicine and director of the Ciccarone Center for the Prevention of Heart Disease at Johns Hopkins University in Baltimore. He had no disclosures. He made these comments in an interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Nissen and his associates did a great job in this study of bringing much more clarity to the issue of muscle-related statin intolerance. Results from observational studies have suggested that this occurs in roughly 10%-20% of patients who start treatment on a statin. The rate has often been much lower in randomized statin trials because statin-intolerant patients are often identified and excluded from participation during a run-in phase before the randomized phase begins.
The first phase of GAUSS-3 showed that significant and treatment-limiting myalgia in response to statin treatment is real, and affects about 40% of patients who have a history of reporting muscle pain while taking statins. This part of the study provides clinicians with an important message about how to determine whether a patient really has muscle-related statin intolerance, and also showed that controlled rechallenge with a statin can identify many patients who can tolerate a statin despite a history of intolerance.
 |
Dr. Roger Blumenthal |
The second phase of GAUSS-3 showed that most patients with a history of muscle-related statin intolerance could nicely tolerate treatment with an effective regimen of either ezetimibe or the PCSK9 inhibitor evolocumab. Evolocumab was especially effective, reducing patient levels of LDL cholesterol by more than 50%.
Currently, the Food and Drug Administration–approved indications for treatment with PCSK9 inhibitors are limited to patients with familial hypercholesterolemia or with poorly-controlled LDL cholesterol levels and clinical atherosclerotic cardiovascular disease. That’s because we still await reports of longer-term follow-up of studies designed to confirm the clinical benefits of lowering LDL cholesterol using a PCSK9 inhibitor. Results from these studies should be available within the next year.
Dr. Roger Blumenthal is professor of medicine and director of the Ciccarone Center for the Prevention of Heart Disease at Johns Hopkins University in Baltimore. He had no disclosures. He made these comments in an interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Statin-associated muscle symptoms are real for roughly 40% of patients with a history of this adverse effect, and for such patients who are truly unable to tolerate a statin treatment, a PCSK9 inhibitor provided an effective and well-tolerated alternative in a randomized trial with more than 500 patients.
“Controversy has surrounded the issue of statin-associated muscle symptoms because of large differences in the incidence of this disorder in randomized trials and observational studies. The GAUSS-3 study results demonstrate that muscle-related intolerance is reproducible during blinded statin rechallenge in a substantial fraction, about 40%, of patients with a history of symptoms,” Dr. Steven E. Nissen said at the annual meeting of the American College of Cardiology. “Alternative approaches to reducing low-density lipoprotein cholesterol in these patients represents an important medical priority.”
Statin intolerance has been a challenging diagnosis for physicians to confirm because no biomarker exists to definitively document it, which led to this study to test a more systematic and objective approach to confirm the diagnosis, explained Dr. Nissen, chairman of the department of cardiology at the Cleveland Clinic. GAUSS-3 (Goal Achievement After Utilizing an Anti-PCSK9 Antibody in Statin Intolerant Subjects 3), run at 53 centers worldwide, included two distinct phases.
In the first phase, researchers enrolled 511 patients with elevated LDL cholesterol levels who had a history of an inability to tolerate treatment with atorvastatin plus at least one other statin or at least three statins of any type. Following a 4-week washout period with no lipid-lowering treatments, they randomized patients to 10 weeks of 20 mg atorvastatin daily or placebo, followed by crossover to the alternative treatment for an additional 10 weeks. The patients averaged 61 years old, with an average LDL cholesterol level of 212 mg/dL.
During this phase, 43% of the patients reported having intolerable muscle symptoms while on atorvastatin, but not on placebo. In addition, 27% reported intolerable muscle symptoms while on placebo but not on atorvastatin, demonstrating the high incidence of psychosomatic muscle symptoms experienced by many patients with this history, Dr. Nissen noted. This placebo-controlled statin rechallenge provides a model for how clinicians can reliably confirm which patients experience statin-specific muscle symptoms.
“This gives physicians a strategy for managing these patients. This was the best strategy we could use to find out who really has intolerance,” Dr. Nissen said.
The second phase included 218 patients who had their muscle symptoms confirmed in the first phase plus a small number of patients with a history of muscle-related statin intolerance who skipped the first phase because their serum creatinine kinase level was greater than 10-times above the upper limit of normal. The researchers randomized these patients to treatment with either a monthly subcutaneous injection with 420 mg of evolocumab (Repatha) or 10 mg of oral ezetimibe (Zetia) given daily. To maintain blinding, all patients received simultaneous placebo treatment that mimicked the drug they were not assigned to receive. The patients enrolled in the second phase had an average entry LDL cholesterol level of about 220 mg/dL.
After 24 weeks on treatment, patients on ezetimibe had an average 17% reduction in their LDL cholesterol level, while those on evolocumab had an average reduction of 53%. An LDL cholesterol level of less than 100 mg/dL was achieved in 2% of the ezetimibe patients and in 64% of those on evolocumab. Muscle-related symptoms occurred in 29% of the ezetimibe patients and in 21% of those on evolocumab, but discontinuations because of muscle symptoms were limited to 1 patient on evolocumab and 5 patients on ezetimibe, Dr. Nissen reported. Concurrent with his report at the meeting, an article with the results appeared online (JAMA. 2016 Apr 3. doi: 10.1001/jama.2016.3608).
“These findings show that it pays to be patient” when dealing with patients who report statin-associated muscle symptoms as more than half of them were able to tolerate the daily 20 mg atorvastatin challenge for 10 weeks, commented Dr. Frederick A. Masoudi, a cardiologist and professor of medicine at the University of Colorado at Denver, Aurora. The report also “gives us a better approach for dealing with patients who have this nonspecific reaction to statin treatment, which remains the mainstay of cholesterol-lowering treatment.”
Dr. Nissen stressed that in his opinion, it is appropriate to use a PCSK9 inhibitor in this off-label way despite the controversial high cost for these drugs. “We have to do something for these patients who say that they cannot take a statin, but have multiple coronary disease risk factors and LDL cholesterol levels above 200 mg/dL. They are an accident waiting to happen. I am unwilling to leave patients with an LDL cholesterol of 200 mg/dL who can’t take statins and just walk away.”
GAUSS-3 was sponsored by Amgen, which markets evolocumab. Dr. Nissen has received research grants from Amgen and several other drug companies. Dr. Masoudi had no disclosures.
On Twitter @mitchelzoler
CHICAGO – Statin-associated muscle symptoms are real for roughly 40% of patients with a history of this adverse effect, and for such patients who are truly unable to tolerate a statin treatment, a PCSK9 inhibitor provided an effective and well-tolerated alternative in a randomized trial with more than 500 patients.
“Controversy has surrounded the issue of statin-associated muscle symptoms because of large differences in the incidence of this disorder in randomized trials and observational studies. The GAUSS-3 study results demonstrate that muscle-related intolerance is reproducible during blinded statin rechallenge in a substantial fraction, about 40%, of patients with a history of symptoms,” Dr. Steven E. Nissen said at the annual meeting of the American College of Cardiology. “Alternative approaches to reducing low-density lipoprotein cholesterol in these patients represents an important medical priority.”
Statin intolerance has been a challenging diagnosis for physicians to confirm because no biomarker exists to definitively document it, which led to this study to test a more systematic and objective approach to confirm the diagnosis, explained Dr. Nissen, chairman of the department of cardiology at the Cleveland Clinic. GAUSS-3 (Goal Achievement After Utilizing an Anti-PCSK9 Antibody in Statin Intolerant Subjects 3), run at 53 centers worldwide, included two distinct phases.
In the first phase, researchers enrolled 511 patients with elevated LDL cholesterol levels who had a history of an inability to tolerate treatment with atorvastatin plus at least one other statin or at least three statins of any type. Following a 4-week washout period with no lipid-lowering treatments, they randomized patients to 10 weeks of 20 mg atorvastatin daily or placebo, followed by crossover to the alternative treatment for an additional 10 weeks. The patients averaged 61 years old, with an average LDL cholesterol level of 212 mg/dL.
During this phase, 43% of the patients reported having intolerable muscle symptoms while on atorvastatin, but not on placebo. In addition, 27% reported intolerable muscle symptoms while on placebo but not on atorvastatin, demonstrating the high incidence of psychosomatic muscle symptoms experienced by many patients with this history, Dr. Nissen noted. This placebo-controlled statin rechallenge provides a model for how clinicians can reliably confirm which patients experience statin-specific muscle symptoms.
“This gives physicians a strategy for managing these patients. This was the best strategy we could use to find out who really has intolerance,” Dr. Nissen said.
The second phase included 218 patients who had their muscle symptoms confirmed in the first phase plus a small number of patients with a history of muscle-related statin intolerance who skipped the first phase because their serum creatinine kinase level was greater than 10-times above the upper limit of normal. The researchers randomized these patients to treatment with either a monthly subcutaneous injection with 420 mg of evolocumab (Repatha) or 10 mg of oral ezetimibe (Zetia) given daily. To maintain blinding, all patients received simultaneous placebo treatment that mimicked the drug they were not assigned to receive. The patients enrolled in the second phase had an average entry LDL cholesterol level of about 220 mg/dL.
After 24 weeks on treatment, patients on ezetimibe had an average 17% reduction in their LDL cholesterol level, while those on evolocumab had an average reduction of 53%. An LDL cholesterol level of less than 100 mg/dL was achieved in 2% of the ezetimibe patients and in 64% of those on evolocumab. Muscle-related symptoms occurred in 29% of the ezetimibe patients and in 21% of those on evolocumab, but discontinuations because of muscle symptoms were limited to 1 patient on evolocumab and 5 patients on ezetimibe, Dr. Nissen reported. Concurrent with his report at the meeting, an article with the results appeared online (JAMA. 2016 Apr 3. doi: 10.1001/jama.2016.3608).
“These findings show that it pays to be patient” when dealing with patients who report statin-associated muscle symptoms as more than half of them were able to tolerate the daily 20 mg atorvastatin challenge for 10 weeks, commented Dr. Frederick A. Masoudi, a cardiologist and professor of medicine at the University of Colorado at Denver, Aurora. The report also “gives us a better approach for dealing with patients who have this nonspecific reaction to statin treatment, which remains the mainstay of cholesterol-lowering treatment.”
Dr. Nissen stressed that in his opinion, it is appropriate to use a PCSK9 inhibitor in this off-label way despite the controversial high cost for these drugs. “We have to do something for these patients who say that they cannot take a statin, but have multiple coronary disease risk factors and LDL cholesterol levels above 200 mg/dL. They are an accident waiting to happen. I am unwilling to leave patients with an LDL cholesterol of 200 mg/dL who can’t take statins and just walk away.”
GAUSS-3 was sponsored by Amgen, which markets evolocumab. Dr. Nissen has received research grants from Amgen and several other drug companies. Dr. Masoudi had no disclosures.
On Twitter @mitchelzoler
AT ACC 16
Key clinical point: Muscle-related statin intolerance was reproducible in many patients, but most could tolerate and respond robustly to a PCSK9 inhibitor.
Major finding: In patients with a history of muscle-related statin intolerance, 43% were intolerant of blinded atorvastatin challenge, but not blinded placebo.
Data source: GAUSS-3, a multicenter, two-phase randomized controlled trial with 511 patients.
Disclosures: GAUSS-3 was sponsored by Amgen, which markets evolocumab. Dr. Nissen has received research grants from Amgen and several other drug companies. Dr. Masoudi had no disclosures.
TAVR matches surgery in intermediate-risk patients
CHICAGO – Transcatheter aortic-valve replacement performed as well as surgical-valve replacement in patients with an intermediate mortality risk in a prospective, randomized trial with more than 2,000 patients followed for 2 years, the first randomized trial to compare the efficacy and safety of transcatheter aortic-valve replacement against surgical replacement in patients who did not have a high mortality risk.
The results “support TAVR [transcatheter aortic-valve replacement] as an alternative to surgery in intermediate-risk patients similar to those included in this trial,” said Dr. Craig R. Smith at the annual meeting of the American College of Cardiology. The findings from the Placement of Aortic Transcatheter Valves (PARTNER) 2 cohort A trial “will increase use of TAVR,” predicted Dr. Smith, professor and chairman of surgery at New York–Presbyterian Hospital/Columbia University in New York.
Until now, TAVR had been compared with surgical aortic-valve replacement in two prospective, randomized trials that both enrolled either high-risk or inoperable patients with severe aortic stenosis, the PARTNER 1 trial that tested the original Sapien TAVR system, and the U.S. CoreValve High-Risk Study that tested the original CoreValve system (often now called CoreValve classic). The average Society of Thoracic Surgeons (STS) operative risk score of high-risk patients enrolled in PARTNER 1 was 11.8%, and the average risk score in patients enrolled in the CoreValve study was 7.3%. In contrast, the design of PARTNER 2A specified that enrolled patients have a STS risk score of 4%-8%, a criterion actually met by 81% of the enrolled patients, and the average STS risk score of all patients enrolled in PARTNER 2A was 5.8%.
Although U.S. labeling for both the Sapien valve and its later iterations, Sapien XT and S3, and for CoreValve and its later iteration, Evolut R, specify that treated patients should have a STS risk score of at least 8%, the labeling also gives the heart teams that perform TAVR the latitude to treat patients with risk scores below 8% when the heart teams identify other patient factors that confer high risk such as frailty or comorbidities. U.S. and European TAVR registries have documented that many patients with STS risk scores below 8% have undergone TAVR since these systems received regulatory approval. The new results from PARTNER 2A may change that by leading to revised labeling that cuts the STS risk-score threshold.
“These findings might lead to a labeling change that would avoid a lot of the patient-evaluation gymnastics that have been used to justify” TAVR treatment, noted Dr. Smith. New labeling like this “would sanction what is already going on” in terms of which patients undergo TAVR.
Others who heard these results at the meeting agreed they were an important milestone in TAVR development and its expanding use.
The new results “make a huge difference,” commented Dr. David R. Holmes Jr., an interventional cardiologist and professor at the Mayo Clinic in Rochester, Minn. “We base many of our guidelines on the results from randomized, controlled trials. It’s true that there are reports of lower-risk patients undergoing TAVR, but we now have results from a well-designed trial with well-controlled and adjudicated endpoints that documents the safety and efficacy of TAVR in intermediate-risk patients,” Dr. Holmes said in an interview.
“The results will have a very important influence on the choice between TAVR and surgery,” commented Dr. Duane S. Pinto, an interventional cardiologist at Beth Israel Deaconess Medical Center in Boston. “It validates the strategy” of using TAVR in patients with a risk score of 4%-8%. “TAVR has already been used in these patients, but these results validate this, especially when used in a transfemoral approach,” Dr. Pinto said in an interview.
One aspect of PARTNER 2A that received a lot of discussion at the meeting was whether enrolled patients could appropriately be characterized as “intermediate” in their risk level. Although their average STS risk score of 5.8% fell squarely within the target range specified for the study, they averaged 82 years old, and other clinical features at baseline suggested a higher risk population. The published report of the PARTNER 2A results that appeared online concurrent with Dr. Smith’s report at the meeting (New Engl J Med 2016;doi:10.1056/NEJMoa1514616) acknowledged that STS risk scores of 4%-8% place the enrolled patients into the upper 20% for risk of all U.S. patients who undergo surgical aortic-valve replacement
“I would characterize the enrolled patients as ‘less high risk’ rather than intermediate risk,” said Dr. Pinto.
But as Dr. Smith explained “even if the enrolled patients are not ‘intermediate’ risk they are at a different risk level” than were the patients enrolled in the prior TAVR randomized trials.
In the PARTNER 1 high-risk trial, the overall 1-year rate of all-cause mortality was 24% and 27% in the TAVR and surgical arms of the study, respectively. In the CoreValve trial these rates were 14% with TAVR and 19% with surgery. In PARTNER 2A 1-year all-cause mortality was 12% with TAVR and 13% with surgery.
Two other notable findings of PARTNER 2A were the superior outcomes of patients who underwent TAVR using a transfemoral approach, and the improved outcomes that all TAVR patients had compared with surgical valve replacement for several secondary outcomes.
The rate of the study’s primary outcome, all-cause death or disabling stroke after 2 years, was cut by a relative 21% in the 77% of TAVR patients who underwent a transfemoral procedure, compared with the surgery patients, a difference that was of borderline statistical significance. In contrast, the entire group of TAVR patients, including those treated via nontransfemoral routes, had an 11% relative reduction of the primary endpoint, compared with surgery, a difference that was not statistically significant but did easily meet the study’s prespecified definition of noninferority. Dr. Smith and others were especially encouraged by these findings as PARTNER 2A used the older Sapien XT TAVR system that is not often used today in U.S. practice. When U.S. patients undergo TAVR with a balloon-expandable valve they most often receive treatment with the S3 system, much smaller than XT and hence much more likely to be used with a transfemoral approach.
Other secondary outcomes included life-threatening or disabling bleeding events, which after 2 years had occurred in 17% of the TAVR patients and 47% of those who underwent surgery; atrial fibrillation, which occurred in 11% of the TAVR patients and 27% of those undergoing surgery; and acute kidney injury which occurred in 4% of TAVR patients and 6% of the surgery patients. With 2-year follow-up, the rate of disabling strokes was 6% in both arms of the study.
PARTNER 2A was sponsored by Edwards Lifesciences, the company that markets the Sapien TAVR systems. Dr. Smith has received travel grants from Edwards. Dr. Holmes had no disclosures, Dr. Pinto has been a consultant to Medtronic.
On Twitter @mitchelzoler
Registries of patients who have undergone transcatheter aortic-valve replacement in Europe and the United States show that this procedure has already been frequently used in selected patients with Society of Thoracic Surgeons operative-risk scores of 4%-8%. Even though regulatory approval specifies using the procedure in high-risk patients with risk scores of at least 8%, the labeling leaves the decision of which patients are at high risk up to local heart teams, and factors other than the risk score play into a patient’s overall risk assessment including frailty and comorbidities.
Despite the prior experience using TAVR in patients with STS risk scores of 4%-8% the results of PARTNER 2A are a game changer because they come from a prospective, randomized, controlled trial.
The PARTNER 2A results are also notable because this is the second randomized trial (in addition to the CoreValve high-risk trial) with results that show or suggest that transcatheter aortic-valve replacement (TAVR) produces better outcomes than surgery, especially in patients who undergo TAVR via a transfemoral approach. Other notable advantages of TAVR over surgery seen in PARTNER 2A include substantial reductions in disabling or life-threatening bleeding events and in new-onset atrial fibrillation, a statistically significant reduction in acute kidney injury, and no significant difference in the incidence of disabling strokes. In the past, we expected stroke rates to be higher with TAVR, but in PARTNER 2A, with neurologists adjudicating the strokes, we saw no difference in the TAVR and surgical stroke rates, a finding that was probably unexpected for many people.
 |
Dr. Ajay J. Kirtane |
The patients enrolled in PARTNER 2A were clearly at lower risk for all-cause mortality than the patients enrolled in the earlier TAVR trials. The operative risk score is just one of several ways to estimate patient risk. The data collected in PARTNER 2A provide a robust resource for finding new, additional ways to assess patients who are at intermediate risk and to match patients seen during routine practice to those who entered this trial.
Dr. Ajay J. Kirtane is an interventional cardiologist and director of the coronary catheterization laboratory at New York–Presbyterian/Columbia University in New York. He was a coinvestigator on prior Sapien TAVR studies but did not participate in PARTNER 2. His institution has received research support from Edwards and from Boston Scientific. He made these comments in an interview.
Registries of patients who have undergone transcatheter aortic-valve replacement in Europe and the United States show that this procedure has already been frequently used in selected patients with Society of Thoracic Surgeons operative-risk scores of 4%-8%. Even though regulatory approval specifies using the procedure in high-risk patients with risk scores of at least 8%, the labeling leaves the decision of which patients are at high risk up to local heart teams, and factors other than the risk score play into a patient’s overall risk assessment including frailty and comorbidities.
Despite the prior experience using TAVR in patients with STS risk scores of 4%-8% the results of PARTNER 2A are a game changer because they come from a prospective, randomized, controlled trial.
The PARTNER 2A results are also notable because this is the second randomized trial (in addition to the CoreValve high-risk trial) with results that show or suggest that transcatheter aortic-valve replacement (TAVR) produces better outcomes than surgery, especially in patients who undergo TAVR via a transfemoral approach. Other notable advantages of TAVR over surgery seen in PARTNER 2A include substantial reductions in disabling or life-threatening bleeding events and in new-onset atrial fibrillation, a statistically significant reduction in acute kidney injury, and no significant difference in the incidence of disabling strokes. In the past, we expected stroke rates to be higher with TAVR, but in PARTNER 2A, with neurologists adjudicating the strokes, we saw no difference in the TAVR and surgical stroke rates, a finding that was probably unexpected for many people.
 |
Dr. Ajay J. Kirtane |
The patients enrolled in PARTNER 2A were clearly at lower risk for all-cause mortality than the patients enrolled in the earlier TAVR trials. The operative risk score is just one of several ways to estimate patient risk. The data collected in PARTNER 2A provide a robust resource for finding new, additional ways to assess patients who are at intermediate risk and to match patients seen during routine practice to those who entered this trial.
Dr. Ajay J. Kirtane is an interventional cardiologist and director of the coronary catheterization laboratory at New York–Presbyterian/Columbia University in New York. He was a coinvestigator on prior Sapien TAVR studies but did not participate in PARTNER 2. His institution has received research support from Edwards and from Boston Scientific. He made these comments in an interview.
Registries of patients who have undergone transcatheter aortic-valve replacement in Europe and the United States show that this procedure has already been frequently used in selected patients with Society of Thoracic Surgeons operative-risk scores of 4%-8%. Even though regulatory approval specifies using the procedure in high-risk patients with risk scores of at least 8%, the labeling leaves the decision of which patients are at high risk up to local heart teams, and factors other than the risk score play into a patient’s overall risk assessment including frailty and comorbidities.
Despite the prior experience using TAVR in patients with STS risk scores of 4%-8% the results of PARTNER 2A are a game changer because they come from a prospective, randomized, controlled trial.
The PARTNER 2A results are also notable because this is the second randomized trial (in addition to the CoreValve high-risk trial) with results that show or suggest that transcatheter aortic-valve replacement (TAVR) produces better outcomes than surgery, especially in patients who undergo TAVR via a transfemoral approach. Other notable advantages of TAVR over surgery seen in PARTNER 2A include substantial reductions in disabling or life-threatening bleeding events and in new-onset atrial fibrillation, a statistically significant reduction in acute kidney injury, and no significant difference in the incidence of disabling strokes. In the past, we expected stroke rates to be higher with TAVR, but in PARTNER 2A, with neurologists adjudicating the strokes, we saw no difference in the TAVR and surgical stroke rates, a finding that was probably unexpected for many people.
 |
Dr. Ajay J. Kirtane |
The patients enrolled in PARTNER 2A were clearly at lower risk for all-cause mortality than the patients enrolled in the earlier TAVR trials. The operative risk score is just one of several ways to estimate patient risk. The data collected in PARTNER 2A provide a robust resource for finding new, additional ways to assess patients who are at intermediate risk and to match patients seen during routine practice to those who entered this trial.
Dr. Ajay J. Kirtane is an interventional cardiologist and director of the coronary catheterization laboratory at New York–Presbyterian/Columbia University in New York. He was a coinvestigator on prior Sapien TAVR studies but did not participate in PARTNER 2. His institution has received research support from Edwards and from Boston Scientific. He made these comments in an interview.
CHICAGO – Transcatheter aortic-valve replacement performed as well as surgical-valve replacement in patients with an intermediate mortality risk in a prospective, randomized trial with more than 2,000 patients followed for 2 years, the first randomized trial to compare the efficacy and safety of transcatheter aortic-valve replacement against surgical replacement in patients who did not have a high mortality risk.
The results “support TAVR [transcatheter aortic-valve replacement] as an alternative to surgery in intermediate-risk patients similar to those included in this trial,” said Dr. Craig R. Smith at the annual meeting of the American College of Cardiology. The findings from the Placement of Aortic Transcatheter Valves (PARTNER) 2 cohort A trial “will increase use of TAVR,” predicted Dr. Smith, professor and chairman of surgery at New York–Presbyterian Hospital/Columbia University in New York.
Until now, TAVR had been compared with surgical aortic-valve replacement in two prospective, randomized trials that both enrolled either high-risk or inoperable patients with severe aortic stenosis, the PARTNER 1 trial that tested the original Sapien TAVR system, and the U.S. CoreValve High-Risk Study that tested the original CoreValve system (often now called CoreValve classic). The average Society of Thoracic Surgeons (STS) operative risk score of high-risk patients enrolled in PARTNER 1 was 11.8%, and the average risk score in patients enrolled in the CoreValve study was 7.3%. In contrast, the design of PARTNER 2A specified that enrolled patients have a STS risk score of 4%-8%, a criterion actually met by 81% of the enrolled patients, and the average STS risk score of all patients enrolled in PARTNER 2A was 5.8%.
Although U.S. labeling for both the Sapien valve and its later iterations, Sapien XT and S3, and for CoreValve and its later iteration, Evolut R, specify that treated patients should have a STS risk score of at least 8%, the labeling also gives the heart teams that perform TAVR the latitude to treat patients with risk scores below 8% when the heart teams identify other patient factors that confer high risk such as frailty or comorbidities. U.S. and European TAVR registries have documented that many patients with STS risk scores below 8% have undergone TAVR since these systems received regulatory approval. The new results from PARTNER 2A may change that by leading to revised labeling that cuts the STS risk-score threshold.
“These findings might lead to a labeling change that would avoid a lot of the patient-evaluation gymnastics that have been used to justify” TAVR treatment, noted Dr. Smith. New labeling like this “would sanction what is already going on” in terms of which patients undergo TAVR.
Others who heard these results at the meeting agreed they were an important milestone in TAVR development and its expanding use.
The new results “make a huge difference,” commented Dr. David R. Holmes Jr., an interventional cardiologist and professor at the Mayo Clinic in Rochester, Minn. “We base many of our guidelines on the results from randomized, controlled trials. It’s true that there are reports of lower-risk patients undergoing TAVR, but we now have results from a well-designed trial with well-controlled and adjudicated endpoints that documents the safety and efficacy of TAVR in intermediate-risk patients,” Dr. Holmes said in an interview.
“The results will have a very important influence on the choice between TAVR and surgery,” commented Dr. Duane S. Pinto, an interventional cardiologist at Beth Israel Deaconess Medical Center in Boston. “It validates the strategy” of using TAVR in patients with a risk score of 4%-8%. “TAVR has already been used in these patients, but these results validate this, especially when used in a transfemoral approach,” Dr. Pinto said in an interview.
One aspect of PARTNER 2A that received a lot of discussion at the meeting was whether enrolled patients could appropriately be characterized as “intermediate” in their risk level. Although their average STS risk score of 5.8% fell squarely within the target range specified for the study, they averaged 82 years old, and other clinical features at baseline suggested a higher risk population. The published report of the PARTNER 2A results that appeared online concurrent with Dr. Smith’s report at the meeting (New Engl J Med 2016;doi:10.1056/NEJMoa1514616) acknowledged that STS risk scores of 4%-8% place the enrolled patients into the upper 20% for risk of all U.S. patients who undergo surgical aortic-valve replacement
“I would characterize the enrolled patients as ‘less high risk’ rather than intermediate risk,” said Dr. Pinto.
But as Dr. Smith explained “even if the enrolled patients are not ‘intermediate’ risk they are at a different risk level” than were the patients enrolled in the prior TAVR randomized trials.
In the PARTNER 1 high-risk trial, the overall 1-year rate of all-cause mortality was 24% and 27% in the TAVR and surgical arms of the study, respectively. In the CoreValve trial these rates were 14% with TAVR and 19% with surgery. In PARTNER 2A 1-year all-cause mortality was 12% with TAVR and 13% with surgery.
Two other notable findings of PARTNER 2A were the superior outcomes of patients who underwent TAVR using a transfemoral approach, and the improved outcomes that all TAVR patients had compared with surgical valve replacement for several secondary outcomes.
The rate of the study’s primary outcome, all-cause death or disabling stroke after 2 years, was cut by a relative 21% in the 77% of TAVR patients who underwent a transfemoral procedure, compared with the surgery patients, a difference that was of borderline statistical significance. In contrast, the entire group of TAVR patients, including those treated via nontransfemoral routes, had an 11% relative reduction of the primary endpoint, compared with surgery, a difference that was not statistically significant but did easily meet the study’s prespecified definition of noninferority. Dr. Smith and others were especially encouraged by these findings as PARTNER 2A used the older Sapien XT TAVR system that is not often used today in U.S. practice. When U.S. patients undergo TAVR with a balloon-expandable valve they most often receive treatment with the S3 system, much smaller than XT and hence much more likely to be used with a transfemoral approach.
Other secondary outcomes included life-threatening or disabling bleeding events, which after 2 years had occurred in 17% of the TAVR patients and 47% of those who underwent surgery; atrial fibrillation, which occurred in 11% of the TAVR patients and 27% of those undergoing surgery; and acute kidney injury which occurred in 4% of TAVR patients and 6% of the surgery patients. With 2-year follow-up, the rate of disabling strokes was 6% in both arms of the study.
PARTNER 2A was sponsored by Edwards Lifesciences, the company that markets the Sapien TAVR systems. Dr. Smith has received travel grants from Edwards. Dr. Holmes had no disclosures, Dr. Pinto has been a consultant to Medtronic.
On Twitter @mitchelzoler
CHICAGO – Transcatheter aortic-valve replacement performed as well as surgical-valve replacement in patients with an intermediate mortality risk in a prospective, randomized trial with more than 2,000 patients followed for 2 years, the first randomized trial to compare the efficacy and safety of transcatheter aortic-valve replacement against surgical replacement in patients who did not have a high mortality risk.
The results “support TAVR [transcatheter aortic-valve replacement] as an alternative to surgery in intermediate-risk patients similar to those included in this trial,” said Dr. Craig R. Smith at the annual meeting of the American College of Cardiology. The findings from the Placement of Aortic Transcatheter Valves (PARTNER) 2 cohort A trial “will increase use of TAVR,” predicted Dr. Smith, professor and chairman of surgery at New York–Presbyterian Hospital/Columbia University in New York.
Until now, TAVR had been compared with surgical aortic-valve replacement in two prospective, randomized trials that both enrolled either high-risk or inoperable patients with severe aortic stenosis, the PARTNER 1 trial that tested the original Sapien TAVR system, and the U.S. CoreValve High-Risk Study that tested the original CoreValve system (often now called CoreValve classic). The average Society of Thoracic Surgeons (STS) operative risk score of high-risk patients enrolled in PARTNER 1 was 11.8%, and the average risk score in patients enrolled in the CoreValve study was 7.3%. In contrast, the design of PARTNER 2A specified that enrolled patients have a STS risk score of 4%-8%, a criterion actually met by 81% of the enrolled patients, and the average STS risk score of all patients enrolled in PARTNER 2A was 5.8%.
Although U.S. labeling for both the Sapien valve and its later iterations, Sapien XT and S3, and for CoreValve and its later iteration, Evolut R, specify that treated patients should have a STS risk score of at least 8%, the labeling also gives the heart teams that perform TAVR the latitude to treat patients with risk scores below 8% when the heart teams identify other patient factors that confer high risk such as frailty or comorbidities. U.S. and European TAVR registries have documented that many patients with STS risk scores below 8% have undergone TAVR since these systems received regulatory approval. The new results from PARTNER 2A may change that by leading to revised labeling that cuts the STS risk-score threshold.
“These findings might lead to a labeling change that would avoid a lot of the patient-evaluation gymnastics that have been used to justify” TAVR treatment, noted Dr. Smith. New labeling like this “would sanction what is already going on” in terms of which patients undergo TAVR.
Others who heard these results at the meeting agreed they were an important milestone in TAVR development and its expanding use.
The new results “make a huge difference,” commented Dr. David R. Holmes Jr., an interventional cardiologist and professor at the Mayo Clinic in Rochester, Minn. “We base many of our guidelines on the results from randomized, controlled trials. It’s true that there are reports of lower-risk patients undergoing TAVR, but we now have results from a well-designed trial with well-controlled and adjudicated endpoints that documents the safety and efficacy of TAVR in intermediate-risk patients,” Dr. Holmes said in an interview.
“The results will have a very important influence on the choice between TAVR and surgery,” commented Dr. Duane S. Pinto, an interventional cardiologist at Beth Israel Deaconess Medical Center in Boston. “It validates the strategy” of using TAVR in patients with a risk score of 4%-8%. “TAVR has already been used in these patients, but these results validate this, especially when used in a transfemoral approach,” Dr. Pinto said in an interview.
One aspect of PARTNER 2A that received a lot of discussion at the meeting was whether enrolled patients could appropriately be characterized as “intermediate” in their risk level. Although their average STS risk score of 5.8% fell squarely within the target range specified for the study, they averaged 82 years old, and other clinical features at baseline suggested a higher risk population. The published report of the PARTNER 2A results that appeared online concurrent with Dr. Smith’s report at the meeting (New Engl J Med 2016;doi:10.1056/NEJMoa1514616) acknowledged that STS risk scores of 4%-8% place the enrolled patients into the upper 20% for risk of all U.S. patients who undergo surgical aortic-valve replacement
“I would characterize the enrolled patients as ‘less high risk’ rather than intermediate risk,” said Dr. Pinto.
But as Dr. Smith explained “even if the enrolled patients are not ‘intermediate’ risk they are at a different risk level” than were the patients enrolled in the prior TAVR randomized trials.
In the PARTNER 1 high-risk trial, the overall 1-year rate of all-cause mortality was 24% and 27% in the TAVR and surgical arms of the study, respectively. In the CoreValve trial these rates were 14% with TAVR and 19% with surgery. In PARTNER 2A 1-year all-cause mortality was 12% with TAVR and 13% with surgery.
Two other notable findings of PARTNER 2A were the superior outcomes of patients who underwent TAVR using a transfemoral approach, and the improved outcomes that all TAVR patients had compared with surgical valve replacement for several secondary outcomes.
The rate of the study’s primary outcome, all-cause death or disabling stroke after 2 years, was cut by a relative 21% in the 77% of TAVR patients who underwent a transfemoral procedure, compared with the surgery patients, a difference that was of borderline statistical significance. In contrast, the entire group of TAVR patients, including those treated via nontransfemoral routes, had an 11% relative reduction of the primary endpoint, compared with surgery, a difference that was not statistically significant but did easily meet the study’s prespecified definition of noninferority. Dr. Smith and others were especially encouraged by these findings as PARTNER 2A used the older Sapien XT TAVR system that is not often used today in U.S. practice. When U.S. patients undergo TAVR with a balloon-expandable valve they most often receive treatment with the S3 system, much smaller than XT and hence much more likely to be used with a transfemoral approach.
Other secondary outcomes included life-threatening or disabling bleeding events, which after 2 years had occurred in 17% of the TAVR patients and 47% of those who underwent surgery; atrial fibrillation, which occurred in 11% of the TAVR patients and 27% of those undergoing surgery; and acute kidney injury which occurred in 4% of TAVR patients and 6% of the surgery patients. With 2-year follow-up, the rate of disabling strokes was 6% in both arms of the study.
PARTNER 2A was sponsored by Edwards Lifesciences, the company that markets the Sapien TAVR systems. Dr. Smith has received travel grants from Edwards. Dr. Holmes had no disclosures, Dr. Pinto has been a consultant to Medtronic.
On Twitter @mitchelzoler
AT ACC 16
Key clinical point: Intermediate-risk patients who had transcatheter aortic valve replacement had a 2-year death or disabling stroke rate that was no different from patients who had surgical valve replacement.
Major finding: The 2-year rate of death or disabling stroke was 19% with transcatheter valve replacement and 21% with surgical replacement.
Data source: PARTNER 2A, a prospective, multicenter, North American trial with 2,032 enrolled patients with severe aortic-valve stenosis.
Disclosures: PARTNER 2A was sponsored by Edwards Lifesciences, the company that markets the Sapien TAVR systems. Dr. Smith has received travel grants from Edwards. Dr. Holmes had no disclosures, Dr. Pinto has been a consultant to Medtronic.
VIDEO: PARTNER 2 results extend TAVR to intermediate-risk patients
CHICAGO – The “groundbreaking” results from the PARTNER 2 trial of transcatheter aortic valve replacement in patients at intermediate risk for death or complications from surgical replacement of a stenotic aortic valve provide substantially increased certainty that the transcatheter approach is at least as good as surgical valve replacement, commented Dr. Roxana Mehran in a video interview at the annual meeting of the American College of Cardiology.
In addition to providing important new data on the equivalence of surgical and transcatheter aortic valve replacement (TAVR) in a new target population--intermediate-risk patients, the findings from the randomized, multicenter PARTNER trial, which enrolled 2,032 patients, may also lead to expansion of the Food and Drug Administration labeling of the balloon-expandable TAVR device used in the study, the Sapien XT, to intermediate-risk patients. This expanded indication may also apply to the newer, smaller and more advanced iteration of this device, the Sapien 3, which has largely replaced the XT in U.S. practice, Dr. Mehran suggested.
Although the results came from the XT TAVR system, “these results have big relevance” to current U.S. practice said Dr. Mehran, professor and director of interventional cardiovascular research at Mount Sinai Hospital in New York.
The primary outcome of the Placement of Aortic Transcatheter Valves (PARTNER) 2 trial showed that all-cause mortality or disabling stroke after 2 years follow-up occurred in 21.2% (695) of the surgery patients and 19.3% (775) of the TAVR patients, meeting the prespecified noninferiority endpoint, with a P value of .001. Full results from the study were published online concurrent with their presentation at the meeting (New Engl J Med 2016;doi:10.1056/NEJMoa1514616).
Dr. Mehran has received consultant fees and honoraria from Abbott Vascular, AstraZeneca, and Bayer.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
CHICAGO – The “groundbreaking” results from the PARTNER 2 trial of transcatheter aortic valve replacement in patients at intermediate risk for death or complications from surgical replacement of a stenotic aortic valve provide substantially increased certainty that the transcatheter approach is at least as good as surgical valve replacement, commented Dr. Roxana Mehran in a video interview at the annual meeting of the American College of Cardiology.
In addition to providing important new data on the equivalence of surgical and transcatheter aortic valve replacement (TAVR) in a new target population--intermediate-risk patients, the findings from the randomized, multicenter PARTNER trial, which enrolled 2,032 patients, may also lead to expansion of the Food and Drug Administration labeling of the balloon-expandable TAVR device used in the study, the Sapien XT, to intermediate-risk patients. This expanded indication may also apply to the newer, smaller and more advanced iteration of this device, the Sapien 3, which has largely replaced the XT in U.S. practice, Dr. Mehran suggested.
Although the results came from the XT TAVR system, “these results have big relevance” to current U.S. practice said Dr. Mehran, professor and director of interventional cardiovascular research at Mount Sinai Hospital in New York.
The primary outcome of the Placement of Aortic Transcatheter Valves (PARTNER) 2 trial showed that all-cause mortality or disabling stroke after 2 years follow-up occurred in 21.2% (695) of the surgery patients and 19.3% (775) of the TAVR patients, meeting the prespecified noninferiority endpoint, with a P value of .001. Full results from the study were published online concurrent with their presentation at the meeting (New Engl J Med 2016;doi:10.1056/NEJMoa1514616).
Dr. Mehran has received consultant fees and honoraria from Abbott Vascular, AstraZeneca, and Bayer.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
CHICAGO – The “groundbreaking” results from the PARTNER 2 trial of transcatheter aortic valve replacement in patients at intermediate risk for death or complications from surgical replacement of a stenotic aortic valve provide substantially increased certainty that the transcatheter approach is at least as good as surgical valve replacement, commented Dr. Roxana Mehran in a video interview at the annual meeting of the American College of Cardiology.
In addition to providing important new data on the equivalence of surgical and transcatheter aortic valve replacement (TAVR) in a new target population--intermediate-risk patients, the findings from the randomized, multicenter PARTNER trial, which enrolled 2,032 patients, may also lead to expansion of the Food and Drug Administration labeling of the balloon-expandable TAVR device used in the study, the Sapien XT, to intermediate-risk patients. This expanded indication may also apply to the newer, smaller and more advanced iteration of this device, the Sapien 3, which has largely replaced the XT in U.S. practice, Dr. Mehran suggested.
Although the results came from the XT TAVR system, “these results have big relevance” to current U.S. practice said Dr. Mehran, professor and director of interventional cardiovascular research at Mount Sinai Hospital in New York.
The primary outcome of the Placement of Aortic Transcatheter Valves (PARTNER) 2 trial showed that all-cause mortality or disabling stroke after 2 years follow-up occurred in 21.2% (695) of the surgery patients and 19.3% (775) of the TAVR patients, meeting the prespecified noninferiority endpoint, with a P value of .001. Full results from the study were published online concurrent with their presentation at the meeting (New Engl J Med 2016;doi:10.1056/NEJMoa1514616).
Dr. Mehran has received consultant fees and honoraria from Abbott Vascular, AstraZeneca, and Bayer.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT ACC 16
Prepsychosis links with elevated metabolic syndrome
MADRID – Untreated people at high risk for developing psychosis also showed an increased prevalence of certain components of metabolic syndrome in data collected from 163 German study participants, a finding that gives new insight into the well-documented but poorly delineated link between schizophrenia and metabolic syndrome.
“The findings point out that a high risk for schizophrenia implies a certain risk for patients to develop metabolic syndrome independent of treatment effects,” said Dr. Joachim Cordes, a psychiatrist at the LVR Clinic of the Heinrich-Heine University in Düsseldorf, Germany. He assumed that genetic factors underlie the shared risk some people face for both developing schizophrenia and metabolic syndrome. “I think there is a direct connection between schizophrenia and metabolic syndrome, an inherent factor like a genetic factor,” Dr. Cordes said in an interview. This understanding should influence how patients with newly diagnosed schizophrenia or those at risk for psychosis are managed, he added.
Dr. Cordes’s report was one of several at the meeting sponsored by the European Psychiatric Association that examined different facets of the complex links that tie schizophrenia to metabolic syndrome, an association that already had lots of evidence, including a recent meta-analysis (Schizophr Bull. 2013 March;39[2]:306-18).
He used data collected on 163 people enrolled in the PREVENT study and at high risk for a first psychotic episode. Run at nine German centers, PREVENT primarily tested very early intervention with drug and behavioral therapy to improve outcomes. Dr. Cordes took data collected from these prepsychosis, high-risk patients to assess their prevalence of metabolic syndrome and of the various individual features that define metabolic syndrome, using a definition published by the American Heart Association and the U.S. National Heart, Lung, and Blood Institute (Circulation. 2005 Oct 18;112[17]:2735-52). He compared these metabolic syndrome rates with the general German population, using data from 35,869 randomly selected German adults in more than 1,500 German primary care practices, the German Metabolic and Cardiovascular Risk Project (GEMCAS).
The findings showed a 9.2% prevalence of metabolic syndrome in the prepsychosis group and a 7.4% rate among the general adult population, Dr. Cordes reported. Among men in the prepsychosis group, the metabolic syndrome definers with the largest increments in prevalence were low HDL, in 21% of the prepsychosis people and in 12% of the general population, and elevated blood glucose in 11%, compared with 6%. Among women, the metabolic syndrome definers with the greatest between-group differences were elevated waist circumference, in 30% of those with prepsychosis, compared with 17% in the general population, and low HDL in 19%, compared with 14%.
This apparently inherent link between a tendency toward psychosis and schizophrenia and a tendency to develop features of metabolic syndrome suggests that patients with newly diagnosed schizophrenia need a preventive approach to weight management, Dr. Cordes said. He also suggested prescribing antipsychotic medications that pose the lowest risk for causing further metabolic derangements in patients.
A second report at the meeting came from an assessment of cognitive function and its relationship to metabolic syndrome in 54 women diagnosed with schizophrenia and on stable treatment. The schizophrenia patients with metabolic syndrome, nearly half of the total group, performed significantly worse than those without metabolic syndrome in tests of verbal memory, executive function, and attention and processing speed, findings that support an increased incidence of selective cognitive impairment in patients with schizophrenia and metabolic syndrome, said Dr. Adela C. Botis, a psychiatrist and researcher at the University of Medicine and Pharmacy in Cluj-Napoca, Romania.
Dr. Botis and her associates studied 54 women diagnosed with schizophrenia who had remitted symptoms for at least 6 months on stable antipsychotic treatment. Using the metabolic syndrome definition of the International Diabetes Federation 25 (46%) had metabolic syndrome, and the other 29 (54%) did not. These numbers document the high prevalence of metabolic syndrome in schizophrenia patients.
A multivariate analysis identified demographic and metabolic factors that significantly linked with decrements in several cognitive domains. Economic status and living situation linked with deficits in verbal memory; elevated systolic blood pressure significantly linked with worsened attention and processing speed; high body mass index linked with loss of motor speed; and less education significantly linked with all these increments as well as four other domains,
A third report used a post-hoc analysis of data from two separate trials to show that treatment with a relatively new antipsychotic drug, lurasidone (Latuda), produced less metabolic syndrome, compared with risperidone or extended-release quetiapine (Seroquel XR), said Dr. Andrei Pikalov, head of global medical affairs at Sunovion Pharmaceuticals, the company that markets Latuda. Lurasidone received approval for treating schizophrenia in 2010.
He took data from two studies designed to assess lurasidone’s efficacy for treating adults with schizophrenia for 12 months, compared with either risperidone in a study with 621 patients, or with quetiapine XR in a study with 292 patients. He applied the same metabolic syndrome definition used by Dr. Cordes to clinical measurements taken at baseline and after 12 months on treatment.
The results showed that treatment with lurasidone produced less than half the rate of new metabolic syndrome cases, compared with risperidone, a statistically significant difference, and less than two-thirds the rate of quetiapine XR, a difference that did not reach statistical significance.
Dr. Cordes said he has been a speaker for Servier. Dr. Botis had no disclosures. Dr. Pikalov is an employee of Sunovion, which markets lurasidone (Latuda).
On Twitter @mitchelzoler
MADRID – Untreated people at high risk for developing psychosis also showed an increased prevalence of certain components of metabolic syndrome in data collected from 163 German study participants, a finding that gives new insight into the well-documented but poorly delineated link between schizophrenia and metabolic syndrome.
“The findings point out that a high risk for schizophrenia implies a certain risk for patients to develop metabolic syndrome independent of treatment effects,” said Dr. Joachim Cordes, a psychiatrist at the LVR Clinic of the Heinrich-Heine University in Düsseldorf, Germany. He assumed that genetic factors underlie the shared risk some people face for both developing schizophrenia and metabolic syndrome. “I think there is a direct connection between schizophrenia and metabolic syndrome, an inherent factor like a genetic factor,” Dr. Cordes said in an interview. This understanding should influence how patients with newly diagnosed schizophrenia or those at risk for psychosis are managed, he added.
Dr. Cordes’s report was one of several at the meeting sponsored by the European Psychiatric Association that examined different facets of the complex links that tie schizophrenia to metabolic syndrome, an association that already had lots of evidence, including a recent meta-analysis (Schizophr Bull. 2013 March;39[2]:306-18).
He used data collected on 163 people enrolled in the PREVENT study and at high risk for a first psychotic episode. Run at nine German centers, PREVENT primarily tested very early intervention with drug and behavioral therapy to improve outcomes. Dr. Cordes took data collected from these prepsychosis, high-risk patients to assess their prevalence of metabolic syndrome and of the various individual features that define metabolic syndrome, using a definition published by the American Heart Association and the U.S. National Heart, Lung, and Blood Institute (Circulation. 2005 Oct 18;112[17]:2735-52). He compared these metabolic syndrome rates with the general German population, using data from 35,869 randomly selected German adults in more than 1,500 German primary care practices, the German Metabolic and Cardiovascular Risk Project (GEMCAS).
The findings showed a 9.2% prevalence of metabolic syndrome in the prepsychosis group and a 7.4% rate among the general adult population, Dr. Cordes reported. Among men in the prepsychosis group, the metabolic syndrome definers with the largest increments in prevalence were low HDL, in 21% of the prepsychosis people and in 12% of the general population, and elevated blood glucose in 11%, compared with 6%. Among women, the metabolic syndrome definers with the greatest between-group differences were elevated waist circumference, in 30% of those with prepsychosis, compared with 17% in the general population, and low HDL in 19%, compared with 14%.
This apparently inherent link between a tendency toward psychosis and schizophrenia and a tendency to develop features of metabolic syndrome suggests that patients with newly diagnosed schizophrenia need a preventive approach to weight management, Dr. Cordes said. He also suggested prescribing antipsychotic medications that pose the lowest risk for causing further metabolic derangements in patients.
A second report at the meeting came from an assessment of cognitive function and its relationship to metabolic syndrome in 54 women diagnosed with schizophrenia and on stable treatment. The schizophrenia patients with metabolic syndrome, nearly half of the total group, performed significantly worse than those without metabolic syndrome in tests of verbal memory, executive function, and attention and processing speed, findings that support an increased incidence of selective cognitive impairment in patients with schizophrenia and metabolic syndrome, said Dr. Adela C. Botis, a psychiatrist and researcher at the University of Medicine and Pharmacy in Cluj-Napoca, Romania.
Dr. Botis and her associates studied 54 women diagnosed with schizophrenia who had remitted symptoms for at least 6 months on stable antipsychotic treatment. Using the metabolic syndrome definition of the International Diabetes Federation 25 (46%) had metabolic syndrome, and the other 29 (54%) did not. These numbers document the high prevalence of metabolic syndrome in schizophrenia patients.
A multivariate analysis identified demographic and metabolic factors that significantly linked with decrements in several cognitive domains. Economic status and living situation linked with deficits in verbal memory; elevated systolic blood pressure significantly linked with worsened attention and processing speed; high body mass index linked with loss of motor speed; and less education significantly linked with all these increments as well as four other domains,
A third report used a post-hoc analysis of data from two separate trials to show that treatment with a relatively new antipsychotic drug, lurasidone (Latuda), produced less metabolic syndrome, compared with risperidone or extended-release quetiapine (Seroquel XR), said Dr. Andrei Pikalov, head of global medical affairs at Sunovion Pharmaceuticals, the company that markets Latuda. Lurasidone received approval for treating schizophrenia in 2010.
He took data from two studies designed to assess lurasidone’s efficacy for treating adults with schizophrenia for 12 months, compared with either risperidone in a study with 621 patients, or with quetiapine XR in a study with 292 patients. He applied the same metabolic syndrome definition used by Dr. Cordes to clinical measurements taken at baseline and after 12 months on treatment.
The results showed that treatment with lurasidone produced less than half the rate of new metabolic syndrome cases, compared with risperidone, a statistically significant difference, and less than two-thirds the rate of quetiapine XR, a difference that did not reach statistical significance.
Dr. Cordes said he has been a speaker for Servier. Dr. Botis had no disclosures. Dr. Pikalov is an employee of Sunovion, which markets lurasidone (Latuda).
On Twitter @mitchelzoler
MADRID – Untreated people at high risk for developing psychosis also showed an increased prevalence of certain components of metabolic syndrome in data collected from 163 German study participants, a finding that gives new insight into the well-documented but poorly delineated link between schizophrenia and metabolic syndrome.
“The findings point out that a high risk for schizophrenia implies a certain risk for patients to develop metabolic syndrome independent of treatment effects,” said Dr. Joachim Cordes, a psychiatrist at the LVR Clinic of the Heinrich-Heine University in Düsseldorf, Germany. He assumed that genetic factors underlie the shared risk some people face for both developing schizophrenia and metabolic syndrome. “I think there is a direct connection between schizophrenia and metabolic syndrome, an inherent factor like a genetic factor,” Dr. Cordes said in an interview. This understanding should influence how patients with newly diagnosed schizophrenia or those at risk for psychosis are managed, he added.
Dr. Cordes’s report was one of several at the meeting sponsored by the European Psychiatric Association that examined different facets of the complex links that tie schizophrenia to metabolic syndrome, an association that already had lots of evidence, including a recent meta-analysis (Schizophr Bull. 2013 March;39[2]:306-18).
He used data collected on 163 people enrolled in the PREVENT study and at high risk for a first psychotic episode. Run at nine German centers, PREVENT primarily tested very early intervention with drug and behavioral therapy to improve outcomes. Dr. Cordes took data collected from these prepsychosis, high-risk patients to assess their prevalence of metabolic syndrome and of the various individual features that define metabolic syndrome, using a definition published by the American Heart Association and the U.S. National Heart, Lung, and Blood Institute (Circulation. 2005 Oct 18;112[17]:2735-52). He compared these metabolic syndrome rates with the general German population, using data from 35,869 randomly selected German adults in more than 1,500 German primary care practices, the German Metabolic and Cardiovascular Risk Project (GEMCAS).
The findings showed a 9.2% prevalence of metabolic syndrome in the prepsychosis group and a 7.4% rate among the general adult population, Dr. Cordes reported. Among men in the prepsychosis group, the metabolic syndrome definers with the largest increments in prevalence were low HDL, in 21% of the prepsychosis people and in 12% of the general population, and elevated blood glucose in 11%, compared with 6%. Among women, the metabolic syndrome definers with the greatest between-group differences were elevated waist circumference, in 30% of those with prepsychosis, compared with 17% in the general population, and low HDL in 19%, compared with 14%.
This apparently inherent link between a tendency toward psychosis and schizophrenia and a tendency to develop features of metabolic syndrome suggests that patients with newly diagnosed schizophrenia need a preventive approach to weight management, Dr. Cordes said. He also suggested prescribing antipsychotic medications that pose the lowest risk for causing further metabolic derangements in patients.
A second report at the meeting came from an assessment of cognitive function and its relationship to metabolic syndrome in 54 women diagnosed with schizophrenia and on stable treatment. The schizophrenia patients with metabolic syndrome, nearly half of the total group, performed significantly worse than those without metabolic syndrome in tests of verbal memory, executive function, and attention and processing speed, findings that support an increased incidence of selective cognitive impairment in patients with schizophrenia and metabolic syndrome, said Dr. Adela C. Botis, a psychiatrist and researcher at the University of Medicine and Pharmacy in Cluj-Napoca, Romania.
Dr. Botis and her associates studied 54 women diagnosed with schizophrenia who had remitted symptoms for at least 6 months on stable antipsychotic treatment. Using the metabolic syndrome definition of the International Diabetes Federation 25 (46%) had metabolic syndrome, and the other 29 (54%) did not. These numbers document the high prevalence of metabolic syndrome in schizophrenia patients.
A multivariate analysis identified demographic and metabolic factors that significantly linked with decrements in several cognitive domains. Economic status and living situation linked with deficits in verbal memory; elevated systolic blood pressure significantly linked with worsened attention and processing speed; high body mass index linked with loss of motor speed; and less education significantly linked with all these increments as well as four other domains,
A third report used a post-hoc analysis of data from two separate trials to show that treatment with a relatively new antipsychotic drug, lurasidone (Latuda), produced less metabolic syndrome, compared with risperidone or extended-release quetiapine (Seroquel XR), said Dr. Andrei Pikalov, head of global medical affairs at Sunovion Pharmaceuticals, the company that markets Latuda. Lurasidone received approval for treating schizophrenia in 2010.
He took data from two studies designed to assess lurasidone’s efficacy for treating adults with schizophrenia for 12 months, compared with either risperidone in a study with 621 patients, or with quetiapine XR in a study with 292 patients. He applied the same metabolic syndrome definition used by Dr. Cordes to clinical measurements taken at baseline and after 12 months on treatment.
The results showed that treatment with lurasidone produced less than half the rate of new metabolic syndrome cases, compared with risperidone, a statistically significant difference, and less than two-thirds the rate of quetiapine XR, a difference that did not reach statistical significance.
Dr. Cordes said he has been a speaker for Servier. Dr. Botis had no disclosures. Dr. Pikalov is an employee of Sunovion, which markets lurasidone (Latuda).
On Twitter @mitchelzoler
AT THE EUROPEAN CONGRESS OF PSYCHIATRY
Key clinical point: People at high risk for a first psychosis episode had an increased prevalence of certain metabolic syndrome components, compared with the general population.
Major finding: Metabolic syndrome was prevalent in 9.2% of the prepsychosis group and in 7.4% of the general population.
Data source: Post-hoc analysis of data from 163 German people with prepsychosis.
Disclosures: Dr. Cordes said he has been a speaker for Servier. Dr. Botis had no disclosures. Dr. Pikalov is an employee of Sunovion, which markets lurasidone (Latuda).
Breast cancer treatment linked to mild systolic dysfunction
AMSTERDAM – Breast cancer patients who underwent chemotherapy or radiotherapy had about a two-fold increased prevalence of mild systolic cardiac dysfunction a median of 10 years after treatment, compared with age-matched controls in a study that included a total of 700 people.
But even longer follow-up of treated breast cancer patients is needed to determine whether the excess mild cardiac dysfunction seen in this analysis eventually progresses to more severe cardiac impairment, Liselotte M. Boerman said at the European Breast Cancer Conference.
Data from the Breast Cancer Long-term Outcome of Cardiac Dysfunction (BLOC) study showed that 175 breast cancer patients who received chemotherapy (and may have also received radiotherapy) had a 2.5-fold higher prevalence of a left ventricular ejection fraction (LVEF) below 54% (95% confidence interval, 1.2-5.4) when measured by echocardiography a median of 10 years after treatment, compared with an equal number of age-matched individuals from the general population.
A separate group of 175 patients treated with radiotherapy only and evaluated by echocardiography a median of 10 years later had a 2.3-fold increased prevalence (1.1-4.7) of a LVEF below 54% when compared with an equal number of age-matched individuals, said Ms. Boerman, an epidemiology researcher at the University of Groningen (the Netherlands).
This degree of left-ventricular dysfunction was found in 15% of the chemotherapy patients and 6% of their controls, and in 16% of the radiotherapy patients and 8% of their controls.
However, the treated breast cancer patients had no long-term increase in their prevalence of more significant systolic cardiac dysfunction, defined as a LVEF of less than 45%, compared with the controls, and the overall rate of systolic dysfunction of this severity was low, affecting fewer than 1% of patients.
Also, the chemotherapy and radiotherapy patients showed no significant increase in the prevalence of diastolic cardiac dysfunction, defined as delayed cardiac relaxation beyond the age-appropriate range. Treated patients did show, after 10 years, a suggestion of an increased prevalence of diagnosed cardiovascular disease, which was 2.3-fold higher (1.0-4.9) in the chemotherapy-receiving patients, compared with their controls; and 70% higher (0.9-3.4) among the patients treated with radiotherapy, compared with their controls, Ms. Boerman said.
The study used data collected from breast cancer patients younger than 80 years old treated after 1980 and controls seen by general practice Dutch physicians. The chemotherapy patients were diagnosed at an average age of 49 years old (range 26-66 years old). About 78% had received treatment with an anthracycline agent and 7% had received trastuzumab (Herceptin). Radiotherapy had also been administered to 70%, while 62% had also received hormonal therapy, and 7% either had a recurrence or developed a tumor in their contralateral breast.
None of the radiotherapy-only patients had received chemotherapy, but 21% had also received hormonal therapy. Their average age at diagnosis was 54 years old (range 32-79 years old), and 10% had a recurrence or a contralateral tumor.
Follow-up echocardiography occurred 5-34 years after the index treatment, at a median age of 60 years old. Echocardiography follow-up occurred in 70% of the chemotherapy breast cancer patients contacted, and in 63% of those who received radiotherapy only. Among controls, about half of those selected by age matching, and contacted, agreed to participate.
Rates of cardiovascular-disease risk factors – dyslipidemia, hypertension, and diabetes – were at roughly similar levels in the cases and controls at the time of breast cancer diagnosis. But the rate of current smoking at the time of diagnosis appeared higher in the cases (30% among those who received chemotherapy and 33% among those on radiotherapy), compared with their respective control groups (22% and 30%). Ms. Boerman said that a multivariate analysis had not yet been run on the data but should occur soon.
“The prevalence of cardiac dysfunction was higher [in treated patients] than I would have expected, but there is potential bias as only 70% of invited patients actually participated,” commented Dr. Robert Mansel, a professor at the Institute of Cancer & Genetics at Cardiff University (Wales). He also noted the very low rate of patients who developed severe cardiac dysfunction.
Ms. Boerman and Dr. Mansel reported having no financial disclosures.
On Twitter @mitchelzoler
AMSTERDAM – Breast cancer patients who underwent chemotherapy or radiotherapy had about a two-fold increased prevalence of mild systolic cardiac dysfunction a median of 10 years after treatment, compared with age-matched controls in a study that included a total of 700 people.
But even longer follow-up of treated breast cancer patients is needed to determine whether the excess mild cardiac dysfunction seen in this analysis eventually progresses to more severe cardiac impairment, Liselotte M. Boerman said at the European Breast Cancer Conference.
Data from the Breast Cancer Long-term Outcome of Cardiac Dysfunction (BLOC) study showed that 175 breast cancer patients who received chemotherapy (and may have also received radiotherapy) had a 2.5-fold higher prevalence of a left ventricular ejection fraction (LVEF) below 54% (95% confidence interval, 1.2-5.4) when measured by echocardiography a median of 10 years after treatment, compared with an equal number of age-matched individuals from the general population.
A separate group of 175 patients treated with radiotherapy only and evaluated by echocardiography a median of 10 years later had a 2.3-fold increased prevalence (1.1-4.7) of a LVEF below 54% when compared with an equal number of age-matched individuals, said Ms. Boerman, an epidemiology researcher at the University of Groningen (the Netherlands).
This degree of left-ventricular dysfunction was found in 15% of the chemotherapy patients and 6% of their controls, and in 16% of the radiotherapy patients and 8% of their controls.
However, the treated breast cancer patients had no long-term increase in their prevalence of more significant systolic cardiac dysfunction, defined as a LVEF of less than 45%, compared with the controls, and the overall rate of systolic dysfunction of this severity was low, affecting fewer than 1% of patients.
Also, the chemotherapy and radiotherapy patients showed no significant increase in the prevalence of diastolic cardiac dysfunction, defined as delayed cardiac relaxation beyond the age-appropriate range. Treated patients did show, after 10 years, a suggestion of an increased prevalence of diagnosed cardiovascular disease, which was 2.3-fold higher (1.0-4.9) in the chemotherapy-receiving patients, compared with their controls; and 70% higher (0.9-3.4) among the patients treated with radiotherapy, compared with their controls, Ms. Boerman said.
The study used data collected from breast cancer patients younger than 80 years old treated after 1980 and controls seen by general practice Dutch physicians. The chemotherapy patients were diagnosed at an average age of 49 years old (range 26-66 years old). About 78% had received treatment with an anthracycline agent and 7% had received trastuzumab (Herceptin). Radiotherapy had also been administered to 70%, while 62% had also received hormonal therapy, and 7% either had a recurrence or developed a tumor in their contralateral breast.
None of the radiotherapy-only patients had received chemotherapy, but 21% had also received hormonal therapy. Their average age at diagnosis was 54 years old (range 32-79 years old), and 10% had a recurrence or a contralateral tumor.
Follow-up echocardiography occurred 5-34 years after the index treatment, at a median age of 60 years old. Echocardiography follow-up occurred in 70% of the chemotherapy breast cancer patients contacted, and in 63% of those who received radiotherapy only. Among controls, about half of those selected by age matching, and contacted, agreed to participate.
Rates of cardiovascular-disease risk factors – dyslipidemia, hypertension, and diabetes – were at roughly similar levels in the cases and controls at the time of breast cancer diagnosis. But the rate of current smoking at the time of diagnosis appeared higher in the cases (30% among those who received chemotherapy and 33% among those on radiotherapy), compared with their respective control groups (22% and 30%). Ms. Boerman said that a multivariate analysis had not yet been run on the data but should occur soon.
“The prevalence of cardiac dysfunction was higher [in treated patients] than I would have expected, but there is potential bias as only 70% of invited patients actually participated,” commented Dr. Robert Mansel, a professor at the Institute of Cancer & Genetics at Cardiff University (Wales). He also noted the very low rate of patients who developed severe cardiac dysfunction.
Ms. Boerman and Dr. Mansel reported having no financial disclosures.
On Twitter @mitchelzoler
AMSTERDAM – Breast cancer patients who underwent chemotherapy or radiotherapy had about a two-fold increased prevalence of mild systolic cardiac dysfunction a median of 10 years after treatment, compared with age-matched controls in a study that included a total of 700 people.
But even longer follow-up of treated breast cancer patients is needed to determine whether the excess mild cardiac dysfunction seen in this analysis eventually progresses to more severe cardiac impairment, Liselotte M. Boerman said at the European Breast Cancer Conference.
Data from the Breast Cancer Long-term Outcome of Cardiac Dysfunction (BLOC) study showed that 175 breast cancer patients who received chemotherapy (and may have also received radiotherapy) had a 2.5-fold higher prevalence of a left ventricular ejection fraction (LVEF) below 54% (95% confidence interval, 1.2-5.4) when measured by echocardiography a median of 10 years after treatment, compared with an equal number of age-matched individuals from the general population.
A separate group of 175 patients treated with radiotherapy only and evaluated by echocardiography a median of 10 years later had a 2.3-fold increased prevalence (1.1-4.7) of a LVEF below 54% when compared with an equal number of age-matched individuals, said Ms. Boerman, an epidemiology researcher at the University of Groningen (the Netherlands).
This degree of left-ventricular dysfunction was found in 15% of the chemotherapy patients and 6% of their controls, and in 16% of the radiotherapy patients and 8% of their controls.
However, the treated breast cancer patients had no long-term increase in their prevalence of more significant systolic cardiac dysfunction, defined as a LVEF of less than 45%, compared with the controls, and the overall rate of systolic dysfunction of this severity was low, affecting fewer than 1% of patients.
Also, the chemotherapy and radiotherapy patients showed no significant increase in the prevalence of diastolic cardiac dysfunction, defined as delayed cardiac relaxation beyond the age-appropriate range. Treated patients did show, after 10 years, a suggestion of an increased prevalence of diagnosed cardiovascular disease, which was 2.3-fold higher (1.0-4.9) in the chemotherapy-receiving patients, compared with their controls; and 70% higher (0.9-3.4) among the patients treated with radiotherapy, compared with their controls, Ms. Boerman said.
The study used data collected from breast cancer patients younger than 80 years old treated after 1980 and controls seen by general practice Dutch physicians. The chemotherapy patients were diagnosed at an average age of 49 years old (range 26-66 years old). About 78% had received treatment with an anthracycline agent and 7% had received trastuzumab (Herceptin). Radiotherapy had also been administered to 70%, while 62% had also received hormonal therapy, and 7% either had a recurrence or developed a tumor in their contralateral breast.
None of the radiotherapy-only patients had received chemotherapy, but 21% had also received hormonal therapy. Their average age at diagnosis was 54 years old (range 32-79 years old), and 10% had a recurrence or a contralateral tumor.
Follow-up echocardiography occurred 5-34 years after the index treatment, at a median age of 60 years old. Echocardiography follow-up occurred in 70% of the chemotherapy breast cancer patients contacted, and in 63% of those who received radiotherapy only. Among controls, about half of those selected by age matching, and contacted, agreed to participate.
Rates of cardiovascular-disease risk factors – dyslipidemia, hypertension, and diabetes – were at roughly similar levels in the cases and controls at the time of breast cancer diagnosis. But the rate of current smoking at the time of diagnosis appeared higher in the cases (30% among those who received chemotherapy and 33% among those on radiotherapy), compared with their respective control groups (22% and 30%). Ms. Boerman said that a multivariate analysis had not yet been run on the data but should occur soon.
“The prevalence of cardiac dysfunction was higher [in treated patients] than I would have expected, but there is potential bias as only 70% of invited patients actually participated,” commented Dr. Robert Mansel, a professor at the Institute of Cancer & Genetics at Cardiff University (Wales). He also noted the very low rate of patients who developed severe cardiac dysfunction.
Ms. Boerman and Dr. Mansel reported having no financial disclosures.
On Twitter @mitchelzoler
AT EBCC10
Key clinical point: Breast cancer patients treated with chemotherapy or radiotherapy showed a doubled rate of mild left-ventricular dysfunction, compared with matched controls 10 years after treatment.
Major finding: Mildly reduced left-ventricular function occurred in 15% of post-chemotherapy patients, compared with 6% of controls.
Data source: Echocardiography examinations conducted on 350 Dutch breast cancer patients and an equal number of age-matched controls.
Disclosures: Ms. Boerman and Dr. Mansel reported having no financial disclosures.
Phone monitoring program helps cut chemotherapy symptom severity
AMSTERDAM – A telephone-based system to monitor chemotherapy-induced symptoms when patients are home and facilitate interventions as needed led to significant cuts in symptom burden in a single-center, randomized trial with 152 breast cancer patients.
“Symptom care at home gives patients symptom care when and where they need it,” Kathi H. Mooney, Ph.D., said at the European Breast Cancer Conference. “Rarely is symptom monitoring extended to when patients are home, but that is when symptoms are most problematic for patients.”
The 30-day program was linked with significant cuts in the number of days with any of seven chemotherapy-induced symptoms. In addition, overall days with any severe symptom fell by 48% (P = .006) and the number of days with any moderate symptoms fell by 38% (P = .011), reported Dr. Mooney, professor of nursing at the University of Utah, Salt Lake City.
She and her associates designed a telephone-based system to address the usual reticence that chemotherapy patients have to report their symptoms. Prior study results had documented that patients with moderate or severe symptoms initiated calls for about 5% of episodes, even when explicitly told to report symptoms. This led the Utah researchers to develop an automated, interactive system that phoned patients daily.
The enrolled patients spanned the full spectrum of breast cancer stages; the average age was 53 years. All patients received a daily, automated call that prompted them to rate each of 11 chemotherapy symptoms on a scale of 0-10.
The calls also provided automated, self-management coaching for problematic symptoms. The investigational Symptom Care at Home intervention involved a nurse practitioner getting back to patients who reported poorly-controlled symptoms. These follow-up calls averaged just under 7 minutes in length, and on average each patient received 11 calls during the 30 days of the intervention.
After 30 days, the 83 patients in the Symptom Care at Home program had statistically-significant reductions in days with moderate or worse episodes for 7 of the 11 symptoms tallied: numbness or tingling, anxiety, nausea, pain, depressed mood, sore mouth, and fatigue. The most robust effects were a 72% drop in days with moderate or worse numbness or tingling, a 66% reduction in anxiety days, and a 61% cut in nausea days.
“I like the intervention used in this study. I think it shows what can happen when you collect symptom information in a way that is patient friendly,” said Dr. Robert Mansel, professor at the Institute of Cancer & Genetics at Cardiff University, South Wales. “I was delighted to see that this intervention really made a difference. The findings show that patients often suffer a lot more from treatment than they are usually prepared to tell us.”
In addition to the efficacy of this intervention, “patients told us that they liked having someone to talk with about their symptoms,” Dr. Mooney said in an interview. “Patients are concerned about their symptoms.”
One aspect of the Symptom Care at Home program that has not yet been analyzed is its cost efficacy. The University of Utah’s Huntsman Cancer Institute, where the program was developed, is awaiting results from a cost-benefit analysis before deciding whether to make the telephone system part of routine practice, she said.
Dr. Mooney and Dr. Mansel reported having no financial disclosures.
On Twitter @mitchelzoler
AMSTERDAM – A telephone-based system to monitor chemotherapy-induced symptoms when patients are home and facilitate interventions as needed led to significant cuts in symptom burden in a single-center, randomized trial with 152 breast cancer patients.
“Symptom care at home gives patients symptom care when and where they need it,” Kathi H. Mooney, Ph.D., said at the European Breast Cancer Conference. “Rarely is symptom monitoring extended to when patients are home, but that is when symptoms are most problematic for patients.”
The 30-day program was linked with significant cuts in the number of days with any of seven chemotherapy-induced symptoms. In addition, overall days with any severe symptom fell by 48% (P = .006) and the number of days with any moderate symptoms fell by 38% (P = .011), reported Dr. Mooney, professor of nursing at the University of Utah, Salt Lake City.
She and her associates designed a telephone-based system to address the usual reticence that chemotherapy patients have to report their symptoms. Prior study results had documented that patients with moderate or severe symptoms initiated calls for about 5% of episodes, even when explicitly told to report symptoms. This led the Utah researchers to develop an automated, interactive system that phoned patients daily.
The enrolled patients spanned the full spectrum of breast cancer stages; the average age was 53 years. All patients received a daily, automated call that prompted them to rate each of 11 chemotherapy symptoms on a scale of 0-10.
The calls also provided automated, self-management coaching for problematic symptoms. The investigational Symptom Care at Home intervention involved a nurse practitioner getting back to patients who reported poorly-controlled symptoms. These follow-up calls averaged just under 7 minutes in length, and on average each patient received 11 calls during the 30 days of the intervention.
After 30 days, the 83 patients in the Symptom Care at Home program had statistically-significant reductions in days with moderate or worse episodes for 7 of the 11 symptoms tallied: numbness or tingling, anxiety, nausea, pain, depressed mood, sore mouth, and fatigue. The most robust effects were a 72% drop in days with moderate or worse numbness or tingling, a 66% reduction in anxiety days, and a 61% cut in nausea days.
“I like the intervention used in this study. I think it shows what can happen when you collect symptom information in a way that is patient friendly,” said Dr. Robert Mansel, professor at the Institute of Cancer & Genetics at Cardiff University, South Wales. “I was delighted to see that this intervention really made a difference. The findings show that patients often suffer a lot more from treatment than they are usually prepared to tell us.”
In addition to the efficacy of this intervention, “patients told us that they liked having someone to talk with about their symptoms,” Dr. Mooney said in an interview. “Patients are concerned about their symptoms.”
One aspect of the Symptom Care at Home program that has not yet been analyzed is its cost efficacy. The University of Utah’s Huntsman Cancer Institute, where the program was developed, is awaiting results from a cost-benefit analysis before deciding whether to make the telephone system part of routine practice, she said.
Dr. Mooney and Dr. Mansel reported having no financial disclosures.
On Twitter @mitchelzoler
AMSTERDAM – A telephone-based system to monitor chemotherapy-induced symptoms when patients are home and facilitate interventions as needed led to significant cuts in symptom burden in a single-center, randomized trial with 152 breast cancer patients.
“Symptom care at home gives patients symptom care when and where they need it,” Kathi H. Mooney, Ph.D., said at the European Breast Cancer Conference. “Rarely is symptom monitoring extended to when patients are home, but that is when symptoms are most problematic for patients.”
The 30-day program was linked with significant cuts in the number of days with any of seven chemotherapy-induced symptoms. In addition, overall days with any severe symptom fell by 48% (P = .006) and the number of days with any moderate symptoms fell by 38% (P = .011), reported Dr. Mooney, professor of nursing at the University of Utah, Salt Lake City.
She and her associates designed a telephone-based system to address the usual reticence that chemotherapy patients have to report their symptoms. Prior study results had documented that patients with moderate or severe symptoms initiated calls for about 5% of episodes, even when explicitly told to report symptoms. This led the Utah researchers to develop an automated, interactive system that phoned patients daily.
The enrolled patients spanned the full spectrum of breast cancer stages; the average age was 53 years. All patients received a daily, automated call that prompted them to rate each of 11 chemotherapy symptoms on a scale of 0-10.
The calls also provided automated, self-management coaching for problematic symptoms. The investigational Symptom Care at Home intervention involved a nurse practitioner getting back to patients who reported poorly-controlled symptoms. These follow-up calls averaged just under 7 minutes in length, and on average each patient received 11 calls during the 30 days of the intervention.
After 30 days, the 83 patients in the Symptom Care at Home program had statistically-significant reductions in days with moderate or worse episodes for 7 of the 11 symptoms tallied: numbness or tingling, anxiety, nausea, pain, depressed mood, sore mouth, and fatigue. The most robust effects were a 72% drop in days with moderate or worse numbness or tingling, a 66% reduction in anxiety days, and a 61% cut in nausea days.
“I like the intervention used in this study. I think it shows what can happen when you collect symptom information in a way that is patient friendly,” said Dr. Robert Mansel, professor at the Institute of Cancer & Genetics at Cardiff University, South Wales. “I was delighted to see that this intervention really made a difference. The findings show that patients often suffer a lot more from treatment than they are usually prepared to tell us.”
In addition to the efficacy of this intervention, “patients told us that they liked having someone to talk with about their symptoms,” Dr. Mooney said in an interview. “Patients are concerned about their symptoms.”
One aspect of the Symptom Care at Home program that has not yet been analyzed is its cost efficacy. The University of Utah’s Huntsman Cancer Institute, where the program was developed, is awaiting results from a cost-benefit analysis before deciding whether to make the telephone system part of routine practice, she said.
Dr. Mooney and Dr. Mansel reported having no financial disclosures.
On Twitter @mitchelzoler
AT EBCC 10
VIDEO: Trastuzumab plus lapatinib erases selected breast cancers
AMSTERDAM – An unexpectedly dramatic benefit from combining trastuzumab and lapatinib when briefly treating women scheduled for breast cancer surgery has researchers focused on the best follow-up study to this promising but preliminary finding from 66 patients.
Among 66 patients with newly diagnosed HER2-positive breast cancer and scheduled for surgery, an average 11 days of treatment with a combination of trastuzumab (Herceptin) and lapatinib (Tykerb) during the period before surgery resulted in a pathologic complete response (pCR) in seven patients (11%) and 11 patients (17%) with minimal residual disease (MRD), Dr. Nigel Bundred reported at the European Breast Cancer Conference.
These patients had breast cancer tumors at baseline with a median diameter of 2 cm that with treatment for not quite 2 weeks resulted in either complete tumor disappearance or shrinkage to less than 5 mm in diameter in 18 (27%) of the patients on dual therapy, said Dr. Bundred, a professor of surgical oncology at the University Hospital of South Manchester (England).
“No cancer has ever disappeared that fast. It was flabbergasting,” Dr. Bundred said in an interview. “We need to confirm the results, and get larger numbers of patients.”
“This was a really surprising finding,” said Judith M. Bliss, professor and director of the Clinical Trials & Statistics unit of the Institute of Cancer Research in London and a co-investigator. “We knew that trastuzumab and lapatinib are effective treatments, but we had not expected to see such a dramatic effect on the structure and size of the tumor in such a short period of time,” Prof. Bliss said in a video interview.
The finding came as part of the Effect of Perioperative Anti-HER2 Therapy on Overall Survival–Biologic Phase (EPHOS-B) trial, designed to assess changes in a marker of cell proliferation (Ki67) and in a marker of cell apoptosis in relation to treatment with trastuzumab, lapatinib, or both when administered during the 10-12 days from the time patients entered the study until their scheduled surgery.
During the first phase of EPHOS-B, when 130 patients received trastuzumab monotherapy, lapatinib monotherapy, or neither, one of the 57 patients on trastuzumab (2%) had a pathologic complete response and one patient (2%) had minimal residual disease. No patients on lapatinib alone or in the control arm with no anti-HER2 drug had this sort of response.
During the second phase, 127 patients received trastuzumab alone, trastuzumab plus lapatinib in combination, or controls who received no anti-HER2 treatment. The substantial number of complete or partial responders in the 66 patients who received combined treatment with trastuzumab and lapatinib contrasted with one minimal residual disease among 32 patients (3%) who received trastuzumab alone and no responders among the 29 controls.
Patients receiving trastuzumab, alone or in the combined regimen, received a standard intravenous loading dosage of 6 mg/kg on days 1 and 8 after entry into the protocol, followed by a third dose after surgery on days 15-19; those also receiving lapatinib received 1 g/day orally for 28 days starting on entry.
“A quarter of the patients seem exquisitely sensitive to the combination of trastuzumab and lapatinib,” said Dr. David Cameron, another collaborator on the EPHOS-B study. “It’s pretty unusual to treat for 10-12 days and have 10% of the tumors disappear.”
Follow-up studies will be needed to determine whether patients with a pathologic complete response or minimal residual disease can forgo some or all of the chemotherapy that would usually follow surgery and still have good long-term disease-free survival. “We will focus on optimizing the short-term effect, and then modulate subsequent treatments,” said Dr. Cameron, professor and clinical director of oncology at the University of Edinburgh.
“We think these are patients who don’t need chemotherapy and are particularly sensitive to anti-HER2 drugs,” but so far that hasn’t been proven, cautioned Ms. Bliss.
The striking efficacy of trastuzumab combined with lapatinib in these 66 patients contrasts with the previously reported results from the ALTTO (Adjuvant Lapatinib and/or Trastuzumab Treatment Optimization) study, which failed to show an advantage in disease-free survival with trastuzumab plus lapatinib, compared with either of these two agents used individually during 1 year of adjuvant treatment in more than 8,000 randomized patients (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.62.1797), But the EPHOS-B results did agree with results from the much smaller NeoALTTO study, which showed in a randomized, multicenter, phase III study with 455 patients a significant incremental increase in pathologic complete response rate in patients on combined trastuzumab plus lapatinib, compared with patients on either drug alone (Lancet. 2012;379 [9816]:633-40).
Another promising finding from EPHOS-B was that among the 64 patients who had their left ventricular ejection fraction assessed prior to the second phase, none of 32 patients on the combined regimen showed signs of cardiotoxicity with a reduced ejection fraction following treatment, Dr. Bundred reported.
Until now, not much was known about the beneficial mechanisms of anti-HER2 drugs, he noted. The results from EPHOS-B “tell us that combined treatment does more than just shut down cell replication. It might be that trastuzumab induces an immune response.” The former tumor beds of patients with pathologic complete response as well as regions with minimal residual disease showed large numbers of tumor infiltrating lymphocytes, a sign of a robust immune response.
Trastuzumab and lapatinib work by different mechanisms, Dr. Bundred stressed. “The only way you can combine drugs is by understanding their mechanisms. We’re still looking for the mechanisms of the anti-HER2 drugs.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
The significant proportion of patients treated with trastuzumab plus lapatinib for about 11 days who developed a pathologic complete response or minimal residual disease was largely unexpected.
The finding raises questions: Can we identify patients after 11 days of treatment who are good responders to this combined treatment and will have an excellent relapse-free survival without ongoing combination anti-HER2 treatment or anti-HER2 escalation, and who will be eligible for chemotherapy de-escalation similar to the regimen tested by Tolaney and her associates (N Engl J Med. 2015 Jan;372:134-41)?
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Hervé Bonnefoi |
We clearly need more data on the impact of the combined anti-HER2 regimen on the rate of long-term, relapse-free survival, and data from many more patients treated with a combined anti-HER2 regimen. The EPHOS-B results seem to contradict the results of the ALTTO study (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.62.1797), but they confirm results of the NeoALTTO study, a randomized, multicenter, phase III study with 455 patients (Lancet. 2012 Jan;379[9816]:633-40).
The EPHOS-B researchers modeled their study after the presurgical treatment studies run using hormonal therapies. The results from studies of anti-HER2 treatments during this presurgical time window have been much harder to interpret.
Dr. Hervé Bonnefoi is a professor of medical oncology at Bordeaux University (France). He reported having no financial disclosures. He made these comments as the designated discussant for the EPHOS-B study.
The significant proportion of patients treated with trastuzumab plus lapatinib for about 11 days who developed a pathologic complete response or minimal residual disease was largely unexpected.
The finding raises questions: Can we identify patients after 11 days of treatment who are good responders to this combined treatment and will have an excellent relapse-free survival without ongoing combination anti-HER2 treatment or anti-HER2 escalation, and who will be eligible for chemotherapy de-escalation similar to the regimen tested by Tolaney and her associates (N Engl J Med. 2015 Jan;372:134-41)?
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Hervé Bonnefoi |
We clearly need more data on the impact of the combined anti-HER2 regimen on the rate of long-term, relapse-free survival, and data from many more patients treated with a combined anti-HER2 regimen. The EPHOS-B results seem to contradict the results of the ALTTO study (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.62.1797), but they confirm results of the NeoALTTO study, a randomized, multicenter, phase III study with 455 patients (Lancet. 2012 Jan;379[9816]:633-40).
The EPHOS-B researchers modeled their study after the presurgical treatment studies run using hormonal therapies. The results from studies of anti-HER2 treatments during this presurgical time window have been much harder to interpret.
Dr. Hervé Bonnefoi is a professor of medical oncology at Bordeaux University (France). He reported having no financial disclosures. He made these comments as the designated discussant for the EPHOS-B study.
The significant proportion of patients treated with trastuzumab plus lapatinib for about 11 days who developed a pathologic complete response or minimal residual disease was largely unexpected.
The finding raises questions: Can we identify patients after 11 days of treatment who are good responders to this combined treatment and will have an excellent relapse-free survival without ongoing combination anti-HER2 treatment or anti-HER2 escalation, and who will be eligible for chemotherapy de-escalation similar to the regimen tested by Tolaney and her associates (N Engl J Med. 2015 Jan;372:134-41)?
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Hervé Bonnefoi |
We clearly need more data on the impact of the combined anti-HER2 regimen on the rate of long-term, relapse-free survival, and data from many more patients treated with a combined anti-HER2 regimen. The EPHOS-B results seem to contradict the results of the ALTTO study (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.62.1797), but they confirm results of the NeoALTTO study, a randomized, multicenter, phase III study with 455 patients (Lancet. 2012 Jan;379[9816]:633-40).
The EPHOS-B researchers modeled their study after the presurgical treatment studies run using hormonal therapies. The results from studies of anti-HER2 treatments during this presurgical time window have been much harder to interpret.
Dr. Hervé Bonnefoi is a professor of medical oncology at Bordeaux University (France). He reported having no financial disclosures. He made these comments as the designated discussant for the EPHOS-B study.
AMSTERDAM – An unexpectedly dramatic benefit from combining trastuzumab and lapatinib when briefly treating women scheduled for breast cancer surgery has researchers focused on the best follow-up study to this promising but preliminary finding from 66 patients.
Among 66 patients with newly diagnosed HER2-positive breast cancer and scheduled for surgery, an average 11 days of treatment with a combination of trastuzumab (Herceptin) and lapatinib (Tykerb) during the period before surgery resulted in a pathologic complete response (pCR) in seven patients (11%) and 11 patients (17%) with minimal residual disease (MRD), Dr. Nigel Bundred reported at the European Breast Cancer Conference.
These patients had breast cancer tumors at baseline with a median diameter of 2 cm that with treatment for not quite 2 weeks resulted in either complete tumor disappearance or shrinkage to less than 5 mm in diameter in 18 (27%) of the patients on dual therapy, said Dr. Bundred, a professor of surgical oncology at the University Hospital of South Manchester (England).
“No cancer has ever disappeared that fast. It was flabbergasting,” Dr. Bundred said in an interview. “We need to confirm the results, and get larger numbers of patients.”
“This was a really surprising finding,” said Judith M. Bliss, professor and director of the Clinical Trials & Statistics unit of the Institute of Cancer Research in London and a co-investigator. “We knew that trastuzumab and lapatinib are effective treatments, but we had not expected to see such a dramatic effect on the structure and size of the tumor in such a short period of time,” Prof. Bliss said in a video interview.
The finding came as part of the Effect of Perioperative Anti-HER2 Therapy on Overall Survival–Biologic Phase (EPHOS-B) trial, designed to assess changes in a marker of cell proliferation (Ki67) and in a marker of cell apoptosis in relation to treatment with trastuzumab, lapatinib, or both when administered during the 10-12 days from the time patients entered the study until their scheduled surgery.
During the first phase of EPHOS-B, when 130 patients received trastuzumab monotherapy, lapatinib monotherapy, or neither, one of the 57 patients on trastuzumab (2%) had a pathologic complete response and one patient (2%) had minimal residual disease. No patients on lapatinib alone or in the control arm with no anti-HER2 drug had this sort of response.
During the second phase, 127 patients received trastuzumab alone, trastuzumab plus lapatinib in combination, or controls who received no anti-HER2 treatment. The substantial number of complete or partial responders in the 66 patients who received combined treatment with trastuzumab and lapatinib contrasted with one minimal residual disease among 32 patients (3%) who received trastuzumab alone and no responders among the 29 controls.
Patients receiving trastuzumab, alone or in the combined regimen, received a standard intravenous loading dosage of 6 mg/kg on days 1 and 8 after entry into the protocol, followed by a third dose after surgery on days 15-19; those also receiving lapatinib received 1 g/day orally for 28 days starting on entry.
“A quarter of the patients seem exquisitely sensitive to the combination of trastuzumab and lapatinib,” said Dr. David Cameron, another collaborator on the EPHOS-B study. “It’s pretty unusual to treat for 10-12 days and have 10% of the tumors disappear.”
Follow-up studies will be needed to determine whether patients with a pathologic complete response or minimal residual disease can forgo some or all of the chemotherapy that would usually follow surgery and still have good long-term disease-free survival. “We will focus on optimizing the short-term effect, and then modulate subsequent treatments,” said Dr. Cameron, professor and clinical director of oncology at the University of Edinburgh.
“We think these are patients who don’t need chemotherapy and are particularly sensitive to anti-HER2 drugs,” but so far that hasn’t been proven, cautioned Ms. Bliss.
The striking efficacy of trastuzumab combined with lapatinib in these 66 patients contrasts with the previously reported results from the ALTTO (Adjuvant Lapatinib and/or Trastuzumab Treatment Optimization) study, which failed to show an advantage in disease-free survival with trastuzumab plus lapatinib, compared with either of these two agents used individually during 1 year of adjuvant treatment in more than 8,000 randomized patients (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.62.1797), But the EPHOS-B results did agree with results from the much smaller NeoALTTO study, which showed in a randomized, multicenter, phase III study with 455 patients a significant incremental increase in pathologic complete response rate in patients on combined trastuzumab plus lapatinib, compared with patients on either drug alone (Lancet. 2012;379 [9816]:633-40).
Another promising finding from EPHOS-B was that among the 64 patients who had their left ventricular ejection fraction assessed prior to the second phase, none of 32 patients on the combined regimen showed signs of cardiotoxicity with a reduced ejection fraction following treatment, Dr. Bundred reported.
Until now, not much was known about the beneficial mechanisms of anti-HER2 drugs, he noted. The results from EPHOS-B “tell us that combined treatment does more than just shut down cell replication. It might be that trastuzumab induces an immune response.” The former tumor beds of patients with pathologic complete response as well as regions with minimal residual disease showed large numbers of tumor infiltrating lymphocytes, a sign of a robust immune response.
Trastuzumab and lapatinib work by different mechanisms, Dr. Bundred stressed. “The only way you can combine drugs is by understanding their mechanisms. We’re still looking for the mechanisms of the anti-HER2 drugs.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AMSTERDAM – An unexpectedly dramatic benefit from combining trastuzumab and lapatinib when briefly treating women scheduled for breast cancer surgery has researchers focused on the best follow-up study to this promising but preliminary finding from 66 patients.
Among 66 patients with newly diagnosed HER2-positive breast cancer and scheduled for surgery, an average 11 days of treatment with a combination of trastuzumab (Herceptin) and lapatinib (Tykerb) during the period before surgery resulted in a pathologic complete response (pCR) in seven patients (11%) and 11 patients (17%) with minimal residual disease (MRD), Dr. Nigel Bundred reported at the European Breast Cancer Conference.
These patients had breast cancer tumors at baseline with a median diameter of 2 cm that with treatment for not quite 2 weeks resulted in either complete tumor disappearance or shrinkage to less than 5 mm in diameter in 18 (27%) of the patients on dual therapy, said Dr. Bundred, a professor of surgical oncology at the University Hospital of South Manchester (England).
“No cancer has ever disappeared that fast. It was flabbergasting,” Dr. Bundred said in an interview. “We need to confirm the results, and get larger numbers of patients.”
“This was a really surprising finding,” said Judith M. Bliss, professor and director of the Clinical Trials & Statistics unit of the Institute of Cancer Research in London and a co-investigator. “We knew that trastuzumab and lapatinib are effective treatments, but we had not expected to see such a dramatic effect on the structure and size of the tumor in such a short period of time,” Prof. Bliss said in a video interview.
The finding came as part of the Effect of Perioperative Anti-HER2 Therapy on Overall Survival–Biologic Phase (EPHOS-B) trial, designed to assess changes in a marker of cell proliferation (Ki67) and in a marker of cell apoptosis in relation to treatment with trastuzumab, lapatinib, or both when administered during the 10-12 days from the time patients entered the study until their scheduled surgery.
During the first phase of EPHOS-B, when 130 patients received trastuzumab monotherapy, lapatinib monotherapy, or neither, one of the 57 patients on trastuzumab (2%) had a pathologic complete response and one patient (2%) had minimal residual disease. No patients on lapatinib alone or in the control arm with no anti-HER2 drug had this sort of response.
During the second phase, 127 patients received trastuzumab alone, trastuzumab plus lapatinib in combination, or controls who received no anti-HER2 treatment. The substantial number of complete or partial responders in the 66 patients who received combined treatment with trastuzumab and lapatinib contrasted with one minimal residual disease among 32 patients (3%) who received trastuzumab alone and no responders among the 29 controls.
Patients receiving trastuzumab, alone or in the combined regimen, received a standard intravenous loading dosage of 6 mg/kg on days 1 and 8 after entry into the protocol, followed by a third dose after surgery on days 15-19; those also receiving lapatinib received 1 g/day orally for 28 days starting on entry.
“A quarter of the patients seem exquisitely sensitive to the combination of trastuzumab and lapatinib,” said Dr. David Cameron, another collaborator on the EPHOS-B study. “It’s pretty unusual to treat for 10-12 days and have 10% of the tumors disappear.”
Follow-up studies will be needed to determine whether patients with a pathologic complete response or minimal residual disease can forgo some or all of the chemotherapy that would usually follow surgery and still have good long-term disease-free survival. “We will focus on optimizing the short-term effect, and then modulate subsequent treatments,” said Dr. Cameron, professor and clinical director of oncology at the University of Edinburgh.
“We think these are patients who don’t need chemotherapy and are particularly sensitive to anti-HER2 drugs,” but so far that hasn’t been proven, cautioned Ms. Bliss.
The striking efficacy of trastuzumab combined with lapatinib in these 66 patients contrasts with the previously reported results from the ALTTO (Adjuvant Lapatinib and/or Trastuzumab Treatment Optimization) study, which failed to show an advantage in disease-free survival with trastuzumab plus lapatinib, compared with either of these two agents used individually during 1 year of adjuvant treatment in more than 8,000 randomized patients (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.62.1797), But the EPHOS-B results did agree with results from the much smaller NeoALTTO study, which showed in a randomized, multicenter, phase III study with 455 patients a significant incremental increase in pathologic complete response rate in patients on combined trastuzumab plus lapatinib, compared with patients on either drug alone (Lancet. 2012;379 [9816]:633-40).
Another promising finding from EPHOS-B was that among the 64 patients who had their left ventricular ejection fraction assessed prior to the second phase, none of 32 patients on the combined regimen showed signs of cardiotoxicity with a reduced ejection fraction following treatment, Dr. Bundred reported.
Until now, not much was known about the beneficial mechanisms of anti-HER2 drugs, he noted. The results from EPHOS-B “tell us that combined treatment does more than just shut down cell replication. It might be that trastuzumab induces an immune response.” The former tumor beds of patients with pathologic complete response as well as regions with minimal residual disease showed large numbers of tumor infiltrating lymphocytes, a sign of a robust immune response.
Trastuzumab and lapatinib work by different mechanisms, Dr. Bundred stressed. “The only way you can combine drugs is by understanding their mechanisms. We’re still looking for the mechanisms of the anti-HER2 drugs.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT EBCC10
Key clinical point: Combined treatment with trastuzumab and lapatinib for 10-12 days led to complete HER2-positive breast cancer disappearance in seven of 66 patients.
Major finding: Pathologic complete responses occurred in seven of 66 patients on trastuzumab plus lapatinib, but none of 32 patients on trastuzumab alone or the 29 controls.
Data source: EPHOS-B, a multicenter, randomized, British study run in two phases with a total of 257 women with HER2-positive breast cancer.
Disclosures: GlaxoSmithKline, which at the time marketed lapatinib (Tykerb, now marketed by Novartis), made an educational grant to the Institute of Cancer Research in association with the EPHOS-B trial. Dr. Bundred served on an advisory board for Roche U.K. Ms. Bliss reported having no financial disclosures. Dr. Cameron has been a consultant to Novartis, GlaxoSmithKline, and Roche, but received no additional compensation.