User login
Mitchel is a reporter for MDedge based in the Philadelphia area. He started with the company in 1992, when it was International Medical News Group (IMNG), and has since covered a range of medical specialties. Mitchel trained as a virologist at Roswell Park Memorial Institute in Buffalo, and then worked briefly as a researcher at Boston Children's Hospital before pivoting to journalism as a AAAS Mass Media Fellow in 1980. His first reporting job was with Science Digest magazine, and from the mid-1980s to early-1990s he was a reporter with Medical World News. @mitchelzoler
TCT: SAPIEN XT TAVR system gains valve-in-valve indication
SAN FRANCISCO – Food and Drug Administration approval of the SAPIEN XT transcatheter aortic valve for the valve-in-valve indication in high–surgical risk patients means that, officially, there are now two options for transcatheter replacement of a faulty prosthetic aortic valve.
CoreValve, the competing device for transcatheter aortic valve replacement (TAVR) in U.S. practice, received FDA approval for the valve-in-valve indication in March.
Researchers reported the data behind SAPIEN XT’s approval from two U.S. registries with a total of 197 high-risk patients at the Transcatheter Cardiovascular Therapeutics annual meeting on Oct. 16, the same day the FDA approval was announced by Edwards Lifesciences. The mortality rate was 4% after 30 days and 13% after 1 year, and the 1-year stroke rate was 4%, Dr. Danny Dvir said at the meeting.
One feature of the 1-year survival data that Dr. Dvir called “quite amazing” was the absence of any deaths during the first 30 days post TAVR with the SAPIEN XT system, and 7% at 1 year among the 100 patients treated during the final 8 months of the registry, who comprised the second half of patients enrolled in the registry. “I think we learned how to choose the right patients for this procedure,” said Dr. Dvir, an interventional cardiologist at St. Paul’s Hospital in Vancouver, B.C.
Given the risk from replacing a failed bioprosthetic valve by open surgery, “TAVR is becoming the preferred approach to valve-in-valve,” commented Dr. Ajay J. Kirtane, director of the cardiac catheterization laboratories at Columbia University in New York.
The registry results also highlighted a key limitation of the SAPIEN XT valve: patients with a bioprosthetic valve with a relatively narrow inner diameter of 21 mm or less.
Because the SAPIEN series of valves are balloon expandable and designed to sit directly in the aortic-valve annulus, the inner diameter of an existing bioprothesis can limit the TAVR options. The CoreValve, self-expanding valves sit in a supravalvular location and better fit through a narrow-frame existing valve.
This geometric limitation means that SAPIEN XT cannot work in patients with existing valves less than 21 mm in inner diameter, and the registry excluded such patients, who generally comprise about 10% of all patients with severe aortic stenosis.
In addition, among the 28% of patients enrolled in the registry who had an existing valve diameter of 21 mm, the 1-year mortality rate was strikingly high – 20% – compared with an 11% mortality rate in patients with existing valve diameters of 23 or 25 mm, Dr. Dvir reported.
“If a patient had a smaller inner diameter I’d definitely go with the supravalvular valve. For a bigger valve you have more choices,” commented Dr. Axel H.P. Linke, codirector of cardiology at the Heart Center at the University of Leipzig (Germany).
“It’s not fair to extrapolate these findings with SAPIEN XT to smaller [existing bioprosthetic] valves. There is the ability to go to lower inner diameters” using CoreValve, commented Dr. Jeffrey J. Popma, who led the U.S. CoreValve studies and is professor at Harvard Medical School and director of interventional cardiology at Beth Israel Deaconess Medical Center in Boston.
The two sequential valve-in-valve U.S. registries for SAPIEN XT ran as part of the PARTNER 2 trial, designed to test the safety and efficacy of SAPIEN XT in patients undergoing TAVR for a de novo aortic valve. The 197 patients in the full registry averaged 79 years of age, 60% were men, their average Society of Thoracic Surgeons mortality risk score was 9.7%, 50% had atrial fibrillation, 95% had New York Heart Association class III or IV symptoms, and baseline screening identified one-third of the patients as frail.
The PARTNER 2 trial valve-in-valve registry and extended registry are sponsored by Edwards Lifesciences, which markets the SAPIEN XT system. Dr. Dvir has been a consultant to Edwards and to Medtronic, the company that markets the CoreValve systems. Dr. Kirtane has received research grants from Boston Scientific, St. Jude, Eli Lilly, GlaxoSmithKline, Abiomed, and Abbott Vascular. Dr. Linke has been a consultant to Boston Scientific, St. Jude, Bard, Edwards, and Medtronic and owns equity in Claret. Dr. Popma has been principal investigator of the CoreValve studies, has been a consultant to Abbott Vascular, Boston Scientific, and Director Flow; he owns equity in Direct Flow, and he has received research grants from Abbott Vascular, Medtronic, Boston Scientific, and Cook Medical.
On Twitter @mitchelzoler
Transcatheter aortic valve replacement is on track to be the preferred treatment for aortic valve-in-valve replacement. How many surgeons are eager to do a reoperation on an aortic valve?
 |
Dr. David L. Brown |
Transcatheter valve replacement is the best way to treat aortic valve-in-valve disease. The results reported by Dr. Dvir further support that notion. One attraction of the balloon-expandable TAVR valve is that it greatly reduces the risk of annular rupture. But it is important to use a TAVR valve that is right sized. If the existing bioprosthesis is narrow then you have no choice but to use a self-expanding valve.
We had already been placing the SAPIEN XT, as well as SAPIEN 3 valves before XT received the valve-in-valve indication. In the past, when we did this we were never sure if the procedure would receive insurance coverage, but now XT should be covered because of the FDA approval, so this is a huge deal for us. It eliminates our economic uncertainty.
Dr. David L. Brown is director of interventional cardiology at the Heart Hospital Baylor Plano, Texas. He had no disclosures. He made these comments as a discussant at the meeting and in an interview.
Transcatheter aortic valve replacement is on track to be the preferred treatment for aortic valve-in-valve replacement. How many surgeons are eager to do a reoperation on an aortic valve?
 |
Dr. David L. Brown |
Transcatheter valve replacement is the best way to treat aortic valve-in-valve disease. The results reported by Dr. Dvir further support that notion. One attraction of the balloon-expandable TAVR valve is that it greatly reduces the risk of annular rupture. But it is important to use a TAVR valve that is right sized. If the existing bioprosthesis is narrow then you have no choice but to use a self-expanding valve.
We had already been placing the SAPIEN XT, as well as SAPIEN 3 valves before XT received the valve-in-valve indication. In the past, when we did this we were never sure if the procedure would receive insurance coverage, but now XT should be covered because of the FDA approval, so this is a huge deal for us. It eliminates our economic uncertainty.
Dr. David L. Brown is director of interventional cardiology at the Heart Hospital Baylor Plano, Texas. He had no disclosures. He made these comments as a discussant at the meeting and in an interview.
Transcatheter aortic valve replacement is on track to be the preferred treatment for aortic valve-in-valve replacement. How many surgeons are eager to do a reoperation on an aortic valve?
 |
Dr. David L. Brown |
Transcatheter valve replacement is the best way to treat aortic valve-in-valve disease. The results reported by Dr. Dvir further support that notion. One attraction of the balloon-expandable TAVR valve is that it greatly reduces the risk of annular rupture. But it is important to use a TAVR valve that is right sized. If the existing bioprosthesis is narrow then you have no choice but to use a self-expanding valve.
We had already been placing the SAPIEN XT, as well as SAPIEN 3 valves before XT received the valve-in-valve indication. In the past, when we did this we were never sure if the procedure would receive insurance coverage, but now XT should be covered because of the FDA approval, so this is a huge deal for us. It eliminates our economic uncertainty.
Dr. David L. Brown is director of interventional cardiology at the Heart Hospital Baylor Plano, Texas. He had no disclosures. He made these comments as a discussant at the meeting and in an interview.
SAN FRANCISCO – Food and Drug Administration approval of the SAPIEN XT transcatheter aortic valve for the valve-in-valve indication in high–surgical risk patients means that, officially, there are now two options for transcatheter replacement of a faulty prosthetic aortic valve.
CoreValve, the competing device for transcatheter aortic valve replacement (TAVR) in U.S. practice, received FDA approval for the valve-in-valve indication in March.
Researchers reported the data behind SAPIEN XT’s approval from two U.S. registries with a total of 197 high-risk patients at the Transcatheter Cardiovascular Therapeutics annual meeting on Oct. 16, the same day the FDA approval was announced by Edwards Lifesciences. The mortality rate was 4% after 30 days and 13% after 1 year, and the 1-year stroke rate was 4%, Dr. Danny Dvir said at the meeting.
One feature of the 1-year survival data that Dr. Dvir called “quite amazing” was the absence of any deaths during the first 30 days post TAVR with the SAPIEN XT system, and 7% at 1 year among the 100 patients treated during the final 8 months of the registry, who comprised the second half of patients enrolled in the registry. “I think we learned how to choose the right patients for this procedure,” said Dr. Dvir, an interventional cardiologist at St. Paul’s Hospital in Vancouver, B.C.
Given the risk from replacing a failed bioprosthetic valve by open surgery, “TAVR is becoming the preferred approach to valve-in-valve,” commented Dr. Ajay J. Kirtane, director of the cardiac catheterization laboratories at Columbia University in New York.
The registry results also highlighted a key limitation of the SAPIEN XT valve: patients with a bioprosthetic valve with a relatively narrow inner diameter of 21 mm or less.
Because the SAPIEN series of valves are balloon expandable and designed to sit directly in the aortic-valve annulus, the inner diameter of an existing bioprothesis can limit the TAVR options. The CoreValve, self-expanding valves sit in a supravalvular location and better fit through a narrow-frame existing valve.
This geometric limitation means that SAPIEN XT cannot work in patients with existing valves less than 21 mm in inner diameter, and the registry excluded such patients, who generally comprise about 10% of all patients with severe aortic stenosis.
In addition, among the 28% of patients enrolled in the registry who had an existing valve diameter of 21 mm, the 1-year mortality rate was strikingly high – 20% – compared with an 11% mortality rate in patients with existing valve diameters of 23 or 25 mm, Dr. Dvir reported.
“If a patient had a smaller inner diameter I’d definitely go with the supravalvular valve. For a bigger valve you have more choices,” commented Dr. Axel H.P. Linke, codirector of cardiology at the Heart Center at the University of Leipzig (Germany).
“It’s not fair to extrapolate these findings with SAPIEN XT to smaller [existing bioprosthetic] valves. There is the ability to go to lower inner diameters” using CoreValve, commented Dr. Jeffrey J. Popma, who led the U.S. CoreValve studies and is professor at Harvard Medical School and director of interventional cardiology at Beth Israel Deaconess Medical Center in Boston.
The two sequential valve-in-valve U.S. registries for SAPIEN XT ran as part of the PARTNER 2 trial, designed to test the safety and efficacy of SAPIEN XT in patients undergoing TAVR for a de novo aortic valve. The 197 patients in the full registry averaged 79 years of age, 60% were men, their average Society of Thoracic Surgeons mortality risk score was 9.7%, 50% had atrial fibrillation, 95% had New York Heart Association class III or IV symptoms, and baseline screening identified one-third of the patients as frail.
The PARTNER 2 trial valve-in-valve registry and extended registry are sponsored by Edwards Lifesciences, which markets the SAPIEN XT system. Dr. Dvir has been a consultant to Edwards and to Medtronic, the company that markets the CoreValve systems. Dr. Kirtane has received research grants from Boston Scientific, St. Jude, Eli Lilly, GlaxoSmithKline, Abiomed, and Abbott Vascular. Dr. Linke has been a consultant to Boston Scientific, St. Jude, Bard, Edwards, and Medtronic and owns equity in Claret. Dr. Popma has been principal investigator of the CoreValve studies, has been a consultant to Abbott Vascular, Boston Scientific, and Director Flow; he owns equity in Direct Flow, and he has received research grants from Abbott Vascular, Medtronic, Boston Scientific, and Cook Medical.
On Twitter @mitchelzoler
SAN FRANCISCO – Food and Drug Administration approval of the SAPIEN XT transcatheter aortic valve for the valve-in-valve indication in high–surgical risk patients means that, officially, there are now two options for transcatheter replacement of a faulty prosthetic aortic valve.
CoreValve, the competing device for transcatheter aortic valve replacement (TAVR) in U.S. practice, received FDA approval for the valve-in-valve indication in March.
Researchers reported the data behind SAPIEN XT’s approval from two U.S. registries with a total of 197 high-risk patients at the Transcatheter Cardiovascular Therapeutics annual meeting on Oct. 16, the same day the FDA approval was announced by Edwards Lifesciences. The mortality rate was 4% after 30 days and 13% after 1 year, and the 1-year stroke rate was 4%, Dr. Danny Dvir said at the meeting.
One feature of the 1-year survival data that Dr. Dvir called “quite amazing” was the absence of any deaths during the first 30 days post TAVR with the SAPIEN XT system, and 7% at 1 year among the 100 patients treated during the final 8 months of the registry, who comprised the second half of patients enrolled in the registry. “I think we learned how to choose the right patients for this procedure,” said Dr. Dvir, an interventional cardiologist at St. Paul’s Hospital in Vancouver, B.C.
Given the risk from replacing a failed bioprosthetic valve by open surgery, “TAVR is becoming the preferred approach to valve-in-valve,” commented Dr. Ajay J. Kirtane, director of the cardiac catheterization laboratories at Columbia University in New York.
The registry results also highlighted a key limitation of the SAPIEN XT valve: patients with a bioprosthetic valve with a relatively narrow inner diameter of 21 mm or less.
Because the SAPIEN series of valves are balloon expandable and designed to sit directly in the aortic-valve annulus, the inner diameter of an existing bioprothesis can limit the TAVR options. The CoreValve, self-expanding valves sit in a supravalvular location and better fit through a narrow-frame existing valve.
This geometric limitation means that SAPIEN XT cannot work in patients with existing valves less than 21 mm in inner diameter, and the registry excluded such patients, who generally comprise about 10% of all patients with severe aortic stenosis.
In addition, among the 28% of patients enrolled in the registry who had an existing valve diameter of 21 mm, the 1-year mortality rate was strikingly high – 20% – compared with an 11% mortality rate in patients with existing valve diameters of 23 or 25 mm, Dr. Dvir reported.
“If a patient had a smaller inner diameter I’d definitely go with the supravalvular valve. For a bigger valve you have more choices,” commented Dr. Axel H.P. Linke, codirector of cardiology at the Heart Center at the University of Leipzig (Germany).
“It’s not fair to extrapolate these findings with SAPIEN XT to smaller [existing bioprosthetic] valves. There is the ability to go to lower inner diameters” using CoreValve, commented Dr. Jeffrey J. Popma, who led the U.S. CoreValve studies and is professor at Harvard Medical School and director of interventional cardiology at Beth Israel Deaconess Medical Center in Boston.
The two sequential valve-in-valve U.S. registries for SAPIEN XT ran as part of the PARTNER 2 trial, designed to test the safety and efficacy of SAPIEN XT in patients undergoing TAVR for a de novo aortic valve. The 197 patients in the full registry averaged 79 years of age, 60% were men, their average Society of Thoracic Surgeons mortality risk score was 9.7%, 50% had atrial fibrillation, 95% had New York Heart Association class III or IV symptoms, and baseline screening identified one-third of the patients as frail.
The PARTNER 2 trial valve-in-valve registry and extended registry are sponsored by Edwards Lifesciences, which markets the SAPIEN XT system. Dr. Dvir has been a consultant to Edwards and to Medtronic, the company that markets the CoreValve systems. Dr. Kirtane has received research grants from Boston Scientific, St. Jude, Eli Lilly, GlaxoSmithKline, Abiomed, and Abbott Vascular. Dr. Linke has been a consultant to Boston Scientific, St. Jude, Bard, Edwards, and Medtronic and owns equity in Claret. Dr. Popma has been principal investigator of the CoreValve studies, has been a consultant to Abbott Vascular, Boston Scientific, and Director Flow; he owns equity in Direct Flow, and he has received research grants from Abbott Vascular, Medtronic, Boston Scientific, and Cook Medical.
On Twitter @mitchelzoler
AT TCT 2015
Key clinical point:The SAPIEN XT balloon-expandable system for transcatheter aortic valve replacement received FDA approval for valve-in-valve use in high-risk patients.
Major finding: High-risk patients treated for aortic valve-in-replacement with SAPIEN XT had a 13% 1-year mortality rate.
Data source: The PARTNER 2 trial valve-in-valve registry and extended registry, a multicenter center based primarily in the United States with 197 high-risk patients.
Disclosures: The PARTNER 2 trial valve-in-valve registry and extended registry are sponsored by Edwards Lifesciences, which markets the SAPIEN XT system. Dr. Dvir has been a consultant to Edwards and to Medtronic, the company that markets the CoreValve systems.
VIDEO: Ultrafiltration’s role for acute heart failure remains uncertain
NATIONAL HARBOR, MD. – The trial designed to definitively test the safety and efficacy of ultrafiltration as an alternative to intravenous diuretics for patients hospitalized with acute decompensated heart failure got cut to about a quarter of its planned enrollment by the company that recently acquired the ultrafiltration technology. This outcomes means that ultrafiltration’s role in acute heart failure remains uncertain and will stay that way for the foreseeable future.
As a consequence, ultrafiltration (also known as aquapheresis), approved for use in the United States by the Food and Drug Administration in 2002, will be used by believers in the treatment on some of the estimated 200,000 or more U.S. heart failure patients who become hospitalized each year with acute, severe congestion that is unresponsive to diuretic treatment. Other clinicians who remain skeptical of ultrafiltration’s safety and efficacy will not use it, and currently no prospect remains to resolve this uncertainty. Also limiting ultrafiltration’s use is its designation as investigational by U.S. health insurers.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Early termination off the AVOID-HF [Aquapheresis Vs. Intravenous Diuretics and Hospitalization for Heart Failure] trial was a tragedy because it is unlikely we will ever see a trial of its size again,” commented Dr. G. Michael Felker during a discussion of treatment for acute heart failure at the at the annual meeting of the Heart Failure Society of America. “We still have no definitive answer” about ultrafiltration,” said Dr. Felker, professor of medicine and a cardiologist specializing in acute heart failure at Duke University in Durham, N.C.
Opinions about ultrafiltration and its role in treating patients with acute decompensated heart failure remain sharply split, although at this point, even proponents of the treatment concede that its use is limited to severely congested decompensated heart failure patients who prove unresponsive to intravenous diuretic therapy.
Ultrafiltration is for patients with “recurrent decompensation (not the first episode) and a large amount of fluid overload (more than 10 pounds) who also have elevated central venous pressure and elevated abdominal pressure that reduces blood flow to the kidneys,” Dr. Maria Rosa Costanzo said in a video interview. Used in these patients at a low rate of 20-50 cc/hour to “gently remove fluid,” the treatment reduces central venous and intra-abdominal pressures, leading to increased urine output and restoration of diuretic sensitivity, said Dr. Costanzo, lead investigator for the AVOID-HF trial and medical director of the heart failure and pulmonary hypertension program at the Advocate Heart Institute in Naperville, Ill.
A dramatically opposing view of ultrafiltration came from Dr. Christopher M. O’Connor, a heart failure cardiologist and CEO of the Inova Heart and Vascular Institute in Falls Church, Va.
“Even in diuretic-resistant, patients I would not use ultrafiltration. It does not anymore fit into management” of acute decompensated heart failure patients, Dr. O’Connor said in an interview. The CARRESS-HF [Cardiorenal Rescue Study in Acute Decompensated Heart Failure] trial targeted patients with diuretic resistance, the very population we would need to treat, and we did not see an advantage to ultrafiltration,” said Dr. O’Connor, a coinvestigator on CARRESS-HF, an earlier trial that compared the two treatment methods (N Engl J Med. 2012 Dec 13;367[24]:2296-304).
“We need to understand who is the right patient” for ultrafiltration. “We need to continue to investigate [ultrafiltration] to know where it best fits,” commented Dr. Clyde W. Yancy, professor and chief of cardiology at Northwestern University in Chicago.
AVOID-HF enrolled and randomized 224 patients with acute decompensated heart failure out of an anticipated enrollment of 810 patients. Analysis of the study’s primary endpoint, time to first heart failure event within the first 90 days following hospital discharge, occurred after an average of 34 days in 108 loop-diuretic treated patients and after an average 62 days in 105 ultrafiltration-treated patients, a difference that did not achieve statistical significance. A heart failure event within the first 90 days occurred in 25% of the ultrafiltration patients and in 35% of those on diuretic treatment, also a nonsignificant difference, Dr. Costanzo reported. Concurrent with her report at the meeting an article appeared online with the results (JACC Heart Fail. 2015;doi: 10.1016/j.jchf.2015.08.005).
Increases in serum creatinine were modest following ultrafiltration and similar to changes seen in the patients who received loop diuretic treatment. The biggest rise in average serum creatinine level occurred at 30 days after randomization, with an average 0.37 mg/dL rise among the ultrafiltration patients.
The abrupt shutdown in the AVOID-HF trial occurred following a change in ownership of the ultrafiltration technology used in the study. Ultrafiltration had been initially developed by CHF Solutions of Brooklyn Park, Minn. In 2010, Gambro, a Swedish company, acquired CHF Solutions and rights to the ultrafiltration system, and Gambro initiated the AVOID-HF trial. Baxter, in Deerfield, Ill., acquired Gambro in September 2013, and in April 2014, Baxter stopped the AVOID-HF trial because of slow projected enrollment, said Dr. Costanzo. But she strongly disagreed with this projection, and said that the trial showed no signs of futility or safety concerns when it came to a stop. Getting the data from Baxter to allow her and her associates to write their report and deliver their findings at the meeting took a lot of persuasion, Dr. Costanzo added.
Dr. Felker has been a consultant to and received research grants from 10 drug or device companies. He was a coinvestigator on the CARRESS-HF trial. Dr. Costanzo, lead investigator of AVOID-HF, said she had no relevant disclosures. Dr. O’Connor has been a consultant to ResMed, Roche Diagnostics, Cardiorentis, Bayer, and Actelion and has received research grants from Otsuka, ResMed, Roche Diagnostics. He was a coinvestigator on the CARESS-HF trial. Dr. Yancy had no disclosures.
On Twitter @mitchelzoler
Patients hospitalized with vascular congestion caused by an acute exacerbation of heart failure universally receive loop diuretics, but most patients continue to have persistent congestion and poor outcomes following treatment. In one recent trial, fewer than 20% of patients left the hospital with adequate decongestion regardless of whether they received high- or low-dose furosemide and whether they received it as a bolus or as a continuous infusion (N Engl J Med. 2011 Mar 3;364[9]:797-805). We need an alternative to decongestion by loop-diuretic treatment.
Ultrafiltration offers a number of potential advantages for treating acute congestion, especially for patients unresponsive to diuretic treatment. It provides a way to quickly and predictably remove isotonic fluid with no effect on electrolytes, no neurohormonal stimulation, and in several trials, no significant effect on renal function. It also can restore diuretic responsiveness,
 |
Dr. Bradley A. Bart |
Critics of ultrafiltration often cite the results of the CARRESS-HF [Cardiorenal Rescue Study in Acute Decompensated Heart Failure] trial, which I led (N Engl J Med 2012 Dec 13;367[24]:2296-304). I’m not convinced that the CARRESS-HF results apply to the large majority of patients with acute heart failure. All of the patients enrolled in this trial had acute kidney injury. Also, in CARRESS-HF, we used a control arm that received diuretic treatment in a stepped pharmacologic way, which is not the dosing strategy we usually see in community practice. In addition, CARRESS-HF did not use variable dosing in the ultrafiltration arm. A better comparison of diuretic treatment and ultrafiltration would use variable dosing in both arms.
That’s the design used in AVOID-HF. In this trial, clinicians adjusted both diuretic and ultrafiltration dosages based on the renal function and hemodynamics of each enrolled patient. Unfortunately, AVOID-HF ended too soon, after enrolling just a quarter of the patients calculated as necessary to produce a statistically significant difference in outcomes between the two treatment arms. This appeared to result in a nonsignificant trend in favor of ultrafiltration for the study’s primary endpoint. Despite being extremely underpowered, the results showed significant benefits for ultrafiltration for several secondary endpoints. The results also showed no deleterious effects on renal function with ultrafiltration.
If AVOID-HF had shown no signal of benefit from ultrafiltration then I think that would have meant to end of ultrafiltration, but that is not what happened. The strong trends in favor of ultrafiltration make the case to keep studying it for patients who have become unresponsive to diuretics. In these patients ultrafiltration is a good alternative. Several questions remain unanswered about the use of ultrafiltration, such as exactly when a patient has become too unresponsive to diuretic treatment to warrant using ultrafiltration, and how to optimally dose ultrafiltration. Despite this lingering uncertainty ultrafiltration remains a viable option that deserves more study.
Dr. Bradley A. Bart is professor of medicine at the University of Minnesota and chief of cardiology at Hennepin County Medical Center, both in Minneapolis. He had no financial disclosures. Dr. Bart was lead investigator for the CARRESS-HF trial and a coinvestigator on the AVOID-HF trial. He made these comments in a talk at the meeting and during an interview.
Patients hospitalized with vascular congestion caused by an acute exacerbation of heart failure universally receive loop diuretics, but most patients continue to have persistent congestion and poor outcomes following treatment. In one recent trial, fewer than 20% of patients left the hospital with adequate decongestion regardless of whether they received high- or low-dose furosemide and whether they received it as a bolus or as a continuous infusion (N Engl J Med. 2011 Mar 3;364[9]:797-805). We need an alternative to decongestion by loop-diuretic treatment.
Ultrafiltration offers a number of potential advantages for treating acute congestion, especially for patients unresponsive to diuretic treatment. It provides a way to quickly and predictably remove isotonic fluid with no effect on electrolytes, no neurohormonal stimulation, and in several trials, no significant effect on renal function. It also can restore diuretic responsiveness,
 |
Dr. Bradley A. Bart |
Critics of ultrafiltration often cite the results of the CARRESS-HF [Cardiorenal Rescue Study in Acute Decompensated Heart Failure] trial, which I led (N Engl J Med 2012 Dec 13;367[24]:2296-304). I’m not convinced that the CARRESS-HF results apply to the large majority of patients with acute heart failure. All of the patients enrolled in this trial had acute kidney injury. Also, in CARRESS-HF, we used a control arm that received diuretic treatment in a stepped pharmacologic way, which is not the dosing strategy we usually see in community practice. In addition, CARRESS-HF did not use variable dosing in the ultrafiltration arm. A better comparison of diuretic treatment and ultrafiltration would use variable dosing in both arms.
That’s the design used in AVOID-HF. In this trial, clinicians adjusted both diuretic and ultrafiltration dosages based on the renal function and hemodynamics of each enrolled patient. Unfortunately, AVOID-HF ended too soon, after enrolling just a quarter of the patients calculated as necessary to produce a statistically significant difference in outcomes between the two treatment arms. This appeared to result in a nonsignificant trend in favor of ultrafiltration for the study’s primary endpoint. Despite being extremely underpowered, the results showed significant benefits for ultrafiltration for several secondary endpoints. The results also showed no deleterious effects on renal function with ultrafiltration.
If AVOID-HF had shown no signal of benefit from ultrafiltration then I think that would have meant to end of ultrafiltration, but that is not what happened. The strong trends in favor of ultrafiltration make the case to keep studying it for patients who have become unresponsive to diuretics. In these patients ultrafiltration is a good alternative. Several questions remain unanswered about the use of ultrafiltration, such as exactly when a patient has become too unresponsive to diuretic treatment to warrant using ultrafiltration, and how to optimally dose ultrafiltration. Despite this lingering uncertainty ultrafiltration remains a viable option that deserves more study.
Dr. Bradley A. Bart is professor of medicine at the University of Minnesota and chief of cardiology at Hennepin County Medical Center, both in Minneapolis. He had no financial disclosures. Dr. Bart was lead investigator for the CARRESS-HF trial and a coinvestigator on the AVOID-HF trial. He made these comments in a talk at the meeting and during an interview.
Patients hospitalized with vascular congestion caused by an acute exacerbation of heart failure universally receive loop diuretics, but most patients continue to have persistent congestion and poor outcomes following treatment. In one recent trial, fewer than 20% of patients left the hospital with adequate decongestion regardless of whether they received high- or low-dose furosemide and whether they received it as a bolus or as a continuous infusion (N Engl J Med. 2011 Mar 3;364[9]:797-805). We need an alternative to decongestion by loop-diuretic treatment.
Ultrafiltration offers a number of potential advantages for treating acute congestion, especially for patients unresponsive to diuretic treatment. It provides a way to quickly and predictably remove isotonic fluid with no effect on electrolytes, no neurohormonal stimulation, and in several trials, no significant effect on renal function. It also can restore diuretic responsiveness,
 |
Dr. Bradley A. Bart |
Critics of ultrafiltration often cite the results of the CARRESS-HF [Cardiorenal Rescue Study in Acute Decompensated Heart Failure] trial, which I led (N Engl J Med 2012 Dec 13;367[24]:2296-304). I’m not convinced that the CARRESS-HF results apply to the large majority of patients with acute heart failure. All of the patients enrolled in this trial had acute kidney injury. Also, in CARRESS-HF, we used a control arm that received diuretic treatment in a stepped pharmacologic way, which is not the dosing strategy we usually see in community practice. In addition, CARRESS-HF did not use variable dosing in the ultrafiltration arm. A better comparison of diuretic treatment and ultrafiltration would use variable dosing in both arms.
That’s the design used in AVOID-HF. In this trial, clinicians adjusted both diuretic and ultrafiltration dosages based on the renal function and hemodynamics of each enrolled patient. Unfortunately, AVOID-HF ended too soon, after enrolling just a quarter of the patients calculated as necessary to produce a statistically significant difference in outcomes between the two treatment arms. This appeared to result in a nonsignificant trend in favor of ultrafiltration for the study’s primary endpoint. Despite being extremely underpowered, the results showed significant benefits for ultrafiltration for several secondary endpoints. The results also showed no deleterious effects on renal function with ultrafiltration.
If AVOID-HF had shown no signal of benefit from ultrafiltration then I think that would have meant to end of ultrafiltration, but that is not what happened. The strong trends in favor of ultrafiltration make the case to keep studying it for patients who have become unresponsive to diuretics. In these patients ultrafiltration is a good alternative. Several questions remain unanswered about the use of ultrafiltration, such as exactly when a patient has become too unresponsive to diuretic treatment to warrant using ultrafiltration, and how to optimally dose ultrafiltration. Despite this lingering uncertainty ultrafiltration remains a viable option that deserves more study.
Dr. Bradley A. Bart is professor of medicine at the University of Minnesota and chief of cardiology at Hennepin County Medical Center, both in Minneapolis. He had no financial disclosures. Dr. Bart was lead investigator for the CARRESS-HF trial and a coinvestigator on the AVOID-HF trial. He made these comments in a talk at the meeting and during an interview.
NATIONAL HARBOR, MD. – The trial designed to definitively test the safety and efficacy of ultrafiltration as an alternative to intravenous diuretics for patients hospitalized with acute decompensated heart failure got cut to about a quarter of its planned enrollment by the company that recently acquired the ultrafiltration technology. This outcomes means that ultrafiltration’s role in acute heart failure remains uncertain and will stay that way for the foreseeable future.
As a consequence, ultrafiltration (also known as aquapheresis), approved for use in the United States by the Food and Drug Administration in 2002, will be used by believers in the treatment on some of the estimated 200,000 or more U.S. heart failure patients who become hospitalized each year with acute, severe congestion that is unresponsive to diuretic treatment. Other clinicians who remain skeptical of ultrafiltration’s safety and efficacy will not use it, and currently no prospect remains to resolve this uncertainty. Also limiting ultrafiltration’s use is its designation as investigational by U.S. health insurers.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Early termination off the AVOID-HF [Aquapheresis Vs. Intravenous Diuretics and Hospitalization for Heart Failure] trial was a tragedy because it is unlikely we will ever see a trial of its size again,” commented Dr. G. Michael Felker during a discussion of treatment for acute heart failure at the at the annual meeting of the Heart Failure Society of America. “We still have no definitive answer” about ultrafiltration,” said Dr. Felker, professor of medicine and a cardiologist specializing in acute heart failure at Duke University in Durham, N.C.
Opinions about ultrafiltration and its role in treating patients with acute decompensated heart failure remain sharply split, although at this point, even proponents of the treatment concede that its use is limited to severely congested decompensated heart failure patients who prove unresponsive to intravenous diuretic therapy.
Ultrafiltration is for patients with “recurrent decompensation (not the first episode) and a large amount of fluid overload (more than 10 pounds) who also have elevated central venous pressure and elevated abdominal pressure that reduces blood flow to the kidneys,” Dr. Maria Rosa Costanzo said in a video interview. Used in these patients at a low rate of 20-50 cc/hour to “gently remove fluid,” the treatment reduces central venous and intra-abdominal pressures, leading to increased urine output and restoration of diuretic sensitivity, said Dr. Costanzo, lead investigator for the AVOID-HF trial and medical director of the heart failure and pulmonary hypertension program at the Advocate Heart Institute in Naperville, Ill.
A dramatically opposing view of ultrafiltration came from Dr. Christopher M. O’Connor, a heart failure cardiologist and CEO of the Inova Heart and Vascular Institute in Falls Church, Va.
“Even in diuretic-resistant, patients I would not use ultrafiltration. It does not anymore fit into management” of acute decompensated heart failure patients, Dr. O’Connor said in an interview. The CARRESS-HF [Cardiorenal Rescue Study in Acute Decompensated Heart Failure] trial targeted patients with diuretic resistance, the very population we would need to treat, and we did not see an advantage to ultrafiltration,” said Dr. O’Connor, a coinvestigator on CARRESS-HF, an earlier trial that compared the two treatment methods (N Engl J Med. 2012 Dec 13;367[24]:2296-304).
“We need to understand who is the right patient” for ultrafiltration. “We need to continue to investigate [ultrafiltration] to know where it best fits,” commented Dr. Clyde W. Yancy, professor and chief of cardiology at Northwestern University in Chicago.
AVOID-HF enrolled and randomized 224 patients with acute decompensated heart failure out of an anticipated enrollment of 810 patients. Analysis of the study’s primary endpoint, time to first heart failure event within the first 90 days following hospital discharge, occurred after an average of 34 days in 108 loop-diuretic treated patients and after an average 62 days in 105 ultrafiltration-treated patients, a difference that did not achieve statistical significance. A heart failure event within the first 90 days occurred in 25% of the ultrafiltration patients and in 35% of those on diuretic treatment, also a nonsignificant difference, Dr. Costanzo reported. Concurrent with her report at the meeting an article appeared online with the results (JACC Heart Fail. 2015;doi: 10.1016/j.jchf.2015.08.005).
Increases in serum creatinine were modest following ultrafiltration and similar to changes seen in the patients who received loop diuretic treatment. The biggest rise in average serum creatinine level occurred at 30 days after randomization, with an average 0.37 mg/dL rise among the ultrafiltration patients.
The abrupt shutdown in the AVOID-HF trial occurred following a change in ownership of the ultrafiltration technology used in the study. Ultrafiltration had been initially developed by CHF Solutions of Brooklyn Park, Minn. In 2010, Gambro, a Swedish company, acquired CHF Solutions and rights to the ultrafiltration system, and Gambro initiated the AVOID-HF trial. Baxter, in Deerfield, Ill., acquired Gambro in September 2013, and in April 2014, Baxter stopped the AVOID-HF trial because of slow projected enrollment, said Dr. Costanzo. But she strongly disagreed with this projection, and said that the trial showed no signs of futility or safety concerns when it came to a stop. Getting the data from Baxter to allow her and her associates to write their report and deliver their findings at the meeting took a lot of persuasion, Dr. Costanzo added.
Dr. Felker has been a consultant to and received research grants from 10 drug or device companies. He was a coinvestigator on the CARRESS-HF trial. Dr. Costanzo, lead investigator of AVOID-HF, said she had no relevant disclosures. Dr. O’Connor has been a consultant to ResMed, Roche Diagnostics, Cardiorentis, Bayer, and Actelion and has received research grants from Otsuka, ResMed, Roche Diagnostics. He was a coinvestigator on the CARESS-HF trial. Dr. Yancy had no disclosures.
On Twitter @mitchelzoler
NATIONAL HARBOR, MD. – The trial designed to definitively test the safety and efficacy of ultrafiltration as an alternative to intravenous diuretics for patients hospitalized with acute decompensated heart failure got cut to about a quarter of its planned enrollment by the company that recently acquired the ultrafiltration technology. This outcomes means that ultrafiltration’s role in acute heart failure remains uncertain and will stay that way for the foreseeable future.
As a consequence, ultrafiltration (also known as aquapheresis), approved for use in the United States by the Food and Drug Administration in 2002, will be used by believers in the treatment on some of the estimated 200,000 or more U.S. heart failure patients who become hospitalized each year with acute, severe congestion that is unresponsive to diuretic treatment. Other clinicians who remain skeptical of ultrafiltration’s safety and efficacy will not use it, and currently no prospect remains to resolve this uncertainty. Also limiting ultrafiltration’s use is its designation as investigational by U.S. health insurers.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Early termination off the AVOID-HF [Aquapheresis Vs. Intravenous Diuretics and Hospitalization for Heart Failure] trial was a tragedy because it is unlikely we will ever see a trial of its size again,” commented Dr. G. Michael Felker during a discussion of treatment for acute heart failure at the at the annual meeting of the Heart Failure Society of America. “We still have no definitive answer” about ultrafiltration,” said Dr. Felker, professor of medicine and a cardiologist specializing in acute heart failure at Duke University in Durham, N.C.
Opinions about ultrafiltration and its role in treating patients with acute decompensated heart failure remain sharply split, although at this point, even proponents of the treatment concede that its use is limited to severely congested decompensated heart failure patients who prove unresponsive to intravenous diuretic therapy.
Ultrafiltration is for patients with “recurrent decompensation (not the first episode) and a large amount of fluid overload (more than 10 pounds) who also have elevated central venous pressure and elevated abdominal pressure that reduces blood flow to the kidneys,” Dr. Maria Rosa Costanzo said in a video interview. Used in these patients at a low rate of 20-50 cc/hour to “gently remove fluid,” the treatment reduces central venous and intra-abdominal pressures, leading to increased urine output and restoration of diuretic sensitivity, said Dr. Costanzo, lead investigator for the AVOID-HF trial and medical director of the heart failure and pulmonary hypertension program at the Advocate Heart Institute in Naperville, Ill.
A dramatically opposing view of ultrafiltration came from Dr. Christopher M. O’Connor, a heart failure cardiologist and CEO of the Inova Heart and Vascular Institute in Falls Church, Va.
“Even in diuretic-resistant, patients I would not use ultrafiltration. It does not anymore fit into management” of acute decompensated heart failure patients, Dr. O’Connor said in an interview. The CARRESS-HF [Cardiorenal Rescue Study in Acute Decompensated Heart Failure] trial targeted patients with diuretic resistance, the very population we would need to treat, and we did not see an advantage to ultrafiltration,” said Dr. O’Connor, a coinvestigator on CARRESS-HF, an earlier trial that compared the two treatment methods (N Engl J Med. 2012 Dec 13;367[24]:2296-304).
“We need to understand who is the right patient” for ultrafiltration. “We need to continue to investigate [ultrafiltration] to know where it best fits,” commented Dr. Clyde W. Yancy, professor and chief of cardiology at Northwestern University in Chicago.
AVOID-HF enrolled and randomized 224 patients with acute decompensated heart failure out of an anticipated enrollment of 810 patients. Analysis of the study’s primary endpoint, time to first heart failure event within the first 90 days following hospital discharge, occurred after an average of 34 days in 108 loop-diuretic treated patients and after an average 62 days in 105 ultrafiltration-treated patients, a difference that did not achieve statistical significance. A heart failure event within the first 90 days occurred in 25% of the ultrafiltration patients and in 35% of those on diuretic treatment, also a nonsignificant difference, Dr. Costanzo reported. Concurrent with her report at the meeting an article appeared online with the results (JACC Heart Fail. 2015;doi: 10.1016/j.jchf.2015.08.005).
Increases in serum creatinine were modest following ultrafiltration and similar to changes seen in the patients who received loop diuretic treatment. The biggest rise in average serum creatinine level occurred at 30 days after randomization, with an average 0.37 mg/dL rise among the ultrafiltration patients.
The abrupt shutdown in the AVOID-HF trial occurred following a change in ownership of the ultrafiltration technology used in the study. Ultrafiltration had been initially developed by CHF Solutions of Brooklyn Park, Minn. In 2010, Gambro, a Swedish company, acquired CHF Solutions and rights to the ultrafiltration system, and Gambro initiated the AVOID-HF trial. Baxter, in Deerfield, Ill., acquired Gambro in September 2013, and in April 2014, Baxter stopped the AVOID-HF trial because of slow projected enrollment, said Dr. Costanzo. But she strongly disagreed with this projection, and said that the trial showed no signs of futility or safety concerns when it came to a stop. Getting the data from Baxter to allow her and her associates to write their report and deliver their findings at the meeting took a lot of persuasion, Dr. Costanzo added.
Dr. Felker has been a consultant to and received research grants from 10 drug or device companies. He was a coinvestigator on the CARRESS-HF trial. Dr. Costanzo, lead investigator of AVOID-HF, said she had no relevant disclosures. Dr. O’Connor has been a consultant to ResMed, Roche Diagnostics, Cardiorentis, Bayer, and Actelion and has received research grants from Otsuka, ResMed, Roche Diagnostics. He was a coinvestigator on the CARESS-HF trial. Dr. Yancy had no disclosures.
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point: Early halt to the AVOID-HF trial prevented the study from definitively comparing ultrafiltration with intravenous diuretic treatment in patients with acute decompensated heart failure.
Major finding: Average time to first heart-failure event was 62 days with ultrafiltration and 34 days with diuretic treatment, a nonsignificant difference.
Data source: AVOID-HF, a randomized trial that enrolled 224 patients at 30 U.S. centers.
Disclosures: AVOID-HF was initially sponsored by Gambro, which was later acquired by Baxter. Dr. Costanzo had no relevant disclosures.
TCT: Scoring balloon boosts efficacy against in-stent restenosis
SAN FRANCISCO – Drug-coated balloons are an option in Europe for treating in-stent restenosis in coronary arteries, and new results from a randomized trial with 252 German patients showed that the efficacy of a drug-coated balloon for treating restenosis jumped significantly when preceded by prepping the in-stent restenosis with a scoring-balloon inflation.
“Neointimal modification with a scoring balloon significantly improved the antirestenotic efficacy of a paclitaxel-coated balloon” measured by angiography 6-8 months after the intervention, Dr. Robert A. Byrne said at the at the Transcatheter Cardiovascular Therapeutics annual meeting.
Using a scoring balloon first led to an average 35% diameter stenosis in the treated segment at follow-up angiography, compared with a 40% average diameter stenosis at follow-up in patients treated with a paclitaxel-coated balloon alone, without the scoring-balloon first.
“We feel that even this modest increased benefit might be relevant for practice,” said Dr. Byrne, an interventional cardiologist at the German Heart Center in Munich. “This is a challenging patient group, particularly patients who develop restenosis inside a drug-eluting stent. Even small gains are worth pursuing.” All patients enrolled in the study had their restenosis inside a drug-eluting stent.
“It was a modest benefit,” but the alternative to treating in-stent restenosis with a drug-eluting balloon is using a stent, which creates a stent-in-stent situation and has relatively poor outcomes, commented Dr. David J. Cohen, director of cardiovascular research at Saint Luke’s Mid America Heart Institute in Kansas City. Dr. Cohen noted that, as of now, no drug-coated balloon has received approval for U.S. marketing.
“The most important message was that if you treat in-stent restenosis with a drug-coated balloon, then lesion preparation is the most important step,” commented Dr. Bruno Scheller, professor and interventional cardiologist at the University Clinic of Saarland in Homburg, Germany.
The ISAR-DESIRE 4 (Intracoronary Stenting and Angiographic Results: Optimizing Treatment of Drug Eluting Stent In-Stent Restenosis 4) trial enrolled 252 patients with restenosis inside a drug-eluting coronary stent at four German centers during June 2012–December 2014. Patients averaged 69 years old, about 85% were men, and about 42% had diabetes. The study randomized patients to pretreatment with either a scoring balloon or a conventional balloon. After that, all lesions received treatment with a paclitaxel-coated balloon (Pantera Lux).
The study’s primary endpoint was average-diameter stenosis on follow-up angiography 6-8 months after treatment. Scoring balloon pretreatment produced a five percentage-point decline in the diameter stenosis at follow-up. In addition, the secondary outcome of binary restenosis – the percentage of patients with at least 50% diameter stenosis at follow-up – occurred at a 19% rate in the 125 patients pretreated with a scoring balloon and a 32% rate in the 127 control patients pretreated with a conventional balloon, Dr. Byrne reported at the meeting, sponsored by the Cardiovascular Research Foundation.
Scoring-balloon pretreatment also produced a trend toward fewer patients undergoing a new revascularization procedure during 1 year of clinical follow-up, with a 17% revascularization rate among patients pretreated with a scoring balloon and a 23% rate among the controls. The primary safety outcome, the combined rate of death and nonfatal MIs during 1-year clinical follow-up, occurred at an identical 3% rate in both treatment arms.
The ISAR-DESIRE 4 trial was cosponsored by Biotronik, which markets the paclitaxel-coated balloon (Pantera Lux) used in the trial. Dr. Byrne said that he has received speaking fees from Biotronik and from Boston Scientific and B. Braun Melsungen. Dr. Cohen has been a consultant to Abbott Vascular and Medtronic, a speaker for AstraZeneca, and he has received research grants from nine companies. Dr. Scheller has several patents involving drug-coated balloons.
On Twitter @mitchelzoler
Stenosis often forms within a stent because initial placement failed to open the stent to its optimal diameter. In these cases, treating the stenosis with a second stent inside the first does not make sense. The more attractive alternative is to treat the stenosis with a couple of balloons, with one balloon aimed at retreating the existing stent to open it more optimally.
 |
Dr. Marco Valgimigli |
Until now, studies designed to show the efficacy of a drug-coated balloon in treating in-stent restenosis have generally not been of high quality, and in Europe, drug-coated balloons have been more expensive than drug-eluting stents and are often not reimbursed by medical coverage programs. But the results from ISAR-DESIRE 4 may change that because they are convincing.
The incremental benefit produced by first using a scoring balloon highlights the importance of preparing a coronary stenosis before treating it with a drug-coated balloon. The effect of the scoring balloon on further opening the existing stent may have been as important or more important than the scoring itself.
Regardless of the exact mechanism of benefit, the treatment method tested in ISAR-DESIRE 4 showed a small but significant incremental benefit from scoring pretreatment, and the benefit was large enough to warrant adoption. In-stent restenosis is very challenging to treat, so any significant gain in efficacy is welcome. It is very important to treat the restenosis optimally the first time, because it is often refractory and keeps recurring and when this happens, the only alternative is coronary bypass surgery. The approach that succeeded in ISAR-DESIRE 4 is worth trying if it can prevent some patients from needing bypass surgery.
Dr. Marco Valgimigli is an interventional cardiologist at Inselspital University Hospital in Bern, Switzerland. He made these comments in an interview. He had no disclosures.
Stenosis often forms within a stent because initial placement failed to open the stent to its optimal diameter. In these cases, treating the stenosis with a second stent inside the first does not make sense. The more attractive alternative is to treat the stenosis with a couple of balloons, with one balloon aimed at retreating the existing stent to open it more optimally.
 |
Dr. Marco Valgimigli |
Until now, studies designed to show the efficacy of a drug-coated balloon in treating in-stent restenosis have generally not been of high quality, and in Europe, drug-coated balloons have been more expensive than drug-eluting stents and are often not reimbursed by medical coverage programs. But the results from ISAR-DESIRE 4 may change that because they are convincing.
The incremental benefit produced by first using a scoring balloon highlights the importance of preparing a coronary stenosis before treating it with a drug-coated balloon. The effect of the scoring balloon on further opening the existing stent may have been as important or more important than the scoring itself.
Regardless of the exact mechanism of benefit, the treatment method tested in ISAR-DESIRE 4 showed a small but significant incremental benefit from scoring pretreatment, and the benefit was large enough to warrant adoption. In-stent restenosis is very challenging to treat, so any significant gain in efficacy is welcome. It is very important to treat the restenosis optimally the first time, because it is often refractory and keeps recurring and when this happens, the only alternative is coronary bypass surgery. The approach that succeeded in ISAR-DESIRE 4 is worth trying if it can prevent some patients from needing bypass surgery.
Dr. Marco Valgimigli is an interventional cardiologist at Inselspital University Hospital in Bern, Switzerland. He made these comments in an interview. He had no disclosures.
Stenosis often forms within a stent because initial placement failed to open the stent to its optimal diameter. In these cases, treating the stenosis with a second stent inside the first does not make sense. The more attractive alternative is to treat the stenosis with a couple of balloons, with one balloon aimed at retreating the existing stent to open it more optimally.
 |
Dr. Marco Valgimigli |
Until now, studies designed to show the efficacy of a drug-coated balloon in treating in-stent restenosis have generally not been of high quality, and in Europe, drug-coated balloons have been more expensive than drug-eluting stents and are often not reimbursed by medical coverage programs. But the results from ISAR-DESIRE 4 may change that because they are convincing.
The incremental benefit produced by first using a scoring balloon highlights the importance of preparing a coronary stenosis before treating it with a drug-coated balloon. The effect of the scoring balloon on further opening the existing stent may have been as important or more important than the scoring itself.
Regardless of the exact mechanism of benefit, the treatment method tested in ISAR-DESIRE 4 showed a small but significant incremental benefit from scoring pretreatment, and the benefit was large enough to warrant adoption. In-stent restenosis is very challenging to treat, so any significant gain in efficacy is welcome. It is very important to treat the restenosis optimally the first time, because it is often refractory and keeps recurring and when this happens, the only alternative is coronary bypass surgery. The approach that succeeded in ISAR-DESIRE 4 is worth trying if it can prevent some patients from needing bypass surgery.
Dr. Marco Valgimigli is an interventional cardiologist at Inselspital University Hospital in Bern, Switzerland. He made these comments in an interview. He had no disclosures.
SAN FRANCISCO – Drug-coated balloons are an option in Europe for treating in-stent restenosis in coronary arteries, and new results from a randomized trial with 252 German patients showed that the efficacy of a drug-coated balloon for treating restenosis jumped significantly when preceded by prepping the in-stent restenosis with a scoring-balloon inflation.
“Neointimal modification with a scoring balloon significantly improved the antirestenotic efficacy of a paclitaxel-coated balloon” measured by angiography 6-8 months after the intervention, Dr. Robert A. Byrne said at the at the Transcatheter Cardiovascular Therapeutics annual meeting.
Using a scoring balloon first led to an average 35% diameter stenosis in the treated segment at follow-up angiography, compared with a 40% average diameter stenosis at follow-up in patients treated with a paclitaxel-coated balloon alone, without the scoring-balloon first.
“We feel that even this modest increased benefit might be relevant for practice,” said Dr. Byrne, an interventional cardiologist at the German Heart Center in Munich. “This is a challenging patient group, particularly patients who develop restenosis inside a drug-eluting stent. Even small gains are worth pursuing.” All patients enrolled in the study had their restenosis inside a drug-eluting stent.
“It was a modest benefit,” but the alternative to treating in-stent restenosis with a drug-eluting balloon is using a stent, which creates a stent-in-stent situation and has relatively poor outcomes, commented Dr. David J. Cohen, director of cardiovascular research at Saint Luke’s Mid America Heart Institute in Kansas City. Dr. Cohen noted that, as of now, no drug-coated balloon has received approval for U.S. marketing.
“The most important message was that if you treat in-stent restenosis with a drug-coated balloon, then lesion preparation is the most important step,” commented Dr. Bruno Scheller, professor and interventional cardiologist at the University Clinic of Saarland in Homburg, Germany.
The ISAR-DESIRE 4 (Intracoronary Stenting and Angiographic Results: Optimizing Treatment of Drug Eluting Stent In-Stent Restenosis 4) trial enrolled 252 patients with restenosis inside a drug-eluting coronary stent at four German centers during June 2012–December 2014. Patients averaged 69 years old, about 85% were men, and about 42% had diabetes. The study randomized patients to pretreatment with either a scoring balloon or a conventional balloon. After that, all lesions received treatment with a paclitaxel-coated balloon (Pantera Lux).
The study’s primary endpoint was average-diameter stenosis on follow-up angiography 6-8 months after treatment. Scoring balloon pretreatment produced a five percentage-point decline in the diameter stenosis at follow-up. In addition, the secondary outcome of binary restenosis – the percentage of patients with at least 50% diameter stenosis at follow-up – occurred at a 19% rate in the 125 patients pretreated with a scoring balloon and a 32% rate in the 127 control patients pretreated with a conventional balloon, Dr. Byrne reported at the meeting, sponsored by the Cardiovascular Research Foundation.
Scoring-balloon pretreatment also produced a trend toward fewer patients undergoing a new revascularization procedure during 1 year of clinical follow-up, with a 17% revascularization rate among patients pretreated with a scoring balloon and a 23% rate among the controls. The primary safety outcome, the combined rate of death and nonfatal MIs during 1-year clinical follow-up, occurred at an identical 3% rate in both treatment arms.
The ISAR-DESIRE 4 trial was cosponsored by Biotronik, which markets the paclitaxel-coated balloon (Pantera Lux) used in the trial. Dr. Byrne said that he has received speaking fees from Biotronik and from Boston Scientific and B. Braun Melsungen. Dr. Cohen has been a consultant to Abbott Vascular and Medtronic, a speaker for AstraZeneca, and he has received research grants from nine companies. Dr. Scheller has several patents involving drug-coated balloons.
On Twitter @mitchelzoler
SAN FRANCISCO – Drug-coated balloons are an option in Europe for treating in-stent restenosis in coronary arteries, and new results from a randomized trial with 252 German patients showed that the efficacy of a drug-coated balloon for treating restenosis jumped significantly when preceded by prepping the in-stent restenosis with a scoring-balloon inflation.
“Neointimal modification with a scoring balloon significantly improved the antirestenotic efficacy of a paclitaxel-coated balloon” measured by angiography 6-8 months after the intervention, Dr. Robert A. Byrne said at the at the Transcatheter Cardiovascular Therapeutics annual meeting.
Using a scoring balloon first led to an average 35% diameter stenosis in the treated segment at follow-up angiography, compared with a 40% average diameter stenosis at follow-up in patients treated with a paclitaxel-coated balloon alone, without the scoring-balloon first.
“We feel that even this modest increased benefit might be relevant for practice,” said Dr. Byrne, an interventional cardiologist at the German Heart Center in Munich. “This is a challenging patient group, particularly patients who develop restenosis inside a drug-eluting stent. Even small gains are worth pursuing.” All patients enrolled in the study had their restenosis inside a drug-eluting stent.
“It was a modest benefit,” but the alternative to treating in-stent restenosis with a drug-eluting balloon is using a stent, which creates a stent-in-stent situation and has relatively poor outcomes, commented Dr. David J. Cohen, director of cardiovascular research at Saint Luke’s Mid America Heart Institute in Kansas City. Dr. Cohen noted that, as of now, no drug-coated balloon has received approval for U.S. marketing.
“The most important message was that if you treat in-stent restenosis with a drug-coated balloon, then lesion preparation is the most important step,” commented Dr. Bruno Scheller, professor and interventional cardiologist at the University Clinic of Saarland in Homburg, Germany.
The ISAR-DESIRE 4 (Intracoronary Stenting and Angiographic Results: Optimizing Treatment of Drug Eluting Stent In-Stent Restenosis 4) trial enrolled 252 patients with restenosis inside a drug-eluting coronary stent at four German centers during June 2012–December 2014. Patients averaged 69 years old, about 85% were men, and about 42% had diabetes. The study randomized patients to pretreatment with either a scoring balloon or a conventional balloon. After that, all lesions received treatment with a paclitaxel-coated balloon (Pantera Lux).
The study’s primary endpoint was average-diameter stenosis on follow-up angiography 6-8 months after treatment. Scoring balloon pretreatment produced a five percentage-point decline in the diameter stenosis at follow-up. In addition, the secondary outcome of binary restenosis – the percentage of patients with at least 50% diameter stenosis at follow-up – occurred at a 19% rate in the 125 patients pretreated with a scoring balloon and a 32% rate in the 127 control patients pretreated with a conventional balloon, Dr. Byrne reported at the meeting, sponsored by the Cardiovascular Research Foundation.
Scoring-balloon pretreatment also produced a trend toward fewer patients undergoing a new revascularization procedure during 1 year of clinical follow-up, with a 17% revascularization rate among patients pretreated with a scoring balloon and a 23% rate among the controls. The primary safety outcome, the combined rate of death and nonfatal MIs during 1-year clinical follow-up, occurred at an identical 3% rate in both treatment arms.
The ISAR-DESIRE 4 trial was cosponsored by Biotronik, which markets the paclitaxel-coated balloon (Pantera Lux) used in the trial. Dr. Byrne said that he has received speaking fees from Biotronik and from Boston Scientific and B. Braun Melsungen. Dr. Cohen has been a consultant to Abbott Vascular and Medtronic, a speaker for AstraZeneca, and he has received research grants from nine companies. Dr. Scheller has several patents involving drug-coated balloons.
On Twitter @mitchelzoler
AT TCT 2015
Key clinical point: Pretreating in-stent restenosis with a scoring balloon before using a drug-coated balloon significantly boosted efficacy.
Major finding: After 6 months, average diameter stenosis following paclitaxel-coated balloon treatment was 35% with a scoring balloon and 40% without.
Data source: ISAR-DESIRE 4, a randomized trial of 252 patients at four German centers.
Disclosures: The ISAR-DESIRE 4 trial was cosponsored by Biotronik, which markets the paclitaxel-coated balloon (Pantera Lux) used in the trial. Dr. Byrne said that he has received speaking fees from Biotronik and from Boston Scientific and B. Braun Melsungen.
TCT: Ranolazine fails to block angina after incomplete revascularization
SAN FRANCISCO – The antianginal drug ranolazine proved safe but completely ineffective at heading off new, severe anginal episodes when used prophylactically in patients who had recently undergone an incomplete revascularization in a prospective trial with more than 2,600 randomized patients.
While the trial failed to identify a new treatment to help these patients, it succeeded in better defining and documenting an at-risk population that could use a new, effective treatment of some kind: patients who have recently undergone incomplete revascularization.
The RIVER-PCI (Ranolazine for Incomplete Vessel Revascularization Post-Percutaneous Coronary Intervention) trial prospectively followed a large group of these patients with just one other qualification: They had to have also experienced at least two anginal episodes during the prior 1-12 months (angina within 30 days of the PCI didn’t count). The study results showed that during an average 1.8 years of follow-up, these patients had a 27% rate of ischemic, anginal episodes severe enough to push them to either hospitalization or another round of revascularization, Dr. Giora Weisz reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
“This event rate is very high. I want to better treat and do something more for these patients” with incomplete revascularization, “So we still need to look for an answer, to look for other options that might improve their outcomes,” said Dr. Weisz, professor and director of cardiology at the Jerusalem Heart Center of Shaare Zedek Medical Center.
Incomplete revascularization – defined in the study as coronary stenoses visible on an angiogram that block at least 50% of a coronary artery that is at least 2 mm in diameter – occurs quite often, Dr. Weisz noted. These significant stenoses exist in roughly half the patients who undergo PCI and in some instances in as many as 80%. These lesions usually go untreated because they seem clinically unimportant at the time of the index procedure, he explained.
“We need to better understand why the prognosis is so bad” in incompletely revascularized patients. “We need to better understand which lesions are the ones that produce poor outcomes and how we can better treat them both pharmacologically and with interventions,” commented Dr. Stefan James, a professor of cardiology at Uppsala (Sweden) University.
The findings also highlighted the limitations of ranolazine (Ranexa) as a treatment for angina and cardiac ischemia, although Dr. Weisz and others remained convinced that it is an effective drug for reducing angina in other situations, specifically patients with recurring episodes of severe angina.
Ranolazine “did not prevent ischemia, but it remains useful for patients with refractory angina; that is a separate indication,” commented Dr. Sanjit S. Jolly of McMaster University, Hamilton, Ont.
Dr. Weisz speculated that one explanation for ranolazine’s lack of efficacy is that the drug doesn’t prevent ischemia and angina directly but rather interrupts the self-exacerbating cycle of angina. The ischemia that produces angina activates “late sodium” channels in myocardial cells, which boosts intracellular calcium levels and increases oxygen demand in cells while also dropping intracellular oxygen supply, thereby triggering further worsening of the ischemia, he explained. “Ischemia aggravates itself, and ranolazine prevents this by blocking the late sodium channels,” but clearly this effect did not prevent new anginal episodes in patients who experienced incomplete revascularization, he said in an interview.
Dr. Weisz and his associates ran RIVER-PCI during November 2011–May 2013 at 245 sites in 15 countries. They randomized and followed 1,317 patients who received 1,000 mg ranolazine twice daily and 1,287 placebo patients. All patients also received all the other medications appropriate for post-PCI patients, including aspirin and another antiplatelet drug, a statin, a beta-blocker, renin-angiotensin-aldosterone system blocking drugs, as well as other blood pressure lowering and vasodilating medications.
During an average follow-up of 1.8 years, patients in the ranolazine arm had a 26% incidence of ischemia-driven hospitalization of revascularization, and patients in the control arm had a 28% rate, a between-group difference that was not statistically significant. Ranolazine treatment had no significant benefit over placebo for any secondary efficacy measure, but it was also safe and generally well tolerated. About 40% of patients in the ranolazine arm and 36% in the placebo arm discontinued their study treatment during the course of follow-up. Concurrent with Dr. Weisz’s report the results also appeared in an article published online (Lancet 2015 Oct 13;doi: 10.1016/S0140-6736[15]00459-6).
During his report of the findings, Dr. Weisz defended the endpoint used in the study, ischemia-driven hospitalization or revascularization, which he conceded could be considered a “soft” endpoint.
“We had a very strict definition of these events, and every episode was reviewed by an independent committee that judged whether or not to include the event. Every patient with an ischemia-driven event had to show characteristic symptoms and objective evidence of ischemia such as an ECG change or elevated enzymes. We tried to approach judging patient symptoms as scientifically as possible,” he said.
On Twitter @mitchelzoler
The adjunctive treatment of patients who undergo incomplete revascularization is a real unmet need. The results from the RIVER-PCI trial showed that about 27% of patients who undergo an incomplete revascularization with percutaneous coronary intervention have a major ischemia-driven event within the next 2 years. In RIVER-PCI, we were unable to prevent these events by giving patients the anti-ischemia drug ranolazine.
In the study, the rates of new MIs and cardiovascular mortality were relatively low. It was recurrent ischemic events that drove the outcome we saw. If nothing else, this study has opened a new avenue for research into this high-risk group of patients.
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Gregg W. Stone |
As interventional cardiologists, we don’t usually think about the coronary disease that we leave behind following a revascularization procedure. Patients who undergo incomplete revascularization may avoid having an excess of future MIs or death, but they still experience a lot of angina, which leads to rehospitalizations and new procedures. I think we could improve the quality of life for our patients if we can come up with new ways to improve revascularization procedures and better approaches to preventing ischemia and angina following these procedures.
Dr. Gregg W. Stone was chairman of the RIVER-PCI trial and is professor and director of cardiovascular research and education at the Center for Interventional Vascular Therapy at Columbia University in New York. He has been a consultant to nine companies but has no relationship with Gilead Sciences and the Menarini Group, the two companies that sponsored the trial and that market ranolazine. He made these comments during the session that discussed the RIVER-PCI results.
The adjunctive treatment of patients who undergo incomplete revascularization is a real unmet need. The results from the RIVER-PCI trial showed that about 27% of patients who undergo an incomplete revascularization with percutaneous coronary intervention have a major ischemia-driven event within the next 2 years. In RIVER-PCI, we were unable to prevent these events by giving patients the anti-ischemia drug ranolazine.
In the study, the rates of new MIs and cardiovascular mortality were relatively low. It was recurrent ischemic events that drove the outcome we saw. If nothing else, this study has opened a new avenue for research into this high-risk group of patients.
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Gregg W. Stone |
As interventional cardiologists, we don’t usually think about the coronary disease that we leave behind following a revascularization procedure. Patients who undergo incomplete revascularization may avoid having an excess of future MIs or death, but they still experience a lot of angina, which leads to rehospitalizations and new procedures. I think we could improve the quality of life for our patients if we can come up with new ways to improve revascularization procedures and better approaches to preventing ischemia and angina following these procedures.
Dr. Gregg W. Stone was chairman of the RIVER-PCI trial and is professor and director of cardiovascular research and education at the Center for Interventional Vascular Therapy at Columbia University in New York. He has been a consultant to nine companies but has no relationship with Gilead Sciences and the Menarini Group, the two companies that sponsored the trial and that market ranolazine. He made these comments during the session that discussed the RIVER-PCI results.
The adjunctive treatment of patients who undergo incomplete revascularization is a real unmet need. The results from the RIVER-PCI trial showed that about 27% of patients who undergo an incomplete revascularization with percutaneous coronary intervention have a major ischemia-driven event within the next 2 years. In RIVER-PCI, we were unable to prevent these events by giving patients the anti-ischemia drug ranolazine.
In the study, the rates of new MIs and cardiovascular mortality were relatively low. It was recurrent ischemic events that drove the outcome we saw. If nothing else, this study has opened a new avenue for research into this high-risk group of patients.
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Gregg W. Stone |
As interventional cardiologists, we don’t usually think about the coronary disease that we leave behind following a revascularization procedure. Patients who undergo incomplete revascularization may avoid having an excess of future MIs or death, but they still experience a lot of angina, which leads to rehospitalizations and new procedures. I think we could improve the quality of life for our patients if we can come up with new ways to improve revascularization procedures and better approaches to preventing ischemia and angina following these procedures.
Dr. Gregg W. Stone was chairman of the RIVER-PCI trial and is professor and director of cardiovascular research and education at the Center for Interventional Vascular Therapy at Columbia University in New York. He has been a consultant to nine companies but has no relationship with Gilead Sciences and the Menarini Group, the two companies that sponsored the trial and that market ranolazine. He made these comments during the session that discussed the RIVER-PCI results.
SAN FRANCISCO – The antianginal drug ranolazine proved safe but completely ineffective at heading off new, severe anginal episodes when used prophylactically in patients who had recently undergone an incomplete revascularization in a prospective trial with more than 2,600 randomized patients.
While the trial failed to identify a new treatment to help these patients, it succeeded in better defining and documenting an at-risk population that could use a new, effective treatment of some kind: patients who have recently undergone incomplete revascularization.
The RIVER-PCI (Ranolazine for Incomplete Vessel Revascularization Post-Percutaneous Coronary Intervention) trial prospectively followed a large group of these patients with just one other qualification: They had to have also experienced at least two anginal episodes during the prior 1-12 months (angina within 30 days of the PCI didn’t count). The study results showed that during an average 1.8 years of follow-up, these patients had a 27% rate of ischemic, anginal episodes severe enough to push them to either hospitalization or another round of revascularization, Dr. Giora Weisz reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
“This event rate is very high. I want to better treat and do something more for these patients” with incomplete revascularization, “So we still need to look for an answer, to look for other options that might improve their outcomes,” said Dr. Weisz, professor and director of cardiology at the Jerusalem Heart Center of Shaare Zedek Medical Center.
Incomplete revascularization – defined in the study as coronary stenoses visible on an angiogram that block at least 50% of a coronary artery that is at least 2 mm in diameter – occurs quite often, Dr. Weisz noted. These significant stenoses exist in roughly half the patients who undergo PCI and in some instances in as many as 80%. These lesions usually go untreated because they seem clinically unimportant at the time of the index procedure, he explained.
“We need to better understand why the prognosis is so bad” in incompletely revascularized patients. “We need to better understand which lesions are the ones that produce poor outcomes and how we can better treat them both pharmacologically and with interventions,” commented Dr. Stefan James, a professor of cardiology at Uppsala (Sweden) University.
The findings also highlighted the limitations of ranolazine (Ranexa) as a treatment for angina and cardiac ischemia, although Dr. Weisz and others remained convinced that it is an effective drug for reducing angina in other situations, specifically patients with recurring episodes of severe angina.
Ranolazine “did not prevent ischemia, but it remains useful for patients with refractory angina; that is a separate indication,” commented Dr. Sanjit S. Jolly of McMaster University, Hamilton, Ont.
Dr. Weisz speculated that one explanation for ranolazine’s lack of efficacy is that the drug doesn’t prevent ischemia and angina directly but rather interrupts the self-exacerbating cycle of angina. The ischemia that produces angina activates “late sodium” channels in myocardial cells, which boosts intracellular calcium levels and increases oxygen demand in cells while also dropping intracellular oxygen supply, thereby triggering further worsening of the ischemia, he explained. “Ischemia aggravates itself, and ranolazine prevents this by blocking the late sodium channels,” but clearly this effect did not prevent new anginal episodes in patients who experienced incomplete revascularization, he said in an interview.
Dr. Weisz and his associates ran RIVER-PCI during November 2011–May 2013 at 245 sites in 15 countries. They randomized and followed 1,317 patients who received 1,000 mg ranolazine twice daily and 1,287 placebo patients. All patients also received all the other medications appropriate for post-PCI patients, including aspirin and another antiplatelet drug, a statin, a beta-blocker, renin-angiotensin-aldosterone system blocking drugs, as well as other blood pressure lowering and vasodilating medications.
During an average follow-up of 1.8 years, patients in the ranolazine arm had a 26% incidence of ischemia-driven hospitalization of revascularization, and patients in the control arm had a 28% rate, a between-group difference that was not statistically significant. Ranolazine treatment had no significant benefit over placebo for any secondary efficacy measure, but it was also safe and generally well tolerated. About 40% of patients in the ranolazine arm and 36% in the placebo arm discontinued their study treatment during the course of follow-up. Concurrent with Dr. Weisz’s report the results also appeared in an article published online (Lancet 2015 Oct 13;doi: 10.1016/S0140-6736[15]00459-6).
During his report of the findings, Dr. Weisz defended the endpoint used in the study, ischemia-driven hospitalization or revascularization, which he conceded could be considered a “soft” endpoint.
“We had a very strict definition of these events, and every episode was reviewed by an independent committee that judged whether or not to include the event. Every patient with an ischemia-driven event had to show characteristic symptoms and objective evidence of ischemia such as an ECG change or elevated enzymes. We tried to approach judging patient symptoms as scientifically as possible,” he said.
On Twitter @mitchelzoler
SAN FRANCISCO – The antianginal drug ranolazine proved safe but completely ineffective at heading off new, severe anginal episodes when used prophylactically in patients who had recently undergone an incomplete revascularization in a prospective trial with more than 2,600 randomized patients.
While the trial failed to identify a new treatment to help these patients, it succeeded in better defining and documenting an at-risk population that could use a new, effective treatment of some kind: patients who have recently undergone incomplete revascularization.
The RIVER-PCI (Ranolazine for Incomplete Vessel Revascularization Post-Percutaneous Coronary Intervention) trial prospectively followed a large group of these patients with just one other qualification: They had to have also experienced at least two anginal episodes during the prior 1-12 months (angina within 30 days of the PCI didn’t count). The study results showed that during an average 1.8 years of follow-up, these patients had a 27% rate of ischemic, anginal episodes severe enough to push them to either hospitalization or another round of revascularization, Dr. Giora Weisz reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
“This event rate is very high. I want to better treat and do something more for these patients” with incomplete revascularization, “So we still need to look for an answer, to look for other options that might improve their outcomes,” said Dr. Weisz, professor and director of cardiology at the Jerusalem Heart Center of Shaare Zedek Medical Center.
Incomplete revascularization – defined in the study as coronary stenoses visible on an angiogram that block at least 50% of a coronary artery that is at least 2 mm in diameter – occurs quite often, Dr. Weisz noted. These significant stenoses exist in roughly half the patients who undergo PCI and in some instances in as many as 80%. These lesions usually go untreated because they seem clinically unimportant at the time of the index procedure, he explained.
“We need to better understand why the prognosis is so bad” in incompletely revascularized patients. “We need to better understand which lesions are the ones that produce poor outcomes and how we can better treat them both pharmacologically and with interventions,” commented Dr. Stefan James, a professor of cardiology at Uppsala (Sweden) University.
The findings also highlighted the limitations of ranolazine (Ranexa) as a treatment for angina and cardiac ischemia, although Dr. Weisz and others remained convinced that it is an effective drug for reducing angina in other situations, specifically patients with recurring episodes of severe angina.
Ranolazine “did not prevent ischemia, but it remains useful for patients with refractory angina; that is a separate indication,” commented Dr. Sanjit S. Jolly of McMaster University, Hamilton, Ont.
Dr. Weisz speculated that one explanation for ranolazine’s lack of efficacy is that the drug doesn’t prevent ischemia and angina directly but rather interrupts the self-exacerbating cycle of angina. The ischemia that produces angina activates “late sodium” channels in myocardial cells, which boosts intracellular calcium levels and increases oxygen demand in cells while also dropping intracellular oxygen supply, thereby triggering further worsening of the ischemia, he explained. “Ischemia aggravates itself, and ranolazine prevents this by blocking the late sodium channels,” but clearly this effect did not prevent new anginal episodes in patients who experienced incomplete revascularization, he said in an interview.
Dr. Weisz and his associates ran RIVER-PCI during November 2011–May 2013 at 245 sites in 15 countries. They randomized and followed 1,317 patients who received 1,000 mg ranolazine twice daily and 1,287 placebo patients. All patients also received all the other medications appropriate for post-PCI patients, including aspirin and another antiplatelet drug, a statin, a beta-blocker, renin-angiotensin-aldosterone system blocking drugs, as well as other blood pressure lowering and vasodilating medications.
During an average follow-up of 1.8 years, patients in the ranolazine arm had a 26% incidence of ischemia-driven hospitalization of revascularization, and patients in the control arm had a 28% rate, a between-group difference that was not statistically significant. Ranolazine treatment had no significant benefit over placebo for any secondary efficacy measure, but it was also safe and generally well tolerated. About 40% of patients in the ranolazine arm and 36% in the placebo arm discontinued their study treatment during the course of follow-up. Concurrent with Dr. Weisz’s report the results also appeared in an article published online (Lancet 2015 Oct 13;doi: 10.1016/S0140-6736[15]00459-6).
During his report of the findings, Dr. Weisz defended the endpoint used in the study, ischemia-driven hospitalization or revascularization, which he conceded could be considered a “soft” endpoint.
“We had a very strict definition of these events, and every episode was reviewed by an independent committee that judged whether or not to include the event. Every patient with an ischemia-driven event had to show characteristic symptoms and objective evidence of ischemia such as an ECG change or elevated enzymes. We tried to approach judging patient symptoms as scientifically as possible,” he said.
On Twitter @mitchelzoler
AT TCT 2015
Key clinical point: Prophylactic ranolazine failed to stop major episodes of angina in patients who had undergone incomplete coronary revascularization.
Major finding: Ischemia-driven hospitalizations or revascularizations occurred in 26% of patients on ranolazine and 28% of patients on placebo.
Data source: RIVER-PCI, a prospective, multicenter, randomized trial with 2,604 patients treated and followed for an average of 1.8 years.
Disclosures: RIVER-PCI was sponsored by Gilead Sciences and the Menarini Group, the companies that market ranolazine (Ranexa). Dr. Weisz said that he had no relevant disclosures. Dr. James has received honoraria from AstraZeneca, the Medicines Company, and Sanofi-Aventis. Dr. Jolly had no relevant disclosures.
TCT: Absorb BVS meets pivotal U.S. noninferiority goal
SAN FRANCISCO – The first bioresorbable vascular scaffold to finish a U.S. pivotal trial met its prespecified noninferiority endpoint, compared with the best-available metallic drug-eluting stent, putting the Absorb scaffold in good position to soon reach the U.S. market.
But, as expected, the results from the pivotal ABSORB III randomized controlled trial also left unaddressed the question of whether bioresorbable vascular scaffolds (BVS) actually offer patients any benefit above the best metallic drug-eluting stent comparator. That part won’t be answered for several more years, until results from an expanded, prospective group of 5,000 randomized patients are followed for something like 5 years, study researchers said.
Until then, favoring the Absorb stent over a metallic model will involve “a leap of faith,” admitted Dr. Dean J. Kereiakes, coprincipal investigator of the trial, who reported the ABSORB III results at the Transcatheter Cardiovascular Therapeutics annual meeting.
“There was no expectation that Absorb would be superior at 1 year,” emphasized Dr. Gregg W. Stone, chairman of the trial during discussion of the results. “The thought is that, as the Absorb BVS disappears over several years, then we’ll start to see improved outcomes,” said Dr. Stone, professor and director of cardiovascular research and education at the Center for Interventional Vascular Therapy of Columbia University in New York.
“The best metallic drug-eluting stents have a total lesion failure rate of about 17% after 5 years, with about half due to the device,” commented Dr. Daniel I. Simon, professor and chief of cardiovascular medicine at University Hospitals Case Medical Center in Cleveland. “This is an unmet need to address. We need to do better for patients, and this is a tool to do that,” he said during a press conference at the meeting.
The ABSORB III trial enrolled 2,008 patients with stable or unstable angina undergoing percutaneous coronary intervention at 193 centers in the United States and Australia. Patients’ coronary lesions received treatment with either the Absorb BVS or the Xience V everolimus-eluting cobalt-chromium stent. The primary endpoint was a test for noninferiority by the Absorb BVS for target-lesion failure after 1 year, defined as the combined rate of cardiovascular death, target-vessel MI, or ischemia-driven target-lesion revascularization.
The 1-year rates were 7.8% in 1,312 Absorb recipients who completed the 12-month follow-up and a 6.1% rate in 677 control patients. The upper statistical limit of the 1.7%-between group difference fell within the 4.5% prespecified difference for noninferiority, Dr. Kereiakes reported at the meeting, sponsored by the Cardiovascular Research Foundation. Concurrent with his report the results appeared online (N Engl J Med. 2015 Oct 12;doi: 10.1056NEJMoa1509038).
Although the results met the study’s primary endpoint, the outcomes showed that the Absorb BVS numerically underperformed the comparator metallic stent by several individual efficacy and safety parameters, including target-vessel MI and stent thrombosis, but none of the differences were statistically significant. Dr. Kereiakes dismissed these as “small, insignificant differences for low-frequency events that were underpowered to show differences.” The results also showed no suggestion that the incidence of angina during 1-year follow-up differed between the two treatment arms, indicating that prior evidence for an angina-reducing benefit with BVS treatment that had been seen in smaller studies had been misleading, Dr. Stone acknowledged.
Dr. Kereiakes stressed that the noninferiority outcome occurred in procedures performed by operators who largely used BVS for the first time. Despite that, the procedural success rate with the BVS was similar to that of the metallic stent. Procedures using a BVS averaged 4 minutes longer than did placement of the metallic stent.
One additional analysis presented by Dr. Kereiakes provided an important lesson about the danger of using the Absorb BVS in coronary arteries less than 2.5 mm in diameter. Even though the study protocol specified not treating vessels less than 2.5 mm in diameter, case records showed that 19% of the BVS target vessels had diameters of 2.25 mm or less, noted Dr. Kereiakes, medical director of the Christ Hospital Heart and Vascular Center in Cincinnati. Within this subgroup, the rate of target-lesion failure ran 13% with BVS and 8% with the metallic stent, while in the 80% of vessels that were properly sized, the primary endpoint occurred in 7% and 6% respectively.
“The lesson is clear: This BVS does not perform well in small vessels when operators do not use the correct methodology with aggressive postdilitation,” commented Dr. Martin B. Leon, director of the Center for Interventional Vascular Therapy of Columbia University in New York.
ABSORB III was sponsored by Abbott Vascular, which markets the Absorb BVS. Dr. Kereiakes has been a consultant to Abbott Vascular as well as to HCRI, Boston Scientific, Svelte, Janssen, and Sanofi-Aventis, and he holds equity interest in Ablative Solution. Dr. Stone has received grant support and consultant fees from Abbott Vascular and has been a consultant to 12 other companies and holds equity options in 8t companies. Dr. Simon has received research grants from and has been a consultant to Medtronic and a consultant to Cordis, Merck, and Janssen. Dr. Leon had no relevant disclosures.
On Twitter @mitchelzoler
SAN FRANCISCO – The first bioresorbable vascular scaffold to finish a U.S. pivotal trial met its prespecified noninferiority endpoint, compared with the best-available metallic drug-eluting stent, putting the Absorb scaffold in good position to soon reach the U.S. market.
But, as expected, the results from the pivotal ABSORB III randomized controlled trial also left unaddressed the question of whether bioresorbable vascular scaffolds (BVS) actually offer patients any benefit above the best metallic drug-eluting stent comparator. That part won’t be answered for several more years, until results from an expanded, prospective group of 5,000 randomized patients are followed for something like 5 years, study researchers said.
Until then, favoring the Absorb stent over a metallic model will involve “a leap of faith,” admitted Dr. Dean J. Kereiakes, coprincipal investigator of the trial, who reported the ABSORB III results at the Transcatheter Cardiovascular Therapeutics annual meeting.
“There was no expectation that Absorb would be superior at 1 year,” emphasized Dr. Gregg W. Stone, chairman of the trial during discussion of the results. “The thought is that, as the Absorb BVS disappears over several years, then we’ll start to see improved outcomes,” said Dr. Stone, professor and director of cardiovascular research and education at the Center for Interventional Vascular Therapy of Columbia University in New York.
“The best metallic drug-eluting stents have a total lesion failure rate of about 17% after 5 years, with about half due to the device,” commented Dr. Daniel I. Simon, professor and chief of cardiovascular medicine at University Hospitals Case Medical Center in Cleveland. “This is an unmet need to address. We need to do better for patients, and this is a tool to do that,” he said during a press conference at the meeting.
The ABSORB III trial enrolled 2,008 patients with stable or unstable angina undergoing percutaneous coronary intervention at 193 centers in the United States and Australia. Patients’ coronary lesions received treatment with either the Absorb BVS or the Xience V everolimus-eluting cobalt-chromium stent. The primary endpoint was a test for noninferiority by the Absorb BVS for target-lesion failure after 1 year, defined as the combined rate of cardiovascular death, target-vessel MI, or ischemia-driven target-lesion revascularization.
The 1-year rates were 7.8% in 1,312 Absorb recipients who completed the 12-month follow-up and a 6.1% rate in 677 control patients. The upper statistical limit of the 1.7%-between group difference fell within the 4.5% prespecified difference for noninferiority, Dr. Kereiakes reported at the meeting, sponsored by the Cardiovascular Research Foundation. Concurrent with his report the results appeared online (N Engl J Med. 2015 Oct 12;doi: 10.1056NEJMoa1509038).
Although the results met the study’s primary endpoint, the outcomes showed that the Absorb BVS numerically underperformed the comparator metallic stent by several individual efficacy and safety parameters, including target-vessel MI and stent thrombosis, but none of the differences were statistically significant. Dr. Kereiakes dismissed these as “small, insignificant differences for low-frequency events that were underpowered to show differences.” The results also showed no suggestion that the incidence of angina during 1-year follow-up differed between the two treatment arms, indicating that prior evidence for an angina-reducing benefit with BVS treatment that had been seen in smaller studies had been misleading, Dr. Stone acknowledged.
Dr. Kereiakes stressed that the noninferiority outcome occurred in procedures performed by operators who largely used BVS for the first time. Despite that, the procedural success rate with the BVS was similar to that of the metallic stent. Procedures using a BVS averaged 4 minutes longer than did placement of the metallic stent.
One additional analysis presented by Dr. Kereiakes provided an important lesson about the danger of using the Absorb BVS in coronary arteries less than 2.5 mm in diameter. Even though the study protocol specified not treating vessels less than 2.5 mm in diameter, case records showed that 19% of the BVS target vessels had diameters of 2.25 mm or less, noted Dr. Kereiakes, medical director of the Christ Hospital Heart and Vascular Center in Cincinnati. Within this subgroup, the rate of target-lesion failure ran 13% with BVS and 8% with the metallic stent, while in the 80% of vessels that were properly sized, the primary endpoint occurred in 7% and 6% respectively.
“The lesson is clear: This BVS does not perform well in small vessels when operators do not use the correct methodology with aggressive postdilitation,” commented Dr. Martin B. Leon, director of the Center for Interventional Vascular Therapy of Columbia University in New York.
ABSORB III was sponsored by Abbott Vascular, which markets the Absorb BVS. Dr. Kereiakes has been a consultant to Abbott Vascular as well as to HCRI, Boston Scientific, Svelte, Janssen, and Sanofi-Aventis, and he holds equity interest in Ablative Solution. Dr. Stone has received grant support and consultant fees from Abbott Vascular and has been a consultant to 12 other companies and holds equity options in 8t companies. Dr. Simon has received research grants from and has been a consultant to Medtronic and a consultant to Cordis, Merck, and Janssen. Dr. Leon had no relevant disclosures.
On Twitter @mitchelzoler
SAN FRANCISCO – The first bioresorbable vascular scaffold to finish a U.S. pivotal trial met its prespecified noninferiority endpoint, compared with the best-available metallic drug-eluting stent, putting the Absorb scaffold in good position to soon reach the U.S. market.
But, as expected, the results from the pivotal ABSORB III randomized controlled trial also left unaddressed the question of whether bioresorbable vascular scaffolds (BVS) actually offer patients any benefit above the best metallic drug-eluting stent comparator. That part won’t be answered for several more years, until results from an expanded, prospective group of 5,000 randomized patients are followed for something like 5 years, study researchers said.
Until then, favoring the Absorb stent over a metallic model will involve “a leap of faith,” admitted Dr. Dean J. Kereiakes, coprincipal investigator of the trial, who reported the ABSORB III results at the Transcatheter Cardiovascular Therapeutics annual meeting.
“There was no expectation that Absorb would be superior at 1 year,” emphasized Dr. Gregg W. Stone, chairman of the trial during discussion of the results. “The thought is that, as the Absorb BVS disappears over several years, then we’ll start to see improved outcomes,” said Dr. Stone, professor and director of cardiovascular research and education at the Center for Interventional Vascular Therapy of Columbia University in New York.
“The best metallic drug-eluting stents have a total lesion failure rate of about 17% after 5 years, with about half due to the device,” commented Dr. Daniel I. Simon, professor and chief of cardiovascular medicine at University Hospitals Case Medical Center in Cleveland. “This is an unmet need to address. We need to do better for patients, and this is a tool to do that,” he said during a press conference at the meeting.
The ABSORB III trial enrolled 2,008 patients with stable or unstable angina undergoing percutaneous coronary intervention at 193 centers in the United States and Australia. Patients’ coronary lesions received treatment with either the Absorb BVS or the Xience V everolimus-eluting cobalt-chromium stent. The primary endpoint was a test for noninferiority by the Absorb BVS for target-lesion failure after 1 year, defined as the combined rate of cardiovascular death, target-vessel MI, or ischemia-driven target-lesion revascularization.
The 1-year rates were 7.8% in 1,312 Absorb recipients who completed the 12-month follow-up and a 6.1% rate in 677 control patients. The upper statistical limit of the 1.7%-between group difference fell within the 4.5% prespecified difference for noninferiority, Dr. Kereiakes reported at the meeting, sponsored by the Cardiovascular Research Foundation. Concurrent with his report the results appeared online (N Engl J Med. 2015 Oct 12;doi: 10.1056NEJMoa1509038).
Although the results met the study’s primary endpoint, the outcomes showed that the Absorb BVS numerically underperformed the comparator metallic stent by several individual efficacy and safety parameters, including target-vessel MI and stent thrombosis, but none of the differences were statistically significant. Dr. Kereiakes dismissed these as “small, insignificant differences for low-frequency events that were underpowered to show differences.” The results also showed no suggestion that the incidence of angina during 1-year follow-up differed between the two treatment arms, indicating that prior evidence for an angina-reducing benefit with BVS treatment that had been seen in smaller studies had been misleading, Dr. Stone acknowledged.
Dr. Kereiakes stressed that the noninferiority outcome occurred in procedures performed by operators who largely used BVS for the first time. Despite that, the procedural success rate with the BVS was similar to that of the metallic stent. Procedures using a BVS averaged 4 minutes longer than did placement of the metallic stent.
One additional analysis presented by Dr. Kereiakes provided an important lesson about the danger of using the Absorb BVS in coronary arteries less than 2.5 mm in diameter. Even though the study protocol specified not treating vessels less than 2.5 mm in diameter, case records showed that 19% of the BVS target vessels had diameters of 2.25 mm or less, noted Dr. Kereiakes, medical director of the Christ Hospital Heart and Vascular Center in Cincinnati. Within this subgroup, the rate of target-lesion failure ran 13% with BVS and 8% with the metallic stent, while in the 80% of vessels that were properly sized, the primary endpoint occurred in 7% and 6% respectively.
“The lesson is clear: This BVS does not perform well in small vessels when operators do not use the correct methodology with aggressive postdilitation,” commented Dr. Martin B. Leon, director of the Center for Interventional Vascular Therapy of Columbia University in New York.
ABSORB III was sponsored by Abbott Vascular, which markets the Absorb BVS. Dr. Kereiakes has been a consultant to Abbott Vascular as well as to HCRI, Boston Scientific, Svelte, Janssen, and Sanofi-Aventis, and he holds equity interest in Ablative Solution. Dr. Stone has received grant support and consultant fees from Abbott Vascular and has been a consultant to 12 other companies and holds equity options in 8t companies. Dr. Simon has received research grants from and has been a consultant to Medtronic and a consultant to Cordis, Merck, and Janssen. Dr. Leon had no relevant disclosures.
On Twitter @mitchelzoler
AT TCT 2015
Key clinical point: The Absorb bioresorbable vascular scaffold met its prespecified noninferiority primary endpoint in its pivotal U.S. trial.
Major finding: Target-lesion failure occurred in 7.8% of Absorb patients and 6.1% of controls on the best metallic drug-eluting stent.
Data source: ABSORB III, a pivotal randomized controlled trial with 2,008 patients run at 193 centers in the United States and Australia.
Disclosures: ABSORB III was sponsored by Abbott Vascular, which markets the Absorb BVS. Dr. Kereiakes has been a consultant to Abbott Vascular as well as to HCRI, Boston Scientific, Svelte, Janssen, and Sanofi-Aventis, and he holds equity interest in Ablative Solution.
Insurance, labeling problems hinder LAA closure in AF patients
The Watchman device, approved for routine use by the Food and Drug Administration in March, gives U.S. atrial fibrillation patients their first alternative to chronic anticoagulant treatment for preventing ischemic stroke.
By closing off the sac-like left-atrial appendage (LAA) with Watchman – a plug-like device placed via percutaneous, transcatheter delivery – blood clots cannot form in the LAA, thereby eliminating the source for most of the thrombi that threaten to cause ischemic strokes in patients with atrial fibrillation (AF).
But while many cardiologists welcome this new option that, for the first time, gives AF patients a way to avoid years or even decades of daily treatment with an anticoagulant, U.S. rollout of the device out has not been seamless. In many regions, health insurers have been unwilling to cover payment for Watchman and its placement, say physicians. Medicare AF patients in particular have been in a state of limbo for receiving a Watchman device while the Centers for Medicare and Medicaid Services (CMS) makes a national coverage determination, a decision not expected until later this year.
In addition, the AF patients who arguably are the best candidates for receiving this device are technically ineligible based on Watchman’s labeling as well as a very limited evidence base. The FDA approved the device specifically for patients judged “suitable for warfarin,” a decision driven largely by the two Watchman trials that led to approval. Each of these trials randomized warfarin-eligible patients either to receive the device along with a 6-week course of warfarin following placement to ensure against acute thromboembolic complications, or to chronic warfarin treatment with no device.
Although this design allowed head-to-head comparison between Watchman and the traditional standard for anticoagulation in AF patients, it left unaddressed the question of how Watchman performs in the AF patient population with the most obvious indication for a mechanical solution to stroke risk: patients who are completely intolerant of anticoagulation treatment. By strict labeling criteria those patients, desperate for an effective means to reduce their stroke risk, are ineligible to receive Watchman.
“It’s approved for patients who can take warfarin, and that’s wrong,” said Dr. Peter R. Kowey, an AF specialist and professor and director of the Center for Clinical Cardiology at the Lankenau Institute for Medical Research in Wynnewood, Pa. “Most of us in clinical practice believe Watchman has the potential to help patients who would be difficult to anticoagulate long term. This is how it’s used around the world.”
Who should get Watchman right now?
With patients with contraindications for anticoagulants excluded by current labeling, who are the right patients to get this device, especially with long-term experience still relatively limited? Many AF experts say they currently see targeting it to AF patients who are clearly at high risk from both stroke and anticoagulation, as well as possibly also patients who face less of a risk from an anticoagulant treatment but express a strong dissatisfaction with having to remain on such therapy for the rest of their lives.
The Watchman-trial results “were quite compelling, and the device fills a large, unmet need for patients who are inappropriately treated or undertreated” with anticoagulation, said Dr. J. Peter Weiss, an electrophysiologist at the Intermountain Heart Institute in Salt Lake City. “The data show it’s as good as warfarin for preventing ischemic stroke, and the 5-year outcome data [from the PREVENT AF trial] showed a survival advantage largely based on a reduced rate of hemorrhagic stroke” compared with patients on warfarin. “The benefit from Watchman is not just in preventing ischemic strokes,” Dr. Weiss said in an interview.
Researchers presented the 5-year outcomes from PROTECT AF to the FDA in October 2014, and while those results remain unpublished, Dr. Shephal K. Doshi, director of cardiac electrophysiology at Saint Johns Health Center in Santa Monica, Calif., presented them at the Heart Rhythm Society annual meeting in Boston in May. The 5-year outcomes showed that compared with patients treated chronically with warfarin, those who had received a Watchman device had a 39% relative risk reduction for the study’s primary, combined endpoint, a 32% relative risk reduction in the incidence of all strokes, and a 56% statistically significant relative risk reduction in cardiovascular deaths plus unexplained deaths. The 4-year follow-up results from PROTECT AF, with a similar mortality advantage for Watchman over warfarin, were published last year (JAMA. 2014 Nov. 19; 312[19]:1988-98).
The patients who could benefit the most from receiving a Watchman device fall into two categories, Dr. Weiss said: AF patients at high risk for both stroke and bleeding, identified by their high scores on both the CHA2DS2-VASc and HAS-BLED formulas, and relatively young AF patients with a high CHA2DS2-VASc score who face the prospect of receiving warfarin or another anticoagulant for a long period of time, possibly several decades. An AF patient who is, for example, 66 years old may have a moderate risk for a serious bleeding event of about 0.5%/year on warfarin or a new oral anticoagulant (NOAC) such as apixaban (Eliquis), dabigatran (Pradaxa), edoxaban (Savaysa), or rivaroxaban (Xarelto), but if that patient were to live for 20 years, the cumulative risk for a major bleeding event could be about 10%, he noted.
Dr. Gordon F. Tomaselli, an electrophysiologist, professor of medicine, and chief of cardiology at Johns Hopkins University in Baltimore, envisions a similar target population: “People who cannot or will not take warfarin or a new oral anticoagulant,” he said. He cited AF patients with a CHA2DS2-VASc score of at least 2, but perhaps in most cases for serious Watchman consideration with an even higher CHA2DS2-VASc score and hence an even greater stroke risk, as well as an inability to received optimal anticoagulant-drug treatment.
“Right now Watchman fills a small but important niche. If a patient is eligible for an oral anticoagulant and not especially averse to taking one I’d go with that, especially if the patient does not closely resemble those enrolled in the trials, because our experience with NOACs is quite good. But once we get good at placing Watchman and our experience grows, you’ll start to see the indications expand,” he predicted.
Dr. Saibal Kar, director of interventional cardiology research at Cedars-Sinai Medical Center in Los Angeles and a lead collaborator on the Watchman pivotal trials, agreed that for the time being as well as the foreseeable future Watchman remains a “second-line” option for patients who clearly fail the first line of treatment with warfarin or a NOAC (although Dr. Kar still prefers warfarin). “I absolutely start patients on warfarin and see how they do” and then he offers Watchman to patients who “for various reasons cannot take warfarin or a NOAC,” which could mean serious bleeding episodes or a clear pattern of noncompliance, Dr. Kar said in an interview. Some patients also opt for Watchman because of lifestyle issues, such as a history of falls, or patients who engage in potentially bruising sports such as skiing, he said.
Dr. Kar highlighted the evidence that with longer follow-up, Watchman is not only comparable to warfarin for safety and efficacy, the endpoint specified in the pivotal trials, but also showed a strong signal for long-term superiority in the 4- and 5-year results from PROTECT AF. “For a lot of patients who have challenges [with bleeding complications] Watchman is a great option. When you prevent life-threatening bleeds, it translates into a mortality benefit.”
A cautionary view for the current role of Watchman came in a June editorial written by two physicians at Beth Israel Deaconess Hospital in Boston, who warned that in selected patients Watchman “may be safe, effective, and preferable to chronic warfarin thromboembolic prophylaxis in AF, but at this point many questions surrounding its safety and long-term efficacy remain unanswered” (J Am Coll Cardiol. 2015 June 23;65[24]:2624-7). Dr. Jonathan W. Waks and Dr. Warren J. Manning went on to say in their commentary that “at this point in time, it appears that patients treated with Watchman may pay early (procedural complications) and may also possibly pay later (late thromboembolism).”
In a reply to this critique, Dr. David R. Holmes Jr., professor of medicine and an electrophysiologist and interventional cardiologist at the Mayo Clinic in Rochester, Minn., and developer of the Watchman device, countered that while extremely long-term outcomes from Watchman, beyond 5 years, are not yet available, the long-term consequences of extremely prolonged chronic anticoagulation that continues for a similarly extended period also remain undocumented. He noted that hemorrhagic stroke poses the greatest stroke danger to patients maintained on anticoagulant therapy, but the meta-analysis of Watchman results that he and his associates published in June – the article that was the subject for the comment by Dr. Waks and Dr. Manning – showed a 78% relative risk reduction in hemorrhagic strokes among Watchman recipients compared with control AF patients who received warfarin (J Am Coll Cardiol. 2015 June 23;65[24]:2614-23).
Dr. Holmes acknowledged that patients treated with Watchman and no anticoagulant can develop ischemic strokes from causes aside from clot formation in the LAA. But he stressed that the meta-analysis he published in June showed a striking 52% relative decrease in cardiovascular or unexplained deaths during and average 2.7 years of follow-up compared with the control patients treated with warfarin.
“It is extraordinarily uncommon to have this magnitude of improved survival in a relatively small number of patients,” and the survival benefit was consistent across both randomized Watchman trials as well as in both continued access cohorts that followed each of the two trials, Dr. Holmes said in an interview.
“I fully accept that we don’t have data beyond 5 years, but the data from PROTECT AF out to 5 years showed no evidence of late strokes or other adverse events,” said Dr. Vivek Y. Reddy, professor of medicine and director of the cardiac arrhythmia service at Mount Sinai Hospital in New York. “In fact, the longer you follow these patients [who received Watchman], the more benefit you see, because these patients are not on an oral anticoagulant long term. Concern about long-term outcomes “is not borne out in the data,” said Dr. Reddy, another leader of the team of interventionalists and electrophysiologists who ran the Watchman trials.
“If a patient with AF comes to me and says ‘I don’t want to take the damn anticoagulants, I want a Watchman,’ and if the patient understands the risks and benefits of Watchman, then I’m 100% fine” facilitating placement of the device in such a patient, explained Dr. Kowey, someone who remains very skeptical of Watchman’s current track record and role. “But what should not happen is for physicians to try to sell Watchman to their patients. Physicians should not tell patients that you don’t need to worry about anticoagulation anymore because I can put in a Watchman and it’s the end of the story. We’re very short of having enough information right now to recommend it to patients” this way. Despite this information shortfall, “I know for a fact” that this sort of promotion of Watchman occurs right now from physicians with an economic incentive to place the device into patients, Dr. Kowey said in an interview.
While some physicians may excessively promote Watchman, they also likely have a receptive audience. “I don’t think it will be hard to find patients who are interested in the device. The challenge will be to figure out if a patient is a good candidate,” said Dr. Paul Varosy, director of electrophysiology at the Denver VA Medical Center. “I have patients and physicians who ask all the time when we will start making the device available. I care for many patients who absolutely despise warfarin and NOACs, and they would love to have a way to get off their medication that does not involve having a risk for a massive stroke,” he said. “What is striking to me is how many patients are interested in this device without being aware of what they would be getting.”
Paying for Watchman
Economic incentives for placing Watchman into patients aside, paying for the device right now and for the procedure that’s involved is no easy matter. Several cardiologists active in Watchman programs scattered around the United States report substantial problems encountered since March with health insurance coverage for the device and placement procedure, and they add that uncertainties about coverage or denied coverage has significantly limited the number of patients who have received the device.
One of the more glaring examples is at the Mayo Clinic in Rochester, Minn., the program led by Dr. Holmes, who helped develop the Watchman technology. He and his associates have placed roughly 20 of the devices since March, but in August he said that his program had “about 40-50 patients” who had been fully screened for the device and looked like they were excellent candidates but were refused coverage by their health insurers. And after some of the 20 patients had already received a Watchman at Mayo, their insurers denied payment, cases that now are on appeal, Dr. Holmes said.
Other active programs report similar difficulties. Dr. Reddy said his program had placed Watchman into about 30-35 patients through the end of August, and while “a majority” of his candidate patients received authorization from their health insurers, others have not received authorization and are on appeal. Insurance coverage is “clearly a problem,” he said in an interview.
Dr. Kar said his Cedars-Sinai program in Los Angles has put Watchman into about 55 patients since last March, and the pace recently accelerated with his treating 13 patients during a 2-day period in August, but he has also seen “lots of problems with insurance,” with appeals usually needed on a case-by-case basis. “We’ve had several appropriate patients who have not received the device because they were not covered,” although most of those cases remain on appeal.
At the University of Kansas in Kansas City, “reimbursement issues have been a major hindrance to widespread use of the device,” and has so far limited placement to just a few patients, said Dr. Dhanunjaya R. Lakkireddy, professor of medicine and director of the University’s Center for Excellence in AF and Complex Arrhythmias. At the Intermountain Heart Institute in Salt Lake City, operators have done just 3 placements since the device’s approval, after doing 128 Watchman placements during the trials and continued access programs. One of the patients paid for the device and procedure completely out of pocket, said Dr. Weiss, a bill that Dr. Kar said runs more than $20,000. The second of the Intermountain patients received Medicare coverage, and in the third case “we met with CMS and are waiting to hear,” Dr. Weiss said. “We are being very cautious to do cases that are very well indicated” to help better ensure that they will receive medical insurance coverage, Dr. Weiss said in an interview.
In May, the CMS began a National Coverage Analysis for Watchman prompted by a request from the device’s manufacturer, Boston Scientific. The appeal for Medicare coverage received support in a June letter written by the presidents of the American College of Cardiology, the Heart Rhythm Society, and the Society for Cardiovascular Angiography and Interventions.
A national coverage determination by the CMS in favor of paying for Medicare patients who undergo Watchman placement “would be a huge benefit,” said Dr. Holmes, who predicted that private insurers would then follow the CMS’ lead and cover the procedure as well. The CMS set Nov. 21, 2015, as the deadline for its decision.
Patients with anticoagulant contraindications will take more time
Even if the CMS decides in favor of reimbursing Watchman placement, the request that it received from Boston Scientific specified coverage for the FDA-approved indication, which stipulates placement in patients able to undergo warfarin treatment. That means for patients who are unable to receive anticoagulant treatment, placement constitutes off-label use that will likely remain unreimbursed, yet these are the very patients that experts agree form an obvious target for Watchman intervention. Currently, these AF patients generally rely on chronic aspirin treatment as their only protection against ischemic stroke.
The only formal, reported experience using Watchman in AF patients who did not also receive warfarin during the first 6 weeks following placement came in a 150-patient, uncontrolled feasibility study, ASAP(ASA Plavix Feasibility Study With WATCHMAN Left Atrial Appendage Closure Technology) run at four centers in Europe (J Am Coll Cardiol. 2013 June 25;61[25]:2551-6). All of the enrolled patients were ineligible to receive warfarin, and instead following Watchman placement these patients received either clopidogrel or ticlopidine for 6 months and chronic treatment with aspirin (dual antiplatelet therapy [DAPT]). Follow-up averaged 14 months, and based on the patients’ average CHA2DS2-VASc score at entry the expected annualized rate of ischemic stroke in these patients was roughly 7%.
However, their observed rate was just 1.7%, and their rate of periprocedural and postprocedural complications roughly matched the rates seen in the first Watchman randomized trial. The researchers who ran the study concluded that the results showed that “Watchman can be safely implanted without a warfarin transition.”
Although the ASAP results showed “Watchman is very effective for stroke prevention” without early anticoagulation following placement, “I’m not sure how one could use Watchman for patients contraindicated for oral anticoagulation,” said Dr. Lakkireddy. “This is a controversial area, and one has to be cautious about cavalier off-label use of the device.”
“I think we need to know more about the [ASAP] data before we’d feel comfortable offering the Watchman device” to patients contraindicated for oral anticoagulation, said Dr. Weiss.
Patients with a total contraindication against treatment with warfarin or a NOAC have the greatest need, said Dr. Reddy. “The problem is, we don’t have much safety data” for these patients, and while the results from the ASAP trial showed the device can be safely placed just using DAPT, the numbers were small and the device is not approved” for use in this setting, said Dr. Reddy, the lead investigator for the ASAP study.
The solution to the dilemma posed by this patient group may lie in the ASAP 2 study, a large, multicenter trial that will enroll AF patients with a contraindication to oral anticoagulation and will compare Watchman placement followed by several months of antiplatelet treatment with DAPT head-to-head with patients randomized to today’s standard treatment of aspirin only. The trial will be sponsored by Boston Scientific, and should start by the end of this year, Dr. Reddy said. He envisions enrolling many of the AF patients he sees with an absolute contraindication to oral anticoagulant treatment in the trial once it starts, though it will mean that only half the enrolled patients will receive a Watchman device.
Dr. Holmes sees registry data as another possible route for eventually expanding the labeled indication for Watchman to patients who can’t receive warfarin or another anticoagulant. He cited the precedent of the FDA broadening the labeled indication for transcatheter aortic-valve replacement in 2013 based in part on U.S. registry data as well as on data collected in Europe.
One potential source of U.S. patients who could wind up receiving only brief warfarin treatment after Watchman placement would be those who develop a major bleed soon after starting on anticoagulation, an event that would prompt most physicians to discontinue and not restart warfarin, Dr. Holmes said. He suggested that in these circumstances patients receive DAPT for 6 months using aspirin and clopidogrel, following the protocol tested in ASAP.
The likely source of registry data would be the database that will be created and maintained by the ACC according to an announcement from the ACC in August. This registry is seen by the ACC as addressing the need for a postapproval safety and efficacy assessment of 1,000 U.S. Watchman recipients that the FDA mandated as part of its device approval last March.
“The registry will function as the postapproval study mandated by the FDA,” said Dr. Varosy of Denver, who led the effort to develop and structure the ACC’s Watchman registry. One goal of the registry “will be to get a better understanding of how the device performs” in patients who can’t take an anticoagulant. “I think that’s where the strongest rationale is for having a device like this,” he said. “It would be great to do something for patients who can’t take warfarin, but until we have data for that group we’ll just have to wait.”
Recommendations detail appropriate Watchman rollout
A recent review of LAA occlusion-device options by the ACC, Heart Rhythm Society, and Society for Cardiovascular Angiography and Interventions was an attempt by these three U.S. professional societies with a stake in AF management and LAA closure to “address issues critical to the appropriate integration of new technologies into the care of patients with AF” (J Am Coll Cardiol. 2015. doi:10.1016/j.jacc.2015.06.028]). One of the review’s most notable features is a section that makes specific recommendations about the composition of the physician team that assesses prospective AF patients for LAA closure and performs the procedure. The document suggests the process involve a team of physicians with expertise in electrophysiology, cardiac catheterization, stroke prevention, echocardiography, x-ray imaging, and possibly anesthesiology if general anesthesia is planned. The panel also recommended having a cardiac surgeon on hand for surgical backup if needed. The review also made recommendations on the facilities needed to safely and effectively perform LAA occlusion, the training that should be in place for the operator who performs the procedure, the protocols that should exist to guide patient management before, during, and after occlusion, the methods used to select AF patients for LAA occlusion, and the need for a U.S.-based LAA registry.
Despite these recommendations, “it is currently too early to tell how Watchman will be introduced into practice with respect to facilities, training, etc.,” Dr. Frederick A. Masoudi, a cardiologist at the University of Colorado in Denver and chair of the review committee, said in an interview. The three professional societies “are separately releasing a statement that focuses in greater detail on recommended operator characteristics and training.” This statement is still pending, he said.
A spokeswoman for Boston Scientific said that the company “supports the recommendations [from Dr. Masoudi’s committee], which are very much in line with our established criteria for new implanting centers. We are committed to the rational dispersion of the technology through a disciplined and highly selective approach to center identification. We will ensure that all implanters and implanting centers meet specific prerequisites including appropriate facilities and a dedicated and experienced team to perform the procedure. In addition, we will require implanters and echocardiographers to complete a rigorous clinical training program.”
As of late August, Boston Scientific identified on its website 32 U.S. centers performing LAA closure using Watchman. The company anticipates that about 100 U.S. centers will be performing the procedure by the end of 2015.
The PREVENT AF and PREVAIL pivotal trials for Watchman and their subsequent continued-access programs were sponsored by Boston Scientific. Dr. Kowey has been a speaker for Boston Scientific and has consulted for several drug companies that market anticoagulants. Dr. Weiss has been a speaker for Boston Scientific and also for St. Jude, Biosense Webster, and Stereotaxis. Dr. Kar has received research grants from Boston Scientific and served as principal investigator for the two continued-access programs that followed the two Watchman pivotal trials. He has also received research grants from Abbott Vascular and St. Jude, and has an equity interest in Coherex. Dr. Holmes and the Mayo Clinic have a financial interest in technology related to Watchman and this technology was licensed to Boston Scientific. Dr. Reddy has been an adviser to and received research grants from Atritech/Boston Scientific. Dr. Lakkireddy, Dr. Varosy, Dr. Masoudi, and Dr. Tomaselli had no disclosures.
On Twitter@mitchelzoler
The Watchman device, approved for routine use by the Food and Drug Administration in March, gives U.S. atrial fibrillation patients their first alternative to chronic anticoagulant treatment for preventing ischemic stroke.
By closing off the sac-like left-atrial appendage (LAA) with Watchman – a plug-like device placed via percutaneous, transcatheter delivery – blood clots cannot form in the LAA, thereby eliminating the source for most of the thrombi that threaten to cause ischemic strokes in patients with atrial fibrillation (AF).
But while many cardiologists welcome this new option that, for the first time, gives AF patients a way to avoid years or even decades of daily treatment with an anticoagulant, U.S. rollout of the device out has not been seamless. In many regions, health insurers have been unwilling to cover payment for Watchman and its placement, say physicians. Medicare AF patients in particular have been in a state of limbo for receiving a Watchman device while the Centers for Medicare and Medicaid Services (CMS) makes a national coverage determination, a decision not expected until later this year.
In addition, the AF patients who arguably are the best candidates for receiving this device are technically ineligible based on Watchman’s labeling as well as a very limited evidence base. The FDA approved the device specifically for patients judged “suitable for warfarin,” a decision driven largely by the two Watchman trials that led to approval. Each of these trials randomized warfarin-eligible patients either to receive the device along with a 6-week course of warfarin following placement to ensure against acute thromboembolic complications, or to chronic warfarin treatment with no device.
Although this design allowed head-to-head comparison between Watchman and the traditional standard for anticoagulation in AF patients, it left unaddressed the question of how Watchman performs in the AF patient population with the most obvious indication for a mechanical solution to stroke risk: patients who are completely intolerant of anticoagulation treatment. By strict labeling criteria those patients, desperate for an effective means to reduce their stroke risk, are ineligible to receive Watchman.
“It’s approved for patients who can take warfarin, and that’s wrong,” said Dr. Peter R. Kowey, an AF specialist and professor and director of the Center for Clinical Cardiology at the Lankenau Institute for Medical Research in Wynnewood, Pa. “Most of us in clinical practice believe Watchman has the potential to help patients who would be difficult to anticoagulate long term. This is how it’s used around the world.”
Who should get Watchman right now?
With patients with contraindications for anticoagulants excluded by current labeling, who are the right patients to get this device, especially with long-term experience still relatively limited? Many AF experts say they currently see targeting it to AF patients who are clearly at high risk from both stroke and anticoagulation, as well as possibly also patients who face less of a risk from an anticoagulant treatment but express a strong dissatisfaction with having to remain on such therapy for the rest of their lives.
The Watchman-trial results “were quite compelling, and the device fills a large, unmet need for patients who are inappropriately treated or undertreated” with anticoagulation, said Dr. J. Peter Weiss, an electrophysiologist at the Intermountain Heart Institute in Salt Lake City. “The data show it’s as good as warfarin for preventing ischemic stroke, and the 5-year outcome data [from the PREVENT AF trial] showed a survival advantage largely based on a reduced rate of hemorrhagic stroke” compared with patients on warfarin. “The benefit from Watchman is not just in preventing ischemic strokes,” Dr. Weiss said in an interview.
Researchers presented the 5-year outcomes from PROTECT AF to the FDA in October 2014, and while those results remain unpublished, Dr. Shephal K. Doshi, director of cardiac electrophysiology at Saint Johns Health Center in Santa Monica, Calif., presented them at the Heart Rhythm Society annual meeting in Boston in May. The 5-year outcomes showed that compared with patients treated chronically with warfarin, those who had received a Watchman device had a 39% relative risk reduction for the study’s primary, combined endpoint, a 32% relative risk reduction in the incidence of all strokes, and a 56% statistically significant relative risk reduction in cardiovascular deaths plus unexplained deaths. The 4-year follow-up results from PROTECT AF, with a similar mortality advantage for Watchman over warfarin, were published last year (JAMA. 2014 Nov. 19; 312[19]:1988-98).
The patients who could benefit the most from receiving a Watchman device fall into two categories, Dr. Weiss said: AF patients at high risk for both stroke and bleeding, identified by their high scores on both the CHA2DS2-VASc and HAS-BLED formulas, and relatively young AF patients with a high CHA2DS2-VASc score who face the prospect of receiving warfarin or another anticoagulant for a long period of time, possibly several decades. An AF patient who is, for example, 66 years old may have a moderate risk for a serious bleeding event of about 0.5%/year on warfarin or a new oral anticoagulant (NOAC) such as apixaban (Eliquis), dabigatran (Pradaxa), edoxaban (Savaysa), or rivaroxaban (Xarelto), but if that patient were to live for 20 years, the cumulative risk for a major bleeding event could be about 10%, he noted.
Dr. Gordon F. Tomaselli, an electrophysiologist, professor of medicine, and chief of cardiology at Johns Hopkins University in Baltimore, envisions a similar target population: “People who cannot or will not take warfarin or a new oral anticoagulant,” he said. He cited AF patients with a CHA2DS2-VASc score of at least 2, but perhaps in most cases for serious Watchman consideration with an even higher CHA2DS2-VASc score and hence an even greater stroke risk, as well as an inability to received optimal anticoagulant-drug treatment.
“Right now Watchman fills a small but important niche. If a patient is eligible for an oral anticoagulant and not especially averse to taking one I’d go with that, especially if the patient does not closely resemble those enrolled in the trials, because our experience with NOACs is quite good. But once we get good at placing Watchman and our experience grows, you’ll start to see the indications expand,” he predicted.
Dr. Saibal Kar, director of interventional cardiology research at Cedars-Sinai Medical Center in Los Angeles and a lead collaborator on the Watchman pivotal trials, agreed that for the time being as well as the foreseeable future Watchman remains a “second-line” option for patients who clearly fail the first line of treatment with warfarin or a NOAC (although Dr. Kar still prefers warfarin). “I absolutely start patients on warfarin and see how they do” and then he offers Watchman to patients who “for various reasons cannot take warfarin or a NOAC,” which could mean serious bleeding episodes or a clear pattern of noncompliance, Dr. Kar said in an interview. Some patients also opt for Watchman because of lifestyle issues, such as a history of falls, or patients who engage in potentially bruising sports such as skiing, he said.
Dr. Kar highlighted the evidence that with longer follow-up, Watchman is not only comparable to warfarin for safety and efficacy, the endpoint specified in the pivotal trials, but also showed a strong signal for long-term superiority in the 4- and 5-year results from PROTECT AF. “For a lot of patients who have challenges [with bleeding complications] Watchman is a great option. When you prevent life-threatening bleeds, it translates into a mortality benefit.”
A cautionary view for the current role of Watchman came in a June editorial written by two physicians at Beth Israel Deaconess Hospital in Boston, who warned that in selected patients Watchman “may be safe, effective, and preferable to chronic warfarin thromboembolic prophylaxis in AF, but at this point many questions surrounding its safety and long-term efficacy remain unanswered” (J Am Coll Cardiol. 2015 June 23;65[24]:2624-7). Dr. Jonathan W. Waks and Dr. Warren J. Manning went on to say in their commentary that “at this point in time, it appears that patients treated with Watchman may pay early (procedural complications) and may also possibly pay later (late thromboembolism).”
In a reply to this critique, Dr. David R. Holmes Jr., professor of medicine and an electrophysiologist and interventional cardiologist at the Mayo Clinic in Rochester, Minn., and developer of the Watchman device, countered that while extremely long-term outcomes from Watchman, beyond 5 years, are not yet available, the long-term consequences of extremely prolonged chronic anticoagulation that continues for a similarly extended period also remain undocumented. He noted that hemorrhagic stroke poses the greatest stroke danger to patients maintained on anticoagulant therapy, but the meta-analysis of Watchman results that he and his associates published in June – the article that was the subject for the comment by Dr. Waks and Dr. Manning – showed a 78% relative risk reduction in hemorrhagic strokes among Watchman recipients compared with control AF patients who received warfarin (J Am Coll Cardiol. 2015 June 23;65[24]:2614-23).
Dr. Holmes acknowledged that patients treated with Watchman and no anticoagulant can develop ischemic strokes from causes aside from clot formation in the LAA. But he stressed that the meta-analysis he published in June showed a striking 52% relative decrease in cardiovascular or unexplained deaths during and average 2.7 years of follow-up compared with the control patients treated with warfarin.
“It is extraordinarily uncommon to have this magnitude of improved survival in a relatively small number of patients,” and the survival benefit was consistent across both randomized Watchman trials as well as in both continued access cohorts that followed each of the two trials, Dr. Holmes said in an interview.
“I fully accept that we don’t have data beyond 5 years, but the data from PROTECT AF out to 5 years showed no evidence of late strokes or other adverse events,” said Dr. Vivek Y. Reddy, professor of medicine and director of the cardiac arrhythmia service at Mount Sinai Hospital in New York. “In fact, the longer you follow these patients [who received Watchman], the more benefit you see, because these patients are not on an oral anticoagulant long term. Concern about long-term outcomes “is not borne out in the data,” said Dr. Reddy, another leader of the team of interventionalists and electrophysiologists who ran the Watchman trials.
“If a patient with AF comes to me and says ‘I don’t want to take the damn anticoagulants, I want a Watchman,’ and if the patient understands the risks and benefits of Watchman, then I’m 100% fine” facilitating placement of the device in such a patient, explained Dr. Kowey, someone who remains very skeptical of Watchman’s current track record and role. “But what should not happen is for physicians to try to sell Watchman to their patients. Physicians should not tell patients that you don’t need to worry about anticoagulation anymore because I can put in a Watchman and it’s the end of the story. We’re very short of having enough information right now to recommend it to patients” this way. Despite this information shortfall, “I know for a fact” that this sort of promotion of Watchman occurs right now from physicians with an economic incentive to place the device into patients, Dr. Kowey said in an interview.
While some physicians may excessively promote Watchman, they also likely have a receptive audience. “I don’t think it will be hard to find patients who are interested in the device. The challenge will be to figure out if a patient is a good candidate,” said Dr. Paul Varosy, director of electrophysiology at the Denver VA Medical Center. “I have patients and physicians who ask all the time when we will start making the device available. I care for many patients who absolutely despise warfarin and NOACs, and they would love to have a way to get off their medication that does not involve having a risk for a massive stroke,” he said. “What is striking to me is how many patients are interested in this device without being aware of what they would be getting.”
Paying for Watchman
Economic incentives for placing Watchman into patients aside, paying for the device right now and for the procedure that’s involved is no easy matter. Several cardiologists active in Watchman programs scattered around the United States report substantial problems encountered since March with health insurance coverage for the device and placement procedure, and they add that uncertainties about coverage or denied coverage has significantly limited the number of patients who have received the device.
One of the more glaring examples is at the Mayo Clinic in Rochester, Minn., the program led by Dr. Holmes, who helped develop the Watchman technology. He and his associates have placed roughly 20 of the devices since March, but in August he said that his program had “about 40-50 patients” who had been fully screened for the device and looked like they were excellent candidates but were refused coverage by their health insurers. And after some of the 20 patients had already received a Watchman at Mayo, their insurers denied payment, cases that now are on appeal, Dr. Holmes said.
Other active programs report similar difficulties. Dr. Reddy said his program had placed Watchman into about 30-35 patients through the end of August, and while “a majority” of his candidate patients received authorization from their health insurers, others have not received authorization and are on appeal. Insurance coverage is “clearly a problem,” he said in an interview.
Dr. Kar said his Cedars-Sinai program in Los Angles has put Watchman into about 55 patients since last March, and the pace recently accelerated with his treating 13 patients during a 2-day period in August, but he has also seen “lots of problems with insurance,” with appeals usually needed on a case-by-case basis. “We’ve had several appropriate patients who have not received the device because they were not covered,” although most of those cases remain on appeal.
At the University of Kansas in Kansas City, “reimbursement issues have been a major hindrance to widespread use of the device,” and has so far limited placement to just a few patients, said Dr. Dhanunjaya R. Lakkireddy, professor of medicine and director of the University’s Center for Excellence in AF and Complex Arrhythmias. At the Intermountain Heart Institute in Salt Lake City, operators have done just 3 placements since the device’s approval, after doing 128 Watchman placements during the trials and continued access programs. One of the patients paid for the device and procedure completely out of pocket, said Dr. Weiss, a bill that Dr. Kar said runs more than $20,000. The second of the Intermountain patients received Medicare coverage, and in the third case “we met with CMS and are waiting to hear,” Dr. Weiss said. “We are being very cautious to do cases that are very well indicated” to help better ensure that they will receive medical insurance coverage, Dr. Weiss said in an interview.
In May, the CMS began a National Coverage Analysis for Watchman prompted by a request from the device’s manufacturer, Boston Scientific. The appeal for Medicare coverage received support in a June letter written by the presidents of the American College of Cardiology, the Heart Rhythm Society, and the Society for Cardiovascular Angiography and Interventions.
A national coverage determination by the CMS in favor of paying for Medicare patients who undergo Watchman placement “would be a huge benefit,” said Dr. Holmes, who predicted that private insurers would then follow the CMS’ lead and cover the procedure as well. The CMS set Nov. 21, 2015, as the deadline for its decision.
Patients with anticoagulant contraindications will take more time
Even if the CMS decides in favor of reimbursing Watchman placement, the request that it received from Boston Scientific specified coverage for the FDA-approved indication, which stipulates placement in patients able to undergo warfarin treatment. That means for patients who are unable to receive anticoagulant treatment, placement constitutes off-label use that will likely remain unreimbursed, yet these are the very patients that experts agree form an obvious target for Watchman intervention. Currently, these AF patients generally rely on chronic aspirin treatment as their only protection against ischemic stroke.
The only formal, reported experience using Watchman in AF patients who did not also receive warfarin during the first 6 weeks following placement came in a 150-patient, uncontrolled feasibility study, ASAP(ASA Plavix Feasibility Study With WATCHMAN Left Atrial Appendage Closure Technology) run at four centers in Europe (J Am Coll Cardiol. 2013 June 25;61[25]:2551-6). All of the enrolled patients were ineligible to receive warfarin, and instead following Watchman placement these patients received either clopidogrel or ticlopidine for 6 months and chronic treatment with aspirin (dual antiplatelet therapy [DAPT]). Follow-up averaged 14 months, and based on the patients’ average CHA2DS2-VASc score at entry the expected annualized rate of ischemic stroke in these patients was roughly 7%.
However, their observed rate was just 1.7%, and their rate of periprocedural and postprocedural complications roughly matched the rates seen in the first Watchman randomized trial. The researchers who ran the study concluded that the results showed that “Watchman can be safely implanted without a warfarin transition.”
Although the ASAP results showed “Watchman is very effective for stroke prevention” without early anticoagulation following placement, “I’m not sure how one could use Watchman for patients contraindicated for oral anticoagulation,” said Dr. Lakkireddy. “This is a controversial area, and one has to be cautious about cavalier off-label use of the device.”
“I think we need to know more about the [ASAP] data before we’d feel comfortable offering the Watchman device” to patients contraindicated for oral anticoagulation, said Dr. Weiss.
Patients with a total contraindication against treatment with warfarin or a NOAC have the greatest need, said Dr. Reddy. “The problem is, we don’t have much safety data” for these patients, and while the results from the ASAP trial showed the device can be safely placed just using DAPT, the numbers were small and the device is not approved” for use in this setting, said Dr. Reddy, the lead investigator for the ASAP study.
The solution to the dilemma posed by this patient group may lie in the ASAP 2 study, a large, multicenter trial that will enroll AF patients with a contraindication to oral anticoagulation and will compare Watchman placement followed by several months of antiplatelet treatment with DAPT head-to-head with patients randomized to today’s standard treatment of aspirin only. The trial will be sponsored by Boston Scientific, and should start by the end of this year, Dr. Reddy said. He envisions enrolling many of the AF patients he sees with an absolute contraindication to oral anticoagulant treatment in the trial once it starts, though it will mean that only half the enrolled patients will receive a Watchman device.
Dr. Holmes sees registry data as another possible route for eventually expanding the labeled indication for Watchman to patients who can’t receive warfarin or another anticoagulant. He cited the precedent of the FDA broadening the labeled indication for transcatheter aortic-valve replacement in 2013 based in part on U.S. registry data as well as on data collected in Europe.
One potential source of U.S. patients who could wind up receiving only brief warfarin treatment after Watchman placement would be those who develop a major bleed soon after starting on anticoagulation, an event that would prompt most physicians to discontinue and not restart warfarin, Dr. Holmes said. He suggested that in these circumstances patients receive DAPT for 6 months using aspirin and clopidogrel, following the protocol tested in ASAP.
The likely source of registry data would be the database that will be created and maintained by the ACC according to an announcement from the ACC in August. This registry is seen by the ACC as addressing the need for a postapproval safety and efficacy assessment of 1,000 U.S. Watchman recipients that the FDA mandated as part of its device approval last March.
“The registry will function as the postapproval study mandated by the FDA,” said Dr. Varosy of Denver, who led the effort to develop and structure the ACC’s Watchman registry. One goal of the registry “will be to get a better understanding of how the device performs” in patients who can’t take an anticoagulant. “I think that’s where the strongest rationale is for having a device like this,” he said. “It would be great to do something for patients who can’t take warfarin, but until we have data for that group we’ll just have to wait.”
Recommendations detail appropriate Watchman rollout
A recent review of LAA occlusion-device options by the ACC, Heart Rhythm Society, and Society for Cardiovascular Angiography and Interventions was an attempt by these three U.S. professional societies with a stake in AF management and LAA closure to “address issues critical to the appropriate integration of new technologies into the care of patients with AF” (J Am Coll Cardiol. 2015. doi:10.1016/j.jacc.2015.06.028]). One of the review’s most notable features is a section that makes specific recommendations about the composition of the physician team that assesses prospective AF patients for LAA closure and performs the procedure. The document suggests the process involve a team of physicians with expertise in electrophysiology, cardiac catheterization, stroke prevention, echocardiography, x-ray imaging, and possibly anesthesiology if general anesthesia is planned. The panel also recommended having a cardiac surgeon on hand for surgical backup if needed. The review also made recommendations on the facilities needed to safely and effectively perform LAA occlusion, the training that should be in place for the operator who performs the procedure, the protocols that should exist to guide patient management before, during, and after occlusion, the methods used to select AF patients for LAA occlusion, and the need for a U.S.-based LAA registry.
Despite these recommendations, “it is currently too early to tell how Watchman will be introduced into practice with respect to facilities, training, etc.,” Dr. Frederick A. Masoudi, a cardiologist at the University of Colorado in Denver and chair of the review committee, said in an interview. The three professional societies “are separately releasing a statement that focuses in greater detail on recommended operator characteristics and training.” This statement is still pending, he said.
A spokeswoman for Boston Scientific said that the company “supports the recommendations [from Dr. Masoudi’s committee], which are very much in line with our established criteria for new implanting centers. We are committed to the rational dispersion of the technology through a disciplined and highly selective approach to center identification. We will ensure that all implanters and implanting centers meet specific prerequisites including appropriate facilities and a dedicated and experienced team to perform the procedure. In addition, we will require implanters and echocardiographers to complete a rigorous clinical training program.”
As of late August, Boston Scientific identified on its website 32 U.S. centers performing LAA closure using Watchman. The company anticipates that about 100 U.S. centers will be performing the procedure by the end of 2015.
The PREVENT AF and PREVAIL pivotal trials for Watchman and their subsequent continued-access programs were sponsored by Boston Scientific. Dr. Kowey has been a speaker for Boston Scientific and has consulted for several drug companies that market anticoagulants. Dr. Weiss has been a speaker for Boston Scientific and also for St. Jude, Biosense Webster, and Stereotaxis. Dr. Kar has received research grants from Boston Scientific and served as principal investigator for the two continued-access programs that followed the two Watchman pivotal trials. He has also received research grants from Abbott Vascular and St. Jude, and has an equity interest in Coherex. Dr. Holmes and the Mayo Clinic have a financial interest in technology related to Watchman and this technology was licensed to Boston Scientific. Dr. Reddy has been an adviser to and received research grants from Atritech/Boston Scientific. Dr. Lakkireddy, Dr. Varosy, Dr. Masoudi, and Dr. Tomaselli had no disclosures.
On Twitter@mitchelzoler
The Watchman device, approved for routine use by the Food and Drug Administration in March, gives U.S. atrial fibrillation patients their first alternative to chronic anticoagulant treatment for preventing ischemic stroke.
By closing off the sac-like left-atrial appendage (LAA) with Watchman – a plug-like device placed via percutaneous, transcatheter delivery – blood clots cannot form in the LAA, thereby eliminating the source for most of the thrombi that threaten to cause ischemic strokes in patients with atrial fibrillation (AF).
But while many cardiologists welcome this new option that, for the first time, gives AF patients a way to avoid years or even decades of daily treatment with an anticoagulant, U.S. rollout of the device out has not been seamless. In many regions, health insurers have been unwilling to cover payment for Watchman and its placement, say physicians. Medicare AF patients in particular have been in a state of limbo for receiving a Watchman device while the Centers for Medicare and Medicaid Services (CMS) makes a national coverage determination, a decision not expected until later this year.
In addition, the AF patients who arguably are the best candidates for receiving this device are technically ineligible based on Watchman’s labeling as well as a very limited evidence base. The FDA approved the device specifically for patients judged “suitable for warfarin,” a decision driven largely by the two Watchman trials that led to approval. Each of these trials randomized warfarin-eligible patients either to receive the device along with a 6-week course of warfarin following placement to ensure against acute thromboembolic complications, or to chronic warfarin treatment with no device.
Although this design allowed head-to-head comparison between Watchman and the traditional standard for anticoagulation in AF patients, it left unaddressed the question of how Watchman performs in the AF patient population with the most obvious indication for a mechanical solution to stroke risk: patients who are completely intolerant of anticoagulation treatment. By strict labeling criteria those patients, desperate for an effective means to reduce their stroke risk, are ineligible to receive Watchman.
“It’s approved for patients who can take warfarin, and that’s wrong,” said Dr. Peter R. Kowey, an AF specialist and professor and director of the Center for Clinical Cardiology at the Lankenau Institute for Medical Research in Wynnewood, Pa. “Most of us in clinical practice believe Watchman has the potential to help patients who would be difficult to anticoagulate long term. This is how it’s used around the world.”
Who should get Watchman right now?
With patients with contraindications for anticoagulants excluded by current labeling, who are the right patients to get this device, especially with long-term experience still relatively limited? Many AF experts say they currently see targeting it to AF patients who are clearly at high risk from both stroke and anticoagulation, as well as possibly also patients who face less of a risk from an anticoagulant treatment but express a strong dissatisfaction with having to remain on such therapy for the rest of their lives.
The Watchman-trial results “were quite compelling, and the device fills a large, unmet need for patients who are inappropriately treated or undertreated” with anticoagulation, said Dr. J. Peter Weiss, an electrophysiologist at the Intermountain Heart Institute in Salt Lake City. “The data show it’s as good as warfarin for preventing ischemic stroke, and the 5-year outcome data [from the PREVENT AF trial] showed a survival advantage largely based on a reduced rate of hemorrhagic stroke” compared with patients on warfarin. “The benefit from Watchman is not just in preventing ischemic strokes,” Dr. Weiss said in an interview.
Researchers presented the 5-year outcomes from PROTECT AF to the FDA in October 2014, and while those results remain unpublished, Dr. Shephal K. Doshi, director of cardiac electrophysiology at Saint Johns Health Center in Santa Monica, Calif., presented them at the Heart Rhythm Society annual meeting in Boston in May. The 5-year outcomes showed that compared with patients treated chronically with warfarin, those who had received a Watchman device had a 39% relative risk reduction for the study’s primary, combined endpoint, a 32% relative risk reduction in the incidence of all strokes, and a 56% statistically significant relative risk reduction in cardiovascular deaths plus unexplained deaths. The 4-year follow-up results from PROTECT AF, with a similar mortality advantage for Watchman over warfarin, were published last year (JAMA. 2014 Nov. 19; 312[19]:1988-98).
The patients who could benefit the most from receiving a Watchman device fall into two categories, Dr. Weiss said: AF patients at high risk for both stroke and bleeding, identified by their high scores on both the CHA2DS2-VASc and HAS-BLED formulas, and relatively young AF patients with a high CHA2DS2-VASc score who face the prospect of receiving warfarin or another anticoagulant for a long period of time, possibly several decades. An AF patient who is, for example, 66 years old may have a moderate risk for a serious bleeding event of about 0.5%/year on warfarin or a new oral anticoagulant (NOAC) such as apixaban (Eliquis), dabigatran (Pradaxa), edoxaban (Savaysa), or rivaroxaban (Xarelto), but if that patient were to live for 20 years, the cumulative risk for a major bleeding event could be about 10%, he noted.
Dr. Gordon F. Tomaselli, an electrophysiologist, professor of medicine, and chief of cardiology at Johns Hopkins University in Baltimore, envisions a similar target population: “People who cannot or will not take warfarin or a new oral anticoagulant,” he said. He cited AF patients with a CHA2DS2-VASc score of at least 2, but perhaps in most cases for serious Watchman consideration with an even higher CHA2DS2-VASc score and hence an even greater stroke risk, as well as an inability to received optimal anticoagulant-drug treatment.
“Right now Watchman fills a small but important niche. If a patient is eligible for an oral anticoagulant and not especially averse to taking one I’d go with that, especially if the patient does not closely resemble those enrolled in the trials, because our experience with NOACs is quite good. But once we get good at placing Watchman and our experience grows, you’ll start to see the indications expand,” he predicted.
Dr. Saibal Kar, director of interventional cardiology research at Cedars-Sinai Medical Center in Los Angeles and a lead collaborator on the Watchman pivotal trials, agreed that for the time being as well as the foreseeable future Watchman remains a “second-line” option for patients who clearly fail the first line of treatment with warfarin or a NOAC (although Dr. Kar still prefers warfarin). “I absolutely start patients on warfarin and see how they do” and then he offers Watchman to patients who “for various reasons cannot take warfarin or a NOAC,” which could mean serious bleeding episodes or a clear pattern of noncompliance, Dr. Kar said in an interview. Some patients also opt for Watchman because of lifestyle issues, such as a history of falls, or patients who engage in potentially bruising sports such as skiing, he said.
Dr. Kar highlighted the evidence that with longer follow-up, Watchman is not only comparable to warfarin for safety and efficacy, the endpoint specified in the pivotal trials, but also showed a strong signal for long-term superiority in the 4- and 5-year results from PROTECT AF. “For a lot of patients who have challenges [with bleeding complications] Watchman is a great option. When you prevent life-threatening bleeds, it translates into a mortality benefit.”
A cautionary view for the current role of Watchman came in a June editorial written by two physicians at Beth Israel Deaconess Hospital in Boston, who warned that in selected patients Watchman “may be safe, effective, and preferable to chronic warfarin thromboembolic prophylaxis in AF, but at this point many questions surrounding its safety and long-term efficacy remain unanswered” (J Am Coll Cardiol. 2015 June 23;65[24]:2624-7). Dr. Jonathan W. Waks and Dr. Warren J. Manning went on to say in their commentary that “at this point in time, it appears that patients treated with Watchman may pay early (procedural complications) and may also possibly pay later (late thromboembolism).”
In a reply to this critique, Dr. David R. Holmes Jr., professor of medicine and an electrophysiologist and interventional cardiologist at the Mayo Clinic in Rochester, Minn., and developer of the Watchman device, countered that while extremely long-term outcomes from Watchman, beyond 5 years, are not yet available, the long-term consequences of extremely prolonged chronic anticoagulation that continues for a similarly extended period also remain undocumented. He noted that hemorrhagic stroke poses the greatest stroke danger to patients maintained on anticoagulant therapy, but the meta-analysis of Watchman results that he and his associates published in June – the article that was the subject for the comment by Dr. Waks and Dr. Manning – showed a 78% relative risk reduction in hemorrhagic strokes among Watchman recipients compared with control AF patients who received warfarin (J Am Coll Cardiol. 2015 June 23;65[24]:2614-23).
Dr. Holmes acknowledged that patients treated with Watchman and no anticoagulant can develop ischemic strokes from causes aside from clot formation in the LAA. But he stressed that the meta-analysis he published in June showed a striking 52% relative decrease in cardiovascular or unexplained deaths during and average 2.7 years of follow-up compared with the control patients treated with warfarin.
“It is extraordinarily uncommon to have this magnitude of improved survival in a relatively small number of patients,” and the survival benefit was consistent across both randomized Watchman trials as well as in both continued access cohorts that followed each of the two trials, Dr. Holmes said in an interview.
“I fully accept that we don’t have data beyond 5 years, but the data from PROTECT AF out to 5 years showed no evidence of late strokes or other adverse events,” said Dr. Vivek Y. Reddy, professor of medicine and director of the cardiac arrhythmia service at Mount Sinai Hospital in New York. “In fact, the longer you follow these patients [who received Watchman], the more benefit you see, because these patients are not on an oral anticoagulant long term. Concern about long-term outcomes “is not borne out in the data,” said Dr. Reddy, another leader of the team of interventionalists and electrophysiologists who ran the Watchman trials.
“If a patient with AF comes to me and says ‘I don’t want to take the damn anticoagulants, I want a Watchman,’ and if the patient understands the risks and benefits of Watchman, then I’m 100% fine” facilitating placement of the device in such a patient, explained Dr. Kowey, someone who remains very skeptical of Watchman’s current track record and role. “But what should not happen is for physicians to try to sell Watchman to their patients. Physicians should not tell patients that you don’t need to worry about anticoagulation anymore because I can put in a Watchman and it’s the end of the story. We’re very short of having enough information right now to recommend it to patients” this way. Despite this information shortfall, “I know for a fact” that this sort of promotion of Watchman occurs right now from physicians with an economic incentive to place the device into patients, Dr. Kowey said in an interview.
While some physicians may excessively promote Watchman, they also likely have a receptive audience. “I don’t think it will be hard to find patients who are interested in the device. The challenge will be to figure out if a patient is a good candidate,” said Dr. Paul Varosy, director of electrophysiology at the Denver VA Medical Center. “I have patients and physicians who ask all the time when we will start making the device available. I care for many patients who absolutely despise warfarin and NOACs, and they would love to have a way to get off their medication that does not involve having a risk for a massive stroke,” he said. “What is striking to me is how many patients are interested in this device without being aware of what they would be getting.”
Paying for Watchman
Economic incentives for placing Watchman into patients aside, paying for the device right now and for the procedure that’s involved is no easy matter. Several cardiologists active in Watchman programs scattered around the United States report substantial problems encountered since March with health insurance coverage for the device and placement procedure, and they add that uncertainties about coverage or denied coverage has significantly limited the number of patients who have received the device.
One of the more glaring examples is at the Mayo Clinic in Rochester, Minn., the program led by Dr. Holmes, who helped develop the Watchman technology. He and his associates have placed roughly 20 of the devices since March, but in August he said that his program had “about 40-50 patients” who had been fully screened for the device and looked like they were excellent candidates but were refused coverage by their health insurers. And after some of the 20 patients had already received a Watchman at Mayo, their insurers denied payment, cases that now are on appeal, Dr. Holmes said.
Other active programs report similar difficulties. Dr. Reddy said his program had placed Watchman into about 30-35 patients through the end of August, and while “a majority” of his candidate patients received authorization from their health insurers, others have not received authorization and are on appeal. Insurance coverage is “clearly a problem,” he said in an interview.
Dr. Kar said his Cedars-Sinai program in Los Angles has put Watchman into about 55 patients since last March, and the pace recently accelerated with his treating 13 patients during a 2-day period in August, but he has also seen “lots of problems with insurance,” with appeals usually needed on a case-by-case basis. “We’ve had several appropriate patients who have not received the device because they were not covered,” although most of those cases remain on appeal.
At the University of Kansas in Kansas City, “reimbursement issues have been a major hindrance to widespread use of the device,” and has so far limited placement to just a few patients, said Dr. Dhanunjaya R. Lakkireddy, professor of medicine and director of the University’s Center for Excellence in AF and Complex Arrhythmias. At the Intermountain Heart Institute in Salt Lake City, operators have done just 3 placements since the device’s approval, after doing 128 Watchman placements during the trials and continued access programs. One of the patients paid for the device and procedure completely out of pocket, said Dr. Weiss, a bill that Dr. Kar said runs more than $20,000. The second of the Intermountain patients received Medicare coverage, and in the third case “we met with CMS and are waiting to hear,” Dr. Weiss said. “We are being very cautious to do cases that are very well indicated” to help better ensure that they will receive medical insurance coverage, Dr. Weiss said in an interview.
In May, the CMS began a National Coverage Analysis for Watchman prompted by a request from the device’s manufacturer, Boston Scientific. The appeal for Medicare coverage received support in a June letter written by the presidents of the American College of Cardiology, the Heart Rhythm Society, and the Society for Cardiovascular Angiography and Interventions.
A national coverage determination by the CMS in favor of paying for Medicare patients who undergo Watchman placement “would be a huge benefit,” said Dr. Holmes, who predicted that private insurers would then follow the CMS’ lead and cover the procedure as well. The CMS set Nov. 21, 2015, as the deadline for its decision.
Patients with anticoagulant contraindications will take more time
Even if the CMS decides in favor of reimbursing Watchman placement, the request that it received from Boston Scientific specified coverage for the FDA-approved indication, which stipulates placement in patients able to undergo warfarin treatment. That means for patients who are unable to receive anticoagulant treatment, placement constitutes off-label use that will likely remain unreimbursed, yet these are the very patients that experts agree form an obvious target for Watchman intervention. Currently, these AF patients generally rely on chronic aspirin treatment as their only protection against ischemic stroke.
The only formal, reported experience using Watchman in AF patients who did not also receive warfarin during the first 6 weeks following placement came in a 150-patient, uncontrolled feasibility study, ASAP(ASA Plavix Feasibility Study With WATCHMAN Left Atrial Appendage Closure Technology) run at four centers in Europe (J Am Coll Cardiol. 2013 June 25;61[25]:2551-6). All of the enrolled patients were ineligible to receive warfarin, and instead following Watchman placement these patients received either clopidogrel or ticlopidine for 6 months and chronic treatment with aspirin (dual antiplatelet therapy [DAPT]). Follow-up averaged 14 months, and based on the patients’ average CHA2DS2-VASc score at entry the expected annualized rate of ischemic stroke in these patients was roughly 7%.
However, their observed rate was just 1.7%, and their rate of periprocedural and postprocedural complications roughly matched the rates seen in the first Watchman randomized trial. The researchers who ran the study concluded that the results showed that “Watchman can be safely implanted without a warfarin transition.”
Although the ASAP results showed “Watchman is very effective for stroke prevention” without early anticoagulation following placement, “I’m not sure how one could use Watchman for patients contraindicated for oral anticoagulation,” said Dr. Lakkireddy. “This is a controversial area, and one has to be cautious about cavalier off-label use of the device.”
“I think we need to know more about the [ASAP] data before we’d feel comfortable offering the Watchman device” to patients contraindicated for oral anticoagulation, said Dr. Weiss.
Patients with a total contraindication against treatment with warfarin or a NOAC have the greatest need, said Dr. Reddy. “The problem is, we don’t have much safety data” for these patients, and while the results from the ASAP trial showed the device can be safely placed just using DAPT, the numbers were small and the device is not approved” for use in this setting, said Dr. Reddy, the lead investigator for the ASAP study.
The solution to the dilemma posed by this patient group may lie in the ASAP 2 study, a large, multicenter trial that will enroll AF patients with a contraindication to oral anticoagulation and will compare Watchman placement followed by several months of antiplatelet treatment with DAPT head-to-head with patients randomized to today’s standard treatment of aspirin only. The trial will be sponsored by Boston Scientific, and should start by the end of this year, Dr. Reddy said. He envisions enrolling many of the AF patients he sees with an absolute contraindication to oral anticoagulant treatment in the trial once it starts, though it will mean that only half the enrolled patients will receive a Watchman device.
Dr. Holmes sees registry data as another possible route for eventually expanding the labeled indication for Watchman to patients who can’t receive warfarin or another anticoagulant. He cited the precedent of the FDA broadening the labeled indication for transcatheter aortic-valve replacement in 2013 based in part on U.S. registry data as well as on data collected in Europe.
One potential source of U.S. patients who could wind up receiving only brief warfarin treatment after Watchman placement would be those who develop a major bleed soon after starting on anticoagulation, an event that would prompt most physicians to discontinue and not restart warfarin, Dr. Holmes said. He suggested that in these circumstances patients receive DAPT for 6 months using aspirin and clopidogrel, following the protocol tested in ASAP.
The likely source of registry data would be the database that will be created and maintained by the ACC according to an announcement from the ACC in August. This registry is seen by the ACC as addressing the need for a postapproval safety and efficacy assessment of 1,000 U.S. Watchman recipients that the FDA mandated as part of its device approval last March.
“The registry will function as the postapproval study mandated by the FDA,” said Dr. Varosy of Denver, who led the effort to develop and structure the ACC’s Watchman registry. One goal of the registry “will be to get a better understanding of how the device performs” in patients who can’t take an anticoagulant. “I think that’s where the strongest rationale is for having a device like this,” he said. “It would be great to do something for patients who can’t take warfarin, but until we have data for that group we’ll just have to wait.”
Recommendations detail appropriate Watchman rollout
A recent review of LAA occlusion-device options by the ACC, Heart Rhythm Society, and Society for Cardiovascular Angiography and Interventions was an attempt by these three U.S. professional societies with a stake in AF management and LAA closure to “address issues critical to the appropriate integration of new technologies into the care of patients with AF” (J Am Coll Cardiol. 2015. doi:10.1016/j.jacc.2015.06.028]). One of the review’s most notable features is a section that makes specific recommendations about the composition of the physician team that assesses prospective AF patients for LAA closure and performs the procedure. The document suggests the process involve a team of physicians with expertise in electrophysiology, cardiac catheterization, stroke prevention, echocardiography, x-ray imaging, and possibly anesthesiology if general anesthesia is planned. The panel also recommended having a cardiac surgeon on hand for surgical backup if needed. The review also made recommendations on the facilities needed to safely and effectively perform LAA occlusion, the training that should be in place for the operator who performs the procedure, the protocols that should exist to guide patient management before, during, and after occlusion, the methods used to select AF patients for LAA occlusion, and the need for a U.S.-based LAA registry.
Despite these recommendations, “it is currently too early to tell how Watchman will be introduced into practice with respect to facilities, training, etc.,” Dr. Frederick A. Masoudi, a cardiologist at the University of Colorado in Denver and chair of the review committee, said in an interview. The three professional societies “are separately releasing a statement that focuses in greater detail on recommended operator characteristics and training.” This statement is still pending, he said.
A spokeswoman for Boston Scientific said that the company “supports the recommendations [from Dr. Masoudi’s committee], which are very much in line with our established criteria for new implanting centers. We are committed to the rational dispersion of the technology through a disciplined and highly selective approach to center identification. We will ensure that all implanters and implanting centers meet specific prerequisites including appropriate facilities and a dedicated and experienced team to perform the procedure. In addition, we will require implanters and echocardiographers to complete a rigorous clinical training program.”
As of late August, Boston Scientific identified on its website 32 U.S. centers performing LAA closure using Watchman. The company anticipates that about 100 U.S. centers will be performing the procedure by the end of 2015.
The PREVENT AF and PREVAIL pivotal trials for Watchman and their subsequent continued-access programs were sponsored by Boston Scientific. Dr. Kowey has been a speaker for Boston Scientific and has consulted for several drug companies that market anticoagulants. Dr. Weiss has been a speaker for Boston Scientific and also for St. Jude, Biosense Webster, and Stereotaxis. Dr. Kar has received research grants from Boston Scientific and served as principal investigator for the two continued-access programs that followed the two Watchman pivotal trials. He has also received research grants from Abbott Vascular and St. Jude, and has an equity interest in Coherex. Dr. Holmes and the Mayo Clinic have a financial interest in technology related to Watchman and this technology was licensed to Boston Scientific. Dr. Reddy has been an adviser to and received research grants from Atritech/Boston Scientific. Dr. Lakkireddy, Dr. Varosy, Dr. Masoudi, and Dr. Tomaselli had no disclosures.
On Twitter@mitchelzoler
BLOG: Cardiologists quickly adopt SPRINT’s 120-mm Hg blood pressure target
Heart failure physicians were quick to embrace the sub–120 mm Hg systolic blood pressure target for both patients and at-risk people fewer than 3 weeks after the early-release news came out from the SPRINT trial that treating to this level produced a significant cut in cardiovascular disease events, compared with a less stringent systolic blood-pressure target of below 140 mm Hg.
At the annual meeting of the Heart Failure Society of America this week – one of the first cardiology gatherings held since the SPRINT announcement on Sept. 11 – at least 10 heart failure specialists offered their opinion at various times during the sessions on what the results have already meant for their practice. What was most striking was their unanimity in accepting this new blood pressure treatment target for heart failure patients and for people at increased risk for developing heart failure, and the rapidity at which they had come to their decision despite the absence so far of details about the trial’s results.
The unifying theme was that these physicians constituted a highly receptive audience for the SPRINT message, several of these specialists said in interviews. They appeared poised to pounce on a scientific rationale as soon as it became available to adopt a more aggressive blood pressure goal. It’s certainly no coincidence that most (if not all) these physicians now see uncontrolled hypertension as one of the top drivers of both heart failure onset and progression.
“We’ve all had some misgivings” about the systolic blood pressure targets set by the JNC 8 panel members last year of less than 150 mm Hg or less than 140 mm Hg (depending on age), and as a result of those misgivings, “I think people were ready to do a reverse and accept a new, lower target,” said Dr. Margaret M. Redfield, a heart failure specialist who was among those at the meeting who voiced endorsement for a new, sub–120 mm Hg target. “We don’t have the [SPRINT] data yet, but it’s very unusual for the NHLBI to release trial information ahead of time, so it must be very dramatic,” she added.
“The data and safety monitoring board had strict rules to govern early stopping,” said Dr. Clyde W. Yancy, a heart failure cardiologist and a member of the SPRINT data and safety monitoring panel. While careful not to prematurely provide any unreleased details of the SPRINT results, Dr. Yancy tried to frame what the September announcement meant in objective terms, while also rationalizing the quick uptake of the finding by so many of his colleagues.
“The decision to stop early must have been driven by some high level of evidence,” he told me, “You can infer a significant scientific rational” for a new target of less than 120 mm Hg “and you have to also surmise that there was no signal of harm.”
And, of course, some cardiologists had decided even before the SPRINT results came out in September that a lower target was better even without any evidence to back up that instinct.
“I love the 120s; a 140-mm Hg target has always been too high for me,” said Dr. Ileana L. Piña, a heart failure specialist at Montefiore Medical Center, Bronx, N.Y.
Another question, following so many endorsements of the 120-mm Hg goal, was whether these physicians believed people stood a good chance to reach this ambitious target.
“It’s a target; it’s not that everyone will get to it, but we need to apply the same rigor for blood pressure control as we use in heart failure clinics,” Dr. Redfield said. “We need to use a system” for patient support and monitoring and to promote adherence to treatment, “and keep pushing” patients to work toward their goal, she said.
Dr. Yancy predicted that a more aggressive blood pressure goal will help generate a stronger and more innovative infrastructure of drugs and monitoring tools to help patients get there.
“If a target blood pressure of 120/80 mm Hg gains credibility in guidelines, I think that industry will respond” with more combined drug formulations, new drugs, and innovative methods for easier blood pressure measurement, he said.
On Twitter @mitchelzoler
Heart failure physicians were quick to embrace the sub–120 mm Hg systolic blood pressure target for both patients and at-risk people fewer than 3 weeks after the early-release news came out from the SPRINT trial that treating to this level produced a significant cut in cardiovascular disease events, compared with a less stringent systolic blood-pressure target of below 140 mm Hg.
At the annual meeting of the Heart Failure Society of America this week – one of the first cardiology gatherings held since the SPRINT announcement on Sept. 11 – at least 10 heart failure specialists offered their opinion at various times during the sessions on what the results have already meant for their practice. What was most striking was their unanimity in accepting this new blood pressure treatment target for heart failure patients and for people at increased risk for developing heart failure, and the rapidity at which they had come to their decision despite the absence so far of details about the trial’s results.
The unifying theme was that these physicians constituted a highly receptive audience for the SPRINT message, several of these specialists said in interviews. They appeared poised to pounce on a scientific rationale as soon as it became available to adopt a more aggressive blood pressure goal. It’s certainly no coincidence that most (if not all) these physicians now see uncontrolled hypertension as one of the top drivers of both heart failure onset and progression.
“We’ve all had some misgivings” about the systolic blood pressure targets set by the JNC 8 panel members last year of less than 150 mm Hg or less than 140 mm Hg (depending on age), and as a result of those misgivings, “I think people were ready to do a reverse and accept a new, lower target,” said Dr. Margaret M. Redfield, a heart failure specialist who was among those at the meeting who voiced endorsement for a new, sub–120 mm Hg target. “We don’t have the [SPRINT] data yet, but it’s very unusual for the NHLBI to release trial information ahead of time, so it must be very dramatic,” she added.
“The data and safety monitoring board had strict rules to govern early stopping,” said Dr. Clyde W. Yancy, a heart failure cardiologist and a member of the SPRINT data and safety monitoring panel. While careful not to prematurely provide any unreleased details of the SPRINT results, Dr. Yancy tried to frame what the September announcement meant in objective terms, while also rationalizing the quick uptake of the finding by so many of his colleagues.
“The decision to stop early must have been driven by some high level of evidence,” he told me, “You can infer a significant scientific rational” for a new target of less than 120 mm Hg “and you have to also surmise that there was no signal of harm.”
And, of course, some cardiologists had decided even before the SPRINT results came out in September that a lower target was better even without any evidence to back up that instinct.
“I love the 120s; a 140-mm Hg target has always been too high for me,” said Dr. Ileana L. Piña, a heart failure specialist at Montefiore Medical Center, Bronx, N.Y.
Another question, following so many endorsements of the 120-mm Hg goal, was whether these physicians believed people stood a good chance to reach this ambitious target.
“It’s a target; it’s not that everyone will get to it, but we need to apply the same rigor for blood pressure control as we use in heart failure clinics,” Dr. Redfield said. “We need to use a system” for patient support and monitoring and to promote adherence to treatment, “and keep pushing” patients to work toward their goal, she said.
Dr. Yancy predicted that a more aggressive blood pressure goal will help generate a stronger and more innovative infrastructure of drugs and monitoring tools to help patients get there.
“If a target blood pressure of 120/80 mm Hg gains credibility in guidelines, I think that industry will respond” with more combined drug formulations, new drugs, and innovative methods for easier blood pressure measurement, he said.
On Twitter @mitchelzoler
Heart failure physicians were quick to embrace the sub–120 mm Hg systolic blood pressure target for both patients and at-risk people fewer than 3 weeks after the early-release news came out from the SPRINT trial that treating to this level produced a significant cut in cardiovascular disease events, compared with a less stringent systolic blood-pressure target of below 140 mm Hg.
At the annual meeting of the Heart Failure Society of America this week – one of the first cardiology gatherings held since the SPRINT announcement on Sept. 11 – at least 10 heart failure specialists offered their opinion at various times during the sessions on what the results have already meant for their practice. What was most striking was their unanimity in accepting this new blood pressure treatment target for heart failure patients and for people at increased risk for developing heart failure, and the rapidity at which they had come to their decision despite the absence so far of details about the trial’s results.
The unifying theme was that these physicians constituted a highly receptive audience for the SPRINT message, several of these specialists said in interviews. They appeared poised to pounce on a scientific rationale as soon as it became available to adopt a more aggressive blood pressure goal. It’s certainly no coincidence that most (if not all) these physicians now see uncontrolled hypertension as one of the top drivers of both heart failure onset and progression.
“We’ve all had some misgivings” about the systolic blood pressure targets set by the JNC 8 panel members last year of less than 150 mm Hg or less than 140 mm Hg (depending on age), and as a result of those misgivings, “I think people were ready to do a reverse and accept a new, lower target,” said Dr. Margaret M. Redfield, a heart failure specialist who was among those at the meeting who voiced endorsement for a new, sub–120 mm Hg target. “We don’t have the [SPRINT] data yet, but it’s very unusual for the NHLBI to release trial information ahead of time, so it must be very dramatic,” she added.
“The data and safety monitoring board had strict rules to govern early stopping,” said Dr. Clyde W. Yancy, a heart failure cardiologist and a member of the SPRINT data and safety monitoring panel. While careful not to prematurely provide any unreleased details of the SPRINT results, Dr. Yancy tried to frame what the September announcement meant in objective terms, while also rationalizing the quick uptake of the finding by so many of his colleagues.
“The decision to stop early must have been driven by some high level of evidence,” he told me, “You can infer a significant scientific rational” for a new target of less than 120 mm Hg “and you have to also surmise that there was no signal of harm.”
And, of course, some cardiologists had decided even before the SPRINT results came out in September that a lower target was better even without any evidence to back up that instinct.
“I love the 120s; a 140-mm Hg target has always been too high for me,” said Dr. Ileana L. Piña, a heart failure specialist at Montefiore Medical Center, Bronx, N.Y.
Another question, following so many endorsements of the 120-mm Hg goal, was whether these physicians believed people stood a good chance to reach this ambitious target.
“It’s a target; it’s not that everyone will get to it, but we need to apply the same rigor for blood pressure control as we use in heart failure clinics,” Dr. Redfield said. “We need to use a system” for patient support and monitoring and to promote adherence to treatment, “and keep pushing” patients to work toward their goal, she said.
Dr. Yancy predicted that a more aggressive blood pressure goal will help generate a stronger and more innovative infrastructure of drugs and monitoring tools to help patients get there.
“If a target blood pressure of 120/80 mm Hg gains credibility in guidelines, I think that industry will respond” with more combined drug formulations, new drugs, and innovative methods for easier blood pressure measurement, he said.
On Twitter @mitchelzoler
ESC: Heart failure patients have increased cancer incidence
LONDON – Adult patients with chronic heart failure had an average 51% increased incidence of all forms of cancer, compared with the general population in an analysis of more than 9,000 Danish patients treated for heart failure during 2002-2009.
Although the study did not address causality, the elevated risk for new-onset cancers in heart failure patients may stem from shared risk factors for the two diseases, Dr. Ann Banke said at the annual congress of the European Society of Cardiology. Smoking, for example, is a potential etiologic factor for both heart failure and certain cancers. Other potential shared risk factors could include other types of unhealthy lifestyle choices, and a heightened inflammatory state, suggested Dr. Banke, a researcher in the department of cardiology at Odense (Denmark) University Hospital.
“Increased awareness of the risk for development of cancer in heart failure patients is warranted,” especially given the relatively long life expectancy now seen among many patients with chronic heart failure, Dr. Banke said.
She and her associates reviewed 9,307 Danish patients with chronic heart failure and no history of cancer who entered a national heart failure cohort during 2002-2009. Their average age was 68 years, 73% were men, 89% had heart failure with reduced ejection fraction, 80% had New York Heart Association class I or II heart failure, and 15% had diabetes. During follow-up through 2013, a total of 975 of these patients received a diagnosis of cancer. The researchers compared the incidence rate of cancer among these heart failure patients with the rate in the general Danish adult population in the same 2002-2013 period, during which the general population developed 330,843 cancers.
In an analysis that adjusted for age and sex, the heart failure patients had a statistically significant 51% increased rate of incidence cancers of all types (P less than .0001). When broken down by cancer site, the heart failure patients showed significantly increased rates for all types of cancers except prostate cancer (see chart). Dr. Banke speculated that the absence of an increased incidence rate in prostate cancer among heart failure patients may reflect the age of the heart failure patients, or perhaps because prostate cancer does not share as many risk factors with heart failure as do the other cancer types.
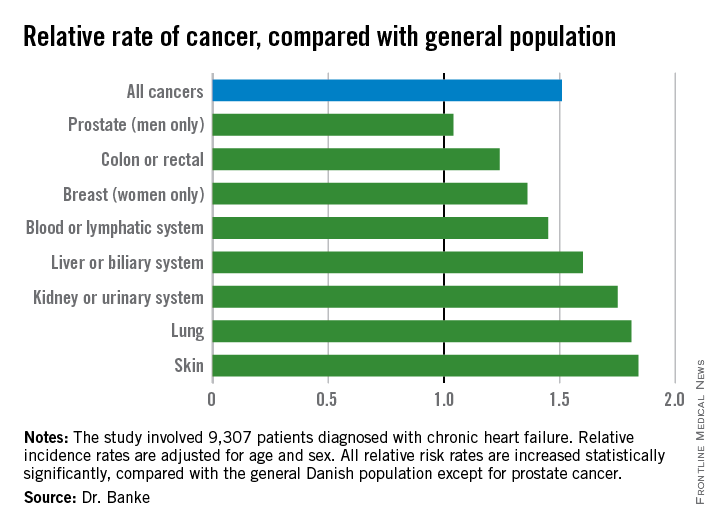
On Twitter @mitchelzoler
LONDON – Adult patients with chronic heart failure had an average 51% increased incidence of all forms of cancer, compared with the general population in an analysis of more than 9,000 Danish patients treated for heart failure during 2002-2009.
Although the study did not address causality, the elevated risk for new-onset cancers in heart failure patients may stem from shared risk factors for the two diseases, Dr. Ann Banke said at the annual congress of the European Society of Cardiology. Smoking, for example, is a potential etiologic factor for both heart failure and certain cancers. Other potential shared risk factors could include other types of unhealthy lifestyle choices, and a heightened inflammatory state, suggested Dr. Banke, a researcher in the department of cardiology at Odense (Denmark) University Hospital.
“Increased awareness of the risk for development of cancer in heart failure patients is warranted,” especially given the relatively long life expectancy now seen among many patients with chronic heart failure, Dr. Banke said.
She and her associates reviewed 9,307 Danish patients with chronic heart failure and no history of cancer who entered a national heart failure cohort during 2002-2009. Their average age was 68 years, 73% were men, 89% had heart failure with reduced ejection fraction, 80% had New York Heart Association class I or II heart failure, and 15% had diabetes. During follow-up through 2013, a total of 975 of these patients received a diagnosis of cancer. The researchers compared the incidence rate of cancer among these heart failure patients with the rate in the general Danish adult population in the same 2002-2013 period, during which the general population developed 330,843 cancers.
In an analysis that adjusted for age and sex, the heart failure patients had a statistically significant 51% increased rate of incidence cancers of all types (P less than .0001). When broken down by cancer site, the heart failure patients showed significantly increased rates for all types of cancers except prostate cancer (see chart). Dr. Banke speculated that the absence of an increased incidence rate in prostate cancer among heart failure patients may reflect the age of the heart failure patients, or perhaps because prostate cancer does not share as many risk factors with heart failure as do the other cancer types.
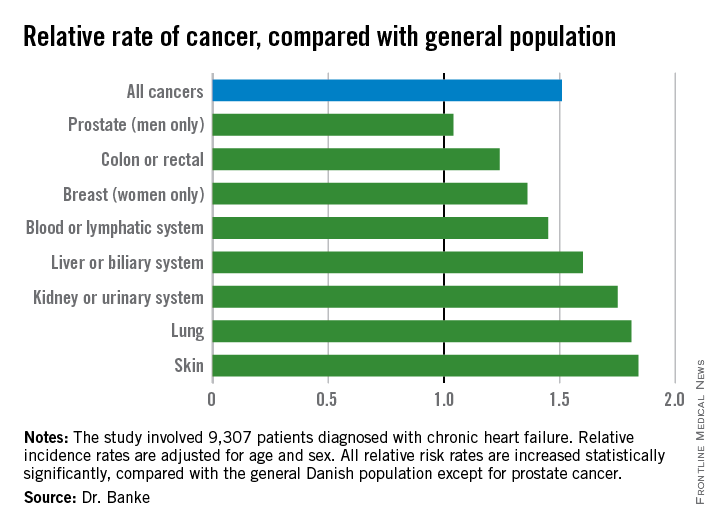
On Twitter @mitchelzoler
LONDON – Adult patients with chronic heart failure had an average 51% increased incidence of all forms of cancer, compared with the general population in an analysis of more than 9,000 Danish patients treated for heart failure during 2002-2009.
Although the study did not address causality, the elevated risk for new-onset cancers in heart failure patients may stem from shared risk factors for the two diseases, Dr. Ann Banke said at the annual congress of the European Society of Cardiology. Smoking, for example, is a potential etiologic factor for both heart failure and certain cancers. Other potential shared risk factors could include other types of unhealthy lifestyle choices, and a heightened inflammatory state, suggested Dr. Banke, a researcher in the department of cardiology at Odense (Denmark) University Hospital.
“Increased awareness of the risk for development of cancer in heart failure patients is warranted,” especially given the relatively long life expectancy now seen among many patients with chronic heart failure, Dr. Banke said.
She and her associates reviewed 9,307 Danish patients with chronic heart failure and no history of cancer who entered a national heart failure cohort during 2002-2009. Their average age was 68 years, 73% were men, 89% had heart failure with reduced ejection fraction, 80% had New York Heart Association class I or II heart failure, and 15% had diabetes. During follow-up through 2013, a total of 975 of these patients received a diagnosis of cancer. The researchers compared the incidence rate of cancer among these heart failure patients with the rate in the general Danish adult population in the same 2002-2013 period, during which the general population developed 330,843 cancers.
In an analysis that adjusted for age and sex, the heart failure patients had a statistically significant 51% increased rate of incidence cancers of all types (P less than .0001). When broken down by cancer site, the heart failure patients showed significantly increased rates for all types of cancers except prostate cancer (see chart). Dr. Banke speculated that the absence of an increased incidence rate in prostate cancer among heart failure patients may reflect the age of the heart failure patients, or perhaps because prostate cancer does not share as many risk factors with heart failure as do the other cancer types.
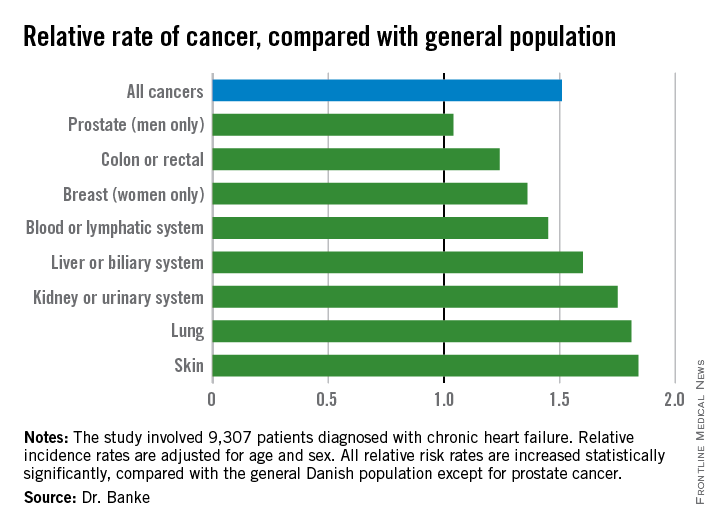
On Twitter @mitchelzoler
AT THE ESC CONGRESS 2015
Key clinical point: Adults with chronic heart failure had a significantly increased incidence of cancer, compared with the general population.
Major finding: Patients with chronic heart failure had an average 51% higher incidence of cancer, compared with the general population.
Data source: A nationwide Danish cohort with 9,307 patients diagnosed with chronic heart failure.
Disclosures: Dr. Banke had no disclosures.
HFSA: In heart failure, beta-blocker dosage trumps heart rate
NATIONAL HARBOR, MD. – In beta-blocker treatment of heart failure, dose matters; heart rate, not so much.
When using beta-blockers to treat patients with heart failure and reduced ejection fraction, administering a high, evidence-backed dosage of the drug had much more beneficial impact than did getting patients to a low heart rate, according to a post hoc analysis of data from more than 2,000 patients.
The finding provides new evidence supporting “titrating the beta-blocker to evidence-based, high dosages of a beta-blocker and not holding back,” Mona Fiuzat, Ph.D., said in an interview at the annual scientific meeting of the Heart Failure Society of America. “It’s not just lowering the heart rate; there is something else, other mechanisms [of beta-blocker effects] that may be of greater benefit” to patients beyond heart-rate reduction when patients they receive the full dosage of beta-blocker treatment that had been shown effective in the randomized trials run about 2 decades ago.
“The point of our report is that if you have [heart failure with reduced ejection fraction] patients on a beta-blocker, they will be better off by increasing the dose” to the target level rather than by adding an additional, non–beta-blocker drug, such as ivabradine (Corlanor), to further reduce heart rate, said Dr. Fiuzat, a clinical pharmacologist and heart-failure researcher at Duke University in Durham, N.C. In the trial that enrolled the 2,320 patients included in the current analysis, half the patients were not on their target beta-blocker dosage.
Some clinicians are too heart-rate focused, she said. “Our results show that there is added benefit from using the full beta-blocker dosage even when the patient’s heart rate is already low.”
The analysis run by Dr. Fiuzat and her associates used data collected in HF-ACTION (Heart Failure: A Controlled Trial Investigating Outcomes of Exercise Training), a randomized, controlled study that assessed the impact of exercise training on patients with heart failure with reduced ejection fraction (JAMA 2009 Apr 8;301[14]:1439-50). All patients received usual care (and the intervention group also received exercise training), which meant they were on whichever beta-blocker and dosage their individual physician prescribed.
The current analysis converted these baseline dosages into carvedilol (Coreg) equivalents and identified the dosage levels as either low, defined as a daily carvedilol equivalent of less than 25 mg/day, or high, a daily equivalent of at least 25 mg/day. The analysis also categorized heart rate at baseline into a high rate defined as at least 70 beats/min, and a low rate of less than 70 beats/min. At entry, 71% of patients were on a high beta-blocker dosage (although in many cases not their full, ideal dosage), and 52% of patients had a high heart rate.
The new analysis showed that after a median follow-up of 2.5 years, the rate of all-cause death and all-cause hospitalization was significantly higher among patients who entered the study on a low beta-blocker dosage and with a high heart rate compared with patients in the other three groups: low dosage/low heart rate, high dosage/high heart rate, and high dosage/low heart rate. In addition, the results showed that a high beta-blocker dosage at baseline mitigated the impact of a high heart rate; patients in this subgroup had outcomes comparable to those of patients on a high beta-blocker dosage with a low heart rate.
In an analysis that adjusted for baseline differences in several clinical and demographic variables, patients on a high beta-blocker dosage had a statistically significant 13% reduced rate of all-cause death or all-cause hospitalization compared with patients on a low-dosage beta-blocker. In contrast, baseline heart rate had no statistically significant impact on outcomes, Dr. Fiuzat and her associates reported in an article published online concurrently with the presentation of the results at the meeting by one of Dr. Fiuzat’s colleagues (JACC: Heart Failure 2015. doi: 10.1016/j.jchf.2015.09.002]).
On Twitter @mitchelzoler
NATIONAL HARBOR, MD. – In beta-blocker treatment of heart failure, dose matters; heart rate, not so much.
When using beta-blockers to treat patients with heart failure and reduced ejection fraction, administering a high, evidence-backed dosage of the drug had much more beneficial impact than did getting patients to a low heart rate, according to a post hoc analysis of data from more than 2,000 patients.
The finding provides new evidence supporting “titrating the beta-blocker to evidence-based, high dosages of a beta-blocker and not holding back,” Mona Fiuzat, Ph.D., said in an interview at the annual scientific meeting of the Heart Failure Society of America. “It’s not just lowering the heart rate; there is something else, other mechanisms [of beta-blocker effects] that may be of greater benefit” to patients beyond heart-rate reduction when patients they receive the full dosage of beta-blocker treatment that had been shown effective in the randomized trials run about 2 decades ago.
“The point of our report is that if you have [heart failure with reduced ejection fraction] patients on a beta-blocker, they will be better off by increasing the dose” to the target level rather than by adding an additional, non–beta-blocker drug, such as ivabradine (Corlanor), to further reduce heart rate, said Dr. Fiuzat, a clinical pharmacologist and heart-failure researcher at Duke University in Durham, N.C. In the trial that enrolled the 2,320 patients included in the current analysis, half the patients were not on their target beta-blocker dosage.
Some clinicians are too heart-rate focused, she said. “Our results show that there is added benefit from using the full beta-blocker dosage even when the patient’s heart rate is already low.”
The analysis run by Dr. Fiuzat and her associates used data collected in HF-ACTION (Heart Failure: A Controlled Trial Investigating Outcomes of Exercise Training), a randomized, controlled study that assessed the impact of exercise training on patients with heart failure with reduced ejection fraction (JAMA 2009 Apr 8;301[14]:1439-50). All patients received usual care (and the intervention group also received exercise training), which meant they were on whichever beta-blocker and dosage their individual physician prescribed.
The current analysis converted these baseline dosages into carvedilol (Coreg) equivalents and identified the dosage levels as either low, defined as a daily carvedilol equivalent of less than 25 mg/day, or high, a daily equivalent of at least 25 mg/day. The analysis also categorized heart rate at baseline into a high rate defined as at least 70 beats/min, and a low rate of less than 70 beats/min. At entry, 71% of patients were on a high beta-blocker dosage (although in many cases not their full, ideal dosage), and 52% of patients had a high heart rate.
The new analysis showed that after a median follow-up of 2.5 years, the rate of all-cause death and all-cause hospitalization was significantly higher among patients who entered the study on a low beta-blocker dosage and with a high heart rate compared with patients in the other three groups: low dosage/low heart rate, high dosage/high heart rate, and high dosage/low heart rate. In addition, the results showed that a high beta-blocker dosage at baseline mitigated the impact of a high heart rate; patients in this subgroup had outcomes comparable to those of patients on a high beta-blocker dosage with a low heart rate.
In an analysis that adjusted for baseline differences in several clinical and demographic variables, patients on a high beta-blocker dosage had a statistically significant 13% reduced rate of all-cause death or all-cause hospitalization compared with patients on a low-dosage beta-blocker. In contrast, baseline heart rate had no statistically significant impact on outcomes, Dr. Fiuzat and her associates reported in an article published online concurrently with the presentation of the results at the meeting by one of Dr. Fiuzat’s colleagues (JACC: Heart Failure 2015. doi: 10.1016/j.jchf.2015.09.002]).
On Twitter @mitchelzoler
NATIONAL HARBOR, MD. – In beta-blocker treatment of heart failure, dose matters; heart rate, not so much.
When using beta-blockers to treat patients with heart failure and reduced ejection fraction, administering a high, evidence-backed dosage of the drug had much more beneficial impact than did getting patients to a low heart rate, according to a post hoc analysis of data from more than 2,000 patients.
The finding provides new evidence supporting “titrating the beta-blocker to evidence-based, high dosages of a beta-blocker and not holding back,” Mona Fiuzat, Ph.D., said in an interview at the annual scientific meeting of the Heart Failure Society of America. “It’s not just lowering the heart rate; there is something else, other mechanisms [of beta-blocker effects] that may be of greater benefit” to patients beyond heart-rate reduction when patients they receive the full dosage of beta-blocker treatment that had been shown effective in the randomized trials run about 2 decades ago.
“The point of our report is that if you have [heart failure with reduced ejection fraction] patients on a beta-blocker, they will be better off by increasing the dose” to the target level rather than by adding an additional, non–beta-blocker drug, such as ivabradine (Corlanor), to further reduce heart rate, said Dr. Fiuzat, a clinical pharmacologist and heart-failure researcher at Duke University in Durham, N.C. In the trial that enrolled the 2,320 patients included in the current analysis, half the patients were not on their target beta-blocker dosage.
Some clinicians are too heart-rate focused, she said. “Our results show that there is added benefit from using the full beta-blocker dosage even when the patient’s heart rate is already low.”
The analysis run by Dr. Fiuzat and her associates used data collected in HF-ACTION (Heart Failure: A Controlled Trial Investigating Outcomes of Exercise Training), a randomized, controlled study that assessed the impact of exercise training on patients with heart failure with reduced ejection fraction (JAMA 2009 Apr 8;301[14]:1439-50). All patients received usual care (and the intervention group also received exercise training), which meant they were on whichever beta-blocker and dosage their individual physician prescribed.
The current analysis converted these baseline dosages into carvedilol (Coreg) equivalents and identified the dosage levels as either low, defined as a daily carvedilol equivalent of less than 25 mg/day, or high, a daily equivalent of at least 25 mg/day. The analysis also categorized heart rate at baseline into a high rate defined as at least 70 beats/min, and a low rate of less than 70 beats/min. At entry, 71% of patients were on a high beta-blocker dosage (although in many cases not their full, ideal dosage), and 52% of patients had a high heart rate.
The new analysis showed that after a median follow-up of 2.5 years, the rate of all-cause death and all-cause hospitalization was significantly higher among patients who entered the study on a low beta-blocker dosage and with a high heart rate compared with patients in the other three groups: low dosage/low heart rate, high dosage/high heart rate, and high dosage/low heart rate. In addition, the results showed that a high beta-blocker dosage at baseline mitigated the impact of a high heart rate; patients in this subgroup had outcomes comparable to those of patients on a high beta-blocker dosage with a low heart rate.
In an analysis that adjusted for baseline differences in several clinical and demographic variables, patients on a high beta-blocker dosage had a statistically significant 13% reduced rate of all-cause death or all-cause hospitalization compared with patients on a low-dosage beta-blocker. In contrast, baseline heart rate had no statistically significant impact on outcomes, Dr. Fiuzat and her associates reported in an article published online concurrently with the presentation of the results at the meeting by one of Dr. Fiuzat’s colleagues (JACC: Heart Failure 2015. doi: 10.1016/j.jchf.2015.09.002]).
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point: High-dose beta-blockers produced significantly better outcomes than did low-dose beta-blockers, while heart rate had no significant impact.
Major finding: Patients on high beta-blocker dosage had a significant 13% reduced rate of bad outcomes compared with low-dosage patients.
Data source: A post hoc analysis of data from the HF-ACTION trial, which enrolled 2,331 patients with heart failure and reduced ejection fraction.
Disclosures: Dr. Fiuzat had no disclosures.
HFSA: Next-generation LVAD meets survival goal
NATIONAL HARBOR, MD. – A next-generation left-ventricular assist device, the HeartMate 3, gave a solid debut performance in an uncontrolled series of the first 50 recipients, which was designed to gain the device CE mark approval in Europe.
In this study, run at 10 sites in Australia, Austria, Canada, Czech Republic, Germany, and Kazakhstan, the new-design left ventricular assist device (LVAD) numerically surpassed the study’s prespecified primary endpoint with 6-month recipient survival of 92%. This bested the target survival rate of 88% that the trial’s designers derived from the survival rate among 50 matched patients who had received a LVAD during 2012-2014 and had entered the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS), Dr. Ivan Netuka said at the annual meeting of the Heart Failure Society of America.
Other notable findings of the HeartMate 3’s performance in the first 50 patients followed for 6 months were no pump malfunctions, no thrombosis within the pump, and no evidence of hemolysis, said Dr. Netuka, deputy director of cardiovascular surgery at IKEM hospital in Prague.
HeartMate 3 features several improvements over the HeartMate II model, such as a fully magnetically levitated rotor designed to eliminate friction and wear within the pump. The device also is engineered to produce an artificial pulse of 30 beats per minute, and it can deliver a wide blood-flow range of 2-10 L/min. Larger and consistent pump gaps are designed to reduced shear stress on blood components.
The study enrolled patients during June-November 2014 with NYHA class IIIB or IV heart failure and stage D heart failure, with a left ventricular ejection fraction of 25% or less. The 50 patients averaged 59 years of age and 90% were men; they were divided about equally between patients who received the device as a bridge to transplant and those who received the LVAD as destination therapy.
During 6 months of follow-up, two patients received a heart transplant. Twenty-one (42%) of the enrolled patients classified as INTERMACS patient profile 3, 20 (40%) as profile 4, and 5 (10%) as profile 2 patients, with the remaining four patients falling into other profile levels. Twenty-one patients had concomitant heart surgery when they received their LVAD, usually valve replacement. All patients received warfarin treatment and aspirin following device placement. Dr. Netuka and his associates calculated an expected 6-month survival of 78% for the enrolled patients without LVAD intervention.
The four deaths included a patient who died from cardiac arrest following a stroke on day 19 – a complication judged attributable to the device-placement procedure, a patient with circulatory failure on day 48, a suicide on day 113, and a patient with multiorgan failure on day 144.
After 6 months of follow-up, notable adverse events included bleeding in 19 patients (38%) – including gastrointestinal bleeds in 4 patients (8%) – strokes in 6 patients (12%), and infections in 18 patients (36%). Most of the adverse events occurred in the first 7 days following LVAD placement. Three of the six strokes were judged procedure associated, Dr. Netuka said.
Following device placement, patients showed improvements in their NYHA class and quality of life; their 6-minute walk distance improved by an average of 231 m.
The HeartMate 3 device is currently undergoing U.S. assessment in comparison to HeartMate II prior to submission to the Food and Drug Administration. The randomized trial, known as MOMENTUM 3, plans to enroll 1,028 patients with completion scheduled for 2018.
The study was sponsored by Thoratec, which is developing the HeartMate 3 device. Dr. Netuka is a speaker for and consultant to Thoratec.
On Twitter @mitchelzoler
It is extremely exciting to see this next-generation left ventricular assist device move forward, but it is important not to overinterpret the findings because the number of patients treated was relatively small and, as a result, the findings are limited by very wide confidence limits.
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Marvin A. Konstam |
The HeartMate 3 device probably represents an important advance beyond currently available technology. Its attractive features include full magnetic levitation of the rotor, production of an artificial pulse, and the ability to deliver a wide range of blood-flow rates. These features may improve performance and could have favorable effects on thrombus and stroke rates.
The device clearly achieved its primary performance goal of 88% 6-month survival. The INTERMACS profiles of the enrolled patients included 40% of patients with profile 4 and 10% with profile 2. This does not exactly mimic the typical U.S. population receiving these devices, which recently had 15% of patients with a level 4 profile and 36% of patients with more severe disease at level 2. I applaud the decision to include patients who received their devices as destination therapy as well as patients who received it as a bridge to transplant.
The technologic advances that this new device represents are a step in the right direction, and the results provide a green light for further assessment. I look forward to seeing results from the U.S. randomized trial.
Dr. Marvin A. Konstam is professor and chief physician executive of the CardioVascular Center at Tufts Medical Center in Boston. He made these comments as designated discussant for Dr. Netuka’s report. Dr. Konstam has been a consultant to Merck, Novartis, Amgen, Johnson & Johnson, Arbor, Mast, and Cardioxyl.
It is extremely exciting to see this next-generation left ventricular assist device move forward, but it is important not to overinterpret the findings because the number of patients treated was relatively small and, as a result, the findings are limited by very wide confidence limits.
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Marvin A. Konstam |
The HeartMate 3 device probably represents an important advance beyond currently available technology. Its attractive features include full magnetic levitation of the rotor, production of an artificial pulse, and the ability to deliver a wide range of blood-flow rates. These features may improve performance and could have favorable effects on thrombus and stroke rates.
The device clearly achieved its primary performance goal of 88% 6-month survival. The INTERMACS profiles of the enrolled patients included 40% of patients with profile 4 and 10% with profile 2. This does not exactly mimic the typical U.S. population receiving these devices, which recently had 15% of patients with a level 4 profile and 36% of patients with more severe disease at level 2. I applaud the decision to include patients who received their devices as destination therapy as well as patients who received it as a bridge to transplant.
The technologic advances that this new device represents are a step in the right direction, and the results provide a green light for further assessment. I look forward to seeing results from the U.S. randomized trial.
Dr. Marvin A. Konstam is professor and chief physician executive of the CardioVascular Center at Tufts Medical Center in Boston. He made these comments as designated discussant for Dr. Netuka’s report. Dr. Konstam has been a consultant to Merck, Novartis, Amgen, Johnson & Johnson, Arbor, Mast, and Cardioxyl.
It is extremely exciting to see this next-generation left ventricular assist device move forward, but it is important not to overinterpret the findings because the number of patients treated was relatively small and, as a result, the findings are limited by very wide confidence limits.
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Marvin A. Konstam |
The HeartMate 3 device probably represents an important advance beyond currently available technology. Its attractive features include full magnetic levitation of the rotor, production of an artificial pulse, and the ability to deliver a wide range of blood-flow rates. These features may improve performance and could have favorable effects on thrombus and stroke rates.
The device clearly achieved its primary performance goal of 88% 6-month survival. The INTERMACS profiles of the enrolled patients included 40% of patients with profile 4 and 10% with profile 2. This does not exactly mimic the typical U.S. population receiving these devices, which recently had 15% of patients with a level 4 profile and 36% of patients with more severe disease at level 2. I applaud the decision to include patients who received their devices as destination therapy as well as patients who received it as a bridge to transplant.
The technologic advances that this new device represents are a step in the right direction, and the results provide a green light for further assessment. I look forward to seeing results from the U.S. randomized trial.
Dr. Marvin A. Konstam is professor and chief physician executive of the CardioVascular Center at Tufts Medical Center in Boston. He made these comments as designated discussant for Dr. Netuka’s report. Dr. Konstam has been a consultant to Merck, Novartis, Amgen, Johnson & Johnson, Arbor, Mast, and Cardioxyl.
NATIONAL HARBOR, MD. – A next-generation left-ventricular assist device, the HeartMate 3, gave a solid debut performance in an uncontrolled series of the first 50 recipients, which was designed to gain the device CE mark approval in Europe.
In this study, run at 10 sites in Australia, Austria, Canada, Czech Republic, Germany, and Kazakhstan, the new-design left ventricular assist device (LVAD) numerically surpassed the study’s prespecified primary endpoint with 6-month recipient survival of 92%. This bested the target survival rate of 88% that the trial’s designers derived from the survival rate among 50 matched patients who had received a LVAD during 2012-2014 and had entered the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS), Dr. Ivan Netuka said at the annual meeting of the Heart Failure Society of America.
Other notable findings of the HeartMate 3’s performance in the first 50 patients followed for 6 months were no pump malfunctions, no thrombosis within the pump, and no evidence of hemolysis, said Dr. Netuka, deputy director of cardiovascular surgery at IKEM hospital in Prague.
HeartMate 3 features several improvements over the HeartMate II model, such as a fully magnetically levitated rotor designed to eliminate friction and wear within the pump. The device also is engineered to produce an artificial pulse of 30 beats per minute, and it can deliver a wide blood-flow range of 2-10 L/min. Larger and consistent pump gaps are designed to reduced shear stress on blood components.
The study enrolled patients during June-November 2014 with NYHA class IIIB or IV heart failure and stage D heart failure, with a left ventricular ejection fraction of 25% or less. The 50 patients averaged 59 years of age and 90% were men; they were divided about equally between patients who received the device as a bridge to transplant and those who received the LVAD as destination therapy.
During 6 months of follow-up, two patients received a heart transplant. Twenty-one (42%) of the enrolled patients classified as INTERMACS patient profile 3, 20 (40%) as profile 4, and 5 (10%) as profile 2 patients, with the remaining four patients falling into other profile levels. Twenty-one patients had concomitant heart surgery when they received their LVAD, usually valve replacement. All patients received warfarin treatment and aspirin following device placement. Dr. Netuka and his associates calculated an expected 6-month survival of 78% for the enrolled patients without LVAD intervention.
The four deaths included a patient who died from cardiac arrest following a stroke on day 19 – a complication judged attributable to the device-placement procedure, a patient with circulatory failure on day 48, a suicide on day 113, and a patient with multiorgan failure on day 144.
After 6 months of follow-up, notable adverse events included bleeding in 19 patients (38%) – including gastrointestinal bleeds in 4 patients (8%) – strokes in 6 patients (12%), and infections in 18 patients (36%). Most of the adverse events occurred in the first 7 days following LVAD placement. Three of the six strokes were judged procedure associated, Dr. Netuka said.
Following device placement, patients showed improvements in their NYHA class and quality of life; their 6-minute walk distance improved by an average of 231 m.
The HeartMate 3 device is currently undergoing U.S. assessment in comparison to HeartMate II prior to submission to the Food and Drug Administration. The randomized trial, known as MOMENTUM 3, plans to enroll 1,028 patients with completion scheduled for 2018.
The study was sponsored by Thoratec, which is developing the HeartMate 3 device. Dr. Netuka is a speaker for and consultant to Thoratec.
On Twitter @mitchelzoler
NATIONAL HARBOR, MD. – A next-generation left-ventricular assist device, the HeartMate 3, gave a solid debut performance in an uncontrolled series of the first 50 recipients, which was designed to gain the device CE mark approval in Europe.
In this study, run at 10 sites in Australia, Austria, Canada, Czech Republic, Germany, and Kazakhstan, the new-design left ventricular assist device (LVAD) numerically surpassed the study’s prespecified primary endpoint with 6-month recipient survival of 92%. This bested the target survival rate of 88% that the trial’s designers derived from the survival rate among 50 matched patients who had received a LVAD during 2012-2014 and had entered the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS), Dr. Ivan Netuka said at the annual meeting of the Heart Failure Society of America.
Other notable findings of the HeartMate 3’s performance in the first 50 patients followed for 6 months were no pump malfunctions, no thrombosis within the pump, and no evidence of hemolysis, said Dr. Netuka, deputy director of cardiovascular surgery at IKEM hospital in Prague.
HeartMate 3 features several improvements over the HeartMate II model, such as a fully magnetically levitated rotor designed to eliminate friction and wear within the pump. The device also is engineered to produce an artificial pulse of 30 beats per minute, and it can deliver a wide blood-flow range of 2-10 L/min. Larger and consistent pump gaps are designed to reduced shear stress on blood components.
The study enrolled patients during June-November 2014 with NYHA class IIIB or IV heart failure and stage D heart failure, with a left ventricular ejection fraction of 25% or less. The 50 patients averaged 59 years of age and 90% were men; they were divided about equally between patients who received the device as a bridge to transplant and those who received the LVAD as destination therapy.
During 6 months of follow-up, two patients received a heart transplant. Twenty-one (42%) of the enrolled patients classified as INTERMACS patient profile 3, 20 (40%) as profile 4, and 5 (10%) as profile 2 patients, with the remaining four patients falling into other profile levels. Twenty-one patients had concomitant heart surgery when they received their LVAD, usually valve replacement. All patients received warfarin treatment and aspirin following device placement. Dr. Netuka and his associates calculated an expected 6-month survival of 78% for the enrolled patients without LVAD intervention.
The four deaths included a patient who died from cardiac arrest following a stroke on day 19 – a complication judged attributable to the device-placement procedure, a patient with circulatory failure on day 48, a suicide on day 113, and a patient with multiorgan failure on day 144.
After 6 months of follow-up, notable adverse events included bleeding in 19 patients (38%) – including gastrointestinal bleeds in 4 patients (8%) – strokes in 6 patients (12%), and infections in 18 patients (36%). Most of the adverse events occurred in the first 7 days following LVAD placement. Three of the six strokes were judged procedure associated, Dr. Netuka said.
Following device placement, patients showed improvements in their NYHA class and quality of life; their 6-minute walk distance improved by an average of 231 m.
The HeartMate 3 device is currently undergoing U.S. assessment in comparison to HeartMate II prior to submission to the Food and Drug Administration. The randomized trial, known as MOMENTUM 3, plans to enroll 1,028 patients with completion scheduled for 2018.
The study was sponsored by Thoratec, which is developing the HeartMate 3 device. Dr. Netuka is a speaker for and consultant to Thoratec.
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point: A next-generation left ventricular assist device, HeartMate 3, met its 6-month survival goal to receive CE mark approval in Europe.
Major finding: The advanced heart failure patients who received the HeartMate 3 LVAD had a 92% survival rate after 6 months.
Data source: A prospective series of 50 patients enrolled at 10 centers in six countries.
Disclosures: The study was sponsored by Thoratec, which is developing the HeartMate 3 device. Dr. Netuka is a speaker for and consultant to Thoratec.