User login
Continuous lenalidomide plus dexamethasone ups progression-free survival
NEW ORLEANS – For patients with newly diagnosed multiple myeloma who are not eligible for stem cell transplants, continuous treatment with lenalidomide and low-dose dexamethasone was associated with significant overall survival and progression-free survival benefits, compared with melphalan-prednisone-thalidomide.
"Overall, we should congratulate [the investigators] for having a new standard of care that is active, convenient, and with excellent tolerability," said invited discussant Dr. Jesús San Miguel from the cancer center at the Hospital Universitario de Salamanca, Spain.
Initial results from the phase III FIRST trial (Front-Line Investigation of Revlimid/Dexamethasone vs. Standard Thalidomide) showed that lenalidomide (Revlimid [RD]) plus low-dose dexamethasone used until disease progression was associated with a median progression-free survival (PFS, the primary endpoint) of 25.5 months, compared with 20.7 months for patients treated with the same combination for 18 cycles over 72 weeks (RD18), and 21.2 months for patients treated with melphalan-prednisone-thalidomide (MPT) for 12 cycles over 72 weeks, reported Dr. Thierry Facon of the Service des Maladies du Sang, Hôpital Claude Huriez and CHRU Lille, France.
At the first interim analysis, patients treated with continuous RD had better overall survival than patients treated with MPT, with a hazard ratio favoring RD of 0.78 (P = .0168). However, there were no significant differences in overall survival between the RD and RD18 groups or between the RD18 and MPT groups, Dr. Facon said at the American Society of Hematology annual meeting.
The FIRST trial investigators enrolled 1,623 patients aged 65 years or older from 246 centers in 18 countries in North America, Europe, Asia, and Australia/New Zealand. Patients were randomly assigned to either continuous RD (535), RD18 (541), or MPT (547). Median follow-up as of May 24, 2013, was 37 months.
Continuous RD offered significantly better PFS, compared with either RD18 or MPT. At 3 years, 42% of patients on continuous RD remained progression free, compared with 23% each in the other two groups. The hazard ratio for continuous RD vs. MPT was 0.72 (P = .00006), and vs. RD18 was 0.70 (P = .00001). There was no significant difference in progression-free survival between RD18 and MPT.
Estimated 4-year overall survival rates were 59.4% in the continuous RD group, 55.7% in the RD18 group, and 51.4% in the MPT group.
"RD was superior to MPT across all other efficacy secondary endpoints," Dr. Facon said in the plenary session. Those secondary endpoints included response, duration of response, time to response, time to treatment failure, time to second-line anti–multiple myeloma therapy, time to progression, safety, and quality of life.
Both versions of the RD regimen were generally comparable to MPT in safety profile, although infections were more frequent with RD, and peripheral sensory neuropathy was more frequent with continuous RD (1.1% vs. 0.4% for the other two regimens).
The incidence of second primary malignancies was lower in both RD groups, consisting of one case each of acute myeloid leukemia and myelodysplasia in each group, compared with four cases of acute myeloid leukemia, six of myelodysplasia, and two cases of myelodysplasia converting to acute myeloid leukemia in the MPT group.
Current treatment approaches for elderly, newly diagnosed patients with multiple myeloma include MPT, which is associated with a PFS of 20.3 months; and bortezomib (Velcade), melphalan, and prednisone (VMP), with a PFS of 18.3 months. MPT and VMP are the preferred regimens recommend by the National Comprehensive Cancer Network for patients who are ineligible for stem cell transplants because of age or other factors, Dr. Facon noted. Typically, drug therapy in this patient population has had a fixed duration because of f concern for toxicities associated with long-term therapy.
Dr. San Miguel noted that the excellent results were achieved without the use of an alkylating agent such as melphalan or cyclophosphamide, which might lead some clinicians to question whether alkylating agents still have a role in this population. He pointed out, however, that the study was not designed to answer that question. To do so, it would be necessary to compare RD with and without an alkylator for the same treatment duration.
"Probably the most challenging question is the duration of the lenalidomide treatment. The data indicate that the best option is to treat until progression. Nevertheless, it would be interesting to know the outcome according to response, because it could be that in patients taking lenalidomide and dexamethasone for 1 year or [1 1/2 years] will achieve a complete response with prolonged disease stability. Additional treatment may not add too much, and this could contribute to increased cost and toxicities of unnecessary prolonged treatment," he said.
Questions that still need to be answered include benefits for specific populations, such as high-risk patients, the very elderly, and those with renal insufficiency. It’s also unclear whether the reduced risk of secondary malignancies is because of the absence of melphalan or the presence of dexamethasone.
It will also be important to find a way to indentify, as early as possible, the 25% of patients who will not achieve at least a partial response, he said.
The study was supported by Celegene Corporation and by the Intergroupe Francophone du Myelome. Dr. Facon disclosed serving on the speakers bureau and being a member on a board of directors/advisory committee for Celgene. Dr. San Miguel reported having no disclosures.
NEW ORLEANS – For patients with newly diagnosed multiple myeloma who are not eligible for stem cell transplants, continuous treatment with lenalidomide and low-dose dexamethasone was associated with significant overall survival and progression-free survival benefits, compared with melphalan-prednisone-thalidomide.
"Overall, we should congratulate [the investigators] for having a new standard of care that is active, convenient, and with excellent tolerability," said invited discussant Dr. Jesús San Miguel from the cancer center at the Hospital Universitario de Salamanca, Spain.
Initial results from the phase III FIRST trial (Front-Line Investigation of Revlimid/Dexamethasone vs. Standard Thalidomide) showed that lenalidomide (Revlimid [RD]) plus low-dose dexamethasone used until disease progression was associated with a median progression-free survival (PFS, the primary endpoint) of 25.5 months, compared with 20.7 months for patients treated with the same combination for 18 cycles over 72 weeks (RD18), and 21.2 months for patients treated with melphalan-prednisone-thalidomide (MPT) for 12 cycles over 72 weeks, reported Dr. Thierry Facon of the Service des Maladies du Sang, Hôpital Claude Huriez and CHRU Lille, France.
At the first interim analysis, patients treated with continuous RD had better overall survival than patients treated with MPT, with a hazard ratio favoring RD of 0.78 (P = .0168). However, there were no significant differences in overall survival between the RD and RD18 groups or between the RD18 and MPT groups, Dr. Facon said at the American Society of Hematology annual meeting.
The FIRST trial investigators enrolled 1,623 patients aged 65 years or older from 246 centers in 18 countries in North America, Europe, Asia, and Australia/New Zealand. Patients were randomly assigned to either continuous RD (535), RD18 (541), or MPT (547). Median follow-up as of May 24, 2013, was 37 months.
Continuous RD offered significantly better PFS, compared with either RD18 or MPT. At 3 years, 42% of patients on continuous RD remained progression free, compared with 23% each in the other two groups. The hazard ratio for continuous RD vs. MPT was 0.72 (P = .00006), and vs. RD18 was 0.70 (P = .00001). There was no significant difference in progression-free survival between RD18 and MPT.
Estimated 4-year overall survival rates were 59.4% in the continuous RD group, 55.7% in the RD18 group, and 51.4% in the MPT group.
"RD was superior to MPT across all other efficacy secondary endpoints," Dr. Facon said in the plenary session. Those secondary endpoints included response, duration of response, time to response, time to treatment failure, time to second-line anti–multiple myeloma therapy, time to progression, safety, and quality of life.
Both versions of the RD regimen were generally comparable to MPT in safety profile, although infections were more frequent with RD, and peripheral sensory neuropathy was more frequent with continuous RD (1.1% vs. 0.4% for the other two regimens).
The incidence of second primary malignancies was lower in both RD groups, consisting of one case each of acute myeloid leukemia and myelodysplasia in each group, compared with four cases of acute myeloid leukemia, six of myelodysplasia, and two cases of myelodysplasia converting to acute myeloid leukemia in the MPT group.
Current treatment approaches for elderly, newly diagnosed patients with multiple myeloma include MPT, which is associated with a PFS of 20.3 months; and bortezomib (Velcade), melphalan, and prednisone (VMP), with a PFS of 18.3 months. MPT and VMP are the preferred regimens recommend by the National Comprehensive Cancer Network for patients who are ineligible for stem cell transplants because of age or other factors, Dr. Facon noted. Typically, drug therapy in this patient population has had a fixed duration because of f concern for toxicities associated with long-term therapy.
Dr. San Miguel noted that the excellent results were achieved without the use of an alkylating agent such as melphalan or cyclophosphamide, which might lead some clinicians to question whether alkylating agents still have a role in this population. He pointed out, however, that the study was not designed to answer that question. To do so, it would be necessary to compare RD with and without an alkylator for the same treatment duration.
"Probably the most challenging question is the duration of the lenalidomide treatment. The data indicate that the best option is to treat until progression. Nevertheless, it would be interesting to know the outcome according to response, because it could be that in patients taking lenalidomide and dexamethasone for 1 year or [1 1/2 years] will achieve a complete response with prolonged disease stability. Additional treatment may not add too much, and this could contribute to increased cost and toxicities of unnecessary prolonged treatment," he said.
Questions that still need to be answered include benefits for specific populations, such as high-risk patients, the very elderly, and those with renal insufficiency. It’s also unclear whether the reduced risk of secondary malignancies is because of the absence of melphalan or the presence of dexamethasone.
It will also be important to find a way to indentify, as early as possible, the 25% of patients who will not achieve at least a partial response, he said.
The study was supported by Celegene Corporation and by the Intergroupe Francophone du Myelome. Dr. Facon disclosed serving on the speakers bureau and being a member on a board of directors/advisory committee for Celgene. Dr. San Miguel reported having no disclosures.
NEW ORLEANS – For patients with newly diagnosed multiple myeloma who are not eligible for stem cell transplants, continuous treatment with lenalidomide and low-dose dexamethasone was associated with significant overall survival and progression-free survival benefits, compared with melphalan-prednisone-thalidomide.
"Overall, we should congratulate [the investigators] for having a new standard of care that is active, convenient, and with excellent tolerability," said invited discussant Dr. Jesús San Miguel from the cancer center at the Hospital Universitario de Salamanca, Spain.
Initial results from the phase III FIRST trial (Front-Line Investigation of Revlimid/Dexamethasone vs. Standard Thalidomide) showed that lenalidomide (Revlimid [RD]) plus low-dose dexamethasone used until disease progression was associated with a median progression-free survival (PFS, the primary endpoint) of 25.5 months, compared with 20.7 months for patients treated with the same combination for 18 cycles over 72 weeks (RD18), and 21.2 months for patients treated with melphalan-prednisone-thalidomide (MPT) for 12 cycles over 72 weeks, reported Dr. Thierry Facon of the Service des Maladies du Sang, Hôpital Claude Huriez and CHRU Lille, France.
At the first interim analysis, patients treated with continuous RD had better overall survival than patients treated with MPT, with a hazard ratio favoring RD of 0.78 (P = .0168). However, there were no significant differences in overall survival between the RD and RD18 groups or between the RD18 and MPT groups, Dr. Facon said at the American Society of Hematology annual meeting.
The FIRST trial investigators enrolled 1,623 patients aged 65 years or older from 246 centers in 18 countries in North America, Europe, Asia, and Australia/New Zealand. Patients were randomly assigned to either continuous RD (535), RD18 (541), or MPT (547). Median follow-up as of May 24, 2013, was 37 months.
Continuous RD offered significantly better PFS, compared with either RD18 or MPT. At 3 years, 42% of patients on continuous RD remained progression free, compared with 23% each in the other two groups. The hazard ratio for continuous RD vs. MPT was 0.72 (P = .00006), and vs. RD18 was 0.70 (P = .00001). There was no significant difference in progression-free survival between RD18 and MPT.
Estimated 4-year overall survival rates were 59.4% in the continuous RD group, 55.7% in the RD18 group, and 51.4% in the MPT group.
"RD was superior to MPT across all other efficacy secondary endpoints," Dr. Facon said in the plenary session. Those secondary endpoints included response, duration of response, time to response, time to treatment failure, time to second-line anti–multiple myeloma therapy, time to progression, safety, and quality of life.
Both versions of the RD regimen were generally comparable to MPT in safety profile, although infections were more frequent with RD, and peripheral sensory neuropathy was more frequent with continuous RD (1.1% vs. 0.4% for the other two regimens).
The incidence of second primary malignancies was lower in both RD groups, consisting of one case each of acute myeloid leukemia and myelodysplasia in each group, compared with four cases of acute myeloid leukemia, six of myelodysplasia, and two cases of myelodysplasia converting to acute myeloid leukemia in the MPT group.
Current treatment approaches for elderly, newly diagnosed patients with multiple myeloma include MPT, which is associated with a PFS of 20.3 months; and bortezomib (Velcade), melphalan, and prednisone (VMP), with a PFS of 18.3 months. MPT and VMP are the preferred regimens recommend by the National Comprehensive Cancer Network for patients who are ineligible for stem cell transplants because of age or other factors, Dr. Facon noted. Typically, drug therapy in this patient population has had a fixed duration because of f concern for toxicities associated with long-term therapy.
Dr. San Miguel noted that the excellent results were achieved without the use of an alkylating agent such as melphalan or cyclophosphamide, which might lead some clinicians to question whether alkylating agents still have a role in this population. He pointed out, however, that the study was not designed to answer that question. To do so, it would be necessary to compare RD with and without an alkylator for the same treatment duration.
"Probably the most challenging question is the duration of the lenalidomide treatment. The data indicate that the best option is to treat until progression. Nevertheless, it would be interesting to know the outcome according to response, because it could be that in patients taking lenalidomide and dexamethasone for 1 year or [1 1/2 years] will achieve a complete response with prolonged disease stability. Additional treatment may not add too much, and this could contribute to increased cost and toxicities of unnecessary prolonged treatment," he said.
Questions that still need to be answered include benefits for specific populations, such as high-risk patients, the very elderly, and those with renal insufficiency. It’s also unclear whether the reduced risk of secondary malignancies is because of the absence of melphalan or the presence of dexamethasone.
It will also be important to find a way to indentify, as early as possible, the 25% of patients who will not achieve at least a partial response, he said.
The study was supported by Celegene Corporation and by the Intergroupe Francophone du Myelome. Dr. Facon disclosed serving on the speakers bureau and being a member on a board of directors/advisory committee for Celgene. Dr. San Miguel reported having no disclosures.
AT ASH 2013
Major finding: Continuous lenalidomide plus dexamethasone was associated with a median progression-free survival of 25.5 months in multiple myeloma patients, compared with 20.7 months for patients treated with the same combination for 18 cycles, and 21.2 months for patients treated with melphalan-prednisone-thalidomide (MPT).
Data source: Randomized, phase III trial of 1,623 patients aged 65 years or older from 246 centers in 18 countries.
Disclosures: The study was supported by Celegene Corporation and by the Intergroupe Francophone du Myelome. Dr. Facon disclosed serving on the speakers bureau and being a member on a board of directors/advisory committee for Celgene. Dr. San Miguel reported having no disclosures.
Resurrected gemtuzumab shows benefit against pediatric AML
NEW ORLEANS – Gemtuzumab, an antileukemia antibody withdrawn from the market in 2010, has been shown to reduce relapse risk and improve event-free survival when added to conventional therapy in children with acute myeloid leukemia.
Among 1,022 children with AML who were followed for a median of 3.6 years, 3-year event-free survival rates were 53% for children and young adults treated with gemtuzumab ozogamicin added to a standard chemotherapy induction/intensification regimen, compared with 47% for patients treated with chemotherapy alone, said Dr. Alan Gamis, associate division director of the section of oncology at Children’s Mercy Hospital in Kansas City, Mo.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
"It would be our thought that [gemtuzumab] would be added to standard therapy at the time of induction for low-risk patients, and it may be a way to enhance the benefits of stem-cell transplant, as we saw for our high-risk patients," Dr. Gamis said in a briefing at the annual meeting of the American Society of Hematology prior to his presentation of data.
Gemtuzumab (formerly marketed as Mylotarg) is a monoclonal antibody linked to the DNA toxin calicheamicin. The antibody targets the CD33 receptor found on the surface of approximately 80%-85% of acute myeloid leukemia (AML) cells and causes both single-stranded and double-stranded DNA breaks.
The agent was voluntarily withdrawn from the market by Pfizer in 2010 at the urging of the U.S. Food and Drug Administration, following a failure to reach the primary endpoint of complete remission in a phase III clinical trial. In that trial, the addition of gemtuzumab to induction therapy was associated with a significantly higher risk of fatal adverse events.
The findings of the current study, however, suggest that gemtuzumab may be worth another look, Dr. Gamis said.
Survival of childhood AML has been gradually improving due to chemotherapy intensification, stem-cell transplants for high-risk patients, and improved supportive care. However, treatment is limited by a relatively high 10%-19% rate of treatment-related mortality. Further, compared with the general population, patients have a 27-fold increased risk for developing late cardiac toxicities from exposure to anthracyclines such as daunorubicin.
"There is also a ceiling to our success. We still, despite the advances in therapy, are only seeing event-free survival between 46% and 59%, and overall survival between 56% and 74% among the best chemotherapy regimens tested throughout the world," Dr. Gamis said.
In the phase III trial, pediatric and adolescent/young adult patients with newly diagnosed AML were randomized to receive induction therapy with the ADE regimen (cytarabine, daunorubicin, and etoposide), with or without gemtuzumab 3 mg/m2 on day 6 of the first induction cycle, and, for those patients not going on to immediate stem-cell transplant, on day 7 of the second intensification cycle. Intensification includes, for some patients, additional cytarabine and etoposide, as well as mitoxantrone.
Patients were risk-stratified following induction, with all low-risk patients and with intermediate-risk patients without matched family donors going on to intensification. Intermediate-risk patients with matched donors went on to stem-cell transplant, and high-risk patients went on to transplant with any suitable donor.
A total of 1,070 patients from infancy to up to age 29 years were enrolled from 181 institutions in the United States and Canada. Of this cohort, 1,022 were eligible for analysis.
Three-year overall survival rates were 69.4% in patients who received gemtuzumab, compared with 65.4% in those who received chemotherapy only, a difference that was not statistically significant.
As noted before, however, 3-year event-free survival was significantly better for patients who received gemtuzumab, with a hazard ratio (HR) of 0.83 (P = .04).
In addition, gemtuzumab was associated with a significantly lower risk of relapse, with a 3-year relapse rate of nearly 33%, compared with slightly more than 41% for no gemtuzumab (HR, 0.73; P = .01).
There were no significant differences in nonleukemic mortality, disease-free survival, or overall survival; there appeared to be a trend in each category favoring gemtuzumab, Dr. Gamis said.
Looking at the individual risk groups, gemtuzumab was significantly associated with a reduced risk for relapse in low-risk patients (HR, 0.58; 95% confidence interval, 0.34-0.97). There was a trend, albeit nonsignificant, toward greater treatment-related mortality, primarily from infections during intensification cycles 2 and 3.
There were no significant differences in intermediate-risk patients or in high-risk patients, although in the latter group there were trends favoring gemtuzumab for reduced relapse risk, disease-free survival, and overall survival.
The risk of relapse was consistently reduced in all groups, Dr. Gamis said, but he noted that in intermediate- and high-risk groups that benefit was limited to transplant recipients. The decreased relapse risk in low-risk patients was offset by increases in treatment-related mortality.
The overall treatment-related mortality rates were 2% during induction and 5% overall, and did not differ by study arm. The incidence of veno-occlusive disease was 3% overall and was severe in 0.6% of patients. There were no differences in incidence of this complication between the study arms.
Dr. Joseph Mikhael, who moderated the briefing, commented that the findings are "exciting" and noted that "this agent not only has efficacy, but is particularly well tolerated in this pediatric population." He is an associate professor of medicine at the Mayo Clinic in Scottsdale, Ariz.
The study was supported by the National Cancer Institute. Dr. Gamis and Dr. Mikhael reported no relevant conflicts of interest.
NEW ORLEANS – Gemtuzumab, an antileukemia antibody withdrawn from the market in 2010, has been shown to reduce relapse risk and improve event-free survival when added to conventional therapy in children with acute myeloid leukemia.
Among 1,022 children with AML who were followed for a median of 3.6 years, 3-year event-free survival rates were 53% for children and young adults treated with gemtuzumab ozogamicin added to a standard chemotherapy induction/intensification regimen, compared with 47% for patients treated with chemotherapy alone, said Dr. Alan Gamis, associate division director of the section of oncology at Children’s Mercy Hospital in Kansas City, Mo.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
"It would be our thought that [gemtuzumab] would be added to standard therapy at the time of induction for low-risk patients, and it may be a way to enhance the benefits of stem-cell transplant, as we saw for our high-risk patients," Dr. Gamis said in a briefing at the annual meeting of the American Society of Hematology prior to his presentation of data.
Gemtuzumab (formerly marketed as Mylotarg) is a monoclonal antibody linked to the DNA toxin calicheamicin. The antibody targets the CD33 receptor found on the surface of approximately 80%-85% of acute myeloid leukemia (AML) cells and causes both single-stranded and double-stranded DNA breaks.
The agent was voluntarily withdrawn from the market by Pfizer in 2010 at the urging of the U.S. Food and Drug Administration, following a failure to reach the primary endpoint of complete remission in a phase III clinical trial. In that trial, the addition of gemtuzumab to induction therapy was associated with a significantly higher risk of fatal adverse events.
The findings of the current study, however, suggest that gemtuzumab may be worth another look, Dr. Gamis said.
Survival of childhood AML has been gradually improving due to chemotherapy intensification, stem-cell transplants for high-risk patients, and improved supportive care. However, treatment is limited by a relatively high 10%-19% rate of treatment-related mortality. Further, compared with the general population, patients have a 27-fold increased risk for developing late cardiac toxicities from exposure to anthracyclines such as daunorubicin.
"There is also a ceiling to our success. We still, despite the advances in therapy, are only seeing event-free survival between 46% and 59%, and overall survival between 56% and 74% among the best chemotherapy regimens tested throughout the world," Dr. Gamis said.
In the phase III trial, pediatric and adolescent/young adult patients with newly diagnosed AML were randomized to receive induction therapy with the ADE regimen (cytarabine, daunorubicin, and etoposide), with or without gemtuzumab 3 mg/m2 on day 6 of the first induction cycle, and, for those patients not going on to immediate stem-cell transplant, on day 7 of the second intensification cycle. Intensification includes, for some patients, additional cytarabine and etoposide, as well as mitoxantrone.
Patients were risk-stratified following induction, with all low-risk patients and with intermediate-risk patients without matched family donors going on to intensification. Intermediate-risk patients with matched donors went on to stem-cell transplant, and high-risk patients went on to transplant with any suitable donor.
A total of 1,070 patients from infancy to up to age 29 years were enrolled from 181 institutions in the United States and Canada. Of this cohort, 1,022 were eligible for analysis.
Three-year overall survival rates were 69.4% in patients who received gemtuzumab, compared with 65.4% in those who received chemotherapy only, a difference that was not statistically significant.
As noted before, however, 3-year event-free survival was significantly better for patients who received gemtuzumab, with a hazard ratio (HR) of 0.83 (P = .04).
In addition, gemtuzumab was associated with a significantly lower risk of relapse, with a 3-year relapse rate of nearly 33%, compared with slightly more than 41% for no gemtuzumab (HR, 0.73; P = .01).
There were no significant differences in nonleukemic mortality, disease-free survival, or overall survival; there appeared to be a trend in each category favoring gemtuzumab, Dr. Gamis said.
Looking at the individual risk groups, gemtuzumab was significantly associated with a reduced risk for relapse in low-risk patients (HR, 0.58; 95% confidence interval, 0.34-0.97). There was a trend, albeit nonsignificant, toward greater treatment-related mortality, primarily from infections during intensification cycles 2 and 3.
There were no significant differences in intermediate-risk patients or in high-risk patients, although in the latter group there were trends favoring gemtuzumab for reduced relapse risk, disease-free survival, and overall survival.
The risk of relapse was consistently reduced in all groups, Dr. Gamis said, but he noted that in intermediate- and high-risk groups that benefit was limited to transplant recipients. The decreased relapse risk in low-risk patients was offset by increases in treatment-related mortality.
The overall treatment-related mortality rates were 2% during induction and 5% overall, and did not differ by study arm. The incidence of veno-occlusive disease was 3% overall and was severe in 0.6% of patients. There were no differences in incidence of this complication between the study arms.
Dr. Joseph Mikhael, who moderated the briefing, commented that the findings are "exciting" and noted that "this agent not only has efficacy, but is particularly well tolerated in this pediatric population." He is an associate professor of medicine at the Mayo Clinic in Scottsdale, Ariz.
The study was supported by the National Cancer Institute. Dr. Gamis and Dr. Mikhael reported no relevant conflicts of interest.
NEW ORLEANS – Gemtuzumab, an antileukemia antibody withdrawn from the market in 2010, has been shown to reduce relapse risk and improve event-free survival when added to conventional therapy in children with acute myeloid leukemia.
Among 1,022 children with AML who were followed for a median of 3.6 years, 3-year event-free survival rates were 53% for children and young adults treated with gemtuzumab ozogamicin added to a standard chemotherapy induction/intensification regimen, compared with 47% for patients treated with chemotherapy alone, said Dr. Alan Gamis, associate division director of the section of oncology at Children’s Mercy Hospital in Kansas City, Mo.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
"It would be our thought that [gemtuzumab] would be added to standard therapy at the time of induction for low-risk patients, and it may be a way to enhance the benefits of stem-cell transplant, as we saw for our high-risk patients," Dr. Gamis said in a briefing at the annual meeting of the American Society of Hematology prior to his presentation of data.
Gemtuzumab (formerly marketed as Mylotarg) is a monoclonal antibody linked to the DNA toxin calicheamicin. The antibody targets the CD33 receptor found on the surface of approximately 80%-85% of acute myeloid leukemia (AML) cells and causes both single-stranded and double-stranded DNA breaks.
The agent was voluntarily withdrawn from the market by Pfizer in 2010 at the urging of the U.S. Food and Drug Administration, following a failure to reach the primary endpoint of complete remission in a phase III clinical trial. In that trial, the addition of gemtuzumab to induction therapy was associated with a significantly higher risk of fatal adverse events.
The findings of the current study, however, suggest that gemtuzumab may be worth another look, Dr. Gamis said.
Survival of childhood AML has been gradually improving due to chemotherapy intensification, stem-cell transplants for high-risk patients, and improved supportive care. However, treatment is limited by a relatively high 10%-19% rate of treatment-related mortality. Further, compared with the general population, patients have a 27-fold increased risk for developing late cardiac toxicities from exposure to anthracyclines such as daunorubicin.
"There is also a ceiling to our success. We still, despite the advances in therapy, are only seeing event-free survival between 46% and 59%, and overall survival between 56% and 74% among the best chemotherapy regimens tested throughout the world," Dr. Gamis said.
In the phase III trial, pediatric and adolescent/young adult patients with newly diagnosed AML were randomized to receive induction therapy with the ADE regimen (cytarabine, daunorubicin, and etoposide), with or without gemtuzumab 3 mg/m2 on day 6 of the first induction cycle, and, for those patients not going on to immediate stem-cell transplant, on day 7 of the second intensification cycle. Intensification includes, for some patients, additional cytarabine and etoposide, as well as mitoxantrone.
Patients were risk-stratified following induction, with all low-risk patients and with intermediate-risk patients without matched family donors going on to intensification. Intermediate-risk patients with matched donors went on to stem-cell transplant, and high-risk patients went on to transplant with any suitable donor.
A total of 1,070 patients from infancy to up to age 29 years were enrolled from 181 institutions in the United States and Canada. Of this cohort, 1,022 were eligible for analysis.
Three-year overall survival rates were 69.4% in patients who received gemtuzumab, compared with 65.4% in those who received chemotherapy only, a difference that was not statistically significant.
As noted before, however, 3-year event-free survival was significantly better for patients who received gemtuzumab, with a hazard ratio (HR) of 0.83 (P = .04).
In addition, gemtuzumab was associated with a significantly lower risk of relapse, with a 3-year relapse rate of nearly 33%, compared with slightly more than 41% for no gemtuzumab (HR, 0.73; P = .01).
There were no significant differences in nonleukemic mortality, disease-free survival, or overall survival; there appeared to be a trend in each category favoring gemtuzumab, Dr. Gamis said.
Looking at the individual risk groups, gemtuzumab was significantly associated with a reduced risk for relapse in low-risk patients (HR, 0.58; 95% confidence interval, 0.34-0.97). There was a trend, albeit nonsignificant, toward greater treatment-related mortality, primarily from infections during intensification cycles 2 and 3.
There were no significant differences in intermediate-risk patients or in high-risk patients, although in the latter group there were trends favoring gemtuzumab for reduced relapse risk, disease-free survival, and overall survival.
The risk of relapse was consistently reduced in all groups, Dr. Gamis said, but he noted that in intermediate- and high-risk groups that benefit was limited to transplant recipients. The decreased relapse risk in low-risk patients was offset by increases in treatment-related mortality.
The overall treatment-related mortality rates were 2% during induction and 5% overall, and did not differ by study arm. The incidence of veno-occlusive disease was 3% overall and was severe in 0.6% of patients. There were no differences in incidence of this complication between the study arms.
Dr. Joseph Mikhael, who moderated the briefing, commented that the findings are "exciting" and noted that "this agent not only has efficacy, but is particularly well tolerated in this pediatric population." He is an associate professor of medicine at the Mayo Clinic in Scottsdale, Ariz.
The study was supported by the National Cancer Institute. Dr. Gamis and Dr. Mikhael reported no relevant conflicts of interest.
AT ASH 2013
Major finding: Three-year event-free survival rates were 53% for children and young adults treated with gemtuzumab ozogamicin added to a standard chemotherapy induction/intensification regimen, compared with 47% for patients treated with chemotherapy alone.
Data source: Randomized phase III trial in 1,070 patients aged 0-29 years with acute myeloid leukemia.
Disclosures: The study was supported by the National Cancer Institute. Dr. Gamis and Dr. Mikhael reported no relevant conflicts of interest.
Treated T-cells induce remissions in chemo-refractory B-cell lymphomas
NEW ORLEANS – A majority of patients with aggressive, treatment-refractory lymphomas had a complete or partial remission after being treated with chemotherapy and T-cells engineered to target the CD-19 receptor, National Cancer Institute investigators reported here.
In a study of 15 patients, 9 of whom had aggressive large-cell lymphomas and 6 of whom had indolent B-cell malignancies, 6 of 13 evaluable patients had a complete remission, 6 had a partial remission, and 1 had stable disease, said Dr. James N. Kochenderfer, an investigator in the Experimental Transplantation and Immunology Branch at the National Cancer Institute in Bethesda, Md.
One patient who, despite having undergone 10 prior therapies -- including 3 rituximab-based chemotherapy regimens -- continued to have lymphoma involvement of the liver and other abdominal areas, remains in complete remission 9 months after treatment with a chimeric antigen receptor (CAR) targeting the B-cell antigen CD19, Dr. Kochenderfer said at the American Society of Hematology annual meeting.
"We’ve chosen to focus on the aggressive large-cell lymphomas, because patients with these lymphomas, such as diffuse large B-cell lymphoma and primary mediastinal B-cell lymphoma, have a very poor prognosis if they are refractory to chemotherapy," he said in a briefing prior to his presentation of the results in oral session.
Commenting on the CAR-T cell strategy, Dr. Laurence Cooper of the University of Texas MD Anderson Cancer Center in Houston, who moderated the briefing, noted that "these patients were mortally wounded – they were all going to die, except that these types of engineered T-cell therapies rescued the patients."
The NCI investigators genetically modify each patient’s T-cells in vitro, using a gammaretroviral vector to induce in the cells expression of an anti-CD19 antibody. The process takes 10 days, during which time the patients receive cyclophosphamide and fludarabine to deplete their endogenous leukocytes.
"There’s extensive evidence in multiple animal models and also in humans that shows that depletion of endogenous lymphocytes dramatically enhances the activity of adoptively transferred T-cells. In mouse models, it’s absolutely critical for effectiveness of these CAR T-cells," Dr. Kochenderfer said.
The patients are then infused with the anti-C19-CAR transduced T-cells.
The investigators thus far have treated 15 patients with the technique, including, as noted before, 9 with chemo-refractory large cell lymphomas.
Treatment toxicities included hypotension and neurological toxicities such as confusion, delirium, and transient aphasia.
"Another thing about this therapy that’s amazing is that the patients do become sick; we previously published that the toxicity correlates with serum cytokine levels. [However] they recover very quickly: they can go from being incredibly ill to completely feeling almost normal within 2 days," Dr. Kochenderfer noted.
He and his colleagues also have used the technique in 10 patients who had persistent B-cell malignancies or other cancers following allogeneic stem cell transplantation as an alternative to donor lymphocyte infusions, which have shown inconsistent efficacy and are associated with significant risk for morbidity and mortality for graft-versus-host disease (GvHD).
Of 10 patients treated to date, 3 had "substantial regression" of their malignancies, and one patient with chronic lymphoctic leukemia (CLL) is still in complete remission 12 months after treatment. Another CLL patient had tumor lysis syndrome as he experienced regression of CLL in his bone marrow, blood, and lymph nodes. A patient with the notoriously treatment-refractory mantle cell lymphoma had a partial remission.
As in the first study, toxicities were manageable and consisted mainly of fever, hypotension, and B-cell depletion. No patients developed GvHD after infusion of the altered T-cells.
The study was funded by the National Cancer Institute and by Kite Pharma. Dr. Kochenderfer and Dr. Cooper reported having no conflicts of interest to disclose.
NEW ORLEANS – A majority of patients with aggressive, treatment-refractory lymphomas had a complete or partial remission after being treated with chemotherapy and T-cells engineered to target the CD-19 receptor, National Cancer Institute investigators reported here.
In a study of 15 patients, 9 of whom had aggressive large-cell lymphomas and 6 of whom had indolent B-cell malignancies, 6 of 13 evaluable patients had a complete remission, 6 had a partial remission, and 1 had stable disease, said Dr. James N. Kochenderfer, an investigator in the Experimental Transplantation and Immunology Branch at the National Cancer Institute in Bethesda, Md.
One patient who, despite having undergone 10 prior therapies -- including 3 rituximab-based chemotherapy regimens -- continued to have lymphoma involvement of the liver and other abdominal areas, remains in complete remission 9 months after treatment with a chimeric antigen receptor (CAR) targeting the B-cell antigen CD19, Dr. Kochenderfer said at the American Society of Hematology annual meeting.
"We’ve chosen to focus on the aggressive large-cell lymphomas, because patients with these lymphomas, such as diffuse large B-cell lymphoma and primary mediastinal B-cell lymphoma, have a very poor prognosis if they are refractory to chemotherapy," he said in a briefing prior to his presentation of the results in oral session.
Commenting on the CAR-T cell strategy, Dr. Laurence Cooper of the University of Texas MD Anderson Cancer Center in Houston, who moderated the briefing, noted that "these patients were mortally wounded – they were all going to die, except that these types of engineered T-cell therapies rescued the patients."
The NCI investigators genetically modify each patient’s T-cells in vitro, using a gammaretroviral vector to induce in the cells expression of an anti-CD19 antibody. The process takes 10 days, during which time the patients receive cyclophosphamide and fludarabine to deplete their endogenous leukocytes.
"There’s extensive evidence in multiple animal models and also in humans that shows that depletion of endogenous lymphocytes dramatically enhances the activity of adoptively transferred T-cells. In mouse models, it’s absolutely critical for effectiveness of these CAR T-cells," Dr. Kochenderfer said.
The patients are then infused with the anti-C19-CAR transduced T-cells.
The investigators thus far have treated 15 patients with the technique, including, as noted before, 9 with chemo-refractory large cell lymphomas.
Treatment toxicities included hypotension and neurological toxicities such as confusion, delirium, and transient aphasia.
"Another thing about this therapy that’s amazing is that the patients do become sick; we previously published that the toxicity correlates with serum cytokine levels. [However] they recover very quickly: they can go from being incredibly ill to completely feeling almost normal within 2 days," Dr. Kochenderfer noted.
He and his colleagues also have used the technique in 10 patients who had persistent B-cell malignancies or other cancers following allogeneic stem cell transplantation as an alternative to donor lymphocyte infusions, which have shown inconsistent efficacy and are associated with significant risk for morbidity and mortality for graft-versus-host disease (GvHD).
Of 10 patients treated to date, 3 had "substantial regression" of their malignancies, and one patient with chronic lymphoctic leukemia (CLL) is still in complete remission 12 months after treatment. Another CLL patient had tumor lysis syndrome as he experienced regression of CLL in his bone marrow, blood, and lymph nodes. A patient with the notoriously treatment-refractory mantle cell lymphoma had a partial remission.
As in the first study, toxicities were manageable and consisted mainly of fever, hypotension, and B-cell depletion. No patients developed GvHD after infusion of the altered T-cells.
The study was funded by the National Cancer Institute and by Kite Pharma. Dr. Kochenderfer and Dr. Cooper reported having no conflicts of interest to disclose.
NEW ORLEANS – A majority of patients with aggressive, treatment-refractory lymphomas had a complete or partial remission after being treated with chemotherapy and T-cells engineered to target the CD-19 receptor, National Cancer Institute investigators reported here.
In a study of 15 patients, 9 of whom had aggressive large-cell lymphomas and 6 of whom had indolent B-cell malignancies, 6 of 13 evaluable patients had a complete remission, 6 had a partial remission, and 1 had stable disease, said Dr. James N. Kochenderfer, an investigator in the Experimental Transplantation and Immunology Branch at the National Cancer Institute in Bethesda, Md.
One patient who, despite having undergone 10 prior therapies -- including 3 rituximab-based chemotherapy regimens -- continued to have lymphoma involvement of the liver and other abdominal areas, remains in complete remission 9 months after treatment with a chimeric antigen receptor (CAR) targeting the B-cell antigen CD19, Dr. Kochenderfer said at the American Society of Hematology annual meeting.
"We’ve chosen to focus on the aggressive large-cell lymphomas, because patients with these lymphomas, such as diffuse large B-cell lymphoma and primary mediastinal B-cell lymphoma, have a very poor prognosis if they are refractory to chemotherapy," he said in a briefing prior to his presentation of the results in oral session.
Commenting on the CAR-T cell strategy, Dr. Laurence Cooper of the University of Texas MD Anderson Cancer Center in Houston, who moderated the briefing, noted that "these patients were mortally wounded – they were all going to die, except that these types of engineered T-cell therapies rescued the patients."
The NCI investigators genetically modify each patient’s T-cells in vitro, using a gammaretroviral vector to induce in the cells expression of an anti-CD19 antibody. The process takes 10 days, during which time the patients receive cyclophosphamide and fludarabine to deplete their endogenous leukocytes.
"There’s extensive evidence in multiple animal models and also in humans that shows that depletion of endogenous lymphocytes dramatically enhances the activity of adoptively transferred T-cells. In mouse models, it’s absolutely critical for effectiveness of these CAR T-cells," Dr. Kochenderfer said.
The patients are then infused with the anti-C19-CAR transduced T-cells.
The investigators thus far have treated 15 patients with the technique, including, as noted before, 9 with chemo-refractory large cell lymphomas.
Treatment toxicities included hypotension and neurological toxicities such as confusion, delirium, and transient aphasia.
"Another thing about this therapy that’s amazing is that the patients do become sick; we previously published that the toxicity correlates with serum cytokine levels. [However] they recover very quickly: they can go from being incredibly ill to completely feeling almost normal within 2 days," Dr. Kochenderfer noted.
He and his colleagues also have used the technique in 10 patients who had persistent B-cell malignancies or other cancers following allogeneic stem cell transplantation as an alternative to donor lymphocyte infusions, which have shown inconsistent efficacy and are associated with significant risk for morbidity and mortality for graft-versus-host disease (GvHD).
Of 10 patients treated to date, 3 had "substantial regression" of their malignancies, and one patient with chronic lymphoctic leukemia (CLL) is still in complete remission 12 months after treatment. Another CLL patient had tumor lysis syndrome as he experienced regression of CLL in his bone marrow, blood, and lymph nodes. A patient with the notoriously treatment-refractory mantle cell lymphoma had a partial remission.
As in the first study, toxicities were manageable and consisted mainly of fever, hypotension, and B-cell depletion. No patients developed GvHD after infusion of the altered T-cells.
The study was funded by the National Cancer Institute and by Kite Pharma. Dr. Kochenderfer and Dr. Cooper reported having no conflicts of interest to disclose.
AT ASH 2013
Major finding: Among evaluable patient treated with chimeric antigen receptor expressing T cells, 12 of 13 had complete or partial remissions, and the remaining patient had stable disease.
Data source: Prospective clinical trial in 15 patients with chemo-resistant aggressive large-cell or indolent lymphomas.
Disclosures: The study was funded by the National Cancer Institute and by Kite Pharma. Dr. Kochenderfer and Dr. Cooper reported having no conflicts of interest to disclose.
Reduced-intensity pre-transplant conditioning found easier on the brain
NEW ORLEANS – Full-intensity conditioning regimens before stem-cell transplants put patients at risk for cognitive problems afterward, investigators reported.
Compared with healthy controls, men and women who underwent allogeneic hematopoietic stem transplants (HCT) with full-intensity pre-transplant conditioning continued to have deficits in executive function for at least 2 years after transplant.
In contrast, patients who had reduced-intensity conditioning before their transplants had initial cognitive deficits but recovered gradually, continued to have significantly better cognitive function than patients who had undergone full-intensity conditioning (P = .01), and had no significant deficits in executive function compared with controls at 2-year follow-up, reported Dr. Smita Bhatia, professor and chair of the department of population sciences at City of Hope in Duarte, Calif.
The investigators also found preliminary evidence to suggest that the length of telomeres, the caps at the end of chromosomes that protect chromosomal integrity through cellular division, also may be associated with risk for post-transplant cognitive problems -- at least in women.
In women, telomeric shortening before HCT was associated with poorer cognitive functioning after HCT in domains of executive function, processing speed, verbal speed, and working memory, Dr. Bhatia reported at the American Society of Hematology annual meeting.
Those especially at risk for post-transplant cognitive problems include older patients, men, Hispanics, people with lower socioeconomic status, those with high levels of fatigue, and those who undergo a full-intensity pre-transplant conditioning regimen.
"This study has identified vulnerable sub-populations, and there is a need to develop future interventions targeted toward these patients, as well as to understand the pathogenesis of this outcome," Dr. Bhatia said in a briefing before the presentation of results.
Dr. Bhatia stressed that clinicians need to educate patients and families about the cognitive consequences of transplantation.
"When these patients come back, and especially younger patients when they are not performing well in their schools or college settings, very often the family blames these patients for being lazy, and that is something which we need to absolutely negate and say that this is the effect of the treatment they received, and we need to offer them services," she said.
The investigators conducted a 2-year prospective longitudinal study comparing patients scheduled for HCT with age and sex-matched healthy controls.
The participants underwent baseline testing with a 2-hour battery of standardized neurocognitive tests assessing 8 cognitive domains. Scores of healthy controls were used to correct the scores of HCT patients for practice effects.
Patients also had pre-transplant blood draws tested by assay for relative telomere length, defined as the ratio of telomeres to single genes.
As the authors had previously shown, allogeneic HCT recipients overall have poorer cognitive function than controls in domains of executive function, processing speed, verbal fluency, and fine motor dexterity.
For example, in an analysis adjusted for age, race, and income, controls had significantly better executive function scores than did transplant recipients (P = .0008).
When the researchers drilled down a little deeper, however, they found that patients who had undergone full-intensity conditioning did especially poorly in domains of executive function, processing speed, verbal speed, and visual memory.
When they looked at telomere length, they found in an analysis adjusted for age, race, income, IQ, diagnosis, risk of relapse, and remission status that women with short telomeres fared worse than women with long telomeres. At a 2-year follow-up women with short telomeres had significantly poorer executive function scores (P = .004).
There were no significant associations between telomere length and cognitive function among men, however.
Dr. Bhatia noted that chemotherapy and radiation both accelerate telomere shortening and that glial cells, which divide, therefore are susceptible to telomere shortening, offering a potential explanation for the association between telomere length and cognitive function.
Although the investigators have not yet sorted out which components of the conditioning regimen contribute to cognitive problems, it appears to be a combination of total body irradiation and high-myeloablative intensity agents, Dr. Bhatia said.
Clinical trials testing behavioral therapy and pharmacologic therapy with agents that support attention and cognitive processing, such as methylphenidate, are underway, she noted.
Dr. Jeffrey Miller, who moderated the briefing at which Dr. Bhatia presented the data, noted that reduced-intensity pre-transplant conditioning is suitable for older, frailer patients, and in this study was shown to offer cognitive protection compared with full-intensity conditioning.
Reduced-intensity conditioning, however, comes with a significant trade-off in terms of increased risk for relapse, said Dr. Miller, deputy director of the Masonic Cancer Center and the Clinical and Translational Sciences Institute, University of Minnesota, Minneapolis.
Dr. Bhatia commented that the most important clinical consideration is which treatment strategy is likely to offer the best relapse-free survival.
"Then we have the luxury of looking at whether we have a mode of therapy that is less toxic down the road," she said.
The study was supported in part by the Leukemia & Lymphoma Society. Dr. Bhatia and Dr. Miller reported having no relevant conflicts of interest to disclose.
NEW ORLEANS – Full-intensity conditioning regimens before stem-cell transplants put patients at risk for cognitive problems afterward, investigators reported.
Compared with healthy controls, men and women who underwent allogeneic hematopoietic stem transplants (HCT) with full-intensity pre-transplant conditioning continued to have deficits in executive function for at least 2 years after transplant.
In contrast, patients who had reduced-intensity conditioning before their transplants had initial cognitive deficits but recovered gradually, continued to have significantly better cognitive function than patients who had undergone full-intensity conditioning (P = .01), and had no significant deficits in executive function compared with controls at 2-year follow-up, reported Dr. Smita Bhatia, professor and chair of the department of population sciences at City of Hope in Duarte, Calif.
The investigators also found preliminary evidence to suggest that the length of telomeres, the caps at the end of chromosomes that protect chromosomal integrity through cellular division, also may be associated with risk for post-transplant cognitive problems -- at least in women.
In women, telomeric shortening before HCT was associated with poorer cognitive functioning after HCT in domains of executive function, processing speed, verbal speed, and working memory, Dr. Bhatia reported at the American Society of Hematology annual meeting.
Those especially at risk for post-transplant cognitive problems include older patients, men, Hispanics, people with lower socioeconomic status, those with high levels of fatigue, and those who undergo a full-intensity pre-transplant conditioning regimen.
"This study has identified vulnerable sub-populations, and there is a need to develop future interventions targeted toward these patients, as well as to understand the pathogenesis of this outcome," Dr. Bhatia said in a briefing before the presentation of results.
Dr. Bhatia stressed that clinicians need to educate patients and families about the cognitive consequences of transplantation.
"When these patients come back, and especially younger patients when they are not performing well in their schools or college settings, very often the family blames these patients for being lazy, and that is something which we need to absolutely negate and say that this is the effect of the treatment they received, and we need to offer them services," she said.
The investigators conducted a 2-year prospective longitudinal study comparing patients scheduled for HCT with age and sex-matched healthy controls.
The participants underwent baseline testing with a 2-hour battery of standardized neurocognitive tests assessing 8 cognitive domains. Scores of healthy controls were used to correct the scores of HCT patients for practice effects.
Patients also had pre-transplant blood draws tested by assay for relative telomere length, defined as the ratio of telomeres to single genes.
As the authors had previously shown, allogeneic HCT recipients overall have poorer cognitive function than controls in domains of executive function, processing speed, verbal fluency, and fine motor dexterity.
For example, in an analysis adjusted for age, race, and income, controls had significantly better executive function scores than did transplant recipients (P = .0008).
When the researchers drilled down a little deeper, however, they found that patients who had undergone full-intensity conditioning did especially poorly in domains of executive function, processing speed, verbal speed, and visual memory.
When they looked at telomere length, they found in an analysis adjusted for age, race, income, IQ, diagnosis, risk of relapse, and remission status that women with short telomeres fared worse than women with long telomeres. At a 2-year follow-up women with short telomeres had significantly poorer executive function scores (P = .004).
There were no significant associations between telomere length and cognitive function among men, however.
Dr. Bhatia noted that chemotherapy and radiation both accelerate telomere shortening and that glial cells, which divide, therefore are susceptible to telomere shortening, offering a potential explanation for the association between telomere length and cognitive function.
Although the investigators have not yet sorted out which components of the conditioning regimen contribute to cognitive problems, it appears to be a combination of total body irradiation and high-myeloablative intensity agents, Dr. Bhatia said.
Clinical trials testing behavioral therapy and pharmacologic therapy with agents that support attention and cognitive processing, such as methylphenidate, are underway, she noted.
Dr. Jeffrey Miller, who moderated the briefing at which Dr. Bhatia presented the data, noted that reduced-intensity pre-transplant conditioning is suitable for older, frailer patients, and in this study was shown to offer cognitive protection compared with full-intensity conditioning.
Reduced-intensity conditioning, however, comes with a significant trade-off in terms of increased risk for relapse, said Dr. Miller, deputy director of the Masonic Cancer Center and the Clinical and Translational Sciences Institute, University of Minnesota, Minneapolis.
Dr. Bhatia commented that the most important clinical consideration is which treatment strategy is likely to offer the best relapse-free survival.
"Then we have the luxury of looking at whether we have a mode of therapy that is less toxic down the road," she said.
The study was supported in part by the Leukemia & Lymphoma Society. Dr. Bhatia and Dr. Miller reported having no relevant conflicts of interest to disclose.
NEW ORLEANS – Full-intensity conditioning regimens before stem-cell transplants put patients at risk for cognitive problems afterward, investigators reported.
Compared with healthy controls, men and women who underwent allogeneic hematopoietic stem transplants (HCT) with full-intensity pre-transplant conditioning continued to have deficits in executive function for at least 2 years after transplant.
In contrast, patients who had reduced-intensity conditioning before their transplants had initial cognitive deficits but recovered gradually, continued to have significantly better cognitive function than patients who had undergone full-intensity conditioning (P = .01), and had no significant deficits in executive function compared with controls at 2-year follow-up, reported Dr. Smita Bhatia, professor and chair of the department of population sciences at City of Hope in Duarte, Calif.
The investigators also found preliminary evidence to suggest that the length of telomeres, the caps at the end of chromosomes that protect chromosomal integrity through cellular division, also may be associated with risk for post-transplant cognitive problems -- at least in women.
In women, telomeric shortening before HCT was associated with poorer cognitive functioning after HCT in domains of executive function, processing speed, verbal speed, and working memory, Dr. Bhatia reported at the American Society of Hematology annual meeting.
Those especially at risk for post-transplant cognitive problems include older patients, men, Hispanics, people with lower socioeconomic status, those with high levels of fatigue, and those who undergo a full-intensity pre-transplant conditioning regimen.
"This study has identified vulnerable sub-populations, and there is a need to develop future interventions targeted toward these patients, as well as to understand the pathogenesis of this outcome," Dr. Bhatia said in a briefing before the presentation of results.
Dr. Bhatia stressed that clinicians need to educate patients and families about the cognitive consequences of transplantation.
"When these patients come back, and especially younger patients when they are not performing well in their schools or college settings, very often the family blames these patients for being lazy, and that is something which we need to absolutely negate and say that this is the effect of the treatment they received, and we need to offer them services," she said.
The investigators conducted a 2-year prospective longitudinal study comparing patients scheduled for HCT with age and sex-matched healthy controls.
The participants underwent baseline testing with a 2-hour battery of standardized neurocognitive tests assessing 8 cognitive domains. Scores of healthy controls were used to correct the scores of HCT patients for practice effects.
Patients also had pre-transplant blood draws tested by assay for relative telomere length, defined as the ratio of telomeres to single genes.
As the authors had previously shown, allogeneic HCT recipients overall have poorer cognitive function than controls in domains of executive function, processing speed, verbal fluency, and fine motor dexterity.
For example, in an analysis adjusted for age, race, and income, controls had significantly better executive function scores than did transplant recipients (P = .0008).
When the researchers drilled down a little deeper, however, they found that patients who had undergone full-intensity conditioning did especially poorly in domains of executive function, processing speed, verbal speed, and visual memory.
When they looked at telomere length, they found in an analysis adjusted for age, race, income, IQ, diagnosis, risk of relapse, and remission status that women with short telomeres fared worse than women with long telomeres. At a 2-year follow-up women with short telomeres had significantly poorer executive function scores (P = .004).
There were no significant associations between telomere length and cognitive function among men, however.
Dr. Bhatia noted that chemotherapy and radiation both accelerate telomere shortening and that glial cells, which divide, therefore are susceptible to telomere shortening, offering a potential explanation for the association between telomere length and cognitive function.
Although the investigators have not yet sorted out which components of the conditioning regimen contribute to cognitive problems, it appears to be a combination of total body irradiation and high-myeloablative intensity agents, Dr. Bhatia said.
Clinical trials testing behavioral therapy and pharmacologic therapy with agents that support attention and cognitive processing, such as methylphenidate, are underway, she noted.
Dr. Jeffrey Miller, who moderated the briefing at which Dr. Bhatia presented the data, noted that reduced-intensity pre-transplant conditioning is suitable for older, frailer patients, and in this study was shown to offer cognitive protection compared with full-intensity conditioning.
Reduced-intensity conditioning, however, comes with a significant trade-off in terms of increased risk for relapse, said Dr. Miller, deputy director of the Masonic Cancer Center and the Clinical and Translational Sciences Institute, University of Minnesota, Minneapolis.
Dr. Bhatia commented that the most important clinical consideration is which treatment strategy is likely to offer the best relapse-free survival.
"Then we have the luxury of looking at whether we have a mode of therapy that is less toxic down the road," she said.
The study was supported in part by the Leukemia & Lymphoma Society. Dr. Bhatia and Dr. Miller reported having no relevant conflicts of interest to disclose.
AT ASH 2013
Vitals: Patients who had reduced-intensity conditioning before transplant had significantly better cognitive function than patients who had undergone full-intensity conditioning (P = .01) and had no significant deficits in executive function compared with controls at 2-year follow-up.
Data source: Prospective, longitudinal follow-up study of 242 hematopoietic stem-cell transplant recipients and 98 healthy matched controls.
Disclosures: The study was supported in part by the Leukemia & Lymphoma Society. Dr. Bhatia and Dr. Miller reported having no relevant conflicts of interest to disclose.
SBRT in marginally operable NSCLC
ATLANTA – For older patients with marginally operable stage 1 non–small cell lung cancer, stereotactic body radiation therapy is significantly more cost effective than surgery.
For patients with clearly operable non–small cell lung cancer (NSCLS) tumors, however, lobectomy is the most cost-effective option, reported Dr. Anand Shah, a radiation oncology resident at Columbia University Medical Center in New York.
The findings, based on cost-effectiveness modeling, were robust over a wide range of assumptions, including various scenarios about treatment efficacies, toxicities, costs, and health state utilities.
"The rationale behind our study was that the traditional treatment for clearly operable patients with stage 1 lung cancer is lobectomy, whereas wedge resection and SBRT [stereotactic body radiation therapy] serve as alternatives in marginally operable patients.
Given an aging population and an increased prevalence of screening, it is likely more people will be diagnosed with stage 1 lung cancer, and thus we felt it was critical to compare the cost-effectiveness of these treatments," he said at the annual meeting of the American Society for Radiation Oncology.
The researchers created a Markov model in which hypothetical patient cohorts transition from one discrete, mutually exclusive health state to another at fixed time increments and at defined probabilities.
For a cohort with marginally operable disease, they compared SBRT with wedge resection, and for a cohort with clearly operable disease, they compared SBRT with lobectomy. Patients in the model were older than age 65
The model assumes that in both cohorts, SBRT will be similarly efficacious, but with higher toxicity for marginally operable patients, who are more likely to experience treatment-related morbidities.
The authors considered both open and less-invasive visually assisted surgical procedures for patients undergoing lobectomy and wedge resection. They considered costs from a Medicare perspective using 2012 dollars.
For the base case, SBRT for the marginally operable cohort cost a mean of $42,084, and the mean quality-adjusted life-year (QALY) gain was 8.03 years. In contrast, wedge resection cost a mean of $51,487, for a QALY gain of 7.93 years. In statistical parlance, SBRT for this cohort was the less costly and most effective strategy.
For clearly operable patients, however, SBRT was less costly than surgery. The mean cost was $40,107 vs. $49,083, but with less efficacy at 8.21 QALY compared with 8.89 for lobectomy. The investigators calculated an incremental cost-effectiveness ratio favoring lobectomy in this cohort, at a cost of $13,200 per QALY gained.
"We conducted a number of sensitivity analyses in which we varied the cost, efficacy, utility, and toxicity data, and in the marginally operable cohort SBRT was nearly always the dominant and thus cost-effective strategy. For patients who were considered clearly operable, lobectomy was the cost-effective treatment in nearly every sensitivity analysis," Dr. Shah said.
Dr. James B. Yu, the invited discussant, said that given current data, the findings of the study generally support current practice.
"However, even if you don’t agree that lobectomy is more cost effective for the clearly operable patient, at the very least this study will illuminate what we disagree about and where better data and clearer goals are needed," he said.
Dr. Yu is a therapeutic radiologist and cancer outcomes researcher at Yale School of Medicine in New Haven, Conn.
The funding source for the study was not disclosed. Dr. Shah and Dr. Yu reported having no relevant financial disclosures.
ATLANTA – For older patients with marginally operable stage 1 non–small cell lung cancer, stereotactic body radiation therapy is significantly more cost effective than surgery.
For patients with clearly operable non–small cell lung cancer (NSCLS) tumors, however, lobectomy is the most cost-effective option, reported Dr. Anand Shah, a radiation oncology resident at Columbia University Medical Center in New York.
The findings, based on cost-effectiveness modeling, were robust over a wide range of assumptions, including various scenarios about treatment efficacies, toxicities, costs, and health state utilities.
"The rationale behind our study was that the traditional treatment for clearly operable patients with stage 1 lung cancer is lobectomy, whereas wedge resection and SBRT [stereotactic body radiation therapy] serve as alternatives in marginally operable patients.
Given an aging population and an increased prevalence of screening, it is likely more people will be diagnosed with stage 1 lung cancer, and thus we felt it was critical to compare the cost-effectiveness of these treatments," he said at the annual meeting of the American Society for Radiation Oncology.
The researchers created a Markov model in which hypothetical patient cohorts transition from one discrete, mutually exclusive health state to another at fixed time increments and at defined probabilities.
For a cohort with marginally operable disease, they compared SBRT with wedge resection, and for a cohort with clearly operable disease, they compared SBRT with lobectomy. Patients in the model were older than age 65
The model assumes that in both cohorts, SBRT will be similarly efficacious, but with higher toxicity for marginally operable patients, who are more likely to experience treatment-related morbidities.
The authors considered both open and less-invasive visually assisted surgical procedures for patients undergoing lobectomy and wedge resection. They considered costs from a Medicare perspective using 2012 dollars.
For the base case, SBRT for the marginally operable cohort cost a mean of $42,084, and the mean quality-adjusted life-year (QALY) gain was 8.03 years. In contrast, wedge resection cost a mean of $51,487, for a QALY gain of 7.93 years. In statistical parlance, SBRT for this cohort was the less costly and most effective strategy.
For clearly operable patients, however, SBRT was less costly than surgery. The mean cost was $40,107 vs. $49,083, but with less efficacy at 8.21 QALY compared with 8.89 for lobectomy. The investigators calculated an incremental cost-effectiveness ratio favoring lobectomy in this cohort, at a cost of $13,200 per QALY gained.
"We conducted a number of sensitivity analyses in which we varied the cost, efficacy, utility, and toxicity data, and in the marginally operable cohort SBRT was nearly always the dominant and thus cost-effective strategy. For patients who were considered clearly operable, lobectomy was the cost-effective treatment in nearly every sensitivity analysis," Dr. Shah said.
Dr. James B. Yu, the invited discussant, said that given current data, the findings of the study generally support current practice.
"However, even if you don’t agree that lobectomy is more cost effective for the clearly operable patient, at the very least this study will illuminate what we disagree about and where better data and clearer goals are needed," he said.
Dr. Yu is a therapeutic radiologist and cancer outcomes researcher at Yale School of Medicine in New Haven, Conn.
The funding source for the study was not disclosed. Dr. Shah and Dr. Yu reported having no relevant financial disclosures.
ATLANTA – For older patients with marginally operable stage 1 non–small cell lung cancer, stereotactic body radiation therapy is significantly more cost effective than surgery.
For patients with clearly operable non–small cell lung cancer (NSCLS) tumors, however, lobectomy is the most cost-effective option, reported Dr. Anand Shah, a radiation oncology resident at Columbia University Medical Center in New York.
The findings, based on cost-effectiveness modeling, were robust over a wide range of assumptions, including various scenarios about treatment efficacies, toxicities, costs, and health state utilities.
"The rationale behind our study was that the traditional treatment for clearly operable patients with stage 1 lung cancer is lobectomy, whereas wedge resection and SBRT [stereotactic body radiation therapy] serve as alternatives in marginally operable patients.
Given an aging population and an increased prevalence of screening, it is likely more people will be diagnosed with stage 1 lung cancer, and thus we felt it was critical to compare the cost-effectiveness of these treatments," he said at the annual meeting of the American Society for Radiation Oncology.
The researchers created a Markov model in which hypothetical patient cohorts transition from one discrete, mutually exclusive health state to another at fixed time increments and at defined probabilities.
For a cohort with marginally operable disease, they compared SBRT with wedge resection, and for a cohort with clearly operable disease, they compared SBRT with lobectomy. Patients in the model were older than age 65
The model assumes that in both cohorts, SBRT will be similarly efficacious, but with higher toxicity for marginally operable patients, who are more likely to experience treatment-related morbidities.
The authors considered both open and less-invasive visually assisted surgical procedures for patients undergoing lobectomy and wedge resection. They considered costs from a Medicare perspective using 2012 dollars.
For the base case, SBRT for the marginally operable cohort cost a mean of $42,084, and the mean quality-adjusted life-year (QALY) gain was 8.03 years. In contrast, wedge resection cost a mean of $51,487, for a QALY gain of 7.93 years. In statistical parlance, SBRT for this cohort was the less costly and most effective strategy.
For clearly operable patients, however, SBRT was less costly than surgery. The mean cost was $40,107 vs. $49,083, but with less efficacy at 8.21 QALY compared with 8.89 for lobectomy. The investigators calculated an incremental cost-effectiveness ratio favoring lobectomy in this cohort, at a cost of $13,200 per QALY gained.
"We conducted a number of sensitivity analyses in which we varied the cost, efficacy, utility, and toxicity data, and in the marginally operable cohort SBRT was nearly always the dominant and thus cost-effective strategy. For patients who were considered clearly operable, lobectomy was the cost-effective treatment in nearly every sensitivity analysis," Dr. Shah said.
Dr. James B. Yu, the invited discussant, said that given current data, the findings of the study generally support current practice.
"However, even if you don’t agree that lobectomy is more cost effective for the clearly operable patient, at the very least this study will illuminate what we disagree about and where better data and clearer goals are needed," he said.
Dr. Yu is a therapeutic radiologist and cancer outcomes researcher at Yale School of Medicine in New Haven, Conn.
The funding source for the study was not disclosed. Dr. Shah and Dr. Yu reported having no relevant financial disclosures.
Younger adults with brain metastases survive longer with radiosurgery alone
ATLANTA – Younger adults with one to three brain metastases survive longer when they are treated with stereotactic radiosurgery alone rather than whole-brain radiation therapy or a combination of both modalities, researchers reported at the annual meeting of the American Society for Radiation Oncology.
Among patients aged 35-50 years, stereotactic radiosurgery (SRS) alone was associated with hazard ratios (HR) for death ranging from 0.46 to 0.64, compared with an age-matched cohort treated with a combination of SRS and whole-brain radiation therapy (WBRT), based on a meta-analysis of data on 389 individual patients in three randomized clinical trials.
For local control, however, the data show a benefit for combined SRS and WBRT. For control of distant brain metastases, the data indicate a benefit for the combined therapies, but only among patients aged 55 years and older, reported Dr. Arjun Sahgal, associate professor of radiation oncology at the University of Toronto.
"Our overall survival results favoring radiosurgery alone in younger patients may be explained by the lack of benefit of whole-brain radiation with respect to distant brain control in this cohort, while still exposing them to the harms of whole-brain radiation with respect to memory function and quality of life," he said.
Dr. Sahgal and his colleagues had previously published an aggregate meta-analysis showing that WBRT and SRS improved distant and local brain control but without overall survival benefit compared with SRS alone.
The current study looked at the raw, individual patient data from the three randomized controlled trials included in the original aggregate analysis. The trials included a 2006 study of 132 patients with an endpoint of brain tumor recurrence, a 2009 trial looking at the effect of SRS/WBRT on neurocognitive function in 58 patients, and a 2011 study examining the effect of adjuvant SRS on World Health Organization performance status scores.
The overall median time to local failure in the trials was 6.6 months for SRS alone, compared with 7.7 months for SRS/WBRT. Time to distant failure was also shorter with SRS alone, at a median of 4.7 vs. 7.7 months, respectively. Median time to death, however, was longer with SRS, at 10 vs. 8.2 months.
In a multivariate model for overall survival, the HR was 0.46 for patients at age 35 years, 0.52 at age 40, 0.58 at age 45, and 0.64 at age 50; all hazard ratios had significant confidence intervals. For patients aged 55 years and older, however, the HR for overall survival was not significant.
Patients with only one metastasis had a significantly lower risk of dying, compared with those who had two or three metastases (HR, 0.72).
The risk of local failure was significantly greater with SRS alone for patients aged 45-70.
The risk of new distant metastases was significant with SRS alone for patients aged 55 years and older, and was significantly lower for patients with one metastasis (HR, 0.63) vs. two or more metastases.
Salvage therapy was performed in 28% of patients who underwent SRS alone and 12% of those who received the combined therapies. Distant brain failures occurred in 54% of those in the SRS alone group, compared with 34% of those in the SRS/WBRT group.
Patients who underwent salvage therapy had significantly greater survival rates than those who did not, and this effect did not vary significantly by age, Dr. Sahgal reported.
The authors did not report specific funding sources. Dr. Sahgal reported having no relevant financial disclosures.
ATLANTA – Younger adults with one to three brain metastases survive longer when they are treated with stereotactic radiosurgery alone rather than whole-brain radiation therapy or a combination of both modalities, researchers reported at the annual meeting of the American Society for Radiation Oncology.
Among patients aged 35-50 years, stereotactic radiosurgery (SRS) alone was associated with hazard ratios (HR) for death ranging from 0.46 to 0.64, compared with an age-matched cohort treated with a combination of SRS and whole-brain radiation therapy (WBRT), based on a meta-analysis of data on 389 individual patients in three randomized clinical trials.
For local control, however, the data show a benefit for combined SRS and WBRT. For control of distant brain metastases, the data indicate a benefit for the combined therapies, but only among patients aged 55 years and older, reported Dr. Arjun Sahgal, associate professor of radiation oncology at the University of Toronto.
"Our overall survival results favoring radiosurgery alone in younger patients may be explained by the lack of benefit of whole-brain radiation with respect to distant brain control in this cohort, while still exposing them to the harms of whole-brain radiation with respect to memory function and quality of life," he said.
Dr. Sahgal and his colleagues had previously published an aggregate meta-analysis showing that WBRT and SRS improved distant and local brain control but without overall survival benefit compared with SRS alone.
The current study looked at the raw, individual patient data from the three randomized controlled trials included in the original aggregate analysis. The trials included a 2006 study of 132 patients with an endpoint of brain tumor recurrence, a 2009 trial looking at the effect of SRS/WBRT on neurocognitive function in 58 patients, and a 2011 study examining the effect of adjuvant SRS on World Health Organization performance status scores.
The overall median time to local failure in the trials was 6.6 months for SRS alone, compared with 7.7 months for SRS/WBRT. Time to distant failure was also shorter with SRS alone, at a median of 4.7 vs. 7.7 months, respectively. Median time to death, however, was longer with SRS, at 10 vs. 8.2 months.
In a multivariate model for overall survival, the HR was 0.46 for patients at age 35 years, 0.52 at age 40, 0.58 at age 45, and 0.64 at age 50; all hazard ratios had significant confidence intervals. For patients aged 55 years and older, however, the HR for overall survival was not significant.
Patients with only one metastasis had a significantly lower risk of dying, compared with those who had two or three metastases (HR, 0.72).
The risk of local failure was significantly greater with SRS alone for patients aged 45-70.
The risk of new distant metastases was significant with SRS alone for patients aged 55 years and older, and was significantly lower for patients with one metastasis (HR, 0.63) vs. two or more metastases.
Salvage therapy was performed in 28% of patients who underwent SRS alone and 12% of those who received the combined therapies. Distant brain failures occurred in 54% of those in the SRS alone group, compared with 34% of those in the SRS/WBRT group.
Patients who underwent salvage therapy had significantly greater survival rates than those who did not, and this effect did not vary significantly by age, Dr. Sahgal reported.
The authors did not report specific funding sources. Dr. Sahgal reported having no relevant financial disclosures.
ATLANTA – Younger adults with one to three brain metastases survive longer when they are treated with stereotactic radiosurgery alone rather than whole-brain radiation therapy or a combination of both modalities, researchers reported at the annual meeting of the American Society for Radiation Oncology.
Among patients aged 35-50 years, stereotactic radiosurgery (SRS) alone was associated with hazard ratios (HR) for death ranging from 0.46 to 0.64, compared with an age-matched cohort treated with a combination of SRS and whole-brain radiation therapy (WBRT), based on a meta-analysis of data on 389 individual patients in three randomized clinical trials.
For local control, however, the data show a benefit for combined SRS and WBRT. For control of distant brain metastases, the data indicate a benefit for the combined therapies, but only among patients aged 55 years and older, reported Dr. Arjun Sahgal, associate professor of radiation oncology at the University of Toronto.
"Our overall survival results favoring radiosurgery alone in younger patients may be explained by the lack of benefit of whole-brain radiation with respect to distant brain control in this cohort, while still exposing them to the harms of whole-brain radiation with respect to memory function and quality of life," he said.
Dr. Sahgal and his colleagues had previously published an aggregate meta-analysis showing that WBRT and SRS improved distant and local brain control but without overall survival benefit compared with SRS alone.
The current study looked at the raw, individual patient data from the three randomized controlled trials included in the original aggregate analysis. The trials included a 2006 study of 132 patients with an endpoint of brain tumor recurrence, a 2009 trial looking at the effect of SRS/WBRT on neurocognitive function in 58 patients, and a 2011 study examining the effect of adjuvant SRS on World Health Organization performance status scores.
The overall median time to local failure in the trials was 6.6 months for SRS alone, compared with 7.7 months for SRS/WBRT. Time to distant failure was also shorter with SRS alone, at a median of 4.7 vs. 7.7 months, respectively. Median time to death, however, was longer with SRS, at 10 vs. 8.2 months.
In a multivariate model for overall survival, the HR was 0.46 for patients at age 35 years, 0.52 at age 40, 0.58 at age 45, and 0.64 at age 50; all hazard ratios had significant confidence intervals. For patients aged 55 years and older, however, the HR for overall survival was not significant.
Patients with only one metastasis had a significantly lower risk of dying, compared with those who had two or three metastases (HR, 0.72).
The risk of local failure was significantly greater with SRS alone for patients aged 45-70.
The risk of new distant metastases was significant with SRS alone for patients aged 55 years and older, and was significantly lower for patients with one metastasis (HR, 0.63) vs. two or more metastases.
Salvage therapy was performed in 28% of patients who underwent SRS alone and 12% of those who received the combined therapies. Distant brain failures occurred in 54% of those in the SRS alone group, compared with 34% of those in the SRS/WBRT group.
Patients who underwent salvage therapy had significantly greater survival rates than those who did not, and this effect did not vary significantly by age, Dr. Sahgal reported.
The authors did not report specific funding sources. Dr. Sahgal reported having no relevant financial disclosures.
AT THE ASTRO ANNUAL MEETING
Major finding: Stereotactic radiosurgery was associated with significantly longer overall survival among patients age 50 years and younger (hazard ratios from 0.46 to 0.64).
Data source: Meta-analysis of individual patient data from three randomized controlled clinical trials enrolling a total of 389 patients.
Disclosures: The authors did not report specific funding sources. Dr. Sahgal reported having no relevant financial disclosures.
Genetic anomalies account for majority of miscarriages
BOSTON – A substantial majority of miscarriages appear to be caused by genetic abnormalities rather than the usual suspects of thrombophilias, antiphospholipid syndromes, immunologic problems, or other maternal factors, study results suggest.
A decade of microscopic studies of placental tissues obtained after pregnancy losses showed that of 615 samples, 495 cases (80.5%) were caused by genetic abnormalities, determined by the presence of markers for genetic abnormalities, said Dr. Harvey J. Kliman, director of the reproductive and placental research unit at Yale University in New Haven, Conn.
Data from a second study of the karyotypes of embryos from spontaneous abortions showed that embryonic chromosomal abnormalities accounted for a significant portion of the miscarriages, and that two-thirds of women with prior loss of an aneuploid embryo went on to have a live birth, said Dr. Ruth B. Lathi, director of the recurrent pregnancy loss program at the Stanford (Calif.) Fertility and Reproductive Medicine Center.
The studies were reported at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Although standard workups fail to identify the cause of recurrent pregnancy losses in more than half of all cases, the findings should be reassuring to patients, Dr. Lathi said in an interview.
"The vast majority of miscarriages are chromosomally or somehow morphologically or genetically abnormal – even if we can’t prove it, we all believe it. Luckily, these genetic abnormalities for the most part are random, and women can have a combination of abnormal pregnancies and normal pregnancies," Dr. Lathi said.
"Each new pregnancy is a new set of genetics: It’s a new egg, it’s a new sperm, and what was wrong in the last pregnancy may not carry over to the next pregnancy," she added.
Dr. Kliman said that if women know that recurrent miscarriages are unlikely to be related to something they have done, such as having a cocktail or smoking marijuana when they weren’t even aware that they were pregnant, they will be better able to cope emotionally and resume trying.
"I have a lot of families that have six pregnancies: three perfectly normal children and three losses, and the losses always happen at the same time, because it’s a programming error; that’s another hint that it’s genetic," he said.
Dr. Kliman and Kristin M. Milano, director of laboratory services in the reproductive and placental research unit at Yale, reported data on 615 pregnancy losses that occurred from 7 to 20 weeks’ gestational age. The samples were fixed, sectioned, stained, and then examined microscopically for abnormalities.
The primary diagnosis in 495 of the 615 samples examined was dysmorphic trophoblastic invaginations and inclusions. In 55 cases (8.9%) there were no chorionic villi, 53 cases (8.6%) had no pathologic abnormalities, 10 cases (1.6%) were apparently due to thrombosis, 1 (0.2%) was due to abruption, and 1 to chronic villitis.
"This study validates the importance of pathologic examination of all pregnancy losses," Dr. Kliman said in a poster.
Dr. Lathi and her colleague, Dr. Jamie Massie, examined the live birth rate by embryonic karyotype among 95 women with a self-reported history of recurrent pregnancy loss.
They found that 40 of the women (42%) had a miscarriage of a euploid embryo, and 55 (58%) lost a pregnancy with an aneuploid embryo. Of the aneuploid abnormalities, 95% were numeric (for example, monosomies and trisomies), and 5% were structural.
In all, 21 of the 40 women (52.5%) with loss of a euploid embryo had a subsequent live birth, compared with 37 of 55 (67.3%) of those with loss of an aneuploid pregnancy.
The findings, which need to be validated in larger studies, suggest that aneuploidy may be a good prognostic indicator for the success of future live births, the investigators concluded.
Dr. Lathi was coauthor of a separate study of 87 women with two or more recurrent pregnancy losses from either explained or unexplained causes, which found that 59.7% of the patients had a healthy term delivery, with obstetrical outcomes similar to those in women with infertility problems.
Dr. Kliman’s study was supported by the reproductive and placental research unit at Yale. He reported having no relevant financial disclosures. The funding sources for Dr. Lathi’s studies were not disclosed. She reported having no relevant conflicts of interest.
BOSTON – A substantial majority of miscarriages appear to be caused by genetic abnormalities rather than the usual suspects of thrombophilias, antiphospholipid syndromes, immunologic problems, or other maternal factors, study results suggest.
A decade of microscopic studies of placental tissues obtained after pregnancy losses showed that of 615 samples, 495 cases (80.5%) were caused by genetic abnormalities, determined by the presence of markers for genetic abnormalities, said Dr. Harvey J. Kliman, director of the reproductive and placental research unit at Yale University in New Haven, Conn.
Data from a second study of the karyotypes of embryos from spontaneous abortions showed that embryonic chromosomal abnormalities accounted for a significant portion of the miscarriages, and that two-thirds of women with prior loss of an aneuploid embryo went on to have a live birth, said Dr. Ruth B. Lathi, director of the recurrent pregnancy loss program at the Stanford (Calif.) Fertility and Reproductive Medicine Center.
The studies were reported at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Although standard workups fail to identify the cause of recurrent pregnancy losses in more than half of all cases, the findings should be reassuring to patients, Dr. Lathi said in an interview.
"The vast majority of miscarriages are chromosomally or somehow morphologically or genetically abnormal – even if we can’t prove it, we all believe it. Luckily, these genetic abnormalities for the most part are random, and women can have a combination of abnormal pregnancies and normal pregnancies," Dr. Lathi said.
"Each new pregnancy is a new set of genetics: It’s a new egg, it’s a new sperm, and what was wrong in the last pregnancy may not carry over to the next pregnancy," she added.
Dr. Kliman said that if women know that recurrent miscarriages are unlikely to be related to something they have done, such as having a cocktail or smoking marijuana when they weren’t even aware that they were pregnant, they will be better able to cope emotionally and resume trying.
"I have a lot of families that have six pregnancies: three perfectly normal children and three losses, and the losses always happen at the same time, because it’s a programming error; that’s another hint that it’s genetic," he said.
Dr. Kliman and Kristin M. Milano, director of laboratory services in the reproductive and placental research unit at Yale, reported data on 615 pregnancy losses that occurred from 7 to 20 weeks’ gestational age. The samples were fixed, sectioned, stained, and then examined microscopically for abnormalities.
The primary diagnosis in 495 of the 615 samples examined was dysmorphic trophoblastic invaginations and inclusions. In 55 cases (8.9%) there were no chorionic villi, 53 cases (8.6%) had no pathologic abnormalities, 10 cases (1.6%) were apparently due to thrombosis, 1 (0.2%) was due to abruption, and 1 to chronic villitis.
"This study validates the importance of pathologic examination of all pregnancy losses," Dr. Kliman said in a poster.
Dr. Lathi and her colleague, Dr. Jamie Massie, examined the live birth rate by embryonic karyotype among 95 women with a self-reported history of recurrent pregnancy loss.
They found that 40 of the women (42%) had a miscarriage of a euploid embryo, and 55 (58%) lost a pregnancy with an aneuploid embryo. Of the aneuploid abnormalities, 95% were numeric (for example, monosomies and trisomies), and 5% were structural.
In all, 21 of the 40 women (52.5%) with loss of a euploid embryo had a subsequent live birth, compared with 37 of 55 (67.3%) of those with loss of an aneuploid pregnancy.
The findings, which need to be validated in larger studies, suggest that aneuploidy may be a good prognostic indicator for the success of future live births, the investigators concluded.
Dr. Lathi was coauthor of a separate study of 87 women with two or more recurrent pregnancy losses from either explained or unexplained causes, which found that 59.7% of the patients had a healthy term delivery, with obstetrical outcomes similar to those in women with infertility problems.
Dr. Kliman’s study was supported by the reproductive and placental research unit at Yale. He reported having no relevant financial disclosures. The funding sources for Dr. Lathi’s studies were not disclosed. She reported having no relevant conflicts of interest.
BOSTON – A substantial majority of miscarriages appear to be caused by genetic abnormalities rather than the usual suspects of thrombophilias, antiphospholipid syndromes, immunologic problems, or other maternal factors, study results suggest.
A decade of microscopic studies of placental tissues obtained after pregnancy losses showed that of 615 samples, 495 cases (80.5%) were caused by genetic abnormalities, determined by the presence of markers for genetic abnormalities, said Dr. Harvey J. Kliman, director of the reproductive and placental research unit at Yale University in New Haven, Conn.
Data from a second study of the karyotypes of embryos from spontaneous abortions showed that embryonic chromosomal abnormalities accounted for a significant portion of the miscarriages, and that two-thirds of women with prior loss of an aneuploid embryo went on to have a live birth, said Dr. Ruth B. Lathi, director of the recurrent pregnancy loss program at the Stanford (Calif.) Fertility and Reproductive Medicine Center.
The studies were reported at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Although standard workups fail to identify the cause of recurrent pregnancy losses in more than half of all cases, the findings should be reassuring to patients, Dr. Lathi said in an interview.
"The vast majority of miscarriages are chromosomally or somehow morphologically or genetically abnormal – even if we can’t prove it, we all believe it. Luckily, these genetic abnormalities for the most part are random, and women can have a combination of abnormal pregnancies and normal pregnancies," Dr. Lathi said.
"Each new pregnancy is a new set of genetics: It’s a new egg, it’s a new sperm, and what was wrong in the last pregnancy may not carry over to the next pregnancy," she added.
Dr. Kliman said that if women know that recurrent miscarriages are unlikely to be related to something they have done, such as having a cocktail or smoking marijuana when they weren’t even aware that they were pregnant, they will be better able to cope emotionally and resume trying.
"I have a lot of families that have six pregnancies: three perfectly normal children and three losses, and the losses always happen at the same time, because it’s a programming error; that’s another hint that it’s genetic," he said.
Dr. Kliman and Kristin M. Milano, director of laboratory services in the reproductive and placental research unit at Yale, reported data on 615 pregnancy losses that occurred from 7 to 20 weeks’ gestational age. The samples were fixed, sectioned, stained, and then examined microscopically for abnormalities.
The primary diagnosis in 495 of the 615 samples examined was dysmorphic trophoblastic invaginations and inclusions. In 55 cases (8.9%) there were no chorionic villi, 53 cases (8.6%) had no pathologic abnormalities, 10 cases (1.6%) were apparently due to thrombosis, 1 (0.2%) was due to abruption, and 1 to chronic villitis.
"This study validates the importance of pathologic examination of all pregnancy losses," Dr. Kliman said in a poster.
Dr. Lathi and her colleague, Dr. Jamie Massie, examined the live birth rate by embryonic karyotype among 95 women with a self-reported history of recurrent pregnancy loss.
They found that 40 of the women (42%) had a miscarriage of a euploid embryo, and 55 (58%) lost a pregnancy with an aneuploid embryo. Of the aneuploid abnormalities, 95% were numeric (for example, monosomies and trisomies), and 5% were structural.
In all, 21 of the 40 women (52.5%) with loss of a euploid embryo had a subsequent live birth, compared with 37 of 55 (67.3%) of those with loss of an aneuploid pregnancy.
The findings, which need to be validated in larger studies, suggest that aneuploidy may be a good prognostic indicator for the success of future live births, the investigators concluded.
Dr. Lathi was coauthor of a separate study of 87 women with two or more recurrent pregnancy losses from either explained or unexplained causes, which found that 59.7% of the patients had a healthy term delivery, with obstetrical outcomes similar to those in women with infertility problems.
Dr. Kliman’s study was supported by the reproductive and placental research unit at Yale. He reported having no relevant financial disclosures. The funding sources for Dr. Lathi’s studies were not disclosed. She reported having no relevant conflicts of interest.
AT THE JOINT IFFS/ASRM MEETING
Major finding: Of 615 spontaneous abortions, 495 (80.5%) were caused by genetic abnormalities in the embryo rather than maternal factors.
Data source: Prospective single-center studies of the contribution of genetic abnormalities to pregnancy loss.
Disclosures: Dr. Kliman’s study was supported by the reproductive and placental research unit at Yale. He reported having no relevant financial disclosures. The funding sources for Dr. Lathi’s studies were not disclosed. She reported having no relevant conflicts of interest.
Radiation of early breast cancer does not increase cardiac death risk
ATLANTA – A decade after treatment for early-stage breast cancer, women who underwent surgery and radiation had higher survival rates than women who had surgery alone, with no increase in radiation-related cardiac or secondary cancer deaths, investigators reported at the annual meeting of the American Society for Radiation Oncology.
An analysis of Surveillance, Epidemiology and End Results (SEER) data on women treated for stage TIA N0 breast cancer in their mid to late 50s showed that after a median follow-up of 14 years, 10-year overall survival among the 2,397 women who received lumpectomy or mastectomy and radiation was 91.6%, compared with 87% for 2,988 women who had lumpectomy or mastectomy only (P less than .001).
Ten-year cardiac cause–specific survival was 96.7% vs. 92.7% (P less than .001), respectively. Breast cancer–specific survival was also higher among women who had undergone radiation, at 97% vs. 95.7% (P = .01), reported Dr. Jason C. Ye, a resident in radiation oncology at Weill Cornell Medical College, New York.
The data also suggest that breast irradiation does not increase the risk of lung cancer death, which occurred in 6 patients (1.9%) who underwent lumpectomy and radiation, and in 48 (1.6%) of those who had lumpectomies only, a difference that was not significant.
Dr. Ye noted, however, that between-group differences may begin to show up with longer follow-up.
"Although 14 years is a long time, studies have found increases in cardiac mortality and secondary cancers at 20 and 30 years after radiation. Also, there might have been a selection bias by physicians treating at the time, based on patients’ comorbidities and the patient’s health status. This might explain why the overall survival and the cardiac cause–specific survival were different between the two groups, with the no-radiation arm doing worse," he said at a media briefing.
In addition, changes in techniques introduced since the 1990s, such as three-dimensional conformal radiation, prone irradiation, hypofractionation, and intensity-modulated radiation therapy, may have effects on cardiac-specific and overall survival rates in the future, Dr. Ye said.
Dr. Ye and his colleagues reviewed SEER records on 5,385 women treated for early breast cancer during 1990-1997, and stratified them according to treatment with external-beam radiation or no radiation.
They included only patients with stage TIA N0 breast cancer identified as their first malignancy.
The authors used cause-of-death codes to identify cardiac deaths (either from cardiac disease or from atherosclerosis, breast cancer mortality, and deaths from second cancers in the chest area).
Radiation was associated with significantly lower overall mortality (relative risk, 0.69; P less than .001), breast cancer mortality (RR, 0.75; P = .02), and cardiac mortality (RR, 0.53; P less than .001).
Women with tumors in the left breast, whose hearts would presumably receive a larger dose of radiation than women with right breast tumors, were not at increased risk for cardiac-specific death. Deaths from second cancers included lung cancer in 2%; lymphomas and leukemias, each in 0.4%; soft-tissue malignancies (including the heart) in 0.06%; and cancer of the esophagus in 0.04%.
There were no significant differences between the radiation and no-radiation groups in incidence of death from second cancers.
The study was supported by the National Cancer Institute. Dr. Ye reported having no relevant disclosures.
 |
|
We’ve heard some reassuring news for our early breast cancer patients, that perhaps they will not have to endure cardiac mortality or death from other cancers because they received radiation to their breast, were thereby able to keep their breast, and were able to be cured without the need for mastectomy. I think that’s great news.
Dr. Beth Erickson is a professor of radiation oncology at the Medical College of Wisconsin in Milwaukee.
 |
|
We’ve heard some reassuring news for our early breast cancer patients, that perhaps they will not have to endure cardiac mortality or death from other cancers because they received radiation to their breast, were thereby able to keep their breast, and were able to be cured without the need for mastectomy. I think that’s great news.
Dr. Beth Erickson is a professor of radiation oncology at the Medical College of Wisconsin in Milwaukee.
 |
|
We’ve heard some reassuring news for our early breast cancer patients, that perhaps they will not have to endure cardiac mortality or death from other cancers because they received radiation to their breast, were thereby able to keep their breast, and were able to be cured without the need for mastectomy. I think that’s great news.
Dr. Beth Erickson is a professor of radiation oncology at the Medical College of Wisconsin in Milwaukee.
ATLANTA – A decade after treatment for early-stage breast cancer, women who underwent surgery and radiation had higher survival rates than women who had surgery alone, with no increase in radiation-related cardiac or secondary cancer deaths, investigators reported at the annual meeting of the American Society for Radiation Oncology.
An analysis of Surveillance, Epidemiology and End Results (SEER) data on women treated for stage TIA N0 breast cancer in their mid to late 50s showed that after a median follow-up of 14 years, 10-year overall survival among the 2,397 women who received lumpectomy or mastectomy and radiation was 91.6%, compared with 87% for 2,988 women who had lumpectomy or mastectomy only (P less than .001).
Ten-year cardiac cause–specific survival was 96.7% vs. 92.7% (P less than .001), respectively. Breast cancer–specific survival was also higher among women who had undergone radiation, at 97% vs. 95.7% (P = .01), reported Dr. Jason C. Ye, a resident in radiation oncology at Weill Cornell Medical College, New York.
The data also suggest that breast irradiation does not increase the risk of lung cancer death, which occurred in 6 patients (1.9%) who underwent lumpectomy and radiation, and in 48 (1.6%) of those who had lumpectomies only, a difference that was not significant.
Dr. Ye noted, however, that between-group differences may begin to show up with longer follow-up.
"Although 14 years is a long time, studies have found increases in cardiac mortality and secondary cancers at 20 and 30 years after radiation. Also, there might have been a selection bias by physicians treating at the time, based on patients’ comorbidities and the patient’s health status. This might explain why the overall survival and the cardiac cause–specific survival were different between the two groups, with the no-radiation arm doing worse," he said at a media briefing.
In addition, changes in techniques introduced since the 1990s, such as three-dimensional conformal radiation, prone irradiation, hypofractionation, and intensity-modulated radiation therapy, may have effects on cardiac-specific and overall survival rates in the future, Dr. Ye said.
Dr. Ye and his colleagues reviewed SEER records on 5,385 women treated for early breast cancer during 1990-1997, and stratified them according to treatment with external-beam radiation or no radiation.
They included only patients with stage TIA N0 breast cancer identified as their first malignancy.
The authors used cause-of-death codes to identify cardiac deaths (either from cardiac disease or from atherosclerosis, breast cancer mortality, and deaths from second cancers in the chest area).
Radiation was associated with significantly lower overall mortality (relative risk, 0.69; P less than .001), breast cancer mortality (RR, 0.75; P = .02), and cardiac mortality (RR, 0.53; P less than .001).
Women with tumors in the left breast, whose hearts would presumably receive a larger dose of radiation than women with right breast tumors, were not at increased risk for cardiac-specific death. Deaths from second cancers included lung cancer in 2%; lymphomas and leukemias, each in 0.4%; soft-tissue malignancies (including the heart) in 0.06%; and cancer of the esophagus in 0.04%.
There were no significant differences between the radiation and no-radiation groups in incidence of death from second cancers.
The study was supported by the National Cancer Institute. Dr. Ye reported having no relevant disclosures.
ATLANTA – A decade after treatment for early-stage breast cancer, women who underwent surgery and radiation had higher survival rates than women who had surgery alone, with no increase in radiation-related cardiac or secondary cancer deaths, investigators reported at the annual meeting of the American Society for Radiation Oncology.
An analysis of Surveillance, Epidemiology and End Results (SEER) data on women treated for stage TIA N0 breast cancer in their mid to late 50s showed that after a median follow-up of 14 years, 10-year overall survival among the 2,397 women who received lumpectomy or mastectomy and radiation was 91.6%, compared with 87% for 2,988 women who had lumpectomy or mastectomy only (P less than .001).
Ten-year cardiac cause–specific survival was 96.7% vs. 92.7% (P less than .001), respectively. Breast cancer–specific survival was also higher among women who had undergone radiation, at 97% vs. 95.7% (P = .01), reported Dr. Jason C. Ye, a resident in radiation oncology at Weill Cornell Medical College, New York.
The data also suggest that breast irradiation does not increase the risk of lung cancer death, which occurred in 6 patients (1.9%) who underwent lumpectomy and radiation, and in 48 (1.6%) of those who had lumpectomies only, a difference that was not significant.
Dr. Ye noted, however, that between-group differences may begin to show up with longer follow-up.
"Although 14 years is a long time, studies have found increases in cardiac mortality and secondary cancers at 20 and 30 years after radiation. Also, there might have been a selection bias by physicians treating at the time, based on patients’ comorbidities and the patient’s health status. This might explain why the overall survival and the cardiac cause–specific survival were different between the two groups, with the no-radiation arm doing worse," he said at a media briefing.
In addition, changes in techniques introduced since the 1990s, such as three-dimensional conformal radiation, prone irradiation, hypofractionation, and intensity-modulated radiation therapy, may have effects on cardiac-specific and overall survival rates in the future, Dr. Ye said.
Dr. Ye and his colleagues reviewed SEER records on 5,385 women treated for early breast cancer during 1990-1997, and stratified them according to treatment with external-beam radiation or no radiation.
They included only patients with stage TIA N0 breast cancer identified as their first malignancy.
The authors used cause-of-death codes to identify cardiac deaths (either from cardiac disease or from atherosclerosis, breast cancer mortality, and deaths from second cancers in the chest area).
Radiation was associated with significantly lower overall mortality (relative risk, 0.69; P less than .001), breast cancer mortality (RR, 0.75; P = .02), and cardiac mortality (RR, 0.53; P less than .001).
Women with tumors in the left breast, whose hearts would presumably receive a larger dose of radiation than women with right breast tumors, were not at increased risk for cardiac-specific death. Deaths from second cancers included lung cancer in 2%; lymphomas and leukemias, each in 0.4%; soft-tissue malignancies (including the heart) in 0.06%; and cancer of the esophagus in 0.04%.
There were no significant differences between the radiation and no-radiation groups in incidence of death from second cancers.
The study was supported by the National Cancer Institute. Dr. Ye reported having no relevant disclosures.
AT THE ASTRO ANNUAL MEETING
Major finding: Ten-year cardiac cause–specific survival was 96.7% for women who had surgery and radiation, compared with 92.7% for women who had surgery alone (P less than .001).
Data source: Retrospective study of SEER data on 5,385 women treated for early breast cancer from 1990 through 1997.
Disclosures: The study was supported by the National Cancer Institute. Dr. Ye and Dr. Erickson reported having no relevant disclosures.
Despite incentives, many couples aim for twins with IVF
BOSTON – For many couples undergoing in vitro fertilization, the desire to rapidly complete a family apparently outweighs concerns over medical risks and the lure of cash savings, according to Dr. Fady I. Sharara.
Despite being offered free gonadotropins (Menopur) for one cycle and a free year of freezing and storage of all extra blastocysts, 48% of couples who were paying out of pocket opted for multiple- rather than single-embryo transfer, and 23.5% of those who had at least one reproductive cycle covered by insurance also refused the free offer, said Dr. Sharara, a reproductive endocrinologist and infertility specialist in group practice in Reston.
The medication alone could cost as much as $6,000, with freezing adding another $1,800 or so and storage, approximately $750, Dr. Sharara said in an interview.
The patients made the decision to proceed with multiples despite being informed about the higher risk of maternal, fetal, and perinatal problems.
"Twins are associated with significant morbidities: early delivery, cerebral palsy, mental retardation if they’re delivered very early, diabetes in the mom, and hypertension, so [there are] a lot of issues, and I tell my patients that twins are not twice the fun," he said.
"We were not meant to bear litters," he added.
New mothers of twins are more susceptible to postpartum depression, especially if they do not have help at home, and parents of twins have been shown in at least one study (Obstet. Gynecol. 2011;117:892-7) to be slightly but significantly more likely to get divorced than parents of singletons.
"One is hard enough; two at the same time is a killer for a lot of people. Some marriages don’t survive this," he said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Dr. Sharara offered patients – all women under age 38 who were proceeding with assisted reproductive technology (ART) – the chance to participate in the study. The free drugs and services were offered without regard to the patient’s insurance coverage or to her ovarian reserve status.
Of 48 couples offered a single-embryo transfer, 18 refused to take part in the trial. Of those who had double-embryo transfer, the ongoing pregnancy rate (approximately 10 weeks’ duration) was 80%, compared with 58.3% for the women who had single-embryo transfer, a difference that was not significant. Dr. Sharara noted, however, that two additional patients who had single-embryo transfer are now pregnant, and he estimated that the updated ongoing pregnancy rate for singletons will be about 60%-65%.
In all, 7 of the 18 women who opted for dual-embryo transfer are pregnant with twins, whereas none of the single-embryo pregnancies have resulted in twins. In a series of 500 single-embryo transfers at his center, the rate of twin pregnancies was 1.5%.
Dr. Sharara noted that some of the women offered single-embryo transfer did not meet the ASRM definitions for good-prognosis patients, including women aged 35 years and older who had a failed prior reproductive cycle, one ovary, prior uterine surgery, or diminished ovarian reserve.
One of the hardest parts of his job, he said, is getting the message through.
"When I sit down and talk to patients about the risks of having twins, they don’t want to hear it," Dr. Sharara said.
The study was supported by Ferring Pharmaceuticals. Dr. Sharara disclosed receiving grants from the company.
BOSTON – For many couples undergoing in vitro fertilization, the desire to rapidly complete a family apparently outweighs concerns over medical risks and the lure of cash savings, according to Dr. Fady I. Sharara.
Despite being offered free gonadotropins (Menopur) for one cycle and a free year of freezing and storage of all extra blastocysts, 48% of couples who were paying out of pocket opted for multiple- rather than single-embryo transfer, and 23.5% of those who had at least one reproductive cycle covered by insurance also refused the free offer, said Dr. Sharara, a reproductive endocrinologist and infertility specialist in group practice in Reston.
The medication alone could cost as much as $6,000, with freezing adding another $1,800 or so and storage, approximately $750, Dr. Sharara said in an interview.
The patients made the decision to proceed with multiples despite being informed about the higher risk of maternal, fetal, and perinatal problems.
"Twins are associated with significant morbidities: early delivery, cerebral palsy, mental retardation if they’re delivered very early, diabetes in the mom, and hypertension, so [there are] a lot of issues, and I tell my patients that twins are not twice the fun," he said.
"We were not meant to bear litters," he added.
New mothers of twins are more susceptible to postpartum depression, especially if they do not have help at home, and parents of twins have been shown in at least one study (Obstet. Gynecol. 2011;117:892-7) to be slightly but significantly more likely to get divorced than parents of singletons.
"One is hard enough; two at the same time is a killer for a lot of people. Some marriages don’t survive this," he said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Dr. Sharara offered patients – all women under age 38 who were proceeding with assisted reproductive technology (ART) – the chance to participate in the study. The free drugs and services were offered without regard to the patient’s insurance coverage or to her ovarian reserve status.
Of 48 couples offered a single-embryo transfer, 18 refused to take part in the trial. Of those who had double-embryo transfer, the ongoing pregnancy rate (approximately 10 weeks’ duration) was 80%, compared with 58.3% for the women who had single-embryo transfer, a difference that was not significant. Dr. Sharara noted, however, that two additional patients who had single-embryo transfer are now pregnant, and he estimated that the updated ongoing pregnancy rate for singletons will be about 60%-65%.
In all, 7 of the 18 women who opted for dual-embryo transfer are pregnant with twins, whereas none of the single-embryo pregnancies have resulted in twins. In a series of 500 single-embryo transfers at his center, the rate of twin pregnancies was 1.5%.
Dr. Sharara noted that some of the women offered single-embryo transfer did not meet the ASRM definitions for good-prognosis patients, including women aged 35 years and older who had a failed prior reproductive cycle, one ovary, prior uterine surgery, or diminished ovarian reserve.
One of the hardest parts of his job, he said, is getting the message through.
"When I sit down and talk to patients about the risks of having twins, they don’t want to hear it," Dr. Sharara said.
The study was supported by Ferring Pharmaceuticals. Dr. Sharara disclosed receiving grants from the company.
BOSTON – For many couples undergoing in vitro fertilization, the desire to rapidly complete a family apparently outweighs concerns over medical risks and the lure of cash savings, according to Dr. Fady I. Sharara.
Despite being offered free gonadotropins (Menopur) for one cycle and a free year of freezing and storage of all extra blastocysts, 48% of couples who were paying out of pocket opted for multiple- rather than single-embryo transfer, and 23.5% of those who had at least one reproductive cycle covered by insurance also refused the free offer, said Dr. Sharara, a reproductive endocrinologist and infertility specialist in group practice in Reston.
The medication alone could cost as much as $6,000, with freezing adding another $1,800 or so and storage, approximately $750, Dr. Sharara said in an interview.
The patients made the decision to proceed with multiples despite being informed about the higher risk of maternal, fetal, and perinatal problems.
"Twins are associated with significant morbidities: early delivery, cerebral palsy, mental retardation if they’re delivered very early, diabetes in the mom, and hypertension, so [there are] a lot of issues, and I tell my patients that twins are not twice the fun," he said.
"We were not meant to bear litters," he added.
New mothers of twins are more susceptible to postpartum depression, especially if they do not have help at home, and parents of twins have been shown in at least one study (Obstet. Gynecol. 2011;117:892-7) to be slightly but significantly more likely to get divorced than parents of singletons.
"One is hard enough; two at the same time is a killer for a lot of people. Some marriages don’t survive this," he said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Dr. Sharara offered patients – all women under age 38 who were proceeding with assisted reproductive technology (ART) – the chance to participate in the study. The free drugs and services were offered without regard to the patient’s insurance coverage or to her ovarian reserve status.
Of 48 couples offered a single-embryo transfer, 18 refused to take part in the trial. Of those who had double-embryo transfer, the ongoing pregnancy rate (approximately 10 weeks’ duration) was 80%, compared with 58.3% for the women who had single-embryo transfer, a difference that was not significant. Dr. Sharara noted, however, that two additional patients who had single-embryo transfer are now pregnant, and he estimated that the updated ongoing pregnancy rate for singletons will be about 60%-65%.
In all, 7 of the 18 women who opted for dual-embryo transfer are pregnant with twins, whereas none of the single-embryo pregnancies have resulted in twins. In a series of 500 single-embryo transfers at his center, the rate of twin pregnancies was 1.5%.
Dr. Sharara noted that some of the women offered single-embryo transfer did not meet the ASRM definitions for good-prognosis patients, including women aged 35 years and older who had a failed prior reproductive cycle, one ovary, prior uterine surgery, or diminished ovarian reserve.
One of the hardest parts of his job, he said, is getting the message through.
"When I sit down and talk to patients about the risks of having twins, they don’t want to hear it," Dr. Sharara said.
The study was supported by Ferring Pharmaceuticals. Dr. Sharara disclosed receiving grants from the company.
AT THE JOINT IFFS/ASRM MEETING
Major finding: Of 48 couples offered approximately $8,500 in savings if they opted for single-embryo transfer, 18 refused and chose dual transfers.
Data source: An ongoing, prospective single-center study of patient attitudes regarding the relative merits of single-embryo transfer in 48 couples.
Disclosures: The study was supported by Ferring Pharmaceuticals. Dr. Sharara disclosed receiving grants from the company.
Many women physicians regret delaying reproduction
BOSTON – Many female physicians say that if they had to do it over again, they might have tried to have children sooner, chosen a different specialty, or elected to have embryos frozen "just in case" they had later fertility problems, an investigator said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Dr. Natalie A. Clark and her colleagues surveyed a random sample of female physicians in the United States to ask about their choices for timing of conception, their basic knowledge of reproductive limitations, and how reproductive choices factor into their professional and personal decision making. The investigators randomly selected 600 women who graduated from medical school from 1995 through 2000 from the American Medical Association (AMA) physicians’ database, and mailed surveys to them. A total of 333 (55.5%) responded.
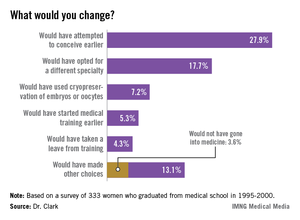
Asked whether they would in retrospect have changed anything about their reproductive choices, 27.9% said they would have attempted to conceive earlier, 17.7% would have opted for a different specialty, 7.2% would have used cryopreservation of embryos or oocytes, 5.3% would have started medical training earlier, and 4.3% would have taken a leave from training. Of the 13.1% who said they would have made other, unspecified choices, 3.6% independently reported that they would not have gone into medicine.
The survey of female physicians highlights the unique challenges that women of childbearing age face when trying to balance the demands of education, training, and career advancement, said Dr. Clark, a third-year resident at the University of Michigan department of obstetrics and gynecology in Ann Arbor.
"We have a number of highly educated patients who come into our clinic who have finished their MDs or PhDs, and have done a great amount of postgraduate work, and they present at very late reproductive ages. They say, "I’m ready to start reproducing, and I don’t want to be too aggressive, but what can I do?’ – not fully realizing that they’ve missed their ideal reproductive window," Dr. Clark said in an interview.
The majority of respondents (55%) work in specialties for women, children, and families, including family medicine, obstetrics and gynecology, and pediatrics; 31% work in other medical specialties; 10% in hospital-based specialties; and 4% in surgical specialties.
In all, 80% of the respondents said they had attempted to conceive, and 77% had at least one biological child. The physicians on average had their first child 7.4 years later than did women in the general population, according to data from the Centers for Disease Control and Prevention.
One-fourth (25%) of all respondents had been diagnosed with infertility. Ovulatory dysfunction was the most common cause, followed by male factor, age-related diminished ovarian reserve, endometriosis, tubal factor, and uterine factor.
"Despite having a medical background, 44% of infertile respondents were surprised about their diagnosis of infertility," Dr. Clark said. In every age range, physicians consistently underestimated their chances for conceiving, she added.
"I think that if we can change the culture of medicine such that we can support those decisions at a biologically advantageous time point, it could change the field of medicine," Dr. Clark said.
The study was supported by a grant from the AMA Joan F. Giambalvo Memorial Scholarship Fund. Dr. Clark was a 2012 recipient of a research award from the fund.
The fact that 25% of physicians have infertility is a slight increase over the percentage of general population (15%), and it reinforces to physicians that they are not immune to the diseases we treat.
The study utilizes graduates from medical school between 1995 and 2000, and it doesn't reflect the working environment that today's graduates face, 13-18 years later. Duty hours, Gen X graduates, and the increasing number of women in medicine, especially in obstetrics and gynecology, have changed the workplace. Residents and young physicians in practice are no longer willing to work the hours that their predecessors did. To me, this is mostly a positive trend, as the desire for work-life balance is something young physicians are teaching older physicians, by example. In my own department, we see many physicians of all ages leading fuller, happier lives because of these changes. That is not to say that being a resident or young physician in practice and being pregnant is easy. It is just more acceptable than it was for the physicians in the study cohort.
 |
| Dr. David Forstein |
As to the option of oocyte freezing early in their career, this option is becoming more and more available to women. We have seen a number of women in their mid- to late 20s, with no partner in place, freeze oocytes "just in case." As the technology improves and allows higher pregnancy rates from unstimulated oocytes, more women will choose this option. Currently, the best pregnancy rates come from frozen embryos, then from oocytes frozen following an ovarian stimulation cycle. The stimulation still requires multiple medication injections, and ultrasound and hormone-level monitoring. These requirements are an additional hurdle for women with busy schedules to navigate.
The cost of an oocyte harvest is significant and not often covered by insurance or, even if it is covered, there are copays and deductibles that make it difficult for residents to manage. This is a challenge to which there are no easy answers.
In my residency program director's role, I have frequently been challenged by resident and attending physicians about what the response to "another pregnant resident" should be. Often frustration ensues amongst the team because a maternity leave stretches the manpower of a program. In my mind, the appropriate response is that as ob.gyns., we should celebrate every pregnancy! If we can't lead by example about how to treat professional women during pregnancy and with their young families, who is going to do it? Respect for the challenge of multitasking a residency or a practice and a family is the way forward.
David Forstein, D.O., is an infertility specialist who is associate professor of obstetrics and gynecology at the University of South Carolina, Greenville. He said he had no financial disclosures relevant to this commentary.
Ob.Gyns. should be leading the way
Regarding this intriguing research performed by Clark and her colleagues, these women physicians had their first child about 7 years later than women in the general population, and just over a quarter of respondents indicated, in retrospect, that they would have attempted to conceive earlier. This paper highlights the bind that professional women often find themselves in - that there is no "ideal" time to have a child.
 |
| Dr. Eve Espey |
Women pursuing professions may be discouraged from childbearing during their education and may hear the message that it is irresponsible to detract from their study time or professional development by having children during their undergraduate education or medical school. During residency, the "system" is not designed to accommodate absences, and fellow residents usually absorb the workload for women taking maternity leave, sometimes leading to resentment and an unspoken bias against childbearing.
Our society is only beginning to accommodate the women who wish to "have it all," both professional fulfillment in a rewarding career and the personal happiness that comes with parenthood.
As women's physicians, ob.gyns. should lead the way in encouraging women professionals to have children whenever during their professional development or careers they see fit, whether that be in college, medical school, residency, or beyond. Because there is no "ideal" time, we should support women in their personal and professional fulfillment, and develop flexible systems that do not punish women for electing to have children at any point in their reproductive lives.
Eve Espey, M.D., is an associate professor of obstetrics and gynecology at the University of New Mexico, Albuquerque. She said she had no financial disclosures relevant to this commentary.
The fact that 25% of physicians have infertility is a slight increase over the percentage of general population (15%), and it reinforces to physicians that they are not immune to the diseases we treat.
The study utilizes graduates from medical school between 1995 and 2000, and it doesn't reflect the working environment that today's graduates face, 13-18 years later. Duty hours, Gen X graduates, and the increasing number of women in medicine, especially in obstetrics and gynecology, have changed the workplace. Residents and young physicians in practice are no longer willing to work the hours that their predecessors did. To me, this is mostly a positive trend, as the desire for work-life balance is something young physicians are teaching older physicians, by example. In my own department, we see many physicians of all ages leading fuller, happier lives because of these changes. That is not to say that being a resident or young physician in practice and being pregnant is easy. It is just more acceptable than it was for the physicians in the study cohort.
 |
| Dr. David Forstein |
As to the option of oocyte freezing early in their career, this option is becoming more and more available to women. We have seen a number of women in their mid- to late 20s, with no partner in place, freeze oocytes "just in case." As the technology improves and allows higher pregnancy rates from unstimulated oocytes, more women will choose this option. Currently, the best pregnancy rates come from frozen embryos, then from oocytes frozen following an ovarian stimulation cycle. The stimulation still requires multiple medication injections, and ultrasound and hormone-level monitoring. These requirements are an additional hurdle for women with busy schedules to navigate.
The cost of an oocyte harvest is significant and not often covered by insurance or, even if it is covered, there are copays and deductibles that make it difficult for residents to manage. This is a challenge to which there are no easy answers.
In my residency program director's role, I have frequently been challenged by resident and attending physicians about what the response to "another pregnant resident" should be. Often frustration ensues amongst the team because a maternity leave stretches the manpower of a program. In my mind, the appropriate response is that as ob.gyns., we should celebrate every pregnancy! If we can't lead by example about how to treat professional women during pregnancy and with their young families, who is going to do it? Respect for the challenge of multitasking a residency or a practice and a family is the way forward.
David Forstein, D.O., is an infertility specialist who is associate professor of obstetrics and gynecology at the University of South Carolina, Greenville. He said he had no financial disclosures relevant to this commentary.
Ob.Gyns. should be leading the way
Regarding this intriguing research performed by Clark and her colleagues, these women physicians had their first child about 7 years later than women in the general population, and just over a quarter of respondents indicated, in retrospect, that they would have attempted to conceive earlier. This paper highlights the bind that professional women often find themselves in - that there is no "ideal" time to have a child.
 |
| Dr. Eve Espey |
Women pursuing professions may be discouraged from childbearing during their education and may hear the message that it is irresponsible to detract from their study time or professional development by having children during their undergraduate education or medical school. During residency, the "system" is not designed to accommodate absences, and fellow residents usually absorb the workload for women taking maternity leave, sometimes leading to resentment and an unspoken bias against childbearing.
Our society is only beginning to accommodate the women who wish to "have it all," both professional fulfillment in a rewarding career and the personal happiness that comes with parenthood.
As women's physicians, ob.gyns. should lead the way in encouraging women professionals to have children whenever during their professional development or careers they see fit, whether that be in college, medical school, residency, or beyond. Because there is no "ideal" time, we should support women in their personal and professional fulfillment, and develop flexible systems that do not punish women for electing to have children at any point in their reproductive lives.
Eve Espey, M.D., is an associate professor of obstetrics and gynecology at the University of New Mexico, Albuquerque. She said she had no financial disclosures relevant to this commentary.
The fact that 25% of physicians have infertility is a slight increase over the percentage of general population (15%), and it reinforces to physicians that they are not immune to the diseases we treat.
The study utilizes graduates from medical school between 1995 and 2000, and it doesn't reflect the working environment that today's graduates face, 13-18 years later. Duty hours, Gen X graduates, and the increasing number of women in medicine, especially in obstetrics and gynecology, have changed the workplace. Residents and young physicians in practice are no longer willing to work the hours that their predecessors did. To me, this is mostly a positive trend, as the desire for work-life balance is something young physicians are teaching older physicians, by example. In my own department, we see many physicians of all ages leading fuller, happier lives because of these changes. That is not to say that being a resident or young physician in practice and being pregnant is easy. It is just more acceptable than it was for the physicians in the study cohort.
 |
| Dr. David Forstein |
As to the option of oocyte freezing early in their career, this option is becoming more and more available to women. We have seen a number of women in their mid- to late 20s, with no partner in place, freeze oocytes "just in case." As the technology improves and allows higher pregnancy rates from unstimulated oocytes, more women will choose this option. Currently, the best pregnancy rates come from frozen embryos, then from oocytes frozen following an ovarian stimulation cycle. The stimulation still requires multiple medication injections, and ultrasound and hormone-level monitoring. These requirements are an additional hurdle for women with busy schedules to navigate.
The cost of an oocyte harvest is significant and not often covered by insurance or, even if it is covered, there are copays and deductibles that make it difficult for residents to manage. This is a challenge to which there are no easy answers.
In my residency program director's role, I have frequently been challenged by resident and attending physicians about what the response to "another pregnant resident" should be. Often frustration ensues amongst the team because a maternity leave stretches the manpower of a program. In my mind, the appropriate response is that as ob.gyns., we should celebrate every pregnancy! If we can't lead by example about how to treat professional women during pregnancy and with their young families, who is going to do it? Respect for the challenge of multitasking a residency or a practice and a family is the way forward.
David Forstein, D.O., is an infertility specialist who is associate professor of obstetrics and gynecology at the University of South Carolina, Greenville. He said he had no financial disclosures relevant to this commentary.
Ob.Gyns. should be leading the way
Regarding this intriguing research performed by Clark and her colleagues, these women physicians had their first child about 7 years later than women in the general population, and just over a quarter of respondents indicated, in retrospect, that they would have attempted to conceive earlier. This paper highlights the bind that professional women often find themselves in - that there is no "ideal" time to have a child.
 |
| Dr. Eve Espey |
Women pursuing professions may be discouraged from childbearing during their education and may hear the message that it is irresponsible to detract from their study time or professional development by having children during their undergraduate education or medical school. During residency, the "system" is not designed to accommodate absences, and fellow residents usually absorb the workload for women taking maternity leave, sometimes leading to resentment and an unspoken bias against childbearing.
Our society is only beginning to accommodate the women who wish to "have it all," both professional fulfillment in a rewarding career and the personal happiness that comes with parenthood.
As women's physicians, ob.gyns. should lead the way in encouraging women professionals to have children whenever during their professional development or careers they see fit, whether that be in college, medical school, residency, or beyond. Because there is no "ideal" time, we should support women in their personal and professional fulfillment, and develop flexible systems that do not punish women for electing to have children at any point in their reproductive lives.
Eve Espey, M.D., is an associate professor of obstetrics and gynecology at the University of New Mexico, Albuquerque. She said she had no financial disclosures relevant to this commentary.
BOSTON – Many female physicians say that if they had to do it over again, they might have tried to have children sooner, chosen a different specialty, or elected to have embryos frozen "just in case" they had later fertility problems, an investigator said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Dr. Natalie A. Clark and her colleagues surveyed a random sample of female physicians in the United States to ask about their choices for timing of conception, their basic knowledge of reproductive limitations, and how reproductive choices factor into their professional and personal decision making. The investigators randomly selected 600 women who graduated from medical school from 1995 through 2000 from the American Medical Association (AMA) physicians’ database, and mailed surveys to them. A total of 333 (55.5%) responded.
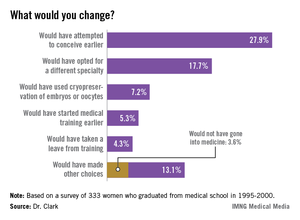
Asked whether they would in retrospect have changed anything about their reproductive choices, 27.9% said they would have attempted to conceive earlier, 17.7% would have opted for a different specialty, 7.2% would have used cryopreservation of embryos or oocytes, 5.3% would have started medical training earlier, and 4.3% would have taken a leave from training. Of the 13.1% who said they would have made other, unspecified choices, 3.6% independently reported that they would not have gone into medicine.
The survey of female physicians highlights the unique challenges that women of childbearing age face when trying to balance the demands of education, training, and career advancement, said Dr. Clark, a third-year resident at the University of Michigan department of obstetrics and gynecology in Ann Arbor.
"We have a number of highly educated patients who come into our clinic who have finished their MDs or PhDs, and have done a great amount of postgraduate work, and they present at very late reproductive ages. They say, "I’m ready to start reproducing, and I don’t want to be too aggressive, but what can I do?’ – not fully realizing that they’ve missed their ideal reproductive window," Dr. Clark said in an interview.
The majority of respondents (55%) work in specialties for women, children, and families, including family medicine, obstetrics and gynecology, and pediatrics; 31% work in other medical specialties; 10% in hospital-based specialties; and 4% in surgical specialties.
In all, 80% of the respondents said they had attempted to conceive, and 77% had at least one biological child. The physicians on average had their first child 7.4 years later than did women in the general population, according to data from the Centers for Disease Control and Prevention.
One-fourth (25%) of all respondents had been diagnosed with infertility. Ovulatory dysfunction was the most common cause, followed by male factor, age-related diminished ovarian reserve, endometriosis, tubal factor, and uterine factor.
"Despite having a medical background, 44% of infertile respondents were surprised about their diagnosis of infertility," Dr. Clark said. In every age range, physicians consistently underestimated their chances for conceiving, she added.
"I think that if we can change the culture of medicine such that we can support those decisions at a biologically advantageous time point, it could change the field of medicine," Dr. Clark said.
The study was supported by a grant from the AMA Joan F. Giambalvo Memorial Scholarship Fund. Dr. Clark was a 2012 recipient of a research award from the fund.
BOSTON – Many female physicians say that if they had to do it over again, they might have tried to have children sooner, chosen a different specialty, or elected to have embryos frozen "just in case" they had later fertility problems, an investigator said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Dr. Natalie A. Clark and her colleagues surveyed a random sample of female physicians in the United States to ask about their choices for timing of conception, their basic knowledge of reproductive limitations, and how reproductive choices factor into their professional and personal decision making. The investigators randomly selected 600 women who graduated from medical school from 1995 through 2000 from the American Medical Association (AMA) physicians’ database, and mailed surveys to them. A total of 333 (55.5%) responded.
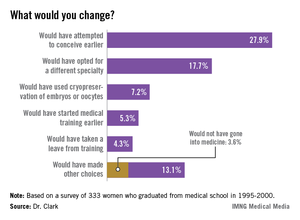
Asked whether they would in retrospect have changed anything about their reproductive choices, 27.9% said they would have attempted to conceive earlier, 17.7% would have opted for a different specialty, 7.2% would have used cryopreservation of embryos or oocytes, 5.3% would have started medical training earlier, and 4.3% would have taken a leave from training. Of the 13.1% who said they would have made other, unspecified choices, 3.6% independently reported that they would not have gone into medicine.
The survey of female physicians highlights the unique challenges that women of childbearing age face when trying to balance the demands of education, training, and career advancement, said Dr. Clark, a third-year resident at the University of Michigan department of obstetrics and gynecology in Ann Arbor.
"We have a number of highly educated patients who come into our clinic who have finished their MDs or PhDs, and have done a great amount of postgraduate work, and they present at very late reproductive ages. They say, "I’m ready to start reproducing, and I don’t want to be too aggressive, but what can I do?’ – not fully realizing that they’ve missed their ideal reproductive window," Dr. Clark said in an interview.
The majority of respondents (55%) work in specialties for women, children, and families, including family medicine, obstetrics and gynecology, and pediatrics; 31% work in other medical specialties; 10% in hospital-based specialties; and 4% in surgical specialties.
In all, 80% of the respondents said they had attempted to conceive, and 77% had at least one biological child. The physicians on average had their first child 7.4 years later than did women in the general population, according to data from the Centers for Disease Control and Prevention.
One-fourth (25%) of all respondents had been diagnosed with infertility. Ovulatory dysfunction was the most common cause, followed by male factor, age-related diminished ovarian reserve, endometriosis, tubal factor, and uterine factor.
"Despite having a medical background, 44% of infertile respondents were surprised about their diagnosis of infertility," Dr. Clark said. In every age range, physicians consistently underestimated their chances for conceiving, she added.
"I think that if we can change the culture of medicine such that we can support those decisions at a biologically advantageous time point, it could change the field of medicine," Dr. Clark said.
The study was supported by a grant from the AMA Joan F. Giambalvo Memorial Scholarship Fund. Dr. Clark was a 2012 recipient of a research award from the fund.
AT THE JOINT IFFS/ASRM MEETING
Major finding: Asked whether they would in retrospect have changed anything about their reproductive choices, 27.9% of female physicians said they would have attempted to conceive earlier, 17.7% would have opted for a different specialty, 7.2% would have used cryopreservation of embryos or oocytes, 5.3% would have started medical training earlier, and 4.3% would have taken a leave from training.
Data source: Mailed survey of 333 U.S. women physicians who graduated from medical school from 1995 through 2000.
Disclosures: The study was supported by a grant from the AMA Joan F. Giambalvo Memorial Scholarship Fund. Dr. Clark was a 2012 recipient of a research award from the fund.