User login
Current Concepts in Lip Augmentation
Historically, a variety of tools have been used to alter one’s appearance for cultural or religious purposes or to conform to standards of beauty. As a defining feature of the face, the lips provide a unique opportunity for facial aesthetic enhancement. There has been a paradigm shift in medicine favoring preventative health and a desire to slow and even reverse the aging process.1 Acknowledging that product technology, skill sets, and cultural ideals continually evolve, this article highlights perioral anatomy, explains aging of the lower face, and reviews techniques to achieve perioral rejuvenation through volume restoration and muscle control.
Perioral Anatomy
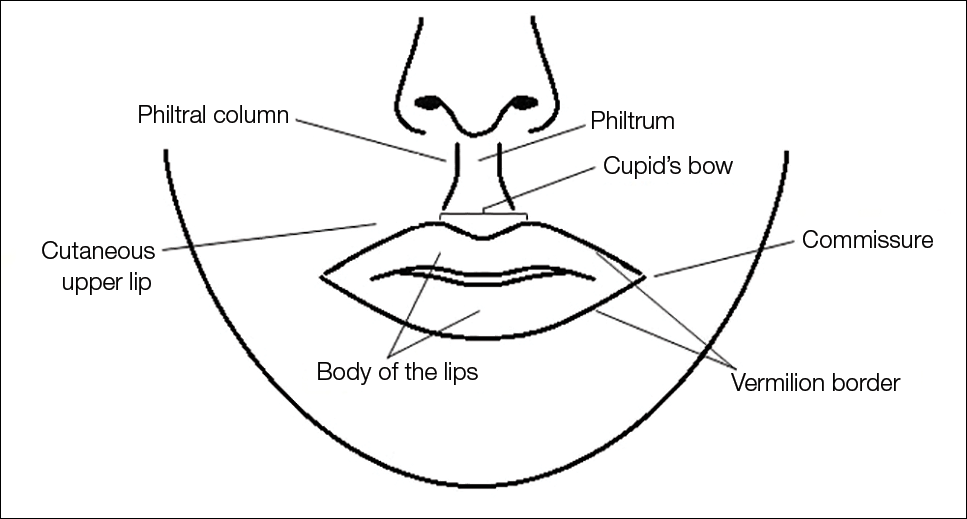
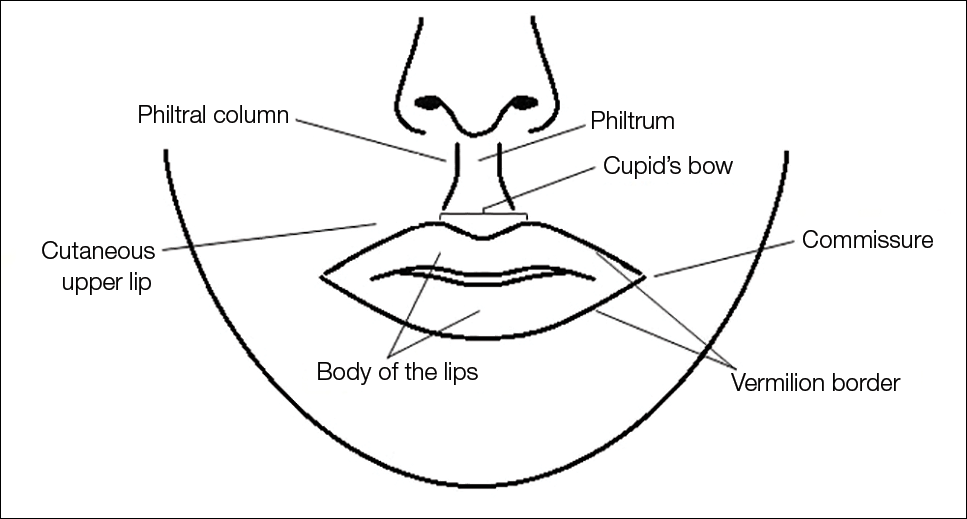
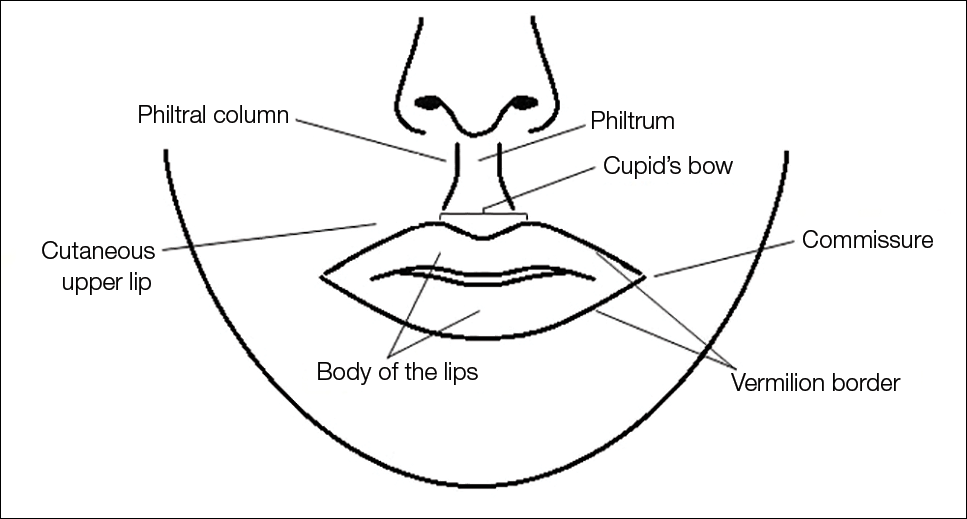
The layers of the lips include the epidermis, subcutaneous tissue, orbicularis oris muscle fibers, and mucosa. The upper lip extends from the base of the nose to the mucosa inferiorly and to the nasolabial folds laterally. The curvilinear lower lip extends from the mucosa to the mandible inferiorly and to the oral commissures laterally.2 Circumferential at the vermilion-cutaneous junction, a raised area of pale skin known as the white roll accentuates the vermilion border and provides an important landmark during lip augmentation.3 At the upper lip, this elevation of the vermilion joins at a V-shaped depression centrally to form the Cupid’s bow. The cutaneous upper lip has 2 raised vertical pillars known as the philtral columns, which are formed from decussating fibers of the orbicularis oris muscle.2 The resultant midline depression is the philtrum. These defining features of the upper lip are to be preserved during augmentation procedures (Figure 1).4
The superior and inferior labial arteries, both branches of the facial artery, supply the upper and lower lip, respectively. The anastomotic arch of the superior labial artery is susceptible to injury from deep injection of the upper lip between the muscle layer and mucosa; therefore, caution must be exercised in this area.5 Injections into the vermilion and lower lip can be safely performed with less concern for vascular compromise. The vermilion derives its red color from the translucency of capillaries in the superficial papillae.2 The capillary plexus at the papillae and rich sensory nerve network render the lip a highly vascular and sensitive structure.
Aging of the Lower Face
Subcutaneous fat atrophy, loss of elasticity, gravitational forces, and remodeling of the skeletal foundation all contribute to aging of the lower face. Starting as early as the third decade of life, intrinsic factors including hormonal changes and genetically determined processes produce alterations in skin quality and structure. Similarly, extrinsic aging through environmental influences, namely exposure to UV radiation and smoking, accelerate the loss of skin integrity.6
The decreased laxity of the skin in combination with repeated contraction of the orbicularis oris muscle results in perioral rhytides.7 For women in particular, vertically oriented perioral rhytides develop above the vermilion; terminal hair follicles, thicker skin, and a greater density of subcutaneous fat are presumptive protective factors for males.8 With time, the cutaneous portion of the upper lip lengthens and there is redistribution of volume with effacement of the upper lip vermilion.9 Additionally, the demarcation of the vermilion becomes blurred secondary to pallor, flattening of the philtral columns, and loss of projection of the Cupid’s bow.10
Downturning of the oral commissures is observed secondary to a combination of gravity, bone resorption, and soft tissue volume loss. Hyperactivity of the depressor anguli oris muscle exacerbates the mesolabial folds, producing marionette lines and a saddened expression.7 With ongoing volume loss and ligament laxity, tissue redistributes near the jaws and chin, giving rise to jowls. Similarly, perioral volume loss and descent of the malar fat-pad deepen the nasolabial folds in the aging midface.6
The main objective of perioral rejuvenation is to reinstate a harmonious refreshed look to the lower face; however, aesthetic analysis should occur within the context of the face as a whole, as the lips should complement the surrounding perioral cosmetic unit and overall skeletal foundation of the face. To accomplish this goal, the dermatologist’s armamentarium contains a broad variety of approaches including restriction of muscle movement, volume restoration, and surface contouring.
Volume Restoration
Treatment Options
In 2015, hyaluronic acid (HA) fillers constituted 80% of all injectable soft-tissue fillers, an 8% increase from 2014.11 Hyaluronic acid has achieved immense popularity as a temporary dermal filler given its biocompatibility, longevity, and reversibility via hyaluronidase.12
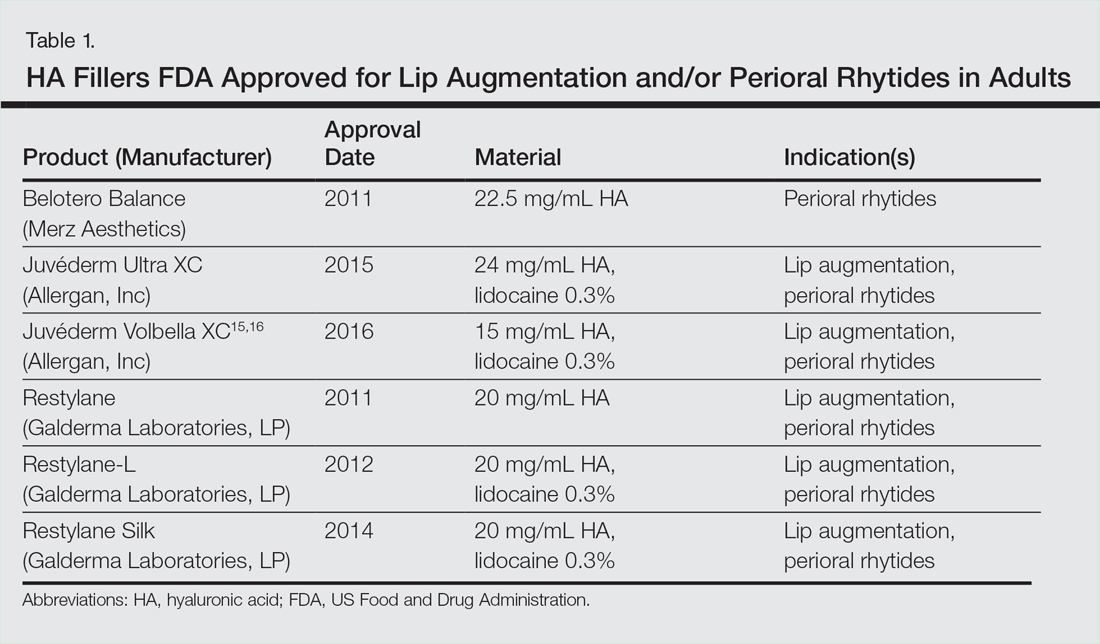
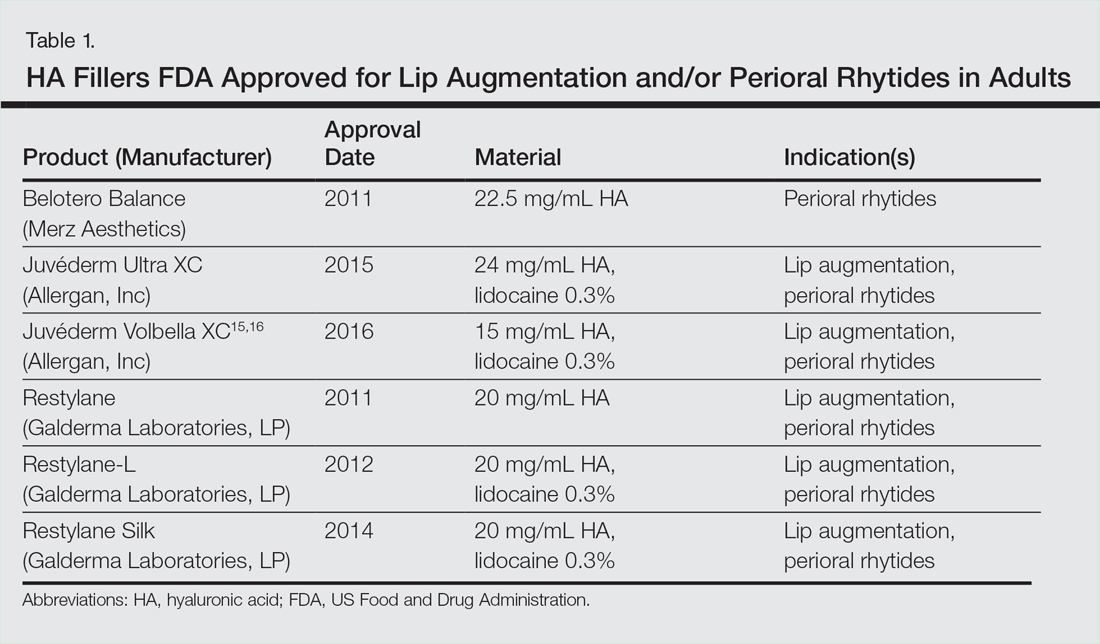
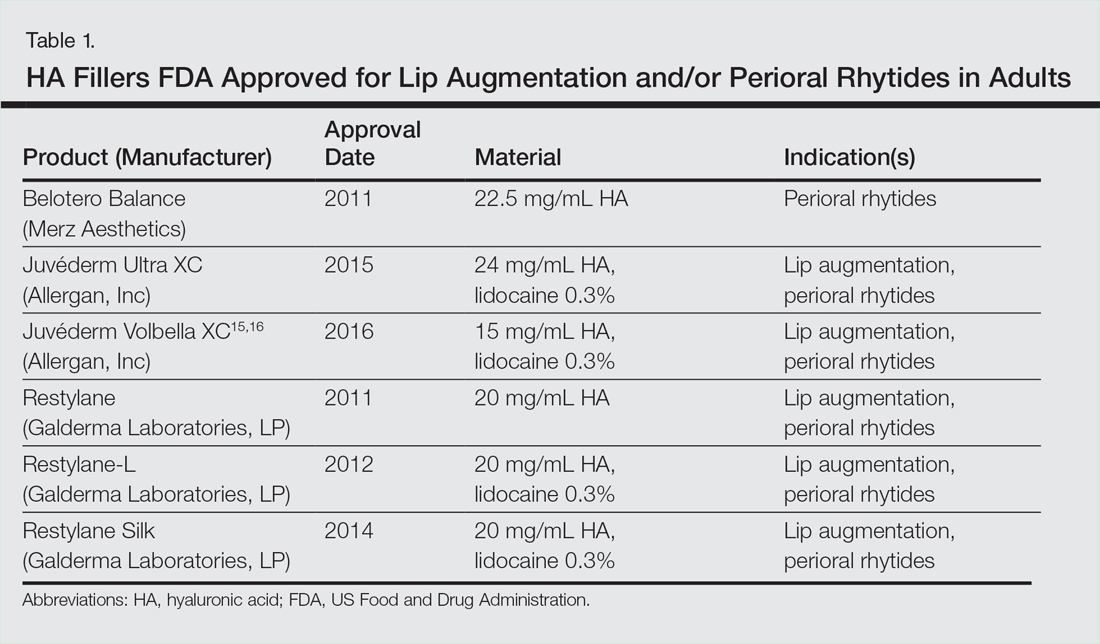
Hyaluronic acid is a naturally occurring glycosaminoglycan that comprises the connective tissue matrix. The molecular composition affords HA its hydrophilic property, which augments dermal volume.7 Endogenous HA has a short half-life, and chemical modification by a cross-linking process extends longevity by 6 to 12 months. The various HA fillers are distinguished by method of purification, size of molecules, concentration and degree of cross-linking, and viscosity.7,13,14 These differences dictate overall clinical performance such as flow properties, longevity, and stability. As a general rule, a high-viscosity product is more appropriate for deeper augmentation; fillers with low viscosity are more appropriate for correction of shallow defects.1 Table 1 lists the HA fillers that are currently approved by the US Food and Drug Administration for lip augmentation and/or perioral rhytides in adults 21 years and older.15-17
Randomized controlled trials comparing the efficacy, longevity, and tolerability of different HA products are lacking in the literature and, where present, have strong industry influence.18,19 The advent of assessment scales has provided an objective evaluation of perioral and lip augmentation, facilitating comparisons between products in both clinical research and practice.20
Semipermanent biostimulatory dermal fillers such as calcium hydroxylapatite and poly-L-lactic acid are not recommended for lip augmentation due to an increased incidence of submucosal nodule formation.6,14,21 Likewise, permanent fillers are not recommended given their irreversibility and risk of nodule formation around the lips.14,22 Nonetheless, liquid silicone (purified polydimethylsiloxane) administered via a microdroplet technique (0.01 mL of silicone at a time, no more than 1 cc per lip per session) has been used off label as a permanent filling agent for lip augmentation with limited complications.23 Regardless, trepidations about its use with respect to reported risks continue to limit its application.22
Similarly, surgical lip implants such as expanded polytetrafluoroethylene is an option for a subset of patients desiring permanent enhancement but are less commonly utilized given the side-effect profile, irreversibility, and relatively invasive nature of the procedure.22 Lastly, autologous fat transfer has been used in correction of the nasolabial and mesolabial folds as well as in lip augmentation; however, irregular surface contours and unpredictable longevity secondary to postinjection resorption (20%–90%) has limited its popularity.3,14,21
HA Injection Technique
With respect to HA fillers in the perioral area, numerous approaches have been described.10,22 The techniques in Table 2 provide a foundation for lip rejuvenation.

Several injection techniques exist, including serial puncture, linear threading, cross-hatching, and fanning in a retrograde or anterograde manner.24 A blunt microcannula (27 gauge, 38 mm) may be used in place of sharp needles and offers the benefit of increased patient comfort, reduced edema and ecchymosis, and shortened recovery period.25,26 Gentle massage of the product after injection can assist with an even contour. Lastly, a key determinant of successful outcomes is using an adequate volume of HA filler (1–2 mL for shaping the vermilion border and volumizing the lips).27 Figure 2 highlights a clinical example of HA filler for lip augmentation.

Fortunately, most complications encountered with HA lip augmentation are mild and transient. The most commonly observed side effects include injection-site reactions such as pain, erythema, and edema. Similarly, most adverse effects are related to injection technique. All HA fillers are prone to the Tyndall effect, a consequence of too superficial an injection plane. Patients with history of recurrent herpes simplex virus infections should receive prophylactic antiviral therapy.12
Muscle Control
An emerging concept in rejuvenation of the lower face recognizes not only restoration of volume but also control of muscle movement. Local injection of botulinum toxin type A induces relaxation of hyperfunctional facial muscles through temporary inhibition of neurotransmitter release.6 The potential for paralysis of the oral cavity may limit the application of botulinum toxin type A in that region.7 Nonetheless, the off-label potential of botulinum toxin type A has expanded to include several targets in the lower face. The orbicularis oris muscle is targeted to soften perioral rhytides. Conservative dosing (1–2 U per lip quadrant or approximately 5 U total) and superficial injection is emphasized in this area.27 Similarly, the depressor anguli oris muscle is targeted by injection of 4 U bilaterally to soften the marionette lines. In the chin area, the mentalis muscle can be targeted by injection of 2 U deep into each belly of the muscle to reduce the mental crease and dimpling.28 Combination treatment with dermal filler and neurotoxin demonstrates effects that last longer than either modality alone without additional adverse events.29 With combination therapy, guidelines suggest treating with filler first.27
Conclusion
A greater understanding of the extrinsic and intrinsic factors that contribute to the structural and surface changes of the aging face coupled with a preference for minimally invasive procedures has revolutionized the dermatologist’s approach to perioral rejuvenation. Serving as a focal point of the face, the lips and perioral skin are well poised to benefit from this paradigm shift. A multifaceted approach utilizing dermal fillers and neurotoxins may be most appropriate and has demonstrated optimal outcomes in facial aesthetics.
- Buck DW, Alam M, Kim JYS. Injectable fillers for facial rejuvenation: a review. J Plast Reconstr Aesthet Surg. 2009;62:11-18.
- Guareschi M, Stella E. Lips. In: Goisis M, ed. Injections in Aesthetic Medicine. Milan, Italy: Springer; 2014:125-136.
- Byrne PJ, Hilger PA. Lip augmentation. Facial Plast Surg. 2004;20:31-38.
- Niamtu J. Rejuvenation of the lip and perioral areas. In: Bell WH, Guerroro CA, eds. Distraction Osteogenesis of the Facial Skeleton. Ontario, Canada: BC Decker Inc; 2007:38-48.
- Tansatit T, Apinuntrum P, Phetudom T. A typical pattern of the labial arteries with implication for lip augmentation with injectable fillers. Aesthet Plast Surg. 2014;38:1083-1089.
- Sadick NS, Karcher C, Palmisano L. Cosmetic dermatology of the aging face. Clin Dermatol. 2009;27(suppl):S3-S12.
- Ali MJ, Ende K, Mass CS. Perioral rejuvenation and lip augmentation. Facial Plast Surg Clin N Am. 2007;15:491-500.
- Chien AL, Qi J, Cheng N, et al. Perioral wrinkles are associated with female gender, aging, and smoking: development of a gender-specific photonumeric scale. J Am Acad Dermatol. 2016;74:924-930.
- Iblher N, Stark GB, Penna V. The aging perioral region—do we really know what is happening? J Nutr Health Aging. 2012;16:581-585.
- Sarnoff DS, Gotkin RH. Six steps to the “perfect” lip. J Drugs Dermatol. 2012;11:1081-1088.
- American Society of Plastic Surgeons. 2015 Cosmetic plastic surgery statistics. https://d2wirczt3b6wjm.cloudfront.net/News/Statistics/2015/cosmetic-procedure-trends-2015.pdf. Published February 26, 2015. Accessed October 5, 2016.
- Abduljabbar MH, Basendwh MA. Complications of hyaluronic acid fillers and their managements. J Dermatol Surg. 2016;20:1-7.
- Luebberding S, Alexiades-Armenakas M. Facial volume augmentation in 2014: overview of different filler options. J Drugs Dermatol. 2013;12:1339-1344.
- Huang Attenello N, Mass CS. Injectable fillers: review of material and properties. Facial Plast Surg. 2015;31:29-34.
- Eccleston D, Murphy DK. Juvéderm Volbella in the perioral area: a 12-month perspective, multicenter, open-label study. Clin Cosmet Investig Dermatol. 2012;5:167-172.
- Raspaldo H, Chantrey J, Belhaouari L, et al. Lip and perioral enhancement: a 12-month prospective, randomized, controlled study. J Drugs Dermatol. 2015;14:1444-1452.
- Soft tissue fillers approved by the center for devices and radiological health. US Food and Drug Administration website. http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/CosmeticDevices/WrinkleFillers/ucm227749.htm. Updated July 27, 2015. Accessed October 5, 2016.
- Butterwick K, Marmur E, Narurkar V, et al. HYC-24L demonstrates greater effectiveness with less pain than CPM-22.5 for treatment of perioral lines in a randomized controlled trial. Dermatol Surg. 2015;41:1351-1360.
- San Miguel Moragas J, Reddy RR, Hernández Alfaro F, et al. Systematic review of “filling” procedures for lip augmentation regarding types of material, outcomes and complications. J Craniomaxillofac Surg. 2015;43:883-906.
- Cohen JL, Thomas J, Paradkar D, et al. An interrater and intrarater reliability study of 3 photographic scales for the classification of perioral aesthetic features. Dermatol Surg. 2014;40:663-670.
- Broder KW, Cohen SR. An overview of permanent and semipermanent fillers. Plast Reconstr Surg. 2006;118(3 suppl):7S-14S.
- Sarnoff DS, Saini R, Gotkin RH. Comparison of filling agents for lip augmentation. Aesthet Surg J. 2008;28:556-563.
- Moscona RA, Fodor L. A retrospective study on liquid injectable silicone for lip augmentation: long-term results and patient satisfaction. J Plast Reconstr Aesthet Surg. 2010;63:1694-1698.
- Bertucci V, Lynde CB. Current concepts in the use of small-particle hyaluronic acid. Plast Reconstr Surg. 2015;136(5 suppl):132S-138S.
- Wilson AJ, Taglienti AJ, Chang CS, et al. Current applications of facial volumization with fillers. Plast Reconstr Surg. 2016;137:E872-E889.
- Dewandre L, Caperton C, Fulton J. Filler injections with the blunt-tip microcannula compared to the sharp hypodermic needle. J Drugs Dermatol. 2012;11:1098-1103.
- Carruthers JD, Glogau RG, Blitzer A; Facial Aesthetics Consensus Group Faculty. Advances in facial rejuvenation: botulinum toxin type A, hyaluronic acid dermal fillers, and combination therapies-consensus recommendations. Plast Reconstr Surg. 2008;121(5 suppl):5S-30S.
- Wu DC, Fabi SG, Goldman MP. Neurotoxins: current concepts in cosmetic use on the face and neck-lower face. Plast Reconstr Surg. 2015;136(5 suppl):76S-79S.
- Carruthers A, Carruthers J, Monheit GD, et al. Multicenter, randomized, parallel-group study of the safety and effectiveness of onabotulinumtoxin A and hyaluronic acid dermal fillers (24-mg/mL smooth, cohesive gel) alone and in combination for lower facial rejuvenation. Dermatol Surg. 2010;36:2121-2134.
Historically, a variety of tools have been used to alter one’s appearance for cultural or religious purposes or to conform to standards of beauty. As a defining feature of the face, the lips provide a unique opportunity for facial aesthetic enhancement. There has been a paradigm shift in medicine favoring preventative health and a desire to slow and even reverse the aging process.1 Acknowledging that product technology, skill sets, and cultural ideals continually evolve, this article highlights perioral anatomy, explains aging of the lower face, and reviews techniques to achieve perioral rejuvenation through volume restoration and muscle control.
Perioral Anatomy
The layers of the lips include the epidermis, subcutaneous tissue, orbicularis oris muscle fibers, and mucosa. The upper lip extends from the base of the nose to the mucosa inferiorly and to the nasolabial folds laterally. The curvilinear lower lip extends from the mucosa to the mandible inferiorly and to the oral commissures laterally.2 Circumferential at the vermilion-cutaneous junction, a raised area of pale skin known as the white roll accentuates the vermilion border and provides an important landmark during lip augmentation.3 At the upper lip, this elevation of the vermilion joins at a V-shaped depression centrally to form the Cupid’s bow. The cutaneous upper lip has 2 raised vertical pillars known as the philtral columns, which are formed from decussating fibers of the orbicularis oris muscle.2 The resultant midline depression is the philtrum. These defining features of the upper lip are to be preserved during augmentation procedures (Figure 1).4
The superior and inferior labial arteries, both branches of the facial artery, supply the upper and lower lip, respectively. The anastomotic arch of the superior labial artery is susceptible to injury from deep injection of the upper lip between the muscle layer and mucosa; therefore, caution must be exercised in this area.5 Injections into the vermilion and lower lip can be safely performed with less concern for vascular compromise. The vermilion derives its red color from the translucency of capillaries in the superficial papillae.2 The capillary plexus at the papillae and rich sensory nerve network render the lip a highly vascular and sensitive structure.
Aging of the Lower Face
Subcutaneous fat atrophy, loss of elasticity, gravitational forces, and remodeling of the skeletal foundation all contribute to aging of the lower face. Starting as early as the third decade of life, intrinsic factors including hormonal changes and genetically determined processes produce alterations in skin quality and structure. Similarly, extrinsic aging through environmental influences, namely exposure to UV radiation and smoking, accelerate the loss of skin integrity.6
The decreased laxity of the skin in combination with repeated contraction of the orbicularis oris muscle results in perioral rhytides.7 For women in particular, vertically oriented perioral rhytides develop above the vermilion; terminal hair follicles, thicker skin, and a greater density of subcutaneous fat are presumptive protective factors for males.8 With time, the cutaneous portion of the upper lip lengthens and there is redistribution of volume with effacement of the upper lip vermilion.9 Additionally, the demarcation of the vermilion becomes blurred secondary to pallor, flattening of the philtral columns, and loss of projection of the Cupid’s bow.10
Downturning of the oral commissures is observed secondary to a combination of gravity, bone resorption, and soft tissue volume loss. Hyperactivity of the depressor anguli oris muscle exacerbates the mesolabial folds, producing marionette lines and a saddened expression.7 With ongoing volume loss and ligament laxity, tissue redistributes near the jaws and chin, giving rise to jowls. Similarly, perioral volume loss and descent of the malar fat-pad deepen the nasolabial folds in the aging midface.6
The main objective of perioral rejuvenation is to reinstate a harmonious refreshed look to the lower face; however, aesthetic analysis should occur within the context of the face as a whole, as the lips should complement the surrounding perioral cosmetic unit and overall skeletal foundation of the face. To accomplish this goal, the dermatologist’s armamentarium contains a broad variety of approaches including restriction of muscle movement, volume restoration, and surface contouring.
Volume Restoration
Treatment Options
In 2015, hyaluronic acid (HA) fillers constituted 80% of all injectable soft-tissue fillers, an 8% increase from 2014.11 Hyaluronic acid has achieved immense popularity as a temporary dermal filler given its biocompatibility, longevity, and reversibility via hyaluronidase.12
Hyaluronic acid is a naturally occurring glycosaminoglycan that comprises the connective tissue matrix. The molecular composition affords HA its hydrophilic property, which augments dermal volume.7 Endogenous HA has a short half-life, and chemical modification by a cross-linking process extends longevity by 6 to 12 months. The various HA fillers are distinguished by method of purification, size of molecules, concentration and degree of cross-linking, and viscosity.7,13,14 These differences dictate overall clinical performance such as flow properties, longevity, and stability. As a general rule, a high-viscosity product is more appropriate for deeper augmentation; fillers with low viscosity are more appropriate for correction of shallow defects.1 Table 1 lists the HA fillers that are currently approved by the US Food and Drug Administration for lip augmentation and/or perioral rhytides in adults 21 years and older.15-17
Randomized controlled trials comparing the efficacy, longevity, and tolerability of different HA products are lacking in the literature and, where present, have strong industry influence.18,19 The advent of assessment scales has provided an objective evaluation of perioral and lip augmentation, facilitating comparisons between products in both clinical research and practice.20
Semipermanent biostimulatory dermal fillers such as calcium hydroxylapatite and poly-L-lactic acid are not recommended for lip augmentation due to an increased incidence of submucosal nodule formation.6,14,21 Likewise, permanent fillers are not recommended given their irreversibility and risk of nodule formation around the lips.14,22 Nonetheless, liquid silicone (purified polydimethylsiloxane) administered via a microdroplet technique (0.01 mL of silicone at a time, no more than 1 cc per lip per session) has been used off label as a permanent filling agent for lip augmentation with limited complications.23 Regardless, trepidations about its use with respect to reported risks continue to limit its application.22
Similarly, surgical lip implants such as expanded polytetrafluoroethylene is an option for a subset of patients desiring permanent enhancement but are less commonly utilized given the side-effect profile, irreversibility, and relatively invasive nature of the procedure.22 Lastly, autologous fat transfer has been used in correction of the nasolabial and mesolabial folds as well as in lip augmentation; however, irregular surface contours and unpredictable longevity secondary to postinjection resorption (20%–90%) has limited its popularity.3,14,21
HA Injection Technique
With respect to HA fillers in the perioral area, numerous approaches have been described.10,22 The techniques in Table 2 provide a foundation for lip rejuvenation.

Several injection techniques exist, including serial puncture, linear threading, cross-hatching, and fanning in a retrograde or anterograde manner.24 A blunt microcannula (27 gauge, 38 mm) may be used in place of sharp needles and offers the benefit of increased patient comfort, reduced edema and ecchymosis, and shortened recovery period.25,26 Gentle massage of the product after injection can assist with an even contour. Lastly, a key determinant of successful outcomes is using an adequate volume of HA filler (1–2 mL for shaping the vermilion border and volumizing the lips).27 Figure 2 highlights a clinical example of HA filler for lip augmentation.

Fortunately, most complications encountered with HA lip augmentation are mild and transient. The most commonly observed side effects include injection-site reactions such as pain, erythema, and edema. Similarly, most adverse effects are related to injection technique. All HA fillers are prone to the Tyndall effect, a consequence of too superficial an injection plane. Patients with history of recurrent herpes simplex virus infections should receive prophylactic antiviral therapy.12
Muscle Control
An emerging concept in rejuvenation of the lower face recognizes not only restoration of volume but also control of muscle movement. Local injection of botulinum toxin type A induces relaxation of hyperfunctional facial muscles through temporary inhibition of neurotransmitter release.6 The potential for paralysis of the oral cavity may limit the application of botulinum toxin type A in that region.7 Nonetheless, the off-label potential of botulinum toxin type A has expanded to include several targets in the lower face. The orbicularis oris muscle is targeted to soften perioral rhytides. Conservative dosing (1–2 U per lip quadrant or approximately 5 U total) and superficial injection is emphasized in this area.27 Similarly, the depressor anguli oris muscle is targeted by injection of 4 U bilaterally to soften the marionette lines. In the chin area, the mentalis muscle can be targeted by injection of 2 U deep into each belly of the muscle to reduce the mental crease and dimpling.28 Combination treatment with dermal filler and neurotoxin demonstrates effects that last longer than either modality alone without additional adverse events.29 With combination therapy, guidelines suggest treating with filler first.27
Conclusion
A greater understanding of the extrinsic and intrinsic factors that contribute to the structural and surface changes of the aging face coupled with a preference for minimally invasive procedures has revolutionized the dermatologist’s approach to perioral rejuvenation. Serving as a focal point of the face, the lips and perioral skin are well poised to benefit from this paradigm shift. A multifaceted approach utilizing dermal fillers and neurotoxins may be most appropriate and has demonstrated optimal outcomes in facial aesthetics.
Historically, a variety of tools have been used to alter one’s appearance for cultural or religious purposes or to conform to standards of beauty. As a defining feature of the face, the lips provide a unique opportunity for facial aesthetic enhancement. There has been a paradigm shift in medicine favoring preventative health and a desire to slow and even reverse the aging process.1 Acknowledging that product technology, skill sets, and cultural ideals continually evolve, this article highlights perioral anatomy, explains aging of the lower face, and reviews techniques to achieve perioral rejuvenation through volume restoration and muscle control.
Perioral Anatomy
The layers of the lips include the epidermis, subcutaneous tissue, orbicularis oris muscle fibers, and mucosa. The upper lip extends from the base of the nose to the mucosa inferiorly and to the nasolabial folds laterally. The curvilinear lower lip extends from the mucosa to the mandible inferiorly and to the oral commissures laterally.2 Circumferential at the vermilion-cutaneous junction, a raised area of pale skin known as the white roll accentuates the vermilion border and provides an important landmark during lip augmentation.3 At the upper lip, this elevation of the vermilion joins at a V-shaped depression centrally to form the Cupid’s bow. The cutaneous upper lip has 2 raised vertical pillars known as the philtral columns, which are formed from decussating fibers of the orbicularis oris muscle.2 The resultant midline depression is the philtrum. These defining features of the upper lip are to be preserved during augmentation procedures (Figure 1).4
The superior and inferior labial arteries, both branches of the facial artery, supply the upper and lower lip, respectively. The anastomotic arch of the superior labial artery is susceptible to injury from deep injection of the upper lip between the muscle layer and mucosa; therefore, caution must be exercised in this area.5 Injections into the vermilion and lower lip can be safely performed with less concern for vascular compromise. The vermilion derives its red color from the translucency of capillaries in the superficial papillae.2 The capillary plexus at the papillae and rich sensory nerve network render the lip a highly vascular and sensitive structure.
Aging of the Lower Face
Subcutaneous fat atrophy, loss of elasticity, gravitational forces, and remodeling of the skeletal foundation all contribute to aging of the lower face. Starting as early as the third decade of life, intrinsic factors including hormonal changes and genetically determined processes produce alterations in skin quality and structure. Similarly, extrinsic aging through environmental influences, namely exposure to UV radiation and smoking, accelerate the loss of skin integrity.6
The decreased laxity of the skin in combination with repeated contraction of the orbicularis oris muscle results in perioral rhytides.7 For women in particular, vertically oriented perioral rhytides develop above the vermilion; terminal hair follicles, thicker skin, and a greater density of subcutaneous fat are presumptive protective factors for males.8 With time, the cutaneous portion of the upper lip lengthens and there is redistribution of volume with effacement of the upper lip vermilion.9 Additionally, the demarcation of the vermilion becomes blurred secondary to pallor, flattening of the philtral columns, and loss of projection of the Cupid’s bow.10
Downturning of the oral commissures is observed secondary to a combination of gravity, bone resorption, and soft tissue volume loss. Hyperactivity of the depressor anguli oris muscle exacerbates the mesolabial folds, producing marionette lines and a saddened expression.7 With ongoing volume loss and ligament laxity, tissue redistributes near the jaws and chin, giving rise to jowls. Similarly, perioral volume loss and descent of the malar fat-pad deepen the nasolabial folds in the aging midface.6
The main objective of perioral rejuvenation is to reinstate a harmonious refreshed look to the lower face; however, aesthetic analysis should occur within the context of the face as a whole, as the lips should complement the surrounding perioral cosmetic unit and overall skeletal foundation of the face. To accomplish this goal, the dermatologist’s armamentarium contains a broad variety of approaches including restriction of muscle movement, volume restoration, and surface contouring.
Volume Restoration
Treatment Options
In 2015, hyaluronic acid (HA) fillers constituted 80% of all injectable soft-tissue fillers, an 8% increase from 2014.11 Hyaluronic acid has achieved immense popularity as a temporary dermal filler given its biocompatibility, longevity, and reversibility via hyaluronidase.12
Hyaluronic acid is a naturally occurring glycosaminoglycan that comprises the connective tissue matrix. The molecular composition affords HA its hydrophilic property, which augments dermal volume.7 Endogenous HA has a short half-life, and chemical modification by a cross-linking process extends longevity by 6 to 12 months. The various HA fillers are distinguished by method of purification, size of molecules, concentration and degree of cross-linking, and viscosity.7,13,14 These differences dictate overall clinical performance such as flow properties, longevity, and stability. As a general rule, a high-viscosity product is more appropriate for deeper augmentation; fillers with low viscosity are more appropriate for correction of shallow defects.1 Table 1 lists the HA fillers that are currently approved by the US Food and Drug Administration for lip augmentation and/or perioral rhytides in adults 21 years and older.15-17
Randomized controlled trials comparing the efficacy, longevity, and tolerability of different HA products are lacking in the literature and, where present, have strong industry influence.18,19 The advent of assessment scales has provided an objective evaluation of perioral and lip augmentation, facilitating comparisons between products in both clinical research and practice.20
Semipermanent biostimulatory dermal fillers such as calcium hydroxylapatite and poly-L-lactic acid are not recommended for lip augmentation due to an increased incidence of submucosal nodule formation.6,14,21 Likewise, permanent fillers are not recommended given their irreversibility and risk of nodule formation around the lips.14,22 Nonetheless, liquid silicone (purified polydimethylsiloxane) administered via a microdroplet technique (0.01 mL of silicone at a time, no more than 1 cc per lip per session) has been used off label as a permanent filling agent for lip augmentation with limited complications.23 Regardless, trepidations about its use with respect to reported risks continue to limit its application.22
Similarly, surgical lip implants such as expanded polytetrafluoroethylene is an option for a subset of patients desiring permanent enhancement but are less commonly utilized given the side-effect profile, irreversibility, and relatively invasive nature of the procedure.22 Lastly, autologous fat transfer has been used in correction of the nasolabial and mesolabial folds as well as in lip augmentation; however, irregular surface contours and unpredictable longevity secondary to postinjection resorption (20%–90%) has limited its popularity.3,14,21
HA Injection Technique
With respect to HA fillers in the perioral area, numerous approaches have been described.10,22 The techniques in Table 2 provide a foundation for lip rejuvenation.

Several injection techniques exist, including serial puncture, linear threading, cross-hatching, and fanning in a retrograde or anterograde manner.24 A blunt microcannula (27 gauge, 38 mm) may be used in place of sharp needles and offers the benefit of increased patient comfort, reduced edema and ecchymosis, and shortened recovery period.25,26 Gentle massage of the product after injection can assist with an even contour. Lastly, a key determinant of successful outcomes is using an adequate volume of HA filler (1–2 mL for shaping the vermilion border and volumizing the lips).27 Figure 2 highlights a clinical example of HA filler for lip augmentation.

Fortunately, most complications encountered with HA lip augmentation are mild and transient. The most commonly observed side effects include injection-site reactions such as pain, erythema, and edema. Similarly, most adverse effects are related to injection technique. All HA fillers are prone to the Tyndall effect, a consequence of too superficial an injection plane. Patients with history of recurrent herpes simplex virus infections should receive prophylactic antiviral therapy.12
Muscle Control
An emerging concept in rejuvenation of the lower face recognizes not only restoration of volume but also control of muscle movement. Local injection of botulinum toxin type A induces relaxation of hyperfunctional facial muscles through temporary inhibition of neurotransmitter release.6 The potential for paralysis of the oral cavity may limit the application of botulinum toxin type A in that region.7 Nonetheless, the off-label potential of botulinum toxin type A has expanded to include several targets in the lower face. The orbicularis oris muscle is targeted to soften perioral rhytides. Conservative dosing (1–2 U per lip quadrant or approximately 5 U total) and superficial injection is emphasized in this area.27 Similarly, the depressor anguli oris muscle is targeted by injection of 4 U bilaterally to soften the marionette lines. In the chin area, the mentalis muscle can be targeted by injection of 2 U deep into each belly of the muscle to reduce the mental crease and dimpling.28 Combination treatment with dermal filler and neurotoxin demonstrates effects that last longer than either modality alone without additional adverse events.29 With combination therapy, guidelines suggest treating with filler first.27
Conclusion
A greater understanding of the extrinsic and intrinsic factors that contribute to the structural and surface changes of the aging face coupled with a preference for minimally invasive procedures has revolutionized the dermatologist’s approach to perioral rejuvenation. Serving as a focal point of the face, the lips and perioral skin are well poised to benefit from this paradigm shift. A multifaceted approach utilizing dermal fillers and neurotoxins may be most appropriate and has demonstrated optimal outcomes in facial aesthetics.
- Buck DW, Alam M, Kim JYS. Injectable fillers for facial rejuvenation: a review. J Plast Reconstr Aesthet Surg. 2009;62:11-18.
- Guareschi M, Stella E. Lips. In: Goisis M, ed. Injections in Aesthetic Medicine. Milan, Italy: Springer; 2014:125-136.
- Byrne PJ, Hilger PA. Lip augmentation. Facial Plast Surg. 2004;20:31-38.
- Niamtu J. Rejuvenation of the lip and perioral areas. In: Bell WH, Guerroro CA, eds. Distraction Osteogenesis of the Facial Skeleton. Ontario, Canada: BC Decker Inc; 2007:38-48.
- Tansatit T, Apinuntrum P, Phetudom T. A typical pattern of the labial arteries with implication for lip augmentation with injectable fillers. Aesthet Plast Surg. 2014;38:1083-1089.
- Sadick NS, Karcher C, Palmisano L. Cosmetic dermatology of the aging face. Clin Dermatol. 2009;27(suppl):S3-S12.
- Ali MJ, Ende K, Mass CS. Perioral rejuvenation and lip augmentation. Facial Plast Surg Clin N Am. 2007;15:491-500.
- Chien AL, Qi J, Cheng N, et al. Perioral wrinkles are associated with female gender, aging, and smoking: development of a gender-specific photonumeric scale. J Am Acad Dermatol. 2016;74:924-930.
- Iblher N, Stark GB, Penna V. The aging perioral region—do we really know what is happening? J Nutr Health Aging. 2012;16:581-585.
- Sarnoff DS, Gotkin RH. Six steps to the “perfect” lip. J Drugs Dermatol. 2012;11:1081-1088.
- American Society of Plastic Surgeons. 2015 Cosmetic plastic surgery statistics. https://d2wirczt3b6wjm.cloudfront.net/News/Statistics/2015/cosmetic-procedure-trends-2015.pdf. Published February 26, 2015. Accessed October 5, 2016.
- Abduljabbar MH, Basendwh MA. Complications of hyaluronic acid fillers and their managements. J Dermatol Surg. 2016;20:1-7.
- Luebberding S, Alexiades-Armenakas M. Facial volume augmentation in 2014: overview of different filler options. J Drugs Dermatol. 2013;12:1339-1344.
- Huang Attenello N, Mass CS. Injectable fillers: review of material and properties. Facial Plast Surg. 2015;31:29-34.
- Eccleston D, Murphy DK. Juvéderm Volbella in the perioral area: a 12-month perspective, multicenter, open-label study. Clin Cosmet Investig Dermatol. 2012;5:167-172.
- Raspaldo H, Chantrey J, Belhaouari L, et al. Lip and perioral enhancement: a 12-month prospective, randomized, controlled study. J Drugs Dermatol. 2015;14:1444-1452.
- Soft tissue fillers approved by the center for devices and radiological health. US Food and Drug Administration website. http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/CosmeticDevices/WrinkleFillers/ucm227749.htm. Updated July 27, 2015. Accessed October 5, 2016.
- Butterwick K, Marmur E, Narurkar V, et al. HYC-24L demonstrates greater effectiveness with less pain than CPM-22.5 for treatment of perioral lines in a randomized controlled trial. Dermatol Surg. 2015;41:1351-1360.
- San Miguel Moragas J, Reddy RR, Hernández Alfaro F, et al. Systematic review of “filling” procedures for lip augmentation regarding types of material, outcomes and complications. J Craniomaxillofac Surg. 2015;43:883-906.
- Cohen JL, Thomas J, Paradkar D, et al. An interrater and intrarater reliability study of 3 photographic scales for the classification of perioral aesthetic features. Dermatol Surg. 2014;40:663-670.
- Broder KW, Cohen SR. An overview of permanent and semipermanent fillers. Plast Reconstr Surg. 2006;118(3 suppl):7S-14S.
- Sarnoff DS, Saini R, Gotkin RH. Comparison of filling agents for lip augmentation. Aesthet Surg J. 2008;28:556-563.
- Moscona RA, Fodor L. A retrospective study on liquid injectable silicone for lip augmentation: long-term results and patient satisfaction. J Plast Reconstr Aesthet Surg. 2010;63:1694-1698.
- Bertucci V, Lynde CB. Current concepts in the use of small-particle hyaluronic acid. Plast Reconstr Surg. 2015;136(5 suppl):132S-138S.
- Wilson AJ, Taglienti AJ, Chang CS, et al. Current applications of facial volumization with fillers. Plast Reconstr Surg. 2016;137:E872-E889.
- Dewandre L, Caperton C, Fulton J. Filler injections with the blunt-tip microcannula compared to the sharp hypodermic needle. J Drugs Dermatol. 2012;11:1098-1103.
- Carruthers JD, Glogau RG, Blitzer A; Facial Aesthetics Consensus Group Faculty. Advances in facial rejuvenation: botulinum toxin type A, hyaluronic acid dermal fillers, and combination therapies-consensus recommendations. Plast Reconstr Surg. 2008;121(5 suppl):5S-30S.
- Wu DC, Fabi SG, Goldman MP. Neurotoxins: current concepts in cosmetic use on the face and neck-lower face. Plast Reconstr Surg. 2015;136(5 suppl):76S-79S.
- Carruthers A, Carruthers J, Monheit GD, et al. Multicenter, randomized, parallel-group study of the safety and effectiveness of onabotulinumtoxin A and hyaluronic acid dermal fillers (24-mg/mL smooth, cohesive gel) alone and in combination for lower facial rejuvenation. Dermatol Surg. 2010;36:2121-2134.
- Buck DW, Alam M, Kim JYS. Injectable fillers for facial rejuvenation: a review. J Plast Reconstr Aesthet Surg. 2009;62:11-18.
- Guareschi M, Stella E. Lips. In: Goisis M, ed. Injections in Aesthetic Medicine. Milan, Italy: Springer; 2014:125-136.
- Byrne PJ, Hilger PA. Lip augmentation. Facial Plast Surg. 2004;20:31-38.
- Niamtu J. Rejuvenation of the lip and perioral areas. In: Bell WH, Guerroro CA, eds. Distraction Osteogenesis of the Facial Skeleton. Ontario, Canada: BC Decker Inc; 2007:38-48.
- Tansatit T, Apinuntrum P, Phetudom T. A typical pattern of the labial arteries with implication for lip augmentation with injectable fillers. Aesthet Plast Surg. 2014;38:1083-1089.
- Sadick NS, Karcher C, Palmisano L. Cosmetic dermatology of the aging face. Clin Dermatol. 2009;27(suppl):S3-S12.
- Ali MJ, Ende K, Mass CS. Perioral rejuvenation and lip augmentation. Facial Plast Surg Clin N Am. 2007;15:491-500.
- Chien AL, Qi J, Cheng N, et al. Perioral wrinkles are associated with female gender, aging, and smoking: development of a gender-specific photonumeric scale. J Am Acad Dermatol. 2016;74:924-930.
- Iblher N, Stark GB, Penna V. The aging perioral region—do we really know what is happening? J Nutr Health Aging. 2012;16:581-585.
- Sarnoff DS, Gotkin RH. Six steps to the “perfect” lip. J Drugs Dermatol. 2012;11:1081-1088.
- American Society of Plastic Surgeons. 2015 Cosmetic plastic surgery statistics. https://d2wirczt3b6wjm.cloudfront.net/News/Statistics/2015/cosmetic-procedure-trends-2015.pdf. Published February 26, 2015. Accessed October 5, 2016.
- Abduljabbar MH, Basendwh MA. Complications of hyaluronic acid fillers and their managements. J Dermatol Surg. 2016;20:1-7.
- Luebberding S, Alexiades-Armenakas M. Facial volume augmentation in 2014: overview of different filler options. J Drugs Dermatol. 2013;12:1339-1344.
- Huang Attenello N, Mass CS. Injectable fillers: review of material and properties. Facial Plast Surg. 2015;31:29-34.
- Eccleston D, Murphy DK. Juvéderm Volbella in the perioral area: a 12-month perspective, multicenter, open-label study. Clin Cosmet Investig Dermatol. 2012;5:167-172.
- Raspaldo H, Chantrey J, Belhaouari L, et al. Lip and perioral enhancement: a 12-month prospective, randomized, controlled study. J Drugs Dermatol. 2015;14:1444-1452.
- Soft tissue fillers approved by the center for devices and radiological health. US Food and Drug Administration website. http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/CosmeticDevices/WrinkleFillers/ucm227749.htm. Updated July 27, 2015. Accessed October 5, 2016.
- Butterwick K, Marmur E, Narurkar V, et al. HYC-24L demonstrates greater effectiveness with less pain than CPM-22.5 for treatment of perioral lines in a randomized controlled trial. Dermatol Surg. 2015;41:1351-1360.
- San Miguel Moragas J, Reddy RR, Hernández Alfaro F, et al. Systematic review of “filling” procedures for lip augmentation regarding types of material, outcomes and complications. J Craniomaxillofac Surg. 2015;43:883-906.
- Cohen JL, Thomas J, Paradkar D, et al. An interrater and intrarater reliability study of 3 photographic scales for the classification of perioral aesthetic features. Dermatol Surg. 2014;40:663-670.
- Broder KW, Cohen SR. An overview of permanent and semipermanent fillers. Plast Reconstr Surg. 2006;118(3 suppl):7S-14S.
- Sarnoff DS, Saini R, Gotkin RH. Comparison of filling agents for lip augmentation. Aesthet Surg J. 2008;28:556-563.
- Moscona RA, Fodor L. A retrospective study on liquid injectable silicone for lip augmentation: long-term results and patient satisfaction. J Plast Reconstr Aesthet Surg. 2010;63:1694-1698.
- Bertucci V, Lynde CB. Current concepts in the use of small-particle hyaluronic acid. Plast Reconstr Surg. 2015;136(5 suppl):132S-138S.
- Wilson AJ, Taglienti AJ, Chang CS, et al. Current applications of facial volumization with fillers. Plast Reconstr Surg. 2016;137:E872-E889.
- Dewandre L, Caperton C, Fulton J. Filler injections with the blunt-tip microcannula compared to the sharp hypodermic needle. J Drugs Dermatol. 2012;11:1098-1103.
- Carruthers JD, Glogau RG, Blitzer A; Facial Aesthetics Consensus Group Faculty. Advances in facial rejuvenation: botulinum toxin type A, hyaluronic acid dermal fillers, and combination therapies-consensus recommendations. Plast Reconstr Surg. 2008;121(5 suppl):5S-30S.
- Wu DC, Fabi SG, Goldman MP. Neurotoxins: current concepts in cosmetic use on the face and neck-lower face. Plast Reconstr Surg. 2015;136(5 suppl):76S-79S.
- Carruthers A, Carruthers J, Monheit GD, et al. Multicenter, randomized, parallel-group study of the safety and effectiveness of onabotulinumtoxin A and hyaluronic acid dermal fillers (24-mg/mL smooth, cohesive gel) alone and in combination for lower facial rejuvenation. Dermatol Surg. 2010;36:2121-2134.
Practice Points
- Hyaluronic acid (HA) fillers are approved by the US Food and Drug Administration for lip augmentation and/or treatment of perioral rhytides in adults 21 years and older.
- Most complications encountered with HA lip augmentation are mild and transient and can include injection-site reactions such as pain, erythema, and edema.
- Combination treatment with dermal fillers and neurotoxins (off label) may demonstrate effects that last longer than either modality alone without additional adverse events.
Evaluation of nail lines: Color and shape hold clues
Inspection of the fingernails and toenails should be part of a complete physical examination. A basic understanding of nail anatomy and recognition of several basic types of nail lines and bands allow the clinician to properly diagnose and treat the nail disease, to recognize possible underlying systemic diseases, and to know when to refer the patient to a dermatologist for specialized evaluation and biopsy.
In this review, we delineate the three basic types of nail lines—white lines (leukonychia striata), brown-black lines (longitudinal melanonychia), and red lines (longitudinal erythronychia)—and the differential diagnosis for each type. We also discuss grooves in the nail plate, or Beau lines.
BASIC NAIL ANATOMY
A fundamental understanding of the anatomy of the nail unit is necessary to understand the origin of nail diseases and underlying pathologic conditions.
The nail unit includes the nail matrix, the lunula, the nail fold, the nail plate, and the nail bed. The nail matrix extends from under the proximal nail fold to the half-moon-shaped area (ie, the lunula) and is responsible for nail plate production. The nail bed lies under the nail plate and on top of the distal phalanx and extends from the lunula to just proximal to the free edge of the nail; its rich blood supply gives it its reddish color.
Nails grow slowly, and this should be kept in mind during the examination. Regrowth of a fingernail takes at least 6 months, and regrowth of a toenail may take 12 to 18 months. Therefore, a defect in the nail plate may reveal an injury that occurred—or a condition that began—several months before.1
NAIL EXAMINATION ESSENTIALS
A complete examination includes all 20 nail units and the periungual skin. Patients should be instructed to remove nail polish from all nails, as it may camouflage dystrophy or disease of the nail. Photography and careful measurement help document changes over time.
LEUKONYCHIA STRIATA: WHITE NAIL LINES
White nail lines or leukonychia is classified as true or apparent, depending on whether the origin is in the nail matrix or the nail bed.
In true leukonychia, there is abnormal keratinization of the underlying nail matrix, resulting in parakeratosis within the nail plate and an opaque appearance on examination.2 The white discoloration is unaffected by pressure, and the opacity moves distally as the nail grows out, which can be documented by serial photography on subsequent visits.
Apparent leukonychia involves abnormal nail bed vasculature, which changes the translucency of the nail plate. The whiteness disappears with pressure, is unaffected by nail growth, and will likely show no change on later visits with serial photography.3
True leukonychia
Leukonychia striata, a subtype of true leukonychia, is characterized by transverse or longitudinal bands. It is most often associated with microtrauma, such as from a manicure.4 Lines due to trauma are typically more apparent in the central part of the nail plate; they spare the lateral portion and lie parallel to the edge of the proximal nail fold.5
Onychomycosis. White longitudinal bands may also be seen in onychomycosis, a fungal infection of the nail accounting for up to 50% of all cases of nail disease. The infection may present as irregular dense longitudinal white or yellowish bands or “spikes” on the nail plate with associated hyperkeratosis, known as a dermatophytoma (Figure 1).
If a fungal infection is suspected, a potassium hydroxide stain can be performed on the subungual debris, which is then examined with direct microscopy.6 Alternatively, the physician can send a nail plate clipping in a 10% buffered formalin container with a request for a fungal stain such as periodic acid-Schiff.7 Microscopic examination of a dermatophytoma shows a dense mass of dermatophyte hyphae, otherwise known as a fungal abscess.8
The physician can play an important role in diagnosis because clinical findings suggestive of a dermatophytoma are associated with a poor response to antifungal therapy.9
Inherited diseases. White longitudinal bands are also an important clue to the rare autosomal dominant genodermatoses Hailey-Hailey disease (from mutations of the ATP2A2 gene) and Darier disease (from mutations of the ATP2C1 gene). Patients with Hailey-Hailey disease may have nails with multiple parallel longitudinal white stripes of variable width originating in the lunula and most prominent on the thumbs.10–12 These patients also have recurrent vesicular eruptions in flexural skin areas, such as the groin, axilla, neck, and periumbilical area causing significant morbidity.
Patients with Darier disease may have nails with alternating red and white longitudinal streaks, described as “candy-cane,”13 as well as wedge-shaped distal subungual keratosis accompanied by flat keratotic papules on the proximal nail fold.14 These nail changes are reported in 92% to 95% of patients with Darier disease.15,16 Patients typically have skin findings characterized by keratotic papules and plaques predominantly in seborrheic areas and palmoplantar pits, as well as secondary infections and malodor causing significant morbidity.15 Therefore, knowing the characteristic nail findings in these diseases may lead to more rapid diagnosis and treatment.
Mees lines. Leukonychia striata can present as transverse white lines, commonly known as Mees lines. They are 1- to 2-mm wide horizontal parallel white bands that span the width of the nail plate, usually affecting all fingernails.17 They are not a common finding and are most often associated with arsenic poisoning. They can also be used to identify the time of poisoning, since they tend to appear 2 months after the initial insult.
Mees lines are also associated with acute systemic stresses, such as acute renal failure, heart failure, ulcerative colitis, breast cancer, infections such as measles and tuberculosis, and systemic lupus erythematosus, and with exposure to toxic metals such as thallium.3
Apparent leukonychia
Apparent leukonychia can alert the physician to systemic diseases, infections, drug side effects, and nutrient deficiencies. Specific nail findings include Muehrcke lines, “half-and-half” nails, and Terry nails.
Muehrcke lines are paired white transverse bands that span the width of the nail bed and run parallel to the distal lunula. They were first described in the fingernails of patients with severe hypoalbuminemia, some of whom also had nephrotic syndrome, which resolved with normalization of the serum albumin level. Muehrcke lines have since been reported in patients with liver disease, malnutrition, chemotherapy, organ transplant, human immunodeficiency virus (HIV) infection, and acquired immunodeficiency syndrome.3,18 They are associated with periods of metabolic stress, ie, when the body’s capacity to synthesize proteins is diminished.19
Half-and-half nails, or Lindsay nails, are characterized by a white band proximally, a pink or red-brown band distally, and a sharp demarcation between the two (Figure 2). They were originally described in association with chronic renal disease,20 and surprisingly, they resolve with kidney transplant but not with hemodialysis treatment or improvement in hemoglobin or albumin levels.21–23 Half-and-half nails have been reported with Kawasaki disease, hepatic cirrhosis, Crohn disease, zinc deficiency, chemotherapy, Behçet disease, and pellagra.3,24,25 They should be distinguished from Terry nails, which are characterized by leukonychia involving more than 80% of the total nail length.26
Terry nails were originally reported in association with hepatic cirrhosis, usually secondary to alcoholism27 but have since been found with heart failure, type 2 diabetes mellitus, pulmonary tuberculosis, reactive arthritis, older age, Hansen disease, and peripheral vascular disease.3,26,28,29
LONGITUDINAL MELANONYCHIA: VERTICAL BROWN-BLACK NAIL LINES
Longitudinal melanonychia is the presence of black-brown vertical lines in the nail plate. They have a variety of causes, including blood from trauma; bacterial, fungal, or HIV infection; drug therapy (eg, from minocycline); endocrine disorders (Addison disease); exogenous pigmentation; or excess melanin production within the nail matrix.30–32 They may also be a sign of a benign condition such as benign melanocytic activation, lentigines, or nevi, or a malignant condition such as melanoma (Figure 3).33,34
When to suspect melanoma and refer
Although melanoma is less commonly associated with brown-black vertical nail lines, awareness of melanoma-associated longitudinal melanonychia reduces the likelihood of delayed diagnosis and improves patient outcomes.35 Also, it is important to remember that although nail melanoma is more common in the 5th and 6th decades of life, it can occur at any age, even in children.36
Findings that raise suspicion of nail melanoma (Table 1)33,37 and that should prompt referral to a dermatologist who specializes in nails include the following:
- A personal or family history of melanoma
- Involvement of a “high-risk” digit (thumb, index finger, great toe),30,31,38 although nail melanoma can occur in any digit
- Any new vertical brown-black nail pigmentation in a fair-skinned patient
- Only one nail affected: involvement of more than one nail is common in people with darker skin, and nearly all patients with darker skin exhibit longitudinal melanonychia by age 5031
- Changes in the band such as darkening, widening, and bleeding
- A bandwidth greater than 6 mm33
- A band that is wider proximally than distally34
- Nonuniform color of the line
- Indistinct lateral borders
- Associated with pigmentation of the nail fold (the Hutchinson sign, representing subungual melanoma),31,39 nail plate dystrophy, bleeding, or ulceration.33
While these features may help distinguish benign from malignant causes of longitudinal melanonychia, the clinical examination alone may not provide a definitive diagnosis. Delayed diagnosis of nail melanoma carries a high mortality rate; the internist can promote early diagnosis by recognizing the risk factors and clinical signs and referring the patient to a dermatologist for further evaluation with nail biopsy.
LONGITUDINAL ERYTHRONYCHIA: VERTICAL RED NAIL LINES
Longitudinal erythronychia—the presence of one or more linear red bands in the nail unit—can be localized (involving only one nail) or polydactylous (involving more than one nail). The localized form is usually due to a neoplastic process, whereas involvement of more than one nail may indicate an underlying regional or systemic disease.13Table 2 lists indications for referral to a nail specialist.
General features on examination
Clinical examination reveals one or more linear, pink-red streaks extending from the proximal nail fold to the distal free edge of the nail plate (Figure 4). The width of the band typically ranges from less than 1 mm to 3 mm.40 Other features may include splinter hemorrhages within a red band, a semitransparent distal matrix, distal V-shaped chipping, splitting, onycholysis of the nail plate, and reactive distal nail bed and hyponychial hyperkeratosis. These features can be visible to the naked eye but may be better viewed with a magnifying glass, a 7× loupe, or a dermatoscope.13
Localized longitudinal erythronychia is usually seen in middle-aged individuals and is most commonly found on the thumbnail, followed by the index finger.41,42 The condition may be asymptomatic, but the patient may present with pain or with concern that the split end of the nail catches on fabrics or small objects.42
Glomus tumor
Intense, pulsatile pain with sensitivity to cold and tenderness to palpation is highly suggestive of glomus tumor,43 a benign neoplasm that originates from a neuromyoarterial glomus body. Glomus bodies are located throughout the body but are more highly concentrated in the fingertips, especially beneath the nails, and they regulate skin circulation. Therefore, the nail unit is the most common site for glomus tumor.44,45 A characteristic feature of subungual glomus tumor is demonstration of tenderness after pin-point palpation of the suspected tumor (positive Love sign).45 While it is typical for glomus tumor to affect only one nail, multiple tumors are associated with neurofibromatosis type 1.46 Confirmation of this diagnosis requires referral to a dermatologist.
Other causes of localized red nail lines
Onychopapilloma, a benign idiopathic tumor, is the most common cause of localized longitudinal erythronychia. Unlike glomus tumor, it is usually asymptomatic.42,47 Less common benign conditions are warts, warty dyskeratoma, benign vascular proliferation, a solitary lesion of lichen planus, hemiplegia, and postsurgical scarring of the nail matrix. In some cases, the lines are idiopathic.42,43
Malignant diseases that can present as localized longitudinal erythronychia include invasive squamous cell carcinoma, squamous cell carcinoma in situ (Bowen disease), and, less frequently, amelanotic melanoma in situ, malignant melanoma, and basal cell carcinoma.42 Squamous cell carcinoma in situ most commonly presents in the 5th decade of life and is the malignancy most commonly associated with localized longitudinal erythronychia. Clinically, there is also often nail dystrophy, such as distal subungual keratosis or onycholysis.43
Patients with asymptomatic, stable localized longitudinal erythronychia may be followed closely with photography and measurements. However, any new lesion or a change in an existing lesion should prompt referral to a dermatologist for biopsy.13
Red streaks on more than one nail
Polydactylous longitudinal erythronychia usually presents in adults as red streaks on multiple nails and, depending on the presence or absence of symptoms (eg, pain, splitting), may be the patient’s chief complaint or an incidental finding noted by the astute clinician. Often, it is associated with systemic disease, most commonly lichen planus or Darier disease.
Lichen planus is a papulosquamous skin disease with nail involvement in 10% of patients and permanent nail dystrophy in 4%. Common nail findings include thinning, longitudinal ridging, and fissuring, as well as scarring of the nail matrix resulting in pterygium. Linear red streaks may accompany these more typical nail findings.13 Patients with Darier disease present with alternating red and white linear bands on multiple nails as in leukonychia striata.
Less frequently, polydactylous longitudinal erythronychia is associated with primary and systemic amyloidosis, hemiplegia, graft-vs-host disease, acantholytic epidermolysis bullosa, acantholytic dyskeratotic epidermal nevus, acrokeratosis verruciformis of Hopf, or pseudobulbar syndrome, or is idiopathic.13,42,48 Therefore, the physician evaluating a patient with these nail findings should focus on a workup for regional or systemic disease or refer the patient to a dermatologist who specializes in nails.
BEAU LINES
Beau lines are a common finding in clinical practice. They are not true lines, but transverse grooves in the nail plate that arise from the temporary suppression of nail growth within the nail matrix that can occur during periods of acute or chronic stress or systemic illness (Figure 5).49
The precipitating event may be local trauma or paronychia, chemotherapeutic agents cytotoxic to the nail matrix, or the abrupt onset of systemic disease.18,50 The grooves have also been associated with rheumatic fever, malaria, pemphigus, Raynaud disease, and myocardial infarction, as well as following deep-sea dives.51–53 The distance of a Beau line from the proximal nail fold can provide an estimate of the time of the acute stress, based on an average growth rate of 3 mm per month for fingernails and 1 mm per month for toenails.49
- Scher RK, Rich P, Pariser D, Elewski B. The epidemiology, etiology, and pathophysiology of onychomycosis. Semin Cutan Med Surg 2013; 32(suppl 1):S2–S4.
- Lawry MA, Haneke E, Strobeck K, Martin S, Zimmer B, Romano PS. Methods for diagnosing onychomycosis: a comparative study and review of the literature. Arch Dermatol 2000; 136:1112–1116.
- Zaiac MN, Walker A. Nail abnormalities associated with systemic pathologies. Clin Dermatol 2013; 31:627–649.
- Zaiac MN, Daniel CR. Nails in systemic disease. Dermatol Ther 2002; 15:99–106.
- Tosti A, Iorizzo M, Piraccini BM, Starace M. The nail in systemic diseases. Dermatol Clin 2006; 24:341–347.
- Scher RK, Daniel CR, eds. Nails Diagnosis, Therapy, Surgery. 3rd ed. Oxford: Elsevier Saunders; 2005.
- Smith MB, McGinnis MR. Diagnostic histopathology. In: Hospenthal DR, Rinaldi MG, eds. Diagnosis and Treatment of Human Mycoses. Totowa, NJ: Humana Press; 2008:37–51.
- Roberts DT, Evans EG. Subungual dermatophytoma complicating dermatophyte onychomycosis. Br J Dermatol 1998; 138:189–190.
- Sigurgeirsson B. Prognostic factors for cure following treatment of onychomycosis. J Eur Acad Dermatol Venereol 2010; 24:679–684.
- Kumar R, Zawar V. Longitudinal leukonychia in Hailey-Hailey disease: a sign not to be missed. Dermatol Online J 2008; 14:17.
- Burge SM. Hailey-Hailey disease: the clinical features, response to treatment and prognosis. Br J Dermatol 1992; 126:275–282.
- Kirtschig G, Effendy I, Happle R. Leukonychia longitudinalis as the primary symptom of Hailey-Hailey disease. Hautarzt 1992; 43:451–452. German.
- Jellinek NJ. Longitudinal erythronychia: suggestions for evaluation and management. J Am Acad Dermatol 2011; 64:167.e1–167.e11
- Zaias N, Ackerman AB. The nail in Darier-White disease. Arch Dermatol 1973; 107:193–199.
- Burge SM, Wilkinson JD. Darier-White disease: a review of the clinical features in 163 patients. J Am Acad Dermatol 1992; 27:40–50.
- Munro CS. The phenotype of Darier's disease: penetrance and expressivity in adults and children. Br J Dermatol 1992; 127:126–130.
- Schwartz RA. Arsenic and the skin. Int J Dermatol 1997; 36:241–250.
- Fawcett RS, Linford S, Stulberg DL. Nail abnormalities: clues to systemic disease. Am Fam Physician 2004; 69:1417–1424.
- Morrison-Bryant M, Gradon JD. Images in clinical medicine. Muehrcke's lines. N Engl J Med 2007; 357:917.
- Daniel CR 3rd, Bower JD, Daniel CR Jr. The “half and half fingernail”: the most significant onychopathological indicator of chronic renal failure. J Miss State Med Assoc 1975; 16:367–370.
- Saray Y, Seckin D, Gulec AT, Akgun S, Haberal M. Nail disorders in hemodialysis patients and renal transplant recipients: a case-control study. J Am Acad Dermatol 2004; 50:197–202.
- Dyachenko P, Monselise A, Shustak A, Ziv M, Rozenman D. Nail disorders in patients with chronic renal failure and undergoing haemodialysis treatment: a case-control study. J Eur Acad Dermatol Venereol 2007; 21:340–344.
- Salem A, Al Mokadem S, Attwa E, Abd El Raoof S, Ebrahim HM, Faheem KT. Nail changes in chronic renal failure patients under haemodialysis. J Eur Acad Dermatol Venereol 2008; 22:1326–1331.
- Zagoni T, Sipos F, Tarjan Z, Peter Z. The half-and-half nail: a new sign of Crohn's disease? Report of four cases. Dis Colon Rectum 2006; 49:1071–1073.
- Nixon DW, Pirozzi D, York RM, Black M, Lawson DH. Dermatologic changes after systemic cancer therapy. Cutis 1981; 27:181–194.
- Holzberg M, Walker HK. Terry's nails: revised definition and new correlations. Lancet 1984; 1:896–899.
- Terry R. White nails in hepatic cirrhosis. Lancet 1954; 266:757–759.
- Coskun BK, Saral Y, Ozturk P, Coskun N. Reiter syndrome accompanied by Terry nail. J Eur Acad Dermatol Venereol 2005; 19:87–89.
- Blyumin M, Khachemoune A, Bourelly P. What is your diagnosis? Terry nails. Cutis 2005; 76:201–202.
- Haneke E, Baran R. Longitudinal melanonychia. Dermatol Surg 2001; 27:580–584.
- Andre J, Lateur N. Pigmented nail disorders. Dermatol Clin 2006; 24:329–339.
- Braun RP, Baran R, Le Gal FA, et al. Diagnosis and management of nail pigmentations. J Am Acad Dermatol 2007; 56:835–847.
- Mannava KA, Mannava S, Koman LA, Robinson-Bostom L, Jellinek N. Longitudinal melanonychia: detection and management of nail melanoma. Hand Surg 2013; 18:133–139.
- Ruben BS. Pigmented lesions of the nail unit: clinical and histopathologic features. Semin Cutan Med Surg 2010; 29:148–158.
- Cohen T, Busam KJ, Patel A, Brady MS. Subungual melanoma: management considerations. Am J Surg 2008; 195:244–248.
- Iorizzo M, Tosti A, Di Chiacchio N, et al. Nail melanoma in children: differential diagnosis and management. Dermatol Surg 2008; 34:974–978.
- Jellinek N. Nail matrix biopsy of longitudinal melanonychia: diagnostic algorithm including the matrix shave biopsy. J Am Acad Dermatol 2007; 56:803–810.
- Husain S, Scher RK, Silvers DN, Ackerman AB. Melanotic macule of nail unit and its clinicopathologic spectrum. J Am Acad Dermatol 2006; 54:664–667.
- Baran R, Kechijian P. Hutchinson's sign: a reappraisal. J Am Acad Dermatol 1996; 34:87–90.
- Baran R. Red nails. Dermatol Online 2005; 11:29.
- Baran R, Perrin C. Longitudinal erythronychia with distal subungual keratosis: onychopapilloma of the nail bed and Bowen’s disease. Br J Dermatol 2000; 143:132–135.
- de Berker DA, Perrin C, Baran R. Localized longitudinal erythronychia: diagnostic significance and physical explanation. Arch Dermatol 2004; 140:1253–1257.
- Cohen PR. Longitudinal erythronychia: individual or multiple linear red bands of the nail plate: a review of clinical features and associated conditions. Am J Clin Dermatol 2011; 12:217–231.
- Van Geertruyden J, Lorea P, Goldschmidt D, et al. Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br 1996; 21:257–260.
- Moon SE, Won JH, Kwon OS, Kim JA. Subungual glomus tumor: clinical manifestations and outcome of surgical treatment. J Dermatol 2004; 31:993–997.
- Okada O, Demitsu T, Manabe M, Yoneda K. A case of multiple subungual glomus tumors associated with neurofibromatosis type 1. J Dermatol 1999; 26:535–537.
- Gee BC, Millard PR, Dawber RP. Onychopapilloma is not a distinct clinicopathological entity. Br J Dermatol 2002; 146:156–157.
- Siragusa M, Del Gracco S, Ferri R, Schepis C. Longitudinal red streaks on the big toenails in a patient with pseudobulbar syndrome. J Eur Acad Dermatol Venereol 2001; 15:85–86.
- Lipner S, Scher RK. Nails. In: Callen J, Jorizzo JL, eds. Dermatological Signs of Systemic Disease. 5th ed: Elsevier; in press.
- Mortimer NJ, Mills J. Images in clinical medicine. Beau’s lines. N Engl J Med 2004; 351:1778.
- Schwartz H. Clinical observation: Beau’s lines on fingernails after deep saturation dives. Undersea Hyperb Med 2006; 33:5–10.
- Gugelmann HM, Gaieski DF. Beau’s lines after cardiac arrest. Ther Hypothermia Temp Manag 2013; 3:199–202.
- Lauber J, Turk K. Beau’s lines and pemphigus vulgaris. Int J Dermatol 1990; 29:309.
Inspection of the fingernails and toenails should be part of a complete physical examination. A basic understanding of nail anatomy and recognition of several basic types of nail lines and bands allow the clinician to properly diagnose and treat the nail disease, to recognize possible underlying systemic diseases, and to know when to refer the patient to a dermatologist for specialized evaluation and biopsy.
In this review, we delineate the three basic types of nail lines—white lines (leukonychia striata), brown-black lines (longitudinal melanonychia), and red lines (longitudinal erythronychia)—and the differential diagnosis for each type. We also discuss grooves in the nail plate, or Beau lines.
BASIC NAIL ANATOMY
A fundamental understanding of the anatomy of the nail unit is necessary to understand the origin of nail diseases and underlying pathologic conditions.
The nail unit includes the nail matrix, the lunula, the nail fold, the nail plate, and the nail bed. The nail matrix extends from under the proximal nail fold to the half-moon-shaped area (ie, the lunula) and is responsible for nail plate production. The nail bed lies under the nail plate and on top of the distal phalanx and extends from the lunula to just proximal to the free edge of the nail; its rich blood supply gives it its reddish color.
Nails grow slowly, and this should be kept in mind during the examination. Regrowth of a fingernail takes at least 6 months, and regrowth of a toenail may take 12 to 18 months. Therefore, a defect in the nail plate may reveal an injury that occurred—or a condition that began—several months before.1
NAIL EXAMINATION ESSENTIALS
A complete examination includes all 20 nail units and the periungual skin. Patients should be instructed to remove nail polish from all nails, as it may camouflage dystrophy or disease of the nail. Photography and careful measurement help document changes over time.
LEUKONYCHIA STRIATA: WHITE NAIL LINES
White nail lines or leukonychia is classified as true or apparent, depending on whether the origin is in the nail matrix or the nail bed.
In true leukonychia, there is abnormal keratinization of the underlying nail matrix, resulting in parakeratosis within the nail plate and an opaque appearance on examination.2 The white discoloration is unaffected by pressure, and the opacity moves distally as the nail grows out, which can be documented by serial photography on subsequent visits.
Apparent leukonychia involves abnormal nail bed vasculature, which changes the translucency of the nail plate. The whiteness disappears with pressure, is unaffected by nail growth, and will likely show no change on later visits with serial photography.3
True leukonychia
Leukonychia striata, a subtype of true leukonychia, is characterized by transverse or longitudinal bands. It is most often associated with microtrauma, such as from a manicure.4 Lines due to trauma are typically more apparent in the central part of the nail plate; they spare the lateral portion and lie parallel to the edge of the proximal nail fold.5
Onychomycosis. White longitudinal bands may also be seen in onychomycosis, a fungal infection of the nail accounting for up to 50% of all cases of nail disease. The infection may present as irregular dense longitudinal white or yellowish bands or “spikes” on the nail plate with associated hyperkeratosis, known as a dermatophytoma (Figure 1).
If a fungal infection is suspected, a potassium hydroxide stain can be performed on the subungual debris, which is then examined with direct microscopy.6 Alternatively, the physician can send a nail plate clipping in a 10% buffered formalin container with a request for a fungal stain such as periodic acid-Schiff.7 Microscopic examination of a dermatophytoma shows a dense mass of dermatophyte hyphae, otherwise known as a fungal abscess.8
The physician can play an important role in diagnosis because clinical findings suggestive of a dermatophytoma are associated with a poor response to antifungal therapy.9
Inherited diseases. White longitudinal bands are also an important clue to the rare autosomal dominant genodermatoses Hailey-Hailey disease (from mutations of the ATP2A2 gene) and Darier disease (from mutations of the ATP2C1 gene). Patients with Hailey-Hailey disease may have nails with multiple parallel longitudinal white stripes of variable width originating in the lunula and most prominent on the thumbs.10–12 These patients also have recurrent vesicular eruptions in flexural skin areas, such as the groin, axilla, neck, and periumbilical area causing significant morbidity.
Patients with Darier disease may have nails with alternating red and white longitudinal streaks, described as “candy-cane,”13 as well as wedge-shaped distal subungual keratosis accompanied by flat keratotic papules on the proximal nail fold.14 These nail changes are reported in 92% to 95% of patients with Darier disease.15,16 Patients typically have skin findings characterized by keratotic papules and plaques predominantly in seborrheic areas and palmoplantar pits, as well as secondary infections and malodor causing significant morbidity.15 Therefore, knowing the characteristic nail findings in these diseases may lead to more rapid diagnosis and treatment.
Mees lines. Leukonychia striata can present as transverse white lines, commonly known as Mees lines. They are 1- to 2-mm wide horizontal parallel white bands that span the width of the nail plate, usually affecting all fingernails.17 They are not a common finding and are most often associated with arsenic poisoning. They can also be used to identify the time of poisoning, since they tend to appear 2 months after the initial insult.
Mees lines are also associated with acute systemic stresses, such as acute renal failure, heart failure, ulcerative colitis, breast cancer, infections such as measles and tuberculosis, and systemic lupus erythematosus, and with exposure to toxic metals such as thallium.3
Apparent leukonychia
Apparent leukonychia can alert the physician to systemic diseases, infections, drug side effects, and nutrient deficiencies. Specific nail findings include Muehrcke lines, “half-and-half” nails, and Terry nails.
Muehrcke lines are paired white transverse bands that span the width of the nail bed and run parallel to the distal lunula. They were first described in the fingernails of patients with severe hypoalbuminemia, some of whom also had nephrotic syndrome, which resolved with normalization of the serum albumin level. Muehrcke lines have since been reported in patients with liver disease, malnutrition, chemotherapy, organ transplant, human immunodeficiency virus (HIV) infection, and acquired immunodeficiency syndrome.3,18 They are associated with periods of metabolic stress, ie, when the body’s capacity to synthesize proteins is diminished.19
Half-and-half nails, or Lindsay nails, are characterized by a white band proximally, a pink or red-brown band distally, and a sharp demarcation between the two (Figure 2). They were originally described in association with chronic renal disease,20 and surprisingly, they resolve with kidney transplant but not with hemodialysis treatment or improvement in hemoglobin or albumin levels.21–23 Half-and-half nails have been reported with Kawasaki disease, hepatic cirrhosis, Crohn disease, zinc deficiency, chemotherapy, Behçet disease, and pellagra.3,24,25 They should be distinguished from Terry nails, which are characterized by leukonychia involving more than 80% of the total nail length.26
Terry nails were originally reported in association with hepatic cirrhosis, usually secondary to alcoholism27 but have since been found with heart failure, type 2 diabetes mellitus, pulmonary tuberculosis, reactive arthritis, older age, Hansen disease, and peripheral vascular disease.3,26,28,29
LONGITUDINAL MELANONYCHIA: VERTICAL BROWN-BLACK NAIL LINES
Longitudinal melanonychia is the presence of black-brown vertical lines in the nail plate. They have a variety of causes, including blood from trauma; bacterial, fungal, or HIV infection; drug therapy (eg, from minocycline); endocrine disorders (Addison disease); exogenous pigmentation; or excess melanin production within the nail matrix.30–32 They may also be a sign of a benign condition such as benign melanocytic activation, lentigines, or nevi, or a malignant condition such as melanoma (Figure 3).33,34
When to suspect melanoma and refer
Although melanoma is less commonly associated with brown-black vertical nail lines, awareness of melanoma-associated longitudinal melanonychia reduces the likelihood of delayed diagnosis and improves patient outcomes.35 Also, it is important to remember that although nail melanoma is more common in the 5th and 6th decades of life, it can occur at any age, even in children.36
Findings that raise suspicion of nail melanoma (Table 1)33,37 and that should prompt referral to a dermatologist who specializes in nails include the following:
- A personal or family history of melanoma
- Involvement of a “high-risk” digit (thumb, index finger, great toe),30,31,38 although nail melanoma can occur in any digit
- Any new vertical brown-black nail pigmentation in a fair-skinned patient
- Only one nail affected: involvement of more than one nail is common in people with darker skin, and nearly all patients with darker skin exhibit longitudinal melanonychia by age 5031
- Changes in the band such as darkening, widening, and bleeding
- A bandwidth greater than 6 mm33
- A band that is wider proximally than distally34
- Nonuniform color of the line
- Indistinct lateral borders
- Associated with pigmentation of the nail fold (the Hutchinson sign, representing subungual melanoma),31,39 nail plate dystrophy, bleeding, or ulceration.33
While these features may help distinguish benign from malignant causes of longitudinal melanonychia, the clinical examination alone may not provide a definitive diagnosis. Delayed diagnosis of nail melanoma carries a high mortality rate; the internist can promote early diagnosis by recognizing the risk factors and clinical signs and referring the patient to a dermatologist for further evaluation with nail biopsy.
LONGITUDINAL ERYTHRONYCHIA: VERTICAL RED NAIL LINES
Longitudinal erythronychia—the presence of one or more linear red bands in the nail unit—can be localized (involving only one nail) or polydactylous (involving more than one nail). The localized form is usually due to a neoplastic process, whereas involvement of more than one nail may indicate an underlying regional or systemic disease.13Table 2 lists indications for referral to a nail specialist.
General features on examination
Clinical examination reveals one or more linear, pink-red streaks extending from the proximal nail fold to the distal free edge of the nail plate (Figure 4). The width of the band typically ranges from less than 1 mm to 3 mm.40 Other features may include splinter hemorrhages within a red band, a semitransparent distal matrix, distal V-shaped chipping, splitting, onycholysis of the nail plate, and reactive distal nail bed and hyponychial hyperkeratosis. These features can be visible to the naked eye but may be better viewed with a magnifying glass, a 7× loupe, or a dermatoscope.13
Localized longitudinal erythronychia is usually seen in middle-aged individuals and is most commonly found on the thumbnail, followed by the index finger.41,42 The condition may be asymptomatic, but the patient may present with pain or with concern that the split end of the nail catches on fabrics or small objects.42
Glomus tumor
Intense, pulsatile pain with sensitivity to cold and tenderness to palpation is highly suggestive of glomus tumor,43 a benign neoplasm that originates from a neuromyoarterial glomus body. Glomus bodies are located throughout the body but are more highly concentrated in the fingertips, especially beneath the nails, and they regulate skin circulation. Therefore, the nail unit is the most common site for glomus tumor.44,45 A characteristic feature of subungual glomus tumor is demonstration of tenderness after pin-point palpation of the suspected tumor (positive Love sign).45 While it is typical for glomus tumor to affect only one nail, multiple tumors are associated with neurofibromatosis type 1.46 Confirmation of this diagnosis requires referral to a dermatologist.
Other causes of localized red nail lines
Onychopapilloma, a benign idiopathic tumor, is the most common cause of localized longitudinal erythronychia. Unlike glomus tumor, it is usually asymptomatic.42,47 Less common benign conditions are warts, warty dyskeratoma, benign vascular proliferation, a solitary lesion of lichen planus, hemiplegia, and postsurgical scarring of the nail matrix. In some cases, the lines are idiopathic.42,43
Malignant diseases that can present as localized longitudinal erythronychia include invasive squamous cell carcinoma, squamous cell carcinoma in situ (Bowen disease), and, less frequently, amelanotic melanoma in situ, malignant melanoma, and basal cell carcinoma.42 Squamous cell carcinoma in situ most commonly presents in the 5th decade of life and is the malignancy most commonly associated with localized longitudinal erythronychia. Clinically, there is also often nail dystrophy, such as distal subungual keratosis or onycholysis.43
Patients with asymptomatic, stable localized longitudinal erythronychia may be followed closely with photography and measurements. However, any new lesion or a change in an existing lesion should prompt referral to a dermatologist for biopsy.13
Red streaks on more than one nail
Polydactylous longitudinal erythronychia usually presents in adults as red streaks on multiple nails and, depending on the presence or absence of symptoms (eg, pain, splitting), may be the patient’s chief complaint or an incidental finding noted by the astute clinician. Often, it is associated with systemic disease, most commonly lichen planus or Darier disease.
Lichen planus is a papulosquamous skin disease with nail involvement in 10% of patients and permanent nail dystrophy in 4%. Common nail findings include thinning, longitudinal ridging, and fissuring, as well as scarring of the nail matrix resulting in pterygium. Linear red streaks may accompany these more typical nail findings.13 Patients with Darier disease present with alternating red and white linear bands on multiple nails as in leukonychia striata.
Less frequently, polydactylous longitudinal erythronychia is associated with primary and systemic amyloidosis, hemiplegia, graft-vs-host disease, acantholytic epidermolysis bullosa, acantholytic dyskeratotic epidermal nevus, acrokeratosis verruciformis of Hopf, or pseudobulbar syndrome, or is idiopathic.13,42,48 Therefore, the physician evaluating a patient with these nail findings should focus on a workup for regional or systemic disease or refer the patient to a dermatologist who specializes in nails.
BEAU LINES
Beau lines are a common finding in clinical practice. They are not true lines, but transverse grooves in the nail plate that arise from the temporary suppression of nail growth within the nail matrix that can occur during periods of acute or chronic stress or systemic illness (Figure 5).49
The precipitating event may be local trauma or paronychia, chemotherapeutic agents cytotoxic to the nail matrix, or the abrupt onset of systemic disease.18,50 The grooves have also been associated with rheumatic fever, malaria, pemphigus, Raynaud disease, and myocardial infarction, as well as following deep-sea dives.51–53 The distance of a Beau line from the proximal nail fold can provide an estimate of the time of the acute stress, based on an average growth rate of 3 mm per month for fingernails and 1 mm per month for toenails.49
Inspection of the fingernails and toenails should be part of a complete physical examination. A basic understanding of nail anatomy and recognition of several basic types of nail lines and bands allow the clinician to properly diagnose and treat the nail disease, to recognize possible underlying systemic diseases, and to know when to refer the patient to a dermatologist for specialized evaluation and biopsy.
In this review, we delineate the three basic types of nail lines—white lines (leukonychia striata), brown-black lines (longitudinal melanonychia), and red lines (longitudinal erythronychia)—and the differential diagnosis for each type. We also discuss grooves in the nail plate, or Beau lines.
BASIC NAIL ANATOMY
A fundamental understanding of the anatomy of the nail unit is necessary to understand the origin of nail diseases and underlying pathologic conditions.
The nail unit includes the nail matrix, the lunula, the nail fold, the nail plate, and the nail bed. The nail matrix extends from under the proximal nail fold to the half-moon-shaped area (ie, the lunula) and is responsible for nail plate production. The nail bed lies under the nail plate and on top of the distal phalanx and extends from the lunula to just proximal to the free edge of the nail; its rich blood supply gives it its reddish color.
Nails grow slowly, and this should be kept in mind during the examination. Regrowth of a fingernail takes at least 6 months, and regrowth of a toenail may take 12 to 18 months. Therefore, a defect in the nail plate may reveal an injury that occurred—or a condition that began—several months before.1
NAIL EXAMINATION ESSENTIALS
A complete examination includes all 20 nail units and the periungual skin. Patients should be instructed to remove nail polish from all nails, as it may camouflage dystrophy or disease of the nail. Photography and careful measurement help document changes over time.
LEUKONYCHIA STRIATA: WHITE NAIL LINES
White nail lines or leukonychia is classified as true or apparent, depending on whether the origin is in the nail matrix or the nail bed.
In true leukonychia, there is abnormal keratinization of the underlying nail matrix, resulting in parakeratosis within the nail plate and an opaque appearance on examination.2 The white discoloration is unaffected by pressure, and the opacity moves distally as the nail grows out, which can be documented by serial photography on subsequent visits.
Apparent leukonychia involves abnormal nail bed vasculature, which changes the translucency of the nail plate. The whiteness disappears with pressure, is unaffected by nail growth, and will likely show no change on later visits with serial photography.3
True leukonychia
Leukonychia striata, a subtype of true leukonychia, is characterized by transverse or longitudinal bands. It is most often associated with microtrauma, such as from a manicure.4 Lines due to trauma are typically more apparent in the central part of the nail plate; they spare the lateral portion and lie parallel to the edge of the proximal nail fold.5
Onychomycosis. White longitudinal bands may also be seen in onychomycosis, a fungal infection of the nail accounting for up to 50% of all cases of nail disease. The infection may present as irregular dense longitudinal white or yellowish bands or “spikes” on the nail plate with associated hyperkeratosis, known as a dermatophytoma (Figure 1).
If a fungal infection is suspected, a potassium hydroxide stain can be performed on the subungual debris, which is then examined with direct microscopy.6 Alternatively, the physician can send a nail plate clipping in a 10% buffered formalin container with a request for a fungal stain such as periodic acid-Schiff.7 Microscopic examination of a dermatophytoma shows a dense mass of dermatophyte hyphae, otherwise known as a fungal abscess.8
The physician can play an important role in diagnosis because clinical findings suggestive of a dermatophytoma are associated with a poor response to antifungal therapy.9
Inherited diseases. White longitudinal bands are also an important clue to the rare autosomal dominant genodermatoses Hailey-Hailey disease (from mutations of the ATP2A2 gene) and Darier disease (from mutations of the ATP2C1 gene). Patients with Hailey-Hailey disease may have nails with multiple parallel longitudinal white stripes of variable width originating in the lunula and most prominent on the thumbs.10–12 These patients also have recurrent vesicular eruptions in flexural skin areas, such as the groin, axilla, neck, and periumbilical area causing significant morbidity.
Patients with Darier disease may have nails with alternating red and white longitudinal streaks, described as “candy-cane,”13 as well as wedge-shaped distal subungual keratosis accompanied by flat keratotic papules on the proximal nail fold.14 These nail changes are reported in 92% to 95% of patients with Darier disease.15,16 Patients typically have skin findings characterized by keratotic papules and plaques predominantly in seborrheic areas and palmoplantar pits, as well as secondary infections and malodor causing significant morbidity.15 Therefore, knowing the characteristic nail findings in these diseases may lead to more rapid diagnosis and treatment.
Mees lines. Leukonychia striata can present as transverse white lines, commonly known as Mees lines. They are 1- to 2-mm wide horizontal parallel white bands that span the width of the nail plate, usually affecting all fingernails.17 They are not a common finding and are most often associated with arsenic poisoning. They can also be used to identify the time of poisoning, since they tend to appear 2 months after the initial insult.
Mees lines are also associated with acute systemic stresses, such as acute renal failure, heart failure, ulcerative colitis, breast cancer, infections such as measles and tuberculosis, and systemic lupus erythematosus, and with exposure to toxic metals such as thallium.3
Apparent leukonychia
Apparent leukonychia can alert the physician to systemic diseases, infections, drug side effects, and nutrient deficiencies. Specific nail findings include Muehrcke lines, “half-and-half” nails, and Terry nails.
Muehrcke lines are paired white transverse bands that span the width of the nail bed and run parallel to the distal lunula. They were first described in the fingernails of patients with severe hypoalbuminemia, some of whom also had nephrotic syndrome, which resolved with normalization of the serum albumin level. Muehrcke lines have since been reported in patients with liver disease, malnutrition, chemotherapy, organ transplant, human immunodeficiency virus (HIV) infection, and acquired immunodeficiency syndrome.3,18 They are associated with periods of metabolic stress, ie, when the body’s capacity to synthesize proteins is diminished.19
Half-and-half nails, or Lindsay nails, are characterized by a white band proximally, a pink or red-brown band distally, and a sharp demarcation between the two (Figure 2). They were originally described in association with chronic renal disease,20 and surprisingly, they resolve with kidney transplant but not with hemodialysis treatment or improvement in hemoglobin or albumin levels.21–23 Half-and-half nails have been reported with Kawasaki disease, hepatic cirrhosis, Crohn disease, zinc deficiency, chemotherapy, Behçet disease, and pellagra.3,24,25 They should be distinguished from Terry nails, which are characterized by leukonychia involving more than 80% of the total nail length.26
Terry nails were originally reported in association with hepatic cirrhosis, usually secondary to alcoholism27 but have since been found with heart failure, type 2 diabetes mellitus, pulmonary tuberculosis, reactive arthritis, older age, Hansen disease, and peripheral vascular disease.3,26,28,29
LONGITUDINAL MELANONYCHIA: VERTICAL BROWN-BLACK NAIL LINES
Longitudinal melanonychia is the presence of black-brown vertical lines in the nail plate. They have a variety of causes, including blood from trauma; bacterial, fungal, or HIV infection; drug therapy (eg, from minocycline); endocrine disorders (Addison disease); exogenous pigmentation; or excess melanin production within the nail matrix.30–32 They may also be a sign of a benign condition such as benign melanocytic activation, lentigines, or nevi, or a malignant condition such as melanoma (Figure 3).33,34
When to suspect melanoma and refer
Although melanoma is less commonly associated with brown-black vertical nail lines, awareness of melanoma-associated longitudinal melanonychia reduces the likelihood of delayed diagnosis and improves patient outcomes.35 Also, it is important to remember that although nail melanoma is more common in the 5th and 6th decades of life, it can occur at any age, even in children.36
Findings that raise suspicion of nail melanoma (Table 1)33,37 and that should prompt referral to a dermatologist who specializes in nails include the following:
- A personal or family history of melanoma
- Involvement of a “high-risk” digit (thumb, index finger, great toe),30,31,38 although nail melanoma can occur in any digit
- Any new vertical brown-black nail pigmentation in a fair-skinned patient
- Only one nail affected: involvement of more than one nail is common in people with darker skin, and nearly all patients with darker skin exhibit longitudinal melanonychia by age 5031
- Changes in the band such as darkening, widening, and bleeding
- A bandwidth greater than 6 mm33
- A band that is wider proximally than distally34
- Nonuniform color of the line
- Indistinct lateral borders
- Associated with pigmentation of the nail fold (the Hutchinson sign, representing subungual melanoma),31,39 nail plate dystrophy, bleeding, or ulceration.33
While these features may help distinguish benign from malignant causes of longitudinal melanonychia, the clinical examination alone may not provide a definitive diagnosis. Delayed diagnosis of nail melanoma carries a high mortality rate; the internist can promote early diagnosis by recognizing the risk factors and clinical signs and referring the patient to a dermatologist for further evaluation with nail biopsy.
LONGITUDINAL ERYTHRONYCHIA: VERTICAL RED NAIL LINES
Longitudinal erythronychia—the presence of one or more linear red bands in the nail unit—can be localized (involving only one nail) or polydactylous (involving more than one nail). The localized form is usually due to a neoplastic process, whereas involvement of more than one nail may indicate an underlying regional or systemic disease.13Table 2 lists indications for referral to a nail specialist.
General features on examination
Clinical examination reveals one or more linear, pink-red streaks extending from the proximal nail fold to the distal free edge of the nail plate (Figure 4). The width of the band typically ranges from less than 1 mm to 3 mm.40 Other features may include splinter hemorrhages within a red band, a semitransparent distal matrix, distal V-shaped chipping, splitting, onycholysis of the nail plate, and reactive distal nail bed and hyponychial hyperkeratosis. These features can be visible to the naked eye but may be better viewed with a magnifying glass, a 7× loupe, or a dermatoscope.13
Localized longitudinal erythronychia is usually seen in middle-aged individuals and is most commonly found on the thumbnail, followed by the index finger.41,42 The condition may be asymptomatic, but the patient may present with pain or with concern that the split end of the nail catches on fabrics or small objects.42
Glomus tumor
Intense, pulsatile pain with sensitivity to cold and tenderness to palpation is highly suggestive of glomus tumor,43 a benign neoplasm that originates from a neuromyoarterial glomus body. Glomus bodies are located throughout the body but are more highly concentrated in the fingertips, especially beneath the nails, and they regulate skin circulation. Therefore, the nail unit is the most common site for glomus tumor.44,45 A characteristic feature of subungual glomus tumor is demonstration of tenderness after pin-point palpation of the suspected tumor (positive Love sign).45 While it is typical for glomus tumor to affect only one nail, multiple tumors are associated with neurofibromatosis type 1.46 Confirmation of this diagnosis requires referral to a dermatologist.
Other causes of localized red nail lines
Onychopapilloma, a benign idiopathic tumor, is the most common cause of localized longitudinal erythronychia. Unlike glomus tumor, it is usually asymptomatic.42,47 Less common benign conditions are warts, warty dyskeratoma, benign vascular proliferation, a solitary lesion of lichen planus, hemiplegia, and postsurgical scarring of the nail matrix. In some cases, the lines are idiopathic.42,43
Malignant diseases that can present as localized longitudinal erythronychia include invasive squamous cell carcinoma, squamous cell carcinoma in situ (Bowen disease), and, less frequently, amelanotic melanoma in situ, malignant melanoma, and basal cell carcinoma.42 Squamous cell carcinoma in situ most commonly presents in the 5th decade of life and is the malignancy most commonly associated with localized longitudinal erythronychia. Clinically, there is also often nail dystrophy, such as distal subungual keratosis or onycholysis.43
Patients with asymptomatic, stable localized longitudinal erythronychia may be followed closely with photography and measurements. However, any new lesion or a change in an existing lesion should prompt referral to a dermatologist for biopsy.13
Red streaks on more than one nail
Polydactylous longitudinal erythronychia usually presents in adults as red streaks on multiple nails and, depending on the presence or absence of symptoms (eg, pain, splitting), may be the patient’s chief complaint or an incidental finding noted by the astute clinician. Often, it is associated with systemic disease, most commonly lichen planus or Darier disease.
Lichen planus is a papulosquamous skin disease with nail involvement in 10% of patients and permanent nail dystrophy in 4%. Common nail findings include thinning, longitudinal ridging, and fissuring, as well as scarring of the nail matrix resulting in pterygium. Linear red streaks may accompany these more typical nail findings.13 Patients with Darier disease present with alternating red and white linear bands on multiple nails as in leukonychia striata.
Less frequently, polydactylous longitudinal erythronychia is associated with primary and systemic amyloidosis, hemiplegia, graft-vs-host disease, acantholytic epidermolysis bullosa, acantholytic dyskeratotic epidermal nevus, acrokeratosis verruciformis of Hopf, or pseudobulbar syndrome, or is idiopathic.13,42,48 Therefore, the physician evaluating a patient with these nail findings should focus on a workup for regional or systemic disease or refer the patient to a dermatologist who specializes in nails.
BEAU LINES
Beau lines are a common finding in clinical practice. They are not true lines, but transverse grooves in the nail plate that arise from the temporary suppression of nail growth within the nail matrix that can occur during periods of acute or chronic stress or systemic illness (Figure 5).49
The precipitating event may be local trauma or paronychia, chemotherapeutic agents cytotoxic to the nail matrix, or the abrupt onset of systemic disease.18,50 The grooves have also been associated with rheumatic fever, malaria, pemphigus, Raynaud disease, and myocardial infarction, as well as following deep-sea dives.51–53 The distance of a Beau line from the proximal nail fold can provide an estimate of the time of the acute stress, based on an average growth rate of 3 mm per month for fingernails and 1 mm per month for toenails.49
- Scher RK, Rich P, Pariser D, Elewski B. The epidemiology, etiology, and pathophysiology of onychomycosis. Semin Cutan Med Surg 2013; 32(suppl 1):S2–S4.
- Lawry MA, Haneke E, Strobeck K, Martin S, Zimmer B, Romano PS. Methods for diagnosing onychomycosis: a comparative study and review of the literature. Arch Dermatol 2000; 136:1112–1116.
- Zaiac MN, Walker A. Nail abnormalities associated with systemic pathologies. Clin Dermatol 2013; 31:627–649.
- Zaiac MN, Daniel CR. Nails in systemic disease. Dermatol Ther 2002; 15:99–106.
- Tosti A, Iorizzo M, Piraccini BM, Starace M. The nail in systemic diseases. Dermatol Clin 2006; 24:341–347.
- Scher RK, Daniel CR, eds. Nails Diagnosis, Therapy, Surgery. 3rd ed. Oxford: Elsevier Saunders; 2005.
- Smith MB, McGinnis MR. Diagnostic histopathology. In: Hospenthal DR, Rinaldi MG, eds. Diagnosis and Treatment of Human Mycoses. Totowa, NJ: Humana Press; 2008:37–51.
- Roberts DT, Evans EG. Subungual dermatophytoma complicating dermatophyte onychomycosis. Br J Dermatol 1998; 138:189–190.
- Sigurgeirsson B. Prognostic factors for cure following treatment of onychomycosis. J Eur Acad Dermatol Venereol 2010; 24:679–684.
- Kumar R, Zawar V. Longitudinal leukonychia in Hailey-Hailey disease: a sign not to be missed. Dermatol Online J 2008; 14:17.
- Burge SM. Hailey-Hailey disease: the clinical features, response to treatment and prognosis. Br J Dermatol 1992; 126:275–282.
- Kirtschig G, Effendy I, Happle R. Leukonychia longitudinalis as the primary symptom of Hailey-Hailey disease. Hautarzt 1992; 43:451–452. German.
- Jellinek NJ. Longitudinal erythronychia: suggestions for evaluation and management. J Am Acad Dermatol 2011; 64:167.e1–167.e11
- Zaias N, Ackerman AB. The nail in Darier-White disease. Arch Dermatol 1973; 107:193–199.
- Burge SM, Wilkinson JD. Darier-White disease: a review of the clinical features in 163 patients. J Am Acad Dermatol 1992; 27:40–50.
- Munro CS. The phenotype of Darier's disease: penetrance and expressivity in adults and children. Br J Dermatol 1992; 127:126–130.
- Schwartz RA. Arsenic and the skin. Int J Dermatol 1997; 36:241–250.
- Fawcett RS, Linford S, Stulberg DL. Nail abnormalities: clues to systemic disease. Am Fam Physician 2004; 69:1417–1424.
- Morrison-Bryant M, Gradon JD. Images in clinical medicine. Muehrcke's lines. N Engl J Med 2007; 357:917.
- Daniel CR 3rd, Bower JD, Daniel CR Jr. The “half and half fingernail”: the most significant onychopathological indicator of chronic renal failure. J Miss State Med Assoc 1975; 16:367–370.
- Saray Y, Seckin D, Gulec AT, Akgun S, Haberal M. Nail disorders in hemodialysis patients and renal transplant recipients: a case-control study. J Am Acad Dermatol 2004; 50:197–202.
- Dyachenko P, Monselise A, Shustak A, Ziv M, Rozenman D. Nail disorders in patients with chronic renal failure and undergoing haemodialysis treatment: a case-control study. J Eur Acad Dermatol Venereol 2007; 21:340–344.
- Salem A, Al Mokadem S, Attwa E, Abd El Raoof S, Ebrahim HM, Faheem KT. Nail changes in chronic renal failure patients under haemodialysis. J Eur Acad Dermatol Venereol 2008; 22:1326–1331.
- Zagoni T, Sipos F, Tarjan Z, Peter Z. The half-and-half nail: a new sign of Crohn's disease? Report of four cases. Dis Colon Rectum 2006; 49:1071–1073.
- Nixon DW, Pirozzi D, York RM, Black M, Lawson DH. Dermatologic changes after systemic cancer therapy. Cutis 1981; 27:181–194.
- Holzberg M, Walker HK. Terry's nails: revised definition and new correlations. Lancet 1984; 1:896–899.
- Terry R. White nails in hepatic cirrhosis. Lancet 1954; 266:757–759.
- Coskun BK, Saral Y, Ozturk P, Coskun N. Reiter syndrome accompanied by Terry nail. J Eur Acad Dermatol Venereol 2005; 19:87–89.
- Blyumin M, Khachemoune A, Bourelly P. What is your diagnosis? Terry nails. Cutis 2005; 76:201–202.
- Haneke E, Baran R. Longitudinal melanonychia. Dermatol Surg 2001; 27:580–584.
- Andre J, Lateur N. Pigmented nail disorders. Dermatol Clin 2006; 24:329–339.
- Braun RP, Baran R, Le Gal FA, et al. Diagnosis and management of nail pigmentations. J Am Acad Dermatol 2007; 56:835–847.
- Mannava KA, Mannava S, Koman LA, Robinson-Bostom L, Jellinek N. Longitudinal melanonychia: detection and management of nail melanoma. Hand Surg 2013; 18:133–139.
- Ruben BS. Pigmented lesions of the nail unit: clinical and histopathologic features. Semin Cutan Med Surg 2010; 29:148–158.
- Cohen T, Busam KJ, Patel A, Brady MS. Subungual melanoma: management considerations. Am J Surg 2008; 195:244–248.
- Iorizzo M, Tosti A, Di Chiacchio N, et al. Nail melanoma in children: differential diagnosis and management. Dermatol Surg 2008; 34:974–978.
- Jellinek N. Nail matrix biopsy of longitudinal melanonychia: diagnostic algorithm including the matrix shave biopsy. J Am Acad Dermatol 2007; 56:803–810.
- Husain S, Scher RK, Silvers DN, Ackerman AB. Melanotic macule of nail unit and its clinicopathologic spectrum. J Am Acad Dermatol 2006; 54:664–667.
- Baran R, Kechijian P. Hutchinson's sign: a reappraisal. J Am Acad Dermatol 1996; 34:87–90.
- Baran R. Red nails. Dermatol Online 2005; 11:29.
- Baran R, Perrin C. Longitudinal erythronychia with distal subungual keratosis: onychopapilloma of the nail bed and Bowen’s disease. Br J Dermatol 2000; 143:132–135.
- de Berker DA, Perrin C, Baran R. Localized longitudinal erythronychia: diagnostic significance and physical explanation. Arch Dermatol 2004; 140:1253–1257.
- Cohen PR. Longitudinal erythronychia: individual or multiple linear red bands of the nail plate: a review of clinical features and associated conditions. Am J Clin Dermatol 2011; 12:217–231.
- Van Geertruyden J, Lorea P, Goldschmidt D, et al. Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br 1996; 21:257–260.
- Moon SE, Won JH, Kwon OS, Kim JA. Subungual glomus tumor: clinical manifestations and outcome of surgical treatment. J Dermatol 2004; 31:993–997.
- Okada O, Demitsu T, Manabe M, Yoneda K. A case of multiple subungual glomus tumors associated with neurofibromatosis type 1. J Dermatol 1999; 26:535–537.
- Gee BC, Millard PR, Dawber RP. Onychopapilloma is not a distinct clinicopathological entity. Br J Dermatol 2002; 146:156–157.
- Siragusa M, Del Gracco S, Ferri R, Schepis C. Longitudinal red streaks on the big toenails in a patient with pseudobulbar syndrome. J Eur Acad Dermatol Venereol 2001; 15:85–86.
- Lipner S, Scher RK. Nails. In: Callen J, Jorizzo JL, eds. Dermatological Signs of Systemic Disease. 5th ed: Elsevier; in press.
- Mortimer NJ, Mills J. Images in clinical medicine. Beau’s lines. N Engl J Med 2004; 351:1778.
- Schwartz H. Clinical observation: Beau’s lines on fingernails after deep saturation dives. Undersea Hyperb Med 2006; 33:5–10.
- Gugelmann HM, Gaieski DF. Beau’s lines after cardiac arrest. Ther Hypothermia Temp Manag 2013; 3:199–202.
- Lauber J, Turk K. Beau’s lines and pemphigus vulgaris. Int J Dermatol 1990; 29:309.
- Scher RK, Rich P, Pariser D, Elewski B. The epidemiology, etiology, and pathophysiology of onychomycosis. Semin Cutan Med Surg 2013; 32(suppl 1):S2–S4.
- Lawry MA, Haneke E, Strobeck K, Martin S, Zimmer B, Romano PS. Methods for diagnosing onychomycosis: a comparative study and review of the literature. Arch Dermatol 2000; 136:1112–1116.
- Zaiac MN, Walker A. Nail abnormalities associated with systemic pathologies. Clin Dermatol 2013; 31:627–649.
- Zaiac MN, Daniel CR. Nails in systemic disease. Dermatol Ther 2002; 15:99–106.
- Tosti A, Iorizzo M, Piraccini BM, Starace M. The nail in systemic diseases. Dermatol Clin 2006; 24:341–347.
- Scher RK, Daniel CR, eds. Nails Diagnosis, Therapy, Surgery. 3rd ed. Oxford: Elsevier Saunders; 2005.
- Smith MB, McGinnis MR. Diagnostic histopathology. In: Hospenthal DR, Rinaldi MG, eds. Diagnosis and Treatment of Human Mycoses. Totowa, NJ: Humana Press; 2008:37–51.
- Roberts DT, Evans EG. Subungual dermatophytoma complicating dermatophyte onychomycosis. Br J Dermatol 1998; 138:189–190.
- Sigurgeirsson B. Prognostic factors for cure following treatment of onychomycosis. J Eur Acad Dermatol Venereol 2010; 24:679–684.
- Kumar R, Zawar V. Longitudinal leukonychia in Hailey-Hailey disease: a sign not to be missed. Dermatol Online J 2008; 14:17.
- Burge SM. Hailey-Hailey disease: the clinical features, response to treatment and prognosis. Br J Dermatol 1992; 126:275–282.
- Kirtschig G, Effendy I, Happle R. Leukonychia longitudinalis as the primary symptom of Hailey-Hailey disease. Hautarzt 1992; 43:451–452. German.
- Jellinek NJ. Longitudinal erythronychia: suggestions for evaluation and management. J Am Acad Dermatol 2011; 64:167.e1–167.e11
- Zaias N, Ackerman AB. The nail in Darier-White disease. Arch Dermatol 1973; 107:193–199.
- Burge SM, Wilkinson JD. Darier-White disease: a review of the clinical features in 163 patients. J Am Acad Dermatol 1992; 27:40–50.
- Munro CS. The phenotype of Darier's disease: penetrance and expressivity in adults and children. Br J Dermatol 1992; 127:126–130.
- Schwartz RA. Arsenic and the skin. Int J Dermatol 1997; 36:241–250.
- Fawcett RS, Linford S, Stulberg DL. Nail abnormalities: clues to systemic disease. Am Fam Physician 2004; 69:1417–1424.
- Morrison-Bryant M, Gradon JD. Images in clinical medicine. Muehrcke's lines. N Engl J Med 2007; 357:917.
- Daniel CR 3rd, Bower JD, Daniel CR Jr. The “half and half fingernail”: the most significant onychopathological indicator of chronic renal failure. J Miss State Med Assoc 1975; 16:367–370.
- Saray Y, Seckin D, Gulec AT, Akgun S, Haberal M. Nail disorders in hemodialysis patients and renal transplant recipients: a case-control study. J Am Acad Dermatol 2004; 50:197–202.
- Dyachenko P, Monselise A, Shustak A, Ziv M, Rozenman D. Nail disorders in patients with chronic renal failure and undergoing haemodialysis treatment: a case-control study. J Eur Acad Dermatol Venereol 2007; 21:340–344.
- Salem A, Al Mokadem S, Attwa E, Abd El Raoof S, Ebrahim HM, Faheem KT. Nail changes in chronic renal failure patients under haemodialysis. J Eur Acad Dermatol Venereol 2008; 22:1326–1331.
- Zagoni T, Sipos F, Tarjan Z, Peter Z. The half-and-half nail: a new sign of Crohn's disease? Report of four cases. Dis Colon Rectum 2006; 49:1071–1073.
- Nixon DW, Pirozzi D, York RM, Black M, Lawson DH. Dermatologic changes after systemic cancer therapy. Cutis 1981; 27:181–194.
- Holzberg M, Walker HK. Terry's nails: revised definition and new correlations. Lancet 1984; 1:896–899.
- Terry R. White nails in hepatic cirrhosis. Lancet 1954; 266:757–759.
- Coskun BK, Saral Y, Ozturk P, Coskun N. Reiter syndrome accompanied by Terry nail. J Eur Acad Dermatol Venereol 2005; 19:87–89.
- Blyumin M, Khachemoune A, Bourelly P. What is your diagnosis? Terry nails. Cutis 2005; 76:201–202.
- Haneke E, Baran R. Longitudinal melanonychia. Dermatol Surg 2001; 27:580–584.
- Andre J, Lateur N. Pigmented nail disorders. Dermatol Clin 2006; 24:329–339.
- Braun RP, Baran R, Le Gal FA, et al. Diagnosis and management of nail pigmentations. J Am Acad Dermatol 2007; 56:835–847.
- Mannava KA, Mannava S, Koman LA, Robinson-Bostom L, Jellinek N. Longitudinal melanonychia: detection and management of nail melanoma. Hand Surg 2013; 18:133–139.
- Ruben BS. Pigmented lesions of the nail unit: clinical and histopathologic features. Semin Cutan Med Surg 2010; 29:148–158.
- Cohen T, Busam KJ, Patel A, Brady MS. Subungual melanoma: management considerations. Am J Surg 2008; 195:244–248.
- Iorizzo M, Tosti A, Di Chiacchio N, et al. Nail melanoma in children: differential diagnosis and management. Dermatol Surg 2008; 34:974–978.
- Jellinek N. Nail matrix biopsy of longitudinal melanonychia: diagnostic algorithm including the matrix shave biopsy. J Am Acad Dermatol 2007; 56:803–810.
- Husain S, Scher RK, Silvers DN, Ackerman AB. Melanotic macule of nail unit and its clinicopathologic spectrum. J Am Acad Dermatol 2006; 54:664–667.
- Baran R, Kechijian P. Hutchinson's sign: a reappraisal. J Am Acad Dermatol 1996; 34:87–90.
- Baran R. Red nails. Dermatol Online 2005; 11:29.
- Baran R, Perrin C. Longitudinal erythronychia with distal subungual keratosis: onychopapilloma of the nail bed and Bowen’s disease. Br J Dermatol 2000; 143:132–135.
- de Berker DA, Perrin C, Baran R. Localized longitudinal erythronychia: diagnostic significance and physical explanation. Arch Dermatol 2004; 140:1253–1257.
- Cohen PR. Longitudinal erythronychia: individual or multiple linear red bands of the nail plate: a review of clinical features and associated conditions. Am J Clin Dermatol 2011; 12:217–231.
- Van Geertruyden J, Lorea P, Goldschmidt D, et al. Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br 1996; 21:257–260.
- Moon SE, Won JH, Kwon OS, Kim JA. Subungual glomus tumor: clinical manifestations and outcome of surgical treatment. J Dermatol 2004; 31:993–997.
- Okada O, Demitsu T, Manabe M, Yoneda K. A case of multiple subungual glomus tumors associated with neurofibromatosis type 1. J Dermatol 1999; 26:535–537.
- Gee BC, Millard PR, Dawber RP. Onychopapilloma is not a distinct clinicopathological entity. Br J Dermatol 2002; 146:156–157.
- Siragusa M, Del Gracco S, Ferri R, Schepis C. Longitudinal red streaks on the big toenails in a patient with pseudobulbar syndrome. J Eur Acad Dermatol Venereol 2001; 15:85–86.
- Lipner S, Scher RK. Nails. In: Callen J, Jorizzo JL, eds. Dermatological Signs of Systemic Disease. 5th ed: Elsevier; in press.
- Mortimer NJ, Mills J. Images in clinical medicine. Beau’s lines. N Engl J Med 2004; 351:1778.
- Schwartz H. Clinical observation: Beau’s lines on fingernails after deep saturation dives. Undersea Hyperb Med 2006; 33:5–10.
- Gugelmann HM, Gaieski DF. Beau’s lines after cardiac arrest. Ther Hypothermia Temp Manag 2013; 3:199–202.
- Lauber J, Turk K. Beau’s lines and pemphigus vulgaris. Int J Dermatol 1990; 29:309.
KEY POINTS
- Transverse white nail lines, or Mees lines, have been associated with acute systemic stress, such as from acute renal failure, heart failure, ulcerative colitis, breast cancer, infection (measles, tuberculosis), and systemic lupus erythematosus, and with exposure to toxic metals such as thallium.
- In true leukonychia, there is abnormal keratinization of the underlying nail matrix, resulting in a white discoloration that is unaffected by pressure. In apparent leukonychia, the white discoloration is due to abnormal nail bed vasculature, and the whiteness disappears with pressure.
- Brown-black nail lines may represent blood from trauma; bacterial, fungal, or viral infection; drug reaction; endocrine disorders; exogenous pigmentation; excess melanin production within the nail matrix; nevi; or melanoma.
Onychomycosis: Current and Investigational Therapies
To the Editor:
Onychomycosis is a fungal infection of the nail plate by dermatophytes, yeasts, and nondermatophyte molds. It is a common problem with a prevalence of 10% to 12% in the United States.1,2 The clinical presentation of onychomycosis is shown in the Figure. Although some patients may have mild asymptomatic cases of onychomycosis and do not inquire about treatment, many will have more advanced cases, presenting with pain and discomfort, secondary infection, unattractive appearance, or problems performing everyday functions. The goal of onychomycosis treatment is to eliminate the fungus, if possible, which usually restores the nail to its normal state when it fully grows out. Patients should be counseled that it is a long process that may take 6 months or more for fingernails and 12 to 18 months for toenails. These estimates are based on a growth rate of 2 to 3 mm per month for fingernails and 1 to 2 mm per month for toenails.3 Nails grow fastest during the teenaged years and slow down with advancing age.4 It should be noted that advanced cases of onychomycosis affecting the nail matrix may cause permanent scarring; therefore, the nail unit may still appear dystrophic after the causative organism is eliminated. The US Food and Drug Administration (FDA) defines a complete cure as negative potassium hydroxide preparation and negative fungal culture plus a completely normal appearance of the nail.
Treatment of onychomycosis poses a number of challenges. First, hyperkeratosis and the fungal mass may limit the delivery of topical and systemic drugs to the source of the infection. In addition, high rates of relapse and reinfection after treatment may be due to residual hyphae or spores.5 Furthermore, the extended length of treatment limits patient adherence and many patients are unwilling to forego wearing nail cosmetics during the course of some of the treatments.
There are 4 approved classes of antifungal drugs for the treatment of onychomycosis: allylamines, azoles, morpholines, and hydroxypyridinones.6 The allylamines (eg, terbinafine) inhibit squalene epoxidase.7 Oral terbinafine (250 mg daily) taken for 6 weeks for fingernails and 12 weeks for toenails is considered the current systemic treatment preference in onychomycosis therapy8 with complete cure rates in 12-week studies of approximately 38%9 and 49%.10
The second class of drugs is the azoles, which inhibit lanosterol 14a-demethylase, a step in the ergosterol biosynthesis pathway.6 Two members of this class that are widely used in treating onychomycosis are oral itraconazole11 and off-label oral fluconazole.12 The approved dose for oral itraconazole is 200 mg daily for 3 months (or an alternative pulse regimen) with a reported complete cure rate of 14%.11 Although fluconazole is not FDA approved for the treatment of onychomycosis in the United States, it is used extensively in other countries and to some extent off label in the United States. In a study of 362 patients with onychomycosis treated with oral fluconazole, complete cure rates were 48% in patients who received 450 mg weekly, 46% in those who received 300 mg weekly, and 37% in those who received 150 mg weekly for up to 9 months.12 It should be noted that several oral triazole antifungals, namely albaconazole,13 posaconazole,14 and ravuconazole,15 have undergone phase 1 and 2 studies for the treatment of onychomycosis and have shown some efficacy.
Another class of antifungals are the morpholines including topical amorolfine, which is approved for use in Europe but not in North America.16 Amorolfine inhibits D14 reductase and D7-D8 isomerase, thus depleting ergosterol.17 In one randomized controlled study, the combination of amorolfine nail lacquer and oral terbinafine compared to oral terbinafine alone resulted in a higher clinical cure rate with the combination (59.2% vs 46%); complete cure rate was not reported.16
Finally, the hydroxypyridinone class includes topical ciclopirox, which has a poorly understood mechanism of action but may involve iron chelation or oxidative damage.18,19 Ciclopirox nail lacquer 8% was approved by the FDA in 1999 and has reported complete cure rates of 5.5% to 8.5% with monthly nail debridement.20
Based on the poor efficacy of many of the currently available treatments and time-consuming treatment courses, it is clear that there is a need for alternative and novel therapies. There has been a greater emphasis on topical agents due to their more favorable side-effect profile and lower risk for drug-drug interactions. Although there are many agents for the treatment of onychomycosis currently in development, many are in vitro studies or phase 1 and 2 studies. However, we will focus on drugs that are further along in phase 3 studies and those that were recently FDA approved.
Efinaconazole is a member of the azole class of drugs and has completed 2 phase 3 clinical trials (study 1, N=870; study 2, N=785).21 Patients in these 2 studies were randomized to receive either efinaconazole nail solution 10% or vehicle for 48 weeks followed by a 4-week washout period. Complete cure rates in the 2 studies were 17.8% and 15.2% in the treated group and 3.3% and 5.5% in the control group. The mycological cure rates were 55.2% and 53.4% in the treated group and 16.8% and 16.9% in the control group. The side-effect profile was minimal, with the most common adverse events being application-site dermatitis and vesiculation, which were not significantly higher in the treated group versus the control group.21 Efinaconazole received FDA approval for the treatment of toenail onychomycosis in June 2014.
There are some notable differences between ciclopirox and efinaconazole that may improve patient compliance with the latter. First, treatment with ciclopirox includes monthly nail debridement, which is not required with efinaconazole. Secondly, although ciclopirox lacquer must be removed weekly, efinaconazole is a solution, so no removal is necessary.
Terbinafine nail solution (TNS) is a member of the allylamine class and has completed phase 3 clinical trials.22 Three studies—2 vehicle controlled and 1 active comparator—were performed. The first compared TNS and vehicle, both applied daily for 24 weeks; the second study repeated the same for 48 weeks; and the third study compared TNS to amorolfine nail lacquer 5% daily for 48 weeks. The best results for complete cure were achieved with TNS for 48 weeks in the vehicle-controlled study with a rate of 2.2% versus 0%. The authors also concluded TNS was not more effective than amorolfine, as complete cure rates were 1.2% for TNS and 0.96% for amorolfine. The most common side effects were headache, nasopharyngitis, and influenza.22
Tavaborole is a member of the new benzoxaborole class, which inhibits protein synthesis by forming an adduct with the aminoacyl–transfer RNA synthetase.23 The topical solution was engineered to have improved penetration through the nail plate. In vitro studies showed better penetration than both ciclopirox and amorolfine.24 Two identical phase 3 randomized, double-blind, vehicle-controlled studies were completed involving 1197 patients who were treated with tavaborole topical solution 5% daily compared to vehicle for 48 weeks followed by a 4-week washout period with promising results.25 The incidence of treatment-related side effects was comparable to the vehicle. The most common adverse events were exfoliation, erythema, and dermatitis, all occurring at the application site.25 Tavaborole was approved by the FDA for the treatment of toenail onychomycosis in July 2014.
Luliconazole is a member of the azole class and a phase 2b/3 clinical trial with a 10% solution involving 334 patients was completed in June 2013.26 Results from this trial are expected in early 2015.
Lasers are a developing area for onychomycosis therapy and the appeal stems from their ability to selectively deliver energy to the target tissue, thus avoiding systemic side effects. Since 2010, the FDA has approved numerous laser devices for the temporary cosmetic improvement of onychomycosis, all of which are Nd:YAG 1064-nm lasers.27,28 It was previously thought that the mechanism of action for the fungicidal effect was achieved with heat,29 but newer in vitro studies have shown that the amount of time and level of heat required to kill Trichophyton rubrum would not be tolerable to patients.30 Although the mechanism of action is poorly understood, some clinical trials have shown success using the Nd:YAG 1064-nm laser for treatment of onychomycosis. However, in a study of 8 patients treated with the Nd:YAG 1064-nm laser for 5 treatment sessions, none had a mycological or clinical cure and there was only mild clinical improvement. In addition, most patients had pain and burning during the treatments requiring many short breaks.30 Although not yet FDA approved for the treatment of onychomycosis, other types of lasers are currently being studied, including CO2, near-infrared diode, and femtosecond-infrared laser systems.3
Plasma therapy is a developing area for the treatment of onychomycosis. Plasma was shown to be fungicidal to T rubrum in an in vitro model (MOE Medical Devices, written communication, July 2012), and a clinical trial to evaluate the safety, tolerability, and efficacy of plasma in human subjects is ongoing (registered on March 22, 2013, at www.clinicaltrials.gov with the identifier NCT01819051).
Onychomycosis is a common problem that increases in prevalence with advancing age. Oral terbinafine is considered the first-line treatment at this point in time.31 Two new topical agents, efinaconazole and tavaborole, were recently FDA approved and may be used for the treatment of toenail onychomycosis without the need for nail debridement. The Nd:YAG laser has shown some promise in earlier clinical studies but was ineffective in a more recent study.
1. Ghannoum MA, Hajjeh RA, Scher R, et al. A large-scale North American study of fungal isolates from nails: the frequency of onychomycosis, fungal distribution, and antifungal susceptibility patterns. J Am Acad Dermatol. 2000;43:641-648.
2. Heikkila H, Stubb S. The prevalence of onychomycosis in Finland. Br J Dermatol. 1995;133:699-703.
3. Scher RK, Rich P, Pariser D, et al. The epidemiology, etiology, and pathophysiology of onychomycosis. Semin Cutan Med Surg. 2013;32(2, suppl 1):S2-S4.
4. Abdullah L, Abbas O. Common nail changes and disorders in older people: diagnosis and management. Can Fam Physician. 2011;57:173-181.
5. Scher RK, Baran R. Onychomycosis in clinical practice: factors contributing to recurrence. Br J Dermatol. 2003;149(suppl 65):5-9.
6. Welsh O, Vera-Cabrera L, Welsh E. Onychomycosis. Clin Dermatol. 2010;28:151-159.
7. Gupta AK, Sauder DN, Shear NH. Antifungal agents: an overview. part II. J Am Acad Dermatol. 1994;30:911-933.
8. Gupta AK, Paquet M, Simpson F, et al. Terbinafine in the treatment of dermatophyte toenail onychomycosis: a meta-analysis of efficacy for continuous and intermittent regimens. J Eur Acad Dermatol Venereol. 2013;27:267-272.
9. Drake LA, Shear NH, Arlette JP, et al. Oral terbinafine in the treatment of toenail onychomycosis: North American multicenter trial. J Am Acad Dermatol. 1997;37:740-745.
10. Evans EG, Sigurgeirsson B. Double blind, randomised study of continuous terbinafine compared with intermittent itraconazole in treatment of toenail onychomycosis. the LION Study Group. BMJ. 1999;318:1031-1035.
11. Sporanox [package insert]. Macquarie Park, Australia: Janssen-Cilag Pty Ltd; 2014.
12. Scher RK, Breneman D, Rich P, et al. Once-weekly fluconazole (150, 300, or 450 mg) in the treatment of distal subungual onychomycosis of the toenail. J Am Acad Dermatol. 1998;38(6, pt 2):S77-S86.
13. Sigurgeirsson B, van Rossem K, Malahias S, et al. A phase II, randomized, double-blind, placebo-controlled, parallel group, dose-ranging study to investigate the efficacy and safety of 4 dose regimens of oral albaconazole in patients with distal subungual onychomycosis. J Am Acad Dermatol. 2013;69:416-425.
14. Elewski B, Pollak R, Ashton S, et al. A randomized, placebo- and active-controlled, parallel-group, multicentre, investigator-blinded study of four treatment regimens of posaconazole in adults with toenail onychomycosis. Br J Dermatol. 2012;166:389-398.
15. Gupta AK, Leonardi C, Stoltz RR, et al. A phase I/II randomized, double-blind, placebo-controlled, dose-ranging study evaluating the efficacy, safety and pharmacokinetics of ravuconazole in the treatment of onychomycosis. J Eur Acad Dermatol Venereol. 2005;19:437-443.
16. Baran R, Sigurgeirsson B, de Berker D, et al. A multicentre, randomized, controlled study of the efficacy, safety and cost-effectiveness of a combination therapy with amorolfine nail lacquer and oral terbinafine compared with oral terbinafine alone for the treatment of onychomycosis with matrix involvement. Br J Dermatol. 2007;157:149-157.
17. Polak A. Preclinical data and mode of action of amorolfine. Dermatology. 1992;184(suppl 1):3-7.
18. Belenky P, Camacho D, Collins JJ. Fungicidal drugs induce a common oxidative-damage cellular death pathway. Cell Rep. 2013;3:350-358.
19. Lee RE, Liu TT, Barker KS, et al. Genome-wide expression profiling of the response to ciclopirox olamine in Candida albicans. J Antimicrob Chemother. 2005;55:655-662.
20. Penlac [package insert]. Bridgewater, NJ: sanofi-aventis; 2006.
21. Elewski BE, Rich P, Pollak R, et al. Efinaconazole 10% solution in the treatment of toenail onychomycosis: two phase III multicenter, randomized, double-blind studies. J Am Acad Dermatol. 2013;68:600-608.
22. Elewski BE, Ghannoum MA, Mayser P, et al. Efficacy, safety and tolerability of topical terbinafine nail solution in patients with mild-to-moderate toenail onychomycosis: results from three randomized studies using double-blind vehicle-controlled and open-label active-controlled designs. J Eur Acad Dermatol Venereol. 2013;27:287-294.
23. Rock FL, Mao W, Yaremchuk A, et al. An antifungal agent inhibits an aminoacyl-tRNA synthetase by trapping tRNA in the editing site. Science. 2007;316:1759-1761.
24. Hui X, Baker SJ, Wester RC, et al. In vitro penetration of a novel oxaborole antifungal (AN2690) into the human nail plate. J Pharm Sci. 2007;96:2622-2631.
25. Elewski BE, Rich P, Wiltz H, et al. Effectiveness and safety of tavaborole, a novel born-based molecule for the treatment of onychomycosis: results from two phase 3 studies. Poster presented at: Women’s & Pediatric Dermatology Seminar; October 4-6, 2013; Newport Beach, CA.
26. The solution study: Topica’s phase 2b/3 clinical trial. Topica Pharmaceuticals Inc Web site. http://www.
topicapharma.com/phase-2b3. Accessed December 2, 2014.
27. Gupta AK, Simpson FC. Medical devices for the treatment of onychomycosis. Dermatol Ther. 2012;25:574-581.
28. Ortiz AE, Avram MM, Wanner MA. A review of lasers and light for the treatment of onychomycosis. Lasers Surg Med. 2014;46:117-124.
29. Vural E, Winfield HL, Shingleton AW, et al. The effects of laser irradiation on Trichophyton rubrum growth. Lasers Med Sci. 2008;23:349-353.
30. Carney C, Cantrell W, Warner J, et al. Treatment of onychomycosis using a submillisecond 1064-nm neodymium:yttrium-aluminum-garnet laser. J Am Acad Dermatol. 2013;69:578-582.
31. Gupta AK, Daigle D, Paquet M. Therapies for onychomycosis: a systematic review and network meta-analysis of mycological cure [published online ahead of print July 17, 2014]. J Am Podiatr Med Assoc. doi:10.7547/13-110.1.
To the Editor:
Onychomycosis is a fungal infection of the nail plate by dermatophytes, yeasts, and nondermatophyte molds. It is a common problem with a prevalence of 10% to 12% in the United States.1,2 The clinical presentation of onychomycosis is shown in the Figure. Although some patients may have mild asymptomatic cases of onychomycosis and do not inquire about treatment, many will have more advanced cases, presenting with pain and discomfort, secondary infection, unattractive appearance, or problems performing everyday functions. The goal of onychomycosis treatment is to eliminate the fungus, if possible, which usually restores the nail to its normal state when it fully grows out. Patients should be counseled that it is a long process that may take 6 months or more for fingernails and 12 to 18 months for toenails. These estimates are based on a growth rate of 2 to 3 mm per month for fingernails and 1 to 2 mm per month for toenails.3 Nails grow fastest during the teenaged years and slow down with advancing age.4 It should be noted that advanced cases of onychomycosis affecting the nail matrix may cause permanent scarring; therefore, the nail unit may still appear dystrophic after the causative organism is eliminated. The US Food and Drug Administration (FDA) defines a complete cure as negative potassium hydroxide preparation and negative fungal culture plus a completely normal appearance of the nail.
Treatment of onychomycosis poses a number of challenges. First, hyperkeratosis and the fungal mass may limit the delivery of topical and systemic drugs to the source of the infection. In addition, high rates of relapse and reinfection after treatment may be due to residual hyphae or spores.5 Furthermore, the extended length of treatment limits patient adherence and many patients are unwilling to forego wearing nail cosmetics during the course of some of the treatments.
There are 4 approved classes of antifungal drugs for the treatment of onychomycosis: allylamines, azoles, morpholines, and hydroxypyridinones.6 The allylamines (eg, terbinafine) inhibit squalene epoxidase.7 Oral terbinafine (250 mg daily) taken for 6 weeks for fingernails and 12 weeks for toenails is considered the current systemic treatment preference in onychomycosis therapy8 with complete cure rates in 12-week studies of approximately 38%9 and 49%.10
The second class of drugs is the azoles, which inhibit lanosterol 14a-demethylase, a step in the ergosterol biosynthesis pathway.6 Two members of this class that are widely used in treating onychomycosis are oral itraconazole11 and off-label oral fluconazole.12 The approved dose for oral itraconazole is 200 mg daily for 3 months (or an alternative pulse regimen) with a reported complete cure rate of 14%.11 Although fluconazole is not FDA approved for the treatment of onychomycosis in the United States, it is used extensively in other countries and to some extent off label in the United States. In a study of 362 patients with onychomycosis treated with oral fluconazole, complete cure rates were 48% in patients who received 450 mg weekly, 46% in those who received 300 mg weekly, and 37% in those who received 150 mg weekly for up to 9 months.12 It should be noted that several oral triazole antifungals, namely albaconazole,13 posaconazole,14 and ravuconazole,15 have undergone phase 1 and 2 studies for the treatment of onychomycosis and have shown some efficacy.
Another class of antifungals are the morpholines including topical amorolfine, which is approved for use in Europe but not in North America.16 Amorolfine inhibits D14 reductase and D7-D8 isomerase, thus depleting ergosterol.17 In one randomized controlled study, the combination of amorolfine nail lacquer and oral terbinafine compared to oral terbinafine alone resulted in a higher clinical cure rate with the combination (59.2% vs 46%); complete cure rate was not reported.16
Finally, the hydroxypyridinone class includes topical ciclopirox, which has a poorly understood mechanism of action but may involve iron chelation or oxidative damage.18,19 Ciclopirox nail lacquer 8% was approved by the FDA in 1999 and has reported complete cure rates of 5.5% to 8.5% with monthly nail debridement.20
Based on the poor efficacy of many of the currently available treatments and time-consuming treatment courses, it is clear that there is a need for alternative and novel therapies. There has been a greater emphasis on topical agents due to their more favorable side-effect profile and lower risk for drug-drug interactions. Although there are many agents for the treatment of onychomycosis currently in development, many are in vitro studies or phase 1 and 2 studies. However, we will focus on drugs that are further along in phase 3 studies and those that were recently FDA approved.
Efinaconazole is a member of the azole class of drugs and has completed 2 phase 3 clinical trials (study 1, N=870; study 2, N=785).21 Patients in these 2 studies were randomized to receive either efinaconazole nail solution 10% or vehicle for 48 weeks followed by a 4-week washout period. Complete cure rates in the 2 studies were 17.8% and 15.2% in the treated group and 3.3% and 5.5% in the control group. The mycological cure rates were 55.2% and 53.4% in the treated group and 16.8% and 16.9% in the control group. The side-effect profile was minimal, with the most common adverse events being application-site dermatitis and vesiculation, which were not significantly higher in the treated group versus the control group.21 Efinaconazole received FDA approval for the treatment of toenail onychomycosis in June 2014.
There are some notable differences between ciclopirox and efinaconazole that may improve patient compliance with the latter. First, treatment with ciclopirox includes monthly nail debridement, which is not required with efinaconazole. Secondly, although ciclopirox lacquer must be removed weekly, efinaconazole is a solution, so no removal is necessary.
Terbinafine nail solution (TNS) is a member of the allylamine class and has completed phase 3 clinical trials.22 Three studies—2 vehicle controlled and 1 active comparator—were performed. The first compared TNS and vehicle, both applied daily for 24 weeks; the second study repeated the same for 48 weeks; and the third study compared TNS to amorolfine nail lacquer 5% daily for 48 weeks. The best results for complete cure were achieved with TNS for 48 weeks in the vehicle-controlled study with a rate of 2.2% versus 0%. The authors also concluded TNS was not more effective than amorolfine, as complete cure rates were 1.2% for TNS and 0.96% for amorolfine. The most common side effects were headache, nasopharyngitis, and influenza.22
Tavaborole is a member of the new benzoxaborole class, which inhibits protein synthesis by forming an adduct with the aminoacyl–transfer RNA synthetase.23 The topical solution was engineered to have improved penetration through the nail plate. In vitro studies showed better penetration than both ciclopirox and amorolfine.24 Two identical phase 3 randomized, double-blind, vehicle-controlled studies were completed involving 1197 patients who were treated with tavaborole topical solution 5% daily compared to vehicle for 48 weeks followed by a 4-week washout period with promising results.25 The incidence of treatment-related side effects was comparable to the vehicle. The most common adverse events were exfoliation, erythema, and dermatitis, all occurring at the application site.25 Tavaborole was approved by the FDA for the treatment of toenail onychomycosis in July 2014.
Luliconazole is a member of the azole class and a phase 2b/3 clinical trial with a 10% solution involving 334 patients was completed in June 2013.26 Results from this trial are expected in early 2015.
Lasers are a developing area for onychomycosis therapy and the appeal stems from their ability to selectively deliver energy to the target tissue, thus avoiding systemic side effects. Since 2010, the FDA has approved numerous laser devices for the temporary cosmetic improvement of onychomycosis, all of which are Nd:YAG 1064-nm lasers.27,28 It was previously thought that the mechanism of action for the fungicidal effect was achieved with heat,29 but newer in vitro studies have shown that the amount of time and level of heat required to kill Trichophyton rubrum would not be tolerable to patients.30 Although the mechanism of action is poorly understood, some clinical trials have shown success using the Nd:YAG 1064-nm laser for treatment of onychomycosis. However, in a study of 8 patients treated with the Nd:YAG 1064-nm laser for 5 treatment sessions, none had a mycological or clinical cure and there was only mild clinical improvement. In addition, most patients had pain and burning during the treatments requiring many short breaks.30 Although not yet FDA approved for the treatment of onychomycosis, other types of lasers are currently being studied, including CO2, near-infrared diode, and femtosecond-infrared laser systems.3
Plasma therapy is a developing area for the treatment of onychomycosis. Plasma was shown to be fungicidal to T rubrum in an in vitro model (MOE Medical Devices, written communication, July 2012), and a clinical trial to evaluate the safety, tolerability, and efficacy of plasma in human subjects is ongoing (registered on March 22, 2013, at www.clinicaltrials.gov with the identifier NCT01819051).
Onychomycosis is a common problem that increases in prevalence with advancing age. Oral terbinafine is considered the first-line treatment at this point in time.31 Two new topical agents, efinaconazole and tavaborole, were recently FDA approved and may be used for the treatment of toenail onychomycosis without the need for nail debridement. The Nd:YAG laser has shown some promise in earlier clinical studies but was ineffective in a more recent study.
To the Editor:
Onychomycosis is a fungal infection of the nail plate by dermatophytes, yeasts, and nondermatophyte molds. It is a common problem with a prevalence of 10% to 12% in the United States.1,2 The clinical presentation of onychomycosis is shown in the Figure. Although some patients may have mild asymptomatic cases of onychomycosis and do not inquire about treatment, many will have more advanced cases, presenting with pain and discomfort, secondary infection, unattractive appearance, or problems performing everyday functions. The goal of onychomycosis treatment is to eliminate the fungus, if possible, which usually restores the nail to its normal state when it fully grows out. Patients should be counseled that it is a long process that may take 6 months or more for fingernails and 12 to 18 months for toenails. These estimates are based on a growth rate of 2 to 3 mm per month for fingernails and 1 to 2 mm per month for toenails.3 Nails grow fastest during the teenaged years and slow down with advancing age.4 It should be noted that advanced cases of onychomycosis affecting the nail matrix may cause permanent scarring; therefore, the nail unit may still appear dystrophic after the causative organism is eliminated. The US Food and Drug Administration (FDA) defines a complete cure as negative potassium hydroxide preparation and negative fungal culture plus a completely normal appearance of the nail.
Treatment of onychomycosis poses a number of challenges. First, hyperkeratosis and the fungal mass may limit the delivery of topical and systemic drugs to the source of the infection. In addition, high rates of relapse and reinfection after treatment may be due to residual hyphae or spores.5 Furthermore, the extended length of treatment limits patient adherence and many patients are unwilling to forego wearing nail cosmetics during the course of some of the treatments.
There are 4 approved classes of antifungal drugs for the treatment of onychomycosis: allylamines, azoles, morpholines, and hydroxypyridinones.6 The allylamines (eg, terbinafine) inhibit squalene epoxidase.7 Oral terbinafine (250 mg daily) taken for 6 weeks for fingernails and 12 weeks for toenails is considered the current systemic treatment preference in onychomycosis therapy8 with complete cure rates in 12-week studies of approximately 38%9 and 49%.10
The second class of drugs is the azoles, which inhibit lanosterol 14a-demethylase, a step in the ergosterol biosynthesis pathway.6 Two members of this class that are widely used in treating onychomycosis are oral itraconazole11 and off-label oral fluconazole.12 The approved dose for oral itraconazole is 200 mg daily for 3 months (or an alternative pulse regimen) with a reported complete cure rate of 14%.11 Although fluconazole is not FDA approved for the treatment of onychomycosis in the United States, it is used extensively in other countries and to some extent off label in the United States. In a study of 362 patients with onychomycosis treated with oral fluconazole, complete cure rates were 48% in patients who received 450 mg weekly, 46% in those who received 300 mg weekly, and 37% in those who received 150 mg weekly for up to 9 months.12 It should be noted that several oral triazole antifungals, namely albaconazole,13 posaconazole,14 and ravuconazole,15 have undergone phase 1 and 2 studies for the treatment of onychomycosis and have shown some efficacy.
Another class of antifungals are the morpholines including topical amorolfine, which is approved for use in Europe but not in North America.16 Amorolfine inhibits D14 reductase and D7-D8 isomerase, thus depleting ergosterol.17 In one randomized controlled study, the combination of amorolfine nail lacquer and oral terbinafine compared to oral terbinafine alone resulted in a higher clinical cure rate with the combination (59.2% vs 46%); complete cure rate was not reported.16
Finally, the hydroxypyridinone class includes topical ciclopirox, which has a poorly understood mechanism of action but may involve iron chelation or oxidative damage.18,19 Ciclopirox nail lacquer 8% was approved by the FDA in 1999 and has reported complete cure rates of 5.5% to 8.5% with monthly nail debridement.20
Based on the poor efficacy of many of the currently available treatments and time-consuming treatment courses, it is clear that there is a need for alternative and novel therapies. There has been a greater emphasis on topical agents due to their more favorable side-effect profile and lower risk for drug-drug interactions. Although there are many agents for the treatment of onychomycosis currently in development, many are in vitro studies or phase 1 and 2 studies. However, we will focus on drugs that are further along in phase 3 studies and those that were recently FDA approved.
Efinaconazole is a member of the azole class of drugs and has completed 2 phase 3 clinical trials (study 1, N=870; study 2, N=785).21 Patients in these 2 studies were randomized to receive either efinaconazole nail solution 10% or vehicle for 48 weeks followed by a 4-week washout period. Complete cure rates in the 2 studies were 17.8% and 15.2% in the treated group and 3.3% and 5.5% in the control group. The mycological cure rates were 55.2% and 53.4% in the treated group and 16.8% and 16.9% in the control group. The side-effect profile was minimal, with the most common adverse events being application-site dermatitis and vesiculation, which were not significantly higher in the treated group versus the control group.21 Efinaconazole received FDA approval for the treatment of toenail onychomycosis in June 2014.
There are some notable differences between ciclopirox and efinaconazole that may improve patient compliance with the latter. First, treatment with ciclopirox includes monthly nail debridement, which is not required with efinaconazole. Secondly, although ciclopirox lacquer must be removed weekly, efinaconazole is a solution, so no removal is necessary.
Terbinafine nail solution (TNS) is a member of the allylamine class and has completed phase 3 clinical trials.22 Three studies—2 vehicle controlled and 1 active comparator—were performed. The first compared TNS and vehicle, both applied daily for 24 weeks; the second study repeated the same for 48 weeks; and the third study compared TNS to amorolfine nail lacquer 5% daily for 48 weeks. The best results for complete cure were achieved with TNS for 48 weeks in the vehicle-controlled study with a rate of 2.2% versus 0%. The authors also concluded TNS was not more effective than amorolfine, as complete cure rates were 1.2% for TNS and 0.96% for amorolfine. The most common side effects were headache, nasopharyngitis, and influenza.22
Tavaborole is a member of the new benzoxaborole class, which inhibits protein synthesis by forming an adduct with the aminoacyl–transfer RNA synthetase.23 The topical solution was engineered to have improved penetration through the nail plate. In vitro studies showed better penetration than both ciclopirox and amorolfine.24 Two identical phase 3 randomized, double-blind, vehicle-controlled studies were completed involving 1197 patients who were treated with tavaborole topical solution 5% daily compared to vehicle for 48 weeks followed by a 4-week washout period with promising results.25 The incidence of treatment-related side effects was comparable to the vehicle. The most common adverse events were exfoliation, erythema, and dermatitis, all occurring at the application site.25 Tavaborole was approved by the FDA for the treatment of toenail onychomycosis in July 2014.
Luliconazole is a member of the azole class and a phase 2b/3 clinical trial with a 10% solution involving 334 patients was completed in June 2013.26 Results from this trial are expected in early 2015.
Lasers are a developing area for onychomycosis therapy and the appeal stems from their ability to selectively deliver energy to the target tissue, thus avoiding systemic side effects. Since 2010, the FDA has approved numerous laser devices for the temporary cosmetic improvement of onychomycosis, all of which are Nd:YAG 1064-nm lasers.27,28 It was previously thought that the mechanism of action for the fungicidal effect was achieved with heat,29 but newer in vitro studies have shown that the amount of time and level of heat required to kill Trichophyton rubrum would not be tolerable to patients.30 Although the mechanism of action is poorly understood, some clinical trials have shown success using the Nd:YAG 1064-nm laser for treatment of onychomycosis. However, in a study of 8 patients treated with the Nd:YAG 1064-nm laser for 5 treatment sessions, none had a mycological or clinical cure and there was only mild clinical improvement. In addition, most patients had pain and burning during the treatments requiring many short breaks.30 Although not yet FDA approved for the treatment of onychomycosis, other types of lasers are currently being studied, including CO2, near-infrared diode, and femtosecond-infrared laser systems.3
Plasma therapy is a developing area for the treatment of onychomycosis. Plasma was shown to be fungicidal to T rubrum in an in vitro model (MOE Medical Devices, written communication, July 2012), and a clinical trial to evaluate the safety, tolerability, and efficacy of plasma in human subjects is ongoing (registered on March 22, 2013, at www.clinicaltrials.gov with the identifier NCT01819051).
Onychomycosis is a common problem that increases in prevalence with advancing age. Oral terbinafine is considered the first-line treatment at this point in time.31 Two new topical agents, efinaconazole and tavaborole, were recently FDA approved and may be used for the treatment of toenail onychomycosis without the need for nail debridement. The Nd:YAG laser has shown some promise in earlier clinical studies but was ineffective in a more recent study.
1. Ghannoum MA, Hajjeh RA, Scher R, et al. A large-scale North American study of fungal isolates from nails: the frequency of onychomycosis, fungal distribution, and antifungal susceptibility patterns. J Am Acad Dermatol. 2000;43:641-648.
2. Heikkila H, Stubb S. The prevalence of onychomycosis in Finland. Br J Dermatol. 1995;133:699-703.
3. Scher RK, Rich P, Pariser D, et al. The epidemiology, etiology, and pathophysiology of onychomycosis. Semin Cutan Med Surg. 2013;32(2, suppl 1):S2-S4.
4. Abdullah L, Abbas O. Common nail changes and disorders in older people: diagnosis and management. Can Fam Physician. 2011;57:173-181.
5. Scher RK, Baran R. Onychomycosis in clinical practice: factors contributing to recurrence. Br J Dermatol. 2003;149(suppl 65):5-9.
6. Welsh O, Vera-Cabrera L, Welsh E. Onychomycosis. Clin Dermatol. 2010;28:151-159.
7. Gupta AK, Sauder DN, Shear NH. Antifungal agents: an overview. part II. J Am Acad Dermatol. 1994;30:911-933.
8. Gupta AK, Paquet M, Simpson F, et al. Terbinafine in the treatment of dermatophyte toenail onychomycosis: a meta-analysis of efficacy for continuous and intermittent regimens. J Eur Acad Dermatol Venereol. 2013;27:267-272.
9. Drake LA, Shear NH, Arlette JP, et al. Oral terbinafine in the treatment of toenail onychomycosis: North American multicenter trial. J Am Acad Dermatol. 1997;37:740-745.
10. Evans EG, Sigurgeirsson B. Double blind, randomised study of continuous terbinafine compared with intermittent itraconazole in treatment of toenail onychomycosis. the LION Study Group. BMJ. 1999;318:1031-1035.
11. Sporanox [package insert]. Macquarie Park, Australia: Janssen-Cilag Pty Ltd; 2014.
12. Scher RK, Breneman D, Rich P, et al. Once-weekly fluconazole (150, 300, or 450 mg) in the treatment of distal subungual onychomycosis of the toenail. J Am Acad Dermatol. 1998;38(6, pt 2):S77-S86.
13. Sigurgeirsson B, van Rossem K, Malahias S, et al. A phase II, randomized, double-blind, placebo-controlled, parallel group, dose-ranging study to investigate the efficacy and safety of 4 dose regimens of oral albaconazole in patients with distal subungual onychomycosis. J Am Acad Dermatol. 2013;69:416-425.
14. Elewski B, Pollak R, Ashton S, et al. A randomized, placebo- and active-controlled, parallel-group, multicentre, investigator-blinded study of four treatment regimens of posaconazole in adults with toenail onychomycosis. Br J Dermatol. 2012;166:389-398.
15. Gupta AK, Leonardi C, Stoltz RR, et al. A phase I/II randomized, double-blind, placebo-controlled, dose-ranging study evaluating the efficacy, safety and pharmacokinetics of ravuconazole in the treatment of onychomycosis. J Eur Acad Dermatol Venereol. 2005;19:437-443.
16. Baran R, Sigurgeirsson B, de Berker D, et al. A multicentre, randomized, controlled study of the efficacy, safety and cost-effectiveness of a combination therapy with amorolfine nail lacquer and oral terbinafine compared with oral terbinafine alone for the treatment of onychomycosis with matrix involvement. Br J Dermatol. 2007;157:149-157.
17. Polak A. Preclinical data and mode of action of amorolfine. Dermatology. 1992;184(suppl 1):3-7.
18. Belenky P, Camacho D, Collins JJ. Fungicidal drugs induce a common oxidative-damage cellular death pathway. Cell Rep. 2013;3:350-358.
19. Lee RE, Liu TT, Barker KS, et al. Genome-wide expression profiling of the response to ciclopirox olamine in Candida albicans. J Antimicrob Chemother. 2005;55:655-662.
20. Penlac [package insert]. Bridgewater, NJ: sanofi-aventis; 2006.
21. Elewski BE, Rich P, Pollak R, et al. Efinaconazole 10% solution in the treatment of toenail onychomycosis: two phase III multicenter, randomized, double-blind studies. J Am Acad Dermatol. 2013;68:600-608.
22. Elewski BE, Ghannoum MA, Mayser P, et al. Efficacy, safety and tolerability of topical terbinafine nail solution in patients with mild-to-moderate toenail onychomycosis: results from three randomized studies using double-blind vehicle-controlled and open-label active-controlled designs. J Eur Acad Dermatol Venereol. 2013;27:287-294.
23. Rock FL, Mao W, Yaremchuk A, et al. An antifungal agent inhibits an aminoacyl-tRNA synthetase by trapping tRNA in the editing site. Science. 2007;316:1759-1761.
24. Hui X, Baker SJ, Wester RC, et al. In vitro penetration of a novel oxaborole antifungal (AN2690) into the human nail plate. J Pharm Sci. 2007;96:2622-2631.
25. Elewski BE, Rich P, Wiltz H, et al. Effectiveness and safety of tavaborole, a novel born-based molecule for the treatment of onychomycosis: results from two phase 3 studies. Poster presented at: Women’s & Pediatric Dermatology Seminar; October 4-6, 2013; Newport Beach, CA.
26. The solution study: Topica’s phase 2b/3 clinical trial. Topica Pharmaceuticals Inc Web site. http://www.
topicapharma.com/phase-2b3. Accessed December 2, 2014.
27. Gupta AK, Simpson FC. Medical devices for the treatment of onychomycosis. Dermatol Ther. 2012;25:574-581.
28. Ortiz AE, Avram MM, Wanner MA. A review of lasers and light for the treatment of onychomycosis. Lasers Surg Med. 2014;46:117-124.
29. Vural E, Winfield HL, Shingleton AW, et al. The effects of laser irradiation on Trichophyton rubrum growth. Lasers Med Sci. 2008;23:349-353.
30. Carney C, Cantrell W, Warner J, et al. Treatment of onychomycosis using a submillisecond 1064-nm neodymium:yttrium-aluminum-garnet laser. J Am Acad Dermatol. 2013;69:578-582.
31. Gupta AK, Daigle D, Paquet M. Therapies for onychomycosis: a systematic review and network meta-analysis of mycological cure [published online ahead of print July 17, 2014]. J Am Podiatr Med Assoc. doi:10.7547/13-110.1.
1. Ghannoum MA, Hajjeh RA, Scher R, et al. A large-scale North American study of fungal isolates from nails: the frequency of onychomycosis, fungal distribution, and antifungal susceptibility patterns. J Am Acad Dermatol. 2000;43:641-648.
2. Heikkila H, Stubb S. The prevalence of onychomycosis in Finland. Br J Dermatol. 1995;133:699-703.
3. Scher RK, Rich P, Pariser D, et al. The epidemiology, etiology, and pathophysiology of onychomycosis. Semin Cutan Med Surg. 2013;32(2, suppl 1):S2-S4.
4. Abdullah L, Abbas O. Common nail changes and disorders in older people: diagnosis and management. Can Fam Physician. 2011;57:173-181.
5. Scher RK, Baran R. Onychomycosis in clinical practice: factors contributing to recurrence. Br J Dermatol. 2003;149(suppl 65):5-9.
6. Welsh O, Vera-Cabrera L, Welsh E. Onychomycosis. Clin Dermatol. 2010;28:151-159.
7. Gupta AK, Sauder DN, Shear NH. Antifungal agents: an overview. part II. J Am Acad Dermatol. 1994;30:911-933.
8. Gupta AK, Paquet M, Simpson F, et al. Terbinafine in the treatment of dermatophyte toenail onychomycosis: a meta-analysis of efficacy for continuous and intermittent regimens. J Eur Acad Dermatol Venereol. 2013;27:267-272.
9. Drake LA, Shear NH, Arlette JP, et al. Oral terbinafine in the treatment of toenail onychomycosis: North American multicenter trial. J Am Acad Dermatol. 1997;37:740-745.
10. Evans EG, Sigurgeirsson B. Double blind, randomised study of continuous terbinafine compared with intermittent itraconazole in treatment of toenail onychomycosis. the LION Study Group. BMJ. 1999;318:1031-1035.
11. Sporanox [package insert]. Macquarie Park, Australia: Janssen-Cilag Pty Ltd; 2014.
12. Scher RK, Breneman D, Rich P, et al. Once-weekly fluconazole (150, 300, or 450 mg) in the treatment of distal subungual onychomycosis of the toenail. J Am Acad Dermatol. 1998;38(6, pt 2):S77-S86.
13. Sigurgeirsson B, van Rossem K, Malahias S, et al. A phase II, randomized, double-blind, placebo-controlled, parallel group, dose-ranging study to investigate the efficacy and safety of 4 dose regimens of oral albaconazole in patients with distal subungual onychomycosis. J Am Acad Dermatol. 2013;69:416-425.
14. Elewski B, Pollak R, Ashton S, et al. A randomized, placebo- and active-controlled, parallel-group, multicentre, investigator-blinded study of four treatment regimens of posaconazole in adults with toenail onychomycosis. Br J Dermatol. 2012;166:389-398.
15. Gupta AK, Leonardi C, Stoltz RR, et al. A phase I/II randomized, double-blind, placebo-controlled, dose-ranging study evaluating the efficacy, safety and pharmacokinetics of ravuconazole in the treatment of onychomycosis. J Eur Acad Dermatol Venereol. 2005;19:437-443.
16. Baran R, Sigurgeirsson B, de Berker D, et al. A multicentre, randomized, controlled study of the efficacy, safety and cost-effectiveness of a combination therapy with amorolfine nail lacquer and oral terbinafine compared with oral terbinafine alone for the treatment of onychomycosis with matrix involvement. Br J Dermatol. 2007;157:149-157.
17. Polak A. Preclinical data and mode of action of amorolfine. Dermatology. 1992;184(suppl 1):3-7.
18. Belenky P, Camacho D, Collins JJ. Fungicidal drugs induce a common oxidative-damage cellular death pathway. Cell Rep. 2013;3:350-358.
19. Lee RE, Liu TT, Barker KS, et al. Genome-wide expression profiling of the response to ciclopirox olamine in Candida albicans. J Antimicrob Chemother. 2005;55:655-662.
20. Penlac [package insert]. Bridgewater, NJ: sanofi-aventis; 2006.
21. Elewski BE, Rich P, Pollak R, et al. Efinaconazole 10% solution in the treatment of toenail onychomycosis: two phase III multicenter, randomized, double-blind studies. J Am Acad Dermatol. 2013;68:600-608.
22. Elewski BE, Ghannoum MA, Mayser P, et al. Efficacy, safety and tolerability of topical terbinafine nail solution in patients with mild-to-moderate toenail onychomycosis: results from three randomized studies using double-blind vehicle-controlled and open-label active-controlled designs. J Eur Acad Dermatol Venereol. 2013;27:287-294.
23. Rock FL, Mao W, Yaremchuk A, et al. An antifungal agent inhibits an aminoacyl-tRNA synthetase by trapping tRNA in the editing site. Science. 2007;316:1759-1761.
24. Hui X, Baker SJ, Wester RC, et al. In vitro penetration of a novel oxaborole antifungal (AN2690) into the human nail plate. J Pharm Sci. 2007;96:2622-2631.
25. Elewski BE, Rich P, Wiltz H, et al. Effectiveness and safety of tavaborole, a novel born-based molecule for the treatment of onychomycosis: results from two phase 3 studies. Poster presented at: Women’s & Pediatric Dermatology Seminar; October 4-6, 2013; Newport Beach, CA.
26. The solution study: Topica’s phase 2b/3 clinical trial. Topica Pharmaceuticals Inc Web site. http://www.
topicapharma.com/phase-2b3. Accessed December 2, 2014.
27. Gupta AK, Simpson FC. Medical devices for the treatment of onychomycosis. Dermatol Ther. 2012;25:574-581.
28. Ortiz AE, Avram MM, Wanner MA. A review of lasers and light for the treatment of onychomycosis. Lasers Surg Med. 2014;46:117-124.
29. Vural E, Winfield HL, Shingleton AW, et al. The effects of laser irradiation on Trichophyton rubrum growth. Lasers Med Sci. 2008;23:349-353.
30. Carney C, Cantrell W, Warner J, et al. Treatment of onychomycosis using a submillisecond 1064-nm neodymium:yttrium-aluminum-garnet laser. J Am Acad Dermatol. 2013;69:578-582.
31. Gupta AK, Daigle D, Paquet M. Therapies for onychomycosis: a systematic review and network meta-analysis of mycological cure [published online ahead of print July 17, 2014]. J Am Podiatr Med Assoc. doi:10.7547/13-110.1.










