User login
Patients and Surgeons Diverge on Disclosures
SAN FRANCISCO – Recent surveys of patients and attending surgeons show differing views on disclosures, Dr. Susan Lee Char said at the clinical congress of the American College of Surgeons.
She and her associates surveyed 353 adult patients at their first postoperative clinic visit and 85 attending surgeons at hospitals affiliated with the University of California, San Francisco. The survey presented a hypothetical case of a patient’s undergoing elective partial hepatectomy and asked respondents to rate the importance of receiving or conveying various items of information on a 6-point Likert scale.
In all, 79% of patients said it’s essential to know if their surgeon would be doing a procedure for the first time on them, but only 55% of attending surgeons felt this was important information to disclose. A total of 63% of patients considered it essential to know the number of times a surgeon had performed a particular procedure and the outcomes in those cases, compared with just 25% and 20% of surgeons, respectively.
"The data suggest that surgeons do have an ethical obligation to disclose volumes and outcomes and if it’s the first time [they’re] doing a procedure," said Dr. Char, a surgical resident at the university who is also a lawyer. "This has possible legal implications."
The main barrier to surgeons’ disclosure may be a practical one, she added. Surgeons often don’t have data on the volumes and outcomes of their procedures.
Patients’ and attending surgeons’ perceptions of the importance of other types of information also differed significantly. A general description of the procedure was rated as important by 65% of patients vs. 58% of surgeons, and technical details of the procedure were important to 48% of patients and 13% of surgeons. Disclosure of risks and benefits of the procedure were deemed essential by 77% and 71% of patients, respectively, compared with 72% and 65% of surgeons, respectively. A total of 41% of patients and 5% of surgeons said the patient should be told the number of times the procedure has been done by other surgeons, and 44% of patients and 20% of surgeons said other surgeons’ outcomes should be disclosed.
A total of 64% of patients and 31% of surgeons believed it was important to discuss any special training by the surgeon doing the procedure. Some 64% of patients said they would want to be informed about the surgeon’s special training for a standard procedure, compared with 68% for a laparoscopic procedure and 71% for a robotic procedure.
Technological innovation made a difference in whether patients deemed certain information essential. Patients scheduled for a laparoscopic or robotic procedure were significantly more likely to want information than those undergoing a standard operation.
In all, 63% of patients said they would want to know the number of times that a standard procedure had been done by their surgeon. That percentage rose to 66% for a laparoscopic procedure and to 68% for a robotic procedure. Outcomes information was considered important by 63% of patients for a standard procedure, 66% for a laparoscopic procedure, and 67% for a robotic procedure. And 24% of patients, compared with 6% of surgeons, said the patient should be told if the surgeon planned to publish an article including the case. Disclosing whether a surgeon is a paid consultant was less important to patients (5%) than to surgeons (40%).
Dr. Char had no conflicts of interest.
This study is an important one for all practicing surgeons. Informed consent is central to the practice of surgery, and disclosure of information is a cornerstone of the consent process. Nevertheless, as Dr. Char’s study so dramatically illustrates, surgeons and patients frequently disagree on which items must be disclosed in order to obtain informed consent.
A few important areas of discrepancy are revealed. For example, patients considered disclosure of how many times a surgeon had performed a specific procedure more important than did surgeons. Similarly, only 55% of surgeons thought it was important to disclose to patients whether they were performing an operation for the first time, whereas 79% of patients said that such information was essential. On the other hand, despite the national movement to disclose financial conflicts of interest, only 5% of patients wanted to know if their surgeon was a paid consultant to industry compared with 40% of surgeons who felt that this is important to disclose.
What conclusions should we draw from these discrepancies between what patients say they want to know and what surgeons say is important to disclose in the informed consent process? Most important, surgeons should realize the difficulties we have in accurately predicting what information will be important to our patients. If we assume that we know how much information our patients want, we will almost certainly guess incorrectly. As a result, a different strategy should be adopted. Surgeons should tailor their disclosure in the consent process to the specific information needs of the individual patient. This can readily be accomplished by asking, "What additional questions do you have?" or "What information do you need in order to feel comfortable consenting to this operation?" If surgeons were to be guided by their patients when tailoring the nature and amount of information they disclose, patients would more likely be satisfied with that disclosure and the consent process would be improved.
Dr. Peter Angelos is an ACS Fellow, professor of surgery, and associate director, MacLean Center for Clinical Medical Ethics, University of Chicago.
This study is an important one for all practicing surgeons. Informed consent is central to the practice of surgery, and disclosure of information is a cornerstone of the consent process. Nevertheless, as Dr. Char’s study so dramatically illustrates, surgeons and patients frequently disagree on which items must be disclosed in order to obtain informed consent.
A few important areas of discrepancy are revealed. For example, patients considered disclosure of how many times a surgeon had performed a specific procedure more important than did surgeons. Similarly, only 55% of surgeons thought it was important to disclose to patients whether they were performing an operation for the first time, whereas 79% of patients said that such information was essential. On the other hand, despite the national movement to disclose financial conflicts of interest, only 5% of patients wanted to know if their surgeon was a paid consultant to industry compared with 40% of surgeons who felt that this is important to disclose.
What conclusions should we draw from these discrepancies between what patients say they want to know and what surgeons say is important to disclose in the informed consent process? Most important, surgeons should realize the difficulties we have in accurately predicting what information will be important to our patients. If we assume that we know how much information our patients want, we will almost certainly guess incorrectly. As a result, a different strategy should be adopted. Surgeons should tailor their disclosure in the consent process to the specific information needs of the individual patient. This can readily be accomplished by asking, "What additional questions do you have?" or "What information do you need in order to feel comfortable consenting to this operation?" If surgeons were to be guided by their patients when tailoring the nature and amount of information they disclose, patients would more likely be satisfied with that disclosure and the consent process would be improved.
Dr. Peter Angelos is an ACS Fellow, professor of surgery, and associate director, MacLean Center for Clinical Medical Ethics, University of Chicago.
This study is an important one for all practicing surgeons. Informed consent is central to the practice of surgery, and disclosure of information is a cornerstone of the consent process. Nevertheless, as Dr. Char’s study so dramatically illustrates, surgeons and patients frequently disagree on which items must be disclosed in order to obtain informed consent.
A few important areas of discrepancy are revealed. For example, patients considered disclosure of how many times a surgeon had performed a specific procedure more important than did surgeons. Similarly, only 55% of surgeons thought it was important to disclose to patients whether they were performing an operation for the first time, whereas 79% of patients said that such information was essential. On the other hand, despite the national movement to disclose financial conflicts of interest, only 5% of patients wanted to know if their surgeon was a paid consultant to industry compared with 40% of surgeons who felt that this is important to disclose.
What conclusions should we draw from these discrepancies between what patients say they want to know and what surgeons say is important to disclose in the informed consent process? Most important, surgeons should realize the difficulties we have in accurately predicting what information will be important to our patients. If we assume that we know how much information our patients want, we will almost certainly guess incorrectly. As a result, a different strategy should be adopted. Surgeons should tailor their disclosure in the consent process to the specific information needs of the individual patient. This can readily be accomplished by asking, "What additional questions do you have?" or "What information do you need in order to feel comfortable consenting to this operation?" If surgeons were to be guided by their patients when tailoring the nature and amount of information they disclose, patients would more likely be satisfied with that disclosure and the consent process would be improved.
Dr. Peter Angelos is an ACS Fellow, professor of surgery, and associate director, MacLean Center for Clinical Medical Ethics, University of Chicago.
SAN FRANCISCO – Recent surveys of patients and attending surgeons show differing views on disclosures, Dr. Susan Lee Char said at the clinical congress of the American College of Surgeons.
She and her associates surveyed 353 adult patients at their first postoperative clinic visit and 85 attending surgeons at hospitals affiliated with the University of California, San Francisco. The survey presented a hypothetical case of a patient’s undergoing elective partial hepatectomy and asked respondents to rate the importance of receiving or conveying various items of information on a 6-point Likert scale.
In all, 79% of patients said it’s essential to know if their surgeon would be doing a procedure for the first time on them, but only 55% of attending surgeons felt this was important information to disclose. A total of 63% of patients considered it essential to know the number of times a surgeon had performed a particular procedure and the outcomes in those cases, compared with just 25% and 20% of surgeons, respectively.
"The data suggest that surgeons do have an ethical obligation to disclose volumes and outcomes and if it’s the first time [they’re] doing a procedure," said Dr. Char, a surgical resident at the university who is also a lawyer. "This has possible legal implications."
The main barrier to surgeons’ disclosure may be a practical one, she added. Surgeons often don’t have data on the volumes and outcomes of their procedures.
Patients’ and attending surgeons’ perceptions of the importance of other types of information also differed significantly. A general description of the procedure was rated as important by 65% of patients vs. 58% of surgeons, and technical details of the procedure were important to 48% of patients and 13% of surgeons. Disclosure of risks and benefits of the procedure were deemed essential by 77% and 71% of patients, respectively, compared with 72% and 65% of surgeons, respectively. A total of 41% of patients and 5% of surgeons said the patient should be told the number of times the procedure has been done by other surgeons, and 44% of patients and 20% of surgeons said other surgeons’ outcomes should be disclosed.
A total of 64% of patients and 31% of surgeons believed it was important to discuss any special training by the surgeon doing the procedure. Some 64% of patients said they would want to be informed about the surgeon’s special training for a standard procedure, compared with 68% for a laparoscopic procedure and 71% for a robotic procedure.
Technological innovation made a difference in whether patients deemed certain information essential. Patients scheduled for a laparoscopic or robotic procedure were significantly more likely to want information than those undergoing a standard operation.
In all, 63% of patients said they would want to know the number of times that a standard procedure had been done by their surgeon. That percentage rose to 66% for a laparoscopic procedure and to 68% for a robotic procedure. Outcomes information was considered important by 63% of patients for a standard procedure, 66% for a laparoscopic procedure, and 67% for a robotic procedure. And 24% of patients, compared with 6% of surgeons, said the patient should be told if the surgeon planned to publish an article including the case. Disclosing whether a surgeon is a paid consultant was less important to patients (5%) than to surgeons (40%).
Dr. Char had no conflicts of interest.
SAN FRANCISCO – Recent surveys of patients and attending surgeons show differing views on disclosures, Dr. Susan Lee Char said at the clinical congress of the American College of Surgeons.
She and her associates surveyed 353 adult patients at their first postoperative clinic visit and 85 attending surgeons at hospitals affiliated with the University of California, San Francisco. The survey presented a hypothetical case of a patient’s undergoing elective partial hepatectomy and asked respondents to rate the importance of receiving or conveying various items of information on a 6-point Likert scale.
In all, 79% of patients said it’s essential to know if their surgeon would be doing a procedure for the first time on them, but only 55% of attending surgeons felt this was important information to disclose. A total of 63% of patients considered it essential to know the number of times a surgeon had performed a particular procedure and the outcomes in those cases, compared with just 25% and 20% of surgeons, respectively.
"The data suggest that surgeons do have an ethical obligation to disclose volumes and outcomes and if it’s the first time [they’re] doing a procedure," said Dr. Char, a surgical resident at the university who is also a lawyer. "This has possible legal implications."
The main barrier to surgeons’ disclosure may be a practical one, she added. Surgeons often don’t have data on the volumes and outcomes of their procedures.
Patients’ and attending surgeons’ perceptions of the importance of other types of information also differed significantly. A general description of the procedure was rated as important by 65% of patients vs. 58% of surgeons, and technical details of the procedure were important to 48% of patients and 13% of surgeons. Disclosure of risks and benefits of the procedure were deemed essential by 77% and 71% of patients, respectively, compared with 72% and 65% of surgeons, respectively. A total of 41% of patients and 5% of surgeons said the patient should be told the number of times the procedure has been done by other surgeons, and 44% of patients and 20% of surgeons said other surgeons’ outcomes should be disclosed.
A total of 64% of patients and 31% of surgeons believed it was important to discuss any special training by the surgeon doing the procedure. Some 64% of patients said they would want to be informed about the surgeon’s special training for a standard procedure, compared with 68% for a laparoscopic procedure and 71% for a robotic procedure.
Technological innovation made a difference in whether patients deemed certain information essential. Patients scheduled for a laparoscopic or robotic procedure were significantly more likely to want information than those undergoing a standard operation.
In all, 63% of patients said they would want to know the number of times that a standard procedure had been done by their surgeon. That percentage rose to 66% for a laparoscopic procedure and to 68% for a robotic procedure. Outcomes information was considered important by 63% of patients for a standard procedure, 66% for a laparoscopic procedure, and 67% for a robotic procedure. And 24% of patients, compared with 6% of surgeons, said the patient should be told if the surgeon planned to publish an article including the case. Disclosing whether a surgeon is a paid consultant was less important to patients (5%) than to surgeons (40%).
Dr. Char had no conflicts of interest.
Major Finding: Only 55% of surgeons believed they should disclose that they would be doing a surgery for the first time on a patient when getting informed consent, compared with 79% of patients.
Data Source: Surveys presenting a hypothetical case to 353 patients at postoperative clinic visits, and to 85 attending surgeons.
Disclosures: Dr. Char said she has no relevant conflicts of interest.
Establishing Acute Pain Service Deemed Worthwhile
PALM SPRINGS, CALIF. – The University of Louisville has had an acute pain service for nearly a decade, but for many hospitals in the United States this still is a new idea.
"What we’re seeing is the birth of a new modality in treatment" and possibly a new specialty, Dr. Laura Clark said.
An acute pain service (APS) primarily manages pain after traumatic injury or surgery. The basic aspects of an APS include standardization of analgesic techniques, increased pain monitoring and assessment, and the ability to respond to inadequate or excessive doses of analgesics.
Establishing an APS, however, takes a lot of persuasion and education, said Dr. Clark, professor of anesthesiology and director of acute pain and regional anesthesia at the University of Louisville (Ky.).
Hospital administrators must be convinced that an APS can benefit the hospital by increasing patient satisfaction (which is strongly associated with adequate pain relief) and by cutting costs through reducing nausea and vomiting, respiratory depression, the incidence of ileus (and thus the length of hospitalization), and the incidence of chronic pain.
Physicians and pharmacists need to be willing to accept an APS as part of the care team. Many anesthesiologists mistakenly think that a single nerve block that dissipates in 10 hours is sufficient acute pain management, she said. But more than anyone, surgeons need convincing, Dr. Clark said at the annual meeting of the American Academy of Pain Medicine.
Currently, a surgeon must request involvement of the APS and that request must be documented in order for the service to be covered by insurers. "That needs to change," she said.
To get surgeons on board, include them in developing protocols for all analgesic techniques, she suggested.
There are two groups that don’t need convincing about the benefits of an APS – patients and nurses, she said. Still, education of nurses and all staff about the APS is essential. Simply asking nurses to follow written orders is not sufficient, especially for the more advanced pain therapies. Good acute pain care requires a change in culture and attitudes; for example, nurses need to change empty bags of analgesics just as they change other bags of fluids.
Nurses can be certified in pain management, and "I recommend that you have your nurses do that," Dr. Clark said.
The need for better acute pain management has been established by major reports in the United States, England, Australia, Germany, Sweden, and elsewhere. At least eight published studies report that an APS improves pain relief, five studies report a lower incidence of side effects, and three studies suggest that an APS may reduce the incidence of persistent pain after surgery, she said.
One study reported reduced postoperative morbidity and mortality with an APS but noted that "the workload is considerable" (Anesthesia 2006;61:24-8).
A recent study concluded that an APS is "likely" to be cost effective, but the investigators "didn’t even study what we do," Dr. Clark said. Key treatment techniques such as peripheral nerve blocks and epidural patient-controlled analgesia were not included in the study (Anesth. Analg. 2010;111:1042-50). Had it included those, she believes the study would have shown that an APS is very cost effective, she said.
Better studies with hard data are needed, she added.
The service ideally is physician directed but multidisciplinary, including physicians, nurses, pharmacists, and physical therapists. The most common but least desirable model of an APS in the United States includes a private physician or regionalist who may not do rounds unless called by a surgeon to manage a problem, Dr. Clark said. A second model that may be the most flexible and cost effective for around-the-clock care involves a nurse-led physician consult, in which the nurse makes daily rounds, reports to the physician, and implements therapy based on standard orders and protocols developed by the pain physician and surgeon.
The most common model in academic centers, and Dr. Clark’s favorite, is a physician-led team with a pain management nurse. The team makes rounds and decides on care. The pain physician may or may not be the regionalist. Medical residents are on call for the pain service. The pain nurse is involved in cases before, during, and after surgery and implements advanced pain management techniques, provides consultations, and coordinates with trauma, surgery, and critical care services.
Once you’ve convinced your institution and colleagues to establish an APS, make sure that someone on the APS can be reached by telephone at any hour of every day. Establish "acute pain champions" on every floor and in every area of the hospital, and make sure that at least one champion is available on every shift.
Running an APS can be challenging, but it’s a therapeutic tool that’s worth the effort, she said: "With our twice-a-day rounds, we often hear from the patients that we talk to them more than any other physician. It can be quite rewarding."
Dr. Clark has been a speaker for Covidien and Cadence and an adviser and researcher for Covidien.
PALM SPRINGS, CALIF. – The University of Louisville has had an acute pain service for nearly a decade, but for many hospitals in the United States this still is a new idea.
"What we’re seeing is the birth of a new modality in treatment" and possibly a new specialty, Dr. Laura Clark said.
An acute pain service (APS) primarily manages pain after traumatic injury or surgery. The basic aspects of an APS include standardization of analgesic techniques, increased pain monitoring and assessment, and the ability to respond to inadequate or excessive doses of analgesics.
Establishing an APS, however, takes a lot of persuasion and education, said Dr. Clark, professor of anesthesiology and director of acute pain and regional anesthesia at the University of Louisville (Ky.).
Hospital administrators must be convinced that an APS can benefit the hospital by increasing patient satisfaction (which is strongly associated with adequate pain relief) and by cutting costs through reducing nausea and vomiting, respiratory depression, the incidence of ileus (and thus the length of hospitalization), and the incidence of chronic pain.
Physicians and pharmacists need to be willing to accept an APS as part of the care team. Many anesthesiologists mistakenly think that a single nerve block that dissipates in 10 hours is sufficient acute pain management, she said. But more than anyone, surgeons need convincing, Dr. Clark said at the annual meeting of the American Academy of Pain Medicine.
Currently, a surgeon must request involvement of the APS and that request must be documented in order for the service to be covered by insurers. "That needs to change," she said.
To get surgeons on board, include them in developing protocols for all analgesic techniques, she suggested.
There are two groups that don’t need convincing about the benefits of an APS – patients and nurses, she said. Still, education of nurses and all staff about the APS is essential. Simply asking nurses to follow written orders is not sufficient, especially for the more advanced pain therapies. Good acute pain care requires a change in culture and attitudes; for example, nurses need to change empty bags of analgesics just as they change other bags of fluids.
Nurses can be certified in pain management, and "I recommend that you have your nurses do that," Dr. Clark said.
The need for better acute pain management has been established by major reports in the United States, England, Australia, Germany, Sweden, and elsewhere. At least eight published studies report that an APS improves pain relief, five studies report a lower incidence of side effects, and three studies suggest that an APS may reduce the incidence of persistent pain after surgery, she said.
One study reported reduced postoperative morbidity and mortality with an APS but noted that "the workload is considerable" (Anesthesia 2006;61:24-8).
A recent study concluded that an APS is "likely" to be cost effective, but the investigators "didn’t even study what we do," Dr. Clark said. Key treatment techniques such as peripheral nerve blocks and epidural patient-controlled analgesia were not included in the study (Anesth. Analg. 2010;111:1042-50). Had it included those, she believes the study would have shown that an APS is very cost effective, she said.
Better studies with hard data are needed, she added.
The service ideally is physician directed but multidisciplinary, including physicians, nurses, pharmacists, and physical therapists. The most common but least desirable model of an APS in the United States includes a private physician or regionalist who may not do rounds unless called by a surgeon to manage a problem, Dr. Clark said. A second model that may be the most flexible and cost effective for around-the-clock care involves a nurse-led physician consult, in which the nurse makes daily rounds, reports to the physician, and implements therapy based on standard orders and protocols developed by the pain physician and surgeon.
The most common model in academic centers, and Dr. Clark’s favorite, is a physician-led team with a pain management nurse. The team makes rounds and decides on care. The pain physician may or may not be the regionalist. Medical residents are on call for the pain service. The pain nurse is involved in cases before, during, and after surgery and implements advanced pain management techniques, provides consultations, and coordinates with trauma, surgery, and critical care services.
Once you’ve convinced your institution and colleagues to establish an APS, make sure that someone on the APS can be reached by telephone at any hour of every day. Establish "acute pain champions" on every floor and in every area of the hospital, and make sure that at least one champion is available on every shift.
Running an APS can be challenging, but it’s a therapeutic tool that’s worth the effort, she said: "With our twice-a-day rounds, we often hear from the patients that we talk to them more than any other physician. It can be quite rewarding."
Dr. Clark has been a speaker for Covidien and Cadence and an adviser and researcher for Covidien.
PALM SPRINGS, CALIF. – The University of Louisville has had an acute pain service for nearly a decade, but for many hospitals in the United States this still is a new idea.
"What we’re seeing is the birth of a new modality in treatment" and possibly a new specialty, Dr. Laura Clark said.
An acute pain service (APS) primarily manages pain after traumatic injury or surgery. The basic aspects of an APS include standardization of analgesic techniques, increased pain monitoring and assessment, and the ability to respond to inadequate or excessive doses of analgesics.
Establishing an APS, however, takes a lot of persuasion and education, said Dr. Clark, professor of anesthesiology and director of acute pain and regional anesthesia at the University of Louisville (Ky.).
Hospital administrators must be convinced that an APS can benefit the hospital by increasing patient satisfaction (which is strongly associated with adequate pain relief) and by cutting costs through reducing nausea and vomiting, respiratory depression, the incidence of ileus (and thus the length of hospitalization), and the incidence of chronic pain.
Physicians and pharmacists need to be willing to accept an APS as part of the care team. Many anesthesiologists mistakenly think that a single nerve block that dissipates in 10 hours is sufficient acute pain management, she said. But more than anyone, surgeons need convincing, Dr. Clark said at the annual meeting of the American Academy of Pain Medicine.
Currently, a surgeon must request involvement of the APS and that request must be documented in order for the service to be covered by insurers. "That needs to change," she said.
To get surgeons on board, include them in developing protocols for all analgesic techniques, she suggested.
There are two groups that don’t need convincing about the benefits of an APS – patients and nurses, she said. Still, education of nurses and all staff about the APS is essential. Simply asking nurses to follow written orders is not sufficient, especially for the more advanced pain therapies. Good acute pain care requires a change in culture and attitudes; for example, nurses need to change empty bags of analgesics just as they change other bags of fluids.
Nurses can be certified in pain management, and "I recommend that you have your nurses do that," Dr. Clark said.
The need for better acute pain management has been established by major reports in the United States, England, Australia, Germany, Sweden, and elsewhere. At least eight published studies report that an APS improves pain relief, five studies report a lower incidence of side effects, and three studies suggest that an APS may reduce the incidence of persistent pain after surgery, she said.
One study reported reduced postoperative morbidity and mortality with an APS but noted that "the workload is considerable" (Anesthesia 2006;61:24-8).
A recent study concluded that an APS is "likely" to be cost effective, but the investigators "didn’t even study what we do," Dr. Clark said. Key treatment techniques such as peripheral nerve blocks and epidural patient-controlled analgesia were not included in the study (Anesth. Analg. 2010;111:1042-50). Had it included those, she believes the study would have shown that an APS is very cost effective, she said.
Better studies with hard data are needed, she added.
The service ideally is physician directed but multidisciplinary, including physicians, nurses, pharmacists, and physical therapists. The most common but least desirable model of an APS in the United States includes a private physician or regionalist who may not do rounds unless called by a surgeon to manage a problem, Dr. Clark said. A second model that may be the most flexible and cost effective for around-the-clock care involves a nurse-led physician consult, in which the nurse makes daily rounds, reports to the physician, and implements therapy based on standard orders and protocols developed by the pain physician and surgeon.
The most common model in academic centers, and Dr. Clark’s favorite, is a physician-led team with a pain management nurse. The team makes rounds and decides on care. The pain physician may or may not be the regionalist. Medical residents are on call for the pain service. The pain nurse is involved in cases before, during, and after surgery and implements advanced pain management techniques, provides consultations, and coordinates with trauma, surgery, and critical care services.
Once you’ve convinced your institution and colleagues to establish an APS, make sure that someone on the APS can be reached by telephone at any hour of every day. Establish "acute pain champions" on every floor and in every area of the hospital, and make sure that at least one champion is available on every shift.
Running an APS can be challenging, but it’s a therapeutic tool that’s worth the effort, she said: "With our twice-a-day rounds, we often hear from the patients that we talk to them more than any other physician. It can be quite rewarding."
Dr. Clark has been a speaker for Covidien and Cadence and an adviser and researcher for Covidien.
FROM THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF PAIN MEDICINE
Side Effects Challenge Opioid Therapy for Acute Pain
PALM SPRINGS, CALIF. – Balancing pain relief against gastrointestinal side effects of opioid analgesics in treating acute pain is a major challenge, a nationwide survey of nearly 6,000 physicians suggests.
A total of 70% of physicians said they "usually" or "often" prescribe opioid analgesics for patients with moderate to severe acute pain. Alongside that, 63% said they also "usually" or "often" prescribe or recommend treatments to manage opioid-related side effects, especially GI side effects, Dr. Bill H. McCarberg and his associates reported in a poster presentation at the annual meeting of the American Academy of Pain Medicine.
The survey also found that 65% of physicians said that patients who receive opioid analgesics for acute pain also take over-the-counter or prescription treatments to manage opioid-related GI side effects. A total of 20% of physicians rated unacceptable GI side effects as the top reason for discontinuing opioid analgesics, and 60% said GI side effects were the top or second-to-the-top reason for discontinuing opioids, reported Dr. McCarberg, a family physician and pain specialist at Kaiser Permanente, San Diego.
The data came from the Physicians Partnering Against Pain survey, which asked 5,982 physicians to identify 10-15 "typical patients who were returning for their first follow-up visits after treatment for moderate to severe acute pain. A majority of respondents (52%) were primary care physicians, 25% were pain specialists, and 23% were other medical specialists.
In all, 55% of physicians ranked unacceptable GI or other side effects as the most common reason patients discontinued opioids. More than 40% of physicians said that patients discontinued opioids, mainly because they believed that their pain had dissipated.
More than 15% of physicians said that they see more than 60 patients with moderate to severe pain in a typical week. More than 20% said they see 31-60 patients per week, more than 35% said they see 16-30 patients per week, and nearly 25% said they see 0-15 patients with moderate to severe pain in a typical week. A majority of physicians (55%) reported that more than 75% of their patients return for a follow-up visit after the initial acute pain treatment.
The participating physicians may not be representative of all U.S. practicing physicians, and there may be some recall bias affecting how well the results represent actual physician behavior.
Despite these limitations, the findings reflect the significant challenges that opioid-related side effects pose for managing moderate to severe acute pain, Dr. McCarberg said.
Janssen Scientific Affairs funded the study and Dr. McCarberg’s associates in the study were Janssen employees. Dr. McCarberg reported having no financial disclosures.
PALM SPRINGS, CALIF. – Balancing pain relief against gastrointestinal side effects of opioid analgesics in treating acute pain is a major challenge, a nationwide survey of nearly 6,000 physicians suggests.
A total of 70% of physicians said they "usually" or "often" prescribe opioid analgesics for patients with moderate to severe acute pain. Alongside that, 63% said they also "usually" or "often" prescribe or recommend treatments to manage opioid-related side effects, especially GI side effects, Dr. Bill H. McCarberg and his associates reported in a poster presentation at the annual meeting of the American Academy of Pain Medicine.
The survey also found that 65% of physicians said that patients who receive opioid analgesics for acute pain also take over-the-counter or prescription treatments to manage opioid-related GI side effects. A total of 20% of physicians rated unacceptable GI side effects as the top reason for discontinuing opioid analgesics, and 60% said GI side effects were the top or second-to-the-top reason for discontinuing opioids, reported Dr. McCarberg, a family physician and pain specialist at Kaiser Permanente, San Diego.
The data came from the Physicians Partnering Against Pain survey, which asked 5,982 physicians to identify 10-15 "typical patients who were returning for their first follow-up visits after treatment for moderate to severe acute pain. A majority of respondents (52%) were primary care physicians, 25% were pain specialists, and 23% were other medical specialists.
In all, 55% of physicians ranked unacceptable GI or other side effects as the most common reason patients discontinued opioids. More than 40% of physicians said that patients discontinued opioids, mainly because they believed that their pain had dissipated.
More than 15% of physicians said that they see more than 60 patients with moderate to severe pain in a typical week. More than 20% said they see 31-60 patients per week, more than 35% said they see 16-30 patients per week, and nearly 25% said they see 0-15 patients with moderate to severe pain in a typical week. A majority of physicians (55%) reported that more than 75% of their patients return for a follow-up visit after the initial acute pain treatment.
The participating physicians may not be representative of all U.S. practicing physicians, and there may be some recall bias affecting how well the results represent actual physician behavior.
Despite these limitations, the findings reflect the significant challenges that opioid-related side effects pose for managing moderate to severe acute pain, Dr. McCarberg said.
Janssen Scientific Affairs funded the study and Dr. McCarberg’s associates in the study were Janssen employees. Dr. McCarberg reported having no financial disclosures.
PALM SPRINGS, CALIF. – Balancing pain relief against gastrointestinal side effects of opioid analgesics in treating acute pain is a major challenge, a nationwide survey of nearly 6,000 physicians suggests.
A total of 70% of physicians said they "usually" or "often" prescribe opioid analgesics for patients with moderate to severe acute pain. Alongside that, 63% said they also "usually" or "often" prescribe or recommend treatments to manage opioid-related side effects, especially GI side effects, Dr. Bill H. McCarberg and his associates reported in a poster presentation at the annual meeting of the American Academy of Pain Medicine.
The survey also found that 65% of physicians said that patients who receive opioid analgesics for acute pain also take over-the-counter or prescription treatments to manage opioid-related GI side effects. A total of 20% of physicians rated unacceptable GI side effects as the top reason for discontinuing opioid analgesics, and 60% said GI side effects were the top or second-to-the-top reason for discontinuing opioids, reported Dr. McCarberg, a family physician and pain specialist at Kaiser Permanente, San Diego.
The data came from the Physicians Partnering Against Pain survey, which asked 5,982 physicians to identify 10-15 "typical patients who were returning for their first follow-up visits after treatment for moderate to severe acute pain. A majority of respondents (52%) were primary care physicians, 25% were pain specialists, and 23% were other medical specialists.
In all, 55% of physicians ranked unacceptable GI or other side effects as the most common reason patients discontinued opioids. More than 40% of physicians said that patients discontinued opioids, mainly because they believed that their pain had dissipated.
More than 15% of physicians said that they see more than 60 patients with moderate to severe pain in a typical week. More than 20% said they see 31-60 patients per week, more than 35% said they see 16-30 patients per week, and nearly 25% said they see 0-15 patients with moderate to severe pain in a typical week. A majority of physicians (55%) reported that more than 75% of their patients return for a follow-up visit after the initial acute pain treatment.
The participating physicians may not be representative of all U.S. practicing physicians, and there may be some recall bias affecting how well the results represent actual physician behavior.
Despite these limitations, the findings reflect the significant challenges that opioid-related side effects pose for managing moderate to severe acute pain, Dr. McCarberg said.
Janssen Scientific Affairs funded the study and Dr. McCarberg’s associates in the study were Janssen employees. Dr. McCarberg reported having no financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF PAIN MEDICINE
Major Finding: In all, 70% of physicians said that they "usually" or "often" prescribe opioid analgesics for patients with moderate to severe pain, and 63% prescribe or recommend treatments to manage opioid-related side effects.
Data Source: The nationwide survey queried 5,982 physicians.
Disclosures: Janssen Scientific Affairs funded the study, and Dr. McCarberg’s associates in the study were Janssen employees. Dr. McCarberg reported having no financial conflicts of interest.
Long-Acting Opioids May Trigger Hypogonadism
PALM SPRINGS, CALIF. – Low testosterone levels were nearly five times more likely in men on long-acting or sustained-release opioids, compared with equipotent short-acting or immediate-release formulations, judging from the findings of a study of 81 men on daily opioids for chronic pain.
Neither the age of the patient nor the total daily dose of opioid significantly affected the risk of hypogonadism, Dr. Andrea Rubenstein reported in her award-winning poster and a plenary presentation at the annual meeting of the American Academy of Pain Medicine.
With her associates, Dr. Rubenstein reviewed records on the morning measurements of total testosterone levels in men who were on a stable dose of an opioid for at least 3 months and who had no history of hypogonadism. In all, 46 of the 81 men had total testosterone levels below 25 ng/dl (57%), consistent with published reports of a high rate of hypogonadism in men on chronic opioid therapy ranging from 54% to 86%.
Previous studies, however, evaluated only men on sustained-release or intrathecal formulations and could not identify what aspect of opioid use may be contributing to hypogonadism.
The current study found that 34 of 46 men on long-acting or sustained-release opioids had low total testosterone levels (74%), compared with 12 of 35 men on short-acting or immediate-release opioids (34%), a significant difference, said Dr. Rubenstein, an anesthesiologist and pain specialist at Kaiser Permanente Medical Group, Santa Rosa, Calif.
After adjusting for the effects of dosage and body mass index (BMI), men on long-acting or sustained-release opioids were 4.8 times more likely to have low testosterone levels, compared with men on short-acting or immediate-release formulations.
Higher BMI had a small but significant association, increasing the risk for hypogonadism by 13%.
Opioid-related androgen deficiency has been documented in one fashion or another since the 1970s, and appears to come on quickly, within days or weeks of starting chronic opioid therapy, she said.
"This phenomenon is not new, even though it’s kind of a hot topic this year," Dr. Rubenstein said.
For the past 20 years, the trend has been to put more and more patients on long-acting opioids because these were believed to be safer than short-acting formulations. If the association between hypogonadism and long-acting opioids holds up in further studies, "it will be the first evidence of a difference in safety, though not in the direction we had thought," she said.
Dr. Steven Linder of the Veterans Affairs Healthcare System Hospital, Palo Alto, Calif., commented on the study in an interview at the poster presentation. The V.A. is seeing a large number of young veterans with spinal and other injuries who are on long-term opioids, and often these patients are not screened for hypogonadism. Dr. Rubenstein’s study is an important reminder to check testosterone levels in men on long-acting or sustained-release opioids, he said.
If unrecognized and untreated, hypogonadism can lead to osteoporosis, low libido, lower function and mood, insulin resistance, increased pain, and obesity. Often, these are managed with other medications that contribute side effects, Dr. Rubenstein said.
"The last thing we need in a guy on 40 mg of methadone for back pain is to get osteoporosis of the spine," she said.
Patients in the study included 25 on hydrocodone, 8 on continuous-release oxycodone, 10 on immediate-release oxycodone, 12 on continuous-release morphine, 4 on the fentanyl patch, 14 on methadone, and 8 on off-label sublingual buprenorphine. (Only the patch form of buprenorphine is approved to treat pain.)
The study was limited by its small size, "but in the opioid literature, 81 is a nice number," she said. The study also is limited by its retrospective design, potential bias if the symptoms of hypogonadism played a role in the initial referral, and questionable generalizability if the men at this tertiary-care pain clinic are not representative of men with chronic pain in the general population.
The investigators next will repeat the study on a much larger sample of patients, and if the association is replicated, will design a prospective study to see if changing opioid therapy modifies the risk for hypogonadism. The findings of the current study are too preliminary to generate recommendations, she said.
The current study excluded patients with a history of cancer, HIV, or endocrine disease other than hypothyroidism.
Dr. Rubenstein and her associates reported having no financial disclosures.
PALM SPRINGS, CALIF. – Low testosterone levels were nearly five times more likely in men on long-acting or sustained-release opioids, compared with equipotent short-acting or immediate-release formulations, judging from the findings of a study of 81 men on daily opioids for chronic pain.
Neither the age of the patient nor the total daily dose of opioid significantly affected the risk of hypogonadism, Dr. Andrea Rubenstein reported in her award-winning poster and a plenary presentation at the annual meeting of the American Academy of Pain Medicine.
With her associates, Dr. Rubenstein reviewed records on the morning measurements of total testosterone levels in men who were on a stable dose of an opioid for at least 3 months and who had no history of hypogonadism. In all, 46 of the 81 men had total testosterone levels below 25 ng/dl (57%), consistent with published reports of a high rate of hypogonadism in men on chronic opioid therapy ranging from 54% to 86%.
Previous studies, however, evaluated only men on sustained-release or intrathecal formulations and could not identify what aspect of opioid use may be contributing to hypogonadism.
The current study found that 34 of 46 men on long-acting or sustained-release opioids had low total testosterone levels (74%), compared with 12 of 35 men on short-acting or immediate-release opioids (34%), a significant difference, said Dr. Rubenstein, an anesthesiologist and pain specialist at Kaiser Permanente Medical Group, Santa Rosa, Calif.
After adjusting for the effects of dosage and body mass index (BMI), men on long-acting or sustained-release opioids were 4.8 times more likely to have low testosterone levels, compared with men on short-acting or immediate-release formulations.
Higher BMI had a small but significant association, increasing the risk for hypogonadism by 13%.
Opioid-related androgen deficiency has been documented in one fashion or another since the 1970s, and appears to come on quickly, within days or weeks of starting chronic opioid therapy, she said.
"This phenomenon is not new, even though it’s kind of a hot topic this year," Dr. Rubenstein said.
For the past 20 years, the trend has been to put more and more patients on long-acting opioids because these were believed to be safer than short-acting formulations. If the association between hypogonadism and long-acting opioids holds up in further studies, "it will be the first evidence of a difference in safety, though not in the direction we had thought," she said.
Dr. Steven Linder of the Veterans Affairs Healthcare System Hospital, Palo Alto, Calif., commented on the study in an interview at the poster presentation. The V.A. is seeing a large number of young veterans with spinal and other injuries who are on long-term opioids, and often these patients are not screened for hypogonadism. Dr. Rubenstein’s study is an important reminder to check testosterone levels in men on long-acting or sustained-release opioids, he said.
If unrecognized and untreated, hypogonadism can lead to osteoporosis, low libido, lower function and mood, insulin resistance, increased pain, and obesity. Often, these are managed with other medications that contribute side effects, Dr. Rubenstein said.
"The last thing we need in a guy on 40 mg of methadone for back pain is to get osteoporosis of the spine," she said.
Patients in the study included 25 on hydrocodone, 8 on continuous-release oxycodone, 10 on immediate-release oxycodone, 12 on continuous-release morphine, 4 on the fentanyl patch, 14 on methadone, and 8 on off-label sublingual buprenorphine. (Only the patch form of buprenorphine is approved to treat pain.)
The study was limited by its small size, "but in the opioid literature, 81 is a nice number," she said. The study also is limited by its retrospective design, potential bias if the symptoms of hypogonadism played a role in the initial referral, and questionable generalizability if the men at this tertiary-care pain clinic are not representative of men with chronic pain in the general population.
The investigators next will repeat the study on a much larger sample of patients, and if the association is replicated, will design a prospective study to see if changing opioid therapy modifies the risk for hypogonadism. The findings of the current study are too preliminary to generate recommendations, she said.
The current study excluded patients with a history of cancer, HIV, or endocrine disease other than hypothyroidism.
Dr. Rubenstein and her associates reported having no financial disclosures.
PALM SPRINGS, CALIF. – Low testosterone levels were nearly five times more likely in men on long-acting or sustained-release opioids, compared with equipotent short-acting or immediate-release formulations, judging from the findings of a study of 81 men on daily opioids for chronic pain.
Neither the age of the patient nor the total daily dose of opioid significantly affected the risk of hypogonadism, Dr. Andrea Rubenstein reported in her award-winning poster and a plenary presentation at the annual meeting of the American Academy of Pain Medicine.
With her associates, Dr. Rubenstein reviewed records on the morning measurements of total testosterone levels in men who were on a stable dose of an opioid for at least 3 months and who had no history of hypogonadism. In all, 46 of the 81 men had total testosterone levels below 25 ng/dl (57%), consistent with published reports of a high rate of hypogonadism in men on chronic opioid therapy ranging from 54% to 86%.
Previous studies, however, evaluated only men on sustained-release or intrathecal formulations and could not identify what aspect of opioid use may be contributing to hypogonadism.
The current study found that 34 of 46 men on long-acting or sustained-release opioids had low total testosterone levels (74%), compared with 12 of 35 men on short-acting or immediate-release opioids (34%), a significant difference, said Dr. Rubenstein, an anesthesiologist and pain specialist at Kaiser Permanente Medical Group, Santa Rosa, Calif.
After adjusting for the effects of dosage and body mass index (BMI), men on long-acting or sustained-release opioids were 4.8 times more likely to have low testosterone levels, compared with men on short-acting or immediate-release formulations.
Higher BMI had a small but significant association, increasing the risk for hypogonadism by 13%.
Opioid-related androgen deficiency has been documented in one fashion or another since the 1970s, and appears to come on quickly, within days or weeks of starting chronic opioid therapy, she said.
"This phenomenon is not new, even though it’s kind of a hot topic this year," Dr. Rubenstein said.
For the past 20 years, the trend has been to put more and more patients on long-acting opioids because these were believed to be safer than short-acting formulations. If the association between hypogonadism and long-acting opioids holds up in further studies, "it will be the first evidence of a difference in safety, though not in the direction we had thought," she said.
Dr. Steven Linder of the Veterans Affairs Healthcare System Hospital, Palo Alto, Calif., commented on the study in an interview at the poster presentation. The V.A. is seeing a large number of young veterans with spinal and other injuries who are on long-term opioids, and often these patients are not screened for hypogonadism. Dr. Rubenstein’s study is an important reminder to check testosterone levels in men on long-acting or sustained-release opioids, he said.
If unrecognized and untreated, hypogonadism can lead to osteoporosis, low libido, lower function and mood, insulin resistance, increased pain, and obesity. Often, these are managed with other medications that contribute side effects, Dr. Rubenstein said.
"The last thing we need in a guy on 40 mg of methadone for back pain is to get osteoporosis of the spine," she said.
Patients in the study included 25 on hydrocodone, 8 on continuous-release oxycodone, 10 on immediate-release oxycodone, 12 on continuous-release morphine, 4 on the fentanyl patch, 14 on methadone, and 8 on off-label sublingual buprenorphine. (Only the patch form of buprenorphine is approved to treat pain.)
The study was limited by its small size, "but in the opioid literature, 81 is a nice number," she said. The study also is limited by its retrospective design, potential bias if the symptoms of hypogonadism played a role in the initial referral, and questionable generalizability if the men at this tertiary-care pain clinic are not representative of men with chronic pain in the general population.
The investigators next will repeat the study on a much larger sample of patients, and if the association is replicated, will design a prospective study to see if changing opioid therapy modifies the risk for hypogonadism. The findings of the current study are too preliminary to generate recommendations, she said.
The current study excluded patients with a history of cancer, HIV, or endocrine disease other than hypothyroidism.
Dr. Rubenstein and her associates reported having no financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF PAIN MEDICINE
Major Finding: Tests found low testosterone levels in 74% of men on long-acting or sustained-release opioids, compared with 34% of men on equipotent short-acting or immediate-release opioids.
Data Source: The review included records on 81 men treated with daily opioids for chronic pain at one institution.
Disclosures: Dr. Rubenstein and her associates reported having no financial disclosures.
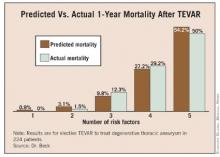
Risk Factors Predict 1-Year Mortality After Elective TEVAR
SCOTTSDALE, ARIZ. – A new model for predicting 1-year survival after elective endovascular repair of degenerative thoracic aortic aneurysm suggests that the risks outweigh potential benefits of the procedure in some older patients with multiple comorbidities.
For patients aged 70 years or older who have multiple comorbidities, there is a very high risk of death in the year following thoracic endovascular aortic aneurysm repair (TEVAR), so it may be best to wait until the aneurysm is large enough that the risk from not doing TEVAR outweighs the risk of performing the procedure, according to Dr. Adam W. Beck.
Dr. Beck, of the University of Florida, Gainesville, and his associates analyzed data from a prospective registry of all 526 consecutive TEVARs performed on patients with intact degenerative, asymptomatic thoracic aneurysms at the university between 2000 and 2010. After excluding urgent or emergent cases, the researchers used data from 224 patients who underwent elective TEVAR to identify predictors of death within a year of TEVAR, and compared predictions to survival data from the Social Security Death Index.
Overall, 3% of patients died within 30 days of TEVAR, and 15% died within 1 year – rates that are comparable to those of many studies reported in the medical literature, Dr. Beck said at the annual meeting of the Southern Association for Vascular Surgery.
In a multivariate analysis of factors associated with mortality, being at least 70 years old conferred nearly a sixfold increase in the predicted 1-year risk of death (hazard ratio, 5.8). Patients who had an adjunctive procedure at the time of TEVAR, such as brachiocephalic/visceral stent placement or concomitant visceral debranching procedures, were 4.5 times more likely to die within a year than were patients without an adjunctive procedure.
The predicted risk of death at 1 year was 3 times higher in patients with peripheral vascular occlusive disease and 2.4 times higher in patients with coronary artery disease than in patients without those diseases. All of these associations were statistically significant. The presence of chronic obstructive pulmonary disease showed a nonsignificant trend toward a 1.9-fold higher risk of death at 1 year (P = .06).
Having a diagnosis of hyperlipidemia appeared to be protective, because it was significantly associated with a 60% decrease in the risk of death at 1 year after TEVAR. When the risk prediction model was created, the lack of a history of hyperlipidemia was considered to be a risk factor.
The risk of death at 1 year rose as the number of significant risk factors increased, and predictive risk correlated well with actual mortality data, Dr. Beck said.
In general, aneurysm diameter was larger in patients with more risk factors, and the risk of death at 1 year increased with aneurysm size and number of risk factors, he added.
The risk of rupture, as reported in the previous literature, is approximately 2% for thoracic aortic aneurysms measuring 5.5 cm in diameter, 10% for aneurysms with a diameter of 6.5 cm, 15% for those measuring 7 cm in diameter, and 45% for aneurysms with a diameter of 8 cm.
When the risk of 1-year mortality is plotted against the number of risk factors, it appears that TEVAR should be delayed in patients with three or more risk factors until their aneurysm diameter is greater than the usual 6-cm threshold commonly used to justify the risk of TEVAR, Dr. Beck said.
"This is an important contribution to our literature," said Dr. Hazim J. Safi, a discussant at the meeting. "Most of us implicitly, when we decide how to manage these patients, would categorize the patient by presumed risk," said Dr. Safi, professor and chair of cardiovascular and thoracic surgery at the University of Texas, Houston. "I congratulate the authors for quantifying the relationship between the risk factors and mortality rate."
Usually, surgeons discuss the annual risk of thoracic aneurysm rupture and compare this with the 30-day operative mortality risk when advising patients who are considering TEVAR, Dr. Beck said. To adequately assess the success of aneurysm repair, however, longer survival should be considered, he said.
"It’s important to note that only 21% of deaths within 1 year of repair occurred within 30 days after the procedure, underscoring the importance of looking beyond the first 30 days to determine the benefit of therapy," Dr. Beck said. Even for the groups with multiple risk factors who are at very high risk, the majority of deaths occurred outside the 30-day window.
The risk prediction model should help clinicians select patients who would benefit most from early TEVAR, and delay TEVAR in patients who might be better managed nonoperatively.
To evaluate whether surgeons at his institution were accounting for higher-risk patients, Dr. Beck and his associates performed a secondary analysis. As the number of risk factors for death within 1 year of TEVAR increased, so did the aneurysm diameter at which patients underwent repair. This suggests that surgeons were taking into account risk factors, at least to some extent, in deciding when to operate on these patients.
Patients in the study had a mean age of 61 years, and 63% were male. The average aneurysm diameter was 6.25 cm. At the time of treatment, 38% of patients had coronary artery disease, 28% had chronic obstructive pulmonary disease, and 12% had peripheral vascular occlusive disease. Nine percent of patients underwent an intraoperative adjunctive procedure.
Among other comorbidities, 85% had hypertension, 51% had dyslipidemia, 14% had diabetes, 11% had chronic renal insufficiency, and 7% had heart failure.
Eighty percent of patients were taking antiplatelet medications, 55% were on statins, and 67% were considered to be in American Society of Anesthesiologists classification 4.
Dr. Beck reported having no financial disclosures.
SCOTTSDALE, ARIZ. – A new model for predicting 1-year survival after elective endovascular repair of degenerative thoracic aortic aneurysm suggests that the risks outweigh potential benefits of the procedure in some older patients with multiple comorbidities.
For patients aged 70 years or older who have multiple comorbidities, there is a very high risk of death in the year following thoracic endovascular aortic aneurysm repair (TEVAR), so it may be best to wait until the aneurysm is large enough that the risk from not doing TEVAR outweighs the risk of performing the procedure, according to Dr. Adam W. Beck.
Dr. Beck, of the University of Florida, Gainesville, and his associates analyzed data from a prospective registry of all 526 consecutive TEVARs performed on patients with intact degenerative, asymptomatic thoracic aneurysms at the university between 2000 and 2010. After excluding urgent or emergent cases, the researchers used data from 224 patients who underwent elective TEVAR to identify predictors of death within a year of TEVAR, and compared predictions to survival data from the Social Security Death Index.
Overall, 3% of patients died within 30 days of TEVAR, and 15% died within 1 year – rates that are comparable to those of many studies reported in the medical literature, Dr. Beck said at the annual meeting of the Southern Association for Vascular Surgery.
In a multivariate analysis of factors associated with mortality, being at least 70 years old conferred nearly a sixfold increase in the predicted 1-year risk of death (hazard ratio, 5.8). Patients who had an adjunctive procedure at the time of TEVAR, such as brachiocephalic/visceral stent placement or concomitant visceral debranching procedures, were 4.5 times more likely to die within a year than were patients without an adjunctive procedure.
The predicted risk of death at 1 year was 3 times higher in patients with peripheral vascular occlusive disease and 2.4 times higher in patients with coronary artery disease than in patients without those diseases. All of these associations were statistically significant. The presence of chronic obstructive pulmonary disease showed a nonsignificant trend toward a 1.9-fold higher risk of death at 1 year (P = .06).
Having a diagnosis of hyperlipidemia appeared to be protective, because it was significantly associated with a 60% decrease in the risk of death at 1 year after TEVAR. When the risk prediction model was created, the lack of a history of hyperlipidemia was considered to be a risk factor.
The risk of death at 1 year rose as the number of significant risk factors increased, and predictive risk correlated well with actual mortality data, Dr. Beck said.
In general, aneurysm diameter was larger in patients with more risk factors, and the risk of death at 1 year increased with aneurysm size and number of risk factors, he added.
The risk of rupture, as reported in the previous literature, is approximately 2% for thoracic aortic aneurysms measuring 5.5 cm in diameter, 10% for aneurysms with a diameter of 6.5 cm, 15% for those measuring 7 cm in diameter, and 45% for aneurysms with a diameter of 8 cm.
When the risk of 1-year mortality is plotted against the number of risk factors, it appears that TEVAR should be delayed in patients with three or more risk factors until their aneurysm diameter is greater than the usual 6-cm threshold commonly used to justify the risk of TEVAR, Dr. Beck said.
"This is an important contribution to our literature," said Dr. Hazim J. Safi, a discussant at the meeting. "Most of us implicitly, when we decide how to manage these patients, would categorize the patient by presumed risk," said Dr. Safi, professor and chair of cardiovascular and thoracic surgery at the University of Texas, Houston. "I congratulate the authors for quantifying the relationship between the risk factors and mortality rate."
Usually, surgeons discuss the annual risk of thoracic aneurysm rupture and compare this with the 30-day operative mortality risk when advising patients who are considering TEVAR, Dr. Beck said. To adequately assess the success of aneurysm repair, however, longer survival should be considered, he said.
"It’s important to note that only 21% of deaths within 1 year of repair occurred within 30 days after the procedure, underscoring the importance of looking beyond the first 30 days to determine the benefit of therapy," Dr. Beck said. Even for the groups with multiple risk factors who are at very high risk, the majority of deaths occurred outside the 30-day window.
The risk prediction model should help clinicians select patients who would benefit most from early TEVAR, and delay TEVAR in patients who might be better managed nonoperatively.
To evaluate whether surgeons at his institution were accounting for higher-risk patients, Dr. Beck and his associates performed a secondary analysis. As the number of risk factors for death within 1 year of TEVAR increased, so did the aneurysm diameter at which patients underwent repair. This suggests that surgeons were taking into account risk factors, at least to some extent, in deciding when to operate on these patients.
Patients in the study had a mean age of 61 years, and 63% were male. The average aneurysm diameter was 6.25 cm. At the time of treatment, 38% of patients had coronary artery disease, 28% had chronic obstructive pulmonary disease, and 12% had peripheral vascular occlusive disease. Nine percent of patients underwent an intraoperative adjunctive procedure.
Among other comorbidities, 85% had hypertension, 51% had dyslipidemia, 14% had diabetes, 11% had chronic renal insufficiency, and 7% had heart failure.
Eighty percent of patients were taking antiplatelet medications, 55% were on statins, and 67% were considered to be in American Society of Anesthesiologists classification 4.
Dr. Beck reported having no financial disclosures.
SCOTTSDALE, ARIZ. – A new model for predicting 1-year survival after elective endovascular repair of degenerative thoracic aortic aneurysm suggests that the risks outweigh potential benefits of the procedure in some older patients with multiple comorbidities.
For patients aged 70 years or older who have multiple comorbidities, there is a very high risk of death in the year following thoracic endovascular aortic aneurysm repair (TEVAR), so it may be best to wait until the aneurysm is large enough that the risk from not doing TEVAR outweighs the risk of performing the procedure, according to Dr. Adam W. Beck.
Dr. Beck, of the University of Florida, Gainesville, and his associates analyzed data from a prospective registry of all 526 consecutive TEVARs performed on patients with intact degenerative, asymptomatic thoracic aneurysms at the university between 2000 and 2010. After excluding urgent or emergent cases, the researchers used data from 224 patients who underwent elective TEVAR to identify predictors of death within a year of TEVAR, and compared predictions to survival data from the Social Security Death Index.
Overall, 3% of patients died within 30 days of TEVAR, and 15% died within 1 year – rates that are comparable to those of many studies reported in the medical literature, Dr. Beck said at the annual meeting of the Southern Association for Vascular Surgery.
In a multivariate analysis of factors associated with mortality, being at least 70 years old conferred nearly a sixfold increase in the predicted 1-year risk of death (hazard ratio, 5.8). Patients who had an adjunctive procedure at the time of TEVAR, such as brachiocephalic/visceral stent placement or concomitant visceral debranching procedures, were 4.5 times more likely to die within a year than were patients without an adjunctive procedure.
The predicted risk of death at 1 year was 3 times higher in patients with peripheral vascular occlusive disease and 2.4 times higher in patients with coronary artery disease than in patients without those diseases. All of these associations were statistically significant. The presence of chronic obstructive pulmonary disease showed a nonsignificant trend toward a 1.9-fold higher risk of death at 1 year (P = .06).
Having a diagnosis of hyperlipidemia appeared to be protective, because it was significantly associated with a 60% decrease in the risk of death at 1 year after TEVAR. When the risk prediction model was created, the lack of a history of hyperlipidemia was considered to be a risk factor.
The risk of death at 1 year rose as the number of significant risk factors increased, and predictive risk correlated well with actual mortality data, Dr. Beck said.
In general, aneurysm diameter was larger in patients with more risk factors, and the risk of death at 1 year increased with aneurysm size and number of risk factors, he added.
The risk of rupture, as reported in the previous literature, is approximately 2% for thoracic aortic aneurysms measuring 5.5 cm in diameter, 10% for aneurysms with a diameter of 6.5 cm, 15% for those measuring 7 cm in diameter, and 45% for aneurysms with a diameter of 8 cm.
When the risk of 1-year mortality is plotted against the number of risk factors, it appears that TEVAR should be delayed in patients with three or more risk factors until their aneurysm diameter is greater than the usual 6-cm threshold commonly used to justify the risk of TEVAR, Dr. Beck said.
"This is an important contribution to our literature," said Dr. Hazim J. Safi, a discussant at the meeting. "Most of us implicitly, when we decide how to manage these patients, would categorize the patient by presumed risk," said Dr. Safi, professor and chair of cardiovascular and thoracic surgery at the University of Texas, Houston. "I congratulate the authors for quantifying the relationship between the risk factors and mortality rate."
Usually, surgeons discuss the annual risk of thoracic aneurysm rupture and compare this with the 30-day operative mortality risk when advising patients who are considering TEVAR, Dr. Beck said. To adequately assess the success of aneurysm repair, however, longer survival should be considered, he said.
"It’s important to note that only 21% of deaths within 1 year of repair occurred within 30 days after the procedure, underscoring the importance of looking beyond the first 30 days to determine the benefit of therapy," Dr. Beck said. Even for the groups with multiple risk factors who are at very high risk, the majority of deaths occurred outside the 30-day window.
The risk prediction model should help clinicians select patients who would benefit most from early TEVAR, and delay TEVAR in patients who might be better managed nonoperatively.
To evaluate whether surgeons at his institution were accounting for higher-risk patients, Dr. Beck and his associates performed a secondary analysis. As the number of risk factors for death within 1 year of TEVAR increased, so did the aneurysm diameter at which patients underwent repair. This suggests that surgeons were taking into account risk factors, at least to some extent, in deciding when to operate on these patients.
Patients in the study had a mean age of 61 years, and 63% were male. The average aneurysm diameter was 6.25 cm. At the time of treatment, 38% of patients had coronary artery disease, 28% had chronic obstructive pulmonary disease, and 12% had peripheral vascular occlusive disease. Nine percent of patients underwent an intraoperative adjunctive procedure.
Among other comorbidities, 85% had hypertension, 51% had dyslipidemia, 14% had diabetes, 11% had chronic renal insufficiency, and 7% had heart failure.
Eighty percent of patients were taking antiplatelet medications, 55% were on statins, and 67% were considered to be in American Society of Anesthesiologists classification 4.
Dr. Beck reported having no financial disclosures.
FROM THE ANNUAL MEETING OF THE SOUTHERN ASSOCIATION FOR VASCULAR SURGERY
Off-label Low-Dose Naltrexone Reduced Fibromyalgia Pain
PALM SPRINGS, CALIF. – Off-label use of daily low-dose naltrexone hydrochloride reduced fibromyalgia pain severity by an average of 48%, compared with a 27% pain reduction on placebo in a double-blind crossover trial in 28 women.
"These are statistically significant results, and I think they are also clinically significant," said Jarred Younger, Ph.D., at the annual meeting of the American Academy of Pain Medicine.
Tolerability ratings of a regimen of 4.5 mg daily of naltrexone and placebo were statistically equivalent, with scores of 89 (of a possible 100, which represented perfectly tolerated treatment) for both naltrexone and placebo. Side effects associated with use of naltrexone were mild and transient, with significantly more patients reporting vivid dreams (37%) and headaches (16%) on the drug compared with placebo (13% and 3%, respectively).
Low-dose naltrexone, an opioid agonist, is not approved by the Food and Drug Administration and must be custom compounded, but the drug is generic and costs less than $40 per month, said Dr. Younger, director of the adult and pediatric pain laboratory at Stanford (Calif.) University.
"We know it’s cheap, and we know it’s easy to get ahold of," he said.
The 22-week study included women aged 23-65 years living near Stanford who fulfilled the American College of Rheumatology’s 1990 criteria for fibromyalgia, including having 11 of 18 tender points. They had had fibromyalgia for a mean of 12 years. Patients were allowed to continue taking their medications as normal, with the exclusion of opioid analgesics.
After a 2-week run-in period, patients were randomized to either 12 weeks of naltrexone or 4 weeks of placebo, taken daily with or without food or water approximately 1 hour before bedtime, in the form of an opaque gelatin capsule with microcrystalline cellulose filler and noncaloric sweetener. The treatment groups then switched to the other regimen for a total of 16 weeks of treatment or placebo, ending with a 4-week follow-up period.
Patients daily rated their pain, fatigue, and other symptoms on a handheld computer; they were assessed every 2 weeks in the laboratory for side effects and were given a new bottle of capsules. Investigators calculated the mean reduction in symptom severity based on measurements in the final 3 days on the drug or placebo.
Three other patients (for a total of 31) were randomized in the study but were excluded from the final analysis, two of them because they stopped taking the capsules.
"Global impression of change" ratings by 30 patients showed that after 12 weeks on naltrexone, 13% reported that their pain was very much improved, 37% said it was much improved, 20% reported minimal improvement, 20% said there was no change in pain, and 10% said pain was minimally worse.
By the end of the naltrexone phase, 57% of patients reported a 30% or greater reduction in pain, Dr. Younger and his associates reported.
Fatigue and sleep quality were not significantly improved on naltrexone, compared with placebo. Patients were not able to guess accurately whether they were receiving the drug or placebo.
The findings confirm results of a 10-patient pilot study by the same investigators (Pain Med. 2009;10:663-72). "We now have two studies" suggesting that low-dose naltrexone reduces the severity of fibromyalgia pain, he said.
Low-dose naltrexone deserves a larger, parallel-group, randomized, controlled trial to further confirm the results in a larger cohort, he added.
Naltrexone is microglia moderator, and the investigators hypothesized that this may be the mechanism of action in reducing fibromyalgia pain. Abnormal functioning of microglia may cause the central sensitivity seen in fibromyalgia and the subsequent overproduction of proinflammatory factors. In-vitro and animal studies have shown that naltrexone reduces microglia hyperexcitability, suppressing the production of proinflammatory cytokines, reducing pain, and serving a neuroprotective function, he said.
Dr. Younger said that future studies also should assess other potential microglia modulators, including ibudilast and 3-hydroxymorphinan. Fluorocitrate, minocycline, and dextromethorphan also are microglia modulators.
A physician in the audience noted that the current study showed a higher-than-usual placebo effect, and wondered about the cause. "I wondered about that very thing," Dr. Younger replied. The previous pilot study found a lower placebo effect, but the results of the pilot study became widely known and may have increased expectations and the effect of placebo in the women who were recruited to the current study, he speculated.
The study excluded women with abnormal or elevated levels of rheumatoid factor, antinuclear antibodies, erythrocyte sedimentation rate, or C-reactive protein; women who were taking opioid analgesics; and women with joint inflammation or a history of autoimmune disease.
Approximately 5% of U.S. women and 2% of men are thought to have fibromyalgia.
Dr. Younger reported having no financial disclosures. Funding for the study came primarily from the American Fibromyalgia Syndrome Association, with other support from Jim and Connie Binns, the Oxnard Foundation, the Chris Redlich Pain Research Endowment, and the Rosekran Pain Research Endowment.
PALM SPRINGS, CALIF. – Off-label use of daily low-dose naltrexone hydrochloride reduced fibromyalgia pain severity by an average of 48%, compared with a 27% pain reduction on placebo in a double-blind crossover trial in 28 women.
"These are statistically significant results, and I think they are also clinically significant," said Jarred Younger, Ph.D., at the annual meeting of the American Academy of Pain Medicine.
Tolerability ratings of a regimen of 4.5 mg daily of naltrexone and placebo were statistically equivalent, with scores of 89 (of a possible 100, which represented perfectly tolerated treatment) for both naltrexone and placebo. Side effects associated with use of naltrexone were mild and transient, with significantly more patients reporting vivid dreams (37%) and headaches (16%) on the drug compared with placebo (13% and 3%, respectively).
Low-dose naltrexone, an opioid agonist, is not approved by the Food and Drug Administration and must be custom compounded, but the drug is generic and costs less than $40 per month, said Dr. Younger, director of the adult and pediatric pain laboratory at Stanford (Calif.) University.
"We know it’s cheap, and we know it’s easy to get ahold of," he said.
The 22-week study included women aged 23-65 years living near Stanford who fulfilled the American College of Rheumatology’s 1990 criteria for fibromyalgia, including having 11 of 18 tender points. They had had fibromyalgia for a mean of 12 years. Patients were allowed to continue taking their medications as normal, with the exclusion of opioid analgesics.
After a 2-week run-in period, patients were randomized to either 12 weeks of naltrexone or 4 weeks of placebo, taken daily with or without food or water approximately 1 hour before bedtime, in the form of an opaque gelatin capsule with microcrystalline cellulose filler and noncaloric sweetener. The treatment groups then switched to the other regimen for a total of 16 weeks of treatment or placebo, ending with a 4-week follow-up period.
Patients daily rated their pain, fatigue, and other symptoms on a handheld computer; they were assessed every 2 weeks in the laboratory for side effects and were given a new bottle of capsules. Investigators calculated the mean reduction in symptom severity based on measurements in the final 3 days on the drug or placebo.
Three other patients (for a total of 31) were randomized in the study but were excluded from the final analysis, two of them because they stopped taking the capsules.
"Global impression of change" ratings by 30 patients showed that after 12 weeks on naltrexone, 13% reported that their pain was very much improved, 37% said it was much improved, 20% reported minimal improvement, 20% said there was no change in pain, and 10% said pain was minimally worse.
By the end of the naltrexone phase, 57% of patients reported a 30% or greater reduction in pain, Dr. Younger and his associates reported.
Fatigue and sleep quality were not significantly improved on naltrexone, compared with placebo. Patients were not able to guess accurately whether they were receiving the drug or placebo.
The findings confirm results of a 10-patient pilot study by the same investigators (Pain Med. 2009;10:663-72). "We now have two studies" suggesting that low-dose naltrexone reduces the severity of fibromyalgia pain, he said.
Low-dose naltrexone deserves a larger, parallel-group, randomized, controlled trial to further confirm the results in a larger cohort, he added.
Naltrexone is microglia moderator, and the investigators hypothesized that this may be the mechanism of action in reducing fibromyalgia pain. Abnormal functioning of microglia may cause the central sensitivity seen in fibromyalgia and the subsequent overproduction of proinflammatory factors. In-vitro and animal studies have shown that naltrexone reduces microglia hyperexcitability, suppressing the production of proinflammatory cytokines, reducing pain, and serving a neuroprotective function, he said.
Dr. Younger said that future studies also should assess other potential microglia modulators, including ibudilast and 3-hydroxymorphinan. Fluorocitrate, minocycline, and dextromethorphan also are microglia modulators.
A physician in the audience noted that the current study showed a higher-than-usual placebo effect, and wondered about the cause. "I wondered about that very thing," Dr. Younger replied. The previous pilot study found a lower placebo effect, but the results of the pilot study became widely known and may have increased expectations and the effect of placebo in the women who were recruited to the current study, he speculated.
The study excluded women with abnormal or elevated levels of rheumatoid factor, antinuclear antibodies, erythrocyte sedimentation rate, or C-reactive protein; women who were taking opioid analgesics; and women with joint inflammation or a history of autoimmune disease.
Approximately 5% of U.S. women and 2% of men are thought to have fibromyalgia.
Dr. Younger reported having no financial disclosures. Funding for the study came primarily from the American Fibromyalgia Syndrome Association, with other support from Jim and Connie Binns, the Oxnard Foundation, the Chris Redlich Pain Research Endowment, and the Rosekran Pain Research Endowment.
PALM SPRINGS, CALIF. – Off-label use of daily low-dose naltrexone hydrochloride reduced fibromyalgia pain severity by an average of 48%, compared with a 27% pain reduction on placebo in a double-blind crossover trial in 28 women.
"These are statistically significant results, and I think they are also clinically significant," said Jarred Younger, Ph.D., at the annual meeting of the American Academy of Pain Medicine.
Tolerability ratings of a regimen of 4.5 mg daily of naltrexone and placebo were statistically equivalent, with scores of 89 (of a possible 100, which represented perfectly tolerated treatment) for both naltrexone and placebo. Side effects associated with use of naltrexone were mild and transient, with significantly more patients reporting vivid dreams (37%) and headaches (16%) on the drug compared with placebo (13% and 3%, respectively).
Low-dose naltrexone, an opioid agonist, is not approved by the Food and Drug Administration and must be custom compounded, but the drug is generic and costs less than $40 per month, said Dr. Younger, director of the adult and pediatric pain laboratory at Stanford (Calif.) University.
"We know it’s cheap, and we know it’s easy to get ahold of," he said.
The 22-week study included women aged 23-65 years living near Stanford who fulfilled the American College of Rheumatology’s 1990 criteria for fibromyalgia, including having 11 of 18 tender points. They had had fibromyalgia for a mean of 12 years. Patients were allowed to continue taking their medications as normal, with the exclusion of opioid analgesics.
After a 2-week run-in period, patients were randomized to either 12 weeks of naltrexone or 4 weeks of placebo, taken daily with or without food or water approximately 1 hour before bedtime, in the form of an opaque gelatin capsule with microcrystalline cellulose filler and noncaloric sweetener. The treatment groups then switched to the other regimen for a total of 16 weeks of treatment or placebo, ending with a 4-week follow-up period.
Patients daily rated their pain, fatigue, and other symptoms on a handheld computer; they were assessed every 2 weeks in the laboratory for side effects and were given a new bottle of capsules. Investigators calculated the mean reduction in symptom severity based on measurements in the final 3 days on the drug or placebo.
Three other patients (for a total of 31) were randomized in the study but were excluded from the final analysis, two of them because they stopped taking the capsules.
"Global impression of change" ratings by 30 patients showed that after 12 weeks on naltrexone, 13% reported that their pain was very much improved, 37% said it was much improved, 20% reported minimal improvement, 20% said there was no change in pain, and 10% said pain was minimally worse.
By the end of the naltrexone phase, 57% of patients reported a 30% or greater reduction in pain, Dr. Younger and his associates reported.
Fatigue and sleep quality were not significantly improved on naltrexone, compared with placebo. Patients were not able to guess accurately whether they were receiving the drug or placebo.
The findings confirm results of a 10-patient pilot study by the same investigators (Pain Med. 2009;10:663-72). "We now have two studies" suggesting that low-dose naltrexone reduces the severity of fibromyalgia pain, he said.
Low-dose naltrexone deserves a larger, parallel-group, randomized, controlled trial to further confirm the results in a larger cohort, he added.
Naltrexone is microglia moderator, and the investigators hypothesized that this may be the mechanism of action in reducing fibromyalgia pain. Abnormal functioning of microglia may cause the central sensitivity seen in fibromyalgia and the subsequent overproduction of proinflammatory factors. In-vitro and animal studies have shown that naltrexone reduces microglia hyperexcitability, suppressing the production of proinflammatory cytokines, reducing pain, and serving a neuroprotective function, he said.
Dr. Younger said that future studies also should assess other potential microglia modulators, including ibudilast and 3-hydroxymorphinan. Fluorocitrate, minocycline, and dextromethorphan also are microglia modulators.
A physician in the audience noted that the current study showed a higher-than-usual placebo effect, and wondered about the cause. "I wondered about that very thing," Dr. Younger replied. The previous pilot study found a lower placebo effect, but the results of the pilot study became widely known and may have increased expectations and the effect of placebo in the women who were recruited to the current study, he speculated.
The study excluded women with abnormal or elevated levels of rheumatoid factor, antinuclear antibodies, erythrocyte sedimentation rate, or C-reactive protein; women who were taking opioid analgesics; and women with joint inflammation or a history of autoimmune disease.
Approximately 5% of U.S. women and 2% of men are thought to have fibromyalgia.
Dr. Younger reported having no financial disclosures. Funding for the study came primarily from the American Fibromyalgia Syndrome Association, with other support from Jim and Connie Binns, the Oxnard Foundation, the Chris Redlich Pain Research Endowment, and the Rosekran Pain Research Endowment.
FROM THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF PAIN MEDICINE
Major Finding: Daily naltrexone (4.5 mg) reduced fibromyalgia pain by 48%, compared with a 27% pain reduction on placebo.
Data Source: Data are from a prospective, double-blind crossover trial in 28 women who met the 1990 criteria for fibromyalgia.
Disclosures: Dr. Younger reported having no financial disclosures. Funding for the study came primarily from the American Fibromyalgia Syndrome Association, with other support from Jim and Connie Binns, the Oxnard Foundation, the Chris Redlich Pain Research Endowment, and the Rosekran Pain Research Endowment.
Endovascular Repair Effective for Inflammatory AAA
SCOTTSDALE, ARIZ. – Inflammatory abdominal aortic aneurysms can be treated safely and effectively by endovascular aneurysm repair, though patients with significant hydronephrosis may have worse outcomes, a retrospective study suggests.
The study included 69 patients who underwent either endovascular repair (10 patients) or open surgical repair (59 patients) at the surgeon’s discretion at Mayo Clinics in Minnesota, Florida, or Arizona between 1999 and 2011.
Previous case series and meta-analyses have reported mixed results with endovascular aneurysm repair (EVAR), but the current study suggests that EVAR is appropriate management for inflammatory abdominal aortic aneurysms (AAAs), Dr. William M. Stone said at the annual meeting of the Southern Association for Vascular Surgery.
In the study’s EVAR group, eight patients presented with symptoms (80%), including one with rupture. In the open-repair group, 31 patients (52%) presented with symptoms, including 3 with rupture (5%).
Ureteral involvement was seen in 23 patients: 2 patients in the EVAR group (20%) and 21 in the open group (34%). Of these 23 patients, 21 underwent preoperative ureteral stent placement (91%). Thirty-six patients in the open-repair group had suprarenal aortic cross clamps (61%).
All of the EVAR procedures were technically successful, and patients were followed for an average of 34 months. The mean aneurysm size in the EVAR group decreased from 5.94 cm preoperatively to 4.73 cm after EVAR, an average change of nearly 18%, reported Dr. Stone of the Mayo Clinic in Phoenix.
Aneurysm size decreased in seven patients (70%), and did not change in two patients (20%) after EVAR. One EVAR patient was lost to follow-up. Preoperative hydronephrosis in one patient (10%) before EVAR did not change after EVAR, and one patient developed new hydronephrosis after EVAR. No patients in the EVAR group died, developed endoleaks, or needed steroids. Two patients developed atrial fibrillation after EVAR and were treated for it.
The inflammatory rind measured 5.4 cm before EVAR and 2.7 cm afterward on average, a mean change of 50%, he said.
In the open-repair group, surgeons used midline incisions in 52 patients (88%), a left flank approach in 6 patients (10%), and a bilateral subcostal approach in 1 (2%) to repair aneurysms with a mean size of 6.3 cm.
One patient in the open-repair group died postoperatively of a ruptured suprarenal inflammatory aneurysm. Major complications were seen in 22 patients (38%), including renal complications in 5 (8%), ischemic colitis in 2 (3%), and ureteral obstruction that required intervention in 3 (5%). A late anastomotic rupture in one patient in the open-surgery group was repaired by EVAR.
During a mean follow-up of 43 months, 17 patients in the open-repair group were lost to follow-up (28%). All of the remaining patients had resolution of their aneurysm sac. Four patients (7%) received steroids, not to treat the aneurysm but for comorbidities.
Among 12 patients in the open-repair group with preoperative hydronephrosis (20%), the hydronephrosis resolved in 7 of the 12 (58%), remained stable in 4 patients (33%), and worsened in 1 patient (8%). The patient with worsening hydronephrosis underwent ureterolysis. Two patients developed renal atrophy.
Although the retrospective study was small, it appeared to show a trend toward less severe complications in the EVAR group, "which is what we intuitively would have guessed," Dr. Stone said.
Previous data from the EUROSTAR (European Collaborators on Stent-Graft Techniques for Abdominal Aortic Aneurysm Repair) registry suggested that inflammatory AAA size decreased by 87% after EVAR, he noted (Semin. Interv. Cardiol. 2000;5:29-33). Aneurysm wall thickness averaged 21 mm preoperatively, 17 mm at intermediate follow-up, and 13 mm with long-term follow-up, which is "consistent with our review," he said.
Patients in the EUROSTAR database had problems with graft limb stenosis that were not seen in the current series, Dr. Stone noted. A ureteral stent and/or ureterolysis were required in 18% of the EUROSTAR patients who underwent EVAR. The rate of ureteral "entrapment" (inflammation around the ureters) improved from 45% to 27% after EVAR.
In a previous meta-analysis of data on 46 patients in 14 studies, EVAR decreased aneurysm size in most patients, with a median decrease of 11 mm. Periaortic fibrosis decreased in 52%, was unchanged in 42%, and progressed in 7% (J. Endovasc. Ther. 2005;12:560-7).
A separate meta-analysis of 56 studies with 1,120 patients compared EVAR with open repair of AAA, and found 1-year all-cause mortality rates of 2% with EVAR and 14% with open repair (Eur. J. Vasc. Endovasc. Surg. 2009;38:291-7). Periaortic fibrosis decreased in 65% of the EVAR group and in 73% of the open-repair group. Hydronephrosis regressed in 38% of the EVAR group and in 69% of the open-repair group.
In the current study, the two groups did not differ significantly in mean age, preoperative aneurysm size, or length of follow-up. In the EVAR group, patients averaged 72 years of age, and eight patients (80%) were male. In the open-repair group, patients averaged 66 years of age, and 45 (77%) were male.
Patients were excluded from endovascular treatment if they had infected aneurysms or aneurysms with inflammation that were not deemed to be true inflammatory aneurysms. The diagnosis of inflammatory aortic aneurysm was confirmed preoperatively by CT scan in the EVAR group or at the time of surgery in the open-repair group.
Dr. Stone reported having no financial disclosures.
SCOTTSDALE, ARIZ. – Inflammatory abdominal aortic aneurysms can be treated safely and effectively by endovascular aneurysm repair, though patients with significant hydronephrosis may have worse outcomes, a retrospective study suggests.
The study included 69 patients who underwent either endovascular repair (10 patients) or open surgical repair (59 patients) at the surgeon’s discretion at Mayo Clinics in Minnesota, Florida, or Arizona between 1999 and 2011.
Previous case series and meta-analyses have reported mixed results with endovascular aneurysm repair (EVAR), but the current study suggests that EVAR is appropriate management for inflammatory abdominal aortic aneurysms (AAAs), Dr. William M. Stone said at the annual meeting of the Southern Association for Vascular Surgery.
In the study’s EVAR group, eight patients presented with symptoms (80%), including one with rupture. In the open-repair group, 31 patients (52%) presented with symptoms, including 3 with rupture (5%).
Ureteral involvement was seen in 23 patients: 2 patients in the EVAR group (20%) and 21 in the open group (34%). Of these 23 patients, 21 underwent preoperative ureteral stent placement (91%). Thirty-six patients in the open-repair group had suprarenal aortic cross clamps (61%).
All of the EVAR procedures were technically successful, and patients were followed for an average of 34 months. The mean aneurysm size in the EVAR group decreased from 5.94 cm preoperatively to 4.73 cm after EVAR, an average change of nearly 18%, reported Dr. Stone of the Mayo Clinic in Phoenix.
Aneurysm size decreased in seven patients (70%), and did not change in two patients (20%) after EVAR. One EVAR patient was lost to follow-up. Preoperative hydronephrosis in one patient (10%) before EVAR did not change after EVAR, and one patient developed new hydronephrosis after EVAR. No patients in the EVAR group died, developed endoleaks, or needed steroids. Two patients developed atrial fibrillation after EVAR and were treated for it.
The inflammatory rind measured 5.4 cm before EVAR and 2.7 cm afterward on average, a mean change of 50%, he said.
In the open-repair group, surgeons used midline incisions in 52 patients (88%), a left flank approach in 6 patients (10%), and a bilateral subcostal approach in 1 (2%) to repair aneurysms with a mean size of 6.3 cm.
One patient in the open-repair group died postoperatively of a ruptured suprarenal inflammatory aneurysm. Major complications were seen in 22 patients (38%), including renal complications in 5 (8%), ischemic colitis in 2 (3%), and ureteral obstruction that required intervention in 3 (5%). A late anastomotic rupture in one patient in the open-surgery group was repaired by EVAR.
During a mean follow-up of 43 months, 17 patients in the open-repair group were lost to follow-up (28%). All of the remaining patients had resolution of their aneurysm sac. Four patients (7%) received steroids, not to treat the aneurysm but for comorbidities.
Among 12 patients in the open-repair group with preoperative hydronephrosis (20%), the hydronephrosis resolved in 7 of the 12 (58%), remained stable in 4 patients (33%), and worsened in 1 patient (8%). The patient with worsening hydronephrosis underwent ureterolysis. Two patients developed renal atrophy.
Although the retrospective study was small, it appeared to show a trend toward less severe complications in the EVAR group, "which is what we intuitively would have guessed," Dr. Stone said.
Previous data from the EUROSTAR (European Collaborators on Stent-Graft Techniques for Abdominal Aortic Aneurysm Repair) registry suggested that inflammatory AAA size decreased by 87% after EVAR, he noted (Semin. Interv. Cardiol. 2000;5:29-33). Aneurysm wall thickness averaged 21 mm preoperatively, 17 mm at intermediate follow-up, and 13 mm with long-term follow-up, which is "consistent with our review," he said.
Patients in the EUROSTAR database had problems with graft limb stenosis that were not seen in the current series, Dr. Stone noted. A ureteral stent and/or ureterolysis were required in 18% of the EUROSTAR patients who underwent EVAR. The rate of ureteral "entrapment" (inflammation around the ureters) improved from 45% to 27% after EVAR.
In a previous meta-analysis of data on 46 patients in 14 studies, EVAR decreased aneurysm size in most patients, with a median decrease of 11 mm. Periaortic fibrosis decreased in 52%, was unchanged in 42%, and progressed in 7% (J. Endovasc. Ther. 2005;12:560-7).
A separate meta-analysis of 56 studies with 1,120 patients compared EVAR with open repair of AAA, and found 1-year all-cause mortality rates of 2% with EVAR and 14% with open repair (Eur. J. Vasc. Endovasc. Surg. 2009;38:291-7). Periaortic fibrosis decreased in 65% of the EVAR group and in 73% of the open-repair group. Hydronephrosis regressed in 38% of the EVAR group and in 69% of the open-repair group.
In the current study, the two groups did not differ significantly in mean age, preoperative aneurysm size, or length of follow-up. In the EVAR group, patients averaged 72 years of age, and eight patients (80%) were male. In the open-repair group, patients averaged 66 years of age, and 45 (77%) were male.
Patients were excluded from endovascular treatment if they had infected aneurysms or aneurysms with inflammation that were not deemed to be true inflammatory aneurysms. The diagnosis of inflammatory aortic aneurysm was confirmed preoperatively by CT scan in the EVAR group or at the time of surgery in the open-repair group.
Dr. Stone reported having no financial disclosures.
SCOTTSDALE, ARIZ. – Inflammatory abdominal aortic aneurysms can be treated safely and effectively by endovascular aneurysm repair, though patients with significant hydronephrosis may have worse outcomes, a retrospective study suggests.
The study included 69 patients who underwent either endovascular repair (10 patients) or open surgical repair (59 patients) at the surgeon’s discretion at Mayo Clinics in Minnesota, Florida, or Arizona between 1999 and 2011.
Previous case series and meta-analyses have reported mixed results with endovascular aneurysm repair (EVAR), but the current study suggests that EVAR is appropriate management for inflammatory abdominal aortic aneurysms (AAAs), Dr. William M. Stone said at the annual meeting of the Southern Association for Vascular Surgery.
In the study’s EVAR group, eight patients presented with symptoms (80%), including one with rupture. In the open-repair group, 31 patients (52%) presented with symptoms, including 3 with rupture (5%).
Ureteral involvement was seen in 23 patients: 2 patients in the EVAR group (20%) and 21 in the open group (34%). Of these 23 patients, 21 underwent preoperative ureteral stent placement (91%). Thirty-six patients in the open-repair group had suprarenal aortic cross clamps (61%).
All of the EVAR procedures were technically successful, and patients were followed for an average of 34 months. The mean aneurysm size in the EVAR group decreased from 5.94 cm preoperatively to 4.73 cm after EVAR, an average change of nearly 18%, reported Dr. Stone of the Mayo Clinic in Phoenix.
Aneurysm size decreased in seven patients (70%), and did not change in two patients (20%) after EVAR. One EVAR patient was lost to follow-up. Preoperative hydronephrosis in one patient (10%) before EVAR did not change after EVAR, and one patient developed new hydronephrosis after EVAR. No patients in the EVAR group died, developed endoleaks, or needed steroids. Two patients developed atrial fibrillation after EVAR and were treated for it.
The inflammatory rind measured 5.4 cm before EVAR and 2.7 cm afterward on average, a mean change of 50%, he said.
In the open-repair group, surgeons used midline incisions in 52 patients (88%), a left flank approach in 6 patients (10%), and a bilateral subcostal approach in 1 (2%) to repair aneurysms with a mean size of 6.3 cm.
One patient in the open-repair group died postoperatively of a ruptured suprarenal inflammatory aneurysm. Major complications were seen in 22 patients (38%), including renal complications in 5 (8%), ischemic colitis in 2 (3%), and ureteral obstruction that required intervention in 3 (5%). A late anastomotic rupture in one patient in the open-surgery group was repaired by EVAR.
During a mean follow-up of 43 months, 17 patients in the open-repair group were lost to follow-up (28%). All of the remaining patients had resolution of their aneurysm sac. Four patients (7%) received steroids, not to treat the aneurysm but for comorbidities.
Among 12 patients in the open-repair group with preoperative hydronephrosis (20%), the hydronephrosis resolved in 7 of the 12 (58%), remained stable in 4 patients (33%), and worsened in 1 patient (8%). The patient with worsening hydronephrosis underwent ureterolysis. Two patients developed renal atrophy.
Although the retrospective study was small, it appeared to show a trend toward less severe complications in the EVAR group, "which is what we intuitively would have guessed," Dr. Stone said.
Previous data from the EUROSTAR (European Collaborators on Stent-Graft Techniques for Abdominal Aortic Aneurysm Repair) registry suggested that inflammatory AAA size decreased by 87% after EVAR, he noted (Semin. Interv. Cardiol. 2000;5:29-33). Aneurysm wall thickness averaged 21 mm preoperatively, 17 mm at intermediate follow-up, and 13 mm with long-term follow-up, which is "consistent with our review," he said.
Patients in the EUROSTAR database had problems with graft limb stenosis that were not seen in the current series, Dr. Stone noted. A ureteral stent and/or ureterolysis were required in 18% of the EUROSTAR patients who underwent EVAR. The rate of ureteral "entrapment" (inflammation around the ureters) improved from 45% to 27% after EVAR.
In a previous meta-analysis of data on 46 patients in 14 studies, EVAR decreased aneurysm size in most patients, with a median decrease of 11 mm. Periaortic fibrosis decreased in 52%, was unchanged in 42%, and progressed in 7% (J. Endovasc. Ther. 2005;12:560-7).
A separate meta-analysis of 56 studies with 1,120 patients compared EVAR with open repair of AAA, and found 1-year all-cause mortality rates of 2% with EVAR and 14% with open repair (Eur. J. Vasc. Endovasc. Surg. 2009;38:291-7). Periaortic fibrosis decreased in 65% of the EVAR group and in 73% of the open-repair group. Hydronephrosis regressed in 38% of the EVAR group and in 69% of the open-repair group.
In the current study, the two groups did not differ significantly in mean age, preoperative aneurysm size, or length of follow-up. In the EVAR group, patients averaged 72 years of age, and eight patients (80%) were male. In the open-repair group, patients averaged 66 years of age, and 45 (77%) were male.
Patients were excluded from endovascular treatment if they had infected aneurysms or aneurysms with inflammation that were not deemed to be true inflammatory aneurysms. The diagnosis of inflammatory aortic aneurysm was confirmed preoperatively by CT scan in the EVAR group or at the time of surgery in the open-repair group.
Dr. Stone reported having no financial disclosures.
FROM THE ANNUAL MEETING OF THE SOUTHERN ASSOCIATION FOR VASCULAR SURGERY
Human Genome Sequencing Affordable, but Practical?
SAN FRANCISCO – The cost of sequencing one person’s genome has shrunk from nearly $3 billion 14 years ago to an anticipated $1,000 within the next year or two, a development that positions human genome sequencing to explode into widespread use by researchers and clinicians.
Or maybe not, depending in part on recommendations to President Obama from the Presidential Commission for the Study of Bioethical Issues, which will submit a report on the topic later this year. In preparation, the Commission conducted a day-long public discussion with multiple experts about the potential for medical discoveries from genome research, and the difficulties of protecting patient privacy.
Excitement in some quarters about the already proven ability to diagnose rare disorders via genome sequencing has been tempered by concerns that the field may be moving too fast for the general good. The ability to collect genome data far exceeds the ability to interpret the data. And the growing use of such tests threatens to bankrupt the medical system if it leads to an avalanche of tests for the worried well and untreatable disorders.
Currently, physicians can order sequencing of an individual’s whole exome (all the expressed genes) or whole genome from a few centers on a very limited basis. Approximately 10,000 people had their genomes sequenced in 2011. Perhaps 100,000 will do the same in 2012, estimated Dr. Richard A. Gibbs, director of the Human Genome Sequencing Center at Baylor College of Medicine, Houston.
While many stakeholders emphasize the importance of free and unrestricted release of human genome data to all researchers, others argue that such open access would also allow third parties to manipulate data to deny individuals insurance or employment, he said. The race is on to try to understand genome data better before uninformed interpreters can do their damage. But clearly, having access to lots of genome data is key to advancing the science, he said.
"Less than 1% of the American public understands" genetics, opening the door to manipulation, said Commission Chair Amy Gutmann, Ph.D., president of the University of Pennsylvania, Philadelphia. "There’s a snake oil salesman out there for everything."
Benefits of Unrestricted Access
Among those arguing in favor of the unrestricted access to human genome data to all researchers is Retta Beery. The Baylor center helped diagnose a rare but treatable disorder in her twins, Alexis and Noah. After years of extremely limited mobility, severe breathing problems, costly emergency department visits, imaging tests, and visits to specialists, genome sequencing identified mutations in a gene called SPR that encodes the enzyme sepiapterin reductase. With proper drug treatment, the twins are healthy and high-functioning teenagers today.
"We believe this saved Alexis’s life," Ms. Beery told the Commission. "Weighing privacy versus life-saving treatment – it didn’t balance out at all." The family started a website to support others with similar challenges dealing with dystonia.
Another proponent of unrestricted access, Dr. Daniel Masys described the PREDICT (Pharmacogenomic Resource for Enhanced Decisions in Care and Treatment) project that he helped launch at Vanderbilt University, Nashville, Tenn., in 2010. The system prospectively gathers genome data from patients’ blood samples and makes clinically useful pharmacogenomic information available to physicians and patients through electronic medical records so that the right drug and dose get chosen for a specific patient.
Researchers there also are starting to analyze genomic data in a way that turns the traditional model on its head. Instead of picking a phenotype and looking for associations among all genetic polymorphisms, they pick a genotype and interrogate the set of all phenotypes (diseases) as recorded in the electronic medical records, Dr. Masys explained. Data from DNA "biorepositories" at seven U.S. centers get shared within the eMERGE (Electronic Medical Records & Genomics) Network for conducting genomic studies.
A Long Way to Go
The good news is we have the human genome. The bad news is it’s largely just a parts list," said Dr. Masys, currently an affiliated professor of biomedical and health informatics at the University of Washington, Seattle. "Our ability to acquire person-specific DNA data far exceeds our understanding of its meaning."
To advance the science quickly, genome data from hundreds of thousands or millions of people will be needed to draw clinical correlations. "The principle impediment is that this is a scale of science that we’ve never seen before," Dr. Masys said. He urged the Commission to not let privacy concerns slow the rapidity of this research.
Computerized clinical decision support is the only effective way to apply genomic variation–based guidance into clinical care because of the complexity of interpreting an individual’s data. And because an individual’s genomic data may evolve with age and other factors, electronic medical records will need to store multiple genomes. This is possible with today’s technology, but less than 2% of U.S. hospitals have fully adopted comprehensive electronic medical records, he said.
"Clearly, adoption of fully functional electronic medical records, including those that have patient-specific clinical decision support that can reason with data such as DNA variation, will be an essential feature of 21st-century health care," Dr. Masys said in an interview. "The sooner we get there, the sooner it will be easier for doctors to deal with what otherwise is an impossible task of trying to read and understand and keep up with this rapidly expanding science."
There is a risk, however, that delving into genomic data will identify numerous "incidentalomas," which will unnecessarily trigger expensive follow-up tests or misguided treatments, he said.
George Annas, J.D., chair of Health Law, Bioethics and Human Rights at Boston University, agreed and questioned whether "personalized medicine" is realistic. "At a time when the cost of health care is the No. 1 issue on the political agenda, it’s kind of bizarre that we would do something that’s the most expensive [thing to do] in medicine," he said.
Patient consent is another important issue, said Mr. Annas, citing the example of Henrietta Lacks, whose cells fueled decades of medical research without her knowledge or consent. "If people want to make their genetic information public, that’s fine with me. But to say everyone must is not the kind of country most people want to live in," he said.
Protections especially are needed for people who are unable to give informed consent, said Mark A. Rothstein, J.D., chair of law and medicine at the University of Louisville, Ky. "Those who are advocating newborn genome sequencing are throwing out long-standing policy in genetics not to test for late-onset disease," he said.
At least 25 million U.S. residents each year must sign authorizations for release of medical records to get a job or insurance or for other reasons, and adding genome data to those records could put them at greater risk. "I don’t think we’re ready for this huge onslaught of additional information, because there’s too much opportunity for misuse," he said.
Developments, such as the phenome-wide association studies at Vanderbilt, are exciting, Commissioner Nelson L. Michael noted in an interview. The human genome "is a new ‘book’ that many of us don’t know how to read very well," but this new approach to research should help translate that book, said the director of retrovirology at the Walter Reed Army Institute of Research, Bethesda, Md. "The better we are able to understand how the book is read and what it means, I think we are going to be able to translate that into clinical benefits" for a reasonable risk/benefit ratio, said Dr. Michael.
Dr. Gibbs reported being an investor in Life Technology and cofounder of the company Seq-Wright. The other speakers and commissioners did not report financial disclosures.
SAN FRANCISCO – The cost of sequencing one person’s genome has shrunk from nearly $3 billion 14 years ago to an anticipated $1,000 within the next year or two, a development that positions human genome sequencing to explode into widespread use by researchers and clinicians.
Or maybe not, depending in part on recommendations to President Obama from the Presidential Commission for the Study of Bioethical Issues, which will submit a report on the topic later this year. In preparation, the Commission conducted a day-long public discussion with multiple experts about the potential for medical discoveries from genome research, and the difficulties of protecting patient privacy.
Excitement in some quarters about the already proven ability to diagnose rare disorders via genome sequencing has been tempered by concerns that the field may be moving too fast for the general good. The ability to collect genome data far exceeds the ability to interpret the data. And the growing use of such tests threatens to bankrupt the medical system if it leads to an avalanche of tests for the worried well and untreatable disorders.
Currently, physicians can order sequencing of an individual’s whole exome (all the expressed genes) or whole genome from a few centers on a very limited basis. Approximately 10,000 people had their genomes sequenced in 2011. Perhaps 100,000 will do the same in 2012, estimated Dr. Richard A. Gibbs, director of the Human Genome Sequencing Center at Baylor College of Medicine, Houston.
While many stakeholders emphasize the importance of free and unrestricted release of human genome data to all researchers, others argue that such open access would also allow third parties to manipulate data to deny individuals insurance or employment, he said. The race is on to try to understand genome data better before uninformed interpreters can do their damage. But clearly, having access to lots of genome data is key to advancing the science, he said.
"Less than 1% of the American public understands" genetics, opening the door to manipulation, said Commission Chair Amy Gutmann, Ph.D., president of the University of Pennsylvania, Philadelphia. "There’s a snake oil salesman out there for everything."
Benefits of Unrestricted Access
Among those arguing in favor of the unrestricted access to human genome data to all researchers is Retta Beery. The Baylor center helped diagnose a rare but treatable disorder in her twins, Alexis and Noah. After years of extremely limited mobility, severe breathing problems, costly emergency department visits, imaging tests, and visits to specialists, genome sequencing identified mutations in a gene called SPR that encodes the enzyme sepiapterin reductase. With proper drug treatment, the twins are healthy and high-functioning teenagers today.
"We believe this saved Alexis’s life," Ms. Beery told the Commission. "Weighing privacy versus life-saving treatment – it didn’t balance out at all." The family started a website to support others with similar challenges dealing with dystonia.
Another proponent of unrestricted access, Dr. Daniel Masys described the PREDICT (Pharmacogenomic Resource for Enhanced Decisions in Care and Treatment) project that he helped launch at Vanderbilt University, Nashville, Tenn., in 2010. The system prospectively gathers genome data from patients’ blood samples and makes clinically useful pharmacogenomic information available to physicians and patients through electronic medical records so that the right drug and dose get chosen for a specific patient.
Researchers there also are starting to analyze genomic data in a way that turns the traditional model on its head. Instead of picking a phenotype and looking for associations among all genetic polymorphisms, they pick a genotype and interrogate the set of all phenotypes (diseases) as recorded in the electronic medical records, Dr. Masys explained. Data from DNA "biorepositories" at seven U.S. centers get shared within the eMERGE (Electronic Medical Records & Genomics) Network for conducting genomic studies.
A Long Way to Go
The good news is we have the human genome. The bad news is it’s largely just a parts list," said Dr. Masys, currently an affiliated professor of biomedical and health informatics at the University of Washington, Seattle. "Our ability to acquire person-specific DNA data far exceeds our understanding of its meaning."
To advance the science quickly, genome data from hundreds of thousands or millions of people will be needed to draw clinical correlations. "The principle impediment is that this is a scale of science that we’ve never seen before," Dr. Masys said. He urged the Commission to not let privacy concerns slow the rapidity of this research.
Computerized clinical decision support is the only effective way to apply genomic variation–based guidance into clinical care because of the complexity of interpreting an individual’s data. And because an individual’s genomic data may evolve with age and other factors, electronic medical records will need to store multiple genomes. This is possible with today’s technology, but less than 2% of U.S. hospitals have fully adopted comprehensive electronic medical records, he said.
"Clearly, adoption of fully functional electronic medical records, including those that have patient-specific clinical decision support that can reason with data such as DNA variation, will be an essential feature of 21st-century health care," Dr. Masys said in an interview. "The sooner we get there, the sooner it will be easier for doctors to deal with what otherwise is an impossible task of trying to read and understand and keep up with this rapidly expanding science."
There is a risk, however, that delving into genomic data will identify numerous "incidentalomas," which will unnecessarily trigger expensive follow-up tests or misguided treatments, he said.
George Annas, J.D., chair of Health Law, Bioethics and Human Rights at Boston University, agreed and questioned whether "personalized medicine" is realistic. "At a time when the cost of health care is the No. 1 issue on the political agenda, it’s kind of bizarre that we would do something that’s the most expensive [thing to do] in medicine," he said.
Patient consent is another important issue, said Mr. Annas, citing the example of Henrietta Lacks, whose cells fueled decades of medical research without her knowledge or consent. "If people want to make their genetic information public, that’s fine with me. But to say everyone must is not the kind of country most people want to live in," he said.
Protections especially are needed for people who are unable to give informed consent, said Mark A. Rothstein, J.D., chair of law and medicine at the University of Louisville, Ky. "Those who are advocating newborn genome sequencing are throwing out long-standing policy in genetics not to test for late-onset disease," he said.
At least 25 million U.S. residents each year must sign authorizations for release of medical records to get a job or insurance or for other reasons, and adding genome data to those records could put them at greater risk. "I don’t think we’re ready for this huge onslaught of additional information, because there’s too much opportunity for misuse," he said.
Developments, such as the phenome-wide association studies at Vanderbilt, are exciting, Commissioner Nelson L. Michael noted in an interview. The human genome "is a new ‘book’ that many of us don’t know how to read very well," but this new approach to research should help translate that book, said the director of retrovirology at the Walter Reed Army Institute of Research, Bethesda, Md. "The better we are able to understand how the book is read and what it means, I think we are going to be able to translate that into clinical benefits" for a reasonable risk/benefit ratio, said Dr. Michael.
Dr. Gibbs reported being an investor in Life Technology and cofounder of the company Seq-Wright. The other speakers and commissioners did not report financial disclosures.
SAN FRANCISCO – The cost of sequencing one person’s genome has shrunk from nearly $3 billion 14 years ago to an anticipated $1,000 within the next year or two, a development that positions human genome sequencing to explode into widespread use by researchers and clinicians.
Or maybe not, depending in part on recommendations to President Obama from the Presidential Commission for the Study of Bioethical Issues, which will submit a report on the topic later this year. In preparation, the Commission conducted a day-long public discussion with multiple experts about the potential for medical discoveries from genome research, and the difficulties of protecting patient privacy.
Excitement in some quarters about the already proven ability to diagnose rare disorders via genome sequencing has been tempered by concerns that the field may be moving too fast for the general good. The ability to collect genome data far exceeds the ability to interpret the data. And the growing use of such tests threatens to bankrupt the medical system if it leads to an avalanche of tests for the worried well and untreatable disorders.
Currently, physicians can order sequencing of an individual’s whole exome (all the expressed genes) or whole genome from a few centers on a very limited basis. Approximately 10,000 people had their genomes sequenced in 2011. Perhaps 100,000 will do the same in 2012, estimated Dr. Richard A. Gibbs, director of the Human Genome Sequencing Center at Baylor College of Medicine, Houston.
While many stakeholders emphasize the importance of free and unrestricted release of human genome data to all researchers, others argue that such open access would also allow third parties to manipulate data to deny individuals insurance or employment, he said. The race is on to try to understand genome data better before uninformed interpreters can do their damage. But clearly, having access to lots of genome data is key to advancing the science, he said.
"Less than 1% of the American public understands" genetics, opening the door to manipulation, said Commission Chair Amy Gutmann, Ph.D., president of the University of Pennsylvania, Philadelphia. "There’s a snake oil salesman out there for everything."
Benefits of Unrestricted Access
Among those arguing in favor of the unrestricted access to human genome data to all researchers is Retta Beery. The Baylor center helped diagnose a rare but treatable disorder in her twins, Alexis and Noah. After years of extremely limited mobility, severe breathing problems, costly emergency department visits, imaging tests, and visits to specialists, genome sequencing identified mutations in a gene called SPR that encodes the enzyme sepiapterin reductase. With proper drug treatment, the twins are healthy and high-functioning teenagers today.
"We believe this saved Alexis’s life," Ms. Beery told the Commission. "Weighing privacy versus life-saving treatment – it didn’t balance out at all." The family started a website to support others with similar challenges dealing with dystonia.
Another proponent of unrestricted access, Dr. Daniel Masys described the PREDICT (Pharmacogenomic Resource for Enhanced Decisions in Care and Treatment) project that he helped launch at Vanderbilt University, Nashville, Tenn., in 2010. The system prospectively gathers genome data from patients’ blood samples and makes clinically useful pharmacogenomic information available to physicians and patients through electronic medical records so that the right drug and dose get chosen for a specific patient.
Researchers there also are starting to analyze genomic data in a way that turns the traditional model on its head. Instead of picking a phenotype and looking for associations among all genetic polymorphisms, they pick a genotype and interrogate the set of all phenotypes (diseases) as recorded in the electronic medical records, Dr. Masys explained. Data from DNA "biorepositories" at seven U.S. centers get shared within the eMERGE (Electronic Medical Records & Genomics) Network for conducting genomic studies.
A Long Way to Go
The good news is we have the human genome. The bad news is it’s largely just a parts list," said Dr. Masys, currently an affiliated professor of biomedical and health informatics at the University of Washington, Seattle. "Our ability to acquire person-specific DNA data far exceeds our understanding of its meaning."
To advance the science quickly, genome data from hundreds of thousands or millions of people will be needed to draw clinical correlations. "The principle impediment is that this is a scale of science that we’ve never seen before," Dr. Masys said. He urged the Commission to not let privacy concerns slow the rapidity of this research.
Computerized clinical decision support is the only effective way to apply genomic variation–based guidance into clinical care because of the complexity of interpreting an individual’s data. And because an individual’s genomic data may evolve with age and other factors, electronic medical records will need to store multiple genomes. This is possible with today’s technology, but less than 2% of U.S. hospitals have fully adopted comprehensive electronic medical records, he said.
"Clearly, adoption of fully functional electronic medical records, including those that have patient-specific clinical decision support that can reason with data such as DNA variation, will be an essential feature of 21st-century health care," Dr. Masys said in an interview. "The sooner we get there, the sooner it will be easier for doctors to deal with what otherwise is an impossible task of trying to read and understand and keep up with this rapidly expanding science."
There is a risk, however, that delving into genomic data will identify numerous "incidentalomas," which will unnecessarily trigger expensive follow-up tests or misguided treatments, he said.
George Annas, J.D., chair of Health Law, Bioethics and Human Rights at Boston University, agreed and questioned whether "personalized medicine" is realistic. "At a time when the cost of health care is the No. 1 issue on the political agenda, it’s kind of bizarre that we would do something that’s the most expensive [thing to do] in medicine," he said.
Patient consent is another important issue, said Mr. Annas, citing the example of Henrietta Lacks, whose cells fueled decades of medical research without her knowledge or consent. "If people want to make their genetic information public, that’s fine with me. But to say everyone must is not the kind of country most people want to live in," he said.
Protections especially are needed for people who are unable to give informed consent, said Mark A. Rothstein, J.D., chair of law and medicine at the University of Louisville, Ky. "Those who are advocating newborn genome sequencing are throwing out long-standing policy in genetics not to test for late-onset disease," he said.
At least 25 million U.S. residents each year must sign authorizations for release of medical records to get a job or insurance or for other reasons, and adding genome data to those records could put them at greater risk. "I don’t think we’re ready for this huge onslaught of additional information, because there’s too much opportunity for misuse," he said.
Developments, such as the phenome-wide association studies at Vanderbilt, are exciting, Commissioner Nelson L. Michael noted in an interview. The human genome "is a new ‘book’ that many of us don’t know how to read very well," but this new approach to research should help translate that book, said the director of retrovirology at the Walter Reed Army Institute of Research, Bethesda, Md. "The better we are able to understand how the book is read and what it means, I think we are going to be able to translate that into clinical benefits" for a reasonable risk/benefit ratio, said Dr. Michael.
Dr. Gibbs reported being an investor in Life Technology and cofounder of the company Seq-Wright. The other speakers and commissioners did not report financial disclosures.
FROM THE EIGHTH MEETING OF THE PRESIDENTIAL COMMISSION FOR THE STUDY OF BIOETHICAL ISSUES
Improving Resident Communication
SAN FRANCISCO – Training residents to notify attending surgeons of any significant change in a patient’s condition greatly reduced the proportion of critical events that were not communicated to attending surgeons, from 33% to 2%, in a prospective study of four hospitals.
The current study was undertaken in response to a previous study by the same research group showing that ambiguity about who is responsible for communications contributed to communication breakdowns between attending surgeons and other members of the team at any point in patient care, Dr. Caprice C. Greenberg said at the annual clinical congress of the American College of Surgeons.
In the previous study, 444 malpractice claims were reviewed, and this process identified 60 cases in which communication breakdown resulted in harm to a patient. Dr. Greenberg and colleagues found that communication breakdowns related to surgery are equally likely to happen during preoperative, intraoperative, and postoperative care, and most commonly involve communications attempted between an attending surgeon and another attending surgeon, a resident, or the patient or family.
Ambiguity about who is responsible for communicating played a role in 58% of communication breakdowns, said Dr. Greenberg, director of the Wisconsin Surgical Outcomes Research Program at the University of Wisconsin, Madison.
Handoffs of patient care from one provider to another contributed to 43% of communication breakdowns, and transferring a patient to a different location contributed to 39% of communication breakdowns. The data also showed that an asymmetry in status between the two communicating parties contributed to 74% of message breakdowns ( J. Am. Coll. Surg. 2007;204:533-40).
Dr. Greenberg and her associates identified "triggers" that should prompt residents or nurses to contact attending surgeons, including a patient’s admission to a hospital, discharge, or a visit to an emergency department, transfer into or out of the ICU, unplanned intubation, or the development of cardiac arrest, new arrhythmia, or hemodynamic instability.
Significant neurologic changes, major wound complications, unplanned blood transfusion, an invasive procedure or operation, or errors in medication or treatment necessitating an intervention also should trigger communication with the attending surgeon. Even simply concern by a surgical trainee or a request from a nurse or another physician to contact the attending surgeon were considered triggers for communication.
The triggers were included in guidelines created by representatives of the four hospitals in Harvard University’s system in a collaboration organized by the system’s malpractice insurers. Under the new guidelines, residents were to notify attending surgeons of any significant changes in a patient’s condition regardless of the day or time. The residents would be trained to understand what qualifies as "significant changes" based in part on specialty-specific definitions, she said.
"What a urologist cares about is probably a little bit different from what a neurosurgeon or cardiac surgeon cares about," she explained.
A study of previous practices found that residents thought that 61 of 80 critical patient events (76%) did not need to be communicated to attending surgeons for safe patient care, and 26 events were not communicated (33%). Of the 54 events that were communicated, discussions with the attending surgeons changed management in 18 cases (33%). Attending surgeons responded to calls 100% of the time ( Ann. Surg. 2009;250:861-5).
"It wasn’t that the attendings didn’t want to be called. It was that residents either felt unempowered to call or they felt that it wasn’t necessary," she said.
Breakdowns in communication are common and play a significant role in adverse events, prior data suggest. One study of 48 surgeries found that 31% of 421 attempted communications between surgical team members failed, and approximately a third of these communication failures potentially jeopardized patient safety (Qual. Saf. Health Care 2004;13:330-4).
Other strategies to reduce the risk of errors during surgery include "workload leveling," Dr. Greenberg added. This means the attending surgeon should communicate frequently to members of the interdisciplinary surgical team about the status of the case and expected progression of the case, so that team members can manage their time and plan to do auxiliary tasks at the appropriate times. It’s probably impossible to avoid all errors, so surgeons need to find the right balance of error prevention and error mitigation through "resilience" – the ability to anticipate, cope with, recover from, and learn from unforeseen developments, she added. "To start to increase resilience, we really need to teach people adaptability and flexibility," she said.
Dr. Mary Klingensmith, a professor of surgery at Washington University, St. Louis, and Dr. John Hanks, a professor of surgery at the University of Virginia, Charlottesville, commented, "The conclusion of this study may seem obvious to those of us no longer in training – namely that residents should communicate critical patient events to attendings. Yet the imperative nature of such communication is not stressed adequately in our surgical training culture. In many training programs, there are some time-honored but outdated concepts in play, such as it is a "sign of weakness" to call the attending. Dr. Greenberg describes residents in this position as feeling "unempowered" to place such a call.
"We need to debunk this myth and explicitly instruct our residents about what we want and expect. Under the new paradigm, this accountability must include rapid and accurate transmittal of information with confidence on both the sending and receiving ends.
"The intervention put into place by Dr. Greenberg’s group did just that, laying out for trainees the patient events that should trigger a call to the attending. Interestingly, they reported that change in patient management, as a result of attending input, occurred in only 33% of cases in which the attending was called – a result suggesting that information transfer was merely that of the "FYI" variety. Yet in all instances, the attending wanted to be called.
"If the patient safety aspect of these communication triggers can be stressed, we can more effectively shape trainee behavior." ☐
Effective communication continues to be a problem as medical teams become more modular in their approach to patient care. Although methods of communication for residents have become ubiquitous, communication to the attending often does not occur in a reliable manner.
This study is an excellent example of improving patient safety by removing potential communication breakdowns. This prospective study by Dr. Greenberg created clear, documented expectations on when the attending should be notified by either a resident or nurse. As such, critical patient events were more effectively delivered to the attending. In a third of these notifications, the patient care plan was then changed. An interesting component of this study was the setting of expectations on both ends; when to call and when to be open to receiving a call.
This study is also a microcosm of the dilemma surgical education finds itself in when attempting to merge ideals of graded resident autonomy with safe patient care. Grey-haired residency stories abound of feats of technical magnificence as their attending slept. Yet, over time, increased scrutiny on accountability and improved outcomes has shortened if not changed the leash trainees are given. Resident autonomy though is based on effective, bi-directional communication guided by an attending.
More hospitals are adopting critical pathways which cause a mandatory notification to the attending. Potential exists for the resident to be marginalized, becoming an outsider in patient care. It is imperative that safety measures implemented in hospital programs include an educational component. Integrating the resident into algorithms that emphasizes their role in diagnosis and implementing a treatment plan is crucial.
Dr. Robroy MacIver is a pediatric cardiothoracic surgery fellow at Seattle Children’s Hospital and a resident editor of Thoracic Surgery News.
Effective communication continues to be a problem as medical teams become more modular in their approach to patient care. Although methods of communication for residents have become ubiquitous, communication to the attending often does not occur in a reliable manner.
This study is an excellent example of improving patient safety by removing potential communication breakdowns. This prospective study by Dr. Greenberg created clear, documented expectations on when the attending should be notified by either a resident or nurse. As such, critical patient events were more effectively delivered to the attending. In a third of these notifications, the patient care plan was then changed. An interesting component of this study was the setting of expectations on both ends; when to call and when to be open to receiving a call.
This study is also a microcosm of the dilemma surgical education finds itself in when attempting to merge ideals of graded resident autonomy with safe patient care. Grey-haired residency stories abound of feats of technical magnificence as their attending slept. Yet, over time, increased scrutiny on accountability and improved outcomes has shortened if not changed the leash trainees are given. Resident autonomy though is based on effective, bi-directional communication guided by an attending.
More hospitals are adopting critical pathways which cause a mandatory notification to the attending. Potential exists for the resident to be marginalized, becoming an outsider in patient care. It is imperative that safety measures implemented in hospital programs include an educational component. Integrating the resident into algorithms that emphasizes their role in diagnosis and implementing a treatment plan is crucial.
Dr. Robroy MacIver is a pediatric cardiothoracic surgery fellow at Seattle Children’s Hospital and a resident editor of Thoracic Surgery News.
Effective communication continues to be a problem as medical teams become more modular in their approach to patient care. Although methods of communication for residents have become ubiquitous, communication to the attending often does not occur in a reliable manner.
This study is an excellent example of improving patient safety by removing potential communication breakdowns. This prospective study by Dr. Greenberg created clear, documented expectations on when the attending should be notified by either a resident or nurse. As such, critical patient events were more effectively delivered to the attending. In a third of these notifications, the patient care plan was then changed. An interesting component of this study was the setting of expectations on both ends; when to call and when to be open to receiving a call.
This study is also a microcosm of the dilemma surgical education finds itself in when attempting to merge ideals of graded resident autonomy with safe patient care. Grey-haired residency stories abound of feats of technical magnificence as their attending slept. Yet, over time, increased scrutiny on accountability and improved outcomes has shortened if not changed the leash trainees are given. Resident autonomy though is based on effective, bi-directional communication guided by an attending.
More hospitals are adopting critical pathways which cause a mandatory notification to the attending. Potential exists for the resident to be marginalized, becoming an outsider in patient care. It is imperative that safety measures implemented in hospital programs include an educational component. Integrating the resident into algorithms that emphasizes their role in diagnosis and implementing a treatment plan is crucial.
Dr. Robroy MacIver is a pediatric cardiothoracic surgery fellow at Seattle Children’s Hospital and a resident editor of Thoracic Surgery News.
SAN FRANCISCO – Training residents to notify attending surgeons of any significant change in a patient’s condition greatly reduced the proportion of critical events that were not communicated to attending surgeons, from 33% to 2%, in a prospective study of four hospitals.
The current study was undertaken in response to a previous study by the same research group showing that ambiguity about who is responsible for communications contributed to communication breakdowns between attending surgeons and other members of the team at any point in patient care, Dr. Caprice C. Greenberg said at the annual clinical congress of the American College of Surgeons.
In the previous study, 444 malpractice claims were reviewed, and this process identified 60 cases in which communication breakdown resulted in harm to a patient. Dr. Greenberg and colleagues found that communication breakdowns related to surgery are equally likely to happen during preoperative, intraoperative, and postoperative care, and most commonly involve communications attempted between an attending surgeon and another attending surgeon, a resident, or the patient or family.
Ambiguity about who is responsible for communicating played a role in 58% of communication breakdowns, said Dr. Greenberg, director of the Wisconsin Surgical Outcomes Research Program at the University of Wisconsin, Madison.
Handoffs of patient care from one provider to another contributed to 43% of communication breakdowns, and transferring a patient to a different location contributed to 39% of communication breakdowns. The data also showed that an asymmetry in status between the two communicating parties contributed to 74% of message breakdowns ( J. Am. Coll. Surg. 2007;204:533-40).
Dr. Greenberg and her associates identified "triggers" that should prompt residents or nurses to contact attending surgeons, including a patient’s admission to a hospital, discharge, or a visit to an emergency department, transfer into or out of the ICU, unplanned intubation, or the development of cardiac arrest, new arrhythmia, or hemodynamic instability.
Significant neurologic changes, major wound complications, unplanned blood transfusion, an invasive procedure or operation, or errors in medication or treatment necessitating an intervention also should trigger communication with the attending surgeon. Even simply concern by a surgical trainee or a request from a nurse or another physician to contact the attending surgeon were considered triggers for communication.
The triggers were included in guidelines created by representatives of the four hospitals in Harvard University’s system in a collaboration organized by the system’s malpractice insurers. Under the new guidelines, residents were to notify attending surgeons of any significant changes in a patient’s condition regardless of the day or time. The residents would be trained to understand what qualifies as "significant changes" based in part on specialty-specific definitions, she said.
"What a urologist cares about is probably a little bit different from what a neurosurgeon or cardiac surgeon cares about," she explained.
A study of previous practices found that residents thought that 61 of 80 critical patient events (76%) did not need to be communicated to attending surgeons for safe patient care, and 26 events were not communicated (33%). Of the 54 events that were communicated, discussions with the attending surgeons changed management in 18 cases (33%). Attending surgeons responded to calls 100% of the time ( Ann. Surg. 2009;250:861-5).
"It wasn’t that the attendings didn’t want to be called. It was that residents either felt unempowered to call or they felt that it wasn’t necessary," she said.
Breakdowns in communication are common and play a significant role in adverse events, prior data suggest. One study of 48 surgeries found that 31% of 421 attempted communications between surgical team members failed, and approximately a third of these communication failures potentially jeopardized patient safety (Qual. Saf. Health Care 2004;13:330-4).
Other strategies to reduce the risk of errors during surgery include "workload leveling," Dr. Greenberg added. This means the attending surgeon should communicate frequently to members of the interdisciplinary surgical team about the status of the case and expected progression of the case, so that team members can manage their time and plan to do auxiliary tasks at the appropriate times. It’s probably impossible to avoid all errors, so surgeons need to find the right balance of error prevention and error mitigation through "resilience" – the ability to anticipate, cope with, recover from, and learn from unforeseen developments, she added. "To start to increase resilience, we really need to teach people adaptability and flexibility," she said.
Dr. Mary Klingensmith, a professor of surgery at Washington University, St. Louis, and Dr. John Hanks, a professor of surgery at the University of Virginia, Charlottesville, commented, "The conclusion of this study may seem obvious to those of us no longer in training – namely that residents should communicate critical patient events to attendings. Yet the imperative nature of such communication is not stressed adequately in our surgical training culture. In many training programs, there are some time-honored but outdated concepts in play, such as it is a "sign of weakness" to call the attending. Dr. Greenberg describes residents in this position as feeling "unempowered" to place such a call.
"We need to debunk this myth and explicitly instruct our residents about what we want and expect. Under the new paradigm, this accountability must include rapid and accurate transmittal of information with confidence on both the sending and receiving ends.
"The intervention put into place by Dr. Greenberg’s group did just that, laying out for trainees the patient events that should trigger a call to the attending. Interestingly, they reported that change in patient management, as a result of attending input, occurred in only 33% of cases in which the attending was called – a result suggesting that information transfer was merely that of the "FYI" variety. Yet in all instances, the attending wanted to be called.
"If the patient safety aspect of these communication triggers can be stressed, we can more effectively shape trainee behavior." ☐
SAN FRANCISCO – Training residents to notify attending surgeons of any significant change in a patient’s condition greatly reduced the proportion of critical events that were not communicated to attending surgeons, from 33% to 2%, in a prospective study of four hospitals.
The current study was undertaken in response to a previous study by the same research group showing that ambiguity about who is responsible for communications contributed to communication breakdowns between attending surgeons and other members of the team at any point in patient care, Dr. Caprice C. Greenberg said at the annual clinical congress of the American College of Surgeons.
In the previous study, 444 malpractice claims were reviewed, and this process identified 60 cases in which communication breakdown resulted in harm to a patient. Dr. Greenberg and colleagues found that communication breakdowns related to surgery are equally likely to happen during preoperative, intraoperative, and postoperative care, and most commonly involve communications attempted between an attending surgeon and another attending surgeon, a resident, or the patient or family.
Ambiguity about who is responsible for communicating played a role in 58% of communication breakdowns, said Dr. Greenberg, director of the Wisconsin Surgical Outcomes Research Program at the University of Wisconsin, Madison.
Handoffs of patient care from one provider to another contributed to 43% of communication breakdowns, and transferring a patient to a different location contributed to 39% of communication breakdowns. The data also showed that an asymmetry in status between the two communicating parties contributed to 74% of message breakdowns ( J. Am. Coll. Surg. 2007;204:533-40).
Dr. Greenberg and her associates identified "triggers" that should prompt residents or nurses to contact attending surgeons, including a patient’s admission to a hospital, discharge, or a visit to an emergency department, transfer into or out of the ICU, unplanned intubation, or the development of cardiac arrest, new arrhythmia, or hemodynamic instability.
Significant neurologic changes, major wound complications, unplanned blood transfusion, an invasive procedure or operation, or errors in medication or treatment necessitating an intervention also should trigger communication with the attending surgeon. Even simply concern by a surgical trainee or a request from a nurse or another physician to contact the attending surgeon were considered triggers for communication.
The triggers were included in guidelines created by representatives of the four hospitals in Harvard University’s system in a collaboration organized by the system’s malpractice insurers. Under the new guidelines, residents were to notify attending surgeons of any significant changes in a patient’s condition regardless of the day or time. The residents would be trained to understand what qualifies as "significant changes" based in part on specialty-specific definitions, she said.
"What a urologist cares about is probably a little bit different from what a neurosurgeon or cardiac surgeon cares about," she explained.
A study of previous practices found that residents thought that 61 of 80 critical patient events (76%) did not need to be communicated to attending surgeons for safe patient care, and 26 events were not communicated (33%). Of the 54 events that were communicated, discussions with the attending surgeons changed management in 18 cases (33%). Attending surgeons responded to calls 100% of the time ( Ann. Surg. 2009;250:861-5).
"It wasn’t that the attendings didn’t want to be called. It was that residents either felt unempowered to call or they felt that it wasn’t necessary," she said.
Breakdowns in communication are common and play a significant role in adverse events, prior data suggest. One study of 48 surgeries found that 31% of 421 attempted communications between surgical team members failed, and approximately a third of these communication failures potentially jeopardized patient safety (Qual. Saf. Health Care 2004;13:330-4).
Other strategies to reduce the risk of errors during surgery include "workload leveling," Dr. Greenberg added. This means the attending surgeon should communicate frequently to members of the interdisciplinary surgical team about the status of the case and expected progression of the case, so that team members can manage their time and plan to do auxiliary tasks at the appropriate times. It’s probably impossible to avoid all errors, so surgeons need to find the right balance of error prevention and error mitigation through "resilience" – the ability to anticipate, cope with, recover from, and learn from unforeseen developments, she added. "To start to increase resilience, we really need to teach people adaptability and flexibility," she said.
Dr. Mary Klingensmith, a professor of surgery at Washington University, St. Louis, and Dr. John Hanks, a professor of surgery at the University of Virginia, Charlottesville, commented, "The conclusion of this study may seem obvious to those of us no longer in training – namely that residents should communicate critical patient events to attendings. Yet the imperative nature of such communication is not stressed adequately in our surgical training culture. In many training programs, there are some time-honored but outdated concepts in play, such as it is a "sign of weakness" to call the attending. Dr. Greenberg describes residents in this position as feeling "unempowered" to place such a call.
"We need to debunk this myth and explicitly instruct our residents about what we want and expect. Under the new paradigm, this accountability must include rapid and accurate transmittal of information with confidence on both the sending and receiving ends.
"The intervention put into place by Dr. Greenberg’s group did just that, laying out for trainees the patient events that should trigger a call to the attending. Interestingly, they reported that change in patient management, as a result of attending input, occurred in only 33% of cases in which the attending was called – a result suggesting that information transfer was merely that of the "FYI" variety. Yet in all instances, the attending wanted to be called.
"If the patient safety aspect of these communication triggers can be stressed, we can more effectively shape trainee behavior." ☐
Major Finding: Residents failed to inform attending surgeons of critical patient events in 26 of 80 cases (33%) before adoption of new guidelines, and in only 1 of 47 cases (2%) after the intervention.
Data Source: Prospective studies at four hospitals before and after adoption of guidelines requiring residents to inform attending surgeons of any significant change in patient status.
Disclosures: Dr. Greenberg said she has no relevant conflicts of interest.
Disclose and Discuss Errors; Don't Defend, Deny
SAN FRANCISCO – Changing the clinical culture so that physicians were more willing to talk with patients about medical and surgical errors increased the number of errors reported, decreased lawsuits and legal costs, and improved safety at one institution.
"It used to be a ‘defend and deny’ culture," said Dr. Darrell A. Campbell Jr., professor of surgery and chief of clinical affairs at the University of Michigan, Ann Arbor. "Now it’s ‘disclose and discuss.’ "
The University of Michigan Health System’s "Disclosure of Unanticipated Outcomes" policy requires physicians to give patients "full disclosure of results, including results that differ significantly from what was anticipated" to allow patients to make informed decisions about future medical care, he said at the annual clinical congress of the American College of Surgeons.
Under the policy’s driving principles, the health system will defend medically appropriate care vigorously but will compensate quickly and fairly when inappropriate medical care causes injury and will learn from mistakes to improve patient safety and communication. The health system can compensate quickly and fairly because it is a closed-staff model covered by a captive insurance company, he said.
Reports of errors and "risk management events" more than doubled since full implementation of the policy in February 2004, from 6,706 in 2004 to 15,650 in 2007, he said. "I think people feel much more comfortable reporting errors" now.
A comparison of data from 2001 (before the policy) and 2005 (after the policy) found that the number of claims and lawsuits fell from 262 to 114, the average time to resolve claims and lawsuits decreased from 21 months to 10 months, and annual litigation costs declined from $3 million to $1 million, he said.
A retrospective study by other investigators looked at the university’s experience from 1995 to 2007 and reported similar findings. The average monthly rate of new legal claims decreased from seven per 100,000 patient encounters to less than five per 100,000 patient encounters after adopting the new policy.
The median time to resolve claims decreased from 1.36 to 0.95 years, and costs decreased for total liability, patient compensation, and legal costs not related to compensation (Ann. Intern. Med. 2010;153:213-21).
Dr. Campbell, a transplantation surgeon, described a case that went awry to illustrate possible responses to the situation. A 9-month-old girl undergoing a liver transplant had a small-diameter hepatic artery. Although the surgeon communicated to the anesthesiologist that the patient should not be overtransfused, the message may have been lost during handoff. The first postoperative hematocrit was 50%, the hepatic artery thrombosed, and the patient required retransplantation.
Prior to the full-disclosure policy, it might have been tempting to tell the patient’s parents, "These things happen," he said. While this is true, and it may avoid litigation, it’s not the whole truth. Caregivers would feel bad about it, the clinical safety culture would suffer, nothing would be learned, and the same problem could happen again.
If the physician instead says to the parents, "I’m concerned about what just happened. Let’s talk," the conversation is more difficult and could lead to litigation, but it’s an honest approach that augments doctor-patient trust and the culture of safety, which should make caregivers feel better, he said.
"Let’s talk" does not mean the surgeon should make reckless comments, Dr. Campbell stressed. It would not be helpful to say, "Anesthesia is incompetent," or "The fellow dropped the ball," or "I should have been notified earlier," or "I did a perfect operation," or "Somebody’s head will roll," for example.
Disclosing an unanticipated outcome should sound something like the following, he suggested: "This was an unexpected result. I am going to investigate fully. You have the right to know the whole story – the facts. I will tell you what I learn, but not right now."
That provides a window for exploring other possible complications in the case he described, he said. There may have been a laboratory or transcription error. An artery may have been open at the time of reexploration and not seen on relatively insensitive ultrasound. A technical error could have been made, or the patient may have had a humorally mediated rejection of the organ.
Dr. Campbell reported he had no relevant conflicts.
Body text
Doctor’s Bio
Body text
Doctor’s Bio
Body text
Doctor’s Bio
SAN FRANCISCO – Changing the clinical culture so that physicians were more willing to talk with patients about medical and surgical errors increased the number of errors reported, decreased lawsuits and legal costs, and improved safety at one institution.
"It used to be a ‘defend and deny’ culture," said Dr. Darrell A. Campbell Jr., professor of surgery and chief of clinical affairs at the University of Michigan, Ann Arbor. "Now it’s ‘disclose and discuss.’ "
The University of Michigan Health System’s "Disclosure of Unanticipated Outcomes" policy requires physicians to give patients "full disclosure of results, including results that differ significantly from what was anticipated" to allow patients to make informed decisions about future medical care, he said at the annual clinical congress of the American College of Surgeons.
Under the policy’s driving principles, the health system will defend medically appropriate care vigorously but will compensate quickly and fairly when inappropriate medical care causes injury and will learn from mistakes to improve patient safety and communication. The health system can compensate quickly and fairly because it is a closed-staff model covered by a captive insurance company, he said.
Reports of errors and "risk management events" more than doubled since full implementation of the policy in February 2004, from 6,706 in 2004 to 15,650 in 2007, he said. "I think people feel much more comfortable reporting errors" now.
A comparison of data from 2001 (before the policy) and 2005 (after the policy) found that the number of claims and lawsuits fell from 262 to 114, the average time to resolve claims and lawsuits decreased from 21 months to 10 months, and annual litigation costs declined from $3 million to $1 million, he said.
A retrospective study by other investigators looked at the university’s experience from 1995 to 2007 and reported similar findings. The average monthly rate of new legal claims decreased from seven per 100,000 patient encounters to less than five per 100,000 patient encounters after adopting the new policy.
The median time to resolve claims decreased from 1.36 to 0.95 years, and costs decreased for total liability, patient compensation, and legal costs not related to compensation (Ann. Intern. Med. 2010;153:213-21).
Dr. Campbell, a transplantation surgeon, described a case that went awry to illustrate possible responses to the situation. A 9-month-old girl undergoing a liver transplant had a small-diameter hepatic artery. Although the surgeon communicated to the anesthesiologist that the patient should not be overtransfused, the message may have been lost during handoff. The first postoperative hematocrit was 50%, the hepatic artery thrombosed, and the patient required retransplantation.
Prior to the full-disclosure policy, it might have been tempting to tell the patient’s parents, "These things happen," he said. While this is true, and it may avoid litigation, it’s not the whole truth. Caregivers would feel bad about it, the clinical safety culture would suffer, nothing would be learned, and the same problem could happen again.
If the physician instead says to the parents, "I’m concerned about what just happened. Let’s talk," the conversation is more difficult and could lead to litigation, but it’s an honest approach that augments doctor-patient trust and the culture of safety, which should make caregivers feel better, he said.
"Let’s talk" does not mean the surgeon should make reckless comments, Dr. Campbell stressed. It would not be helpful to say, "Anesthesia is incompetent," or "The fellow dropped the ball," or "I should have been notified earlier," or "I did a perfect operation," or "Somebody’s head will roll," for example.
Disclosing an unanticipated outcome should sound something like the following, he suggested: "This was an unexpected result. I am going to investigate fully. You have the right to know the whole story – the facts. I will tell you what I learn, but not right now."
That provides a window for exploring other possible complications in the case he described, he said. There may have been a laboratory or transcription error. An artery may have been open at the time of reexploration and not seen on relatively insensitive ultrasound. A technical error could have been made, or the patient may have had a humorally mediated rejection of the organ.
Dr. Campbell reported he had no relevant conflicts.
SAN FRANCISCO – Changing the clinical culture so that physicians were more willing to talk with patients about medical and surgical errors increased the number of errors reported, decreased lawsuits and legal costs, and improved safety at one institution.
"It used to be a ‘defend and deny’ culture," said Dr. Darrell A. Campbell Jr., professor of surgery and chief of clinical affairs at the University of Michigan, Ann Arbor. "Now it’s ‘disclose and discuss.’ "
The University of Michigan Health System’s "Disclosure of Unanticipated Outcomes" policy requires physicians to give patients "full disclosure of results, including results that differ significantly from what was anticipated" to allow patients to make informed decisions about future medical care, he said at the annual clinical congress of the American College of Surgeons.
Under the policy’s driving principles, the health system will defend medically appropriate care vigorously but will compensate quickly and fairly when inappropriate medical care causes injury and will learn from mistakes to improve patient safety and communication. The health system can compensate quickly and fairly because it is a closed-staff model covered by a captive insurance company, he said.
Reports of errors and "risk management events" more than doubled since full implementation of the policy in February 2004, from 6,706 in 2004 to 15,650 in 2007, he said. "I think people feel much more comfortable reporting errors" now.
A comparison of data from 2001 (before the policy) and 2005 (after the policy) found that the number of claims and lawsuits fell from 262 to 114, the average time to resolve claims and lawsuits decreased from 21 months to 10 months, and annual litigation costs declined from $3 million to $1 million, he said.
A retrospective study by other investigators looked at the university’s experience from 1995 to 2007 and reported similar findings. The average monthly rate of new legal claims decreased from seven per 100,000 patient encounters to less than five per 100,000 patient encounters after adopting the new policy.
The median time to resolve claims decreased from 1.36 to 0.95 years, and costs decreased for total liability, patient compensation, and legal costs not related to compensation (Ann. Intern. Med. 2010;153:213-21).
Dr. Campbell, a transplantation surgeon, described a case that went awry to illustrate possible responses to the situation. A 9-month-old girl undergoing a liver transplant had a small-diameter hepatic artery. Although the surgeon communicated to the anesthesiologist that the patient should not be overtransfused, the message may have been lost during handoff. The first postoperative hematocrit was 50%, the hepatic artery thrombosed, and the patient required retransplantation.
Prior to the full-disclosure policy, it might have been tempting to tell the patient’s parents, "These things happen," he said. While this is true, and it may avoid litigation, it’s not the whole truth. Caregivers would feel bad about it, the clinical safety culture would suffer, nothing would be learned, and the same problem could happen again.
If the physician instead says to the parents, "I’m concerned about what just happened. Let’s talk," the conversation is more difficult and could lead to litigation, but it’s an honest approach that augments doctor-patient trust and the culture of safety, which should make caregivers feel better, he said.
"Let’s talk" does not mean the surgeon should make reckless comments, Dr. Campbell stressed. It would not be helpful to say, "Anesthesia is incompetent," or "The fellow dropped the ball," or "I should have been notified earlier," or "I did a perfect operation," or "Somebody’s head will roll," for example.
Disclosing an unanticipated outcome should sound something like the following, he suggested: "This was an unexpected result. I am going to investigate fully. You have the right to know the whole story – the facts. I will tell you what I learn, but not right now."
That provides a window for exploring other possible complications in the case he described, he said. There may have been a laboratory or transcription error. An artery may have been open at the time of reexploration and not seen on relatively insensitive ultrasound. A technical error could have been made, or the patient may have had a humorally mediated rejection of the organ.
Dr. Campbell reported he had no relevant conflicts.
Major Finding:
Data Source:
Disclosures: