User login
Cosmeceutical Experts Agree on Best Antiaging Products
The skin care market may pull in $9 billion per year, but three cosmeceutical experts agreed that the best over-the-counter antiaging products come down to two words: "moisturizer" and "sunscreen."
Speaking in separate presentations at the annual meeting of the American Society of Cosmetic Dermatology and Aesthetic Surgery (ASCDAS), Dr. Zoe D. Draelos, Dr. Ellen S. Marmur, and Dr. Michael H. Gold agreed that there is little science to back up claims made by cosmeceutical companies.
Cosmeceuticals fall somewhere between cosmetics and pharmaceuticals; therefore, they are not regulated, and manufacturers are not required to show evidence of antiaging effectiveness. When evidence does exist, it generally points back to the moisturizer and sunscreen properties.
Dr. Draelos, a dermatologist in High Point, N.C., and a consulting professor of dermatology at Duke University in Durham, N.C., studied the ingredients in over-the-counter skin care products. She found that 80% of products are basically moisturizers that serve as a vehicle to deliver a high-profile ingredient being touted by the manufacturer (Plast. Reconstr. Surg. 2010;125:719-24).
"Hands down, it’s the moisturizer" that’s the most important cosmeceutical choice, she said. "All the products that make antiaging claims are making moisturizer claims," and most antiaging products also have sunscreen ingredients in them.
Dr. Michael Gold said he has been dispensing cosmeceuticals for 22 years and has seen the market explode. "There is now a $700 moisturizer," he said. "There may be no difference" between that and a $10 moisturizer, "but some people will pay the $700 because it’s $700."
Dr. Gold, the founder and medical director of a skin care center based in Nashville, Tenn., urged his colleagues, "If you dispense, do it ethically."
Dermatologists have an important role to play by assessing the marketing claims of cosmeceuticals, not just listening to them. "Even though we don’t have a lot of good research right now, patients want something their doctor feels good about," said Dr. Marmur of Mount Sinai School of Medicine, New York, who is also president of the ASCDAS.
She took that approach in her book, written with Gina Way, "Simple Skin Beauty: Every Woman’s Guide to a Lifetime of Healthy, Gorgeous Skin" (Atria Books, 2009). The book "perhaps put me at odds with some of the industry, but we’re challenging them to produce better science," she said.
Dr. Marmur and her associates are conducting the first independent, randomized, blinded, controlled trial comparing over-the-counter antiaging creams. With more than 130 subjects enrolled, the study will evaluate 28 biomarkers in seven lines of products, with the people who apply the products blinded to the product being used.
Not all antiaging cream manufacturers are included, however, "Some brands refused to participate" perhaps because they were afraid that the study would show that their product is effective but is a pharmaceutical, she said.
Dr. Draelos echoed that observation during a question-and-answer session. "The industry doesn’t want closer scrutiny," she said.
Dr. Draelos also spoke at the 2011 Skin Disease Education Foundation's Women's and Pediatric Dermatology Seminar. She said she recommends that her patients start with a moisturizer containing dimethicone, glycerin, or petrolatum. "The most robust moisturizer known to man has these three ingredients," she said.
For antiaging, she suggested recommending sunscreens containing avobenzone, oxybenzone, octocrylene, reflecting spheres, or antioxidant botanicals.
How does that translate into over-the-counter product recommendations for patients? For hands, Dr. Draelos favors Neutrogena Norwegian Formula Hand Cream. For the face, she recommends Johnson & Johnson’s Aveeno Positively Radiant Daily Moisturizer SPF 30, and for the body, she suggests Galderma’s Cetaphil Cream.
In separate interviews, the three dermatologists agreed that more research is needed on the efficacy of cosmeceuticals, and delved into the nuances of ingredients in antiaging skin-care regimens. They also agreed that dermatologists need to be patients’ advocates and educators first and foremost.
Moisturizers and sunscreen undoubtedly are the main ingredients in most cosmeceutical regimens, but there are good data to support other ingredients, said Dr. Paul F. Lizzul of Tufts Medical Center, Boston. Randomized clinical trials have shown that retinoids, for example, can be beneficial, but patients probably are better served by prescription-strength retinoids to get "a better bang for their buck," compared with over-the-counter products, he said.
For other cosmeceutical ingredients, however, there may be in vitro or in vivo data but no rigorous clinical studies to back them up. "Even as a well-trained academic dermatologist with an extensive scientific and clinical research background, I, at times, am at a loss to understand the claims made by some cosmeceutical manufacturers," he said.
Dr. Lizzul does not believe that most of the questionable "active ingredients" penetrate the stratum corneum to be able to have the claimed effects on the dermis or epidermis. In some cases, if the ingredient magically penetrated to the dermis, it could be harmful, not helpful, he added.
"It is curious to me that at many of our meetings, research presented to support product claims is oftentimes no more than anecdotal evidence. If you critically look at the presentation and the actual data, you would be remiss to believe that product X actually works," he said.
On the other hand, the lack of double-blind studies of a particular product or ingredient does not mean that it isn’t helpful. By reviewing the biochemistry, basic science, and clinical observations of a treatment, dermatologists can steer patients toward a potential treatment, said Dr. Wendy E. Roberts, a dermatologist in Rancho Mirage, Calif.
She compared her approach to cosmeceuticals to the correlations she makes as a dermatopathologist. "Under the microscope it could be many things, but you match it with the clinical information and come up with a diagnosis. We can kind of use that model with cosmeceuticals," she said. "With our expertise, we know that there’s this body of evidence, we know the activity, and we have our living lab, which is our patients [whom we] see every day. Those observations can lead to further observations."
Many reports in the medical literature describe antiaging benefits from ingredients like peptides, vitamin C, alpha and beta hydroxy acids, lactic acid, retinol, niacinamide, and other ingredients, which can be incorporated into moisturizer formulas, Dr. Roberts said.
Although the three pillars of cosmeceutical regimens are cleansers, moisturizers, and sunscreen, limiting the discussion to those vague terms is "so 1990s," she said. "As a cosmetic dermatologist, it is my job to be able to know the science of a product and recommend the cosmeceutical for that skin type. Working in the capital of sun-damaged skin, I see how certain cosmeceuticals alone can improve skin qualities."
Dr. Leslie Baumann of Miami Beach also said that ingredients other than moisturizer and sunscreen are necessary, depending on the patient’s skin type. She has patients complete a questionnaire to help determine skin type, and matches ingredients to that type.
Sensitive skin types, for example, need anti-inflammatory ingredients, she said. Aged skin benefits from retinoids. Lighteners can help skin with unwanted pigment.
Dermatologists have an ethical responsibility to advise patients on the best cosmeceutical options and on more affordable options if they exist. "Sometimes cheaper products will suffice, and sometimes they will not," Dr. Baumann said.
Dr. Draelos has been a consultant and researcher for Avon, Dial, Johnson & Johnson, L’Oréal, Nu Skin, Procter & Gamble, and Stiefel. Dr. Marmur disclosed financial relationships with Allergan, DUSA Pharmaceuticals, Genentech, Medicis, Merz, and Sanofi-Aventis. Dr. Gold has been a consultant or researcher for Allergan, Medicis, Mentor (Johnson & Johnson), Merz, Galderma, and numerous other companies.
Dr. Roberts has had financial relationships with Allergan, Johnson & Johnson, L’Oréal, La Roche–Posay, and Ortho Dermatologics. Dr. Baumann has led or participated in research trials for more than 50 cosmetic and pharmaceutical companies. Dr. Lizzul had no relevant disclosures.
SDEF and this news organization are owned by Elsevier.
The skin care market may pull in $9 billion per year, but three cosmeceutical experts agreed that the best over-the-counter antiaging products come down to two words: "moisturizer" and "sunscreen."
Speaking in separate presentations at the annual meeting of the American Society of Cosmetic Dermatology and Aesthetic Surgery (ASCDAS), Dr. Zoe D. Draelos, Dr. Ellen S. Marmur, and Dr. Michael H. Gold agreed that there is little science to back up claims made by cosmeceutical companies.
Cosmeceuticals fall somewhere between cosmetics and pharmaceuticals; therefore, they are not regulated, and manufacturers are not required to show evidence of antiaging effectiveness. When evidence does exist, it generally points back to the moisturizer and sunscreen properties.
Dr. Draelos, a dermatologist in High Point, N.C., and a consulting professor of dermatology at Duke University in Durham, N.C., studied the ingredients in over-the-counter skin care products. She found that 80% of products are basically moisturizers that serve as a vehicle to deliver a high-profile ingredient being touted by the manufacturer (Plast. Reconstr. Surg. 2010;125:719-24).
"Hands down, it’s the moisturizer" that’s the most important cosmeceutical choice, she said. "All the products that make antiaging claims are making moisturizer claims," and most antiaging products also have sunscreen ingredients in them.
Dr. Michael Gold said he has been dispensing cosmeceuticals for 22 years and has seen the market explode. "There is now a $700 moisturizer," he said. "There may be no difference" between that and a $10 moisturizer, "but some people will pay the $700 because it’s $700."
Dr. Gold, the founder and medical director of a skin care center based in Nashville, Tenn., urged his colleagues, "If you dispense, do it ethically."
Dermatologists have an important role to play by assessing the marketing claims of cosmeceuticals, not just listening to them. "Even though we don’t have a lot of good research right now, patients want something their doctor feels good about," said Dr. Marmur of Mount Sinai School of Medicine, New York, who is also president of the ASCDAS.
She took that approach in her book, written with Gina Way, "Simple Skin Beauty: Every Woman’s Guide to a Lifetime of Healthy, Gorgeous Skin" (Atria Books, 2009). The book "perhaps put me at odds with some of the industry, but we’re challenging them to produce better science," she said.
Dr. Marmur and her associates are conducting the first independent, randomized, blinded, controlled trial comparing over-the-counter antiaging creams. With more than 130 subjects enrolled, the study will evaluate 28 biomarkers in seven lines of products, with the people who apply the products blinded to the product being used.
Not all antiaging cream manufacturers are included, however, "Some brands refused to participate" perhaps because they were afraid that the study would show that their product is effective but is a pharmaceutical, she said.
Dr. Draelos echoed that observation during a question-and-answer session. "The industry doesn’t want closer scrutiny," she said.
Dr. Draelos also spoke at the 2011 Skin Disease Education Foundation's Women's and Pediatric Dermatology Seminar. She said she recommends that her patients start with a moisturizer containing dimethicone, glycerin, or petrolatum. "The most robust moisturizer known to man has these three ingredients," she said.
For antiaging, she suggested recommending sunscreens containing avobenzone, oxybenzone, octocrylene, reflecting spheres, or antioxidant botanicals.
How does that translate into over-the-counter product recommendations for patients? For hands, Dr. Draelos favors Neutrogena Norwegian Formula Hand Cream. For the face, she recommends Johnson & Johnson’s Aveeno Positively Radiant Daily Moisturizer SPF 30, and for the body, she suggests Galderma’s Cetaphil Cream.
In separate interviews, the three dermatologists agreed that more research is needed on the efficacy of cosmeceuticals, and delved into the nuances of ingredients in antiaging skin-care regimens. They also agreed that dermatologists need to be patients’ advocates and educators first and foremost.
Moisturizers and sunscreen undoubtedly are the main ingredients in most cosmeceutical regimens, but there are good data to support other ingredients, said Dr. Paul F. Lizzul of Tufts Medical Center, Boston. Randomized clinical trials have shown that retinoids, for example, can be beneficial, but patients probably are better served by prescription-strength retinoids to get "a better bang for their buck," compared with over-the-counter products, he said.
For other cosmeceutical ingredients, however, there may be in vitro or in vivo data but no rigorous clinical studies to back them up. "Even as a well-trained academic dermatologist with an extensive scientific and clinical research background, I, at times, am at a loss to understand the claims made by some cosmeceutical manufacturers," he said.
Dr. Lizzul does not believe that most of the questionable "active ingredients" penetrate the stratum corneum to be able to have the claimed effects on the dermis or epidermis. In some cases, if the ingredient magically penetrated to the dermis, it could be harmful, not helpful, he added.
"It is curious to me that at many of our meetings, research presented to support product claims is oftentimes no more than anecdotal evidence. If you critically look at the presentation and the actual data, you would be remiss to believe that product X actually works," he said.
On the other hand, the lack of double-blind studies of a particular product or ingredient does not mean that it isn’t helpful. By reviewing the biochemistry, basic science, and clinical observations of a treatment, dermatologists can steer patients toward a potential treatment, said Dr. Wendy E. Roberts, a dermatologist in Rancho Mirage, Calif.
She compared her approach to cosmeceuticals to the correlations she makes as a dermatopathologist. "Under the microscope it could be many things, but you match it with the clinical information and come up with a diagnosis. We can kind of use that model with cosmeceuticals," she said. "With our expertise, we know that there’s this body of evidence, we know the activity, and we have our living lab, which is our patients [whom we] see every day. Those observations can lead to further observations."
Many reports in the medical literature describe antiaging benefits from ingredients like peptides, vitamin C, alpha and beta hydroxy acids, lactic acid, retinol, niacinamide, and other ingredients, which can be incorporated into moisturizer formulas, Dr. Roberts said.
Although the three pillars of cosmeceutical regimens are cleansers, moisturizers, and sunscreen, limiting the discussion to those vague terms is "so 1990s," she said. "As a cosmetic dermatologist, it is my job to be able to know the science of a product and recommend the cosmeceutical for that skin type. Working in the capital of sun-damaged skin, I see how certain cosmeceuticals alone can improve skin qualities."
Dr. Leslie Baumann of Miami Beach also said that ingredients other than moisturizer and sunscreen are necessary, depending on the patient’s skin type. She has patients complete a questionnaire to help determine skin type, and matches ingredients to that type.
Sensitive skin types, for example, need anti-inflammatory ingredients, she said. Aged skin benefits from retinoids. Lighteners can help skin with unwanted pigment.
Dermatologists have an ethical responsibility to advise patients on the best cosmeceutical options and on more affordable options if they exist. "Sometimes cheaper products will suffice, and sometimes they will not," Dr. Baumann said.
Dr. Draelos has been a consultant and researcher for Avon, Dial, Johnson & Johnson, L’Oréal, Nu Skin, Procter & Gamble, and Stiefel. Dr. Marmur disclosed financial relationships with Allergan, DUSA Pharmaceuticals, Genentech, Medicis, Merz, and Sanofi-Aventis. Dr. Gold has been a consultant or researcher for Allergan, Medicis, Mentor (Johnson & Johnson), Merz, Galderma, and numerous other companies.
Dr. Roberts has had financial relationships with Allergan, Johnson & Johnson, L’Oréal, La Roche–Posay, and Ortho Dermatologics. Dr. Baumann has led or participated in research trials for more than 50 cosmetic and pharmaceutical companies. Dr. Lizzul had no relevant disclosures.
SDEF and this news organization are owned by Elsevier.
The skin care market may pull in $9 billion per year, but three cosmeceutical experts agreed that the best over-the-counter antiaging products come down to two words: "moisturizer" and "sunscreen."
Speaking in separate presentations at the annual meeting of the American Society of Cosmetic Dermatology and Aesthetic Surgery (ASCDAS), Dr. Zoe D. Draelos, Dr. Ellen S. Marmur, and Dr. Michael H. Gold agreed that there is little science to back up claims made by cosmeceutical companies.
Cosmeceuticals fall somewhere between cosmetics and pharmaceuticals; therefore, they are not regulated, and manufacturers are not required to show evidence of antiaging effectiveness. When evidence does exist, it generally points back to the moisturizer and sunscreen properties.
Dr. Draelos, a dermatologist in High Point, N.C., and a consulting professor of dermatology at Duke University in Durham, N.C., studied the ingredients in over-the-counter skin care products. She found that 80% of products are basically moisturizers that serve as a vehicle to deliver a high-profile ingredient being touted by the manufacturer (Plast. Reconstr. Surg. 2010;125:719-24).
"Hands down, it’s the moisturizer" that’s the most important cosmeceutical choice, she said. "All the products that make antiaging claims are making moisturizer claims," and most antiaging products also have sunscreen ingredients in them.
Dr. Michael Gold said he has been dispensing cosmeceuticals for 22 years and has seen the market explode. "There is now a $700 moisturizer," he said. "There may be no difference" between that and a $10 moisturizer, "but some people will pay the $700 because it’s $700."
Dr. Gold, the founder and medical director of a skin care center based in Nashville, Tenn., urged his colleagues, "If you dispense, do it ethically."
Dermatologists have an important role to play by assessing the marketing claims of cosmeceuticals, not just listening to them. "Even though we don’t have a lot of good research right now, patients want something their doctor feels good about," said Dr. Marmur of Mount Sinai School of Medicine, New York, who is also president of the ASCDAS.
She took that approach in her book, written with Gina Way, "Simple Skin Beauty: Every Woman’s Guide to a Lifetime of Healthy, Gorgeous Skin" (Atria Books, 2009). The book "perhaps put me at odds with some of the industry, but we’re challenging them to produce better science," she said.
Dr. Marmur and her associates are conducting the first independent, randomized, blinded, controlled trial comparing over-the-counter antiaging creams. With more than 130 subjects enrolled, the study will evaluate 28 biomarkers in seven lines of products, with the people who apply the products blinded to the product being used.
Not all antiaging cream manufacturers are included, however, "Some brands refused to participate" perhaps because they were afraid that the study would show that their product is effective but is a pharmaceutical, she said.
Dr. Draelos echoed that observation during a question-and-answer session. "The industry doesn’t want closer scrutiny," she said.
Dr. Draelos also spoke at the 2011 Skin Disease Education Foundation's Women's and Pediatric Dermatology Seminar. She said she recommends that her patients start with a moisturizer containing dimethicone, glycerin, or petrolatum. "The most robust moisturizer known to man has these three ingredients," she said.
For antiaging, she suggested recommending sunscreens containing avobenzone, oxybenzone, octocrylene, reflecting spheres, or antioxidant botanicals.
How does that translate into over-the-counter product recommendations for patients? For hands, Dr. Draelos favors Neutrogena Norwegian Formula Hand Cream. For the face, she recommends Johnson & Johnson’s Aveeno Positively Radiant Daily Moisturizer SPF 30, and for the body, she suggests Galderma’s Cetaphil Cream.
In separate interviews, the three dermatologists agreed that more research is needed on the efficacy of cosmeceuticals, and delved into the nuances of ingredients in antiaging skin-care regimens. They also agreed that dermatologists need to be patients’ advocates and educators first and foremost.
Moisturizers and sunscreen undoubtedly are the main ingredients in most cosmeceutical regimens, but there are good data to support other ingredients, said Dr. Paul F. Lizzul of Tufts Medical Center, Boston. Randomized clinical trials have shown that retinoids, for example, can be beneficial, but patients probably are better served by prescription-strength retinoids to get "a better bang for their buck," compared with over-the-counter products, he said.
For other cosmeceutical ingredients, however, there may be in vitro or in vivo data but no rigorous clinical studies to back them up. "Even as a well-trained academic dermatologist with an extensive scientific and clinical research background, I, at times, am at a loss to understand the claims made by some cosmeceutical manufacturers," he said.
Dr. Lizzul does not believe that most of the questionable "active ingredients" penetrate the stratum corneum to be able to have the claimed effects on the dermis or epidermis. In some cases, if the ingredient magically penetrated to the dermis, it could be harmful, not helpful, he added.
"It is curious to me that at many of our meetings, research presented to support product claims is oftentimes no more than anecdotal evidence. If you critically look at the presentation and the actual data, you would be remiss to believe that product X actually works," he said.
On the other hand, the lack of double-blind studies of a particular product or ingredient does not mean that it isn’t helpful. By reviewing the biochemistry, basic science, and clinical observations of a treatment, dermatologists can steer patients toward a potential treatment, said Dr. Wendy E. Roberts, a dermatologist in Rancho Mirage, Calif.
She compared her approach to cosmeceuticals to the correlations she makes as a dermatopathologist. "Under the microscope it could be many things, but you match it with the clinical information and come up with a diagnosis. We can kind of use that model with cosmeceuticals," she said. "With our expertise, we know that there’s this body of evidence, we know the activity, and we have our living lab, which is our patients [whom we] see every day. Those observations can lead to further observations."
Many reports in the medical literature describe antiaging benefits from ingredients like peptides, vitamin C, alpha and beta hydroxy acids, lactic acid, retinol, niacinamide, and other ingredients, which can be incorporated into moisturizer formulas, Dr. Roberts said.
Although the three pillars of cosmeceutical regimens are cleansers, moisturizers, and sunscreen, limiting the discussion to those vague terms is "so 1990s," she said. "As a cosmetic dermatologist, it is my job to be able to know the science of a product and recommend the cosmeceutical for that skin type. Working in the capital of sun-damaged skin, I see how certain cosmeceuticals alone can improve skin qualities."
Dr. Leslie Baumann of Miami Beach also said that ingredients other than moisturizer and sunscreen are necessary, depending on the patient’s skin type. She has patients complete a questionnaire to help determine skin type, and matches ingredients to that type.
Sensitive skin types, for example, need anti-inflammatory ingredients, she said. Aged skin benefits from retinoids. Lighteners can help skin with unwanted pigment.
Dermatologists have an ethical responsibility to advise patients on the best cosmeceutical options and on more affordable options if they exist. "Sometimes cheaper products will suffice, and sometimes they will not," Dr. Baumann said.
Dr. Draelos has been a consultant and researcher for Avon, Dial, Johnson & Johnson, L’Oréal, Nu Skin, Procter & Gamble, and Stiefel. Dr. Marmur disclosed financial relationships with Allergan, DUSA Pharmaceuticals, Genentech, Medicis, Merz, and Sanofi-Aventis. Dr. Gold has been a consultant or researcher for Allergan, Medicis, Mentor (Johnson & Johnson), Merz, Galderma, and numerous other companies.
Dr. Roberts has had financial relationships with Allergan, Johnson & Johnson, L’Oréal, La Roche–Posay, and Ortho Dermatologics. Dr. Baumann has led or participated in research trials for more than 50 cosmetic and pharmaceutical companies. Dr. Lizzul had no relevant disclosures.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF COSMETIC DERMATOLOGY AND AESTHETIC SURGERY
Off-Label Fillers Help Reposition Aging Eyes
LAS VEGAS – Off-label use of hyaluronic acid fillers can help reposition aging eyes for a younger look.
As bones of the orbital socket dissolve with age, the globe of the eyeball descends and shifts laterally, shifting the balance of the gaze. Permanent fillers such as silicone have been used in the retro-orbital space to lift up the globe, but that doesn’t help move the globe from a lateral to a more medial position, Dr. Ellen S. Marmur said at the annual meeting of the American Society of Cosmetic Dermatology and Aesthetic Surgery.
For a typical patient who has malar flattening and complains of looking tired all the time, Dr. Marmur uses a "two-point technique." She injects two perpendicular boluses of hyaluronic acid filler under the muscles below each eye and molds the filler upward.
She starts medially to the infraorbital foramen and stays deep, using the fewest injections to cause the fewest bruises and to give a smooth finish.
For patients who are older, she may extend the two-point technique into a five-point technique or even a circumferential technique.
"I start medially and then continue on laterally throughout the upper cheek, all the way up to near the medial canthus," said Dr. Marmur of Mount Sinai School of Medicine, New York. It’s hard to stay under the muscle all the way, so she injects using a threading technique with the bevel down so the filler is being pushed down.
Even dermatologists who are experienced in these techniques will cause bruising in approximately half of patients, she said. The worst bruising and swelling happens in the lateral aspect of the orbit because of the vessels and the histamine released there.
"You should be worried about occlusion, so try to avoid the vasculature," Dr. Marmur said.
If there is lidocaine in the injections, it will numb some of the muscle and the area might get "a little bit twitchy" during the injection.
"Once you fill these areas, you realize it’s a continuum and you want to go around" the lateral orbit itself, she said. "Some people get almost a little ‘V’ of the lateral canthus. Just filling that in also helps reassert the nice dimension and the width of the gaze and makes people look a little less serious. We start looking really serious when we’re getting older."
The eyes are considered a "danger zone" of the face because injections can tract bacteria into the cavernous sinus, she cautioned. "I’ve never seen it happen, and it hasn’t been reported, but be very clean in the area."
Filler injections also can produce a Tyndall effect, a discoloration that can get worse as the filler degrades. "I’m not exactly sure why that is," said Dr. Marmur, adding that she looks forward to newer hyaluronic acid fillers that won’t show the blue hue.
Injections also can take on a "festoonlike appearance," caused either by the filler itself or when the filler grabs water that needs to be massaged away, she said.
Dr. Marmur always talks to patients about the option of using hyaluronidase to reverse the hyaluronic acid filler. "There’s no shame in having it in your office and using it whenever you want," she said. "It’s a nice, comfortable option for people, especially if they’re doing their eyes for the first time.
Dermatologists will be learning from each other about which of the many approved hyaluronic acid fillers are good to use in different areas of the face, but the specialty really needs some well-designed, head-to-head, randomized trials comparing the strengths and weaknesses of these fillers, she said. The studies should compare the fillers for use in patients of different facial types and ages.
Planning cosmetic facial injections for aged patients involves thinking about how they may have looked when they were younger, and understanding the effects of aging, such as bone degradation, muscle thinning, skin laxity, and drooping fat. It also involves understanding the ideals of beauty that might be achieved without changing how the patient looks. Dermatologists also must commit themselves "to not overdoing it and not letting our patients push us into overdoing it," she said.
Dr. Marmur disclosed financial ties with Allergan, DUSA Pharmaceuticals, Genentech, Medicis, Merz, and Sanofi-Aventis.
LAS VEGAS – Off-label use of hyaluronic acid fillers can help reposition aging eyes for a younger look.
As bones of the orbital socket dissolve with age, the globe of the eyeball descends and shifts laterally, shifting the balance of the gaze. Permanent fillers such as silicone have been used in the retro-orbital space to lift up the globe, but that doesn’t help move the globe from a lateral to a more medial position, Dr. Ellen S. Marmur said at the annual meeting of the American Society of Cosmetic Dermatology and Aesthetic Surgery.
For a typical patient who has malar flattening and complains of looking tired all the time, Dr. Marmur uses a "two-point technique." She injects two perpendicular boluses of hyaluronic acid filler under the muscles below each eye and molds the filler upward.
She starts medially to the infraorbital foramen and stays deep, using the fewest injections to cause the fewest bruises and to give a smooth finish.
For patients who are older, she may extend the two-point technique into a five-point technique or even a circumferential technique.
"I start medially and then continue on laterally throughout the upper cheek, all the way up to near the medial canthus," said Dr. Marmur of Mount Sinai School of Medicine, New York. It’s hard to stay under the muscle all the way, so she injects using a threading technique with the bevel down so the filler is being pushed down.
Even dermatologists who are experienced in these techniques will cause bruising in approximately half of patients, she said. The worst bruising and swelling happens in the lateral aspect of the orbit because of the vessels and the histamine released there.
"You should be worried about occlusion, so try to avoid the vasculature," Dr. Marmur said.
If there is lidocaine in the injections, it will numb some of the muscle and the area might get "a little bit twitchy" during the injection.
"Once you fill these areas, you realize it’s a continuum and you want to go around" the lateral orbit itself, she said. "Some people get almost a little ‘V’ of the lateral canthus. Just filling that in also helps reassert the nice dimension and the width of the gaze and makes people look a little less serious. We start looking really serious when we’re getting older."
The eyes are considered a "danger zone" of the face because injections can tract bacteria into the cavernous sinus, she cautioned. "I’ve never seen it happen, and it hasn’t been reported, but be very clean in the area."
Filler injections also can produce a Tyndall effect, a discoloration that can get worse as the filler degrades. "I’m not exactly sure why that is," said Dr. Marmur, adding that she looks forward to newer hyaluronic acid fillers that won’t show the blue hue.
Injections also can take on a "festoonlike appearance," caused either by the filler itself or when the filler grabs water that needs to be massaged away, she said.
Dr. Marmur always talks to patients about the option of using hyaluronidase to reverse the hyaluronic acid filler. "There’s no shame in having it in your office and using it whenever you want," she said. "It’s a nice, comfortable option for people, especially if they’re doing their eyes for the first time.
Dermatologists will be learning from each other about which of the many approved hyaluronic acid fillers are good to use in different areas of the face, but the specialty really needs some well-designed, head-to-head, randomized trials comparing the strengths and weaknesses of these fillers, she said. The studies should compare the fillers for use in patients of different facial types and ages.
Planning cosmetic facial injections for aged patients involves thinking about how they may have looked when they were younger, and understanding the effects of aging, such as bone degradation, muscle thinning, skin laxity, and drooping fat. It also involves understanding the ideals of beauty that might be achieved without changing how the patient looks. Dermatologists also must commit themselves "to not overdoing it and not letting our patients push us into overdoing it," she said.
Dr. Marmur disclosed financial ties with Allergan, DUSA Pharmaceuticals, Genentech, Medicis, Merz, and Sanofi-Aventis.
LAS VEGAS – Off-label use of hyaluronic acid fillers can help reposition aging eyes for a younger look.
As bones of the orbital socket dissolve with age, the globe of the eyeball descends and shifts laterally, shifting the balance of the gaze. Permanent fillers such as silicone have been used in the retro-orbital space to lift up the globe, but that doesn’t help move the globe from a lateral to a more medial position, Dr. Ellen S. Marmur said at the annual meeting of the American Society of Cosmetic Dermatology and Aesthetic Surgery.
For a typical patient who has malar flattening and complains of looking tired all the time, Dr. Marmur uses a "two-point technique." She injects two perpendicular boluses of hyaluronic acid filler under the muscles below each eye and molds the filler upward.
She starts medially to the infraorbital foramen and stays deep, using the fewest injections to cause the fewest bruises and to give a smooth finish.
For patients who are older, she may extend the two-point technique into a five-point technique or even a circumferential technique.
"I start medially and then continue on laterally throughout the upper cheek, all the way up to near the medial canthus," said Dr. Marmur of Mount Sinai School of Medicine, New York. It’s hard to stay under the muscle all the way, so she injects using a threading technique with the bevel down so the filler is being pushed down.
Even dermatologists who are experienced in these techniques will cause bruising in approximately half of patients, she said. The worst bruising and swelling happens in the lateral aspect of the orbit because of the vessels and the histamine released there.
"You should be worried about occlusion, so try to avoid the vasculature," Dr. Marmur said.
If there is lidocaine in the injections, it will numb some of the muscle and the area might get "a little bit twitchy" during the injection.
"Once you fill these areas, you realize it’s a continuum and you want to go around" the lateral orbit itself, she said. "Some people get almost a little ‘V’ of the lateral canthus. Just filling that in also helps reassert the nice dimension and the width of the gaze and makes people look a little less serious. We start looking really serious when we’re getting older."
The eyes are considered a "danger zone" of the face because injections can tract bacteria into the cavernous sinus, she cautioned. "I’ve never seen it happen, and it hasn’t been reported, but be very clean in the area."
Filler injections also can produce a Tyndall effect, a discoloration that can get worse as the filler degrades. "I’m not exactly sure why that is," said Dr. Marmur, adding that she looks forward to newer hyaluronic acid fillers that won’t show the blue hue.
Injections also can take on a "festoonlike appearance," caused either by the filler itself or when the filler grabs water that needs to be massaged away, she said.
Dr. Marmur always talks to patients about the option of using hyaluronidase to reverse the hyaluronic acid filler. "There’s no shame in having it in your office and using it whenever you want," she said. "It’s a nice, comfortable option for people, especially if they’re doing their eyes for the first time.
Dermatologists will be learning from each other about which of the many approved hyaluronic acid fillers are good to use in different areas of the face, but the specialty really needs some well-designed, head-to-head, randomized trials comparing the strengths and weaknesses of these fillers, she said. The studies should compare the fillers for use in patients of different facial types and ages.
Planning cosmetic facial injections for aged patients involves thinking about how they may have looked when they were younger, and understanding the effects of aging, such as bone degradation, muscle thinning, skin laxity, and drooping fat. It also involves understanding the ideals of beauty that might be achieved without changing how the patient looks. Dermatologists also must commit themselves "to not overdoing it and not letting our patients push us into overdoing it," she said.
Dr. Marmur disclosed financial ties with Allergan, DUSA Pharmaceuticals, Genentech, Medicis, Merz, and Sanofi-Aventis.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF COSMETIC DERMATOLOGY AND AESTHETIC SURGERY
Virtual Reality Allows Patient-Specific Surgery Simulation
Physicians and patients heading into the operating room have to hope that the surgeon or proceduralist does the job right the first time. Generally, needing a do-over is not a good thing.
Soon, however, vascular and cardiac surgeons at Cleveland Clinic will be able to take several consequences-free do-overs that should lower risk for the patient. Some of the latest advances in imaging and technology are being incorporated into new simulation rooms built adjacent to a few new ORs. In these rooms physicians can rehearse the procedure they’re about to do on a three-dimensional simulation of the patient, who is being prepared for surgery next door.
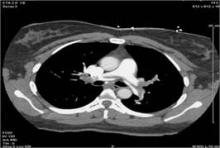
For example, “fusion” imaging can help in the repair of aortic aneurysms. The results of an angiogram taken at the time of the procedure are superimposed on a preoperative CT scan of the patient to create three-dimensional imaging studies “telling us where all the arteries are without using any contrast,” Dr. Roy K. Greenberg said at the annual meeting of the Southern Association for Vascular Surgery. Not having to use catheters and wires to figure that out makes the procedure much easier, said Dr. Greenberg of the Cleveland Clinic Foundation.
His talk on “Aortic Care for the 21st Century” at the meeting was the first Jesse E. Thompson, M.D. Distinguished Guest Lecture.
“The imaging can be loaded in patient-specific simulators, providing a means to ‘test’ the procedures in virtual reality, train the team, and problem-solve `off-line’ ” with less risk to the patient, he said.
The Cleveland Clinic is no slouch when it comes to simulation. Their doctors-in-training practice on mannequins, robots, and other virtual stand-ins for patients. There is an Anesthesia Simulation Lab. The Clinic is even building an entire Center for Multidisciplinary Simulation.
The two new ORs that Dr. Greenberg described take simulation to the next level. The simulators are not in a remote room, they’re not in a separate building, and they’re not at a course that physicians go to for two or three days before the surgery. “I think they have to be integrated into the actual work flow and case,” he said.
The ORs should be finished in the fourth quarter of 2012, and will feature a control room behind each OR. Behind each control room will be a simulator room.
Dr. Greenberg described the work flow for a fenestrated endovascular aneurysm repair as something like this: The preoperative CT scan is used for patient selection and device design, and is imported into the OR and the simulator before the patient arrives. The CT scan and fluoroscopic imaging studies are used in fusion imaging in the OR, minimizing the use of contrast agents and radiation.
Standard clinic procedures required team sign-ins when the patient is on the table. Each team members signs in, introduces themselves, and makes sure they're operating on the correct anatomic part. Then “we have that obligatory 2.5 hours while anesthesia gets everything else ready,” during which the operative team goes to the simulator room. Residents, fellows, and the rest of the team get to practice the procedure using the repair device on a simulation of that particular patient.
“So there’s no question about what steps are next” during the live surgery, he said. If something doesn’t seem right during rehearsal, “you can say, `Why not?’ Is that a problem with the simulator, or is it going to be a problem with the procedure?”
Dr. Greenberg said he doesn’t know of any other institutions doing patient-specific simulations like this, but “I hope they will.”
Dr. Greenberg disclosed receiving royalties for intellectual property licensed to Cook, Inc. and funds for research and travel from Cook.
Physicians and patients heading into the operating room have to hope that the surgeon or proceduralist does the job right the first time. Generally, needing a do-over is not a good thing.
Soon, however, vascular and cardiac surgeons at Cleveland Clinic will be able to take several consequences-free do-overs that should lower risk for the patient. Some of the latest advances in imaging and technology are being incorporated into new simulation rooms built adjacent to a few new ORs. In these rooms physicians can rehearse the procedure they’re about to do on a three-dimensional simulation of the patient, who is being prepared for surgery next door.
For example, “fusion” imaging can help in the repair of aortic aneurysms. The results of an angiogram taken at the time of the procedure are superimposed on a preoperative CT scan of the patient to create three-dimensional imaging studies “telling us where all the arteries are without using any contrast,” Dr. Roy K. Greenberg said at the annual meeting of the Southern Association for Vascular Surgery. Not having to use catheters and wires to figure that out makes the procedure much easier, said Dr. Greenberg of the Cleveland Clinic Foundation.
His talk on “Aortic Care for the 21st Century” at the meeting was the first Jesse E. Thompson, M.D. Distinguished Guest Lecture.
“The imaging can be loaded in patient-specific simulators, providing a means to ‘test’ the procedures in virtual reality, train the team, and problem-solve `off-line’ ” with less risk to the patient, he said.
The Cleveland Clinic is no slouch when it comes to simulation. Their doctors-in-training practice on mannequins, robots, and other virtual stand-ins for patients. There is an Anesthesia Simulation Lab. The Clinic is even building an entire Center for Multidisciplinary Simulation.
The two new ORs that Dr. Greenberg described take simulation to the next level. The simulators are not in a remote room, they’re not in a separate building, and they’re not at a course that physicians go to for two or three days before the surgery. “I think they have to be integrated into the actual work flow and case,” he said.
The ORs should be finished in the fourth quarter of 2012, and will feature a control room behind each OR. Behind each control room will be a simulator room.
Dr. Greenberg described the work flow for a fenestrated endovascular aneurysm repair as something like this: The preoperative CT scan is used for patient selection and device design, and is imported into the OR and the simulator before the patient arrives. The CT scan and fluoroscopic imaging studies are used in fusion imaging in the OR, minimizing the use of contrast agents and radiation.
Standard clinic procedures required team sign-ins when the patient is on the table. Each team members signs in, introduces themselves, and makes sure they're operating on the correct anatomic part. Then “we have that obligatory 2.5 hours while anesthesia gets everything else ready,” during which the operative team goes to the simulator room. Residents, fellows, and the rest of the team get to practice the procedure using the repair device on a simulation of that particular patient.
“So there’s no question about what steps are next” during the live surgery, he said. If something doesn’t seem right during rehearsal, “you can say, `Why not?’ Is that a problem with the simulator, or is it going to be a problem with the procedure?”
Dr. Greenberg said he doesn’t know of any other institutions doing patient-specific simulations like this, but “I hope they will.”
Dr. Greenberg disclosed receiving royalties for intellectual property licensed to Cook, Inc. and funds for research and travel from Cook.
Physicians and patients heading into the operating room have to hope that the surgeon or proceduralist does the job right the first time. Generally, needing a do-over is not a good thing.
Soon, however, vascular and cardiac surgeons at Cleveland Clinic will be able to take several consequences-free do-overs that should lower risk for the patient. Some of the latest advances in imaging and technology are being incorporated into new simulation rooms built adjacent to a few new ORs. In these rooms physicians can rehearse the procedure they’re about to do on a three-dimensional simulation of the patient, who is being prepared for surgery next door.
For example, “fusion” imaging can help in the repair of aortic aneurysms. The results of an angiogram taken at the time of the procedure are superimposed on a preoperative CT scan of the patient to create three-dimensional imaging studies “telling us where all the arteries are without using any contrast,” Dr. Roy K. Greenberg said at the annual meeting of the Southern Association for Vascular Surgery. Not having to use catheters and wires to figure that out makes the procedure much easier, said Dr. Greenberg of the Cleveland Clinic Foundation.
His talk on “Aortic Care for the 21st Century” at the meeting was the first Jesse E. Thompson, M.D. Distinguished Guest Lecture.
“The imaging can be loaded in patient-specific simulators, providing a means to ‘test’ the procedures in virtual reality, train the team, and problem-solve `off-line’ ” with less risk to the patient, he said.
The Cleveland Clinic is no slouch when it comes to simulation. Their doctors-in-training practice on mannequins, robots, and other virtual stand-ins for patients. There is an Anesthesia Simulation Lab. The Clinic is even building an entire Center for Multidisciplinary Simulation.
The two new ORs that Dr. Greenberg described take simulation to the next level. The simulators are not in a remote room, they’re not in a separate building, and they’re not at a course that physicians go to for two or three days before the surgery. “I think they have to be integrated into the actual work flow and case,” he said.
The ORs should be finished in the fourth quarter of 2012, and will feature a control room behind each OR. Behind each control room will be a simulator room.
Dr. Greenberg described the work flow for a fenestrated endovascular aneurysm repair as something like this: The preoperative CT scan is used for patient selection and device design, and is imported into the OR and the simulator before the patient arrives. The CT scan and fluoroscopic imaging studies are used in fusion imaging in the OR, minimizing the use of contrast agents and radiation.
Standard clinic procedures required team sign-ins when the patient is on the table. Each team members signs in, introduces themselves, and makes sure they're operating on the correct anatomic part. Then “we have that obligatory 2.5 hours while anesthesia gets everything else ready,” during which the operative team goes to the simulator room. Residents, fellows, and the rest of the team get to practice the procedure using the repair device on a simulation of that particular patient.
“So there’s no question about what steps are next” during the live surgery, he said. If something doesn’t seem right during rehearsal, “you can say, `Why not?’ Is that a problem with the simulator, or is it going to be a problem with the procedure?”
Dr. Greenberg said he doesn’t know of any other institutions doing patient-specific simulations like this, but “I hope they will.”
Dr. Greenberg disclosed receiving royalties for intellectual property licensed to Cook, Inc. and funds for research and travel from Cook.
Blog: Human Genome Sequencing vs. Privacy Examined
Human genome sequencing. Facebook. Informed consent. “The Lion, the Witch and the Wardrobe.” Rare diseases. “Hotel California.” Cost-effective medicine.
It was all in a day’s work for the Presidential Commission for the Study of Bioethical Issues in its eighth meeting, this time at the University of California, San Francisco. The focus: What policies or programs should be in place (if any) to guide the ethical use of human genome sequencing, a kind of testing that’s positioned to explode into widespread use.
The cost of sequencing one person’s genome has shrunk from nearly $3 billion a mere 14 years ago to an anticipated $1,000 within the next year or two, Richard A. Gibbs, Ph.D. told the Commission. He and other experts testified in preparation for the Commission’s third report as advisors to the President. (See previous reports on separate topics here).
Today, physicians can order human genome sequencing at a handful of specialized centers. Approximately 10,000 humans had their genomes sequenced in 2011. Perhaps 100,000 will do the same in 2012, estimated Dr. Gibbs, director of the Human Genome Sequencing Center at Baylor College. He disclosed being an investor in Life Technology and co-founder of the company Seq-Wright.
Researchers and families with genetic diseases are salivating at the possibility of access to the gold mine of data this could provide, potentially improving diagnoses, identifying unknown causes of diseases, and helping people and their physicians know which drugs they will or won’t respond to, among other possible benefits.
Retta Beery is one example – she described the agonizing journey of her twins, Alexis and Noah, to a correct diagnosis of their rare but treatable genetic condition. After years of extremely limited mobility, severe breathing problems, costly ER visits, imaging tests, visits to specialists, and more, genome sequencing at Dr. Gibbs’ Center identified mutations in a gene called SPR that encodes the enzyme sepiapterin reductase. With proper treatment, the twins are healthy and high-functioning teenagers today, as Ms. Beery chronicles on a website she started to support other families with similar challenges.
Scientists are in the infant stages of understanding all the data that genome sequencing produces, however. “The good news is we have the human genome. The bad news is it’s largely just a parts list,” said Dr. Daniel Masys of the University of Washington. “Our ability to acquire person-specific DNA data far exceeds our understanding of its meaning.”
Learning how to “read” genomes will require sophisticated studies of vast amounts of data from millions of people, a scale of research never seen before, he said. Limiting access to genome data could stifle the many discoveries sure to be made by this work.
Meanwhile, who will be interpreting genome data? How will patients understand the potential risks and benefits of making their genome data available to others? Can the data ever be safely protected in today’s interconnected world? Every human has multiple genetic variations, and “worried well” patients could bankrupt the medical system by demanding tests or cures for things that may not really be a problem.
“There’s a snake oil salesman out there for everything,” said Commission Chair Amy Gutmann, Ph.D., president of the University of Pennsylvania.
Several speakers cautioned that it may be impossible to prevent someone from connecting even “protected” genome sequencing data to an individual and using that for commercial purposes or to limit access to insurance or health care.
“I don’t think we’re ready for this huge onslaught of additional information, because there’s too much opportunity for misuse,” said Mark A. Rothstein, J.D., chair of law and medicine at the University of Louisville.
Given the concerns about privacy, it was only a matter of time before Facebook analogies became part of the discussion. “The privacy settings are set so you don’t have any,” and users must “crank down” the settings to establish any privacy on Facebook, said Jane Kaye, D.Phil, director of the Centre for Law, Health and Emerging Technologies at the University of Oxford, U.K. “I don’t think we want to be in a society which is like that.”
Privacy should be a right in human society with ways for people to crank down their privacy limits if they want to share their information, she said. Finding mechanisms to ensure that would protect all people, not just people who are able to make decisions on their own behalf.
The future of digital information will be networks within networks of information, she predicted. Opening one “portal” may give access to information that you didn’t even know was there, like the portal between worlds in C.S. Lewis’ book, “The Lion, the Witch and the Wardrobe,” Dr. Kaye said.
And how do you get truly informed consent from a patient if you can’t say what the data may be used to study in the future? Dr. Kaye argued for a “consent for governance” in which patients are educated about the rules of the game, which will be refereed by research ethics committees and oversight bodies, and the patients agree that once they release their data, the lose individual control in some ways.
“It’s a bit like `Hotel California,’” she said. “You can check out any time you like, but you can never leave.”
The chief of the New York County District Attorney’s Forensic Sciences/Cold Case Unit brought the discussion back down to earth by describing how they convicted a criminal by matching his DNA to a specimen from tea cup that he left behind. (“We only catch the dumb ones,” she said as an aside.)
“Opponents of forensic DNA databases say this will allow government, employers and insurers to deny benefits. They’re just wrong,” said Melissa Mourges, J.D. Nearly 15 years of experience with the FBI’s Combined DNA Index System (CODIS) is “enough to prove you can have privacy and security” while allowing access to some genetic information.
Read more details from the meeting in blog posts by Commission staff on Ms. Beery, on comments by various speakers, on Ms. Mourges’s show-and-tell, and on the speakers’ final thoughts. The Commission’s report should be finished by late 2012.
--Sherry Boschert (@SherryBoschert on Twitter)
Human genome sequencing. Facebook. Informed consent. “The Lion, the Witch and the Wardrobe.” Rare diseases. “Hotel California.” Cost-effective medicine.
It was all in a day’s work for the Presidential Commission for the Study of Bioethical Issues in its eighth meeting, this time at the University of California, San Francisco. The focus: What policies or programs should be in place (if any) to guide the ethical use of human genome sequencing, a kind of testing that’s positioned to explode into widespread use.
The cost of sequencing one person’s genome has shrunk from nearly $3 billion a mere 14 years ago to an anticipated $1,000 within the next year or two, Richard A. Gibbs, Ph.D. told the Commission. He and other experts testified in preparation for the Commission’s third report as advisors to the President. (See previous reports on separate topics here).
Today, physicians can order human genome sequencing at a handful of specialized centers. Approximately 10,000 humans had their genomes sequenced in 2011. Perhaps 100,000 will do the same in 2012, estimated Dr. Gibbs, director of the Human Genome Sequencing Center at Baylor College. He disclosed being an investor in Life Technology and co-founder of the company Seq-Wright.
Researchers and families with genetic diseases are salivating at the possibility of access to the gold mine of data this could provide, potentially improving diagnoses, identifying unknown causes of diseases, and helping people and their physicians know which drugs they will or won’t respond to, among other possible benefits.
Retta Beery is one example – she described the agonizing journey of her twins, Alexis and Noah, to a correct diagnosis of their rare but treatable genetic condition. After years of extremely limited mobility, severe breathing problems, costly ER visits, imaging tests, visits to specialists, and more, genome sequencing at Dr. Gibbs’ Center identified mutations in a gene called SPR that encodes the enzyme sepiapterin reductase. With proper treatment, the twins are healthy and high-functioning teenagers today, as Ms. Beery chronicles on a website she started to support other families with similar challenges.
Scientists are in the infant stages of understanding all the data that genome sequencing produces, however. “The good news is we have the human genome. The bad news is it’s largely just a parts list,” said Dr. Daniel Masys of the University of Washington. “Our ability to acquire person-specific DNA data far exceeds our understanding of its meaning.”
Learning how to “read” genomes will require sophisticated studies of vast amounts of data from millions of people, a scale of research never seen before, he said. Limiting access to genome data could stifle the many discoveries sure to be made by this work.
Meanwhile, who will be interpreting genome data? How will patients understand the potential risks and benefits of making their genome data available to others? Can the data ever be safely protected in today’s interconnected world? Every human has multiple genetic variations, and “worried well” patients could bankrupt the medical system by demanding tests or cures for things that may not really be a problem.
“There’s a snake oil salesman out there for everything,” said Commission Chair Amy Gutmann, Ph.D., president of the University of Pennsylvania.
Several speakers cautioned that it may be impossible to prevent someone from connecting even “protected” genome sequencing data to an individual and using that for commercial purposes or to limit access to insurance or health care.
“I don’t think we’re ready for this huge onslaught of additional information, because there’s too much opportunity for misuse,” said Mark A. Rothstein, J.D., chair of law and medicine at the University of Louisville.
Given the concerns about privacy, it was only a matter of time before Facebook analogies became part of the discussion. “The privacy settings are set so you don’t have any,” and users must “crank down” the settings to establish any privacy on Facebook, said Jane Kaye, D.Phil, director of the Centre for Law, Health and Emerging Technologies at the University of Oxford, U.K. “I don’t think we want to be in a society which is like that.”
Privacy should be a right in human society with ways for people to crank down their privacy limits if they want to share their information, she said. Finding mechanisms to ensure that would protect all people, not just people who are able to make decisions on their own behalf.
The future of digital information will be networks within networks of information, she predicted. Opening one “portal” may give access to information that you didn’t even know was there, like the portal between worlds in C.S. Lewis’ book, “The Lion, the Witch and the Wardrobe,” Dr. Kaye said.
And how do you get truly informed consent from a patient if you can’t say what the data may be used to study in the future? Dr. Kaye argued for a “consent for governance” in which patients are educated about the rules of the game, which will be refereed by research ethics committees and oversight bodies, and the patients agree that once they release their data, the lose individual control in some ways.
“It’s a bit like `Hotel California,’” she said. “You can check out any time you like, but you can never leave.”
The chief of the New York County District Attorney’s Forensic Sciences/Cold Case Unit brought the discussion back down to earth by describing how they convicted a criminal by matching his DNA to a specimen from tea cup that he left behind. (“We only catch the dumb ones,” she said as an aside.)
“Opponents of forensic DNA databases say this will allow government, employers and insurers to deny benefits. They’re just wrong,” said Melissa Mourges, J.D. Nearly 15 years of experience with the FBI’s Combined DNA Index System (CODIS) is “enough to prove you can have privacy and security” while allowing access to some genetic information.
Read more details from the meeting in blog posts by Commission staff on Ms. Beery, on comments by various speakers, on Ms. Mourges’s show-and-tell, and on the speakers’ final thoughts. The Commission’s report should be finished by late 2012.
--Sherry Boschert (@SherryBoschert on Twitter)
Human genome sequencing. Facebook. Informed consent. “The Lion, the Witch and the Wardrobe.” Rare diseases. “Hotel California.” Cost-effective medicine.
It was all in a day’s work for the Presidential Commission for the Study of Bioethical Issues in its eighth meeting, this time at the University of California, San Francisco. The focus: What policies or programs should be in place (if any) to guide the ethical use of human genome sequencing, a kind of testing that’s positioned to explode into widespread use.
The cost of sequencing one person’s genome has shrunk from nearly $3 billion a mere 14 years ago to an anticipated $1,000 within the next year or two, Richard A. Gibbs, Ph.D. told the Commission. He and other experts testified in preparation for the Commission’s third report as advisors to the President. (See previous reports on separate topics here).
Today, physicians can order human genome sequencing at a handful of specialized centers. Approximately 10,000 humans had their genomes sequenced in 2011. Perhaps 100,000 will do the same in 2012, estimated Dr. Gibbs, director of the Human Genome Sequencing Center at Baylor College. He disclosed being an investor in Life Technology and co-founder of the company Seq-Wright.
Researchers and families with genetic diseases are salivating at the possibility of access to the gold mine of data this could provide, potentially improving diagnoses, identifying unknown causes of diseases, and helping people and their physicians know which drugs they will or won’t respond to, among other possible benefits.
Retta Beery is one example – she described the agonizing journey of her twins, Alexis and Noah, to a correct diagnosis of their rare but treatable genetic condition. After years of extremely limited mobility, severe breathing problems, costly ER visits, imaging tests, visits to specialists, and more, genome sequencing at Dr. Gibbs’ Center identified mutations in a gene called SPR that encodes the enzyme sepiapterin reductase. With proper treatment, the twins are healthy and high-functioning teenagers today, as Ms. Beery chronicles on a website she started to support other families with similar challenges.
Scientists are in the infant stages of understanding all the data that genome sequencing produces, however. “The good news is we have the human genome. The bad news is it’s largely just a parts list,” said Dr. Daniel Masys of the University of Washington. “Our ability to acquire person-specific DNA data far exceeds our understanding of its meaning.”
Learning how to “read” genomes will require sophisticated studies of vast amounts of data from millions of people, a scale of research never seen before, he said. Limiting access to genome data could stifle the many discoveries sure to be made by this work.
Meanwhile, who will be interpreting genome data? How will patients understand the potential risks and benefits of making their genome data available to others? Can the data ever be safely protected in today’s interconnected world? Every human has multiple genetic variations, and “worried well” patients could bankrupt the medical system by demanding tests or cures for things that may not really be a problem.
“There’s a snake oil salesman out there for everything,” said Commission Chair Amy Gutmann, Ph.D., president of the University of Pennsylvania.
Several speakers cautioned that it may be impossible to prevent someone from connecting even “protected” genome sequencing data to an individual and using that for commercial purposes or to limit access to insurance or health care.
“I don’t think we’re ready for this huge onslaught of additional information, because there’s too much opportunity for misuse,” said Mark A. Rothstein, J.D., chair of law and medicine at the University of Louisville.
Given the concerns about privacy, it was only a matter of time before Facebook analogies became part of the discussion. “The privacy settings are set so you don’t have any,” and users must “crank down” the settings to establish any privacy on Facebook, said Jane Kaye, D.Phil, director of the Centre for Law, Health and Emerging Technologies at the University of Oxford, U.K. “I don’t think we want to be in a society which is like that.”
Privacy should be a right in human society with ways for people to crank down their privacy limits if they want to share their information, she said. Finding mechanisms to ensure that would protect all people, not just people who are able to make decisions on their own behalf.
The future of digital information will be networks within networks of information, she predicted. Opening one “portal” may give access to information that you didn’t even know was there, like the portal between worlds in C.S. Lewis’ book, “The Lion, the Witch and the Wardrobe,” Dr. Kaye said.
And how do you get truly informed consent from a patient if you can’t say what the data may be used to study in the future? Dr. Kaye argued for a “consent for governance” in which patients are educated about the rules of the game, which will be refereed by research ethics committees and oversight bodies, and the patients agree that once they release their data, the lose individual control in some ways.
“It’s a bit like `Hotel California,’” she said. “You can check out any time you like, but you can never leave.”
The chief of the New York County District Attorney’s Forensic Sciences/Cold Case Unit brought the discussion back down to earth by describing how they convicted a criminal by matching his DNA to a specimen from tea cup that he left behind. (“We only catch the dumb ones,” she said as an aside.)
“Opponents of forensic DNA databases say this will allow government, employers and insurers to deny benefits. They’re just wrong,” said Melissa Mourges, J.D. Nearly 15 years of experience with the FBI’s Combined DNA Index System (CODIS) is “enough to prove you can have privacy and security” while allowing access to some genetic information.
Read more details from the meeting in blog posts by Commission staff on Ms. Beery, on comments by various speakers, on Ms. Mourges’s show-and-tell, and on the speakers’ final thoughts. The Commission’s report should be finished by late 2012.
--Sherry Boschert (@SherryBoschert on Twitter)
Human Genome Sequencing vs. Privacy Examined
Human genome sequencing. Facebook. Informed consent. “The Lion, the Witch and the Wardrobe.” Rare diseases. “Hotel California.” Cost-effective medicine.
It was all in a day’s work for the Presidential Commission for the Study of Bioethical Issues in its eighth meeting, this time at the University of California, San Francisco. The focus: What policies or programs should be in place (if any) to guide the ethical use of human genome sequencing, a kind of testing that’s positioned to explode into widespread use.
The cost of sequencing one person’s genome has shrunk from nearly $3 billion a mere 14 years ago to an anticipated $1,000 within the next year or two, Richard A. Gibbs, Ph.D. told the Commission. He and other experts testified in preparation for the Commission’s third report as advisors to the President. (See previous reports on separate topics here).
Today, physicians can order human genome sequencing at a handful of specialized centers. Approximately 10,000 humans had their genomes sequenced in 2011. Perhaps 100,000 will do the same in 2012, estimated Dr. Gibbs, director of the Human Genome Sequencing Center at Baylor College. He disclosed being an investor in Life Technology and co-founder of the company Seq-Wright.
Researchers and families with genetic diseases are salivating at the possibility of access to the gold mine of data this could provide, potentially improving diagnoses, identifying unknown causes of diseases, and helping people and their physicians know which drugs they will or won’t respond to, among other possible benefits.
Retta Beery is one example – she described the agonizing journey of her twins, Alexis and Noah, to a correct diagnosis of their rare but treatable genetic condition. After years of extremely limited mobility, severe breathing problems, costly ER visits, imaging tests, visits to specialists, and more, genome sequencing at Dr. Gibbs’ Center identified mutations in a gene called SPR that encodes the enzyme sepiapterin reductase. With proper treatment, the twins are healthy and high-functioning teenagers today, as Ms. Beery chronicles on a website she started to support other families with similar challenges.
Scientists are in the infant stages of understanding all the data that genome sequencing produces, however. “The good news is we have the human genome. The bad news is it’s largely just a parts list,” said Dr. Daniel Masys of the University of Washington. “Our ability to acquire person-specific DNA data far exceeds our understanding of its meaning.”
Learning how to “read” genomes will require sophisticated studies of vast amounts of data from millions of people, a scale of research never seen before, he said. Limiting access to genome data could stifle the many discoveries sure to be made by this work.
Meanwhile, who will be interpreting genome data? How will patients understand the potential risks and benefits of making their genome data available to others? Can the data ever be safely protected in today’s interconnected world? Every human has multiple genetic variations, and “worried well” patients could bankrupt the medical system by demanding tests or cures for things that may not really be a problem.
“There’s a snake oil salesman out there for everything,” said Commission Chair Amy Gutmann, Ph.D., president of the University of Pennsylvania.
Several speakers cautioned that it may be impossible to prevent someone from connecting even “protected” genome sequencing data to an individual and using that for commercial purposes or to limit access to insurance or health care.
“I don’t think we’re ready for this huge onslaught of additional information, because there’s too much opportunity for misuse,” said Mark A. Rothstein, J.D., chair of law and medicine at the University of Louisville.
Given the concerns about privacy, it was only a matter of time before Facebook analogies became part of the discussion. “The privacy settings are set so you don’t have any,” and users must “crank down” the settings to establish any privacy on Facebook, said Jane Kaye, D.Phil, director of the Centre for Law, Health and Emerging Technologies at the University of Oxford, U.K. “I don’t think we want to be in a society which is like that.”
Privacy should be a right in human society with ways for people to crank down their privacy limits if they want to share their information, she said. Finding mechanisms to ensure that would protect all people, not just people who are able to make decisions on their own behalf.
The future of digital information will be networks within networks of information, she predicted. Opening one “portal” may give access to information that you didn’t even know was there, like the portal between worlds in C.S. Lewis’ book, “The Lion, the Witch and the Wardrobe,” Dr. Kaye said.
And how do you get truly informed consent from a patient if you can’t say what the data may be used to study in the future? Dr. Kaye argued for a “consent for governance” in which patients are educated about the rules of the game, which will be refereed by research ethics committees and oversight bodies, and the patients agree that once they release their data, the lose individual control in some ways.
“It’s a bit like `Hotel California,’” she said. “You can check out any time you like, but you can never leave.”
The chief of the New York County District Attorney’s Forensic Sciences/Cold Case Unit brought the discussion back down to earth by describing how they convicted a criminal by matching his DNA to a specimen from tea cup that he left behind. (“We only catch the dumb ones,” she said as an aside.)
“Opponents of forensic DNA databases say this will allow government, employers and insurers to deny benefits. They’re just wrong,” said Melissa Mourges, J.D. Nearly 15 years of experience with the FBI’s Combined DNA Index System (CODIS) is “enough to prove you can have privacy and security” while allowing access to some genetic information.
Read more details from the meeting in blog posts by Commission staff on Ms. Beery, on comments by various speakers, on Ms. Mourges’s show-and-tell, and on the speakers’ final thoughts. The Commission’s report should be finished by late 2012.
--Sherry Boschert (@SherryBoschert on Twitter)
Human genome sequencing. Facebook. Informed consent. “The Lion, the Witch and the Wardrobe.” Rare diseases. “Hotel California.” Cost-effective medicine.
It was all in a day’s work for the Presidential Commission for the Study of Bioethical Issues in its eighth meeting, this time at the University of California, San Francisco. The focus: What policies or programs should be in place (if any) to guide the ethical use of human genome sequencing, a kind of testing that’s positioned to explode into widespread use.
The cost of sequencing one person’s genome has shrunk from nearly $3 billion a mere 14 years ago to an anticipated $1,000 within the next year or two, Richard A. Gibbs, Ph.D. told the Commission. He and other experts testified in preparation for the Commission’s third report as advisors to the President. (See previous reports on separate topics here).
Today, physicians can order human genome sequencing at a handful of specialized centers. Approximately 10,000 humans had their genomes sequenced in 2011. Perhaps 100,000 will do the same in 2012, estimated Dr. Gibbs, director of the Human Genome Sequencing Center at Baylor College. He disclosed being an investor in Life Technology and co-founder of the company Seq-Wright.
Researchers and families with genetic diseases are salivating at the possibility of access to the gold mine of data this could provide, potentially improving diagnoses, identifying unknown causes of diseases, and helping people and their physicians know which drugs they will or won’t respond to, among other possible benefits.
Retta Beery is one example – she described the agonizing journey of her twins, Alexis and Noah, to a correct diagnosis of their rare but treatable genetic condition. After years of extremely limited mobility, severe breathing problems, costly ER visits, imaging tests, visits to specialists, and more, genome sequencing at Dr. Gibbs’ Center identified mutations in a gene called SPR that encodes the enzyme sepiapterin reductase. With proper treatment, the twins are healthy and high-functioning teenagers today, as Ms. Beery chronicles on a website she started to support other families with similar challenges.
Scientists are in the infant stages of understanding all the data that genome sequencing produces, however. “The good news is we have the human genome. The bad news is it’s largely just a parts list,” said Dr. Daniel Masys of the University of Washington. “Our ability to acquire person-specific DNA data far exceeds our understanding of its meaning.”
Learning how to “read” genomes will require sophisticated studies of vast amounts of data from millions of people, a scale of research never seen before, he said. Limiting access to genome data could stifle the many discoveries sure to be made by this work.
Meanwhile, who will be interpreting genome data? How will patients understand the potential risks and benefits of making their genome data available to others? Can the data ever be safely protected in today’s interconnected world? Every human has multiple genetic variations, and “worried well” patients could bankrupt the medical system by demanding tests or cures for things that may not really be a problem.
“There’s a snake oil salesman out there for everything,” said Commission Chair Amy Gutmann, Ph.D., president of the University of Pennsylvania.
Several speakers cautioned that it may be impossible to prevent someone from connecting even “protected” genome sequencing data to an individual and using that for commercial purposes or to limit access to insurance or health care.
“I don’t think we’re ready for this huge onslaught of additional information, because there’s too much opportunity for misuse,” said Mark A. Rothstein, J.D., chair of law and medicine at the University of Louisville.
Given the concerns about privacy, it was only a matter of time before Facebook analogies became part of the discussion. “The privacy settings are set so you don’t have any,” and users must “crank down” the settings to establish any privacy on Facebook, said Jane Kaye, D.Phil, director of the Centre for Law, Health and Emerging Technologies at the University of Oxford, U.K. “I don’t think we want to be in a society which is like that.”
Privacy should be a right in human society with ways for people to crank down their privacy limits if they want to share their information, she said. Finding mechanisms to ensure that would protect all people, not just people who are able to make decisions on their own behalf.
The future of digital information will be networks within networks of information, she predicted. Opening one “portal” may give access to information that you didn’t even know was there, like the portal between worlds in C.S. Lewis’ book, “The Lion, the Witch and the Wardrobe,” Dr. Kaye said.
And how do you get truly informed consent from a patient if you can’t say what the data may be used to study in the future? Dr. Kaye argued for a “consent for governance” in which patients are educated about the rules of the game, which will be refereed by research ethics committees and oversight bodies, and the patients agree that once they release their data, the lose individual control in some ways.
“It’s a bit like `Hotel California,’” she said. “You can check out any time you like, but you can never leave.”
The chief of the New York County District Attorney’s Forensic Sciences/Cold Case Unit brought the discussion back down to earth by describing how they convicted a criminal by matching his DNA to a specimen from tea cup that he left behind. (“We only catch the dumb ones,” she said as an aside.)
“Opponents of forensic DNA databases say this will allow government, employers and insurers to deny benefits. They’re just wrong,” said Melissa Mourges, J.D. Nearly 15 years of experience with the FBI’s Combined DNA Index System (CODIS) is “enough to prove you can have privacy and security” while allowing access to some genetic information.
Read more details from the meeting in blog posts by Commission staff on Ms. Beery, on comments by various speakers, on Ms. Mourges’s show-and-tell, and on the speakers’ final thoughts. The Commission’s report should be finished by late 2012.
--Sherry Boschert (@SherryBoschert on Twitter)
Human genome sequencing. Facebook. Informed consent. “The Lion, the Witch and the Wardrobe.” Rare diseases. “Hotel California.” Cost-effective medicine.
It was all in a day’s work for the Presidential Commission for the Study of Bioethical Issues in its eighth meeting, this time at the University of California, San Francisco. The focus: What policies or programs should be in place (if any) to guide the ethical use of human genome sequencing, a kind of testing that’s positioned to explode into widespread use.
The cost of sequencing one person’s genome has shrunk from nearly $3 billion a mere 14 years ago to an anticipated $1,000 within the next year or two, Richard A. Gibbs, Ph.D. told the Commission. He and other experts testified in preparation for the Commission’s third report as advisors to the President. (See previous reports on separate topics here).
Today, physicians can order human genome sequencing at a handful of specialized centers. Approximately 10,000 humans had their genomes sequenced in 2011. Perhaps 100,000 will do the same in 2012, estimated Dr. Gibbs, director of the Human Genome Sequencing Center at Baylor College. He disclosed being an investor in Life Technology and co-founder of the company Seq-Wright.
Researchers and families with genetic diseases are salivating at the possibility of access to the gold mine of data this could provide, potentially improving diagnoses, identifying unknown causes of diseases, and helping people and their physicians know which drugs they will or won’t respond to, among other possible benefits.
Retta Beery is one example – she described the agonizing journey of her twins, Alexis and Noah, to a correct diagnosis of their rare but treatable genetic condition. After years of extremely limited mobility, severe breathing problems, costly ER visits, imaging tests, visits to specialists, and more, genome sequencing at Dr. Gibbs’ Center identified mutations in a gene called SPR that encodes the enzyme sepiapterin reductase. With proper treatment, the twins are healthy and high-functioning teenagers today, as Ms. Beery chronicles on a website she started to support other families with similar challenges.
Scientists are in the infant stages of understanding all the data that genome sequencing produces, however. “The good news is we have the human genome. The bad news is it’s largely just a parts list,” said Dr. Daniel Masys of the University of Washington. “Our ability to acquire person-specific DNA data far exceeds our understanding of its meaning.”
Learning how to “read” genomes will require sophisticated studies of vast amounts of data from millions of people, a scale of research never seen before, he said. Limiting access to genome data could stifle the many discoveries sure to be made by this work.
Meanwhile, who will be interpreting genome data? How will patients understand the potential risks and benefits of making their genome data available to others? Can the data ever be safely protected in today’s interconnected world? Every human has multiple genetic variations, and “worried well” patients could bankrupt the medical system by demanding tests or cures for things that may not really be a problem.
“There’s a snake oil salesman out there for everything,” said Commission Chair Amy Gutmann, Ph.D., president of the University of Pennsylvania.
Several speakers cautioned that it may be impossible to prevent someone from connecting even “protected” genome sequencing data to an individual and using that for commercial purposes or to limit access to insurance or health care.
“I don’t think we’re ready for this huge onslaught of additional information, because there’s too much opportunity for misuse,” said Mark A. Rothstein, J.D., chair of law and medicine at the University of Louisville.
Given the concerns about privacy, it was only a matter of time before Facebook analogies became part of the discussion. “The privacy settings are set so you don’t have any,” and users must “crank down” the settings to establish any privacy on Facebook, said Jane Kaye, D.Phil, director of the Centre for Law, Health and Emerging Technologies at the University of Oxford, U.K. “I don’t think we want to be in a society which is like that.”
Privacy should be a right in human society with ways for people to crank down their privacy limits if they want to share their information, she said. Finding mechanisms to ensure that would protect all people, not just people who are able to make decisions on their own behalf.
The future of digital information will be networks within networks of information, she predicted. Opening one “portal” may give access to information that you didn’t even know was there, like the portal between worlds in C.S. Lewis’ book, “The Lion, the Witch and the Wardrobe,” Dr. Kaye said.
And how do you get truly informed consent from a patient if you can’t say what the data may be used to study in the future? Dr. Kaye argued for a “consent for governance” in which patients are educated about the rules of the game, which will be refereed by research ethics committees and oversight bodies, and the patients agree that once they release their data, the lose individual control in some ways.
“It’s a bit like `Hotel California,’” she said. “You can check out any time you like, but you can never leave.”
The chief of the New York County District Attorney’s Forensic Sciences/Cold Case Unit brought the discussion back down to earth by describing how they convicted a criminal by matching his DNA to a specimen from tea cup that he left behind. (“We only catch the dumb ones,” she said as an aside.)
“Opponents of forensic DNA databases say this will allow government, employers and insurers to deny benefits. They’re just wrong,” said Melissa Mourges, J.D. Nearly 15 years of experience with the FBI’s Combined DNA Index System (CODIS) is “enough to prove you can have privacy and security” while allowing access to some genetic information.
Read more details from the meeting in blog posts by Commission staff on Ms. Beery, on comments by various speakers, on Ms. Mourges’s show-and-tell, and on the speakers’ final thoughts. The Commission’s report should be finished by late 2012.
--Sherry Boschert (@SherryBoschert on Twitter)
Community Hospital Offers Catheter-Directed Pulmonary Thrombolysis
Few, if any, vascular specialists are aggressively treating massive or submassive pulmonary embolism with catheter-directed thrombolytic therapy at community hospitals, but it is feasible and can have good outcomes with proper planning and preparation, according to Dr. Jeffrey Y. Wang.
Catheter-directed thrombolytic therapy for massive or submassive pulmonary embolism (PE) can shorten stays in the ICU and the hospital, reduce or eliminate the need for home oxygen therapy, and help restore right heart function, he said. However, catheter-directed interventions for these patients is rare outside of academic or tertiary-care settings, probably because of a lack of randomized trials, little retrospective data, and lack of expertise, he said.
For physicians considering this treatment at their own community hospitals, Dr. Wang emphasized that preparing the hospital and protocols are as important as is technical expertise in doing the procedure. The fluoroscopy suite must be available on an emergency basis, for example.
"In our institution, we use the same protocols for call-in and transport to the cath lab as for ST-elevation myocardial infarction, which allows us to get the patient up and into the fluoroscopy suite within 30 minutes," said Dr. Wang of Shady Grove Adventist Hospital, Rockville, Md.
Before doing his first case, he made sure that protocols were in place in the emergency department, in the ICU, and with the hospitalist team for the early detection of deep vein thrombosis and PE, notification of the appropriate staff, and posttreatment care of patients.
Systemic anticoagulation has been the mainstay of treatment for PE, but the American Heart Association and the American College of Chest Physicians have recommended more aggressive therapy for massive and submassive PEs, Dr. Wang said. Up to 60% of patients with massive PE die, data suggest, with two-thirds of the deaths occurring in the first hour of embolism formation. Within 30 days of submassive PE formation, 15%-20% of patients die secondary to pulmonary hypertension and subsequent cor pulmonale.
Approximately 30% of all 500,000 symptomatic PEs diagnosed each year in the United States lead to death. Even among inpatients who are diagnosed with a PE while in the hospital, the mortality rate is approximately 10%-15%, he said.
Until recently, there was no Food and Drug Administration–approved device for catheter-directed thrombolytic therapy. "There’s also not a purpose-built device to help you with these types of procedures," Dr. Wang said.
At the annual meeting of the Southern Association for Vascular Surgery, he described treating nine women and three men who had a total of seven massive and five submassive PEs. Catheter-directed thrombolytic therapy was offered to patients with massive or submassive PE if they were hemodynamically unstable or had right heart dysfunction, elevated troponin levels, or pulmonary artery pressures greater than 70 mm Hg, or if they were not being weaned off intubation for oxygen within 5 days, Dr. Wang said. He excluded patients who were actively bleeding or who were not able to tolerate any systemic anticoagulation – "not even aspirin," he said.
Recent surgery was not a disqualifying factor. "Typically those patients were orthopedic in nature, with a hip or knee replacement," Dr. Wang said. The patient would develop a big PE, and the orthopedist would give him the green light for aggressive treatment.
All procedures were technically successful. One patient developed hemodynamically significant bradycardia, but all were off supplemental oxygen within 24 hours of the procedure, and there were no bleeding events.
One patient died 14 hours after the procedure, most likely due to a paradoxical embolism to the intestine, Dr. Wang said. The 11 surviving patients were discharged to home within 48 hours of the intervention.
His technique includes accessing the internal jugular vein to get to the pulmonary artery, placing a vena cava filter, and giving tissue plasminogen activator as the lytic agent. All patients had a spiral CT scan before going to the catheterization lab, so pulmonary angiography was not routinely performed.
He reserved mechanical (catheter) thrombectomy for some patients with massive thromboembolism. Instead of being guided by angiography, he determined the duration of mechanical thrombectomy by the patient’s blood pressure, pulse, and oxygen saturation.
"I discontinued mechanical thrombectomy once oxygen saturation was above 95%, they’re weaning off their inotropes, and the pulse rate was trending toward normal," he said.
For some patients who developed nonsinus arrhythmias due to the wire manipulations within the heart and pulmonary arteries, he removed the wire device, waited for it to resolve, and continued. A minority of patients whose arrhythmias continued to occur during the intervention received calcium blockade or beta blockade.
Patients who received mechanical thrombectomy developed dark or bloody urine that resolved within 48 hours with hydration.
Follow-up at 2 weeks assessed general function and access sites, and patients had a repeat echocardiogram at 1 month. If they were doing well functionally and pulmonary hypertension had resolved, Dr. Wang offered to remove the vena cava filter. All but one patient accepted. All were to remain on systemic anticoagulation for 6-12 months, and patients with massive PE underwent hematologic workups.
Dr. Wang reported having no financial disclosures.
It amazes me that over many decades, the treatment of pulmonary embolism has remained stagnant. There have been no significant changes in the way we treat these patients. Most are treated with systemic anticoagulation and prolonged warfarin therapy.
There are many limitations to the use of systemic thrombolysis. The most important one is a high incidence of bleeding complications, about 20%-40%. Surgical thrombectomy also has limitations and is performed in a very limited number of centers, with mortality rates of about 10%-20%.
There is no question in my mind that there is a large potential benefit in treating patients with catheter-directed thrombolysis, particularly patients with massive pulmonary embolism. There’s also a potential benefit from catheter-directed thrombolysis in a large subgroup of patients with submassive pulmonary embolism. Those patients may benefit the most in terms of prevention of pulmonary hypertension.
Many of these questions are being investigated now in a European prospective, randomized trial comparing catheter-guided pulmonary thrombolysis to chemical thrombolysis. In the Unites States, there are a couple of registries for these patients, and a randomized trial is expected to start in the near future. I encourage vascular specialists to enroll patients in these.
Dr. Juan Ayerdi is a clinical assistant professor of vascular surgery at the Medical Center of Central Georgia, Macon. He made these remarks as the discussant of Dr. Wang’s presentation at the meeting. Dr. Ayerdi reported having no financial disclosures.
It amazes me that over many decades, the treatment of pulmonary embolism has remained stagnant. There have been no significant changes in the way we treat these patients. Most are treated with systemic anticoagulation and prolonged warfarin therapy.
There are many limitations to the use of systemic thrombolysis. The most important one is a high incidence of bleeding complications, about 20%-40%. Surgical thrombectomy also has limitations and is performed in a very limited number of centers, with mortality rates of about 10%-20%.
There is no question in my mind that there is a large potential benefit in treating patients with catheter-directed thrombolysis, particularly patients with massive pulmonary embolism. There’s also a potential benefit from catheter-directed thrombolysis in a large subgroup of patients with submassive pulmonary embolism. Those patients may benefit the most in terms of prevention of pulmonary hypertension.
Many of these questions are being investigated now in a European prospective, randomized trial comparing catheter-guided pulmonary thrombolysis to chemical thrombolysis. In the Unites States, there are a couple of registries for these patients, and a randomized trial is expected to start in the near future. I encourage vascular specialists to enroll patients in these.
Dr. Juan Ayerdi is a clinical assistant professor of vascular surgery at the Medical Center of Central Georgia, Macon. He made these remarks as the discussant of Dr. Wang’s presentation at the meeting. Dr. Ayerdi reported having no financial disclosures.
It amazes me that over many decades, the treatment of pulmonary embolism has remained stagnant. There have been no significant changes in the way we treat these patients. Most are treated with systemic anticoagulation and prolonged warfarin therapy.
There are many limitations to the use of systemic thrombolysis. The most important one is a high incidence of bleeding complications, about 20%-40%. Surgical thrombectomy also has limitations and is performed in a very limited number of centers, with mortality rates of about 10%-20%.
There is no question in my mind that there is a large potential benefit in treating patients with catheter-directed thrombolysis, particularly patients with massive pulmonary embolism. There’s also a potential benefit from catheter-directed thrombolysis in a large subgroup of patients with submassive pulmonary embolism. Those patients may benefit the most in terms of prevention of pulmonary hypertension.
Many of these questions are being investigated now in a European prospective, randomized trial comparing catheter-guided pulmonary thrombolysis to chemical thrombolysis. In the Unites States, there are a couple of registries for these patients, and a randomized trial is expected to start in the near future. I encourage vascular specialists to enroll patients in these.
Dr. Juan Ayerdi is a clinical assistant professor of vascular surgery at the Medical Center of Central Georgia, Macon. He made these remarks as the discussant of Dr. Wang’s presentation at the meeting. Dr. Ayerdi reported having no financial disclosures.
Few, if any, vascular specialists are aggressively treating massive or submassive pulmonary embolism with catheter-directed thrombolytic therapy at community hospitals, but it is feasible and can have good outcomes with proper planning and preparation, according to Dr. Jeffrey Y. Wang.
Catheter-directed thrombolytic therapy for massive or submassive pulmonary embolism (PE) can shorten stays in the ICU and the hospital, reduce or eliminate the need for home oxygen therapy, and help restore right heart function, he said. However, catheter-directed interventions for these patients is rare outside of academic or tertiary-care settings, probably because of a lack of randomized trials, little retrospective data, and lack of expertise, he said.
For physicians considering this treatment at their own community hospitals, Dr. Wang emphasized that preparing the hospital and protocols are as important as is technical expertise in doing the procedure. The fluoroscopy suite must be available on an emergency basis, for example.
"In our institution, we use the same protocols for call-in and transport to the cath lab as for ST-elevation myocardial infarction, which allows us to get the patient up and into the fluoroscopy suite within 30 minutes," said Dr. Wang of Shady Grove Adventist Hospital, Rockville, Md.
Before doing his first case, he made sure that protocols were in place in the emergency department, in the ICU, and with the hospitalist team for the early detection of deep vein thrombosis and PE, notification of the appropriate staff, and posttreatment care of patients.
Systemic anticoagulation has been the mainstay of treatment for PE, but the American Heart Association and the American College of Chest Physicians have recommended more aggressive therapy for massive and submassive PEs, Dr. Wang said. Up to 60% of patients with massive PE die, data suggest, with two-thirds of the deaths occurring in the first hour of embolism formation. Within 30 days of submassive PE formation, 15%-20% of patients die secondary to pulmonary hypertension and subsequent cor pulmonale.
Approximately 30% of all 500,000 symptomatic PEs diagnosed each year in the United States lead to death. Even among inpatients who are diagnosed with a PE while in the hospital, the mortality rate is approximately 10%-15%, he said.
Until recently, there was no Food and Drug Administration–approved device for catheter-directed thrombolytic therapy. "There’s also not a purpose-built device to help you with these types of procedures," Dr. Wang said.
At the annual meeting of the Southern Association for Vascular Surgery, he described treating nine women and three men who had a total of seven massive and five submassive PEs. Catheter-directed thrombolytic therapy was offered to patients with massive or submassive PE if they were hemodynamically unstable or had right heart dysfunction, elevated troponin levels, or pulmonary artery pressures greater than 70 mm Hg, or if they were not being weaned off intubation for oxygen within 5 days, Dr. Wang said. He excluded patients who were actively bleeding or who were not able to tolerate any systemic anticoagulation – "not even aspirin," he said.
Recent surgery was not a disqualifying factor. "Typically those patients were orthopedic in nature, with a hip or knee replacement," Dr. Wang said. The patient would develop a big PE, and the orthopedist would give him the green light for aggressive treatment.
All procedures were technically successful. One patient developed hemodynamically significant bradycardia, but all were off supplemental oxygen within 24 hours of the procedure, and there were no bleeding events.
One patient died 14 hours after the procedure, most likely due to a paradoxical embolism to the intestine, Dr. Wang said. The 11 surviving patients were discharged to home within 48 hours of the intervention.
His technique includes accessing the internal jugular vein to get to the pulmonary artery, placing a vena cava filter, and giving tissue plasminogen activator as the lytic agent. All patients had a spiral CT scan before going to the catheterization lab, so pulmonary angiography was not routinely performed.
He reserved mechanical (catheter) thrombectomy for some patients with massive thromboembolism. Instead of being guided by angiography, he determined the duration of mechanical thrombectomy by the patient’s blood pressure, pulse, and oxygen saturation.
"I discontinued mechanical thrombectomy once oxygen saturation was above 95%, they’re weaning off their inotropes, and the pulse rate was trending toward normal," he said.
For some patients who developed nonsinus arrhythmias due to the wire manipulations within the heart and pulmonary arteries, he removed the wire device, waited for it to resolve, and continued. A minority of patients whose arrhythmias continued to occur during the intervention received calcium blockade or beta blockade.
Patients who received mechanical thrombectomy developed dark or bloody urine that resolved within 48 hours with hydration.
Follow-up at 2 weeks assessed general function and access sites, and patients had a repeat echocardiogram at 1 month. If they were doing well functionally and pulmonary hypertension had resolved, Dr. Wang offered to remove the vena cava filter. All but one patient accepted. All were to remain on systemic anticoagulation for 6-12 months, and patients with massive PE underwent hematologic workups.
Dr. Wang reported having no financial disclosures.
Few, if any, vascular specialists are aggressively treating massive or submassive pulmonary embolism with catheter-directed thrombolytic therapy at community hospitals, but it is feasible and can have good outcomes with proper planning and preparation, according to Dr. Jeffrey Y. Wang.
Catheter-directed thrombolytic therapy for massive or submassive pulmonary embolism (PE) can shorten stays in the ICU and the hospital, reduce or eliminate the need for home oxygen therapy, and help restore right heart function, he said. However, catheter-directed interventions for these patients is rare outside of academic or tertiary-care settings, probably because of a lack of randomized trials, little retrospective data, and lack of expertise, he said.
For physicians considering this treatment at their own community hospitals, Dr. Wang emphasized that preparing the hospital and protocols are as important as is technical expertise in doing the procedure. The fluoroscopy suite must be available on an emergency basis, for example.
"In our institution, we use the same protocols for call-in and transport to the cath lab as for ST-elevation myocardial infarction, which allows us to get the patient up and into the fluoroscopy suite within 30 minutes," said Dr. Wang of Shady Grove Adventist Hospital, Rockville, Md.
Before doing his first case, he made sure that protocols were in place in the emergency department, in the ICU, and with the hospitalist team for the early detection of deep vein thrombosis and PE, notification of the appropriate staff, and posttreatment care of patients.
Systemic anticoagulation has been the mainstay of treatment for PE, but the American Heart Association and the American College of Chest Physicians have recommended more aggressive therapy for massive and submassive PEs, Dr. Wang said. Up to 60% of patients with massive PE die, data suggest, with two-thirds of the deaths occurring in the first hour of embolism formation. Within 30 days of submassive PE formation, 15%-20% of patients die secondary to pulmonary hypertension and subsequent cor pulmonale.
Approximately 30% of all 500,000 symptomatic PEs diagnosed each year in the United States lead to death. Even among inpatients who are diagnosed with a PE while in the hospital, the mortality rate is approximately 10%-15%, he said.
Until recently, there was no Food and Drug Administration–approved device for catheter-directed thrombolytic therapy. "There’s also not a purpose-built device to help you with these types of procedures," Dr. Wang said.
At the annual meeting of the Southern Association for Vascular Surgery, he described treating nine women and three men who had a total of seven massive and five submassive PEs. Catheter-directed thrombolytic therapy was offered to patients with massive or submassive PE if they were hemodynamically unstable or had right heart dysfunction, elevated troponin levels, or pulmonary artery pressures greater than 70 mm Hg, or if they were not being weaned off intubation for oxygen within 5 days, Dr. Wang said. He excluded patients who were actively bleeding or who were not able to tolerate any systemic anticoagulation – "not even aspirin," he said.
Recent surgery was not a disqualifying factor. "Typically those patients were orthopedic in nature, with a hip or knee replacement," Dr. Wang said. The patient would develop a big PE, and the orthopedist would give him the green light for aggressive treatment.
All procedures were technically successful. One patient developed hemodynamically significant bradycardia, but all were off supplemental oxygen within 24 hours of the procedure, and there were no bleeding events.
One patient died 14 hours after the procedure, most likely due to a paradoxical embolism to the intestine, Dr. Wang said. The 11 surviving patients were discharged to home within 48 hours of the intervention.
His technique includes accessing the internal jugular vein to get to the pulmonary artery, placing a vena cava filter, and giving tissue plasminogen activator as the lytic agent. All patients had a spiral CT scan before going to the catheterization lab, so pulmonary angiography was not routinely performed.
He reserved mechanical (catheter) thrombectomy for some patients with massive thromboembolism. Instead of being guided by angiography, he determined the duration of mechanical thrombectomy by the patient’s blood pressure, pulse, and oxygen saturation.
"I discontinued mechanical thrombectomy once oxygen saturation was above 95%, they’re weaning off their inotropes, and the pulse rate was trending toward normal," he said.
For some patients who developed nonsinus arrhythmias due to the wire manipulations within the heart and pulmonary arteries, he removed the wire device, waited for it to resolve, and continued. A minority of patients whose arrhythmias continued to occur during the intervention received calcium blockade or beta blockade.
Patients who received mechanical thrombectomy developed dark or bloody urine that resolved within 48 hours with hydration.
Follow-up at 2 weeks assessed general function and access sites, and patients had a repeat echocardiogram at 1 month. If they were doing well functionally and pulmonary hypertension had resolved, Dr. Wang offered to remove the vena cava filter. All but one patient accepted. All were to remain on systemic anticoagulation for 6-12 months, and patients with massive PE underwent hematologic workups.
Dr. Wang reported having no financial disclosures.
Human Genome Sequencing vs. Privacy Examined
Human genome sequencing. Facebook. Informed consent. “The Lion, the Witch and the Wardrobe.” Rare diseases. “Hotel California.” Cost-effective medicine.
It was all in a day’s work for the Presidential Commission for the Study of Bioethical Issues in its eighth meeting, this time at the University of California, San Francisco. The focus: What policies or programs should be in place (if any) to guide the ethical use of human genome sequencing, a kind of testing that’s positioned to explode into widespread use.
The cost of sequencing one person’s genome has shrunk from nearly $3 billion a mere 14 years ago to an anticipated $1,000 within the next year or two, Richard A. Gibbs, Ph.D. told the Commission. He and other experts testified in preparation for the Commission’s third report as advisors to the President. (See previous reports on separate topics here).
Today, physicians can order human genome sequencing at a handful of specialized centers. Approximately 10,000 humans had their genomes sequenced in 2011. Perhaps 100,000 will do the same in 2012, estimated Dr. Gibbs, director of the Human Genome Sequencing Center at Baylor College. He disclosed being an investor in Life Technology and co-founder of the company Seq-Wright.
Researchers and families with genetic diseases are salivating at the possibility of access to the gold mine of data this could provide, potentially improving diagnoses, identifying unknown causes of diseases, and helping people and their physicians know which drugs they will or won’t respond to, among other possible benefits.
Retta Beery is one example – she described the agonizing journey of her twins, Alexis and Noah, to a correct diagnosis of their rare but treatable genetic condition. After years of extremely limited mobility, severe breathing problems, costly ER visits, imaging tests, visits to specialists, and more, genome sequencing at Dr. Gibbs’ Center identified mutations in a gene called SPR that encodes the enzyme sepiapterin reductase. With proper treatment, the twins are healthy and high-functioning teenagers today, as Ms. Beery chronicles on a website she started to support other families with similar challenges.
Scientists are in the infant stages of understanding all the data that genome sequencing produces, however. “The good news is we have the human genome. The bad news is it’s largely just a parts list,” said Dr. Daniel Masys of the University of Washington. “Our ability to acquire person-specific DNA data far exceeds our understanding of its meaning.”
Learning how to “read” genomes will require sophisticated studies of vast amounts of data from millions of people, a scale of research never seen before, he said. Limiting access to genome data could stifle the many discoveries sure to be made by this work.
Meanwhile, who will be interpreting genome data? How will patients understand the potential risks and benefits of making their genome data available to others? Can the data ever be safely protected in today’s interconnected world? Every human has multiple genetic variations, and “worried well” patients could bankrupt the medical system by demanding tests or cures for things that may not really be a problem.
“There’s a snake oil salesman out there for everything,” said Commission Chair Amy Gutmann, Ph.D., president of the University of Pennsylvania.
Several speakers cautioned that it may be impossible to prevent someone from connecting even “protected” genome sequencing data to an individual and using that for commercial purposes or to limit access to insurance or health care.
“I don’t think we’re ready for this huge onslaught of additional information, because there’s too much opportunity for misuse,” said Mark A. Rothstein, J.D., chair of law and medicine at the University of Louisville.
Given the concerns about privacy, it was only a matter of time before Facebook analogies became part of the discussion. “The privacy settings are set so you don’t have any,” and users must “crank down” the settings to establish any privacy on Facebook, said Jane Kaye, D.Phil, director of the Centre for Law, Health and Emerging Technologies at the University of Oxford, U.K. “I don’t think we want to be in a society which is like that.”
Privacy should be a right in human society with ways for people to crank down their privacy limits if they want to share their information, she said. Finding mechanisms to ensure that would protect all people, not just people who are able to make decisions on their own behalf.
The future of digital information will be networks within networks of information, she predicted. Opening one “portal” may give access to information that you didn’t even know was there, like the portal between worlds in C.S. Lewis’ book, “The Lion, the Witch and the Wardrobe,” Dr. Kaye said.
And how do you get truly informed consent from a patient if you can’t say what the data may be used to study in the future? Dr. Kaye argued for a “consent for governance” in which patients are educated about the rules of the game, which will be refereed by research ethics committees and oversight bodies, and the patients agree that once they release their data, the lose individual control in some ways.
“It’s a bit like `Hotel California,’” she said. “You can check out any time you like, but you can never leave.”
The chief of the New York County District Attorney’s Forensic Sciences/Cold Case Unit brought the discussion back down to earth by describing how they convicted a criminal by matching his DNA to a specimen from tea cup that he left behind. (“We only catch the dumb ones,” she said as an aside.)
“Opponents of forensic DNA databases say this will allow government, employers and insurers to deny benefits. They’re just wrong,” said Melissa Mourges, J.D. Nearly 15 years of experience with the FBI’s Combined DNA Index System (CODIS) is “enough to prove you can have privacy and security” while allowing access to some genetic information.
Read more details from the meeting in blog posts by Commission staff on Ms. Beery, on comments by various speakers, on Ms. Mourges’s show-and-tell, and on the speakers’ final thoughts. The Commission’s report should be finished by late 2012.
--Sherry Boschert (@SherryBoschert on Twitter)
Human genome sequencing. Facebook. Informed consent. “The Lion, the Witch and the Wardrobe.” Rare diseases. “Hotel California.” Cost-effective medicine.
It was all in a day’s work for the Presidential Commission for the Study of Bioethical Issues in its eighth meeting, this time at the University of California, San Francisco. The focus: What policies or programs should be in place (if any) to guide the ethical use of human genome sequencing, a kind of testing that’s positioned to explode into widespread use.
The cost of sequencing one person’s genome has shrunk from nearly $3 billion a mere 14 years ago to an anticipated $1,000 within the next year or two, Richard A. Gibbs, Ph.D. told the Commission. He and other experts testified in preparation for the Commission’s third report as advisors to the President. (See previous reports on separate topics here).
Today, physicians can order human genome sequencing at a handful of specialized centers. Approximately 10,000 humans had their genomes sequenced in 2011. Perhaps 100,000 will do the same in 2012, estimated Dr. Gibbs, director of the Human Genome Sequencing Center at Baylor College. He disclosed being an investor in Life Technology and co-founder of the company Seq-Wright.
Researchers and families with genetic diseases are salivating at the possibility of access to the gold mine of data this could provide, potentially improving diagnoses, identifying unknown causes of diseases, and helping people and their physicians know which drugs they will or won’t respond to, among other possible benefits.
Retta Beery is one example – she described the agonizing journey of her twins, Alexis and Noah, to a correct diagnosis of their rare but treatable genetic condition. After years of extremely limited mobility, severe breathing problems, costly ER visits, imaging tests, visits to specialists, and more, genome sequencing at Dr. Gibbs’ Center identified mutations in a gene called SPR that encodes the enzyme sepiapterin reductase. With proper treatment, the twins are healthy and high-functioning teenagers today, as Ms. Beery chronicles on a website she started to support other families with similar challenges.
Scientists are in the infant stages of understanding all the data that genome sequencing produces, however. “The good news is we have the human genome. The bad news is it’s largely just a parts list,” said Dr. Daniel Masys of the University of Washington. “Our ability to acquire person-specific DNA data far exceeds our understanding of its meaning.”
Learning how to “read” genomes will require sophisticated studies of vast amounts of data from millions of people, a scale of research never seen before, he said. Limiting access to genome data could stifle the many discoveries sure to be made by this work.
Meanwhile, who will be interpreting genome data? How will patients understand the potential risks and benefits of making their genome data available to others? Can the data ever be safely protected in today’s interconnected world? Every human has multiple genetic variations, and “worried well” patients could bankrupt the medical system by demanding tests or cures for things that may not really be a problem.
“There’s a snake oil salesman out there for everything,” said Commission Chair Amy Gutmann, Ph.D., president of the University of Pennsylvania.
Several speakers cautioned that it may be impossible to prevent someone from connecting even “protected” genome sequencing data to an individual and using that for commercial purposes or to limit access to insurance or health care.
“I don’t think we’re ready for this huge onslaught of additional information, because there’s too much opportunity for misuse,” said Mark A. Rothstein, J.D., chair of law and medicine at the University of Louisville.
Given the concerns about privacy, it was only a matter of time before Facebook analogies became part of the discussion. “The privacy settings are set so you don’t have any,” and users must “crank down” the settings to establish any privacy on Facebook, said Jane Kaye, D.Phil, director of the Centre for Law, Health and Emerging Technologies at the University of Oxford, U.K. “I don’t think we want to be in a society which is like that.”
Privacy should be a right in human society with ways for people to crank down their privacy limits if they want to share their information, she said. Finding mechanisms to ensure that would protect all people, not just people who are able to make decisions on their own behalf.
The future of digital information will be networks within networks of information, she predicted. Opening one “portal” may give access to information that you didn’t even know was there, like the portal between worlds in C.S. Lewis’ book, “The Lion, the Witch and the Wardrobe,” Dr. Kaye said.
And how do you get truly informed consent from a patient if you can’t say what the data may be used to study in the future? Dr. Kaye argued for a “consent for governance” in which patients are educated about the rules of the game, which will be refereed by research ethics committees and oversight bodies, and the patients agree that once they release their data, the lose individual control in some ways.
“It’s a bit like `Hotel California,’” she said. “You can check out any time you like, but you can never leave.”
The chief of the New York County District Attorney’s Forensic Sciences/Cold Case Unit brought the discussion back down to earth by describing how they convicted a criminal by matching his DNA to a specimen from tea cup that he left behind. (“We only catch the dumb ones,” she said as an aside.)
“Opponents of forensic DNA databases say this will allow government, employers and insurers to deny benefits. They’re just wrong,” said Melissa Mourges, J.D. Nearly 15 years of experience with the FBI’s Combined DNA Index System (CODIS) is “enough to prove you can have privacy and security” while allowing access to some genetic information.
Read more details from the meeting in blog posts by Commission staff on Ms. Beery, on comments by various speakers, on Ms. Mourges’s show-and-tell, and on the speakers’ final thoughts. The Commission’s report should be finished by late 2012.
--Sherry Boschert (@SherryBoschert on Twitter)
Human genome sequencing. Facebook. Informed consent. “The Lion, the Witch and the Wardrobe.” Rare diseases. “Hotel California.” Cost-effective medicine.
It was all in a day’s work for the Presidential Commission for the Study of Bioethical Issues in its eighth meeting, this time at the University of California, San Francisco. The focus: What policies or programs should be in place (if any) to guide the ethical use of human genome sequencing, a kind of testing that’s positioned to explode into widespread use.
The cost of sequencing one person’s genome has shrunk from nearly $3 billion a mere 14 years ago to an anticipated $1,000 within the next year or two, Richard A. Gibbs, Ph.D. told the Commission. He and other experts testified in preparation for the Commission’s third report as advisors to the President. (See previous reports on separate topics here).
Today, physicians can order human genome sequencing at a handful of specialized centers. Approximately 10,000 humans had their genomes sequenced in 2011. Perhaps 100,000 will do the same in 2012, estimated Dr. Gibbs, director of the Human Genome Sequencing Center at Baylor College. He disclosed being an investor in Life Technology and co-founder of the company Seq-Wright.
Researchers and families with genetic diseases are salivating at the possibility of access to the gold mine of data this could provide, potentially improving diagnoses, identifying unknown causes of diseases, and helping people and their physicians know which drugs they will or won’t respond to, among other possible benefits.
Retta Beery is one example – she described the agonizing journey of her twins, Alexis and Noah, to a correct diagnosis of their rare but treatable genetic condition. After years of extremely limited mobility, severe breathing problems, costly ER visits, imaging tests, visits to specialists, and more, genome sequencing at Dr. Gibbs’ Center identified mutations in a gene called SPR that encodes the enzyme sepiapterin reductase. With proper treatment, the twins are healthy and high-functioning teenagers today, as Ms. Beery chronicles on a website she started to support other families with similar challenges.
Scientists are in the infant stages of understanding all the data that genome sequencing produces, however. “The good news is we have the human genome. The bad news is it’s largely just a parts list,” said Dr. Daniel Masys of the University of Washington. “Our ability to acquire person-specific DNA data far exceeds our understanding of its meaning.”
Learning how to “read” genomes will require sophisticated studies of vast amounts of data from millions of people, a scale of research never seen before, he said. Limiting access to genome data could stifle the many discoveries sure to be made by this work.
Meanwhile, who will be interpreting genome data? How will patients understand the potential risks and benefits of making their genome data available to others? Can the data ever be safely protected in today’s interconnected world? Every human has multiple genetic variations, and “worried well” patients could bankrupt the medical system by demanding tests or cures for things that may not really be a problem.
“There’s a snake oil salesman out there for everything,” said Commission Chair Amy Gutmann, Ph.D., president of the University of Pennsylvania.
Several speakers cautioned that it may be impossible to prevent someone from connecting even “protected” genome sequencing data to an individual and using that for commercial purposes or to limit access to insurance or health care.
“I don’t think we’re ready for this huge onslaught of additional information, because there’s too much opportunity for misuse,” said Mark A. Rothstein, J.D., chair of law and medicine at the University of Louisville.
Given the concerns about privacy, it was only a matter of time before Facebook analogies became part of the discussion. “The privacy settings are set so you don’t have any,” and users must “crank down” the settings to establish any privacy on Facebook, said Jane Kaye, D.Phil, director of the Centre for Law, Health and Emerging Technologies at the University of Oxford, U.K. “I don’t think we want to be in a society which is like that.”
Privacy should be a right in human society with ways for people to crank down their privacy limits if they want to share their information, she said. Finding mechanisms to ensure that would protect all people, not just people who are able to make decisions on their own behalf.
The future of digital information will be networks within networks of information, she predicted. Opening one “portal” may give access to information that you didn’t even know was there, like the portal between worlds in C.S. Lewis’ book, “The Lion, the Witch and the Wardrobe,” Dr. Kaye said.
And how do you get truly informed consent from a patient if you can’t say what the data may be used to study in the future? Dr. Kaye argued for a “consent for governance” in which patients are educated about the rules of the game, which will be refereed by research ethics committees and oversight bodies, and the patients agree that once they release their data, the lose individual control in some ways.
“It’s a bit like `Hotel California,’” she said. “You can check out any time you like, but you can never leave.”
The chief of the New York County District Attorney’s Forensic Sciences/Cold Case Unit brought the discussion back down to earth by describing how they convicted a criminal by matching his DNA to a specimen from tea cup that he left behind. (“We only catch the dumb ones,” she said as an aside.)
“Opponents of forensic DNA databases say this will allow government, employers and insurers to deny benefits. They’re just wrong,” said Melissa Mourges, J.D. Nearly 15 years of experience with the FBI’s Combined DNA Index System (CODIS) is “enough to prove you can have privacy and security” while allowing access to some genetic information.
Read more details from the meeting in blog posts by Commission staff on Ms. Beery, on comments by various speakers, on Ms. Mourges’s show-and-tell, and on the speakers’ final thoughts. The Commission’s report should be finished by late 2012.
--Sherry Boschert (@SherryBoschert on Twitter)
Carotid Endarterectomy More Cost Effective Than Stenting
SCOTTSDALE, ARIZ. – The cost of materials makes carotid artery stenting 40% more expensive than carotid endarterectomy with no relative clinical advantage, a retrospective study of 306 cases found.
Coronary artery stenting is not cost effective in the routine management of carotid disease, Dr. Gregory D. Crenshaw and his associates reported at the annual meeting of the Southern Association for Vascular Surgery. The study won an award as the best study presented at the meeting.
The investigators compared 30-day clinical outcomes and hospital costs for 174 patients who underwent carotid endarterectomy (CEA) and 132 who underwent carotid artery stenting (CAS) with embolic protection at a single tertiary-care institution during January 2008–September 2010. Nine other patients who underwent CAS during that time were excluded because they had additional procedures that could bias the economic analysis.
Hospital costs in 2010 dollars averaged $9,426 for CAS, 40% higher than the mean $6,734 cost of CEA, said Dr. Crenshaw, a vascular and endovascular surgery fellow at the Ochsner Clinic Foundation, New Orleans.
Supply costs drove most of the difference, with supplies for CAS procedures averaging $3,667 more than for CEA. In 2010 terms, a carotid stent in the study cost $2,100-$2,495 and an embolic protection device cost $1,594-$1,695, compared with a cost of $90-$100 for a synthetic carotid patch used with endarterectomy.
Rates of adverse events did not differ significantly between groups. Stroke, MI, or death occurred in 2.3% of patients undergoing CEA and 3.8% of patients undergoing CAS.
Analyses of subgroups found the same trends in all subgroups – higher cost but no clinical advantage with carotid artery stenting, compared with carotid endarterectomy.
The investigators assessed hospital costs (not charges) by creating relative value units (RVUs) for expenses in the categories of labor, supplies, facility or equipment, and miscellaneous. The RVUs in the study were not related to Medicare work RVU valuations. The analysis did not include professional fees. Total expenses were normalized to 2010 costs based on the medical consumer price index.
The findings support previous studies suggesting similar clinical results from the two treatments but higher costs with carotid artery stenting.
The 2,502-patient Carotid Revascularization Endarterectomy Versus Stenting (CREST) trial found rates of 6.8% for CEA and 7.2% for CAS for a composite end point of periprocedural stroke, MI, death, or an ipsilateral stroke within 4 years (N. Engl. J. Med. 2010;363:11-23). In six studies between 1998 and 2010, the cost of carotid artery stenting exceeded that of carotid endarterectomy by 5%-118%, Dr. Crenshaw said.
When there is "clinical equipoise" between two therapies, costs become increasingly important, especially in the current era of rising health care costs and the need for efficient use of health care dollars, he said.
In Dr. Crenshaw’s study, the CEA group had a higher proportion of symptomatic patients (44%) and urgent cases (13%), compared with the CAS group (34% and 10%, respectively), but these differences did not achieve statistical significance. Compared with the endarterectomy group, the stenting group had significantly higher prevalences of coronary artery disease (61% vs. 37%) and congestive heart failure (18% vs. 5%).
Hospital costs were significantly higher with carotid artery stenting than with carotid endarterectomy for symptomatic or asymptomatic patients and for elective surgeries. Higher hospital costs for urgent cases treated by stenting compared with endarterectomy did not reach statistical significance.
Higher costs for symptomatic patients compared with asymptomatic patients in each subgroup were due to longer stays in the hospital and possibly due in part to extra costs for diagnostic imaging, he said. Overall, length of hospitalization was similar between the endarterectomy and stenting groups, a mean of 2 days in each.
Although the study was limited by not including professional fees in the analysis, including professional fees likely would not have changed the conclusions, he said. Medicare reimbursement for carotid artery stenting and for carotid endarterectomy is identical (averaging $1,167 in 2011). The average Medicare reimbursement for anesthesia for carotid endarterectomy is $350-$425, which also would not have changed the results significantly.
Dr. Crenshaw said he has no relevant conflicts of interest.
SCOTTSDALE, ARIZ. – The cost of materials makes carotid artery stenting 40% more expensive than carotid endarterectomy with no relative clinical advantage, a retrospective study of 306 cases found.
Coronary artery stenting is not cost effective in the routine management of carotid disease, Dr. Gregory D. Crenshaw and his associates reported at the annual meeting of the Southern Association for Vascular Surgery. The study won an award as the best study presented at the meeting.
The investigators compared 30-day clinical outcomes and hospital costs for 174 patients who underwent carotid endarterectomy (CEA) and 132 who underwent carotid artery stenting (CAS) with embolic protection at a single tertiary-care institution during January 2008–September 2010. Nine other patients who underwent CAS during that time were excluded because they had additional procedures that could bias the economic analysis.
Hospital costs in 2010 dollars averaged $9,426 for CAS, 40% higher than the mean $6,734 cost of CEA, said Dr. Crenshaw, a vascular and endovascular surgery fellow at the Ochsner Clinic Foundation, New Orleans.
Supply costs drove most of the difference, with supplies for CAS procedures averaging $3,667 more than for CEA. In 2010 terms, a carotid stent in the study cost $2,100-$2,495 and an embolic protection device cost $1,594-$1,695, compared with a cost of $90-$100 for a synthetic carotid patch used with endarterectomy.
Rates of adverse events did not differ significantly between groups. Stroke, MI, or death occurred in 2.3% of patients undergoing CEA and 3.8% of patients undergoing CAS.
Analyses of subgroups found the same trends in all subgroups – higher cost but no clinical advantage with carotid artery stenting, compared with carotid endarterectomy.
The investigators assessed hospital costs (not charges) by creating relative value units (RVUs) for expenses in the categories of labor, supplies, facility or equipment, and miscellaneous. The RVUs in the study were not related to Medicare work RVU valuations. The analysis did not include professional fees. Total expenses were normalized to 2010 costs based on the medical consumer price index.
The findings support previous studies suggesting similar clinical results from the two treatments but higher costs with carotid artery stenting.
The 2,502-patient Carotid Revascularization Endarterectomy Versus Stenting (CREST) trial found rates of 6.8% for CEA and 7.2% for CAS for a composite end point of periprocedural stroke, MI, death, or an ipsilateral stroke within 4 years (N. Engl. J. Med. 2010;363:11-23). In six studies between 1998 and 2010, the cost of carotid artery stenting exceeded that of carotid endarterectomy by 5%-118%, Dr. Crenshaw said.
When there is "clinical equipoise" between two therapies, costs become increasingly important, especially in the current era of rising health care costs and the need for efficient use of health care dollars, he said.
In Dr. Crenshaw’s study, the CEA group had a higher proportion of symptomatic patients (44%) and urgent cases (13%), compared with the CAS group (34% and 10%, respectively), but these differences did not achieve statistical significance. Compared with the endarterectomy group, the stenting group had significantly higher prevalences of coronary artery disease (61% vs. 37%) and congestive heart failure (18% vs. 5%).
Hospital costs were significantly higher with carotid artery stenting than with carotid endarterectomy for symptomatic or asymptomatic patients and for elective surgeries. Higher hospital costs for urgent cases treated by stenting compared with endarterectomy did not reach statistical significance.
Higher costs for symptomatic patients compared with asymptomatic patients in each subgroup were due to longer stays in the hospital and possibly due in part to extra costs for diagnostic imaging, he said. Overall, length of hospitalization was similar between the endarterectomy and stenting groups, a mean of 2 days in each.
Although the study was limited by not including professional fees in the analysis, including professional fees likely would not have changed the conclusions, he said. Medicare reimbursement for carotid artery stenting and for carotid endarterectomy is identical (averaging $1,167 in 2011). The average Medicare reimbursement for anesthesia for carotid endarterectomy is $350-$425, which also would not have changed the results significantly.
Dr. Crenshaw said he has no relevant conflicts of interest.
SCOTTSDALE, ARIZ. – The cost of materials makes carotid artery stenting 40% more expensive than carotid endarterectomy with no relative clinical advantage, a retrospective study of 306 cases found.
Coronary artery stenting is not cost effective in the routine management of carotid disease, Dr. Gregory D. Crenshaw and his associates reported at the annual meeting of the Southern Association for Vascular Surgery. The study won an award as the best study presented at the meeting.
The investigators compared 30-day clinical outcomes and hospital costs for 174 patients who underwent carotid endarterectomy (CEA) and 132 who underwent carotid artery stenting (CAS) with embolic protection at a single tertiary-care institution during January 2008–September 2010. Nine other patients who underwent CAS during that time were excluded because they had additional procedures that could bias the economic analysis.
Hospital costs in 2010 dollars averaged $9,426 for CAS, 40% higher than the mean $6,734 cost of CEA, said Dr. Crenshaw, a vascular and endovascular surgery fellow at the Ochsner Clinic Foundation, New Orleans.
Supply costs drove most of the difference, with supplies for CAS procedures averaging $3,667 more than for CEA. In 2010 terms, a carotid stent in the study cost $2,100-$2,495 and an embolic protection device cost $1,594-$1,695, compared with a cost of $90-$100 for a synthetic carotid patch used with endarterectomy.
Rates of adverse events did not differ significantly between groups. Stroke, MI, or death occurred in 2.3% of patients undergoing CEA and 3.8% of patients undergoing CAS.
Analyses of subgroups found the same trends in all subgroups – higher cost but no clinical advantage with carotid artery stenting, compared with carotid endarterectomy.
The investigators assessed hospital costs (not charges) by creating relative value units (RVUs) for expenses in the categories of labor, supplies, facility or equipment, and miscellaneous. The RVUs in the study were not related to Medicare work RVU valuations. The analysis did not include professional fees. Total expenses were normalized to 2010 costs based on the medical consumer price index.
The findings support previous studies suggesting similar clinical results from the two treatments but higher costs with carotid artery stenting.
The 2,502-patient Carotid Revascularization Endarterectomy Versus Stenting (CREST) trial found rates of 6.8% for CEA and 7.2% for CAS for a composite end point of periprocedural stroke, MI, death, or an ipsilateral stroke within 4 years (N. Engl. J. Med. 2010;363:11-23). In six studies between 1998 and 2010, the cost of carotid artery stenting exceeded that of carotid endarterectomy by 5%-118%, Dr. Crenshaw said.
When there is "clinical equipoise" between two therapies, costs become increasingly important, especially in the current era of rising health care costs and the need for efficient use of health care dollars, he said.
In Dr. Crenshaw’s study, the CEA group had a higher proportion of symptomatic patients (44%) and urgent cases (13%), compared with the CAS group (34% and 10%, respectively), but these differences did not achieve statistical significance. Compared with the endarterectomy group, the stenting group had significantly higher prevalences of coronary artery disease (61% vs. 37%) and congestive heart failure (18% vs. 5%).
Hospital costs were significantly higher with carotid artery stenting than with carotid endarterectomy for symptomatic or asymptomatic patients and for elective surgeries. Higher hospital costs for urgent cases treated by stenting compared with endarterectomy did not reach statistical significance.
Higher costs for symptomatic patients compared with asymptomatic patients in each subgroup were due to longer stays in the hospital and possibly due in part to extra costs for diagnostic imaging, he said. Overall, length of hospitalization was similar between the endarterectomy and stenting groups, a mean of 2 days in each.
Although the study was limited by not including professional fees in the analysis, including professional fees likely would not have changed the conclusions, he said. Medicare reimbursement for carotid artery stenting and for carotid endarterectomy is identical (averaging $1,167 in 2011). The average Medicare reimbursement for anesthesia for carotid endarterectomy is $350-$425, which also would not have changed the results significantly.
Dr. Crenshaw said he has no relevant conflicts of interest.
FROM THE ANNUAL MEETING OF THE SOUTHERN ASSOCIATION FOR VASCULAR SURGERY
Employee Embezzlement in Private Practice Runs High
LAS VEGAS – More medical practices will be victims of embezzlement than not, so physicians must be on top of all financial affairs in their practice, said Dr. David A. Laub.
In a 2009 survey of members of the Medical Group Management Association, 83% of 945 respondents reported being affiliated with a medical practice that had been the victim of employee theft or embezzlement.
Given that figure, it’s important to have an accountant that can be trusted, ideally one who specializes in medical practices, and to monitor the accountant’s reports at least quarterly, Dr. David A. Laub said at the annual meeting of the American Society of Cosmetic Dermatology and Aesthetic Surgery.
If someone is embezzling, most often it’s the office manager, usually by taking copays and petty cash, said Dr. Laub. Secret bank accounts hurt the most, so be wary if someone from the office staff interrupts a busy day to have a form quickly signed with a brief rationale for opening another account.
"You need to be the one signing every check and the one reviewing the credit card statements. It’s a lot of work, but unfortunately you have to monitor this" as part of financial discipline, said Dr. Laub, who practices dermatology in Mill Valley, Calif.
He suggested watching for signs of embezzlement, such as disparities between billing and collections, or an increasing number of accounts written off as unpaid. If there are increasing overhead costs but not increasing revenues related to products, the embezzler may be taking the products. On the more blatant side, if your office manager shows up at work one day in a Jaguar or makes some other lavish lifestyle change – well, you have to wonder.
Other potential signs include disorganized books or computer entries, or an office manager who suggests changing accountants or who declines vacation time, perhaps hoping to stay in control and not get caught, he said. Be alert also for duplicate payables – checks already signed but the manager asks for another one to be signed, which gets altered later for the embezzler’s gain.
Another tip for preventing theft is to separate duties. The person who takes checks from the mail should not be the same one who enters the data into the computer, he said. Get an electronic time clock to stamp the date and time on everything. Design a system for inventory and review it monthly, either through electronic medical records or a ledger in the back office. Insist on signing all checks.
"As long as you show you’re interested and are following what’s going on, it will stop a lot of problems," Dr. Laub said.
From his experience running his solo practice with two* physician assistants, three medical assistants,* three staff members answering phones, a billing administrator, and an office manager, Dr. Laub offered another tip for running a successful practice: positive leadership.
"If I’m not in a good mood, it brings the staff down, and all of a sudden everybody is inefficient," he said. Enter the office with a smile and ask staff members how their morning or weekend went.
To maintain his positive energy, Dr. Laub decided in his 40s to start taking a half-day off per week for each subsequent 5 years of practice. Now in his mid-50s, Dr. Laub is about to change from 4.5 to 4 days of work per week.
Dr. Laub said that when he first started a practice, all of his staff members were full-time employees, but he said that he has found a part-time staff is more efficient. Now his staff is composed of 80% part-time employees and 20% full-time employees, and they stay with him for 7 years on average. "These staffers are much happier," he said.
Offer complimentary staff treatments if possible, perhaps one treatment per quarter for each employee so they are exposed to services offered, he suggested.
Also, identify what’s important to individual staff members – professional growth, or getting home to the family each day – to help inform scheduling and goal setting. Praise staff publicly but critique them in private, always sandwiching criticisms between positive statements.
Dr. Laub did not disclose any conflicts of interest.
*03/26/2012 Information updated to reflect correct staff numbers and titles.
LAS VEGAS – More medical practices will be victims of embezzlement than not, so physicians must be on top of all financial affairs in their practice, said Dr. David A. Laub.
In a 2009 survey of members of the Medical Group Management Association, 83% of 945 respondents reported being affiliated with a medical practice that had been the victim of employee theft or embezzlement.
Given that figure, it’s important to have an accountant that can be trusted, ideally one who specializes in medical practices, and to monitor the accountant’s reports at least quarterly, Dr. David A. Laub said at the annual meeting of the American Society of Cosmetic Dermatology and Aesthetic Surgery.
If someone is embezzling, most often it’s the office manager, usually by taking copays and petty cash, said Dr. Laub. Secret bank accounts hurt the most, so be wary if someone from the office staff interrupts a busy day to have a form quickly signed with a brief rationale for opening another account.
"You need to be the one signing every check and the one reviewing the credit card statements. It’s a lot of work, but unfortunately you have to monitor this" as part of financial discipline, said Dr. Laub, who practices dermatology in Mill Valley, Calif.
He suggested watching for signs of embezzlement, such as disparities between billing and collections, or an increasing number of accounts written off as unpaid. If there are increasing overhead costs but not increasing revenues related to products, the embezzler may be taking the products. On the more blatant side, if your office manager shows up at work one day in a Jaguar or makes some other lavish lifestyle change – well, you have to wonder.
Other potential signs include disorganized books or computer entries, or an office manager who suggests changing accountants or who declines vacation time, perhaps hoping to stay in control and not get caught, he said. Be alert also for duplicate payables – checks already signed but the manager asks for another one to be signed, which gets altered later for the embezzler’s gain.
Another tip for preventing theft is to separate duties. The person who takes checks from the mail should not be the same one who enters the data into the computer, he said. Get an electronic time clock to stamp the date and time on everything. Design a system for inventory and review it monthly, either through electronic medical records or a ledger in the back office. Insist on signing all checks.
"As long as you show you’re interested and are following what’s going on, it will stop a lot of problems," Dr. Laub said.
From his experience running his solo practice with two* physician assistants, three medical assistants,* three staff members answering phones, a billing administrator, and an office manager, Dr. Laub offered another tip for running a successful practice: positive leadership.
"If I’m not in a good mood, it brings the staff down, and all of a sudden everybody is inefficient," he said. Enter the office with a smile and ask staff members how their morning or weekend went.
To maintain his positive energy, Dr. Laub decided in his 40s to start taking a half-day off per week for each subsequent 5 years of practice. Now in his mid-50s, Dr. Laub is about to change from 4.5 to 4 days of work per week.
Dr. Laub said that when he first started a practice, all of his staff members were full-time employees, but he said that he has found a part-time staff is more efficient. Now his staff is composed of 80% part-time employees and 20% full-time employees, and they stay with him for 7 years on average. "These staffers are much happier," he said.
Offer complimentary staff treatments if possible, perhaps one treatment per quarter for each employee so they are exposed to services offered, he suggested.
Also, identify what’s important to individual staff members – professional growth, or getting home to the family each day – to help inform scheduling and goal setting. Praise staff publicly but critique them in private, always sandwiching criticisms between positive statements.
Dr. Laub did not disclose any conflicts of interest.
*03/26/2012 Information updated to reflect correct staff numbers and titles.
LAS VEGAS – More medical practices will be victims of embezzlement than not, so physicians must be on top of all financial affairs in their practice, said Dr. David A. Laub.
In a 2009 survey of members of the Medical Group Management Association, 83% of 945 respondents reported being affiliated with a medical practice that had been the victim of employee theft or embezzlement.
Given that figure, it’s important to have an accountant that can be trusted, ideally one who specializes in medical practices, and to monitor the accountant’s reports at least quarterly, Dr. David A. Laub said at the annual meeting of the American Society of Cosmetic Dermatology and Aesthetic Surgery.
If someone is embezzling, most often it’s the office manager, usually by taking copays and petty cash, said Dr. Laub. Secret bank accounts hurt the most, so be wary if someone from the office staff interrupts a busy day to have a form quickly signed with a brief rationale for opening another account.
"You need to be the one signing every check and the one reviewing the credit card statements. It’s a lot of work, but unfortunately you have to monitor this" as part of financial discipline, said Dr. Laub, who practices dermatology in Mill Valley, Calif.
He suggested watching for signs of embezzlement, such as disparities between billing and collections, or an increasing number of accounts written off as unpaid. If there are increasing overhead costs but not increasing revenues related to products, the embezzler may be taking the products. On the more blatant side, if your office manager shows up at work one day in a Jaguar or makes some other lavish lifestyle change – well, you have to wonder.
Other potential signs include disorganized books or computer entries, or an office manager who suggests changing accountants or who declines vacation time, perhaps hoping to stay in control and not get caught, he said. Be alert also for duplicate payables – checks already signed but the manager asks for another one to be signed, which gets altered later for the embezzler’s gain.
Another tip for preventing theft is to separate duties. The person who takes checks from the mail should not be the same one who enters the data into the computer, he said. Get an electronic time clock to stamp the date and time on everything. Design a system for inventory and review it monthly, either through electronic medical records or a ledger in the back office. Insist on signing all checks.
"As long as you show you’re interested and are following what’s going on, it will stop a lot of problems," Dr. Laub said.
From his experience running his solo practice with two* physician assistants, three medical assistants,* three staff members answering phones, a billing administrator, and an office manager, Dr. Laub offered another tip for running a successful practice: positive leadership.
"If I’m not in a good mood, it brings the staff down, and all of a sudden everybody is inefficient," he said. Enter the office with a smile and ask staff members how their morning or weekend went.
To maintain his positive energy, Dr. Laub decided in his 40s to start taking a half-day off per week for each subsequent 5 years of practice. Now in his mid-50s, Dr. Laub is about to change from 4.5 to 4 days of work per week.
Dr. Laub said that when he first started a practice, all of his staff members were full-time employees, but he said that he has found a part-time staff is more efficient. Now his staff is composed of 80% part-time employees and 20% full-time employees, and they stay with him for 7 years on average. "These staffers are much happier," he said.
Offer complimentary staff treatments if possible, perhaps one treatment per quarter for each employee so they are exposed to services offered, he suggested.
Also, identify what’s important to individual staff members – professional growth, or getting home to the family each day – to help inform scheduling and goal setting. Praise staff publicly but critique them in private, always sandwiching criticisms between positive statements.
Dr. Laub did not disclose any conflicts of interest.
*03/26/2012 Information updated to reflect correct staff numbers and titles.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF COSMETIC DERMATOLOGY AND AESTHETIC SURGERY
Patients and Surgeons Diverge on Importance of Disclosures
SAN FRANCISCO – The medical community has long debated whether surgeons need to disclose their operative volumes and outcomes to patients when obtaining informed consent, and legal rulings in court cases offer mixed opinions.
Recent surveys administered to patients and attending surgeons have indicated that although patients want to know about their surgeon’s expertise and surgical outcomes during preoperative discussions for informed consent, attendings are significantly less likely to think that such information is important to disclose, Dr. Susan Lee Char said at the annual clinical congress of the American College of Surgeons.
Dr. Char and her associates surveyed 353 adult patients at their first postoperative clinic visit and 85 attending surgeons at hospitals affiliated with the University of California, San Francisco. The survey, which presented a hypothetical case of a patient’s undergoing elective partial hepatectomy, asked respondents to rate the importance of receiving or conveying various items of information on a 6-point Likert scale (with a score of 1 indicating "completely unimportant" and a score of 6 indicating "extremely important").
In all, 79% of patients said it’s essential to know if their surgeon would be doing a procedure for the first time on them, but only 55% of attending surgeons felt that this was important information to disclose. A total of 63% of patients considered it essential to know the number of times a surgeon had performed a particular procedure and the outcomes in those cases, compared with just 25% and 20% of surgeons, respectively.
"The data suggest that surgeons do have an ethical obligation to disclose volumes and outcomes and if it’s the first time [they’re] doing a procedure," said Dr. Char, a surgical resident at the university who is also a lawyer. "This has possible legal implications."
The main barrier to surgeons’ disclosing such information may be a practical one, she added. Surgeons often don’t have data on the volumes and outcomes of their procedures.
Patients’ and attending surgeons’ perceptions of the importance of other types of information also differed significantly. A general description of the procedure was rated as important by 65% of patients vs. 58% of surgeons, and technical details of the procedure were important to 48% of patients, as compared with 13% of surgeons. Disclosure of risks and benefits of the procedure were deemed essential by 77% and 71% of patients, respectively, compared with 72% and 65% of surgeons, respectively.
A total of 41% of patients and 5% of surgeons said the patient should be told the number of times that the procedure has been done by other surgeons, and 44% of patients and 20% of surgeons said other surgeons’ outcomes should be disclosed. A total of 64% of patients and 31% of surgeons believed it was important to discuss any special training obtained by the surgeon doing the procedure. Some 64% of patients said they would want to be informed about the surgeon’s special training for a standard procedure, compared with 68% for a laparoscopic procedure and 71% for a robotic procedure.
Technological innovation made a difference in whether patients deemed certain information essential, Dr. Char added. Patients who were scheduled for a laparoscopic or robotic procedure were significantly more likely to want information than were those undergoing a standard operation.
In all, 63% of patients said they would want to know the number of times that a standard procedure had been done by their surgeon. That percentage rose to 66% for a laparoscopic procedure and to 68% for a robotic procedure. Outcomes information was considered important by 63% of patients for a standard procedure, 66% for a laparoscopic procedure, and 67% for a robotic procedure.
And 24% of patients, compared with 6% of surgeons, said the patient should be told if the surgeon planned to publish an article including the case. Disclosing whether a surgeon is a paid consultant was less important to patients (5%) than to surgeons (40%).
The study was limited because it used a hypothetical case scenario rather than real informed-consent discussions, and it included only one type of surgery. Because most of the patients were well-educated women, the results may not be generalizable.
Dr. Char said she had no conflicts.
This study raises a number of issues and is both interesting and worrying. It illustrates a major mis-match between views of patients and the doctors who are treating them, which uncorrected is likely to be the source of future problems.
Of course the study has limitations in that we are not aware of any previous information that was given to the patients about their procedure or the previous health care experiences of the patients. However, it is apparent that the views of the patients about what they should expect to be told and those of the treating doctors are quite different. This is particularly true of outcome data and numbers of cases undertaken by the doctor.
The UK is still living with the consequences of the Bristol Heart Enquiry in which a number of children died when operated on by teams not experienced with complex pediatric cardiac surgery, who continued despite poor results. One of the messages that came out of this was the need for high quality outcome data that was in the public domain. Cardiac Surgery has responded well with regularly published outcome data which has also seen an improvement in cardiac surgery outcomes nationally. Other surgical specialties have been slow, hiding behind the excuses of lack of resources and case variation and complexity. Again medical complacency was shaken in 2010 when one of our national papers ran a series of articles on poorly performing vascular surgical units.
The message is clear and this study emphasizes it. The patient is our customer and we must listen to what they want; they want information and honesty. Unless we respond to this there will further erosion of public trust in our profession.
Dr. C.P. Shearman is a professor of vascular surgery at University of Southampton, Southampton, U.K. He is one of two new international associate medical editors of Vascular Specialist.
This study raises a number of issues and is both interesting and worrying. It illustrates a major mis-match between views of patients and the doctors who are treating them, which uncorrected is likely to be the source of future problems.
Of course the study has limitations in that we are not aware of any previous information that was given to the patients about their procedure or the previous health care experiences of the patients. However, it is apparent that the views of the patients about what they should expect to be told and those of the treating doctors are quite different. This is particularly true of outcome data and numbers of cases undertaken by the doctor.
The UK is still living with the consequences of the Bristol Heart Enquiry in which a number of children died when operated on by teams not experienced with complex pediatric cardiac surgery, who continued despite poor results. One of the messages that came out of this was the need for high quality outcome data that was in the public domain. Cardiac Surgery has responded well with regularly published outcome data which has also seen an improvement in cardiac surgery outcomes nationally. Other surgical specialties have been slow, hiding behind the excuses of lack of resources and case variation and complexity. Again medical complacency was shaken in 2010 when one of our national papers ran a series of articles on poorly performing vascular surgical units.
The message is clear and this study emphasizes it. The patient is our customer and we must listen to what they want; they want information and honesty. Unless we respond to this there will further erosion of public trust in our profession.
Dr. C.P. Shearman is a professor of vascular surgery at University of Southampton, Southampton, U.K. He is one of two new international associate medical editors of Vascular Specialist.
This study raises a number of issues and is both interesting and worrying. It illustrates a major mis-match between views of patients and the doctors who are treating them, which uncorrected is likely to be the source of future problems.
Of course the study has limitations in that we are not aware of any previous information that was given to the patients about their procedure or the previous health care experiences of the patients. However, it is apparent that the views of the patients about what they should expect to be told and those of the treating doctors are quite different. This is particularly true of outcome data and numbers of cases undertaken by the doctor.
The UK is still living with the consequences of the Bristol Heart Enquiry in which a number of children died when operated on by teams not experienced with complex pediatric cardiac surgery, who continued despite poor results. One of the messages that came out of this was the need for high quality outcome data that was in the public domain. Cardiac Surgery has responded well with regularly published outcome data which has also seen an improvement in cardiac surgery outcomes nationally. Other surgical specialties have been slow, hiding behind the excuses of lack of resources and case variation and complexity. Again medical complacency was shaken in 2010 when one of our national papers ran a series of articles on poorly performing vascular surgical units.
The message is clear and this study emphasizes it. The patient is our customer and we must listen to what they want; they want information and honesty. Unless we respond to this there will further erosion of public trust in our profession.
Dr. C.P. Shearman is a professor of vascular surgery at University of Southampton, Southampton, U.K. He is one of two new international associate medical editors of Vascular Specialist.
SAN FRANCISCO – The medical community has long debated whether surgeons need to disclose their operative volumes and outcomes to patients when obtaining informed consent, and legal rulings in court cases offer mixed opinions.
Recent surveys administered to patients and attending surgeons have indicated that although patients want to know about their surgeon’s expertise and surgical outcomes during preoperative discussions for informed consent, attendings are significantly less likely to think that such information is important to disclose, Dr. Susan Lee Char said at the annual clinical congress of the American College of Surgeons.
Dr. Char and her associates surveyed 353 adult patients at their first postoperative clinic visit and 85 attending surgeons at hospitals affiliated with the University of California, San Francisco. The survey, which presented a hypothetical case of a patient’s undergoing elective partial hepatectomy, asked respondents to rate the importance of receiving or conveying various items of information on a 6-point Likert scale (with a score of 1 indicating "completely unimportant" and a score of 6 indicating "extremely important").
In all, 79% of patients said it’s essential to know if their surgeon would be doing a procedure for the first time on them, but only 55% of attending surgeons felt that this was important information to disclose. A total of 63% of patients considered it essential to know the number of times a surgeon had performed a particular procedure and the outcomes in those cases, compared with just 25% and 20% of surgeons, respectively.
"The data suggest that surgeons do have an ethical obligation to disclose volumes and outcomes and if it’s the first time [they’re] doing a procedure," said Dr. Char, a surgical resident at the university who is also a lawyer. "This has possible legal implications."
The main barrier to surgeons’ disclosing such information may be a practical one, she added. Surgeons often don’t have data on the volumes and outcomes of their procedures.
Patients’ and attending surgeons’ perceptions of the importance of other types of information also differed significantly. A general description of the procedure was rated as important by 65% of patients vs. 58% of surgeons, and technical details of the procedure were important to 48% of patients, as compared with 13% of surgeons. Disclosure of risks and benefits of the procedure were deemed essential by 77% and 71% of patients, respectively, compared with 72% and 65% of surgeons, respectively.
A total of 41% of patients and 5% of surgeons said the patient should be told the number of times that the procedure has been done by other surgeons, and 44% of patients and 20% of surgeons said other surgeons’ outcomes should be disclosed. A total of 64% of patients and 31% of surgeons believed it was important to discuss any special training obtained by the surgeon doing the procedure. Some 64% of patients said they would want to be informed about the surgeon’s special training for a standard procedure, compared with 68% for a laparoscopic procedure and 71% for a robotic procedure.
Technological innovation made a difference in whether patients deemed certain information essential, Dr. Char added. Patients who were scheduled for a laparoscopic or robotic procedure were significantly more likely to want information than were those undergoing a standard operation.
In all, 63% of patients said they would want to know the number of times that a standard procedure had been done by their surgeon. That percentage rose to 66% for a laparoscopic procedure and to 68% for a robotic procedure. Outcomes information was considered important by 63% of patients for a standard procedure, 66% for a laparoscopic procedure, and 67% for a robotic procedure.
And 24% of patients, compared with 6% of surgeons, said the patient should be told if the surgeon planned to publish an article including the case. Disclosing whether a surgeon is a paid consultant was less important to patients (5%) than to surgeons (40%).
The study was limited because it used a hypothetical case scenario rather than real informed-consent discussions, and it included only one type of surgery. Because most of the patients were well-educated women, the results may not be generalizable.
Dr. Char said she had no conflicts.
SAN FRANCISCO – The medical community has long debated whether surgeons need to disclose their operative volumes and outcomes to patients when obtaining informed consent, and legal rulings in court cases offer mixed opinions.
Recent surveys administered to patients and attending surgeons have indicated that although patients want to know about their surgeon’s expertise and surgical outcomes during preoperative discussions for informed consent, attendings are significantly less likely to think that such information is important to disclose, Dr. Susan Lee Char said at the annual clinical congress of the American College of Surgeons.
Dr. Char and her associates surveyed 353 adult patients at their first postoperative clinic visit and 85 attending surgeons at hospitals affiliated with the University of California, San Francisco. The survey, which presented a hypothetical case of a patient’s undergoing elective partial hepatectomy, asked respondents to rate the importance of receiving or conveying various items of information on a 6-point Likert scale (with a score of 1 indicating "completely unimportant" and a score of 6 indicating "extremely important").
In all, 79% of patients said it’s essential to know if their surgeon would be doing a procedure for the first time on them, but only 55% of attending surgeons felt that this was important information to disclose. A total of 63% of patients considered it essential to know the number of times a surgeon had performed a particular procedure and the outcomes in those cases, compared with just 25% and 20% of surgeons, respectively.
"The data suggest that surgeons do have an ethical obligation to disclose volumes and outcomes and if it’s the first time [they’re] doing a procedure," said Dr. Char, a surgical resident at the university who is also a lawyer. "This has possible legal implications."
The main barrier to surgeons’ disclosing such information may be a practical one, she added. Surgeons often don’t have data on the volumes and outcomes of their procedures.
Patients’ and attending surgeons’ perceptions of the importance of other types of information also differed significantly. A general description of the procedure was rated as important by 65% of patients vs. 58% of surgeons, and technical details of the procedure were important to 48% of patients, as compared with 13% of surgeons. Disclosure of risks and benefits of the procedure were deemed essential by 77% and 71% of patients, respectively, compared with 72% and 65% of surgeons, respectively.
A total of 41% of patients and 5% of surgeons said the patient should be told the number of times that the procedure has been done by other surgeons, and 44% of patients and 20% of surgeons said other surgeons’ outcomes should be disclosed. A total of 64% of patients and 31% of surgeons believed it was important to discuss any special training obtained by the surgeon doing the procedure. Some 64% of patients said they would want to be informed about the surgeon’s special training for a standard procedure, compared with 68% for a laparoscopic procedure and 71% for a robotic procedure.
Technological innovation made a difference in whether patients deemed certain information essential, Dr. Char added. Patients who were scheduled for a laparoscopic or robotic procedure were significantly more likely to want information than were those undergoing a standard operation.
In all, 63% of patients said they would want to know the number of times that a standard procedure had been done by their surgeon. That percentage rose to 66% for a laparoscopic procedure and to 68% for a robotic procedure. Outcomes information was considered important by 63% of patients for a standard procedure, 66% for a laparoscopic procedure, and 67% for a robotic procedure.
And 24% of patients, compared with 6% of surgeons, said the patient should be told if the surgeon planned to publish an article including the case. Disclosing whether a surgeon is a paid consultant was less important to patients (5%) than to surgeons (40%).
The study was limited because it used a hypothetical case scenario rather than real informed-consent discussions, and it included only one type of surgery. Because most of the patients were well-educated women, the results may not be generalizable.
Dr. Char said she had no conflicts.
Major Finding: Only 55% of surgeons believed they should disclose that they would be doing a surgery for the first time on a patient when getting informed consent, compared with 79% of patients.
Data Source: Surveys presenting a hypothetical case to 353 patients at postoperative clinic visits, and to 85 attending surgeons.
Disclosures: Dr. Char said she has no relevant conflicts of interest.