User login
Recurrent Headache in Young May Be Tied to Vitamin D Deficiency
LOS ANGELES – Vitamin D deficiency was detected in 37% of 497 children and adolescents presenting to a tertiary care center for recurrent headache that required preventive treatment. Vitamin D insufficiency was found in 87%.
These results of routinely measuring baseline serum 25-hydroxyvitamin D (25[OH]D) levels at new patient visits or at follow-up visits suggest that pediatric patients with recurrent headaches may be at increased risk for vitamin D insufficiency or deficiency compared with the general healthy population, Dr. Hope L. O'Brien and her associates reported in a poster presentation at the meeting.
Vitamin D deficiency was defined as a serum 25(OH)D level of less than 20 ng/mL. Vitamin D insufficiency was defined as a level below 30 ng/mL.
Serum 25(OH)D levels averaged 24 ng/mL in patients presenting with episodic migraine and 23 ng/mL in patients presenting with chronic migraine, reported Dr. O'Brien of the University of Cincinnati.
Studies have suggested a link between low vitamin D levels and migraine or chronic tension-type headache in adults, but this may be the first study to assess this association in children and adolescents. Patients in the current study had a mean age of 14 years (range 4–25).
The implications of these findings are unclear, but it's possible that vitamin D supplementation might help improve headaches and overall health, Dr. O'Brien said. Studies in adults have linked low vitamin D levels with medical problems such as heart disease, diabetes, cancer, autoimmune disease, chronic pain, and osteoporosis, with some evidence suggesting poorer outcomes in patients with these problems and low vitamin D levels.
More studies are needed to confirm a relationship between vitamin D levels and headache frequency in children and adolescents and to explore whether vitamin supplementation may improve headache, she said.
Dr. O'Brien did not list any disclosures in her poster and did not respond to attempts to contact her.
LOS ANGELES – Vitamin D deficiency was detected in 37% of 497 children and adolescents presenting to a tertiary care center for recurrent headache that required preventive treatment. Vitamin D insufficiency was found in 87%.
These results of routinely measuring baseline serum 25-hydroxyvitamin D (25[OH]D) levels at new patient visits or at follow-up visits suggest that pediatric patients with recurrent headaches may be at increased risk for vitamin D insufficiency or deficiency compared with the general healthy population, Dr. Hope L. O'Brien and her associates reported in a poster presentation at the meeting.
Vitamin D deficiency was defined as a serum 25(OH)D level of less than 20 ng/mL. Vitamin D insufficiency was defined as a level below 30 ng/mL.
Serum 25(OH)D levels averaged 24 ng/mL in patients presenting with episodic migraine and 23 ng/mL in patients presenting with chronic migraine, reported Dr. O'Brien of the University of Cincinnati.
Studies have suggested a link between low vitamin D levels and migraine or chronic tension-type headache in adults, but this may be the first study to assess this association in children and adolescents. Patients in the current study had a mean age of 14 years (range 4–25).
The implications of these findings are unclear, but it's possible that vitamin D supplementation might help improve headaches and overall health, Dr. O'Brien said. Studies in adults have linked low vitamin D levels with medical problems such as heart disease, diabetes, cancer, autoimmune disease, chronic pain, and osteoporosis, with some evidence suggesting poorer outcomes in patients with these problems and low vitamin D levels.
More studies are needed to confirm a relationship between vitamin D levels and headache frequency in children and adolescents and to explore whether vitamin supplementation may improve headache, she said.
Dr. O'Brien did not list any disclosures in her poster and did not respond to attempts to contact her.
LOS ANGELES – Vitamin D deficiency was detected in 37% of 497 children and adolescents presenting to a tertiary care center for recurrent headache that required preventive treatment. Vitamin D insufficiency was found in 87%.
These results of routinely measuring baseline serum 25-hydroxyvitamin D (25[OH]D) levels at new patient visits or at follow-up visits suggest that pediatric patients with recurrent headaches may be at increased risk for vitamin D insufficiency or deficiency compared with the general healthy population, Dr. Hope L. O'Brien and her associates reported in a poster presentation at the meeting.
Vitamin D deficiency was defined as a serum 25(OH)D level of less than 20 ng/mL. Vitamin D insufficiency was defined as a level below 30 ng/mL.
Serum 25(OH)D levels averaged 24 ng/mL in patients presenting with episodic migraine and 23 ng/mL in patients presenting with chronic migraine, reported Dr. O'Brien of the University of Cincinnati.
Studies have suggested a link between low vitamin D levels and migraine or chronic tension-type headache in adults, but this may be the first study to assess this association in children and adolescents. Patients in the current study had a mean age of 14 years (range 4–25).
The implications of these findings are unclear, but it's possible that vitamin D supplementation might help improve headaches and overall health, Dr. O'Brien said. Studies in adults have linked low vitamin D levels with medical problems such as heart disease, diabetes, cancer, autoimmune disease, chronic pain, and osteoporosis, with some evidence suggesting poorer outcomes in patients with these problems and low vitamin D levels.
More studies are needed to confirm a relationship between vitamin D levels and headache frequency in children and adolescents and to explore whether vitamin supplementation may improve headache, she said.
Dr. O'Brien did not list any disclosures in her poster and did not respond to attempts to contact her.
Chronic Headache, Pain Disorders in Girls Linked
LOS ANGELES – Three-fourths of 82 adolescent girls with chronic daily headache also fulfilled diagnostic criteria for fibromyalgia, and other pain-related disorders and comorbidities were common in a screening study.
Although adults with chronic daily headache are known to be at higher risk for pain in other body regions, compared with adults without chronic daily headache, it has not been known whether this phenomenon also applies to adolescents, or to what extent.
Dr. Daniel J. Lacey screened for “central sensitization” pain comorbidities in adolescent girls with chronic daily headache seen in the chronic pain or adolescent headache clinics at a Midwestern children's hospital. He also screened for more commonly recognized comorbidities – anxiety, depression, and sleep disorders – in children with chronic headache, as well as for neck and back pain, orthostatic intolerance, dysmenorrhea, pelvic pain, and joint pain or swelling.
In all, 62 patients (75%) had more than five positive fibromyalgia syndrome tender points, although only 25 of these patients complained of chronic widespread pain (40% of screen-positive patients), he reported in a poster presentation at the meeting In addition, 49 patients (60%) screened positive for irritable bowel disease, and 37 patients (45%) reported at least moderate neck and/or back pain. Most patients complained of significant chronic tiredness, and 12 (15%) screened positive for chronic fatigue syndrome, reported Dr. Lacey of Wright State University in Dayton, Ohio.
Almost the entire cohort had mild orthostatic intolerance, and 16 patients (19%) felt that it was disruptive. Five patients (6%) had postural orthostatic tachycardia syndrome. Although 19 patients (23%) said that anxiety and/or depression were significant issues, mothers of the patients rated these two problems as much more consequential, he said.
Nearly all patients complained of at least moderate levels of nonrestorative sleep. Dysmenorrhea was common. School absences were a significant problem for 25 patients (30%), and many others were being homeschooled or were pursuing online education.
“Clinicians who treat teens with chronic daily headache also need to screen for other pain disorders in addition to other pain comorbidities,” Dr. Lacey stated in the poster. “Those adolescents who have chronic daily headache and irritable bowel syndrome are at highest risk for central sensitization disorders such as fibromyalgia syndrome, chronic fatigue, and disturbed sleep. If these are not recognized and adequately treated, restoration of normal functioning may be limited.”
Cognitive problems were only infrequently seen in this cohort.
Chronic daily headache was the initial manifestation of headache disorder in 19 patients (23%). Most patients had episodic, intense migraines in addition to their usually migrainous chronic daily headache.
Because of the small number of patients and the multiple and different medications being used by patients, Dr. Lacey could not rigorously compare the efficacies of treatments for chronic daily headache in patients with or without pain comorbidities. His experience suggests, however, that medications used primarily for headaches may not be as effective for adolescents who also have comorbid pain disorders.
When amitriptyline monotherapy was used to treat chronic daily headache, the headaches improved similarly in patients with or without other pain comorbidities. When topiramate or valproate monotherapy was used, however, these agents seemed to be less successful at improving headaches in patients with other pain comorbidities, compared with patients who had chronic daily headache alone, said Dr. Lacey, who indicated that he had no conflicts of interest.
LOS ANGELES – Three-fourths of 82 adolescent girls with chronic daily headache also fulfilled diagnostic criteria for fibromyalgia, and other pain-related disorders and comorbidities were common in a screening study.
Although adults with chronic daily headache are known to be at higher risk for pain in other body regions, compared with adults without chronic daily headache, it has not been known whether this phenomenon also applies to adolescents, or to what extent.
Dr. Daniel J. Lacey screened for “central sensitization” pain comorbidities in adolescent girls with chronic daily headache seen in the chronic pain or adolescent headache clinics at a Midwestern children's hospital. He also screened for more commonly recognized comorbidities – anxiety, depression, and sleep disorders – in children with chronic headache, as well as for neck and back pain, orthostatic intolerance, dysmenorrhea, pelvic pain, and joint pain or swelling.
In all, 62 patients (75%) had more than five positive fibromyalgia syndrome tender points, although only 25 of these patients complained of chronic widespread pain (40% of screen-positive patients), he reported in a poster presentation at the meeting In addition, 49 patients (60%) screened positive for irritable bowel disease, and 37 patients (45%) reported at least moderate neck and/or back pain. Most patients complained of significant chronic tiredness, and 12 (15%) screened positive for chronic fatigue syndrome, reported Dr. Lacey of Wright State University in Dayton, Ohio.
Almost the entire cohort had mild orthostatic intolerance, and 16 patients (19%) felt that it was disruptive. Five patients (6%) had postural orthostatic tachycardia syndrome. Although 19 patients (23%) said that anxiety and/or depression were significant issues, mothers of the patients rated these two problems as much more consequential, he said.
Nearly all patients complained of at least moderate levels of nonrestorative sleep. Dysmenorrhea was common. School absences were a significant problem for 25 patients (30%), and many others were being homeschooled or were pursuing online education.
“Clinicians who treat teens with chronic daily headache also need to screen for other pain disorders in addition to other pain comorbidities,” Dr. Lacey stated in the poster. “Those adolescents who have chronic daily headache and irritable bowel syndrome are at highest risk for central sensitization disorders such as fibromyalgia syndrome, chronic fatigue, and disturbed sleep. If these are not recognized and adequately treated, restoration of normal functioning may be limited.”
Cognitive problems were only infrequently seen in this cohort.
Chronic daily headache was the initial manifestation of headache disorder in 19 patients (23%). Most patients had episodic, intense migraines in addition to their usually migrainous chronic daily headache.
Because of the small number of patients and the multiple and different medications being used by patients, Dr. Lacey could not rigorously compare the efficacies of treatments for chronic daily headache in patients with or without pain comorbidities. His experience suggests, however, that medications used primarily for headaches may not be as effective for adolescents who also have comorbid pain disorders.
When amitriptyline monotherapy was used to treat chronic daily headache, the headaches improved similarly in patients with or without other pain comorbidities. When topiramate or valproate monotherapy was used, however, these agents seemed to be less successful at improving headaches in patients with other pain comorbidities, compared with patients who had chronic daily headache alone, said Dr. Lacey, who indicated that he had no conflicts of interest.
LOS ANGELES – Three-fourths of 82 adolescent girls with chronic daily headache also fulfilled diagnostic criteria for fibromyalgia, and other pain-related disorders and comorbidities were common in a screening study.
Although adults with chronic daily headache are known to be at higher risk for pain in other body regions, compared with adults without chronic daily headache, it has not been known whether this phenomenon also applies to adolescents, or to what extent.
Dr. Daniel J. Lacey screened for “central sensitization” pain comorbidities in adolescent girls with chronic daily headache seen in the chronic pain or adolescent headache clinics at a Midwestern children's hospital. He also screened for more commonly recognized comorbidities – anxiety, depression, and sleep disorders – in children with chronic headache, as well as for neck and back pain, orthostatic intolerance, dysmenorrhea, pelvic pain, and joint pain or swelling.
In all, 62 patients (75%) had more than five positive fibromyalgia syndrome tender points, although only 25 of these patients complained of chronic widespread pain (40% of screen-positive patients), he reported in a poster presentation at the meeting In addition, 49 patients (60%) screened positive for irritable bowel disease, and 37 patients (45%) reported at least moderate neck and/or back pain. Most patients complained of significant chronic tiredness, and 12 (15%) screened positive for chronic fatigue syndrome, reported Dr. Lacey of Wright State University in Dayton, Ohio.
Almost the entire cohort had mild orthostatic intolerance, and 16 patients (19%) felt that it was disruptive. Five patients (6%) had postural orthostatic tachycardia syndrome. Although 19 patients (23%) said that anxiety and/or depression were significant issues, mothers of the patients rated these two problems as much more consequential, he said.
Nearly all patients complained of at least moderate levels of nonrestorative sleep. Dysmenorrhea was common. School absences were a significant problem for 25 patients (30%), and many others were being homeschooled or were pursuing online education.
“Clinicians who treat teens with chronic daily headache also need to screen for other pain disorders in addition to other pain comorbidities,” Dr. Lacey stated in the poster. “Those adolescents who have chronic daily headache and irritable bowel syndrome are at highest risk for central sensitization disorders such as fibromyalgia syndrome, chronic fatigue, and disturbed sleep. If these are not recognized and adequately treated, restoration of normal functioning may be limited.”
Cognitive problems were only infrequently seen in this cohort.
Chronic daily headache was the initial manifestation of headache disorder in 19 patients (23%). Most patients had episodic, intense migraines in addition to their usually migrainous chronic daily headache.
Because of the small number of patients and the multiple and different medications being used by patients, Dr. Lacey could not rigorously compare the efficacies of treatments for chronic daily headache in patients with or without pain comorbidities. His experience suggests, however, that medications used primarily for headaches may not be as effective for adolescents who also have comorbid pain disorders.
When amitriptyline monotherapy was used to treat chronic daily headache, the headaches improved similarly in patients with or without other pain comorbidities. When topiramate or valproate monotherapy was used, however, these agents seemed to be less successful at improving headaches in patients with other pain comorbidities, compared with patients who had chronic daily headache alone, said Dr. Lacey, who indicated that he had no conflicts of interest.
Nursing Home Residents Who Reject Care Require Screening
LONG BEACH, CALIF. – Rejection of care by nursing home residents was associated with four potentially modifiable factors in an analysis of data on 3,230 residents.
Clinicians should screen for the conditions – delusion, delirium, minor or major depression, and severe or worse pain – when residents reject care such as taking medications and accepting assistance with activities of daily living, Dr. Shinya Ishii and associates reported in the top prize–winning poster presentation at the meeting.
If the associations observed in the study are causal, appropriate interventions may improve residents' willingness to accept care, the researchers suggested. The team analyzed data on residents scheduled for Minimum Data Set assessments in 71 nursing homes in eight states. Nurses identified residents who were rejecting care.
The likelihood of doing so increased fourfold in the presence of delusion and doubled in the presence of delirium, depression, or severe-to-horrible pain, reported Dr. Ishii of the Department of Veterans Affairs' geriatric research education and clinical center, Los Angeles.
Among the 312 residents who exhibited rejection-of-care behaviors, 18% had delusions, 35% had delirium, 32% had minor depression, 15% had major depression, and 30% had severe to “horrible” pain. Some symptoms overlapped. An attributable-risk analysis suggested that 19% of care-rejecting behavior could be eliminated if delusions were stopped and that 5% of care rejection might end if delirium were reversed.
Treating minor depression might eliminate 7% of care-rejecting behavior, reversing major depression might eliminate 10% of care-rejecting behavior, and ending severe or worse pain might eliminate 5% of care-rejecting behavior, Dr. Ishii reported.
Several covariates also were associated with rejection of care, including being male and having moderate or severe cognitive impairment.
Factors that were not associated with rejection of care included hallucination, mild to moderate pain, hearing and vision impairment, and infections (including urinary tract infection, pneumonia, wound infection, HIV, tuberculosis, and viral hepatitis).
The large, geographically diverse sample of residents strengthened the findings of the study, but its cross-sectional design did not allow examination of temporal sequences.
Also, the lack of any significant association between care rejection and infection might be attributable to different time frames for reporting infection, compared with those governing the other variables.
The investigators reported having no disclosures.
LONG BEACH, CALIF. – Rejection of care by nursing home residents was associated with four potentially modifiable factors in an analysis of data on 3,230 residents.
Clinicians should screen for the conditions – delusion, delirium, minor or major depression, and severe or worse pain – when residents reject care such as taking medications and accepting assistance with activities of daily living, Dr. Shinya Ishii and associates reported in the top prize–winning poster presentation at the meeting.
If the associations observed in the study are causal, appropriate interventions may improve residents' willingness to accept care, the researchers suggested. The team analyzed data on residents scheduled for Minimum Data Set assessments in 71 nursing homes in eight states. Nurses identified residents who were rejecting care.
The likelihood of doing so increased fourfold in the presence of delusion and doubled in the presence of delirium, depression, or severe-to-horrible pain, reported Dr. Ishii of the Department of Veterans Affairs' geriatric research education and clinical center, Los Angeles.
Among the 312 residents who exhibited rejection-of-care behaviors, 18% had delusions, 35% had delirium, 32% had minor depression, 15% had major depression, and 30% had severe to “horrible” pain. Some symptoms overlapped. An attributable-risk analysis suggested that 19% of care-rejecting behavior could be eliminated if delusions were stopped and that 5% of care rejection might end if delirium were reversed.
Treating minor depression might eliminate 7% of care-rejecting behavior, reversing major depression might eliminate 10% of care-rejecting behavior, and ending severe or worse pain might eliminate 5% of care-rejecting behavior, Dr. Ishii reported.
Several covariates also were associated with rejection of care, including being male and having moderate or severe cognitive impairment.
Factors that were not associated with rejection of care included hallucination, mild to moderate pain, hearing and vision impairment, and infections (including urinary tract infection, pneumonia, wound infection, HIV, tuberculosis, and viral hepatitis).
The large, geographically diverse sample of residents strengthened the findings of the study, but its cross-sectional design did not allow examination of temporal sequences.
Also, the lack of any significant association between care rejection and infection might be attributable to different time frames for reporting infection, compared with those governing the other variables.
The investigators reported having no disclosures.
LONG BEACH, CALIF. – Rejection of care by nursing home residents was associated with four potentially modifiable factors in an analysis of data on 3,230 residents.
Clinicians should screen for the conditions – delusion, delirium, minor or major depression, and severe or worse pain – when residents reject care such as taking medications and accepting assistance with activities of daily living, Dr. Shinya Ishii and associates reported in the top prize–winning poster presentation at the meeting.
If the associations observed in the study are causal, appropriate interventions may improve residents' willingness to accept care, the researchers suggested. The team analyzed data on residents scheduled for Minimum Data Set assessments in 71 nursing homes in eight states. Nurses identified residents who were rejecting care.
The likelihood of doing so increased fourfold in the presence of delusion and doubled in the presence of delirium, depression, or severe-to-horrible pain, reported Dr. Ishii of the Department of Veterans Affairs' geriatric research education and clinical center, Los Angeles.
Among the 312 residents who exhibited rejection-of-care behaviors, 18% had delusions, 35% had delirium, 32% had minor depression, 15% had major depression, and 30% had severe to “horrible” pain. Some symptoms overlapped. An attributable-risk analysis suggested that 19% of care-rejecting behavior could be eliminated if delusions were stopped and that 5% of care rejection might end if delirium were reversed.
Treating minor depression might eliminate 7% of care-rejecting behavior, reversing major depression might eliminate 10% of care-rejecting behavior, and ending severe or worse pain might eliminate 5% of care-rejecting behavior, Dr. Ishii reported.
Several covariates also were associated with rejection of care, including being male and having moderate or severe cognitive impairment.
Factors that were not associated with rejection of care included hallucination, mild to moderate pain, hearing and vision impairment, and infections (including urinary tract infection, pneumonia, wound infection, HIV, tuberculosis, and viral hepatitis).
The large, geographically diverse sample of residents strengthened the findings of the study, but its cross-sectional design did not allow examination of temporal sequences.
Also, the lack of any significant association between care rejection and infection might be attributable to different time frames for reporting infection, compared with those governing the other variables.
The investigators reported having no disclosures.
FROM THE ANNUAL SYMPOSIUM OF THE AMERICAN MEDICAL DIRECTORS ASSOCIATION
Address Adherence at Initial Visit for Acne
SAN FRANCISCO – For best outcomes in acne patients, address specific factors that affect the likelihood of adherence for an individual and incorporate that information into the larger treatment plan, advises Dr. Christina Kim, a dermatologist at the University of California, Los Angeles.
"On the initial visit, it’s worthwhile to spend a little bit of extra time on thinking about patient adherence." In medicine as a whole, 20%-50% of patients do not take medications as directed. "That number is probably much higher in dermatology, as topical therapies are notorious for their lack of adherence or compliance," Dr. Kim said at the annual meeting of the Pacific Dermatologic Association.
To assist adherence, consider cost, patient preferences, and convenience. Choose medications that the patient can afford. "Once-daily formulations are more user friendly. If there’s an inconvenience aspect to a therapy – like having to take a [product] out of the refrigerator when it’s time for application – the likelihood of adherence decreases."
Patients expect to get better fast – usually within 4-6 weeks – so it’s important to explain that acne is a chronic disease, and to describe the time frame for treatment response.
"Usually I tell my patients that my strategy is to improve their acne in the next couple of months with pills. Then they will be on creams for many months after that, to keep their skin clear. Their acne will not go away for several years, and only time will tell when it will resolve," Dr. Kim said.
If you don’t manage patient expectations, they will move on to another physician when the acne doesn’t improve as quickly as they want.
"If patients feel they’re getting better, they’re much more likely to continue treatment. Studies show if a patient is pleased with the physician, if they know that you care, that you are working to improve their disease, they’re also more likely to use the treatment that you recommend," she said.
Discuss with patients not only how to apply their acne medication, but what to do and not do in their non-acne skin care, she added. "If they’re using everything under the sun that’s over the counter, their skin is going to get irritated, they’re not going to continue with their treatment, and adherence will go down."
Schedule the first follow-up visit soon after the initial visit, she advised. "Even though you don’t expect your therapeutics to take effect sometimes for several months, it’s worthwhile to see your patient back in 4-6 weeks to see if they are using the products, to see if there are any side effects or any barriers to their use."
At each visit, ask about adherence, using open-ended, nonjudgmental questions that help establish trust and confidence in your patient. "I usually ask, `How did you find the treatment? Have you been able to do it? Do you find it bothersome? What about the treatment do you not like? What about the treatment do you like?’" Dr. Kim said. "It seems obvious, but I think it’s something we don’t always do. It turns out that when you ask, either verbally or in questionnaires, patients will be very open with you."
You may discover, for example, that the patient used the samples you provided, but hated the product and didn’t buy any more. "That’s why their skin didn’t get better. They weren’t using the treatment," she said.
Dr. Kim said she had no financial conflicts of interest.
SAN FRANCISCO – For best outcomes in acne patients, address specific factors that affect the likelihood of adherence for an individual and incorporate that information into the larger treatment plan, advises Dr. Christina Kim, a dermatologist at the University of California, Los Angeles.
"On the initial visit, it’s worthwhile to spend a little bit of extra time on thinking about patient adherence." In medicine as a whole, 20%-50% of patients do not take medications as directed. "That number is probably much higher in dermatology, as topical therapies are notorious for their lack of adherence or compliance," Dr. Kim said at the annual meeting of the Pacific Dermatologic Association.
To assist adherence, consider cost, patient preferences, and convenience. Choose medications that the patient can afford. "Once-daily formulations are more user friendly. If there’s an inconvenience aspect to a therapy – like having to take a [product] out of the refrigerator when it’s time for application – the likelihood of adherence decreases."
Patients expect to get better fast – usually within 4-6 weeks – so it’s important to explain that acne is a chronic disease, and to describe the time frame for treatment response.
"Usually I tell my patients that my strategy is to improve their acne in the next couple of months with pills. Then they will be on creams for many months after that, to keep their skin clear. Their acne will not go away for several years, and only time will tell when it will resolve," Dr. Kim said.
If you don’t manage patient expectations, they will move on to another physician when the acne doesn’t improve as quickly as they want.
"If patients feel they’re getting better, they’re much more likely to continue treatment. Studies show if a patient is pleased with the physician, if they know that you care, that you are working to improve their disease, they’re also more likely to use the treatment that you recommend," she said.
Discuss with patients not only how to apply their acne medication, but what to do and not do in their non-acne skin care, she added. "If they’re using everything under the sun that’s over the counter, their skin is going to get irritated, they’re not going to continue with their treatment, and adherence will go down."
Schedule the first follow-up visit soon after the initial visit, she advised. "Even though you don’t expect your therapeutics to take effect sometimes for several months, it’s worthwhile to see your patient back in 4-6 weeks to see if they are using the products, to see if there are any side effects or any barriers to their use."
At each visit, ask about adherence, using open-ended, nonjudgmental questions that help establish trust and confidence in your patient. "I usually ask, `How did you find the treatment? Have you been able to do it? Do you find it bothersome? What about the treatment do you not like? What about the treatment do you like?’" Dr. Kim said. "It seems obvious, but I think it’s something we don’t always do. It turns out that when you ask, either verbally or in questionnaires, patients will be very open with you."
You may discover, for example, that the patient used the samples you provided, but hated the product and didn’t buy any more. "That’s why their skin didn’t get better. They weren’t using the treatment," she said.
Dr. Kim said she had no financial conflicts of interest.
SAN FRANCISCO – For best outcomes in acne patients, address specific factors that affect the likelihood of adherence for an individual and incorporate that information into the larger treatment plan, advises Dr. Christina Kim, a dermatologist at the University of California, Los Angeles.
"On the initial visit, it’s worthwhile to spend a little bit of extra time on thinking about patient adherence." In medicine as a whole, 20%-50% of patients do not take medications as directed. "That number is probably much higher in dermatology, as topical therapies are notorious for their lack of adherence or compliance," Dr. Kim said at the annual meeting of the Pacific Dermatologic Association.
To assist adherence, consider cost, patient preferences, and convenience. Choose medications that the patient can afford. "Once-daily formulations are more user friendly. If there’s an inconvenience aspect to a therapy – like having to take a [product] out of the refrigerator when it’s time for application – the likelihood of adherence decreases."
Patients expect to get better fast – usually within 4-6 weeks – so it’s important to explain that acne is a chronic disease, and to describe the time frame for treatment response.
"Usually I tell my patients that my strategy is to improve their acne in the next couple of months with pills. Then they will be on creams for many months after that, to keep their skin clear. Their acne will not go away for several years, and only time will tell when it will resolve," Dr. Kim said.
If you don’t manage patient expectations, they will move on to another physician when the acne doesn’t improve as quickly as they want.
"If patients feel they’re getting better, they’re much more likely to continue treatment. Studies show if a patient is pleased with the physician, if they know that you care, that you are working to improve their disease, they’re also more likely to use the treatment that you recommend," she said.
Discuss with patients not only how to apply their acne medication, but what to do and not do in their non-acne skin care, she added. "If they’re using everything under the sun that’s over the counter, their skin is going to get irritated, they’re not going to continue with their treatment, and adherence will go down."
Schedule the first follow-up visit soon after the initial visit, she advised. "Even though you don’t expect your therapeutics to take effect sometimes for several months, it’s worthwhile to see your patient back in 4-6 weeks to see if they are using the products, to see if there are any side effects or any barriers to their use."
At each visit, ask about adherence, using open-ended, nonjudgmental questions that help establish trust and confidence in your patient. "I usually ask, `How did you find the treatment? Have you been able to do it? Do you find it bothersome? What about the treatment do you not like? What about the treatment do you like?’" Dr. Kim said. "It seems obvious, but I think it’s something we don’t always do. It turns out that when you ask, either verbally or in questionnaires, patients will be very open with you."
You may discover, for example, that the patient used the samples you provided, but hated the product and didn’t buy any more. "That’s why their skin didn’t get better. They weren’t using the treatment," she said.
Dr. Kim said she had no financial conflicts of interest.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE PACIFIC DERMATOLOGIC ASSOCIATION
Children Help Themselves by Helping Others
SAN FRANCISCO – Look around at the next black-tie fundraiser for your hospital. See any children?
Dr. Ronald Marino, director of general pediatrics at Winthrop-University Hospital, Mineola, N.Y., saw only adults at hospital benefit events. He realized that involving children in supporting his department could be a win-win-win for the participants, the patients, and the community.
He picked one of his passions – swimming – as a focus for a new event and launched an annual swim-a-thon that has raised more than $120,000 over the past 9 years. The funds benefit the hospital’s Child Life Program, which gives pediatric patients the opportunity to talk at length with hospital physicians and staff about the tests and procedures they’re facing in an effort to dispel some of their fears.
The money is a small part of the benefits produced by the swim-a-thon, he said.
The children who help organize and participate in the event learn ways to become involved in their community. They gain leadership and planning skills, get public speaking experience as they promote the event, and learn about health care careers from their adult co-organizers. In addition, the children design the event logo and are involved in creating publicity materials, gaining practical experience. Dr. Marino said he has seen boosts to the children’s pride and self-esteem, and the focus on swimming promotes their health and well-being.
A month or so after the day of swimming, an awards celebration for all who were involved features public recognition for participants, food, music, and a clown or superhero entertainer, followed by a tour of the hospital and its pediatric services.
"Kids really love seeing what nurseries look like, what the pediatric wards look like. They love seeing where their money goes," Dr. Marino said.
The event also has inspired some of the hospital’s doctors, nurses, and staff to support children’s health and development outside of the clinical setting. One of the nurse participants this year decided to mentor a child with Down syndrome separately from the swim-a-thon, to teach the child how to swim.
Swimming itself is a great equalizer, Dr. Marino added. Some children with disabilities that severely limit their motion on land become more graceful in the pool. "So often in our society we’re separated from people with disabilities," he noted.
Plus, because the usual signs of socioeconomic status are left in the locker room when swimmers shed their clothing for swimsuits, "it demonstrates that we’re all the same," Dr. Marino said. In addition to getting 95 swimmers to take part this year, targeted outreach to the community has drawn people of all ages and races to participate in many different roles.
The swim-a-thon has attracted community support from corporations, lifeguards, swim coaches, bands that play during the event, raffle donors, the medical school’s pediatrics club, and many volunteers who contribute in their own ways. One teenager who didn’t swim made a slideshow to promote the swim-a-thon. Another nonswimmer started his own nonprofit organization to auction off sports memorabilia and donate the proceeds to charity, including the hospital.
Swimmers are grouped in four categories by age, ranging from 4 years to more than 60 years of age. The minimal expenses of the event – for towels, pool rental, and some promotion – keep overhead low. Swimmers pay a small fee varying by age (from $3 to $10).
Physicians who want to start a similar event in their community should pick one of their own passions as a focus, Dr. Marino advised: "For me, it was children, swimming, and community service. I put them all together." Try to make it a grassroots effort. Cast a wide net for organizers and participants, and build relationships in the process, he said. Start small, and be patient. "You’ll find that it just takes off on its own once it gets going."
Events like the swim-a-thon help realize several aspects of the five key promises that our society should give to its children, Dr. Marino said – caring adults, safe places, a healthy start, an effective education, and opportunities to help others.
"Empowering kids strengthens our communities and ensures a brighter future," he said.
Dr. Marino said he had no pertinent conflicts of interest.
SAN FRANCISCO – Look around at the next black-tie fundraiser for your hospital. See any children?
Dr. Ronald Marino, director of general pediatrics at Winthrop-University Hospital, Mineola, N.Y., saw only adults at hospital benefit events. He realized that involving children in supporting his department could be a win-win-win for the participants, the patients, and the community.
He picked one of his passions – swimming – as a focus for a new event and launched an annual swim-a-thon that has raised more than $120,000 over the past 9 years. The funds benefit the hospital’s Child Life Program, which gives pediatric patients the opportunity to talk at length with hospital physicians and staff about the tests and procedures they’re facing in an effort to dispel some of their fears.
The money is a small part of the benefits produced by the swim-a-thon, he said.
The children who help organize and participate in the event learn ways to become involved in their community. They gain leadership and planning skills, get public speaking experience as they promote the event, and learn about health care careers from their adult co-organizers. In addition, the children design the event logo and are involved in creating publicity materials, gaining practical experience. Dr. Marino said he has seen boosts to the children’s pride and self-esteem, and the focus on swimming promotes their health and well-being.
A month or so after the day of swimming, an awards celebration for all who were involved features public recognition for participants, food, music, and a clown or superhero entertainer, followed by a tour of the hospital and its pediatric services.
"Kids really love seeing what nurseries look like, what the pediatric wards look like. They love seeing where their money goes," Dr. Marino said.
The event also has inspired some of the hospital’s doctors, nurses, and staff to support children’s health and development outside of the clinical setting. One of the nurse participants this year decided to mentor a child with Down syndrome separately from the swim-a-thon, to teach the child how to swim.
Swimming itself is a great equalizer, Dr. Marino added. Some children with disabilities that severely limit their motion on land become more graceful in the pool. "So often in our society we’re separated from people with disabilities," he noted.
Plus, because the usual signs of socioeconomic status are left in the locker room when swimmers shed their clothing for swimsuits, "it demonstrates that we’re all the same," Dr. Marino said. In addition to getting 95 swimmers to take part this year, targeted outreach to the community has drawn people of all ages and races to participate in many different roles.
The swim-a-thon has attracted community support from corporations, lifeguards, swim coaches, bands that play during the event, raffle donors, the medical school’s pediatrics club, and many volunteers who contribute in their own ways. One teenager who didn’t swim made a slideshow to promote the swim-a-thon. Another nonswimmer started his own nonprofit organization to auction off sports memorabilia and donate the proceeds to charity, including the hospital.
Swimmers are grouped in four categories by age, ranging from 4 years to more than 60 years of age. The minimal expenses of the event – for towels, pool rental, and some promotion – keep overhead low. Swimmers pay a small fee varying by age (from $3 to $10).
Physicians who want to start a similar event in their community should pick one of their own passions as a focus, Dr. Marino advised: "For me, it was children, swimming, and community service. I put them all together." Try to make it a grassroots effort. Cast a wide net for organizers and participants, and build relationships in the process, he said. Start small, and be patient. "You’ll find that it just takes off on its own once it gets going."
Events like the swim-a-thon help realize several aspects of the five key promises that our society should give to its children, Dr. Marino said – caring adults, safe places, a healthy start, an effective education, and opportunities to help others.
"Empowering kids strengthens our communities and ensures a brighter future," he said.
Dr. Marino said he had no pertinent conflicts of interest.
SAN FRANCISCO – Look around at the next black-tie fundraiser for your hospital. See any children?
Dr. Ronald Marino, director of general pediatrics at Winthrop-University Hospital, Mineola, N.Y., saw only adults at hospital benefit events. He realized that involving children in supporting his department could be a win-win-win for the participants, the patients, and the community.
He picked one of his passions – swimming – as a focus for a new event and launched an annual swim-a-thon that has raised more than $120,000 over the past 9 years. The funds benefit the hospital’s Child Life Program, which gives pediatric patients the opportunity to talk at length with hospital physicians and staff about the tests and procedures they’re facing in an effort to dispel some of their fears.
The money is a small part of the benefits produced by the swim-a-thon, he said.
The children who help organize and participate in the event learn ways to become involved in their community. They gain leadership and planning skills, get public speaking experience as they promote the event, and learn about health care careers from their adult co-organizers. In addition, the children design the event logo and are involved in creating publicity materials, gaining practical experience. Dr. Marino said he has seen boosts to the children’s pride and self-esteem, and the focus on swimming promotes their health and well-being.
A month or so after the day of swimming, an awards celebration for all who were involved features public recognition for participants, food, music, and a clown or superhero entertainer, followed by a tour of the hospital and its pediatric services.
"Kids really love seeing what nurseries look like, what the pediatric wards look like. They love seeing where their money goes," Dr. Marino said.
The event also has inspired some of the hospital’s doctors, nurses, and staff to support children’s health and development outside of the clinical setting. One of the nurse participants this year decided to mentor a child with Down syndrome separately from the swim-a-thon, to teach the child how to swim.
Swimming itself is a great equalizer, Dr. Marino added. Some children with disabilities that severely limit their motion on land become more graceful in the pool. "So often in our society we’re separated from people with disabilities," he noted.
Plus, because the usual signs of socioeconomic status are left in the locker room when swimmers shed their clothing for swimsuits, "it demonstrates that we’re all the same," Dr. Marino said. In addition to getting 95 swimmers to take part this year, targeted outreach to the community has drawn people of all ages and races to participate in many different roles.
The swim-a-thon has attracted community support from corporations, lifeguards, swim coaches, bands that play during the event, raffle donors, the medical school’s pediatrics club, and many volunteers who contribute in their own ways. One teenager who didn’t swim made a slideshow to promote the swim-a-thon. Another nonswimmer started his own nonprofit organization to auction off sports memorabilia and donate the proceeds to charity, including the hospital.
Swimmers are grouped in four categories by age, ranging from 4 years to more than 60 years of age. The minimal expenses of the event – for towels, pool rental, and some promotion – keep overhead low. Swimmers pay a small fee varying by age (from $3 to $10).
Physicians who want to start a similar event in their community should pick one of their own passions as a focus, Dr. Marino advised: "For me, it was children, swimming, and community service. I put them all together." Try to make it a grassroots effort. Cast a wide net for organizers and participants, and build relationships in the process, he said. Start small, and be patient. "You’ll find that it just takes off on its own once it gets going."
Events like the swim-a-thon help realize several aspects of the five key promises that our society should give to its children, Dr. Marino said – caring adults, safe places, a healthy start, an effective education, and opportunities to help others.
"Empowering kids strengthens our communities and ensures a brighter future," he said.
Dr. Marino said he had no pertinent conflicts of interest.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF PEDIATRICS
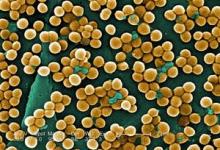
Daily Antiretroviral Prophylaxis Reduced Risk of HIV Infection
Taking a daily pill containing two antiretroviral drugs plus exposure to conventional HIV prevention strategies reduced the risk of acquiring HIV by an average of 44% in the people at highest risk of getting infected – men and transgender women who have sex with men, based on a study published online Nov. 23 in the New England Journal of Medicine.
The Preexposure Prophylaxis Initiative (iPrEx) study randomized 2,499 subjects in six countries to take a daily pill containing placebo or a combination of emtricitabine and tenofovir disoproxil fumarate (FTC-TDF). All subjects also received regular HIV testing, condoms, counseling on reducing risks for HIV, and management of sexually transmitted infections (N. Engl. J. Med. 2010 Nov. 23 [doi:10.1056/NEJMoa1011205]).
During a median follow-up of 1.2 years (and a maximum of 2.8 years), 36 of 1,251 subjects in the FTC-TDF group (3%) acquired HIV, compared with 64 of 1,248 subjects in the placebo group (5%). The preventive efficacy of FTC-TDF was significant but not as high as investigators had hoped, Dr. Robert M. Grant of the University of California, San Francisco, and his associates reported.
Although most subjects reported taking the pills, objective measures of exposure to the drugs suggested substantially lower adherence rates. When intracellular assays showed that subjects had been exposed to FTC-TDF, they were much less likely to acquire HIV. Evidence of FTC-TDF was seen in only 3 of 34 HIV-infected subjects (9%), compared with 22 of 43 HIV-negative subjects (51%) in the FTC-TDF group.
"It’s very exciting news," Dr. Moupali Das said in an interview. "These are extremely promising results," said Dr. Das of the University of California, San Francisco, and director of research in the HIV prevention section of the San Francisco Department of Public Health. She was not involved in the iPrEx study.
The findings are consistent with results from a separate preexposure prophylaxis trial reported earlier in 2010 showing an overall 39% reduction in HIV infections in women who agreed to apply a 1% tenofovir gel vaginally before and after sex, she noted. The randomized, double-blind placebo-controlled Centre for the AIDS Programme of Research in South Africa (CAPRISA) 004 trial studied 889 sexually active African women (Science 2010;329:1168-74).
The iPrEx study enrolled subjects at multiple centers in the United States, South Africa, Brazil, Ecuador, Peru, and Thailand.
Patients in the FTC-TDF group were significantly more likely to develop nausea (2%) in the first 4 weeks of treatment, compared with the placebo group (less than 1%).
"It’s a groundbreaking study," but several factors will temper excitement among clinicians, said Dr. Grant Colfax, director of HIV prevention for the San Francisco Department of Public Health. He was not involved in the iPrEx study.
The FTC-TDF pill is expensive, costing $750 per month or more in the United States, he noted in an interview. Subjects in the study got comprehensive care with monthly HIV testing, state-of-the-art prevention counseling, free condoms and more, which might not be representative of the real world.
"This was not just giving someone a pill and walking out of the office," Dr. Colfax said.
Two subjects in the FTC-TDF group who later were found to have had HIV at enrollment both developed resistance to FTC, compared with one of eight subjects on placebo with HIV at enrollment. People at risk for HIV should not start taking FTC-TDF without reviewing the risks and benefits with their physician, Dr. Colfax said.
The study does not answer questions about the advisability of implementing this prevention strategy in all or even most HIV-negative people at risk for acquiring the infection, Dr. Das agreed. "It will be important to see the results of the upcoming trials on different ways to provide preexposure prophylaxis," results of which should be available in the near future, she said. The Web site of the nonprofit group AVAC: Global Advocacy for HIV Prevention provides a timeline of expected efficacy trial results.
In the meantime, there might be some specific populations in whom preexposure prophylaxis with FTC-TDF makes sense while research continues, she added. Some clinicians already offer preexposure prophylaxis to HIV-negative people whose sexual partners have HIV or to serodiscordant couples who can’t use other modes of preventing infection.
Further research might identify ways to reduce the frequency and expense of preexposure prophylaxis, Dr. Das suggested, such as perhaps taking FTC-TDF only during high-risk periods of life, similar to the way women use contraceptives mainly during the sexually active years.
The main obstacle for most people will be cost, especially for the low-income or indigent patients Dr. Das sees in her practice. "I could write a prescription, but I don’t know how they would be able to pay for it," she said. Still, FTC-TDF is "another potential tool in our prevention toolkit."
The rate of HIV infection has been climbing since the early 1990s in U.S. men and transgender women who have sex with men, especially in black and Hispanic populations, the investigators in the iPrEx study noted. In almost all countries, the prevalence of HIV is higher among men and transgender women who have sex with men, compared with other groups.
The U.S. National Institutes of Health and the Bill and Melinda Gates Foundation funded the study. Gilead Sciences donated the FTC-TDF and placebo tablets, and provided some travel funding for investigators. Two of the investigators worked for Gilead. Disclosures for all the investigators are posted with the article. Dr. Das and Dr. Colfax said they have no relevant conflicts of interest.
Taking a daily pill containing two antiretroviral drugs plus exposure to conventional HIV prevention strategies reduced the risk of acquiring HIV by an average of 44% in the people at highest risk of getting infected – men and transgender women who have sex with men, based on a study published online Nov. 23 in the New England Journal of Medicine.
The Preexposure Prophylaxis Initiative (iPrEx) study randomized 2,499 subjects in six countries to take a daily pill containing placebo or a combination of emtricitabine and tenofovir disoproxil fumarate (FTC-TDF). All subjects also received regular HIV testing, condoms, counseling on reducing risks for HIV, and management of sexually transmitted infections (N. Engl. J. Med. 2010 Nov. 23 [doi:10.1056/NEJMoa1011205]).
During a median follow-up of 1.2 years (and a maximum of 2.8 years), 36 of 1,251 subjects in the FTC-TDF group (3%) acquired HIV, compared with 64 of 1,248 subjects in the placebo group (5%). The preventive efficacy of FTC-TDF was significant but not as high as investigators had hoped, Dr. Robert M. Grant of the University of California, San Francisco, and his associates reported.
Although most subjects reported taking the pills, objective measures of exposure to the drugs suggested substantially lower adherence rates. When intracellular assays showed that subjects had been exposed to FTC-TDF, they were much less likely to acquire HIV. Evidence of FTC-TDF was seen in only 3 of 34 HIV-infected subjects (9%), compared with 22 of 43 HIV-negative subjects (51%) in the FTC-TDF group.
"It’s very exciting news," Dr. Moupali Das said in an interview. "These are extremely promising results," said Dr. Das of the University of California, San Francisco, and director of research in the HIV prevention section of the San Francisco Department of Public Health. She was not involved in the iPrEx study.
The findings are consistent with results from a separate preexposure prophylaxis trial reported earlier in 2010 showing an overall 39% reduction in HIV infections in women who agreed to apply a 1% tenofovir gel vaginally before and after sex, she noted. The randomized, double-blind placebo-controlled Centre for the AIDS Programme of Research in South Africa (CAPRISA) 004 trial studied 889 sexually active African women (Science 2010;329:1168-74).
The iPrEx study enrolled subjects at multiple centers in the United States, South Africa, Brazil, Ecuador, Peru, and Thailand.
Patients in the FTC-TDF group were significantly more likely to develop nausea (2%) in the first 4 weeks of treatment, compared with the placebo group (less than 1%).
"It’s a groundbreaking study," but several factors will temper excitement among clinicians, said Dr. Grant Colfax, director of HIV prevention for the San Francisco Department of Public Health. He was not involved in the iPrEx study.
The FTC-TDF pill is expensive, costing $750 per month or more in the United States, he noted in an interview. Subjects in the study got comprehensive care with monthly HIV testing, state-of-the-art prevention counseling, free condoms and more, which might not be representative of the real world.
"This was not just giving someone a pill and walking out of the office," Dr. Colfax said.
Two subjects in the FTC-TDF group who later were found to have had HIV at enrollment both developed resistance to FTC, compared with one of eight subjects on placebo with HIV at enrollment. People at risk for HIV should not start taking FTC-TDF without reviewing the risks and benefits with their physician, Dr. Colfax said.
The study does not answer questions about the advisability of implementing this prevention strategy in all or even most HIV-negative people at risk for acquiring the infection, Dr. Das agreed. "It will be important to see the results of the upcoming trials on different ways to provide preexposure prophylaxis," results of which should be available in the near future, she said. The Web site of the nonprofit group AVAC: Global Advocacy for HIV Prevention provides a timeline of expected efficacy trial results.
In the meantime, there might be some specific populations in whom preexposure prophylaxis with FTC-TDF makes sense while research continues, she added. Some clinicians already offer preexposure prophylaxis to HIV-negative people whose sexual partners have HIV or to serodiscordant couples who can’t use other modes of preventing infection.
Further research might identify ways to reduce the frequency and expense of preexposure prophylaxis, Dr. Das suggested, such as perhaps taking FTC-TDF only during high-risk periods of life, similar to the way women use contraceptives mainly during the sexually active years.
The main obstacle for most people will be cost, especially for the low-income or indigent patients Dr. Das sees in her practice. "I could write a prescription, but I don’t know how they would be able to pay for it," she said. Still, FTC-TDF is "another potential tool in our prevention toolkit."
The rate of HIV infection has been climbing since the early 1990s in U.S. men and transgender women who have sex with men, especially in black and Hispanic populations, the investigators in the iPrEx study noted. In almost all countries, the prevalence of HIV is higher among men and transgender women who have sex with men, compared with other groups.
The U.S. National Institutes of Health and the Bill and Melinda Gates Foundation funded the study. Gilead Sciences donated the FTC-TDF and placebo tablets, and provided some travel funding for investigators. Two of the investigators worked for Gilead. Disclosures for all the investigators are posted with the article. Dr. Das and Dr. Colfax said they have no relevant conflicts of interest.
Taking a daily pill containing two antiretroviral drugs plus exposure to conventional HIV prevention strategies reduced the risk of acquiring HIV by an average of 44% in the people at highest risk of getting infected – men and transgender women who have sex with men, based on a study published online Nov. 23 in the New England Journal of Medicine.
The Preexposure Prophylaxis Initiative (iPrEx) study randomized 2,499 subjects in six countries to take a daily pill containing placebo or a combination of emtricitabine and tenofovir disoproxil fumarate (FTC-TDF). All subjects also received regular HIV testing, condoms, counseling on reducing risks for HIV, and management of sexually transmitted infections (N. Engl. J. Med. 2010 Nov. 23 [doi:10.1056/NEJMoa1011205]).
During a median follow-up of 1.2 years (and a maximum of 2.8 years), 36 of 1,251 subjects in the FTC-TDF group (3%) acquired HIV, compared with 64 of 1,248 subjects in the placebo group (5%). The preventive efficacy of FTC-TDF was significant but not as high as investigators had hoped, Dr. Robert M. Grant of the University of California, San Francisco, and his associates reported.
Although most subjects reported taking the pills, objective measures of exposure to the drugs suggested substantially lower adherence rates. When intracellular assays showed that subjects had been exposed to FTC-TDF, they were much less likely to acquire HIV. Evidence of FTC-TDF was seen in only 3 of 34 HIV-infected subjects (9%), compared with 22 of 43 HIV-negative subjects (51%) in the FTC-TDF group.
"It’s very exciting news," Dr. Moupali Das said in an interview. "These are extremely promising results," said Dr. Das of the University of California, San Francisco, and director of research in the HIV prevention section of the San Francisco Department of Public Health. She was not involved in the iPrEx study.
The findings are consistent with results from a separate preexposure prophylaxis trial reported earlier in 2010 showing an overall 39% reduction in HIV infections in women who agreed to apply a 1% tenofovir gel vaginally before and after sex, she noted. The randomized, double-blind placebo-controlled Centre for the AIDS Programme of Research in South Africa (CAPRISA) 004 trial studied 889 sexually active African women (Science 2010;329:1168-74).
The iPrEx study enrolled subjects at multiple centers in the United States, South Africa, Brazil, Ecuador, Peru, and Thailand.
Patients in the FTC-TDF group were significantly more likely to develop nausea (2%) in the first 4 weeks of treatment, compared with the placebo group (less than 1%).
"It’s a groundbreaking study," but several factors will temper excitement among clinicians, said Dr. Grant Colfax, director of HIV prevention for the San Francisco Department of Public Health. He was not involved in the iPrEx study.
The FTC-TDF pill is expensive, costing $750 per month or more in the United States, he noted in an interview. Subjects in the study got comprehensive care with monthly HIV testing, state-of-the-art prevention counseling, free condoms and more, which might not be representative of the real world.
"This was not just giving someone a pill and walking out of the office," Dr. Colfax said.
Two subjects in the FTC-TDF group who later were found to have had HIV at enrollment both developed resistance to FTC, compared with one of eight subjects on placebo with HIV at enrollment. People at risk for HIV should not start taking FTC-TDF without reviewing the risks and benefits with their physician, Dr. Colfax said.
The study does not answer questions about the advisability of implementing this prevention strategy in all or even most HIV-negative people at risk for acquiring the infection, Dr. Das agreed. "It will be important to see the results of the upcoming trials on different ways to provide preexposure prophylaxis," results of which should be available in the near future, she said. The Web site of the nonprofit group AVAC: Global Advocacy for HIV Prevention provides a timeline of expected efficacy trial results.
In the meantime, there might be some specific populations in whom preexposure prophylaxis with FTC-TDF makes sense while research continues, she added. Some clinicians already offer preexposure prophylaxis to HIV-negative people whose sexual partners have HIV or to serodiscordant couples who can’t use other modes of preventing infection.
Further research might identify ways to reduce the frequency and expense of preexposure prophylaxis, Dr. Das suggested, such as perhaps taking FTC-TDF only during high-risk periods of life, similar to the way women use contraceptives mainly during the sexually active years.
The main obstacle for most people will be cost, especially for the low-income or indigent patients Dr. Das sees in her practice. "I could write a prescription, but I don’t know how they would be able to pay for it," she said. Still, FTC-TDF is "another potential tool in our prevention toolkit."
The rate of HIV infection has been climbing since the early 1990s in U.S. men and transgender women who have sex with men, especially in black and Hispanic populations, the investigators in the iPrEx study noted. In almost all countries, the prevalence of HIV is higher among men and transgender women who have sex with men, compared with other groups.
The U.S. National Institutes of Health and the Bill and Melinda Gates Foundation funded the study. Gilead Sciences donated the FTC-TDF and placebo tablets, and provided some travel funding for investigators. Two of the investigators worked for Gilead. Disclosures for all the investigators are posted with the article. Dr. Das and Dr. Colfax said they have no relevant conflicts of interest.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Daily Antiretroviral Prophylaxis Reduced Risk of HIV Infection
Taking a daily pill containing two antiretroviral drugs plus exposure to conventional HIV prevention strategies reduced the risk of acquiring HIV by an average of 44% in the people at highest risk of getting infected – men and transgender women who have sex with men, based on a study published online Nov. 23 in the New England Journal of Medicine.
The Preexposure Prophylaxis Initiative (iPrEx) study randomized 2,499 subjects in six countries to take a daily pill containing placebo or a combination of emtricitabine and tenofovir disoproxil fumarate (FTC-TDF). All subjects also received regular HIV testing, condoms, counseling on reducing risks for HIV, and management of sexually transmitted infections (N. Engl. J. Med. 2010 Nov. 23 [doi:10.1056/NEJMoa1011205]).
During a median follow-up of 1.2 years (and a maximum of 2.8 years), 36 of 1,251 subjects in the FTC-TDF group (3%) acquired HIV, compared with 64 of 1,248 subjects in the placebo group (5%). The preventive efficacy of FTC-TDF was significant but not as high as investigators had hoped, Dr. Robert M. Grant of the University of California, San Francisco, and his associates reported.
Although most subjects reported taking the pills, objective measures of exposure to the drugs suggested substantially lower adherence rates. When intracellular assays showed that subjects had been exposed to FTC-TDF, they were much less likely to acquire HIV. Evidence of FTC-TDF was seen in only 3 of 34 HIV-infected subjects (9%), compared with 22 of 43 HIV-negative subjects (51%) in the FTC-TDF group.
"It’s very exciting news," Dr. Moupali Das said in an interview. "These are extremely promising results," said Dr. Das of the University of California, San Francisco, and director of research in the HIV prevention section of the San Francisco Department of Public Health. She was not involved in the iPrEx study.
The findings are consistent with results from a separate preexposure prophylaxis trial reported earlier in 2010 showing an overall 39% reduction in HIV infections in women who agreed to apply a 1% tenofovir gel vaginally before and after sex, she noted. The randomized, double-blind placebo-controlled Centre for the AIDS Programme of Research in South Africa (CAPRISA) 004 trial studied 889 sexually active African women (Science 2010;329:1168-74).
The iPrEx study enrolled subjects at multiple centers in the United States, South Africa, Brazil, Ecuador, Peru, and Thailand.
Patients in the FTC-TDF group were significantly more likely to develop nausea (2%) in the first 4 weeks of treatment, compared with the placebo group (less than 1%).
"It’s a groundbreaking study," but several factors will temper excitement among clinicians, said Dr. Grant Colfax, director of HIV prevention for the San Francisco Department of Public Health. He was not involved in the iPrEx study.
The FTC-TDF pill is expensive, costing $750 per month or more in the United States, he noted in an interview. Subjects in the study got comprehensive care with monthly HIV testing, state-of-the-art prevention counseling, free condoms and more, which might not be representative of the real world.
"This was not just giving someone a pill and walking out of the office," Dr. Colfax said.
Two subjects in the FTC-TDF group who later were found to have had HIV at enrollment both developed resistance to FTC, compared with one of eight subjects on placebo with HIV at enrollment. People at risk for HIV should not start taking FTC-TDF without reviewing the risks and benefits with their physician, Dr. Colfax said.
The study does not answer questions about the advisability of implementing this prevention strategy in all or even most HIV-negative people at risk for acquiring the infection, Dr. Das agreed. "It will be important to see the results of the upcoming trials on different ways to provide preexposure prophylaxis," results of which should be available in the near future, she said. The Web site of the nonprofit group AVAC: Global Advocacy for HIV Prevention provides a timeline of expected efficacy trial results.
In the meantime, there might be some specific populations in whom preexposure prophylaxis with FTC-TDF makes sense while research continues, she added. Some clinicians already offer preexposure prophylaxis to HIV-negative people whose sexual partners have HIV or to serodiscordant couples who can’t use other modes of preventing infection.
Further research might identify ways to reduce the frequency and expense of preexposure prophylaxis, Dr. Das suggested, such as perhaps taking FTC-TDF only during high-risk periods of life, similar to the way women use contraceptives mainly during the sexually active years.
The main obstacle for most people will be cost, especially for the low-income or indigent patients Dr. Das sees in her practice. "I could write a prescription, but I don’t know how they would be able to pay for it," she said. Still, FTC-TDF is "another potential tool in our prevention toolkit."
The rate of HIV infection has been climbing since the early 1990s in U.S. men and transgender women who have sex with men, especially in black and Hispanic populations, the investigators in the iPrEx study noted. In almost all countries, the prevalence of HIV is higher among men and transgender women who have sex with men, compared with other groups.
The U.S. National Institutes of Health and the Bill and Melinda Gates Foundation funded the study. Gilead Sciences donated the FTC-TDF and placebo tablets, and provided some travel funding for investigators. Two of the investigators worked for Gilead. Disclosures for all the investigators are posted with the article. Dr. Das and Dr. Colfax said they have no relevant conflicts of interest.
Taking a daily pill containing two antiretroviral drugs plus exposure to conventional HIV prevention strategies reduced the risk of acquiring HIV by an average of 44% in the people at highest risk of getting infected – men and transgender women who have sex with men, based on a study published online Nov. 23 in the New England Journal of Medicine.
The Preexposure Prophylaxis Initiative (iPrEx) study randomized 2,499 subjects in six countries to take a daily pill containing placebo or a combination of emtricitabine and tenofovir disoproxil fumarate (FTC-TDF). All subjects also received regular HIV testing, condoms, counseling on reducing risks for HIV, and management of sexually transmitted infections (N. Engl. J. Med. 2010 Nov. 23 [doi:10.1056/NEJMoa1011205]).
During a median follow-up of 1.2 years (and a maximum of 2.8 years), 36 of 1,251 subjects in the FTC-TDF group (3%) acquired HIV, compared with 64 of 1,248 subjects in the placebo group (5%). The preventive efficacy of FTC-TDF was significant but not as high as investigators had hoped, Dr. Robert M. Grant of the University of California, San Francisco, and his associates reported.
Although most subjects reported taking the pills, objective measures of exposure to the drugs suggested substantially lower adherence rates. When intracellular assays showed that subjects had been exposed to FTC-TDF, they were much less likely to acquire HIV. Evidence of FTC-TDF was seen in only 3 of 34 HIV-infected subjects (9%), compared with 22 of 43 HIV-negative subjects (51%) in the FTC-TDF group.
"It’s very exciting news," Dr. Moupali Das said in an interview. "These are extremely promising results," said Dr. Das of the University of California, San Francisco, and director of research in the HIV prevention section of the San Francisco Department of Public Health. She was not involved in the iPrEx study.
The findings are consistent with results from a separate preexposure prophylaxis trial reported earlier in 2010 showing an overall 39% reduction in HIV infections in women who agreed to apply a 1% tenofovir gel vaginally before and after sex, she noted. The randomized, double-blind placebo-controlled Centre for the AIDS Programme of Research in South Africa (CAPRISA) 004 trial studied 889 sexually active African women (Science 2010;329:1168-74).
The iPrEx study enrolled subjects at multiple centers in the United States, South Africa, Brazil, Ecuador, Peru, and Thailand.
Patients in the FTC-TDF group were significantly more likely to develop nausea (2%) in the first 4 weeks of treatment, compared with the placebo group (less than 1%).
"It’s a groundbreaking study," but several factors will temper excitement among clinicians, said Dr. Grant Colfax, director of HIV prevention for the San Francisco Department of Public Health. He was not involved in the iPrEx study.
The FTC-TDF pill is expensive, costing $750 per month or more in the United States, he noted in an interview. Subjects in the study got comprehensive care with monthly HIV testing, state-of-the-art prevention counseling, free condoms and more, which might not be representative of the real world.
"This was not just giving someone a pill and walking out of the office," Dr. Colfax said.
Two subjects in the FTC-TDF group who later were found to have had HIV at enrollment both developed resistance to FTC, compared with one of eight subjects on placebo with HIV at enrollment. People at risk for HIV should not start taking FTC-TDF without reviewing the risks and benefits with their physician, Dr. Colfax said.
The study does not answer questions about the advisability of implementing this prevention strategy in all or even most HIV-negative people at risk for acquiring the infection, Dr. Das agreed. "It will be important to see the results of the upcoming trials on different ways to provide preexposure prophylaxis," results of which should be available in the near future, she said. The Web site of the nonprofit group AVAC: Global Advocacy for HIV Prevention provides a timeline of expected efficacy trial results.
In the meantime, there might be some specific populations in whom preexposure prophylaxis with FTC-TDF makes sense while research continues, she added. Some clinicians already offer preexposure prophylaxis to HIV-negative people whose sexual partners have HIV or to serodiscordant couples who can’t use other modes of preventing infection.
Further research might identify ways to reduce the frequency and expense of preexposure prophylaxis, Dr. Das suggested, such as perhaps taking FTC-TDF only during high-risk periods of life, similar to the way women use contraceptives mainly during the sexually active years.
The main obstacle for most people will be cost, especially for the low-income or indigent patients Dr. Das sees in her practice. "I could write a prescription, but I don’t know how they would be able to pay for it," she said. Still, FTC-TDF is "another potential tool in our prevention toolkit."
The rate of HIV infection has been climbing since the early 1990s in U.S. men and transgender women who have sex with men, especially in black and Hispanic populations, the investigators in the iPrEx study noted. In almost all countries, the prevalence of HIV is higher among men and transgender women who have sex with men, compared with other groups.
The U.S. National Institutes of Health and the Bill and Melinda Gates Foundation funded the study. Gilead Sciences donated the FTC-TDF and placebo tablets, and provided some travel funding for investigators. Two of the investigators worked for Gilead. Disclosures for all the investigators are posted with the article. Dr. Das and Dr. Colfax said they have no relevant conflicts of interest.
Taking a daily pill containing two antiretroviral drugs plus exposure to conventional HIV prevention strategies reduced the risk of acquiring HIV by an average of 44% in the people at highest risk of getting infected – men and transgender women who have sex with men, based on a study published online Nov. 23 in the New England Journal of Medicine.
The Preexposure Prophylaxis Initiative (iPrEx) study randomized 2,499 subjects in six countries to take a daily pill containing placebo or a combination of emtricitabine and tenofovir disoproxil fumarate (FTC-TDF). All subjects also received regular HIV testing, condoms, counseling on reducing risks for HIV, and management of sexually transmitted infections (N. Engl. J. Med. 2010 Nov. 23 [doi:10.1056/NEJMoa1011205]).
During a median follow-up of 1.2 years (and a maximum of 2.8 years), 36 of 1,251 subjects in the FTC-TDF group (3%) acquired HIV, compared with 64 of 1,248 subjects in the placebo group (5%). The preventive efficacy of FTC-TDF was significant but not as high as investigators had hoped, Dr. Robert M. Grant of the University of California, San Francisco, and his associates reported.
Although most subjects reported taking the pills, objective measures of exposure to the drugs suggested substantially lower adherence rates. When intracellular assays showed that subjects had been exposed to FTC-TDF, they were much less likely to acquire HIV. Evidence of FTC-TDF was seen in only 3 of 34 HIV-infected subjects (9%), compared with 22 of 43 HIV-negative subjects (51%) in the FTC-TDF group.
"It’s very exciting news," Dr. Moupali Das said in an interview. "These are extremely promising results," said Dr. Das of the University of California, San Francisco, and director of research in the HIV prevention section of the San Francisco Department of Public Health. She was not involved in the iPrEx study.
The findings are consistent with results from a separate preexposure prophylaxis trial reported earlier in 2010 showing an overall 39% reduction in HIV infections in women who agreed to apply a 1% tenofovir gel vaginally before and after sex, she noted. The randomized, double-blind placebo-controlled Centre for the AIDS Programme of Research in South Africa (CAPRISA) 004 trial studied 889 sexually active African women (Science 2010;329:1168-74).
The iPrEx study enrolled subjects at multiple centers in the United States, South Africa, Brazil, Ecuador, Peru, and Thailand.
Patients in the FTC-TDF group were significantly more likely to develop nausea (2%) in the first 4 weeks of treatment, compared with the placebo group (less than 1%).
"It’s a groundbreaking study," but several factors will temper excitement among clinicians, said Dr. Grant Colfax, director of HIV prevention for the San Francisco Department of Public Health. He was not involved in the iPrEx study.
The FTC-TDF pill is expensive, costing $750 per month or more in the United States, he noted in an interview. Subjects in the study got comprehensive care with monthly HIV testing, state-of-the-art prevention counseling, free condoms and more, which might not be representative of the real world.
"This was not just giving someone a pill and walking out of the office," Dr. Colfax said.
Two subjects in the FTC-TDF group who later were found to have had HIV at enrollment both developed resistance to FTC, compared with one of eight subjects on placebo with HIV at enrollment. People at risk for HIV should not start taking FTC-TDF without reviewing the risks and benefits with their physician, Dr. Colfax said.
The study does not answer questions about the advisability of implementing this prevention strategy in all or even most HIV-negative people at risk for acquiring the infection, Dr. Das agreed. "It will be important to see the results of the upcoming trials on different ways to provide preexposure prophylaxis," results of which should be available in the near future, she said. The Web site of the nonprofit group AVAC: Global Advocacy for HIV Prevention provides a timeline of expected efficacy trial results.
In the meantime, there might be some specific populations in whom preexposure prophylaxis with FTC-TDF makes sense while research continues, she added. Some clinicians already offer preexposure prophylaxis to HIV-negative people whose sexual partners have HIV or to serodiscordant couples who can’t use other modes of preventing infection.
Further research might identify ways to reduce the frequency and expense of preexposure prophylaxis, Dr. Das suggested, such as perhaps taking FTC-TDF only during high-risk periods of life, similar to the way women use contraceptives mainly during the sexually active years.
The main obstacle for most people will be cost, especially for the low-income or indigent patients Dr. Das sees in her practice. "I could write a prescription, but I don’t know how they would be able to pay for it," she said. Still, FTC-TDF is "another potential tool in our prevention toolkit."
The rate of HIV infection has been climbing since the early 1990s in U.S. men and transgender women who have sex with men, especially in black and Hispanic populations, the investigators in the iPrEx study noted. In almost all countries, the prevalence of HIV is higher among men and transgender women who have sex with men, compared with other groups.
The U.S. National Institutes of Health and the Bill and Melinda Gates Foundation funded the study. Gilead Sciences donated the FTC-TDF and placebo tablets, and provided some travel funding for investigators. Two of the investigators worked for Gilead. Disclosures for all the investigators are posted with the article. Dr. Das and Dr. Colfax said they have no relevant conflicts of interest.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: Taking a daily pill containing the antiretroviral drugs emtricitabine and tenofovir along with using conventional HIV prevention strategies reduced the risk of acquiring HIV by 44% on average in men or transgender women who have sex with men.
Data Source: Randomized, blinded placebo-controlled trial in 2,499 subjects in six countries.
Disclosures: The National Institutes of Health and the Bill and Melinda Gates Foundation funded the study. Gilead Sciences donated the FTC-TDF and placebo tablets, and provided some travel funding for investigators. Two of the investigators worked for Gilead. Disclosures for individual investigators are posted with the article at www.nejm.org. Dr. Das and Dr. Colfax said they have no relevant conflicts of interest.
Assume Skin and Soft Tissue Infection to Be MRSA
PASADENA, CALIF. – Clinicians should assume community-acquired skin and soft tissue infections are due to methicillin-resistant Staphylococcus aureus infection unless proved otherwise, according to Dr. Paul D. Holtom.
For years, most hospital-associated S. aureus infections have been resistant to methicillin, and now the same has been found for community-acquired S. aureus in studies done mostly in adults, Dr. Holtom of the University of Southern California, Los Angeles, said at the meeting.
At his institution, he said, 70% of people presenting to the emergency department with skin and soft tissue infections have community-acquired MRSA. And a multistate study of 422 patients seen in EDs for skin and soft tissue infections found MRSA in 59%, with rates ranging from 32% to 74% in various states, except for an inexplicably low outlier rate of 15% in New York (N. Engl. J. Med. 2006;355:666-74).
Enough risk factors have been identified for community-acquired MRSA that "you might say that almost everyone is now at risk," he said. Risk factors include intravenous drug use, men having sex with men, residence in correctional institutions, being homeless or marginally housed, various athletic sports, and postinfluenza pneumonia.
A study of 812 U.S. soldiers found that 28% had nasal colonization of methicillin-susceptible S. aureus (MSSA) and 3% had MRSA in their nares. Those colonized with MRSA, however, were significantly more likely to develop soft tissue infection – 9 of 24 soldiers (38%), compared with infections in 8 of 229 soldiers (3%) with MSSA colonization (Clin. Infect. Dis. 2004;39:971-9).
After a "very serious outbreak" of MRSA infections in 928 of 165,000 inmates in the Los Angeles County Jail in 2002, 66 inmates were hospitalized, most with skin and soft tissue infections, and 10 had invasive disease. Subsequent implementation of preventive measures was ineffective, Dr. Holtom said. The number of MRSA infections increased to 1,849 in 2003 and 2,480 in 2004. "It’s not only being spread in the jail, but it’s being brought in. It is throughout the community," he said.
There have been many reports of MRSA infections being spread among competitive athletes, including wrestlers, fencers, and collegiate football players. "This has continued to be a problem. It’s not only collegiate teams but now has moved to high school teams as well," Dr. Holtom said.
Assume that skin and soft tissue infections are due to MRSA, he advised, and get culture and sensitivity testing if you want to understand the epidemiology in your area. When appropriate, treat with surgical drainage of the infection site. Studies suggest that adding antibiotics for patients treated with irrigation and drainage does not improve rates of healing but may help the abscesses heal faster, he said.
When treating suspected S. aureus infection with empiric antibiotics, choose carefully, he added. The infection most likely is due to MRSA, so drugs like cephalexin and dicloxacillin probably will not be effective.
"The good news is that unlike hospital-associated MRSA, community-associated MRSA is frequently sensitive to multiple old-fashioned, inexpensive drugs," including trimethoprim/sulfamethoxazole (TMP/SMX), tetracyclines, or clindamycin, Dr. Holtom said.
TMP/SMX is not very active against Streptococcus pyogenes, the other most likely cause of skin and soft tissue infections and abscesses, so many clinicians combine TMP/SMX with rifampin for synergistic activity against S. aureus and activity against S. pyogenes. Others use TMP/SMX and cephalexin, he said.
The tetracycline drugs doxycycline and minocycline are active against S. aureus. Clindamycin also is a popular choice, but rates of resistance are increasing. At Dr. Holtom’s institution, he said, 8%-10% of S. aureus infections are now resistant to clindamycin.
Dr. Holtom reported having no disclosures or conflicts of interest.
PASADENA, CALIF. – Clinicians should assume community-acquired skin and soft tissue infections are due to methicillin-resistant Staphylococcus aureus infection unless proved otherwise, according to Dr. Paul D. Holtom.
For years, most hospital-associated S. aureus infections have been resistant to methicillin, and now the same has been found for community-acquired S. aureus in studies done mostly in adults, Dr. Holtom of the University of Southern California, Los Angeles, said at the meeting.
At his institution, he said, 70% of people presenting to the emergency department with skin and soft tissue infections have community-acquired MRSA. And a multistate study of 422 patients seen in EDs for skin and soft tissue infections found MRSA in 59%, with rates ranging from 32% to 74% in various states, except for an inexplicably low outlier rate of 15% in New York (N. Engl. J. Med. 2006;355:666-74).
Enough risk factors have been identified for community-acquired MRSA that "you might say that almost everyone is now at risk," he said. Risk factors include intravenous drug use, men having sex with men, residence in correctional institutions, being homeless or marginally housed, various athletic sports, and postinfluenza pneumonia.
A study of 812 U.S. soldiers found that 28% had nasal colonization of methicillin-susceptible S. aureus (MSSA) and 3% had MRSA in their nares. Those colonized with MRSA, however, were significantly more likely to develop soft tissue infection – 9 of 24 soldiers (38%), compared with infections in 8 of 229 soldiers (3%) with MSSA colonization (Clin. Infect. Dis. 2004;39:971-9).
After a "very serious outbreak" of MRSA infections in 928 of 165,000 inmates in the Los Angeles County Jail in 2002, 66 inmates were hospitalized, most with skin and soft tissue infections, and 10 had invasive disease. Subsequent implementation of preventive measures was ineffective, Dr. Holtom said. The number of MRSA infections increased to 1,849 in 2003 and 2,480 in 2004. "It’s not only being spread in the jail, but it’s being brought in. It is throughout the community," he said.
There have been many reports of MRSA infections being spread among competitive athletes, including wrestlers, fencers, and collegiate football players. "This has continued to be a problem. It’s not only collegiate teams but now has moved to high school teams as well," Dr. Holtom said.
Assume that skin and soft tissue infections are due to MRSA, he advised, and get culture and sensitivity testing if you want to understand the epidemiology in your area. When appropriate, treat with surgical drainage of the infection site. Studies suggest that adding antibiotics for patients treated with irrigation and drainage does not improve rates of healing but may help the abscesses heal faster, he said.
When treating suspected S. aureus infection with empiric antibiotics, choose carefully, he added. The infection most likely is due to MRSA, so drugs like cephalexin and dicloxacillin probably will not be effective.
"The good news is that unlike hospital-associated MRSA, community-associated MRSA is frequently sensitive to multiple old-fashioned, inexpensive drugs," including trimethoprim/sulfamethoxazole (TMP/SMX), tetracyclines, or clindamycin, Dr. Holtom said.
TMP/SMX is not very active against Streptococcus pyogenes, the other most likely cause of skin and soft tissue infections and abscesses, so many clinicians combine TMP/SMX with rifampin for synergistic activity against S. aureus and activity against S. pyogenes. Others use TMP/SMX and cephalexin, he said.
The tetracycline drugs doxycycline and minocycline are active against S. aureus. Clindamycin also is a popular choice, but rates of resistance are increasing. At Dr. Holtom’s institution, he said, 8%-10% of S. aureus infections are now resistant to clindamycin.
Dr. Holtom reported having no disclosures or conflicts of interest.
PASADENA, CALIF. – Clinicians should assume community-acquired skin and soft tissue infections are due to methicillin-resistant Staphylococcus aureus infection unless proved otherwise, according to Dr. Paul D. Holtom.
For years, most hospital-associated S. aureus infections have been resistant to methicillin, and now the same has been found for community-acquired S. aureus in studies done mostly in adults, Dr. Holtom of the University of Southern California, Los Angeles, said at the meeting.
At his institution, he said, 70% of people presenting to the emergency department with skin and soft tissue infections have community-acquired MRSA. And a multistate study of 422 patients seen in EDs for skin and soft tissue infections found MRSA in 59%, with rates ranging from 32% to 74% in various states, except for an inexplicably low outlier rate of 15% in New York (N. Engl. J. Med. 2006;355:666-74).
Enough risk factors have been identified for community-acquired MRSA that "you might say that almost everyone is now at risk," he said. Risk factors include intravenous drug use, men having sex with men, residence in correctional institutions, being homeless or marginally housed, various athletic sports, and postinfluenza pneumonia.
A study of 812 U.S. soldiers found that 28% had nasal colonization of methicillin-susceptible S. aureus (MSSA) and 3% had MRSA in their nares. Those colonized with MRSA, however, were significantly more likely to develop soft tissue infection – 9 of 24 soldiers (38%), compared with infections in 8 of 229 soldiers (3%) with MSSA colonization (Clin. Infect. Dis. 2004;39:971-9).
After a "very serious outbreak" of MRSA infections in 928 of 165,000 inmates in the Los Angeles County Jail in 2002, 66 inmates were hospitalized, most with skin and soft tissue infections, and 10 had invasive disease. Subsequent implementation of preventive measures was ineffective, Dr. Holtom said. The number of MRSA infections increased to 1,849 in 2003 and 2,480 in 2004. "It’s not only being spread in the jail, but it’s being brought in. It is throughout the community," he said.
There have been many reports of MRSA infections being spread among competitive athletes, including wrestlers, fencers, and collegiate football players. "This has continued to be a problem. It’s not only collegiate teams but now has moved to high school teams as well," Dr. Holtom said.
Assume that skin and soft tissue infections are due to MRSA, he advised, and get culture and sensitivity testing if you want to understand the epidemiology in your area. When appropriate, treat with surgical drainage of the infection site. Studies suggest that adding antibiotics for patients treated with irrigation and drainage does not improve rates of healing but may help the abscesses heal faster, he said.
When treating suspected S. aureus infection with empiric antibiotics, choose carefully, he added. The infection most likely is due to MRSA, so drugs like cephalexin and dicloxacillin probably will not be effective.
"The good news is that unlike hospital-associated MRSA, community-associated MRSA is frequently sensitive to multiple old-fashioned, inexpensive drugs," including trimethoprim/sulfamethoxazole (TMP/SMX), tetracyclines, or clindamycin, Dr. Holtom said.
TMP/SMX is not very active against Streptococcus pyogenes, the other most likely cause of skin and soft tissue infections and abscesses, so many clinicians combine TMP/SMX with rifampin for synergistic activity against S. aureus and activity against S. pyogenes. Others use TMP/SMX and cephalexin, he said.
The tetracycline drugs doxycycline and minocycline are active against S. aureus. Clindamycin also is a popular choice, but rates of resistance are increasing. At Dr. Holtom’s institution, he said, 8%-10% of S. aureus infections are now resistant to clindamycin.
Dr. Holtom reported having no disclosures or conflicts of interest.
FROM THE ANNUAL MEETING OF THE PACIFIC DERMATOLOGIC ASSOCIATION
Assume Skin and Soft Tissue Infection to Be MRSA
PASADENA, CALIF. – Clinicians should assume community-acquired skin and soft tissue infections are due to methicillin-resistant Staphylococcus aureus infection unless proved otherwise, according to Dr. Paul D. Holtom.
For years, most hospital-associated S. aureus infections have been resistant to methicillin, and now the same has been found for community-acquired S. aureus in studies done mostly in adults, Dr. Holtom of the University of Southern California, Los Angeles, said at the meeting.
At his institution, he said, 70% of people presenting to the emergency department with skin and soft tissue infections have community-acquired MRSA. And a multistate study of 422 patients seen in EDs for skin and soft tissue infections found MRSA in 59%, with rates ranging from 32% to 74% in various states, except for an inexplicably low outlier rate of 15% in New York (N. Engl. J. Med. 2006;355:666-74).
Enough risk factors have been identified for community-acquired MRSA that "you might say that almost everyone is now at risk," he said. Risk factors include intravenous drug use, men having sex with men, residence in correctional institutions, being homeless or marginally housed, various athletic sports, and postinfluenza pneumonia.
A study of 812 U.S. soldiers found that 28% had nasal colonization of methicillin-susceptible S. aureus (MSSA) and 3% had MRSA in their nares. Those colonized with MRSA, however, were significantly more likely to develop soft tissue infection – 9 of 24 soldiers (38%), compared with infections in 8 of 229 soldiers (3%) with MSSA colonization (Clin. Infect. Dis. 2004;39:971-9).
After a "very serious outbreak" of MRSA infections in 928 of 165,000 inmates in the Los Angeles County Jail in 2002, 66 inmates were hospitalized, most with skin and soft tissue infections, and 10 had invasive disease. Subsequent implementation of preventive measures was ineffective, Dr. Holtom said. The number of MRSA infections increased to 1,849 in 2003 and 2,480 in 2004. "It’s not only being spread in the jail, but it’s being brought in. It is throughout the community," he said.
There have been many reports of MRSA infections being spread among competitive athletes, including wrestlers, fencers, and collegiate football players. "This has continued to be a problem. It’s not only collegiate teams but now has moved to high school teams as well," Dr. Holtom said.
Assume that skin and soft tissue infections are due to MRSA, he advised, and get culture and sensitivity testing if you want to understand the epidemiology in your area. When appropriate, treat with surgical drainage of the infection site. Studies suggest that adding antibiotics for patients treated with irrigation and drainage does not improve rates of healing but may help the abscesses heal faster, he said.
When treating suspected S. aureus infection with empiric antibiotics, choose carefully, he added. The infection most likely is due to MRSA, so drugs like cephalexin and dicloxacillin probably will not be effective.
"The good news is that unlike hospital-associated MRSA, community-associated MRSA is frequently sensitive to multiple old-fashioned, inexpensive drugs," including trimethoprim/sulfamethoxazole (TMP/SMX), tetracyclines, or clindamycin, Dr. Holtom said.
TMP/SMX is not very active against Streptococcus pyogenes, the other most likely cause of skin and soft tissue infections and abscesses, so many clinicians combine TMP/SMX with rifampin for synergistic activity against S. aureus and activity against S. pyogenes. Others use TMP/SMX and cephalexin, he said.
The tetracycline drugs doxycycline and minocycline are active against S. aureus. Clindamycin also is a popular choice, but rates of resistance are increasing. At Dr. Holtom’s institution, he said, 8%-10% of S. aureus infections are now resistant to clindamycin.
Dr. Holtom reported having no disclosures or conflicts of interest.
PASADENA, CALIF. – Clinicians should assume community-acquired skin and soft tissue infections are due to methicillin-resistant Staphylococcus aureus infection unless proved otherwise, according to Dr. Paul D. Holtom.
For years, most hospital-associated S. aureus infections have been resistant to methicillin, and now the same has been found for community-acquired S. aureus in studies done mostly in adults, Dr. Holtom of the University of Southern California, Los Angeles, said at the meeting.
At his institution, he said, 70% of people presenting to the emergency department with skin and soft tissue infections have community-acquired MRSA. And a multistate study of 422 patients seen in EDs for skin and soft tissue infections found MRSA in 59%, with rates ranging from 32% to 74% in various states, except for an inexplicably low outlier rate of 15% in New York (N. Engl. J. Med. 2006;355:666-74).
Enough risk factors have been identified for community-acquired MRSA that "you might say that almost everyone is now at risk," he said. Risk factors include intravenous drug use, men having sex with men, residence in correctional institutions, being homeless or marginally housed, various athletic sports, and postinfluenza pneumonia.
A study of 812 U.S. soldiers found that 28% had nasal colonization of methicillin-susceptible S. aureus (MSSA) and 3% had MRSA in their nares. Those colonized with MRSA, however, were significantly more likely to develop soft tissue infection – 9 of 24 soldiers (38%), compared with infections in 8 of 229 soldiers (3%) with MSSA colonization (Clin. Infect. Dis. 2004;39:971-9).
After a "very serious outbreak" of MRSA infections in 928 of 165,000 inmates in the Los Angeles County Jail in 2002, 66 inmates were hospitalized, most with skin and soft tissue infections, and 10 had invasive disease. Subsequent implementation of preventive measures was ineffective, Dr. Holtom said. The number of MRSA infections increased to 1,849 in 2003 and 2,480 in 2004. "It’s not only being spread in the jail, but it’s being brought in. It is throughout the community," he said.
There have been many reports of MRSA infections being spread among competitive athletes, including wrestlers, fencers, and collegiate football players. "This has continued to be a problem. It’s not only collegiate teams but now has moved to high school teams as well," Dr. Holtom said.
Assume that skin and soft tissue infections are due to MRSA, he advised, and get culture and sensitivity testing if you want to understand the epidemiology in your area. When appropriate, treat with surgical drainage of the infection site. Studies suggest that adding antibiotics for patients treated with irrigation and drainage does not improve rates of healing but may help the abscesses heal faster, he said.
When treating suspected S. aureus infection with empiric antibiotics, choose carefully, he added. The infection most likely is due to MRSA, so drugs like cephalexin and dicloxacillin probably will not be effective.
"The good news is that unlike hospital-associated MRSA, community-associated MRSA is frequently sensitive to multiple old-fashioned, inexpensive drugs," including trimethoprim/sulfamethoxazole (TMP/SMX), tetracyclines, or clindamycin, Dr. Holtom said.
TMP/SMX is not very active against Streptococcus pyogenes, the other most likely cause of skin and soft tissue infections and abscesses, so many clinicians combine TMP/SMX with rifampin for synergistic activity against S. aureus and activity against S. pyogenes. Others use TMP/SMX and cephalexin, he said.
The tetracycline drugs doxycycline and minocycline are active against S. aureus. Clindamycin also is a popular choice, but rates of resistance are increasing. At Dr. Holtom’s institution, he said, 8%-10% of S. aureus infections are now resistant to clindamycin.
Dr. Holtom reported having no disclosures or conflicts of interest.
PASADENA, CALIF. – Clinicians should assume community-acquired skin and soft tissue infections are due to methicillin-resistant Staphylococcus aureus infection unless proved otherwise, according to Dr. Paul D. Holtom.
For years, most hospital-associated S. aureus infections have been resistant to methicillin, and now the same has been found for community-acquired S. aureus in studies done mostly in adults, Dr. Holtom of the University of Southern California, Los Angeles, said at the meeting.
At his institution, he said, 70% of people presenting to the emergency department with skin and soft tissue infections have community-acquired MRSA. And a multistate study of 422 patients seen in EDs for skin and soft tissue infections found MRSA in 59%, with rates ranging from 32% to 74% in various states, except for an inexplicably low outlier rate of 15% in New York (N. Engl. J. Med. 2006;355:666-74).
Enough risk factors have been identified for community-acquired MRSA that "you might say that almost everyone is now at risk," he said. Risk factors include intravenous drug use, men having sex with men, residence in correctional institutions, being homeless or marginally housed, various athletic sports, and postinfluenza pneumonia.
A study of 812 U.S. soldiers found that 28% had nasal colonization of methicillin-susceptible S. aureus (MSSA) and 3% had MRSA in their nares. Those colonized with MRSA, however, were significantly more likely to develop soft tissue infection – 9 of 24 soldiers (38%), compared with infections in 8 of 229 soldiers (3%) with MSSA colonization (Clin. Infect. Dis. 2004;39:971-9).
After a "very serious outbreak" of MRSA infections in 928 of 165,000 inmates in the Los Angeles County Jail in 2002, 66 inmates were hospitalized, most with skin and soft tissue infections, and 10 had invasive disease. Subsequent implementation of preventive measures was ineffective, Dr. Holtom said. The number of MRSA infections increased to 1,849 in 2003 and 2,480 in 2004. "It’s not only being spread in the jail, but it’s being brought in. It is throughout the community," he said.
There have been many reports of MRSA infections being spread among competitive athletes, including wrestlers, fencers, and collegiate football players. "This has continued to be a problem. It’s not only collegiate teams but now has moved to high school teams as well," Dr. Holtom said.
Assume that skin and soft tissue infections are due to MRSA, he advised, and get culture and sensitivity testing if you want to understand the epidemiology in your area. When appropriate, treat with surgical drainage of the infection site. Studies suggest that adding antibiotics for patients treated with irrigation and drainage does not improve rates of healing but may help the abscesses heal faster, he said.
When treating suspected S. aureus infection with empiric antibiotics, choose carefully, he added. The infection most likely is due to MRSA, so drugs like cephalexin and dicloxacillin probably will not be effective.
"The good news is that unlike hospital-associated MRSA, community-associated MRSA is frequently sensitive to multiple old-fashioned, inexpensive drugs," including trimethoprim/sulfamethoxazole (TMP/SMX), tetracyclines, or clindamycin, Dr. Holtom said.
TMP/SMX is not very active against Streptococcus pyogenes, the other most likely cause of skin and soft tissue infections and abscesses, so many clinicians combine TMP/SMX with rifampin for synergistic activity against S. aureus and activity against S. pyogenes. Others use TMP/SMX and cephalexin, he said.
The tetracycline drugs doxycycline and minocycline are active against S. aureus. Clindamycin also is a popular choice, but rates of resistance are increasing. At Dr. Holtom’s institution, he said, 8%-10% of S. aureus infections are now resistant to clindamycin.
Dr. Holtom reported having no disclosures or conflicts of interest.
FROM THE ANNUAL MEETING OF THE PACIFIC DERMATOLOGIC ASSOCIATION
Coal Tar Making a Psoriasis Comeback
LAS VEGAS – Topical tar therapy for psoriasis may be making a comeback thanks to more user-friendly formulations.
That trend is happening in Europe and may be replicated in the United States, Dr. Linda Stein Gold said at a dermatology seminar sponsored by Skin Disease Education Foundation (SDEF).
"Topical therapy is the bread and butter of psoriasis treatment," and coal tar has been used for centuries to control the symptoms of plaque psoriasis, said Dr. Stein Gold, director of dermatology research at Henry Ford Hospital, Detroit.
The Goeckerman regimen, a combination of topical tar and ultraviolet light therapy in use since the 1920s, proved "exceptionally" effective and durable, she noted, with an average time of 18 days to 90% clearing of psoriatic lesions and 90% of patients remaining clear for up to 8 months.
But tar therapy was time consuming, a logistical hassle, and aesthetically unpleasing, and its use declined in recent decades with the advent of systemic biologic medications. "People weren't using tar before because it's messy and it smelled. Now we have some better options," Dr. Stein Gold said.
One of the newer topical solutions is a transparent gel of 15% liquor carbonis distillate (LCD), the equivalent of 2.3% coal tar (Psorent, NeoStrata Co.). "It doesn’t discolor bleached hair" when used for scalp psoriasis, it is quick-drying, and it comes in bottles with "dab-on" applicators, she said.
In a controlled comparison with calcipotriol cream in 12 weeks of treatment of 60 adults with moderate plaque psoriasis, the LCD solution was more effective and led to fewer relapses 6 weeks after treatment. Among 55 patients with complete data, mean Psoriasis Area Severity Index (PASI) scores improved by 58% in the LCD solution group and 37% in the calcipotriol group, a significant difference (J. Am. Acad. Dermatol. 2009;60:Ab174 [doi: 10.1016/j.jaad.2008.11.757]).
A 75% improvement in PASI scores was seen in 11 of 27 (41%) of the LCD solution group and none of the 28 patients on calcipotriol. A 50% improvement in PASI scores was seen in 18 of 27 (67%) in the LCD group and 10 of 28 (36%) in the calcipotriol group. These differences between groups were statistically significant.
Among 42 patients with Physician Global Assessment (PGA) scores 6 weeks after treatment, the PGA scores worsened to baseline in 5 of 22 patients (23%) in the LCD solution group and in 14 of 20 patients (70%) in the calcipotriol group, again a significant difference.
A separate study compared the LCD solution in combination with UVB therapy on one side of the body with UVB light therapy alone on the other side of the body in 12 patients in 4 weeks of therapy. "Very quickly, the combo therapy gets more rapid and complete efficacy compared with UVB alone," said Dr. Stein Gold (J. Drugs. Dermatol. 2009;8 [4]:351-7).
Another relatively user-friendly product is an over-the-counter 2% coal tar formulation in a foam base (Scytera, Promius Pharma). The foam is "a much more cosmetically elegant" treatment compared with older tar therapies, she said. It spreads easily, dries quickly, and has an acceptable fragrance, Dr. Stein Gold added.
In a randomized, observer-blind study of 38 patients with chronic plaque-type psoriasis, two lesions on each patient were treated for 8 weeks with a 1% coal tar foam or calcipotriol cream. The treatments appeared to be comparably effective. More patients reported itching, unpleasant odor or staining with the tar foam than with calcipotriol cream, but the foam is considerably less expensive, the investigators noted (Br. J. Dermatol. 2003;149:350-53).
"Tar is something we probably should look at again," Dr. Stein Gold said.
Other useful topical therapies include corticosteroids, she said. While studies with objective measures of atrophy have proved that potent topical corticosteroids do lead to thinning of the skin over time, often this effect is not clinically noticeable, and it reverses over time once treatment is stopped.
Topical vitamin D is complementary to topical steroids for psoriasis therapy and helps counteract some of the side effects of topical steroids on skin.
Dr. Stein Gold said she has had financial associations with Leo Pharma, Medicis Pharmaceutical Corp., Stiefel Laboratories, Galderma, and Novartis. SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Topical tar therapy for psoriasis may be making a comeback thanks to more user-friendly formulations.
That trend is happening in Europe and may be replicated in the United States, Dr. Linda Stein Gold said at a dermatology seminar sponsored by Skin Disease Education Foundation (SDEF).
"Topical therapy is the bread and butter of psoriasis treatment," and coal tar has been used for centuries to control the symptoms of plaque psoriasis, said Dr. Stein Gold, director of dermatology research at Henry Ford Hospital, Detroit.
The Goeckerman regimen, a combination of topical tar and ultraviolet light therapy in use since the 1920s, proved "exceptionally" effective and durable, she noted, with an average time of 18 days to 90% clearing of psoriatic lesions and 90% of patients remaining clear for up to 8 months.
But tar therapy was time consuming, a logistical hassle, and aesthetically unpleasing, and its use declined in recent decades with the advent of systemic biologic medications. "People weren't using tar before because it's messy and it smelled. Now we have some better options," Dr. Stein Gold said.
One of the newer topical solutions is a transparent gel of 15% liquor carbonis distillate (LCD), the equivalent of 2.3% coal tar (Psorent, NeoStrata Co.). "It doesn’t discolor bleached hair" when used for scalp psoriasis, it is quick-drying, and it comes in bottles with "dab-on" applicators, she said.
In a controlled comparison with calcipotriol cream in 12 weeks of treatment of 60 adults with moderate plaque psoriasis, the LCD solution was more effective and led to fewer relapses 6 weeks after treatment. Among 55 patients with complete data, mean Psoriasis Area Severity Index (PASI) scores improved by 58% in the LCD solution group and 37% in the calcipotriol group, a significant difference (J. Am. Acad. Dermatol. 2009;60:Ab174 [doi: 10.1016/j.jaad.2008.11.757]).
A 75% improvement in PASI scores was seen in 11 of 27 (41%) of the LCD solution group and none of the 28 patients on calcipotriol. A 50% improvement in PASI scores was seen in 18 of 27 (67%) in the LCD group and 10 of 28 (36%) in the calcipotriol group. These differences between groups were statistically significant.
Among 42 patients with Physician Global Assessment (PGA) scores 6 weeks after treatment, the PGA scores worsened to baseline in 5 of 22 patients (23%) in the LCD solution group and in 14 of 20 patients (70%) in the calcipotriol group, again a significant difference.
A separate study compared the LCD solution in combination with UVB therapy on one side of the body with UVB light therapy alone on the other side of the body in 12 patients in 4 weeks of therapy. "Very quickly, the combo therapy gets more rapid and complete efficacy compared with UVB alone," said Dr. Stein Gold (J. Drugs. Dermatol. 2009;8 [4]:351-7).
Another relatively user-friendly product is an over-the-counter 2% coal tar formulation in a foam base (Scytera, Promius Pharma). The foam is "a much more cosmetically elegant" treatment compared with older tar therapies, she said. It spreads easily, dries quickly, and has an acceptable fragrance, Dr. Stein Gold added.
In a randomized, observer-blind study of 38 patients with chronic plaque-type psoriasis, two lesions on each patient were treated for 8 weeks with a 1% coal tar foam or calcipotriol cream. The treatments appeared to be comparably effective. More patients reported itching, unpleasant odor or staining with the tar foam than with calcipotriol cream, but the foam is considerably less expensive, the investigators noted (Br. J. Dermatol. 2003;149:350-53).
"Tar is something we probably should look at again," Dr. Stein Gold said.
Other useful topical therapies include corticosteroids, she said. While studies with objective measures of atrophy have proved that potent topical corticosteroids do lead to thinning of the skin over time, often this effect is not clinically noticeable, and it reverses over time once treatment is stopped.
Topical vitamin D is complementary to topical steroids for psoriasis therapy and helps counteract some of the side effects of topical steroids on skin.
Dr. Stein Gold said she has had financial associations with Leo Pharma, Medicis Pharmaceutical Corp., Stiefel Laboratories, Galderma, and Novartis. SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Topical tar therapy for psoriasis may be making a comeback thanks to more user-friendly formulations.
That trend is happening in Europe and may be replicated in the United States, Dr. Linda Stein Gold said at a dermatology seminar sponsored by Skin Disease Education Foundation (SDEF).
"Topical therapy is the bread and butter of psoriasis treatment," and coal tar has been used for centuries to control the symptoms of plaque psoriasis, said Dr. Stein Gold, director of dermatology research at Henry Ford Hospital, Detroit.
The Goeckerman regimen, a combination of topical tar and ultraviolet light therapy in use since the 1920s, proved "exceptionally" effective and durable, she noted, with an average time of 18 days to 90% clearing of psoriatic lesions and 90% of patients remaining clear for up to 8 months.
But tar therapy was time consuming, a logistical hassle, and aesthetically unpleasing, and its use declined in recent decades with the advent of systemic biologic medications. "People weren't using tar before because it's messy and it smelled. Now we have some better options," Dr. Stein Gold said.
One of the newer topical solutions is a transparent gel of 15% liquor carbonis distillate (LCD), the equivalent of 2.3% coal tar (Psorent, NeoStrata Co.). "It doesn’t discolor bleached hair" when used for scalp psoriasis, it is quick-drying, and it comes in bottles with "dab-on" applicators, she said.
In a controlled comparison with calcipotriol cream in 12 weeks of treatment of 60 adults with moderate plaque psoriasis, the LCD solution was more effective and led to fewer relapses 6 weeks after treatment. Among 55 patients with complete data, mean Psoriasis Area Severity Index (PASI) scores improved by 58% in the LCD solution group and 37% in the calcipotriol group, a significant difference (J. Am. Acad. Dermatol. 2009;60:Ab174 [doi: 10.1016/j.jaad.2008.11.757]).
A 75% improvement in PASI scores was seen in 11 of 27 (41%) of the LCD solution group and none of the 28 patients on calcipotriol. A 50% improvement in PASI scores was seen in 18 of 27 (67%) in the LCD group and 10 of 28 (36%) in the calcipotriol group. These differences between groups were statistically significant.
Among 42 patients with Physician Global Assessment (PGA) scores 6 weeks after treatment, the PGA scores worsened to baseline in 5 of 22 patients (23%) in the LCD solution group and in 14 of 20 patients (70%) in the calcipotriol group, again a significant difference.
A separate study compared the LCD solution in combination with UVB therapy on one side of the body with UVB light therapy alone on the other side of the body in 12 patients in 4 weeks of therapy. "Very quickly, the combo therapy gets more rapid and complete efficacy compared with UVB alone," said Dr. Stein Gold (J. Drugs. Dermatol. 2009;8 [4]:351-7).
Another relatively user-friendly product is an over-the-counter 2% coal tar formulation in a foam base (Scytera, Promius Pharma). The foam is "a much more cosmetically elegant" treatment compared with older tar therapies, she said. It spreads easily, dries quickly, and has an acceptable fragrance, Dr. Stein Gold added.
In a randomized, observer-blind study of 38 patients with chronic plaque-type psoriasis, two lesions on each patient were treated for 8 weeks with a 1% coal tar foam or calcipotriol cream. The treatments appeared to be comparably effective. More patients reported itching, unpleasant odor or staining with the tar foam than with calcipotriol cream, but the foam is considerably less expensive, the investigators noted (Br. J. Dermatol. 2003;149:350-53).
"Tar is something we probably should look at again," Dr. Stein Gold said.
Other useful topical therapies include corticosteroids, she said. While studies with objective measures of atrophy have proved that potent topical corticosteroids do lead to thinning of the skin over time, often this effect is not clinically noticeable, and it reverses over time once treatment is stopped.
Topical vitamin D is complementary to topical steroids for psoriasis therapy and helps counteract some of the side effects of topical steroids on skin.
Dr. Stein Gold said she has had financial associations with Leo Pharma, Medicis Pharmaceutical Corp., Stiefel Laboratories, Galderma, and Novartis. SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM A DERMATOLOGY SEMINAR SPONSORED BY SKIN DISEASE EDUCATION FOUNDATION