User login
Tivozanib has PFS benefit over sorafenib in hard-to-treat RCC
SAN FRANCISCO – The risk-benefit profile of the novel vascular endothelial growth factor (VEGF) inhibitor tivozanib when used as later-line therapy for renal cell carcinoma (RCC) appears to be similar to when it is used earlier, according to eagerly awaited results of the TIVO-3 trial.
Tivozanib, an oral tyrosine kinase inhibitor of the VEGF family of receptors with a long half-life, is designed both to optimize receptor blockade and minimize off-target toxicities, lead investigator Brian I. Rini, MD, said at the the 2019 Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Positive progression-free survival results of the TIVO-1 trial (J Clin Oncol. 2013;31:3791-9) led to approval of this agent as first-line therapy for RCC in Europe. However, the Food and Drug Administration rejected approval because of a trend toward poorer overall survival, which was likely related to imbalanced cross-over to active treatment.
The TIVO-3 trial enrolled 350 patients with advanced clear-cell RCC who had experienced failure of two or three prior regimens, including a VEGF receptor tyrosine kinase inhibitor. They were randomized evenly to open-label tivozanib (1.5 mg q.d., 3 weeks on and 1 week off) or sorafenib (Nexavar) (400 mg b.i.d. continuously).
Main results showed that progression-free survival was about 2 months longer with tivozanib, compared with sorafenib. The difference translated to a 27% reduction in risk of events, reported Dr. Rini, professor of medicine at Case Western Reserve University, Cleveland, and leader of the genitourinary oncology program at the Cleveland Clinic.
The benefit was similar for most subgroups. The tivozanib group had a higher incidence of hypertension, but lower incidences of diarrhea, hand-foot syndrome, and rash.
“Tivozanib significantly improved progression-free survival and objective response rate compared to sorafenib in patients with treatment-refractory advanced RCC. It was superior in the subset of patients previously treated with checkpoint inhibitors, as well as the subset who had had two prior TKIs,” Dr. Rini said. “Responses to tivozanib, perhaps most impressively, were more durable than those with sorafenib. Tivozanib was very well tolerated, with on-target hypertension as the most common adverse event, but lower rates of off-target toxicities.”
Overall survival data at present show a trend toward shorter survival with tivozanib, but are not yet mature. Definitive results are expected later this year.
Study details
About 60% of patients in TIVO-3 had received two prior lines of therapy, Dr. Rini reported at the symposium. The proportion stopping study treatment because of adverse events was 13% in the tivozanib group and 23% in the sorafenib group.
Median progression-free survival according to an independent review committee was 5.6 months and 3.9 months, respectively (hazard ratio, 0.73; P = .0165). Corresponding 1-year rates were 28% and 11%.
Among patients previously treated with an immune checkpoint inhibitor, median progression-free survival according to an independent review committee was 7.3 months with tivozanib and 5.1 months with sorafenib (hazard ratio, 0.55; P = .028). Corresponding 1-year rates were 35% and 4%.
In the entire trial population, the overall response rate was 18% for tivozanib versus 8% for sorafenib (P = .02). Median duration of response was not reached, compared with 5.7 months.
An interim analysis showed a median overall survival of 16.4 months in the tivozanib group and 19.7 months in the sorafenib group.
The rate of any-grade treatment-related adverse events was 84% with tivozanib and 94% with sorafenib. Tivozanib had a higher rate of grade 3 or 4 hypertension (20% vs. 14%), but lower rates of grade 3 or 4 diarrhea (2% vs. 9%), hand-foot syndrome (1% vs. 10%), and rash (0% vs. 8%).
Dr. Rini reported that he has a consulting role with Aveo, which sponsored the trial, and financial relationships with several other companies.
SOURCE: Rini BI et al. GUCS 2019, Abstract 541.
SAN FRANCISCO – The risk-benefit profile of the novel vascular endothelial growth factor (VEGF) inhibitor tivozanib when used as later-line therapy for renal cell carcinoma (RCC) appears to be similar to when it is used earlier, according to eagerly awaited results of the TIVO-3 trial.
Tivozanib, an oral tyrosine kinase inhibitor of the VEGF family of receptors with a long half-life, is designed both to optimize receptor blockade and minimize off-target toxicities, lead investigator Brian I. Rini, MD, said at the the 2019 Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Positive progression-free survival results of the TIVO-1 trial (J Clin Oncol. 2013;31:3791-9) led to approval of this agent as first-line therapy for RCC in Europe. However, the Food and Drug Administration rejected approval because of a trend toward poorer overall survival, which was likely related to imbalanced cross-over to active treatment.
The TIVO-3 trial enrolled 350 patients with advanced clear-cell RCC who had experienced failure of two or three prior regimens, including a VEGF receptor tyrosine kinase inhibitor. They were randomized evenly to open-label tivozanib (1.5 mg q.d., 3 weeks on and 1 week off) or sorafenib (Nexavar) (400 mg b.i.d. continuously).
Main results showed that progression-free survival was about 2 months longer with tivozanib, compared with sorafenib. The difference translated to a 27% reduction in risk of events, reported Dr. Rini, professor of medicine at Case Western Reserve University, Cleveland, and leader of the genitourinary oncology program at the Cleveland Clinic.
The benefit was similar for most subgroups. The tivozanib group had a higher incidence of hypertension, but lower incidences of diarrhea, hand-foot syndrome, and rash.
“Tivozanib significantly improved progression-free survival and objective response rate compared to sorafenib in patients with treatment-refractory advanced RCC. It was superior in the subset of patients previously treated with checkpoint inhibitors, as well as the subset who had had two prior TKIs,” Dr. Rini said. “Responses to tivozanib, perhaps most impressively, were more durable than those with sorafenib. Tivozanib was very well tolerated, with on-target hypertension as the most common adverse event, but lower rates of off-target toxicities.”
Overall survival data at present show a trend toward shorter survival with tivozanib, but are not yet mature. Definitive results are expected later this year.
Study details
About 60% of patients in TIVO-3 had received two prior lines of therapy, Dr. Rini reported at the symposium. The proportion stopping study treatment because of adverse events was 13% in the tivozanib group and 23% in the sorafenib group.
Median progression-free survival according to an independent review committee was 5.6 months and 3.9 months, respectively (hazard ratio, 0.73; P = .0165). Corresponding 1-year rates were 28% and 11%.
Among patients previously treated with an immune checkpoint inhibitor, median progression-free survival according to an independent review committee was 7.3 months with tivozanib and 5.1 months with sorafenib (hazard ratio, 0.55; P = .028). Corresponding 1-year rates were 35% and 4%.
In the entire trial population, the overall response rate was 18% for tivozanib versus 8% for sorafenib (P = .02). Median duration of response was not reached, compared with 5.7 months.
An interim analysis showed a median overall survival of 16.4 months in the tivozanib group and 19.7 months in the sorafenib group.
The rate of any-grade treatment-related adverse events was 84% with tivozanib and 94% with sorafenib. Tivozanib had a higher rate of grade 3 or 4 hypertension (20% vs. 14%), but lower rates of grade 3 or 4 diarrhea (2% vs. 9%), hand-foot syndrome (1% vs. 10%), and rash (0% vs. 8%).
Dr. Rini reported that he has a consulting role with Aveo, which sponsored the trial, and financial relationships with several other companies.
SOURCE: Rini BI et al. GUCS 2019, Abstract 541.
SAN FRANCISCO – The risk-benefit profile of the novel vascular endothelial growth factor (VEGF) inhibitor tivozanib when used as later-line therapy for renal cell carcinoma (RCC) appears to be similar to when it is used earlier, according to eagerly awaited results of the TIVO-3 trial.
Tivozanib, an oral tyrosine kinase inhibitor of the VEGF family of receptors with a long half-life, is designed both to optimize receptor blockade and minimize off-target toxicities, lead investigator Brian I. Rini, MD, said at the the 2019 Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Positive progression-free survival results of the TIVO-1 trial (J Clin Oncol. 2013;31:3791-9) led to approval of this agent as first-line therapy for RCC in Europe. However, the Food and Drug Administration rejected approval because of a trend toward poorer overall survival, which was likely related to imbalanced cross-over to active treatment.
The TIVO-3 trial enrolled 350 patients with advanced clear-cell RCC who had experienced failure of two or three prior regimens, including a VEGF receptor tyrosine kinase inhibitor. They were randomized evenly to open-label tivozanib (1.5 mg q.d., 3 weeks on and 1 week off) or sorafenib (Nexavar) (400 mg b.i.d. continuously).
Main results showed that progression-free survival was about 2 months longer with tivozanib, compared with sorafenib. The difference translated to a 27% reduction in risk of events, reported Dr. Rini, professor of medicine at Case Western Reserve University, Cleveland, and leader of the genitourinary oncology program at the Cleveland Clinic.
The benefit was similar for most subgroups. The tivozanib group had a higher incidence of hypertension, but lower incidences of diarrhea, hand-foot syndrome, and rash.
“Tivozanib significantly improved progression-free survival and objective response rate compared to sorafenib in patients with treatment-refractory advanced RCC. It was superior in the subset of patients previously treated with checkpoint inhibitors, as well as the subset who had had two prior TKIs,” Dr. Rini said. “Responses to tivozanib, perhaps most impressively, were more durable than those with sorafenib. Tivozanib was very well tolerated, with on-target hypertension as the most common adverse event, but lower rates of off-target toxicities.”
Overall survival data at present show a trend toward shorter survival with tivozanib, but are not yet mature. Definitive results are expected later this year.
Study details
About 60% of patients in TIVO-3 had received two prior lines of therapy, Dr. Rini reported at the symposium. The proportion stopping study treatment because of adverse events was 13% in the tivozanib group and 23% in the sorafenib group.
Median progression-free survival according to an independent review committee was 5.6 months and 3.9 months, respectively (hazard ratio, 0.73; P = .0165). Corresponding 1-year rates were 28% and 11%.
Among patients previously treated with an immune checkpoint inhibitor, median progression-free survival according to an independent review committee was 7.3 months with tivozanib and 5.1 months with sorafenib (hazard ratio, 0.55; P = .028). Corresponding 1-year rates were 35% and 4%.
In the entire trial population, the overall response rate was 18% for tivozanib versus 8% for sorafenib (P = .02). Median duration of response was not reached, compared with 5.7 months.
An interim analysis showed a median overall survival of 16.4 months in the tivozanib group and 19.7 months in the sorafenib group.
The rate of any-grade treatment-related adverse events was 84% with tivozanib and 94% with sorafenib. Tivozanib had a higher rate of grade 3 or 4 hypertension (20% vs. 14%), but lower rates of grade 3 or 4 diarrhea (2% vs. 9%), hand-foot syndrome (1% vs. 10%), and rash (0% vs. 8%).
Dr. Rini reported that he has a consulting role with Aveo, which sponsored the trial, and financial relationships with several other companies.
SOURCE: Rini BI et al. GUCS 2019, Abstract 541.
REPORTING FROM GUCS 2019
Dual-targeted CAR T shows ‘clinical signal’ in NHL
HOUSTON – A dual-targeted, locally manufactured, anti-CD19/CD20 chimeric antigen receptor (CAR) T-cell therapy was safe and produced ongoing complete responses in a phase 1 study of heavily pretreated non-Hodgkin lymphoma patients, an investigator reported.
The bispecific CAR T-cell product, designed to limit relapses due to loss of target antigen, was produced at the point of care with a 100% success rate for these heavily pretreated patients, the first of whom has now maintained a complete response for 19 months, said Parameswaran Hari, MD, of the Medical College of Wisconsin, Milwaukee.
“So far, this trial has demonstrated safety for this bispecific vector and suggests a clinical signal, with 7 out of 12 patients with ongoing CR, and with minimal toxicity,” Dr. Hari said at the Transplantation & Cellular Therapy Meetings.
“Point of care delivery, we think, allowed patients to have fresh infusion of CAR T cells, with the avoidance of cryopreservation,” added Dr. Hari, who presented the results on behalf of coinvestigators at the Medical College of Wisconsin and Lentigen Technology.
There was no grade 3 or 4 neurotoxicity or cytokine release syndrome among the 12 patients reported to date in the phase 1, dose-escalation trial, and no patient required intensive care, according to Dr. Hari. Grade 1 and 2 neurotoxicity occurred in two and one patients, respectively, while grade 1 and 2 cytokine release syndrome was observed in three patients each.
Among the 12 patients treated to date, the overall response rate was 81% at day 28, Dr. Hari said, noting that of 6 patients treated at the goal dose of 2.5 x 106 cells/kg, 5 remain in ongoing complete remission.
The median age of patients enrolled in the study was 55 years. Six patients had diffuse large B-cell lymphoma, five had mantle cell lymphoma, and two had chronic lymphocytic leukemia. All but one patient underwent fludarabine/cyclophosphamide lymphodepletion prior to receiving the inpatient CAR T-cell infusions, given over the course of 2 days.
Dr. Hari specifically highlighted the mantle cell lymphoma patient subset, noting that four out of five patients were in complete remission at day 28, and remained in ongoing complete remission at times ranging from 1 to 16 months.
With a set manufacturing time of 14 days, production was successful in all 12 patients, and 10 were able to receive fresh product, while 3 received cryopreserved product due to illness-related delays and a holiday, according to the investigators.
“The time to actual delivery of CAR T cell in the patient is actually shortened dramatically,” Dr. Hari said. “We hope to get it down to day 10.”
Local manufacturing can also reduce some costs associated with CAR T-cell production, such as shipping and courier costs, he added.
Taken together, these findings suggest that locally manufactured anti-CD19/CD20 CAR T cells could improve clinical outcomes for patients with relapsed and refractory B-cell NHL, with efficiency through point-of-care delivery, Dr. Hari concluded.
Further studies are planned to evaluate the efficacy of the product and to investigate the mechanism of relapse or progression in patients who experience treatment failure, he said.
Dr. Hari reported disclosures related to Juno, Kite, Spectrum, Janssen, Takeda, Celgene, and BMS. Several study coauthors reported that they were employed by Lentigen Technology, a Miltenyi Biotec Company.
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
SOURCE: Shah NN et al. TCT 2019, Abstract 80.
HOUSTON – A dual-targeted, locally manufactured, anti-CD19/CD20 chimeric antigen receptor (CAR) T-cell therapy was safe and produced ongoing complete responses in a phase 1 study of heavily pretreated non-Hodgkin lymphoma patients, an investigator reported.
The bispecific CAR T-cell product, designed to limit relapses due to loss of target antigen, was produced at the point of care with a 100% success rate for these heavily pretreated patients, the first of whom has now maintained a complete response for 19 months, said Parameswaran Hari, MD, of the Medical College of Wisconsin, Milwaukee.
“So far, this trial has demonstrated safety for this bispecific vector and suggests a clinical signal, with 7 out of 12 patients with ongoing CR, and with minimal toxicity,” Dr. Hari said at the Transplantation & Cellular Therapy Meetings.
“Point of care delivery, we think, allowed patients to have fresh infusion of CAR T cells, with the avoidance of cryopreservation,” added Dr. Hari, who presented the results on behalf of coinvestigators at the Medical College of Wisconsin and Lentigen Technology.
There was no grade 3 or 4 neurotoxicity or cytokine release syndrome among the 12 patients reported to date in the phase 1, dose-escalation trial, and no patient required intensive care, according to Dr. Hari. Grade 1 and 2 neurotoxicity occurred in two and one patients, respectively, while grade 1 and 2 cytokine release syndrome was observed in three patients each.
Among the 12 patients treated to date, the overall response rate was 81% at day 28, Dr. Hari said, noting that of 6 patients treated at the goal dose of 2.5 x 106 cells/kg, 5 remain in ongoing complete remission.
The median age of patients enrolled in the study was 55 years. Six patients had diffuse large B-cell lymphoma, five had mantle cell lymphoma, and two had chronic lymphocytic leukemia. All but one patient underwent fludarabine/cyclophosphamide lymphodepletion prior to receiving the inpatient CAR T-cell infusions, given over the course of 2 days.
Dr. Hari specifically highlighted the mantle cell lymphoma patient subset, noting that four out of five patients were in complete remission at day 28, and remained in ongoing complete remission at times ranging from 1 to 16 months.
With a set manufacturing time of 14 days, production was successful in all 12 patients, and 10 were able to receive fresh product, while 3 received cryopreserved product due to illness-related delays and a holiday, according to the investigators.
“The time to actual delivery of CAR T cell in the patient is actually shortened dramatically,” Dr. Hari said. “We hope to get it down to day 10.”
Local manufacturing can also reduce some costs associated with CAR T-cell production, such as shipping and courier costs, he added.
Taken together, these findings suggest that locally manufactured anti-CD19/CD20 CAR T cells could improve clinical outcomes for patients with relapsed and refractory B-cell NHL, with efficiency through point-of-care delivery, Dr. Hari concluded.
Further studies are planned to evaluate the efficacy of the product and to investigate the mechanism of relapse or progression in patients who experience treatment failure, he said.
Dr. Hari reported disclosures related to Juno, Kite, Spectrum, Janssen, Takeda, Celgene, and BMS. Several study coauthors reported that they were employed by Lentigen Technology, a Miltenyi Biotec Company.
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
SOURCE: Shah NN et al. TCT 2019, Abstract 80.
HOUSTON – A dual-targeted, locally manufactured, anti-CD19/CD20 chimeric antigen receptor (CAR) T-cell therapy was safe and produced ongoing complete responses in a phase 1 study of heavily pretreated non-Hodgkin lymphoma patients, an investigator reported.
The bispecific CAR T-cell product, designed to limit relapses due to loss of target antigen, was produced at the point of care with a 100% success rate for these heavily pretreated patients, the first of whom has now maintained a complete response for 19 months, said Parameswaran Hari, MD, of the Medical College of Wisconsin, Milwaukee.
“So far, this trial has demonstrated safety for this bispecific vector and suggests a clinical signal, with 7 out of 12 patients with ongoing CR, and with minimal toxicity,” Dr. Hari said at the Transplantation & Cellular Therapy Meetings.
“Point of care delivery, we think, allowed patients to have fresh infusion of CAR T cells, with the avoidance of cryopreservation,” added Dr. Hari, who presented the results on behalf of coinvestigators at the Medical College of Wisconsin and Lentigen Technology.
There was no grade 3 or 4 neurotoxicity or cytokine release syndrome among the 12 patients reported to date in the phase 1, dose-escalation trial, and no patient required intensive care, according to Dr. Hari. Grade 1 and 2 neurotoxicity occurred in two and one patients, respectively, while grade 1 and 2 cytokine release syndrome was observed in three patients each.
Among the 12 patients treated to date, the overall response rate was 81% at day 28, Dr. Hari said, noting that of 6 patients treated at the goal dose of 2.5 x 106 cells/kg, 5 remain in ongoing complete remission.
The median age of patients enrolled in the study was 55 years. Six patients had diffuse large B-cell lymphoma, five had mantle cell lymphoma, and two had chronic lymphocytic leukemia. All but one patient underwent fludarabine/cyclophosphamide lymphodepletion prior to receiving the inpatient CAR T-cell infusions, given over the course of 2 days.
Dr. Hari specifically highlighted the mantle cell lymphoma patient subset, noting that four out of five patients were in complete remission at day 28, and remained in ongoing complete remission at times ranging from 1 to 16 months.
With a set manufacturing time of 14 days, production was successful in all 12 patients, and 10 were able to receive fresh product, while 3 received cryopreserved product due to illness-related delays and a holiday, according to the investigators.
“The time to actual delivery of CAR T cell in the patient is actually shortened dramatically,” Dr. Hari said. “We hope to get it down to day 10.”
Local manufacturing can also reduce some costs associated with CAR T-cell production, such as shipping and courier costs, he added.
Taken together, these findings suggest that locally manufactured anti-CD19/CD20 CAR T cells could improve clinical outcomes for patients with relapsed and refractory B-cell NHL, with efficiency through point-of-care delivery, Dr. Hari concluded.
Further studies are planned to evaluate the efficacy of the product and to investigate the mechanism of relapse or progression in patients who experience treatment failure, he said.
Dr. Hari reported disclosures related to Juno, Kite, Spectrum, Janssen, Takeda, Celgene, and BMS. Several study coauthors reported that they were employed by Lentigen Technology, a Miltenyi Biotec Company.
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
SOURCE: Shah NN et al. TCT 2019, Abstract 80.
REPORTING FROM TCT 2019
AlloBMT should be option for older adults with hematologic malignancies
HOUSTON – Allogeneic blood and marrow transplantation (alloBMT) with posttransplant cyclophosphamide (PTCy) is relatively safe and feasible in septuagenarians with hematologic malignancies and should be considered in this population, findings from a review of 108 cases suggest.
The main difference in outcomes in older versus younger patients is a higher – but still low – rate of nonrelapse mortality (NRM) that appears to be due in part to age-related causes, Philip Hollingsworth Imus, MD, of Johns Hopkins University and the Sidney Kimmel Comprehensive Cancer Center, Baltimore, reported at the Transplantation & Cellular Therapy Meetings.
Overall survival (OS) among the 108 consecutive patients over age 70 years who underwent alloBMT at Johns Hopkins from Jan. 1, 2009, through March 31, 2018, was 64% at 1 year and 43% at 3 years, and progression-free survival (PFS) was 50% at 1 year and 32% at 3 years, Dr. Imus said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
NRM, especially later NRM, however, seemed to be increased, he said, noting that 6-month NRM was acceptable at 14%, but at 1 and 3 years it was 20% and 29%, respectively.
“In contrast to younger patients, [hematopoietic cell transplantation–specific comorbidity index] did not seem to predict NRM in our cohort,” he said.
Early causes of NRM were “in keeping with what we typically see,” and included pneumonia, sepsis, and a few cases of cytokine release syndrome, but later causes of NRM included some that are commonly seen in older patients without hematologic malignancies, such as secondary malignancies, dementia, falls, and cerebrovascular accidents, he said.
Based on frailty research suggesting that weight loss and gain may contribute to outcomes in older patients, Dr. Imus and his colleagues also performed a landmark analysis looking at weight change at 6 months versus pretreatment weight, and found that OS was 31 months in those with greater than the median loss of 4.4 kg, compared with 79 months in those who maintained or regained weight and who therefore had less than the median weight loss at 6 months.
The patients in this series had a median age of 72 years, and the refined disease risk index was low in 9% of patients, intermediate in 77%, and high or very high in 13%. All received nonmyeloablative (NMA) conditioning, PTCy and mycophenolate mofetil prophylaxis from day 5 to day 35, and either tacrolimus and sirolimus from day 5 to day 60-180.
The graft source was bone marrow in 75% of patients.
Engraftment in this population was acceptable and similar to that seen in younger patients; there were seven graft failures, with most occurring in patients who received bone marrow grafts, Dr. Imus said.
The incidence of severe, acute, and chronic graft-versus-host disease was about 10% for each, and was also similar to what is seen in younger patients, he noted.
The findings are of interest because many hematologic malignancies in septuagenarians are associated with very poor survival in the absence of alloBMT. It has only been in recent years that advances in NMA conditioning and haploidentical donor use have made alloBMT more available to older patients, he explained.
With increasing numbers of patients over age 70 years being offered the therapy – about 10% of adult alloBMT recipients at Johns Hopkins are over age 70 now – it was of interest to look at these outcomes, he said, adding that the findings demonstrate that hematologic malignancies in older patients are curable with alloBMT.
“Patients should not be denied therapy based on age alone,” Dr. Imus said, noting that in an effort to address the finding of increased graft failures in those receiving bone marrow grafts at Johns Hopkins, peripheral blood is now being used in certain cases.
“Nonrelapse mortality continues to be a major challenge in this group. It rivals relapse for poor outcomes, especially for late nonrelapse mortality,” he said, concluding that prospective studies looking at NRM are warranted.
Dr. Imus reported having no financial disclosures.
SOURCE: Imus P et al. TCT 2019, Abstract 42.
HOUSTON – Allogeneic blood and marrow transplantation (alloBMT) with posttransplant cyclophosphamide (PTCy) is relatively safe and feasible in septuagenarians with hematologic malignancies and should be considered in this population, findings from a review of 108 cases suggest.
The main difference in outcomes in older versus younger patients is a higher – but still low – rate of nonrelapse mortality (NRM) that appears to be due in part to age-related causes, Philip Hollingsworth Imus, MD, of Johns Hopkins University and the Sidney Kimmel Comprehensive Cancer Center, Baltimore, reported at the Transplantation & Cellular Therapy Meetings.
Overall survival (OS) among the 108 consecutive patients over age 70 years who underwent alloBMT at Johns Hopkins from Jan. 1, 2009, through March 31, 2018, was 64% at 1 year and 43% at 3 years, and progression-free survival (PFS) was 50% at 1 year and 32% at 3 years, Dr. Imus said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
NRM, especially later NRM, however, seemed to be increased, he said, noting that 6-month NRM was acceptable at 14%, but at 1 and 3 years it was 20% and 29%, respectively.
“In contrast to younger patients, [hematopoietic cell transplantation–specific comorbidity index] did not seem to predict NRM in our cohort,” he said.
Early causes of NRM were “in keeping with what we typically see,” and included pneumonia, sepsis, and a few cases of cytokine release syndrome, but later causes of NRM included some that are commonly seen in older patients without hematologic malignancies, such as secondary malignancies, dementia, falls, and cerebrovascular accidents, he said.
Based on frailty research suggesting that weight loss and gain may contribute to outcomes in older patients, Dr. Imus and his colleagues also performed a landmark analysis looking at weight change at 6 months versus pretreatment weight, and found that OS was 31 months in those with greater than the median loss of 4.4 kg, compared with 79 months in those who maintained or regained weight and who therefore had less than the median weight loss at 6 months.
The patients in this series had a median age of 72 years, and the refined disease risk index was low in 9% of patients, intermediate in 77%, and high or very high in 13%. All received nonmyeloablative (NMA) conditioning, PTCy and mycophenolate mofetil prophylaxis from day 5 to day 35, and either tacrolimus and sirolimus from day 5 to day 60-180.
The graft source was bone marrow in 75% of patients.
Engraftment in this population was acceptable and similar to that seen in younger patients; there were seven graft failures, with most occurring in patients who received bone marrow grafts, Dr. Imus said.
The incidence of severe, acute, and chronic graft-versus-host disease was about 10% for each, and was also similar to what is seen in younger patients, he noted.
The findings are of interest because many hematologic malignancies in septuagenarians are associated with very poor survival in the absence of alloBMT. It has only been in recent years that advances in NMA conditioning and haploidentical donor use have made alloBMT more available to older patients, he explained.
With increasing numbers of patients over age 70 years being offered the therapy – about 10% of adult alloBMT recipients at Johns Hopkins are over age 70 now – it was of interest to look at these outcomes, he said, adding that the findings demonstrate that hematologic malignancies in older patients are curable with alloBMT.
“Patients should not be denied therapy based on age alone,” Dr. Imus said, noting that in an effort to address the finding of increased graft failures in those receiving bone marrow grafts at Johns Hopkins, peripheral blood is now being used in certain cases.
“Nonrelapse mortality continues to be a major challenge in this group. It rivals relapse for poor outcomes, especially for late nonrelapse mortality,” he said, concluding that prospective studies looking at NRM are warranted.
Dr. Imus reported having no financial disclosures.
SOURCE: Imus P et al. TCT 2019, Abstract 42.
HOUSTON – Allogeneic blood and marrow transplantation (alloBMT) with posttransplant cyclophosphamide (PTCy) is relatively safe and feasible in septuagenarians with hematologic malignancies and should be considered in this population, findings from a review of 108 cases suggest.
The main difference in outcomes in older versus younger patients is a higher – but still low – rate of nonrelapse mortality (NRM) that appears to be due in part to age-related causes, Philip Hollingsworth Imus, MD, of Johns Hopkins University and the Sidney Kimmel Comprehensive Cancer Center, Baltimore, reported at the Transplantation & Cellular Therapy Meetings.
Overall survival (OS) among the 108 consecutive patients over age 70 years who underwent alloBMT at Johns Hopkins from Jan. 1, 2009, through March 31, 2018, was 64% at 1 year and 43% at 3 years, and progression-free survival (PFS) was 50% at 1 year and 32% at 3 years, Dr. Imus said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
NRM, especially later NRM, however, seemed to be increased, he said, noting that 6-month NRM was acceptable at 14%, but at 1 and 3 years it was 20% and 29%, respectively.
“In contrast to younger patients, [hematopoietic cell transplantation–specific comorbidity index] did not seem to predict NRM in our cohort,” he said.
Early causes of NRM were “in keeping with what we typically see,” and included pneumonia, sepsis, and a few cases of cytokine release syndrome, but later causes of NRM included some that are commonly seen in older patients without hematologic malignancies, such as secondary malignancies, dementia, falls, and cerebrovascular accidents, he said.
Based on frailty research suggesting that weight loss and gain may contribute to outcomes in older patients, Dr. Imus and his colleagues also performed a landmark analysis looking at weight change at 6 months versus pretreatment weight, and found that OS was 31 months in those with greater than the median loss of 4.4 kg, compared with 79 months in those who maintained or regained weight and who therefore had less than the median weight loss at 6 months.
The patients in this series had a median age of 72 years, and the refined disease risk index was low in 9% of patients, intermediate in 77%, and high or very high in 13%. All received nonmyeloablative (NMA) conditioning, PTCy and mycophenolate mofetil prophylaxis from day 5 to day 35, and either tacrolimus and sirolimus from day 5 to day 60-180.
The graft source was bone marrow in 75% of patients.
Engraftment in this population was acceptable and similar to that seen in younger patients; there were seven graft failures, with most occurring in patients who received bone marrow grafts, Dr. Imus said.
The incidence of severe, acute, and chronic graft-versus-host disease was about 10% for each, and was also similar to what is seen in younger patients, he noted.
The findings are of interest because many hematologic malignancies in septuagenarians are associated with very poor survival in the absence of alloBMT. It has only been in recent years that advances in NMA conditioning and haploidentical donor use have made alloBMT more available to older patients, he explained.
With increasing numbers of patients over age 70 years being offered the therapy – about 10% of adult alloBMT recipients at Johns Hopkins are over age 70 now – it was of interest to look at these outcomes, he said, adding that the findings demonstrate that hematologic malignancies in older patients are curable with alloBMT.
“Patients should not be denied therapy based on age alone,” Dr. Imus said, noting that in an effort to address the finding of increased graft failures in those receiving bone marrow grafts at Johns Hopkins, peripheral blood is now being used in certain cases.
“Nonrelapse mortality continues to be a major challenge in this group. It rivals relapse for poor outcomes, especially for late nonrelapse mortality,” he said, concluding that prospective studies looking at NRM are warranted.
Dr. Imus reported having no financial disclosures.
SOURCE: Imus P et al. TCT 2019, Abstract 42.
REPORTING FROM TCT 2019
Dupilumab relieves severe sinusitis with polyposis
SAN FRANCISCO – Dupilumab, an anti-inflammatory drug already approved for use in the United States, met its efficacy endpoints for treating chronic rhinosinusitis with nasal polyps in a pivotal trial with 276 patients.
The results make it likely that dupilumab (Dupixent) will receive a new indication from the Food and Drug Administration, pending similar results in a second pivotal trial for nasal polyps that researchers will report soon. Dupilumab, which works by blocking a receptor for both interleukin 4 and interleukin 13 and thereby shutting down type 2 inflammation, is already approved in the United States for treating atopic dermatitis and asthma.
Type 2 inflammation drives polyp formation in patients with chronic rhinosinusitis that can produce severe nasal congestion, breathing difficulty, and substantially reduced quality of life.
In the new trial, the drug showed efficacy by significantly improving both the nasal congestion score reported by patients and the nasal polyp score measured by sinus endoscopy after 24 weeks on treatment, when compared with control patients on placebo, Joseph K. Han, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Patients enrolled in the study had chronic, severe sinusitis and nasal polyps that remained uncontrolled despite prior surgery, for 75% of enrolled patients, or treatment with systemic corticosteroids, used on about 90% of the patients within the prior 2 years.
During the 24 weeks of treatment, 23% of patients in the control arm had to restart systemic corticosteroid treatment or have surgery, compared with 7% of patients on dupilumab treatment, a statistically significant difference.
The new drug is a “game changer,” for these patients, Dr. Han said in a video interview.
In some patients, treatment produced complete polyp resolution. He and his colleagues in the otolaryngology field are now trying to decide exactly which patients with polyps secondary to sinusitis will be good candidates for dupilumab after it receives an expected indication for shrinking nasal polyps.
Roughly 4% of the adult population has chronic rhinosinusitis that generates polyps. How many of these patients are affected severely enough to warrant dupilumab treatment is not clear, but will likely include several hundreds of thousands of U.S. adults, said Dr. Han, professor of otolaryngology and chief of the division of allergy at Eastern Virginia Medical School in Norfolk.
The SINUS-24 (A Controlled Clinical Study of Dupilumab in Patients With Nasal Polyps) trial enrolled patients at 76 sites in the United States and in several European countries. The study randomized 143 patients who received standard treatment plus a 300-mg dupilumab subcutaneous injection every 2 weeks, and 133 patients who received standard treatment plus placebo injections. Standard treatment included a nasal corticosteroid spray.
After 24 weeks of treatment, the endoscopically-measured nasal polyp score, which averaged about 6 at baseline on a scale of 0-8, fell by an average of 2.06 points, compared with controls, which was a statistically significant and clinically meaningful change, said Dr. Han.
The second primary endpoint, patient self-assessment of nasal congestion on a scale of 0-3, showed an average 0.89 improvement, compared with controls, which was also a statistically significant and meaningful change from the average baseline score of about 2.4.
Other efficacy measures also showed benefits from treatment, including a substantial improvement compared with controls in a quality-of-life measure. The safety profile was benign compared with placebo, and consistent with existing safety data for the drug.SINUS-24 was funded by Regeneron and Sanofi, the companies that market dupilumab. Dr. Han has been an adviser to Regeneron and Sanofi.
SOURCE: Han JK et al. AAAAI 2019, Abstract L4.
SAN FRANCISCO – Dupilumab, an anti-inflammatory drug already approved for use in the United States, met its efficacy endpoints for treating chronic rhinosinusitis with nasal polyps in a pivotal trial with 276 patients.
The results make it likely that dupilumab (Dupixent) will receive a new indication from the Food and Drug Administration, pending similar results in a second pivotal trial for nasal polyps that researchers will report soon. Dupilumab, which works by blocking a receptor for both interleukin 4 and interleukin 13 and thereby shutting down type 2 inflammation, is already approved in the United States for treating atopic dermatitis and asthma.
Type 2 inflammation drives polyp formation in patients with chronic rhinosinusitis that can produce severe nasal congestion, breathing difficulty, and substantially reduced quality of life.
In the new trial, the drug showed efficacy by significantly improving both the nasal congestion score reported by patients and the nasal polyp score measured by sinus endoscopy after 24 weeks on treatment, when compared with control patients on placebo, Joseph K. Han, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Patients enrolled in the study had chronic, severe sinusitis and nasal polyps that remained uncontrolled despite prior surgery, for 75% of enrolled patients, or treatment with systemic corticosteroids, used on about 90% of the patients within the prior 2 years.
During the 24 weeks of treatment, 23% of patients in the control arm had to restart systemic corticosteroid treatment or have surgery, compared with 7% of patients on dupilumab treatment, a statistically significant difference.
The new drug is a “game changer,” for these patients, Dr. Han said in a video interview.
In some patients, treatment produced complete polyp resolution. He and his colleagues in the otolaryngology field are now trying to decide exactly which patients with polyps secondary to sinusitis will be good candidates for dupilumab after it receives an expected indication for shrinking nasal polyps.
Roughly 4% of the adult population has chronic rhinosinusitis that generates polyps. How many of these patients are affected severely enough to warrant dupilumab treatment is not clear, but will likely include several hundreds of thousands of U.S. adults, said Dr. Han, professor of otolaryngology and chief of the division of allergy at Eastern Virginia Medical School in Norfolk.
The SINUS-24 (A Controlled Clinical Study of Dupilumab in Patients With Nasal Polyps) trial enrolled patients at 76 sites in the United States and in several European countries. The study randomized 143 patients who received standard treatment plus a 300-mg dupilumab subcutaneous injection every 2 weeks, and 133 patients who received standard treatment plus placebo injections. Standard treatment included a nasal corticosteroid spray.
After 24 weeks of treatment, the endoscopically-measured nasal polyp score, which averaged about 6 at baseline on a scale of 0-8, fell by an average of 2.06 points, compared with controls, which was a statistically significant and clinically meaningful change, said Dr. Han.
The second primary endpoint, patient self-assessment of nasal congestion on a scale of 0-3, showed an average 0.89 improvement, compared with controls, which was also a statistically significant and meaningful change from the average baseline score of about 2.4.
Other efficacy measures also showed benefits from treatment, including a substantial improvement compared with controls in a quality-of-life measure. The safety profile was benign compared with placebo, and consistent with existing safety data for the drug.SINUS-24 was funded by Regeneron and Sanofi, the companies that market dupilumab. Dr. Han has been an adviser to Regeneron and Sanofi.
SOURCE: Han JK et al. AAAAI 2019, Abstract L4.
SAN FRANCISCO – Dupilumab, an anti-inflammatory drug already approved for use in the United States, met its efficacy endpoints for treating chronic rhinosinusitis with nasal polyps in a pivotal trial with 276 patients.
The results make it likely that dupilumab (Dupixent) will receive a new indication from the Food and Drug Administration, pending similar results in a second pivotal trial for nasal polyps that researchers will report soon. Dupilumab, which works by blocking a receptor for both interleukin 4 and interleukin 13 and thereby shutting down type 2 inflammation, is already approved in the United States for treating atopic dermatitis and asthma.
Type 2 inflammation drives polyp formation in patients with chronic rhinosinusitis that can produce severe nasal congestion, breathing difficulty, and substantially reduced quality of life.
In the new trial, the drug showed efficacy by significantly improving both the nasal congestion score reported by patients and the nasal polyp score measured by sinus endoscopy after 24 weeks on treatment, when compared with control patients on placebo, Joseph K. Han, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Patients enrolled in the study had chronic, severe sinusitis and nasal polyps that remained uncontrolled despite prior surgery, for 75% of enrolled patients, or treatment with systemic corticosteroids, used on about 90% of the patients within the prior 2 years.
During the 24 weeks of treatment, 23% of patients in the control arm had to restart systemic corticosteroid treatment or have surgery, compared with 7% of patients on dupilumab treatment, a statistically significant difference.
The new drug is a “game changer,” for these patients, Dr. Han said in a video interview.
In some patients, treatment produced complete polyp resolution. He and his colleagues in the otolaryngology field are now trying to decide exactly which patients with polyps secondary to sinusitis will be good candidates for dupilumab after it receives an expected indication for shrinking nasal polyps.
Roughly 4% of the adult population has chronic rhinosinusitis that generates polyps. How many of these patients are affected severely enough to warrant dupilumab treatment is not clear, but will likely include several hundreds of thousands of U.S. adults, said Dr. Han, professor of otolaryngology and chief of the division of allergy at Eastern Virginia Medical School in Norfolk.
The SINUS-24 (A Controlled Clinical Study of Dupilumab in Patients With Nasal Polyps) trial enrolled patients at 76 sites in the United States and in several European countries. The study randomized 143 patients who received standard treatment plus a 300-mg dupilumab subcutaneous injection every 2 weeks, and 133 patients who received standard treatment plus placebo injections. Standard treatment included a nasal corticosteroid spray.
After 24 weeks of treatment, the endoscopically-measured nasal polyp score, which averaged about 6 at baseline on a scale of 0-8, fell by an average of 2.06 points, compared with controls, which was a statistically significant and clinically meaningful change, said Dr. Han.
The second primary endpoint, patient self-assessment of nasal congestion on a scale of 0-3, showed an average 0.89 improvement, compared with controls, which was also a statistically significant and meaningful change from the average baseline score of about 2.4.
Other efficacy measures also showed benefits from treatment, including a substantial improvement compared with controls in a quality-of-life measure. The safety profile was benign compared with placebo, and consistent with existing safety data for the drug.SINUS-24 was funded by Regeneron and Sanofi, the companies that market dupilumab. Dr. Han has been an adviser to Regeneron and Sanofi.
SOURCE: Han JK et al. AAAAI 2019, Abstract L4.
REPORTING FROM AAAAI
Getting Started on SVSConnect
Complete your profile, post your first message, upload a resource or find another member – getting started has never been easier on SVSConnect. New “easy” buttons on the home page will help guide users as they begin activity on the online community. After getting started, you’ll be able to join discussions on hot topics, including carotid surveillance imaging or office based labs. Log in with your SVS credentials to begin. If you encounter sign-in difficulties, email communications@vascularsociety.org or call 312-334-2300.
Complete your profile, post your first message, upload a resource or find another member – getting started has never been easier on SVSConnect. New “easy” buttons on the home page will help guide users as they begin activity on the online community. After getting started, you’ll be able to join discussions on hot topics, including carotid surveillance imaging or office based labs. Log in with your SVS credentials to begin. If you encounter sign-in difficulties, email communications@vascularsociety.org or call 312-334-2300.
Complete your profile, post your first message, upload a resource or find another member – getting started has never been easier on SVSConnect. New “easy” buttons on the home page will help guide users as they begin activity on the online community. After getting started, you’ll be able to join discussions on hot topics, including carotid surveillance imaging or office based labs. Log in with your SVS credentials to begin. If you encounter sign-in difficulties, email communications@vascularsociety.org or call 312-334-2300.
MRD negativity linked to survival in MM after auto-HCT
HOUSTON – Minimal residual disease (MRD) negativity by multiparameter flow cytometry was linked to survival benefit in multiple myeloma patients undergoing autologous transplantation, according to results of the first U.S.-based study evaluating this endpoint as part of a national randomized clinical trial.
MRD-negative status was prognostic for improved progression-free survival at all time points measured over the course of 1 year post transplant, in this ancillary study of patients in the randomized, 3-arm STAMiNA trial.
Moreover, there was an overall survival benefit for MRD-negative status at 1 year post transplant, investigator Theresa A. Hahn, PhD, of Roswell Park Comprehensive Cancer Center, Buffalo, N.Y., reported at the Transplantation & Cellular Therapy Meetings.
There was no significant difference in rate of conversion to MRD negativity in the arms of the trial, which evaluated several different upfront approaches to autologous hematopoietic stem cell transplantation (HCT).
Assessments of MRD beyond 1 year post transplant may be valuable in future trials, Dr. Hahn said.
“Trials are needed incorporating MRD as an endpoint for treatment decisions to augment, change, or discontinue therapy,” she added.
Results of the ancillary study known as PRIMeR (Prognostic Immunophenotyping for Myeloma Response) included 445 patients from STAMiNA who underwent MRD assessment at baseline, prior to maintenance, and at 1 year post transplantation.
As part of the overall STAMiNA trial, they were randomized to single autologous hematopoietic cell transplantation (HCT); autologous HCT followed by a second autologous HCT (tandem autologous HCT); or single autologous HCT followed by four cycles of consolidation with lenalidomide, bortezomib, and dexamethasone (RVD). All three arms continued on lenalidomide maintenance after those interventions.
Overall results of the STAMiNA trial, previously reported, showed no significant differences in progression-free survival or overall survival among the three transplant strategies (J Clin Oncol. 2019 Jan 17. doi: 10.1200/JCO.18.00685).
In this PRIMeR substudy, by contrast, progression-free survival was significantly increased for patients who were MRD negative at all three time points measured, Dr. Hahn reported, while overall survival was significantly improved based on MRD status measured at the 1-year time point.
The rate of MRD negativity did not differ significantly between arms at baseline or premaintenance time points, Dr. Hahn said. Those rates were 42%, 47%, and 40%, respectively, for the single transplant, tandem transplant, and single transplant plus consolidation arms, while the premaintenance MRD negativity rates were 77%, 83%, and 76%.
At 1 year, MRD negativity rates were significantly different between arms, but only in the intent-to-treat analysis.
Most of the difference was due to an increased rate of MRD negativity in the tandem-transplant arm, compared to a single auto-transplant. However, about 30% of patients in the tandem transplant arm did not receive the therapy, so in the analysis by actual treatment received, the rates of MRD negativity were 81% for single transplant, 90% for tandem transplant, and 85% for single transplant plus consolidation (P = 0.2).
Dr. Hahn said she and her colleagues will be updating their analysis of the PRIMeR study to assess the predictive value of MRD status in patients who were negative at all time points evaluated, versus those who converted to MRD negativity at the 1-year analysis.
The MRD assessments used in this trial have been incorporated into the recently completed BMT CTN 1401 trial and the ongoing BMT CTN 1302 study of allogeneic HCT plus ixazomib in high-risk myeloma, she added.
Dr. Hahn reported research funding from Celgene and the National Institutes of Health.
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
SOURCE: Hahn TE et al. TCT 2019, Abstract 6.
HOUSTON – Minimal residual disease (MRD) negativity by multiparameter flow cytometry was linked to survival benefit in multiple myeloma patients undergoing autologous transplantation, according to results of the first U.S.-based study evaluating this endpoint as part of a national randomized clinical trial.
MRD-negative status was prognostic for improved progression-free survival at all time points measured over the course of 1 year post transplant, in this ancillary study of patients in the randomized, 3-arm STAMiNA trial.
Moreover, there was an overall survival benefit for MRD-negative status at 1 year post transplant, investigator Theresa A. Hahn, PhD, of Roswell Park Comprehensive Cancer Center, Buffalo, N.Y., reported at the Transplantation & Cellular Therapy Meetings.
There was no significant difference in rate of conversion to MRD negativity in the arms of the trial, which evaluated several different upfront approaches to autologous hematopoietic stem cell transplantation (HCT).
Assessments of MRD beyond 1 year post transplant may be valuable in future trials, Dr. Hahn said.
“Trials are needed incorporating MRD as an endpoint for treatment decisions to augment, change, or discontinue therapy,” she added.
Results of the ancillary study known as PRIMeR (Prognostic Immunophenotyping for Myeloma Response) included 445 patients from STAMiNA who underwent MRD assessment at baseline, prior to maintenance, and at 1 year post transplantation.
As part of the overall STAMiNA trial, they were randomized to single autologous hematopoietic cell transplantation (HCT); autologous HCT followed by a second autologous HCT (tandem autologous HCT); or single autologous HCT followed by four cycles of consolidation with lenalidomide, bortezomib, and dexamethasone (RVD). All three arms continued on lenalidomide maintenance after those interventions.
Overall results of the STAMiNA trial, previously reported, showed no significant differences in progression-free survival or overall survival among the three transplant strategies (J Clin Oncol. 2019 Jan 17. doi: 10.1200/JCO.18.00685).
In this PRIMeR substudy, by contrast, progression-free survival was significantly increased for patients who were MRD negative at all three time points measured, Dr. Hahn reported, while overall survival was significantly improved based on MRD status measured at the 1-year time point.
The rate of MRD negativity did not differ significantly between arms at baseline or premaintenance time points, Dr. Hahn said. Those rates were 42%, 47%, and 40%, respectively, for the single transplant, tandem transplant, and single transplant plus consolidation arms, while the premaintenance MRD negativity rates were 77%, 83%, and 76%.
At 1 year, MRD negativity rates were significantly different between arms, but only in the intent-to-treat analysis.
Most of the difference was due to an increased rate of MRD negativity in the tandem-transplant arm, compared to a single auto-transplant. However, about 30% of patients in the tandem transplant arm did not receive the therapy, so in the analysis by actual treatment received, the rates of MRD negativity were 81% for single transplant, 90% for tandem transplant, and 85% for single transplant plus consolidation (P = 0.2).
Dr. Hahn said she and her colleagues will be updating their analysis of the PRIMeR study to assess the predictive value of MRD status in patients who were negative at all time points evaluated, versus those who converted to MRD negativity at the 1-year analysis.
The MRD assessments used in this trial have been incorporated into the recently completed BMT CTN 1401 trial and the ongoing BMT CTN 1302 study of allogeneic HCT plus ixazomib in high-risk myeloma, she added.
Dr. Hahn reported research funding from Celgene and the National Institutes of Health.
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
SOURCE: Hahn TE et al. TCT 2019, Abstract 6.
HOUSTON – Minimal residual disease (MRD) negativity by multiparameter flow cytometry was linked to survival benefit in multiple myeloma patients undergoing autologous transplantation, according to results of the first U.S.-based study evaluating this endpoint as part of a national randomized clinical trial.
MRD-negative status was prognostic for improved progression-free survival at all time points measured over the course of 1 year post transplant, in this ancillary study of patients in the randomized, 3-arm STAMiNA trial.
Moreover, there was an overall survival benefit for MRD-negative status at 1 year post transplant, investigator Theresa A. Hahn, PhD, of Roswell Park Comprehensive Cancer Center, Buffalo, N.Y., reported at the Transplantation & Cellular Therapy Meetings.
There was no significant difference in rate of conversion to MRD negativity in the arms of the trial, which evaluated several different upfront approaches to autologous hematopoietic stem cell transplantation (HCT).
Assessments of MRD beyond 1 year post transplant may be valuable in future trials, Dr. Hahn said.
“Trials are needed incorporating MRD as an endpoint for treatment decisions to augment, change, or discontinue therapy,” she added.
Results of the ancillary study known as PRIMeR (Prognostic Immunophenotyping for Myeloma Response) included 445 patients from STAMiNA who underwent MRD assessment at baseline, prior to maintenance, and at 1 year post transplantation.
As part of the overall STAMiNA trial, they were randomized to single autologous hematopoietic cell transplantation (HCT); autologous HCT followed by a second autologous HCT (tandem autologous HCT); or single autologous HCT followed by four cycles of consolidation with lenalidomide, bortezomib, and dexamethasone (RVD). All three arms continued on lenalidomide maintenance after those interventions.
Overall results of the STAMiNA trial, previously reported, showed no significant differences in progression-free survival or overall survival among the three transplant strategies (J Clin Oncol. 2019 Jan 17. doi: 10.1200/JCO.18.00685).
In this PRIMeR substudy, by contrast, progression-free survival was significantly increased for patients who were MRD negative at all three time points measured, Dr. Hahn reported, while overall survival was significantly improved based on MRD status measured at the 1-year time point.
The rate of MRD negativity did not differ significantly between arms at baseline or premaintenance time points, Dr. Hahn said. Those rates were 42%, 47%, and 40%, respectively, for the single transplant, tandem transplant, and single transplant plus consolidation arms, while the premaintenance MRD negativity rates were 77%, 83%, and 76%.
At 1 year, MRD negativity rates were significantly different between arms, but only in the intent-to-treat analysis.
Most of the difference was due to an increased rate of MRD negativity in the tandem-transplant arm, compared to a single auto-transplant. However, about 30% of patients in the tandem transplant arm did not receive the therapy, so in the analysis by actual treatment received, the rates of MRD negativity were 81% for single transplant, 90% for tandem transplant, and 85% for single transplant plus consolidation (P = 0.2).
Dr. Hahn said she and her colleagues will be updating their analysis of the PRIMeR study to assess the predictive value of MRD status in patients who were negative at all time points evaluated, versus those who converted to MRD negativity at the 1-year analysis.
The MRD assessments used in this trial have been incorporated into the recently completed BMT CTN 1401 trial and the ongoing BMT CTN 1302 study of allogeneic HCT plus ixazomib in high-risk myeloma, she added.
Dr. Hahn reported research funding from Celgene and the National Institutes of Health.
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
SOURCE: Hahn TE et al. TCT 2019, Abstract 6.
REPORTING FROM TCT 2019
Anti-GM-CSF antibody reduced CAR T-cell toxicity
HOUSTON – Neutralizing granulocyte-macrophage colony-stimulating factor (GM-CSF) may be an effective strategy not only to manage toxicities associated with chimeric antigen receptor (CAR) T-cell therapy, but also to enhance CAR-T cell function, an investigator reported at the Transplantation & Cellular Therapy Meetings.
The GM-CSF targeted monoclonal antibody lenzilumab reduced neurotoxicity and cytokine release syndrome (CRS) related to CD19-targeted CAR T-cell therapy in a patient-derived xenograft model, said investigator Rosalie M. Sterner, an MD-PhD student in the department of immunology at Mayo Clinic, Rochester, Minn.
Other investigations showed that neutralizing or knocking out GM-CSF enhanced the antitumor functions of the CAR T cells, Ms. Sterner said in a podium presentation at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
“GM-CSF blockade does not impair CAR T-cell effector function, and in fact, enhances CAR T-cell effector functions in certain models, and actually can help to ameliorate CAR T-cell associated toxicities,” Ms. Sterner said.
Based on these early findings, the investigators have designed a phase 2 clinical trial to see if lenzilumab can prevent CAR T cell-related toxicities in patients with diffuse large B-cell lymphoma.
GM-CSF, a cytokine produced by T cells and myeloid cells, is the most statistically significantly elevated serum marker in patients with severe neurotoxicity related to CAR T-cell therapy, Ms. Sterner told attendees.
Investigations have shown that the combination of lenzilumab plus CD19-targeted T-cell therapy did not impair CAR T-cell function in vivo or in vitro, she said.
In other studies, they investigated the impact of GM-CSF neutralization in mice engrafted with primary acute lymphocytic leukemia (ALL) blasts and treated with high doses of CD19 CAR T-cells, lenzilumab, and a murine GM-CSF blocking antibody to neutralize the mouse GM-CSF. That strategy prevented weight loss, decreased myeloid cytokines, reduced cerebral edema, and enhanced disease control, Ms. Sterner said.
Investigators also reported on CD19 CAR T-cells with reduced GM-CSF secretion due to CRISPR/Cas9 gene editing of the GM-CSF gene during the CAR T-cell manufacturing process. Xenograft model results showed a slight enhancement of disease control for those GM-CSF knockout CAR T cells versus standard CAR T cells.
More details of the investigations were recently published in Blood (2019;133:697-709).
Taken together, the investigations highlight GM-CSF inhibition as a novel approach to reducing neurotoxicity and CRS that may also enhance CAR T-cell effector functions, Ms. Sterner said.
Ms. Sterner reported having no financial disclosures related to her presentation.
SOURCE: Sterner R et al. TCT 2019, Abstract 5.
HOUSTON – Neutralizing granulocyte-macrophage colony-stimulating factor (GM-CSF) may be an effective strategy not only to manage toxicities associated with chimeric antigen receptor (CAR) T-cell therapy, but also to enhance CAR-T cell function, an investigator reported at the Transplantation & Cellular Therapy Meetings.
The GM-CSF targeted monoclonal antibody lenzilumab reduced neurotoxicity and cytokine release syndrome (CRS) related to CD19-targeted CAR T-cell therapy in a patient-derived xenograft model, said investigator Rosalie M. Sterner, an MD-PhD student in the department of immunology at Mayo Clinic, Rochester, Minn.
Other investigations showed that neutralizing or knocking out GM-CSF enhanced the antitumor functions of the CAR T cells, Ms. Sterner said in a podium presentation at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
“GM-CSF blockade does not impair CAR T-cell effector function, and in fact, enhances CAR T-cell effector functions in certain models, and actually can help to ameliorate CAR T-cell associated toxicities,” Ms. Sterner said.
Based on these early findings, the investigators have designed a phase 2 clinical trial to see if lenzilumab can prevent CAR T cell-related toxicities in patients with diffuse large B-cell lymphoma.
GM-CSF, a cytokine produced by T cells and myeloid cells, is the most statistically significantly elevated serum marker in patients with severe neurotoxicity related to CAR T-cell therapy, Ms. Sterner told attendees.
Investigations have shown that the combination of lenzilumab plus CD19-targeted T-cell therapy did not impair CAR T-cell function in vivo or in vitro, she said.
In other studies, they investigated the impact of GM-CSF neutralization in mice engrafted with primary acute lymphocytic leukemia (ALL) blasts and treated with high doses of CD19 CAR T-cells, lenzilumab, and a murine GM-CSF blocking antibody to neutralize the mouse GM-CSF. That strategy prevented weight loss, decreased myeloid cytokines, reduced cerebral edema, and enhanced disease control, Ms. Sterner said.
Investigators also reported on CD19 CAR T-cells with reduced GM-CSF secretion due to CRISPR/Cas9 gene editing of the GM-CSF gene during the CAR T-cell manufacturing process. Xenograft model results showed a slight enhancement of disease control for those GM-CSF knockout CAR T cells versus standard CAR T cells.
More details of the investigations were recently published in Blood (2019;133:697-709).
Taken together, the investigations highlight GM-CSF inhibition as a novel approach to reducing neurotoxicity and CRS that may also enhance CAR T-cell effector functions, Ms. Sterner said.
Ms. Sterner reported having no financial disclosures related to her presentation.
SOURCE: Sterner R et al. TCT 2019, Abstract 5.
HOUSTON – Neutralizing granulocyte-macrophage colony-stimulating factor (GM-CSF) may be an effective strategy not only to manage toxicities associated with chimeric antigen receptor (CAR) T-cell therapy, but also to enhance CAR-T cell function, an investigator reported at the Transplantation & Cellular Therapy Meetings.
The GM-CSF targeted monoclonal antibody lenzilumab reduced neurotoxicity and cytokine release syndrome (CRS) related to CD19-targeted CAR T-cell therapy in a patient-derived xenograft model, said investigator Rosalie M. Sterner, an MD-PhD student in the department of immunology at Mayo Clinic, Rochester, Minn.
Other investigations showed that neutralizing or knocking out GM-CSF enhanced the antitumor functions of the CAR T cells, Ms. Sterner said in a podium presentation at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
“GM-CSF blockade does not impair CAR T-cell effector function, and in fact, enhances CAR T-cell effector functions in certain models, and actually can help to ameliorate CAR T-cell associated toxicities,” Ms. Sterner said.
Based on these early findings, the investigators have designed a phase 2 clinical trial to see if lenzilumab can prevent CAR T cell-related toxicities in patients with diffuse large B-cell lymphoma.
GM-CSF, a cytokine produced by T cells and myeloid cells, is the most statistically significantly elevated serum marker in patients with severe neurotoxicity related to CAR T-cell therapy, Ms. Sterner told attendees.
Investigations have shown that the combination of lenzilumab plus CD19-targeted T-cell therapy did not impair CAR T-cell function in vivo or in vitro, she said.
In other studies, they investigated the impact of GM-CSF neutralization in mice engrafted with primary acute lymphocytic leukemia (ALL) blasts and treated with high doses of CD19 CAR T-cells, lenzilumab, and a murine GM-CSF blocking antibody to neutralize the mouse GM-CSF. That strategy prevented weight loss, decreased myeloid cytokines, reduced cerebral edema, and enhanced disease control, Ms. Sterner said.
Investigators also reported on CD19 CAR T-cells with reduced GM-CSF secretion due to CRISPR/Cas9 gene editing of the GM-CSF gene during the CAR T-cell manufacturing process. Xenograft model results showed a slight enhancement of disease control for those GM-CSF knockout CAR T cells versus standard CAR T cells.
More details of the investigations were recently published in Blood (2019;133:697-709).
Taken together, the investigations highlight GM-CSF inhibition as a novel approach to reducing neurotoxicity and CRS that may also enhance CAR T-cell effector functions, Ms. Sterner said.
Ms. Sterner reported having no financial disclosures related to her presentation.
SOURCE: Sterner R et al. TCT 2019, Abstract 5.
REPORTING FROM TCT 2019
Female Sexual Dysfunction
Treosulfan may become standard in allo-HCT for AML/MDS
HOUSTON – A treosulfan-based conditioning regimen could become standard prior to allogeneic transplant in elderly or comorbid patients with acute myeloid leukemia or myelodysplastic syndromes, according to the lead investigator in a phase 3 trial.
The treosulfan/fludarabine myeloablative conditioning regimen had noninferior event-free survival, compared with a reduced-intensity busulfan-based regimen in the large, randomized trial that included elderly patients and those with multiple comorbidities, said researcher Dietrich Wilhelm Beelen, MD, PhD.
The experimental regimen was superior to busulfan in overall survival, nonrelapse mortality, and complete donor chimerism in the trial, added Dr. Beelen, who is with the department of bone marrow transplantation at the West German Cancer Center, University Hospital of Essen, Germany.
“The study results point to a potential benefit of the treosulfan/fludarabine regimen, while the early safety profile, engraftment kinetics, acute or chronic graft-versus-host-disease (GvHD), and the relapse risk of both regimens appear comparable,” Dr. Beelen said at the Transplantation & Cellular Therapy Meetings.
Allogeneic hematopoietic cell transplantation (HCT) is challenging in elderly and comorbid patients, who have an increased risk of nonrelapse mortality with standard myeloablative regimens, according to Dr. Beelen, who presented results on behalf of investigators from the international MC-FludT.14/L Study Group.
Their phase 3 randomized trial included patients who were 50-70 years of age, or who had a Hematopoietic Cell Transplantation Comorbidity Index of 2 or greater. The final analysis included 551 patients (352 with AML and 199 with MDS).
The primary endpoint of the study was event-free survival at 2 years. That endpoint comprised relapse/progression of disease, graft failure, or death.
Patient enrollment was terminated early the MC-FludT.14/L study following an interim analysis that investigators said “clearly demonstrated” the noninferiority of the treosulfan/fludarabine regimen versus the reduced intensity busulfan/fludarabine regimen.
In the final analysis, event-free survival at 2 years was about 14.5 percentage points higher in the treosulfan group, at 65.7% versus 51.2% (P = .0000001), Dr. Beelen reported at the meeting.
A number of other secondary endpoints also favored treosulfan/fludarabine over busulfan, including overall survival (P = .0037), nonrelapse mortality (P = .0343), and survival free of chronic GvHD or relapse (P = .0030).
These results help establish the new treosulfan/fludarabine regimen as a “relatively well-tolerable and effective preparative regimen” in elderly or comorbid AML/MDS patients, Dr. Beelen said.
However, treosulfan has not been authorized for use in allogeneic HCT conditioning regimens, and so should be considered experimental in this setting, he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Beelen reported honoraria, travel support, and trial documentation support provided by medac GmbH, which sponsored the trial.
SOURCE: Beelen DW et al. TCT 2019, Abstract 4.
HOUSTON – A treosulfan-based conditioning regimen could become standard prior to allogeneic transplant in elderly or comorbid patients with acute myeloid leukemia or myelodysplastic syndromes, according to the lead investigator in a phase 3 trial.
The treosulfan/fludarabine myeloablative conditioning regimen had noninferior event-free survival, compared with a reduced-intensity busulfan-based regimen in the large, randomized trial that included elderly patients and those with multiple comorbidities, said researcher Dietrich Wilhelm Beelen, MD, PhD.
The experimental regimen was superior to busulfan in overall survival, nonrelapse mortality, and complete donor chimerism in the trial, added Dr. Beelen, who is with the department of bone marrow transplantation at the West German Cancer Center, University Hospital of Essen, Germany.
“The study results point to a potential benefit of the treosulfan/fludarabine regimen, while the early safety profile, engraftment kinetics, acute or chronic graft-versus-host-disease (GvHD), and the relapse risk of both regimens appear comparable,” Dr. Beelen said at the Transplantation & Cellular Therapy Meetings.
Allogeneic hematopoietic cell transplantation (HCT) is challenging in elderly and comorbid patients, who have an increased risk of nonrelapse mortality with standard myeloablative regimens, according to Dr. Beelen, who presented results on behalf of investigators from the international MC-FludT.14/L Study Group.
Their phase 3 randomized trial included patients who were 50-70 years of age, or who had a Hematopoietic Cell Transplantation Comorbidity Index of 2 or greater. The final analysis included 551 patients (352 with AML and 199 with MDS).
The primary endpoint of the study was event-free survival at 2 years. That endpoint comprised relapse/progression of disease, graft failure, or death.
Patient enrollment was terminated early the MC-FludT.14/L study following an interim analysis that investigators said “clearly demonstrated” the noninferiority of the treosulfan/fludarabine regimen versus the reduced intensity busulfan/fludarabine regimen.
In the final analysis, event-free survival at 2 years was about 14.5 percentage points higher in the treosulfan group, at 65.7% versus 51.2% (P = .0000001), Dr. Beelen reported at the meeting.
A number of other secondary endpoints also favored treosulfan/fludarabine over busulfan, including overall survival (P = .0037), nonrelapse mortality (P = .0343), and survival free of chronic GvHD or relapse (P = .0030).
These results help establish the new treosulfan/fludarabine regimen as a “relatively well-tolerable and effective preparative regimen” in elderly or comorbid AML/MDS patients, Dr. Beelen said.
However, treosulfan has not been authorized for use in allogeneic HCT conditioning regimens, and so should be considered experimental in this setting, he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Beelen reported honoraria, travel support, and trial documentation support provided by medac GmbH, which sponsored the trial.
SOURCE: Beelen DW et al. TCT 2019, Abstract 4.
HOUSTON – A treosulfan-based conditioning regimen could become standard prior to allogeneic transplant in elderly or comorbid patients with acute myeloid leukemia or myelodysplastic syndromes, according to the lead investigator in a phase 3 trial.
The treosulfan/fludarabine myeloablative conditioning regimen had noninferior event-free survival, compared with a reduced-intensity busulfan-based regimen in the large, randomized trial that included elderly patients and those with multiple comorbidities, said researcher Dietrich Wilhelm Beelen, MD, PhD.
The experimental regimen was superior to busulfan in overall survival, nonrelapse mortality, and complete donor chimerism in the trial, added Dr. Beelen, who is with the department of bone marrow transplantation at the West German Cancer Center, University Hospital of Essen, Germany.
“The study results point to a potential benefit of the treosulfan/fludarabine regimen, while the early safety profile, engraftment kinetics, acute or chronic graft-versus-host-disease (GvHD), and the relapse risk of both regimens appear comparable,” Dr. Beelen said at the Transplantation & Cellular Therapy Meetings.
Allogeneic hematopoietic cell transplantation (HCT) is challenging in elderly and comorbid patients, who have an increased risk of nonrelapse mortality with standard myeloablative regimens, according to Dr. Beelen, who presented results on behalf of investigators from the international MC-FludT.14/L Study Group.
Their phase 3 randomized trial included patients who were 50-70 years of age, or who had a Hematopoietic Cell Transplantation Comorbidity Index of 2 or greater. The final analysis included 551 patients (352 with AML and 199 with MDS).
The primary endpoint of the study was event-free survival at 2 years. That endpoint comprised relapse/progression of disease, graft failure, or death.
Patient enrollment was terminated early the MC-FludT.14/L study following an interim analysis that investigators said “clearly demonstrated” the noninferiority of the treosulfan/fludarabine regimen versus the reduced intensity busulfan/fludarabine regimen.
In the final analysis, event-free survival at 2 years was about 14.5 percentage points higher in the treosulfan group, at 65.7% versus 51.2% (P = .0000001), Dr. Beelen reported at the meeting.
A number of other secondary endpoints also favored treosulfan/fludarabine over busulfan, including overall survival (P = .0037), nonrelapse mortality (P = .0343), and survival free of chronic GvHD or relapse (P = .0030).
These results help establish the new treosulfan/fludarabine regimen as a “relatively well-tolerable and effective preparative regimen” in elderly or comorbid AML/MDS patients, Dr. Beelen said.
However, treosulfan has not been authorized for use in allogeneic HCT conditioning regimens, and so should be considered experimental in this setting, he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Beelen reported honoraria, travel support, and trial documentation support provided by medac GmbH, which sponsored the trial.
SOURCE: Beelen DW et al. TCT 2019, Abstract 4.
REPORTING FROM TCT 2019
Ixekizumab psoriasis outcomes, sliced and diced
WAIKOLOA, HAWAII – The highly selective interleukin-17A subunit inhibitor in the long-term extension phase of the randomized, controlled UNCOVER-3 (NCT01646177) trial, Craig L. Leonardi, MD, reported at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
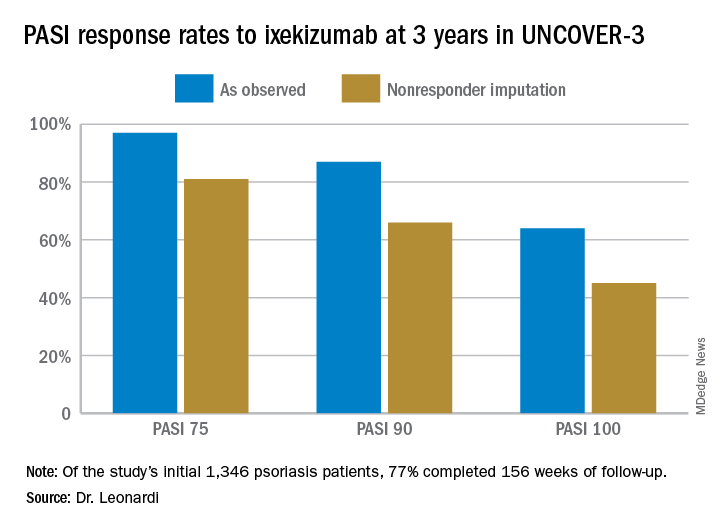
However, the strict inclusion and exclusion criteria employed in randomized trials such as this raise questions about the broader applicability of the results in real-world clinical practice. So separately at the Hawaii seminar, Dr. Leonardi presented a single-center retrospective observational cohort study of the rapidity and duration of response to ixekizumab in his own clinical practice after the biologic received Food and Drug Administration marketing approval. Those results, too, were impressive and, in his view, highly generalizable.
“It is expected that this study cohort is generally representative of patients who are routinely seen at dermatology referral practices in the U.S.,” commented Dr. Leonardi, of Saint Louis University.
UNCOVER-3 included 1,346 psoriasis patients initially randomized 2:2:2:1 to double-blind subcutaneous ixekizumab (Taltz) at 80 mg either every 2 weeks or every 4 weeks after a 160-mg loading dose; subcutaneous etanercept at 50 mg twice weekly; or placebo for 12 weeks, followed by a switch to ixekizumab at 80 mg every 4 weeks from week 12 out to 3 years. The long-term efficacy analysis was restricted to patients who received the biologic according to what ultimately became the approved dosing schedule: a 160-mg loading dose, followed by 80 mg every 2 weeks through week 12, then 80 mg every 4 weeks. The safety analysis, in contrast, included everybody.
Dr. Leonardi presented the efficacy data using several different statistical methodologies, thereby providing an instructive lesson regarding the importance of examining the fine print when viewing clinical trial results. At one extreme is the as-observed analysis. Under this methodology, if a patient dropped out of UNCOVER-3 at, for example, week 11, the last measurement of treatment response, recorded at week 8, is carried forward by investigators and assumed to be valid for the rest of the study. Since week 8 may have been the last time the patient was doing well on the drug, the as-observed analysis can create a distorted overly favorable picture of the drug’s performance.
“Patients fall out because the drug isn’t working well or they’re having a side effect, so over time, you tend to enrich for patients who are doing very well with the as-observed analysis,” the dermatologist explained.
Historically, many industry-sponsored clinical trials reported efficacy outcomes using the as-observed analysis; however, the FDA is increasingly unwilling to accept that approach as the sole analytic method.
At the other extreme is the nonresponder imputation method.
“This is the most stringent statistical package that exists. In fact, when a patient isn’t observed at one of the observation points – for example, at week 8 say the patient has a flat tire and can’t make it to the clinic – they’re counted as a treatment failure. So it’s a very tough statistical package,” according to Dr. Leonardi.
Seventy-seven percent of the initial 1,346 randomized patients in UNCOVER-3 completed 156 weeks of follow-up. To illustrate the importance of paying attention to the details of statistical methodology utilized in reporting efficacy outcomes, he noted that the PASI 75 rate at 156 weeks in study completers on the approved dosing regimen was 97% by the as-observed method, dropping to a still robust 81% by nonresponder imputation. The PASI 90 and -100 rates and static Physician’s Global Assessment (sPGA) results followed suit (see graphic).
Real-world performance
Dr. Leonard’s analysis of ixekizumab’s performance in his own practice included 106 patients placed on the drug following its FDA approval in March 2016, 74% of whom were still on the drug 12 months later. The cohort had a mean disease duration of 15 years. Three-quarters of them had previously received biologic therapy for their psoriasis, most often a tumor necrosis factor inhibitor. The study efficacy endpoints were the sPGA and Dermatology Life Quality Index (DLQI).
Already at 1 month, 30% of ixekizumab-treated patients had an sPGA score of 0, meaning their skin was totally clear. Another 29% had an sPGA of 1, meaning almost clear. At 3 months, 53% of patients had an sPGA of 0 and 21% had an sPGA of 1. Among patients on treatment at 12 months, the rates were 39% and 24% for sPGAs of 0 and 1, respectively. And in patients with an sPGA of 0/1 at 3 months, 73% maintained that score at 12 months, including 47% with an sPGA of 0.
A DLQI score of 0/1, indicative of little or no disease effect upon a patient’s life, was present in 63% of ixekizumab-treated patients at 1 month, 84% at 3 months, and 73% at 12 months.
The value in pushing for PASI 100
The ixekizumab experience in the phase-3 UNCOVER clinical trial program provided the first-ever evidence that incrementally improving psoriasis also provides stepwise improvement in DLQI, a key patient-reported outcome. At week 12 under double-blind conditions, only 4% of ixekizumab-treated patients with less than a PASI 50 response had a DLQI of 0/1. The rate rose to 18.8% in those with a PASI 50 to less than PASI 75 response. In patients with a week-12 PASI 75 to less than PASI 90 response, the DLQI 0/1 rate climbed to 52.3%. At a PASI 90 to less than PASI 100 response, the rate was 66.9%. And 82.9% of patients with a PASI 100 had a DLQI of 0/1. Every step of the way, those DLQI rates were significantly different from each other.
These data are “fascinating,” Dr. Leonardi commented. “If you ever get any inquiries from the friendly insurance carrier and they want to know if you’re improving your patient’s life, this is the kind of data that supports that they’re being improved dramatically.”
Dr. Leonardi noted that ixekizumab isn’t unique in its high rate of clinical effectiveness. That distinction is shared by the other approved IL-17 inhibitors, secukinumab (Cosentyx) and brodalumab (Siliq), as well as the IL-23 inhibitor guselkumab (Tremfya). He refers to these biologics collectively as “high-performance skin-clearance drugs.” He has calculated the number needed to treat (NNT) to achieve a PASI 100 response – complete clearance of the disease – based upon clinical trial data filed with the FDA and/or in the package inserts. The numbers are eye-opening: an NTT of 2.6 for ixekizumab based upon data from the UNCOVER-2 trial, 2.4 for brodalumab, 2.7 for guselkumab, and 3.6 for secukinumab. To help put that into perspective, the NNTs for methotrexate and etanercept (Enbrel) – not so long ago considered state of the art medications for moderate to severe psoriasis – are 25 and 23.3, respectively.
The UNCOVER trial portfolio and Dr. Leonardi’s single-center retrospective study were funded by Eli Lilly, which markets ixekizumab. He reported serving as a consultant to and receiving research funding from that company and more than a dozen others.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – The highly selective interleukin-17A subunit inhibitor in the long-term extension phase of the randomized, controlled UNCOVER-3 (NCT01646177) trial, Craig L. Leonardi, MD, reported at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
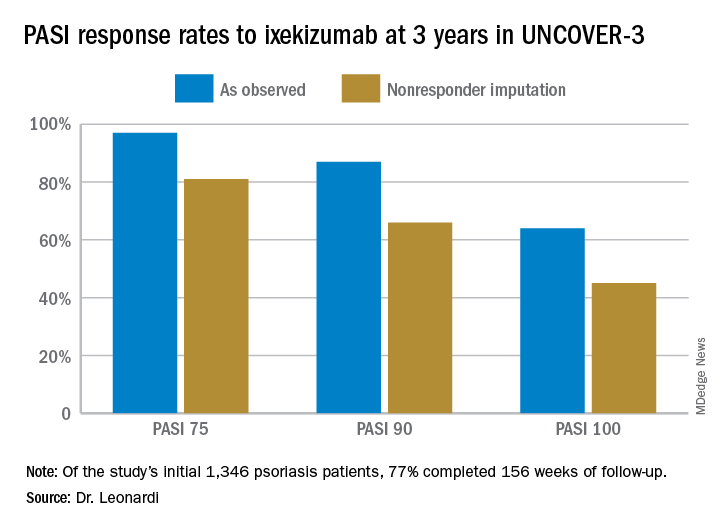
However, the strict inclusion and exclusion criteria employed in randomized trials such as this raise questions about the broader applicability of the results in real-world clinical practice. So separately at the Hawaii seminar, Dr. Leonardi presented a single-center retrospective observational cohort study of the rapidity and duration of response to ixekizumab in his own clinical practice after the biologic received Food and Drug Administration marketing approval. Those results, too, were impressive and, in his view, highly generalizable.
“It is expected that this study cohort is generally representative of patients who are routinely seen at dermatology referral practices in the U.S.,” commented Dr. Leonardi, of Saint Louis University.
UNCOVER-3 included 1,346 psoriasis patients initially randomized 2:2:2:1 to double-blind subcutaneous ixekizumab (Taltz) at 80 mg either every 2 weeks or every 4 weeks after a 160-mg loading dose; subcutaneous etanercept at 50 mg twice weekly; or placebo for 12 weeks, followed by a switch to ixekizumab at 80 mg every 4 weeks from week 12 out to 3 years. The long-term efficacy analysis was restricted to patients who received the biologic according to what ultimately became the approved dosing schedule: a 160-mg loading dose, followed by 80 mg every 2 weeks through week 12, then 80 mg every 4 weeks. The safety analysis, in contrast, included everybody.
Dr. Leonardi presented the efficacy data using several different statistical methodologies, thereby providing an instructive lesson regarding the importance of examining the fine print when viewing clinical trial results. At one extreme is the as-observed analysis. Under this methodology, if a patient dropped out of UNCOVER-3 at, for example, week 11, the last measurement of treatment response, recorded at week 8, is carried forward by investigators and assumed to be valid for the rest of the study. Since week 8 may have been the last time the patient was doing well on the drug, the as-observed analysis can create a distorted overly favorable picture of the drug’s performance.
“Patients fall out because the drug isn’t working well or they’re having a side effect, so over time, you tend to enrich for patients who are doing very well with the as-observed analysis,” the dermatologist explained.
Historically, many industry-sponsored clinical trials reported efficacy outcomes using the as-observed analysis; however, the FDA is increasingly unwilling to accept that approach as the sole analytic method.
At the other extreme is the nonresponder imputation method.
“This is the most stringent statistical package that exists. In fact, when a patient isn’t observed at one of the observation points – for example, at week 8 say the patient has a flat tire and can’t make it to the clinic – they’re counted as a treatment failure. So it’s a very tough statistical package,” according to Dr. Leonardi.
Seventy-seven percent of the initial 1,346 randomized patients in UNCOVER-3 completed 156 weeks of follow-up. To illustrate the importance of paying attention to the details of statistical methodology utilized in reporting efficacy outcomes, he noted that the PASI 75 rate at 156 weeks in study completers on the approved dosing regimen was 97% by the as-observed method, dropping to a still robust 81% by nonresponder imputation. The PASI 90 and -100 rates and static Physician’s Global Assessment (sPGA) results followed suit (see graphic).
Real-world performance
Dr. Leonard’s analysis of ixekizumab’s performance in his own practice included 106 patients placed on the drug following its FDA approval in March 2016, 74% of whom were still on the drug 12 months later. The cohort had a mean disease duration of 15 years. Three-quarters of them had previously received biologic therapy for their psoriasis, most often a tumor necrosis factor inhibitor. The study efficacy endpoints were the sPGA and Dermatology Life Quality Index (DLQI).
Already at 1 month, 30% of ixekizumab-treated patients had an sPGA score of 0, meaning their skin was totally clear. Another 29% had an sPGA of 1, meaning almost clear. At 3 months, 53% of patients had an sPGA of 0 and 21% had an sPGA of 1. Among patients on treatment at 12 months, the rates were 39% and 24% for sPGAs of 0 and 1, respectively. And in patients with an sPGA of 0/1 at 3 months, 73% maintained that score at 12 months, including 47% with an sPGA of 0.
A DLQI score of 0/1, indicative of little or no disease effect upon a patient’s life, was present in 63% of ixekizumab-treated patients at 1 month, 84% at 3 months, and 73% at 12 months.
The value in pushing for PASI 100
The ixekizumab experience in the phase-3 UNCOVER clinical trial program provided the first-ever evidence that incrementally improving psoriasis also provides stepwise improvement in DLQI, a key patient-reported outcome. At week 12 under double-blind conditions, only 4% of ixekizumab-treated patients with less than a PASI 50 response had a DLQI of 0/1. The rate rose to 18.8% in those with a PASI 50 to less than PASI 75 response. In patients with a week-12 PASI 75 to less than PASI 90 response, the DLQI 0/1 rate climbed to 52.3%. At a PASI 90 to less than PASI 100 response, the rate was 66.9%. And 82.9% of patients with a PASI 100 had a DLQI of 0/1. Every step of the way, those DLQI rates were significantly different from each other.
These data are “fascinating,” Dr. Leonardi commented. “If you ever get any inquiries from the friendly insurance carrier and they want to know if you’re improving your patient’s life, this is the kind of data that supports that they’re being improved dramatically.”
Dr. Leonardi noted that ixekizumab isn’t unique in its high rate of clinical effectiveness. That distinction is shared by the other approved IL-17 inhibitors, secukinumab (Cosentyx) and brodalumab (Siliq), as well as the IL-23 inhibitor guselkumab (Tremfya). He refers to these biologics collectively as “high-performance skin-clearance drugs.” He has calculated the number needed to treat (NNT) to achieve a PASI 100 response – complete clearance of the disease – based upon clinical trial data filed with the FDA and/or in the package inserts. The numbers are eye-opening: an NTT of 2.6 for ixekizumab based upon data from the UNCOVER-2 trial, 2.4 for brodalumab, 2.7 for guselkumab, and 3.6 for secukinumab. To help put that into perspective, the NNTs for methotrexate and etanercept (Enbrel) – not so long ago considered state of the art medications for moderate to severe psoriasis – are 25 and 23.3, respectively.
The UNCOVER trial portfolio and Dr. Leonardi’s single-center retrospective study were funded by Eli Lilly, which markets ixekizumab. He reported serving as a consultant to and receiving research funding from that company and more than a dozen others.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – The highly selective interleukin-17A subunit inhibitor in the long-term extension phase of the randomized, controlled UNCOVER-3 (NCT01646177) trial, Craig L. Leonardi, MD, reported at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
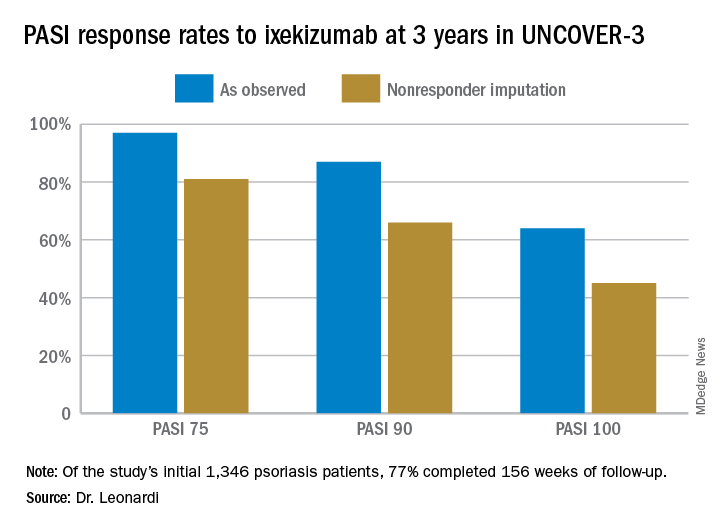
However, the strict inclusion and exclusion criteria employed in randomized trials such as this raise questions about the broader applicability of the results in real-world clinical practice. So separately at the Hawaii seminar, Dr. Leonardi presented a single-center retrospective observational cohort study of the rapidity and duration of response to ixekizumab in his own clinical practice after the biologic received Food and Drug Administration marketing approval. Those results, too, were impressive and, in his view, highly generalizable.
“It is expected that this study cohort is generally representative of patients who are routinely seen at dermatology referral practices in the U.S.,” commented Dr. Leonardi, of Saint Louis University.
UNCOVER-3 included 1,346 psoriasis patients initially randomized 2:2:2:1 to double-blind subcutaneous ixekizumab (Taltz) at 80 mg either every 2 weeks or every 4 weeks after a 160-mg loading dose; subcutaneous etanercept at 50 mg twice weekly; or placebo for 12 weeks, followed by a switch to ixekizumab at 80 mg every 4 weeks from week 12 out to 3 years. The long-term efficacy analysis was restricted to patients who received the biologic according to what ultimately became the approved dosing schedule: a 160-mg loading dose, followed by 80 mg every 2 weeks through week 12, then 80 mg every 4 weeks. The safety analysis, in contrast, included everybody.
Dr. Leonardi presented the efficacy data using several different statistical methodologies, thereby providing an instructive lesson regarding the importance of examining the fine print when viewing clinical trial results. At one extreme is the as-observed analysis. Under this methodology, if a patient dropped out of UNCOVER-3 at, for example, week 11, the last measurement of treatment response, recorded at week 8, is carried forward by investigators and assumed to be valid for the rest of the study. Since week 8 may have been the last time the patient was doing well on the drug, the as-observed analysis can create a distorted overly favorable picture of the drug’s performance.
“Patients fall out because the drug isn’t working well or they’re having a side effect, so over time, you tend to enrich for patients who are doing very well with the as-observed analysis,” the dermatologist explained.
Historically, many industry-sponsored clinical trials reported efficacy outcomes using the as-observed analysis; however, the FDA is increasingly unwilling to accept that approach as the sole analytic method.
At the other extreme is the nonresponder imputation method.
“This is the most stringent statistical package that exists. In fact, when a patient isn’t observed at one of the observation points – for example, at week 8 say the patient has a flat tire and can’t make it to the clinic – they’re counted as a treatment failure. So it’s a very tough statistical package,” according to Dr. Leonardi.
Seventy-seven percent of the initial 1,346 randomized patients in UNCOVER-3 completed 156 weeks of follow-up. To illustrate the importance of paying attention to the details of statistical methodology utilized in reporting efficacy outcomes, he noted that the PASI 75 rate at 156 weeks in study completers on the approved dosing regimen was 97% by the as-observed method, dropping to a still robust 81% by nonresponder imputation. The PASI 90 and -100 rates and static Physician’s Global Assessment (sPGA) results followed suit (see graphic).
Real-world performance
Dr. Leonard’s analysis of ixekizumab’s performance in his own practice included 106 patients placed on the drug following its FDA approval in March 2016, 74% of whom were still on the drug 12 months later. The cohort had a mean disease duration of 15 years. Three-quarters of them had previously received biologic therapy for their psoriasis, most often a tumor necrosis factor inhibitor. The study efficacy endpoints were the sPGA and Dermatology Life Quality Index (DLQI).
Already at 1 month, 30% of ixekizumab-treated patients had an sPGA score of 0, meaning their skin was totally clear. Another 29% had an sPGA of 1, meaning almost clear. At 3 months, 53% of patients had an sPGA of 0 and 21% had an sPGA of 1. Among patients on treatment at 12 months, the rates were 39% and 24% for sPGAs of 0 and 1, respectively. And in patients with an sPGA of 0/1 at 3 months, 73% maintained that score at 12 months, including 47% with an sPGA of 0.
A DLQI score of 0/1, indicative of little or no disease effect upon a patient’s life, was present in 63% of ixekizumab-treated patients at 1 month, 84% at 3 months, and 73% at 12 months.
The value in pushing for PASI 100
The ixekizumab experience in the phase-3 UNCOVER clinical trial program provided the first-ever evidence that incrementally improving psoriasis also provides stepwise improvement in DLQI, a key patient-reported outcome. At week 12 under double-blind conditions, only 4% of ixekizumab-treated patients with less than a PASI 50 response had a DLQI of 0/1. The rate rose to 18.8% in those with a PASI 50 to less than PASI 75 response. In patients with a week-12 PASI 75 to less than PASI 90 response, the DLQI 0/1 rate climbed to 52.3%. At a PASI 90 to less than PASI 100 response, the rate was 66.9%. And 82.9% of patients with a PASI 100 had a DLQI of 0/1. Every step of the way, those DLQI rates were significantly different from each other.
These data are “fascinating,” Dr. Leonardi commented. “If you ever get any inquiries from the friendly insurance carrier and they want to know if you’re improving your patient’s life, this is the kind of data that supports that they’re being improved dramatically.”
Dr. Leonardi noted that ixekizumab isn’t unique in its high rate of clinical effectiveness. That distinction is shared by the other approved IL-17 inhibitors, secukinumab (Cosentyx) and brodalumab (Siliq), as well as the IL-23 inhibitor guselkumab (Tremfya). He refers to these biologics collectively as “high-performance skin-clearance drugs.” He has calculated the number needed to treat (NNT) to achieve a PASI 100 response – complete clearance of the disease – based upon clinical trial data filed with the FDA and/or in the package inserts. The numbers are eye-opening: an NTT of 2.6 for ixekizumab based upon data from the UNCOVER-2 trial, 2.4 for brodalumab, 2.7 for guselkumab, and 3.6 for secukinumab. To help put that into perspective, the NNTs for methotrexate and etanercept (Enbrel) – not so long ago considered state of the art medications for moderate to severe psoriasis – are 25 and 23.3, respectively.
The UNCOVER trial portfolio and Dr. Leonardi’s single-center retrospective study were funded by Eli Lilly, which markets ixekizumab. He reported serving as a consultant to and receiving research funding from that company and more than a dozen others.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
REPORTING FROM SDEF HAWAII DERMATOLOGY SEMINAR












