User login
From the Washington Office: A guide to in-district meetings with your representatives and senators
WHY should surgeons take time out of their busy schedules to meet with legislators?
To become an effective surgeon advocate, nothing is more important than establishing a personal relationship with your legislators. Conversely, to a legislator, there is nothing more valuable than the input and support of constituents. After all, constituents are VOTERS. Meeting with policy makers and/or their staff is extremely valuable in advancing the overall advocacy agenda of The American College of Surgeons and provides surgeons with the opportunity to develop key contacts in the offices of their legislators.
WHERE do such meetings take place?
All U.S. Representatives and Senators have one or more offices for constituent service in their home districts or states. These offices serve as a readily accessible meeting point. As an alternative, legislators frequently will schedule meetings with constituents in mutually convenient locations such as a coffee shop, or during a local legislative event such as a town hall.
WHEN is it most feasible to schedule in-district meetings?
You might be surprised to discover how much time is allotted by both the House and Senate for in-district work periods. Typical times include periods around President’s Day in February, Easter/Passover in March/April, Memorial Day, Independence Day, and summer recess (late July and the month of August). If Congress does not officially adjourn in early October, additional work periods include time around Columbus Day in October, Veteran’s Day in November, and Thanksgiving. Congress will usually adjourn for the year in December. A specific schedule for each legislative body for the year 2016 can be found at:
House of Representatives: http://www.majorityleader.gov/wp-content/uploads/2011/07/2016_ANNUAL_CALENDAR.pdf
Senate: http://www.senate.gov/legislative/resources/pdf/2016_calendar.pdf
HOW does one schedule an in-district meeting?
To set up a meeting you should first search the websites of your representatives (www.house.gov) and senators (www.senate.gov) for information as to the preferred scheduling procedures. Expect each office’s procedure to be a bit different. You will be asked to provide your name, address, and basic contact information as well as to briefly describe what issue(s) you wish to discuss. Be sure to mention that you are a surgeon and also whether you have previously met with the representative or senator.
If several days pass and staff from the office have not followed up, you should not hesitate to call or contact the office again. Remember, persistence is key! Keep in mind that legislators typically maintain busy schedules during the in-district work period and accordingly, the scheduled appointment time will be brief and subject to change, perhaps on short notice.
If you experience difficulty or simply would like to have assistance in scheduling an in-district meeting, staff in the ACS Division of Advocacy and Health Policy are available to assist and may be contacted by e-mail at surgeonsvoice.org.
WHAT should one discuss?
As a surgeon advocate, your most powerful tool is frequent contact and meetings with your elected officials. Meetings provide an opportunity to offer knowledge and perspective to educate legislators on key topics important to ensuring access to quality surgical care. Your personal experience brings a personal, human touch to issues about which legislators only have knowledge based upon raw numbers and impersonal policy jargon. Most legislators, as well as their staff, will be grateful to have the reliable resource of a constituent’s experience and perspective on complicated medical issues.
To maximize the opportunity for a successful meeting and thereby lay the foundation for the development of a mutually beneficial future relationship, I would offer the following three tips:
1) KNOW YOUR LEGISLATOR: Visit your legislators’ websites, read their biographies, ascertain to what congressional committees they are assigned, and what leadership roles they may have. All of this serves to help determine what issues are important to them and what positions they have previously taken on such issues.
2) KNOW YOUR ISSUE and be able to FRAME IT: Nothing substitutes for a solid knowledge base of the issue and the position you are trying to convey. Be focused and resist the temptation to try to cover too many topics in any one visit. When presenting your argument, “frame it” in layman’s terms much as you would explain it to a patient. Including examples of real-life, anecdotal experiences demonstrating how the status quo or the proposed legislation (depending upon the circumstance) is impacting providers and patients is particularly important.
3) HAVE AN ASK: It is imperative that you always be clear with your legislators about what you want them to do. This serves to reinforce the importance of your having taken time out of your schedule to communicate with them and also serves to hold the legislator accountable. “Asks” can be as specific as a request to cosponsor and support legislation or simply making the offer to serve as a resource to them as a constituent with expertise in health care.
Lastly, I would respectfully request that when surgeons meet with their legislators they inform the ACS Division of Advocacy and Health Policy. Having basic information about the outcome of the meeting, whether knowing that the legislator committed to taking a specific action or knowing that the legislator has requested additional information, is incredibly valuable to us in our ongoing advocacy efforts on behalf of surgeons and their patients here in Washington, DC.
Until next month ….
Dr. Patrick V. Bailey is an ACS Fellow, a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy, in the ACS offices in Washington, D.C.
WHY should surgeons take time out of their busy schedules to meet with legislators?
To become an effective surgeon advocate, nothing is more important than establishing a personal relationship with your legislators. Conversely, to a legislator, there is nothing more valuable than the input and support of constituents. After all, constituents are VOTERS. Meeting with policy makers and/or their staff is extremely valuable in advancing the overall advocacy agenda of The American College of Surgeons and provides surgeons with the opportunity to develop key contacts in the offices of their legislators.
WHERE do such meetings take place?
All U.S. Representatives and Senators have one or more offices for constituent service in their home districts or states. These offices serve as a readily accessible meeting point. As an alternative, legislators frequently will schedule meetings with constituents in mutually convenient locations such as a coffee shop, or during a local legislative event such as a town hall.
WHEN is it most feasible to schedule in-district meetings?
You might be surprised to discover how much time is allotted by both the House and Senate for in-district work periods. Typical times include periods around President’s Day in February, Easter/Passover in March/April, Memorial Day, Independence Day, and summer recess (late July and the month of August). If Congress does not officially adjourn in early October, additional work periods include time around Columbus Day in October, Veteran’s Day in November, and Thanksgiving. Congress will usually adjourn for the year in December. A specific schedule for each legislative body for the year 2016 can be found at:
House of Representatives: http://www.majorityleader.gov/wp-content/uploads/2011/07/2016_ANNUAL_CALENDAR.pdf
Senate: http://www.senate.gov/legislative/resources/pdf/2016_calendar.pdf
HOW does one schedule an in-district meeting?
To set up a meeting you should first search the websites of your representatives (www.house.gov) and senators (www.senate.gov) for information as to the preferred scheduling procedures. Expect each office’s procedure to be a bit different. You will be asked to provide your name, address, and basic contact information as well as to briefly describe what issue(s) you wish to discuss. Be sure to mention that you are a surgeon and also whether you have previously met with the representative or senator.
If several days pass and staff from the office have not followed up, you should not hesitate to call or contact the office again. Remember, persistence is key! Keep in mind that legislators typically maintain busy schedules during the in-district work period and accordingly, the scheduled appointment time will be brief and subject to change, perhaps on short notice.
If you experience difficulty or simply would like to have assistance in scheduling an in-district meeting, staff in the ACS Division of Advocacy and Health Policy are available to assist and may be contacted by e-mail at surgeonsvoice.org.
WHAT should one discuss?
As a surgeon advocate, your most powerful tool is frequent contact and meetings with your elected officials. Meetings provide an opportunity to offer knowledge and perspective to educate legislators on key topics important to ensuring access to quality surgical care. Your personal experience brings a personal, human touch to issues about which legislators only have knowledge based upon raw numbers and impersonal policy jargon. Most legislators, as well as their staff, will be grateful to have the reliable resource of a constituent’s experience and perspective on complicated medical issues.
To maximize the opportunity for a successful meeting and thereby lay the foundation for the development of a mutually beneficial future relationship, I would offer the following three tips:
1) KNOW YOUR LEGISLATOR: Visit your legislators’ websites, read their biographies, ascertain to what congressional committees they are assigned, and what leadership roles they may have. All of this serves to help determine what issues are important to them and what positions they have previously taken on such issues.
2) KNOW YOUR ISSUE and be able to FRAME IT: Nothing substitutes for a solid knowledge base of the issue and the position you are trying to convey. Be focused and resist the temptation to try to cover too many topics in any one visit. When presenting your argument, “frame it” in layman’s terms much as you would explain it to a patient. Including examples of real-life, anecdotal experiences demonstrating how the status quo or the proposed legislation (depending upon the circumstance) is impacting providers and patients is particularly important.
3) HAVE AN ASK: It is imperative that you always be clear with your legislators about what you want them to do. This serves to reinforce the importance of your having taken time out of your schedule to communicate with them and also serves to hold the legislator accountable. “Asks” can be as specific as a request to cosponsor and support legislation or simply making the offer to serve as a resource to them as a constituent with expertise in health care.
Lastly, I would respectfully request that when surgeons meet with their legislators they inform the ACS Division of Advocacy and Health Policy. Having basic information about the outcome of the meeting, whether knowing that the legislator committed to taking a specific action or knowing that the legislator has requested additional information, is incredibly valuable to us in our ongoing advocacy efforts on behalf of surgeons and their patients here in Washington, DC.
Until next month ….
Dr. Patrick V. Bailey is an ACS Fellow, a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy, in the ACS offices in Washington, D.C.
WHY should surgeons take time out of their busy schedules to meet with legislators?
To become an effective surgeon advocate, nothing is more important than establishing a personal relationship with your legislators. Conversely, to a legislator, there is nothing more valuable than the input and support of constituents. After all, constituents are VOTERS. Meeting with policy makers and/or their staff is extremely valuable in advancing the overall advocacy agenda of The American College of Surgeons and provides surgeons with the opportunity to develop key contacts in the offices of their legislators.
WHERE do such meetings take place?
All U.S. Representatives and Senators have one or more offices for constituent service in their home districts or states. These offices serve as a readily accessible meeting point. As an alternative, legislators frequently will schedule meetings with constituents in mutually convenient locations such as a coffee shop, or during a local legislative event such as a town hall.
WHEN is it most feasible to schedule in-district meetings?
You might be surprised to discover how much time is allotted by both the House and Senate for in-district work periods. Typical times include periods around President’s Day in February, Easter/Passover in March/April, Memorial Day, Independence Day, and summer recess (late July and the month of August). If Congress does not officially adjourn in early October, additional work periods include time around Columbus Day in October, Veteran’s Day in November, and Thanksgiving. Congress will usually adjourn for the year in December. A specific schedule for each legislative body for the year 2016 can be found at:
House of Representatives: http://www.majorityleader.gov/wp-content/uploads/2011/07/2016_ANNUAL_CALENDAR.pdf
Senate: http://www.senate.gov/legislative/resources/pdf/2016_calendar.pdf
HOW does one schedule an in-district meeting?
To set up a meeting you should first search the websites of your representatives (www.house.gov) and senators (www.senate.gov) for information as to the preferred scheduling procedures. Expect each office’s procedure to be a bit different. You will be asked to provide your name, address, and basic contact information as well as to briefly describe what issue(s) you wish to discuss. Be sure to mention that you are a surgeon and also whether you have previously met with the representative or senator.
If several days pass and staff from the office have not followed up, you should not hesitate to call or contact the office again. Remember, persistence is key! Keep in mind that legislators typically maintain busy schedules during the in-district work period and accordingly, the scheduled appointment time will be brief and subject to change, perhaps on short notice.
If you experience difficulty or simply would like to have assistance in scheduling an in-district meeting, staff in the ACS Division of Advocacy and Health Policy are available to assist and may be contacted by e-mail at surgeonsvoice.org.
WHAT should one discuss?
As a surgeon advocate, your most powerful tool is frequent contact and meetings with your elected officials. Meetings provide an opportunity to offer knowledge and perspective to educate legislators on key topics important to ensuring access to quality surgical care. Your personal experience brings a personal, human touch to issues about which legislators only have knowledge based upon raw numbers and impersonal policy jargon. Most legislators, as well as their staff, will be grateful to have the reliable resource of a constituent’s experience and perspective on complicated medical issues.
To maximize the opportunity for a successful meeting and thereby lay the foundation for the development of a mutually beneficial future relationship, I would offer the following three tips:
1) KNOW YOUR LEGISLATOR: Visit your legislators’ websites, read their biographies, ascertain to what congressional committees they are assigned, and what leadership roles they may have. All of this serves to help determine what issues are important to them and what positions they have previously taken on such issues.
2) KNOW YOUR ISSUE and be able to FRAME IT: Nothing substitutes for a solid knowledge base of the issue and the position you are trying to convey. Be focused and resist the temptation to try to cover too many topics in any one visit. When presenting your argument, “frame it” in layman’s terms much as you would explain it to a patient. Including examples of real-life, anecdotal experiences demonstrating how the status quo or the proposed legislation (depending upon the circumstance) is impacting providers and patients is particularly important.
3) HAVE AN ASK: It is imperative that you always be clear with your legislators about what you want them to do. This serves to reinforce the importance of your having taken time out of your schedule to communicate with them and also serves to hold the legislator accountable. “Asks” can be as specific as a request to cosponsor and support legislation or simply making the offer to serve as a resource to them as a constituent with expertise in health care.
Lastly, I would respectfully request that when surgeons meet with their legislators they inform the ACS Division of Advocacy and Health Policy. Having basic information about the outcome of the meeting, whether knowing that the legislator committed to taking a specific action or knowing that the legislator has requested additional information, is incredibly valuable to us in our ongoing advocacy efforts on behalf of surgeons and their patients here in Washington, DC.
Until next month ….
Dr. Patrick V. Bailey is an ACS Fellow, a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy, in the ACS offices in Washington, D.C.
C. difficile transmission linked to antibiotic use in long-term care facilities
Antibiotic use may drive Clostridium difficile transmission within long-term care facilities, according to the results of a recent study published in Annals of Internal Medicine.
Dr. Kevin A. Brown of Public Health Ontario in Toronto, and his coauthors, assessed long-term care–onset C. difficile infection in the largest and most comprehensive study of its kind to date. The retrospective study included 86 Veterans Health Administration health care regions and examined long-term care residents from January 2006 through December 2012. Study results indicated large variations in regional rates of C. difficile infection, regional antibiotic use, and importation of cases of acute care C. difficile infection (Ann Intern Med. 2016 Apr 19. doi: 10.7326/M15-1754).
The total study population included 6,012 cases with a C. difficile infection incidence of 3.7 cases per 10,000 resident days. The regional variability in the incidence of long-term care–onset C. difficile infection was found to be attributable in large part (75%) to antibiotic use and importation from acute care facilities. The data also showed that regional differences in both the prescription of antibiotics and the individual receipt of antibiotics contributed to resident risk, suggesting increased risk for both acquiring and spreading C. difficile.
A potential mechanism offered by the authors for the transmission of C. difficile in facilities with high antibiotic use may be the increased prevalence of residents with asymptomatic C. difficile colonization who become more effective at shedding C. difficile spores when exposed to antibiotics.
Dr. Brown and his colleagues said that efforts designed to reduce C. difficile infection in long-term care should focus on the reduction of total antibiotic use, and that infection control teams may need to take special measures in long-term care facilities that receive residents from hospitals with elevated rates of C. difficile infection.
This study was funded by the U.S. Department of Veterans Affairs and the Centers for Disease Control and Prevention. Dr. Brown reported grants from AstraZeneca outside the submitted work, and another coauthor disclosed grant support from the funding source during the conduct of the study. The remaining coauthors disclosed no conflicts of interest.
Antibiotic use may drive Clostridium difficile transmission within long-term care facilities, according to the results of a recent study published in Annals of Internal Medicine.
Dr. Kevin A. Brown of Public Health Ontario in Toronto, and his coauthors, assessed long-term care–onset C. difficile infection in the largest and most comprehensive study of its kind to date. The retrospective study included 86 Veterans Health Administration health care regions and examined long-term care residents from January 2006 through December 2012. Study results indicated large variations in regional rates of C. difficile infection, regional antibiotic use, and importation of cases of acute care C. difficile infection (Ann Intern Med. 2016 Apr 19. doi: 10.7326/M15-1754).
The total study population included 6,012 cases with a C. difficile infection incidence of 3.7 cases per 10,000 resident days. The regional variability in the incidence of long-term care–onset C. difficile infection was found to be attributable in large part (75%) to antibiotic use and importation from acute care facilities. The data also showed that regional differences in both the prescription of antibiotics and the individual receipt of antibiotics contributed to resident risk, suggesting increased risk for both acquiring and spreading C. difficile.
A potential mechanism offered by the authors for the transmission of C. difficile in facilities with high antibiotic use may be the increased prevalence of residents with asymptomatic C. difficile colonization who become more effective at shedding C. difficile spores when exposed to antibiotics.
Dr. Brown and his colleagues said that efforts designed to reduce C. difficile infection in long-term care should focus on the reduction of total antibiotic use, and that infection control teams may need to take special measures in long-term care facilities that receive residents from hospitals with elevated rates of C. difficile infection.
This study was funded by the U.S. Department of Veterans Affairs and the Centers for Disease Control and Prevention. Dr. Brown reported grants from AstraZeneca outside the submitted work, and another coauthor disclosed grant support from the funding source during the conduct of the study. The remaining coauthors disclosed no conflicts of interest.
Antibiotic use may drive Clostridium difficile transmission within long-term care facilities, according to the results of a recent study published in Annals of Internal Medicine.
Dr. Kevin A. Brown of Public Health Ontario in Toronto, and his coauthors, assessed long-term care–onset C. difficile infection in the largest and most comprehensive study of its kind to date. The retrospective study included 86 Veterans Health Administration health care regions and examined long-term care residents from January 2006 through December 2012. Study results indicated large variations in regional rates of C. difficile infection, regional antibiotic use, and importation of cases of acute care C. difficile infection (Ann Intern Med. 2016 Apr 19. doi: 10.7326/M15-1754).
The total study population included 6,012 cases with a C. difficile infection incidence of 3.7 cases per 10,000 resident days. The regional variability in the incidence of long-term care–onset C. difficile infection was found to be attributable in large part (75%) to antibiotic use and importation from acute care facilities. The data also showed that regional differences in both the prescription of antibiotics and the individual receipt of antibiotics contributed to resident risk, suggesting increased risk for both acquiring and spreading C. difficile.
A potential mechanism offered by the authors for the transmission of C. difficile in facilities with high antibiotic use may be the increased prevalence of residents with asymptomatic C. difficile colonization who become more effective at shedding C. difficile spores when exposed to antibiotics.
Dr. Brown and his colleagues said that efforts designed to reduce C. difficile infection in long-term care should focus on the reduction of total antibiotic use, and that infection control teams may need to take special measures in long-term care facilities that receive residents from hospitals with elevated rates of C. difficile infection.
This study was funded by the U.S. Department of Veterans Affairs and the Centers for Disease Control and Prevention. Dr. Brown reported grants from AstraZeneca outside the submitted work, and another coauthor disclosed grant support from the funding source during the conduct of the study. The remaining coauthors disclosed no conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point:C. difficile transmission may be driven by antibiotic use in long-term care facilities.
Major finding: The majority (75%) of the regional variability in the incidence of long-term care–onset C. difficile infection was attributable to antibiotic use and importation.
Data sources: Retrospective study of long-term care residents from 86 Veterans Health Administration health care regions examined from January 2006 through December 2012.
Disclosures: This study was funded by the U.S. Department of Veterans Affairs and the Centers for Disease Control and Prevention. Dr. Brown reported grants from AstraZeneca outside the submitted work, and another coauthor disclosed grant support from the funding source during the conduct of the study. The remaining coauthors disclosed no conflicts of interest.
New Model May Predict Risk of Acute Kidney Injury in Orthopedic Patients
Clinical question: What is the risk of acute kidney injury after orthopedic surgery, and does it impact mortality?
Background: Current studies show that acute kidney injury is associated with increased long-term mortality, future development of chronic kidney disease, and increased healthcare costs. However, no externally validated models are available to predict patients undergoing non-cardiac surgery at risk of postoperative acute kidney injury.
Study design: Observational, cohort study.
Setting: Teaching and private hospitals in the National Health Service (NHS) in the Tayside region of Scotland.
Synopsis: Investigators enrolled 10,615 adults >18 years of age undergoing orthopedic surgery into two groups: development cohort (6,220 patients) and validation cohort (4,395 patients). Using the development cohort, seven predictors were identified in the risk model: age at operation, male sex, diabetes, lower estimated glomerular filtration rate (GFR), use of ACE inhibitor/ARB, number of prescribing drugs, and American Society of Anesthesiologists (ASA) grade.
The model’s predictive performance for discrimination was good in the development cohort (C statistic 0.74; 95% CI, 0.72–0.76) and validation cohort (C statistic 0.7). Calibration was good in the development cohort but overestimated the risk in the validation cohort. Postoperative acute kidney injury developed in 672 (10.8%) patients in the development cohort and 295 (6.7%) in the validation cohort. Thirty percent (3,166) of the 10,615 patients enrolled in this study died over the median follow-up of 4.58 years. Survival was worse in the patients with acute kidney injury (adjusted hazard ratio 1.53; 95% CI, 1.38–1.70), worse in the short term (90-day adjusted hazard ratio 2.36; 95% CI, 1.94–2.87), and diminished over time.
Bottom line: A predictive model using age, male sex, diabetes, lower GFR, use of ACE inhibitor/ARB, multiple medications, and ASA grades might predict risk of postoperative acute kidney injury in orthopedic patients.
Citation: Bell S, Dekker FW, Vadiveloo T, et al. Risk of postoperative acute kidney injury in patients undergoing orthopaedic surgery—development and validation of a risk score and effect of acute kidney injury on survival: observational cohort study. BMJ 2015; 351:h5639.
Clinical question: What is the risk of acute kidney injury after orthopedic surgery, and does it impact mortality?
Background: Current studies show that acute kidney injury is associated with increased long-term mortality, future development of chronic kidney disease, and increased healthcare costs. However, no externally validated models are available to predict patients undergoing non-cardiac surgery at risk of postoperative acute kidney injury.
Study design: Observational, cohort study.
Setting: Teaching and private hospitals in the National Health Service (NHS) in the Tayside region of Scotland.
Synopsis: Investigators enrolled 10,615 adults >18 years of age undergoing orthopedic surgery into two groups: development cohort (6,220 patients) and validation cohort (4,395 patients). Using the development cohort, seven predictors were identified in the risk model: age at operation, male sex, diabetes, lower estimated glomerular filtration rate (GFR), use of ACE inhibitor/ARB, number of prescribing drugs, and American Society of Anesthesiologists (ASA) grade.
The model’s predictive performance for discrimination was good in the development cohort (C statistic 0.74; 95% CI, 0.72–0.76) and validation cohort (C statistic 0.7). Calibration was good in the development cohort but overestimated the risk in the validation cohort. Postoperative acute kidney injury developed in 672 (10.8%) patients in the development cohort and 295 (6.7%) in the validation cohort. Thirty percent (3,166) of the 10,615 patients enrolled in this study died over the median follow-up of 4.58 years. Survival was worse in the patients with acute kidney injury (adjusted hazard ratio 1.53; 95% CI, 1.38–1.70), worse in the short term (90-day adjusted hazard ratio 2.36; 95% CI, 1.94–2.87), and diminished over time.
Bottom line: A predictive model using age, male sex, diabetes, lower GFR, use of ACE inhibitor/ARB, multiple medications, and ASA grades might predict risk of postoperative acute kidney injury in orthopedic patients.
Citation: Bell S, Dekker FW, Vadiveloo T, et al. Risk of postoperative acute kidney injury in patients undergoing orthopaedic surgery—development and validation of a risk score and effect of acute kidney injury on survival: observational cohort study. BMJ 2015; 351:h5639.
Clinical question: What is the risk of acute kidney injury after orthopedic surgery, and does it impact mortality?
Background: Current studies show that acute kidney injury is associated with increased long-term mortality, future development of chronic kidney disease, and increased healthcare costs. However, no externally validated models are available to predict patients undergoing non-cardiac surgery at risk of postoperative acute kidney injury.
Study design: Observational, cohort study.
Setting: Teaching and private hospitals in the National Health Service (NHS) in the Tayside region of Scotland.
Synopsis: Investigators enrolled 10,615 adults >18 years of age undergoing orthopedic surgery into two groups: development cohort (6,220 patients) and validation cohort (4,395 patients). Using the development cohort, seven predictors were identified in the risk model: age at operation, male sex, diabetes, lower estimated glomerular filtration rate (GFR), use of ACE inhibitor/ARB, number of prescribing drugs, and American Society of Anesthesiologists (ASA) grade.
The model’s predictive performance for discrimination was good in the development cohort (C statistic 0.74; 95% CI, 0.72–0.76) and validation cohort (C statistic 0.7). Calibration was good in the development cohort but overestimated the risk in the validation cohort. Postoperative acute kidney injury developed in 672 (10.8%) patients in the development cohort and 295 (6.7%) in the validation cohort. Thirty percent (3,166) of the 10,615 patients enrolled in this study died over the median follow-up of 4.58 years. Survival was worse in the patients with acute kidney injury (adjusted hazard ratio 1.53; 95% CI, 1.38–1.70), worse in the short term (90-day adjusted hazard ratio 2.36; 95% CI, 1.94–2.87), and diminished over time.
Bottom line: A predictive model using age, male sex, diabetes, lower GFR, use of ACE inhibitor/ARB, multiple medications, and ASA grades might predict risk of postoperative acute kidney injury in orthopedic patients.
Citation: Bell S, Dekker FW, Vadiveloo T, et al. Risk of postoperative acute kidney injury in patients undergoing orthopaedic surgery—development and validation of a risk score and effect of acute kidney injury on survival: observational cohort study. BMJ 2015; 351:h5639.
Treating Asymptomatic Bacteriuria Can Be Dangerous
Clinical question: Does treating asymptomatic bacteriuria (AB) cause harm in women?
Background: In women with recurrent UTIs, AB is often treated, increasing the risk of multi-drug-resistant bacteria. At the same time, little data exist on the relationship between AB treatment and risk of higher antibiotic resistance in women with recurrent UTIs.
Study design: Follow-up observational, analytical, longitudinal study on a previously randomized clinical trial (RCT).
Setting: Sexually transmitted disease (STD) center in Florence, Italy.
Synopsis: Using the patients from the authors’ previous RCT, the study followed 550 women with recurrent UTIs and AB for a mean of 38.8 months in parallel groups: One group had AB treated, and the other group did not. In the group of women treated with antibiotics, the recurrence rate was 69.6% versus 37.7% in the group not treated (P<0.001). In addition, E. coli isolates showed more resistance to amoxicillin/clavulanic acid (P=0.03), trimethoprim/sulfamethazole (P=0.01), and ciprofloxacin (P=0.03) in the group previously treated with antibiotics.
Given the observational design of the study, data must be interpreted with caution in determining a causal relationship. However, prior studies have shown this relationship, and current Infectious Diseases Society of America guidelines support neither screening nor treating AB.
Bottom line: In women with recurrent UTIs, previous treatment of AB is associated with higher rates of antibiotic-resistant bacteria, causing symptomatic UTIs.
Citation: Cai T, Nsei G, Mazzoli S, et al. Asymptomatic bacteriuria treatment is associated with a higher prevalence of antibiotic resistant strains in women with urinary tract infection. Clin Infect Dis. 2015;61(11):1655-1661.
Short Take
National Healthcare Spending Increased in 2014
Led by expansions under the Affordable Care Act, healthcare spending increased 5.3% from the previous year and now totals $3 trillion, which represents 17.5% of the gross domestic product.
Citation: Martin AB, Hartman M, Benson J, Catlin A. National health spending in 2014: faster growth drive by coverage expansion and prescription drug spending. Health Aff. 2016;35(1):150-160.
Clinical question: Does treating asymptomatic bacteriuria (AB) cause harm in women?
Background: In women with recurrent UTIs, AB is often treated, increasing the risk of multi-drug-resistant bacteria. At the same time, little data exist on the relationship between AB treatment and risk of higher antibiotic resistance in women with recurrent UTIs.
Study design: Follow-up observational, analytical, longitudinal study on a previously randomized clinical trial (RCT).
Setting: Sexually transmitted disease (STD) center in Florence, Italy.
Synopsis: Using the patients from the authors’ previous RCT, the study followed 550 women with recurrent UTIs and AB for a mean of 38.8 months in parallel groups: One group had AB treated, and the other group did not. In the group of women treated with antibiotics, the recurrence rate was 69.6% versus 37.7% in the group not treated (P<0.001). In addition, E. coli isolates showed more resistance to amoxicillin/clavulanic acid (P=0.03), trimethoprim/sulfamethazole (P=0.01), and ciprofloxacin (P=0.03) in the group previously treated with antibiotics.
Given the observational design of the study, data must be interpreted with caution in determining a causal relationship. However, prior studies have shown this relationship, and current Infectious Diseases Society of America guidelines support neither screening nor treating AB.
Bottom line: In women with recurrent UTIs, previous treatment of AB is associated with higher rates of antibiotic-resistant bacteria, causing symptomatic UTIs.
Citation: Cai T, Nsei G, Mazzoli S, et al. Asymptomatic bacteriuria treatment is associated with a higher prevalence of antibiotic resistant strains in women with urinary tract infection. Clin Infect Dis. 2015;61(11):1655-1661.
Short Take
National Healthcare Spending Increased in 2014
Led by expansions under the Affordable Care Act, healthcare spending increased 5.3% from the previous year and now totals $3 trillion, which represents 17.5% of the gross domestic product.
Citation: Martin AB, Hartman M, Benson J, Catlin A. National health spending in 2014: faster growth drive by coverage expansion and prescription drug spending. Health Aff. 2016;35(1):150-160.
Clinical question: Does treating asymptomatic bacteriuria (AB) cause harm in women?
Background: In women with recurrent UTIs, AB is often treated, increasing the risk of multi-drug-resistant bacteria. At the same time, little data exist on the relationship between AB treatment and risk of higher antibiotic resistance in women with recurrent UTIs.
Study design: Follow-up observational, analytical, longitudinal study on a previously randomized clinical trial (RCT).
Setting: Sexually transmitted disease (STD) center in Florence, Italy.
Synopsis: Using the patients from the authors’ previous RCT, the study followed 550 women with recurrent UTIs and AB for a mean of 38.8 months in parallel groups: One group had AB treated, and the other group did not. In the group of women treated with antibiotics, the recurrence rate was 69.6% versus 37.7% in the group not treated (P<0.001). In addition, E. coli isolates showed more resistance to amoxicillin/clavulanic acid (P=0.03), trimethoprim/sulfamethazole (P=0.01), and ciprofloxacin (P=0.03) in the group previously treated with antibiotics.
Given the observational design of the study, data must be interpreted with caution in determining a causal relationship. However, prior studies have shown this relationship, and current Infectious Diseases Society of America guidelines support neither screening nor treating AB.
Bottom line: In women with recurrent UTIs, previous treatment of AB is associated with higher rates of antibiotic-resistant bacteria, causing symptomatic UTIs.
Citation: Cai T, Nsei G, Mazzoli S, et al. Asymptomatic bacteriuria treatment is associated with a higher prevalence of antibiotic resistant strains in women with urinary tract infection. Clin Infect Dis. 2015;61(11):1655-1661.
Short Take
National Healthcare Spending Increased in 2014
Led by expansions under the Affordable Care Act, healthcare spending increased 5.3% from the previous year and now totals $3 trillion, which represents 17.5% of the gross domestic product.
Citation: Martin AB, Hartman M, Benson J, Catlin A. National health spending in 2014: faster growth drive by coverage expansion and prescription drug spending. Health Aff. 2016;35(1):150-160.
Targeted corticosteroids cut GVHD incidence
Short-term low-dose corticosteroid prophylaxis reduces the incidence of graft-vs.-host disease in patients who undergo allogeneic haploidentical stem-cell transplantation to treat hematologic neoplasms, according to a report published online April 18 in the Journal of Clinical Oncology.
The key to selecting patients most likely to benefit from the corticosteroid therapy is to identify those at high risk for graft-vs.-host disease (GVHD) using two biomarkers: high levels of CD56bright natural killer cells in allogeneic grafts or high CD4:CD8 ratios in bone marrow grafts, according to Dr. Ying-Jun Chang of Peking University People’s Hospital, Beijing, and associates.
The investigators performed an open-label trial involving 228 patients aged 15-60 years treated at a single medical center during an 18-month period for acute myeloid leukemia, acute lymphoblastic leukemia, chronic myeloid leukemia, myelodysplastic syndrome, or other hematologic neoplasms. Using the two biomarkers, the patients were categorized as either high or low risk for developing GVHD. They were randomly assigned to three study groups: 72 high-risk patients who received short-term low-dose corticosteroids, 73 high-risk patients who received usual care, and 83 low-risk patients who received usual care.
The cumulative 100-day incidence of acute grade-II to grade-IV GVHD was significantly lower in the high-risk patients who received prophylaxis (21%) than in the high-risk patients who did not receive prophylaxis (48%). In fact, corticosteroids decreased the rate of GVHD so that it was comparable with that in the low-risk patients (26%), Dr. Chang and associates said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.63l.8817).
Moreover, in the high-risk patients the median interval until GVHD developed was 25 days for those who took corticosteroids, compared with only 15 days for those who did not. Median times to myeloid recovery and platelet recovery were significantly shorter for high-risk patients who received corticosteroids than for either of the other study groups. However, 3-year overall survival and leukemia-free survival were comparable among the three study groups.
The short-term low-dose regimen of corticosteroids did not raise the rate of adverse events, including infection, which suggests that it is preferable to standard corticosteroid regimens in this patient population. The incidences of cytomegalovirus or Epstein-Barr virus reactivation, post-transplantation lymphoproliferative disorder, hemorrhagic cystitis, bacteremia, and invasive fungal infections were comparable among the three study groups. Of note, the incidences of osteonecrosis of the femoral head and secondary hypertension were significantly lower among high-risk patients who received corticosteroid prophylaxis than among those who did not.
“These results provide the first test, to our knowledge, of a novel risk-stratification-directed prophylaxis strategy that effectively prevented acute GVHD among patients who were at high risk for GVHD, without unnecessarily exposing patients who were at low risk to excessive toxicity from additional immunosuppressive agents,” Dr. Chang and associates said.
Despite the encouraging results of Chang et al, it would be premature to routinely use corticosteroid prophylaxis to prevent GVHD until further studies are completed.
This study wasn’t sufficiently powered to determine whether corticosteroids reduced treatment-specific mortality or improved overall survival. Future studies must examine these end points, as well as relapse rates, before this method of prophylaxis is widely adopted.
Dr. Edwin P. Alyea is at Dana-Farber Cancer Institute, Boston. He reported having no relevant financial disclosures. Dr. Alyea made these remarks in an editorial accompanying Dr. Chang’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.66.0902).
Despite the encouraging results of Chang et al, it would be premature to routinely use corticosteroid prophylaxis to prevent GVHD until further studies are completed.
This study wasn’t sufficiently powered to determine whether corticosteroids reduced treatment-specific mortality or improved overall survival. Future studies must examine these end points, as well as relapse rates, before this method of prophylaxis is widely adopted.
Dr. Edwin P. Alyea is at Dana-Farber Cancer Institute, Boston. He reported having no relevant financial disclosures. Dr. Alyea made these remarks in an editorial accompanying Dr. Chang’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.66.0902).
Despite the encouraging results of Chang et al, it would be premature to routinely use corticosteroid prophylaxis to prevent GVHD until further studies are completed.
This study wasn’t sufficiently powered to determine whether corticosteroids reduced treatment-specific mortality or improved overall survival. Future studies must examine these end points, as well as relapse rates, before this method of prophylaxis is widely adopted.
Dr. Edwin P. Alyea is at Dana-Farber Cancer Institute, Boston. He reported having no relevant financial disclosures. Dr. Alyea made these remarks in an editorial accompanying Dr. Chang’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.66.0902).
Short-term low-dose corticosteroid prophylaxis reduces the incidence of graft-vs.-host disease in patients who undergo allogeneic haploidentical stem-cell transplantation to treat hematologic neoplasms, according to a report published online April 18 in the Journal of Clinical Oncology.
The key to selecting patients most likely to benefit from the corticosteroid therapy is to identify those at high risk for graft-vs.-host disease (GVHD) using two biomarkers: high levels of CD56bright natural killer cells in allogeneic grafts or high CD4:CD8 ratios in bone marrow grafts, according to Dr. Ying-Jun Chang of Peking University People’s Hospital, Beijing, and associates.
The investigators performed an open-label trial involving 228 patients aged 15-60 years treated at a single medical center during an 18-month period for acute myeloid leukemia, acute lymphoblastic leukemia, chronic myeloid leukemia, myelodysplastic syndrome, or other hematologic neoplasms. Using the two biomarkers, the patients were categorized as either high or low risk for developing GVHD. They were randomly assigned to three study groups: 72 high-risk patients who received short-term low-dose corticosteroids, 73 high-risk patients who received usual care, and 83 low-risk patients who received usual care.
The cumulative 100-day incidence of acute grade-II to grade-IV GVHD was significantly lower in the high-risk patients who received prophylaxis (21%) than in the high-risk patients who did not receive prophylaxis (48%). In fact, corticosteroids decreased the rate of GVHD so that it was comparable with that in the low-risk patients (26%), Dr. Chang and associates said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.63l.8817).
Moreover, in the high-risk patients the median interval until GVHD developed was 25 days for those who took corticosteroids, compared with only 15 days for those who did not. Median times to myeloid recovery and platelet recovery were significantly shorter for high-risk patients who received corticosteroids than for either of the other study groups. However, 3-year overall survival and leukemia-free survival were comparable among the three study groups.
The short-term low-dose regimen of corticosteroids did not raise the rate of adverse events, including infection, which suggests that it is preferable to standard corticosteroid regimens in this patient population. The incidences of cytomegalovirus or Epstein-Barr virus reactivation, post-transplantation lymphoproliferative disorder, hemorrhagic cystitis, bacteremia, and invasive fungal infections were comparable among the three study groups. Of note, the incidences of osteonecrosis of the femoral head and secondary hypertension were significantly lower among high-risk patients who received corticosteroid prophylaxis than among those who did not.
“These results provide the first test, to our knowledge, of a novel risk-stratification-directed prophylaxis strategy that effectively prevented acute GVHD among patients who were at high risk for GVHD, without unnecessarily exposing patients who were at low risk to excessive toxicity from additional immunosuppressive agents,” Dr. Chang and associates said.
Short-term low-dose corticosteroid prophylaxis reduces the incidence of graft-vs.-host disease in patients who undergo allogeneic haploidentical stem-cell transplantation to treat hematologic neoplasms, according to a report published online April 18 in the Journal of Clinical Oncology.
The key to selecting patients most likely to benefit from the corticosteroid therapy is to identify those at high risk for graft-vs.-host disease (GVHD) using two biomarkers: high levels of CD56bright natural killer cells in allogeneic grafts or high CD4:CD8 ratios in bone marrow grafts, according to Dr. Ying-Jun Chang of Peking University People’s Hospital, Beijing, and associates.
The investigators performed an open-label trial involving 228 patients aged 15-60 years treated at a single medical center during an 18-month period for acute myeloid leukemia, acute lymphoblastic leukemia, chronic myeloid leukemia, myelodysplastic syndrome, or other hematologic neoplasms. Using the two biomarkers, the patients were categorized as either high or low risk for developing GVHD. They were randomly assigned to three study groups: 72 high-risk patients who received short-term low-dose corticosteroids, 73 high-risk patients who received usual care, and 83 low-risk patients who received usual care.
The cumulative 100-day incidence of acute grade-II to grade-IV GVHD was significantly lower in the high-risk patients who received prophylaxis (21%) than in the high-risk patients who did not receive prophylaxis (48%). In fact, corticosteroids decreased the rate of GVHD so that it was comparable with that in the low-risk patients (26%), Dr. Chang and associates said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.63l.8817).
Moreover, in the high-risk patients the median interval until GVHD developed was 25 days for those who took corticosteroids, compared with only 15 days for those who did not. Median times to myeloid recovery and platelet recovery were significantly shorter for high-risk patients who received corticosteroids than for either of the other study groups. However, 3-year overall survival and leukemia-free survival were comparable among the three study groups.
The short-term low-dose regimen of corticosteroids did not raise the rate of adverse events, including infection, which suggests that it is preferable to standard corticosteroid regimens in this patient population. The incidences of cytomegalovirus or Epstein-Barr virus reactivation, post-transplantation lymphoproliferative disorder, hemorrhagic cystitis, bacteremia, and invasive fungal infections were comparable among the three study groups. Of note, the incidences of osteonecrosis of the femoral head and secondary hypertension were significantly lower among high-risk patients who received corticosteroid prophylaxis than among those who did not.
“These results provide the first test, to our knowledge, of a novel risk-stratification-directed prophylaxis strategy that effectively prevented acute GVHD among patients who were at high risk for GVHD, without unnecessarily exposing patients who were at low risk to excessive toxicity from additional immunosuppressive agents,” Dr. Chang and associates said.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Short-term low-dose corticosteroid prophylaxis reduces the incidence of the GVHD in patients who undergo haploidentical stem-cell transplantation to treat hematologic neoplasms.
Major finding: The 100-day incidence of acute GVHD was significantly lower in the high-risk patients who received corticosteroid prophylaxis (21%) than in the high-risk patients who did not (48%).
Data source: An open-label randomized controlled trial involving 228 Chinese patients who underwent stem-cell transplantation.
Disclosures: This study was supported by the Beijing Committee of Science and Technology, the National High Technology Research and Development Program of China, and the National Natural Science Foundation of China. Dr. Chang and associates reported having no relevant financial disclosures.
Donor EBV status affects recipient graft-vs-host disease risk
In allogeneic hematopoietic stem-cell transplantation, the donor’s status regarding Epstein-Barr virus affects the recipient’s risk of developing graft-vs-host disease – a “completely new and striking” finding, according to a report published online April 18 in the Journal of Clinical Oncology.
Approximately 80% of the general population has been infected with EBV and carries persistent virus in memory B cells. When viral material is transmitted to stem-cell recipients, it is known to cause posttransplantation lymphoproliferative disorder. Until now, however, no data were available to examine EBV serology’s effect on other posttransplantation outcomes, said Dr. Jan Styczynski of the department of pediatric hematology and oncology at Nicolaus Copernicus University, Bydgoszcz, Poland, and his associates.
They analyzed information in the European Society of Blood and Marrow Transplantation database for 11,364 patients with acute lymphoblastic leukemia or acute myeloblastic leukemia who underwent stem-cell transplantation between 1997 and 2012 and who were followed for approximately 5 years. Most of the donors (82%) were seropositive for EBV. Acute graft-vs-host disease (GVHD) developed in 32% and chronic GVHD developed in 40% of these stem cell–transplant recipients.
The incidence of chronic GVHD was significantly higher when the donor was EBV-seropositive (41%) than when the donor was EBV-seronegative (31%). Similarly, the incidence of acute GVHD was significantly higher when the donor was EBV-seropositive (32% vs 30%), but the magnitude of the difference between the two groups was smaller. The risk for GVHD increased even though patients receiving transplants from EBV-seropositive donors underwent more intensive GVHD prophylaxis than did those who had seronegative donors, the investigators said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.64.2405).
In contrast, the transplant recipients’ EBV status did not affect their risk of developing GVHD.
“Despite the effect of donor EBV serostatus on GVHD, we did not observe a corresponding GVHD-related death rate, and as a result, there was no effect on overall survival, relapse-free survival, relapse incidence, and nonrelapse mortality. However, it should be kept in mind that many other pre- and posttransplantation factors play a role in contributing to final transplantation outcomes,” Dr. Styczynski and his associates noted.
The current recommendation to monitor transplantation recipients for EBV and to give them “preemptive” rituximab to stave off the development of posttransplantation lymphoproliferative disorder might prove useful in also preventing GVHD, they added.
The findings of Dr. Styczynski and his associates raise the possibility that we may be able to prevent or treat GVHD in transplant recipients by controlling EBV infection.
Selecting only EBV-negative donors would be one way to accomplish this, but that would be impractical given the high seroprevalence of EBV in the general population. Depleting memory B cells, the reservoir of EBV infection, using monoclonal antibodies may prove helpful, and these agents might provide additional therapeutic effects. And novel antivirals such as retroviral integrase inhibitors may be more specific at targeting EBV than acyclovir and related agents, which have limited activity against latently infected B cells. These novel drugs, however, are not without risks and adverse effects.
A promising alternative might be to boost immunity to EBV using vaccination or adoptive transfer of ex vivo expanded EBV-specific cytotoxic T cells.
Dr. Katayoun Rezvani and Dr. Richard E. Champlin are with the University of Texas MD Andersen Cancer Center, Houston. Their financial disclosures are available at www.jco.org. They made these remarks in an editorial accompanying Dr. Styczynski’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2016.66.6099).
The findings of Dr. Styczynski and his associates raise the possibility that we may be able to prevent or treat GVHD in transplant recipients by controlling EBV infection.
Selecting only EBV-negative donors would be one way to accomplish this, but that would be impractical given the high seroprevalence of EBV in the general population. Depleting memory B cells, the reservoir of EBV infection, using monoclonal antibodies may prove helpful, and these agents might provide additional therapeutic effects. And novel antivirals such as retroviral integrase inhibitors may be more specific at targeting EBV than acyclovir and related agents, which have limited activity against latently infected B cells. These novel drugs, however, are not without risks and adverse effects.
A promising alternative might be to boost immunity to EBV using vaccination or adoptive transfer of ex vivo expanded EBV-specific cytotoxic T cells.
Dr. Katayoun Rezvani and Dr. Richard E. Champlin are with the University of Texas MD Andersen Cancer Center, Houston. Their financial disclosures are available at www.jco.org. They made these remarks in an editorial accompanying Dr. Styczynski’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2016.66.6099).
The findings of Dr. Styczynski and his associates raise the possibility that we may be able to prevent or treat GVHD in transplant recipients by controlling EBV infection.
Selecting only EBV-negative donors would be one way to accomplish this, but that would be impractical given the high seroprevalence of EBV in the general population. Depleting memory B cells, the reservoir of EBV infection, using monoclonal antibodies may prove helpful, and these agents might provide additional therapeutic effects. And novel antivirals such as retroviral integrase inhibitors may be more specific at targeting EBV than acyclovir and related agents, which have limited activity against latently infected B cells. These novel drugs, however, are not without risks and adverse effects.
A promising alternative might be to boost immunity to EBV using vaccination or adoptive transfer of ex vivo expanded EBV-specific cytotoxic T cells.
Dr. Katayoun Rezvani and Dr. Richard E. Champlin are with the University of Texas MD Andersen Cancer Center, Houston. Their financial disclosures are available at www.jco.org. They made these remarks in an editorial accompanying Dr. Styczynski’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2016.66.6099).
In allogeneic hematopoietic stem-cell transplantation, the donor’s status regarding Epstein-Barr virus affects the recipient’s risk of developing graft-vs-host disease – a “completely new and striking” finding, according to a report published online April 18 in the Journal of Clinical Oncology.
Approximately 80% of the general population has been infected with EBV and carries persistent virus in memory B cells. When viral material is transmitted to stem-cell recipients, it is known to cause posttransplantation lymphoproliferative disorder. Until now, however, no data were available to examine EBV serology’s effect on other posttransplantation outcomes, said Dr. Jan Styczynski of the department of pediatric hematology and oncology at Nicolaus Copernicus University, Bydgoszcz, Poland, and his associates.
They analyzed information in the European Society of Blood and Marrow Transplantation database for 11,364 patients with acute lymphoblastic leukemia or acute myeloblastic leukemia who underwent stem-cell transplantation between 1997 and 2012 and who were followed for approximately 5 years. Most of the donors (82%) were seropositive for EBV. Acute graft-vs-host disease (GVHD) developed in 32% and chronic GVHD developed in 40% of these stem cell–transplant recipients.
The incidence of chronic GVHD was significantly higher when the donor was EBV-seropositive (41%) than when the donor was EBV-seronegative (31%). Similarly, the incidence of acute GVHD was significantly higher when the donor was EBV-seropositive (32% vs 30%), but the magnitude of the difference between the two groups was smaller. The risk for GVHD increased even though patients receiving transplants from EBV-seropositive donors underwent more intensive GVHD prophylaxis than did those who had seronegative donors, the investigators said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.64.2405).
In contrast, the transplant recipients’ EBV status did not affect their risk of developing GVHD.
“Despite the effect of donor EBV serostatus on GVHD, we did not observe a corresponding GVHD-related death rate, and as a result, there was no effect on overall survival, relapse-free survival, relapse incidence, and nonrelapse mortality. However, it should be kept in mind that many other pre- and posttransplantation factors play a role in contributing to final transplantation outcomes,” Dr. Styczynski and his associates noted.
The current recommendation to monitor transplantation recipients for EBV and to give them “preemptive” rituximab to stave off the development of posttransplantation lymphoproliferative disorder might prove useful in also preventing GVHD, they added.
In allogeneic hematopoietic stem-cell transplantation, the donor’s status regarding Epstein-Barr virus affects the recipient’s risk of developing graft-vs-host disease – a “completely new and striking” finding, according to a report published online April 18 in the Journal of Clinical Oncology.
Approximately 80% of the general population has been infected with EBV and carries persistent virus in memory B cells. When viral material is transmitted to stem-cell recipients, it is known to cause posttransplantation lymphoproliferative disorder. Until now, however, no data were available to examine EBV serology’s effect on other posttransplantation outcomes, said Dr. Jan Styczynski of the department of pediatric hematology and oncology at Nicolaus Copernicus University, Bydgoszcz, Poland, and his associates.
They analyzed information in the European Society of Blood and Marrow Transplantation database for 11,364 patients with acute lymphoblastic leukemia or acute myeloblastic leukemia who underwent stem-cell transplantation between 1997 and 2012 and who were followed for approximately 5 years. Most of the donors (82%) were seropositive for EBV. Acute graft-vs-host disease (GVHD) developed in 32% and chronic GVHD developed in 40% of these stem cell–transplant recipients.
The incidence of chronic GVHD was significantly higher when the donor was EBV-seropositive (41%) than when the donor was EBV-seronegative (31%). Similarly, the incidence of acute GVHD was significantly higher when the donor was EBV-seropositive (32% vs 30%), but the magnitude of the difference between the two groups was smaller. The risk for GVHD increased even though patients receiving transplants from EBV-seropositive donors underwent more intensive GVHD prophylaxis than did those who had seronegative donors, the investigators said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.64.2405).
In contrast, the transplant recipients’ EBV status did not affect their risk of developing GVHD.
“Despite the effect of donor EBV serostatus on GVHD, we did not observe a corresponding GVHD-related death rate, and as a result, there was no effect on overall survival, relapse-free survival, relapse incidence, and nonrelapse mortality. However, it should be kept in mind that many other pre- and posttransplantation factors play a role in contributing to final transplantation outcomes,” Dr. Styczynski and his associates noted.
The current recommendation to monitor transplantation recipients for EBV and to give them “preemptive” rituximab to stave off the development of posttransplantation lymphoproliferative disorder might prove useful in also preventing GVHD, they added.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: In allogeneic hematopoietic stem-cell transplantation, the donor’s EBV status affects the recipient’s risk of developing GVHD.
Major finding: Chronic GVHD was significantly more likely to develop when the donor was EBV-seropositive (41%) than EBV-seronegative (31%).
Data source: A retrospective analysis of data regarding 11,364 European patients with acute leukemia who underwent stem-cell transplantation and were followed for 5 years.
Disclosures: No study sponsor was identified. Dr. Styczynski reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
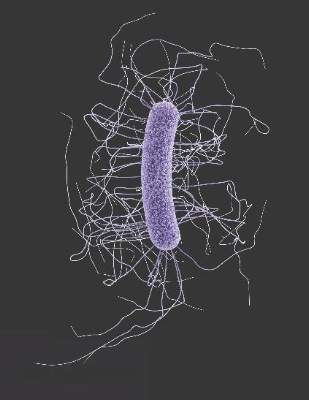
Targeting T and B Cells as a Therapeutic Approach for Multiple Sclerosis
Immunotherapies that target abnormally activated T and B cells may represent a unique combination and promising DMT strategy for patients with RRMS and have the greatest potential for long-term success. Targeting T cells in MS may help attenuate initiation and maintenance of inflammatory attacks by reducing the production of pro-inflammatory cytokines, recruitment of innate immune cells, stimulation of antibody production, and direct attack of myelin. Targeting B cells in MS may attenuate secretion of autoantibodies and pro-inflammatory cytokines, as well as presentation of self-antigen to T cells.
Click here to read the digital edition.
Immunotherapies that target abnormally activated T and B cells may represent a unique combination and promising DMT strategy for patients with RRMS and have the greatest potential for long-term success. Targeting T cells in MS may help attenuate initiation and maintenance of inflammatory attacks by reducing the production of pro-inflammatory cytokines, recruitment of innate immune cells, stimulation of antibody production, and direct attack of myelin. Targeting B cells in MS may attenuate secretion of autoantibodies and pro-inflammatory cytokines, as well as presentation of self-antigen to T cells.
Click here to read the digital edition.
Immunotherapies that target abnormally activated T and B cells may represent a unique combination and promising DMT strategy for patients with RRMS and have the greatest potential for long-term success. Targeting T cells in MS may help attenuate initiation and maintenance of inflammatory attacks by reducing the production of pro-inflammatory cytokines, recruitment of innate immune cells, stimulation of antibody production, and direct attack of myelin. Targeting B cells in MS may attenuate secretion of autoantibodies and pro-inflammatory cytokines, as well as presentation of self-antigen to T cells.
Click here to read the digital edition.
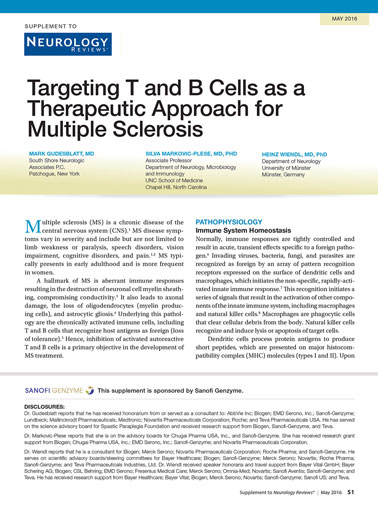
U.S. flu activity down again, except in New Jersey
Overall activity of influenza-like illness (ILI) in the United States continued to fall, but New Jersey took a turn for the worse during the week ending April 9, 2016, according to the Centers for Disease Control and Prevention.
New Jersey’s ILI activity level went from 8 the previous week to 10 on the CDC’s 1-10 scale. For the week ending April 9, it was the only U.S. state in the “high” range, with Hawaii the next highest at level 6 – the only state in the “moderate” range, the CDC reported.
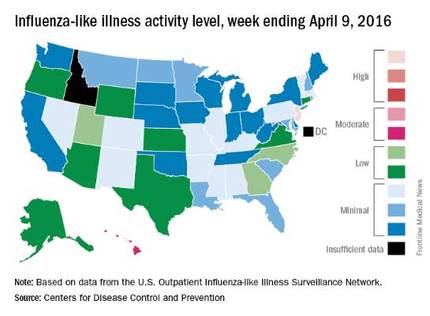
Nationwide, the proportion of outpatient visits for ILI was 2.1%, which is at the national baseline of 2.1% and down from 2.5% the week before. That number has now dropped for 4 consecutive weeks since hitting a season high of 3.7% for the week ending March 12. The CDC also reported a cumulative rate of 26.6 influenza-associated hospitalizations per 100,000 population.
Ten flu-related pediatric deaths were reported during the week, of which only one occurred during the week. A total of 50 flu-related pediatric deaths have been reported during the 2015-2016 season, the CDC said. The overall proportion of deaths attributed to pneumonia and influenza was below the system-specific threshold in the National Center for Health Statistics Mortality Surveillance System, but above the system-specific threshold in the 122 Cities Mortality Reporting System.
Overall activity of influenza-like illness (ILI) in the United States continued to fall, but New Jersey took a turn for the worse during the week ending April 9, 2016, according to the Centers for Disease Control and Prevention.
New Jersey’s ILI activity level went from 8 the previous week to 10 on the CDC’s 1-10 scale. For the week ending April 9, it was the only U.S. state in the “high” range, with Hawaii the next highest at level 6 – the only state in the “moderate” range, the CDC reported.
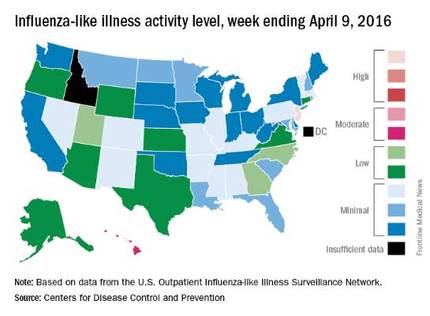
Nationwide, the proportion of outpatient visits for ILI was 2.1%, which is at the national baseline of 2.1% and down from 2.5% the week before. That number has now dropped for 4 consecutive weeks since hitting a season high of 3.7% for the week ending March 12. The CDC also reported a cumulative rate of 26.6 influenza-associated hospitalizations per 100,000 population.
Ten flu-related pediatric deaths were reported during the week, of which only one occurred during the week. A total of 50 flu-related pediatric deaths have been reported during the 2015-2016 season, the CDC said. The overall proportion of deaths attributed to pneumonia and influenza was below the system-specific threshold in the National Center for Health Statistics Mortality Surveillance System, but above the system-specific threshold in the 122 Cities Mortality Reporting System.
Overall activity of influenza-like illness (ILI) in the United States continued to fall, but New Jersey took a turn for the worse during the week ending April 9, 2016, according to the Centers for Disease Control and Prevention.
New Jersey’s ILI activity level went from 8 the previous week to 10 on the CDC’s 1-10 scale. For the week ending April 9, it was the only U.S. state in the “high” range, with Hawaii the next highest at level 6 – the only state in the “moderate” range, the CDC reported.
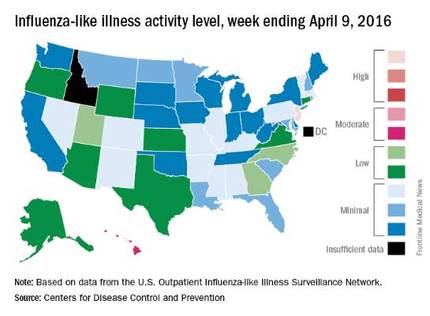
Nationwide, the proportion of outpatient visits for ILI was 2.1%, which is at the national baseline of 2.1% and down from 2.5% the week before. That number has now dropped for 4 consecutive weeks since hitting a season high of 3.7% for the week ending March 12. The CDC also reported a cumulative rate of 26.6 influenza-associated hospitalizations per 100,000 population.
Ten flu-related pediatric deaths were reported during the week, of which only one occurred during the week. A total of 50 flu-related pediatric deaths have been reported during the 2015-2016 season, the CDC said. The overall proportion of deaths attributed to pneumonia and influenza was below the system-specific threshold in the National Center for Health Statistics Mortality Surveillance System, but above the system-specific threshold in the 122 Cities Mortality Reporting System.
Pregnancy Considerations for Women With Epilepsy—The WEPOD Study
VANCOUVER—Women with epilepsy seeking pregnancy had comparable likelihood of achieving pregnancy, time to achieve pregnancy, and pregnancy outcomes, compared with a group of healthy peers, according to study findings presented at the 68th Annual Meeting of the American Academy of Neurology. "These findings should reassure women with epilepsy and clinicians when counseling women with epilepsy who are planning pregnancy," said Page B. Pennell, MD, Associate Professor of Neurology at Brigham and Women's Hospital and Harvard Medical School in Boston, and her research colleagues.
Page B. Pennell, MD, Associate Professor of Neurology at Brigham and Women's Hospital and Harvard Medical School in Boston, and her research colleagues.
Previous studies suggested that women with epilepsy have lower fertility compared with healthy controls. Dr. Pennell and colleagues sought to compare time to pregnancy and outcomes (eg, live birth, miscarriage) among women with epilepsy and healthy controls. The Women with Epilepsy: Pregnancy Outcomes and Deliveries (WEPOD) study was a multicenter, prospective, observational study of women with epilepsy and healthy controls.
Dr. Pennell and colleagues enrolled and prospectively followed women with epilepsy and healthy controls, ages 18 to 41, seeking pregnancy within six months of discontinuing contraception. The customized WEPOD electronicdiary captured medication use, seizures, sexual activity, and menstrual bleeding. Pregnancy tests were performed if there was no menses by cycle day 35. Outcomes included proportions of women who achieved pregnancy and time to pregnancy from cessation of birth control. The researchers used a proportional hazard model to evaluate the association between time to pregnancy and certain baseline characteristics.
Enrolled in the study were 88 women with epilepsy and 109 healthy controls with similar demographic characteristics. Among women with epilepsy, 61.4% achieved pregnancy versus 60.6% for healthy controls. Median time to pregnancy was six months in women with epilepsy, compared with nine months for healthy controls. Time to pregnancy was no different across the two groups after controlling for age, BMI, parity, and race. Race and parity were significantly associated with time to pregnancy.
Of the pregnancies that occurred, a similar proportion resulted in miscarriage (12.9% among women with epilepsy and 19.7% among controls), live birth (80.0% among women with epilepsy and 80.3% controls) or other outcome (5.0% versus 0.0%).
The WEPOD study was supported by the Epilepsy Foundation.
VANCOUVER—Women with epilepsy seeking pregnancy had comparable likelihood of achieving pregnancy, time to achieve pregnancy, and pregnancy outcomes, compared with a group of healthy peers, according to study findings presented at the 68th Annual Meeting of the American Academy of Neurology. "These findings should reassure women with epilepsy and clinicians when counseling women with epilepsy who are planning pregnancy," said Page B. Pennell, MD, Associate Professor of Neurology at Brigham and Women's Hospital and Harvard Medical School in Boston, and her research colleagues.
Page B. Pennell, MD, Associate Professor of Neurology at Brigham and Women's Hospital and Harvard Medical School in Boston, and her research colleagues.
Previous studies suggested that women with epilepsy have lower fertility compared with healthy controls. Dr. Pennell and colleagues sought to compare time to pregnancy and outcomes (eg, live birth, miscarriage) among women with epilepsy and healthy controls. The Women with Epilepsy: Pregnancy Outcomes and Deliveries (WEPOD) study was a multicenter, prospective, observational study of women with epilepsy and healthy controls.
Dr. Pennell and colleagues enrolled and prospectively followed women with epilepsy and healthy controls, ages 18 to 41, seeking pregnancy within six months of discontinuing contraception. The customized WEPOD electronicdiary captured medication use, seizures, sexual activity, and menstrual bleeding. Pregnancy tests were performed if there was no menses by cycle day 35. Outcomes included proportions of women who achieved pregnancy and time to pregnancy from cessation of birth control. The researchers used a proportional hazard model to evaluate the association between time to pregnancy and certain baseline characteristics.
Enrolled in the study were 88 women with epilepsy and 109 healthy controls with similar demographic characteristics. Among women with epilepsy, 61.4% achieved pregnancy versus 60.6% for healthy controls. Median time to pregnancy was six months in women with epilepsy, compared with nine months for healthy controls. Time to pregnancy was no different across the two groups after controlling for age, BMI, parity, and race. Race and parity were significantly associated with time to pregnancy.
Of the pregnancies that occurred, a similar proportion resulted in miscarriage (12.9% among women with epilepsy and 19.7% among controls), live birth (80.0% among women with epilepsy and 80.3% controls) or other outcome (5.0% versus 0.0%).
The WEPOD study was supported by the Epilepsy Foundation.
VANCOUVER—Women with epilepsy seeking pregnancy had comparable likelihood of achieving pregnancy, time to achieve pregnancy, and pregnancy outcomes, compared with a group of healthy peers, according to study findings presented at the 68th Annual Meeting of the American Academy of Neurology. "These findings should reassure women with epilepsy and clinicians when counseling women with epilepsy who are planning pregnancy," said Page B. Pennell, MD, Associate Professor of Neurology at Brigham and Women's Hospital and Harvard Medical School in Boston, and her research colleagues.
Page B. Pennell, MD, Associate Professor of Neurology at Brigham and Women's Hospital and Harvard Medical School in Boston, and her research colleagues.
Previous studies suggested that women with epilepsy have lower fertility compared with healthy controls. Dr. Pennell and colleagues sought to compare time to pregnancy and outcomes (eg, live birth, miscarriage) among women with epilepsy and healthy controls. The Women with Epilepsy: Pregnancy Outcomes and Deliveries (WEPOD) study was a multicenter, prospective, observational study of women with epilepsy and healthy controls.
Dr. Pennell and colleagues enrolled and prospectively followed women with epilepsy and healthy controls, ages 18 to 41, seeking pregnancy within six months of discontinuing contraception. The customized WEPOD electronicdiary captured medication use, seizures, sexual activity, and menstrual bleeding. Pregnancy tests were performed if there was no menses by cycle day 35. Outcomes included proportions of women who achieved pregnancy and time to pregnancy from cessation of birth control. The researchers used a proportional hazard model to evaluate the association between time to pregnancy and certain baseline characteristics.
Enrolled in the study were 88 women with epilepsy and 109 healthy controls with similar demographic characteristics. Among women with epilepsy, 61.4% achieved pregnancy versus 60.6% for healthy controls. Median time to pregnancy was six months in women with epilepsy, compared with nine months for healthy controls. Time to pregnancy was no different across the two groups after controlling for age, BMI, parity, and race. Race and parity were significantly associated with time to pregnancy.
Of the pregnancies that occurred, a similar proportion resulted in miscarriage (12.9% among women with epilepsy and 19.7% among controls), live birth (80.0% among women with epilepsy and 80.3% controls) or other outcome (5.0% versus 0.0%).
The WEPOD study was supported by the Epilepsy Foundation.
VRIC is Just Around the Corner
The Vascular Research Initiatives Conference - VRIC - is less than three weeks away. The one-day conference, on May 4 in Nashville, focuses on translational research. This year’s theme is “Outside In: Paradigm Shifts in Vascular Disease.”
VRIC takes place the day before the American Heart Association’s Arteriosclerosis, Thrombosis and Vascular Biology (ATVB) Scientific Sessions, and at the same venue in Nashville. VRIC is considered a key event for meeting and reconnecting with vascular research collaborators.
The Vascular Research Initiatives Conference - VRIC - is less than three weeks away. The one-day conference, on May 4 in Nashville, focuses on translational research. This year’s theme is “Outside In: Paradigm Shifts in Vascular Disease.”
VRIC takes place the day before the American Heart Association’s Arteriosclerosis, Thrombosis and Vascular Biology (ATVB) Scientific Sessions, and at the same venue in Nashville. VRIC is considered a key event for meeting and reconnecting with vascular research collaborators.
The Vascular Research Initiatives Conference - VRIC - is less than three weeks away. The one-day conference, on May 4 in Nashville, focuses on translational research. This year’s theme is “Outside In: Paradigm Shifts in Vascular Disease.”
VRIC takes place the day before the American Heart Association’s Arteriosclerosis, Thrombosis and Vascular Biology (ATVB) Scientific Sessions, and at the same venue in Nashville. VRIC is considered a key event for meeting and reconnecting with vascular research collaborators.