User login
New and Noteworthy Information—September 2015
Emergency medical services (EMS) use for stroke differs by race, ethnicity, and sex, according to a study published in the August issue of the Journal of the American Heart Association. Data were analyzed from 398,798 stroke patients who were admitted to 1,613 Get With The Guidelines–Stroke participating hospitals between October 2011 and March 2014. Multivariable logistic regression was used to evaluate the associations between combinations of racial, ethnic, and sex groups with EMS use, adjusting for potential confounders including demographics, medical history, and stroke symptoms. White women were most likely to use EMS to get to the hospital (62%). Hispanic men were least likely to use EMS (52%). Hispanic and Asian men and women had 20% to 29% lower adjusted odds of using EMS compared with their white counterparts. Black women were less likely than white women to use EMS.
For patients who take sleeping pills to treat chronic insomnia, new study findings suggest that they may be able to get relief from as little as half of the drugs, and may even be helped by including placebos in the treatment plan. The study was published online July 7 in Sleep Medicine. In all, 74 subjects with chronic insomnia were treated with 10 mg of zolpidem for four weeks. Treatment responders were then randomized to nightly dosing with 10 mg or 5 mg, intermittent dosing (3 to 5 days weekly) with 10 mg, or partial reinforcement dosing (nightly pills with 50% active meds and 50% placebo) with 10 mg for 12 weeks. In compliant subjects, all of the treatment strategies maintained treatment response. For the subjects that remained in remission, the subjects in the intermittent dosing group exhibited poorer sleep continuity. “Our research found that changing the industry standard for maintenance therapy can maintain treatment responses and lower the incidence of side effects,” said the researchers.
Hospitals often overestimate their ability to deliver timely t-PA to treated patients, according to a study published in the July issue of the Journal of the American Heart Association. Researchers surveyed staff in 141 hospitals that treated 48,201 stroke patients in 2009 and 2010. Data included the onset of stroke symptoms, hospital arrival time, treatments, initiation of t-PA, and complications from the drug. Hospital performance was based on “door-to-needle” time. Only 29% of hospital staff accurately identified their door-to-needle performance; 42% of middle-performing hospitals and 85% of low-performing hospitals overestimated their abilities to quickly administer t-PA and nearly 20% of low-performing hospitals believed their door-to-needle time was above the national average. Hospitals that overestimated their performance had lower volumes of t-PA administration.
Incidence rates for Alzheimer’s disease and other dementias among African Americans age 70 or older have decreased over the last two decades, but the incidence rates for these conditions among Africans has remained unchanged over the same time period. According to a study published online ahead of print July 23 in Alzheimer’s & Dementia, dementia and Alzheimer’s disease incidence rates among African Americans were significantly lower in 2001 than in 1992, except for the oldest group. The cohorts consisted of 1,440 African Americans residing in Indianapolis and 1,774 Yoruba in Ibadan, Nigeria, in 1992, and 1,835 African Americans and 1,895 Yoruba in 2001. The overall dementia incidence rates among the African Americans were 3.6% in the 1992 cohort and 1.4% in the 2001 cohort. “The reason for the significant decline in new cases of Alzheimer’s disease and other dementias in the African Americans we studied is not yet entirely clear but we believe it may be possible that medications for cardiovascular conditions contributed to the decline,” the study authors said.
Lower executive function, but not memory, is associated with higher risk of coronary heart disease and stroke, according to a study published online ahead of print August 5 in Neurology. Included in this study were 3,926 participants with a mean age of 75, who were 44% male, and at risk for cardiovascular diseases. During 3.2 years of follow-up, incidence rates of coronary heart disease and stroke were 30.5 and 12.4 per 1,000 person-years, respectively. In multivariable models, participants in the lowest third of executive function, compared with participants in the highest third, had 1.85-fold higher risk of coronary heart disease and 1.51-fold higher risk of stroke. Participants in the lowest third of memory had no increased risk of coronary heart disease or stroke.
The Quick Dementia Rating System (QDRS) differentiates between individuals with and without dementia, accurately stages dementia without extensive tester training or clinician input, and is highly correlated with gold standard measures, according to a study published in the June issue of Alzheimer’s & Dementia. The QDRS was used in 267 patient-caregiver dyads compared with Clinical Dementia Ratings (CDR), neuropsychologic testing, and gold standard measures of function, mood, and behavior. The QDRS scores increased with higher CDR staging and poorer neuropsychologic performance. The QDRS demonstrated low floor and ceiling effects; excellent known-groups validity across CDR stages; construct validity against cognitive, behavioral, and functional measures; and reliability. The QDRS demonstrated differential scores across different dementia etiologies. The QDRS is copyrighted and permission is required to use it. The QDRS is available at no cost to clinicians, researchers, and not-for-profit organizations.
A drug used to treat diabetes may also reduce the risk of Parkinson’s disease, according to a study published July 21 in PLOS Medicine. Researchers conducted a retrospective cohort study in which individuals with diabetes who were prescribed glitazone antidiabetes drugs (rosiglitazone or pioglitazone) were matched by age, sex, practice, and diabetes treatment stage with up to five people who were taking other diabetes treatments. Patients were followed up from 1999 until the first recording of a Parkinson’s disease diagnosis, end of observation in the database, or the end of the study (August 1, 2013). In all, 44,597 glitazone-exposed individuals were matched to 120,373 other antidiabetic users. The incidence rate of Parkinson’s disease in the glitazone-exposed group was 6.4 per 10,000 patient years compared with 8.8 per 10,000 years in those prescribed other antidiabetic treatments.
Day-of-injury serum brain-derived neurotrophic factor (BDNF) is associated with traumatic brain injury (TBI) diagnosis and provides six-month prognostic information regarding recovery, according to a study published online ahead of print July 10 in the Journal of Neurotrauma. Researchers examined BDNF in 300 patients drawn from two independent cohorts of TBI cases presenting to two emergency departments and 150 patients without brain injuries. Among Transforming Research and Clinical Knowledge in TBI (TRACK-TBI) pilot study subjects, median BDNF concentrations were higher in mild than in moderate or severe TBI. In the TRACK-TBI cohort, the subjects with very low BDNF values had higher odds of incomplete recovery than those without very low values. According to the researchers, their results suggest that a test for BDNF levels, administered in the emergency department, could help stratify patients.
Children with multiple sclerosis (MS) are less physically active than children with monophasic acquired demyelinating syndrome, according to a study published online ahead of print August 12 in Neurology. In this cross-sectional study of consecutive patients attending a specialized pediatric MS clinic, researchers administered the PedsQL Multidimensional Fatigue Scale, Center for Epidemiological Studies Depression Scale, and Godin Leisure-Time Exercise Questionnaire. A total of 110 patients were included. Patients with MS reported less strenuous and total physical activity than those with monophasic acquired demyelinating syndrome. Patients with MS who reported greater amounts of moderate physical activity metabolic equivalents had fewer sleep/rest fatigue symptoms. Participation in strenuous physical activity was associated with smaller T2 lesion volumes and lower annualized relapse rate.
—Kimberly Williams
Emergency medical services (EMS) use for stroke differs by race, ethnicity, and sex, according to a study published in the August issue of the Journal of the American Heart Association. Data were analyzed from 398,798 stroke patients who were admitted to 1,613 Get With The Guidelines–Stroke participating hospitals between October 2011 and March 2014. Multivariable logistic regression was used to evaluate the associations between combinations of racial, ethnic, and sex groups with EMS use, adjusting for potential confounders including demographics, medical history, and stroke symptoms. White women were most likely to use EMS to get to the hospital (62%). Hispanic men were least likely to use EMS (52%). Hispanic and Asian men and women had 20% to 29% lower adjusted odds of using EMS compared with their white counterparts. Black women were less likely than white women to use EMS.
For patients who take sleeping pills to treat chronic insomnia, new study findings suggest that they may be able to get relief from as little as half of the drugs, and may even be helped by including placebos in the treatment plan. The study was published online July 7 in Sleep Medicine. In all, 74 subjects with chronic insomnia were treated with 10 mg of zolpidem for four weeks. Treatment responders were then randomized to nightly dosing with 10 mg or 5 mg, intermittent dosing (3 to 5 days weekly) with 10 mg, or partial reinforcement dosing (nightly pills with 50% active meds and 50% placebo) with 10 mg for 12 weeks. In compliant subjects, all of the treatment strategies maintained treatment response. For the subjects that remained in remission, the subjects in the intermittent dosing group exhibited poorer sleep continuity. “Our research found that changing the industry standard for maintenance therapy can maintain treatment responses and lower the incidence of side effects,” said the researchers.
Hospitals often overestimate their ability to deliver timely t-PA to treated patients, according to a study published in the July issue of the Journal of the American Heart Association. Researchers surveyed staff in 141 hospitals that treated 48,201 stroke patients in 2009 and 2010. Data included the onset of stroke symptoms, hospital arrival time, treatments, initiation of t-PA, and complications from the drug. Hospital performance was based on “door-to-needle” time. Only 29% of hospital staff accurately identified their door-to-needle performance; 42% of middle-performing hospitals and 85% of low-performing hospitals overestimated their abilities to quickly administer t-PA and nearly 20% of low-performing hospitals believed their door-to-needle time was above the national average. Hospitals that overestimated their performance had lower volumes of t-PA administration.
Incidence rates for Alzheimer’s disease and other dementias among African Americans age 70 or older have decreased over the last two decades, but the incidence rates for these conditions among Africans has remained unchanged over the same time period. According to a study published online ahead of print July 23 in Alzheimer’s & Dementia, dementia and Alzheimer’s disease incidence rates among African Americans were significantly lower in 2001 than in 1992, except for the oldest group. The cohorts consisted of 1,440 African Americans residing in Indianapolis and 1,774 Yoruba in Ibadan, Nigeria, in 1992, and 1,835 African Americans and 1,895 Yoruba in 2001. The overall dementia incidence rates among the African Americans were 3.6% in the 1992 cohort and 1.4% in the 2001 cohort. “The reason for the significant decline in new cases of Alzheimer’s disease and other dementias in the African Americans we studied is not yet entirely clear but we believe it may be possible that medications for cardiovascular conditions contributed to the decline,” the study authors said.
Lower executive function, but not memory, is associated with higher risk of coronary heart disease and stroke, according to a study published online ahead of print August 5 in Neurology. Included in this study were 3,926 participants with a mean age of 75, who were 44% male, and at risk for cardiovascular diseases. During 3.2 years of follow-up, incidence rates of coronary heart disease and stroke were 30.5 and 12.4 per 1,000 person-years, respectively. In multivariable models, participants in the lowest third of executive function, compared with participants in the highest third, had 1.85-fold higher risk of coronary heart disease and 1.51-fold higher risk of stroke. Participants in the lowest third of memory had no increased risk of coronary heart disease or stroke.
The Quick Dementia Rating System (QDRS) differentiates between individuals with and without dementia, accurately stages dementia without extensive tester training or clinician input, and is highly correlated with gold standard measures, according to a study published in the June issue of Alzheimer’s & Dementia. The QDRS was used in 267 patient-caregiver dyads compared with Clinical Dementia Ratings (CDR), neuropsychologic testing, and gold standard measures of function, mood, and behavior. The QDRS scores increased with higher CDR staging and poorer neuropsychologic performance. The QDRS demonstrated low floor and ceiling effects; excellent known-groups validity across CDR stages; construct validity against cognitive, behavioral, and functional measures; and reliability. The QDRS demonstrated differential scores across different dementia etiologies. The QDRS is copyrighted and permission is required to use it. The QDRS is available at no cost to clinicians, researchers, and not-for-profit organizations.
A drug used to treat diabetes may also reduce the risk of Parkinson’s disease, according to a study published July 21 in PLOS Medicine. Researchers conducted a retrospective cohort study in which individuals with diabetes who were prescribed glitazone antidiabetes drugs (rosiglitazone or pioglitazone) were matched by age, sex, practice, and diabetes treatment stage with up to five people who were taking other diabetes treatments. Patients were followed up from 1999 until the first recording of a Parkinson’s disease diagnosis, end of observation in the database, or the end of the study (August 1, 2013). In all, 44,597 glitazone-exposed individuals were matched to 120,373 other antidiabetic users. The incidence rate of Parkinson’s disease in the glitazone-exposed group was 6.4 per 10,000 patient years compared with 8.8 per 10,000 years in those prescribed other antidiabetic treatments.
Day-of-injury serum brain-derived neurotrophic factor (BDNF) is associated with traumatic brain injury (TBI) diagnosis and provides six-month prognostic information regarding recovery, according to a study published online ahead of print July 10 in the Journal of Neurotrauma. Researchers examined BDNF in 300 patients drawn from two independent cohorts of TBI cases presenting to two emergency departments and 150 patients without brain injuries. Among Transforming Research and Clinical Knowledge in TBI (TRACK-TBI) pilot study subjects, median BDNF concentrations were higher in mild than in moderate or severe TBI. In the TRACK-TBI cohort, the subjects with very low BDNF values had higher odds of incomplete recovery than those without very low values. According to the researchers, their results suggest that a test for BDNF levels, administered in the emergency department, could help stratify patients.
Children with multiple sclerosis (MS) are less physically active than children with monophasic acquired demyelinating syndrome, according to a study published online ahead of print August 12 in Neurology. In this cross-sectional study of consecutive patients attending a specialized pediatric MS clinic, researchers administered the PedsQL Multidimensional Fatigue Scale, Center for Epidemiological Studies Depression Scale, and Godin Leisure-Time Exercise Questionnaire. A total of 110 patients were included. Patients with MS reported less strenuous and total physical activity than those with monophasic acquired demyelinating syndrome. Patients with MS who reported greater amounts of moderate physical activity metabolic equivalents had fewer sleep/rest fatigue symptoms. Participation in strenuous physical activity was associated with smaller T2 lesion volumes and lower annualized relapse rate.
—Kimberly Williams
Emergency medical services (EMS) use for stroke differs by race, ethnicity, and sex, according to a study published in the August issue of the Journal of the American Heart Association. Data were analyzed from 398,798 stroke patients who were admitted to 1,613 Get With The Guidelines–Stroke participating hospitals between October 2011 and March 2014. Multivariable logistic regression was used to evaluate the associations between combinations of racial, ethnic, and sex groups with EMS use, adjusting for potential confounders including demographics, medical history, and stroke symptoms. White women were most likely to use EMS to get to the hospital (62%). Hispanic men were least likely to use EMS (52%). Hispanic and Asian men and women had 20% to 29% lower adjusted odds of using EMS compared with their white counterparts. Black women were less likely than white women to use EMS.
For patients who take sleeping pills to treat chronic insomnia, new study findings suggest that they may be able to get relief from as little as half of the drugs, and may even be helped by including placebos in the treatment plan. The study was published online July 7 in Sleep Medicine. In all, 74 subjects with chronic insomnia were treated with 10 mg of zolpidem for four weeks. Treatment responders were then randomized to nightly dosing with 10 mg or 5 mg, intermittent dosing (3 to 5 days weekly) with 10 mg, or partial reinforcement dosing (nightly pills with 50% active meds and 50% placebo) with 10 mg for 12 weeks. In compliant subjects, all of the treatment strategies maintained treatment response. For the subjects that remained in remission, the subjects in the intermittent dosing group exhibited poorer sleep continuity. “Our research found that changing the industry standard for maintenance therapy can maintain treatment responses and lower the incidence of side effects,” said the researchers.
Hospitals often overestimate their ability to deliver timely t-PA to treated patients, according to a study published in the July issue of the Journal of the American Heart Association. Researchers surveyed staff in 141 hospitals that treated 48,201 stroke patients in 2009 and 2010. Data included the onset of stroke symptoms, hospital arrival time, treatments, initiation of t-PA, and complications from the drug. Hospital performance was based on “door-to-needle” time. Only 29% of hospital staff accurately identified their door-to-needle performance; 42% of middle-performing hospitals and 85% of low-performing hospitals overestimated their abilities to quickly administer t-PA and nearly 20% of low-performing hospitals believed their door-to-needle time was above the national average. Hospitals that overestimated their performance had lower volumes of t-PA administration.
Incidence rates for Alzheimer’s disease and other dementias among African Americans age 70 or older have decreased over the last two decades, but the incidence rates for these conditions among Africans has remained unchanged over the same time period. According to a study published online ahead of print July 23 in Alzheimer’s & Dementia, dementia and Alzheimer’s disease incidence rates among African Americans were significantly lower in 2001 than in 1992, except for the oldest group. The cohorts consisted of 1,440 African Americans residing in Indianapolis and 1,774 Yoruba in Ibadan, Nigeria, in 1992, and 1,835 African Americans and 1,895 Yoruba in 2001. The overall dementia incidence rates among the African Americans were 3.6% in the 1992 cohort and 1.4% in the 2001 cohort. “The reason for the significant decline in new cases of Alzheimer’s disease and other dementias in the African Americans we studied is not yet entirely clear but we believe it may be possible that medications for cardiovascular conditions contributed to the decline,” the study authors said.
Lower executive function, but not memory, is associated with higher risk of coronary heart disease and stroke, according to a study published online ahead of print August 5 in Neurology. Included in this study were 3,926 participants with a mean age of 75, who were 44% male, and at risk for cardiovascular diseases. During 3.2 years of follow-up, incidence rates of coronary heart disease and stroke were 30.5 and 12.4 per 1,000 person-years, respectively. In multivariable models, participants in the lowest third of executive function, compared with participants in the highest third, had 1.85-fold higher risk of coronary heart disease and 1.51-fold higher risk of stroke. Participants in the lowest third of memory had no increased risk of coronary heart disease or stroke.
The Quick Dementia Rating System (QDRS) differentiates between individuals with and without dementia, accurately stages dementia without extensive tester training or clinician input, and is highly correlated with gold standard measures, according to a study published in the June issue of Alzheimer’s & Dementia. The QDRS was used in 267 patient-caregiver dyads compared with Clinical Dementia Ratings (CDR), neuropsychologic testing, and gold standard measures of function, mood, and behavior. The QDRS scores increased with higher CDR staging and poorer neuropsychologic performance. The QDRS demonstrated low floor and ceiling effects; excellent known-groups validity across CDR stages; construct validity against cognitive, behavioral, and functional measures; and reliability. The QDRS demonstrated differential scores across different dementia etiologies. The QDRS is copyrighted and permission is required to use it. The QDRS is available at no cost to clinicians, researchers, and not-for-profit organizations.
A drug used to treat diabetes may also reduce the risk of Parkinson’s disease, according to a study published July 21 in PLOS Medicine. Researchers conducted a retrospective cohort study in which individuals with diabetes who were prescribed glitazone antidiabetes drugs (rosiglitazone or pioglitazone) were matched by age, sex, practice, and diabetes treatment stage with up to five people who were taking other diabetes treatments. Patients were followed up from 1999 until the first recording of a Parkinson’s disease diagnosis, end of observation in the database, or the end of the study (August 1, 2013). In all, 44,597 glitazone-exposed individuals were matched to 120,373 other antidiabetic users. The incidence rate of Parkinson’s disease in the glitazone-exposed group was 6.4 per 10,000 patient years compared with 8.8 per 10,000 years in those prescribed other antidiabetic treatments.
Day-of-injury serum brain-derived neurotrophic factor (BDNF) is associated with traumatic brain injury (TBI) diagnosis and provides six-month prognostic information regarding recovery, according to a study published online ahead of print July 10 in the Journal of Neurotrauma. Researchers examined BDNF in 300 patients drawn from two independent cohorts of TBI cases presenting to two emergency departments and 150 patients without brain injuries. Among Transforming Research and Clinical Knowledge in TBI (TRACK-TBI) pilot study subjects, median BDNF concentrations were higher in mild than in moderate or severe TBI. In the TRACK-TBI cohort, the subjects with very low BDNF values had higher odds of incomplete recovery than those without very low values. According to the researchers, their results suggest that a test for BDNF levels, administered in the emergency department, could help stratify patients.
Children with multiple sclerosis (MS) are less physically active than children with monophasic acquired demyelinating syndrome, according to a study published online ahead of print August 12 in Neurology. In this cross-sectional study of consecutive patients attending a specialized pediatric MS clinic, researchers administered the PedsQL Multidimensional Fatigue Scale, Center for Epidemiological Studies Depression Scale, and Godin Leisure-Time Exercise Questionnaire. A total of 110 patients were included. Patients with MS reported less strenuous and total physical activity than those with monophasic acquired demyelinating syndrome. Patients with MS who reported greater amounts of moderate physical activity metabolic equivalents had fewer sleep/rest fatigue symptoms. Participation in strenuous physical activity was associated with smaller T2 lesion volumes and lower annualized relapse rate.
—Kimberly Williams
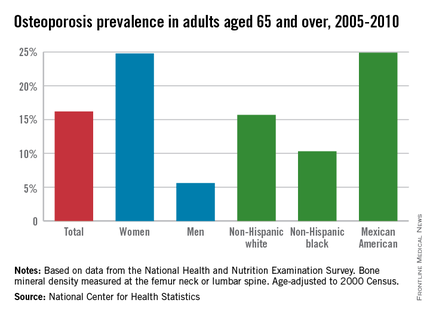
Osteoporosis Trends Collide for Mexican American Women
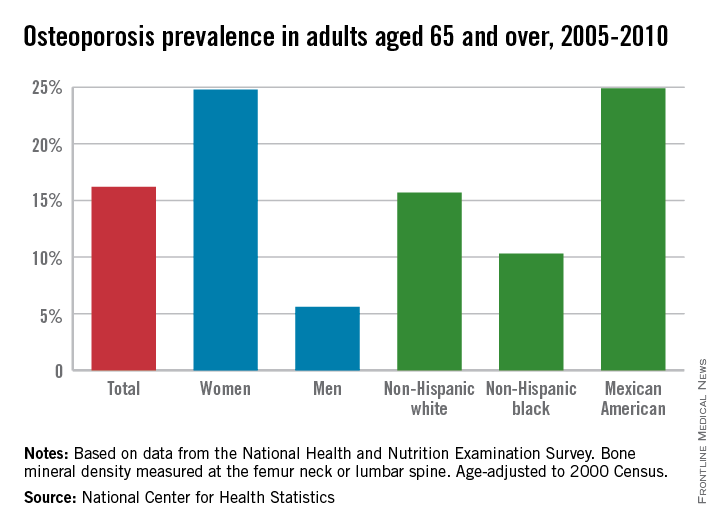
Among adults aged 65 years and over, women were 4.4 times as likely as men to have osteoporosis, and Mexican Americans were 2.4 times more likely than were blacks to have osteoporosis from 2005 to 2010, the National Center for Health Statistics reported.
So where does leave those who are both women and Mexican American?
First, a little background: The age-adjusted prevalence of osteoporosis measured at either the lumbar spine or femur neck among adults aged 65 years and over was 24.8% for women and 5.6% for men, for an overall prevalence of 16.2%. Adults aged 65-79 years had an unadjusted prevalence of 12.8%, compared with 25.7% for those aged 80 years and over, according to data from the 2005-2010 National Health and Nutrition Examination Survey.
Age-adjusted prevalence over that time period for Mexican Americans aged 65 years and older was 24.9%, compared with 15.7% for non-Hispanic whites and 10.3% for non-Hispanic blacks.
Mexican American women, who find themselves at the intersection of these two trends, had an adjusted osteoporosis rate of 36.8%, the NCHS reported.
Osteoporosis was defined as a bone mineral density value that was more than 2.5 standard deviations below the mean value for young, non-Hispanic white females.
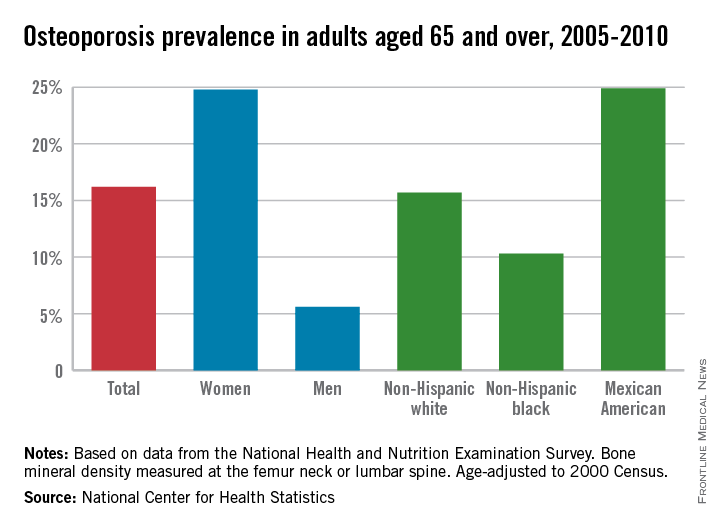
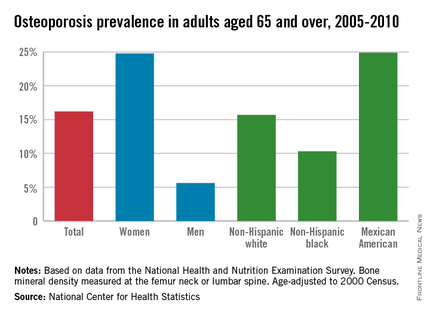
Among adults aged 65 years and over, women were 4.4 times as likely as men to have osteoporosis, and Mexican Americans were 2.4 times more likely than were blacks to have osteoporosis from 2005 to 2010, the National Center for Health Statistics reported.
So where does leave those who are both women and Mexican American?
First, a little background: The age-adjusted prevalence of osteoporosis measured at either the lumbar spine or femur neck among adults aged 65 years and over was 24.8% for women and 5.6% for men, for an overall prevalence of 16.2%. Adults aged 65-79 years had an unadjusted prevalence of 12.8%, compared with 25.7% for those aged 80 years and over, according to data from the 2005-2010 National Health and Nutrition Examination Survey.
Age-adjusted prevalence over that time period for Mexican Americans aged 65 years and older was 24.9%, compared with 15.7% for non-Hispanic whites and 10.3% for non-Hispanic blacks.
Mexican American women, who find themselves at the intersection of these two trends, had an adjusted osteoporosis rate of 36.8%, the NCHS reported.
Osteoporosis was defined as a bone mineral density value that was more than 2.5 standard deviations below the mean value for young, non-Hispanic white females.
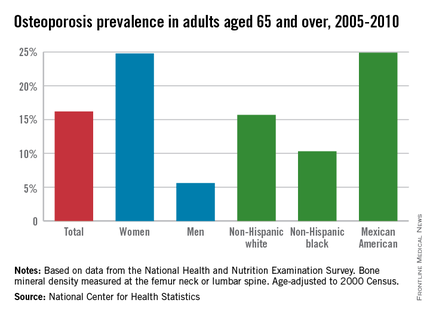
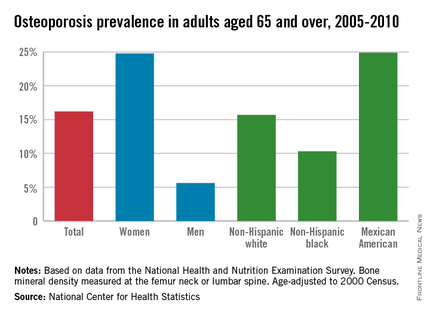
Among adults aged 65 years and over, women were 4.4 times as likely as men to have osteoporosis, and Mexican Americans were 2.4 times more likely than were blacks to have osteoporosis from 2005 to 2010, the National Center for Health Statistics reported.
So where does leave those who are both women and Mexican American?
First, a little background: The age-adjusted prevalence of osteoporosis measured at either the lumbar spine or femur neck among adults aged 65 years and over was 24.8% for women and 5.6% for men, for an overall prevalence of 16.2%. Adults aged 65-79 years had an unadjusted prevalence of 12.8%, compared with 25.7% for those aged 80 years and over, according to data from the 2005-2010 National Health and Nutrition Examination Survey.
Age-adjusted prevalence over that time period for Mexican Americans aged 65 years and older was 24.9%, compared with 15.7% for non-Hispanic whites and 10.3% for non-Hispanic blacks.
Mexican American women, who find themselves at the intersection of these two trends, had an adjusted osteoporosis rate of 36.8%, the NCHS reported.
Osteoporosis was defined as a bone mineral density value that was more than 2.5 standard deviations below the mean value for young, non-Hispanic white females.
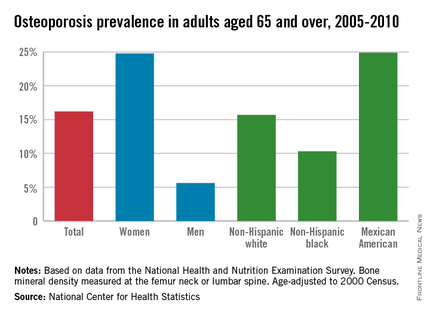
Osteoporosis trends collide for Mexican American women
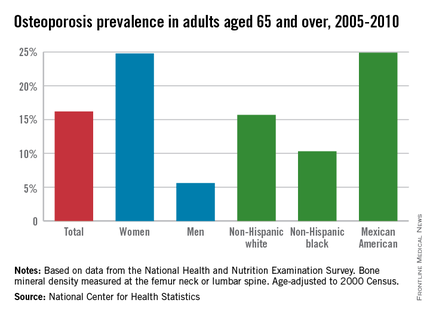
Among adults aged 65 years and over, women were 4.4 times as likely as men to have osteoporosis, and Mexican Americans were 2.4 times more likely than were blacks to have osteoporosis from 2005 to 2010, the National Center for Health Statistics reported.
So where does leave those who are both women and Mexican American?
First, a little background: The age-adjusted prevalence of osteoporosis measured at either the lumbar spine or femur neck among adults aged 65 years and over was 24.8% for women and 5.6% for men, for an overall prevalence of 16.2%. Adults aged 65-79 years had an unadjusted prevalence of 12.8%, compared with 25.7% for those aged 80 years and over, according to data from the 2005-2010 National Health and Nutrition Examination Survey.
Age-adjusted prevalence over that time period for Mexican Americans aged 65 years and older was 24.9%, compared with 15.7% for non-Hispanic whites and 10.3% for non-Hispanic blacks.
Mexican American women, who find themselves at the intersection of these two trends, had an adjusted osteoporosis rate of 36.8%, the NCHS reported.
Osteoporosis was defined as a bone mineral density value that was more than 2.5 standard deviations below the mean value for young, non-Hispanic white females.
Among adults aged 65 years and over, women were 4.4 times as likely as men to have osteoporosis, and Mexican Americans were 2.4 times more likely than were blacks to have osteoporosis from 2005 to 2010, the National Center for Health Statistics reported.
So where does leave those who are both women and Mexican American?
First, a little background: The age-adjusted prevalence of osteoporosis measured at either the lumbar spine or femur neck among adults aged 65 years and over was 24.8% for women and 5.6% for men, for an overall prevalence of 16.2%. Adults aged 65-79 years had an unadjusted prevalence of 12.8%, compared with 25.7% for those aged 80 years and over, according to data from the 2005-2010 National Health and Nutrition Examination Survey.
Age-adjusted prevalence over that time period for Mexican Americans aged 65 years and older was 24.9%, compared with 15.7% for non-Hispanic whites and 10.3% for non-Hispanic blacks.
Mexican American women, who find themselves at the intersection of these two trends, had an adjusted osteoporosis rate of 36.8%, the NCHS reported.
Osteoporosis was defined as a bone mineral density value that was more than 2.5 standard deviations below the mean value for young, non-Hispanic white females.
Among adults aged 65 years and over, women were 4.4 times as likely as men to have osteoporosis, and Mexican Americans were 2.4 times more likely than were blacks to have osteoporosis from 2005 to 2010, the National Center for Health Statistics reported.
So where does leave those who are both women and Mexican American?
First, a little background: The age-adjusted prevalence of osteoporosis measured at either the lumbar spine or femur neck among adults aged 65 years and over was 24.8% for women and 5.6% for men, for an overall prevalence of 16.2%. Adults aged 65-79 years had an unadjusted prevalence of 12.8%, compared with 25.7% for those aged 80 years and over, according to data from the 2005-2010 National Health and Nutrition Examination Survey.
Age-adjusted prevalence over that time period for Mexican Americans aged 65 years and older was 24.9%, compared with 15.7% for non-Hispanic whites and 10.3% for non-Hispanic blacks.
Mexican American women, who find themselves at the intersection of these two trends, had an adjusted osteoporosis rate of 36.8%, the NCHS reported.
Osteoporosis was defined as a bone mineral density value that was more than 2.5 standard deviations below the mean value for young, non-Hispanic white females.
Migraine Can Significantly Impact Family Activities and Dynamics
WASHINGTON, DC—While migraine is debilitating on an individual and societal level, its effects on the entire family can be substantial, as well. In a survey of migraineurs and their spouse/partners, migraine was found to impact family activities, inspire worries about financial security, and influence the nature of personal interactions. Lead author Dawn C. Buse, PhD, Associate Professor of Clinical Neurology at Albert Einstein College of Medicine and Montefiore Medical Center in the Bronx, New York, reported the study results at the American Headache Society’s 57th Annual Meeting. The study also assessed differences in family impact based on headache frequency. Previously, there had been little data to shed light on this topic.
Online Search for Study Participants In an attempt to represent US population demography, the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study used Web-based cross-sectional modules to identify potential participants from a panel of 2.4 million people. Dr. Buse and her research colleagues sent e-mail invitations to nearly 490,000 individuals who met study criteria—namely, meeting criteria for migraine using the American Migraine Study/American Migraine Prevalence and Prevention Study Diagnostic Module and chronic migraine using modified Silberstein-Lipton criteria. In addition to the migraine respondents (probands), their spouse/partners (a spouse, partner, or significant other living in the same household for ≥ 2 months) also were invited to participate.
Categories for headache days per month were divided into low-, moderate-, and high-frequency episodic migraine: 0 to 4, 5 to 9, and 10 to 14, respectively. Chronic migraine was defined as 15 or more headache days per month. The number of headache days per month was averaged over the preceding 90 days.
Survey items assessed four domains of interest: reduced participation in family activities, missed or canceled events, financial impact, and spouse interactions. Reduced participation and missed or canceled events were assessed on a Likert-type scale ranging from 1 (disagree completely) to 4 (agree completely).
After determining usable returns, the researchers included responses for 4,022 proband-spouse dyads in the final analysis. Of the probands, 73.3% were women and 72.9% of spouses were men. The mean age of probands and spouses were 43 and 44, respectively; 14.6% of participants were nonwhite.
Disrupted Relationships
Nearly half of probands (49.4%) on average reported not participating in family activity at home because of headache in the past 30 days, and nearly a third (29.8%) of their spouses reported not participating due to the proband’s headache. A total of 53.5% and 33.6% of probands and spouses, respectively, reported reduced enjoyment in family activity more than once during the past 30 days, and 51.4% and 53.6%, respectively, reported that one-on-one time was disrupted more than once during the past month due to the proband’s headaches.
On average, one in five probands reported missing a holiday or religious event due to headache. The frequency of that response among those with chronic migraine was four times that of those with low-frequency episodic migraine (0 to 4 headache days per month)—40.8% vs 10.7%, respectively. About 38% of probands with chronic migraine and 32% of spouses reported canceling an important celebration at home in the past month. Nearly 40% of probands with chronic migraine and 29% of spouses reported missing a wedding, graduation, retirement celebration, or other important event.
Worry about covering household expenses or about being fired or laid off from a job was prevalent among probands and spouses. Such concern increased with increased headache frequency. The researchers noted that as many as a quarter of probands with low-frequency episodic migraine worried about overall long-term financial security, as did 59.5% of those with chronic migraine.
About one-third of all spouses and nearly half of spouses of those with chronic migraine reported avoiding the proband because of headache. About 24% of probands with 0 to 4 headaches per month and 44% of those with chronic migraine had the perception that their spouses do not believe them about their headaches.
“The CaMEO Study results offer a unique view into migraine impact because both the probands’ and spouses’ perspectives were gathered,” the researchers said. “Existing data and clinical experience suggest that the impact of migraine is pervasive and extends beyond the individual with migraine.”
—Adriene Marshall
Suggested Reading
Buse DC, Lipton RB. Global perspectives on the burden of episodic and chronic migraine. Cephalalgia. 2013;33(11):885-890.
Adams AM, Serrano D, Buse DC, et al. The impact of chronic migraine: The Chronic Migraine Epidemiology and Outcomes (CaMEO) Study methods and baseline results. Cephalalgia. 2015;35(7):563-578.
Lanteri-Minet M. Economic burden and costs of chronic migraine. Curr Pain Headache Rep. 2014;18(1):385.
WASHINGTON, DC—While migraine is debilitating on an individual and societal level, its effects on the entire family can be substantial, as well. In a survey of migraineurs and their spouse/partners, migraine was found to impact family activities, inspire worries about financial security, and influence the nature of personal interactions. Lead author Dawn C. Buse, PhD, Associate Professor of Clinical Neurology at Albert Einstein College of Medicine and Montefiore Medical Center in the Bronx, New York, reported the study results at the American Headache Society’s 57th Annual Meeting. The study also assessed differences in family impact based on headache frequency. Previously, there had been little data to shed light on this topic.
Online Search for Study Participants In an attempt to represent US population demography, the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study used Web-based cross-sectional modules to identify potential participants from a panel of 2.4 million people. Dr. Buse and her research colleagues sent e-mail invitations to nearly 490,000 individuals who met study criteria—namely, meeting criteria for migraine using the American Migraine Study/American Migraine Prevalence and Prevention Study Diagnostic Module and chronic migraine using modified Silberstein-Lipton criteria. In addition to the migraine respondents (probands), their spouse/partners (a spouse, partner, or significant other living in the same household for ≥ 2 months) also were invited to participate.
Categories for headache days per month were divided into low-, moderate-, and high-frequency episodic migraine: 0 to 4, 5 to 9, and 10 to 14, respectively. Chronic migraine was defined as 15 or more headache days per month. The number of headache days per month was averaged over the preceding 90 days.
Survey items assessed four domains of interest: reduced participation in family activities, missed or canceled events, financial impact, and spouse interactions. Reduced participation and missed or canceled events were assessed on a Likert-type scale ranging from 1 (disagree completely) to 4 (agree completely).
After determining usable returns, the researchers included responses for 4,022 proband-spouse dyads in the final analysis. Of the probands, 73.3% were women and 72.9% of spouses were men. The mean age of probands and spouses were 43 and 44, respectively; 14.6% of participants were nonwhite.
Disrupted Relationships
Nearly half of probands (49.4%) on average reported not participating in family activity at home because of headache in the past 30 days, and nearly a third (29.8%) of their spouses reported not participating due to the proband’s headache. A total of 53.5% and 33.6% of probands and spouses, respectively, reported reduced enjoyment in family activity more than once during the past 30 days, and 51.4% and 53.6%, respectively, reported that one-on-one time was disrupted more than once during the past month due to the proband’s headaches.
On average, one in five probands reported missing a holiday or religious event due to headache. The frequency of that response among those with chronic migraine was four times that of those with low-frequency episodic migraine (0 to 4 headache days per month)—40.8% vs 10.7%, respectively. About 38% of probands with chronic migraine and 32% of spouses reported canceling an important celebration at home in the past month. Nearly 40% of probands with chronic migraine and 29% of spouses reported missing a wedding, graduation, retirement celebration, or other important event.
Worry about covering household expenses or about being fired or laid off from a job was prevalent among probands and spouses. Such concern increased with increased headache frequency. The researchers noted that as many as a quarter of probands with low-frequency episodic migraine worried about overall long-term financial security, as did 59.5% of those with chronic migraine.
About one-third of all spouses and nearly half of spouses of those with chronic migraine reported avoiding the proband because of headache. About 24% of probands with 0 to 4 headaches per month and 44% of those with chronic migraine had the perception that their spouses do not believe them about their headaches.
“The CaMEO Study results offer a unique view into migraine impact because both the probands’ and spouses’ perspectives were gathered,” the researchers said. “Existing data and clinical experience suggest that the impact of migraine is pervasive and extends beyond the individual with migraine.”
—Adriene Marshall
WASHINGTON, DC—While migraine is debilitating on an individual and societal level, its effects on the entire family can be substantial, as well. In a survey of migraineurs and their spouse/partners, migraine was found to impact family activities, inspire worries about financial security, and influence the nature of personal interactions. Lead author Dawn C. Buse, PhD, Associate Professor of Clinical Neurology at Albert Einstein College of Medicine and Montefiore Medical Center in the Bronx, New York, reported the study results at the American Headache Society’s 57th Annual Meeting. The study also assessed differences in family impact based on headache frequency. Previously, there had been little data to shed light on this topic.
Online Search for Study Participants In an attempt to represent US population demography, the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study used Web-based cross-sectional modules to identify potential participants from a panel of 2.4 million people. Dr. Buse and her research colleagues sent e-mail invitations to nearly 490,000 individuals who met study criteria—namely, meeting criteria for migraine using the American Migraine Study/American Migraine Prevalence and Prevention Study Diagnostic Module and chronic migraine using modified Silberstein-Lipton criteria. In addition to the migraine respondents (probands), their spouse/partners (a spouse, partner, or significant other living in the same household for ≥ 2 months) also were invited to participate.
Categories for headache days per month were divided into low-, moderate-, and high-frequency episodic migraine: 0 to 4, 5 to 9, and 10 to 14, respectively. Chronic migraine was defined as 15 or more headache days per month. The number of headache days per month was averaged over the preceding 90 days.
Survey items assessed four domains of interest: reduced participation in family activities, missed or canceled events, financial impact, and spouse interactions. Reduced participation and missed or canceled events were assessed on a Likert-type scale ranging from 1 (disagree completely) to 4 (agree completely).
After determining usable returns, the researchers included responses for 4,022 proband-spouse dyads in the final analysis. Of the probands, 73.3% were women and 72.9% of spouses were men. The mean age of probands and spouses were 43 and 44, respectively; 14.6% of participants were nonwhite.
Disrupted Relationships
Nearly half of probands (49.4%) on average reported not participating in family activity at home because of headache in the past 30 days, and nearly a third (29.8%) of their spouses reported not participating due to the proband’s headache. A total of 53.5% and 33.6% of probands and spouses, respectively, reported reduced enjoyment in family activity more than once during the past 30 days, and 51.4% and 53.6%, respectively, reported that one-on-one time was disrupted more than once during the past month due to the proband’s headaches.
On average, one in five probands reported missing a holiday or religious event due to headache. The frequency of that response among those with chronic migraine was four times that of those with low-frequency episodic migraine (0 to 4 headache days per month)—40.8% vs 10.7%, respectively. About 38% of probands with chronic migraine and 32% of spouses reported canceling an important celebration at home in the past month. Nearly 40% of probands with chronic migraine and 29% of spouses reported missing a wedding, graduation, retirement celebration, or other important event.
Worry about covering household expenses or about being fired or laid off from a job was prevalent among probands and spouses. Such concern increased with increased headache frequency. The researchers noted that as many as a quarter of probands with low-frequency episodic migraine worried about overall long-term financial security, as did 59.5% of those with chronic migraine.
About one-third of all spouses and nearly half of spouses of those with chronic migraine reported avoiding the proband because of headache. About 24% of probands with 0 to 4 headaches per month and 44% of those with chronic migraine had the perception that their spouses do not believe them about their headaches.
“The CaMEO Study results offer a unique view into migraine impact because both the probands’ and spouses’ perspectives were gathered,” the researchers said. “Existing data and clinical experience suggest that the impact of migraine is pervasive and extends beyond the individual with migraine.”
—Adriene Marshall
Suggested Reading
Buse DC, Lipton RB. Global perspectives on the burden of episodic and chronic migraine. Cephalalgia. 2013;33(11):885-890.
Adams AM, Serrano D, Buse DC, et al. The impact of chronic migraine: The Chronic Migraine Epidemiology and Outcomes (CaMEO) Study methods and baseline results. Cephalalgia. 2015;35(7):563-578.
Lanteri-Minet M. Economic burden and costs of chronic migraine. Curr Pain Headache Rep. 2014;18(1):385.
Suggested Reading
Buse DC, Lipton RB. Global perspectives on the burden of episodic and chronic migraine. Cephalalgia. 2013;33(11):885-890.
Adams AM, Serrano D, Buse DC, et al. The impact of chronic migraine: The Chronic Migraine Epidemiology and Outcomes (CaMEO) Study methods and baseline results. Cephalalgia. 2015;35(7):563-578.
Lanteri-Minet M. Economic burden and costs of chronic migraine. Curr Pain Headache Rep. 2014;18(1):385.
TBI Biomarker Development on the Horizon
A number of advanced efforts in traumatic brain injury (TBI) research are on the verge of reporting new data, according to a roundtable discussion that took place during the Military Health System Research Symposium on August 19. Among the most notable is in the area of biomarker development.
A 2,000-patient pivotal trial recently closed, and analysis should be completed by the end of the year. By March 2016, the research team expects to submit for FDA clearance a first-ever blood test for TBI. In addition, TBI research is currently being conducted in the areas of eye movement and balance.
Related: Brain Training for TBI Patients
A problem with assessing and treating the complexities of TBI up to this point is that although there are hundreds of measures of brain function, the evidence isn’t strong enough to provide a gold standard. “The whole area of drugs in neuroscience has been very difficult,” said Col. Dallas Hack, MD, senior medical advisor to the principal assistant for research and technology. “We have a couple of major efforts that are aimed at solving the problems of achieving results that can be measured according to the standards required to have them approved.”
Related: Stopping TBI-Related Brain Degeneration
To address the lack of a gold standard, the TBI Endpoints Development multiyear effort is making progress to give validity to the many existing measures of brain injury. Another effort is the VA/DoD Chronic Effects of Neurotrauma Consortium (CENC), a federally funded program that identifies gaps in research and provides support services for scientific, clinical, and translational research projects focused on the long-term effects of mild TBI in veterans and active-duty service members.
For information about the CENC, click here.
A number of advanced efforts in traumatic brain injury (TBI) research are on the verge of reporting new data, according to a roundtable discussion that took place during the Military Health System Research Symposium on August 19. Among the most notable is in the area of biomarker development.
A 2,000-patient pivotal trial recently closed, and analysis should be completed by the end of the year. By March 2016, the research team expects to submit for FDA clearance a first-ever blood test for TBI. In addition, TBI research is currently being conducted in the areas of eye movement and balance.
Related: Brain Training for TBI Patients
A problem with assessing and treating the complexities of TBI up to this point is that although there are hundreds of measures of brain function, the evidence isn’t strong enough to provide a gold standard. “The whole area of drugs in neuroscience has been very difficult,” said Col. Dallas Hack, MD, senior medical advisor to the principal assistant for research and technology. “We have a couple of major efforts that are aimed at solving the problems of achieving results that can be measured according to the standards required to have them approved.”
Related: Stopping TBI-Related Brain Degeneration
To address the lack of a gold standard, the TBI Endpoints Development multiyear effort is making progress to give validity to the many existing measures of brain injury. Another effort is the VA/DoD Chronic Effects of Neurotrauma Consortium (CENC), a federally funded program that identifies gaps in research and provides support services for scientific, clinical, and translational research projects focused on the long-term effects of mild TBI in veterans and active-duty service members.
For information about the CENC, click here.
A number of advanced efforts in traumatic brain injury (TBI) research are on the verge of reporting new data, according to a roundtable discussion that took place during the Military Health System Research Symposium on August 19. Among the most notable is in the area of biomarker development.
A 2,000-patient pivotal trial recently closed, and analysis should be completed by the end of the year. By March 2016, the research team expects to submit for FDA clearance a first-ever blood test for TBI. In addition, TBI research is currently being conducted in the areas of eye movement and balance.
Related: Brain Training for TBI Patients
A problem with assessing and treating the complexities of TBI up to this point is that although there are hundreds of measures of brain function, the evidence isn’t strong enough to provide a gold standard. “The whole area of drugs in neuroscience has been very difficult,” said Col. Dallas Hack, MD, senior medical advisor to the principal assistant for research and technology. “We have a couple of major efforts that are aimed at solving the problems of achieving results that can be measured according to the standards required to have them approved.”
Related: Stopping TBI-Related Brain Degeneration
To address the lack of a gold standard, the TBI Endpoints Development multiyear effort is making progress to give validity to the many existing measures of brain injury. Another effort is the VA/DoD Chronic Effects of Neurotrauma Consortium (CENC), a federally funded program that identifies gaps in research and provides support services for scientific, clinical, and translational research projects focused on the long-term effects of mild TBI in veterans and active-duty service members.
For information about the CENC, click here.
Persistent mutations tied to relapse, death in AML

Mutations that persist after initial chemotherapy may confer an increased risk of relapse and poor survival in patients with acute myeloid leukemia (AML), according to research published in JAMA.
Investigators found that patients who still had leukemia-specific mutations 30 days after they began chemotherapy had significantly shorter event-free and overall survival than patients whose bone marrow was free of these mutations.
These findings suggest genetic profiling of AML and other cancers may be more effective if it is focused less on the specific set of mutations present in a patient’s tumor at the time of diagnosis and more on whether those mutations are cleared by initial treatment with chemotherapy.
“If our results are confirmed in larger, prospective studies, genetic profiling after initial chemotherapy could help oncologists predict prognosis early in the course of a patient’s leukemia and determine whether that patient has responded to the chemotherapy, without having to wait for the cancer to recur,” said study author Jeffery M. Klco, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“This approach to genetic profiling, which focuses on performing genome sequencing after a patient’s initial treatment, also may be useful for other cancers.”
To investigate the utility of this approach, Dr Klco and his colleagues conducted a retrospective study of AML patients. The team began with bone marrow samples from 71 AML patients treated with standard induction chemotherapy.
The investigators first sequenced these samples, which were obtained at the time of diagnosis, to see if the presence of mutations correlated with the outcome of chemotherapy. They found that mutations were no more informative than standard methods used to predict patient outcomes.
So the team sequenced samples obtained from 50 AML patients at the time of diagnosis and again 30 days after the initiation of chemotherapy, when the patients were in remission. Twenty-five of the 50 patients were from the first cohort of 71 patients, and 25 were new cases.
Analyzing these samples, the investigators found that 24 patients (48%) had persistent mutations in at least 5% of bone marrow cells after chemotherapy, even though, by standard clinical measures, they were in remission.
These patients had inferior event-free and overall survival when compared to the patients whose mutations had been cleared by initial chemotherapy.
The median event-free survival was 6 months and 17.9 months in patients with and without mutations, respectively (P<0.001). And the median overall survival was 10.5 months and 42 months, respectively (P=0.004).
The investigators noted that only a subset of the persistent mutations were in recurrently mutated AML genes (NPM1, FLT3, DNMT3A, etc.).
“These findings build on studies performed more than a decade ago that suggested the failure to clear leukemia cells bearing chromosomal abnormalities was associated with increased risk of relapse,” said study author Timothy J. Ley, MD, of the Washington University School of Medicine in St. Louis, Missouri.
“But that technology was applicable only for the subset of patients with abnormal chromosomes, while genome sequencing can detect mutations in virtually all patients and is much more sensitive and specific. This new approach gives us a way to think about how to use genomics to evaluate the risk of relapse for nearly all AML patients.” ![]()

Mutations that persist after initial chemotherapy may confer an increased risk of relapse and poor survival in patients with acute myeloid leukemia (AML), according to research published in JAMA.
Investigators found that patients who still had leukemia-specific mutations 30 days after they began chemotherapy had significantly shorter event-free and overall survival than patients whose bone marrow was free of these mutations.
These findings suggest genetic profiling of AML and other cancers may be more effective if it is focused less on the specific set of mutations present in a patient’s tumor at the time of diagnosis and more on whether those mutations are cleared by initial treatment with chemotherapy.
“If our results are confirmed in larger, prospective studies, genetic profiling after initial chemotherapy could help oncologists predict prognosis early in the course of a patient’s leukemia and determine whether that patient has responded to the chemotherapy, without having to wait for the cancer to recur,” said study author Jeffery M. Klco, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“This approach to genetic profiling, which focuses on performing genome sequencing after a patient’s initial treatment, also may be useful for other cancers.”
To investigate the utility of this approach, Dr Klco and his colleagues conducted a retrospective study of AML patients. The team began with bone marrow samples from 71 AML patients treated with standard induction chemotherapy.
The investigators first sequenced these samples, which were obtained at the time of diagnosis, to see if the presence of mutations correlated with the outcome of chemotherapy. They found that mutations were no more informative than standard methods used to predict patient outcomes.
So the team sequenced samples obtained from 50 AML patients at the time of diagnosis and again 30 days after the initiation of chemotherapy, when the patients were in remission. Twenty-five of the 50 patients were from the first cohort of 71 patients, and 25 were new cases.
Analyzing these samples, the investigators found that 24 patients (48%) had persistent mutations in at least 5% of bone marrow cells after chemotherapy, even though, by standard clinical measures, they were in remission.
These patients had inferior event-free and overall survival when compared to the patients whose mutations had been cleared by initial chemotherapy.
The median event-free survival was 6 months and 17.9 months in patients with and without mutations, respectively (P<0.001). And the median overall survival was 10.5 months and 42 months, respectively (P=0.004).
The investigators noted that only a subset of the persistent mutations were in recurrently mutated AML genes (NPM1, FLT3, DNMT3A, etc.).
“These findings build on studies performed more than a decade ago that suggested the failure to clear leukemia cells bearing chromosomal abnormalities was associated with increased risk of relapse,” said study author Timothy J. Ley, MD, of the Washington University School of Medicine in St. Louis, Missouri.
“But that technology was applicable only for the subset of patients with abnormal chromosomes, while genome sequencing can detect mutations in virtually all patients and is much more sensitive and specific. This new approach gives us a way to think about how to use genomics to evaluate the risk of relapse for nearly all AML patients.” ![]()

Mutations that persist after initial chemotherapy may confer an increased risk of relapse and poor survival in patients with acute myeloid leukemia (AML), according to research published in JAMA.
Investigators found that patients who still had leukemia-specific mutations 30 days after they began chemotherapy had significantly shorter event-free and overall survival than patients whose bone marrow was free of these mutations.
These findings suggest genetic profiling of AML and other cancers may be more effective if it is focused less on the specific set of mutations present in a patient’s tumor at the time of diagnosis and more on whether those mutations are cleared by initial treatment with chemotherapy.
“If our results are confirmed in larger, prospective studies, genetic profiling after initial chemotherapy could help oncologists predict prognosis early in the course of a patient’s leukemia and determine whether that patient has responded to the chemotherapy, without having to wait for the cancer to recur,” said study author Jeffery M. Klco, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“This approach to genetic profiling, which focuses on performing genome sequencing after a patient’s initial treatment, also may be useful for other cancers.”
To investigate the utility of this approach, Dr Klco and his colleagues conducted a retrospective study of AML patients. The team began with bone marrow samples from 71 AML patients treated with standard induction chemotherapy.
The investigators first sequenced these samples, which were obtained at the time of diagnosis, to see if the presence of mutations correlated with the outcome of chemotherapy. They found that mutations were no more informative than standard methods used to predict patient outcomes.
So the team sequenced samples obtained from 50 AML patients at the time of diagnosis and again 30 days after the initiation of chemotherapy, when the patients were in remission. Twenty-five of the 50 patients were from the first cohort of 71 patients, and 25 were new cases.
Analyzing these samples, the investigators found that 24 patients (48%) had persistent mutations in at least 5% of bone marrow cells after chemotherapy, even though, by standard clinical measures, they were in remission.
These patients had inferior event-free and overall survival when compared to the patients whose mutations had been cleared by initial chemotherapy.
The median event-free survival was 6 months and 17.9 months in patients with and without mutations, respectively (P<0.001). And the median overall survival was 10.5 months and 42 months, respectively (P=0.004).
The investigators noted that only a subset of the persistent mutations were in recurrently mutated AML genes (NPM1, FLT3, DNMT3A, etc.).
“These findings build on studies performed more than a decade ago that suggested the failure to clear leukemia cells bearing chromosomal abnormalities was associated with increased risk of relapse,” said study author Timothy J. Ley, MD, of the Washington University School of Medicine in St. Louis, Missouri.
“But that technology was applicable only for the subset of patients with abnormal chromosomes, while genome sequencing can detect mutations in virtually all patients and is much more sensitive and specific. This new approach gives us a way to think about how to use genomics to evaluate the risk of relapse for nearly all AML patients.” ![]()
Treatment appears feasible for acute PE

Image courtesy of the
Medical College of Georgia
New research suggests that ultrasound-facilitated, catheter-directed, low-dose thrombolysis can produce positive results in patients with acute pulmonary embolism (PE).
In the SEATTLE II study, this treatment prompted significant decreases in thrombus burden, pulmonary hypertension, and the right ventricular-to-left ventricular (RV/LV) diameter ratio.
Major bleeds occurred in 10% of patients, but there were no cases of intracranial hemorrhage.
These results were published in JACC: Cardiovascular Interventions.
The SEATTLE II study was designed to evaluate ultrasound-facilitated, catheter-directed, low-dose thrombolysis using the EKOS EkoSonic® Endovascular System. The research was sponsored by EKOS Corporation, the company developing the system.
The trial included 150 patients diagnosed with acute massive (n=31) or submassive (n=119) PE. Patients received low-dose (24 mg) tissue plasminogen activator for 24 hours with a unilateral catheter or for 12 hours with bilateral catheters.
By 48 hours after treatment initiation, the mean RV/LV diameter ratio had significantly decreased, from 1.55 to 1.13 (P<0.0001).
The mean pulmonary artery systolic pressure decreased significantly as well, from 51.4 mm Hg to 36.9 mm Hg (P<0.0001).
And there was a significant decrease in modified Miller angiographic obstruction index score, from 22.5 to 15.8 (P<0.0001).
There were no intracranial hemorrhages and no fatal bleeding events. Major bleeds occurred in 15 patients (10%) and consisted of 1 severe bleed and 16 moderate bleeds.
Six of the major bleeds occurred in patients with comorbidities known to be associated with an increased risk of bleeding during thrombolytic therapy.
There were 3 serious adverse events that were considered potentially related to the EkoSonic Endovascular System. And 2 serious adverse events were potentially related to tissue plasminogen activator.
At 30 days post-treatment, there were 4 deaths. Three occurred in-hospital, and 1 was directly attributed to PE.
The researchers pointed out that 31 patients presented with massive PE, syncope, and hypotension. And all 31 survived the 30-day follow-up period.
“The SEATTLE II findings establish a new rationale for considering ultrasound-facilitated, catheter-directed, low-dose thrombolysis in both massive and submassive PE,” said study author Gregory Piazza, MD, of Brigham and Woman’s Hospital in Boston, Massachusetts.
“Without any intracranial hemorrhage and using a much-reduced lytic dose, a substantial and clinically meaningful reduction of the RV/LV ratio was achieved.” ![]()

Image courtesy of the
Medical College of Georgia
New research suggests that ultrasound-facilitated, catheter-directed, low-dose thrombolysis can produce positive results in patients with acute pulmonary embolism (PE).
In the SEATTLE II study, this treatment prompted significant decreases in thrombus burden, pulmonary hypertension, and the right ventricular-to-left ventricular (RV/LV) diameter ratio.
Major bleeds occurred in 10% of patients, but there were no cases of intracranial hemorrhage.
These results were published in JACC: Cardiovascular Interventions.
The SEATTLE II study was designed to evaluate ultrasound-facilitated, catheter-directed, low-dose thrombolysis using the EKOS EkoSonic® Endovascular System. The research was sponsored by EKOS Corporation, the company developing the system.
The trial included 150 patients diagnosed with acute massive (n=31) or submassive (n=119) PE. Patients received low-dose (24 mg) tissue plasminogen activator for 24 hours with a unilateral catheter or for 12 hours with bilateral catheters.
By 48 hours after treatment initiation, the mean RV/LV diameter ratio had significantly decreased, from 1.55 to 1.13 (P<0.0001).
The mean pulmonary artery systolic pressure decreased significantly as well, from 51.4 mm Hg to 36.9 mm Hg (P<0.0001).
And there was a significant decrease in modified Miller angiographic obstruction index score, from 22.5 to 15.8 (P<0.0001).
There were no intracranial hemorrhages and no fatal bleeding events. Major bleeds occurred in 15 patients (10%) and consisted of 1 severe bleed and 16 moderate bleeds.
Six of the major bleeds occurred in patients with comorbidities known to be associated with an increased risk of bleeding during thrombolytic therapy.
There were 3 serious adverse events that were considered potentially related to the EkoSonic Endovascular System. And 2 serious adverse events were potentially related to tissue plasminogen activator.
At 30 days post-treatment, there were 4 deaths. Three occurred in-hospital, and 1 was directly attributed to PE.
The researchers pointed out that 31 patients presented with massive PE, syncope, and hypotension. And all 31 survived the 30-day follow-up period.
“The SEATTLE II findings establish a new rationale for considering ultrasound-facilitated, catheter-directed, low-dose thrombolysis in both massive and submassive PE,” said study author Gregory Piazza, MD, of Brigham and Woman’s Hospital in Boston, Massachusetts.
“Without any intracranial hemorrhage and using a much-reduced lytic dose, a substantial and clinically meaningful reduction of the RV/LV ratio was achieved.” ![]()

Image courtesy of the
Medical College of Georgia
New research suggests that ultrasound-facilitated, catheter-directed, low-dose thrombolysis can produce positive results in patients with acute pulmonary embolism (PE).
In the SEATTLE II study, this treatment prompted significant decreases in thrombus burden, pulmonary hypertension, and the right ventricular-to-left ventricular (RV/LV) diameter ratio.
Major bleeds occurred in 10% of patients, but there were no cases of intracranial hemorrhage.
These results were published in JACC: Cardiovascular Interventions.
The SEATTLE II study was designed to evaluate ultrasound-facilitated, catheter-directed, low-dose thrombolysis using the EKOS EkoSonic® Endovascular System. The research was sponsored by EKOS Corporation, the company developing the system.
The trial included 150 patients diagnosed with acute massive (n=31) or submassive (n=119) PE. Patients received low-dose (24 mg) tissue plasminogen activator for 24 hours with a unilateral catheter or for 12 hours with bilateral catheters.
By 48 hours after treatment initiation, the mean RV/LV diameter ratio had significantly decreased, from 1.55 to 1.13 (P<0.0001).
The mean pulmonary artery systolic pressure decreased significantly as well, from 51.4 mm Hg to 36.9 mm Hg (P<0.0001).
And there was a significant decrease in modified Miller angiographic obstruction index score, from 22.5 to 15.8 (P<0.0001).
There were no intracranial hemorrhages and no fatal bleeding events. Major bleeds occurred in 15 patients (10%) and consisted of 1 severe bleed and 16 moderate bleeds.
Six of the major bleeds occurred in patients with comorbidities known to be associated with an increased risk of bleeding during thrombolytic therapy.
There were 3 serious adverse events that were considered potentially related to the EkoSonic Endovascular System. And 2 serious adverse events were potentially related to tissue plasminogen activator.
At 30 days post-treatment, there were 4 deaths. Three occurred in-hospital, and 1 was directly attributed to PE.
The researchers pointed out that 31 patients presented with massive PE, syncope, and hypotension. And all 31 survived the 30-day follow-up period.
“The SEATTLE II findings establish a new rationale for considering ultrasound-facilitated, catheter-directed, low-dose thrombolysis in both massive and submassive PE,” said study author Gregory Piazza, MD, of Brigham and Woman’s Hospital in Boston, Massachusetts.
“Without any intracranial hemorrhage and using a much-reduced lytic dose, a substantial and clinically meaningful reduction of the RV/LV ratio was achieved.” ![]()
Study reveals approaches to aid, prevent apoptosis

apoptosis in cancer cells
Scientists say they have gained new insight into the role Bax plays in apoptosis.
The Bax protein is known to be a key regulator of apoptosis, mediating the release of cytochrome c to the cytosol via oligomerization in the outer mitochondrial membrane before pore formation.
But the exact mechanism of Bax assembly was previously unclear.
Now, research published in Nature Communications has provided some clarity.
Katia Cosentino, PhD, of the Max Planck Institute for Intelligent Systems in Stuttgart, Germany, and her colleagues conducted this research, examining how the mitochondrial membrane becomes permeable.
The team’s experiments on artificial membrane systems showed that Bax is initially inserted into the membrane as a single molecule.
Once inserted, one Bax molecule will join up with a second Bax molecule to form a stable complex, the Bax dimers. From these dimers, larger complexes are formed.
“Surprisingly, Bax complexes have no standard size, but we observed a mixture of different-sized Bax species, and these species are mostly based on dimer units,” Dr Cosentino said.
She and her colleagues noted that these Bax complexes form the pores through which cytochrome c exits the mitochondrial membrane.
But the process of pore formation is finely controlled by other proteins. Some (such as cBid) enable the assembly of Bax elements, while others (such as Bcl-xL) induce their dismantling.
“The differing size of the Bax complexes in the pore formation is likely part of the reason why earlier investigations on pore formation conveyed contradictory results,” Dr Cosentino said.
She and her colleagues believe that, based on these findings, they can make some initial recommendations for medical intervention in the apoptotic process.
They think that, to promote apoptosis, it should be enough to initiate the first step of activating Bax proteins because the subsequent steps of self-organization will then happen automatically.
Conversely, the team’s findings suggest apoptosis can be prevented when drugs force the dismantling of the Bax dimers into their individual elements. ![]()

apoptosis in cancer cells
Scientists say they have gained new insight into the role Bax plays in apoptosis.
The Bax protein is known to be a key regulator of apoptosis, mediating the release of cytochrome c to the cytosol via oligomerization in the outer mitochondrial membrane before pore formation.
But the exact mechanism of Bax assembly was previously unclear.
Now, research published in Nature Communications has provided some clarity.
Katia Cosentino, PhD, of the Max Planck Institute for Intelligent Systems in Stuttgart, Germany, and her colleagues conducted this research, examining how the mitochondrial membrane becomes permeable.
The team’s experiments on artificial membrane systems showed that Bax is initially inserted into the membrane as a single molecule.
Once inserted, one Bax molecule will join up with a second Bax molecule to form a stable complex, the Bax dimers. From these dimers, larger complexes are formed.
“Surprisingly, Bax complexes have no standard size, but we observed a mixture of different-sized Bax species, and these species are mostly based on dimer units,” Dr Cosentino said.
She and her colleagues noted that these Bax complexes form the pores through which cytochrome c exits the mitochondrial membrane.
But the process of pore formation is finely controlled by other proteins. Some (such as cBid) enable the assembly of Bax elements, while others (such as Bcl-xL) induce their dismantling.
“The differing size of the Bax complexes in the pore formation is likely part of the reason why earlier investigations on pore formation conveyed contradictory results,” Dr Cosentino said.
She and her colleagues believe that, based on these findings, they can make some initial recommendations for medical intervention in the apoptotic process.
They think that, to promote apoptosis, it should be enough to initiate the first step of activating Bax proteins because the subsequent steps of self-organization will then happen automatically.
Conversely, the team’s findings suggest apoptosis can be prevented when drugs force the dismantling of the Bax dimers into their individual elements. ![]()

apoptosis in cancer cells
Scientists say they have gained new insight into the role Bax plays in apoptosis.
The Bax protein is known to be a key regulator of apoptosis, mediating the release of cytochrome c to the cytosol via oligomerization in the outer mitochondrial membrane before pore formation.
But the exact mechanism of Bax assembly was previously unclear.
Now, research published in Nature Communications has provided some clarity.
Katia Cosentino, PhD, of the Max Planck Institute for Intelligent Systems in Stuttgart, Germany, and her colleagues conducted this research, examining how the mitochondrial membrane becomes permeable.
The team’s experiments on artificial membrane systems showed that Bax is initially inserted into the membrane as a single molecule.
Once inserted, one Bax molecule will join up with a second Bax molecule to form a stable complex, the Bax dimers. From these dimers, larger complexes are formed.
“Surprisingly, Bax complexes have no standard size, but we observed a mixture of different-sized Bax species, and these species are mostly based on dimer units,” Dr Cosentino said.
She and her colleagues noted that these Bax complexes form the pores through which cytochrome c exits the mitochondrial membrane.
But the process of pore formation is finely controlled by other proteins. Some (such as cBid) enable the assembly of Bax elements, while others (such as Bcl-xL) induce their dismantling.
“The differing size of the Bax complexes in the pore formation is likely part of the reason why earlier investigations on pore formation conveyed contradictory results,” Dr Cosentino said.
She and her colleagues believe that, based on these findings, they can make some initial recommendations for medical intervention in the apoptotic process.
They think that, to promote apoptosis, it should be enough to initiate the first step of activating Bax proteins because the subsequent steps of self-organization will then happen automatically.
Conversely, the team’s findings suggest apoptosis can be prevented when drugs force the dismantling of the Bax dimers into their individual elements. ![]()
New proteasome inhibitor exhibits activity against MM

A novel, cancer-selective proteasome inhibitor has shown early promise for treating multiple myeloma (MM) and breast cancer, according to researchers.
The drug, known as VR23, is a quinoline-sulfonyl hybrid proteasome inhibitor.
In preclinical experiments, VR23 preferentially targeted MM cells and breast cancer cells, demonstrated synergy with bortezomib or paclitaxel, and shrank both MM and breast cancer tumors in mice.
Hoyun Lee, PhD, of the Advanced Medical Research Institute of Canada (AMRIC) in Sudbury, Ontario, and his colleagues described these experiments in Cancer Research.
The team noted that VR23 is structurally distinct from other known proteasome inhibitors, and it “potently inhibits” the activities of trypsin-like proteasomes, chymotrypsin-like proteasomes, and caspase-like proteasomes.
In several experiments, VR23 proved active against breast cancer.
In experiments with MM cell lines, VR23 exhibited activity as a single agent and demonstrated synergy with bortezomib. VR23 proved more effective against bortezomib-resistant cells than bortezomib-naïve cells.
When the researchers introduced treatments to bortezomib-naïve RPMI-8226 cells, they found the cell growth rate was 79.3% with VR23, 12.5% with bortezomib, and 1.6% with both drugs. In bortezomib-resistant RPMI-8226 cells, the cell growth rate was 47% with VR23, 109.7% with bortezomib, and -8.6% with both drugs.
In KAS6/1 cells, the cell growth rate was 65% with VR23, 92% with bortezomib, and 26.5% with both drugs. In bortezomib-resistant ANBL6 cells, the cell growth rate was 94% with VR23, 102.9% with bortezomib, and 48.9% with both drugs.
The researchers also tested VR23 in mice engrafted with RPMI-8226 MM cells. At 24 days after treatment, the tumor volume for VR23-treated mice was 19.1% that of placebo-treated mice.
The team noted that VR23 selectively killed cancer cells via apoptosis. Cancer cells exposed to the drug underwent an abnormal centrosome amplification cycle caused by the accumulation of ubiquitinated cyclin E.
Dr Lee and his colleagues are now planning to work with the US National Cancer Institute to test VR23 in additional cancers. The team is hoping to progress to clinical trials with the drug in the next 3 years.
AMRIC has applied for international intellectual property protection for VR23 and licensed commercial rights to Ramsey Lake Pharmaceutical Corporation (www.ramseylakepharma.com), an operation of AMRIC. ![]()

A novel, cancer-selective proteasome inhibitor has shown early promise for treating multiple myeloma (MM) and breast cancer, according to researchers.
The drug, known as VR23, is a quinoline-sulfonyl hybrid proteasome inhibitor.
In preclinical experiments, VR23 preferentially targeted MM cells and breast cancer cells, demonstrated synergy with bortezomib or paclitaxel, and shrank both MM and breast cancer tumors in mice.
Hoyun Lee, PhD, of the Advanced Medical Research Institute of Canada (AMRIC) in Sudbury, Ontario, and his colleagues described these experiments in Cancer Research.
The team noted that VR23 is structurally distinct from other known proteasome inhibitors, and it “potently inhibits” the activities of trypsin-like proteasomes, chymotrypsin-like proteasomes, and caspase-like proteasomes.
In several experiments, VR23 proved active against breast cancer.
In experiments with MM cell lines, VR23 exhibited activity as a single agent and demonstrated synergy with bortezomib. VR23 proved more effective against bortezomib-resistant cells than bortezomib-naïve cells.
When the researchers introduced treatments to bortezomib-naïve RPMI-8226 cells, they found the cell growth rate was 79.3% with VR23, 12.5% with bortezomib, and 1.6% with both drugs. In bortezomib-resistant RPMI-8226 cells, the cell growth rate was 47% with VR23, 109.7% with bortezomib, and -8.6% with both drugs.
In KAS6/1 cells, the cell growth rate was 65% with VR23, 92% with bortezomib, and 26.5% with both drugs. In bortezomib-resistant ANBL6 cells, the cell growth rate was 94% with VR23, 102.9% with bortezomib, and 48.9% with both drugs.
The researchers also tested VR23 in mice engrafted with RPMI-8226 MM cells. At 24 days after treatment, the tumor volume for VR23-treated mice was 19.1% that of placebo-treated mice.
The team noted that VR23 selectively killed cancer cells via apoptosis. Cancer cells exposed to the drug underwent an abnormal centrosome amplification cycle caused by the accumulation of ubiquitinated cyclin E.
Dr Lee and his colleagues are now planning to work with the US National Cancer Institute to test VR23 in additional cancers. The team is hoping to progress to clinical trials with the drug in the next 3 years.
AMRIC has applied for international intellectual property protection for VR23 and licensed commercial rights to Ramsey Lake Pharmaceutical Corporation (www.ramseylakepharma.com), an operation of AMRIC. ![]()

A novel, cancer-selective proteasome inhibitor has shown early promise for treating multiple myeloma (MM) and breast cancer, according to researchers.
The drug, known as VR23, is a quinoline-sulfonyl hybrid proteasome inhibitor.
In preclinical experiments, VR23 preferentially targeted MM cells and breast cancer cells, demonstrated synergy with bortezomib or paclitaxel, and shrank both MM and breast cancer tumors in mice.
Hoyun Lee, PhD, of the Advanced Medical Research Institute of Canada (AMRIC) in Sudbury, Ontario, and his colleagues described these experiments in Cancer Research.
The team noted that VR23 is structurally distinct from other known proteasome inhibitors, and it “potently inhibits” the activities of trypsin-like proteasomes, chymotrypsin-like proteasomes, and caspase-like proteasomes.
In several experiments, VR23 proved active against breast cancer.
In experiments with MM cell lines, VR23 exhibited activity as a single agent and demonstrated synergy with bortezomib. VR23 proved more effective against bortezomib-resistant cells than bortezomib-naïve cells.
When the researchers introduced treatments to bortezomib-naïve RPMI-8226 cells, they found the cell growth rate was 79.3% with VR23, 12.5% with bortezomib, and 1.6% with both drugs. In bortezomib-resistant RPMI-8226 cells, the cell growth rate was 47% with VR23, 109.7% with bortezomib, and -8.6% with both drugs.
In KAS6/1 cells, the cell growth rate was 65% with VR23, 92% with bortezomib, and 26.5% with both drugs. In bortezomib-resistant ANBL6 cells, the cell growth rate was 94% with VR23, 102.9% with bortezomib, and 48.9% with both drugs.
The researchers also tested VR23 in mice engrafted with RPMI-8226 MM cells. At 24 days after treatment, the tumor volume for VR23-treated mice was 19.1% that of placebo-treated mice.
The team noted that VR23 selectively killed cancer cells via apoptosis. Cancer cells exposed to the drug underwent an abnormal centrosome amplification cycle caused by the accumulation of ubiquitinated cyclin E.
Dr Lee and his colleagues are now planning to work with the US National Cancer Institute to test VR23 in additional cancers. The team is hoping to progress to clinical trials with the drug in the next 3 years.
AMRIC has applied for international intellectual property protection for VR23 and licensed commercial rights to Ramsey Lake Pharmaceutical Corporation (www.ramseylakepharma.com), an operation of AMRIC. ![]()
Corticosteroids Show Benefit in Community-Acquired Pneumonia
Clinical question: Does corticosteroid treatment shorten systemic illness in patients admitted to the hospital for community-acquired pneumonia (CAP)?
Background: Pneumonia is the third-leading cause of death worldwide. Studies have yielded conflicting data about the benefit of adding systemic corticosteroids for treatment of CAP.
Study design: Double-blind, multicenter, randomized, placebo-controlled trial.
Setting: Seven tertiary-care hospitals in Switzerland.
Synopsis: A group of 784 patients hospitalized for CAP were randomized to receive either oral prednisone 50 mg daily for seven days or placebo, with the primary endpoint being time to stable vital signs. The intention-to-treat analysis found that the median time to clinical stability was 1.4 days earlier in the prednisone group (hazard ratio 1.33; 95% CI, 1.15–1.50, P <0.0001) and that length of stay and IV antibiotics were reduced by one day; this effect was valid across all PSI classes and was not dependent on age. Pneumonia-associated complications in the two groups did not differ at 30 days, though the prednisone group had a higher incidence of hyperglycemia requiring insulin. Because all study locations were in a single, fairly homogenous northern European country, care should be taken when hospitalists apply these findings to their patient population, and the risks of hyperglycemia requiring insulin should be taken into consideration.
Bottom line: Systemic steroids may reduce the time to clinical stability in patients with CAP.
Citation: Blum CA, Nigro N, Briel M, et al. Adjunct prednisone therapy for patients with community-acquired pneumonia: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet. 2015;385(9977):1511–1518.
Clinical question: Does corticosteroid treatment shorten systemic illness in patients admitted to the hospital for community-acquired pneumonia (CAP)?
Background: Pneumonia is the third-leading cause of death worldwide. Studies have yielded conflicting data about the benefit of adding systemic corticosteroids for treatment of CAP.
Study design: Double-blind, multicenter, randomized, placebo-controlled trial.
Setting: Seven tertiary-care hospitals in Switzerland.
Synopsis: A group of 784 patients hospitalized for CAP were randomized to receive either oral prednisone 50 mg daily for seven days or placebo, with the primary endpoint being time to stable vital signs. The intention-to-treat analysis found that the median time to clinical stability was 1.4 days earlier in the prednisone group (hazard ratio 1.33; 95% CI, 1.15–1.50, P <0.0001) and that length of stay and IV antibiotics were reduced by one day; this effect was valid across all PSI classes and was not dependent on age. Pneumonia-associated complications in the two groups did not differ at 30 days, though the prednisone group had a higher incidence of hyperglycemia requiring insulin. Because all study locations were in a single, fairly homogenous northern European country, care should be taken when hospitalists apply these findings to their patient population, and the risks of hyperglycemia requiring insulin should be taken into consideration.
Bottom line: Systemic steroids may reduce the time to clinical stability in patients with CAP.
Citation: Blum CA, Nigro N, Briel M, et al. Adjunct prednisone therapy for patients with community-acquired pneumonia: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet. 2015;385(9977):1511–1518.
Clinical question: Does corticosteroid treatment shorten systemic illness in patients admitted to the hospital for community-acquired pneumonia (CAP)?
Background: Pneumonia is the third-leading cause of death worldwide. Studies have yielded conflicting data about the benefit of adding systemic corticosteroids for treatment of CAP.
Study design: Double-blind, multicenter, randomized, placebo-controlled trial.
Setting: Seven tertiary-care hospitals in Switzerland.
Synopsis: A group of 784 patients hospitalized for CAP were randomized to receive either oral prednisone 50 mg daily for seven days or placebo, with the primary endpoint being time to stable vital signs. The intention-to-treat analysis found that the median time to clinical stability was 1.4 days earlier in the prednisone group (hazard ratio 1.33; 95% CI, 1.15–1.50, P <0.0001) and that length of stay and IV antibiotics were reduced by one day; this effect was valid across all PSI classes and was not dependent on age. Pneumonia-associated complications in the two groups did not differ at 30 days, though the prednisone group had a higher incidence of hyperglycemia requiring insulin. Because all study locations were in a single, fairly homogenous northern European country, care should be taken when hospitalists apply these findings to their patient population, and the risks of hyperglycemia requiring insulin should be taken into consideration.
Bottom line: Systemic steroids may reduce the time to clinical stability in patients with CAP.
Citation: Blum CA, Nigro N, Briel M, et al. Adjunct prednisone therapy for patients with community-acquired pneumonia: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet. 2015;385(9977):1511–1518.