User login
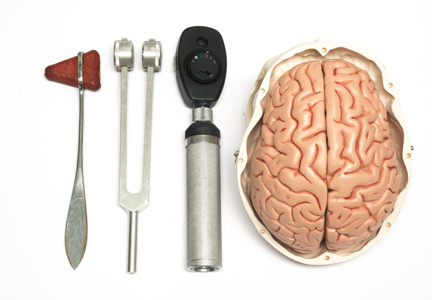
Is a detailed neurologic physical examination always necessary?
The article in this issue by Shikino et al1 on a mimic of Bell palsy gives us an opportunity to discuss the question posed by the title of this editorial. The obvious short answer is “no.”
Any experienced clinician will acknowledge that the extent of the physical examination and the extent of information obtained during the history should be determined by the problem being evaluated at the time and by the setting in which it takes place. The difficulty, of course, is that this relies on the judgment of the clinician, and this may or may not pass the test of hindsight.
Verghese et al2 have eloquently emphasized the hazards of an incomplete or inadequate physical examination. Their study was not designed to determine the prevalence of deficient physical examination, either in its extent or its accuracy. Their purpose was to promote the necessity of proper teaching and performance of examination technique.
The neurologic examination is one of the last bastions of physical assessment.3 Despite remarkable advances in imaging and physiologic techniques, the neurologic physical assessment remains critical for diagnosis and management of the neurologic patient. One of my mentors in neurology used to urge residents to examine patients and record the results of the examination as if every patient would subsequently be the subject of a clinicopathologic conference. Anyone who has reviewed a case for a conference or a case report can identify with that sentiment, wishing that some missing piece of information were available. Yet everyone also recognizes the difficulties, if not the impossibility, of achieving that ideal result.
But recording information obtained during the history or physical examination is important even in the course of a daily routine evaluation. I find myself wishing that a previous examiner had commented on whether the muscle stretch reflexes were somewhat hypoactive (eg, “1+”) or on the brisk side (“3+”) rather than “physiologic.” Was the right leg actually globally weak (“4/5”), or was there a discrepancy between proximal and distal muscles or between the physiologic flexors and the extensors?
This can make a big difference in following a patient’s neurologic progress, even over a short time span. It might tell us whether we are dealing with weakness from a peripheral neuromuscular disorder (eg, Guillain-Barré syndrome) or from a myelopathy due to impending spinal cord compression.
It should be mentioned that although Guillain-Barré syndrome is characterized as an ascending paralysis, ie, beginning distally and spreading rostrally, it is one of the few peripheral neuropathies that can present with predominant proximal weakness. It is, in fact, a radiculoneuropathy. But spinal cord (upper motor neuron) disorders preferentially weaken the physiologic flexors of the lower limbs (hamstrings and ankle dorsiflexors), leading to the characteristic extensor posture of the spastic leg. Other findings that can help differential peripheral vs spinal cord disorders include distal sensory loss and hypoactive or absent muscle stretch reflexes in a peripheral neuropathy, compared with dissociated sensory loss (eg, impaired pain and temperature sensation in one leg with reduced vibration perception and proprioception in the other) along with hyperreflexia with cord lesions.
Therefore, a careful neurologic examination may tell us whether magnetic resonance imaging of the spine or an electrodiagnostic study should be the next step.
Shikino et al describe a patient who presented with what looked like idiopathic facial palsy (Bell palsy) but turned out to be the result of a primary central nervous system (CNS) cause. Would a more detailed neurologic examination have identified this as a CNS disorder? Would more specific information about the degree and distribution of facial paresis have facilitated earlier recognition of a progressive process, making idiopathic facial palsy less likely? How much elevation of the eyebrow occurred with voluntary activation, how many millimeters of sclera were visible with gentle eyelid closure? How much space remained between the lips on attempted lip closure?
Upper facial muscle weakness is typically not seen in CNS disorders, although facial nerve or nucleus involvement at the pontine level can impair eyelid and frontalis function. Such lesions would usually be accompanied by “neighborhood” signs such as subtle ipsilateral lateral rectus or abducens palsy, involvement of the vestibular nuclei with vertigo, or facial sensory impairment from disruption of the descending trigeminal nucleus and tract. These would be “pertinent negatives” for excluding a brainstem lesion, and ipsilateral motor, sensory, or “higher cortical” functions would obviously signal a supratentorial CNS disorder.
In the case described by Shikino et al, observation and recording of the amount of facial motor function at the initial visit, 3 days after onset, could facilitate recognition of an aberrant course even a few days later and prompt further investigation at an early follow-up visit (idiopathic palsy is almost invariably maximal by 72 hours). I would assume that no additional clinical information was available to the subsequent examiner in this case, 2 months later, rather than suggesting that such information was omitted for the sake of parsimony.
Would any of this have made a difference? Probably not, but we need all the help we can get in medicine. Remember that every bit of information you obtain from your history or physical examination that you do not record disappears with you and is irretrievably lost.
- Shikino K, Suzuki S, Uehara T, Ikusaka M. Primary central nervous system lymphoma mimicking Bell palsy. Cleve Clin J Med 2018: 85(6)442–443. doi:10.3949/ccjm.85a.17061
- Verghese A, Charlton B, Kassirer JP, Ramsey M, Ioannidis JP. Inadequacies of physical examination as a cause of medical errors and adverse events: a collection of vignettes. Am J Med 2015; 128(12):1322–1324.e3. doi:10.1016/j.amjmed.2015.06.004
- Berger JR. Neurologists: the last bedside physician-scientists. JAMA Neurol 2013; 70(8):965–966. doi:10.1001/jamaneurol.2013.2977
The article in this issue by Shikino et al1 on a mimic of Bell palsy gives us an opportunity to discuss the question posed by the title of this editorial. The obvious short answer is “no.”
Any experienced clinician will acknowledge that the extent of the physical examination and the extent of information obtained during the history should be determined by the problem being evaluated at the time and by the setting in which it takes place. The difficulty, of course, is that this relies on the judgment of the clinician, and this may or may not pass the test of hindsight.
Verghese et al2 have eloquently emphasized the hazards of an incomplete or inadequate physical examination. Their study was not designed to determine the prevalence of deficient physical examination, either in its extent or its accuracy. Their purpose was to promote the necessity of proper teaching and performance of examination technique.
The neurologic examination is one of the last bastions of physical assessment.3 Despite remarkable advances in imaging and physiologic techniques, the neurologic physical assessment remains critical for diagnosis and management of the neurologic patient. One of my mentors in neurology used to urge residents to examine patients and record the results of the examination as if every patient would subsequently be the subject of a clinicopathologic conference. Anyone who has reviewed a case for a conference or a case report can identify with that sentiment, wishing that some missing piece of information were available. Yet everyone also recognizes the difficulties, if not the impossibility, of achieving that ideal result.
But recording information obtained during the history or physical examination is important even in the course of a daily routine evaluation. I find myself wishing that a previous examiner had commented on whether the muscle stretch reflexes were somewhat hypoactive (eg, “1+”) or on the brisk side (“3+”) rather than “physiologic.” Was the right leg actually globally weak (“4/5”), or was there a discrepancy between proximal and distal muscles or between the physiologic flexors and the extensors?
This can make a big difference in following a patient’s neurologic progress, even over a short time span. It might tell us whether we are dealing with weakness from a peripheral neuromuscular disorder (eg, Guillain-Barré syndrome) or from a myelopathy due to impending spinal cord compression.
It should be mentioned that although Guillain-Barré syndrome is characterized as an ascending paralysis, ie, beginning distally and spreading rostrally, it is one of the few peripheral neuropathies that can present with predominant proximal weakness. It is, in fact, a radiculoneuropathy. But spinal cord (upper motor neuron) disorders preferentially weaken the physiologic flexors of the lower limbs (hamstrings and ankle dorsiflexors), leading to the characteristic extensor posture of the spastic leg. Other findings that can help differential peripheral vs spinal cord disorders include distal sensory loss and hypoactive or absent muscle stretch reflexes in a peripheral neuropathy, compared with dissociated sensory loss (eg, impaired pain and temperature sensation in one leg with reduced vibration perception and proprioception in the other) along with hyperreflexia with cord lesions.
Therefore, a careful neurologic examination may tell us whether magnetic resonance imaging of the spine or an electrodiagnostic study should be the next step.
Shikino et al describe a patient who presented with what looked like idiopathic facial palsy (Bell palsy) but turned out to be the result of a primary central nervous system (CNS) cause. Would a more detailed neurologic examination have identified this as a CNS disorder? Would more specific information about the degree and distribution of facial paresis have facilitated earlier recognition of a progressive process, making idiopathic facial palsy less likely? How much elevation of the eyebrow occurred with voluntary activation, how many millimeters of sclera were visible with gentle eyelid closure? How much space remained between the lips on attempted lip closure?
Upper facial muscle weakness is typically not seen in CNS disorders, although facial nerve or nucleus involvement at the pontine level can impair eyelid and frontalis function. Such lesions would usually be accompanied by “neighborhood” signs such as subtle ipsilateral lateral rectus or abducens palsy, involvement of the vestibular nuclei with vertigo, or facial sensory impairment from disruption of the descending trigeminal nucleus and tract. These would be “pertinent negatives” for excluding a brainstem lesion, and ipsilateral motor, sensory, or “higher cortical” functions would obviously signal a supratentorial CNS disorder.
In the case described by Shikino et al, observation and recording of the amount of facial motor function at the initial visit, 3 days after onset, could facilitate recognition of an aberrant course even a few days later and prompt further investigation at an early follow-up visit (idiopathic palsy is almost invariably maximal by 72 hours). I would assume that no additional clinical information was available to the subsequent examiner in this case, 2 months later, rather than suggesting that such information was omitted for the sake of parsimony.
Would any of this have made a difference? Probably not, but we need all the help we can get in medicine. Remember that every bit of information you obtain from your history or physical examination that you do not record disappears with you and is irretrievably lost.
The article in this issue by Shikino et al1 on a mimic of Bell palsy gives us an opportunity to discuss the question posed by the title of this editorial. The obvious short answer is “no.”
Any experienced clinician will acknowledge that the extent of the physical examination and the extent of information obtained during the history should be determined by the problem being evaluated at the time and by the setting in which it takes place. The difficulty, of course, is that this relies on the judgment of the clinician, and this may or may not pass the test of hindsight.
Verghese et al2 have eloquently emphasized the hazards of an incomplete or inadequate physical examination. Their study was not designed to determine the prevalence of deficient physical examination, either in its extent or its accuracy. Their purpose was to promote the necessity of proper teaching and performance of examination technique.
The neurologic examination is one of the last bastions of physical assessment.3 Despite remarkable advances in imaging and physiologic techniques, the neurologic physical assessment remains critical for diagnosis and management of the neurologic patient. One of my mentors in neurology used to urge residents to examine patients and record the results of the examination as if every patient would subsequently be the subject of a clinicopathologic conference. Anyone who has reviewed a case for a conference or a case report can identify with that sentiment, wishing that some missing piece of information were available. Yet everyone also recognizes the difficulties, if not the impossibility, of achieving that ideal result.
But recording information obtained during the history or physical examination is important even in the course of a daily routine evaluation. I find myself wishing that a previous examiner had commented on whether the muscle stretch reflexes were somewhat hypoactive (eg, “1+”) or on the brisk side (“3+”) rather than “physiologic.” Was the right leg actually globally weak (“4/5”), or was there a discrepancy between proximal and distal muscles or between the physiologic flexors and the extensors?
This can make a big difference in following a patient’s neurologic progress, even over a short time span. It might tell us whether we are dealing with weakness from a peripheral neuromuscular disorder (eg, Guillain-Barré syndrome) or from a myelopathy due to impending spinal cord compression.
It should be mentioned that although Guillain-Barré syndrome is characterized as an ascending paralysis, ie, beginning distally and spreading rostrally, it is one of the few peripheral neuropathies that can present with predominant proximal weakness. It is, in fact, a radiculoneuropathy. But spinal cord (upper motor neuron) disorders preferentially weaken the physiologic flexors of the lower limbs (hamstrings and ankle dorsiflexors), leading to the characteristic extensor posture of the spastic leg. Other findings that can help differential peripheral vs spinal cord disorders include distal sensory loss and hypoactive or absent muscle stretch reflexes in a peripheral neuropathy, compared with dissociated sensory loss (eg, impaired pain and temperature sensation in one leg with reduced vibration perception and proprioception in the other) along with hyperreflexia with cord lesions.
Therefore, a careful neurologic examination may tell us whether magnetic resonance imaging of the spine or an electrodiagnostic study should be the next step.
Shikino et al describe a patient who presented with what looked like idiopathic facial palsy (Bell palsy) but turned out to be the result of a primary central nervous system (CNS) cause. Would a more detailed neurologic examination have identified this as a CNS disorder? Would more specific information about the degree and distribution of facial paresis have facilitated earlier recognition of a progressive process, making idiopathic facial palsy less likely? How much elevation of the eyebrow occurred with voluntary activation, how many millimeters of sclera were visible with gentle eyelid closure? How much space remained between the lips on attempted lip closure?
Upper facial muscle weakness is typically not seen in CNS disorders, although facial nerve or nucleus involvement at the pontine level can impair eyelid and frontalis function. Such lesions would usually be accompanied by “neighborhood” signs such as subtle ipsilateral lateral rectus or abducens palsy, involvement of the vestibular nuclei with vertigo, or facial sensory impairment from disruption of the descending trigeminal nucleus and tract. These would be “pertinent negatives” for excluding a brainstem lesion, and ipsilateral motor, sensory, or “higher cortical” functions would obviously signal a supratentorial CNS disorder.
In the case described by Shikino et al, observation and recording of the amount of facial motor function at the initial visit, 3 days after onset, could facilitate recognition of an aberrant course even a few days later and prompt further investigation at an early follow-up visit (idiopathic palsy is almost invariably maximal by 72 hours). I would assume that no additional clinical information was available to the subsequent examiner in this case, 2 months later, rather than suggesting that such information was omitted for the sake of parsimony.
Would any of this have made a difference? Probably not, but we need all the help we can get in medicine. Remember that every bit of information you obtain from your history or physical examination that you do not record disappears with you and is irretrievably lost.
- Shikino K, Suzuki S, Uehara T, Ikusaka M. Primary central nervous system lymphoma mimicking Bell palsy. Cleve Clin J Med 2018: 85(6)442–443. doi:10.3949/ccjm.85a.17061
- Verghese A, Charlton B, Kassirer JP, Ramsey M, Ioannidis JP. Inadequacies of physical examination as a cause of medical errors and adverse events: a collection of vignettes. Am J Med 2015; 128(12):1322–1324.e3. doi:10.1016/j.amjmed.2015.06.004
- Berger JR. Neurologists: the last bedside physician-scientists. JAMA Neurol 2013; 70(8):965–966. doi:10.1001/jamaneurol.2013.2977
- Shikino K, Suzuki S, Uehara T, Ikusaka M. Primary central nervous system lymphoma mimicking Bell palsy. Cleve Clin J Med 2018: 85(6)442–443. doi:10.3949/ccjm.85a.17061
- Verghese A, Charlton B, Kassirer JP, Ramsey M, Ioannidis JP. Inadequacies of physical examination as a cause of medical errors and adverse events: a collection of vignettes. Am J Med 2015; 128(12):1322–1324.e3. doi:10.1016/j.amjmed.2015.06.004
- Berger JR. Neurologists: the last bedside physician-scientists. JAMA Neurol 2013; 70(8):965–966. doi:10.1001/jamaneurol.2013.2977
Inpatient Portals: The Questions that Remain
Personal health records (PHRs) are a broad group of applications “through which individuals can access, manage, and share their health information,” and are intended as a means to increase consumer health awareness, activation, safety, and self-efficacy.1 Patient portals—PHRs that are tethered to an electronic health record (EHR)—have expanded over the past decade, driven in part by the “Meaningful Use” EHR Incentive Program of the Centers for Medicare and Medicaid Services.2 This has been particularly true in the outpatient setting. Unfortunately, despite increased adoption and a large number of research studies, it is not clear whether outpatient portal use is associated with improved clinical outcomes.3
Both the use of portals in the inpatient setting and the research thereof are at a more nascent stage. In this issue of the Journal of Hospital Medicine, Kelly et al.4 provide a systematic review of the existing research on the implementation of inpatient portals. The authors identified 17 studies and categorized the papers’ findings into the following 3 themes: design, use and usability, and impact. Most of the studies elicited feedback from patients, caregivers, and/or providers – sometimes in multiple phases as portals were redesigned – allowing the authors to offer the following recommendations for inpatient portal design: portals should present timely information, include the care plan in ways patients can understand, and facilitate identification and communication with the care team.4 Most of the included studies focused on portal design and use, thereby limiting knowledge regarding impact on the outcomes portals are intended to target. All findings should be interpreted with caution, as many of the included studies were small and qualitative, most of them used convenience samples and subject-reported outcomes, and all were conducted at a single center. Many sites also used customized portals, thus limiting generalizability.
Participants often found portals to be useful, but this finding is of uncertain value in the absence of robust evidence on outcomes. In addition, providers included in the reviewed studies expressed concerns that have not yet been well studied, such as the potential impact of portals on workload and on patient anxiety. Some studies reported that provider concerns lessened following a portal rollout, but few studies evaluated physician input on features such as direct communication and test result reporting in active use. The outpatient portal literature suggests potential harm related to how results are delivered, thus placing importance on conducting additional inpatient studies. Patients value online access to their health information5 and in previous literature have indicated a preference for immediate access to results even if abnormal results would then be given without explanation.6 However, in a recent study, even normal findings delivered without context were a cause of negative emotions and increased calls to physicians.7 This effect could be more pronounced in inpatient settings, given the large volume of tests and abnormal results, the rapidly evolving treatment plans, and generally higher acuity and medical uncertainty.
This review and other current literature highlight challenges for vendors and hospitals. Vendors must ensure that patient health information is contextualized and delivered in a manner that meets individual learning styles.8 Patients and caregivers need clinical decision support to process today’s large amount of data, just as providers do. We must be careful not to implement patient portals in ways that increase cognitive load and generate anxiety and confusion. Hospitals have infrastructural challenges if portals are to be successful. Care provider information must be accurately registered in the EHR to route patient-to-provider communications, a difficult task across frequent handoffs and staffing changes.
We now have the beginnings of an informed vision for inpatient portal design. Future research and industry directions include greater exploration of recognized concerns and how to best reconcile these concerns with the benefits of portals espoused by consumer health advocates and experienced by patients, caregivers, and providers in the reviewed studies. Specifically, we need a better understanding of how best to incorporate inpatient portals into routine care delivery in ways that are useful to both patients and providers. We also need a better understanding of why patients opt out of portal use. Most of the studies to date report on the set of patients who decided to use the portals, leaving a knowledge gap in design and use implications for patients who opted out. Studies should include comparisons of patient outcomes between users and nonusers. Although inpatient portals show promise, many questions remain.
Disclosures
The authors declare no conflicts of interest.
1. Markle Foundation. Connecting Americans to their healthcare. Working group on policies for electronic information sharing between doctors and patients final report. https://www.markle.org/sites/default/files/CnctAmerHC_fullreport.pdf. Accessed February 18, 2018.
2. Centers for Medicare and Medicaid Services. Electronic health records (EHR) incentive programs. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/EHRIncentivePrograms. Accessed February 18, 2018.
3. Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res. 2015;17(2):e44-e48. DOI:10.2196/jmir.3171. PubMed
4. Kelly MM, Coller RJ, Hoonakker PLT. Inpatient portals for hospitalized patients and caregivers: a systematic review. J Hosp Med. 2018;13(5):405-412.Published online first December 20, 2017. PubMed
5. Peacock S, Reddy A, Leveille SG, et al. Patient portals and personal health information online: perception, access, and use by US adults. J Am Med Inform Assoc. 2017;24(e1):e173-e177. DOI:10.1093/jamia/ocw095. PubMed
6. Johnson AJ, Easterling D, Nelson R, Chen MY, Frankel RM. Access to radiologic reports via a patient portal: clinical simulations to investigate patient preferences. JACR. 2012;9(4):256-263. DOI:10.1016/j.jacr.2011.12.023. PubMed
7. Giardina TD, Baldwin J, Nystrom DT, Sittig DF, Singh H. Patient perceptions of receiving test results via online portals: a mixed-methods study. J Am Med Inform Assoc. 2018;25(4)440-446. DOI:10.1093/jamia/ocx140. PubMed
8. Dalal AK, Bates DW, Collins S. Opportunities and challenges for improving the patient experience in the acute and post–acute care setting using patient portals: the patient’s perspective. J Hosp Med. 2017;12(12):1012-1016. DOI:10.12788/jhm.2860. PubMed
Personal health records (PHRs) are a broad group of applications “through which individuals can access, manage, and share their health information,” and are intended as a means to increase consumer health awareness, activation, safety, and self-efficacy.1 Patient portals—PHRs that are tethered to an electronic health record (EHR)—have expanded over the past decade, driven in part by the “Meaningful Use” EHR Incentive Program of the Centers for Medicare and Medicaid Services.2 This has been particularly true in the outpatient setting. Unfortunately, despite increased adoption and a large number of research studies, it is not clear whether outpatient portal use is associated with improved clinical outcomes.3
Both the use of portals in the inpatient setting and the research thereof are at a more nascent stage. In this issue of the Journal of Hospital Medicine, Kelly et al.4 provide a systematic review of the existing research on the implementation of inpatient portals. The authors identified 17 studies and categorized the papers’ findings into the following 3 themes: design, use and usability, and impact. Most of the studies elicited feedback from patients, caregivers, and/or providers – sometimes in multiple phases as portals were redesigned – allowing the authors to offer the following recommendations for inpatient portal design: portals should present timely information, include the care plan in ways patients can understand, and facilitate identification and communication with the care team.4 Most of the included studies focused on portal design and use, thereby limiting knowledge regarding impact on the outcomes portals are intended to target. All findings should be interpreted with caution, as many of the included studies were small and qualitative, most of them used convenience samples and subject-reported outcomes, and all were conducted at a single center. Many sites also used customized portals, thus limiting generalizability.
Participants often found portals to be useful, but this finding is of uncertain value in the absence of robust evidence on outcomes. In addition, providers included in the reviewed studies expressed concerns that have not yet been well studied, such as the potential impact of portals on workload and on patient anxiety. Some studies reported that provider concerns lessened following a portal rollout, but few studies evaluated physician input on features such as direct communication and test result reporting in active use. The outpatient portal literature suggests potential harm related to how results are delivered, thus placing importance on conducting additional inpatient studies. Patients value online access to their health information5 and in previous literature have indicated a preference for immediate access to results even if abnormal results would then be given without explanation.6 However, in a recent study, even normal findings delivered without context were a cause of negative emotions and increased calls to physicians.7 This effect could be more pronounced in inpatient settings, given the large volume of tests and abnormal results, the rapidly evolving treatment plans, and generally higher acuity and medical uncertainty.
This review and other current literature highlight challenges for vendors and hospitals. Vendors must ensure that patient health information is contextualized and delivered in a manner that meets individual learning styles.8 Patients and caregivers need clinical decision support to process today’s large amount of data, just as providers do. We must be careful not to implement patient portals in ways that increase cognitive load and generate anxiety and confusion. Hospitals have infrastructural challenges if portals are to be successful. Care provider information must be accurately registered in the EHR to route patient-to-provider communications, a difficult task across frequent handoffs and staffing changes.
We now have the beginnings of an informed vision for inpatient portal design. Future research and industry directions include greater exploration of recognized concerns and how to best reconcile these concerns with the benefits of portals espoused by consumer health advocates and experienced by patients, caregivers, and providers in the reviewed studies. Specifically, we need a better understanding of how best to incorporate inpatient portals into routine care delivery in ways that are useful to both patients and providers. We also need a better understanding of why patients opt out of portal use. Most of the studies to date report on the set of patients who decided to use the portals, leaving a knowledge gap in design and use implications for patients who opted out. Studies should include comparisons of patient outcomes between users and nonusers. Although inpatient portals show promise, many questions remain.
Disclosures
The authors declare no conflicts of interest.
Personal health records (PHRs) are a broad group of applications “through which individuals can access, manage, and share their health information,” and are intended as a means to increase consumer health awareness, activation, safety, and self-efficacy.1 Patient portals—PHRs that are tethered to an electronic health record (EHR)—have expanded over the past decade, driven in part by the “Meaningful Use” EHR Incentive Program of the Centers for Medicare and Medicaid Services.2 This has been particularly true in the outpatient setting. Unfortunately, despite increased adoption and a large number of research studies, it is not clear whether outpatient portal use is associated with improved clinical outcomes.3
Both the use of portals in the inpatient setting and the research thereof are at a more nascent stage. In this issue of the Journal of Hospital Medicine, Kelly et al.4 provide a systematic review of the existing research on the implementation of inpatient portals. The authors identified 17 studies and categorized the papers’ findings into the following 3 themes: design, use and usability, and impact. Most of the studies elicited feedback from patients, caregivers, and/or providers – sometimes in multiple phases as portals were redesigned – allowing the authors to offer the following recommendations for inpatient portal design: portals should present timely information, include the care plan in ways patients can understand, and facilitate identification and communication with the care team.4 Most of the included studies focused on portal design and use, thereby limiting knowledge regarding impact on the outcomes portals are intended to target. All findings should be interpreted with caution, as many of the included studies were small and qualitative, most of them used convenience samples and subject-reported outcomes, and all were conducted at a single center. Many sites also used customized portals, thus limiting generalizability.
Participants often found portals to be useful, but this finding is of uncertain value in the absence of robust evidence on outcomes. In addition, providers included in the reviewed studies expressed concerns that have not yet been well studied, such as the potential impact of portals on workload and on patient anxiety. Some studies reported that provider concerns lessened following a portal rollout, but few studies evaluated physician input on features such as direct communication and test result reporting in active use. The outpatient portal literature suggests potential harm related to how results are delivered, thus placing importance on conducting additional inpatient studies. Patients value online access to their health information5 and in previous literature have indicated a preference for immediate access to results even if abnormal results would then be given without explanation.6 However, in a recent study, even normal findings delivered without context were a cause of negative emotions and increased calls to physicians.7 This effect could be more pronounced in inpatient settings, given the large volume of tests and abnormal results, the rapidly evolving treatment plans, and generally higher acuity and medical uncertainty.
This review and other current literature highlight challenges for vendors and hospitals. Vendors must ensure that patient health information is contextualized and delivered in a manner that meets individual learning styles.8 Patients and caregivers need clinical decision support to process today’s large amount of data, just as providers do. We must be careful not to implement patient portals in ways that increase cognitive load and generate anxiety and confusion. Hospitals have infrastructural challenges if portals are to be successful. Care provider information must be accurately registered in the EHR to route patient-to-provider communications, a difficult task across frequent handoffs and staffing changes.
We now have the beginnings of an informed vision for inpatient portal design. Future research and industry directions include greater exploration of recognized concerns and how to best reconcile these concerns with the benefits of portals espoused by consumer health advocates and experienced by patients, caregivers, and providers in the reviewed studies. Specifically, we need a better understanding of how best to incorporate inpatient portals into routine care delivery in ways that are useful to both patients and providers. We also need a better understanding of why patients opt out of portal use. Most of the studies to date report on the set of patients who decided to use the portals, leaving a knowledge gap in design and use implications for patients who opted out. Studies should include comparisons of patient outcomes between users and nonusers. Although inpatient portals show promise, many questions remain.
Disclosures
The authors declare no conflicts of interest.
1. Markle Foundation. Connecting Americans to their healthcare. Working group on policies for electronic information sharing between doctors and patients final report. https://www.markle.org/sites/default/files/CnctAmerHC_fullreport.pdf. Accessed February 18, 2018.
2. Centers for Medicare and Medicaid Services. Electronic health records (EHR) incentive programs. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/EHRIncentivePrograms. Accessed February 18, 2018.
3. Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res. 2015;17(2):e44-e48. DOI:10.2196/jmir.3171. PubMed
4. Kelly MM, Coller RJ, Hoonakker PLT. Inpatient portals for hospitalized patients and caregivers: a systematic review. J Hosp Med. 2018;13(5):405-412.Published online first December 20, 2017. PubMed
5. Peacock S, Reddy A, Leveille SG, et al. Patient portals and personal health information online: perception, access, and use by US adults. J Am Med Inform Assoc. 2017;24(e1):e173-e177. DOI:10.1093/jamia/ocw095. PubMed
6. Johnson AJ, Easterling D, Nelson R, Chen MY, Frankel RM. Access to radiologic reports via a patient portal: clinical simulations to investigate patient preferences. JACR. 2012;9(4):256-263. DOI:10.1016/j.jacr.2011.12.023. PubMed
7. Giardina TD, Baldwin J, Nystrom DT, Sittig DF, Singh H. Patient perceptions of receiving test results via online portals: a mixed-methods study. J Am Med Inform Assoc. 2018;25(4)440-446. DOI:10.1093/jamia/ocx140. PubMed
8. Dalal AK, Bates DW, Collins S. Opportunities and challenges for improving the patient experience in the acute and post–acute care setting using patient portals: the patient’s perspective. J Hosp Med. 2017;12(12):1012-1016. DOI:10.12788/jhm.2860. PubMed
1. Markle Foundation. Connecting Americans to their healthcare. Working group on policies for electronic information sharing between doctors and patients final report. https://www.markle.org/sites/default/files/CnctAmerHC_fullreport.pdf. Accessed February 18, 2018.
2. Centers for Medicare and Medicaid Services. Electronic health records (EHR) incentive programs. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/EHRIncentivePrograms. Accessed February 18, 2018.
3. Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res. 2015;17(2):e44-e48. DOI:10.2196/jmir.3171. PubMed
4. Kelly MM, Coller RJ, Hoonakker PLT. Inpatient portals for hospitalized patients and caregivers: a systematic review. J Hosp Med. 2018;13(5):405-412.Published online first December 20, 2017. PubMed
5. Peacock S, Reddy A, Leveille SG, et al. Patient portals and personal health information online: perception, access, and use by US adults. J Am Med Inform Assoc. 2017;24(e1):e173-e177. DOI:10.1093/jamia/ocw095. PubMed
6. Johnson AJ, Easterling D, Nelson R, Chen MY, Frankel RM. Access to radiologic reports via a patient portal: clinical simulations to investigate patient preferences. JACR. 2012;9(4):256-263. DOI:10.1016/j.jacr.2011.12.023. PubMed
7. Giardina TD, Baldwin J, Nystrom DT, Sittig DF, Singh H. Patient perceptions of receiving test results via online portals: a mixed-methods study. J Am Med Inform Assoc. 2018;25(4)440-446. DOI:10.1093/jamia/ocx140. PubMed
8. Dalal AK, Bates DW, Collins S. Opportunities and challenges for improving the patient experience in the acute and post–acute care setting using patient portals: the patient’s perspective. J Hosp Med. 2017;12(12):1012-1016. DOI:10.12788/jhm.2860. PubMed
© 2018 Society of Hospital Medicine
Is it Time to Re-Examine the Physical Exam?
“Am I supposed to have such a hard time feeling the kidneys?” “I think I’m doing it wrong,” echoed another classmate. The frustration of these first-year students, who were already overwhelmed by the three pages of physical exam techniques that they were responsible for, became increasingly visible as they palpated the abdomens of their standardized patients. Then, they asked the dreaded question: “How often do you do this on real patients?”
When we teach first-year medical students the physical exam, these students are already aware that they have never observed physicians perform these maneuvers in their own medical care. “How come I’ve never seen my doctor do this before?” is a common question that we are often asked. We as faculty struggle with demonstrating and defending techniques that we hardly ever use given their variable utility in daily clinical practice. However, students are told that they must be familiar with the various “tools” in the repertoire, and they are led to believe that these skills will be a fundamental part of their future practice as physicians. Of course, when they begin their clerkships, the truth is revealed: the currency on the wards revolves around the computer. The experienced and passionate clinicians who may astonish them with the bedside exam are the exception and are hardly the rule.
In this issue of Journal of Hospital Medicine, Bergl et al.1 found that when medical students rotated on their internal medicine clerkship, patients were rarely examined during attending rounds and were even examined less often when these rounds were not at the bedside. Although the students themselves consistently incorporated the physical exam into patient assessments and presentations, neither their findings nor those of the residents were ever validated by the attending physician or by others. Notably, the physical exam did not influence clinical decision making as much as one might expect.
These findings should not come as a surprise. The current generation of residents and junior attendings today are more accustomed to emphasizing labs, imaging studies, pathology reports, and other data within the electronic health record (EHR) and with formulating initial plans before having met the patient.2 Physicians become uneasy when asked to decide without the reassurance of daily lab results, as if the information in the EHR is highly fundamental to patient care. Caring for the “iPatient” often trumps revisiting and reexamining the real patient.3 Medical teams are also bombarded with increasing demands for their attention and time and are pushed to expedite patient discharges while constantly responding to documentation queries in the EHR. Emphasis on patient throughput, quality metrics, and multidisciplinary communication is essential to provide effective patient care but often feels at odds with opportunities for bedside teaching.
Although discussions on these obstacles have increased in recent years, time-motion studies spanning decades and even preceding the duty-hours era have consistently shown that physicians reserve little time for physical examination and direct patient care.4 In other words, the challenges in bringing physicians to the bedside might have less to do with environmental barriers than we think.
Much of what we teach about physical diagnosis is imperfect,5 and the routine annual exam might well be eliminated given its low yield.6 Nevertheless, we cannot discount the importance of the physical exam in fostering the bond between the patient and the healthcare provider, particularly in patients with acute illnesses, and in making the interaction meaningful to the practitioner.
Many of us can easily recall embarrassing examples of obvious physical exam findings that were critical and overlooked with consequences – the missed incarcerated hernia in a patient labeled with gastritis and vomiting, or the patient with chest pain who had to undergo catheterization because the shingles rash was missed. The confidence in normal findings that might save a patient from unnecessary lab tests, imaging, or consultation is often not discussed. The burden is on us to retire maneuvers that have outlived their usefulness and to demonstrate to students the hazards and consequences of poor examination skills. We must also further what we know and understand about the physical exam as Osler, Laennec, and others before us once did. Point-of-care ultrasound is only one example of how innovation can bring trainees to the bedside, excite learners, engage patients, and affect care in a meaningful way while enhancing the nonultrasound-based skills of practitioners.7
It is promising that the students in this study consistently examined their patients each day. As future physicians, they can be very enthusiastic learners eager to apply the physical exam skills they have recently acquired during their early years of training. However, this excitement can taper off if not actively encouraged and reinforced, especially if role models are unintentionally sending the message that the physical exam does not matter or emphasizing exam maneuvers that do not serve a meaningful purpose. New technology will hopefully help us develop novel exam skills. If we can advance what we can diagnose at the bedside, students will remain motivated to improve and learn exam skills that truly affect patient-care decisions. After all, one day, they too will serve as role models for the next generation of physicians and hopefully will be the ones taking care of us at the bedside.
Disclosures
The authors declare no conflicts of interest.
1. Bergl PA, Taylor AC, Klumb J, et al. Teaching physical examination to medical students on inpatient medicine reams: A prospective mixed-methods descriptive study. J Hosp Med. 2018;13:399-402. PubMed
2. Chi J, Verghese A. Clinical education and the electronic health record: the flipped patient. JAMA. 2010;312(22):2331-2332. DOI: 10.1001/jama.2014.12820. PubMed
2. Verghese A. Culture shock—patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. DOI: 10.1056/NEJMp0807461 PubMed
3. Czernik Z, Lin CT. A piece of my mind. Time at the bedside (Computing). JAMA. 2016;315(22):2399-2400. DOI: 10.1001/jama.2016.1722 PubMed
5. Jauhar S. The demise of the physical exam. N Engl J Med. 2006;354(6):548-551. DOI: 10.1056/NEJMp068013 PubMed
6. Mehrotra A, Prochazka A. Improving value in health care--against the annual physical. N Engl J Med. 2015;373(16):1485-1487. DOI: 10.1056/NEJMp1507485 PubMed
7. Kugler J. Price and the evolution of the physical examination. JAMA Cardiol. 2018. DOI: 10.1001/jamacardio.2018.0002. [Epub ahead of print] PubMed
“Am I supposed to have such a hard time feeling the kidneys?” “I think I’m doing it wrong,” echoed another classmate. The frustration of these first-year students, who were already overwhelmed by the three pages of physical exam techniques that they were responsible for, became increasingly visible as they palpated the abdomens of their standardized patients. Then, they asked the dreaded question: “How often do you do this on real patients?”
When we teach first-year medical students the physical exam, these students are already aware that they have never observed physicians perform these maneuvers in their own medical care. “How come I’ve never seen my doctor do this before?” is a common question that we are often asked. We as faculty struggle with demonstrating and defending techniques that we hardly ever use given their variable utility in daily clinical practice. However, students are told that they must be familiar with the various “tools” in the repertoire, and they are led to believe that these skills will be a fundamental part of their future practice as physicians. Of course, when they begin their clerkships, the truth is revealed: the currency on the wards revolves around the computer. The experienced and passionate clinicians who may astonish them with the bedside exam are the exception and are hardly the rule.
In this issue of Journal of Hospital Medicine, Bergl et al.1 found that when medical students rotated on their internal medicine clerkship, patients were rarely examined during attending rounds and were even examined less often when these rounds were not at the bedside. Although the students themselves consistently incorporated the physical exam into patient assessments and presentations, neither their findings nor those of the residents were ever validated by the attending physician or by others. Notably, the physical exam did not influence clinical decision making as much as one might expect.
These findings should not come as a surprise. The current generation of residents and junior attendings today are more accustomed to emphasizing labs, imaging studies, pathology reports, and other data within the electronic health record (EHR) and with formulating initial plans before having met the patient.2 Physicians become uneasy when asked to decide without the reassurance of daily lab results, as if the information in the EHR is highly fundamental to patient care. Caring for the “iPatient” often trumps revisiting and reexamining the real patient.3 Medical teams are also bombarded with increasing demands for their attention and time and are pushed to expedite patient discharges while constantly responding to documentation queries in the EHR. Emphasis on patient throughput, quality metrics, and multidisciplinary communication is essential to provide effective patient care but often feels at odds with opportunities for bedside teaching.
Although discussions on these obstacles have increased in recent years, time-motion studies spanning decades and even preceding the duty-hours era have consistently shown that physicians reserve little time for physical examination and direct patient care.4 In other words, the challenges in bringing physicians to the bedside might have less to do with environmental barriers than we think.
Much of what we teach about physical diagnosis is imperfect,5 and the routine annual exam might well be eliminated given its low yield.6 Nevertheless, we cannot discount the importance of the physical exam in fostering the bond between the patient and the healthcare provider, particularly in patients with acute illnesses, and in making the interaction meaningful to the practitioner.
Many of us can easily recall embarrassing examples of obvious physical exam findings that were critical and overlooked with consequences – the missed incarcerated hernia in a patient labeled with gastritis and vomiting, or the patient with chest pain who had to undergo catheterization because the shingles rash was missed. The confidence in normal findings that might save a patient from unnecessary lab tests, imaging, or consultation is often not discussed. The burden is on us to retire maneuvers that have outlived their usefulness and to demonstrate to students the hazards and consequences of poor examination skills. We must also further what we know and understand about the physical exam as Osler, Laennec, and others before us once did. Point-of-care ultrasound is only one example of how innovation can bring trainees to the bedside, excite learners, engage patients, and affect care in a meaningful way while enhancing the nonultrasound-based skills of practitioners.7
It is promising that the students in this study consistently examined their patients each day. As future physicians, they can be very enthusiastic learners eager to apply the physical exam skills they have recently acquired during their early years of training. However, this excitement can taper off if not actively encouraged and reinforced, especially if role models are unintentionally sending the message that the physical exam does not matter or emphasizing exam maneuvers that do not serve a meaningful purpose. New technology will hopefully help us develop novel exam skills. If we can advance what we can diagnose at the bedside, students will remain motivated to improve and learn exam skills that truly affect patient-care decisions. After all, one day, they too will serve as role models for the next generation of physicians and hopefully will be the ones taking care of us at the bedside.
Disclosures
The authors declare no conflicts of interest.
“Am I supposed to have such a hard time feeling the kidneys?” “I think I’m doing it wrong,” echoed another classmate. The frustration of these first-year students, who were already overwhelmed by the three pages of physical exam techniques that they were responsible for, became increasingly visible as they palpated the abdomens of their standardized patients. Then, they asked the dreaded question: “How often do you do this on real patients?”
When we teach first-year medical students the physical exam, these students are already aware that they have never observed physicians perform these maneuvers in their own medical care. “How come I’ve never seen my doctor do this before?” is a common question that we are often asked. We as faculty struggle with demonstrating and defending techniques that we hardly ever use given their variable utility in daily clinical practice. However, students are told that they must be familiar with the various “tools” in the repertoire, and they are led to believe that these skills will be a fundamental part of their future practice as physicians. Of course, when they begin their clerkships, the truth is revealed: the currency on the wards revolves around the computer. The experienced and passionate clinicians who may astonish them with the bedside exam are the exception and are hardly the rule.
In this issue of Journal of Hospital Medicine, Bergl et al.1 found that when medical students rotated on their internal medicine clerkship, patients were rarely examined during attending rounds and were even examined less often when these rounds were not at the bedside. Although the students themselves consistently incorporated the physical exam into patient assessments and presentations, neither their findings nor those of the residents were ever validated by the attending physician or by others. Notably, the physical exam did not influence clinical decision making as much as one might expect.
These findings should not come as a surprise. The current generation of residents and junior attendings today are more accustomed to emphasizing labs, imaging studies, pathology reports, and other data within the electronic health record (EHR) and with formulating initial plans before having met the patient.2 Physicians become uneasy when asked to decide without the reassurance of daily lab results, as if the information in the EHR is highly fundamental to patient care. Caring for the “iPatient” often trumps revisiting and reexamining the real patient.3 Medical teams are also bombarded with increasing demands for their attention and time and are pushed to expedite patient discharges while constantly responding to documentation queries in the EHR. Emphasis on patient throughput, quality metrics, and multidisciplinary communication is essential to provide effective patient care but often feels at odds with opportunities for bedside teaching.
Although discussions on these obstacles have increased in recent years, time-motion studies spanning decades and even preceding the duty-hours era have consistently shown that physicians reserve little time for physical examination and direct patient care.4 In other words, the challenges in bringing physicians to the bedside might have less to do with environmental barriers than we think.
Much of what we teach about physical diagnosis is imperfect,5 and the routine annual exam might well be eliminated given its low yield.6 Nevertheless, we cannot discount the importance of the physical exam in fostering the bond between the patient and the healthcare provider, particularly in patients with acute illnesses, and in making the interaction meaningful to the practitioner.
Many of us can easily recall embarrassing examples of obvious physical exam findings that were critical and overlooked with consequences – the missed incarcerated hernia in a patient labeled with gastritis and vomiting, or the patient with chest pain who had to undergo catheterization because the shingles rash was missed. The confidence in normal findings that might save a patient from unnecessary lab tests, imaging, or consultation is often not discussed. The burden is on us to retire maneuvers that have outlived their usefulness and to demonstrate to students the hazards and consequences of poor examination skills. We must also further what we know and understand about the physical exam as Osler, Laennec, and others before us once did. Point-of-care ultrasound is only one example of how innovation can bring trainees to the bedside, excite learners, engage patients, and affect care in a meaningful way while enhancing the nonultrasound-based skills of practitioners.7
It is promising that the students in this study consistently examined their patients each day. As future physicians, they can be very enthusiastic learners eager to apply the physical exam skills they have recently acquired during their early years of training. However, this excitement can taper off if not actively encouraged and reinforced, especially if role models are unintentionally sending the message that the physical exam does not matter or emphasizing exam maneuvers that do not serve a meaningful purpose. New technology will hopefully help us develop novel exam skills. If we can advance what we can diagnose at the bedside, students will remain motivated to improve and learn exam skills that truly affect patient-care decisions. After all, one day, they too will serve as role models for the next generation of physicians and hopefully will be the ones taking care of us at the bedside.
Disclosures
The authors declare no conflicts of interest.
1. Bergl PA, Taylor AC, Klumb J, et al. Teaching physical examination to medical students on inpatient medicine reams: A prospective mixed-methods descriptive study. J Hosp Med. 2018;13:399-402. PubMed
2. Chi J, Verghese A. Clinical education and the electronic health record: the flipped patient. JAMA. 2010;312(22):2331-2332. DOI: 10.1001/jama.2014.12820. PubMed
2. Verghese A. Culture shock—patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. DOI: 10.1056/NEJMp0807461 PubMed
3. Czernik Z, Lin CT. A piece of my mind. Time at the bedside (Computing). JAMA. 2016;315(22):2399-2400. DOI: 10.1001/jama.2016.1722 PubMed
5. Jauhar S. The demise of the physical exam. N Engl J Med. 2006;354(6):548-551. DOI: 10.1056/NEJMp068013 PubMed
6. Mehrotra A, Prochazka A. Improving value in health care--against the annual physical. N Engl J Med. 2015;373(16):1485-1487. DOI: 10.1056/NEJMp1507485 PubMed
7. Kugler J. Price and the evolution of the physical examination. JAMA Cardiol. 2018. DOI: 10.1001/jamacardio.2018.0002. [Epub ahead of print] PubMed
1. Bergl PA, Taylor AC, Klumb J, et al. Teaching physical examination to medical students on inpatient medicine reams: A prospective mixed-methods descriptive study. J Hosp Med. 2018;13:399-402. PubMed
2. Chi J, Verghese A. Clinical education and the electronic health record: the flipped patient. JAMA. 2010;312(22):2331-2332. DOI: 10.1001/jama.2014.12820. PubMed
2. Verghese A. Culture shock—patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. DOI: 10.1056/NEJMp0807461 PubMed
3. Czernik Z, Lin CT. A piece of my mind. Time at the bedside (Computing). JAMA. 2016;315(22):2399-2400. DOI: 10.1001/jama.2016.1722 PubMed
5. Jauhar S. The demise of the physical exam. N Engl J Med. 2006;354(6):548-551. DOI: 10.1056/NEJMp068013 PubMed
6. Mehrotra A, Prochazka A. Improving value in health care--against the annual physical. N Engl J Med. 2015;373(16):1485-1487. DOI: 10.1056/NEJMp1507485 PubMed
7. Kugler J. Price and the evolution of the physical examination. JAMA Cardiol. 2018. DOI: 10.1001/jamacardio.2018.0002. [Epub ahead of print] PubMed
©2018 Society of Hospital Medicine
Faculty Development for Hospitalists: A Call to Arms
Over the past two decades, the field of hospital medicine has gone from relative obscurity to a viable career pathway for approximately 50,000 physicians in this country.1 A subset of hospitalists pursue careers in academic medicine, which is a pathway that traditionally includes education and scholarship in addition to patient care. While the academic career pathway is well paved in many clinical specialties, it is still relatively underdeveloped for academic hospitalists, and thus what defines career success for this group is even less clear.
In this issue of the Journal of Hospital Medicine, Cumbler et al. performed a qualitative analysis to explore how early career academic hospitalists self-define and perceive their career success.2 Drawing on interviews with 17 early-career hospitalists at 3 academic medical centers, the authors created a theoretical framework organized around a traditional conceptual model of career success that is divided into intrinsic and extrinsic motivating factors. They found that early-career academic hospitalists, (clinician-educators in first 2-5 years), defined their career success almost exclusively around factors intrinsic to their day-to-day job. These factors included such things as excitement about their daily work, developing proficiency in the delivery of high-quality clinical care, and passion for doing work that is meaningful to them. In addition to these immediate job satisfiers, many hospitalists emphasized long-term career success factors such as becoming an expert in a particular domain of hospital medicine and gaining respect and recognition within their local or national environment. Surprisingly, compensation and career advancement through promotion, two traditional external career success factors, were not uniformly valued.
These findings come at a critical time for our field in which early-career faculty outnumber mid- and late-career faculty by an order of magnitude. Indeed, how to develop, promote, sustain, and retain young hospitalists is a topic on the minds of most hospital medicine group directors. Putting aside the impact of hospitalist turnover on productivity, patient care outcomes, and morale within an individual hospital medicine group, we agree with the authors that understanding and cultivating career success for academic hospitalists is imperative for the future of our field. For this reason, we launched a formal faculty development program at Penn this year, which focuses on supporting the growth of hospitalists in their first two years on faculty. The findings of this study provide interesting new perspectives and encourage us to continue our focus on early-career academic hospitalists. We laud the previous efforts in this area and hope that the paper by Cumbler et al. encourages and inspires other programs to start or accelerate their hospitalist faculty development efforts.3-5
However, some findings from this study are somewhat perplexing or even a bit discouraging for those who are invested in faculty development in academia. For example, the authors raise the possibility that there may be a disconnect in the minds of early-career hospitalists as it pertains to their thoughts on career success. On the one hand, the hospitalists interviewed in this study are happy doing their clinical work and cite this as a primary driver of their career success. On the other hand, they equate career success with things such as developing expertise within a particular domain of hospital medicine, acquiring leadership roles, collaborating academically with other specialties or professions, or developing new innovations. Presumably this is part of the reason that they selected a job in an academic setting as opposed to a community setting. However, in order to achieve these goals, one must devote time and effort to purposefully developing them. Therefore, identifying and developing mentors who can assist early-career hospitalists with identifying, articulating, and developing strategies to achieve both their short- and long-term career goals is critical. One mentor–mentee conversation may reveal that an individual hospitalist values being an excellent clinician and has little interest in developing a niche within hospital medicine; another may reveal a lack of awareness of available professional development resources; still another may uncover a lack of realism regarding the time or skills it takes to achieve a particular career goal. These realities highlight an imperative for our field to develop robust and sustainable mentorship programs for not only early-career hospitalists but also some mid-career hospitalists whose careers may not yet be fully developed. Indeed, one of the biggest challenges that have emerged in our experience with a faculty development program at Penn is creating meaningful mentorship and career development advice for mid-career hospitalists (late assistant or early associate professors who are typically 5-10 years into their careers).
We found it interesting that the hospitalists interviewed did not mention three of the four pillars of career satisfaction outlined in the white paper on Hospitalist Career Satisfaction from the Society for Hospital Medicine: workload schedule, autonomy control, and community/environment.6 Perhaps this is because hospitalists, like many other professionals, recognize that feeling satisfied in one’s career is not the same as feeling successful. Satisfaction in one’s career refers to the foundational needs that one requires in order to feel content, whereas success is more often equated with achievement, even if that achievement is simply the acquisition of one’s goals for themselves. The reality is that given the constant growth and change within teaching hospitals, and therefore academic hospital medicine groups, tending to the satisfiers for hospitalists (eg, schedule and workload) often takes a front seat to assisting faculty in achieving their individual career potential. We assert that despite the inherent difficulty, academic hospital medicine group leaders need to focus their attention on both the satisfaction and career success of their early-career faculty.
Finally, this paper raises many interesting questions
In conclusion, the findings of Cumbler et al. should promote unrest among leaders of academic hospital medicine groups and their departments of medicine. While it is inspiring to see so many early-career hospitalists focused on their daily happiness at work, we are unsure about whether they have the knowledge, tools, and guidance to achieve their self-professed academic goals, which many equate with career success. Given the continued growth of the hospital medicine workforce, we view this important new work as a national call to arms for the purposeful development of academic hospitalist faculty development programs.
Disclosures
Dr. Myers and Dr. Greysen have nothing to disclose.
1. Wachter RM, Goldman L. Zero to 50,000-The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. PubMed
2. Cumbler E, Yirdaw E, Kneeland P, et al. What is career success for academic hospitalists? A qualitative analysis of early-career faculty perspectives. J Hosp Med. 2018;13(5):372-377. doi: 10.12788/jhm.2924. Published online first January 31, 2018. PubMed
3. Nagarur A, O’Neill RM, Lawton D, Greenwald JL. Supporting faculty development in hospital medicine: design and implementation of a personalized structured mentoring program. J Hosp Med. 2018;13(2):96-99. PubMed
4. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. PubMed
5. Howell E, Kravet S, Kisuule F, Wright SM. An innovative approach to supporting hospitalist physicians towards academic success. J Hosp Med. 2008;3(4):314-318. PubMed
6. Society of Hospital Medicine Career Satisfaction Taskforce: A Challenge for a new Specialty. A White paper on hospitalist career satisfaction. http://dev.hospitalmedicine.org/Web/Media_Center/shm_white_papers.aspx . Accessed February 9, 2018.
Over the past two decades, the field of hospital medicine has gone from relative obscurity to a viable career pathway for approximately 50,000 physicians in this country.1 A subset of hospitalists pursue careers in academic medicine, which is a pathway that traditionally includes education and scholarship in addition to patient care. While the academic career pathway is well paved in many clinical specialties, it is still relatively underdeveloped for academic hospitalists, and thus what defines career success for this group is even less clear.
In this issue of the Journal of Hospital Medicine, Cumbler et al. performed a qualitative analysis to explore how early career academic hospitalists self-define and perceive their career success.2 Drawing on interviews with 17 early-career hospitalists at 3 academic medical centers, the authors created a theoretical framework organized around a traditional conceptual model of career success that is divided into intrinsic and extrinsic motivating factors. They found that early-career academic hospitalists, (clinician-educators in first 2-5 years), defined their career success almost exclusively around factors intrinsic to their day-to-day job. These factors included such things as excitement about their daily work, developing proficiency in the delivery of high-quality clinical care, and passion for doing work that is meaningful to them. In addition to these immediate job satisfiers, many hospitalists emphasized long-term career success factors such as becoming an expert in a particular domain of hospital medicine and gaining respect and recognition within their local or national environment. Surprisingly, compensation and career advancement through promotion, two traditional external career success factors, were not uniformly valued.
These findings come at a critical time for our field in which early-career faculty outnumber mid- and late-career faculty by an order of magnitude. Indeed, how to develop, promote, sustain, and retain young hospitalists is a topic on the minds of most hospital medicine group directors. Putting aside the impact of hospitalist turnover on productivity, patient care outcomes, and morale within an individual hospital medicine group, we agree with the authors that understanding and cultivating career success for academic hospitalists is imperative for the future of our field. For this reason, we launched a formal faculty development program at Penn this year, which focuses on supporting the growth of hospitalists in their first two years on faculty. The findings of this study provide interesting new perspectives and encourage us to continue our focus on early-career academic hospitalists. We laud the previous efforts in this area and hope that the paper by Cumbler et al. encourages and inspires other programs to start or accelerate their hospitalist faculty development efforts.3-5
However, some findings from this study are somewhat perplexing or even a bit discouraging for those who are invested in faculty development in academia. For example, the authors raise the possibility that there may be a disconnect in the minds of early-career hospitalists as it pertains to their thoughts on career success. On the one hand, the hospitalists interviewed in this study are happy doing their clinical work and cite this as a primary driver of their career success. On the other hand, they equate career success with things such as developing expertise within a particular domain of hospital medicine, acquiring leadership roles, collaborating academically with other specialties or professions, or developing new innovations. Presumably this is part of the reason that they selected a job in an academic setting as opposed to a community setting. However, in order to achieve these goals, one must devote time and effort to purposefully developing them. Therefore, identifying and developing mentors who can assist early-career hospitalists with identifying, articulating, and developing strategies to achieve both their short- and long-term career goals is critical. One mentor–mentee conversation may reveal that an individual hospitalist values being an excellent clinician and has little interest in developing a niche within hospital medicine; another may reveal a lack of awareness of available professional development resources; still another may uncover a lack of realism regarding the time or skills it takes to achieve a particular career goal. These realities highlight an imperative for our field to develop robust and sustainable mentorship programs for not only early-career hospitalists but also some mid-career hospitalists whose careers may not yet be fully developed. Indeed, one of the biggest challenges that have emerged in our experience with a faculty development program at Penn is creating meaningful mentorship and career development advice for mid-career hospitalists (late assistant or early associate professors who are typically 5-10 years into their careers).
We found it interesting that the hospitalists interviewed did not mention three of the four pillars of career satisfaction outlined in the white paper on Hospitalist Career Satisfaction from the Society for Hospital Medicine: workload schedule, autonomy control, and community/environment.6 Perhaps this is because hospitalists, like many other professionals, recognize that feeling satisfied in one’s career is not the same as feeling successful. Satisfaction in one’s career refers to the foundational needs that one requires in order to feel content, whereas success is more often equated with achievement, even if that achievement is simply the acquisition of one’s goals for themselves. The reality is that given the constant growth and change within teaching hospitals, and therefore academic hospital medicine groups, tending to the satisfiers for hospitalists (eg, schedule and workload) often takes a front seat to assisting faculty in achieving their individual career potential. We assert that despite the inherent difficulty, academic hospital medicine group leaders need to focus their attention on both the satisfaction and career success of their early-career faculty.
Finally, this paper raises many interesting questions
In conclusion, the findings of Cumbler et al. should promote unrest among leaders of academic hospital medicine groups and their departments of medicine. While it is inspiring to see so many early-career hospitalists focused on their daily happiness at work, we are unsure about whether they have the knowledge, tools, and guidance to achieve their self-professed academic goals, which many equate with career success. Given the continued growth of the hospital medicine workforce, we view this important new work as a national call to arms for the purposeful development of academic hospitalist faculty development programs.
Disclosures
Dr. Myers and Dr. Greysen have nothing to disclose.
Over the past two decades, the field of hospital medicine has gone from relative obscurity to a viable career pathway for approximately 50,000 physicians in this country.1 A subset of hospitalists pursue careers in academic medicine, which is a pathway that traditionally includes education and scholarship in addition to patient care. While the academic career pathway is well paved in many clinical specialties, it is still relatively underdeveloped for academic hospitalists, and thus what defines career success for this group is even less clear.
In this issue of the Journal of Hospital Medicine, Cumbler et al. performed a qualitative analysis to explore how early career academic hospitalists self-define and perceive their career success.2 Drawing on interviews with 17 early-career hospitalists at 3 academic medical centers, the authors created a theoretical framework organized around a traditional conceptual model of career success that is divided into intrinsic and extrinsic motivating factors. They found that early-career academic hospitalists, (clinician-educators in first 2-5 years), defined their career success almost exclusively around factors intrinsic to their day-to-day job. These factors included such things as excitement about their daily work, developing proficiency in the delivery of high-quality clinical care, and passion for doing work that is meaningful to them. In addition to these immediate job satisfiers, many hospitalists emphasized long-term career success factors such as becoming an expert in a particular domain of hospital medicine and gaining respect and recognition within their local or national environment. Surprisingly, compensation and career advancement through promotion, two traditional external career success factors, were not uniformly valued.
These findings come at a critical time for our field in which early-career faculty outnumber mid- and late-career faculty by an order of magnitude. Indeed, how to develop, promote, sustain, and retain young hospitalists is a topic on the minds of most hospital medicine group directors. Putting aside the impact of hospitalist turnover on productivity, patient care outcomes, and morale within an individual hospital medicine group, we agree with the authors that understanding and cultivating career success for academic hospitalists is imperative for the future of our field. For this reason, we launched a formal faculty development program at Penn this year, which focuses on supporting the growth of hospitalists in their first two years on faculty. The findings of this study provide interesting new perspectives and encourage us to continue our focus on early-career academic hospitalists. We laud the previous efforts in this area and hope that the paper by Cumbler et al. encourages and inspires other programs to start or accelerate their hospitalist faculty development efforts.3-5
However, some findings from this study are somewhat perplexing or even a bit discouraging for those who are invested in faculty development in academia. For example, the authors raise the possibility that there may be a disconnect in the minds of early-career hospitalists as it pertains to their thoughts on career success. On the one hand, the hospitalists interviewed in this study are happy doing their clinical work and cite this as a primary driver of their career success. On the other hand, they equate career success with things such as developing expertise within a particular domain of hospital medicine, acquiring leadership roles, collaborating academically with other specialties or professions, or developing new innovations. Presumably this is part of the reason that they selected a job in an academic setting as opposed to a community setting. However, in order to achieve these goals, one must devote time and effort to purposefully developing them. Therefore, identifying and developing mentors who can assist early-career hospitalists with identifying, articulating, and developing strategies to achieve both their short- and long-term career goals is critical. One mentor–mentee conversation may reveal that an individual hospitalist values being an excellent clinician and has little interest in developing a niche within hospital medicine; another may reveal a lack of awareness of available professional development resources; still another may uncover a lack of realism regarding the time or skills it takes to achieve a particular career goal. These realities highlight an imperative for our field to develop robust and sustainable mentorship programs for not only early-career hospitalists but also some mid-career hospitalists whose careers may not yet be fully developed. Indeed, one of the biggest challenges that have emerged in our experience with a faculty development program at Penn is creating meaningful mentorship and career development advice for mid-career hospitalists (late assistant or early associate professors who are typically 5-10 years into their careers).
We found it interesting that the hospitalists interviewed did not mention three of the four pillars of career satisfaction outlined in the white paper on Hospitalist Career Satisfaction from the Society for Hospital Medicine: workload schedule, autonomy control, and community/environment.6 Perhaps this is because hospitalists, like many other professionals, recognize that feeling satisfied in one’s career is not the same as feeling successful. Satisfaction in one’s career refers to the foundational needs that one requires in order to feel content, whereas success is more often equated with achievement, even if that achievement is simply the acquisition of one’s goals for themselves. The reality is that given the constant growth and change within teaching hospitals, and therefore academic hospital medicine groups, tending to the satisfiers for hospitalists (eg, schedule and workload) often takes a front seat to assisting faculty in achieving their individual career potential. We assert that despite the inherent difficulty, academic hospital medicine group leaders need to focus their attention on both the satisfaction and career success of their early-career faculty.
Finally, this paper raises many interesting questions
In conclusion, the findings of Cumbler et al. should promote unrest among leaders of academic hospital medicine groups and their departments of medicine. While it is inspiring to see so many early-career hospitalists focused on their daily happiness at work, we are unsure about whether they have the knowledge, tools, and guidance to achieve their self-professed academic goals, which many equate with career success. Given the continued growth of the hospital medicine workforce, we view this important new work as a national call to arms for the purposeful development of academic hospitalist faculty development programs.
Disclosures
Dr. Myers and Dr. Greysen have nothing to disclose.
1. Wachter RM, Goldman L. Zero to 50,000-The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. PubMed
2. Cumbler E, Yirdaw E, Kneeland P, et al. What is career success for academic hospitalists? A qualitative analysis of early-career faculty perspectives. J Hosp Med. 2018;13(5):372-377. doi: 10.12788/jhm.2924. Published online first January 31, 2018. PubMed
3. Nagarur A, O’Neill RM, Lawton D, Greenwald JL. Supporting faculty development in hospital medicine: design and implementation of a personalized structured mentoring program. J Hosp Med. 2018;13(2):96-99. PubMed
4. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. PubMed
5. Howell E, Kravet S, Kisuule F, Wright SM. An innovative approach to supporting hospitalist physicians towards academic success. J Hosp Med. 2008;3(4):314-318. PubMed
6. Society of Hospital Medicine Career Satisfaction Taskforce: A Challenge for a new Specialty. A White paper on hospitalist career satisfaction. http://dev.hospitalmedicine.org/Web/Media_Center/shm_white_papers.aspx . Accessed February 9, 2018.
1. Wachter RM, Goldman L. Zero to 50,000-The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. PubMed
2. Cumbler E, Yirdaw E, Kneeland P, et al. What is career success for academic hospitalists? A qualitative analysis of early-career faculty perspectives. J Hosp Med. 2018;13(5):372-377. doi: 10.12788/jhm.2924. Published online first January 31, 2018. PubMed
3. Nagarur A, O’Neill RM, Lawton D, Greenwald JL. Supporting faculty development in hospital medicine: design and implementation of a personalized structured mentoring program. J Hosp Med. 2018;13(2):96-99. PubMed
4. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. PubMed
5. Howell E, Kravet S, Kisuule F, Wright SM. An innovative approach to supporting hospitalist physicians towards academic success. J Hosp Med. 2008;3(4):314-318. PubMed
6. Society of Hospital Medicine Career Satisfaction Taskforce: A Challenge for a new Specialty. A White paper on hospitalist career satisfaction. http://dev.hospitalmedicine.org/Web/Media_Center/shm_white_papers.aspx . Accessed February 9, 2018.
©2018 Society of Hospital Medicine
Commentary: Shifting the care delivery paradigm to diabetes-depression collaborative care models
Significant depressive symptoms affect approximately one in four adults with type 1 and type 2 diabetes while a formal diagnosis of depressive disorders is made in approximately 10%-15% of individuals with diabetes.1 The combination of diabetes and depression presents a major clinical challenge because the outcomes of each condition is worsened by the presence of the other, which results in worsened quality of life, impaired diabetes self-management, and poor clinical outcomes.1 While the costs of treatment are high for both individual patients and health economies, these costs do not necessarily result in significant improvements in disease or quality of life outcomes.1 This raises the question, “What is the best approach to managing patients with comorbid depression and diabetes?”
Strategies associated with at least a 0.5% reduction in hemoglobin A1c include team changes (–0.67%) and case management (–0.52%).2 The most effective team changes were those that included multidisciplinary, interactive teams with shared care between specialists and primary care providers.2 Such a collaborative care model that integrates specialty psychiatric care into primary care has been successfully demonstrated for patients with depression and poorly controlled type 2 diabetes or coronary heart disease.3
In this study, patients at 14 primary care clinics in an integrated health care system in Washington State received either a multidisciplinary, team-based intervention or usual care.3 Components of the intervention in these clinics included the following:
- Three part-time registered nurses who had diabetes education training (certified diabetes educators), as well as training on depression management, behavioral strategies, and glycemic, hypertension, and lipid control.
- Combined support for self-care with pharmacotherapy to control depression, hyperglycemia, hypertension, and hyperlipidemia with algorithm guidance.
- Motivational and encouraging coaching for problem-solving and adherence to self-care.
- Weekly nurse supervision with a psychiatrist, primary care physician, and psychologist, with a nurse communicating recommendations back to the primary care team.
An endocrinologist/diabetologist was also incorporated for consultation when needed. After 12 months, patients in the intervention group had greater reduction in hemoglobin A1c (0.58%), LDL cholesterol (6.9 mg/dL), systolic blood pressure (5.1 mm Hg), and depression scores than did those in the usual care group. Patients in the intervention group were also more likely to have adjustments made to insulin, antihypertensive medications, and antidepressants.
The success of this intervention, known as TEAMCare, highlights the critical need to incorporate mental health care into primary care and endocrinology practice. Currently, psychiatric and psychological care are largely administered separately from medical care for diabetes, despite evidence showing the success of an integrated care delivery model. In order to address the important interaction between mental health disorders, such as depression, and diabetes, it is critical that evaluation and treatment of mental health be integrated into medical practice.
What can we – endocrinologists and psychiatrists – do to facilitate adoption of such models? First, we can lobby our health systems to support reorganization of our health care delivery approach for patients with comorbid depression and diabetes so that endocrinologists, psychiatrists, and behavioral specialists are incorporated into primary care practices. This will facilitate better alignment of specialists and primary care providers and also enable patients to receive care in a clinical environment where they are most comfortable and have established relationships. Instead of the primary care physician referring the patient separately to psychiatry and endocrinology and awaiting feedback, which can sometimes take several weeks, the psychiatrist and endocrinologist would meet weekly with the primary care physician and nurse case manager team to review the entire patient panel, make timely adjustments in diabetes and antidepressant medications, and recommend behavioral therapy. This population health strategy would enable our two specialties to make a greater impact on a larger number of patients than we can in a half-day clinic session.
Second, our other critical role is to collaborate with payers to develop a sustainable financial reimbursement model to support the psychiatrist and endocrinologist in this novel health care delivery approach, which departs from the traditional fee-for-service model.
Finally, diabetes remains highly prevalent in the United States and worldwide, and depression is now a widely recognized comorbidity of diabetes. Many behavioral specialists are not trained to address the complexities of diabetes management experienced by patients who also have mental health comorbidities. To this end, the American Diabetes Association and the American Psychological Association established a partnership to build the ADA-APA Mental Health Provider Diabetes Education Program to prepare mental health providers with the knowledge and tools and treat diabetes-related psychosocial factors. Let us join them in supporting this important step toward developing diabetes-mental health collaborative health care delivery models.
Dr. Golden is the Hugh P. McCormick Family Professor of Endocrinology and Metabolism and executive vice-chair of the department of medicine at Johns Hopkins University, Baltimore.
References
1. Holt RIG et al. Current Diabetes Reports. 2014;14(6):491.
2. Shojania KG et al. JAMA. 2006;296(4):427-40.
3. Katon WJ et al. N Eng J Med. 2010;363(27):2611-20.
Significant depressive symptoms affect approximately one in four adults with type 1 and type 2 diabetes while a formal diagnosis of depressive disorders is made in approximately 10%-15% of individuals with diabetes.1 The combination of diabetes and depression presents a major clinical challenge because the outcomes of each condition is worsened by the presence of the other, which results in worsened quality of life, impaired diabetes self-management, and poor clinical outcomes.1 While the costs of treatment are high for both individual patients and health economies, these costs do not necessarily result in significant improvements in disease or quality of life outcomes.1 This raises the question, “What is the best approach to managing patients with comorbid depression and diabetes?”
Strategies associated with at least a 0.5% reduction in hemoglobin A1c include team changes (–0.67%) and case management (–0.52%).2 The most effective team changes were those that included multidisciplinary, interactive teams with shared care between specialists and primary care providers.2 Such a collaborative care model that integrates specialty psychiatric care into primary care has been successfully demonstrated for patients with depression and poorly controlled type 2 diabetes or coronary heart disease.3
In this study, patients at 14 primary care clinics in an integrated health care system in Washington State received either a multidisciplinary, team-based intervention or usual care.3 Components of the intervention in these clinics included the following:
- Three part-time registered nurses who had diabetes education training (certified diabetes educators), as well as training on depression management, behavioral strategies, and glycemic, hypertension, and lipid control.
- Combined support for self-care with pharmacotherapy to control depression, hyperglycemia, hypertension, and hyperlipidemia with algorithm guidance.
- Motivational and encouraging coaching for problem-solving and adherence to self-care.
- Weekly nurse supervision with a psychiatrist, primary care physician, and psychologist, with a nurse communicating recommendations back to the primary care team.
An endocrinologist/diabetologist was also incorporated for consultation when needed. After 12 months, patients in the intervention group had greater reduction in hemoglobin A1c (0.58%), LDL cholesterol (6.9 mg/dL), systolic blood pressure (5.1 mm Hg), and depression scores than did those in the usual care group. Patients in the intervention group were also more likely to have adjustments made to insulin, antihypertensive medications, and antidepressants.
The success of this intervention, known as TEAMCare, highlights the critical need to incorporate mental health care into primary care and endocrinology practice. Currently, psychiatric and psychological care are largely administered separately from medical care for diabetes, despite evidence showing the success of an integrated care delivery model. In order to address the important interaction between mental health disorders, such as depression, and diabetes, it is critical that evaluation and treatment of mental health be integrated into medical practice.
What can we – endocrinologists and psychiatrists – do to facilitate adoption of such models? First, we can lobby our health systems to support reorganization of our health care delivery approach for patients with comorbid depression and diabetes so that endocrinologists, psychiatrists, and behavioral specialists are incorporated into primary care practices. This will facilitate better alignment of specialists and primary care providers and also enable patients to receive care in a clinical environment where they are most comfortable and have established relationships. Instead of the primary care physician referring the patient separately to psychiatry and endocrinology and awaiting feedback, which can sometimes take several weeks, the psychiatrist and endocrinologist would meet weekly with the primary care physician and nurse case manager team to review the entire patient panel, make timely adjustments in diabetes and antidepressant medications, and recommend behavioral therapy. This population health strategy would enable our two specialties to make a greater impact on a larger number of patients than we can in a half-day clinic session.
Second, our other critical role is to collaborate with payers to develop a sustainable financial reimbursement model to support the psychiatrist and endocrinologist in this novel health care delivery approach, which departs from the traditional fee-for-service model.
Finally, diabetes remains highly prevalent in the United States and worldwide, and depression is now a widely recognized comorbidity of diabetes. Many behavioral specialists are not trained to address the complexities of diabetes management experienced by patients who also have mental health comorbidities. To this end, the American Diabetes Association and the American Psychological Association established a partnership to build the ADA-APA Mental Health Provider Diabetes Education Program to prepare mental health providers with the knowledge and tools and treat diabetes-related psychosocial factors. Let us join them in supporting this important step toward developing diabetes-mental health collaborative health care delivery models.
Dr. Golden is the Hugh P. McCormick Family Professor of Endocrinology and Metabolism and executive vice-chair of the department of medicine at Johns Hopkins University, Baltimore.
References
1. Holt RIG et al. Current Diabetes Reports. 2014;14(6):491.
2. Shojania KG et al. JAMA. 2006;296(4):427-40.
3. Katon WJ et al. N Eng J Med. 2010;363(27):2611-20.
Significant depressive symptoms affect approximately one in four adults with type 1 and type 2 diabetes while a formal diagnosis of depressive disorders is made in approximately 10%-15% of individuals with diabetes.1 The combination of diabetes and depression presents a major clinical challenge because the outcomes of each condition is worsened by the presence of the other, which results in worsened quality of life, impaired diabetes self-management, and poor clinical outcomes.1 While the costs of treatment are high for both individual patients and health economies, these costs do not necessarily result in significant improvements in disease or quality of life outcomes.1 This raises the question, “What is the best approach to managing patients with comorbid depression and diabetes?”
Strategies associated with at least a 0.5% reduction in hemoglobin A1c include team changes (–0.67%) and case management (–0.52%).2 The most effective team changes were those that included multidisciplinary, interactive teams with shared care between specialists and primary care providers.2 Such a collaborative care model that integrates specialty psychiatric care into primary care has been successfully demonstrated for patients with depression and poorly controlled type 2 diabetes or coronary heart disease.3
In this study, patients at 14 primary care clinics in an integrated health care system in Washington State received either a multidisciplinary, team-based intervention or usual care.3 Components of the intervention in these clinics included the following:
- Three part-time registered nurses who had diabetes education training (certified diabetes educators), as well as training on depression management, behavioral strategies, and glycemic, hypertension, and lipid control.
- Combined support for self-care with pharmacotherapy to control depression, hyperglycemia, hypertension, and hyperlipidemia with algorithm guidance.
- Motivational and encouraging coaching for problem-solving and adherence to self-care.
- Weekly nurse supervision with a psychiatrist, primary care physician, and psychologist, with a nurse communicating recommendations back to the primary care team.
An endocrinologist/diabetologist was also incorporated for consultation when needed. After 12 months, patients in the intervention group had greater reduction in hemoglobin A1c (0.58%), LDL cholesterol (6.9 mg/dL), systolic blood pressure (5.1 mm Hg), and depression scores than did those in the usual care group. Patients in the intervention group were also more likely to have adjustments made to insulin, antihypertensive medications, and antidepressants.
The success of this intervention, known as TEAMCare, highlights the critical need to incorporate mental health care into primary care and endocrinology practice. Currently, psychiatric and psychological care are largely administered separately from medical care for diabetes, despite evidence showing the success of an integrated care delivery model. In order to address the important interaction between mental health disorders, such as depression, and diabetes, it is critical that evaluation and treatment of mental health be integrated into medical practice.
What can we – endocrinologists and psychiatrists – do to facilitate adoption of such models? First, we can lobby our health systems to support reorganization of our health care delivery approach for patients with comorbid depression and diabetes so that endocrinologists, psychiatrists, and behavioral specialists are incorporated into primary care practices. This will facilitate better alignment of specialists and primary care providers and also enable patients to receive care in a clinical environment where they are most comfortable and have established relationships. Instead of the primary care physician referring the patient separately to psychiatry and endocrinology and awaiting feedback, which can sometimes take several weeks, the psychiatrist and endocrinologist would meet weekly with the primary care physician and nurse case manager team to review the entire patient panel, make timely adjustments in diabetes and antidepressant medications, and recommend behavioral therapy. This population health strategy would enable our two specialties to make a greater impact on a larger number of patients than we can in a half-day clinic session.
Second, our other critical role is to collaborate with payers to develop a sustainable financial reimbursement model to support the psychiatrist and endocrinologist in this novel health care delivery approach, which departs from the traditional fee-for-service model.
Finally, diabetes remains highly prevalent in the United States and worldwide, and depression is now a widely recognized comorbidity of diabetes. Many behavioral specialists are not trained to address the complexities of diabetes management experienced by patients who also have mental health comorbidities. To this end, the American Diabetes Association and the American Psychological Association established a partnership to build the ADA-APA Mental Health Provider Diabetes Education Program to prepare mental health providers with the knowledge and tools and treat diabetes-related psychosocial factors. Let us join them in supporting this important step toward developing diabetes-mental health collaborative health care delivery models.
Dr. Golden is the Hugh P. McCormick Family Professor of Endocrinology and Metabolism and executive vice-chair of the department of medicine at Johns Hopkins University, Baltimore.
References
1. Holt RIG et al. Current Diabetes Reports. 2014;14(6):491.
2. Shojania KG et al. JAMA. 2006;296(4):427-40.
3. Katon WJ et al. N Eng J Med. 2010;363(27):2611-20.
It takes a village to care for the patient with idiopathic pulmonary fibrosis
Idiopathic pulmonary fibrosis (IPF) is a devastating progressive fibrosing interstitial lung disease associated with a high burden of morbidity and death.1 A clinical diagnosis of IPF is made only after careful interpretation of integrated clinical, radiologic, and often histopathologic data.
Interstitial lung disease encompasses a broad spectrum of parenchymal lung diseases, and a classification of IPF is restricted to a lung injury pattern of usual interstitial pneumonia (UIP) based on high-resolution computed tomography or surgical lung biopsy, after all known causes of UIP have been excluded.1
However, a lung injury pattern of UIP is not synonymous with IPF, as UIP can be seen with connective tissue disease, chronic hypersensitivity pneumonitis, drug toxicity, and sarcoidosis.1 As such, rendering a diagnosis of IPF requires a thorough evaluation to exclude such diverse potential etiologies.
In this issue of the Cleveland Clinic Journal of Medicine, Tolle and colleagues2 provide an up-to-date, broad overview of IPF focused on what the primary care provider needs to know about the disease. Their review is timely and serves as a useful primer for the practicing clinician.
The field of IPF is actively evolving, as this era has been witness to a recent paradigm shift in pharmacologic management. Immunosuppression is no longer recommended3 and may even be harmful.4 And the US Food and Drug Administration has approved 2 antifibrotic drugs—pirfenidone and nintedanib—that have been shown to delay progression of IPF.5,6
Primary care providers have a unique opportunity to play an integral role in the evaluation and care of patients with IPF, in particular with earlier disease recognition, initial disease assessment, and timely specialty consultative referral—as well as implementing a comprehensive longitudinal care plan.
EARLIER DISEASE RECOGNITION
IPF is a rare disease primarily affecting men over the age of 65.1 It is reasonable to presume that many or most of these individuals ultimately diagnosed with IPF are already seeking routine care for existing common medical conditions such as hypertension or dyslipidemia—or at least having periodic routine health maintenance assessments. Such evaluations may offer an opportunity for earlier recognition of an underlying fibrotic lung disease that may be subclinical in nature.
IPF has a lower-lung zone predominance. The importance of chest auscultation, particularly listening carefully to the lung bases, is poignantly highlighted in a recent editorial: “It is time that the stethoscope draped around the neck of physicians, which tends to be used for identification purposes rather than for medical diagnosis, be also the (presently only) genuine tool for an earlier diagnosis of IPF.”7
Advances in imaging also provide an opportunity for earlier diagnosis. Many patients undergo screening computed tomography for coronary calcium scoring or lung cancer surveillance, and these studies may incidentally identify subtle interstitial lung abnormalities. These incidental findings should lead to further investigation, as they have been shown to be functionally important and carry risk of progression to clinical interstitial lung disease.8
INITIAL ASSESSMENT, TIMELY REFERRAL
But whether evidence of interstitial lung disease is detected incidentally or during testing for respiratory symptoms, further evaluation is necessary. Primary care providers are uniquely positioned to initiate the assessment and to expedite and guide further evaluation and specialty referral consultation to ensure an accurate diagnosis. They can also help grade the severity of the disease with pulmonary function testing, oxygen assessments at rest and with ambulation, and ordering thoracic high-resolution computed tomography to provide valuable information about disease extent and interstitial lung disease pattern.
General practitioners may assess for features suggesting connective tissue disease that would warrant specific serologic testing and dedicated rheumatologic consultation.
Finally, given the rarity, complexity, and challenges of interstitial lung disease, an effective multidisciplinary team consisting of clinicians, radiologists, and pathologists enhances diagnostic accuracy.9 This may also help general practitioners deviate from normal patterns of referral to general pulmonary providers, and instead refer patients to specialized centers with dedicated clinical and research expertise in interstitial lung disease.
IMPLEMENTING A COMPREHENSIVE, LONGITUDINAL CARE PLAN
The primary care practitioner often has developed long-term relationships with patients ultimately diagnosed with IPF, and because of this is particularly well positioned to help implement a collaborative and comprehensive care plan. Logistical realities such as distance to a specialty center, limited insurance coverage for specialty visits, and limited specialty availability all reinforce the central role that primary care practitioners play in ensuring that patients adhere to a comprehensive treatment program.
Primary providers may be very experienced and more inclined to manage a number of the common and often important comorbid conditions seen in patients with IPF, such as gastroesophageal reflux disease, obstructive sleep apnea, and depression. Reinforcing to the patient the need to adhere to adjunctive therapies such as supplemental oxygen and pulmonary rehabilitation is another key opportunity to actively engage in the management of patients with IPF.
Primary providers may also play a central role in IPF care through prevention strategies such as smoking cessation and ensuring appropriate immunization against seasonal influenza, pneumococcal pneumonia, and pertussis, among other age-appropriate vaccinations.
With the introduction and expansion of use of nintedanib and pirfenidone for IPF over the past few years, general practitioners may be called on to help manage common gastrointestinal side effects associated with pirfenidone (primarily nausea) and nintedanib (primarily diarrhea), and to be aware of potential drug-drug interactions and other medication-related toxicities.
Finally, as IPF remains a progressive disease, primary care practitioners are often well positioned to help implement palliative care, hospice care, and end-of-life care.
Despite recent advances in treatment, IPF remains a devastating lung disease with a high degree of morbidity and mortality. It takes a village to help care for the IPF patient. And as key members of the healthcare team, primary care providers have unique and important opportunities to help in the early recognition, thorough assessment, and comprehensive management of patients with IPF.
- Raghu G, Collard HR, Egan JJ, et al; ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011; 183(6):788–824. doi:10.1164/rccm.2009-040GL
- Tolle L, Southern BD, Culver D, Horowitz JC. Idiopathic pulmonary fibrosis: what primary care physicians need to know. Cleve Clin J Med 2018; 85(5):377–386. doi:10.3949/ccjm.85a.17018
- Raghu G, Richeldi L. Current approaches to the management of idiopathic pulmonary fibrosis. Respir Med 2017; 129:24–30. doi:10.1016/j.rmed.2017.05.017
- Idiopathic Pulmonary Fibrosis Clinical Research Network; Raghu G, Anstrom KJ, King TE Jr, Lasky JA, Martinez FJ. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med 2012; 366(21):1968–1977. doi:10.1056/NEJMoa1113354
- King TE Jr, Bradford WZ, Castro-Bernardini S, et al; ASCEND Study Group. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med 2014; 370(22):2083–2092. doi:10.1056/NEJMoa1402582
- Richeldi L, du Bois RM, Raghu G, et al; INPULSIS Trial Investigators. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med 2014; 370(22):2071–2082. doi:10.1056/NEJMoa1402584
- Cottin V, Cordier JF. Velcro crackles: the key for early diagnosis of idiopathic pulmonary fibrosis? Eur Respir J 2012; 40(3):519–521. doi:10.1183/09031936.00001612
- Doyle TJ, Hunninghake GM, Rosas IO. Subclinical interstitial lung disease: why you should care. Am J Respir Crit Care Med 2012; 185(11):1147–1153. doi:10.1164/rccm.201108-1420PP
- Walsh SLF, Maher TM, Kolb M, et al; IPF Project Consortium. Diagnostic accuracy of a clinical diagnosis of idiopathic pulmonary fibrosis: an international case-cohort study. Eur Respir J 2017; 50(2):1700936. doi:10.1183/13993003.00936-2017
Idiopathic pulmonary fibrosis (IPF) is a devastating progressive fibrosing interstitial lung disease associated with a high burden of morbidity and death.1 A clinical diagnosis of IPF is made only after careful interpretation of integrated clinical, radiologic, and often histopathologic data.
Interstitial lung disease encompasses a broad spectrum of parenchymal lung diseases, and a classification of IPF is restricted to a lung injury pattern of usual interstitial pneumonia (UIP) based on high-resolution computed tomography or surgical lung biopsy, after all known causes of UIP have been excluded.1
However, a lung injury pattern of UIP is not synonymous with IPF, as UIP can be seen with connective tissue disease, chronic hypersensitivity pneumonitis, drug toxicity, and sarcoidosis.1 As such, rendering a diagnosis of IPF requires a thorough evaluation to exclude such diverse potential etiologies.
In this issue of the Cleveland Clinic Journal of Medicine, Tolle and colleagues2 provide an up-to-date, broad overview of IPF focused on what the primary care provider needs to know about the disease. Their review is timely and serves as a useful primer for the practicing clinician.
The field of IPF is actively evolving, as this era has been witness to a recent paradigm shift in pharmacologic management. Immunosuppression is no longer recommended3 and may even be harmful.4 And the US Food and Drug Administration has approved 2 antifibrotic drugs—pirfenidone and nintedanib—that have been shown to delay progression of IPF.5,6
Primary care providers have a unique opportunity to play an integral role in the evaluation and care of patients with IPF, in particular with earlier disease recognition, initial disease assessment, and timely specialty consultative referral—as well as implementing a comprehensive longitudinal care plan.
EARLIER DISEASE RECOGNITION
IPF is a rare disease primarily affecting men over the age of 65.1 It is reasonable to presume that many or most of these individuals ultimately diagnosed with IPF are already seeking routine care for existing common medical conditions such as hypertension or dyslipidemia—or at least having periodic routine health maintenance assessments. Such evaluations may offer an opportunity for earlier recognition of an underlying fibrotic lung disease that may be subclinical in nature.
IPF has a lower-lung zone predominance. The importance of chest auscultation, particularly listening carefully to the lung bases, is poignantly highlighted in a recent editorial: “It is time that the stethoscope draped around the neck of physicians, which tends to be used for identification purposes rather than for medical diagnosis, be also the (presently only) genuine tool for an earlier diagnosis of IPF.”7
Advances in imaging also provide an opportunity for earlier diagnosis. Many patients undergo screening computed tomography for coronary calcium scoring or lung cancer surveillance, and these studies may incidentally identify subtle interstitial lung abnormalities. These incidental findings should lead to further investigation, as they have been shown to be functionally important and carry risk of progression to clinical interstitial lung disease.8
INITIAL ASSESSMENT, TIMELY REFERRAL
But whether evidence of interstitial lung disease is detected incidentally or during testing for respiratory symptoms, further evaluation is necessary. Primary care providers are uniquely positioned to initiate the assessment and to expedite and guide further evaluation and specialty referral consultation to ensure an accurate diagnosis. They can also help grade the severity of the disease with pulmonary function testing, oxygen assessments at rest and with ambulation, and ordering thoracic high-resolution computed tomography to provide valuable information about disease extent and interstitial lung disease pattern.
General practitioners may assess for features suggesting connective tissue disease that would warrant specific serologic testing and dedicated rheumatologic consultation.
Finally, given the rarity, complexity, and challenges of interstitial lung disease, an effective multidisciplinary team consisting of clinicians, radiologists, and pathologists enhances diagnostic accuracy.9 This may also help general practitioners deviate from normal patterns of referral to general pulmonary providers, and instead refer patients to specialized centers with dedicated clinical and research expertise in interstitial lung disease.
IMPLEMENTING A COMPREHENSIVE, LONGITUDINAL CARE PLAN
The primary care practitioner often has developed long-term relationships with patients ultimately diagnosed with IPF, and because of this is particularly well positioned to help implement a collaborative and comprehensive care plan. Logistical realities such as distance to a specialty center, limited insurance coverage for specialty visits, and limited specialty availability all reinforce the central role that primary care practitioners play in ensuring that patients adhere to a comprehensive treatment program.
Primary providers may be very experienced and more inclined to manage a number of the common and often important comorbid conditions seen in patients with IPF, such as gastroesophageal reflux disease, obstructive sleep apnea, and depression. Reinforcing to the patient the need to adhere to adjunctive therapies such as supplemental oxygen and pulmonary rehabilitation is another key opportunity to actively engage in the management of patients with IPF.
Primary providers may also play a central role in IPF care through prevention strategies such as smoking cessation and ensuring appropriate immunization against seasonal influenza, pneumococcal pneumonia, and pertussis, among other age-appropriate vaccinations.
With the introduction and expansion of use of nintedanib and pirfenidone for IPF over the past few years, general practitioners may be called on to help manage common gastrointestinal side effects associated with pirfenidone (primarily nausea) and nintedanib (primarily diarrhea), and to be aware of potential drug-drug interactions and other medication-related toxicities.
Finally, as IPF remains a progressive disease, primary care practitioners are often well positioned to help implement palliative care, hospice care, and end-of-life care.
Despite recent advances in treatment, IPF remains a devastating lung disease with a high degree of morbidity and mortality. It takes a village to help care for the IPF patient. And as key members of the healthcare team, primary care providers have unique and important opportunities to help in the early recognition, thorough assessment, and comprehensive management of patients with IPF.
Idiopathic pulmonary fibrosis (IPF) is a devastating progressive fibrosing interstitial lung disease associated with a high burden of morbidity and death.1 A clinical diagnosis of IPF is made only after careful interpretation of integrated clinical, radiologic, and often histopathologic data.
Interstitial lung disease encompasses a broad spectrum of parenchymal lung diseases, and a classification of IPF is restricted to a lung injury pattern of usual interstitial pneumonia (UIP) based on high-resolution computed tomography or surgical lung biopsy, after all known causes of UIP have been excluded.1
However, a lung injury pattern of UIP is not synonymous with IPF, as UIP can be seen with connective tissue disease, chronic hypersensitivity pneumonitis, drug toxicity, and sarcoidosis.1 As such, rendering a diagnosis of IPF requires a thorough evaluation to exclude such diverse potential etiologies.
In this issue of the Cleveland Clinic Journal of Medicine, Tolle and colleagues2 provide an up-to-date, broad overview of IPF focused on what the primary care provider needs to know about the disease. Their review is timely and serves as a useful primer for the practicing clinician.
The field of IPF is actively evolving, as this era has been witness to a recent paradigm shift in pharmacologic management. Immunosuppression is no longer recommended3 and may even be harmful.4 And the US Food and Drug Administration has approved 2 antifibrotic drugs—pirfenidone and nintedanib—that have been shown to delay progression of IPF.5,6
Primary care providers have a unique opportunity to play an integral role in the evaluation and care of patients with IPF, in particular with earlier disease recognition, initial disease assessment, and timely specialty consultative referral—as well as implementing a comprehensive longitudinal care plan.
EARLIER DISEASE RECOGNITION
IPF is a rare disease primarily affecting men over the age of 65.1 It is reasonable to presume that many or most of these individuals ultimately diagnosed with IPF are already seeking routine care for existing common medical conditions such as hypertension or dyslipidemia—or at least having periodic routine health maintenance assessments. Such evaluations may offer an opportunity for earlier recognition of an underlying fibrotic lung disease that may be subclinical in nature.
IPF has a lower-lung zone predominance. The importance of chest auscultation, particularly listening carefully to the lung bases, is poignantly highlighted in a recent editorial: “It is time that the stethoscope draped around the neck of physicians, which tends to be used for identification purposes rather than for medical diagnosis, be also the (presently only) genuine tool for an earlier diagnosis of IPF.”7
Advances in imaging also provide an opportunity for earlier diagnosis. Many patients undergo screening computed tomography for coronary calcium scoring or lung cancer surveillance, and these studies may incidentally identify subtle interstitial lung abnormalities. These incidental findings should lead to further investigation, as they have been shown to be functionally important and carry risk of progression to clinical interstitial lung disease.8
INITIAL ASSESSMENT, TIMELY REFERRAL
But whether evidence of interstitial lung disease is detected incidentally or during testing for respiratory symptoms, further evaluation is necessary. Primary care providers are uniquely positioned to initiate the assessment and to expedite and guide further evaluation and specialty referral consultation to ensure an accurate diagnosis. They can also help grade the severity of the disease with pulmonary function testing, oxygen assessments at rest and with ambulation, and ordering thoracic high-resolution computed tomography to provide valuable information about disease extent and interstitial lung disease pattern.
General practitioners may assess for features suggesting connective tissue disease that would warrant specific serologic testing and dedicated rheumatologic consultation.
Finally, given the rarity, complexity, and challenges of interstitial lung disease, an effective multidisciplinary team consisting of clinicians, radiologists, and pathologists enhances diagnostic accuracy.9 This may also help general practitioners deviate from normal patterns of referral to general pulmonary providers, and instead refer patients to specialized centers with dedicated clinical and research expertise in interstitial lung disease.
IMPLEMENTING A COMPREHENSIVE, LONGITUDINAL CARE PLAN
The primary care practitioner often has developed long-term relationships with patients ultimately diagnosed with IPF, and because of this is particularly well positioned to help implement a collaborative and comprehensive care plan. Logistical realities such as distance to a specialty center, limited insurance coverage for specialty visits, and limited specialty availability all reinforce the central role that primary care practitioners play in ensuring that patients adhere to a comprehensive treatment program.
Primary providers may be very experienced and more inclined to manage a number of the common and often important comorbid conditions seen in patients with IPF, such as gastroesophageal reflux disease, obstructive sleep apnea, and depression. Reinforcing to the patient the need to adhere to adjunctive therapies such as supplemental oxygen and pulmonary rehabilitation is another key opportunity to actively engage in the management of patients with IPF.
Primary providers may also play a central role in IPF care through prevention strategies such as smoking cessation and ensuring appropriate immunization against seasonal influenza, pneumococcal pneumonia, and pertussis, among other age-appropriate vaccinations.
With the introduction and expansion of use of nintedanib and pirfenidone for IPF over the past few years, general practitioners may be called on to help manage common gastrointestinal side effects associated with pirfenidone (primarily nausea) and nintedanib (primarily diarrhea), and to be aware of potential drug-drug interactions and other medication-related toxicities.
Finally, as IPF remains a progressive disease, primary care practitioners are often well positioned to help implement palliative care, hospice care, and end-of-life care.
Despite recent advances in treatment, IPF remains a devastating lung disease with a high degree of morbidity and mortality. It takes a village to help care for the IPF patient. And as key members of the healthcare team, primary care providers have unique and important opportunities to help in the early recognition, thorough assessment, and comprehensive management of patients with IPF.
- Raghu G, Collard HR, Egan JJ, et al; ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011; 183(6):788–824. doi:10.1164/rccm.2009-040GL
- Tolle L, Southern BD, Culver D, Horowitz JC. Idiopathic pulmonary fibrosis: what primary care physicians need to know. Cleve Clin J Med 2018; 85(5):377–386. doi:10.3949/ccjm.85a.17018
- Raghu G, Richeldi L. Current approaches to the management of idiopathic pulmonary fibrosis. Respir Med 2017; 129:24–30. doi:10.1016/j.rmed.2017.05.017
- Idiopathic Pulmonary Fibrosis Clinical Research Network; Raghu G, Anstrom KJ, King TE Jr, Lasky JA, Martinez FJ. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med 2012; 366(21):1968–1977. doi:10.1056/NEJMoa1113354
- King TE Jr, Bradford WZ, Castro-Bernardini S, et al; ASCEND Study Group. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med 2014; 370(22):2083–2092. doi:10.1056/NEJMoa1402582
- Richeldi L, du Bois RM, Raghu G, et al; INPULSIS Trial Investigators. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med 2014; 370(22):2071–2082. doi:10.1056/NEJMoa1402584
- Cottin V, Cordier JF. Velcro crackles: the key for early diagnosis of idiopathic pulmonary fibrosis? Eur Respir J 2012; 40(3):519–521. doi:10.1183/09031936.00001612
- Doyle TJ, Hunninghake GM, Rosas IO. Subclinical interstitial lung disease: why you should care. Am J Respir Crit Care Med 2012; 185(11):1147–1153. doi:10.1164/rccm.201108-1420PP
- Walsh SLF, Maher TM, Kolb M, et al; IPF Project Consortium. Diagnostic accuracy of a clinical diagnosis of idiopathic pulmonary fibrosis: an international case-cohort study. Eur Respir J 2017; 50(2):1700936. doi:10.1183/13993003.00936-2017
- Raghu G, Collard HR, Egan JJ, et al; ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011; 183(6):788–824. doi:10.1164/rccm.2009-040GL
- Tolle L, Southern BD, Culver D, Horowitz JC. Idiopathic pulmonary fibrosis: what primary care physicians need to know. Cleve Clin J Med 2018; 85(5):377–386. doi:10.3949/ccjm.85a.17018
- Raghu G, Richeldi L. Current approaches to the management of idiopathic pulmonary fibrosis. Respir Med 2017; 129:24–30. doi:10.1016/j.rmed.2017.05.017
- Idiopathic Pulmonary Fibrosis Clinical Research Network; Raghu G, Anstrom KJ, King TE Jr, Lasky JA, Martinez FJ. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med 2012; 366(21):1968–1977. doi:10.1056/NEJMoa1113354
- King TE Jr, Bradford WZ, Castro-Bernardini S, et al; ASCEND Study Group. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med 2014; 370(22):2083–2092. doi:10.1056/NEJMoa1402582
- Richeldi L, du Bois RM, Raghu G, et al; INPULSIS Trial Investigators. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med 2014; 370(22):2071–2082. doi:10.1056/NEJMoa1402584
- Cottin V, Cordier JF. Velcro crackles: the key for early diagnosis of idiopathic pulmonary fibrosis? Eur Respir J 2012; 40(3):519–521. doi:10.1183/09031936.00001612
- Doyle TJ, Hunninghake GM, Rosas IO. Subclinical interstitial lung disease: why you should care. Am J Respir Crit Care Med 2012; 185(11):1147–1153. doi:10.1164/rccm.201108-1420PP
- Walsh SLF, Maher TM, Kolb M, et al; IPF Project Consortium. Diagnostic accuracy of a clinical diagnosis of idiopathic pulmonary fibrosis: an international case-cohort study. Eur Respir J 2017; 50(2):1700936. doi:10.1183/13993003.00936-2017
Infective endocarditis: Refer for expert team care as soon as possible
In this issue of the Journal, Soud et al discuss the timing of referral of patients with infective endocarditis to surgery.1 When having this discussion, it is important to understand the nature of the disease and the role of surgery in its treatment.
Unless successfully treated and cured, infective endocarditis is fatal. It is associated with septic embolism (systemic with left-sided infective endocarditis and pulmonary with right-sided infective endocarditis), destruction of valve tissue, and invasion outside the aortic root or into the atrioventricular groove. Antimicrobials kill sensitive and exposed organisms but cannot reach those hiding in vegetations or biofilm, on foreign material, or in invaded extravascular tissue.
The objectives of surgery are to eliminate the source of embolism, debride and remove infected tissue and foreign material, expose and make residual organisms vulnerable to antimicrobials, and restore functional valves and cardiac integrity. Surgery to treat infective endocarditis is difficult and high-risk and requires an experienced surgeon. But final cure of the infection is still by antimicrobial treatment.
INFECTIVE ENDOCARDITIS NEEDS MULTIDISCIPLINARY CARE
Every aspect of infective endocarditis—diagnosis, medical management, management of complications, and surgery—is difficult. Recent guidelines2–6 therefore favor care by a multidisciplinary team that includes an infectious disease specialist, cardiologist, and cardiac surgeon from the very beginning, with access to any other needed discipline, often including neurology, neurosurgery, nephrology, and dependence specialists. Patients with infective endocarditis should be referred early to a center with access to a full endocarditis treatment team. The need for surgery and the optimal timing of it are team decisions. The American Association for Thoracic Surgery infective endocarditis guidelines are question-based and address most aspects that surgeons must consider before, during, and after operation.2
IF SURGERY IS INDICATED, IT IS BEST DONE SOONER
Once there is an indication to operate, the operation should be expedited. Delays mean continued risk of disease progression, invasion, heart block, and embolic events. Determining the timing of surgery is difficult in patients who have suffered an embolic stroke—nonhemorrhagic or hemorrhagic—or who have suffered brain bleeding; management of these issues has recently triggered expert opinion and review articles.7,8 The recommendation for early surgery is based on the conviction that once the patient has been stabilized (or has overwhelming mechanical hemodynamic problems requiring emergency surgery) and adequate antimicrobial coverage is on board, there are no additional benefits to delaying surgery.9 When the indication to operate is large mobile vegetations associated with a high risk of stroke, surgery before another event can make all the difference.
In the operating room, the first aspect addressed is adequate debridement. There is wide agreement that repair is preferable to replacement for the mitral and tricuspid valves, but there is no agreement that an allograft (although favored by our team) is the best replacement alternative for a destroyed aortic root. The key is that surgeons and their surgical teams must have the experience and tools that work for them.
Our recommendation is to refer all patients with infective endocarditis to a center with access to a full team of experienced experts able to address all aspects of the disease and its complications.
- Soud M, Pacha HM, Alraies MC. How soon should patients with infective endocarditis be referred for valve surgery? Cleve Clin J Med 2018; 85(5):362–364. doi:10.3949/ccjm.85a:17052
- Pettersson GB, Coselli JS, Pettersson GB, et al. 2016 The American Association for Thoracic Surgery (AATS) consensus guidelines: surgical treatment of infective endocarditis: executive summary. J Thorac Cardiovasc Surg 2017; 153(6):1241–1258.e29. doi:10.1016/j.jtcvs.2016.09.093
- Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 2015; 132(15):1435–1486. doi:10.1161/CIR.0000000000000296
- Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC guidelines for the management of infective endocarditis: the Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015; 36(44):3075–3128. doi:10.1093/eurheartj/ehv319
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease:executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129(23):2440–2492. doi:10.1161/CIR.0000000000000029
- Byrne JG, Rezai K, Sanchez JA, et al. Surgical management of endocarditis: the Society of Thoracic Surgeons clinical practice guideline. Ann Thorac Surg 2011; 91(6):2012–2019. doi:10.1016/j.athoracsur.2011.01.106
- Yanagawa B, Pettersson GB, Habib G, et al. Surgical management of infective endocarditis complicated by embolic stroke: practical recommendations for clinicians. Circulation 2016; 134(17):1280–1292. doi:10.1161/CIRCULATIONAHA.116.024156
- Cahill TJ , Baddour LM, Habib G, et al. Challenges in infective endocarditis. J Am Coll Cardiol 2017; 69(3):325–344. doi:10.1016/j.jacc.2016.10.066
- Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med 2012; 366(26):2466–2473. doi:10.1056/NEJMoa1112843
In this issue of the Journal, Soud et al discuss the timing of referral of patients with infective endocarditis to surgery.1 When having this discussion, it is important to understand the nature of the disease and the role of surgery in its treatment.
Unless successfully treated and cured, infective endocarditis is fatal. It is associated with septic embolism (systemic with left-sided infective endocarditis and pulmonary with right-sided infective endocarditis), destruction of valve tissue, and invasion outside the aortic root or into the atrioventricular groove. Antimicrobials kill sensitive and exposed organisms but cannot reach those hiding in vegetations or biofilm, on foreign material, or in invaded extravascular tissue.
The objectives of surgery are to eliminate the source of embolism, debride and remove infected tissue and foreign material, expose and make residual organisms vulnerable to antimicrobials, and restore functional valves and cardiac integrity. Surgery to treat infective endocarditis is difficult and high-risk and requires an experienced surgeon. But final cure of the infection is still by antimicrobial treatment.
INFECTIVE ENDOCARDITIS NEEDS MULTIDISCIPLINARY CARE
Every aspect of infective endocarditis—diagnosis, medical management, management of complications, and surgery—is difficult. Recent guidelines2–6 therefore favor care by a multidisciplinary team that includes an infectious disease specialist, cardiologist, and cardiac surgeon from the very beginning, with access to any other needed discipline, often including neurology, neurosurgery, nephrology, and dependence specialists. Patients with infective endocarditis should be referred early to a center with access to a full endocarditis treatment team. The need for surgery and the optimal timing of it are team decisions. The American Association for Thoracic Surgery infective endocarditis guidelines are question-based and address most aspects that surgeons must consider before, during, and after operation.2
IF SURGERY IS INDICATED, IT IS BEST DONE SOONER
Once there is an indication to operate, the operation should be expedited. Delays mean continued risk of disease progression, invasion, heart block, and embolic events. Determining the timing of surgery is difficult in patients who have suffered an embolic stroke—nonhemorrhagic or hemorrhagic—or who have suffered brain bleeding; management of these issues has recently triggered expert opinion and review articles.7,8 The recommendation for early surgery is based on the conviction that once the patient has been stabilized (or has overwhelming mechanical hemodynamic problems requiring emergency surgery) and adequate antimicrobial coverage is on board, there are no additional benefits to delaying surgery.9 When the indication to operate is large mobile vegetations associated with a high risk of stroke, surgery before another event can make all the difference.
In the operating room, the first aspect addressed is adequate debridement. There is wide agreement that repair is preferable to replacement for the mitral and tricuspid valves, but there is no agreement that an allograft (although favored by our team) is the best replacement alternative for a destroyed aortic root. The key is that surgeons and their surgical teams must have the experience and tools that work for them.
Our recommendation is to refer all patients with infective endocarditis to a center with access to a full team of experienced experts able to address all aspects of the disease and its complications.
In this issue of the Journal, Soud et al discuss the timing of referral of patients with infective endocarditis to surgery.1 When having this discussion, it is important to understand the nature of the disease and the role of surgery in its treatment.
Unless successfully treated and cured, infective endocarditis is fatal. It is associated with septic embolism (systemic with left-sided infective endocarditis and pulmonary with right-sided infective endocarditis), destruction of valve tissue, and invasion outside the aortic root or into the atrioventricular groove. Antimicrobials kill sensitive and exposed organisms but cannot reach those hiding in vegetations or biofilm, on foreign material, or in invaded extravascular tissue.
The objectives of surgery are to eliminate the source of embolism, debride and remove infected tissue and foreign material, expose and make residual organisms vulnerable to antimicrobials, and restore functional valves and cardiac integrity. Surgery to treat infective endocarditis is difficult and high-risk and requires an experienced surgeon. But final cure of the infection is still by antimicrobial treatment.
INFECTIVE ENDOCARDITIS NEEDS MULTIDISCIPLINARY CARE
Every aspect of infective endocarditis—diagnosis, medical management, management of complications, and surgery—is difficult. Recent guidelines2–6 therefore favor care by a multidisciplinary team that includes an infectious disease specialist, cardiologist, and cardiac surgeon from the very beginning, with access to any other needed discipline, often including neurology, neurosurgery, nephrology, and dependence specialists. Patients with infective endocarditis should be referred early to a center with access to a full endocarditis treatment team. The need for surgery and the optimal timing of it are team decisions. The American Association for Thoracic Surgery infective endocarditis guidelines are question-based and address most aspects that surgeons must consider before, during, and after operation.2
IF SURGERY IS INDICATED, IT IS BEST DONE SOONER
Once there is an indication to operate, the operation should be expedited. Delays mean continued risk of disease progression, invasion, heart block, and embolic events. Determining the timing of surgery is difficult in patients who have suffered an embolic stroke—nonhemorrhagic or hemorrhagic—or who have suffered brain bleeding; management of these issues has recently triggered expert opinion and review articles.7,8 The recommendation for early surgery is based on the conviction that once the patient has been stabilized (or has overwhelming mechanical hemodynamic problems requiring emergency surgery) and adequate antimicrobial coverage is on board, there are no additional benefits to delaying surgery.9 When the indication to operate is large mobile vegetations associated with a high risk of stroke, surgery before another event can make all the difference.
In the operating room, the first aspect addressed is adequate debridement. There is wide agreement that repair is preferable to replacement for the mitral and tricuspid valves, but there is no agreement that an allograft (although favored by our team) is the best replacement alternative for a destroyed aortic root. The key is that surgeons and their surgical teams must have the experience and tools that work for them.
Our recommendation is to refer all patients with infective endocarditis to a center with access to a full team of experienced experts able to address all aspects of the disease and its complications.
- Soud M, Pacha HM, Alraies MC. How soon should patients with infective endocarditis be referred for valve surgery? Cleve Clin J Med 2018; 85(5):362–364. doi:10.3949/ccjm.85a:17052
- Pettersson GB, Coselli JS, Pettersson GB, et al. 2016 The American Association for Thoracic Surgery (AATS) consensus guidelines: surgical treatment of infective endocarditis: executive summary. J Thorac Cardiovasc Surg 2017; 153(6):1241–1258.e29. doi:10.1016/j.jtcvs.2016.09.093
- Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 2015; 132(15):1435–1486. doi:10.1161/CIR.0000000000000296
- Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC guidelines for the management of infective endocarditis: the Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015; 36(44):3075–3128. doi:10.1093/eurheartj/ehv319
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease:executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129(23):2440–2492. doi:10.1161/CIR.0000000000000029
- Byrne JG, Rezai K, Sanchez JA, et al. Surgical management of endocarditis: the Society of Thoracic Surgeons clinical practice guideline. Ann Thorac Surg 2011; 91(6):2012–2019. doi:10.1016/j.athoracsur.2011.01.106
- Yanagawa B, Pettersson GB, Habib G, et al. Surgical management of infective endocarditis complicated by embolic stroke: practical recommendations for clinicians. Circulation 2016; 134(17):1280–1292. doi:10.1161/CIRCULATIONAHA.116.024156
- Cahill TJ , Baddour LM, Habib G, et al. Challenges in infective endocarditis. J Am Coll Cardiol 2017; 69(3):325–344. doi:10.1016/j.jacc.2016.10.066
- Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med 2012; 366(26):2466–2473. doi:10.1056/NEJMoa1112843
- Soud M, Pacha HM, Alraies MC. How soon should patients with infective endocarditis be referred for valve surgery? Cleve Clin J Med 2018; 85(5):362–364. doi:10.3949/ccjm.85a:17052
- Pettersson GB, Coselli JS, Pettersson GB, et al. 2016 The American Association for Thoracic Surgery (AATS) consensus guidelines: surgical treatment of infective endocarditis: executive summary. J Thorac Cardiovasc Surg 2017; 153(6):1241–1258.e29. doi:10.1016/j.jtcvs.2016.09.093
- Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 2015; 132(15):1435–1486. doi:10.1161/CIR.0000000000000296
- Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC guidelines for the management of infective endocarditis: the Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015; 36(44):3075–3128. doi:10.1093/eurheartj/ehv319
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease:executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129(23):2440–2492. doi:10.1161/CIR.0000000000000029
- Byrne JG, Rezai K, Sanchez JA, et al. Surgical management of endocarditis: the Society of Thoracic Surgeons clinical practice guideline. Ann Thorac Surg 2011; 91(6):2012–2019. doi:10.1016/j.athoracsur.2011.01.106
- Yanagawa B, Pettersson GB, Habib G, et al. Surgical management of infective endocarditis complicated by embolic stroke: practical recommendations for clinicians. Circulation 2016; 134(17):1280–1292. doi:10.1161/CIRCULATIONAHA.116.024156
- Cahill TJ , Baddour LM, Habib G, et al. Challenges in infective endocarditis. J Am Coll Cardiol 2017; 69(3):325–344. doi:10.1016/j.jacc.2016.10.066
- Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med 2012; 366(26):2466–2473. doi:10.1056/NEJMoa1112843
Patient-Centered, Payer-Centered, or Both? The 30-Day Readmission Metric
There is little doubt that preventing 30-day readmissions to the hospital results in lower costs for payers. However, reducing costs alone does not make this metric a measure of “high value” care.1 Rather, it is the improvement in the effectiveness of the discharge process that occurs alongside lower costs that makes readmission reduction efforts “high value” – or a “win-win” for patients and payers.
However, the article by Nuckols and colleagues in this month’s issue of the Journal of Hospital Medicine (JHM) suggests that it might not be that simple and adds nuance to the ongoing discussion about the 30-day readmission metric.2 The study used data collected by the federal government to examine changes not only in 30-day readmission rates between 2009-2010 and 2013-2014 but also changes in emergency department (ED) and observation unit visits. What they found is important. In general, despite reductions in 30-day readmissions for patients served by Medicare and private insurance, there were increases in observation unit and ED visits across all payer types (including Medicare and private insurance). These increases in observation unit and ED visits resulted in statistically higher overall “revisit” rates for the uninsured and those insured by Medicaid and offset any improvements in the “revisit” rates resulting from reductions in 30-day readmissions for those with private insurance. Those insured by Medicare—representing about 300,000 of the 420,000 visits analyzed—still had a statistically lower “revisit” rate, but it was only marginally lower (25.0% in 2013-2014 versus 25.3% in 2009-2010).2
The generalizability of the Nuckols’ study was limited in that it examined only index admissions for acute myocardial infarction (AMI), heart failure (HF), and pneumonia and used data from only Georgia, Nebraska, South Carolina, and Tennessee—the four states where observation and ED visit data were available in the federal database.2 The study also did not examine hospital-level revisit data; hence, it was not able to determine if hospitals with greater reductions in readmission rates had greater increases in observation or ED visits, as one might predict. Despite these limitations, the rigor of the study was noteworthy. The authors used matching techniques to ensure that the populations examined in the two time periods were comparable. Unlike previous research,3,4 they also used a comprehensive definition of a hospital “revisit” (including both observation and ED visits) and measured “revisit” rates across several payer types, rather than focusing exclusively on those covered by fee for service Medicare, as in past studies.4,5
What the study by Nuckols and colleagues suggests is that even though patients may be readmitted less, they may be coming back to the ED or getting admitted to the observation unit more, resulting in overall “revisit” rates that are marginally lower for Medicare patients, but often the same or even higher for other payer groups, particularly disadvantaged payer groups who are uninsured or insured by Medicaid.2 Although the authors do not assert causality for these trends, it is worth noting that the much-discussed Hospital Readmission Reduction Program (or “readmission penalty”) applies only to Medicare patients aged more than 65 years. It is likely that this program influenced the differences identified between payer groups in this article.
Beyond the policy implications of these findings, the experience of patients cared for in these different settings is of paramount importance. Unfortunately, there are limited data comparing patient perceptions, preferences, or outcomes resulting from readmission to an inpatient service versus an observation unit or ED visit within 30 days of discharge. However, there is reason to believe that costs could be higher for some patients treated in the ED or an observation unit as compared to those in the inpatient setting,6 and that care continuity and quality may be different across these settings. In a recent white paper on observation care published by the Society of Hospital Medicine (SHM) Public Policy Committee,7 the SHM reported the results of a 2017 survey of its members about observation care. The results were concerning. An overwhelming majority of respondents (87%) believed that the rules for observation are unclear for patients, and 68% of respondents believed that policy changes mandating informing patients of their observation status have created conflict between the provider and the patient.7 As shared by one respondent, “the observation issue can severely damage the therapeutic bond with patient/family, who may conclude that the hospitalist has more interest in saving someone money at the expense of patient care.”7 Thus, there is significant concern about the nature of observation stays and the experience for patients and providers. We should take care to better understand these experiences given that readmission reduction efforts may funnel more patients into observation care.
As a next step, we recommend further examination of how “revisit” rates have changed over time for patients with any discharge diagnosis, and not just those with pneumonia, AMI, or HF.8 Such examinations should be stratified by payer to identify differential impacts on those with lower socioeconomic status. Analyses should also examine changes in “revisit” types at the hospital level to better understand if hospitals with reductions in readmission rates are simply shifting revisits to the observation unit or ED. It is possible that inpatient readmissions for any given hospital are decreasing without concomitant increases in observation visits, as there are forces independent of the readmission penalty, such as the Recovery Audit Contractor program, that are driving hospitals to more frequently code patients as observation visits rather than inpatient admissions.9 Thus, readmissions could decrease and observation unit visits could increase independent of one another. We also recommend further research to examine differences in care quality, clinical outcomes, and costs for those readmitted to the hospital within 30 days of discharge versus those cared for in observation units or the ED. The challenge of such studies will be to identify and examine comparable populations of patients across these three settings. Examining patient perceptions and preferences across these settings is also critical. Finally, when assessing interventions to reduce inpatient readmissions, we need to consider “revisits” as a whole, not simply readmissions.10 Otherwise, we may simply be promoting the use of interventions that shift inpatient readmissions to observation unit or ED revisits, and there is little that is patient-centered or high value about that.9
Disclosures
The authors have nothing to disclose.
1. Smith M, Saunders R, Stuckhardt L, McGinnis JM, eds. Best care at lower cost: the path to continuously learning health care in America. Washington, DC: National Academies Press; 2013. PubMed
2. Nuckols TK, Fingar KR, Barrett ML, et al. Returns to emergency department, observation, or inpatient care within 30 days after hospitalization in 4 states, 2009 and 2010 versus 2013 and 2014. J Hosp Med. 2018;13(5):296-303. PubMed
3. Fingar KR, Washington R. Trends in Hospital Readmissions for Four High-Volume Conditions, 2009–2013. Statistical Brief No. 196. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb196-Readmissions-Trends-High-Volume-Conditions.pdf. Accessed March 5, 2018.
4. Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374(16):1543-1551. DOI: 10.1056/NEJMsa1513024. PubMed
5. Gerhardt G, Yemane A, Apostle K, Oelschlaeger A, Rollins E, Brennan N. Evaluating whether changes in utilization of hospital outpatient services contributed to lower Medicare readmission rate. Medicare Medicaid Res Rev. 2014;4(1). DOI: 10.5600/mmrr2014-004-01-b03 PubMed
6. Kangovi S, Cafardi SG, Smith RA, Kulkarni R, Grande D. Patient financial responsibility for observation care. J Hosp Med. 2015;10(11):718-723. DOI: 10.1002/jhm.2436. PubMed
7. The Hospital Observation Care Problem: Perspectives and Solutions from the Society of Hospital Medicine. Society of Hospital Medicine Public Policy Committee. https://www.hospitalmedicine.org/globalassets/policy-and-advocacy/advocacy-pdf/shms-observation-white-paper-2017. Accessed February 12, 2018.
8. Rosen AK, Chen Q, Shwartz M, et al. Does use of a hospital-wide readmission measure versus condition-specific readmission measures make a difference for hospital profiling and payment penalties? Medical Care. 2016;54(2):155-161. DOI: 10.1097/MLR.0000000000000455. PubMed
9. Baugh CW, Schuur JD. Observation care-high-value care or a cost-shifting loophole? N Engl J Med. 2013;369(4):302-305. DOI: 10.1056/NEJMp1304493. PubMed
10. Cassel CK, Conway PH, Delbanco SF, Jha AK, Saunders RS, Lee TH. Getting more performance from performance measurement. N Engl J Med. 2014;371(23):2145-2147. DOI: 10.1056/NEJMp1408345. PubMed
There is little doubt that preventing 30-day readmissions to the hospital results in lower costs for payers. However, reducing costs alone does not make this metric a measure of “high value” care.1 Rather, it is the improvement in the effectiveness of the discharge process that occurs alongside lower costs that makes readmission reduction efforts “high value” – or a “win-win” for patients and payers.
However, the article by Nuckols and colleagues in this month’s issue of the Journal of Hospital Medicine (JHM) suggests that it might not be that simple and adds nuance to the ongoing discussion about the 30-day readmission metric.2 The study used data collected by the federal government to examine changes not only in 30-day readmission rates between 2009-2010 and 2013-2014 but also changes in emergency department (ED) and observation unit visits. What they found is important. In general, despite reductions in 30-day readmissions for patients served by Medicare and private insurance, there were increases in observation unit and ED visits across all payer types (including Medicare and private insurance). These increases in observation unit and ED visits resulted in statistically higher overall “revisit” rates for the uninsured and those insured by Medicaid and offset any improvements in the “revisit” rates resulting from reductions in 30-day readmissions for those with private insurance. Those insured by Medicare—representing about 300,000 of the 420,000 visits analyzed—still had a statistically lower “revisit” rate, but it was only marginally lower (25.0% in 2013-2014 versus 25.3% in 2009-2010).2
The generalizability of the Nuckols’ study was limited in that it examined only index admissions for acute myocardial infarction (AMI), heart failure (HF), and pneumonia and used data from only Georgia, Nebraska, South Carolina, and Tennessee—the four states where observation and ED visit data were available in the federal database.2 The study also did not examine hospital-level revisit data; hence, it was not able to determine if hospitals with greater reductions in readmission rates had greater increases in observation or ED visits, as one might predict. Despite these limitations, the rigor of the study was noteworthy. The authors used matching techniques to ensure that the populations examined in the two time periods were comparable. Unlike previous research,3,4 they also used a comprehensive definition of a hospital “revisit” (including both observation and ED visits) and measured “revisit” rates across several payer types, rather than focusing exclusively on those covered by fee for service Medicare, as in past studies.4,5
What the study by Nuckols and colleagues suggests is that even though patients may be readmitted less, they may be coming back to the ED or getting admitted to the observation unit more, resulting in overall “revisit” rates that are marginally lower for Medicare patients, but often the same or even higher for other payer groups, particularly disadvantaged payer groups who are uninsured or insured by Medicaid.2 Although the authors do not assert causality for these trends, it is worth noting that the much-discussed Hospital Readmission Reduction Program (or “readmission penalty”) applies only to Medicare patients aged more than 65 years. It is likely that this program influenced the differences identified between payer groups in this article.
Beyond the policy implications of these findings, the experience of patients cared for in these different settings is of paramount importance. Unfortunately, there are limited data comparing patient perceptions, preferences, or outcomes resulting from readmission to an inpatient service versus an observation unit or ED visit within 30 days of discharge. However, there is reason to believe that costs could be higher for some patients treated in the ED or an observation unit as compared to those in the inpatient setting,6 and that care continuity and quality may be different across these settings. In a recent white paper on observation care published by the Society of Hospital Medicine (SHM) Public Policy Committee,7 the SHM reported the results of a 2017 survey of its members about observation care. The results were concerning. An overwhelming majority of respondents (87%) believed that the rules for observation are unclear for patients, and 68% of respondents believed that policy changes mandating informing patients of their observation status have created conflict between the provider and the patient.7 As shared by one respondent, “the observation issue can severely damage the therapeutic bond with patient/family, who may conclude that the hospitalist has more interest in saving someone money at the expense of patient care.”7 Thus, there is significant concern about the nature of observation stays and the experience for patients and providers. We should take care to better understand these experiences given that readmission reduction efforts may funnel more patients into observation care.
As a next step, we recommend further examination of how “revisit” rates have changed over time for patients with any discharge diagnosis, and not just those with pneumonia, AMI, or HF.8 Such examinations should be stratified by payer to identify differential impacts on those with lower socioeconomic status. Analyses should also examine changes in “revisit” types at the hospital level to better understand if hospitals with reductions in readmission rates are simply shifting revisits to the observation unit or ED. It is possible that inpatient readmissions for any given hospital are decreasing without concomitant increases in observation visits, as there are forces independent of the readmission penalty, such as the Recovery Audit Contractor program, that are driving hospitals to more frequently code patients as observation visits rather than inpatient admissions.9 Thus, readmissions could decrease and observation unit visits could increase independent of one another. We also recommend further research to examine differences in care quality, clinical outcomes, and costs for those readmitted to the hospital within 30 days of discharge versus those cared for in observation units or the ED. The challenge of such studies will be to identify and examine comparable populations of patients across these three settings. Examining patient perceptions and preferences across these settings is also critical. Finally, when assessing interventions to reduce inpatient readmissions, we need to consider “revisits” as a whole, not simply readmissions.10 Otherwise, we may simply be promoting the use of interventions that shift inpatient readmissions to observation unit or ED revisits, and there is little that is patient-centered or high value about that.9
Disclosures
The authors have nothing to disclose.
There is little doubt that preventing 30-day readmissions to the hospital results in lower costs for payers. However, reducing costs alone does not make this metric a measure of “high value” care.1 Rather, it is the improvement in the effectiveness of the discharge process that occurs alongside lower costs that makes readmission reduction efforts “high value” – or a “win-win” for patients and payers.
However, the article by Nuckols and colleagues in this month’s issue of the Journal of Hospital Medicine (JHM) suggests that it might not be that simple and adds nuance to the ongoing discussion about the 30-day readmission metric.2 The study used data collected by the federal government to examine changes not only in 30-day readmission rates between 2009-2010 and 2013-2014 but also changes in emergency department (ED) and observation unit visits. What they found is important. In general, despite reductions in 30-day readmissions for patients served by Medicare and private insurance, there were increases in observation unit and ED visits across all payer types (including Medicare and private insurance). These increases in observation unit and ED visits resulted in statistically higher overall “revisit” rates for the uninsured and those insured by Medicaid and offset any improvements in the “revisit” rates resulting from reductions in 30-day readmissions for those with private insurance. Those insured by Medicare—representing about 300,000 of the 420,000 visits analyzed—still had a statistically lower “revisit” rate, but it was only marginally lower (25.0% in 2013-2014 versus 25.3% in 2009-2010).2
The generalizability of the Nuckols’ study was limited in that it examined only index admissions for acute myocardial infarction (AMI), heart failure (HF), and pneumonia and used data from only Georgia, Nebraska, South Carolina, and Tennessee—the four states where observation and ED visit data were available in the federal database.2 The study also did not examine hospital-level revisit data; hence, it was not able to determine if hospitals with greater reductions in readmission rates had greater increases in observation or ED visits, as one might predict. Despite these limitations, the rigor of the study was noteworthy. The authors used matching techniques to ensure that the populations examined in the two time periods were comparable. Unlike previous research,3,4 they also used a comprehensive definition of a hospital “revisit” (including both observation and ED visits) and measured “revisit” rates across several payer types, rather than focusing exclusively on those covered by fee for service Medicare, as in past studies.4,5
What the study by Nuckols and colleagues suggests is that even though patients may be readmitted less, they may be coming back to the ED or getting admitted to the observation unit more, resulting in overall “revisit” rates that are marginally lower for Medicare patients, but often the same or even higher for other payer groups, particularly disadvantaged payer groups who are uninsured or insured by Medicaid.2 Although the authors do not assert causality for these trends, it is worth noting that the much-discussed Hospital Readmission Reduction Program (or “readmission penalty”) applies only to Medicare patients aged more than 65 years. It is likely that this program influenced the differences identified between payer groups in this article.
Beyond the policy implications of these findings, the experience of patients cared for in these different settings is of paramount importance. Unfortunately, there are limited data comparing patient perceptions, preferences, or outcomes resulting from readmission to an inpatient service versus an observation unit or ED visit within 30 days of discharge. However, there is reason to believe that costs could be higher for some patients treated in the ED or an observation unit as compared to those in the inpatient setting,6 and that care continuity and quality may be different across these settings. In a recent white paper on observation care published by the Society of Hospital Medicine (SHM) Public Policy Committee,7 the SHM reported the results of a 2017 survey of its members about observation care. The results were concerning. An overwhelming majority of respondents (87%) believed that the rules for observation are unclear for patients, and 68% of respondents believed that policy changes mandating informing patients of their observation status have created conflict between the provider and the patient.7 As shared by one respondent, “the observation issue can severely damage the therapeutic bond with patient/family, who may conclude that the hospitalist has more interest in saving someone money at the expense of patient care.”7 Thus, there is significant concern about the nature of observation stays and the experience for patients and providers. We should take care to better understand these experiences given that readmission reduction efforts may funnel more patients into observation care.
As a next step, we recommend further examination of how “revisit” rates have changed over time for patients with any discharge diagnosis, and not just those with pneumonia, AMI, or HF.8 Such examinations should be stratified by payer to identify differential impacts on those with lower socioeconomic status. Analyses should also examine changes in “revisit” types at the hospital level to better understand if hospitals with reductions in readmission rates are simply shifting revisits to the observation unit or ED. It is possible that inpatient readmissions for any given hospital are decreasing without concomitant increases in observation visits, as there are forces independent of the readmission penalty, such as the Recovery Audit Contractor program, that are driving hospitals to more frequently code patients as observation visits rather than inpatient admissions.9 Thus, readmissions could decrease and observation unit visits could increase independent of one another. We also recommend further research to examine differences in care quality, clinical outcomes, and costs for those readmitted to the hospital within 30 days of discharge versus those cared for in observation units or the ED. The challenge of such studies will be to identify and examine comparable populations of patients across these three settings. Examining patient perceptions and preferences across these settings is also critical. Finally, when assessing interventions to reduce inpatient readmissions, we need to consider “revisits” as a whole, not simply readmissions.10 Otherwise, we may simply be promoting the use of interventions that shift inpatient readmissions to observation unit or ED revisits, and there is little that is patient-centered or high value about that.9
Disclosures
The authors have nothing to disclose.
1. Smith M, Saunders R, Stuckhardt L, McGinnis JM, eds. Best care at lower cost: the path to continuously learning health care in America. Washington, DC: National Academies Press; 2013. PubMed
2. Nuckols TK, Fingar KR, Barrett ML, et al. Returns to emergency department, observation, or inpatient care within 30 days after hospitalization in 4 states, 2009 and 2010 versus 2013 and 2014. J Hosp Med. 2018;13(5):296-303. PubMed
3. Fingar KR, Washington R. Trends in Hospital Readmissions for Four High-Volume Conditions, 2009–2013. Statistical Brief No. 196. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb196-Readmissions-Trends-High-Volume-Conditions.pdf. Accessed March 5, 2018.
4. Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374(16):1543-1551. DOI: 10.1056/NEJMsa1513024. PubMed
5. Gerhardt G, Yemane A, Apostle K, Oelschlaeger A, Rollins E, Brennan N. Evaluating whether changes in utilization of hospital outpatient services contributed to lower Medicare readmission rate. Medicare Medicaid Res Rev. 2014;4(1). DOI: 10.5600/mmrr2014-004-01-b03 PubMed
6. Kangovi S, Cafardi SG, Smith RA, Kulkarni R, Grande D. Patient financial responsibility for observation care. J Hosp Med. 2015;10(11):718-723. DOI: 10.1002/jhm.2436. PubMed
7. The Hospital Observation Care Problem: Perspectives and Solutions from the Society of Hospital Medicine. Society of Hospital Medicine Public Policy Committee. https://www.hospitalmedicine.org/globalassets/policy-and-advocacy/advocacy-pdf/shms-observation-white-paper-2017. Accessed February 12, 2018.
8. Rosen AK, Chen Q, Shwartz M, et al. Does use of a hospital-wide readmission measure versus condition-specific readmission measures make a difference for hospital profiling and payment penalties? Medical Care. 2016;54(2):155-161. DOI: 10.1097/MLR.0000000000000455. PubMed
9. Baugh CW, Schuur JD. Observation care-high-value care or a cost-shifting loophole? N Engl J Med. 2013;369(4):302-305. DOI: 10.1056/NEJMp1304493. PubMed
10. Cassel CK, Conway PH, Delbanco SF, Jha AK, Saunders RS, Lee TH. Getting more performance from performance measurement. N Engl J Med. 2014;371(23):2145-2147. DOI: 10.1056/NEJMp1408345. PubMed
1. Smith M, Saunders R, Stuckhardt L, McGinnis JM, eds. Best care at lower cost: the path to continuously learning health care in America. Washington, DC: National Academies Press; 2013. PubMed
2. Nuckols TK, Fingar KR, Barrett ML, et al. Returns to emergency department, observation, or inpatient care within 30 days after hospitalization in 4 states, 2009 and 2010 versus 2013 and 2014. J Hosp Med. 2018;13(5):296-303. PubMed
3. Fingar KR, Washington R. Trends in Hospital Readmissions for Four High-Volume Conditions, 2009–2013. Statistical Brief No. 196. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb196-Readmissions-Trends-High-Volume-Conditions.pdf. Accessed March 5, 2018.
4. Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374(16):1543-1551. DOI: 10.1056/NEJMsa1513024. PubMed
5. Gerhardt G, Yemane A, Apostle K, Oelschlaeger A, Rollins E, Brennan N. Evaluating whether changes in utilization of hospital outpatient services contributed to lower Medicare readmission rate. Medicare Medicaid Res Rev. 2014;4(1). DOI: 10.5600/mmrr2014-004-01-b03 PubMed
6. Kangovi S, Cafardi SG, Smith RA, Kulkarni R, Grande D. Patient financial responsibility for observation care. J Hosp Med. 2015;10(11):718-723. DOI: 10.1002/jhm.2436. PubMed
7. The Hospital Observation Care Problem: Perspectives and Solutions from the Society of Hospital Medicine. Society of Hospital Medicine Public Policy Committee. https://www.hospitalmedicine.org/globalassets/policy-and-advocacy/advocacy-pdf/shms-observation-white-paper-2017. Accessed February 12, 2018.
8. Rosen AK, Chen Q, Shwartz M, et al. Does use of a hospital-wide readmission measure versus condition-specific readmission measures make a difference for hospital profiling and payment penalties? Medical Care. 2016;54(2):155-161. DOI: 10.1097/MLR.0000000000000455. PubMed
9. Baugh CW, Schuur JD. Observation care-high-value care or a cost-shifting loophole? N Engl J Med. 2013;369(4):302-305. DOI: 10.1056/NEJMp1304493. PubMed
10. Cassel CK, Conway PH, Delbanco SF, Jha AK, Saunders RS, Lee TH. Getting more performance from performance measurement. N Engl J Med. 2014;371(23):2145-2147. DOI: 10.1056/NEJMp1408345. PubMed
© 2018 Society of Hospital Medicine