User login
Schizoaffective disorder: A challenging diagnosis
Mr. C, age 34, presented to the emergency department with his wife because of increasingly bizarre behavior. He reported auditory and visual hallucinations, and believed that the “mob had ordered a hit” against him. He had threatened to shoot his wife and children, which led to his arrest and being briefly jailed. In jail, he was agitated, defecated on the floor, and disrobed. His wife reported that Mr. C had a long history of bipolar disorder and had experienced his first manic episode and hospitalization at age 17. Since then, he had been treated with many different antidepressants, antipsychotics, and mood stabilizers.
Mr. C was admitted to the hospital, where he developed a catatonic syndrome that was treated with a course of electroconvulsive therapy. He was eventually stabilized with
Over the next 8 years, Mr. C was often noncompliant with medication and frequently was hospitalized for mania. His symptoms included poor sleep, grandiosity, pressured speech, racing and disorganized thoughts, increased risk-taking behavior (ie, driving at excessive speeds), and hyperreligiosity (ie, speaking with God). Mr. C also occasionally used methamphetamine, cannabis, and cocaine. Although he had responded well to treatment early in the course of his illness, as he entered his late 30s, his response was less complete, and by his 40s, Mr. C was no longer able to function independently. He eventually was prescribed a long-acting injectable antipsychotic, paliperidone palmitate, 156 mg monthly. Eventually, his family was no longer able to care for him at home, so he was admitted to a residential care facility.
In this facility, based on the long-standing nature of Mr. C’s psychotic disorder and frequency with which he presented with mania, his clinicians changed his diagnosis to schizoaffective disorder, bipolar type. It had become clear that mood symptoms comprised >50% of the total duration of his illness.
Schizoaffective disorder (SAD) often has been used as a diagnosis for patients who have an admixture of mood and psychotic symptoms whose diagnosis is uncertain. Its hallmark is the presence of symptoms of a major mood episode (either a depressive or manic episode) concurrent with symptoms characteristic of schizophrenia, such as delusions, hallucinations, or disorganized speech.1
SAD is a controversial diagnosis. There has been inadequate research regarding the epidemiology, course, etiologic factors, and treatment of this disorder. Debate continues to swirl around its conceptualization; some experts view SAD as an independent disorder, while others see SAD as either a form of schizophrenia or a mood disorder.1 In this review, we describe the classification of SAD and its features, diagnosis, and treatment.
An evolving diagnosis
The term schizoaffective was first used by Jacob Kasanin, MD, in 1933.2 He described 9 patients with “acute schizoaffective psychoses,” each of whom had an abrupt onset. The term was used in the first edition of the DSM as a subtype of schizophrenia.3 In DSM-I, the “schizo-affective type” was defined as a diagnosis for patients with a “significant admixture of schizophrenic and affective reactions.”3 Diagnostic criteria for SAD were developed for DSM-III-R, published in 1987.4 These criteria continued to evolve with subsequent editions of the DSM.
Continue to: DSM-5 provides...
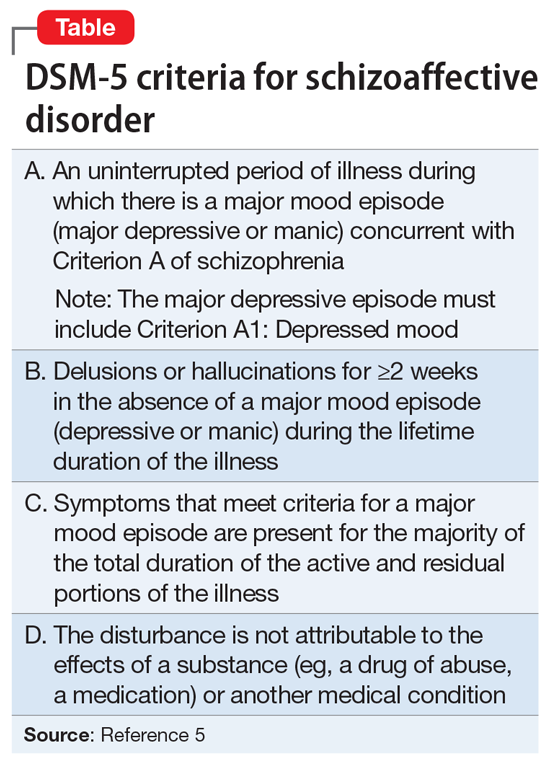
DSM-5 provides a clearer separation between schizophrenia with mood symptoms, bipolar disorder, and SAD (Table5). In addition, DSM-5 shifts away from the DSM-IV diagnosis of SAD as an episode, and instead focuses more on the longitudinal course of the illness. It has been suggested that this change will likely lead to reduced rates of diagnosis of SAD.6 Despite improvements in classification, the diagnosis remains controversial (Box7-11).
Box 1
Despite improvements in classification, controversy continues to swirl around the question of whether schizoaffective disorder (SAD) represents an independent disorder that stands apart from schizophrenia and bipolar disorder, whether it is a form of schizophrenia, or whether it is a form of bipolar disorder or a depressive disorder.7,8 Other possibilities are that SAD is heterogeneous or that it represents a middle point on a spectrum that bridges mood and psychotic disorders. While the merits of each possibility are beyond the scope of this review, it is safe to say that each possibility has its proponents. For these reasons, some argue that the concept itself lacks validity and shows the pitfalls of our classification system.7
Poor diagnostic reliability is one reason for concerns about validity. Most recently, a field trial using DSM-5 criteria produced a kappa of 0.50, which is moderate,9 but earlier definitions produced relatively poor results. Wilson et al10 point out that Criterion C, which concerns duration of mood symptoms, produces a particularly low kappa. Another reason is diagnostic switching, whereby patients initially diagnosed with 1 disorder receive a different diagnosis at followup. Diagnostic switching is especially problematic for SAD. In a large meta-analysis by Santelmann et al,11 36% of patients initially diagnosed with SAD had their diagnosis changed when reassessed. This diagnostic shift tended more toward schizophrenia than bipolar disorder. In addition, more than one-half of all patients initially diagnosed with schizophrenia, bipolar disorder, or major depressive disorder were re-diagnosed with SAD when reassessed.
DSM-5 subtypes and specifiers
In DSM-5,SAD has 2 subtypes5:
- Bipolar type. The bipolar type is marked by the presence of a manic episode (major depressive episodes may also occur)
- Depressive type. The depressive type is marked by the presence of only major depressive episodes.
SAD also includes several specifiers, with the express purpose of giving clinicians greater descriptive ability. The course of SAD can be described as either “first episode,” defined as the first manifestation of the disorder, or as having “multiple episodes,” defined as a minimum of 2 episodes with 1 relapse. In addition, SAD can be described as an acute episode, in partial remission, or in full remission. The course can be described as “continuous” if it is clear that symptoms have been present for the majority of the illness with very brief subthreshold periods. The course is designated as “unspecified” when information is unavailable or lacking. The 5-point Clinician-Rated Dimensions of Psychosis Symptoms was introduced to enable clinicians to make a quantitative assessment of the psychotic symptoms, although its use is not required.
Epidemiology and gender ratio
The epidemiology of SAD has not been well studied. DSM-5 estimates that SAD is approximately one-third as common as schizophrenia, which has a lifetime prevalence of 0.5% to 0.8%.5 This is similar to an estimate by Perälä et al12 of a 0.32% lifetime prevalence based on a nationally representative sample of persons in Finland age ≥30. Scully et al13 calculated a prevalence estimate of 1.1% in a representative sample of adults in rural Ireland. Based on pooled clinical data, Keck et al14 estimated the prevalence in clinical settings at 16%, similar to the figure of 19% reported by Levinson et al15 based on data from New York State psychiatric hospitals. In clinical practice, the diagnosis of SAD is used frequently when there is diagnostic uncertainty, which potentially inflates estimates of lifetime prevalence.
The prevalence of SAD is higher in women than men, with a sex ratio of about 2:1, similar to that seen in mood disorders.13,16-19 There are an equal number of men and women with the bipolar subtype, but a female preponderance with the depressive subtype.5 The bipolar subtype is more common in younger patients, while the depressive subtype is more common in older patients. SAD is a rare diagnosis in children.20
Continue to: Course and outcome
Course and outcome
The onset of SAD typically occurs in early adulthood, but can range from childhood to senescence. Approximately one-third of patients are diagnosed before age 25, one-third between age 25 and 35, and one-third after age 35.21-23 Based on a literature review, Cheniaux et al7 concluded that that age at onset for patients with SAD is between those with schizophrenia and those with mood disorders.
The course of SAD is variable but represents a middle ground between that of schizophrenia and the mood disorders. In a 4- to 5-year follow-up,24 patients with SAD had a better overall course than patients with schizophrenia but had poorer functioning than those with bipolar mania, and much poorer than those with unipolar depression. Mood-incongruent psychotic features predict a particularly worse outcome. These findings were reaffirmed at a 10-year follow-up.25 Mood symptoms portend a better outcome than do symptoms of schizophrenia.
The lifetime suicide risk for patients with SAD is estimated at 5%, with a higher risk associated with the presence of depressive symptoms.26 One study found that women with SAD had a 17.5-year reduced life expectancy (64.1 years) compared with a reduction of 8.0 years for men (69.4 years).27
Comorbidity
Patients with SAD are commonly diagnosed with other psychiatric disorders, including anxiety disorders, obsessive-compulsive disorder, posttraumatic stress disorder, and substance use disorders.21,28,29 When compared with the general population, patients with SAD are at higher risk for coronary heart disease, stroke, obesity, and smoking, likely contributing to their decreased life expectancy.27,30 Because second-generation antipsychotics (SGAs) are often used to treat SAD, patients with SAD are at risk for metabolic syndrome and diabetes mellitus.30
Clinical assessment
Because there are no diagnostic, laboratory, or neuroimaging tests for SAD, the most important basis for making the diagnosis is the patient’s history, supplemented by collateral history from family members or friends, and medical records. Determining the percentage of time spent in a mood episode (DSM-5 Criterion C) is especially important.31 This requires the clinician to pay close attention to the temporal relationship of psychotic and mood symptoms.
Continue to: Differential diagnosis
Differential diagnosis
The differential diagnosis for SAD is broad because it includes all of the possibilities usually considered for major mood disorders and for psychotic disorders5:
- schizophrenia
- bipolar disorder with psychotic features
- major depressive disorder with psychotic features
- depressive or bipolar disorders with catatonic features
- personality disorders (especially the schizotypal, paranoid, and borderline types)
- major neurocognitive disorders in which there are mood and psychotic symptoms
- substance/medication-induced psychotic disorder
- disorders induced by medical conditions.
With schizophrenia, the duration of all episodes of a mood syndrome is brief (<50% of the total duration of the illness) relative to the duration of the psychotic symptoms. Although psychotic symptoms may occur in persons with mood disorders, they are generally not present in the absence of depression or mania, helping to set the boundary between SAD and psychotic mania or depression. As for personality disorders, the individual will not have a true psychosis, although some symptoms, such as feelings of unreality, paranoia, or magical thinking, may cause diagnostic confusion.
Medical conditions also can present with psychotic and mood symptoms and need to be ruled out. These include psychotic disorder due to another medical condition, and delirium. A thorough medical workup should be performed to rule out any possible medical causes for the symptoms.
Substance use should also be ruled out as the cause of the symptoms because many substances are associated with mood and psychotic symptoms. It is usually clear from the history, physical examination, or laboratory tests when a medication/illicit substance has initiated and maintained the disorder.
Neurologic conditions. If a neurologic condition is suspected, a neurologic evaluation may be warranted, including laboratory tests, brain imaging to identify specific anatomical abnormalities, lumbar puncture with cerebrospinal fluid analysis, and an electroencephalogram to rule out a convulsive disorder.
Continue to: Clinical symptoms
Clinical symptoms
The signs and symptoms of SAD include those typically seen in schizophrenia and the mood disorders. Thus, the patient may exhibit elated mood and/or grandiosity, or severe depression, combined with mood-incongruent psychotic features such as paranoid delusions. The symptoms may present together or in an alternating fashion, and psychotic symptoms may be mood-congruent or mood-incongruent. Mr. C’s case illustrates some of the symptoms of the disorder.
Brain imaging
Significant changes have been reported to occur in the brain structure and function in persons with SAD. Neuroimaging studies using voxel-based morphometry have shown significant reductions in gray matter volume in several areas of the brain, including the medial prefrontal cortex, insula, Rolandic operculum, parts of the temporal lobe, and the hippocampus.32-35 Amann et al32 found that patients with SAD and schizophrenia had widespread and overlapping areas of significant volume reduction, but patients with bipolar disorder did not. These studies suggest that at least from a neuroimaging standpoint, SAD is more closely related to schizophrenia than bipolar disorder, and could represent a variant of schizophrenia.
Treatment of SAD
The pharmacotherapy of SAD is mostly empirical because of the lack of randomized controlled trials. Clinicians have traditionally prescribed an antipsychotic agent along with either a mood stabilizer (eg,
Since that exhaustive review,
Patients with SAD will require maintenance treatment for ongoing symptom control. Medication that is effective for treatment of an acute episode should be considered for maintenance treatment. Both the extended-release and long-acting injectable (LAI) formulations of paliperidone have been shown to be efficacious in the maintenance treatment of patients with SAD.40 The LAI form of paliperidone significantly delayed psychotic, depressive, and manic relapses, improved clinical rating scale scores, and increased medication adherence.41,42 In an open-label study, olanzapine LAI was effective in long-term maintenance treatment, although approximately 40% of patients experienced significant weight gain.43 One concern with olanzapine is the possible occurrence of a post-injection delirium/sedation syndrome. For that reason, patients receiving olanzapine must be monitored for at least 3 hours post-injection. The paliperidone LAI does not require monitoring after injection.
Continue to: There is a single clinical trial...
There is a single clinical trial showing that patients with SAD can be successfully switched from other antipsychotics to
Other approaches
Electroconvulsive therapy (ECT) should be considered for patients with SAD who are acutely ill and have failed to respond adequately to medication. ECT is especially relevant in the setting of acute mood symptoms (ie, depressive or manic symptoms co-occurring with psychosis or in the absence of psychosis).45
As currently conceptualized, the diagnosis of SAD is made in persons having an admixture of mood and psychotic symptoms, although by definition mood symptoms must take up the majority (≥50%) of the total duration of the illness. Unfortunately, SAD has been inadequately researched due to the unreliability of its definition and concerns about its validity. The long-term course of SAD is midway between mood and psychotic disorders, and the disorder can cause significant disability.
Bottom Line
Schizoaffective disorder (SAD) is characterized by the presence of symptoms of a major mood episode (a depressive or manic episode) concurrent with symptoms of schizophrenia. The most important basis for establishing the diagnosis is the patient’s history. Determining the percentage of time spent in a mood episode is especially important. Treatment usually consists of an antipsychotic plus a mood stabilizer or antidepressant. Electroconvulsive therapy is an option for patients with SAD who do not respond well to medication.
Related Resources
- Wy TJP, Saadabadi A. Schizoaffective disorder. NCBI Bookshelf: StatPearls Publishing. Published January 2020. https://www.ncbi.nlm.nih.gov/books/NBK541012/. Updated April 15, 2020.
- Parker G. How well does the DSM-5 capture schizoaffective disorder? Can J Psychiatry. 2019;64(9):607-610.
Drug Brand Names
Aripiprazole • Abilify
Lithium • Eskalith, Lithobid
Lurasidone • Latuda
Olanzapine • Zyprexa
Olanzapine long-acting injectable • Zyprexa Relprevv
Paliperidone • Invega
Paliperidone palmitate • Invega sustenna
Valproate • Depacon
1. Miller JN, Black DW. Schizoaffective disorder: a review. Ann Clin Psychiatry. 2019;31(1):47-53.
2. Kasanin J. The acute schizoaffective psychoses. Am J Psychiatry. 1933;90:97-126.
3. Diagnostic and statistical manual of mental disorders, 1st ed. Washington, DC: American Psychiatric Association; 1952.
4. Diagnostic and statistical manual of mental disorders, 3rd ed, revision. Washington, DC: American Psychiatric Association; 1987.
5. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
6. Malaspina D, Owen M, Heckers S, et al. Schizoaffective disorder in the DSM-5. Schizophr Res. 2013;150:21-25.
7. Cheniaux E, Landeria-Fernandez J, Telles LL, et al. Does schizoaffective disorder really exist? A systematic review of the studies that compared schizoaffective disorder with schizophrenia or mood disorders. J Affect Disord. 2008;106:209-217.
8. Kantrowitz JT, Citrome L. Schizoaffective disorder: a review of current research themes and pharmacologic management. CNS Drugs. 2011;25:317-331.
9. Regier DA, Narrow WE, Clarke DE, et al. DSM-5 field trials in the United States and Canada, Part II: test-retest reliability of selected categorical diagnoses. Am J Psychiatry. 2013;170:59-70.
10. Wilson JE, Nian H, Heckers S. The schizoaffective disorder diagnosis: a conundrum in the clinical setting. Eur Arch Psychiatry Clin Neurosci. 2014;264:29-34.
11. Santelmann H, Franklin J, Bußhoff J, Baethge C. Test-retest reliability of schizoaffective disorder compared with schizophrenia, bipolar disorder, and unipolar depression--a systematic review and meta-analysis. Bipolar Disord. 2015;17:753-768.
12. Perälä J, Suvisaari J, Saarni SI, et al. Lifetime Prevalence of psychotic and bipolar I disorders in a general population. JAMA Psychiatry. 2007;64:19-28.
13. Scully PJ, Owens JM, Kinsella A, et al. Schizophrenia, schizoaffective and bipolar disorder within an epidemiologically complete, homogeneous population in rural Ireland: small area variation in rate. Schizophr Res. 2004;67:143-155.
14. Keck PE Jr, McElroy SE, Strakowski SM, et al. Pharmacologic treatment of schizoaffective disorder. Psychopharmacol. 1994;114:529-538.
15. Levinson DF, Umapathy C, Musthaq M. Treatment of schizoaffective disorder and schizophrenia with mood symptoms. Am J Psychiatry. 1999;156:1138-1148.
16. Angst J, Felder W, Lohmeyer B. Course of schizoaffective psychoses: results of a follow-up study. Schizophr Bull. 1980;6:579-585.
17. Lenz G, Simhandl C, Thau K, et al. Temporal stability of diagnostic criteria for functional psychoses. Psychopathol. 1991;24:328-335.
18. Malhi GS, Green M, Fagiolini A, et al. Schizoaffective disorder: diagnostic issues and future recommendations. Bipolar Disord. 2008;10:215-230.
19. Marneros A, Deister A, Rohde A. Psychopathological and social status of patients with affective, schizophrenic and schizoaffective disorders after long‐term course. Acta Psychiatr Scand. 1990;82:352-358.
20. Werry JS, McClellan JM, Chard L. Childhood and adolescent schizophrenic, bipolar, and schizoaffective disorders: a clinical and outcome study. J Am Acad Child Adolesc Psychiatry. 1991;30:457-465.
21. Abrams DJ, Rojas DC, Arciniegas DB. Is schizoaffective disorder a distinct categorical diagnosis? A critical review of the literature. Neuropsychiatr Dis Treat. 2008;4:1089-1109.
22. Bromet EJ, Kotov R, Fochtmann LJ, et al. Diagnostic shifts during the decade following first admission for psychosis. Am J Psychiatry. 2011;168:1186-1194.
23. Salvatore P, Baldessarini RJ, Tohen M, et al. The McLean-Harvard First Episode Project: two-year stability of DSM-IV diagnoses in 500 first-episode psychotic disorder patients. J Clin Psychiatry. 2009;70:458-466.
24. Grossman LS, Harrow M, Goldberg JF, et al. Outcome of schizoaffective disorder at two long term follow-ups: comparisons with outcome of schizophrenia and affective disorders. Am J Psychiatry. 1991;148:1359-1365.
25. Harrow M, Grossman L, Herbener E, et al. Ten-year outcome: patients with schizoaffective disorders, schizophrenia, affective disorders and mood-incongruent psychotic symptoms. Br J Psychiatry. 2000;177:421-426.
26. Hor K, Taylor M. Review: suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24:81-90.
27. Chang CK, Hayes RD, Perera G, et al. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS ONE. 2011;6:e19590.
28. Byerly M, Goodman W, Acholonu W, et al. Obsessive compulsive symptoms in schizophrenia: frequency and clinical features. Schizophr Res. 2005;76:309-316.
29. Strauss JL, Calhoun PS, Marx CE, et al. Comorbid posttraumatic stress disorder is associated with suicidality in male veterans with schizophrenia or schizoaffective disorder. Schizophr Res. 2006;84:165-169.
30. Fagiolini A, Goracci A. The effects of undertreated chronic medical illnesses in patients with severe mental disorders. J Clin Psychiatry. 2009;70:22-29.
31. Black DW, Grant JE. DSM-5 guidebook: the essential companion to the diagnostic and statistical manual of mental disorders, 5th edition. Washington, DC: American Psychiatric Publishing; 2014.
32. Amann BL, Canales-Rodríguez EJ, Madre M, et al. Brain structural changes in schizoaffective disorder compared to schizophrenia and bipolar disorder. Acta Psychiatr Scand. 2016;133:23-33.
33. Ivleva EI, Bidesi AS, Keshavan MS, et al. Gray matter volume as an intermediate phenotype for psychosis: Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP). Am J Psychiatry. 2013;170:1285-1296.
34. Ivleva EI, Bidesi AS, Thomas BP, et al. Brain gray matter phenotypes across the psychosis dimension. Psychiatry Res. 2012;204:13-24.
35. Radonic
36. Jäger M, Becker T, Weinmann S, et al. Treatment of schizoaffective disorder - a challenge for evidence-based psychiatry. Acta Psychiatr Scand. 2010;121:22-32.
37. Glick ID, Mankosli R, Eudicone JM, et al. The efficacy, safety, and tolerability of aripiprazole for the treatment of schizoaffective disorder: results from a pooled analysis of a sub-population of subjects from two randomized, double-blind, placebo controlled, pivotal trials. J Affect Disord. 2009;115:18-26.
38. Canuso CM, Lindenmayer JP, Kosik-Gonzalez C, et al. A randomized, double-blind, placebo controlled study of 2 dose ranges of paliperidone extended-release in the treatment of subjects with schizoaffective disorder. J Clin Psychiatry. 2010;71:587-598.
39. Canuso CM, Schooler NR, Carothers J, et al. Paliperidone extended-release in schizoaffective disorder: a randomized controlled trial comparing a flexible-dose with placebo in patients treated with and without antidepressants and/or mood stabilizers. J Clin Psychopharmacol. 2010;30:487-495.
40. Lindenmayer JP, Kaur A. Antipsychotic management of schizoaffective disorder: a review. Drugs. 2016;76:589-604.
41. Alphs L, Fu DJ, Turkoz I. Paliperidone for the treatment of schizoaffective disorder. Expert Opin Pharmacother. 2016;176:871-883.
42. Bossie CA, Turkoz I, Alphs L, et al. Paliperidone palmitate once-monthly treatment in recent onset and chronic illness patients with schizoaffective disorder. J Nerv Ment Dis. 2017;205:324-328.
43. McDonnell DP, Landry J, Detke HC. Long-term safety and efficacy of olanzapine long-acting injection in patients with schizophrenia or schizoaffective disorder: a 6-year, multinational, single-arm, open-label study. Int Clin Psychopharmacol. 2014;29:322-331.
44. McEvoy JP, Citrome L, Hernandez D, et al. Effectiveness of lurasidone in patients with schizophrenia or schizoaffective disorder switched from other antipsychotics: a randomized, 6-week, open-label study. J Clin Psychiatry. 2013;74:170-179.
45. Mankad MV, Beyer JL, Wiener RD, et al. Manual of electroconvulsive therapy. Washington, DC: American Psychiatric Publishing; 2010.
Mr. C, age 34, presented to the emergency department with his wife because of increasingly bizarre behavior. He reported auditory and visual hallucinations, and believed that the “mob had ordered a hit” against him. He had threatened to shoot his wife and children, which led to his arrest and being briefly jailed. In jail, he was agitated, defecated on the floor, and disrobed. His wife reported that Mr. C had a long history of bipolar disorder and had experienced his first manic episode and hospitalization at age 17. Since then, he had been treated with many different antidepressants, antipsychotics, and mood stabilizers.
Mr. C was admitted to the hospital, where he developed a catatonic syndrome that was treated with a course of electroconvulsive therapy. He was eventually stabilized with
Over the next 8 years, Mr. C was often noncompliant with medication and frequently was hospitalized for mania. His symptoms included poor sleep, grandiosity, pressured speech, racing and disorganized thoughts, increased risk-taking behavior (ie, driving at excessive speeds), and hyperreligiosity (ie, speaking with God). Mr. C also occasionally used methamphetamine, cannabis, and cocaine. Although he had responded well to treatment early in the course of his illness, as he entered his late 30s, his response was less complete, and by his 40s, Mr. C was no longer able to function independently. He eventually was prescribed a long-acting injectable antipsychotic, paliperidone palmitate, 156 mg monthly. Eventually, his family was no longer able to care for him at home, so he was admitted to a residential care facility.
In this facility, based on the long-standing nature of Mr. C’s psychotic disorder and frequency with which he presented with mania, his clinicians changed his diagnosis to schizoaffective disorder, bipolar type. It had become clear that mood symptoms comprised >50% of the total duration of his illness.
Schizoaffective disorder (SAD) often has been used as a diagnosis for patients who have an admixture of mood and psychotic symptoms whose diagnosis is uncertain. Its hallmark is the presence of symptoms of a major mood episode (either a depressive or manic episode) concurrent with symptoms characteristic of schizophrenia, such as delusions, hallucinations, or disorganized speech.1
SAD is a controversial diagnosis. There has been inadequate research regarding the epidemiology, course, etiologic factors, and treatment of this disorder. Debate continues to swirl around its conceptualization; some experts view SAD as an independent disorder, while others see SAD as either a form of schizophrenia or a mood disorder.1 In this review, we describe the classification of SAD and its features, diagnosis, and treatment.
An evolving diagnosis
The term schizoaffective was first used by Jacob Kasanin, MD, in 1933.2 He described 9 patients with “acute schizoaffective psychoses,” each of whom had an abrupt onset. The term was used in the first edition of the DSM as a subtype of schizophrenia.3 In DSM-I, the “schizo-affective type” was defined as a diagnosis for patients with a “significant admixture of schizophrenic and affective reactions.”3 Diagnostic criteria for SAD were developed for DSM-III-R, published in 1987.4 These criteria continued to evolve with subsequent editions of the DSM.
Continue to: DSM-5 provides...
DSM-5 provides a clearer separation between schizophrenia with mood symptoms, bipolar disorder, and SAD (Table5). In addition, DSM-5 shifts away from the DSM-IV diagnosis of SAD as an episode, and instead focuses more on the longitudinal course of the illness. It has been suggested that this change will likely lead to reduced rates of diagnosis of SAD.6 Despite improvements in classification, the diagnosis remains controversial (Box7-11).
Box 1
Despite improvements in classification, controversy continues to swirl around the question of whether schizoaffective disorder (SAD) represents an independent disorder that stands apart from schizophrenia and bipolar disorder, whether it is a form of schizophrenia, or whether it is a form of bipolar disorder or a depressive disorder.7,8 Other possibilities are that SAD is heterogeneous or that it represents a middle point on a spectrum that bridges mood and psychotic disorders. While the merits of each possibility are beyond the scope of this review, it is safe to say that each possibility has its proponents. For these reasons, some argue that the concept itself lacks validity and shows the pitfalls of our classification system.7
Poor diagnostic reliability is one reason for concerns about validity. Most recently, a field trial using DSM-5 criteria produced a kappa of 0.50, which is moderate,9 but earlier definitions produced relatively poor results. Wilson et al10 point out that Criterion C, which concerns duration of mood symptoms, produces a particularly low kappa. Another reason is diagnostic switching, whereby patients initially diagnosed with 1 disorder receive a different diagnosis at followup. Diagnostic switching is especially problematic for SAD. In a large meta-analysis by Santelmann et al,11 36% of patients initially diagnosed with SAD had their diagnosis changed when reassessed. This diagnostic shift tended more toward schizophrenia than bipolar disorder. In addition, more than one-half of all patients initially diagnosed with schizophrenia, bipolar disorder, or major depressive disorder were re-diagnosed with SAD when reassessed.
DSM-5 subtypes and specifiers
In DSM-5,SAD has 2 subtypes5:
- Bipolar type. The bipolar type is marked by the presence of a manic episode (major depressive episodes may also occur)
- Depressive type. The depressive type is marked by the presence of only major depressive episodes.
SAD also includes several specifiers, with the express purpose of giving clinicians greater descriptive ability. The course of SAD can be described as either “first episode,” defined as the first manifestation of the disorder, or as having “multiple episodes,” defined as a minimum of 2 episodes with 1 relapse. In addition, SAD can be described as an acute episode, in partial remission, or in full remission. The course can be described as “continuous” if it is clear that symptoms have been present for the majority of the illness with very brief subthreshold periods. The course is designated as “unspecified” when information is unavailable or lacking. The 5-point Clinician-Rated Dimensions of Psychosis Symptoms was introduced to enable clinicians to make a quantitative assessment of the psychotic symptoms, although its use is not required.
Epidemiology and gender ratio
The epidemiology of SAD has not been well studied. DSM-5 estimates that SAD is approximately one-third as common as schizophrenia, which has a lifetime prevalence of 0.5% to 0.8%.5 This is similar to an estimate by Perälä et al12 of a 0.32% lifetime prevalence based on a nationally representative sample of persons in Finland age ≥30. Scully et al13 calculated a prevalence estimate of 1.1% in a representative sample of adults in rural Ireland. Based on pooled clinical data, Keck et al14 estimated the prevalence in clinical settings at 16%, similar to the figure of 19% reported by Levinson et al15 based on data from New York State psychiatric hospitals. In clinical practice, the diagnosis of SAD is used frequently when there is diagnostic uncertainty, which potentially inflates estimates of lifetime prevalence.
The prevalence of SAD is higher in women than men, with a sex ratio of about 2:1, similar to that seen in mood disorders.13,16-19 There are an equal number of men and women with the bipolar subtype, but a female preponderance with the depressive subtype.5 The bipolar subtype is more common in younger patients, while the depressive subtype is more common in older patients. SAD is a rare diagnosis in children.20
Continue to: Course and outcome
Course and outcome
The onset of SAD typically occurs in early adulthood, but can range from childhood to senescence. Approximately one-third of patients are diagnosed before age 25, one-third between age 25 and 35, and one-third after age 35.21-23 Based on a literature review, Cheniaux et al7 concluded that that age at onset for patients with SAD is between those with schizophrenia and those with mood disorders.
The course of SAD is variable but represents a middle ground between that of schizophrenia and the mood disorders. In a 4- to 5-year follow-up,24 patients with SAD had a better overall course than patients with schizophrenia but had poorer functioning than those with bipolar mania, and much poorer than those with unipolar depression. Mood-incongruent psychotic features predict a particularly worse outcome. These findings were reaffirmed at a 10-year follow-up.25 Mood symptoms portend a better outcome than do symptoms of schizophrenia.
The lifetime suicide risk for patients with SAD is estimated at 5%, with a higher risk associated with the presence of depressive symptoms.26 One study found that women with SAD had a 17.5-year reduced life expectancy (64.1 years) compared with a reduction of 8.0 years for men (69.4 years).27
Comorbidity
Patients with SAD are commonly diagnosed with other psychiatric disorders, including anxiety disorders, obsessive-compulsive disorder, posttraumatic stress disorder, and substance use disorders.21,28,29 When compared with the general population, patients with SAD are at higher risk for coronary heart disease, stroke, obesity, and smoking, likely contributing to their decreased life expectancy.27,30 Because second-generation antipsychotics (SGAs) are often used to treat SAD, patients with SAD are at risk for metabolic syndrome and diabetes mellitus.30
Clinical assessment
Because there are no diagnostic, laboratory, or neuroimaging tests for SAD, the most important basis for making the diagnosis is the patient’s history, supplemented by collateral history from family members or friends, and medical records. Determining the percentage of time spent in a mood episode (DSM-5 Criterion C) is especially important.31 This requires the clinician to pay close attention to the temporal relationship of psychotic and mood symptoms.
Continue to: Differential diagnosis
Differential diagnosis
The differential diagnosis for SAD is broad because it includes all of the possibilities usually considered for major mood disorders and for psychotic disorders5:
- schizophrenia
- bipolar disorder with psychotic features
- major depressive disorder with psychotic features
- depressive or bipolar disorders with catatonic features
- personality disorders (especially the schizotypal, paranoid, and borderline types)
- major neurocognitive disorders in which there are mood and psychotic symptoms
- substance/medication-induced psychotic disorder
- disorders induced by medical conditions.
With schizophrenia, the duration of all episodes of a mood syndrome is brief (<50% of the total duration of the illness) relative to the duration of the psychotic symptoms. Although psychotic symptoms may occur in persons with mood disorders, they are generally not present in the absence of depression or mania, helping to set the boundary between SAD and psychotic mania or depression. As for personality disorders, the individual will not have a true psychosis, although some symptoms, such as feelings of unreality, paranoia, or magical thinking, may cause diagnostic confusion.
Medical conditions also can present with psychotic and mood symptoms and need to be ruled out. These include psychotic disorder due to another medical condition, and delirium. A thorough medical workup should be performed to rule out any possible medical causes for the symptoms.
Substance use should also be ruled out as the cause of the symptoms because many substances are associated with mood and psychotic symptoms. It is usually clear from the history, physical examination, or laboratory tests when a medication/illicit substance has initiated and maintained the disorder.
Neurologic conditions. If a neurologic condition is suspected, a neurologic evaluation may be warranted, including laboratory tests, brain imaging to identify specific anatomical abnormalities, lumbar puncture with cerebrospinal fluid analysis, and an electroencephalogram to rule out a convulsive disorder.
Continue to: Clinical symptoms
Clinical symptoms
The signs and symptoms of SAD include those typically seen in schizophrenia and the mood disorders. Thus, the patient may exhibit elated mood and/or grandiosity, or severe depression, combined with mood-incongruent psychotic features such as paranoid delusions. The symptoms may present together or in an alternating fashion, and psychotic symptoms may be mood-congruent or mood-incongruent. Mr. C’s case illustrates some of the symptoms of the disorder.
Brain imaging
Significant changes have been reported to occur in the brain structure and function in persons with SAD. Neuroimaging studies using voxel-based morphometry have shown significant reductions in gray matter volume in several areas of the brain, including the medial prefrontal cortex, insula, Rolandic operculum, parts of the temporal lobe, and the hippocampus.32-35 Amann et al32 found that patients with SAD and schizophrenia had widespread and overlapping areas of significant volume reduction, but patients with bipolar disorder did not. These studies suggest that at least from a neuroimaging standpoint, SAD is more closely related to schizophrenia than bipolar disorder, and could represent a variant of schizophrenia.
Treatment of SAD
The pharmacotherapy of SAD is mostly empirical because of the lack of randomized controlled trials. Clinicians have traditionally prescribed an antipsychotic agent along with either a mood stabilizer (eg,
Since that exhaustive review,
Patients with SAD will require maintenance treatment for ongoing symptom control. Medication that is effective for treatment of an acute episode should be considered for maintenance treatment. Both the extended-release and long-acting injectable (LAI) formulations of paliperidone have been shown to be efficacious in the maintenance treatment of patients with SAD.40 The LAI form of paliperidone significantly delayed psychotic, depressive, and manic relapses, improved clinical rating scale scores, and increased medication adherence.41,42 In an open-label study, olanzapine LAI was effective in long-term maintenance treatment, although approximately 40% of patients experienced significant weight gain.43 One concern with olanzapine is the possible occurrence of a post-injection delirium/sedation syndrome. For that reason, patients receiving olanzapine must be monitored for at least 3 hours post-injection. The paliperidone LAI does not require monitoring after injection.
Continue to: There is a single clinical trial...
There is a single clinical trial showing that patients with SAD can be successfully switched from other antipsychotics to
Other approaches
Electroconvulsive therapy (ECT) should be considered for patients with SAD who are acutely ill and have failed to respond adequately to medication. ECT is especially relevant in the setting of acute mood symptoms (ie, depressive or manic symptoms co-occurring with psychosis or in the absence of psychosis).45
As currently conceptualized, the diagnosis of SAD is made in persons having an admixture of mood and psychotic symptoms, although by definition mood symptoms must take up the majority (≥50%) of the total duration of the illness. Unfortunately, SAD has been inadequately researched due to the unreliability of its definition and concerns about its validity. The long-term course of SAD is midway between mood and psychotic disorders, and the disorder can cause significant disability.
Bottom Line
Schizoaffective disorder (SAD) is characterized by the presence of symptoms of a major mood episode (a depressive or manic episode) concurrent with symptoms of schizophrenia. The most important basis for establishing the diagnosis is the patient’s history. Determining the percentage of time spent in a mood episode is especially important. Treatment usually consists of an antipsychotic plus a mood stabilizer or antidepressant. Electroconvulsive therapy is an option for patients with SAD who do not respond well to medication.
Related Resources
- Wy TJP, Saadabadi A. Schizoaffective disorder. NCBI Bookshelf: StatPearls Publishing. Published January 2020. https://www.ncbi.nlm.nih.gov/books/NBK541012/. Updated April 15, 2020.
- Parker G. How well does the DSM-5 capture schizoaffective disorder? Can J Psychiatry. 2019;64(9):607-610.
Drug Brand Names
Aripiprazole • Abilify
Lithium • Eskalith, Lithobid
Lurasidone • Latuda
Olanzapine • Zyprexa
Olanzapine long-acting injectable • Zyprexa Relprevv
Paliperidone • Invega
Paliperidone palmitate • Invega sustenna
Valproate • Depacon
Mr. C, age 34, presented to the emergency department with his wife because of increasingly bizarre behavior. He reported auditory and visual hallucinations, and believed that the “mob had ordered a hit” against him. He had threatened to shoot his wife and children, which led to his arrest and being briefly jailed. In jail, he was agitated, defecated on the floor, and disrobed. His wife reported that Mr. C had a long history of bipolar disorder and had experienced his first manic episode and hospitalization at age 17. Since then, he had been treated with many different antidepressants, antipsychotics, and mood stabilizers.
Mr. C was admitted to the hospital, where he developed a catatonic syndrome that was treated with a course of electroconvulsive therapy. He was eventually stabilized with
Over the next 8 years, Mr. C was often noncompliant with medication and frequently was hospitalized for mania. His symptoms included poor sleep, grandiosity, pressured speech, racing and disorganized thoughts, increased risk-taking behavior (ie, driving at excessive speeds), and hyperreligiosity (ie, speaking with God). Mr. C also occasionally used methamphetamine, cannabis, and cocaine. Although he had responded well to treatment early in the course of his illness, as he entered his late 30s, his response was less complete, and by his 40s, Mr. C was no longer able to function independently. He eventually was prescribed a long-acting injectable antipsychotic, paliperidone palmitate, 156 mg monthly. Eventually, his family was no longer able to care for him at home, so he was admitted to a residential care facility.
In this facility, based on the long-standing nature of Mr. C’s psychotic disorder and frequency with which he presented with mania, his clinicians changed his diagnosis to schizoaffective disorder, bipolar type. It had become clear that mood symptoms comprised >50% of the total duration of his illness.
Schizoaffective disorder (SAD) often has been used as a diagnosis for patients who have an admixture of mood and psychotic symptoms whose diagnosis is uncertain. Its hallmark is the presence of symptoms of a major mood episode (either a depressive or manic episode) concurrent with symptoms characteristic of schizophrenia, such as delusions, hallucinations, or disorganized speech.1
SAD is a controversial diagnosis. There has been inadequate research regarding the epidemiology, course, etiologic factors, and treatment of this disorder. Debate continues to swirl around its conceptualization; some experts view SAD as an independent disorder, while others see SAD as either a form of schizophrenia or a mood disorder.1 In this review, we describe the classification of SAD and its features, diagnosis, and treatment.
An evolving diagnosis
The term schizoaffective was first used by Jacob Kasanin, MD, in 1933.2 He described 9 patients with “acute schizoaffective psychoses,” each of whom had an abrupt onset. The term was used in the first edition of the DSM as a subtype of schizophrenia.3 In DSM-I, the “schizo-affective type” was defined as a diagnosis for patients with a “significant admixture of schizophrenic and affective reactions.”3 Diagnostic criteria for SAD were developed for DSM-III-R, published in 1987.4 These criteria continued to evolve with subsequent editions of the DSM.
Continue to: DSM-5 provides...
DSM-5 provides a clearer separation between schizophrenia with mood symptoms, bipolar disorder, and SAD (Table5). In addition, DSM-5 shifts away from the DSM-IV diagnosis of SAD as an episode, and instead focuses more on the longitudinal course of the illness. It has been suggested that this change will likely lead to reduced rates of diagnosis of SAD.6 Despite improvements in classification, the diagnosis remains controversial (Box7-11).
Box 1
Despite improvements in classification, controversy continues to swirl around the question of whether schizoaffective disorder (SAD) represents an independent disorder that stands apart from schizophrenia and bipolar disorder, whether it is a form of schizophrenia, or whether it is a form of bipolar disorder or a depressive disorder.7,8 Other possibilities are that SAD is heterogeneous or that it represents a middle point on a spectrum that bridges mood and psychotic disorders. While the merits of each possibility are beyond the scope of this review, it is safe to say that each possibility has its proponents. For these reasons, some argue that the concept itself lacks validity and shows the pitfalls of our classification system.7
Poor diagnostic reliability is one reason for concerns about validity. Most recently, a field trial using DSM-5 criteria produced a kappa of 0.50, which is moderate,9 but earlier definitions produced relatively poor results. Wilson et al10 point out that Criterion C, which concerns duration of mood symptoms, produces a particularly low kappa. Another reason is diagnostic switching, whereby patients initially diagnosed with 1 disorder receive a different diagnosis at followup. Diagnostic switching is especially problematic for SAD. In a large meta-analysis by Santelmann et al,11 36% of patients initially diagnosed with SAD had their diagnosis changed when reassessed. This diagnostic shift tended more toward schizophrenia than bipolar disorder. In addition, more than one-half of all patients initially diagnosed with schizophrenia, bipolar disorder, or major depressive disorder were re-diagnosed with SAD when reassessed.
DSM-5 subtypes and specifiers
In DSM-5,SAD has 2 subtypes5:
- Bipolar type. The bipolar type is marked by the presence of a manic episode (major depressive episodes may also occur)
- Depressive type. The depressive type is marked by the presence of only major depressive episodes.
SAD also includes several specifiers, with the express purpose of giving clinicians greater descriptive ability. The course of SAD can be described as either “first episode,” defined as the first manifestation of the disorder, or as having “multiple episodes,” defined as a minimum of 2 episodes with 1 relapse. In addition, SAD can be described as an acute episode, in partial remission, or in full remission. The course can be described as “continuous” if it is clear that symptoms have been present for the majority of the illness with very brief subthreshold periods. The course is designated as “unspecified” when information is unavailable or lacking. The 5-point Clinician-Rated Dimensions of Psychosis Symptoms was introduced to enable clinicians to make a quantitative assessment of the psychotic symptoms, although its use is not required.
Epidemiology and gender ratio
The epidemiology of SAD has not been well studied. DSM-5 estimates that SAD is approximately one-third as common as schizophrenia, which has a lifetime prevalence of 0.5% to 0.8%.5 This is similar to an estimate by Perälä et al12 of a 0.32% lifetime prevalence based on a nationally representative sample of persons in Finland age ≥30. Scully et al13 calculated a prevalence estimate of 1.1% in a representative sample of adults in rural Ireland. Based on pooled clinical data, Keck et al14 estimated the prevalence in clinical settings at 16%, similar to the figure of 19% reported by Levinson et al15 based on data from New York State psychiatric hospitals. In clinical practice, the diagnosis of SAD is used frequently when there is diagnostic uncertainty, which potentially inflates estimates of lifetime prevalence.
The prevalence of SAD is higher in women than men, with a sex ratio of about 2:1, similar to that seen in mood disorders.13,16-19 There are an equal number of men and women with the bipolar subtype, but a female preponderance with the depressive subtype.5 The bipolar subtype is more common in younger patients, while the depressive subtype is more common in older patients. SAD is a rare diagnosis in children.20
Continue to: Course and outcome
Course and outcome
The onset of SAD typically occurs in early adulthood, but can range from childhood to senescence. Approximately one-third of patients are diagnosed before age 25, one-third between age 25 and 35, and one-third after age 35.21-23 Based on a literature review, Cheniaux et al7 concluded that that age at onset for patients with SAD is between those with schizophrenia and those with mood disorders.
The course of SAD is variable but represents a middle ground between that of schizophrenia and the mood disorders. In a 4- to 5-year follow-up,24 patients with SAD had a better overall course than patients with schizophrenia but had poorer functioning than those with bipolar mania, and much poorer than those with unipolar depression. Mood-incongruent psychotic features predict a particularly worse outcome. These findings were reaffirmed at a 10-year follow-up.25 Mood symptoms portend a better outcome than do symptoms of schizophrenia.
The lifetime suicide risk for patients with SAD is estimated at 5%, with a higher risk associated with the presence of depressive symptoms.26 One study found that women with SAD had a 17.5-year reduced life expectancy (64.1 years) compared with a reduction of 8.0 years for men (69.4 years).27
Comorbidity
Patients with SAD are commonly diagnosed with other psychiatric disorders, including anxiety disorders, obsessive-compulsive disorder, posttraumatic stress disorder, and substance use disorders.21,28,29 When compared with the general population, patients with SAD are at higher risk for coronary heart disease, stroke, obesity, and smoking, likely contributing to their decreased life expectancy.27,30 Because second-generation antipsychotics (SGAs) are often used to treat SAD, patients with SAD are at risk for metabolic syndrome and diabetes mellitus.30
Clinical assessment
Because there are no diagnostic, laboratory, or neuroimaging tests for SAD, the most important basis for making the diagnosis is the patient’s history, supplemented by collateral history from family members or friends, and medical records. Determining the percentage of time spent in a mood episode (DSM-5 Criterion C) is especially important.31 This requires the clinician to pay close attention to the temporal relationship of psychotic and mood symptoms.
Continue to: Differential diagnosis
Differential diagnosis
The differential diagnosis for SAD is broad because it includes all of the possibilities usually considered for major mood disorders and for psychotic disorders5:
- schizophrenia
- bipolar disorder with psychotic features
- major depressive disorder with psychotic features
- depressive or bipolar disorders with catatonic features
- personality disorders (especially the schizotypal, paranoid, and borderline types)
- major neurocognitive disorders in which there are mood and psychotic symptoms
- substance/medication-induced psychotic disorder
- disorders induced by medical conditions.
With schizophrenia, the duration of all episodes of a mood syndrome is brief (<50% of the total duration of the illness) relative to the duration of the psychotic symptoms. Although psychotic symptoms may occur in persons with mood disorders, they are generally not present in the absence of depression or mania, helping to set the boundary between SAD and psychotic mania or depression. As for personality disorders, the individual will not have a true psychosis, although some symptoms, such as feelings of unreality, paranoia, or magical thinking, may cause diagnostic confusion.
Medical conditions also can present with psychotic and mood symptoms and need to be ruled out. These include psychotic disorder due to another medical condition, and delirium. A thorough medical workup should be performed to rule out any possible medical causes for the symptoms.
Substance use should also be ruled out as the cause of the symptoms because many substances are associated with mood and psychotic symptoms. It is usually clear from the history, physical examination, or laboratory tests when a medication/illicit substance has initiated and maintained the disorder.
Neurologic conditions. If a neurologic condition is suspected, a neurologic evaluation may be warranted, including laboratory tests, brain imaging to identify specific anatomical abnormalities, lumbar puncture with cerebrospinal fluid analysis, and an electroencephalogram to rule out a convulsive disorder.
Continue to: Clinical symptoms
Clinical symptoms
The signs and symptoms of SAD include those typically seen in schizophrenia and the mood disorders. Thus, the patient may exhibit elated mood and/or grandiosity, or severe depression, combined with mood-incongruent psychotic features such as paranoid delusions. The symptoms may present together or in an alternating fashion, and psychotic symptoms may be mood-congruent or mood-incongruent. Mr. C’s case illustrates some of the symptoms of the disorder.
Brain imaging
Significant changes have been reported to occur in the brain structure and function in persons with SAD. Neuroimaging studies using voxel-based morphometry have shown significant reductions in gray matter volume in several areas of the brain, including the medial prefrontal cortex, insula, Rolandic operculum, parts of the temporal lobe, and the hippocampus.32-35 Amann et al32 found that patients with SAD and schizophrenia had widespread and overlapping areas of significant volume reduction, but patients with bipolar disorder did not. These studies suggest that at least from a neuroimaging standpoint, SAD is more closely related to schizophrenia than bipolar disorder, and could represent a variant of schizophrenia.
Treatment of SAD
The pharmacotherapy of SAD is mostly empirical because of the lack of randomized controlled trials. Clinicians have traditionally prescribed an antipsychotic agent along with either a mood stabilizer (eg,
Since that exhaustive review,
Patients with SAD will require maintenance treatment for ongoing symptom control. Medication that is effective for treatment of an acute episode should be considered for maintenance treatment. Both the extended-release and long-acting injectable (LAI) formulations of paliperidone have been shown to be efficacious in the maintenance treatment of patients with SAD.40 The LAI form of paliperidone significantly delayed psychotic, depressive, and manic relapses, improved clinical rating scale scores, and increased medication adherence.41,42 In an open-label study, olanzapine LAI was effective in long-term maintenance treatment, although approximately 40% of patients experienced significant weight gain.43 One concern with olanzapine is the possible occurrence of a post-injection delirium/sedation syndrome. For that reason, patients receiving olanzapine must be monitored for at least 3 hours post-injection. The paliperidone LAI does not require monitoring after injection.
Continue to: There is a single clinical trial...
There is a single clinical trial showing that patients with SAD can be successfully switched from other antipsychotics to
Other approaches
Electroconvulsive therapy (ECT) should be considered for patients with SAD who are acutely ill and have failed to respond adequately to medication. ECT is especially relevant in the setting of acute mood symptoms (ie, depressive or manic symptoms co-occurring with psychosis or in the absence of psychosis).45
As currently conceptualized, the diagnosis of SAD is made in persons having an admixture of mood and psychotic symptoms, although by definition mood symptoms must take up the majority (≥50%) of the total duration of the illness. Unfortunately, SAD has been inadequately researched due to the unreliability of its definition and concerns about its validity. The long-term course of SAD is midway between mood and psychotic disorders, and the disorder can cause significant disability.
Bottom Line
Schizoaffective disorder (SAD) is characterized by the presence of symptoms of a major mood episode (a depressive or manic episode) concurrent with symptoms of schizophrenia. The most important basis for establishing the diagnosis is the patient’s history. Determining the percentage of time spent in a mood episode is especially important. Treatment usually consists of an antipsychotic plus a mood stabilizer or antidepressant. Electroconvulsive therapy is an option for patients with SAD who do not respond well to medication.
Related Resources
- Wy TJP, Saadabadi A. Schizoaffective disorder. NCBI Bookshelf: StatPearls Publishing. Published January 2020. https://www.ncbi.nlm.nih.gov/books/NBK541012/. Updated April 15, 2020.
- Parker G. How well does the DSM-5 capture schizoaffective disorder? Can J Psychiatry. 2019;64(9):607-610.
Drug Brand Names
Aripiprazole • Abilify
Lithium • Eskalith, Lithobid
Lurasidone • Latuda
Olanzapine • Zyprexa
Olanzapine long-acting injectable • Zyprexa Relprevv
Paliperidone • Invega
Paliperidone palmitate • Invega sustenna
Valproate • Depacon
1. Miller JN, Black DW. Schizoaffective disorder: a review. Ann Clin Psychiatry. 2019;31(1):47-53.
2. Kasanin J. The acute schizoaffective psychoses. Am J Psychiatry. 1933;90:97-126.
3. Diagnostic and statistical manual of mental disorders, 1st ed. Washington, DC: American Psychiatric Association; 1952.
4. Diagnostic and statistical manual of mental disorders, 3rd ed, revision. Washington, DC: American Psychiatric Association; 1987.
5. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
6. Malaspina D, Owen M, Heckers S, et al. Schizoaffective disorder in the DSM-5. Schizophr Res. 2013;150:21-25.
7. Cheniaux E, Landeria-Fernandez J, Telles LL, et al. Does schizoaffective disorder really exist? A systematic review of the studies that compared schizoaffective disorder with schizophrenia or mood disorders. J Affect Disord. 2008;106:209-217.
8. Kantrowitz JT, Citrome L. Schizoaffective disorder: a review of current research themes and pharmacologic management. CNS Drugs. 2011;25:317-331.
9. Regier DA, Narrow WE, Clarke DE, et al. DSM-5 field trials in the United States and Canada, Part II: test-retest reliability of selected categorical diagnoses. Am J Psychiatry. 2013;170:59-70.
10. Wilson JE, Nian H, Heckers S. The schizoaffective disorder diagnosis: a conundrum in the clinical setting. Eur Arch Psychiatry Clin Neurosci. 2014;264:29-34.
11. Santelmann H, Franklin J, Bußhoff J, Baethge C. Test-retest reliability of schizoaffective disorder compared with schizophrenia, bipolar disorder, and unipolar depression--a systematic review and meta-analysis. Bipolar Disord. 2015;17:753-768.
12. Perälä J, Suvisaari J, Saarni SI, et al. Lifetime Prevalence of psychotic and bipolar I disorders in a general population. JAMA Psychiatry. 2007;64:19-28.
13. Scully PJ, Owens JM, Kinsella A, et al. Schizophrenia, schizoaffective and bipolar disorder within an epidemiologically complete, homogeneous population in rural Ireland: small area variation in rate. Schizophr Res. 2004;67:143-155.
14. Keck PE Jr, McElroy SE, Strakowski SM, et al. Pharmacologic treatment of schizoaffective disorder. Psychopharmacol. 1994;114:529-538.
15. Levinson DF, Umapathy C, Musthaq M. Treatment of schizoaffective disorder and schizophrenia with mood symptoms. Am J Psychiatry. 1999;156:1138-1148.
16. Angst J, Felder W, Lohmeyer B. Course of schizoaffective psychoses: results of a follow-up study. Schizophr Bull. 1980;6:579-585.
17. Lenz G, Simhandl C, Thau K, et al. Temporal stability of diagnostic criteria for functional psychoses. Psychopathol. 1991;24:328-335.
18. Malhi GS, Green M, Fagiolini A, et al. Schizoaffective disorder: diagnostic issues and future recommendations. Bipolar Disord. 2008;10:215-230.
19. Marneros A, Deister A, Rohde A. Psychopathological and social status of patients with affective, schizophrenic and schizoaffective disorders after long‐term course. Acta Psychiatr Scand. 1990;82:352-358.
20. Werry JS, McClellan JM, Chard L. Childhood and adolescent schizophrenic, bipolar, and schizoaffective disorders: a clinical and outcome study. J Am Acad Child Adolesc Psychiatry. 1991;30:457-465.
21. Abrams DJ, Rojas DC, Arciniegas DB. Is schizoaffective disorder a distinct categorical diagnosis? A critical review of the literature. Neuropsychiatr Dis Treat. 2008;4:1089-1109.
22. Bromet EJ, Kotov R, Fochtmann LJ, et al. Diagnostic shifts during the decade following first admission for psychosis. Am J Psychiatry. 2011;168:1186-1194.
23. Salvatore P, Baldessarini RJ, Tohen M, et al. The McLean-Harvard First Episode Project: two-year stability of DSM-IV diagnoses in 500 first-episode psychotic disorder patients. J Clin Psychiatry. 2009;70:458-466.
24. Grossman LS, Harrow M, Goldberg JF, et al. Outcome of schizoaffective disorder at two long term follow-ups: comparisons with outcome of schizophrenia and affective disorders. Am J Psychiatry. 1991;148:1359-1365.
25. Harrow M, Grossman L, Herbener E, et al. Ten-year outcome: patients with schizoaffective disorders, schizophrenia, affective disorders and mood-incongruent psychotic symptoms. Br J Psychiatry. 2000;177:421-426.
26. Hor K, Taylor M. Review: suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24:81-90.
27. Chang CK, Hayes RD, Perera G, et al. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS ONE. 2011;6:e19590.
28. Byerly M, Goodman W, Acholonu W, et al. Obsessive compulsive symptoms in schizophrenia: frequency and clinical features. Schizophr Res. 2005;76:309-316.
29. Strauss JL, Calhoun PS, Marx CE, et al. Comorbid posttraumatic stress disorder is associated with suicidality in male veterans with schizophrenia or schizoaffective disorder. Schizophr Res. 2006;84:165-169.
30. Fagiolini A, Goracci A. The effects of undertreated chronic medical illnesses in patients with severe mental disorders. J Clin Psychiatry. 2009;70:22-29.
31. Black DW, Grant JE. DSM-5 guidebook: the essential companion to the diagnostic and statistical manual of mental disorders, 5th edition. Washington, DC: American Psychiatric Publishing; 2014.
32. Amann BL, Canales-Rodríguez EJ, Madre M, et al. Brain structural changes in schizoaffective disorder compared to schizophrenia and bipolar disorder. Acta Psychiatr Scand. 2016;133:23-33.
33. Ivleva EI, Bidesi AS, Keshavan MS, et al. Gray matter volume as an intermediate phenotype for psychosis: Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP). Am J Psychiatry. 2013;170:1285-1296.
34. Ivleva EI, Bidesi AS, Thomas BP, et al. Brain gray matter phenotypes across the psychosis dimension. Psychiatry Res. 2012;204:13-24.
35. Radonic
36. Jäger M, Becker T, Weinmann S, et al. Treatment of schizoaffective disorder - a challenge for evidence-based psychiatry. Acta Psychiatr Scand. 2010;121:22-32.
37. Glick ID, Mankosli R, Eudicone JM, et al. The efficacy, safety, and tolerability of aripiprazole for the treatment of schizoaffective disorder: results from a pooled analysis of a sub-population of subjects from two randomized, double-blind, placebo controlled, pivotal trials. J Affect Disord. 2009;115:18-26.
38. Canuso CM, Lindenmayer JP, Kosik-Gonzalez C, et al. A randomized, double-blind, placebo controlled study of 2 dose ranges of paliperidone extended-release in the treatment of subjects with schizoaffective disorder. J Clin Psychiatry. 2010;71:587-598.
39. Canuso CM, Schooler NR, Carothers J, et al. Paliperidone extended-release in schizoaffective disorder: a randomized controlled trial comparing a flexible-dose with placebo in patients treated with and without antidepressants and/or mood stabilizers. J Clin Psychopharmacol. 2010;30:487-495.
40. Lindenmayer JP, Kaur A. Antipsychotic management of schizoaffective disorder: a review. Drugs. 2016;76:589-604.
41. Alphs L, Fu DJ, Turkoz I. Paliperidone for the treatment of schizoaffective disorder. Expert Opin Pharmacother. 2016;176:871-883.
42. Bossie CA, Turkoz I, Alphs L, et al. Paliperidone palmitate once-monthly treatment in recent onset and chronic illness patients with schizoaffective disorder. J Nerv Ment Dis. 2017;205:324-328.
43. McDonnell DP, Landry J, Detke HC. Long-term safety and efficacy of olanzapine long-acting injection in patients with schizophrenia or schizoaffective disorder: a 6-year, multinational, single-arm, open-label study. Int Clin Psychopharmacol. 2014;29:322-331.
44. McEvoy JP, Citrome L, Hernandez D, et al. Effectiveness of lurasidone in patients with schizophrenia or schizoaffective disorder switched from other antipsychotics: a randomized, 6-week, open-label study. J Clin Psychiatry. 2013;74:170-179.
45. Mankad MV, Beyer JL, Wiener RD, et al. Manual of electroconvulsive therapy. Washington, DC: American Psychiatric Publishing; 2010.
1. Miller JN, Black DW. Schizoaffective disorder: a review. Ann Clin Psychiatry. 2019;31(1):47-53.
2. Kasanin J. The acute schizoaffective psychoses. Am J Psychiatry. 1933;90:97-126.
3. Diagnostic and statistical manual of mental disorders, 1st ed. Washington, DC: American Psychiatric Association; 1952.
4. Diagnostic and statistical manual of mental disorders, 3rd ed, revision. Washington, DC: American Psychiatric Association; 1987.
5. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
6. Malaspina D, Owen M, Heckers S, et al. Schizoaffective disorder in the DSM-5. Schizophr Res. 2013;150:21-25.
7. Cheniaux E, Landeria-Fernandez J, Telles LL, et al. Does schizoaffective disorder really exist? A systematic review of the studies that compared schizoaffective disorder with schizophrenia or mood disorders. J Affect Disord. 2008;106:209-217.
8. Kantrowitz JT, Citrome L. Schizoaffective disorder: a review of current research themes and pharmacologic management. CNS Drugs. 2011;25:317-331.
9. Regier DA, Narrow WE, Clarke DE, et al. DSM-5 field trials in the United States and Canada, Part II: test-retest reliability of selected categorical diagnoses. Am J Psychiatry. 2013;170:59-70.
10. Wilson JE, Nian H, Heckers S. The schizoaffective disorder diagnosis: a conundrum in the clinical setting. Eur Arch Psychiatry Clin Neurosci. 2014;264:29-34.
11. Santelmann H, Franklin J, Bußhoff J, Baethge C. Test-retest reliability of schizoaffective disorder compared with schizophrenia, bipolar disorder, and unipolar depression--a systematic review and meta-analysis. Bipolar Disord. 2015;17:753-768.
12. Perälä J, Suvisaari J, Saarni SI, et al. Lifetime Prevalence of psychotic and bipolar I disorders in a general population. JAMA Psychiatry. 2007;64:19-28.
13. Scully PJ, Owens JM, Kinsella A, et al. Schizophrenia, schizoaffective and bipolar disorder within an epidemiologically complete, homogeneous population in rural Ireland: small area variation in rate. Schizophr Res. 2004;67:143-155.
14. Keck PE Jr, McElroy SE, Strakowski SM, et al. Pharmacologic treatment of schizoaffective disorder. Psychopharmacol. 1994;114:529-538.
15. Levinson DF, Umapathy C, Musthaq M. Treatment of schizoaffective disorder and schizophrenia with mood symptoms. Am J Psychiatry. 1999;156:1138-1148.
16. Angst J, Felder W, Lohmeyer B. Course of schizoaffective psychoses: results of a follow-up study. Schizophr Bull. 1980;6:579-585.
17. Lenz G, Simhandl C, Thau K, et al. Temporal stability of diagnostic criteria for functional psychoses. Psychopathol. 1991;24:328-335.
18. Malhi GS, Green M, Fagiolini A, et al. Schizoaffective disorder: diagnostic issues and future recommendations. Bipolar Disord. 2008;10:215-230.
19. Marneros A, Deister A, Rohde A. Psychopathological and social status of patients with affective, schizophrenic and schizoaffective disorders after long‐term course. Acta Psychiatr Scand. 1990;82:352-358.
20. Werry JS, McClellan JM, Chard L. Childhood and adolescent schizophrenic, bipolar, and schizoaffective disorders: a clinical and outcome study. J Am Acad Child Adolesc Psychiatry. 1991;30:457-465.
21. Abrams DJ, Rojas DC, Arciniegas DB. Is schizoaffective disorder a distinct categorical diagnosis? A critical review of the literature. Neuropsychiatr Dis Treat. 2008;4:1089-1109.
22. Bromet EJ, Kotov R, Fochtmann LJ, et al. Diagnostic shifts during the decade following first admission for psychosis. Am J Psychiatry. 2011;168:1186-1194.
23. Salvatore P, Baldessarini RJ, Tohen M, et al. The McLean-Harvard First Episode Project: two-year stability of DSM-IV diagnoses in 500 first-episode psychotic disorder patients. J Clin Psychiatry. 2009;70:458-466.
24. Grossman LS, Harrow M, Goldberg JF, et al. Outcome of schizoaffective disorder at two long term follow-ups: comparisons with outcome of schizophrenia and affective disorders. Am J Psychiatry. 1991;148:1359-1365.
25. Harrow M, Grossman L, Herbener E, et al. Ten-year outcome: patients with schizoaffective disorders, schizophrenia, affective disorders and mood-incongruent psychotic symptoms. Br J Psychiatry. 2000;177:421-426.
26. Hor K, Taylor M. Review: suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24:81-90.
27. Chang CK, Hayes RD, Perera G, et al. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS ONE. 2011;6:e19590.
28. Byerly M, Goodman W, Acholonu W, et al. Obsessive compulsive symptoms in schizophrenia: frequency and clinical features. Schizophr Res. 2005;76:309-316.
29. Strauss JL, Calhoun PS, Marx CE, et al. Comorbid posttraumatic stress disorder is associated with suicidality in male veterans with schizophrenia or schizoaffective disorder. Schizophr Res. 2006;84:165-169.
30. Fagiolini A, Goracci A. The effects of undertreated chronic medical illnesses in patients with severe mental disorders. J Clin Psychiatry. 2009;70:22-29.
31. Black DW, Grant JE. DSM-5 guidebook: the essential companion to the diagnostic and statistical manual of mental disorders, 5th edition. Washington, DC: American Psychiatric Publishing; 2014.
32. Amann BL, Canales-Rodríguez EJ, Madre M, et al. Brain structural changes in schizoaffective disorder compared to schizophrenia and bipolar disorder. Acta Psychiatr Scand. 2016;133:23-33.
33. Ivleva EI, Bidesi AS, Keshavan MS, et al. Gray matter volume as an intermediate phenotype for psychosis: Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP). Am J Psychiatry. 2013;170:1285-1296.
34. Ivleva EI, Bidesi AS, Thomas BP, et al. Brain gray matter phenotypes across the psychosis dimension. Psychiatry Res. 2012;204:13-24.
35. Radonic
36. Jäger M, Becker T, Weinmann S, et al. Treatment of schizoaffective disorder - a challenge for evidence-based psychiatry. Acta Psychiatr Scand. 2010;121:22-32.
37. Glick ID, Mankosli R, Eudicone JM, et al. The efficacy, safety, and tolerability of aripiprazole for the treatment of schizoaffective disorder: results from a pooled analysis of a sub-population of subjects from two randomized, double-blind, placebo controlled, pivotal trials. J Affect Disord. 2009;115:18-26.
38. Canuso CM, Lindenmayer JP, Kosik-Gonzalez C, et al. A randomized, double-blind, placebo controlled study of 2 dose ranges of paliperidone extended-release in the treatment of subjects with schizoaffective disorder. J Clin Psychiatry. 2010;71:587-598.
39. Canuso CM, Schooler NR, Carothers J, et al. Paliperidone extended-release in schizoaffective disorder: a randomized controlled trial comparing a flexible-dose with placebo in patients treated with and without antidepressants and/or mood stabilizers. J Clin Psychopharmacol. 2010;30:487-495.
40. Lindenmayer JP, Kaur A. Antipsychotic management of schizoaffective disorder: a review. Drugs. 2016;76:589-604.
41. Alphs L, Fu DJ, Turkoz I. Paliperidone for the treatment of schizoaffective disorder. Expert Opin Pharmacother. 2016;176:871-883.
42. Bossie CA, Turkoz I, Alphs L, et al. Paliperidone palmitate once-monthly treatment in recent onset and chronic illness patients with schizoaffective disorder. J Nerv Ment Dis. 2017;205:324-328.
43. McDonnell DP, Landry J, Detke HC. Long-term safety and efficacy of olanzapine long-acting injection in patients with schizophrenia or schizoaffective disorder: a 6-year, multinational, single-arm, open-label study. Int Clin Psychopharmacol. 2014;29:322-331.
44. McEvoy JP, Citrome L, Hernandez D, et al. Effectiveness of lurasidone in patients with schizophrenia or schizoaffective disorder switched from other antipsychotics: a randomized, 6-week, open-label study. J Clin Psychiatry. 2013;74:170-179.
45. Mankad MV, Beyer JL, Wiener RD, et al. Manual of electroconvulsive therapy. Washington, DC: American Psychiatric Publishing; 2010.
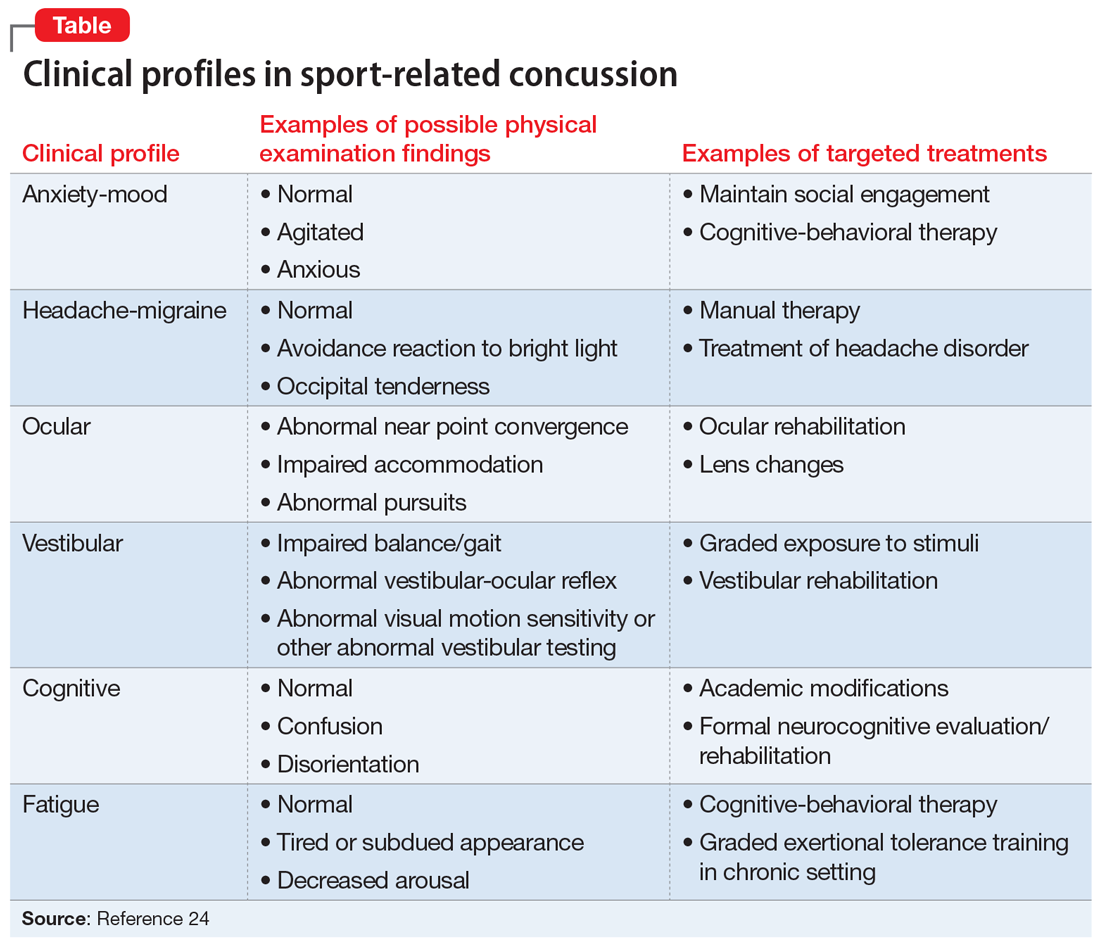
Psychiatric manifestations of sport-related concussion
Ms. J, age 19, is a Division I collegiate volleyball player who recently sustained her third sport-related concussion (SRC). She has no psychiatric history but does have a history of migraine, and her headaches have worsened since the most recent SRC. She has a family history of depression (mother and her sole sibling). Ms. J recently experienced the loss of her coach, someone she greatly admired, in a motor vehicle accident. She is referred to outpatient psychiatry for assessment of mood symptoms that are persisting 1 month after the SRC. Upon assessment, she is found to meet 8 of the 9 criteria for a major depressive episode, including suicidality with vague plans but no intent to end her life.
Although Ms. J does not have a history of psychiatric illness, her psychiatrist recognizes that she has factors that increase her risk of developing depression post-SRC, and of poor recovery from SRC. These include pre-existing symptoms, such as her history of migraine, which is common in patients after SRC. Additionally, a family history of psychiatric disorders and high life stressors (eg, recent loss of her coach) are risk factors for a poor SRC recovery.1 Due to these risk factors and the severity of Ms. J’s symptoms—which include suicidal ideation—the psychiatrist believes that her depressive symptoms might be unlikely to improve in the coming weeks, so he establishes a diagnosis of “depressive disorder due to another medical condition (concussion)” because the development of her depressive symptoms coincided with the SRC. If Ms. J had a pre-existing mood disorder, or if her depression had not developed until later in the post-injury period, it would have been more difficult to establish confidently that the depressive episode was a direct physiologic consequence of the SRC; if that had been the case, the diagnosis probably would have been unspecified or other specified depressive disorder.2
SRC is a traumatic brain injury (TBI) induced by biomechanical forces, typically resulting in short-lived impairment of neurologic function, although signs and symptoms may evolve over minutes to hours.3 It largely reflects functional, rather than structural, brain disturbances.3 SRC has been deemed a “neuropsychiatric syndrome” because psychiatric manifestations are common.4 There may be a myriad of biopsychosocial factors involved in the etiology of psychiatric symptoms in an individual who sustains an SRC. For example, SRC may have a direct physiologic cause of psychiatric symptoms based on the location and degree of injury to the brain. Additionally, pre-existing psychiatric symptoms might increase the likelihood of sustaining an SRC. Finally, as with any major injury, illness, or event, stressors associated with SRC may cause psychiatric symptoms.
Regardless of causal factors, psychiatrists should be comfortable with managing psychiatric symptoms that commonly accompany this condition. This article highlights possible psychiatric manifestations of SRC and delineates high-yield management considerations. Although it focuses on concussions that occur in the context of sport, much of the information applies to patients who experience concussions from other causes.
SRC and depression
Changes in mood, emotion, and behavior are common following SRC. On the Sport Concussion Assessment Tool 5 (SCAT5),5 which is a standardized tool used to evaluate athletes suspected of having sustained a concussion, most symptoms overlap with those attributable to anxiety and depression.4,6 These include5:
- feeling slowed down
- “not feeling right”
- difficulty concentrating
- fatigue or loss of energy
- feeling more emotional
- irritability
- sadness
- feeling nervous or anxious
- difficulty falling asleep.
A recent systematic review of mental health outcomes of SRC in athletes found that the most commonly described and studied psychiatric symptoms following SRC were depression, anxiety, and impulsivity.7 The most rigorous study included in this review found depressive symptoms in 20% of collegiate athletes following SRC (all tested within 41 days of the SRC) vs 5% in the control group.8 These researchers delineated factors that predicted depressive symptoms after SRC (Box 18). Data were insufficient to draw conclusions about the association between SRC and other psychiatric symptoms, such as anxiety.8
Box 1
- Baseline depressive symptoms
- Baseline “post-concussion” symptoms
- Lower estimated premorbid intelligence
- Nonwhite ethnicity
- Increased number of games missed following injury
- Age of first participation in organized sport (more depression in athletes with fewer years of experience)
Source: Reference 8
Psychiatric manifestations of concussion in retired athletes may shed light on the long-term impact of SRC on psychiatric disorders, particularly depression. Hutchison et al9 conducted a systematic review of mental health outcomes of SRC in retired athletes.Two of the included studies that measured clinically diagnosed disorders found positive associations between self-reported concussion and clinically diagnosed depression.10,11 Hutchison et al9 found insufficient data to draw conclusions about depression and a lifetime history of subconcussive impacts—a topic that is receiving growing attention.
Continue to: Regarding a dose-response relationship...
Regarding a dose-response relationship in retired athletes, Guskiewicz et al11 reported a 3-fold increased risk of depression among retired professional football players who had experienced ≥3 SRCs. Five years later, the same research group reported a 5.8-fold increased risk of depression in retired professional football players after 5 to 9 concussions.10 In sum, there is evidence to suggest that the more SRCs an athlete sustains, the more likely they are to develop depression. Moreover, depression may persist or develop long after an SRC occurs.
Suicide risk
While suicide among athletes, especially football players, who have experienced concussion has received relatively widespread media attention, the risk of suicide in former professional football players appears to be significantly lower than in the general population.12 A recent large systematic review and meta-analysis reported on 713,706 individuals diagnosed with concussion and/or mild TBI and 6,236,010 individuals with no such diagnoses.13 It found a 2-fold higher risk of suicide in individuals who experienced concussion and/or mild TBI, but because participants were not necessarily athletes, it is difficult to extrapolate these findings to the athlete population.
Other psychiatric symptoms associated with SRC
Posttraumatic stress disorder (PTSD). Some athletes experience PTSD symptoms shortly after SRC, and these can be missed if clinicians do not specifically ask about them.14 For example, substantial proportions of athletes who have had an SRC report making efforts to avoid sport situations that are similar to how and where their SRC occurred (19%), having trouble keeping thoughts about sustaining the SRC out of their heads (18%), experiencing flashbacks of sustaining the SRC (13%), and having nightmares about sustaining the SRC (8%).14 Posttraumatic stress disorder may have a negative impact on an athlete’s performance because a fear of re-injury might lead them to avoid rehabilitation exercises and inhibit their effort.15-18
Attention-deficit/hyperactivity disorder (ADHD) is commonly comorbid with SRC.19,20 It is not known if pre-existing ADHD makes sustaining a concussion more likely (eg, because the athlete is distractible and thus does not notice when an opponent is about to hit them hard) and/or if a history of concussion makes ADHD more likely to develop (eg, because something about the concussed brain is changed in a way that leads to ADHD). Additionally, in some cases, ADHD has been associated with prolonged recovery from SRC.3,21
Immediate medical evaluation and cognitive assessment
Any patient in whom an SRC is suspected should undergo a medical evaluation immediately, whether in a physician’s office, emergency department, or on the sideline of a sports event. This medical evaluation should incorporate a clinical neurologic assessment, including evaluation of mental status/cognition, oculomotor function, gross sensorimotor, coordination, gait, vestibular function, and balance.3
Continue to: There is no single guideline...
There is no single guideline on how and when a neuropsychology referral is warranted.22 Insurance coverage for neurocognitive testing varies. Regardless of formal referral to neuropsychology, assessment of cognitive function is an important aspect of SRC management and is a factor in return-to-school and return-to-play decisions.3,22 Screening tools, such as the SCAT5, are useful in acute and subacute settings (ie, up to 3 to 5 days after injury); clinicians often use serial monitoring to track the resolution of symptoms.3 If pre-season baseline cognitive test results are available, clinicians may compare them to post-SRC results, but this should not be the sole basis of management decisions.3,22
Diagnosing psychiatric disorders in patients with SRC
Diagnosis of psychiatric symptoms and disorders associated with SRC can be challenging.7 There are no concussion-specific rating scales or diagnostic criteria for psychiatric disorders unique to patients who have sustained SRC. As a result, clinicians are left to use standard DSM-5 criteria for the diagnosis of psychiatric disorders in patients with SRC. Importantly, psychiatric symptoms must be distinguished from disorders. For example, Kontos et al23 reported significantly worse depressive symptoms following SRC, but not at the level to meet the criteria for major depressive disorder. This is an important distinction, because a psychiatrist might be less likely to initiate pharmacotherapy for a patient with SRC who has only a few depressive symptoms and is only 1 week post-SRC, vs for one who has had most symptoms of a major depressive episode for several weeks.
The American Medical Society for Sports Medicine has proposed 6 overlapping clinical profiles in patients with SRC (see the Table).24 Most patients with SRC have features of multiple clinical profiles.24 Anxiety/mood is one of these profiles. The impetus for developing these profiles was the recognition of heterogeneity among concussion presentations. Identification of the clinical profile(s) into which a patient’s symptoms fall might allow for more specific prognostication and targeted treatment.24 For example, referral to a psychiatrist obviously would be appropriate for a patient for whom anxiety/mood symptoms are prominent.
Treatment options for psychiatric sequelae of SRC
Both psychosocial and medical principles of management of psychiatric manifestations of SRC are important. Psychosocially, clinicians should address factors that may contribute to delayed SRC recovery (Box 225-30).
Box 2
- Recommend a progressive increase in exercise after a brief period of rest (often ameliorates psychiatric symptoms, as opposed to the historical approach of “cocoon therapy” in which the patient was to rest for prolonged periods of time in a darkened room so as to minimize brain stimulation)25
- Allow social activities, including team meetings (restriction of such activities has been associated with increased post-SRC depression)26
- Encourage members of the athlete’s “entourage” (team physicians, athletic trainers, coaches, teammates, and parents) to provide support27
- Educate coaches and teammates about how to make supportive statements because they often have trouble knowing how to do so27
- Recommend psychotherapy for mental and other physical symptoms of SRC that are moderate to severe or that persist longer than 4 weeks after the SRC28
- Recommend minimization of use of alcohol and other substances29,30
SRC: sport-related concussion
No medications are FDA-approved for SRC or associated psychiatric symptoms, and there is minimal evidence to support the use of specific medications.31 Most athletes with SRC recover quickly—typically within 2 weeks—and do not need medication.4,32 When medications are needed, start with low dosing and titrate slowly.33,34
Continue to: For patients with SRC who experience insomnia...
For patients with SRC who experience insomnia, clinicians should focus on sleep hygiene and, if needed, cognitive-behavioral therapy for insomnia (CBT-I).31 If medication is needed, melatonin may be a first-line agent.31,35,36 Trazodone may be a second option.32 Benzodiazepines typically are avoided because of their negative impact on cognition.31
For patients with SRC who have depression, selective serotonin reuptake inhibitors (SSRIs) may simultaneously improve depressed mood31 and cognition.37 Tricyclic antidepressants (TCAs) are sometimes used to treat headaches, depression, anxiety, and/or insomnia after SRC,32 but adverse effects such as sedation and weight gain may limit their use in athletes. Theoretically, serotonin-norepinephrine reuptake inhibitors might have some of the same benefits as TCAs with fewer adverse effects, but they have not been well studied in patients with SRC.
For patients with SRC who have cognitive dysfunction (eg, deficits in attention and processing speed), there is some evidence for treatment with stimulants.31,37 However, these medications are prohibited by many athletic governing organizations, including professional sports leagues, the National Collegiate Athletic Association (NCAA), and the World Anti-Doping Agency.4 If an athlete was receiving stimulants for ADHD before sustaining an SRC, there is no evidence that these medications should be stopped.
Consider interdisciplinary collaboration
Throughout the course of management, psychiatrists should consider if and when it is necessary to consult with other specialties such as primary care, sports medicine, neurology, and neuropsychology. As with many psychiatric symptoms and disorders, collaboration with an interdisciplinary team is recommended. Primary care, sports medicine, or neurology should be involved in the management of patients with SRC. Choice of which of those 3 specialties in particular will depend on comfort level and experience with managing SRC of the individual providers in question as well as availability of each provider type in a given community.
Additionally, psychiatrists may wonder if and when they should refer patients with SRC for neuroimaging. Because SRC is a functional, rather than structural, brain disturbance, neuroimaging is not typically pursued because results would be expected to be normal.3 However, when in doubt, consultation with the interdisciplinary team can guide this decision. Factors that may lead to a decision to obtain neuroimaging include:
- an abnormal neurologic examination
- prolonged loss of consciousness
- unexpected persistence of symptoms (eg, 6 to 12 weeks)
- worsening symptoms.22
Continue to: If imaging is deemed necessary...
If imaging is deemed necessary for a patient with an acute SRC, brain CT is typically the imaging modality of choice; however, if imaging is deemed necessary due to the persistence of symptoms, then MRI is often the preferred test because it provides more detailed information and does not expose the patient to ionizing radiation.22 While results are often normal, the ordering clinician should be prepared for the possibility of incidental findings, such as cysts or aneurysms, and the need for further consultation with other clinicians to weigh in on such findings.22
CASE CONTINUED
Ms. J is prescribed extended-release venlafaxine, 37.5 mg every morning for 5 days, and then is switched to 75 mg every morning. The psychiatrist hopes that venlafaxine might simultaneously offer benefit for Ms. J’s depression and migraine headaches. Venlafaxine is not FDA-approved for migraine, and there is more evidence supporting TCAs for preventing migraine. However, Ms. J is adamant that she does not want to take a medication, such as a TCA, that could cause weight gain or sedation, which could be problematic in her sport. The psychiatrist also tells Ms. J to avoid substances of abuse, and emphasizes the importance of good sleep hygiene. Finally, the psychiatrist communicates with the interdisciplinary medical team, which is helping Ms. J with gradual return-to-school and return-to-sport strategies and ensuring continued social involvement with the team even as she is held out from sport.
Ultimately, Ms. J’s extended-release venlafaxine is titrated to 150 mg every morning. After 2 months on this dose, her depressive symptoms remit. After her other symptoms remit, Ms. J has difficulty returning to certain practice drills that remind her of what she was doing when she sustained the SRC. She says that while participating in these drills, she has intrusive thoughts and images of the experience of her most recent concussion. She works with her psychiatrist on a gradual program of exposure therapy so she can return to all types of practice. Ms. J says she wishes to continue playing volleyball; however, together with her parents and treatment team, she decides that any additional SRCs might lead her to retire from the sport.
Bottom Line
Psychiatric symptoms are common after sport-related concussion (SRC). The nature of the relationship between concussion and mental health is not firmly established. Post-SRC psychiatric symptoms need to be carefully managed to avoid unnecessary treatment or restrictions.
Related Resources
- National Collegiate Athletic Association. Concussion. www.ncaa.org/sport-science-institute/concussion.
- American Academy of Neurology. Sports concussion resources. www.aan.com/tools-and-resources/practicing-neurologists-administrators/patient-resources/sports-concussion-resources. Published 2020.
Drug Brand Names
Trazodone • Desyrel
Venlafaxine • Effexor
1. Morgan CD, Zuckerman SL, Lee YM, et al. Predictors of postconcussion syndrome after sports-related concussion in young athletes: a matched case-control study. J Neurosurg Pediatr. 2015;15(6):589-598.
2. Jorge RE, Arciniegas DB. Mood disorders after TBI. Psychiatr Clin North Am. 2014;37(1):13-29.
3. McCrory P, Meeuwisse W, Dvor˘ák J, et al. Consensus statement on concussion in sport—the 5th International Conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838-847.
4. Reardon CL, Hainline B, Aron CM, et al. Mental health in elite athletes: International Olympic Committee consensus statement (2019). Br J Sports Med. 2019;53(11):667-699.
5. Echemendia RJ, Meeuwisse W, McCrory P, et al. The sport concussion assessment tool 5th edition (SCAT5): background and rationale. Br J Sports Med. 2017;51:848-850.
6. Thompson E. Hamilton rating scale for anxiety (HAM-A). Occup Med. 2015;65(7):601.
7. Rice SM, Parker AG, Rosenbaum S, et al. Sport-related concussion outcomes in elite athletes: a systematic review. Sports Med. 2018;48(2):447-465.
8. Vargas G, Rabinowitz A, Meyer J, et al. Predictors and prevalence of postconcussion depression symptoms in collegiate athletes. J Athl Train. 2015;50(3):250-255.
9. Hutchison MG, Di Battista AP, McCoskey J, et al. Systematic review of mental health measures associated with concussive and subconcussive head trauma in former athletes. Int J Psychophysiol. 2018;132(Pt A):55-61.
10. Kerr GA, Stirling AE. Parents’ reflections on their child’s experiences of emotionally abusive coaching practices. J Appl Sport Psychol. 2012;24(2):191-206.
11. Guskiewicz KM, Marshall SW, Bailes J, et al. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exerc. 2007;39(6):903-909.
12. Lehman EJ, Hein MJ, Gersic CM. Suicide mortality among retired National Football League players who played 5 or more seasons. Am J Sports Med. 2016;44(10):2486-2491.
13. Fralick M, Sy E, Hassan A, et al. Association of concussion with the risk of suicide: a systematic review and meta-analysis. JAMA Neurol. 2018;76(2):144-151.
14. Brassil HE, Salvatore AP. The frequency of post-traumatic stress disorder symptoms in athletes with and without sports related concussion. Clin Transl Med. 2018;7:25.
15. Bateman A, Morgan KAD. The postinjury psychological sequelae of high-level Jamaican athletes: exploration of a posttraumatic stress disorder-self-efficacy conceptualization. J Sport Rehabil. 2019;28(2):144-152.
16. Brewer BW, Van Raalte JL, Cornelius AE, et al. Psychological factors, rehabilitation adherence, and rehabilitation outcome after anterior cruciate ligament reconstruction. Rehabil Psychol. 2000;45(1):20-37.
17. Putukian M, Echemendia RJ. Psychological aspects of serious head injury in the competitive athlete. Clin Sports Med. 2003;22(33):617-630.
18. James LM, Strom TQ, Leskela J. Risk-taking behaviors and impulsivity among Veterans with and without PTSD and mild TBI. Mil Med. 2014;179(4):357-363.
19. Harmon KG, Drezner J, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Clin J Sport Med. 2013;47(1):15-26.
20. Nelson LD, Guskiewicz KM, Marshall SW, et al. Multiple self-reported concussions are more prevalent in athletes with ADHD and learning disability. Clin J Sport Med. 2016;26(2):120-127.
21. Esfandiari A, Broshek DK, Freeman JR. Psychiatric and neuropsychological issues in sports medicine. Clin Sports Med. 2011;30(3):611-627.
22. Mahooti N. Sport-related concussion: acute management and chronic postconcussive issues. Chld Adolesc Psychiatric Clin N Am. 2018;27(1):93-108.
23. Kontos AP, Covassin T, Elbin RJ, et al. Depression and neurocognitive performance after concussion among male and female high school and collegiate athletes. Arch Phys Med Rehabil. 2012;93(10):1751-1756.
24. Harmon KG, Clugston JR, Dec K, et al. American Medical Society for Sports Medicine position statement on concussion in sport. Clin J Sport Med. 2019;29(2):87-100.
25. Leddy JJ, Willer B. Use of graded exercise testing in concussion and return-to-activity management. Current Sports Medicine Reports. 2013;12(6):370-376.
26. Schneider KJ, Iverson GL, Emery CA, et al. The effects of rest and treatment following sport-related concussion: a systematic review of the literature. Br J Sports Med. 2013;47(5):304-307.
27. Wayment HA, Huffman AH. Psychosocial experiences of concussed collegiate athletes: the role of emotional support in the recovery process. J Am Coll Health. 2020;68(4):438-443.
28. Todd R, Bhalerao S, Vu MT, et al. Understanding the psychiatric effects of concussion on constructed identity in hockey players: implications for health professionals. PLoS ONE. 2018;13(2):e0192125.
29. Iverson GL, Silverberg ND, Mannix R, et al. Factors associated with concussion-like symptom reporting in high school athletes. JAMA Pediatr. 2015;169(12):1132-1140.
30. Gaetz M. The multi-factorial origins of chronic traumatic encephalopathy (CTE) symptomatology in post-career athletes: the athlete post-career adjustment (AP-CA) model. Med Hypotheses. 2017;102:130-143.
31. Meehan WP. Medical therapies for concussion. Clin Sports Med. 2011;30(1):115-124.
32. Broglio SP, Collins MW, Williams RM, et al. Current and emerging rehabilitation for concussion: a review of the evidence. Clin Sports Med. 2015;34(2):213-231.
33. Arciniegas DB, Silver JM, McAllister TW. Stimulants and acetylcholinesterase inhibitors for the treatment of cognitive impairment after traumatic brain injury. Psychopharm Review. 2008;43(12):91-97.
34. Warden DL, Gordon B, McAllister TW, et al. Guidelines for the pharmacologic treatment of neurobehavioral sequelae of traumatic brain injury. J Neurotrauma. 2006;23(10):1468-1501.
35. Maldonado MD, Murillo-Cabezas F, Terron MP, et al. The potential of melatonin in reducing morbidity/mortality after craniocerebral trauma. J Pineal Res. 2007;42(1):1-11.
36. Samantaray S, Das A, Thakore NP, et al. Therapeutic potential of melatonin in traumatic central nervous system injury. J Pineal Res. 2009;47(2):134-142.
37. Chew E, Zafonte RD. Pharmacological management of neurobehavioral disorders following traumatic brain injury—a state-of-the-art review. J Rehabil Res Dev. 2009;46(6):851-879.
Ms. J, age 19, is a Division I collegiate volleyball player who recently sustained her third sport-related concussion (SRC). She has no psychiatric history but does have a history of migraine, and her headaches have worsened since the most recent SRC. She has a family history of depression (mother and her sole sibling). Ms. J recently experienced the loss of her coach, someone she greatly admired, in a motor vehicle accident. She is referred to outpatient psychiatry for assessment of mood symptoms that are persisting 1 month after the SRC. Upon assessment, she is found to meet 8 of the 9 criteria for a major depressive episode, including suicidality with vague plans but no intent to end her life.
Although Ms. J does not have a history of psychiatric illness, her psychiatrist recognizes that she has factors that increase her risk of developing depression post-SRC, and of poor recovery from SRC. These include pre-existing symptoms, such as her history of migraine, which is common in patients after SRC. Additionally, a family history of psychiatric disorders and high life stressors (eg, recent loss of her coach) are risk factors for a poor SRC recovery.1 Due to these risk factors and the severity of Ms. J’s symptoms—which include suicidal ideation—the psychiatrist believes that her depressive symptoms might be unlikely to improve in the coming weeks, so he establishes a diagnosis of “depressive disorder due to another medical condition (concussion)” because the development of her depressive symptoms coincided with the SRC. If Ms. J had a pre-existing mood disorder, or if her depression had not developed until later in the post-injury period, it would have been more difficult to establish confidently that the depressive episode was a direct physiologic consequence of the SRC; if that had been the case, the diagnosis probably would have been unspecified or other specified depressive disorder.2
SRC is a traumatic brain injury (TBI) induced by biomechanical forces, typically resulting in short-lived impairment of neurologic function, although signs and symptoms may evolve over minutes to hours.3 It largely reflects functional, rather than structural, brain disturbances.3 SRC has been deemed a “neuropsychiatric syndrome” because psychiatric manifestations are common.4 There may be a myriad of biopsychosocial factors involved in the etiology of psychiatric symptoms in an individual who sustains an SRC. For example, SRC may have a direct physiologic cause of psychiatric symptoms based on the location and degree of injury to the brain. Additionally, pre-existing psychiatric symptoms might increase the likelihood of sustaining an SRC. Finally, as with any major injury, illness, or event, stressors associated with SRC may cause psychiatric symptoms.
Regardless of causal factors, psychiatrists should be comfortable with managing psychiatric symptoms that commonly accompany this condition. This article highlights possible psychiatric manifestations of SRC and delineates high-yield management considerations. Although it focuses on concussions that occur in the context of sport, much of the information applies to patients who experience concussions from other causes.
SRC and depression
Changes in mood, emotion, and behavior are common following SRC. On the Sport Concussion Assessment Tool 5 (SCAT5),5 which is a standardized tool used to evaluate athletes suspected of having sustained a concussion, most symptoms overlap with those attributable to anxiety and depression.4,6 These include5:
- feeling slowed down
- “not feeling right”
- difficulty concentrating
- fatigue or loss of energy
- feeling more emotional
- irritability
- sadness
- feeling nervous or anxious
- difficulty falling asleep.
A recent systematic review of mental health outcomes of SRC in athletes found that the most commonly described and studied psychiatric symptoms following SRC were depression, anxiety, and impulsivity.7 The most rigorous study included in this review found depressive symptoms in 20% of collegiate athletes following SRC (all tested within 41 days of the SRC) vs 5% in the control group.8 These researchers delineated factors that predicted depressive symptoms after SRC (Box 18). Data were insufficient to draw conclusions about the association between SRC and other psychiatric symptoms, such as anxiety.8
Box 1
- Baseline depressive symptoms
- Baseline “post-concussion” symptoms
- Lower estimated premorbid intelligence
- Nonwhite ethnicity
- Increased number of games missed following injury
- Age of first participation in organized sport (more depression in athletes with fewer years of experience)
Source: Reference 8
Psychiatric manifestations of concussion in retired athletes may shed light on the long-term impact of SRC on psychiatric disorders, particularly depression. Hutchison et al9 conducted a systematic review of mental health outcomes of SRC in retired athletes.Two of the included studies that measured clinically diagnosed disorders found positive associations between self-reported concussion and clinically diagnosed depression.10,11 Hutchison et al9 found insufficient data to draw conclusions about depression and a lifetime history of subconcussive impacts—a topic that is receiving growing attention.
Continue to: Regarding a dose-response relationship...
Regarding a dose-response relationship in retired athletes, Guskiewicz et al11 reported a 3-fold increased risk of depression among retired professional football players who had experienced ≥3 SRCs. Five years later, the same research group reported a 5.8-fold increased risk of depression in retired professional football players after 5 to 9 concussions.10 In sum, there is evidence to suggest that the more SRCs an athlete sustains, the more likely they are to develop depression. Moreover, depression may persist or develop long after an SRC occurs.
Suicide risk
While suicide among athletes, especially football players, who have experienced concussion has received relatively widespread media attention, the risk of suicide in former professional football players appears to be significantly lower than in the general population.12 A recent large systematic review and meta-analysis reported on 713,706 individuals diagnosed with concussion and/or mild TBI and 6,236,010 individuals with no such diagnoses.13 It found a 2-fold higher risk of suicide in individuals who experienced concussion and/or mild TBI, but because participants were not necessarily athletes, it is difficult to extrapolate these findings to the athlete population.
Other psychiatric symptoms associated with SRC
Posttraumatic stress disorder (PTSD). Some athletes experience PTSD symptoms shortly after SRC, and these can be missed if clinicians do not specifically ask about them.14 For example, substantial proportions of athletes who have had an SRC report making efforts to avoid sport situations that are similar to how and where their SRC occurred (19%), having trouble keeping thoughts about sustaining the SRC out of their heads (18%), experiencing flashbacks of sustaining the SRC (13%), and having nightmares about sustaining the SRC (8%).14 Posttraumatic stress disorder may have a negative impact on an athlete’s performance because a fear of re-injury might lead them to avoid rehabilitation exercises and inhibit their effort.15-18
Attention-deficit/hyperactivity disorder (ADHD) is commonly comorbid with SRC.19,20 It is not known if pre-existing ADHD makes sustaining a concussion more likely (eg, because the athlete is distractible and thus does not notice when an opponent is about to hit them hard) and/or if a history of concussion makes ADHD more likely to develop (eg, because something about the concussed brain is changed in a way that leads to ADHD). Additionally, in some cases, ADHD has been associated with prolonged recovery from SRC.3,21
Immediate medical evaluation and cognitive assessment
Any patient in whom an SRC is suspected should undergo a medical evaluation immediately, whether in a physician’s office, emergency department, or on the sideline of a sports event. This medical evaluation should incorporate a clinical neurologic assessment, including evaluation of mental status/cognition, oculomotor function, gross sensorimotor, coordination, gait, vestibular function, and balance.3
Continue to: There is no single guideline...
There is no single guideline on how and when a neuropsychology referral is warranted.22 Insurance coverage for neurocognitive testing varies. Regardless of formal referral to neuropsychology, assessment of cognitive function is an important aspect of SRC management and is a factor in return-to-school and return-to-play decisions.3,22 Screening tools, such as the SCAT5, are useful in acute and subacute settings (ie, up to 3 to 5 days after injury); clinicians often use serial monitoring to track the resolution of symptoms.3 If pre-season baseline cognitive test results are available, clinicians may compare them to post-SRC results, but this should not be the sole basis of management decisions.3,22
Diagnosing psychiatric disorders in patients with SRC
Diagnosis of psychiatric symptoms and disorders associated with SRC can be challenging.7 There are no concussion-specific rating scales or diagnostic criteria for psychiatric disorders unique to patients who have sustained SRC. As a result, clinicians are left to use standard DSM-5 criteria for the diagnosis of psychiatric disorders in patients with SRC. Importantly, psychiatric symptoms must be distinguished from disorders. For example, Kontos et al23 reported significantly worse depressive symptoms following SRC, but not at the level to meet the criteria for major depressive disorder. This is an important distinction, because a psychiatrist might be less likely to initiate pharmacotherapy for a patient with SRC who has only a few depressive symptoms and is only 1 week post-SRC, vs for one who has had most symptoms of a major depressive episode for several weeks.
The American Medical Society for Sports Medicine has proposed 6 overlapping clinical profiles in patients with SRC (see the Table).24 Most patients with SRC have features of multiple clinical profiles.24 Anxiety/mood is one of these profiles. The impetus for developing these profiles was the recognition of heterogeneity among concussion presentations. Identification of the clinical profile(s) into which a patient’s symptoms fall might allow for more specific prognostication and targeted treatment.24 For example, referral to a psychiatrist obviously would be appropriate for a patient for whom anxiety/mood symptoms are prominent.
Treatment options for psychiatric sequelae of SRC
Both psychosocial and medical principles of management of psychiatric manifestations of SRC are important. Psychosocially, clinicians should address factors that may contribute to delayed SRC recovery (Box 225-30).
Box 2
- Recommend a progressive increase in exercise after a brief period of rest (often ameliorates psychiatric symptoms, as opposed to the historical approach of “cocoon therapy” in which the patient was to rest for prolonged periods of time in a darkened room so as to minimize brain stimulation)25
- Allow social activities, including team meetings (restriction of such activities has been associated with increased post-SRC depression)26
- Encourage members of the athlete’s “entourage” (team physicians, athletic trainers, coaches, teammates, and parents) to provide support27
- Educate coaches and teammates about how to make supportive statements because they often have trouble knowing how to do so27
- Recommend psychotherapy for mental and other physical symptoms of SRC that are moderate to severe or that persist longer than 4 weeks after the SRC28
- Recommend minimization of use of alcohol and other substances29,30
SRC: sport-related concussion
No medications are FDA-approved for SRC or associated psychiatric symptoms, and there is minimal evidence to support the use of specific medications.31 Most athletes with SRC recover quickly—typically within 2 weeks—and do not need medication.4,32 When medications are needed, start with low dosing and titrate slowly.33,34
Continue to: For patients with SRC who experience insomnia...
For patients with SRC who experience insomnia, clinicians should focus on sleep hygiene and, if needed, cognitive-behavioral therapy for insomnia (CBT-I).31 If medication is needed, melatonin may be a first-line agent.31,35,36 Trazodone may be a second option.32 Benzodiazepines typically are avoided because of their negative impact on cognition.31
For patients with SRC who have depression, selective serotonin reuptake inhibitors (SSRIs) may simultaneously improve depressed mood31 and cognition.37 Tricyclic antidepressants (TCAs) are sometimes used to treat headaches, depression, anxiety, and/or insomnia after SRC,32 but adverse effects such as sedation and weight gain may limit their use in athletes. Theoretically, serotonin-norepinephrine reuptake inhibitors might have some of the same benefits as TCAs with fewer adverse effects, but they have not been well studied in patients with SRC.
For patients with SRC who have cognitive dysfunction (eg, deficits in attention and processing speed), there is some evidence for treatment with stimulants.31,37 However, these medications are prohibited by many athletic governing organizations, including professional sports leagues, the National Collegiate Athletic Association (NCAA), and the World Anti-Doping Agency.4 If an athlete was receiving stimulants for ADHD before sustaining an SRC, there is no evidence that these medications should be stopped.
Consider interdisciplinary collaboration
Throughout the course of management, psychiatrists should consider if and when it is necessary to consult with other specialties such as primary care, sports medicine, neurology, and neuropsychology. As with many psychiatric symptoms and disorders, collaboration with an interdisciplinary team is recommended. Primary care, sports medicine, or neurology should be involved in the management of patients with SRC. Choice of which of those 3 specialties in particular will depend on comfort level and experience with managing SRC of the individual providers in question as well as availability of each provider type in a given community.
Additionally, psychiatrists may wonder if and when they should refer patients with SRC for neuroimaging. Because SRC is a functional, rather than structural, brain disturbance, neuroimaging is not typically pursued because results would be expected to be normal.3 However, when in doubt, consultation with the interdisciplinary team can guide this decision. Factors that may lead to a decision to obtain neuroimaging include:
- an abnormal neurologic examination
- prolonged loss of consciousness
- unexpected persistence of symptoms (eg, 6 to 12 weeks)
- worsening symptoms.22
Continue to: If imaging is deemed necessary...
If imaging is deemed necessary for a patient with an acute SRC, brain CT is typically the imaging modality of choice; however, if imaging is deemed necessary due to the persistence of symptoms, then MRI is often the preferred test because it provides more detailed information and does not expose the patient to ionizing radiation.22 While results are often normal, the ordering clinician should be prepared for the possibility of incidental findings, such as cysts or aneurysms, and the need for further consultation with other clinicians to weigh in on such findings.22
CASE CONTINUED
Ms. J is prescribed extended-release venlafaxine, 37.5 mg every morning for 5 days, and then is switched to 75 mg every morning. The psychiatrist hopes that venlafaxine might simultaneously offer benefit for Ms. J’s depression and migraine headaches. Venlafaxine is not FDA-approved for migraine, and there is more evidence supporting TCAs for preventing migraine. However, Ms. J is adamant that she does not want to take a medication, such as a TCA, that could cause weight gain or sedation, which could be problematic in her sport. The psychiatrist also tells Ms. J to avoid substances of abuse, and emphasizes the importance of good sleep hygiene. Finally, the psychiatrist communicates with the interdisciplinary medical team, which is helping Ms. J with gradual return-to-school and return-to-sport strategies and ensuring continued social involvement with the team even as she is held out from sport.
Ultimately, Ms. J’s extended-release venlafaxine is titrated to 150 mg every morning. After 2 months on this dose, her depressive symptoms remit. After her other symptoms remit, Ms. J has difficulty returning to certain practice drills that remind her of what she was doing when she sustained the SRC. She says that while participating in these drills, she has intrusive thoughts and images of the experience of her most recent concussion. She works with her psychiatrist on a gradual program of exposure therapy so she can return to all types of practice. Ms. J says she wishes to continue playing volleyball; however, together with her parents and treatment team, she decides that any additional SRCs might lead her to retire from the sport.
Bottom Line
Psychiatric symptoms are common after sport-related concussion (SRC). The nature of the relationship between concussion and mental health is not firmly established. Post-SRC psychiatric symptoms need to be carefully managed to avoid unnecessary treatment or restrictions.
Related Resources
- National Collegiate Athletic Association. Concussion. www.ncaa.org/sport-science-institute/concussion.
- American Academy of Neurology. Sports concussion resources. www.aan.com/tools-and-resources/practicing-neurologists-administrators/patient-resources/sports-concussion-resources. Published 2020.
Drug Brand Names
Trazodone • Desyrel
Venlafaxine • Effexor
Ms. J, age 19, is a Division I collegiate volleyball player who recently sustained her third sport-related concussion (SRC). She has no psychiatric history but does have a history of migraine, and her headaches have worsened since the most recent SRC. She has a family history of depression (mother and her sole sibling). Ms. J recently experienced the loss of her coach, someone she greatly admired, in a motor vehicle accident. She is referred to outpatient psychiatry for assessment of mood symptoms that are persisting 1 month after the SRC. Upon assessment, she is found to meet 8 of the 9 criteria for a major depressive episode, including suicidality with vague plans but no intent to end her life.
Although Ms. J does not have a history of psychiatric illness, her psychiatrist recognizes that she has factors that increase her risk of developing depression post-SRC, and of poor recovery from SRC. These include pre-existing symptoms, such as her history of migraine, which is common in patients after SRC. Additionally, a family history of psychiatric disorders and high life stressors (eg, recent loss of her coach) are risk factors for a poor SRC recovery.1 Due to these risk factors and the severity of Ms. J’s symptoms—which include suicidal ideation—the psychiatrist believes that her depressive symptoms might be unlikely to improve in the coming weeks, so he establishes a diagnosis of “depressive disorder due to another medical condition (concussion)” because the development of her depressive symptoms coincided with the SRC. If Ms. J had a pre-existing mood disorder, or if her depression had not developed until later in the post-injury period, it would have been more difficult to establish confidently that the depressive episode was a direct physiologic consequence of the SRC; if that had been the case, the diagnosis probably would have been unspecified or other specified depressive disorder.2
SRC is a traumatic brain injury (TBI) induced by biomechanical forces, typically resulting in short-lived impairment of neurologic function, although signs and symptoms may evolve over minutes to hours.3 It largely reflects functional, rather than structural, brain disturbances.3 SRC has been deemed a “neuropsychiatric syndrome” because psychiatric manifestations are common.4 There may be a myriad of biopsychosocial factors involved in the etiology of psychiatric symptoms in an individual who sustains an SRC. For example, SRC may have a direct physiologic cause of psychiatric symptoms based on the location and degree of injury to the brain. Additionally, pre-existing psychiatric symptoms might increase the likelihood of sustaining an SRC. Finally, as with any major injury, illness, or event, stressors associated with SRC may cause psychiatric symptoms.
Regardless of causal factors, psychiatrists should be comfortable with managing psychiatric symptoms that commonly accompany this condition. This article highlights possible psychiatric manifestations of SRC and delineates high-yield management considerations. Although it focuses on concussions that occur in the context of sport, much of the information applies to patients who experience concussions from other causes.
SRC and depression
Changes in mood, emotion, and behavior are common following SRC. On the Sport Concussion Assessment Tool 5 (SCAT5),5 which is a standardized tool used to evaluate athletes suspected of having sustained a concussion, most symptoms overlap with those attributable to anxiety and depression.4,6 These include5:
- feeling slowed down
- “not feeling right”
- difficulty concentrating
- fatigue or loss of energy
- feeling more emotional
- irritability
- sadness
- feeling nervous or anxious
- difficulty falling asleep.
A recent systematic review of mental health outcomes of SRC in athletes found that the most commonly described and studied psychiatric symptoms following SRC were depression, anxiety, and impulsivity.7 The most rigorous study included in this review found depressive symptoms in 20% of collegiate athletes following SRC (all tested within 41 days of the SRC) vs 5% in the control group.8 These researchers delineated factors that predicted depressive symptoms after SRC (Box 18). Data were insufficient to draw conclusions about the association between SRC and other psychiatric symptoms, such as anxiety.8
Box 1
- Baseline depressive symptoms
- Baseline “post-concussion” symptoms
- Lower estimated premorbid intelligence
- Nonwhite ethnicity
- Increased number of games missed following injury
- Age of first participation in organized sport (more depression in athletes with fewer years of experience)
Source: Reference 8
Psychiatric manifestations of concussion in retired athletes may shed light on the long-term impact of SRC on psychiatric disorders, particularly depression. Hutchison et al9 conducted a systematic review of mental health outcomes of SRC in retired athletes.Two of the included studies that measured clinically diagnosed disorders found positive associations between self-reported concussion and clinically diagnosed depression.10,11 Hutchison et al9 found insufficient data to draw conclusions about depression and a lifetime history of subconcussive impacts—a topic that is receiving growing attention.
Continue to: Regarding a dose-response relationship...
Regarding a dose-response relationship in retired athletes, Guskiewicz et al11 reported a 3-fold increased risk of depression among retired professional football players who had experienced ≥3 SRCs. Five years later, the same research group reported a 5.8-fold increased risk of depression in retired professional football players after 5 to 9 concussions.10 In sum, there is evidence to suggest that the more SRCs an athlete sustains, the more likely they are to develop depression. Moreover, depression may persist or develop long after an SRC occurs.
Suicide risk
While suicide among athletes, especially football players, who have experienced concussion has received relatively widespread media attention, the risk of suicide in former professional football players appears to be significantly lower than in the general population.12 A recent large systematic review and meta-analysis reported on 713,706 individuals diagnosed with concussion and/or mild TBI and 6,236,010 individuals with no such diagnoses.13 It found a 2-fold higher risk of suicide in individuals who experienced concussion and/or mild TBI, but because participants were not necessarily athletes, it is difficult to extrapolate these findings to the athlete population.
Other psychiatric symptoms associated with SRC
Posttraumatic stress disorder (PTSD). Some athletes experience PTSD symptoms shortly after SRC, and these can be missed if clinicians do not specifically ask about them.14 For example, substantial proportions of athletes who have had an SRC report making efforts to avoid sport situations that are similar to how and where their SRC occurred (19%), having trouble keeping thoughts about sustaining the SRC out of their heads (18%), experiencing flashbacks of sustaining the SRC (13%), and having nightmares about sustaining the SRC (8%).14 Posttraumatic stress disorder may have a negative impact on an athlete’s performance because a fear of re-injury might lead them to avoid rehabilitation exercises and inhibit their effort.15-18
Attention-deficit/hyperactivity disorder (ADHD) is commonly comorbid with SRC.19,20 It is not known if pre-existing ADHD makes sustaining a concussion more likely (eg, because the athlete is distractible and thus does not notice when an opponent is about to hit them hard) and/or if a history of concussion makes ADHD more likely to develop (eg, because something about the concussed brain is changed in a way that leads to ADHD). Additionally, in some cases, ADHD has been associated with prolonged recovery from SRC.3,21
Immediate medical evaluation and cognitive assessment
Any patient in whom an SRC is suspected should undergo a medical evaluation immediately, whether in a physician’s office, emergency department, or on the sideline of a sports event. This medical evaluation should incorporate a clinical neurologic assessment, including evaluation of mental status/cognition, oculomotor function, gross sensorimotor, coordination, gait, vestibular function, and balance.3
Continue to: There is no single guideline...
There is no single guideline on how and when a neuropsychology referral is warranted.22 Insurance coverage for neurocognitive testing varies. Regardless of formal referral to neuropsychology, assessment of cognitive function is an important aspect of SRC management and is a factor in return-to-school and return-to-play decisions.3,22 Screening tools, such as the SCAT5, are useful in acute and subacute settings (ie, up to 3 to 5 days after injury); clinicians often use serial monitoring to track the resolution of symptoms.3 If pre-season baseline cognitive test results are available, clinicians may compare them to post-SRC results, but this should not be the sole basis of management decisions.3,22
Diagnosing psychiatric disorders in patients with SRC
Diagnosis of psychiatric symptoms and disorders associated with SRC can be challenging.7 There are no concussion-specific rating scales or diagnostic criteria for psychiatric disorders unique to patients who have sustained SRC. As a result, clinicians are left to use standard DSM-5 criteria for the diagnosis of psychiatric disorders in patients with SRC. Importantly, psychiatric symptoms must be distinguished from disorders. For example, Kontos et al23 reported significantly worse depressive symptoms following SRC, but not at the level to meet the criteria for major depressive disorder. This is an important distinction, because a psychiatrist might be less likely to initiate pharmacotherapy for a patient with SRC who has only a few depressive symptoms and is only 1 week post-SRC, vs for one who has had most symptoms of a major depressive episode for several weeks.
The American Medical Society for Sports Medicine has proposed 6 overlapping clinical profiles in patients with SRC (see the Table).24 Most patients with SRC have features of multiple clinical profiles.24 Anxiety/mood is one of these profiles. The impetus for developing these profiles was the recognition of heterogeneity among concussion presentations. Identification of the clinical profile(s) into which a patient’s symptoms fall might allow for more specific prognostication and targeted treatment.24 For example, referral to a psychiatrist obviously would be appropriate for a patient for whom anxiety/mood symptoms are prominent.
Treatment options for psychiatric sequelae of SRC
Both psychosocial and medical principles of management of psychiatric manifestations of SRC are important. Psychosocially, clinicians should address factors that may contribute to delayed SRC recovery (Box 225-30).
Box 2
- Recommend a progressive increase in exercise after a brief period of rest (often ameliorates psychiatric symptoms, as opposed to the historical approach of “cocoon therapy” in which the patient was to rest for prolonged periods of time in a darkened room so as to minimize brain stimulation)25
- Allow social activities, including team meetings (restriction of such activities has been associated with increased post-SRC depression)26
- Encourage members of the athlete’s “entourage” (team physicians, athletic trainers, coaches, teammates, and parents) to provide support27
- Educate coaches and teammates about how to make supportive statements because they often have trouble knowing how to do so27
- Recommend psychotherapy for mental and other physical symptoms of SRC that are moderate to severe or that persist longer than 4 weeks after the SRC28
- Recommend minimization of use of alcohol and other substances29,30
SRC: sport-related concussion
No medications are FDA-approved for SRC or associated psychiatric symptoms, and there is minimal evidence to support the use of specific medications.31 Most athletes with SRC recover quickly—typically within 2 weeks—and do not need medication.4,32 When medications are needed, start with low dosing and titrate slowly.33,34
Continue to: For patients with SRC who experience insomnia...
For patients with SRC who experience insomnia, clinicians should focus on sleep hygiene and, if needed, cognitive-behavioral therapy for insomnia (CBT-I).31 If medication is needed, melatonin may be a first-line agent.31,35,36 Trazodone may be a second option.32 Benzodiazepines typically are avoided because of their negative impact on cognition.31
For patients with SRC who have depression, selective serotonin reuptake inhibitors (SSRIs) may simultaneously improve depressed mood31 and cognition.37 Tricyclic antidepressants (TCAs) are sometimes used to treat headaches, depression, anxiety, and/or insomnia after SRC,32 but adverse effects such as sedation and weight gain may limit their use in athletes. Theoretically, serotonin-norepinephrine reuptake inhibitors might have some of the same benefits as TCAs with fewer adverse effects, but they have not been well studied in patients with SRC.
For patients with SRC who have cognitive dysfunction (eg, deficits in attention and processing speed), there is some evidence for treatment with stimulants.31,37 However, these medications are prohibited by many athletic governing organizations, including professional sports leagues, the National Collegiate Athletic Association (NCAA), and the World Anti-Doping Agency.4 If an athlete was receiving stimulants for ADHD before sustaining an SRC, there is no evidence that these medications should be stopped.
Consider interdisciplinary collaboration
Throughout the course of management, psychiatrists should consider if and when it is necessary to consult with other specialties such as primary care, sports medicine, neurology, and neuropsychology. As with many psychiatric symptoms and disorders, collaboration with an interdisciplinary team is recommended. Primary care, sports medicine, or neurology should be involved in the management of patients with SRC. Choice of which of those 3 specialties in particular will depend on comfort level and experience with managing SRC of the individual providers in question as well as availability of each provider type in a given community.
Additionally, psychiatrists may wonder if and when they should refer patients with SRC for neuroimaging. Because SRC is a functional, rather than structural, brain disturbance, neuroimaging is not typically pursued because results would be expected to be normal.3 However, when in doubt, consultation with the interdisciplinary team can guide this decision. Factors that may lead to a decision to obtain neuroimaging include:
- an abnormal neurologic examination
- prolonged loss of consciousness
- unexpected persistence of symptoms (eg, 6 to 12 weeks)
- worsening symptoms.22
Continue to: If imaging is deemed necessary...
If imaging is deemed necessary for a patient with an acute SRC, brain CT is typically the imaging modality of choice; however, if imaging is deemed necessary due to the persistence of symptoms, then MRI is often the preferred test because it provides more detailed information and does not expose the patient to ionizing radiation.22 While results are often normal, the ordering clinician should be prepared for the possibility of incidental findings, such as cysts or aneurysms, and the need for further consultation with other clinicians to weigh in on such findings.22
CASE CONTINUED
Ms. J is prescribed extended-release venlafaxine, 37.5 mg every morning for 5 days, and then is switched to 75 mg every morning. The psychiatrist hopes that venlafaxine might simultaneously offer benefit for Ms. J’s depression and migraine headaches. Venlafaxine is not FDA-approved for migraine, and there is more evidence supporting TCAs for preventing migraine. However, Ms. J is adamant that she does not want to take a medication, such as a TCA, that could cause weight gain or sedation, which could be problematic in her sport. The psychiatrist also tells Ms. J to avoid substances of abuse, and emphasizes the importance of good sleep hygiene. Finally, the psychiatrist communicates with the interdisciplinary medical team, which is helping Ms. J with gradual return-to-school and return-to-sport strategies and ensuring continued social involvement with the team even as she is held out from sport.
Ultimately, Ms. J’s extended-release venlafaxine is titrated to 150 mg every morning. After 2 months on this dose, her depressive symptoms remit. After her other symptoms remit, Ms. J has difficulty returning to certain practice drills that remind her of what she was doing when she sustained the SRC. She says that while participating in these drills, she has intrusive thoughts and images of the experience of her most recent concussion. She works with her psychiatrist on a gradual program of exposure therapy so she can return to all types of practice. Ms. J says she wishes to continue playing volleyball; however, together with her parents and treatment team, she decides that any additional SRCs might lead her to retire from the sport.
Bottom Line
Psychiatric symptoms are common after sport-related concussion (SRC). The nature of the relationship between concussion and mental health is not firmly established. Post-SRC psychiatric symptoms need to be carefully managed to avoid unnecessary treatment or restrictions.
Related Resources
- National Collegiate Athletic Association. Concussion. www.ncaa.org/sport-science-institute/concussion.
- American Academy of Neurology. Sports concussion resources. www.aan.com/tools-and-resources/practicing-neurologists-administrators/patient-resources/sports-concussion-resources. Published 2020.
Drug Brand Names
Trazodone • Desyrel
Venlafaxine • Effexor
1. Morgan CD, Zuckerman SL, Lee YM, et al. Predictors of postconcussion syndrome after sports-related concussion in young athletes: a matched case-control study. J Neurosurg Pediatr. 2015;15(6):589-598.
2. Jorge RE, Arciniegas DB. Mood disorders after TBI. Psychiatr Clin North Am. 2014;37(1):13-29.
3. McCrory P, Meeuwisse W, Dvor˘ák J, et al. Consensus statement on concussion in sport—the 5th International Conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838-847.
4. Reardon CL, Hainline B, Aron CM, et al. Mental health in elite athletes: International Olympic Committee consensus statement (2019). Br J Sports Med. 2019;53(11):667-699.
5. Echemendia RJ, Meeuwisse W, McCrory P, et al. The sport concussion assessment tool 5th edition (SCAT5): background and rationale. Br J Sports Med. 2017;51:848-850.
6. Thompson E. Hamilton rating scale for anxiety (HAM-A). Occup Med. 2015;65(7):601.
7. Rice SM, Parker AG, Rosenbaum S, et al. Sport-related concussion outcomes in elite athletes: a systematic review. Sports Med. 2018;48(2):447-465.
8. Vargas G, Rabinowitz A, Meyer J, et al. Predictors and prevalence of postconcussion depression symptoms in collegiate athletes. J Athl Train. 2015;50(3):250-255.
9. Hutchison MG, Di Battista AP, McCoskey J, et al. Systematic review of mental health measures associated with concussive and subconcussive head trauma in former athletes. Int J Psychophysiol. 2018;132(Pt A):55-61.
10. Kerr GA, Stirling AE. Parents’ reflections on their child’s experiences of emotionally abusive coaching practices. J Appl Sport Psychol. 2012;24(2):191-206.
11. Guskiewicz KM, Marshall SW, Bailes J, et al. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exerc. 2007;39(6):903-909.
12. Lehman EJ, Hein MJ, Gersic CM. Suicide mortality among retired National Football League players who played 5 or more seasons. Am J Sports Med. 2016;44(10):2486-2491.
13. Fralick M, Sy E, Hassan A, et al. Association of concussion with the risk of suicide: a systematic review and meta-analysis. JAMA Neurol. 2018;76(2):144-151.
14. Brassil HE, Salvatore AP. The frequency of post-traumatic stress disorder symptoms in athletes with and without sports related concussion. Clin Transl Med. 2018;7:25.
15. Bateman A, Morgan KAD. The postinjury psychological sequelae of high-level Jamaican athletes: exploration of a posttraumatic stress disorder-self-efficacy conceptualization. J Sport Rehabil. 2019;28(2):144-152.
16. Brewer BW, Van Raalte JL, Cornelius AE, et al. Psychological factors, rehabilitation adherence, and rehabilitation outcome after anterior cruciate ligament reconstruction. Rehabil Psychol. 2000;45(1):20-37.
17. Putukian M, Echemendia RJ. Psychological aspects of serious head injury in the competitive athlete. Clin Sports Med. 2003;22(33):617-630.
18. James LM, Strom TQ, Leskela J. Risk-taking behaviors and impulsivity among Veterans with and without PTSD and mild TBI. Mil Med. 2014;179(4):357-363.
19. Harmon KG, Drezner J, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Clin J Sport Med. 2013;47(1):15-26.
20. Nelson LD, Guskiewicz KM, Marshall SW, et al. Multiple self-reported concussions are more prevalent in athletes with ADHD and learning disability. Clin J Sport Med. 2016;26(2):120-127.
21. Esfandiari A, Broshek DK, Freeman JR. Psychiatric and neuropsychological issues in sports medicine. Clin Sports Med. 2011;30(3):611-627.
22. Mahooti N. Sport-related concussion: acute management and chronic postconcussive issues. Chld Adolesc Psychiatric Clin N Am. 2018;27(1):93-108.
23. Kontos AP, Covassin T, Elbin RJ, et al. Depression and neurocognitive performance after concussion among male and female high school and collegiate athletes. Arch Phys Med Rehabil. 2012;93(10):1751-1756.
24. Harmon KG, Clugston JR, Dec K, et al. American Medical Society for Sports Medicine position statement on concussion in sport. Clin J Sport Med. 2019;29(2):87-100.
25. Leddy JJ, Willer B. Use of graded exercise testing in concussion and return-to-activity management. Current Sports Medicine Reports. 2013;12(6):370-376.
26. Schneider KJ, Iverson GL, Emery CA, et al. The effects of rest and treatment following sport-related concussion: a systematic review of the literature. Br J Sports Med. 2013;47(5):304-307.
27. Wayment HA, Huffman AH. Psychosocial experiences of concussed collegiate athletes: the role of emotional support in the recovery process. J Am Coll Health. 2020;68(4):438-443.
28. Todd R, Bhalerao S, Vu MT, et al. Understanding the psychiatric effects of concussion on constructed identity in hockey players: implications for health professionals. PLoS ONE. 2018;13(2):e0192125.
29. Iverson GL, Silverberg ND, Mannix R, et al. Factors associated with concussion-like symptom reporting in high school athletes. JAMA Pediatr. 2015;169(12):1132-1140.
30. Gaetz M. The multi-factorial origins of chronic traumatic encephalopathy (CTE) symptomatology in post-career athletes: the athlete post-career adjustment (AP-CA) model. Med Hypotheses. 2017;102:130-143.
31. Meehan WP. Medical therapies for concussion. Clin Sports Med. 2011;30(1):115-124.
32. Broglio SP, Collins MW, Williams RM, et al. Current and emerging rehabilitation for concussion: a review of the evidence. Clin Sports Med. 2015;34(2):213-231.
33. Arciniegas DB, Silver JM, McAllister TW. Stimulants and acetylcholinesterase inhibitors for the treatment of cognitive impairment after traumatic brain injury. Psychopharm Review. 2008;43(12):91-97.
34. Warden DL, Gordon B, McAllister TW, et al. Guidelines for the pharmacologic treatment of neurobehavioral sequelae of traumatic brain injury. J Neurotrauma. 2006;23(10):1468-1501.
35. Maldonado MD, Murillo-Cabezas F, Terron MP, et al. The potential of melatonin in reducing morbidity/mortality after craniocerebral trauma. J Pineal Res. 2007;42(1):1-11.
36. Samantaray S, Das A, Thakore NP, et al. Therapeutic potential of melatonin in traumatic central nervous system injury. J Pineal Res. 2009;47(2):134-142.
37. Chew E, Zafonte RD. Pharmacological management of neurobehavioral disorders following traumatic brain injury—a state-of-the-art review. J Rehabil Res Dev. 2009;46(6):851-879.
1. Morgan CD, Zuckerman SL, Lee YM, et al. Predictors of postconcussion syndrome after sports-related concussion in young athletes: a matched case-control study. J Neurosurg Pediatr. 2015;15(6):589-598.
2. Jorge RE, Arciniegas DB. Mood disorders after TBI. Psychiatr Clin North Am. 2014;37(1):13-29.
3. McCrory P, Meeuwisse W, Dvor˘ák J, et al. Consensus statement on concussion in sport—the 5th International Conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838-847.
4. Reardon CL, Hainline B, Aron CM, et al. Mental health in elite athletes: International Olympic Committee consensus statement (2019). Br J Sports Med. 2019;53(11):667-699.
5. Echemendia RJ, Meeuwisse W, McCrory P, et al. The sport concussion assessment tool 5th edition (SCAT5): background and rationale. Br J Sports Med. 2017;51:848-850.
6. Thompson E. Hamilton rating scale for anxiety (HAM-A). Occup Med. 2015;65(7):601.
7. Rice SM, Parker AG, Rosenbaum S, et al. Sport-related concussion outcomes in elite athletes: a systematic review. Sports Med. 2018;48(2):447-465.
8. Vargas G, Rabinowitz A, Meyer J, et al. Predictors and prevalence of postconcussion depression symptoms in collegiate athletes. J Athl Train. 2015;50(3):250-255.
9. Hutchison MG, Di Battista AP, McCoskey J, et al. Systematic review of mental health measures associated with concussive and subconcussive head trauma in former athletes. Int J Psychophysiol. 2018;132(Pt A):55-61.
10. Kerr GA, Stirling AE. Parents’ reflections on their child’s experiences of emotionally abusive coaching practices. J Appl Sport Psychol. 2012;24(2):191-206.
11. Guskiewicz KM, Marshall SW, Bailes J, et al. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exerc. 2007;39(6):903-909.
12. Lehman EJ, Hein MJ, Gersic CM. Suicide mortality among retired National Football League players who played 5 or more seasons. Am J Sports Med. 2016;44(10):2486-2491.
13. Fralick M, Sy E, Hassan A, et al. Association of concussion with the risk of suicide: a systematic review and meta-analysis. JAMA Neurol. 2018;76(2):144-151.
14. Brassil HE, Salvatore AP. The frequency of post-traumatic stress disorder symptoms in athletes with and without sports related concussion. Clin Transl Med. 2018;7:25.
15. Bateman A, Morgan KAD. The postinjury psychological sequelae of high-level Jamaican athletes: exploration of a posttraumatic stress disorder-self-efficacy conceptualization. J Sport Rehabil. 2019;28(2):144-152.
16. Brewer BW, Van Raalte JL, Cornelius AE, et al. Psychological factors, rehabilitation adherence, and rehabilitation outcome after anterior cruciate ligament reconstruction. Rehabil Psychol. 2000;45(1):20-37.
17. Putukian M, Echemendia RJ. Psychological aspects of serious head injury in the competitive athlete. Clin Sports Med. 2003;22(33):617-630.
18. James LM, Strom TQ, Leskela J. Risk-taking behaviors and impulsivity among Veterans with and without PTSD and mild TBI. Mil Med. 2014;179(4):357-363.
19. Harmon KG, Drezner J, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Clin J Sport Med. 2013;47(1):15-26.
20. Nelson LD, Guskiewicz KM, Marshall SW, et al. Multiple self-reported concussions are more prevalent in athletes with ADHD and learning disability. Clin J Sport Med. 2016;26(2):120-127.
21. Esfandiari A, Broshek DK, Freeman JR. Psychiatric and neuropsychological issues in sports medicine. Clin Sports Med. 2011;30(3):611-627.
22. Mahooti N. Sport-related concussion: acute management and chronic postconcussive issues. Chld Adolesc Psychiatric Clin N Am. 2018;27(1):93-108.
23. Kontos AP, Covassin T, Elbin RJ, et al. Depression and neurocognitive performance after concussion among male and female high school and collegiate athletes. Arch Phys Med Rehabil. 2012;93(10):1751-1756.
24. Harmon KG, Clugston JR, Dec K, et al. American Medical Society for Sports Medicine position statement on concussion in sport. Clin J Sport Med. 2019;29(2):87-100.
25. Leddy JJ, Willer B. Use of graded exercise testing in concussion and return-to-activity management. Current Sports Medicine Reports. 2013;12(6):370-376.
26. Schneider KJ, Iverson GL, Emery CA, et al. The effects of rest and treatment following sport-related concussion: a systematic review of the literature. Br J Sports Med. 2013;47(5):304-307.
27. Wayment HA, Huffman AH. Psychosocial experiences of concussed collegiate athletes: the role of emotional support in the recovery process. J Am Coll Health. 2020;68(4):438-443.
28. Todd R, Bhalerao S, Vu MT, et al. Understanding the psychiatric effects of concussion on constructed identity in hockey players: implications for health professionals. PLoS ONE. 2018;13(2):e0192125.
29. Iverson GL, Silverberg ND, Mannix R, et al. Factors associated with concussion-like symptom reporting in high school athletes. JAMA Pediatr. 2015;169(12):1132-1140.
30. Gaetz M. The multi-factorial origins of chronic traumatic encephalopathy (CTE) symptomatology in post-career athletes: the athlete post-career adjustment (AP-CA) model. Med Hypotheses. 2017;102:130-143.
31. Meehan WP. Medical therapies for concussion. Clin Sports Med. 2011;30(1):115-124.
32. Broglio SP, Collins MW, Williams RM, et al. Current and emerging rehabilitation for concussion: a review of the evidence. Clin Sports Med. 2015;34(2):213-231.
33. Arciniegas DB, Silver JM, McAllister TW. Stimulants and acetylcholinesterase inhibitors for the treatment of cognitive impairment after traumatic brain injury. Psychopharm Review. 2008;43(12):91-97.
34. Warden DL, Gordon B, McAllister TW, et al. Guidelines for the pharmacologic treatment of neurobehavioral sequelae of traumatic brain injury. J Neurotrauma. 2006;23(10):1468-1501.
35. Maldonado MD, Murillo-Cabezas F, Terron MP, et al. The potential of melatonin in reducing morbidity/mortality after craniocerebral trauma. J Pineal Res. 2007;42(1):1-11.
36. Samantaray S, Das A, Thakore NP, et al. Therapeutic potential of melatonin in traumatic central nervous system injury. J Pineal Res. 2009;47(2):134-142.
37. Chew E, Zafonte RD. Pharmacological management of neurobehavioral disorders following traumatic brain injury—a state-of-the-art review. J Rehabil Res Dev. 2009;46(6):851-879.
Anorexia nervosa and COVID-19
Recent concerns surrounding coronavirus disease 2019 (COVID-19) make it timely to reexamine the complex findings related to eating disorders and the immune system, and the risks for and detection of infection in patients with anorexia nervosa (AN) and similar disorders. To date, there are no published studies evaluating patients with eating disorders and COVID-19. However, it may be helpful to review the data on the infectious process in this patient population to improve patient communication, enhance surveillance and detection, and possibly reduce morbidity and mortality.
The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) issued warnings that individuals who are older, have underlying medical conditions, and/or are immunocompromised face the greatest risk of serious complications and death as a result of COVID-19, the disease process caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Due to malnutrition, patients with eating disorders, especially AN, may be perceived to have an increased risk of medical conditions and infection. Despite many studies on specific changes and differences in the immune system of patients with eating disorders, the consequences of these changes remain controversial and inconclusive.
This article reviews research on eating disorders, focusing on published data regarding the effects of AN on the immune system, susceptibility to infections, infectious detection, and morbidity. We also discuss clinical considerations related to COVID-19 and patients with AN.
Infection risks: Conflicting data
In a 1981 study that included 9 participants, Golla et al1 concluded that patients with AN may have “resistance” to infections based on a suggested protective factor within the immune system of these patients. Because this study has been cited repeatedly in multiple articles about AN and cell-mediated immunity,2-7 some clinicians have accepted this evidence of resistance to infection in patients with AN, which may lower their suspicion for and detection of infections in patients with AN.
However, studies published both before and after Golla et al1 have shown statistically significant results that contradict those researchers’ conclusion. A study that compared the medical records of 68 patients with AN with those who did not have AN found no significant difference, and concluded that the rate of infection among patients with AN is the same as among controls.8 These researchers noted that infection rates may be higher among patients with later-stage, more severe AN. In a 1986 study of 12 patients with AN, Cason et al9 concluded that while cellular immunity function is abnormal in patients with AN, their results were not compatible with prior studies that suggested AN patients were more resistant to infection.1,2,8
More recently, researchers compared 1,592 patients with eating disorders with 6,368 matched controls; they reviewed prescriptions of antibacterial, antifungal, and antiviral medications as a measure of infection rates.10 Compared with controls, patients with binge eating disorder (BED), patients with bulimia nervosa (BN), and males with AN more often received prescriptions for antimicrobial medications. There was no statistically significant difference between controls and females with AN, which is consistent with other reports of no increased or decreased risk of infection among females with AN. In terms of antiviral use, this study showed an increased prescription of antivirals only in the BN group.
Several other studies examining the rate of infection in patients with AN concluded that there is neither an increased nor decreased rate of infection in patients with AN, and that the rate of infection in this population is similar to that of the general population.8,10-12 Because studies that have included patients with AN have evaluated only symptomatic viral infections, some researchers have proposed that patients with AN may show lower rates of symptomatic viral infection but higher rates of asymptomatic infection, as evidenced by higher viral titers.6 Further research is required. Despite controversy regarding infection rates, studies have found that patients with AN have increased rates of morbidity and mortality from infections.6,12-16
Continue to: Obstacles to detecting infections
Obstacles to detecting infections
Several factors can complicate the surveillance and detection of infections in patients with eating disorders, especially those with AN. These include:
- an accepted predisposition to infection secondary to malnutrition
- a lack of visual or reported infectious symptoms
- misrepresentation and assumptions from published research.
Clinicians who report fewer observed cases of infections among patients with AN may be overlooking comorbid disease processes due to a bias from the literature and/or a lack of awareness of symptom parameters in patients with AN.
Features of AN include a loss of adipose tissue responsible for pro-inflammatory cytokines, and excessive exercise, which stimulates anti-inflammatory myokines. This can modulate the experience of illness that impacts the core features of disease,17 possibly reducing symptomatic presentation of infections.
Fever. The presence and intensity of fever may be altered in patients with eating disorders, especially those with AN. In a study of 311 inpatients with AN, researchers found that patients with AN had a significant delay in fever response in AN.12 Of 23 patients with an active bacterial infection, all but 5 had a fever <37°C, with some as low as 35.5°C. A detectable fever response and unexplained fevers were found in 2 of the 6 patients with a viral infection. A series of case studies found that patients with AN with bacterial infections also had a delayed fever response.18
For patients with infections that commonly present with fever, such as COVID-19, a delayed fever response can delay or evade the detection of infection, thus increasing potential complications as well viral exposure to others. Thus, clinicians should use caution when ruling out COVID-19 or other infections because of a lack of significant fever.
Continue to: Overlapping symptoms
Overlapping symptoms. The symptoms of viral infection can mimic the symptoms of AN, which further complicates screening and diagnosis of infection in these patients. Although up to 80% of individuals infected with COVID-19 may be asymptomatic or have a mild presentation, the most common reported symptoms are fever (92.6%), shortness of breath (50.8%), expectoration (41.4%), fatigue (46.4%), dry cough (33.3%), and myalgia (21.4%).19-21 Gastrointestinal (GI) symptoms have been reported in patients with COVID-19, as well as a loss of taste and smell.
Commonly reported physical symptoms of AN include an intolerance to cold, general fatigue, muscle aches and pains, restlessness, emesis, and a multitude of GI complaints. Patients with AN also have been reported to experience shortness of breath due to conditions such as respiratory muscle weakness,22 nutritional emphysema,23 and anxiety and panic attack.24 These conditions could lead to an increased susceptibility to COVID-19 and increased complications during treatment. Cardiac abnormalities, which are common in patients with AN and BN, may increase the risk of adverse events. While these symptoms may be an important part of screening for diseases such as COVID-19, suspicion of infection also may be lower because of the overlap of AN symptomology, underlying conditions, and a delayed fever response.
Laboratory findings. Laboratory testing results for patients with COVID-19 include lower lymphocyte counts, higher leukocyte counts, elevated levels of infection-related biomarkers and inflammatory cytokines, and significantly decreased T-cell counts.19 Similar values are also found in patients with AN.
The similar clinical presentations and laboratory values of AN and COVID-19 could lead to delayed diagnosis, increased disease transmission, cross-contamination of facilities, and higher incidences of medical complications and mortality.
The immunology of AN and correlations with COVID-19
Many studies examining the immune system of patients with eating disorders, especially those with AN, have discovered changes and differences in both cell-mediated and humoral response to infections.1,3,5,7,9,11,16,21,25-27 Whether these differences represent a dysfunctional immune system, an immunocompromised state, or even a protective factor remains unclear.
Continue to: While some studies have reported...
While some studies have reported that AN represents an immunocompromised state, others describe the immune system of patients with AN as dysfunctional or simply altered.9,11,22,28 Some studies have found that patients with AN had delayed reactions to pathogen skin exposures compared with healthy controls, which provides evidence of an impaired cell-mediated immune system.9,27,29
Some studies have considered the consequences of infection and immunologic findings as markers of or contributing to the onset of AN.2,30,31 Numerous studies have noted abnormalities in AN with regards to cell-mediated immunity, the humoral system, the lymphoreticular system, and the innate immune system, and potential contributions from increased oxidative stress, a chronically activated sympathetic nervous system and hypothalamic-pituitary-adrenal axis, altered intestinal microbiota, and an abnormal bone marrow microenvironment.2
Box 1
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a new beta-coronavirus that is still being studied for its effects on the immune system. It may take years to fully understand the nature of the pathogen and the response of the human immune system. To better understand COVID19, researchers have been turning to what they learned from the past outbreaks of severe acute respiratory syndrome (SARS) in 2003- 2004 and Middle East respiratory syndrome (MERS) in 2011, both caused by betacoronaviruses with a zoonotic origin.25,32
The proposed pathogenesis for infection of SARS-CoV-2 is similar to SARS and occurs when aerosolized droplets containing the virus enter the host.32 While currently there is only initial data on the host innate immune status of patients infected with SARS-CoV-2, initial findings of a report on 99 cases in Wuhan, China included increased total neutrophils (38%), reduced total lymphocytes (35%), increased serum interleukin-6 (52%), and increased C-reactive protein (84%).33 Additional findings were decreased percentages of monocytes, eosinophils, and basophils, as well as significantly decreased levels of cytokines and T-cells in more severe cases.19 Past research with SARS reported similar T-cell findings, with a more frequent CD8+ response and a greater magnitude of CD4+.34
Box 119,25,32-34 describes some of the initial immunologic findings reported in patients with COVID-19. In Box 2,5,8,11,13,14,19,26,28,35-40 we discuss reports that describe the immunologic overlay of COVID-19 and AN.
Box 2
Leukopenia (low leukocyte levels) is a common finding in patients with anorexia nervosa (AN),8 and often leads clinicians to lower their suspicion for infection. A 2008 Hungarian study that evaluated lymphocyte activation parameters and clinical status in 11 adolescents (10 girls and 1 boy) with AN, 12 obese adolescents, and 10 healthy controls did not find any association between the variables.35 While many studies have focused on adults, it is important to note that leukopenia is a common finding in adolescents (age 12 to 17) with AN.36
Leukocyte counts are elevated in coronavirus disease 2019 (COVID-19), possibly offsetting AN’s leukopenia. In addition, neutrophil counts are elevated and monocyte, eosinophil, basophil, and especially lymphocyte counts are significantly decreased. A meta-analysis that included 22 studies and 924 participants (512 with AN and 412 controls) examined common inflammatory cytokine findings in patients with AN.11 Compared with healthy controls, patients with AN had significantly elevated levels of tumor necrosis factor alpha (TNF-alpha), interleukin (IL)-1, IL-6, and TNF-receptor II, and significantly decreased levels of C-reactive protein and IL-6 receptor. Elevated levels of TNF-alpha and IL-6 also have been reported in patients with COVID-19.19 These findings may mask suspicion for infection in patients with AN.19
In patients with AN and those with bulimia nervosa, CD4+-to-CD8+ ratios also have been found to be low as a result of normal-tohigher levels of CD4+ cells and lower levels of CD8+ cells.36-39 Researchers have also proposed that the lymphocytosis observed in AN is a result of increased naïve CD4+.36 In AN, total lymphocyte counts have been found to correlate positively with a patient’s body mass index (BMI), while the CD4+ T-lymphocyte correlated negatively with BMI and were critically low in patients with severe malnutrition.26,40 In patients with COVID-19, CD4+ levels have reported to be within normal range, naïve CD4+ cells were elevated, and CD8+ cells were slightly decreased,19 which is similar to the findings in AN.
Fewer studies have evaluated humoral immune response in AN, and results have varied. One study (N = 46) found elevated B-cell counts in adolescents with AN-restricting type,36 while another (N = 40) reported normal levels of B-cells.5 Specific decreases in immunoglobulin (Ig) G and IgM have also been reported in AN, while IgA, IgG, and IgM usually are normal in COVID-19.19
Despite differences in immune system function, cellular immunity appears to remain relatively intact in patients with AN, but can become compromised with severe malnutrition or with advanced weight loss.28,40 This compromised immunity related to severe AN with a very low BMI likely leads to the increased morbidity and mortality.8,13,14
Malnutrition and the immune system
Differences in the type of malnutrition observed in low-weight patients with AN may help explain why patients with AN can maintain a relatively intact cell-mediated immune system.1 Protein-energy malnutrition (PEM), which is found in typical states of starvation, consists of deficiencies in multiple vitamins, protein, and energy (caloric content), whereas the dietary habits of patients with AN usually result in a deficiency of carbohydrates and fats.41 Studies that examined the impact of PEM on immunity to influenza infection have suggested that balanced protein energy replenishment may be a strategy for boosting immunity against influenza viral infections.42 However, carbohydrates are the primary nutrients for human bone marrow fat cells, which play a crucial role in the maturation of white blood cells. This may account for the leukopenia that is common in patients with AN.6,43 The protein-sparing aspect of the typical AN diet may account for the immune system changes observed in patients with AN.44
Although some studies have proposed that immune deficiencies observed in patients with AN are secondary to malnutrition and return to normal with refeeding,5,40,45 others have concluded that immune function is not compromised by factors such as nutritional status or body weight in AN.26,43,46
Continue to: Clinical considerations
Clinical considerations
Neither the CDC nor the WHO have issued a specific protocol for monitoring for and treating COVID-19 in patients with eating disorders; however, the guidelines offered by these organizations for the general population should be followed for patients with eating disorders.
When screening a patient with an eating disorder, keep in mind that the symptoms of eating disorders, such as AN, may mimic an infectious process. Mood symptoms, such as depression or anxiety, could represent physiological responses to infection. Patients with GI symptoms that typically are considered part of the pathology of an eating disorder should be more carefully considered for COVID-19. Monitor a patient’s basal body temperature, and be mindful that a patient with AN may exhibit a delayed fever response. Be vigilant for a recent loss of taste or smell, which should raise suspicion for COVID-19. When monitoring vital signs, pay careful attention for any decompensation in a patient’s pulse oximetry. Whenever possible, order COVID-19 testing for any patient you suspect may be infected.
Outpatient clinicians should work closely in a collaborative manner with a patient’s eating disorder treatment team. Psychiatrists, primary care physicians, psychotherapists, nutritionists, and other clinicians should all follow CDC/WHO guidelines regarding COVID-19, provide surveillance, and communicate any suspicions to the medical team. Eating disorder treatment programs, including residential centers, partial hospital programs (PHP), and intensive outpatient programs (IOP), must enhance monitoring for COVID-19, and exercise caution by practicing social distancing and providing adequate personal protective equipment for patients and staff. To reduce the spread of COVID-19, many IOPs and PHPs have transitioned to virtual treatment. Residential centers must carefully screen patients before admission to weigh the risks and benefits of inpatient vs outpatient care.
Bottom Line
Differences in the immune system of patients with an eating disorder do not necessarily confer a higher or lower risk of infection. Symptoms of some infections can mimic the symptoms of anorexia nervosa. Recognizing infections in patients with eating disorders is critical because compared with the general population, they have higher rates of infection-related morbidity and mortality.
Related Resources
- Congress J, Madaan V. 6 ‘M’s to keep in mind when you next see a patient with anorexia nervosa. Current Psychiatry. 2014;13(5):58-59.
- Westmoreland P. Eating disorders: Masterclass lecture part I. Psychcast (podcast). https://www.mdedge.com/podcasts/psychcast/eating-disorders-masterclass-lecture-part-i.
1. Golla JA, Larson LA, Anderson CF, et al. An immunological assessment of patients with anorexia nervosa. Am J Clin Nutr. 1981;34(12):2756-2762.
2. Gibson D, Mehler PS. Anorexia nervosa and the immune system—a narrative review. J Clin Med. 2019;8(11):1915. doi: 10.3390/jcm8111915.
3. Słotwin
4. Nova E, Samartín S, Gómez S, et al. The adaptive response of the immune system to the particular malnutrition of eating disorders. Eur J Clin Nutr. 2002;56(suppl 3):S34-S37.
5. Allende LM, Corell A, Manzanares J, et al. Immunodeficiency associated with anorexia nervosa is secondary and improves after refeeding. Immunology. 1998;94(4):543-551.
6. Brown RF, Bartrop R, Birmingham CL. Immunological disturbance and infectious disease in anorexia nervosa: a review. Acta Neuropsychiatr. 2008;20(3):117-128.
7. Polack E, Nahmod VE, Emeric-Sauval E, et al. Low lymphocyte interferon-gamma production and variable proliferative response in anorexia nervosa patients. J Clin Immunol. 1993;13(6):445-451.
8. Bowers TK, Eckert E. Leukopenia in anorexia nervosa. Lack of increased risk of infection. Arch Intern Med. 1978;138(10):1520-1523.
9. Cason J, Ainley CC, Wolstencroft RA, et al. Cell-mediated immunity in anorexia nervosa. Clin Exp Immunol. 1986;64(2):370-375.
10. Raevuori A, Lukkariniemi L, Suokas JT, et al. Increased use of antimicrobial medication in bulimia nervosa and binge-eating disorder prior to the eating disorder treatment. Int J Eat Disord. 2016;49(6):542-552.
11. Solmi M, Veronese N, Favaro A, et al. Inflammatory cytokines and anorexia nervosa: a meta-analysis of cross-sectional and longitudinal studies. Psychoneuroendocrinology. 2015;51:237-252.
12. Brown RF, Bartrop R, Beumont P, et al. Bacterial infections in anorexia nervosa: delayed recognition increases complications. Int J Eat Disord. 2005;37(3):261-265.
13. Theander S. Anorexia nervosa. A psychiatric investigation of 94 female patients. Acta Psychiatr Scand Suppl. 1970;214:1-194.
14. Warren MP, Vande Wiele RL. Clinical and metabolic features of anorexia nervosa. Am J Obstet Gynecol. 1973;117(3):435-449.
15. Copeland PM, Herzog DB. Hypoglycemia and death in anorexia nervosa. Psychother Psychosom. 1987;48(1-4):146-150.
16. Devuyst O, Lambert M, Rodhain J, et al. Haematological changes and infectious complications in anorexia nervosa: a case-control study. Q J Med. 1993;86(12):791-799.
17. Pisetsky DS, Trace SE, Brownley KA, et al. The expression of cytokines and chemokines in the blood of patients with severe weight loss from anorexia nervosa: an exploratory study. Cytokine. 2014;69(1):110-115.
18. Birmingham CL, Hodgson DM, Fung J, et al. Reduced febrile response to bacterial infection in anorexia nervosa patients. Int J Eat Disord. 2003;34(2):269-272.
19. Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China [published online March 12, 2020]. Clin Infect Dis. doi: 10.1093/cid/ciaa248.
20. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
21. Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514-523.
22. Birmingham CL, Tan AO. Respiratory muscle weakness and anorexia nervosa. Int J Eat Disord. 2003;33(2):230-233.
23. Cook VJ, Coxson HO, Mason AG, et al. Bullae, bronchiectasis and nutritional emphysema in severe anorexia nervosa. Can Respir J. 2001;8(5):361-365.
24. Khalsa SS, Hassanpour MS, Strober M, et al. Interoceptive anxiety and body representation in anorexia nervosa [published online September 21, 2018]. Front Psychiatry. 2018;9:444. doi: 10.3389/fpsyt.2018.00444.
25. van West D, Maes M. Cytokines in de obsessief compulsieve stoornis en in anorexia nervosa: een overzicht. Acta Neuropsychiatr. 1999;11(4):125-129.
26. Komorowska-Pietrzykowska R, Rajewski A, Wiktorowicz K, et al. Czynnos
27. Marcos A, Varela P, Toro O, et al. Interactions between nutrition and immunity in anorexia nervosa: a 1-y follow-up study. Am J Clin Nutr. 1997;66(2):485S-490S.
28. Pertschuk MJ, Crosby LO, Barot L, et al. Immunocompetency in anorexia nervosa. Am J Clin Nutr. 1982;35(5):968-972.
29. Varela P, Marcos A, Navarro MP. Zinc status in anorexia nervosa. Ann Nutr Metab. 1992;36(4):197-202.
30. Breithaupt L, Köhler-Forsberg O, Larsen JT, et al. Association of exposure to infections in childhood with risk of eating disorders in adolescent girls. JAMA Psychiatry. 2019;76(8):800-809.
31. Brambilla F, Monti D, Franceschi C. Plasma concentrations of interleukin-1-beta, interleukin-6 and tumor necrosis factor-alpha, and of their soluble receptors and receptor antagonist in anorexia nervosa. Psychiatry Res. 2001;103(2-3):107-114.
32. Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic [published online February 27, 2020]. Asian Pac J Allergy Immunol. doi: 10.12932/AP-200220-0772.
33. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270-273.
34. Li CK, Wu H, Yan H, et al. T cell responses to whole SARS coronavirus in humans. J Immunol. 2008;181(8):5490-5500.
35. Páli AA, Pászthy B. Az immunrendszer muködésének megváltozása a táplálkozási magatartás zavarai esetén [Changes of the immune functions in patients with eating disorders]. Ideggyogy Sz. 2008;61(11-12):381‐384.
36. Elegido A, Graell M, Andrés P, et al. Increased naive CD4+ and B lymphocyte subsets are associated with body mass loss and drive relative lymphocytosis in anorexia nervosa patients. Nutr Res. 2017;39:43-50.
37. Marcos A, Varela P, Santacruz I, et al. Nutritional status and immunocompetence in eating disorders. A comparative study. Eur J Clin Nutr. 1993;47(11):787-793.
38. Mustafa A, Ward A, Treasure J, et al. T lymphocyte subpopulations in anorexia nervosa and refeeding. Clin Immunol Immunopathol. 1997;82(3):282-289.
39. Nagata T, Kiriike N, Tobitani W, et al. Lymphocyte subset, lymphocyte proliferative response, and soluble interleukin-2 receptor in anorexic patients. Biol Psychiatry. 1999;45(4):471-474.
40. Saito H, Nomura K, Hotta M, et al. Malnutrition induces dissociated changes in lymphocyte count and subset proportion in patients with anorexia nervosa. Int J Eat Disord. 2007;40(6):575-579.
41. Nova E, Varela P, López-Vidriero I, et al. A one-year follow-up study in anorexia nervosa. Dietary pattern and anthropometrical evolution. Eur J Clin Nutr. 2001;55(7):547-554.
42. Taylor AK, Cao W, Vora KP, et al. Protein energy malnutrition decreases immunity and increases susceptibility to influenza infection in mice. J Infect Dis. 2013;207(3):501-510.
43. Mant MJ, Faragher BS. The hematology of anorexia nervosa. Br J Haematol. 1972;23(6):737-749.
44. Marcos A. The immune system in eating disorders: an overview. Nutrition. 1997;13(10):853-862.
45. Schattner A, Tepper R, Steinbock M, et al. TNF, interferon-gamma and cell-mediated cytotoxicity in anorexia nervosa; effect of refeeding. J Clin Lab Immunol. 1990;32(4):183-184.
46. Nagata T, Tobitani W, Kiriike N, et al. Capacity to produce cytokines during weight restoration in patients with anorexia nervosa. Psychosom Med. 1999;61(3):371-377.
Recent concerns surrounding coronavirus disease 2019 (COVID-19) make it timely to reexamine the complex findings related to eating disorders and the immune system, and the risks for and detection of infection in patients with anorexia nervosa (AN) and similar disorders. To date, there are no published studies evaluating patients with eating disorders and COVID-19. However, it may be helpful to review the data on the infectious process in this patient population to improve patient communication, enhance surveillance and detection, and possibly reduce morbidity and mortality.
The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) issued warnings that individuals who are older, have underlying medical conditions, and/or are immunocompromised face the greatest risk of serious complications and death as a result of COVID-19, the disease process caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Due to malnutrition, patients with eating disorders, especially AN, may be perceived to have an increased risk of medical conditions and infection. Despite many studies on specific changes and differences in the immune system of patients with eating disorders, the consequences of these changes remain controversial and inconclusive.
This article reviews research on eating disorders, focusing on published data regarding the effects of AN on the immune system, susceptibility to infections, infectious detection, and morbidity. We also discuss clinical considerations related to COVID-19 and patients with AN.
Infection risks: Conflicting data
In a 1981 study that included 9 participants, Golla et al1 concluded that patients with AN may have “resistance” to infections based on a suggested protective factor within the immune system of these patients. Because this study has been cited repeatedly in multiple articles about AN and cell-mediated immunity,2-7 some clinicians have accepted this evidence of resistance to infection in patients with AN, which may lower their suspicion for and detection of infections in patients with AN.
However, studies published both before and after Golla et al1 have shown statistically significant results that contradict those researchers’ conclusion. A study that compared the medical records of 68 patients with AN with those who did not have AN found no significant difference, and concluded that the rate of infection among patients with AN is the same as among controls.8 These researchers noted that infection rates may be higher among patients with later-stage, more severe AN. In a 1986 study of 12 patients with AN, Cason et al9 concluded that while cellular immunity function is abnormal in patients with AN, their results were not compatible with prior studies that suggested AN patients were more resistant to infection.1,2,8
More recently, researchers compared 1,592 patients with eating disorders with 6,368 matched controls; they reviewed prescriptions of antibacterial, antifungal, and antiviral medications as a measure of infection rates.10 Compared with controls, patients with binge eating disorder (BED), patients with bulimia nervosa (BN), and males with AN more often received prescriptions for antimicrobial medications. There was no statistically significant difference between controls and females with AN, which is consistent with other reports of no increased or decreased risk of infection among females with AN. In terms of antiviral use, this study showed an increased prescription of antivirals only in the BN group.
Several other studies examining the rate of infection in patients with AN concluded that there is neither an increased nor decreased rate of infection in patients with AN, and that the rate of infection in this population is similar to that of the general population.8,10-12 Because studies that have included patients with AN have evaluated only symptomatic viral infections, some researchers have proposed that patients with AN may show lower rates of symptomatic viral infection but higher rates of asymptomatic infection, as evidenced by higher viral titers.6 Further research is required. Despite controversy regarding infection rates, studies have found that patients with AN have increased rates of morbidity and mortality from infections.6,12-16
Continue to: Obstacles to detecting infections
Obstacles to detecting infections
Several factors can complicate the surveillance and detection of infections in patients with eating disorders, especially those with AN. These include:
- an accepted predisposition to infection secondary to malnutrition
- a lack of visual or reported infectious symptoms
- misrepresentation and assumptions from published research.
Clinicians who report fewer observed cases of infections among patients with AN may be overlooking comorbid disease processes due to a bias from the literature and/or a lack of awareness of symptom parameters in patients with AN.
Features of AN include a loss of adipose tissue responsible for pro-inflammatory cytokines, and excessive exercise, which stimulates anti-inflammatory myokines. This can modulate the experience of illness that impacts the core features of disease,17 possibly reducing symptomatic presentation of infections.
Fever. The presence and intensity of fever may be altered in patients with eating disorders, especially those with AN. In a study of 311 inpatients with AN, researchers found that patients with AN had a significant delay in fever response in AN.12 Of 23 patients with an active bacterial infection, all but 5 had a fever <37°C, with some as low as 35.5°C. A detectable fever response and unexplained fevers were found in 2 of the 6 patients with a viral infection. A series of case studies found that patients with AN with bacterial infections also had a delayed fever response.18
For patients with infections that commonly present with fever, such as COVID-19, a delayed fever response can delay or evade the detection of infection, thus increasing potential complications as well viral exposure to others. Thus, clinicians should use caution when ruling out COVID-19 or other infections because of a lack of significant fever.
Continue to: Overlapping symptoms
Overlapping symptoms. The symptoms of viral infection can mimic the symptoms of AN, which further complicates screening and diagnosis of infection in these patients. Although up to 80% of individuals infected with COVID-19 may be asymptomatic or have a mild presentation, the most common reported symptoms are fever (92.6%), shortness of breath (50.8%), expectoration (41.4%), fatigue (46.4%), dry cough (33.3%), and myalgia (21.4%).19-21 Gastrointestinal (GI) symptoms have been reported in patients with COVID-19, as well as a loss of taste and smell.
Commonly reported physical symptoms of AN include an intolerance to cold, general fatigue, muscle aches and pains, restlessness, emesis, and a multitude of GI complaints. Patients with AN also have been reported to experience shortness of breath due to conditions such as respiratory muscle weakness,22 nutritional emphysema,23 and anxiety and panic attack.24 These conditions could lead to an increased susceptibility to COVID-19 and increased complications during treatment. Cardiac abnormalities, which are common in patients with AN and BN, may increase the risk of adverse events. While these symptoms may be an important part of screening for diseases such as COVID-19, suspicion of infection also may be lower because of the overlap of AN symptomology, underlying conditions, and a delayed fever response.
Laboratory findings. Laboratory testing results for patients with COVID-19 include lower lymphocyte counts, higher leukocyte counts, elevated levels of infection-related biomarkers and inflammatory cytokines, and significantly decreased T-cell counts.19 Similar values are also found in patients with AN.
The similar clinical presentations and laboratory values of AN and COVID-19 could lead to delayed diagnosis, increased disease transmission, cross-contamination of facilities, and higher incidences of medical complications and mortality.
The immunology of AN and correlations with COVID-19
Many studies examining the immune system of patients with eating disorders, especially those with AN, have discovered changes and differences in both cell-mediated and humoral response to infections.1,3,5,7,9,11,16,21,25-27 Whether these differences represent a dysfunctional immune system, an immunocompromised state, or even a protective factor remains unclear.
Continue to: While some studies have reported...
While some studies have reported that AN represents an immunocompromised state, others describe the immune system of patients with AN as dysfunctional or simply altered.9,11,22,28 Some studies have found that patients with AN had delayed reactions to pathogen skin exposures compared with healthy controls, which provides evidence of an impaired cell-mediated immune system.9,27,29
Some studies have considered the consequences of infection and immunologic findings as markers of or contributing to the onset of AN.2,30,31 Numerous studies have noted abnormalities in AN with regards to cell-mediated immunity, the humoral system, the lymphoreticular system, and the innate immune system, and potential contributions from increased oxidative stress, a chronically activated sympathetic nervous system and hypothalamic-pituitary-adrenal axis, altered intestinal microbiota, and an abnormal bone marrow microenvironment.2
Box 1
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a new beta-coronavirus that is still being studied for its effects on the immune system. It may take years to fully understand the nature of the pathogen and the response of the human immune system. To better understand COVID19, researchers have been turning to what they learned from the past outbreaks of severe acute respiratory syndrome (SARS) in 2003- 2004 and Middle East respiratory syndrome (MERS) in 2011, both caused by betacoronaviruses with a zoonotic origin.25,32
The proposed pathogenesis for infection of SARS-CoV-2 is similar to SARS and occurs when aerosolized droplets containing the virus enter the host.32 While currently there is only initial data on the host innate immune status of patients infected with SARS-CoV-2, initial findings of a report on 99 cases in Wuhan, China included increased total neutrophils (38%), reduced total lymphocytes (35%), increased serum interleukin-6 (52%), and increased C-reactive protein (84%).33 Additional findings were decreased percentages of monocytes, eosinophils, and basophils, as well as significantly decreased levels of cytokines and T-cells in more severe cases.19 Past research with SARS reported similar T-cell findings, with a more frequent CD8+ response and a greater magnitude of CD4+.34
Box 119,25,32-34 describes some of the initial immunologic findings reported in patients with COVID-19. In Box 2,5,8,11,13,14,19,26,28,35-40 we discuss reports that describe the immunologic overlay of COVID-19 and AN.
Box 2
Leukopenia (low leukocyte levels) is a common finding in patients with anorexia nervosa (AN),8 and often leads clinicians to lower their suspicion for infection. A 2008 Hungarian study that evaluated lymphocyte activation parameters and clinical status in 11 adolescents (10 girls and 1 boy) with AN, 12 obese adolescents, and 10 healthy controls did not find any association between the variables.35 While many studies have focused on adults, it is important to note that leukopenia is a common finding in adolescents (age 12 to 17) with AN.36
Leukocyte counts are elevated in coronavirus disease 2019 (COVID-19), possibly offsetting AN’s leukopenia. In addition, neutrophil counts are elevated and monocyte, eosinophil, basophil, and especially lymphocyte counts are significantly decreased. A meta-analysis that included 22 studies and 924 participants (512 with AN and 412 controls) examined common inflammatory cytokine findings in patients with AN.11 Compared with healthy controls, patients with AN had significantly elevated levels of tumor necrosis factor alpha (TNF-alpha), interleukin (IL)-1, IL-6, and TNF-receptor II, and significantly decreased levels of C-reactive protein and IL-6 receptor. Elevated levels of TNF-alpha and IL-6 also have been reported in patients with COVID-19.19 These findings may mask suspicion for infection in patients with AN.19
In patients with AN and those with bulimia nervosa, CD4+-to-CD8+ ratios also have been found to be low as a result of normal-tohigher levels of CD4+ cells and lower levels of CD8+ cells.36-39 Researchers have also proposed that the lymphocytosis observed in AN is a result of increased naïve CD4+.36 In AN, total lymphocyte counts have been found to correlate positively with a patient’s body mass index (BMI), while the CD4+ T-lymphocyte correlated negatively with BMI and were critically low in patients with severe malnutrition.26,40 In patients with COVID-19, CD4+ levels have reported to be within normal range, naïve CD4+ cells were elevated, and CD8+ cells were slightly decreased,19 which is similar to the findings in AN.
Fewer studies have evaluated humoral immune response in AN, and results have varied. One study (N = 46) found elevated B-cell counts in adolescents with AN-restricting type,36 while another (N = 40) reported normal levels of B-cells.5 Specific decreases in immunoglobulin (Ig) G and IgM have also been reported in AN, while IgA, IgG, and IgM usually are normal in COVID-19.19
Despite differences in immune system function, cellular immunity appears to remain relatively intact in patients with AN, but can become compromised with severe malnutrition or with advanced weight loss.28,40 This compromised immunity related to severe AN with a very low BMI likely leads to the increased morbidity and mortality.8,13,14
Malnutrition and the immune system
Differences in the type of malnutrition observed in low-weight patients with AN may help explain why patients with AN can maintain a relatively intact cell-mediated immune system.1 Protein-energy malnutrition (PEM), which is found in typical states of starvation, consists of deficiencies in multiple vitamins, protein, and energy (caloric content), whereas the dietary habits of patients with AN usually result in a deficiency of carbohydrates and fats.41 Studies that examined the impact of PEM on immunity to influenza infection have suggested that balanced protein energy replenishment may be a strategy for boosting immunity against influenza viral infections.42 However, carbohydrates are the primary nutrients for human bone marrow fat cells, which play a crucial role in the maturation of white blood cells. This may account for the leukopenia that is common in patients with AN.6,43 The protein-sparing aspect of the typical AN diet may account for the immune system changes observed in patients with AN.44
Although some studies have proposed that immune deficiencies observed in patients with AN are secondary to malnutrition and return to normal with refeeding,5,40,45 others have concluded that immune function is not compromised by factors such as nutritional status or body weight in AN.26,43,46
Continue to: Clinical considerations
Clinical considerations
Neither the CDC nor the WHO have issued a specific protocol for monitoring for and treating COVID-19 in patients with eating disorders; however, the guidelines offered by these organizations for the general population should be followed for patients with eating disorders.
When screening a patient with an eating disorder, keep in mind that the symptoms of eating disorders, such as AN, may mimic an infectious process. Mood symptoms, such as depression or anxiety, could represent physiological responses to infection. Patients with GI symptoms that typically are considered part of the pathology of an eating disorder should be more carefully considered for COVID-19. Monitor a patient’s basal body temperature, and be mindful that a patient with AN may exhibit a delayed fever response. Be vigilant for a recent loss of taste or smell, which should raise suspicion for COVID-19. When monitoring vital signs, pay careful attention for any decompensation in a patient’s pulse oximetry. Whenever possible, order COVID-19 testing for any patient you suspect may be infected.
Outpatient clinicians should work closely in a collaborative manner with a patient’s eating disorder treatment team. Psychiatrists, primary care physicians, psychotherapists, nutritionists, and other clinicians should all follow CDC/WHO guidelines regarding COVID-19, provide surveillance, and communicate any suspicions to the medical team. Eating disorder treatment programs, including residential centers, partial hospital programs (PHP), and intensive outpatient programs (IOP), must enhance monitoring for COVID-19, and exercise caution by practicing social distancing and providing adequate personal protective equipment for patients and staff. To reduce the spread of COVID-19, many IOPs and PHPs have transitioned to virtual treatment. Residential centers must carefully screen patients before admission to weigh the risks and benefits of inpatient vs outpatient care.
Bottom Line
Differences in the immune system of patients with an eating disorder do not necessarily confer a higher or lower risk of infection. Symptoms of some infections can mimic the symptoms of anorexia nervosa. Recognizing infections in patients with eating disorders is critical because compared with the general population, they have higher rates of infection-related morbidity and mortality.
Related Resources
- Congress J, Madaan V. 6 ‘M’s to keep in mind when you next see a patient with anorexia nervosa. Current Psychiatry. 2014;13(5):58-59.
- Westmoreland P. Eating disorders: Masterclass lecture part I. Psychcast (podcast). https://www.mdedge.com/podcasts/psychcast/eating-disorders-masterclass-lecture-part-i.
Recent concerns surrounding coronavirus disease 2019 (COVID-19) make it timely to reexamine the complex findings related to eating disorders and the immune system, and the risks for and detection of infection in patients with anorexia nervosa (AN) and similar disorders. To date, there are no published studies evaluating patients with eating disorders and COVID-19. However, it may be helpful to review the data on the infectious process in this patient population to improve patient communication, enhance surveillance and detection, and possibly reduce morbidity and mortality.
The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) issued warnings that individuals who are older, have underlying medical conditions, and/or are immunocompromised face the greatest risk of serious complications and death as a result of COVID-19, the disease process caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Due to malnutrition, patients with eating disorders, especially AN, may be perceived to have an increased risk of medical conditions and infection. Despite many studies on specific changes and differences in the immune system of patients with eating disorders, the consequences of these changes remain controversial and inconclusive.
This article reviews research on eating disorders, focusing on published data regarding the effects of AN on the immune system, susceptibility to infections, infectious detection, and morbidity. We also discuss clinical considerations related to COVID-19 and patients with AN.
Infection risks: Conflicting data
In a 1981 study that included 9 participants, Golla et al1 concluded that patients with AN may have “resistance” to infections based on a suggested protective factor within the immune system of these patients. Because this study has been cited repeatedly in multiple articles about AN and cell-mediated immunity,2-7 some clinicians have accepted this evidence of resistance to infection in patients with AN, which may lower their suspicion for and detection of infections in patients with AN.
However, studies published both before and after Golla et al1 have shown statistically significant results that contradict those researchers’ conclusion. A study that compared the medical records of 68 patients with AN with those who did not have AN found no significant difference, and concluded that the rate of infection among patients with AN is the same as among controls.8 These researchers noted that infection rates may be higher among patients with later-stage, more severe AN. In a 1986 study of 12 patients with AN, Cason et al9 concluded that while cellular immunity function is abnormal in patients with AN, their results were not compatible with prior studies that suggested AN patients were more resistant to infection.1,2,8
More recently, researchers compared 1,592 patients with eating disorders with 6,368 matched controls; they reviewed prescriptions of antibacterial, antifungal, and antiviral medications as a measure of infection rates.10 Compared with controls, patients with binge eating disorder (BED), patients with bulimia nervosa (BN), and males with AN more often received prescriptions for antimicrobial medications. There was no statistically significant difference between controls and females with AN, which is consistent with other reports of no increased or decreased risk of infection among females with AN. In terms of antiviral use, this study showed an increased prescription of antivirals only in the BN group.
Several other studies examining the rate of infection in patients with AN concluded that there is neither an increased nor decreased rate of infection in patients with AN, and that the rate of infection in this population is similar to that of the general population.8,10-12 Because studies that have included patients with AN have evaluated only symptomatic viral infections, some researchers have proposed that patients with AN may show lower rates of symptomatic viral infection but higher rates of asymptomatic infection, as evidenced by higher viral titers.6 Further research is required. Despite controversy regarding infection rates, studies have found that patients with AN have increased rates of morbidity and mortality from infections.6,12-16
Continue to: Obstacles to detecting infections
Obstacles to detecting infections
Several factors can complicate the surveillance and detection of infections in patients with eating disorders, especially those with AN. These include:
- an accepted predisposition to infection secondary to malnutrition
- a lack of visual or reported infectious symptoms
- misrepresentation and assumptions from published research.
Clinicians who report fewer observed cases of infections among patients with AN may be overlooking comorbid disease processes due to a bias from the literature and/or a lack of awareness of symptom parameters in patients with AN.
Features of AN include a loss of adipose tissue responsible for pro-inflammatory cytokines, and excessive exercise, which stimulates anti-inflammatory myokines. This can modulate the experience of illness that impacts the core features of disease,17 possibly reducing symptomatic presentation of infections.
Fever. The presence and intensity of fever may be altered in patients with eating disorders, especially those with AN. In a study of 311 inpatients with AN, researchers found that patients with AN had a significant delay in fever response in AN.12 Of 23 patients with an active bacterial infection, all but 5 had a fever <37°C, with some as low as 35.5°C. A detectable fever response and unexplained fevers were found in 2 of the 6 patients with a viral infection. A series of case studies found that patients with AN with bacterial infections also had a delayed fever response.18
For patients with infections that commonly present with fever, such as COVID-19, a delayed fever response can delay or evade the detection of infection, thus increasing potential complications as well viral exposure to others. Thus, clinicians should use caution when ruling out COVID-19 or other infections because of a lack of significant fever.
Continue to: Overlapping symptoms
Overlapping symptoms. The symptoms of viral infection can mimic the symptoms of AN, which further complicates screening and diagnosis of infection in these patients. Although up to 80% of individuals infected with COVID-19 may be asymptomatic or have a mild presentation, the most common reported symptoms are fever (92.6%), shortness of breath (50.8%), expectoration (41.4%), fatigue (46.4%), dry cough (33.3%), and myalgia (21.4%).19-21 Gastrointestinal (GI) symptoms have been reported in patients with COVID-19, as well as a loss of taste and smell.
Commonly reported physical symptoms of AN include an intolerance to cold, general fatigue, muscle aches and pains, restlessness, emesis, and a multitude of GI complaints. Patients with AN also have been reported to experience shortness of breath due to conditions such as respiratory muscle weakness,22 nutritional emphysema,23 and anxiety and panic attack.24 These conditions could lead to an increased susceptibility to COVID-19 and increased complications during treatment. Cardiac abnormalities, which are common in patients with AN and BN, may increase the risk of adverse events. While these symptoms may be an important part of screening for diseases such as COVID-19, suspicion of infection also may be lower because of the overlap of AN symptomology, underlying conditions, and a delayed fever response.
Laboratory findings. Laboratory testing results for patients with COVID-19 include lower lymphocyte counts, higher leukocyte counts, elevated levels of infection-related biomarkers and inflammatory cytokines, and significantly decreased T-cell counts.19 Similar values are also found in patients with AN.
The similar clinical presentations and laboratory values of AN and COVID-19 could lead to delayed diagnosis, increased disease transmission, cross-contamination of facilities, and higher incidences of medical complications and mortality.
The immunology of AN and correlations with COVID-19
Many studies examining the immune system of patients with eating disorders, especially those with AN, have discovered changes and differences in both cell-mediated and humoral response to infections.1,3,5,7,9,11,16,21,25-27 Whether these differences represent a dysfunctional immune system, an immunocompromised state, or even a protective factor remains unclear.
Continue to: While some studies have reported...
While some studies have reported that AN represents an immunocompromised state, others describe the immune system of patients with AN as dysfunctional or simply altered.9,11,22,28 Some studies have found that patients with AN had delayed reactions to pathogen skin exposures compared with healthy controls, which provides evidence of an impaired cell-mediated immune system.9,27,29
Some studies have considered the consequences of infection and immunologic findings as markers of or contributing to the onset of AN.2,30,31 Numerous studies have noted abnormalities in AN with regards to cell-mediated immunity, the humoral system, the lymphoreticular system, and the innate immune system, and potential contributions from increased oxidative stress, a chronically activated sympathetic nervous system and hypothalamic-pituitary-adrenal axis, altered intestinal microbiota, and an abnormal bone marrow microenvironment.2
Box 1
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a new beta-coronavirus that is still being studied for its effects on the immune system. It may take years to fully understand the nature of the pathogen and the response of the human immune system. To better understand COVID19, researchers have been turning to what they learned from the past outbreaks of severe acute respiratory syndrome (SARS) in 2003- 2004 and Middle East respiratory syndrome (MERS) in 2011, both caused by betacoronaviruses with a zoonotic origin.25,32
The proposed pathogenesis for infection of SARS-CoV-2 is similar to SARS and occurs when aerosolized droplets containing the virus enter the host.32 While currently there is only initial data on the host innate immune status of patients infected with SARS-CoV-2, initial findings of a report on 99 cases in Wuhan, China included increased total neutrophils (38%), reduced total lymphocytes (35%), increased serum interleukin-6 (52%), and increased C-reactive protein (84%).33 Additional findings were decreased percentages of monocytes, eosinophils, and basophils, as well as significantly decreased levels of cytokines and T-cells in more severe cases.19 Past research with SARS reported similar T-cell findings, with a more frequent CD8+ response and a greater magnitude of CD4+.34
Box 119,25,32-34 describes some of the initial immunologic findings reported in patients with COVID-19. In Box 2,5,8,11,13,14,19,26,28,35-40 we discuss reports that describe the immunologic overlay of COVID-19 and AN.
Box 2
Leukopenia (low leukocyte levels) is a common finding in patients with anorexia nervosa (AN),8 and often leads clinicians to lower their suspicion for infection. A 2008 Hungarian study that evaluated lymphocyte activation parameters and clinical status in 11 adolescents (10 girls and 1 boy) with AN, 12 obese adolescents, and 10 healthy controls did not find any association between the variables.35 While many studies have focused on adults, it is important to note that leukopenia is a common finding in adolescents (age 12 to 17) with AN.36
Leukocyte counts are elevated in coronavirus disease 2019 (COVID-19), possibly offsetting AN’s leukopenia. In addition, neutrophil counts are elevated and monocyte, eosinophil, basophil, and especially lymphocyte counts are significantly decreased. A meta-analysis that included 22 studies and 924 participants (512 with AN and 412 controls) examined common inflammatory cytokine findings in patients with AN.11 Compared with healthy controls, patients with AN had significantly elevated levels of tumor necrosis factor alpha (TNF-alpha), interleukin (IL)-1, IL-6, and TNF-receptor II, and significantly decreased levels of C-reactive protein and IL-6 receptor. Elevated levels of TNF-alpha and IL-6 also have been reported in patients with COVID-19.19 These findings may mask suspicion for infection in patients with AN.19
In patients with AN and those with bulimia nervosa, CD4+-to-CD8+ ratios also have been found to be low as a result of normal-tohigher levels of CD4+ cells and lower levels of CD8+ cells.36-39 Researchers have also proposed that the lymphocytosis observed in AN is a result of increased naïve CD4+.36 In AN, total lymphocyte counts have been found to correlate positively with a patient’s body mass index (BMI), while the CD4+ T-lymphocyte correlated negatively with BMI and were critically low in patients with severe malnutrition.26,40 In patients with COVID-19, CD4+ levels have reported to be within normal range, naïve CD4+ cells were elevated, and CD8+ cells were slightly decreased,19 which is similar to the findings in AN.
Fewer studies have evaluated humoral immune response in AN, and results have varied. One study (N = 46) found elevated B-cell counts in adolescents with AN-restricting type,36 while another (N = 40) reported normal levels of B-cells.5 Specific decreases in immunoglobulin (Ig) G and IgM have also been reported in AN, while IgA, IgG, and IgM usually are normal in COVID-19.19
Despite differences in immune system function, cellular immunity appears to remain relatively intact in patients with AN, but can become compromised with severe malnutrition or with advanced weight loss.28,40 This compromised immunity related to severe AN with a very low BMI likely leads to the increased morbidity and mortality.8,13,14
Malnutrition and the immune system
Differences in the type of malnutrition observed in low-weight patients with AN may help explain why patients with AN can maintain a relatively intact cell-mediated immune system.1 Protein-energy malnutrition (PEM), which is found in typical states of starvation, consists of deficiencies in multiple vitamins, protein, and energy (caloric content), whereas the dietary habits of patients with AN usually result in a deficiency of carbohydrates and fats.41 Studies that examined the impact of PEM on immunity to influenza infection have suggested that balanced protein energy replenishment may be a strategy for boosting immunity against influenza viral infections.42 However, carbohydrates are the primary nutrients for human bone marrow fat cells, which play a crucial role in the maturation of white blood cells. This may account for the leukopenia that is common in patients with AN.6,43 The protein-sparing aspect of the typical AN diet may account for the immune system changes observed in patients with AN.44
Although some studies have proposed that immune deficiencies observed in patients with AN are secondary to malnutrition and return to normal with refeeding,5,40,45 others have concluded that immune function is not compromised by factors such as nutritional status or body weight in AN.26,43,46
Continue to: Clinical considerations
Clinical considerations
Neither the CDC nor the WHO have issued a specific protocol for monitoring for and treating COVID-19 in patients with eating disorders; however, the guidelines offered by these organizations for the general population should be followed for patients with eating disorders.
When screening a patient with an eating disorder, keep in mind that the symptoms of eating disorders, such as AN, may mimic an infectious process. Mood symptoms, such as depression or anxiety, could represent physiological responses to infection. Patients with GI symptoms that typically are considered part of the pathology of an eating disorder should be more carefully considered for COVID-19. Monitor a patient’s basal body temperature, and be mindful that a patient with AN may exhibit a delayed fever response. Be vigilant for a recent loss of taste or smell, which should raise suspicion for COVID-19. When monitoring vital signs, pay careful attention for any decompensation in a patient’s pulse oximetry. Whenever possible, order COVID-19 testing for any patient you suspect may be infected.
Outpatient clinicians should work closely in a collaborative manner with a patient’s eating disorder treatment team. Psychiatrists, primary care physicians, psychotherapists, nutritionists, and other clinicians should all follow CDC/WHO guidelines regarding COVID-19, provide surveillance, and communicate any suspicions to the medical team. Eating disorder treatment programs, including residential centers, partial hospital programs (PHP), and intensive outpatient programs (IOP), must enhance monitoring for COVID-19, and exercise caution by practicing social distancing and providing adequate personal protective equipment for patients and staff. To reduce the spread of COVID-19, many IOPs and PHPs have transitioned to virtual treatment. Residential centers must carefully screen patients before admission to weigh the risks and benefits of inpatient vs outpatient care.
Bottom Line
Differences in the immune system of patients with an eating disorder do not necessarily confer a higher or lower risk of infection. Symptoms of some infections can mimic the symptoms of anorexia nervosa. Recognizing infections in patients with eating disorders is critical because compared with the general population, they have higher rates of infection-related morbidity and mortality.
Related Resources
- Congress J, Madaan V. 6 ‘M’s to keep in mind when you next see a patient with anorexia nervosa. Current Psychiatry. 2014;13(5):58-59.
- Westmoreland P. Eating disorders: Masterclass lecture part I. Psychcast (podcast). https://www.mdedge.com/podcasts/psychcast/eating-disorders-masterclass-lecture-part-i.
1. Golla JA, Larson LA, Anderson CF, et al. An immunological assessment of patients with anorexia nervosa. Am J Clin Nutr. 1981;34(12):2756-2762.
2. Gibson D, Mehler PS. Anorexia nervosa and the immune system—a narrative review. J Clin Med. 2019;8(11):1915. doi: 10.3390/jcm8111915.
3. Słotwin
4. Nova E, Samartín S, Gómez S, et al. The adaptive response of the immune system to the particular malnutrition of eating disorders. Eur J Clin Nutr. 2002;56(suppl 3):S34-S37.
5. Allende LM, Corell A, Manzanares J, et al. Immunodeficiency associated with anorexia nervosa is secondary and improves after refeeding. Immunology. 1998;94(4):543-551.
6. Brown RF, Bartrop R, Birmingham CL. Immunological disturbance and infectious disease in anorexia nervosa: a review. Acta Neuropsychiatr. 2008;20(3):117-128.
7. Polack E, Nahmod VE, Emeric-Sauval E, et al. Low lymphocyte interferon-gamma production and variable proliferative response in anorexia nervosa patients. J Clin Immunol. 1993;13(6):445-451.
8. Bowers TK, Eckert E. Leukopenia in anorexia nervosa. Lack of increased risk of infection. Arch Intern Med. 1978;138(10):1520-1523.
9. Cason J, Ainley CC, Wolstencroft RA, et al. Cell-mediated immunity in anorexia nervosa. Clin Exp Immunol. 1986;64(2):370-375.
10. Raevuori A, Lukkariniemi L, Suokas JT, et al. Increased use of antimicrobial medication in bulimia nervosa and binge-eating disorder prior to the eating disorder treatment. Int J Eat Disord. 2016;49(6):542-552.
11. Solmi M, Veronese N, Favaro A, et al. Inflammatory cytokines and anorexia nervosa: a meta-analysis of cross-sectional and longitudinal studies. Psychoneuroendocrinology. 2015;51:237-252.
12. Brown RF, Bartrop R, Beumont P, et al. Bacterial infections in anorexia nervosa: delayed recognition increases complications. Int J Eat Disord. 2005;37(3):261-265.
13. Theander S. Anorexia nervosa. A psychiatric investigation of 94 female patients. Acta Psychiatr Scand Suppl. 1970;214:1-194.
14. Warren MP, Vande Wiele RL. Clinical and metabolic features of anorexia nervosa. Am J Obstet Gynecol. 1973;117(3):435-449.
15. Copeland PM, Herzog DB. Hypoglycemia and death in anorexia nervosa. Psychother Psychosom. 1987;48(1-4):146-150.
16. Devuyst O, Lambert M, Rodhain J, et al. Haematological changes and infectious complications in anorexia nervosa: a case-control study. Q J Med. 1993;86(12):791-799.
17. Pisetsky DS, Trace SE, Brownley KA, et al. The expression of cytokines and chemokines in the blood of patients with severe weight loss from anorexia nervosa: an exploratory study. Cytokine. 2014;69(1):110-115.
18. Birmingham CL, Hodgson DM, Fung J, et al. Reduced febrile response to bacterial infection in anorexia nervosa patients. Int J Eat Disord. 2003;34(2):269-272.
19. Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China [published online March 12, 2020]. Clin Infect Dis. doi: 10.1093/cid/ciaa248.
20. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
21. Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514-523.
22. Birmingham CL, Tan AO. Respiratory muscle weakness and anorexia nervosa. Int J Eat Disord. 2003;33(2):230-233.
23. Cook VJ, Coxson HO, Mason AG, et al. Bullae, bronchiectasis and nutritional emphysema in severe anorexia nervosa. Can Respir J. 2001;8(5):361-365.
24. Khalsa SS, Hassanpour MS, Strober M, et al. Interoceptive anxiety and body representation in anorexia nervosa [published online September 21, 2018]. Front Psychiatry. 2018;9:444. doi: 10.3389/fpsyt.2018.00444.
25. van West D, Maes M. Cytokines in de obsessief compulsieve stoornis en in anorexia nervosa: een overzicht. Acta Neuropsychiatr. 1999;11(4):125-129.
26. Komorowska-Pietrzykowska R, Rajewski A, Wiktorowicz K, et al. Czynnos
27. Marcos A, Varela P, Toro O, et al. Interactions between nutrition and immunity in anorexia nervosa: a 1-y follow-up study. Am J Clin Nutr. 1997;66(2):485S-490S.
28. Pertschuk MJ, Crosby LO, Barot L, et al. Immunocompetency in anorexia nervosa. Am J Clin Nutr. 1982;35(5):968-972.
29. Varela P, Marcos A, Navarro MP. Zinc status in anorexia nervosa. Ann Nutr Metab. 1992;36(4):197-202.
30. Breithaupt L, Köhler-Forsberg O, Larsen JT, et al. Association of exposure to infections in childhood with risk of eating disorders in adolescent girls. JAMA Psychiatry. 2019;76(8):800-809.
31. Brambilla F, Monti D, Franceschi C. Plasma concentrations of interleukin-1-beta, interleukin-6 and tumor necrosis factor-alpha, and of their soluble receptors and receptor antagonist in anorexia nervosa. Psychiatry Res. 2001;103(2-3):107-114.
32. Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic [published online February 27, 2020]. Asian Pac J Allergy Immunol. doi: 10.12932/AP-200220-0772.
33. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270-273.
34. Li CK, Wu H, Yan H, et al. T cell responses to whole SARS coronavirus in humans. J Immunol. 2008;181(8):5490-5500.
35. Páli AA, Pászthy B. Az immunrendszer muködésének megváltozása a táplálkozási magatartás zavarai esetén [Changes of the immune functions in patients with eating disorders]. Ideggyogy Sz. 2008;61(11-12):381‐384.
36. Elegido A, Graell M, Andrés P, et al. Increased naive CD4+ and B lymphocyte subsets are associated with body mass loss and drive relative lymphocytosis in anorexia nervosa patients. Nutr Res. 2017;39:43-50.
37. Marcos A, Varela P, Santacruz I, et al. Nutritional status and immunocompetence in eating disorders. A comparative study. Eur J Clin Nutr. 1993;47(11):787-793.
38. Mustafa A, Ward A, Treasure J, et al. T lymphocyte subpopulations in anorexia nervosa and refeeding. Clin Immunol Immunopathol. 1997;82(3):282-289.
39. Nagata T, Kiriike N, Tobitani W, et al. Lymphocyte subset, lymphocyte proliferative response, and soluble interleukin-2 receptor in anorexic patients. Biol Psychiatry. 1999;45(4):471-474.
40. Saito H, Nomura K, Hotta M, et al. Malnutrition induces dissociated changes in lymphocyte count and subset proportion in patients with anorexia nervosa. Int J Eat Disord. 2007;40(6):575-579.
41. Nova E, Varela P, López-Vidriero I, et al. A one-year follow-up study in anorexia nervosa. Dietary pattern and anthropometrical evolution. Eur J Clin Nutr. 2001;55(7):547-554.
42. Taylor AK, Cao W, Vora KP, et al. Protein energy malnutrition decreases immunity and increases susceptibility to influenza infection in mice. J Infect Dis. 2013;207(3):501-510.
43. Mant MJ, Faragher BS. The hematology of anorexia nervosa. Br J Haematol. 1972;23(6):737-749.
44. Marcos A. The immune system in eating disorders: an overview. Nutrition. 1997;13(10):853-862.
45. Schattner A, Tepper R, Steinbock M, et al. TNF, interferon-gamma and cell-mediated cytotoxicity in anorexia nervosa; effect of refeeding. J Clin Lab Immunol. 1990;32(4):183-184.
46. Nagata T, Tobitani W, Kiriike N, et al. Capacity to produce cytokines during weight restoration in patients with anorexia nervosa. Psychosom Med. 1999;61(3):371-377.
1. Golla JA, Larson LA, Anderson CF, et al. An immunological assessment of patients with anorexia nervosa. Am J Clin Nutr. 1981;34(12):2756-2762.
2. Gibson D, Mehler PS. Anorexia nervosa and the immune system—a narrative review. J Clin Med. 2019;8(11):1915. doi: 10.3390/jcm8111915.
3. Słotwin
4. Nova E, Samartín S, Gómez S, et al. The adaptive response of the immune system to the particular malnutrition of eating disorders. Eur J Clin Nutr. 2002;56(suppl 3):S34-S37.
5. Allende LM, Corell A, Manzanares J, et al. Immunodeficiency associated with anorexia nervosa is secondary and improves after refeeding. Immunology. 1998;94(4):543-551.
6. Brown RF, Bartrop R, Birmingham CL. Immunological disturbance and infectious disease in anorexia nervosa: a review. Acta Neuropsychiatr. 2008;20(3):117-128.
7. Polack E, Nahmod VE, Emeric-Sauval E, et al. Low lymphocyte interferon-gamma production and variable proliferative response in anorexia nervosa patients. J Clin Immunol. 1993;13(6):445-451.
8. Bowers TK, Eckert E. Leukopenia in anorexia nervosa. Lack of increased risk of infection. Arch Intern Med. 1978;138(10):1520-1523.
9. Cason J, Ainley CC, Wolstencroft RA, et al. Cell-mediated immunity in anorexia nervosa. Clin Exp Immunol. 1986;64(2):370-375.
10. Raevuori A, Lukkariniemi L, Suokas JT, et al. Increased use of antimicrobial medication in bulimia nervosa and binge-eating disorder prior to the eating disorder treatment. Int J Eat Disord. 2016;49(6):542-552.
11. Solmi M, Veronese N, Favaro A, et al. Inflammatory cytokines and anorexia nervosa: a meta-analysis of cross-sectional and longitudinal studies. Psychoneuroendocrinology. 2015;51:237-252.
12. Brown RF, Bartrop R, Beumont P, et al. Bacterial infections in anorexia nervosa: delayed recognition increases complications. Int J Eat Disord. 2005;37(3):261-265.
13. Theander S. Anorexia nervosa. A psychiatric investigation of 94 female patients. Acta Psychiatr Scand Suppl. 1970;214:1-194.
14. Warren MP, Vande Wiele RL. Clinical and metabolic features of anorexia nervosa. Am J Obstet Gynecol. 1973;117(3):435-449.
15. Copeland PM, Herzog DB. Hypoglycemia and death in anorexia nervosa. Psychother Psychosom. 1987;48(1-4):146-150.
16. Devuyst O, Lambert M, Rodhain J, et al. Haematological changes and infectious complications in anorexia nervosa: a case-control study. Q J Med. 1993;86(12):791-799.
17. Pisetsky DS, Trace SE, Brownley KA, et al. The expression of cytokines and chemokines in the blood of patients with severe weight loss from anorexia nervosa: an exploratory study. Cytokine. 2014;69(1):110-115.
18. Birmingham CL, Hodgson DM, Fung J, et al. Reduced febrile response to bacterial infection in anorexia nervosa patients. Int J Eat Disord. 2003;34(2):269-272.
19. Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China [published online March 12, 2020]. Clin Infect Dis. doi: 10.1093/cid/ciaa248.
20. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
21. Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514-523.
22. Birmingham CL, Tan AO. Respiratory muscle weakness and anorexia nervosa. Int J Eat Disord. 2003;33(2):230-233.
23. Cook VJ, Coxson HO, Mason AG, et al. Bullae, bronchiectasis and nutritional emphysema in severe anorexia nervosa. Can Respir J. 2001;8(5):361-365.
24. Khalsa SS, Hassanpour MS, Strober M, et al. Interoceptive anxiety and body representation in anorexia nervosa [published online September 21, 2018]. Front Psychiatry. 2018;9:444. doi: 10.3389/fpsyt.2018.00444.
25. van West D, Maes M. Cytokines in de obsessief compulsieve stoornis en in anorexia nervosa: een overzicht. Acta Neuropsychiatr. 1999;11(4):125-129.
26. Komorowska-Pietrzykowska R, Rajewski A, Wiktorowicz K, et al. Czynnos
27. Marcos A, Varela P, Toro O, et al. Interactions between nutrition and immunity in anorexia nervosa: a 1-y follow-up study. Am J Clin Nutr. 1997;66(2):485S-490S.
28. Pertschuk MJ, Crosby LO, Barot L, et al. Immunocompetency in anorexia nervosa. Am J Clin Nutr. 1982;35(5):968-972.
29. Varela P, Marcos A, Navarro MP. Zinc status in anorexia nervosa. Ann Nutr Metab. 1992;36(4):197-202.
30. Breithaupt L, Köhler-Forsberg O, Larsen JT, et al. Association of exposure to infections in childhood with risk of eating disorders in adolescent girls. JAMA Psychiatry. 2019;76(8):800-809.
31. Brambilla F, Monti D, Franceschi C. Plasma concentrations of interleukin-1-beta, interleukin-6 and tumor necrosis factor-alpha, and of their soluble receptors and receptor antagonist in anorexia nervosa. Psychiatry Res. 2001;103(2-3):107-114.
32. Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic [published online February 27, 2020]. Asian Pac J Allergy Immunol. doi: 10.12932/AP-200220-0772.
33. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270-273.
34. Li CK, Wu H, Yan H, et al. T cell responses to whole SARS coronavirus in humans. J Immunol. 2008;181(8):5490-5500.
35. Páli AA, Pászthy B. Az immunrendszer muködésének megváltozása a táplálkozási magatartás zavarai esetén [Changes of the immune functions in patients with eating disorders]. Ideggyogy Sz. 2008;61(11-12):381‐384.
36. Elegido A, Graell M, Andrés P, et al. Increased naive CD4+ and B lymphocyte subsets are associated with body mass loss and drive relative lymphocytosis in anorexia nervosa patients. Nutr Res. 2017;39:43-50.
37. Marcos A, Varela P, Santacruz I, et al. Nutritional status and immunocompetence in eating disorders. A comparative study. Eur J Clin Nutr. 1993;47(11):787-793.
38. Mustafa A, Ward A, Treasure J, et al. T lymphocyte subpopulations in anorexia nervosa and refeeding. Clin Immunol Immunopathol. 1997;82(3):282-289.
39. Nagata T, Kiriike N, Tobitani W, et al. Lymphocyte subset, lymphocyte proliferative response, and soluble interleukin-2 receptor in anorexic patients. Biol Psychiatry. 1999;45(4):471-474.
40. Saito H, Nomura K, Hotta M, et al. Malnutrition induces dissociated changes in lymphocyte count and subset proportion in patients with anorexia nervosa. Int J Eat Disord. 2007;40(6):575-579.
41. Nova E, Varela P, López-Vidriero I, et al. A one-year follow-up study in anorexia nervosa. Dietary pattern and anthropometrical evolution. Eur J Clin Nutr. 2001;55(7):547-554.
42. Taylor AK, Cao W, Vora KP, et al. Protein energy malnutrition decreases immunity and increases susceptibility to influenza infection in mice. J Infect Dis. 2013;207(3):501-510.
43. Mant MJ, Faragher BS. The hematology of anorexia nervosa. Br J Haematol. 1972;23(6):737-749.
44. Marcos A. The immune system in eating disorders: an overview. Nutrition. 1997;13(10):853-862.
45. Schattner A, Tepper R, Steinbock M, et al. TNF, interferon-gamma and cell-mediated cytotoxicity in anorexia nervosa; effect of refeeding. J Clin Lab Immunol. 1990;32(4):183-184.
46. Nagata T, Tobitani W, Kiriike N, et al. Capacity to produce cytokines during weight restoration in patients with anorexia nervosa. Psychosom Med. 1999;61(3):371-377.
Telepsychiatry: What you need to know
The need for mental health services has never been greater. Unfortunately, many patients have limited access to psychiatric treatment, especially those who live in rural areas. Telepsychiatry—the delivery of psychiatric services through telecommunications technology, usually video conferencing—may help address this problem. Even before the onset of the coronavirus disease 2019 (COVID-19) pandemic, telepsychiatry was becoming increasingly common. A survey of US mental health facilities found that the proportion of facilities offering telepsychiatry nearly doubled from 2010 to 2017, from 15.2% to 29.2%.1
In this article, we describe examples of where and how telepsychiatry is being used successfully, and its potential advantages. We discuss concerns about its use, its impact on the therapeutic alliance, and patients’ and clinicians’ perceptions of it. We also discuss the legal, technological, and financial aspects of using telepsychiatry. With an increased understanding of these issues, psychiatric clinicians will be better able to integrate telepsychiatry into their practices.
How and where is telepsychiatry being used
In addition to being used to provide psychotherapy, telepsychiatry is being employed for diagnosis and evaluation; clinical consultations; research; supervision, mentoring, and education of trainees; development of treatment programs; and public health. Telepsychiatry is an excellent mechanism to provide high-level second opinions to primary care physicians and psychiatrists on complex cases for both diagnostic purposes and treatment.
Evidence suggests that telepsychiatry can play a beneficial role in a variety of settings, and for a range of patient populations.
Emergency departments (EDs). Using telepsychiatry for psychiatric consultations in EDs could result in a quicker disposition of patients and reduced crowding and wait times. A survey of on-call clinicians in a pediatric ED found that using telepsychiatry for on-site psychiatric consultations decreased patients’ length of stay, improved resident on-call burden, and reduced factors related to physician burnout.2 In this study, telepsychiatry use reduced travel for face-to-face evaluations by 75% and saved more than 2 hours per call day.2
Medical clinics. Using telepsychiatry to deliver cognitive-behavioral therapy significantly reduced symptoms of depression or anxiety among 203 primary care patients.3 Incorporating telepsychiatry into existing integrated primary care settings is becoming more common. For example, an integrated-care model that includes telepsychiatry is serving the needs of complex patients in a high-volume, urban primary care clinic in Colorado.4
Assertive Community Treatment (ACT) teams. Telepsychiatry is being used by ACT teams for crisis intervention and to reduce inpatient hospitalizations.5
Continue to: Correctional facilities
Correctional facilities. With the downsizing and closure of many state psychiatric hospitals across the United States over the last several decades, jails and prisons have become de facto mental health hospitals. This situation presents many challenges, including access to mental health care and the need to avoid medications with the potential for abuse. Using telepsychiatry for psychiatric consultations in correctional facilities can improve access to mental health care.
Geriatric patients.
Children and adolescents. The Michigan Child Collaborative Care (MC3) program is a telepsychiatry consultation service that has been able to provide cost-effective, timely, remote consultation to primary care clinicians who care for youth and perinatal women.8 New York has a pediatric collaborative care program, the Child and Adolescent Psychiatry for Primary Care (CAP PC), that incorporates telepsychiatry consultations for families who live >1 hour away from one of the program’s treatment sites.9
Patients with cancer. A literature review that included 9 studies found no statistically significant differences between standard face-to-face interventions and telepsychiatry for improving quality-of-life scores among patients receiving treatment for cancer.10
Patients with insomnia. Cognitive-behavioral therapy for insomnia (CBT-I) is often recommended as a first-line treatment, but is not available for many patients. A recent study showed that CBT-I provided via telepsychiatry for patients with shift work sleep disorder was as effective as face-to-face therapy.11 Increasing the availability of this treatment could decrease reliance on pharmacotherapy for sleep.
Patients with opioid use disorder (OUD). Treatment for patients with OUD is limited by access to, and availability of, psychiatric clinicians. Telepsychiatry can help bridge this gap. One example of such use is in Ontario, Canada, where more than 10,000 patients with concurrent opiate abuse and other mental health disorders have received care via telepsychiatry since 2008.12
Continue to: Increasing access to cost-effective care where it is needed most
Increasing access to cost-effective care where it is needed most
There is a crisis in mental health care in rural areas of the United States. A study assessing delivery of care to US residents who live in rural areas found these patients’ mental health–related quality of life was 2.5 standard deviations below the national mean.13 Additionally, the need for treatment is expected to rise as the number of psychiatrists falls. According to a 2017 National Council for Behavioral Health report,14 by 2025, demand may outstrip supply by 6,090 to 15,600 psychiatrists. While telepsychiatry cannot improve this shortage per se, it can help increase access to psychiatric services. The potential benefits of telepsychiatry for patients are summarized in Table 1.15
Telepsychiatry may be more cost-effective than traditional face-to-face treatment. A cost analysis of an expanding, multistate behavioral telehealth intervention program for rural American Indian/Alaska Native populations found substantial cost savings associated with telepsychiatry.16 In this analysis, the estimated cost efficiencies of telepsychiatry were more evident in rural communities, and having a multistate center was less expensive than each state operating independently.16
Most importantly, evidence suggests that treatment delivered via telepsychiatry is at least as effective as traditional face-to-face care. In a review that included >150 studies, Bashshur et al17 concluded, “Effective approaches to the long-term management of mental illness include monitoring, surveillance, mental health promotion, mental illness prevention, and biopsychosocial treatment programs. The empirical evidence … demonstrates the capability of [telepsychiatry] to perform these functions more efficiently and as well as or more effectively than in-person care
Clinician and patient attitudes toward telepsychiatry
Clinicians have legitimate concerns about the quality of care being delivered when using telepsychiatry. Are patients satisfied with treatment delivered via telepsychiatry? Can a therapeutic alliance be established and maintained? It appears that clinicians may have more concerns than patients do.18
A study of telepsychiatry consultations for patients in rural primary care clinics performed by clinicians at an urban health center found that patients and clinicians were highly satisfied with telepsychiatry.19 Both patients and clinicians believed that telepsychiatry provided patients with better access to care. There was a high degree of agreement between patients and clinician responses.19
Continue to: In a review of...
In a review of 452 telepsychiatry studies, Hubley et al20 focused on satisfaction, reliability, treatment outcomes, implementation outcomes, cost effectiveness, and legal issues. They concluded that patients and clinicians are generally satisfied with telepsychiatry services. Interestingly, clinicians expressed more concerns about the potential adverse effects of telepsychiatry on therapeutic rapport. Hubley et al20 found no published reports of adverse events associated with telepsychiatry use.
In a study of school-based telepsychiatry in an urban setting, Mayworm et al21 found that patients were highly satisfied with both in-person and telepsychiatry services, and there were no significant differences in preference. This study also found that telepsychiatry services were more time-efficient than in-person services.
A study of using telepsychiatry to treat unipolar depression found that patient satisfaction scores improved with increasing number of video-based sessions, and were similar among all age groups.22 An analysis of this study found that total satisfaction scores were higher for patients than for clinicians.23
In a study of satisfaction with telepsychiatry among community-dwelling older veterans, 90% of participants reported liking or even preferring telepsychiatry, even though the experience was novel for most of them.24
As always, patients’ preferences need to be kept in mind when considering what services can and should be provided via telepsychiatry, because not all patients will find it acceptable. For example, in a study of veterans’ attitudes toward treatment via telepsychiatry, Goetter et al25 found that interest was mixed. Twenty-six percent of patients were “not at all comfortable,” while 13% were “extremely comfortable” using telepsychiatry from home. Notably, 33% indicated a clear preference for telepsychiatry compared to in-person mental health visits.
Continue to: Legal aspects of telepsychiatry
Legal aspects of telepsychiatry
Box 1
As part of the efforts to contain the spread of coronavirus disease 2019 (COVID-19), the use of telemedicine, including telepsychiatry, has increased substantially. Here are a few key facts to keep in mind while practicing telepsychiatry during this pandemic:
- The Centers for Medicare and Medicaid Services relaxed requirements for telehealth starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency. Under this new waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country and including in patient’s places of residence. For details, see www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. This fact sheet reviews relevant information, including billing codes.
- Health Insurance Portability and Accountability Act requirements, specifically those for secure communications, will not be enforced when telehealth is used under the new waiver. Because of this, popular but unsecure software applications, such as Apple’s FaceTime, Microsoft’s Teams, or Facebook’s Messenger, WhatsApp, and Messenger Rooms, can be used.
- Informed consent for the use of telepsychiatry in this situation should be obtained from the patient or his/her guardian, and documented in the patient’s medical record. For example: “Informed consent received for providing services via video teleconferencing to the home in order to protect the patient from COVID-19 exposure. Confidentiality issues were discussed.”
Licensure. State licensing and medical regulatory organizations consider the care provided via telepsychiatry to be rendered where the patient is physically located when services are rendered. Because of this, psychiatrists who use telepsychiatry generally need to hold a license in the state where their patients are located, regardless of where the psychiatrist is located.
Some states offer special telemedicine licenses. Typically, these licenses allow clinicians to practice across state lines without having to obtain a full professional license from the state. Be sure to check with the relevant state medical board where you intend to practice.
Because state laws related to telepsychiatry are continuously evolving, we suggest that clinicians continually check these laws and obtain a regulatory response in writing so there is ongoing documentation. For more information on this topic, see “Telepsychiatry during COVID-19: Understanding the rules” at MDedge.com/psychiatry.
Malpractice insurance. Some insurance companies offer coverage that includes the practice of telepsychiatry, whereas other carriers require the purchase of additional coverage for telepsychiatry. There may be additional requirements for practicing across state lines. Be sure to check with your insurer.
Continue to: Technical requirements and costs
Technical requirements and costs
In order to perform telepsychiatry, one needs Internet access, appropriate hardware such as a desktop or laptop computer or tablet, and a video conferencing application. Software must be HIPAA-compliant, although this requirement is not being enforced during the COVID-19 pandemic. Several popular video conferencing platforms were designed for or have versions suitable for telemedicine, including Zoom, Doxy.me, Vidyo, and Skype.
The use of different electronic health record (EHR) systems by various health care systems is a barrier to using telepsychiatry.
Box 2
The North Carolina Statewide Telepsychiatry Program (NC-STeP) began in 2013 by providing telepsychiatry services in hospital emergency departments (EDs) to individuals experiencing an acute behavioral health crisis. In 2018, the program expanded to include community-based primary care sites using a “hybrid” collaborative-care model. This model benefits patients by improving access to mental health specialty care; reducing the need for trips to the ED and inpatient admissions, thus decompressing EDs; improving compliance with treatment; reducing delays in care; reducing stigma; and improving continuity of care and follow-up. East Carolina University’s Center for Telepsychiatry and E-Behavioral Health is the home for this program, which is connecting hospital EDs and community-based primary care sites across North Carolina.
NC-STeP provides patients with a faceto-face interaction with a clinician through real-time video conferencing that is facilitated using mobile carts and desktop units. A web portal combines scheduling, electronic medical records, health information exchange functions, and data management systems.
NC-STeP has significantly reduced patient length of stay in EDs, provided cost savings to the health care delivery system through overturned involuntary commitments, improved ED throughout, and reduced patient boarding time; and has achieved high rates of patient, staff, and clinician satisfaction. Highlights of the program include:
- 57 hospitals and 8 communitybased sites in the network (as of January 1, 2020)
- 8 clinical hubs are operational, with 53 consultant clinicians
- 40,573 telepsychiatry assessments (as of January 1, 2020)
- 5,631 involuntary commitments overturned, thus preventing unnecessary hospitalizations representing a saving of $30,407,400 to the state
- Since program inception, >40% of ED patients who received telepsychiatry services were discharged to home
- 32% of the patients served had no insurance coverage
- Currently, the average consult elapsed time (in queue to consult complete) is 3 hours 9 minutes.
For more information about this program, see www.ecu.edu/cs-dhs/ncstep.
Our practice has extensive experience with telepsychiatry (Box 3), and for us, the specific costs associated with providing telepsychiatry services include maintenance of infrastructure and the purchase of hardware (eg, computers, smartphones, tablets), a video conferencing application (some free versions are available), EHR systems, and Internet access.
Box 3
Our practice (Rural Psychiatry Associates, Grand Forks, North Dakota) and our close associates have provided telepsychiatry services to >200 mental health clinics, hospitals, Native American villages, prisons, and nursing homes, mostly in rural and underserved areas. To provide these services, in addition to physicians, we also utilize nurse practitioners and physician assistants, for whom we provide extensive education, training, and supervision. We also provide education to the staff at the facilities where we provide services.
For nursing homes, we often use what is referred to as a “blended mode,” where we combine telepsychiatry visits with in-person, on-site visits, alternating monthly. In this model, we also typically alternate one physician with one nonphysician clinician at each facility. For continuity of care, the same clinicians service the same facilities. For very distant facilities with only a few patients, only telepsychiatry is utilized. However, initial services are always provided by a physician to establish a relationship, discuss policies and procedures, and evaluate patients face-to-face.
Telepsychiatry is increasingly used for education and mentoring. We have found telepsychiatry to be especially useful when working with psychiatric residents on a realtime basis as they evaluate and treat patients at a different location.
Reimbursement for telepsychiatry
Private insurance reimbursement for treatment delivered via telepsychiatry obviously depends on the specific insurance company. Some facilities, such as nursing homes, hospitals, medical clinics, and correctional facilities, offer lump-sum fees to clinicians for providing contracted services. Some clinicians are providing telepsychiatry as direct-bill or concierge services, which require direct payment from the patient without any reimbursement from insurance.
Medicare Part B covers some telepsychiatry services, but only under certain conditions.28 Previously, reimbursement was limited to services provided to patients who live in rural areas. However, on November 1, 2019, eligibility for telehealth services for Medicare Advantage (MA) recipients was expanded to include patients in both urban and rural locations. Patients covered by MA also can receive telehealth services from their home, instead of having to drive to a Centers for Medicare and Medicaid Services–qualified telehealth service center.
Continue to: Medicaid is the single...
Medicaid is the single largest payer for mental health services in the United States,29 and all Medicaid programs reimburse for some telepsychiatry services. As with all Medicaid health care, fees paid for telepsychiatry are state-specific. Since 2013, several state Medicaid programs, including New York,30 have expanded the list of eligible telehealth sites to include schools, thereby giving children virtual access to mental health clinicians.
Getting started
Clinicians who are interested in starting to provide treatment via telepsychiatry can begin by reviewing the American Psychiatric Association’s Telepsychiatry Toolkit at www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit. This toolkit, which is being continually updated, features numerous training videos for clinicians new to telepsychiatry, such as Learning To Do Telemental Health (www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit/learning-telemental-health) and The Credentialing Process (www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit/credentialing-process). Before starting, also consider reviewing the steps listed in Table 2.
Bottom Line
Evidence suggests telepsychiatry can be beneficial for a wide range of patient populations and settings. Most patients accept its use, and some actually prefer it to face-to-face care. Telepsychiatry may be especially useful for patients who have limited access to psychiatric treatment, such as those who live in rural areas. Factors to consider before incorporating telepsychiatry into your practice include addressing various legal, technological, and financial requirements.
Related Resources
- Von Hafften A. Telepsychiatry practice guidelines. American Psychiatric Association. https://www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit/practice-guidelines.
- Centers for Disease Control and Prevention. Telehealth and telemedicine: a research anthology of law and policy resources. https://www.cdc.gov/phlp/publications/topic/anthologies/anthologies-telehealth.html. Reviewed July 31, 2019.
- American Telemedicine Association. https://www.americantelemed.org/.
1. Spivak S, Spivak A, Cullen B, et al. Telepsychiatry use in U.S. mental health facilities, 2010-2017. Psychiatr Serv. 2019;71(2):appips201900261. doi: 10.1176/appi.ps.201900261.
2. Reliford A, Adebanjo B. Use of telepsychiatry in pediatric emergency room to decrease length of stay for psychiatric patients, improve resident on-call burden, and reduce factors related to physician burnout. Telemed J E Health. 2019;25(9):828-832.
3. Mathiasen K, Riper H, Andersen TE, et al. Guided internet-based cognitive behavioral therapy for adult depression and anxiety in routine secondary care: observational study. J Med Internet Res. 2018;20(11):e10927. doi: 10.2196/10927.
4. Waugh M, Calderone J, Brown Levey S, et al. Using telepsychiatry to enrich existing integrated primary care. Telemed J E Health. 2019;25(8):762-768.
5. Swanson CL, Trestman RL. Rural assertive community treatment and telepsychiatry. J Psychiatr Pract. 2018;24(4):269-273.
6. Gentry MT, Lapid MI, Rummans TA. Geriatric telepsychiatry: systematic review and policy considerations. Am J Geriatr Psychiatry. 2019;27(2):109-127.
7. Christensen LF, Moller AM, Hansen JP, et al. Patients’ and providers’ experiences with video consultations used in the treatment of older patients with unipolar depression: a systematic review. J Psychiatr Ment Health Nurs. 2020;27(3):258-271.
8. Marcus S, Malas N, Dopp R, et al. The Michigan Child Collaborative Care program: building a telepsychiatry consultation service. Psychiatr Serv. 2019;70(9):849-852.
9. Kaye DL, Fornari V, Scharf M, et al. Description of a multi-university education and collaborative care child psychiatry access program: New York State’s CAP PC. Gen Hosp Psychiatry. 2017;48:32-36.
10. Larson JL, Rosen AB, Wilson FA. The effect of telehealth interventions on quality of life of cancer patients: a systematic review and meta-analysis. Telemed J E Health. 2018;24(6):397-405.
11. Peter L, Reindl R, Zauter S, et al. Effectiveness of an online CBT-I intervention and a face-to-face treatment for shift work sleep disorder: a comparison of sleep diary data. Int J Environ Res Public Health. 2019;16(17):E3081. doi: 10.3390/ijerph16173081.
12. LaBelle B, Franklyn AM, Pkh Nguyen V, et al. Characterizing the use of telepsychiatry for patients with opioid use disorder and cooccurring mental health disorders in Ontario, Canada. Int J Telemed Appl. 2018;2018(3):1-7.
13. Fortney JC, Heagerty PJ, Bauer AM, et al. Study to promote innovation in rural integrated telepsychiatry (SPIRIT): rationale and design of a randomized comparative effectiveness trial of managing complex psychiatric disorders in rural primary care clinics. Contemp Clin Trials. 2020;90:105873. doi: 10.1016/j.cct.2019.105873.
14. Weiner S. Addressing the escalating psychiatrist shortage. AAMC. https://www.aamc.org/news-insights/addressing-escalating-psychiatrist-shortage. Published February 12, 2018. Accessed May 14, 2020.
15. American Psychiatric Association. What is telepsychiatry? https://www.psychiatry.org/patients-families/what-is-telepsychiatry. Published 2017. Accessed May 14, 2020.
16. Yilmaz SK, Horn BP, Fore C, et al. An economic cost analysis of an expanding, multi-state behavioural telehealth intervention. J Telemed Telecare. 2019;25(6):353-364.
17. Bashshur RL, Shannon GW, Bashshur N, et al. The empirical evidence for telemedicine interventions in mental disorders. Telemed J E Health. 2016;22(2):87-113.
18. Lopez A, Schwenk S, Schneck CD, et al. Technology-based mental health treatment and the impact on the therapeutic alliance. Curr Psychiatry Rep. 2019;21(8):76.
19. Schubert NJ, Backman PJ, Bhatla R, et al. Telepsychiatry and patient-provider concordance. Can J Rural Med. 2019;24(3):75-82.
20. Hubley S, Lynch SB, Schneck C, et al. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6(2):269-282.
21. Mayworm AM, Lever N, Gloff N, et al. School-based telepsychiatry in an urban setting: efficiency and satisfaction with care. Telemed J E Health. 2020;26(4):446-454.
22. Christensen LF, Gildberg FA, Sibbersen C, et al. Videoconferences and treatment of depression: satisfaction score correlated with number of sessions attended but not with age [published online October 31, 2019]. Telemed J E Health. 2019. doi: 10.1089/tmj.2019.0129.
23. Christensen LF, Gildberg FA, Sibbersen C, et al. Disagreement in satisfaction between patients and providers in the use of videoconferences by depressed adults. Telemed J E Health. 2020;26(5):614-620.
24. Hantke N, Lajoy M, Gould CE, et al. Patient satisfaction with geriatric psychiatry services via video teleconference. Am J Geriatr Psychiatry. 2020;28(4):491-494.
25. Goetter EM, Blackburn AM, Bui E, et al. Veterans’ prospective attitudes about mental health treatment using telehealth. J Psychosoc Nurs Ment Health Serv. 2019;57(9):38-43.
26. Vanderpool D. Top 10 myths about telepsychiatry. Innov Clin Neurosci. 2017;14(9-10):13-15.
27. Butterfield A. Telepsychiatric evaluation and consultation in emergency care settings. Child Adolesc Psychiatr Clin N Am. 2018;27(3):467-478.
28. Medicare.gov. Telehealth. https://www.medicare.gov/coverage/telehealth. Accessed May 14, 2020.
29. Centers for Medicare & Medicaid Services. Behavioral Health Services. https://www.medicaid.gov/medicaid/benefits/bhs/index.html. Accessed May 14, 2020.
30. New York Pub Health Law §2999-cc (2017).
The need for mental health services has never been greater. Unfortunately, many patients have limited access to psychiatric treatment, especially those who live in rural areas. Telepsychiatry—the delivery of psychiatric services through telecommunications technology, usually video conferencing—may help address this problem. Even before the onset of the coronavirus disease 2019 (COVID-19) pandemic, telepsychiatry was becoming increasingly common. A survey of US mental health facilities found that the proportion of facilities offering telepsychiatry nearly doubled from 2010 to 2017, from 15.2% to 29.2%.1
In this article, we describe examples of where and how telepsychiatry is being used successfully, and its potential advantages. We discuss concerns about its use, its impact on the therapeutic alliance, and patients’ and clinicians’ perceptions of it. We also discuss the legal, technological, and financial aspects of using telepsychiatry. With an increased understanding of these issues, psychiatric clinicians will be better able to integrate telepsychiatry into their practices.
How and where is telepsychiatry being used
In addition to being used to provide psychotherapy, telepsychiatry is being employed for diagnosis and evaluation; clinical consultations; research; supervision, mentoring, and education of trainees; development of treatment programs; and public health. Telepsychiatry is an excellent mechanism to provide high-level second opinions to primary care physicians and psychiatrists on complex cases for both diagnostic purposes and treatment.
Evidence suggests that telepsychiatry can play a beneficial role in a variety of settings, and for a range of patient populations.
Emergency departments (EDs). Using telepsychiatry for psychiatric consultations in EDs could result in a quicker disposition of patients and reduced crowding and wait times. A survey of on-call clinicians in a pediatric ED found that using telepsychiatry for on-site psychiatric consultations decreased patients’ length of stay, improved resident on-call burden, and reduced factors related to physician burnout.2 In this study, telepsychiatry use reduced travel for face-to-face evaluations by 75% and saved more than 2 hours per call day.2
Medical clinics. Using telepsychiatry to deliver cognitive-behavioral therapy significantly reduced symptoms of depression or anxiety among 203 primary care patients.3 Incorporating telepsychiatry into existing integrated primary care settings is becoming more common. For example, an integrated-care model that includes telepsychiatry is serving the needs of complex patients in a high-volume, urban primary care clinic in Colorado.4
Assertive Community Treatment (ACT) teams. Telepsychiatry is being used by ACT teams for crisis intervention and to reduce inpatient hospitalizations.5
Continue to: Correctional facilities
Correctional facilities. With the downsizing and closure of many state psychiatric hospitals across the United States over the last several decades, jails and prisons have become de facto mental health hospitals. This situation presents many challenges, including access to mental health care and the need to avoid medications with the potential for abuse. Using telepsychiatry for psychiatric consultations in correctional facilities can improve access to mental health care.
Geriatric patients.
Children and adolescents. The Michigan Child Collaborative Care (MC3) program is a telepsychiatry consultation service that has been able to provide cost-effective, timely, remote consultation to primary care clinicians who care for youth and perinatal women.8 New York has a pediatric collaborative care program, the Child and Adolescent Psychiatry for Primary Care (CAP PC), that incorporates telepsychiatry consultations for families who live >1 hour away from one of the program’s treatment sites.9
Patients with cancer. A literature review that included 9 studies found no statistically significant differences between standard face-to-face interventions and telepsychiatry for improving quality-of-life scores among patients receiving treatment for cancer.10
Patients with insomnia. Cognitive-behavioral therapy for insomnia (CBT-I) is often recommended as a first-line treatment, but is not available for many patients. A recent study showed that CBT-I provided via telepsychiatry for patients with shift work sleep disorder was as effective as face-to-face therapy.11 Increasing the availability of this treatment could decrease reliance on pharmacotherapy for sleep.
Patients with opioid use disorder (OUD). Treatment for patients with OUD is limited by access to, and availability of, psychiatric clinicians. Telepsychiatry can help bridge this gap. One example of such use is in Ontario, Canada, where more than 10,000 patients with concurrent opiate abuse and other mental health disorders have received care via telepsychiatry since 2008.12
Continue to: Increasing access to cost-effective care where it is needed most
Increasing access to cost-effective care where it is needed most
There is a crisis in mental health care in rural areas of the United States. A study assessing delivery of care to US residents who live in rural areas found these patients’ mental health–related quality of life was 2.5 standard deviations below the national mean.13 Additionally, the need for treatment is expected to rise as the number of psychiatrists falls. According to a 2017 National Council for Behavioral Health report,14 by 2025, demand may outstrip supply by 6,090 to 15,600 psychiatrists. While telepsychiatry cannot improve this shortage per se, it can help increase access to psychiatric services. The potential benefits of telepsychiatry for patients are summarized in Table 1.15
Telepsychiatry may be more cost-effective than traditional face-to-face treatment. A cost analysis of an expanding, multistate behavioral telehealth intervention program for rural American Indian/Alaska Native populations found substantial cost savings associated with telepsychiatry.16 In this analysis, the estimated cost efficiencies of telepsychiatry were more evident in rural communities, and having a multistate center was less expensive than each state operating independently.16
Most importantly, evidence suggests that treatment delivered via telepsychiatry is at least as effective as traditional face-to-face care. In a review that included >150 studies, Bashshur et al17 concluded, “Effective approaches to the long-term management of mental illness include monitoring, surveillance, mental health promotion, mental illness prevention, and biopsychosocial treatment programs. The empirical evidence … demonstrates the capability of [telepsychiatry] to perform these functions more efficiently and as well as or more effectively than in-person care
Clinician and patient attitudes toward telepsychiatry
Clinicians have legitimate concerns about the quality of care being delivered when using telepsychiatry. Are patients satisfied with treatment delivered via telepsychiatry? Can a therapeutic alliance be established and maintained? It appears that clinicians may have more concerns than patients do.18
A study of telepsychiatry consultations for patients in rural primary care clinics performed by clinicians at an urban health center found that patients and clinicians were highly satisfied with telepsychiatry.19 Both patients and clinicians believed that telepsychiatry provided patients with better access to care. There was a high degree of agreement between patients and clinician responses.19
Continue to: In a review of...
In a review of 452 telepsychiatry studies, Hubley et al20 focused on satisfaction, reliability, treatment outcomes, implementation outcomes, cost effectiveness, and legal issues. They concluded that patients and clinicians are generally satisfied with telepsychiatry services. Interestingly, clinicians expressed more concerns about the potential adverse effects of telepsychiatry on therapeutic rapport. Hubley et al20 found no published reports of adverse events associated with telepsychiatry use.
In a study of school-based telepsychiatry in an urban setting, Mayworm et al21 found that patients were highly satisfied with both in-person and telepsychiatry services, and there were no significant differences in preference. This study also found that telepsychiatry services were more time-efficient than in-person services.
A study of using telepsychiatry to treat unipolar depression found that patient satisfaction scores improved with increasing number of video-based sessions, and were similar among all age groups.22 An analysis of this study found that total satisfaction scores were higher for patients than for clinicians.23
In a study of satisfaction with telepsychiatry among community-dwelling older veterans, 90% of participants reported liking or even preferring telepsychiatry, even though the experience was novel for most of them.24
As always, patients’ preferences need to be kept in mind when considering what services can and should be provided via telepsychiatry, because not all patients will find it acceptable. For example, in a study of veterans’ attitudes toward treatment via telepsychiatry, Goetter et al25 found that interest was mixed. Twenty-six percent of patients were “not at all comfortable,” while 13% were “extremely comfortable” using telepsychiatry from home. Notably, 33% indicated a clear preference for telepsychiatry compared to in-person mental health visits.
Continue to: Legal aspects of telepsychiatry
Legal aspects of telepsychiatry
Box 1
As part of the efforts to contain the spread of coronavirus disease 2019 (COVID-19), the use of telemedicine, including telepsychiatry, has increased substantially. Here are a few key facts to keep in mind while practicing telepsychiatry during this pandemic:
- The Centers for Medicare and Medicaid Services relaxed requirements for telehealth starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency. Under this new waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country and including in patient’s places of residence. For details, see www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. This fact sheet reviews relevant information, including billing codes.
- Health Insurance Portability and Accountability Act requirements, specifically those for secure communications, will not be enforced when telehealth is used under the new waiver. Because of this, popular but unsecure software applications, such as Apple’s FaceTime, Microsoft’s Teams, or Facebook’s Messenger, WhatsApp, and Messenger Rooms, can be used.
- Informed consent for the use of telepsychiatry in this situation should be obtained from the patient or his/her guardian, and documented in the patient’s medical record. For example: “Informed consent received for providing services via video teleconferencing to the home in order to protect the patient from COVID-19 exposure. Confidentiality issues were discussed.”
Licensure. State licensing and medical regulatory organizations consider the care provided via telepsychiatry to be rendered where the patient is physically located when services are rendered. Because of this, psychiatrists who use telepsychiatry generally need to hold a license in the state where their patients are located, regardless of where the psychiatrist is located.
Some states offer special telemedicine licenses. Typically, these licenses allow clinicians to practice across state lines without having to obtain a full professional license from the state. Be sure to check with the relevant state medical board where you intend to practice.
Because state laws related to telepsychiatry are continuously evolving, we suggest that clinicians continually check these laws and obtain a regulatory response in writing so there is ongoing documentation. For more information on this topic, see “Telepsychiatry during COVID-19: Understanding the rules” at MDedge.com/psychiatry.
Malpractice insurance. Some insurance companies offer coverage that includes the practice of telepsychiatry, whereas other carriers require the purchase of additional coverage for telepsychiatry. There may be additional requirements for practicing across state lines. Be sure to check with your insurer.
Continue to: Technical requirements and costs
Technical requirements and costs
In order to perform telepsychiatry, one needs Internet access, appropriate hardware such as a desktop or laptop computer or tablet, and a video conferencing application. Software must be HIPAA-compliant, although this requirement is not being enforced during the COVID-19 pandemic. Several popular video conferencing platforms were designed for or have versions suitable for telemedicine, including Zoom, Doxy.me, Vidyo, and Skype.
The use of different electronic health record (EHR) systems by various health care systems is a barrier to using telepsychiatry.
Box 2
The North Carolina Statewide Telepsychiatry Program (NC-STeP) began in 2013 by providing telepsychiatry services in hospital emergency departments (EDs) to individuals experiencing an acute behavioral health crisis. In 2018, the program expanded to include community-based primary care sites using a “hybrid” collaborative-care model. This model benefits patients by improving access to mental health specialty care; reducing the need for trips to the ED and inpatient admissions, thus decompressing EDs; improving compliance with treatment; reducing delays in care; reducing stigma; and improving continuity of care and follow-up. East Carolina University’s Center for Telepsychiatry and E-Behavioral Health is the home for this program, which is connecting hospital EDs and community-based primary care sites across North Carolina.
NC-STeP provides patients with a faceto-face interaction with a clinician through real-time video conferencing that is facilitated using mobile carts and desktop units. A web portal combines scheduling, electronic medical records, health information exchange functions, and data management systems.
NC-STeP has significantly reduced patient length of stay in EDs, provided cost savings to the health care delivery system through overturned involuntary commitments, improved ED throughout, and reduced patient boarding time; and has achieved high rates of patient, staff, and clinician satisfaction. Highlights of the program include:
- 57 hospitals and 8 communitybased sites in the network (as of January 1, 2020)
- 8 clinical hubs are operational, with 53 consultant clinicians
- 40,573 telepsychiatry assessments (as of January 1, 2020)
- 5,631 involuntary commitments overturned, thus preventing unnecessary hospitalizations representing a saving of $30,407,400 to the state
- Since program inception, >40% of ED patients who received telepsychiatry services were discharged to home
- 32% of the patients served had no insurance coverage
- Currently, the average consult elapsed time (in queue to consult complete) is 3 hours 9 minutes.
For more information about this program, see www.ecu.edu/cs-dhs/ncstep.
Our practice has extensive experience with telepsychiatry (Box 3), and for us, the specific costs associated with providing telepsychiatry services include maintenance of infrastructure and the purchase of hardware (eg, computers, smartphones, tablets), a video conferencing application (some free versions are available), EHR systems, and Internet access.
Box 3
Our practice (Rural Psychiatry Associates, Grand Forks, North Dakota) and our close associates have provided telepsychiatry services to >200 mental health clinics, hospitals, Native American villages, prisons, and nursing homes, mostly in rural and underserved areas. To provide these services, in addition to physicians, we also utilize nurse practitioners and physician assistants, for whom we provide extensive education, training, and supervision. We also provide education to the staff at the facilities where we provide services.
For nursing homes, we often use what is referred to as a “blended mode,” where we combine telepsychiatry visits with in-person, on-site visits, alternating monthly. In this model, we also typically alternate one physician with one nonphysician clinician at each facility. For continuity of care, the same clinicians service the same facilities. For very distant facilities with only a few patients, only telepsychiatry is utilized. However, initial services are always provided by a physician to establish a relationship, discuss policies and procedures, and evaluate patients face-to-face.
Telepsychiatry is increasingly used for education and mentoring. We have found telepsychiatry to be especially useful when working with psychiatric residents on a realtime basis as they evaluate and treat patients at a different location.
Reimbursement for telepsychiatry
Private insurance reimbursement for treatment delivered via telepsychiatry obviously depends on the specific insurance company. Some facilities, such as nursing homes, hospitals, medical clinics, and correctional facilities, offer lump-sum fees to clinicians for providing contracted services. Some clinicians are providing telepsychiatry as direct-bill or concierge services, which require direct payment from the patient without any reimbursement from insurance.
Medicare Part B covers some telepsychiatry services, but only under certain conditions.28 Previously, reimbursement was limited to services provided to patients who live in rural areas. However, on November 1, 2019, eligibility for telehealth services for Medicare Advantage (MA) recipients was expanded to include patients in both urban and rural locations. Patients covered by MA also can receive telehealth services from their home, instead of having to drive to a Centers for Medicare and Medicaid Services–qualified telehealth service center.
Continue to: Medicaid is the single...
Medicaid is the single largest payer for mental health services in the United States,29 and all Medicaid programs reimburse for some telepsychiatry services. As with all Medicaid health care, fees paid for telepsychiatry are state-specific. Since 2013, several state Medicaid programs, including New York,30 have expanded the list of eligible telehealth sites to include schools, thereby giving children virtual access to mental health clinicians.
Getting started
Clinicians who are interested in starting to provide treatment via telepsychiatry can begin by reviewing the American Psychiatric Association’s Telepsychiatry Toolkit at www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit. This toolkit, which is being continually updated, features numerous training videos for clinicians new to telepsychiatry, such as Learning To Do Telemental Health (www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit/learning-telemental-health) and The Credentialing Process (www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit/credentialing-process). Before starting, also consider reviewing the steps listed in Table 2.
Bottom Line
Evidence suggests telepsychiatry can be beneficial for a wide range of patient populations and settings. Most patients accept its use, and some actually prefer it to face-to-face care. Telepsychiatry may be especially useful for patients who have limited access to psychiatric treatment, such as those who live in rural areas. Factors to consider before incorporating telepsychiatry into your practice include addressing various legal, technological, and financial requirements.
Related Resources
- Von Hafften A. Telepsychiatry practice guidelines. American Psychiatric Association. https://www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit/practice-guidelines.
- Centers for Disease Control and Prevention. Telehealth and telemedicine: a research anthology of law and policy resources. https://www.cdc.gov/phlp/publications/topic/anthologies/anthologies-telehealth.html. Reviewed July 31, 2019.
- American Telemedicine Association. https://www.americantelemed.org/.
The need for mental health services has never been greater. Unfortunately, many patients have limited access to psychiatric treatment, especially those who live in rural areas. Telepsychiatry—the delivery of psychiatric services through telecommunications technology, usually video conferencing—may help address this problem. Even before the onset of the coronavirus disease 2019 (COVID-19) pandemic, telepsychiatry was becoming increasingly common. A survey of US mental health facilities found that the proportion of facilities offering telepsychiatry nearly doubled from 2010 to 2017, from 15.2% to 29.2%.1
In this article, we describe examples of where and how telepsychiatry is being used successfully, and its potential advantages. We discuss concerns about its use, its impact on the therapeutic alliance, and patients’ and clinicians’ perceptions of it. We also discuss the legal, technological, and financial aspects of using telepsychiatry. With an increased understanding of these issues, psychiatric clinicians will be better able to integrate telepsychiatry into their practices.
How and where is telepsychiatry being used
In addition to being used to provide psychotherapy, telepsychiatry is being employed for diagnosis and evaluation; clinical consultations; research; supervision, mentoring, and education of trainees; development of treatment programs; and public health. Telepsychiatry is an excellent mechanism to provide high-level second opinions to primary care physicians and psychiatrists on complex cases for both diagnostic purposes and treatment.
Evidence suggests that telepsychiatry can play a beneficial role in a variety of settings, and for a range of patient populations.
Emergency departments (EDs). Using telepsychiatry for psychiatric consultations in EDs could result in a quicker disposition of patients and reduced crowding and wait times. A survey of on-call clinicians in a pediatric ED found that using telepsychiatry for on-site psychiatric consultations decreased patients’ length of stay, improved resident on-call burden, and reduced factors related to physician burnout.2 In this study, telepsychiatry use reduced travel for face-to-face evaluations by 75% and saved more than 2 hours per call day.2
Medical clinics. Using telepsychiatry to deliver cognitive-behavioral therapy significantly reduced symptoms of depression or anxiety among 203 primary care patients.3 Incorporating telepsychiatry into existing integrated primary care settings is becoming more common. For example, an integrated-care model that includes telepsychiatry is serving the needs of complex patients in a high-volume, urban primary care clinic in Colorado.4
Assertive Community Treatment (ACT) teams. Telepsychiatry is being used by ACT teams for crisis intervention and to reduce inpatient hospitalizations.5
Continue to: Correctional facilities
Correctional facilities. With the downsizing and closure of many state psychiatric hospitals across the United States over the last several decades, jails and prisons have become de facto mental health hospitals. This situation presents many challenges, including access to mental health care and the need to avoid medications with the potential for abuse. Using telepsychiatry for psychiatric consultations in correctional facilities can improve access to mental health care.
Geriatric patients.
Children and adolescents. The Michigan Child Collaborative Care (MC3) program is a telepsychiatry consultation service that has been able to provide cost-effective, timely, remote consultation to primary care clinicians who care for youth and perinatal women.8 New York has a pediatric collaborative care program, the Child and Adolescent Psychiatry for Primary Care (CAP PC), that incorporates telepsychiatry consultations for families who live >1 hour away from one of the program’s treatment sites.9
Patients with cancer. A literature review that included 9 studies found no statistically significant differences between standard face-to-face interventions and telepsychiatry for improving quality-of-life scores among patients receiving treatment for cancer.10
Patients with insomnia. Cognitive-behavioral therapy for insomnia (CBT-I) is often recommended as a first-line treatment, but is not available for many patients. A recent study showed that CBT-I provided via telepsychiatry for patients with shift work sleep disorder was as effective as face-to-face therapy.11 Increasing the availability of this treatment could decrease reliance on pharmacotherapy for sleep.
Patients with opioid use disorder (OUD). Treatment for patients with OUD is limited by access to, and availability of, psychiatric clinicians. Telepsychiatry can help bridge this gap. One example of such use is in Ontario, Canada, where more than 10,000 patients with concurrent opiate abuse and other mental health disorders have received care via telepsychiatry since 2008.12
Continue to: Increasing access to cost-effective care where it is needed most
Increasing access to cost-effective care where it is needed most
There is a crisis in mental health care in rural areas of the United States. A study assessing delivery of care to US residents who live in rural areas found these patients’ mental health–related quality of life was 2.5 standard deviations below the national mean.13 Additionally, the need for treatment is expected to rise as the number of psychiatrists falls. According to a 2017 National Council for Behavioral Health report,14 by 2025, demand may outstrip supply by 6,090 to 15,600 psychiatrists. While telepsychiatry cannot improve this shortage per se, it can help increase access to psychiatric services. The potential benefits of telepsychiatry for patients are summarized in Table 1.15
Telepsychiatry may be more cost-effective than traditional face-to-face treatment. A cost analysis of an expanding, multistate behavioral telehealth intervention program for rural American Indian/Alaska Native populations found substantial cost savings associated with telepsychiatry.16 In this analysis, the estimated cost efficiencies of telepsychiatry were more evident in rural communities, and having a multistate center was less expensive than each state operating independently.16
Most importantly, evidence suggests that treatment delivered via telepsychiatry is at least as effective as traditional face-to-face care. In a review that included >150 studies, Bashshur et al17 concluded, “Effective approaches to the long-term management of mental illness include monitoring, surveillance, mental health promotion, mental illness prevention, and biopsychosocial treatment programs. The empirical evidence … demonstrates the capability of [telepsychiatry] to perform these functions more efficiently and as well as or more effectively than in-person care
Clinician and patient attitudes toward telepsychiatry
Clinicians have legitimate concerns about the quality of care being delivered when using telepsychiatry. Are patients satisfied with treatment delivered via telepsychiatry? Can a therapeutic alliance be established and maintained? It appears that clinicians may have more concerns than patients do.18
A study of telepsychiatry consultations for patients in rural primary care clinics performed by clinicians at an urban health center found that patients and clinicians were highly satisfied with telepsychiatry.19 Both patients and clinicians believed that telepsychiatry provided patients with better access to care. There was a high degree of agreement between patients and clinician responses.19
Continue to: In a review of...
In a review of 452 telepsychiatry studies, Hubley et al20 focused on satisfaction, reliability, treatment outcomes, implementation outcomes, cost effectiveness, and legal issues. They concluded that patients and clinicians are generally satisfied with telepsychiatry services. Interestingly, clinicians expressed more concerns about the potential adverse effects of telepsychiatry on therapeutic rapport. Hubley et al20 found no published reports of adverse events associated with telepsychiatry use.
In a study of school-based telepsychiatry in an urban setting, Mayworm et al21 found that patients were highly satisfied with both in-person and telepsychiatry services, and there were no significant differences in preference. This study also found that telepsychiatry services were more time-efficient than in-person services.
A study of using telepsychiatry to treat unipolar depression found that patient satisfaction scores improved with increasing number of video-based sessions, and were similar among all age groups.22 An analysis of this study found that total satisfaction scores were higher for patients than for clinicians.23
In a study of satisfaction with telepsychiatry among community-dwelling older veterans, 90% of participants reported liking or even preferring telepsychiatry, even though the experience was novel for most of them.24
As always, patients’ preferences need to be kept in mind when considering what services can and should be provided via telepsychiatry, because not all patients will find it acceptable. For example, in a study of veterans’ attitudes toward treatment via telepsychiatry, Goetter et al25 found that interest was mixed. Twenty-six percent of patients were “not at all comfortable,” while 13% were “extremely comfortable” using telepsychiatry from home. Notably, 33% indicated a clear preference for telepsychiatry compared to in-person mental health visits.
Continue to: Legal aspects of telepsychiatry
Legal aspects of telepsychiatry
Box 1
As part of the efforts to contain the spread of coronavirus disease 2019 (COVID-19), the use of telemedicine, including telepsychiatry, has increased substantially. Here are a few key facts to keep in mind while practicing telepsychiatry during this pandemic:
- The Centers for Medicare and Medicaid Services relaxed requirements for telehealth starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency. Under this new waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country and including in patient’s places of residence. For details, see www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. This fact sheet reviews relevant information, including billing codes.
- Health Insurance Portability and Accountability Act requirements, specifically those for secure communications, will not be enforced when telehealth is used under the new waiver. Because of this, popular but unsecure software applications, such as Apple’s FaceTime, Microsoft’s Teams, or Facebook’s Messenger, WhatsApp, and Messenger Rooms, can be used.
- Informed consent for the use of telepsychiatry in this situation should be obtained from the patient or his/her guardian, and documented in the patient’s medical record. For example: “Informed consent received for providing services via video teleconferencing to the home in order to protect the patient from COVID-19 exposure. Confidentiality issues were discussed.”
Licensure. State licensing and medical regulatory organizations consider the care provided via telepsychiatry to be rendered where the patient is physically located when services are rendered. Because of this, psychiatrists who use telepsychiatry generally need to hold a license in the state where their patients are located, regardless of where the psychiatrist is located.
Some states offer special telemedicine licenses. Typically, these licenses allow clinicians to practice across state lines without having to obtain a full professional license from the state. Be sure to check with the relevant state medical board where you intend to practice.
Because state laws related to telepsychiatry are continuously evolving, we suggest that clinicians continually check these laws and obtain a regulatory response in writing so there is ongoing documentation. For more information on this topic, see “Telepsychiatry during COVID-19: Understanding the rules” at MDedge.com/psychiatry.
Malpractice insurance. Some insurance companies offer coverage that includes the practice of telepsychiatry, whereas other carriers require the purchase of additional coverage for telepsychiatry. There may be additional requirements for practicing across state lines. Be sure to check with your insurer.
Continue to: Technical requirements and costs
Technical requirements and costs
In order to perform telepsychiatry, one needs Internet access, appropriate hardware such as a desktop or laptop computer or tablet, and a video conferencing application. Software must be HIPAA-compliant, although this requirement is not being enforced during the COVID-19 pandemic. Several popular video conferencing platforms were designed for or have versions suitable for telemedicine, including Zoom, Doxy.me, Vidyo, and Skype.
The use of different electronic health record (EHR) systems by various health care systems is a barrier to using telepsychiatry.
Box 2
The North Carolina Statewide Telepsychiatry Program (NC-STeP) began in 2013 by providing telepsychiatry services in hospital emergency departments (EDs) to individuals experiencing an acute behavioral health crisis. In 2018, the program expanded to include community-based primary care sites using a “hybrid” collaborative-care model. This model benefits patients by improving access to mental health specialty care; reducing the need for trips to the ED and inpatient admissions, thus decompressing EDs; improving compliance with treatment; reducing delays in care; reducing stigma; and improving continuity of care and follow-up. East Carolina University’s Center for Telepsychiatry and E-Behavioral Health is the home for this program, which is connecting hospital EDs and community-based primary care sites across North Carolina.
NC-STeP provides patients with a faceto-face interaction with a clinician through real-time video conferencing that is facilitated using mobile carts and desktop units. A web portal combines scheduling, electronic medical records, health information exchange functions, and data management systems.
NC-STeP has significantly reduced patient length of stay in EDs, provided cost savings to the health care delivery system through overturned involuntary commitments, improved ED throughout, and reduced patient boarding time; and has achieved high rates of patient, staff, and clinician satisfaction. Highlights of the program include:
- 57 hospitals and 8 communitybased sites in the network (as of January 1, 2020)
- 8 clinical hubs are operational, with 53 consultant clinicians
- 40,573 telepsychiatry assessments (as of January 1, 2020)
- 5,631 involuntary commitments overturned, thus preventing unnecessary hospitalizations representing a saving of $30,407,400 to the state
- Since program inception, >40% of ED patients who received telepsychiatry services were discharged to home
- 32% of the patients served had no insurance coverage
- Currently, the average consult elapsed time (in queue to consult complete) is 3 hours 9 minutes.
For more information about this program, see www.ecu.edu/cs-dhs/ncstep.
Our practice has extensive experience with telepsychiatry (Box 3), and for us, the specific costs associated with providing telepsychiatry services include maintenance of infrastructure and the purchase of hardware (eg, computers, smartphones, tablets), a video conferencing application (some free versions are available), EHR systems, and Internet access.
Box 3
Our practice (Rural Psychiatry Associates, Grand Forks, North Dakota) and our close associates have provided telepsychiatry services to >200 mental health clinics, hospitals, Native American villages, prisons, and nursing homes, mostly in rural and underserved areas. To provide these services, in addition to physicians, we also utilize nurse practitioners and physician assistants, for whom we provide extensive education, training, and supervision. We also provide education to the staff at the facilities where we provide services.
For nursing homes, we often use what is referred to as a “blended mode,” where we combine telepsychiatry visits with in-person, on-site visits, alternating monthly. In this model, we also typically alternate one physician with one nonphysician clinician at each facility. For continuity of care, the same clinicians service the same facilities. For very distant facilities with only a few patients, only telepsychiatry is utilized. However, initial services are always provided by a physician to establish a relationship, discuss policies and procedures, and evaluate patients face-to-face.
Telepsychiatry is increasingly used for education and mentoring. We have found telepsychiatry to be especially useful when working with psychiatric residents on a realtime basis as they evaluate and treat patients at a different location.
Reimbursement for telepsychiatry
Private insurance reimbursement for treatment delivered via telepsychiatry obviously depends on the specific insurance company. Some facilities, such as nursing homes, hospitals, medical clinics, and correctional facilities, offer lump-sum fees to clinicians for providing contracted services. Some clinicians are providing telepsychiatry as direct-bill or concierge services, which require direct payment from the patient without any reimbursement from insurance.
Medicare Part B covers some telepsychiatry services, but only under certain conditions.28 Previously, reimbursement was limited to services provided to patients who live in rural areas. However, on November 1, 2019, eligibility for telehealth services for Medicare Advantage (MA) recipients was expanded to include patients in both urban and rural locations. Patients covered by MA also can receive telehealth services from their home, instead of having to drive to a Centers for Medicare and Medicaid Services–qualified telehealth service center.
Continue to: Medicaid is the single...
Medicaid is the single largest payer for mental health services in the United States,29 and all Medicaid programs reimburse for some telepsychiatry services. As with all Medicaid health care, fees paid for telepsychiatry are state-specific. Since 2013, several state Medicaid programs, including New York,30 have expanded the list of eligible telehealth sites to include schools, thereby giving children virtual access to mental health clinicians.
Getting started
Clinicians who are interested in starting to provide treatment via telepsychiatry can begin by reviewing the American Psychiatric Association’s Telepsychiatry Toolkit at www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit. This toolkit, which is being continually updated, features numerous training videos for clinicians new to telepsychiatry, such as Learning To Do Telemental Health (www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit/learning-telemental-health) and The Credentialing Process (www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit/credentialing-process). Before starting, also consider reviewing the steps listed in Table 2.
Bottom Line
Evidence suggests telepsychiatry can be beneficial for a wide range of patient populations and settings. Most patients accept its use, and some actually prefer it to face-to-face care. Telepsychiatry may be especially useful for patients who have limited access to psychiatric treatment, such as those who live in rural areas. Factors to consider before incorporating telepsychiatry into your practice include addressing various legal, technological, and financial requirements.
Related Resources
- Von Hafften A. Telepsychiatry practice guidelines. American Psychiatric Association. https://www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit/practice-guidelines.
- Centers for Disease Control and Prevention. Telehealth and telemedicine: a research anthology of law and policy resources. https://www.cdc.gov/phlp/publications/topic/anthologies/anthologies-telehealth.html. Reviewed July 31, 2019.
- American Telemedicine Association. https://www.americantelemed.org/.
1. Spivak S, Spivak A, Cullen B, et al. Telepsychiatry use in U.S. mental health facilities, 2010-2017. Psychiatr Serv. 2019;71(2):appips201900261. doi: 10.1176/appi.ps.201900261.
2. Reliford A, Adebanjo B. Use of telepsychiatry in pediatric emergency room to decrease length of stay for psychiatric patients, improve resident on-call burden, and reduce factors related to physician burnout. Telemed J E Health. 2019;25(9):828-832.
3. Mathiasen K, Riper H, Andersen TE, et al. Guided internet-based cognitive behavioral therapy for adult depression and anxiety in routine secondary care: observational study. J Med Internet Res. 2018;20(11):e10927. doi: 10.2196/10927.
4. Waugh M, Calderone J, Brown Levey S, et al. Using telepsychiatry to enrich existing integrated primary care. Telemed J E Health. 2019;25(8):762-768.
5. Swanson CL, Trestman RL. Rural assertive community treatment and telepsychiatry. J Psychiatr Pract. 2018;24(4):269-273.
6. Gentry MT, Lapid MI, Rummans TA. Geriatric telepsychiatry: systematic review and policy considerations. Am J Geriatr Psychiatry. 2019;27(2):109-127.
7. Christensen LF, Moller AM, Hansen JP, et al. Patients’ and providers’ experiences with video consultations used in the treatment of older patients with unipolar depression: a systematic review. J Psychiatr Ment Health Nurs. 2020;27(3):258-271.
8. Marcus S, Malas N, Dopp R, et al. The Michigan Child Collaborative Care program: building a telepsychiatry consultation service. Psychiatr Serv. 2019;70(9):849-852.
9. Kaye DL, Fornari V, Scharf M, et al. Description of a multi-university education and collaborative care child psychiatry access program: New York State’s CAP PC. Gen Hosp Psychiatry. 2017;48:32-36.
10. Larson JL, Rosen AB, Wilson FA. The effect of telehealth interventions on quality of life of cancer patients: a systematic review and meta-analysis. Telemed J E Health. 2018;24(6):397-405.
11. Peter L, Reindl R, Zauter S, et al. Effectiveness of an online CBT-I intervention and a face-to-face treatment for shift work sleep disorder: a comparison of sleep diary data. Int J Environ Res Public Health. 2019;16(17):E3081. doi: 10.3390/ijerph16173081.
12. LaBelle B, Franklyn AM, Pkh Nguyen V, et al. Characterizing the use of telepsychiatry for patients with opioid use disorder and cooccurring mental health disorders in Ontario, Canada. Int J Telemed Appl. 2018;2018(3):1-7.
13. Fortney JC, Heagerty PJ, Bauer AM, et al. Study to promote innovation in rural integrated telepsychiatry (SPIRIT): rationale and design of a randomized comparative effectiveness trial of managing complex psychiatric disorders in rural primary care clinics. Contemp Clin Trials. 2020;90:105873. doi: 10.1016/j.cct.2019.105873.
14. Weiner S. Addressing the escalating psychiatrist shortage. AAMC. https://www.aamc.org/news-insights/addressing-escalating-psychiatrist-shortage. Published February 12, 2018. Accessed May 14, 2020.
15. American Psychiatric Association. What is telepsychiatry? https://www.psychiatry.org/patients-families/what-is-telepsychiatry. Published 2017. Accessed May 14, 2020.
16. Yilmaz SK, Horn BP, Fore C, et al. An economic cost analysis of an expanding, multi-state behavioural telehealth intervention. J Telemed Telecare. 2019;25(6):353-364.
17. Bashshur RL, Shannon GW, Bashshur N, et al. The empirical evidence for telemedicine interventions in mental disorders. Telemed J E Health. 2016;22(2):87-113.
18. Lopez A, Schwenk S, Schneck CD, et al. Technology-based mental health treatment and the impact on the therapeutic alliance. Curr Psychiatry Rep. 2019;21(8):76.
19. Schubert NJ, Backman PJ, Bhatla R, et al. Telepsychiatry and patient-provider concordance. Can J Rural Med. 2019;24(3):75-82.
20. Hubley S, Lynch SB, Schneck C, et al. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6(2):269-282.
21. Mayworm AM, Lever N, Gloff N, et al. School-based telepsychiatry in an urban setting: efficiency and satisfaction with care. Telemed J E Health. 2020;26(4):446-454.
22. Christensen LF, Gildberg FA, Sibbersen C, et al. Videoconferences and treatment of depression: satisfaction score correlated with number of sessions attended but not with age [published online October 31, 2019]. Telemed J E Health. 2019. doi: 10.1089/tmj.2019.0129.
23. Christensen LF, Gildberg FA, Sibbersen C, et al. Disagreement in satisfaction between patients and providers in the use of videoconferences by depressed adults. Telemed J E Health. 2020;26(5):614-620.
24. Hantke N, Lajoy M, Gould CE, et al. Patient satisfaction with geriatric psychiatry services via video teleconference. Am J Geriatr Psychiatry. 2020;28(4):491-494.
25. Goetter EM, Blackburn AM, Bui E, et al. Veterans’ prospective attitudes about mental health treatment using telehealth. J Psychosoc Nurs Ment Health Serv. 2019;57(9):38-43.
26. Vanderpool D. Top 10 myths about telepsychiatry. Innov Clin Neurosci. 2017;14(9-10):13-15.
27. Butterfield A. Telepsychiatric evaluation and consultation in emergency care settings. Child Adolesc Psychiatr Clin N Am. 2018;27(3):467-478.
28. Medicare.gov. Telehealth. https://www.medicare.gov/coverage/telehealth. Accessed May 14, 2020.
29. Centers for Medicare & Medicaid Services. Behavioral Health Services. https://www.medicaid.gov/medicaid/benefits/bhs/index.html. Accessed May 14, 2020.
30. New York Pub Health Law §2999-cc (2017).
1. Spivak S, Spivak A, Cullen B, et al. Telepsychiatry use in U.S. mental health facilities, 2010-2017. Psychiatr Serv. 2019;71(2):appips201900261. doi: 10.1176/appi.ps.201900261.
2. Reliford A, Adebanjo B. Use of telepsychiatry in pediatric emergency room to decrease length of stay for psychiatric patients, improve resident on-call burden, and reduce factors related to physician burnout. Telemed J E Health. 2019;25(9):828-832.
3. Mathiasen K, Riper H, Andersen TE, et al. Guided internet-based cognitive behavioral therapy for adult depression and anxiety in routine secondary care: observational study. J Med Internet Res. 2018;20(11):e10927. doi: 10.2196/10927.
4. Waugh M, Calderone J, Brown Levey S, et al. Using telepsychiatry to enrich existing integrated primary care. Telemed J E Health. 2019;25(8):762-768.
5. Swanson CL, Trestman RL. Rural assertive community treatment and telepsychiatry. J Psychiatr Pract. 2018;24(4):269-273.
6. Gentry MT, Lapid MI, Rummans TA. Geriatric telepsychiatry: systematic review and policy considerations. Am J Geriatr Psychiatry. 2019;27(2):109-127.
7. Christensen LF, Moller AM, Hansen JP, et al. Patients’ and providers’ experiences with video consultations used in the treatment of older patients with unipolar depression: a systematic review. J Psychiatr Ment Health Nurs. 2020;27(3):258-271.
8. Marcus S, Malas N, Dopp R, et al. The Michigan Child Collaborative Care program: building a telepsychiatry consultation service. Psychiatr Serv. 2019;70(9):849-852.
9. Kaye DL, Fornari V, Scharf M, et al. Description of a multi-university education and collaborative care child psychiatry access program: New York State’s CAP PC. Gen Hosp Psychiatry. 2017;48:32-36.
10. Larson JL, Rosen AB, Wilson FA. The effect of telehealth interventions on quality of life of cancer patients: a systematic review and meta-analysis. Telemed J E Health. 2018;24(6):397-405.
11. Peter L, Reindl R, Zauter S, et al. Effectiveness of an online CBT-I intervention and a face-to-face treatment for shift work sleep disorder: a comparison of sleep diary data. Int J Environ Res Public Health. 2019;16(17):E3081. doi: 10.3390/ijerph16173081.
12. LaBelle B, Franklyn AM, Pkh Nguyen V, et al. Characterizing the use of telepsychiatry for patients with opioid use disorder and cooccurring mental health disorders in Ontario, Canada. Int J Telemed Appl. 2018;2018(3):1-7.
13. Fortney JC, Heagerty PJ, Bauer AM, et al. Study to promote innovation in rural integrated telepsychiatry (SPIRIT): rationale and design of a randomized comparative effectiveness trial of managing complex psychiatric disorders in rural primary care clinics. Contemp Clin Trials. 2020;90:105873. doi: 10.1016/j.cct.2019.105873.
14. Weiner S. Addressing the escalating psychiatrist shortage. AAMC. https://www.aamc.org/news-insights/addressing-escalating-psychiatrist-shortage. Published February 12, 2018. Accessed May 14, 2020.
15. American Psychiatric Association. What is telepsychiatry? https://www.psychiatry.org/patients-families/what-is-telepsychiatry. Published 2017. Accessed May 14, 2020.
16. Yilmaz SK, Horn BP, Fore C, et al. An economic cost analysis of an expanding, multi-state behavioural telehealth intervention. J Telemed Telecare. 2019;25(6):353-364.
17. Bashshur RL, Shannon GW, Bashshur N, et al. The empirical evidence for telemedicine interventions in mental disorders. Telemed J E Health. 2016;22(2):87-113.
18. Lopez A, Schwenk S, Schneck CD, et al. Technology-based mental health treatment and the impact on the therapeutic alliance. Curr Psychiatry Rep. 2019;21(8):76.
19. Schubert NJ, Backman PJ, Bhatla R, et al. Telepsychiatry and patient-provider concordance. Can J Rural Med. 2019;24(3):75-82.
20. Hubley S, Lynch SB, Schneck C, et al. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6(2):269-282.
21. Mayworm AM, Lever N, Gloff N, et al. School-based telepsychiatry in an urban setting: efficiency and satisfaction with care. Telemed J E Health. 2020;26(4):446-454.
22. Christensen LF, Gildberg FA, Sibbersen C, et al. Videoconferences and treatment of depression: satisfaction score correlated with number of sessions attended but not with age [published online October 31, 2019]. Telemed J E Health. 2019. doi: 10.1089/tmj.2019.0129.
23. Christensen LF, Gildberg FA, Sibbersen C, et al. Disagreement in satisfaction between patients and providers in the use of videoconferences by depressed adults. Telemed J E Health. 2020;26(5):614-620.
24. Hantke N, Lajoy M, Gould CE, et al. Patient satisfaction with geriatric psychiatry services via video teleconference. Am J Geriatr Psychiatry. 2020;28(4):491-494.
25. Goetter EM, Blackburn AM, Bui E, et al. Veterans’ prospective attitudes about mental health treatment using telehealth. J Psychosoc Nurs Ment Health Serv. 2019;57(9):38-43.
26. Vanderpool D. Top 10 myths about telepsychiatry. Innov Clin Neurosci. 2017;14(9-10):13-15.
27. Butterfield A. Telepsychiatric evaluation and consultation in emergency care settings. Child Adolesc Psychiatr Clin N Am. 2018;27(3):467-478.
28. Medicare.gov. Telehealth. https://www.medicare.gov/coverage/telehealth. Accessed May 14, 2020.
29. Centers for Medicare & Medicaid Services. Behavioral Health Services. https://www.medicaid.gov/medicaid/benefits/bhs/index.html. Accessed May 14, 2020.
30. New York Pub Health Law §2999-cc (2017).
Cannabidiol for psychosis: A review of 4 studies
There has been increasing interest in the medicinal use of cannabidiol (CBD) for a wide variety of health conditions. CBD is one of more than 80 chemicals identified in the Cannabis sativa plant, otherwise known as marijuana or hemp. Delta-9-tetrahydrocannabinol (THC) is the psychoactive ingredient found in marijuana that produces a “high.” CBD, which is one of the most abundant cannabinoids in Cannabis sativa, does not produce any psychotomimetic effects.
The strongest scientific evidence supporting CBD for medicinal purposes is for its effectiveness in treating certain childhood epilepsy syndromes that typically do not respond to antiseizure medications. Currently, the only FDA-approved CBD product is a prescription oil cannabidiol (brand name: Epidiolex) for treating 2 types of epilepsy. Aside from Epidiolex, state laws governing the use of CBD vary. CBD is being studied as a treatment for a wide range of psychiatric conditions, including bipolar disorder, schizophrenia, dystonia, insomnia, and anxiety. Research supporting CBD’s benefits is limited, and the US National Library of Medicine’s MedlinePlus indicates there is “insufficient evidence to rate effectiveness” for these indications.1
Despite having been legalized for medicinal use in many states, CBD is classified as a Schedule I controlled substance by the US Drug Enforcement Agency. Because of this classification, little has been done to regulate and oversee the sale of products containing CBD. In a 2017 study of 84 CBD products sold by 31 companies online, Bonn-Miller et al2 found that nearly 70% percent of products were inaccurately labeled. In this study, blind testing found that only approximately 31% of products contained within 10% of the amount of CBD that was listed on the label. These researchers also found that some products contained components not listed on the label, including THC.2
The relationship between cannabis and psychosis or psychotic symptoms has been investigated for decades. Some recent studies that examined the effects of CBD on psychosis found that individuals who use CBD may experience fewer positive psychotic symptoms compared with placebo. This raises the question of whether CBD may have a role in the treatment of schizophrenia and other psychotic disorders. One of the first studies on this issue was conducted by Leweke et al,3 who compared oral CBD, up to 800 mg/d, with the antipsychotic amisulpride, up to 800 mg/d, in 39 patients with an acute exacerbation of psychotic symptoms. Amisulpride is used outside the United States to treat psychosis, but is FDA-approved only as an antiemetic. Patients were treated for 4 weeks. By Day 28, there was a significant reduction in positive symptoms as measured using the Positive and Negative Syndrome Scale (PANSS), with no significant difference in efficacy between the treatments. Similar findings emerged for negative, total, and general symptoms, with significant reductions by Day 28 in both treatment arms, and no significant between-treatment differences.
These findings were the first robust indication that CBD may have antipsychotic efficacy. However, of greater interest may be CBD’s markedly superior adverse effect profile. Predictably, amisulpride significantly increased extrapyramidal symptoms (EPS), weight gain, and prolactin levels from baseline to Day 28. However, no significant change was found in any of these adverse effects in the CBD group, and the between-treatment difference was significant (all P < .01).
Here we review 4 recent studies that evaluated CBD as a treatment for schizophrenia. These studies are summarized in the Table.4-7
Continue to: McGuire P, et al...
1. McGuire P, Robson P, Cubala WJ, et al. Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: a multicenter randomized controlled trial. Am J Psychiatry. 2018;175(3):225-231.
Antipsychotic medications act through blockade of central dopamine D2 receptors. For most patients, antipsychotics effectively treat positive psychotic symptoms, which are driven by elevated dopamine function. However, these medications have minimal effects on negative symptoms and cognitive impairment, features of schizophrenia that are not driven by elevated dopamine. Compounds exhibiting a mechanism of action unlike that of current antipsychotics may improve the treatment and outcomes of patients with schizophrenia. The mechanism of action of CBD is unclear, but it does not appear to involve the direct antagonism of dopamine receptors. Human and animal research study findings indicate that CBD has antipsychotic properties. McGuire et al4 assessed the safety and effectiveness of CBD as an adjunctive treatment of schizophrenia.
Study design
- In this double-blind parallel-group trial conducted at 15 hospitals in the United Kingdom, Romania, and Poland, 88 patients with schizophrenia received CBD (1,000 mg/d; N = 43) or placebo (N = 45) as adjunct to the antipsychotic medication they had been prescribed. Patients had previously demonstrated at least a partial response to antipsychotic treatment, and were taking stable doses of an antipsychotic for ≥4 weeks.
- Evaluations of symptoms, general functioning, cognitive performance, and EPS were completed at baseline and on Days 8, 22, and 43 (± 3 days). Current substance use was assessed using a semi-structured interview, and reassessed at the end of treatment.
- The key endpoints were the patients’ level of functioning, severity of symptoms, and cognitive performance. Participants were assessed before and after treatment using the PANSS, the Brief Assessment of Cognition in Schizophrenia (BACS), the Global Assessment of Functioning scale (GAF), and the improvement and severity scales of the Clinical Global Impressions Scale (CGI-I and CGI-S, respectively).
- The clinicians’ impression of illness severity and symptom improvement and patient- or caregiver-reported impressions of general functioning and sleep also were noted.
Outcomes
- After 6 weeks, compared with the placebo group, the CBD group had lower levels of positive psychotic symptoms and were more likely to be rated as improved and as not severely unwell by the treating clinician. Patients in the CBD group also showed greater improvements in cognitive performance and in overall functioning, although these were not statistically significant.
- Similar levels of negative psychotic symptoms, overall psychopathology, and general psychopathology were observed in the CBD and placebo groups. The CBD group had a higher proportion of treatment responders (≥20% improvement in PANSS total score) than did the placebo group; however, the total number of responders per group was small (12 and 6 patients, respectively). At baseline, most patients in both groups were classified as moderately, markedly, or severely ill (83.4% in the CBD group vs 79.6% in placebo group). By the end of treatment, this decreased to 54.8% in the CBD group and 63.6% in the placebo group. Clinicians rated 78.6% of patients in the CBD group as “improved” on the CGI-I, compared with 54.6% of patients in the placebo group.
Conclusion
- CBD treatment adjunctive to antipsychotics was associated with significant effects on positive psychotic symptoms and on CGI-I and illness severity. Improvements in cognitive performance and level of overall functioning were also seen, but were not statistically significant.
- Although the effect on positive symptoms was modest, improvement occurred in patients being treated with appropriate dosages of antipsychotics, which suggests CBD provided benefits over and above the effect of antipsychotic treatment. Moreover, the changes in CGI-I and CGI-S scores indicated that the improvement was evident to the treating psychiatrists, and may therefore be clinically meaningful.
Continue to: Boggs DL, et al...
2. Boggs DL, Surti T, Gupta A, et al. The effects of cannabidiol (CBD) on cognition and symptoms in outpatients with chronic schizophrenia a randomized placebo controlled trial. Psychopharmacology (Berl). 2018;235(7):1923-1932.
Schizophrenia is associated with cognitive deficits in learning, recall, attention, working memory, and executive function. The cognitive impairments associated with schizophrenia (CIAS) are independent of phase of illness and often persist after other symptoms have been effectively treated. These impairments are the strongest predictor of functional outcome, even more so than psychotic symptoms.
Antipsychotics have limited efficacy for CIAS, which highlights the need for CIAS treatments that target other nondopaminergic neurotransmitter systems. The endocannabinoid system, which has been implicated in schizophrenia and in cognition, is a potential target. Several cannabinoids impair memory and attention. The main psychoactive component of marijuana, THC, is a cannabinoid receptor type 1 (CB1R) partial agonist. Administration of THC produces significant deficits in verbal learning, attention, and working memory.
Researchers have hypothesized that CB1R blockade or modulation of cannabinoid levels may offer a novel target for treating CIAS. Boggs et al5 compared the cognitive, symptomatic, and adverse effects of CBD vs placebo.
Study design
- In this 6-week, randomized, placebo-controlled study conducted in Connecticut from September 2009 to May 2012, 36 stable patients with schizophrenia who were treated with antipsychotics were randomized to also receive oral CBD, 600 mg/d, or placebo.
- Cognition was assessed using the t score of the MATRICS Consensus Cognitive Battery (MCCB) composite and subscales at baseline and the end of study. An increase in MCCB t score indicates an improvement in cognitive ability. Psychotic symptoms were assessed using the PANSS at baseline, Week 2, Week 4, and Week 6.
Outcomes
- CBD augmentation did not improve MCCB performance or psychotic symptoms. There was no main effect of time or medication on MCCB composite score, but a significant drug × time effect was observed.
- Post-hoc analyses revealed that only patients who received placebo improved over time. The lack of a similar improvement with CBD might be related to the greater incidence of sedation among the CBD group (20%) vs the placebo group (5%). Both the MCCB composite score and reasoning and problem-solving domain scores were higher at baseline and endpoint for patients who received CBD, which suggests that the observed improvement in the placebo group could represent a regression to the mean.
- There was a significant decrease in PANSS scores over time, but there was no significant drug × time interaction.
Conclusion
- CBD augmentation was not associated with an improvement in MCCB score. This is consistent with data from other clinical trials4,8 that suggested that CBD (at a wide range of doses) does not have significant beneficial effects on cognition in patients with schizophrenia.
- Additionally, CBD did not improve psychotic symptoms. These results are in contrast to published case reports9,10 and 2 published clinical trials3,4 that found CBD (800 mg/d) was as efficacious as amisulpride in reducing positive psychotic symptoms, and a small but statistically significant improvement in PANSS positive scores with CBD (1,000 mg/d) compared with placebo. However, these results are similar to those of a separate study11 that evaluated the same 600-mg/d dose of CBD used by Boggs et al.5 At 600 mg/d, CBD produced very small improvements in PANSS total scores (~2.4) that were not statistically significant. A higher CBD dose may be needed to reduce psychotic symptoms in patients with schizophrenia.
Continue to: O’Neill A, et al...
3. O’Neill A, Wilson R, Blest-Hopley G, et al. Normalization of mediotemporal and prefrontal activity, and mediotemporal-striatal connectivity, may underlie antipsychotic effects of cannabidiol in psychosis. Psychol Med. 2020;1-11. doi: 10.1017/S0033291719003519.
In addition to their key roles in the psychopathology of psychosis, the mediotemporal and prefrontal cortices are involved in learning and memory, and the striatum plays a role in encoding contextual information associated with memories. Because deficits in verbal learning and memory are one of the most commonly reported impairments in patients with psychosis, O’Neill et al6 used functional MRI (fMRI) to examine brain activity during a verbal learning task in patients with psychosis after taking CBD or placebo.
Study design
- In a double-blind, randomized, placebo-controlled, crossover study, researchers investigated the effects of a single dose of CBD in 15 patients with psychosis who were treated with antipsychotics. Three hours after taking a 600-mg dose of CBD or placebo, these participants were scanned using fMRI while performing a verbal paired associate (VPA) learning task. Nineteen healthy controls underwent fMRI in identical conditions, but without any medication administration.
- The fMRI measured brain activation using the blood oxygen level–dependent (BOLD) hemodynamic responses of the brain. The fMRI signals were studied in the mediotemporal, prefrontal, and striatal regions.
- The VPA task presented word pairs visually, and the accuracy of responses were recorded online. The VPA task was comprised of 3 conditions: encoding, recall, and baseline.
- Results during each phase of the VPA task were compared.
Outcomes
- While completing the VPA task after taking placebo, compared with healthy controls, patients with psychosis demonstrated a different pattern of activity in the prefrontal and mediotemporal brain areas. Specifically, during verbal encoding, the placebo group showed altered activation in prefrontal regions. During verbal recall, the placebo group showed altered activation in prefrontal and mediotemporal regions, as well as increased mediotemporal-striatal functional connectivity.
- After participants received CBD, activation in these brain areas became more like the activation seen in controls. CBD attenuated dysfunction in these regions such that activation was intermediate between the placebo condition and the control group. CBD also attenuated functional connectivity between the hippocampus and striatum, and lead to reduced symptoms in patients with psychosis (as measured by PANSS total score).
Conclusion
- Altered activation in prefrontal and mediotemporal regions during verbal learning in patients with psychosis appeared to be partially normalized after a single 600-mg dose of CBD. Results also showed improvement in PANSS total score with CBD.
- These findings suggest that a single dose of CBD may partially attenuate the dysfunctional prefrontal and mediotemporal activation that is believed to underlie the dopamine dysfunction that leads to psychotic symptoms. These effects, along with a reduction in psychotic symptoms, suggest that normalization of altered prefrontal and mediotemporal function and mediotemporal-striatal connectivity may underlie the antipsychotic effects of CBD in established psychosis.
Continue to: Bhattacharyya S, et al...
4. Bhattacharyya S, Wilson R, Appiah-Kusi E, et al. Effect of cannabidiol on medial temporal, midbrain, and striatal dysfunction in people at clinical high risk of psychosis: a randomized clinical trial. JAMA Psychiatry. 2018;75(11):1107-1117.
Current preclinical models suggest that psychosis involves a disturbance of activity in the medial temporal lobe (MTL) that drives dopamine dysfunction in the striatum and midbrain. THC, which produces psychotomimetic effects, impacts the function of the striatum (verbal memoryand salience processing) andamygdala (emotional processing), and alters the functional connectivity of these regions. Compared with THC, CBD has broadly opposite neural and behavioral effects, including opposing effects on the activation of these regions. Bhattacharyya et al7 examined the neurocognitive mechanisms that underlie the therapeutic effects of CBD in psychosis and sought to understand whether CBD would attenuate functional abnormalities in the MTL, midbrain, and striatum.
Study design
- A randomized, double-blind, placebo-controlled trial examined 33 antipsychotic-naïve participants at clinical high risk (CHR) for psychosis and 19 healthy controls. The CHR group was randomized to CBD, 600 mg, or placebo.
- Three hours after taking CBD or placebo, CHR participants were studied using fMRI while performing a VPA learning task, which engages verbal learning and recall in the MTL, midbrain and striatum. Control participants did not receive any medication but underwent fMRI while performing the VPA task.
- The VPA task presented word pairs visually, and the accuracy of responses was recorded online. It was comprised of 3 conditions: encoding, recall, and baseline.
Outcomes
- Brain activation was analyzed in 15 participants in the CBD group, 16 in the placebo group, and 19 in the control group. Activation during encoding was observed in the striatum (specifically, the right caudate). Activation during recall was observed in the midbrain and the MTL (specifically, the parahippocampus).
- Brain activation levels in all 3 regions were lowest in the placebo group, intermediate in the CBD group, and greatest in the healthy control group. For all participants, the total recall score was directly correlated with the activation level in the left MTL (parahippocampus) during recall.
Conclusion
- Relative to controls, CHR participants exhibited different levels of activation in several regions, including the 3 areas thought to be critical to the pathophysiology of psychosis: the striatum during verbal encoding, and the MTL and midbrain during verbal recall.
- Compared with those who received placebo, CHR participants who received CBD before completing the VPA task demonstrated greater levels of brain activation and higher recall score.
- These findings suggest that CBD may partially normalize alterations in MTL, striatal, and midbrain function associated with CHR of psychosis. Because these regions are implicated in the pathophysiology of psychosis, the impact of CBD at these sites may contribute to the therapeutic effects of CBD that have been reported by some patients with psychosis.
Continue to: Conflicting data highlights...
Conflicting data highlights the need for longer, larger studies
Research findings on the use of CBD for psychotic symptoms in patients with schizophrenia have been conflicting. Some early research suggests that taking CBD 4 times daily for 4 weeks improves psychotic symptoms and might be as effective as the antipsychotic amisulpride. However, other early research suggests that taking CBD for 14 days is not beneficial. The conflicting results might be related to the CBD dose used and duration of treatment.
Davies and Bhattacharya12 recently reviewed evidence regarding the efficacy of CBD as a potential novel treatment for psychotic disorders.They concluded that CBD represents a promising potential novel treatment for patients with psychosis. It also appears that CBD may improve the disease trajectory of individuals with early psychosis and comorbid cannabis misuse.13 CBD use has also been associated with a decrease in symptoms of psychosis and changes in brain activity during verbal memory tasks in patients at high risk of psychosis.6 However, before CBD can become a viable treatment option for psychosis, the promising findings in these initial clinical studies must be replicated in large-scale trials with appropriate treatment duration.
1. US National Library of Medicine. MedlinePlus. Cannabidiol (CBD). https://medlineplus.gov/druginfo/natural/1439.html. Accessed May 14, 2020.
2. Bonn-Miller MO, Loflin MJE, Thomas BF, et al. Labeling accuracy of cannabidiol extracts sold online. JAMA. 2017;318(17):1708-1709.
3. Leweke FM, Piomelli D, Pahlisch F, et al. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl Psychiatry. 2012;2(3):e94.
4. McGuire P, Robson P, Cubala WJ, et al. Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: a multicenter randomized controlled trial. Am J Psychiatry. 2018;175(3):225-231.
5. Boggs DL, Surti T, Gupta A, et al. The effects of cannabidiol (CBD) on cognition and symptoms in outpatients with chronic schizophrenia a randomized placebo controlled trial. Psychopharmacology (Berl). 2018;235(7):1923-1932.
6. O’Neill A, Wilson R, Blest-Hopley G, et al. Normalization of mediotemporal and prefrontal activity, and mediotemporal-striatal connectivity, may underlie antipsychotic effects of cannabidiol in psychosis. Psychol Med. 2020;1-11. doi: 10.1017/S0033291719003519.
7. Bhattacharyya S, Wilson R, Appiah-Kusi E, et al. Effect of cannabidiol on medial temporal, midbrain, and striatal dysfunction in people at clinical high risk of psychosis: a randomized clinical trial. JAMA Psychiatry. 2018;75(11):1107-1117.
8. Hallak JE, Machado-de-Sousa JP, Crippa JAS, et al. Performance of schizophrenic patients in the Stroop color word test and electrodermal responsiveness after acute administration of cannabidiol (CBD). Rev Bras Psiquiatr. 2010;32(1):56-61.
9. Zuardi AW, Morais SL, Guimaraes FS, et al. Antipsychotic effect of cannabidiol. J Clin Psychiatry. 1995;56(10):485-486.
10. Zuardi AW, Hallak JE, Dursun SM, et al. Cannabidiol monotherapy for treatment-resistant schizophrenia. J Psychopharmacol. 2006;20(5):683-686.
11. Leweke FM, Hellmich M, Pahlisch F, et al. Modulation of the endocannabinoid system as a potential new target in the treatment of schizophrenia. Schizophr Res. 2014; 153(1):S47.
12. Davies C, Bhattacharyya S. Cannabidiol as a potential treatment for psychosis. Ther Adv Psychopharmacol. 2019;9. doi:10.1177/2045125319881916.
13. Hahn B. The potential of cannabidiol treatment for cannabis users with recent-onset psychosis. Schizophr Bull. 2018;44(1):46-53.
There has been increasing interest in the medicinal use of cannabidiol (CBD) for a wide variety of health conditions. CBD is one of more than 80 chemicals identified in the Cannabis sativa plant, otherwise known as marijuana or hemp. Delta-9-tetrahydrocannabinol (THC) is the psychoactive ingredient found in marijuana that produces a “high.” CBD, which is one of the most abundant cannabinoids in Cannabis sativa, does not produce any psychotomimetic effects.
The strongest scientific evidence supporting CBD for medicinal purposes is for its effectiveness in treating certain childhood epilepsy syndromes that typically do not respond to antiseizure medications. Currently, the only FDA-approved CBD product is a prescription oil cannabidiol (brand name: Epidiolex) for treating 2 types of epilepsy. Aside from Epidiolex, state laws governing the use of CBD vary. CBD is being studied as a treatment for a wide range of psychiatric conditions, including bipolar disorder, schizophrenia, dystonia, insomnia, and anxiety. Research supporting CBD’s benefits is limited, and the US National Library of Medicine’s MedlinePlus indicates there is “insufficient evidence to rate effectiveness” for these indications.1
Despite having been legalized for medicinal use in many states, CBD is classified as a Schedule I controlled substance by the US Drug Enforcement Agency. Because of this classification, little has been done to regulate and oversee the sale of products containing CBD. In a 2017 study of 84 CBD products sold by 31 companies online, Bonn-Miller et al2 found that nearly 70% percent of products were inaccurately labeled. In this study, blind testing found that only approximately 31% of products contained within 10% of the amount of CBD that was listed on the label. These researchers also found that some products contained components not listed on the label, including THC.2
The relationship between cannabis and psychosis or psychotic symptoms has been investigated for decades. Some recent studies that examined the effects of CBD on psychosis found that individuals who use CBD may experience fewer positive psychotic symptoms compared with placebo. This raises the question of whether CBD may have a role in the treatment of schizophrenia and other psychotic disorders. One of the first studies on this issue was conducted by Leweke et al,3 who compared oral CBD, up to 800 mg/d, with the antipsychotic amisulpride, up to 800 mg/d, in 39 patients with an acute exacerbation of psychotic symptoms. Amisulpride is used outside the United States to treat psychosis, but is FDA-approved only as an antiemetic. Patients were treated for 4 weeks. By Day 28, there was a significant reduction in positive symptoms as measured using the Positive and Negative Syndrome Scale (PANSS), with no significant difference in efficacy between the treatments. Similar findings emerged for negative, total, and general symptoms, with significant reductions by Day 28 in both treatment arms, and no significant between-treatment differences.
These findings were the first robust indication that CBD may have antipsychotic efficacy. However, of greater interest may be CBD’s markedly superior adverse effect profile. Predictably, amisulpride significantly increased extrapyramidal symptoms (EPS), weight gain, and prolactin levels from baseline to Day 28. However, no significant change was found in any of these adverse effects in the CBD group, and the between-treatment difference was significant (all P < .01).
Here we review 4 recent studies that evaluated CBD as a treatment for schizophrenia. These studies are summarized in the Table.4-7
Continue to: McGuire P, et al...
1. McGuire P, Robson P, Cubala WJ, et al. Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: a multicenter randomized controlled trial. Am J Psychiatry. 2018;175(3):225-231.
Antipsychotic medications act through blockade of central dopamine D2 receptors. For most patients, antipsychotics effectively treat positive psychotic symptoms, which are driven by elevated dopamine function. However, these medications have minimal effects on negative symptoms and cognitive impairment, features of schizophrenia that are not driven by elevated dopamine. Compounds exhibiting a mechanism of action unlike that of current antipsychotics may improve the treatment and outcomes of patients with schizophrenia. The mechanism of action of CBD is unclear, but it does not appear to involve the direct antagonism of dopamine receptors. Human and animal research study findings indicate that CBD has antipsychotic properties. McGuire et al4 assessed the safety and effectiveness of CBD as an adjunctive treatment of schizophrenia.
Study design
- In this double-blind parallel-group trial conducted at 15 hospitals in the United Kingdom, Romania, and Poland, 88 patients with schizophrenia received CBD (1,000 mg/d; N = 43) or placebo (N = 45) as adjunct to the antipsychotic medication they had been prescribed. Patients had previously demonstrated at least a partial response to antipsychotic treatment, and were taking stable doses of an antipsychotic for ≥4 weeks.
- Evaluations of symptoms, general functioning, cognitive performance, and EPS were completed at baseline and on Days 8, 22, and 43 (± 3 days). Current substance use was assessed using a semi-structured interview, and reassessed at the end of treatment.
- The key endpoints were the patients’ level of functioning, severity of symptoms, and cognitive performance. Participants were assessed before and after treatment using the PANSS, the Brief Assessment of Cognition in Schizophrenia (BACS), the Global Assessment of Functioning scale (GAF), and the improvement and severity scales of the Clinical Global Impressions Scale (CGI-I and CGI-S, respectively).
- The clinicians’ impression of illness severity and symptom improvement and patient- or caregiver-reported impressions of general functioning and sleep also were noted.
Outcomes
- After 6 weeks, compared with the placebo group, the CBD group had lower levels of positive psychotic symptoms and were more likely to be rated as improved and as not severely unwell by the treating clinician. Patients in the CBD group also showed greater improvements in cognitive performance and in overall functioning, although these were not statistically significant.
- Similar levels of negative psychotic symptoms, overall psychopathology, and general psychopathology were observed in the CBD and placebo groups. The CBD group had a higher proportion of treatment responders (≥20% improvement in PANSS total score) than did the placebo group; however, the total number of responders per group was small (12 and 6 patients, respectively). At baseline, most patients in both groups were classified as moderately, markedly, or severely ill (83.4% in the CBD group vs 79.6% in placebo group). By the end of treatment, this decreased to 54.8% in the CBD group and 63.6% in the placebo group. Clinicians rated 78.6% of patients in the CBD group as “improved” on the CGI-I, compared with 54.6% of patients in the placebo group.
Conclusion
- CBD treatment adjunctive to antipsychotics was associated with significant effects on positive psychotic symptoms and on CGI-I and illness severity. Improvements in cognitive performance and level of overall functioning were also seen, but were not statistically significant.
- Although the effect on positive symptoms was modest, improvement occurred in patients being treated with appropriate dosages of antipsychotics, which suggests CBD provided benefits over and above the effect of antipsychotic treatment. Moreover, the changes in CGI-I and CGI-S scores indicated that the improvement was evident to the treating psychiatrists, and may therefore be clinically meaningful.
Continue to: Boggs DL, et al...
2. Boggs DL, Surti T, Gupta A, et al. The effects of cannabidiol (CBD) on cognition and symptoms in outpatients with chronic schizophrenia a randomized placebo controlled trial. Psychopharmacology (Berl). 2018;235(7):1923-1932.
Schizophrenia is associated with cognitive deficits in learning, recall, attention, working memory, and executive function. The cognitive impairments associated with schizophrenia (CIAS) are independent of phase of illness and often persist after other symptoms have been effectively treated. These impairments are the strongest predictor of functional outcome, even more so than psychotic symptoms.
Antipsychotics have limited efficacy for CIAS, which highlights the need for CIAS treatments that target other nondopaminergic neurotransmitter systems. The endocannabinoid system, which has been implicated in schizophrenia and in cognition, is a potential target. Several cannabinoids impair memory and attention. The main psychoactive component of marijuana, THC, is a cannabinoid receptor type 1 (CB1R) partial agonist. Administration of THC produces significant deficits in verbal learning, attention, and working memory.
Researchers have hypothesized that CB1R blockade or modulation of cannabinoid levels may offer a novel target for treating CIAS. Boggs et al5 compared the cognitive, symptomatic, and adverse effects of CBD vs placebo.
Study design
- In this 6-week, randomized, placebo-controlled study conducted in Connecticut from September 2009 to May 2012, 36 stable patients with schizophrenia who were treated with antipsychotics were randomized to also receive oral CBD, 600 mg/d, or placebo.
- Cognition was assessed using the t score of the MATRICS Consensus Cognitive Battery (MCCB) composite and subscales at baseline and the end of study. An increase in MCCB t score indicates an improvement in cognitive ability. Psychotic symptoms were assessed using the PANSS at baseline, Week 2, Week 4, and Week 6.
Outcomes
- CBD augmentation did not improve MCCB performance or psychotic symptoms. There was no main effect of time or medication on MCCB composite score, but a significant drug × time effect was observed.
- Post-hoc analyses revealed that only patients who received placebo improved over time. The lack of a similar improvement with CBD might be related to the greater incidence of sedation among the CBD group (20%) vs the placebo group (5%). Both the MCCB composite score and reasoning and problem-solving domain scores were higher at baseline and endpoint for patients who received CBD, which suggests that the observed improvement in the placebo group could represent a regression to the mean.
- There was a significant decrease in PANSS scores over time, but there was no significant drug × time interaction.
Conclusion
- CBD augmentation was not associated with an improvement in MCCB score. This is consistent with data from other clinical trials4,8 that suggested that CBD (at a wide range of doses) does not have significant beneficial effects on cognition in patients with schizophrenia.
- Additionally, CBD did not improve psychotic symptoms. These results are in contrast to published case reports9,10 and 2 published clinical trials3,4 that found CBD (800 mg/d) was as efficacious as amisulpride in reducing positive psychotic symptoms, and a small but statistically significant improvement in PANSS positive scores with CBD (1,000 mg/d) compared with placebo. However, these results are similar to those of a separate study11 that evaluated the same 600-mg/d dose of CBD used by Boggs et al.5 At 600 mg/d, CBD produced very small improvements in PANSS total scores (~2.4) that were not statistically significant. A higher CBD dose may be needed to reduce psychotic symptoms in patients with schizophrenia.
Continue to: O’Neill A, et al...
3. O’Neill A, Wilson R, Blest-Hopley G, et al. Normalization of mediotemporal and prefrontal activity, and mediotemporal-striatal connectivity, may underlie antipsychotic effects of cannabidiol in psychosis. Psychol Med. 2020;1-11. doi: 10.1017/S0033291719003519.
In addition to their key roles in the psychopathology of psychosis, the mediotemporal and prefrontal cortices are involved in learning and memory, and the striatum plays a role in encoding contextual information associated with memories. Because deficits in verbal learning and memory are one of the most commonly reported impairments in patients with psychosis, O’Neill et al6 used functional MRI (fMRI) to examine brain activity during a verbal learning task in patients with psychosis after taking CBD or placebo.
Study design
- In a double-blind, randomized, placebo-controlled, crossover study, researchers investigated the effects of a single dose of CBD in 15 patients with psychosis who were treated with antipsychotics. Three hours after taking a 600-mg dose of CBD or placebo, these participants were scanned using fMRI while performing a verbal paired associate (VPA) learning task. Nineteen healthy controls underwent fMRI in identical conditions, but without any medication administration.
- The fMRI measured brain activation using the blood oxygen level–dependent (BOLD) hemodynamic responses of the brain. The fMRI signals were studied in the mediotemporal, prefrontal, and striatal regions.
- The VPA task presented word pairs visually, and the accuracy of responses were recorded online. The VPA task was comprised of 3 conditions: encoding, recall, and baseline.
- Results during each phase of the VPA task were compared.
Outcomes
- While completing the VPA task after taking placebo, compared with healthy controls, patients with psychosis demonstrated a different pattern of activity in the prefrontal and mediotemporal brain areas. Specifically, during verbal encoding, the placebo group showed altered activation in prefrontal regions. During verbal recall, the placebo group showed altered activation in prefrontal and mediotemporal regions, as well as increased mediotemporal-striatal functional connectivity.
- After participants received CBD, activation in these brain areas became more like the activation seen in controls. CBD attenuated dysfunction in these regions such that activation was intermediate between the placebo condition and the control group. CBD also attenuated functional connectivity between the hippocampus and striatum, and lead to reduced symptoms in patients with psychosis (as measured by PANSS total score).
Conclusion
- Altered activation in prefrontal and mediotemporal regions during verbal learning in patients with psychosis appeared to be partially normalized after a single 600-mg dose of CBD. Results also showed improvement in PANSS total score with CBD.
- These findings suggest that a single dose of CBD may partially attenuate the dysfunctional prefrontal and mediotemporal activation that is believed to underlie the dopamine dysfunction that leads to psychotic symptoms. These effects, along with a reduction in psychotic symptoms, suggest that normalization of altered prefrontal and mediotemporal function and mediotemporal-striatal connectivity may underlie the antipsychotic effects of CBD in established psychosis.
Continue to: Bhattacharyya S, et al...
4. Bhattacharyya S, Wilson R, Appiah-Kusi E, et al. Effect of cannabidiol on medial temporal, midbrain, and striatal dysfunction in people at clinical high risk of psychosis: a randomized clinical trial. JAMA Psychiatry. 2018;75(11):1107-1117.
Current preclinical models suggest that psychosis involves a disturbance of activity in the medial temporal lobe (MTL) that drives dopamine dysfunction in the striatum and midbrain. THC, which produces psychotomimetic effects, impacts the function of the striatum (verbal memoryand salience processing) andamygdala (emotional processing), and alters the functional connectivity of these regions. Compared with THC, CBD has broadly opposite neural and behavioral effects, including opposing effects on the activation of these regions. Bhattacharyya et al7 examined the neurocognitive mechanisms that underlie the therapeutic effects of CBD in psychosis and sought to understand whether CBD would attenuate functional abnormalities in the MTL, midbrain, and striatum.
Study design
- A randomized, double-blind, placebo-controlled trial examined 33 antipsychotic-naïve participants at clinical high risk (CHR) for psychosis and 19 healthy controls. The CHR group was randomized to CBD, 600 mg, or placebo.
- Three hours after taking CBD or placebo, CHR participants were studied using fMRI while performing a VPA learning task, which engages verbal learning and recall in the MTL, midbrain and striatum. Control participants did not receive any medication but underwent fMRI while performing the VPA task.
- The VPA task presented word pairs visually, and the accuracy of responses was recorded online. It was comprised of 3 conditions: encoding, recall, and baseline.
Outcomes
- Brain activation was analyzed in 15 participants in the CBD group, 16 in the placebo group, and 19 in the control group. Activation during encoding was observed in the striatum (specifically, the right caudate). Activation during recall was observed in the midbrain and the MTL (specifically, the parahippocampus).
- Brain activation levels in all 3 regions were lowest in the placebo group, intermediate in the CBD group, and greatest in the healthy control group. For all participants, the total recall score was directly correlated with the activation level in the left MTL (parahippocampus) during recall.
Conclusion
- Relative to controls, CHR participants exhibited different levels of activation in several regions, including the 3 areas thought to be critical to the pathophysiology of psychosis: the striatum during verbal encoding, and the MTL and midbrain during verbal recall.
- Compared with those who received placebo, CHR participants who received CBD before completing the VPA task demonstrated greater levels of brain activation and higher recall score.
- These findings suggest that CBD may partially normalize alterations in MTL, striatal, and midbrain function associated with CHR of psychosis. Because these regions are implicated in the pathophysiology of psychosis, the impact of CBD at these sites may contribute to the therapeutic effects of CBD that have been reported by some patients with psychosis.
Continue to: Conflicting data highlights...
Conflicting data highlights the need for longer, larger studies
Research findings on the use of CBD for psychotic symptoms in patients with schizophrenia have been conflicting. Some early research suggests that taking CBD 4 times daily for 4 weeks improves psychotic symptoms and might be as effective as the antipsychotic amisulpride. However, other early research suggests that taking CBD for 14 days is not beneficial. The conflicting results might be related to the CBD dose used and duration of treatment.
Davies and Bhattacharya12 recently reviewed evidence regarding the efficacy of CBD as a potential novel treatment for psychotic disorders.They concluded that CBD represents a promising potential novel treatment for patients with psychosis. It also appears that CBD may improve the disease trajectory of individuals with early psychosis and comorbid cannabis misuse.13 CBD use has also been associated with a decrease in symptoms of psychosis and changes in brain activity during verbal memory tasks in patients at high risk of psychosis.6 However, before CBD can become a viable treatment option for psychosis, the promising findings in these initial clinical studies must be replicated in large-scale trials with appropriate treatment duration.
There has been increasing interest in the medicinal use of cannabidiol (CBD) for a wide variety of health conditions. CBD is one of more than 80 chemicals identified in the Cannabis sativa plant, otherwise known as marijuana or hemp. Delta-9-tetrahydrocannabinol (THC) is the psychoactive ingredient found in marijuana that produces a “high.” CBD, which is one of the most abundant cannabinoids in Cannabis sativa, does not produce any psychotomimetic effects.
The strongest scientific evidence supporting CBD for medicinal purposes is for its effectiveness in treating certain childhood epilepsy syndromes that typically do not respond to antiseizure medications. Currently, the only FDA-approved CBD product is a prescription oil cannabidiol (brand name: Epidiolex) for treating 2 types of epilepsy. Aside from Epidiolex, state laws governing the use of CBD vary. CBD is being studied as a treatment for a wide range of psychiatric conditions, including bipolar disorder, schizophrenia, dystonia, insomnia, and anxiety. Research supporting CBD’s benefits is limited, and the US National Library of Medicine’s MedlinePlus indicates there is “insufficient evidence to rate effectiveness” for these indications.1
Despite having been legalized for medicinal use in many states, CBD is classified as a Schedule I controlled substance by the US Drug Enforcement Agency. Because of this classification, little has been done to regulate and oversee the sale of products containing CBD. In a 2017 study of 84 CBD products sold by 31 companies online, Bonn-Miller et al2 found that nearly 70% percent of products were inaccurately labeled. In this study, blind testing found that only approximately 31% of products contained within 10% of the amount of CBD that was listed on the label. These researchers also found that some products contained components not listed on the label, including THC.2
The relationship between cannabis and psychosis or psychotic symptoms has been investigated for decades. Some recent studies that examined the effects of CBD on psychosis found that individuals who use CBD may experience fewer positive psychotic symptoms compared with placebo. This raises the question of whether CBD may have a role in the treatment of schizophrenia and other psychotic disorders. One of the first studies on this issue was conducted by Leweke et al,3 who compared oral CBD, up to 800 mg/d, with the antipsychotic amisulpride, up to 800 mg/d, in 39 patients with an acute exacerbation of psychotic symptoms. Amisulpride is used outside the United States to treat psychosis, but is FDA-approved only as an antiemetic. Patients were treated for 4 weeks. By Day 28, there was a significant reduction in positive symptoms as measured using the Positive and Negative Syndrome Scale (PANSS), with no significant difference in efficacy between the treatments. Similar findings emerged for negative, total, and general symptoms, with significant reductions by Day 28 in both treatment arms, and no significant between-treatment differences.
These findings were the first robust indication that CBD may have antipsychotic efficacy. However, of greater interest may be CBD’s markedly superior adverse effect profile. Predictably, amisulpride significantly increased extrapyramidal symptoms (EPS), weight gain, and prolactin levels from baseline to Day 28. However, no significant change was found in any of these adverse effects in the CBD group, and the between-treatment difference was significant (all P < .01).
Here we review 4 recent studies that evaluated CBD as a treatment for schizophrenia. These studies are summarized in the Table.4-7
Continue to: McGuire P, et al...
1. McGuire P, Robson P, Cubala WJ, et al. Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: a multicenter randomized controlled trial. Am J Psychiatry. 2018;175(3):225-231.
Antipsychotic medications act through blockade of central dopamine D2 receptors. For most patients, antipsychotics effectively treat positive psychotic symptoms, which are driven by elevated dopamine function. However, these medications have minimal effects on negative symptoms and cognitive impairment, features of schizophrenia that are not driven by elevated dopamine. Compounds exhibiting a mechanism of action unlike that of current antipsychotics may improve the treatment and outcomes of patients with schizophrenia. The mechanism of action of CBD is unclear, but it does not appear to involve the direct antagonism of dopamine receptors. Human and animal research study findings indicate that CBD has antipsychotic properties. McGuire et al4 assessed the safety and effectiveness of CBD as an adjunctive treatment of schizophrenia.
Study design
- In this double-blind parallel-group trial conducted at 15 hospitals in the United Kingdom, Romania, and Poland, 88 patients with schizophrenia received CBD (1,000 mg/d; N = 43) or placebo (N = 45) as adjunct to the antipsychotic medication they had been prescribed. Patients had previously demonstrated at least a partial response to antipsychotic treatment, and were taking stable doses of an antipsychotic for ≥4 weeks.
- Evaluations of symptoms, general functioning, cognitive performance, and EPS were completed at baseline and on Days 8, 22, and 43 (± 3 days). Current substance use was assessed using a semi-structured interview, and reassessed at the end of treatment.
- The key endpoints were the patients’ level of functioning, severity of symptoms, and cognitive performance. Participants were assessed before and after treatment using the PANSS, the Brief Assessment of Cognition in Schizophrenia (BACS), the Global Assessment of Functioning scale (GAF), and the improvement and severity scales of the Clinical Global Impressions Scale (CGI-I and CGI-S, respectively).
- The clinicians’ impression of illness severity and symptom improvement and patient- or caregiver-reported impressions of general functioning and sleep also were noted.
Outcomes
- After 6 weeks, compared with the placebo group, the CBD group had lower levels of positive psychotic symptoms and were more likely to be rated as improved and as not severely unwell by the treating clinician. Patients in the CBD group also showed greater improvements in cognitive performance and in overall functioning, although these were not statistically significant.
- Similar levels of negative psychotic symptoms, overall psychopathology, and general psychopathology were observed in the CBD and placebo groups. The CBD group had a higher proportion of treatment responders (≥20% improvement in PANSS total score) than did the placebo group; however, the total number of responders per group was small (12 and 6 patients, respectively). At baseline, most patients in both groups were classified as moderately, markedly, or severely ill (83.4% in the CBD group vs 79.6% in placebo group). By the end of treatment, this decreased to 54.8% in the CBD group and 63.6% in the placebo group. Clinicians rated 78.6% of patients in the CBD group as “improved” on the CGI-I, compared with 54.6% of patients in the placebo group.
Conclusion
- CBD treatment adjunctive to antipsychotics was associated with significant effects on positive psychotic symptoms and on CGI-I and illness severity. Improvements in cognitive performance and level of overall functioning were also seen, but were not statistically significant.
- Although the effect on positive symptoms was modest, improvement occurred in patients being treated with appropriate dosages of antipsychotics, which suggests CBD provided benefits over and above the effect of antipsychotic treatment. Moreover, the changes in CGI-I and CGI-S scores indicated that the improvement was evident to the treating psychiatrists, and may therefore be clinically meaningful.
Continue to: Boggs DL, et al...
2. Boggs DL, Surti T, Gupta A, et al. The effects of cannabidiol (CBD) on cognition and symptoms in outpatients with chronic schizophrenia a randomized placebo controlled trial. Psychopharmacology (Berl). 2018;235(7):1923-1932.
Schizophrenia is associated with cognitive deficits in learning, recall, attention, working memory, and executive function. The cognitive impairments associated with schizophrenia (CIAS) are independent of phase of illness and often persist after other symptoms have been effectively treated. These impairments are the strongest predictor of functional outcome, even more so than psychotic symptoms.
Antipsychotics have limited efficacy for CIAS, which highlights the need for CIAS treatments that target other nondopaminergic neurotransmitter systems. The endocannabinoid system, which has been implicated in schizophrenia and in cognition, is a potential target. Several cannabinoids impair memory and attention. The main psychoactive component of marijuana, THC, is a cannabinoid receptor type 1 (CB1R) partial agonist. Administration of THC produces significant deficits in verbal learning, attention, and working memory.
Researchers have hypothesized that CB1R blockade or modulation of cannabinoid levels may offer a novel target for treating CIAS. Boggs et al5 compared the cognitive, symptomatic, and adverse effects of CBD vs placebo.
Study design
- In this 6-week, randomized, placebo-controlled study conducted in Connecticut from September 2009 to May 2012, 36 stable patients with schizophrenia who were treated with antipsychotics were randomized to also receive oral CBD, 600 mg/d, or placebo.
- Cognition was assessed using the t score of the MATRICS Consensus Cognitive Battery (MCCB) composite and subscales at baseline and the end of study. An increase in MCCB t score indicates an improvement in cognitive ability. Psychotic symptoms were assessed using the PANSS at baseline, Week 2, Week 4, and Week 6.
Outcomes
- CBD augmentation did not improve MCCB performance or psychotic symptoms. There was no main effect of time or medication on MCCB composite score, but a significant drug × time effect was observed.
- Post-hoc analyses revealed that only patients who received placebo improved over time. The lack of a similar improvement with CBD might be related to the greater incidence of sedation among the CBD group (20%) vs the placebo group (5%). Both the MCCB composite score and reasoning and problem-solving domain scores were higher at baseline and endpoint for patients who received CBD, which suggests that the observed improvement in the placebo group could represent a regression to the mean.
- There was a significant decrease in PANSS scores over time, but there was no significant drug × time interaction.
Conclusion
- CBD augmentation was not associated with an improvement in MCCB score. This is consistent with data from other clinical trials4,8 that suggested that CBD (at a wide range of doses) does not have significant beneficial effects on cognition in patients with schizophrenia.
- Additionally, CBD did not improve psychotic symptoms. These results are in contrast to published case reports9,10 and 2 published clinical trials3,4 that found CBD (800 mg/d) was as efficacious as amisulpride in reducing positive psychotic symptoms, and a small but statistically significant improvement in PANSS positive scores with CBD (1,000 mg/d) compared with placebo. However, these results are similar to those of a separate study11 that evaluated the same 600-mg/d dose of CBD used by Boggs et al.5 At 600 mg/d, CBD produced very small improvements in PANSS total scores (~2.4) that were not statistically significant. A higher CBD dose may be needed to reduce psychotic symptoms in patients with schizophrenia.
Continue to: O’Neill A, et al...
3. O’Neill A, Wilson R, Blest-Hopley G, et al. Normalization of mediotemporal and prefrontal activity, and mediotemporal-striatal connectivity, may underlie antipsychotic effects of cannabidiol in psychosis. Psychol Med. 2020;1-11. doi: 10.1017/S0033291719003519.
In addition to their key roles in the psychopathology of psychosis, the mediotemporal and prefrontal cortices are involved in learning and memory, and the striatum plays a role in encoding contextual information associated with memories. Because deficits in verbal learning and memory are one of the most commonly reported impairments in patients with psychosis, O’Neill et al6 used functional MRI (fMRI) to examine brain activity during a verbal learning task in patients with psychosis after taking CBD or placebo.
Study design
- In a double-blind, randomized, placebo-controlled, crossover study, researchers investigated the effects of a single dose of CBD in 15 patients with psychosis who were treated with antipsychotics. Three hours after taking a 600-mg dose of CBD or placebo, these participants were scanned using fMRI while performing a verbal paired associate (VPA) learning task. Nineteen healthy controls underwent fMRI in identical conditions, but without any medication administration.
- The fMRI measured brain activation using the blood oxygen level–dependent (BOLD) hemodynamic responses of the brain. The fMRI signals were studied in the mediotemporal, prefrontal, and striatal regions.
- The VPA task presented word pairs visually, and the accuracy of responses were recorded online. The VPA task was comprised of 3 conditions: encoding, recall, and baseline.
- Results during each phase of the VPA task were compared.
Outcomes
- While completing the VPA task after taking placebo, compared with healthy controls, patients with psychosis demonstrated a different pattern of activity in the prefrontal and mediotemporal brain areas. Specifically, during verbal encoding, the placebo group showed altered activation in prefrontal regions. During verbal recall, the placebo group showed altered activation in prefrontal and mediotemporal regions, as well as increased mediotemporal-striatal functional connectivity.
- After participants received CBD, activation in these brain areas became more like the activation seen in controls. CBD attenuated dysfunction in these regions such that activation was intermediate between the placebo condition and the control group. CBD also attenuated functional connectivity between the hippocampus and striatum, and lead to reduced symptoms in patients with psychosis (as measured by PANSS total score).
Conclusion
- Altered activation in prefrontal and mediotemporal regions during verbal learning in patients with psychosis appeared to be partially normalized after a single 600-mg dose of CBD. Results also showed improvement in PANSS total score with CBD.
- These findings suggest that a single dose of CBD may partially attenuate the dysfunctional prefrontal and mediotemporal activation that is believed to underlie the dopamine dysfunction that leads to psychotic symptoms. These effects, along with a reduction in psychotic symptoms, suggest that normalization of altered prefrontal and mediotemporal function and mediotemporal-striatal connectivity may underlie the antipsychotic effects of CBD in established psychosis.
Continue to: Bhattacharyya S, et al...
4. Bhattacharyya S, Wilson R, Appiah-Kusi E, et al. Effect of cannabidiol on medial temporal, midbrain, and striatal dysfunction in people at clinical high risk of psychosis: a randomized clinical trial. JAMA Psychiatry. 2018;75(11):1107-1117.
Current preclinical models suggest that psychosis involves a disturbance of activity in the medial temporal lobe (MTL) that drives dopamine dysfunction in the striatum and midbrain. THC, which produces psychotomimetic effects, impacts the function of the striatum (verbal memoryand salience processing) andamygdala (emotional processing), and alters the functional connectivity of these regions. Compared with THC, CBD has broadly opposite neural and behavioral effects, including opposing effects on the activation of these regions. Bhattacharyya et al7 examined the neurocognitive mechanisms that underlie the therapeutic effects of CBD in psychosis and sought to understand whether CBD would attenuate functional abnormalities in the MTL, midbrain, and striatum.
Study design
- A randomized, double-blind, placebo-controlled trial examined 33 antipsychotic-naïve participants at clinical high risk (CHR) for psychosis and 19 healthy controls. The CHR group was randomized to CBD, 600 mg, or placebo.
- Three hours after taking CBD or placebo, CHR participants were studied using fMRI while performing a VPA learning task, which engages verbal learning and recall in the MTL, midbrain and striatum. Control participants did not receive any medication but underwent fMRI while performing the VPA task.
- The VPA task presented word pairs visually, and the accuracy of responses was recorded online. It was comprised of 3 conditions: encoding, recall, and baseline.
Outcomes
- Brain activation was analyzed in 15 participants in the CBD group, 16 in the placebo group, and 19 in the control group. Activation during encoding was observed in the striatum (specifically, the right caudate). Activation during recall was observed in the midbrain and the MTL (specifically, the parahippocampus).
- Brain activation levels in all 3 regions were lowest in the placebo group, intermediate in the CBD group, and greatest in the healthy control group. For all participants, the total recall score was directly correlated with the activation level in the left MTL (parahippocampus) during recall.
Conclusion
- Relative to controls, CHR participants exhibited different levels of activation in several regions, including the 3 areas thought to be critical to the pathophysiology of psychosis: the striatum during verbal encoding, and the MTL and midbrain during verbal recall.
- Compared with those who received placebo, CHR participants who received CBD before completing the VPA task demonstrated greater levels of brain activation and higher recall score.
- These findings suggest that CBD may partially normalize alterations in MTL, striatal, and midbrain function associated with CHR of psychosis. Because these regions are implicated in the pathophysiology of psychosis, the impact of CBD at these sites may contribute to the therapeutic effects of CBD that have been reported by some patients with psychosis.
Continue to: Conflicting data highlights...
Conflicting data highlights the need for longer, larger studies
Research findings on the use of CBD for psychotic symptoms in patients with schizophrenia have been conflicting. Some early research suggests that taking CBD 4 times daily for 4 weeks improves psychotic symptoms and might be as effective as the antipsychotic amisulpride. However, other early research suggests that taking CBD for 14 days is not beneficial. The conflicting results might be related to the CBD dose used and duration of treatment.
Davies and Bhattacharya12 recently reviewed evidence regarding the efficacy of CBD as a potential novel treatment for psychotic disorders.They concluded that CBD represents a promising potential novel treatment for patients with psychosis. It also appears that CBD may improve the disease trajectory of individuals with early psychosis and comorbid cannabis misuse.13 CBD use has also been associated with a decrease in symptoms of psychosis and changes in brain activity during verbal memory tasks in patients at high risk of psychosis.6 However, before CBD can become a viable treatment option for psychosis, the promising findings in these initial clinical studies must be replicated in large-scale trials with appropriate treatment duration.
1. US National Library of Medicine. MedlinePlus. Cannabidiol (CBD). https://medlineplus.gov/druginfo/natural/1439.html. Accessed May 14, 2020.
2. Bonn-Miller MO, Loflin MJE, Thomas BF, et al. Labeling accuracy of cannabidiol extracts sold online. JAMA. 2017;318(17):1708-1709.
3. Leweke FM, Piomelli D, Pahlisch F, et al. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl Psychiatry. 2012;2(3):e94.
4. McGuire P, Robson P, Cubala WJ, et al. Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: a multicenter randomized controlled trial. Am J Psychiatry. 2018;175(3):225-231.
5. Boggs DL, Surti T, Gupta A, et al. The effects of cannabidiol (CBD) on cognition and symptoms in outpatients with chronic schizophrenia a randomized placebo controlled trial. Psychopharmacology (Berl). 2018;235(7):1923-1932.
6. O’Neill A, Wilson R, Blest-Hopley G, et al. Normalization of mediotemporal and prefrontal activity, and mediotemporal-striatal connectivity, may underlie antipsychotic effects of cannabidiol in psychosis. Psychol Med. 2020;1-11. doi: 10.1017/S0033291719003519.
7. Bhattacharyya S, Wilson R, Appiah-Kusi E, et al. Effect of cannabidiol on medial temporal, midbrain, and striatal dysfunction in people at clinical high risk of psychosis: a randomized clinical trial. JAMA Psychiatry. 2018;75(11):1107-1117.
8. Hallak JE, Machado-de-Sousa JP, Crippa JAS, et al. Performance of schizophrenic patients in the Stroop color word test and electrodermal responsiveness after acute administration of cannabidiol (CBD). Rev Bras Psiquiatr. 2010;32(1):56-61.
9. Zuardi AW, Morais SL, Guimaraes FS, et al. Antipsychotic effect of cannabidiol. J Clin Psychiatry. 1995;56(10):485-486.
10. Zuardi AW, Hallak JE, Dursun SM, et al. Cannabidiol monotherapy for treatment-resistant schizophrenia. J Psychopharmacol. 2006;20(5):683-686.
11. Leweke FM, Hellmich M, Pahlisch F, et al. Modulation of the endocannabinoid system as a potential new target in the treatment of schizophrenia. Schizophr Res. 2014; 153(1):S47.
12. Davies C, Bhattacharyya S. Cannabidiol as a potential treatment for psychosis. Ther Adv Psychopharmacol. 2019;9. doi:10.1177/2045125319881916.
13. Hahn B. The potential of cannabidiol treatment for cannabis users with recent-onset psychosis. Schizophr Bull. 2018;44(1):46-53.
1. US National Library of Medicine. MedlinePlus. Cannabidiol (CBD). https://medlineplus.gov/druginfo/natural/1439.html. Accessed May 14, 2020.
2. Bonn-Miller MO, Loflin MJE, Thomas BF, et al. Labeling accuracy of cannabidiol extracts sold online. JAMA. 2017;318(17):1708-1709.
3. Leweke FM, Piomelli D, Pahlisch F, et al. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl Psychiatry. 2012;2(3):e94.
4. McGuire P, Robson P, Cubala WJ, et al. Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: a multicenter randomized controlled trial. Am J Psychiatry. 2018;175(3):225-231.
5. Boggs DL, Surti T, Gupta A, et al. The effects of cannabidiol (CBD) on cognition and symptoms in outpatients with chronic schizophrenia a randomized placebo controlled trial. Psychopharmacology (Berl). 2018;235(7):1923-1932.
6. O’Neill A, Wilson R, Blest-Hopley G, et al. Normalization of mediotemporal and prefrontal activity, and mediotemporal-striatal connectivity, may underlie antipsychotic effects of cannabidiol in psychosis. Psychol Med. 2020;1-11. doi: 10.1017/S0033291719003519.
7. Bhattacharyya S, Wilson R, Appiah-Kusi E, et al. Effect of cannabidiol on medial temporal, midbrain, and striatal dysfunction in people at clinical high risk of psychosis: a randomized clinical trial. JAMA Psychiatry. 2018;75(11):1107-1117.
8. Hallak JE, Machado-de-Sousa JP, Crippa JAS, et al. Performance of schizophrenic patients in the Stroop color word test and electrodermal responsiveness after acute administration of cannabidiol (CBD). Rev Bras Psiquiatr. 2010;32(1):56-61.
9. Zuardi AW, Morais SL, Guimaraes FS, et al. Antipsychotic effect of cannabidiol. J Clin Psychiatry. 1995;56(10):485-486.
10. Zuardi AW, Hallak JE, Dursun SM, et al. Cannabidiol monotherapy for treatment-resistant schizophrenia. J Psychopharmacol. 2006;20(5):683-686.
11. Leweke FM, Hellmich M, Pahlisch F, et al. Modulation of the endocannabinoid system as a potential new target in the treatment of schizophrenia. Schizophr Res. 2014; 153(1):S47.
12. Davies C, Bhattacharyya S. Cannabidiol as a potential treatment for psychosis. Ther Adv Psychopharmacol. 2019;9. doi:10.1177/2045125319881916.
13. Hahn B. The potential of cannabidiol treatment for cannabis users with recent-onset psychosis. Schizophr Bull. 2018;44(1):46-53.
Time to retire haloperidol?
For more than half a century, haloperidol has been used as a first-line medication for psychiatric agitation constituting a “behavioral emergency” when a patient cannot or will not take oral medication. Today, haloperidol is most commonly administered as an IM injection along with an anticholinergic medication to minimize extrapyramidal symptoms (EPS) and a benzodiazepine for additional sedation. The multiple-medication “cocktail” is often referred to by double-entendre nicknames, such as “B-52” or “5250” (ie, haloperidol, 5 mg; lorazepam, 2 mg; and
Earlier evidence of haloperidol’s efficacy
The initial “discovery” of antipsychotic medications was made in 1951 based on the inadvertent observation that chlorpromazine had the potential to calm surgical patients with autonomic activation. This calming effect, described as “désintéressment” (meaning a kind of “indifference to the world”),1 resulted in a new class of medications replacing barbiturates and bromides as go-to options to achieve “rapid tranquilization” of psychiatric agitation.2 Although the ability of antipsychotic medications to gradually reduce positive symptoms, such as delusions and hallucinations, has been attributed to dopamine (D2) antagonism, their more immediate sedating and anti-agitation effects are the result of broader effects as histamine (H1) and alpha-1 adrenergic antagonists.
In the 1970s, haloperidol emerged as a first-line option to manage agitation due to its IM and IV availability, as well as its relative lack of sedation and orthostasis compared with low-potency D2 antagonists such as chlorpromazine. However, haloperidol was observed to have a significant risk of acute EPS, including dystonic reactions.2 From the 1970s to the 1990s, numerous prospective clinical trials of haloperidol for the treatment of acute psychotic agitation, including several randomized controlled trials (RCTs) comparing haloperidol to lorazepam, were conducted.3 The design and outcomes of the haloperidol vs lorazepam RCTs were fairly consistent4-7:
- adult participants with acute agitation and a variety of psychiatric diagnoses, for whom informed consent often was waived due to agitation severity
- randomization to either IM haloperidol, 5 mg, or IM lorazepam, 2 mg, administered every 30 minutes until agitation resolved
- behavioral outcomes measured over several hours using various rating scales, without consistent assessment of EPS
- equivalent efficacy of haloperidol and lorazepam, with symptom resolution usually achieved after 1 to 2 doses (in 30 to 60 minutes), but sometimes longer
- anticholinergic “rescue” allowed for EPS, but not administered prophylactically
- EPS, including dystonia and akathisia, were significantly more frequent with haloperidol compared with lorazepam.8
In recognition of the greater risk of EPS with haloperidol compared with lorazepam, and the fact that most study participants were already taking standing doses of antipsychotic medications, some researchers have recommended using benzodiazepines alone as the optimal treatment for agitation.4,9 A 2012 Cochrane review concluded that the involuntary use of haloperidol alone “could be considered unethical.”10,11 However, other studies that examined the combination of haloperidol and lorazepam compared with either medication alone found that the combination of the 2 medications was associated with a more rapid resolution of symptoms, which suggests a superior synergistic effect.6,7,12 By the late 1990s, combined haloperidol and lorazepam, often mixed within a single injection, became the most common strategy to achieve rapid tranquilization in the psychiatric emergency setting.13 However, while the combination has been justified as a way to reduce the antipsychotic medication dose and EPS risk,2 few studies have compared combinations containing <5 mg of haloperidol. As a result, the apparent superiority of combined haloperidol and lorazepam compared with either medication alone may be a simple cumulative dose effect rather than true synergism. It is also important to note that adding lorazepam to haloperidol does not mitigate the risk of EPS such as dystonia in the absence of anticholinergic medication.8 To date, however, there have been no clinical trials investigating the efficacy of IM haloperidol, lorazepam, and
Newer RCTs tell a different story
With the availability of second-generation antipsychotics (SGAs) in IM formulations, clinical trials over the past 2 decades have focused on comparing SGAs with haloperidol alone as the “gold standard” control for acute agitation. Compared with previous trials of
- Study participants who signed informed consent (and were likely less agitated)
- IM haloperidol doses typically >5 mg (eg, 6.5 to 10 mg).
As with studies comparing lorazepam with haloperidol, the results of these RCTs revealed that IM
An updated 2017 Cochrane review of haloperidol for psychosis-induced aggression or agitation concluded that9:
- haloperidol is an effective intervention, although the evidence is “weak”
- significant treatment effects may take as long as 1 to 2 hours following multiple IM injections
- in contrast to SGAs, treatment with haloperidol carries a significant risk of EPS
- adding a benzodiazepine “does not have strong evidence of benefit and carries risk of additional harm.”
Continue to: Haloperidol's well-known toxicity
Haloperidol’s well-known toxicity
Haloperidol has been associated with numerous adverse effects:
Akathisia and other acute EPS. Treatment with even a single dose of IM haloperidol can result in acute EPS, including dystonia and akathisia. At best, such adverse effects are subjectively troubling and unpleasant; at worst, akathisia can exacerbate and be mistaken for agitation, leading to administration of more medication23 and the possible development of suicidal or violent behavior.24-25 In the studies reviewed above, the overall rate of EPS was as high as 21% after treatment with haloperidol,16 with parkinsonism occurring in up to 17% of patients,19 dystonia in up to 11%,7 and akathisia in up to 10%.15 However, because specific EPS were assessed inconsistently, and sometimes not at all, the rate of akathisia—arguably the most relevant and counter-therapeutic adverse effect related to agitation—remains unclear.
In another study that specifically assessed for akathisia in patients treated with haloperidol, up to 40% experienced akathisia 6 hours after a single oral dose of 5 mg.26 Even a single dose of IV
Although anticholinergic medications or benzodiazepinesare often administered as part of a haloperidol “cocktail,” these medications often do not adequately resolve emergent akathisia.26,28 No clinical trials of IM haloperidol combined with benztropine or diphenhydramine have been published, but several studies suggest that combining haloperidol with
Cardiotoxicity. Although low-potency antipsychotic medications such as
Continue to: Although there is no direct evidence...
Although there is no direct evidence that the cardiac risks associated with IV haloperidol apply to IM administration, epidemiologic studies indicate that oral haloperidol carries an elevated risk of ventricular arrhythmia and sudden cardiac death,35,36 with 1 study reporting greater risk compared with other SGAs.37 Haloperidol, whether administered orally or IM, may therefore be an especially poor choice for patients with agitation who are at risk for arrhythmia, including those with relevant medical comorbidities or delirium.34
Neuronal cell death. Several lines of research evidence have demonstrated that haloperidol can cause cellular injury or death in neuronal tissue in a dose-dependent fashion through a variety of mechanisms.38 By contrast, SGAs have been shown to have neuroprotective effects.39 While these findings have mostly come from studies conducted in animals or in vitro human tumor cell lines, some researchers have nonetheless called for haloperidol to be banned, noting that if its neurotoxic effects were more widely known, “we would realize what a travesty it is to use [such] a brain-unfriendly drug.”40
Several reasonable alternatives
Echoing the earlier Cochrane review of haloperidol for psychosis-induced aggression or agitation,10 a 2017 update concluded, “If no other alternative exists, sole use of intramuscular haloperidol could be life-saving. Where additional drugs are available, sole use of haloperidol for extreme emergency could be considered unethical.”9
What then are reasonable alternatives to replace IM haloperidol for agitation? Clinicians should consider the following nonpharmacologic and pharmacologic interventions:
Nonpharmacologic interventions. Several behavioral interventions have been demonstrated to be effective for managing acute agitation, including verbal de-escalation, enhanced “programming” on the inpatient units, and the judicious use of seclusion.41-43 While such interventions may demand additional staff or resources, they have the potential to lower long-term costs, reduce injuries to patients and staff, and improve the quality of care.43 The use of IM haloperidol as a form of “chemical restraint” does not represent standard-of-care treatment,3 and from an ethical perspective, should never be implemented punitively or to compensate for substandard care in the form of inadequate staffing or staff training.
Continue to: Benzodiazepines
Benzodiazepines. Lorazepam offers an attractive alternative to haloperidol without the risk of EPS.2,4,8 However, lorazepam alone may be perceived as less efficacious than a haloperidol “cocktail” because it represents less overall medication. Some evidence has suggested that lorazepam, 4 mg, might be the most appropriate dose, although it has only rarely been studied in clinical trials of acute agitation.3
Respiratory depression is frequently cited as an argument against using lorazepam for agitation, as if the therapeutic window is extremely narrow with ineffectiveness at 2 mg, but potential lethality beyond that dose. In fact, serious respiratory depression with lorazepam is unlikely in the absence of chronic obstructive pulmonary disease (COPD), obstructive sleep apnea, or concomitant alcohol or other sedative use.46 Case reports have documented therapeutic lorazepam dosing of 2 to 4 mg every 2 hours up to 20 to 30 mg/d in patients with manic agitation.47 Even in patients with COPD, significant respiratory depression tends not to occur at doses <8 mg.48 A more evidence-based concern about lorazepam dosing is that 2 mg might be ineffective in patients with established tolerance. For example, 1 report described a patient in acute alcohol withdrawal who required dosing lorazepam to 1,600 mg within 24 hours.49 Collectively, these reports suggest that lorazepam has a much wider therapeutic window than is typically perceived, and that dosing with 3 to 4 mg IM is a reasonable option for agitation when 2 mg is likely to be inadequate.
Paradoxical disinhibition is another concern that might prevent benzodiazepines from being used alone as a first-line intervention for emergency treatment of agitation. However, similar to respiratory depression, this adverse event is relatively rare and tends to occur in children and geriatric patients, individuals intoxicated with alcohol or other sedatives, and patients with brain injury, developmental delay, or dementia.23,46 Although exacerbation of aggression has not been demonstrated in the RCTs examining benzodiazepines for agitation reviewed above, based on other research, some clinicians have expressed concerns about the potential for benzodiazepines to exacerbate aggression in patients with impulse control disorders and a history of violent behavior.50
The 2005 Expert Consensus Panel for Behavioral Emergencies51 recommended the use of lorazepam alone over haloperidol for agitation for patients for whom the diagnosis is unknown or includes the following:
- stimulant intoxication
- personality disorder
- comorbid obesity
- comorbid cardiac arrhythmia
- a history of akathisia and other EPS
- a history of amenorrhea/galactorrhea
- a history of seizures.
In surveys, patients have ranked lorazepam as the preferred medication for emergency agitation, whereas haloperidol was ranked as one of the least-preferred options.51,52
Continue to: Second-generation antipsychotics
Second-generation antipsychotics. The SGAs available in IM formulations, such as aripiprazole, olanzapine, and ziprasidone, have been shown to be at least as effective as haloperidol for the treatment of acute agitation (in 2015, the short-acting injectable formulation of aripiprazole was discontinued in the United States independent of safety or efficacy issues53). A review of RCTs examining IM SGAs for the treatment of agitation concluded that the number needed to treat for response compared with placebo was 5 for aripiprazole, 3 for olanzapine, and 3 for ziprasidone.54 In terms of safety, a meta-analysis of studies examining IM medications for agitation confirmed that the risk of acute EPS, including dystonia, akathisia, and parkinsonism, is significantly lower with SGAs compared with haloperidol.55 An RCT comparing IM ziprasidone with haloperidol found equivalently modest effects on QTc prolongation.56 Therefore, SGAs are an obvious and evidence-based option for replacing haloperidol as a treatment for acute agitation.
Unfortunately, for clinicians hoping to replace haloperidol within a multiple-medication IM “cocktail,” there have been no published controlled trials of SGAs combined with benzodiazepines. Although a short report indicated that aripiprazole and lorazepam are chemically compatible to be combined within a single injection,57 the package insert for aripiprazole warns that “If parenteral benzodiazepine therapy is deemed necessary in addition to ABILIFY injection treatment, patients should be monitored for excessive sedation and for orthostatic hypotension.”58 The package insert for olanzapine likewise lists the combination of lorazepam and olanzapine as a drug interaction that can potentiate sedation, and the manufacturer issued specific warnings about parenteral combination.59,60 A single published case of significant hypotension with combined IM olanzapine and lorazepam,60 together with the fact that IM olanzapine can cause hypotension by itself,61 has discouraged the coadministration of these medications. Nonetheless, the combination is used in some emergency settings, with several retrospective studies failing to provide evidence of hypotension or respiratory depression as adverse effects.62-64
Droperidol.
Over the past decade, however, droperidol has returned to the US market68 and its IV and IM usage has been revitalized for managing patients with agitation within or en route to the ED. Studies have demonstrated droperidol efficacy comparable to midazolam, ziprasidone, or olanzapine, as well as effectiveness as an IV adjunct to midazolam.69-71 In contrast to the FDA black-box warning, retrospective studies and RCTs of both IV and IM droperidol suggest that QTc prolongation and torsades de pointes are rare events that do not occur any more frequently than they do with haloperidol, even at doses >10 mg.72,73 However, in studies involving patients with drug intoxication and treatment with multiple medications, oversedation to the point of needing rescue intervention was reported. In an emergency setting where these issues are relatively easily managed, such risks may be better tolerated than in psychiatric settings.
With earlier studies examining the use of droperidol in an acute psychiatric setting that reported a more rapid onset of action than haloperidol,65-67 a 2016 Cochrane review concluded that there was high-quality evidence to support droperidol’s use for psychosis-induced agitation.74 However, a 2015 RCT comparing IM droperidol, 10 mg, to haloperidol, 10 mg, found equivalent efficacy and response times (with maximal response occurring within 2 hours) and concluded that droperidol had no advantage over haloperidol.75 Because none of the clinical trials that evaluated droperidol have included assessments for EPS, its risk of akathisia remains uncertain.
Continue to: Ketamine
Ketamine. In recent years, ketamine has been used to treat acute agitation within or en route to the ED. Preliminary observational studies support ketamine’s efficacy when administered via IV or IM routes,76 with more rapid symptomatic improvement compared with haloperidol, lorazepam, or midazolam alone.77 Reported adverse effects of ketamine include dissociation, psychotic exacerbation, and respiratory depression,76 although 1 small naturalistic study found no evidence of exacerbation of psychotic or other psychiatric symptoms.78 An ongoing RCT is comparing IM ketamine, 5 mg/kg, to combined IM haloperidol, 5 mg, and midazolam, 5 mg.79 Although various ketamine formulations are increasingly being used in psychiatry, active psychosis is generally regarded as a contraindication. It is premature to recommend parenteral ketamine administration for agitation within most psychiatric settings until more research on safety has been completed.
Haloperidol, or something else? Practical considerations
Consider the following factors when deciding whether to use haloperidol or one of its alternatives:
Limitations of the evidence. Modern clinical trials requiring informed consent often do not include the kind of severe agitation that clinicians encounter in acute psychiatric, emergency, or forensic settings. In addition, standard interventions, such as 3-medication haloperidol “cocktails,” have not been evaluated in clinical trials. Clinicians are therefore often in the dark about optimal evidence-based practices.
Treatment goals. Psychiatric agitation has many causes, with a range of severity that warrants a commensurate range of responses. Protocols for managing acute agitation should include graded interventions that begin with nonpharmacologic interventions and voluntary oral medications, and move to involuntary IM medications when necessary.
While treatment guidelines clearly recommend against IM medications as “chemical restraint” with a goal of sedating a patient until he/she is unconscious,3,51 such outcomes are nonetheless often sought by staff who are concerned about the risk of injuries during a behavioral emergency. In such instances, the risks of violence towards patients and staff may outweigh concerns about adverse effects in a risk-benefit analysis. Consequently, clinicians may be prone to “skip over” graded interventions because they assume they “won’t work” in favor of administering involuntary multiple-medication haloperidol “cocktails” despite risks of excess sedation, EPS, and cardiotoxicity. Treatment settings should critically evaluate such biased preferences, with a goal of developing tailored, evidence-based strategies that maximize benefits while minimizing excess sedation and other untoward adverse effects, with an eye towards promoting better overall patient care and reducing length of stay.42,43,80
Continue to: Limitations of available medications
Limitations of available medications. There is no perfect medication for the management of acute agitation. Evidence indicates that pharmacologic options take 15 minutes to several hours to resolve acute agitation, even potentially more rapid-acting medications such as midazolam and droperidol. This is well beyond most clinicians’ desired window for response time in a behavioral emergency. Multiple-medication “cocktails” may be used with the hope of hastening response time, but may not achieve this goal at the expense of increasing the risk of adverse effects and the likelihood that a patient will remain sedated for a prolonged time. In the real world, this often means that by the time a psychiatrist comes to evaluate a patient who has been given emergency medications, the patient cannot be aroused for an interview. Ideally, medications would calm an agitated patient rapidly, without excess or prolonged sedation.80 Less-sedating SGAs, such as ziprasidone, might have this potential, but can sometimes be perceived as ineffective.
Avoiding akathisia. Akathisia’s potential to worsen and be mistaken for agitation makes it an especially concerning, if underappreciated, adverse effect of haloperidol that is often not adequately assessed in clinical trials or practice. In light of evidence that akathisia can occur in nearly half of patients receiving a single 5 mg-dose of haloperidol, it is difficult to justify the use of this medication for agitation when equally effective options exist with a lower risk of EPS.
While haloperidol-induced akathisia could in theory be mitigated by adding anticholinergic medications or benzodiazepines, previous studies have found that such strategies have limited effectiveness compared to “gold standard” treatment with propranolol.28,81,82 Furthermore, the half-lives of anticholinergic medications, such as benztropine or diphenhydramine, are significantly shorter than that of a single dose of haloperidol, which can be as long as 37 hours.83 Therefore, akathisia and other EPS could emerge or worsen several hours or even days after receiving an IM haloperidol “cocktail” as the shorter-acting medications wear off. Akathisia is best minimized by avoiding FGAs, such as haloperidol, when treating acute agitation.
Promoting adherence. Although haloperidol is often recommended for acute agitation in patients with schizophrenia or bipolar disorder on the basis that it would treat the underlying condition, many patients who receive IM medications for acute agitation are already prescribed standing doses of oral medication, which increases the risk of cumulative toxicity. In addition, receiving a medication likely to cause acute EPS that is ranked near the bottom of patient preferences may erode the potential for a therapeutic alliance and hamper longer-term antipsychotic medication adherence.
Time for a change
For nearly half a century, haloperidol has been a “gold standard” intervention for IM control in patients with agitation. However, given its potential to produce adverse effects, including a significant risk of akathisia that can worsen agitation, along with the availability of newer pharmacologic options that are at least as effective (Table 1, and Table 2), haloperidol should be retired as a first-line medication for the treatment of agitation. Clinicians would benefit from RCTs investigating the safety and efficacy of novel interventions including frequently-used, but untested medication combinations, as well as nonpharmacologic interventions.
Continue to: Bottom Line
Bottom Line
Although there is no perfect IM medication to treat acute agitation, haloperidol’s higher risk of adverse effects relative to newer alternatives suggest that it should no longer be considered a first-line intervention.
Related Resources
- Zun LS. Evidence-based review of pharmacotherapy for acute agitation. Part 1: onset of efficacy. J Emerg Med. 2018;54(3):364-374.
- Zun LS. Evidence-based review of pharmacotherapy for acute agitation. Part 2: safety. J Emerg Med. 2018;54(4): 522-532.
Drug Brand Names
Aripiprazole • Abilify
Benztropine • Cogentin
Chlorpromazine • Thorazine
Diphenhydramine • Benadryl
Droperidol • Inapsine
Haloperidol • Haldol
Ketamine • Ketalar
Lorazepam • Ativan
Midazolam • Versed
Olanzapine • Zyprexa
Prochlorperazine • Compazine
Promethazine • Phenergan
Propranolol • Inderal, Pronol
Ziprasidone • Geodon
1. Shorter E. A history of psychiatry. New York, NY: John Wiley & Sons, Inc.; 1997:249.
2. Salzman C, Green AI, Rodriguez-Villa F, et al. Benzodiazepines combined with neuroleptics for management of severe disruptive behavior. Psychosomatics. 1986;27(suppl 1):17-22.
3. Allen MH. Managing the agitated psychotic patient: a reappraisal of the evidence. J Clin Psychiatr. 2000;61(suppl 14):11-20.
4. Salzman C, Solomon D, Miyawaki E, et al. Parenteral lorazepam versus parenteral haloperidol for the control of psychotic disruptive behavior. J Clin Psychiatr. 1991:52(4):177-180.
5. Allen MH, Currier GW, Hughes DH, et al. The expert consensus guideline series: treatment of behavioral emergencies. Postgrad Med. 2001;(Spec No):1-88; quiz 89-90.
6. Foster S, Kessel J, Berman ME, et al. Efficacy of lorazepam and haloperidol for rapid tranquilization in a psychiatric emergency room setting. Int Clin Psychopharmacol. 1997;12(3):175-179.
7. Garza-Trevino WS, Hollister LE, Overall JE, et al. Efficacy of combinations of intramuscular antipsychotics and sedative-hypnotics for control of psychotic agitation. Am J Psychiatr. 1989:146(12):1598-1601.
8. Battaglia J, Moss S, Rush J, et al. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective double-blind, emergency study. Am J Emerg Med 1997;15(4):335-340.
9. Ostinelli EG, Brooke-Powney MJ, Li X, et al. Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2017; 7:CD009377. doi: 10.1002/14651858.CD009377.pub3.
10. Powney MJ, Adams CE, Jones H. Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2012;11:CD009377. doi: 10.1002/14651858.CD009377.pub2.
11. Citrome L. Review: limited evidence on effects of haloperidol alone for rapid tranquillisation in psychosis-induced aggression. Evid Based Ment Health. 2013;16(2):47.
12. Bienek SA, Ownby R, Penalver A, et al. A double-blind study of lorazepam versus the combination of haloperidol and lorazepam in managing agitation. Pharmacother. 1998;18(1):57-62.
13. Binder RL, McNiel DE. Contemporary practices in managing acutely violent patients in 20 psychiatric emergency rooms. Psychiatric Serv. 1999;50(2):1553-1554.
14. Andrezina R, Josiassen RC, Marcus RN, et al. Intramuscular aripiprazole for the treatment of acute agitation in patients with schizophrenia or schizoaffective disorder: a double-blind, placebo-controlled comparison with intramuscular haloperidol. Psychopharmacology (Berl). 2006;188(3):281-292.
15. Tran-Johnson TK, Sack DA, Marcus RN, et al. Efficacy and safety of intramuscular aripiprazole in patients with acute agitation: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatr. 2007;68(1):111-119.
16. Brook S, Lucey JV, Gunn KP. Intramuscular ziprasidone compared with intramuscular haloperidol in the treatment of acute psychosis. J Clin Psychiatr. 2000;61(12):933-941.
17. Brook S, Walden J, Benattia I, et al. Ziprasidone and haloperidol in the treatment of acute exacerbation of schizophrenia and schizoaffective disorder: comparison of intramuscular and oral formulations in a 6-week, randomized, blinded-assessment study. Psychopharmacology (Berl). 2005;178(4):514-523.
18. Wright P, Birkett M, David SR, et al. Double-blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation in schizophrenia. Am J Psychiatr. 2001;158(7):1149-1151.
19. Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psych. 2002;59(5):441-448.
20. Hsu W, Huang S, Lee B, et al. Comparison of intramuscular olanzapine, orally disintegrating olanzapine tablets, oral risperidone solution, and intramuscular haloperidol in the management of acute agitation in an acute care psychiatric ward in Taiwan. J Clin Psychopharmacol. 2010;30(3):230-234.
21. Chan H, Ree S, Su L, et al. A double-blind, randomized comparison study of efficacy and safety of intramuscular olanzapine and intramuscular haloperidol in patients with schizophrenia and acute agitated behavior. J Clin Psychopharmacol. 2014;34(3):355-358.
22. Baldaçara L, Sanches M, Cordeiro DC, et al. Rapid tranquilization for agitated patients in emergency psychiatric rooms: a randomized trial of olanzapine, ziprasidone, haloperidol plus promethazine, haloperidol plus midazolam and haloperidol alone. Braz J Psychiatry. 2011;33(1):30-39.
23. Hillard JR. Defusing patient violence. Current Psychiatry. 2002;1(4):22-29.
24. Seemüller F, Schennach R, Mayr A, et al. Akathisia and suicidal ideation in first-episode schizophrenia. J Clin Psychopharmacol. 2012;32(5):694-698.
25. Eikelenboom-Schieveld SJM, Lucire Y, Fogleman JC. The relevance of cytochrome P450 polymorphism in forensic medicine and akathisia-related violence and suicide. J Forens Leg Med. 2016;41:65-71.
26. Van Putten T, May PRA, Marder SR. Akathisia with haloperidol and thiothixene. Arch Gen Psych. 1984;41:1036-1039.
27. Drotts DL, Vinson DR. Prochlorperazine induced akathisia in emergency patients. Ann Emerg Med. 1999;34(4):469-475.
28. Salem H, Negpal C, Pigott T. Revisiting antipsychotic-induced akathisia: current issues and prospective challenges. Curr Neuropharmacol. 2017;15(5):789-798.
29. Huf G, Coutinho ESF, Adams CE. Rapid tranquilization in psychiatric emergency settings in Brazil: pragmatic randomized controlled trial of intramuscular haloperidol versus intramuscular haloperidol plus promethazine. BMJ. 2007;335(7625):869.
30. Mantovani C, Labate CM, Sponholz A, et al. Are low doses of antipsychotics effective in the management of psychomotor agitation? A randomized, rated-blind trial of 4 intramuscular interventions. J Clin Psychopharmacol. 2013;33(3):306-312.
31. Darwish H, Grant R, Haslam R, et al. Promethazine-induced acute dystonic reactions. Am J Dis Child. 1980;134(10):990-991.
32. Jyothi CH, Rudraiah HGM, Vidya HK, et al. Promethazine induced acute dystonia: a case report. Manipal J Med Sci. 2016;1(2):63-64.
33. Ames D, Carr-Lopez SM, Gutierrez MA, et al. Detecting and managing adverse effects of antipsychotic medications: current state of play. Psychiatr Clin North Am. 2016;39(2):275-311.
34. Meyer-Massetti C, Cheng CM, Sharpe MA, et al. The FDA extended warning for intravenous haloperidol and torsades de pointes: how should institutions respond? J Hosp Med. 2010;5(4):E8-E16. doi: 10.1002/jhm.691.
35. Wu C, Tsai Y, Tsai H. Antipsychotic drugs and the risk of ventricular arrhythmia and/or sudden cardiac death: a nation-wide case-crossover study. J Am Heart Dis. 2015;4(2):e001568. doi: 10.1161/JAHA.114.001568.
36. Beach SR, Celano CM, Sugrue AM, et al. QT prolongation, torsades de pointe, and psychotropic medications: a 5-year update. Psychosomatics. 2018;59(1):105-122.
37. Leonard CE, Freeman CP, Newcomb CW, et al. Antipsychotics and the risks of sudden cardiac death and all-cause death: cohort studies in Medicaid and dually-eligible Medicaid-Medicare beneficiaries of five states. J Clin Exp Cardiol. 2013;suppl 10(6):1-9.
38. Nasrallah H, Chen AT. Multiple neurotoxic effects of haloperidol resulting in neuronal death. Ann Clin Psychiatr. 2017;29(3):195-202.
39. Chen AT, Nasrallah HA. Neuroprotective effects of the second generation antipsychotics. Schizophr Res. 2019;208:1-7.
40. Nasrallah HA. Haloperidol clearly is neurotoxic. Should it be banned? Current Psychiatry. 2013;12(7):7-8.
41. Corrigan PW, Yudofsky SC, Silver JM. Pharmacological and behavioral treatments for aggressive psychiatric inpatients. Hosp Comm Psychiatr. 1993;44(2):125-133.
42. Zeller SL, Citrome L. Managing agitation associated with schizophrenia and bipolar disorder in the emergency setting. West J Emerg Med. 2016;17(2):165-172.
43. Vieta E, Garriga M, Cardete L, et al. Protocol for the management of psychiatric patients with psychomotor agitation. BMC Psychiatr. 2017;17:328.
44. Nobay F, Simon BC, Levitt A, et al. A prospective, double-blind, randomized trial of midazolam versus haloperidol versus lorazepam in the chemical restraint of violent and severely agitated patients. Acad Emerg Med. 2004;11(7):744-749.
45. Klein LR, Driver BE, Miner JR, et al. Intramuscular midazolam, olanzapine, ziprasidone, or haloperidol for treating acute agitation in the emergency department. Ann Emerg Med. 2018;72(4):374-385.
46. Hillard JR. Emergency treatment of acute psychosis. J Clin Psychiatr. 1998;59(suppl 1):57-60.
47. Modell JG, Lenox RH, Weiner S. Inpatient clinical trial of lorazepam for the management of manic agitation. J Clin Psychopharmacol. 1985;5(2):109-110.
48. Denaut M, Yernault JC, De Coster A. Double-blind comparison of the respiratory effects of parenteral lorazepam and diazepam in patients with chronic obstructive lung disease. Curr Med Res Opin. 1975;2(10):611-615.
49. Kahn DR, Barnhorst AV, Bourgeois JA. A case of alcohol withdrawal requiring 1,600 mg of lorazepam in 24 hours. CNS Spectr. 2009;14(7):385-389.
50. Jones KA. Benzodiazepines: their role in aggression and why GPs should prescribe with caution. Austral Fam Physician. 2011;40(11):862-865.
51. Allen MH, Currier GW, Carpenter D, et al. The expert consensus guideline series. Treatment of behavioral emergencies 2005. J Psychiatr Pract. 2005;11(suppl 1):5-108.
52. Allen MH, Carpenter D, Sheets JL, et al. What do consumers say they want and need during a psychiatric emergency? J Psychiatr Pract. 2003;9(1):39-58.
53. Han DH. Some Abilify formulations to discontinue in 2015. MPR. https://www.empr.com/home/news/some-abilify-formulations-to-discontinue-in-2015/. Published January 13, 2015. Accessed April 17, 2020.
54. Citrome L. Comparison of intramuscular ziprasidone, olanzapine, or aripiprazole for agitation: a quantitative review of efficacy and safety. J Clin Psychiatry. 2007;68(12):1876-1885.
55. Satterthwaite TD, Wolf DH, Rosenheck RA, et al. A meta-analysis of the risk of acute extrapyramidal symptoms with intramuscular antipsychotics for the treatment for agitation. J Clin Psychiatr. 2008;69(12):1869-1879.
56. Miceli JJ, Tensfeldt TG, Shiovitz T, et al. Effects of high-dose ziprasidone and haloperidol on the QTc interval after intramuscular administration: a randomized, single-blind, parallel-group study in patients with schizophrenia or schizoaffective disorder. Clin Ther. 2010;32(3):472-491.
57. Kovalick LJ, Pikalov AA, Ni N, et al. Short-term physical compatibility of intramuscular aripiprazole with intramuscular lorazepam. Am J Health-Syst Pharm. 2008;65(21):2007-2008.
58. Abilify [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2014.
59. Zyprexa [package insert]. Indianapolis, IN: Lilly Research Laboratories; 2005.
60. Zacher JL, Roche-Desilets J. Hypotension secondary to the combination of intramuscular olanzapine and intramuscular lorazepam. J Clin Psychiatr. 2005;66(12):1614-1615.
61. Marder SR, Sorsaburu S, Dunayevich E, et al. Case reports of postmarketing adverse event experiences with olanzapine intramuscular treatment in patients with agitation. J Clin Psychiatr 2010;71(4):433-441.
62. Wilson MP, MacDonald K, Vilke GM, et al. A comparison of the safety of olanzapine and haloperidol in combination with benzodiazepines in emergency department patients with acute agitation. J Emerg Med. 2012;43(5):790-797.
63. Wilson MP, MacDonald K, Vilke GM, et al. Potential complications of combining intramuscular olanzapine with benzodiazepines in emergency department patients. J Emerg Med. 2012;43(5):889-896.
64. Williams AM. Coadministration of intramuscular olanzapine and benzodiazepines in agitated patients with mental illness. Ment Health Clin [Internet]. 2018;8(5):208-213.
65. Resnick M, Burton BT. Droperidol vs. haloperidol in the initial management of acutely agitated patients. J Clin Psychiatry. 1984;45(7):298-299.
66. Thomas H, Schwartz E, Petrilli R. Droperidol versus haloperidol for chemical restraint of agitated and combative patients. Ann Emerg Med. 1992;21(4):407-413.
67. Richards JR, Derlet RW, Duncan DR. Chemical restraint for the agitated patient in the emergency department: lorazepam versus droperidol. J Emerg Med. 1998;16(4):567-573.
68. Boyer EW. Droperidol is back (and here’s what you need to know). ACEP Now. https://www.acepnow.com/article/droperidol-is-back-and-heres-what-you-need-to-know/. Published September 16, 2019. Accessed April 17, 2020.
69. Martel M, Sterzinger A, Miner J, et al. Management of acute undifferentiated agitation in the emergency department: a randomized double-blind trial of droperidol, ziprasidone, and midazolam. Acad Emerg Med. 2005;12(12):1167-1172.
70. Chan EW, Taylor DM, Knott JC, et al. Intravenous droperidol or olanzapine as an adjunct to midazolam for the acutely agitated patient: a multicenter, randomized, double-blind, placebo-controlled clinical trial. Ann Emerg Med. 2013;61(1):72-81.
71. Isbister GK, Calver LA, Page CB, et al. Randomized controlled trial of intramuscular droperidol versus midazolam for violence and acute behavioral disturbance: the DORM study. Ann Emerg Med. 2010;56(4):392-401.
72. Macht M, Mull AC, McVaney KE, et al. Comparison of droperidol and haloperidol for use by paramedics assessment of safety and effectiveness. Prehosp Emerg Care. 2014;18(3):375-380.
73. Calver L, Page CB, Downes MA, et al. The safety and effectiveness of droperidol for sedation of acute behavioral disturbance in the emergency department. Ann Emerg Med. 2015;66(3):230-238.
74. Kohokar MA, Rathbone J. Droperidol for psychosis-induced aggression or agitation. Cochrane Database Syst Rev. 2016;12:CD002830.
75. Calver L, Drinkwater V, Gupta R, et al. Droperidol v. haloperidol for sedation of aggressive behavior in acute mental health: randomized controlled trial. Brit J Psychiatr. 2015;206(3):223-228.
76. Hopper AB, Vilke GM, Castillo EM, et al. Ketamine use for acute agitation in the emergency department. J Emerg Med. 2015;48(6):712-719.
77. Riddell J, Tran A, Bengiamin R, et al. Ketamine as a first-line treatment for severely agitated emergency department patients. Am J Emerg Med. 2017;35:1000-1004.
78. Lebin JA, Akhavan AR, Hippe DS, et al. Psychiatric outcomes of patients with severe agitation following administration of prehospital ketamine. Acad Emerg Med. 2019;26(8):889-896.
79. Barbic D, Andolfatto G, Grunau B, et al. Rapid agitation control with ketamine in the emergency department (RACKED): a randomized controlled trial protocol. Trials. 2018;19(1):651.
80. Garriga M, Pacchiarotti I, Kasper S, et al. Assessment and management of agitation in psychiatry: expert consensus. World J Biol Psychiatr. 2016;17(2):86-128.
81. Adler L, Angrist B, Peselow E, et al. Efficacy of propranolol in neuroleptic-induced akathesia. J Clin Psychopharmacol. 1985;5(3):164-166.
82. Adler LA, Reiter S, Corwin J, et al. Neuroleptic-induced akathisia: propranolol versus benztropine. Biol Psychiatry. 1988;23(2):211-213.
83. de Leon J, Diaz FJ, Wedlund P, et al. Haloperidol half-life after chronic dosing. J Clin Psychopharmacol. 2004;24(6):656-660.
For more than half a century, haloperidol has been used as a first-line medication for psychiatric agitation constituting a “behavioral emergency” when a patient cannot or will not take oral medication. Today, haloperidol is most commonly administered as an IM injection along with an anticholinergic medication to minimize extrapyramidal symptoms (EPS) and a benzodiazepine for additional sedation. The multiple-medication “cocktail” is often referred to by double-entendre nicknames, such as “B-52” or “5250” (ie, haloperidol, 5 mg; lorazepam, 2 mg; and
Earlier evidence of haloperidol’s efficacy
The initial “discovery” of antipsychotic medications was made in 1951 based on the inadvertent observation that chlorpromazine had the potential to calm surgical patients with autonomic activation. This calming effect, described as “désintéressment” (meaning a kind of “indifference to the world”),1 resulted in a new class of medications replacing barbiturates and bromides as go-to options to achieve “rapid tranquilization” of psychiatric agitation.2 Although the ability of antipsychotic medications to gradually reduce positive symptoms, such as delusions and hallucinations, has been attributed to dopamine (D2) antagonism, their more immediate sedating and anti-agitation effects are the result of broader effects as histamine (H1) and alpha-1 adrenergic antagonists.
In the 1970s, haloperidol emerged as a first-line option to manage agitation due to its IM and IV availability, as well as its relative lack of sedation and orthostasis compared with low-potency D2 antagonists such as chlorpromazine. However, haloperidol was observed to have a significant risk of acute EPS, including dystonic reactions.2 From the 1970s to the 1990s, numerous prospective clinical trials of haloperidol for the treatment of acute psychotic agitation, including several randomized controlled trials (RCTs) comparing haloperidol to lorazepam, were conducted.3 The design and outcomes of the haloperidol vs lorazepam RCTs were fairly consistent4-7:
- adult participants with acute agitation and a variety of psychiatric diagnoses, for whom informed consent often was waived due to agitation severity
- randomization to either IM haloperidol, 5 mg, or IM lorazepam, 2 mg, administered every 30 minutes until agitation resolved
- behavioral outcomes measured over several hours using various rating scales, without consistent assessment of EPS
- equivalent efficacy of haloperidol and lorazepam, with symptom resolution usually achieved after 1 to 2 doses (in 30 to 60 minutes), but sometimes longer
- anticholinergic “rescue” allowed for EPS, but not administered prophylactically
- EPS, including dystonia and akathisia, were significantly more frequent with haloperidol compared with lorazepam.8
In recognition of the greater risk of EPS with haloperidol compared with lorazepam, and the fact that most study participants were already taking standing doses of antipsychotic medications, some researchers have recommended using benzodiazepines alone as the optimal treatment for agitation.4,9 A 2012 Cochrane review concluded that the involuntary use of haloperidol alone “could be considered unethical.”10,11 However, other studies that examined the combination of haloperidol and lorazepam compared with either medication alone found that the combination of the 2 medications was associated with a more rapid resolution of symptoms, which suggests a superior synergistic effect.6,7,12 By the late 1990s, combined haloperidol and lorazepam, often mixed within a single injection, became the most common strategy to achieve rapid tranquilization in the psychiatric emergency setting.13 However, while the combination has been justified as a way to reduce the antipsychotic medication dose and EPS risk,2 few studies have compared combinations containing <5 mg of haloperidol. As a result, the apparent superiority of combined haloperidol and lorazepam compared with either medication alone may be a simple cumulative dose effect rather than true synergism. It is also important to note that adding lorazepam to haloperidol does not mitigate the risk of EPS such as dystonia in the absence of anticholinergic medication.8 To date, however, there have been no clinical trials investigating the efficacy of IM haloperidol, lorazepam, and
Newer RCTs tell a different story
With the availability of second-generation antipsychotics (SGAs) in IM formulations, clinical trials over the past 2 decades have focused on comparing SGAs with haloperidol alone as the “gold standard” control for acute agitation. Compared with previous trials of
- Study participants who signed informed consent (and were likely less agitated)
- IM haloperidol doses typically >5 mg (eg, 6.5 to 10 mg).
As with studies comparing lorazepam with haloperidol, the results of these RCTs revealed that IM
An updated 2017 Cochrane review of haloperidol for psychosis-induced aggression or agitation concluded that9:
- haloperidol is an effective intervention, although the evidence is “weak”
- significant treatment effects may take as long as 1 to 2 hours following multiple IM injections
- in contrast to SGAs, treatment with haloperidol carries a significant risk of EPS
- adding a benzodiazepine “does not have strong evidence of benefit and carries risk of additional harm.”
Continue to: Haloperidol's well-known toxicity
Haloperidol’s well-known toxicity
Haloperidol has been associated with numerous adverse effects:
Akathisia and other acute EPS. Treatment with even a single dose of IM haloperidol can result in acute EPS, including dystonia and akathisia. At best, such adverse effects are subjectively troubling and unpleasant; at worst, akathisia can exacerbate and be mistaken for agitation, leading to administration of more medication23 and the possible development of suicidal or violent behavior.24-25 In the studies reviewed above, the overall rate of EPS was as high as 21% after treatment with haloperidol,16 with parkinsonism occurring in up to 17% of patients,19 dystonia in up to 11%,7 and akathisia in up to 10%.15 However, because specific EPS were assessed inconsistently, and sometimes not at all, the rate of akathisia—arguably the most relevant and counter-therapeutic adverse effect related to agitation—remains unclear.
In another study that specifically assessed for akathisia in patients treated with haloperidol, up to 40% experienced akathisia 6 hours after a single oral dose of 5 mg.26 Even a single dose of IV
Although anticholinergic medications or benzodiazepinesare often administered as part of a haloperidol “cocktail,” these medications often do not adequately resolve emergent akathisia.26,28 No clinical trials of IM haloperidol combined with benztropine or diphenhydramine have been published, but several studies suggest that combining haloperidol with
Cardiotoxicity. Although low-potency antipsychotic medications such as
Continue to: Although there is no direct evidence...
Although there is no direct evidence that the cardiac risks associated with IV haloperidol apply to IM administration, epidemiologic studies indicate that oral haloperidol carries an elevated risk of ventricular arrhythmia and sudden cardiac death,35,36 with 1 study reporting greater risk compared with other SGAs.37 Haloperidol, whether administered orally or IM, may therefore be an especially poor choice for patients with agitation who are at risk for arrhythmia, including those with relevant medical comorbidities or delirium.34
Neuronal cell death. Several lines of research evidence have demonstrated that haloperidol can cause cellular injury or death in neuronal tissue in a dose-dependent fashion through a variety of mechanisms.38 By contrast, SGAs have been shown to have neuroprotective effects.39 While these findings have mostly come from studies conducted in animals or in vitro human tumor cell lines, some researchers have nonetheless called for haloperidol to be banned, noting that if its neurotoxic effects were more widely known, “we would realize what a travesty it is to use [such] a brain-unfriendly drug.”40
Several reasonable alternatives
Echoing the earlier Cochrane review of haloperidol for psychosis-induced aggression or agitation,10 a 2017 update concluded, “If no other alternative exists, sole use of intramuscular haloperidol could be life-saving. Where additional drugs are available, sole use of haloperidol for extreme emergency could be considered unethical.”9
What then are reasonable alternatives to replace IM haloperidol for agitation? Clinicians should consider the following nonpharmacologic and pharmacologic interventions:
Nonpharmacologic interventions. Several behavioral interventions have been demonstrated to be effective for managing acute agitation, including verbal de-escalation, enhanced “programming” on the inpatient units, and the judicious use of seclusion.41-43 While such interventions may demand additional staff or resources, they have the potential to lower long-term costs, reduce injuries to patients and staff, and improve the quality of care.43 The use of IM haloperidol as a form of “chemical restraint” does not represent standard-of-care treatment,3 and from an ethical perspective, should never be implemented punitively or to compensate for substandard care in the form of inadequate staffing or staff training.
Continue to: Benzodiazepines
Benzodiazepines. Lorazepam offers an attractive alternative to haloperidol without the risk of EPS.2,4,8 However, lorazepam alone may be perceived as less efficacious than a haloperidol “cocktail” because it represents less overall medication. Some evidence has suggested that lorazepam, 4 mg, might be the most appropriate dose, although it has only rarely been studied in clinical trials of acute agitation.3
Respiratory depression is frequently cited as an argument against using lorazepam for agitation, as if the therapeutic window is extremely narrow with ineffectiveness at 2 mg, but potential lethality beyond that dose. In fact, serious respiratory depression with lorazepam is unlikely in the absence of chronic obstructive pulmonary disease (COPD), obstructive sleep apnea, or concomitant alcohol or other sedative use.46 Case reports have documented therapeutic lorazepam dosing of 2 to 4 mg every 2 hours up to 20 to 30 mg/d in patients with manic agitation.47 Even in patients with COPD, significant respiratory depression tends not to occur at doses <8 mg.48 A more evidence-based concern about lorazepam dosing is that 2 mg might be ineffective in patients with established tolerance. For example, 1 report described a patient in acute alcohol withdrawal who required dosing lorazepam to 1,600 mg within 24 hours.49 Collectively, these reports suggest that lorazepam has a much wider therapeutic window than is typically perceived, and that dosing with 3 to 4 mg IM is a reasonable option for agitation when 2 mg is likely to be inadequate.
Paradoxical disinhibition is another concern that might prevent benzodiazepines from being used alone as a first-line intervention for emergency treatment of agitation. However, similar to respiratory depression, this adverse event is relatively rare and tends to occur in children and geriatric patients, individuals intoxicated with alcohol or other sedatives, and patients with brain injury, developmental delay, or dementia.23,46 Although exacerbation of aggression has not been demonstrated in the RCTs examining benzodiazepines for agitation reviewed above, based on other research, some clinicians have expressed concerns about the potential for benzodiazepines to exacerbate aggression in patients with impulse control disorders and a history of violent behavior.50
The 2005 Expert Consensus Panel for Behavioral Emergencies51 recommended the use of lorazepam alone over haloperidol for agitation for patients for whom the diagnosis is unknown or includes the following:
- stimulant intoxication
- personality disorder
- comorbid obesity
- comorbid cardiac arrhythmia
- a history of akathisia and other EPS
- a history of amenorrhea/galactorrhea
- a history of seizures.
In surveys, patients have ranked lorazepam as the preferred medication for emergency agitation, whereas haloperidol was ranked as one of the least-preferred options.51,52
Continue to: Second-generation antipsychotics
Second-generation antipsychotics. The SGAs available in IM formulations, such as aripiprazole, olanzapine, and ziprasidone, have been shown to be at least as effective as haloperidol for the treatment of acute agitation (in 2015, the short-acting injectable formulation of aripiprazole was discontinued in the United States independent of safety or efficacy issues53). A review of RCTs examining IM SGAs for the treatment of agitation concluded that the number needed to treat for response compared with placebo was 5 for aripiprazole, 3 for olanzapine, and 3 for ziprasidone.54 In terms of safety, a meta-analysis of studies examining IM medications for agitation confirmed that the risk of acute EPS, including dystonia, akathisia, and parkinsonism, is significantly lower with SGAs compared with haloperidol.55 An RCT comparing IM ziprasidone with haloperidol found equivalently modest effects on QTc prolongation.56 Therefore, SGAs are an obvious and evidence-based option for replacing haloperidol as a treatment for acute agitation.
Unfortunately, for clinicians hoping to replace haloperidol within a multiple-medication IM “cocktail,” there have been no published controlled trials of SGAs combined with benzodiazepines. Although a short report indicated that aripiprazole and lorazepam are chemically compatible to be combined within a single injection,57 the package insert for aripiprazole warns that “If parenteral benzodiazepine therapy is deemed necessary in addition to ABILIFY injection treatment, patients should be monitored for excessive sedation and for orthostatic hypotension.”58 The package insert for olanzapine likewise lists the combination of lorazepam and olanzapine as a drug interaction that can potentiate sedation, and the manufacturer issued specific warnings about parenteral combination.59,60 A single published case of significant hypotension with combined IM olanzapine and lorazepam,60 together with the fact that IM olanzapine can cause hypotension by itself,61 has discouraged the coadministration of these medications. Nonetheless, the combination is used in some emergency settings, with several retrospective studies failing to provide evidence of hypotension or respiratory depression as adverse effects.62-64
Droperidol.
Over the past decade, however, droperidol has returned to the US market68 and its IV and IM usage has been revitalized for managing patients with agitation within or en route to the ED. Studies have demonstrated droperidol efficacy comparable to midazolam, ziprasidone, or olanzapine, as well as effectiveness as an IV adjunct to midazolam.69-71 In contrast to the FDA black-box warning, retrospective studies and RCTs of both IV and IM droperidol suggest that QTc prolongation and torsades de pointes are rare events that do not occur any more frequently than they do with haloperidol, even at doses >10 mg.72,73 However, in studies involving patients with drug intoxication and treatment with multiple medications, oversedation to the point of needing rescue intervention was reported. In an emergency setting where these issues are relatively easily managed, such risks may be better tolerated than in psychiatric settings.
With earlier studies examining the use of droperidol in an acute psychiatric setting that reported a more rapid onset of action than haloperidol,65-67 a 2016 Cochrane review concluded that there was high-quality evidence to support droperidol’s use for psychosis-induced agitation.74 However, a 2015 RCT comparing IM droperidol, 10 mg, to haloperidol, 10 mg, found equivalent efficacy and response times (with maximal response occurring within 2 hours) and concluded that droperidol had no advantage over haloperidol.75 Because none of the clinical trials that evaluated droperidol have included assessments for EPS, its risk of akathisia remains uncertain.
Continue to: Ketamine
Ketamine. In recent years, ketamine has been used to treat acute agitation within or en route to the ED. Preliminary observational studies support ketamine’s efficacy when administered via IV or IM routes,76 with more rapid symptomatic improvement compared with haloperidol, lorazepam, or midazolam alone.77 Reported adverse effects of ketamine include dissociation, psychotic exacerbation, and respiratory depression,76 although 1 small naturalistic study found no evidence of exacerbation of psychotic or other psychiatric symptoms.78 An ongoing RCT is comparing IM ketamine, 5 mg/kg, to combined IM haloperidol, 5 mg, and midazolam, 5 mg.79 Although various ketamine formulations are increasingly being used in psychiatry, active psychosis is generally regarded as a contraindication. It is premature to recommend parenteral ketamine administration for agitation within most psychiatric settings until more research on safety has been completed.
Haloperidol, or something else? Practical considerations
Consider the following factors when deciding whether to use haloperidol or one of its alternatives:
Limitations of the evidence. Modern clinical trials requiring informed consent often do not include the kind of severe agitation that clinicians encounter in acute psychiatric, emergency, or forensic settings. In addition, standard interventions, such as 3-medication haloperidol “cocktails,” have not been evaluated in clinical trials. Clinicians are therefore often in the dark about optimal evidence-based practices.
Treatment goals. Psychiatric agitation has many causes, with a range of severity that warrants a commensurate range of responses. Protocols for managing acute agitation should include graded interventions that begin with nonpharmacologic interventions and voluntary oral medications, and move to involuntary IM medications when necessary.
While treatment guidelines clearly recommend against IM medications as “chemical restraint” with a goal of sedating a patient until he/she is unconscious,3,51 such outcomes are nonetheless often sought by staff who are concerned about the risk of injuries during a behavioral emergency. In such instances, the risks of violence towards patients and staff may outweigh concerns about adverse effects in a risk-benefit analysis. Consequently, clinicians may be prone to “skip over” graded interventions because they assume they “won’t work” in favor of administering involuntary multiple-medication haloperidol “cocktails” despite risks of excess sedation, EPS, and cardiotoxicity. Treatment settings should critically evaluate such biased preferences, with a goal of developing tailored, evidence-based strategies that maximize benefits while minimizing excess sedation and other untoward adverse effects, with an eye towards promoting better overall patient care and reducing length of stay.42,43,80
Continue to: Limitations of available medications
Limitations of available medications. There is no perfect medication for the management of acute agitation. Evidence indicates that pharmacologic options take 15 minutes to several hours to resolve acute agitation, even potentially more rapid-acting medications such as midazolam and droperidol. This is well beyond most clinicians’ desired window for response time in a behavioral emergency. Multiple-medication “cocktails” may be used with the hope of hastening response time, but may not achieve this goal at the expense of increasing the risk of adverse effects and the likelihood that a patient will remain sedated for a prolonged time. In the real world, this often means that by the time a psychiatrist comes to evaluate a patient who has been given emergency medications, the patient cannot be aroused for an interview. Ideally, medications would calm an agitated patient rapidly, without excess or prolonged sedation.80 Less-sedating SGAs, such as ziprasidone, might have this potential, but can sometimes be perceived as ineffective.
Avoiding akathisia. Akathisia’s potential to worsen and be mistaken for agitation makes it an especially concerning, if underappreciated, adverse effect of haloperidol that is often not adequately assessed in clinical trials or practice. In light of evidence that akathisia can occur in nearly half of patients receiving a single 5 mg-dose of haloperidol, it is difficult to justify the use of this medication for agitation when equally effective options exist with a lower risk of EPS.
While haloperidol-induced akathisia could in theory be mitigated by adding anticholinergic medications or benzodiazepines, previous studies have found that such strategies have limited effectiveness compared to “gold standard” treatment with propranolol.28,81,82 Furthermore, the half-lives of anticholinergic medications, such as benztropine or diphenhydramine, are significantly shorter than that of a single dose of haloperidol, which can be as long as 37 hours.83 Therefore, akathisia and other EPS could emerge or worsen several hours or even days after receiving an IM haloperidol “cocktail” as the shorter-acting medications wear off. Akathisia is best minimized by avoiding FGAs, such as haloperidol, when treating acute agitation.
Promoting adherence. Although haloperidol is often recommended for acute agitation in patients with schizophrenia or bipolar disorder on the basis that it would treat the underlying condition, many patients who receive IM medications for acute agitation are already prescribed standing doses of oral medication, which increases the risk of cumulative toxicity. In addition, receiving a medication likely to cause acute EPS that is ranked near the bottom of patient preferences may erode the potential for a therapeutic alliance and hamper longer-term antipsychotic medication adherence.
Time for a change
For nearly half a century, haloperidol has been a “gold standard” intervention for IM control in patients with agitation. However, given its potential to produce adverse effects, including a significant risk of akathisia that can worsen agitation, along with the availability of newer pharmacologic options that are at least as effective (Table 1, and Table 2), haloperidol should be retired as a first-line medication for the treatment of agitation. Clinicians would benefit from RCTs investigating the safety and efficacy of novel interventions including frequently-used, but untested medication combinations, as well as nonpharmacologic interventions.
Continue to: Bottom Line
Bottom Line
Although there is no perfect IM medication to treat acute agitation, haloperidol’s higher risk of adverse effects relative to newer alternatives suggest that it should no longer be considered a first-line intervention.
Related Resources
- Zun LS. Evidence-based review of pharmacotherapy for acute agitation. Part 1: onset of efficacy. J Emerg Med. 2018;54(3):364-374.
- Zun LS. Evidence-based review of pharmacotherapy for acute agitation. Part 2: safety. J Emerg Med. 2018;54(4): 522-532.
Drug Brand Names
Aripiprazole • Abilify
Benztropine • Cogentin
Chlorpromazine • Thorazine
Diphenhydramine • Benadryl
Droperidol • Inapsine
Haloperidol • Haldol
Ketamine • Ketalar
Lorazepam • Ativan
Midazolam • Versed
Olanzapine • Zyprexa
Prochlorperazine • Compazine
Promethazine • Phenergan
Propranolol • Inderal, Pronol
Ziprasidone • Geodon
For more than half a century, haloperidol has been used as a first-line medication for psychiatric agitation constituting a “behavioral emergency” when a patient cannot or will not take oral medication. Today, haloperidol is most commonly administered as an IM injection along with an anticholinergic medication to minimize extrapyramidal symptoms (EPS) and a benzodiazepine for additional sedation. The multiple-medication “cocktail” is often referred to by double-entendre nicknames, such as “B-52” or “5250” (ie, haloperidol, 5 mg; lorazepam, 2 mg; and
Earlier evidence of haloperidol’s efficacy
The initial “discovery” of antipsychotic medications was made in 1951 based on the inadvertent observation that chlorpromazine had the potential to calm surgical patients with autonomic activation. This calming effect, described as “désintéressment” (meaning a kind of “indifference to the world”),1 resulted in a new class of medications replacing barbiturates and bromides as go-to options to achieve “rapid tranquilization” of psychiatric agitation.2 Although the ability of antipsychotic medications to gradually reduce positive symptoms, such as delusions and hallucinations, has been attributed to dopamine (D2) antagonism, their more immediate sedating and anti-agitation effects are the result of broader effects as histamine (H1) and alpha-1 adrenergic antagonists.
In the 1970s, haloperidol emerged as a first-line option to manage agitation due to its IM and IV availability, as well as its relative lack of sedation and orthostasis compared with low-potency D2 antagonists such as chlorpromazine. However, haloperidol was observed to have a significant risk of acute EPS, including dystonic reactions.2 From the 1970s to the 1990s, numerous prospective clinical trials of haloperidol for the treatment of acute psychotic agitation, including several randomized controlled trials (RCTs) comparing haloperidol to lorazepam, were conducted.3 The design and outcomes of the haloperidol vs lorazepam RCTs were fairly consistent4-7:
- adult participants with acute agitation and a variety of psychiatric diagnoses, for whom informed consent often was waived due to agitation severity
- randomization to either IM haloperidol, 5 mg, or IM lorazepam, 2 mg, administered every 30 minutes until agitation resolved
- behavioral outcomes measured over several hours using various rating scales, without consistent assessment of EPS
- equivalent efficacy of haloperidol and lorazepam, with symptom resolution usually achieved after 1 to 2 doses (in 30 to 60 minutes), but sometimes longer
- anticholinergic “rescue” allowed for EPS, but not administered prophylactically
- EPS, including dystonia and akathisia, were significantly more frequent with haloperidol compared with lorazepam.8
In recognition of the greater risk of EPS with haloperidol compared with lorazepam, and the fact that most study participants were already taking standing doses of antipsychotic medications, some researchers have recommended using benzodiazepines alone as the optimal treatment for agitation.4,9 A 2012 Cochrane review concluded that the involuntary use of haloperidol alone “could be considered unethical.”10,11 However, other studies that examined the combination of haloperidol and lorazepam compared with either medication alone found that the combination of the 2 medications was associated with a more rapid resolution of symptoms, which suggests a superior synergistic effect.6,7,12 By the late 1990s, combined haloperidol and lorazepam, often mixed within a single injection, became the most common strategy to achieve rapid tranquilization in the psychiatric emergency setting.13 However, while the combination has been justified as a way to reduce the antipsychotic medication dose and EPS risk,2 few studies have compared combinations containing <5 mg of haloperidol. As a result, the apparent superiority of combined haloperidol and lorazepam compared with either medication alone may be a simple cumulative dose effect rather than true synergism. It is also important to note that adding lorazepam to haloperidol does not mitigate the risk of EPS such as dystonia in the absence of anticholinergic medication.8 To date, however, there have been no clinical trials investigating the efficacy of IM haloperidol, lorazepam, and
Newer RCTs tell a different story
With the availability of second-generation antipsychotics (SGAs) in IM formulations, clinical trials over the past 2 decades have focused on comparing SGAs with haloperidol alone as the “gold standard” control for acute agitation. Compared with previous trials of
- Study participants who signed informed consent (and were likely less agitated)
- IM haloperidol doses typically >5 mg (eg, 6.5 to 10 mg).
As with studies comparing lorazepam with haloperidol, the results of these RCTs revealed that IM
An updated 2017 Cochrane review of haloperidol for psychosis-induced aggression or agitation concluded that9:
- haloperidol is an effective intervention, although the evidence is “weak”
- significant treatment effects may take as long as 1 to 2 hours following multiple IM injections
- in contrast to SGAs, treatment with haloperidol carries a significant risk of EPS
- adding a benzodiazepine “does not have strong evidence of benefit and carries risk of additional harm.”
Continue to: Haloperidol's well-known toxicity
Haloperidol’s well-known toxicity
Haloperidol has been associated with numerous adverse effects:
Akathisia and other acute EPS. Treatment with even a single dose of IM haloperidol can result in acute EPS, including dystonia and akathisia. At best, such adverse effects are subjectively troubling and unpleasant; at worst, akathisia can exacerbate and be mistaken for agitation, leading to administration of more medication23 and the possible development of suicidal or violent behavior.24-25 In the studies reviewed above, the overall rate of EPS was as high as 21% after treatment with haloperidol,16 with parkinsonism occurring in up to 17% of patients,19 dystonia in up to 11%,7 and akathisia in up to 10%.15 However, because specific EPS were assessed inconsistently, and sometimes not at all, the rate of akathisia—arguably the most relevant and counter-therapeutic adverse effect related to agitation—remains unclear.
In another study that specifically assessed for akathisia in patients treated with haloperidol, up to 40% experienced akathisia 6 hours after a single oral dose of 5 mg.26 Even a single dose of IV
Although anticholinergic medications or benzodiazepinesare often administered as part of a haloperidol “cocktail,” these medications often do not adequately resolve emergent akathisia.26,28 No clinical trials of IM haloperidol combined with benztropine or diphenhydramine have been published, but several studies suggest that combining haloperidol with
Cardiotoxicity. Although low-potency antipsychotic medications such as
Continue to: Although there is no direct evidence...
Although there is no direct evidence that the cardiac risks associated with IV haloperidol apply to IM administration, epidemiologic studies indicate that oral haloperidol carries an elevated risk of ventricular arrhythmia and sudden cardiac death,35,36 with 1 study reporting greater risk compared with other SGAs.37 Haloperidol, whether administered orally or IM, may therefore be an especially poor choice for patients with agitation who are at risk for arrhythmia, including those with relevant medical comorbidities or delirium.34
Neuronal cell death. Several lines of research evidence have demonstrated that haloperidol can cause cellular injury or death in neuronal tissue in a dose-dependent fashion through a variety of mechanisms.38 By contrast, SGAs have been shown to have neuroprotective effects.39 While these findings have mostly come from studies conducted in animals or in vitro human tumor cell lines, some researchers have nonetheless called for haloperidol to be banned, noting that if its neurotoxic effects were more widely known, “we would realize what a travesty it is to use [such] a brain-unfriendly drug.”40
Several reasonable alternatives
Echoing the earlier Cochrane review of haloperidol for psychosis-induced aggression or agitation,10 a 2017 update concluded, “If no other alternative exists, sole use of intramuscular haloperidol could be life-saving. Where additional drugs are available, sole use of haloperidol for extreme emergency could be considered unethical.”9
What then are reasonable alternatives to replace IM haloperidol for agitation? Clinicians should consider the following nonpharmacologic and pharmacologic interventions:
Nonpharmacologic interventions. Several behavioral interventions have been demonstrated to be effective for managing acute agitation, including verbal de-escalation, enhanced “programming” on the inpatient units, and the judicious use of seclusion.41-43 While such interventions may demand additional staff or resources, they have the potential to lower long-term costs, reduce injuries to patients and staff, and improve the quality of care.43 The use of IM haloperidol as a form of “chemical restraint” does not represent standard-of-care treatment,3 and from an ethical perspective, should never be implemented punitively or to compensate for substandard care in the form of inadequate staffing or staff training.
Continue to: Benzodiazepines
Benzodiazepines. Lorazepam offers an attractive alternative to haloperidol without the risk of EPS.2,4,8 However, lorazepam alone may be perceived as less efficacious than a haloperidol “cocktail” because it represents less overall medication. Some evidence has suggested that lorazepam, 4 mg, might be the most appropriate dose, although it has only rarely been studied in clinical trials of acute agitation.3
Respiratory depression is frequently cited as an argument against using lorazepam for agitation, as if the therapeutic window is extremely narrow with ineffectiveness at 2 mg, but potential lethality beyond that dose. In fact, serious respiratory depression with lorazepam is unlikely in the absence of chronic obstructive pulmonary disease (COPD), obstructive sleep apnea, or concomitant alcohol or other sedative use.46 Case reports have documented therapeutic lorazepam dosing of 2 to 4 mg every 2 hours up to 20 to 30 mg/d in patients with manic agitation.47 Even in patients with COPD, significant respiratory depression tends not to occur at doses <8 mg.48 A more evidence-based concern about lorazepam dosing is that 2 mg might be ineffective in patients with established tolerance. For example, 1 report described a patient in acute alcohol withdrawal who required dosing lorazepam to 1,600 mg within 24 hours.49 Collectively, these reports suggest that lorazepam has a much wider therapeutic window than is typically perceived, and that dosing with 3 to 4 mg IM is a reasonable option for agitation when 2 mg is likely to be inadequate.
Paradoxical disinhibition is another concern that might prevent benzodiazepines from being used alone as a first-line intervention for emergency treatment of agitation. However, similar to respiratory depression, this adverse event is relatively rare and tends to occur in children and geriatric patients, individuals intoxicated with alcohol or other sedatives, and patients with brain injury, developmental delay, or dementia.23,46 Although exacerbation of aggression has not been demonstrated in the RCTs examining benzodiazepines for agitation reviewed above, based on other research, some clinicians have expressed concerns about the potential for benzodiazepines to exacerbate aggression in patients with impulse control disorders and a history of violent behavior.50
The 2005 Expert Consensus Panel for Behavioral Emergencies51 recommended the use of lorazepam alone over haloperidol for agitation for patients for whom the diagnosis is unknown or includes the following:
- stimulant intoxication
- personality disorder
- comorbid obesity
- comorbid cardiac arrhythmia
- a history of akathisia and other EPS
- a history of amenorrhea/galactorrhea
- a history of seizures.
In surveys, patients have ranked lorazepam as the preferred medication for emergency agitation, whereas haloperidol was ranked as one of the least-preferred options.51,52
Continue to: Second-generation antipsychotics
Second-generation antipsychotics. The SGAs available in IM formulations, such as aripiprazole, olanzapine, and ziprasidone, have been shown to be at least as effective as haloperidol for the treatment of acute agitation (in 2015, the short-acting injectable formulation of aripiprazole was discontinued in the United States independent of safety or efficacy issues53). A review of RCTs examining IM SGAs for the treatment of agitation concluded that the number needed to treat for response compared with placebo was 5 for aripiprazole, 3 for olanzapine, and 3 for ziprasidone.54 In terms of safety, a meta-analysis of studies examining IM medications for agitation confirmed that the risk of acute EPS, including dystonia, akathisia, and parkinsonism, is significantly lower with SGAs compared with haloperidol.55 An RCT comparing IM ziprasidone with haloperidol found equivalently modest effects on QTc prolongation.56 Therefore, SGAs are an obvious and evidence-based option for replacing haloperidol as a treatment for acute agitation.
Unfortunately, for clinicians hoping to replace haloperidol within a multiple-medication IM “cocktail,” there have been no published controlled trials of SGAs combined with benzodiazepines. Although a short report indicated that aripiprazole and lorazepam are chemically compatible to be combined within a single injection,57 the package insert for aripiprazole warns that “If parenteral benzodiazepine therapy is deemed necessary in addition to ABILIFY injection treatment, patients should be monitored for excessive sedation and for orthostatic hypotension.”58 The package insert for olanzapine likewise lists the combination of lorazepam and olanzapine as a drug interaction that can potentiate sedation, and the manufacturer issued specific warnings about parenteral combination.59,60 A single published case of significant hypotension with combined IM olanzapine and lorazepam,60 together with the fact that IM olanzapine can cause hypotension by itself,61 has discouraged the coadministration of these medications. Nonetheless, the combination is used in some emergency settings, with several retrospective studies failing to provide evidence of hypotension or respiratory depression as adverse effects.62-64
Droperidol.
Over the past decade, however, droperidol has returned to the US market68 and its IV and IM usage has been revitalized for managing patients with agitation within or en route to the ED. Studies have demonstrated droperidol efficacy comparable to midazolam, ziprasidone, or olanzapine, as well as effectiveness as an IV adjunct to midazolam.69-71 In contrast to the FDA black-box warning, retrospective studies and RCTs of both IV and IM droperidol suggest that QTc prolongation and torsades de pointes are rare events that do not occur any more frequently than they do with haloperidol, even at doses >10 mg.72,73 However, in studies involving patients with drug intoxication and treatment with multiple medications, oversedation to the point of needing rescue intervention was reported. In an emergency setting where these issues are relatively easily managed, such risks may be better tolerated than in psychiatric settings.
With earlier studies examining the use of droperidol in an acute psychiatric setting that reported a more rapid onset of action than haloperidol,65-67 a 2016 Cochrane review concluded that there was high-quality evidence to support droperidol’s use for psychosis-induced agitation.74 However, a 2015 RCT comparing IM droperidol, 10 mg, to haloperidol, 10 mg, found equivalent efficacy and response times (with maximal response occurring within 2 hours) and concluded that droperidol had no advantage over haloperidol.75 Because none of the clinical trials that evaluated droperidol have included assessments for EPS, its risk of akathisia remains uncertain.
Continue to: Ketamine
Ketamine. In recent years, ketamine has been used to treat acute agitation within or en route to the ED. Preliminary observational studies support ketamine’s efficacy when administered via IV or IM routes,76 with more rapid symptomatic improvement compared with haloperidol, lorazepam, or midazolam alone.77 Reported adverse effects of ketamine include dissociation, psychotic exacerbation, and respiratory depression,76 although 1 small naturalistic study found no evidence of exacerbation of psychotic or other psychiatric symptoms.78 An ongoing RCT is comparing IM ketamine, 5 mg/kg, to combined IM haloperidol, 5 mg, and midazolam, 5 mg.79 Although various ketamine formulations are increasingly being used in psychiatry, active psychosis is generally regarded as a contraindication. It is premature to recommend parenteral ketamine administration for agitation within most psychiatric settings until more research on safety has been completed.
Haloperidol, or something else? Practical considerations
Consider the following factors when deciding whether to use haloperidol or one of its alternatives:
Limitations of the evidence. Modern clinical trials requiring informed consent often do not include the kind of severe agitation that clinicians encounter in acute psychiatric, emergency, or forensic settings. In addition, standard interventions, such as 3-medication haloperidol “cocktails,” have not been evaluated in clinical trials. Clinicians are therefore often in the dark about optimal evidence-based practices.
Treatment goals. Psychiatric agitation has many causes, with a range of severity that warrants a commensurate range of responses. Protocols for managing acute agitation should include graded interventions that begin with nonpharmacologic interventions and voluntary oral medications, and move to involuntary IM medications when necessary.
While treatment guidelines clearly recommend against IM medications as “chemical restraint” with a goal of sedating a patient until he/she is unconscious,3,51 such outcomes are nonetheless often sought by staff who are concerned about the risk of injuries during a behavioral emergency. In such instances, the risks of violence towards patients and staff may outweigh concerns about adverse effects in a risk-benefit analysis. Consequently, clinicians may be prone to “skip over” graded interventions because they assume they “won’t work” in favor of administering involuntary multiple-medication haloperidol “cocktails” despite risks of excess sedation, EPS, and cardiotoxicity. Treatment settings should critically evaluate such biased preferences, with a goal of developing tailored, evidence-based strategies that maximize benefits while minimizing excess sedation and other untoward adverse effects, with an eye towards promoting better overall patient care and reducing length of stay.42,43,80
Continue to: Limitations of available medications
Limitations of available medications. There is no perfect medication for the management of acute agitation. Evidence indicates that pharmacologic options take 15 minutes to several hours to resolve acute agitation, even potentially more rapid-acting medications such as midazolam and droperidol. This is well beyond most clinicians’ desired window for response time in a behavioral emergency. Multiple-medication “cocktails” may be used with the hope of hastening response time, but may not achieve this goal at the expense of increasing the risk of adverse effects and the likelihood that a patient will remain sedated for a prolonged time. In the real world, this often means that by the time a psychiatrist comes to evaluate a patient who has been given emergency medications, the patient cannot be aroused for an interview. Ideally, medications would calm an agitated patient rapidly, without excess or prolonged sedation.80 Less-sedating SGAs, such as ziprasidone, might have this potential, but can sometimes be perceived as ineffective.
Avoiding akathisia. Akathisia’s potential to worsen and be mistaken for agitation makes it an especially concerning, if underappreciated, adverse effect of haloperidol that is often not adequately assessed in clinical trials or practice. In light of evidence that akathisia can occur in nearly half of patients receiving a single 5 mg-dose of haloperidol, it is difficult to justify the use of this medication for agitation when equally effective options exist with a lower risk of EPS.
While haloperidol-induced akathisia could in theory be mitigated by adding anticholinergic medications or benzodiazepines, previous studies have found that such strategies have limited effectiveness compared to “gold standard” treatment with propranolol.28,81,82 Furthermore, the half-lives of anticholinergic medications, such as benztropine or diphenhydramine, are significantly shorter than that of a single dose of haloperidol, which can be as long as 37 hours.83 Therefore, akathisia and other EPS could emerge or worsen several hours or even days after receiving an IM haloperidol “cocktail” as the shorter-acting medications wear off. Akathisia is best minimized by avoiding FGAs, such as haloperidol, when treating acute agitation.
Promoting adherence. Although haloperidol is often recommended for acute agitation in patients with schizophrenia or bipolar disorder on the basis that it would treat the underlying condition, many patients who receive IM medications for acute agitation are already prescribed standing doses of oral medication, which increases the risk of cumulative toxicity. In addition, receiving a medication likely to cause acute EPS that is ranked near the bottom of patient preferences may erode the potential for a therapeutic alliance and hamper longer-term antipsychotic medication adherence.
Time for a change
For nearly half a century, haloperidol has been a “gold standard” intervention for IM control in patients with agitation. However, given its potential to produce adverse effects, including a significant risk of akathisia that can worsen agitation, along with the availability of newer pharmacologic options that are at least as effective (Table 1, and Table 2), haloperidol should be retired as a first-line medication for the treatment of agitation. Clinicians would benefit from RCTs investigating the safety and efficacy of novel interventions including frequently-used, but untested medication combinations, as well as nonpharmacologic interventions.
Continue to: Bottom Line
Bottom Line
Although there is no perfect IM medication to treat acute agitation, haloperidol’s higher risk of adverse effects relative to newer alternatives suggest that it should no longer be considered a first-line intervention.
Related Resources
- Zun LS. Evidence-based review of pharmacotherapy for acute agitation. Part 1: onset of efficacy. J Emerg Med. 2018;54(3):364-374.
- Zun LS. Evidence-based review of pharmacotherapy for acute agitation. Part 2: safety. J Emerg Med. 2018;54(4): 522-532.
Drug Brand Names
Aripiprazole • Abilify
Benztropine • Cogentin
Chlorpromazine • Thorazine
Diphenhydramine • Benadryl
Droperidol • Inapsine
Haloperidol • Haldol
Ketamine • Ketalar
Lorazepam • Ativan
Midazolam • Versed
Olanzapine • Zyprexa
Prochlorperazine • Compazine
Promethazine • Phenergan
Propranolol • Inderal, Pronol
Ziprasidone • Geodon
1. Shorter E. A history of psychiatry. New York, NY: John Wiley & Sons, Inc.; 1997:249.
2. Salzman C, Green AI, Rodriguez-Villa F, et al. Benzodiazepines combined with neuroleptics for management of severe disruptive behavior. Psychosomatics. 1986;27(suppl 1):17-22.
3. Allen MH. Managing the agitated psychotic patient: a reappraisal of the evidence. J Clin Psychiatr. 2000;61(suppl 14):11-20.
4. Salzman C, Solomon D, Miyawaki E, et al. Parenteral lorazepam versus parenteral haloperidol for the control of psychotic disruptive behavior. J Clin Psychiatr. 1991:52(4):177-180.
5. Allen MH, Currier GW, Hughes DH, et al. The expert consensus guideline series: treatment of behavioral emergencies. Postgrad Med. 2001;(Spec No):1-88; quiz 89-90.
6. Foster S, Kessel J, Berman ME, et al. Efficacy of lorazepam and haloperidol for rapid tranquilization in a psychiatric emergency room setting. Int Clin Psychopharmacol. 1997;12(3):175-179.
7. Garza-Trevino WS, Hollister LE, Overall JE, et al. Efficacy of combinations of intramuscular antipsychotics and sedative-hypnotics for control of psychotic agitation. Am J Psychiatr. 1989:146(12):1598-1601.
8. Battaglia J, Moss S, Rush J, et al. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective double-blind, emergency study. Am J Emerg Med 1997;15(4):335-340.
9. Ostinelli EG, Brooke-Powney MJ, Li X, et al. Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2017; 7:CD009377. doi: 10.1002/14651858.CD009377.pub3.
10. Powney MJ, Adams CE, Jones H. Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2012;11:CD009377. doi: 10.1002/14651858.CD009377.pub2.
11. Citrome L. Review: limited evidence on effects of haloperidol alone for rapid tranquillisation in psychosis-induced aggression. Evid Based Ment Health. 2013;16(2):47.
12. Bienek SA, Ownby R, Penalver A, et al. A double-blind study of lorazepam versus the combination of haloperidol and lorazepam in managing agitation. Pharmacother. 1998;18(1):57-62.
13. Binder RL, McNiel DE. Contemporary practices in managing acutely violent patients in 20 psychiatric emergency rooms. Psychiatric Serv. 1999;50(2):1553-1554.
14. Andrezina R, Josiassen RC, Marcus RN, et al. Intramuscular aripiprazole for the treatment of acute agitation in patients with schizophrenia or schizoaffective disorder: a double-blind, placebo-controlled comparison with intramuscular haloperidol. Psychopharmacology (Berl). 2006;188(3):281-292.
15. Tran-Johnson TK, Sack DA, Marcus RN, et al. Efficacy and safety of intramuscular aripiprazole in patients with acute agitation: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatr. 2007;68(1):111-119.
16. Brook S, Lucey JV, Gunn KP. Intramuscular ziprasidone compared with intramuscular haloperidol in the treatment of acute psychosis. J Clin Psychiatr. 2000;61(12):933-941.
17. Brook S, Walden J, Benattia I, et al. Ziprasidone and haloperidol in the treatment of acute exacerbation of schizophrenia and schizoaffective disorder: comparison of intramuscular and oral formulations in a 6-week, randomized, blinded-assessment study. Psychopharmacology (Berl). 2005;178(4):514-523.
18. Wright P, Birkett M, David SR, et al. Double-blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation in schizophrenia. Am J Psychiatr. 2001;158(7):1149-1151.
19. Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psych. 2002;59(5):441-448.
20. Hsu W, Huang S, Lee B, et al. Comparison of intramuscular olanzapine, orally disintegrating olanzapine tablets, oral risperidone solution, and intramuscular haloperidol in the management of acute agitation in an acute care psychiatric ward in Taiwan. J Clin Psychopharmacol. 2010;30(3):230-234.
21. Chan H, Ree S, Su L, et al. A double-blind, randomized comparison study of efficacy and safety of intramuscular olanzapine and intramuscular haloperidol in patients with schizophrenia and acute agitated behavior. J Clin Psychopharmacol. 2014;34(3):355-358.
22. Baldaçara L, Sanches M, Cordeiro DC, et al. Rapid tranquilization for agitated patients in emergency psychiatric rooms: a randomized trial of olanzapine, ziprasidone, haloperidol plus promethazine, haloperidol plus midazolam and haloperidol alone. Braz J Psychiatry. 2011;33(1):30-39.
23. Hillard JR. Defusing patient violence. Current Psychiatry. 2002;1(4):22-29.
24. Seemüller F, Schennach R, Mayr A, et al. Akathisia and suicidal ideation in first-episode schizophrenia. J Clin Psychopharmacol. 2012;32(5):694-698.
25. Eikelenboom-Schieveld SJM, Lucire Y, Fogleman JC. The relevance of cytochrome P450 polymorphism in forensic medicine and akathisia-related violence and suicide. J Forens Leg Med. 2016;41:65-71.
26. Van Putten T, May PRA, Marder SR. Akathisia with haloperidol and thiothixene. Arch Gen Psych. 1984;41:1036-1039.
27. Drotts DL, Vinson DR. Prochlorperazine induced akathisia in emergency patients. Ann Emerg Med. 1999;34(4):469-475.
28. Salem H, Negpal C, Pigott T. Revisiting antipsychotic-induced akathisia: current issues and prospective challenges. Curr Neuropharmacol. 2017;15(5):789-798.
29. Huf G, Coutinho ESF, Adams CE. Rapid tranquilization in psychiatric emergency settings in Brazil: pragmatic randomized controlled trial of intramuscular haloperidol versus intramuscular haloperidol plus promethazine. BMJ. 2007;335(7625):869.
30. Mantovani C, Labate CM, Sponholz A, et al. Are low doses of antipsychotics effective in the management of psychomotor agitation? A randomized, rated-blind trial of 4 intramuscular interventions. J Clin Psychopharmacol. 2013;33(3):306-312.
31. Darwish H, Grant R, Haslam R, et al. Promethazine-induced acute dystonic reactions. Am J Dis Child. 1980;134(10):990-991.
32. Jyothi CH, Rudraiah HGM, Vidya HK, et al. Promethazine induced acute dystonia: a case report. Manipal J Med Sci. 2016;1(2):63-64.
33. Ames D, Carr-Lopez SM, Gutierrez MA, et al. Detecting and managing adverse effects of antipsychotic medications: current state of play. Psychiatr Clin North Am. 2016;39(2):275-311.
34. Meyer-Massetti C, Cheng CM, Sharpe MA, et al. The FDA extended warning for intravenous haloperidol and torsades de pointes: how should institutions respond? J Hosp Med. 2010;5(4):E8-E16. doi: 10.1002/jhm.691.
35. Wu C, Tsai Y, Tsai H. Antipsychotic drugs and the risk of ventricular arrhythmia and/or sudden cardiac death: a nation-wide case-crossover study. J Am Heart Dis. 2015;4(2):e001568. doi: 10.1161/JAHA.114.001568.
36. Beach SR, Celano CM, Sugrue AM, et al. QT prolongation, torsades de pointe, and psychotropic medications: a 5-year update. Psychosomatics. 2018;59(1):105-122.
37. Leonard CE, Freeman CP, Newcomb CW, et al. Antipsychotics and the risks of sudden cardiac death and all-cause death: cohort studies in Medicaid and dually-eligible Medicaid-Medicare beneficiaries of five states. J Clin Exp Cardiol. 2013;suppl 10(6):1-9.
38. Nasrallah H, Chen AT. Multiple neurotoxic effects of haloperidol resulting in neuronal death. Ann Clin Psychiatr. 2017;29(3):195-202.
39. Chen AT, Nasrallah HA. Neuroprotective effects of the second generation antipsychotics. Schizophr Res. 2019;208:1-7.
40. Nasrallah HA. Haloperidol clearly is neurotoxic. Should it be banned? Current Psychiatry. 2013;12(7):7-8.
41. Corrigan PW, Yudofsky SC, Silver JM. Pharmacological and behavioral treatments for aggressive psychiatric inpatients. Hosp Comm Psychiatr. 1993;44(2):125-133.
42. Zeller SL, Citrome L. Managing agitation associated with schizophrenia and bipolar disorder in the emergency setting. West J Emerg Med. 2016;17(2):165-172.
43. Vieta E, Garriga M, Cardete L, et al. Protocol for the management of psychiatric patients with psychomotor agitation. BMC Psychiatr. 2017;17:328.
44. Nobay F, Simon BC, Levitt A, et al. A prospective, double-blind, randomized trial of midazolam versus haloperidol versus lorazepam in the chemical restraint of violent and severely agitated patients. Acad Emerg Med. 2004;11(7):744-749.
45. Klein LR, Driver BE, Miner JR, et al. Intramuscular midazolam, olanzapine, ziprasidone, or haloperidol for treating acute agitation in the emergency department. Ann Emerg Med. 2018;72(4):374-385.
46. Hillard JR. Emergency treatment of acute psychosis. J Clin Psychiatr. 1998;59(suppl 1):57-60.
47. Modell JG, Lenox RH, Weiner S. Inpatient clinical trial of lorazepam for the management of manic agitation. J Clin Psychopharmacol. 1985;5(2):109-110.
48. Denaut M, Yernault JC, De Coster A. Double-blind comparison of the respiratory effects of parenteral lorazepam and diazepam in patients with chronic obstructive lung disease. Curr Med Res Opin. 1975;2(10):611-615.
49. Kahn DR, Barnhorst AV, Bourgeois JA. A case of alcohol withdrawal requiring 1,600 mg of lorazepam in 24 hours. CNS Spectr. 2009;14(7):385-389.
50. Jones KA. Benzodiazepines: their role in aggression and why GPs should prescribe with caution. Austral Fam Physician. 2011;40(11):862-865.
51. Allen MH, Currier GW, Carpenter D, et al. The expert consensus guideline series. Treatment of behavioral emergencies 2005. J Psychiatr Pract. 2005;11(suppl 1):5-108.
52. Allen MH, Carpenter D, Sheets JL, et al. What do consumers say they want and need during a psychiatric emergency? J Psychiatr Pract. 2003;9(1):39-58.
53. Han DH. Some Abilify formulations to discontinue in 2015. MPR. https://www.empr.com/home/news/some-abilify-formulations-to-discontinue-in-2015/. Published January 13, 2015. Accessed April 17, 2020.
54. Citrome L. Comparison of intramuscular ziprasidone, olanzapine, or aripiprazole for agitation: a quantitative review of efficacy and safety. J Clin Psychiatry. 2007;68(12):1876-1885.
55. Satterthwaite TD, Wolf DH, Rosenheck RA, et al. A meta-analysis of the risk of acute extrapyramidal symptoms with intramuscular antipsychotics for the treatment for agitation. J Clin Psychiatr. 2008;69(12):1869-1879.
56. Miceli JJ, Tensfeldt TG, Shiovitz T, et al. Effects of high-dose ziprasidone and haloperidol on the QTc interval after intramuscular administration: a randomized, single-blind, parallel-group study in patients with schizophrenia or schizoaffective disorder. Clin Ther. 2010;32(3):472-491.
57. Kovalick LJ, Pikalov AA, Ni N, et al. Short-term physical compatibility of intramuscular aripiprazole with intramuscular lorazepam. Am J Health-Syst Pharm. 2008;65(21):2007-2008.
58. Abilify [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2014.
59. Zyprexa [package insert]. Indianapolis, IN: Lilly Research Laboratories; 2005.
60. Zacher JL, Roche-Desilets J. Hypotension secondary to the combination of intramuscular olanzapine and intramuscular lorazepam. J Clin Psychiatr. 2005;66(12):1614-1615.
61. Marder SR, Sorsaburu S, Dunayevich E, et al. Case reports of postmarketing adverse event experiences with olanzapine intramuscular treatment in patients with agitation. J Clin Psychiatr 2010;71(4):433-441.
62. Wilson MP, MacDonald K, Vilke GM, et al. A comparison of the safety of olanzapine and haloperidol in combination with benzodiazepines in emergency department patients with acute agitation. J Emerg Med. 2012;43(5):790-797.
63. Wilson MP, MacDonald K, Vilke GM, et al. Potential complications of combining intramuscular olanzapine with benzodiazepines in emergency department patients. J Emerg Med. 2012;43(5):889-896.
64. Williams AM. Coadministration of intramuscular olanzapine and benzodiazepines in agitated patients with mental illness. Ment Health Clin [Internet]. 2018;8(5):208-213.
65. Resnick M, Burton BT. Droperidol vs. haloperidol in the initial management of acutely agitated patients. J Clin Psychiatry. 1984;45(7):298-299.
66. Thomas H, Schwartz E, Petrilli R. Droperidol versus haloperidol for chemical restraint of agitated and combative patients. Ann Emerg Med. 1992;21(4):407-413.
67. Richards JR, Derlet RW, Duncan DR. Chemical restraint for the agitated patient in the emergency department: lorazepam versus droperidol. J Emerg Med. 1998;16(4):567-573.
68. Boyer EW. Droperidol is back (and here’s what you need to know). ACEP Now. https://www.acepnow.com/article/droperidol-is-back-and-heres-what-you-need-to-know/. Published September 16, 2019. Accessed April 17, 2020.
69. Martel M, Sterzinger A, Miner J, et al. Management of acute undifferentiated agitation in the emergency department: a randomized double-blind trial of droperidol, ziprasidone, and midazolam. Acad Emerg Med. 2005;12(12):1167-1172.
70. Chan EW, Taylor DM, Knott JC, et al. Intravenous droperidol or olanzapine as an adjunct to midazolam for the acutely agitated patient: a multicenter, randomized, double-blind, placebo-controlled clinical trial. Ann Emerg Med. 2013;61(1):72-81.
71. Isbister GK, Calver LA, Page CB, et al. Randomized controlled trial of intramuscular droperidol versus midazolam for violence and acute behavioral disturbance: the DORM study. Ann Emerg Med. 2010;56(4):392-401.
72. Macht M, Mull AC, McVaney KE, et al. Comparison of droperidol and haloperidol for use by paramedics assessment of safety and effectiveness. Prehosp Emerg Care. 2014;18(3):375-380.
73. Calver L, Page CB, Downes MA, et al. The safety and effectiveness of droperidol for sedation of acute behavioral disturbance in the emergency department. Ann Emerg Med. 2015;66(3):230-238.
74. Kohokar MA, Rathbone J. Droperidol for psychosis-induced aggression or agitation. Cochrane Database Syst Rev. 2016;12:CD002830.
75. Calver L, Drinkwater V, Gupta R, et al. Droperidol v. haloperidol for sedation of aggressive behavior in acute mental health: randomized controlled trial. Brit J Psychiatr. 2015;206(3):223-228.
76. Hopper AB, Vilke GM, Castillo EM, et al. Ketamine use for acute agitation in the emergency department. J Emerg Med. 2015;48(6):712-719.
77. Riddell J, Tran A, Bengiamin R, et al. Ketamine as a first-line treatment for severely agitated emergency department patients. Am J Emerg Med. 2017;35:1000-1004.
78. Lebin JA, Akhavan AR, Hippe DS, et al. Psychiatric outcomes of patients with severe agitation following administration of prehospital ketamine. Acad Emerg Med. 2019;26(8):889-896.
79. Barbic D, Andolfatto G, Grunau B, et al. Rapid agitation control with ketamine in the emergency department (RACKED): a randomized controlled trial protocol. Trials. 2018;19(1):651.
80. Garriga M, Pacchiarotti I, Kasper S, et al. Assessment and management of agitation in psychiatry: expert consensus. World J Biol Psychiatr. 2016;17(2):86-128.
81. Adler L, Angrist B, Peselow E, et al. Efficacy of propranolol in neuroleptic-induced akathesia. J Clin Psychopharmacol. 1985;5(3):164-166.
82. Adler LA, Reiter S, Corwin J, et al. Neuroleptic-induced akathisia: propranolol versus benztropine. Biol Psychiatry. 1988;23(2):211-213.
83. de Leon J, Diaz FJ, Wedlund P, et al. Haloperidol half-life after chronic dosing. J Clin Psychopharmacol. 2004;24(6):656-660.
1. Shorter E. A history of psychiatry. New York, NY: John Wiley & Sons, Inc.; 1997:249.
2. Salzman C, Green AI, Rodriguez-Villa F, et al. Benzodiazepines combined with neuroleptics for management of severe disruptive behavior. Psychosomatics. 1986;27(suppl 1):17-22.
3. Allen MH. Managing the agitated psychotic patient: a reappraisal of the evidence. J Clin Psychiatr. 2000;61(suppl 14):11-20.
4. Salzman C, Solomon D, Miyawaki E, et al. Parenteral lorazepam versus parenteral haloperidol for the control of psychotic disruptive behavior. J Clin Psychiatr. 1991:52(4):177-180.
5. Allen MH, Currier GW, Hughes DH, et al. The expert consensus guideline series: treatment of behavioral emergencies. Postgrad Med. 2001;(Spec No):1-88; quiz 89-90.
6. Foster S, Kessel J, Berman ME, et al. Efficacy of lorazepam and haloperidol for rapid tranquilization in a psychiatric emergency room setting. Int Clin Psychopharmacol. 1997;12(3):175-179.
7. Garza-Trevino WS, Hollister LE, Overall JE, et al. Efficacy of combinations of intramuscular antipsychotics and sedative-hypnotics for control of psychotic agitation. Am J Psychiatr. 1989:146(12):1598-1601.
8. Battaglia J, Moss S, Rush J, et al. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective double-blind, emergency study. Am J Emerg Med 1997;15(4):335-340.
9. Ostinelli EG, Brooke-Powney MJ, Li X, et al. Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2017; 7:CD009377. doi: 10.1002/14651858.CD009377.pub3.
10. Powney MJ, Adams CE, Jones H. Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2012;11:CD009377. doi: 10.1002/14651858.CD009377.pub2.
11. Citrome L. Review: limited evidence on effects of haloperidol alone for rapid tranquillisation in psychosis-induced aggression. Evid Based Ment Health. 2013;16(2):47.
12. Bienek SA, Ownby R, Penalver A, et al. A double-blind study of lorazepam versus the combination of haloperidol and lorazepam in managing agitation. Pharmacother. 1998;18(1):57-62.
13. Binder RL, McNiel DE. Contemporary practices in managing acutely violent patients in 20 psychiatric emergency rooms. Psychiatric Serv. 1999;50(2):1553-1554.
14. Andrezina R, Josiassen RC, Marcus RN, et al. Intramuscular aripiprazole for the treatment of acute agitation in patients with schizophrenia or schizoaffective disorder: a double-blind, placebo-controlled comparison with intramuscular haloperidol. Psychopharmacology (Berl). 2006;188(3):281-292.
15. Tran-Johnson TK, Sack DA, Marcus RN, et al. Efficacy and safety of intramuscular aripiprazole in patients with acute agitation: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatr. 2007;68(1):111-119.
16. Brook S, Lucey JV, Gunn KP. Intramuscular ziprasidone compared with intramuscular haloperidol in the treatment of acute psychosis. J Clin Psychiatr. 2000;61(12):933-941.
17. Brook S, Walden J, Benattia I, et al. Ziprasidone and haloperidol in the treatment of acute exacerbation of schizophrenia and schizoaffective disorder: comparison of intramuscular and oral formulations in a 6-week, randomized, blinded-assessment study. Psychopharmacology (Berl). 2005;178(4):514-523.
18. Wright P, Birkett M, David SR, et al. Double-blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation in schizophrenia. Am J Psychiatr. 2001;158(7):1149-1151.
19. Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psych. 2002;59(5):441-448.
20. Hsu W, Huang S, Lee B, et al. Comparison of intramuscular olanzapine, orally disintegrating olanzapine tablets, oral risperidone solution, and intramuscular haloperidol in the management of acute agitation in an acute care psychiatric ward in Taiwan. J Clin Psychopharmacol. 2010;30(3):230-234.
21. Chan H, Ree S, Su L, et al. A double-blind, randomized comparison study of efficacy and safety of intramuscular olanzapine and intramuscular haloperidol in patients with schizophrenia and acute agitated behavior. J Clin Psychopharmacol. 2014;34(3):355-358.
22. Baldaçara L, Sanches M, Cordeiro DC, et al. Rapid tranquilization for agitated patients in emergency psychiatric rooms: a randomized trial of olanzapine, ziprasidone, haloperidol plus promethazine, haloperidol plus midazolam and haloperidol alone. Braz J Psychiatry. 2011;33(1):30-39.
23. Hillard JR. Defusing patient violence. Current Psychiatry. 2002;1(4):22-29.
24. Seemüller F, Schennach R, Mayr A, et al. Akathisia and suicidal ideation in first-episode schizophrenia. J Clin Psychopharmacol. 2012;32(5):694-698.
25. Eikelenboom-Schieveld SJM, Lucire Y, Fogleman JC. The relevance of cytochrome P450 polymorphism in forensic medicine and akathisia-related violence and suicide. J Forens Leg Med. 2016;41:65-71.
26. Van Putten T, May PRA, Marder SR. Akathisia with haloperidol and thiothixene. Arch Gen Psych. 1984;41:1036-1039.
27. Drotts DL, Vinson DR. Prochlorperazine induced akathisia in emergency patients. Ann Emerg Med. 1999;34(4):469-475.
28. Salem H, Negpal C, Pigott T. Revisiting antipsychotic-induced akathisia: current issues and prospective challenges. Curr Neuropharmacol. 2017;15(5):789-798.
29. Huf G, Coutinho ESF, Adams CE. Rapid tranquilization in psychiatric emergency settings in Brazil: pragmatic randomized controlled trial of intramuscular haloperidol versus intramuscular haloperidol plus promethazine. BMJ. 2007;335(7625):869.
30. Mantovani C, Labate CM, Sponholz A, et al. Are low doses of antipsychotics effective in the management of psychomotor agitation? A randomized, rated-blind trial of 4 intramuscular interventions. J Clin Psychopharmacol. 2013;33(3):306-312.
31. Darwish H, Grant R, Haslam R, et al. Promethazine-induced acute dystonic reactions. Am J Dis Child. 1980;134(10):990-991.
32. Jyothi CH, Rudraiah HGM, Vidya HK, et al. Promethazine induced acute dystonia: a case report. Manipal J Med Sci. 2016;1(2):63-64.
33. Ames D, Carr-Lopez SM, Gutierrez MA, et al. Detecting and managing adverse effects of antipsychotic medications: current state of play. Psychiatr Clin North Am. 2016;39(2):275-311.
34. Meyer-Massetti C, Cheng CM, Sharpe MA, et al. The FDA extended warning for intravenous haloperidol and torsades de pointes: how should institutions respond? J Hosp Med. 2010;5(4):E8-E16. doi: 10.1002/jhm.691.
35. Wu C, Tsai Y, Tsai H. Antipsychotic drugs and the risk of ventricular arrhythmia and/or sudden cardiac death: a nation-wide case-crossover study. J Am Heart Dis. 2015;4(2):e001568. doi: 10.1161/JAHA.114.001568.
36. Beach SR, Celano CM, Sugrue AM, et al. QT prolongation, torsades de pointe, and psychotropic medications: a 5-year update. Psychosomatics. 2018;59(1):105-122.
37. Leonard CE, Freeman CP, Newcomb CW, et al. Antipsychotics and the risks of sudden cardiac death and all-cause death: cohort studies in Medicaid and dually-eligible Medicaid-Medicare beneficiaries of five states. J Clin Exp Cardiol. 2013;suppl 10(6):1-9.
38. Nasrallah H, Chen AT. Multiple neurotoxic effects of haloperidol resulting in neuronal death. Ann Clin Psychiatr. 2017;29(3):195-202.
39. Chen AT, Nasrallah HA. Neuroprotective effects of the second generation antipsychotics. Schizophr Res. 2019;208:1-7.
40. Nasrallah HA. Haloperidol clearly is neurotoxic. Should it be banned? Current Psychiatry. 2013;12(7):7-8.
41. Corrigan PW, Yudofsky SC, Silver JM. Pharmacological and behavioral treatments for aggressive psychiatric inpatients. Hosp Comm Psychiatr. 1993;44(2):125-133.
42. Zeller SL, Citrome L. Managing agitation associated with schizophrenia and bipolar disorder in the emergency setting. West J Emerg Med. 2016;17(2):165-172.
43. Vieta E, Garriga M, Cardete L, et al. Protocol for the management of psychiatric patients with psychomotor agitation. BMC Psychiatr. 2017;17:328.
44. Nobay F, Simon BC, Levitt A, et al. A prospective, double-blind, randomized trial of midazolam versus haloperidol versus lorazepam in the chemical restraint of violent and severely agitated patients. Acad Emerg Med. 2004;11(7):744-749.
45. Klein LR, Driver BE, Miner JR, et al. Intramuscular midazolam, olanzapine, ziprasidone, or haloperidol for treating acute agitation in the emergency department. Ann Emerg Med. 2018;72(4):374-385.
46. Hillard JR. Emergency treatment of acute psychosis. J Clin Psychiatr. 1998;59(suppl 1):57-60.
47. Modell JG, Lenox RH, Weiner S. Inpatient clinical trial of lorazepam for the management of manic agitation. J Clin Psychopharmacol. 1985;5(2):109-110.
48. Denaut M, Yernault JC, De Coster A. Double-blind comparison of the respiratory effects of parenteral lorazepam and diazepam in patients with chronic obstructive lung disease. Curr Med Res Opin. 1975;2(10):611-615.
49. Kahn DR, Barnhorst AV, Bourgeois JA. A case of alcohol withdrawal requiring 1,600 mg of lorazepam in 24 hours. CNS Spectr. 2009;14(7):385-389.
50. Jones KA. Benzodiazepines: their role in aggression and why GPs should prescribe with caution. Austral Fam Physician. 2011;40(11):862-865.
51. Allen MH, Currier GW, Carpenter D, et al. The expert consensus guideline series. Treatment of behavioral emergencies 2005. J Psychiatr Pract. 2005;11(suppl 1):5-108.
52. Allen MH, Carpenter D, Sheets JL, et al. What do consumers say they want and need during a psychiatric emergency? J Psychiatr Pract. 2003;9(1):39-58.
53. Han DH. Some Abilify formulations to discontinue in 2015. MPR. https://www.empr.com/home/news/some-abilify-formulations-to-discontinue-in-2015/. Published January 13, 2015. Accessed April 17, 2020.
54. Citrome L. Comparison of intramuscular ziprasidone, olanzapine, or aripiprazole for agitation: a quantitative review of efficacy and safety. J Clin Psychiatry. 2007;68(12):1876-1885.
55. Satterthwaite TD, Wolf DH, Rosenheck RA, et al. A meta-analysis of the risk of acute extrapyramidal symptoms with intramuscular antipsychotics for the treatment for agitation. J Clin Psychiatr. 2008;69(12):1869-1879.
56. Miceli JJ, Tensfeldt TG, Shiovitz T, et al. Effects of high-dose ziprasidone and haloperidol on the QTc interval after intramuscular administration: a randomized, single-blind, parallel-group study in patients with schizophrenia or schizoaffective disorder. Clin Ther. 2010;32(3):472-491.
57. Kovalick LJ, Pikalov AA, Ni N, et al. Short-term physical compatibility of intramuscular aripiprazole with intramuscular lorazepam. Am J Health-Syst Pharm. 2008;65(21):2007-2008.
58. Abilify [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2014.
59. Zyprexa [package insert]. Indianapolis, IN: Lilly Research Laboratories; 2005.
60. Zacher JL, Roche-Desilets J. Hypotension secondary to the combination of intramuscular olanzapine and intramuscular lorazepam. J Clin Psychiatr. 2005;66(12):1614-1615.
61. Marder SR, Sorsaburu S, Dunayevich E, et al. Case reports of postmarketing adverse event experiences with olanzapine intramuscular treatment in patients with agitation. J Clin Psychiatr 2010;71(4):433-441.
62. Wilson MP, MacDonald K, Vilke GM, et al. A comparison of the safety of olanzapine and haloperidol in combination with benzodiazepines in emergency department patients with acute agitation. J Emerg Med. 2012;43(5):790-797.
63. Wilson MP, MacDonald K, Vilke GM, et al. Potential complications of combining intramuscular olanzapine with benzodiazepines in emergency department patients. J Emerg Med. 2012;43(5):889-896.
64. Williams AM. Coadministration of intramuscular olanzapine and benzodiazepines in agitated patients with mental illness. Ment Health Clin [Internet]. 2018;8(5):208-213.
65. Resnick M, Burton BT. Droperidol vs. haloperidol in the initial management of acutely agitated patients. J Clin Psychiatry. 1984;45(7):298-299.
66. Thomas H, Schwartz E, Petrilli R. Droperidol versus haloperidol for chemical restraint of agitated and combative patients. Ann Emerg Med. 1992;21(4):407-413.
67. Richards JR, Derlet RW, Duncan DR. Chemical restraint for the agitated patient in the emergency department: lorazepam versus droperidol. J Emerg Med. 1998;16(4):567-573.
68. Boyer EW. Droperidol is back (and here’s what you need to know). ACEP Now. https://www.acepnow.com/article/droperidol-is-back-and-heres-what-you-need-to-know/. Published September 16, 2019. Accessed April 17, 2020.
69. Martel M, Sterzinger A, Miner J, et al. Management of acute undifferentiated agitation in the emergency department: a randomized double-blind trial of droperidol, ziprasidone, and midazolam. Acad Emerg Med. 2005;12(12):1167-1172.
70. Chan EW, Taylor DM, Knott JC, et al. Intravenous droperidol or olanzapine as an adjunct to midazolam for the acutely agitated patient: a multicenter, randomized, double-blind, placebo-controlled clinical trial. Ann Emerg Med. 2013;61(1):72-81.
71. Isbister GK, Calver LA, Page CB, et al. Randomized controlled trial of intramuscular droperidol versus midazolam for violence and acute behavioral disturbance: the DORM study. Ann Emerg Med. 2010;56(4):392-401.
72. Macht M, Mull AC, McVaney KE, et al. Comparison of droperidol and haloperidol for use by paramedics assessment of safety and effectiveness. Prehosp Emerg Care. 2014;18(3):375-380.
73. Calver L, Page CB, Downes MA, et al. The safety and effectiveness of droperidol for sedation of acute behavioral disturbance in the emergency department. Ann Emerg Med. 2015;66(3):230-238.
74. Kohokar MA, Rathbone J. Droperidol for psychosis-induced aggression or agitation. Cochrane Database Syst Rev. 2016;12:CD002830.
75. Calver L, Drinkwater V, Gupta R, et al. Droperidol v. haloperidol for sedation of aggressive behavior in acute mental health: randomized controlled trial. Brit J Psychiatr. 2015;206(3):223-228.
76. Hopper AB, Vilke GM, Castillo EM, et al. Ketamine use for acute agitation in the emergency department. J Emerg Med. 2015;48(6):712-719.
77. Riddell J, Tran A, Bengiamin R, et al. Ketamine as a first-line treatment for severely agitated emergency department patients. Am J Emerg Med. 2017;35:1000-1004.
78. Lebin JA, Akhavan AR, Hippe DS, et al. Psychiatric outcomes of patients with severe agitation following administration of prehospital ketamine. Acad Emerg Med. 2019;26(8):889-896.
79. Barbic D, Andolfatto G, Grunau B, et al. Rapid agitation control with ketamine in the emergency department (RACKED): a randomized controlled trial protocol. Trials. 2018;19(1):651.
80. Garriga M, Pacchiarotti I, Kasper S, et al. Assessment and management of agitation in psychiatry: expert consensus. World J Biol Psychiatr. 2016;17(2):86-128.
81. Adler L, Angrist B, Peselow E, et al. Efficacy of propranolol in neuroleptic-induced akathesia. J Clin Psychopharmacol. 1985;5(3):164-166.
82. Adler LA, Reiter S, Corwin J, et al. Neuroleptic-induced akathisia: propranolol versus benztropine. Biol Psychiatry. 1988;23(2):211-213.
83. de Leon J, Diaz FJ, Wedlund P, et al. Haloperidol half-life after chronic dosing. J Clin Psychopharmacol. 2004;24(6):656-660.