User login
Tackling the massive threat of climate change
Soon after moving to Pittsburgh for my pulmonary and critical care medicine fellowship in 2014, I began noticing a theme: So many of my patients expressed a sense that the air they breathed was harming them or was in some way responsible for the severity of their lung disease.
In this city, the legacy of the steel industry from the last century fostered economic prosperity but resulted in a profound legacy of pollution as well. Unfortunately, due to a combination of fossil fuel dependence for electricity generation and transportation, industrial particulate matter (PM) generation and greenhouse gas emissions, temperature inversions related to the topography of the region, and, most recently, smoke from Canadian wildfires in the summer of 2023, the air quality in Pittsburgh ranks among the 25 least healthy US cities. Our patients are bearing the burden of climate change.
I remember a patient in clinic talking about how on the days he could see a film of particulate on all the cars and the street outside, he knew he would feel more shortness of breath. Patients share about how when they had lived in different neighborhoods in town or traveled outside of Pittsburgh, their breathing improved.
Patients tell me that their asthma or COPD that did not use to cause them frequent trouble is now less well controlled despite better therapies available. Patients who used to experience seasonal allergies in just the fall or the spring now are plagued by their allergy symptoms year-round because of a warming climate yielding excess pollen throughout all seasons.
A recent study of patients with pulmonary fibrosis demonstrated that exposure to excess PM2.5 in this region resulted in more rapid clinical deterioration and premature death compared with patients with the same disease in other parts of North America with better air quality. The common denominator is human-generated climate change’s negative impact on health.
In particular, those who are already vulnerable because of underlying chronic disease or socioeconomic disparity are at greater risk and feel these repercussions disproportionately. Black and brown communities are more heavily exposed to air pollution due to the history of redlining and ongoing structural racism and, as a result, have worse health outcomes than other groups. There is an urgency and moral imperative for us as clinicians to address generations of environmental injustice.
While these themes floated around in the background during the early stage of my career as a pulmonologist, I didn’t have language or deep knowledge around these structural environmental issues. As a profession, we are gradually recognizing that the health impacts of climate change on which to advocate are within our wheelhouse as clinicians.
Our patients and our trainees are increasingly aware of these issues, and, as a result, we as currently practicing clinicians and educators must urgently learn about the lived experiences of our patients and how their diseases interplay with their exposures.
Nowadays, I think more about how to mitigate the impact of air pollution, which did not previously factor into my training or the early years of my clinical practice. We know that some patients, particularly those with underlying lung disease and young children, are at greater risk when exposed to more polluted air and may need to take different steps to limit their exposure. We now consider advising these patients with chronic respiratory disease to be aware of air quality advisories and limit their time outdoors on worse air quality days. We anticipate that when the air quality is worse, we will see more complications of cardiovascular and pulmonary disease.
As lifelong learners, we thirst for the latest data to incorporate into our clinical decision-making. Similarly, colleagues and I are now also voraciously reading and starting to have conversations with peers about the convergence of climate change and disease. But no matter how compelling and urgent these issues are, one clinician cannot tackle the massive threat of climate change and complexity of health care sustainability in isolation.
I am fortunate to work with several like-minded and highly motivated colleagues at my own institution. We have been able to organize effectively to spark local change toward reducing our system’s carbon emissions. Similarly, through professional organizations like CHEST, I have been able to collaborate with other pulmonary and critical care clinicians who share these passions and are doing similar advocacy work across the country. I am honored to serve as CHEST’s representative to the Medical Society Consortium on Climate and Health as another avenue to keep advancing this cause at scale in collaboration with advocates across all specialties.
While I worry every day for my patients, our communities, and my children as we face the accelerating threat of climate change, knowing that I am actively engaging in these efforts in pursuit of environmental justice and mitigating health care’s climate change contribution gives me a sense of empowerment and solidarity with others also striving to lessen our burden on the planet.
This article was adapted from the Winter 2024 online issue of CHEST Advocates. For the full article — and to engage with the other content from this issue — visit https://chestnet.org/chest-advocates.
Soon after moving to Pittsburgh for my pulmonary and critical care medicine fellowship in 2014, I began noticing a theme: So many of my patients expressed a sense that the air they breathed was harming them or was in some way responsible for the severity of their lung disease.
In this city, the legacy of the steel industry from the last century fostered economic prosperity but resulted in a profound legacy of pollution as well. Unfortunately, due to a combination of fossil fuel dependence for electricity generation and transportation, industrial particulate matter (PM) generation and greenhouse gas emissions, temperature inversions related to the topography of the region, and, most recently, smoke from Canadian wildfires in the summer of 2023, the air quality in Pittsburgh ranks among the 25 least healthy US cities. Our patients are bearing the burden of climate change.
I remember a patient in clinic talking about how on the days he could see a film of particulate on all the cars and the street outside, he knew he would feel more shortness of breath. Patients share about how when they had lived in different neighborhoods in town or traveled outside of Pittsburgh, their breathing improved.
Patients tell me that their asthma or COPD that did not use to cause them frequent trouble is now less well controlled despite better therapies available. Patients who used to experience seasonal allergies in just the fall or the spring now are plagued by their allergy symptoms year-round because of a warming climate yielding excess pollen throughout all seasons.
A recent study of patients with pulmonary fibrosis demonstrated that exposure to excess PM2.5 in this region resulted in more rapid clinical deterioration and premature death compared with patients with the same disease in other parts of North America with better air quality. The common denominator is human-generated climate change’s negative impact on health.
In particular, those who are already vulnerable because of underlying chronic disease or socioeconomic disparity are at greater risk and feel these repercussions disproportionately. Black and brown communities are more heavily exposed to air pollution due to the history of redlining and ongoing structural racism and, as a result, have worse health outcomes than other groups. There is an urgency and moral imperative for us as clinicians to address generations of environmental injustice.
While these themes floated around in the background during the early stage of my career as a pulmonologist, I didn’t have language or deep knowledge around these structural environmental issues. As a profession, we are gradually recognizing that the health impacts of climate change on which to advocate are within our wheelhouse as clinicians.
Our patients and our trainees are increasingly aware of these issues, and, as a result, we as currently practicing clinicians and educators must urgently learn about the lived experiences of our patients and how their diseases interplay with their exposures.
Nowadays, I think more about how to mitigate the impact of air pollution, which did not previously factor into my training or the early years of my clinical practice. We know that some patients, particularly those with underlying lung disease and young children, are at greater risk when exposed to more polluted air and may need to take different steps to limit their exposure. We now consider advising these patients with chronic respiratory disease to be aware of air quality advisories and limit their time outdoors on worse air quality days. We anticipate that when the air quality is worse, we will see more complications of cardiovascular and pulmonary disease.
As lifelong learners, we thirst for the latest data to incorporate into our clinical decision-making. Similarly, colleagues and I are now also voraciously reading and starting to have conversations with peers about the convergence of climate change and disease. But no matter how compelling and urgent these issues are, one clinician cannot tackle the massive threat of climate change and complexity of health care sustainability in isolation.
I am fortunate to work with several like-minded and highly motivated colleagues at my own institution. We have been able to organize effectively to spark local change toward reducing our system’s carbon emissions. Similarly, through professional organizations like CHEST, I have been able to collaborate with other pulmonary and critical care clinicians who share these passions and are doing similar advocacy work across the country. I am honored to serve as CHEST’s representative to the Medical Society Consortium on Climate and Health as another avenue to keep advancing this cause at scale in collaboration with advocates across all specialties.
While I worry every day for my patients, our communities, and my children as we face the accelerating threat of climate change, knowing that I am actively engaging in these efforts in pursuit of environmental justice and mitigating health care’s climate change contribution gives me a sense of empowerment and solidarity with others also striving to lessen our burden on the planet.
This article was adapted from the Winter 2024 online issue of CHEST Advocates. For the full article — and to engage with the other content from this issue — visit https://chestnet.org/chest-advocates.
Soon after moving to Pittsburgh for my pulmonary and critical care medicine fellowship in 2014, I began noticing a theme: So many of my patients expressed a sense that the air they breathed was harming them or was in some way responsible for the severity of their lung disease.
In this city, the legacy of the steel industry from the last century fostered economic prosperity but resulted in a profound legacy of pollution as well. Unfortunately, due to a combination of fossil fuel dependence for electricity generation and transportation, industrial particulate matter (PM) generation and greenhouse gas emissions, temperature inversions related to the topography of the region, and, most recently, smoke from Canadian wildfires in the summer of 2023, the air quality in Pittsburgh ranks among the 25 least healthy US cities. Our patients are bearing the burden of climate change.
I remember a patient in clinic talking about how on the days he could see a film of particulate on all the cars and the street outside, he knew he would feel more shortness of breath. Patients share about how when they had lived in different neighborhoods in town or traveled outside of Pittsburgh, their breathing improved.
Patients tell me that their asthma or COPD that did not use to cause them frequent trouble is now less well controlled despite better therapies available. Patients who used to experience seasonal allergies in just the fall or the spring now are plagued by their allergy symptoms year-round because of a warming climate yielding excess pollen throughout all seasons.
A recent study of patients with pulmonary fibrosis demonstrated that exposure to excess PM2.5 in this region resulted in more rapid clinical deterioration and premature death compared with patients with the same disease in other parts of North America with better air quality. The common denominator is human-generated climate change’s negative impact on health.
In particular, those who are already vulnerable because of underlying chronic disease or socioeconomic disparity are at greater risk and feel these repercussions disproportionately. Black and brown communities are more heavily exposed to air pollution due to the history of redlining and ongoing structural racism and, as a result, have worse health outcomes than other groups. There is an urgency and moral imperative for us as clinicians to address generations of environmental injustice.
While these themes floated around in the background during the early stage of my career as a pulmonologist, I didn’t have language or deep knowledge around these structural environmental issues. As a profession, we are gradually recognizing that the health impacts of climate change on which to advocate are within our wheelhouse as clinicians.
Our patients and our trainees are increasingly aware of these issues, and, as a result, we as currently practicing clinicians and educators must urgently learn about the lived experiences of our patients and how their diseases interplay with their exposures.
Nowadays, I think more about how to mitigate the impact of air pollution, which did not previously factor into my training or the early years of my clinical practice. We know that some patients, particularly those with underlying lung disease and young children, are at greater risk when exposed to more polluted air and may need to take different steps to limit their exposure. We now consider advising these patients with chronic respiratory disease to be aware of air quality advisories and limit their time outdoors on worse air quality days. We anticipate that when the air quality is worse, we will see more complications of cardiovascular and pulmonary disease.
As lifelong learners, we thirst for the latest data to incorporate into our clinical decision-making. Similarly, colleagues and I are now also voraciously reading and starting to have conversations with peers about the convergence of climate change and disease. But no matter how compelling and urgent these issues are, one clinician cannot tackle the massive threat of climate change and complexity of health care sustainability in isolation.
I am fortunate to work with several like-minded and highly motivated colleagues at my own institution. We have been able to organize effectively to spark local change toward reducing our system’s carbon emissions. Similarly, through professional organizations like CHEST, I have been able to collaborate with other pulmonary and critical care clinicians who share these passions and are doing similar advocacy work across the country. I am honored to serve as CHEST’s representative to the Medical Society Consortium on Climate and Health as another avenue to keep advancing this cause at scale in collaboration with advocates across all specialties.
While I worry every day for my patients, our communities, and my children as we face the accelerating threat of climate change, knowing that I am actively engaging in these efforts in pursuit of environmental justice and mitigating health care’s climate change contribution gives me a sense of empowerment and solidarity with others also striving to lessen our burden on the planet.
This article was adapted from the Winter 2024 online issue of CHEST Advocates. For the full article — and to engage with the other content from this issue — visit https://chestnet.org/chest-advocates.
CHEST grant recipient studying increase in lung cancer diagnoses among Chinese American women
In his prior research, Chien-Ching Li, PhD, MPH, focused on promoting lung cancer screening in Chinese American men, a population that frequently smokes heavily. But last year, he applied for a CHEST grant that’s shifting his focus to another demographic: Chinese American women who do not smoke, especially those with limited English proficiency.
“They are developing lung cancer, and we don’t know why,” said Dr. Li, an associate professor of Health Systems Management at Rush University.
In fact, 57% of Asian American women diagnosed with lung cancer never smoked cigarettes.
What’s behind this rise in lung cancer in women who have never smoked compared with men, and particularly in Asian American women? One possibility: While Chinese American women may never smoke themselves, they frequently live with partners or family members who do. (About 28% of Chinese American men smoke heavily, Dr. Li said.)
“We think secondhand smoke might be one of the key risk factors, because they’re living with people who smoke,” Dr. Li said. His prior research shows that the majority of Chinese American men in greater Chicagoland—89%—are married, and many of them smoke or have a history of smoking.
With the CHEST grant Dr. Li received in October 2023, he’s working to increase awareness among Chinese American women about the risks of secondhand smoke and “reduce the health disparity in lung cancer among women,” Dr. Li said.
Developing culturally sensitive materials for a high-risk group
While many lung cancer reduction efforts focus on people who smoke, there are plenty of pamphlets designed to inform about the risks incurred when breathing in secondhand smoke.
These handouts, however, aren’t always available in languages spoken by Chinese Americans. Nor is it as simple as hiring a translator; doing so may make the pamphlets readable to the women, but it won’t necessarily make the text culturally appropriate.
This is what Dr. Li—along with his coinvestigators, Alicia Matthews, PhD, a professor of clinical psychology at Columbia University, and Hong Liu, PhD, of the Midwest Asian Health Association—seeks to change, with funding from the CHEST grant. Their goal is four-pronged:
1. Discovery: Dr. Li and his team are currently surveying Chinese American women who have never smoked but who live with people who smoke in greater Chicagoland. These surveys will help them learn more about what (if anything) this group knows about the health risks associated with secondhand smoke and other types of environmental smoke.
2. Identify: These surveys, along with focus group interviews with select participants, will help reveal barriers standing in the way of reducing the women’s exposure to secondhand smoke—as well as ways to encourage habits to reduce risk.
3. Develop: All the information gained through surveys and conversations will then be analyzed and used to craft targeted, translated, and culturally appropriate materials on secondhand smoke, conveying communication strategies the women can use to persuade their partners to quit smoking and ways to build a smoke-free household.
4. Evaluate: The effectiveness of the new materials will be tested to assess the change in the women’s knowledge, as well as any uptick in taking steps to reduce exposure or sign up for screening.
Using the CHEST grant as a building block to more grants—and more information
Dr. Li and his collaborators are still in the early stages of using the CHEST grant: gathering up participants and surveying them.
But there’s much ahead. With the CHEST grant in hand, Dr. Li plans to apply for grants from the National Institutes of Health (NIH): first, an NIH Exploratory/Developmental Research Grant Award (R21) to help achieve that fourth aim of evaluating how the intervention works. And next, they’ll apply for an NIH Research Project Grant Program (R01), which will fund an even larger trial.
“Not many studies focus on identifying the risk factors with lung cancer associated with Chinese American [women who have never smoked],” Dr. Li said. “This is why we want to focus on this area to provide more knowledge and make more contributions to research.”
Projects like this are made possible by generous contributions from CHEST donors. Support the future of chest medicine by visiting https://chestnet.org/donate.
In his prior research, Chien-Ching Li, PhD, MPH, focused on promoting lung cancer screening in Chinese American men, a population that frequently smokes heavily. But last year, he applied for a CHEST grant that’s shifting his focus to another demographic: Chinese American women who do not smoke, especially those with limited English proficiency.
“They are developing lung cancer, and we don’t know why,” said Dr. Li, an associate professor of Health Systems Management at Rush University.
In fact, 57% of Asian American women diagnosed with lung cancer never smoked cigarettes.
What’s behind this rise in lung cancer in women who have never smoked compared with men, and particularly in Asian American women? One possibility: While Chinese American women may never smoke themselves, they frequently live with partners or family members who do. (About 28% of Chinese American men smoke heavily, Dr. Li said.)
“We think secondhand smoke might be one of the key risk factors, because they’re living with people who smoke,” Dr. Li said. His prior research shows that the majority of Chinese American men in greater Chicagoland—89%—are married, and many of them smoke or have a history of smoking.
With the CHEST grant Dr. Li received in October 2023, he’s working to increase awareness among Chinese American women about the risks of secondhand smoke and “reduce the health disparity in lung cancer among women,” Dr. Li said.
Developing culturally sensitive materials for a high-risk group
While many lung cancer reduction efforts focus on people who smoke, there are plenty of pamphlets designed to inform about the risks incurred when breathing in secondhand smoke.
These handouts, however, aren’t always available in languages spoken by Chinese Americans. Nor is it as simple as hiring a translator; doing so may make the pamphlets readable to the women, but it won’t necessarily make the text culturally appropriate.
This is what Dr. Li—along with his coinvestigators, Alicia Matthews, PhD, a professor of clinical psychology at Columbia University, and Hong Liu, PhD, of the Midwest Asian Health Association—seeks to change, with funding from the CHEST grant. Their goal is four-pronged:
1. Discovery: Dr. Li and his team are currently surveying Chinese American women who have never smoked but who live with people who smoke in greater Chicagoland. These surveys will help them learn more about what (if anything) this group knows about the health risks associated with secondhand smoke and other types of environmental smoke.
2. Identify: These surveys, along with focus group interviews with select participants, will help reveal barriers standing in the way of reducing the women’s exposure to secondhand smoke—as well as ways to encourage habits to reduce risk.
3. Develop: All the information gained through surveys and conversations will then be analyzed and used to craft targeted, translated, and culturally appropriate materials on secondhand smoke, conveying communication strategies the women can use to persuade their partners to quit smoking and ways to build a smoke-free household.
4. Evaluate: The effectiveness of the new materials will be tested to assess the change in the women’s knowledge, as well as any uptick in taking steps to reduce exposure or sign up for screening.
Using the CHEST grant as a building block to more grants—and more information
Dr. Li and his collaborators are still in the early stages of using the CHEST grant: gathering up participants and surveying them.
But there’s much ahead. With the CHEST grant in hand, Dr. Li plans to apply for grants from the National Institutes of Health (NIH): first, an NIH Exploratory/Developmental Research Grant Award (R21) to help achieve that fourth aim of evaluating how the intervention works. And next, they’ll apply for an NIH Research Project Grant Program (R01), which will fund an even larger trial.
“Not many studies focus on identifying the risk factors with lung cancer associated with Chinese American [women who have never smoked],” Dr. Li said. “This is why we want to focus on this area to provide more knowledge and make more contributions to research.”
Projects like this are made possible by generous contributions from CHEST donors. Support the future of chest medicine by visiting https://chestnet.org/donate.
In his prior research, Chien-Ching Li, PhD, MPH, focused on promoting lung cancer screening in Chinese American men, a population that frequently smokes heavily. But last year, he applied for a CHEST grant that’s shifting his focus to another demographic: Chinese American women who do not smoke, especially those with limited English proficiency.
“They are developing lung cancer, and we don’t know why,” said Dr. Li, an associate professor of Health Systems Management at Rush University.
In fact, 57% of Asian American women diagnosed with lung cancer never smoked cigarettes.
What’s behind this rise in lung cancer in women who have never smoked compared with men, and particularly in Asian American women? One possibility: While Chinese American women may never smoke themselves, they frequently live with partners or family members who do. (About 28% of Chinese American men smoke heavily, Dr. Li said.)
“We think secondhand smoke might be one of the key risk factors, because they’re living with people who smoke,” Dr. Li said. His prior research shows that the majority of Chinese American men in greater Chicagoland—89%—are married, and many of them smoke or have a history of smoking.
With the CHEST grant Dr. Li received in October 2023, he’s working to increase awareness among Chinese American women about the risks of secondhand smoke and “reduce the health disparity in lung cancer among women,” Dr. Li said.
Developing culturally sensitive materials for a high-risk group
While many lung cancer reduction efforts focus on people who smoke, there are plenty of pamphlets designed to inform about the risks incurred when breathing in secondhand smoke.
These handouts, however, aren’t always available in languages spoken by Chinese Americans. Nor is it as simple as hiring a translator; doing so may make the pamphlets readable to the women, but it won’t necessarily make the text culturally appropriate.
This is what Dr. Li—along with his coinvestigators, Alicia Matthews, PhD, a professor of clinical psychology at Columbia University, and Hong Liu, PhD, of the Midwest Asian Health Association—seeks to change, with funding from the CHEST grant. Their goal is four-pronged:
1. Discovery: Dr. Li and his team are currently surveying Chinese American women who have never smoked but who live with people who smoke in greater Chicagoland. These surveys will help them learn more about what (if anything) this group knows about the health risks associated with secondhand smoke and other types of environmental smoke.
2. Identify: These surveys, along with focus group interviews with select participants, will help reveal barriers standing in the way of reducing the women’s exposure to secondhand smoke—as well as ways to encourage habits to reduce risk.
3. Develop: All the information gained through surveys and conversations will then be analyzed and used to craft targeted, translated, and culturally appropriate materials on secondhand smoke, conveying communication strategies the women can use to persuade their partners to quit smoking and ways to build a smoke-free household.
4. Evaluate: The effectiveness of the new materials will be tested to assess the change in the women’s knowledge, as well as any uptick in taking steps to reduce exposure or sign up for screening.
Using the CHEST grant as a building block to more grants—and more information
Dr. Li and his collaborators are still in the early stages of using the CHEST grant: gathering up participants and surveying them.
But there’s much ahead. With the CHEST grant in hand, Dr. Li plans to apply for grants from the National Institutes of Health (NIH): first, an NIH Exploratory/Developmental Research Grant Award (R21) to help achieve that fourth aim of evaluating how the intervention works. And next, they’ll apply for an NIH Research Project Grant Program (R01), which will fund an even larger trial.
“Not many studies focus on identifying the risk factors with lung cancer associated with Chinese American [women who have never smoked],” Dr. Li said. “This is why we want to focus on this area to provide more knowledge and make more contributions to research.”
Projects like this are made possible by generous contributions from CHEST donors. Support the future of chest medicine by visiting https://chestnet.org/donate.
Find your community with CHEST Interest Groups
Learn about the LGBTQ+ at CHEST, Respiratory Care, and Women in Chest Medicine Interest Groups
, we were proud to add Interest Groups to our member offerings in 2023.
The introduction of Interest Groups has proven to be an effective way to organically connect CHEST members with shared interests and passions. Membership in one of these groups allows for networking in a smaller setting, with the goals of supporting career development and enriching an individual’s professional path.
To learn more about the three existing Interest Groups, we spoke with each group’s chair: Margaret Pisani, MD, FCCP, Chair of the Women in Chest Medicine Interest Group; Kevin O’Neil, MD, FCCP, Chair of the Respiratory Care Interest Group; and Mauricio Danckers, MD, FCCP, Chair of the LGBTQ+ at CHEST Interest Group.
1) Tell us about the key issues that your Interest Group is trying to address and who should join this group.
Mauricio Danckers: Our LGBTQ+ community continues to be the target of unrelenting discrimination. Current disparities toward sexual and gender-diverse individuals persistently hinder their personal and professional growth. There are several key issues currently affecting the LGBTQ+ community; among those are ongoing health care disparities, lack of education of our providers on LGBTQ+ health issues, underrepresentation of scientific research in the LGBTQ+ community, and scarce opportunities for mentorship and networking among LGBTQ+ health professionals. Our Interest Group seeks to provide a space to work together to overcome these shortcomings. Through the exchange of ideas, the opportunity for interprofessional collaborations, resource development and dissemination, scholar productivity, organic mentoring, and patient and provider advocacy, we seek to create change and better serve the LGBTQ+ identity in our CHEST community.
Anyone who is ready to make a change for the LGBTQ+ community, their care, and their well-being is encouraged to join. Self-identification as a member of the LGBTQ+ community is not a prerequisite for joining our group. We welcome individuals committed to advancing gender-affirming health, wellness, and education approaches to reduce health disparities.
Kevin O’Neil: The Respiratory Care Interest Group is invested in a number of focus areas, including improving collaboration between pulmonary/critical care/sleep physicians and respiratory care providers with a goal of improved and more efficient patient care, addressing critical shortages in the respiratory therapist (RT) workforce in collaboration with respiratory care organizations by identifying and supporting strategies to grow the workforce, and promoting wellness in all members of the community by providing tools and resources to mitigate stress and reduce burnout.
This Interest Group is for any CHEST member with an interest in respiratory care education or care delivery.
Margaret Pisani: The Women in Chest Medicine Interest Group has two overarching goals. The first is focused on ensuring that content around sex as a biologic variable and the impact of gender—as they relate to lung disease and critical care—are addressed in the educational activities of CHEST. The second is to provide mentorship and aid with career advancement for women in pulmonary, critical care, and sleep medicine (PCCSM) who are members of CHEST.
Anyone who does research on the impact of sex and gender as biologic variables—and the importance of these variables in lung disease—is welcome in this Interest Group. Persons who would like to be involved in mentoring the next generation of women and junior members who would like to learn more about how to be active at CHEST are also encouraged to join.
2) What motivated you to lead an Interest Group?
Danckers: My path in medicine as an LGBTQ+ individual has been unique and personal. It has opened the opportunity to witness the urgency of the changes needed to serve our LGBTQ+ community better. I wanted to lead this Interest Group to connect to other members interested in advancing health care equity for LGBTQ+ individuals, to inspire one another to achieve major changes in LGBTQ+ health education, and to ignite an educational and social initiative supported by CHEST to witness the LGBTQ+ medical community thriving while grounded on mentoring and advocacy.
O’Neil: I’ve been a CHEST member for more than 35 years and involved with respiratory care almost as long. The relationship between pulmonary/critical care physicians and RTs is unique, and RTs are critically important to my ability to care for my patients. I am committed to facilitating opportunities for collaboration between the two groups.
Pisani: I am motivated by my passion to ensure we are providing the best possible education to our members and patients and supporting the next generation of leaders in the PCCSM community.
3) What are the goals for your Interest Group in 2024?
Danckers: 2024 will be an exciting year, no doubt about it! Our goals for 2024 are: 1) to connect talented individuals with professional goals that align with the ones from the Interest Group and CHEST, 2) to increase the presence of the LGBTQ+ identity representation in our CHEST scientific meetings and educational offerings, 3) to build a resource platform for LGBTQ+ health education with the innovative approach CHEST is known to provide, and 4) to provide venues to inspire and support scholarly work within the LGBTQ+ community.
O’Neil: Growing the Interest Group membership and increasing opportunities for RTs to participate in CHEST activities by providing a landing space for new RT members are key initiatives for us. We are also hoping to increase the visibility of the Interest Group through events at the annual meeting, educational offerings, and other opportunities as they arise. We will also focus on improving communication between CHEST and other respiratory organizations.
Pisani: We are focused on ensuring that sex and gender topics are addressed during scientific presentations when relevant to research and patient care and developing resources on specific topics where there is data regarding the impact of sex and gender in lung disease.
To learn more about Interest Groups and how to join, go to chestnet.org/interest-groups.
Learn about the LGBTQ+ at CHEST, Respiratory Care, and Women in Chest Medicine Interest Groups
Learn about the LGBTQ+ at CHEST, Respiratory Care, and Women in Chest Medicine Interest Groups
, we were proud to add Interest Groups to our member offerings in 2023.
The introduction of Interest Groups has proven to be an effective way to organically connect CHEST members with shared interests and passions. Membership in one of these groups allows for networking in a smaller setting, with the goals of supporting career development and enriching an individual’s professional path.
To learn more about the three existing Interest Groups, we spoke with each group’s chair: Margaret Pisani, MD, FCCP, Chair of the Women in Chest Medicine Interest Group; Kevin O’Neil, MD, FCCP, Chair of the Respiratory Care Interest Group; and Mauricio Danckers, MD, FCCP, Chair of the LGBTQ+ at CHEST Interest Group.
1) Tell us about the key issues that your Interest Group is trying to address and who should join this group.
Mauricio Danckers: Our LGBTQ+ community continues to be the target of unrelenting discrimination. Current disparities toward sexual and gender-diverse individuals persistently hinder their personal and professional growth. There are several key issues currently affecting the LGBTQ+ community; among those are ongoing health care disparities, lack of education of our providers on LGBTQ+ health issues, underrepresentation of scientific research in the LGBTQ+ community, and scarce opportunities for mentorship and networking among LGBTQ+ health professionals. Our Interest Group seeks to provide a space to work together to overcome these shortcomings. Through the exchange of ideas, the opportunity for interprofessional collaborations, resource development and dissemination, scholar productivity, organic mentoring, and patient and provider advocacy, we seek to create change and better serve the LGBTQ+ identity in our CHEST community.
Anyone who is ready to make a change for the LGBTQ+ community, their care, and their well-being is encouraged to join. Self-identification as a member of the LGBTQ+ community is not a prerequisite for joining our group. We welcome individuals committed to advancing gender-affirming health, wellness, and education approaches to reduce health disparities.
Kevin O’Neil: The Respiratory Care Interest Group is invested in a number of focus areas, including improving collaboration between pulmonary/critical care/sleep physicians and respiratory care providers with a goal of improved and more efficient patient care, addressing critical shortages in the respiratory therapist (RT) workforce in collaboration with respiratory care organizations by identifying and supporting strategies to grow the workforce, and promoting wellness in all members of the community by providing tools and resources to mitigate stress and reduce burnout.
This Interest Group is for any CHEST member with an interest in respiratory care education or care delivery.
Margaret Pisani: The Women in Chest Medicine Interest Group has two overarching goals. The first is focused on ensuring that content around sex as a biologic variable and the impact of gender—as they relate to lung disease and critical care—are addressed in the educational activities of CHEST. The second is to provide mentorship and aid with career advancement for women in pulmonary, critical care, and sleep medicine (PCCSM) who are members of CHEST.
Anyone who does research on the impact of sex and gender as biologic variables—and the importance of these variables in lung disease—is welcome in this Interest Group. Persons who would like to be involved in mentoring the next generation of women and junior members who would like to learn more about how to be active at CHEST are also encouraged to join.
2) What motivated you to lead an Interest Group?
Danckers: My path in medicine as an LGBTQ+ individual has been unique and personal. It has opened the opportunity to witness the urgency of the changes needed to serve our LGBTQ+ community better. I wanted to lead this Interest Group to connect to other members interested in advancing health care equity for LGBTQ+ individuals, to inspire one another to achieve major changes in LGBTQ+ health education, and to ignite an educational and social initiative supported by CHEST to witness the LGBTQ+ medical community thriving while grounded on mentoring and advocacy.
O’Neil: I’ve been a CHEST member for more than 35 years and involved with respiratory care almost as long. The relationship between pulmonary/critical care physicians and RTs is unique, and RTs are critically important to my ability to care for my patients. I am committed to facilitating opportunities for collaboration between the two groups.
Pisani: I am motivated by my passion to ensure we are providing the best possible education to our members and patients and supporting the next generation of leaders in the PCCSM community.
3) What are the goals for your Interest Group in 2024?
Danckers: 2024 will be an exciting year, no doubt about it! Our goals for 2024 are: 1) to connect talented individuals with professional goals that align with the ones from the Interest Group and CHEST, 2) to increase the presence of the LGBTQ+ identity representation in our CHEST scientific meetings and educational offerings, 3) to build a resource platform for LGBTQ+ health education with the innovative approach CHEST is known to provide, and 4) to provide venues to inspire and support scholarly work within the LGBTQ+ community.
O’Neil: Growing the Interest Group membership and increasing opportunities for RTs to participate in CHEST activities by providing a landing space for new RT members are key initiatives for us. We are also hoping to increase the visibility of the Interest Group through events at the annual meeting, educational offerings, and other opportunities as they arise. We will also focus on improving communication between CHEST and other respiratory organizations.
Pisani: We are focused on ensuring that sex and gender topics are addressed during scientific presentations when relevant to research and patient care and developing resources on specific topics where there is data regarding the impact of sex and gender in lung disease.
To learn more about Interest Groups and how to join, go to chestnet.org/interest-groups.
, we were proud to add Interest Groups to our member offerings in 2023.
The introduction of Interest Groups has proven to be an effective way to organically connect CHEST members with shared interests and passions. Membership in one of these groups allows for networking in a smaller setting, with the goals of supporting career development and enriching an individual’s professional path.
To learn more about the three existing Interest Groups, we spoke with each group’s chair: Margaret Pisani, MD, FCCP, Chair of the Women in Chest Medicine Interest Group; Kevin O’Neil, MD, FCCP, Chair of the Respiratory Care Interest Group; and Mauricio Danckers, MD, FCCP, Chair of the LGBTQ+ at CHEST Interest Group.
1) Tell us about the key issues that your Interest Group is trying to address and who should join this group.
Mauricio Danckers: Our LGBTQ+ community continues to be the target of unrelenting discrimination. Current disparities toward sexual and gender-diverse individuals persistently hinder their personal and professional growth. There are several key issues currently affecting the LGBTQ+ community; among those are ongoing health care disparities, lack of education of our providers on LGBTQ+ health issues, underrepresentation of scientific research in the LGBTQ+ community, and scarce opportunities for mentorship and networking among LGBTQ+ health professionals. Our Interest Group seeks to provide a space to work together to overcome these shortcomings. Through the exchange of ideas, the opportunity for interprofessional collaborations, resource development and dissemination, scholar productivity, organic mentoring, and patient and provider advocacy, we seek to create change and better serve the LGBTQ+ identity in our CHEST community.
Anyone who is ready to make a change for the LGBTQ+ community, their care, and their well-being is encouraged to join. Self-identification as a member of the LGBTQ+ community is not a prerequisite for joining our group. We welcome individuals committed to advancing gender-affirming health, wellness, and education approaches to reduce health disparities.
Kevin O’Neil: The Respiratory Care Interest Group is invested in a number of focus areas, including improving collaboration between pulmonary/critical care/sleep physicians and respiratory care providers with a goal of improved and more efficient patient care, addressing critical shortages in the respiratory therapist (RT) workforce in collaboration with respiratory care organizations by identifying and supporting strategies to grow the workforce, and promoting wellness in all members of the community by providing tools and resources to mitigate stress and reduce burnout.
This Interest Group is for any CHEST member with an interest in respiratory care education or care delivery.
Margaret Pisani: The Women in Chest Medicine Interest Group has two overarching goals. The first is focused on ensuring that content around sex as a biologic variable and the impact of gender—as they relate to lung disease and critical care—are addressed in the educational activities of CHEST. The second is to provide mentorship and aid with career advancement for women in pulmonary, critical care, and sleep medicine (PCCSM) who are members of CHEST.
Anyone who does research on the impact of sex and gender as biologic variables—and the importance of these variables in lung disease—is welcome in this Interest Group. Persons who would like to be involved in mentoring the next generation of women and junior members who would like to learn more about how to be active at CHEST are also encouraged to join.
2) What motivated you to lead an Interest Group?
Danckers: My path in medicine as an LGBTQ+ individual has been unique and personal. It has opened the opportunity to witness the urgency of the changes needed to serve our LGBTQ+ community better. I wanted to lead this Interest Group to connect to other members interested in advancing health care equity for LGBTQ+ individuals, to inspire one another to achieve major changes in LGBTQ+ health education, and to ignite an educational and social initiative supported by CHEST to witness the LGBTQ+ medical community thriving while grounded on mentoring and advocacy.
O’Neil: I’ve been a CHEST member for more than 35 years and involved with respiratory care almost as long. The relationship between pulmonary/critical care physicians and RTs is unique, and RTs are critically important to my ability to care for my patients. I am committed to facilitating opportunities for collaboration between the two groups.
Pisani: I am motivated by my passion to ensure we are providing the best possible education to our members and patients and supporting the next generation of leaders in the PCCSM community.
3) What are the goals for your Interest Group in 2024?
Danckers: 2024 will be an exciting year, no doubt about it! Our goals for 2024 are: 1) to connect talented individuals with professional goals that align with the ones from the Interest Group and CHEST, 2) to increase the presence of the LGBTQ+ identity representation in our CHEST scientific meetings and educational offerings, 3) to build a resource platform for LGBTQ+ health education with the innovative approach CHEST is known to provide, and 4) to provide venues to inspire and support scholarly work within the LGBTQ+ community.
O’Neil: Growing the Interest Group membership and increasing opportunities for RTs to participate in CHEST activities by providing a landing space for new RT members are key initiatives for us. We are also hoping to increase the visibility of the Interest Group through events at the annual meeting, educational offerings, and other opportunities as they arise. We will also focus on improving communication between CHEST and other respiratory organizations.
Pisani: We are focused on ensuring that sex and gender topics are addressed during scientific presentations when relevant to research and patient care and developing resources on specific topics where there is data regarding the impact of sex and gender in lung disease.
To learn more about Interest Groups and how to join, go to chestnet.org/interest-groups.
Leading with integrity: A values-driven year
As the President of the American College of Chest Physicians (CHEST), I have the privilege of regularly addressing CHEST members through a quarterly column where I can share updates and expand on topics that we hold in high regard.
As such, I’d like to focus on the CHEST commitment to social responsibility and the work we have done and will continue to do throughout this year and beyond.
In 2023, under the leadership of my predecessor, Doreen Addrizzo-Harris, MD, FCCP, CHEST made strong changes to our organizational focus, including cementing Social Responsibility as a formal pillar of CHEST. In addition to our other four pillars—Education, People, Products, and Growth—this new pillar is a sign of our stronger commitment to be more explicit in our aspirations, measure our success, and move the bar higher.
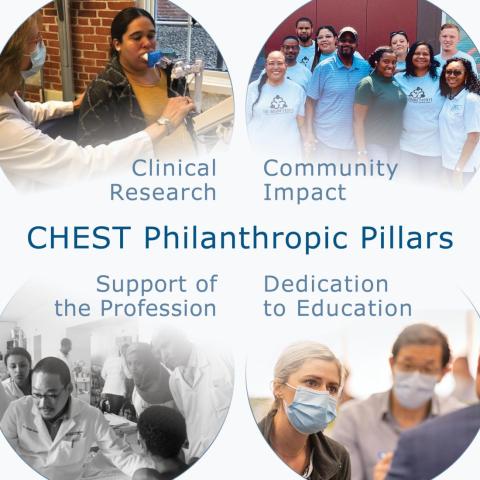
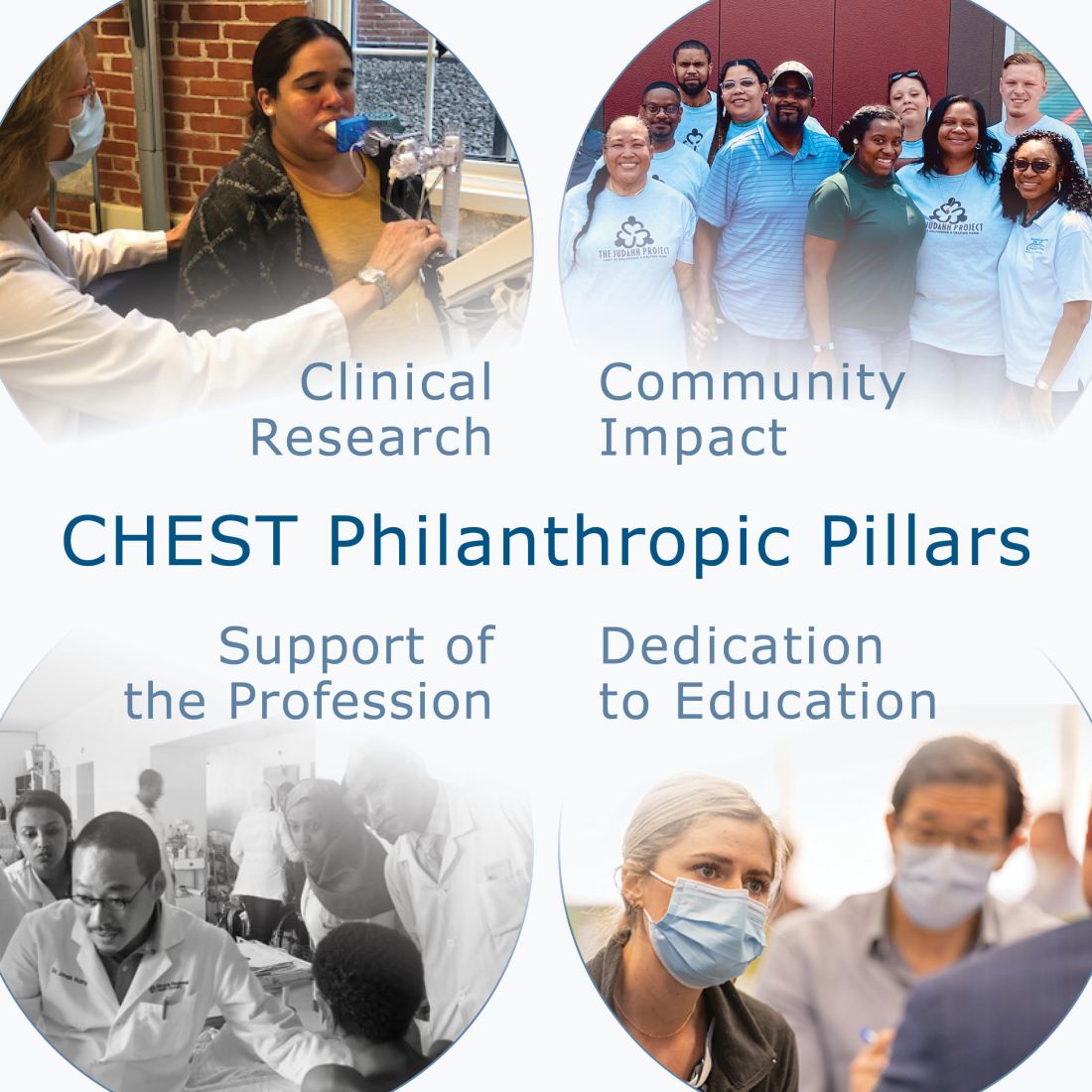
As part of the new social responsibility pillar, CHEST philanthropy evolved from what was known as the CHEST Foundation and defined a new giving strategy that reflects our organizational commitment to clinical research, community impact, support for the profession, and fostering education. Through growth in our research support and furthering community impact, 2024 will be a strong year of providing grant support aligned to this new giving strategy.
In addition, we formalized how CHEST will pursue our new social responsibility pillar. In 2023, we articulated our organizational values—Community, Inclusivity, Innovation, Advocacy, and Integrity—which will serve as a consistent reminder of who we are as an organization and guide us in decisions as we pursue our mission.
Led by these values, CHEST will use its voice and capabilities to promote change that equitably impacts our community. In 2024 specifically, the organization looks forward to engaging actively with social responsibility by expanding volunteer opportunities local to CHEST headquarters and in conjunction with the location of the annual meeting.
It is also my hope that 2024 will be known as a year of member input, starring feedback from none other than you, our members.
For those who recall my address from the Opening Session at CHEST 2023, I very much encourage you to reach out to share with me your thoughts, your CHEST experience, and more at president@chestnet.org. I look forward to having this regular touchpoint with all of you, and I welcome your input on topics you’d like to hear more on.
Until next time,
Jack D. Buckley, MD, MPH, FCCP
As the President of the American College of Chest Physicians (CHEST), I have the privilege of regularly addressing CHEST members through a quarterly column where I can share updates and expand on topics that we hold in high regard.
As such, I’d like to focus on the CHEST commitment to social responsibility and the work we have done and will continue to do throughout this year and beyond.
In 2023, under the leadership of my predecessor, Doreen Addrizzo-Harris, MD, FCCP, CHEST made strong changes to our organizational focus, including cementing Social Responsibility as a formal pillar of CHEST. In addition to our other four pillars—Education, People, Products, and Growth—this new pillar is a sign of our stronger commitment to be more explicit in our aspirations, measure our success, and move the bar higher.
As part of the new social responsibility pillar, CHEST philanthropy evolved from what was known as the CHEST Foundation and defined a new giving strategy that reflects our organizational commitment to clinical research, community impact, support for the profession, and fostering education. Through growth in our research support and furthering community impact, 2024 will be a strong year of providing grant support aligned to this new giving strategy.
In addition, we formalized how CHEST will pursue our new social responsibility pillar. In 2023, we articulated our organizational values—Community, Inclusivity, Innovation, Advocacy, and Integrity—which will serve as a consistent reminder of who we are as an organization and guide us in decisions as we pursue our mission.
Led by these values, CHEST will use its voice and capabilities to promote change that equitably impacts our community. In 2024 specifically, the organization looks forward to engaging actively with social responsibility by expanding volunteer opportunities local to CHEST headquarters and in conjunction with the location of the annual meeting.
It is also my hope that 2024 will be known as a year of member input, starring feedback from none other than you, our members.
For those who recall my address from the Opening Session at CHEST 2023, I very much encourage you to reach out to share with me your thoughts, your CHEST experience, and more at president@chestnet.org. I look forward to having this regular touchpoint with all of you, and I welcome your input on topics you’d like to hear more on.
Until next time,
Jack D. Buckley, MD, MPH, FCCP
As the President of the American College of Chest Physicians (CHEST), I have the privilege of regularly addressing CHEST members through a quarterly column where I can share updates and expand on topics that we hold in high regard.
As such, I’d like to focus on the CHEST commitment to social responsibility and the work we have done and will continue to do throughout this year and beyond.
In 2023, under the leadership of my predecessor, Doreen Addrizzo-Harris, MD, FCCP, CHEST made strong changes to our organizational focus, including cementing Social Responsibility as a formal pillar of CHEST. In addition to our other four pillars—Education, People, Products, and Growth—this new pillar is a sign of our stronger commitment to be more explicit in our aspirations, measure our success, and move the bar higher.
As part of the new social responsibility pillar, CHEST philanthropy evolved from what was known as the CHEST Foundation and defined a new giving strategy that reflects our organizational commitment to clinical research, community impact, support for the profession, and fostering education. Through growth in our research support and furthering community impact, 2024 will be a strong year of providing grant support aligned to this new giving strategy.
In addition, we formalized how CHEST will pursue our new social responsibility pillar. In 2023, we articulated our organizational values—Community, Inclusivity, Innovation, Advocacy, and Integrity—which will serve as a consistent reminder of who we are as an organization and guide us in decisions as we pursue our mission.
Led by these values, CHEST will use its voice and capabilities to promote change that equitably impacts our community. In 2024 specifically, the organization looks forward to engaging actively with social responsibility by expanding volunteer opportunities local to CHEST headquarters and in conjunction with the location of the annual meeting.
It is also my hope that 2024 will be known as a year of member input, starring feedback from none other than you, our members.
For those who recall my address from the Opening Session at CHEST 2023, I very much encourage you to reach out to share with me your thoughts, your CHEST experience, and more at president@chestnet.org. I look forward to having this regular touchpoint with all of you, and I welcome your input on topics you’d like to hear more on.
Until next time,
Jack D. Buckley, MD, MPH, FCCP
New age of CHEST philanthropy to focus on education, impact, community
In a time echoing with the constant call for transformation, CHEST delved deep into its essence, questioning its potential for impact. This pivotal introspection led to a crucial inquiry…
Are we harnessing every opportunity to make a difference?
It’s a familiar question, yet its resonance urged a deeper evaluation.
Philanthropy has long been entwined in CHEST’s identity. Commemorating 25 years of the CHEST Foundation at CHEST 2022 spotlighted our history of generosity. Stories of transformative community initiatives and pivotal clinical research grants narrated a tale of empowered change and fostering healthier communities worldwide.
However, amid these achievements, more pressing inquiries surfaced:
- What unique role can CHEST play?
- Where do unmet needs persist?
- Which causes deeply resonate within our community?
CHEST’s leadership and dedicated staff embarked on a comprehensive review, scrutinizing past triumphs, donor commitments, and the evolving aspirations of our members. Themes of social responsibility, professional diversity, community impact, and expanded partnerships emerged as pivotal points. This extensive process, spanning nearly a year, resembled a reflective pause amid the rapid cadence of change.
Achieving these aspirations meant reimagining our approach, thereby streamlining efforts for maximal impact by…
- Integrating philanthropy as an integral facet of our mission, and amplifying the culture of giving within CHEST
- Consolidating philanthropic initiatives under CHEST to maximize resources for direct, substantial impact
- Defining clear avenues for giving that deeply resonate with our members
With endorsement from the Board of Regents, the CHEST Foundation seamlessly merged into CHEST, inaugurating a new chapter in our philanthropic endeavors.
Central to this transformative shift is the crystallization of our giving strategy, fortified by four pillars: Clinical Research, Community Impact, Support to the Profession, and Dedication to Education. These pillars encapsulate our commitment to nurturing clinicians, supporting trainees, and enhancing patient care.
Clinical Research emerges as the cornerstone, transcending boundaries to empower researchers in their pursuit of groundbreaking insights. Through strategic grants, we embolden early career investigators to delve into uncharted territories, unraveling mysteries that underpin advancements in chest medicine. The ripple effect extends beyond labs; it traverses communities, amplifying equitable health care solutions and bridging disparities in patient care. Our commitment to nurturing this pillar springs from the belief that every breakthrough, regardless of scale, is a catalyst for transformative change.
Community Impact extends CHEST’s reach far beyond clinical settings, fostering alliances with local organizations. Together, we forge a tapestry of collaboration, weaving essential services and imparting knowledge on crucial lung health issues into the fabric of diverse communities. This engagement not only elevates awareness but also empowers individuals and communities to take charge of their respiratory well-being. It’s the grassroots unity that amplifies our impact, creating enduring shifts in local landscapes.
Support of the Profession epitomizes our dedication to fortifying the backbone of pulmonary, critical care, and sleep medicine. By offering unparalleled clinical education and mentorship, we empower emerging clinicians from diverse backgrounds with the latest knowledge and resources. Fueling their professional growth is pivotal to nurturing a robust and inclusive cadre of health care professionals, ensuring comprehensive and culturally sensitive care for patients worldwide.
Dedication to Education isn’t just a commitment—it’s a bridge spanning the gap between knowledge and application, patient and clinician. Strengthening this connection involves equipping clinicians with tools for effective communication and partnering with patient-centered organizations. Our focus transcends textbooks; it embodies a relentless pursuit to refine patient-clinician interactions, enhancing patient understanding and, ultimately, elevating their quality of life.
CHEST’s philanthropic evolution signifies not just growth but a resolute commitment to effecting tangible change in chest medicine and patient care. These pillars stand as guiding beacons, steering us toward a future that mirrors our mission, vision, and values. Each pillar represents a pathway to meaningful, enduring change within chest medicine, ensuring a lasting impact on patient well-being.
In a time echoing with the constant call for transformation, CHEST delved deep into its essence, questioning its potential for impact. This pivotal introspection led to a crucial inquiry…
Are we harnessing every opportunity to make a difference?
It’s a familiar question, yet its resonance urged a deeper evaluation.
Philanthropy has long been entwined in CHEST’s identity. Commemorating 25 years of the CHEST Foundation at CHEST 2022 spotlighted our history of generosity. Stories of transformative community initiatives and pivotal clinical research grants narrated a tale of empowered change and fostering healthier communities worldwide.
However, amid these achievements, more pressing inquiries surfaced:
- What unique role can CHEST play?
- Where do unmet needs persist?
- Which causes deeply resonate within our community?
CHEST’s leadership and dedicated staff embarked on a comprehensive review, scrutinizing past triumphs, donor commitments, and the evolving aspirations of our members. Themes of social responsibility, professional diversity, community impact, and expanded partnerships emerged as pivotal points. This extensive process, spanning nearly a year, resembled a reflective pause amid the rapid cadence of change.
Achieving these aspirations meant reimagining our approach, thereby streamlining efforts for maximal impact by…
- Integrating philanthropy as an integral facet of our mission, and amplifying the culture of giving within CHEST
- Consolidating philanthropic initiatives under CHEST to maximize resources for direct, substantial impact
- Defining clear avenues for giving that deeply resonate with our members
With endorsement from the Board of Regents, the CHEST Foundation seamlessly merged into CHEST, inaugurating a new chapter in our philanthropic endeavors.
Central to this transformative shift is the crystallization of our giving strategy, fortified by four pillars: Clinical Research, Community Impact, Support to the Profession, and Dedication to Education. These pillars encapsulate our commitment to nurturing clinicians, supporting trainees, and enhancing patient care.
Clinical Research emerges as the cornerstone, transcending boundaries to empower researchers in their pursuit of groundbreaking insights. Through strategic grants, we embolden early career investigators to delve into uncharted territories, unraveling mysteries that underpin advancements in chest medicine. The ripple effect extends beyond labs; it traverses communities, amplifying equitable health care solutions and bridging disparities in patient care. Our commitment to nurturing this pillar springs from the belief that every breakthrough, regardless of scale, is a catalyst for transformative change.
Community Impact extends CHEST’s reach far beyond clinical settings, fostering alliances with local organizations. Together, we forge a tapestry of collaboration, weaving essential services and imparting knowledge on crucial lung health issues into the fabric of diverse communities. This engagement not only elevates awareness but also empowers individuals and communities to take charge of their respiratory well-being. It’s the grassroots unity that amplifies our impact, creating enduring shifts in local landscapes.
Support of the Profession epitomizes our dedication to fortifying the backbone of pulmonary, critical care, and sleep medicine. By offering unparalleled clinical education and mentorship, we empower emerging clinicians from diverse backgrounds with the latest knowledge and resources. Fueling their professional growth is pivotal to nurturing a robust and inclusive cadre of health care professionals, ensuring comprehensive and culturally sensitive care for patients worldwide.
Dedication to Education isn’t just a commitment—it’s a bridge spanning the gap between knowledge and application, patient and clinician. Strengthening this connection involves equipping clinicians with tools for effective communication and partnering with patient-centered organizations. Our focus transcends textbooks; it embodies a relentless pursuit to refine patient-clinician interactions, enhancing patient understanding and, ultimately, elevating their quality of life.
CHEST’s philanthropic evolution signifies not just growth but a resolute commitment to effecting tangible change in chest medicine and patient care. These pillars stand as guiding beacons, steering us toward a future that mirrors our mission, vision, and values. Each pillar represents a pathway to meaningful, enduring change within chest medicine, ensuring a lasting impact on patient well-being.
In a time echoing with the constant call for transformation, CHEST delved deep into its essence, questioning its potential for impact. This pivotal introspection led to a crucial inquiry…
Are we harnessing every opportunity to make a difference?
It’s a familiar question, yet its resonance urged a deeper evaluation.
Philanthropy has long been entwined in CHEST’s identity. Commemorating 25 years of the CHEST Foundation at CHEST 2022 spotlighted our history of generosity. Stories of transformative community initiatives and pivotal clinical research grants narrated a tale of empowered change and fostering healthier communities worldwide.
However, amid these achievements, more pressing inquiries surfaced:
- What unique role can CHEST play?
- Where do unmet needs persist?
- Which causes deeply resonate within our community?
CHEST’s leadership and dedicated staff embarked on a comprehensive review, scrutinizing past triumphs, donor commitments, and the evolving aspirations of our members. Themes of social responsibility, professional diversity, community impact, and expanded partnerships emerged as pivotal points. This extensive process, spanning nearly a year, resembled a reflective pause amid the rapid cadence of change.
Achieving these aspirations meant reimagining our approach, thereby streamlining efforts for maximal impact by…
- Integrating philanthropy as an integral facet of our mission, and amplifying the culture of giving within CHEST
- Consolidating philanthropic initiatives under CHEST to maximize resources for direct, substantial impact
- Defining clear avenues for giving that deeply resonate with our members
With endorsement from the Board of Regents, the CHEST Foundation seamlessly merged into CHEST, inaugurating a new chapter in our philanthropic endeavors.
Central to this transformative shift is the crystallization of our giving strategy, fortified by four pillars: Clinical Research, Community Impact, Support to the Profession, and Dedication to Education. These pillars encapsulate our commitment to nurturing clinicians, supporting trainees, and enhancing patient care.
Clinical Research emerges as the cornerstone, transcending boundaries to empower researchers in their pursuit of groundbreaking insights. Through strategic grants, we embolden early career investigators to delve into uncharted territories, unraveling mysteries that underpin advancements in chest medicine. The ripple effect extends beyond labs; it traverses communities, amplifying equitable health care solutions and bridging disparities in patient care. Our commitment to nurturing this pillar springs from the belief that every breakthrough, regardless of scale, is a catalyst for transformative change.
Community Impact extends CHEST’s reach far beyond clinical settings, fostering alliances with local organizations. Together, we forge a tapestry of collaboration, weaving essential services and imparting knowledge on crucial lung health issues into the fabric of diverse communities. This engagement not only elevates awareness but also empowers individuals and communities to take charge of their respiratory well-being. It’s the grassroots unity that amplifies our impact, creating enduring shifts in local landscapes.
Support of the Profession epitomizes our dedication to fortifying the backbone of pulmonary, critical care, and sleep medicine. By offering unparalleled clinical education and mentorship, we empower emerging clinicians from diverse backgrounds with the latest knowledge and resources. Fueling their professional growth is pivotal to nurturing a robust and inclusive cadre of health care professionals, ensuring comprehensive and culturally sensitive care for patients worldwide.
Dedication to Education isn’t just a commitment—it’s a bridge spanning the gap between knowledge and application, patient and clinician. Strengthening this connection involves equipping clinicians with tools for effective communication and partnering with patient-centered organizations. Our focus transcends textbooks; it embodies a relentless pursuit to refine patient-clinician interactions, enhancing patient understanding and, ultimately, elevating their quality of life.
CHEST’s philanthropic evolution signifies not just growth but a resolute commitment to effecting tangible change in chest medicine and patient care. These pillars stand as guiding beacons, steering us toward a future that mirrors our mission, vision, and values. Each pillar represents a pathway to meaningful, enduring change within chest medicine, ensuring a lasting impact on patient well-being.
Biomarker checklist seeks to expedite NSCLC diagnoses
Drs. Tamer Said Ahmed and Adam Fox receive funding for quality improvement projects in biomarker testing
Establishing a systematic biomarker testing program for patients with suspected non-small cell lung cancer (NSCLC) takes both time and collaboration across specialties. To standardize this process, the American College of Chest Physicians (CHEST) created two clinician checklists for use in practice.
The case-by-case checklist helps guide physicians to ensure timely and comprehensive biomarker testing for individual patients, and the programmatic/institutional checklist is for multidisciplinary teams to enable clear expectations and processes across hand-offs to aid in the testing process.
To substantiate best practices for ordering biomarker tests using the checklists, CHEST issued quality improvement demonstration grants for implementation at two institutions. This year, Tamer Said Ahmed, MD, FCCP, pulmonary and sleep physician at Toledo Hospital (ProMedica Health System) and Assistant Professor at the University of Toledo, and Adam Fox, MD, MS, Assistant Professor of Medicine at the Medical University of South Carolina, will begin projects to improve biomarker testing.
“Biomarker testing allows for tailored treatment plans that drastically impact the progression of lung cancer, but every hospital system and practice is following a different procedure for testing,” Dr. Said Ahmed said. “To best serve the patient, our project aims to streamline the approach to biomarker testing to bridge health care inconsistencies. Given the intense progression of some forms of lung cancer where every week matters, the more streamlined we can make the biomarker testing process, the earlier we will get to an accurate diagnosis, begin treatment, and likely extend the life of a patient.”
Discrepancies in the testing process stem from existing silos between specialties, including pathology, oncology, interventional radiology, and more. Care is fragmented, leading to delays like repeat biopsies because a large enough sample was not taken the first time.
This is the exact problem that checklist implementation will seek to solve.
“By intent, these checklists help to provide a systematic approach to timely and comprehensive biomarker testing,” said Dr. Fox, who was also part of the team that developed the checklists. “What we need now is to implement them into clinical practice to gain metrics that can be studied, identified, and will lead to the process being widely accepted. To truly impact practice, we need to be able to provide strong evidence for interventions that work for clinicians to implement.”
To learn more and download the checklists, visit CHEST’s Thoracic Oncology Topic Collection onlineThis project is supported in part by AstraZeneca, Sanofi, and Pfizer.
Drs. Tamer Said Ahmed and Adam Fox receive funding for quality improvement projects in biomarker testing
Drs. Tamer Said Ahmed and Adam Fox receive funding for quality improvement projects in biomarker testing
Establishing a systematic biomarker testing program for patients with suspected non-small cell lung cancer (NSCLC) takes both time and collaboration across specialties. To standardize this process, the American College of Chest Physicians (CHEST) created two clinician checklists for use in practice.
The case-by-case checklist helps guide physicians to ensure timely and comprehensive biomarker testing for individual patients, and the programmatic/institutional checklist is for multidisciplinary teams to enable clear expectations and processes across hand-offs to aid in the testing process.
To substantiate best practices for ordering biomarker tests using the checklists, CHEST issued quality improvement demonstration grants for implementation at two institutions. This year, Tamer Said Ahmed, MD, FCCP, pulmonary and sleep physician at Toledo Hospital (ProMedica Health System) and Assistant Professor at the University of Toledo, and Adam Fox, MD, MS, Assistant Professor of Medicine at the Medical University of South Carolina, will begin projects to improve biomarker testing.
“Biomarker testing allows for tailored treatment plans that drastically impact the progression of lung cancer, but every hospital system and practice is following a different procedure for testing,” Dr. Said Ahmed said. “To best serve the patient, our project aims to streamline the approach to biomarker testing to bridge health care inconsistencies. Given the intense progression of some forms of lung cancer where every week matters, the more streamlined we can make the biomarker testing process, the earlier we will get to an accurate diagnosis, begin treatment, and likely extend the life of a patient.”
Discrepancies in the testing process stem from existing silos between specialties, including pathology, oncology, interventional radiology, and more. Care is fragmented, leading to delays like repeat biopsies because a large enough sample was not taken the first time.
This is the exact problem that checklist implementation will seek to solve.
“By intent, these checklists help to provide a systematic approach to timely and comprehensive biomarker testing,” said Dr. Fox, who was also part of the team that developed the checklists. “What we need now is to implement them into clinical practice to gain metrics that can be studied, identified, and will lead to the process being widely accepted. To truly impact practice, we need to be able to provide strong evidence for interventions that work for clinicians to implement.”
To learn more and download the checklists, visit CHEST’s Thoracic Oncology Topic Collection onlineThis project is supported in part by AstraZeneca, Sanofi, and Pfizer.
Establishing a systematic biomarker testing program for patients with suspected non-small cell lung cancer (NSCLC) takes both time and collaboration across specialties. To standardize this process, the American College of Chest Physicians (CHEST) created two clinician checklists for use in practice.
The case-by-case checklist helps guide physicians to ensure timely and comprehensive biomarker testing for individual patients, and the programmatic/institutional checklist is for multidisciplinary teams to enable clear expectations and processes across hand-offs to aid in the testing process.
To substantiate best practices for ordering biomarker tests using the checklists, CHEST issued quality improvement demonstration grants for implementation at two institutions. This year, Tamer Said Ahmed, MD, FCCP, pulmonary and sleep physician at Toledo Hospital (ProMedica Health System) and Assistant Professor at the University of Toledo, and Adam Fox, MD, MS, Assistant Professor of Medicine at the Medical University of South Carolina, will begin projects to improve biomarker testing.
“Biomarker testing allows for tailored treatment plans that drastically impact the progression of lung cancer, but every hospital system and practice is following a different procedure for testing,” Dr. Said Ahmed said. “To best serve the patient, our project aims to streamline the approach to biomarker testing to bridge health care inconsistencies. Given the intense progression of some forms of lung cancer where every week matters, the more streamlined we can make the biomarker testing process, the earlier we will get to an accurate diagnosis, begin treatment, and likely extend the life of a patient.”
Discrepancies in the testing process stem from existing silos between specialties, including pathology, oncology, interventional radiology, and more. Care is fragmented, leading to delays like repeat biopsies because a large enough sample was not taken the first time.
This is the exact problem that checklist implementation will seek to solve.
“By intent, these checklists help to provide a systematic approach to timely and comprehensive biomarker testing,” said Dr. Fox, who was also part of the team that developed the checklists. “What we need now is to implement them into clinical practice to gain metrics that can be studied, identified, and will lead to the process being widely accepted. To truly impact practice, we need to be able to provide strong evidence for interventions that work for clinicians to implement.”
To learn more and download the checklists, visit CHEST’s Thoracic Oncology Topic Collection onlineThis project is supported in part by AstraZeneca, Sanofi, and Pfizer.
CHEST grant winners to study health inequities related to air pollution, medication nonadherence, and more
In 2023, CHEST awarded $300,000 in clinical research and community impact grants to 15 individuals. Grant recipients are recognized for their scientifically meritorious achievements, with rigorous metrics to track their project’s progress, and have innovative, novel approaches to addressing their research topic.
CHEST grants have made a difference in patients’ lives by leading to breakthroughs in the treatment and/or management of chest diseases and patient care. This year’s grant-funded projects run the gamut of topics within chest medicine, ranging from lung cancer and COPD to tuberculosis and idiopathic pulmonary fibrosis.
Here’s a glimpse into two of this year’s grant winners and their projects.
For a full list of the 2023 grant winners, visit chestnet.org/grant-recipients.
Air pollution in sarcoidosis
This year, the John R. Addrizzo, MD, FCCP Research Grant in Sarcoidosis was awarded to Ali Mustafa, MD, of the Johns Hopkins Hospital in Baltimore, MD, for his project “Air Pollution in Sarcoidosis.”
The project’s aim is to investigate the feasibility of studying indoor and outdoor air pollution in patients with pulmonary sarcoidosis.
According to Dr. Mustafa’s application, pulmonary sarcoidosis is one of the most common interstitial lung diseases in the United States, and mortality due to sarcoidosis has risen by more than 3% in recent decades.
While the etiology of sarcoidosis remains elusive, evidence points toward a combination of genetic predisposition with external environmental triggers affecting disease onset. One small study of 16 individuals with fibrotic pulmonary sarcoidosis assessed the association between local levels of outdoor air pollutants to clinical outcomes. This study found that increased short-term exposure was associated with increased respiratory symptom severity and worse health-related quality of life.
Additionally, significant health disparities exist in sarcoidosis. Black individuals with sarcoidosis have worse pulmonary function, higher rates of multiorgan disease, and as much as a 12-fold increase in mortality compared with non-Hispanic White individuals with sarcoidosis. Socioeconomic status and Black race have also been associated with increased exposure to air pollution and closer proximity to high toxic emission facilities, suggesting higher exposure to outdoor air pollution.
Racial disparities are present and particularly important in sarcoidosis. Black individuals are more likely to have more advanced disease at diagnosis, have a six-fold increase in hospitalization, and a 12-fold increase in mortality compared with non-Hispanic White individuals with sarcoidosis. Little is known about the drivers of these disparities; however, environmental exposure has been implicated in sarcoidosis pathogenesis and incidence and may be an important contributor.
Dr. Mustafa’s preliminary work suggests disparities in exposure to air pollution among individuals with sarcoidosis may be contributing to inequities in clinical outcomes.
Determinants of medication non-adherence among adults with chronic obstructive pulmonary disease
The CHEST/ALA/ATS Respiratory Health Equity Research Award was given to Stephanie LaBedz, MD, of the University of Illinois Chicago. The Respiratory Health Equity Research Award is jointly supported by the American Lung Association, the American Thoracic Society, and CHEST.
Dr. LaBedz’s project, “Determinants of Medication Non-Adherence Among Adults With Chronic Obstructive Pulmonary Disease,” aims to use behavioral science theory to identify barriers and facilitators to COPD medication adherence.
Studies suggest racial minorities and individuals of low socioeconomic status (SES) are less likely to be adherent to COPD medications compared with White and high SES patients with COPD. Interventions designed to improve COPD medication adherence must address barriers to adherence experienced by these groups to avoid perpetuating disparities in adherence and downstream outcomes disparities.
For her project, Dr. LaBedz will focus on examining barriers and facilitators of COPD medication adherence, including social determinants of health and other structural barriers faced by these vulnerable populations. She will use the information gained from the qualitative study to design interventions that address the barriers to adherence faced by these groups.
Her long-term goal is to improve COPD medication adherence in vulnerable patients with COPD in order to improve the health status and reduce health disparities experienced by racial/ethnic minority and low SES patients with COPD.
In 2023, CHEST awarded $300,000 in clinical research and community impact grants to 15 individuals. Grant recipients are recognized for their scientifically meritorious achievements, with rigorous metrics to track their project’s progress, and have innovative, novel approaches to addressing their research topic.
CHEST grants have made a difference in patients’ lives by leading to breakthroughs in the treatment and/or management of chest diseases and patient care. This year’s grant-funded projects run the gamut of topics within chest medicine, ranging from lung cancer and COPD to tuberculosis and idiopathic pulmonary fibrosis.
Here’s a glimpse into two of this year’s grant winners and their projects.
For a full list of the 2023 grant winners, visit chestnet.org/grant-recipients.
Air pollution in sarcoidosis
This year, the John R. Addrizzo, MD, FCCP Research Grant in Sarcoidosis was awarded to Ali Mustafa, MD, of the Johns Hopkins Hospital in Baltimore, MD, for his project “Air Pollution in Sarcoidosis.”
The project’s aim is to investigate the feasibility of studying indoor and outdoor air pollution in patients with pulmonary sarcoidosis.
According to Dr. Mustafa’s application, pulmonary sarcoidosis is one of the most common interstitial lung diseases in the United States, and mortality due to sarcoidosis has risen by more than 3% in recent decades.
While the etiology of sarcoidosis remains elusive, evidence points toward a combination of genetic predisposition with external environmental triggers affecting disease onset. One small study of 16 individuals with fibrotic pulmonary sarcoidosis assessed the association between local levels of outdoor air pollutants to clinical outcomes. This study found that increased short-term exposure was associated with increased respiratory symptom severity and worse health-related quality of life.
Additionally, significant health disparities exist in sarcoidosis. Black individuals with sarcoidosis have worse pulmonary function, higher rates of multiorgan disease, and as much as a 12-fold increase in mortality compared with non-Hispanic White individuals with sarcoidosis. Socioeconomic status and Black race have also been associated with increased exposure to air pollution and closer proximity to high toxic emission facilities, suggesting higher exposure to outdoor air pollution.
Racial disparities are present and particularly important in sarcoidosis. Black individuals are more likely to have more advanced disease at diagnosis, have a six-fold increase in hospitalization, and a 12-fold increase in mortality compared with non-Hispanic White individuals with sarcoidosis. Little is known about the drivers of these disparities; however, environmental exposure has been implicated in sarcoidosis pathogenesis and incidence and may be an important contributor.
Dr. Mustafa’s preliminary work suggests disparities in exposure to air pollution among individuals with sarcoidosis may be contributing to inequities in clinical outcomes.
Determinants of medication non-adherence among adults with chronic obstructive pulmonary disease
The CHEST/ALA/ATS Respiratory Health Equity Research Award was given to Stephanie LaBedz, MD, of the University of Illinois Chicago. The Respiratory Health Equity Research Award is jointly supported by the American Lung Association, the American Thoracic Society, and CHEST.
Dr. LaBedz’s project, “Determinants of Medication Non-Adherence Among Adults With Chronic Obstructive Pulmonary Disease,” aims to use behavioral science theory to identify barriers and facilitators to COPD medication adherence.
Studies suggest racial minorities and individuals of low socioeconomic status (SES) are less likely to be adherent to COPD medications compared with White and high SES patients with COPD. Interventions designed to improve COPD medication adherence must address barriers to adherence experienced by these groups to avoid perpetuating disparities in adherence and downstream outcomes disparities.
For her project, Dr. LaBedz will focus on examining barriers and facilitators of COPD medication adherence, including social determinants of health and other structural barriers faced by these vulnerable populations. She will use the information gained from the qualitative study to design interventions that address the barriers to adherence faced by these groups.
Her long-term goal is to improve COPD medication adherence in vulnerable patients with COPD in order to improve the health status and reduce health disparities experienced by racial/ethnic minority and low SES patients with COPD.
In 2023, CHEST awarded $300,000 in clinical research and community impact grants to 15 individuals. Grant recipients are recognized for their scientifically meritorious achievements, with rigorous metrics to track their project’s progress, and have innovative, novel approaches to addressing their research topic.
CHEST grants have made a difference in patients’ lives by leading to breakthroughs in the treatment and/or management of chest diseases and patient care. This year’s grant-funded projects run the gamut of topics within chest medicine, ranging from lung cancer and COPD to tuberculosis and idiopathic pulmonary fibrosis.
Here’s a glimpse into two of this year’s grant winners and their projects.
For a full list of the 2023 grant winners, visit chestnet.org/grant-recipients.
Air pollution in sarcoidosis
This year, the John R. Addrizzo, MD, FCCP Research Grant in Sarcoidosis was awarded to Ali Mustafa, MD, of the Johns Hopkins Hospital in Baltimore, MD, for his project “Air Pollution in Sarcoidosis.”
The project’s aim is to investigate the feasibility of studying indoor and outdoor air pollution in patients with pulmonary sarcoidosis.
According to Dr. Mustafa’s application, pulmonary sarcoidosis is one of the most common interstitial lung diseases in the United States, and mortality due to sarcoidosis has risen by more than 3% in recent decades.
While the etiology of sarcoidosis remains elusive, evidence points toward a combination of genetic predisposition with external environmental triggers affecting disease onset. One small study of 16 individuals with fibrotic pulmonary sarcoidosis assessed the association between local levels of outdoor air pollutants to clinical outcomes. This study found that increased short-term exposure was associated with increased respiratory symptom severity and worse health-related quality of life.
Additionally, significant health disparities exist in sarcoidosis. Black individuals with sarcoidosis have worse pulmonary function, higher rates of multiorgan disease, and as much as a 12-fold increase in mortality compared with non-Hispanic White individuals with sarcoidosis. Socioeconomic status and Black race have also been associated with increased exposure to air pollution and closer proximity to high toxic emission facilities, suggesting higher exposure to outdoor air pollution.
Racial disparities are present and particularly important in sarcoidosis. Black individuals are more likely to have more advanced disease at diagnosis, have a six-fold increase in hospitalization, and a 12-fold increase in mortality compared with non-Hispanic White individuals with sarcoidosis. Little is known about the drivers of these disparities; however, environmental exposure has been implicated in sarcoidosis pathogenesis and incidence and may be an important contributor.
Dr. Mustafa’s preliminary work suggests disparities in exposure to air pollution among individuals with sarcoidosis may be contributing to inequities in clinical outcomes.
Determinants of medication non-adherence among adults with chronic obstructive pulmonary disease
The CHEST/ALA/ATS Respiratory Health Equity Research Award was given to Stephanie LaBedz, MD, of the University of Illinois Chicago. The Respiratory Health Equity Research Award is jointly supported by the American Lung Association, the American Thoracic Society, and CHEST.
Dr. LaBedz’s project, “Determinants of Medication Non-Adherence Among Adults With Chronic Obstructive Pulmonary Disease,” aims to use behavioral science theory to identify barriers and facilitators to COPD medication adherence.
Studies suggest racial minorities and individuals of low socioeconomic status (SES) are less likely to be adherent to COPD medications compared with White and high SES patients with COPD. Interventions designed to improve COPD medication adherence must address barriers to adherence experienced by these groups to avoid perpetuating disparities in adherence and downstream outcomes disparities.
For her project, Dr. LaBedz will focus on examining barriers and facilitators of COPD medication adherence, including social determinants of health and other structural barriers faced by these vulnerable populations. She will use the information gained from the qualitative study to design interventions that address the barriers to adherence faced by these groups.
Her long-term goal is to improve COPD medication adherence in vulnerable patients with COPD in order to improve the health status and reduce health disparities experienced by racial/ethnic minority and low SES patients with COPD.
CHEST introduces five core organizational values
Looking ahead to 2024, one notable accomplishment of the past 12 months that will guide our organization for years to come was to establish CHEST organizational values. The result of a collaborative process that was led by the Value-Setting Work Group and informed by CHEST leaders, members, and staff, the CHEST values are Community, Inclusivity, Innovation, Advocacy, and Integrity.
The process to arrive at these values was intentionally designed to ensure input from all corners of the organization. Over the course of 5 months, CHEST members had the opportunity to participate in focus groups or submit written feedback about the proposed values. The feedback shaped subsequent iterations of the values that the work group produced, finally arriving at these five.
“These values are meant to be reflective of the CHEST organization and all of its leaders, members, and staff,” said Co-Chair of the Value-Setting Work Group and CHEST Board of Regents Member Nneka Sederstrom, PhD, FCCP. “As a society, we’ve come to a point where we can’t pretend that real life issues don’t matter to our patients and to our members. It’s become a pivotal point in our world for our systems to be clear on who they are. All too often, the question of, ‘Is this our lane?’ comes up. These values are a succinct way to show not only what falls into our ‘lane,’ but that we celebrate where we stand. It was a big undertaking, but seeing the collaboration and passion was exceptional.”
The work group was co-chaired by Dr. Sederstrom and Elizabeth Stigler, PhD, and was supported by David Zielinski, MD, FCCP; Bravein Amalakuhan, MD; Alisha Young, MD; Steven Simpson, MD, FCCP; Nehan Sher, MD; and CHEST staff members, Teresa Rodriguez, Manager, CHEST Annual Meeting; Terri Horton-O’Connell, MSW, Director, Grant and Proposal Development; and Vanessa Rancine, Recruiting Specialist.
Beyond solidifying the five succinct values, the work group strategically defined each value to clarify its intent.
- Community: We invest in the support, growth, and development of everyone involved with CHEST, both individually and collectively, and are tireless champions for one another.
- Inclusivity: We cherish the diverse perspectives and experiences of our community members and amplify their unique voices.
- Innovation: We strive for excellence in all that we do with an adaptable and ever-evolving perspective. We pursue bold, future-oriented possibilities for constant improvement and continual growth.
- Advocacy: We courageously and intentionally create and foster positive changes for our patients and their families, our members and staff, and the next generation of CHEST clinicians.
- Integrity: We take pride in acting responsibly with respect, honesty, and accountability that engenders trust.
“With the new values in place, hopefully, our members will feel a shift in how we, as an organization, show up when anything occurs,” Dr. Sederstrom said. “The values will be reflected through community engagement and support and will be deeply integrated into the CHEST Annual Meeting. When someone asks CHEST, ‘Who are you?’ -we can now answer it with certitude.”
Looking ahead to 2024, one notable accomplishment of the past 12 months that will guide our organization for years to come was to establish CHEST organizational values. The result of a collaborative process that was led by the Value-Setting Work Group and informed by CHEST leaders, members, and staff, the CHEST values are Community, Inclusivity, Innovation, Advocacy, and Integrity.
The process to arrive at these values was intentionally designed to ensure input from all corners of the organization. Over the course of 5 months, CHEST members had the opportunity to participate in focus groups or submit written feedback about the proposed values. The feedback shaped subsequent iterations of the values that the work group produced, finally arriving at these five.
“These values are meant to be reflective of the CHEST organization and all of its leaders, members, and staff,” said Co-Chair of the Value-Setting Work Group and CHEST Board of Regents Member Nneka Sederstrom, PhD, FCCP. “As a society, we’ve come to a point where we can’t pretend that real life issues don’t matter to our patients and to our members. It’s become a pivotal point in our world for our systems to be clear on who they are. All too often, the question of, ‘Is this our lane?’ comes up. These values are a succinct way to show not only what falls into our ‘lane,’ but that we celebrate where we stand. It was a big undertaking, but seeing the collaboration and passion was exceptional.”
The work group was co-chaired by Dr. Sederstrom and Elizabeth Stigler, PhD, and was supported by David Zielinski, MD, FCCP; Bravein Amalakuhan, MD; Alisha Young, MD; Steven Simpson, MD, FCCP; Nehan Sher, MD; and CHEST staff members, Teresa Rodriguez, Manager, CHEST Annual Meeting; Terri Horton-O’Connell, MSW, Director, Grant and Proposal Development; and Vanessa Rancine, Recruiting Specialist.
Beyond solidifying the five succinct values, the work group strategically defined each value to clarify its intent.
- Community: We invest in the support, growth, and development of everyone involved with CHEST, both individually and collectively, and are tireless champions for one another.
- Inclusivity: We cherish the diverse perspectives and experiences of our community members and amplify their unique voices.
- Innovation: We strive for excellence in all that we do with an adaptable and ever-evolving perspective. We pursue bold, future-oriented possibilities for constant improvement and continual growth.
- Advocacy: We courageously and intentionally create and foster positive changes for our patients and their families, our members and staff, and the next generation of CHEST clinicians.
- Integrity: We take pride in acting responsibly with respect, honesty, and accountability that engenders trust.
“With the new values in place, hopefully, our members will feel a shift in how we, as an organization, show up when anything occurs,” Dr. Sederstrom said. “The values will be reflected through community engagement and support and will be deeply integrated into the CHEST Annual Meeting. When someone asks CHEST, ‘Who are you?’ -we can now answer it with certitude.”
Looking ahead to 2024, one notable accomplishment of the past 12 months that will guide our organization for years to come was to establish CHEST organizational values. The result of a collaborative process that was led by the Value-Setting Work Group and informed by CHEST leaders, members, and staff, the CHEST values are Community, Inclusivity, Innovation, Advocacy, and Integrity.
The process to arrive at these values was intentionally designed to ensure input from all corners of the organization. Over the course of 5 months, CHEST members had the opportunity to participate in focus groups or submit written feedback about the proposed values. The feedback shaped subsequent iterations of the values that the work group produced, finally arriving at these five.
“These values are meant to be reflective of the CHEST organization and all of its leaders, members, and staff,” said Co-Chair of the Value-Setting Work Group and CHEST Board of Regents Member Nneka Sederstrom, PhD, FCCP. “As a society, we’ve come to a point where we can’t pretend that real life issues don’t matter to our patients and to our members. It’s become a pivotal point in our world for our systems to be clear on who they are. All too often, the question of, ‘Is this our lane?’ comes up. These values are a succinct way to show not only what falls into our ‘lane,’ but that we celebrate where we stand. It was a big undertaking, but seeing the collaboration and passion was exceptional.”
The work group was co-chaired by Dr. Sederstrom and Elizabeth Stigler, PhD, and was supported by David Zielinski, MD, FCCP; Bravein Amalakuhan, MD; Alisha Young, MD; Steven Simpson, MD, FCCP; Nehan Sher, MD; and CHEST staff members, Teresa Rodriguez, Manager, CHEST Annual Meeting; Terri Horton-O’Connell, MSW, Director, Grant and Proposal Development; and Vanessa Rancine, Recruiting Specialist.
Beyond solidifying the five succinct values, the work group strategically defined each value to clarify its intent.
- Community: We invest in the support, growth, and development of everyone involved with CHEST, both individually and collectively, and are tireless champions for one another.
- Inclusivity: We cherish the diverse perspectives and experiences of our community members and amplify their unique voices.
- Innovation: We strive for excellence in all that we do with an adaptable and ever-evolving perspective. We pursue bold, future-oriented possibilities for constant improvement and continual growth.
- Advocacy: We courageously and intentionally create and foster positive changes for our patients and their families, our members and staff, and the next generation of CHEST clinicians.
- Integrity: We take pride in acting responsibly with respect, honesty, and accountability that engenders trust.
“With the new values in place, hopefully, our members will feel a shift in how we, as an organization, show up when anything occurs,” Dr. Sederstrom said. “The values will be reflected through community engagement and support and will be deeply integrated into the CHEST Annual Meeting. When someone asks CHEST, ‘Who are you?’ -we can now answer it with certitude.”
University of Washington Fellowship director announced as mentor for Medical Educator Fellowship
It wasn’t until Başak Çoruh, MD, FCCP, was a mentee herself that she realized the value of structured mentoring. And now, she has more to give.
Dr. Çoruh, Associate Professor of Pulmonary, Critical Care, and Sleep Medicine and Director of the Pulmonary and Critical Care Medicine fellowship program at the University of Washington, was named as the mentor for the Medical Educator Diversity Scholarship Fellowship.
It was created to support a fellow who intends to pursue a career in medical education but who may have limited resources to train in teaching, formal medical education curricula, and medical education research.
“The fellowship is an incredible opportunity to increase the diversity of our medical education community,” Dr. Çoruh said.
The fellowship also closely aligns with CHEST’s newly established philanthropic pillar of “Support of the profession.” CHEST is devoted to elevating the field of chest medicine through top-notch clinical education and empowering early career clinicians from diverse backgrounds with the latest knowledge.
“I’m particularly excited to serve as a mentor for an aspiring medical educator without access to resources for coursework, teaching activities, or scholarship at their home institution,” Dr. Çoruh said. “I am fortunate to be a part of a large and welcoming education community at the University of Washington that I’m excited to share with my mentee.”
The importance of mentorship cannot be overstated, as it can shape the rest of a clinician’s career. There is immense value in not only the funding and research aspect but in the wisdom-sharing and motivational side, as well.
“It wasn’t until my own fellowship that I experienced the value of structured mentoring, and the mentoring I have received has impacted my career in countless ways. I look forward to helping [the fellow] achieve their goals.”
The fellowship recipient will be announced in early 2024.
It wasn’t until Başak Çoruh, MD, FCCP, was a mentee herself that she realized the value of structured mentoring. And now, she has more to give.
Dr. Çoruh, Associate Professor of Pulmonary, Critical Care, and Sleep Medicine and Director of the Pulmonary and Critical Care Medicine fellowship program at the University of Washington, was named as the mentor for the Medical Educator Diversity Scholarship Fellowship.
It was created to support a fellow who intends to pursue a career in medical education but who may have limited resources to train in teaching, formal medical education curricula, and medical education research.
“The fellowship is an incredible opportunity to increase the diversity of our medical education community,” Dr. Çoruh said.
The fellowship also closely aligns with CHEST’s newly established philanthropic pillar of “Support of the profession.” CHEST is devoted to elevating the field of chest medicine through top-notch clinical education and empowering early career clinicians from diverse backgrounds with the latest knowledge.
“I’m particularly excited to serve as a mentor for an aspiring medical educator without access to resources for coursework, teaching activities, or scholarship at their home institution,” Dr. Çoruh said. “I am fortunate to be a part of a large and welcoming education community at the University of Washington that I’m excited to share with my mentee.”
The importance of mentorship cannot be overstated, as it can shape the rest of a clinician’s career. There is immense value in not only the funding and research aspect but in the wisdom-sharing and motivational side, as well.
“It wasn’t until my own fellowship that I experienced the value of structured mentoring, and the mentoring I have received has impacted my career in countless ways. I look forward to helping [the fellow] achieve their goals.”
The fellowship recipient will be announced in early 2024.
It wasn’t until Başak Çoruh, MD, FCCP, was a mentee herself that she realized the value of structured mentoring. And now, she has more to give.
Dr. Çoruh, Associate Professor of Pulmonary, Critical Care, and Sleep Medicine and Director of the Pulmonary and Critical Care Medicine fellowship program at the University of Washington, was named as the mentor for the Medical Educator Diversity Scholarship Fellowship.
It was created to support a fellow who intends to pursue a career in medical education but who may have limited resources to train in teaching, formal medical education curricula, and medical education research.
“The fellowship is an incredible opportunity to increase the diversity of our medical education community,” Dr. Çoruh said.
The fellowship also closely aligns with CHEST’s newly established philanthropic pillar of “Support of the profession.” CHEST is devoted to elevating the field of chest medicine through top-notch clinical education and empowering early career clinicians from diverse backgrounds with the latest knowledge.
“I’m particularly excited to serve as a mentor for an aspiring medical educator without access to resources for coursework, teaching activities, or scholarship at their home institution,” Dr. Çoruh said. “I am fortunate to be a part of a large and welcoming education community at the University of Washington that I’m excited to share with my mentee.”
The importance of mentorship cannot be overstated, as it can shape the rest of a clinician’s career. There is immense value in not only the funding and research aspect but in the wisdom-sharing and motivational side, as well.
“It wasn’t until my own fellowship that I experienced the value of structured mentoring, and the mentoring I have received has impacted my career in countless ways. I look forward to helping [the fellow] achieve their goals.”
The fellowship recipient will be announced in early 2024.
Get to know incoming CHEST President John “Jack” D. Buckley, MD, MPH, FCCP
Starting January 1, 2024, current President-Elect John “Jack” D. Buckley, MD, MPH, FCCP, will become the new President of CHEST. Dr. Buckley is a pulmonologist and critical care physician with an extensive background in education, and he has served on the Board of Regents for the College for 8 years collectively.
What would you like to accomplish as President of CHEST?
I mentioned this in my address during the CHEST Annual Meeting in Honolulu, but the role of President is to guide the Board of Regents as we provide governance and direct the organization to fulfill our mission. With that in mind, my job is to advance CHEST by following our strategic plan, continuing the great work already being done, and preparing for what comes next.
As our world changes around us, we must not only adapt to the current environment but anticipate the future and take the lead by influencing the direction we believe to be important. This is the role of the Board of Regents, and we need input from CHEST’s members.
In 2023, with the guidance of an advisory board, and a tremendous amount of time and effort encompassing input from a wide range of CHEST members, leaders and staff, the organization defined its core values. The values – Community, Inclusivity, Innovation, Advocacy, and Integrity – are reflective of the CHEST organization and will guide decisions for years to come.
While looking forward, it’s also important to reflect on the past. CHEST started as an organization centered on preventing and treating tuberculosis. As progress was made, the entire pulmonary field evolved from tuberculosis experts and, from there, critical care emerged and continues to evolve. Now we’re seeing tremendous growth in the roles of advanced practice providers in our ICUs and, most recently, a resurgence of cardiology-critical care. We are excited to welcome these colleagues into CHEST as we move forward.
What do you consider to be CHEST’s greatest strength, and how will you build upon this during your presidency?
The strength of CHEST is in our community and our educational programs. Our emphasis is on delivering relevant information to our members in ways that are immediately clinically applicable – something I think we do better than anyone – to improve the care we’re able to provide to our patients. Through expanding our community and continuing to produce quality medical education, this will continue to be a focus for years to come.
What are some challenges facing CHEST, and how will you address them?
The challenges facing CHEST are the same challenges facing the whole of health care. Predominantly, providers and patients are both caught navigating complex health systems and insurance programs, costs of care, and access. The latter is particularly concerning for us as the burnout of health care providers has worsened, and people are leaving the clinical setting.
While there is no simple solution, CHEST has demonstrated commitments to making an impact through initiatives like First 5 Minutes®, which was created to address implicit bias, establish trust, and form a stronger connection between patients and their clinicians more quickly.
This will be a growing focus for CHEST, and it is reflected in the formal addition of social responsibility to our organizational pillars. The work being done in philanthropy and through our diversity, equity, inclusion, and belonging efforts will continue to develop and are now a core element of the organization.
And finally, what do you ask of the members and Fellows of CHEST to support you during your presidency?
I cannot stress enough that every person reading this should join the conversation. Meant to represent the whole of pulmonary, critical care, and sleep medicine clinicians, CHEST is stronger with every voice. Conveniently, an email address exists for this very purpose. The address president@chestnet.org is a direct way to communicate with me, and I very much encourage you to take me up on this.
Let me know what you would like to see change in 2024 or what you think we’re doing well. I’d also like to hear if there is something neat you’re doing for the field; beyond my personal interest, CHEST loves to celebrate the accomplishments of members.
I look forward to elevating your voice and am truly elated to serve as the next President of CHEST.
Starting January 1, 2024, current President-Elect John “Jack” D. Buckley, MD, MPH, FCCP, will become the new President of CHEST. Dr. Buckley is a pulmonologist and critical care physician with an extensive background in education, and he has served on the Board of Regents for the College for 8 years collectively.
What would you like to accomplish as President of CHEST?
I mentioned this in my address during the CHEST Annual Meeting in Honolulu, but the role of President is to guide the Board of Regents as we provide governance and direct the organization to fulfill our mission. With that in mind, my job is to advance CHEST by following our strategic plan, continuing the great work already being done, and preparing for what comes next.
As our world changes around us, we must not only adapt to the current environment but anticipate the future and take the lead by influencing the direction we believe to be important. This is the role of the Board of Regents, and we need input from CHEST’s members.
In 2023, with the guidance of an advisory board, and a tremendous amount of time and effort encompassing input from a wide range of CHEST members, leaders and staff, the organization defined its core values. The values – Community, Inclusivity, Innovation, Advocacy, and Integrity – are reflective of the CHEST organization and will guide decisions for years to come.
While looking forward, it’s also important to reflect on the past. CHEST started as an organization centered on preventing and treating tuberculosis. As progress was made, the entire pulmonary field evolved from tuberculosis experts and, from there, critical care emerged and continues to evolve. Now we’re seeing tremendous growth in the roles of advanced practice providers in our ICUs and, most recently, a resurgence of cardiology-critical care. We are excited to welcome these colleagues into CHEST as we move forward.
What do you consider to be CHEST’s greatest strength, and how will you build upon this during your presidency?
The strength of CHEST is in our community and our educational programs. Our emphasis is on delivering relevant information to our members in ways that are immediately clinically applicable – something I think we do better than anyone – to improve the care we’re able to provide to our patients. Through expanding our community and continuing to produce quality medical education, this will continue to be a focus for years to come.
What are some challenges facing CHEST, and how will you address them?
The challenges facing CHEST are the same challenges facing the whole of health care. Predominantly, providers and patients are both caught navigating complex health systems and insurance programs, costs of care, and access. The latter is particularly concerning for us as the burnout of health care providers has worsened, and people are leaving the clinical setting.
While there is no simple solution, CHEST has demonstrated commitments to making an impact through initiatives like First 5 Minutes®, which was created to address implicit bias, establish trust, and form a stronger connection between patients and their clinicians more quickly.
This will be a growing focus for CHEST, and it is reflected in the formal addition of social responsibility to our organizational pillars. The work being done in philanthropy and through our diversity, equity, inclusion, and belonging efforts will continue to develop and are now a core element of the organization.
And finally, what do you ask of the members and Fellows of CHEST to support you during your presidency?
I cannot stress enough that every person reading this should join the conversation. Meant to represent the whole of pulmonary, critical care, and sleep medicine clinicians, CHEST is stronger with every voice. Conveniently, an email address exists for this very purpose. The address president@chestnet.org is a direct way to communicate with me, and I very much encourage you to take me up on this.
Let me know what you would like to see change in 2024 or what you think we’re doing well. I’d also like to hear if there is something neat you’re doing for the field; beyond my personal interest, CHEST loves to celebrate the accomplishments of members.
I look forward to elevating your voice and am truly elated to serve as the next President of CHEST.
Starting January 1, 2024, current President-Elect John “Jack” D. Buckley, MD, MPH, FCCP, will become the new President of CHEST. Dr. Buckley is a pulmonologist and critical care physician with an extensive background in education, and he has served on the Board of Regents for the College for 8 years collectively.
What would you like to accomplish as President of CHEST?
I mentioned this in my address during the CHEST Annual Meeting in Honolulu, but the role of President is to guide the Board of Regents as we provide governance and direct the organization to fulfill our mission. With that in mind, my job is to advance CHEST by following our strategic plan, continuing the great work already being done, and preparing for what comes next.
As our world changes around us, we must not only adapt to the current environment but anticipate the future and take the lead by influencing the direction we believe to be important. This is the role of the Board of Regents, and we need input from CHEST’s members.
In 2023, with the guidance of an advisory board, and a tremendous amount of time and effort encompassing input from a wide range of CHEST members, leaders and staff, the organization defined its core values. The values – Community, Inclusivity, Innovation, Advocacy, and Integrity – are reflective of the CHEST organization and will guide decisions for years to come.
While looking forward, it’s also important to reflect on the past. CHEST started as an organization centered on preventing and treating tuberculosis. As progress was made, the entire pulmonary field evolved from tuberculosis experts and, from there, critical care emerged and continues to evolve. Now we’re seeing tremendous growth in the roles of advanced practice providers in our ICUs and, most recently, a resurgence of cardiology-critical care. We are excited to welcome these colleagues into CHEST as we move forward.
What do you consider to be CHEST’s greatest strength, and how will you build upon this during your presidency?
The strength of CHEST is in our community and our educational programs. Our emphasis is on delivering relevant information to our members in ways that are immediately clinically applicable – something I think we do better than anyone – to improve the care we’re able to provide to our patients. Through expanding our community and continuing to produce quality medical education, this will continue to be a focus for years to come.
What are some challenges facing CHEST, and how will you address them?
The challenges facing CHEST are the same challenges facing the whole of health care. Predominantly, providers and patients are both caught navigating complex health systems and insurance programs, costs of care, and access. The latter is particularly concerning for us as the burnout of health care providers has worsened, and people are leaving the clinical setting.
While there is no simple solution, CHEST has demonstrated commitments to making an impact through initiatives like First 5 Minutes®, which was created to address implicit bias, establish trust, and form a stronger connection between patients and their clinicians more quickly.
This will be a growing focus for CHEST, and it is reflected in the formal addition of social responsibility to our organizational pillars. The work being done in philanthropy and through our diversity, equity, inclusion, and belonging efforts will continue to develop and are now a core element of the organization.
And finally, what do you ask of the members and Fellows of CHEST to support you during your presidency?
I cannot stress enough that every person reading this should join the conversation. Meant to represent the whole of pulmonary, critical care, and sleep medicine clinicians, CHEST is stronger with every voice. Conveniently, an email address exists for this very purpose. The address president@chestnet.org is a direct way to communicate with me, and I very much encourage you to take me up on this.
Let me know what you would like to see change in 2024 or what you think we’re doing well. I’d also like to hear if there is something neat you’re doing for the field; beyond my personal interest, CHEST loves to celebrate the accomplishments of members.
I look forward to elevating your voice and am truly elated to serve as the next President of CHEST.