User login
Perspectives of Clinicians at Skilled Nursing Facilities on 30-Day Hospital Readmissions: A Qualitative Study
Skilled nursing facilities (SNFs) play a crucial role in the hospital readmission process.Approximately 1 in 4 Medicare beneficiaries discharged from an acute care hospital is admitted to a SNF instead of returning directly home. Of these patients, 1 in 4 will be readmitted within 30 days,1 a rate significantly higher than the readmission rate of the inpatient population as a whole.2 The 2014 Protecting Access to Medicare Act created a value-based purchasing program that will use quality measures to steer funds to, or away from, individual SNFs. When the program takes effect in 2018, the Centers for Medicare & Medicaid Services will use SNFs’ 30-day all-cause readmission rate to determine which SNFs receive payments and which receive penalties.3 The Affordable Care Act, passed in 2010, has also established penalties for hospitals with higher than expected readmission rates for Medicare patients.4
Despite this intensifying regulatory focus, relatively little is known about the factors that drive readmissions from SNFs. A prospective review of data from SNFs in 4 states has shown that SNFs staffed by nurse practitioners or physician assistants and those equipped to provide intravenous therapy were less likely to transfer patients to the hospital for ambulatory care-sensitive diagnoses.5 Qualitative studies have provided useful insight into the causes of SNF-to-hospital transfers but have not focused on 30-day readmissions.6,7 A single survey-based study has examined the causes of SNF-to-hospital readmissions.8 However, survey-based methodologies have limited ability to capture the complex perspectives of SNF clinicians, who play a critical role in determining which SNF patients require evaluation or treatment in an acute care setting.
To address this gap in knowledge about factors contributing to SNF readmissions, we conducted a qualitative study examining SNF clinicians’ perspectives on patients readmitted to the hospital within 30 days of discharge. We used a structured interview tool to explore the root causes of readmission with frontline SNF staff, with the goal of using this knowledge to inform future hospital quality improvement (QI) efforts.
METHODS
Case Identification
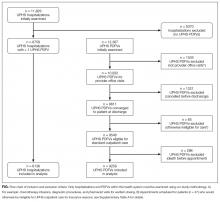
Hospital data-tracking software (Allscripts) was used to identify patients who experienced a 30-day, unplanned readmission from SNFs to an academic medical center. We restricted our search to patients whose index admission and readmission were to the medical center’s inpatient general medicine service. A study team member (BWC) monitored the dataset on a weekly basis and contacted SNF clinicians by e-mail and telephone to arrange interviews at times of mutual convenience. To mitigate against recall bias, interviews were conducted within 30 days of the readmission in question. A total of 32 cases were identified. No SNF clinicians refused a request for interview. For 8 of these cases, it was not possible to find a time of mutual convenience within the specified 30-day window. The remaining 24 cases involved patients from 15 SNFs across Connecticut. Interviews were conducted from August 2015 to November 2015.
The project was reviewed by our institution’s Human Investigation Committee and was exempted from Institutional Review Board review.
Study Participants
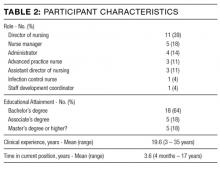
Interviews were conducted on-site at SNFs with groups of 1 to 4 SNF clinicians and administrators. SNF participants were informed of interviewer credentials and the study’s QI goals prior to participation. Participation was voluntary and did not affect the clinician’s relationship with the hospital or the SNF. Participants were not paid.
DATA COLLECTION
Interventions to Reduce Acute Care Transfers (INTERACT) is a QI program that includes training for clinicians, communication tools, and advance care planning tools.9 INTERACT is currently used in 138 Connecticut SNFs as part of a statewide QI effort funded by the Connecticut State Department of Public Health. In prospective QI studies,10,11 implementation of INTERACT has been associated with decreased transfers from SNFs to acute care hospitals. The INTERACT Quality Improvement Tool, one part of the INTERACT bundle of interventions, is a 26-item questionnaire used to identify root causes of transfers from SNFs to acute care hospitals. It includes both checklists and open-ended questions about patient factors, SNF procedures, and SNF clinical decision-making.
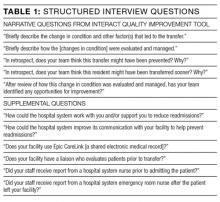
We used the INTERACT QI Tool12 to conduct structured interviews with nurses and administrators at SNFs. Interviewers used a hard copy of the tool to maintain field notes, and all parts of the questionnaire were completed in each interview. Although the questionnaire elicits baseline demographic and medical information, such as the patient’s age and vital signs prior to readmission, the majority of each interview was dedicated to discussion of the open-ended questions in Table 1. Upon completion of the INTERACT QI Tool, the interviewer asked 2 open-ended questions about reducing readmissions and 4 closed-ended questions regarding SNF admission procedures. (Table 1) The supplemental questions were added after preliminary interviews with SNF clinicians revealed concerns about the SNF referral process and about communication between the hospital, emergency department (ED) and SNFs—issues not included in the INTERACT questionnaire. Interviewers used phatic communication, probing questions, and follow-up questions to elicit detailed information from participants, and participant responses were not limited to topics in the questionnaire and the list of supplemental questions.
Interviews were conducted by a hospital clinical integration coordinator, social worker, and a physician (KB, MCB, BWC). All interviewers received formal training in qualitative research methods prior to the study.
All interviews were audio recorded, with permission from the participants, and were professionally transcribed. Field notes were maintained to ensure accuracy of INTERACT QI Tool data. Participant interviews covered no more than two cases per session and lasted from 18 to 71 minutes (mean duration, 38 minutes).
Analysis
Analysis of transcripts was inductive and informed by grounded theory methodology, in which data is reviewed for repeating ideas, which are then analyzed and grouped to develop a theoretical understanding of the phenomenon under investigation.13,14
A preliminary codebook was developed using transcripts of the first 11 interviews. All statements relevant to the readmission process were extracted from the raw interview transcript and collected into a single list. This list was then reviewed for statements sharing a particular idea or concern. Such statements were grouped together under the heading of a repeating idea, and each repeating idea was assigned a code. Using this codebook, each transcript was independently reviewed and coded by three study team members with formal training in inductive qualitative analysis (KB, KTM, BWC). Reviewers assigned codes to sections of relevant text. Discrepancies in code assignment were discussed among the 3 analysts until consensus was reached. Using the method of constant comparison described in grounded theory,the codebook was updated continuously as the process of coding transcripts proceeded.12 Changes to the codebook were discussed among the coding team until consensus was achieved. The process of data acquisition and coding continued until theoretical saturation was reached. Themes relating to underlying factors associated with readmissions were then identified based on shared properties among repeating ideas. ATLAS.ti (Scientific Software, Berlin, Germany, Version 7) was used to facilitate data organization and retrieval.
RESULTS
The SNFs in our study included 12 for-profit and 3 non-profit facilities. The number of licensed beds in each facility ranged from 73 to 360, with a mean of 148 beds. The SNFs had CMS Nursing Home Compare ratings ranging from 1 star, the lowest possible rating, to 5 stars, the highest possible,15 with a mean rating of 2.9 stars. Our analysis did not reveal differences in perceived contributions to readmissions from large vs. small or highly rated vs poorly rated SNFs.
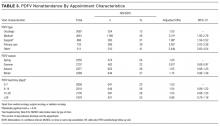
The patients in our analysis represented a highly comorbid and medically complex population (Table 3). Many had barriers to communication with clinical staff, including non–English-speaking status and underlying dementia.
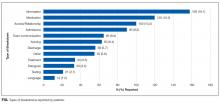
Five main themes emerged from our analysis: (1) lack of coordination between EDs and SNFs; (2) incompletely addressed goals of care; (3) mismatch between patient clinical needs and SNF capabilities; (4) important clinical information not effectively communicated by hospital; and (5) challenges in SNF processes and culture.
Emergent transitions: Lack of coordination between ED and SNF
SNF clinicians frequently encountered situations in which a relatively stable patient was readmitted to the hospital after being transferred to the ED, despite the fact that SNF clinicians believed the patient should have returned to the SNF once a specific test was performed or service rendered at the ED. Commonly cited clinical scenarios that resulted in such readmissions included placement of urinary catheters and evaluation for cystitis. An assistant director of nursing reported that “the ER doesn’t want to hear my side of the story,” making it difficult for her to provide information that would prevent such readmissions. Other SNF clinicians reported similar difficulties in communicating with ED clinicians.
Code status: Incompletely addressed goals of care
The SNF clinicians in our study described cases in which patients with end-stage lung disease and disseminated cancer were readmitted to the hospital, despite SNF efforts to prevent readmission and provide palliative care within the SNF. For example, a SNF advanced practice nurse described a case in which a patient with widely metastatic cancer requested readmission to the hospital for treatment of deep vein thrombosis, despite longstanding recommendations from SNF staff that the patient forego hospitalization and enroll in hospice care. After discussion of code status and goals of care with hospital clinicians, the patient chose to enroll in hospice care and not to continue anticoagulation. SNF clinicians often perceived that, in the words of one administrator, “the palliative talks in the hospital outweigh our talks by a lot.” Numerous SNF clinicians believed that in-depth clarification of goals of care prior to discharge could prevent some readmissions.
Wrong patient, wrong place: Mismatch between clinical needs and SNF capabilities
One director of nursing stated that “[when] you read a referral, there’s a huge difference sometimes between what you read and what you see.” SNF clinicians reported that this discrepancy between clinical report and clinical reality often leads to patients being placed in SNFs that are unequipped to care for them. Many patients were perceived as being too ill for discharge from the acute-care setting in the first place. A nurse manager described this as a pattern of “pushing patients out of the hospital.” However, mismatches in clinical disposition were also seen as contributing to readmissions for medically stable patients, such as those with dementia, for whom SNFs frequently lack adequate staffing and physical safeguards.
Missing links: Important clinical information not effectively communicated by hospital
SNF clinicians described numerous challenges in formulating plans of care based on hospital discharge documentation. Discrepancies between discharge summaries and patient instructions were perceived as common and potential causes of readmissions. For patients discharged from the academic medical center in this study, medication instructions are included in both the discharge summary sent to the SNF and in a patient instruction packet. Several SNF clinicians said that it was common for a course of antibiotics to be listed on the discharge summary but not the patient instruction packet, or vice versa. SNF clinicians, who usually lack access to the hospital’s electronic medical record, have limited means for determining the correct document. Other important clinical data points, such as intermittent intravenous (IV) furosemide dosing and suppressive antibiotic regimens, were omitted from discharge paperwork altogether. SNF clinicians had difficulty reaching hospital clinicians who could clarify these clinical questions. “Good luck finding the person that took care of [the patient] three days before,” said one director of nursing.
Change starts at home: Challenges in SNF processes and culture
Many clinicians in our study reported that their facilities had recently added clinical capabilities in an effort to care for patients with complex medical problems. For example, to prevent transfers of patients with decompensated heart failure, several facilities in our study had recently obtained certification to give IV diuretics. However, as one director of nursing stated, these efforts require “buy-in” from doctors to decrease readmissions. That buy-in has not always been forthcoming. SNF clinicians also reported difficulty convincing patients and families that their facilities are capable of providing care that, in the past, might only have been available in acute-care settings.
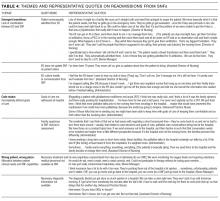
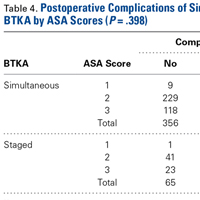
These themes, along with associated sub-themes and representative quotations, are shown above (Table 4).
DISCUSSION
Our study suggests that the interaction between EDs and SNFs is an important and understudied domain in the spectrum of events leading to readmission. Prior studies have documented inadequacies in patient information provided by SNFs to EDs.16,17 Efforts to improve SNF-to-ED information sharing have focused on making sure that ED clinicians have important baseline information about patients transferred from a SNF.18,19 However, many of the clinicians in our study reported taking proactive steps to communicate with ED clinicians. These efforts encountered logistical and cultural barriers, with information that might have prevented readmission failing to reach ED providers. Many of the SNF clinicians in our study perceived this failure as a common cause of readmission, especially for relatively stable SNF patients.
Previous studies have pointed to a role for goals of care discussions in reducing hospital readmissions.20 Our data underscore an important qualification to these findings: Location matters. The SNF clinicians in our study reported frequent and detailed goals of care discussions with their patients. However, they also reported that goals of care discussions held in the subacute setting carried less weight with patients and families than discussions held in the hospital. SNF clinicians described a number of cases in which patients were willing to adjust code status or goals of care only after being readmitted to the hospital.
Our study also points to the implications of existing research showing that patients are discharged from acute care hospitals “quicker and sicker” than they had been prior to the 1983 adoption of Medicare’s prospective payment system.21 Specifically, the SNF clinicians we interviewed perceived a strong link between patient acuity at the time of transfer and SNFs’ persistently high readmission rates. As SNFs have worked to expand their clinical capabilities, they struggle to win buy-in from physicians and families, many of whom view SNFs as incapable of managing acute illness. Many SNF clinicians also pointed to deficiencies in their own referral and admission processes as a recurring cause of readmissions. For example, several patients in our analysis suffered from dementia. Although these patients were stable enough to leave the acute care setting, the SNF clinicians responsible for their readmissions felt that their SNFs were not well-equipped to care for patients with dementia and that the patients should instead have been transferred to facilities with more robust resources for dementia care.
Finally, our findings highlight a fundamental tension between hospitals and SNFs: Which facility ought to shoulder the responsibility and cost for services that may prevent a readmission—the hospital or the SNF? For example, does responsibility for coordinating subspecialist evaluation of a patient’s chronic condition fall to the hospital or to the SNF? If such an evaluation is undertaken during a hospitalization, it prolongs the patient’s hospital stay and happens at the hospital’s expense. If the patient is discharged to a SNF and sees the subspecialist in clinic, then the SNF must pay for transportation to and from the clinic appointment. SNF clinicians expressed near unanimity that fragmented models of care and high barriers to communication made it difficult to design solutions to these dilemmas.
Strengths and limitations
To our knowledge, this is the first interview-based study examining SNF clinicians’ perspectives on unplanned, 30-day hospital readmissions. We gathered information from clinicians with a range of clinical experience, all of whom had cared directly for the patient who had been readmitted. Our data came from clinicians at 15 SNFs of varying sizes and quality ratings, allowing us to identify a broad range of factors contributing to readmissions.
Because this study relied on qualitative methods, it should be viewed as hypothesis-generating rather than hypothesis-confirming. Further research is needed to determine whether variables related to the themes above are causally linked to SNF readmissions. We identified cases for review using convenience sampling of a cohort of readmitted patients at a single tertiary-care hospital, and all participating SNFs were located in Connecticut. These factors may limit the generalizability of our findings. Although the clinicians we interviewed occupied diverse roles within their respective SNFs, our sample did not include direct-care staff without managerial responsibility, such as certified nursing assistants or licensed practical nurses. This prevented our study from identifying themes into which managers would have limited insight, especially those involving cultural and management practices leading to poor communication between them and their staff. Because our study examines cases in which discharge and readmission were to a general medicine service, it may not describe factors relevant to patients discharged from subspecialist or surgical services.
Implications for future QI efforts and research
Several clinicians we interviewed suggested that readmissions might be reduced by dedicating the services of a hospital professional, such as a nurse or case manager, to monitoring the clinical course of medically complex patients after discharge. A dedicated “transition coach” could clarify deficiencies in discharge paperwork, facilitate necessary follow-up appointments, liaise with staff at both the hospital and the SNF, or coordinate acquisition of necessary equipment. Prospective trials have demonstrated that such interventions can decrease readmission rates among hospitalized patients,22,23 but formal studies have not been carried out among cohorts of SNF patients.
Prior efforts to improve SNF-ED information sharing have focused on making sure that ED clinicians have important baseline information about patients transferred from a SNF.24,25 The experiences of SNF clinicians in our study suggest that important information also fails to make its way from ED providers to SNFs and that this failure results in unnecessary readmissions of relatively stable SNF patients. Thus, hospitals may be able to prevent SNF readmissions by creating lines of communication between EDs and SNFs and by ensuring that ED physicians and mid-level providers are familiar with the clinical capabilities of local SNFs.
Future research and QI work should also investigate approaches to care coordination that ensure that complex patients are placed in SNFs with resources adequate to address their comorbidities. Potential interventions might include increased use of SNF “liaisons,” who would evaluate patients in-person prior to approving transfer to a given SNF. As has been previously suggested,26 hospitals might also reduce readmissions by narrowing the pool of facilities to which they transfer patients, thereby building more robust, interconnected relationships with a smaller number of SNFs.
CONCLUSION
SNF clinicians identified areas for improvement at almost every point in the chain of events spanning hospitalization, discharge, and transfer. Among the most frequently cited contributors to readmissions were clinical instability at the time of discharge and omission of clinically important information from discharge documentation. Improved communication between hospitals, ED clinicians, and SNFs, as well as more thoroughly defined goals of care at the time of discharge, were seen as promising ways of decreasing readmissions. Successful interventions for reducing readmissions from SNFs will likely require multifaceted approaches to these problems.
Disclosure: This research was supported by a grant (#P30HS023554-01) from the Agency for Healthcare Research and Quality (AHRQ) and received support from Yale New Haven Hospital and the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (#P30AG021342 NIH/NIA).
1. Mor V, Intrator O, Feng Z, et al. The revolving door of rehospitalization from skilled nursing facilities. Health Aff. 2010;29(1):57-64. PubMed
2. Department of Health and Human Services. Medicare.gov Hospital Compare. https://medicare .gov/hospitalcompare/compare. Accessed October 21, 2015.
3. Centers for Medicare and Medicaid Services. Proposed fiscal year 2016 payment and policy changes for Medicare Skilled Nursing Facilities. https://cms.gov. Accessed October 21, 2015.
4. The Patient Protection and Affordable Care Act: Detailed Summary. Democratic Policy and Communications Committee website. http://www.dpc.senate.gov/healthreformbill/healthbill04.pdf. Accessed August 22, 2016.
5. Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J Am Geriatr Soc. 2004;52:1730-1736. PubMed
6. Ouslander JG, Lamb G, Perloe M, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes and costs. J Am Geriatr Soc. 2010;58:627-635. PubMed
7. Lamb G, Tappen R, Diaz S, et al. Avoidability of hospital transfers of nursing home residents: perspectives of frontline staff. J Am Geriatr Soc. 2011;59:1665-1672. PubMed
8. Ouslander JG, Naharci I, Engstrom G, et al. Hospital transfers of skilled nursing facility (SNF) patients within 48 hours and 30 days after SNF admission. J Am Med Dir Assoc. 2016; doi: 10.1016/j.jamda.2016.05.021. PubMed
9. Ouslander JG, Lamb G, Tappen R et al. Interventions to reduce hospitalizations from nursing homes: Evaluation of the INTERACT II collaborative quality improvement project. J Am Geriatr Soc. 2011; 59:745-753. PubMed
10. Ouslander JG, Perloe M, Givens JH et al. Reducing potentially avoidable hospitalization of nursing home residents: Results of a pilot quality improvement project. J Am Med Dir Assoc. 2009; 10:644-652. PubMed
11. Tena-Nelson R, Santos K, Weingast E et al. Reducing preventable hospital transfers: Results from a thirty nursing home collaborative. J Am Med Dir Assoc. 2012; 13:651-656. PubMed
12. Florida Atlantic University. Interventions to Reduce Acute Care Transfers. https://interact2.net/docs/INTERACT%20Version%204.0%20Tools/INTERACT%204.0%20NH%20Tools%206_17_15/148604%20QI_Tool%20for%20Review%20Acute%20Care%20Transf_AL.pdf
13. Oktay, Julianne. Grounded Theory. New York: Oxford University Press, 2012.
14. Auerbach, Carl and Silverstein, Louise B. Qualitative Data. New York: NYU Press, 2003.
15. Department of Health and Human Services. Medicare.gov Nursing Home Compare. https://medicare .gov/nursinghomecompare. Accessed April 4, 2016.
16. Jones JS, Dwyer PR, White LJ, et al. Patient transfer from nursing home to emergency department: outcomes and policy implications. Acad Emerg Med. 1997 Sep;4(9):908-15. PubMed
17. Lahn M, Friedman B, Bijur P, et al. Advance directives in skilled nursing facility residents transferred to emergency departments. Acad Emerg Med. 2001 Dec;8(12):1158-62. PubMed
18. Madden C, Garrett J, Busby-Whitehead J. The interface between nursing homes and emergency departments: a community effort to improve transfer of information. Acad Emerg Med. 1998 Nov;5(11):1123-6. PubMed
19. Hustey FM, Palmer RM. An internet-based communication network for information transfer during patient transitions from skilled nursing facility to the emergency department. J Am Geriatr Soc. 2010 Jun;58(6):1148-52. PubMed
20. O’Connor N, Moyer ME, Behta M, et al. The Impact of Inpatient Palliative Care Consultations on 30-Day Hospital Readmissions. J Pall Med. 2015 Nov 1; 18(11):956-961. PubMed
21. Qian X, Russell LB, Valiyeva E, et al. “Quicker and sicker” under Medicare’s prospective payment system for hospitals: new evidence on an old issue from a national longitudinal survey. Bull Econ Res. 2011;63(1):1-27. PubMed
22. Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004 May;52(5):675-84. PubMed
23. Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006 Sep 25;166(17):1822-1828. PubMed
24. Madden C, Garrett J, Busby-Whitehead J. The interface between nursing homes and emergency departments: a community effort to improve transfer of information. Acad Emerg Med. 1998 Nov;5(11):1123-6. PubMed
25. Hustey FM, Palmer RM. An internet-based communication network for information transfer during patient transitions from skilled nursing facility to the emergency department. J Am Geriatr Soc. 2010 Jun;58(6):1148-52. PubMed
26. Rahman M, Foster AD, Grabowski DC, Zinn JS, Mor V. Effect of hospital-SNF referral linkages on rehospitalization. Health Serv Res. 2013 Dec;48(6 Pt 1):1898-919. PubMed
Skilled nursing facilities (SNFs) play a crucial role in the hospital readmission process.Approximately 1 in 4 Medicare beneficiaries discharged from an acute care hospital is admitted to a SNF instead of returning directly home. Of these patients, 1 in 4 will be readmitted within 30 days,1 a rate significantly higher than the readmission rate of the inpatient population as a whole.2 The 2014 Protecting Access to Medicare Act created a value-based purchasing program that will use quality measures to steer funds to, or away from, individual SNFs. When the program takes effect in 2018, the Centers for Medicare & Medicaid Services will use SNFs’ 30-day all-cause readmission rate to determine which SNFs receive payments and which receive penalties.3 The Affordable Care Act, passed in 2010, has also established penalties for hospitals with higher than expected readmission rates for Medicare patients.4
Despite this intensifying regulatory focus, relatively little is known about the factors that drive readmissions from SNFs. A prospective review of data from SNFs in 4 states has shown that SNFs staffed by nurse practitioners or physician assistants and those equipped to provide intravenous therapy were less likely to transfer patients to the hospital for ambulatory care-sensitive diagnoses.5 Qualitative studies have provided useful insight into the causes of SNF-to-hospital transfers but have not focused on 30-day readmissions.6,7 A single survey-based study has examined the causes of SNF-to-hospital readmissions.8 However, survey-based methodologies have limited ability to capture the complex perspectives of SNF clinicians, who play a critical role in determining which SNF patients require evaluation or treatment in an acute care setting.
To address this gap in knowledge about factors contributing to SNF readmissions, we conducted a qualitative study examining SNF clinicians’ perspectives on patients readmitted to the hospital within 30 days of discharge. We used a structured interview tool to explore the root causes of readmission with frontline SNF staff, with the goal of using this knowledge to inform future hospital quality improvement (QI) efforts.
METHODS
Case Identification
Hospital data-tracking software (Allscripts) was used to identify patients who experienced a 30-day, unplanned readmission from SNFs to an academic medical center. We restricted our search to patients whose index admission and readmission were to the medical center’s inpatient general medicine service. A study team member (BWC) monitored the dataset on a weekly basis and contacted SNF clinicians by e-mail and telephone to arrange interviews at times of mutual convenience. To mitigate against recall bias, interviews were conducted within 30 days of the readmission in question. A total of 32 cases were identified. No SNF clinicians refused a request for interview. For 8 of these cases, it was not possible to find a time of mutual convenience within the specified 30-day window. The remaining 24 cases involved patients from 15 SNFs across Connecticut. Interviews were conducted from August 2015 to November 2015.
The project was reviewed by our institution’s Human Investigation Committee and was exempted from Institutional Review Board review.
Study Participants
Interviews were conducted on-site at SNFs with groups of 1 to 4 SNF clinicians and administrators. SNF participants were informed of interviewer credentials and the study’s QI goals prior to participation. Participation was voluntary and did not affect the clinician’s relationship with the hospital or the SNF. Participants were not paid.
DATA COLLECTION
Interventions to Reduce Acute Care Transfers (INTERACT) is a QI program that includes training for clinicians, communication tools, and advance care planning tools.9 INTERACT is currently used in 138 Connecticut SNFs as part of a statewide QI effort funded by the Connecticut State Department of Public Health. In prospective QI studies,10,11 implementation of INTERACT has been associated with decreased transfers from SNFs to acute care hospitals. The INTERACT Quality Improvement Tool, one part of the INTERACT bundle of interventions, is a 26-item questionnaire used to identify root causes of transfers from SNFs to acute care hospitals. It includes both checklists and open-ended questions about patient factors, SNF procedures, and SNF clinical decision-making.
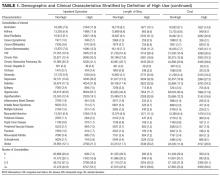
We used the INTERACT QI Tool12 to conduct structured interviews with nurses and administrators at SNFs. Interviewers used a hard copy of the tool to maintain field notes, and all parts of the questionnaire were completed in each interview. Although the questionnaire elicits baseline demographic and medical information, such as the patient’s age and vital signs prior to readmission, the majority of each interview was dedicated to discussion of the open-ended questions in Table 1. Upon completion of the INTERACT QI Tool, the interviewer asked 2 open-ended questions about reducing readmissions and 4 closed-ended questions regarding SNF admission procedures. (Table 1) The supplemental questions were added after preliminary interviews with SNF clinicians revealed concerns about the SNF referral process and about communication between the hospital, emergency department (ED) and SNFs—issues not included in the INTERACT questionnaire. Interviewers used phatic communication, probing questions, and follow-up questions to elicit detailed information from participants, and participant responses were not limited to topics in the questionnaire and the list of supplemental questions.
Interviews were conducted by a hospital clinical integration coordinator, social worker, and a physician (KB, MCB, BWC). All interviewers received formal training in qualitative research methods prior to the study.
All interviews were audio recorded, with permission from the participants, and were professionally transcribed. Field notes were maintained to ensure accuracy of INTERACT QI Tool data. Participant interviews covered no more than two cases per session and lasted from 18 to 71 minutes (mean duration, 38 minutes).
Analysis
Analysis of transcripts was inductive and informed by grounded theory methodology, in which data is reviewed for repeating ideas, which are then analyzed and grouped to develop a theoretical understanding of the phenomenon under investigation.13,14
A preliminary codebook was developed using transcripts of the first 11 interviews. All statements relevant to the readmission process were extracted from the raw interview transcript and collected into a single list. This list was then reviewed for statements sharing a particular idea or concern. Such statements were grouped together under the heading of a repeating idea, and each repeating idea was assigned a code. Using this codebook, each transcript was independently reviewed and coded by three study team members with formal training in inductive qualitative analysis (KB, KTM, BWC). Reviewers assigned codes to sections of relevant text. Discrepancies in code assignment were discussed among the 3 analysts until consensus was reached. Using the method of constant comparison described in grounded theory,the codebook was updated continuously as the process of coding transcripts proceeded.12 Changes to the codebook were discussed among the coding team until consensus was achieved. The process of data acquisition and coding continued until theoretical saturation was reached. Themes relating to underlying factors associated with readmissions were then identified based on shared properties among repeating ideas. ATLAS.ti (Scientific Software, Berlin, Germany, Version 7) was used to facilitate data organization and retrieval.
RESULTS
The SNFs in our study included 12 for-profit and 3 non-profit facilities. The number of licensed beds in each facility ranged from 73 to 360, with a mean of 148 beds. The SNFs had CMS Nursing Home Compare ratings ranging from 1 star, the lowest possible rating, to 5 stars, the highest possible,15 with a mean rating of 2.9 stars. Our analysis did not reveal differences in perceived contributions to readmissions from large vs. small or highly rated vs poorly rated SNFs.
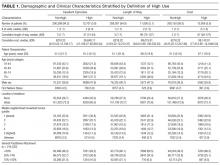
The patients in our analysis represented a highly comorbid and medically complex population (Table 3). Many had barriers to communication with clinical staff, including non–English-speaking status and underlying dementia.
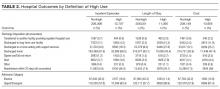
Five main themes emerged from our analysis: (1) lack of coordination between EDs and SNFs; (2) incompletely addressed goals of care; (3) mismatch between patient clinical needs and SNF capabilities; (4) important clinical information not effectively communicated by hospital; and (5) challenges in SNF processes and culture.
Emergent transitions: Lack of coordination between ED and SNF
SNF clinicians frequently encountered situations in which a relatively stable patient was readmitted to the hospital after being transferred to the ED, despite the fact that SNF clinicians believed the patient should have returned to the SNF once a specific test was performed or service rendered at the ED. Commonly cited clinical scenarios that resulted in such readmissions included placement of urinary catheters and evaluation for cystitis. An assistant director of nursing reported that “the ER doesn’t want to hear my side of the story,” making it difficult for her to provide information that would prevent such readmissions. Other SNF clinicians reported similar difficulties in communicating with ED clinicians.
Code status: Incompletely addressed goals of care
The SNF clinicians in our study described cases in which patients with end-stage lung disease and disseminated cancer were readmitted to the hospital, despite SNF efforts to prevent readmission and provide palliative care within the SNF. For example, a SNF advanced practice nurse described a case in which a patient with widely metastatic cancer requested readmission to the hospital for treatment of deep vein thrombosis, despite longstanding recommendations from SNF staff that the patient forego hospitalization and enroll in hospice care. After discussion of code status and goals of care with hospital clinicians, the patient chose to enroll in hospice care and not to continue anticoagulation. SNF clinicians often perceived that, in the words of one administrator, “the palliative talks in the hospital outweigh our talks by a lot.” Numerous SNF clinicians believed that in-depth clarification of goals of care prior to discharge could prevent some readmissions.
Wrong patient, wrong place: Mismatch between clinical needs and SNF capabilities
One director of nursing stated that “[when] you read a referral, there’s a huge difference sometimes between what you read and what you see.” SNF clinicians reported that this discrepancy between clinical report and clinical reality often leads to patients being placed in SNFs that are unequipped to care for them. Many patients were perceived as being too ill for discharge from the acute-care setting in the first place. A nurse manager described this as a pattern of “pushing patients out of the hospital.” However, mismatches in clinical disposition were also seen as contributing to readmissions for medically stable patients, such as those with dementia, for whom SNFs frequently lack adequate staffing and physical safeguards.
Missing links: Important clinical information not effectively communicated by hospital
SNF clinicians described numerous challenges in formulating plans of care based on hospital discharge documentation. Discrepancies between discharge summaries and patient instructions were perceived as common and potential causes of readmissions. For patients discharged from the academic medical center in this study, medication instructions are included in both the discharge summary sent to the SNF and in a patient instruction packet. Several SNF clinicians said that it was common for a course of antibiotics to be listed on the discharge summary but not the patient instruction packet, or vice versa. SNF clinicians, who usually lack access to the hospital’s electronic medical record, have limited means for determining the correct document. Other important clinical data points, such as intermittent intravenous (IV) furosemide dosing and suppressive antibiotic regimens, were omitted from discharge paperwork altogether. SNF clinicians had difficulty reaching hospital clinicians who could clarify these clinical questions. “Good luck finding the person that took care of [the patient] three days before,” said one director of nursing.
Change starts at home: Challenges in SNF processes and culture
Many clinicians in our study reported that their facilities had recently added clinical capabilities in an effort to care for patients with complex medical problems. For example, to prevent transfers of patients with decompensated heart failure, several facilities in our study had recently obtained certification to give IV diuretics. However, as one director of nursing stated, these efforts require “buy-in” from doctors to decrease readmissions. That buy-in has not always been forthcoming. SNF clinicians also reported difficulty convincing patients and families that their facilities are capable of providing care that, in the past, might only have been available in acute-care settings.
These themes, along with associated sub-themes and representative quotations, are shown above (Table 4).
DISCUSSION
Our study suggests that the interaction between EDs and SNFs is an important and understudied domain in the spectrum of events leading to readmission. Prior studies have documented inadequacies in patient information provided by SNFs to EDs.16,17 Efforts to improve SNF-to-ED information sharing have focused on making sure that ED clinicians have important baseline information about patients transferred from a SNF.18,19 However, many of the clinicians in our study reported taking proactive steps to communicate with ED clinicians. These efforts encountered logistical and cultural barriers, with information that might have prevented readmission failing to reach ED providers. Many of the SNF clinicians in our study perceived this failure as a common cause of readmission, especially for relatively stable SNF patients.
Previous studies have pointed to a role for goals of care discussions in reducing hospital readmissions.20 Our data underscore an important qualification to these findings: Location matters. The SNF clinicians in our study reported frequent and detailed goals of care discussions with their patients. However, they also reported that goals of care discussions held in the subacute setting carried less weight with patients and families than discussions held in the hospital. SNF clinicians described a number of cases in which patients were willing to adjust code status or goals of care only after being readmitted to the hospital.
Our study also points to the implications of existing research showing that patients are discharged from acute care hospitals “quicker and sicker” than they had been prior to the 1983 adoption of Medicare’s prospective payment system.21 Specifically, the SNF clinicians we interviewed perceived a strong link between patient acuity at the time of transfer and SNFs’ persistently high readmission rates. As SNFs have worked to expand their clinical capabilities, they struggle to win buy-in from physicians and families, many of whom view SNFs as incapable of managing acute illness. Many SNF clinicians also pointed to deficiencies in their own referral and admission processes as a recurring cause of readmissions. For example, several patients in our analysis suffered from dementia. Although these patients were stable enough to leave the acute care setting, the SNF clinicians responsible for their readmissions felt that their SNFs were not well-equipped to care for patients with dementia and that the patients should instead have been transferred to facilities with more robust resources for dementia care.
Finally, our findings highlight a fundamental tension between hospitals and SNFs: Which facility ought to shoulder the responsibility and cost for services that may prevent a readmission—the hospital or the SNF? For example, does responsibility for coordinating subspecialist evaluation of a patient’s chronic condition fall to the hospital or to the SNF? If such an evaluation is undertaken during a hospitalization, it prolongs the patient’s hospital stay and happens at the hospital’s expense. If the patient is discharged to a SNF and sees the subspecialist in clinic, then the SNF must pay for transportation to and from the clinic appointment. SNF clinicians expressed near unanimity that fragmented models of care and high barriers to communication made it difficult to design solutions to these dilemmas.
Strengths and limitations
To our knowledge, this is the first interview-based study examining SNF clinicians’ perspectives on unplanned, 30-day hospital readmissions. We gathered information from clinicians with a range of clinical experience, all of whom had cared directly for the patient who had been readmitted. Our data came from clinicians at 15 SNFs of varying sizes and quality ratings, allowing us to identify a broad range of factors contributing to readmissions.
Because this study relied on qualitative methods, it should be viewed as hypothesis-generating rather than hypothesis-confirming. Further research is needed to determine whether variables related to the themes above are causally linked to SNF readmissions. We identified cases for review using convenience sampling of a cohort of readmitted patients at a single tertiary-care hospital, and all participating SNFs were located in Connecticut. These factors may limit the generalizability of our findings. Although the clinicians we interviewed occupied diverse roles within their respective SNFs, our sample did not include direct-care staff without managerial responsibility, such as certified nursing assistants or licensed practical nurses. This prevented our study from identifying themes into which managers would have limited insight, especially those involving cultural and management practices leading to poor communication between them and their staff. Because our study examines cases in which discharge and readmission were to a general medicine service, it may not describe factors relevant to patients discharged from subspecialist or surgical services.
Implications for future QI efforts and research
Several clinicians we interviewed suggested that readmissions might be reduced by dedicating the services of a hospital professional, such as a nurse or case manager, to monitoring the clinical course of medically complex patients after discharge. A dedicated “transition coach” could clarify deficiencies in discharge paperwork, facilitate necessary follow-up appointments, liaise with staff at both the hospital and the SNF, or coordinate acquisition of necessary equipment. Prospective trials have demonstrated that such interventions can decrease readmission rates among hospitalized patients,22,23 but formal studies have not been carried out among cohorts of SNF patients.
Prior efforts to improve SNF-ED information sharing have focused on making sure that ED clinicians have important baseline information about patients transferred from a SNF.24,25 The experiences of SNF clinicians in our study suggest that important information also fails to make its way from ED providers to SNFs and that this failure results in unnecessary readmissions of relatively stable SNF patients. Thus, hospitals may be able to prevent SNF readmissions by creating lines of communication between EDs and SNFs and by ensuring that ED physicians and mid-level providers are familiar with the clinical capabilities of local SNFs.
Future research and QI work should also investigate approaches to care coordination that ensure that complex patients are placed in SNFs with resources adequate to address their comorbidities. Potential interventions might include increased use of SNF “liaisons,” who would evaluate patients in-person prior to approving transfer to a given SNF. As has been previously suggested,26 hospitals might also reduce readmissions by narrowing the pool of facilities to which they transfer patients, thereby building more robust, interconnected relationships with a smaller number of SNFs.
CONCLUSION
SNF clinicians identified areas for improvement at almost every point in the chain of events spanning hospitalization, discharge, and transfer. Among the most frequently cited contributors to readmissions were clinical instability at the time of discharge and omission of clinically important information from discharge documentation. Improved communication between hospitals, ED clinicians, and SNFs, as well as more thoroughly defined goals of care at the time of discharge, were seen as promising ways of decreasing readmissions. Successful interventions for reducing readmissions from SNFs will likely require multifaceted approaches to these problems.
Disclosure: This research was supported by a grant (#P30HS023554-01) from the Agency for Healthcare Research and Quality (AHRQ) and received support from Yale New Haven Hospital and the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (#P30AG021342 NIH/NIA).
Skilled nursing facilities (SNFs) play a crucial role in the hospital readmission process.Approximately 1 in 4 Medicare beneficiaries discharged from an acute care hospital is admitted to a SNF instead of returning directly home. Of these patients, 1 in 4 will be readmitted within 30 days,1 a rate significantly higher than the readmission rate of the inpatient population as a whole.2 The 2014 Protecting Access to Medicare Act created a value-based purchasing program that will use quality measures to steer funds to, or away from, individual SNFs. When the program takes effect in 2018, the Centers for Medicare & Medicaid Services will use SNFs’ 30-day all-cause readmission rate to determine which SNFs receive payments and which receive penalties.3 The Affordable Care Act, passed in 2010, has also established penalties for hospitals with higher than expected readmission rates for Medicare patients.4
Despite this intensifying regulatory focus, relatively little is known about the factors that drive readmissions from SNFs. A prospective review of data from SNFs in 4 states has shown that SNFs staffed by nurse practitioners or physician assistants and those equipped to provide intravenous therapy were less likely to transfer patients to the hospital for ambulatory care-sensitive diagnoses.5 Qualitative studies have provided useful insight into the causes of SNF-to-hospital transfers but have not focused on 30-day readmissions.6,7 A single survey-based study has examined the causes of SNF-to-hospital readmissions.8 However, survey-based methodologies have limited ability to capture the complex perspectives of SNF clinicians, who play a critical role in determining which SNF patients require evaluation or treatment in an acute care setting.
To address this gap in knowledge about factors contributing to SNF readmissions, we conducted a qualitative study examining SNF clinicians’ perspectives on patients readmitted to the hospital within 30 days of discharge. We used a structured interview tool to explore the root causes of readmission with frontline SNF staff, with the goal of using this knowledge to inform future hospital quality improvement (QI) efforts.
METHODS
Case Identification
Hospital data-tracking software (Allscripts) was used to identify patients who experienced a 30-day, unplanned readmission from SNFs to an academic medical center. We restricted our search to patients whose index admission and readmission were to the medical center’s inpatient general medicine service. A study team member (BWC) monitored the dataset on a weekly basis and contacted SNF clinicians by e-mail and telephone to arrange interviews at times of mutual convenience. To mitigate against recall bias, interviews were conducted within 30 days of the readmission in question. A total of 32 cases were identified. No SNF clinicians refused a request for interview. For 8 of these cases, it was not possible to find a time of mutual convenience within the specified 30-day window. The remaining 24 cases involved patients from 15 SNFs across Connecticut. Interviews were conducted from August 2015 to November 2015.
The project was reviewed by our institution’s Human Investigation Committee and was exempted from Institutional Review Board review.
Study Participants
Interviews were conducted on-site at SNFs with groups of 1 to 4 SNF clinicians and administrators. SNF participants were informed of interviewer credentials and the study’s QI goals prior to participation. Participation was voluntary and did not affect the clinician’s relationship with the hospital or the SNF. Participants were not paid.
DATA COLLECTION
Interventions to Reduce Acute Care Transfers (INTERACT) is a QI program that includes training for clinicians, communication tools, and advance care planning tools.9 INTERACT is currently used in 138 Connecticut SNFs as part of a statewide QI effort funded by the Connecticut State Department of Public Health. In prospective QI studies,10,11 implementation of INTERACT has been associated with decreased transfers from SNFs to acute care hospitals. The INTERACT Quality Improvement Tool, one part of the INTERACT bundle of interventions, is a 26-item questionnaire used to identify root causes of transfers from SNFs to acute care hospitals. It includes both checklists and open-ended questions about patient factors, SNF procedures, and SNF clinical decision-making.
We used the INTERACT QI Tool12 to conduct structured interviews with nurses and administrators at SNFs. Interviewers used a hard copy of the tool to maintain field notes, and all parts of the questionnaire were completed in each interview. Although the questionnaire elicits baseline demographic and medical information, such as the patient’s age and vital signs prior to readmission, the majority of each interview was dedicated to discussion of the open-ended questions in Table 1. Upon completion of the INTERACT QI Tool, the interviewer asked 2 open-ended questions about reducing readmissions and 4 closed-ended questions regarding SNF admission procedures. (Table 1) The supplemental questions were added after preliminary interviews with SNF clinicians revealed concerns about the SNF referral process and about communication between the hospital, emergency department (ED) and SNFs—issues not included in the INTERACT questionnaire. Interviewers used phatic communication, probing questions, and follow-up questions to elicit detailed information from participants, and participant responses were not limited to topics in the questionnaire and the list of supplemental questions.
Interviews were conducted by a hospital clinical integration coordinator, social worker, and a physician (KB, MCB, BWC). All interviewers received formal training in qualitative research methods prior to the study.
All interviews were audio recorded, with permission from the participants, and were professionally transcribed. Field notes were maintained to ensure accuracy of INTERACT QI Tool data. Participant interviews covered no more than two cases per session and lasted from 18 to 71 minutes (mean duration, 38 minutes).
Analysis
Analysis of transcripts was inductive and informed by grounded theory methodology, in which data is reviewed for repeating ideas, which are then analyzed and grouped to develop a theoretical understanding of the phenomenon under investigation.13,14
A preliminary codebook was developed using transcripts of the first 11 interviews. All statements relevant to the readmission process were extracted from the raw interview transcript and collected into a single list. This list was then reviewed for statements sharing a particular idea or concern. Such statements were grouped together under the heading of a repeating idea, and each repeating idea was assigned a code. Using this codebook, each transcript was independently reviewed and coded by three study team members with formal training in inductive qualitative analysis (KB, KTM, BWC). Reviewers assigned codes to sections of relevant text. Discrepancies in code assignment were discussed among the 3 analysts until consensus was reached. Using the method of constant comparison described in grounded theory,the codebook was updated continuously as the process of coding transcripts proceeded.12 Changes to the codebook were discussed among the coding team until consensus was achieved. The process of data acquisition and coding continued until theoretical saturation was reached. Themes relating to underlying factors associated with readmissions were then identified based on shared properties among repeating ideas. ATLAS.ti (Scientific Software, Berlin, Germany, Version 7) was used to facilitate data organization and retrieval.
RESULTS
The SNFs in our study included 12 for-profit and 3 non-profit facilities. The number of licensed beds in each facility ranged from 73 to 360, with a mean of 148 beds. The SNFs had CMS Nursing Home Compare ratings ranging from 1 star, the lowest possible rating, to 5 stars, the highest possible,15 with a mean rating of 2.9 stars. Our analysis did not reveal differences in perceived contributions to readmissions from large vs. small or highly rated vs poorly rated SNFs.
The patients in our analysis represented a highly comorbid and medically complex population (Table 3). Many had barriers to communication with clinical staff, including non–English-speaking status and underlying dementia.
Five main themes emerged from our analysis: (1) lack of coordination between EDs and SNFs; (2) incompletely addressed goals of care; (3) mismatch between patient clinical needs and SNF capabilities; (4) important clinical information not effectively communicated by hospital; and (5) challenges in SNF processes and culture.
Emergent transitions: Lack of coordination between ED and SNF
SNF clinicians frequently encountered situations in which a relatively stable patient was readmitted to the hospital after being transferred to the ED, despite the fact that SNF clinicians believed the patient should have returned to the SNF once a specific test was performed or service rendered at the ED. Commonly cited clinical scenarios that resulted in such readmissions included placement of urinary catheters and evaluation for cystitis. An assistant director of nursing reported that “the ER doesn’t want to hear my side of the story,” making it difficult for her to provide information that would prevent such readmissions. Other SNF clinicians reported similar difficulties in communicating with ED clinicians.
Code status: Incompletely addressed goals of care
The SNF clinicians in our study described cases in which patients with end-stage lung disease and disseminated cancer were readmitted to the hospital, despite SNF efforts to prevent readmission and provide palliative care within the SNF. For example, a SNF advanced practice nurse described a case in which a patient with widely metastatic cancer requested readmission to the hospital for treatment of deep vein thrombosis, despite longstanding recommendations from SNF staff that the patient forego hospitalization and enroll in hospice care. After discussion of code status and goals of care with hospital clinicians, the patient chose to enroll in hospice care and not to continue anticoagulation. SNF clinicians often perceived that, in the words of one administrator, “the palliative talks in the hospital outweigh our talks by a lot.” Numerous SNF clinicians believed that in-depth clarification of goals of care prior to discharge could prevent some readmissions.
Wrong patient, wrong place: Mismatch between clinical needs and SNF capabilities
One director of nursing stated that “[when] you read a referral, there’s a huge difference sometimes between what you read and what you see.” SNF clinicians reported that this discrepancy between clinical report and clinical reality often leads to patients being placed in SNFs that are unequipped to care for them. Many patients were perceived as being too ill for discharge from the acute-care setting in the first place. A nurse manager described this as a pattern of “pushing patients out of the hospital.” However, mismatches in clinical disposition were also seen as contributing to readmissions for medically stable patients, such as those with dementia, for whom SNFs frequently lack adequate staffing and physical safeguards.
Missing links: Important clinical information not effectively communicated by hospital
SNF clinicians described numerous challenges in formulating plans of care based on hospital discharge documentation. Discrepancies between discharge summaries and patient instructions were perceived as common and potential causes of readmissions. For patients discharged from the academic medical center in this study, medication instructions are included in both the discharge summary sent to the SNF and in a patient instruction packet. Several SNF clinicians said that it was common for a course of antibiotics to be listed on the discharge summary but not the patient instruction packet, or vice versa. SNF clinicians, who usually lack access to the hospital’s electronic medical record, have limited means for determining the correct document. Other important clinical data points, such as intermittent intravenous (IV) furosemide dosing and suppressive antibiotic regimens, were omitted from discharge paperwork altogether. SNF clinicians had difficulty reaching hospital clinicians who could clarify these clinical questions. “Good luck finding the person that took care of [the patient] three days before,” said one director of nursing.
Change starts at home: Challenges in SNF processes and culture
Many clinicians in our study reported that their facilities had recently added clinical capabilities in an effort to care for patients with complex medical problems. For example, to prevent transfers of patients with decompensated heart failure, several facilities in our study had recently obtained certification to give IV diuretics. However, as one director of nursing stated, these efforts require “buy-in” from doctors to decrease readmissions. That buy-in has not always been forthcoming. SNF clinicians also reported difficulty convincing patients and families that their facilities are capable of providing care that, in the past, might only have been available in acute-care settings.
These themes, along with associated sub-themes and representative quotations, are shown above (Table 4).
DISCUSSION
Our study suggests that the interaction between EDs and SNFs is an important and understudied domain in the spectrum of events leading to readmission. Prior studies have documented inadequacies in patient information provided by SNFs to EDs.16,17 Efforts to improve SNF-to-ED information sharing have focused on making sure that ED clinicians have important baseline information about patients transferred from a SNF.18,19 However, many of the clinicians in our study reported taking proactive steps to communicate with ED clinicians. These efforts encountered logistical and cultural barriers, with information that might have prevented readmission failing to reach ED providers. Many of the SNF clinicians in our study perceived this failure as a common cause of readmission, especially for relatively stable SNF patients.
Previous studies have pointed to a role for goals of care discussions in reducing hospital readmissions.20 Our data underscore an important qualification to these findings: Location matters. The SNF clinicians in our study reported frequent and detailed goals of care discussions with their patients. However, they also reported that goals of care discussions held in the subacute setting carried less weight with patients and families than discussions held in the hospital. SNF clinicians described a number of cases in which patients were willing to adjust code status or goals of care only after being readmitted to the hospital.
Our study also points to the implications of existing research showing that patients are discharged from acute care hospitals “quicker and sicker” than they had been prior to the 1983 adoption of Medicare’s prospective payment system.21 Specifically, the SNF clinicians we interviewed perceived a strong link between patient acuity at the time of transfer and SNFs’ persistently high readmission rates. As SNFs have worked to expand their clinical capabilities, they struggle to win buy-in from physicians and families, many of whom view SNFs as incapable of managing acute illness. Many SNF clinicians also pointed to deficiencies in their own referral and admission processes as a recurring cause of readmissions. For example, several patients in our analysis suffered from dementia. Although these patients were stable enough to leave the acute care setting, the SNF clinicians responsible for their readmissions felt that their SNFs were not well-equipped to care for patients with dementia and that the patients should instead have been transferred to facilities with more robust resources for dementia care.
Finally, our findings highlight a fundamental tension between hospitals and SNFs: Which facility ought to shoulder the responsibility and cost for services that may prevent a readmission—the hospital or the SNF? For example, does responsibility for coordinating subspecialist evaluation of a patient’s chronic condition fall to the hospital or to the SNF? If such an evaluation is undertaken during a hospitalization, it prolongs the patient’s hospital stay and happens at the hospital’s expense. If the patient is discharged to a SNF and sees the subspecialist in clinic, then the SNF must pay for transportation to and from the clinic appointment. SNF clinicians expressed near unanimity that fragmented models of care and high barriers to communication made it difficult to design solutions to these dilemmas.
Strengths and limitations
To our knowledge, this is the first interview-based study examining SNF clinicians’ perspectives on unplanned, 30-day hospital readmissions. We gathered information from clinicians with a range of clinical experience, all of whom had cared directly for the patient who had been readmitted. Our data came from clinicians at 15 SNFs of varying sizes and quality ratings, allowing us to identify a broad range of factors contributing to readmissions.
Because this study relied on qualitative methods, it should be viewed as hypothesis-generating rather than hypothesis-confirming. Further research is needed to determine whether variables related to the themes above are causally linked to SNF readmissions. We identified cases for review using convenience sampling of a cohort of readmitted patients at a single tertiary-care hospital, and all participating SNFs were located in Connecticut. These factors may limit the generalizability of our findings. Although the clinicians we interviewed occupied diverse roles within their respective SNFs, our sample did not include direct-care staff without managerial responsibility, such as certified nursing assistants or licensed practical nurses. This prevented our study from identifying themes into which managers would have limited insight, especially those involving cultural and management practices leading to poor communication between them and their staff. Because our study examines cases in which discharge and readmission were to a general medicine service, it may not describe factors relevant to patients discharged from subspecialist or surgical services.
Implications for future QI efforts and research
Several clinicians we interviewed suggested that readmissions might be reduced by dedicating the services of a hospital professional, such as a nurse or case manager, to monitoring the clinical course of medically complex patients after discharge. A dedicated “transition coach” could clarify deficiencies in discharge paperwork, facilitate necessary follow-up appointments, liaise with staff at both the hospital and the SNF, or coordinate acquisition of necessary equipment. Prospective trials have demonstrated that such interventions can decrease readmission rates among hospitalized patients,22,23 but formal studies have not been carried out among cohorts of SNF patients.
Prior efforts to improve SNF-ED information sharing have focused on making sure that ED clinicians have important baseline information about patients transferred from a SNF.24,25 The experiences of SNF clinicians in our study suggest that important information also fails to make its way from ED providers to SNFs and that this failure results in unnecessary readmissions of relatively stable SNF patients. Thus, hospitals may be able to prevent SNF readmissions by creating lines of communication between EDs and SNFs and by ensuring that ED physicians and mid-level providers are familiar with the clinical capabilities of local SNFs.
Future research and QI work should also investigate approaches to care coordination that ensure that complex patients are placed in SNFs with resources adequate to address their comorbidities. Potential interventions might include increased use of SNF “liaisons,” who would evaluate patients in-person prior to approving transfer to a given SNF. As has been previously suggested,26 hospitals might also reduce readmissions by narrowing the pool of facilities to which they transfer patients, thereby building more robust, interconnected relationships with a smaller number of SNFs.
CONCLUSION
SNF clinicians identified areas for improvement at almost every point in the chain of events spanning hospitalization, discharge, and transfer. Among the most frequently cited contributors to readmissions were clinical instability at the time of discharge and omission of clinically important information from discharge documentation. Improved communication between hospitals, ED clinicians, and SNFs, as well as more thoroughly defined goals of care at the time of discharge, were seen as promising ways of decreasing readmissions. Successful interventions for reducing readmissions from SNFs will likely require multifaceted approaches to these problems.
Disclosure: This research was supported by a grant (#P30HS023554-01) from the Agency for Healthcare Research and Quality (AHRQ) and received support from Yale New Haven Hospital and the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (#P30AG021342 NIH/NIA).
1. Mor V, Intrator O, Feng Z, et al. The revolving door of rehospitalization from skilled nursing facilities. Health Aff. 2010;29(1):57-64. PubMed
2. Department of Health and Human Services. Medicare.gov Hospital Compare. https://medicare .gov/hospitalcompare/compare. Accessed October 21, 2015.
3. Centers for Medicare and Medicaid Services. Proposed fiscal year 2016 payment and policy changes for Medicare Skilled Nursing Facilities. https://cms.gov. Accessed October 21, 2015.
4. The Patient Protection and Affordable Care Act: Detailed Summary. Democratic Policy and Communications Committee website. http://www.dpc.senate.gov/healthreformbill/healthbill04.pdf. Accessed August 22, 2016.
5. Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J Am Geriatr Soc. 2004;52:1730-1736. PubMed
6. Ouslander JG, Lamb G, Perloe M, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes and costs. J Am Geriatr Soc. 2010;58:627-635. PubMed
7. Lamb G, Tappen R, Diaz S, et al. Avoidability of hospital transfers of nursing home residents: perspectives of frontline staff. J Am Geriatr Soc. 2011;59:1665-1672. PubMed
8. Ouslander JG, Naharci I, Engstrom G, et al. Hospital transfers of skilled nursing facility (SNF) patients within 48 hours and 30 days after SNF admission. J Am Med Dir Assoc. 2016; doi: 10.1016/j.jamda.2016.05.021. PubMed
9. Ouslander JG, Lamb G, Tappen R et al. Interventions to reduce hospitalizations from nursing homes: Evaluation of the INTERACT II collaborative quality improvement project. J Am Geriatr Soc. 2011; 59:745-753. PubMed
10. Ouslander JG, Perloe M, Givens JH et al. Reducing potentially avoidable hospitalization of nursing home residents: Results of a pilot quality improvement project. J Am Med Dir Assoc. 2009; 10:644-652. PubMed
11. Tena-Nelson R, Santos K, Weingast E et al. Reducing preventable hospital transfers: Results from a thirty nursing home collaborative. J Am Med Dir Assoc. 2012; 13:651-656. PubMed
12. Florida Atlantic University. Interventions to Reduce Acute Care Transfers. https://interact2.net/docs/INTERACT%20Version%204.0%20Tools/INTERACT%204.0%20NH%20Tools%206_17_15/148604%20QI_Tool%20for%20Review%20Acute%20Care%20Transf_AL.pdf
13. Oktay, Julianne. Grounded Theory. New York: Oxford University Press, 2012.
14. Auerbach, Carl and Silverstein, Louise B. Qualitative Data. New York: NYU Press, 2003.
15. Department of Health and Human Services. Medicare.gov Nursing Home Compare. https://medicare .gov/nursinghomecompare. Accessed April 4, 2016.
16. Jones JS, Dwyer PR, White LJ, et al. Patient transfer from nursing home to emergency department: outcomes and policy implications. Acad Emerg Med. 1997 Sep;4(9):908-15. PubMed
17. Lahn M, Friedman B, Bijur P, et al. Advance directives in skilled nursing facility residents transferred to emergency departments. Acad Emerg Med. 2001 Dec;8(12):1158-62. PubMed
18. Madden C, Garrett J, Busby-Whitehead J. The interface between nursing homes and emergency departments: a community effort to improve transfer of information. Acad Emerg Med. 1998 Nov;5(11):1123-6. PubMed
19. Hustey FM, Palmer RM. An internet-based communication network for information transfer during patient transitions from skilled nursing facility to the emergency department. J Am Geriatr Soc. 2010 Jun;58(6):1148-52. PubMed
20. O’Connor N, Moyer ME, Behta M, et al. The Impact of Inpatient Palliative Care Consultations on 30-Day Hospital Readmissions. J Pall Med. 2015 Nov 1; 18(11):956-961. PubMed
21. Qian X, Russell LB, Valiyeva E, et al. “Quicker and sicker” under Medicare’s prospective payment system for hospitals: new evidence on an old issue from a national longitudinal survey. Bull Econ Res. 2011;63(1):1-27. PubMed
22. Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004 May;52(5):675-84. PubMed
23. Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006 Sep 25;166(17):1822-1828. PubMed
24. Madden C, Garrett J, Busby-Whitehead J. The interface between nursing homes and emergency departments: a community effort to improve transfer of information. Acad Emerg Med. 1998 Nov;5(11):1123-6. PubMed
25. Hustey FM, Palmer RM. An internet-based communication network for information transfer during patient transitions from skilled nursing facility to the emergency department. J Am Geriatr Soc. 2010 Jun;58(6):1148-52. PubMed
26. Rahman M, Foster AD, Grabowski DC, Zinn JS, Mor V. Effect of hospital-SNF referral linkages on rehospitalization. Health Serv Res. 2013 Dec;48(6 Pt 1):1898-919. PubMed
1. Mor V, Intrator O, Feng Z, et al. The revolving door of rehospitalization from skilled nursing facilities. Health Aff. 2010;29(1):57-64. PubMed
2. Department of Health and Human Services. Medicare.gov Hospital Compare. https://medicare .gov/hospitalcompare/compare. Accessed October 21, 2015.
3. Centers for Medicare and Medicaid Services. Proposed fiscal year 2016 payment and policy changes for Medicare Skilled Nursing Facilities. https://cms.gov. Accessed October 21, 2015.
4. The Patient Protection and Affordable Care Act: Detailed Summary. Democratic Policy and Communications Committee website. http://www.dpc.senate.gov/healthreformbill/healthbill04.pdf. Accessed August 22, 2016.
5. Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J Am Geriatr Soc. 2004;52:1730-1736. PubMed
6. Ouslander JG, Lamb G, Perloe M, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes and costs. J Am Geriatr Soc. 2010;58:627-635. PubMed
7. Lamb G, Tappen R, Diaz S, et al. Avoidability of hospital transfers of nursing home residents: perspectives of frontline staff. J Am Geriatr Soc. 2011;59:1665-1672. PubMed
8. Ouslander JG, Naharci I, Engstrom G, et al. Hospital transfers of skilled nursing facility (SNF) patients within 48 hours and 30 days after SNF admission. J Am Med Dir Assoc. 2016; doi: 10.1016/j.jamda.2016.05.021. PubMed
9. Ouslander JG, Lamb G, Tappen R et al. Interventions to reduce hospitalizations from nursing homes: Evaluation of the INTERACT II collaborative quality improvement project. J Am Geriatr Soc. 2011; 59:745-753. PubMed
10. Ouslander JG, Perloe M, Givens JH et al. Reducing potentially avoidable hospitalization of nursing home residents: Results of a pilot quality improvement project. J Am Med Dir Assoc. 2009; 10:644-652. PubMed
11. Tena-Nelson R, Santos K, Weingast E et al. Reducing preventable hospital transfers: Results from a thirty nursing home collaborative. J Am Med Dir Assoc. 2012; 13:651-656. PubMed
12. Florida Atlantic University. Interventions to Reduce Acute Care Transfers. https://interact2.net/docs/INTERACT%20Version%204.0%20Tools/INTERACT%204.0%20NH%20Tools%206_17_15/148604%20QI_Tool%20for%20Review%20Acute%20Care%20Transf_AL.pdf
13. Oktay, Julianne. Grounded Theory. New York: Oxford University Press, 2012.
14. Auerbach, Carl and Silverstein, Louise B. Qualitative Data. New York: NYU Press, 2003.
15. Department of Health and Human Services. Medicare.gov Nursing Home Compare. https://medicare .gov/nursinghomecompare. Accessed April 4, 2016.
16. Jones JS, Dwyer PR, White LJ, et al. Patient transfer from nursing home to emergency department: outcomes and policy implications. Acad Emerg Med. 1997 Sep;4(9):908-15. PubMed
17. Lahn M, Friedman B, Bijur P, et al. Advance directives in skilled nursing facility residents transferred to emergency departments. Acad Emerg Med. 2001 Dec;8(12):1158-62. PubMed
18. Madden C, Garrett J, Busby-Whitehead J. The interface between nursing homes and emergency departments: a community effort to improve transfer of information. Acad Emerg Med. 1998 Nov;5(11):1123-6. PubMed
19. Hustey FM, Palmer RM. An internet-based communication network for information transfer during patient transitions from skilled nursing facility to the emergency department. J Am Geriatr Soc. 2010 Jun;58(6):1148-52. PubMed
20. O’Connor N, Moyer ME, Behta M, et al. The Impact of Inpatient Palliative Care Consultations on 30-Day Hospital Readmissions. J Pall Med. 2015 Nov 1; 18(11):956-961. PubMed
21. Qian X, Russell LB, Valiyeva E, et al. “Quicker and sicker” under Medicare’s prospective payment system for hospitals: new evidence on an old issue from a national longitudinal survey. Bull Econ Res. 2011;63(1):1-27. PubMed
22. Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004 May;52(5):675-84. PubMed
23. Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006 Sep 25;166(17):1822-1828. PubMed
24. Madden C, Garrett J, Busby-Whitehead J. The interface between nursing homes and emergency departments: a community effort to improve transfer of information. Acad Emerg Med. 1998 Nov;5(11):1123-6. PubMed
25. Hustey FM, Palmer RM. An internet-based communication network for information transfer during patient transitions from skilled nursing facility to the emergency department. J Am Geriatr Soc. 2010 Jun;58(6):1148-52. PubMed
26. Rahman M, Foster AD, Grabowski DC, Zinn JS, Mor V. Effect of hospital-SNF referral linkages on rehospitalization. Health Serv Res. 2013 Dec;48(6 Pt 1):1898-919. PubMed
© 2017 Society of Hospital Medicine
Use of Post-Acute Facility Care in Children Hospitalized With Acute Respiratory Illness
Respiratory illness (RI) is one of the most common reasons for pediatric hospitalization.1 Examples of RI include acute illness, such as bronchiolitis, bacterial pneumonia, and asthma, as well as chronic conditions, such as obstructive sleep apnea and chronic respiratory insufficiency. Hospital care for RI includes monitoring and treatment to optimize oxygenation, ventilation, hydration, and other body functions. Most previously healthy children hospitalized with RI stay in the hospital for a limited duration (eg, a few days) because the severity of their illness is short lived and they quickly return to their previous healthy status.2 However, hospital care is increasing for children with fragile and tenuous health due to complex medical conditions.3 RI is a common reason for hospitalization among these children as well and recovery of respiratory health and function can be slow and protracted for some of them.4 Weeks, months, or longer periods of time may be necessary for the children to return to their previous respiratory baseline health and function after hospital discharge; other children may not return to their baseline.5,6
Hospitalized older adults with high-severity RI are routinely streamlined for transfer to post-acute facility care (PAC) shortly (eg, a few days) after acute-care hospitalization. Nearly 70% of elderly Medicare beneficiaries use PAC following a brief length of stay (LOS) in the acute-care hospital.7 It is believed that PAC helps optimize the patients’ health and functional status and relieves the family caregiving burden that would have occurred at home.8-10 PAC use also helps to shorten acute-care hospitalization for RI while avoiding readmission.8-10 In contrast with adult patients, use of PAC for hospitalized children is not routine.11 While PAC use in children is infrequent, RI is one of the most common reasons for acute admission among children who use it.12
For some children with RI, PAC might be positioned to offer a safe, therapeutic, and high-value setting for pulmonary rehabilitation, as well as related medical, nutritional, functional, and family cares.6 PAC, by design, could possibly help some of the children transition back into their homes and communities. As studies continue to emerge that assess the value of PAC in children, it is important to learn more about the use of PAC in children hospitalized with RI. The objectives were to (1) assess which children admitted with RI are the most likely to use PAC services for recovery and (2) estimate how many hospitalized children not using PAC had the same characteristics as those who did.
METHODS
Study Design, Setting, and Population
We conducted a retrospective cohort analysis of 609,800 hospitalizations for RI occurring from January 1, 2010 to December 31, 2015, in 43 freestanding children’s hospitals in the Pediatric Health Information Systems (PHIS) dataset. All hospitals participating in PHIS are members of the Children’s Hospital Association.13 The Boston Children’s Hospital Institutional Review Board approved this study with a waiver for informed consent.
RI was identified using the Agency for Healthcare Research and Quality (AHRQ) Clinical Classification System (CCS).14 Using diagnosis CCS category 8 (“Diseases of the Respiratory System”) and the procedure CCS category 6 (“Operations on the Respiratory System”), we identified all hospitalizations from the participating hospitals with a principal diagnosis or procedure International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code for an RI.
Main Outcome Measure
Discharge disposition following the acute-care hospitalization for RI was the main outcome measure. We used PHIS uniform disposition coding to classify the discharge disposition as transfer to PAC (ie, rehabilitation facility, skilled nursing facility, etc.) vs all other dispositions (ie, routine to home, against medical advice, etc.).12 The PAC disposition category was derived from the Centers for Medicare & Medicaid Services Patient Discharge Status Codes and Hospital Transfer Policies as informed by the National Uniform Billing Committee Official UB-04 Data Specifications Manual, 2008. PAC transfer included disposition to external PAC facilities, as well as to internal, embedded PAC units residing in a few of the acute-care children’s hospitals included in the cohort.
Demographic and Clinical Characteristics
We assessed patient demographic and clinical characteristics that might correlate with PAC use following acute-care hospitalization for RI. Demographic characteristics included gender, age at admission in years, payer (public, private, and other), and race/ethnicity (Hispanic, non-Hispanic black, non-Hispanic white, other).
Clinical characteristics included chronic conditions (type and number) and assistance with medical technology. Chronic condition and medical technology characteristics were assessed with ICD-9-CM diagnosis codes. PHIS contain up to 41 ICD-9-CM diagnosis codes per hospital discharge record. To identify the presence and number of chronic conditions, we used the AHRQ Chronic Condition Indicator system, which categorizes over 14,000 ICD-9-CM diagnosis codes into chronic vs non-chronic conditions.14,15 Children hospitalized with a chronic condition were further classified as having a complex chronic condition (CCC) using Feudtner and colleagues’ ICD-9-CM diagnosis classification scheme.16 CCCs represent defined diagnosis groupings expected to last longer than 12 months and involving either a single organ system, severe enough to require specialty pediatric care and hospitalization, or multiple organ systems.17,18 Hospitalized children who were assisted with medical technology were identified with ICD-9-CM codes indicating the use of a medical device to manage and treat a chronic illness (eg, ventricular shunt to treat hydrocephalus) or to maintain basic body functions necessary for sustaining life (eg, a tracheostomy tube for breathing).19,20 We distinguished children undergoing tracheotomy during hospitalization using ICD-9-CM procedure codes 31.1 and 31.2.
Acute-Care Hospitalization Characteristics
We also assessed the relationship between acute-care hospitalization characteristics and use of PAC after discharge, including US census region, LOS, use of intensive care, number of medication classes administered, and use of enhanced respiratory support. Enhanced respiratory support was defined as use of continuous or bilevel positive airway pressure (CPAP or BiPAP) or mechanical ventilation during the acute-care hospitalization for RI. These respiratory supports were identified using billing data in PHIS.
Statistical Analysis
In bivariable analysis, we compared demographic, clinical, and hospitalization characteristics of hospitalized children with vs without discharge to PAC using Rao-Scott chi-square tests and Wilcoxon rank-sum tests as appropriate. In multivariable analysis, we derived a generalized linear mix effects model with fixed effects for demographic, clinical, and hospitalization characteristics that were associated with PAC at P < 0.1 in bivariable analysis (ie, age, gender, race/ethnicity, payer, medical technology, use of intensive care unit [ICU], use of positive pressure or mechanical ventilation, hospital region, LOS, new tracheostomy, existing tracheostomy, other technologies, number of medications, number of chronic conditions [of any complexity], and type of complex chronic conditions). We controlled for clustering of patients within hospitals by including a random intercept for each hospital. We also assessed combinations of patient characteristics on the likelihood of PAC use with classification and regression tree (CART) modeling. Using CART, we determined which characteristic combinations were associated with the highest and lowest use of PAC using binary split and post-pruning, goodness of fit rules.21 All statistical analyses were performed using SAS v.9.4 (SAS Institute, Cary, NC), and R v.3.2 (R Foundation for Statistical Computing, Vienna, Austria) using the “party” package. The threshold for statistical significance was set at P < 0.05.
RESULTS
Of the 609,800 hospitalizations for RI, PAC use after discharge occurred for 2660 (0.4%). RI discharges to PAC accounted for 2.1% (n = 67,405) of hospital days and 2.7% ($280 million) of hospital cost of all RI hospitalizations. For discharges to PAC, the most common RI were pneumonia (29.1% [n = 773]), respiratory failure or insufficiency (unspecified reason; 22.0% [n = 584]), and upper respiratory infection (12.2% [n = 323]).
Demographic Characteristics
Median age at acute-care admission was higher for PAC vs non-PAC discharges (6 years [interquartile range {IQR} 1-15] vs 2 years [0-7], P < 0.001; Table 1). Hispanic patients accounted for a smaller percentage of RI discharges to PAC vs non-PAC (14.1% vs 21.8%, P < 0.001) and a higher percentage to PAC were for patients with public insurance (75.9% vs 62.5, P < 0.001; Table 1).
Clinical Characteristics
A greater percentage of RI hospitalizations discharged to PAC vs not-PAC had ≥1 CCC (94.9% vs 33.5%), including a neuromuscular CCC (57.5% vs 8.9%) or respiratory CCC (62.5% vs 12.0%), P < 0.001 for all (Table 2). A greater percentage discharged to PAC was assisted with medical technology (83.2% vs 15.1%), including respiratory technology (eg, tracheostomy; 53.8% vs 5.4%) and gastrointestinal technology (eg, gastrostomy; 71.9% vs 11.8%), P < 0.001 for all. Of the children with respiratory technology, 14.8% (n = 394) underwent tracheotomy during the acute-care hospitalization. Children discharged to PAC had a higher percentage of multiple chronic conditions. For example, the percentages of children discharged to PAC vs not with ≥7 conditions were 54.5% vs 7.0% (P < 0.001; Table 2). The most common chronic conditions experienced by children discharged to PAC included epilepsy (41.2%), gastroesophageal reflux (36.6%), cerebral palsy (28.2%), and asthma (18.2%).
Hospitalization Characteristics
Acute-care RI hospitalization median LOS was longer for discharges to PAC vs non-PAC (10 days [IQR 4-27] vs 2 days [IQR 1-4], P < 0.001; Table 1). A greater percentage of discharges to PAC were administered medications from multiple classes during the acute-care RI admission (eg, 54.8% vs 13.4% used medications from ≥7 classes, P < 0.001). A greater percentage of discharges to PAC used intensive care services during the acute-care admission (65.6% vs 22.4%, P < 0.001). A greater percentage of discharges to PAC received CPAP (10.6 vs 5.0%), BiPAP (19.8% vs 11.4%), or mechanical ventilation (52.7% vs 9.1%) during the acute-care RI hospitalization (P < 0.001 for all; Table 1).
Multivariable Analysis of the Likelihood of Post-Acute Care Use Following Discharge
In multivariable analysis, the patient characteristics associated with the highest likelihood of discharge to PAC included ≥11 vs no chronic conditions (odds ratio [OR] 11.8 , 95% CI, 8.0-17.2), ≥9 classes vs no classes of medications administered during the acute-care hospitalization (OR 4.8 , 95% CI, 1.8-13.0), and existing tracheostomy (OR 3.0, [95% CI, 2.6-3.5; Figure 2 and eTable). Patient characteristics associated with a more modest likelihood of discharge to PAC included public vs private insurance (OR 1.8, 95% CI, 1.6-2.0), neuromuscular complex chronic condition (OR 1.6, 95% CI, 1.5-1.8), new tracheostomy (OR 1.9, 95% CI, 1.7-2.2), and use of any enhanced respiratory support (ie, CPAP/BiPAP/mechanical ventilation) during the acute-care hospitalization (OR 1.4, 95% CI, 1.3-1.6; Figure 2 and Supplementary Table).
Classification and Regression Tree Analysis
In the CART analysis, the highest percentage (6.3%) of children hospitalized with RI who were discharged to PAC had the following combination of characteristics: ≥6 chronic conditions, ≥7 classes of medications administered, and respiratory technology. Median (IQR) length of acute-care LOS for children with these attributes who were transferred to PAC was 19 (IQR 8-56; range 1-1005) days; LOS remained long (median 13 days [IQR 6-41, range 1-1413]) for children with the same attributes not transferred to PAC (n = 9448). Between these children transferred vs not to PAC, 79.3% vs 65.9% received ICU services; 74.4% vs 73.5% received CPAP, BiPAP, or mechanical ventilation; and 31.0% vs 22.7% underwent tracheotomy during the acute-care hospitalization. Of these children who were not transferred to PAC, 18.9% were discharged to home nursing services.
DISCUSSION
The findings from the present study suggest that patients with RI hospitalization in children’s hospitals who use PAC are medically complex, with high rates of multiple chronic conditions—including cerebral palsy, asthma, chronic respiratory insufficiency, dysphagia, epilepsy, and gastroesophageal reflux—and high rates of technology assistance including enterostomy and tracheostomy. The characteristics of patients most likely to use PAC include long LOS, a large number of chronic conditions, many types of medications administered during the acute-care hospitalization, respiratory technology use, and an underlying neuromuscular condition. Specifically, the highest percentage of children hospitalized with RI who were discharged to PAC had ≥6 chronic conditions, ≥7 classes of medications administered, and respiratory technology. Our analysis suggests that there may be a large population of children with these same characteristics who experienced a prolonged LOS but were not transferred to PAC.
There are several reasons to explain why children hospitalized with RI who rely on medical technology, such as existing tracheostomy, are more likely to use PAC. Tracheostomy often indicates the presence of life-limiting impairment in oxygenation or ventilation, thereby representing a high degree of medical fragility. Tracheostomy, in some cases, offers enhanced ability to assist with RI treatment, including establishment of airway clearance of secretions (ie, suctioning and chest physiotherapy), administration of antimicrobials (eg, nebulized antibiotics), and optimization of ventilation (eg, non-invasive positive airway pressure). However, not all acute-care inpatient clinicians have experience and clinical proficiencies in the care of children with pediatric tracheostomy.23 As a result, a more cautious approach, with prolonged LOS and gradual arrival to hospital discharge, is often taken in the acute-care hospital setting for children with tracheostomy. Tracheostomy care delivered during recovery from RI by trained and experienced teams of providers in the PAC setting may be best positioned to help optimize respiratory health and ensure proper family education and readiness to continue care at home.6
Further investigation is needed of the long LOS in children not transferred to PAC who had similar characteristics to those who were transferred. In hospitalized adult patients with RI, PAC is routinely introduced early in the admission process, with anticipated transfer within a few days into the hospitalization. In the current study, LOS was nearly 2 weeks or longer in many children not transferred to PAC who had similar characteristics to those who were transferred. Perhaps some of the children not transferred experienced long LOS in the acute-care hospital because of a limited number of pediatric PAC beds in their local area. Some families of these children may have been offered but declined use of PAC. PAC may not have been offered to some because illness acuity was too high or there was lack of PAC awareness as a possible setting for recovery.
There are several limitations to this study. PHIS does not contain non-freestanding children’s hospitals; therefore, the study results may generalize best to children’s hospitals. PHIS does not contain information on the amount (eg, number of days used), cost, or treatments provided in PAC. Therefore, we were unable to determine the true reasons why children used PAC services following RI hospitalization (eg, for respiratory rehabilitation vs other reasons, such as epilepsy or nutrition/hydration management). Moreover, we could not assess which children truly used PAC for short-term recovery vs longer-term care because they were unable to reside at home (eg, they were too medically complex). We were unable to assess PAC availability (eg, number of beds) in the surrounding areas of the acute-care hospitals in the PHIS database. Although we assessed use of medical technology, PHIS does not contain data on functional status or activities of daily living, which correlate with the use of PAC in adults. We could not distinguish whether children receiving BiPAP, CPAP, or mechanical ventilation during hospitalization were using it chronically. Although higher PAC use was associated with public insurance, due to absent information on the children’s home, family, and social environment, we were unable to assess whether PAC use was influenced by limited caregiving support or resources.
Data on the type and number of chronic conditions are limited by the ICD-9-CM codes available to distinguish them. Although several patient demographic and clinical characteristics were significantly associated with the use of PAC, significance may have occurred because of the large sample size and consequent robust statistical power. This is why we elected to highlight and discuss the characteristics with the strongest and most clinically meaningful associations (eg, multiple chronic conditions). There may be additional characteristics, including social, familial, and community resources, that are not available to assess in PHIS that could have affected PAC use.
Despite these limitations, the current study suggests that the characteristics of children hospitalized with RI who use PAC for recovery are evident and that there is a large population of children with these characteristics who experienced a prolonged LOS that did not result in transfer to PAC. These findings could be used in subsequent studies to help create the base of a matched cohort of children with similar clinical, demographic, and hospitalization characteristics who used vs didn’t use PAC. Comparison of the functional status, health trajectory, and family and/or social attributes of these 2 groups of children, as well as their post-discharge outcomes and utilization (eg, length of PAC stay, emergency department revisits, and acute-care hospital readmissions), could occur with chart review, clinician and parent interview, and other methods. This body of work might ultimately lead to an assessment of value in PAC and potentially help us understand the need for PAC capacity in various communities. In the meantime, clinicians may find it useful to consider the results of the current study when contemplating PAC use in their hospitalized children with RI, including exploration of health system opportunities of clinical collaboration between acute-care children’s hospitals and PAC facilities. Ultimately, all of this work will generate meaningful knowledge regarding the most appropriate, safe, and cost-effective settings for hospitalized children with RI to regain their health.
Acknowledgments
Dr. Berry was supported by the Agency for Healthcare Research and Quality (R21 HS023092-01), the Lucile Packard Foundation for Children’s Health, and Franciscan Hospital for Children. The funders were not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclosure: The authors have no financial relationships relevant to this article to disclose.
1. Friedman B, Berdahl T, Simpson LA, et al. Annual report on health care for children and youth in the United States: focus on trends in hospital use and quality. Acad Pediatr. 2011;11(4):263-279. PubMed
2. Srivastava R, Homer CJ. Length of stay for common pediatric conditions: teaching versus nonteaching hospitals. Pediatrics. 2003;112(2):278-281. PubMed
3. Berry JG, Hall M, Hall DE, et al. Inpatient growth and resource use in 28 children’s hospitals: a longitudinal, multi-institutional study. JAMA Pediatr. 2013;167(2):170-177. PubMed
4. Gold JM, Hall M, Shah SS, et al. Long length of hospital stay in children with medical complexity. J Hosp Med. 2016;11(11):750-756. PubMed
5. Faultner J. Integrating medical plans within family life. JAMA Pediatr. 2014;168(10):891-892. PubMed
6. O’Brien JE, Haley SM, Dumas HM, et al. Outcomes of post-acute hospital episodes for young children requiring airway support. Dev Neurorehabil. 2007;10(3):241-247. PubMed
7. Morley M, Bogasky S, Gage B, et al. Medicare post-acute care episodes and payment bundling. Medicare Medicaid Res Rev. 2014;4(1):mmrr.004.01.b02. PubMed
8. Mentro AM, Steward DK. Caring for medically fragile children in the home: an alternative theoretical approach. Res Theory Nurs Pract. 2002;16(3):161-177. PubMed
9. Thyen U, Kuhlthau K, Perrin JM. Employment, child care, and mental health of mothers caring for children assisted by technology. Pediatrics. 1999;103(6 Pt 1):1235-1242. PubMed
10. Thyen U, Terres NM, Yazdgerdi SR, Perrin JM. Impact of long-term care of children assisted by technology on maternal health. J Dev Behav Pediatr. 1998;19(4):273-282. PubMed
11. O’Brien JE, Berry J, Dumas H. Pediatric Post-acute hospital care: striving for identity and value. Hosp Pediatr. 2015;5(10):548-551. PubMed
12. Berry JG, Hall M, Dumas H, et al. Pediatric hospital discharges to home health and postacute facility care: a national study. JAMA Pediatr. 2016;170(4):326-333. PubMed
13. Children’s Hospital Association. Pediatric Health Information System. https://childrenshospitals.org/Programs-and-Services/Data-Analytics-and-Research/Pediatric-Analytic-Solutions/Pediatric-Health-Information-System. Accessed June 12, 2017.
14. Agency for Healthcare Research and Quality. Chronic Condition Indicator. http://www.hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp. Accessed on June 19, 2017.
15. Berry JG, Ash AS, Cohen E, Hasan F, Feudtner C, Hall M. Contributions of children with multiple chronic conditions to pediatric hospitalizations in the United States: A Retrospective Cohort Analysis [published online ahead of print June 20, 2017]. Hosp Pediatr. 2017 Jun 20. doi: 10.1542/hpeds.2016-0179. PubMed
16. Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:199. PubMed
17. Cohen E, Kuo DZ, Agrawal R, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529-538. PubMed
18. Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980-1997. Pediatrics. 2000;106(1 Pt 2):205-209. PubMed
19. Palfrey JS, Walker DK, Haynie M, et al. Technology’s children: report of a statewide census of children dependent on medical supports. Pediatrics. 1991;87(5):611-618. PubMed
20. Feudtner C, Villareale NL, Morray B, Sharp V, Hays RM, Neff JM. Technology-dependency among patients discharged from a children’s hospital: a retrospective cohort study. BMC Pediatr. 2005;5(1):8. PubMed
21. Breiman L, Freidman J, Stone CJ, Olshen RA. Classification and Regression Trees. Belmont, CA: Wadsworth International; 1984.
22. Thomson J, Hall M, Ambroggio L, et al. Aspiration and Non-Aspiration Pneumonia in Hospitalized Children With Neurologic Impairment. Pediatrics. 2016;137(2):e20151612. PubMed
23. Berry JG, Goldmann DA, Mandl KD, et al. Health information management and perceptions of the quality of care for children with tracheotomy: a qualitative study. BMC Health Serv Res. 2011;11:117. PubMed
Respiratory illness (RI) is one of the most common reasons for pediatric hospitalization.1 Examples of RI include acute illness, such as bronchiolitis, bacterial pneumonia, and asthma, as well as chronic conditions, such as obstructive sleep apnea and chronic respiratory insufficiency. Hospital care for RI includes monitoring and treatment to optimize oxygenation, ventilation, hydration, and other body functions. Most previously healthy children hospitalized with RI stay in the hospital for a limited duration (eg, a few days) because the severity of their illness is short lived and they quickly return to their previous healthy status.2 However, hospital care is increasing for children with fragile and tenuous health due to complex medical conditions.3 RI is a common reason for hospitalization among these children as well and recovery of respiratory health and function can be slow and protracted for some of them.4 Weeks, months, or longer periods of time may be necessary for the children to return to their previous respiratory baseline health and function after hospital discharge; other children may not return to their baseline.5,6
Hospitalized older adults with high-severity RI are routinely streamlined for transfer to post-acute facility care (PAC) shortly (eg, a few days) after acute-care hospitalization. Nearly 70% of elderly Medicare beneficiaries use PAC following a brief length of stay (LOS) in the acute-care hospital.7 It is believed that PAC helps optimize the patients’ health and functional status and relieves the family caregiving burden that would have occurred at home.8-10 PAC use also helps to shorten acute-care hospitalization for RI while avoiding readmission.8-10 In contrast with adult patients, use of PAC for hospitalized children is not routine.11 While PAC use in children is infrequent, RI is one of the most common reasons for acute admission among children who use it.12
For some children with RI, PAC might be positioned to offer a safe, therapeutic, and high-value setting for pulmonary rehabilitation, as well as related medical, nutritional, functional, and family cares.6 PAC, by design, could possibly help some of the children transition back into their homes and communities. As studies continue to emerge that assess the value of PAC in children, it is important to learn more about the use of PAC in children hospitalized with RI. The objectives were to (1) assess which children admitted with RI are the most likely to use PAC services for recovery and (2) estimate how many hospitalized children not using PAC had the same characteristics as those who did.
METHODS
Study Design, Setting, and Population
We conducted a retrospective cohort analysis of 609,800 hospitalizations for RI occurring from January 1, 2010 to December 31, 2015, in 43 freestanding children’s hospitals in the Pediatric Health Information Systems (PHIS) dataset. All hospitals participating in PHIS are members of the Children’s Hospital Association.13 The Boston Children’s Hospital Institutional Review Board approved this study with a waiver for informed consent.
RI was identified using the Agency for Healthcare Research and Quality (AHRQ) Clinical Classification System (CCS).14 Using diagnosis CCS category 8 (“Diseases of the Respiratory System”) and the procedure CCS category 6 (“Operations on the Respiratory System”), we identified all hospitalizations from the participating hospitals with a principal diagnosis or procedure International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code for an RI.
Main Outcome Measure
Discharge disposition following the acute-care hospitalization for RI was the main outcome measure. We used PHIS uniform disposition coding to classify the discharge disposition as transfer to PAC (ie, rehabilitation facility, skilled nursing facility, etc.) vs all other dispositions (ie, routine to home, against medical advice, etc.).12 The PAC disposition category was derived from the Centers for Medicare & Medicaid Services Patient Discharge Status Codes and Hospital Transfer Policies as informed by the National Uniform Billing Committee Official UB-04 Data Specifications Manual, 2008. PAC transfer included disposition to external PAC facilities, as well as to internal, embedded PAC units residing in a few of the acute-care children’s hospitals included in the cohort.
Demographic and Clinical Characteristics
We assessed patient demographic and clinical characteristics that might correlate with PAC use following acute-care hospitalization for RI. Demographic characteristics included gender, age at admission in years, payer (public, private, and other), and race/ethnicity (Hispanic, non-Hispanic black, non-Hispanic white, other).
Clinical characteristics included chronic conditions (type and number) and assistance with medical technology. Chronic condition and medical technology characteristics were assessed with ICD-9-CM diagnosis codes. PHIS contain up to 41 ICD-9-CM diagnosis codes per hospital discharge record. To identify the presence and number of chronic conditions, we used the AHRQ Chronic Condition Indicator system, which categorizes over 14,000 ICD-9-CM diagnosis codes into chronic vs non-chronic conditions.14,15 Children hospitalized with a chronic condition were further classified as having a complex chronic condition (CCC) using Feudtner and colleagues’ ICD-9-CM diagnosis classification scheme.16 CCCs represent defined diagnosis groupings expected to last longer than 12 months and involving either a single organ system, severe enough to require specialty pediatric care and hospitalization, or multiple organ systems.17,18 Hospitalized children who were assisted with medical technology were identified with ICD-9-CM codes indicating the use of a medical device to manage and treat a chronic illness (eg, ventricular shunt to treat hydrocephalus) or to maintain basic body functions necessary for sustaining life (eg, a tracheostomy tube for breathing).19,20 We distinguished children undergoing tracheotomy during hospitalization using ICD-9-CM procedure codes 31.1 and 31.2.
Acute-Care Hospitalization Characteristics
We also assessed the relationship between acute-care hospitalization characteristics and use of PAC after discharge, including US census region, LOS, use of intensive care, number of medication classes administered, and use of enhanced respiratory support. Enhanced respiratory support was defined as use of continuous or bilevel positive airway pressure (CPAP or BiPAP) or mechanical ventilation during the acute-care hospitalization for RI. These respiratory supports were identified using billing data in PHIS.
Statistical Analysis
In bivariable analysis, we compared demographic, clinical, and hospitalization characteristics of hospitalized children with vs without discharge to PAC using Rao-Scott chi-square tests and Wilcoxon rank-sum tests as appropriate. In multivariable analysis, we derived a generalized linear mix effects model with fixed effects for demographic, clinical, and hospitalization characteristics that were associated with PAC at P < 0.1 in bivariable analysis (ie, age, gender, race/ethnicity, payer, medical technology, use of intensive care unit [ICU], use of positive pressure or mechanical ventilation, hospital region, LOS, new tracheostomy, existing tracheostomy, other technologies, number of medications, number of chronic conditions [of any complexity], and type of complex chronic conditions). We controlled for clustering of patients within hospitals by including a random intercept for each hospital. We also assessed combinations of patient characteristics on the likelihood of PAC use with classification and regression tree (CART) modeling. Using CART, we determined which characteristic combinations were associated with the highest and lowest use of PAC using binary split and post-pruning, goodness of fit rules.21 All statistical analyses were performed using SAS v.9.4 (SAS Institute, Cary, NC), and R v.3.2 (R Foundation for Statistical Computing, Vienna, Austria) using the “party” package. The threshold for statistical significance was set at P < 0.05.
RESULTS
Of the 609,800 hospitalizations for RI, PAC use after discharge occurred for 2660 (0.4%). RI discharges to PAC accounted for 2.1% (n = 67,405) of hospital days and 2.7% ($280 million) of hospital cost of all RI hospitalizations. For discharges to PAC, the most common RI were pneumonia (29.1% [n = 773]), respiratory failure or insufficiency (unspecified reason; 22.0% [n = 584]), and upper respiratory infection (12.2% [n = 323]).
Demographic Characteristics
Median age at acute-care admission was higher for PAC vs non-PAC discharges (6 years [interquartile range {IQR} 1-15] vs 2 years [0-7], P < 0.001; Table 1). Hispanic patients accounted for a smaller percentage of RI discharges to PAC vs non-PAC (14.1% vs 21.8%, P < 0.001) and a higher percentage to PAC were for patients with public insurance (75.9% vs 62.5, P < 0.001; Table 1).
Clinical Characteristics
A greater percentage of RI hospitalizations discharged to PAC vs not-PAC had ≥1 CCC (94.9% vs 33.5%), including a neuromuscular CCC (57.5% vs 8.9%) or respiratory CCC (62.5% vs 12.0%), P < 0.001 for all (Table 2). A greater percentage discharged to PAC was assisted with medical technology (83.2% vs 15.1%), including respiratory technology (eg, tracheostomy; 53.8% vs 5.4%) and gastrointestinal technology (eg, gastrostomy; 71.9% vs 11.8%), P < 0.001 for all. Of the children with respiratory technology, 14.8% (n = 394) underwent tracheotomy during the acute-care hospitalization. Children discharged to PAC had a higher percentage of multiple chronic conditions. For example, the percentages of children discharged to PAC vs not with ≥7 conditions were 54.5% vs 7.0% (P < 0.001; Table 2). The most common chronic conditions experienced by children discharged to PAC included epilepsy (41.2%), gastroesophageal reflux (36.6%), cerebral palsy (28.2%), and asthma (18.2%).
Hospitalization Characteristics
Acute-care RI hospitalization median LOS was longer for discharges to PAC vs non-PAC (10 days [IQR 4-27] vs 2 days [IQR 1-4], P < 0.001; Table 1). A greater percentage of discharges to PAC were administered medications from multiple classes during the acute-care RI admission (eg, 54.8% vs 13.4% used medications from ≥7 classes, P < 0.001). A greater percentage of discharges to PAC used intensive care services during the acute-care admission (65.6% vs 22.4%, P < 0.001). A greater percentage of discharges to PAC received CPAP (10.6 vs 5.0%), BiPAP (19.8% vs 11.4%), or mechanical ventilation (52.7% vs 9.1%) during the acute-care RI hospitalization (P < 0.001 for all; Table 1).
Multivariable Analysis of the Likelihood of Post-Acute Care Use Following Discharge
In multivariable analysis, the patient characteristics associated with the highest likelihood of discharge to PAC included ≥11 vs no chronic conditions (odds ratio [OR] 11.8 , 95% CI, 8.0-17.2), ≥9 classes vs no classes of medications administered during the acute-care hospitalization (OR 4.8 , 95% CI, 1.8-13.0), and existing tracheostomy (OR 3.0, [95% CI, 2.6-3.5; Figure 2 and eTable). Patient characteristics associated with a more modest likelihood of discharge to PAC included public vs private insurance (OR 1.8, 95% CI, 1.6-2.0), neuromuscular complex chronic condition (OR 1.6, 95% CI, 1.5-1.8), new tracheostomy (OR 1.9, 95% CI, 1.7-2.2), and use of any enhanced respiratory support (ie, CPAP/BiPAP/mechanical ventilation) during the acute-care hospitalization (OR 1.4, 95% CI, 1.3-1.6; Figure 2 and Supplementary Table).
Classification and Regression Tree Analysis
In the CART analysis, the highest percentage (6.3%) of children hospitalized with RI who were discharged to PAC had the following combination of characteristics: ≥6 chronic conditions, ≥7 classes of medications administered, and respiratory technology. Median (IQR) length of acute-care LOS for children with these attributes who were transferred to PAC was 19 (IQR 8-56; range 1-1005) days; LOS remained long (median 13 days [IQR 6-41, range 1-1413]) for children with the same attributes not transferred to PAC (n = 9448). Between these children transferred vs not to PAC, 79.3% vs 65.9% received ICU services; 74.4% vs 73.5% received CPAP, BiPAP, or mechanical ventilation; and 31.0% vs 22.7% underwent tracheotomy during the acute-care hospitalization. Of these children who were not transferred to PAC, 18.9% were discharged to home nursing services.
DISCUSSION
The findings from the present study suggest that patients with RI hospitalization in children’s hospitals who use PAC are medically complex, with high rates of multiple chronic conditions—including cerebral palsy, asthma, chronic respiratory insufficiency, dysphagia, epilepsy, and gastroesophageal reflux—and high rates of technology assistance including enterostomy and tracheostomy. The characteristics of patients most likely to use PAC include long LOS, a large number of chronic conditions, many types of medications administered during the acute-care hospitalization, respiratory technology use, and an underlying neuromuscular condition. Specifically, the highest percentage of children hospitalized with RI who were discharged to PAC had ≥6 chronic conditions, ≥7 classes of medications administered, and respiratory technology. Our analysis suggests that there may be a large population of children with these same characteristics who experienced a prolonged LOS but were not transferred to PAC.
There are several reasons to explain why children hospitalized with RI who rely on medical technology, such as existing tracheostomy, are more likely to use PAC. Tracheostomy often indicates the presence of life-limiting impairment in oxygenation or ventilation, thereby representing a high degree of medical fragility. Tracheostomy, in some cases, offers enhanced ability to assist with RI treatment, including establishment of airway clearance of secretions (ie, suctioning and chest physiotherapy), administration of antimicrobials (eg, nebulized antibiotics), and optimization of ventilation (eg, non-invasive positive airway pressure). However, not all acute-care inpatient clinicians have experience and clinical proficiencies in the care of children with pediatric tracheostomy.23 As a result, a more cautious approach, with prolonged LOS and gradual arrival to hospital discharge, is often taken in the acute-care hospital setting for children with tracheostomy. Tracheostomy care delivered during recovery from RI by trained and experienced teams of providers in the PAC setting may be best positioned to help optimize respiratory health and ensure proper family education and readiness to continue care at home.6
Further investigation is needed of the long LOS in children not transferred to PAC who had similar characteristics to those who were transferred. In hospitalized adult patients with RI, PAC is routinely introduced early in the admission process, with anticipated transfer within a few days into the hospitalization. In the current study, LOS was nearly 2 weeks or longer in many children not transferred to PAC who had similar characteristics to those who were transferred. Perhaps some of the children not transferred experienced long LOS in the acute-care hospital because of a limited number of pediatric PAC beds in their local area. Some families of these children may have been offered but declined use of PAC. PAC may not have been offered to some because illness acuity was too high or there was lack of PAC awareness as a possible setting for recovery.
There are several limitations to this study. PHIS does not contain non-freestanding children’s hospitals; therefore, the study results may generalize best to children’s hospitals. PHIS does not contain information on the amount (eg, number of days used), cost, or treatments provided in PAC. Therefore, we were unable to determine the true reasons why children used PAC services following RI hospitalization (eg, for respiratory rehabilitation vs other reasons, such as epilepsy or nutrition/hydration management). Moreover, we could not assess which children truly used PAC for short-term recovery vs longer-term care because they were unable to reside at home (eg, they were too medically complex). We were unable to assess PAC availability (eg, number of beds) in the surrounding areas of the acute-care hospitals in the PHIS database. Although we assessed use of medical technology, PHIS does not contain data on functional status or activities of daily living, which correlate with the use of PAC in adults. We could not distinguish whether children receiving BiPAP, CPAP, or mechanical ventilation during hospitalization were using it chronically. Although higher PAC use was associated with public insurance, due to absent information on the children’s home, family, and social environment, we were unable to assess whether PAC use was influenced by limited caregiving support or resources.
Data on the type and number of chronic conditions are limited by the ICD-9-CM codes available to distinguish them. Although several patient demographic and clinical characteristics were significantly associated with the use of PAC, significance may have occurred because of the large sample size and consequent robust statistical power. This is why we elected to highlight and discuss the characteristics with the strongest and most clinically meaningful associations (eg, multiple chronic conditions). There may be additional characteristics, including social, familial, and community resources, that are not available to assess in PHIS that could have affected PAC use.
Despite these limitations, the current study suggests that the characteristics of children hospitalized with RI who use PAC for recovery are evident and that there is a large population of children with these characteristics who experienced a prolonged LOS that did not result in transfer to PAC. These findings could be used in subsequent studies to help create the base of a matched cohort of children with similar clinical, demographic, and hospitalization characteristics who used vs didn’t use PAC. Comparison of the functional status, health trajectory, and family and/or social attributes of these 2 groups of children, as well as their post-discharge outcomes and utilization (eg, length of PAC stay, emergency department revisits, and acute-care hospital readmissions), could occur with chart review, clinician and parent interview, and other methods. This body of work might ultimately lead to an assessment of value in PAC and potentially help us understand the need for PAC capacity in various communities. In the meantime, clinicians may find it useful to consider the results of the current study when contemplating PAC use in their hospitalized children with RI, including exploration of health system opportunities of clinical collaboration between acute-care children’s hospitals and PAC facilities. Ultimately, all of this work will generate meaningful knowledge regarding the most appropriate, safe, and cost-effective settings for hospitalized children with RI to regain their health.
Acknowledgments
Dr. Berry was supported by the Agency for Healthcare Research and Quality (R21 HS023092-01), the Lucile Packard Foundation for Children’s Health, and Franciscan Hospital for Children. The funders were not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclosure: The authors have no financial relationships relevant to this article to disclose.
Respiratory illness (RI) is one of the most common reasons for pediatric hospitalization.1 Examples of RI include acute illness, such as bronchiolitis, bacterial pneumonia, and asthma, as well as chronic conditions, such as obstructive sleep apnea and chronic respiratory insufficiency. Hospital care for RI includes monitoring and treatment to optimize oxygenation, ventilation, hydration, and other body functions. Most previously healthy children hospitalized with RI stay in the hospital for a limited duration (eg, a few days) because the severity of their illness is short lived and they quickly return to their previous healthy status.2 However, hospital care is increasing for children with fragile and tenuous health due to complex medical conditions.3 RI is a common reason for hospitalization among these children as well and recovery of respiratory health and function can be slow and protracted for some of them.4 Weeks, months, or longer periods of time may be necessary for the children to return to their previous respiratory baseline health and function after hospital discharge; other children may not return to their baseline.5,6
Hospitalized older adults with high-severity RI are routinely streamlined for transfer to post-acute facility care (PAC) shortly (eg, a few days) after acute-care hospitalization. Nearly 70% of elderly Medicare beneficiaries use PAC following a brief length of stay (LOS) in the acute-care hospital.7 It is believed that PAC helps optimize the patients’ health and functional status and relieves the family caregiving burden that would have occurred at home.8-10 PAC use also helps to shorten acute-care hospitalization for RI while avoiding readmission.8-10 In contrast with adult patients, use of PAC for hospitalized children is not routine.11 While PAC use in children is infrequent, RI is one of the most common reasons for acute admission among children who use it.12
For some children with RI, PAC might be positioned to offer a safe, therapeutic, and high-value setting for pulmonary rehabilitation, as well as related medical, nutritional, functional, and family cares.6 PAC, by design, could possibly help some of the children transition back into their homes and communities. As studies continue to emerge that assess the value of PAC in children, it is important to learn more about the use of PAC in children hospitalized with RI. The objectives were to (1) assess which children admitted with RI are the most likely to use PAC services for recovery and (2) estimate how many hospitalized children not using PAC had the same characteristics as those who did.
METHODS
Study Design, Setting, and Population
We conducted a retrospective cohort analysis of 609,800 hospitalizations for RI occurring from January 1, 2010 to December 31, 2015, in 43 freestanding children’s hospitals in the Pediatric Health Information Systems (PHIS) dataset. All hospitals participating in PHIS are members of the Children’s Hospital Association.13 The Boston Children’s Hospital Institutional Review Board approved this study with a waiver for informed consent.
RI was identified using the Agency for Healthcare Research and Quality (AHRQ) Clinical Classification System (CCS).14 Using diagnosis CCS category 8 (“Diseases of the Respiratory System”) and the procedure CCS category 6 (“Operations on the Respiratory System”), we identified all hospitalizations from the participating hospitals with a principal diagnosis or procedure International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code for an RI.
Main Outcome Measure
Discharge disposition following the acute-care hospitalization for RI was the main outcome measure. We used PHIS uniform disposition coding to classify the discharge disposition as transfer to PAC (ie, rehabilitation facility, skilled nursing facility, etc.) vs all other dispositions (ie, routine to home, against medical advice, etc.).12 The PAC disposition category was derived from the Centers for Medicare & Medicaid Services Patient Discharge Status Codes and Hospital Transfer Policies as informed by the National Uniform Billing Committee Official UB-04 Data Specifications Manual, 2008. PAC transfer included disposition to external PAC facilities, as well as to internal, embedded PAC units residing in a few of the acute-care children’s hospitals included in the cohort.
Demographic and Clinical Characteristics
We assessed patient demographic and clinical characteristics that might correlate with PAC use following acute-care hospitalization for RI. Demographic characteristics included gender, age at admission in years, payer (public, private, and other), and race/ethnicity (Hispanic, non-Hispanic black, non-Hispanic white, other).
Clinical characteristics included chronic conditions (type and number) and assistance with medical technology. Chronic condition and medical technology characteristics were assessed with ICD-9-CM diagnosis codes. PHIS contain up to 41 ICD-9-CM diagnosis codes per hospital discharge record. To identify the presence and number of chronic conditions, we used the AHRQ Chronic Condition Indicator system, which categorizes over 14,000 ICD-9-CM diagnosis codes into chronic vs non-chronic conditions.14,15 Children hospitalized with a chronic condition were further classified as having a complex chronic condition (CCC) using Feudtner and colleagues’ ICD-9-CM diagnosis classification scheme.16 CCCs represent defined diagnosis groupings expected to last longer than 12 months and involving either a single organ system, severe enough to require specialty pediatric care and hospitalization, or multiple organ systems.17,18 Hospitalized children who were assisted with medical technology were identified with ICD-9-CM codes indicating the use of a medical device to manage and treat a chronic illness (eg, ventricular shunt to treat hydrocephalus) or to maintain basic body functions necessary for sustaining life (eg, a tracheostomy tube for breathing).19,20 We distinguished children undergoing tracheotomy during hospitalization using ICD-9-CM procedure codes 31.1 and 31.2.
Acute-Care Hospitalization Characteristics
We also assessed the relationship between acute-care hospitalization characteristics and use of PAC after discharge, including US census region, LOS, use of intensive care, number of medication classes administered, and use of enhanced respiratory support. Enhanced respiratory support was defined as use of continuous or bilevel positive airway pressure (CPAP or BiPAP) or mechanical ventilation during the acute-care hospitalization for RI. These respiratory supports were identified using billing data in PHIS.
Statistical Analysis
In bivariable analysis, we compared demographic, clinical, and hospitalization characteristics of hospitalized children with vs without discharge to PAC using Rao-Scott chi-square tests and Wilcoxon rank-sum tests as appropriate. In multivariable analysis, we derived a generalized linear mix effects model with fixed effects for demographic, clinical, and hospitalization characteristics that were associated with PAC at P < 0.1 in bivariable analysis (ie, age, gender, race/ethnicity, payer, medical technology, use of intensive care unit [ICU], use of positive pressure or mechanical ventilation, hospital region, LOS, new tracheostomy, existing tracheostomy, other technologies, number of medications, number of chronic conditions [of any complexity], and type of complex chronic conditions). We controlled for clustering of patients within hospitals by including a random intercept for each hospital. We also assessed combinations of patient characteristics on the likelihood of PAC use with classification and regression tree (CART) modeling. Using CART, we determined which characteristic combinations were associated with the highest and lowest use of PAC using binary split and post-pruning, goodness of fit rules.21 All statistical analyses were performed using SAS v.9.4 (SAS Institute, Cary, NC), and R v.3.2 (R Foundation for Statistical Computing, Vienna, Austria) using the “party” package. The threshold for statistical significance was set at P < 0.05.
RESULTS
Of the 609,800 hospitalizations for RI, PAC use after discharge occurred for 2660 (0.4%). RI discharges to PAC accounted for 2.1% (n = 67,405) of hospital days and 2.7% ($280 million) of hospital cost of all RI hospitalizations. For discharges to PAC, the most common RI were pneumonia (29.1% [n = 773]), respiratory failure or insufficiency (unspecified reason; 22.0% [n = 584]), and upper respiratory infection (12.2% [n = 323]).
Demographic Characteristics
Median age at acute-care admission was higher for PAC vs non-PAC discharges (6 years [interquartile range {IQR} 1-15] vs 2 years [0-7], P < 0.001; Table 1). Hispanic patients accounted for a smaller percentage of RI discharges to PAC vs non-PAC (14.1% vs 21.8%, P < 0.001) and a higher percentage to PAC were for patients with public insurance (75.9% vs 62.5, P < 0.001; Table 1).
Clinical Characteristics
A greater percentage of RI hospitalizations discharged to PAC vs not-PAC had ≥1 CCC (94.9% vs 33.5%), including a neuromuscular CCC (57.5% vs 8.9%) or respiratory CCC (62.5% vs 12.0%), P < 0.001 for all (Table 2). A greater percentage discharged to PAC was assisted with medical technology (83.2% vs 15.1%), including respiratory technology (eg, tracheostomy; 53.8% vs 5.4%) and gastrointestinal technology (eg, gastrostomy; 71.9% vs 11.8%), P < 0.001 for all. Of the children with respiratory technology, 14.8% (n = 394) underwent tracheotomy during the acute-care hospitalization. Children discharged to PAC had a higher percentage of multiple chronic conditions. For example, the percentages of children discharged to PAC vs not with ≥7 conditions were 54.5% vs 7.0% (P < 0.001; Table 2). The most common chronic conditions experienced by children discharged to PAC included epilepsy (41.2%), gastroesophageal reflux (36.6%), cerebral palsy (28.2%), and asthma (18.2%).
Hospitalization Characteristics
Acute-care RI hospitalization median LOS was longer for discharges to PAC vs non-PAC (10 days [IQR 4-27] vs 2 days [IQR 1-4], P < 0.001; Table 1). A greater percentage of discharges to PAC were administered medications from multiple classes during the acute-care RI admission (eg, 54.8% vs 13.4% used medications from ≥7 classes, P < 0.001). A greater percentage of discharges to PAC used intensive care services during the acute-care admission (65.6% vs 22.4%, P < 0.001). A greater percentage of discharges to PAC received CPAP (10.6 vs 5.0%), BiPAP (19.8% vs 11.4%), or mechanical ventilation (52.7% vs 9.1%) during the acute-care RI hospitalization (P < 0.001 for all; Table 1).
Multivariable Analysis of the Likelihood of Post-Acute Care Use Following Discharge
In multivariable analysis, the patient characteristics associated with the highest likelihood of discharge to PAC included ≥11 vs no chronic conditions (odds ratio [OR] 11.8 , 95% CI, 8.0-17.2), ≥9 classes vs no classes of medications administered during the acute-care hospitalization (OR 4.8 , 95% CI, 1.8-13.0), and existing tracheostomy (OR 3.0, [95% CI, 2.6-3.5; Figure 2 and eTable). Patient characteristics associated with a more modest likelihood of discharge to PAC included public vs private insurance (OR 1.8, 95% CI, 1.6-2.0), neuromuscular complex chronic condition (OR 1.6, 95% CI, 1.5-1.8), new tracheostomy (OR 1.9, 95% CI, 1.7-2.2), and use of any enhanced respiratory support (ie, CPAP/BiPAP/mechanical ventilation) during the acute-care hospitalization (OR 1.4, 95% CI, 1.3-1.6; Figure 2 and Supplementary Table).
Classification and Regression Tree Analysis
In the CART analysis, the highest percentage (6.3%) of children hospitalized with RI who were discharged to PAC had the following combination of characteristics: ≥6 chronic conditions, ≥7 classes of medications administered, and respiratory technology. Median (IQR) length of acute-care LOS for children with these attributes who were transferred to PAC was 19 (IQR 8-56; range 1-1005) days; LOS remained long (median 13 days [IQR 6-41, range 1-1413]) for children with the same attributes not transferred to PAC (n = 9448). Between these children transferred vs not to PAC, 79.3% vs 65.9% received ICU services; 74.4% vs 73.5% received CPAP, BiPAP, or mechanical ventilation; and 31.0% vs 22.7% underwent tracheotomy during the acute-care hospitalization. Of these children who were not transferred to PAC, 18.9% were discharged to home nursing services.
DISCUSSION
The findings from the present study suggest that patients with RI hospitalization in children’s hospitals who use PAC are medically complex, with high rates of multiple chronic conditions—including cerebral palsy, asthma, chronic respiratory insufficiency, dysphagia, epilepsy, and gastroesophageal reflux—and high rates of technology assistance including enterostomy and tracheostomy. The characteristics of patients most likely to use PAC include long LOS, a large number of chronic conditions, many types of medications administered during the acute-care hospitalization, respiratory technology use, and an underlying neuromuscular condition. Specifically, the highest percentage of children hospitalized with RI who were discharged to PAC had ≥6 chronic conditions, ≥7 classes of medications administered, and respiratory technology. Our analysis suggests that there may be a large population of children with these same characteristics who experienced a prolonged LOS but were not transferred to PAC.
There are several reasons to explain why children hospitalized with RI who rely on medical technology, such as existing tracheostomy, are more likely to use PAC. Tracheostomy often indicates the presence of life-limiting impairment in oxygenation or ventilation, thereby representing a high degree of medical fragility. Tracheostomy, in some cases, offers enhanced ability to assist with RI treatment, including establishment of airway clearance of secretions (ie, suctioning and chest physiotherapy), administration of antimicrobials (eg, nebulized antibiotics), and optimization of ventilation (eg, non-invasive positive airway pressure). However, not all acute-care inpatient clinicians have experience and clinical proficiencies in the care of children with pediatric tracheostomy.23 As a result, a more cautious approach, with prolonged LOS and gradual arrival to hospital discharge, is often taken in the acute-care hospital setting for children with tracheostomy. Tracheostomy care delivered during recovery from RI by trained and experienced teams of providers in the PAC setting may be best positioned to help optimize respiratory health and ensure proper family education and readiness to continue care at home.6
Further investigation is needed of the long LOS in children not transferred to PAC who had similar characteristics to those who were transferred. In hospitalized adult patients with RI, PAC is routinely introduced early in the admission process, with anticipated transfer within a few days into the hospitalization. In the current study, LOS was nearly 2 weeks or longer in many children not transferred to PAC who had similar characteristics to those who were transferred. Perhaps some of the children not transferred experienced long LOS in the acute-care hospital because of a limited number of pediatric PAC beds in their local area. Some families of these children may have been offered but declined use of PAC. PAC may not have been offered to some because illness acuity was too high or there was lack of PAC awareness as a possible setting for recovery.
There are several limitations to this study. PHIS does not contain non-freestanding children’s hospitals; therefore, the study results may generalize best to children’s hospitals. PHIS does not contain information on the amount (eg, number of days used), cost, or treatments provided in PAC. Therefore, we were unable to determine the true reasons why children used PAC services following RI hospitalization (eg, for respiratory rehabilitation vs other reasons, such as epilepsy or nutrition/hydration management). Moreover, we could not assess which children truly used PAC for short-term recovery vs longer-term care because they were unable to reside at home (eg, they were too medically complex). We were unable to assess PAC availability (eg, number of beds) in the surrounding areas of the acute-care hospitals in the PHIS database. Although we assessed use of medical technology, PHIS does not contain data on functional status or activities of daily living, which correlate with the use of PAC in adults. We could not distinguish whether children receiving BiPAP, CPAP, or mechanical ventilation during hospitalization were using it chronically. Although higher PAC use was associated with public insurance, due to absent information on the children’s home, family, and social environment, we were unable to assess whether PAC use was influenced by limited caregiving support or resources.
Data on the type and number of chronic conditions are limited by the ICD-9-CM codes available to distinguish them. Although several patient demographic and clinical characteristics were significantly associated with the use of PAC, significance may have occurred because of the large sample size and consequent robust statistical power. This is why we elected to highlight and discuss the characteristics with the strongest and most clinically meaningful associations (eg, multiple chronic conditions). There may be additional characteristics, including social, familial, and community resources, that are not available to assess in PHIS that could have affected PAC use.
Despite these limitations, the current study suggests that the characteristics of children hospitalized with RI who use PAC for recovery are evident and that there is a large population of children with these characteristics who experienced a prolonged LOS that did not result in transfer to PAC. These findings could be used in subsequent studies to help create the base of a matched cohort of children with similar clinical, demographic, and hospitalization characteristics who used vs didn’t use PAC. Comparison of the functional status, health trajectory, and family and/or social attributes of these 2 groups of children, as well as their post-discharge outcomes and utilization (eg, length of PAC stay, emergency department revisits, and acute-care hospital readmissions), could occur with chart review, clinician and parent interview, and other methods. This body of work might ultimately lead to an assessment of value in PAC and potentially help us understand the need for PAC capacity in various communities. In the meantime, clinicians may find it useful to consider the results of the current study when contemplating PAC use in their hospitalized children with RI, including exploration of health system opportunities of clinical collaboration between acute-care children’s hospitals and PAC facilities. Ultimately, all of this work will generate meaningful knowledge regarding the most appropriate, safe, and cost-effective settings for hospitalized children with RI to regain their health.
Acknowledgments
Dr. Berry was supported by the Agency for Healthcare Research and Quality (R21 HS023092-01), the Lucile Packard Foundation for Children’s Health, and Franciscan Hospital for Children. The funders were not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclosure: The authors have no financial relationships relevant to this article to disclose.
1. Friedman B, Berdahl T, Simpson LA, et al. Annual report on health care for children and youth in the United States: focus on trends in hospital use and quality. Acad Pediatr. 2011;11(4):263-279. PubMed
2. Srivastava R, Homer CJ. Length of stay for common pediatric conditions: teaching versus nonteaching hospitals. Pediatrics. 2003;112(2):278-281. PubMed
3. Berry JG, Hall M, Hall DE, et al. Inpatient growth and resource use in 28 children’s hospitals: a longitudinal, multi-institutional study. JAMA Pediatr. 2013;167(2):170-177. PubMed
4. Gold JM, Hall M, Shah SS, et al. Long length of hospital stay in children with medical complexity. J Hosp Med. 2016;11(11):750-756. PubMed
5. Faultner J. Integrating medical plans within family life. JAMA Pediatr. 2014;168(10):891-892. PubMed
6. O’Brien JE, Haley SM, Dumas HM, et al. Outcomes of post-acute hospital episodes for young children requiring airway support. Dev Neurorehabil. 2007;10(3):241-247. PubMed
7. Morley M, Bogasky S, Gage B, et al. Medicare post-acute care episodes and payment bundling. Medicare Medicaid Res Rev. 2014;4(1):mmrr.004.01.b02. PubMed
8. Mentro AM, Steward DK. Caring for medically fragile children in the home: an alternative theoretical approach. Res Theory Nurs Pract. 2002;16(3):161-177. PubMed
9. Thyen U, Kuhlthau K, Perrin JM. Employment, child care, and mental health of mothers caring for children assisted by technology. Pediatrics. 1999;103(6 Pt 1):1235-1242. PubMed
10. Thyen U, Terres NM, Yazdgerdi SR, Perrin JM. Impact of long-term care of children assisted by technology on maternal health. J Dev Behav Pediatr. 1998;19(4):273-282. PubMed
11. O’Brien JE, Berry J, Dumas H. Pediatric Post-acute hospital care: striving for identity and value. Hosp Pediatr. 2015;5(10):548-551. PubMed
12. Berry JG, Hall M, Dumas H, et al. Pediatric hospital discharges to home health and postacute facility care: a national study. JAMA Pediatr. 2016;170(4):326-333. PubMed
13. Children’s Hospital Association. Pediatric Health Information System. https://childrenshospitals.org/Programs-and-Services/Data-Analytics-and-Research/Pediatric-Analytic-Solutions/Pediatric-Health-Information-System. Accessed June 12, 2017.
14. Agency for Healthcare Research and Quality. Chronic Condition Indicator. http://www.hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp. Accessed on June 19, 2017.
15. Berry JG, Ash AS, Cohen E, Hasan F, Feudtner C, Hall M. Contributions of children with multiple chronic conditions to pediatric hospitalizations in the United States: A Retrospective Cohort Analysis [published online ahead of print June 20, 2017]. Hosp Pediatr. 2017 Jun 20. doi: 10.1542/hpeds.2016-0179. PubMed
16. Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:199. PubMed
17. Cohen E, Kuo DZ, Agrawal R, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529-538. PubMed
18. Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980-1997. Pediatrics. 2000;106(1 Pt 2):205-209. PubMed
19. Palfrey JS, Walker DK, Haynie M, et al. Technology’s children: report of a statewide census of children dependent on medical supports. Pediatrics. 1991;87(5):611-618. PubMed
20. Feudtner C, Villareale NL, Morray B, Sharp V, Hays RM, Neff JM. Technology-dependency among patients discharged from a children’s hospital: a retrospective cohort study. BMC Pediatr. 2005;5(1):8. PubMed
21. Breiman L, Freidman J, Stone CJ, Olshen RA. Classification and Regression Trees. Belmont, CA: Wadsworth International; 1984.
22. Thomson J, Hall M, Ambroggio L, et al. Aspiration and Non-Aspiration Pneumonia in Hospitalized Children With Neurologic Impairment. Pediatrics. 2016;137(2):e20151612. PubMed
23. Berry JG, Goldmann DA, Mandl KD, et al. Health information management and perceptions of the quality of care for children with tracheotomy: a qualitative study. BMC Health Serv Res. 2011;11:117. PubMed
1. Friedman B, Berdahl T, Simpson LA, et al. Annual report on health care for children and youth in the United States: focus on trends in hospital use and quality. Acad Pediatr. 2011;11(4):263-279. PubMed
2. Srivastava R, Homer CJ. Length of stay for common pediatric conditions: teaching versus nonteaching hospitals. Pediatrics. 2003;112(2):278-281. PubMed
3. Berry JG, Hall M, Hall DE, et al. Inpatient growth and resource use in 28 children’s hospitals: a longitudinal, multi-institutional study. JAMA Pediatr. 2013;167(2):170-177. PubMed
4. Gold JM, Hall M, Shah SS, et al. Long length of hospital stay in children with medical complexity. J Hosp Med. 2016;11(11):750-756. PubMed
5. Faultner J. Integrating medical plans within family life. JAMA Pediatr. 2014;168(10):891-892. PubMed
6. O’Brien JE, Haley SM, Dumas HM, et al. Outcomes of post-acute hospital episodes for young children requiring airway support. Dev Neurorehabil. 2007;10(3):241-247. PubMed
7. Morley M, Bogasky S, Gage B, et al. Medicare post-acute care episodes and payment bundling. Medicare Medicaid Res Rev. 2014;4(1):mmrr.004.01.b02. PubMed
8. Mentro AM, Steward DK. Caring for medically fragile children in the home: an alternative theoretical approach. Res Theory Nurs Pract. 2002;16(3):161-177. PubMed
9. Thyen U, Kuhlthau K, Perrin JM. Employment, child care, and mental health of mothers caring for children assisted by technology. Pediatrics. 1999;103(6 Pt 1):1235-1242. PubMed
10. Thyen U, Terres NM, Yazdgerdi SR, Perrin JM. Impact of long-term care of children assisted by technology on maternal health. J Dev Behav Pediatr. 1998;19(4):273-282. PubMed
11. O’Brien JE, Berry J, Dumas H. Pediatric Post-acute hospital care: striving for identity and value. Hosp Pediatr. 2015;5(10):548-551. PubMed
12. Berry JG, Hall M, Dumas H, et al. Pediatric hospital discharges to home health and postacute facility care: a national study. JAMA Pediatr. 2016;170(4):326-333. PubMed
13. Children’s Hospital Association. Pediatric Health Information System. https://childrenshospitals.org/Programs-and-Services/Data-Analytics-and-Research/Pediatric-Analytic-Solutions/Pediatric-Health-Information-System. Accessed June 12, 2017.
14. Agency for Healthcare Research and Quality. Chronic Condition Indicator. http://www.hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp. Accessed on June 19, 2017.
15. Berry JG, Ash AS, Cohen E, Hasan F, Feudtner C, Hall M. Contributions of children with multiple chronic conditions to pediatric hospitalizations in the United States: A Retrospective Cohort Analysis [published online ahead of print June 20, 2017]. Hosp Pediatr. 2017 Jun 20. doi: 10.1542/hpeds.2016-0179. PubMed
16. Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:199. PubMed
17. Cohen E, Kuo DZ, Agrawal R, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529-538. PubMed
18. Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980-1997. Pediatrics. 2000;106(1 Pt 2):205-209. PubMed
19. Palfrey JS, Walker DK, Haynie M, et al. Technology’s children: report of a statewide census of children dependent on medical supports. Pediatrics. 1991;87(5):611-618. PubMed
20. Feudtner C, Villareale NL, Morray B, Sharp V, Hays RM, Neff JM. Technology-dependency among patients discharged from a children’s hospital: a retrospective cohort study. BMC Pediatr. 2005;5(1):8. PubMed
21. Breiman L, Freidman J, Stone CJ, Olshen RA. Classification and Regression Trees. Belmont, CA: Wadsworth International; 1984.
22. Thomson J, Hall M, Ambroggio L, et al. Aspiration and Non-Aspiration Pneumonia in Hospitalized Children With Neurologic Impairment. Pediatrics. 2016;137(2):e20151612. PubMed
23. Berry JG, Goldmann DA, Mandl KD, et al. Health information management and perceptions of the quality of care for children with tracheotomy: a qualitative study. BMC Health Serv Res. 2011;11:117. PubMed
© 2017 Society of Hospital Medicine
If You Book It, Will They Come? Attendance at Postdischarge Follow-Up Visits Scheduled by Inpatient Providers
Given growing incentives to reduce readmission rates, predischarge checklists and bundles have recommended that inpatient providers schedule postdischarge follow-up visits (PDFVs) for their hospitalized patients.1-4 PDFVs have been linked to lower readmission rates in patients with chronic conditions, including congestive heart failure, psychiatric illnesses, and chronic obstructive pulmonary disease.5-8 In contrast, the impact of PDFVs on readmissions in hospitalized general medicine populations has been mixed.9-12 Beyond the presence or absence of PDFVs, it may be a patient’s inability to keep scheduled PDFVs that contributes more strongly to preventable readmissions.11
This challenge, dealing with the 12% to 37% of patients who miss their visits (“no-shows”), is not new.13-17 In high-risk patient populations, such as those with substance abuse, diabetes, or human immunodeficiency virus, no-shows (NSs) have been linked to poorer short-term and long-term clinical outcomes.16,18-20 Additionally, NSs pose a challenge for outpatient clinics and the healthcare system at large. The financial cost of NSs ranges from approximately $200 per patient in 2 analyses to $7 million in cumulative lost revenue per year at 1 large academic health system.13,17,21 As such, increasing attendance at PDFVs is a potential target for improving both patient outcomes and clinic productivity.
Most prior PDFV research has focused on readmission risk rather than PDFV attendance as the primary outcome.5-12 However, given the patient-oriented benefits of attending PDFVs and the clinic-oriented benefits of avoiding vacant time slots, NS PDFVs represent an important missed opportunity for our healthcare delivery system. To our knowledge, risk factors for PDFV nonattendance have not yet been systematically studied. The aim of our study was to analyze PDFV nonattendance, particularly NSs and same-day cancellations (SDCs), for hospitalizations and clinics within our healthcare system.
METHODS
Study Design
We conducted an observational cohort study of adult patients from 10 medical units at the Hospital of the University of Pennsylvania (a 789-bed quaternary-care hospital within an urban, academic medical system) who were scheduled with at least 1 PDFV. Specifically, the patients included in our analysis were hospitalized on general internal medicine services or medical subspecialty services with discharge dates between April 1, 2014, and March 31, 2015. Hospitalizations included in our study had at least 1 PDFV scheduled with an outpatient provider affiliated with the University of Pennsylvania Health System (UPHS). PDFVs scheduled with unaffiliated providers were not examined.
Each PDFV was requested by a patient’s inpatient care team. Once the care team had determined that a PDFV was clinically warranted, a member of the team (generally a resident, advanced practice provider, medical student, or designee) either called the UPHS clinic to schedule an appointment time or e-mailed the outpatient UPHS provider directly to facilitate a more urgent PDFV appointment time. Once a PDFV time was confirmed, PDFV details (ie, date, time, location, and phone number) were electronically entered into the patient’s discharge instructions by the inpatient care team. At the time of discharge, nurses reviewed these instructions with their patients. All patients left the hospital with a physical copy of these instructions. As part of routine care at our institution, patients then received automated telephone reminders from their UPHS-affiliated outpatient clinic 48 hours prior to each PDFV.
Data Collection
Our study was determined to meet criteria for quality improvement by the University of Pennsylvania’s Institutional Review Board. We used our healthcare system’s integrated electronic medical record system to track the dates of initial PDFV requests, the dates of hospitalization, and actual PDFV dates. PDFVs were included if the appointment request was made while a patient was hospitalized, including the day of discharge. Our study methodology only allowed us to investigate PDFVs scheduled with UPHS outpatient providers. We did not review discharge instructions or survey non-UPHS clinics to quantify visits scheduled with other providers, for example, community health centers or external private practices.
Exclusion criteria included the following: (1) office visits with nonproviders, for example, scheduled diagnostic procedures or pharmacist appointments for warfarin dosing; (2) visits cancelled by inpatient providers prior to discharge; (3) visits for patients not otherwise eligible for UPHS outpatient care because of insurance reasons; and (4) visits scheduled for dates after a patient’s death. Our motivation for the third exclusion criterion was the infrequent and irregular process by which PDFVs were authorized for these patients. These patients and their characteristics are described in Supplementary Table 1 in more detail.
For each PDFV, we recorded age, gender, race, insurance status, driving distance, length of stay for index hospitalization, discharging service (general internal medicine vs subspecialty), postdischarge disposition (home, home with home care services such as nursing or physical therapy, or facility), the number of PDFVs scheduled per index hospitalization, PDFV specialty type (oncologic subspecialty, nononcologic medical subspecialty, nononcologic surgical subspecialty, primary care, or other specialty), PDFV season, and PDFV lead time (the number of days between the discharge date and PDFV). We consolidated oncologic specialties into 1 group given the integrated nature of our healthcare system’s comprehensive cancer center. “Other” PDFV specialty subtypes are described in Supplementary Table 2. Driving distances between patient postal codes and our hospital were calculated using Excel VBA Master (Salt Lake City, Utah) and were subsequently categorized into patient-level quartiles for further analysis. For cancelled PDFVs, we collected dates of cancellation relative to the date of the appointment itself.
Study Outcomes
The primary study outcome was PDFV attendance. Each PDFV’s status was categorized by outpatient clinic staff as attended, cancelled, or NS. For cancelled appointments, cancellation dates and reasons (if entered by clinic representatives) were collected. In keeping with prior studies investigating outpatient nonattendance,we calculated collective NS/SDC rates for the variables listed above.17,22-25 We additionally calculated NS/SDC and attendance-as-scheduled rates stratified by the number of PDFVs per patient to assess for a “high-utilizer” effect with regard to PDFV attendance.
Statistical Analysis
We used multivariable mixed-effects regression with a logit link to assess associations between age, gender, race, insurance, driving distance quartile, length of stay, discharging service, postdischarge disposition, the number of PDFVs per hospitalization, PDFV specialty type, PDFV season, PDFV lead time, and our NS/SDC outcome. The mixed-effects approach was used to account for correlation structures induced by patients who had multiple visits and for patients with multiple hospitalizations. Specifically, our model specified 2 levels of nesting (PDFVs nested within each hospitalization, which were nested within each patient) to obtain appropriate standard error estimates for our adjusted odds ratios (ORs). Correlation matrices and multivariable variance inflation factors were used to assess collinearity among the predictor variables. These assessments did not indicate strong collinearity; hence, all predictors were included in the model. Only driving distance had a small amount of missing data (0.18% of driving distances were unavailable), so multiple imputation was not undertaken. Analyses were performed using R version 3.3.1 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Baseline Characteristics
During the 1-year study period, there were 11,829 discrete hospitalizations in medical units at our hospital. Of these hospitalizations, 6136 (52%) had at least 1 UPHS-affiliated PDFV meeting our inclusion and exclusion criteria, as detailed in the Figure. Across these hospitalizations, 9258 PDFVs were scheduled on behalf of 4653 patients. Demographic characteristics for these patients, hospitalizations, and visits are detailed in Table 1. The median age of patients in our cohort was 61 years old (interquartile range [IQR] 49-70, range 18-101). The median driving distance was 17 miles (IQR 4.3-38.8, range 0-2891). For hospitalizations, the median length of stay was 5 days (IQR 3-10, range 0-97). The median PDFV lead time, which is defined as the number of days between discharge and PDFV, was 12 days (IQR 6-23, range 1-60). Overall, 41% of patients (n = 1927) attended all of their PDFVs as scheduled; Supplementary Figure 1 lists patient-level PDFV attendance-as-scheduled percentages in more detail.
Incidence of NSs and SDCs
Twenty-five percent of PDFVs (n = 2303) were ultimately NS/SDCs; this included 1658 NSs (18% of all appointments) and 645 SDCs (7% of all appointments). Fifty-two percent of PDFVs (n = 4847) were kept as scheduled, while 23% (n = 2108) were cancelled before the day of the visit. Of the 2558 cancellations with valid cancellation dates, 49% (n = 1252) were cancelled 2 or fewer days beforehand, as shown in Supplementary Figure 2.
The presence of exactly 2 PDFVs per hospitalization was also associated with higher NS/SDC rates (OR 1.17, 95% CI, 1.01-1.36), compared to a single PDFV per hospitalization; however, the presence of more than 2 PDFVs per hospitalization was associated with lower NS/SDC rates (OR 0.82, 95% CI, 0.69-0.98). A separate analysis (data not shown) of potential high utilizers revealed a 15% NS/SDC rate for the top 0.5% of patients (median: 18 PDFVs each) and an 18% NS/SDC rate for the top 1% of patients (median: 14 PDFVs each) with regard to the numbers of PDFVs scheduled, compared to the 25% overall NS/SDC rate for all patients.
NS/SDC rates and adjusted ORs with regard to individual PDFV characteristics are displayed in Table 3. Nononcologic visits had higher NS/SDC rates than oncologic visits; for example, the NS/SDC rate for primary care visits was 39% (OR 2.62, 95% CI, 2.03-3.38), compared to 12% for oncologic visits. Appointments in the “other” specialty category also had high nonattendance rates, as further described in Supplementary Table B. Summertime appointments were more likely to be attended (OR 0.81, 95% CI, 0.68-0.97) compared to those in the spring. PDFV lead time (the time interval between the discharge date and appointment date) was not associated with changes in visit attendance.
DISCUSSION
When comparing PDFV characteristics themselves, oncologic visits had the lowest NS/SDC incidence of any group analyzed in our study. This may be related to the inherent life-altering nature of a cancer diagnosis or our cancer center’s use of patient navigators.23,30 In contrast, primary care clinics suffered from NS/SDC rates approaching 40%, which is a concerning finding given the importance of primary care coordination in the posthospitalization period.9,31 Why are primary care appointments so commonly missed? Some studies suggest that forgetting about a primary care appointment is a leading reason.15,32,33 For PDFVs, this phenomenon may be augmented because the visits are not scheduled by patients themselves. Additionally, patients may paradoxically undervalue the benefit of an all-encompassing primary care visit, compared to a PDFV focused on a specific problem, (eg, a cardiology follow-up appointment for a patient with congestive heart failure). In particular, patients with limited health literacy may potentially undervalue the capabilities of their primary care clinics.34,35
The low absolute number of primary care PDFVs (only 8% of all visits) scheduled for patients at our hospital was an unexpected finding. This low percentage is likely a function of the patient population hospitalized at our large, urban quaternary-care facility. First, an unknown number of patients may have had PDFVs manually scheduled with primary care providers external to our health system; these PDFVs were not captured within our study. Second, 71% of the hospitalizations in our study occurred in subspecialty services, for which specific primary care follow-up may not be as urgent. Supporting this fact, further analysis of the 6136 hospitalizations in our study (data not shown) revealed that 28% of the hospitalizations in general internal medicine were scheduled with at least 1 primary care PDFV as opposed to only 5% of subspecialty-service hospitalizations.
In contrast to several previous studies of outpatient nonattendance,we did not find that visits scheduled for time points further in the future were more likely to be missed.14,24,25,36,37 Unlike other appointments, it may be that PDFV lead time does not affect attendance because of the unique manner in which PDFV times are scheduled and conveyed to patients. Unlike other appointments, patients do not schedule PDFVs themselves but instead learn about their PDFV dates as part of a large set of discharge instructions. This practice may result in poor recall of PDFV dates in recently hospitalized patients38, regardless of the lead time between discharge and the visit itself.
Supplementary Table 1 details a 51% NS/SDC rate for the small number of PDFVs (n = 65) that were excluded a priori from our analysis because of general ineligibility for UPHS outpatient care. We specifically chose to exclude this population because of the infrequent and irregular process by which these PDFVs were authorized on a case-by-case basis, typically via active engagement by our hospital’s social work department. We did not study this population further but postulate that the 51% NS/SDC rate may reflect other social determinants of health that contribute to appointment nonadherence in a predominantly uninsured population.
Beyond their effect on patient outcomes, improving PDFV-related processes has the potential to boost both inpatient and outpatient provider satisfaction. From the standpoint of frontline inpatient providers (often resident physicians), calling outpatient clinics to request PDFVs is viewed as 1 of the top 5 administrative tasks that interfere with house staff education.39 Future interventions that involve patients in the PDFV scheduling process may improve inpatient workflow while simultaneously engaging patients in their own care. For example, asking clinic representatives to directly schedule PDFVs with hospitalized patients, either by phone or in person, has been shown in pilot studies to improve PDFV attendance and decrease readmissions.40-42 Conversely, NS/SDC visits harm outpatient provider productivity and decrease provider availability for other patients.13,17,43 Strategies to mitigate the impact of unfilled appointment slots (eg, deliberately overbooking time slots in advance) carry their own risks, including provider burnout.44 As such, preventing NSs may be superior to curing their adverse impacts. Many such strategies exist in the ambulatory setting,13,43,45 for example, better communication with patients through texting or goal-directed, personalized phone reminders.46-48Our study methodology has several limitations. Most importantly, we were unable to measure PDFVs made with providers unaffiliated with UPHS. As previously noted, our low proportion of primary care PDFVs may specifically reflect patients with primary care providers outside of our health system. Similarly, our low percentage of Medicaid patients receiving PDFVs may be related to follow-up visits with nonaffiliated community health centers. We were unable to measure patient acuity and health literacy as potential predictors of NS/SDC rates. Driving distances were calculated from patient postal codes to our hospital, not to individual outpatient clinics. However, the majority of our hospital-affiliated clinics are located adjacent to our hospital; additionally, we grouped driving distances into quartiles for our analysis. We had initially attempted to differentiate between clinic-initiated and patient-initiated cancellations, but unfortunately, we found that the data were too unreliable to be used for further analysis (outlined in Supplementary Table 3). Lastly, because we studied patients in medical units at a single large, urban, academic center, our results are not generalizable to other settings (eg, community hospitals, hospitals with smaller networks of outpatient providers, or patients being discharged from surgical services or observation units).
CONCLUSION
Given national efforts to enhance postdischarge transitions of care, we aimed to analyze attendance at provider-scheduled PDFV appointments. Our finding that 25% of PDFVs resulted in NS/SDCs raises both questions and opportunities for inpatient and outpatient providers. Further research is needed to understand why so many patients miss their PDFVs, and we should work as a field to develop creative solutions to improve PDFV scheduling and attendance.
Acknowledgments
The authors acknowledge Marie Synnestvedt, PhD, and Manik Chhabra, MD, for their assistance with data gathering and statistical analysis. They also acknowledge Allison DeKosky, MD, Michael Serpa, BS, Michael McFall, and Scott Schlegel, MBA, for their assistance with researching this topic. They did not receive external compensation for their assistance outside of their usual salary support.
DISCLOSURE
Nothing to report.
1. Halasyamani L, Kripalani S, Coleman E, et al. Transition of care for hospitalized elderly patients - development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354-360. PubMed
2. Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218. PubMed
3. Soong C, Daub S, Lee JG, et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013;8(8):444-449. PubMed
4. Rice YB, Barnes CA, Rastogi R, Hillstrom TJ, Steinkeler CN. Tackling 30-day, all-cause readmissions with a patient-centered transitional care bundle. Popul Health Manag. 2016;19(1):56-62. PubMed
5. Nelson EA, Maruish MM, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psych Serv. 2000;51(7):885-889. PubMed
6. Gavish R, Levy A, Dekel OK, Karp E, Maimon N. The association between hospital readmission and pulmonologist follow-up visits in patients with chronic obstructive pulmonary disease. Chest. 2015;148(2):375-381. PubMed
7. Jackson C, Shahsahebi M, Wedlake T, DuBard CA. Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med. 2015;13(2):115-122. PubMed
8. Donaho EK, Hall AC, Gass JA, et al. Protocol-driven allied health post-discharge transition clinic to reduce hospital readmissions in heart failure. J Am Heart Assoc. 2015;4(12):e002296. PubMed
9. Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392-397. PubMed
10. Grafft CA, McDonald FS, Ruud KL, Liesinger JT, Johnson MG, Naessens JM. Effect of hospital follow-up appointment on clinical event outcomes and mortality. Arch Intern Med. 2010;171(11):955-960. PubMed
11. Auerbach AD, Kripalani S, Vasilevskis EE, et al. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med. 2016;176(4):484-493. PubMed
12. Field TS, Ogarek J, Garber L, Reed G, Gurwitz JH. Association of early post-discharge follow-up by a primary care physician and 30-day rehospitalization among older adults. J Gen Intern Med. 2015;30(5):565-571. PubMed
13. Quinn K. It’s no-show time! Med Group Manage Assoc Connexion. 2007;7(6):44-49. PubMed
14. Whittle J, Schectman G, Lu N, Baar B, Mayo-Smith MF. Relationship of scheduling interval to missed and cancelled clinic appointments. J Ambulatory Care Manage. 2008;31(4):290-302. PubMed
15. Kaplan-Lewis E, Percac-Lima S. No-show to primary care appointments: Why patients do not come. J Prim Care Community Health. 2013;4(4):251-255. PubMed
16. Molfenter T. Reducing appointment no-shows: Going from theory to practice. Subst Use Misuse. 2013;48(9):743-749. PubMed
17. Kheirkhah P, Feng Q, Travis LM, Tavakoli-Tabasi S, Sharafkhaneh A. Prevalence, predictors and economic consequences of no-shows. BMC Health Serv Res. 2016;16(1):13. PubMed
18. Colubi MM, Perez-Elias MJ, Elias L, et al. Missing scheduled visits in the outpatient clinic as a marker of short-term admissions and death. HIV Clin Trials. 2012;13(5):289-295. PubMed
19. Obialo CI, Hunt WC, Bashir K, Zager PG. Relationship of missed and shortened hemodialysis treatments to hospitalization and mortality: Observations from a US dialysis network. Clin Kidney J. 2012;5(4):315-319. PubMed
20. Hwang AS, Atlas SJ, Cronin P, et al. Appointment “no-shows” are an independent predictor of subsequent quality of care and resource utilization outcomes. J Gen Intern Med. 2015;30(10):1426-1433. PubMed
21. Perez FD, Xie J, Sin A, et al. Characteristics and direct costs of academic pediatric subspecialty outpatient no-show events. J Healthc Qual. 2014;36(4):32-42. PubMed
22. Huang Y, Zuniga P. Effective cancellation policy to reduce the negative impact of patient no-show. Journal of the Operational Research Society. 2013;65(5):605-615.
23. Percac-Lima S, Cronin PR, Ryan DP, Chabner BA, Daly EA, Kimball AB. Patient navigation based on predictive modeling decreases no-show rates in cancer care. Cancer. 2015;121(10):1662-1670. PubMed
24. Torres O, Rothberg MB, Garb J, Ogunneye O, Onyema J, Higgins T. Risk factor model to predict a missed clinic appointment in an urban, academic, and underserved setting. Popul Health Manag. 2015;18(2):131-136. PubMed
25. Eid WE, Shehata SF, Cole DA, Doerman KL. Predictors of nonattendance at an endocrinology outpatient clinic. Endocr Pract. 2016;22(8):983-989. PubMed
26. Kashiwagi DT, Burton MC, Kirkland LL, Cha S, Varkey P. Do timely outpatient follow-up visits decrease hospital readmission rates? Am J Med Qual. 2012;27(1):11-15. PubMed
27. Miller AJ, Chae E, Peterson E, Ko AB. Predictors of repeated “no-showing” to clinic appointments. Am J Otolaryngol. 2015;36(3):411-414. PubMed
28. ASCO. Billing challenges for residents of Skilled Nursing Facilities. J Oncol Pract. 2008;4(5):245-248. PubMed
29. Centers for Medicare & Medicaid Services (2013). “SE0433: Skilled Nursing Facility consolidated billing as it relates to ambulance services.” Medicare Learning Network Matters. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/se0433.pdf. Accessed on February 14, 2017.
30. Luckett R, Pena N, Vitonis A, Bernstein MR, Feldman S. Effect of patient navigator program on no-show rates at an academic referral colposcopy clinic. J Womens Health (Larchmt). 2015;24(7):608-615. PubMed
31. Jones CD, Vu MB, O’Donnell CM, et al. A failure to communicate: A qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations. J Gen Intern Med. 2015;30(4):417-424. PubMed
32. George A, Rubin G. Non-attendance in general practice: a systematic review and its implications for access to primary health care. Fam Pract. 2003;20(2):178-184. 2016;31(12):1460-1466.J Gen Intern Med. PubMed
48. Shah SJ, Cronin P, Hong CS, et al. Targeted reminder phone calls to patients at high risk of no-show for primary care appointment: A randomized trial. 2010;123(6):542-548.Am J Med. PubMed
47. Parikh A, Gupta K, Wilson AC, Fields K, Cosgrove NM, Kostis JB. The effectiveness of outpatient appointment reminder systems in reducing no-show rates. 2009;20:142-144.Int J STD AIDS. PubMed
46. Price H, Waters AM, Mighty D, et al. Texting appointment reminders reduces ‘Did not attend’ rates, is popular with patients and is cost-effective. 2009;25(3):166-170.J Med Practice Management. PubMed
45. Hills LS. How to handle patients who miss appointments or show up late.
2009;39(3):271-287.Interfaces. PubMed
44. Kros J, Dellana S, West D. Overbooking Increases Patient Access at East Carolina University’s Student Health Services Clinic. 2012;344(3):211-219.Am J Med Sci.
43. Stubbs ND, Geraci SA, Stephenson PL, Jones DB, Sanders S. Methods to reduce outpatient non-attendance. PubMed
42. Haftka A, Cerasale MT, Paje D. Direct patient participation in discharge follow-up appointment scheduling. Paper presented at: Society of Hospital Medicine, Annual Meeting 2015; National Harbor, MD. 2012;5(1):27-32.Patient.
41. Chang R, Spahlinger D, Kim CS. Re-engineering the post-discharge appointment process for general medicine patients. PubMed
40. Coffey C, Kufta J. Patient-centered post-discharge appointment scheduling improves readmission rates. Paper presented at: Society of Hospital Medicine, Annual Meeting 2011; Grapevine, Texas. 2006;81(1):76-81.Acad Med.
39. Vidyarthi AR, Katz PP, Wall SD, Wachter RM, Auerbach AD. Impact of reduced duty hours on residents’ education satistfaction at the University of California, San Francisco.
2013;173(18):1715-1722.JAMA Intern Med. PubMed
38. Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center. 2010;16(4):246-259.Health Informatics J. PubMed
37. Daggy J, Lawley M, Willis D, et al. Using no-show modeling to improve clinic performance. 2005;5:51.BMC Health Serv Res. PubMed
36. Lee VJ, Earnest A, Chen MI, Krishnan B. Predictors of failed attendances in a multi-specialty outpatient centre using electronic databases. 2013;3(9):e003212.BMJ Open. PubMed
35. Long T, Genao I, Horwitz LI. Reasons for readmission in an underserved high-risk population: A qualitative analysis of a series of inpatient interviews. 2013;32(7):1196-1203.Health Aff (Millwood). PubMed
34. Kangovi S, Barg FK, Carter T, Long JA, Shannon R, Grande D. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. 2015;54(10):976-982.Clin Pediatr (Phila). PubMed
33. Samuels RC, Ward VL, Melvin P, et al. Missed Appointments: Factors Contributing to High No-Show Rates in an Urban Pediatrics Primary Care Clinic. PubMed
Given growing incentives to reduce readmission rates, predischarge checklists and bundles have recommended that inpatient providers schedule postdischarge follow-up visits (PDFVs) for their hospitalized patients.1-4 PDFVs have been linked to lower readmission rates in patients with chronic conditions, including congestive heart failure, psychiatric illnesses, and chronic obstructive pulmonary disease.5-8 In contrast, the impact of PDFVs on readmissions in hospitalized general medicine populations has been mixed.9-12 Beyond the presence or absence of PDFVs, it may be a patient’s inability to keep scheduled PDFVs that contributes more strongly to preventable readmissions.11
This challenge, dealing with the 12% to 37% of patients who miss their visits (“no-shows”), is not new.13-17 In high-risk patient populations, such as those with substance abuse, diabetes, or human immunodeficiency virus, no-shows (NSs) have been linked to poorer short-term and long-term clinical outcomes.16,18-20 Additionally, NSs pose a challenge for outpatient clinics and the healthcare system at large. The financial cost of NSs ranges from approximately $200 per patient in 2 analyses to $7 million in cumulative lost revenue per year at 1 large academic health system.13,17,21 As such, increasing attendance at PDFVs is a potential target for improving both patient outcomes and clinic productivity.
Most prior PDFV research has focused on readmission risk rather than PDFV attendance as the primary outcome.5-12 However, given the patient-oriented benefits of attending PDFVs and the clinic-oriented benefits of avoiding vacant time slots, NS PDFVs represent an important missed opportunity for our healthcare delivery system. To our knowledge, risk factors for PDFV nonattendance have not yet been systematically studied. The aim of our study was to analyze PDFV nonattendance, particularly NSs and same-day cancellations (SDCs), for hospitalizations and clinics within our healthcare system.
METHODS
Study Design
We conducted an observational cohort study of adult patients from 10 medical units at the Hospital of the University of Pennsylvania (a 789-bed quaternary-care hospital within an urban, academic medical system) who were scheduled with at least 1 PDFV. Specifically, the patients included in our analysis were hospitalized on general internal medicine services or medical subspecialty services with discharge dates between April 1, 2014, and March 31, 2015. Hospitalizations included in our study had at least 1 PDFV scheduled with an outpatient provider affiliated with the University of Pennsylvania Health System (UPHS). PDFVs scheduled with unaffiliated providers were not examined.
Each PDFV was requested by a patient’s inpatient care team. Once the care team had determined that a PDFV was clinically warranted, a member of the team (generally a resident, advanced practice provider, medical student, or designee) either called the UPHS clinic to schedule an appointment time or e-mailed the outpatient UPHS provider directly to facilitate a more urgent PDFV appointment time. Once a PDFV time was confirmed, PDFV details (ie, date, time, location, and phone number) were electronically entered into the patient’s discharge instructions by the inpatient care team. At the time of discharge, nurses reviewed these instructions with their patients. All patients left the hospital with a physical copy of these instructions. As part of routine care at our institution, patients then received automated telephone reminders from their UPHS-affiliated outpatient clinic 48 hours prior to each PDFV.
Data Collection
Our study was determined to meet criteria for quality improvement by the University of Pennsylvania’s Institutional Review Board. We used our healthcare system’s integrated electronic medical record system to track the dates of initial PDFV requests, the dates of hospitalization, and actual PDFV dates. PDFVs were included if the appointment request was made while a patient was hospitalized, including the day of discharge. Our study methodology only allowed us to investigate PDFVs scheduled with UPHS outpatient providers. We did not review discharge instructions or survey non-UPHS clinics to quantify visits scheduled with other providers, for example, community health centers or external private practices.
Exclusion criteria included the following: (1) office visits with nonproviders, for example, scheduled diagnostic procedures or pharmacist appointments for warfarin dosing; (2) visits cancelled by inpatient providers prior to discharge; (3) visits for patients not otherwise eligible for UPHS outpatient care because of insurance reasons; and (4) visits scheduled for dates after a patient’s death. Our motivation for the third exclusion criterion was the infrequent and irregular process by which PDFVs were authorized for these patients. These patients and their characteristics are described in Supplementary Table 1 in more detail.
For each PDFV, we recorded age, gender, race, insurance status, driving distance, length of stay for index hospitalization, discharging service (general internal medicine vs subspecialty), postdischarge disposition (home, home with home care services such as nursing or physical therapy, or facility), the number of PDFVs scheduled per index hospitalization, PDFV specialty type (oncologic subspecialty, nononcologic medical subspecialty, nononcologic surgical subspecialty, primary care, or other specialty), PDFV season, and PDFV lead time (the number of days between the discharge date and PDFV). We consolidated oncologic specialties into 1 group given the integrated nature of our healthcare system’s comprehensive cancer center. “Other” PDFV specialty subtypes are described in Supplementary Table 2. Driving distances between patient postal codes and our hospital were calculated using Excel VBA Master (Salt Lake City, Utah) and were subsequently categorized into patient-level quartiles for further analysis. For cancelled PDFVs, we collected dates of cancellation relative to the date of the appointment itself.
Study Outcomes
The primary study outcome was PDFV attendance. Each PDFV’s status was categorized by outpatient clinic staff as attended, cancelled, or NS. For cancelled appointments, cancellation dates and reasons (if entered by clinic representatives) were collected. In keeping with prior studies investigating outpatient nonattendance,we calculated collective NS/SDC rates for the variables listed above.17,22-25 We additionally calculated NS/SDC and attendance-as-scheduled rates stratified by the number of PDFVs per patient to assess for a “high-utilizer” effect with regard to PDFV attendance.
Statistical Analysis
We used multivariable mixed-effects regression with a logit link to assess associations between age, gender, race, insurance, driving distance quartile, length of stay, discharging service, postdischarge disposition, the number of PDFVs per hospitalization, PDFV specialty type, PDFV season, PDFV lead time, and our NS/SDC outcome. The mixed-effects approach was used to account for correlation structures induced by patients who had multiple visits and for patients with multiple hospitalizations. Specifically, our model specified 2 levels of nesting (PDFVs nested within each hospitalization, which were nested within each patient) to obtain appropriate standard error estimates for our adjusted odds ratios (ORs). Correlation matrices and multivariable variance inflation factors were used to assess collinearity among the predictor variables. These assessments did not indicate strong collinearity; hence, all predictors were included in the model. Only driving distance had a small amount of missing data (0.18% of driving distances were unavailable), so multiple imputation was not undertaken. Analyses were performed using R version 3.3.1 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Baseline Characteristics
During the 1-year study period, there were 11,829 discrete hospitalizations in medical units at our hospital. Of these hospitalizations, 6136 (52%) had at least 1 UPHS-affiliated PDFV meeting our inclusion and exclusion criteria, as detailed in the Figure. Across these hospitalizations, 9258 PDFVs were scheduled on behalf of 4653 patients. Demographic characteristics for these patients, hospitalizations, and visits are detailed in Table 1. The median age of patients in our cohort was 61 years old (interquartile range [IQR] 49-70, range 18-101). The median driving distance was 17 miles (IQR 4.3-38.8, range 0-2891). For hospitalizations, the median length of stay was 5 days (IQR 3-10, range 0-97). The median PDFV lead time, which is defined as the number of days between discharge and PDFV, was 12 days (IQR 6-23, range 1-60). Overall, 41% of patients (n = 1927) attended all of their PDFVs as scheduled; Supplementary Figure 1 lists patient-level PDFV attendance-as-scheduled percentages in more detail.
Incidence of NSs and SDCs
Twenty-five percent of PDFVs (n = 2303) were ultimately NS/SDCs; this included 1658 NSs (18% of all appointments) and 645 SDCs (7% of all appointments). Fifty-two percent of PDFVs (n = 4847) were kept as scheduled, while 23% (n = 2108) were cancelled before the day of the visit. Of the 2558 cancellations with valid cancellation dates, 49% (n = 1252) were cancelled 2 or fewer days beforehand, as shown in Supplementary Figure 2.
The presence of exactly 2 PDFVs per hospitalization was also associated with higher NS/SDC rates (OR 1.17, 95% CI, 1.01-1.36), compared to a single PDFV per hospitalization; however, the presence of more than 2 PDFVs per hospitalization was associated with lower NS/SDC rates (OR 0.82, 95% CI, 0.69-0.98). A separate analysis (data not shown) of potential high utilizers revealed a 15% NS/SDC rate for the top 0.5% of patients (median: 18 PDFVs each) and an 18% NS/SDC rate for the top 1% of patients (median: 14 PDFVs each) with regard to the numbers of PDFVs scheduled, compared to the 25% overall NS/SDC rate for all patients.
NS/SDC rates and adjusted ORs with regard to individual PDFV characteristics are displayed in Table 3. Nononcologic visits had higher NS/SDC rates than oncologic visits; for example, the NS/SDC rate for primary care visits was 39% (OR 2.62, 95% CI, 2.03-3.38), compared to 12% for oncologic visits. Appointments in the “other” specialty category also had high nonattendance rates, as further described in Supplementary Table B. Summertime appointments were more likely to be attended (OR 0.81, 95% CI, 0.68-0.97) compared to those in the spring. PDFV lead time (the time interval between the discharge date and appointment date) was not associated with changes in visit attendance.
DISCUSSION
When comparing PDFV characteristics themselves, oncologic visits had the lowest NS/SDC incidence of any group analyzed in our study. This may be related to the inherent life-altering nature of a cancer diagnosis or our cancer center’s use of patient navigators.23,30 In contrast, primary care clinics suffered from NS/SDC rates approaching 40%, which is a concerning finding given the importance of primary care coordination in the posthospitalization period.9,31 Why are primary care appointments so commonly missed? Some studies suggest that forgetting about a primary care appointment is a leading reason.15,32,33 For PDFVs, this phenomenon may be augmented because the visits are not scheduled by patients themselves. Additionally, patients may paradoxically undervalue the benefit of an all-encompassing primary care visit, compared to a PDFV focused on a specific problem, (eg, a cardiology follow-up appointment for a patient with congestive heart failure). In particular, patients with limited health literacy may potentially undervalue the capabilities of their primary care clinics.34,35
The low absolute number of primary care PDFVs (only 8% of all visits) scheduled for patients at our hospital was an unexpected finding. This low percentage is likely a function of the patient population hospitalized at our large, urban quaternary-care facility. First, an unknown number of patients may have had PDFVs manually scheduled with primary care providers external to our health system; these PDFVs were not captured within our study. Second, 71% of the hospitalizations in our study occurred in subspecialty services, for which specific primary care follow-up may not be as urgent. Supporting this fact, further analysis of the 6136 hospitalizations in our study (data not shown) revealed that 28% of the hospitalizations in general internal medicine were scheduled with at least 1 primary care PDFV as opposed to only 5% of subspecialty-service hospitalizations.
In contrast to several previous studies of outpatient nonattendance,we did not find that visits scheduled for time points further in the future were more likely to be missed.14,24,25,36,37 Unlike other appointments, it may be that PDFV lead time does not affect attendance because of the unique manner in which PDFV times are scheduled and conveyed to patients. Unlike other appointments, patients do not schedule PDFVs themselves but instead learn about their PDFV dates as part of a large set of discharge instructions. This practice may result in poor recall of PDFV dates in recently hospitalized patients38, regardless of the lead time between discharge and the visit itself.
Supplementary Table 1 details a 51% NS/SDC rate for the small number of PDFVs (n = 65) that were excluded a priori from our analysis because of general ineligibility for UPHS outpatient care. We specifically chose to exclude this population because of the infrequent and irregular process by which these PDFVs were authorized on a case-by-case basis, typically via active engagement by our hospital’s social work department. We did not study this population further but postulate that the 51% NS/SDC rate may reflect other social determinants of health that contribute to appointment nonadherence in a predominantly uninsured population.
Beyond their effect on patient outcomes, improving PDFV-related processes has the potential to boost both inpatient and outpatient provider satisfaction. From the standpoint of frontline inpatient providers (often resident physicians), calling outpatient clinics to request PDFVs is viewed as 1 of the top 5 administrative tasks that interfere with house staff education.39 Future interventions that involve patients in the PDFV scheduling process may improve inpatient workflow while simultaneously engaging patients in their own care. For example, asking clinic representatives to directly schedule PDFVs with hospitalized patients, either by phone or in person, has been shown in pilot studies to improve PDFV attendance and decrease readmissions.40-42 Conversely, NS/SDC visits harm outpatient provider productivity and decrease provider availability for other patients.13,17,43 Strategies to mitigate the impact of unfilled appointment slots (eg, deliberately overbooking time slots in advance) carry their own risks, including provider burnout.44 As such, preventing NSs may be superior to curing their adverse impacts. Many such strategies exist in the ambulatory setting,13,43,45 for example, better communication with patients through texting or goal-directed, personalized phone reminders.46-48Our study methodology has several limitations. Most importantly, we were unable to measure PDFVs made with providers unaffiliated with UPHS. As previously noted, our low proportion of primary care PDFVs may specifically reflect patients with primary care providers outside of our health system. Similarly, our low percentage of Medicaid patients receiving PDFVs may be related to follow-up visits with nonaffiliated community health centers. We were unable to measure patient acuity and health literacy as potential predictors of NS/SDC rates. Driving distances were calculated from patient postal codes to our hospital, not to individual outpatient clinics. However, the majority of our hospital-affiliated clinics are located adjacent to our hospital; additionally, we grouped driving distances into quartiles for our analysis. We had initially attempted to differentiate between clinic-initiated and patient-initiated cancellations, but unfortunately, we found that the data were too unreliable to be used for further analysis (outlined in Supplementary Table 3). Lastly, because we studied patients in medical units at a single large, urban, academic center, our results are not generalizable to other settings (eg, community hospitals, hospitals with smaller networks of outpatient providers, or patients being discharged from surgical services or observation units).
CONCLUSION
Given national efforts to enhance postdischarge transitions of care, we aimed to analyze attendance at provider-scheduled PDFV appointments. Our finding that 25% of PDFVs resulted in NS/SDCs raises both questions and opportunities for inpatient and outpatient providers. Further research is needed to understand why so many patients miss their PDFVs, and we should work as a field to develop creative solutions to improve PDFV scheduling and attendance.
Acknowledgments
The authors acknowledge Marie Synnestvedt, PhD, and Manik Chhabra, MD, for their assistance with data gathering and statistical analysis. They also acknowledge Allison DeKosky, MD, Michael Serpa, BS, Michael McFall, and Scott Schlegel, MBA, for their assistance with researching this topic. They did not receive external compensation for their assistance outside of their usual salary support.
DISCLOSURE
Nothing to report.
Given growing incentives to reduce readmission rates, predischarge checklists and bundles have recommended that inpatient providers schedule postdischarge follow-up visits (PDFVs) for their hospitalized patients.1-4 PDFVs have been linked to lower readmission rates in patients with chronic conditions, including congestive heart failure, psychiatric illnesses, and chronic obstructive pulmonary disease.5-8 In contrast, the impact of PDFVs on readmissions in hospitalized general medicine populations has been mixed.9-12 Beyond the presence or absence of PDFVs, it may be a patient’s inability to keep scheduled PDFVs that contributes more strongly to preventable readmissions.11
This challenge, dealing with the 12% to 37% of patients who miss their visits (“no-shows”), is not new.13-17 In high-risk patient populations, such as those with substance abuse, diabetes, or human immunodeficiency virus, no-shows (NSs) have been linked to poorer short-term and long-term clinical outcomes.16,18-20 Additionally, NSs pose a challenge for outpatient clinics and the healthcare system at large. The financial cost of NSs ranges from approximately $200 per patient in 2 analyses to $7 million in cumulative lost revenue per year at 1 large academic health system.13,17,21 As such, increasing attendance at PDFVs is a potential target for improving both patient outcomes and clinic productivity.
Most prior PDFV research has focused on readmission risk rather than PDFV attendance as the primary outcome.5-12 However, given the patient-oriented benefits of attending PDFVs and the clinic-oriented benefits of avoiding vacant time slots, NS PDFVs represent an important missed opportunity for our healthcare delivery system. To our knowledge, risk factors for PDFV nonattendance have not yet been systematically studied. The aim of our study was to analyze PDFV nonattendance, particularly NSs and same-day cancellations (SDCs), for hospitalizations and clinics within our healthcare system.
METHODS
Study Design
We conducted an observational cohort study of adult patients from 10 medical units at the Hospital of the University of Pennsylvania (a 789-bed quaternary-care hospital within an urban, academic medical system) who were scheduled with at least 1 PDFV. Specifically, the patients included in our analysis were hospitalized on general internal medicine services or medical subspecialty services with discharge dates between April 1, 2014, and March 31, 2015. Hospitalizations included in our study had at least 1 PDFV scheduled with an outpatient provider affiliated with the University of Pennsylvania Health System (UPHS). PDFVs scheduled with unaffiliated providers were not examined.
Each PDFV was requested by a patient’s inpatient care team. Once the care team had determined that a PDFV was clinically warranted, a member of the team (generally a resident, advanced practice provider, medical student, or designee) either called the UPHS clinic to schedule an appointment time or e-mailed the outpatient UPHS provider directly to facilitate a more urgent PDFV appointment time. Once a PDFV time was confirmed, PDFV details (ie, date, time, location, and phone number) were electronically entered into the patient’s discharge instructions by the inpatient care team. At the time of discharge, nurses reviewed these instructions with their patients. All patients left the hospital with a physical copy of these instructions. As part of routine care at our institution, patients then received automated telephone reminders from their UPHS-affiliated outpatient clinic 48 hours prior to each PDFV.
Data Collection
Our study was determined to meet criteria for quality improvement by the University of Pennsylvania’s Institutional Review Board. We used our healthcare system’s integrated electronic medical record system to track the dates of initial PDFV requests, the dates of hospitalization, and actual PDFV dates. PDFVs were included if the appointment request was made while a patient was hospitalized, including the day of discharge. Our study methodology only allowed us to investigate PDFVs scheduled with UPHS outpatient providers. We did not review discharge instructions or survey non-UPHS clinics to quantify visits scheduled with other providers, for example, community health centers or external private practices.
Exclusion criteria included the following: (1) office visits with nonproviders, for example, scheduled diagnostic procedures or pharmacist appointments for warfarin dosing; (2) visits cancelled by inpatient providers prior to discharge; (3) visits for patients not otherwise eligible for UPHS outpatient care because of insurance reasons; and (4) visits scheduled for dates after a patient’s death. Our motivation for the third exclusion criterion was the infrequent and irregular process by which PDFVs were authorized for these patients. These patients and their characteristics are described in Supplementary Table 1 in more detail.
For each PDFV, we recorded age, gender, race, insurance status, driving distance, length of stay for index hospitalization, discharging service (general internal medicine vs subspecialty), postdischarge disposition (home, home with home care services such as nursing or physical therapy, or facility), the number of PDFVs scheduled per index hospitalization, PDFV specialty type (oncologic subspecialty, nononcologic medical subspecialty, nononcologic surgical subspecialty, primary care, or other specialty), PDFV season, and PDFV lead time (the number of days between the discharge date and PDFV). We consolidated oncologic specialties into 1 group given the integrated nature of our healthcare system’s comprehensive cancer center. “Other” PDFV specialty subtypes are described in Supplementary Table 2. Driving distances between patient postal codes and our hospital were calculated using Excel VBA Master (Salt Lake City, Utah) and were subsequently categorized into patient-level quartiles for further analysis. For cancelled PDFVs, we collected dates of cancellation relative to the date of the appointment itself.
Study Outcomes
The primary study outcome was PDFV attendance. Each PDFV’s status was categorized by outpatient clinic staff as attended, cancelled, or NS. For cancelled appointments, cancellation dates and reasons (if entered by clinic representatives) were collected. In keeping with prior studies investigating outpatient nonattendance,we calculated collective NS/SDC rates for the variables listed above.17,22-25 We additionally calculated NS/SDC and attendance-as-scheduled rates stratified by the number of PDFVs per patient to assess for a “high-utilizer” effect with regard to PDFV attendance.
Statistical Analysis
We used multivariable mixed-effects regression with a logit link to assess associations between age, gender, race, insurance, driving distance quartile, length of stay, discharging service, postdischarge disposition, the number of PDFVs per hospitalization, PDFV specialty type, PDFV season, PDFV lead time, and our NS/SDC outcome. The mixed-effects approach was used to account for correlation structures induced by patients who had multiple visits and for patients with multiple hospitalizations. Specifically, our model specified 2 levels of nesting (PDFVs nested within each hospitalization, which were nested within each patient) to obtain appropriate standard error estimates for our adjusted odds ratios (ORs). Correlation matrices and multivariable variance inflation factors were used to assess collinearity among the predictor variables. These assessments did not indicate strong collinearity; hence, all predictors were included in the model. Only driving distance had a small amount of missing data (0.18% of driving distances were unavailable), so multiple imputation was not undertaken. Analyses were performed using R version 3.3.1 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Baseline Characteristics
During the 1-year study period, there were 11,829 discrete hospitalizations in medical units at our hospital. Of these hospitalizations, 6136 (52%) had at least 1 UPHS-affiliated PDFV meeting our inclusion and exclusion criteria, as detailed in the Figure. Across these hospitalizations, 9258 PDFVs were scheduled on behalf of 4653 patients. Demographic characteristics for these patients, hospitalizations, and visits are detailed in Table 1. The median age of patients in our cohort was 61 years old (interquartile range [IQR] 49-70, range 18-101). The median driving distance was 17 miles (IQR 4.3-38.8, range 0-2891). For hospitalizations, the median length of stay was 5 days (IQR 3-10, range 0-97). The median PDFV lead time, which is defined as the number of days between discharge and PDFV, was 12 days (IQR 6-23, range 1-60). Overall, 41% of patients (n = 1927) attended all of their PDFVs as scheduled; Supplementary Figure 1 lists patient-level PDFV attendance-as-scheduled percentages in more detail.
Incidence of NSs and SDCs
Twenty-five percent of PDFVs (n = 2303) were ultimately NS/SDCs; this included 1658 NSs (18% of all appointments) and 645 SDCs (7% of all appointments). Fifty-two percent of PDFVs (n = 4847) were kept as scheduled, while 23% (n = 2108) were cancelled before the day of the visit. Of the 2558 cancellations with valid cancellation dates, 49% (n = 1252) were cancelled 2 or fewer days beforehand, as shown in Supplementary Figure 2.
The presence of exactly 2 PDFVs per hospitalization was also associated with higher NS/SDC rates (OR 1.17, 95% CI, 1.01-1.36), compared to a single PDFV per hospitalization; however, the presence of more than 2 PDFVs per hospitalization was associated with lower NS/SDC rates (OR 0.82, 95% CI, 0.69-0.98). A separate analysis (data not shown) of potential high utilizers revealed a 15% NS/SDC rate for the top 0.5% of patients (median: 18 PDFVs each) and an 18% NS/SDC rate for the top 1% of patients (median: 14 PDFVs each) with regard to the numbers of PDFVs scheduled, compared to the 25% overall NS/SDC rate for all patients.
NS/SDC rates and adjusted ORs with regard to individual PDFV characteristics are displayed in Table 3. Nononcologic visits had higher NS/SDC rates than oncologic visits; for example, the NS/SDC rate for primary care visits was 39% (OR 2.62, 95% CI, 2.03-3.38), compared to 12% for oncologic visits. Appointments in the “other” specialty category also had high nonattendance rates, as further described in Supplementary Table B. Summertime appointments were more likely to be attended (OR 0.81, 95% CI, 0.68-0.97) compared to those in the spring. PDFV lead time (the time interval between the discharge date and appointment date) was not associated with changes in visit attendance.
DISCUSSION
When comparing PDFV characteristics themselves, oncologic visits had the lowest NS/SDC incidence of any group analyzed in our study. This may be related to the inherent life-altering nature of a cancer diagnosis or our cancer center’s use of patient navigators.23,30 In contrast, primary care clinics suffered from NS/SDC rates approaching 40%, which is a concerning finding given the importance of primary care coordination in the posthospitalization period.9,31 Why are primary care appointments so commonly missed? Some studies suggest that forgetting about a primary care appointment is a leading reason.15,32,33 For PDFVs, this phenomenon may be augmented because the visits are not scheduled by patients themselves. Additionally, patients may paradoxically undervalue the benefit of an all-encompassing primary care visit, compared to a PDFV focused on a specific problem, (eg, a cardiology follow-up appointment for a patient with congestive heart failure). In particular, patients with limited health literacy may potentially undervalue the capabilities of their primary care clinics.34,35
The low absolute number of primary care PDFVs (only 8% of all visits) scheduled for patients at our hospital was an unexpected finding. This low percentage is likely a function of the patient population hospitalized at our large, urban quaternary-care facility. First, an unknown number of patients may have had PDFVs manually scheduled with primary care providers external to our health system; these PDFVs were not captured within our study. Second, 71% of the hospitalizations in our study occurred in subspecialty services, for which specific primary care follow-up may not be as urgent. Supporting this fact, further analysis of the 6136 hospitalizations in our study (data not shown) revealed that 28% of the hospitalizations in general internal medicine were scheduled with at least 1 primary care PDFV as opposed to only 5% of subspecialty-service hospitalizations.
In contrast to several previous studies of outpatient nonattendance,we did not find that visits scheduled for time points further in the future were more likely to be missed.14,24,25,36,37 Unlike other appointments, it may be that PDFV lead time does not affect attendance because of the unique manner in which PDFV times are scheduled and conveyed to patients. Unlike other appointments, patients do not schedule PDFVs themselves but instead learn about their PDFV dates as part of a large set of discharge instructions. This practice may result in poor recall of PDFV dates in recently hospitalized patients38, regardless of the lead time between discharge and the visit itself.
Supplementary Table 1 details a 51% NS/SDC rate for the small number of PDFVs (n = 65) that were excluded a priori from our analysis because of general ineligibility for UPHS outpatient care. We specifically chose to exclude this population because of the infrequent and irregular process by which these PDFVs were authorized on a case-by-case basis, typically via active engagement by our hospital’s social work department. We did not study this population further but postulate that the 51% NS/SDC rate may reflect other social determinants of health that contribute to appointment nonadherence in a predominantly uninsured population.
Beyond their effect on patient outcomes, improving PDFV-related processes has the potential to boost both inpatient and outpatient provider satisfaction. From the standpoint of frontline inpatient providers (often resident physicians), calling outpatient clinics to request PDFVs is viewed as 1 of the top 5 administrative tasks that interfere with house staff education.39 Future interventions that involve patients in the PDFV scheduling process may improve inpatient workflow while simultaneously engaging patients in their own care. For example, asking clinic representatives to directly schedule PDFVs with hospitalized patients, either by phone or in person, has been shown in pilot studies to improve PDFV attendance and decrease readmissions.40-42 Conversely, NS/SDC visits harm outpatient provider productivity and decrease provider availability for other patients.13,17,43 Strategies to mitigate the impact of unfilled appointment slots (eg, deliberately overbooking time slots in advance) carry their own risks, including provider burnout.44 As such, preventing NSs may be superior to curing their adverse impacts. Many such strategies exist in the ambulatory setting,13,43,45 for example, better communication with patients through texting or goal-directed, personalized phone reminders.46-48Our study methodology has several limitations. Most importantly, we were unable to measure PDFVs made with providers unaffiliated with UPHS. As previously noted, our low proportion of primary care PDFVs may specifically reflect patients with primary care providers outside of our health system. Similarly, our low percentage of Medicaid patients receiving PDFVs may be related to follow-up visits with nonaffiliated community health centers. We were unable to measure patient acuity and health literacy as potential predictors of NS/SDC rates. Driving distances were calculated from patient postal codes to our hospital, not to individual outpatient clinics. However, the majority of our hospital-affiliated clinics are located adjacent to our hospital; additionally, we grouped driving distances into quartiles for our analysis. We had initially attempted to differentiate between clinic-initiated and patient-initiated cancellations, but unfortunately, we found that the data were too unreliable to be used for further analysis (outlined in Supplementary Table 3). Lastly, because we studied patients in medical units at a single large, urban, academic center, our results are not generalizable to other settings (eg, community hospitals, hospitals with smaller networks of outpatient providers, or patients being discharged from surgical services or observation units).
CONCLUSION
Given national efforts to enhance postdischarge transitions of care, we aimed to analyze attendance at provider-scheduled PDFV appointments. Our finding that 25% of PDFVs resulted in NS/SDCs raises both questions and opportunities for inpatient and outpatient providers. Further research is needed to understand why so many patients miss their PDFVs, and we should work as a field to develop creative solutions to improve PDFV scheduling and attendance.
Acknowledgments
The authors acknowledge Marie Synnestvedt, PhD, and Manik Chhabra, MD, for their assistance with data gathering and statistical analysis. They also acknowledge Allison DeKosky, MD, Michael Serpa, BS, Michael McFall, and Scott Schlegel, MBA, for their assistance with researching this topic. They did not receive external compensation for their assistance outside of their usual salary support.
DISCLOSURE
Nothing to report.
1. Halasyamani L, Kripalani S, Coleman E, et al. Transition of care for hospitalized elderly patients - development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354-360. PubMed
2. Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218. PubMed
3. Soong C, Daub S, Lee JG, et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013;8(8):444-449. PubMed
4. Rice YB, Barnes CA, Rastogi R, Hillstrom TJ, Steinkeler CN. Tackling 30-day, all-cause readmissions with a patient-centered transitional care bundle. Popul Health Manag. 2016;19(1):56-62. PubMed
5. Nelson EA, Maruish MM, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psych Serv. 2000;51(7):885-889. PubMed
6. Gavish R, Levy A, Dekel OK, Karp E, Maimon N. The association between hospital readmission and pulmonologist follow-up visits in patients with chronic obstructive pulmonary disease. Chest. 2015;148(2):375-381. PubMed
7. Jackson C, Shahsahebi M, Wedlake T, DuBard CA. Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med. 2015;13(2):115-122. PubMed
8. Donaho EK, Hall AC, Gass JA, et al. Protocol-driven allied health post-discharge transition clinic to reduce hospital readmissions in heart failure. J Am Heart Assoc. 2015;4(12):e002296. PubMed
9. Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392-397. PubMed
10. Grafft CA, McDonald FS, Ruud KL, Liesinger JT, Johnson MG, Naessens JM. Effect of hospital follow-up appointment on clinical event outcomes and mortality. Arch Intern Med. 2010;171(11):955-960. PubMed
11. Auerbach AD, Kripalani S, Vasilevskis EE, et al. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med. 2016;176(4):484-493. PubMed
12. Field TS, Ogarek J, Garber L, Reed G, Gurwitz JH. Association of early post-discharge follow-up by a primary care physician and 30-day rehospitalization among older adults. J Gen Intern Med. 2015;30(5):565-571. PubMed
13. Quinn K. It’s no-show time! Med Group Manage Assoc Connexion. 2007;7(6):44-49. PubMed
14. Whittle J, Schectman G, Lu N, Baar B, Mayo-Smith MF. Relationship of scheduling interval to missed and cancelled clinic appointments. J Ambulatory Care Manage. 2008;31(4):290-302. PubMed
15. Kaplan-Lewis E, Percac-Lima S. No-show to primary care appointments: Why patients do not come. J Prim Care Community Health. 2013;4(4):251-255. PubMed
16. Molfenter T. Reducing appointment no-shows: Going from theory to practice. Subst Use Misuse. 2013;48(9):743-749. PubMed
17. Kheirkhah P, Feng Q, Travis LM, Tavakoli-Tabasi S, Sharafkhaneh A. Prevalence, predictors and economic consequences of no-shows. BMC Health Serv Res. 2016;16(1):13. PubMed
18. Colubi MM, Perez-Elias MJ, Elias L, et al. Missing scheduled visits in the outpatient clinic as a marker of short-term admissions and death. HIV Clin Trials. 2012;13(5):289-295. PubMed
19. Obialo CI, Hunt WC, Bashir K, Zager PG. Relationship of missed and shortened hemodialysis treatments to hospitalization and mortality: Observations from a US dialysis network. Clin Kidney J. 2012;5(4):315-319. PubMed
20. Hwang AS, Atlas SJ, Cronin P, et al. Appointment “no-shows” are an independent predictor of subsequent quality of care and resource utilization outcomes. J Gen Intern Med. 2015;30(10):1426-1433. PubMed
21. Perez FD, Xie J, Sin A, et al. Characteristics and direct costs of academic pediatric subspecialty outpatient no-show events. J Healthc Qual. 2014;36(4):32-42. PubMed
22. Huang Y, Zuniga P. Effective cancellation policy to reduce the negative impact of patient no-show. Journal of the Operational Research Society. 2013;65(5):605-615.
23. Percac-Lima S, Cronin PR, Ryan DP, Chabner BA, Daly EA, Kimball AB. Patient navigation based on predictive modeling decreases no-show rates in cancer care. Cancer. 2015;121(10):1662-1670. PubMed
24. Torres O, Rothberg MB, Garb J, Ogunneye O, Onyema J, Higgins T. Risk factor model to predict a missed clinic appointment in an urban, academic, and underserved setting. Popul Health Manag. 2015;18(2):131-136. PubMed
25. Eid WE, Shehata SF, Cole DA, Doerman KL. Predictors of nonattendance at an endocrinology outpatient clinic. Endocr Pract. 2016;22(8):983-989. PubMed
26. Kashiwagi DT, Burton MC, Kirkland LL, Cha S, Varkey P. Do timely outpatient follow-up visits decrease hospital readmission rates? Am J Med Qual. 2012;27(1):11-15. PubMed
27. Miller AJ, Chae E, Peterson E, Ko AB. Predictors of repeated “no-showing” to clinic appointments. Am J Otolaryngol. 2015;36(3):411-414. PubMed
28. ASCO. Billing challenges for residents of Skilled Nursing Facilities. J Oncol Pract. 2008;4(5):245-248. PubMed
29. Centers for Medicare & Medicaid Services (2013). “SE0433: Skilled Nursing Facility consolidated billing as it relates to ambulance services.” Medicare Learning Network Matters. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/se0433.pdf. Accessed on February 14, 2017.
30. Luckett R, Pena N, Vitonis A, Bernstein MR, Feldman S. Effect of patient navigator program on no-show rates at an academic referral colposcopy clinic. J Womens Health (Larchmt). 2015;24(7):608-615. PubMed
31. Jones CD, Vu MB, O’Donnell CM, et al. A failure to communicate: A qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations. J Gen Intern Med. 2015;30(4):417-424. PubMed
32. George A, Rubin G. Non-attendance in general practice: a systematic review and its implications for access to primary health care. Fam Pract. 2003;20(2):178-184. 2016;31(12):1460-1466.J Gen Intern Med. PubMed
48. Shah SJ, Cronin P, Hong CS, et al. Targeted reminder phone calls to patients at high risk of no-show for primary care appointment: A randomized trial. 2010;123(6):542-548.Am J Med. PubMed
47. Parikh A, Gupta K, Wilson AC, Fields K, Cosgrove NM, Kostis JB. The effectiveness of outpatient appointment reminder systems in reducing no-show rates. 2009;20:142-144.Int J STD AIDS. PubMed
46. Price H, Waters AM, Mighty D, et al. Texting appointment reminders reduces ‘Did not attend’ rates, is popular with patients and is cost-effective. 2009;25(3):166-170.J Med Practice Management. PubMed
45. Hills LS. How to handle patients who miss appointments or show up late.
2009;39(3):271-287.Interfaces. PubMed
44. Kros J, Dellana S, West D. Overbooking Increases Patient Access at East Carolina University’s Student Health Services Clinic. 2012;344(3):211-219.Am J Med Sci.
43. Stubbs ND, Geraci SA, Stephenson PL, Jones DB, Sanders S. Methods to reduce outpatient non-attendance. PubMed
42. Haftka A, Cerasale MT, Paje D. Direct patient participation in discharge follow-up appointment scheduling. Paper presented at: Society of Hospital Medicine, Annual Meeting 2015; National Harbor, MD. 2012;5(1):27-32.Patient.
41. Chang R, Spahlinger D, Kim CS. Re-engineering the post-discharge appointment process for general medicine patients. PubMed
40. Coffey C, Kufta J. Patient-centered post-discharge appointment scheduling improves readmission rates. Paper presented at: Society of Hospital Medicine, Annual Meeting 2011; Grapevine, Texas. 2006;81(1):76-81.Acad Med.
39. Vidyarthi AR, Katz PP, Wall SD, Wachter RM, Auerbach AD. Impact of reduced duty hours on residents’ education satistfaction at the University of California, San Francisco.
2013;173(18):1715-1722.JAMA Intern Med. PubMed
38. Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center. 2010;16(4):246-259.Health Informatics J. PubMed
37. Daggy J, Lawley M, Willis D, et al. Using no-show modeling to improve clinic performance. 2005;5:51.BMC Health Serv Res. PubMed
36. Lee VJ, Earnest A, Chen MI, Krishnan B. Predictors of failed attendances in a multi-specialty outpatient centre using electronic databases. 2013;3(9):e003212.BMJ Open. PubMed
35. Long T, Genao I, Horwitz LI. Reasons for readmission in an underserved high-risk population: A qualitative analysis of a series of inpatient interviews. 2013;32(7):1196-1203.Health Aff (Millwood). PubMed
34. Kangovi S, Barg FK, Carter T, Long JA, Shannon R, Grande D. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. 2015;54(10):976-982.Clin Pediatr (Phila). PubMed
33. Samuels RC, Ward VL, Melvin P, et al. Missed Appointments: Factors Contributing to High No-Show Rates in an Urban Pediatrics Primary Care Clinic. PubMed
1. Halasyamani L, Kripalani S, Coleman E, et al. Transition of care for hospitalized elderly patients - development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354-360. PubMed
2. Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218. PubMed
3. Soong C, Daub S, Lee JG, et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013;8(8):444-449. PubMed
4. Rice YB, Barnes CA, Rastogi R, Hillstrom TJ, Steinkeler CN. Tackling 30-day, all-cause readmissions with a patient-centered transitional care bundle. Popul Health Manag. 2016;19(1):56-62. PubMed
5. Nelson EA, Maruish MM, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psych Serv. 2000;51(7):885-889. PubMed
6. Gavish R, Levy A, Dekel OK, Karp E, Maimon N. The association between hospital readmission and pulmonologist follow-up visits in patients with chronic obstructive pulmonary disease. Chest. 2015;148(2):375-381. PubMed
7. Jackson C, Shahsahebi M, Wedlake T, DuBard CA. Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med. 2015;13(2):115-122. PubMed
8. Donaho EK, Hall AC, Gass JA, et al. Protocol-driven allied health post-discharge transition clinic to reduce hospital readmissions in heart failure. J Am Heart Assoc. 2015;4(12):e002296. PubMed
9. Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392-397. PubMed
10. Grafft CA, McDonald FS, Ruud KL, Liesinger JT, Johnson MG, Naessens JM. Effect of hospital follow-up appointment on clinical event outcomes and mortality. Arch Intern Med. 2010;171(11):955-960. PubMed
11. Auerbach AD, Kripalani S, Vasilevskis EE, et al. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med. 2016;176(4):484-493. PubMed
12. Field TS, Ogarek J, Garber L, Reed G, Gurwitz JH. Association of early post-discharge follow-up by a primary care physician and 30-day rehospitalization among older adults. J Gen Intern Med. 2015;30(5):565-571. PubMed
13. Quinn K. It’s no-show time! Med Group Manage Assoc Connexion. 2007;7(6):44-49. PubMed
14. Whittle J, Schectman G, Lu N, Baar B, Mayo-Smith MF. Relationship of scheduling interval to missed and cancelled clinic appointments. J Ambulatory Care Manage. 2008;31(4):290-302. PubMed
15. Kaplan-Lewis E, Percac-Lima S. No-show to primary care appointments: Why patients do not come. J Prim Care Community Health. 2013;4(4):251-255. PubMed
16. Molfenter T. Reducing appointment no-shows: Going from theory to practice. Subst Use Misuse. 2013;48(9):743-749. PubMed
17. Kheirkhah P, Feng Q, Travis LM, Tavakoli-Tabasi S, Sharafkhaneh A. Prevalence, predictors and economic consequences of no-shows. BMC Health Serv Res. 2016;16(1):13. PubMed
18. Colubi MM, Perez-Elias MJ, Elias L, et al. Missing scheduled visits in the outpatient clinic as a marker of short-term admissions and death. HIV Clin Trials. 2012;13(5):289-295. PubMed
19. Obialo CI, Hunt WC, Bashir K, Zager PG. Relationship of missed and shortened hemodialysis treatments to hospitalization and mortality: Observations from a US dialysis network. Clin Kidney J. 2012;5(4):315-319. PubMed
20. Hwang AS, Atlas SJ, Cronin P, et al. Appointment “no-shows” are an independent predictor of subsequent quality of care and resource utilization outcomes. J Gen Intern Med. 2015;30(10):1426-1433. PubMed
21. Perez FD, Xie J, Sin A, et al. Characteristics and direct costs of academic pediatric subspecialty outpatient no-show events. J Healthc Qual. 2014;36(4):32-42. PubMed
22. Huang Y, Zuniga P. Effective cancellation policy to reduce the negative impact of patient no-show. Journal of the Operational Research Society. 2013;65(5):605-615.
23. Percac-Lima S, Cronin PR, Ryan DP, Chabner BA, Daly EA, Kimball AB. Patient navigation based on predictive modeling decreases no-show rates in cancer care. Cancer. 2015;121(10):1662-1670. PubMed
24. Torres O, Rothberg MB, Garb J, Ogunneye O, Onyema J, Higgins T. Risk factor model to predict a missed clinic appointment in an urban, academic, and underserved setting. Popul Health Manag. 2015;18(2):131-136. PubMed
25. Eid WE, Shehata SF, Cole DA, Doerman KL. Predictors of nonattendance at an endocrinology outpatient clinic. Endocr Pract. 2016;22(8):983-989. PubMed
26. Kashiwagi DT, Burton MC, Kirkland LL, Cha S, Varkey P. Do timely outpatient follow-up visits decrease hospital readmission rates? Am J Med Qual. 2012;27(1):11-15. PubMed
27. Miller AJ, Chae E, Peterson E, Ko AB. Predictors of repeated “no-showing” to clinic appointments. Am J Otolaryngol. 2015;36(3):411-414. PubMed
28. ASCO. Billing challenges for residents of Skilled Nursing Facilities. J Oncol Pract. 2008;4(5):245-248. PubMed
29. Centers for Medicare & Medicaid Services (2013). “SE0433: Skilled Nursing Facility consolidated billing as it relates to ambulance services.” Medicare Learning Network Matters. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/se0433.pdf. Accessed on February 14, 2017.
30. Luckett R, Pena N, Vitonis A, Bernstein MR, Feldman S. Effect of patient navigator program on no-show rates at an academic referral colposcopy clinic. J Womens Health (Larchmt). 2015;24(7):608-615. PubMed
31. Jones CD, Vu MB, O’Donnell CM, et al. A failure to communicate: A qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations. J Gen Intern Med. 2015;30(4):417-424. PubMed
32. George A, Rubin G. Non-attendance in general practice: a systematic review and its implications for access to primary health care. Fam Pract. 2003;20(2):178-184. 2016;31(12):1460-1466.J Gen Intern Med. PubMed
48. Shah SJ, Cronin P, Hong CS, et al. Targeted reminder phone calls to patients at high risk of no-show for primary care appointment: A randomized trial. 2010;123(6):542-548.Am J Med. PubMed
47. Parikh A, Gupta K, Wilson AC, Fields K, Cosgrove NM, Kostis JB. The effectiveness of outpatient appointment reminder systems in reducing no-show rates. 2009;20:142-144.Int J STD AIDS. PubMed
46. Price H, Waters AM, Mighty D, et al. Texting appointment reminders reduces ‘Did not attend’ rates, is popular with patients and is cost-effective. 2009;25(3):166-170.J Med Practice Management. PubMed
45. Hills LS. How to handle patients who miss appointments or show up late.
2009;39(3):271-287.Interfaces. PubMed
44. Kros J, Dellana S, West D. Overbooking Increases Patient Access at East Carolina University’s Student Health Services Clinic. 2012;344(3):211-219.Am J Med Sci.
43. Stubbs ND, Geraci SA, Stephenson PL, Jones DB, Sanders S. Methods to reduce outpatient non-attendance. PubMed
42. Haftka A, Cerasale MT, Paje D. Direct patient participation in discharge follow-up appointment scheduling. Paper presented at: Society of Hospital Medicine, Annual Meeting 2015; National Harbor, MD. 2012;5(1):27-32.Patient.
41. Chang R, Spahlinger D, Kim CS. Re-engineering the post-discharge appointment process for general medicine patients. PubMed
40. Coffey C, Kufta J. Patient-centered post-discharge appointment scheduling improves readmission rates. Paper presented at: Society of Hospital Medicine, Annual Meeting 2011; Grapevine, Texas. 2006;81(1):76-81.Acad Med.
39. Vidyarthi AR, Katz PP, Wall SD, Wachter RM, Auerbach AD. Impact of reduced duty hours on residents’ education satistfaction at the University of California, San Francisco.
2013;173(18):1715-1722.JAMA Intern Med. PubMed
38. Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center. 2010;16(4):246-259.Health Informatics J. PubMed
37. Daggy J, Lawley M, Willis D, et al. Using no-show modeling to improve clinic performance. 2005;5:51.BMC Health Serv Res. PubMed
36. Lee VJ, Earnest A, Chen MI, Krishnan B. Predictors of failed attendances in a multi-specialty outpatient centre using electronic databases. 2013;3(9):e003212.BMJ Open. PubMed
35. Long T, Genao I, Horwitz LI. Reasons for readmission in an underserved high-risk population: A qualitative analysis of a series of inpatient interviews. 2013;32(7):1196-1203.Health Aff (Millwood). PubMed
34. Kangovi S, Barg FK, Carter T, Long JA, Shannon R, Grande D. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. 2015;54(10):976-982.Clin Pediatr (Phila). PubMed
33. Samuels RC, Ward VL, Melvin P, et al. Missed Appointments: Factors Contributing to High No-Show Rates in an Urban Pediatrics Primary Care Clinic. PubMed
662-7919; E-mail: rahul.banerjee.md@gmail.com
Excess Readmission vs Excess Penalties: Maximum Readmission Penalties as a Function of Socioeconomics and Geography
INTRODUCTION
According to Centers for Medicare & Medicaid Services (CMS), approximately 1 in 5 patients discharged from a hospital will be readmitted within 30 days.1 The Hospital Readmission Reduction Program (HRRP) is designed to reduce readmission by withholding up to 3% of all Medicare reimbursement from hospitals with “excess” readmissions; however, absent from the HRRP is adjustment for socioeconomic status (SES), which CMS holds may undermine incentives to reduce health disparities and institutionalize lower standards for hospitals serving disadvantaged populations.2
Lack of SES adjustment has been criticized by those who point to evidence highlighting postdischarge environment and patient SES as drivers of readmission and suggest hospitals that serve low SES individuals will bear a disproportionate share of penalties.3-6 Single-center,3,7,8 regional,9,10 and nationwide6,11 studies highlight census tract level socioeconomic variables as predictive of readmission. Single-center studies, robust in controlling for confounders, including staffing, training, electronic medical record utilization, and transitional care processes, do not allow comparisons between hospitals, limiting utility in HRRP evaluation. Multicenter cohorts, on the other hand, allow for comparisons between high and low penalty hospitals, pioneered by Joynt et al12 after the first round of HRRP penalties; yet this technique may not account for confounding caused by extensive demographic, socioeconomic, and hospital characteristic heterogeneity inherent in a national cohort. Analysis of the 2015 HRRP penalty data by Sjoding et al.6 revealed higher chronic obstructive pulmonary disease (COPD) readmission rates in the Mid-Atlantic, Midwest, and South relative to other regions; however, the magnitude of small-area variation and its relationship to population SES have yet to be characterized.
Therefore, we conducted a matched case-control design, whereby each maximum penalty hospital was matched to a nonpenalty hospital using key hospital characteristics. We then used geographic matching to isolate SES factors predictive of readmission within specific geographies in an effort to control for regional population differences. We hypothesized that, among both matched and localized hospital pairs, the disparities in population SES are the most significant predictors of a maximum penalty. Now in the 3rd year of the HRRP with approximately 75% of eligible hospitals to receive penalties worth an estimated $428 million in the 2015 fiscal year,13 we offer a small-area analysis of bipolar extremes to inform debate surrounding the HRRP with evidence regarding the causes and implications of readmission penalties.
METHODS
Study Design and Sample
This study relies on a case-control design. The cases were defined as US hospitals to receive the maximum 3% HRRP penalty in fiscal year 2015. Controls were drawn from the cohort of hospitals potentially subject to HRRP penalties that received no readmission penalty in the 2015 fiscal year with at least 1 admission for any of the following conditions: heart failure (HF), acute myocardial infarction (AMI), pneumonia (PN), total knee arthroscopy or total hip arthroscopy (THA/TKA), or chronic obstructive pulmonary disease (COPD).
Data Sources
Penalty data were drawn from the 2015 master penalty file,14 which were accessed via CMS.gov. County-level demographic and socioeconomic data were gathered from the 2015 American Community Survey (ACS), a subsidiary of the US Census. Data on hospital characteristics, capacity, and regional healthcare utilization were drawn from 2012 Dartmouth Atlas,15 2012 Medicare Cost Report,16 2012 American Hospital Association Hospital Statistics Database, and 2014 Hospital Care Downloadable Database.
Hospital-level CMS data were linked to the master 2015 penalty file. Dartmouth Atlas data were subsequently linked to the file using the Dartmouth Atlas “Hospital to HSA/HRR Crosswalk” file (accessed via DartmouthAtlas.org.) Each hospital was assigned the profile of the hospital service area (HSA) and hospital referral region (HRR) in which it is located. An HSA is a geographic region defined by hospital admissions; the majority, but not entirety, of residents of a given HSA utilize the corresponding hospital. Similarly, an HRR is a geographic region defined by referrals for major cardiovascular and neurosurgery procedures. County-level socioeconomic data were linked to the dataset by county name; thus, hospital socioeconomic profiles are based on the county in which they are located.
Case-Control Matching
In the primary analysis, coarsened exact matching (CEM) matched controls to cases by potential confounding hospital characteristics, including the following: ownership, number of beds, case mix index (measure of acuity), ambulatory care visit rates within 14 days of discharge, and total number of penalty-eligible cases, including HF, AMI, COPD, PN, and THA/TKA.
In the secondary analysis, hospitals were geocoded by zip code. Geographic Information Systems mapping software (ESRI ArcGIS, Redlands, CA) relied upon Euclidean allocation distance spatial analysis17,18 to match each maximum-penalty hospital to the nearest nonpenalty hospital. Each case was matched to a distinct control; duplicate controls were replaced with the nearest unmatched no-penalty hospital.
Statistical Analysis
Univariate analyses utilized unpaired Student t tests (primary analysis) and paired Student t tests (secondary analysis). The CEM algorithm matches by strata rather than pairs, precluding paired Student t tests in the primary analysis. Statistical analyses were conducted using STATA (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX).
RESULTS
Maximum Penalty and Nonpenalty Hospital Matching
Of 3383 hospitals eligible for the HRRP, 39 received the maximum penalty and 770 received no penalty. Thirty-eight control hospitals were identified using CEM algorithm; 1 maximum-penalty hospital could not be matched and was excluded from primary analy
Hospital Characteristics
Case and control profiles are presented in Table 1. Cases and controls were matched by characteristics which may impact readmission rates (Table 1). CEM yielded cohorts similar across a spectrum of metrics, and identical in terms of matching criteria including ownership, beds (quartile), case mix index (above median), ambulatory care visit within 14 days of discharge (above median), and total number of penalty-eligible cases (above median). Relative to no-penalty hospitals, maximum-penalty hospitals were more likely rural (n = 9 vs n = 2, P = 0.022) and have a less profitable operating margin (0.1% vs 6.9%), and location within HSAs with higher age, sex, and race adjusted hospital-wide mortality rate (5.3% vs 4.9%, P = 0.009) and higher rates of discharge for ambulatory care sensitive conditions (108 vs 63 discharges per 1000 Medicare enrollees).
Demographic and Socioeconomic Characteristics
As presented in Table 2, cases a
Secondary Analysis: Geographical Matching
Secondary analysis matched each maximum-penalty hospital to the nearest no-penalty hospital using a global information system vector analysis algorithm. As shown in the Figure, median distance between the case and the control was 42.5 miles (interquartile range: 25th percentile, 15.4 miles; 75th percentile, 98.4 miles). Seventeen pairs (44%) were in the same HRR, 6 of which were in the same HSA. Seven pairs (18%) were within the same county
Secondary Analysis: Economic and Demographic Profiles of Geographically Matched Pairs
Demographic and socioeconomic profiles are presented in Table 3. The cases and controls are in counties with similar age, sex, and ethnicity distributions. Relative to no-penalty hospitals, maximum-penalty hospitals are in counties with lower socioeconomic profiles, including increased rates of poverty (15.6% vs 19.2%, P = 0.007) and lower rates of high school (86.4% vs 82.1%, P = 0.005) or college graduation (22.3% vs 28.1%, P = 0.002). Seven pairs were in the same county; a sensitivity analysis excluding these hospitals revealed similarly lower SES profile in cases relative to controls (Supplementary Table 1).
DISCUSSION
Our analysis reveals that county-level socioeconomic profiles are predictors of maximum HRRP penalties. Specifically, after matching cases and controls on 5 hospital characteristics that may influence readmission, maximum-penalty hospitals were more likely to be in rural counties with higher rates of poverty and lower rates of education relative to no-penalty hospitals. We observed no difference between cases and controls with respect to age, sex, or ethnicity.
Our study complement
Maximum Penalties as a Function of Population Health
The Dartmouth Atlas of Healthcare measures health outcomes, which are regionally aggregated among local hospitals by either HSA or HRR; see Methods. Such small-area aggregation does not precisely reflect outcomes from a specific hospital, but rather it describes the health status of localities. Disparities in health outcomes exist between maximum-penalty and no-penalty HSAs. Complication rates were slightly higher in maximum penalty HSAs, consistent with studies highlighting complications as drivers of surgical readmissions.22,23 Moreover, hospital-wide mortality rates were higher in maximum-penalty areas relative to nonpenalty HSAs (5.3 vs 4.9, P = 0.009).
Using national data, Krumholz et al. found no correlation between rates of readmission and mortality for HF, AMI, and PN24, which is a phenomenon acknowledged by the Medicare Payment Advisory Commission (MedPac) in a 2013 report titled, “Refining the hospital readmission reduction program.”25 In large national studies, others have shown low SES to be associated with elevated readmission but not mortality.10,11 In contrast, we restricted our analysis to matched cohorts and are, to our knowledge, the first to present evidence of an association between readmission and hospital-wide mortality adjusted for age, sex, and ethnicity.
Our results suggest maximum readmission penalties are a function of population health and public health capacity. The rates of ambulatory care sensitive condition (ACSC) discharges were substantially higher in HSAs of maximum penalty hospitals relative to nonpenalty hospitals (108 vs 63 per 1000 Medicare enrollees, P < 0.001). ACSC discharges have been used to measure primary care quality for 30 years, with the assumption being that admission for chronic conditions, such as HF, can be prevented with effective primary care.26,27 Moreover, patients discharged from maximum-penalty hospitals were more likely to have an emergency room visit within 30 days of discharge (20.8% vs 18.4%, P < 0.001). Higher rates of ACSCs and postdischarge emergency department visits suggest outpatient resources in maximum-penalty service areas struggle to manage the disease burden of high-risk populations. Geography may be a contributor; maximum-penalty hospitals were more likely to be rural than no-penalty hospitals (24% vs 5%, P = 0.022).
Our findings suggest hospitals providing care to vulnerable communities (defined by low income, low education, and high rates of ambulatory sensitive discharges) are disproportionately penalized. McHugh et al. revealed high nurse staffing levels to be protective against readmission penalties28, yet high penalties to low-margin hospitals may encourage reduced rather than increased staff. It may be better policy to direct resources rather than penalties to underserved communities; our findings echo others with concern about disproportionate penalties to hospitals serving low SES patients.2,5,6,29
Secondary Analysis: Geographic Matching
Geographic matching paired each maximum-penalty hospital to the nearest no-penalty hospital in an attempt to control for unmeasured regional factors that may confound an association between socioeconomic profile and health outcomes. For example, cost of living 30, 31 and obesity 32,33 vary regionally. Our study was unequipped to assess potential regional confounders; we attempted to control for them with geographical matching.
Median distance between maximum-penalty and no-penalty hospitals was 42.5 miles. Seven pairs were located within the same county, thus both case and control were assigned the same socioeconomic profile. Despite close proximity and identical SES profile in 7 of 39 pairs, maximum-penalty hospitals were in counties with lower income and lower rates of education, strengthening the association between SES and maximum readmission penalties.
Implications and Future Directions
In response to criticism surrounding the HRRP, the National Quality Forum endorsed the general concept of SES adjustment for hospital quality measures.34 Subsequently, in a briefing dated March 24, 2015, MedPAC, a government agency which provides Medicare policy analysis to Congress, proposed an SES adjustment methodology of “dividing hospitals into peer groups based on their overall share of low-income Medicare patients, and then setting a benchmark readmissions target for each peer group”;35 in other words, lower standards for hospitals that serve low-income populations. MedPAC’s proposal will reduce penalties to “safety net” institutions, which is progress but not a solution. Although the HRRP appears to be working, according to the US Department of Health and Human Services, readmissions fell by 150,000 between January 2012 and February 2013,36 we are concerned neither the HRRP nor the MedPac revision proposal considers geographic and environmental components of readmission. The HRRP promotes national improvement in exchange for regional regression.
Fair quality measures are key to value-based reimbursement models; yet, implicit in penalties for excess readmissions is the assumed ability to calculate hospital performance targets. Benchmarks for safety, timely care, and patient satisfaction can be uniform; rates of central line infections should not be influenced by patient mix. However, 9 of the 39 maximum-penalty hospitals under the HRRP are in rural Kentucky; one could hypothesize many reasons why rural Kentucky is a hotbed for excess readmission, including the regional production of tobacco and bourbon.
The fundamental question raised by our study is whether poor performance on quality measures is a function of underperforming hospitals or a manifestation of underserved communities. Moving forward, we encourage data systems and study designs that focus research on geospatial distribution of population health within the context of social and behavioral health determinants.37 Small-area studies of factors that drive health outcomes will inform rational alignment of healthcare policies and resources (including penalties and incentives) with underlying population needs.
Strengths and Weaknesses
Matching is a strength of the study. Primary analysis matched case and controls by hospital characteristics, generating cohorts similar across a spectrum of hospital metrics. Therefore, variation in readmission rates was less likely confounded by hospital characteristics. The secondary analysis was matched by geography in an effort to adjust for unmeasured, regional factors, including obesity and cost of living that may confound an association between SES and health outcomes. Geographic matching adds strength to our assertion that SES drives distinction between maximum-penalty hospitals and nonpenalty hospitals.
One weakness was the regional unit of analysis for socioeconomic and Dartmouth Atlas data, which is not a precise profile of the corresponding hospital. Each hospital was assigned a county-level socioeconomic profile. A more robust methodology would analyze patient-level SES data; this was impractical given a cohort of 78 hospitals. Regional health outcomes data limits analysis of readmission penalties as a function of hospital quality. Instead, regional data facilitated associations between readmission and population health, consistent with the aim of our study.
We analyzed 116 of 3668 hospitals eligible for the HRRP (3.2%), limiting the generalizability of our findings. Eighty-four percent of hospitals in the primary analysis have below the median number of beds, and none of them are teaching hospitals. Our analysis, restricted to maximum-penalty and no-penalty cohorts, does not address potential association between submaximal readmission penalties and socioeconomics.
Both matching techniques potentially controlled for similar SES factors and skewed our results towards null, especially in terms of race and ethnicity. Geographic matching generated 7 pairs (18%) within in the same county; both maximum-penalty and no-penalty hospitals were assigned the same socioeconomic profile, as well as 6 pairs (15%) within the same HSA, and both cases and controls had identical Dartmouth Atlas health outcomes profiles. We retained these pairs in our analysis to avoid artificially inflating SES and population health differences between cohorts.
Thirty-nine hospitals received a maximum penalty in the 3rd year of the HRRP. Relative to geographically matched no-penalty hospitals, maximum-penalty hospitals were more likely to be rural and located in counties with less educational attainment, more poverty and more poorly controlled chronic disease. In contrast to nationwide studies, a matched analysis plan revealed no difference between the cohorts in terms of race and ethnicity and provided evidence that maximum penalty hospitals had higher rates of age-, sex-, and race-adjusted hospital-wide mortality.
Our results highlight potential consequences of nationally derived benchmarks for phenomena underpinned by social, behavioral, and environmental factors and raise the question of whether maximum HRRP penalties are a consequence of underperforming hospitals or a manifestation of underserved communities. We are encouraged by MedPAC’s proposal to stratify HRRP by SES, yet recommend further small-area geographic analyses to better align quality measures, penalties, and incentives with resources and needs of distinct populations.
Acknowledgments
The authors thank William Hisey, who laid the foundation for the analysis and without whom the project would not have been possible.
DISCLOSURE
The authors certify that none of the material in this manuscript has been previously published and that none of this material is currently under consideration for publication elsewhere. This project received no funding. None of the authors on this manuscript have any commercial relationships to disclose in relation to this manuscript. All authors have reviewed and approved this manuscript and have contributed significantly to the design, conduct, and/or analysis of the research. No authors have any financial interests to disclose. No authors have any potential conflicts of interest to disclose. No authors have financial or personal relationships with any of the subject material presented in the manuscript.
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. PubMed
30. Bethell C, Simpson L, Stumbo S, Carle AC, Gombojav N. National, state and local disparities in childhood obesity. Health Aff. 2010; 29(3): 347-356. PubMed
31. Singh GK, Kogan MD, van Dyck PC. Changes in state-specific childhood obesity and overweight prevalence in the United States from 2003 to 2007. Arch Pediatr Adolesc Med. 2010;164(7):598-607. PubMed
32. Aten BH, Figueroa EB, Martin TB. Regional Price Parities for States and Metropolitan Areas, 2006–2010. Survey of Current Business 2012;92:229-242.
33. Dubay L, Wheaton L, Zedlewski S. Geographic variation in the cost of living: implications for poverty guidelines and program eligibility. Urban Institute. 2013. https://aspe.hhs.gov/system/files/pdf/174186/UrbanGeographicVariation.pdf. Accessed on February 22, 2017. Last accessed July 10, 2017
34. National Quality Forum. Risk Adjustment for Socioeconomic Status or Other Sociodemographic Factors: a Technical Report. 2014. http://www.qualityforum. org/Publications/2014/08/Risk_Adjustment_for_Socioeconomic_Status_or_Other_Sociodemographic_Factors.aspx. Accessed July 10, 2017.
36. Services CfMaM. New HHS Data Shows Major Strides Made in Patient Safety, Leading to Improved Care and Savings. In: Services USDoHaH, ed. https://innovation.cms.gov/Files/reports/patient-safety-results.pdf. Accessed July 10, 2017.
37. Harrison KM, Dean HD. Use of data systems to address social determinants of health: a need to do more. Public Health Reports (Washington, DC:1974). 2011;126 Suppl 3:1-5. PubMed
INTRODUCTION
According to Centers for Medicare & Medicaid Services (CMS), approximately 1 in 5 patients discharged from a hospital will be readmitted within 30 days.1 The Hospital Readmission Reduction Program (HRRP) is designed to reduce readmission by withholding up to 3% of all Medicare reimbursement from hospitals with “excess” readmissions; however, absent from the HRRP is adjustment for socioeconomic status (SES), which CMS holds may undermine incentives to reduce health disparities and institutionalize lower standards for hospitals serving disadvantaged populations.2
Lack of SES adjustment has been criticized by those who point to evidence highlighting postdischarge environment and patient SES as drivers of readmission and suggest hospitals that serve low SES individuals will bear a disproportionate share of penalties.3-6 Single-center,3,7,8 regional,9,10 and nationwide6,11 studies highlight census tract level socioeconomic variables as predictive of readmission. Single-center studies, robust in controlling for confounders, including staffing, training, electronic medical record utilization, and transitional care processes, do not allow comparisons between hospitals, limiting utility in HRRP evaluation. Multicenter cohorts, on the other hand, allow for comparisons between high and low penalty hospitals, pioneered by Joynt et al12 after the first round of HRRP penalties; yet this technique may not account for confounding caused by extensive demographic, socioeconomic, and hospital characteristic heterogeneity inherent in a national cohort. Analysis of the 2015 HRRP penalty data by Sjoding et al.6 revealed higher chronic obstructive pulmonary disease (COPD) readmission rates in the Mid-Atlantic, Midwest, and South relative to other regions; however, the magnitude of small-area variation and its relationship to population SES have yet to be characterized.
Therefore, we conducted a matched case-control design, whereby each maximum penalty hospital was matched to a nonpenalty hospital using key hospital characteristics. We then used geographic matching to isolate SES factors predictive of readmission within specific geographies in an effort to control for regional population differences. We hypothesized that, among both matched and localized hospital pairs, the disparities in population SES are the most significant predictors of a maximum penalty. Now in the 3rd year of the HRRP with approximately 75% of eligible hospitals to receive penalties worth an estimated $428 million in the 2015 fiscal year,13 we offer a small-area analysis of bipolar extremes to inform debate surrounding the HRRP with evidence regarding the causes and implications of readmission penalties.
METHODS
Study Design and Sample
This study relies on a case-control design. The cases were defined as US hospitals to receive the maximum 3% HRRP penalty in fiscal year 2015. Controls were drawn from the cohort of hospitals potentially subject to HRRP penalties that received no readmission penalty in the 2015 fiscal year with at least 1 admission for any of the following conditions: heart failure (HF), acute myocardial infarction (AMI), pneumonia (PN), total knee arthroscopy or total hip arthroscopy (THA/TKA), or chronic obstructive pulmonary disease (COPD).
Data Sources
Penalty data were drawn from the 2015 master penalty file,14 which were accessed via CMS.gov. County-level demographic and socioeconomic data were gathered from the 2015 American Community Survey (ACS), a subsidiary of the US Census. Data on hospital characteristics, capacity, and regional healthcare utilization were drawn from 2012 Dartmouth Atlas,15 2012 Medicare Cost Report,16 2012 American Hospital Association Hospital Statistics Database, and 2014 Hospital Care Downloadable Database.
Hospital-level CMS data were linked to the master 2015 penalty file. Dartmouth Atlas data were subsequently linked to the file using the Dartmouth Atlas “Hospital to HSA/HRR Crosswalk” file (accessed via DartmouthAtlas.org.) Each hospital was assigned the profile of the hospital service area (HSA) and hospital referral region (HRR) in which it is located. An HSA is a geographic region defined by hospital admissions; the majority, but not entirety, of residents of a given HSA utilize the corresponding hospital. Similarly, an HRR is a geographic region defined by referrals for major cardiovascular and neurosurgery procedures. County-level socioeconomic data were linked to the dataset by county name; thus, hospital socioeconomic profiles are based on the county in which they are located.
Case-Control Matching
In the primary analysis, coarsened exact matching (CEM) matched controls to cases by potential confounding hospital characteristics, including the following: ownership, number of beds, case mix index (measure of acuity), ambulatory care visit rates within 14 days of discharge, and total number of penalty-eligible cases, including HF, AMI, COPD, PN, and THA/TKA.
In the secondary analysis, hospitals were geocoded by zip code. Geographic Information Systems mapping software (ESRI ArcGIS, Redlands, CA) relied upon Euclidean allocation distance spatial analysis17,18 to match each maximum-penalty hospital to the nearest nonpenalty hospital. Each case was matched to a distinct control; duplicate controls were replaced with the nearest unmatched no-penalty hospital.
Statistical Analysis
Univariate analyses utilized unpaired Student t tests (primary analysis) and paired Student t tests (secondary analysis). The CEM algorithm matches by strata rather than pairs, precluding paired Student t tests in the primary analysis. Statistical analyses were conducted using STATA (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX).
RESULTS
Maximum Penalty and Nonpenalty Hospital Matching
Of 3383 hospitals eligible for the HRRP, 39 received the maximum penalty and 770 received no penalty. Thirty-eight control hospitals were identified using CEM algorithm; 1 maximum-penalty hospital could not be matched and was excluded from primary analy
Hospital Characteristics
Case and control profiles are presented in Table 1. Cases and controls were matched by characteristics which may impact readmission rates (Table 1). CEM yielded cohorts similar across a spectrum of metrics, and identical in terms of matching criteria including ownership, beds (quartile), case mix index (above median), ambulatory care visit within 14 days of discharge (above median), and total number of penalty-eligible cases (above median). Relative to no-penalty hospitals, maximum-penalty hospitals were more likely rural (n = 9 vs n = 2, P = 0.022) and have a less profitable operating margin (0.1% vs 6.9%), and location within HSAs with higher age, sex, and race adjusted hospital-wide mortality rate (5.3% vs 4.9%, P = 0.009) and higher rates of discharge for ambulatory care sensitive conditions (108 vs 63 discharges per 1000 Medicare enrollees).
Demographic and Socioeconomic Characteristics
As presented in Table 2, cases a
Secondary Analysis: Geographical Matching
Secondary analysis matched each maximum-penalty hospital to the nearest no-penalty hospital using a global information system vector analysis algorithm. As shown in the Figure, median distance between the case and the control was 42.5 miles (interquartile range: 25th percentile, 15.4 miles; 75th percentile, 98.4 miles). Seventeen pairs (44%) were in the same HRR, 6 of which were in the same HSA. Seven pairs (18%) were within the same county
Secondary Analysis: Economic and Demographic Profiles of Geographically Matched Pairs
Demographic and socioeconomic profiles are presented in Table 3. The cases and controls are in counties with similar age, sex, and ethnicity distributions. Relative to no-penalty hospitals, maximum-penalty hospitals are in counties with lower socioeconomic profiles, including increased rates of poverty (15.6% vs 19.2%, P = 0.007) and lower rates of high school (86.4% vs 82.1%, P = 0.005) or college graduation (22.3% vs 28.1%, P = 0.002). Seven pairs were in the same county; a sensitivity analysis excluding these hospitals revealed similarly lower SES profile in cases relative to controls (Supplementary Table 1).
DISCUSSION
Our analysis reveals that county-level socioeconomic profiles are predictors of maximum HRRP penalties. Specifically, after matching cases and controls on 5 hospital characteristics that may influence readmission, maximum-penalty hospitals were more likely to be in rural counties with higher rates of poverty and lower rates of education relative to no-penalty hospitals. We observed no difference between cases and controls with respect to age, sex, or ethnicity.
Our study complement
Maximum Penalties as a Function of Population Health
The Dartmouth Atlas of Healthcare measures health outcomes, which are regionally aggregated among local hospitals by either HSA or HRR; see Methods. Such small-area aggregation does not precisely reflect outcomes from a specific hospital, but rather it describes the health status of localities. Disparities in health outcomes exist between maximum-penalty and no-penalty HSAs. Complication rates were slightly higher in maximum penalty HSAs, consistent with studies highlighting complications as drivers of surgical readmissions.22,23 Moreover, hospital-wide mortality rates were higher in maximum-penalty areas relative to nonpenalty HSAs (5.3 vs 4.9, P = 0.009).
Using national data, Krumholz et al. found no correlation between rates of readmission and mortality for HF, AMI, and PN24, which is a phenomenon acknowledged by the Medicare Payment Advisory Commission (MedPac) in a 2013 report titled, “Refining the hospital readmission reduction program.”25 In large national studies, others have shown low SES to be associated with elevated readmission but not mortality.10,11 In contrast, we restricted our analysis to matched cohorts and are, to our knowledge, the first to present evidence of an association between readmission and hospital-wide mortality adjusted for age, sex, and ethnicity.
Our results suggest maximum readmission penalties are a function of population health and public health capacity. The rates of ambulatory care sensitive condition (ACSC) discharges were substantially higher in HSAs of maximum penalty hospitals relative to nonpenalty hospitals (108 vs 63 per 1000 Medicare enrollees, P < 0.001). ACSC discharges have been used to measure primary care quality for 30 years, with the assumption being that admission for chronic conditions, such as HF, can be prevented with effective primary care.26,27 Moreover, patients discharged from maximum-penalty hospitals were more likely to have an emergency room visit within 30 days of discharge (20.8% vs 18.4%, P < 0.001). Higher rates of ACSCs and postdischarge emergency department visits suggest outpatient resources in maximum-penalty service areas struggle to manage the disease burden of high-risk populations. Geography may be a contributor; maximum-penalty hospitals were more likely to be rural than no-penalty hospitals (24% vs 5%, P = 0.022).
Our findings suggest hospitals providing care to vulnerable communities (defined by low income, low education, and high rates of ambulatory sensitive discharges) are disproportionately penalized. McHugh et al. revealed high nurse staffing levels to be protective against readmission penalties28, yet high penalties to low-margin hospitals may encourage reduced rather than increased staff. It may be better policy to direct resources rather than penalties to underserved communities; our findings echo others with concern about disproportionate penalties to hospitals serving low SES patients.2,5,6,29
Secondary Analysis: Geographic Matching
Geographic matching paired each maximum-penalty hospital to the nearest no-penalty hospital in an attempt to control for unmeasured regional factors that may confound an association between socioeconomic profile and health outcomes. For example, cost of living 30, 31 and obesity 32,33 vary regionally. Our study was unequipped to assess potential regional confounders; we attempted to control for them with geographical matching.
Median distance between maximum-penalty and no-penalty hospitals was 42.5 miles. Seven pairs were located within the same county, thus both case and control were assigned the same socioeconomic profile. Despite close proximity and identical SES profile in 7 of 39 pairs, maximum-penalty hospitals were in counties with lower income and lower rates of education, strengthening the association between SES and maximum readmission penalties.
Implications and Future Directions
In response to criticism surrounding the HRRP, the National Quality Forum endorsed the general concept of SES adjustment for hospital quality measures.34 Subsequently, in a briefing dated March 24, 2015, MedPAC, a government agency which provides Medicare policy analysis to Congress, proposed an SES adjustment methodology of “dividing hospitals into peer groups based on their overall share of low-income Medicare patients, and then setting a benchmark readmissions target for each peer group”;35 in other words, lower standards for hospitals that serve low-income populations. MedPAC’s proposal will reduce penalties to “safety net” institutions, which is progress but not a solution. Although the HRRP appears to be working, according to the US Department of Health and Human Services, readmissions fell by 150,000 between January 2012 and February 2013,36 we are concerned neither the HRRP nor the MedPac revision proposal considers geographic and environmental components of readmission. The HRRP promotes national improvement in exchange for regional regression.
Fair quality measures are key to value-based reimbursement models; yet, implicit in penalties for excess readmissions is the assumed ability to calculate hospital performance targets. Benchmarks for safety, timely care, and patient satisfaction can be uniform; rates of central line infections should not be influenced by patient mix. However, 9 of the 39 maximum-penalty hospitals under the HRRP are in rural Kentucky; one could hypothesize many reasons why rural Kentucky is a hotbed for excess readmission, including the regional production of tobacco and bourbon.
The fundamental question raised by our study is whether poor performance on quality measures is a function of underperforming hospitals or a manifestation of underserved communities. Moving forward, we encourage data systems and study designs that focus research on geospatial distribution of population health within the context of social and behavioral health determinants.37 Small-area studies of factors that drive health outcomes will inform rational alignment of healthcare policies and resources (including penalties and incentives) with underlying population needs.
Strengths and Weaknesses
Matching is a strength of the study. Primary analysis matched case and controls by hospital characteristics, generating cohorts similar across a spectrum of hospital metrics. Therefore, variation in readmission rates was less likely confounded by hospital characteristics. The secondary analysis was matched by geography in an effort to adjust for unmeasured, regional factors, including obesity and cost of living that may confound an association between SES and health outcomes. Geographic matching adds strength to our assertion that SES drives distinction between maximum-penalty hospitals and nonpenalty hospitals.
One weakness was the regional unit of analysis for socioeconomic and Dartmouth Atlas data, which is not a precise profile of the corresponding hospital. Each hospital was assigned a county-level socioeconomic profile. A more robust methodology would analyze patient-level SES data; this was impractical given a cohort of 78 hospitals. Regional health outcomes data limits analysis of readmission penalties as a function of hospital quality. Instead, regional data facilitated associations between readmission and population health, consistent with the aim of our study.
We analyzed 116 of 3668 hospitals eligible for the HRRP (3.2%), limiting the generalizability of our findings. Eighty-four percent of hospitals in the primary analysis have below the median number of beds, and none of them are teaching hospitals. Our analysis, restricted to maximum-penalty and no-penalty cohorts, does not address potential association between submaximal readmission penalties and socioeconomics.
Both matching techniques potentially controlled for similar SES factors and skewed our results towards null, especially in terms of race and ethnicity. Geographic matching generated 7 pairs (18%) within in the same county; both maximum-penalty and no-penalty hospitals were assigned the same socioeconomic profile, as well as 6 pairs (15%) within the same HSA, and both cases and controls had identical Dartmouth Atlas health outcomes profiles. We retained these pairs in our analysis to avoid artificially inflating SES and population health differences between cohorts.
Thirty-nine hospitals received a maximum penalty in the 3rd year of the HRRP. Relative to geographically matched no-penalty hospitals, maximum-penalty hospitals were more likely to be rural and located in counties with less educational attainment, more poverty and more poorly controlled chronic disease. In contrast to nationwide studies, a matched analysis plan revealed no difference between the cohorts in terms of race and ethnicity and provided evidence that maximum penalty hospitals had higher rates of age-, sex-, and race-adjusted hospital-wide mortality.
Our results highlight potential consequences of nationally derived benchmarks for phenomena underpinned by social, behavioral, and environmental factors and raise the question of whether maximum HRRP penalties are a consequence of underperforming hospitals or a manifestation of underserved communities. We are encouraged by MedPAC’s proposal to stratify HRRP by SES, yet recommend further small-area geographic analyses to better align quality measures, penalties, and incentives with resources and needs of distinct populations.
Acknowledgments
The authors thank William Hisey, who laid the foundation for the analysis and without whom the project would not have been possible.
DISCLOSURE
The authors certify that none of the material in this manuscript has been previously published and that none of this material is currently under consideration for publication elsewhere. This project received no funding. None of the authors on this manuscript have any commercial relationships to disclose in relation to this manuscript. All authors have reviewed and approved this manuscript and have contributed significantly to the design, conduct, and/or analysis of the research. No authors have any financial interests to disclose. No authors have any potential conflicts of interest to disclose. No authors have financial or personal relationships with any of the subject material presented in the manuscript.
INTRODUCTION
According to Centers for Medicare & Medicaid Services (CMS), approximately 1 in 5 patients discharged from a hospital will be readmitted within 30 days.1 The Hospital Readmission Reduction Program (HRRP) is designed to reduce readmission by withholding up to 3% of all Medicare reimbursement from hospitals with “excess” readmissions; however, absent from the HRRP is adjustment for socioeconomic status (SES), which CMS holds may undermine incentives to reduce health disparities and institutionalize lower standards for hospitals serving disadvantaged populations.2
Lack of SES adjustment has been criticized by those who point to evidence highlighting postdischarge environment and patient SES as drivers of readmission and suggest hospitals that serve low SES individuals will bear a disproportionate share of penalties.3-6 Single-center,3,7,8 regional,9,10 and nationwide6,11 studies highlight census tract level socioeconomic variables as predictive of readmission. Single-center studies, robust in controlling for confounders, including staffing, training, electronic medical record utilization, and transitional care processes, do not allow comparisons between hospitals, limiting utility in HRRP evaluation. Multicenter cohorts, on the other hand, allow for comparisons between high and low penalty hospitals, pioneered by Joynt et al12 after the first round of HRRP penalties; yet this technique may not account for confounding caused by extensive demographic, socioeconomic, and hospital characteristic heterogeneity inherent in a national cohort. Analysis of the 2015 HRRP penalty data by Sjoding et al.6 revealed higher chronic obstructive pulmonary disease (COPD) readmission rates in the Mid-Atlantic, Midwest, and South relative to other regions; however, the magnitude of small-area variation and its relationship to population SES have yet to be characterized.
Therefore, we conducted a matched case-control design, whereby each maximum penalty hospital was matched to a nonpenalty hospital using key hospital characteristics. We then used geographic matching to isolate SES factors predictive of readmission within specific geographies in an effort to control for regional population differences. We hypothesized that, among both matched and localized hospital pairs, the disparities in population SES are the most significant predictors of a maximum penalty. Now in the 3rd year of the HRRP with approximately 75% of eligible hospitals to receive penalties worth an estimated $428 million in the 2015 fiscal year,13 we offer a small-area analysis of bipolar extremes to inform debate surrounding the HRRP with evidence regarding the causes and implications of readmission penalties.
METHODS
Study Design and Sample
This study relies on a case-control design. The cases were defined as US hospitals to receive the maximum 3% HRRP penalty in fiscal year 2015. Controls were drawn from the cohort of hospitals potentially subject to HRRP penalties that received no readmission penalty in the 2015 fiscal year with at least 1 admission for any of the following conditions: heart failure (HF), acute myocardial infarction (AMI), pneumonia (PN), total knee arthroscopy or total hip arthroscopy (THA/TKA), or chronic obstructive pulmonary disease (COPD).
Data Sources
Penalty data were drawn from the 2015 master penalty file,14 which were accessed via CMS.gov. County-level demographic and socioeconomic data were gathered from the 2015 American Community Survey (ACS), a subsidiary of the US Census. Data on hospital characteristics, capacity, and regional healthcare utilization were drawn from 2012 Dartmouth Atlas,15 2012 Medicare Cost Report,16 2012 American Hospital Association Hospital Statistics Database, and 2014 Hospital Care Downloadable Database.
Hospital-level CMS data were linked to the master 2015 penalty file. Dartmouth Atlas data were subsequently linked to the file using the Dartmouth Atlas “Hospital to HSA/HRR Crosswalk” file (accessed via DartmouthAtlas.org.) Each hospital was assigned the profile of the hospital service area (HSA) and hospital referral region (HRR) in which it is located. An HSA is a geographic region defined by hospital admissions; the majority, but not entirety, of residents of a given HSA utilize the corresponding hospital. Similarly, an HRR is a geographic region defined by referrals for major cardiovascular and neurosurgery procedures. County-level socioeconomic data were linked to the dataset by county name; thus, hospital socioeconomic profiles are based on the county in which they are located.
Case-Control Matching
In the primary analysis, coarsened exact matching (CEM) matched controls to cases by potential confounding hospital characteristics, including the following: ownership, number of beds, case mix index (measure of acuity), ambulatory care visit rates within 14 days of discharge, and total number of penalty-eligible cases, including HF, AMI, COPD, PN, and THA/TKA.
In the secondary analysis, hospitals were geocoded by zip code. Geographic Information Systems mapping software (ESRI ArcGIS, Redlands, CA) relied upon Euclidean allocation distance spatial analysis17,18 to match each maximum-penalty hospital to the nearest nonpenalty hospital. Each case was matched to a distinct control; duplicate controls were replaced with the nearest unmatched no-penalty hospital.
Statistical Analysis
Univariate analyses utilized unpaired Student t tests (primary analysis) and paired Student t tests (secondary analysis). The CEM algorithm matches by strata rather than pairs, precluding paired Student t tests in the primary analysis. Statistical analyses were conducted using STATA (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX).
RESULTS
Maximum Penalty and Nonpenalty Hospital Matching
Of 3383 hospitals eligible for the HRRP, 39 received the maximum penalty and 770 received no penalty. Thirty-eight control hospitals were identified using CEM algorithm; 1 maximum-penalty hospital could not be matched and was excluded from primary analy
Hospital Characteristics
Case and control profiles are presented in Table 1. Cases and controls were matched by characteristics which may impact readmission rates (Table 1). CEM yielded cohorts similar across a spectrum of metrics, and identical in terms of matching criteria including ownership, beds (quartile), case mix index (above median), ambulatory care visit within 14 days of discharge (above median), and total number of penalty-eligible cases (above median). Relative to no-penalty hospitals, maximum-penalty hospitals were more likely rural (n = 9 vs n = 2, P = 0.022) and have a less profitable operating margin (0.1% vs 6.9%), and location within HSAs with higher age, sex, and race adjusted hospital-wide mortality rate (5.3% vs 4.9%, P = 0.009) and higher rates of discharge for ambulatory care sensitive conditions (108 vs 63 discharges per 1000 Medicare enrollees).
Demographic and Socioeconomic Characteristics
As presented in Table 2, cases a
Secondary Analysis: Geographical Matching
Secondary analysis matched each maximum-penalty hospital to the nearest no-penalty hospital using a global information system vector analysis algorithm. As shown in the Figure, median distance between the case and the control was 42.5 miles (interquartile range: 25th percentile, 15.4 miles; 75th percentile, 98.4 miles). Seventeen pairs (44%) were in the same HRR, 6 of which were in the same HSA. Seven pairs (18%) were within the same county
Secondary Analysis: Economic and Demographic Profiles of Geographically Matched Pairs
Demographic and socioeconomic profiles are presented in Table 3. The cases and controls are in counties with similar age, sex, and ethnicity distributions. Relative to no-penalty hospitals, maximum-penalty hospitals are in counties with lower socioeconomic profiles, including increased rates of poverty (15.6% vs 19.2%, P = 0.007) and lower rates of high school (86.4% vs 82.1%, P = 0.005) or college graduation (22.3% vs 28.1%, P = 0.002). Seven pairs were in the same county; a sensitivity analysis excluding these hospitals revealed similarly lower SES profile in cases relative to controls (Supplementary Table 1).
DISCUSSION
Our analysis reveals that county-level socioeconomic profiles are predictors of maximum HRRP penalties. Specifically, after matching cases and controls on 5 hospital characteristics that may influence readmission, maximum-penalty hospitals were more likely to be in rural counties with higher rates of poverty and lower rates of education relative to no-penalty hospitals. We observed no difference between cases and controls with respect to age, sex, or ethnicity.
Our study complement
Maximum Penalties as a Function of Population Health
The Dartmouth Atlas of Healthcare measures health outcomes, which are regionally aggregated among local hospitals by either HSA or HRR; see Methods. Such small-area aggregation does not precisely reflect outcomes from a specific hospital, but rather it describes the health status of localities. Disparities in health outcomes exist between maximum-penalty and no-penalty HSAs. Complication rates were slightly higher in maximum penalty HSAs, consistent with studies highlighting complications as drivers of surgical readmissions.22,23 Moreover, hospital-wide mortality rates were higher in maximum-penalty areas relative to nonpenalty HSAs (5.3 vs 4.9, P = 0.009).
Using national data, Krumholz et al. found no correlation between rates of readmission and mortality for HF, AMI, and PN24, which is a phenomenon acknowledged by the Medicare Payment Advisory Commission (MedPac) in a 2013 report titled, “Refining the hospital readmission reduction program.”25 In large national studies, others have shown low SES to be associated with elevated readmission but not mortality.10,11 In contrast, we restricted our analysis to matched cohorts and are, to our knowledge, the first to present evidence of an association between readmission and hospital-wide mortality adjusted for age, sex, and ethnicity.
Our results suggest maximum readmission penalties are a function of population health and public health capacity. The rates of ambulatory care sensitive condition (ACSC) discharges were substantially higher in HSAs of maximum penalty hospitals relative to nonpenalty hospitals (108 vs 63 per 1000 Medicare enrollees, P < 0.001). ACSC discharges have been used to measure primary care quality for 30 years, with the assumption being that admission for chronic conditions, such as HF, can be prevented with effective primary care.26,27 Moreover, patients discharged from maximum-penalty hospitals were more likely to have an emergency room visit within 30 days of discharge (20.8% vs 18.4%, P < 0.001). Higher rates of ACSCs and postdischarge emergency department visits suggest outpatient resources in maximum-penalty service areas struggle to manage the disease burden of high-risk populations. Geography may be a contributor; maximum-penalty hospitals were more likely to be rural than no-penalty hospitals (24% vs 5%, P = 0.022).
Our findings suggest hospitals providing care to vulnerable communities (defined by low income, low education, and high rates of ambulatory sensitive discharges) are disproportionately penalized. McHugh et al. revealed high nurse staffing levels to be protective against readmission penalties28, yet high penalties to low-margin hospitals may encourage reduced rather than increased staff. It may be better policy to direct resources rather than penalties to underserved communities; our findings echo others with concern about disproportionate penalties to hospitals serving low SES patients.2,5,6,29
Secondary Analysis: Geographic Matching
Geographic matching paired each maximum-penalty hospital to the nearest no-penalty hospital in an attempt to control for unmeasured regional factors that may confound an association between socioeconomic profile and health outcomes. For example, cost of living 30, 31 and obesity 32,33 vary regionally. Our study was unequipped to assess potential regional confounders; we attempted to control for them with geographical matching.
Median distance between maximum-penalty and no-penalty hospitals was 42.5 miles. Seven pairs were located within the same county, thus both case and control were assigned the same socioeconomic profile. Despite close proximity and identical SES profile in 7 of 39 pairs, maximum-penalty hospitals were in counties with lower income and lower rates of education, strengthening the association between SES and maximum readmission penalties.
Implications and Future Directions
In response to criticism surrounding the HRRP, the National Quality Forum endorsed the general concept of SES adjustment for hospital quality measures.34 Subsequently, in a briefing dated March 24, 2015, MedPAC, a government agency which provides Medicare policy analysis to Congress, proposed an SES adjustment methodology of “dividing hospitals into peer groups based on their overall share of low-income Medicare patients, and then setting a benchmark readmissions target for each peer group”;35 in other words, lower standards for hospitals that serve low-income populations. MedPAC’s proposal will reduce penalties to “safety net” institutions, which is progress but not a solution. Although the HRRP appears to be working, according to the US Department of Health and Human Services, readmissions fell by 150,000 between January 2012 and February 2013,36 we are concerned neither the HRRP nor the MedPac revision proposal considers geographic and environmental components of readmission. The HRRP promotes national improvement in exchange for regional regression.
Fair quality measures are key to value-based reimbursement models; yet, implicit in penalties for excess readmissions is the assumed ability to calculate hospital performance targets. Benchmarks for safety, timely care, and patient satisfaction can be uniform; rates of central line infections should not be influenced by patient mix. However, 9 of the 39 maximum-penalty hospitals under the HRRP are in rural Kentucky; one could hypothesize many reasons why rural Kentucky is a hotbed for excess readmission, including the regional production of tobacco and bourbon.
The fundamental question raised by our study is whether poor performance on quality measures is a function of underperforming hospitals or a manifestation of underserved communities. Moving forward, we encourage data systems and study designs that focus research on geospatial distribution of population health within the context of social and behavioral health determinants.37 Small-area studies of factors that drive health outcomes will inform rational alignment of healthcare policies and resources (including penalties and incentives) with underlying population needs.
Strengths and Weaknesses
Matching is a strength of the study. Primary analysis matched case and controls by hospital characteristics, generating cohorts similar across a spectrum of hospital metrics. Therefore, variation in readmission rates was less likely confounded by hospital characteristics. The secondary analysis was matched by geography in an effort to adjust for unmeasured, regional factors, including obesity and cost of living that may confound an association between SES and health outcomes. Geographic matching adds strength to our assertion that SES drives distinction between maximum-penalty hospitals and nonpenalty hospitals.
One weakness was the regional unit of analysis for socioeconomic and Dartmouth Atlas data, which is not a precise profile of the corresponding hospital. Each hospital was assigned a county-level socioeconomic profile. A more robust methodology would analyze patient-level SES data; this was impractical given a cohort of 78 hospitals. Regional health outcomes data limits analysis of readmission penalties as a function of hospital quality. Instead, regional data facilitated associations between readmission and population health, consistent with the aim of our study.
We analyzed 116 of 3668 hospitals eligible for the HRRP (3.2%), limiting the generalizability of our findings. Eighty-four percent of hospitals in the primary analysis have below the median number of beds, and none of them are teaching hospitals. Our analysis, restricted to maximum-penalty and no-penalty cohorts, does not address potential association between submaximal readmission penalties and socioeconomics.
Both matching techniques potentially controlled for similar SES factors and skewed our results towards null, especially in terms of race and ethnicity. Geographic matching generated 7 pairs (18%) within in the same county; both maximum-penalty and no-penalty hospitals were assigned the same socioeconomic profile, as well as 6 pairs (15%) within the same HSA, and both cases and controls had identical Dartmouth Atlas health outcomes profiles. We retained these pairs in our analysis to avoid artificially inflating SES and population health differences between cohorts.
Thirty-nine hospitals received a maximum penalty in the 3rd year of the HRRP. Relative to geographically matched no-penalty hospitals, maximum-penalty hospitals were more likely to be rural and located in counties with less educational attainment, more poverty and more poorly controlled chronic disease. In contrast to nationwide studies, a matched analysis plan revealed no difference between the cohorts in terms of race and ethnicity and provided evidence that maximum penalty hospitals had higher rates of age-, sex-, and race-adjusted hospital-wide mortality.
Our results highlight potential consequences of nationally derived benchmarks for phenomena underpinned by social, behavioral, and environmental factors and raise the question of whether maximum HRRP penalties are a consequence of underperforming hospitals or a manifestation of underserved communities. We are encouraged by MedPAC’s proposal to stratify HRRP by SES, yet recommend further small-area geographic analyses to better align quality measures, penalties, and incentives with resources and needs of distinct populations.
Acknowledgments
The authors thank William Hisey, who laid the foundation for the analysis and without whom the project would not have been possible.
DISCLOSURE
The authors certify that none of the material in this manuscript has been previously published and that none of this material is currently under consideration for publication elsewhere. This project received no funding. None of the authors on this manuscript have any commercial relationships to disclose in relation to this manuscript. All authors have reviewed and approved this manuscript and have contributed significantly to the design, conduct, and/or analysis of the research. No authors have any financial interests to disclose. No authors have any potential conflicts of interest to disclose. No authors have financial or personal relationships with any of the subject material presented in the manuscript.
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. PubMed
30. Bethell C, Simpson L, Stumbo S, Carle AC, Gombojav N. National, state and local disparities in childhood obesity. Health Aff. 2010; 29(3): 347-356. PubMed
31. Singh GK, Kogan MD, van Dyck PC. Changes in state-specific childhood obesity and overweight prevalence in the United States from 2003 to 2007. Arch Pediatr Adolesc Med. 2010;164(7):598-607. PubMed
32. Aten BH, Figueroa EB, Martin TB. Regional Price Parities for States and Metropolitan Areas, 2006–2010. Survey of Current Business 2012;92:229-242.
33. Dubay L, Wheaton L, Zedlewski S. Geographic variation in the cost of living: implications for poverty guidelines and program eligibility. Urban Institute. 2013. https://aspe.hhs.gov/system/files/pdf/174186/UrbanGeographicVariation.pdf. Accessed on February 22, 2017. Last accessed July 10, 2017
34. National Quality Forum. Risk Adjustment for Socioeconomic Status or Other Sociodemographic Factors: a Technical Report. 2014. http://www.qualityforum. org/Publications/2014/08/Risk_Adjustment_for_Socioeconomic_Status_or_Other_Sociodemographic_Factors.aspx. Accessed July 10, 2017.
36. Services CfMaM. New HHS Data Shows Major Strides Made in Patient Safety, Leading to Improved Care and Savings. In: Services USDoHaH, ed. https://innovation.cms.gov/Files/reports/patient-safety-results.pdf. Accessed July 10, 2017.
37. Harrison KM, Dean HD. Use of data systems to address social determinants of health: a need to do more. Public Health Reports (Washington, DC:1974). 2011;126 Suppl 3:1-5. PubMed
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. PubMed
30. Bethell C, Simpson L, Stumbo S, Carle AC, Gombojav N. National, state and local disparities in childhood obesity. Health Aff. 2010; 29(3): 347-356. PubMed
31. Singh GK, Kogan MD, van Dyck PC. Changes in state-specific childhood obesity and overweight prevalence in the United States from 2003 to 2007. Arch Pediatr Adolesc Med. 2010;164(7):598-607. PubMed
32. Aten BH, Figueroa EB, Martin TB. Regional Price Parities for States and Metropolitan Areas, 2006–2010. Survey of Current Business 2012;92:229-242.
33. Dubay L, Wheaton L, Zedlewski S. Geographic variation in the cost of living: implications for poverty guidelines and program eligibility. Urban Institute. 2013. https://aspe.hhs.gov/system/files/pdf/174186/UrbanGeographicVariation.pdf. Accessed on February 22, 2017. Last accessed July 10, 2017
34. National Quality Forum. Risk Adjustment for Socioeconomic Status or Other Sociodemographic Factors: a Technical Report. 2014. http://www.qualityforum. org/Publications/2014/08/Risk_Adjustment_for_Socioeconomic_Status_or_Other_Sociodemographic_Factors.aspx. Accessed July 10, 2017.
36. Services CfMaM. New HHS Data Shows Major Strides Made in Patient Safety, Leading to Improved Care and Savings. In: Services USDoHaH, ed. https://innovation.cms.gov/Files/reports/patient-safety-results.pdf. Accessed July 10, 2017.
37. Harrison KM, Dean HD. Use of data systems to address social determinants of health: a need to do more. Public Health Reports (Washington, DC:1974). 2011;126 Suppl 3:1-5. PubMed
We Want to Know: Eliciting Hospitalized Patients’ Perspectives on Breakdowns in Care
There is growing recognition that patients and family members have critical insights into healthcare experiences. As consumers of healthcare, patient experience is the definitive gauge of whether healthcare is patient centered. In addition, patients may know things about their healthcare that the care team does not. Several studies have demonstrated that patients have knowledge of adverse events and medical errors that are not detected by other methods.1-5 For these reasons, systems designed to elicit patient perspectives of care and detect patient-perceived breakdowns in care could be used to improve healthcare safety and quality, including the patient experience.
Historically, hospitals have relied on patient-initiated reporting via complaints or legal action as the main source of information regarding patient-perceived breakdowns in care. However, many patients are hesitant to speak up about problems or uncertain about how to report concerns.6-8 As a result, healthcare systems often only learn of the most severe breakdowns in care from a subset of activated patients, thus underestimating how widespread patient-perceived breakdowns are.
To overcome these limitations of patient-initiated reporting, hospitals could conduct outreach to patients to actively identify and learn about patient-perceived breakdowns in care. Potential benefits of outreach to patients include more reliable detection of patient-perceived breakdowns in care, identification of a broader range of types of breakdowns commonly experienced by patients, and recognition of problems in real-time when there is more opportunity for redress. Indeed, some hospitals have adopted active outreach programs such as structured nurse manager rounding or postdischarge phone calls.9
It is possible that outreach will not overcome patients’ reluctance to speak up, or patients may not share serious or actionable breakdowns. The manner in which outreach is conducted is likely to influence the information patients are willing to share. Prior studies examining patient perspectives of healthcare have primarily taken a structured approach with close-ended questions or a focus on specific aspects of care.1,10,11 Limited data collected using an open-ended approach suggest patient-perceived breakdowns in care may be very common.2,12,13 However, the impact of such breakdowns on patients has not been well characterized.
In order to design systems that can optimally detect patient-perceived breakdowns in care, additional information is needed to understand whether patients will report breakdowns in response to outreach programs, what types of problems they will report, and how these problems impact them. Understanding such issues will allow healthcare systems to respond to calls by federal health agencies to develop mechanisms for patients to report concerns about breakdowns in care, thereby providing truly patient-centered care.14 Therefore, we undertook this study with the overall goal of describing what may be learned from an open-ended outreach approach that directly asks patients about problems they have encountered during hospitalization. Specifically, we aim to (1) describe the types of problems reported by patients in response to this outreach approach and (2) characterize patients’ perceptions of the impact of these events.
METHODS
Setting
We conducted this study in 2 hospitals between June 2014 and February 2015. One participating hospital is a large, urban, tertiary care medical center serving a predominantly white (78%) patient population in Baltimore, Maryland. The second hospital is a large, inner city, tertiary care medical center serving a predominantly African-American (71%) patient population in Washington, DC.
Three medical-surgical units (MSUs) at each hospital participated. We selected MSUs because MSU patients interact with a variety of clinicians, often have long stays, and are at risk for adverse events. Hospitalists were part of the clinical care team in each of the participating units, serving either as the attending of record or by comanaging patients.
Patient Eligibility
Patients were potentially eligible if they were at least 18 years old, able to speak English or Spanish, and admitted to the hospital for more than 24 hours. Ineligibility criteria included the following: imminent discharge, observation (noninpatient) status, on hospice, on infection precautions (for inpatient interviews only), psychiatric or violence concerns, prisoner status, significant confusion, or inability to provide informed consent.
Eligible patients in each unit were randomized. Interviewers consecutively approached patients according to their random assignment. If a patient was not available, the interviewer proceeded to the next room. Interviewers returned to rooms of missed patients when possible. Recruitment in the unit ended when the recruitment target for that unit was achieved.
Interviewers
Five interviewers conducted interviews. One author (KS) provided interviewer training that included didactic instruction, observation, feedback, and modeling. Interviewers participated in weekly debriefing sessions. One interviewer speaks Spanish fluently and was able to conduct interviews in Spanish. Translator services were available for the other interviewers.
Interview Process
Interviews were conducted in person while the patients were hospitalized or via telephone 7 - 30 days postdischarge. A patient who had completed an interview while hospitalized was not eligible for a postdischarge telephone interview. Family members or friends present at the time of the interviews could also participate in addition to or in lieu of the patients with the patients’ assent. Interviewers obtained verbal, informed consent at the start of each interview.
The interview domains and sample questions were developed specifically for the current study and are listed in Table 1. The goal of the interview was to elicit the patient’s (or family member’s) perception of their care experiences and their perceptions of the consequences of any problems with their care. The interviewer sought to obtain sufficient detail to understand the patient’s concerns and to determine what, if any, action might be needed to remediate problems reported by patients. Interviewers captured patient responses by taking detailed notes on a case report form or by directly entering patient responses using a computer or iPad at the time of interview at the discretion of the interviewer.
We defined a patient-perceived breakdown as something that went wrong during the hospitalization according to the patient. If a patient-perceived breakdown in care was identified, the interviewer attempted to resolve the concern. Some breakdowns had occurred in the past, making further resolution impossible (eg, a long wait in the emergency department). Other breakdowns were active and addressable, such as the patient having clinical questions that had not been answered. In such cases, the interviewer attempted to address the patient’s concerns, typically by working with unit nursing staff. For patients interviewed postdischarge, the interviewer worked to resolve ongoing patient concerns with the assistance of the patient safety, quality, and compliance teams as needed. The interviewer provided a brief narrative summary of all interviews to unit nursing leadership within 24 hours. Positive comments were sent to leadership but not captured systematically for research purposes. Further details of the process of responding to patients’ concerns will be reported elsewhere. All data were entered into REDCap to facilitate data management and reporting.15
The MedStar Health Research Institute Institutional Review Board reviewed and approved this study.
Categorizing Patients’ Responses: The Patient Experience Coding Tool
Using directed content analysis,16 we deductively created the Patient Experience Coding Tool (PECT) in order to summarize the narrative information captured during the interviews and categorize patient-perceived breakdowns in care. First, we referred to our prior interviews of patients’ views on breakdowns in cancer care6 and surrogate decision-makers’ views on breakdowns in intensive care units13 to create the initial categories. We then applied the resultant framework to the interviews in the present study and refined the categories. This involved applying the categorization to an initial set of interviews to check the sufficiency of the coding categories. We clarified the scope of each category (ie, what types of events fit under each category) and created additional categories (eg, medication-related problems) to capture patient experiences that were not included in the initial framework.
We then coded each interview using the PECT. A minimum of 2 readers reviewed the narrative notes for each interview. The first reader provided an initial categorization; the second reader reviewed the narrative and confirmed or questioned the initial categorization to improve coding accuracy. If a reader was uncertain about the correct categorization, it was discussed by three readers until an agreement was achieved. Because facilities-related problems (eg, food or parking) fall outside the realm of provider-based hospital care, such comments were not the focus of the outreach efforts and were not consistently recorded. Therefore, they were not included in the PECT and are not reported here.
Analyses
We computed simple, descriptive statistics including the number and percentage of patients identifying at least one breakdown, as well as the number and percent reporting each type of breakdown. We also computed the number and percentage of patients reporting any harm and each type of harm. We computed the percentage of patients reporting at least 1 breakdown by hospital, type of interview (postdischarge vs inpatient), selected patient demographic characteristics (eg, gender, age, education, race), and interviewee (patient vs someone other than the patient interviewed or present during the interview) using the chi-square statistic to test the statistical significance of the resulting differences. All statistical analyses were performed using SPSS version 22.
RESULTS
A total of 979 outreach interviews were conducted. Of these, 349 were conducted via telephone postdischarge, and 630 were conducted in person during hospitalization. The average interview duration was 8.5 minutes for telephone interviews and 12.2 minutes for in-person interviews. Of the patients approached to participate, 67% completed an interview (61% in person, 83% via telephone). Patient characteristics are summarized in Table 2.
Overall, 386 of 979 interviewees (39.4%) believed they had experienced at least one breakdown in care. The types of patient-perceived breakdowns reported were categorized using the PECT and are summarized in Table 3 and the Figure. The most common concern involved information exchange. Approximately 1 in 10 patients (n = 105, 10.7%) felt that they had not received the information they needed when they needed it. Medication-related concerns were reported by 12.3% (n = 120) of interviewees and predominantly included concerns about what medications were being administered (5.7%) and inadequately treated pain (5.6%). Many of the patients expressing concerns about what medications were administered questioned why they were not receiving their outpatient medications or did not understand why a different medication was being administered, suggesting that many of these instances were related to breakdowns in communication as well. Other relatively common concerns were delays in the admissions process (reported by 9.2% of interviewees), poor team communication (reported by 6.6% of interviewees), healthcare providers with a rude or uncaring manner (reported by 6.3% of interviewees), and problems related to discharge (reported by 5.7% of interviewees).
Of the 386 interviewees who perceived a breakdown in care, 140 (36.3%) perceived harm associated with the event (Table 3). The most common harms were physical (eg, pain; n = 66) and emotional (eg, distress, worry; n = 60). In addition, patients reported instances of damage to relationships with providers (n = 28) resulting in a loss of trust, with participants citing breakdowns as a reason for not coming back to a particular hospital or provider. In other cases, patients believed that breakdowns in care resulted in the need for additional care or a prolonged hospital stay.
We found no difference between the 2 hospitals where the study was conducted in the percentage of interviewees reporting at least 1 breakdown (39.1% vs 39.9%, P = 0.80). We also found no difference between interview method, (ie, in person vs telephone; 40.6% vs 37.2%, respectively, P = 0.30), patient gender (40.6% and 38.8% for men and women, respectively, P = 0.57), race (41.0% and 36.8% for white and black or African-American, respectively, P = 0.20) or between interviewers (P = 0.37). We did identify differences in rates of reporting at least 1 breakdown in care related to age (45.4% of patients aged 60 years or younger vs 34.5% of patients older than 60 years, P < 0.001) and education (32.7% of patients with a high school education or less vs 46.8% of those with at least some college education, P < 0.001). Patients interviewed alone reported fewer breakdowns than if another person was present during the interview or was interviewed in lieu of the patient (37.8% vs 53.4%, P = 0.002). The rate of reporting breakdowns for patients interviewed alone in the hospital is very similar to the rates of those interviewed via telephone (37.8% vs 37.2%). For most types of breakdowns, there were no differences in reporting for in-person vs postdischarge interviews. Discharge-related problems were more frequently reported among patients interviewed postdischarge (8.9% postdischarge vs 4.0% in person, P = 0.002). Patients interviewed in person were more likely to report problems with information exchange compared to patients interviewed postdischarge (17.6% vs 13.5%, respectively; P = 0.09), although this did not reach statistical significance.
DISCUSSION
Through interviews with nearly 1000 patients, we have found that approximately 4 in 10 hospitalized patients believed they experienced a breakdown in care. Not only are patient-perceived breakdowns in care distressingly common, more than one-third of these events resulted in harm according to the patient. Patients reported a diverse range of breakdowns, including problems related to patient experience, as well as breakdowns in technical aspects of medical care. Collectively, these findings illustrate a striking need to identify and address these frequent and potentially harmful breakdowns.
Our findings are consistent with prior studies in which 20% to 50% of patients identified a problem during hospitalization. For example, Weingart et al. interviewed patients in a single general medical unit and found that 20% experienced an adverse event, near miss, or medical error, while nearly 40% experienced what was defined as a service quality incident.2,12 Of note, both our study and the study by Weingart et al. systematically elicited patients’ perspectives of breakdowns in care with explicit questions about problems or breakdowns in care.2,12 Because patients are often reluctant to speak up about problems in care,without such efforts to actively identify problems, providers and leaders are likely to be unaware of the majority of these concerns.6-8 These findings suggest that hospital-based providers should at least consider routinely asking patients about breakdowns in care to identify and respond to patients’ concerns.
Not only are patient-perceived breakdowns common, more than one-third of patients who experienced a breakdown considered it to be harmful. This suggests that our outreach approach identified predominantly nontrivial concerns. We adopted a broad definition of harm that includes emotional distress, damage to the relationship with providers, and life disruption. This differs from other studies examining patient reports of breakdowns in care, in which harm was restricted to physical injury.1,2 We consider this inclusive definition of harm to be a strength of the present study as it provides the most complete picture of the impact of such events on patients. This approach is supported by other studies demonstrating that patients place great emphasis on the psychological consequences of adverse events.17-19 Thus, it is clear from our work and other studies that nonphysical harm is important and warrants concerted efforts to address.
Patients in our study reported a variety of breakdowns, including breakdowns related to patient experience (eg, communication, relationship with providers) and technical aspects of healthcare delivery (eg, diagnosis, treatment). This is consistent with other studies examining patient perspectives of breakdowns in care. Weingart et al.found that hospitalized patients reported a broad range of problems, including adverse events, medical errors, communication breakdowns, and problems with food.2,12 This variety of events suggests a need for integration between the various hospital groups that handle patient-perceived breakdowns, including bedside providers, risk management, patient relations, patient advocates, and quality and safety groups, in order to provide a coordinated and effective response to the full spectrum of patient-perceived breakdowns in care.
Patients in our study were more likely to report breakdowns related to communication and relationships with providers than those related to technical aspects of care. Similarly, Kuzel et al.found that the most common problems cited by patients in the primary care setting were breakdowns in the clinician-patient relationship and access-related problems.17This is not surprising, as patients are likely to have more direct knowledge about communication and interpersonal relationships than about technical aspects of care.
We identified several factors associated with the likelihood of reporting a breakdown in care. Most strikingly, involving a friend or family member in the interview was strongly associated with reporting a breakdown. Other work has also suggested that patients’ friends and family members are an important source of information about safety concerns.20,21 In addition, several patient characteristics were associated with an increased likelihood of reporting a breakdown, including being younger and better educated. These findings highlight the importance of engaging patients’ friends and families in efforts to elicit patient concerns about healthcare, and they confirm recommendations for patients to bring a friend or family member to healthcare encounters.22 In addition, they illustrate the need to better understand how patient characteristics affect perceptions of breakdowns in care and their willingness to speak up, as this could inform efforts to target outreach to especially vulnerable patients.
A strength of this study is the number of interviews completed (almost 1000), which provides a diverse range of patient views and experiences, as evidenced by the demographic characteristics of participants. Interviews were conducted at two hospitals that differ substantially with regard to populations served, further enhancing the generalizability of our findings. Despite the large number of interviews and diverse patient characteristics, patients were drawn from only 3 units at 2 hospitals, which may limit generalizability.
We did not conduct medical record reviews to validate patients’ reports of problems, which may be viewed as a limitation. While such a comparison would be informative, the intent of the current study was to elicit patients’ perceptions of care, including aspects of care that are not typically captured in the medical record, such as communication. Other studies have demonstrated that patients’ reports of medical errors and adverse events tend to differ from providers’ reports of the same subjects.19,23 Therefore, we considered the patients’ perceptions of care to be a useful endpoint in and of itself. We did not determine the extent to which providers were already aware of patients’ concerns or whether they considered patients’ concerns valid. A related limitation is our inability to determine whether the differences we identified in the rates of breakdown reporting based on patient characteristics reflect differences in willingness to report or differences in experiences. Because we included patients in an MSU, it is possible that breakdowns were related to medical care, surgical care, or both. We did not follow patients longitudinally and therefore only captured harm perceived by a patient at the time of the interview. It is possible that patients may have experienced harm later in their hospitalization or following discharge that was not measured. Lastly, we did not measure interrater reliability of the interview coding and therefore do not present the PECT as a validated instrument. These important questions should be targeted for future study.
CONCLUSION
When directly asked about their experiences, almost 4 out of 10 hospitalized patients reported a breakdown in their care, many of which were perceived to be harmful. Not all hospitals will have the resources to implement the intensive approach used in this study to elicit patient-perceived breakdowns. Therefore, further work is needed to develop sustainable methods to overcome patients’ reluctance to report breakdowns in care. Engaging patients’ families and friends may be a particularly fruitful strategy. We offer the PECT as a tool that hospitals could use to summarize a variety of sources of patient feedback such as complaints, responses to surveys, and consumer reviews. Hospitals that effectively encourage patients and their family members to speak up about perceived breakdowns will identify many opportunities to address patient concerns, potentially leading to improved patient safety and experience.
1. Weissman JS, Schneider EC, Weingart SN, et al. Comparing patient-reported hospital adverse events with medical record review: Do patients know something that hospitals do not? Ann Intern Med. 2008;149(2):100-108. PubMed
2. Weingart SN, Pagovich O, Sands DZ, et al. What can hospitalized patients tell us about adverse events? learning from patient-reported incidents. J Gen Intern Med. 2005;20(9):830-836. PubMed
3. Wetzels R, Wolters R, van Weel C, Wensing M. Mix of methods is needed to identify adverse events in general practice: A prospective observational study. BMC Fam Pract. 2008;9:35. PubMed
4. Friedman SM, Provan D, Moore S, Hanneman K. Errors, near misses and adverse events in the emergency department: What can patients tell us? CJEM. 2008;10(5):421-427. PubMed
5. Iedema R, Allen S, Britton K, Gallagher TH. What do patients and relatives know about problems and failures in care? BMJ Qual Saf. 2012;21(3):198-205. PubMed
6. Mazor KM, Roblin DW, Greene SM, et al. Toward patient-centered cancer care: Patient perceptions of problematic events, impact, and response. J Clin Oncol. 2012;30(15):1784-1790. PubMed
7. Frosch DL, May SG, Rendle KA, Tietbohl C, Elwyn G. Authoritarian physicians and patients’ fear of being labeled ‘difficult’ among key obstacles to shared decision making. Health Aff (Millwood). 2012;31(5):1030-1038. PubMed
8. Entwistle VA, McCaughan D, Watt IS, et al. Speaking up about safety concerns: Multi-setting qualitative study of patients’ views and experiences. Qual Saf Health Care. 2010;19(6):e33. PubMed
9. Tan M, Lang D. Effectiveness of nurse leader rounding and post-discharge telephone calls in patient satisfaction: A systematic review. JBI database of systematic reviews and implementation reports. 2015;13(7):154-176. PubMed
10. Garbutt J, Bose D, McCawley BA, Burroughs T, Medoff G. Soliciting patient complaints to improve performance. Jt Comm J Qual Saf. 2003;29(3):103-112. PubMed
11. Agoritsas T, Bovier PA, Perneger TV. Patient reports of undesirable events during hospitalization. J Gen Intern Med. 2005;20(10):922-928. PubMed
12. Weingart SN, Pagovich O, Sands DZ, et al. Patient-reported service quality on a medicine unit. Int J Qual Health Care. 2006;18(2):95-101. PubMed
13. Fisher KA, Ahmad S, Jackson M, Mazor KM. Surrogate decision makers’ perspectives on preventable breakdowns in care among critically ill patients: A qualitative study. Patient Educ Couns. 2016;99(10):1685-1693. PubMed
14. Halpern MT, Roussel AE, Treiman K, Nerz PA, Hatlie MJ, Sheridan S. Designing consumer reporting systems for patient safety events. Final Report (Prepared by RTI International and Consumers Advancing Patient Safety under Contract No. 290-06-00001-5). AHRQ Publication No. 11-0060-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
15. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. PubMed
16. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-1288. PubMed
17. Kuzel AJ, Woolf SH, Gilchrist VJ, et al. Patient reports of preventable problems and harms in primary health care. Ann Fam Med. 2004;2(4):333-340. PubMed
18. Sokol-Hessner L, Folcarelli PH, Sands KE. Emotional harm from disrespect: The neglected preventable harm. BMJ Qual Saf. 2015;24(9):550-553. PubMed
19. Masso Guijarro P, Aranaz Andres JM, Mira JJ, Perdiguero E, Aibar C. Adverse events in hospitals: The patient’s point of view. Qual Saf Health Care. 2010;19(2):144-147. PubMed
20. Bardach NS, Lyndon A, Asteria-Penaloza R, Goldman LE, Lin GA, Dudley RA. From the closest observers of patient care: A thematic analysis of online narrative reviews of hospitals. BMJ Qual Saf. 2015. PubMed
21. Schneider EC, Ridgely MS, Quigley DD, et al. Developing and testing the health care safety hotline: A prototype consumer reporting system for patient safety events. Final Report (Prepared by RAND Corporation under contract HHSA2902010000171). Rockvelle, MD: Agency for Healthcare Research and Quality; May 2016.
22. Shekelle PG, Pronovost PJ, Wachter RM, et al. The top patient safety strategies that can be encouraged for adoption now. Ann Intern Med. 2013;158(5 Pt 2):365-368. PubMed
23. Lawton R, O’Hara JK, Sheard L, et al. Can staff and patient perspectives on hospital safety predict harm-free care? an analysis of staff and patient survey data and routinely collected outcomes. BMJ Qual Saf. 2015;24(6):369-376. PubMed
There is growing recognition that patients and family members have critical insights into healthcare experiences. As consumers of healthcare, patient experience is the definitive gauge of whether healthcare is patient centered. In addition, patients may know things about their healthcare that the care team does not. Several studies have demonstrated that patients have knowledge of adverse events and medical errors that are not detected by other methods.1-5 For these reasons, systems designed to elicit patient perspectives of care and detect patient-perceived breakdowns in care could be used to improve healthcare safety and quality, including the patient experience.
Historically, hospitals have relied on patient-initiated reporting via complaints or legal action as the main source of information regarding patient-perceived breakdowns in care. However, many patients are hesitant to speak up about problems or uncertain about how to report concerns.6-8 As a result, healthcare systems often only learn of the most severe breakdowns in care from a subset of activated patients, thus underestimating how widespread patient-perceived breakdowns are.
To overcome these limitations of patient-initiated reporting, hospitals could conduct outreach to patients to actively identify and learn about patient-perceived breakdowns in care. Potential benefits of outreach to patients include more reliable detection of patient-perceived breakdowns in care, identification of a broader range of types of breakdowns commonly experienced by patients, and recognition of problems in real-time when there is more opportunity for redress. Indeed, some hospitals have adopted active outreach programs such as structured nurse manager rounding or postdischarge phone calls.9
It is possible that outreach will not overcome patients’ reluctance to speak up, or patients may not share serious or actionable breakdowns. The manner in which outreach is conducted is likely to influence the information patients are willing to share. Prior studies examining patient perspectives of healthcare have primarily taken a structured approach with close-ended questions or a focus on specific aspects of care.1,10,11 Limited data collected using an open-ended approach suggest patient-perceived breakdowns in care may be very common.2,12,13 However, the impact of such breakdowns on patients has not been well characterized.
In order to design systems that can optimally detect patient-perceived breakdowns in care, additional information is needed to understand whether patients will report breakdowns in response to outreach programs, what types of problems they will report, and how these problems impact them. Understanding such issues will allow healthcare systems to respond to calls by federal health agencies to develop mechanisms for patients to report concerns about breakdowns in care, thereby providing truly patient-centered care.14 Therefore, we undertook this study with the overall goal of describing what may be learned from an open-ended outreach approach that directly asks patients about problems they have encountered during hospitalization. Specifically, we aim to (1) describe the types of problems reported by patients in response to this outreach approach and (2) characterize patients’ perceptions of the impact of these events.
METHODS
Setting
We conducted this study in 2 hospitals between June 2014 and February 2015. One participating hospital is a large, urban, tertiary care medical center serving a predominantly white (78%) patient population in Baltimore, Maryland. The second hospital is a large, inner city, tertiary care medical center serving a predominantly African-American (71%) patient population in Washington, DC.
Three medical-surgical units (MSUs) at each hospital participated. We selected MSUs because MSU patients interact with a variety of clinicians, often have long stays, and are at risk for adverse events. Hospitalists were part of the clinical care team in each of the participating units, serving either as the attending of record or by comanaging patients.
Patient Eligibility
Patients were potentially eligible if they were at least 18 years old, able to speak English or Spanish, and admitted to the hospital for more than 24 hours. Ineligibility criteria included the following: imminent discharge, observation (noninpatient) status, on hospice, on infection precautions (for inpatient interviews only), psychiatric or violence concerns, prisoner status, significant confusion, or inability to provide informed consent.
Eligible patients in each unit were randomized. Interviewers consecutively approached patients according to their random assignment. If a patient was not available, the interviewer proceeded to the next room. Interviewers returned to rooms of missed patients when possible. Recruitment in the unit ended when the recruitment target for that unit was achieved.
Interviewers
Five interviewers conducted interviews. One author (KS) provided interviewer training that included didactic instruction, observation, feedback, and modeling. Interviewers participated in weekly debriefing sessions. One interviewer speaks Spanish fluently and was able to conduct interviews in Spanish. Translator services were available for the other interviewers.
Interview Process
Interviews were conducted in person while the patients were hospitalized or via telephone 7 - 30 days postdischarge. A patient who had completed an interview while hospitalized was not eligible for a postdischarge telephone interview. Family members or friends present at the time of the interviews could also participate in addition to or in lieu of the patients with the patients’ assent. Interviewers obtained verbal, informed consent at the start of each interview.
The interview domains and sample questions were developed specifically for the current study and are listed in Table 1. The goal of the interview was to elicit the patient’s (or family member’s) perception of their care experiences and their perceptions of the consequences of any problems with their care. The interviewer sought to obtain sufficient detail to understand the patient’s concerns and to determine what, if any, action might be needed to remediate problems reported by patients. Interviewers captured patient responses by taking detailed notes on a case report form or by directly entering patient responses using a computer or iPad at the time of interview at the discretion of the interviewer.
We defined a patient-perceived breakdown as something that went wrong during the hospitalization according to the patient. If a patient-perceived breakdown in care was identified, the interviewer attempted to resolve the concern. Some breakdowns had occurred in the past, making further resolution impossible (eg, a long wait in the emergency department). Other breakdowns were active and addressable, such as the patient having clinical questions that had not been answered. In such cases, the interviewer attempted to address the patient’s concerns, typically by working with unit nursing staff. For patients interviewed postdischarge, the interviewer worked to resolve ongoing patient concerns with the assistance of the patient safety, quality, and compliance teams as needed. The interviewer provided a brief narrative summary of all interviews to unit nursing leadership within 24 hours. Positive comments were sent to leadership but not captured systematically for research purposes. Further details of the process of responding to patients’ concerns will be reported elsewhere. All data were entered into REDCap to facilitate data management and reporting.15
The MedStar Health Research Institute Institutional Review Board reviewed and approved this study.
Categorizing Patients’ Responses: The Patient Experience Coding Tool
Using directed content analysis,16 we deductively created the Patient Experience Coding Tool (PECT) in order to summarize the narrative information captured during the interviews and categorize patient-perceived breakdowns in care. First, we referred to our prior interviews of patients’ views on breakdowns in cancer care6 and surrogate decision-makers’ views on breakdowns in intensive care units13 to create the initial categories. We then applied the resultant framework to the interviews in the present study and refined the categories. This involved applying the categorization to an initial set of interviews to check the sufficiency of the coding categories. We clarified the scope of each category (ie, what types of events fit under each category) and created additional categories (eg, medication-related problems) to capture patient experiences that were not included in the initial framework.
We then coded each interview using the PECT. A minimum of 2 readers reviewed the narrative notes for each interview. The first reader provided an initial categorization; the second reader reviewed the narrative and confirmed or questioned the initial categorization to improve coding accuracy. If a reader was uncertain about the correct categorization, it was discussed by three readers until an agreement was achieved. Because facilities-related problems (eg, food or parking) fall outside the realm of provider-based hospital care, such comments were not the focus of the outreach efforts and were not consistently recorded. Therefore, they were not included in the PECT and are not reported here.
Analyses
We computed simple, descriptive statistics including the number and percentage of patients identifying at least one breakdown, as well as the number and percent reporting each type of breakdown. We also computed the number and percentage of patients reporting any harm and each type of harm. We computed the percentage of patients reporting at least 1 breakdown by hospital, type of interview (postdischarge vs inpatient), selected patient demographic characteristics (eg, gender, age, education, race), and interviewee (patient vs someone other than the patient interviewed or present during the interview) using the chi-square statistic to test the statistical significance of the resulting differences. All statistical analyses were performed using SPSS version 22.
RESULTS
A total of 979 outreach interviews were conducted. Of these, 349 were conducted via telephone postdischarge, and 630 were conducted in person during hospitalization. The average interview duration was 8.5 minutes for telephone interviews and 12.2 minutes for in-person interviews. Of the patients approached to participate, 67% completed an interview (61% in person, 83% via telephone). Patient characteristics are summarized in Table 2.
Overall, 386 of 979 interviewees (39.4%) believed they had experienced at least one breakdown in care. The types of patient-perceived breakdowns reported were categorized using the PECT and are summarized in Table 3 and the Figure. The most common concern involved information exchange. Approximately 1 in 10 patients (n = 105, 10.7%) felt that they had not received the information they needed when they needed it. Medication-related concerns were reported by 12.3% (n = 120) of interviewees and predominantly included concerns about what medications were being administered (5.7%) and inadequately treated pain (5.6%). Many of the patients expressing concerns about what medications were administered questioned why they were not receiving their outpatient medications or did not understand why a different medication was being administered, suggesting that many of these instances were related to breakdowns in communication as well. Other relatively common concerns were delays in the admissions process (reported by 9.2% of interviewees), poor team communication (reported by 6.6% of interviewees), healthcare providers with a rude or uncaring manner (reported by 6.3% of interviewees), and problems related to discharge (reported by 5.7% of interviewees).
Of the 386 interviewees who perceived a breakdown in care, 140 (36.3%) perceived harm associated with the event (Table 3). The most common harms were physical (eg, pain; n = 66) and emotional (eg, distress, worry; n = 60). In addition, patients reported instances of damage to relationships with providers (n = 28) resulting in a loss of trust, with participants citing breakdowns as a reason for not coming back to a particular hospital or provider. In other cases, patients believed that breakdowns in care resulted in the need for additional care or a prolonged hospital stay.
We found no difference between the 2 hospitals where the study was conducted in the percentage of interviewees reporting at least 1 breakdown (39.1% vs 39.9%, P = 0.80). We also found no difference between interview method, (ie, in person vs telephone; 40.6% vs 37.2%, respectively, P = 0.30), patient gender (40.6% and 38.8% for men and women, respectively, P = 0.57), race (41.0% and 36.8% for white and black or African-American, respectively, P = 0.20) or between interviewers (P = 0.37). We did identify differences in rates of reporting at least 1 breakdown in care related to age (45.4% of patients aged 60 years or younger vs 34.5% of patients older than 60 years, P < 0.001) and education (32.7% of patients with a high school education or less vs 46.8% of those with at least some college education, P < 0.001). Patients interviewed alone reported fewer breakdowns than if another person was present during the interview or was interviewed in lieu of the patient (37.8% vs 53.4%, P = 0.002). The rate of reporting breakdowns for patients interviewed alone in the hospital is very similar to the rates of those interviewed via telephone (37.8% vs 37.2%). For most types of breakdowns, there were no differences in reporting for in-person vs postdischarge interviews. Discharge-related problems were more frequently reported among patients interviewed postdischarge (8.9% postdischarge vs 4.0% in person, P = 0.002). Patients interviewed in person were more likely to report problems with information exchange compared to patients interviewed postdischarge (17.6% vs 13.5%, respectively; P = 0.09), although this did not reach statistical significance.
DISCUSSION
Through interviews with nearly 1000 patients, we have found that approximately 4 in 10 hospitalized patients believed they experienced a breakdown in care. Not only are patient-perceived breakdowns in care distressingly common, more than one-third of these events resulted in harm according to the patient. Patients reported a diverse range of breakdowns, including problems related to patient experience, as well as breakdowns in technical aspects of medical care. Collectively, these findings illustrate a striking need to identify and address these frequent and potentially harmful breakdowns.
Our findings are consistent with prior studies in which 20% to 50% of patients identified a problem during hospitalization. For example, Weingart et al. interviewed patients in a single general medical unit and found that 20% experienced an adverse event, near miss, or medical error, while nearly 40% experienced what was defined as a service quality incident.2,12 Of note, both our study and the study by Weingart et al. systematically elicited patients’ perspectives of breakdowns in care with explicit questions about problems or breakdowns in care.2,12 Because patients are often reluctant to speak up about problems in care,without such efforts to actively identify problems, providers and leaders are likely to be unaware of the majority of these concerns.6-8 These findings suggest that hospital-based providers should at least consider routinely asking patients about breakdowns in care to identify and respond to patients’ concerns.
Not only are patient-perceived breakdowns common, more than one-third of patients who experienced a breakdown considered it to be harmful. This suggests that our outreach approach identified predominantly nontrivial concerns. We adopted a broad definition of harm that includes emotional distress, damage to the relationship with providers, and life disruption. This differs from other studies examining patient reports of breakdowns in care, in which harm was restricted to physical injury.1,2 We consider this inclusive definition of harm to be a strength of the present study as it provides the most complete picture of the impact of such events on patients. This approach is supported by other studies demonstrating that patients place great emphasis on the psychological consequences of adverse events.17-19 Thus, it is clear from our work and other studies that nonphysical harm is important and warrants concerted efforts to address.
Patients in our study reported a variety of breakdowns, including breakdowns related to patient experience (eg, communication, relationship with providers) and technical aspects of healthcare delivery (eg, diagnosis, treatment). This is consistent with other studies examining patient perspectives of breakdowns in care. Weingart et al.found that hospitalized patients reported a broad range of problems, including adverse events, medical errors, communication breakdowns, and problems with food.2,12 This variety of events suggests a need for integration between the various hospital groups that handle patient-perceived breakdowns, including bedside providers, risk management, patient relations, patient advocates, and quality and safety groups, in order to provide a coordinated and effective response to the full spectrum of patient-perceived breakdowns in care.
Patients in our study were more likely to report breakdowns related to communication and relationships with providers than those related to technical aspects of care. Similarly, Kuzel et al.found that the most common problems cited by patients in the primary care setting were breakdowns in the clinician-patient relationship and access-related problems.17This is not surprising, as patients are likely to have more direct knowledge about communication and interpersonal relationships than about technical aspects of care.
We identified several factors associated with the likelihood of reporting a breakdown in care. Most strikingly, involving a friend or family member in the interview was strongly associated with reporting a breakdown. Other work has also suggested that patients’ friends and family members are an important source of information about safety concerns.20,21 In addition, several patient characteristics were associated with an increased likelihood of reporting a breakdown, including being younger and better educated. These findings highlight the importance of engaging patients’ friends and families in efforts to elicit patient concerns about healthcare, and they confirm recommendations for patients to bring a friend or family member to healthcare encounters.22 In addition, they illustrate the need to better understand how patient characteristics affect perceptions of breakdowns in care and their willingness to speak up, as this could inform efforts to target outreach to especially vulnerable patients.
A strength of this study is the number of interviews completed (almost 1000), which provides a diverse range of patient views and experiences, as evidenced by the demographic characteristics of participants. Interviews were conducted at two hospitals that differ substantially with regard to populations served, further enhancing the generalizability of our findings. Despite the large number of interviews and diverse patient characteristics, patients were drawn from only 3 units at 2 hospitals, which may limit generalizability.
We did not conduct medical record reviews to validate patients’ reports of problems, which may be viewed as a limitation. While such a comparison would be informative, the intent of the current study was to elicit patients’ perceptions of care, including aspects of care that are not typically captured in the medical record, such as communication. Other studies have demonstrated that patients’ reports of medical errors and adverse events tend to differ from providers’ reports of the same subjects.19,23 Therefore, we considered the patients’ perceptions of care to be a useful endpoint in and of itself. We did not determine the extent to which providers were already aware of patients’ concerns or whether they considered patients’ concerns valid. A related limitation is our inability to determine whether the differences we identified in the rates of breakdown reporting based on patient characteristics reflect differences in willingness to report or differences in experiences. Because we included patients in an MSU, it is possible that breakdowns were related to medical care, surgical care, or both. We did not follow patients longitudinally and therefore only captured harm perceived by a patient at the time of the interview. It is possible that patients may have experienced harm later in their hospitalization or following discharge that was not measured. Lastly, we did not measure interrater reliability of the interview coding and therefore do not present the PECT as a validated instrument. These important questions should be targeted for future study.
CONCLUSION
When directly asked about their experiences, almost 4 out of 10 hospitalized patients reported a breakdown in their care, many of which were perceived to be harmful. Not all hospitals will have the resources to implement the intensive approach used in this study to elicit patient-perceived breakdowns. Therefore, further work is needed to develop sustainable methods to overcome patients’ reluctance to report breakdowns in care. Engaging patients’ families and friends may be a particularly fruitful strategy. We offer the PECT as a tool that hospitals could use to summarize a variety of sources of patient feedback such as complaints, responses to surveys, and consumer reviews. Hospitals that effectively encourage patients and their family members to speak up about perceived breakdowns will identify many opportunities to address patient concerns, potentially leading to improved patient safety and experience.
There is growing recognition that patients and family members have critical insights into healthcare experiences. As consumers of healthcare, patient experience is the definitive gauge of whether healthcare is patient centered. In addition, patients may know things about their healthcare that the care team does not. Several studies have demonstrated that patients have knowledge of adverse events and medical errors that are not detected by other methods.1-5 For these reasons, systems designed to elicit patient perspectives of care and detect patient-perceived breakdowns in care could be used to improve healthcare safety and quality, including the patient experience.
Historically, hospitals have relied on patient-initiated reporting via complaints or legal action as the main source of information regarding patient-perceived breakdowns in care. However, many patients are hesitant to speak up about problems or uncertain about how to report concerns.6-8 As a result, healthcare systems often only learn of the most severe breakdowns in care from a subset of activated patients, thus underestimating how widespread patient-perceived breakdowns are.
To overcome these limitations of patient-initiated reporting, hospitals could conduct outreach to patients to actively identify and learn about patient-perceived breakdowns in care. Potential benefits of outreach to patients include more reliable detection of patient-perceived breakdowns in care, identification of a broader range of types of breakdowns commonly experienced by patients, and recognition of problems in real-time when there is more opportunity for redress. Indeed, some hospitals have adopted active outreach programs such as structured nurse manager rounding or postdischarge phone calls.9
It is possible that outreach will not overcome patients’ reluctance to speak up, or patients may not share serious or actionable breakdowns. The manner in which outreach is conducted is likely to influence the information patients are willing to share. Prior studies examining patient perspectives of healthcare have primarily taken a structured approach with close-ended questions or a focus on specific aspects of care.1,10,11 Limited data collected using an open-ended approach suggest patient-perceived breakdowns in care may be very common.2,12,13 However, the impact of such breakdowns on patients has not been well characterized.
In order to design systems that can optimally detect patient-perceived breakdowns in care, additional information is needed to understand whether patients will report breakdowns in response to outreach programs, what types of problems they will report, and how these problems impact them. Understanding such issues will allow healthcare systems to respond to calls by federal health agencies to develop mechanisms for patients to report concerns about breakdowns in care, thereby providing truly patient-centered care.14 Therefore, we undertook this study with the overall goal of describing what may be learned from an open-ended outreach approach that directly asks patients about problems they have encountered during hospitalization. Specifically, we aim to (1) describe the types of problems reported by patients in response to this outreach approach and (2) characterize patients’ perceptions of the impact of these events.
METHODS
Setting
We conducted this study in 2 hospitals between June 2014 and February 2015. One participating hospital is a large, urban, tertiary care medical center serving a predominantly white (78%) patient population in Baltimore, Maryland. The second hospital is a large, inner city, tertiary care medical center serving a predominantly African-American (71%) patient population in Washington, DC.
Three medical-surgical units (MSUs) at each hospital participated. We selected MSUs because MSU patients interact with a variety of clinicians, often have long stays, and are at risk for adverse events. Hospitalists were part of the clinical care team in each of the participating units, serving either as the attending of record or by comanaging patients.
Patient Eligibility
Patients were potentially eligible if they were at least 18 years old, able to speak English or Spanish, and admitted to the hospital for more than 24 hours. Ineligibility criteria included the following: imminent discharge, observation (noninpatient) status, on hospice, on infection precautions (for inpatient interviews only), psychiatric or violence concerns, prisoner status, significant confusion, or inability to provide informed consent.
Eligible patients in each unit were randomized. Interviewers consecutively approached patients according to their random assignment. If a patient was not available, the interviewer proceeded to the next room. Interviewers returned to rooms of missed patients when possible. Recruitment in the unit ended when the recruitment target for that unit was achieved.
Interviewers
Five interviewers conducted interviews. One author (KS) provided interviewer training that included didactic instruction, observation, feedback, and modeling. Interviewers participated in weekly debriefing sessions. One interviewer speaks Spanish fluently and was able to conduct interviews in Spanish. Translator services were available for the other interviewers.
Interview Process
Interviews were conducted in person while the patients were hospitalized or via telephone 7 - 30 days postdischarge. A patient who had completed an interview while hospitalized was not eligible for a postdischarge telephone interview. Family members or friends present at the time of the interviews could also participate in addition to or in lieu of the patients with the patients’ assent. Interviewers obtained verbal, informed consent at the start of each interview.
The interview domains and sample questions were developed specifically for the current study and are listed in Table 1. The goal of the interview was to elicit the patient’s (or family member’s) perception of their care experiences and their perceptions of the consequences of any problems with their care. The interviewer sought to obtain sufficient detail to understand the patient’s concerns and to determine what, if any, action might be needed to remediate problems reported by patients. Interviewers captured patient responses by taking detailed notes on a case report form or by directly entering patient responses using a computer or iPad at the time of interview at the discretion of the interviewer.
We defined a patient-perceived breakdown as something that went wrong during the hospitalization according to the patient. If a patient-perceived breakdown in care was identified, the interviewer attempted to resolve the concern. Some breakdowns had occurred in the past, making further resolution impossible (eg, a long wait in the emergency department). Other breakdowns were active and addressable, such as the patient having clinical questions that had not been answered. In such cases, the interviewer attempted to address the patient’s concerns, typically by working with unit nursing staff. For patients interviewed postdischarge, the interviewer worked to resolve ongoing patient concerns with the assistance of the patient safety, quality, and compliance teams as needed. The interviewer provided a brief narrative summary of all interviews to unit nursing leadership within 24 hours. Positive comments were sent to leadership but not captured systematically for research purposes. Further details of the process of responding to patients’ concerns will be reported elsewhere. All data were entered into REDCap to facilitate data management and reporting.15
The MedStar Health Research Institute Institutional Review Board reviewed and approved this study.
Categorizing Patients’ Responses: The Patient Experience Coding Tool
Using directed content analysis,16 we deductively created the Patient Experience Coding Tool (PECT) in order to summarize the narrative information captured during the interviews and categorize patient-perceived breakdowns in care. First, we referred to our prior interviews of patients’ views on breakdowns in cancer care6 and surrogate decision-makers’ views on breakdowns in intensive care units13 to create the initial categories. We then applied the resultant framework to the interviews in the present study and refined the categories. This involved applying the categorization to an initial set of interviews to check the sufficiency of the coding categories. We clarified the scope of each category (ie, what types of events fit under each category) and created additional categories (eg, medication-related problems) to capture patient experiences that were not included in the initial framework.
We then coded each interview using the PECT. A minimum of 2 readers reviewed the narrative notes for each interview. The first reader provided an initial categorization; the second reader reviewed the narrative and confirmed or questioned the initial categorization to improve coding accuracy. If a reader was uncertain about the correct categorization, it was discussed by three readers until an agreement was achieved. Because facilities-related problems (eg, food or parking) fall outside the realm of provider-based hospital care, such comments were not the focus of the outreach efforts and were not consistently recorded. Therefore, they were not included in the PECT and are not reported here.
Analyses
We computed simple, descriptive statistics including the number and percentage of patients identifying at least one breakdown, as well as the number and percent reporting each type of breakdown. We also computed the number and percentage of patients reporting any harm and each type of harm. We computed the percentage of patients reporting at least 1 breakdown by hospital, type of interview (postdischarge vs inpatient), selected patient demographic characteristics (eg, gender, age, education, race), and interviewee (patient vs someone other than the patient interviewed or present during the interview) using the chi-square statistic to test the statistical significance of the resulting differences. All statistical analyses were performed using SPSS version 22.
RESULTS
A total of 979 outreach interviews were conducted. Of these, 349 were conducted via telephone postdischarge, and 630 were conducted in person during hospitalization. The average interview duration was 8.5 minutes for telephone interviews and 12.2 minutes for in-person interviews. Of the patients approached to participate, 67% completed an interview (61% in person, 83% via telephone). Patient characteristics are summarized in Table 2.
Overall, 386 of 979 interviewees (39.4%) believed they had experienced at least one breakdown in care. The types of patient-perceived breakdowns reported were categorized using the PECT and are summarized in Table 3 and the Figure. The most common concern involved information exchange. Approximately 1 in 10 patients (n = 105, 10.7%) felt that they had not received the information they needed when they needed it. Medication-related concerns were reported by 12.3% (n = 120) of interviewees and predominantly included concerns about what medications were being administered (5.7%) and inadequately treated pain (5.6%). Many of the patients expressing concerns about what medications were administered questioned why they were not receiving their outpatient medications or did not understand why a different medication was being administered, suggesting that many of these instances were related to breakdowns in communication as well. Other relatively common concerns were delays in the admissions process (reported by 9.2% of interviewees), poor team communication (reported by 6.6% of interviewees), healthcare providers with a rude or uncaring manner (reported by 6.3% of interviewees), and problems related to discharge (reported by 5.7% of interviewees).
Of the 386 interviewees who perceived a breakdown in care, 140 (36.3%) perceived harm associated with the event (Table 3). The most common harms were physical (eg, pain; n = 66) and emotional (eg, distress, worry; n = 60). In addition, patients reported instances of damage to relationships with providers (n = 28) resulting in a loss of trust, with participants citing breakdowns as a reason for not coming back to a particular hospital or provider. In other cases, patients believed that breakdowns in care resulted in the need for additional care or a prolonged hospital stay.
We found no difference between the 2 hospitals where the study was conducted in the percentage of interviewees reporting at least 1 breakdown (39.1% vs 39.9%, P = 0.80). We also found no difference between interview method, (ie, in person vs telephone; 40.6% vs 37.2%, respectively, P = 0.30), patient gender (40.6% and 38.8% for men and women, respectively, P = 0.57), race (41.0% and 36.8% for white and black or African-American, respectively, P = 0.20) or between interviewers (P = 0.37). We did identify differences in rates of reporting at least 1 breakdown in care related to age (45.4% of patients aged 60 years or younger vs 34.5% of patients older than 60 years, P < 0.001) and education (32.7% of patients with a high school education or less vs 46.8% of those with at least some college education, P < 0.001). Patients interviewed alone reported fewer breakdowns than if another person was present during the interview or was interviewed in lieu of the patient (37.8% vs 53.4%, P = 0.002). The rate of reporting breakdowns for patients interviewed alone in the hospital is very similar to the rates of those interviewed via telephone (37.8% vs 37.2%). For most types of breakdowns, there were no differences in reporting for in-person vs postdischarge interviews. Discharge-related problems were more frequently reported among patients interviewed postdischarge (8.9% postdischarge vs 4.0% in person, P = 0.002). Patients interviewed in person were more likely to report problems with information exchange compared to patients interviewed postdischarge (17.6% vs 13.5%, respectively; P = 0.09), although this did not reach statistical significance.
DISCUSSION
Through interviews with nearly 1000 patients, we have found that approximately 4 in 10 hospitalized patients believed they experienced a breakdown in care. Not only are patient-perceived breakdowns in care distressingly common, more than one-third of these events resulted in harm according to the patient. Patients reported a diverse range of breakdowns, including problems related to patient experience, as well as breakdowns in technical aspects of medical care. Collectively, these findings illustrate a striking need to identify and address these frequent and potentially harmful breakdowns.
Our findings are consistent with prior studies in which 20% to 50% of patients identified a problem during hospitalization. For example, Weingart et al. interviewed patients in a single general medical unit and found that 20% experienced an adverse event, near miss, or medical error, while nearly 40% experienced what was defined as a service quality incident.2,12 Of note, both our study and the study by Weingart et al. systematically elicited patients’ perspectives of breakdowns in care with explicit questions about problems or breakdowns in care.2,12 Because patients are often reluctant to speak up about problems in care,without such efforts to actively identify problems, providers and leaders are likely to be unaware of the majority of these concerns.6-8 These findings suggest that hospital-based providers should at least consider routinely asking patients about breakdowns in care to identify and respond to patients’ concerns.
Not only are patient-perceived breakdowns common, more than one-third of patients who experienced a breakdown considered it to be harmful. This suggests that our outreach approach identified predominantly nontrivial concerns. We adopted a broad definition of harm that includes emotional distress, damage to the relationship with providers, and life disruption. This differs from other studies examining patient reports of breakdowns in care, in which harm was restricted to physical injury.1,2 We consider this inclusive definition of harm to be a strength of the present study as it provides the most complete picture of the impact of such events on patients. This approach is supported by other studies demonstrating that patients place great emphasis on the psychological consequences of adverse events.17-19 Thus, it is clear from our work and other studies that nonphysical harm is important and warrants concerted efforts to address.
Patients in our study reported a variety of breakdowns, including breakdowns related to patient experience (eg, communication, relationship with providers) and technical aspects of healthcare delivery (eg, diagnosis, treatment). This is consistent with other studies examining patient perspectives of breakdowns in care. Weingart et al.found that hospitalized patients reported a broad range of problems, including adverse events, medical errors, communication breakdowns, and problems with food.2,12 This variety of events suggests a need for integration between the various hospital groups that handle patient-perceived breakdowns, including bedside providers, risk management, patient relations, patient advocates, and quality and safety groups, in order to provide a coordinated and effective response to the full spectrum of patient-perceived breakdowns in care.
Patients in our study were more likely to report breakdowns related to communication and relationships with providers than those related to technical aspects of care. Similarly, Kuzel et al.found that the most common problems cited by patients in the primary care setting were breakdowns in the clinician-patient relationship and access-related problems.17This is not surprising, as patients are likely to have more direct knowledge about communication and interpersonal relationships than about technical aspects of care.
We identified several factors associated with the likelihood of reporting a breakdown in care. Most strikingly, involving a friend or family member in the interview was strongly associated with reporting a breakdown. Other work has also suggested that patients’ friends and family members are an important source of information about safety concerns.20,21 In addition, several patient characteristics were associated with an increased likelihood of reporting a breakdown, including being younger and better educated. These findings highlight the importance of engaging patients’ friends and families in efforts to elicit patient concerns about healthcare, and they confirm recommendations for patients to bring a friend or family member to healthcare encounters.22 In addition, they illustrate the need to better understand how patient characteristics affect perceptions of breakdowns in care and their willingness to speak up, as this could inform efforts to target outreach to especially vulnerable patients.
A strength of this study is the number of interviews completed (almost 1000), which provides a diverse range of patient views and experiences, as evidenced by the demographic characteristics of participants. Interviews were conducted at two hospitals that differ substantially with regard to populations served, further enhancing the generalizability of our findings. Despite the large number of interviews and diverse patient characteristics, patients were drawn from only 3 units at 2 hospitals, which may limit generalizability.
We did not conduct medical record reviews to validate patients’ reports of problems, which may be viewed as a limitation. While such a comparison would be informative, the intent of the current study was to elicit patients’ perceptions of care, including aspects of care that are not typically captured in the medical record, such as communication. Other studies have demonstrated that patients’ reports of medical errors and adverse events tend to differ from providers’ reports of the same subjects.19,23 Therefore, we considered the patients’ perceptions of care to be a useful endpoint in and of itself. We did not determine the extent to which providers were already aware of patients’ concerns or whether they considered patients’ concerns valid. A related limitation is our inability to determine whether the differences we identified in the rates of breakdown reporting based on patient characteristics reflect differences in willingness to report or differences in experiences. Because we included patients in an MSU, it is possible that breakdowns were related to medical care, surgical care, or both. We did not follow patients longitudinally and therefore only captured harm perceived by a patient at the time of the interview. It is possible that patients may have experienced harm later in their hospitalization or following discharge that was not measured. Lastly, we did not measure interrater reliability of the interview coding and therefore do not present the PECT as a validated instrument. These important questions should be targeted for future study.
CONCLUSION
When directly asked about their experiences, almost 4 out of 10 hospitalized patients reported a breakdown in their care, many of which were perceived to be harmful. Not all hospitals will have the resources to implement the intensive approach used in this study to elicit patient-perceived breakdowns. Therefore, further work is needed to develop sustainable methods to overcome patients’ reluctance to report breakdowns in care. Engaging patients’ families and friends may be a particularly fruitful strategy. We offer the PECT as a tool that hospitals could use to summarize a variety of sources of patient feedback such as complaints, responses to surveys, and consumer reviews. Hospitals that effectively encourage patients and their family members to speak up about perceived breakdowns will identify many opportunities to address patient concerns, potentially leading to improved patient safety and experience.
1. Weissman JS, Schneider EC, Weingart SN, et al. Comparing patient-reported hospital adverse events with medical record review: Do patients know something that hospitals do not? Ann Intern Med. 2008;149(2):100-108. PubMed
2. Weingart SN, Pagovich O, Sands DZ, et al. What can hospitalized patients tell us about adverse events? learning from patient-reported incidents. J Gen Intern Med. 2005;20(9):830-836. PubMed
3. Wetzels R, Wolters R, van Weel C, Wensing M. Mix of methods is needed to identify adverse events in general practice: A prospective observational study. BMC Fam Pract. 2008;9:35. PubMed
4. Friedman SM, Provan D, Moore S, Hanneman K. Errors, near misses and adverse events in the emergency department: What can patients tell us? CJEM. 2008;10(5):421-427. PubMed
5. Iedema R, Allen S, Britton K, Gallagher TH. What do patients and relatives know about problems and failures in care? BMJ Qual Saf. 2012;21(3):198-205. PubMed
6. Mazor KM, Roblin DW, Greene SM, et al. Toward patient-centered cancer care: Patient perceptions of problematic events, impact, and response. J Clin Oncol. 2012;30(15):1784-1790. PubMed
7. Frosch DL, May SG, Rendle KA, Tietbohl C, Elwyn G. Authoritarian physicians and patients’ fear of being labeled ‘difficult’ among key obstacles to shared decision making. Health Aff (Millwood). 2012;31(5):1030-1038. PubMed
8. Entwistle VA, McCaughan D, Watt IS, et al. Speaking up about safety concerns: Multi-setting qualitative study of patients’ views and experiences. Qual Saf Health Care. 2010;19(6):e33. PubMed
9. Tan M, Lang D. Effectiveness of nurse leader rounding and post-discharge telephone calls in patient satisfaction: A systematic review. JBI database of systematic reviews and implementation reports. 2015;13(7):154-176. PubMed
10. Garbutt J, Bose D, McCawley BA, Burroughs T, Medoff G. Soliciting patient complaints to improve performance. Jt Comm J Qual Saf. 2003;29(3):103-112. PubMed
11. Agoritsas T, Bovier PA, Perneger TV. Patient reports of undesirable events during hospitalization. J Gen Intern Med. 2005;20(10):922-928. PubMed
12. Weingart SN, Pagovich O, Sands DZ, et al. Patient-reported service quality on a medicine unit. Int J Qual Health Care. 2006;18(2):95-101. PubMed
13. Fisher KA, Ahmad S, Jackson M, Mazor KM. Surrogate decision makers’ perspectives on preventable breakdowns in care among critically ill patients: A qualitative study. Patient Educ Couns. 2016;99(10):1685-1693. PubMed
14. Halpern MT, Roussel AE, Treiman K, Nerz PA, Hatlie MJ, Sheridan S. Designing consumer reporting systems for patient safety events. Final Report (Prepared by RTI International and Consumers Advancing Patient Safety under Contract No. 290-06-00001-5). AHRQ Publication No. 11-0060-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
15. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. PubMed
16. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-1288. PubMed
17. Kuzel AJ, Woolf SH, Gilchrist VJ, et al. Patient reports of preventable problems and harms in primary health care. Ann Fam Med. 2004;2(4):333-340. PubMed
18. Sokol-Hessner L, Folcarelli PH, Sands KE. Emotional harm from disrespect: The neglected preventable harm. BMJ Qual Saf. 2015;24(9):550-553. PubMed
19. Masso Guijarro P, Aranaz Andres JM, Mira JJ, Perdiguero E, Aibar C. Adverse events in hospitals: The patient’s point of view. Qual Saf Health Care. 2010;19(2):144-147. PubMed
20. Bardach NS, Lyndon A, Asteria-Penaloza R, Goldman LE, Lin GA, Dudley RA. From the closest observers of patient care: A thematic analysis of online narrative reviews of hospitals. BMJ Qual Saf. 2015. PubMed
21. Schneider EC, Ridgely MS, Quigley DD, et al. Developing and testing the health care safety hotline: A prototype consumer reporting system for patient safety events. Final Report (Prepared by RAND Corporation under contract HHSA2902010000171). Rockvelle, MD: Agency for Healthcare Research and Quality; May 2016.
22. Shekelle PG, Pronovost PJ, Wachter RM, et al. The top patient safety strategies that can be encouraged for adoption now. Ann Intern Med. 2013;158(5 Pt 2):365-368. PubMed
23. Lawton R, O’Hara JK, Sheard L, et al. Can staff and patient perspectives on hospital safety predict harm-free care? an analysis of staff and patient survey data and routinely collected outcomes. BMJ Qual Saf. 2015;24(6):369-376. PubMed
1. Weissman JS, Schneider EC, Weingart SN, et al. Comparing patient-reported hospital adverse events with medical record review: Do patients know something that hospitals do not? Ann Intern Med. 2008;149(2):100-108. PubMed
2. Weingart SN, Pagovich O, Sands DZ, et al. What can hospitalized patients tell us about adverse events? learning from patient-reported incidents. J Gen Intern Med. 2005;20(9):830-836. PubMed
3. Wetzels R, Wolters R, van Weel C, Wensing M. Mix of methods is needed to identify adverse events in general practice: A prospective observational study. BMC Fam Pract. 2008;9:35. PubMed
4. Friedman SM, Provan D, Moore S, Hanneman K. Errors, near misses and adverse events in the emergency department: What can patients tell us? CJEM. 2008;10(5):421-427. PubMed
5. Iedema R, Allen S, Britton K, Gallagher TH. What do patients and relatives know about problems and failures in care? BMJ Qual Saf. 2012;21(3):198-205. PubMed
6. Mazor KM, Roblin DW, Greene SM, et al. Toward patient-centered cancer care: Patient perceptions of problematic events, impact, and response. J Clin Oncol. 2012;30(15):1784-1790. PubMed
7. Frosch DL, May SG, Rendle KA, Tietbohl C, Elwyn G. Authoritarian physicians and patients’ fear of being labeled ‘difficult’ among key obstacles to shared decision making. Health Aff (Millwood). 2012;31(5):1030-1038. PubMed
8. Entwistle VA, McCaughan D, Watt IS, et al. Speaking up about safety concerns: Multi-setting qualitative study of patients’ views and experiences. Qual Saf Health Care. 2010;19(6):e33. PubMed
9. Tan M, Lang D. Effectiveness of nurse leader rounding and post-discharge telephone calls in patient satisfaction: A systematic review. JBI database of systematic reviews and implementation reports. 2015;13(7):154-176. PubMed
10. Garbutt J, Bose D, McCawley BA, Burroughs T, Medoff G. Soliciting patient complaints to improve performance. Jt Comm J Qual Saf. 2003;29(3):103-112. PubMed
11. Agoritsas T, Bovier PA, Perneger TV. Patient reports of undesirable events during hospitalization. J Gen Intern Med. 2005;20(10):922-928. PubMed
12. Weingart SN, Pagovich O, Sands DZ, et al. Patient-reported service quality on a medicine unit. Int J Qual Health Care. 2006;18(2):95-101. PubMed
13. Fisher KA, Ahmad S, Jackson M, Mazor KM. Surrogate decision makers’ perspectives on preventable breakdowns in care among critically ill patients: A qualitative study. Patient Educ Couns. 2016;99(10):1685-1693. PubMed
14. Halpern MT, Roussel AE, Treiman K, Nerz PA, Hatlie MJ, Sheridan S. Designing consumer reporting systems for patient safety events. Final Report (Prepared by RTI International and Consumers Advancing Patient Safety under Contract No. 290-06-00001-5). AHRQ Publication No. 11-0060-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
15. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. PubMed
16. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-1288. PubMed
17. Kuzel AJ, Woolf SH, Gilchrist VJ, et al. Patient reports of preventable problems and harms in primary health care. Ann Fam Med. 2004;2(4):333-340. PubMed
18. Sokol-Hessner L, Folcarelli PH, Sands KE. Emotional harm from disrespect: The neglected preventable harm. BMJ Qual Saf. 2015;24(9):550-553. PubMed
19. Masso Guijarro P, Aranaz Andres JM, Mira JJ, Perdiguero E, Aibar C. Adverse events in hospitals: The patient’s point of view. Qual Saf Health Care. 2010;19(2):144-147. PubMed
20. Bardach NS, Lyndon A, Asteria-Penaloza R, Goldman LE, Lin GA, Dudley RA. From the closest observers of patient care: A thematic analysis of online narrative reviews of hospitals. BMJ Qual Saf. 2015. PubMed
21. Schneider EC, Ridgely MS, Quigley DD, et al. Developing and testing the health care safety hotline: A prototype consumer reporting system for patient safety events. Final Report (Prepared by RAND Corporation under contract HHSA2902010000171). Rockvelle, MD: Agency for Healthcare Research and Quality; May 2016.
22. Shekelle PG, Pronovost PJ, Wachter RM, et al. The top patient safety strategies that can be encouraged for adoption now. Ann Intern Med. 2013;158(5 Pt 2):365-368. PubMed
23. Lawton R, O’Hara JK, Sheard L, et al. Can staff and patient perspectives on hospital safety predict harm-free care? an analysis of staff and patient survey data and routinely collected outcomes. BMJ Qual Saf. 2015;24(6):369-376. PubMed
© 2017 Society of Hospital Medicine
Comparison of Methods to Define High Use of Inpatient Services Using Population-Based Data
As healthcare system use and costs continue to rise, increased importance has been placed on identifying the small subgroup of patients that drive this trend.1 It is estimated that 5% of healthcare users account for over 60% of healthcare spending.2-6 Furthermore, care for these “high users” is expensive due to an over-reliance on inpatient services. Approximately 40% of all health spending is for inpatient care, the largest single category of health spending, which is similarly skewed toward high users.1,3,5 Improving our understanding of this population may provide an opportunity to direct improvement efforts to a select group of patients with a potentially high benefit, as well as move care away from the costly inpatient setting.
However, the development of effective interventions to improve patient experience and outcomes while decreasing costs (referred to as the “Triple Aim” by the Institute for Health Improvement) for high users of inpatient services hinges on the methodology used to identify this high-risk population.7 There is substantial variability in definitions of high users; the most common definitions are based on the number of hospital encounters, days spent in the hospital, and hospital costs.8-15 Definitions have intrinsic differences in their implications around appropriateness, efficiency, and financial sustainability of inpatient resource use. Though the constructs underlying these definitions are highly variable, direct comparisons of differences in patient capture are limited.
A recent study from a single US center explored the clinical characteristics of hospital patients based on definitions of use vs cost and observed important differences in patients’ profiles and outcomes.12 While this suggests that the choice of definition may have major implications for whom to target (and the efficacy of any proposed interventions), this concept has not been explored at the population level. Therefore, we used population-based administrative data from a single-payer healthcare system to compare 3 common definitions of high inpatient service use and their influence on patient capture, health outcomes, and inpatient system burden.
METHODS
Data Sources and Study Population
We conducted a retrospective population-based study using administrative and clinical data for the province of Alberta, including the discharge abstracts database, physician claims, ambulatory care records, population health registry file, and aggregated data from the Canadian census.16 We identified all adults who had 1 or more hospitalizations with a discharge date between April 1, 2012, and March 31, 2013, though the admission date could be prior to April 1, 2012.
Definition of High-Inpatient Use
High-inpatient use was defined using 3 metrics: number of inpatient episodes, length of stay, and cost. As in prior studies, for each definition, individuals in the upper5th percentile of the relevant distribution were designated “high users,”2,15 while patients in the lower 95th percentile were considered “nonhigh users.” Patients could be defined as a high user in more than 1 definition.
Patients with 3 or more hospital episodes were defined as high users for the “number of inpatient episodes” definition. A hospital episode of care was defined as an event that resulted in discharge (or death) from an inpatient facility. If an individual was admitted to a hospital and transferred to another facility within 1 day of discharge, the hospitalizations were considered part of the same episode of care.
The “length of stay” definition refers to the cumulative number of days spent in an inpatient facility for all eligible episodes of care. Patients with 56 or more days in hospital during the study period were considered high users. Day of admission and discharge were considered full inpatient days, regardless of the time of admission and discharge.
The “cost” definition considered the cumulative estimated cost of every eligible episode of care. We estimated costs for each hospitalization using resource intensity weights (RIW). This is a relative weighted value for the average inpatient case after taking factors such as age, comorbidity, and procedures into account. The RIW for each episode was multiplied by the national average inpatient cost.17 Based on this definition, patients with a cumulative hospital cost of ≥ $63,597 were deemed high users. All costs were calculated in Canadian Dollars (CAD, $) and adjusted to 2013 dollars based on Statistics Canada’s Consumer Price Index.18
Demographic, Clinical, and Encounter Characteristics
Individual characteristics were measured using a combination of provincial administrative data sources. All measures were recorded as of the admission date of the first eligible hospitalization. Demographic characteristics included age, sex, First Nations status, urban/rural status (based on the individual’s residential postal code), and median neighborhood income quintile. Clinical characteristics included 28 comorbid conditions defined based on separate validated International Statistical Classification of Disease and Health Related Problems, Tenth Revision, Canada (ICD-10-CA) coding algorithms reported individually and cumulatively (categorized as 0, 1, 2–3, and 4+).19 Primary care attachment was defined as the percentage of all outpatient primary care visits made to a single practitioner in the 2-year period prior to their first hospitalization (among those with ≥3 visits). Attachment was categorized as 75%-100% (good attachment), 50%-74% (moderate attachment), or <50% (low attachment).20,21
We also identified hospital encounter-level characteristics. These included the most responsible diagnosis, admission category (elective or urgent/emergent), and discharge disposition for each hospital episode. Reported health outcomes included the proportion of patients with in-hospital mortality and those with at least one 30-day, all-cause readmission to hospital.
Analysis
Patient characteristics were described using proportions and means (standard deviation) as appropriate for high users and nonhigh users within and across each definition. Encounter characteristics were also described and stratified by age category (18-64 or 65+ years). Comparison of patient capture was then analyzed among patients who were high use by at least 1 definition. The overlap and agreement of the 3 definitions were compared using a Venn diagram and kappa statistic. The 10 most responsible diagnoses (based on frequency) were also compared across definitions and stratified by age.
Finally, the percentage of system burden accounted for by each measure was calculated as the amount used by high users divided by the total amount used by the entire study population (x 100). To assess the potential modifying effect of age, results were stratified by age category for each definition.
All analyses were conducted using Stata 11.2 (StataCorp LP, College Station, TX).22 The Conjoint Health Research Ethics Board of the University of Calgary approved this study and granted waiver of patient consent. This manuscript is written in accordance with reporting guidelines for studies conducted using observational routinely collected health data (RECORD statement).23
RESULTS
Comparison of Patient and Encounter-level Characterist
ics
A total of 219,106 adults had 283,204 inpatient episodes of care within the study timeframe. There were 12,707 (5.8%), 11,095 (5.1%), and 10,956 (5.0%) patients defined as high users based on number of inpatient episodes, length of stay, and cost, respectively (supplementary Figure 1). Regardless of definition, when compared to their non–high use counterparts, patients classified as high use were more likely to be male, older, in a lower median neighborhood income quintile, and have a higher level of comorbidity. Comparing across definitions of high use, those defined by number of inpatient episodes were more likely to be younger, live in rural areas, have better primary care attachment, and have fewer comorbidities, compared to the other definitions. High users by length of stay were more likely to be older and had a higher proportion of mental health–related comorbidities, including dementia and depression, as compared with the other definitions. Results were largely similar for those defined by cost (Table 1).
Encounter-level analyses
Comparison of Patient Capture and Inpatient Burden
Of the 22,691 individuals who were defined as high use by at least 1 definition, 2,331 (10.3%) were consistently high use across all 3 definitions (kappa = 0.38; Figure 1). Of the 13,682 individuals classified as high use by at least 1 of length of stay or cost, 8369 (61.2%) were defined as high use by both definitions (kappa = 0.75). However, of the 12,707 defined as high use by the number of inpatient episodes, only 3698 (29.1%) were also defined as high use by another definition. Exploration of the most responsible diagnoses across definitions showed that congestive heart failure (2.8%-3.5%), chronic obstructive pulmonary disease (1.6%-3.2%), and dementia (0.6%-2.2%) were the most frequent. Acute medical conditions (eg, pneumonia [1.8%] or gastroenteritis [0.7%]) that may result in multiple shorter hospitalizations were observed at higher frequencies among high users defined by inpatient episodes, while conditions commonly requiring rehabilitation (eg, fracture [1.8%] and stroke [1.7%]) were more common among high users defined by length of stay and cost (supplementary Table 2). Stratification by age showed marked differences in the diagnoses across high-use definitions. Among hi
When assessing inpatient system burden, high users by number of inpatient episodes accounted for 47,044 (16.6%) of the 283,204 episodes. High users defined by length of stay accounted for 1,286,539 (46.4%) days of 2,773,561 total days, while high users defined by cost accumulated $1.4 billion (38.9%) of the estimated $3.7 billion in inpatient expenditures. High users defined by cost and length of stay each accounted for comparatively few episode
DISCUSSION
Using a large population-based cohort of all adults with at least 1 hospitalization in the province of Alberta, Canada, within a 12-month period, we compared 3 commonly used definitions of high inpatient use. The choice of definition had a substantial influence on the types of patients categorized as high use, as well as the proportion of total inpatient utilization that was associated with high users. The definition based on number of inpatient episodes captured a distinct population of high users, while the populations identified using cumulative length of stay or cost were similar.
Differences within and between definitions were especially apparent in age-stratified analyses: Greater length of stay or higher cost among patients aged 18-64 years identifies a large proportion of psychological conditions, while a greater number of inpatient episodes identifies acute conditions and childbirth or labor-related complications. Conversely, definitions based on length of stay and cost in the elderly (65+) identified groups with chronic conditions that result in progressive functional decline (often requiring increasing supportive services upon discharge) or conditions that require significant rehabilitation prior to discharge. Regarding inpatient system burden, high users defined by number of inpatient episodes accounted for a small proportion of total inpatient episodes, while high users defined by length of stay and cost accounted for nearly half of the accumulated hospital days and cost for each. These findings highlight the need for careful consideration of how high use is defined when studying high-user populations and implications for targeting subpopulations for intervention.
Our results add to those from previous studies. A US-based, single-center study of 2566 individuals compared definitions of high inpatient use based on cost and frequency of admission and found that patients defined by cost were predominantly hospitalized for surgical conditions, while those fulfilling the episode-based definition were often hospitalized for medical conditions.12 The most responsible diagnoses for patient hospitalizations in our study reflect this. We extended this comparison to consider the impact of age on outcomes and inpatient system burden and found that older age was also linked to poorer outcomes and increased burden. We also considered a third definition (cumulative length of stay), which provided another opportunity for comparison. The presence of chronic conditions requiring rehabilitation and possible alternate level of care days within our cohort highlights the utility of this length of stay-based approach when considering definitions. Although there were similarities between patients defined by length of stay and cost, partly due to cost being largely a function of length of stay, there were also important differences in their patient profiles. Those defined by cost tended to have conditions requiring surgical procedures not requiring extended in-hospital rehabilitation. Furthermore, the higher proportion of in-hospital mortality among those defined by cost may also reflect the fact that patients tend to accrue the majority of their healthcare expenditures during the final 120 days of life.24
Each definition of high use identified complex patients; however, the differences between the various types of high users identified by these definitions suggest that they are not interchangeable. Arguably, selection of the most appropriate definition should depend on the objective of measuring high users, particularly if an intervention is planned. Interventions for high users are complex, requiring both medical and nonmedical components. The current literature in this area has often focused on case management programs, collaboration with community-based social support programs, and improving coordination and transitions of care.25-27 While many of these approaches require considerable involvement outside of the inpatient setting, these interventions can be informed by defining who high users of inpatient services are. Our findings show several possible subgroups of high users, which could be targeted for intervention. For example, an inpatient episode-based definition, which identifies patients with frequent encounters for acute conditions (eg, pneumonia and urinary tract infections), would be informative if an intervention targeted reductions in inpatient use and readmission rates. Alternatively, an intervention designed to improve community-based mental health programs would best be informed by a definition based on length of stay in which high users with underlying mental health conditions were prevalent. Such interventions are rarely mutually exclusive and require multiple perspectives to inform their objectives. A well-designed intervention will not only address the medical characteristics of high users but also the social determinants of health that place patients at risk of high inpatient use.
Our study should be interpreted in light of its limitations. First, measures of disease severity were not available to further characterize similarities and differences across high-use groups. Furthermore, we were unable to account for other social determinants of health that may be relevant to inpatient system usage. Second, direct cost of hospitalizations was estimated based on RIW and is thus reflective of expected rather than actual costs. However, this will have minimal impact on capture, as patients defined by this metric require substantial costs to be included in the top fifth percentile, and thus deviations in individual hospitalization costs will have minimal influence on the cumulative cost. Finally, while inpatient spending makes up a large proportion of healthcare spending, there is likely a number of different high-use profiles found outside of the acute care setting. Despite these limitations, our study includes several key strengths. The use of population-level data allows for analysis that is robust and more generalizable than studies from single centers. Additionally, the comparison of 3 independent definitions allows for a greater comparison of the nuances of each definition. Our study also considers the important impact of age as an effect modifier of inpatient use in the general population and identifies distinct patient profiles that exist across each definition.
CONCLUSIONS
Definitions of high use of inpatient services based on number of inpatient episodes, days spent in hospital, and total hospital costs identify patient populations with different characteristics and differ substantially in their impact on health outcomes and inpatient burden. These results highlight the need for careful consideration of the context of the study or intervention and the implications of selecting a specific definition of high inpatient use at study conception. Ultimately, the performance of an intervention in high-use populations is likely to be conditional on the fit of the patient population generated by the chosen definition of high inpatient use to the objectives of a study.
Acknowledgments
This study is based in part on data provided by Alberta Health and Alberta Health Services. The interpretation and conclusions are those of the researchers and do not represent the views of the Government of Alberta. Neither the Government of Alberta nor Alberta Health express any opinion in relation to this study.
Disclosure
Dr. Hemmelgarn is supported by the Roy and Vi Baay Chair in Kidney Research. Dr. Manns is supported by the Svare Professorship in Health Economics and by a Health Scholar Award by Alberta Innovates Health Solutions (AIHS). Dr. Tonelli is supported by the David Freeze chair in Health Services Research. The Interdisciplinary Chronic Disease Collaboration is funded by AIHS—Collaborative Research and Innovation Opportunity (CRIO) Team Grants Program.
1. National Health Expenditure Trends, 1975 to 2015. Canadian Institute for Health Information. 2015. https://secure.cihi.ca/free_products/nhex_trends_narrative_report_2015_en.pdf. Accessed on June 23, 2016.
2. Berk ML, Monheit AC. The concentration of health care expenditures, revisited. Health Aff (Millwood). 2001;20:9-18. PubMed
3. Wodchis WP, Austin PC, Henry DA. A 3-year study of high-cost users of health care. CMAJ. 2016;188(3):182-188. PubMed
4. Forget EL, Roos LL, Deber RB, Wald R. Variations in Lifetime Healthcare Costs across a Population. Healthc Policy. 2008;4:e148-e167. PubMed
5. Joynt KE, Gawande AA, Orav EJ, Jha AK. Contribution of preventable acute care spending to total spending for high-cost Medicare patients. JAMA. 2013;309:2572-2578. PubMed
6. Riley GF. Long-term trends in the concentration of Medicare spending. Health Aff (Millwood). 2007;26:808-816. PubMed
7. IHI Triple Aim Initiative. Institute for Healthcare Improvement. 2015. http://www.ihi.org/engage/initiatives/TripleAim/Pages/default.aspx. Accessed on June 17, 2016.
8. Johansen H, Nair C, Bond J. Who goes to the hospital? An investigation of high users of hospital days. Health Reports. 1994;6(2):253-277. PubMed
9. Conwell LJ, Cohen JW. Characteristics of persons with high medical expenditures in the US civilian noninstitutionalized population. MEPS Statistical Brief# 73. 2002.
10. Lemstra M, Mackenbach J, Neudorf C, Nannapaneni U. High health care utilization and costs associated with lower socio-economic status: Results from a linked dataset. CJPH. 2009;100(3):180-183. PubMed
11. Macnee CL, McCabe S, Clarke PN, Fiske M, Campbell S. Typology of high users of health services among a rural medicaid population. Pub Health Nurs. 2009;26(5):396-404. PubMed
12. Nguyen OK, Tang N, Hillman JM, Gonzales R. What’s cost got to do with it? Association between hospital costs and frequency of admissions among “high users” of hospital care. J. Hosp Med. 2013;8(12):665-671. PubMed
13. Rosella LC, Fitzpatrick T, Wodchis WP, Calzavara A, Manson H, Goel V. High-cost health care users in Ontario, Canada: Demographic, socio-economic, and health status characteristics. BMC Health Serv Res. 2014;14(1):532. PubMed
14. Cohen SB. The Concentration of Health Care Expenditures and Related Expenses for Costly Medical Conditions, 2009. Agency for Healthcare Research and Quality Statistical Brief #359; 2012.
15. Ronksley PE, McKay JA, Kobewka DM, Mulpuru S, Forster AJ. Patterns of health care use in a high-cost inpatient population in Ottawa, Ontario: A retrospective observational study. CMAJ Open. 2015; 3:E111-E118. PubMed
16. Hemmelgarn BR, Clement F, Manns BJ, et al. Overview of the Alberta Kidney Disease Network. BMC Nephrol. 2009;10:30. PubMed
17. DAD Resource Intensity Weights and Expected Length of Stay. Canadian Institute for Health Information. 2016. https://www.cihi.ca/en/data-and-standards/standards/case-mix/resource-indicators-dad-resource-intensity-weights-and. Accessed on June 24, 2016.
18. Statistics Canada. The Canadian Consumer Price Index Reference Paper, Statistics Canada Catalogue no. 62-553-X.
19. Tonelli M, Wiebe N, Fortin M, et al. Methods for identifying 30 chronic conditions: Application to administrative data. BMC Med Inform Decis Mak. 2015;17:15(1):1. PubMed
20. Jaakkimainen RL, Klein-Geltink J, Guttmann A, Barnsley J, Jagorski B, Kopp A. Indicators of primary care based on administrative data. In Primary Care in Ontario: ICES Atlas. Toronto, Ontario: Institute for Clinical Evaluative Sciences; 2006.
21. Jee SH, Cabana MD. Indices for continuity of care: A systematic review of the literature. Med Care Res Rev. 2006;63:158-188. PubMed
22. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP. 2009.
23. Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. PubMed
24. Tanuseputro P, Wodchis WP, Fowler R, et al. The health care cost of dying: A population-based retrospective cohort study of the last year of life in ontario, canada. PLoS One. 2015;10(3):e0121759. PubMed
25. Hong CS, Siegel AL, Ferris TG. Caring for high-need, high-cost patients: What makes for a successful care management program? Issue Brief (Commonw Fund). 2014;19:1-19. PubMed
26. Birnbaum M, Halper DE. Rethinking service delivery for high-cost Medicaid patients. Medicaid Institute. 2009. http://shnny.org/research/rethinking-service-delivery-for-high-cost-medicaid-patients/. Accessed on Jan 11, 2017.
27. Pan-Canadian forum on high users of health care. Canadian Institute for Health Information. 2014. https://secure.cihi.ca/free_products/highusers_summary_report_revised_EN_web.pdf. Accessed on Jan 11, 2017.
As healthcare system use and costs continue to rise, increased importance has been placed on identifying the small subgroup of patients that drive this trend.1 It is estimated that 5% of healthcare users account for over 60% of healthcare spending.2-6 Furthermore, care for these “high users” is expensive due to an over-reliance on inpatient services. Approximately 40% of all health spending is for inpatient care, the largest single category of health spending, which is similarly skewed toward high users.1,3,5 Improving our understanding of this population may provide an opportunity to direct improvement efforts to a select group of patients with a potentially high benefit, as well as move care away from the costly inpatient setting.
However, the development of effective interventions to improve patient experience and outcomes while decreasing costs (referred to as the “Triple Aim” by the Institute for Health Improvement) for high users of inpatient services hinges on the methodology used to identify this high-risk population.7 There is substantial variability in definitions of high users; the most common definitions are based on the number of hospital encounters, days spent in the hospital, and hospital costs.8-15 Definitions have intrinsic differences in their implications around appropriateness, efficiency, and financial sustainability of inpatient resource use. Though the constructs underlying these definitions are highly variable, direct comparisons of differences in patient capture are limited.
A recent study from a single US center explored the clinical characteristics of hospital patients based on definitions of use vs cost and observed important differences in patients’ profiles and outcomes.12 While this suggests that the choice of definition may have major implications for whom to target (and the efficacy of any proposed interventions), this concept has not been explored at the population level. Therefore, we used population-based administrative data from a single-payer healthcare system to compare 3 common definitions of high inpatient service use and their influence on patient capture, health outcomes, and inpatient system burden.
METHODS
Data Sources and Study Population
We conducted a retrospective population-based study using administrative and clinical data for the province of Alberta, including the discharge abstracts database, physician claims, ambulatory care records, population health registry file, and aggregated data from the Canadian census.16 We identified all adults who had 1 or more hospitalizations with a discharge date between April 1, 2012, and March 31, 2013, though the admission date could be prior to April 1, 2012.
Definition of High-Inpatient Use
High-inpatient use was defined using 3 metrics: number of inpatient episodes, length of stay, and cost. As in prior studies, for each definition, individuals in the upper5th percentile of the relevant distribution were designated “high users,”2,15 while patients in the lower 95th percentile were considered “nonhigh users.” Patients could be defined as a high user in more than 1 definition.
Patients with 3 or more hospital episodes were defined as high users for the “number of inpatient episodes” definition. A hospital episode of care was defined as an event that resulted in discharge (or death) from an inpatient facility. If an individual was admitted to a hospital and transferred to another facility within 1 day of discharge, the hospitalizations were considered part of the same episode of care.
The “length of stay” definition refers to the cumulative number of days spent in an inpatient facility for all eligible episodes of care. Patients with 56 or more days in hospital during the study period were considered high users. Day of admission and discharge were considered full inpatient days, regardless of the time of admission and discharge.
The “cost” definition considered the cumulative estimated cost of every eligible episode of care. We estimated costs for each hospitalization using resource intensity weights (RIW). This is a relative weighted value for the average inpatient case after taking factors such as age, comorbidity, and procedures into account. The RIW for each episode was multiplied by the national average inpatient cost.17 Based on this definition, patients with a cumulative hospital cost of ≥ $63,597 were deemed high users. All costs were calculated in Canadian Dollars (CAD, $) and adjusted to 2013 dollars based on Statistics Canada’s Consumer Price Index.18
Demographic, Clinical, and Encounter Characteristics
Individual characteristics were measured using a combination of provincial administrative data sources. All measures were recorded as of the admission date of the first eligible hospitalization. Demographic characteristics included age, sex, First Nations status, urban/rural status (based on the individual’s residential postal code), and median neighborhood income quintile. Clinical characteristics included 28 comorbid conditions defined based on separate validated International Statistical Classification of Disease and Health Related Problems, Tenth Revision, Canada (ICD-10-CA) coding algorithms reported individually and cumulatively (categorized as 0, 1, 2–3, and 4+).19 Primary care attachment was defined as the percentage of all outpatient primary care visits made to a single practitioner in the 2-year period prior to their first hospitalization (among those with ≥3 visits). Attachment was categorized as 75%-100% (good attachment), 50%-74% (moderate attachment), or <50% (low attachment).20,21
We also identified hospital encounter-level characteristics. These included the most responsible diagnosis, admission category (elective or urgent/emergent), and discharge disposition for each hospital episode. Reported health outcomes included the proportion of patients with in-hospital mortality and those with at least one 30-day, all-cause readmission to hospital.
Analysis
Patient characteristics were described using proportions and means (standard deviation) as appropriate for high users and nonhigh users within and across each definition. Encounter characteristics were also described and stratified by age category (18-64 or 65+ years). Comparison of patient capture was then analyzed among patients who were high use by at least 1 definition. The overlap and agreement of the 3 definitions were compared using a Venn diagram and kappa statistic. The 10 most responsible diagnoses (based on frequency) were also compared across definitions and stratified by age.
Finally, the percentage of system burden accounted for by each measure was calculated as the amount used by high users divided by the total amount used by the entire study population (x 100). To assess the potential modifying effect of age, results were stratified by age category for each definition.
All analyses were conducted using Stata 11.2 (StataCorp LP, College Station, TX).22 The Conjoint Health Research Ethics Board of the University of Calgary approved this study and granted waiver of patient consent. This manuscript is written in accordance with reporting guidelines for studies conducted using observational routinely collected health data (RECORD statement).23
RESULTS
Comparison of Patient and Encounter-level Characterist
ics
A total of 219,106 adults had 283,204 inpatient episodes of care within the study timeframe. There were 12,707 (5.8%), 11,095 (5.1%), and 10,956 (5.0%) patients defined as high users based on number of inpatient episodes, length of stay, and cost, respectively (supplementary Figure 1). Regardless of definition, when compared to their non–high use counterparts, patients classified as high use were more likely to be male, older, in a lower median neighborhood income quintile, and have a higher level of comorbidity. Comparing across definitions of high use, those defined by number of inpatient episodes were more likely to be younger, live in rural areas, have better primary care attachment, and have fewer comorbidities, compared to the other definitions. High users by length of stay were more likely to be older and had a higher proportion of mental health–related comorbidities, including dementia and depression, as compared with the other definitions. Results were largely similar for those defined by cost (Table 1).
Encounter-level analyses
Comparison of Patient Capture and Inpatient Burden
Of the 22,691 individuals who were defined as high use by at least 1 definition, 2,331 (10.3%) were consistently high use across all 3 definitions (kappa = 0.38; Figure 1). Of the 13,682 individuals classified as high use by at least 1 of length of stay or cost, 8369 (61.2%) were defined as high use by both definitions (kappa = 0.75). However, of the 12,707 defined as high use by the number of inpatient episodes, only 3698 (29.1%) were also defined as high use by another definition. Exploration of the most responsible diagnoses across definitions showed that congestive heart failure (2.8%-3.5%), chronic obstructive pulmonary disease (1.6%-3.2%), and dementia (0.6%-2.2%) were the most frequent. Acute medical conditions (eg, pneumonia [1.8%] or gastroenteritis [0.7%]) that may result in multiple shorter hospitalizations were observed at higher frequencies among high users defined by inpatient episodes, while conditions commonly requiring rehabilitation (eg, fracture [1.8%] and stroke [1.7%]) were more common among high users defined by length of stay and cost (supplementary Table 2). Stratification by age showed marked differences in the diagnoses across high-use definitions. Among hi
When assessing inpatient system burden, high users by number of inpatient episodes accounted for 47,044 (16.6%) of the 283,204 episodes. High users defined by length of stay accounted for 1,286,539 (46.4%) days of 2,773,561 total days, while high users defined by cost accumulated $1.4 billion (38.9%) of the estimated $3.7 billion in inpatient expenditures. High users defined by cost and length of stay each accounted for comparatively few episode
DISCUSSION
Using a large population-based cohort of all adults with at least 1 hospitalization in the province of Alberta, Canada, within a 12-month period, we compared 3 commonly used definitions of high inpatient use. The choice of definition had a substantial influence on the types of patients categorized as high use, as well as the proportion of total inpatient utilization that was associated with high users. The definition based on number of inpatient episodes captured a distinct population of high users, while the populations identified using cumulative length of stay or cost were similar.
Differences within and between definitions were especially apparent in age-stratified analyses: Greater length of stay or higher cost among patients aged 18-64 years identifies a large proportion of psychological conditions, while a greater number of inpatient episodes identifies acute conditions and childbirth or labor-related complications. Conversely, definitions based on length of stay and cost in the elderly (65+) identified groups with chronic conditions that result in progressive functional decline (often requiring increasing supportive services upon discharge) or conditions that require significant rehabilitation prior to discharge. Regarding inpatient system burden, high users defined by number of inpatient episodes accounted for a small proportion of total inpatient episodes, while high users defined by length of stay and cost accounted for nearly half of the accumulated hospital days and cost for each. These findings highlight the need for careful consideration of how high use is defined when studying high-user populations and implications for targeting subpopulations for intervention.
Our results add to those from previous studies. A US-based, single-center study of 2566 individuals compared definitions of high inpatient use based on cost and frequency of admission and found that patients defined by cost were predominantly hospitalized for surgical conditions, while those fulfilling the episode-based definition were often hospitalized for medical conditions.12 The most responsible diagnoses for patient hospitalizations in our study reflect this. We extended this comparison to consider the impact of age on outcomes and inpatient system burden and found that older age was also linked to poorer outcomes and increased burden. We also considered a third definition (cumulative length of stay), which provided another opportunity for comparison. The presence of chronic conditions requiring rehabilitation and possible alternate level of care days within our cohort highlights the utility of this length of stay-based approach when considering definitions. Although there were similarities between patients defined by length of stay and cost, partly due to cost being largely a function of length of stay, there were also important differences in their patient profiles. Those defined by cost tended to have conditions requiring surgical procedures not requiring extended in-hospital rehabilitation. Furthermore, the higher proportion of in-hospital mortality among those defined by cost may also reflect the fact that patients tend to accrue the majority of their healthcare expenditures during the final 120 days of life.24
Each definition of high use identified complex patients; however, the differences between the various types of high users identified by these definitions suggest that they are not interchangeable. Arguably, selection of the most appropriate definition should depend on the objective of measuring high users, particularly if an intervention is planned. Interventions for high users are complex, requiring both medical and nonmedical components. The current literature in this area has often focused on case management programs, collaboration with community-based social support programs, and improving coordination and transitions of care.25-27 While many of these approaches require considerable involvement outside of the inpatient setting, these interventions can be informed by defining who high users of inpatient services are. Our findings show several possible subgroups of high users, which could be targeted for intervention. For example, an inpatient episode-based definition, which identifies patients with frequent encounters for acute conditions (eg, pneumonia and urinary tract infections), would be informative if an intervention targeted reductions in inpatient use and readmission rates. Alternatively, an intervention designed to improve community-based mental health programs would best be informed by a definition based on length of stay in which high users with underlying mental health conditions were prevalent. Such interventions are rarely mutually exclusive and require multiple perspectives to inform their objectives. A well-designed intervention will not only address the medical characteristics of high users but also the social determinants of health that place patients at risk of high inpatient use.
Our study should be interpreted in light of its limitations. First, measures of disease severity were not available to further characterize similarities and differences across high-use groups. Furthermore, we were unable to account for other social determinants of health that may be relevant to inpatient system usage. Second, direct cost of hospitalizations was estimated based on RIW and is thus reflective of expected rather than actual costs. However, this will have minimal impact on capture, as patients defined by this metric require substantial costs to be included in the top fifth percentile, and thus deviations in individual hospitalization costs will have minimal influence on the cumulative cost. Finally, while inpatient spending makes up a large proportion of healthcare spending, there is likely a number of different high-use profiles found outside of the acute care setting. Despite these limitations, our study includes several key strengths. The use of population-level data allows for analysis that is robust and more generalizable than studies from single centers. Additionally, the comparison of 3 independent definitions allows for a greater comparison of the nuances of each definition. Our study also considers the important impact of age as an effect modifier of inpatient use in the general population and identifies distinct patient profiles that exist across each definition.
CONCLUSIONS
Definitions of high use of inpatient services based on number of inpatient episodes, days spent in hospital, and total hospital costs identify patient populations with different characteristics and differ substantially in their impact on health outcomes and inpatient burden. These results highlight the need for careful consideration of the context of the study or intervention and the implications of selecting a specific definition of high inpatient use at study conception. Ultimately, the performance of an intervention in high-use populations is likely to be conditional on the fit of the patient population generated by the chosen definition of high inpatient use to the objectives of a study.
Acknowledgments
This study is based in part on data provided by Alberta Health and Alberta Health Services. The interpretation and conclusions are those of the researchers and do not represent the views of the Government of Alberta. Neither the Government of Alberta nor Alberta Health express any opinion in relation to this study.
Disclosure
Dr. Hemmelgarn is supported by the Roy and Vi Baay Chair in Kidney Research. Dr. Manns is supported by the Svare Professorship in Health Economics and by a Health Scholar Award by Alberta Innovates Health Solutions (AIHS). Dr. Tonelli is supported by the David Freeze chair in Health Services Research. The Interdisciplinary Chronic Disease Collaboration is funded by AIHS—Collaborative Research and Innovation Opportunity (CRIO) Team Grants Program.
As healthcare system use and costs continue to rise, increased importance has been placed on identifying the small subgroup of patients that drive this trend.1 It is estimated that 5% of healthcare users account for over 60% of healthcare spending.2-6 Furthermore, care for these “high users” is expensive due to an over-reliance on inpatient services. Approximately 40% of all health spending is for inpatient care, the largest single category of health spending, which is similarly skewed toward high users.1,3,5 Improving our understanding of this population may provide an opportunity to direct improvement efforts to a select group of patients with a potentially high benefit, as well as move care away from the costly inpatient setting.
However, the development of effective interventions to improve patient experience and outcomes while decreasing costs (referred to as the “Triple Aim” by the Institute for Health Improvement) for high users of inpatient services hinges on the methodology used to identify this high-risk population.7 There is substantial variability in definitions of high users; the most common definitions are based on the number of hospital encounters, days spent in the hospital, and hospital costs.8-15 Definitions have intrinsic differences in their implications around appropriateness, efficiency, and financial sustainability of inpatient resource use. Though the constructs underlying these definitions are highly variable, direct comparisons of differences in patient capture are limited.
A recent study from a single US center explored the clinical characteristics of hospital patients based on definitions of use vs cost and observed important differences in patients’ profiles and outcomes.12 While this suggests that the choice of definition may have major implications for whom to target (and the efficacy of any proposed interventions), this concept has not been explored at the population level. Therefore, we used population-based administrative data from a single-payer healthcare system to compare 3 common definitions of high inpatient service use and their influence on patient capture, health outcomes, and inpatient system burden.
METHODS
Data Sources and Study Population
We conducted a retrospective population-based study using administrative and clinical data for the province of Alberta, including the discharge abstracts database, physician claims, ambulatory care records, population health registry file, and aggregated data from the Canadian census.16 We identified all adults who had 1 or more hospitalizations with a discharge date between April 1, 2012, and March 31, 2013, though the admission date could be prior to April 1, 2012.
Definition of High-Inpatient Use
High-inpatient use was defined using 3 metrics: number of inpatient episodes, length of stay, and cost. As in prior studies, for each definition, individuals in the upper5th percentile of the relevant distribution were designated “high users,”2,15 while patients in the lower 95th percentile were considered “nonhigh users.” Patients could be defined as a high user in more than 1 definition.
Patients with 3 or more hospital episodes were defined as high users for the “number of inpatient episodes” definition. A hospital episode of care was defined as an event that resulted in discharge (or death) from an inpatient facility. If an individual was admitted to a hospital and transferred to another facility within 1 day of discharge, the hospitalizations were considered part of the same episode of care.
The “length of stay” definition refers to the cumulative number of days spent in an inpatient facility for all eligible episodes of care. Patients with 56 or more days in hospital during the study period were considered high users. Day of admission and discharge were considered full inpatient days, regardless of the time of admission and discharge.
The “cost” definition considered the cumulative estimated cost of every eligible episode of care. We estimated costs for each hospitalization using resource intensity weights (RIW). This is a relative weighted value for the average inpatient case after taking factors such as age, comorbidity, and procedures into account. The RIW for each episode was multiplied by the national average inpatient cost.17 Based on this definition, patients with a cumulative hospital cost of ≥ $63,597 were deemed high users. All costs were calculated in Canadian Dollars (CAD, $) and adjusted to 2013 dollars based on Statistics Canada’s Consumer Price Index.18
Demographic, Clinical, and Encounter Characteristics
Individual characteristics were measured using a combination of provincial administrative data sources. All measures were recorded as of the admission date of the first eligible hospitalization. Demographic characteristics included age, sex, First Nations status, urban/rural status (based on the individual’s residential postal code), and median neighborhood income quintile. Clinical characteristics included 28 comorbid conditions defined based on separate validated International Statistical Classification of Disease and Health Related Problems, Tenth Revision, Canada (ICD-10-CA) coding algorithms reported individually and cumulatively (categorized as 0, 1, 2–3, and 4+).19 Primary care attachment was defined as the percentage of all outpatient primary care visits made to a single practitioner in the 2-year period prior to their first hospitalization (among those with ≥3 visits). Attachment was categorized as 75%-100% (good attachment), 50%-74% (moderate attachment), or <50% (low attachment).20,21
We also identified hospital encounter-level characteristics. These included the most responsible diagnosis, admission category (elective or urgent/emergent), and discharge disposition for each hospital episode. Reported health outcomes included the proportion of patients with in-hospital mortality and those with at least one 30-day, all-cause readmission to hospital.
Analysis
Patient characteristics were described using proportions and means (standard deviation) as appropriate for high users and nonhigh users within and across each definition. Encounter characteristics were also described and stratified by age category (18-64 or 65+ years). Comparison of patient capture was then analyzed among patients who were high use by at least 1 definition. The overlap and agreement of the 3 definitions were compared using a Venn diagram and kappa statistic. The 10 most responsible diagnoses (based on frequency) were also compared across definitions and stratified by age.
Finally, the percentage of system burden accounted for by each measure was calculated as the amount used by high users divided by the total amount used by the entire study population (x 100). To assess the potential modifying effect of age, results were stratified by age category for each definition.
All analyses were conducted using Stata 11.2 (StataCorp LP, College Station, TX).22 The Conjoint Health Research Ethics Board of the University of Calgary approved this study and granted waiver of patient consent. This manuscript is written in accordance with reporting guidelines for studies conducted using observational routinely collected health data (RECORD statement).23
RESULTS
Comparison of Patient and Encounter-level Characterist
ics
A total of 219,106 adults had 283,204 inpatient episodes of care within the study timeframe. There were 12,707 (5.8%), 11,095 (5.1%), and 10,956 (5.0%) patients defined as high users based on number of inpatient episodes, length of stay, and cost, respectively (supplementary Figure 1). Regardless of definition, when compared to their non–high use counterparts, patients classified as high use were more likely to be male, older, in a lower median neighborhood income quintile, and have a higher level of comorbidity. Comparing across definitions of high use, those defined by number of inpatient episodes were more likely to be younger, live in rural areas, have better primary care attachment, and have fewer comorbidities, compared to the other definitions. High users by length of stay were more likely to be older and had a higher proportion of mental health–related comorbidities, including dementia and depression, as compared with the other definitions. Results were largely similar for those defined by cost (Table 1).
Encounter-level analyses
Comparison of Patient Capture and Inpatient Burden
Of the 22,691 individuals who were defined as high use by at least 1 definition, 2,331 (10.3%) were consistently high use across all 3 definitions (kappa = 0.38; Figure 1). Of the 13,682 individuals classified as high use by at least 1 of length of stay or cost, 8369 (61.2%) were defined as high use by both definitions (kappa = 0.75). However, of the 12,707 defined as high use by the number of inpatient episodes, only 3698 (29.1%) were also defined as high use by another definition. Exploration of the most responsible diagnoses across definitions showed that congestive heart failure (2.8%-3.5%), chronic obstructive pulmonary disease (1.6%-3.2%), and dementia (0.6%-2.2%) were the most frequent. Acute medical conditions (eg, pneumonia [1.8%] or gastroenteritis [0.7%]) that may result in multiple shorter hospitalizations were observed at higher frequencies among high users defined by inpatient episodes, while conditions commonly requiring rehabilitation (eg, fracture [1.8%] and stroke [1.7%]) were more common among high users defined by length of stay and cost (supplementary Table 2). Stratification by age showed marked differences in the diagnoses across high-use definitions. Among hi
When assessing inpatient system burden, high users by number of inpatient episodes accounted for 47,044 (16.6%) of the 283,204 episodes. High users defined by length of stay accounted for 1,286,539 (46.4%) days of 2,773,561 total days, while high users defined by cost accumulated $1.4 billion (38.9%) of the estimated $3.7 billion in inpatient expenditures. High users defined by cost and length of stay each accounted for comparatively few episode
DISCUSSION
Using a large population-based cohort of all adults with at least 1 hospitalization in the province of Alberta, Canada, within a 12-month period, we compared 3 commonly used definitions of high inpatient use. The choice of definition had a substantial influence on the types of patients categorized as high use, as well as the proportion of total inpatient utilization that was associated with high users. The definition based on number of inpatient episodes captured a distinct population of high users, while the populations identified using cumulative length of stay or cost were similar.
Differences within and between definitions were especially apparent in age-stratified analyses: Greater length of stay or higher cost among patients aged 18-64 years identifies a large proportion of psychological conditions, while a greater number of inpatient episodes identifies acute conditions and childbirth or labor-related complications. Conversely, definitions based on length of stay and cost in the elderly (65+) identified groups with chronic conditions that result in progressive functional decline (often requiring increasing supportive services upon discharge) or conditions that require significant rehabilitation prior to discharge. Regarding inpatient system burden, high users defined by number of inpatient episodes accounted for a small proportion of total inpatient episodes, while high users defined by length of stay and cost accounted for nearly half of the accumulated hospital days and cost for each. These findings highlight the need for careful consideration of how high use is defined when studying high-user populations and implications for targeting subpopulations for intervention.
Our results add to those from previous studies. A US-based, single-center study of 2566 individuals compared definitions of high inpatient use based on cost and frequency of admission and found that patients defined by cost were predominantly hospitalized for surgical conditions, while those fulfilling the episode-based definition were often hospitalized for medical conditions.12 The most responsible diagnoses for patient hospitalizations in our study reflect this. We extended this comparison to consider the impact of age on outcomes and inpatient system burden and found that older age was also linked to poorer outcomes and increased burden. We also considered a third definition (cumulative length of stay), which provided another opportunity for comparison. The presence of chronic conditions requiring rehabilitation and possible alternate level of care days within our cohort highlights the utility of this length of stay-based approach when considering definitions. Although there were similarities between patients defined by length of stay and cost, partly due to cost being largely a function of length of stay, there were also important differences in their patient profiles. Those defined by cost tended to have conditions requiring surgical procedures not requiring extended in-hospital rehabilitation. Furthermore, the higher proportion of in-hospital mortality among those defined by cost may also reflect the fact that patients tend to accrue the majority of their healthcare expenditures during the final 120 days of life.24
Each definition of high use identified complex patients; however, the differences between the various types of high users identified by these definitions suggest that they are not interchangeable. Arguably, selection of the most appropriate definition should depend on the objective of measuring high users, particularly if an intervention is planned. Interventions for high users are complex, requiring both medical and nonmedical components. The current literature in this area has often focused on case management programs, collaboration with community-based social support programs, and improving coordination and transitions of care.25-27 While many of these approaches require considerable involvement outside of the inpatient setting, these interventions can be informed by defining who high users of inpatient services are. Our findings show several possible subgroups of high users, which could be targeted for intervention. For example, an inpatient episode-based definition, which identifies patients with frequent encounters for acute conditions (eg, pneumonia and urinary tract infections), would be informative if an intervention targeted reductions in inpatient use and readmission rates. Alternatively, an intervention designed to improve community-based mental health programs would best be informed by a definition based on length of stay in which high users with underlying mental health conditions were prevalent. Such interventions are rarely mutually exclusive and require multiple perspectives to inform their objectives. A well-designed intervention will not only address the medical characteristics of high users but also the social determinants of health that place patients at risk of high inpatient use.
Our study should be interpreted in light of its limitations. First, measures of disease severity were not available to further characterize similarities and differences across high-use groups. Furthermore, we were unable to account for other social determinants of health that may be relevant to inpatient system usage. Second, direct cost of hospitalizations was estimated based on RIW and is thus reflective of expected rather than actual costs. However, this will have minimal impact on capture, as patients defined by this metric require substantial costs to be included in the top fifth percentile, and thus deviations in individual hospitalization costs will have minimal influence on the cumulative cost. Finally, while inpatient spending makes up a large proportion of healthcare spending, there is likely a number of different high-use profiles found outside of the acute care setting. Despite these limitations, our study includes several key strengths. The use of population-level data allows for analysis that is robust and more generalizable than studies from single centers. Additionally, the comparison of 3 independent definitions allows for a greater comparison of the nuances of each definition. Our study also considers the important impact of age as an effect modifier of inpatient use in the general population and identifies distinct patient profiles that exist across each definition.
CONCLUSIONS
Definitions of high use of inpatient services based on number of inpatient episodes, days spent in hospital, and total hospital costs identify patient populations with different characteristics and differ substantially in their impact on health outcomes and inpatient burden. These results highlight the need for careful consideration of the context of the study or intervention and the implications of selecting a specific definition of high inpatient use at study conception. Ultimately, the performance of an intervention in high-use populations is likely to be conditional on the fit of the patient population generated by the chosen definition of high inpatient use to the objectives of a study.
Acknowledgments
This study is based in part on data provided by Alberta Health and Alberta Health Services. The interpretation and conclusions are those of the researchers and do not represent the views of the Government of Alberta. Neither the Government of Alberta nor Alberta Health express any opinion in relation to this study.
Disclosure
Dr. Hemmelgarn is supported by the Roy and Vi Baay Chair in Kidney Research. Dr. Manns is supported by the Svare Professorship in Health Economics and by a Health Scholar Award by Alberta Innovates Health Solutions (AIHS). Dr. Tonelli is supported by the David Freeze chair in Health Services Research. The Interdisciplinary Chronic Disease Collaboration is funded by AIHS—Collaborative Research and Innovation Opportunity (CRIO) Team Grants Program.
1. National Health Expenditure Trends, 1975 to 2015. Canadian Institute for Health Information. 2015. https://secure.cihi.ca/free_products/nhex_trends_narrative_report_2015_en.pdf. Accessed on June 23, 2016.
2. Berk ML, Monheit AC. The concentration of health care expenditures, revisited. Health Aff (Millwood). 2001;20:9-18. PubMed
3. Wodchis WP, Austin PC, Henry DA. A 3-year study of high-cost users of health care. CMAJ. 2016;188(3):182-188. PubMed
4. Forget EL, Roos LL, Deber RB, Wald R. Variations in Lifetime Healthcare Costs across a Population. Healthc Policy. 2008;4:e148-e167. PubMed
5. Joynt KE, Gawande AA, Orav EJ, Jha AK. Contribution of preventable acute care spending to total spending for high-cost Medicare patients. JAMA. 2013;309:2572-2578. PubMed
6. Riley GF. Long-term trends in the concentration of Medicare spending. Health Aff (Millwood). 2007;26:808-816. PubMed
7. IHI Triple Aim Initiative. Institute for Healthcare Improvement. 2015. http://www.ihi.org/engage/initiatives/TripleAim/Pages/default.aspx. Accessed on June 17, 2016.
8. Johansen H, Nair C, Bond J. Who goes to the hospital? An investigation of high users of hospital days. Health Reports. 1994;6(2):253-277. PubMed
9. Conwell LJ, Cohen JW. Characteristics of persons with high medical expenditures in the US civilian noninstitutionalized population. MEPS Statistical Brief# 73. 2002.
10. Lemstra M, Mackenbach J, Neudorf C, Nannapaneni U. High health care utilization and costs associated with lower socio-economic status: Results from a linked dataset. CJPH. 2009;100(3):180-183. PubMed
11. Macnee CL, McCabe S, Clarke PN, Fiske M, Campbell S. Typology of high users of health services among a rural medicaid population. Pub Health Nurs. 2009;26(5):396-404. PubMed
12. Nguyen OK, Tang N, Hillman JM, Gonzales R. What’s cost got to do with it? Association between hospital costs and frequency of admissions among “high users” of hospital care. J. Hosp Med. 2013;8(12):665-671. PubMed
13. Rosella LC, Fitzpatrick T, Wodchis WP, Calzavara A, Manson H, Goel V. High-cost health care users in Ontario, Canada: Demographic, socio-economic, and health status characteristics. BMC Health Serv Res. 2014;14(1):532. PubMed
14. Cohen SB. The Concentration of Health Care Expenditures and Related Expenses for Costly Medical Conditions, 2009. Agency for Healthcare Research and Quality Statistical Brief #359; 2012.
15. Ronksley PE, McKay JA, Kobewka DM, Mulpuru S, Forster AJ. Patterns of health care use in a high-cost inpatient population in Ottawa, Ontario: A retrospective observational study. CMAJ Open. 2015; 3:E111-E118. PubMed
16. Hemmelgarn BR, Clement F, Manns BJ, et al. Overview of the Alberta Kidney Disease Network. BMC Nephrol. 2009;10:30. PubMed
17. DAD Resource Intensity Weights and Expected Length of Stay. Canadian Institute for Health Information. 2016. https://www.cihi.ca/en/data-and-standards/standards/case-mix/resource-indicators-dad-resource-intensity-weights-and. Accessed on June 24, 2016.
18. Statistics Canada. The Canadian Consumer Price Index Reference Paper, Statistics Canada Catalogue no. 62-553-X.
19. Tonelli M, Wiebe N, Fortin M, et al. Methods for identifying 30 chronic conditions: Application to administrative data. BMC Med Inform Decis Mak. 2015;17:15(1):1. PubMed
20. Jaakkimainen RL, Klein-Geltink J, Guttmann A, Barnsley J, Jagorski B, Kopp A. Indicators of primary care based on administrative data. In Primary Care in Ontario: ICES Atlas. Toronto, Ontario: Institute for Clinical Evaluative Sciences; 2006.
21. Jee SH, Cabana MD. Indices for continuity of care: A systematic review of the literature. Med Care Res Rev. 2006;63:158-188. PubMed
22. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP. 2009.
23. Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. PubMed
24. Tanuseputro P, Wodchis WP, Fowler R, et al. The health care cost of dying: A population-based retrospective cohort study of the last year of life in ontario, canada. PLoS One. 2015;10(3):e0121759. PubMed
25. Hong CS, Siegel AL, Ferris TG. Caring for high-need, high-cost patients: What makes for a successful care management program? Issue Brief (Commonw Fund). 2014;19:1-19. PubMed
26. Birnbaum M, Halper DE. Rethinking service delivery for high-cost Medicaid patients. Medicaid Institute. 2009. http://shnny.org/research/rethinking-service-delivery-for-high-cost-medicaid-patients/. Accessed on Jan 11, 2017.
27. Pan-Canadian forum on high users of health care. Canadian Institute for Health Information. 2014. https://secure.cihi.ca/free_products/highusers_summary_report_revised_EN_web.pdf. Accessed on Jan 11, 2017.
1. National Health Expenditure Trends, 1975 to 2015. Canadian Institute for Health Information. 2015. https://secure.cihi.ca/free_products/nhex_trends_narrative_report_2015_en.pdf. Accessed on June 23, 2016.
2. Berk ML, Monheit AC. The concentration of health care expenditures, revisited. Health Aff (Millwood). 2001;20:9-18. PubMed
3. Wodchis WP, Austin PC, Henry DA. A 3-year study of high-cost users of health care. CMAJ. 2016;188(3):182-188. PubMed
4. Forget EL, Roos LL, Deber RB, Wald R. Variations in Lifetime Healthcare Costs across a Population. Healthc Policy. 2008;4:e148-e167. PubMed
5. Joynt KE, Gawande AA, Orav EJ, Jha AK. Contribution of preventable acute care spending to total spending for high-cost Medicare patients. JAMA. 2013;309:2572-2578. PubMed
6. Riley GF. Long-term trends in the concentration of Medicare spending. Health Aff (Millwood). 2007;26:808-816. PubMed
7. IHI Triple Aim Initiative. Institute for Healthcare Improvement. 2015. http://www.ihi.org/engage/initiatives/TripleAim/Pages/default.aspx. Accessed on June 17, 2016.
8. Johansen H, Nair C, Bond J. Who goes to the hospital? An investigation of high users of hospital days. Health Reports. 1994;6(2):253-277. PubMed
9. Conwell LJ, Cohen JW. Characteristics of persons with high medical expenditures in the US civilian noninstitutionalized population. MEPS Statistical Brief# 73. 2002.
10. Lemstra M, Mackenbach J, Neudorf C, Nannapaneni U. High health care utilization and costs associated with lower socio-economic status: Results from a linked dataset. CJPH. 2009;100(3):180-183. PubMed
11. Macnee CL, McCabe S, Clarke PN, Fiske M, Campbell S. Typology of high users of health services among a rural medicaid population. Pub Health Nurs. 2009;26(5):396-404. PubMed
12. Nguyen OK, Tang N, Hillman JM, Gonzales R. What’s cost got to do with it? Association between hospital costs and frequency of admissions among “high users” of hospital care. J. Hosp Med. 2013;8(12):665-671. PubMed
13. Rosella LC, Fitzpatrick T, Wodchis WP, Calzavara A, Manson H, Goel V. High-cost health care users in Ontario, Canada: Demographic, socio-economic, and health status characteristics. BMC Health Serv Res. 2014;14(1):532. PubMed
14. Cohen SB. The Concentration of Health Care Expenditures and Related Expenses for Costly Medical Conditions, 2009. Agency for Healthcare Research and Quality Statistical Brief #359; 2012.
15. Ronksley PE, McKay JA, Kobewka DM, Mulpuru S, Forster AJ. Patterns of health care use in a high-cost inpatient population in Ottawa, Ontario: A retrospective observational study. CMAJ Open. 2015; 3:E111-E118. PubMed
16. Hemmelgarn BR, Clement F, Manns BJ, et al. Overview of the Alberta Kidney Disease Network. BMC Nephrol. 2009;10:30. PubMed
17. DAD Resource Intensity Weights and Expected Length of Stay. Canadian Institute for Health Information. 2016. https://www.cihi.ca/en/data-and-standards/standards/case-mix/resource-indicators-dad-resource-intensity-weights-and. Accessed on June 24, 2016.
18. Statistics Canada. The Canadian Consumer Price Index Reference Paper, Statistics Canada Catalogue no. 62-553-X.
19. Tonelli M, Wiebe N, Fortin M, et al. Methods for identifying 30 chronic conditions: Application to administrative data. BMC Med Inform Decis Mak. 2015;17:15(1):1. PubMed
20. Jaakkimainen RL, Klein-Geltink J, Guttmann A, Barnsley J, Jagorski B, Kopp A. Indicators of primary care based on administrative data. In Primary Care in Ontario: ICES Atlas. Toronto, Ontario: Institute for Clinical Evaluative Sciences; 2006.
21. Jee SH, Cabana MD. Indices for continuity of care: A systematic review of the literature. Med Care Res Rev. 2006;63:158-188. PubMed
22. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP. 2009.
23. Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. PubMed
24. Tanuseputro P, Wodchis WP, Fowler R, et al. The health care cost of dying: A population-based retrospective cohort study of the last year of life in ontario, canada. PLoS One. 2015;10(3):e0121759. PubMed
25. Hong CS, Siegel AL, Ferris TG. Caring for high-need, high-cost patients: What makes for a successful care management program? Issue Brief (Commonw Fund). 2014;19:1-19. PubMed
26. Birnbaum M, Halper DE. Rethinking service delivery for high-cost Medicaid patients. Medicaid Institute. 2009. http://shnny.org/research/rethinking-service-delivery-for-high-cost-medicaid-patients/. Accessed on Jan 11, 2017.
27. Pan-Canadian forum on high users of health care. Canadian Institute for Health Information. 2014. https://secure.cihi.ca/free_products/highusers_summary_report_revised_EN_web.pdf. Accessed on Jan 11, 2017.
© 2017 Society of Hospital Medicine
Is Simultaneous Bilateral Total Knee Arthroplasty (BTKA) as Safe as Staged BTKA?
Take-Home Points
- Complication rates did not statistically significantly differ between simultaneous and staged TKA.
- Length of stay of 2 TKA admissions was greater than 1 BTKA admission.
- Transfusion requirements were greater in BTKA.
- Avoid bilateral procedures in ASA 3 patients.
- Develop institutional protocols for BTKA with multidisciplinary input.
In the United States, osteoarthritis is the most common cause of knee pain and one of the leading causes of disability.1 Total knee arthroplasty (TKA) is an effective treatment for end-stage osteoarthritis of the knee.2 Whether patients with severe, debilitating bilateral disease should undergo simultaneous bilateral TKA (BTKA) or staged BTKA (2 separate procedures during separate hospital admissions) continues to be debated. The relative risks and benefits of simultaneous BTKA relative to staged BTKA or unilateral TKA are controversial.3-6 Proponents of simultaneous BTKA have argued that this surgery results in shorter hospital length of stay (LOS) and higher patient satisfaction without increased risk of perioperative complications,7-9 and opponents have argued that it leads to increased perioperative mortality and complications and should not be performed routinely.10,11
The safety of simultaneous BTKA cannot necessarily be extrapolated from data on unilateral TKA. Authors have argued that the complication rate for simultaneous BTKA is not comparable to the rate for unilateral TKA but instead is double the rate.12 Although a doubled rate may more closely approximate the true risk of simultaneous BTKA, it still does not account for the increased surgical impact of 2 procedures (vs 1 procedure) on a patient. In this regard, comparing simultaneous and staged BTKA provides a more accurate assessment of risk, as long as the interval between surgeries is not excessive. The major stress experienced during TKA affects the cardiovascular, pulmonary, and musculoskeletal systems, and full recovery may take up to 6 months.13-15 Outcome studies have found significant improvement in validated measures of function and pain up to but not past 6 months.13,15 Furthermore, a large study comparing American Society of Anesthesiologists (ASA) scores with morbidity and mortality rates recorded in the New Zealand Total Joint Database established 6 months as a best approximation of postoperative mortality and morbidity risk.14 Given these data, we propose that the most accurate analysis of postoperative morbidity and mortality would be a comparison of simultaneous BTKA with BTKA staged <6 months apart. The staged procedures fall within the crucial postoperative period when increased morbidity and mortality would more likely be present. A between-surgeries interval >6 months would effectively separate the 2 procedures, rendering their risks not truly representative.
We retrospectively analyzed all simultaneous BTKA and staged BTKA (<6 months apart) surgeries performed at our orthopedic specialty hospital between 2005 and 2009. We hypothesized there would be no significant difference in perioperative morbidity or mortality between the groups.
Methods and Materials
Our institution’s Institutional Review Board approved this study. All patients who underwent either simultaneous BTKA or staged BTKA (<6 months apart) at a single orthopedic specialty hospital between 2005 and 2009 were retrospectively identified. Twenty-five surgeons performed the procedures. Which procedure to perform (simultaneous or staged) was decided by the attending surgeon in consultation with an anesthesiologist. Preoperative medical diagnostic testing was determined by the internist, who provided medical clearance, and was subject to review by the anesthesiologist. A patient was excluded from simultaneous BTKA only if the medical or anesthesiology consultant deemed the patient too high risk for bilateral procedures. Revision TKAs were excluded from the study.
Implant, approach, tourniquet use, and TKA technique were selected by the individual surgeons. Strategies for the simultaneous procedures were (1) single surgeon, single team, sequential, start second knee after closure of first, and (2) single surgeon, single team, sequential, start second knee after implantation of first but before closure. The decision to proceed with the second knee was confirmed in consultation with the anesthesiologist after implantation and deflation of the tourniquet on the first knee.
Individual electronic patient charts were reviewed for information on demographics, comorbidities, anesthesia type, antibiotics, and postoperative venous thromboembolism prophylaxis. Demographic variables included age, sex, height, weight, and body mass index (BMI). Comorbidities recorded were diabetes mellitus, coronary artery disease, prior myocardial infarction, stroke, and endocrinopathies. In addition, available ASA scores were recorded. The primary outcome was perioperative complications, defined as any complications that occurred within 6 months after surgery. These included death, pulmonary embolism (PE), and deep surgical-site infections (SSIs). Secondary outcome measures were LOS, discharge location (rehabilitation or home), and blood transfusion requirements.
The 2 groups (simultaneous BTKA, staged BTKA) were compared using Student t test for continuous variables and χ2 test for categorical variables. Subgroup analysis was performed to compare healthier patients (ASA score 1 or 2) with patients who had more severe comorbidities (ASA score 3). Statistical significance was set at P < .05.
Results
Between 2005 and 2009, 371 patients had simultaneous BTKA, and 67 had staged BTKA (134 procedures) <6 months apart (Table 1).
Most surgeries (84.4% simultaneous, 90.3% staged) were performed with the patient under spinal anesthesia, and there was a trend (P = .167) toward more frequent use of general anesthesia in the simultaneous group relative to the staged group (Table 2).
The 2 cohorts’ perioperative complication rates were not statistically significantly different (P = .97) (Table 3).
There was no statistically significant difference (P = .398) in occurrence of postoperative complications between the 2 cohorts compared on ASA scores, and the difference between patients with ASA score 1 or 2 and those with ASA score 3 was not statistically significant (P = .200) (Table 4).
Discussion
Although there was no significant difference in postoperative complication rates within 6 months after surgery between the simultaneous and staged BTKA groups, the incidence of complications in the simultaneous group was notable. The disproportionate size of the 2 comparison groups limited the power of our study to analyze individual perioperative complications. This study may be underpowered to detect differences in complications occurring relatively infrequently, which may explain why the difference in number of complications (13 in simultaneous group, 1 in staged group) did not achieve statistical significance (β = 0.89). Post hoc power analysis showed 956 patients would be needed in each group to adequately power for such small complication rates. However, our results are consistent with those of other studies.13-15 The 1.9% PE rate in our simultaneous BTKA group does not vary from the average PE rate for TKA in the literature and is actually lower than the PE rate in a previous study at our institution.16 Fat embolism traditionally is considered more of a concern in bilateral cases than in unilateral cases. Although fat embolism surely is inherent to the physiologic alterations caused by TKA, we did not find clinically significant fat embolism in either cohort.
Similarly, the 1.08% rate of deep SSIs is within the range for postoperative TKA infections at our institution and others.17 Our staged BTKA group’s complication rate, 0.75% (1 SSI), was slightly lower than expected. However, 0.75% is in keeping with institutional norms (typical rate, ~1%). We would have expected a nonzero rate for venous thromboembolism, and perhaps such a rate would have come with an inclusion period longer than 6 months. Last, the death in the simultaneous BTKA group was not an outlier, given the published rate of mortality after elective total joint surgery.18The characteristics of our simultaneous and staged BTKA groups were very similar (Table 1), though the larger number of staged-group patients with diabetes mellitus and coronary artery disease may represent selection bias. Nevertheless, the proportions of patients with each of 3 ASA scores were similar. It is also important to note that, in this context, a high percentage of patients in each group (33.6% simultaneous, 37.5% staged) received ASA score 3 from the anesthesiologist (P > .05). This may be an important factor in explaining the larger though not statistically significant number of complications in the simultaneous group (13) relative to the staged group (1).
Other authors have studied the safety of simultaneous vs staged BTKA and drawn conflicting conclusions.11,19-21 Walmsley and colleagues21 found no differences in 90-day mortality between 3 groups: patients with simultaneous BTKA, patients with BTKA staged within 5 years, and patients with unilateral TKA. Stefánsdóttir and colleagues11 found that, compared with simultaneous BTKA, BTKA staged within 1 year had a lower 30-day mortality rate. Meehan and colleagues20 compared simultaneous BTKA with BTKA staged within 1 year and found a lower risk of infection and device malfunction and a higher risk of adverse cardiovascular outcomes in the simultaneous group. A recent meta-analysis found that, compared with staged BTKA, simultaneous BTKA had a higher risk of perioperative complications.19 A systematic review of retrospective studies found simultaneous BTKA had higher rates of mortality, PE, and transfusion and lower rates of deep SSI and revision.22 A survey of Medicare data found higher 90-day mortality and myocardial infarction rates for simultaneous BTKA but no difference in infection and revision rates.23 Clearly, there is no consensus as to whether simultaneous BTKA carries higher risks relative to staged BTKA.
The amount of blood transfused in our simultaneous BTKA group was more than double that in the 2 staged TKAs combined. It is intuitive that the blood loss in 2 concurrent TKAs is always more than in 1 TKA, but the clinical relevance of this fact is unknown. Transfusions have potential complications, and this risk needs to be addressed in the preoperative discussion.
LOS for simultaneous BTKA was on average 4 days shorter than the combined LOS (2 hospitalizations) for staged BTKA. This shorter LOS has been shown to provide the healthcare system with a cost savings.8 However, not considered in the equation is the difference in cost of rehabilitations, 2 vs 1. In the present study, 92.7% of simultaneous BTKA patients and only 50.7% of staged BTKA patients were discharged to an inpatient acute rehabilitation unit. Interestingly, the majority of the staged patients who went to inpatient rehabilitation did so after the second surgery. At our institution at the time of this study, simultaneous BTKA patients, and staged BTKA patients with the second surgery completed, were more likely than unilateral TKA patients to qualify for inpatient acute rehabilitation. Staged BTKA patients’ higher cost for 2 rehabilitations, rather than 1, adds to the cost savings realized with simultaneous BTKA. In the context of an episode-based payment system, the cost of posthospital rehabilitation enters the overall cost equation and may lead to an increase in the number of simultaneous BTKAs being performed.
Conclusion
In this study, the incidence of postoperative complications was higher for simultaneous BTKA than for staged BTKA performed <6 months apart, but the difference was not significantly different. There were significant differences in LOS and blood transfusion rates between the groups, as expected. At present, only patients with ASA score 1 or 2 are considered for simultaneous BTKA at our institution. Patients with ASA score 3 or higher are not eligible.
Am J Orthop. 2017;46(4):E224-E229. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006;54(1):226-229.
2. Kolettis GT, Wixson RL, Peruzzi WT, Blake MJ, Wardell S, Stulberg SD. Safety of 1-stage bilateral total knee arthroplasty. Clin Orthop Relat Res. 1994;(309):102-109.
3. Kim YH, Choi YW, Kim JS. Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Joint Surg Br. 2009;91(1):64-68.
4. Luscombe JC, Theivendran K, Abudu A, Carter SR. The relative safety of one-stage bilateral total knee arthroplasty. Int Orthop. 2009;33(1):101-104.
5. Memtsoudis SG, Ma Y, González Della Valle A, et al. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology. 2009;111(6):1206-1216.
6. Zeni JA Jr, Snyder-Mackler L. Clinical outcomes after simultaneous bilateral total knee arthroplasty: comparison to unilateral total knee arthroplasty and healthy controls. J Arthroplasty. 2010;25(4):541-546.
7. March LM, Cross M, Tribe KL, et al; Arthritis C.O.S.T. Study Project Group. Two knees or not two knees? Patient costs and outcomes following bilateral and unilateral total knee joint replacement surgery for OA. Osteoarthritis Cartilage. 2004;12(5):400-408.
8. Reuben JD, Meyers SJ, Cox DD, Elliott M, Watson M, Shim SD. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty. 1998;13(2):172-179.
9. Ritter MA, Harty LD. Debate: simultaneous bilateral knee replacements: the outcomes justify its use. Clin Orthop Relat Res. 2004;(428):84-86.
10. Restrepo C, Parvizi J, Dietrich T, Einhorn TA. Safety of simultaneous bilateral total knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2007;89(6):1220-1226.
11. Stefánsdóttir A, Lidgren L, Robertsson O. Higher early mortality with simultaneous rather than staged bilateral TKAs: results from the Swedish Knee Arthroplasty Register. Clin Orthop Relat Res. 2008;466(12):3066-3070.
12. Noble J, Goodall J, Noble D. Simultaneous bilateral total knee replacement: a persistent controversy. Knee. 2009;16(6):420-426.
13. Fortin PR, Penrod JR, Clarke AE, et al. Timing of total joint replacement affects clinical outcomes among patients with osteoarthritis of the hip or knee. Arthritis Rheum. 2002;46(12):3327-3330.
14. Hooper GJ, Rothwell AG, Hooper NM, Frampton C. The relationship between the American Society of Anesthesiologists physical rating and outcome following total hip and knee arthroplasty: an analysis of the New Zealand Joint Registry. J Bone Joint Surg Am. 2012;94(12):1065-1070.
15. MacWilliam CH, Yood MU, Verner JJ, McCarthy BD, Ward RE. Patient-related risk factors that predict poor outcome after total hip replacement. Health Serv Res. 1996;31(5):623-638.
16. Hadley SR, Lee M, Reid M, Dweck E, Steiger D. Predictors of pulmonary embolism in orthopaedic patient population. Abstract presented at: 43rd Annual Meeting of the Eastern Orthopaedic Association; June 20-23, 2012; Bolton Landing, NY.
17. Hadley S, Immerman I, Hutzler L, Slover J, Bosco J. Staphylococcus aureus decolonization protocol decreases surgical site infections for total joint replacement. Arthritis. 2010;2010:924518.
18. Singh JA, Lewallen DG. Ninety-day mortality in patients undergoing elective total hip or total knee arthroplasty. J Arthroplasty. 2012;27(8):1417-1422.e1.
19. Hu J, Liu Y, Lv Z, Li X, Qin X, Fan W. Mortality and morbidity associated with simultaneous bilateral or staged bilateral total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg. 2011;131(9):1291-1298.
20. Meehan JP, Danielsen B, Tancredi DJ, Kim S, Jamali AA, White RH. A population-based comparison of the incidence of adverse outcomes after simultaneous-bilateral and staged-bilateral total knee arthroplasty. J Bone Joint Surg Am. 2011;93(23):2203-2213.
21. Walmsley P, Murray A, Brenkel IJ. The practice of bilateral, simultaneous total knee replacement in Scotland over the last decade. Data from the Scottish Arthroplasty Project. Knee. 2006;13(2):102-105.
22. Fu D, Li G, Chen K, Zeng H, Zhang X, Cai Z. Comparison of clinical outcome between simultaneous-bilateral and staged-bilateral total knee arthroplasty: a systematic review of retrospective studies. J Arthroplasty. 2013;28(7):1141-1147.
23. Bolognesi MP, Watters TS, Attarian DE, Wellman SS, Setoguchi S. Simultaneous vs staged bilateral total knee arthroplasty among Medicare beneficiaries, 2000–2009. J Arthroplasty. 2013;28(8 suppl):87-91.
Take-Home Points
- Complication rates did not statistically significantly differ between simultaneous and staged TKA.
- Length of stay of 2 TKA admissions was greater than 1 BTKA admission.
- Transfusion requirements were greater in BTKA.
- Avoid bilateral procedures in ASA 3 patients.
- Develop institutional protocols for BTKA with multidisciplinary input.
In the United States, osteoarthritis is the most common cause of knee pain and one of the leading causes of disability.1 Total knee arthroplasty (TKA) is an effective treatment for end-stage osteoarthritis of the knee.2 Whether patients with severe, debilitating bilateral disease should undergo simultaneous bilateral TKA (BTKA) or staged BTKA (2 separate procedures during separate hospital admissions) continues to be debated. The relative risks and benefits of simultaneous BTKA relative to staged BTKA or unilateral TKA are controversial.3-6 Proponents of simultaneous BTKA have argued that this surgery results in shorter hospital length of stay (LOS) and higher patient satisfaction without increased risk of perioperative complications,7-9 and opponents have argued that it leads to increased perioperative mortality and complications and should not be performed routinely.10,11
The safety of simultaneous BTKA cannot necessarily be extrapolated from data on unilateral TKA. Authors have argued that the complication rate for simultaneous BTKA is not comparable to the rate for unilateral TKA but instead is double the rate.12 Although a doubled rate may more closely approximate the true risk of simultaneous BTKA, it still does not account for the increased surgical impact of 2 procedures (vs 1 procedure) on a patient. In this regard, comparing simultaneous and staged BTKA provides a more accurate assessment of risk, as long as the interval between surgeries is not excessive. The major stress experienced during TKA affects the cardiovascular, pulmonary, and musculoskeletal systems, and full recovery may take up to 6 months.13-15 Outcome studies have found significant improvement in validated measures of function and pain up to but not past 6 months.13,15 Furthermore, a large study comparing American Society of Anesthesiologists (ASA) scores with morbidity and mortality rates recorded in the New Zealand Total Joint Database established 6 months as a best approximation of postoperative mortality and morbidity risk.14 Given these data, we propose that the most accurate analysis of postoperative morbidity and mortality would be a comparison of simultaneous BTKA with BTKA staged <6 months apart. The staged procedures fall within the crucial postoperative period when increased morbidity and mortality would more likely be present. A between-surgeries interval >6 months would effectively separate the 2 procedures, rendering their risks not truly representative.
We retrospectively analyzed all simultaneous BTKA and staged BTKA (<6 months apart) surgeries performed at our orthopedic specialty hospital between 2005 and 2009. We hypothesized there would be no significant difference in perioperative morbidity or mortality between the groups.
Methods and Materials
Our institution’s Institutional Review Board approved this study. All patients who underwent either simultaneous BTKA or staged BTKA (<6 months apart) at a single orthopedic specialty hospital between 2005 and 2009 were retrospectively identified. Twenty-five surgeons performed the procedures. Which procedure to perform (simultaneous or staged) was decided by the attending surgeon in consultation with an anesthesiologist. Preoperative medical diagnostic testing was determined by the internist, who provided medical clearance, and was subject to review by the anesthesiologist. A patient was excluded from simultaneous BTKA only if the medical or anesthesiology consultant deemed the patient too high risk for bilateral procedures. Revision TKAs were excluded from the study.
Implant, approach, tourniquet use, and TKA technique were selected by the individual surgeons. Strategies for the simultaneous procedures were (1) single surgeon, single team, sequential, start second knee after closure of first, and (2) single surgeon, single team, sequential, start second knee after implantation of first but before closure. The decision to proceed with the second knee was confirmed in consultation with the anesthesiologist after implantation and deflation of the tourniquet on the first knee.
Individual electronic patient charts were reviewed for information on demographics, comorbidities, anesthesia type, antibiotics, and postoperative venous thromboembolism prophylaxis. Demographic variables included age, sex, height, weight, and body mass index (BMI). Comorbidities recorded were diabetes mellitus, coronary artery disease, prior myocardial infarction, stroke, and endocrinopathies. In addition, available ASA scores were recorded. The primary outcome was perioperative complications, defined as any complications that occurred within 6 months after surgery. These included death, pulmonary embolism (PE), and deep surgical-site infections (SSIs). Secondary outcome measures were LOS, discharge location (rehabilitation or home), and blood transfusion requirements.
The 2 groups (simultaneous BTKA, staged BTKA) were compared using Student t test for continuous variables and χ2 test for categorical variables. Subgroup analysis was performed to compare healthier patients (ASA score 1 or 2) with patients who had more severe comorbidities (ASA score 3). Statistical significance was set at P < .05.
Results
Between 2005 and 2009, 371 patients had simultaneous BTKA, and 67 had staged BTKA (134 procedures) <6 months apart (Table 1).
Most surgeries (84.4% simultaneous, 90.3% staged) were performed with the patient under spinal anesthesia, and there was a trend (P = .167) toward more frequent use of general anesthesia in the simultaneous group relative to the staged group (Table 2).
The 2 cohorts’ perioperative complication rates were not statistically significantly different (P = .97) (Table 3).
There was no statistically significant difference (P = .398) in occurrence of postoperative complications between the 2 cohorts compared on ASA scores, and the difference between patients with ASA score 1 or 2 and those with ASA score 3 was not statistically significant (P = .200) (Table 4).
Discussion
Although there was no significant difference in postoperative complication rates within 6 months after surgery between the simultaneous and staged BTKA groups, the incidence of complications in the simultaneous group was notable. The disproportionate size of the 2 comparison groups limited the power of our study to analyze individual perioperative complications. This study may be underpowered to detect differences in complications occurring relatively infrequently, which may explain why the difference in number of complications (13 in simultaneous group, 1 in staged group) did not achieve statistical significance (β = 0.89). Post hoc power analysis showed 956 patients would be needed in each group to adequately power for such small complication rates. However, our results are consistent with those of other studies.13-15 The 1.9% PE rate in our simultaneous BTKA group does not vary from the average PE rate for TKA in the literature and is actually lower than the PE rate in a previous study at our institution.16 Fat embolism traditionally is considered more of a concern in bilateral cases than in unilateral cases. Although fat embolism surely is inherent to the physiologic alterations caused by TKA, we did not find clinically significant fat embolism in either cohort.
Similarly, the 1.08% rate of deep SSIs is within the range for postoperative TKA infections at our institution and others.17 Our staged BTKA group’s complication rate, 0.75% (1 SSI), was slightly lower than expected. However, 0.75% is in keeping with institutional norms (typical rate, ~1%). We would have expected a nonzero rate for venous thromboembolism, and perhaps such a rate would have come with an inclusion period longer than 6 months. Last, the death in the simultaneous BTKA group was not an outlier, given the published rate of mortality after elective total joint surgery.18The characteristics of our simultaneous and staged BTKA groups were very similar (Table 1), though the larger number of staged-group patients with diabetes mellitus and coronary artery disease may represent selection bias. Nevertheless, the proportions of patients with each of 3 ASA scores were similar. It is also important to note that, in this context, a high percentage of patients in each group (33.6% simultaneous, 37.5% staged) received ASA score 3 from the anesthesiologist (P > .05). This may be an important factor in explaining the larger though not statistically significant number of complications in the simultaneous group (13) relative to the staged group (1).
Other authors have studied the safety of simultaneous vs staged BTKA and drawn conflicting conclusions.11,19-21 Walmsley and colleagues21 found no differences in 90-day mortality between 3 groups: patients with simultaneous BTKA, patients with BTKA staged within 5 years, and patients with unilateral TKA. Stefánsdóttir and colleagues11 found that, compared with simultaneous BTKA, BTKA staged within 1 year had a lower 30-day mortality rate. Meehan and colleagues20 compared simultaneous BTKA with BTKA staged within 1 year and found a lower risk of infection and device malfunction and a higher risk of adverse cardiovascular outcomes in the simultaneous group. A recent meta-analysis found that, compared with staged BTKA, simultaneous BTKA had a higher risk of perioperative complications.19 A systematic review of retrospective studies found simultaneous BTKA had higher rates of mortality, PE, and transfusion and lower rates of deep SSI and revision.22 A survey of Medicare data found higher 90-day mortality and myocardial infarction rates for simultaneous BTKA but no difference in infection and revision rates.23 Clearly, there is no consensus as to whether simultaneous BTKA carries higher risks relative to staged BTKA.
The amount of blood transfused in our simultaneous BTKA group was more than double that in the 2 staged TKAs combined. It is intuitive that the blood loss in 2 concurrent TKAs is always more than in 1 TKA, but the clinical relevance of this fact is unknown. Transfusions have potential complications, and this risk needs to be addressed in the preoperative discussion.
LOS for simultaneous BTKA was on average 4 days shorter than the combined LOS (2 hospitalizations) for staged BTKA. This shorter LOS has been shown to provide the healthcare system with a cost savings.8 However, not considered in the equation is the difference in cost of rehabilitations, 2 vs 1. In the present study, 92.7% of simultaneous BTKA patients and only 50.7% of staged BTKA patients were discharged to an inpatient acute rehabilitation unit. Interestingly, the majority of the staged patients who went to inpatient rehabilitation did so after the second surgery. At our institution at the time of this study, simultaneous BTKA patients, and staged BTKA patients with the second surgery completed, were more likely than unilateral TKA patients to qualify for inpatient acute rehabilitation. Staged BTKA patients’ higher cost for 2 rehabilitations, rather than 1, adds to the cost savings realized with simultaneous BTKA. In the context of an episode-based payment system, the cost of posthospital rehabilitation enters the overall cost equation and may lead to an increase in the number of simultaneous BTKAs being performed.
Conclusion
In this study, the incidence of postoperative complications was higher for simultaneous BTKA than for staged BTKA performed <6 months apart, but the difference was not significantly different. There were significant differences in LOS and blood transfusion rates between the groups, as expected. At present, only patients with ASA score 1 or 2 are considered for simultaneous BTKA at our institution. Patients with ASA score 3 or higher are not eligible.
Am J Orthop. 2017;46(4):E224-E229. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Take-Home Points
- Complication rates did not statistically significantly differ between simultaneous and staged TKA.
- Length of stay of 2 TKA admissions was greater than 1 BTKA admission.
- Transfusion requirements were greater in BTKA.
- Avoid bilateral procedures in ASA 3 patients.
- Develop institutional protocols for BTKA with multidisciplinary input.
In the United States, osteoarthritis is the most common cause of knee pain and one of the leading causes of disability.1 Total knee arthroplasty (TKA) is an effective treatment for end-stage osteoarthritis of the knee.2 Whether patients with severe, debilitating bilateral disease should undergo simultaneous bilateral TKA (BTKA) or staged BTKA (2 separate procedures during separate hospital admissions) continues to be debated. The relative risks and benefits of simultaneous BTKA relative to staged BTKA or unilateral TKA are controversial.3-6 Proponents of simultaneous BTKA have argued that this surgery results in shorter hospital length of stay (LOS) and higher patient satisfaction without increased risk of perioperative complications,7-9 and opponents have argued that it leads to increased perioperative mortality and complications and should not be performed routinely.10,11
The safety of simultaneous BTKA cannot necessarily be extrapolated from data on unilateral TKA. Authors have argued that the complication rate for simultaneous BTKA is not comparable to the rate for unilateral TKA but instead is double the rate.12 Although a doubled rate may more closely approximate the true risk of simultaneous BTKA, it still does not account for the increased surgical impact of 2 procedures (vs 1 procedure) on a patient. In this regard, comparing simultaneous and staged BTKA provides a more accurate assessment of risk, as long as the interval between surgeries is not excessive. The major stress experienced during TKA affects the cardiovascular, pulmonary, and musculoskeletal systems, and full recovery may take up to 6 months.13-15 Outcome studies have found significant improvement in validated measures of function and pain up to but not past 6 months.13,15 Furthermore, a large study comparing American Society of Anesthesiologists (ASA) scores with morbidity and mortality rates recorded in the New Zealand Total Joint Database established 6 months as a best approximation of postoperative mortality and morbidity risk.14 Given these data, we propose that the most accurate analysis of postoperative morbidity and mortality would be a comparison of simultaneous BTKA with BTKA staged <6 months apart. The staged procedures fall within the crucial postoperative period when increased morbidity and mortality would more likely be present. A between-surgeries interval >6 months would effectively separate the 2 procedures, rendering their risks not truly representative.
We retrospectively analyzed all simultaneous BTKA and staged BTKA (<6 months apart) surgeries performed at our orthopedic specialty hospital between 2005 and 2009. We hypothesized there would be no significant difference in perioperative morbidity or mortality between the groups.
Methods and Materials
Our institution’s Institutional Review Board approved this study. All patients who underwent either simultaneous BTKA or staged BTKA (<6 months apart) at a single orthopedic specialty hospital between 2005 and 2009 were retrospectively identified. Twenty-five surgeons performed the procedures. Which procedure to perform (simultaneous or staged) was decided by the attending surgeon in consultation with an anesthesiologist. Preoperative medical diagnostic testing was determined by the internist, who provided medical clearance, and was subject to review by the anesthesiologist. A patient was excluded from simultaneous BTKA only if the medical or anesthesiology consultant deemed the patient too high risk for bilateral procedures. Revision TKAs were excluded from the study.
Implant, approach, tourniquet use, and TKA technique were selected by the individual surgeons. Strategies for the simultaneous procedures were (1) single surgeon, single team, sequential, start second knee after closure of first, and (2) single surgeon, single team, sequential, start second knee after implantation of first but before closure. The decision to proceed with the second knee was confirmed in consultation with the anesthesiologist after implantation and deflation of the tourniquet on the first knee.
Individual electronic patient charts were reviewed for information on demographics, comorbidities, anesthesia type, antibiotics, and postoperative venous thromboembolism prophylaxis. Demographic variables included age, sex, height, weight, and body mass index (BMI). Comorbidities recorded were diabetes mellitus, coronary artery disease, prior myocardial infarction, stroke, and endocrinopathies. In addition, available ASA scores were recorded. The primary outcome was perioperative complications, defined as any complications that occurred within 6 months after surgery. These included death, pulmonary embolism (PE), and deep surgical-site infections (SSIs). Secondary outcome measures were LOS, discharge location (rehabilitation or home), and blood transfusion requirements.
The 2 groups (simultaneous BTKA, staged BTKA) were compared using Student t test for continuous variables and χ2 test for categorical variables. Subgroup analysis was performed to compare healthier patients (ASA score 1 or 2) with patients who had more severe comorbidities (ASA score 3). Statistical significance was set at P < .05.
Results
Between 2005 and 2009, 371 patients had simultaneous BTKA, and 67 had staged BTKA (134 procedures) <6 months apart (Table 1).
Most surgeries (84.4% simultaneous, 90.3% staged) were performed with the patient under spinal anesthesia, and there was a trend (P = .167) toward more frequent use of general anesthesia in the simultaneous group relative to the staged group (Table 2).
The 2 cohorts’ perioperative complication rates were not statistically significantly different (P = .97) (Table 3).
There was no statistically significant difference (P = .398) in occurrence of postoperative complications between the 2 cohorts compared on ASA scores, and the difference between patients with ASA score 1 or 2 and those with ASA score 3 was not statistically significant (P = .200) (Table 4).
Discussion
Although there was no significant difference in postoperative complication rates within 6 months after surgery between the simultaneous and staged BTKA groups, the incidence of complications in the simultaneous group was notable. The disproportionate size of the 2 comparison groups limited the power of our study to analyze individual perioperative complications. This study may be underpowered to detect differences in complications occurring relatively infrequently, which may explain why the difference in number of complications (13 in simultaneous group, 1 in staged group) did not achieve statistical significance (β = 0.89). Post hoc power analysis showed 956 patients would be needed in each group to adequately power for such small complication rates. However, our results are consistent with those of other studies.13-15 The 1.9% PE rate in our simultaneous BTKA group does not vary from the average PE rate for TKA in the literature and is actually lower than the PE rate in a previous study at our institution.16 Fat embolism traditionally is considered more of a concern in bilateral cases than in unilateral cases. Although fat embolism surely is inherent to the physiologic alterations caused by TKA, we did not find clinically significant fat embolism in either cohort.
Similarly, the 1.08% rate of deep SSIs is within the range for postoperative TKA infections at our institution and others.17 Our staged BTKA group’s complication rate, 0.75% (1 SSI), was slightly lower than expected. However, 0.75% is in keeping with institutional norms (typical rate, ~1%). We would have expected a nonzero rate for venous thromboembolism, and perhaps such a rate would have come with an inclusion period longer than 6 months. Last, the death in the simultaneous BTKA group was not an outlier, given the published rate of mortality after elective total joint surgery.18The characteristics of our simultaneous and staged BTKA groups were very similar (Table 1), though the larger number of staged-group patients with diabetes mellitus and coronary artery disease may represent selection bias. Nevertheless, the proportions of patients with each of 3 ASA scores were similar. It is also important to note that, in this context, a high percentage of patients in each group (33.6% simultaneous, 37.5% staged) received ASA score 3 from the anesthesiologist (P > .05). This may be an important factor in explaining the larger though not statistically significant number of complications in the simultaneous group (13) relative to the staged group (1).
Other authors have studied the safety of simultaneous vs staged BTKA and drawn conflicting conclusions.11,19-21 Walmsley and colleagues21 found no differences in 90-day mortality between 3 groups: patients with simultaneous BTKA, patients with BTKA staged within 5 years, and patients with unilateral TKA. Stefánsdóttir and colleagues11 found that, compared with simultaneous BTKA, BTKA staged within 1 year had a lower 30-day mortality rate. Meehan and colleagues20 compared simultaneous BTKA with BTKA staged within 1 year and found a lower risk of infection and device malfunction and a higher risk of adverse cardiovascular outcomes in the simultaneous group. A recent meta-analysis found that, compared with staged BTKA, simultaneous BTKA had a higher risk of perioperative complications.19 A systematic review of retrospective studies found simultaneous BTKA had higher rates of mortality, PE, and transfusion and lower rates of deep SSI and revision.22 A survey of Medicare data found higher 90-day mortality and myocardial infarction rates for simultaneous BTKA but no difference in infection and revision rates.23 Clearly, there is no consensus as to whether simultaneous BTKA carries higher risks relative to staged BTKA.
The amount of blood transfused in our simultaneous BTKA group was more than double that in the 2 staged TKAs combined. It is intuitive that the blood loss in 2 concurrent TKAs is always more than in 1 TKA, but the clinical relevance of this fact is unknown. Transfusions have potential complications, and this risk needs to be addressed in the preoperative discussion.
LOS for simultaneous BTKA was on average 4 days shorter than the combined LOS (2 hospitalizations) for staged BTKA. This shorter LOS has been shown to provide the healthcare system with a cost savings.8 However, not considered in the equation is the difference in cost of rehabilitations, 2 vs 1. In the present study, 92.7% of simultaneous BTKA patients and only 50.7% of staged BTKA patients were discharged to an inpatient acute rehabilitation unit. Interestingly, the majority of the staged patients who went to inpatient rehabilitation did so after the second surgery. At our institution at the time of this study, simultaneous BTKA patients, and staged BTKA patients with the second surgery completed, were more likely than unilateral TKA patients to qualify for inpatient acute rehabilitation. Staged BTKA patients’ higher cost for 2 rehabilitations, rather than 1, adds to the cost savings realized with simultaneous BTKA. In the context of an episode-based payment system, the cost of posthospital rehabilitation enters the overall cost equation and may lead to an increase in the number of simultaneous BTKAs being performed.
Conclusion
In this study, the incidence of postoperative complications was higher for simultaneous BTKA than for staged BTKA performed <6 months apart, but the difference was not significantly different. There were significant differences in LOS and blood transfusion rates between the groups, as expected. At present, only patients with ASA score 1 or 2 are considered for simultaneous BTKA at our institution. Patients with ASA score 3 or higher are not eligible.
Am J Orthop. 2017;46(4):E224-E229. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006;54(1):226-229.
2. Kolettis GT, Wixson RL, Peruzzi WT, Blake MJ, Wardell S, Stulberg SD. Safety of 1-stage bilateral total knee arthroplasty. Clin Orthop Relat Res. 1994;(309):102-109.
3. Kim YH, Choi YW, Kim JS. Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Joint Surg Br. 2009;91(1):64-68.
4. Luscombe JC, Theivendran K, Abudu A, Carter SR. The relative safety of one-stage bilateral total knee arthroplasty. Int Orthop. 2009;33(1):101-104.
5. Memtsoudis SG, Ma Y, González Della Valle A, et al. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology. 2009;111(6):1206-1216.
6. Zeni JA Jr, Snyder-Mackler L. Clinical outcomes after simultaneous bilateral total knee arthroplasty: comparison to unilateral total knee arthroplasty and healthy controls. J Arthroplasty. 2010;25(4):541-546.
7. March LM, Cross M, Tribe KL, et al; Arthritis C.O.S.T. Study Project Group. Two knees or not two knees? Patient costs and outcomes following bilateral and unilateral total knee joint replacement surgery for OA. Osteoarthritis Cartilage. 2004;12(5):400-408.
8. Reuben JD, Meyers SJ, Cox DD, Elliott M, Watson M, Shim SD. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty. 1998;13(2):172-179.
9. Ritter MA, Harty LD. Debate: simultaneous bilateral knee replacements: the outcomes justify its use. Clin Orthop Relat Res. 2004;(428):84-86.
10. Restrepo C, Parvizi J, Dietrich T, Einhorn TA. Safety of simultaneous bilateral total knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2007;89(6):1220-1226.
11. Stefánsdóttir A, Lidgren L, Robertsson O. Higher early mortality with simultaneous rather than staged bilateral TKAs: results from the Swedish Knee Arthroplasty Register. Clin Orthop Relat Res. 2008;466(12):3066-3070.
12. Noble J, Goodall J, Noble D. Simultaneous bilateral total knee replacement: a persistent controversy. Knee. 2009;16(6):420-426.
13. Fortin PR, Penrod JR, Clarke AE, et al. Timing of total joint replacement affects clinical outcomes among patients with osteoarthritis of the hip or knee. Arthritis Rheum. 2002;46(12):3327-3330.
14. Hooper GJ, Rothwell AG, Hooper NM, Frampton C. The relationship between the American Society of Anesthesiologists physical rating and outcome following total hip and knee arthroplasty: an analysis of the New Zealand Joint Registry. J Bone Joint Surg Am. 2012;94(12):1065-1070.
15. MacWilliam CH, Yood MU, Verner JJ, McCarthy BD, Ward RE. Patient-related risk factors that predict poor outcome after total hip replacement. Health Serv Res. 1996;31(5):623-638.
16. Hadley SR, Lee M, Reid M, Dweck E, Steiger D. Predictors of pulmonary embolism in orthopaedic patient population. Abstract presented at: 43rd Annual Meeting of the Eastern Orthopaedic Association; June 20-23, 2012; Bolton Landing, NY.
17. Hadley S, Immerman I, Hutzler L, Slover J, Bosco J. Staphylococcus aureus decolonization protocol decreases surgical site infections for total joint replacement. Arthritis. 2010;2010:924518.
18. Singh JA, Lewallen DG. Ninety-day mortality in patients undergoing elective total hip or total knee arthroplasty. J Arthroplasty. 2012;27(8):1417-1422.e1.
19. Hu J, Liu Y, Lv Z, Li X, Qin X, Fan W. Mortality and morbidity associated with simultaneous bilateral or staged bilateral total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg. 2011;131(9):1291-1298.
20. Meehan JP, Danielsen B, Tancredi DJ, Kim S, Jamali AA, White RH. A population-based comparison of the incidence of adverse outcomes after simultaneous-bilateral and staged-bilateral total knee arthroplasty. J Bone Joint Surg Am. 2011;93(23):2203-2213.
21. Walmsley P, Murray A, Brenkel IJ. The practice of bilateral, simultaneous total knee replacement in Scotland over the last decade. Data from the Scottish Arthroplasty Project. Knee. 2006;13(2):102-105.
22. Fu D, Li G, Chen K, Zeng H, Zhang X, Cai Z. Comparison of clinical outcome between simultaneous-bilateral and staged-bilateral total knee arthroplasty: a systematic review of retrospective studies. J Arthroplasty. 2013;28(7):1141-1147.
23. Bolognesi MP, Watters TS, Attarian DE, Wellman SS, Setoguchi S. Simultaneous vs staged bilateral total knee arthroplasty among Medicare beneficiaries, 2000–2009. J Arthroplasty. 2013;28(8 suppl):87-91.
1. Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006;54(1):226-229.
2. Kolettis GT, Wixson RL, Peruzzi WT, Blake MJ, Wardell S, Stulberg SD. Safety of 1-stage bilateral total knee arthroplasty. Clin Orthop Relat Res. 1994;(309):102-109.
3. Kim YH, Choi YW, Kim JS. Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Joint Surg Br. 2009;91(1):64-68.
4. Luscombe JC, Theivendran K, Abudu A, Carter SR. The relative safety of one-stage bilateral total knee arthroplasty. Int Orthop. 2009;33(1):101-104.
5. Memtsoudis SG, Ma Y, González Della Valle A, et al. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology. 2009;111(6):1206-1216.
6. Zeni JA Jr, Snyder-Mackler L. Clinical outcomes after simultaneous bilateral total knee arthroplasty: comparison to unilateral total knee arthroplasty and healthy controls. J Arthroplasty. 2010;25(4):541-546.
7. March LM, Cross M, Tribe KL, et al; Arthritis C.O.S.T. Study Project Group. Two knees or not two knees? Patient costs and outcomes following bilateral and unilateral total knee joint replacement surgery for OA. Osteoarthritis Cartilage. 2004;12(5):400-408.
8. Reuben JD, Meyers SJ, Cox DD, Elliott M, Watson M, Shim SD. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty. 1998;13(2):172-179.
9. Ritter MA, Harty LD. Debate: simultaneous bilateral knee replacements: the outcomes justify its use. Clin Orthop Relat Res. 2004;(428):84-86.
10. Restrepo C, Parvizi J, Dietrich T, Einhorn TA. Safety of simultaneous bilateral total knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2007;89(6):1220-1226.
11. Stefánsdóttir A, Lidgren L, Robertsson O. Higher early mortality with simultaneous rather than staged bilateral TKAs: results from the Swedish Knee Arthroplasty Register. Clin Orthop Relat Res. 2008;466(12):3066-3070.
12. Noble J, Goodall J, Noble D. Simultaneous bilateral total knee replacement: a persistent controversy. Knee. 2009;16(6):420-426.
13. Fortin PR, Penrod JR, Clarke AE, et al. Timing of total joint replacement affects clinical outcomes among patients with osteoarthritis of the hip or knee. Arthritis Rheum. 2002;46(12):3327-3330.
14. Hooper GJ, Rothwell AG, Hooper NM, Frampton C. The relationship between the American Society of Anesthesiologists physical rating and outcome following total hip and knee arthroplasty: an analysis of the New Zealand Joint Registry. J Bone Joint Surg Am. 2012;94(12):1065-1070.
15. MacWilliam CH, Yood MU, Verner JJ, McCarthy BD, Ward RE. Patient-related risk factors that predict poor outcome after total hip replacement. Health Serv Res. 1996;31(5):623-638.
16. Hadley SR, Lee M, Reid M, Dweck E, Steiger D. Predictors of pulmonary embolism in orthopaedic patient population. Abstract presented at: 43rd Annual Meeting of the Eastern Orthopaedic Association; June 20-23, 2012; Bolton Landing, NY.
17. Hadley S, Immerman I, Hutzler L, Slover J, Bosco J. Staphylococcus aureus decolonization protocol decreases surgical site infections for total joint replacement. Arthritis. 2010;2010:924518.
18. Singh JA, Lewallen DG. Ninety-day mortality in patients undergoing elective total hip or total knee arthroplasty. J Arthroplasty. 2012;27(8):1417-1422.e1.
19. Hu J, Liu Y, Lv Z, Li X, Qin X, Fan W. Mortality and morbidity associated with simultaneous bilateral or staged bilateral total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg. 2011;131(9):1291-1298.
20. Meehan JP, Danielsen B, Tancredi DJ, Kim S, Jamali AA, White RH. A population-based comparison of the incidence of adverse outcomes after simultaneous-bilateral and staged-bilateral total knee arthroplasty. J Bone Joint Surg Am. 2011;93(23):2203-2213.
21. Walmsley P, Murray A, Brenkel IJ. The practice of bilateral, simultaneous total knee replacement in Scotland over the last decade. Data from the Scottish Arthroplasty Project. Knee. 2006;13(2):102-105.
22. Fu D, Li G, Chen K, Zeng H, Zhang X, Cai Z. Comparison of clinical outcome between simultaneous-bilateral and staged-bilateral total knee arthroplasty: a systematic review of retrospective studies. J Arthroplasty. 2013;28(7):1141-1147.
23. Bolognesi MP, Watters TS, Attarian DE, Wellman SS, Setoguchi S. Simultaneous vs staged bilateral total knee arthroplasty among Medicare beneficiaries, 2000–2009. J Arthroplasty. 2013;28(8 suppl):87-91.
Biceps Tenodesis: An Evolution of Treatment
Take-Home Points
- The LHB tendon has been shown to be a significant pain generator in the shoulder.
- At our institution, the number of LHB tenodeses significantly increased from 2004 to 2014.
- The age of patients who underwent a LHB tenodesis did not change significantly over the study period.
- Furthermore, the percentage of shoulder procedures that involved a LHB tenodesis significantly increased over the study period.
- Biceps tenodesis has become a more common procedure to treat shoulder pathology.
Although the exact function of the long head of the biceps (LHB) tendon is not completely understood, it is accepted that the LHB tendon can be a significant source of pain within the shoulder.1-4 Patients with symptoms related to biceps pathology often present with anterior shoulder pain that worsens with flexion and supination of the affected elbow and wrist.5 Although the sensitivity and specificity of physical examination maneuvers have been called into question, special tests have been developed to aid in the diagnosis of tendonitis of the LHB. These tests include the Speed, Yergason, bear hug, and uppercut tests as well as the O’Brien test (cross-body adduction).6,7 Recent studies have found LHB pathology in 45% of patients who undergo rotator cuff repair and in 63% of patients with a subscapularis tear.8,9
Pathology of the LHB tendon, including superior labrum anterior to posterior (SLAP) tears, can be treated in many ways.5,10,11 Options include SLAP repair, biceps tenodesis, débridement, and biceps tenotomy.11,12 Results of SLAP repairs have been less than optimal, but biceps tenodesis has been effective, and avoids the issue of cramping as can be seen with biceps tenotomy and débridement.10,12,13 Surgical methods for biceps tenodesis include open subpectoral and all-arthroscopic.11,12 Both methods have had good, reliable outcomes, but the all-arthroscopic technique is relatively new.11,12,14We conducted a study to determine LHB tenodesis trends, including patient age at time of surgery. We used surgical data from fellowship-trained sports or shoulder/elbow orthopedic surgeons at a busy subspecialty-based shoulder orthopedic practice. We hypothesized that the rate of LHB tenodesis would increase significantly over time and that there would be no significant change in the age of patients who underwent LHB tenodesis.
Methods
Our Institutional Review Board exempted this study. To determine the number of LHB tenodesis procedures performed at our institution, overall and in comparison with other common arthroscopic shoulder procedures, we queried the surgical database of 4 fellowship-trained orthopedic surgeons (shoulder/elbow, Drs. Nicholson and Cole; sports, Drs. Romeo and Verma) for the period January 1, 2004 to December 31, 2014. We used Current Procedural Terminology (CPT) code 23430 to determine the number of LHB tenodesis cases, as the surgeons primarily perform an open subpectoral biceps tenodesis. Patient age at time of surgery and the date of surgery were recorded. All patients who underwent LHB tenodesis between January 1, 2004 and December 31, 2014 were included. Number of procedures performed each year by each surgeon was recorded, as were concomitant procedures performed at the same time as the LHB tenodesis. To get the denominator (and reference point) for the number of arthroscopic shoulder surgeries performed by these 4 surgeons during the study period, and thereby determine the rate of LHB tenodesis, we selected the most common shoulder arthroscopy CPT codes used in our practice: 23430, 29806, 29807, 29822, 29823, 29825, 29826, and 29827. For a patient who underwent multiple procedures on the same day (multiple CPT codes entered on the same day), only one code was counted for that day. If 23430 was among the codes, it was included, and the case was placed in the numerator; if 23430 was not among the codes, the case was placed in the denominator.
The Arthroscopy Association of North America provides descriptions for the CPT codes: 23430 (tenodesis of long tendon of biceps), 29806 (arthroscopy, shoulder, surgical; capsulorrhaphy), 29807 (arthroscopy, shoulder, surgical; repair of SLAP lesion), 29822 (arthroscopy, shoulder, surgical; débridement, limited), 29823 (arthroscopy, shoulder, surgical; débridement, extensive), 29825 (arthroscopy, shoulder, surgical; with lysis and resection of adhesions, with or without manipulation), 29826 (arthroscopy, shoulder, surgical; decompression of subacromial space with partial acromioplasty, with or without coracoacromial release), and 29827 (arthroscopy, shoulder, surgical; with rotator cuff repair).
For analysis, we divided the data into total number of arthroscopic shoulder procedures performed by each surgeon each year and number of LHB tenodesis procedures performed by each surgeon each year. Total number of patients who had an arthroscopic procedure was used to create a denominator, and number of LHB tenodesis procedures showed the percentage of arthroscopic shoulder surgery patients who underwent LHB tenodesis. (All patients who undergo biceps tenodesis also have, at the least, diagnostic shoulder arthroscopy with or without tenotomy; if the tendon is ruptured, tenotomy is unnecessary.)
Descriptive statistics were calculated as means (SDs) for continuous variables and as frequencies with percentages for categorical variables. Linear regression analysis was used to determine whether the number of LHB tenodesis procedures changed during the study period and whether patient age changed over time. Significance was set at P < .05.
Results
Of the 7640 patients who underwent arthroscopic shoulder procedures between 2004 and 2014, 2125 had LHB tenodesis (CPT code 23430).
Discussion
Tenodesis has become a common treatment option for several pathologic shoulder conditions involving the LHB tendon.5 We set out to determine trends in LHB tenodesis at a subspecialty-focused shoulder orthopedic practice and hypothesized that the rate of LHB tenodesis would increase significantly over time and that there would be no significant change in the age of patients who underwent LHB tenodesis. Our hypotheses were confirmed: The number of LHB tenodesis cases increased significantly without a significant change in patient age.
Treatment options for LHB pathology and SLAP tears include simple tenotomy, débridement, open biceps tenodesis, and arthroscopic tenodesis.11,12,15
Recent evidence has called into question the results of SLAP repairs and suggested biceps tenodesis may be a better treatment option for SLAP tears.10,13,21 Studies have found excellent outcomes with open subpectoral biceps tenodesis in the treatment of SLAP tears, and others have found better restoration of pitchers’ thoracic rotation with open subpectoral biceps tenodesis than with SLAP repair.13,14 Similarly, comparison studies have largely favored biceps tenodesis over SLAP repair, particularly in patients older than 35 years to 40 years.22 Given these results, it is not surprising that, querying the American Board of Orthopaedic Surgeons (ABOS) part II database for isolated SLAP lesions treated between 2002 and 2011, Patterson and colleagues23 found the percentage of SLAP repairs decreased from 69.3% to 44.8% (P < .0001), whereas the percentage of biceps tenodesis procedures increased from 1.9% to 18.8% (P < .0001), indicating the realization of improved outcomes with LHB tenodesis in the treatment of SLAP tears. On the other hand, in the ABOS part II database for the period 2003 to 2008, Weber and colleagues24 found that, despite a decrease in the percentage of SLAP repairs, total number of SLAP repairs increased from 9.4% to 10.1% (P = .0163). According to our study results, the number of SLAP repairs is decreasing over time, whereas the number of LHB tenodesis procedures is continuing to rise. The practice patterns seen in our study correlate with those in previous studies of the treatment of SLAP tears: good results in tenodesis groups and poor results in SLAP repair groups.10,13Werner and colleagues25 recently used the large PearlDiver database, which includes information from both private payers and Medicare, to determine overall LHB tenodesis trends in the United States for the period 2008 to 2011. Over those years, the incidence of LHB tenodesis increased 1.7-fold, and the rate of arthroscopic LHB tenodesis increased significantly more than the rate of open LHB tenodesis. These results are similar to ours in that the number of LHB tenodesis cases increased significantly over time. However, as the overwhelming majority of patients in our practice undergo open biceps tenodesis, the faster rate of growth in the arthroscopic cohort relative to the open cohort cannot be assessed. Additional randomized studies comparing biceps tenodesis, both open and arthroscopic, with SLAP repair are needed to properly determine the superiority of LHB tenodesis over SLAP repair.
One strength of this database study was the number of patients: more than 7000, 2125 of whom underwent biceps tenodesis performed by 1 of 4 fellowship-trained orthopedic surgeons. There were several study limitations. First, because the original diagnoses were not recorded, it was unclear exactly which pathologies were treated with tenodesis, limiting our ability to make recommendations regarding treatment trends for specific pathologies. Similarly, we did not assess outcome variables, which would have allowed us to draw conclusions about the effectiveness of the biceps tenodesis procedures. Furthermore, some procedures may have been coded incorrectly, and therefore some patients may have been erroneously included or excluded. In addition, using data from only one institution may have introduced bias into our conclusions, though the results are consistent with national trends. Finally, there was some variability among the 4 surgeons in the number of LHB tenodesis procedures performed, and this variability may have confounded results, though these surgeons treat biceps pathology in similar ways.
Am J Orthop. 2017;46(4):E219-E223. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Denard PJ, Dai X, Hanypsiak BT, Burkhart SS. Anatomy of the biceps tendon: implications for restoring physiological length–tension relation during biceps tenodesis with interference screw fixation. Arthroscopy. 2012;28(10):1352-1358.
2. Ejnisman B, Monteiro GC, Andreoli CV, de Castro Pochini A. Disorder of the long head of the biceps tendon. Br J Sports Med. 2010;44(5):347-354.
3. Mellano CR, Shin JJ, Yanke AB, Verma NN. Disorders of the long head of the biceps tendon. Instr Course Lect. 2015;64:567-576.
4. Szabo I, Boileau P, Walch G. The proximal biceps as a pain generator and results of tenotomy. Sports Med Arthrosc Rev. 2008;16(3):180-186.
5. Harwin SF, Birns ME, Mbabuike JJ, Porter DA, Galano GJ. Arthroscopic tenodesis of the long head of the biceps. Orthopedics. 2014;37(11):743-747.
6. Holtby R, Razmjou H. Accuracy of the Speed’s and Yergason’s tests in detecting biceps pathology and SLAP lesions: comparison with arthroscopic findings. Arthroscopy. 2004;20(3):231-236.
7. Ben Kibler W, Sciascia AD, Hester P, Dome D, Jacobs C. Clinical utility of traditional and new tests in the diagnosis of biceps tendon injuries and superior labrum anterior and posterior lesions in the shoulder. Am J Sports Med. 2009;37(9):1840-1847.
8. Lafosse L, Reiland Y, Baier GP, Toussaint B, Jost B. Anterior and posterior instability of the long head of the biceps tendon in rotator cuff tears: a new classification based on arthroscopic observations. Arthroscopy. 2007;23(1):73-80.
9. Adams CR, Schoolfield JD, Burkhart SS. The results of arthroscopic subscapularis tendon repairs. Arthroscopy. 2008;24(12):1381-1389.
10. Provencher MT, McCormick F, Dewing C, McIntire S, Solomon D. A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: outcomes and factors associated with success and failure. Am J Sports Med. 2013;41(4):880-886.
11. Gombera MM, Kahlenberg CA, Nair R, Saltzman MD, Terry MA. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Med. 2015;43(5):1077-1083.
12. Delle Rose G, Borroni M, Silvestro A, et al. The long head of biceps as a source of pain in active population: tenotomy or tenodesis? A comparison of 2 case series with isolated lesions. Musculoskelet Surg. 2012;96(suppl 1):S47-S52.
13. Chalmers PN, Trombley R, Cip J, et al. Postoperative restoration of upper extremity motion and neuromuscular control during the overhand pitch: evaluation of tenodesis and repair for superior labral anterior-posterior tears. Am J Sports Med. 2014;42(12):2825-2836.
14. Gupta AK, Chalmers PN, Klosterman EL, et al. Subpectoral biceps tenodesis for bicipital tendonitis with SLAP tear. Orthopedics. 2015;38(1):e48-e53.
15. Ge H, Zhang Q, Sun Y, Li J, Sun L, Cheng B. Tenotomy or tenodesis for the long head of biceps lesions in shoulders: a systematic review and meta-analysis. PLoS One. 2015;10(3):e0121286.
16. Kaback LA, Gowda AL, Paller D, Green A, Blaine T. Long head biceps tenodesis with a knotless cinch suture anchor: a biomechanical analysis. Arthroscopy. 2015;31(5):831-835.
17. Kany J, Guinand R, Amaravathi RS, Alassaf I. The keyhole technique for arthroscopic tenodesis of the long head of the biceps tendon. In vivo prospective study with a radio-opaque marker. Orthop Traumatol Surg Res. 2015;101(1):31-34.
18. Mazzocca AD, Cote MP, Arciero CL, Romeo AA, Arciero RA. Clinical outcomes after subpectoral biceps tenodesis with an interference screw. Am J Sports Med. 2008;36(10):1922-1929.
19. Provencher MT, LeClere LE, Romeo AA. Subpectoral biceps tenodesis. Sports Med Arthrosc Rev. 2008;16(3):170-176.
20. Erickson BJ, Jain A, Abrams GD, et al. SLAP lesions: trends in treatment. Arthroscopy. 2016;32(6):976-981.
21. Erickson J, Lavery K, Monica J, Gatt C, Dhawan A. Surgical treatment of symptomatic superior labrum anterior-posterior tears in patients older than 40 years: a systematic review. Am J Sports Med. 2015;43(5):1274-1282.
22. Denard PJ, Ladermann A, Parsley BK, Burkhart SS. Arthroscopic biceps tenodesis compared with repair of isolated type II SLAP lesions in patients older than 35 years. Orthopedics. 2014;37(3):e292-e297.
23. Patterson BM, Creighton RA, Spang JT, Roberson JR, Kamath GV. Surgical trends in the treatment of superior labrum anterior and posterior lesions of the shoulder: analysis of data from the American Board of Orthopaedic Surgery certification examination database. Am J Sports Med. 2014;42(8):1904-1910.
24. Weber SC, Martin DF, Seiler JG 3rd, Harrast JJ. Superior labrum anterior and posterior lesions of the shoulder: incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery. Part II candidates. Am J Sports Med. 2012;40(7):1538-1543.
25. Werner BC, Brockmeier SF, Gwathmey FW. Trends in long head biceps tenodesis. Am J Sports Med. 2015;43(3):570-578.
Take-Home Points
- The LHB tendon has been shown to be a significant pain generator in the shoulder.
- At our institution, the number of LHB tenodeses significantly increased from 2004 to 2014.
- The age of patients who underwent a LHB tenodesis did not change significantly over the study period.
- Furthermore, the percentage of shoulder procedures that involved a LHB tenodesis significantly increased over the study period.
- Biceps tenodesis has become a more common procedure to treat shoulder pathology.
Although the exact function of the long head of the biceps (LHB) tendon is not completely understood, it is accepted that the LHB tendon can be a significant source of pain within the shoulder.1-4 Patients with symptoms related to biceps pathology often present with anterior shoulder pain that worsens with flexion and supination of the affected elbow and wrist.5 Although the sensitivity and specificity of physical examination maneuvers have been called into question, special tests have been developed to aid in the diagnosis of tendonitis of the LHB. These tests include the Speed, Yergason, bear hug, and uppercut tests as well as the O’Brien test (cross-body adduction).6,7 Recent studies have found LHB pathology in 45% of patients who undergo rotator cuff repair and in 63% of patients with a subscapularis tear.8,9
Pathology of the LHB tendon, including superior labrum anterior to posterior (SLAP) tears, can be treated in many ways.5,10,11 Options include SLAP repair, biceps tenodesis, débridement, and biceps tenotomy.11,12 Results of SLAP repairs have been less than optimal, but biceps tenodesis has been effective, and avoids the issue of cramping as can be seen with biceps tenotomy and débridement.10,12,13 Surgical methods for biceps tenodesis include open subpectoral and all-arthroscopic.11,12 Both methods have had good, reliable outcomes, but the all-arthroscopic technique is relatively new.11,12,14We conducted a study to determine LHB tenodesis trends, including patient age at time of surgery. We used surgical data from fellowship-trained sports or shoulder/elbow orthopedic surgeons at a busy subspecialty-based shoulder orthopedic practice. We hypothesized that the rate of LHB tenodesis would increase significantly over time and that there would be no significant change in the age of patients who underwent LHB tenodesis.
Methods
Our Institutional Review Board exempted this study. To determine the number of LHB tenodesis procedures performed at our institution, overall and in comparison with other common arthroscopic shoulder procedures, we queried the surgical database of 4 fellowship-trained orthopedic surgeons (shoulder/elbow, Drs. Nicholson and Cole; sports, Drs. Romeo and Verma) for the period January 1, 2004 to December 31, 2014. We used Current Procedural Terminology (CPT) code 23430 to determine the number of LHB tenodesis cases, as the surgeons primarily perform an open subpectoral biceps tenodesis. Patient age at time of surgery and the date of surgery were recorded. All patients who underwent LHB tenodesis between January 1, 2004 and December 31, 2014 were included. Number of procedures performed each year by each surgeon was recorded, as were concomitant procedures performed at the same time as the LHB tenodesis. To get the denominator (and reference point) for the number of arthroscopic shoulder surgeries performed by these 4 surgeons during the study period, and thereby determine the rate of LHB tenodesis, we selected the most common shoulder arthroscopy CPT codes used in our practice: 23430, 29806, 29807, 29822, 29823, 29825, 29826, and 29827. For a patient who underwent multiple procedures on the same day (multiple CPT codes entered on the same day), only one code was counted for that day. If 23430 was among the codes, it was included, and the case was placed in the numerator; if 23430 was not among the codes, the case was placed in the denominator.
The Arthroscopy Association of North America provides descriptions for the CPT codes: 23430 (tenodesis of long tendon of biceps), 29806 (arthroscopy, shoulder, surgical; capsulorrhaphy), 29807 (arthroscopy, shoulder, surgical; repair of SLAP lesion), 29822 (arthroscopy, shoulder, surgical; débridement, limited), 29823 (arthroscopy, shoulder, surgical; débridement, extensive), 29825 (arthroscopy, shoulder, surgical; with lysis and resection of adhesions, with or without manipulation), 29826 (arthroscopy, shoulder, surgical; decompression of subacromial space with partial acromioplasty, with or without coracoacromial release), and 29827 (arthroscopy, shoulder, surgical; with rotator cuff repair).
For analysis, we divided the data into total number of arthroscopic shoulder procedures performed by each surgeon each year and number of LHB tenodesis procedures performed by each surgeon each year. Total number of patients who had an arthroscopic procedure was used to create a denominator, and number of LHB tenodesis procedures showed the percentage of arthroscopic shoulder surgery patients who underwent LHB tenodesis. (All patients who undergo biceps tenodesis also have, at the least, diagnostic shoulder arthroscopy with or without tenotomy; if the tendon is ruptured, tenotomy is unnecessary.)
Descriptive statistics were calculated as means (SDs) for continuous variables and as frequencies with percentages for categorical variables. Linear regression analysis was used to determine whether the number of LHB tenodesis procedures changed during the study period and whether patient age changed over time. Significance was set at P < .05.
Results
Of the 7640 patients who underwent arthroscopic shoulder procedures between 2004 and 2014, 2125 had LHB tenodesis (CPT code 23430).
Discussion
Tenodesis has become a common treatment option for several pathologic shoulder conditions involving the LHB tendon.5 We set out to determine trends in LHB tenodesis at a subspecialty-focused shoulder orthopedic practice and hypothesized that the rate of LHB tenodesis would increase significantly over time and that there would be no significant change in the age of patients who underwent LHB tenodesis. Our hypotheses were confirmed: The number of LHB tenodesis cases increased significantly without a significant change in patient age.
Treatment options for LHB pathology and SLAP tears include simple tenotomy, débridement, open biceps tenodesis, and arthroscopic tenodesis.11,12,15
Recent evidence has called into question the results of SLAP repairs and suggested biceps tenodesis may be a better treatment option for SLAP tears.10,13,21 Studies have found excellent outcomes with open subpectoral biceps tenodesis in the treatment of SLAP tears, and others have found better restoration of pitchers’ thoracic rotation with open subpectoral biceps tenodesis than with SLAP repair.13,14 Similarly, comparison studies have largely favored biceps tenodesis over SLAP repair, particularly in patients older than 35 years to 40 years.22 Given these results, it is not surprising that, querying the American Board of Orthopaedic Surgeons (ABOS) part II database for isolated SLAP lesions treated between 2002 and 2011, Patterson and colleagues23 found the percentage of SLAP repairs decreased from 69.3% to 44.8% (P < .0001), whereas the percentage of biceps tenodesis procedures increased from 1.9% to 18.8% (P < .0001), indicating the realization of improved outcomes with LHB tenodesis in the treatment of SLAP tears. On the other hand, in the ABOS part II database for the period 2003 to 2008, Weber and colleagues24 found that, despite a decrease in the percentage of SLAP repairs, total number of SLAP repairs increased from 9.4% to 10.1% (P = .0163). According to our study results, the number of SLAP repairs is decreasing over time, whereas the number of LHB tenodesis procedures is continuing to rise. The practice patterns seen in our study correlate with those in previous studies of the treatment of SLAP tears: good results in tenodesis groups and poor results in SLAP repair groups.10,13Werner and colleagues25 recently used the large PearlDiver database, which includes information from both private payers and Medicare, to determine overall LHB tenodesis trends in the United States for the period 2008 to 2011. Over those years, the incidence of LHB tenodesis increased 1.7-fold, and the rate of arthroscopic LHB tenodesis increased significantly more than the rate of open LHB tenodesis. These results are similar to ours in that the number of LHB tenodesis cases increased significantly over time. However, as the overwhelming majority of patients in our practice undergo open biceps tenodesis, the faster rate of growth in the arthroscopic cohort relative to the open cohort cannot be assessed. Additional randomized studies comparing biceps tenodesis, both open and arthroscopic, with SLAP repair are needed to properly determine the superiority of LHB tenodesis over SLAP repair.
One strength of this database study was the number of patients: more than 7000, 2125 of whom underwent biceps tenodesis performed by 1 of 4 fellowship-trained orthopedic surgeons. There were several study limitations. First, because the original diagnoses were not recorded, it was unclear exactly which pathologies were treated with tenodesis, limiting our ability to make recommendations regarding treatment trends for specific pathologies. Similarly, we did not assess outcome variables, which would have allowed us to draw conclusions about the effectiveness of the biceps tenodesis procedures. Furthermore, some procedures may have been coded incorrectly, and therefore some patients may have been erroneously included or excluded. In addition, using data from only one institution may have introduced bias into our conclusions, though the results are consistent with national trends. Finally, there was some variability among the 4 surgeons in the number of LHB tenodesis procedures performed, and this variability may have confounded results, though these surgeons treat biceps pathology in similar ways.
Am J Orthop. 2017;46(4):E219-E223. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Take-Home Points
- The LHB tendon has been shown to be a significant pain generator in the shoulder.
- At our institution, the number of LHB tenodeses significantly increased from 2004 to 2014.
- The age of patients who underwent a LHB tenodesis did not change significantly over the study period.
- Furthermore, the percentage of shoulder procedures that involved a LHB tenodesis significantly increased over the study period.
- Biceps tenodesis has become a more common procedure to treat shoulder pathology.
Although the exact function of the long head of the biceps (LHB) tendon is not completely understood, it is accepted that the LHB tendon can be a significant source of pain within the shoulder.1-4 Patients with symptoms related to biceps pathology often present with anterior shoulder pain that worsens with flexion and supination of the affected elbow and wrist.5 Although the sensitivity and specificity of physical examination maneuvers have been called into question, special tests have been developed to aid in the diagnosis of tendonitis of the LHB. These tests include the Speed, Yergason, bear hug, and uppercut tests as well as the O’Brien test (cross-body adduction).6,7 Recent studies have found LHB pathology in 45% of patients who undergo rotator cuff repair and in 63% of patients with a subscapularis tear.8,9
Pathology of the LHB tendon, including superior labrum anterior to posterior (SLAP) tears, can be treated in many ways.5,10,11 Options include SLAP repair, biceps tenodesis, débridement, and biceps tenotomy.11,12 Results of SLAP repairs have been less than optimal, but biceps tenodesis has been effective, and avoids the issue of cramping as can be seen with biceps tenotomy and débridement.10,12,13 Surgical methods for biceps tenodesis include open subpectoral and all-arthroscopic.11,12 Both methods have had good, reliable outcomes, but the all-arthroscopic technique is relatively new.11,12,14We conducted a study to determine LHB tenodesis trends, including patient age at time of surgery. We used surgical data from fellowship-trained sports or shoulder/elbow orthopedic surgeons at a busy subspecialty-based shoulder orthopedic practice. We hypothesized that the rate of LHB tenodesis would increase significantly over time and that there would be no significant change in the age of patients who underwent LHB tenodesis.
Methods
Our Institutional Review Board exempted this study. To determine the number of LHB tenodesis procedures performed at our institution, overall and in comparison with other common arthroscopic shoulder procedures, we queried the surgical database of 4 fellowship-trained orthopedic surgeons (shoulder/elbow, Drs. Nicholson and Cole; sports, Drs. Romeo and Verma) for the period January 1, 2004 to December 31, 2014. We used Current Procedural Terminology (CPT) code 23430 to determine the number of LHB tenodesis cases, as the surgeons primarily perform an open subpectoral biceps tenodesis. Patient age at time of surgery and the date of surgery were recorded. All patients who underwent LHB tenodesis between January 1, 2004 and December 31, 2014 were included. Number of procedures performed each year by each surgeon was recorded, as were concomitant procedures performed at the same time as the LHB tenodesis. To get the denominator (and reference point) for the number of arthroscopic shoulder surgeries performed by these 4 surgeons during the study period, and thereby determine the rate of LHB tenodesis, we selected the most common shoulder arthroscopy CPT codes used in our practice: 23430, 29806, 29807, 29822, 29823, 29825, 29826, and 29827. For a patient who underwent multiple procedures on the same day (multiple CPT codes entered on the same day), only one code was counted for that day. If 23430 was among the codes, it was included, and the case was placed in the numerator; if 23430 was not among the codes, the case was placed in the denominator.
The Arthroscopy Association of North America provides descriptions for the CPT codes: 23430 (tenodesis of long tendon of biceps), 29806 (arthroscopy, shoulder, surgical; capsulorrhaphy), 29807 (arthroscopy, shoulder, surgical; repair of SLAP lesion), 29822 (arthroscopy, shoulder, surgical; débridement, limited), 29823 (arthroscopy, shoulder, surgical; débridement, extensive), 29825 (arthroscopy, shoulder, surgical; with lysis and resection of adhesions, with or without manipulation), 29826 (arthroscopy, shoulder, surgical; decompression of subacromial space with partial acromioplasty, with or without coracoacromial release), and 29827 (arthroscopy, shoulder, surgical; with rotator cuff repair).
For analysis, we divided the data into total number of arthroscopic shoulder procedures performed by each surgeon each year and number of LHB tenodesis procedures performed by each surgeon each year. Total number of patients who had an arthroscopic procedure was used to create a denominator, and number of LHB tenodesis procedures showed the percentage of arthroscopic shoulder surgery patients who underwent LHB tenodesis. (All patients who undergo biceps tenodesis also have, at the least, diagnostic shoulder arthroscopy with or without tenotomy; if the tendon is ruptured, tenotomy is unnecessary.)
Descriptive statistics were calculated as means (SDs) for continuous variables and as frequencies with percentages for categorical variables. Linear regression analysis was used to determine whether the number of LHB tenodesis procedures changed during the study period and whether patient age changed over time. Significance was set at P < .05.
Results
Of the 7640 patients who underwent arthroscopic shoulder procedures between 2004 and 2014, 2125 had LHB tenodesis (CPT code 23430).
Discussion
Tenodesis has become a common treatment option for several pathologic shoulder conditions involving the LHB tendon.5 We set out to determine trends in LHB tenodesis at a subspecialty-focused shoulder orthopedic practice and hypothesized that the rate of LHB tenodesis would increase significantly over time and that there would be no significant change in the age of patients who underwent LHB tenodesis. Our hypotheses were confirmed: The number of LHB tenodesis cases increased significantly without a significant change in patient age.
Treatment options for LHB pathology and SLAP tears include simple tenotomy, débridement, open biceps tenodesis, and arthroscopic tenodesis.11,12,15
Recent evidence has called into question the results of SLAP repairs and suggested biceps tenodesis may be a better treatment option for SLAP tears.10,13,21 Studies have found excellent outcomes with open subpectoral biceps tenodesis in the treatment of SLAP tears, and others have found better restoration of pitchers’ thoracic rotation with open subpectoral biceps tenodesis than with SLAP repair.13,14 Similarly, comparison studies have largely favored biceps tenodesis over SLAP repair, particularly in patients older than 35 years to 40 years.22 Given these results, it is not surprising that, querying the American Board of Orthopaedic Surgeons (ABOS) part II database for isolated SLAP lesions treated between 2002 and 2011, Patterson and colleagues23 found the percentage of SLAP repairs decreased from 69.3% to 44.8% (P < .0001), whereas the percentage of biceps tenodesis procedures increased from 1.9% to 18.8% (P < .0001), indicating the realization of improved outcomes with LHB tenodesis in the treatment of SLAP tears. On the other hand, in the ABOS part II database for the period 2003 to 2008, Weber and colleagues24 found that, despite a decrease in the percentage of SLAP repairs, total number of SLAP repairs increased from 9.4% to 10.1% (P = .0163). According to our study results, the number of SLAP repairs is decreasing over time, whereas the number of LHB tenodesis procedures is continuing to rise. The practice patterns seen in our study correlate with those in previous studies of the treatment of SLAP tears: good results in tenodesis groups and poor results in SLAP repair groups.10,13Werner and colleagues25 recently used the large PearlDiver database, which includes information from both private payers and Medicare, to determine overall LHB tenodesis trends in the United States for the period 2008 to 2011. Over those years, the incidence of LHB tenodesis increased 1.7-fold, and the rate of arthroscopic LHB tenodesis increased significantly more than the rate of open LHB tenodesis. These results are similar to ours in that the number of LHB tenodesis cases increased significantly over time. However, as the overwhelming majority of patients in our practice undergo open biceps tenodesis, the faster rate of growth in the arthroscopic cohort relative to the open cohort cannot be assessed. Additional randomized studies comparing biceps tenodesis, both open and arthroscopic, with SLAP repair are needed to properly determine the superiority of LHB tenodesis over SLAP repair.
One strength of this database study was the number of patients: more than 7000, 2125 of whom underwent biceps tenodesis performed by 1 of 4 fellowship-trained orthopedic surgeons. There were several study limitations. First, because the original diagnoses were not recorded, it was unclear exactly which pathologies were treated with tenodesis, limiting our ability to make recommendations regarding treatment trends for specific pathologies. Similarly, we did not assess outcome variables, which would have allowed us to draw conclusions about the effectiveness of the biceps tenodesis procedures. Furthermore, some procedures may have been coded incorrectly, and therefore some patients may have been erroneously included or excluded. In addition, using data from only one institution may have introduced bias into our conclusions, though the results are consistent with national trends. Finally, there was some variability among the 4 surgeons in the number of LHB tenodesis procedures performed, and this variability may have confounded results, though these surgeons treat biceps pathology in similar ways.
Am J Orthop. 2017;46(4):E219-E223. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Denard PJ, Dai X, Hanypsiak BT, Burkhart SS. Anatomy of the biceps tendon: implications for restoring physiological length–tension relation during biceps tenodesis with interference screw fixation. Arthroscopy. 2012;28(10):1352-1358.
2. Ejnisman B, Monteiro GC, Andreoli CV, de Castro Pochini A. Disorder of the long head of the biceps tendon. Br J Sports Med. 2010;44(5):347-354.
3. Mellano CR, Shin JJ, Yanke AB, Verma NN. Disorders of the long head of the biceps tendon. Instr Course Lect. 2015;64:567-576.
4. Szabo I, Boileau P, Walch G. The proximal biceps as a pain generator and results of tenotomy. Sports Med Arthrosc Rev. 2008;16(3):180-186.
5. Harwin SF, Birns ME, Mbabuike JJ, Porter DA, Galano GJ. Arthroscopic tenodesis of the long head of the biceps. Orthopedics. 2014;37(11):743-747.
6. Holtby R, Razmjou H. Accuracy of the Speed’s and Yergason’s tests in detecting biceps pathology and SLAP lesions: comparison with arthroscopic findings. Arthroscopy. 2004;20(3):231-236.
7. Ben Kibler W, Sciascia AD, Hester P, Dome D, Jacobs C. Clinical utility of traditional and new tests in the diagnosis of biceps tendon injuries and superior labrum anterior and posterior lesions in the shoulder. Am J Sports Med. 2009;37(9):1840-1847.
8. Lafosse L, Reiland Y, Baier GP, Toussaint B, Jost B. Anterior and posterior instability of the long head of the biceps tendon in rotator cuff tears: a new classification based on arthroscopic observations. Arthroscopy. 2007;23(1):73-80.
9. Adams CR, Schoolfield JD, Burkhart SS. The results of arthroscopic subscapularis tendon repairs. Arthroscopy. 2008;24(12):1381-1389.
10. Provencher MT, McCormick F, Dewing C, McIntire S, Solomon D. A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: outcomes and factors associated with success and failure. Am J Sports Med. 2013;41(4):880-886.
11. Gombera MM, Kahlenberg CA, Nair R, Saltzman MD, Terry MA. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Med. 2015;43(5):1077-1083.
12. Delle Rose G, Borroni M, Silvestro A, et al. The long head of biceps as a source of pain in active population: tenotomy or tenodesis? A comparison of 2 case series with isolated lesions. Musculoskelet Surg. 2012;96(suppl 1):S47-S52.
13. Chalmers PN, Trombley R, Cip J, et al. Postoperative restoration of upper extremity motion and neuromuscular control during the overhand pitch: evaluation of tenodesis and repair for superior labral anterior-posterior tears. Am J Sports Med. 2014;42(12):2825-2836.
14. Gupta AK, Chalmers PN, Klosterman EL, et al. Subpectoral biceps tenodesis for bicipital tendonitis with SLAP tear. Orthopedics. 2015;38(1):e48-e53.
15. Ge H, Zhang Q, Sun Y, Li J, Sun L, Cheng B. Tenotomy or tenodesis for the long head of biceps lesions in shoulders: a systematic review and meta-analysis. PLoS One. 2015;10(3):e0121286.
16. Kaback LA, Gowda AL, Paller D, Green A, Blaine T. Long head biceps tenodesis with a knotless cinch suture anchor: a biomechanical analysis. Arthroscopy. 2015;31(5):831-835.
17. Kany J, Guinand R, Amaravathi RS, Alassaf I. The keyhole technique for arthroscopic tenodesis of the long head of the biceps tendon. In vivo prospective study with a radio-opaque marker. Orthop Traumatol Surg Res. 2015;101(1):31-34.
18. Mazzocca AD, Cote MP, Arciero CL, Romeo AA, Arciero RA. Clinical outcomes after subpectoral biceps tenodesis with an interference screw. Am J Sports Med. 2008;36(10):1922-1929.
19. Provencher MT, LeClere LE, Romeo AA. Subpectoral biceps tenodesis. Sports Med Arthrosc Rev. 2008;16(3):170-176.
20. Erickson BJ, Jain A, Abrams GD, et al. SLAP lesions: trends in treatment. Arthroscopy. 2016;32(6):976-981.
21. Erickson J, Lavery K, Monica J, Gatt C, Dhawan A. Surgical treatment of symptomatic superior labrum anterior-posterior tears in patients older than 40 years: a systematic review. Am J Sports Med. 2015;43(5):1274-1282.
22. Denard PJ, Ladermann A, Parsley BK, Burkhart SS. Arthroscopic biceps tenodesis compared with repair of isolated type II SLAP lesions in patients older than 35 years. Orthopedics. 2014;37(3):e292-e297.
23. Patterson BM, Creighton RA, Spang JT, Roberson JR, Kamath GV. Surgical trends in the treatment of superior labrum anterior and posterior lesions of the shoulder: analysis of data from the American Board of Orthopaedic Surgery certification examination database. Am J Sports Med. 2014;42(8):1904-1910.
24. Weber SC, Martin DF, Seiler JG 3rd, Harrast JJ. Superior labrum anterior and posterior lesions of the shoulder: incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery. Part II candidates. Am J Sports Med. 2012;40(7):1538-1543.
25. Werner BC, Brockmeier SF, Gwathmey FW. Trends in long head biceps tenodesis. Am J Sports Med. 2015;43(3):570-578.
1. Denard PJ, Dai X, Hanypsiak BT, Burkhart SS. Anatomy of the biceps tendon: implications for restoring physiological length–tension relation during biceps tenodesis with interference screw fixation. Arthroscopy. 2012;28(10):1352-1358.
2. Ejnisman B, Monteiro GC, Andreoli CV, de Castro Pochini A. Disorder of the long head of the biceps tendon. Br J Sports Med. 2010;44(5):347-354.
3. Mellano CR, Shin JJ, Yanke AB, Verma NN. Disorders of the long head of the biceps tendon. Instr Course Lect. 2015;64:567-576.
4. Szabo I, Boileau P, Walch G. The proximal biceps as a pain generator and results of tenotomy. Sports Med Arthrosc Rev. 2008;16(3):180-186.
5. Harwin SF, Birns ME, Mbabuike JJ, Porter DA, Galano GJ. Arthroscopic tenodesis of the long head of the biceps. Orthopedics. 2014;37(11):743-747.
6. Holtby R, Razmjou H. Accuracy of the Speed’s and Yergason’s tests in detecting biceps pathology and SLAP lesions: comparison with arthroscopic findings. Arthroscopy. 2004;20(3):231-236.
7. Ben Kibler W, Sciascia AD, Hester P, Dome D, Jacobs C. Clinical utility of traditional and new tests in the diagnosis of biceps tendon injuries and superior labrum anterior and posterior lesions in the shoulder. Am J Sports Med. 2009;37(9):1840-1847.
8. Lafosse L, Reiland Y, Baier GP, Toussaint B, Jost B. Anterior and posterior instability of the long head of the biceps tendon in rotator cuff tears: a new classification based on arthroscopic observations. Arthroscopy. 2007;23(1):73-80.
9. Adams CR, Schoolfield JD, Burkhart SS. The results of arthroscopic subscapularis tendon repairs. Arthroscopy. 2008;24(12):1381-1389.
10. Provencher MT, McCormick F, Dewing C, McIntire S, Solomon D. A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: outcomes and factors associated with success and failure. Am J Sports Med. 2013;41(4):880-886.
11. Gombera MM, Kahlenberg CA, Nair R, Saltzman MD, Terry MA. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Med. 2015;43(5):1077-1083.
12. Delle Rose G, Borroni M, Silvestro A, et al. The long head of biceps as a source of pain in active population: tenotomy or tenodesis? A comparison of 2 case series with isolated lesions. Musculoskelet Surg. 2012;96(suppl 1):S47-S52.
13. Chalmers PN, Trombley R, Cip J, et al. Postoperative restoration of upper extremity motion and neuromuscular control during the overhand pitch: evaluation of tenodesis and repair for superior labral anterior-posterior tears. Am J Sports Med. 2014;42(12):2825-2836.
14. Gupta AK, Chalmers PN, Klosterman EL, et al. Subpectoral biceps tenodesis for bicipital tendonitis with SLAP tear. Orthopedics. 2015;38(1):e48-e53.
15. Ge H, Zhang Q, Sun Y, Li J, Sun L, Cheng B. Tenotomy or tenodesis for the long head of biceps lesions in shoulders: a systematic review and meta-analysis. PLoS One. 2015;10(3):e0121286.
16. Kaback LA, Gowda AL, Paller D, Green A, Blaine T. Long head biceps tenodesis with a knotless cinch suture anchor: a biomechanical analysis. Arthroscopy. 2015;31(5):831-835.
17. Kany J, Guinand R, Amaravathi RS, Alassaf I. The keyhole technique for arthroscopic tenodesis of the long head of the biceps tendon. In vivo prospective study with a radio-opaque marker. Orthop Traumatol Surg Res. 2015;101(1):31-34.
18. Mazzocca AD, Cote MP, Arciero CL, Romeo AA, Arciero RA. Clinical outcomes after subpectoral biceps tenodesis with an interference screw. Am J Sports Med. 2008;36(10):1922-1929.
19. Provencher MT, LeClere LE, Romeo AA. Subpectoral biceps tenodesis. Sports Med Arthrosc Rev. 2008;16(3):170-176.
20. Erickson BJ, Jain A, Abrams GD, et al. SLAP lesions: trends in treatment. Arthroscopy. 2016;32(6):976-981.
21. Erickson J, Lavery K, Monica J, Gatt C, Dhawan A. Surgical treatment of symptomatic superior labrum anterior-posterior tears in patients older than 40 years: a systematic review. Am J Sports Med. 2015;43(5):1274-1282.
22. Denard PJ, Ladermann A, Parsley BK, Burkhart SS. Arthroscopic biceps tenodesis compared with repair of isolated type II SLAP lesions in patients older than 35 years. Orthopedics. 2014;37(3):e292-e297.
23. Patterson BM, Creighton RA, Spang JT, Roberson JR, Kamath GV. Surgical trends in the treatment of superior labrum anterior and posterior lesions of the shoulder: analysis of data from the American Board of Orthopaedic Surgery certification examination database. Am J Sports Med. 2014;42(8):1904-1910.
24. Weber SC, Martin DF, Seiler JG 3rd, Harrast JJ. Superior labrum anterior and posterior lesions of the shoulder: incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery. Part II candidates. Am J Sports Med. 2012;40(7):1538-1543.
25. Werner BC, Brockmeier SF, Gwathmey FW. Trends in long head biceps tenodesis. Am J Sports Med. 2015;43(3):570-578.
Sarcopenia and the New ICD-10-CM Code: Screening, Staging, and Diagnosis Considerations
Sarcopenia is an age-related loss of skeletal muscle that may result in diminished muscle strength and functional performance. The prevalence of sarcopenia varies based on the cohort and the assessment criteria. According to the Health Aging and Body Composition (ABC) study, the prevalence of sarcopenia in community-dwelling older adults is about 14% to 18%, whereas the estimate may exceed 30% for those in longterm care.1,2 This geriatric syndrome may disproportionately affect veterans given that they are older than the civilian population and may have disabling comorbid conditions associated with military service.3
Recently, there has been a call to action to systematically address sarcopenia by interdisciplinary organizations such as the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the International Working Group on Sarcopenia (IWGS).4,5 This call to action is due to the association of sarcopenia with increased health care costs, higher disability incidence, and elevated risk of mortality.6,7 The consequences of sarcopenia may include serious complications, such as hip fracture or a loss of functional independence.8,9 The CDC now recognizes sarcopenia as an independently reportable medical condition. Consequently, physicians, nurse practitioners (NPs), and other associated health professionals within the VA will need to better understand clinically viable and valid methods to screen and diagnose this geriatric syndrome.
The purpose of this paper is to inform practitioners how sarcopenia screening is aided by the new ICD-10-CM code and briefly review recent VA initiatives for proactive care. Additional objectives include identifying common methods used to assess sarcopenia and providing general recommendations to the VHA National Center for Health Promotion and Disease Prevention (NCP) concerning the management of sarcopenia.
Addressing Sarcopenia
While the age-related decline in muscle size and performance has long been recognized by geriatricians, sustained advocacy by several organizations was required to realize the formal recognition of sarcopenia. Aging in Motion (AIM), a coalition of organizations focused on advancing research and treatment for conditions associated with age-related muscle dysfunction, sought the formal recognition of sarcopenia. The CDC established the ICD-10-CM code for sarcopenia in October of 2016, which allowed the syndrome to be designated as a primary or secondary condition.10
The ubiquitous nature of agerelated changes in muscle and the mandate to engage in proactive care by all levels of VA leadership led to the focus on addressing sarcopenia. The recognition of sarcopenia by the CDC comes at an opportune time given recent VA efforts to transform itself from a facilitator mainly of care delivery to an active partner in fostering the health and well-being of veterans. Initiatives that are emblematic of this attempt to shift the organizational culture across the VHA include establishing the VA Center for Innovation (VACI) and issuing guidance documents, such as the Blueprint for Excellence, which was introduced in 2014 by then VA Secretary Robert McDonald.11,12 Many of the following Blueprint themes and strategies potentially impact sarcopenia screening and treatment within the VA:
- Delivering high-quality, veteran-centered care: A major Blueprint theme is attaining the “Triple Aims” of a health care system by promoting better health among veterans, improving the provision of care, and lowering costs through operational efficiency. The management of sarcopenia has clear clinical value given the association of age-related muscle loss with fall risk and decreased mobility.13 Financial value also may be associated with the effort to decrease disability related to sarcopenia and the use of a team approach featuring associated health professionals to help screen for this geriatric syndrome.14,15 (Strategy 2)
- Leveraging health care informatics to optimize individual and population health outcomes: The inclusion of the most basic muscle performance and functional status measures in the electronic medical record (EMR), such as grip strength and gait speed, would help to identify the risk factors and determinants of sarcopenia among the veteran population. (Strategy 3)
- Advancing personalized, proactive health care that fosters a high level of health and well-being: The long-term promotion of musculoskeletal health and optimal management of sarcopenia cannot be sustained through episodic medical interactions. Instead, a contemporary approach to health services marked by the continuous promotion of health education, physical activity and exercise, and proper nutrition has demonstrated value in the management of chronic conditions.16,17 (Strategy 6)
The new sarcopenia ICD-10-CM code along with elements of the VHA Blueprint can serve to support the systematic assessment and management of veterans with age-related muscle dysfunction. Nevertheless, renewed calls for health promotion and screening programs are often counterbalanced by the need for cost containment and the cautionary tales concerning the potential harms or errors associated with some forms of medical screening. The American Board of Internal Medicine Foundation has spearheaded the Choosing Wisely campaign to raise awareness about excessive medical testing. However, the Institute of Medicine has linked the provision of quality health care to a diagnostic process that is both timely and accurate.18 Careful consideration of these health care challenges may help guide practitioners within the VA concerning the screening and diagnosis of sarcopenia.
Sarcopenia Assessment
Sarcopenia can have several underlying causes in some individuals and result in varied patterns of clinical presentation and differing degrees of severity. The European Working Group on Sarcopenia in Older People first met in 2009 and used a consensus-based decision-making process to determine operational definitions for sarcopenia and create a staging algorithm for the syndrome.19 This consensus group developed a conceptual staging model with 3 categories: presarcopenia, sarcopenia, and severe sarcopenia (Table 1). The impetus for sarcopenia staging was the emerging research findings suggesting that lean body mass (LBM) alone did not provide a high degree of clinical value in outpatient settings due to the nonlinear relationship between LBM and muscle function in older adults.20,21 Using the consensus model approach, an individual is classified as sarcopenic on presenting with both low LBM and low muscle function.
Screening: A Place to Start
Findings from the Health ABC Study suggested that older adults who maintained high levels of LBM were less likely to become sarcopenic. Whereas, older adults in the cohort with low levels of LBM tended to remain in a sarcopenic state.6 Consequently, the early detection of sarcopenia may have important health promotion implications for older adults. Sarcopenia is a syndrome with a continuum of clinical features; it is not a disease with a clear or singular etiololgy. Therefore, the result of the screening examination should identify those who would most benefit from a formal diagnostic assessment.
One approach to screening for sarcopenia involves the use of questionnaires, such as the SARC-F (sluggishness, assistance in walking, rise from a chair, climb stairs, falls), which is a brief 5-item questionnaire with Likert scoring for patient responses.13 In a cohort of National Health and Nutrition Examination Survey (NHANES) participants, SARC-F scores ≥ 4 were associated with slower gait speed, lower strength, and an increased likelihood of hospitalization within a year of the test response.22 However, rather than stratify patients by risk, the SARC-F exhibits a high degree of test specificity regarding the major consensus-based sarcopenia classification criteria (specificity = 94.2% to 99.1%; sensitivity = 3.8% to 9.9%).13 Given the known limitations of screening tools with low sensitivity, organizations such as the ESCEO have recommended supplementing the SARC-F questionnaire with other forms of assessment.4 Supplements to the screening examination may range from the use of “red flag” questions concerning changes in nutritional status, body weight, and physical activity, to conducting standard gait speed and grip-strength testing.4,19,23
Performance-based testing, including habitual gait speed and grip-strength dynamometry, also may be used in both the screening and classification of sarcopenia.2 Although walking speed below 1.0 m/s has been used by the IWGS as a criterion to prompt further assessment, many people within the VA health care system may have gait abnormalities independent of LBM status, and others may be nonambulatory.24,25 As a result, grip-strength testing should be considered as a supplementary or alternate screening assessment tool.26,27
Hand-grip dynamometry is often used diagnostically given its previous test validation, low expense, and ease of use.23 Moreover, recent evidence suggests that muscle strength surpasses gait speed as a means of identifying people with sarcopenia. Grip strength is associated with all-cause mortality, even when adjusting for age, sex, and body size,28 while slow gait speed (< .82 m/s) has a reported sensitivity of 63% and specificity of 70% for mortality in population-based studies involving older adults.29
Gait speed (in those who are ambulatory) and grip-strength values could be entered into the EMR evaluation note by the primary care provider (PCP). Elements of the VA EMR, such as the ability to review the diagnosis of sarcopenia on the Problem List or the nominal enhancement of providing LBM estimates within the Cumulative Vitals and Measurements Report would support the management of sarcopenia. See Table 2 for cutoff values for frequently used sarcopenia screening and staging tests.
The pitfalls of excessive or inappropriate screening are well documented. The efforts to screen for prostate cancer have highlighted instances when inappropriate followup tests and treatment fail to alter mortality rates and ultimately yield more harm than good.30 However, there are several points of departure concerning the screening for sarcopenia vs screening for prostate cancer. The screening assessments for sarcopenia are low-cost procedures that are associated with a low patient burden. These procedures may include questionnaires, functional testing, or the assessment of muscle performance. Additionally, there is a low propensity for adverse effects stemming from treatment due to disease misclassification given the common nonpharmacologic approaches used to manage sarcopenia.31 Nonetheless, the best screening examination—even one that has low patient burden and cost—may prove to be a poor use of medical resources if the process is not linked to a viable intervention.
Screening people aged ≥ 65 years may strike a balance between controlling health care expenditures and identifying people with the initial signs of sarcopenia early enough to begin monitoring key outcomes and providing a formalized exercise prescription. Presuming an annual age-related decline in LBM of 1.5%, and considering the standard error measurement of the most frequently used methods of strength and LBM assessment, recurrent screening could occur every 2 years.21,32
Earlier screening may be considered for patient populations with a higher pretest probability. These groups include those with conditions associated with accelerated muscle loss, such as chronic kidney disease, peripheral artery disease, and diabetes mellitus (DM).32 Although accelerated muscle loss characterized by an inflammatory motif (eg, cancer-related cachexia) may share some features of the sarcopenia screening and assessment approach, important differences exist regarding the etiology, medical evaluation, and ICD-10-CM code designation.
Staging and Classification
Staging criteria are generally used to denote the severity of a given disease or syndrome, whereas classification criteria are used to define homogenous patient groups based on specific pathologic or clinical features of a disorder. Although classification schemes may incorporate an element of severity, they are primarily used to characterize fairly distinct phenotypic forms of disease or specific clinical presentation patterns associated with a well-defined syndrome. Although not universally adopted, the European consensus group sarcopenia staging criteria are increasingly used to provide a staging algorithm presumably driven by the severity of the condition.19
The assessment of functional performance for use in sarcopenia staging often involves measuring habitual gait speed or completing the Short Physical Performance Battery (SPPB).23 The SPPB involves a variety of performance-based activities for balance, gait, strength, and endurance. This test has predictive validity for the onset of disability and adverse health events, and it has been extensively used in research and clinical settings.33 Additional tests used to characterize function during the staging or diagnostic process include the timed get up and go test (TGUG) and the timed sit to stand test.34,35 The TGUG provides an estimate of dynamic balance, and the sit to stand test has been used as very basic proxy measure of muscular power.36 The sit to stand test and habitual gait speed are items included in the SPPB.33
Accepted methods to obtain the traditional index measure of sarcopenia—based on estimates of LBM—include bioimpedance analysis (BIA) and dual X-ray absorptiometry (DXA). The BIA uses the electrical impedance of body tissues and its 2 components, resistance and reactance, to derive its body composition estimates.37 Segmental BIA allows for isolated measurements of the limbs, which may be calibrated to DXA appendicular lean body mass (ALM) or magnetic resonance imaging-based estimates of LBM. This instrument is relatively safe for use, inexpensive for medical facilities, and useful for longitudinal studies, but it can be confounded by issues, such as varying levels of hydration, which may affect measurement validity in some instances.
Despite the precision of DXA for estimating densities for whole body composition analysis, the equipment is not very portable and involves low levels of radiation exposure, which limits its utility in some clinical settings. While each body composition assessment method has its advantages and disadvantages, DXA is regarded as an acceptable form of measurement for hospital settings, and BIA is frequently used in outpatient clinics and community settings. Other methods used to estimate LBM with greater accuracy, such as peripheral quantitative computed tomography, doubly labeled water, and whole body gamma ray counting, are not viable for clinical use. Other accessible methods such as anthropometric measures and skinfold measures have not been embraced by sarcopenia classification consensus groups.23,37
Alternative methods of estimating LBM, such as diagnostic ultrasound and multifrequency electrical impedance myography, are featured outcomes in ongoing clinical trials that involve veteran participants. These modalities may soon provide a clinically viable approach to assessing muscle quality via estimates of muscle tissue composition.37,38 Similar to the management of other geriatric syndromes, interprofessional collaboration provides an optimal approach to the assessment of sarcopenia. Physicians and other health care providers may draw on the standardized assessment of strength and function (via the SPPB and hand-grip dynamometry) by physical therapists (PTs), questionnaires administered by nursing staff (the SARC-F), or body composition estimates from other health professionals (ranging from BIA to DXA) to aid the diagnostic process and facilitate appropriate case management (Table 2).
Competing staging and classification definitions have been cited as a primary factor behind the CDC’s delayed recognition of the sarcopenia diagnosis, which in turn posed a barrier to formal clinical recognition by geriatricians.24 However, this reaction to the evolving sarcopenia staging criteria also may reveal the larger misapplication of the staging process to the diagnostic process. The application of classification and staging criteria results in a homogenous group of patients, whereas the application of diagnostic criteria results in a heterogeneous group of patients to account for variations in clinical presentation associated with a given disorder. Classification criteria may be equivalent to objective measures that are used in the diagnostic process when a given disease is characterized by a well-established biomarker.39
However, this is not the case for most geriatric syndromes and other disorders marked by varied clinical presentation patterns. On considering the commonly used sarcopenia staging criteria of LBM ≤ 8.50 kg/m2 or grip strength < 30 kg in men and LBM ≤ 5.75 kg/m2 or grip strength < 20 kg in women, it is easy to understand that such general cutoff values are far from diagnostic.40,41 Moreover, stringent cutoff values associated with classification and staging may not adequately capture those with an atypical presentation of the syndrome (eg, someone who exhibits age-related muscle weakness but has retained adequate LBM). Such criteria often prove to have high specificity and low sensitivity, which may yield a false negative rate that is appropriate for clinical research eligibility and group assignment but inadequate for clinical care.
Screening, staging, and classification criteria with high specificity may indeed be desirable for confirmatory imaging tests associated with radiation exposure concerns or for managing risk in experimental clinical trials involving pharmacologic treatment. For example, a SARC-F score ≥ 4 may prompt the formal assessment of LBM via a DXA examination.4 In contrast, those with a SARC-F score ≤ 3 with low gait speed or grip strength may benefit from consultation regarding regular physical activity and nutrition recommendations. Given the challenges of establishing sarcopenia classification criteria that perform consistently across populations and geographic regions, classification and staging criteria may be best viewed as clinical reasoning tools that supplement, but not supplant, the diagnostic process.7,42
Diagnosis
Geriatric syndromes do not lend themselves to a simple diagnostic process. Syndromes such as frailty and sarcopenia are multifactorial and lack a single distinguishing clinical feature or biomarker. The oft-cited refrain that sarcopenia is an underdiagnosed condition is partially explained by the recent ICD-10-CM code and varied classification and diagnostic criteria.5 This circumstance highlights the need to distinctly contrast the diagnostic process with the screening and staging classifications.
The diagnostic process involves the interpretation of the patient history, signs, and symptoms within the context of individual factors, local or regional disease prevalence, and the results of the best available and most appropriate laboratory tests. After all, a patient that presents with low LBM and a gradual loss of strength without a precipitating event would necessitate further workup to rule out many clinical possibilities under the aegis of a differential diagnosis. Clinical features, such as the magnitude of weakness and pattern of strength loss or muscle atrophy along with the determination of neurologic or autoimmune involvement, are among the key elements of the differential examination for a case involving the observation of frank muscle weakness. Older adults with low muscle strength may have additional risk factors for sarcopenia such as obesity, pain, poor nutrition, previous bone fracture, and a sedentary lifestyle. However, disease etiology with lower probabilities, such as myogenic or neurogenic conditions associated with advancing age, also may be under consideration during the clinical assessment.6
In many instances, the cutoff scores associated with the sarcopenia staging criteria may help to guide the diagnostic process and aid clinical decision making. Since individuals with a positive screening result based on the SARC-F questionnaire (score ≥ 4) have a high likelihood of meeting the staging criteria for severe sarcopenia, a PCP may opt to obtain a confirmatory estimate of LBM both to support the clinical assessment and to monitor change over the course of rehabilitation. Whereas people who present with a decline in strength (ie, grip strength < 30 kg for a male) without an observable loss of function or a positive SARC-F score may benefit from consultation from the physician, NP, or rehabilitation health professional regarding modifiable risk factors associated with sarcopenia.
Incorporating less frequently used sarcopenia classification schemes such as identifying those with sarcopenic obesity or secondary sarcopenia due to mitigating factors such as chronic kidney disease or DM (Table 3) may engender a more comprehensive approach to intervention that targets the primary disease while also addressing important secondary sequelae. Nevertheless, staging or classification criteria cannot be deemed equivalent to diagnostic criteria for sarcopenia due to the challenges posed by syndromes that have a heterogeneous clinical presentation.
The refinement of the staging and classification criteria along with the advances in imaging technology and mechanistic research are not unique to sarcopenia. Practitioners involved in the care of people with rheumatologic conditions or osteoporosis also have contended with continued refinements to their classification criteria and approach to risk stratification.39,43,44 Primary care providers will now have the option to use a new ICD-10-CM code (M62.84) for sarcopenia, which will allow them to properly document the clinical distinctions between people with impaired strength or function largely due to age-related muscle changes and those who have impaired muscle function due to cachexia, inflammatory myopathies, or forms of neuromuscular disease.
The ability to identify and document this geriatric syndrome in veterans will help to better define the scope of the problem within the VA health care system. The median age of veterans is 62 years compared with 43 years for nonveterans.3 Consequently, there may be value in the adoption of a formal approach to screening and diagnosis for sarcopenia among veterans who receive their primary care from VA facilities.7 Indeed, the exchange between the patient and the health professional regarding the screening and diagnostic process will provide valuable opportunities to promote exercise interventions before patients incur significant impairments.
One of the biggest threats burdening global health is noncommunicable diseases, and many chronic conditions, such as sarcopenia, can be prevented and managed with appropriate levels of physical activity.17 Increased physician involvement may prove to be critical given the identification of physical inactivity as a top 5 risk factor for general morbidity and mortality by World Health Organization and consensus group recommendations calling for physicians to serve a more prominent role in the provision of exercise and physical activity recommendations.16,17
This developing health care role should include NPs, PTs, physician assistants, and other associated health professionals. It also should include collaborative efforts between physicians and rehabilitation practitioners concerning provision of the formal exercise prescriptionprescription and monitoring of patient outcomes.
Individuals with severe forms of sarcopenia rarely improve without intervention.6 Although no pharmacologic treatment exists to specifically address sarcopenia, strengthening exercise has been shown to be an effective mode of prevention and conservative management.8 Progressive resistance exercise cannot abate the expected age-related changes in skeletal muscle, but it can significantly reverse the loss of LBM and strength in untrained older adults and slow the age-related decline in muscle performance in older adult athletes and trained individuals.45
Local senior centers and community organizations may prove to be valuable resources concerning group exercise options, and they provide the added benefit of social engagement and peer group accountability. Federal resources include the Go4Life exercise guide and online videos provided by the National Institute on Aging and the MOVE! Weight Management and Health Program provided at select VA community-based outpatient clinics. Ultimately, collaborative efforts with exercise specialists may serve to reduce the PCP burden during the provision of health services, minimize diagnostic errors associated with sarcopenia assessment and help to connect patients to valuable health promotion resources.17,18
Conclusion
While practitioners should remain keenly aware of the pernicious effects of overdiagnosis, sarcopenia has long existed as a known, but undiagnosed, condition. Of course, geriatricians have traditionally managed poor muscle performance and mobility limitations by addressing treatable symptoms and providing referrals to physical medicine specialists when warranted. Nevertheless, the advent of ICD-10-CM code M62.84 provides the VA with an opportunity to take a leading role in systematically addressing this geriatric syndrome within an aging veteran population.
The following items should be considered by NCP for the development of guidelines and recommendations concerning sarcopenia screening:
- Consider screening veterans aged > 65 years for sarcopenia every 2 years. Those with mitigating systemic conditions (eg, chronic kidney disease, DM, or malnutrition) or significant mobility limitations may be screened at any age.
- Sarcopenia screening procedures should include at a minimum the SARC-F questionnaire and gait speed (when appropriate). Including gait speed or grip strength testing in the screening exam is recommended given the low sensitivity of the SARC-F questionnaire.
- Veterans with positive SARC-F results (≥ 4) merit a physical therapy referral. In addition, these veterans should obtain confirmatory standardized assessments for LBM and functional status.
- Veterans at risk for sarcopenia based on patient age, medical history, and the physical examination (eg, obesity, sedentary lifestyle, a previous fracture, self-reported physical decline), but with negative SARC-F results should receive a formal exercise prescription from their PCP. Baseline assessment measures may be used for comparison with serial measures obtained during subsequent screening visits to support long-term case management.
- Interprofessional collaboration involving geriatricians, PTs, nurses, radiologists, and other health care professionals should be involved in the screening, diagnosis, and case management of veterans with sarcopenia.
- The VA EMR should be systematically documented with sarcopenia assessment data obtained from the gait speed tests, SARCF, SPPB, grip strength tests, and LBM estimates to better characterize this condition within the veteran population.
Any expansion in the provision of health care comes with anticipated benefits and potential costs. Broad guidance from NCP may encourage veterans to pursue selected screening tests, promote the appropriate use of preventative services, and facilitate timely treatment when needed.31 Clinicians who are informed about the screening, staging, classification, and diagnostic process for sarcopenia may partner with patients to make reasoned decisions about how to best manage this syndrome within the VA medical center environment.
1. Newman AB, Kupelian V, Visser M, et al; Health ABC Study Investigators. Sarcopenia: alternative definitions and associations with lower extremity function. J Am Geriatr Soc. 2003;51(11):1602-1609.
2. Cruz-Jentoft AJ, Landi F, Schneider SM, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014;43(6):748-759.
3. U.S. Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Profile of veterans: 2009. Data from the American Community Survey. http://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2009_FINAL.pdf. Published January 2011. Accessed May 18, 2017.
4. Beaudart C, McCloskey E, Bruyère O, et al. Sarcopenia in daily practice: assessment and management. BMC Geriatr. 2016;16(1):170.
5. Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249-256.
6. Murphy RA, Ip EH, Zhang Q, et al; Health, Aging, and Body Composition Study. Transition to sarcopenia and determinants of transitions in older adults: a population-based study. J Gerontol A Biol Sci Med Sci. 2014;69(6):751-758.
7. Harris-Love MO, Adams B, Hernandez HJ, DiPietro L, Blackman MR. Disparities in the consequences of sarcopenia: implications for African American veterans. Front Physiol. 2014;5:250.
8. Morley JE. Sarcopenia in the elderly. Fam Pract. 2012;29(suppl 1):i44-i48.
9. Fragala MS, Dam TT, Barber V, et al. Strength and function response to clinical interventions of older women categorized by weakness and low lean mass using classifications from the Foundation for the National Institute of Health sarcopenia project. J Gerontol A Biol Sci Med Sci. 2015;70(2):202-209.
10. Aging in Motion. AIM coalition announces establishment of ICD-10-CM Code for Sarcopenia
by the Centers for Disease Control and Prevention [press release]. http://aginginmotion.org/news/2388-2/. Published April 28, 2016. Accessed June 7, 2017.
11. U.S. Department of Veterans Affairs, Veterans Health Administration. Blueprint for excellence. https://www.va.gov/HEALTH/docs/VHA _Blueprint_for_Excellence.pdf. Published September 21, 2014. Accessed June 7, 2017.
12. U.S. Department of Veterans Affairs. VA Center of Innovation 2010–2012 stakeholder report. https://www.innovation.va.gov/docs/VACI_2010-2012_Stakeholder_Report.pdf. Published 2012. Accessed June 14, 2017.
13. Woo J, Leung J, Morley JE. Validating the SARCF: a suitable community screening tool for sarcopenia? J Am Med Dir Assoc. 2014;15(9):630-634.
14. Sousa AS, Guerra RS, Fonseca I, Pichel F, Ferreira S, Amaral TF. Financial impact of sarcopenia on hospitalization costs. Eur J Clin Nutr. 2016;70(9):1046-1051.
15. Janssen I, Shepard DS, Katzmarzyk PT, Roubenoff R. The healthcare costs of sarcopenia in the United States. J Am Geriatr Soc. 2004;52(1):80-85.
16. Ekelund U, Steene-Johannessen J, Brown WJ, et al; Lancet Physical Activity Series 2 Executive Committe; Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302-1310.
17. Thornton JS, Frémont P, Khan K, et al. Physical activity prescription: a critical opportunity to address a modifiable risk factor for the prevention and management of chronic disease: a position statement by the Canadian Academy of Sport and Exercise Medicine. Clin J Sport Med.
2016;26(4):259-265.
18. The National Academies of Sciences, Engineering, and Medicine; Committee on Diagnostic Error in Health Care, Board on Health Care Services; Institute of Medicine. Improving Diagnosis in Health Care. Washington, DC: National Academies Press;2015.
19. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al; European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412-423.
20. Ferrucci L, Guralnik JM, Buchner D, et al. Departures from linearity in the relationship between measures of muscular strength and physical performance of the lower extremities: the Women’s Health and Aging Study. J Gerontol A Biol Sci Med Sci. 1997;52(5):M275-M285.
21. Goodpaster BH, Park SW, Harris TB, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the Health, Aging and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2006;61(10):1059-1064.
22. Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle. 2016;7(1):28-36.
23. Cooper C, Fielding R, Visser M, et al. Tools in the assessment of sarcopenia. Calcif Tissue Int. 2013;93(3):201-210.
24. Lee WJ, Liu LK, Peng LN, Lin MH, Chen LK; ILAS Research Group. Comparisons of sarcopenia defined by IWGS and EWGSOP criteria among older people: results from the I-Lan longitudinal aging study. J Am Med Dir Assoc. 2013;14(7):528.e1-e7.
25. Cesari M, Kritchevsky SB, Penninx BW, et al. Prognostic value of usual gait speed in well-functioning older people—results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53(10):1675-1680.
26. Rossi AP, Fantin F, Micciolo R, et al. Identifying sarcopenia in acute care setting patients. J Am Med Dir Assoc. 2014;15(4):303.e7-e12.
27. Sánchez-Rodríguez D, Marco E, Miralles R, et al. Does gait speed contribute to sarcopenia casefinding in a postacute rehabilitation setting? Arch Gerontol Geriatr. 2015;61(2):176-181.
28. Strand BH, Cooper R, Bergland A, et al. The association of grip strength from midlife onwards with all-cause and cause-specific mortality over 17 years of follow-up in the Tromsø Study. J Epidemiol Community Health. 2016;70:1214-1221.
29. Stanaway FF, Gnjidic D, Blyth FM, et al. How fast does the Grim Reaper walk? Receiver operating characteristics curve analysis in healthy men aged 70 and over. BMJ. 2011;343:d7679.
30. Reiter RE. Risk stratification of prostate cancer 2016. Scand J Clin Lab Invest Suppl. 2016;245:S54-S59.
31. U.S. Department of Veterans Affairs, National Center for Health Promotion and Disease Prevention. Get recommended screening tests and immunizations. https://www.prevention.va.gov/Healthy_Living/Get_Recommended_Screening_Tests_and_Immunizations.asp. Updated September 9, 2016. Accessed June 7, 2017.
32. Buford TW, Anton SD, Judge AR, et al. Models of accelerated sarcopenia: critical pieces for solving the puzzle of age-related muscle atrophy. Ageing Res Rev. 2010;9(4):369-383.
33. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85-M94.
34. Daubney ME, Culham EG. Lower-extremity muscle force and balance performance in adults aged 65 years and older. Phys Ther. 1999;79(12):1177-1185.
35. Bohannon RW. Reference values for the fiverepetition sit-to-stand test: a descriptive metaanalysis of data from elders. Percept Mot Skills. 2006;103(1):215-222.
36. Correa-de-Araujo R, Harris-Love MO, Miljkovic I, Fragala MS, Anthony BW, Manini TM. The need for standardized assessment of muscle quality in skeletal muscle function deficit and other agingrelated muscle dysfunctions: a symposium report. Front Physiol. 2017;8:87.
37. Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J. Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc. 2015;74(4):355-366.
38. Harris-Love MO, Monfaredi R, Ismail C, Blackman MR, Cleary K. Quantitative ultrasound: measurement considerations for the assessment of muscular dystrophy and sarcopenia. Front Aging Neurosci. 2014;6:172.
39. Fries JF, Hochberg MC, Medsger TA Jr, Hunder GG, Bombardier C. Criteria for rheumatic disease. Different types and different functions. The American College of Rheumatology Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum. 1994;37(4):454-462.
40. Janssen I, Baumgartner RN, Ross R, Rosenberg IH, Roubenoff R. Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. Am J Epidemiol.
2004;159(4):413-421.
41. Ismail C, Zabal J, Hernandez HJ, et al. Diagnostic ultrasound estimates of muscle mass and muscle quality discriminate between women with and without sarcopenia. Front Physiol. 2015;6:302.
42. Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15(2):95-101.
43. Aggarwal R, Ringold S, Khanna D, et al. Distinctions between diagnostic and classification criteria? Arthritis Care Res (Hoboken). 2015;67(7):891-897.
44. Licata A. Bone density vs bone quality: what’s a clinician to do? Cleve Clin J Med. 2009;76(6):331-336.
45. Pollock ML, Mengelkoch LJ, Graves JE, et al. Twenty-year follow-up of aerobic power and body composition of older track athletes. J Appl Physiol. 1997;82(5):1508-1516.
Sarcopenia is an age-related loss of skeletal muscle that may result in diminished muscle strength and functional performance. The prevalence of sarcopenia varies based on the cohort and the assessment criteria. According to the Health Aging and Body Composition (ABC) study, the prevalence of sarcopenia in community-dwelling older adults is about 14% to 18%, whereas the estimate may exceed 30% for those in longterm care.1,2 This geriatric syndrome may disproportionately affect veterans given that they are older than the civilian population and may have disabling comorbid conditions associated with military service.3
Recently, there has been a call to action to systematically address sarcopenia by interdisciplinary organizations such as the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the International Working Group on Sarcopenia (IWGS).4,5 This call to action is due to the association of sarcopenia with increased health care costs, higher disability incidence, and elevated risk of mortality.6,7 The consequences of sarcopenia may include serious complications, such as hip fracture or a loss of functional independence.8,9 The CDC now recognizes sarcopenia as an independently reportable medical condition. Consequently, physicians, nurse practitioners (NPs), and other associated health professionals within the VA will need to better understand clinically viable and valid methods to screen and diagnose this geriatric syndrome.
The purpose of this paper is to inform practitioners how sarcopenia screening is aided by the new ICD-10-CM code and briefly review recent VA initiatives for proactive care. Additional objectives include identifying common methods used to assess sarcopenia and providing general recommendations to the VHA National Center for Health Promotion and Disease Prevention (NCP) concerning the management of sarcopenia.
Addressing Sarcopenia
While the age-related decline in muscle size and performance has long been recognized by geriatricians, sustained advocacy by several organizations was required to realize the formal recognition of sarcopenia. Aging in Motion (AIM), a coalition of organizations focused on advancing research and treatment for conditions associated with age-related muscle dysfunction, sought the formal recognition of sarcopenia. The CDC established the ICD-10-CM code for sarcopenia in October of 2016, which allowed the syndrome to be designated as a primary or secondary condition.10
The ubiquitous nature of agerelated changes in muscle and the mandate to engage in proactive care by all levels of VA leadership led to the focus on addressing sarcopenia. The recognition of sarcopenia by the CDC comes at an opportune time given recent VA efforts to transform itself from a facilitator mainly of care delivery to an active partner in fostering the health and well-being of veterans. Initiatives that are emblematic of this attempt to shift the organizational culture across the VHA include establishing the VA Center for Innovation (VACI) and issuing guidance documents, such as the Blueprint for Excellence, which was introduced in 2014 by then VA Secretary Robert McDonald.11,12 Many of the following Blueprint themes and strategies potentially impact sarcopenia screening and treatment within the VA:
- Delivering high-quality, veteran-centered care: A major Blueprint theme is attaining the “Triple Aims” of a health care system by promoting better health among veterans, improving the provision of care, and lowering costs through operational efficiency. The management of sarcopenia has clear clinical value given the association of age-related muscle loss with fall risk and decreased mobility.13 Financial value also may be associated with the effort to decrease disability related to sarcopenia and the use of a team approach featuring associated health professionals to help screen for this geriatric syndrome.14,15 (Strategy 2)
- Leveraging health care informatics to optimize individual and population health outcomes: The inclusion of the most basic muscle performance and functional status measures in the electronic medical record (EMR), such as grip strength and gait speed, would help to identify the risk factors and determinants of sarcopenia among the veteran population. (Strategy 3)
- Advancing personalized, proactive health care that fosters a high level of health and well-being: The long-term promotion of musculoskeletal health and optimal management of sarcopenia cannot be sustained through episodic medical interactions. Instead, a contemporary approach to health services marked by the continuous promotion of health education, physical activity and exercise, and proper nutrition has demonstrated value in the management of chronic conditions.16,17 (Strategy 6)
The new sarcopenia ICD-10-CM code along with elements of the VHA Blueprint can serve to support the systematic assessment and management of veterans with age-related muscle dysfunction. Nevertheless, renewed calls for health promotion and screening programs are often counterbalanced by the need for cost containment and the cautionary tales concerning the potential harms or errors associated with some forms of medical screening. The American Board of Internal Medicine Foundation has spearheaded the Choosing Wisely campaign to raise awareness about excessive medical testing. However, the Institute of Medicine has linked the provision of quality health care to a diagnostic process that is both timely and accurate.18 Careful consideration of these health care challenges may help guide practitioners within the VA concerning the screening and diagnosis of sarcopenia.
Sarcopenia Assessment
Sarcopenia can have several underlying causes in some individuals and result in varied patterns of clinical presentation and differing degrees of severity. The European Working Group on Sarcopenia in Older People first met in 2009 and used a consensus-based decision-making process to determine operational definitions for sarcopenia and create a staging algorithm for the syndrome.19 This consensus group developed a conceptual staging model with 3 categories: presarcopenia, sarcopenia, and severe sarcopenia (Table 1). The impetus for sarcopenia staging was the emerging research findings suggesting that lean body mass (LBM) alone did not provide a high degree of clinical value in outpatient settings due to the nonlinear relationship between LBM and muscle function in older adults.20,21 Using the consensus model approach, an individual is classified as sarcopenic on presenting with both low LBM and low muscle function.
Screening: A Place to Start
Findings from the Health ABC Study suggested that older adults who maintained high levels of LBM were less likely to become sarcopenic. Whereas, older adults in the cohort with low levels of LBM tended to remain in a sarcopenic state.6 Consequently, the early detection of sarcopenia may have important health promotion implications for older adults. Sarcopenia is a syndrome with a continuum of clinical features; it is not a disease with a clear or singular etiololgy. Therefore, the result of the screening examination should identify those who would most benefit from a formal diagnostic assessment.
One approach to screening for sarcopenia involves the use of questionnaires, such as the SARC-F (sluggishness, assistance in walking, rise from a chair, climb stairs, falls), which is a brief 5-item questionnaire with Likert scoring for patient responses.13 In a cohort of National Health and Nutrition Examination Survey (NHANES) participants, SARC-F scores ≥ 4 were associated with slower gait speed, lower strength, and an increased likelihood of hospitalization within a year of the test response.22 However, rather than stratify patients by risk, the SARC-F exhibits a high degree of test specificity regarding the major consensus-based sarcopenia classification criteria (specificity = 94.2% to 99.1%; sensitivity = 3.8% to 9.9%).13 Given the known limitations of screening tools with low sensitivity, organizations such as the ESCEO have recommended supplementing the SARC-F questionnaire with other forms of assessment.4 Supplements to the screening examination may range from the use of “red flag” questions concerning changes in nutritional status, body weight, and physical activity, to conducting standard gait speed and grip-strength testing.4,19,23
Performance-based testing, including habitual gait speed and grip-strength dynamometry, also may be used in both the screening and classification of sarcopenia.2 Although walking speed below 1.0 m/s has been used by the IWGS as a criterion to prompt further assessment, many people within the VA health care system may have gait abnormalities independent of LBM status, and others may be nonambulatory.24,25 As a result, grip-strength testing should be considered as a supplementary or alternate screening assessment tool.26,27
Hand-grip dynamometry is often used diagnostically given its previous test validation, low expense, and ease of use.23 Moreover, recent evidence suggests that muscle strength surpasses gait speed as a means of identifying people with sarcopenia. Grip strength is associated with all-cause mortality, even when adjusting for age, sex, and body size,28 while slow gait speed (< .82 m/s) has a reported sensitivity of 63% and specificity of 70% for mortality in population-based studies involving older adults.29
Gait speed (in those who are ambulatory) and grip-strength values could be entered into the EMR evaluation note by the primary care provider (PCP). Elements of the VA EMR, such as the ability to review the diagnosis of sarcopenia on the Problem List or the nominal enhancement of providing LBM estimates within the Cumulative Vitals and Measurements Report would support the management of sarcopenia. See Table 2 for cutoff values for frequently used sarcopenia screening and staging tests.
The pitfalls of excessive or inappropriate screening are well documented. The efforts to screen for prostate cancer have highlighted instances when inappropriate followup tests and treatment fail to alter mortality rates and ultimately yield more harm than good.30 However, there are several points of departure concerning the screening for sarcopenia vs screening for prostate cancer. The screening assessments for sarcopenia are low-cost procedures that are associated with a low patient burden. These procedures may include questionnaires, functional testing, or the assessment of muscle performance. Additionally, there is a low propensity for adverse effects stemming from treatment due to disease misclassification given the common nonpharmacologic approaches used to manage sarcopenia.31 Nonetheless, the best screening examination—even one that has low patient burden and cost—may prove to be a poor use of medical resources if the process is not linked to a viable intervention.
Screening people aged ≥ 65 years may strike a balance between controlling health care expenditures and identifying people with the initial signs of sarcopenia early enough to begin monitoring key outcomes and providing a formalized exercise prescription. Presuming an annual age-related decline in LBM of 1.5%, and considering the standard error measurement of the most frequently used methods of strength and LBM assessment, recurrent screening could occur every 2 years.21,32
Earlier screening may be considered for patient populations with a higher pretest probability. These groups include those with conditions associated with accelerated muscle loss, such as chronic kidney disease, peripheral artery disease, and diabetes mellitus (DM).32 Although accelerated muscle loss characterized by an inflammatory motif (eg, cancer-related cachexia) may share some features of the sarcopenia screening and assessment approach, important differences exist regarding the etiology, medical evaluation, and ICD-10-CM code designation.
Staging and Classification
Staging criteria are generally used to denote the severity of a given disease or syndrome, whereas classification criteria are used to define homogenous patient groups based on specific pathologic or clinical features of a disorder. Although classification schemes may incorporate an element of severity, they are primarily used to characterize fairly distinct phenotypic forms of disease or specific clinical presentation patterns associated with a well-defined syndrome. Although not universally adopted, the European consensus group sarcopenia staging criteria are increasingly used to provide a staging algorithm presumably driven by the severity of the condition.19
The assessment of functional performance for use in sarcopenia staging often involves measuring habitual gait speed or completing the Short Physical Performance Battery (SPPB).23 The SPPB involves a variety of performance-based activities for balance, gait, strength, and endurance. This test has predictive validity for the onset of disability and adverse health events, and it has been extensively used in research and clinical settings.33 Additional tests used to characterize function during the staging or diagnostic process include the timed get up and go test (TGUG) and the timed sit to stand test.34,35 The TGUG provides an estimate of dynamic balance, and the sit to stand test has been used as very basic proxy measure of muscular power.36 The sit to stand test and habitual gait speed are items included in the SPPB.33
Accepted methods to obtain the traditional index measure of sarcopenia—based on estimates of LBM—include bioimpedance analysis (BIA) and dual X-ray absorptiometry (DXA). The BIA uses the electrical impedance of body tissues and its 2 components, resistance and reactance, to derive its body composition estimates.37 Segmental BIA allows for isolated measurements of the limbs, which may be calibrated to DXA appendicular lean body mass (ALM) or magnetic resonance imaging-based estimates of LBM. This instrument is relatively safe for use, inexpensive for medical facilities, and useful for longitudinal studies, but it can be confounded by issues, such as varying levels of hydration, which may affect measurement validity in some instances.
Despite the precision of DXA for estimating densities for whole body composition analysis, the equipment is not very portable and involves low levels of radiation exposure, which limits its utility in some clinical settings. While each body composition assessment method has its advantages and disadvantages, DXA is regarded as an acceptable form of measurement for hospital settings, and BIA is frequently used in outpatient clinics and community settings. Other methods used to estimate LBM with greater accuracy, such as peripheral quantitative computed tomography, doubly labeled water, and whole body gamma ray counting, are not viable for clinical use. Other accessible methods such as anthropometric measures and skinfold measures have not been embraced by sarcopenia classification consensus groups.23,37
Alternative methods of estimating LBM, such as diagnostic ultrasound and multifrequency electrical impedance myography, are featured outcomes in ongoing clinical trials that involve veteran participants. These modalities may soon provide a clinically viable approach to assessing muscle quality via estimates of muscle tissue composition.37,38 Similar to the management of other geriatric syndromes, interprofessional collaboration provides an optimal approach to the assessment of sarcopenia. Physicians and other health care providers may draw on the standardized assessment of strength and function (via the SPPB and hand-grip dynamometry) by physical therapists (PTs), questionnaires administered by nursing staff (the SARC-F), or body composition estimates from other health professionals (ranging from BIA to DXA) to aid the diagnostic process and facilitate appropriate case management (Table 2).
Competing staging and classification definitions have been cited as a primary factor behind the CDC’s delayed recognition of the sarcopenia diagnosis, which in turn posed a barrier to formal clinical recognition by geriatricians.24 However, this reaction to the evolving sarcopenia staging criteria also may reveal the larger misapplication of the staging process to the diagnostic process. The application of classification and staging criteria results in a homogenous group of patients, whereas the application of diagnostic criteria results in a heterogeneous group of patients to account for variations in clinical presentation associated with a given disorder. Classification criteria may be equivalent to objective measures that are used in the diagnostic process when a given disease is characterized by a well-established biomarker.39
However, this is not the case for most geriatric syndromes and other disorders marked by varied clinical presentation patterns. On considering the commonly used sarcopenia staging criteria of LBM ≤ 8.50 kg/m2 or grip strength < 30 kg in men and LBM ≤ 5.75 kg/m2 or grip strength < 20 kg in women, it is easy to understand that such general cutoff values are far from diagnostic.40,41 Moreover, stringent cutoff values associated with classification and staging may not adequately capture those with an atypical presentation of the syndrome (eg, someone who exhibits age-related muscle weakness but has retained adequate LBM). Such criteria often prove to have high specificity and low sensitivity, which may yield a false negative rate that is appropriate for clinical research eligibility and group assignment but inadequate for clinical care.
Screening, staging, and classification criteria with high specificity may indeed be desirable for confirmatory imaging tests associated with radiation exposure concerns or for managing risk in experimental clinical trials involving pharmacologic treatment. For example, a SARC-F score ≥ 4 may prompt the formal assessment of LBM via a DXA examination.4 In contrast, those with a SARC-F score ≤ 3 with low gait speed or grip strength may benefit from consultation regarding regular physical activity and nutrition recommendations. Given the challenges of establishing sarcopenia classification criteria that perform consistently across populations and geographic regions, classification and staging criteria may be best viewed as clinical reasoning tools that supplement, but not supplant, the diagnostic process.7,42
Diagnosis
Geriatric syndromes do not lend themselves to a simple diagnostic process. Syndromes such as frailty and sarcopenia are multifactorial and lack a single distinguishing clinical feature or biomarker. The oft-cited refrain that sarcopenia is an underdiagnosed condition is partially explained by the recent ICD-10-CM code and varied classification and diagnostic criteria.5 This circumstance highlights the need to distinctly contrast the diagnostic process with the screening and staging classifications.
The diagnostic process involves the interpretation of the patient history, signs, and symptoms within the context of individual factors, local or regional disease prevalence, and the results of the best available and most appropriate laboratory tests. After all, a patient that presents with low LBM and a gradual loss of strength without a precipitating event would necessitate further workup to rule out many clinical possibilities under the aegis of a differential diagnosis. Clinical features, such as the magnitude of weakness and pattern of strength loss or muscle atrophy along with the determination of neurologic or autoimmune involvement, are among the key elements of the differential examination for a case involving the observation of frank muscle weakness. Older adults with low muscle strength may have additional risk factors for sarcopenia such as obesity, pain, poor nutrition, previous bone fracture, and a sedentary lifestyle. However, disease etiology with lower probabilities, such as myogenic or neurogenic conditions associated with advancing age, also may be under consideration during the clinical assessment.6
In many instances, the cutoff scores associated with the sarcopenia staging criteria may help to guide the diagnostic process and aid clinical decision making. Since individuals with a positive screening result based on the SARC-F questionnaire (score ≥ 4) have a high likelihood of meeting the staging criteria for severe sarcopenia, a PCP may opt to obtain a confirmatory estimate of LBM both to support the clinical assessment and to monitor change over the course of rehabilitation. Whereas people who present with a decline in strength (ie, grip strength < 30 kg for a male) without an observable loss of function or a positive SARC-F score may benefit from consultation from the physician, NP, or rehabilitation health professional regarding modifiable risk factors associated with sarcopenia.
Incorporating less frequently used sarcopenia classification schemes such as identifying those with sarcopenic obesity or secondary sarcopenia due to mitigating factors such as chronic kidney disease or DM (Table 3) may engender a more comprehensive approach to intervention that targets the primary disease while also addressing important secondary sequelae. Nevertheless, staging or classification criteria cannot be deemed equivalent to diagnostic criteria for sarcopenia due to the challenges posed by syndromes that have a heterogeneous clinical presentation.
The refinement of the staging and classification criteria along with the advances in imaging technology and mechanistic research are not unique to sarcopenia. Practitioners involved in the care of people with rheumatologic conditions or osteoporosis also have contended with continued refinements to their classification criteria and approach to risk stratification.39,43,44 Primary care providers will now have the option to use a new ICD-10-CM code (M62.84) for sarcopenia, which will allow them to properly document the clinical distinctions between people with impaired strength or function largely due to age-related muscle changes and those who have impaired muscle function due to cachexia, inflammatory myopathies, or forms of neuromuscular disease.
The ability to identify and document this geriatric syndrome in veterans will help to better define the scope of the problem within the VA health care system. The median age of veterans is 62 years compared with 43 years for nonveterans.3 Consequently, there may be value in the adoption of a formal approach to screening and diagnosis for sarcopenia among veterans who receive their primary care from VA facilities.7 Indeed, the exchange between the patient and the health professional regarding the screening and diagnostic process will provide valuable opportunities to promote exercise interventions before patients incur significant impairments.
One of the biggest threats burdening global health is noncommunicable diseases, and many chronic conditions, such as sarcopenia, can be prevented and managed with appropriate levels of physical activity.17 Increased physician involvement may prove to be critical given the identification of physical inactivity as a top 5 risk factor for general morbidity and mortality by World Health Organization and consensus group recommendations calling for physicians to serve a more prominent role in the provision of exercise and physical activity recommendations.16,17
This developing health care role should include NPs, PTs, physician assistants, and other associated health professionals. It also should include collaborative efforts between physicians and rehabilitation practitioners concerning provision of the formal exercise prescriptionprescription and monitoring of patient outcomes.
Individuals with severe forms of sarcopenia rarely improve without intervention.6 Although no pharmacologic treatment exists to specifically address sarcopenia, strengthening exercise has been shown to be an effective mode of prevention and conservative management.8 Progressive resistance exercise cannot abate the expected age-related changes in skeletal muscle, but it can significantly reverse the loss of LBM and strength in untrained older adults and slow the age-related decline in muscle performance in older adult athletes and trained individuals.45
Local senior centers and community organizations may prove to be valuable resources concerning group exercise options, and they provide the added benefit of social engagement and peer group accountability. Federal resources include the Go4Life exercise guide and online videos provided by the National Institute on Aging and the MOVE! Weight Management and Health Program provided at select VA community-based outpatient clinics. Ultimately, collaborative efforts with exercise specialists may serve to reduce the PCP burden during the provision of health services, minimize diagnostic errors associated with sarcopenia assessment and help to connect patients to valuable health promotion resources.17,18
Conclusion
While practitioners should remain keenly aware of the pernicious effects of overdiagnosis, sarcopenia has long existed as a known, but undiagnosed, condition. Of course, geriatricians have traditionally managed poor muscle performance and mobility limitations by addressing treatable symptoms and providing referrals to physical medicine specialists when warranted. Nevertheless, the advent of ICD-10-CM code M62.84 provides the VA with an opportunity to take a leading role in systematically addressing this geriatric syndrome within an aging veteran population.
The following items should be considered by NCP for the development of guidelines and recommendations concerning sarcopenia screening:
- Consider screening veterans aged > 65 years for sarcopenia every 2 years. Those with mitigating systemic conditions (eg, chronic kidney disease, DM, or malnutrition) or significant mobility limitations may be screened at any age.
- Sarcopenia screening procedures should include at a minimum the SARC-F questionnaire and gait speed (when appropriate). Including gait speed or grip strength testing in the screening exam is recommended given the low sensitivity of the SARC-F questionnaire.
- Veterans with positive SARC-F results (≥ 4) merit a physical therapy referral. In addition, these veterans should obtain confirmatory standardized assessments for LBM and functional status.
- Veterans at risk for sarcopenia based on patient age, medical history, and the physical examination (eg, obesity, sedentary lifestyle, a previous fracture, self-reported physical decline), but with negative SARC-F results should receive a formal exercise prescription from their PCP. Baseline assessment measures may be used for comparison with serial measures obtained during subsequent screening visits to support long-term case management.
- Interprofessional collaboration involving geriatricians, PTs, nurses, radiologists, and other health care professionals should be involved in the screening, diagnosis, and case management of veterans with sarcopenia.
- The VA EMR should be systematically documented with sarcopenia assessment data obtained from the gait speed tests, SARCF, SPPB, grip strength tests, and LBM estimates to better characterize this condition within the veteran population.
Any expansion in the provision of health care comes with anticipated benefits and potential costs. Broad guidance from NCP may encourage veterans to pursue selected screening tests, promote the appropriate use of preventative services, and facilitate timely treatment when needed.31 Clinicians who are informed about the screening, staging, classification, and diagnostic process for sarcopenia may partner with patients to make reasoned decisions about how to best manage this syndrome within the VA medical center environment.
Sarcopenia is an age-related loss of skeletal muscle that may result in diminished muscle strength and functional performance. The prevalence of sarcopenia varies based on the cohort and the assessment criteria. According to the Health Aging and Body Composition (ABC) study, the prevalence of sarcopenia in community-dwelling older adults is about 14% to 18%, whereas the estimate may exceed 30% for those in longterm care.1,2 This geriatric syndrome may disproportionately affect veterans given that they are older than the civilian population and may have disabling comorbid conditions associated with military service.3
Recently, there has been a call to action to systematically address sarcopenia by interdisciplinary organizations such as the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the International Working Group on Sarcopenia (IWGS).4,5 This call to action is due to the association of sarcopenia with increased health care costs, higher disability incidence, and elevated risk of mortality.6,7 The consequences of sarcopenia may include serious complications, such as hip fracture or a loss of functional independence.8,9 The CDC now recognizes sarcopenia as an independently reportable medical condition. Consequently, physicians, nurse practitioners (NPs), and other associated health professionals within the VA will need to better understand clinically viable and valid methods to screen and diagnose this geriatric syndrome.
The purpose of this paper is to inform practitioners how sarcopenia screening is aided by the new ICD-10-CM code and briefly review recent VA initiatives for proactive care. Additional objectives include identifying common methods used to assess sarcopenia and providing general recommendations to the VHA National Center for Health Promotion and Disease Prevention (NCP) concerning the management of sarcopenia.
Addressing Sarcopenia
While the age-related decline in muscle size and performance has long been recognized by geriatricians, sustained advocacy by several organizations was required to realize the formal recognition of sarcopenia. Aging in Motion (AIM), a coalition of organizations focused on advancing research and treatment for conditions associated with age-related muscle dysfunction, sought the formal recognition of sarcopenia. The CDC established the ICD-10-CM code for sarcopenia in October of 2016, which allowed the syndrome to be designated as a primary or secondary condition.10
The ubiquitous nature of agerelated changes in muscle and the mandate to engage in proactive care by all levels of VA leadership led to the focus on addressing sarcopenia. The recognition of sarcopenia by the CDC comes at an opportune time given recent VA efforts to transform itself from a facilitator mainly of care delivery to an active partner in fostering the health and well-being of veterans. Initiatives that are emblematic of this attempt to shift the organizational culture across the VHA include establishing the VA Center for Innovation (VACI) and issuing guidance documents, such as the Blueprint for Excellence, which was introduced in 2014 by then VA Secretary Robert McDonald.11,12 Many of the following Blueprint themes and strategies potentially impact sarcopenia screening and treatment within the VA:
- Delivering high-quality, veteran-centered care: A major Blueprint theme is attaining the “Triple Aims” of a health care system by promoting better health among veterans, improving the provision of care, and lowering costs through operational efficiency. The management of sarcopenia has clear clinical value given the association of age-related muscle loss with fall risk and decreased mobility.13 Financial value also may be associated with the effort to decrease disability related to sarcopenia and the use of a team approach featuring associated health professionals to help screen for this geriatric syndrome.14,15 (Strategy 2)
- Leveraging health care informatics to optimize individual and population health outcomes: The inclusion of the most basic muscle performance and functional status measures in the electronic medical record (EMR), such as grip strength and gait speed, would help to identify the risk factors and determinants of sarcopenia among the veteran population. (Strategy 3)
- Advancing personalized, proactive health care that fosters a high level of health and well-being: The long-term promotion of musculoskeletal health and optimal management of sarcopenia cannot be sustained through episodic medical interactions. Instead, a contemporary approach to health services marked by the continuous promotion of health education, physical activity and exercise, and proper nutrition has demonstrated value in the management of chronic conditions.16,17 (Strategy 6)
The new sarcopenia ICD-10-CM code along with elements of the VHA Blueprint can serve to support the systematic assessment and management of veterans with age-related muscle dysfunction. Nevertheless, renewed calls for health promotion and screening programs are often counterbalanced by the need for cost containment and the cautionary tales concerning the potential harms or errors associated with some forms of medical screening. The American Board of Internal Medicine Foundation has spearheaded the Choosing Wisely campaign to raise awareness about excessive medical testing. However, the Institute of Medicine has linked the provision of quality health care to a diagnostic process that is both timely and accurate.18 Careful consideration of these health care challenges may help guide practitioners within the VA concerning the screening and diagnosis of sarcopenia.
Sarcopenia Assessment
Sarcopenia can have several underlying causes in some individuals and result in varied patterns of clinical presentation and differing degrees of severity. The European Working Group on Sarcopenia in Older People first met in 2009 and used a consensus-based decision-making process to determine operational definitions for sarcopenia and create a staging algorithm for the syndrome.19 This consensus group developed a conceptual staging model with 3 categories: presarcopenia, sarcopenia, and severe sarcopenia (Table 1). The impetus for sarcopenia staging was the emerging research findings suggesting that lean body mass (LBM) alone did not provide a high degree of clinical value in outpatient settings due to the nonlinear relationship between LBM and muscle function in older adults.20,21 Using the consensus model approach, an individual is classified as sarcopenic on presenting with both low LBM and low muscle function.
Screening: A Place to Start
Findings from the Health ABC Study suggested that older adults who maintained high levels of LBM were less likely to become sarcopenic. Whereas, older adults in the cohort with low levels of LBM tended to remain in a sarcopenic state.6 Consequently, the early detection of sarcopenia may have important health promotion implications for older adults. Sarcopenia is a syndrome with a continuum of clinical features; it is not a disease with a clear or singular etiololgy. Therefore, the result of the screening examination should identify those who would most benefit from a formal diagnostic assessment.
One approach to screening for sarcopenia involves the use of questionnaires, such as the SARC-F (sluggishness, assistance in walking, rise from a chair, climb stairs, falls), which is a brief 5-item questionnaire with Likert scoring for patient responses.13 In a cohort of National Health and Nutrition Examination Survey (NHANES) participants, SARC-F scores ≥ 4 were associated with slower gait speed, lower strength, and an increased likelihood of hospitalization within a year of the test response.22 However, rather than stratify patients by risk, the SARC-F exhibits a high degree of test specificity regarding the major consensus-based sarcopenia classification criteria (specificity = 94.2% to 99.1%; sensitivity = 3.8% to 9.9%).13 Given the known limitations of screening tools with low sensitivity, organizations such as the ESCEO have recommended supplementing the SARC-F questionnaire with other forms of assessment.4 Supplements to the screening examination may range from the use of “red flag” questions concerning changes in nutritional status, body weight, and physical activity, to conducting standard gait speed and grip-strength testing.4,19,23
Performance-based testing, including habitual gait speed and grip-strength dynamometry, also may be used in both the screening and classification of sarcopenia.2 Although walking speed below 1.0 m/s has been used by the IWGS as a criterion to prompt further assessment, many people within the VA health care system may have gait abnormalities independent of LBM status, and others may be nonambulatory.24,25 As a result, grip-strength testing should be considered as a supplementary or alternate screening assessment tool.26,27
Hand-grip dynamometry is often used diagnostically given its previous test validation, low expense, and ease of use.23 Moreover, recent evidence suggests that muscle strength surpasses gait speed as a means of identifying people with sarcopenia. Grip strength is associated with all-cause mortality, even when adjusting for age, sex, and body size,28 while slow gait speed (< .82 m/s) has a reported sensitivity of 63% and specificity of 70% for mortality in population-based studies involving older adults.29
Gait speed (in those who are ambulatory) and grip-strength values could be entered into the EMR evaluation note by the primary care provider (PCP). Elements of the VA EMR, such as the ability to review the diagnosis of sarcopenia on the Problem List or the nominal enhancement of providing LBM estimates within the Cumulative Vitals and Measurements Report would support the management of sarcopenia. See Table 2 for cutoff values for frequently used sarcopenia screening and staging tests.
The pitfalls of excessive or inappropriate screening are well documented. The efforts to screen for prostate cancer have highlighted instances when inappropriate followup tests and treatment fail to alter mortality rates and ultimately yield more harm than good.30 However, there are several points of departure concerning the screening for sarcopenia vs screening for prostate cancer. The screening assessments for sarcopenia are low-cost procedures that are associated with a low patient burden. These procedures may include questionnaires, functional testing, or the assessment of muscle performance. Additionally, there is a low propensity for adverse effects stemming from treatment due to disease misclassification given the common nonpharmacologic approaches used to manage sarcopenia.31 Nonetheless, the best screening examination—even one that has low patient burden and cost—may prove to be a poor use of medical resources if the process is not linked to a viable intervention.
Screening people aged ≥ 65 years may strike a balance between controlling health care expenditures and identifying people with the initial signs of sarcopenia early enough to begin monitoring key outcomes and providing a formalized exercise prescription. Presuming an annual age-related decline in LBM of 1.5%, and considering the standard error measurement of the most frequently used methods of strength and LBM assessment, recurrent screening could occur every 2 years.21,32
Earlier screening may be considered for patient populations with a higher pretest probability. These groups include those with conditions associated with accelerated muscle loss, such as chronic kidney disease, peripheral artery disease, and diabetes mellitus (DM).32 Although accelerated muscle loss characterized by an inflammatory motif (eg, cancer-related cachexia) may share some features of the sarcopenia screening and assessment approach, important differences exist regarding the etiology, medical evaluation, and ICD-10-CM code designation.
Staging and Classification
Staging criteria are generally used to denote the severity of a given disease or syndrome, whereas classification criteria are used to define homogenous patient groups based on specific pathologic or clinical features of a disorder. Although classification schemes may incorporate an element of severity, they are primarily used to characterize fairly distinct phenotypic forms of disease or specific clinical presentation patterns associated with a well-defined syndrome. Although not universally adopted, the European consensus group sarcopenia staging criteria are increasingly used to provide a staging algorithm presumably driven by the severity of the condition.19
The assessment of functional performance for use in sarcopenia staging often involves measuring habitual gait speed or completing the Short Physical Performance Battery (SPPB).23 The SPPB involves a variety of performance-based activities for balance, gait, strength, and endurance. This test has predictive validity for the onset of disability and adverse health events, and it has been extensively used in research and clinical settings.33 Additional tests used to characterize function during the staging or diagnostic process include the timed get up and go test (TGUG) and the timed sit to stand test.34,35 The TGUG provides an estimate of dynamic balance, and the sit to stand test has been used as very basic proxy measure of muscular power.36 The sit to stand test and habitual gait speed are items included in the SPPB.33
Accepted methods to obtain the traditional index measure of sarcopenia—based on estimates of LBM—include bioimpedance analysis (BIA) and dual X-ray absorptiometry (DXA). The BIA uses the electrical impedance of body tissues and its 2 components, resistance and reactance, to derive its body composition estimates.37 Segmental BIA allows for isolated measurements of the limbs, which may be calibrated to DXA appendicular lean body mass (ALM) or magnetic resonance imaging-based estimates of LBM. This instrument is relatively safe for use, inexpensive for medical facilities, and useful for longitudinal studies, but it can be confounded by issues, such as varying levels of hydration, which may affect measurement validity in some instances.
Despite the precision of DXA for estimating densities for whole body composition analysis, the equipment is not very portable and involves low levels of radiation exposure, which limits its utility in some clinical settings. While each body composition assessment method has its advantages and disadvantages, DXA is regarded as an acceptable form of measurement for hospital settings, and BIA is frequently used in outpatient clinics and community settings. Other methods used to estimate LBM with greater accuracy, such as peripheral quantitative computed tomography, doubly labeled water, and whole body gamma ray counting, are not viable for clinical use. Other accessible methods such as anthropometric measures and skinfold measures have not been embraced by sarcopenia classification consensus groups.23,37
Alternative methods of estimating LBM, such as diagnostic ultrasound and multifrequency electrical impedance myography, are featured outcomes in ongoing clinical trials that involve veteran participants. These modalities may soon provide a clinically viable approach to assessing muscle quality via estimates of muscle tissue composition.37,38 Similar to the management of other geriatric syndromes, interprofessional collaboration provides an optimal approach to the assessment of sarcopenia. Physicians and other health care providers may draw on the standardized assessment of strength and function (via the SPPB and hand-grip dynamometry) by physical therapists (PTs), questionnaires administered by nursing staff (the SARC-F), or body composition estimates from other health professionals (ranging from BIA to DXA) to aid the diagnostic process and facilitate appropriate case management (Table 2).
Competing staging and classification definitions have been cited as a primary factor behind the CDC’s delayed recognition of the sarcopenia diagnosis, which in turn posed a barrier to formal clinical recognition by geriatricians.24 However, this reaction to the evolving sarcopenia staging criteria also may reveal the larger misapplication of the staging process to the diagnostic process. The application of classification and staging criteria results in a homogenous group of patients, whereas the application of diagnostic criteria results in a heterogeneous group of patients to account for variations in clinical presentation associated with a given disorder. Classification criteria may be equivalent to objective measures that are used in the diagnostic process when a given disease is characterized by a well-established biomarker.39
However, this is not the case for most geriatric syndromes and other disorders marked by varied clinical presentation patterns. On considering the commonly used sarcopenia staging criteria of LBM ≤ 8.50 kg/m2 or grip strength < 30 kg in men and LBM ≤ 5.75 kg/m2 or grip strength < 20 kg in women, it is easy to understand that such general cutoff values are far from diagnostic.40,41 Moreover, stringent cutoff values associated with classification and staging may not adequately capture those with an atypical presentation of the syndrome (eg, someone who exhibits age-related muscle weakness but has retained adequate LBM). Such criteria often prove to have high specificity and low sensitivity, which may yield a false negative rate that is appropriate for clinical research eligibility and group assignment but inadequate for clinical care.
Screening, staging, and classification criteria with high specificity may indeed be desirable for confirmatory imaging tests associated with radiation exposure concerns or for managing risk in experimental clinical trials involving pharmacologic treatment. For example, a SARC-F score ≥ 4 may prompt the formal assessment of LBM via a DXA examination.4 In contrast, those with a SARC-F score ≤ 3 with low gait speed or grip strength may benefit from consultation regarding regular physical activity and nutrition recommendations. Given the challenges of establishing sarcopenia classification criteria that perform consistently across populations and geographic regions, classification and staging criteria may be best viewed as clinical reasoning tools that supplement, but not supplant, the diagnostic process.7,42
Diagnosis
Geriatric syndromes do not lend themselves to a simple diagnostic process. Syndromes such as frailty and sarcopenia are multifactorial and lack a single distinguishing clinical feature or biomarker. The oft-cited refrain that sarcopenia is an underdiagnosed condition is partially explained by the recent ICD-10-CM code and varied classification and diagnostic criteria.5 This circumstance highlights the need to distinctly contrast the diagnostic process with the screening and staging classifications.
The diagnostic process involves the interpretation of the patient history, signs, and symptoms within the context of individual factors, local or regional disease prevalence, and the results of the best available and most appropriate laboratory tests. After all, a patient that presents with low LBM and a gradual loss of strength without a precipitating event would necessitate further workup to rule out many clinical possibilities under the aegis of a differential diagnosis. Clinical features, such as the magnitude of weakness and pattern of strength loss or muscle atrophy along with the determination of neurologic or autoimmune involvement, are among the key elements of the differential examination for a case involving the observation of frank muscle weakness. Older adults with low muscle strength may have additional risk factors for sarcopenia such as obesity, pain, poor nutrition, previous bone fracture, and a sedentary lifestyle. However, disease etiology with lower probabilities, such as myogenic or neurogenic conditions associated with advancing age, also may be under consideration during the clinical assessment.6
In many instances, the cutoff scores associated with the sarcopenia staging criteria may help to guide the diagnostic process and aid clinical decision making. Since individuals with a positive screening result based on the SARC-F questionnaire (score ≥ 4) have a high likelihood of meeting the staging criteria for severe sarcopenia, a PCP may opt to obtain a confirmatory estimate of LBM both to support the clinical assessment and to monitor change over the course of rehabilitation. Whereas people who present with a decline in strength (ie, grip strength < 30 kg for a male) without an observable loss of function or a positive SARC-F score may benefit from consultation from the physician, NP, or rehabilitation health professional regarding modifiable risk factors associated with sarcopenia.
Incorporating less frequently used sarcopenia classification schemes such as identifying those with sarcopenic obesity or secondary sarcopenia due to mitigating factors such as chronic kidney disease or DM (Table 3) may engender a more comprehensive approach to intervention that targets the primary disease while also addressing important secondary sequelae. Nevertheless, staging or classification criteria cannot be deemed equivalent to diagnostic criteria for sarcopenia due to the challenges posed by syndromes that have a heterogeneous clinical presentation.
The refinement of the staging and classification criteria along with the advances in imaging technology and mechanistic research are not unique to sarcopenia. Practitioners involved in the care of people with rheumatologic conditions or osteoporosis also have contended with continued refinements to their classification criteria and approach to risk stratification.39,43,44 Primary care providers will now have the option to use a new ICD-10-CM code (M62.84) for sarcopenia, which will allow them to properly document the clinical distinctions between people with impaired strength or function largely due to age-related muscle changes and those who have impaired muscle function due to cachexia, inflammatory myopathies, or forms of neuromuscular disease.
The ability to identify and document this geriatric syndrome in veterans will help to better define the scope of the problem within the VA health care system. The median age of veterans is 62 years compared with 43 years for nonveterans.3 Consequently, there may be value in the adoption of a formal approach to screening and diagnosis for sarcopenia among veterans who receive their primary care from VA facilities.7 Indeed, the exchange between the patient and the health professional regarding the screening and diagnostic process will provide valuable opportunities to promote exercise interventions before patients incur significant impairments.
One of the biggest threats burdening global health is noncommunicable diseases, and many chronic conditions, such as sarcopenia, can be prevented and managed with appropriate levels of physical activity.17 Increased physician involvement may prove to be critical given the identification of physical inactivity as a top 5 risk factor for general morbidity and mortality by World Health Organization and consensus group recommendations calling for physicians to serve a more prominent role in the provision of exercise and physical activity recommendations.16,17
This developing health care role should include NPs, PTs, physician assistants, and other associated health professionals. It also should include collaborative efforts between physicians and rehabilitation practitioners concerning provision of the formal exercise prescriptionprescription and monitoring of patient outcomes.
Individuals with severe forms of sarcopenia rarely improve without intervention.6 Although no pharmacologic treatment exists to specifically address sarcopenia, strengthening exercise has been shown to be an effective mode of prevention and conservative management.8 Progressive resistance exercise cannot abate the expected age-related changes in skeletal muscle, but it can significantly reverse the loss of LBM and strength in untrained older adults and slow the age-related decline in muscle performance in older adult athletes and trained individuals.45
Local senior centers and community organizations may prove to be valuable resources concerning group exercise options, and they provide the added benefit of social engagement and peer group accountability. Federal resources include the Go4Life exercise guide and online videos provided by the National Institute on Aging and the MOVE! Weight Management and Health Program provided at select VA community-based outpatient clinics. Ultimately, collaborative efforts with exercise specialists may serve to reduce the PCP burden during the provision of health services, minimize diagnostic errors associated with sarcopenia assessment and help to connect patients to valuable health promotion resources.17,18
Conclusion
While practitioners should remain keenly aware of the pernicious effects of overdiagnosis, sarcopenia has long existed as a known, but undiagnosed, condition. Of course, geriatricians have traditionally managed poor muscle performance and mobility limitations by addressing treatable symptoms and providing referrals to physical medicine specialists when warranted. Nevertheless, the advent of ICD-10-CM code M62.84 provides the VA with an opportunity to take a leading role in systematically addressing this geriatric syndrome within an aging veteran population.
The following items should be considered by NCP for the development of guidelines and recommendations concerning sarcopenia screening:
- Consider screening veterans aged > 65 years for sarcopenia every 2 years. Those with mitigating systemic conditions (eg, chronic kidney disease, DM, or malnutrition) or significant mobility limitations may be screened at any age.
- Sarcopenia screening procedures should include at a minimum the SARC-F questionnaire and gait speed (when appropriate). Including gait speed or grip strength testing in the screening exam is recommended given the low sensitivity of the SARC-F questionnaire.
- Veterans with positive SARC-F results (≥ 4) merit a physical therapy referral. In addition, these veterans should obtain confirmatory standardized assessments for LBM and functional status.
- Veterans at risk for sarcopenia based on patient age, medical history, and the physical examination (eg, obesity, sedentary lifestyle, a previous fracture, self-reported physical decline), but with negative SARC-F results should receive a formal exercise prescription from their PCP. Baseline assessment measures may be used for comparison with serial measures obtained during subsequent screening visits to support long-term case management.
- Interprofessional collaboration involving geriatricians, PTs, nurses, radiologists, and other health care professionals should be involved in the screening, diagnosis, and case management of veterans with sarcopenia.
- The VA EMR should be systematically documented with sarcopenia assessment data obtained from the gait speed tests, SARCF, SPPB, grip strength tests, and LBM estimates to better characterize this condition within the veteran population.
Any expansion in the provision of health care comes with anticipated benefits and potential costs. Broad guidance from NCP may encourage veterans to pursue selected screening tests, promote the appropriate use of preventative services, and facilitate timely treatment when needed.31 Clinicians who are informed about the screening, staging, classification, and diagnostic process for sarcopenia may partner with patients to make reasoned decisions about how to best manage this syndrome within the VA medical center environment.
1. Newman AB, Kupelian V, Visser M, et al; Health ABC Study Investigators. Sarcopenia: alternative definitions and associations with lower extremity function. J Am Geriatr Soc. 2003;51(11):1602-1609.
2. Cruz-Jentoft AJ, Landi F, Schneider SM, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014;43(6):748-759.
3. U.S. Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Profile of veterans: 2009. Data from the American Community Survey. http://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2009_FINAL.pdf. Published January 2011. Accessed May 18, 2017.
4. Beaudart C, McCloskey E, Bruyère O, et al. Sarcopenia in daily practice: assessment and management. BMC Geriatr. 2016;16(1):170.
5. Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249-256.
6. Murphy RA, Ip EH, Zhang Q, et al; Health, Aging, and Body Composition Study. Transition to sarcopenia and determinants of transitions in older adults: a population-based study. J Gerontol A Biol Sci Med Sci. 2014;69(6):751-758.
7. Harris-Love MO, Adams B, Hernandez HJ, DiPietro L, Blackman MR. Disparities in the consequences of sarcopenia: implications for African American veterans. Front Physiol. 2014;5:250.
8. Morley JE. Sarcopenia in the elderly. Fam Pract. 2012;29(suppl 1):i44-i48.
9. Fragala MS, Dam TT, Barber V, et al. Strength and function response to clinical interventions of older women categorized by weakness and low lean mass using classifications from the Foundation for the National Institute of Health sarcopenia project. J Gerontol A Biol Sci Med Sci. 2015;70(2):202-209.
10. Aging in Motion. AIM coalition announces establishment of ICD-10-CM Code for Sarcopenia
by the Centers for Disease Control and Prevention [press release]. http://aginginmotion.org/news/2388-2/. Published April 28, 2016. Accessed June 7, 2017.
11. U.S. Department of Veterans Affairs, Veterans Health Administration. Blueprint for excellence. https://www.va.gov/HEALTH/docs/VHA _Blueprint_for_Excellence.pdf. Published September 21, 2014. Accessed June 7, 2017.
12. U.S. Department of Veterans Affairs. VA Center of Innovation 2010–2012 stakeholder report. https://www.innovation.va.gov/docs/VACI_2010-2012_Stakeholder_Report.pdf. Published 2012. Accessed June 14, 2017.
13. Woo J, Leung J, Morley JE. Validating the SARCF: a suitable community screening tool for sarcopenia? J Am Med Dir Assoc. 2014;15(9):630-634.
14. Sousa AS, Guerra RS, Fonseca I, Pichel F, Ferreira S, Amaral TF. Financial impact of sarcopenia on hospitalization costs. Eur J Clin Nutr. 2016;70(9):1046-1051.
15. Janssen I, Shepard DS, Katzmarzyk PT, Roubenoff R. The healthcare costs of sarcopenia in the United States. J Am Geriatr Soc. 2004;52(1):80-85.
16. Ekelund U, Steene-Johannessen J, Brown WJ, et al; Lancet Physical Activity Series 2 Executive Committe; Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302-1310.
17. Thornton JS, Frémont P, Khan K, et al. Physical activity prescription: a critical opportunity to address a modifiable risk factor for the prevention and management of chronic disease: a position statement by the Canadian Academy of Sport and Exercise Medicine. Clin J Sport Med.
2016;26(4):259-265.
18. The National Academies of Sciences, Engineering, and Medicine; Committee on Diagnostic Error in Health Care, Board on Health Care Services; Institute of Medicine. Improving Diagnosis in Health Care. Washington, DC: National Academies Press;2015.
19. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al; European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412-423.
20. Ferrucci L, Guralnik JM, Buchner D, et al. Departures from linearity in the relationship between measures of muscular strength and physical performance of the lower extremities: the Women’s Health and Aging Study. J Gerontol A Biol Sci Med Sci. 1997;52(5):M275-M285.
21. Goodpaster BH, Park SW, Harris TB, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the Health, Aging and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2006;61(10):1059-1064.
22. Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle. 2016;7(1):28-36.
23. Cooper C, Fielding R, Visser M, et al. Tools in the assessment of sarcopenia. Calcif Tissue Int. 2013;93(3):201-210.
24. Lee WJ, Liu LK, Peng LN, Lin MH, Chen LK; ILAS Research Group. Comparisons of sarcopenia defined by IWGS and EWGSOP criteria among older people: results from the I-Lan longitudinal aging study. J Am Med Dir Assoc. 2013;14(7):528.e1-e7.
25. Cesari M, Kritchevsky SB, Penninx BW, et al. Prognostic value of usual gait speed in well-functioning older people—results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53(10):1675-1680.
26. Rossi AP, Fantin F, Micciolo R, et al. Identifying sarcopenia in acute care setting patients. J Am Med Dir Assoc. 2014;15(4):303.e7-e12.
27. Sánchez-Rodríguez D, Marco E, Miralles R, et al. Does gait speed contribute to sarcopenia casefinding in a postacute rehabilitation setting? Arch Gerontol Geriatr. 2015;61(2):176-181.
28. Strand BH, Cooper R, Bergland A, et al. The association of grip strength from midlife onwards with all-cause and cause-specific mortality over 17 years of follow-up in the Tromsø Study. J Epidemiol Community Health. 2016;70:1214-1221.
29. Stanaway FF, Gnjidic D, Blyth FM, et al. How fast does the Grim Reaper walk? Receiver operating characteristics curve analysis in healthy men aged 70 and over. BMJ. 2011;343:d7679.
30. Reiter RE. Risk stratification of prostate cancer 2016. Scand J Clin Lab Invest Suppl. 2016;245:S54-S59.
31. U.S. Department of Veterans Affairs, National Center for Health Promotion and Disease Prevention. Get recommended screening tests and immunizations. https://www.prevention.va.gov/Healthy_Living/Get_Recommended_Screening_Tests_and_Immunizations.asp. Updated September 9, 2016. Accessed June 7, 2017.
32. Buford TW, Anton SD, Judge AR, et al. Models of accelerated sarcopenia: critical pieces for solving the puzzle of age-related muscle atrophy. Ageing Res Rev. 2010;9(4):369-383.
33. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85-M94.
34. Daubney ME, Culham EG. Lower-extremity muscle force and balance performance in adults aged 65 years and older. Phys Ther. 1999;79(12):1177-1185.
35. Bohannon RW. Reference values for the fiverepetition sit-to-stand test: a descriptive metaanalysis of data from elders. Percept Mot Skills. 2006;103(1):215-222.
36. Correa-de-Araujo R, Harris-Love MO, Miljkovic I, Fragala MS, Anthony BW, Manini TM. The need for standardized assessment of muscle quality in skeletal muscle function deficit and other agingrelated muscle dysfunctions: a symposium report. Front Physiol. 2017;8:87.
37. Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J. Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc. 2015;74(4):355-366.
38. Harris-Love MO, Monfaredi R, Ismail C, Blackman MR, Cleary K. Quantitative ultrasound: measurement considerations for the assessment of muscular dystrophy and sarcopenia. Front Aging Neurosci. 2014;6:172.
39. Fries JF, Hochberg MC, Medsger TA Jr, Hunder GG, Bombardier C. Criteria for rheumatic disease. Different types and different functions. The American College of Rheumatology Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum. 1994;37(4):454-462.
40. Janssen I, Baumgartner RN, Ross R, Rosenberg IH, Roubenoff R. Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. Am J Epidemiol.
2004;159(4):413-421.
41. Ismail C, Zabal J, Hernandez HJ, et al. Diagnostic ultrasound estimates of muscle mass and muscle quality discriminate between women with and without sarcopenia. Front Physiol. 2015;6:302.
42. Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15(2):95-101.
43. Aggarwal R, Ringold S, Khanna D, et al. Distinctions between diagnostic and classification criteria? Arthritis Care Res (Hoboken). 2015;67(7):891-897.
44. Licata A. Bone density vs bone quality: what’s a clinician to do? Cleve Clin J Med. 2009;76(6):331-336.
45. Pollock ML, Mengelkoch LJ, Graves JE, et al. Twenty-year follow-up of aerobic power and body composition of older track athletes. J Appl Physiol. 1997;82(5):1508-1516.
1. Newman AB, Kupelian V, Visser M, et al; Health ABC Study Investigators. Sarcopenia: alternative definitions and associations with lower extremity function. J Am Geriatr Soc. 2003;51(11):1602-1609.
2. Cruz-Jentoft AJ, Landi F, Schneider SM, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014;43(6):748-759.
3. U.S. Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Profile of veterans: 2009. Data from the American Community Survey. http://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2009_FINAL.pdf. Published January 2011. Accessed May 18, 2017.
4. Beaudart C, McCloskey E, Bruyère O, et al. Sarcopenia in daily practice: assessment and management. BMC Geriatr. 2016;16(1):170.
5. Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249-256.
6. Murphy RA, Ip EH, Zhang Q, et al; Health, Aging, and Body Composition Study. Transition to sarcopenia and determinants of transitions in older adults: a population-based study. J Gerontol A Biol Sci Med Sci. 2014;69(6):751-758.
7. Harris-Love MO, Adams B, Hernandez HJ, DiPietro L, Blackman MR. Disparities in the consequences of sarcopenia: implications for African American veterans. Front Physiol. 2014;5:250.
8. Morley JE. Sarcopenia in the elderly. Fam Pract. 2012;29(suppl 1):i44-i48.
9. Fragala MS, Dam TT, Barber V, et al. Strength and function response to clinical interventions of older women categorized by weakness and low lean mass using classifications from the Foundation for the National Institute of Health sarcopenia project. J Gerontol A Biol Sci Med Sci. 2015;70(2):202-209.
10. Aging in Motion. AIM coalition announces establishment of ICD-10-CM Code for Sarcopenia
by the Centers for Disease Control and Prevention [press release]. http://aginginmotion.org/news/2388-2/. Published April 28, 2016. Accessed June 7, 2017.
11. U.S. Department of Veterans Affairs, Veterans Health Administration. Blueprint for excellence. https://www.va.gov/HEALTH/docs/VHA _Blueprint_for_Excellence.pdf. Published September 21, 2014. Accessed June 7, 2017.
12. U.S. Department of Veterans Affairs. VA Center of Innovation 2010–2012 stakeholder report. https://www.innovation.va.gov/docs/VACI_2010-2012_Stakeholder_Report.pdf. Published 2012. Accessed June 14, 2017.
13. Woo J, Leung J, Morley JE. Validating the SARCF: a suitable community screening tool for sarcopenia? J Am Med Dir Assoc. 2014;15(9):630-634.
14. Sousa AS, Guerra RS, Fonseca I, Pichel F, Ferreira S, Amaral TF. Financial impact of sarcopenia on hospitalization costs. Eur J Clin Nutr. 2016;70(9):1046-1051.
15. Janssen I, Shepard DS, Katzmarzyk PT, Roubenoff R. The healthcare costs of sarcopenia in the United States. J Am Geriatr Soc. 2004;52(1):80-85.
16. Ekelund U, Steene-Johannessen J, Brown WJ, et al; Lancet Physical Activity Series 2 Executive Committe; Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302-1310.
17. Thornton JS, Frémont P, Khan K, et al. Physical activity prescription: a critical opportunity to address a modifiable risk factor for the prevention and management of chronic disease: a position statement by the Canadian Academy of Sport and Exercise Medicine. Clin J Sport Med.
2016;26(4):259-265.
18. The National Academies of Sciences, Engineering, and Medicine; Committee on Diagnostic Error in Health Care, Board on Health Care Services; Institute of Medicine. Improving Diagnosis in Health Care. Washington, DC: National Academies Press;2015.
19. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al; European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412-423.
20. Ferrucci L, Guralnik JM, Buchner D, et al. Departures from linearity in the relationship between measures of muscular strength and physical performance of the lower extremities: the Women’s Health and Aging Study. J Gerontol A Biol Sci Med Sci. 1997;52(5):M275-M285.
21. Goodpaster BH, Park SW, Harris TB, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the Health, Aging and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2006;61(10):1059-1064.
22. Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle. 2016;7(1):28-36.
23. Cooper C, Fielding R, Visser M, et al. Tools in the assessment of sarcopenia. Calcif Tissue Int. 2013;93(3):201-210.
24. Lee WJ, Liu LK, Peng LN, Lin MH, Chen LK; ILAS Research Group. Comparisons of sarcopenia defined by IWGS and EWGSOP criteria among older people: results from the I-Lan longitudinal aging study. J Am Med Dir Assoc. 2013;14(7):528.e1-e7.
25. Cesari M, Kritchevsky SB, Penninx BW, et al. Prognostic value of usual gait speed in well-functioning older people—results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53(10):1675-1680.
26. Rossi AP, Fantin F, Micciolo R, et al. Identifying sarcopenia in acute care setting patients. J Am Med Dir Assoc. 2014;15(4):303.e7-e12.
27. Sánchez-Rodríguez D, Marco E, Miralles R, et al. Does gait speed contribute to sarcopenia casefinding in a postacute rehabilitation setting? Arch Gerontol Geriatr. 2015;61(2):176-181.
28. Strand BH, Cooper R, Bergland A, et al. The association of grip strength from midlife onwards with all-cause and cause-specific mortality over 17 years of follow-up in the Tromsø Study. J Epidemiol Community Health. 2016;70:1214-1221.
29. Stanaway FF, Gnjidic D, Blyth FM, et al. How fast does the Grim Reaper walk? Receiver operating characteristics curve analysis in healthy men aged 70 and over. BMJ. 2011;343:d7679.
30. Reiter RE. Risk stratification of prostate cancer 2016. Scand J Clin Lab Invest Suppl. 2016;245:S54-S59.
31. U.S. Department of Veterans Affairs, National Center for Health Promotion and Disease Prevention. Get recommended screening tests and immunizations. https://www.prevention.va.gov/Healthy_Living/Get_Recommended_Screening_Tests_and_Immunizations.asp. Updated September 9, 2016. Accessed June 7, 2017.
32. Buford TW, Anton SD, Judge AR, et al. Models of accelerated sarcopenia: critical pieces for solving the puzzle of age-related muscle atrophy. Ageing Res Rev. 2010;9(4):369-383.
33. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85-M94.
34. Daubney ME, Culham EG. Lower-extremity muscle force and balance performance in adults aged 65 years and older. Phys Ther. 1999;79(12):1177-1185.
35. Bohannon RW. Reference values for the fiverepetition sit-to-stand test: a descriptive metaanalysis of data from elders. Percept Mot Skills. 2006;103(1):215-222.
36. Correa-de-Araujo R, Harris-Love MO, Miljkovic I, Fragala MS, Anthony BW, Manini TM. The need for standardized assessment of muscle quality in skeletal muscle function deficit and other agingrelated muscle dysfunctions: a symposium report. Front Physiol. 2017;8:87.
37. Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J. Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc. 2015;74(4):355-366.
38. Harris-Love MO, Monfaredi R, Ismail C, Blackman MR, Cleary K. Quantitative ultrasound: measurement considerations for the assessment of muscular dystrophy and sarcopenia. Front Aging Neurosci. 2014;6:172.
39. Fries JF, Hochberg MC, Medsger TA Jr, Hunder GG, Bombardier C. Criteria for rheumatic disease. Different types and different functions. The American College of Rheumatology Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum. 1994;37(4):454-462.
40. Janssen I, Baumgartner RN, Ross R, Rosenberg IH, Roubenoff R. Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. Am J Epidemiol.
2004;159(4):413-421.
41. Ismail C, Zabal J, Hernandez HJ, et al. Diagnostic ultrasound estimates of muscle mass and muscle quality discriminate between women with and without sarcopenia. Front Physiol. 2015;6:302.
42. Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15(2):95-101.
43. Aggarwal R, Ringold S, Khanna D, et al. Distinctions between diagnostic and classification criteria? Arthritis Care Res (Hoboken). 2015;67(7):891-897.
44. Licata A. Bone density vs bone quality: what’s a clinician to do? Cleve Clin J Med. 2009;76(6):331-336.
45. Pollock ML, Mengelkoch LJ, Graves JE, et al. Twenty-year follow-up of aerobic power and body composition of older track athletes. J Appl Physiol. 1997;82(5):1508-1516.
Lack of Significant Anti-inflammatory Activity With Clindamycin in the Treatment of Rosacea: Results of 2 Randomized, Vehicle-Controlled Trials
Rosacea is a chronic inflammatory skin disease characterized by central facial erythema with or without intermittent papules and pustules (described as the inflammatory lesions of rosacea). Although twice-daily clindamycin 1% solution or gel has been used in the treatment of acne, few studies have investigated the use of clindamycin in rosacea.1,2 In one study comparing twice-daily clindamycin lotion 1% with oral tetracycline in 43 rosacea patients, clindamycin was found to be superior in the eradication of pustules.3 A combination therapy of clindamycin 1% and benzoyl peroxide 5% was found to be more effective than the vehicle in inflammatory lesions and erythema of rosacea in a 12-week randomized controlled trial; however, a definitive advantage over US Food and Drug Administration-approved topical agents used to treat papulopustular rosacea was not established.4,5 Two further studies evaluated clindamycin phosphate 1.2%-tretinoin 0.025% combination gel in the treatment of rosacea, but only 1 showed any effect on papulopustular lesions.6-8 The objective of the studies reported here was to evaluate the efficacy and safety of clindamycin in the treatment of patients with moderate to severe rosacea.
Methods
Study Design
Two multicenter (study A, 20 centers; study B, 10 centers), randomized, investigator-blinded, vehicle-controlled studies were conducted in the United States between 1999 and 2002 in accordance with the Declaration of Helsinki, International Conference on Harmonisation Good Clinical Practice guidelines, and local regulatory requirements. The studies were reviewed and approved by the respective institutional review boards, and all participants provided written informed consent.
In study A, moderate to severe rosacea patients with erythema, telangiectasia, and at least 8 inflammatory lesions were randomized to receive clindamycin cream 1% or vehicle cream once (in the evening) or twice daily (in the morning and evening) or clindamycin cream 0.3% once daily (in the evening) for 12 weeks (1:1:1:1:1 ratio). All study treatments were supplied in identical tubes with blinded labels.
In study B, patients with moderate to severe rosacea and at least 8 inflammatory lesions were randomized in a 1:1 ratio with instructions to apply clindamycin gel 1% or vehicle gel to the affected areas twice daily (morning and evening) for 12 weeks.
Efficacy Evaluation
Evaluations were performed at baseline and weeks 2, 4, 8, and 12 on the intention-to-treat population with the last observation carried forward.
Efficacy assessments in both studies included inflammatory lesion counts (papules and pustules) of 5 facial regions--forehead, chin, nose, right cheek, left cheek--counted separately and then combined to give the total inflammatory lesion count (both studies), as well as improvement in the investigator global rosacea severity score (0=none/clear; 1=mild, detectable erythema with ≤7 papules/pustules; 2=moderate, prominent erythema with ≥8 papules/pustules; 3=severe, intense erythema with ≥10 to <50 papules/pustules; 3.5 [study A] or 4 [study B]=very severe, intense erythema with >50 papules/pustules). In study B, the proportion of participants dichotomized to success (a score of 0 [none/clear] or 1 [mild/almost clear]) or failure (a score of ≥2) on the 5-point investigator global rosacea severity scale at week 12 was evaluated. In study A, investigator global improvement assessment at week 12, based on photographs taken at baseline, was graded on a 7-point scale (from -1 [worse], 0 [no change], and 1 [minimal improvement] to 5 [clear]). In both studies, erythema severity was graded on a 7-point scale in increments of 0.5 (from 0=no erythema to 3.5=very severe redness, very intense redness). Skin irritation also was graded as none, mild, moderate, or severe.
Safety Evaluation
Safety was assessed by the incidence of adverse events (AEs).
Statistical Analysis
Studies were powered assuming 60% reduction in inflammatory lesion counts with active and 40% with vehicle, based on historical data from a prior study with metronidazole cream 0.75% versus vehicle; 64 participants were required in each treatment group to detect this effect using a 2-sided t test (α=.017). Pairwise comparisons (clindamycin vs respective vehicle) were performed using the Cochran-Mantel-Haenszel test for combined lesion count percentage change.
Results
Participant Disposition and Baseline Characteristics
Overall, a total of 629 participants were randomized across both studies. In study A, a total of 416 participants were randomized into 5 treatment arms, with 369 participants (88.7%) completing the study; 47 (11.3%) participants discontinued study A, mainly due to participant request (19/47 [40.4%]) or lost to follow-up (11/47 [23.4%]). In study B, a total of 213 participants were randomized to receive either clindamycin gel 1% (n=109 [51.2%]) twice daily or vehicle gel (n=104 [48.8%]) twice daily, with 193 participants (90.6%) completing the study; 20 (9.4%) participants discontinued study B, mainly due to participant request (6/20 [30%]) or lost to follow-up (4/20 [20%]). Participants in studies A and B were similar in demographics and baseline disease characteristics (Table). The majority of participants were white females.
Efficacy
No statistically significant difference was observed in all pairwise comparisons (clindamycin cream twice daily vs vehicle twice daily, clindamycin cream once daily vs vehicle once daily, clindamycin gel vs vehicle gel) for the primary end point of mean percentage change from baseline in inflammatory lesion counts at week 12 (Figure 1; P>.5 for all pairwise comparisons).
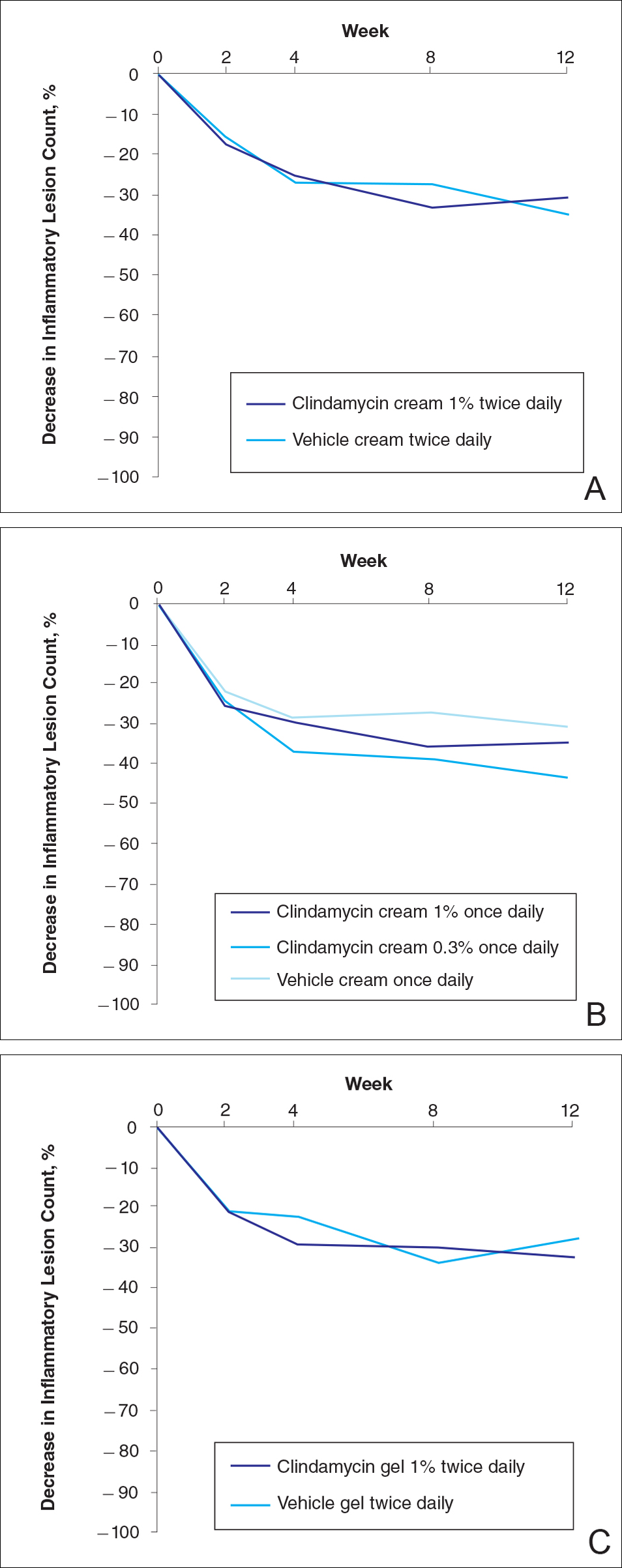
At week 12, the proportion of participants in study B deemed as a success (none/clear or mild/almost clear [investigator global rosacea severity score of 0 or 1]) in the clindamycin gel 1% and vehicle gel groups were 45% versus 38%, respectively (P=.347) (Figure 2).
For the secondary end point of mean investigator global rosacea severity assessment at week 12 (study A), there were no significant differences between the active and vehicle control groups (P>.5 for all pairwise comparisons)(Figure 3). Also, the proportion of participants with at least a moderate investigator global improvement assessment from baseline to week 12 ranged from 45% for clindamycin cream 1% twice daily to 56% for clindamycin cream 0.3% cream once daily and from 45% for vehicle cream once daily to 51% for vehicle cream twice daily (P>.5 for all pairwise comparisons).
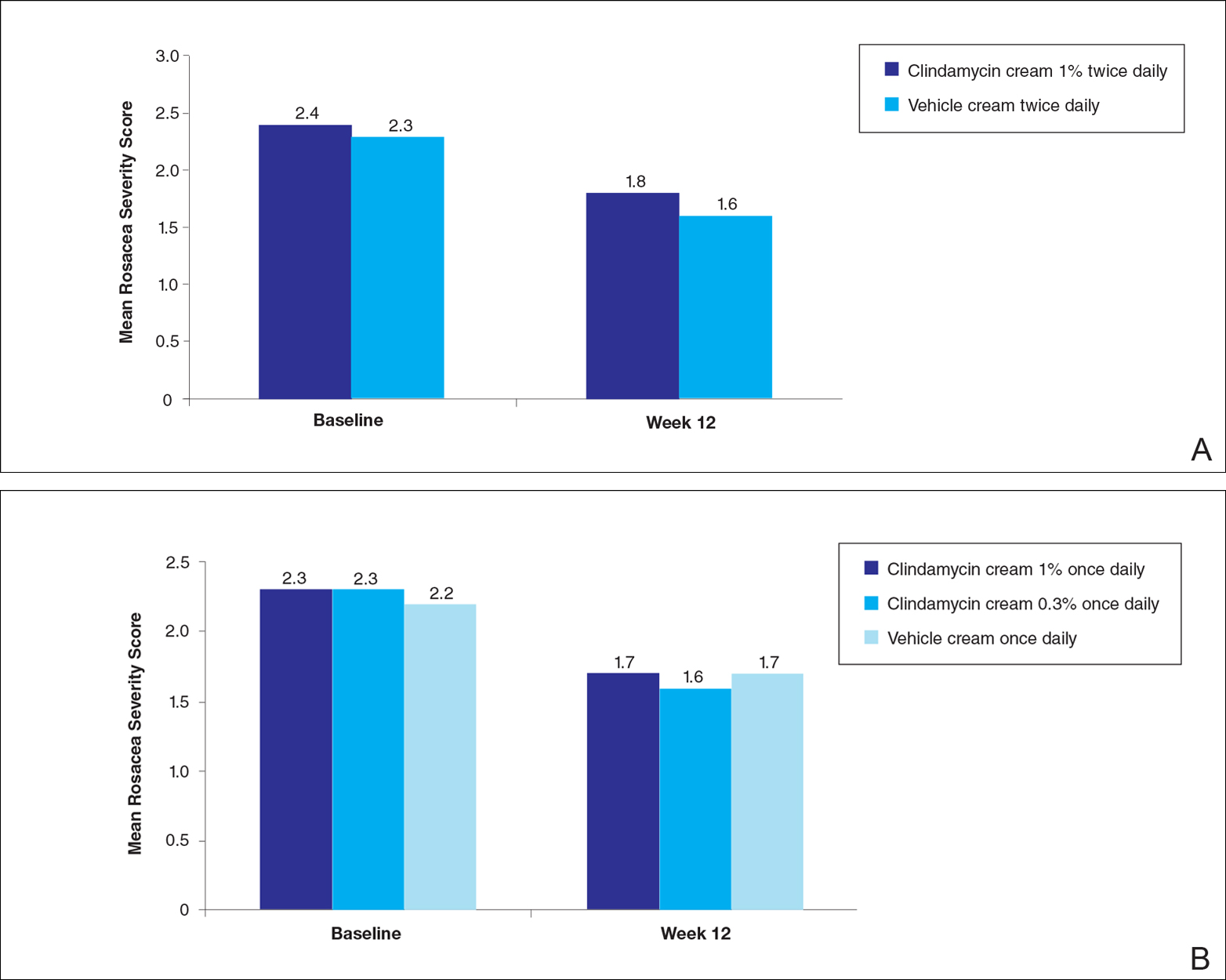
There were no significant differences in the mean total erythema severity scores at week 12 for clindamycin cream 1% twice daily versus vehicle cream twice daily (6.3 vs 6.0; P>.5), clindamycin cream 1% once daily versus vehicle cream once daily (6.2 vs 6.0; P>.5), clindamycin cream 0.3% once daily versus vehicle cream once daily (5.9 vs 6.0; P>.5), and clindamycin gel 1% twice daily versus vehicle gel twice daily (6.7 vs 6.2; P>.5).
There were no relevant differences between any of the clindamycin cream groups and their respective vehicle group at week 12 for skin irritation, including desquamation, edema, dryness, pruritus, and stinging/burning.
Safety
In study A, the majority of AEs in all 5 treatment arms were nondermatologic, mild in intensity, and not considered to be related to the study treatment by the investigator. Overall, 12 participants had AEs considered by the investigator as possibly or probably related to the study treatment: 4.9% in the clindamycin cream 1% twice daily group, 4.6% in the clindamycin cream 1% once daily group, 3.7% in the vehicle cream twice daily group, 1.2% in the clindamycin cream 0.3% once daily group, and 0% in the vehicle cream once daily group. Two treatment-related AEs led to treatment discontinuation, including dermatitis in 1 participant from the clindamycin cream 1% once daily group and contact dermatitis in 1 participant from the clindamycin cream 1% twice daily group.
Comment
No evidence of increased efficacy over the respective vehicles was observed with clindamycin cream or gel, whatever the regimen, in the treatment of rosacea patients in either of these well-designed and well-powered, blinded studies. Slight improvements in the various efficacy criteria were observed, even in the vehicle groups, highlighting the importance of using a good basic skin care regimen in the management of rosacea.9 In contrast to our observations of lack of efficacy in the treatment of rosacea, clinical efficacy of clindamycin has been demonstrated in acne,10-12 albeit with low efficacy for clindamycin monotherapy.13 It is noteworthy that oral or topical antibiotics are no longer recommended as monotherapy for acne to prevent and minimize antibiotic resistance and to preserve the therapeutic value of antibiotics.14
Acne and rosacea are both chronic inflammatory disorders of the skin associated with papules and pustules, and they share some common inflammatory patterns.15-19 Furthermore, the intrinsic anti-inflammatory activity of clindamycin in addition to its antibiotic effects has been suggested by some authors as the main reason for treating acne with clindamycin.20 However, the relative contributions of antibacterial and/or anti-inflammatory properties remain to be fully elucidated, and evidence for direct anti-inflammatory effects of clindamycin remains heterogeneous.21,22 Several pathophysiological factors have been implicated in acne, including hormonal effects, abnormal keratinocyte function, increased sebum production, and microbial components (eg, hypercolonization of the skin follicles by Propionibacterium acnes).23,24 The antibiotic activity of clindamycin against P acnes may be the key factor responsible for the clinical effects in acne.25,26 Although clindamycin may have anti-inflammatory effects in acne via a different inflammatory pathway not shared by rosacea, a purely antibiotic mechanism of action of clindamycin also could explain why we observed no evidence of efficacy in the treatment of rosacea, as no causative bacterial component has been clearly demonstrated in rosacea.27
Conclusion
In these studies, clindamycin cream 0.3% once daily, clindamycin cream 1% once or twice daily, and clindamycin gel 1% twice daily were all well tolerated; however, they were no more effective than the vehicles in the treatment of moderate to severe rosacea.
Acknowledgment
The authors would like to thank Helen Simpson, PhD, of Galderma R&D (Sophia Antipolis, France), for editorial and medical writing assistance.
- Whitney KM, Ditre CM. Anti-inflammatory properties of clindamycin: a review of its use in the treatment of acne vulgaris. Clinical Medicine Insights: Dermatology. 2011;4:27-41.
- Mays RM, Gordon RA, Wilson JM, et al. New antibiotic therapies for acne and rosacea. Dermatol Ther. 2012;25:23-37.
- Wilkin JK, DeWitt S. Treatment of rosacea: topical clindamycin versus oral tetracycline. Int J Dermatol. 1993;32:65-67.
- Breneman D, Savin R, VandePol C, et al. Double-blind, randomized, vehicle-controlled clinical trial of once-daily benzoyl peroxide/clindamycin topical gel in the treatment of patients with moderate to severe rosacea. Int J Dermatol. 2004;43:381-387.
- Leyden JJ, Thiboutot D, Shalita A. Photographic review of results from a clinical study comparing benzoyl peroxide 5%/clindamycin 1% topical gel with vehicle in the treatment of rosacea. Cutis. 2004;73(6 suppl):11-17.
- Chang AL, Alora-Palli M, Lima XT, et al. A randomized, double-blind, placebo-controlled, pilot study to assess the efficacy and safety of clindamycin 1.2% and tretinoin 0.025% combination gel for the treatment of acne rosacea over 12 weeks. J Drugs Dermatol. 2012;11:333-339.
- Freeman SA, Moon SD, Spencer JM. Clindamycin phosphate 1.2% and tretinoin 0.025% gel for rosacea: summary of a placebo-controlled, double-blind trial. J Drugs Dermatol. 2012;11:1410-1414.
- van Zuuren EJ, Fedorowicz Z, Carter B, et al. Interventions for rosacea. Cochrane Database Syst Rev. 2015;4:CD003262.
- Laquieze S, Czernielewski J, Baltas E. Beneficial use of Cetaphil moisturizing cream as part of a daily skin care regimen for individuals with rosacea. J Dermatolog Treat. 2007;18:158-162.
- Lookingbill DP, Chalker DK, Lindholm JS, et al. Treatment of acne with a combination clindamycin/benzoyl peroxide gel compared with clindamycin gel, benzoyl peroxide gel and vehicle gel: combined results of two double-blind investigations. J Am Acad Dermatol. 1997;37:590-595.
- Alirezaï M, Gerlach B, Horvath A, et al. Results of a randomised, multicentre study comparing a new water-based gel of clindamycin 1% versus clindamycin 1% topical solution in the treatment of acne vulgaris. Eur J Dermatol. 2005;15:274-278.
- Jarratt MT, Brundage T. Efficacy and safety of clindamycin-tretinoin gel versus clindamycin or tretinoin alone in acne vulgaris: a randomized, double-blind, vehicle-controlled study. J Drugs Dermatol. 2012;11:318-326.
- Benzaclin. Med Library website. http://medlibrary.org/lib/rx/meds/benzaclin-3. Updated May 8, 2013. Accessed January 24, 2017.
- Walsh TR, Efthimiou J, Dréno B. Systematic review of antibiotic resistance in acne: an increasing topical and oral threat. Lancet Infect Dis. 2016;16:E23-E33.
- Jeremy AH, Holland DB, Roberts SG, et al. Inflammatory events are involved in acne lesion initiation. J Invest Dermatol. 2003;121:20-27.
- Kircik LH. Re-evaluating treatment targets in acne vulgaris: adapting to a new understanding of pathophysiology. J Drugs Dermatol. 2014;13:S57-S60.
- Salzer S, Kresse S, Hirai Y, et al. Cathelicidin peptide LL-37 increases UVB-triggered inflammasome activation: possible implications for rosacea. J Dermatol Sci. 2014;76:173-179.
- Buhl T, Sulk M, Nowak P, et al. Molecular and morphological characterization of inflammatory infiltrate in rosacea reveals activation of Th1/Th17 pathways. J Invest Dermatol. 2015;135:2198-2208.
- Kistowska M, Meier B, Proust T, et al. Propionibacterium acnes promotes Th17 and Th17/Th1 responses in acne patients. J Invest Dermatol. 2015;135:110-118.
- Zeichner JA. Inflammatory acne treatment: review of current and new topical therapeutic options. J Drugs Dermatol. 2016;15(1 suppl 1):S11-S16.
- Nakano T, Hiramatsu K, Kishi K, et al. Clindamycin modulates inflammatory-cytokine induction in lipopolysaccharide-stimulated mouse peritoneal macrophages. Antimicrob Agents Chemother. 2003;47:363-367.
- Orman KL, English BK. Effects of antibiotic class on the macrophage inflammatory response to Streptococcus pneumoniae. J Infect Dis. 2000;182:1561-1565.
- Taylor M, Gonzalez M, Porter R. Pathways to inflammation: acne pathophysiology. Eur J Dermatol. 2011;21:323-333.
- Del Rosso JQ, Kircik LH. The sequence of inflammation, relevant biomarkers, and the pathogenesis of acne vulgaris: what does recent research show and what does it mean to the clinician? J Drugs Dermatol. 2013;12(8 suppl):S109-S115.
- Leyden J, Kaidbey K, Levy SF. The combination formulation of clindamycin 1% plus benzoyl peroxide 5% versus 3 different formulations of topical clindamycin alone in the reduction of Propionibacterium acnes. an in vivo comparative study. Am J Clin Dermatol. 2001;2:263-266.
- Wang WL, Everett ED, Johnson M, et al. Susceptibility of Propionibacterium acnes to seventeen antibiotics. Antimicrob Agents Chemother. 1977;11:171-173.
- Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013;69(6 suppl 1):S15-S26.
Rosacea is a chronic inflammatory skin disease characterized by central facial erythema with or without intermittent papules and pustules (described as the inflammatory lesions of rosacea). Although twice-daily clindamycin 1% solution or gel has been used in the treatment of acne, few studies have investigated the use of clindamycin in rosacea.1,2 In one study comparing twice-daily clindamycin lotion 1% with oral tetracycline in 43 rosacea patients, clindamycin was found to be superior in the eradication of pustules.3 A combination therapy of clindamycin 1% and benzoyl peroxide 5% was found to be more effective than the vehicle in inflammatory lesions and erythema of rosacea in a 12-week randomized controlled trial; however, a definitive advantage over US Food and Drug Administration-approved topical agents used to treat papulopustular rosacea was not established.4,5 Two further studies evaluated clindamycin phosphate 1.2%-tretinoin 0.025% combination gel in the treatment of rosacea, but only 1 showed any effect on papulopustular lesions.6-8 The objective of the studies reported here was to evaluate the efficacy and safety of clindamycin in the treatment of patients with moderate to severe rosacea.
Methods
Study Design
Two multicenter (study A, 20 centers; study B, 10 centers), randomized, investigator-blinded, vehicle-controlled studies were conducted in the United States between 1999 and 2002 in accordance with the Declaration of Helsinki, International Conference on Harmonisation Good Clinical Practice guidelines, and local regulatory requirements. The studies were reviewed and approved by the respective institutional review boards, and all participants provided written informed consent.
In study A, moderate to severe rosacea patients with erythema, telangiectasia, and at least 8 inflammatory lesions were randomized to receive clindamycin cream 1% or vehicle cream once (in the evening) or twice daily (in the morning and evening) or clindamycin cream 0.3% once daily (in the evening) for 12 weeks (1:1:1:1:1 ratio). All study treatments were supplied in identical tubes with blinded labels.
In study B, patients with moderate to severe rosacea and at least 8 inflammatory lesions were randomized in a 1:1 ratio with instructions to apply clindamycin gel 1% or vehicle gel to the affected areas twice daily (morning and evening) for 12 weeks.
Efficacy Evaluation
Evaluations were performed at baseline and weeks 2, 4, 8, and 12 on the intention-to-treat population with the last observation carried forward.
Efficacy assessments in both studies included inflammatory lesion counts (papules and pustules) of 5 facial regions--forehead, chin, nose, right cheek, left cheek--counted separately and then combined to give the total inflammatory lesion count (both studies), as well as improvement in the investigator global rosacea severity score (0=none/clear; 1=mild, detectable erythema with ≤7 papules/pustules; 2=moderate, prominent erythema with ≥8 papules/pustules; 3=severe, intense erythema with ≥10 to <50 papules/pustules; 3.5 [study A] or 4 [study B]=very severe, intense erythema with >50 papules/pustules). In study B, the proportion of participants dichotomized to success (a score of 0 [none/clear] or 1 [mild/almost clear]) or failure (a score of ≥2) on the 5-point investigator global rosacea severity scale at week 12 was evaluated. In study A, investigator global improvement assessment at week 12, based on photographs taken at baseline, was graded on a 7-point scale (from -1 [worse], 0 [no change], and 1 [minimal improvement] to 5 [clear]). In both studies, erythema severity was graded on a 7-point scale in increments of 0.5 (from 0=no erythema to 3.5=very severe redness, very intense redness). Skin irritation also was graded as none, mild, moderate, or severe.
Safety Evaluation
Safety was assessed by the incidence of adverse events (AEs).
Statistical Analysis
Studies were powered assuming 60% reduction in inflammatory lesion counts with active and 40% with vehicle, based on historical data from a prior study with metronidazole cream 0.75% versus vehicle; 64 participants were required in each treatment group to detect this effect using a 2-sided t test (α=.017). Pairwise comparisons (clindamycin vs respective vehicle) were performed using the Cochran-Mantel-Haenszel test for combined lesion count percentage change.
Results
Participant Disposition and Baseline Characteristics
Overall, a total of 629 participants were randomized across both studies. In study A, a total of 416 participants were randomized into 5 treatment arms, with 369 participants (88.7%) completing the study; 47 (11.3%) participants discontinued study A, mainly due to participant request (19/47 [40.4%]) or lost to follow-up (11/47 [23.4%]). In study B, a total of 213 participants were randomized to receive either clindamycin gel 1% (n=109 [51.2%]) twice daily or vehicle gel (n=104 [48.8%]) twice daily, with 193 participants (90.6%) completing the study; 20 (9.4%) participants discontinued study B, mainly due to participant request (6/20 [30%]) or lost to follow-up (4/20 [20%]). Participants in studies A and B were similar in demographics and baseline disease characteristics (Table). The majority of participants were white females.
Efficacy
No statistically significant difference was observed in all pairwise comparisons (clindamycin cream twice daily vs vehicle twice daily, clindamycin cream once daily vs vehicle once daily, clindamycin gel vs vehicle gel) for the primary end point of mean percentage change from baseline in inflammatory lesion counts at week 12 (Figure 1; P>.5 for all pairwise comparisons).
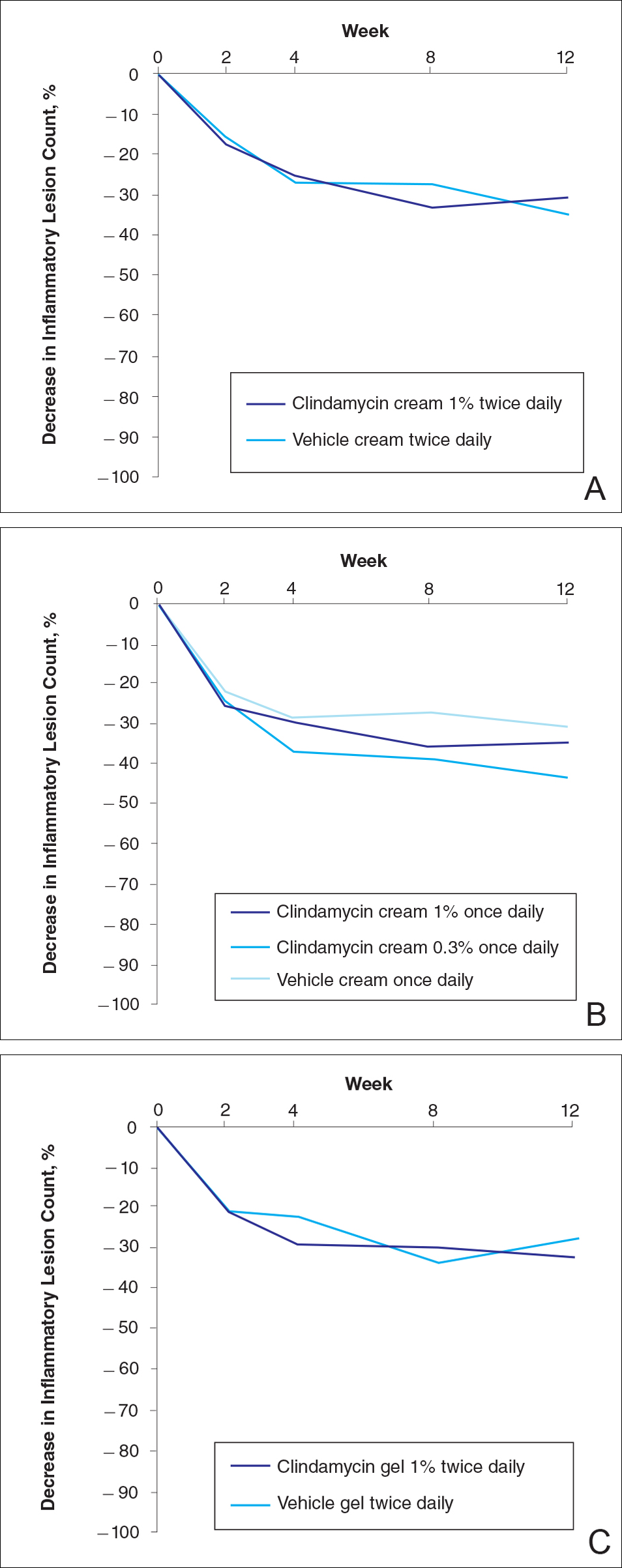
At week 12, the proportion of participants in study B deemed as a success (none/clear or mild/almost clear [investigator global rosacea severity score of 0 or 1]) in the clindamycin gel 1% and vehicle gel groups were 45% versus 38%, respectively (P=.347) (Figure 2).
For the secondary end point of mean investigator global rosacea severity assessment at week 12 (study A), there were no significant differences between the active and vehicle control groups (P>.5 for all pairwise comparisons)(Figure 3). Also, the proportion of participants with at least a moderate investigator global improvement assessment from baseline to week 12 ranged from 45% for clindamycin cream 1% twice daily to 56% for clindamycin cream 0.3% cream once daily and from 45% for vehicle cream once daily to 51% for vehicle cream twice daily (P>.5 for all pairwise comparisons).
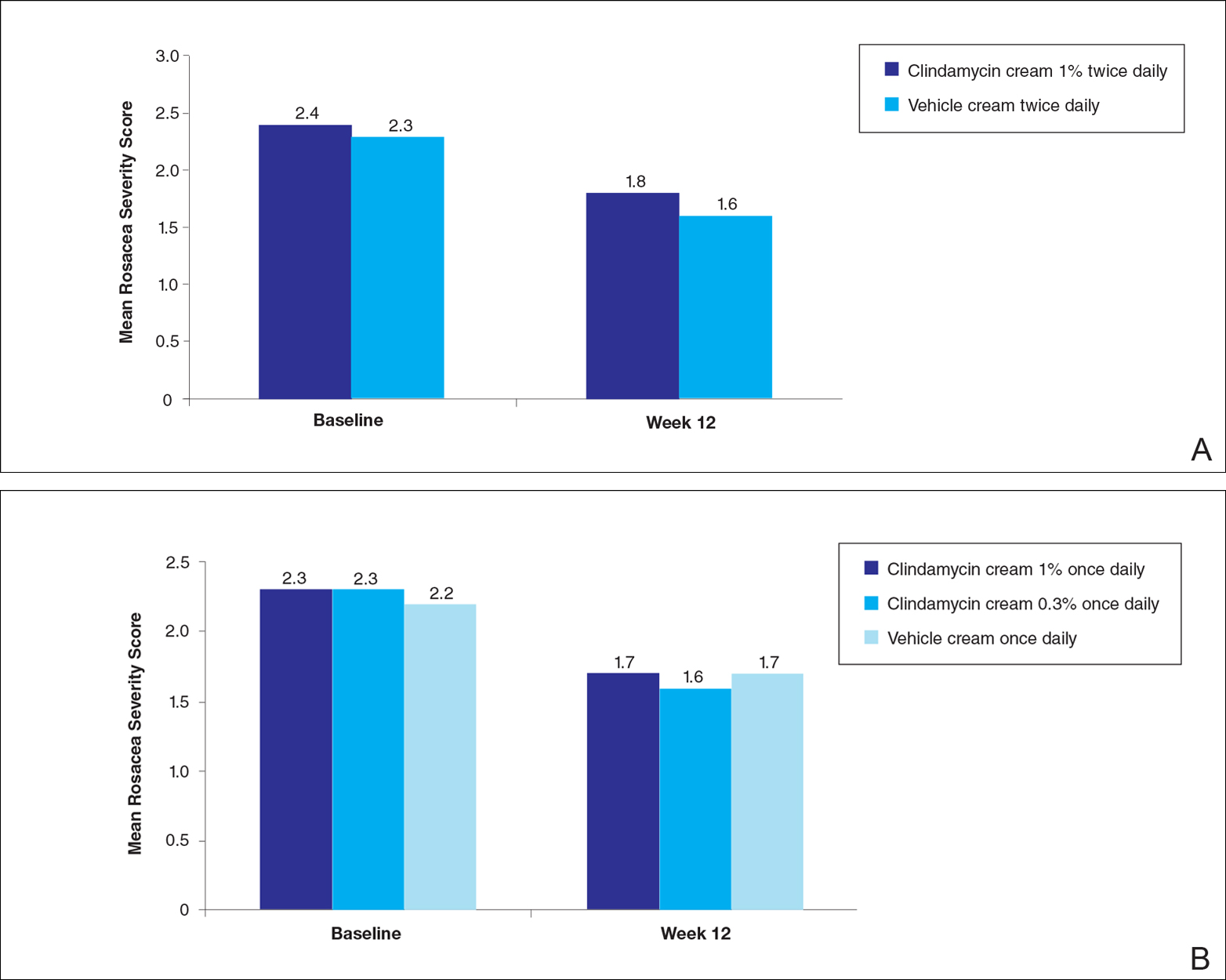
There were no significant differences in the mean total erythema severity scores at week 12 for clindamycin cream 1% twice daily versus vehicle cream twice daily (6.3 vs 6.0; P>.5), clindamycin cream 1% once daily versus vehicle cream once daily (6.2 vs 6.0; P>.5), clindamycin cream 0.3% once daily versus vehicle cream once daily (5.9 vs 6.0; P>.5), and clindamycin gel 1% twice daily versus vehicle gel twice daily (6.7 vs 6.2; P>.5).
There were no relevant differences between any of the clindamycin cream groups and their respective vehicle group at week 12 for skin irritation, including desquamation, edema, dryness, pruritus, and stinging/burning.
Safety
In study A, the majority of AEs in all 5 treatment arms were nondermatologic, mild in intensity, and not considered to be related to the study treatment by the investigator. Overall, 12 participants had AEs considered by the investigator as possibly or probably related to the study treatment: 4.9% in the clindamycin cream 1% twice daily group, 4.6% in the clindamycin cream 1% once daily group, 3.7% in the vehicle cream twice daily group, 1.2% in the clindamycin cream 0.3% once daily group, and 0% in the vehicle cream once daily group. Two treatment-related AEs led to treatment discontinuation, including dermatitis in 1 participant from the clindamycin cream 1% once daily group and contact dermatitis in 1 participant from the clindamycin cream 1% twice daily group.
Comment
No evidence of increased efficacy over the respective vehicles was observed with clindamycin cream or gel, whatever the regimen, in the treatment of rosacea patients in either of these well-designed and well-powered, blinded studies. Slight improvements in the various efficacy criteria were observed, even in the vehicle groups, highlighting the importance of using a good basic skin care regimen in the management of rosacea.9 In contrast to our observations of lack of efficacy in the treatment of rosacea, clinical efficacy of clindamycin has been demonstrated in acne,10-12 albeit with low efficacy for clindamycin monotherapy.13 It is noteworthy that oral or topical antibiotics are no longer recommended as monotherapy for acne to prevent and minimize antibiotic resistance and to preserve the therapeutic value of antibiotics.14
Acne and rosacea are both chronic inflammatory disorders of the skin associated with papules and pustules, and they share some common inflammatory patterns.15-19 Furthermore, the intrinsic anti-inflammatory activity of clindamycin in addition to its antibiotic effects has been suggested by some authors as the main reason for treating acne with clindamycin.20 However, the relative contributions of antibacterial and/or anti-inflammatory properties remain to be fully elucidated, and evidence for direct anti-inflammatory effects of clindamycin remains heterogeneous.21,22 Several pathophysiological factors have been implicated in acne, including hormonal effects, abnormal keratinocyte function, increased sebum production, and microbial components (eg, hypercolonization of the skin follicles by Propionibacterium acnes).23,24 The antibiotic activity of clindamycin against P acnes may be the key factor responsible for the clinical effects in acne.25,26 Although clindamycin may have anti-inflammatory effects in acne via a different inflammatory pathway not shared by rosacea, a purely antibiotic mechanism of action of clindamycin also could explain why we observed no evidence of efficacy in the treatment of rosacea, as no causative bacterial component has been clearly demonstrated in rosacea.27
Conclusion
In these studies, clindamycin cream 0.3% once daily, clindamycin cream 1% once or twice daily, and clindamycin gel 1% twice daily were all well tolerated; however, they were no more effective than the vehicles in the treatment of moderate to severe rosacea.
Acknowledgment
The authors would like to thank Helen Simpson, PhD, of Galderma R&D (Sophia Antipolis, France), for editorial and medical writing assistance.
Rosacea is a chronic inflammatory skin disease characterized by central facial erythema with or without intermittent papules and pustules (described as the inflammatory lesions of rosacea). Although twice-daily clindamycin 1% solution or gel has been used in the treatment of acne, few studies have investigated the use of clindamycin in rosacea.1,2 In one study comparing twice-daily clindamycin lotion 1% with oral tetracycline in 43 rosacea patients, clindamycin was found to be superior in the eradication of pustules.3 A combination therapy of clindamycin 1% and benzoyl peroxide 5% was found to be more effective than the vehicle in inflammatory lesions and erythema of rosacea in a 12-week randomized controlled trial; however, a definitive advantage over US Food and Drug Administration-approved topical agents used to treat papulopustular rosacea was not established.4,5 Two further studies evaluated clindamycin phosphate 1.2%-tretinoin 0.025% combination gel in the treatment of rosacea, but only 1 showed any effect on papulopustular lesions.6-8 The objective of the studies reported here was to evaluate the efficacy and safety of clindamycin in the treatment of patients with moderate to severe rosacea.
Methods
Study Design
Two multicenter (study A, 20 centers; study B, 10 centers), randomized, investigator-blinded, vehicle-controlled studies were conducted in the United States between 1999 and 2002 in accordance with the Declaration of Helsinki, International Conference on Harmonisation Good Clinical Practice guidelines, and local regulatory requirements. The studies were reviewed and approved by the respective institutional review boards, and all participants provided written informed consent.
In study A, moderate to severe rosacea patients with erythema, telangiectasia, and at least 8 inflammatory lesions were randomized to receive clindamycin cream 1% or vehicle cream once (in the evening) or twice daily (in the morning and evening) or clindamycin cream 0.3% once daily (in the evening) for 12 weeks (1:1:1:1:1 ratio). All study treatments were supplied in identical tubes with blinded labels.
In study B, patients with moderate to severe rosacea and at least 8 inflammatory lesions were randomized in a 1:1 ratio with instructions to apply clindamycin gel 1% or vehicle gel to the affected areas twice daily (morning and evening) for 12 weeks.
Efficacy Evaluation
Evaluations were performed at baseline and weeks 2, 4, 8, and 12 on the intention-to-treat population with the last observation carried forward.
Efficacy assessments in both studies included inflammatory lesion counts (papules and pustules) of 5 facial regions--forehead, chin, nose, right cheek, left cheek--counted separately and then combined to give the total inflammatory lesion count (both studies), as well as improvement in the investigator global rosacea severity score (0=none/clear; 1=mild, detectable erythema with ≤7 papules/pustules; 2=moderate, prominent erythema with ≥8 papules/pustules; 3=severe, intense erythema with ≥10 to <50 papules/pustules; 3.5 [study A] or 4 [study B]=very severe, intense erythema with >50 papules/pustules). In study B, the proportion of participants dichotomized to success (a score of 0 [none/clear] or 1 [mild/almost clear]) or failure (a score of ≥2) on the 5-point investigator global rosacea severity scale at week 12 was evaluated. In study A, investigator global improvement assessment at week 12, based on photographs taken at baseline, was graded on a 7-point scale (from -1 [worse], 0 [no change], and 1 [minimal improvement] to 5 [clear]). In both studies, erythema severity was graded on a 7-point scale in increments of 0.5 (from 0=no erythema to 3.5=very severe redness, very intense redness). Skin irritation also was graded as none, mild, moderate, or severe.
Safety Evaluation
Safety was assessed by the incidence of adverse events (AEs).
Statistical Analysis
Studies were powered assuming 60% reduction in inflammatory lesion counts with active and 40% with vehicle, based on historical data from a prior study with metronidazole cream 0.75% versus vehicle; 64 participants were required in each treatment group to detect this effect using a 2-sided t test (α=.017). Pairwise comparisons (clindamycin vs respective vehicle) were performed using the Cochran-Mantel-Haenszel test for combined lesion count percentage change.
Results
Participant Disposition and Baseline Characteristics
Overall, a total of 629 participants were randomized across both studies. In study A, a total of 416 participants were randomized into 5 treatment arms, with 369 participants (88.7%) completing the study; 47 (11.3%) participants discontinued study A, mainly due to participant request (19/47 [40.4%]) or lost to follow-up (11/47 [23.4%]). In study B, a total of 213 participants were randomized to receive either clindamycin gel 1% (n=109 [51.2%]) twice daily or vehicle gel (n=104 [48.8%]) twice daily, with 193 participants (90.6%) completing the study; 20 (9.4%) participants discontinued study B, mainly due to participant request (6/20 [30%]) or lost to follow-up (4/20 [20%]). Participants in studies A and B were similar in demographics and baseline disease characteristics (Table). The majority of participants were white females.
Efficacy
No statistically significant difference was observed in all pairwise comparisons (clindamycin cream twice daily vs vehicle twice daily, clindamycin cream once daily vs vehicle once daily, clindamycin gel vs vehicle gel) for the primary end point of mean percentage change from baseline in inflammatory lesion counts at week 12 (Figure 1; P>.5 for all pairwise comparisons).
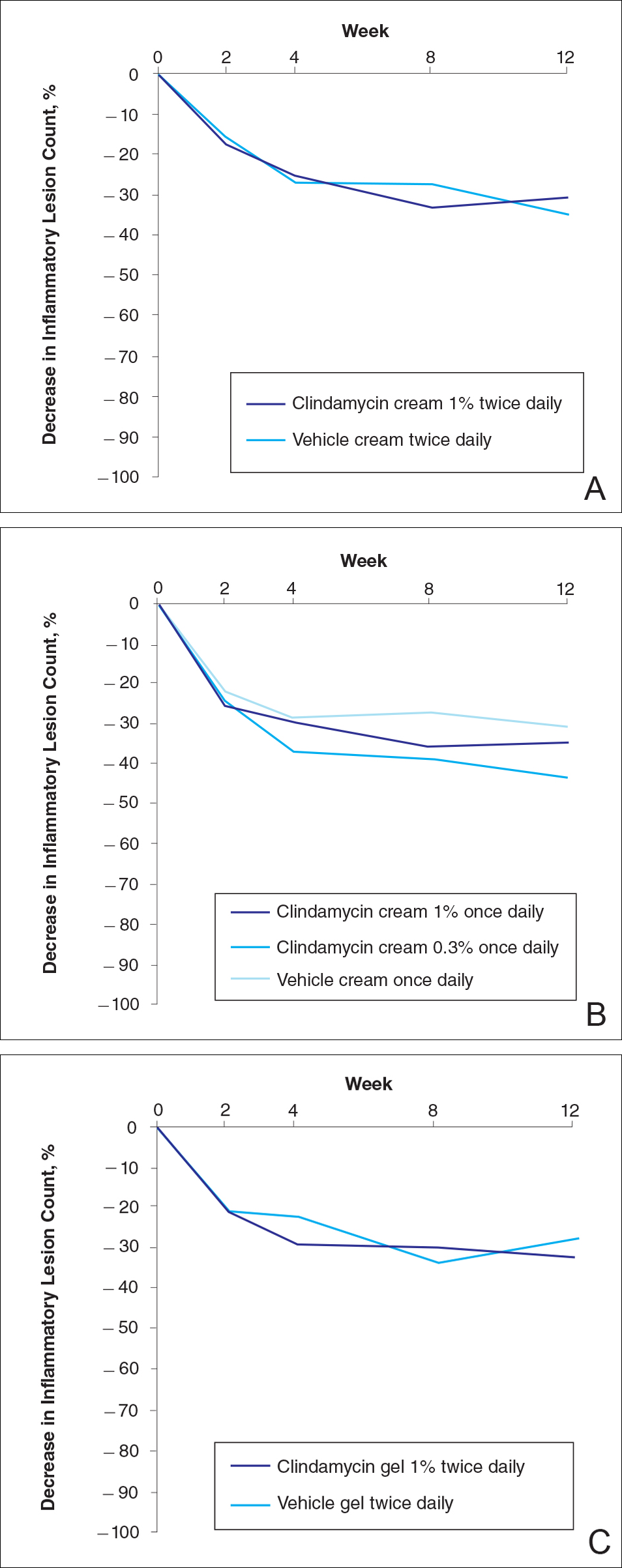
At week 12, the proportion of participants in study B deemed as a success (none/clear or mild/almost clear [investigator global rosacea severity score of 0 or 1]) in the clindamycin gel 1% and vehicle gel groups were 45% versus 38%, respectively (P=.347) (Figure 2).
For the secondary end point of mean investigator global rosacea severity assessment at week 12 (study A), there were no significant differences between the active and vehicle control groups (P>.5 for all pairwise comparisons)(Figure 3). Also, the proportion of participants with at least a moderate investigator global improvement assessment from baseline to week 12 ranged from 45% for clindamycin cream 1% twice daily to 56% for clindamycin cream 0.3% cream once daily and from 45% for vehicle cream once daily to 51% for vehicle cream twice daily (P>.5 for all pairwise comparisons).
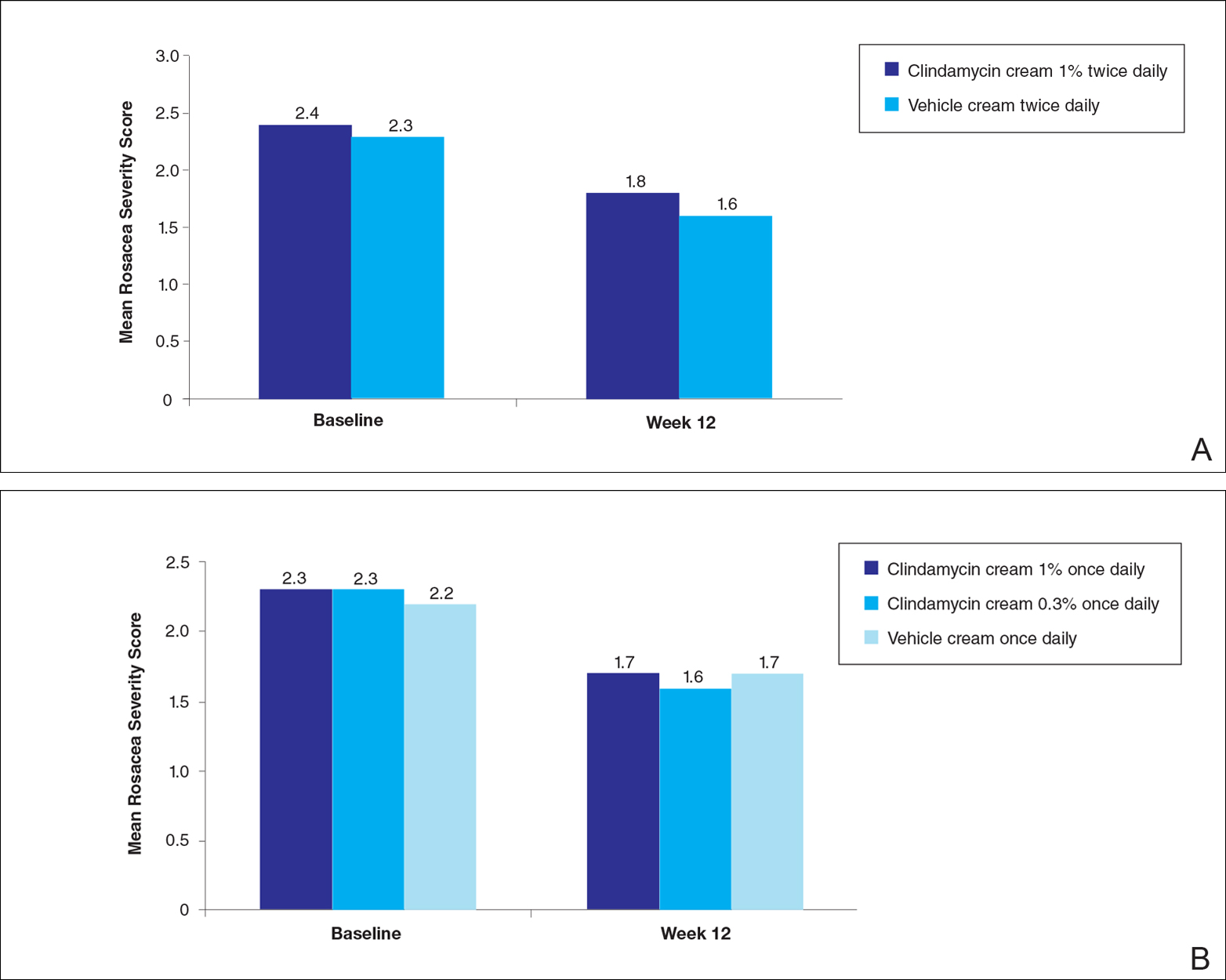
There were no significant differences in the mean total erythema severity scores at week 12 for clindamycin cream 1% twice daily versus vehicle cream twice daily (6.3 vs 6.0; P>.5), clindamycin cream 1% once daily versus vehicle cream once daily (6.2 vs 6.0; P>.5), clindamycin cream 0.3% once daily versus vehicle cream once daily (5.9 vs 6.0; P>.5), and clindamycin gel 1% twice daily versus vehicle gel twice daily (6.7 vs 6.2; P>.5).
There were no relevant differences between any of the clindamycin cream groups and their respective vehicle group at week 12 for skin irritation, including desquamation, edema, dryness, pruritus, and stinging/burning.
Safety
In study A, the majority of AEs in all 5 treatment arms were nondermatologic, mild in intensity, and not considered to be related to the study treatment by the investigator. Overall, 12 participants had AEs considered by the investigator as possibly or probably related to the study treatment: 4.9% in the clindamycin cream 1% twice daily group, 4.6% in the clindamycin cream 1% once daily group, 3.7% in the vehicle cream twice daily group, 1.2% in the clindamycin cream 0.3% once daily group, and 0% in the vehicle cream once daily group. Two treatment-related AEs led to treatment discontinuation, including dermatitis in 1 participant from the clindamycin cream 1% once daily group and contact dermatitis in 1 participant from the clindamycin cream 1% twice daily group.
Comment
No evidence of increased efficacy over the respective vehicles was observed with clindamycin cream or gel, whatever the regimen, in the treatment of rosacea patients in either of these well-designed and well-powered, blinded studies. Slight improvements in the various efficacy criteria were observed, even in the vehicle groups, highlighting the importance of using a good basic skin care regimen in the management of rosacea.9 In contrast to our observations of lack of efficacy in the treatment of rosacea, clinical efficacy of clindamycin has been demonstrated in acne,10-12 albeit with low efficacy for clindamycin monotherapy.13 It is noteworthy that oral or topical antibiotics are no longer recommended as monotherapy for acne to prevent and minimize antibiotic resistance and to preserve the therapeutic value of antibiotics.14
Acne and rosacea are both chronic inflammatory disorders of the skin associated with papules and pustules, and they share some common inflammatory patterns.15-19 Furthermore, the intrinsic anti-inflammatory activity of clindamycin in addition to its antibiotic effects has been suggested by some authors as the main reason for treating acne with clindamycin.20 However, the relative contributions of antibacterial and/or anti-inflammatory properties remain to be fully elucidated, and evidence for direct anti-inflammatory effects of clindamycin remains heterogeneous.21,22 Several pathophysiological factors have been implicated in acne, including hormonal effects, abnormal keratinocyte function, increased sebum production, and microbial components (eg, hypercolonization of the skin follicles by Propionibacterium acnes).23,24 The antibiotic activity of clindamycin against P acnes may be the key factor responsible for the clinical effects in acne.25,26 Although clindamycin may have anti-inflammatory effects in acne via a different inflammatory pathway not shared by rosacea, a purely antibiotic mechanism of action of clindamycin also could explain why we observed no evidence of efficacy in the treatment of rosacea, as no causative bacterial component has been clearly demonstrated in rosacea.27
Conclusion
In these studies, clindamycin cream 0.3% once daily, clindamycin cream 1% once or twice daily, and clindamycin gel 1% twice daily were all well tolerated; however, they were no more effective than the vehicles in the treatment of moderate to severe rosacea.
Acknowledgment
The authors would like to thank Helen Simpson, PhD, of Galderma R&D (Sophia Antipolis, France), for editorial and medical writing assistance.
- Whitney KM, Ditre CM. Anti-inflammatory properties of clindamycin: a review of its use in the treatment of acne vulgaris. Clinical Medicine Insights: Dermatology. 2011;4:27-41.
- Mays RM, Gordon RA, Wilson JM, et al. New antibiotic therapies for acne and rosacea. Dermatol Ther. 2012;25:23-37.
- Wilkin JK, DeWitt S. Treatment of rosacea: topical clindamycin versus oral tetracycline. Int J Dermatol. 1993;32:65-67.
- Breneman D, Savin R, VandePol C, et al. Double-blind, randomized, vehicle-controlled clinical trial of once-daily benzoyl peroxide/clindamycin topical gel in the treatment of patients with moderate to severe rosacea. Int J Dermatol. 2004;43:381-387.
- Leyden JJ, Thiboutot D, Shalita A. Photographic review of results from a clinical study comparing benzoyl peroxide 5%/clindamycin 1% topical gel with vehicle in the treatment of rosacea. Cutis. 2004;73(6 suppl):11-17.
- Chang AL, Alora-Palli M, Lima XT, et al. A randomized, double-blind, placebo-controlled, pilot study to assess the efficacy and safety of clindamycin 1.2% and tretinoin 0.025% combination gel for the treatment of acne rosacea over 12 weeks. J Drugs Dermatol. 2012;11:333-339.
- Freeman SA, Moon SD, Spencer JM. Clindamycin phosphate 1.2% and tretinoin 0.025% gel for rosacea: summary of a placebo-controlled, double-blind trial. J Drugs Dermatol. 2012;11:1410-1414.
- van Zuuren EJ, Fedorowicz Z, Carter B, et al. Interventions for rosacea. Cochrane Database Syst Rev. 2015;4:CD003262.
- Laquieze S, Czernielewski J, Baltas E. Beneficial use of Cetaphil moisturizing cream as part of a daily skin care regimen for individuals with rosacea. J Dermatolog Treat. 2007;18:158-162.
- Lookingbill DP, Chalker DK, Lindholm JS, et al. Treatment of acne with a combination clindamycin/benzoyl peroxide gel compared with clindamycin gel, benzoyl peroxide gel and vehicle gel: combined results of two double-blind investigations. J Am Acad Dermatol. 1997;37:590-595.
- Alirezaï M, Gerlach B, Horvath A, et al. Results of a randomised, multicentre study comparing a new water-based gel of clindamycin 1% versus clindamycin 1% topical solution in the treatment of acne vulgaris. Eur J Dermatol. 2005;15:274-278.
- Jarratt MT, Brundage T. Efficacy and safety of clindamycin-tretinoin gel versus clindamycin or tretinoin alone in acne vulgaris: a randomized, double-blind, vehicle-controlled study. J Drugs Dermatol. 2012;11:318-326.
- Benzaclin. Med Library website. http://medlibrary.org/lib/rx/meds/benzaclin-3. Updated May 8, 2013. Accessed January 24, 2017.
- Walsh TR, Efthimiou J, Dréno B. Systematic review of antibiotic resistance in acne: an increasing topical and oral threat. Lancet Infect Dis. 2016;16:E23-E33.
- Jeremy AH, Holland DB, Roberts SG, et al. Inflammatory events are involved in acne lesion initiation. J Invest Dermatol. 2003;121:20-27.
- Kircik LH. Re-evaluating treatment targets in acne vulgaris: adapting to a new understanding of pathophysiology. J Drugs Dermatol. 2014;13:S57-S60.
- Salzer S, Kresse S, Hirai Y, et al. Cathelicidin peptide LL-37 increases UVB-triggered inflammasome activation: possible implications for rosacea. J Dermatol Sci. 2014;76:173-179.
- Buhl T, Sulk M, Nowak P, et al. Molecular and morphological characterization of inflammatory infiltrate in rosacea reveals activation of Th1/Th17 pathways. J Invest Dermatol. 2015;135:2198-2208.
- Kistowska M, Meier B, Proust T, et al. Propionibacterium acnes promotes Th17 and Th17/Th1 responses in acne patients. J Invest Dermatol. 2015;135:110-118.
- Zeichner JA. Inflammatory acne treatment: review of current and new topical therapeutic options. J Drugs Dermatol. 2016;15(1 suppl 1):S11-S16.
- Nakano T, Hiramatsu K, Kishi K, et al. Clindamycin modulates inflammatory-cytokine induction in lipopolysaccharide-stimulated mouse peritoneal macrophages. Antimicrob Agents Chemother. 2003;47:363-367.
- Orman KL, English BK. Effects of antibiotic class on the macrophage inflammatory response to Streptococcus pneumoniae. J Infect Dis. 2000;182:1561-1565.
- Taylor M, Gonzalez M, Porter R. Pathways to inflammation: acne pathophysiology. Eur J Dermatol. 2011;21:323-333.
- Del Rosso JQ, Kircik LH. The sequence of inflammation, relevant biomarkers, and the pathogenesis of acne vulgaris: what does recent research show and what does it mean to the clinician? J Drugs Dermatol. 2013;12(8 suppl):S109-S115.
- Leyden J, Kaidbey K, Levy SF. The combination formulation of clindamycin 1% plus benzoyl peroxide 5% versus 3 different formulations of topical clindamycin alone in the reduction of Propionibacterium acnes. an in vivo comparative study. Am J Clin Dermatol. 2001;2:263-266.
- Wang WL, Everett ED, Johnson M, et al. Susceptibility of Propionibacterium acnes to seventeen antibiotics. Antimicrob Agents Chemother. 1977;11:171-173.
- Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013;69(6 suppl 1):S15-S26.
- Whitney KM, Ditre CM. Anti-inflammatory properties of clindamycin: a review of its use in the treatment of acne vulgaris. Clinical Medicine Insights: Dermatology. 2011;4:27-41.
- Mays RM, Gordon RA, Wilson JM, et al. New antibiotic therapies for acne and rosacea. Dermatol Ther. 2012;25:23-37.
- Wilkin JK, DeWitt S. Treatment of rosacea: topical clindamycin versus oral tetracycline. Int J Dermatol. 1993;32:65-67.
- Breneman D, Savin R, VandePol C, et al. Double-blind, randomized, vehicle-controlled clinical trial of once-daily benzoyl peroxide/clindamycin topical gel in the treatment of patients with moderate to severe rosacea. Int J Dermatol. 2004;43:381-387.
- Leyden JJ, Thiboutot D, Shalita A. Photographic review of results from a clinical study comparing benzoyl peroxide 5%/clindamycin 1% topical gel with vehicle in the treatment of rosacea. Cutis. 2004;73(6 suppl):11-17.
- Chang AL, Alora-Palli M, Lima XT, et al. A randomized, double-blind, placebo-controlled, pilot study to assess the efficacy and safety of clindamycin 1.2% and tretinoin 0.025% combination gel for the treatment of acne rosacea over 12 weeks. J Drugs Dermatol. 2012;11:333-339.
- Freeman SA, Moon SD, Spencer JM. Clindamycin phosphate 1.2% and tretinoin 0.025% gel for rosacea: summary of a placebo-controlled, double-blind trial. J Drugs Dermatol. 2012;11:1410-1414.
- van Zuuren EJ, Fedorowicz Z, Carter B, et al. Interventions for rosacea. Cochrane Database Syst Rev. 2015;4:CD003262.
- Laquieze S, Czernielewski J, Baltas E. Beneficial use of Cetaphil moisturizing cream as part of a daily skin care regimen for individuals with rosacea. J Dermatolog Treat. 2007;18:158-162.
- Lookingbill DP, Chalker DK, Lindholm JS, et al. Treatment of acne with a combination clindamycin/benzoyl peroxide gel compared with clindamycin gel, benzoyl peroxide gel and vehicle gel: combined results of two double-blind investigations. J Am Acad Dermatol. 1997;37:590-595.
- Alirezaï M, Gerlach B, Horvath A, et al. Results of a randomised, multicentre study comparing a new water-based gel of clindamycin 1% versus clindamycin 1% topical solution in the treatment of acne vulgaris. Eur J Dermatol. 2005;15:274-278.
- Jarratt MT, Brundage T. Efficacy and safety of clindamycin-tretinoin gel versus clindamycin or tretinoin alone in acne vulgaris: a randomized, double-blind, vehicle-controlled study. J Drugs Dermatol. 2012;11:318-326.
- Benzaclin. Med Library website. http://medlibrary.org/lib/rx/meds/benzaclin-3. Updated May 8, 2013. Accessed January 24, 2017.
- Walsh TR, Efthimiou J, Dréno B. Systematic review of antibiotic resistance in acne: an increasing topical and oral threat. Lancet Infect Dis. 2016;16:E23-E33.
- Jeremy AH, Holland DB, Roberts SG, et al. Inflammatory events are involved in acne lesion initiation. J Invest Dermatol. 2003;121:20-27.
- Kircik LH. Re-evaluating treatment targets in acne vulgaris: adapting to a new understanding of pathophysiology. J Drugs Dermatol. 2014;13:S57-S60.
- Salzer S, Kresse S, Hirai Y, et al. Cathelicidin peptide LL-37 increases UVB-triggered inflammasome activation: possible implications for rosacea. J Dermatol Sci. 2014;76:173-179.
- Buhl T, Sulk M, Nowak P, et al. Molecular and morphological characterization of inflammatory infiltrate in rosacea reveals activation of Th1/Th17 pathways. J Invest Dermatol. 2015;135:2198-2208.
- Kistowska M, Meier B, Proust T, et al. Propionibacterium acnes promotes Th17 and Th17/Th1 responses in acne patients. J Invest Dermatol. 2015;135:110-118.
- Zeichner JA. Inflammatory acne treatment: review of current and new topical therapeutic options. J Drugs Dermatol. 2016;15(1 suppl 1):S11-S16.
- Nakano T, Hiramatsu K, Kishi K, et al. Clindamycin modulates inflammatory-cytokine induction in lipopolysaccharide-stimulated mouse peritoneal macrophages. Antimicrob Agents Chemother. 2003;47:363-367.
- Orman KL, English BK. Effects of antibiotic class on the macrophage inflammatory response to Streptococcus pneumoniae. J Infect Dis. 2000;182:1561-1565.
- Taylor M, Gonzalez M, Porter R. Pathways to inflammation: acne pathophysiology. Eur J Dermatol. 2011;21:323-333.
- Del Rosso JQ, Kircik LH. The sequence of inflammation, relevant biomarkers, and the pathogenesis of acne vulgaris: what does recent research show and what does it mean to the clinician? J Drugs Dermatol. 2013;12(8 suppl):S109-S115.
- Leyden J, Kaidbey K, Levy SF. The combination formulation of clindamycin 1% plus benzoyl peroxide 5% versus 3 different formulations of topical clindamycin alone in the reduction of Propionibacterium acnes. an in vivo comparative study. Am J Clin Dermatol. 2001;2:263-266.
- Wang WL, Everett ED, Johnson M, et al. Susceptibility of Propionibacterium acnes to seventeen antibiotics. Antimicrob Agents Chemother. 1977;11:171-173.
- Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013;69(6 suppl 1):S15-S26.
Practice Points
- Clindamycin cream 0.3% and 1% and clindamycin gel 1% were no more effective than their respective vehicles in the treatment of moderate to severe rosacea.
- Clindamycin may have no intrinsic anti-inflammatory activity in rosacea.