User login
SHM Allies with Leading Health Care Groups to Advance Hospital Patient Nutrition
SHM announced in May the launch of a new interdisciplinary partnership, the Alliance to Advance Patient Nutrition, in conjunction with four other organizations. The alliance’s mission is to improve patient outcomes through nutrition intervention in the hospital.
Representing more than 100,000 dietitians, nurses, hospitalists, and other physicians and clinicians from across the nation, the following organizations have come together with SHM to champion for early nutrition screening, assessment, and intervention in hospitals:
- Academy of Medical-Surgical Nurses (AMSN);
- Academy of Nutrition and Dietetics (AND);
- American Society for Parenteral and Enteral Nutrition (ASPEN); and
- Abbott Nutrition.
Malnutrition increases costs, length of stay, and unfavorable outcomes. Properly addressing hospital malnutrition creates an opportunity to improve quality of care while also reducing healthcare costs. Additional clinical research finds that malnourished patients are two times more likely to develop a pressure ulcer, while patients with malnutrition have three times the rate of infection.
Yet when hospitalized patients are provided intervention via oral nutrition supplements, health economic research finds associated benefits:
Nutrition intervention can reduce hospital length of stay by an average of two days, and nutrition intervention has been shown to reduce patient hospitalization costs by 21.6%, or $4,734 per episode.
Additionally, there was a 6.7% reduction in the probability of 30-day readmission with patients who had at least one known subsequent readmission and were offered oral nutrition supplements during hospitalization.
“There is a growing body of evidence supporting the positive impact nutrition has on improving patient outcomes,” says hospitalist Melissa Parkhurst, MD, FHM, who serves as medical director for the University of Kansas Hospital’s hospitalist section and its nutrition support service. “We are seeing that early intervention can make a significant difference. As physicians, we need to work with the entire clinician team to ensure that nutrition is an integral part of our patients’ treatment plans.”
The alliance launched a website at www.malnutrition.org to provide hospital-based clinicians with the following resources:
- Research and fact sheets about malnutrition and the positive impact nutrition intervention has on patient care and outcomes;
- The Alliance Nutrition Toolkit, which facilitates clinician collaboration and nutrition integration; and
- Information about educational events, such as quick learning modules, continuing medical education (CME) programs.
The Alliance to Advance Patient Nutrition is made possible with support from Abbott’s nutrition business.
SHM announced in May the launch of a new interdisciplinary partnership, the Alliance to Advance Patient Nutrition, in conjunction with four other organizations. The alliance’s mission is to improve patient outcomes through nutrition intervention in the hospital.
Representing more than 100,000 dietitians, nurses, hospitalists, and other physicians and clinicians from across the nation, the following organizations have come together with SHM to champion for early nutrition screening, assessment, and intervention in hospitals:
- Academy of Medical-Surgical Nurses (AMSN);
- Academy of Nutrition and Dietetics (AND);
- American Society for Parenteral and Enteral Nutrition (ASPEN); and
- Abbott Nutrition.
Malnutrition increases costs, length of stay, and unfavorable outcomes. Properly addressing hospital malnutrition creates an opportunity to improve quality of care while also reducing healthcare costs. Additional clinical research finds that malnourished patients are two times more likely to develop a pressure ulcer, while patients with malnutrition have three times the rate of infection.
Yet when hospitalized patients are provided intervention via oral nutrition supplements, health economic research finds associated benefits:
Nutrition intervention can reduce hospital length of stay by an average of two days, and nutrition intervention has been shown to reduce patient hospitalization costs by 21.6%, or $4,734 per episode.
Additionally, there was a 6.7% reduction in the probability of 30-day readmission with patients who had at least one known subsequent readmission and were offered oral nutrition supplements during hospitalization.
“There is a growing body of evidence supporting the positive impact nutrition has on improving patient outcomes,” says hospitalist Melissa Parkhurst, MD, FHM, who serves as medical director for the University of Kansas Hospital’s hospitalist section and its nutrition support service. “We are seeing that early intervention can make a significant difference. As physicians, we need to work with the entire clinician team to ensure that nutrition is an integral part of our patients’ treatment plans.”
The alliance launched a website at www.malnutrition.org to provide hospital-based clinicians with the following resources:
- Research and fact sheets about malnutrition and the positive impact nutrition intervention has on patient care and outcomes;
- The Alliance Nutrition Toolkit, which facilitates clinician collaboration and nutrition integration; and
- Information about educational events, such as quick learning modules, continuing medical education (CME) programs.
The Alliance to Advance Patient Nutrition is made possible with support from Abbott’s nutrition business.
SHM announced in May the launch of a new interdisciplinary partnership, the Alliance to Advance Patient Nutrition, in conjunction with four other organizations. The alliance’s mission is to improve patient outcomes through nutrition intervention in the hospital.
Representing more than 100,000 dietitians, nurses, hospitalists, and other physicians and clinicians from across the nation, the following organizations have come together with SHM to champion for early nutrition screening, assessment, and intervention in hospitals:
- Academy of Medical-Surgical Nurses (AMSN);
- Academy of Nutrition and Dietetics (AND);
- American Society for Parenteral and Enteral Nutrition (ASPEN); and
- Abbott Nutrition.
Malnutrition increases costs, length of stay, and unfavorable outcomes. Properly addressing hospital malnutrition creates an opportunity to improve quality of care while also reducing healthcare costs. Additional clinical research finds that malnourished patients are two times more likely to develop a pressure ulcer, while patients with malnutrition have three times the rate of infection.
Yet when hospitalized patients are provided intervention via oral nutrition supplements, health economic research finds associated benefits:
Nutrition intervention can reduce hospital length of stay by an average of two days, and nutrition intervention has been shown to reduce patient hospitalization costs by 21.6%, or $4,734 per episode.
Additionally, there was a 6.7% reduction in the probability of 30-day readmission with patients who had at least one known subsequent readmission and were offered oral nutrition supplements during hospitalization.
“There is a growing body of evidence supporting the positive impact nutrition has on improving patient outcomes,” says hospitalist Melissa Parkhurst, MD, FHM, who serves as medical director for the University of Kansas Hospital’s hospitalist section and its nutrition support service. “We are seeing that early intervention can make a significant difference. As physicians, we need to work with the entire clinician team to ensure that nutrition is an integral part of our patients’ treatment plans.”
The alliance launched a website at www.malnutrition.org to provide hospital-based clinicians with the following resources:
- Research and fact sheets about malnutrition and the positive impact nutrition intervention has on patient care and outcomes;
- The Alliance Nutrition Toolkit, which facilitates clinician collaboration and nutrition integration; and
- Information about educational events, such as quick learning modules, continuing medical education (CME) programs.
The Alliance to Advance Patient Nutrition is made possible with support from Abbott’s nutrition business.
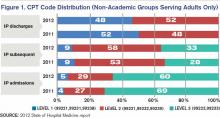
Hospitalist-Specific Data Shows Rise in Use of Some CPT Codes
Before 2011, hospitalists had only Centers for Medicare & Medicaid Services’ (CMS) specialty-specific CPT distribution data, and no hospitalist-specific data, available when looking for benchmarks against which to compare their billing practices. Thanks to recent State of Hospital Medicine surveys, however, we now have hospitalist-specific data for the distribution of commonly used CPT codes. It’s interesting to analyze how 2011 data compares to 2012, and how the use of high-level codes varies by geographic region, employment model, compensation structure, and practice size.
In 2012, the use of the higher-level inpatient (IP) discharge code (99239) increased to 52% from 48% in 2011 among HM groups serving adults only, and the use of the highest-level IP subsequent code (99233) increased to 33% from 28% in the same comparison. This increase is in keeping with national trends. According to a May 2012 report by the Department of Health and Human Services’ Office of Inspector General, from 2001 to 2010, physicians’ billing shifted from lower-level to higher-level codes. For example, the billing of the lowest-level code (99231) decreased 16%, while the billing of the two higher-level codes (99232 and 99233) increased 6% and 9%, respectively.
Possible drivers of this change include:
- Expanded use of electronic health records (EHRs);
- Increased physician education about documentation requirements; and
- A sicker hospitalized patient population due to expanded outpatient care capabilities.
Although the proportion of high-level subsequent and discharge codes reported by SHM increased in 2012, the percent of highest-level IP admission codes (99223) actually decreased to 66% from 69%. There are many possible reasons for this. First, the elimination of consult codes by CMS in 2010 increased the overall use of admission codes but might have decreased the proportion of highest-level admission codes. Additionally, there may be an increased use of higher RVU-generating critical-care codes preferentially over billing of the highest-level admission codes. Third, there is the possibility that the extra documentation required for high-level admissions is a billing deterrent. Similarly, higher-level codes may be downcoded if documentation is lacking or incomplete.
Source: 2012 State of Hospital Medicine report
Comparatively, my health system, Allina Health, showed an increase in the use of highest-level codes for all three CPT codes analyzed.
With the increasing sophistication of EHRs and coding technology tools, it will be interesting to see the future impact on coding distribution as providers adapt to new documentation processes that support health information exchange across systems.
Comparing geographic regions, the West uses the highest proportion of high-level codes for admission, follow-up, and discharge, followed by the Midwest.
Interestingly, variation in billing by group size is only correlated directly to admission codes, but not to follow-up or discharge codes—with larger services tending to bill more of the highest-level admission codes.
Admission code use correlates directly with compensation structure; groups providing 100% of total compensation in the form of salary bill the lowest percentage of high-level admission codes. As compensation trends away from straight salaries, the percentage of high-level admission codes increases. The picture is less clear for high-level follow-up and discharge codes.
Comparing academic and nonacademic HM groups shows greater use of the highest- level admission, follow-up, and discharge codes for nonacademic HM groups. This is likely because academic hospitalists can only bill for their own time and not for time spent by medical residents.
Employment model (e.g. hospital system, private hospitalist-only groups, management companies, etc.) showed no categorical effect on CPT distribution.
Dr. Stephan is regional hospitalist medical director for Allina Health in Minneapolis and the incoming chair of SHM’s Practice Analysis Committee.
Before 2011, hospitalists had only Centers for Medicare & Medicaid Services’ (CMS) specialty-specific CPT distribution data, and no hospitalist-specific data, available when looking for benchmarks against which to compare their billing practices. Thanks to recent State of Hospital Medicine surveys, however, we now have hospitalist-specific data for the distribution of commonly used CPT codes. It’s interesting to analyze how 2011 data compares to 2012, and how the use of high-level codes varies by geographic region, employment model, compensation structure, and practice size.
In 2012, the use of the higher-level inpatient (IP) discharge code (99239) increased to 52% from 48% in 2011 among HM groups serving adults only, and the use of the highest-level IP subsequent code (99233) increased to 33% from 28% in the same comparison. This increase is in keeping with national trends. According to a May 2012 report by the Department of Health and Human Services’ Office of Inspector General, from 2001 to 2010, physicians’ billing shifted from lower-level to higher-level codes. For example, the billing of the lowest-level code (99231) decreased 16%, while the billing of the two higher-level codes (99232 and 99233) increased 6% and 9%, respectively.
Possible drivers of this change include:
- Expanded use of electronic health records (EHRs);
- Increased physician education about documentation requirements; and
- A sicker hospitalized patient population due to expanded outpatient care capabilities.
Although the proportion of high-level subsequent and discharge codes reported by SHM increased in 2012, the percent of highest-level IP admission codes (99223) actually decreased to 66% from 69%. There are many possible reasons for this. First, the elimination of consult codes by CMS in 2010 increased the overall use of admission codes but might have decreased the proportion of highest-level admission codes. Additionally, there may be an increased use of higher RVU-generating critical-care codes preferentially over billing of the highest-level admission codes. Third, there is the possibility that the extra documentation required for high-level admissions is a billing deterrent. Similarly, higher-level codes may be downcoded if documentation is lacking or incomplete.
Source: 2012 State of Hospital Medicine report
Comparatively, my health system, Allina Health, showed an increase in the use of highest-level codes for all three CPT codes analyzed.
With the increasing sophistication of EHRs and coding technology tools, it will be interesting to see the future impact on coding distribution as providers adapt to new documentation processes that support health information exchange across systems.
Comparing geographic regions, the West uses the highest proportion of high-level codes for admission, follow-up, and discharge, followed by the Midwest.
Interestingly, variation in billing by group size is only correlated directly to admission codes, but not to follow-up or discharge codes—with larger services tending to bill more of the highest-level admission codes.
Admission code use correlates directly with compensation structure; groups providing 100% of total compensation in the form of salary bill the lowest percentage of high-level admission codes. As compensation trends away from straight salaries, the percentage of high-level admission codes increases. The picture is less clear for high-level follow-up and discharge codes.
Comparing academic and nonacademic HM groups shows greater use of the highest- level admission, follow-up, and discharge codes for nonacademic HM groups. This is likely because academic hospitalists can only bill for their own time and not for time spent by medical residents.
Employment model (e.g. hospital system, private hospitalist-only groups, management companies, etc.) showed no categorical effect on CPT distribution.
Dr. Stephan is regional hospitalist medical director for Allina Health in Minneapolis and the incoming chair of SHM’s Practice Analysis Committee.
Before 2011, hospitalists had only Centers for Medicare & Medicaid Services’ (CMS) specialty-specific CPT distribution data, and no hospitalist-specific data, available when looking for benchmarks against which to compare their billing practices. Thanks to recent State of Hospital Medicine surveys, however, we now have hospitalist-specific data for the distribution of commonly used CPT codes. It’s interesting to analyze how 2011 data compares to 2012, and how the use of high-level codes varies by geographic region, employment model, compensation structure, and practice size.
In 2012, the use of the higher-level inpatient (IP) discharge code (99239) increased to 52% from 48% in 2011 among HM groups serving adults only, and the use of the highest-level IP subsequent code (99233) increased to 33% from 28% in the same comparison. This increase is in keeping with national trends. According to a May 2012 report by the Department of Health and Human Services’ Office of Inspector General, from 2001 to 2010, physicians’ billing shifted from lower-level to higher-level codes. For example, the billing of the lowest-level code (99231) decreased 16%, while the billing of the two higher-level codes (99232 and 99233) increased 6% and 9%, respectively.
Possible drivers of this change include:
- Expanded use of electronic health records (EHRs);
- Increased physician education about documentation requirements; and
- A sicker hospitalized patient population due to expanded outpatient care capabilities.
Although the proportion of high-level subsequent and discharge codes reported by SHM increased in 2012, the percent of highest-level IP admission codes (99223) actually decreased to 66% from 69%. There are many possible reasons for this. First, the elimination of consult codes by CMS in 2010 increased the overall use of admission codes but might have decreased the proportion of highest-level admission codes. Additionally, there may be an increased use of higher RVU-generating critical-care codes preferentially over billing of the highest-level admission codes. Third, there is the possibility that the extra documentation required for high-level admissions is a billing deterrent. Similarly, higher-level codes may be downcoded if documentation is lacking or incomplete.
Source: 2012 State of Hospital Medicine report
Comparatively, my health system, Allina Health, showed an increase in the use of highest-level codes for all three CPT codes analyzed.
With the increasing sophistication of EHRs and coding technology tools, it will be interesting to see the future impact on coding distribution as providers adapt to new documentation processes that support health information exchange across systems.
Comparing geographic regions, the West uses the highest proportion of high-level codes for admission, follow-up, and discharge, followed by the Midwest.
Interestingly, variation in billing by group size is only correlated directly to admission codes, but not to follow-up or discharge codes—with larger services tending to bill more of the highest-level admission codes.
Admission code use correlates directly with compensation structure; groups providing 100% of total compensation in the form of salary bill the lowest percentage of high-level admission codes. As compensation trends away from straight salaries, the percentage of high-level admission codes increases. The picture is less clear for high-level follow-up and discharge codes.
Comparing academic and nonacademic HM groups shows greater use of the highest- level admission, follow-up, and discharge codes for nonacademic HM groups. This is likely because academic hospitalists can only bill for their own time and not for time spent by medical residents.
Employment model (e.g. hospital system, private hospitalist-only groups, management companies, etc.) showed no categorical effect on CPT distribution.
Dr. Stephan is regional hospitalist medical director for Allina Health in Minneapolis and the incoming chair of SHM’s Practice Analysis Committee.
Peer Benchmarking Network May Reduce Overutilization in Pediatric Bronchiolitis
Clinical question: What is the impact of a peer benchmarking network on resource utilization in acute bronchiolitis?
Background: Acute bronchiolitis is the most common illness requiring hospitalization in children. Despite the publication of national evidence-based guidelines, variation and overuse of common therapies remains. Despite one report of successful implementation of evidence-based guidelines in a collaborative of freestanding children’s hospitals, most children are hospitalized outside of such institutions, and large-scale, lower-resource efforts have not been described.
Study design: Voluntary, quality-improvement (QI), and benchmarking collaborative.
Setting: Seventeen hospitals, including both community and freestanding children’s facilities.
Synopsis: Over a four-year period, data on 11,568 bronchiolitis hospitalizations were collected. The collaborative facilitated sharing of resources (e.g. scoring tools, guidelines), celebrated high performers on an annual basis, and encouraged regular data collection, primarily via conference calls and email. Notably, a common bundle of interventions were not used; groups worked on local improvement cycles, with only a few groups forming a small subcollaborative utilizing a shared pathway. A significant decrease in bronchodilator utilization and chest physiotherapy was seen over the course of the collaborative, although no change in chest radiography, steroid utilization, and RSV testing was noted.
This voluntary and low-resource effort by similarly motivated peers across a variety of inpatient settings demonstrated improvement over time. It is particularly notable as inpatient collaboratives with face-to-face meeting requirements, and annual fees, become more commonplace.
Study limitations include the lack of a conceptual model for studying contextual factors that might have led to improvement in the varied settings and secular changes over this time period. Additionally, EDs were not included in this initiative, which likely accounted for the lack of improvement in chest radiography and RSV testing. Nonetheless, scalable innovations such as this will become increasingly important as hospitalists search for value in health care.
Bottom line: Creating a national community of practice may reduce overutilization in bronchiolitis.
Citation: Ralston S, Garber M, Narang S, et al. Decreasing unnecessary utilization in acute bronchiolitis care: results from the Value in Inpatient Pediatrics Network. J Hosp Med. 2013;8(1):25-30.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Clinical question: What is the impact of a peer benchmarking network on resource utilization in acute bronchiolitis?
Background: Acute bronchiolitis is the most common illness requiring hospitalization in children. Despite the publication of national evidence-based guidelines, variation and overuse of common therapies remains. Despite one report of successful implementation of evidence-based guidelines in a collaborative of freestanding children’s hospitals, most children are hospitalized outside of such institutions, and large-scale, lower-resource efforts have not been described.
Study design: Voluntary, quality-improvement (QI), and benchmarking collaborative.
Setting: Seventeen hospitals, including both community and freestanding children’s facilities.
Synopsis: Over a four-year period, data on 11,568 bronchiolitis hospitalizations were collected. The collaborative facilitated sharing of resources (e.g. scoring tools, guidelines), celebrated high performers on an annual basis, and encouraged regular data collection, primarily via conference calls and email. Notably, a common bundle of interventions were not used; groups worked on local improvement cycles, with only a few groups forming a small subcollaborative utilizing a shared pathway. A significant decrease in bronchodilator utilization and chest physiotherapy was seen over the course of the collaborative, although no change in chest radiography, steroid utilization, and RSV testing was noted.
This voluntary and low-resource effort by similarly motivated peers across a variety of inpatient settings demonstrated improvement over time. It is particularly notable as inpatient collaboratives with face-to-face meeting requirements, and annual fees, become more commonplace.
Study limitations include the lack of a conceptual model for studying contextual factors that might have led to improvement in the varied settings and secular changes over this time period. Additionally, EDs were not included in this initiative, which likely accounted for the lack of improvement in chest radiography and RSV testing. Nonetheless, scalable innovations such as this will become increasingly important as hospitalists search for value in health care.
Bottom line: Creating a national community of practice may reduce overutilization in bronchiolitis.
Citation: Ralston S, Garber M, Narang S, et al. Decreasing unnecessary utilization in acute bronchiolitis care: results from the Value in Inpatient Pediatrics Network. J Hosp Med. 2013;8(1):25-30.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Clinical question: What is the impact of a peer benchmarking network on resource utilization in acute bronchiolitis?
Background: Acute bronchiolitis is the most common illness requiring hospitalization in children. Despite the publication of national evidence-based guidelines, variation and overuse of common therapies remains. Despite one report of successful implementation of evidence-based guidelines in a collaborative of freestanding children’s hospitals, most children are hospitalized outside of such institutions, and large-scale, lower-resource efforts have not been described.
Study design: Voluntary, quality-improvement (QI), and benchmarking collaborative.
Setting: Seventeen hospitals, including both community and freestanding children’s facilities.
Synopsis: Over a four-year period, data on 11,568 bronchiolitis hospitalizations were collected. The collaborative facilitated sharing of resources (e.g. scoring tools, guidelines), celebrated high performers on an annual basis, and encouraged regular data collection, primarily via conference calls and email. Notably, a common bundle of interventions were not used; groups worked on local improvement cycles, with only a few groups forming a small subcollaborative utilizing a shared pathway. A significant decrease in bronchodilator utilization and chest physiotherapy was seen over the course of the collaborative, although no change in chest radiography, steroid utilization, and RSV testing was noted.
This voluntary and low-resource effort by similarly motivated peers across a variety of inpatient settings demonstrated improvement over time. It is particularly notable as inpatient collaboratives with face-to-face meeting requirements, and annual fees, become more commonplace.
Study limitations include the lack of a conceptual model for studying contextual factors that might have led to improvement in the varied settings and secular changes over this time period. Additionally, EDs were not included in this initiative, which likely accounted for the lack of improvement in chest radiography and RSV testing. Nonetheless, scalable innovations such as this will become increasingly important as hospitalists search for value in health care.
Bottom line: Creating a national community of practice may reduce overutilization in bronchiolitis.
Citation: Ralston S, Garber M, Narang S, et al. Decreasing unnecessary utilization in acute bronchiolitis care: results from the Value in Inpatient Pediatrics Network. J Hosp Med. 2013;8(1):25-30.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Commemorating Round-the-Clock Hospital Medicine Programs
The steam engine. The telephone. Television. ATMs. The Internet. Smartphones. The 24/7 hospitalist program.
Perhaps the single most important innovation along the road to where we are now in HM has been the development of the hospital-sponsored, 24/7, on-site hospitalist program. And the father of this invention may be the most significant figure in HM you’ve never heard of: John Holbrook, MD, FACEP. An emergency-medicine physician since the mid-1970s, Dr. Holbrook did something in July 1993 that was considered off the wall, yet proved to be revolutionary: From nothing, he launched a 24/7 hospitalist program staffed with board-eligible and board-certified internists at Mercy Hospital in Springfield, Mass. The inpatient physicians (this was before the word “hospitalist” came to be) were employed by a subsidiary of the hospital and worked in place of community primary-care physicians (PCPs), taking care of hospitalized patients who did not have a PCP, or whose PCP chose not to come to the hospital.
Of great significance, from the beginning, and perhaps by unintentional design, these physicians were agents of change and improvement for the hospital itself.
To be sure, in places like Southern California, 24/7, on-site hospitalist programs were in place in the late 1980s. Some claim those programs may have been the birthplace of the hospitalist model. However, such programs came to be in order to help medical groups manage full capitated risk delegated to them from HMOs on a population of patients, and were not supported by the hospital, per se. This is distinct from hospitalist programs—such as Mercy’s—sponsored by hospitals (whether employed or contracted) in predominantly fee-for-service markets, which then comprised the lion’s share of the U.S. market.
I had the extraordinary good fortune to happen along in July 1994, get hired by Dr. Holbrook, and soon after begin serving as medical director for the Mercy program, which I would do for the next decade. To this day, Dr. Holbrook is a mentor and trusted advisor to me. I caught up with him in recognition of the 20th anniversary of the Mercy Inpatient Medicine Service.
Question: What gave you the idea to launch what was, at the time, considered such an unconventional program?
Answer: Before the specialty of emergency medicine, a patient’s private physician would be called in most cases when a patient present in the ED: 25 or 50 doctors might be called over 24 hours, each to see one patient each. The inefficiency and disruption caused by this system was a natural and logical stimulus to develop the specialty of emergency medicine. I saw hospitalist medicine as an exact analogy.
Q: What were you observing in the healthcare environment that drove you to create the Mercy Inpatient Medicine Service?
A: Working for many years in the emergency department of a community hospital without a house staff, the ED docs would admit a patient at night or on the weekend and the attending physician would often plan to see the patient “in the morning.” When the patient would decompensate in the middle of the night, the ED doc would get a call to run to the floor to “Band-Aid” the situation.
Q: How did you convince the board of trustees to fund it?
A: The reasons were primarily economic. No. 1, the hospital was losing market share because local physicians would prefer to admit to the teaching hospital [a nearby competitor], where they were not required to come in during the middle of the night. No. 2, the cost of a hospitalization managed by a hospitalist was less expensive than either a hospital stay managed by house staff or managed over the telephone by a private attending at home.
Q: What was the most difficult operational challenge for the program?
A: Effective and timely communication with the community physicians was the most difficult operational challenge. Access to outpatient medical treatment immediately prior to a hospitalization and timely communication to the community physician were both challenges that we never adequately solved in the early days. I understand that these issues can still be problematic.
Q: How was it received by patients?
A: Overall, patients were very happy with the system. In the old system, with a typical four-physician practice, a patient had only a 1 in 4 chance of being admitted by the doctor who was familiar with the case. The fact that the hospitalist was available in the hospital made the improvement in quality apparent to most patients.
Q: How did you get the medical staff to buy into the program?
A: I personally visited every private physician who participated. Physicians were given the option of not participating, or of part-time participation—for example, on weekends or holidays only. The word spread. Physicians came up to me and told me that the program enabled them to continue practicing for another five years. Physicians’ spouses thanked me.
Q: Are you surprised HM as a field has grown so quickly?
A: I am not really that surprised. It is a better way to organize health care. I am surprised that it did not occur sooner. We talked about instituting this system for 10 years before 1993.
Q: What big challenges remain for hospital medicine? What are some solutions?
A: I believe that the biggest global challenge for hospital medicine remains communication with community-based providers, both before the hospitalization as well as during hospitalization and immediately after discharge. In the era of the EMR, the Internet, and the iPhone and Android, this should be easier. HIPAA has not helped.
The other growing challenge will become apparent as hospitalists age in the profession: Disruption of the diurnal sleep cycle becomes increasingly problematic for many physicians after the age of 50 and can easily lead to burnout. The early hospitalists were all in their 30s. The attractive lifestyle choice for the 30-year-old can lead to burnout for the 55-year-old. The emergency-medicine literature has noted a similar problem of shift work/sleep fragmentation.
Final Thoughts
I believe Dr. Holbrook’s assessments on the future of our specialty are on target. As HM continues to mature, we need to continue to focus on how we communicate with providers outside the four walls of the hospital and how to address barriers to making HM a sustainable career.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at wfwhit@comcast.net.
(Editor's note: Updated July 12, 2013.)
The steam engine. The telephone. Television. ATMs. The Internet. Smartphones. The 24/7 hospitalist program.
Perhaps the single most important innovation along the road to where we are now in HM has been the development of the hospital-sponsored, 24/7, on-site hospitalist program. And the father of this invention may be the most significant figure in HM you’ve never heard of: John Holbrook, MD, FACEP. An emergency-medicine physician since the mid-1970s, Dr. Holbrook did something in July 1993 that was considered off the wall, yet proved to be revolutionary: From nothing, he launched a 24/7 hospitalist program staffed with board-eligible and board-certified internists at Mercy Hospital in Springfield, Mass. The inpatient physicians (this was before the word “hospitalist” came to be) were employed by a subsidiary of the hospital and worked in place of community primary-care physicians (PCPs), taking care of hospitalized patients who did not have a PCP, or whose PCP chose not to come to the hospital.
Of great significance, from the beginning, and perhaps by unintentional design, these physicians were agents of change and improvement for the hospital itself.
To be sure, in places like Southern California, 24/7, on-site hospitalist programs were in place in the late 1980s. Some claim those programs may have been the birthplace of the hospitalist model. However, such programs came to be in order to help medical groups manage full capitated risk delegated to them from HMOs on a population of patients, and were not supported by the hospital, per se. This is distinct from hospitalist programs—such as Mercy’s—sponsored by hospitals (whether employed or contracted) in predominantly fee-for-service markets, which then comprised the lion’s share of the U.S. market.
I had the extraordinary good fortune to happen along in July 1994, get hired by Dr. Holbrook, and soon after begin serving as medical director for the Mercy program, which I would do for the next decade. To this day, Dr. Holbrook is a mentor and trusted advisor to me. I caught up with him in recognition of the 20th anniversary of the Mercy Inpatient Medicine Service.
Question: What gave you the idea to launch what was, at the time, considered such an unconventional program?
Answer: Before the specialty of emergency medicine, a patient’s private physician would be called in most cases when a patient present in the ED: 25 or 50 doctors might be called over 24 hours, each to see one patient each. The inefficiency and disruption caused by this system was a natural and logical stimulus to develop the specialty of emergency medicine. I saw hospitalist medicine as an exact analogy.
Q: What were you observing in the healthcare environment that drove you to create the Mercy Inpatient Medicine Service?
A: Working for many years in the emergency department of a community hospital without a house staff, the ED docs would admit a patient at night or on the weekend and the attending physician would often plan to see the patient “in the morning.” When the patient would decompensate in the middle of the night, the ED doc would get a call to run to the floor to “Band-Aid” the situation.
Q: How did you convince the board of trustees to fund it?
A: The reasons were primarily economic. No. 1, the hospital was losing market share because local physicians would prefer to admit to the teaching hospital [a nearby competitor], where they were not required to come in during the middle of the night. No. 2, the cost of a hospitalization managed by a hospitalist was less expensive than either a hospital stay managed by house staff or managed over the telephone by a private attending at home.
Q: What was the most difficult operational challenge for the program?
A: Effective and timely communication with the community physicians was the most difficult operational challenge. Access to outpatient medical treatment immediately prior to a hospitalization and timely communication to the community physician were both challenges that we never adequately solved in the early days. I understand that these issues can still be problematic.
Q: How was it received by patients?
A: Overall, patients were very happy with the system. In the old system, with a typical four-physician practice, a patient had only a 1 in 4 chance of being admitted by the doctor who was familiar with the case. The fact that the hospitalist was available in the hospital made the improvement in quality apparent to most patients.
Q: How did you get the medical staff to buy into the program?
A: I personally visited every private physician who participated. Physicians were given the option of not participating, or of part-time participation—for example, on weekends or holidays only. The word spread. Physicians came up to me and told me that the program enabled them to continue practicing for another five years. Physicians’ spouses thanked me.
Q: Are you surprised HM as a field has grown so quickly?
A: I am not really that surprised. It is a better way to organize health care. I am surprised that it did not occur sooner. We talked about instituting this system for 10 years before 1993.
Q: What big challenges remain for hospital medicine? What are some solutions?
A: I believe that the biggest global challenge for hospital medicine remains communication with community-based providers, both before the hospitalization as well as during hospitalization and immediately after discharge. In the era of the EMR, the Internet, and the iPhone and Android, this should be easier. HIPAA has not helped.
The other growing challenge will become apparent as hospitalists age in the profession: Disruption of the diurnal sleep cycle becomes increasingly problematic for many physicians after the age of 50 and can easily lead to burnout. The early hospitalists were all in their 30s. The attractive lifestyle choice for the 30-year-old can lead to burnout for the 55-year-old. The emergency-medicine literature has noted a similar problem of shift work/sleep fragmentation.
Final Thoughts
I believe Dr. Holbrook’s assessments on the future of our specialty are on target. As HM continues to mature, we need to continue to focus on how we communicate with providers outside the four walls of the hospital and how to address barriers to making HM a sustainable career.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at wfwhit@comcast.net.
(Editor's note: Updated July 12, 2013.)
The steam engine. The telephone. Television. ATMs. The Internet. Smartphones. The 24/7 hospitalist program.
Perhaps the single most important innovation along the road to where we are now in HM has been the development of the hospital-sponsored, 24/7, on-site hospitalist program. And the father of this invention may be the most significant figure in HM you’ve never heard of: John Holbrook, MD, FACEP. An emergency-medicine physician since the mid-1970s, Dr. Holbrook did something in July 1993 that was considered off the wall, yet proved to be revolutionary: From nothing, he launched a 24/7 hospitalist program staffed with board-eligible and board-certified internists at Mercy Hospital in Springfield, Mass. The inpatient physicians (this was before the word “hospitalist” came to be) were employed by a subsidiary of the hospital and worked in place of community primary-care physicians (PCPs), taking care of hospitalized patients who did not have a PCP, or whose PCP chose not to come to the hospital.
Of great significance, from the beginning, and perhaps by unintentional design, these physicians were agents of change and improvement for the hospital itself.
To be sure, in places like Southern California, 24/7, on-site hospitalist programs were in place in the late 1980s. Some claim those programs may have been the birthplace of the hospitalist model. However, such programs came to be in order to help medical groups manage full capitated risk delegated to them from HMOs on a population of patients, and were not supported by the hospital, per se. This is distinct from hospitalist programs—such as Mercy’s—sponsored by hospitals (whether employed or contracted) in predominantly fee-for-service markets, which then comprised the lion’s share of the U.S. market.
I had the extraordinary good fortune to happen along in July 1994, get hired by Dr. Holbrook, and soon after begin serving as medical director for the Mercy program, which I would do for the next decade. To this day, Dr. Holbrook is a mentor and trusted advisor to me. I caught up with him in recognition of the 20th anniversary of the Mercy Inpatient Medicine Service.
Question: What gave you the idea to launch what was, at the time, considered such an unconventional program?
Answer: Before the specialty of emergency medicine, a patient’s private physician would be called in most cases when a patient present in the ED: 25 or 50 doctors might be called over 24 hours, each to see one patient each. The inefficiency and disruption caused by this system was a natural and logical stimulus to develop the specialty of emergency medicine. I saw hospitalist medicine as an exact analogy.
Q: What were you observing in the healthcare environment that drove you to create the Mercy Inpatient Medicine Service?
A: Working for many years in the emergency department of a community hospital without a house staff, the ED docs would admit a patient at night or on the weekend and the attending physician would often plan to see the patient “in the morning.” When the patient would decompensate in the middle of the night, the ED doc would get a call to run to the floor to “Band-Aid” the situation.
Q: How did you convince the board of trustees to fund it?
A: The reasons were primarily economic. No. 1, the hospital was losing market share because local physicians would prefer to admit to the teaching hospital [a nearby competitor], where they were not required to come in during the middle of the night. No. 2, the cost of a hospitalization managed by a hospitalist was less expensive than either a hospital stay managed by house staff or managed over the telephone by a private attending at home.
Q: What was the most difficult operational challenge for the program?
A: Effective and timely communication with the community physicians was the most difficult operational challenge. Access to outpatient medical treatment immediately prior to a hospitalization and timely communication to the community physician were both challenges that we never adequately solved in the early days. I understand that these issues can still be problematic.
Q: How was it received by patients?
A: Overall, patients were very happy with the system. In the old system, with a typical four-physician practice, a patient had only a 1 in 4 chance of being admitted by the doctor who was familiar with the case. The fact that the hospitalist was available in the hospital made the improvement in quality apparent to most patients.
Q: How did you get the medical staff to buy into the program?
A: I personally visited every private physician who participated. Physicians were given the option of not participating, or of part-time participation—for example, on weekends or holidays only. The word spread. Physicians came up to me and told me that the program enabled them to continue practicing for another five years. Physicians’ spouses thanked me.
Q: Are you surprised HM as a field has grown so quickly?
A: I am not really that surprised. It is a better way to organize health care. I am surprised that it did not occur sooner. We talked about instituting this system for 10 years before 1993.
Q: What big challenges remain for hospital medicine? What are some solutions?
A: I believe that the biggest global challenge for hospital medicine remains communication with community-based providers, both before the hospitalization as well as during hospitalization and immediately after discharge. In the era of the EMR, the Internet, and the iPhone and Android, this should be easier. HIPAA has not helped.
The other growing challenge will become apparent as hospitalists age in the profession: Disruption of the diurnal sleep cycle becomes increasingly problematic for many physicians after the age of 50 and can easily lead to burnout. The early hospitalists were all in their 30s. The attractive lifestyle choice for the 30-year-old can lead to burnout for the 55-year-old. The emergency-medicine literature has noted a similar problem of shift work/sleep fragmentation.
Final Thoughts
I believe Dr. Holbrook’s assessments on the future of our specialty are on target. As HM continues to mature, we need to continue to focus on how we communicate with providers outside the four walls of the hospital and how to address barriers to making HM a sustainable career.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at wfwhit@comcast.net.
(Editor's note: Updated July 12, 2013.)
IPC-UCSF Fellowship for Hospitalist Group Leaders Demands a Stretch
The yearlong IPC-UCSF Fellowship for Hospitalist Leaders brings about 40 IPC: The Hospitalist Company group leaders together for a series of three-day training sessions and ongoing distance learning, executive coaching, and project mentoring.
The program emphasizes role plays and simulations, and even involves an acting coach to help participants learn to make more effective presentations, such as harnessing the power of storytelling, says Niraj L. Sehgal, MD, MPH, a hospitalist at the University of California at San Francisco (UCSF) who directs the fellowship through UCSF’s Center for Health Professions.
The first class graduated in November 2011, and the third is in session. Participants implement a mentored project in their home facility, with measurable results, as a vehicle for leadership development in such areas as quality improvement (QI), patient safety, or readmissions prevention. But the specific project is not as important as whether or not that project is well-designed to stretch the individual in areas where they weren’t comfortable before, Dr. Sehgal says.
Through her QI project, Jasmin Baleva, MD, of Memorial Hermann Memorial City Medical Center in Houston, a 2012 participant, found an alternate to the costly nocturnist model while maintaining the time it takes for the first hospitalist encounter with newly admitted patients. “I think the IPC-UCSF project gave my proposal a little more legitimacy,” she tells TH. “They also taught me how to present it in an effective package and to approach the C-suite feeling less intimidated.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
The yearlong IPC-UCSF Fellowship for Hospitalist Leaders brings about 40 IPC: The Hospitalist Company group leaders together for a series of three-day training sessions and ongoing distance learning, executive coaching, and project mentoring.
The program emphasizes role plays and simulations, and even involves an acting coach to help participants learn to make more effective presentations, such as harnessing the power of storytelling, says Niraj L. Sehgal, MD, MPH, a hospitalist at the University of California at San Francisco (UCSF) who directs the fellowship through UCSF’s Center for Health Professions.
The first class graduated in November 2011, and the third is in session. Participants implement a mentored project in their home facility, with measurable results, as a vehicle for leadership development in such areas as quality improvement (QI), patient safety, or readmissions prevention. But the specific project is not as important as whether or not that project is well-designed to stretch the individual in areas where they weren’t comfortable before, Dr. Sehgal says.
Through her QI project, Jasmin Baleva, MD, of Memorial Hermann Memorial City Medical Center in Houston, a 2012 participant, found an alternate to the costly nocturnist model while maintaining the time it takes for the first hospitalist encounter with newly admitted patients. “I think the IPC-UCSF project gave my proposal a little more legitimacy,” she tells TH. “They also taught me how to present it in an effective package and to approach the C-suite feeling less intimidated.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
The yearlong IPC-UCSF Fellowship for Hospitalist Leaders brings about 40 IPC: The Hospitalist Company group leaders together for a series of three-day training sessions and ongoing distance learning, executive coaching, and project mentoring.
The program emphasizes role plays and simulations, and even involves an acting coach to help participants learn to make more effective presentations, such as harnessing the power of storytelling, says Niraj L. Sehgal, MD, MPH, a hospitalist at the University of California at San Francisco (UCSF) who directs the fellowship through UCSF’s Center for Health Professions.
The first class graduated in November 2011, and the third is in session. Participants implement a mentored project in their home facility, with measurable results, as a vehicle for leadership development in such areas as quality improvement (QI), patient safety, or readmissions prevention. But the specific project is not as important as whether or not that project is well-designed to stretch the individual in areas where they weren’t comfortable before, Dr. Sehgal says.
Through her QI project, Jasmin Baleva, MD, of Memorial Hermann Memorial City Medical Center in Houston, a 2012 participant, found an alternate to the costly nocturnist model while maintaining the time it takes for the first hospitalist encounter with newly admitted patients. “I think the IPC-UCSF project gave my proposal a little more legitimacy,” she tells TH. “They also taught me how to present it in an effective package and to approach the C-suite feeling less intimidated.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
Hospital ICUs Chart Progress in Preventing Central-Line-Associated Bloodstream Infections
New CDC research published in the June issue of Infection Control and Hospital Epidemiology estimates that as many as 200,000 central-line-associated bloodstream infections (CLABSIs) in ICUs nationally have been prevented since 1990.3 The report indicates much of the success is due to U.S. hospitals adopting successful prevention strategies, namely the dissemination of guideline-supported central-line insertion and maintenance best practices, infection-control treatment bundles, and widespread availability of alcohol-based hand rubs.
Between 462,000 and 636,000 CLABSIs occurred in non-neonatal ICU patients from 1990-2010, CDC estimates, about 104,000 to 198,000 less CLABSIs than would have occurred if rates had remained the same as they were in 1990.
“These findings suggest that technical innovations and dissemination of evidence-based CLABSI prevention practices have likely been effective on a national scale,” Matthew Wise, PhD, lead author of the study, said in a statement.
At the same time, a CLABSI-reduction intervention in a hospital in Hawaii found that while the costs of care were much higher for patients who developed a CLABSI, reimbursement and the hospital’s margin also were higher (margin of $54,906 vs. $6,506).4 The authors conclude that current reimbursement practices offer a perverse incentive for hospitals to have more line infections, “while an optimal reimbursement system would reward them for prevention rather than treating illness.”
Lead author Eugene Hsu, MD, MBA, of Johns Hopkins University School of Medicine said in an email that the study demonstrates how a quality initiative led by providers and funded by a major commercial insurer can save both lives and money. “Hospitalists, like all healthcare providers, must be aware of the distorted financial incentives that may affect how they provide care to patients,” Dr. Hsu said.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
New CDC research published in the June issue of Infection Control and Hospital Epidemiology estimates that as many as 200,000 central-line-associated bloodstream infections (CLABSIs) in ICUs nationally have been prevented since 1990.3 The report indicates much of the success is due to U.S. hospitals adopting successful prevention strategies, namely the dissemination of guideline-supported central-line insertion and maintenance best practices, infection-control treatment bundles, and widespread availability of alcohol-based hand rubs.
Between 462,000 and 636,000 CLABSIs occurred in non-neonatal ICU patients from 1990-2010, CDC estimates, about 104,000 to 198,000 less CLABSIs than would have occurred if rates had remained the same as they were in 1990.
“These findings suggest that technical innovations and dissemination of evidence-based CLABSI prevention practices have likely been effective on a national scale,” Matthew Wise, PhD, lead author of the study, said in a statement.
At the same time, a CLABSI-reduction intervention in a hospital in Hawaii found that while the costs of care were much higher for patients who developed a CLABSI, reimbursement and the hospital’s margin also were higher (margin of $54,906 vs. $6,506).4 The authors conclude that current reimbursement practices offer a perverse incentive for hospitals to have more line infections, “while an optimal reimbursement system would reward them for prevention rather than treating illness.”
Lead author Eugene Hsu, MD, MBA, of Johns Hopkins University School of Medicine said in an email that the study demonstrates how a quality initiative led by providers and funded by a major commercial insurer can save both lives and money. “Hospitalists, like all healthcare providers, must be aware of the distorted financial incentives that may affect how they provide care to patients,” Dr. Hsu said.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
New CDC research published in the June issue of Infection Control and Hospital Epidemiology estimates that as many as 200,000 central-line-associated bloodstream infections (CLABSIs) in ICUs nationally have been prevented since 1990.3 The report indicates much of the success is due to U.S. hospitals adopting successful prevention strategies, namely the dissemination of guideline-supported central-line insertion and maintenance best practices, infection-control treatment bundles, and widespread availability of alcohol-based hand rubs.
Between 462,000 and 636,000 CLABSIs occurred in non-neonatal ICU patients from 1990-2010, CDC estimates, about 104,000 to 198,000 less CLABSIs than would have occurred if rates had remained the same as they were in 1990.
“These findings suggest that technical innovations and dissemination of evidence-based CLABSI prevention practices have likely been effective on a national scale,” Matthew Wise, PhD, lead author of the study, said in a statement.
At the same time, a CLABSI-reduction intervention in a hospital in Hawaii found that while the costs of care were much higher for patients who developed a CLABSI, reimbursement and the hospital’s margin also were higher (margin of $54,906 vs. $6,506).4 The authors conclude that current reimbursement practices offer a perverse incentive for hospitals to have more line infections, “while an optimal reimbursement system would reward them for prevention rather than treating illness.”
Lead author Eugene Hsu, MD, MBA, of Johns Hopkins University School of Medicine said in an email that the study demonstrates how a quality initiative led by providers and funded by a major commercial insurer can save both lives and money. “Hospitalists, like all healthcare providers, must be aware of the distorted financial incentives that may affect how they provide care to patients,” Dr. Hsu said.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
Hospitals' Battle Against Superbugs Goes Robotic
One in 20 hospitalized patients picks up an infection in the hospital, and a recent article by the Associated Press describes the emergence of new technologies to fight antibiotic-resistant superbugs: “They sweep. They swab. They sterilize. And still the germs persist.”1
Hospitals across the country are testing new approaches to stop the spread of superbugs, which are tied to an estimated 100,000 deaths per year, according to the CDC. New approaches include robotlike machines that emit ultraviolet light or hydrogen-peroxide vapors, germ-resistant copper bed rails and call buttons, antimicrobial linens and wall paint, and hydrogel post-surgical dressings infused with silver ions that have antimicrobial properties.
Research firm Frost & Sullivan estimates that the market for bug-killing products and technologies will grow to $80 million from $30 million in the next three years. And yet evidence of positive outcomes from them continues to be debated.
“In short, escalating antimicrobial-resistance issues have us facing the prospect of untreatable bacterial pathogens, particularly involving gram-negative organisms,” James Pile, MD, FACP, SFHM, a hospital medicine and infectious diseases physician at Cleveland Clinic, wrote in an email. “In fact, many of our hospitals already deal with a limited number of infections caused by bacteria we have no clearly effective antibiotics against; the issue is only going to get worse.”
As an example, the CDC recently issued a warning about carbapenum-resistant Enterobacteriaceae (CRE), which has a 40% mortality rate and last year was reported in 4.6% of U.S. hospitals.2 CDC recommends that hospitals use more of the existing prevention measures against CRE, including active-case detection and segregation of patients and the staff who care for them. Dr. Pile says health facilities need to do a better job of preventing infections involving multi-drug-resistant pathogens, but in the meantime, “proven technologies such as proper hand hygiene and antimicrobial stewardship are more important than ever.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
One in 20 hospitalized patients picks up an infection in the hospital, and a recent article by the Associated Press describes the emergence of new technologies to fight antibiotic-resistant superbugs: “They sweep. They swab. They sterilize. And still the germs persist.”1
Hospitals across the country are testing new approaches to stop the spread of superbugs, which are tied to an estimated 100,000 deaths per year, according to the CDC. New approaches include robotlike machines that emit ultraviolet light or hydrogen-peroxide vapors, germ-resistant copper bed rails and call buttons, antimicrobial linens and wall paint, and hydrogel post-surgical dressings infused with silver ions that have antimicrobial properties.
Research firm Frost & Sullivan estimates that the market for bug-killing products and technologies will grow to $80 million from $30 million in the next three years. And yet evidence of positive outcomes from them continues to be debated.
“In short, escalating antimicrobial-resistance issues have us facing the prospect of untreatable bacterial pathogens, particularly involving gram-negative organisms,” James Pile, MD, FACP, SFHM, a hospital medicine and infectious diseases physician at Cleveland Clinic, wrote in an email. “In fact, many of our hospitals already deal with a limited number of infections caused by bacteria we have no clearly effective antibiotics against; the issue is only going to get worse.”
As an example, the CDC recently issued a warning about carbapenum-resistant Enterobacteriaceae (CRE), which has a 40% mortality rate and last year was reported in 4.6% of U.S. hospitals.2 CDC recommends that hospitals use more of the existing prevention measures against CRE, including active-case detection and segregation of patients and the staff who care for them. Dr. Pile says health facilities need to do a better job of preventing infections involving multi-drug-resistant pathogens, but in the meantime, “proven technologies such as proper hand hygiene and antimicrobial stewardship are more important than ever.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
One in 20 hospitalized patients picks up an infection in the hospital, and a recent article by the Associated Press describes the emergence of new technologies to fight antibiotic-resistant superbugs: “They sweep. They swab. They sterilize. And still the germs persist.”1
Hospitals across the country are testing new approaches to stop the spread of superbugs, which are tied to an estimated 100,000 deaths per year, according to the CDC. New approaches include robotlike machines that emit ultraviolet light or hydrogen-peroxide vapors, germ-resistant copper bed rails and call buttons, antimicrobial linens and wall paint, and hydrogel post-surgical dressings infused with silver ions that have antimicrobial properties.
Research firm Frost & Sullivan estimates that the market for bug-killing products and technologies will grow to $80 million from $30 million in the next three years. And yet evidence of positive outcomes from them continues to be debated.
“In short, escalating antimicrobial-resistance issues have us facing the prospect of untreatable bacterial pathogens, particularly involving gram-negative organisms,” James Pile, MD, FACP, SFHM, a hospital medicine and infectious diseases physician at Cleveland Clinic, wrote in an email. “In fact, many of our hospitals already deal with a limited number of infections caused by bacteria we have no clearly effective antibiotics against; the issue is only going to get worse.”
As an example, the CDC recently issued a warning about carbapenum-resistant Enterobacteriaceae (CRE), which has a 40% mortality rate and last year was reported in 4.6% of U.S. hospitals.2 CDC recommends that hospitals use more of the existing prevention measures against CRE, including active-case detection and segregation of patients and the staff who care for them. Dr. Pile says health facilities need to do a better job of preventing infections involving multi-drug-resistant pathogens, but in the meantime, “proven technologies such as proper hand hygiene and antimicrobial stewardship are more important than ever.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
Nutritional Intervention Can Improve Hospital Patients' Outcome, Reduce Costs
Health-care reform is on everyone’s mind these days, and SHM, along with numerous other groups, believes some reform goals can be achieved through the stomach.
Data show an effective program of nutritional intervention during a patient’s hospital stay can go a long way toward improving patient outcomes and reducing costs.1 Hospitalists, however, often have little formal nutrition training. A multidisciplinary approach to patient nutrition that brings together multiple stakeholders—hospitalists, nurses, and dietitians—might effectively address this need with a team tactic, according to Melissa Parkhurst, MD, medical director of the hospital medicine section at the University of Kansas Medical Center in Kansas City.1
Between 20% and 50% of inpatients suffer from malnutrition.2 Many patients, especially the elderly, are malnourished on admission. Many more become malnourished within a few days of their hospital stay due to NPO orders and the effects of disease on metabolism.2 Malnutrition has been associated with worsened discharge status, longer length of stay, higher costs, and greater mortality, as well as increased risk of:2
- Nosocomial infections;
- Falls;
- Pressure ulcers; and
- 30-day readmissions.
To address malnutrition prevalence and its detrimental effects, SHM and the Academy of Medical-Surgical Nurses (AMSN), the Academy of Nutrition and Dietetics (AND), the American Society of Parenteral and Enteral Nutrition (ASPEN), and Abbott Nutrition have formed the Alliance for Patient Nutrition. Kelly Tappenden, MD, PhD, professor of food science and human nutrition at the University of Illinois at Urbana, says the alliance aims to raise awareness of the impact nutrition can have on patient outcomes (see “Three Steps to Better Nutrition,” below).
The campaign is being initiated with the publication of a consensus paper in several peer-reviewed journals. A baseline survey will be conducted among professionals represented in the alliance to assess their familiarity with the prevalence of malnutrition in a hospital setting. The next step is to foster this change in patient care by providing resources on the alliance’s website (www.malnutrition.com), including malnutrition screening tools, a toolkit to facilitate multidisciplinary collaboration, and continuing medical education (CME) information.
As a founding member of the alliance, SHM is communicating this message to its members, encouraging hospitalists to lead the way in transforming hospital culture to recognize the critical role nutrition plays in patient care.
“Nutrition matters,” Dr. Parkhurst says. “You can be winning the battle and losing the war if you are not paying attention to patient nutrition.”
Team Approach
Beth Quatrara, DNP, RN, director of the nursing research program at the University of Virginia Health System in Charlottesville and nursing spokesperson for the alliance, says several shortcomings can be identified in the nutritional care U.S. hospitals provide from admission through discharge and beyond. For example, the Joint Commission requires that all patients be screened for malnutrition risk within 48 hours of admission. But screening is often as cursory as looking at the patient and deciding that he or she “looks fine.” Diets often are set for patients with no thought to taste, texture, or cultural preferences, or even to such practical matters as ascertaining whether the patient has dentures, Quatrara says. Meal trays are left when patients are out of their rooms for procedures and retrieved by dietary staff before patients return. And except for calorie count orders, accurate records often are not kept of actual food consumption.
The alliance, which is made possible with support from Abbott's nutrition business, recommends that physicians implement a three-step plan to improve patient outcomes. The approach begins with an evaluation of a patient’s nutritional status on admission using a simple, validated screening tool, such as the Malnutrition Screening Tool. When an at-risk status is determined, a more in-depth screening is performed. “When patients at risk for malnutrition can be identified faster, appropriate interventions can be put into place sooner,” Quatrara says.
The second step is nutrition intervention with a personalized nutritional care plan that takes into account the individual’s health conditions, caloric needs, physical limitations, tastes, and preferences. An interdisciplinary team approach can transform hospital nutrition, bringing together hospitalists, nurses, nursing assistants, registered dietitians, and the dietary staff to collaboratively develop a nutrition care plan that will be central to patient’s overall treatment, Dr. Tappenden says.
“There is a science behind nutrition and metabolic care,” Dr. Tappenden says. “Just like any other aspect of patient care, we can’t just throw out a blanket solution.”
But nutritional care cannot stop with developing this plan at the outset. Patients must be rescreened throughout their time at the hospital to measure any changes in nutritional status due to disease progression or treatment success.
For optimal impact, all members of the nutritional care team—nurses, nursing assistants, dietary support staff, and family members—should take responsibility for an essential component of the patient’s care: tracking and reporting consumption to the physician to open a dialogue about balancing an individual’s needs with tastes and preferences.
The hospitalist’s final step is developing a discharge plan that includes nutrition care and education so that patients, families, and caregivers can implement better nutrition at home.
“Nutrition makes sense,” Dr. Tappenden says. “Everything we are working toward in healthcare reform can be achieved by taking more care to make nutrition part of the solution.”
Maybelle Cowan-Lincoln is a freelance writer in New Jersey.
References
- Kirkland LL, Kashiwagi DT, Brantley S, Scheurer D, Varkey P. Nutrition in the hospitalized patient. J Hosp Med. 2013;8:52-58.
- Alliance for Patient Nutrition. Malnutrition Backgrounder.
- Banks M, Bauer J, Graves N, Ash S. Malnutrition and pressure ulcer risk in adults in Australian health care facilities. Clin Nutr. 2010;26:896-901.
- Fry DE, Pine M, Jones BL, Meimban RJ. Patient characteristics and the occurrence of never events. Arch Surg. 2010;145:148-151.
- Gariballa S, Forster S, Walters S, Powers H. A randomized, double-blind, placebo-controlled trial of nutritional supplementation during acute illness. Am J Med. 2006;119:693-699.
- Neelemaat F, Lips P, Bosmans J, Thijs A, Seidell JC, van Bokhorst-de van der Schuerer MA. Short-term oral nutritional intervention with protein and vitamin D decreases falls in malnourished older adults. J Am Geriatr Soc. 2012;60:691-699.
- Brugler L, DiPrinzio MJ, Bernstein L. The five-year evolution of a malnutrition treatment program in a community hospital. J Qual Improv. 1999;25:191-206.
- Stratton PJ, et al. Enteral nutritional support in prevention and treatment of pressure ulcers: a systematic review and meta-analysis. Ageing Res Rev. 2005;4:422-450.
- Lawson RM, Doshi MK, Barton JR, Cobden I. The effect of unselected post-operative nutritional supplementation on nutritional status and clinical outcomes of elderly orthopaedic patients. Clin Nutr. 2003;22:39-46.
Health-care reform is on everyone’s mind these days, and SHM, along with numerous other groups, believes some reform goals can be achieved through the stomach.
Data show an effective program of nutritional intervention during a patient’s hospital stay can go a long way toward improving patient outcomes and reducing costs.1 Hospitalists, however, often have little formal nutrition training. A multidisciplinary approach to patient nutrition that brings together multiple stakeholders—hospitalists, nurses, and dietitians—might effectively address this need with a team tactic, according to Melissa Parkhurst, MD, medical director of the hospital medicine section at the University of Kansas Medical Center in Kansas City.1
Between 20% and 50% of inpatients suffer from malnutrition.2 Many patients, especially the elderly, are malnourished on admission. Many more become malnourished within a few days of their hospital stay due to NPO orders and the effects of disease on metabolism.2 Malnutrition has been associated with worsened discharge status, longer length of stay, higher costs, and greater mortality, as well as increased risk of:2
- Nosocomial infections;
- Falls;
- Pressure ulcers; and
- 30-day readmissions.
To address malnutrition prevalence and its detrimental effects, SHM and the Academy of Medical-Surgical Nurses (AMSN), the Academy of Nutrition and Dietetics (AND), the American Society of Parenteral and Enteral Nutrition (ASPEN), and Abbott Nutrition have formed the Alliance for Patient Nutrition. Kelly Tappenden, MD, PhD, professor of food science and human nutrition at the University of Illinois at Urbana, says the alliance aims to raise awareness of the impact nutrition can have on patient outcomes (see “Three Steps to Better Nutrition,” below).
The campaign is being initiated with the publication of a consensus paper in several peer-reviewed journals. A baseline survey will be conducted among professionals represented in the alliance to assess their familiarity with the prevalence of malnutrition in a hospital setting. The next step is to foster this change in patient care by providing resources on the alliance’s website (www.malnutrition.com), including malnutrition screening tools, a toolkit to facilitate multidisciplinary collaboration, and continuing medical education (CME) information.
As a founding member of the alliance, SHM is communicating this message to its members, encouraging hospitalists to lead the way in transforming hospital culture to recognize the critical role nutrition plays in patient care.
“Nutrition matters,” Dr. Parkhurst says. “You can be winning the battle and losing the war if you are not paying attention to patient nutrition.”
Team Approach
Beth Quatrara, DNP, RN, director of the nursing research program at the University of Virginia Health System in Charlottesville and nursing spokesperson for the alliance, says several shortcomings can be identified in the nutritional care U.S. hospitals provide from admission through discharge and beyond. For example, the Joint Commission requires that all patients be screened for malnutrition risk within 48 hours of admission. But screening is often as cursory as looking at the patient and deciding that he or she “looks fine.” Diets often are set for patients with no thought to taste, texture, or cultural preferences, or even to such practical matters as ascertaining whether the patient has dentures, Quatrara says. Meal trays are left when patients are out of their rooms for procedures and retrieved by dietary staff before patients return. And except for calorie count orders, accurate records often are not kept of actual food consumption.
The alliance, which is made possible with support from Abbott's nutrition business, recommends that physicians implement a three-step plan to improve patient outcomes. The approach begins with an evaluation of a patient’s nutritional status on admission using a simple, validated screening tool, such as the Malnutrition Screening Tool. When an at-risk status is determined, a more in-depth screening is performed. “When patients at risk for malnutrition can be identified faster, appropriate interventions can be put into place sooner,” Quatrara says.
The second step is nutrition intervention with a personalized nutritional care plan that takes into account the individual’s health conditions, caloric needs, physical limitations, tastes, and preferences. An interdisciplinary team approach can transform hospital nutrition, bringing together hospitalists, nurses, nursing assistants, registered dietitians, and the dietary staff to collaboratively develop a nutrition care plan that will be central to patient’s overall treatment, Dr. Tappenden says.
“There is a science behind nutrition and metabolic care,” Dr. Tappenden says. “Just like any other aspect of patient care, we can’t just throw out a blanket solution.”
But nutritional care cannot stop with developing this plan at the outset. Patients must be rescreened throughout their time at the hospital to measure any changes in nutritional status due to disease progression or treatment success.
For optimal impact, all members of the nutritional care team—nurses, nursing assistants, dietary support staff, and family members—should take responsibility for an essential component of the patient’s care: tracking and reporting consumption to the physician to open a dialogue about balancing an individual’s needs with tastes and preferences.
The hospitalist’s final step is developing a discharge plan that includes nutrition care and education so that patients, families, and caregivers can implement better nutrition at home.
“Nutrition makes sense,” Dr. Tappenden says. “Everything we are working toward in healthcare reform can be achieved by taking more care to make nutrition part of the solution.”
Maybelle Cowan-Lincoln is a freelance writer in New Jersey.
References
- Kirkland LL, Kashiwagi DT, Brantley S, Scheurer D, Varkey P. Nutrition in the hospitalized patient. J Hosp Med. 2013;8:52-58.
- Alliance for Patient Nutrition. Malnutrition Backgrounder.
- Banks M, Bauer J, Graves N, Ash S. Malnutrition and pressure ulcer risk in adults in Australian health care facilities. Clin Nutr. 2010;26:896-901.
- Fry DE, Pine M, Jones BL, Meimban RJ. Patient characteristics and the occurrence of never events. Arch Surg. 2010;145:148-151.
- Gariballa S, Forster S, Walters S, Powers H. A randomized, double-blind, placebo-controlled trial of nutritional supplementation during acute illness. Am J Med. 2006;119:693-699.
- Neelemaat F, Lips P, Bosmans J, Thijs A, Seidell JC, van Bokhorst-de van der Schuerer MA. Short-term oral nutritional intervention with protein and vitamin D decreases falls in malnourished older adults. J Am Geriatr Soc. 2012;60:691-699.
- Brugler L, DiPrinzio MJ, Bernstein L. The five-year evolution of a malnutrition treatment program in a community hospital. J Qual Improv. 1999;25:191-206.
- Stratton PJ, et al. Enteral nutritional support in prevention and treatment of pressure ulcers: a systematic review and meta-analysis. Ageing Res Rev. 2005;4:422-450.
- Lawson RM, Doshi MK, Barton JR, Cobden I. The effect of unselected post-operative nutritional supplementation on nutritional status and clinical outcomes of elderly orthopaedic patients. Clin Nutr. 2003;22:39-46.
Health-care reform is on everyone’s mind these days, and SHM, along with numerous other groups, believes some reform goals can be achieved through the stomach.
Data show an effective program of nutritional intervention during a patient’s hospital stay can go a long way toward improving patient outcomes and reducing costs.1 Hospitalists, however, often have little formal nutrition training. A multidisciplinary approach to patient nutrition that brings together multiple stakeholders—hospitalists, nurses, and dietitians—might effectively address this need with a team tactic, according to Melissa Parkhurst, MD, medical director of the hospital medicine section at the University of Kansas Medical Center in Kansas City.1
Between 20% and 50% of inpatients suffer from malnutrition.2 Many patients, especially the elderly, are malnourished on admission. Many more become malnourished within a few days of their hospital stay due to NPO orders and the effects of disease on metabolism.2 Malnutrition has been associated with worsened discharge status, longer length of stay, higher costs, and greater mortality, as well as increased risk of:2
- Nosocomial infections;
- Falls;
- Pressure ulcers; and
- 30-day readmissions.
To address malnutrition prevalence and its detrimental effects, SHM and the Academy of Medical-Surgical Nurses (AMSN), the Academy of Nutrition and Dietetics (AND), the American Society of Parenteral and Enteral Nutrition (ASPEN), and Abbott Nutrition have formed the Alliance for Patient Nutrition. Kelly Tappenden, MD, PhD, professor of food science and human nutrition at the University of Illinois at Urbana, says the alliance aims to raise awareness of the impact nutrition can have on patient outcomes (see “Three Steps to Better Nutrition,” below).
The campaign is being initiated with the publication of a consensus paper in several peer-reviewed journals. A baseline survey will be conducted among professionals represented in the alliance to assess their familiarity with the prevalence of malnutrition in a hospital setting. The next step is to foster this change in patient care by providing resources on the alliance’s website (www.malnutrition.com), including malnutrition screening tools, a toolkit to facilitate multidisciplinary collaboration, and continuing medical education (CME) information.
As a founding member of the alliance, SHM is communicating this message to its members, encouraging hospitalists to lead the way in transforming hospital culture to recognize the critical role nutrition plays in patient care.
“Nutrition matters,” Dr. Parkhurst says. “You can be winning the battle and losing the war if you are not paying attention to patient nutrition.”
Team Approach
Beth Quatrara, DNP, RN, director of the nursing research program at the University of Virginia Health System in Charlottesville and nursing spokesperson for the alliance, says several shortcomings can be identified in the nutritional care U.S. hospitals provide from admission through discharge and beyond. For example, the Joint Commission requires that all patients be screened for malnutrition risk within 48 hours of admission. But screening is often as cursory as looking at the patient and deciding that he or she “looks fine.” Diets often are set for patients with no thought to taste, texture, or cultural preferences, or even to such practical matters as ascertaining whether the patient has dentures, Quatrara says. Meal trays are left when patients are out of their rooms for procedures and retrieved by dietary staff before patients return. And except for calorie count orders, accurate records often are not kept of actual food consumption.
The alliance, which is made possible with support from Abbott's nutrition business, recommends that physicians implement a three-step plan to improve patient outcomes. The approach begins with an evaluation of a patient’s nutritional status on admission using a simple, validated screening tool, such as the Malnutrition Screening Tool. When an at-risk status is determined, a more in-depth screening is performed. “When patients at risk for malnutrition can be identified faster, appropriate interventions can be put into place sooner,” Quatrara says.
The second step is nutrition intervention with a personalized nutritional care plan that takes into account the individual’s health conditions, caloric needs, physical limitations, tastes, and preferences. An interdisciplinary team approach can transform hospital nutrition, bringing together hospitalists, nurses, nursing assistants, registered dietitians, and the dietary staff to collaboratively develop a nutrition care plan that will be central to patient’s overall treatment, Dr. Tappenden says.
“There is a science behind nutrition and metabolic care,” Dr. Tappenden says. “Just like any other aspect of patient care, we can’t just throw out a blanket solution.”
But nutritional care cannot stop with developing this plan at the outset. Patients must be rescreened throughout their time at the hospital to measure any changes in nutritional status due to disease progression or treatment success.
For optimal impact, all members of the nutritional care team—nurses, nursing assistants, dietary support staff, and family members—should take responsibility for an essential component of the patient’s care: tracking and reporting consumption to the physician to open a dialogue about balancing an individual’s needs with tastes and preferences.
The hospitalist’s final step is developing a discharge plan that includes nutrition care and education so that patients, families, and caregivers can implement better nutrition at home.
“Nutrition makes sense,” Dr. Tappenden says. “Everything we are working toward in healthcare reform can be achieved by taking more care to make nutrition part of the solution.”
Maybelle Cowan-Lincoln is a freelance writer in New Jersey.
References
- Kirkland LL, Kashiwagi DT, Brantley S, Scheurer D, Varkey P. Nutrition in the hospitalized patient. J Hosp Med. 2013;8:52-58.
- Alliance for Patient Nutrition. Malnutrition Backgrounder.
- Banks M, Bauer J, Graves N, Ash S. Malnutrition and pressure ulcer risk in adults in Australian health care facilities. Clin Nutr. 2010;26:896-901.
- Fry DE, Pine M, Jones BL, Meimban RJ. Patient characteristics and the occurrence of never events. Arch Surg. 2010;145:148-151.
- Gariballa S, Forster S, Walters S, Powers H. A randomized, double-blind, placebo-controlled trial of nutritional supplementation during acute illness. Am J Med. 2006;119:693-699.
- Neelemaat F, Lips P, Bosmans J, Thijs A, Seidell JC, van Bokhorst-de van der Schuerer MA. Short-term oral nutritional intervention with protein and vitamin D decreases falls in malnourished older adults. J Am Geriatr Soc. 2012;60:691-699.
- Brugler L, DiPrinzio MJ, Bernstein L. The five-year evolution of a malnutrition treatment program in a community hospital. J Qual Improv. 1999;25:191-206.
- Stratton PJ, et al. Enteral nutritional support in prevention and treatment of pressure ulcers: a systematic review and meta-analysis. Ageing Res Rev. 2005;4:422-450.
- Lawson RM, Doshi MK, Barton JR, Cobden I. The effect of unselected post-operative nutritional supplementation on nutritional status and clinical outcomes of elderly orthopaedic patients. Clin Nutr. 2003;22:39-46.
Empathy Can Help Hospitalists Improve Patient Experience, Outcomes
Empathy: ability to understand and share the feelings of another.
In today’s increasingly hyper-measured healthcare world, we are looking more and more at measures of patient outcomes. The Institute for Healthcare Improvement (IHI) touts the Triple Aim principle as the lens through which we should be approaching our work. The Triple Aim is the three-part goal and simultaneous focus of improving the health of the community and our patients, improving affordability of care, and finally and perhaps most elusively, improving the patient experience. Who wouldn’t want to hit on these admirable goals? How do we do it?
In approaching the health aspect of the Triple Aim, we, as hospitalists, have tried-and-true frameworks of process improvement. Clinical research and peer-reviewed publication advance the knowledge of what medicines and procedures can improve care. Although powerful and generally truthful, this system results in a slow diffusion of practice improvement, not to mention idiosyncratic and nonstandardized care. This has led to a new toolkit of improvement techniques: continuous quality improvement, Lean, and Six Sigma. We learn and adopt these and watch our scores go up at a steady pace.
Improving affordability has its challenges, some huge, like our basic cultural ethos that “more is better.” Yet affordability is still something we can grasp. It is rooted in systems we are all familiar with, from basic personal finance to resource allocation to generally accepted accounting principles. We all can grasp that the current system of pay for widgets is teetering at the edge, just waiting for a shove from CMS to send it to its doom. Once this happens, affordability likely will become something we can start to make serious headway against.
Improving the experience of patients and families is perhaps the toughest of the three and where I would like to focus.
Patients First
First, a question: Are experience scores reflective of the true experience of a patient?
Two weeks after discharge, when patients receive their HCAHPS questionnaire in the mail, do they remember the details of their stay? And who was their doctor anyway? The cardiologist who placed a stent? The on-call doctor? The hospitalist who visited them every morning? If all we focus on is the scores, and we lack faith that the scores represent the true experience of patients, then how can we ever truly create a more satisfying experience for our patients?
I believe that the answer lies with empathy. What’s unique about this part of the Triple Aim is that many of the answers are within us. Gaining empathy with our patients requires us to ask questions of them and also to ask questions of ourselves. It requires us to invoke ancient methods of learning and thinking, like walking in another’s shoes for a day or using the Golden Rule. Experience doesn’t lend itself to being taught by PowerPoint. It must be lived and channeled back and out through our emotional selves as empathy.
Using the wisdom of patients themselves is one way to understand their needs and develop the empathy to motivate us to change how we do things in health care. Many organizations around the country have used some form of patient focus group to help learn from patients. Park Nicollet, a large health system in Minnesota, has incorporated family councils in nearly every clinic and care area. They usually are patients or caregivers from the area, bound together by a common disease or location. They dedicate their time, often meeting monthly, to share their stories, give opinions on care processes, and even to shape the design of a care area. Currently, there are more than 100 patient councils in the system, and the number continues to grow.
Film, when done skillfully, is a powerful tool in helping us gain empathy. The Cleveland Clinic has produced an amazing short film called “Empathy: The Human Connection to Patient Care.” It follows patients, families, and staff through the care system. As the camera focuses on each person, floating text appears near them, explaining their situation, inner thoughts, or fears, all overlaid by an emotional piano score. Tears will flow. Understanding follows.
Jim Merlino, MD, Cleveland Clinic’s chief experience officer, explains, “We need to understand that being on the other side of health care is frightening, and our job, our responsibility as people responsible for other people, is to help ease that fear.” Cleveland Clinic has done a remarkable job in reminding us why we went in to health care.
Morgan Spurlock of “Super Size Me” fame produced a reality series called “30 Days.” In each episode, a participant spent 30 days in the shoes of another. In the “Life in a Wheelchair” episode, Super Bowl-winning football player Ray Crockett lives in a wheelchair for 30 days and explores what it is like going through recovery and the healthcare system. He meets several rehabbing paraplegics and quadriplegics and accompanies them through their daily lives at home and the hospital. Viewers gain empathy directly in seeing these patients struggle to get better and work with the healthcare system. We also gain empathy watching Crockett gain empathy. The combination is powerful.
In Patients’ Shoes
In addition to listening and observation, we can begin to literally walk in the shoes of our patients.
I recently attended IHI’s International Forum in London. The National Health Service (NHS) in England is using a new tool to help providers understand what it is like for geriatric patients who must navigate the healthcare system with diminished senses and capabilities. Providers put on an age-simulation suit (www.age-simulation-suit.com) that mimics the impairments of aging. Special goggles fog the vision and narrow the visual field. Head mobility is reduced so that it becomes difficult to see beyond the field cuts. Earmuffs reduce high-frequency hearing and the ability to understand speech clearly. The overall suit impedes motion and reduces strength. Thick gloves make it difficult to coordinate fine motions. Wearing this suit and trying to go through a hospital or clinic setting instantly makes the wearer gain empathy for our patients’ needs.
Most important, be a patient. SHM immediate past president Shaun Frost, MD, SFHM, whose personal mission during his tenure was to help the society understand patient experience, explained it best to me. “In one episode in the hospital with a family member, I learned more about patient experience than all the reading and self-educating I have been doing for the last year.”
I think any of us who have been a patient in the hospital, or accompanied a loved one, comes out frustrated that the healthcare system is so convoluted and lacking in clarity for patients. Then there is often a sense of renewal, hopefully,followed by evangelism to spread their newfound empathy to others in the system.
In our busy work lives as hospitalists, it isn’t easy turning our daily focus away from efficiency and productivity. Yet we must always remain mindful of that core idea every one of us wrote down as the heart of our personal statements on our applications to medical school. Do you remember writing something like this? “I want to help people and relieve suffering in their time of need.”
Empathy is the start of our work.
Dr. Kealey is medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn. He is an SHM board member and SHM president-elect.
Empathy: ability to understand and share the feelings of another.
In today’s increasingly hyper-measured healthcare world, we are looking more and more at measures of patient outcomes. The Institute for Healthcare Improvement (IHI) touts the Triple Aim principle as the lens through which we should be approaching our work. The Triple Aim is the three-part goal and simultaneous focus of improving the health of the community and our patients, improving affordability of care, and finally and perhaps most elusively, improving the patient experience. Who wouldn’t want to hit on these admirable goals? How do we do it?
In approaching the health aspect of the Triple Aim, we, as hospitalists, have tried-and-true frameworks of process improvement. Clinical research and peer-reviewed publication advance the knowledge of what medicines and procedures can improve care. Although powerful and generally truthful, this system results in a slow diffusion of practice improvement, not to mention idiosyncratic and nonstandardized care. This has led to a new toolkit of improvement techniques: continuous quality improvement, Lean, and Six Sigma. We learn and adopt these and watch our scores go up at a steady pace.
Improving affordability has its challenges, some huge, like our basic cultural ethos that “more is better.” Yet affordability is still something we can grasp. It is rooted in systems we are all familiar with, from basic personal finance to resource allocation to generally accepted accounting principles. We all can grasp that the current system of pay for widgets is teetering at the edge, just waiting for a shove from CMS to send it to its doom. Once this happens, affordability likely will become something we can start to make serious headway against.
Improving the experience of patients and families is perhaps the toughest of the three and where I would like to focus.
Patients First
First, a question: Are experience scores reflective of the true experience of a patient?
Two weeks after discharge, when patients receive their HCAHPS questionnaire in the mail, do they remember the details of their stay? And who was their doctor anyway? The cardiologist who placed a stent? The on-call doctor? The hospitalist who visited them every morning? If all we focus on is the scores, and we lack faith that the scores represent the true experience of patients, then how can we ever truly create a more satisfying experience for our patients?
I believe that the answer lies with empathy. What’s unique about this part of the Triple Aim is that many of the answers are within us. Gaining empathy with our patients requires us to ask questions of them and also to ask questions of ourselves. It requires us to invoke ancient methods of learning and thinking, like walking in another’s shoes for a day or using the Golden Rule. Experience doesn’t lend itself to being taught by PowerPoint. It must be lived and channeled back and out through our emotional selves as empathy.
Using the wisdom of patients themselves is one way to understand their needs and develop the empathy to motivate us to change how we do things in health care. Many organizations around the country have used some form of patient focus group to help learn from patients. Park Nicollet, a large health system in Minnesota, has incorporated family councils in nearly every clinic and care area. They usually are patients or caregivers from the area, bound together by a common disease or location. They dedicate their time, often meeting monthly, to share their stories, give opinions on care processes, and even to shape the design of a care area. Currently, there are more than 100 patient councils in the system, and the number continues to grow.
Film, when done skillfully, is a powerful tool in helping us gain empathy. The Cleveland Clinic has produced an amazing short film called “Empathy: The Human Connection to Patient Care.” It follows patients, families, and staff through the care system. As the camera focuses on each person, floating text appears near them, explaining their situation, inner thoughts, or fears, all overlaid by an emotional piano score. Tears will flow. Understanding follows.
Jim Merlino, MD, Cleveland Clinic’s chief experience officer, explains, “We need to understand that being on the other side of health care is frightening, and our job, our responsibility as people responsible for other people, is to help ease that fear.” Cleveland Clinic has done a remarkable job in reminding us why we went in to health care.
Morgan Spurlock of “Super Size Me” fame produced a reality series called “30 Days.” In each episode, a participant spent 30 days in the shoes of another. In the “Life in a Wheelchair” episode, Super Bowl-winning football player Ray Crockett lives in a wheelchair for 30 days and explores what it is like going through recovery and the healthcare system. He meets several rehabbing paraplegics and quadriplegics and accompanies them through their daily lives at home and the hospital. Viewers gain empathy directly in seeing these patients struggle to get better and work with the healthcare system. We also gain empathy watching Crockett gain empathy. The combination is powerful.
In Patients’ Shoes
In addition to listening and observation, we can begin to literally walk in the shoes of our patients.
I recently attended IHI’s International Forum in London. The National Health Service (NHS) in England is using a new tool to help providers understand what it is like for geriatric patients who must navigate the healthcare system with diminished senses and capabilities. Providers put on an age-simulation suit (www.age-simulation-suit.com) that mimics the impairments of aging. Special goggles fog the vision and narrow the visual field. Head mobility is reduced so that it becomes difficult to see beyond the field cuts. Earmuffs reduce high-frequency hearing and the ability to understand speech clearly. The overall suit impedes motion and reduces strength. Thick gloves make it difficult to coordinate fine motions. Wearing this suit and trying to go through a hospital or clinic setting instantly makes the wearer gain empathy for our patients’ needs.
Most important, be a patient. SHM immediate past president Shaun Frost, MD, SFHM, whose personal mission during his tenure was to help the society understand patient experience, explained it best to me. “In one episode in the hospital with a family member, I learned more about patient experience than all the reading and self-educating I have been doing for the last year.”
I think any of us who have been a patient in the hospital, or accompanied a loved one, comes out frustrated that the healthcare system is so convoluted and lacking in clarity for patients. Then there is often a sense of renewal, hopefully,followed by evangelism to spread their newfound empathy to others in the system.
In our busy work lives as hospitalists, it isn’t easy turning our daily focus away from efficiency and productivity. Yet we must always remain mindful of that core idea every one of us wrote down as the heart of our personal statements on our applications to medical school. Do you remember writing something like this? “I want to help people and relieve suffering in their time of need.”
Empathy is the start of our work.
Dr. Kealey is medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn. He is an SHM board member and SHM president-elect.
Empathy: ability to understand and share the feelings of another.
In today’s increasingly hyper-measured healthcare world, we are looking more and more at measures of patient outcomes. The Institute for Healthcare Improvement (IHI) touts the Triple Aim principle as the lens through which we should be approaching our work. The Triple Aim is the three-part goal and simultaneous focus of improving the health of the community and our patients, improving affordability of care, and finally and perhaps most elusively, improving the patient experience. Who wouldn’t want to hit on these admirable goals? How do we do it?
In approaching the health aspect of the Triple Aim, we, as hospitalists, have tried-and-true frameworks of process improvement. Clinical research and peer-reviewed publication advance the knowledge of what medicines and procedures can improve care. Although powerful and generally truthful, this system results in a slow diffusion of practice improvement, not to mention idiosyncratic and nonstandardized care. This has led to a new toolkit of improvement techniques: continuous quality improvement, Lean, and Six Sigma. We learn and adopt these and watch our scores go up at a steady pace.
Improving affordability has its challenges, some huge, like our basic cultural ethos that “more is better.” Yet affordability is still something we can grasp. It is rooted in systems we are all familiar with, from basic personal finance to resource allocation to generally accepted accounting principles. We all can grasp that the current system of pay for widgets is teetering at the edge, just waiting for a shove from CMS to send it to its doom. Once this happens, affordability likely will become something we can start to make serious headway against.
Improving the experience of patients and families is perhaps the toughest of the three and where I would like to focus.
Patients First
First, a question: Are experience scores reflective of the true experience of a patient?
Two weeks after discharge, when patients receive their HCAHPS questionnaire in the mail, do they remember the details of their stay? And who was their doctor anyway? The cardiologist who placed a stent? The on-call doctor? The hospitalist who visited them every morning? If all we focus on is the scores, and we lack faith that the scores represent the true experience of patients, then how can we ever truly create a more satisfying experience for our patients?
I believe that the answer lies with empathy. What’s unique about this part of the Triple Aim is that many of the answers are within us. Gaining empathy with our patients requires us to ask questions of them and also to ask questions of ourselves. It requires us to invoke ancient methods of learning and thinking, like walking in another’s shoes for a day or using the Golden Rule. Experience doesn’t lend itself to being taught by PowerPoint. It must be lived and channeled back and out through our emotional selves as empathy.
Using the wisdom of patients themselves is one way to understand their needs and develop the empathy to motivate us to change how we do things in health care. Many organizations around the country have used some form of patient focus group to help learn from patients. Park Nicollet, a large health system in Minnesota, has incorporated family councils in nearly every clinic and care area. They usually are patients or caregivers from the area, bound together by a common disease or location. They dedicate their time, often meeting monthly, to share their stories, give opinions on care processes, and even to shape the design of a care area. Currently, there are more than 100 patient councils in the system, and the number continues to grow.
Film, when done skillfully, is a powerful tool in helping us gain empathy. The Cleveland Clinic has produced an amazing short film called “Empathy: The Human Connection to Patient Care.” It follows patients, families, and staff through the care system. As the camera focuses on each person, floating text appears near them, explaining their situation, inner thoughts, or fears, all overlaid by an emotional piano score. Tears will flow. Understanding follows.
Jim Merlino, MD, Cleveland Clinic’s chief experience officer, explains, “We need to understand that being on the other side of health care is frightening, and our job, our responsibility as people responsible for other people, is to help ease that fear.” Cleveland Clinic has done a remarkable job in reminding us why we went in to health care.
Morgan Spurlock of “Super Size Me” fame produced a reality series called “30 Days.” In each episode, a participant spent 30 days in the shoes of another. In the “Life in a Wheelchair” episode, Super Bowl-winning football player Ray Crockett lives in a wheelchair for 30 days and explores what it is like going through recovery and the healthcare system. He meets several rehabbing paraplegics and quadriplegics and accompanies them through their daily lives at home and the hospital. Viewers gain empathy directly in seeing these patients struggle to get better and work with the healthcare system. We also gain empathy watching Crockett gain empathy. The combination is powerful.
In Patients’ Shoes
In addition to listening and observation, we can begin to literally walk in the shoes of our patients.
I recently attended IHI’s International Forum in London. The National Health Service (NHS) in England is using a new tool to help providers understand what it is like for geriatric patients who must navigate the healthcare system with diminished senses and capabilities. Providers put on an age-simulation suit (www.age-simulation-suit.com) that mimics the impairments of aging. Special goggles fog the vision and narrow the visual field. Head mobility is reduced so that it becomes difficult to see beyond the field cuts. Earmuffs reduce high-frequency hearing and the ability to understand speech clearly. The overall suit impedes motion and reduces strength. Thick gloves make it difficult to coordinate fine motions. Wearing this suit and trying to go through a hospital or clinic setting instantly makes the wearer gain empathy for our patients’ needs.
Most important, be a patient. SHM immediate past president Shaun Frost, MD, SFHM, whose personal mission during his tenure was to help the society understand patient experience, explained it best to me. “In one episode in the hospital with a family member, I learned more about patient experience than all the reading and self-educating I have been doing for the last year.”
I think any of us who have been a patient in the hospital, or accompanied a loved one, comes out frustrated that the healthcare system is so convoluted and lacking in clarity for patients. Then there is often a sense of renewal, hopefully,followed by evangelism to spread their newfound empathy to others in the system.
In our busy work lives as hospitalists, it isn’t easy turning our daily focus away from efficiency and productivity. Yet we must always remain mindful of that core idea every one of us wrote down as the heart of our personal statements on our applications to medical school. Do you remember writing something like this? “I want to help people and relieve suffering in their time of need.”
Empathy is the start of our work.
Dr. Kealey is medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn. He is an SHM board member and SHM president-elect.
Steps Hospitalists Should Take to Reduce Turnaround Time of Death Certificates
Funeral-home representatives sometimes make multiple trips to a hospital or doctor’s office to get a death certificate signed, often waiting in the lobby for hours. I first realized this in the 1980s when starting post-residency practice as a hospitalist. I began asking these guys (they are nearly always men, in my experience) how much time they typically invest getting each certificate signed. They told of walking halfway across a golf course to catch the doctor on the 13th hole or making the 90-minute drive (each way) to a doctor’s office, sometimes finding the doctor had just left, only to repeat the process several times before getting the signature.
When the Clinton administration made electronic signatures via the Internet valid, I thought about starting a business charging funeral homes something like $200 for getting the doctor to sign it electronically within 48 hours. I would use about half of the $200 to provide an incentive for the doctor to sign quickly (sign within 48 hours, and you’ll get a $100 gift card!), then use the rest to fund the company. Since funeral homes probably spend much more than $200 per certificate paying their staff to drive around getting signatures on paper, I thought they would jump at this idea.
I never pursued it, but that doesn’t stop me from loudly proclaiming to friends and family that it was a “can’t-miss” blockbuster Internet business idea. Of course, I never tested that theory, but it makes for fun chest-thumping at parties.
A number of states, including Florida, Texas, and others, now have in place online completion of death certificates. Indiana has required use of its online death certificate since 2011; there is no option to use paper. I suspect nearly every state will do the same before long. But that alone won’t ensure timely completion. Doctors and others who complete the certificates need to ensure they respond quickly, something they often fail to do.
It Really Matters
Lack of a death certificate can hold up burial or cremation, and things like life-insurance payouts and estate settlement are delayed. For a grieving family, these things only add to their pain.
I’m aware of a tragic case from a few years ago in which a certificate was passed around to a number of doctors, each of whom thought with some justification that someone else should sign it. It sat in two different mailboxes for many days while the intended recipients were vacationing. All of this delayed the burial, and the poor family had to send updates to loved ones saying, “We don’t know when Dad’s funeral will be.” About three weeks later, the certificate was completed and the funeral held. What a terribly sad story!
Some states have laws governing how quickly certificates must be signed. A thought-provoking 2004 Medical Staff Update from Stanford University says that California requires a signature within 15 hours of death, though I wonder how often this is enforced.
Improving Turnaround Time
There are several things hospitalists could consider to improve timely completion of death certificates:
- Ensure doctors liberally complete them for one another. Don’t let one doctor’s absence delay, even for a day, getting it completed and signed. This means the “covering” doctor has access to the discharge (death) summary in the medical record.
- When several doctors in different specialties are caring for a patient at the time of death, nearly any of them could reasonably sign the certificate. It might be appropriate to adopt a policy that whichever doctor (e.g. hospitalist, intensivist, or oncologist) who had contact with the patient and is presented with the certificate should go ahead and sign it rather than passing it along to one of the other specialties, regardless of which served as attending.
- Consider creating a central access point at your hospital for receipt of death certificates. Ideally, a funeral-home representative can deliver it to one person at the hospital who will do the leg work of getting a doctor to sign it quickly. Delays are likely if the funeral-home representative has to “shop it around” to different departments and physician offices. A hospital staffer should be able to navigate this quickly.
- Pressure EMR vendors to include some sort of death-certificate functionality in the future. I don’t know if some have it already, but it seems like it shouldn’t be too difficult for an EMR to spit out a prefilled certificate in much the same way e-prescribing works. It could even be delivered electronically to the funeral home.
- For hospitalists with 24-hour, on-site presence, it could be reasonable to have an on-duty hospitalist complete the certificate at the time of death rather than waiting for the funeral home to initiate the process. This was standard when I was a resident, and it may be a practical approach in many settings.
- Consider copying one hospital I worked with previously: They created a hospitalist salary bonus for timely completion. I assure you this policy was very effective.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Funeral-home representatives sometimes make multiple trips to a hospital or doctor’s office to get a death certificate signed, often waiting in the lobby for hours. I first realized this in the 1980s when starting post-residency practice as a hospitalist. I began asking these guys (they are nearly always men, in my experience) how much time they typically invest getting each certificate signed. They told of walking halfway across a golf course to catch the doctor on the 13th hole or making the 90-minute drive (each way) to a doctor’s office, sometimes finding the doctor had just left, only to repeat the process several times before getting the signature.
When the Clinton administration made electronic signatures via the Internet valid, I thought about starting a business charging funeral homes something like $200 for getting the doctor to sign it electronically within 48 hours. I would use about half of the $200 to provide an incentive for the doctor to sign quickly (sign within 48 hours, and you’ll get a $100 gift card!), then use the rest to fund the company. Since funeral homes probably spend much more than $200 per certificate paying their staff to drive around getting signatures on paper, I thought they would jump at this idea.
I never pursued it, but that doesn’t stop me from loudly proclaiming to friends and family that it was a “can’t-miss” blockbuster Internet business idea. Of course, I never tested that theory, but it makes for fun chest-thumping at parties.
A number of states, including Florida, Texas, and others, now have in place online completion of death certificates. Indiana has required use of its online death certificate since 2011; there is no option to use paper. I suspect nearly every state will do the same before long. But that alone won’t ensure timely completion. Doctors and others who complete the certificates need to ensure they respond quickly, something they often fail to do.
It Really Matters
Lack of a death certificate can hold up burial or cremation, and things like life-insurance payouts and estate settlement are delayed. For a grieving family, these things only add to their pain.
I’m aware of a tragic case from a few years ago in which a certificate was passed around to a number of doctors, each of whom thought with some justification that someone else should sign it. It sat in two different mailboxes for many days while the intended recipients were vacationing. All of this delayed the burial, and the poor family had to send updates to loved ones saying, “We don’t know when Dad’s funeral will be.” About three weeks later, the certificate was completed and the funeral held. What a terribly sad story!
Some states have laws governing how quickly certificates must be signed. A thought-provoking 2004 Medical Staff Update from Stanford University says that California requires a signature within 15 hours of death, though I wonder how often this is enforced.
Improving Turnaround Time
There are several things hospitalists could consider to improve timely completion of death certificates:
- Ensure doctors liberally complete them for one another. Don’t let one doctor’s absence delay, even for a day, getting it completed and signed. This means the “covering” doctor has access to the discharge (death) summary in the medical record.
- When several doctors in different specialties are caring for a patient at the time of death, nearly any of them could reasonably sign the certificate. It might be appropriate to adopt a policy that whichever doctor (e.g. hospitalist, intensivist, or oncologist) who had contact with the patient and is presented with the certificate should go ahead and sign it rather than passing it along to one of the other specialties, regardless of which served as attending.
- Consider creating a central access point at your hospital for receipt of death certificates. Ideally, a funeral-home representative can deliver it to one person at the hospital who will do the leg work of getting a doctor to sign it quickly. Delays are likely if the funeral-home representative has to “shop it around” to different departments and physician offices. A hospital staffer should be able to navigate this quickly.
- Pressure EMR vendors to include some sort of death-certificate functionality in the future. I don’t know if some have it already, but it seems like it shouldn’t be too difficult for an EMR to spit out a prefilled certificate in much the same way e-prescribing works. It could even be delivered electronically to the funeral home.
- For hospitalists with 24-hour, on-site presence, it could be reasonable to have an on-duty hospitalist complete the certificate at the time of death rather than waiting for the funeral home to initiate the process. This was standard when I was a resident, and it may be a practical approach in many settings.
- Consider copying one hospital I worked with previously: They created a hospitalist salary bonus for timely completion. I assure you this policy was very effective.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Funeral-home representatives sometimes make multiple trips to a hospital or doctor’s office to get a death certificate signed, often waiting in the lobby for hours. I first realized this in the 1980s when starting post-residency practice as a hospitalist. I began asking these guys (they are nearly always men, in my experience) how much time they typically invest getting each certificate signed. They told of walking halfway across a golf course to catch the doctor on the 13th hole or making the 90-minute drive (each way) to a doctor’s office, sometimes finding the doctor had just left, only to repeat the process several times before getting the signature.
When the Clinton administration made electronic signatures via the Internet valid, I thought about starting a business charging funeral homes something like $200 for getting the doctor to sign it electronically within 48 hours. I would use about half of the $200 to provide an incentive for the doctor to sign quickly (sign within 48 hours, and you’ll get a $100 gift card!), then use the rest to fund the company. Since funeral homes probably spend much more than $200 per certificate paying their staff to drive around getting signatures on paper, I thought they would jump at this idea.
I never pursued it, but that doesn’t stop me from loudly proclaiming to friends and family that it was a “can’t-miss” blockbuster Internet business idea. Of course, I never tested that theory, but it makes for fun chest-thumping at parties.
A number of states, including Florida, Texas, and others, now have in place online completion of death certificates. Indiana has required use of its online death certificate since 2011; there is no option to use paper. I suspect nearly every state will do the same before long. But that alone won’t ensure timely completion. Doctors and others who complete the certificates need to ensure they respond quickly, something they often fail to do.
It Really Matters
Lack of a death certificate can hold up burial or cremation, and things like life-insurance payouts and estate settlement are delayed. For a grieving family, these things only add to their pain.
I’m aware of a tragic case from a few years ago in which a certificate was passed around to a number of doctors, each of whom thought with some justification that someone else should sign it. It sat in two different mailboxes for many days while the intended recipients were vacationing. All of this delayed the burial, and the poor family had to send updates to loved ones saying, “We don’t know when Dad’s funeral will be.” About three weeks later, the certificate was completed and the funeral held. What a terribly sad story!
Some states have laws governing how quickly certificates must be signed. A thought-provoking 2004 Medical Staff Update from Stanford University says that California requires a signature within 15 hours of death, though I wonder how often this is enforced.
Improving Turnaround Time
There are several things hospitalists could consider to improve timely completion of death certificates:
- Ensure doctors liberally complete them for one another. Don’t let one doctor’s absence delay, even for a day, getting it completed and signed. This means the “covering” doctor has access to the discharge (death) summary in the medical record.
- When several doctors in different specialties are caring for a patient at the time of death, nearly any of them could reasonably sign the certificate. It might be appropriate to adopt a policy that whichever doctor (e.g. hospitalist, intensivist, or oncologist) who had contact with the patient and is presented with the certificate should go ahead and sign it rather than passing it along to one of the other specialties, regardless of which served as attending.
- Consider creating a central access point at your hospital for receipt of death certificates. Ideally, a funeral-home representative can deliver it to one person at the hospital who will do the leg work of getting a doctor to sign it quickly. Delays are likely if the funeral-home representative has to “shop it around” to different departments and physician offices. A hospital staffer should be able to navigate this quickly.
- Pressure EMR vendors to include some sort of death-certificate functionality in the future. I don’t know if some have it already, but it seems like it shouldn’t be too difficult for an EMR to spit out a prefilled certificate in much the same way e-prescribing works. It could even be delivered electronically to the funeral home.
- For hospitalists with 24-hour, on-site presence, it could be reasonable to have an on-duty hospitalist complete the certificate at the time of death rather than waiting for the funeral home to initiate the process. This was standard when I was a resident, and it may be a practical approach in many settings.
- Consider copying one hospital I worked with previously: They created a hospitalist salary bonus for timely completion. I assure you this policy was very effective.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.