User login
How to prevent misuse of psychotropics among college students
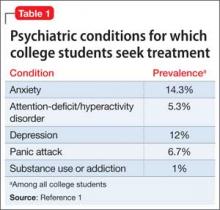
Many college students suffer from mental illness (Table 1),1 which can have a negative impact on academic performance. Although psychotropic medications are an important part of treatment for many college students, the potential for misuse always is present. Drug misuse occurs when patients use medications for reasons inconsistent with legal or medical guidelines.2 For example, patients may take a medication that has not been prescribed for them or in a manner that is inconsistent with the prescriber’s instructions, including administration with other substances.3
Misuse of psychotropic drugs is prevalent among college students. A study of 14,175 students from 26 campuses reported that 14.7% of students taking a psychotropic are doing so without a prescription, including stimulants (52.6%), anxiolytics (38.4%), and antidepressants (17.4%).4 Another study states that more than one-third of responders reported misuse of >1 class of medication.5
Psychotropic misuse is concerning because it increases the risk of adverse events. Nearly one-half of medication errors are associated with writing and dispensing the prescription, which means that prescribers can work to reduce these errors.6 However, nonadherence, prescription misuse, and failure to disclose use of over-the-counter drugs, illicit drugs, and herbal products makes preventing most adverse events difficult, if not impossible, for prescribers.7,8
Psychotropic drug misuse among college students is highly variable and unpredictable. Students misuse medications, including stimulants, benzodiazepines, and antidepressants, for a variety of reasons, such as study enhancement, experimentation, intoxication, self-medication, relaxation, and stress management.8 One survey reported that >70% of students taking a psychotropic medication took it with alcohol or another illicit drug.9
However, <20% of those using a psychotropic medication with alcohol or other illicit drugs told their health care provider(s),9 making it impossible for clinicians to predict a patient’s risk of drug− drug interactions and subsequent adverse events. Additionally, additive effects could occur10 and changes in a patient’s presentation could be caused by a reaction to a combination of medications, rather than a new symptom of mental illness.
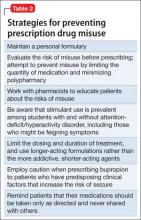
This article will examine common issues associated with drug misuse among college-age students and review prevention strategies (Table 2).
Stimulants
Stimulants have the highest rate of diversion; 61.7% of college students prescribed stimulants have shared or sold their medication.11 A survey of 115 students from 2 universities reported that the most common reason for stimulant misuse was to enhance academic performance.12 The same survey showed that some students take stimulants with Cannabis (17%) and alcohol (30%).12 As a result, in addition to lowering grade point average (GPA) and other academic difficulties,13 students misusing stimulants are at risk of drug interactions.14
It is critical to ascertain the route of drug administration, because non-oral routes, including crushing then snorting or injecting, are associated with additional health concerns, such as accidental death or blood-borne illnesses.15,16 Cardiac adverse effects of stimulants include hypertension, vasospasm, tachycardia, and dysrhythmia; psychiatric and other effects include serotonin syndrome, hallucinations, anxiety, paranoia, seizures, tics, hyperthermia, and tremor.17 Health care providers prescribing or caring for people taking a stimulant should monitor for these potential effects.
The risk of switch to mania might not be apparent to those who prescribe stimulants or to young people who take non-prescribed stimulants for academic enhancement or to achieve medication-induced euphoria. Adolescent stimulant use is associated with symptoms of early-onset bipolar disorder in patients who have attention-deficit/ hyperactivity disorder (ADHD) and undiagnosed bipolarity.18
The cardiovascular risk associated with stimulant use is debatable. Although several studies have been conducted,19-21 methodological factors limit their applicability. To minimize potential risks, several precautions should be taken before prescribing a stimulant to treat ADHD.
First, obtain a detailed personal and family medical history, asking about possible cardiovascular disease. Second, carefully scrutinize the patient’s cardiovascular system during the physical exam. Third, consider additional testing, such as an electrocardiogram, if the patient’s history or physical exam indicates possible risk.22
As a prescriber, you should be aware of the prevalence of stimulant use among students with and without ADHD, including those who could be feigning ADHD symptoms.15 Diversion could occur through sharing medications or selling them to friends and family.11 It also is possible that these medications may be used with other illicit substances, such as Cannabis, ecstasy, cocaine, and opiates.23 Students also could misuse stimulants by taking more than the prescribed dosage.24
Risk factors for misuse of stimulants include: heavy alcohol use, previous illicit drug use, white race, fraternity or sorority membership, low GPA, increased hyperactivity symptoms, and attendance at a competitive college or university.25-27
Benzodiazepines
Misuse of benzodiazepine is a significant component of prescription drug abuse and often occurs with other medications and alcohol.28 Additional methods of misuse include increased dosage and non-oral routes of administration.29
A 2001 national survey reported that 7.8% of college students have misused benzodiazepines.23 Common characteristics of benzodiazepine abusers include young age, male sex, personality characteristics of impulsivity and hopelessness, and abuse of other drugs, including cocaine and methadone.28,29
Benzodiazepines are prescribed for their anxiolytic and hypnotic properties and students could use these drugs with other agents to augment the euphoric effects or diminish withdrawal symptoms.30 Patients taking benzodiazepines for anxiety might self-medicate with alcohol, which increases sedation and depression, and can contribute to the risk for respiratory depression.10 Misuse of benzodiazepines can result in cognitive and psychomotor impairment and increase the risk of accidents and overdose.29,31
Although overdose with monotherapy is rare, the risk increases when a benzodiazepine is used with alcohol10 or another respiratory depressants, such as opioids, because combination use can produce additive effects.28 You should therefore avoid prescribing benzodiazepines to patients who have a history of significant substance abuse and consider using alternative, non-addictive agents, such as selective serotonin reuptake inhibitors, or non-pharmaceutical treatment when such patients present with an anxiety disorder. The risk of adverse effects of benzodiazepines can be reduced by limiting the dosing and the duration of the treatment, and by using longer-acting rather than the more addictive, shorter-acting, agents.
Antidepressants
Health care providers should be aware that, despite the relative absence of physically addictive properties, antidepressants from most classes are abusable agents sought by young people for non-medical use. In particular, the literature highlights monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, and bupropion as the antidepressants most likely to be misused for their amphetamine-like euphoric effects or serotonin-induced dissociative effects.32 However, compared with other drug classes discussed in this article, the rate of antidepressant misuse is relatively low among college students.
Regardless of the antidepressant selected, clinicians should be concerned about alcohol use among college-age patients. Persons with depression are at increased risk of alcoholism compared with the general population.33 This combination can increase depressive symptoms and sedation, and decrease coordination, judgment, and reaction time.33
Excessive alcohol use can increase the risk of seizures in patients taking antidepressants such as buproprion.34 Employ caution when prescribing bupropion to patients who have a predisposing clinical factor that increases seizure risk, such as excessive alcohol use and abrupt cessation, use of other medications that may lower seizure threshold (eg, theophylline, amphetamines, phenothiazines), and a history of head trauma.34
To minimize the risk of seizures with bupropion, titrate up the dosage slowly. Furthermore, using a low dosage during dual therapy for antidepressant augmentation further decreases the risk of seizure.35 For these reasons, we recommend that you avoid bupropion in patients who are at risk of binge drinking, and give careful consideration to providing alternative therapies for them.
Prescribers and patients should also keep in mind that hypertensive crisis could occur if MAOIs are combined with certain types of alcoholic beverages containing tyramine, including some wines and draft beer.33
How you can identify and prevent misuse
Careful communication between health care provider and patient that is necessary to minimize the risk of adverse drug events with psychotropic medications often is lacking. For example, 24% of study college-age participants did not remember if their physician provided a diagnosis and 28.8% could not recall being informed about side effects and, perhaps as a result, many students did not take their medications as prescribed.9
Further, prescribers should ask college-age patients who are undergoing stimulant treatment if they believe that they are being adequately treated. They should inquire about how they are taking their medications.11 These questions can lead to discussion of the need for these medications and reevaluation of their perceived indication.11
Remind patients to take their medication only as directed.36 Highlight the need to:
• store medications in a discreet location
• properly dispose of unused medications
• keep tabs on the quantity of pills
• know how to resist requests for diversion from peers.
The Substance Abuse and Mental Health Services Administration offers additional useful strategies,37 and pharmacists also can be partners in substance use education and prevention.38 These are examples of how health care providers can take an active role in providing patients with a thorough and detailed understanding of (1) their conditions and (2) their prescribed medications to improve efficacy and safety while preventing misuse.8
A study found that the most common method of obtaining these medications without a prescription is acquiring them from peers; 54% of undergraduate patients with stimulant prescriptions have been approached by peers to give, trade, or sell their drugs.25 Other methods include purchasing medications online or faking prescriptions.39 Health care providers should remind patients of the legal ramifications of sharing or selling their prescribed medications. Finally, providers must be vigilant for students who may feign symptoms to obtain a prescription:
• be wary if symptom presentation sounds too “textbook”
• seek collateral history from family. Adults with ADHD should have shown symptoms during childhood
• use external verification such as neuropsychological testing for ADHD. A neuropsychologist can detect deception by analyzing the pattern of responses to questions.
Patient assessment is a key step to in preventing abuse of psychotropic medications. Gentle inquiry about school-related stress and other risk factors for misuse can help practitioners determine if students are at risk of diversion and if additional screening is necessary.
In response to these issues, Stone and Merlo8 have suggested that, in addition to the educational programs held on college campuses on alcohol, illicit drugs, and prescription painkillers, patients should be better informed on the appropriate use of prescription psychiatric medications, instructed to avoid sharing with family and friends, and assessed for abuse risk at regular intervals.
To further protect patients from adverse outcomes during treatment, you can employ conservative and safe prescribing techniques. One strategy might be to keep a personal formulary that lists key medications you use in everyday practice, including knowledge about each drug’s dosage, potential adverse effects, key warnings, and drug−drug interactions.40
Furthermore, maintain healthy caution about newly approved medications and carefully consider how they measure up to existing agents—in other words, practice evidence-based medicine, particularly when students request a particular agent.40,41 Prescribers should evaluate the risk of abuse before prescribing and attempt to prevent misuse by limiting quantities and minimizing polypharmacy.
Last, pharmacists can be key allies for consultation and appropriate medication selection.
Bottom Line
Psychotropic medications are necessary to treat the variety of conditions—anxiety, attention-deficit/hyperactivity disorder, depression, and panic disorder—common among college students. However, students are at risk of combining their prescribed medications with other medications, drugs, and alcohol or could sell or share their medication with peers. Proper counseling and identification of risk factors can be important tools for preventing such events.
Related Resources
• American College Health Association-National College Health Assessment. www.acha-ncha.org.
• Schwartz VI. College mental health: How to provide care for students in need. Current Psychiatry. 2011;10(12):22-29.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Methadone • Methadose, Dolophine
Theophylline • Theo-24, Theolair, Uniphyl
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. http://www.acha-ncha.org/docs/ACHA-NCHA-II_ReferenceGroup_ExecutiveSummary_ Spring2014.pdf. Published 2014. Accessed January 13, 2015.
2. World Health Organization. Management of substance abuse. http://www.who.int/substance_abuse/terminology/ abuse/en. Accessed June 4, 2015.
3. U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. http://www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm. Published July 28, 2010. Accessed June 18, 2014.
4. Eisenberg D, Hunt J, Speer N, et al. Mental health service utilization among college students in the United States. J Nerv Ment Dis. 2011;199(5):301-308.
5. Peralta RL, Steele JL. Nonmedical prescription drug use among US college students at a Midwest university: a partial test of social learning theory. Subst Use Misuse. 2010;45(6):865-887.
6. Agency for Healthcare Research and Quality. Reducing and preventing adverse drug events to decrease hospital costs: Research in action. http://www.ahrq.gov/research/ findings/factsheets/errors-safety/aderia/index.html. Updated March 2001. Accessed June 21, 2014.
7. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2010;24(7):595-609.
8. Stone AM, Merlo LJ. Attitudes of college students toward mental illness stigma and the misuse of psychiatric medications. J Clin Psychiatry. 2011;72(2):134-139.
9. Oberleitner LM, Tzilos GK, Zumberg KM, et al. Psychotropic drug use among college students: patterns of use, misuse, and medical monitoring. J Am Coll Health. 2011;59(7):658-661.
10. Linnoila MI. Benzodiazepines and alcohol. J Psychiatr Res. 1990;24(suppl 2):121-127.
11. Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71(3):262-269.
12. Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144-153.
13. Arria AM. Nonmedical use of prescription stimulants and analgesics: associations with social and academic behaviors among college students. J Drug Issues. 2008; 38(4):1045-1060.
14. Arria AM, Caldeira KM, O’Grady KE, et al. Nonmedical use of prescription stimulants among college students: associations with attention-deficit-hyperactivity disorder and polydrug use. Pharmacotherapy. 2008;28(2):156-169.
15. Rabiner DL. Stimulant prescription cautions: addressing misuse, diversion and malingering. Curr Psychiatry Rep. 2013;15(7):375.
16. Sepúlveda DR, Thomas LM, McCabe SE, et al. Misuse of prescribed stimulant medication for ADHD and associated patterns of substance use: preliminary analysis among college students. J Pharm Pract. 2011;24(6):551-560.
17. Greydanus DE. Stimulant misuse: strategies to manage a growing problem. http://www.acha.org/Continuing_ Education/docs/ACHA_Use_Misuse_of_Stimulants_ Article2.pdf. Accessed June 29, 2015.
18. Vergne D, Whitham E, Barroilhet S, et al. Adult ADHD and amphetamines: a new paradigm. Neuropsychiatry. 2011;1(6):591-598.
19. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306(24):2673-2683.
20. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365(20):1896-1904.
21. Schelleman H, Bilker WB, Kimmel SE, et al. Methylphenidate and risk of serious cardiovascular events in adults. Am J Psychiatry. 2012;169(2):178-185.
22. U.S. Food and Drug Administration. Communication about an ongoing safety review of stimulant medications used in children with attention-deficit/hyperactivity disorder (ADHD). http://www.fda.gov/Drugs/Drug Safety/PostmarketDrugSafetyInformationforPatients andProviders/DrugSafetyInformationforHeathcare Professionals/ucm165858.htm. Updated August 15, 2013. Accessed June 25, 2014.
23. McCabe SE, Knight JR, Teter CJ, et al. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96-106.
24. McNiel AD, Muzzin KB, DeWald JP, et al. The nonmedical use of prescription stimulants among dental and dental hygiene students. J Dent Educ. 2011;75(3):365-376.
25. McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. J Psychoactive Drugs. 2006;38(1):43-56.
26. Arria AM, Garnier-Dykstra LM, Caldeira KM, et al. Persistent nonmedical use of prescription stimulants among college students: possible association with ADHD symptoms. J Atten Disord. 2011;15(5):347-356.
27. Teter CJ, McCabe SE, Boyd CJ, et al. Illicit methylphenidate use in an undergraduate student sample: prevalence and risk factors. Pharmacotherapy. 2003;23(5):609-617.
28. Hernandez SH, Nelson LS. Prescription drug abuse: insight into the epidemic. Clin Pharmacol Ther. 2010; 88(3):307-317.
29. McLarnon ME, Monaghan TL, Stewart SH, et al. Drug misuse and diversion in adults prescribed anxiolytics and sedatives. Pharmacotherapy. 2011;31(3):262-272.
30. Woods JH, Katz JL, Winger G. Benzodiazepines: use, abuse, and consequences. Pharmacol Rev. 1992;44(2):151-347.
31. Buffett-Jerrott SE, Stewart SH. Cognitive and sedative effects of benzodiazepine use. Curr Pharm Des. 2002;8(1):45-58.
32. Evans EA, Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil. 2014;5:107-120.
33. Hall-Flavin DK. Why is it bad to mix antidepressants and alcohol? http://www.mayoclinic.com/health/antidepressants-and-alcohol/AN01653. Updated June 12, 2014. Accessed June 20, 2014.
34. Wellbutrin [package insert]. Research Triangle Park, NC: GlaxoSmithKline LLC; 2014.
35. Davidson J. Seizures and bupropion: a review. J Clin Psychiatry. 1989;50(7):256-261.
36. Maddox JC, Levi M, Thompson C. The compliance with antidepressants in general practice. J Psychopharmacol. 1994;8(1):48-52.
37. Substance Abuse and Mental Health Services Administration. You’re in control: using prescription medication responsibly. http://store.samhsa.gov/shin/content/SMA12-4678B3/SMA12-4678B3.pdf. Accessed June 5, 2015.
38. ASHP statement on the pharmacist’s role in substance abuse prevention, education, and assistance. Am J Health Syst Pharm. 2014;71(3):243-246.
39. Inciardi JA, Surratt HL, Cicero TJ, et al. Prescription drugs purchased through the internet: who are the end users? Drug Alcohol Depend. 2010;110(1-2):21-29.
40. Preskorn SH, Flockhart D. 2006 Guide to psychiatric drug interactions. Primary Psychiatry. 2006;13(4):35-64.
41. Schiff GD, Galanter WL, Duhig J, et al. Principles of conservative prescribing. Arch Intern Med. 2011;171(16): 1433-1440.
Many college students suffer from mental illness (Table 1),1 which can have a negative impact on academic performance. Although psychotropic medications are an important part of treatment for many college students, the potential for misuse always is present. Drug misuse occurs when patients use medications for reasons inconsistent with legal or medical guidelines.2 For example, patients may take a medication that has not been prescribed for them or in a manner that is inconsistent with the prescriber’s instructions, including administration with other substances.3
Misuse of psychotropic drugs is prevalent among college students. A study of 14,175 students from 26 campuses reported that 14.7% of students taking a psychotropic are doing so without a prescription, including stimulants (52.6%), anxiolytics (38.4%), and antidepressants (17.4%).4 Another study states that more than one-third of responders reported misuse of >1 class of medication.5
Psychotropic misuse is concerning because it increases the risk of adverse events. Nearly one-half of medication errors are associated with writing and dispensing the prescription, which means that prescribers can work to reduce these errors.6 However, nonadherence, prescription misuse, and failure to disclose use of over-the-counter drugs, illicit drugs, and herbal products makes preventing most adverse events difficult, if not impossible, for prescribers.7,8
Psychotropic drug misuse among college students is highly variable and unpredictable. Students misuse medications, including stimulants, benzodiazepines, and antidepressants, for a variety of reasons, such as study enhancement, experimentation, intoxication, self-medication, relaxation, and stress management.8 One survey reported that >70% of students taking a psychotropic medication took it with alcohol or another illicit drug.9
However, <20% of those using a psychotropic medication with alcohol or other illicit drugs told their health care provider(s),9 making it impossible for clinicians to predict a patient’s risk of drug− drug interactions and subsequent adverse events. Additionally, additive effects could occur10 and changes in a patient’s presentation could be caused by a reaction to a combination of medications, rather than a new symptom of mental illness.
This article will examine common issues associated with drug misuse among college-age students and review prevention strategies (Table 2).
Stimulants
Stimulants have the highest rate of diversion; 61.7% of college students prescribed stimulants have shared or sold their medication.11 A survey of 115 students from 2 universities reported that the most common reason for stimulant misuse was to enhance academic performance.12 The same survey showed that some students take stimulants with Cannabis (17%) and alcohol (30%).12 As a result, in addition to lowering grade point average (GPA) and other academic difficulties,13 students misusing stimulants are at risk of drug interactions.14
It is critical to ascertain the route of drug administration, because non-oral routes, including crushing then snorting or injecting, are associated with additional health concerns, such as accidental death or blood-borne illnesses.15,16 Cardiac adverse effects of stimulants include hypertension, vasospasm, tachycardia, and dysrhythmia; psychiatric and other effects include serotonin syndrome, hallucinations, anxiety, paranoia, seizures, tics, hyperthermia, and tremor.17 Health care providers prescribing or caring for people taking a stimulant should monitor for these potential effects.
The risk of switch to mania might not be apparent to those who prescribe stimulants or to young people who take non-prescribed stimulants for academic enhancement or to achieve medication-induced euphoria. Adolescent stimulant use is associated with symptoms of early-onset bipolar disorder in patients who have attention-deficit/ hyperactivity disorder (ADHD) and undiagnosed bipolarity.18
The cardiovascular risk associated with stimulant use is debatable. Although several studies have been conducted,19-21 methodological factors limit their applicability. To minimize potential risks, several precautions should be taken before prescribing a stimulant to treat ADHD.
First, obtain a detailed personal and family medical history, asking about possible cardiovascular disease. Second, carefully scrutinize the patient’s cardiovascular system during the physical exam. Third, consider additional testing, such as an electrocardiogram, if the patient’s history or physical exam indicates possible risk.22
As a prescriber, you should be aware of the prevalence of stimulant use among students with and without ADHD, including those who could be feigning ADHD symptoms.15 Diversion could occur through sharing medications or selling them to friends and family.11 It also is possible that these medications may be used with other illicit substances, such as Cannabis, ecstasy, cocaine, and opiates.23 Students also could misuse stimulants by taking more than the prescribed dosage.24
Risk factors for misuse of stimulants include: heavy alcohol use, previous illicit drug use, white race, fraternity or sorority membership, low GPA, increased hyperactivity symptoms, and attendance at a competitive college or university.25-27
Benzodiazepines
Misuse of benzodiazepine is a significant component of prescription drug abuse and often occurs with other medications and alcohol.28 Additional methods of misuse include increased dosage and non-oral routes of administration.29
A 2001 national survey reported that 7.8% of college students have misused benzodiazepines.23 Common characteristics of benzodiazepine abusers include young age, male sex, personality characteristics of impulsivity and hopelessness, and abuse of other drugs, including cocaine and methadone.28,29
Benzodiazepines are prescribed for their anxiolytic and hypnotic properties and students could use these drugs with other agents to augment the euphoric effects or diminish withdrawal symptoms.30 Patients taking benzodiazepines for anxiety might self-medicate with alcohol, which increases sedation and depression, and can contribute to the risk for respiratory depression.10 Misuse of benzodiazepines can result in cognitive and psychomotor impairment and increase the risk of accidents and overdose.29,31
Although overdose with monotherapy is rare, the risk increases when a benzodiazepine is used with alcohol10 or another respiratory depressants, such as opioids, because combination use can produce additive effects.28 You should therefore avoid prescribing benzodiazepines to patients who have a history of significant substance abuse and consider using alternative, non-addictive agents, such as selective serotonin reuptake inhibitors, or non-pharmaceutical treatment when such patients present with an anxiety disorder. The risk of adverse effects of benzodiazepines can be reduced by limiting the dosing and the duration of the treatment, and by using longer-acting rather than the more addictive, shorter-acting, agents.
Antidepressants
Health care providers should be aware that, despite the relative absence of physically addictive properties, antidepressants from most classes are abusable agents sought by young people for non-medical use. In particular, the literature highlights monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, and bupropion as the antidepressants most likely to be misused for their amphetamine-like euphoric effects or serotonin-induced dissociative effects.32 However, compared with other drug classes discussed in this article, the rate of antidepressant misuse is relatively low among college students.
Regardless of the antidepressant selected, clinicians should be concerned about alcohol use among college-age patients. Persons with depression are at increased risk of alcoholism compared with the general population.33 This combination can increase depressive symptoms and sedation, and decrease coordination, judgment, and reaction time.33
Excessive alcohol use can increase the risk of seizures in patients taking antidepressants such as buproprion.34 Employ caution when prescribing bupropion to patients who have a predisposing clinical factor that increases seizure risk, such as excessive alcohol use and abrupt cessation, use of other medications that may lower seizure threshold (eg, theophylline, amphetamines, phenothiazines), and a history of head trauma.34
To minimize the risk of seizures with bupropion, titrate up the dosage slowly. Furthermore, using a low dosage during dual therapy for antidepressant augmentation further decreases the risk of seizure.35 For these reasons, we recommend that you avoid bupropion in patients who are at risk of binge drinking, and give careful consideration to providing alternative therapies for them.
Prescribers and patients should also keep in mind that hypertensive crisis could occur if MAOIs are combined with certain types of alcoholic beverages containing tyramine, including some wines and draft beer.33
How you can identify and prevent misuse
Careful communication between health care provider and patient that is necessary to minimize the risk of adverse drug events with psychotropic medications often is lacking. For example, 24% of study college-age participants did not remember if their physician provided a diagnosis and 28.8% could not recall being informed about side effects and, perhaps as a result, many students did not take their medications as prescribed.9
Further, prescribers should ask college-age patients who are undergoing stimulant treatment if they believe that they are being adequately treated. They should inquire about how they are taking their medications.11 These questions can lead to discussion of the need for these medications and reevaluation of their perceived indication.11
Remind patients to take their medication only as directed.36 Highlight the need to:
• store medications in a discreet location
• properly dispose of unused medications
• keep tabs on the quantity of pills
• know how to resist requests for diversion from peers.
The Substance Abuse and Mental Health Services Administration offers additional useful strategies,37 and pharmacists also can be partners in substance use education and prevention.38 These are examples of how health care providers can take an active role in providing patients with a thorough and detailed understanding of (1) their conditions and (2) their prescribed medications to improve efficacy and safety while preventing misuse.8
A study found that the most common method of obtaining these medications without a prescription is acquiring them from peers; 54% of undergraduate patients with stimulant prescriptions have been approached by peers to give, trade, or sell their drugs.25 Other methods include purchasing medications online or faking prescriptions.39 Health care providers should remind patients of the legal ramifications of sharing or selling their prescribed medications. Finally, providers must be vigilant for students who may feign symptoms to obtain a prescription:
• be wary if symptom presentation sounds too “textbook”
• seek collateral history from family. Adults with ADHD should have shown symptoms during childhood
• use external verification such as neuropsychological testing for ADHD. A neuropsychologist can detect deception by analyzing the pattern of responses to questions.
Patient assessment is a key step to in preventing abuse of psychotropic medications. Gentle inquiry about school-related stress and other risk factors for misuse can help practitioners determine if students are at risk of diversion and if additional screening is necessary.
In response to these issues, Stone and Merlo8 have suggested that, in addition to the educational programs held on college campuses on alcohol, illicit drugs, and prescription painkillers, patients should be better informed on the appropriate use of prescription psychiatric medications, instructed to avoid sharing with family and friends, and assessed for abuse risk at regular intervals.
To further protect patients from adverse outcomes during treatment, you can employ conservative and safe prescribing techniques. One strategy might be to keep a personal formulary that lists key medications you use in everyday practice, including knowledge about each drug’s dosage, potential adverse effects, key warnings, and drug−drug interactions.40
Furthermore, maintain healthy caution about newly approved medications and carefully consider how they measure up to existing agents—in other words, practice evidence-based medicine, particularly when students request a particular agent.40,41 Prescribers should evaluate the risk of abuse before prescribing and attempt to prevent misuse by limiting quantities and minimizing polypharmacy.
Last, pharmacists can be key allies for consultation and appropriate medication selection.
Bottom Line
Psychotropic medications are necessary to treat the variety of conditions—anxiety, attention-deficit/hyperactivity disorder, depression, and panic disorder—common among college students. However, students are at risk of combining their prescribed medications with other medications, drugs, and alcohol or could sell or share their medication with peers. Proper counseling and identification of risk factors can be important tools for preventing such events.
Related Resources
• American College Health Association-National College Health Assessment. www.acha-ncha.org.
• Schwartz VI. College mental health: How to provide care for students in need. Current Psychiatry. 2011;10(12):22-29.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Methadone • Methadose, Dolophine
Theophylline • Theo-24, Theolair, Uniphyl
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Many college students suffer from mental illness (Table 1),1 which can have a negative impact on academic performance. Although psychotropic medications are an important part of treatment for many college students, the potential for misuse always is present. Drug misuse occurs when patients use medications for reasons inconsistent with legal or medical guidelines.2 For example, patients may take a medication that has not been prescribed for them or in a manner that is inconsistent with the prescriber’s instructions, including administration with other substances.3
Misuse of psychotropic drugs is prevalent among college students. A study of 14,175 students from 26 campuses reported that 14.7% of students taking a psychotropic are doing so without a prescription, including stimulants (52.6%), anxiolytics (38.4%), and antidepressants (17.4%).4 Another study states that more than one-third of responders reported misuse of >1 class of medication.5
Psychotropic misuse is concerning because it increases the risk of adverse events. Nearly one-half of medication errors are associated with writing and dispensing the prescription, which means that prescribers can work to reduce these errors.6 However, nonadherence, prescription misuse, and failure to disclose use of over-the-counter drugs, illicit drugs, and herbal products makes preventing most adverse events difficult, if not impossible, for prescribers.7,8
Psychotropic drug misuse among college students is highly variable and unpredictable. Students misuse medications, including stimulants, benzodiazepines, and antidepressants, for a variety of reasons, such as study enhancement, experimentation, intoxication, self-medication, relaxation, and stress management.8 One survey reported that >70% of students taking a psychotropic medication took it with alcohol or another illicit drug.9
However, <20% of those using a psychotropic medication with alcohol or other illicit drugs told their health care provider(s),9 making it impossible for clinicians to predict a patient’s risk of drug− drug interactions and subsequent adverse events. Additionally, additive effects could occur10 and changes in a patient’s presentation could be caused by a reaction to a combination of medications, rather than a new symptom of mental illness.
This article will examine common issues associated with drug misuse among college-age students and review prevention strategies (Table 2).
Stimulants
Stimulants have the highest rate of diversion; 61.7% of college students prescribed stimulants have shared or sold their medication.11 A survey of 115 students from 2 universities reported that the most common reason for stimulant misuse was to enhance academic performance.12 The same survey showed that some students take stimulants with Cannabis (17%) and alcohol (30%).12 As a result, in addition to lowering grade point average (GPA) and other academic difficulties,13 students misusing stimulants are at risk of drug interactions.14
It is critical to ascertain the route of drug administration, because non-oral routes, including crushing then snorting or injecting, are associated with additional health concerns, such as accidental death or blood-borne illnesses.15,16 Cardiac adverse effects of stimulants include hypertension, vasospasm, tachycardia, and dysrhythmia; psychiatric and other effects include serotonin syndrome, hallucinations, anxiety, paranoia, seizures, tics, hyperthermia, and tremor.17 Health care providers prescribing or caring for people taking a stimulant should monitor for these potential effects.
The risk of switch to mania might not be apparent to those who prescribe stimulants or to young people who take non-prescribed stimulants for academic enhancement or to achieve medication-induced euphoria. Adolescent stimulant use is associated with symptoms of early-onset bipolar disorder in patients who have attention-deficit/ hyperactivity disorder (ADHD) and undiagnosed bipolarity.18
The cardiovascular risk associated with stimulant use is debatable. Although several studies have been conducted,19-21 methodological factors limit their applicability. To minimize potential risks, several precautions should be taken before prescribing a stimulant to treat ADHD.
First, obtain a detailed personal and family medical history, asking about possible cardiovascular disease. Second, carefully scrutinize the patient’s cardiovascular system during the physical exam. Third, consider additional testing, such as an electrocardiogram, if the patient’s history or physical exam indicates possible risk.22
As a prescriber, you should be aware of the prevalence of stimulant use among students with and without ADHD, including those who could be feigning ADHD symptoms.15 Diversion could occur through sharing medications or selling them to friends and family.11 It also is possible that these medications may be used with other illicit substances, such as Cannabis, ecstasy, cocaine, and opiates.23 Students also could misuse stimulants by taking more than the prescribed dosage.24
Risk factors for misuse of stimulants include: heavy alcohol use, previous illicit drug use, white race, fraternity or sorority membership, low GPA, increased hyperactivity symptoms, and attendance at a competitive college or university.25-27
Benzodiazepines
Misuse of benzodiazepine is a significant component of prescription drug abuse and often occurs with other medications and alcohol.28 Additional methods of misuse include increased dosage and non-oral routes of administration.29
A 2001 national survey reported that 7.8% of college students have misused benzodiazepines.23 Common characteristics of benzodiazepine abusers include young age, male sex, personality characteristics of impulsivity and hopelessness, and abuse of other drugs, including cocaine and methadone.28,29
Benzodiazepines are prescribed for their anxiolytic and hypnotic properties and students could use these drugs with other agents to augment the euphoric effects or diminish withdrawal symptoms.30 Patients taking benzodiazepines for anxiety might self-medicate with alcohol, which increases sedation and depression, and can contribute to the risk for respiratory depression.10 Misuse of benzodiazepines can result in cognitive and psychomotor impairment and increase the risk of accidents and overdose.29,31
Although overdose with monotherapy is rare, the risk increases when a benzodiazepine is used with alcohol10 or another respiratory depressants, such as opioids, because combination use can produce additive effects.28 You should therefore avoid prescribing benzodiazepines to patients who have a history of significant substance abuse and consider using alternative, non-addictive agents, such as selective serotonin reuptake inhibitors, or non-pharmaceutical treatment when such patients present with an anxiety disorder. The risk of adverse effects of benzodiazepines can be reduced by limiting the dosing and the duration of the treatment, and by using longer-acting rather than the more addictive, shorter-acting, agents.
Antidepressants
Health care providers should be aware that, despite the relative absence of physically addictive properties, antidepressants from most classes are abusable agents sought by young people for non-medical use. In particular, the literature highlights monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, and bupropion as the antidepressants most likely to be misused for their amphetamine-like euphoric effects or serotonin-induced dissociative effects.32 However, compared with other drug classes discussed in this article, the rate of antidepressant misuse is relatively low among college students.
Regardless of the antidepressant selected, clinicians should be concerned about alcohol use among college-age patients. Persons with depression are at increased risk of alcoholism compared with the general population.33 This combination can increase depressive symptoms and sedation, and decrease coordination, judgment, and reaction time.33
Excessive alcohol use can increase the risk of seizures in patients taking antidepressants such as buproprion.34 Employ caution when prescribing bupropion to patients who have a predisposing clinical factor that increases seizure risk, such as excessive alcohol use and abrupt cessation, use of other medications that may lower seizure threshold (eg, theophylline, amphetamines, phenothiazines), and a history of head trauma.34
To minimize the risk of seizures with bupropion, titrate up the dosage slowly. Furthermore, using a low dosage during dual therapy for antidepressant augmentation further decreases the risk of seizure.35 For these reasons, we recommend that you avoid bupropion in patients who are at risk of binge drinking, and give careful consideration to providing alternative therapies for them.
Prescribers and patients should also keep in mind that hypertensive crisis could occur if MAOIs are combined with certain types of alcoholic beverages containing tyramine, including some wines and draft beer.33
How you can identify and prevent misuse
Careful communication between health care provider and patient that is necessary to minimize the risk of adverse drug events with psychotropic medications often is lacking. For example, 24% of study college-age participants did not remember if their physician provided a diagnosis and 28.8% could not recall being informed about side effects and, perhaps as a result, many students did not take their medications as prescribed.9
Further, prescribers should ask college-age patients who are undergoing stimulant treatment if they believe that they are being adequately treated. They should inquire about how they are taking their medications.11 These questions can lead to discussion of the need for these medications and reevaluation of their perceived indication.11
Remind patients to take their medication only as directed.36 Highlight the need to:
• store medications in a discreet location
• properly dispose of unused medications
• keep tabs on the quantity of pills
• know how to resist requests for diversion from peers.
The Substance Abuse and Mental Health Services Administration offers additional useful strategies,37 and pharmacists also can be partners in substance use education and prevention.38 These are examples of how health care providers can take an active role in providing patients with a thorough and detailed understanding of (1) their conditions and (2) their prescribed medications to improve efficacy and safety while preventing misuse.8
A study found that the most common method of obtaining these medications without a prescription is acquiring them from peers; 54% of undergraduate patients with stimulant prescriptions have been approached by peers to give, trade, or sell their drugs.25 Other methods include purchasing medications online or faking prescriptions.39 Health care providers should remind patients of the legal ramifications of sharing or selling their prescribed medications. Finally, providers must be vigilant for students who may feign symptoms to obtain a prescription:
• be wary if symptom presentation sounds too “textbook”
• seek collateral history from family. Adults with ADHD should have shown symptoms during childhood
• use external verification such as neuropsychological testing for ADHD. A neuropsychologist can detect deception by analyzing the pattern of responses to questions.
Patient assessment is a key step to in preventing abuse of psychotropic medications. Gentle inquiry about school-related stress and other risk factors for misuse can help practitioners determine if students are at risk of diversion and if additional screening is necessary.
In response to these issues, Stone and Merlo8 have suggested that, in addition to the educational programs held on college campuses on alcohol, illicit drugs, and prescription painkillers, patients should be better informed on the appropriate use of prescription psychiatric medications, instructed to avoid sharing with family and friends, and assessed for abuse risk at regular intervals.
To further protect patients from adverse outcomes during treatment, you can employ conservative and safe prescribing techniques. One strategy might be to keep a personal formulary that lists key medications you use in everyday practice, including knowledge about each drug’s dosage, potential adverse effects, key warnings, and drug−drug interactions.40
Furthermore, maintain healthy caution about newly approved medications and carefully consider how they measure up to existing agents—in other words, practice evidence-based medicine, particularly when students request a particular agent.40,41 Prescribers should evaluate the risk of abuse before prescribing and attempt to prevent misuse by limiting quantities and minimizing polypharmacy.
Last, pharmacists can be key allies for consultation and appropriate medication selection.
Bottom Line
Psychotropic medications are necessary to treat the variety of conditions—anxiety, attention-deficit/hyperactivity disorder, depression, and panic disorder—common among college students. However, students are at risk of combining their prescribed medications with other medications, drugs, and alcohol or could sell or share their medication with peers. Proper counseling and identification of risk factors can be important tools for preventing such events.
Related Resources
• American College Health Association-National College Health Assessment. www.acha-ncha.org.
• Schwartz VI. College mental health: How to provide care for students in need. Current Psychiatry. 2011;10(12):22-29.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Methadone • Methadose, Dolophine
Theophylline • Theo-24, Theolair, Uniphyl
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. http://www.acha-ncha.org/docs/ACHA-NCHA-II_ReferenceGroup_ExecutiveSummary_ Spring2014.pdf. Published 2014. Accessed January 13, 2015.
2. World Health Organization. Management of substance abuse. http://www.who.int/substance_abuse/terminology/ abuse/en. Accessed June 4, 2015.
3. U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. http://www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm. Published July 28, 2010. Accessed June 18, 2014.
4. Eisenberg D, Hunt J, Speer N, et al. Mental health service utilization among college students in the United States. J Nerv Ment Dis. 2011;199(5):301-308.
5. Peralta RL, Steele JL. Nonmedical prescription drug use among US college students at a Midwest university: a partial test of social learning theory. Subst Use Misuse. 2010;45(6):865-887.
6. Agency for Healthcare Research and Quality. Reducing and preventing adverse drug events to decrease hospital costs: Research in action. http://www.ahrq.gov/research/ findings/factsheets/errors-safety/aderia/index.html. Updated March 2001. Accessed June 21, 2014.
7. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2010;24(7):595-609.
8. Stone AM, Merlo LJ. Attitudes of college students toward mental illness stigma and the misuse of psychiatric medications. J Clin Psychiatry. 2011;72(2):134-139.
9. Oberleitner LM, Tzilos GK, Zumberg KM, et al. Psychotropic drug use among college students: patterns of use, misuse, and medical monitoring. J Am Coll Health. 2011;59(7):658-661.
10. Linnoila MI. Benzodiazepines and alcohol. J Psychiatr Res. 1990;24(suppl 2):121-127.
11. Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71(3):262-269.
12. Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144-153.
13. Arria AM. Nonmedical use of prescription stimulants and analgesics: associations with social and academic behaviors among college students. J Drug Issues. 2008; 38(4):1045-1060.
14. Arria AM, Caldeira KM, O’Grady KE, et al. Nonmedical use of prescription stimulants among college students: associations with attention-deficit-hyperactivity disorder and polydrug use. Pharmacotherapy. 2008;28(2):156-169.
15. Rabiner DL. Stimulant prescription cautions: addressing misuse, diversion and malingering. Curr Psychiatry Rep. 2013;15(7):375.
16. Sepúlveda DR, Thomas LM, McCabe SE, et al. Misuse of prescribed stimulant medication for ADHD and associated patterns of substance use: preliminary analysis among college students. J Pharm Pract. 2011;24(6):551-560.
17. Greydanus DE. Stimulant misuse: strategies to manage a growing problem. http://www.acha.org/Continuing_ Education/docs/ACHA_Use_Misuse_of_Stimulants_ Article2.pdf. Accessed June 29, 2015.
18. Vergne D, Whitham E, Barroilhet S, et al. Adult ADHD and amphetamines: a new paradigm. Neuropsychiatry. 2011;1(6):591-598.
19. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306(24):2673-2683.
20. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365(20):1896-1904.
21. Schelleman H, Bilker WB, Kimmel SE, et al. Methylphenidate and risk of serious cardiovascular events in adults. Am J Psychiatry. 2012;169(2):178-185.
22. U.S. Food and Drug Administration. Communication about an ongoing safety review of stimulant medications used in children with attention-deficit/hyperactivity disorder (ADHD). http://www.fda.gov/Drugs/Drug Safety/PostmarketDrugSafetyInformationforPatients andProviders/DrugSafetyInformationforHeathcare Professionals/ucm165858.htm. Updated August 15, 2013. Accessed June 25, 2014.
23. McCabe SE, Knight JR, Teter CJ, et al. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96-106.
24. McNiel AD, Muzzin KB, DeWald JP, et al. The nonmedical use of prescription stimulants among dental and dental hygiene students. J Dent Educ. 2011;75(3):365-376.
25. McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. J Psychoactive Drugs. 2006;38(1):43-56.
26. Arria AM, Garnier-Dykstra LM, Caldeira KM, et al. Persistent nonmedical use of prescription stimulants among college students: possible association with ADHD symptoms. J Atten Disord. 2011;15(5):347-356.
27. Teter CJ, McCabe SE, Boyd CJ, et al. Illicit methylphenidate use in an undergraduate student sample: prevalence and risk factors. Pharmacotherapy. 2003;23(5):609-617.
28. Hernandez SH, Nelson LS. Prescription drug abuse: insight into the epidemic. Clin Pharmacol Ther. 2010; 88(3):307-317.
29. McLarnon ME, Monaghan TL, Stewart SH, et al. Drug misuse and diversion in adults prescribed anxiolytics and sedatives. Pharmacotherapy. 2011;31(3):262-272.
30. Woods JH, Katz JL, Winger G. Benzodiazepines: use, abuse, and consequences. Pharmacol Rev. 1992;44(2):151-347.
31. Buffett-Jerrott SE, Stewart SH. Cognitive and sedative effects of benzodiazepine use. Curr Pharm Des. 2002;8(1):45-58.
32. Evans EA, Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil. 2014;5:107-120.
33. Hall-Flavin DK. Why is it bad to mix antidepressants and alcohol? http://www.mayoclinic.com/health/antidepressants-and-alcohol/AN01653. Updated June 12, 2014. Accessed June 20, 2014.
34. Wellbutrin [package insert]. Research Triangle Park, NC: GlaxoSmithKline LLC; 2014.
35. Davidson J. Seizures and bupropion: a review. J Clin Psychiatry. 1989;50(7):256-261.
36. Maddox JC, Levi M, Thompson C. The compliance with antidepressants in general practice. J Psychopharmacol. 1994;8(1):48-52.
37. Substance Abuse and Mental Health Services Administration. You’re in control: using prescription medication responsibly. http://store.samhsa.gov/shin/content/SMA12-4678B3/SMA12-4678B3.pdf. Accessed June 5, 2015.
38. ASHP statement on the pharmacist’s role in substance abuse prevention, education, and assistance. Am J Health Syst Pharm. 2014;71(3):243-246.
39. Inciardi JA, Surratt HL, Cicero TJ, et al. Prescription drugs purchased through the internet: who are the end users? Drug Alcohol Depend. 2010;110(1-2):21-29.
40. Preskorn SH, Flockhart D. 2006 Guide to psychiatric drug interactions. Primary Psychiatry. 2006;13(4):35-64.
41. Schiff GD, Galanter WL, Duhig J, et al. Principles of conservative prescribing. Arch Intern Med. 2011;171(16): 1433-1440.
1. American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. http://www.acha-ncha.org/docs/ACHA-NCHA-II_ReferenceGroup_ExecutiveSummary_ Spring2014.pdf. Published 2014. Accessed January 13, 2015.
2. World Health Organization. Management of substance abuse. http://www.who.int/substance_abuse/terminology/ abuse/en. Accessed June 4, 2015.
3. U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. http://www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm. Published July 28, 2010. Accessed June 18, 2014.
4. Eisenberg D, Hunt J, Speer N, et al. Mental health service utilization among college students in the United States. J Nerv Ment Dis. 2011;199(5):301-308.
5. Peralta RL, Steele JL. Nonmedical prescription drug use among US college students at a Midwest university: a partial test of social learning theory. Subst Use Misuse. 2010;45(6):865-887.
6. Agency for Healthcare Research and Quality. Reducing and preventing adverse drug events to decrease hospital costs: Research in action. http://www.ahrq.gov/research/ findings/factsheets/errors-safety/aderia/index.html. Updated March 2001. Accessed June 21, 2014.
7. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2010;24(7):595-609.
8. Stone AM, Merlo LJ. Attitudes of college students toward mental illness stigma and the misuse of psychiatric medications. J Clin Psychiatry. 2011;72(2):134-139.
9. Oberleitner LM, Tzilos GK, Zumberg KM, et al. Psychotropic drug use among college students: patterns of use, misuse, and medical monitoring. J Am Coll Health. 2011;59(7):658-661.
10. Linnoila MI. Benzodiazepines and alcohol. J Psychiatr Res. 1990;24(suppl 2):121-127.
11. Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71(3):262-269.
12. Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144-153.
13. Arria AM. Nonmedical use of prescription stimulants and analgesics: associations with social and academic behaviors among college students. J Drug Issues. 2008; 38(4):1045-1060.
14. Arria AM, Caldeira KM, O’Grady KE, et al. Nonmedical use of prescription stimulants among college students: associations with attention-deficit-hyperactivity disorder and polydrug use. Pharmacotherapy. 2008;28(2):156-169.
15. Rabiner DL. Stimulant prescription cautions: addressing misuse, diversion and malingering. Curr Psychiatry Rep. 2013;15(7):375.
16. Sepúlveda DR, Thomas LM, McCabe SE, et al. Misuse of prescribed stimulant medication for ADHD and associated patterns of substance use: preliminary analysis among college students. J Pharm Pract. 2011;24(6):551-560.
17. Greydanus DE. Stimulant misuse: strategies to manage a growing problem. http://www.acha.org/Continuing_ Education/docs/ACHA_Use_Misuse_of_Stimulants_ Article2.pdf. Accessed June 29, 2015.
18. Vergne D, Whitham E, Barroilhet S, et al. Adult ADHD and amphetamines: a new paradigm. Neuropsychiatry. 2011;1(6):591-598.
19. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306(24):2673-2683.
20. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365(20):1896-1904.
21. Schelleman H, Bilker WB, Kimmel SE, et al. Methylphenidate and risk of serious cardiovascular events in adults. Am J Psychiatry. 2012;169(2):178-185.
22. U.S. Food and Drug Administration. Communication about an ongoing safety review of stimulant medications used in children with attention-deficit/hyperactivity disorder (ADHD). http://www.fda.gov/Drugs/Drug Safety/PostmarketDrugSafetyInformationforPatients andProviders/DrugSafetyInformationforHeathcare Professionals/ucm165858.htm. Updated August 15, 2013. Accessed June 25, 2014.
23. McCabe SE, Knight JR, Teter CJ, et al. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96-106.
24. McNiel AD, Muzzin KB, DeWald JP, et al. The nonmedical use of prescription stimulants among dental and dental hygiene students. J Dent Educ. 2011;75(3):365-376.
25. McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. J Psychoactive Drugs. 2006;38(1):43-56.
26. Arria AM, Garnier-Dykstra LM, Caldeira KM, et al. Persistent nonmedical use of prescription stimulants among college students: possible association with ADHD symptoms. J Atten Disord. 2011;15(5):347-356.
27. Teter CJ, McCabe SE, Boyd CJ, et al. Illicit methylphenidate use in an undergraduate student sample: prevalence and risk factors. Pharmacotherapy. 2003;23(5):609-617.
28. Hernandez SH, Nelson LS. Prescription drug abuse: insight into the epidemic. Clin Pharmacol Ther. 2010; 88(3):307-317.
29. McLarnon ME, Monaghan TL, Stewart SH, et al. Drug misuse and diversion in adults prescribed anxiolytics and sedatives. Pharmacotherapy. 2011;31(3):262-272.
30. Woods JH, Katz JL, Winger G. Benzodiazepines: use, abuse, and consequences. Pharmacol Rev. 1992;44(2):151-347.
31. Buffett-Jerrott SE, Stewart SH. Cognitive and sedative effects of benzodiazepine use. Curr Pharm Des. 2002;8(1):45-58.
32. Evans EA, Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil. 2014;5:107-120.
33. Hall-Flavin DK. Why is it bad to mix antidepressants and alcohol? http://www.mayoclinic.com/health/antidepressants-and-alcohol/AN01653. Updated June 12, 2014. Accessed June 20, 2014.
34. Wellbutrin [package insert]. Research Triangle Park, NC: GlaxoSmithKline LLC; 2014.
35. Davidson J. Seizures and bupropion: a review. J Clin Psychiatry. 1989;50(7):256-261.
36. Maddox JC, Levi M, Thompson C. The compliance with antidepressants in general practice. J Psychopharmacol. 1994;8(1):48-52.
37. Substance Abuse and Mental Health Services Administration. You’re in control: using prescription medication responsibly. http://store.samhsa.gov/shin/content/SMA12-4678B3/SMA12-4678B3.pdf. Accessed June 5, 2015.
38. ASHP statement on the pharmacist’s role in substance abuse prevention, education, and assistance. Am J Health Syst Pharm. 2014;71(3):243-246.
39. Inciardi JA, Surratt HL, Cicero TJ, et al. Prescription drugs purchased through the internet: who are the end users? Drug Alcohol Depend. 2010;110(1-2):21-29.
40. Preskorn SH, Flockhart D. 2006 Guide to psychiatric drug interactions. Primary Psychiatry. 2006;13(4):35-64.
41. Schiff GD, Galanter WL, Duhig J, et al. Principles of conservative prescribing. Arch Intern Med. 2011;171(16): 1433-1440.
What do >700 letters to a mass murderer tell us about the people who wrote them?
Little is known about people who write to criminals incarcerated for a violent crime. However, existence of Web sites such as WriteAPrisoner.com, Meet-An-Inmate.com, and PrisonPenPals.com suggests some appetite among the public for corresponding with the incarcerated. Writers of letters might be drawn to the “bad boy” image of prisoners. Furthermore, much has been written of the willingness of some battered women to remain in an abusive domestic relationship, leading them to correspond with their abusers even after those abusers are incarcerated.1,2
To our knowledge, no examination of letters written to a mass murderer has been published. Therefore, we categorized and analyzed 784 letters sent to a high-profile male mass murderer whose crime was committed during the past decade. Here is a description of the study and what we found, as well as discussion of how our findings might offer utility in a psychiatric practice.
Goals of the study
We hypothesized that a large percentage of those letters could be classified as “Romantic,” given the lay perception that it is women who write to mass murderers. We also sought to evaluate follow-up letters sent by these writers to test the assumption that their individual goals would be constant over time.
We performed this study in the hope that the research could assist psychiatric practitioners in treating patients who seek to associate with a violent person (see “Treatment considerations,”). We thought it might be helpful for practitioners to get a better understanding of the nature of people who write to a violent offender or express a desire to do so.
Methods of study
Two authors (R.S.J. and D.P.G.) evaluated 819 letters that had been written by non-incarcerated, non-family adults to 1 mass murderer. The initial letter and follow-up letters written by each unique writer (n = 333) were categorized as follows:
• state or country from which the letter was sent
• age
• sex
• number of letters sent by each writer
• whether a photograph was enclosed
• whether additional items were enclosed (eg, gifts, drawings)
• whether the letter was rejected by prison authorities
• the writer’s purpose.
The study was approved by the institutional review board of Baylor College of Medicine.
Letters were assigned to 1 of 5 categories:
Acquaintance letters sought ongoing correspondence relationship with the murderer. They focused largely on conveying information about the writer.
Show of support letters also sought an ongoing correspondence relationship with the murderer, but instead focused on him, not the writer.
Romance letters used words that conveyed romantic or non-platonic affection.
Spiritual letters gave advice to the murderer with a religious tone.
Words of wisdom letters offered advice but lacked a religious tone.
Given the nonstandardized nature of categorization and the lack of a formal questionnaire, we were unable to perform an exploratory factor analysis on our categorizations. Inter-rater reliability of letter categorization was 0.79.
Results: Writer profiles, purpose for writing
In all, we reviewed 819 letters:
• Thirty-five letters were excluded because they were written by family members, children, or other prisoners
• Of the remaining 784 letters, there were 333 unique writers
• Two-hundred sixty letters were written by women, 61 by men; 2 were co-written by both sexes; sex could not be determined for 10.
Women were more likely than men to write a letter (P = .014) and to write ≥3 letters (P = .001). The age of the writer was determined for 117 (35.1%) letters; mean age was 27.8 (± 8.9) years (range, 18 to 59 years).
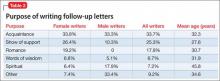
The purpose of the letters differed by sex (P < .001) but not by the writer’s age (P = .058). Women were more likely than men to write letters categorized as “Acquaintance,” “Romance,” and “Show of support”; in contrast, men were more likely than women to write a letter categorized as “Spiritual” (Table 1). Approximately 95% of letters were handwritten. Letters averaged 3 pages (range, 1 to 16 pages).
Two-hundred sixteen writers wrote a single letter; 53 wrote 2 letters; 18 wrote 3 letters; 11 wrote 4 letters; 30 wrote 5 to 10 letters; and 9 wrote 11 to 43 letters. The purpose of follow-up letters was associated with the age of the writer (P < .001) and with the writer’s sex (P < .001). Women were more likely to write “Show of support” and “Romance” follow-up letters; men were more likely to write “Spiritual” follow-up letters (Table 2).
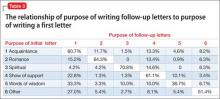
Results suggested that the purpose of the initial letter was a reasonable predictor of the purpose of follow-up letters (P < .001) (Table 3). The murderer never responded to any letters. Letters were most often written from his state of incarceration; next, from contiguous states; then, from non-contiguous states; and, last, from international locations (P < .001).
Of the initial letters from writers who wrote ≥10, 60% were categorized as “Acquaintance” and 20% as “Romance.” The writer who wrote the most letters (43) moved during the course of her letter-writing to live in the same state as the murderer; she stated in her letters that she did so to be closer to him and to be able to attend his court hearings. Four other writers, each of whom wrote >5 letters, stated that they had traveled to the murderer’s state of incarceration to attend some of his hearings in person.
Composite examples of more common categories of letters
Names and other pertinent identifying information have been changed.
Acquaintance. Hi, Steve. I’ve been following your case and just wanted to write you so that maybe we could be friends or keep in touch since you’re probably pretty bored. I’m a 27-year-old college student studying marketing and working at Applebee’s as a waitress (for now) until I can land my dream job. I’ve enclosed a picture of me and my dachshund along with a photo of my favorite beach in the world. Write me back if you want. Jenny.
Show of support. Steve: I’ve been really worried about you since first seeing you on TV. You look different lately and I hope they’re treating you OK and feeding you decent food. In case they’re not, I’ve enclosed a little something to buy yourself a treat. Just know that there are many of us that care about you and are really pulling for you to be strong in this tough situation you’re in. Yours truly, Karen.
Romance. Dearest Steven: My mind has been filled with thoughts of you and of us since I last saw you in my dreams! Be strong, because you are going to beat this once they understand that you are not responsible for what happened! Don’t you see, sweetie, the system failed you, and now you’re caught up in something that you will soon overcome. When I think of the day that you get released, and how we’ll be able to settle down somewhere together, it gets me incredibly excited. You and I are meant to be together, because I understand you and can help you get better. I love you, Steven! Please write me back so that I know we’re on the same page about our plans for the future. Love, ♥ Your sweetie, Rachel.
Spiritual. Dear Child of God: The Lord has a plan for you. I know that things right now might be confusing, and you’re in a black place, but He is there right beside you. If you need some reading materials to give you comfort, just let me know and I can get a Bible to you along with some other books to give you solace and strengthen your walk with Him. God forgives you and he loves you so much! Much love in Christ, Mary.
Discussion
Given that the mass murderer in this study was a young man, it is not surprising that 78% of writers of initial letters were women. However, it is interesting that, among women’s initial letters, 44% were “Acquaintance” letters and only 15% were categorized as “Romance.”
Given the severity of the murderer’s crime, it is remarkable that he received only 1 “Hate mail” letter.
Initial “Spiritual” letters were more likely to be followed by letters of the same category than any other category; “Romance” letters were a close second. This demonstrates the consistent efforts of writers in these 2 categories. Highly persistent writers (≥10 letters) were most likely to fall into “Acquaintance” and “Romance” categories. The persistence of these writers is remarkable, in view of the fact that none of their letters were answered. We hypothesize that the killer did not reply because he had no interest in correspondence.
Similarities to stalking. Given that 9 writers wrote >10 letters each and 2 wrote >20 each, elements of their behavior are not unlike what is seen in stalkers.3 Consistent with the stalking literature and Mullen et al4 stalker typology, many writers in this study appeared to seek intimacy with the perpetrator through “Romance” or “Show of support” letters, and might be akin to Mullen’s so-called intimacy-seeking stalker. Such stalkers’ behavior arises out of loneliness, with a strong desire for a relationship with the target; a significant percentage of such stalkers suffer a delusional disorder.
Mullen’s so-called incompetent suitor stalker is similar to the intimacy-seeking type but, instead, has an interest in a short-term relationship and is far less persistent in his (her) stalking behavior4; this type might apply to the writers in this study who wrote >1 but <10 letters.
Two additional observations also are notable when trying to characterize people who write letters: (1) A high percentage of people who stalk a celebrity suffer a psychotic disorder5,6; (2) 4 letter-writers traveled, and 1 relocated, to the murderer’s state of incarceration to attend his hearings and be closer to him.
This study has limitations:
• categorization of letters is inherently subjective and the categories themselves were created by the researchers
• the nature and categorization of such letters might vary considerably with the age and sex of the violent criminal; our findings in this case are not generalizable.
Last, researchers who plan to study writers of letters to incarcerated criminals should consider sending a personality test and other questionnaires to those writers to understand this population better.
Treatment considerations
Psychiatrists treating patients who seek a romantic attachment with a violent person should consider psychotherapy as a means of treating possible character pathology. The desire for romance with a violent criminal was greater among repeat writers (20%) than in initial letters (15%), suggesting that people who have a strong inclination to associate with a violent person might benefit from exploring romantic feelings in therapy. Specifically, therapists would be wise to explore with such patients the possibility that they experienced violence or verbal abuse in childhood or adulthood.
To the extent that evidence of prior abuse exists, a diagnosis of posttraumatic stress disorder (PTSD) might be appropriate; specialized therapy for men and women with a history of abuse might be indicated. It is important to provide validation for patients who are victims when they describe their abuse, and to stress that they did nothing to provoke the violence. Furthermore, investigation of why the patient feels drawn romantically toward a violent criminal is helpful, as well as an examination of how such behavior is self-defeating.
There might be value in having patients keep a journal in lieu of actually sending letters; there is evidence that “journaling” can reduce substance use recidivism.7 This work can be performed in conjunction with group or individual psychotherapy that addresses any history of abuse and subsequent PTSD.
Many patients are reluctant to discuss their romantic feelings toward a violent criminal until the psychiatrist has established a strong doctor−patient relationship. Last, clinicians should not hesitate to refer these patients to a therapist who specializes in domestic violence.
Related Resource
• Marazziti D, Falaschi V, Lombardi A, et al. Stalking: a neurobiological perspective. Riv Psichiatr. 2015;50(1):12-18.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Mouradian VE. Women’s stay-leave decisions in relationships involving intimate partner violence. Wellesley, MA: Wellesley Centers for Women Publications; 2004:3,4.
2. Bell KM, Naugle AE. Understanding stay/leave decisions in violent relationships: a behavior analytic approach. Behav Soc Issues. 2005;14(1):21-46.
3. Westrup D, Fremouw WJ. Stalking behavior: a literature review and suggested functional analytic assessment technology. Aggression and Violent Behavior. 1998;3: 255-274.
4. Mullen PE, Pathé M, Purcell R, et al. Study of stalkers. Am J Psychiatry. 1999;156(8):1244-1249.
5. West SG, Friedman SH. These boots are made for stalking: characteristics of female stalkers. Psychiatry (Edgmont). 2008;5(8):37-42.
6. Nadkarni R, Grubin D. Stalking: why do people do it? BMJ. 2000;320(7248):1486-1487.
7. Proctor SL, Hoffmann NG, Allison S. The effectiveness of interactive journaling in reducing recidivism among substance-dependent jail inmates. Int J Offender Ther Comp Criminol. 2012;56(2):317-332.
Little is known about people who write to criminals incarcerated for a violent crime. However, existence of Web sites such as WriteAPrisoner.com, Meet-An-Inmate.com, and PrisonPenPals.com suggests some appetite among the public for corresponding with the incarcerated. Writers of letters might be drawn to the “bad boy” image of prisoners. Furthermore, much has been written of the willingness of some battered women to remain in an abusive domestic relationship, leading them to correspond with their abusers even after those abusers are incarcerated.1,2
To our knowledge, no examination of letters written to a mass murderer has been published. Therefore, we categorized and analyzed 784 letters sent to a high-profile male mass murderer whose crime was committed during the past decade. Here is a description of the study and what we found, as well as discussion of how our findings might offer utility in a psychiatric practice.
Goals of the study
We hypothesized that a large percentage of those letters could be classified as “Romantic,” given the lay perception that it is women who write to mass murderers. We also sought to evaluate follow-up letters sent by these writers to test the assumption that their individual goals would be constant over time.
We performed this study in the hope that the research could assist psychiatric practitioners in treating patients who seek to associate with a violent person (see “Treatment considerations,”). We thought it might be helpful for practitioners to get a better understanding of the nature of people who write to a violent offender or express a desire to do so.
Methods of study
Two authors (R.S.J. and D.P.G.) evaluated 819 letters that had been written by non-incarcerated, non-family adults to 1 mass murderer. The initial letter and follow-up letters written by each unique writer (n = 333) were categorized as follows:
• state or country from which the letter was sent
• age
• sex
• number of letters sent by each writer
• whether a photograph was enclosed
• whether additional items were enclosed (eg, gifts, drawings)
• whether the letter was rejected by prison authorities
• the writer’s purpose.
The study was approved by the institutional review board of Baylor College of Medicine.
Letters were assigned to 1 of 5 categories:
Acquaintance letters sought ongoing correspondence relationship with the murderer. They focused largely on conveying information about the writer.
Show of support letters also sought an ongoing correspondence relationship with the murderer, but instead focused on him, not the writer.
Romance letters used words that conveyed romantic or non-platonic affection.
Spiritual letters gave advice to the murderer with a religious tone.
Words of wisdom letters offered advice but lacked a religious tone.
Given the nonstandardized nature of categorization and the lack of a formal questionnaire, we were unable to perform an exploratory factor analysis on our categorizations. Inter-rater reliability of letter categorization was 0.79.
Results: Writer profiles, purpose for writing
In all, we reviewed 819 letters:
• Thirty-five letters were excluded because they were written by family members, children, or other prisoners
• Of the remaining 784 letters, there were 333 unique writers
• Two-hundred sixty letters were written by women, 61 by men; 2 were co-written by both sexes; sex could not be determined for 10.
Women were more likely than men to write a letter (P = .014) and to write ≥3 letters (P = .001). The age of the writer was determined for 117 (35.1%) letters; mean age was 27.8 (± 8.9) years (range, 18 to 59 years).
The purpose of the letters differed by sex (P < .001) but not by the writer’s age (P = .058). Women were more likely than men to write letters categorized as “Acquaintance,” “Romance,” and “Show of support”; in contrast, men were more likely than women to write a letter categorized as “Spiritual” (Table 1). Approximately 95% of letters were handwritten. Letters averaged 3 pages (range, 1 to 16 pages).
Two-hundred sixteen writers wrote a single letter; 53 wrote 2 letters; 18 wrote 3 letters; 11 wrote 4 letters; 30 wrote 5 to 10 letters; and 9 wrote 11 to 43 letters. The purpose of follow-up letters was associated with the age of the writer (P < .001) and with the writer’s sex (P < .001). Women were more likely to write “Show of support” and “Romance” follow-up letters; men were more likely to write “Spiritual” follow-up letters (Table 2).
Results suggested that the purpose of the initial letter was a reasonable predictor of the purpose of follow-up letters (P < .001) (Table 3). The murderer never responded to any letters. Letters were most often written from his state of incarceration; next, from contiguous states; then, from non-contiguous states; and, last, from international locations (P < .001).
Of the initial letters from writers who wrote ≥10, 60% were categorized as “Acquaintance” and 20% as “Romance.” The writer who wrote the most letters (43) moved during the course of her letter-writing to live in the same state as the murderer; she stated in her letters that she did so to be closer to him and to be able to attend his court hearings. Four other writers, each of whom wrote >5 letters, stated that they had traveled to the murderer’s state of incarceration to attend some of his hearings in person.
Composite examples of more common categories of letters
Names and other pertinent identifying information have been changed.
Acquaintance. Hi, Steve. I’ve been following your case and just wanted to write you so that maybe we could be friends or keep in touch since you’re probably pretty bored. I’m a 27-year-old college student studying marketing and working at Applebee’s as a waitress (for now) until I can land my dream job. I’ve enclosed a picture of me and my dachshund along with a photo of my favorite beach in the world. Write me back if you want. Jenny.
Show of support. Steve: I’ve been really worried about you since first seeing you on TV. You look different lately and I hope they’re treating you OK and feeding you decent food. In case they’re not, I’ve enclosed a little something to buy yourself a treat. Just know that there are many of us that care about you and are really pulling for you to be strong in this tough situation you’re in. Yours truly, Karen.
Romance. Dearest Steven: My mind has been filled with thoughts of you and of us since I last saw you in my dreams! Be strong, because you are going to beat this once they understand that you are not responsible for what happened! Don’t you see, sweetie, the system failed you, and now you’re caught up in something that you will soon overcome. When I think of the day that you get released, and how we’ll be able to settle down somewhere together, it gets me incredibly excited. You and I are meant to be together, because I understand you and can help you get better. I love you, Steven! Please write me back so that I know we’re on the same page about our plans for the future. Love, ♥ Your sweetie, Rachel.
Spiritual. Dear Child of God: The Lord has a plan for you. I know that things right now might be confusing, and you’re in a black place, but He is there right beside you. If you need some reading materials to give you comfort, just let me know and I can get a Bible to you along with some other books to give you solace and strengthen your walk with Him. God forgives you and he loves you so much! Much love in Christ, Mary.
Discussion
Given that the mass murderer in this study was a young man, it is not surprising that 78% of writers of initial letters were women. However, it is interesting that, among women’s initial letters, 44% were “Acquaintance” letters and only 15% were categorized as “Romance.”
Given the severity of the murderer’s crime, it is remarkable that he received only 1 “Hate mail” letter.
Initial “Spiritual” letters were more likely to be followed by letters of the same category than any other category; “Romance” letters were a close second. This demonstrates the consistent efforts of writers in these 2 categories. Highly persistent writers (≥10 letters) were most likely to fall into “Acquaintance” and “Romance” categories. The persistence of these writers is remarkable, in view of the fact that none of their letters were answered. We hypothesize that the killer did not reply because he had no interest in correspondence.
Similarities to stalking. Given that 9 writers wrote >10 letters each and 2 wrote >20 each, elements of their behavior are not unlike what is seen in stalkers.3 Consistent with the stalking literature and Mullen et al4 stalker typology, many writers in this study appeared to seek intimacy with the perpetrator through “Romance” or “Show of support” letters, and might be akin to Mullen’s so-called intimacy-seeking stalker. Such stalkers’ behavior arises out of loneliness, with a strong desire for a relationship with the target; a significant percentage of such stalkers suffer a delusional disorder.
Mullen’s so-called incompetent suitor stalker is similar to the intimacy-seeking type but, instead, has an interest in a short-term relationship and is far less persistent in his (her) stalking behavior4; this type might apply to the writers in this study who wrote >1 but <10 letters.
Two additional observations also are notable when trying to characterize people who write letters: (1) A high percentage of people who stalk a celebrity suffer a psychotic disorder5,6; (2) 4 letter-writers traveled, and 1 relocated, to the murderer’s state of incarceration to attend his hearings and be closer to him.
This study has limitations:
• categorization of letters is inherently subjective and the categories themselves were created by the researchers
• the nature and categorization of such letters might vary considerably with the age and sex of the violent criminal; our findings in this case are not generalizable.
Last, researchers who plan to study writers of letters to incarcerated criminals should consider sending a personality test and other questionnaires to those writers to understand this population better.
Treatment considerations
Psychiatrists treating patients who seek a romantic attachment with a violent person should consider psychotherapy as a means of treating possible character pathology. The desire for romance with a violent criminal was greater among repeat writers (20%) than in initial letters (15%), suggesting that people who have a strong inclination to associate with a violent person might benefit from exploring romantic feelings in therapy. Specifically, therapists would be wise to explore with such patients the possibility that they experienced violence or verbal abuse in childhood or adulthood.
To the extent that evidence of prior abuse exists, a diagnosis of posttraumatic stress disorder (PTSD) might be appropriate; specialized therapy for men and women with a history of abuse might be indicated. It is important to provide validation for patients who are victims when they describe their abuse, and to stress that they did nothing to provoke the violence. Furthermore, investigation of why the patient feels drawn romantically toward a violent criminal is helpful, as well as an examination of how such behavior is self-defeating.
There might be value in having patients keep a journal in lieu of actually sending letters; there is evidence that “journaling” can reduce substance use recidivism.7 This work can be performed in conjunction with group or individual psychotherapy that addresses any history of abuse and subsequent PTSD.
Many patients are reluctant to discuss their romantic feelings toward a violent criminal until the psychiatrist has established a strong doctor−patient relationship. Last, clinicians should not hesitate to refer these patients to a therapist who specializes in domestic violence.
Related Resource
• Marazziti D, Falaschi V, Lombardi A, et al. Stalking: a neurobiological perspective. Riv Psichiatr. 2015;50(1):12-18.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Little is known about people who write to criminals incarcerated for a violent crime. However, existence of Web sites such as WriteAPrisoner.com, Meet-An-Inmate.com, and PrisonPenPals.com suggests some appetite among the public for corresponding with the incarcerated. Writers of letters might be drawn to the “bad boy” image of prisoners. Furthermore, much has been written of the willingness of some battered women to remain in an abusive domestic relationship, leading them to correspond with their abusers even after those abusers are incarcerated.1,2
To our knowledge, no examination of letters written to a mass murderer has been published. Therefore, we categorized and analyzed 784 letters sent to a high-profile male mass murderer whose crime was committed during the past decade. Here is a description of the study and what we found, as well as discussion of how our findings might offer utility in a psychiatric practice.
Goals of the study
We hypothesized that a large percentage of those letters could be classified as “Romantic,” given the lay perception that it is women who write to mass murderers. We also sought to evaluate follow-up letters sent by these writers to test the assumption that their individual goals would be constant over time.
We performed this study in the hope that the research could assist psychiatric practitioners in treating patients who seek to associate with a violent person (see “Treatment considerations,”). We thought it might be helpful for practitioners to get a better understanding of the nature of people who write to a violent offender or express a desire to do so.
Methods of study
Two authors (R.S.J. and D.P.G.) evaluated 819 letters that had been written by non-incarcerated, non-family adults to 1 mass murderer. The initial letter and follow-up letters written by each unique writer (n = 333) were categorized as follows:
• state or country from which the letter was sent
• age
• sex
• number of letters sent by each writer
• whether a photograph was enclosed
• whether additional items were enclosed (eg, gifts, drawings)
• whether the letter was rejected by prison authorities
• the writer’s purpose.
The study was approved by the institutional review board of Baylor College of Medicine.
Letters were assigned to 1 of 5 categories:
Acquaintance letters sought ongoing correspondence relationship with the murderer. They focused largely on conveying information about the writer.
Show of support letters also sought an ongoing correspondence relationship with the murderer, but instead focused on him, not the writer.
Romance letters used words that conveyed romantic or non-platonic affection.
Spiritual letters gave advice to the murderer with a religious tone.
Words of wisdom letters offered advice but lacked a religious tone.
Given the nonstandardized nature of categorization and the lack of a formal questionnaire, we were unable to perform an exploratory factor analysis on our categorizations. Inter-rater reliability of letter categorization was 0.79.
Results: Writer profiles, purpose for writing
In all, we reviewed 819 letters:
• Thirty-five letters were excluded because they were written by family members, children, or other prisoners
• Of the remaining 784 letters, there were 333 unique writers
• Two-hundred sixty letters were written by women, 61 by men; 2 were co-written by both sexes; sex could not be determined for 10.
Women were more likely than men to write a letter (P = .014) and to write ≥3 letters (P = .001). The age of the writer was determined for 117 (35.1%) letters; mean age was 27.8 (± 8.9) years (range, 18 to 59 years).
The purpose of the letters differed by sex (P < .001) but not by the writer’s age (P = .058). Women were more likely than men to write letters categorized as “Acquaintance,” “Romance,” and “Show of support”; in contrast, men were more likely than women to write a letter categorized as “Spiritual” (Table 1). Approximately 95% of letters were handwritten. Letters averaged 3 pages (range, 1 to 16 pages).
Two-hundred sixteen writers wrote a single letter; 53 wrote 2 letters; 18 wrote 3 letters; 11 wrote 4 letters; 30 wrote 5 to 10 letters; and 9 wrote 11 to 43 letters. The purpose of follow-up letters was associated with the age of the writer (P < .001) and with the writer’s sex (P < .001). Women were more likely to write “Show of support” and “Romance” follow-up letters; men were more likely to write “Spiritual” follow-up letters (Table 2).
Results suggested that the purpose of the initial letter was a reasonable predictor of the purpose of follow-up letters (P < .001) (Table 3). The murderer never responded to any letters. Letters were most often written from his state of incarceration; next, from contiguous states; then, from non-contiguous states; and, last, from international locations (P < .001).
Of the initial letters from writers who wrote ≥10, 60% were categorized as “Acquaintance” and 20% as “Romance.” The writer who wrote the most letters (43) moved during the course of her letter-writing to live in the same state as the murderer; she stated in her letters that she did so to be closer to him and to be able to attend his court hearings. Four other writers, each of whom wrote >5 letters, stated that they had traveled to the murderer’s state of incarceration to attend some of his hearings in person.
Composite examples of more common categories of letters
Names and other pertinent identifying information have been changed.
Acquaintance. Hi, Steve. I’ve been following your case and just wanted to write you so that maybe we could be friends or keep in touch since you’re probably pretty bored. I’m a 27-year-old college student studying marketing and working at Applebee’s as a waitress (for now) until I can land my dream job. I’ve enclosed a picture of me and my dachshund along with a photo of my favorite beach in the world. Write me back if you want. Jenny.
Show of support. Steve: I’ve been really worried about you since first seeing you on TV. You look different lately and I hope they’re treating you OK and feeding you decent food. In case they’re not, I’ve enclosed a little something to buy yourself a treat. Just know that there are many of us that care about you and are really pulling for you to be strong in this tough situation you’re in. Yours truly, Karen.
Romance. Dearest Steven: My mind has been filled with thoughts of you and of us since I last saw you in my dreams! Be strong, because you are going to beat this once they understand that you are not responsible for what happened! Don’t you see, sweetie, the system failed you, and now you’re caught up in something that you will soon overcome. When I think of the day that you get released, and how we’ll be able to settle down somewhere together, it gets me incredibly excited. You and I are meant to be together, because I understand you and can help you get better. I love you, Steven! Please write me back so that I know we’re on the same page about our plans for the future. Love, ♥ Your sweetie, Rachel.
Spiritual. Dear Child of God: The Lord has a plan for you. I know that things right now might be confusing, and you’re in a black place, but He is there right beside you. If you need some reading materials to give you comfort, just let me know and I can get a Bible to you along with some other books to give you solace and strengthen your walk with Him. God forgives you and he loves you so much! Much love in Christ, Mary.
Discussion
Given that the mass murderer in this study was a young man, it is not surprising that 78% of writers of initial letters were women. However, it is interesting that, among women’s initial letters, 44% were “Acquaintance” letters and only 15% were categorized as “Romance.”
Given the severity of the murderer’s crime, it is remarkable that he received only 1 “Hate mail” letter.
Initial “Spiritual” letters were more likely to be followed by letters of the same category than any other category; “Romance” letters were a close second. This demonstrates the consistent efforts of writers in these 2 categories. Highly persistent writers (≥10 letters) were most likely to fall into “Acquaintance” and “Romance” categories. The persistence of these writers is remarkable, in view of the fact that none of their letters were answered. We hypothesize that the killer did not reply because he had no interest in correspondence.
Similarities to stalking. Given that 9 writers wrote >10 letters each and 2 wrote >20 each, elements of their behavior are not unlike what is seen in stalkers.3 Consistent with the stalking literature and Mullen et al4 stalker typology, many writers in this study appeared to seek intimacy with the perpetrator through “Romance” or “Show of support” letters, and might be akin to Mullen’s so-called intimacy-seeking stalker. Such stalkers’ behavior arises out of loneliness, with a strong desire for a relationship with the target; a significant percentage of such stalkers suffer a delusional disorder.
Mullen’s so-called incompetent suitor stalker is similar to the intimacy-seeking type but, instead, has an interest in a short-term relationship and is far less persistent in his (her) stalking behavior4; this type might apply to the writers in this study who wrote >1 but <10 letters.
Two additional observations also are notable when trying to characterize people who write letters: (1) A high percentage of people who stalk a celebrity suffer a psychotic disorder5,6; (2) 4 letter-writers traveled, and 1 relocated, to the murderer’s state of incarceration to attend his hearings and be closer to him.
This study has limitations:
• categorization of letters is inherently subjective and the categories themselves were created by the researchers
• the nature and categorization of such letters might vary considerably with the age and sex of the violent criminal; our findings in this case are not generalizable.
Last, researchers who plan to study writers of letters to incarcerated criminals should consider sending a personality test and other questionnaires to those writers to understand this population better.
Treatment considerations
Psychiatrists treating patients who seek a romantic attachment with a violent person should consider psychotherapy as a means of treating possible character pathology. The desire for romance with a violent criminal was greater among repeat writers (20%) than in initial letters (15%), suggesting that people who have a strong inclination to associate with a violent person might benefit from exploring romantic feelings in therapy. Specifically, therapists would be wise to explore with such patients the possibility that they experienced violence or verbal abuse in childhood or adulthood.
To the extent that evidence of prior abuse exists, a diagnosis of posttraumatic stress disorder (PTSD) might be appropriate; specialized therapy for men and women with a history of abuse might be indicated. It is important to provide validation for patients who are victims when they describe their abuse, and to stress that they did nothing to provoke the violence. Furthermore, investigation of why the patient feels drawn romantically toward a violent criminal is helpful, as well as an examination of how such behavior is self-defeating.
There might be value in having patients keep a journal in lieu of actually sending letters; there is evidence that “journaling” can reduce substance use recidivism.7 This work can be performed in conjunction with group or individual psychotherapy that addresses any history of abuse and subsequent PTSD.
Many patients are reluctant to discuss their romantic feelings toward a violent criminal until the psychiatrist has established a strong doctor−patient relationship. Last, clinicians should not hesitate to refer these patients to a therapist who specializes in domestic violence.
Related Resource
• Marazziti D, Falaschi V, Lombardi A, et al. Stalking: a neurobiological perspective. Riv Psichiatr. 2015;50(1):12-18.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Mouradian VE. Women’s stay-leave decisions in relationships involving intimate partner violence. Wellesley, MA: Wellesley Centers for Women Publications; 2004:3,4.
2. Bell KM, Naugle AE. Understanding stay/leave decisions in violent relationships: a behavior analytic approach. Behav Soc Issues. 2005;14(1):21-46.
3. Westrup D, Fremouw WJ. Stalking behavior: a literature review and suggested functional analytic assessment technology. Aggression and Violent Behavior. 1998;3: 255-274.
4. Mullen PE, Pathé M, Purcell R, et al. Study of stalkers. Am J Psychiatry. 1999;156(8):1244-1249.
5. West SG, Friedman SH. These boots are made for stalking: characteristics of female stalkers. Psychiatry (Edgmont). 2008;5(8):37-42.
6. Nadkarni R, Grubin D. Stalking: why do people do it? BMJ. 2000;320(7248):1486-1487.
7. Proctor SL, Hoffmann NG, Allison S. The effectiveness of interactive journaling in reducing recidivism among substance-dependent jail inmates. Int J Offender Ther Comp Criminol. 2012;56(2):317-332.
1. Mouradian VE. Women’s stay-leave decisions in relationships involving intimate partner violence. Wellesley, MA: Wellesley Centers for Women Publications; 2004:3,4.
2. Bell KM, Naugle AE. Understanding stay/leave decisions in violent relationships: a behavior analytic approach. Behav Soc Issues. 2005;14(1):21-46.
3. Westrup D, Fremouw WJ. Stalking behavior: a literature review and suggested functional analytic assessment technology. Aggression and Violent Behavior. 1998;3: 255-274.
4. Mullen PE, Pathé M, Purcell R, et al. Study of stalkers. Am J Psychiatry. 1999;156(8):1244-1249.
5. West SG, Friedman SH. These boots are made for stalking: characteristics of female stalkers. Psychiatry (Edgmont). 2008;5(8):37-42.
6. Nadkarni R, Grubin D. Stalking: why do people do it? BMJ. 2000;320(7248):1486-1487.
7. Proctor SL, Hoffmann NG, Allison S. The effectiveness of interactive journaling in reducing recidivism among substance-dependent jail inmates. Int J Offender Ther Comp Criminol. 2012;56(2):317-332.
Get more patients with backlinks
The medical profession has its jargon. So does the Internet world. Some of that jargon can be important to your success. “Backlinks” or “inbound links” are terms that should get your attention.
Why?
By developing them, you can attract more patients to your practice.
Backlinks are one piece of the Internet marketing puzzle that can help get your Web site on the first page of Google search results.
And just how important is it to be on page 1?
Well, consider that 91.5% of Web surfers do not go beyond the first page of results. That’s what an online advertising network called Chitika found when it examined tens of millions of online ad impressions in which the user was referred to the page via a Google search.1
Just what are backlinks? They are links to your Web page from another site. In basic link terminology, a backlink is any link received by a Web page, directory, Web site, or top-level domain from another, similar site. In this article we discuss the importance of these links and ways to use them in your social media to attract new patients to your site and your practice.
Start with good site design
If you can get listed on the first page of Google search results for the keywords your patients are using, more traffic will come to your Web site. That won’t help if you have a poorly designed site that has no patient conversion strategies, techniques, and systems to transform Web site visitors to patients.
You see, everything has to work together in a coordinated, integrated manner if you want to increase the number of patients who are looking for your services online. We’ve covered many of the basics in earlier articles on Web site design and improvement (see the box below). If you have a nonoptimal site, consider starting with these articles.
Articles on Web design and Internet usage by Ron Romano and Neil H. Baum, MD
5 ways to wake up your Web site
April 2015
Using the Internet in your practice
Part 1: Why social media are important and how to get started
February 2014
Part 2: Generating new patients using social media
April 2014
Part 3: Maximizing your online reach through SEO and pay-per-click
September 2014
Part 4: Reputation management: How to gather kudos and combat negative online reviews
December 2014
These articles are available in the archive at obgmanagement.com
Why backlinks are important
Google uses more than 200 algorithms to rank your Web site. Some are more important than others and have a greater influence on search engine positioning. Backlinks are one of those important influencers.
The number of backlinks you have is an indication of the popularity or importance of your Web site. Google considers a site more significant or relevant than others if it has a large number of quality backlinks from other directories, ezines, blogs, and social media Web sites. These backlinks must be relevant to your keywords. For example, because you are a medical professional, a link to your site from the American Cancer Society or the Mayo Clinic is considered more credible than a link from a local spa or health club.
A search engine such as Google considers the content of the sites it places at the top of the search results page. When links to your site come from other credible and popular sites, and those sites have content related to your site, these backlinks are considered more relevant to your site.
If backlinks come from sites with unrelated content, they are considered less relevant. You may even be penalized by Google for adding backlinks that have no content value.
For example, if a Web master has a site that focuses on urinary incontinence and receives a backlink from another site with information or articles about urinary incontinence, that backlink will be considered more relevant than a link from a site about mortgages that somehow also includes urinary incontinence on its page. Therefore, the higher the relevance of the site linking back to yours, the better the quality of that link.
Top 7 inbound links—and how to obtain them
1. Directories
Directories are indexes of online sites, typically organized by category. You want to ensure that each of your keywords is manually submitted to each directory so it is listed separately. This way you get maximum link value for each keyword.
Links back to your site from directories such as Yahoo Directory and DMOZ.org are valuable. DMOZ.org is edited by humans. Although it is free, it may take some time for your site to be added. A listing in Yahoo’s Directory costs $299 per year.
2. Press releases
If you are writing press releases, make sure they contain keywords that someone would use to find a business like yours. Also ensure that they include links back to your site.
Once the press release is written, submit it to all the news agencies. Then you must wait and see if any of them pick it up and publish it.
You may want to consider having a press release professionally written and distributed by a public relations firm to boost your chances of having the release picked up. PRWeb.com has an excellent reputation. Its distribution network includes the search engines Google, Yahoo, and Bing; media outlets such as USA Today, CNN, and the Wall Street Journal; Associated Press distribution through major newspapers; and health and medical digests such as the Mayo Clinic, WebMD, Women’s Health, and many more.
3. Article directories
By writing and distributing articles through high-traffic article directories, such as EzineArticles.com, Articles.org, and Hubpages.com, you can attract valuable inbound links from a high-traffic site. Craft an effective link at the close of your article to drive traffic back to your site. An example of what your link might say is, “To view a short video on Kegel exercises for pelvic organ prolapse, visit our Web site at www.neilbaum.com/videos.”
4. Social bookmarking
Like Web browser bookmarks, social bookmarking sites such as Digg.com, Reddit.com, and Del.icio.us.com store individual pages (bookmarks) online and allow users to tag (with keywords), organize, search, and manage these bookmarks as well as share them with others. If you bookmark your content on these sites, you get a link from the service. By producing content that your readers enjoy and bookmark to their friends, you gain a link that increases in search engine optimization (SEO) value.
5. Blog comments
To find blog posts on which to comment, you can use blog-specific search engines such as Google Blog Search. Make sure these are blogs read by your target market, not your colleagues. Brand yourself by always using the same name and remember to link back to your site. Always leave a comment that adds to the conversation.
6. Social media
Google also indexes your Twitter updates and social networking profiles. Add that to Web 2.0 hubsites like Scribd or HubPage and you’ve got a way to create many inbound links in a very short time. Scribd is a digital library featuring an ebook and audiobook subscription service that includes New York Times best sellers and classics. HubPages is a user-generated content, revenue-sharing Web site.
7. Video syndication
YouTube is one of the most visited sites online, and the number of sites that syndicate videos is growing every day. These sites often allow you to link to your site in your video’s description, on your profile page, or both.
The importance of being consistent—and honest
For best results, you need to build these links monthly with regularity, and over time, you will reap the benefits of improved rankings. While it is fairly easy to modify your Web pages to make them more SEO-friendly, it is harder to influence other Web sites and get them to link to yours. This is the reason search engines consider backlinks such an important factor.
Moreover, search engines’ criteria for quality backlinks have gotten tougher, thanks to unscrupulous Web masters trying to achieve these backlinks by deceptive techniques, such as hidden links or automatically generated pages whose sole purpose is to provide backlinks to Web sites. These pages are called link farms. Not only are they disregarded by search engines, but linking to one could get your site banned entirely. This strategy is often referred to as “black hat” linking and is to be avoided.
“White hat” methods to increase backlinks
Blog posting is one of the easiest, least expensive, and most effective ways to garner links from other sites. However, to reap this benefit, you must post blog entries consistently. We suggest posting at least once weekly. Your blog will gain more attention if you have something newsworthy to report. For example, if you attend a meeting where a revolutionary new development is reported, and you write about it before the media, you can be sure others will want to connect and link to your site.
Conduct a survey and share your results on your site. Others will want to link to your report.
Share any templates your office uses to be more efficient and productive. For example, Dr. Baum has a template, or checklist, for starting and ending every day in the office. It is shared on his Web site so that other sites can link to it and make use of it.
Show your funny bone. Humor often travels in a viral direction. If something funny happens in your practice, share it with others and they will frequently link to the source.
Join a forum. Forums are a great source of high-quality traffic and links. You can use a forum to reach out to a specific community.By placing valid, useful contributions, you gain legitimate authority for your site.
The bottom line
You want to attract as many visitors to your Web site as possible. Your own content and the frequency of your postings are mainstays of making your Web site relevant to existing and potential patients. Also useful are backlinks. The number and quality of your inbound links are major factors in SEO. Search engines place high value on trust and authority, and an inbound link from a very high-ranking and trusted Web site tells the search engine that someone trusted also trusts you. So start linking.
Reference
1. The value of Google result positioning. Chitika.com. http://chitika.com/google-positioning-value. Updated June 12, 2013. Accessed June 9, 2015.
The medical profession has its jargon. So does the Internet world. Some of that jargon can be important to your success. “Backlinks” or “inbound links” are terms that should get your attention.
Why?
By developing them, you can attract more patients to your practice.
Backlinks are one piece of the Internet marketing puzzle that can help get your Web site on the first page of Google search results.
And just how important is it to be on page 1?
Well, consider that 91.5% of Web surfers do not go beyond the first page of results. That’s what an online advertising network called Chitika found when it examined tens of millions of online ad impressions in which the user was referred to the page via a Google search.1
Just what are backlinks? They are links to your Web page from another site. In basic link terminology, a backlink is any link received by a Web page, directory, Web site, or top-level domain from another, similar site. In this article we discuss the importance of these links and ways to use them in your social media to attract new patients to your site and your practice.
Start with good site design
If you can get listed on the first page of Google search results for the keywords your patients are using, more traffic will come to your Web site. That won’t help if you have a poorly designed site that has no patient conversion strategies, techniques, and systems to transform Web site visitors to patients.
You see, everything has to work together in a coordinated, integrated manner if you want to increase the number of patients who are looking for your services online. We’ve covered many of the basics in earlier articles on Web site design and improvement (see the box below). If you have a nonoptimal site, consider starting with these articles.
Articles on Web design and Internet usage by Ron Romano and Neil H. Baum, MD
5 ways to wake up your Web site
April 2015
Using the Internet in your practice
Part 1: Why social media are important and how to get started
February 2014
Part 2: Generating new patients using social media
April 2014
Part 3: Maximizing your online reach through SEO and pay-per-click
September 2014
Part 4: Reputation management: How to gather kudos and combat negative online reviews
December 2014
These articles are available in the archive at obgmanagement.com
Why backlinks are important
Google uses more than 200 algorithms to rank your Web site. Some are more important than others and have a greater influence on search engine positioning. Backlinks are one of those important influencers.
The number of backlinks you have is an indication of the popularity or importance of your Web site. Google considers a site more significant or relevant than others if it has a large number of quality backlinks from other directories, ezines, blogs, and social media Web sites. These backlinks must be relevant to your keywords. For example, because you are a medical professional, a link to your site from the American Cancer Society or the Mayo Clinic is considered more credible than a link from a local spa or health club.
A search engine such as Google considers the content of the sites it places at the top of the search results page. When links to your site come from other credible and popular sites, and those sites have content related to your site, these backlinks are considered more relevant to your site.
If backlinks come from sites with unrelated content, they are considered less relevant. You may even be penalized by Google for adding backlinks that have no content value.
For example, if a Web master has a site that focuses on urinary incontinence and receives a backlink from another site with information or articles about urinary incontinence, that backlink will be considered more relevant than a link from a site about mortgages that somehow also includes urinary incontinence on its page. Therefore, the higher the relevance of the site linking back to yours, the better the quality of that link.
Top 7 inbound links—and how to obtain them
1. Directories
Directories are indexes of online sites, typically organized by category. You want to ensure that each of your keywords is manually submitted to each directory so it is listed separately. This way you get maximum link value for each keyword.
Links back to your site from directories such as Yahoo Directory and DMOZ.org are valuable. DMOZ.org is edited by humans. Although it is free, it may take some time for your site to be added. A listing in Yahoo’s Directory costs $299 per year.
2. Press releases
If you are writing press releases, make sure they contain keywords that someone would use to find a business like yours. Also ensure that they include links back to your site.
Once the press release is written, submit it to all the news agencies. Then you must wait and see if any of them pick it up and publish it.
You may want to consider having a press release professionally written and distributed by a public relations firm to boost your chances of having the release picked up. PRWeb.com has an excellent reputation. Its distribution network includes the search engines Google, Yahoo, and Bing; media outlets such as USA Today, CNN, and the Wall Street Journal; Associated Press distribution through major newspapers; and health and medical digests such as the Mayo Clinic, WebMD, Women’s Health, and many more.
3. Article directories
By writing and distributing articles through high-traffic article directories, such as EzineArticles.com, Articles.org, and Hubpages.com, you can attract valuable inbound links from a high-traffic site. Craft an effective link at the close of your article to drive traffic back to your site. An example of what your link might say is, “To view a short video on Kegel exercises for pelvic organ prolapse, visit our Web site at www.neilbaum.com/videos.”
4. Social bookmarking
Like Web browser bookmarks, social bookmarking sites such as Digg.com, Reddit.com, and Del.icio.us.com store individual pages (bookmarks) online and allow users to tag (with keywords), organize, search, and manage these bookmarks as well as share them with others. If you bookmark your content on these sites, you get a link from the service. By producing content that your readers enjoy and bookmark to their friends, you gain a link that increases in search engine optimization (SEO) value.
5. Blog comments
To find blog posts on which to comment, you can use blog-specific search engines such as Google Blog Search. Make sure these are blogs read by your target market, not your colleagues. Brand yourself by always using the same name and remember to link back to your site. Always leave a comment that adds to the conversation.
6. Social media
Google also indexes your Twitter updates and social networking profiles. Add that to Web 2.0 hubsites like Scribd or HubPage and you’ve got a way to create many inbound links in a very short time. Scribd is a digital library featuring an ebook and audiobook subscription service that includes New York Times best sellers and classics. HubPages is a user-generated content, revenue-sharing Web site.
7. Video syndication
YouTube is one of the most visited sites online, and the number of sites that syndicate videos is growing every day. These sites often allow you to link to your site in your video’s description, on your profile page, or both.
The importance of being consistent—and honest
For best results, you need to build these links monthly with regularity, and over time, you will reap the benefits of improved rankings. While it is fairly easy to modify your Web pages to make them more SEO-friendly, it is harder to influence other Web sites and get them to link to yours. This is the reason search engines consider backlinks such an important factor.
Moreover, search engines’ criteria for quality backlinks have gotten tougher, thanks to unscrupulous Web masters trying to achieve these backlinks by deceptive techniques, such as hidden links or automatically generated pages whose sole purpose is to provide backlinks to Web sites. These pages are called link farms. Not only are they disregarded by search engines, but linking to one could get your site banned entirely. This strategy is often referred to as “black hat” linking and is to be avoided.
“White hat” methods to increase backlinks
Blog posting is one of the easiest, least expensive, and most effective ways to garner links from other sites. However, to reap this benefit, you must post blog entries consistently. We suggest posting at least once weekly. Your blog will gain more attention if you have something newsworthy to report. For example, if you attend a meeting where a revolutionary new development is reported, and you write about it before the media, you can be sure others will want to connect and link to your site.
Conduct a survey and share your results on your site. Others will want to link to your report.
Share any templates your office uses to be more efficient and productive. For example, Dr. Baum has a template, or checklist, for starting and ending every day in the office. It is shared on his Web site so that other sites can link to it and make use of it.
Show your funny bone. Humor often travels in a viral direction. If something funny happens in your practice, share it with others and they will frequently link to the source.
Join a forum. Forums are a great source of high-quality traffic and links. You can use a forum to reach out to a specific community.By placing valid, useful contributions, you gain legitimate authority for your site.
The bottom line
You want to attract as many visitors to your Web site as possible. Your own content and the frequency of your postings are mainstays of making your Web site relevant to existing and potential patients. Also useful are backlinks. The number and quality of your inbound links are major factors in SEO. Search engines place high value on trust and authority, and an inbound link from a very high-ranking and trusted Web site tells the search engine that someone trusted also trusts you. So start linking.
The medical profession has its jargon. So does the Internet world. Some of that jargon can be important to your success. “Backlinks” or “inbound links” are terms that should get your attention.
Why?
By developing them, you can attract more patients to your practice.
Backlinks are one piece of the Internet marketing puzzle that can help get your Web site on the first page of Google search results.
And just how important is it to be on page 1?
Well, consider that 91.5% of Web surfers do not go beyond the first page of results. That’s what an online advertising network called Chitika found when it examined tens of millions of online ad impressions in which the user was referred to the page via a Google search.1
Just what are backlinks? They are links to your Web page from another site. In basic link terminology, a backlink is any link received by a Web page, directory, Web site, or top-level domain from another, similar site. In this article we discuss the importance of these links and ways to use them in your social media to attract new patients to your site and your practice.
Start with good site design
If you can get listed on the first page of Google search results for the keywords your patients are using, more traffic will come to your Web site. That won’t help if you have a poorly designed site that has no patient conversion strategies, techniques, and systems to transform Web site visitors to patients.
You see, everything has to work together in a coordinated, integrated manner if you want to increase the number of patients who are looking for your services online. We’ve covered many of the basics in earlier articles on Web site design and improvement (see the box below). If you have a nonoptimal site, consider starting with these articles.
Articles on Web design and Internet usage by Ron Romano and Neil H. Baum, MD
5 ways to wake up your Web site
April 2015
Using the Internet in your practice
Part 1: Why social media are important and how to get started
February 2014
Part 2: Generating new patients using social media
April 2014
Part 3: Maximizing your online reach through SEO and pay-per-click
September 2014
Part 4: Reputation management: How to gather kudos and combat negative online reviews
December 2014
These articles are available in the archive at obgmanagement.com
Why backlinks are important
Google uses more than 200 algorithms to rank your Web site. Some are more important than others and have a greater influence on search engine positioning. Backlinks are one of those important influencers.
The number of backlinks you have is an indication of the popularity or importance of your Web site. Google considers a site more significant or relevant than others if it has a large number of quality backlinks from other directories, ezines, blogs, and social media Web sites. These backlinks must be relevant to your keywords. For example, because you are a medical professional, a link to your site from the American Cancer Society or the Mayo Clinic is considered more credible than a link from a local spa or health club.
A search engine such as Google considers the content of the sites it places at the top of the search results page. When links to your site come from other credible and popular sites, and those sites have content related to your site, these backlinks are considered more relevant to your site.
If backlinks come from sites with unrelated content, they are considered less relevant. You may even be penalized by Google for adding backlinks that have no content value.
For example, if a Web master has a site that focuses on urinary incontinence and receives a backlink from another site with information or articles about urinary incontinence, that backlink will be considered more relevant than a link from a site about mortgages that somehow also includes urinary incontinence on its page. Therefore, the higher the relevance of the site linking back to yours, the better the quality of that link.
Top 7 inbound links—and how to obtain them
1. Directories
Directories are indexes of online sites, typically organized by category. You want to ensure that each of your keywords is manually submitted to each directory so it is listed separately. This way you get maximum link value for each keyword.
Links back to your site from directories such as Yahoo Directory and DMOZ.org are valuable. DMOZ.org is edited by humans. Although it is free, it may take some time for your site to be added. A listing in Yahoo’s Directory costs $299 per year.
2. Press releases
If you are writing press releases, make sure they contain keywords that someone would use to find a business like yours. Also ensure that they include links back to your site.
Once the press release is written, submit it to all the news agencies. Then you must wait and see if any of them pick it up and publish it.
You may want to consider having a press release professionally written and distributed by a public relations firm to boost your chances of having the release picked up. PRWeb.com has an excellent reputation. Its distribution network includes the search engines Google, Yahoo, and Bing; media outlets such as USA Today, CNN, and the Wall Street Journal; Associated Press distribution through major newspapers; and health and medical digests such as the Mayo Clinic, WebMD, Women’s Health, and many more.
3. Article directories
By writing and distributing articles through high-traffic article directories, such as EzineArticles.com, Articles.org, and Hubpages.com, you can attract valuable inbound links from a high-traffic site. Craft an effective link at the close of your article to drive traffic back to your site. An example of what your link might say is, “To view a short video on Kegel exercises for pelvic organ prolapse, visit our Web site at www.neilbaum.com/videos.”
4. Social bookmarking
Like Web browser bookmarks, social bookmarking sites such as Digg.com, Reddit.com, and Del.icio.us.com store individual pages (bookmarks) online and allow users to tag (with keywords), organize, search, and manage these bookmarks as well as share them with others. If you bookmark your content on these sites, you get a link from the service. By producing content that your readers enjoy and bookmark to their friends, you gain a link that increases in search engine optimization (SEO) value.
5. Blog comments
To find blog posts on which to comment, you can use blog-specific search engines such as Google Blog Search. Make sure these are blogs read by your target market, not your colleagues. Brand yourself by always using the same name and remember to link back to your site. Always leave a comment that adds to the conversation.
6. Social media
Google also indexes your Twitter updates and social networking profiles. Add that to Web 2.0 hubsites like Scribd or HubPage and you’ve got a way to create many inbound links in a very short time. Scribd is a digital library featuring an ebook and audiobook subscription service that includes New York Times best sellers and classics. HubPages is a user-generated content, revenue-sharing Web site.
7. Video syndication
YouTube is one of the most visited sites online, and the number of sites that syndicate videos is growing every day. These sites often allow you to link to your site in your video’s description, on your profile page, or both.
The importance of being consistent—and honest
For best results, you need to build these links monthly with regularity, and over time, you will reap the benefits of improved rankings. While it is fairly easy to modify your Web pages to make them more SEO-friendly, it is harder to influence other Web sites and get them to link to yours. This is the reason search engines consider backlinks such an important factor.
Moreover, search engines’ criteria for quality backlinks have gotten tougher, thanks to unscrupulous Web masters trying to achieve these backlinks by deceptive techniques, such as hidden links or automatically generated pages whose sole purpose is to provide backlinks to Web sites. These pages are called link farms. Not only are they disregarded by search engines, but linking to one could get your site banned entirely. This strategy is often referred to as “black hat” linking and is to be avoided.
“White hat” methods to increase backlinks
Blog posting is one of the easiest, least expensive, and most effective ways to garner links from other sites. However, to reap this benefit, you must post blog entries consistently. We suggest posting at least once weekly. Your blog will gain more attention if you have something newsworthy to report. For example, if you attend a meeting where a revolutionary new development is reported, and you write about it before the media, you can be sure others will want to connect and link to your site.
Conduct a survey and share your results on your site. Others will want to link to your report.
Share any templates your office uses to be more efficient and productive. For example, Dr. Baum has a template, or checklist, for starting and ending every day in the office. It is shared on his Web site so that other sites can link to it and make use of it.
Show your funny bone. Humor often travels in a viral direction. If something funny happens in your practice, share it with others and they will frequently link to the source.
Join a forum. Forums are a great source of high-quality traffic and links. You can use a forum to reach out to a specific community.By placing valid, useful contributions, you gain legitimate authority for your site.
The bottom line
You want to attract as many visitors to your Web site as possible. Your own content and the frequency of your postings are mainstays of making your Web site relevant to existing and potential patients. Also useful are backlinks. The number and quality of your inbound links are major factors in SEO. Search engines place high value on trust and authority, and an inbound link from a very high-ranking and trusted Web site tells the search engine that someone trusted also trusts you. So start linking.
Reference
1. The value of Google result positioning. Chitika.com. http://chitika.com/google-positioning-value. Updated June 12, 2013. Accessed June 9, 2015.
Reference
1. The value of Google result positioning. Chitika.com. http://chitika.com/google-positioning-value. Updated June 12, 2013. Accessed June 9, 2015.
Chronic Myeloid Leukemia
The first connection between cancer and a patient’s genome was documented by Peter Nowell and David Hungerford when they identified a unique chromosome in the metaphase spread of 7 patients diagnosed with chronic myeloid leukemia (CML). In 1973, renowned cytopathologist Janet Rowley determined that this chromosome is part of a chromosomal translocation between chromosome 9 and chromosome 22. Further delineation of this translocation showed that the gene ABL1, normally located on chromosome 9, is translocated to the Philadelphia (Ph+) chromosome in patients with CML. ABL1 was found to be located downstream of a specific genetic region in each patient, and this region became known as the BCR, or “breakpoint cluster region.” The BCR-ABL1 translocation found in patients with CML creates a constitutively active tyrosine kinase necessary for cellular transformation.
To read the full article in PDF:
The first connection between cancer and a patient’s genome was documented by Peter Nowell and David Hungerford when they identified a unique chromosome in the metaphase spread of 7 patients diagnosed with chronic myeloid leukemia (CML). In 1973, renowned cytopathologist Janet Rowley determined that this chromosome is part of a chromosomal translocation between chromosome 9 and chromosome 22. Further delineation of this translocation showed that the gene ABL1, normally located on chromosome 9, is translocated to the Philadelphia (Ph+) chromosome in patients with CML. ABL1 was found to be located downstream of a specific genetic region in each patient, and this region became known as the BCR, or “breakpoint cluster region.” The BCR-ABL1 translocation found in patients with CML creates a constitutively active tyrosine kinase necessary for cellular transformation.
To read the full article in PDF:
The first connection between cancer and a patient’s genome was documented by Peter Nowell and David Hungerford when they identified a unique chromosome in the metaphase spread of 7 patients diagnosed with chronic myeloid leukemia (CML). In 1973, renowned cytopathologist Janet Rowley determined that this chromosome is part of a chromosomal translocation between chromosome 9 and chromosome 22. Further delineation of this translocation showed that the gene ABL1, normally located on chromosome 9, is translocated to the Philadelphia (Ph+) chromosome in patients with CML. ABL1 was found to be located downstream of a specific genetic region in each patient, and this region became known as the BCR, or “breakpoint cluster region.” The BCR-ABL1 translocation found in patients with CML creates a constitutively active tyrosine kinase necessary for cellular transformation.
To read the full article in PDF:
Urologic applications of botulinum toxin
Patients with loss of bladder control experience discomfort, embarrassment, personal care and health issues, and, often, significant pain, all with a decidedly negative impact on quality of life. Although some patients may find lifestyle modifications, drug therapy, and self-catheterization acceptable and effective, there is a clear need for more options.
Botulinum toxin, or onabotulinumtoxinA, is currently approved by the US Food and Drug Administration (FDA) for neurogenic detrusor overactivity and overactive bladder refractory to drug therapy. Studies so far have shown botulinum toxin injection to be safe and effective for these conditions, and these results have led to interest in off-label uses, eg, for detrusor external sphincter dyssynergia (DESD), motor and sensory urgency, and painful bladder syndrome/interstitial cystitis (Table 1).
Although more data from clinical trials are needed, botulinum toxin injection offers patients a much-needed treatment option.
HOW BOTULINUM TOXIN WORKS
Seven serotypes identified
Discovered in 1897, botulinum toxin is a neurotoxin produced by the gram-positive, rod-shaped anaerobic bacterium Clostridium botulinum1 and is the most poisonous naturally occurring toxin known.2 Seven immunologically distinct antigenic serotypes have been identified (A, B, C1, D, E, F, and G),1 but only types A and B are available for clinical use.
Most research into potential therapeutic uses has focused on type A, which has the longest duration of action, a clinical advantage.3 Recently, work has been done to further characterize other serotypes and to isolate additional variants of botulinum toxin. For example, serotype E, the predominant serotype associated with foodborne botulism, is being studied in an effort to prevent future outbreaks.4
Our discussion focuses on clinical uses of the serotype A botulinum toxin preparation, which we will refer to simply as botulinum toxin.
Studies exploring how it works
Botulinum toxin exerts its effects by binding to peripheral cholinergic terminals, inhibiting release of acetylcholine at the neuromuscular junction. Flaccid paralysis ensues as a result.
Results of animal studies have shed additional light on the specific actions of botulinum toxin A:
- It may alter levels of nerve growth factor and transient receptor potential vanilloid 1 in rats, and this may provide an additional mechanism of reducing bladder detrusor overactivity.5
- In addition to blocking acetylcholine release from motor neurons, it inhibits the release of neurotransmitters involved in bladder sensory afferent pathways.6
- It inhibits the release of substance P and glutamate, neuropeptides involved in sensory and nociceptive pathways.6,7
- It promotes apoptosis in prostatic tissue; however, this effect has not been shown in the bladder.3
The time necessary to recover function after botulinum toxin paralysis depends on the subtype of botulinum toxin as well as on the type of nerve terminal. Chemodenervation lasts from 3 to 6 months when the toxin is injected into the neuromuscular junction of skeletal muscle, and considerably longer (up to 1 year) when injected into the autonomic neurons of smooth muscle.2,6
TREATMENT OF NEUROGENIC DETRUSOR OVERACTIVITY
Neurogenic detrusor overactivity involves involuntary contractions of the bladder resulting from spinal cord injury, multiple sclerosis, and other neurologic conditions. An estimated 273,000 people in the United States have a spinal cord injury, and 81% of them have urologic symptoms ranging from areflexia to overactivity.8 From 75% to 100% of patients with multiple sclerosis have urologic symptoms, and detrusor overactivity is the most common.9
Detrusor overactivity can cause urinary urgency, urinary frequency, and urgency incontinence, significantly affecting quality of life and leading to skin breakdown, sacral ulcerations, and challenges with personal care.
Anticholinergic drugs have been the mainstay of therapy. If drug therapy failed, the next option was reconstructive surgery, often augmentation cystoplasty. Thus, botulinum toxin injection is an important advance in treatment options.
Studies that showed effectiveness
Botulinum toxin for neurogenic detrusor overactivity was first studied by Schurch et al.10 In their study, 200 U or 300 U was injected into the trigone of 21 patients with spinal cord injury and urgency incontinence managed with intermittent self-catheterization.10 At 6 weeks after injection, 17 of the 19 patients seen at follow-up visits were completely continent. Urodynamic evaluation revealed significant increases in maximum cystometric capacity and in volume at first involuntary detrusor contraction, and a decrease in detrusor voiding pressure. Of the 11 patients available for follow-up at 16 and 36 weeks, improvements in measures of incontinence and urodynamic function persisted.
In addition, two small randomized controlled trials11,12 showed significant increases in cystometric bladder capacity, significant improvement in quality-of-life measures, and reduction in episodes of urgency incontinence.
In 2011 and 2012, two multicenter double-blind randomized controlled trials reported on patients with multiple sclerosis and spinal cord injury with neurogenic detrusor overactivity inadequately managed with drug therapy. The patients were randomized to botulinum toxin injection (200 U or 300 U) or placebo injection.13,14 The primary end point for both studies was the change from baseline in episodes of urinary incontinence per week at week 6. Secondary end points were maximum cystometric capacity, maximum detrusor pressure during first involuntary detrusor contraction, and score on the Incontinence Quality of Life scale.15
In both studies, the mean number of urinary incontinence episodes per week was 33 at baseline. At week 6, Cruz et al14 found that patients who received botulinum toxin injection had significantly fewer episodes per week (21.8 fewer with 200 U, 19.4 fewer with 300 U) than those in the placebo group, who had 13.2 fewer episodes per week (P < .01). Ginsberg et al13 reported decreases in the mean number of episodes of urinary incontinence of 21, 23, and 9 episodes per week in the 200 U, 300 U, and placebo groups, respectively (P < .001). The patients who received botulinum toxin had statistically significant improvements in maximum cystometric capacity, maximum detrusor pressure during first involuntary detrusor contraction, and Incontinence Quality of Life scores compared with placebo (P < .001). Thirty-eight percent of patients in the treatment group were fully continent.13,14
Safety and adverse effects
The most frequently reported adverse events were urinary tract infection (24% of patients)13,14 and urinary retention requiring initiation of clean intermittent catheterization. In the study by Cruz et al,14 these were reported in 30% with 200 U, 42% with 300 U, and 12% with placebo, while in the study by Ginsberg et al13 they were reported in 35% with 200 U, 42% with 300 U, and 10% with placebo.
In a study of long-term safety and efficacy of botulinum toxin injection in patients with neurogenic detrusor overactivity, Kennelly et al16 found that patients undergoing repeat injections had sustained reductions in episodes of incontinence and increases in the maximum cystometric capacity and quality of life scores, with no increase in adverse events over time.16
But is it cost-effective?
While botulinum toxin injection may be safe and effective for neurogenic detrusor overactivity, is it cost-effective?
Carlson et al17 used a Markov State Transition model to assess the cost of refractory neurogenic detrusor overactivity in patients receiving botulinum toxin vs best supportive care (incontinence pads, medications, intermittent self-catheterization).17 They found that the injections were more expensive than supportive care but were cost-effective when considering the reduction in episodes of incontinence, the reduced need for incontinence products, and improvement in measures of quality of life.
What the evidence indicates
Trials of botulinum toxin injection for neurogenic detrusor overactivity have shown that it improves continence, maximum cystometric capacity, detrusor pressures, and quality of life. The main adverse effects are urinary tract infection and urinary retention requiring intermittent self-catheterization.
Although many patients with this condition are already self-catheterizing, the physician must discuss this before botulinum toxin therapy to ensure that the patient or a family member is able to perform catheterization. Studies have shown that patients have an increase in urinary tract infections after botulinum injections. But in these studies, a urinary tract infection was defined as 100,000 colony-forming units or the presence of leukocytosis with or without symptoms. It is important to remember that patients on intermittent catheterization have bacteriuria and should be treated only for symptomatic, not asymptomatic, bacteriuria.
TREATMENT OF IDIOPATHIC OVERACTIVE BLADDER
Patients with idiopathic overactive bladder have urinary urgency accompanied by urgency incontinence, nocturia, or urinary frequency.18 The prevalence of this condition has been reported to range from 1.7% to 13.3% in men age 30 and older and 7% to 30.3% in women of similar ages. About one-third of women with overactive bladder also have detrusor overactivity.19 Overactive bladder presents a significant economic and medical burden on the healthcare system, as well as having a negative impact on quality of life.
The FDA approved botulinum toxin injection for treatment of idiopathic overactive bladder in January 2013.
Evidence of effectiveness
Two multicenter randomized controlled trials20,21 of botulinum toxin 100 U enrolled patients age 18 and older who had more than three episodes of urinary urgency incontinence in a 3-day period or more than eight micturitions per day inadequately managed by anticholinergic drug therapy. Primary end points were the change from baseline in the number of episodes of urinary incontinence per day and the proportion of patients with a positive response on the Treatment Benefit Scale22 at week 12. Secondary end points included episodes of urinary urgency incontinence, micturition, urgency, and nocturia, and scores on health-related quality of life questionnaires (Incontinence Quality of Life scale, King’s Health Questionnaire).
In both studies, patients receiving botulinum toxin had significantly fewer episodes of incontinence compared with placebo (−2.65 vs −0.87; P < .001 and −2.95 vs −1.03; P < .001).20,21 Reductions from baseline in all other symptoms of overactive bladder, a positive treatment response on the treatment benefit scale, and improvements in quality-of-life scores were also significantly greater with botulinum toxin injection than with placebo (P ≤ .01).
As in the studies of neurogenic detrusor overactivity, the most common adverse effects were urinary tract infection (occurring in 15.5%20 and 24.1%21 of patients) and urinary retention requiring self-catheterization (5.4%20 and 6.9%21).
The largest study to date of anticholinergic therapy vs botulinum toxin injection23 in women with urinary urgency incontinence, published in 2012, studied nearly 250 women who had five or more episodes of idiopathic urgency incontinence in a 3-day period. They were randomized either to daily oral therapy (solifenacin 5 mg with possible escalation to 10 mg and, if necessary, a subsequent switch to extended-release trospium 60 mg) plus one intradetrusor injection of saline, or to a daily oral placebo plus one injection of botulinum toxin 100 U.23
The dropout rate was low in both groups, with 93% of patients in both groups completing the 6-month protocol. Women experienced a mean reduction in urgency incontinence episodes of 3.4 per day (baseline 5) in the anticholinergic group vs 3.3 episodes in the botulinum toxin group (P = .81). However, more patients achieved complete resolution of urinary urgency incontinence in the botulinum toxin group than in the anticholinergic therapy group (27% vs 13%; P = .003). Quality of life improved in both groups without a significant difference between the groups. The botulinum toxin group had higher rates of initiation of self-catheterization (5% vs 0%, P = .01) and urinary tract infection (33% vs 13%, P < .001).23
Botulinum toxin as a third-line therapy
In May 2014, the American Urological Association updated its guidelines on idiopathic overactive bladder24 to include botulinum toxin injection as standard third-line therapy for patients in whom behavioral and medical management (ie, anticholinergics and beta-3-agonists) failed.
Interpreting the evidence to date
Overall, studies in idiopathic overactive bladder have shown a reduction in episodes of urgency incontinence and other symptoms, with some data also demonstrating a corresponding improvement in quality of life.
As in neurogenic detrusor overactivity, the main risks associated with botulinum toxin injection are urinary tract infection and the need to initiate self-catheterization. Although 94% of patients studied did not require self-catheterization after injection, the patient’s ability to perform self-catheterization should be determined before proceeding with botulinum toxin injections.
DETRUSOR EXTERNAL SPHINCTER DYSSYNERGIA
Botulinum toxin has been used not only to improve bladder storage but also to facilitate bladder emptying, as in patients with DESD, a lack of coordination between the bladder and the urinary sphincter. Normal voiding involves relaxation of the urinary sphincter and contraction of the bladder; in DESD the sphincter contracts and works against the bladder’s ability to empty. This leads not only to difficulty emptying the bladder but also to elevated bladder pressure, which can cause renal damage if untreated.
DESD can be seen after injury between the pontine micturition center, which coordinates activity between the bladder and the sphincter, and the caudal spinal cord. This can occur in spinal cord injury, multiple sclerosis, myelomeningocele, and transverse myelitis and can cause significant morbidity for the patient.
Treatment options include drug therapy, injection of botulinum toxin into the sphincter, clean intermittent catheterization, indwelling catheterization, urethral stenting, sphincterotomy, and reconstructive surgery such as urinary diversion.25
The goals of therapy are to avoid the need for clean intermittent catheterization in patients who have difficulty with manual dexterity, and to avoid the need for surgical procedures such as sphincterotomy and urinary diversion. The efficacy of urethral stenting is low, and medical management can be limited.26
In the first published report on botulinum toxin for DESD (in 1988),27 of 11 patients with spinal cord injury and DESD who received botulinum toxin injected into the external urethral sphincter, 10 showed signs of sphincter denervation on electromyography and reductions in urethral pressure profiles and postvoid residual volumes. Schurch et al28 and de Sèze et al29 also reported reductions in postvoid residual volume and maximal urethral pressures in patients with spinal cord injury and DESD.
In 2005, Gallien et al30 reported what is still the largest multicenter randomized controlled trial of botulinum toxin injection in DESD. Eighty-six patients with multiple sclerosis, DESD, and chronic urinary retention were randomized to receive either a single transperineal botulinum toxin injection of 100 U plus the alpha-1-blocker alfuzosin, or a placebo injection plus alfuzosin. Botulinum toxin treatment was associated with significantly increased voided volumes and reduced premicturition and maximal detrusor pressures, but no significant decrease in postvoid residual volume.30
More study needed
Despite these findings, a Cochrane Review concluded that, given the limited experience with intrasphincteric injection of botulinum toxin, data from larger randomized controlled trials are needed before making definitive recommendations.25 In the meantime, the clinician must weigh the low morbidity of the procedure against the limited options in the treatment of these patients.
OFF-LABEL UROLOGIC INDICATIONS
Botulinum toxin injection has been studied off-label for painful bladder syndrome/interstitial cystitis and for chronic prostatic pain. Patients with these conditions often describe pain with filling of the bladder, which leads to urinary frequency in an attempt to relieve the pain.
These pain syndromes can be difficult to treat and can have a devastating impact on quality of life. Treatment options include pain management, stress management, physical therapy, intravesical therapies, cystoscopy with hydrodistention, neuromodulation, cyclosporine, urinary diversion surgery, and botulinum toxin injection (an off-label use).31
In painful bladder syndrome/interstitial cystitis, botulinum toxin is thought to act on sensory afferent pathways, as well as to inhibit the release of substance P and glutamate, neuropeptides involved in sensory and nociceptive pathways.6 In animal studies,32 botulinum toxin was found to inhibit the afferent neural response by inhibiting mechanoreceptor-mediated release of adenosine triphosphate and by causing a decrease in calcitonin gene-related peptide, which helps regulate micturition and mediates painful bladder sensation.
Clinical studies to date in pelvic pain syndromes
Data from clinical studies of botulinum toxin injection for pelvic pain syndromes are limited. Zermann et al33 performed transurethral perisphincteric injection in 11 men with chronic prostatic pain, 9 of whom reported subjective pain relief, with an average decrease from 7.2 to 1.6 on a visual analogue scale. Postinjection urodynamic studies showed a decrease in functional urethral length, urethral closure pressure, and postvoid residual volume, and an increase in the peak and average flow rates.33
Abbott et al34 evaluated the effect of botulinum toxin injection into the levator ani in 12 women with chronic pelvic pain and pelvic floor hypertonicity. Pelvic floor manometry showed significant reduction in resting muscle pressures and improvements in dyspareunia and nonmenstrual pain. There were also improvements in quality of life and dyschezia, but these were not statistically significant.
Smith et al35 injected botulinum toxin into the detrusor of 13 women with refractory painful bladder syndrome and interstitial cystitis,35 and 9 women (69%) noted statistically significant improvements in the Interstitial Cystitis Symptom Index and Interstitial Cystitis Problem Index, daytime frequency, nocturia, pain, and urodynamic parameters (volume at first desire to void, and maximum cystometric capacity).
In a prospective randomized study of patients with refractory painful bladder syndrome and interstitial cystitis, Kuo and Chancellor36 compared suburothelial injection of 200 U or 100 U of botulinum toxin plus hydrodistention against hydrodistention alone.Patients who received botulinum toxin had increased bladder capacity and improved long-term pain relief, but no difference was noted between 200 U and 100 U, and more adverse effects were seen with the higher dose.36
Pinto et al37 treated 16 women with refractory painful bladder syndrome and interstitial cystitis with intratrigonal injections of botulinum toxin and reported improvements in pain scores, symptom scores, urinary frequency, and quality-of-life measures. The effect lasted 9.9 months (± 2.4 months) and persisted with successive injections.37
More study needed
Although these studies show that botulinum toxin injection for pelvic pain syndromes has the potential to improve pain, urinary frequency, bladder sensation, bladder capacity, and quality of life, larger randomized controlled trials are needed.
Again, the treatment options are limited for refractory painful bladder syndrome and interstitial cystitis. Patients may be desperate for relief from their symptoms. Practitioners must manage expectations and properly inform patients of the potential risks of treatments, especially with patients who will easily agree to further treatment with the smallest hope of relief.
INJECTION TECHNIQUES
For general points about the procedure to discuss with patients, see “What to tell patients.”
Cystoscopic detrusor injection
This procedure is usually done on an outpatient basis (eg, office, ambulatory surgery center). With the patient in the lithotomy position, 100 mL of 2% lidocaine is instilled into the bladder and is allowed 15 to 20 minutes to take effect. A flexible or rigid cystoscope can be used. Depending on the indication, the bladder is injected with 100 U to 300 U of botulinum toxin. The ideal depth of injection is 2 mm in the detrusor muscle, with each injection spaced about 1 cm apart. The recommended administration for 100 U is to inject 20 sites with 0.5 U per mL of saline and, for 200 U, to inject 30 sites with about 0.67 U per mL of saline.38 The location of the injections into the detrusor can vary, as long as adequate spacing is assured.
Injection sites vary. Proponents of injecting the trigone argue that as it is an area of greater nerve density, patients will have a better clinical response. Opponents argue that trigonal injection could result in distal ureteral paralysis and subsequent ureteral reflux. However, this theoretical concern has not been observed clinically.
Urethral injection (off-label use)
The urethra can be injected cystoscopically or periurethrally. Cystoscopic injection involves localization of the external sphincter using the rigid cystoscope and collagen needle; a total of 100 U is injected into the sphincter under direct vision, typically at the 3 o’clock and 9 o’clock positions.35 The periurethral technique is an option in women and involves a spinal needle with 100 U to 200 U of botulinum toxin injected into the external sphincter muscle at the 2 o’clock and 10 o’clock positions.
ADVERSE EFFECTS AND CONTRAINDICATIONS
Adverse effects are rare for urologic applications. The injections are localized, with little systemic absorption, and the doses are 1/1,000th of the theorized lethal dose in a 70-kg male.2 The maximum recommended dose for a 3-month period is 360 U.
Generalized muscle weakness has been reported in a paraplegic patient and in a tetraplegic patient after detrusor injections.2 Interestingly, both patients had return of bladder spasticity within 2 months, prompting speculation about diffusion of botulinum toxin through the bladder wall.2
Repeat injections can cause an immune response in up to 5% of patients.6 Patients undergoing repeat injections are at risk of forming neutralizing antibodies that can interfere with the efficacy of botulinum toxin.6 In a study by Schulte-Baukloh et al, all patients with antibodies to botulinum toxin had a history of recurrent urinary tract infection.39
Botulinum toxin injection is contraindicated in patients with preexisting neuromuscular disease, such as myasthenia gravis, Eaton-Lambert syndrome, and amyotrophic lateral sclerosis. It should also be avoided in patients who are breastfeeding, pregnant, or using agents that potentiate neuromuscular weakness, such as aminoglycosides.
Patients should be informed that some formulations of botulinum toxin include a stabilizer such as albumin derived from human blood, as this may be of religious or cultural significance.
- Leippold T, Reitz A, Schurch B. Botulinum toxin as a new therapy option for voiding disorders: current state of the art. Eur Urol 2003; 44:165–174.
- Sahai A, Khan M, Fowler CJ, Dasgupta P. Botulinum toxin for the treatment of lower urinary tract symptoms: a review. Neurourol Urodyn 2005; 24:2–12.
- Cruz F. Targets for botulinum toxin in the lower urinary tract. Neurourol Urodyn 2014; 33:31–38.
- Weedmark KA, Lambert DL, Mabon P, et al. Two novel toxin variants revealed by whole-genome sequencing of 175 Clostridium botulinum type E strains. Appl Environ Microbiol 2014; 80:6334–6345.
- Ha US, Park EY, Kim JC. Effect of botulinum toxin on expression of nerve growth factor and transient receptor potential vanilloid 1 in urothelium and detrusor muscle of rats with bladder outlet obstruction-induced detrusor overactivity. Urology 2011; 78:721.e1–721.e6
- Frenkl TL, Rackley RR. Injectable neuromodulatory agents: botulinum toxin therapy. Urol Clin North Am 2005; 32:89–99.
- Ikeda Y, Zabbarova IV, Birder LA, et al. Botulinum neurotoxin serotype A suppresses neurotransmitter release from afferent as well as efferent nerves in the urinary bladder. Eur Urol 2012; 62:1157–1164.
- Goldmark E, Niver B, Ginsberg DA. Neurogenic bladder: from diagnosis to management. Curr Urol Rep 2014; 15:448.
- Andersson KE. Current and future drugs for treatment of MS-associated bladder dysfunction. Ann Phys Rehabil Med 2014; 57:321–328.
- Schurch B, Stöhrer M, Kramer G, Schmid DM, Gaul G, Hauri D. Botulinum-A toxin for treating detrusor hyperreflexia in spinal cord injured patients: a new alternative to anticholinergic drugs? Preliminary results. J Urol 2000; 164:692–697.
- Schurch B, de Sèze M, Denys P, et al; Botox Detrusor Hyperreflexia Study Team. Botulinum toxin type a is a safe and effective treatment for neurogenic urinary incontinence: results of a single treatment, randomized, placebo controlled 6-month study. J Urol 2005; 174:196–200.
- Ehren I, Volz D, Farrelly E, et al. Efficacy and impact of botulinum toxin A on quality of life in patients with neurogenic detrusor overactivity: a randomised, placebo-controlled, double-blind study. Scand J Urol Nephrol 2007; 41:335–340.
- Ginsberg D, Gousse A, Keppenne V, et al. Phase 3 efficacy and tolerability study of onabotulinumtoxinA for urinary incontinence from neurogenic detrusor overactivity. J Urol 2012; 187:2131–2139.
- Cruz F, Herschorn S, Aliotta P, et al. Efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: a randomised, double-blind, placebo-controlled trial. Eur Urol 2011; 60:742–750.
- Wagner TH, Patrick DL, Bavendam TG, Martin ML, Buesching DP. Quality of life of persons with urinary incontinence: development of a new measure. Urology 1996: 47:67–71.
- Kennelly M, Dmochowski R, Ethans K, et al. Long-term efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: an interim analysis. Urology 2013; 81:491–497.
- Carlson JJ, Hansen RN, Dmochowski RR, Globe DR, Colayco DC, Sullivan SD. Estimating the cost-effectiveness of onabotulinumtoxinA for neurogenic detrusor overactivity in the United States. Clin Ther 2013; 35:414–424.
- Abrams P, Cardozo L, Fall M, et al; Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 2003; 61:37–49.
- Milsom I, Coyne KS, Nicholson S, Kvasz M, Chen CI, Wein AJ. Global prevalence and economic burden of urgency urinary incontinence: a systematic review. Eur Urol 2014; 65:79–95.
- Nitti VW, Dmochowski R, Herschorn S, et al; EMBARK Study Group. OnabotulinumtoxinA for the treatment of patients with overactive bladder and urinary incontinence: results of a phase 3, randomized, placebo controlled trial. J Urol 2013; 189:2186–2193.
- Chapple C, Sievert KD, MacDiarmid S, et al. OnabotulinumtoxinA 100 U significantly improves all idiopathic overactive bladder symptoms and quality of life in patients with overactive bladder and urinary incontinence: a randomised, double-blind, placebo-controlled trial. Eur Urol 2013; 64:249–256.
- Colman S, Chapple C, Nitti V, Haag-Molkenteller C, Hastedt C, Massow U. Validation of Treatment Benefit Scale for assessing subjective outcomes in treatment of overactive bladder. Urology 2008; 72:803–807.
- Visco AG, Brubaker L, Richter HE, et al; Pelvic Floor Disorders Network. Anticholinergic therapy vs onabotulinumtoxinA for urgency urinary incontinence. N Engl J Med 2012; 367:1803–1813.
- Gormley EA, Lightner DJ, Burgio KL, et al. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU Guideline. www.auanet.org/education/guidelines/overactive-bladder.cfm. Accessed June 11, 2015.
- Utomo E, Groen J, Blok BF. Surgical management of functional bladder outlet obstruction in adults with neurogenic bladder dysfunction. Cochrane Database Syst Rev 2014; 5:CD004927.
- Mahfouz W, Corcos J. Management of detrusor external sphincter dyssynergia in neurogenic bladder. Eur J Phys Rehabil Med 2011; 47:639–650.
- Dykstra DD, Sidi AA, Scott AB, Pagel JM, Goldish GD. Effects of botulinum A toxin on detrusor-sphincter dyssynergia in spinal cord injury patients. J Urol 1988; 139:919–922.
- Schurch B, Hauri D, Rodic B, Curt A, Meyer M, Rossier AB. Botulinum-A toxin as a treatment of detrusor-sphincter dyssynergia: a prospective study in 24 spinal cord injury patients. J Urol 1996; 155:1023–1029.
- de Sèze M, Petit H, Gallien, de Sèze MP, Joseph PA, Mazaux JM, Barat M. Botulinum a toxin and detrusor sphincter dyssynergia: a double-blind lidocaine-controlled study in 13 patients with spinal cord disease. Eur Urol 2002; 42:56–62.
- Gallien P, Reymann JM, Amarenco G, Nicolas B, de Sèze M, Bellissant E. Placebo controlled, randomised, double blind study of the effects of botulinum A toxin on detrusor sphincter dyssynergia in multiple sclerosis patients. J Neurol Neurosurg Psychiatry 2005; 76:1670–1676.
- Hanno PM, Burks DA, Clemens JQ, et al; Interstitial Cystitis Guidelines Panel of the American Urological Association Education and Research, Inc. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol 2011; 185:2162–2170.
- Chuang YC, Yoshimura N, Huang CC, Chiang PH, Chancellor MB. Intravesical botulinum toxin a administration produces analgesia against acetic acid induced bladder pain responses in rats. J Urol 2004; 172:1529–1532.
- Zermann DH, Ishigooka M, Schubert J, Schmidt RA. Perisphincteric injection of botulinum toxin type A. A treatment option for patients with chronic prostatic pain? Eur Urol 2000; 38:393–399.
- Abbott JA, Jarvis SK, Lyons SD, Thomson A, Vancaille TG. Botulinum toxin type A for chronic pain and pelvic floor spasm in women: a randomized controlled trial. Obstet Gynecol 2006; 108:915–923.
- Smith CP, Radziszewski P, Borkowski A, Somogyi GT, Boone TB, Chancellor MB. Botulinum toxin A has antinociceptive effects in treating interstitial cystitis. Urology 2004; 64:871–875.
- Kuo HC, Chancellor MB. Comparison of intravesical botulinum toxin type A injections plus hydrodistention with hydrodistention alone for the treatment of refractory interstitial cystitis/painful bladder syndrome. BJU Int 2009: 104:657–661.
- Pinto R, Lopes T, Silva J, Silva C, Dinis P, Cruz F. Persistent therapeutic effect of repeated injections of onabotulinum toxin a in refractory bladder pain syndrome/interstitial cystitis. J Urol 2013; 189:548–553.
- Rovner E. Chapter 6: Practical aspects of administration of onabotulinumtoxinA. Neurourol Urodyn 2014; 33(suppl 3):S32–S37.
- Schulte-Baukloh H, Herholz J, Bigalke H, Miller K, Knispel HH. Results of a BoNT/A antibody study in children and adolescents after onabotulinumtoxin A (Botox®) detrusor injection. Urol Int 2011; 87:434–438.
Patients with loss of bladder control experience discomfort, embarrassment, personal care and health issues, and, often, significant pain, all with a decidedly negative impact on quality of life. Although some patients may find lifestyle modifications, drug therapy, and self-catheterization acceptable and effective, there is a clear need for more options.
Botulinum toxin, or onabotulinumtoxinA, is currently approved by the US Food and Drug Administration (FDA) for neurogenic detrusor overactivity and overactive bladder refractory to drug therapy. Studies so far have shown botulinum toxin injection to be safe and effective for these conditions, and these results have led to interest in off-label uses, eg, for detrusor external sphincter dyssynergia (DESD), motor and sensory urgency, and painful bladder syndrome/interstitial cystitis (Table 1).
Although more data from clinical trials are needed, botulinum toxin injection offers patients a much-needed treatment option.
HOW BOTULINUM TOXIN WORKS
Seven serotypes identified
Discovered in 1897, botulinum toxin is a neurotoxin produced by the gram-positive, rod-shaped anaerobic bacterium Clostridium botulinum1 and is the most poisonous naturally occurring toxin known.2 Seven immunologically distinct antigenic serotypes have been identified (A, B, C1, D, E, F, and G),1 but only types A and B are available for clinical use.
Most research into potential therapeutic uses has focused on type A, which has the longest duration of action, a clinical advantage.3 Recently, work has been done to further characterize other serotypes and to isolate additional variants of botulinum toxin. For example, serotype E, the predominant serotype associated with foodborne botulism, is being studied in an effort to prevent future outbreaks.4
Our discussion focuses on clinical uses of the serotype A botulinum toxin preparation, which we will refer to simply as botulinum toxin.
Studies exploring how it works
Botulinum toxin exerts its effects by binding to peripheral cholinergic terminals, inhibiting release of acetylcholine at the neuromuscular junction. Flaccid paralysis ensues as a result.
Results of animal studies have shed additional light on the specific actions of botulinum toxin A:
- It may alter levels of nerve growth factor and transient receptor potential vanilloid 1 in rats, and this may provide an additional mechanism of reducing bladder detrusor overactivity.5
- In addition to blocking acetylcholine release from motor neurons, it inhibits the release of neurotransmitters involved in bladder sensory afferent pathways.6
- It inhibits the release of substance P and glutamate, neuropeptides involved in sensory and nociceptive pathways.6,7
- It promotes apoptosis in prostatic tissue; however, this effect has not been shown in the bladder.3
The time necessary to recover function after botulinum toxin paralysis depends on the subtype of botulinum toxin as well as on the type of nerve terminal. Chemodenervation lasts from 3 to 6 months when the toxin is injected into the neuromuscular junction of skeletal muscle, and considerably longer (up to 1 year) when injected into the autonomic neurons of smooth muscle.2,6
TREATMENT OF NEUROGENIC DETRUSOR OVERACTIVITY
Neurogenic detrusor overactivity involves involuntary contractions of the bladder resulting from spinal cord injury, multiple sclerosis, and other neurologic conditions. An estimated 273,000 people in the United States have a spinal cord injury, and 81% of them have urologic symptoms ranging from areflexia to overactivity.8 From 75% to 100% of patients with multiple sclerosis have urologic symptoms, and detrusor overactivity is the most common.9
Detrusor overactivity can cause urinary urgency, urinary frequency, and urgency incontinence, significantly affecting quality of life and leading to skin breakdown, sacral ulcerations, and challenges with personal care.
Anticholinergic drugs have been the mainstay of therapy. If drug therapy failed, the next option was reconstructive surgery, often augmentation cystoplasty. Thus, botulinum toxin injection is an important advance in treatment options.
Studies that showed effectiveness
Botulinum toxin for neurogenic detrusor overactivity was first studied by Schurch et al.10 In their study, 200 U or 300 U was injected into the trigone of 21 patients with spinal cord injury and urgency incontinence managed with intermittent self-catheterization.10 At 6 weeks after injection, 17 of the 19 patients seen at follow-up visits were completely continent. Urodynamic evaluation revealed significant increases in maximum cystometric capacity and in volume at first involuntary detrusor contraction, and a decrease in detrusor voiding pressure. Of the 11 patients available for follow-up at 16 and 36 weeks, improvements in measures of incontinence and urodynamic function persisted.
In addition, two small randomized controlled trials11,12 showed significant increases in cystometric bladder capacity, significant improvement in quality-of-life measures, and reduction in episodes of urgency incontinence.
In 2011 and 2012, two multicenter double-blind randomized controlled trials reported on patients with multiple sclerosis and spinal cord injury with neurogenic detrusor overactivity inadequately managed with drug therapy. The patients were randomized to botulinum toxin injection (200 U or 300 U) or placebo injection.13,14 The primary end point for both studies was the change from baseline in episodes of urinary incontinence per week at week 6. Secondary end points were maximum cystometric capacity, maximum detrusor pressure during first involuntary detrusor contraction, and score on the Incontinence Quality of Life scale.15
In both studies, the mean number of urinary incontinence episodes per week was 33 at baseline. At week 6, Cruz et al14 found that patients who received botulinum toxin injection had significantly fewer episodes per week (21.8 fewer with 200 U, 19.4 fewer with 300 U) than those in the placebo group, who had 13.2 fewer episodes per week (P < .01). Ginsberg et al13 reported decreases in the mean number of episodes of urinary incontinence of 21, 23, and 9 episodes per week in the 200 U, 300 U, and placebo groups, respectively (P < .001). The patients who received botulinum toxin had statistically significant improvements in maximum cystometric capacity, maximum detrusor pressure during first involuntary detrusor contraction, and Incontinence Quality of Life scores compared with placebo (P < .001). Thirty-eight percent of patients in the treatment group were fully continent.13,14
Safety and adverse effects
The most frequently reported adverse events were urinary tract infection (24% of patients)13,14 and urinary retention requiring initiation of clean intermittent catheterization. In the study by Cruz et al,14 these were reported in 30% with 200 U, 42% with 300 U, and 12% with placebo, while in the study by Ginsberg et al13 they were reported in 35% with 200 U, 42% with 300 U, and 10% with placebo.
In a study of long-term safety and efficacy of botulinum toxin injection in patients with neurogenic detrusor overactivity, Kennelly et al16 found that patients undergoing repeat injections had sustained reductions in episodes of incontinence and increases in the maximum cystometric capacity and quality of life scores, with no increase in adverse events over time.16
But is it cost-effective?
While botulinum toxin injection may be safe and effective for neurogenic detrusor overactivity, is it cost-effective?
Carlson et al17 used a Markov State Transition model to assess the cost of refractory neurogenic detrusor overactivity in patients receiving botulinum toxin vs best supportive care (incontinence pads, medications, intermittent self-catheterization).17 They found that the injections were more expensive than supportive care but were cost-effective when considering the reduction in episodes of incontinence, the reduced need for incontinence products, and improvement in measures of quality of life.
What the evidence indicates
Trials of botulinum toxin injection for neurogenic detrusor overactivity have shown that it improves continence, maximum cystometric capacity, detrusor pressures, and quality of life. The main adverse effects are urinary tract infection and urinary retention requiring intermittent self-catheterization.
Although many patients with this condition are already self-catheterizing, the physician must discuss this before botulinum toxin therapy to ensure that the patient or a family member is able to perform catheterization. Studies have shown that patients have an increase in urinary tract infections after botulinum injections. But in these studies, a urinary tract infection was defined as 100,000 colony-forming units or the presence of leukocytosis with or without symptoms. It is important to remember that patients on intermittent catheterization have bacteriuria and should be treated only for symptomatic, not asymptomatic, bacteriuria.
TREATMENT OF IDIOPATHIC OVERACTIVE BLADDER
Patients with idiopathic overactive bladder have urinary urgency accompanied by urgency incontinence, nocturia, or urinary frequency.18 The prevalence of this condition has been reported to range from 1.7% to 13.3% in men age 30 and older and 7% to 30.3% in women of similar ages. About one-third of women with overactive bladder also have detrusor overactivity.19 Overactive bladder presents a significant economic and medical burden on the healthcare system, as well as having a negative impact on quality of life.
The FDA approved botulinum toxin injection for treatment of idiopathic overactive bladder in January 2013.
Evidence of effectiveness
Two multicenter randomized controlled trials20,21 of botulinum toxin 100 U enrolled patients age 18 and older who had more than three episodes of urinary urgency incontinence in a 3-day period or more than eight micturitions per day inadequately managed by anticholinergic drug therapy. Primary end points were the change from baseline in the number of episodes of urinary incontinence per day and the proportion of patients with a positive response on the Treatment Benefit Scale22 at week 12. Secondary end points included episodes of urinary urgency incontinence, micturition, urgency, and nocturia, and scores on health-related quality of life questionnaires (Incontinence Quality of Life scale, King’s Health Questionnaire).
In both studies, patients receiving botulinum toxin had significantly fewer episodes of incontinence compared with placebo (−2.65 vs −0.87; P < .001 and −2.95 vs −1.03; P < .001).20,21 Reductions from baseline in all other symptoms of overactive bladder, a positive treatment response on the treatment benefit scale, and improvements in quality-of-life scores were also significantly greater with botulinum toxin injection than with placebo (P ≤ .01).
As in the studies of neurogenic detrusor overactivity, the most common adverse effects were urinary tract infection (occurring in 15.5%20 and 24.1%21 of patients) and urinary retention requiring self-catheterization (5.4%20 and 6.9%21).
The largest study to date of anticholinergic therapy vs botulinum toxin injection23 in women with urinary urgency incontinence, published in 2012, studied nearly 250 women who had five or more episodes of idiopathic urgency incontinence in a 3-day period. They were randomized either to daily oral therapy (solifenacin 5 mg with possible escalation to 10 mg and, if necessary, a subsequent switch to extended-release trospium 60 mg) plus one intradetrusor injection of saline, or to a daily oral placebo plus one injection of botulinum toxin 100 U.23
The dropout rate was low in both groups, with 93% of patients in both groups completing the 6-month protocol. Women experienced a mean reduction in urgency incontinence episodes of 3.4 per day (baseline 5) in the anticholinergic group vs 3.3 episodes in the botulinum toxin group (P = .81). However, more patients achieved complete resolution of urinary urgency incontinence in the botulinum toxin group than in the anticholinergic therapy group (27% vs 13%; P = .003). Quality of life improved in both groups without a significant difference between the groups. The botulinum toxin group had higher rates of initiation of self-catheterization (5% vs 0%, P = .01) and urinary tract infection (33% vs 13%, P < .001).23
Botulinum toxin as a third-line therapy
In May 2014, the American Urological Association updated its guidelines on idiopathic overactive bladder24 to include botulinum toxin injection as standard third-line therapy for patients in whom behavioral and medical management (ie, anticholinergics and beta-3-agonists) failed.
Interpreting the evidence to date
Overall, studies in idiopathic overactive bladder have shown a reduction in episodes of urgency incontinence and other symptoms, with some data also demonstrating a corresponding improvement in quality of life.
As in neurogenic detrusor overactivity, the main risks associated with botulinum toxin injection are urinary tract infection and the need to initiate self-catheterization. Although 94% of patients studied did not require self-catheterization after injection, the patient’s ability to perform self-catheterization should be determined before proceeding with botulinum toxin injections.
DETRUSOR EXTERNAL SPHINCTER DYSSYNERGIA
Botulinum toxin has been used not only to improve bladder storage but also to facilitate bladder emptying, as in patients with DESD, a lack of coordination between the bladder and the urinary sphincter. Normal voiding involves relaxation of the urinary sphincter and contraction of the bladder; in DESD the sphincter contracts and works against the bladder’s ability to empty. This leads not only to difficulty emptying the bladder but also to elevated bladder pressure, which can cause renal damage if untreated.
DESD can be seen after injury between the pontine micturition center, which coordinates activity between the bladder and the sphincter, and the caudal spinal cord. This can occur in spinal cord injury, multiple sclerosis, myelomeningocele, and transverse myelitis and can cause significant morbidity for the patient.
Treatment options include drug therapy, injection of botulinum toxin into the sphincter, clean intermittent catheterization, indwelling catheterization, urethral stenting, sphincterotomy, and reconstructive surgery such as urinary diversion.25
The goals of therapy are to avoid the need for clean intermittent catheterization in patients who have difficulty with manual dexterity, and to avoid the need for surgical procedures such as sphincterotomy and urinary diversion. The efficacy of urethral stenting is low, and medical management can be limited.26
In the first published report on botulinum toxin for DESD (in 1988),27 of 11 patients with spinal cord injury and DESD who received botulinum toxin injected into the external urethral sphincter, 10 showed signs of sphincter denervation on electromyography and reductions in urethral pressure profiles and postvoid residual volumes. Schurch et al28 and de Sèze et al29 also reported reductions in postvoid residual volume and maximal urethral pressures in patients with spinal cord injury and DESD.
In 2005, Gallien et al30 reported what is still the largest multicenter randomized controlled trial of botulinum toxin injection in DESD. Eighty-six patients with multiple sclerosis, DESD, and chronic urinary retention were randomized to receive either a single transperineal botulinum toxin injection of 100 U plus the alpha-1-blocker alfuzosin, or a placebo injection plus alfuzosin. Botulinum toxin treatment was associated with significantly increased voided volumes and reduced premicturition and maximal detrusor pressures, but no significant decrease in postvoid residual volume.30
More study needed
Despite these findings, a Cochrane Review concluded that, given the limited experience with intrasphincteric injection of botulinum toxin, data from larger randomized controlled trials are needed before making definitive recommendations.25 In the meantime, the clinician must weigh the low morbidity of the procedure against the limited options in the treatment of these patients.
OFF-LABEL UROLOGIC INDICATIONS
Botulinum toxin injection has been studied off-label for painful bladder syndrome/interstitial cystitis and for chronic prostatic pain. Patients with these conditions often describe pain with filling of the bladder, which leads to urinary frequency in an attempt to relieve the pain.
These pain syndromes can be difficult to treat and can have a devastating impact on quality of life. Treatment options include pain management, stress management, physical therapy, intravesical therapies, cystoscopy with hydrodistention, neuromodulation, cyclosporine, urinary diversion surgery, and botulinum toxin injection (an off-label use).31
In painful bladder syndrome/interstitial cystitis, botulinum toxin is thought to act on sensory afferent pathways, as well as to inhibit the release of substance P and glutamate, neuropeptides involved in sensory and nociceptive pathways.6 In animal studies,32 botulinum toxin was found to inhibit the afferent neural response by inhibiting mechanoreceptor-mediated release of adenosine triphosphate and by causing a decrease in calcitonin gene-related peptide, which helps regulate micturition and mediates painful bladder sensation.
Clinical studies to date in pelvic pain syndromes
Data from clinical studies of botulinum toxin injection for pelvic pain syndromes are limited. Zermann et al33 performed transurethral perisphincteric injection in 11 men with chronic prostatic pain, 9 of whom reported subjective pain relief, with an average decrease from 7.2 to 1.6 on a visual analogue scale. Postinjection urodynamic studies showed a decrease in functional urethral length, urethral closure pressure, and postvoid residual volume, and an increase in the peak and average flow rates.33
Abbott et al34 evaluated the effect of botulinum toxin injection into the levator ani in 12 women with chronic pelvic pain and pelvic floor hypertonicity. Pelvic floor manometry showed significant reduction in resting muscle pressures and improvements in dyspareunia and nonmenstrual pain. There were also improvements in quality of life and dyschezia, but these were not statistically significant.
Smith et al35 injected botulinum toxin into the detrusor of 13 women with refractory painful bladder syndrome and interstitial cystitis,35 and 9 women (69%) noted statistically significant improvements in the Interstitial Cystitis Symptom Index and Interstitial Cystitis Problem Index, daytime frequency, nocturia, pain, and urodynamic parameters (volume at first desire to void, and maximum cystometric capacity).
In a prospective randomized study of patients with refractory painful bladder syndrome and interstitial cystitis, Kuo and Chancellor36 compared suburothelial injection of 200 U or 100 U of botulinum toxin plus hydrodistention against hydrodistention alone.Patients who received botulinum toxin had increased bladder capacity and improved long-term pain relief, but no difference was noted between 200 U and 100 U, and more adverse effects were seen with the higher dose.36
Pinto et al37 treated 16 women with refractory painful bladder syndrome and interstitial cystitis with intratrigonal injections of botulinum toxin and reported improvements in pain scores, symptom scores, urinary frequency, and quality-of-life measures. The effect lasted 9.9 months (± 2.4 months) and persisted with successive injections.37
More study needed
Although these studies show that botulinum toxin injection for pelvic pain syndromes has the potential to improve pain, urinary frequency, bladder sensation, bladder capacity, and quality of life, larger randomized controlled trials are needed.
Again, the treatment options are limited for refractory painful bladder syndrome and interstitial cystitis. Patients may be desperate for relief from their symptoms. Practitioners must manage expectations and properly inform patients of the potential risks of treatments, especially with patients who will easily agree to further treatment with the smallest hope of relief.
INJECTION TECHNIQUES
For general points about the procedure to discuss with patients, see “What to tell patients.”
Cystoscopic detrusor injection
This procedure is usually done on an outpatient basis (eg, office, ambulatory surgery center). With the patient in the lithotomy position, 100 mL of 2% lidocaine is instilled into the bladder and is allowed 15 to 20 minutes to take effect. A flexible or rigid cystoscope can be used. Depending on the indication, the bladder is injected with 100 U to 300 U of botulinum toxin. The ideal depth of injection is 2 mm in the detrusor muscle, with each injection spaced about 1 cm apart. The recommended administration for 100 U is to inject 20 sites with 0.5 U per mL of saline and, for 200 U, to inject 30 sites with about 0.67 U per mL of saline.38 The location of the injections into the detrusor can vary, as long as adequate spacing is assured.
Injection sites vary. Proponents of injecting the trigone argue that as it is an area of greater nerve density, patients will have a better clinical response. Opponents argue that trigonal injection could result in distal ureteral paralysis and subsequent ureteral reflux. However, this theoretical concern has not been observed clinically.
Urethral injection (off-label use)
The urethra can be injected cystoscopically or periurethrally. Cystoscopic injection involves localization of the external sphincter using the rigid cystoscope and collagen needle; a total of 100 U is injected into the sphincter under direct vision, typically at the 3 o’clock and 9 o’clock positions.35 The periurethral technique is an option in women and involves a spinal needle with 100 U to 200 U of botulinum toxin injected into the external sphincter muscle at the 2 o’clock and 10 o’clock positions.
ADVERSE EFFECTS AND CONTRAINDICATIONS
Adverse effects are rare for urologic applications. The injections are localized, with little systemic absorption, and the doses are 1/1,000th of the theorized lethal dose in a 70-kg male.2 The maximum recommended dose for a 3-month period is 360 U.
Generalized muscle weakness has been reported in a paraplegic patient and in a tetraplegic patient after detrusor injections.2 Interestingly, both patients had return of bladder spasticity within 2 months, prompting speculation about diffusion of botulinum toxin through the bladder wall.2
Repeat injections can cause an immune response in up to 5% of patients.6 Patients undergoing repeat injections are at risk of forming neutralizing antibodies that can interfere with the efficacy of botulinum toxin.6 In a study by Schulte-Baukloh et al, all patients with antibodies to botulinum toxin had a history of recurrent urinary tract infection.39
Botulinum toxin injection is contraindicated in patients with preexisting neuromuscular disease, such as myasthenia gravis, Eaton-Lambert syndrome, and amyotrophic lateral sclerosis. It should also be avoided in patients who are breastfeeding, pregnant, or using agents that potentiate neuromuscular weakness, such as aminoglycosides.
Patients should be informed that some formulations of botulinum toxin include a stabilizer such as albumin derived from human blood, as this may be of religious or cultural significance.
Patients with loss of bladder control experience discomfort, embarrassment, personal care and health issues, and, often, significant pain, all with a decidedly negative impact on quality of life. Although some patients may find lifestyle modifications, drug therapy, and self-catheterization acceptable and effective, there is a clear need for more options.
Botulinum toxin, or onabotulinumtoxinA, is currently approved by the US Food and Drug Administration (FDA) for neurogenic detrusor overactivity and overactive bladder refractory to drug therapy. Studies so far have shown botulinum toxin injection to be safe and effective for these conditions, and these results have led to interest in off-label uses, eg, for detrusor external sphincter dyssynergia (DESD), motor and sensory urgency, and painful bladder syndrome/interstitial cystitis (Table 1).
Although more data from clinical trials are needed, botulinum toxin injection offers patients a much-needed treatment option.
HOW BOTULINUM TOXIN WORKS
Seven serotypes identified
Discovered in 1897, botulinum toxin is a neurotoxin produced by the gram-positive, rod-shaped anaerobic bacterium Clostridium botulinum1 and is the most poisonous naturally occurring toxin known.2 Seven immunologically distinct antigenic serotypes have been identified (A, B, C1, D, E, F, and G),1 but only types A and B are available for clinical use.
Most research into potential therapeutic uses has focused on type A, which has the longest duration of action, a clinical advantage.3 Recently, work has been done to further characterize other serotypes and to isolate additional variants of botulinum toxin. For example, serotype E, the predominant serotype associated with foodborne botulism, is being studied in an effort to prevent future outbreaks.4
Our discussion focuses on clinical uses of the serotype A botulinum toxin preparation, which we will refer to simply as botulinum toxin.
Studies exploring how it works
Botulinum toxin exerts its effects by binding to peripheral cholinergic terminals, inhibiting release of acetylcholine at the neuromuscular junction. Flaccid paralysis ensues as a result.
Results of animal studies have shed additional light on the specific actions of botulinum toxin A:
- It may alter levels of nerve growth factor and transient receptor potential vanilloid 1 in rats, and this may provide an additional mechanism of reducing bladder detrusor overactivity.5
- In addition to blocking acetylcholine release from motor neurons, it inhibits the release of neurotransmitters involved in bladder sensory afferent pathways.6
- It inhibits the release of substance P and glutamate, neuropeptides involved in sensory and nociceptive pathways.6,7
- It promotes apoptosis in prostatic tissue; however, this effect has not been shown in the bladder.3
The time necessary to recover function after botulinum toxin paralysis depends on the subtype of botulinum toxin as well as on the type of nerve terminal. Chemodenervation lasts from 3 to 6 months when the toxin is injected into the neuromuscular junction of skeletal muscle, and considerably longer (up to 1 year) when injected into the autonomic neurons of smooth muscle.2,6
TREATMENT OF NEUROGENIC DETRUSOR OVERACTIVITY
Neurogenic detrusor overactivity involves involuntary contractions of the bladder resulting from spinal cord injury, multiple sclerosis, and other neurologic conditions. An estimated 273,000 people in the United States have a spinal cord injury, and 81% of them have urologic symptoms ranging from areflexia to overactivity.8 From 75% to 100% of patients with multiple sclerosis have urologic symptoms, and detrusor overactivity is the most common.9
Detrusor overactivity can cause urinary urgency, urinary frequency, and urgency incontinence, significantly affecting quality of life and leading to skin breakdown, sacral ulcerations, and challenges with personal care.
Anticholinergic drugs have been the mainstay of therapy. If drug therapy failed, the next option was reconstructive surgery, often augmentation cystoplasty. Thus, botulinum toxin injection is an important advance in treatment options.
Studies that showed effectiveness
Botulinum toxin for neurogenic detrusor overactivity was first studied by Schurch et al.10 In their study, 200 U or 300 U was injected into the trigone of 21 patients with spinal cord injury and urgency incontinence managed with intermittent self-catheterization.10 At 6 weeks after injection, 17 of the 19 patients seen at follow-up visits were completely continent. Urodynamic evaluation revealed significant increases in maximum cystometric capacity and in volume at first involuntary detrusor contraction, and a decrease in detrusor voiding pressure. Of the 11 patients available for follow-up at 16 and 36 weeks, improvements in measures of incontinence and urodynamic function persisted.
In addition, two small randomized controlled trials11,12 showed significant increases in cystometric bladder capacity, significant improvement in quality-of-life measures, and reduction in episodes of urgency incontinence.
In 2011 and 2012, two multicenter double-blind randomized controlled trials reported on patients with multiple sclerosis and spinal cord injury with neurogenic detrusor overactivity inadequately managed with drug therapy. The patients were randomized to botulinum toxin injection (200 U or 300 U) or placebo injection.13,14 The primary end point for both studies was the change from baseline in episodes of urinary incontinence per week at week 6. Secondary end points were maximum cystometric capacity, maximum detrusor pressure during first involuntary detrusor contraction, and score on the Incontinence Quality of Life scale.15
In both studies, the mean number of urinary incontinence episodes per week was 33 at baseline. At week 6, Cruz et al14 found that patients who received botulinum toxin injection had significantly fewer episodes per week (21.8 fewer with 200 U, 19.4 fewer with 300 U) than those in the placebo group, who had 13.2 fewer episodes per week (P < .01). Ginsberg et al13 reported decreases in the mean number of episodes of urinary incontinence of 21, 23, and 9 episodes per week in the 200 U, 300 U, and placebo groups, respectively (P < .001). The patients who received botulinum toxin had statistically significant improvements in maximum cystometric capacity, maximum detrusor pressure during first involuntary detrusor contraction, and Incontinence Quality of Life scores compared with placebo (P < .001). Thirty-eight percent of patients in the treatment group were fully continent.13,14
Safety and adverse effects
The most frequently reported adverse events were urinary tract infection (24% of patients)13,14 and urinary retention requiring initiation of clean intermittent catheterization. In the study by Cruz et al,14 these were reported in 30% with 200 U, 42% with 300 U, and 12% with placebo, while in the study by Ginsberg et al13 they were reported in 35% with 200 U, 42% with 300 U, and 10% with placebo.
In a study of long-term safety and efficacy of botulinum toxin injection in patients with neurogenic detrusor overactivity, Kennelly et al16 found that patients undergoing repeat injections had sustained reductions in episodes of incontinence and increases in the maximum cystometric capacity and quality of life scores, with no increase in adverse events over time.16
But is it cost-effective?
While botulinum toxin injection may be safe and effective for neurogenic detrusor overactivity, is it cost-effective?
Carlson et al17 used a Markov State Transition model to assess the cost of refractory neurogenic detrusor overactivity in patients receiving botulinum toxin vs best supportive care (incontinence pads, medications, intermittent self-catheterization).17 They found that the injections were more expensive than supportive care but were cost-effective when considering the reduction in episodes of incontinence, the reduced need for incontinence products, and improvement in measures of quality of life.
What the evidence indicates
Trials of botulinum toxin injection for neurogenic detrusor overactivity have shown that it improves continence, maximum cystometric capacity, detrusor pressures, and quality of life. The main adverse effects are urinary tract infection and urinary retention requiring intermittent self-catheterization.
Although many patients with this condition are already self-catheterizing, the physician must discuss this before botulinum toxin therapy to ensure that the patient or a family member is able to perform catheterization. Studies have shown that patients have an increase in urinary tract infections after botulinum injections. But in these studies, a urinary tract infection was defined as 100,000 colony-forming units or the presence of leukocytosis with or without symptoms. It is important to remember that patients on intermittent catheterization have bacteriuria and should be treated only for symptomatic, not asymptomatic, bacteriuria.
TREATMENT OF IDIOPATHIC OVERACTIVE BLADDER
Patients with idiopathic overactive bladder have urinary urgency accompanied by urgency incontinence, nocturia, or urinary frequency.18 The prevalence of this condition has been reported to range from 1.7% to 13.3% in men age 30 and older and 7% to 30.3% in women of similar ages. About one-third of women with overactive bladder also have detrusor overactivity.19 Overactive bladder presents a significant economic and medical burden on the healthcare system, as well as having a negative impact on quality of life.
The FDA approved botulinum toxin injection for treatment of idiopathic overactive bladder in January 2013.
Evidence of effectiveness
Two multicenter randomized controlled trials20,21 of botulinum toxin 100 U enrolled patients age 18 and older who had more than three episodes of urinary urgency incontinence in a 3-day period or more than eight micturitions per day inadequately managed by anticholinergic drug therapy. Primary end points were the change from baseline in the number of episodes of urinary incontinence per day and the proportion of patients with a positive response on the Treatment Benefit Scale22 at week 12. Secondary end points included episodes of urinary urgency incontinence, micturition, urgency, and nocturia, and scores on health-related quality of life questionnaires (Incontinence Quality of Life scale, King’s Health Questionnaire).
In both studies, patients receiving botulinum toxin had significantly fewer episodes of incontinence compared with placebo (−2.65 vs −0.87; P < .001 and −2.95 vs −1.03; P < .001).20,21 Reductions from baseline in all other symptoms of overactive bladder, a positive treatment response on the treatment benefit scale, and improvements in quality-of-life scores were also significantly greater with botulinum toxin injection than with placebo (P ≤ .01).
As in the studies of neurogenic detrusor overactivity, the most common adverse effects were urinary tract infection (occurring in 15.5%20 and 24.1%21 of patients) and urinary retention requiring self-catheterization (5.4%20 and 6.9%21).
The largest study to date of anticholinergic therapy vs botulinum toxin injection23 in women with urinary urgency incontinence, published in 2012, studied nearly 250 women who had five or more episodes of idiopathic urgency incontinence in a 3-day period. They were randomized either to daily oral therapy (solifenacin 5 mg with possible escalation to 10 mg and, if necessary, a subsequent switch to extended-release trospium 60 mg) plus one intradetrusor injection of saline, or to a daily oral placebo plus one injection of botulinum toxin 100 U.23
The dropout rate was low in both groups, with 93% of patients in both groups completing the 6-month protocol. Women experienced a mean reduction in urgency incontinence episodes of 3.4 per day (baseline 5) in the anticholinergic group vs 3.3 episodes in the botulinum toxin group (P = .81). However, more patients achieved complete resolution of urinary urgency incontinence in the botulinum toxin group than in the anticholinergic therapy group (27% vs 13%; P = .003). Quality of life improved in both groups without a significant difference between the groups. The botulinum toxin group had higher rates of initiation of self-catheterization (5% vs 0%, P = .01) and urinary tract infection (33% vs 13%, P < .001).23
Botulinum toxin as a third-line therapy
In May 2014, the American Urological Association updated its guidelines on idiopathic overactive bladder24 to include botulinum toxin injection as standard third-line therapy for patients in whom behavioral and medical management (ie, anticholinergics and beta-3-agonists) failed.
Interpreting the evidence to date
Overall, studies in idiopathic overactive bladder have shown a reduction in episodes of urgency incontinence and other symptoms, with some data also demonstrating a corresponding improvement in quality of life.
As in neurogenic detrusor overactivity, the main risks associated with botulinum toxin injection are urinary tract infection and the need to initiate self-catheterization. Although 94% of patients studied did not require self-catheterization after injection, the patient’s ability to perform self-catheterization should be determined before proceeding with botulinum toxin injections.
DETRUSOR EXTERNAL SPHINCTER DYSSYNERGIA
Botulinum toxin has been used not only to improve bladder storage but also to facilitate bladder emptying, as in patients with DESD, a lack of coordination between the bladder and the urinary sphincter. Normal voiding involves relaxation of the urinary sphincter and contraction of the bladder; in DESD the sphincter contracts and works against the bladder’s ability to empty. This leads not only to difficulty emptying the bladder but also to elevated bladder pressure, which can cause renal damage if untreated.
DESD can be seen after injury between the pontine micturition center, which coordinates activity between the bladder and the sphincter, and the caudal spinal cord. This can occur in spinal cord injury, multiple sclerosis, myelomeningocele, and transverse myelitis and can cause significant morbidity for the patient.
Treatment options include drug therapy, injection of botulinum toxin into the sphincter, clean intermittent catheterization, indwelling catheterization, urethral stenting, sphincterotomy, and reconstructive surgery such as urinary diversion.25
The goals of therapy are to avoid the need for clean intermittent catheterization in patients who have difficulty with manual dexterity, and to avoid the need for surgical procedures such as sphincterotomy and urinary diversion. The efficacy of urethral stenting is low, and medical management can be limited.26
In the first published report on botulinum toxin for DESD (in 1988),27 of 11 patients with spinal cord injury and DESD who received botulinum toxin injected into the external urethral sphincter, 10 showed signs of sphincter denervation on electromyography and reductions in urethral pressure profiles and postvoid residual volumes. Schurch et al28 and de Sèze et al29 also reported reductions in postvoid residual volume and maximal urethral pressures in patients with spinal cord injury and DESD.
In 2005, Gallien et al30 reported what is still the largest multicenter randomized controlled trial of botulinum toxin injection in DESD. Eighty-six patients with multiple sclerosis, DESD, and chronic urinary retention were randomized to receive either a single transperineal botulinum toxin injection of 100 U plus the alpha-1-blocker alfuzosin, or a placebo injection plus alfuzosin. Botulinum toxin treatment was associated with significantly increased voided volumes and reduced premicturition and maximal detrusor pressures, but no significant decrease in postvoid residual volume.30
More study needed
Despite these findings, a Cochrane Review concluded that, given the limited experience with intrasphincteric injection of botulinum toxin, data from larger randomized controlled trials are needed before making definitive recommendations.25 In the meantime, the clinician must weigh the low morbidity of the procedure against the limited options in the treatment of these patients.
OFF-LABEL UROLOGIC INDICATIONS
Botulinum toxin injection has been studied off-label for painful bladder syndrome/interstitial cystitis and for chronic prostatic pain. Patients with these conditions often describe pain with filling of the bladder, which leads to urinary frequency in an attempt to relieve the pain.
These pain syndromes can be difficult to treat and can have a devastating impact on quality of life. Treatment options include pain management, stress management, physical therapy, intravesical therapies, cystoscopy with hydrodistention, neuromodulation, cyclosporine, urinary diversion surgery, and botulinum toxin injection (an off-label use).31
In painful bladder syndrome/interstitial cystitis, botulinum toxin is thought to act on sensory afferent pathways, as well as to inhibit the release of substance P and glutamate, neuropeptides involved in sensory and nociceptive pathways.6 In animal studies,32 botulinum toxin was found to inhibit the afferent neural response by inhibiting mechanoreceptor-mediated release of adenosine triphosphate and by causing a decrease in calcitonin gene-related peptide, which helps regulate micturition and mediates painful bladder sensation.
Clinical studies to date in pelvic pain syndromes
Data from clinical studies of botulinum toxin injection for pelvic pain syndromes are limited. Zermann et al33 performed transurethral perisphincteric injection in 11 men with chronic prostatic pain, 9 of whom reported subjective pain relief, with an average decrease from 7.2 to 1.6 on a visual analogue scale. Postinjection urodynamic studies showed a decrease in functional urethral length, urethral closure pressure, and postvoid residual volume, and an increase in the peak and average flow rates.33
Abbott et al34 evaluated the effect of botulinum toxin injection into the levator ani in 12 women with chronic pelvic pain and pelvic floor hypertonicity. Pelvic floor manometry showed significant reduction in resting muscle pressures and improvements in dyspareunia and nonmenstrual pain. There were also improvements in quality of life and dyschezia, but these were not statistically significant.
Smith et al35 injected botulinum toxin into the detrusor of 13 women with refractory painful bladder syndrome and interstitial cystitis,35 and 9 women (69%) noted statistically significant improvements in the Interstitial Cystitis Symptom Index and Interstitial Cystitis Problem Index, daytime frequency, nocturia, pain, and urodynamic parameters (volume at first desire to void, and maximum cystometric capacity).
In a prospective randomized study of patients with refractory painful bladder syndrome and interstitial cystitis, Kuo and Chancellor36 compared suburothelial injection of 200 U or 100 U of botulinum toxin plus hydrodistention against hydrodistention alone.Patients who received botulinum toxin had increased bladder capacity and improved long-term pain relief, but no difference was noted between 200 U and 100 U, and more adverse effects were seen with the higher dose.36
Pinto et al37 treated 16 women with refractory painful bladder syndrome and interstitial cystitis with intratrigonal injections of botulinum toxin and reported improvements in pain scores, symptom scores, urinary frequency, and quality-of-life measures. The effect lasted 9.9 months (± 2.4 months) and persisted with successive injections.37
More study needed
Although these studies show that botulinum toxin injection for pelvic pain syndromes has the potential to improve pain, urinary frequency, bladder sensation, bladder capacity, and quality of life, larger randomized controlled trials are needed.
Again, the treatment options are limited for refractory painful bladder syndrome and interstitial cystitis. Patients may be desperate for relief from their symptoms. Practitioners must manage expectations and properly inform patients of the potential risks of treatments, especially with patients who will easily agree to further treatment with the smallest hope of relief.
INJECTION TECHNIQUES
For general points about the procedure to discuss with patients, see “What to tell patients.”
Cystoscopic detrusor injection
This procedure is usually done on an outpatient basis (eg, office, ambulatory surgery center). With the patient in the lithotomy position, 100 mL of 2% lidocaine is instilled into the bladder and is allowed 15 to 20 minutes to take effect. A flexible or rigid cystoscope can be used. Depending on the indication, the bladder is injected with 100 U to 300 U of botulinum toxin. The ideal depth of injection is 2 mm in the detrusor muscle, with each injection spaced about 1 cm apart. The recommended administration for 100 U is to inject 20 sites with 0.5 U per mL of saline and, for 200 U, to inject 30 sites with about 0.67 U per mL of saline.38 The location of the injections into the detrusor can vary, as long as adequate spacing is assured.
Injection sites vary. Proponents of injecting the trigone argue that as it is an area of greater nerve density, patients will have a better clinical response. Opponents argue that trigonal injection could result in distal ureteral paralysis and subsequent ureteral reflux. However, this theoretical concern has not been observed clinically.
Urethral injection (off-label use)
The urethra can be injected cystoscopically or periurethrally. Cystoscopic injection involves localization of the external sphincter using the rigid cystoscope and collagen needle; a total of 100 U is injected into the sphincter under direct vision, typically at the 3 o’clock and 9 o’clock positions.35 The periurethral technique is an option in women and involves a spinal needle with 100 U to 200 U of botulinum toxin injected into the external sphincter muscle at the 2 o’clock and 10 o’clock positions.
ADVERSE EFFECTS AND CONTRAINDICATIONS
Adverse effects are rare for urologic applications. The injections are localized, with little systemic absorption, and the doses are 1/1,000th of the theorized lethal dose in a 70-kg male.2 The maximum recommended dose for a 3-month period is 360 U.
Generalized muscle weakness has been reported in a paraplegic patient and in a tetraplegic patient after detrusor injections.2 Interestingly, both patients had return of bladder spasticity within 2 months, prompting speculation about diffusion of botulinum toxin through the bladder wall.2
Repeat injections can cause an immune response in up to 5% of patients.6 Patients undergoing repeat injections are at risk of forming neutralizing antibodies that can interfere with the efficacy of botulinum toxin.6 In a study by Schulte-Baukloh et al, all patients with antibodies to botulinum toxin had a history of recurrent urinary tract infection.39
Botulinum toxin injection is contraindicated in patients with preexisting neuromuscular disease, such as myasthenia gravis, Eaton-Lambert syndrome, and amyotrophic lateral sclerosis. It should also be avoided in patients who are breastfeeding, pregnant, or using agents that potentiate neuromuscular weakness, such as aminoglycosides.
Patients should be informed that some formulations of botulinum toxin include a stabilizer such as albumin derived from human blood, as this may be of religious or cultural significance.
- Leippold T, Reitz A, Schurch B. Botulinum toxin as a new therapy option for voiding disorders: current state of the art. Eur Urol 2003; 44:165–174.
- Sahai A, Khan M, Fowler CJ, Dasgupta P. Botulinum toxin for the treatment of lower urinary tract symptoms: a review. Neurourol Urodyn 2005; 24:2–12.
- Cruz F. Targets for botulinum toxin in the lower urinary tract. Neurourol Urodyn 2014; 33:31–38.
- Weedmark KA, Lambert DL, Mabon P, et al. Two novel toxin variants revealed by whole-genome sequencing of 175 Clostridium botulinum type E strains. Appl Environ Microbiol 2014; 80:6334–6345.
- Ha US, Park EY, Kim JC. Effect of botulinum toxin on expression of nerve growth factor and transient receptor potential vanilloid 1 in urothelium and detrusor muscle of rats with bladder outlet obstruction-induced detrusor overactivity. Urology 2011; 78:721.e1–721.e6
- Frenkl TL, Rackley RR. Injectable neuromodulatory agents: botulinum toxin therapy. Urol Clin North Am 2005; 32:89–99.
- Ikeda Y, Zabbarova IV, Birder LA, et al. Botulinum neurotoxin serotype A suppresses neurotransmitter release from afferent as well as efferent nerves in the urinary bladder. Eur Urol 2012; 62:1157–1164.
- Goldmark E, Niver B, Ginsberg DA. Neurogenic bladder: from diagnosis to management. Curr Urol Rep 2014; 15:448.
- Andersson KE. Current and future drugs for treatment of MS-associated bladder dysfunction. Ann Phys Rehabil Med 2014; 57:321–328.
- Schurch B, Stöhrer M, Kramer G, Schmid DM, Gaul G, Hauri D. Botulinum-A toxin for treating detrusor hyperreflexia in spinal cord injured patients: a new alternative to anticholinergic drugs? Preliminary results. J Urol 2000; 164:692–697.
- Schurch B, de Sèze M, Denys P, et al; Botox Detrusor Hyperreflexia Study Team. Botulinum toxin type a is a safe and effective treatment for neurogenic urinary incontinence: results of a single treatment, randomized, placebo controlled 6-month study. J Urol 2005; 174:196–200.
- Ehren I, Volz D, Farrelly E, et al. Efficacy and impact of botulinum toxin A on quality of life in patients with neurogenic detrusor overactivity: a randomised, placebo-controlled, double-blind study. Scand J Urol Nephrol 2007; 41:335–340.
- Ginsberg D, Gousse A, Keppenne V, et al. Phase 3 efficacy and tolerability study of onabotulinumtoxinA for urinary incontinence from neurogenic detrusor overactivity. J Urol 2012; 187:2131–2139.
- Cruz F, Herschorn S, Aliotta P, et al. Efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: a randomised, double-blind, placebo-controlled trial. Eur Urol 2011; 60:742–750.
- Wagner TH, Patrick DL, Bavendam TG, Martin ML, Buesching DP. Quality of life of persons with urinary incontinence: development of a new measure. Urology 1996: 47:67–71.
- Kennelly M, Dmochowski R, Ethans K, et al. Long-term efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: an interim analysis. Urology 2013; 81:491–497.
- Carlson JJ, Hansen RN, Dmochowski RR, Globe DR, Colayco DC, Sullivan SD. Estimating the cost-effectiveness of onabotulinumtoxinA for neurogenic detrusor overactivity in the United States. Clin Ther 2013; 35:414–424.
- Abrams P, Cardozo L, Fall M, et al; Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 2003; 61:37–49.
- Milsom I, Coyne KS, Nicholson S, Kvasz M, Chen CI, Wein AJ. Global prevalence and economic burden of urgency urinary incontinence: a systematic review. Eur Urol 2014; 65:79–95.
- Nitti VW, Dmochowski R, Herschorn S, et al; EMBARK Study Group. OnabotulinumtoxinA for the treatment of patients with overactive bladder and urinary incontinence: results of a phase 3, randomized, placebo controlled trial. J Urol 2013; 189:2186–2193.
- Chapple C, Sievert KD, MacDiarmid S, et al. OnabotulinumtoxinA 100 U significantly improves all idiopathic overactive bladder symptoms and quality of life in patients with overactive bladder and urinary incontinence: a randomised, double-blind, placebo-controlled trial. Eur Urol 2013; 64:249–256.
- Colman S, Chapple C, Nitti V, Haag-Molkenteller C, Hastedt C, Massow U. Validation of Treatment Benefit Scale for assessing subjective outcomes in treatment of overactive bladder. Urology 2008; 72:803–807.
- Visco AG, Brubaker L, Richter HE, et al; Pelvic Floor Disorders Network. Anticholinergic therapy vs onabotulinumtoxinA for urgency urinary incontinence. N Engl J Med 2012; 367:1803–1813.
- Gormley EA, Lightner DJ, Burgio KL, et al. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU Guideline. www.auanet.org/education/guidelines/overactive-bladder.cfm. Accessed June 11, 2015.
- Utomo E, Groen J, Blok BF. Surgical management of functional bladder outlet obstruction in adults with neurogenic bladder dysfunction. Cochrane Database Syst Rev 2014; 5:CD004927.
- Mahfouz W, Corcos J. Management of detrusor external sphincter dyssynergia in neurogenic bladder. Eur J Phys Rehabil Med 2011; 47:639–650.
- Dykstra DD, Sidi AA, Scott AB, Pagel JM, Goldish GD. Effects of botulinum A toxin on detrusor-sphincter dyssynergia in spinal cord injury patients. J Urol 1988; 139:919–922.
- Schurch B, Hauri D, Rodic B, Curt A, Meyer M, Rossier AB. Botulinum-A toxin as a treatment of detrusor-sphincter dyssynergia: a prospective study in 24 spinal cord injury patients. J Urol 1996; 155:1023–1029.
- de Sèze M, Petit H, Gallien, de Sèze MP, Joseph PA, Mazaux JM, Barat M. Botulinum a toxin and detrusor sphincter dyssynergia: a double-blind lidocaine-controlled study in 13 patients with spinal cord disease. Eur Urol 2002; 42:56–62.
- Gallien P, Reymann JM, Amarenco G, Nicolas B, de Sèze M, Bellissant E. Placebo controlled, randomised, double blind study of the effects of botulinum A toxin on detrusor sphincter dyssynergia in multiple sclerosis patients. J Neurol Neurosurg Psychiatry 2005; 76:1670–1676.
- Hanno PM, Burks DA, Clemens JQ, et al; Interstitial Cystitis Guidelines Panel of the American Urological Association Education and Research, Inc. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol 2011; 185:2162–2170.
- Chuang YC, Yoshimura N, Huang CC, Chiang PH, Chancellor MB. Intravesical botulinum toxin a administration produces analgesia against acetic acid induced bladder pain responses in rats. J Urol 2004; 172:1529–1532.
- Zermann DH, Ishigooka M, Schubert J, Schmidt RA. Perisphincteric injection of botulinum toxin type A. A treatment option for patients with chronic prostatic pain? Eur Urol 2000; 38:393–399.
- Abbott JA, Jarvis SK, Lyons SD, Thomson A, Vancaille TG. Botulinum toxin type A for chronic pain and pelvic floor spasm in women: a randomized controlled trial. Obstet Gynecol 2006; 108:915–923.
- Smith CP, Radziszewski P, Borkowski A, Somogyi GT, Boone TB, Chancellor MB. Botulinum toxin A has antinociceptive effects in treating interstitial cystitis. Urology 2004; 64:871–875.
- Kuo HC, Chancellor MB. Comparison of intravesical botulinum toxin type A injections plus hydrodistention with hydrodistention alone for the treatment of refractory interstitial cystitis/painful bladder syndrome. BJU Int 2009: 104:657–661.
- Pinto R, Lopes T, Silva J, Silva C, Dinis P, Cruz F. Persistent therapeutic effect of repeated injections of onabotulinum toxin a in refractory bladder pain syndrome/interstitial cystitis. J Urol 2013; 189:548–553.
- Rovner E. Chapter 6: Practical aspects of administration of onabotulinumtoxinA. Neurourol Urodyn 2014; 33(suppl 3):S32–S37.
- Schulte-Baukloh H, Herholz J, Bigalke H, Miller K, Knispel HH. Results of a BoNT/A antibody study in children and adolescents after onabotulinumtoxin A (Botox®) detrusor injection. Urol Int 2011; 87:434–438.
- Leippold T, Reitz A, Schurch B. Botulinum toxin as a new therapy option for voiding disorders: current state of the art. Eur Urol 2003; 44:165–174.
- Sahai A, Khan M, Fowler CJ, Dasgupta P. Botulinum toxin for the treatment of lower urinary tract symptoms: a review. Neurourol Urodyn 2005; 24:2–12.
- Cruz F. Targets for botulinum toxin in the lower urinary tract. Neurourol Urodyn 2014; 33:31–38.
- Weedmark KA, Lambert DL, Mabon P, et al. Two novel toxin variants revealed by whole-genome sequencing of 175 Clostridium botulinum type E strains. Appl Environ Microbiol 2014; 80:6334–6345.
- Ha US, Park EY, Kim JC. Effect of botulinum toxin on expression of nerve growth factor and transient receptor potential vanilloid 1 in urothelium and detrusor muscle of rats with bladder outlet obstruction-induced detrusor overactivity. Urology 2011; 78:721.e1–721.e6
- Frenkl TL, Rackley RR. Injectable neuromodulatory agents: botulinum toxin therapy. Urol Clin North Am 2005; 32:89–99.
- Ikeda Y, Zabbarova IV, Birder LA, et al. Botulinum neurotoxin serotype A suppresses neurotransmitter release from afferent as well as efferent nerves in the urinary bladder. Eur Urol 2012; 62:1157–1164.
- Goldmark E, Niver B, Ginsberg DA. Neurogenic bladder: from diagnosis to management. Curr Urol Rep 2014; 15:448.
- Andersson KE. Current and future drugs for treatment of MS-associated bladder dysfunction. Ann Phys Rehabil Med 2014; 57:321–328.
- Schurch B, Stöhrer M, Kramer G, Schmid DM, Gaul G, Hauri D. Botulinum-A toxin for treating detrusor hyperreflexia in spinal cord injured patients: a new alternative to anticholinergic drugs? Preliminary results. J Urol 2000; 164:692–697.
- Schurch B, de Sèze M, Denys P, et al; Botox Detrusor Hyperreflexia Study Team. Botulinum toxin type a is a safe and effective treatment for neurogenic urinary incontinence: results of a single treatment, randomized, placebo controlled 6-month study. J Urol 2005; 174:196–200.
- Ehren I, Volz D, Farrelly E, et al. Efficacy and impact of botulinum toxin A on quality of life in patients with neurogenic detrusor overactivity: a randomised, placebo-controlled, double-blind study. Scand J Urol Nephrol 2007; 41:335–340.
- Ginsberg D, Gousse A, Keppenne V, et al. Phase 3 efficacy and tolerability study of onabotulinumtoxinA for urinary incontinence from neurogenic detrusor overactivity. J Urol 2012; 187:2131–2139.
- Cruz F, Herschorn S, Aliotta P, et al. Efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: a randomised, double-blind, placebo-controlled trial. Eur Urol 2011; 60:742–750.
- Wagner TH, Patrick DL, Bavendam TG, Martin ML, Buesching DP. Quality of life of persons with urinary incontinence: development of a new measure. Urology 1996: 47:67–71.
- Kennelly M, Dmochowski R, Ethans K, et al. Long-term efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: an interim analysis. Urology 2013; 81:491–497.
- Carlson JJ, Hansen RN, Dmochowski RR, Globe DR, Colayco DC, Sullivan SD. Estimating the cost-effectiveness of onabotulinumtoxinA for neurogenic detrusor overactivity in the United States. Clin Ther 2013; 35:414–424.
- Abrams P, Cardozo L, Fall M, et al; Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 2003; 61:37–49.
- Milsom I, Coyne KS, Nicholson S, Kvasz M, Chen CI, Wein AJ. Global prevalence and economic burden of urgency urinary incontinence: a systematic review. Eur Urol 2014; 65:79–95.
- Nitti VW, Dmochowski R, Herschorn S, et al; EMBARK Study Group. OnabotulinumtoxinA for the treatment of patients with overactive bladder and urinary incontinence: results of a phase 3, randomized, placebo controlled trial. J Urol 2013; 189:2186–2193.
- Chapple C, Sievert KD, MacDiarmid S, et al. OnabotulinumtoxinA 100 U significantly improves all idiopathic overactive bladder symptoms and quality of life in patients with overactive bladder and urinary incontinence: a randomised, double-blind, placebo-controlled trial. Eur Urol 2013; 64:249–256.
- Colman S, Chapple C, Nitti V, Haag-Molkenteller C, Hastedt C, Massow U. Validation of Treatment Benefit Scale for assessing subjective outcomes in treatment of overactive bladder. Urology 2008; 72:803–807.
- Visco AG, Brubaker L, Richter HE, et al; Pelvic Floor Disorders Network. Anticholinergic therapy vs onabotulinumtoxinA for urgency urinary incontinence. N Engl J Med 2012; 367:1803–1813.
- Gormley EA, Lightner DJ, Burgio KL, et al. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU Guideline. www.auanet.org/education/guidelines/overactive-bladder.cfm. Accessed June 11, 2015.
- Utomo E, Groen J, Blok BF. Surgical management of functional bladder outlet obstruction in adults with neurogenic bladder dysfunction. Cochrane Database Syst Rev 2014; 5:CD004927.
- Mahfouz W, Corcos J. Management of detrusor external sphincter dyssynergia in neurogenic bladder. Eur J Phys Rehabil Med 2011; 47:639–650.
- Dykstra DD, Sidi AA, Scott AB, Pagel JM, Goldish GD. Effects of botulinum A toxin on detrusor-sphincter dyssynergia in spinal cord injury patients. J Urol 1988; 139:919–922.
- Schurch B, Hauri D, Rodic B, Curt A, Meyer M, Rossier AB. Botulinum-A toxin as a treatment of detrusor-sphincter dyssynergia: a prospective study in 24 spinal cord injury patients. J Urol 1996; 155:1023–1029.
- de Sèze M, Petit H, Gallien, de Sèze MP, Joseph PA, Mazaux JM, Barat M. Botulinum a toxin and detrusor sphincter dyssynergia: a double-blind lidocaine-controlled study in 13 patients with spinal cord disease. Eur Urol 2002; 42:56–62.
- Gallien P, Reymann JM, Amarenco G, Nicolas B, de Sèze M, Bellissant E. Placebo controlled, randomised, double blind study of the effects of botulinum A toxin on detrusor sphincter dyssynergia in multiple sclerosis patients. J Neurol Neurosurg Psychiatry 2005; 76:1670–1676.
- Hanno PM, Burks DA, Clemens JQ, et al; Interstitial Cystitis Guidelines Panel of the American Urological Association Education and Research, Inc. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol 2011; 185:2162–2170.
- Chuang YC, Yoshimura N, Huang CC, Chiang PH, Chancellor MB. Intravesical botulinum toxin a administration produces analgesia against acetic acid induced bladder pain responses in rats. J Urol 2004; 172:1529–1532.
- Zermann DH, Ishigooka M, Schubert J, Schmidt RA. Perisphincteric injection of botulinum toxin type A. A treatment option for patients with chronic prostatic pain? Eur Urol 2000; 38:393–399.
- Abbott JA, Jarvis SK, Lyons SD, Thomson A, Vancaille TG. Botulinum toxin type A for chronic pain and pelvic floor spasm in women: a randomized controlled trial. Obstet Gynecol 2006; 108:915–923.
- Smith CP, Radziszewski P, Borkowski A, Somogyi GT, Boone TB, Chancellor MB. Botulinum toxin A has antinociceptive effects in treating interstitial cystitis. Urology 2004; 64:871–875.
- Kuo HC, Chancellor MB. Comparison of intravesical botulinum toxin type A injections plus hydrodistention with hydrodistention alone for the treatment of refractory interstitial cystitis/painful bladder syndrome. BJU Int 2009: 104:657–661.
- Pinto R, Lopes T, Silva J, Silva C, Dinis P, Cruz F. Persistent therapeutic effect of repeated injections of onabotulinum toxin a in refractory bladder pain syndrome/interstitial cystitis. J Urol 2013; 189:548–553.
- Rovner E. Chapter 6: Practical aspects of administration of onabotulinumtoxinA. Neurourol Urodyn 2014; 33(suppl 3):S32–S37.
- Schulte-Baukloh H, Herholz J, Bigalke H, Miller K, Knispel HH. Results of a BoNT/A antibody study in children and adolescents after onabotulinumtoxin A (Botox®) detrusor injection. Urol Int 2011; 87:434–438.
KEY POINTS
- Anticholinergic drugs have been the first-line therapy for neurogenic detrusor overactivity. If drug therapy failed, the next option was reconstructive surgery such as cystoplasty. Botulinum toxin injection may be an option in select patients.
- Urinary tract infection and urinary retention requiring intermittent self-catheterization are the most common adverse events of botulinum toxin injection in trials of patients with neurogenic detrusor overactivity or idiopathic overactive bladder.
- Small studies have shown that botulinum toxin injection for painful bladder syndrome/interstitial cystitis can improve pain, urinary frequency, and quality of life. But larger randomized controlled trials are needed.
Care of the aging HIV patient
In the 1980s, human immunodeficiency virus (HIV) infection was considered untreatable and predictably lethal. Today, with highly effective antiretroviral therapy, it has become a chronic condition in which patients have a life expectancy comparable to that in the general population.
This change has led to new challenges for primary care physicians, many of whom now find themselves either the sole medical provider for or the comanager of aging HIV-infected patients. Given that about one-fifth of new HIV diagnoses are now in people over the age of 50, it is crucial that primary care providers be able to recognize and diagnose the disease in this population. In addition, they need to effectively manage the polypharmacy and subsequent drug interactions prevalent in older HIV-infected patients. Finally, the clinician must address comorbid diseases common in the elderly, specifically neurologic, cardiovascular, metabolic, and endocrine disorders, as well as performing routine cancer screening.
Take-home point
- As the number of people age 50 and older with HIV infection increases, primary care providers must be able to both recognize and manage the condition.
RISING PREVALENCE OF HIV IN THE ELDERLY
Globally, about 2.5 million people received a new diagnosis of HIV infection in 2011, and about 35 million people worldwide are currently living with it.1 An estimated 1.1 million Americans are living with HIV, and of these, about 16% do not know they are infected.2
Antiretroviral therapy has greatly improved the life expectancy of HIV-infected patients, and the number of HIV-infected people over age 50 continues to rise. A successfully treated HIV-positive person with a CD4 count higher than 350 × 106/L and a suppressed viral load now has a normal life expectancy.3 In 2011, nearly 20% of newly diagnosed HIV-infected people in the United States were over age 50, as were nearly 25% of those with a new diagnosis of acquired immune deficiency syndrome (AIDS).4 This year (2015), we expect that more than half of all HIV-infected people in the United States will be over age 50.5
The rising prevalence of HIV infection in this age group has prompted reevaluation of screening guidelines. The US Preventive Services Task Force recommends screening for HIV in all people ages 15 to 65, and also after age 65 in people at ongoing risk of infection.6 The American College of Physicians has suggested that the range for routine HIV screening be expanded to age 75.7 The cost-effectiveness of expanded and more frequent HIV testing appears to justify it.8
Take-home points
- An HIV-infected patient who is compliant with an appropriate antiretroviral regimen and has a CD4 count higher than 350 × 106/L and a suppressed viral load now has a normal life expectancy.
- Today, nearly 20% of newly diagnosed HIV-infected people and more than 50% of all HIV-infected people in the United States are over the age of 50.
- The age range for routine screening for HIV infection should be expanded.
HIGH-RISK GROUPS AMONG THE ELDERLY
Early in the HIV epidemic, older patients acquired HIV from blood transfusions received because of hemophilia and other disorders. However, this rapidly ceased after blood banks began screening blood products. Today, people over age 50 who acquire HIV have many of the same risk factors as younger people.
Men who have sex with men are the largest subgroup of HIV-infected people in the United States, even among those over age 50. In particular, white men who have sex with men now constitute the largest demographic group among the HIV-infected elderly.4
Intravenous drug users make up about 15% of older people with HIV.
Women who have sex with infected men or with men at risk of HIV infection make up the largest group of older women with HIV.4
Sex and the older person
Many older HIV-infected people remain sexually active and continue to engage in unprotected sexual intercourse far into advanced age. According to one survey, 53% of Americans ages 65 to 74 are engaging in sexual activity regularly; however, they are not using protective measures with up to 91% of casual partners and 70% of new partners.9,10 Many widowed and divorced people are dating again, and they may be unfamiliar with condom use or may be reluctant to use condoms because condoms can often make it difficult to maintain an erection.
Drugs for erectile dysfunction are making it easier for the elderly to engage in both vaginal and anal intercourse, but often without a condom.9 Older women who no longer worry about getting pregnant may be less likely to insist their partners use a condom and to practice safe sex. In addition, age-related thinning and dryness can cause vaginal tears, increasing the risk of HIV transmission.11
Take-home points
- People older than 50 have risk factors for HIV similar to those in younger people.
- Men who have sex with men compose the largest group of HIV-infected individuals in the elderly population.
- Unprotected sexual intercourse is common in the elderly for several reasons: unfamiliarity with condom use, difficulty maintaining an erection, lack of concern about possible pregnancy, and vaginal thinning and dryness in women.
UNDERDIAGNOSIS AND LATE DIAGNOSIS IN THE ELDERLY
The cumulative number of AIDS cases in adults age 50 and older increased nearly ninefold from 1990 to the end of 2009. Even more worrisome, one-half of HIV-positive adults over age 50 are diagnosed with AIDS simultaneously or within 1 year of their HIV diagnosis.4 This late diagnosis—and therefore late initiation of treatment—is associated with poorer health outcomes and more rapid disease progression.12
HIV infection in older adults often goes undiagnosed, for several reasons.
Providers may underestimate the risk in this population and therefore may not discuss HIV transmission or perform testing. Despite a US Centers for Disease Control and Prevention recommendation that people ages 13 to 64 be tested at least once, and more often if sexually active, only 35% of adults ages 45 to 64 have ever been tested for HIV infection.13
Older patients may not perceive themselves to be at risk of HIV infection because of lack of insight and information about its prevention and transmission. They are also less likely than younger adults to discuss their sexual habits or drug use with providers.14 In addition, compared with the young sexually active population, very little HIV prevention education is targeted to older people.15 Social stigmatization is also a concern for many HIV-infected elderly, as a perceived negative reputation within their community may prevent them from seeking care and disclosing their HIV status.
Take-home points
Reasons that HIV infection is underdiagnosed in the elderly include lack of:
- Provider recognition
- Insight and information about HIV prevention and transmission
- HIV-prevention education targeting the elderly
- Disclosure because of the social stigma of HIV infection.
HIV ACCELERATES AGING, AGING REDUCES IMMUNITY
Many HIV-positive people can expect to live as long as people in the general population, but those who are diagnosed late and thus are started on antiretroviral therapy later in the course of their infection have a reduced life expectancy. Longevity depends on both restoring the CD4 count to near-normal and suppressing the viral load to undetectable levels.3,16 This is especially important for older adults, as HIV may accelerate aging, and aging itself may speed the progression of HIV disease, so that therapy may result in delayed or only partial restoration of immunity.
Older age at the time of HIV infection is a strong predictor of accelerated HIV disease progression in the absence of therapy.17 Left untreated, older patients with HIV lose CD4 cells and progress to AIDS and death faster than younger patients. The deleterious effects of chronic immune activation in the course of HIV infection, combined with the immune senescence of aging, are thought to promote this accelerated course.18
Recent data indicate that starting antiretroviral therapy early can help prevent the CD4-cell impairment that occurs with aging.19 However, in adults over age 50, the capacity to restore the CD4 count with antiretroviral therapy apears to be reduced, despite demonstrated viral load suppression and better adherence.20 Although mean adherence rates appear higher in older HIV-infected patients, they are worse in those with neurocognitive impairment, highlighting the importance of evaluating neurocognition in this population.21
Decreased immune recovery and the subsequent increased risk of serious AIDS events are factors that now favor starting antiretroviral therapy in all HIV patients over age 50, regardless of CD4 count.
Take-home points
- Without treatment, HIV infection in older patients progresses more rapidly to AIDS and death than in younger patients.
- HIV-positive people over age 50 who have never received antiretroviral therapy should be strongly considered for it, regardless of the CD4 count.
SO MANY DRUGS, SO MANY INTERACTIONS
Since HIV patients are now living longer thanks to antiretroviral therapy, they are now experiencing more disease- and treatment-related problems. This has led to an increased likelihood of polypharmacy, defined here as the use of six or more medications.
In general, polypharmacy in the elderly is associated with adverse drug events, drug interactions, inappropriate medication use, delirium, falls, fractures, and poor medication adherence.22,23 But it becomes even more of a problem in HIV-infected elderly patients, as various drug interactions can alter the effectiveness of the antiretroviral regimen and can result in drug toxicity.
The most common classes of medications used in the elderly are antihypertensives, lipid-lowering agents, antiplatelet medications, antidepressants, anxiolytics, sedatives, and analgesics, and many of these have notable interactions with current antiretroviral regimens.24,25 Most medications, including antiretrovirals, are cleared by the liver or kidneys, and the function of these organs often decreases with age, resulting in impaired elimination and in drug accumulation.
Information on drug interactions is readily available from the US Department of Health and Human Services,26 drug interaction databases,27,28 and drug interaction software. The combination of antiretroviral therapy and preexisting polypharmacy significantly increases the risk of serious interactions, which can lead to drug toxicity, poorer adherence with antiretroviral therapy, loss of efficacy of the coadministered medication, or resurgence of HIV infection due to drug-drug interactions affecting the metabolism and ultimate efficacy of the antiretroviral therapy. An increased awareness of common drug-drug interactions can prevent coadministration of potentially harmful medications in elderly HIV patients.
Important interactions between antiretroviral drugs and other drug classes are summarized in Table 1.25–28 Most notably:
- Simvastatin and lovastatin are contraindicated with any protease inhibitor.
- Proton pump inhibitors are not recommended for patients taking ritonavir-boosted atazanavir. If a proton pump inhibitor is necessary, the daily dose should not exceed 20 mg of omeprazole or its equivalent in patients who have never taken a protease inhibitor, and it should be taken 12 hours before boosted atazanavir.26
- Corticosteroids, whether systemic, inhaled, or intranasal (eg, fluticasone, budesonide), should be avoided in combination with any protease inhibitor, as they can cause iatrogenic Cushing syndrome and also pose the risk of adrenal crisis during acute illness.27
Take-home points
- In cases of preexisting polypharmacy, antiretroviral therapy can lead to significant drug toxicity, poor adherence to medications, and resurgence of HIV infection.
- Increased provider awareness of common drug-drug interactions can prevent the prescribing of potentially harmful drug combinations to HIV-infected elderly patients.
COMORBIDITIES
In recent years, more than half of the deaths in HIV patients on antiretroviral therapy have been from noninfectious comorbidities such as cardiovascular disease, bone disease, and renal failure, which often coexist and are associated with advanced age.29 In fact, both older age and each additional year of antiretroviral therapy are independent predictors of polypathology (simultaneous occurrence of two or more defined diseases).30 The Antiretroviral Therapy Cohort Collaboration found that age greater than 50 was strongly associated with increasing rates of non–AIDS-related malignancy and cardiovascular disease.31
CARDIOVASCULAR DISEASE
With the increasing life expectancy of HIV-infected adults on antiretroviral therapy, cardiovascular disease has become an important concern. HIV-infected adults appear to have a significantly greater risk of myocardial infarction and coronary artery disease than age-matched HIV-negative individuals.32 Strikingly, being older than 50 itself increases the risk of hospitalization for cardiovascular disease fivefold (incidence rate ratio 5.01, 95% confidence interval 3.41–7.38).33 In addition, HIV infection is associated with a risk of acute myocardial infarction 50% higher than that explained by recognized risk factors.34
This high prevalence of coronary artery disease is likely from a combination of factors, including increasing age and the chronic inflammation and immune activation associated with HIV infection.35 An association between untreated HIV disease and markers of risk for cardiovascular disease has been identified.36,37
In addition, antiretroviral therapy is associated with dyslipidemia, which is most pronounced with protease inhibitor regimens. Whether specific lipid changes associated with individual antiretroviral drugs affect cardiovascular risk remains uncertain. In the Data Collection on Adverse Events of Anti-HIV Drugs studies,38 only cumulative exposure to indinavir, lopinavir-ritonavir, and didanosine was associated with an increased risk of myocardial infarction.38
Traditional risk factors such as obesity, tobacco use, and genetic predisposition also apply to HIV-infected people.39 In fact, the prevalence of traditional risk factors such as smoking and dyslipidemia is generally higher in HIV-infected people than in the general population, although this situation may be improving.40
Science needs to elucidate the relationship between traditional and nontraditional risk factors for cardiovascular disease in older HIV-infected adults. In the meantime, older patients with HIV require aggressive management of modifiable risk factors.
Tools for assessing cardiovascular risk include the Framingham risk score41 and the Data Collection on Adverse Events of Anti-HIV Drugs 5-year risk calculator.42 The European AIDS Clinical Society guidelines recommend considering changing the antiretroviral regimen if the patient’s 10-year risk of cardiovascular disease is more than 20%.43 Recommended strategies for reducing cardiovascular risk in elderly patients with HIV infection include counseling about smoking cessation and weight loss at every clinic visit and optimally controlling dyslipidemia and hypertension using nationally accepted standardized guidelines.44
Take-home points
- HIV infection is associated with a 50% higher risk of acute myocardial infarction beyond that explained by traditional risk factors.
- Chronic inflammation, immune activation, and dyslipidemia associated with antiretroviral therapy all contribute to cardiovascular disease in HIV-infected patients.
- HIV-infected elderly patients require aggressive management of modifiable risk factors for cardiovascular disease.
ENDOCRINE DISEASE
Diabetes mellitus
The estimated prevalence of diabetes mellitus is 3% in HIV-infected people who have never received antiretroviral therapy, but glucose intolerance increases to the range of 10% to 25% in those who have started it.45 Glucose disorders are associated with traditional risk factors as well as with HIV-associated factors such as lipodystrophy and antiretroviral therapy, specifically long-term use of protease inhibitors.46 Although increasing age and obesity clearly play a role in the development of diabetes mellitus in this population, HIV-specific factors may also allow diabetes to develop at a lower level of adiposity than in people without HIV infection.47
Strategies for preventing type 2 diabetes mellitus in HIV-infected patients focus on avoiding excessive weight gain, especially after starting antiretroviral therapy; regularly screening for diabetes using hemoglobin A1c, both before and after starting antiretroviral therapy; and continuing to check hemoglobin A1c every 6 months. The target hemoglobin A1c should be less than 7.0%. This threshold should be increased to 8% in frail elderly adults if their anticipated life expectancy is less than 5 years, given their higher risk of hypoglycemia, polypharmacy, and drug interactions.48 In addition, as in HIV-negative patients, diabetes screening should be performed if systolic blood pressure exceeds 135/80 mm Hg.
Insulin sensitizers such as metformin and thiazolidinediones should be considered for treating diabetes in HIV-infected patients if no contraindications exist. Consideration may also be given to switching the antiretroviral regimen from a protease inhibitor-based regimen to a nonnucleoside reverse transcriptase inhibitor-based regimen.48
Take-home points
- Glucose intolerance has been associated with HIV-specific factors, including lipodystrophy and antiretroviral therapy.
- Avoiding excessive weight gain, use of insulin-sensitizing medications, and alteration in antiretroviral regimens should be considered for the treatment of diabetes mellitus in HIV infection.
Osteoporosis
Osteoporotic bone disease disproportionately affects patients with advanced HIV infection compared with patients of similar age.49 Bone mineral density is lower and the fracture rate is higher in HIV-infected individuals.
The pathogenesis of bone disease appears to be multifactorial. Traditional risk factors include hypogonadism, smoking, alcohol use, and low body weight, while HIV-related risk factors include chronic immune activation and antiretroviral therapy.50
Several antiretroviral regimens have been linked to clinically significant bone loss, including both tenofovir-based and protease inhibitor-based regimens.51 Most studies have shown that bone mineral density decreases by 2% to 6% in the first 2 years after starting these regimens52; however, long-term effects on bone loss are unknown.
Questions remain. For example, what are the exact mechanisms that lead to the acute decrease in bone mineral density after starting antiretroviral therapy? And why is vitamin D deficiency is so prevalent in HIV infection, with low vitamin D levels seen in up to 60% to 75% of elderly HIV-infected patients?53
Both the Work Group for the HIV and Aging Consensus Project54 and the European AIDS Clinical Society43 recommend screening for and treating causes of secondary low bone mineral density in HIV-infected men over age 50 and postmenopausal HIV-infected women. These causes include vitamin D deficiency. As of 2013, the National Osteoporosis Foundation guidelines include HIV infection and antiretroviral therapy as osteoporosis risk factors that should trigger screening for low bone mineral density with dual-energy x-ray absorptiometry (DXA).55
As in the general population, the preferred treatment for low bone mineral density in people with HIV is a bisphosphonate, in addition to ensuring adequate calcium and vitamin D intake. It is important to repeat DXA imaging every 2 years and to reassess the need for continued bisphosphonate therapy after 3 to 5 years because of a possible increased risk of fracture with prolonged use.
Take-home points
- Osteoporosis and vitamin D deficiency both appear to be more prevalent with HIV infection.
- HIV infection and antiretroviral therapy are risk factors that should prompt DXA screening to evaluate for osteoporosis.
NEUROCOGNITIVE DISORDERS
HIV-associated neurocognitive disorders are common, with an estimated 50% of HIV-infected patients experiencing some degree of cognitive loss and some progressing to dementia.56 Unfortunately, studies suggest that cognitive disorders can occur despite good HIV control with antiretroviral therapy, with one report demonstrating that 84% of patients with cognitive complaints and 64% without complaints were affected by an HIV-associated neurocognitive disorder.57
HIV-associated dementia is often subcortical, with fluctuating symptoms such as psychomotor retardation, difficulty multitasking, and apathy. In contrast to dementia syndromes such as Alzheimer disease, relentless progression is less common in HIV-infected patients who receive antiretroviral therapy.
The Mini-Mental State Examination should not be used to screen for HIV-associated neurocognitive disorders, as it does not assess the domains that are typically impaired. The Montreal Cognitive Assessment has been suggested as the best screening instrument in elderly HIV-infected patients; it is available at no cost at www.mocatest.org.58
As HIV-associated neurocognitive disorder is a diagnosis of exclusion, an evaluation for alternative diagnoses such as syphilis, hypothyroidism, and depression is recommended. If an HIV-associated neurocognitive disorder is diagnosed, referral to specialty care should be considered, as interventions such as lumbar puncture to assess cerebrospinal fluid viral escape and changing the antiretroviral regimen to improve central nervous system penetration are possible options under study.
Patients with poorly controlled HIV and a depressed CD4 count are at risk of a number of central nervous system complications in addition to HIV-associated neurocognitive disorders, eg, central nervous system toxoplasmosis, cryptococcal meningitis, progressive multifocal leukoencephalopathy, and primary central nervous system lymphoma. Adherence to an effective antiretroviral regimen is the primary prevention strategy.
Take-home points
- HIV-associated neurocognitive disorders and dementia can occur despite appropriate HIV control and adherence to antiretroviral therapy.
- Adherence to antiretroviral therapy is the primary prevention against most central nervous system complications in HIV infection.
GERIATRIC SYNDROMES
The aging HIV-infected adult may also be at increased risk of geriatric syndromes.
In particular, a frailty-related phenotype of weight loss, exhaustion, slowness, and low physical activity was more common in HIV-infected elderly than in noninfected elderly.59 HIV-infected men are 4.5 to 10 times more likely than age-matched controls to be frail, and the likelihood of frailty increases with age, duration of HIV infection, having a CD4 count lower than 350 × 106/L, and having uncontrolled HIV replication.60,61
Other geriatric syndromes such as falls, urinary incontinence, and functional impairment have been identified in 25% to 56% of older HIV-infected patients.62 Indeed, the combination of HIV and older age may adversely affect performance of instrumental activities of daily living.63 Also, as previously mentioned, nondisclosure, fear of HIV-related social stigmatization, and a desire to be self-reliant are all factors that perpetuate the social isolation that is common among the HIV-infected elderly.
For these reasons, a comprehensive approach involving a geriatrician, an infectious disease specialist, and community social workers is needed to manage the care of this aging population.
Take-home point
- Geriatric syndromes have an important impact on health in aging HIV patients.
CANCER SCREENING IN HIV PATIENTS
People with HIV have an elevated risk of cancer. Specifically, compared with the general population, their risk is:
- 3,640 times higher for Kaposi sarcoma
- 77 times higher for non-Hodgkin lymphomas
- 6 times higher for cervical cancer.64,65
These cancers are considered “AIDS-defining,” and fortunately, the development of effective antiretroviral therapy in the 1990s has led to a marked reduction in their incidence. However, the aging HIV population is now experiencing a rise in the incidence of non–AIDS-defining cancers, such as cancers of the lung, liver, kidney, anus, head and neck, and skin, as well as Hodgkin lymphoma.66 Table 2 shows the standardized incidence ratio of selected non–AIDS-defining cancers in HIV-infected patients as reported in several large international studies.65,67,68 The etiology for the increased risk of non–AIDS-defining cancers in the HIV-infected population is not clear, but possible explanations include the virus itself, antiretroviral therapy, and co-infection with other viruses such as hepatitis B, hepatitis C, and Epstein-Barr virus.
Guidelines for cancer screening vary by organization, and the American Cancer Society, the National Cancer Institute, and the US Preventive Services Task Force do not have formal screening guidelines for the most common non–AIDS-defining cancers. The European AIDS Clinical Society, however, has proposed some screening recommendations for selected malignancies.43
In general, screening recommendations are similar to those for HIV-negative patients. A specific difference for HIV-infected patients is in cervical cancer screening. HIV-infected women should undergo a Papanicolaou smear at 6-month intervals during the first year after diagnosis of HIV infection and, if the results are normal, annually thereafter. There is no consensus as to whether human papillomavirus testing should be performed routinely on HIV-infected women.
At the time of this writing, there are no recommendations for routine screening for anal cancer, although some specialists recommend anal cytologic screening for HIV-positive men and women, and an annual digital anal examination may be useful to detect masses that could be anal cancer.69
Take-home points
- The incidence of non–AIDS-defining cancers is rising in the aging HIV population.
- There are currently no formal recommendations for routine screening for anal cancer.
FINAL WORD
Because patients with HIV are living longer as a result of newer effective combination antiretroviral therapies, physicians face a new challenge of managing conditions in these patients that are traditionally associated with aging. Providers will need to improve their understanding of drug-drug interactions and polypharmacy issues and be able to address the complex medical and psychosocial issues in this growing population. As patients with HIV on effective antiretroviral therapy grow older, the burden of comorbid medical disease will continue to increase.
- World Health Organization. HIV/AIDS: fact sheet. www.who.int/mediacentre/factsheets/fs360/en/. Accessed April 16, 2015.
- Centers for Disease Control and Prevention (CDC). HIV/AIDS: basic statistics. www.cdc.gov/hiv/basics/statistics.html. Accessed April 16, 2015.
- May MT, Gompels M, Delpech V, et al; UK Collaborative HIV Cohort (UK CHIC) Study. Impact on life expectancy of HIV-1 positive individuals of CD4+ cell count and viral load response to antiretroviral therapy. AIDS 2014; 28:1193–1202.
- Centers for Disease Control and Prevention (CDC). Diagnoses of HIV infection in the United States and dependent areas: HIV surveillance report. www.cdc.gov/hiv/library/reports/surveillance/2011/surveillance_Report_vol_23.html. Accessed April 16, 2015.
- Effros RB, Fletcher CV, Gebo K, et al. Aging and infectious diseases: workshop on HIV infection and aging: what is known and future research directions. Clin Infect Dis 2008; 47:542–553.
- Moyer VA; US Preventive Services Task Force. Screening for HIV: US Preventive Services Task Force Recommendation Statement. Ann Intern Med 2013; 159:51–60.
- Qaseem A, Snow V, Shekelle P, Hopkins R Jr, Owens DK; Clinical Efficacy Assessment Subcommittee, American College of Physicians. Screening for HIV in health care settings: a guidance statement from the American College of Physicians and HIV Medicine Association. Ann Intern Med 2009; 150:125–131.
- Lucas A, Armbruster B. The cost-effectiveness of expanded HIV screening in the United States. AIDS 2013; 27:795–801.
- Lindau ST, Schumm LP, Laumann EO, Levinson W, O’Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the United States. N Engl J Med 2007; 357:762–774.
- Schick V, Herbenick D, Reece M, et al. Sexual behaviors, condom use, and sexual health of Americans over 50: implications for sexual health promotion for older adults. J Sex Med 2010; 7(suppl 5):315–329.
- US Department of Health and Human Services, HIV/AIDS Bureau. The Ryan White HIV/AIDS program: population fact sheet: August 2010. Older adults. http://hab.hrsa.gov/abouthab/populations/olderadultsfacts.pdf. Accessed April 16, 2015.
- May M, Gompels M, Delpech V, et al. Impact of late diagnosis and treatment on life expectancy in people with HIV-1: UK Collaborative HIV Cohort (UK CHIC) Study. BMJ 2011; 343:d6016.
- Branson BM, Handsfield HH, Lampe MA, et al; Centers for Disease Control and Prevention (CDC). Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep 2006; 55:1–17.
- Health Resources and Services Administration (HRSA); HIV/AIDS Bureau. HRSA CAREAction. The graying of HIV. http://hab.hrsa.gov/newspublications/careactionnewsletter/february2009.pdf. Accessed April 16, 2015.
- AIDS InfoNet. Fact sheet number 616: Older people and HIV. http://aidsinfonet.org/fact_sheets/view/616. Accessed April 16, 2015.
- Rodger AJ, Lodwick R, Schechter M, et al; INSIGHT SMART, ESPRIT Study Groups. Mortality in well controlled HIV in the continuous antiretroviral therapy arms of the SMART and ESPRIT trials compared with the general population. AIDS 2013; 27:973–979.
- Kitahata MM, Gange SJ, Abraham AG, et al; NA-ACCORD Investigators. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med 2009; 360:1815–1826.
- Cao W, Jamieson BD, Hultin LE, Hultin PM, Effros RB, Detels R. Premature aging of T cells is associated with faster HIV-1 disease progression. J Acquir Immune Defic Syndr 2009; 50:137–147.
- Allers K, Bösel D, Epple HJ, et al. Effect of age on the CD4+ T-cell impairment in HIV-infected persons without and with cART. J Acquir Immune Defic Syndr 2014; 66:7–15.
- Kalayjian RC, Spritzler J, Matining RM, et al. Older HIV-infected patients on antiretroviral therapy have B-cell expansion and attenuated CD4 cell increases with immune activation reduction. AIDS 2013; 27:1563–1571.
- Althoff KN, Gebo KA, Gange SJ, et al; North American AIDS Cohort Collaboration on Research and Design. CD4 count at presentation for HIV care in the United States and Canada: are those over 50 years more likely to have a delayed presentation? AIDS Res Ther 2010; 7:45.
- Freeland KN, Thompson AN, Zhao Y, Leal JE, Mauldin PD, Moran WP. Medication use and associated risk of falling in a geriatric outpatient population. Ann Pharmacother 2012; 46:1188–1192.
- Steinman MA, Hanlon JT. Managing medications in clinically complex elders: “There’s got to be a happy medium.” JAMA 2010; 304:1592–1601.
- Marzolini C, Elzi L, Gibbons S, et al; Swiss HIV Cohort Study. Prevalence of comedications and effect of potential drug-drug interactions in the Swiss HIV Cohort Study. Antivir Ther 2010; 15:413–423.
- Greene M, Justice AC, Lampiris HW, Valcour V. Management of human immunodeficiency virus infection in advanced age. JAMA 2013; 309:1397–1405.
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. http://aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf. Accessed April 16, 2015.
- UCSF Center for HIV Information. HIVInSite. Comprehensive, up-to-date information on HIV/AIDS treatment, prevention, and policy from the University of California San Francisco: database of antiretroviral drug interactions. http://hivinsite.ucsf.edu/. Accessed April 16, 2015.
- The University of Liverpool. Drug interaction charts. www.hiv-druginteractions.org. Accessed April 16, 2015.
- Vance DE, Mugavero M, Willig J, Raper JL, Saag MS. Aging with HIV: a cross-sectional study of comorbidity prevalence and clinical characteristics across decades of life. J Assoc Nurses AIDS Care 2011; 22:17–25.
- Guaraldi G, Orlando G, Zona S, et al. Premature age-related comorbidities among HIV-infected persons compared with the general population. Clin Infect Dis 2011; 53:1120–1126.
- Antiretroviral Therapy Cohort Collaboration. Causes of death in HIV-1-infected patients treated with antiretroviral therapy, 1996-2006: collaborative analysis of 13 HIV cohort studies. Clin Infect Dis 2010; 50:1387–1396.
- Currier JS, Taylor A, Boyd F, et al. Coronary heart disease in HIV-infected individuals. J Acquir Immune Defic Syndr 2003; 33:506–512.
- Berry SA, Fleishman JA, Moore RD, Gebo KA; HIV Research Network. Trends in reasons for hospitalization in a multisite United States cohort of persons living with HIV, 2001-2008. J Acquir Immune Defic Syndr 2012; 59:368–375.
- Freiberg MS, Chang CC, Kuller LH, et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med 2013; 173:614–622.
- Triant VA, Lee H, Hadigan C, Grinspoon SK. Increased acute myocardial infarction rates and cardiovascular risk factors among patients with human immunodeficiency virus disease. J Clin Endocrinol Metab 2007; 92:2506–2512.
- Calmy A, Gayet-Ageron A, Montecucco F, et al; STACCATO Study Group. HIV increases markers of cardiovascular risk: results from a randomized, treatment interruption trial. AIDS 2009; 23:929–939.
- Phillips AN, Carr A, Neuhaus J, et al. Interruption of antiretroviral therapy and risk of cardiovascular disease in persons with HIV-1 infection: exploratory analyses from the SMART trial. Antivir Ther 2008; 13:177–187.
- Worm SW, Sabin C, Weber R, et al. Risk of myocardial infarction in patients with HIV infection exposed to specific individual antiretroviral drugs from the 3 major drug classes: the Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study. J Infect Dis 2010; 201:318–330.
- Lake JE, Currier JS. Metabolic disease in HIV infection. Lancet Infect Dis 2013; 13:964–975.
- Data Collection on Adverse Events of Anti-HIV Drugs Study Group; Sabin CA, d’Arminio Monforte A, Friis-Moller N, et al. Changes over time in risk factors for cardiovascular disease and use of lipid-lowering drugs in HIV-infected individuals and impact on myocardial infarction. Clin Infect Dis 2008; 46:1101–1110.
- Falcone EL, Mangili A, Skinner S, Alam A, Polak JF, Wanke CA. Framingham risk score and early markers of atherosclerosis in a cohort of adults infected with HIV. Antivir Ther 2011; 16:1–8.
- Friis-Møller N, Thiébaut R, Reiss P, et al; DAD study group. Predicting the risk of cardiovascular disease in HIV-infected patients: the Data Collection on Adverse Effects of Anti-HIV Drugs study. Eur J Cardiovasc Prev Rehabil 2010; 17:491–501.
- European AIDS Clinical Society Guidelines (EACS). www.eacsociety.org/guidelines/eacs-guidelines/eacs-guidelines.html. Accessed April 16, 2015.
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311:507–520.
- Samaras K. The burden of diabetes and hyperlipidemia in treated HIV infection and approaches for cardiometabolic care. Curr HIV/AIDS Rep 2012; 9:206–217.
- Rasmussen LD, Mathiesen ER, Kronborg G, Pedersen C, Gerstoft J, Obel N. Risk of diabetes mellitus in persons with and without HIV: a Danish nationwide population-based cohort study. PLoS One 2012; 7:e44575.
- Capeau J, Bouteloup V, Katlama C, et al; ANRS CO8 APROCO-COPILOTE Cohort Study Group. Ten-year diabetes incidence in 1,046 HIV-infected patients started on a combination antiretroviral treatment. AIDS 2012; 26:303–314.
- American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care 2013; 36(suppl 1):S11–S66.
- Brown TT, Qaqish RB. Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a meta-analytic review. AIDS 2006; 20:2165–2174.
- Rothman MS, Bessesen MT. HIV infection and osteoporosis: pathophysiology, diagnosis, and treatment options. Curr Osteoporos Rep 2012; 10:270–277.
- Bedimo R, Maalouf NM, Zhang S, Drechsler H, Tebas P. Osteoporotic fracture risk associated with cumulative exposure to tenofovir and other antiretroviral agents. AIDS 2012; 26:825–831.
- Brown TT, McComsey GA, King MS, Qaqish RB, Bernstein BM, da Silva BA. Loss of bone mineral density after antiretroviral therapy initiation, independent of antiretroviral regimen. J Acquir Immune Defic Syndr 2009; 51:554–561.
- Rodríguez M, Daniels B, Gunawardene S, Robbins GK. High frequency of vitamin D deficiency in ambulatory HIV-positive patients. AIDS Res Hum Retroviruses 2009; 25:9–14.
- Work Group for HIV and Aging Consensus Project. Summary report from the Human Immunodeficiency Virus and Aging Consensus Project: treatment strategies for clinicians managing older individuals with the human immunodeficiency virus. J Am Geriatr Soc 2012; 60:974–979.
- National Osteoporosis Foundation. Clinician’s guide to prevention and treatment of osteoporosis. 2013 Issue, Version 3. http://nof.org/files/nof/public/content/file/2791/upload/919.pdf. Accessed April 16, 2015.
- Heaton RK, Clifford DB, Franklin DR Jr, et al; CHARTER Group. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology 2010; 75:2087–2096.
- Simioni S, Cavassini M, Annoni JM, et al. Cognitive dysfunction in HIV patients despite long-standing suppression of viremia. AIDS 2010; 24:1243–1250.
- Valcour VG. Evaluating cognitive impairment in the clinical setting: practical screening and assessment tools. Top Antivir Med 2011; 19:175–180.
- Desquilbet L, Jacobson LP, Fried LP, et al; Multicenter AIDS Cohort Study. HIV-1 infection is associated with an earlier occurrence of a phenotype related to frailty. J Gerontol A Biol Sci Med Sci 2007; 62:1279–1286.
- Desquilbet L, Jacobson LP, Fried LP, et al. A frailty-related phenotype before HAART initiation as an independent risk factor for AIDS or death after HAART among HIV-infected men. J Gerontol A Biol Sci Med Sci 2011; 66:1030–1038.
- Fried LP, Tangen CM, Walston J, et al; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56:M146–M156.
- Greene M, Valcour V, Miao Y, et al. Geriatric syndromes are common among older HIV-infected adults. 21st Conference on Retroviruses and Opportunistic Infections (CROI) 2014 March 3-6, Boston MA.
- Morgan EE, Iudicello JE, Weber E, et al; HIV Neurobehavioral Research Program (HNRP) Group. Synergistic effects of HIV infection and older age on daily functioning. J Acquir Immune Defic Syndr 2012; 61:341–348.
- Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet 2007; 370:59–67.
- Shiels MS, Pfeiffer RM, Gail MH, et al. Cancer burden in the HIV-infected population in the United States. J Natl Cancer Inst 2011; 103:753–762.
- Deeken JF, Tjen-A-Looi A, Rudek MA, et al. The rising challenge of non-AIDS-defining cancers in HIV-infected patients. Clin Infect Dis 2012; 55:1228–1235.
- Powles T, Robinson D, Stebbing J, et al. Highly active antiretroviral therapy and the incidence of non-AIDS-defining cancers in people with HIV infection. J Clin Oncol 2009; 27:884–890.
- Patel P, Hanson DL, Sullivan PS, et al; Adult and Adolescent Spectrum of Disease Project and HIV Outpatient Study Investigators. Incidence of types of cancer among HIV-infected persons compared with the general population in the United States, 1992-2003. Ann Intern Med 2008; 148:728–736.
- Kaplan JE, Benson C, Holmes KK, Brooks JT, Pau A, Masur H; Centers for Disease Control and Prevention (CDC); National Institutes of Health; HIV Medicine Association of the Infectious Diseases Society of America. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep 2009; 58:1–207.
In the 1980s, human immunodeficiency virus (HIV) infection was considered untreatable and predictably lethal. Today, with highly effective antiretroviral therapy, it has become a chronic condition in which patients have a life expectancy comparable to that in the general population.
This change has led to new challenges for primary care physicians, many of whom now find themselves either the sole medical provider for or the comanager of aging HIV-infected patients. Given that about one-fifth of new HIV diagnoses are now in people over the age of 50, it is crucial that primary care providers be able to recognize and diagnose the disease in this population. In addition, they need to effectively manage the polypharmacy and subsequent drug interactions prevalent in older HIV-infected patients. Finally, the clinician must address comorbid diseases common in the elderly, specifically neurologic, cardiovascular, metabolic, and endocrine disorders, as well as performing routine cancer screening.
Take-home point
- As the number of people age 50 and older with HIV infection increases, primary care providers must be able to both recognize and manage the condition.
RISING PREVALENCE OF HIV IN THE ELDERLY
Globally, about 2.5 million people received a new diagnosis of HIV infection in 2011, and about 35 million people worldwide are currently living with it.1 An estimated 1.1 million Americans are living with HIV, and of these, about 16% do not know they are infected.2
Antiretroviral therapy has greatly improved the life expectancy of HIV-infected patients, and the number of HIV-infected people over age 50 continues to rise. A successfully treated HIV-positive person with a CD4 count higher than 350 × 106/L and a suppressed viral load now has a normal life expectancy.3 In 2011, nearly 20% of newly diagnosed HIV-infected people in the United States were over age 50, as were nearly 25% of those with a new diagnosis of acquired immune deficiency syndrome (AIDS).4 This year (2015), we expect that more than half of all HIV-infected people in the United States will be over age 50.5
The rising prevalence of HIV infection in this age group has prompted reevaluation of screening guidelines. The US Preventive Services Task Force recommends screening for HIV in all people ages 15 to 65, and also after age 65 in people at ongoing risk of infection.6 The American College of Physicians has suggested that the range for routine HIV screening be expanded to age 75.7 The cost-effectiveness of expanded and more frequent HIV testing appears to justify it.8
Take-home points
- An HIV-infected patient who is compliant with an appropriate antiretroviral regimen and has a CD4 count higher than 350 × 106/L and a suppressed viral load now has a normal life expectancy.
- Today, nearly 20% of newly diagnosed HIV-infected people and more than 50% of all HIV-infected people in the United States are over the age of 50.
- The age range for routine screening for HIV infection should be expanded.
HIGH-RISK GROUPS AMONG THE ELDERLY
Early in the HIV epidemic, older patients acquired HIV from blood transfusions received because of hemophilia and other disorders. However, this rapidly ceased after blood banks began screening blood products. Today, people over age 50 who acquire HIV have many of the same risk factors as younger people.
Men who have sex with men are the largest subgroup of HIV-infected people in the United States, even among those over age 50. In particular, white men who have sex with men now constitute the largest demographic group among the HIV-infected elderly.4
Intravenous drug users make up about 15% of older people with HIV.
Women who have sex with infected men or with men at risk of HIV infection make up the largest group of older women with HIV.4
Sex and the older person
Many older HIV-infected people remain sexually active and continue to engage in unprotected sexual intercourse far into advanced age. According to one survey, 53% of Americans ages 65 to 74 are engaging in sexual activity regularly; however, they are not using protective measures with up to 91% of casual partners and 70% of new partners.9,10 Many widowed and divorced people are dating again, and they may be unfamiliar with condom use or may be reluctant to use condoms because condoms can often make it difficult to maintain an erection.
Drugs for erectile dysfunction are making it easier for the elderly to engage in both vaginal and anal intercourse, but often without a condom.9 Older women who no longer worry about getting pregnant may be less likely to insist their partners use a condom and to practice safe sex. In addition, age-related thinning and dryness can cause vaginal tears, increasing the risk of HIV transmission.11
Take-home points
- People older than 50 have risk factors for HIV similar to those in younger people.
- Men who have sex with men compose the largest group of HIV-infected individuals in the elderly population.
- Unprotected sexual intercourse is common in the elderly for several reasons: unfamiliarity with condom use, difficulty maintaining an erection, lack of concern about possible pregnancy, and vaginal thinning and dryness in women.
UNDERDIAGNOSIS AND LATE DIAGNOSIS IN THE ELDERLY
The cumulative number of AIDS cases in adults age 50 and older increased nearly ninefold from 1990 to the end of 2009. Even more worrisome, one-half of HIV-positive adults over age 50 are diagnosed with AIDS simultaneously or within 1 year of their HIV diagnosis.4 This late diagnosis—and therefore late initiation of treatment—is associated with poorer health outcomes and more rapid disease progression.12
HIV infection in older adults often goes undiagnosed, for several reasons.
Providers may underestimate the risk in this population and therefore may not discuss HIV transmission or perform testing. Despite a US Centers for Disease Control and Prevention recommendation that people ages 13 to 64 be tested at least once, and more often if sexually active, only 35% of adults ages 45 to 64 have ever been tested for HIV infection.13
Older patients may not perceive themselves to be at risk of HIV infection because of lack of insight and information about its prevention and transmission. They are also less likely than younger adults to discuss their sexual habits or drug use with providers.14 In addition, compared with the young sexually active population, very little HIV prevention education is targeted to older people.15 Social stigmatization is also a concern for many HIV-infected elderly, as a perceived negative reputation within their community may prevent them from seeking care and disclosing their HIV status.
Take-home points
Reasons that HIV infection is underdiagnosed in the elderly include lack of:
- Provider recognition
- Insight and information about HIV prevention and transmission
- HIV-prevention education targeting the elderly
- Disclosure because of the social stigma of HIV infection.
HIV ACCELERATES AGING, AGING REDUCES IMMUNITY
Many HIV-positive people can expect to live as long as people in the general population, but those who are diagnosed late and thus are started on antiretroviral therapy later in the course of their infection have a reduced life expectancy. Longevity depends on both restoring the CD4 count to near-normal and suppressing the viral load to undetectable levels.3,16 This is especially important for older adults, as HIV may accelerate aging, and aging itself may speed the progression of HIV disease, so that therapy may result in delayed or only partial restoration of immunity.
Older age at the time of HIV infection is a strong predictor of accelerated HIV disease progression in the absence of therapy.17 Left untreated, older patients with HIV lose CD4 cells and progress to AIDS and death faster than younger patients. The deleterious effects of chronic immune activation in the course of HIV infection, combined with the immune senescence of aging, are thought to promote this accelerated course.18
Recent data indicate that starting antiretroviral therapy early can help prevent the CD4-cell impairment that occurs with aging.19 However, in adults over age 50, the capacity to restore the CD4 count with antiretroviral therapy apears to be reduced, despite demonstrated viral load suppression and better adherence.20 Although mean adherence rates appear higher in older HIV-infected patients, they are worse in those with neurocognitive impairment, highlighting the importance of evaluating neurocognition in this population.21
Decreased immune recovery and the subsequent increased risk of serious AIDS events are factors that now favor starting antiretroviral therapy in all HIV patients over age 50, regardless of CD4 count.
Take-home points
- Without treatment, HIV infection in older patients progresses more rapidly to AIDS and death than in younger patients.
- HIV-positive people over age 50 who have never received antiretroviral therapy should be strongly considered for it, regardless of the CD4 count.
SO MANY DRUGS, SO MANY INTERACTIONS
Since HIV patients are now living longer thanks to antiretroviral therapy, they are now experiencing more disease- and treatment-related problems. This has led to an increased likelihood of polypharmacy, defined here as the use of six or more medications.
In general, polypharmacy in the elderly is associated with adverse drug events, drug interactions, inappropriate medication use, delirium, falls, fractures, and poor medication adherence.22,23 But it becomes even more of a problem in HIV-infected elderly patients, as various drug interactions can alter the effectiveness of the antiretroviral regimen and can result in drug toxicity.
The most common classes of medications used in the elderly are antihypertensives, lipid-lowering agents, antiplatelet medications, antidepressants, anxiolytics, sedatives, and analgesics, and many of these have notable interactions with current antiretroviral regimens.24,25 Most medications, including antiretrovirals, are cleared by the liver or kidneys, and the function of these organs often decreases with age, resulting in impaired elimination and in drug accumulation.
Information on drug interactions is readily available from the US Department of Health and Human Services,26 drug interaction databases,27,28 and drug interaction software. The combination of antiretroviral therapy and preexisting polypharmacy significantly increases the risk of serious interactions, which can lead to drug toxicity, poorer adherence with antiretroviral therapy, loss of efficacy of the coadministered medication, or resurgence of HIV infection due to drug-drug interactions affecting the metabolism and ultimate efficacy of the antiretroviral therapy. An increased awareness of common drug-drug interactions can prevent coadministration of potentially harmful medications in elderly HIV patients.
Important interactions between antiretroviral drugs and other drug classes are summarized in Table 1.25–28 Most notably:
- Simvastatin and lovastatin are contraindicated with any protease inhibitor.
- Proton pump inhibitors are not recommended for patients taking ritonavir-boosted atazanavir. If a proton pump inhibitor is necessary, the daily dose should not exceed 20 mg of omeprazole or its equivalent in patients who have never taken a protease inhibitor, and it should be taken 12 hours before boosted atazanavir.26
- Corticosteroids, whether systemic, inhaled, or intranasal (eg, fluticasone, budesonide), should be avoided in combination with any protease inhibitor, as they can cause iatrogenic Cushing syndrome and also pose the risk of adrenal crisis during acute illness.27
Take-home points
- In cases of preexisting polypharmacy, antiretroviral therapy can lead to significant drug toxicity, poor adherence to medications, and resurgence of HIV infection.
- Increased provider awareness of common drug-drug interactions can prevent the prescribing of potentially harmful drug combinations to HIV-infected elderly patients.
COMORBIDITIES
In recent years, more than half of the deaths in HIV patients on antiretroviral therapy have been from noninfectious comorbidities such as cardiovascular disease, bone disease, and renal failure, which often coexist and are associated with advanced age.29 In fact, both older age and each additional year of antiretroviral therapy are independent predictors of polypathology (simultaneous occurrence of two or more defined diseases).30 The Antiretroviral Therapy Cohort Collaboration found that age greater than 50 was strongly associated with increasing rates of non–AIDS-related malignancy and cardiovascular disease.31
CARDIOVASCULAR DISEASE
With the increasing life expectancy of HIV-infected adults on antiretroviral therapy, cardiovascular disease has become an important concern. HIV-infected adults appear to have a significantly greater risk of myocardial infarction and coronary artery disease than age-matched HIV-negative individuals.32 Strikingly, being older than 50 itself increases the risk of hospitalization for cardiovascular disease fivefold (incidence rate ratio 5.01, 95% confidence interval 3.41–7.38).33 In addition, HIV infection is associated with a risk of acute myocardial infarction 50% higher than that explained by recognized risk factors.34
This high prevalence of coronary artery disease is likely from a combination of factors, including increasing age and the chronic inflammation and immune activation associated with HIV infection.35 An association between untreated HIV disease and markers of risk for cardiovascular disease has been identified.36,37
In addition, antiretroviral therapy is associated with dyslipidemia, which is most pronounced with protease inhibitor regimens. Whether specific lipid changes associated with individual antiretroviral drugs affect cardiovascular risk remains uncertain. In the Data Collection on Adverse Events of Anti-HIV Drugs studies,38 only cumulative exposure to indinavir, lopinavir-ritonavir, and didanosine was associated with an increased risk of myocardial infarction.38
Traditional risk factors such as obesity, tobacco use, and genetic predisposition also apply to HIV-infected people.39 In fact, the prevalence of traditional risk factors such as smoking and dyslipidemia is generally higher in HIV-infected people than in the general population, although this situation may be improving.40
Science needs to elucidate the relationship between traditional and nontraditional risk factors for cardiovascular disease in older HIV-infected adults. In the meantime, older patients with HIV require aggressive management of modifiable risk factors.
Tools for assessing cardiovascular risk include the Framingham risk score41 and the Data Collection on Adverse Events of Anti-HIV Drugs 5-year risk calculator.42 The European AIDS Clinical Society guidelines recommend considering changing the antiretroviral regimen if the patient’s 10-year risk of cardiovascular disease is more than 20%.43 Recommended strategies for reducing cardiovascular risk in elderly patients with HIV infection include counseling about smoking cessation and weight loss at every clinic visit and optimally controlling dyslipidemia and hypertension using nationally accepted standardized guidelines.44
Take-home points
- HIV infection is associated with a 50% higher risk of acute myocardial infarction beyond that explained by traditional risk factors.
- Chronic inflammation, immune activation, and dyslipidemia associated with antiretroviral therapy all contribute to cardiovascular disease in HIV-infected patients.
- HIV-infected elderly patients require aggressive management of modifiable risk factors for cardiovascular disease.
ENDOCRINE DISEASE
Diabetes mellitus
The estimated prevalence of diabetes mellitus is 3% in HIV-infected people who have never received antiretroviral therapy, but glucose intolerance increases to the range of 10% to 25% in those who have started it.45 Glucose disorders are associated with traditional risk factors as well as with HIV-associated factors such as lipodystrophy and antiretroviral therapy, specifically long-term use of protease inhibitors.46 Although increasing age and obesity clearly play a role in the development of diabetes mellitus in this population, HIV-specific factors may also allow diabetes to develop at a lower level of adiposity than in people without HIV infection.47
Strategies for preventing type 2 diabetes mellitus in HIV-infected patients focus on avoiding excessive weight gain, especially after starting antiretroviral therapy; regularly screening for diabetes using hemoglobin A1c, both before and after starting antiretroviral therapy; and continuing to check hemoglobin A1c every 6 months. The target hemoglobin A1c should be less than 7.0%. This threshold should be increased to 8% in frail elderly adults if their anticipated life expectancy is less than 5 years, given their higher risk of hypoglycemia, polypharmacy, and drug interactions.48 In addition, as in HIV-negative patients, diabetes screening should be performed if systolic blood pressure exceeds 135/80 mm Hg.
Insulin sensitizers such as metformin and thiazolidinediones should be considered for treating diabetes in HIV-infected patients if no contraindications exist. Consideration may also be given to switching the antiretroviral regimen from a protease inhibitor-based regimen to a nonnucleoside reverse transcriptase inhibitor-based regimen.48
Take-home points
- Glucose intolerance has been associated with HIV-specific factors, including lipodystrophy and antiretroviral therapy.
- Avoiding excessive weight gain, use of insulin-sensitizing medications, and alteration in antiretroviral regimens should be considered for the treatment of diabetes mellitus in HIV infection.
Osteoporosis
Osteoporotic bone disease disproportionately affects patients with advanced HIV infection compared with patients of similar age.49 Bone mineral density is lower and the fracture rate is higher in HIV-infected individuals.
The pathogenesis of bone disease appears to be multifactorial. Traditional risk factors include hypogonadism, smoking, alcohol use, and low body weight, while HIV-related risk factors include chronic immune activation and antiretroviral therapy.50
Several antiretroviral regimens have been linked to clinically significant bone loss, including both tenofovir-based and protease inhibitor-based regimens.51 Most studies have shown that bone mineral density decreases by 2% to 6% in the first 2 years after starting these regimens52; however, long-term effects on bone loss are unknown.
Questions remain. For example, what are the exact mechanisms that lead to the acute decrease in bone mineral density after starting antiretroviral therapy? And why is vitamin D deficiency is so prevalent in HIV infection, with low vitamin D levels seen in up to 60% to 75% of elderly HIV-infected patients?53
Both the Work Group for the HIV and Aging Consensus Project54 and the European AIDS Clinical Society43 recommend screening for and treating causes of secondary low bone mineral density in HIV-infected men over age 50 and postmenopausal HIV-infected women. These causes include vitamin D deficiency. As of 2013, the National Osteoporosis Foundation guidelines include HIV infection and antiretroviral therapy as osteoporosis risk factors that should trigger screening for low bone mineral density with dual-energy x-ray absorptiometry (DXA).55
As in the general population, the preferred treatment for low bone mineral density in people with HIV is a bisphosphonate, in addition to ensuring adequate calcium and vitamin D intake. It is important to repeat DXA imaging every 2 years and to reassess the need for continued bisphosphonate therapy after 3 to 5 years because of a possible increased risk of fracture with prolonged use.
Take-home points
- Osteoporosis and vitamin D deficiency both appear to be more prevalent with HIV infection.
- HIV infection and antiretroviral therapy are risk factors that should prompt DXA screening to evaluate for osteoporosis.
NEUROCOGNITIVE DISORDERS
HIV-associated neurocognitive disorders are common, with an estimated 50% of HIV-infected patients experiencing some degree of cognitive loss and some progressing to dementia.56 Unfortunately, studies suggest that cognitive disorders can occur despite good HIV control with antiretroviral therapy, with one report demonstrating that 84% of patients with cognitive complaints and 64% without complaints were affected by an HIV-associated neurocognitive disorder.57
HIV-associated dementia is often subcortical, with fluctuating symptoms such as psychomotor retardation, difficulty multitasking, and apathy. In contrast to dementia syndromes such as Alzheimer disease, relentless progression is less common in HIV-infected patients who receive antiretroviral therapy.
The Mini-Mental State Examination should not be used to screen for HIV-associated neurocognitive disorders, as it does not assess the domains that are typically impaired. The Montreal Cognitive Assessment has been suggested as the best screening instrument in elderly HIV-infected patients; it is available at no cost at www.mocatest.org.58
As HIV-associated neurocognitive disorder is a diagnosis of exclusion, an evaluation for alternative diagnoses such as syphilis, hypothyroidism, and depression is recommended. If an HIV-associated neurocognitive disorder is diagnosed, referral to specialty care should be considered, as interventions such as lumbar puncture to assess cerebrospinal fluid viral escape and changing the antiretroviral regimen to improve central nervous system penetration are possible options under study.
Patients with poorly controlled HIV and a depressed CD4 count are at risk of a number of central nervous system complications in addition to HIV-associated neurocognitive disorders, eg, central nervous system toxoplasmosis, cryptococcal meningitis, progressive multifocal leukoencephalopathy, and primary central nervous system lymphoma. Adherence to an effective antiretroviral regimen is the primary prevention strategy.
Take-home points
- HIV-associated neurocognitive disorders and dementia can occur despite appropriate HIV control and adherence to antiretroviral therapy.
- Adherence to antiretroviral therapy is the primary prevention against most central nervous system complications in HIV infection.
GERIATRIC SYNDROMES
The aging HIV-infected adult may also be at increased risk of geriatric syndromes.
In particular, a frailty-related phenotype of weight loss, exhaustion, slowness, and low physical activity was more common in HIV-infected elderly than in noninfected elderly.59 HIV-infected men are 4.5 to 10 times more likely than age-matched controls to be frail, and the likelihood of frailty increases with age, duration of HIV infection, having a CD4 count lower than 350 × 106/L, and having uncontrolled HIV replication.60,61
Other geriatric syndromes such as falls, urinary incontinence, and functional impairment have been identified in 25% to 56% of older HIV-infected patients.62 Indeed, the combination of HIV and older age may adversely affect performance of instrumental activities of daily living.63 Also, as previously mentioned, nondisclosure, fear of HIV-related social stigmatization, and a desire to be self-reliant are all factors that perpetuate the social isolation that is common among the HIV-infected elderly.
For these reasons, a comprehensive approach involving a geriatrician, an infectious disease specialist, and community social workers is needed to manage the care of this aging population.
Take-home point
- Geriatric syndromes have an important impact on health in aging HIV patients.
CANCER SCREENING IN HIV PATIENTS
People with HIV have an elevated risk of cancer. Specifically, compared with the general population, their risk is:
- 3,640 times higher for Kaposi sarcoma
- 77 times higher for non-Hodgkin lymphomas
- 6 times higher for cervical cancer.64,65
These cancers are considered “AIDS-defining,” and fortunately, the development of effective antiretroviral therapy in the 1990s has led to a marked reduction in their incidence. However, the aging HIV population is now experiencing a rise in the incidence of non–AIDS-defining cancers, such as cancers of the lung, liver, kidney, anus, head and neck, and skin, as well as Hodgkin lymphoma.66 Table 2 shows the standardized incidence ratio of selected non–AIDS-defining cancers in HIV-infected patients as reported in several large international studies.65,67,68 The etiology for the increased risk of non–AIDS-defining cancers in the HIV-infected population is not clear, but possible explanations include the virus itself, antiretroviral therapy, and co-infection with other viruses such as hepatitis B, hepatitis C, and Epstein-Barr virus.
Guidelines for cancer screening vary by organization, and the American Cancer Society, the National Cancer Institute, and the US Preventive Services Task Force do not have formal screening guidelines for the most common non–AIDS-defining cancers. The European AIDS Clinical Society, however, has proposed some screening recommendations for selected malignancies.43
In general, screening recommendations are similar to those for HIV-negative patients. A specific difference for HIV-infected patients is in cervical cancer screening. HIV-infected women should undergo a Papanicolaou smear at 6-month intervals during the first year after diagnosis of HIV infection and, if the results are normal, annually thereafter. There is no consensus as to whether human papillomavirus testing should be performed routinely on HIV-infected women.
At the time of this writing, there are no recommendations for routine screening for anal cancer, although some specialists recommend anal cytologic screening for HIV-positive men and women, and an annual digital anal examination may be useful to detect masses that could be anal cancer.69
Take-home points
- The incidence of non–AIDS-defining cancers is rising in the aging HIV population.
- There are currently no formal recommendations for routine screening for anal cancer.
FINAL WORD
Because patients with HIV are living longer as a result of newer effective combination antiretroviral therapies, physicians face a new challenge of managing conditions in these patients that are traditionally associated with aging. Providers will need to improve their understanding of drug-drug interactions and polypharmacy issues and be able to address the complex medical and psychosocial issues in this growing population. As patients with HIV on effective antiretroviral therapy grow older, the burden of comorbid medical disease will continue to increase.
In the 1980s, human immunodeficiency virus (HIV) infection was considered untreatable and predictably lethal. Today, with highly effective antiretroviral therapy, it has become a chronic condition in which patients have a life expectancy comparable to that in the general population.
This change has led to new challenges for primary care physicians, many of whom now find themselves either the sole medical provider for or the comanager of aging HIV-infected patients. Given that about one-fifth of new HIV diagnoses are now in people over the age of 50, it is crucial that primary care providers be able to recognize and diagnose the disease in this population. In addition, they need to effectively manage the polypharmacy and subsequent drug interactions prevalent in older HIV-infected patients. Finally, the clinician must address comorbid diseases common in the elderly, specifically neurologic, cardiovascular, metabolic, and endocrine disorders, as well as performing routine cancer screening.
Take-home point
- As the number of people age 50 and older with HIV infection increases, primary care providers must be able to both recognize and manage the condition.
RISING PREVALENCE OF HIV IN THE ELDERLY
Globally, about 2.5 million people received a new diagnosis of HIV infection in 2011, and about 35 million people worldwide are currently living with it.1 An estimated 1.1 million Americans are living with HIV, and of these, about 16% do not know they are infected.2
Antiretroviral therapy has greatly improved the life expectancy of HIV-infected patients, and the number of HIV-infected people over age 50 continues to rise. A successfully treated HIV-positive person with a CD4 count higher than 350 × 106/L and a suppressed viral load now has a normal life expectancy.3 In 2011, nearly 20% of newly diagnosed HIV-infected people in the United States were over age 50, as were nearly 25% of those with a new diagnosis of acquired immune deficiency syndrome (AIDS).4 This year (2015), we expect that more than half of all HIV-infected people in the United States will be over age 50.5
The rising prevalence of HIV infection in this age group has prompted reevaluation of screening guidelines. The US Preventive Services Task Force recommends screening for HIV in all people ages 15 to 65, and also after age 65 in people at ongoing risk of infection.6 The American College of Physicians has suggested that the range for routine HIV screening be expanded to age 75.7 The cost-effectiveness of expanded and more frequent HIV testing appears to justify it.8
Take-home points
- An HIV-infected patient who is compliant with an appropriate antiretroviral regimen and has a CD4 count higher than 350 × 106/L and a suppressed viral load now has a normal life expectancy.
- Today, nearly 20% of newly diagnosed HIV-infected people and more than 50% of all HIV-infected people in the United States are over the age of 50.
- The age range for routine screening for HIV infection should be expanded.
HIGH-RISK GROUPS AMONG THE ELDERLY
Early in the HIV epidemic, older patients acquired HIV from blood transfusions received because of hemophilia and other disorders. However, this rapidly ceased after blood banks began screening blood products. Today, people over age 50 who acquire HIV have many of the same risk factors as younger people.
Men who have sex with men are the largest subgroup of HIV-infected people in the United States, even among those over age 50. In particular, white men who have sex with men now constitute the largest demographic group among the HIV-infected elderly.4
Intravenous drug users make up about 15% of older people with HIV.
Women who have sex with infected men or with men at risk of HIV infection make up the largest group of older women with HIV.4
Sex and the older person
Many older HIV-infected people remain sexually active and continue to engage in unprotected sexual intercourse far into advanced age. According to one survey, 53% of Americans ages 65 to 74 are engaging in sexual activity regularly; however, they are not using protective measures with up to 91% of casual partners and 70% of new partners.9,10 Many widowed and divorced people are dating again, and they may be unfamiliar with condom use or may be reluctant to use condoms because condoms can often make it difficult to maintain an erection.
Drugs for erectile dysfunction are making it easier for the elderly to engage in both vaginal and anal intercourse, but often without a condom.9 Older women who no longer worry about getting pregnant may be less likely to insist their partners use a condom and to practice safe sex. In addition, age-related thinning and dryness can cause vaginal tears, increasing the risk of HIV transmission.11
Take-home points
- People older than 50 have risk factors for HIV similar to those in younger people.
- Men who have sex with men compose the largest group of HIV-infected individuals in the elderly population.
- Unprotected sexual intercourse is common in the elderly for several reasons: unfamiliarity with condom use, difficulty maintaining an erection, lack of concern about possible pregnancy, and vaginal thinning and dryness in women.
UNDERDIAGNOSIS AND LATE DIAGNOSIS IN THE ELDERLY
The cumulative number of AIDS cases in adults age 50 and older increased nearly ninefold from 1990 to the end of 2009. Even more worrisome, one-half of HIV-positive adults over age 50 are diagnosed with AIDS simultaneously or within 1 year of their HIV diagnosis.4 This late diagnosis—and therefore late initiation of treatment—is associated with poorer health outcomes and more rapid disease progression.12
HIV infection in older adults often goes undiagnosed, for several reasons.
Providers may underestimate the risk in this population and therefore may not discuss HIV transmission or perform testing. Despite a US Centers for Disease Control and Prevention recommendation that people ages 13 to 64 be tested at least once, and more often if sexually active, only 35% of adults ages 45 to 64 have ever been tested for HIV infection.13
Older patients may not perceive themselves to be at risk of HIV infection because of lack of insight and information about its prevention and transmission. They are also less likely than younger adults to discuss their sexual habits or drug use with providers.14 In addition, compared with the young sexually active population, very little HIV prevention education is targeted to older people.15 Social stigmatization is also a concern for many HIV-infected elderly, as a perceived negative reputation within their community may prevent them from seeking care and disclosing their HIV status.
Take-home points
Reasons that HIV infection is underdiagnosed in the elderly include lack of:
- Provider recognition
- Insight and information about HIV prevention and transmission
- HIV-prevention education targeting the elderly
- Disclosure because of the social stigma of HIV infection.
HIV ACCELERATES AGING, AGING REDUCES IMMUNITY
Many HIV-positive people can expect to live as long as people in the general population, but those who are diagnosed late and thus are started on antiretroviral therapy later in the course of their infection have a reduced life expectancy. Longevity depends on both restoring the CD4 count to near-normal and suppressing the viral load to undetectable levels.3,16 This is especially important for older adults, as HIV may accelerate aging, and aging itself may speed the progression of HIV disease, so that therapy may result in delayed or only partial restoration of immunity.
Older age at the time of HIV infection is a strong predictor of accelerated HIV disease progression in the absence of therapy.17 Left untreated, older patients with HIV lose CD4 cells and progress to AIDS and death faster than younger patients. The deleterious effects of chronic immune activation in the course of HIV infection, combined with the immune senescence of aging, are thought to promote this accelerated course.18
Recent data indicate that starting antiretroviral therapy early can help prevent the CD4-cell impairment that occurs with aging.19 However, in adults over age 50, the capacity to restore the CD4 count with antiretroviral therapy apears to be reduced, despite demonstrated viral load suppression and better adherence.20 Although mean adherence rates appear higher in older HIV-infected patients, they are worse in those with neurocognitive impairment, highlighting the importance of evaluating neurocognition in this population.21
Decreased immune recovery and the subsequent increased risk of serious AIDS events are factors that now favor starting antiretroviral therapy in all HIV patients over age 50, regardless of CD4 count.
Take-home points
- Without treatment, HIV infection in older patients progresses more rapidly to AIDS and death than in younger patients.
- HIV-positive people over age 50 who have never received antiretroviral therapy should be strongly considered for it, regardless of the CD4 count.
SO MANY DRUGS, SO MANY INTERACTIONS
Since HIV patients are now living longer thanks to antiretroviral therapy, they are now experiencing more disease- and treatment-related problems. This has led to an increased likelihood of polypharmacy, defined here as the use of six or more medications.
In general, polypharmacy in the elderly is associated with adverse drug events, drug interactions, inappropriate medication use, delirium, falls, fractures, and poor medication adherence.22,23 But it becomes even more of a problem in HIV-infected elderly patients, as various drug interactions can alter the effectiveness of the antiretroviral regimen and can result in drug toxicity.
The most common classes of medications used in the elderly are antihypertensives, lipid-lowering agents, antiplatelet medications, antidepressants, anxiolytics, sedatives, and analgesics, and many of these have notable interactions with current antiretroviral regimens.24,25 Most medications, including antiretrovirals, are cleared by the liver or kidneys, and the function of these organs often decreases with age, resulting in impaired elimination and in drug accumulation.
Information on drug interactions is readily available from the US Department of Health and Human Services,26 drug interaction databases,27,28 and drug interaction software. The combination of antiretroviral therapy and preexisting polypharmacy significantly increases the risk of serious interactions, which can lead to drug toxicity, poorer adherence with antiretroviral therapy, loss of efficacy of the coadministered medication, or resurgence of HIV infection due to drug-drug interactions affecting the metabolism and ultimate efficacy of the antiretroviral therapy. An increased awareness of common drug-drug interactions can prevent coadministration of potentially harmful medications in elderly HIV patients.
Important interactions between antiretroviral drugs and other drug classes are summarized in Table 1.25–28 Most notably:
- Simvastatin and lovastatin are contraindicated with any protease inhibitor.
- Proton pump inhibitors are not recommended for patients taking ritonavir-boosted atazanavir. If a proton pump inhibitor is necessary, the daily dose should not exceed 20 mg of omeprazole or its equivalent in patients who have never taken a protease inhibitor, and it should be taken 12 hours before boosted atazanavir.26
- Corticosteroids, whether systemic, inhaled, or intranasal (eg, fluticasone, budesonide), should be avoided in combination with any protease inhibitor, as they can cause iatrogenic Cushing syndrome and also pose the risk of adrenal crisis during acute illness.27
Take-home points
- In cases of preexisting polypharmacy, antiretroviral therapy can lead to significant drug toxicity, poor adherence to medications, and resurgence of HIV infection.
- Increased provider awareness of common drug-drug interactions can prevent the prescribing of potentially harmful drug combinations to HIV-infected elderly patients.
COMORBIDITIES
In recent years, more than half of the deaths in HIV patients on antiretroviral therapy have been from noninfectious comorbidities such as cardiovascular disease, bone disease, and renal failure, which often coexist and are associated with advanced age.29 In fact, both older age and each additional year of antiretroviral therapy are independent predictors of polypathology (simultaneous occurrence of two or more defined diseases).30 The Antiretroviral Therapy Cohort Collaboration found that age greater than 50 was strongly associated with increasing rates of non–AIDS-related malignancy and cardiovascular disease.31
CARDIOVASCULAR DISEASE
With the increasing life expectancy of HIV-infected adults on antiretroviral therapy, cardiovascular disease has become an important concern. HIV-infected adults appear to have a significantly greater risk of myocardial infarction and coronary artery disease than age-matched HIV-negative individuals.32 Strikingly, being older than 50 itself increases the risk of hospitalization for cardiovascular disease fivefold (incidence rate ratio 5.01, 95% confidence interval 3.41–7.38).33 In addition, HIV infection is associated with a risk of acute myocardial infarction 50% higher than that explained by recognized risk factors.34
This high prevalence of coronary artery disease is likely from a combination of factors, including increasing age and the chronic inflammation and immune activation associated with HIV infection.35 An association between untreated HIV disease and markers of risk for cardiovascular disease has been identified.36,37
In addition, antiretroviral therapy is associated with dyslipidemia, which is most pronounced with protease inhibitor regimens. Whether specific lipid changes associated with individual antiretroviral drugs affect cardiovascular risk remains uncertain. In the Data Collection on Adverse Events of Anti-HIV Drugs studies,38 only cumulative exposure to indinavir, lopinavir-ritonavir, and didanosine was associated with an increased risk of myocardial infarction.38
Traditional risk factors such as obesity, tobacco use, and genetic predisposition also apply to HIV-infected people.39 In fact, the prevalence of traditional risk factors such as smoking and dyslipidemia is generally higher in HIV-infected people than in the general population, although this situation may be improving.40
Science needs to elucidate the relationship between traditional and nontraditional risk factors for cardiovascular disease in older HIV-infected adults. In the meantime, older patients with HIV require aggressive management of modifiable risk factors.
Tools for assessing cardiovascular risk include the Framingham risk score41 and the Data Collection on Adverse Events of Anti-HIV Drugs 5-year risk calculator.42 The European AIDS Clinical Society guidelines recommend considering changing the antiretroviral regimen if the patient’s 10-year risk of cardiovascular disease is more than 20%.43 Recommended strategies for reducing cardiovascular risk in elderly patients with HIV infection include counseling about smoking cessation and weight loss at every clinic visit and optimally controlling dyslipidemia and hypertension using nationally accepted standardized guidelines.44
Take-home points
- HIV infection is associated with a 50% higher risk of acute myocardial infarction beyond that explained by traditional risk factors.
- Chronic inflammation, immune activation, and dyslipidemia associated with antiretroviral therapy all contribute to cardiovascular disease in HIV-infected patients.
- HIV-infected elderly patients require aggressive management of modifiable risk factors for cardiovascular disease.
ENDOCRINE DISEASE
Diabetes mellitus
The estimated prevalence of diabetes mellitus is 3% in HIV-infected people who have never received antiretroviral therapy, but glucose intolerance increases to the range of 10% to 25% in those who have started it.45 Glucose disorders are associated with traditional risk factors as well as with HIV-associated factors such as lipodystrophy and antiretroviral therapy, specifically long-term use of protease inhibitors.46 Although increasing age and obesity clearly play a role in the development of diabetes mellitus in this population, HIV-specific factors may also allow diabetes to develop at a lower level of adiposity than in people without HIV infection.47
Strategies for preventing type 2 diabetes mellitus in HIV-infected patients focus on avoiding excessive weight gain, especially after starting antiretroviral therapy; regularly screening for diabetes using hemoglobin A1c, both before and after starting antiretroviral therapy; and continuing to check hemoglobin A1c every 6 months. The target hemoglobin A1c should be less than 7.0%. This threshold should be increased to 8% in frail elderly adults if their anticipated life expectancy is less than 5 years, given their higher risk of hypoglycemia, polypharmacy, and drug interactions.48 In addition, as in HIV-negative patients, diabetes screening should be performed if systolic blood pressure exceeds 135/80 mm Hg.
Insulin sensitizers such as metformin and thiazolidinediones should be considered for treating diabetes in HIV-infected patients if no contraindications exist. Consideration may also be given to switching the antiretroviral regimen from a protease inhibitor-based regimen to a nonnucleoside reverse transcriptase inhibitor-based regimen.48
Take-home points
- Glucose intolerance has been associated with HIV-specific factors, including lipodystrophy and antiretroviral therapy.
- Avoiding excessive weight gain, use of insulin-sensitizing medications, and alteration in antiretroviral regimens should be considered for the treatment of diabetes mellitus in HIV infection.
Osteoporosis
Osteoporotic bone disease disproportionately affects patients with advanced HIV infection compared with patients of similar age.49 Bone mineral density is lower and the fracture rate is higher in HIV-infected individuals.
The pathogenesis of bone disease appears to be multifactorial. Traditional risk factors include hypogonadism, smoking, alcohol use, and low body weight, while HIV-related risk factors include chronic immune activation and antiretroviral therapy.50
Several antiretroviral regimens have been linked to clinically significant bone loss, including both tenofovir-based and protease inhibitor-based regimens.51 Most studies have shown that bone mineral density decreases by 2% to 6% in the first 2 years after starting these regimens52; however, long-term effects on bone loss are unknown.
Questions remain. For example, what are the exact mechanisms that lead to the acute decrease in bone mineral density after starting antiretroviral therapy? And why is vitamin D deficiency is so prevalent in HIV infection, with low vitamin D levels seen in up to 60% to 75% of elderly HIV-infected patients?53
Both the Work Group for the HIV and Aging Consensus Project54 and the European AIDS Clinical Society43 recommend screening for and treating causes of secondary low bone mineral density in HIV-infected men over age 50 and postmenopausal HIV-infected women. These causes include vitamin D deficiency. As of 2013, the National Osteoporosis Foundation guidelines include HIV infection and antiretroviral therapy as osteoporosis risk factors that should trigger screening for low bone mineral density with dual-energy x-ray absorptiometry (DXA).55
As in the general population, the preferred treatment for low bone mineral density in people with HIV is a bisphosphonate, in addition to ensuring adequate calcium and vitamin D intake. It is important to repeat DXA imaging every 2 years and to reassess the need for continued bisphosphonate therapy after 3 to 5 years because of a possible increased risk of fracture with prolonged use.
Take-home points
- Osteoporosis and vitamin D deficiency both appear to be more prevalent with HIV infection.
- HIV infection and antiretroviral therapy are risk factors that should prompt DXA screening to evaluate for osteoporosis.
NEUROCOGNITIVE DISORDERS
HIV-associated neurocognitive disorders are common, with an estimated 50% of HIV-infected patients experiencing some degree of cognitive loss and some progressing to dementia.56 Unfortunately, studies suggest that cognitive disorders can occur despite good HIV control with antiretroviral therapy, with one report demonstrating that 84% of patients with cognitive complaints and 64% without complaints were affected by an HIV-associated neurocognitive disorder.57
HIV-associated dementia is often subcortical, with fluctuating symptoms such as psychomotor retardation, difficulty multitasking, and apathy. In contrast to dementia syndromes such as Alzheimer disease, relentless progression is less common in HIV-infected patients who receive antiretroviral therapy.
The Mini-Mental State Examination should not be used to screen for HIV-associated neurocognitive disorders, as it does not assess the domains that are typically impaired. The Montreal Cognitive Assessment has been suggested as the best screening instrument in elderly HIV-infected patients; it is available at no cost at www.mocatest.org.58
As HIV-associated neurocognitive disorder is a diagnosis of exclusion, an evaluation for alternative diagnoses such as syphilis, hypothyroidism, and depression is recommended. If an HIV-associated neurocognitive disorder is diagnosed, referral to specialty care should be considered, as interventions such as lumbar puncture to assess cerebrospinal fluid viral escape and changing the antiretroviral regimen to improve central nervous system penetration are possible options under study.
Patients with poorly controlled HIV and a depressed CD4 count are at risk of a number of central nervous system complications in addition to HIV-associated neurocognitive disorders, eg, central nervous system toxoplasmosis, cryptococcal meningitis, progressive multifocal leukoencephalopathy, and primary central nervous system lymphoma. Adherence to an effective antiretroviral regimen is the primary prevention strategy.
Take-home points
- HIV-associated neurocognitive disorders and dementia can occur despite appropriate HIV control and adherence to antiretroviral therapy.
- Adherence to antiretroviral therapy is the primary prevention against most central nervous system complications in HIV infection.
GERIATRIC SYNDROMES
The aging HIV-infected adult may also be at increased risk of geriatric syndromes.
In particular, a frailty-related phenotype of weight loss, exhaustion, slowness, and low physical activity was more common in HIV-infected elderly than in noninfected elderly.59 HIV-infected men are 4.5 to 10 times more likely than age-matched controls to be frail, and the likelihood of frailty increases with age, duration of HIV infection, having a CD4 count lower than 350 × 106/L, and having uncontrolled HIV replication.60,61
Other geriatric syndromes such as falls, urinary incontinence, and functional impairment have been identified in 25% to 56% of older HIV-infected patients.62 Indeed, the combination of HIV and older age may adversely affect performance of instrumental activities of daily living.63 Also, as previously mentioned, nondisclosure, fear of HIV-related social stigmatization, and a desire to be self-reliant are all factors that perpetuate the social isolation that is common among the HIV-infected elderly.
For these reasons, a comprehensive approach involving a geriatrician, an infectious disease specialist, and community social workers is needed to manage the care of this aging population.
Take-home point
- Geriatric syndromes have an important impact on health in aging HIV patients.
CANCER SCREENING IN HIV PATIENTS
People with HIV have an elevated risk of cancer. Specifically, compared with the general population, their risk is:
- 3,640 times higher for Kaposi sarcoma
- 77 times higher for non-Hodgkin lymphomas
- 6 times higher for cervical cancer.64,65
These cancers are considered “AIDS-defining,” and fortunately, the development of effective antiretroviral therapy in the 1990s has led to a marked reduction in their incidence. However, the aging HIV population is now experiencing a rise in the incidence of non–AIDS-defining cancers, such as cancers of the lung, liver, kidney, anus, head and neck, and skin, as well as Hodgkin lymphoma.66 Table 2 shows the standardized incidence ratio of selected non–AIDS-defining cancers in HIV-infected patients as reported in several large international studies.65,67,68 The etiology for the increased risk of non–AIDS-defining cancers in the HIV-infected population is not clear, but possible explanations include the virus itself, antiretroviral therapy, and co-infection with other viruses such as hepatitis B, hepatitis C, and Epstein-Barr virus.
Guidelines for cancer screening vary by organization, and the American Cancer Society, the National Cancer Institute, and the US Preventive Services Task Force do not have formal screening guidelines for the most common non–AIDS-defining cancers. The European AIDS Clinical Society, however, has proposed some screening recommendations for selected malignancies.43
In general, screening recommendations are similar to those for HIV-negative patients. A specific difference for HIV-infected patients is in cervical cancer screening. HIV-infected women should undergo a Papanicolaou smear at 6-month intervals during the first year after diagnosis of HIV infection and, if the results are normal, annually thereafter. There is no consensus as to whether human papillomavirus testing should be performed routinely on HIV-infected women.
At the time of this writing, there are no recommendations for routine screening for anal cancer, although some specialists recommend anal cytologic screening for HIV-positive men and women, and an annual digital anal examination may be useful to detect masses that could be anal cancer.69
Take-home points
- The incidence of non–AIDS-defining cancers is rising in the aging HIV population.
- There are currently no formal recommendations for routine screening for anal cancer.
FINAL WORD
Because patients with HIV are living longer as a result of newer effective combination antiretroviral therapies, physicians face a new challenge of managing conditions in these patients that are traditionally associated with aging. Providers will need to improve their understanding of drug-drug interactions and polypharmacy issues and be able to address the complex medical and psychosocial issues in this growing population. As patients with HIV on effective antiretroviral therapy grow older, the burden of comorbid medical disease will continue to increase.
- World Health Organization. HIV/AIDS: fact sheet. www.who.int/mediacentre/factsheets/fs360/en/. Accessed April 16, 2015.
- Centers for Disease Control and Prevention (CDC). HIV/AIDS: basic statistics. www.cdc.gov/hiv/basics/statistics.html. Accessed April 16, 2015.
- May MT, Gompels M, Delpech V, et al; UK Collaborative HIV Cohort (UK CHIC) Study. Impact on life expectancy of HIV-1 positive individuals of CD4+ cell count and viral load response to antiretroviral therapy. AIDS 2014; 28:1193–1202.
- Centers for Disease Control and Prevention (CDC). Diagnoses of HIV infection in the United States and dependent areas: HIV surveillance report. www.cdc.gov/hiv/library/reports/surveillance/2011/surveillance_Report_vol_23.html. Accessed April 16, 2015.
- Effros RB, Fletcher CV, Gebo K, et al. Aging and infectious diseases: workshop on HIV infection and aging: what is known and future research directions. Clin Infect Dis 2008; 47:542–553.
- Moyer VA; US Preventive Services Task Force. Screening for HIV: US Preventive Services Task Force Recommendation Statement. Ann Intern Med 2013; 159:51–60.
- Qaseem A, Snow V, Shekelle P, Hopkins R Jr, Owens DK; Clinical Efficacy Assessment Subcommittee, American College of Physicians. Screening for HIV in health care settings: a guidance statement from the American College of Physicians and HIV Medicine Association. Ann Intern Med 2009; 150:125–131.
- Lucas A, Armbruster B. The cost-effectiveness of expanded HIV screening in the United States. AIDS 2013; 27:795–801.
- Lindau ST, Schumm LP, Laumann EO, Levinson W, O’Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the United States. N Engl J Med 2007; 357:762–774.
- Schick V, Herbenick D, Reece M, et al. Sexual behaviors, condom use, and sexual health of Americans over 50: implications for sexual health promotion for older adults. J Sex Med 2010; 7(suppl 5):315–329.
- US Department of Health and Human Services, HIV/AIDS Bureau. The Ryan White HIV/AIDS program: population fact sheet: August 2010. Older adults. http://hab.hrsa.gov/abouthab/populations/olderadultsfacts.pdf. Accessed April 16, 2015.
- May M, Gompels M, Delpech V, et al. Impact of late diagnosis and treatment on life expectancy in people with HIV-1: UK Collaborative HIV Cohort (UK CHIC) Study. BMJ 2011; 343:d6016.
- Branson BM, Handsfield HH, Lampe MA, et al; Centers for Disease Control and Prevention (CDC). Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep 2006; 55:1–17.
- Health Resources and Services Administration (HRSA); HIV/AIDS Bureau. HRSA CAREAction. The graying of HIV. http://hab.hrsa.gov/newspublications/careactionnewsletter/february2009.pdf. Accessed April 16, 2015.
- AIDS InfoNet. Fact sheet number 616: Older people and HIV. http://aidsinfonet.org/fact_sheets/view/616. Accessed April 16, 2015.
- Rodger AJ, Lodwick R, Schechter M, et al; INSIGHT SMART, ESPRIT Study Groups. Mortality in well controlled HIV in the continuous antiretroviral therapy arms of the SMART and ESPRIT trials compared with the general population. AIDS 2013; 27:973–979.
- Kitahata MM, Gange SJ, Abraham AG, et al; NA-ACCORD Investigators. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med 2009; 360:1815–1826.
- Cao W, Jamieson BD, Hultin LE, Hultin PM, Effros RB, Detels R. Premature aging of T cells is associated with faster HIV-1 disease progression. J Acquir Immune Defic Syndr 2009; 50:137–147.
- Allers K, Bösel D, Epple HJ, et al. Effect of age on the CD4+ T-cell impairment in HIV-infected persons without and with cART. J Acquir Immune Defic Syndr 2014; 66:7–15.
- Kalayjian RC, Spritzler J, Matining RM, et al. Older HIV-infected patients on antiretroviral therapy have B-cell expansion and attenuated CD4 cell increases with immune activation reduction. AIDS 2013; 27:1563–1571.
- Althoff KN, Gebo KA, Gange SJ, et al; North American AIDS Cohort Collaboration on Research and Design. CD4 count at presentation for HIV care in the United States and Canada: are those over 50 years more likely to have a delayed presentation? AIDS Res Ther 2010; 7:45.
- Freeland KN, Thompson AN, Zhao Y, Leal JE, Mauldin PD, Moran WP. Medication use and associated risk of falling in a geriatric outpatient population. Ann Pharmacother 2012; 46:1188–1192.
- Steinman MA, Hanlon JT. Managing medications in clinically complex elders: “There’s got to be a happy medium.” JAMA 2010; 304:1592–1601.
- Marzolini C, Elzi L, Gibbons S, et al; Swiss HIV Cohort Study. Prevalence of comedications and effect of potential drug-drug interactions in the Swiss HIV Cohort Study. Antivir Ther 2010; 15:413–423.
- Greene M, Justice AC, Lampiris HW, Valcour V. Management of human immunodeficiency virus infection in advanced age. JAMA 2013; 309:1397–1405.
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. http://aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf. Accessed April 16, 2015.
- UCSF Center for HIV Information. HIVInSite. Comprehensive, up-to-date information on HIV/AIDS treatment, prevention, and policy from the University of California San Francisco: database of antiretroviral drug interactions. http://hivinsite.ucsf.edu/. Accessed April 16, 2015.
- The University of Liverpool. Drug interaction charts. www.hiv-druginteractions.org. Accessed April 16, 2015.
- Vance DE, Mugavero M, Willig J, Raper JL, Saag MS. Aging with HIV: a cross-sectional study of comorbidity prevalence and clinical characteristics across decades of life. J Assoc Nurses AIDS Care 2011; 22:17–25.
- Guaraldi G, Orlando G, Zona S, et al. Premature age-related comorbidities among HIV-infected persons compared with the general population. Clin Infect Dis 2011; 53:1120–1126.
- Antiretroviral Therapy Cohort Collaboration. Causes of death in HIV-1-infected patients treated with antiretroviral therapy, 1996-2006: collaborative analysis of 13 HIV cohort studies. Clin Infect Dis 2010; 50:1387–1396.
- Currier JS, Taylor A, Boyd F, et al. Coronary heart disease in HIV-infected individuals. J Acquir Immune Defic Syndr 2003; 33:506–512.
- Berry SA, Fleishman JA, Moore RD, Gebo KA; HIV Research Network. Trends in reasons for hospitalization in a multisite United States cohort of persons living with HIV, 2001-2008. J Acquir Immune Defic Syndr 2012; 59:368–375.
- Freiberg MS, Chang CC, Kuller LH, et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med 2013; 173:614–622.
- Triant VA, Lee H, Hadigan C, Grinspoon SK. Increased acute myocardial infarction rates and cardiovascular risk factors among patients with human immunodeficiency virus disease. J Clin Endocrinol Metab 2007; 92:2506–2512.
- Calmy A, Gayet-Ageron A, Montecucco F, et al; STACCATO Study Group. HIV increases markers of cardiovascular risk: results from a randomized, treatment interruption trial. AIDS 2009; 23:929–939.
- Phillips AN, Carr A, Neuhaus J, et al. Interruption of antiretroviral therapy and risk of cardiovascular disease in persons with HIV-1 infection: exploratory analyses from the SMART trial. Antivir Ther 2008; 13:177–187.
- Worm SW, Sabin C, Weber R, et al. Risk of myocardial infarction in patients with HIV infection exposed to specific individual antiretroviral drugs from the 3 major drug classes: the Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study. J Infect Dis 2010; 201:318–330.
- Lake JE, Currier JS. Metabolic disease in HIV infection. Lancet Infect Dis 2013; 13:964–975.
- Data Collection on Adverse Events of Anti-HIV Drugs Study Group; Sabin CA, d’Arminio Monforte A, Friis-Moller N, et al. Changes over time in risk factors for cardiovascular disease and use of lipid-lowering drugs in HIV-infected individuals and impact on myocardial infarction. Clin Infect Dis 2008; 46:1101–1110.
- Falcone EL, Mangili A, Skinner S, Alam A, Polak JF, Wanke CA. Framingham risk score and early markers of atherosclerosis in a cohort of adults infected with HIV. Antivir Ther 2011; 16:1–8.
- Friis-Møller N, Thiébaut R, Reiss P, et al; DAD study group. Predicting the risk of cardiovascular disease in HIV-infected patients: the Data Collection on Adverse Effects of Anti-HIV Drugs study. Eur J Cardiovasc Prev Rehabil 2010; 17:491–501.
- European AIDS Clinical Society Guidelines (EACS). www.eacsociety.org/guidelines/eacs-guidelines/eacs-guidelines.html. Accessed April 16, 2015.
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311:507–520.
- Samaras K. The burden of diabetes and hyperlipidemia in treated HIV infection and approaches for cardiometabolic care. Curr HIV/AIDS Rep 2012; 9:206–217.
- Rasmussen LD, Mathiesen ER, Kronborg G, Pedersen C, Gerstoft J, Obel N. Risk of diabetes mellitus in persons with and without HIV: a Danish nationwide population-based cohort study. PLoS One 2012; 7:e44575.
- Capeau J, Bouteloup V, Katlama C, et al; ANRS CO8 APROCO-COPILOTE Cohort Study Group. Ten-year diabetes incidence in 1,046 HIV-infected patients started on a combination antiretroviral treatment. AIDS 2012; 26:303–314.
- American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care 2013; 36(suppl 1):S11–S66.
- Brown TT, Qaqish RB. Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a meta-analytic review. AIDS 2006; 20:2165–2174.
- Rothman MS, Bessesen MT. HIV infection and osteoporosis: pathophysiology, diagnosis, and treatment options. Curr Osteoporos Rep 2012; 10:270–277.
- Bedimo R, Maalouf NM, Zhang S, Drechsler H, Tebas P. Osteoporotic fracture risk associated with cumulative exposure to tenofovir and other antiretroviral agents. AIDS 2012; 26:825–831.
- Brown TT, McComsey GA, King MS, Qaqish RB, Bernstein BM, da Silva BA. Loss of bone mineral density after antiretroviral therapy initiation, independent of antiretroviral regimen. J Acquir Immune Defic Syndr 2009; 51:554–561.
- Rodríguez M, Daniels B, Gunawardene S, Robbins GK. High frequency of vitamin D deficiency in ambulatory HIV-positive patients. AIDS Res Hum Retroviruses 2009; 25:9–14.
- Work Group for HIV and Aging Consensus Project. Summary report from the Human Immunodeficiency Virus and Aging Consensus Project: treatment strategies for clinicians managing older individuals with the human immunodeficiency virus. J Am Geriatr Soc 2012; 60:974–979.
- National Osteoporosis Foundation. Clinician’s guide to prevention and treatment of osteoporosis. 2013 Issue, Version 3. http://nof.org/files/nof/public/content/file/2791/upload/919.pdf. Accessed April 16, 2015.
- Heaton RK, Clifford DB, Franklin DR Jr, et al; CHARTER Group. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology 2010; 75:2087–2096.
- Simioni S, Cavassini M, Annoni JM, et al. Cognitive dysfunction in HIV patients despite long-standing suppression of viremia. AIDS 2010; 24:1243–1250.
- Valcour VG. Evaluating cognitive impairment in the clinical setting: practical screening and assessment tools. Top Antivir Med 2011; 19:175–180.
- Desquilbet L, Jacobson LP, Fried LP, et al; Multicenter AIDS Cohort Study. HIV-1 infection is associated with an earlier occurrence of a phenotype related to frailty. J Gerontol A Biol Sci Med Sci 2007; 62:1279–1286.
- Desquilbet L, Jacobson LP, Fried LP, et al. A frailty-related phenotype before HAART initiation as an independent risk factor for AIDS or death after HAART among HIV-infected men. J Gerontol A Biol Sci Med Sci 2011; 66:1030–1038.
- Fried LP, Tangen CM, Walston J, et al; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56:M146–M156.
- Greene M, Valcour V, Miao Y, et al. Geriatric syndromes are common among older HIV-infected adults. 21st Conference on Retroviruses and Opportunistic Infections (CROI) 2014 March 3-6, Boston MA.
- Morgan EE, Iudicello JE, Weber E, et al; HIV Neurobehavioral Research Program (HNRP) Group. Synergistic effects of HIV infection and older age on daily functioning. J Acquir Immune Defic Syndr 2012; 61:341–348.
- Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet 2007; 370:59–67.
- Shiels MS, Pfeiffer RM, Gail MH, et al. Cancer burden in the HIV-infected population in the United States. J Natl Cancer Inst 2011; 103:753–762.
- Deeken JF, Tjen-A-Looi A, Rudek MA, et al. The rising challenge of non-AIDS-defining cancers in HIV-infected patients. Clin Infect Dis 2012; 55:1228–1235.
- Powles T, Robinson D, Stebbing J, et al. Highly active antiretroviral therapy and the incidence of non-AIDS-defining cancers in people with HIV infection. J Clin Oncol 2009; 27:884–890.
- Patel P, Hanson DL, Sullivan PS, et al; Adult and Adolescent Spectrum of Disease Project and HIV Outpatient Study Investigators. Incidence of types of cancer among HIV-infected persons compared with the general population in the United States, 1992-2003. Ann Intern Med 2008; 148:728–736.
- Kaplan JE, Benson C, Holmes KK, Brooks JT, Pau A, Masur H; Centers for Disease Control and Prevention (CDC); National Institutes of Health; HIV Medicine Association of the Infectious Diseases Society of America. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep 2009; 58:1–207.
- World Health Organization. HIV/AIDS: fact sheet. www.who.int/mediacentre/factsheets/fs360/en/. Accessed April 16, 2015.
- Centers for Disease Control and Prevention (CDC). HIV/AIDS: basic statistics. www.cdc.gov/hiv/basics/statistics.html. Accessed April 16, 2015.
- May MT, Gompels M, Delpech V, et al; UK Collaborative HIV Cohort (UK CHIC) Study. Impact on life expectancy of HIV-1 positive individuals of CD4+ cell count and viral load response to antiretroviral therapy. AIDS 2014; 28:1193–1202.
- Centers for Disease Control and Prevention (CDC). Diagnoses of HIV infection in the United States and dependent areas: HIV surveillance report. www.cdc.gov/hiv/library/reports/surveillance/2011/surveillance_Report_vol_23.html. Accessed April 16, 2015.
- Effros RB, Fletcher CV, Gebo K, et al. Aging and infectious diseases: workshop on HIV infection and aging: what is known and future research directions. Clin Infect Dis 2008; 47:542–553.
- Moyer VA; US Preventive Services Task Force. Screening for HIV: US Preventive Services Task Force Recommendation Statement. Ann Intern Med 2013; 159:51–60.
- Qaseem A, Snow V, Shekelle P, Hopkins R Jr, Owens DK; Clinical Efficacy Assessment Subcommittee, American College of Physicians. Screening for HIV in health care settings: a guidance statement from the American College of Physicians and HIV Medicine Association. Ann Intern Med 2009; 150:125–131.
- Lucas A, Armbruster B. The cost-effectiveness of expanded HIV screening in the United States. AIDS 2013; 27:795–801.
- Lindau ST, Schumm LP, Laumann EO, Levinson W, O’Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the United States. N Engl J Med 2007; 357:762–774.
- Schick V, Herbenick D, Reece M, et al. Sexual behaviors, condom use, and sexual health of Americans over 50: implications for sexual health promotion for older adults. J Sex Med 2010; 7(suppl 5):315–329.
- US Department of Health and Human Services, HIV/AIDS Bureau. The Ryan White HIV/AIDS program: population fact sheet: August 2010. Older adults. http://hab.hrsa.gov/abouthab/populations/olderadultsfacts.pdf. Accessed April 16, 2015.
- May M, Gompels M, Delpech V, et al. Impact of late diagnosis and treatment on life expectancy in people with HIV-1: UK Collaborative HIV Cohort (UK CHIC) Study. BMJ 2011; 343:d6016.
- Branson BM, Handsfield HH, Lampe MA, et al; Centers for Disease Control and Prevention (CDC). Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep 2006; 55:1–17.
- Health Resources and Services Administration (HRSA); HIV/AIDS Bureau. HRSA CAREAction. The graying of HIV. http://hab.hrsa.gov/newspublications/careactionnewsletter/february2009.pdf. Accessed April 16, 2015.
- AIDS InfoNet. Fact sheet number 616: Older people and HIV. http://aidsinfonet.org/fact_sheets/view/616. Accessed April 16, 2015.
- Rodger AJ, Lodwick R, Schechter M, et al; INSIGHT SMART, ESPRIT Study Groups. Mortality in well controlled HIV in the continuous antiretroviral therapy arms of the SMART and ESPRIT trials compared with the general population. AIDS 2013; 27:973–979.
- Kitahata MM, Gange SJ, Abraham AG, et al; NA-ACCORD Investigators. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med 2009; 360:1815–1826.
- Cao W, Jamieson BD, Hultin LE, Hultin PM, Effros RB, Detels R. Premature aging of T cells is associated with faster HIV-1 disease progression. J Acquir Immune Defic Syndr 2009; 50:137–147.
- Allers K, Bösel D, Epple HJ, et al. Effect of age on the CD4+ T-cell impairment in HIV-infected persons without and with cART. J Acquir Immune Defic Syndr 2014; 66:7–15.
- Kalayjian RC, Spritzler J, Matining RM, et al. Older HIV-infected patients on antiretroviral therapy have B-cell expansion and attenuated CD4 cell increases with immune activation reduction. AIDS 2013; 27:1563–1571.
- Althoff KN, Gebo KA, Gange SJ, et al; North American AIDS Cohort Collaboration on Research and Design. CD4 count at presentation for HIV care in the United States and Canada: are those over 50 years more likely to have a delayed presentation? AIDS Res Ther 2010; 7:45.
- Freeland KN, Thompson AN, Zhao Y, Leal JE, Mauldin PD, Moran WP. Medication use and associated risk of falling in a geriatric outpatient population. Ann Pharmacother 2012; 46:1188–1192.
- Steinman MA, Hanlon JT. Managing medications in clinically complex elders: “There’s got to be a happy medium.” JAMA 2010; 304:1592–1601.
- Marzolini C, Elzi L, Gibbons S, et al; Swiss HIV Cohort Study. Prevalence of comedications and effect of potential drug-drug interactions in the Swiss HIV Cohort Study. Antivir Ther 2010; 15:413–423.
- Greene M, Justice AC, Lampiris HW, Valcour V. Management of human immunodeficiency virus infection in advanced age. JAMA 2013; 309:1397–1405.
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. http://aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf. Accessed April 16, 2015.
- UCSF Center for HIV Information. HIVInSite. Comprehensive, up-to-date information on HIV/AIDS treatment, prevention, and policy from the University of California San Francisco: database of antiretroviral drug interactions. http://hivinsite.ucsf.edu/. Accessed April 16, 2015.
- The University of Liverpool. Drug interaction charts. www.hiv-druginteractions.org. Accessed April 16, 2015.
- Vance DE, Mugavero M, Willig J, Raper JL, Saag MS. Aging with HIV: a cross-sectional study of comorbidity prevalence and clinical characteristics across decades of life. J Assoc Nurses AIDS Care 2011; 22:17–25.
- Guaraldi G, Orlando G, Zona S, et al. Premature age-related comorbidities among HIV-infected persons compared with the general population. Clin Infect Dis 2011; 53:1120–1126.
- Antiretroviral Therapy Cohort Collaboration. Causes of death in HIV-1-infected patients treated with antiretroviral therapy, 1996-2006: collaborative analysis of 13 HIV cohort studies. Clin Infect Dis 2010; 50:1387–1396.
- Currier JS, Taylor A, Boyd F, et al. Coronary heart disease in HIV-infected individuals. J Acquir Immune Defic Syndr 2003; 33:506–512.
- Berry SA, Fleishman JA, Moore RD, Gebo KA; HIV Research Network. Trends in reasons for hospitalization in a multisite United States cohort of persons living with HIV, 2001-2008. J Acquir Immune Defic Syndr 2012; 59:368–375.
- Freiberg MS, Chang CC, Kuller LH, et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med 2013; 173:614–622.
- Triant VA, Lee H, Hadigan C, Grinspoon SK. Increased acute myocardial infarction rates and cardiovascular risk factors among patients with human immunodeficiency virus disease. J Clin Endocrinol Metab 2007; 92:2506–2512.
- Calmy A, Gayet-Ageron A, Montecucco F, et al; STACCATO Study Group. HIV increases markers of cardiovascular risk: results from a randomized, treatment interruption trial. AIDS 2009; 23:929–939.
- Phillips AN, Carr A, Neuhaus J, et al. Interruption of antiretroviral therapy and risk of cardiovascular disease in persons with HIV-1 infection: exploratory analyses from the SMART trial. Antivir Ther 2008; 13:177–187.
- Worm SW, Sabin C, Weber R, et al. Risk of myocardial infarction in patients with HIV infection exposed to specific individual antiretroviral drugs from the 3 major drug classes: the Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study. J Infect Dis 2010; 201:318–330.
- Lake JE, Currier JS. Metabolic disease in HIV infection. Lancet Infect Dis 2013; 13:964–975.
- Data Collection on Adverse Events of Anti-HIV Drugs Study Group; Sabin CA, d’Arminio Monforte A, Friis-Moller N, et al. Changes over time in risk factors for cardiovascular disease and use of lipid-lowering drugs in HIV-infected individuals and impact on myocardial infarction. Clin Infect Dis 2008; 46:1101–1110.
- Falcone EL, Mangili A, Skinner S, Alam A, Polak JF, Wanke CA. Framingham risk score and early markers of atherosclerosis in a cohort of adults infected with HIV. Antivir Ther 2011; 16:1–8.
- Friis-Møller N, Thiébaut R, Reiss P, et al; DAD study group. Predicting the risk of cardiovascular disease in HIV-infected patients: the Data Collection on Adverse Effects of Anti-HIV Drugs study. Eur J Cardiovasc Prev Rehabil 2010; 17:491–501.
- European AIDS Clinical Society Guidelines (EACS). www.eacsociety.org/guidelines/eacs-guidelines/eacs-guidelines.html. Accessed April 16, 2015.
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311:507–520.
- Samaras K. The burden of diabetes and hyperlipidemia in treated HIV infection and approaches for cardiometabolic care. Curr HIV/AIDS Rep 2012; 9:206–217.
- Rasmussen LD, Mathiesen ER, Kronborg G, Pedersen C, Gerstoft J, Obel N. Risk of diabetes mellitus in persons with and without HIV: a Danish nationwide population-based cohort study. PLoS One 2012; 7:e44575.
- Capeau J, Bouteloup V, Katlama C, et al; ANRS CO8 APROCO-COPILOTE Cohort Study Group. Ten-year diabetes incidence in 1,046 HIV-infected patients started on a combination antiretroviral treatment. AIDS 2012; 26:303–314.
- American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care 2013; 36(suppl 1):S11–S66.
- Brown TT, Qaqish RB. Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a meta-analytic review. AIDS 2006; 20:2165–2174.
- Rothman MS, Bessesen MT. HIV infection and osteoporosis: pathophysiology, diagnosis, and treatment options. Curr Osteoporos Rep 2012; 10:270–277.
- Bedimo R, Maalouf NM, Zhang S, Drechsler H, Tebas P. Osteoporotic fracture risk associated with cumulative exposure to tenofovir and other antiretroviral agents. AIDS 2012; 26:825–831.
- Brown TT, McComsey GA, King MS, Qaqish RB, Bernstein BM, da Silva BA. Loss of bone mineral density after antiretroviral therapy initiation, independent of antiretroviral regimen. J Acquir Immune Defic Syndr 2009; 51:554–561.
- Rodríguez M, Daniels B, Gunawardene S, Robbins GK. High frequency of vitamin D deficiency in ambulatory HIV-positive patients. AIDS Res Hum Retroviruses 2009; 25:9–14.
- Work Group for HIV and Aging Consensus Project. Summary report from the Human Immunodeficiency Virus and Aging Consensus Project: treatment strategies for clinicians managing older individuals with the human immunodeficiency virus. J Am Geriatr Soc 2012; 60:974–979.
- National Osteoporosis Foundation. Clinician’s guide to prevention and treatment of osteoporosis. 2013 Issue, Version 3. http://nof.org/files/nof/public/content/file/2791/upload/919.pdf. Accessed April 16, 2015.
- Heaton RK, Clifford DB, Franklin DR Jr, et al; CHARTER Group. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology 2010; 75:2087–2096.
- Simioni S, Cavassini M, Annoni JM, et al. Cognitive dysfunction in HIV patients despite long-standing suppression of viremia. AIDS 2010; 24:1243–1250.
- Valcour VG. Evaluating cognitive impairment in the clinical setting: practical screening and assessment tools. Top Antivir Med 2011; 19:175–180.
- Desquilbet L, Jacobson LP, Fried LP, et al; Multicenter AIDS Cohort Study. HIV-1 infection is associated with an earlier occurrence of a phenotype related to frailty. J Gerontol A Biol Sci Med Sci 2007; 62:1279–1286.
- Desquilbet L, Jacobson LP, Fried LP, et al. A frailty-related phenotype before HAART initiation as an independent risk factor for AIDS or death after HAART among HIV-infected men. J Gerontol A Biol Sci Med Sci 2011; 66:1030–1038.
- Fried LP, Tangen CM, Walston J, et al; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56:M146–M156.
- Greene M, Valcour V, Miao Y, et al. Geriatric syndromes are common among older HIV-infected adults. 21st Conference on Retroviruses and Opportunistic Infections (CROI) 2014 March 3-6, Boston MA.
- Morgan EE, Iudicello JE, Weber E, et al; HIV Neurobehavioral Research Program (HNRP) Group. Synergistic effects of HIV infection and older age on daily functioning. J Acquir Immune Defic Syndr 2012; 61:341–348.
- Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet 2007; 370:59–67.
- Shiels MS, Pfeiffer RM, Gail MH, et al. Cancer burden in the HIV-infected population in the United States. J Natl Cancer Inst 2011; 103:753–762.
- Deeken JF, Tjen-A-Looi A, Rudek MA, et al. The rising challenge of non-AIDS-defining cancers in HIV-infected patients. Clin Infect Dis 2012; 55:1228–1235.
- Powles T, Robinson D, Stebbing J, et al. Highly active antiretroviral therapy and the incidence of non-AIDS-defining cancers in people with HIV infection. J Clin Oncol 2009; 27:884–890.
- Patel P, Hanson DL, Sullivan PS, et al; Adult and Adolescent Spectrum of Disease Project and HIV Outpatient Study Investigators. Incidence of types of cancer among HIV-infected persons compared with the general population in the United States, 1992-2003. Ann Intern Med 2008; 148:728–736.
- Kaplan JE, Benson C, Holmes KK, Brooks JT, Pau A, Masur H; Centers for Disease Control and Prevention (CDC); National Institutes of Health; HIV Medicine Association of the Infectious Diseases Society of America. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep 2009; 58:1–207.
KEY POINTS
- Today, nearly 20% of newly diagnosed HIV-infected people and more than 50% of all HIV-infected people in the United States are over age 50.
- The diagnosis and treatment of HIV tends to be delayed in elderly patients, with deleterious effects.
- Antiretroviral drugs have a number of interactions with drugs commonly used in elderly patients.
- Several diseases are more common in HIV-positive patients, including cardiovascular disease, diabetes mellitus, osteoporosis, dementia, and various malignant diseases. These merit aggressive screening and preventive measures.
Cannabinoid hyperemesis syndrome: Marijuana is both antiemetic and proemetic
With the growing use of marijuana, reports have appeared of a newly recognized condition in long-term heavy users termed cannabinoid hyperemesis syndrome.1
This syndrome is interesting for at least two reasons. First, paradoxically, marijuana appears to have an emetic effect with chronic use, whereas it usually has the opposite effect and is used as an antiemetic in patients undergoing chemotherapy. Second, patients develop a compulsion to bathe or shower in extremely hot water to relieve the symptoms.
In this article, we review the pathophysiology, clinical presentation, diagnosis, and management of this emerging condition.
MARIJUANA USE ON THE RISE
Marijuana is the most widely used illicit drug worldwide. Although statistics on its use vary, a report from the Pew Research Center2 stated that 49% of Americans say they have tried it. Several states now allow the use of marijuana for medicinal purposes, and Colorado and Washington have legalized it for recreational use. This marks a major turning point and may accelerate the slow-growing acceptance of marijuana use in the United States.
Marijuana has been used to treat HIV-associated anorexia and wasting, convulsions, glaucoma, headache, and chemotherapy-induced nausea and vomiting.3–5
Cannabinoid hyperemesis syndrome was first described in 2004 in South Australia.1 Since its recognition, an increasing number of cases have been identified worldwide. However, there are still no population-based studies to estimate its exact prevalence.
THC PREVENTS VOMITING—AND CAUSES IT
Delta-9-tetrahydrocannabinol (THC) is the principal psychoactive component in marijuana.6,7 There are two types of cannabinoid receptors in humans: CB1 and CB2. Both are found in the central nervous system and autonomic nervous system. Activation of CB1 receptors is responsible for the psychoactive effects of cannabinoids such as altered consciousness, euphoria, relaxation, perceptual disturbances, intensified sensory experiences, cognitive impairment, and increased reaction time. The physiologic role of CB2 is not known.
THC as an antiemetic
The antiemetic property of THC is not well understood but has been linked to activation of CB1 receptors found on the enteric plexus, presynaptic parasympathetic system, and central nervous system, particularly the cerebellum, hypothalamus, and vomiting center in the medulla.1,8–12 Stimulation and blockade of CB1 receptors can inhibit and induce vomiting in a dose-dependent manner, implicating endogenous cannabinoids in emetic circuits.12
THC as a proemetic
The mechanism of the paradoxical hyperemetic effect of THC is unknown, but several concepts have been proposed.
Chronic cannabis use can lead to down-regulation of CB1 receptors.13 Simonetto et al10 suggested that the central effects of long-term cannabis use on the hypothalamic-pituitary-adrenal axis may play a central role in the development of hyperemesis.10
Cannabinoids have a long half-life and are lipophilic.1 When used infrequently, they prevent vomiting. But with chronic use, high concentrations of THC can accumulate in the body, including cerebral fat, and can cause severe nausea and vomiting.8,9 This paradoxic hyperemesis was observed in people using intravenous crude marijuana extract.7 The same response was also noted in ferrets injected with 2-arachidonoylglycerol, a potent cannabinoid agonist.11
Patients who experience hyperemesis from chronic cannabis use may also have a genetic variation in their hepatic drug-transforming enzymes that results in excessive levels of cannabis metabolites that promote emesis.1,14
Delayed gastric emptying has also been linked to the proemetic effect of THC. However, this association became controversial when a large case series study showed that only 30% of patients with cannabinoid hyperemesis syndrome had delayed emptying on gastric scintigraphy.10
It is also possible that excessive stimulation of cannabinoid receptors in the gut can cause diffuse splanchnic vasodilation and contribute to the abdominal pain.13
DIAGNOSING CANNABINOID HYPEREMESIS SYNDROME
Cannabinoid hyperemesis syndrome is a clinical diagnosis typically seen in young patients (under age 50) with a long history of marijuana use. They present with severe, cyclic nausea and vomiting and admit to compulsively taking extremely hot showers or baths. Most patients report using marijuana for more than a year before developing episodes of severe vomiting. However, one study found that as many as 32% of patients had used it less than 1 year before experiencing symptoms.10
Other associated nonspecific symptoms are diaphoresis, bloating, abdominal discomfort, flushing, and weight loss. Symptoms are relieved with long, hot showers or baths and cessation of marijuana use. Taking a complete history is key to making the diagnosis.
In 2004, Allen et al1 first defined cannabinoid hyperemesis as excessive marijuana use associated with cyclical vomiting and abdominal pain.1 In 2012, Simonetto et al10 proposed diagnostic criteria (Table 1). Although not yet validated, these criteria are based on the largest series of cases of cannabinoid hyperemesis syndrome to date (98 patients).10
THE THREE PHASES OF CANNABINOID HYPEREMESIS
The clinical presentation of cannabinoid hyperemesis syndrome can be divided into three phases: prodromal, vomiting, and resolution.
Prodromal phase
During this phase, patients often appear anxious and agitated and display a spectrum of autonomic symptoms such as sweating, flushing, and constantly sipping water due to thirst. They may sometimes have abdominal pain that is usually epigastric but may also be diffuse. Their symptoms are associated with severe nausea, usually early in the morning or when they see or smell food. Appetite and eating patterns remain normal. Compulsive hot bathing or showering is minimal at this phase.
Vomiting phase
In this next phase, patients experience incapacitating nausea and vomiting that may occur without warning and are resistant to conventional antiemetics such as ondansetron and promethazine.14 However, patients eventually learn that hot baths or showers relieve the symptoms, and this behavior eventually becomes a compulsion. The higher the temperature of the water, the better the effect on symptoms.1 Low-grade pyrexia, excessive thirst, orthostasis, abdominal tenderness, weight loss, and sometimes even superficial skin burns have been reported.1,9,15–18
Recovery phase
During the final phase of cannabinoid hyperemesis syndrome, most patients experience marked resolution of symptoms after 24 to 48 hours of conservative management (bowel rest until symptoms resolve, slowly advancing diet as tolerated, intravenous fluids, and electrolyte monitoring and repletion as necessary), and most importantly, cessation of cannabis use. However, the time from cessation of marijuana use to resolution of symptoms may be as long as 1 week to 1 month.1,10,14 Patients begin to resume their normal diet and daily activities. The bathing-showering compulsion subsides, and patients regain lost weight after 3 to 6 months.1
In all case series and reports, resumption of cannabis use causes the symptoms to recur. This recurrence is compelling evidence that cannabis is the cause of the hyperemesis and should be part of the essential criteria for the diagnosis of cannabinoid hyperemesis syndrome.
WHY COMPULSIVE HOT BATHING?
The mechanism behind this unique characteristic of cannabinoid hyperemesis syndrome is not known. Several theories have been suggested, but no study has identified the exact explanation for this phenomenon.1,9,10,13–15,17–31
One suggested mechanism is a response by the thermoregulatory center of the brain to the dose-dependent hypothermic effects of THC, or even a direct effect of CB1 receptor activation in the hypothalamus.9 Cannabis toxicity could disrupt the equilibrium of satiety, thirst, digestive, and thermoregulatory systems of the hypothalamus, and this interference could resolve with hot bathing.1
The so-called “cutaneous steal” syndrome has also been proposed, in which cutaneous vasodilation caused by hot water decreases the blood volume available for the splanchnic circulation thought to be responsible for the abdominal pain and vomiting.13 The compulsive hot bathing may also be a response by the brain to the anxiety or psychological stress induced by severe nausea and vomiting.14
DIFFERENTIAL DIAGNOSIS
The differential diagnosis of cannabinoid hyperemesis syndrome includes mainly cyclic vomiting syndrome and psychogenic vomiting. A careful history is useful, as is ruling out medication-induced reactions, toxins, pregnancy, and gastrointestinal, neurologic, metabolic, and endocrine causes. All three of these vomiting syndromes can present with a cyclic pattern of nausea and vomiting. Cannabis use is common in all three and so is not helpful in differentiating them. But the characteristic compulsive hot bathing and showering is unique and pathognomonic of cannabinoid hyperemesis syndrome.32
Endoscopic examination may reveal esophagitis and gastritis from severe bouts of retching.26
Cyclic vomiting syndrome
The Rome III criteria for the diagnosis of cyclic vomiting syndrome include three or more stereotypic episodes of acute-onset nausea and vomiting lasting less than 1 week, alternating with intervals of completely normal health. The criteria should be fulfilled for the previous 3 months with symptom onset at least 6 months before diagnosis.33
In a series of 17 patients with adult-onset cyclic vomiting syndrome,18 the average age at onset was 30, and 13 (76%) of the patients were women. Fifteen (88%) of the patients experienced a prodrome or aura of abdominal pain or headache, and in this group, a trigger such as emotional stress and infection could also be identified in 9 (60%).
Unlike in cannabinoid hyperemesis syndrome, most patients with cyclic vomiting syndrome have a family history of migraine headache, and the prevalence of psychological stressors is high.31 Also, patients with cannabinoid hyperemesis syndrome do not respond to medications that usually abort migraine episodes,15 whereas patients with cyclic vomiting syndrome, especially those who have a family history of migraines, may respond to antimigraine medications such as triptans. There is evidence of clinical psychological overlap between cyclic vomiting syndrome, abdominal migraine, and migraine headaches. Some authors recommend antimigraine therapy even in the absence of a family or personal history of migraine if, after a careful history and physical examination, the diagnosis of cyclic vomiting syndrome seems likely. Moreover, nonmedical management such as sleep, dark rooms, and quiet environment are not as effective in cannabinoid hyperemesis syndrome as they are in cyclic vomiting syndrome.18
Psychogenic vomiting
Psychogenic vomiting is classically defined as vomiting caused by psychological mechanisms without any obvious organic cause.13 It occurs most commonly in patients with major depressive disorder or conversion disorder.34 The mechanism appears to be a combination of past organic or gastrointestinal functional abnormalities and emotional problems, and multiple patterns of vomiting can occur. Most of these patients can be treated with behavioral therapy, antidepressant drug therapy, and supportive psychotherapy.34,35
ASKING A SERIES OF QUESTIONS
Most patients with cannabinoid hyperemesis syndrome have a history of frequent visits to emergency departments or clinics for persistent nausea and vomiting, and they may have undergone extensive diagnostic workups to exclude structural, inflammatory, infectious, and functional diseases of the bowel.23,24
To prevent unnecessary testing and use of healthcare resources, Wallace et al32 proposed an algorithm to help guide clinicians in diagnosing and treating patients with suspected cannabinoid hyperemesis syndrome. A patient presenting with severe nausea and vomiting should prompt a series of questions:
Do the signs and symptoms suggest a severe underlying medical cause? If so, this should be pursued.
Do symptoms improve while taking a hot shower or bath? If not, pursue an appropriate diagnostic evaluation and treatment for conditions other than cannabinoid hyperemesis syndrome.
Is the bathing compulsive? If not, consider other diagnoses, but remain suspicious about cannabinoid hyperemesis syndrome.
Does the patient currently use cannabis daily or almost daily, and has the patient done so for at least the past year? If the patient denies using cannabis, a urine drug screen for THC may be useful. If the patient admits to use, a presumptive diagnosis of cannabinoid hyperemesis syndrome can be made.
Does the patient have signs or symptoms of volume depletion, or is the patient unable to tolerate oral hydration? Encourage oral hydration or provide intravenous hydration, and provide cannabis cessation counseling.
Do the symptoms improve? If yes, great! Provide cessation counseling, resources, and follow-up. If not:
Is the patient still using cannabis? If not, it is time to rethink the diagnosis.
Treatment in the acute setting is supportive and includes intravenous hydration and correction of electrolytes. Conventional antiemetics such as ondansetron, metoclopramide, prochlorperazine, and promethazine have not been effective in relieving hyperemesis.9,12,14 This implies that the mechanism of emesis likely does not involve dopaminergic and serotonin pathways in the central and autonomic nervous systems.
Cessation of cannabis use is key for long-term resolution of symptoms. Efforts should be made to provide counseling and encourage patients to stop using the drug entirely (Figure 1).
SOMETHING TO THINK ABOUT
With the high prevalence of chronic cannabis abuse and the recent legalization of recreational marijuana use, we will all likely encounter a patient with cannabinoid hyperemesis. With adequate knowledge of this phenomenon, we can avoid unnecessary workups and inappropriate medical and surgical treatment in patients presenting with recurrent vomiting of unknown cause. The diagnosis can easily be made by simply asking for a history of chronic marijuana use and symptoms related to cannabinoid hyperemesis syndrome, such as relief of symptoms with hot baths or showers and with marijuana cessation.
Conservative management and fluid resuscitation is important in the acute setting, but cessation of marijuana use and follow-up counseling are the key components for treating patients with cannabinoid hyperemesis syndrome and for preventing recurrence.
- Allen JH, de Moore GM, Heddle R, Twartz JC. Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis abuse. Gut 2004; 53:1566–1570.
- Motel S. 6 facts about marijuana. Factank. News in the Numbers Pew Research Center. www.pewresearch.org/fact-tank/2015/04/14/6-facts-about-marijuana/. Accessed June 2, 2015.
- Walsh D, Nelson KA, Mahmoud FA. Established and potential therapeutic applications of cannabinoids in oncology. Support Care Cancer 2003; 11:137–143.
- Tramèr MR, Carroll D, Campbell FA, Reynolds DJ, Moore RA, McQuay HJ. Cannabinoids for control of chemotherapy induced nausea and vomiting: quantitative systematic review. BMJ 2001; 323:16–21.
- Davis M, Maida V, Daeninck P, Pergolizzi J. The emerging role of cannabinoid neuromodulators in symptom management. Support Care Cancer 2007; 15:63–71.
- National Institutes of Health (NIH). National Institute on Drug Abuse. Drug facts: marijuana. www.nida.nih.gov/infofacts/marijuana. Accessed April 29, 2015.
- Vaziri ND, Thomas R, Sterling M, et al. Toxicity with intravenous injection of crude marijuana extract. Clin Toxicol 1981; 18:353–366.
- Devane WA, Hanus L, Breuer A, et al. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science 1992; 258:1946–1949.
- Chang YH, Windish DM. Cannabinoid hyperemesis relieved by compulsive bathing. Mayo Clin Proc 2009; 84:76–78.
- Simonetto DA, Oxentenko AS, Herman ML, Szostek JH. Cannabinoid hyperemesis: a case series of 98 patients. Mayo Clin Proc 2012; 87:114–119.
- Darmani NA. The potent emetogenic effects of the endocannabinoid, 2-AG (2-arachidonoylglycerol) are blocked by delta(9)-tetrahydrocannabinol and other cannnabinoids. J Pharmacol Exp Ther 2002; 300:34–42.
- Darmani NA, Sim-Selley LJ, Martin BR, et al. Antiemetic and motor-depressive actions of CP55,940: cannabinoid CB1 receptor characterization, distribution, and G-protein activation. Eur J Pharmacol 2003; 459:83–95.
- Leibovich MA. Psychogenic vomiting. Psychotherapeutic considerations. Psychother Psychosom 1973; 22:263–268.
- Soriano-Co M, Batke M, Cappell MS. The cannabis hyperemesis syndrome characterized by persistent nausea and vomiting, abdominal pain, and compulsive bathing associated with chronic marijuana use: a report of eight cases in the United States. Dig Dis Sci 2010; 55:3113–3119.
- Sontineni SP, Chaudhary S, Sontineni V, Lanspa SJ. Cannabinoid hyperemesis syndrome: clinical diagnosis of an underrecognised manifestation of chronic cannabis abuse. World J Gastroenterol 2009; 15:1264–1266.
- Cox B, Chhabra A, Adler M, Simmons J, Randlett D. Cannabinoid hyperemesis syndrome: case report of a paradoxical reaction with heavy marijuana use. Case Rep Med 2012; 2012:757696.
- Price SL, Fisher C, Kumar R, Hilgerson A. Cannabinoid hyperemesis syndrome as the underlying cause of intractable nausea and vomiting. J Am Osteopath Assoc 2011; 111:166–169.
- Lee LY, Abbott L, Moodie S, Anderson S. Cyclic vomiting syndrome in 28 patients: demographics, features and outcomes. Eur J Gastroenterol Hepatol 2012; 24:939–943.
- Wallace D, Martin AL, Park B. Cannabinoid hyperemesis: marijuana puts patients in hot water. Australas Psychiatry 2007; 15:156–158.
- Ashton CH. Adverse effects of cannabis and cannabinoids. Br J Anaesth 1999; 83:637–649.
- Cota D, Steiner MA, Marsicano G, et al. Requirement of cannabinoid receptor type 1 for the basal modulation of hypothalamic-pituitary-adrenal axis function. Endocrinology 2007; 148:1574–1581.
- McCallum RW, Soykan I, Sridhar KR, Ricci DA, Lange RC, Plankey MW. Delta-9-tetrahydrocannabinol delays the gastric emptying of solid food in humans: a double-blind, randomized study. Aliment Pharmacol Ther 1999; 13:77–80.
- Donnino MW, Cocchi MN, Miller J, Fisher J. Cannabinoid hyperemesis: a case series. J Emerg Med 2011; 40:e63–e66.
- Singh E, Coyle W. Cannabinoid hyperemesis. Am J Gastroenterol 2008; 103:1048–1049.
- Carnett JB. Intercostal neuralgia as a cause of abdominal pain and tenderness. Surg Gynecol Obstet 1926; 42:625–632.
- Patterson DA, Smith E, Monahan M, et al. Cannabinoid hyperemesis and compulsive bathing: a case series and paradoxical pathophysiological explanation. J Am Board Fam Med 2010; 23:790–793.
- Izzo AA, Camilleri M. Emerging role of cannabinoids in gastrointestinal and liver diseases: basic and clinical aspects. Gut 2008; 57:1140–1155.
- Pertwee RG. Cannabinoids and the gastrointestinal tract. Gut 2001; 48:859–867.
- Choung RS, Locke GR 3rd, Lee RM, Schleck CD, Zinsmeister AR, Talley NJ. Cyclic vomiting syndrome and functional vomiting in adults: association with cannabinoid use in males. Neurogastroenterol Motil 2012; 24:20–26,e1.
- Nicolson SE, Denysenko L, Mulcare JL, Vito JP, Chabon B. Cannabinoid hyperemesis syndrome: a case series and review of previous reports. Psychosomatics 2012; 53:212–219.
- Miller JB, Walsh M, Patel PA, et al. Pediatric cannabinoid hyperemesis: two cases. Pediatr Emerg Care 2010; 26:919–920.
- Wallace EA, Andrews SE, Garmany CL, Jelley MJ. Cannabinoid hyperemesis syndrome: literature review and proposed diagnosis and treatment algorithm. South Med J 2011; 104:659–664.
- Tack J, Taley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology 2006; 130:1466–1479.
- Muraoka M, Mine K, Matsumoto K, Nakai Y, Nakagawa T. Psychogenic vomiting: the relation between patterns of vomiting and psychiatric diagnoses. Gut 1990; 31:526–528.
- Stravynski A. Behavioral treatment of psychogenic vomiting in the context of social phobia. J Nerv Ment Dis 1983; 171:448–451.
With the growing use of marijuana, reports have appeared of a newly recognized condition in long-term heavy users termed cannabinoid hyperemesis syndrome.1
This syndrome is interesting for at least two reasons. First, paradoxically, marijuana appears to have an emetic effect with chronic use, whereas it usually has the opposite effect and is used as an antiemetic in patients undergoing chemotherapy. Second, patients develop a compulsion to bathe or shower in extremely hot water to relieve the symptoms.
In this article, we review the pathophysiology, clinical presentation, diagnosis, and management of this emerging condition.
MARIJUANA USE ON THE RISE
Marijuana is the most widely used illicit drug worldwide. Although statistics on its use vary, a report from the Pew Research Center2 stated that 49% of Americans say they have tried it. Several states now allow the use of marijuana for medicinal purposes, and Colorado and Washington have legalized it for recreational use. This marks a major turning point and may accelerate the slow-growing acceptance of marijuana use in the United States.
Marijuana has been used to treat HIV-associated anorexia and wasting, convulsions, glaucoma, headache, and chemotherapy-induced nausea and vomiting.3–5
Cannabinoid hyperemesis syndrome was first described in 2004 in South Australia.1 Since its recognition, an increasing number of cases have been identified worldwide. However, there are still no population-based studies to estimate its exact prevalence.
THC PREVENTS VOMITING—AND CAUSES IT
Delta-9-tetrahydrocannabinol (THC) is the principal psychoactive component in marijuana.6,7 There are two types of cannabinoid receptors in humans: CB1 and CB2. Both are found in the central nervous system and autonomic nervous system. Activation of CB1 receptors is responsible for the psychoactive effects of cannabinoids such as altered consciousness, euphoria, relaxation, perceptual disturbances, intensified sensory experiences, cognitive impairment, and increased reaction time. The physiologic role of CB2 is not known.
THC as an antiemetic
The antiemetic property of THC is not well understood but has been linked to activation of CB1 receptors found on the enteric plexus, presynaptic parasympathetic system, and central nervous system, particularly the cerebellum, hypothalamus, and vomiting center in the medulla.1,8–12 Stimulation and blockade of CB1 receptors can inhibit and induce vomiting in a dose-dependent manner, implicating endogenous cannabinoids in emetic circuits.12
THC as a proemetic
The mechanism of the paradoxical hyperemetic effect of THC is unknown, but several concepts have been proposed.
Chronic cannabis use can lead to down-regulation of CB1 receptors.13 Simonetto et al10 suggested that the central effects of long-term cannabis use on the hypothalamic-pituitary-adrenal axis may play a central role in the development of hyperemesis.10
Cannabinoids have a long half-life and are lipophilic.1 When used infrequently, they prevent vomiting. But with chronic use, high concentrations of THC can accumulate in the body, including cerebral fat, and can cause severe nausea and vomiting.8,9 This paradoxic hyperemesis was observed in people using intravenous crude marijuana extract.7 The same response was also noted in ferrets injected with 2-arachidonoylglycerol, a potent cannabinoid agonist.11
Patients who experience hyperemesis from chronic cannabis use may also have a genetic variation in their hepatic drug-transforming enzymes that results in excessive levels of cannabis metabolites that promote emesis.1,14
Delayed gastric emptying has also been linked to the proemetic effect of THC. However, this association became controversial when a large case series study showed that only 30% of patients with cannabinoid hyperemesis syndrome had delayed emptying on gastric scintigraphy.10
It is also possible that excessive stimulation of cannabinoid receptors in the gut can cause diffuse splanchnic vasodilation and contribute to the abdominal pain.13
DIAGNOSING CANNABINOID HYPEREMESIS SYNDROME
Cannabinoid hyperemesis syndrome is a clinical diagnosis typically seen in young patients (under age 50) with a long history of marijuana use. They present with severe, cyclic nausea and vomiting and admit to compulsively taking extremely hot showers or baths. Most patients report using marijuana for more than a year before developing episodes of severe vomiting. However, one study found that as many as 32% of patients had used it less than 1 year before experiencing symptoms.10
Other associated nonspecific symptoms are diaphoresis, bloating, abdominal discomfort, flushing, and weight loss. Symptoms are relieved with long, hot showers or baths and cessation of marijuana use. Taking a complete history is key to making the diagnosis.
In 2004, Allen et al1 first defined cannabinoid hyperemesis as excessive marijuana use associated with cyclical vomiting and abdominal pain.1 In 2012, Simonetto et al10 proposed diagnostic criteria (Table 1). Although not yet validated, these criteria are based on the largest series of cases of cannabinoid hyperemesis syndrome to date (98 patients).10
THE THREE PHASES OF CANNABINOID HYPEREMESIS
The clinical presentation of cannabinoid hyperemesis syndrome can be divided into three phases: prodromal, vomiting, and resolution.
Prodromal phase
During this phase, patients often appear anxious and agitated and display a spectrum of autonomic symptoms such as sweating, flushing, and constantly sipping water due to thirst. They may sometimes have abdominal pain that is usually epigastric but may also be diffuse. Their symptoms are associated with severe nausea, usually early in the morning or when they see or smell food. Appetite and eating patterns remain normal. Compulsive hot bathing or showering is minimal at this phase.
Vomiting phase
In this next phase, patients experience incapacitating nausea and vomiting that may occur without warning and are resistant to conventional antiemetics such as ondansetron and promethazine.14 However, patients eventually learn that hot baths or showers relieve the symptoms, and this behavior eventually becomes a compulsion. The higher the temperature of the water, the better the effect on symptoms.1 Low-grade pyrexia, excessive thirst, orthostasis, abdominal tenderness, weight loss, and sometimes even superficial skin burns have been reported.1,9,15–18
Recovery phase
During the final phase of cannabinoid hyperemesis syndrome, most patients experience marked resolution of symptoms after 24 to 48 hours of conservative management (bowel rest until symptoms resolve, slowly advancing diet as tolerated, intravenous fluids, and electrolyte monitoring and repletion as necessary), and most importantly, cessation of cannabis use. However, the time from cessation of marijuana use to resolution of symptoms may be as long as 1 week to 1 month.1,10,14 Patients begin to resume their normal diet and daily activities. The bathing-showering compulsion subsides, and patients regain lost weight after 3 to 6 months.1
In all case series and reports, resumption of cannabis use causes the symptoms to recur. This recurrence is compelling evidence that cannabis is the cause of the hyperemesis and should be part of the essential criteria for the diagnosis of cannabinoid hyperemesis syndrome.
WHY COMPULSIVE HOT BATHING?
The mechanism behind this unique characteristic of cannabinoid hyperemesis syndrome is not known. Several theories have been suggested, but no study has identified the exact explanation for this phenomenon.1,9,10,13–15,17–31
One suggested mechanism is a response by the thermoregulatory center of the brain to the dose-dependent hypothermic effects of THC, or even a direct effect of CB1 receptor activation in the hypothalamus.9 Cannabis toxicity could disrupt the equilibrium of satiety, thirst, digestive, and thermoregulatory systems of the hypothalamus, and this interference could resolve with hot bathing.1
The so-called “cutaneous steal” syndrome has also been proposed, in which cutaneous vasodilation caused by hot water decreases the blood volume available for the splanchnic circulation thought to be responsible for the abdominal pain and vomiting.13 The compulsive hot bathing may also be a response by the brain to the anxiety or psychological stress induced by severe nausea and vomiting.14
DIFFERENTIAL DIAGNOSIS
The differential diagnosis of cannabinoid hyperemesis syndrome includes mainly cyclic vomiting syndrome and psychogenic vomiting. A careful history is useful, as is ruling out medication-induced reactions, toxins, pregnancy, and gastrointestinal, neurologic, metabolic, and endocrine causes. All three of these vomiting syndromes can present with a cyclic pattern of nausea and vomiting. Cannabis use is common in all three and so is not helpful in differentiating them. But the characteristic compulsive hot bathing and showering is unique and pathognomonic of cannabinoid hyperemesis syndrome.32
Endoscopic examination may reveal esophagitis and gastritis from severe bouts of retching.26
Cyclic vomiting syndrome
The Rome III criteria for the diagnosis of cyclic vomiting syndrome include three or more stereotypic episodes of acute-onset nausea and vomiting lasting less than 1 week, alternating with intervals of completely normal health. The criteria should be fulfilled for the previous 3 months with symptom onset at least 6 months before diagnosis.33
In a series of 17 patients with adult-onset cyclic vomiting syndrome,18 the average age at onset was 30, and 13 (76%) of the patients were women. Fifteen (88%) of the patients experienced a prodrome or aura of abdominal pain or headache, and in this group, a trigger such as emotional stress and infection could also be identified in 9 (60%).
Unlike in cannabinoid hyperemesis syndrome, most patients with cyclic vomiting syndrome have a family history of migraine headache, and the prevalence of psychological stressors is high.31 Also, patients with cannabinoid hyperemesis syndrome do not respond to medications that usually abort migraine episodes,15 whereas patients with cyclic vomiting syndrome, especially those who have a family history of migraines, may respond to antimigraine medications such as triptans. There is evidence of clinical psychological overlap between cyclic vomiting syndrome, abdominal migraine, and migraine headaches. Some authors recommend antimigraine therapy even in the absence of a family or personal history of migraine if, after a careful history and physical examination, the diagnosis of cyclic vomiting syndrome seems likely. Moreover, nonmedical management such as sleep, dark rooms, and quiet environment are not as effective in cannabinoid hyperemesis syndrome as they are in cyclic vomiting syndrome.18
Psychogenic vomiting
Psychogenic vomiting is classically defined as vomiting caused by psychological mechanisms without any obvious organic cause.13 It occurs most commonly in patients with major depressive disorder or conversion disorder.34 The mechanism appears to be a combination of past organic or gastrointestinal functional abnormalities and emotional problems, and multiple patterns of vomiting can occur. Most of these patients can be treated with behavioral therapy, antidepressant drug therapy, and supportive psychotherapy.34,35
ASKING A SERIES OF QUESTIONS
Most patients with cannabinoid hyperemesis syndrome have a history of frequent visits to emergency departments or clinics for persistent nausea and vomiting, and they may have undergone extensive diagnostic workups to exclude structural, inflammatory, infectious, and functional diseases of the bowel.23,24
To prevent unnecessary testing and use of healthcare resources, Wallace et al32 proposed an algorithm to help guide clinicians in diagnosing and treating patients with suspected cannabinoid hyperemesis syndrome. A patient presenting with severe nausea and vomiting should prompt a series of questions:
Do the signs and symptoms suggest a severe underlying medical cause? If so, this should be pursued.
Do symptoms improve while taking a hot shower or bath? If not, pursue an appropriate diagnostic evaluation and treatment for conditions other than cannabinoid hyperemesis syndrome.
Is the bathing compulsive? If not, consider other diagnoses, but remain suspicious about cannabinoid hyperemesis syndrome.
Does the patient currently use cannabis daily or almost daily, and has the patient done so for at least the past year? If the patient denies using cannabis, a urine drug screen for THC may be useful. If the patient admits to use, a presumptive diagnosis of cannabinoid hyperemesis syndrome can be made.
Does the patient have signs or symptoms of volume depletion, or is the patient unable to tolerate oral hydration? Encourage oral hydration or provide intravenous hydration, and provide cannabis cessation counseling.
Do the symptoms improve? If yes, great! Provide cessation counseling, resources, and follow-up. If not:
Is the patient still using cannabis? If not, it is time to rethink the diagnosis.
Treatment in the acute setting is supportive and includes intravenous hydration and correction of electrolytes. Conventional antiemetics such as ondansetron, metoclopramide, prochlorperazine, and promethazine have not been effective in relieving hyperemesis.9,12,14 This implies that the mechanism of emesis likely does not involve dopaminergic and serotonin pathways in the central and autonomic nervous systems.
Cessation of cannabis use is key for long-term resolution of symptoms. Efforts should be made to provide counseling and encourage patients to stop using the drug entirely (Figure 1).
SOMETHING TO THINK ABOUT
With the high prevalence of chronic cannabis abuse and the recent legalization of recreational marijuana use, we will all likely encounter a patient with cannabinoid hyperemesis. With adequate knowledge of this phenomenon, we can avoid unnecessary workups and inappropriate medical and surgical treatment in patients presenting with recurrent vomiting of unknown cause. The diagnosis can easily be made by simply asking for a history of chronic marijuana use and symptoms related to cannabinoid hyperemesis syndrome, such as relief of symptoms with hot baths or showers and with marijuana cessation.
Conservative management and fluid resuscitation is important in the acute setting, but cessation of marijuana use and follow-up counseling are the key components for treating patients with cannabinoid hyperemesis syndrome and for preventing recurrence.
With the growing use of marijuana, reports have appeared of a newly recognized condition in long-term heavy users termed cannabinoid hyperemesis syndrome.1
This syndrome is interesting for at least two reasons. First, paradoxically, marijuana appears to have an emetic effect with chronic use, whereas it usually has the opposite effect and is used as an antiemetic in patients undergoing chemotherapy. Second, patients develop a compulsion to bathe or shower in extremely hot water to relieve the symptoms.
In this article, we review the pathophysiology, clinical presentation, diagnosis, and management of this emerging condition.
MARIJUANA USE ON THE RISE
Marijuana is the most widely used illicit drug worldwide. Although statistics on its use vary, a report from the Pew Research Center2 stated that 49% of Americans say they have tried it. Several states now allow the use of marijuana for medicinal purposes, and Colorado and Washington have legalized it for recreational use. This marks a major turning point and may accelerate the slow-growing acceptance of marijuana use in the United States.
Marijuana has been used to treat HIV-associated anorexia and wasting, convulsions, glaucoma, headache, and chemotherapy-induced nausea and vomiting.3–5
Cannabinoid hyperemesis syndrome was first described in 2004 in South Australia.1 Since its recognition, an increasing number of cases have been identified worldwide. However, there are still no population-based studies to estimate its exact prevalence.
THC PREVENTS VOMITING—AND CAUSES IT
Delta-9-tetrahydrocannabinol (THC) is the principal psychoactive component in marijuana.6,7 There are two types of cannabinoid receptors in humans: CB1 and CB2. Both are found in the central nervous system and autonomic nervous system. Activation of CB1 receptors is responsible for the psychoactive effects of cannabinoids such as altered consciousness, euphoria, relaxation, perceptual disturbances, intensified sensory experiences, cognitive impairment, and increased reaction time. The physiologic role of CB2 is not known.
THC as an antiemetic
The antiemetic property of THC is not well understood but has been linked to activation of CB1 receptors found on the enteric plexus, presynaptic parasympathetic system, and central nervous system, particularly the cerebellum, hypothalamus, and vomiting center in the medulla.1,8–12 Stimulation and blockade of CB1 receptors can inhibit and induce vomiting in a dose-dependent manner, implicating endogenous cannabinoids in emetic circuits.12
THC as a proemetic
The mechanism of the paradoxical hyperemetic effect of THC is unknown, but several concepts have been proposed.
Chronic cannabis use can lead to down-regulation of CB1 receptors.13 Simonetto et al10 suggested that the central effects of long-term cannabis use on the hypothalamic-pituitary-adrenal axis may play a central role in the development of hyperemesis.10
Cannabinoids have a long half-life and are lipophilic.1 When used infrequently, they prevent vomiting. But with chronic use, high concentrations of THC can accumulate in the body, including cerebral fat, and can cause severe nausea and vomiting.8,9 This paradoxic hyperemesis was observed in people using intravenous crude marijuana extract.7 The same response was also noted in ferrets injected with 2-arachidonoylglycerol, a potent cannabinoid agonist.11
Patients who experience hyperemesis from chronic cannabis use may also have a genetic variation in their hepatic drug-transforming enzymes that results in excessive levels of cannabis metabolites that promote emesis.1,14
Delayed gastric emptying has also been linked to the proemetic effect of THC. However, this association became controversial when a large case series study showed that only 30% of patients with cannabinoid hyperemesis syndrome had delayed emptying on gastric scintigraphy.10
It is also possible that excessive stimulation of cannabinoid receptors in the gut can cause diffuse splanchnic vasodilation and contribute to the abdominal pain.13
DIAGNOSING CANNABINOID HYPEREMESIS SYNDROME
Cannabinoid hyperemesis syndrome is a clinical diagnosis typically seen in young patients (under age 50) with a long history of marijuana use. They present with severe, cyclic nausea and vomiting and admit to compulsively taking extremely hot showers or baths. Most patients report using marijuana for more than a year before developing episodes of severe vomiting. However, one study found that as many as 32% of patients had used it less than 1 year before experiencing symptoms.10
Other associated nonspecific symptoms are diaphoresis, bloating, abdominal discomfort, flushing, and weight loss. Symptoms are relieved with long, hot showers or baths and cessation of marijuana use. Taking a complete history is key to making the diagnosis.
In 2004, Allen et al1 first defined cannabinoid hyperemesis as excessive marijuana use associated with cyclical vomiting and abdominal pain.1 In 2012, Simonetto et al10 proposed diagnostic criteria (Table 1). Although not yet validated, these criteria are based on the largest series of cases of cannabinoid hyperemesis syndrome to date (98 patients).10
THE THREE PHASES OF CANNABINOID HYPEREMESIS
The clinical presentation of cannabinoid hyperemesis syndrome can be divided into three phases: prodromal, vomiting, and resolution.
Prodromal phase
During this phase, patients often appear anxious and agitated and display a spectrum of autonomic symptoms such as sweating, flushing, and constantly sipping water due to thirst. They may sometimes have abdominal pain that is usually epigastric but may also be diffuse. Their symptoms are associated with severe nausea, usually early in the morning or when they see or smell food. Appetite and eating patterns remain normal. Compulsive hot bathing or showering is minimal at this phase.
Vomiting phase
In this next phase, patients experience incapacitating nausea and vomiting that may occur without warning and are resistant to conventional antiemetics such as ondansetron and promethazine.14 However, patients eventually learn that hot baths or showers relieve the symptoms, and this behavior eventually becomes a compulsion. The higher the temperature of the water, the better the effect on symptoms.1 Low-grade pyrexia, excessive thirst, orthostasis, abdominal tenderness, weight loss, and sometimes even superficial skin burns have been reported.1,9,15–18
Recovery phase
During the final phase of cannabinoid hyperemesis syndrome, most patients experience marked resolution of symptoms after 24 to 48 hours of conservative management (bowel rest until symptoms resolve, slowly advancing diet as tolerated, intravenous fluids, and electrolyte monitoring and repletion as necessary), and most importantly, cessation of cannabis use. However, the time from cessation of marijuana use to resolution of symptoms may be as long as 1 week to 1 month.1,10,14 Patients begin to resume their normal diet and daily activities. The bathing-showering compulsion subsides, and patients regain lost weight after 3 to 6 months.1
In all case series and reports, resumption of cannabis use causes the symptoms to recur. This recurrence is compelling evidence that cannabis is the cause of the hyperemesis and should be part of the essential criteria for the diagnosis of cannabinoid hyperemesis syndrome.
WHY COMPULSIVE HOT BATHING?
The mechanism behind this unique characteristic of cannabinoid hyperemesis syndrome is not known. Several theories have been suggested, but no study has identified the exact explanation for this phenomenon.1,9,10,13–15,17–31
One suggested mechanism is a response by the thermoregulatory center of the brain to the dose-dependent hypothermic effects of THC, or even a direct effect of CB1 receptor activation in the hypothalamus.9 Cannabis toxicity could disrupt the equilibrium of satiety, thirst, digestive, and thermoregulatory systems of the hypothalamus, and this interference could resolve with hot bathing.1
The so-called “cutaneous steal” syndrome has also been proposed, in which cutaneous vasodilation caused by hot water decreases the blood volume available for the splanchnic circulation thought to be responsible for the abdominal pain and vomiting.13 The compulsive hot bathing may also be a response by the brain to the anxiety or psychological stress induced by severe nausea and vomiting.14
DIFFERENTIAL DIAGNOSIS
The differential diagnosis of cannabinoid hyperemesis syndrome includes mainly cyclic vomiting syndrome and psychogenic vomiting. A careful history is useful, as is ruling out medication-induced reactions, toxins, pregnancy, and gastrointestinal, neurologic, metabolic, and endocrine causes. All three of these vomiting syndromes can present with a cyclic pattern of nausea and vomiting. Cannabis use is common in all three and so is not helpful in differentiating them. But the characteristic compulsive hot bathing and showering is unique and pathognomonic of cannabinoid hyperemesis syndrome.32
Endoscopic examination may reveal esophagitis and gastritis from severe bouts of retching.26
Cyclic vomiting syndrome
The Rome III criteria for the diagnosis of cyclic vomiting syndrome include three or more stereotypic episodes of acute-onset nausea and vomiting lasting less than 1 week, alternating with intervals of completely normal health. The criteria should be fulfilled for the previous 3 months with symptom onset at least 6 months before diagnosis.33
In a series of 17 patients with adult-onset cyclic vomiting syndrome,18 the average age at onset was 30, and 13 (76%) of the patients were women. Fifteen (88%) of the patients experienced a prodrome or aura of abdominal pain or headache, and in this group, a trigger such as emotional stress and infection could also be identified in 9 (60%).
Unlike in cannabinoid hyperemesis syndrome, most patients with cyclic vomiting syndrome have a family history of migraine headache, and the prevalence of psychological stressors is high.31 Also, patients with cannabinoid hyperemesis syndrome do not respond to medications that usually abort migraine episodes,15 whereas patients with cyclic vomiting syndrome, especially those who have a family history of migraines, may respond to antimigraine medications such as triptans. There is evidence of clinical psychological overlap between cyclic vomiting syndrome, abdominal migraine, and migraine headaches. Some authors recommend antimigraine therapy even in the absence of a family or personal history of migraine if, after a careful history and physical examination, the diagnosis of cyclic vomiting syndrome seems likely. Moreover, nonmedical management such as sleep, dark rooms, and quiet environment are not as effective in cannabinoid hyperemesis syndrome as they are in cyclic vomiting syndrome.18
Psychogenic vomiting
Psychogenic vomiting is classically defined as vomiting caused by psychological mechanisms without any obvious organic cause.13 It occurs most commonly in patients with major depressive disorder or conversion disorder.34 The mechanism appears to be a combination of past organic or gastrointestinal functional abnormalities and emotional problems, and multiple patterns of vomiting can occur. Most of these patients can be treated with behavioral therapy, antidepressant drug therapy, and supportive psychotherapy.34,35
ASKING A SERIES OF QUESTIONS
Most patients with cannabinoid hyperemesis syndrome have a history of frequent visits to emergency departments or clinics for persistent nausea and vomiting, and they may have undergone extensive diagnostic workups to exclude structural, inflammatory, infectious, and functional diseases of the bowel.23,24
To prevent unnecessary testing and use of healthcare resources, Wallace et al32 proposed an algorithm to help guide clinicians in diagnosing and treating patients with suspected cannabinoid hyperemesis syndrome. A patient presenting with severe nausea and vomiting should prompt a series of questions:
Do the signs and symptoms suggest a severe underlying medical cause? If so, this should be pursued.
Do symptoms improve while taking a hot shower or bath? If not, pursue an appropriate diagnostic evaluation and treatment for conditions other than cannabinoid hyperemesis syndrome.
Is the bathing compulsive? If not, consider other diagnoses, but remain suspicious about cannabinoid hyperemesis syndrome.
Does the patient currently use cannabis daily or almost daily, and has the patient done so for at least the past year? If the patient denies using cannabis, a urine drug screen for THC may be useful. If the patient admits to use, a presumptive diagnosis of cannabinoid hyperemesis syndrome can be made.
Does the patient have signs or symptoms of volume depletion, or is the patient unable to tolerate oral hydration? Encourage oral hydration or provide intravenous hydration, and provide cannabis cessation counseling.
Do the symptoms improve? If yes, great! Provide cessation counseling, resources, and follow-up. If not:
Is the patient still using cannabis? If not, it is time to rethink the diagnosis.
Treatment in the acute setting is supportive and includes intravenous hydration and correction of electrolytes. Conventional antiemetics such as ondansetron, metoclopramide, prochlorperazine, and promethazine have not been effective in relieving hyperemesis.9,12,14 This implies that the mechanism of emesis likely does not involve dopaminergic and serotonin pathways in the central and autonomic nervous systems.
Cessation of cannabis use is key for long-term resolution of symptoms. Efforts should be made to provide counseling and encourage patients to stop using the drug entirely (Figure 1).
SOMETHING TO THINK ABOUT
With the high prevalence of chronic cannabis abuse and the recent legalization of recreational marijuana use, we will all likely encounter a patient with cannabinoid hyperemesis. With adequate knowledge of this phenomenon, we can avoid unnecessary workups and inappropriate medical and surgical treatment in patients presenting with recurrent vomiting of unknown cause. The diagnosis can easily be made by simply asking for a history of chronic marijuana use and symptoms related to cannabinoid hyperemesis syndrome, such as relief of symptoms with hot baths or showers and with marijuana cessation.
Conservative management and fluid resuscitation is important in the acute setting, but cessation of marijuana use and follow-up counseling are the key components for treating patients with cannabinoid hyperemesis syndrome and for preventing recurrence.
- Allen JH, de Moore GM, Heddle R, Twartz JC. Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis abuse. Gut 2004; 53:1566–1570.
- Motel S. 6 facts about marijuana. Factank. News in the Numbers Pew Research Center. www.pewresearch.org/fact-tank/2015/04/14/6-facts-about-marijuana/. Accessed June 2, 2015.
- Walsh D, Nelson KA, Mahmoud FA. Established and potential therapeutic applications of cannabinoids in oncology. Support Care Cancer 2003; 11:137–143.
- Tramèr MR, Carroll D, Campbell FA, Reynolds DJ, Moore RA, McQuay HJ. Cannabinoids for control of chemotherapy induced nausea and vomiting: quantitative systematic review. BMJ 2001; 323:16–21.
- Davis M, Maida V, Daeninck P, Pergolizzi J. The emerging role of cannabinoid neuromodulators in symptom management. Support Care Cancer 2007; 15:63–71.
- National Institutes of Health (NIH). National Institute on Drug Abuse. Drug facts: marijuana. www.nida.nih.gov/infofacts/marijuana. Accessed April 29, 2015.
- Vaziri ND, Thomas R, Sterling M, et al. Toxicity with intravenous injection of crude marijuana extract. Clin Toxicol 1981; 18:353–366.
- Devane WA, Hanus L, Breuer A, et al. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science 1992; 258:1946–1949.
- Chang YH, Windish DM. Cannabinoid hyperemesis relieved by compulsive bathing. Mayo Clin Proc 2009; 84:76–78.
- Simonetto DA, Oxentenko AS, Herman ML, Szostek JH. Cannabinoid hyperemesis: a case series of 98 patients. Mayo Clin Proc 2012; 87:114–119.
- Darmani NA. The potent emetogenic effects of the endocannabinoid, 2-AG (2-arachidonoylglycerol) are blocked by delta(9)-tetrahydrocannabinol and other cannnabinoids. J Pharmacol Exp Ther 2002; 300:34–42.
- Darmani NA, Sim-Selley LJ, Martin BR, et al. Antiemetic and motor-depressive actions of CP55,940: cannabinoid CB1 receptor characterization, distribution, and G-protein activation. Eur J Pharmacol 2003; 459:83–95.
- Leibovich MA. Psychogenic vomiting. Psychotherapeutic considerations. Psychother Psychosom 1973; 22:263–268.
- Soriano-Co M, Batke M, Cappell MS. The cannabis hyperemesis syndrome characterized by persistent nausea and vomiting, abdominal pain, and compulsive bathing associated with chronic marijuana use: a report of eight cases in the United States. Dig Dis Sci 2010; 55:3113–3119.
- Sontineni SP, Chaudhary S, Sontineni V, Lanspa SJ. Cannabinoid hyperemesis syndrome: clinical diagnosis of an underrecognised manifestation of chronic cannabis abuse. World J Gastroenterol 2009; 15:1264–1266.
- Cox B, Chhabra A, Adler M, Simmons J, Randlett D. Cannabinoid hyperemesis syndrome: case report of a paradoxical reaction with heavy marijuana use. Case Rep Med 2012; 2012:757696.
- Price SL, Fisher C, Kumar R, Hilgerson A. Cannabinoid hyperemesis syndrome as the underlying cause of intractable nausea and vomiting. J Am Osteopath Assoc 2011; 111:166–169.
- Lee LY, Abbott L, Moodie S, Anderson S. Cyclic vomiting syndrome in 28 patients: demographics, features and outcomes. Eur J Gastroenterol Hepatol 2012; 24:939–943.
- Wallace D, Martin AL, Park B. Cannabinoid hyperemesis: marijuana puts patients in hot water. Australas Psychiatry 2007; 15:156–158.
- Ashton CH. Adverse effects of cannabis and cannabinoids. Br J Anaesth 1999; 83:637–649.
- Cota D, Steiner MA, Marsicano G, et al. Requirement of cannabinoid receptor type 1 for the basal modulation of hypothalamic-pituitary-adrenal axis function. Endocrinology 2007; 148:1574–1581.
- McCallum RW, Soykan I, Sridhar KR, Ricci DA, Lange RC, Plankey MW. Delta-9-tetrahydrocannabinol delays the gastric emptying of solid food in humans: a double-blind, randomized study. Aliment Pharmacol Ther 1999; 13:77–80.
- Donnino MW, Cocchi MN, Miller J, Fisher J. Cannabinoid hyperemesis: a case series. J Emerg Med 2011; 40:e63–e66.
- Singh E, Coyle W. Cannabinoid hyperemesis. Am J Gastroenterol 2008; 103:1048–1049.
- Carnett JB. Intercostal neuralgia as a cause of abdominal pain and tenderness. Surg Gynecol Obstet 1926; 42:625–632.
- Patterson DA, Smith E, Monahan M, et al. Cannabinoid hyperemesis and compulsive bathing: a case series and paradoxical pathophysiological explanation. J Am Board Fam Med 2010; 23:790–793.
- Izzo AA, Camilleri M. Emerging role of cannabinoids in gastrointestinal and liver diseases: basic and clinical aspects. Gut 2008; 57:1140–1155.
- Pertwee RG. Cannabinoids and the gastrointestinal tract. Gut 2001; 48:859–867.
- Choung RS, Locke GR 3rd, Lee RM, Schleck CD, Zinsmeister AR, Talley NJ. Cyclic vomiting syndrome and functional vomiting in adults: association with cannabinoid use in males. Neurogastroenterol Motil 2012; 24:20–26,e1.
- Nicolson SE, Denysenko L, Mulcare JL, Vito JP, Chabon B. Cannabinoid hyperemesis syndrome: a case series and review of previous reports. Psychosomatics 2012; 53:212–219.
- Miller JB, Walsh M, Patel PA, et al. Pediatric cannabinoid hyperemesis: two cases. Pediatr Emerg Care 2010; 26:919–920.
- Wallace EA, Andrews SE, Garmany CL, Jelley MJ. Cannabinoid hyperemesis syndrome: literature review and proposed diagnosis and treatment algorithm. South Med J 2011; 104:659–664.
- Tack J, Taley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology 2006; 130:1466–1479.
- Muraoka M, Mine K, Matsumoto K, Nakai Y, Nakagawa T. Psychogenic vomiting: the relation between patterns of vomiting and psychiatric diagnoses. Gut 1990; 31:526–528.
- Stravynski A. Behavioral treatment of psychogenic vomiting in the context of social phobia. J Nerv Ment Dis 1983; 171:448–451.
- Allen JH, de Moore GM, Heddle R, Twartz JC. Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis abuse. Gut 2004; 53:1566–1570.
- Motel S. 6 facts about marijuana. Factank. News in the Numbers Pew Research Center. www.pewresearch.org/fact-tank/2015/04/14/6-facts-about-marijuana/. Accessed June 2, 2015.
- Walsh D, Nelson KA, Mahmoud FA. Established and potential therapeutic applications of cannabinoids in oncology. Support Care Cancer 2003; 11:137–143.
- Tramèr MR, Carroll D, Campbell FA, Reynolds DJ, Moore RA, McQuay HJ. Cannabinoids for control of chemotherapy induced nausea and vomiting: quantitative systematic review. BMJ 2001; 323:16–21.
- Davis M, Maida V, Daeninck P, Pergolizzi J. The emerging role of cannabinoid neuromodulators in symptom management. Support Care Cancer 2007; 15:63–71.
- National Institutes of Health (NIH). National Institute on Drug Abuse. Drug facts: marijuana. www.nida.nih.gov/infofacts/marijuana. Accessed April 29, 2015.
- Vaziri ND, Thomas R, Sterling M, et al. Toxicity with intravenous injection of crude marijuana extract. Clin Toxicol 1981; 18:353–366.
- Devane WA, Hanus L, Breuer A, et al. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science 1992; 258:1946–1949.
- Chang YH, Windish DM. Cannabinoid hyperemesis relieved by compulsive bathing. Mayo Clin Proc 2009; 84:76–78.
- Simonetto DA, Oxentenko AS, Herman ML, Szostek JH. Cannabinoid hyperemesis: a case series of 98 patients. Mayo Clin Proc 2012; 87:114–119.
- Darmani NA. The potent emetogenic effects of the endocannabinoid, 2-AG (2-arachidonoylglycerol) are blocked by delta(9)-tetrahydrocannabinol and other cannnabinoids. J Pharmacol Exp Ther 2002; 300:34–42.
- Darmani NA, Sim-Selley LJ, Martin BR, et al. Antiemetic and motor-depressive actions of CP55,940: cannabinoid CB1 receptor characterization, distribution, and G-protein activation. Eur J Pharmacol 2003; 459:83–95.
- Leibovich MA. Psychogenic vomiting. Psychotherapeutic considerations. Psychother Psychosom 1973; 22:263–268.
- Soriano-Co M, Batke M, Cappell MS. The cannabis hyperemesis syndrome characterized by persistent nausea and vomiting, abdominal pain, and compulsive bathing associated with chronic marijuana use: a report of eight cases in the United States. Dig Dis Sci 2010; 55:3113–3119.
- Sontineni SP, Chaudhary S, Sontineni V, Lanspa SJ. Cannabinoid hyperemesis syndrome: clinical diagnosis of an underrecognised manifestation of chronic cannabis abuse. World J Gastroenterol 2009; 15:1264–1266.
- Cox B, Chhabra A, Adler M, Simmons J, Randlett D. Cannabinoid hyperemesis syndrome: case report of a paradoxical reaction with heavy marijuana use. Case Rep Med 2012; 2012:757696.
- Price SL, Fisher C, Kumar R, Hilgerson A. Cannabinoid hyperemesis syndrome as the underlying cause of intractable nausea and vomiting. J Am Osteopath Assoc 2011; 111:166–169.
- Lee LY, Abbott L, Moodie S, Anderson S. Cyclic vomiting syndrome in 28 patients: demographics, features and outcomes. Eur J Gastroenterol Hepatol 2012; 24:939–943.
- Wallace D, Martin AL, Park B. Cannabinoid hyperemesis: marijuana puts patients in hot water. Australas Psychiatry 2007; 15:156–158.
- Ashton CH. Adverse effects of cannabis and cannabinoids. Br J Anaesth 1999; 83:637–649.
- Cota D, Steiner MA, Marsicano G, et al. Requirement of cannabinoid receptor type 1 for the basal modulation of hypothalamic-pituitary-adrenal axis function. Endocrinology 2007; 148:1574–1581.
- McCallum RW, Soykan I, Sridhar KR, Ricci DA, Lange RC, Plankey MW. Delta-9-tetrahydrocannabinol delays the gastric emptying of solid food in humans: a double-blind, randomized study. Aliment Pharmacol Ther 1999; 13:77–80.
- Donnino MW, Cocchi MN, Miller J, Fisher J. Cannabinoid hyperemesis: a case series. J Emerg Med 2011; 40:e63–e66.
- Singh E, Coyle W. Cannabinoid hyperemesis. Am J Gastroenterol 2008; 103:1048–1049.
- Carnett JB. Intercostal neuralgia as a cause of abdominal pain and tenderness. Surg Gynecol Obstet 1926; 42:625–632.
- Patterson DA, Smith E, Monahan M, et al. Cannabinoid hyperemesis and compulsive bathing: a case series and paradoxical pathophysiological explanation. J Am Board Fam Med 2010; 23:790–793.
- Izzo AA, Camilleri M. Emerging role of cannabinoids in gastrointestinal and liver diseases: basic and clinical aspects. Gut 2008; 57:1140–1155.
- Pertwee RG. Cannabinoids and the gastrointestinal tract. Gut 2001; 48:859–867.
- Choung RS, Locke GR 3rd, Lee RM, Schleck CD, Zinsmeister AR, Talley NJ. Cyclic vomiting syndrome and functional vomiting in adults: association with cannabinoid use in males. Neurogastroenterol Motil 2012; 24:20–26,e1.
- Nicolson SE, Denysenko L, Mulcare JL, Vito JP, Chabon B. Cannabinoid hyperemesis syndrome: a case series and review of previous reports. Psychosomatics 2012; 53:212–219.
- Miller JB, Walsh M, Patel PA, et al. Pediatric cannabinoid hyperemesis: two cases. Pediatr Emerg Care 2010; 26:919–920.
- Wallace EA, Andrews SE, Garmany CL, Jelley MJ. Cannabinoid hyperemesis syndrome: literature review and proposed diagnosis and treatment algorithm. South Med J 2011; 104:659–664.
- Tack J, Taley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology 2006; 130:1466–1479.
- Muraoka M, Mine K, Matsumoto K, Nakai Y, Nakagawa T. Psychogenic vomiting: the relation between patterns of vomiting and psychiatric diagnoses. Gut 1990; 31:526–528.
- Stravynski A. Behavioral treatment of psychogenic vomiting in the context of social phobia. J Nerv Ment Dis 1983; 171:448–451.
KEY POINTS
- The prodromal phase is characterized by severe anxiety and agitation. Patients display a spectrum of autonomic symptoms such as sweating, flushing, constantly sipping water due to thirst, and colicky abdominal pain.
- In the second phase, patients develop incapacitating nausea and vomiting that may occur without warning and is usually resistant to conventional antiemetics such as ondansetron and promethazine. During this phase, patients learn the immediate relieving effects of taking hot baths.
- After 24 to 48 hours of conservative management, intravenous fluid replacement, and, most importantly, cessation of cannabis use, patients experience marked resolution of symptoms. The compulsive hot-bathing behavior subsides. However, eventually, patients go back to using marijuana, and the cycle of symptoms recurs.
Bell palsy: Clinical examination and management
Bell palsy is an idiopathic peripheral nerve disorder involving the facial nerve (ie, cranial nerve VII) and manifesting as acute, ipsilateral facial muscle weakness. It is named after Sir Charles Bell, who in 1821 first described the anatomy of the facial nerve.1 Although the disorder is clinically benign, patients can be devastated by its disfigurement.
The annual incidence of Bell palsy is 20 per 100,000, with no predilection for sex or ethnicity. It can affect people at any age, but the incidence is slightly higher after age 40.2,3 Risk factors include diabetes, pregnancy, severe preeclampsia, obesity, and hypertension.4–7
THE FACIAL NERVE IS VULNERABLE TO TRAUMA AND COMPRESSION
A basic understanding of the neuroanatomy of the facial nerve provides clues for distinguishing a central lesion from a peripheral lesion. This differentiation is important because the causes and management differ.
The facial nerve is a mixed sensory and motor nerve, carrying fibers involved in facial expression, taste, lacrimation, salivation, and sensation of the ear. It originates in the lower pons and exits the brainstem ventrally at the pontomedullary junction. After entering the internal acoustic meatus, it travels 20 to 30 mm in the facial canal, the longest bony course of any cranial nerve, making it highly susceptible to trauma and compression by edema.8
In the facial canal, it makes a posterior and inferior turn, forming a bend (ie, the genu of the facial nerve). The genu is proximal to the geniculate ganglion, which contains the facial nerve’s primary sensory neurons for taste and sensation. The motor branch of the facial nerve then exits the cranium via the stylomastoid foramen and passes through the parotid gland, where it divides into temporofacial and cervicofacial trunks.9
The facial nerve has five terminal branches that innervate the muscles of facial expression:
- The temporal branch (muscles of the forehead and superior part of the orbicularis oculi)
- The zygomatic branch (muscles of the nasolabial fold and cheek, eg, nasalis and zygomaticus).
- The buccal branch (the buccinators and inferior part of the orbicularis oculi)
- The marginal mandibular branch (the depressors of the mouth, eg, depressor anguli and mentalis)
- The cervical branch (the platysma muscle).
INFLAMMATION IS BELIEVED TO BE RESPONSIBLE
Although the precise cause of Bell palsy is not known, one theory is that inflammation of the nerve causes focal edema, demyelination, and ischemia. Several studies have suggested that herpes virus simplex type 1 infection may be involved.10
FACIAL DROOPING, EYELID WEAKNESS, OTHER SYMPTOMS
Symptoms of Bell palsy include ipsilateral sagging of the eyebrow, drooping of the face, flattening of the nasolabial fold, and inability to fully close the eye, pucker the lips, or raise the corner of the mouth (Figure 1). Symptoms develop within hours and are maximal by 3 days.
About 70% of patients have associated ipsilateral pain around the ear. If facial pain is present with sensory and hearing loss, a tumor of the parotid gland or viral otitis must be considered.11 Other complaints may include hyperacusis due to disruption of nerve fibers to the stapedius muscle, changes in taste, and dry eye from parasympathetic dysfunction. Some patients report paresthesias over the face, which most often represent motor symptoms misconstrued as sensory changes.
PHYSICAL EXAMINATION
The clinical examination should include a complete neurologic and general examination, including otoscopy and attention to the skin and parotid gland. Vesicles or scabbing around the ear should prompt testing for herpes zoster. Careful observation during the interview while the patient is talking may reveal subtle signs of weakness and provide additional clues.
A systematic approach to the assessment of a patient with suspected Bell palsy is recommended (Table 1) and outlined below:
Does the patient have peripheral facial palsy?
In Bell palsy, wrinkling of the forehead on the affected side when raising the eyebrows is either asymmetrical or absent.
If the forehead muscles are spared and the lower face is weak, this signifies a central lesion such as a stroke or other structural abnormality and not a peripheral lesion of the facial nerve (eg, Bell palsy).
Can the patient close the eyes tightly?
Normally, the patient should be able to close both eyes tightly, and the eyelashes should be buried between the eyelids. In Bell palsy, when the patient attempts to close the eyes, the affected side shows incomplete closure and the eye may remain partly open.
Assess the strength of the orbicularis oculi by trying to open the eyes. The patient who is attempting to close the eyelids tightly but cannot will demonstrate the Bell phenomenon, ie, the examiner is able to force open the eyelids, and the eyes are deviated upward and laterally.
Closely observe the blink pattern, as the involved side in Bell palsy may slightly lag behind the normal eye, and the patient may be unable to close the eye completely.
Is the smile symmetric?
Note flattening of the nasolabial fold on one side, which indicates facial weakness.
Can the patient puff out the cheeks?
Ask the patient to hold air in the mouth against resistance. This assesses the strength of the buccinator muscle.
Can the patient purse the lips?
Ask the patient to pucker or purse the lips and observe for asymmetry or weakness on the affected side.
Test the orbicularis oris muscle by trying to spread the lips apart while the patient resists, and observe for weakness on one side.
Is there a symmetric grimace?
This will test the muscles involved in depressing the angles of the mouth and platysma.
Are taste, sensation, and hearing intact?
Other testable functions of the facial nerve, including taste, sensation, and hearing, do not always need to be assessed but can be in patients with specific sensory deficits.
Abnormalities in taste can support localization of the problem either proximal or distal to the branch point of fibers mediating taste. The facial nerve supplies taste fibers to the anterior two-thirds of the tongue. Sweet and salty taste can be screened with sugar and salt. Tell the patient to close the eyes, and using a tongue blade, apply a small amount of sugar or salt on the side of the tongue. Ask the patient to identify the taste and repeat with the other sample after he or she has rinsed the mouth.
Somatic sensory fibers supplied by the facial nerve innervate the inner ear and a small area behind the ear, but these may be difficult to assess objectively. Formal audiologic testing may be needed if hearing is impaired.
Facial nerve reflexes
A number of facial reflexes can be tested, including the orbicularis oculi, palpebral-oculogyric, and corneal reflexes.12
The orbicularis oculi reflex is tested by gentle finger percussion of the glabella while observing for involuntary blinking with each stimulus. The afferent branch of this reflex is carried by the trigeminal nerve, while the efferent response is carried by the facial nerve. In peripheral facial nerve palsy, this reflex is weakened or absent on the affected side.
The palpebral-oculogyric reflex, or Bell phenomenon, produces upward and lateral deviation of the eyes when attempting forceful eyelid closure. In this reflex, the afferent fibers are carried by the facial nerve and the efferent fibers travel in the oculomotor nerve to the superior rectus muscle. In Bell palsy, this reflex is visible because of failure of adequate eyelid closure.
The corneal reflex is elicited by stimulating the cornea with a wisp of cotton, causing reflexive closure of the both eyes. The affected side may show slowed or absent lid closure when tested on either side. The sensory afferent fibers are carried by the trigeminal nerve, and the motor efferent fibers are carried by the facial nerve.
Grading of facial paralysis
The House-Brackmann scale is the most widely used tool for grading the degree of facial paralysis and for predicting recovery. Grades are I to VI, with grade I indicating normal function, and grade VI, complete paralysis.
Patients with some preserved motor function generally have good recovery, but those with complete paralysis may have long-term residual deficits.13
A DIAGNOSIS OF EXCLUSION
The diagnosis of Bell palsy is made by excluding other causes of unilateral facial paralysis, and 30% to 60% of cases of facial palsy are caused by an underlying disorder that mimics Bell palsy, including central nervous system lesion (eg, stroke, demyelinating disease), parotid gland tumor, Lyme disease, Ramsay Hunt syndrome, granulomatous disease, otitis media, cholesteatoma, diabetes, trauma, and Guillain-Barré syndrome (Table 2).14,15 Many of these conditions have associated features that help distinguish them from Bell palsy. Facial palsy that does not improve after 3 weeks should prompt referral to a neurologist.
Brain lesions
It is uncommon to have isolated facial palsy with a cortical or subcortical brain lesion, since the corticobulbar and corticospinal tracts travel in close proximity. Cortical signs such as hemiparesis, hemisensory loss, neglect, and dysarthria suggest a lesion of the cerebral cortex. Additionally, forehead muscle sparing is expected in supranuclear lesions.
Brainstem lesions can manifest with multiple ipsilateral cranial nerve palsies and contralateral limb weakness. Sarcoidosis and leptomeningeal carcinomatosis tend to involve the skull base and present with multiple cranial neuropathies.
Tumors of the brain or parotid gland have an insidious onset and may cause systemic signs such as fevers, chills, and weight loss. Headache, seizures, and hearing loss indicate an intracranial lesion. A palpable mass near the ear, neck, or parotid gland requires imaging of the face to look for a parotid gland tumor.
Infection
A number of infections can cause acute facial paralysis. The most common is herpes simplex virus, and the next most common is varicella zoster.14 Herpes simplex virus, Ramsay Hunt syndrome, and Lyme disease may have associated pain and skin changes. Erythema of the tympanic membrane suggests otitis media, especially in the setting of ear pain and hearing loss.
Ramsay Hunt syndrome is caused by reactivation of the herpes zoster virus from the geniculate ganglion, affecting the facial nerve. Careful examination of the ear canal and the oropharynx may show vesicles.
In Lyme disease, facial palsy is the most common cranial neuropathy, seen in 50% to 63% of patients with Borrelia burgdorferi meningitis.16,17 In people with a history of rash, arthralgia, tick bite, or travel to an endemic region, Lyme titers should be checked before starting the patient on corticosteroids.
Bilateral facial palsy is rare and occurs in fewer than 1% of patients. It has been reported in patients with Lyme disease, Guillain-Barré syndrome, sarcoidosis, diabetes mellitus, viral infection, and pontine glioma.18
DIAGNOSTIC EVALUATION
Serologic testing, electrodiagnostic studies, and imaging are not routinely necessary to diagnose Bell palsy. However, referral to the appropriate specialist (neurologist, otolaryngologist, optometrist, ophthalmologist) is advised if the patient has sparing of the forehead muscle, multiple cranial neuropathies, signs of infection, or persistent weakness without significant improvement at 3 weeks.
Laboratory testing
A complete blood cell count with differential may point to infection or a lymphoproliferative disorder. When indicated, screening for diabetes mellitus with fasting blood glucose or hemoglobin A1c may be helpful. In Lyme-endemic regions, patients should undergo an enzyme-linked immunosorbent assay or an indirect fluorescent antibody test to screen for the disease. If positive, the diagnosis of Lyme disease should be confirmed by Western blot. If vesicles are present on examination, check serum antibodies for herpes zoster. In the appropriate clinical setting, angiotensin-converting enzyme, human immunodeficiency virus, and inflammatory markers can be tested.
Cerebrospinal fluid analysis is generally not helpful in diagnosing Bell palsy but can differentiate it from Guillain-Barré syndrome, leptomeningeal carcinomatosis, and infection involving the central nervous system.
Imaging
Imaging is not recommended in the initial evaluation of Bell palsy unless symptoms and the examination are atypical. From 5% to 7% of cases of facial palsy are caused by a tumor (eg, facial neuroma, cholesteatoma, hemangioma, meningioma), whether benign or malignant.14,15 Therefore, in patients with insidious onset of symptoms that do not improve in about 3 weeks, contrast-enhanced computed tomography or gadolinium-enhanced magnetic resonance imaging of the internal auditory canal and face is warranted.
Electrodiagnostic studies
Electrodiagnostic testing is typically not part of the evaluation of acute Bell palsy, but in patients with complete paralysis, it may help assess the degree of nerve injury and the chances of recovery, especially since patients with complete paralysis have a higher risk of incomplete recovery.19 Electrodiagnostic studies should be performed at least 1 week after symptom onset to avoid false-negative results.
TREATMENT
The treatment of Bell palsy focuses on maximizing recovery and minimizing associated complications.
Protect the eyes
Patients who cannot completely close their eyes should be given instructions on ocular protective care to prevent exposure keratopathy. Frequent application of lubricant eyedrops with artificial tears during the day or ophthalmic ointment at bedtime is recommended. The physician should also recommend protective eyewear such as sunglasses during the day. Eye patching or taping at night may be useful but could be harmful if applied too loosely or too tightly. Patients with vision loss or eye irritation should be referred to an ophthalmologist.19
Corticosteroids are recommended in the first 72 hours
In two randomized clinical trials (conducted by Sullivan et al20 in 511 patients and Engström et al21 in 829 patients), prednisolone was found to be beneficial if started within 72 hours of symptom onset.
In a double-blind, randomized, placebo-controlled study of prednisone in 58 patients, those who received the drug recovered faster, although long-term outcomes in these patients were not significantly different than those in the control group.22 The American Academy of Neurology23 rated this study as class II, ie, not meeting all of its criteria for the highest level of evidence, class I. Nevertheless, although prednisone lacks class I evidence, its use is recommended because it is a precursor to its active metabolite, prednisolone, which has been studied extensively.
The current guidelines of the American Academy of Neurology, updated in 2012, state, “For patients with new-onset Bell palsy, steroids are highly likely to be effective and should be offered to increase the probability of recovery of facial nerve function”23 (level A evidence, ie, established as effective). They also concluded that adverse effects of corticosteroids were generally minor and temporary.
Similarly, the guidelines of the American Academy of Otolaryngology–Head and Neck Surgery, published in 2013, recommend oral corticosteroids within 72 hours of onset of symptoms of Bell palsy for patients age 16 and older.19 The recommendation is for a 10-day course of corticosteroids with at least 5 days at a high dose (prednisolone 50 mg orally daily for 10 days, or prednisone 60 mg orally daily for 5 days, followed by a 5-day taper). The benefit of corticosteroids after 72 hours is unclear (Table 3).19
Even though the guidelines recommend corticosteroids, the decision to use them in diabetic patients and pregnant women should be individualized. Discretion is advised, as not all patients with Bell palsy need to be treated. Most recover spontaneously, especially those with mild symptoms.
Antiviral therapy may offer modest benefit
Antiviral therapy has not been shown to be beneficial in Bell palsy, and current guidelines do not recommend oral antiviral therapy alone.19 However, an antiviral combined with a corticosteroid may offer modest benefit if started within 72 hours of symptom onset (level C evidence, ie, possibly effective).23 Patients starting antiviral therapy should understand that its benefit has not been established.
Surgical decompression remains controversial
A Cochrane systematic review in 2011 found insufficient evidence regarding the safety and efficacy of surgical intervention in Bell palsy.24 Surgery should be considered only for patients with complete paralysis with a greater than 90% reduction in motor amplitude on a nerve conduction study compared with the unaffected side, and absent volitional activity on needle examination.19,25
Acupuncture: No recommendation
Currently, there is no recommendation for acupuncture in the treatment of Bell palsy.19 A recent randomized clinical trial suggests benefit from acupuncture combined with corticosteroids,26 but high-quality studies to support its use are lacking.26
Physical therapy: Insufficient evidence
There is insufficient evidence to show that physical therapy has benefit—or harm—in Bell palsy. However, some low-quality studies indicated that facial exercises and mime therapy may improve function in patients with moderate paralysis.27
Follow-up
Patients should be instructed to call at 2 weeks to report progress of symptoms and to be reevaluated within or at 1 month, with close attention to facial weakness and eye irritation. Further evaluation is needed if there has been no improvement, if symptoms have worsened, or if new symptoms have appeared.
The psychosocial impact of Bell palsy cannot be discounted, as the disfigurement can have negative implications for self-esteem and social relationships. Appropriate referral to an ophthalmologist, neurologist, otolaryngologist, social worker, or a plastic surgeon may be necessary.
COMPLICATIONS AND PROGNOSIS
Most patients with Bell palsy recover completely, but up to 30% have residual symptoms at 6 months.14,20 Furthermore, although Bell palsy usually has a monophasic course, 7% to 12% of patients have a recurrence.3,15
Long-term complications can include residual facial weakness, facial synkinesis, facial contracture, and facial spasm.14,28 Incomplete eye closure may benefit from surgery (tarsorrhaphy or gold-weight implantation) to prevent corneal ulceration. Facial synkinesis is due to aberrant nerve regeneration and occurs in 15% to 20% of patients after recovery from Bell palsy.29 Patients may describe tearing while chewing (“crocodile tears”), involuntary movement of the corners of the mouth with blinking, or ipsilateral eye-closing when the jaw opens (“jaw-winking”). Facial contracture, facial synkinesis, and facial spasm can be treated with botulinum toxin injection.30
- Grzybowski A, Kaufman MH. Sir Charles Bell (1774-1842): contributions to neuro-ophthalmology. Acta Ophthalmol Scand 2007; 85:897–901.
- De Diego-Sastre JI, Prim-Espada MP, Fernández-García F. The epidemiology of Bell’s palsy. Rev Neurol 2005; 41:287–290. In Spanish.
- Morris AM, Deeks SL, Hill MD, et al. Annualized incidence and spectrum of illness from an outbreak investigation of Bell’s palsy. Neuroepidemiology 2002; 21:255–261.
- Bosco D, Plastino M, Bosco F, et al. Bell’s palsy: a manifestation of prediabetes? Acta Neurol Scand 2011; 123:68–72.
- Riga M, Kefalidis G, Danielides V. The role of diabetes mellitus in the clinical presentation and prognosis of Bell palsy. J Am Board Fam Med 2012; 25:819–826.
- Hilsinger RL Jr, Adour KK, Doty HE. Idiopathic facial paralysis, pregnancy, and the menstrual cycle. Ann Otol Rhinol Laryngol 1975; 84:433–442.
- Savadi-Oskouei D, Abedi A, Sadeghi-Bazargani H. Independent role of hypertension in Bell’s palsy: a case-control study. Eur Neurol 2008; 60:253–257.
- Murai A, Kariya S, Tamura K, et al. The facial nerve canal in patients with Bell’s palsy: an investigation by high-resolution computed tomography with multiplanar reconstruction. Eur Arch Otorhinolaryngol 2013; 270:2035–2038.
- Blumenfeld H. Neuroanatomy Through Clinical Cases. 1st ed. Sunderland, MA: Sinauer; 2002:479–484.
- Murakami S, Mizobuchi M, Nakashiro Y, Doi T, Hato N, Yanagihara N. Bell palsy and herpes simplex virus: identification of viral DNA in endoneurial fluid and muscle. Ann Intern Med 1996; 124:27–30.
- Boahene DO, Olsen KD, Driscoll C, Lewis JE, McDonald TJ. Facial nerve paralysis secondary to occult malignant neoplasms. Otolaryngol Head Neck Surg 2004; 130:459–465.
- DeJong RN. The Neurologic Examination: Incorporating the fundamentals of neuroanatomy and neurophysiology. 4th ed. New York, NY: Harper & Row; 1979:178–198.
- House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg 1985; 93:146–147.
- Peitersen E. Bell’s palsy: the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Otolaryngol Suppl 2002; 549:4–30.
- Hohman MH, Hadlock TA. Etiology, diagnosis, and management of facial palsy: 2000 patients at a facial nerve center. Laryngoscope 2014; 124:E283–E293.
- Ackermann R, Hörstrup P, Schmidt R. Tick-borne meningopolyneuritis (Garin-Bujadoux, Bannwarth). Yale J Biol Med 1984; 57:485–490.
- Pachner AR, Steere AC. The triad of neurologic manifestations of Lyme disease: meningitis, cranial neuritis, and radiculoneuritis. Neurology 1985; 35:47–53.
- Keane JR. Bilateral seventh nerve palsy: analysis of 43 cases and review of the literature. Neurology 1994; 44:1198–1202.
- Baugh RF, Basura GJ, Ishii LE, et al. Clinical practice guideline: Bell’s palsy. Otolaryngol Head Neck Surg 2013; 149(suppl 3):S1–S27.
- Sullivan FM, Swan IR, Donnan PT, et al. Early treatment with prednisolone or acyclovir in Bell’s palsy. N Engl J Med 2007; 357:1598–1607.
- Engström M, Berg T, Stjernquist-Desatnik A, et al. Prednisolone and valaciclovir in Bell’s palsy: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet Neurol 2008; 7:993–1000.
- Lagalla G, Logullo F, Di Bella P, Provinciali L, Ceravolo MG. Influence of early high-dose steroid treatment on Bell’s palsy evolution. Neurol Sci 2002; 23:107–112.
- Gronseth GS, Paduga R; American Academy of Neurology. Evidence-based guideline update: steroids and antivirals for Bell palsy: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 2012; 79:2209–2213.
- McAllister K, Walker D, Donnan PT, Swan I. Surgical interventions for the early management of Bell’s palsy. Cochrane Database Syst Rev 2011; 2:CD007468.
- Gantz BJ, Rubinstein JT, Gidley P, Woodworth GG. Surgical management of Bell’s palsy. Laryngoscope 1999; 109:1177–1188.
- Xu SB, Huang B, Zhang CY, et al. Effectiveness of strengthened stimulation during acupuncture for the treatment of Bell palsy: a randomized controlled trial. CMAJ 2013; 185:473–479.
- Teixeira LJ, Valbuza JS, Prado GF. Physical therapy for Bell’s palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 2011; 12:CD006283.
- Yaltho TC, Jankovic J. The many faces of hemifacial spasm: differential diagnosis of unilateral facial spasms. Mov Disord 2011; 26:1582–1592.
- Celik M, Forta H, Vural C. The development of synkinesis after facial nerve paralysis. Eur Neurol 2000; 43:147–151.
- Chua CN, Quhill F, Jones E, Voon LW, Ahad M, Rowson N. Treatment of aberrant facial nerve regeneration with botulinum toxin A. Orbit 2004; 23:213–218.
Bell palsy is an idiopathic peripheral nerve disorder involving the facial nerve (ie, cranial nerve VII) and manifesting as acute, ipsilateral facial muscle weakness. It is named after Sir Charles Bell, who in 1821 first described the anatomy of the facial nerve.1 Although the disorder is clinically benign, patients can be devastated by its disfigurement.
The annual incidence of Bell palsy is 20 per 100,000, with no predilection for sex or ethnicity. It can affect people at any age, but the incidence is slightly higher after age 40.2,3 Risk factors include diabetes, pregnancy, severe preeclampsia, obesity, and hypertension.4–7
THE FACIAL NERVE IS VULNERABLE TO TRAUMA AND COMPRESSION
A basic understanding of the neuroanatomy of the facial nerve provides clues for distinguishing a central lesion from a peripheral lesion. This differentiation is important because the causes and management differ.
The facial nerve is a mixed sensory and motor nerve, carrying fibers involved in facial expression, taste, lacrimation, salivation, and sensation of the ear. It originates in the lower pons and exits the brainstem ventrally at the pontomedullary junction. After entering the internal acoustic meatus, it travels 20 to 30 mm in the facial canal, the longest bony course of any cranial nerve, making it highly susceptible to trauma and compression by edema.8
In the facial canal, it makes a posterior and inferior turn, forming a bend (ie, the genu of the facial nerve). The genu is proximal to the geniculate ganglion, which contains the facial nerve’s primary sensory neurons for taste and sensation. The motor branch of the facial nerve then exits the cranium via the stylomastoid foramen and passes through the parotid gland, where it divides into temporofacial and cervicofacial trunks.9
The facial nerve has five terminal branches that innervate the muscles of facial expression:
- The temporal branch (muscles of the forehead and superior part of the orbicularis oculi)
- The zygomatic branch (muscles of the nasolabial fold and cheek, eg, nasalis and zygomaticus).
- The buccal branch (the buccinators and inferior part of the orbicularis oculi)
- The marginal mandibular branch (the depressors of the mouth, eg, depressor anguli and mentalis)
- The cervical branch (the platysma muscle).
INFLAMMATION IS BELIEVED TO BE RESPONSIBLE
Although the precise cause of Bell palsy is not known, one theory is that inflammation of the nerve causes focal edema, demyelination, and ischemia. Several studies have suggested that herpes virus simplex type 1 infection may be involved.10
FACIAL DROOPING, EYELID WEAKNESS, OTHER SYMPTOMS
Symptoms of Bell palsy include ipsilateral sagging of the eyebrow, drooping of the face, flattening of the nasolabial fold, and inability to fully close the eye, pucker the lips, or raise the corner of the mouth (Figure 1). Symptoms develop within hours and are maximal by 3 days.
About 70% of patients have associated ipsilateral pain around the ear. If facial pain is present with sensory and hearing loss, a tumor of the parotid gland or viral otitis must be considered.11 Other complaints may include hyperacusis due to disruption of nerve fibers to the stapedius muscle, changes in taste, and dry eye from parasympathetic dysfunction. Some patients report paresthesias over the face, which most often represent motor symptoms misconstrued as sensory changes.
PHYSICAL EXAMINATION
The clinical examination should include a complete neurologic and general examination, including otoscopy and attention to the skin and parotid gland. Vesicles or scabbing around the ear should prompt testing for herpes zoster. Careful observation during the interview while the patient is talking may reveal subtle signs of weakness and provide additional clues.
A systematic approach to the assessment of a patient with suspected Bell palsy is recommended (Table 1) and outlined below:
Does the patient have peripheral facial palsy?
In Bell palsy, wrinkling of the forehead on the affected side when raising the eyebrows is either asymmetrical or absent.
If the forehead muscles are spared and the lower face is weak, this signifies a central lesion such as a stroke or other structural abnormality and not a peripheral lesion of the facial nerve (eg, Bell palsy).
Can the patient close the eyes tightly?
Normally, the patient should be able to close both eyes tightly, and the eyelashes should be buried between the eyelids. In Bell palsy, when the patient attempts to close the eyes, the affected side shows incomplete closure and the eye may remain partly open.
Assess the strength of the orbicularis oculi by trying to open the eyes. The patient who is attempting to close the eyelids tightly but cannot will demonstrate the Bell phenomenon, ie, the examiner is able to force open the eyelids, and the eyes are deviated upward and laterally.
Closely observe the blink pattern, as the involved side in Bell palsy may slightly lag behind the normal eye, and the patient may be unable to close the eye completely.
Is the smile symmetric?
Note flattening of the nasolabial fold on one side, which indicates facial weakness.
Can the patient puff out the cheeks?
Ask the patient to hold air in the mouth against resistance. This assesses the strength of the buccinator muscle.
Can the patient purse the lips?
Ask the patient to pucker or purse the lips and observe for asymmetry or weakness on the affected side.
Test the orbicularis oris muscle by trying to spread the lips apart while the patient resists, and observe for weakness on one side.
Is there a symmetric grimace?
This will test the muscles involved in depressing the angles of the mouth and platysma.
Are taste, sensation, and hearing intact?
Other testable functions of the facial nerve, including taste, sensation, and hearing, do not always need to be assessed but can be in patients with specific sensory deficits.
Abnormalities in taste can support localization of the problem either proximal or distal to the branch point of fibers mediating taste. The facial nerve supplies taste fibers to the anterior two-thirds of the tongue. Sweet and salty taste can be screened with sugar and salt. Tell the patient to close the eyes, and using a tongue blade, apply a small amount of sugar or salt on the side of the tongue. Ask the patient to identify the taste and repeat with the other sample after he or she has rinsed the mouth.
Somatic sensory fibers supplied by the facial nerve innervate the inner ear and a small area behind the ear, but these may be difficult to assess objectively. Formal audiologic testing may be needed if hearing is impaired.
Facial nerve reflexes
A number of facial reflexes can be tested, including the orbicularis oculi, palpebral-oculogyric, and corneal reflexes.12
The orbicularis oculi reflex is tested by gentle finger percussion of the glabella while observing for involuntary blinking with each stimulus. The afferent branch of this reflex is carried by the trigeminal nerve, while the efferent response is carried by the facial nerve. In peripheral facial nerve palsy, this reflex is weakened or absent on the affected side.
The palpebral-oculogyric reflex, or Bell phenomenon, produces upward and lateral deviation of the eyes when attempting forceful eyelid closure. In this reflex, the afferent fibers are carried by the facial nerve and the efferent fibers travel in the oculomotor nerve to the superior rectus muscle. In Bell palsy, this reflex is visible because of failure of adequate eyelid closure.
The corneal reflex is elicited by stimulating the cornea with a wisp of cotton, causing reflexive closure of the both eyes. The affected side may show slowed or absent lid closure when tested on either side. The sensory afferent fibers are carried by the trigeminal nerve, and the motor efferent fibers are carried by the facial nerve.
Grading of facial paralysis
The House-Brackmann scale is the most widely used tool for grading the degree of facial paralysis and for predicting recovery. Grades are I to VI, with grade I indicating normal function, and grade VI, complete paralysis.
Patients with some preserved motor function generally have good recovery, but those with complete paralysis may have long-term residual deficits.13
A DIAGNOSIS OF EXCLUSION
The diagnosis of Bell palsy is made by excluding other causes of unilateral facial paralysis, and 30% to 60% of cases of facial palsy are caused by an underlying disorder that mimics Bell palsy, including central nervous system lesion (eg, stroke, demyelinating disease), parotid gland tumor, Lyme disease, Ramsay Hunt syndrome, granulomatous disease, otitis media, cholesteatoma, diabetes, trauma, and Guillain-Barré syndrome (Table 2).14,15 Many of these conditions have associated features that help distinguish them from Bell palsy. Facial palsy that does not improve after 3 weeks should prompt referral to a neurologist.
Brain lesions
It is uncommon to have isolated facial palsy with a cortical or subcortical brain lesion, since the corticobulbar and corticospinal tracts travel in close proximity. Cortical signs such as hemiparesis, hemisensory loss, neglect, and dysarthria suggest a lesion of the cerebral cortex. Additionally, forehead muscle sparing is expected in supranuclear lesions.
Brainstem lesions can manifest with multiple ipsilateral cranial nerve palsies and contralateral limb weakness. Sarcoidosis and leptomeningeal carcinomatosis tend to involve the skull base and present with multiple cranial neuropathies.
Tumors of the brain or parotid gland have an insidious onset and may cause systemic signs such as fevers, chills, and weight loss. Headache, seizures, and hearing loss indicate an intracranial lesion. A palpable mass near the ear, neck, or parotid gland requires imaging of the face to look for a parotid gland tumor.
Infection
A number of infections can cause acute facial paralysis. The most common is herpes simplex virus, and the next most common is varicella zoster.14 Herpes simplex virus, Ramsay Hunt syndrome, and Lyme disease may have associated pain and skin changes. Erythema of the tympanic membrane suggests otitis media, especially in the setting of ear pain and hearing loss.
Ramsay Hunt syndrome is caused by reactivation of the herpes zoster virus from the geniculate ganglion, affecting the facial nerve. Careful examination of the ear canal and the oropharynx may show vesicles.
In Lyme disease, facial palsy is the most common cranial neuropathy, seen in 50% to 63% of patients with Borrelia burgdorferi meningitis.16,17 In people with a history of rash, arthralgia, tick bite, or travel to an endemic region, Lyme titers should be checked before starting the patient on corticosteroids.
Bilateral facial palsy is rare and occurs in fewer than 1% of patients. It has been reported in patients with Lyme disease, Guillain-Barré syndrome, sarcoidosis, diabetes mellitus, viral infection, and pontine glioma.18
DIAGNOSTIC EVALUATION
Serologic testing, electrodiagnostic studies, and imaging are not routinely necessary to diagnose Bell palsy. However, referral to the appropriate specialist (neurologist, otolaryngologist, optometrist, ophthalmologist) is advised if the patient has sparing of the forehead muscle, multiple cranial neuropathies, signs of infection, or persistent weakness without significant improvement at 3 weeks.
Laboratory testing
A complete blood cell count with differential may point to infection or a lymphoproliferative disorder. When indicated, screening for diabetes mellitus with fasting blood glucose or hemoglobin A1c may be helpful. In Lyme-endemic regions, patients should undergo an enzyme-linked immunosorbent assay or an indirect fluorescent antibody test to screen for the disease. If positive, the diagnosis of Lyme disease should be confirmed by Western blot. If vesicles are present on examination, check serum antibodies for herpes zoster. In the appropriate clinical setting, angiotensin-converting enzyme, human immunodeficiency virus, and inflammatory markers can be tested.
Cerebrospinal fluid analysis is generally not helpful in diagnosing Bell palsy but can differentiate it from Guillain-Barré syndrome, leptomeningeal carcinomatosis, and infection involving the central nervous system.
Imaging
Imaging is not recommended in the initial evaluation of Bell palsy unless symptoms and the examination are atypical. From 5% to 7% of cases of facial palsy are caused by a tumor (eg, facial neuroma, cholesteatoma, hemangioma, meningioma), whether benign or malignant.14,15 Therefore, in patients with insidious onset of symptoms that do not improve in about 3 weeks, contrast-enhanced computed tomography or gadolinium-enhanced magnetic resonance imaging of the internal auditory canal and face is warranted.
Electrodiagnostic studies
Electrodiagnostic testing is typically not part of the evaluation of acute Bell palsy, but in patients with complete paralysis, it may help assess the degree of nerve injury and the chances of recovery, especially since patients with complete paralysis have a higher risk of incomplete recovery.19 Electrodiagnostic studies should be performed at least 1 week after symptom onset to avoid false-negative results.
TREATMENT
The treatment of Bell palsy focuses on maximizing recovery and minimizing associated complications.
Protect the eyes
Patients who cannot completely close their eyes should be given instructions on ocular protective care to prevent exposure keratopathy. Frequent application of lubricant eyedrops with artificial tears during the day or ophthalmic ointment at bedtime is recommended. The physician should also recommend protective eyewear such as sunglasses during the day. Eye patching or taping at night may be useful but could be harmful if applied too loosely or too tightly. Patients with vision loss or eye irritation should be referred to an ophthalmologist.19
Corticosteroids are recommended in the first 72 hours
In two randomized clinical trials (conducted by Sullivan et al20 in 511 patients and Engström et al21 in 829 patients), prednisolone was found to be beneficial if started within 72 hours of symptom onset.
In a double-blind, randomized, placebo-controlled study of prednisone in 58 patients, those who received the drug recovered faster, although long-term outcomes in these patients were not significantly different than those in the control group.22 The American Academy of Neurology23 rated this study as class II, ie, not meeting all of its criteria for the highest level of evidence, class I. Nevertheless, although prednisone lacks class I evidence, its use is recommended because it is a precursor to its active metabolite, prednisolone, which has been studied extensively.
The current guidelines of the American Academy of Neurology, updated in 2012, state, “For patients with new-onset Bell palsy, steroids are highly likely to be effective and should be offered to increase the probability of recovery of facial nerve function”23 (level A evidence, ie, established as effective). They also concluded that adverse effects of corticosteroids were generally minor and temporary.
Similarly, the guidelines of the American Academy of Otolaryngology–Head and Neck Surgery, published in 2013, recommend oral corticosteroids within 72 hours of onset of symptoms of Bell palsy for patients age 16 and older.19 The recommendation is for a 10-day course of corticosteroids with at least 5 days at a high dose (prednisolone 50 mg orally daily for 10 days, or prednisone 60 mg orally daily for 5 days, followed by a 5-day taper). The benefit of corticosteroids after 72 hours is unclear (Table 3).19
Even though the guidelines recommend corticosteroids, the decision to use them in diabetic patients and pregnant women should be individualized. Discretion is advised, as not all patients with Bell palsy need to be treated. Most recover spontaneously, especially those with mild symptoms.
Antiviral therapy may offer modest benefit
Antiviral therapy has not been shown to be beneficial in Bell palsy, and current guidelines do not recommend oral antiviral therapy alone.19 However, an antiviral combined with a corticosteroid may offer modest benefit if started within 72 hours of symptom onset (level C evidence, ie, possibly effective).23 Patients starting antiviral therapy should understand that its benefit has not been established.
Surgical decompression remains controversial
A Cochrane systematic review in 2011 found insufficient evidence regarding the safety and efficacy of surgical intervention in Bell palsy.24 Surgery should be considered only for patients with complete paralysis with a greater than 90% reduction in motor amplitude on a nerve conduction study compared with the unaffected side, and absent volitional activity on needle examination.19,25
Acupuncture: No recommendation
Currently, there is no recommendation for acupuncture in the treatment of Bell palsy.19 A recent randomized clinical trial suggests benefit from acupuncture combined with corticosteroids,26 but high-quality studies to support its use are lacking.26
Physical therapy: Insufficient evidence
There is insufficient evidence to show that physical therapy has benefit—or harm—in Bell palsy. However, some low-quality studies indicated that facial exercises and mime therapy may improve function in patients with moderate paralysis.27
Follow-up
Patients should be instructed to call at 2 weeks to report progress of symptoms and to be reevaluated within or at 1 month, with close attention to facial weakness and eye irritation. Further evaluation is needed if there has been no improvement, if symptoms have worsened, or if new symptoms have appeared.
The psychosocial impact of Bell palsy cannot be discounted, as the disfigurement can have negative implications for self-esteem and social relationships. Appropriate referral to an ophthalmologist, neurologist, otolaryngologist, social worker, or a plastic surgeon may be necessary.
COMPLICATIONS AND PROGNOSIS
Most patients with Bell palsy recover completely, but up to 30% have residual symptoms at 6 months.14,20 Furthermore, although Bell palsy usually has a monophasic course, 7% to 12% of patients have a recurrence.3,15
Long-term complications can include residual facial weakness, facial synkinesis, facial contracture, and facial spasm.14,28 Incomplete eye closure may benefit from surgery (tarsorrhaphy or gold-weight implantation) to prevent corneal ulceration. Facial synkinesis is due to aberrant nerve regeneration and occurs in 15% to 20% of patients after recovery from Bell palsy.29 Patients may describe tearing while chewing (“crocodile tears”), involuntary movement of the corners of the mouth with blinking, or ipsilateral eye-closing when the jaw opens (“jaw-winking”). Facial contracture, facial synkinesis, and facial spasm can be treated with botulinum toxin injection.30
Bell palsy is an idiopathic peripheral nerve disorder involving the facial nerve (ie, cranial nerve VII) and manifesting as acute, ipsilateral facial muscle weakness. It is named after Sir Charles Bell, who in 1821 first described the anatomy of the facial nerve.1 Although the disorder is clinically benign, patients can be devastated by its disfigurement.
The annual incidence of Bell palsy is 20 per 100,000, with no predilection for sex or ethnicity. It can affect people at any age, but the incidence is slightly higher after age 40.2,3 Risk factors include diabetes, pregnancy, severe preeclampsia, obesity, and hypertension.4–7
THE FACIAL NERVE IS VULNERABLE TO TRAUMA AND COMPRESSION
A basic understanding of the neuroanatomy of the facial nerve provides clues for distinguishing a central lesion from a peripheral lesion. This differentiation is important because the causes and management differ.
The facial nerve is a mixed sensory and motor nerve, carrying fibers involved in facial expression, taste, lacrimation, salivation, and sensation of the ear. It originates in the lower pons and exits the brainstem ventrally at the pontomedullary junction. After entering the internal acoustic meatus, it travels 20 to 30 mm in the facial canal, the longest bony course of any cranial nerve, making it highly susceptible to trauma and compression by edema.8
In the facial canal, it makes a posterior and inferior turn, forming a bend (ie, the genu of the facial nerve). The genu is proximal to the geniculate ganglion, which contains the facial nerve’s primary sensory neurons for taste and sensation. The motor branch of the facial nerve then exits the cranium via the stylomastoid foramen and passes through the parotid gland, where it divides into temporofacial and cervicofacial trunks.9
The facial nerve has five terminal branches that innervate the muscles of facial expression:
- The temporal branch (muscles of the forehead and superior part of the orbicularis oculi)
- The zygomatic branch (muscles of the nasolabial fold and cheek, eg, nasalis and zygomaticus).
- The buccal branch (the buccinators and inferior part of the orbicularis oculi)
- The marginal mandibular branch (the depressors of the mouth, eg, depressor anguli and mentalis)
- The cervical branch (the platysma muscle).
INFLAMMATION IS BELIEVED TO BE RESPONSIBLE
Although the precise cause of Bell palsy is not known, one theory is that inflammation of the nerve causes focal edema, demyelination, and ischemia. Several studies have suggested that herpes virus simplex type 1 infection may be involved.10
FACIAL DROOPING, EYELID WEAKNESS, OTHER SYMPTOMS
Symptoms of Bell palsy include ipsilateral sagging of the eyebrow, drooping of the face, flattening of the nasolabial fold, and inability to fully close the eye, pucker the lips, or raise the corner of the mouth (Figure 1). Symptoms develop within hours and are maximal by 3 days.
About 70% of patients have associated ipsilateral pain around the ear. If facial pain is present with sensory and hearing loss, a tumor of the parotid gland or viral otitis must be considered.11 Other complaints may include hyperacusis due to disruption of nerve fibers to the stapedius muscle, changes in taste, and dry eye from parasympathetic dysfunction. Some patients report paresthesias over the face, which most often represent motor symptoms misconstrued as sensory changes.
PHYSICAL EXAMINATION
The clinical examination should include a complete neurologic and general examination, including otoscopy and attention to the skin and parotid gland. Vesicles or scabbing around the ear should prompt testing for herpes zoster. Careful observation during the interview while the patient is talking may reveal subtle signs of weakness and provide additional clues.
A systematic approach to the assessment of a patient with suspected Bell palsy is recommended (Table 1) and outlined below:
Does the patient have peripheral facial palsy?
In Bell palsy, wrinkling of the forehead on the affected side when raising the eyebrows is either asymmetrical or absent.
If the forehead muscles are spared and the lower face is weak, this signifies a central lesion such as a stroke or other structural abnormality and not a peripheral lesion of the facial nerve (eg, Bell palsy).
Can the patient close the eyes tightly?
Normally, the patient should be able to close both eyes tightly, and the eyelashes should be buried between the eyelids. In Bell palsy, when the patient attempts to close the eyes, the affected side shows incomplete closure and the eye may remain partly open.
Assess the strength of the orbicularis oculi by trying to open the eyes. The patient who is attempting to close the eyelids tightly but cannot will demonstrate the Bell phenomenon, ie, the examiner is able to force open the eyelids, and the eyes are deviated upward and laterally.
Closely observe the blink pattern, as the involved side in Bell palsy may slightly lag behind the normal eye, and the patient may be unable to close the eye completely.
Is the smile symmetric?
Note flattening of the nasolabial fold on one side, which indicates facial weakness.
Can the patient puff out the cheeks?
Ask the patient to hold air in the mouth against resistance. This assesses the strength of the buccinator muscle.
Can the patient purse the lips?
Ask the patient to pucker or purse the lips and observe for asymmetry or weakness on the affected side.
Test the orbicularis oris muscle by trying to spread the lips apart while the patient resists, and observe for weakness on one side.
Is there a symmetric grimace?
This will test the muscles involved in depressing the angles of the mouth and platysma.
Are taste, sensation, and hearing intact?
Other testable functions of the facial nerve, including taste, sensation, and hearing, do not always need to be assessed but can be in patients with specific sensory deficits.
Abnormalities in taste can support localization of the problem either proximal or distal to the branch point of fibers mediating taste. The facial nerve supplies taste fibers to the anterior two-thirds of the tongue. Sweet and salty taste can be screened with sugar and salt. Tell the patient to close the eyes, and using a tongue blade, apply a small amount of sugar or salt on the side of the tongue. Ask the patient to identify the taste and repeat with the other sample after he or she has rinsed the mouth.
Somatic sensory fibers supplied by the facial nerve innervate the inner ear and a small area behind the ear, but these may be difficult to assess objectively. Formal audiologic testing may be needed if hearing is impaired.
Facial nerve reflexes
A number of facial reflexes can be tested, including the orbicularis oculi, palpebral-oculogyric, and corneal reflexes.12
The orbicularis oculi reflex is tested by gentle finger percussion of the glabella while observing for involuntary blinking with each stimulus. The afferent branch of this reflex is carried by the trigeminal nerve, while the efferent response is carried by the facial nerve. In peripheral facial nerve palsy, this reflex is weakened or absent on the affected side.
The palpebral-oculogyric reflex, or Bell phenomenon, produces upward and lateral deviation of the eyes when attempting forceful eyelid closure. In this reflex, the afferent fibers are carried by the facial nerve and the efferent fibers travel in the oculomotor nerve to the superior rectus muscle. In Bell palsy, this reflex is visible because of failure of adequate eyelid closure.
The corneal reflex is elicited by stimulating the cornea with a wisp of cotton, causing reflexive closure of the both eyes. The affected side may show slowed or absent lid closure when tested on either side. The sensory afferent fibers are carried by the trigeminal nerve, and the motor efferent fibers are carried by the facial nerve.
Grading of facial paralysis
The House-Brackmann scale is the most widely used tool for grading the degree of facial paralysis and for predicting recovery. Grades are I to VI, with grade I indicating normal function, and grade VI, complete paralysis.
Patients with some preserved motor function generally have good recovery, but those with complete paralysis may have long-term residual deficits.13
A DIAGNOSIS OF EXCLUSION
The diagnosis of Bell palsy is made by excluding other causes of unilateral facial paralysis, and 30% to 60% of cases of facial palsy are caused by an underlying disorder that mimics Bell palsy, including central nervous system lesion (eg, stroke, demyelinating disease), parotid gland tumor, Lyme disease, Ramsay Hunt syndrome, granulomatous disease, otitis media, cholesteatoma, diabetes, trauma, and Guillain-Barré syndrome (Table 2).14,15 Many of these conditions have associated features that help distinguish them from Bell palsy. Facial palsy that does not improve after 3 weeks should prompt referral to a neurologist.
Brain lesions
It is uncommon to have isolated facial palsy with a cortical or subcortical brain lesion, since the corticobulbar and corticospinal tracts travel in close proximity. Cortical signs such as hemiparesis, hemisensory loss, neglect, and dysarthria suggest a lesion of the cerebral cortex. Additionally, forehead muscle sparing is expected in supranuclear lesions.
Brainstem lesions can manifest with multiple ipsilateral cranial nerve palsies and contralateral limb weakness. Sarcoidosis and leptomeningeal carcinomatosis tend to involve the skull base and present with multiple cranial neuropathies.
Tumors of the brain or parotid gland have an insidious onset and may cause systemic signs such as fevers, chills, and weight loss. Headache, seizures, and hearing loss indicate an intracranial lesion. A palpable mass near the ear, neck, or parotid gland requires imaging of the face to look for a parotid gland tumor.
Infection
A number of infections can cause acute facial paralysis. The most common is herpes simplex virus, and the next most common is varicella zoster.14 Herpes simplex virus, Ramsay Hunt syndrome, and Lyme disease may have associated pain and skin changes. Erythema of the tympanic membrane suggests otitis media, especially in the setting of ear pain and hearing loss.
Ramsay Hunt syndrome is caused by reactivation of the herpes zoster virus from the geniculate ganglion, affecting the facial nerve. Careful examination of the ear canal and the oropharynx may show vesicles.
In Lyme disease, facial palsy is the most common cranial neuropathy, seen in 50% to 63% of patients with Borrelia burgdorferi meningitis.16,17 In people with a history of rash, arthralgia, tick bite, or travel to an endemic region, Lyme titers should be checked before starting the patient on corticosteroids.
Bilateral facial palsy is rare and occurs in fewer than 1% of patients. It has been reported in patients with Lyme disease, Guillain-Barré syndrome, sarcoidosis, diabetes mellitus, viral infection, and pontine glioma.18
DIAGNOSTIC EVALUATION
Serologic testing, electrodiagnostic studies, and imaging are not routinely necessary to diagnose Bell palsy. However, referral to the appropriate specialist (neurologist, otolaryngologist, optometrist, ophthalmologist) is advised if the patient has sparing of the forehead muscle, multiple cranial neuropathies, signs of infection, or persistent weakness without significant improvement at 3 weeks.
Laboratory testing
A complete blood cell count with differential may point to infection or a lymphoproliferative disorder. When indicated, screening for diabetes mellitus with fasting blood glucose or hemoglobin A1c may be helpful. In Lyme-endemic regions, patients should undergo an enzyme-linked immunosorbent assay or an indirect fluorescent antibody test to screen for the disease. If positive, the diagnosis of Lyme disease should be confirmed by Western blot. If vesicles are present on examination, check serum antibodies for herpes zoster. In the appropriate clinical setting, angiotensin-converting enzyme, human immunodeficiency virus, and inflammatory markers can be tested.
Cerebrospinal fluid analysis is generally not helpful in diagnosing Bell palsy but can differentiate it from Guillain-Barré syndrome, leptomeningeal carcinomatosis, and infection involving the central nervous system.
Imaging
Imaging is not recommended in the initial evaluation of Bell palsy unless symptoms and the examination are atypical. From 5% to 7% of cases of facial palsy are caused by a tumor (eg, facial neuroma, cholesteatoma, hemangioma, meningioma), whether benign or malignant.14,15 Therefore, in patients with insidious onset of symptoms that do not improve in about 3 weeks, contrast-enhanced computed tomography or gadolinium-enhanced magnetic resonance imaging of the internal auditory canal and face is warranted.
Electrodiagnostic studies
Electrodiagnostic testing is typically not part of the evaluation of acute Bell palsy, but in patients with complete paralysis, it may help assess the degree of nerve injury and the chances of recovery, especially since patients with complete paralysis have a higher risk of incomplete recovery.19 Electrodiagnostic studies should be performed at least 1 week after symptom onset to avoid false-negative results.
TREATMENT
The treatment of Bell palsy focuses on maximizing recovery and minimizing associated complications.
Protect the eyes
Patients who cannot completely close their eyes should be given instructions on ocular protective care to prevent exposure keratopathy. Frequent application of lubricant eyedrops with artificial tears during the day or ophthalmic ointment at bedtime is recommended. The physician should also recommend protective eyewear such as sunglasses during the day. Eye patching or taping at night may be useful but could be harmful if applied too loosely or too tightly. Patients with vision loss or eye irritation should be referred to an ophthalmologist.19
Corticosteroids are recommended in the first 72 hours
In two randomized clinical trials (conducted by Sullivan et al20 in 511 patients and Engström et al21 in 829 patients), prednisolone was found to be beneficial if started within 72 hours of symptom onset.
In a double-blind, randomized, placebo-controlled study of prednisone in 58 patients, those who received the drug recovered faster, although long-term outcomes in these patients were not significantly different than those in the control group.22 The American Academy of Neurology23 rated this study as class II, ie, not meeting all of its criteria for the highest level of evidence, class I. Nevertheless, although prednisone lacks class I evidence, its use is recommended because it is a precursor to its active metabolite, prednisolone, which has been studied extensively.
The current guidelines of the American Academy of Neurology, updated in 2012, state, “For patients with new-onset Bell palsy, steroids are highly likely to be effective and should be offered to increase the probability of recovery of facial nerve function”23 (level A evidence, ie, established as effective). They also concluded that adverse effects of corticosteroids were generally minor and temporary.
Similarly, the guidelines of the American Academy of Otolaryngology–Head and Neck Surgery, published in 2013, recommend oral corticosteroids within 72 hours of onset of symptoms of Bell palsy for patients age 16 and older.19 The recommendation is for a 10-day course of corticosteroids with at least 5 days at a high dose (prednisolone 50 mg orally daily for 10 days, or prednisone 60 mg orally daily for 5 days, followed by a 5-day taper). The benefit of corticosteroids after 72 hours is unclear (Table 3).19
Even though the guidelines recommend corticosteroids, the decision to use them in diabetic patients and pregnant women should be individualized. Discretion is advised, as not all patients with Bell palsy need to be treated. Most recover spontaneously, especially those with mild symptoms.
Antiviral therapy may offer modest benefit
Antiviral therapy has not been shown to be beneficial in Bell palsy, and current guidelines do not recommend oral antiviral therapy alone.19 However, an antiviral combined with a corticosteroid may offer modest benefit if started within 72 hours of symptom onset (level C evidence, ie, possibly effective).23 Patients starting antiviral therapy should understand that its benefit has not been established.
Surgical decompression remains controversial
A Cochrane systematic review in 2011 found insufficient evidence regarding the safety and efficacy of surgical intervention in Bell palsy.24 Surgery should be considered only for patients with complete paralysis with a greater than 90% reduction in motor amplitude on a nerve conduction study compared with the unaffected side, and absent volitional activity on needle examination.19,25
Acupuncture: No recommendation
Currently, there is no recommendation for acupuncture in the treatment of Bell palsy.19 A recent randomized clinical trial suggests benefit from acupuncture combined with corticosteroids,26 but high-quality studies to support its use are lacking.26
Physical therapy: Insufficient evidence
There is insufficient evidence to show that physical therapy has benefit—or harm—in Bell palsy. However, some low-quality studies indicated that facial exercises and mime therapy may improve function in patients with moderate paralysis.27
Follow-up
Patients should be instructed to call at 2 weeks to report progress of symptoms and to be reevaluated within or at 1 month, with close attention to facial weakness and eye irritation. Further evaluation is needed if there has been no improvement, if symptoms have worsened, or if new symptoms have appeared.
The psychosocial impact of Bell palsy cannot be discounted, as the disfigurement can have negative implications for self-esteem and social relationships. Appropriate referral to an ophthalmologist, neurologist, otolaryngologist, social worker, or a plastic surgeon may be necessary.
COMPLICATIONS AND PROGNOSIS
Most patients with Bell palsy recover completely, but up to 30% have residual symptoms at 6 months.14,20 Furthermore, although Bell palsy usually has a monophasic course, 7% to 12% of patients have a recurrence.3,15
Long-term complications can include residual facial weakness, facial synkinesis, facial contracture, and facial spasm.14,28 Incomplete eye closure may benefit from surgery (tarsorrhaphy or gold-weight implantation) to prevent corneal ulceration. Facial synkinesis is due to aberrant nerve regeneration and occurs in 15% to 20% of patients after recovery from Bell palsy.29 Patients may describe tearing while chewing (“crocodile tears”), involuntary movement of the corners of the mouth with blinking, or ipsilateral eye-closing when the jaw opens (“jaw-winking”). Facial contracture, facial synkinesis, and facial spasm can be treated with botulinum toxin injection.30
- Grzybowski A, Kaufman MH. Sir Charles Bell (1774-1842): contributions to neuro-ophthalmology. Acta Ophthalmol Scand 2007; 85:897–901.
- De Diego-Sastre JI, Prim-Espada MP, Fernández-García F. The epidemiology of Bell’s palsy. Rev Neurol 2005; 41:287–290. In Spanish.
- Morris AM, Deeks SL, Hill MD, et al. Annualized incidence and spectrum of illness from an outbreak investigation of Bell’s palsy. Neuroepidemiology 2002; 21:255–261.
- Bosco D, Plastino M, Bosco F, et al. Bell’s palsy: a manifestation of prediabetes? Acta Neurol Scand 2011; 123:68–72.
- Riga M, Kefalidis G, Danielides V. The role of diabetes mellitus in the clinical presentation and prognosis of Bell palsy. J Am Board Fam Med 2012; 25:819–826.
- Hilsinger RL Jr, Adour KK, Doty HE. Idiopathic facial paralysis, pregnancy, and the menstrual cycle. Ann Otol Rhinol Laryngol 1975; 84:433–442.
- Savadi-Oskouei D, Abedi A, Sadeghi-Bazargani H. Independent role of hypertension in Bell’s palsy: a case-control study. Eur Neurol 2008; 60:253–257.
- Murai A, Kariya S, Tamura K, et al. The facial nerve canal in patients with Bell’s palsy: an investigation by high-resolution computed tomography with multiplanar reconstruction. Eur Arch Otorhinolaryngol 2013; 270:2035–2038.
- Blumenfeld H. Neuroanatomy Through Clinical Cases. 1st ed. Sunderland, MA: Sinauer; 2002:479–484.
- Murakami S, Mizobuchi M, Nakashiro Y, Doi T, Hato N, Yanagihara N. Bell palsy and herpes simplex virus: identification of viral DNA in endoneurial fluid and muscle. Ann Intern Med 1996; 124:27–30.
- Boahene DO, Olsen KD, Driscoll C, Lewis JE, McDonald TJ. Facial nerve paralysis secondary to occult malignant neoplasms. Otolaryngol Head Neck Surg 2004; 130:459–465.
- DeJong RN. The Neurologic Examination: Incorporating the fundamentals of neuroanatomy and neurophysiology. 4th ed. New York, NY: Harper & Row; 1979:178–198.
- House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg 1985; 93:146–147.
- Peitersen E. Bell’s palsy: the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Otolaryngol Suppl 2002; 549:4–30.
- Hohman MH, Hadlock TA. Etiology, diagnosis, and management of facial palsy: 2000 patients at a facial nerve center. Laryngoscope 2014; 124:E283–E293.
- Ackermann R, Hörstrup P, Schmidt R. Tick-borne meningopolyneuritis (Garin-Bujadoux, Bannwarth). Yale J Biol Med 1984; 57:485–490.
- Pachner AR, Steere AC. The triad of neurologic manifestations of Lyme disease: meningitis, cranial neuritis, and radiculoneuritis. Neurology 1985; 35:47–53.
- Keane JR. Bilateral seventh nerve palsy: analysis of 43 cases and review of the literature. Neurology 1994; 44:1198–1202.
- Baugh RF, Basura GJ, Ishii LE, et al. Clinical practice guideline: Bell’s palsy. Otolaryngol Head Neck Surg 2013; 149(suppl 3):S1–S27.
- Sullivan FM, Swan IR, Donnan PT, et al. Early treatment with prednisolone or acyclovir in Bell’s palsy. N Engl J Med 2007; 357:1598–1607.
- Engström M, Berg T, Stjernquist-Desatnik A, et al. Prednisolone and valaciclovir in Bell’s palsy: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet Neurol 2008; 7:993–1000.
- Lagalla G, Logullo F, Di Bella P, Provinciali L, Ceravolo MG. Influence of early high-dose steroid treatment on Bell’s palsy evolution. Neurol Sci 2002; 23:107–112.
- Gronseth GS, Paduga R; American Academy of Neurology. Evidence-based guideline update: steroids and antivirals for Bell palsy: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 2012; 79:2209–2213.
- McAllister K, Walker D, Donnan PT, Swan I. Surgical interventions for the early management of Bell’s palsy. Cochrane Database Syst Rev 2011; 2:CD007468.
- Gantz BJ, Rubinstein JT, Gidley P, Woodworth GG. Surgical management of Bell’s palsy. Laryngoscope 1999; 109:1177–1188.
- Xu SB, Huang B, Zhang CY, et al. Effectiveness of strengthened stimulation during acupuncture for the treatment of Bell palsy: a randomized controlled trial. CMAJ 2013; 185:473–479.
- Teixeira LJ, Valbuza JS, Prado GF. Physical therapy for Bell’s palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 2011; 12:CD006283.
- Yaltho TC, Jankovic J. The many faces of hemifacial spasm: differential diagnosis of unilateral facial spasms. Mov Disord 2011; 26:1582–1592.
- Celik M, Forta H, Vural C. The development of synkinesis after facial nerve paralysis. Eur Neurol 2000; 43:147–151.
- Chua CN, Quhill F, Jones E, Voon LW, Ahad M, Rowson N. Treatment of aberrant facial nerve regeneration with botulinum toxin A. Orbit 2004; 23:213–218.
- Grzybowski A, Kaufman MH. Sir Charles Bell (1774-1842): contributions to neuro-ophthalmology. Acta Ophthalmol Scand 2007; 85:897–901.
- De Diego-Sastre JI, Prim-Espada MP, Fernández-García F. The epidemiology of Bell’s palsy. Rev Neurol 2005; 41:287–290. In Spanish.
- Morris AM, Deeks SL, Hill MD, et al. Annualized incidence and spectrum of illness from an outbreak investigation of Bell’s palsy. Neuroepidemiology 2002; 21:255–261.
- Bosco D, Plastino M, Bosco F, et al. Bell’s palsy: a manifestation of prediabetes? Acta Neurol Scand 2011; 123:68–72.
- Riga M, Kefalidis G, Danielides V. The role of diabetes mellitus in the clinical presentation and prognosis of Bell palsy. J Am Board Fam Med 2012; 25:819–826.
- Hilsinger RL Jr, Adour KK, Doty HE. Idiopathic facial paralysis, pregnancy, and the menstrual cycle. Ann Otol Rhinol Laryngol 1975; 84:433–442.
- Savadi-Oskouei D, Abedi A, Sadeghi-Bazargani H. Independent role of hypertension in Bell’s palsy: a case-control study. Eur Neurol 2008; 60:253–257.
- Murai A, Kariya S, Tamura K, et al. The facial nerve canal in patients with Bell’s palsy: an investigation by high-resolution computed tomography with multiplanar reconstruction. Eur Arch Otorhinolaryngol 2013; 270:2035–2038.
- Blumenfeld H. Neuroanatomy Through Clinical Cases. 1st ed. Sunderland, MA: Sinauer; 2002:479–484.
- Murakami S, Mizobuchi M, Nakashiro Y, Doi T, Hato N, Yanagihara N. Bell palsy and herpes simplex virus: identification of viral DNA in endoneurial fluid and muscle. Ann Intern Med 1996; 124:27–30.
- Boahene DO, Olsen KD, Driscoll C, Lewis JE, McDonald TJ. Facial nerve paralysis secondary to occult malignant neoplasms. Otolaryngol Head Neck Surg 2004; 130:459–465.
- DeJong RN. The Neurologic Examination: Incorporating the fundamentals of neuroanatomy and neurophysiology. 4th ed. New York, NY: Harper & Row; 1979:178–198.
- House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg 1985; 93:146–147.
- Peitersen E. Bell’s palsy: the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Otolaryngol Suppl 2002; 549:4–30.
- Hohman MH, Hadlock TA. Etiology, diagnosis, and management of facial palsy: 2000 patients at a facial nerve center. Laryngoscope 2014; 124:E283–E293.
- Ackermann R, Hörstrup P, Schmidt R. Tick-borne meningopolyneuritis (Garin-Bujadoux, Bannwarth). Yale J Biol Med 1984; 57:485–490.
- Pachner AR, Steere AC. The triad of neurologic manifestations of Lyme disease: meningitis, cranial neuritis, and radiculoneuritis. Neurology 1985; 35:47–53.
- Keane JR. Bilateral seventh nerve palsy: analysis of 43 cases and review of the literature. Neurology 1994; 44:1198–1202.
- Baugh RF, Basura GJ, Ishii LE, et al. Clinical practice guideline: Bell’s palsy. Otolaryngol Head Neck Surg 2013; 149(suppl 3):S1–S27.
- Sullivan FM, Swan IR, Donnan PT, et al. Early treatment with prednisolone or acyclovir in Bell’s palsy. N Engl J Med 2007; 357:1598–1607.
- Engström M, Berg T, Stjernquist-Desatnik A, et al. Prednisolone and valaciclovir in Bell’s palsy: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet Neurol 2008; 7:993–1000.
- Lagalla G, Logullo F, Di Bella P, Provinciali L, Ceravolo MG. Influence of early high-dose steroid treatment on Bell’s palsy evolution. Neurol Sci 2002; 23:107–112.
- Gronseth GS, Paduga R; American Academy of Neurology. Evidence-based guideline update: steroids and antivirals for Bell palsy: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 2012; 79:2209–2213.
- McAllister K, Walker D, Donnan PT, Swan I. Surgical interventions for the early management of Bell’s palsy. Cochrane Database Syst Rev 2011; 2:CD007468.
- Gantz BJ, Rubinstein JT, Gidley P, Woodworth GG. Surgical management of Bell’s palsy. Laryngoscope 1999; 109:1177–1188.
- Xu SB, Huang B, Zhang CY, et al. Effectiveness of strengthened stimulation during acupuncture for the treatment of Bell palsy: a randomized controlled trial. CMAJ 2013; 185:473–479.
- Teixeira LJ, Valbuza JS, Prado GF. Physical therapy for Bell’s palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 2011; 12:CD006283.
- Yaltho TC, Jankovic J. The many faces of hemifacial spasm: differential diagnosis of unilateral facial spasms. Mov Disord 2011; 26:1582–1592.
- Celik M, Forta H, Vural C. The development of synkinesis after facial nerve paralysis. Eur Neurol 2000; 43:147–151.
- Chua CN, Quhill F, Jones E, Voon LW, Ahad M, Rowson N. Treatment of aberrant facial nerve regeneration with botulinum toxin A. Orbit 2004; 23:213–218.
KEY POINTS
- Bell palsy is an acute disorder of the facial nerve causing unilateral facial weakness, pain, abnormal taste, and reduced tearing.
- Although herpes simplex virus reactivation is suspected in the pathogenesis, the exact cause is unknown.
- An additional workup is warranted for abnormalities beyond isolated facial nerve palsy.
- Guidelines recommend starting corticosteroids for patients who present within 3 days of symptom onset. There is no compelling evidence to support antiviral therapy, physical therapy, acupuncture, or surgical decompression.
ObGyn salaries continue gradual improvement
The mean income for ObGyns rose by 2% in 2014 over 2013 to $249,000, according to the 2015 Medscape Compensation Report.1 This slight rise continues a gradual increase over the past few years ($242,000 in 2012; $220,000 in 2011).1–4 The 2015 report took into account survey responses from 19,657 physicians across 26 specialties, 5% (982) of whom were ObGyns.
The highest earners among all physician specialties were orthopedists ($421,000), cardiologists, and gastroenterologists. The lowest earners were pediatricians, family physicians, endocrinologists, and internists ($196,000). The highest ObGyn earners lived in the Northwest ($289,000) and Great Lakes ($268,000) regions; the lowest earners lived in the Mid-Atlantic ($230,000) and Northeast ($235,000) areas.1
Survey findings
Career satisfaction for ObGyns is dipping
In 2011, 69%, 53%, and 48% of ObGyns indicated they would choose a career in medicine again, select the same specialty, and pick the same practice setting, respectively.4 In the 2015 survey, 67% of ObGyns reported that they would still choose medicine; however, only 40% would pick obstetrics and gynecology as their specialty, and only 22% would select the same practice setting.1
Employment over private practice: Who feels best compensated?
Overall, 63% of all physicians are now employed, with only 23% reporting to be in private practice. Employment appears to be more popular for women: 59% of men and 72% of women responded that they work for a salary. Slightly more than a third (36%) of men and about a quarter (23%) of women are self-employed.5
The gender picture. Half of all ObGyns are women, and almost half of medical school graduates are women, yet male ObGyns continue to make more money than their female counterparts.1,5,6 The 9% difference between compensation rates for self-employed male and female ObGyns ($265,000 vs $242,000, respectively) is less than the 14% difference between their employed colleagues ($266,000 vs $229,000, respectively).1 Women tend to work shorter hours, fewer weeks, and see fewer patients than men, which could account for the lower compensation rate for female ObGyns. Studies suggest that greater schedule flexibility and fewer hours are key factors that improve satisfaction rates for female physicians.5
Male and female ObGyns tend to agree on their income satisfaction: less than half are satisfied (male, 44%; female, 46%). Many more employed ObGyns (55%) than self-employed ObGyns (31%) believe that they are fairly compensated.1
Which practice settings pay better?
Compensation rates for ObGyns in 2015 are greatest for those in office-based multispecialty group practice ($280,000), followed by those who work in1:
- health care organizations ($269,000)
- office-based single-specialty group practices ($266,000)
- outpatient clinics ($223,000)
- academic settings (nonhospital), research, military, and government ($219,000).
The lowest paid practice settings are office-based solo practices ($218,000) and hospital-employed ObGyns ($209,000).
In 2013, ObGyns who earned the most worked for health care organizations ($273,000); those who earned the least worked for outpatient clinics ($207,000).1
Do you take insurance, Medicare, Medicaid?
More employed (82%) than self-employed (53%) ObGyns will continue to take new and current Medicare or Medicaid patients, which is a rise from data published in the 2014 report (employed, 72%; self-employed, 46%).1
More than half (58%) of all physicians received less than $100 from private insurers for a new-patient office visit in 2014. Among ObGyns, 26% said they would drop insurers that pay poorly; 29% replied that they would not drop an insurer because they need all payers.1
The rate of participation in Accountable Care Organizations (ACOs) has increased from 25% in 2013 to 35% in 2014, with 8% more expecting to join an ACO in 2015. Concierge practice (2%) and cash-only practice (5%) were reportedly not significant payment models for ObGyns in 2014.1
Only 26% of ObGyns are planning to participate in health insurance exchanges; 23% said they are not participating, and 51% are not sure whether they will participate. Close to half (41%) of ObGyns believe their income will decrease because of health insurance exchanges, whereas 54% do not anticipate a change in income.1
Do you offer ancillary services?
When asked, 11% of employed ObGyns and 28% of self-employed ObGyns revealed that they have offered new ancillary services within the past 3 years. These ancillary services can include mammography, bone density testing, ultrasound, in-house laboratory services, bioidentical hormone replacement therapy, and weight management.1
How much time do you spend with patients?
In 2014, 62% of ObGyns reported spending 9 to 16 minutes with a patient during a visit. This is compared to 56% of family physicians and 44% of internists (TABLE).1,5
More than one-half (52%) of ObGynsspend 30 to 45 hours per week seeing patients. Fewer (38%) spend more than 45 hours per week, and 9% spend less than 30 hours per week with patients. This decline may be due to the increasing proportion of women and older physicians who tend to work shorter hours and fewer weeks.1
In the general physician population, 24% of women and 13% of men work part time, whereas 16% of both male and female ObGyns work part time. ObGyns aged 65 years or older constitute 35% of part-timers; 9% of those aged 35 to 49 years, and 11% of those aged 50 to 64 years, work part time. Only 2% of those younger than age 35 work part time.1
Would you select a career in obstetrics and gynecology all over again?
If given a second chance, would you rather choose orthopedic surgery as your specialty, or even choose medicine as a career again? OBG Management recently asked readers to weigh in, through its Quick Poll posted at obgmanagement.com, on whether or not they would choose ObGyn all over again. Ninety-one readers answered “yes” and 70 answered “no,” for a total of 161 respondents.
When this same question was posed to OBG Management’s Virtual Board of Editors (VBE), the perspectives were as split as the Quick Poll results:
- “No, no, no, I would not choose ObGyn all over again.”
- “Yes, I still love what I do.”
- “Yes, it is still the most unique specialty in medicine because it involves both surgery and primary care.”
- “Yes, for all the reasons I first loved the specialty: every week’s schedule, and every day is different. There is a mix of office care, surgery, and call.”
- “No! There is constant concern of litigation for complications, poor reimbursement, and compromised lifestyle.”
“There are much easier ways to make a living,” said one respondent, and another replied, “Work is very tough right now and the payment is too low.”
“The specialty has changed,” said Mary Vanko, MD, who practices in the suburbs of “blue collar Indiana.” “The public has very little idea of the breadth of our knowledge. The ObGyn generalist has the ability to serve as a woman’s doctor throughout her lifetime, not just perform the deliveries and surgeries. All of a sudden we are excluded from primary care status and people have to fight to see us. The newbies will never experience what it used to be as an ObGyn, the woman’s primary. Now we are the doctors to see when someone wants an IUD or is bleeding or pregnant. Big difference.”
Wesley Hambright, MD, practices in a small community hospital, but feels that “a larger hospital with more specialties may offer more flexibility and support in dealing with external pressures.” Tameka O’Neal, MD, is currently hospital employed but feels “as though I have little say in my practice.” Shaukat Ashai, MD, who is retired after 35 years in practice, says he would have preferred an academic setting on a full-time basis, citing long hours and poor compensation.
Robert del Rosario, MD, is in a large single-specialty suburban practice and would choose this practice setting again, although he would not choose a career as an ObGyn again. “The work demands have taken away too much from family,” he says. In addition, “as a male ObGyn, I am regularly faced with patients who choose their doctors based on gender rather than on skill. Our colleagues are no better. Early in my career and until the present, I hear people say, ‘Oh, I can’t hire Dr. X because we’re looking to hire a female.’”
Joe Walsh, MD, of Philadelphia, Pennsylvania, expresses similar discontent as a male ObGyn practicing in today’s female-populated specialty. In a letter to the editor in response to Editor in Chief Robert L. Barbieri, MD’s Editorial in the May 2015 issue, “Why is obstetrics and gynecology a popular choice for medical students?” Dr. Walsh states: “The unaddressed question is why is it unpopular for half of medical students? Ninety-three percent of resident graduates in the field are women, while women account for half of medical student graduates. Men rarely go into the field today. Perhaps job advertisements touting physician opportunities in ‘all female groups’ discourage men. Perhaps hospitals’ ‘Women’s Health Centers’ with such slogans as ‘Women taking care of women’ discourage men. Perhaps receptionists’ asking patients whether they prefer a male or female physician discourages male ObGyns.”
Many VBE members express some frustrations—with their practice setting, compensation, and longer work hours—but say that the patient relationships are the most rewarding aspect of their jobs. After 29 years in practice, Patrick Pevoto, MD, says the most rewarding aspect of his job is “being part of the legacy in people’s lives.”
Others say what keeps them engaged is:
- Enjoying “good outcomes.”
- “The patient contact. It’s fun having someone come up to me in the grocery store and introduce me to a teenager that I delivered 15 years ago.”
- “Surgery.”
- “Helping patients and teaching fellows.”
- “Knowing that I am making a difference in people’s lives.”
What is most rewarding?
When given several choices to select as the most rewarding aspect of their jobs, more female ObGyns (47%) than males (41%) reported that their physician-patient relationships are the major source of satisfaction. More men (10%) than women (7%) cite that making good money at a job they like is most gratifying. Only 3% of men and 2% of women reported no reward to being an ObGyn.1
Survey methodology
Medscape reports that the recruitment period for the 2015 Physician Compensation Report was from December 30, 2014, through March 11, 2015. Data were collected via a third-party online survey collection site. The margin of error for the survey was ±0.69%.1
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Peckham C. Medscape OB/GYN Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed May 13, 2015.
2. Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
3. Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
4. Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
5. Peckham C. Medscape Physician Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/public/overview. Published April 21, 2015. Accessed May 13, 2015.
6. Distribution of medical school graduates by gender. Henry Kaiser Family Foundation Web site. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Accessed May 13, 2015.
The mean income for ObGyns rose by 2% in 2014 over 2013 to $249,000, according to the 2015 Medscape Compensation Report.1 This slight rise continues a gradual increase over the past few years ($242,000 in 2012; $220,000 in 2011).1–4 The 2015 report took into account survey responses from 19,657 physicians across 26 specialties, 5% (982) of whom were ObGyns.
The highest earners among all physician specialties were orthopedists ($421,000), cardiologists, and gastroenterologists. The lowest earners were pediatricians, family physicians, endocrinologists, and internists ($196,000). The highest ObGyn earners lived in the Northwest ($289,000) and Great Lakes ($268,000) regions; the lowest earners lived in the Mid-Atlantic ($230,000) and Northeast ($235,000) areas.1
Survey findings
Career satisfaction for ObGyns is dipping
In 2011, 69%, 53%, and 48% of ObGyns indicated they would choose a career in medicine again, select the same specialty, and pick the same practice setting, respectively.4 In the 2015 survey, 67% of ObGyns reported that they would still choose medicine; however, only 40% would pick obstetrics and gynecology as their specialty, and only 22% would select the same practice setting.1
Employment over private practice: Who feels best compensated?
Overall, 63% of all physicians are now employed, with only 23% reporting to be in private practice. Employment appears to be more popular for women: 59% of men and 72% of women responded that they work for a salary. Slightly more than a third (36%) of men and about a quarter (23%) of women are self-employed.5
The gender picture. Half of all ObGyns are women, and almost half of medical school graduates are women, yet male ObGyns continue to make more money than their female counterparts.1,5,6 The 9% difference between compensation rates for self-employed male and female ObGyns ($265,000 vs $242,000, respectively) is less than the 14% difference between their employed colleagues ($266,000 vs $229,000, respectively).1 Women tend to work shorter hours, fewer weeks, and see fewer patients than men, which could account for the lower compensation rate for female ObGyns. Studies suggest that greater schedule flexibility and fewer hours are key factors that improve satisfaction rates for female physicians.5
Male and female ObGyns tend to agree on their income satisfaction: less than half are satisfied (male, 44%; female, 46%). Many more employed ObGyns (55%) than self-employed ObGyns (31%) believe that they are fairly compensated.1
Which practice settings pay better?
Compensation rates for ObGyns in 2015 are greatest for those in office-based multispecialty group practice ($280,000), followed by those who work in1:
- health care organizations ($269,000)
- office-based single-specialty group practices ($266,000)
- outpatient clinics ($223,000)
- academic settings (nonhospital), research, military, and government ($219,000).
The lowest paid practice settings are office-based solo practices ($218,000) and hospital-employed ObGyns ($209,000).
In 2013, ObGyns who earned the most worked for health care organizations ($273,000); those who earned the least worked for outpatient clinics ($207,000).1
Do you take insurance, Medicare, Medicaid?
More employed (82%) than self-employed (53%) ObGyns will continue to take new and current Medicare or Medicaid patients, which is a rise from data published in the 2014 report (employed, 72%; self-employed, 46%).1
More than half (58%) of all physicians received less than $100 from private insurers for a new-patient office visit in 2014. Among ObGyns, 26% said they would drop insurers that pay poorly; 29% replied that they would not drop an insurer because they need all payers.1
The rate of participation in Accountable Care Organizations (ACOs) has increased from 25% in 2013 to 35% in 2014, with 8% more expecting to join an ACO in 2015. Concierge practice (2%) and cash-only practice (5%) were reportedly not significant payment models for ObGyns in 2014.1
Only 26% of ObGyns are planning to participate in health insurance exchanges; 23% said they are not participating, and 51% are not sure whether they will participate. Close to half (41%) of ObGyns believe their income will decrease because of health insurance exchanges, whereas 54% do not anticipate a change in income.1
Do you offer ancillary services?
When asked, 11% of employed ObGyns and 28% of self-employed ObGyns revealed that they have offered new ancillary services within the past 3 years. These ancillary services can include mammography, bone density testing, ultrasound, in-house laboratory services, bioidentical hormone replacement therapy, and weight management.1
How much time do you spend with patients?
In 2014, 62% of ObGyns reported spending 9 to 16 minutes with a patient during a visit. This is compared to 56% of family physicians and 44% of internists (TABLE).1,5
More than one-half (52%) of ObGynsspend 30 to 45 hours per week seeing patients. Fewer (38%) spend more than 45 hours per week, and 9% spend less than 30 hours per week with patients. This decline may be due to the increasing proportion of women and older physicians who tend to work shorter hours and fewer weeks.1
In the general physician population, 24% of women and 13% of men work part time, whereas 16% of both male and female ObGyns work part time. ObGyns aged 65 years or older constitute 35% of part-timers; 9% of those aged 35 to 49 years, and 11% of those aged 50 to 64 years, work part time. Only 2% of those younger than age 35 work part time.1
Would you select a career in obstetrics and gynecology all over again?
If given a second chance, would you rather choose orthopedic surgery as your specialty, or even choose medicine as a career again? OBG Management recently asked readers to weigh in, through its Quick Poll posted at obgmanagement.com, on whether or not they would choose ObGyn all over again. Ninety-one readers answered “yes” and 70 answered “no,” for a total of 161 respondents.
When this same question was posed to OBG Management’s Virtual Board of Editors (VBE), the perspectives were as split as the Quick Poll results:
- “No, no, no, I would not choose ObGyn all over again.”
- “Yes, I still love what I do.”
- “Yes, it is still the most unique specialty in medicine because it involves both surgery and primary care.”
- “Yes, for all the reasons I first loved the specialty: every week’s schedule, and every day is different. There is a mix of office care, surgery, and call.”
- “No! There is constant concern of litigation for complications, poor reimbursement, and compromised lifestyle.”
“There are much easier ways to make a living,” said one respondent, and another replied, “Work is very tough right now and the payment is too low.”
“The specialty has changed,” said Mary Vanko, MD, who practices in the suburbs of “blue collar Indiana.” “The public has very little idea of the breadth of our knowledge. The ObGyn generalist has the ability to serve as a woman’s doctor throughout her lifetime, not just perform the deliveries and surgeries. All of a sudden we are excluded from primary care status and people have to fight to see us. The newbies will never experience what it used to be as an ObGyn, the woman’s primary. Now we are the doctors to see when someone wants an IUD or is bleeding or pregnant. Big difference.”
Wesley Hambright, MD, practices in a small community hospital, but feels that “a larger hospital with more specialties may offer more flexibility and support in dealing with external pressures.” Tameka O’Neal, MD, is currently hospital employed but feels “as though I have little say in my practice.” Shaukat Ashai, MD, who is retired after 35 years in practice, says he would have preferred an academic setting on a full-time basis, citing long hours and poor compensation.
Robert del Rosario, MD, is in a large single-specialty suburban practice and would choose this practice setting again, although he would not choose a career as an ObGyn again. “The work demands have taken away too much from family,” he says. In addition, “as a male ObGyn, I am regularly faced with patients who choose their doctors based on gender rather than on skill. Our colleagues are no better. Early in my career and until the present, I hear people say, ‘Oh, I can’t hire Dr. X because we’re looking to hire a female.’”
Joe Walsh, MD, of Philadelphia, Pennsylvania, expresses similar discontent as a male ObGyn practicing in today’s female-populated specialty. In a letter to the editor in response to Editor in Chief Robert L. Barbieri, MD’s Editorial in the May 2015 issue, “Why is obstetrics and gynecology a popular choice for medical students?” Dr. Walsh states: “The unaddressed question is why is it unpopular for half of medical students? Ninety-three percent of resident graduates in the field are women, while women account for half of medical student graduates. Men rarely go into the field today. Perhaps job advertisements touting physician opportunities in ‘all female groups’ discourage men. Perhaps hospitals’ ‘Women’s Health Centers’ with such slogans as ‘Women taking care of women’ discourage men. Perhaps receptionists’ asking patients whether they prefer a male or female physician discourages male ObGyns.”
Many VBE members express some frustrations—with their practice setting, compensation, and longer work hours—but say that the patient relationships are the most rewarding aspect of their jobs. After 29 years in practice, Patrick Pevoto, MD, says the most rewarding aspect of his job is “being part of the legacy in people’s lives.”
Others say what keeps them engaged is:
- Enjoying “good outcomes.”
- “The patient contact. It’s fun having someone come up to me in the grocery store and introduce me to a teenager that I delivered 15 years ago.”
- “Surgery.”
- “Helping patients and teaching fellows.”
- “Knowing that I am making a difference in people’s lives.”
What is most rewarding?
When given several choices to select as the most rewarding aspect of their jobs, more female ObGyns (47%) than males (41%) reported that their physician-patient relationships are the major source of satisfaction. More men (10%) than women (7%) cite that making good money at a job they like is most gratifying. Only 3% of men and 2% of women reported no reward to being an ObGyn.1
Survey methodology
Medscape reports that the recruitment period for the 2015 Physician Compensation Report was from December 30, 2014, through March 11, 2015. Data were collected via a third-party online survey collection site. The margin of error for the survey was ±0.69%.1
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
The mean income for ObGyns rose by 2% in 2014 over 2013 to $249,000, according to the 2015 Medscape Compensation Report.1 This slight rise continues a gradual increase over the past few years ($242,000 in 2012; $220,000 in 2011).1–4 The 2015 report took into account survey responses from 19,657 physicians across 26 specialties, 5% (982) of whom were ObGyns.
The highest earners among all physician specialties were orthopedists ($421,000), cardiologists, and gastroenterologists. The lowest earners were pediatricians, family physicians, endocrinologists, and internists ($196,000). The highest ObGyn earners lived in the Northwest ($289,000) and Great Lakes ($268,000) regions; the lowest earners lived in the Mid-Atlantic ($230,000) and Northeast ($235,000) areas.1
Survey findings
Career satisfaction for ObGyns is dipping
In 2011, 69%, 53%, and 48% of ObGyns indicated they would choose a career in medicine again, select the same specialty, and pick the same practice setting, respectively.4 In the 2015 survey, 67% of ObGyns reported that they would still choose medicine; however, only 40% would pick obstetrics and gynecology as their specialty, and only 22% would select the same practice setting.1
Employment over private practice: Who feels best compensated?
Overall, 63% of all physicians are now employed, with only 23% reporting to be in private practice. Employment appears to be more popular for women: 59% of men and 72% of women responded that they work for a salary. Slightly more than a third (36%) of men and about a quarter (23%) of women are self-employed.5
The gender picture. Half of all ObGyns are women, and almost half of medical school graduates are women, yet male ObGyns continue to make more money than their female counterparts.1,5,6 The 9% difference between compensation rates for self-employed male and female ObGyns ($265,000 vs $242,000, respectively) is less than the 14% difference between their employed colleagues ($266,000 vs $229,000, respectively).1 Women tend to work shorter hours, fewer weeks, and see fewer patients than men, which could account for the lower compensation rate for female ObGyns. Studies suggest that greater schedule flexibility and fewer hours are key factors that improve satisfaction rates for female physicians.5
Male and female ObGyns tend to agree on their income satisfaction: less than half are satisfied (male, 44%; female, 46%). Many more employed ObGyns (55%) than self-employed ObGyns (31%) believe that they are fairly compensated.1
Which practice settings pay better?
Compensation rates for ObGyns in 2015 are greatest for those in office-based multispecialty group practice ($280,000), followed by those who work in1:
- health care organizations ($269,000)
- office-based single-specialty group practices ($266,000)
- outpatient clinics ($223,000)
- academic settings (nonhospital), research, military, and government ($219,000).
The lowest paid practice settings are office-based solo practices ($218,000) and hospital-employed ObGyns ($209,000).
In 2013, ObGyns who earned the most worked for health care organizations ($273,000); those who earned the least worked for outpatient clinics ($207,000).1
Do you take insurance, Medicare, Medicaid?
More employed (82%) than self-employed (53%) ObGyns will continue to take new and current Medicare or Medicaid patients, which is a rise from data published in the 2014 report (employed, 72%; self-employed, 46%).1
More than half (58%) of all physicians received less than $100 from private insurers for a new-patient office visit in 2014. Among ObGyns, 26% said they would drop insurers that pay poorly; 29% replied that they would not drop an insurer because they need all payers.1
The rate of participation in Accountable Care Organizations (ACOs) has increased from 25% in 2013 to 35% in 2014, with 8% more expecting to join an ACO in 2015. Concierge practice (2%) and cash-only practice (5%) were reportedly not significant payment models for ObGyns in 2014.1
Only 26% of ObGyns are planning to participate in health insurance exchanges; 23% said they are not participating, and 51% are not sure whether they will participate. Close to half (41%) of ObGyns believe their income will decrease because of health insurance exchanges, whereas 54% do not anticipate a change in income.1
Do you offer ancillary services?
When asked, 11% of employed ObGyns and 28% of self-employed ObGyns revealed that they have offered new ancillary services within the past 3 years. These ancillary services can include mammography, bone density testing, ultrasound, in-house laboratory services, bioidentical hormone replacement therapy, and weight management.1
How much time do you spend with patients?
In 2014, 62% of ObGyns reported spending 9 to 16 minutes with a patient during a visit. This is compared to 56% of family physicians and 44% of internists (TABLE).1,5
More than one-half (52%) of ObGynsspend 30 to 45 hours per week seeing patients. Fewer (38%) spend more than 45 hours per week, and 9% spend less than 30 hours per week with patients. This decline may be due to the increasing proportion of women and older physicians who tend to work shorter hours and fewer weeks.1
In the general physician population, 24% of women and 13% of men work part time, whereas 16% of both male and female ObGyns work part time. ObGyns aged 65 years or older constitute 35% of part-timers; 9% of those aged 35 to 49 years, and 11% of those aged 50 to 64 years, work part time. Only 2% of those younger than age 35 work part time.1
Would you select a career in obstetrics and gynecology all over again?
If given a second chance, would you rather choose orthopedic surgery as your specialty, or even choose medicine as a career again? OBG Management recently asked readers to weigh in, through its Quick Poll posted at obgmanagement.com, on whether or not they would choose ObGyn all over again. Ninety-one readers answered “yes” and 70 answered “no,” for a total of 161 respondents.
When this same question was posed to OBG Management’s Virtual Board of Editors (VBE), the perspectives were as split as the Quick Poll results:
- “No, no, no, I would not choose ObGyn all over again.”
- “Yes, I still love what I do.”
- “Yes, it is still the most unique specialty in medicine because it involves both surgery and primary care.”
- “Yes, for all the reasons I first loved the specialty: every week’s schedule, and every day is different. There is a mix of office care, surgery, and call.”
- “No! There is constant concern of litigation for complications, poor reimbursement, and compromised lifestyle.”
“There are much easier ways to make a living,” said one respondent, and another replied, “Work is very tough right now and the payment is too low.”
“The specialty has changed,” said Mary Vanko, MD, who practices in the suburbs of “blue collar Indiana.” “The public has very little idea of the breadth of our knowledge. The ObGyn generalist has the ability to serve as a woman’s doctor throughout her lifetime, not just perform the deliveries and surgeries. All of a sudden we are excluded from primary care status and people have to fight to see us. The newbies will never experience what it used to be as an ObGyn, the woman’s primary. Now we are the doctors to see when someone wants an IUD or is bleeding or pregnant. Big difference.”
Wesley Hambright, MD, practices in a small community hospital, but feels that “a larger hospital with more specialties may offer more flexibility and support in dealing with external pressures.” Tameka O’Neal, MD, is currently hospital employed but feels “as though I have little say in my practice.” Shaukat Ashai, MD, who is retired after 35 years in practice, says he would have preferred an academic setting on a full-time basis, citing long hours and poor compensation.
Robert del Rosario, MD, is in a large single-specialty suburban practice and would choose this practice setting again, although he would not choose a career as an ObGyn again. “The work demands have taken away too much from family,” he says. In addition, “as a male ObGyn, I am regularly faced with patients who choose their doctors based on gender rather than on skill. Our colleagues are no better. Early in my career and until the present, I hear people say, ‘Oh, I can’t hire Dr. X because we’re looking to hire a female.’”
Joe Walsh, MD, of Philadelphia, Pennsylvania, expresses similar discontent as a male ObGyn practicing in today’s female-populated specialty. In a letter to the editor in response to Editor in Chief Robert L. Barbieri, MD’s Editorial in the May 2015 issue, “Why is obstetrics and gynecology a popular choice for medical students?” Dr. Walsh states: “The unaddressed question is why is it unpopular for half of medical students? Ninety-three percent of resident graduates in the field are women, while women account for half of medical student graduates. Men rarely go into the field today. Perhaps job advertisements touting physician opportunities in ‘all female groups’ discourage men. Perhaps hospitals’ ‘Women’s Health Centers’ with such slogans as ‘Women taking care of women’ discourage men. Perhaps receptionists’ asking patients whether they prefer a male or female physician discourages male ObGyns.”
Many VBE members express some frustrations—with their practice setting, compensation, and longer work hours—but say that the patient relationships are the most rewarding aspect of their jobs. After 29 years in practice, Patrick Pevoto, MD, says the most rewarding aspect of his job is “being part of the legacy in people’s lives.”
Others say what keeps them engaged is:
- Enjoying “good outcomes.”
- “The patient contact. It’s fun having someone come up to me in the grocery store and introduce me to a teenager that I delivered 15 years ago.”
- “Surgery.”
- “Helping patients and teaching fellows.”
- “Knowing that I am making a difference in people’s lives.”
What is most rewarding?
When given several choices to select as the most rewarding aspect of their jobs, more female ObGyns (47%) than males (41%) reported that their physician-patient relationships are the major source of satisfaction. More men (10%) than women (7%) cite that making good money at a job they like is most gratifying. Only 3% of men and 2% of women reported no reward to being an ObGyn.1
Survey methodology
Medscape reports that the recruitment period for the 2015 Physician Compensation Report was from December 30, 2014, through March 11, 2015. Data were collected via a third-party online survey collection site. The margin of error for the survey was ±0.69%.1
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Peckham C. Medscape OB/GYN Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed May 13, 2015.
2. Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
3. Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
4. Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
5. Peckham C. Medscape Physician Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/public/overview. Published April 21, 2015. Accessed May 13, 2015.
6. Distribution of medical school graduates by gender. Henry Kaiser Family Foundation Web site. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Accessed May 13, 2015.
1. Peckham C. Medscape OB/GYN Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed May 13, 2015.
2. Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
3. Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
4. Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
5. Peckham C. Medscape Physician Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/public/overview. Published April 21, 2015. Accessed May 13, 2015.
6. Distribution of medical school graduates by gender. Henry Kaiser Family Foundation Web site. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Accessed May 13, 2015.
In this article
- Which practice settings pay better?
- Would you select a career in ObGyn again?
- Comparing time spent with patients
Consider telehealth technology to perform reliable and valid cognitive screening
Brief cognitive screening is essential for assessing neurocognitive disorders. Such screening can give clinicians a snapshot of patients’ cognitive abilities across a range of disorders and help tailor interventions to yield better outcomes. Appropriate administration of a brief cognitive screening using telehealth technology can improve access to care and treatment planning.
Neurocognitive decline can be a barrier to treatment
Persons with neurocognitive impairment, regardless of the cause, often face barriers when they seek treatment. Memory and attention difficulties often interfere with attending appointments; driving restrictions, smaller social networks, caregiver burden, and medical conditions limit access to care. For such patients, telehealth assessment is a tool that physicians can use to help patients overcome these barriers.
Cognitive screening tools
Brief cognitive assessments need to demonstrate (1) consistent and accurate scores over time (reliability) and (2) that they are measuring the intended cognitive domain (validity). The Mini-Mental State Examination is used often; the Montreal Cognitive Assessment and the Short Blessed Test are additional cognitive screeners that have support in the literature for use with telehealth technology.1
Telehealth assessment modalities
Modalities for telehealth assessment2 include:
• Audio-based systems. Pro: Telephone-based telehealth screening usually does not require extra equipment or advanced planning. Con: Visual information is absent and there is overreliance on verbal tasks.
• Video-based systems. Pro: Using videophones or video conferencing systems allow physicians to observe patients’ behaviors and their ability to complete tasks on paper. Con: A video system often requires more planning and effort to set up than other types of systems.
• Web-based systems. Pro: Web sites on which patient and provider can interact in real time—through a combination of audio, video, and programmed applications—offer immediate access to a patient’s responses and test results, thus providing a wealth of clinical information such as exact timing and calculation of patients’ responses, ability to record and review patients’ approach to construction tasks, and the capability to adapt test batteries in real-time based on patients’ ongoing performance. Con: Such systems require specialized software and infrastructure.
Support for telehealth screening
Our patients report feeling comfortable with telehealth screening; they overwhelmingly report that they prefer telehealth services to in-person services that require travel. Studies on the reliability and validity of using cognitive screeners have shown that telehealth screening is a feasible and acceptable practice.3 Although the telehealth approaches mentioned here can all be used effectively, we have found that video-based cognitive screening might offer the best balance of flexibility, accessibility, and ease of use at this time.
Our recommendations
Consider your resources, patient population, and the scope of available telehealth services to guide your approach. Use validated measures that fit the limitations of the modality you have chosen:
• Telephone-based screenings should use verbally based measures (eg, the Short Blessed Test and the Telephone Interview for Cognitive Status).
• Video-based screenings can include visual elements, but you need to decide how to best administer, record, and score the patient’s written responses. You might need to mail portions of tests along with a writing utensil and paper to their home. Patients can hold up their responses to the camera or send back the completed tests for scoring.
• Adapt testing to the constraints of a particular situation, but modifications to tests should be limited as much as possible to minimize decreases in reliability and validity.
• Have a clear policy for dealing with unexpected events, such as technological malfunctions, patient privacy concerns, and mental health emergencies.
Acknowledgement
This article was supported by the facilities and resources of the Salem VA Medical Center. The views expressed in this article are those of the authors and not necessarily those of the Department of Veterans Affairs.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or wiith manufacturers of competing products.
1. Martin-Khan M, Wootton R, Gray L. A systematic review of the reliability of screening for cognitive impairment in older adults by use of standardised assessment tools administered via the telephone. J Telemed Telecare. 2010;16(8):422-428.
2. Pramuka M, van Roosmalen L. Telerehabilitation technologies: accessibility and usability. International Journal of Telerehabilitation. 2009;1(1):85-97.
3. Morgan D, Crossley M, Basran J, et al. Evaluation of telehealth for preclinic assessment and follow-up in an interprofessional rural and remote memory clinic. J Appl Gerontol. 2011;30(3):304-331.
Brief cognitive screening is essential for assessing neurocognitive disorders. Such screening can give clinicians a snapshot of patients’ cognitive abilities across a range of disorders and help tailor interventions to yield better outcomes. Appropriate administration of a brief cognitive screening using telehealth technology can improve access to care and treatment planning.
Neurocognitive decline can be a barrier to treatment
Persons with neurocognitive impairment, regardless of the cause, often face barriers when they seek treatment. Memory and attention difficulties often interfere with attending appointments; driving restrictions, smaller social networks, caregiver burden, and medical conditions limit access to care. For such patients, telehealth assessment is a tool that physicians can use to help patients overcome these barriers.
Cognitive screening tools
Brief cognitive assessments need to demonstrate (1) consistent and accurate scores over time (reliability) and (2) that they are measuring the intended cognitive domain (validity). The Mini-Mental State Examination is used often; the Montreal Cognitive Assessment and the Short Blessed Test are additional cognitive screeners that have support in the literature for use with telehealth technology.1
Telehealth assessment modalities
Modalities for telehealth assessment2 include:
• Audio-based systems. Pro: Telephone-based telehealth screening usually does not require extra equipment or advanced planning. Con: Visual information is absent and there is overreliance on verbal tasks.
• Video-based systems. Pro: Using videophones or video conferencing systems allow physicians to observe patients’ behaviors and their ability to complete tasks on paper. Con: A video system often requires more planning and effort to set up than other types of systems.
• Web-based systems. Pro: Web sites on which patient and provider can interact in real time—through a combination of audio, video, and programmed applications—offer immediate access to a patient’s responses and test results, thus providing a wealth of clinical information such as exact timing and calculation of patients’ responses, ability to record and review patients’ approach to construction tasks, and the capability to adapt test batteries in real-time based on patients’ ongoing performance. Con: Such systems require specialized software and infrastructure.
Support for telehealth screening
Our patients report feeling comfortable with telehealth screening; they overwhelmingly report that they prefer telehealth services to in-person services that require travel. Studies on the reliability and validity of using cognitive screeners have shown that telehealth screening is a feasible and acceptable practice.3 Although the telehealth approaches mentioned here can all be used effectively, we have found that video-based cognitive screening might offer the best balance of flexibility, accessibility, and ease of use at this time.
Our recommendations
Consider your resources, patient population, and the scope of available telehealth services to guide your approach. Use validated measures that fit the limitations of the modality you have chosen:
• Telephone-based screenings should use verbally based measures (eg, the Short Blessed Test and the Telephone Interview for Cognitive Status).
• Video-based screenings can include visual elements, but you need to decide how to best administer, record, and score the patient’s written responses. You might need to mail portions of tests along with a writing utensil and paper to their home. Patients can hold up their responses to the camera or send back the completed tests for scoring.
• Adapt testing to the constraints of a particular situation, but modifications to tests should be limited as much as possible to minimize decreases in reliability and validity.
• Have a clear policy for dealing with unexpected events, such as technological malfunctions, patient privacy concerns, and mental health emergencies.
Acknowledgement
This article was supported by the facilities and resources of the Salem VA Medical Center. The views expressed in this article are those of the authors and not necessarily those of the Department of Veterans Affairs.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or wiith manufacturers of competing products.
Brief cognitive screening is essential for assessing neurocognitive disorders. Such screening can give clinicians a snapshot of patients’ cognitive abilities across a range of disorders and help tailor interventions to yield better outcomes. Appropriate administration of a brief cognitive screening using telehealth technology can improve access to care and treatment planning.
Neurocognitive decline can be a barrier to treatment
Persons with neurocognitive impairment, regardless of the cause, often face barriers when they seek treatment. Memory and attention difficulties often interfere with attending appointments; driving restrictions, smaller social networks, caregiver burden, and medical conditions limit access to care. For such patients, telehealth assessment is a tool that physicians can use to help patients overcome these barriers.
Cognitive screening tools
Brief cognitive assessments need to demonstrate (1) consistent and accurate scores over time (reliability) and (2) that they are measuring the intended cognitive domain (validity). The Mini-Mental State Examination is used often; the Montreal Cognitive Assessment and the Short Blessed Test are additional cognitive screeners that have support in the literature for use with telehealth technology.1
Telehealth assessment modalities
Modalities for telehealth assessment2 include:
• Audio-based systems. Pro: Telephone-based telehealth screening usually does not require extra equipment or advanced planning. Con: Visual information is absent and there is overreliance on verbal tasks.
• Video-based systems. Pro: Using videophones or video conferencing systems allow physicians to observe patients’ behaviors and their ability to complete tasks on paper. Con: A video system often requires more planning and effort to set up than other types of systems.
• Web-based systems. Pro: Web sites on which patient and provider can interact in real time—through a combination of audio, video, and programmed applications—offer immediate access to a patient’s responses and test results, thus providing a wealth of clinical information such as exact timing and calculation of patients’ responses, ability to record and review patients’ approach to construction tasks, and the capability to adapt test batteries in real-time based on patients’ ongoing performance. Con: Such systems require specialized software and infrastructure.
Support for telehealth screening
Our patients report feeling comfortable with telehealth screening; they overwhelmingly report that they prefer telehealth services to in-person services that require travel. Studies on the reliability and validity of using cognitive screeners have shown that telehealth screening is a feasible and acceptable practice.3 Although the telehealth approaches mentioned here can all be used effectively, we have found that video-based cognitive screening might offer the best balance of flexibility, accessibility, and ease of use at this time.
Our recommendations
Consider your resources, patient population, and the scope of available telehealth services to guide your approach. Use validated measures that fit the limitations of the modality you have chosen:
• Telephone-based screenings should use verbally based measures (eg, the Short Blessed Test and the Telephone Interview for Cognitive Status).
• Video-based screenings can include visual elements, but you need to decide how to best administer, record, and score the patient’s written responses. You might need to mail portions of tests along with a writing utensil and paper to their home. Patients can hold up their responses to the camera or send back the completed tests for scoring.
• Adapt testing to the constraints of a particular situation, but modifications to tests should be limited as much as possible to minimize decreases in reliability and validity.
• Have a clear policy for dealing with unexpected events, such as technological malfunctions, patient privacy concerns, and mental health emergencies.
Acknowledgement
This article was supported by the facilities and resources of the Salem VA Medical Center. The views expressed in this article are those of the authors and not necessarily those of the Department of Veterans Affairs.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or wiith manufacturers of competing products.
1. Martin-Khan M, Wootton R, Gray L. A systematic review of the reliability of screening for cognitive impairment in older adults by use of standardised assessment tools administered via the telephone. J Telemed Telecare. 2010;16(8):422-428.
2. Pramuka M, van Roosmalen L. Telerehabilitation technologies: accessibility and usability. International Journal of Telerehabilitation. 2009;1(1):85-97.
3. Morgan D, Crossley M, Basran J, et al. Evaluation of telehealth for preclinic assessment and follow-up in an interprofessional rural and remote memory clinic. J Appl Gerontol. 2011;30(3):304-331.
1. Martin-Khan M, Wootton R, Gray L. A systematic review of the reliability of screening for cognitive impairment in older adults by use of standardised assessment tools administered via the telephone. J Telemed Telecare. 2010;16(8):422-428.
2. Pramuka M, van Roosmalen L. Telerehabilitation technologies: accessibility and usability. International Journal of Telerehabilitation. 2009;1(1):85-97.
3. Morgan D, Crossley M, Basran J, et al. Evaluation of telehealth for preclinic assessment and follow-up in an interprofessional rural and remote memory clinic. J Appl Gerontol. 2011;30(3):304-331.