User login
The pendulum swings in favor of corticosteroids
Critical Care Network
Sepsis/Shock Section
The pendulum swings in favor of corticosteroids and endorses the colloquialism among intensivists that no patient shall die without steroids, especially as it relates to sepsis and septic shock.
In 2018, we saw divergence among randomized controlled trials in the use of glucocorticoids for adults with septic shock such that hydrocortisone without the use of fludrocortisone showed no 90-day mortality benefit; however, hydrocortisone with fludrocortisone showed a 90-day mortality benefit.1,2 The Surviving Sepsis Guidelines in 2021 favored using low-dose corticosteroids in those with persistent vasopressor requirements in whom other core interventions had been instituted.
In 2023, a patient-level meta-analysis of low-dose hydrocortisone in adults with septic shock included seven trials and failed to demonstrate a mortality benefit by relative risk in those who received hydrocortisone compared with placebo. Separately, a network meta-analysis with hydrocortisone plus enteral fludrocortisone was associated with a 90-day all-cause mortality. Of the secondary outcomes, these results offered a possible association of hydrocortisone with a decreased risk of ICU mortality and with increased vasopressor-free days.3
The 2024 Society of Critical Care Medicine recently shared an update of focused guidelines on the use of corticosteroids in sepsis, acute respiratory distress syndrome, and community-acquired pneumonia. These included a conditional recommendation to administer corticosteroids for patients with septic shock but recommended against high-dose/short-duration administration of corticosteroids in these patients. These guidelines were supported by data from 46 randomized controlled trials, which showed that corticosteroid use may reduce hospital/long-term mortality and ICU/short-term mortality, as well as result in higher rates of shock reversal and reduced organ dysfunction.
With the results of these meta-analyses and randomized controlled trials, clinicians should consider low-dose corticosteroids paired with fludrocortisone as a tool in treating patients with septic shock given that the short- and long-term benefits may exceed any risks.
References
1. Venkatesh B, et al. Adjunctive glucocorticoid therapy in patients with septic shock. N Engl J Med. 2018;378:797-808.
2. Annane D, et al. Hydrocortisone plus fludrocortisone for adults with septic shock. N Engl J Med. 2018;378:809-818.
3. Pirracchio R, et al. Patient-level meta-analysis of low-dose hydrocortisone in adults with septic shock. NEJM Evid. 2023;2(6).
Critical Care Network
Sepsis/Shock Section
The pendulum swings in favor of corticosteroids and endorses the colloquialism among intensivists that no patient shall die without steroids, especially as it relates to sepsis and septic shock.
In 2018, we saw divergence among randomized controlled trials in the use of glucocorticoids for adults with septic shock such that hydrocortisone without the use of fludrocortisone showed no 90-day mortality benefit; however, hydrocortisone with fludrocortisone showed a 90-day mortality benefit.1,2 The Surviving Sepsis Guidelines in 2021 favored using low-dose corticosteroids in those with persistent vasopressor requirements in whom other core interventions had been instituted.
In 2023, a patient-level meta-analysis of low-dose hydrocortisone in adults with septic shock included seven trials and failed to demonstrate a mortality benefit by relative risk in those who received hydrocortisone compared with placebo. Separately, a network meta-analysis with hydrocortisone plus enteral fludrocortisone was associated with a 90-day all-cause mortality. Of the secondary outcomes, these results offered a possible association of hydrocortisone with a decreased risk of ICU mortality and with increased vasopressor-free days.3
The 2024 Society of Critical Care Medicine recently shared an update of focused guidelines on the use of corticosteroids in sepsis, acute respiratory distress syndrome, and community-acquired pneumonia. These included a conditional recommendation to administer corticosteroids for patients with septic shock but recommended against high-dose/short-duration administration of corticosteroids in these patients. These guidelines were supported by data from 46 randomized controlled trials, which showed that corticosteroid use may reduce hospital/long-term mortality and ICU/short-term mortality, as well as result in higher rates of shock reversal and reduced organ dysfunction.
With the results of these meta-analyses and randomized controlled trials, clinicians should consider low-dose corticosteroids paired with fludrocortisone as a tool in treating patients with septic shock given that the short- and long-term benefits may exceed any risks.
References
1. Venkatesh B, et al. Adjunctive glucocorticoid therapy in patients with septic shock. N Engl J Med. 2018;378:797-808.
2. Annane D, et al. Hydrocortisone plus fludrocortisone for adults with septic shock. N Engl J Med. 2018;378:809-818.
3. Pirracchio R, et al. Patient-level meta-analysis of low-dose hydrocortisone in adults with septic shock. NEJM Evid. 2023;2(6).
Critical Care Network
Sepsis/Shock Section
The pendulum swings in favor of corticosteroids and endorses the colloquialism among intensivists that no patient shall die without steroids, especially as it relates to sepsis and septic shock.
In 2018, we saw divergence among randomized controlled trials in the use of glucocorticoids for adults with septic shock such that hydrocortisone without the use of fludrocortisone showed no 90-day mortality benefit; however, hydrocortisone with fludrocortisone showed a 90-day mortality benefit.1,2 The Surviving Sepsis Guidelines in 2021 favored using low-dose corticosteroids in those with persistent vasopressor requirements in whom other core interventions had been instituted.
In 2023, a patient-level meta-analysis of low-dose hydrocortisone in adults with septic shock included seven trials and failed to demonstrate a mortality benefit by relative risk in those who received hydrocortisone compared with placebo. Separately, a network meta-analysis with hydrocortisone plus enteral fludrocortisone was associated with a 90-day all-cause mortality. Of the secondary outcomes, these results offered a possible association of hydrocortisone with a decreased risk of ICU mortality and with increased vasopressor-free days.3
The 2024 Society of Critical Care Medicine recently shared an update of focused guidelines on the use of corticosteroids in sepsis, acute respiratory distress syndrome, and community-acquired pneumonia. These included a conditional recommendation to administer corticosteroids for patients with septic shock but recommended against high-dose/short-duration administration of corticosteroids in these patients. These guidelines were supported by data from 46 randomized controlled trials, which showed that corticosteroid use may reduce hospital/long-term mortality and ICU/short-term mortality, as well as result in higher rates of shock reversal and reduced organ dysfunction.
With the results of these meta-analyses and randomized controlled trials, clinicians should consider low-dose corticosteroids paired with fludrocortisone as a tool in treating patients with septic shock given that the short- and long-term benefits may exceed any risks.
References
1. Venkatesh B, et al. Adjunctive glucocorticoid therapy in patients with septic shock. N Engl J Med. 2018;378:797-808.
2. Annane D, et al. Hydrocortisone plus fludrocortisone for adults with septic shock. N Engl J Med. 2018;378:809-818.
3. Pirracchio R, et al. Patient-level meta-analysis of low-dose hydrocortisone in adults with septic shock. NEJM Evid. 2023;2(6).
Which Emergencies Are Genuine Emergencies?
WIESBADEN, GERMANY — Crowded waiting rooms, long wait times, irritable patients, and aggression toward nursing staff and doctors are increasingly the reality in German emergency rooms. Clearly, emergencies belong in the emergency room. However, “In about half of all patients in the emergency room, there is no urgent medical emergency,” Norbert Schütz, MD, director of geriatrics and rheumatology at Helios Dr. Horst Schmidt Hospital in Wiesbaden, Germany, said at a press conference for the 130th Annual Meeting of the German Society of Internal Medicine (DGIM).
“In our daily medical practice, we repeatedly experience people either accessing our emergency departments and ambulances too quickly or lingering at home for too long when they have severe symptoms,” said Dr. Schütz, who organized the Patient Day during the Internist Congress.
DGIM Educates Patients
What is an emergency? “I think the public is quite well informed about conditions associated with loss of consciousness, severe pain, chest pain, or paralysis: Think stroke or heart attack. This is undoubtedly a success of recent years. The difficulty arises with everything in between. For instance, should I go to the hospital with severe headaches?” asked Dr. Schütz.
When is a patient a case for the emergency room, the physician on-call service, or the general practitioner? At the Patient Day in Wiesbaden, DGIM aims to educate and train interested parties with a dedicated lecture. The focus is on recognizing an emergency, specifically emergencies in children and mental illnesses.
“Our Patient Day aims to contribute to making the right decisions. We want to inform, answer questions, and alleviate fears,” said Dr. Schütz. Interested parties can refresh their emergency knowledge, tour ambulances, and have the equipment explained. The public also has the opportunity to learn about resuscitation techniques theoretically and practically.
“Should, for whatever reason, the general practitioner not be reachable, the physician on-call service can be reached,” said Dr. Schütz. It may happen, however, that neither the general practitioner nor the on-call physician is immediately available.
What Are Emergencies?
In cases of severe health impairment, urgency is required, and a severe emergency should be assumed in the following cases:
- Chest pain
- Circulatory disorder
- Disorders of consciousness
- Breathing difficulties
- Sudden weakness or numbness/paralysis
- Severe bleeding
- Allergic shock
“In such cases, the emergency departments of the hospitals are available around the clock, and if necessary, an emergency doctor should be present during transportation to the hospital,” said Dr. Schütz.
Classifying emergencies is challenging, especially with children. “Children often find it difficult to clearly categorize or describe symptoms,” said Dr. Schütz. A situation is critical if, for example, the child’s breathing or consciousness is impaired.
Mental emergencies pose a particular challenge for patients and relatives because the patient and relatives are often overwhelmed by the situation. If there are suicidal thoughts, the patient should present him- or herself immediately to an emergency room.
“Patients who come to the emergency room because they cannot get appointments with their general practitioner or specialist, for whatever reason, are no emergency. We also see this in the emergency room from time to time,” said Dr. Schütz. Emergency rooms are not intended for this purpose. “And generally, these are not emergencies.”
Four of 10 Cases
The number of patients in emergency rooms has steadily increased in recent years. Statistically, only 4 out of 10 cases are genuine emergencies, as detailed surveys of patients in the emergency rooms of northern German hospitals have shown.
In the PiNo Nord cross-sectional study, Martin Scherer, MD, of University Hospital Hamburg-Eppendorf in Hamburg, Germany, and his team examined the reasons why patients visit the emergency room. They interviewed 1175 patients in five hospitals and documented the medical diagnoses. Patients classified as “immediately” or “very urgently” in need of treatment were excluded.
The surveyed patients were on average 41.8 years old, 52.9% were men, and 54.7% of the patients indicated a low urgency of treatment. About 41% of the patients visited the emergency room on their own initiative, 17% stated they were referred or entrusted by their general practitioner, and 8% were referred by a specialist in the emergency room.
The strongest predictors for low subjective treatment urgency were musculoskeletal trauma (odds ratio [OR], 2.18), skin afflictions (OR, 2.15), and the unavailability of an open general practitioner’s office (OR, 1.70).
According to Dr. Scherer and his colleagues, the reasons for visiting an emergency room are diverse and can be based on the perceived structural conditions and individual patient preferences in addition to the urgency of the health problem.
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
WIESBADEN, GERMANY — Crowded waiting rooms, long wait times, irritable patients, and aggression toward nursing staff and doctors are increasingly the reality in German emergency rooms. Clearly, emergencies belong in the emergency room. However, “In about half of all patients in the emergency room, there is no urgent medical emergency,” Norbert Schütz, MD, director of geriatrics and rheumatology at Helios Dr. Horst Schmidt Hospital in Wiesbaden, Germany, said at a press conference for the 130th Annual Meeting of the German Society of Internal Medicine (DGIM).
“In our daily medical practice, we repeatedly experience people either accessing our emergency departments and ambulances too quickly or lingering at home for too long when they have severe symptoms,” said Dr. Schütz, who organized the Patient Day during the Internist Congress.
DGIM Educates Patients
What is an emergency? “I think the public is quite well informed about conditions associated with loss of consciousness, severe pain, chest pain, or paralysis: Think stroke or heart attack. This is undoubtedly a success of recent years. The difficulty arises with everything in between. For instance, should I go to the hospital with severe headaches?” asked Dr. Schütz.
When is a patient a case for the emergency room, the physician on-call service, or the general practitioner? At the Patient Day in Wiesbaden, DGIM aims to educate and train interested parties with a dedicated lecture. The focus is on recognizing an emergency, specifically emergencies in children and mental illnesses.
“Our Patient Day aims to contribute to making the right decisions. We want to inform, answer questions, and alleviate fears,” said Dr. Schütz. Interested parties can refresh their emergency knowledge, tour ambulances, and have the equipment explained. The public also has the opportunity to learn about resuscitation techniques theoretically and practically.
“Should, for whatever reason, the general practitioner not be reachable, the physician on-call service can be reached,” said Dr. Schütz. It may happen, however, that neither the general practitioner nor the on-call physician is immediately available.
What Are Emergencies?
In cases of severe health impairment, urgency is required, and a severe emergency should be assumed in the following cases:
- Chest pain
- Circulatory disorder
- Disorders of consciousness
- Breathing difficulties
- Sudden weakness or numbness/paralysis
- Severe bleeding
- Allergic shock
“In such cases, the emergency departments of the hospitals are available around the clock, and if necessary, an emergency doctor should be present during transportation to the hospital,” said Dr. Schütz.
Classifying emergencies is challenging, especially with children. “Children often find it difficult to clearly categorize or describe symptoms,” said Dr. Schütz. A situation is critical if, for example, the child’s breathing or consciousness is impaired.
Mental emergencies pose a particular challenge for patients and relatives because the patient and relatives are often overwhelmed by the situation. If there are suicidal thoughts, the patient should present him- or herself immediately to an emergency room.
“Patients who come to the emergency room because they cannot get appointments with their general practitioner or specialist, for whatever reason, are no emergency. We also see this in the emergency room from time to time,” said Dr. Schütz. Emergency rooms are not intended for this purpose. “And generally, these are not emergencies.”
Four of 10 Cases
The number of patients in emergency rooms has steadily increased in recent years. Statistically, only 4 out of 10 cases are genuine emergencies, as detailed surveys of patients in the emergency rooms of northern German hospitals have shown.
In the PiNo Nord cross-sectional study, Martin Scherer, MD, of University Hospital Hamburg-Eppendorf in Hamburg, Germany, and his team examined the reasons why patients visit the emergency room. They interviewed 1175 patients in five hospitals and documented the medical diagnoses. Patients classified as “immediately” or “very urgently” in need of treatment were excluded.
The surveyed patients were on average 41.8 years old, 52.9% were men, and 54.7% of the patients indicated a low urgency of treatment. About 41% of the patients visited the emergency room on their own initiative, 17% stated they were referred or entrusted by their general practitioner, and 8% were referred by a specialist in the emergency room.
The strongest predictors for low subjective treatment urgency were musculoskeletal trauma (odds ratio [OR], 2.18), skin afflictions (OR, 2.15), and the unavailability of an open general practitioner’s office (OR, 1.70).
According to Dr. Scherer and his colleagues, the reasons for visiting an emergency room are diverse and can be based on the perceived structural conditions and individual patient preferences in addition to the urgency of the health problem.
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
WIESBADEN, GERMANY — Crowded waiting rooms, long wait times, irritable patients, and aggression toward nursing staff and doctors are increasingly the reality in German emergency rooms. Clearly, emergencies belong in the emergency room. However, “In about half of all patients in the emergency room, there is no urgent medical emergency,” Norbert Schütz, MD, director of geriatrics and rheumatology at Helios Dr. Horst Schmidt Hospital in Wiesbaden, Germany, said at a press conference for the 130th Annual Meeting of the German Society of Internal Medicine (DGIM).
“In our daily medical practice, we repeatedly experience people either accessing our emergency departments and ambulances too quickly or lingering at home for too long when they have severe symptoms,” said Dr. Schütz, who organized the Patient Day during the Internist Congress.
DGIM Educates Patients
What is an emergency? “I think the public is quite well informed about conditions associated with loss of consciousness, severe pain, chest pain, or paralysis: Think stroke or heart attack. This is undoubtedly a success of recent years. The difficulty arises with everything in between. For instance, should I go to the hospital with severe headaches?” asked Dr. Schütz.
When is a patient a case for the emergency room, the physician on-call service, or the general practitioner? At the Patient Day in Wiesbaden, DGIM aims to educate and train interested parties with a dedicated lecture. The focus is on recognizing an emergency, specifically emergencies in children and mental illnesses.
“Our Patient Day aims to contribute to making the right decisions. We want to inform, answer questions, and alleviate fears,” said Dr. Schütz. Interested parties can refresh their emergency knowledge, tour ambulances, and have the equipment explained. The public also has the opportunity to learn about resuscitation techniques theoretically and practically.
“Should, for whatever reason, the general practitioner not be reachable, the physician on-call service can be reached,” said Dr. Schütz. It may happen, however, that neither the general practitioner nor the on-call physician is immediately available.
What Are Emergencies?
In cases of severe health impairment, urgency is required, and a severe emergency should be assumed in the following cases:
- Chest pain
- Circulatory disorder
- Disorders of consciousness
- Breathing difficulties
- Sudden weakness or numbness/paralysis
- Severe bleeding
- Allergic shock
“In such cases, the emergency departments of the hospitals are available around the clock, and if necessary, an emergency doctor should be present during transportation to the hospital,” said Dr. Schütz.
Classifying emergencies is challenging, especially with children. “Children often find it difficult to clearly categorize or describe symptoms,” said Dr. Schütz. A situation is critical if, for example, the child’s breathing or consciousness is impaired.
Mental emergencies pose a particular challenge for patients and relatives because the patient and relatives are often overwhelmed by the situation. If there are suicidal thoughts, the patient should present him- or herself immediately to an emergency room.
“Patients who come to the emergency room because they cannot get appointments with their general practitioner or specialist, for whatever reason, are no emergency. We also see this in the emergency room from time to time,” said Dr. Schütz. Emergency rooms are not intended for this purpose. “And generally, these are not emergencies.”
Four of 10 Cases
The number of patients in emergency rooms has steadily increased in recent years. Statistically, only 4 out of 10 cases are genuine emergencies, as detailed surveys of patients in the emergency rooms of northern German hospitals have shown.
In the PiNo Nord cross-sectional study, Martin Scherer, MD, of University Hospital Hamburg-Eppendorf in Hamburg, Germany, and his team examined the reasons why patients visit the emergency room. They interviewed 1175 patients in five hospitals and documented the medical diagnoses. Patients classified as “immediately” or “very urgently” in need of treatment were excluded.
The surveyed patients were on average 41.8 years old, 52.9% were men, and 54.7% of the patients indicated a low urgency of treatment. About 41% of the patients visited the emergency room on their own initiative, 17% stated they were referred or entrusted by their general practitioner, and 8% were referred by a specialist in the emergency room.
The strongest predictors for low subjective treatment urgency were musculoskeletal trauma (odds ratio [OR], 2.18), skin afflictions (OR, 2.15), and the unavailability of an open general practitioner’s office (OR, 1.70).
According to Dr. Scherer and his colleagues, the reasons for visiting an emergency room are diverse and can be based on the perceived structural conditions and individual patient preferences in addition to the urgency of the health problem.
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
‘No Pulse’: An MD’s First Night Off in 2 Weeks Turns Grave
Emergencies happen anywhere, anytime, and sometimes, medical professionals find themselves in situations where they are the only ones who can help. Is There a Doctor in the House? is a series by this news organization that tells these stories.
It was my first night off after 12 days. It was a Friday night, and I went to a bar in Naples to get a beer with some friends. As it turned out, it wasn’t a night off after all.
As soon as we got inside, we heard over the speaker that they needed medical personnel and to please go to the left side of the bar. I thought it would be syncope or something like that.
I went over there and saw a woman holding up a man. He was basically leaning all over her. The light was low, and the music was pounding. I started to assess him and tried to get him to answer me. No response. I checked for pulses — nothing.
The woman helped me lower him to the floor. I checked again for a pulse. Still nothing. I said, “Call 911,” and started compressions.
The difficult part was the place was completely dark. I knew where his body was on the floor. I could see his chest. But I couldn’t see his face at all.
It was also extremely loud with the music thumping. After a while, they finally shut it off.
Pretty soon, the security personnel from the bar brought me an automated external defibrillator, and it showed the man was having V-fib arrest. I shocked him. Still no pulse. I continued with cardiopulmonary resuscitation (CPR).
I hadn’t noticed, but lots of people were crowding around us. Somebody came up and said, “He’s my friend. He has a 9-year-old daughter. He can’t die. Let me help with the compressions.” I was like, “Go for it.”
The guy started kind of pushing on the man’s abdomen. He had no idea how to do compressions. I said, “Okay, let me take over again.”
Out of the crowd, nobody else volunteered to help. No one asked me, “Hey, what can I do?” Meanwhile, I found out later that someone was filming the whole thing on their phone.
But what the guy said about the man’s young daughter stayed in my brain. I thought, we need to keep going.
I did more compressions and shocked him again. Still no pulse. At that point, the police and emergency medical services showed up. They checked, nothing had changed, so they got him into the ambulance.
I asked one of the paramedics, “Where are you taking him? I can call ahead.”
But he said, “That’s HIPAA. We can’t tell you.” They also wouldn’t let me go with him in the ambulance.
“I have an active Florida license, and I work in the ICU [intensive care unit],” I said.
“No, we need to follow our protocol,” he replied.
I understood that, but I just wanted to help.
It was around 10:30 PM by then, and I was drenched in sweat. I had to go home. The first thing I did after taking a shower was open the computer and check my system. I needed to find out what happened to the guy.
I was looking for admissions, and I didn’t see him. I called the main hospital downtown and the one in North Naples. I couldn’t find him anywhere. I stayed up until almost 1:00 AM checking for his name. At that point I thought, okay, maybe he died.
The next night, Saturday, I was home and got a call from one of my colleagues. “Hey, were you in a bar yesterday? Did you do CPR on somebody?”
“How did you know?” I said.
He said the paramedics had described me — “a tall doctor with glasses who was a nice guy.” It was funny that he knew that was me.
He told me, “The guy’s alive. He’s sick and needs to be put on dialysis, but he’s alive.”
Apparently, the guy had gone to the emergency department at North Naples, and the doctors in the emergency room (ER) worked on him for over an hour. They did continuous CPR and shocked him for close to 40 minutes. They finally got his pulse back, and after that, he was transferred to the main hospital ICU. They didn’t admit him at the ER, which was why I couldn’t find his name.
On Sunday, I was checking my patients’ charts for the ICU that coming week. And there he was. I saw his name and the documentation by the ED that CPR was provided by a critical care doctor in the field. He was still alive. That gave me so much joy.
So, the man I had helped became my patient. When I saw him on Monday, he was intubated and needed dialysis. I finally saw his face and thought, Oh, so that’s what you look like. I hadn’t realized he was only 39 years old.
When he was awake, I explained to him I was the doctor that provided CPR at the bar. He was very grateful, but of course, he didn’t remember anything.
Eventually, I met his daughter, and she just said, “Thank you for allowing me to have my dad.”
The funny part is that he broke his leg. Well, that’s not funny, but no one had any idea how it happened. That was his only complaint. He was asking me, “Doctor, how did you break my leg?”
“Hey, I have no idea how you broke your leg,” I replied. “I was trying to save your life.”
He was in the hospital for almost a month but made a full recovery. The amazing part: After all the evaluations, he has no neurological deficits. He’s back to a normal life now.
They never found a cause for the cardiac arrest. I mean, he had an ejection fraction of 10%. All my money was on something drug related, but that wasn’t the case. They’d done a cardiac cut, and there was no obstruction. They couldn’t find a reason.
We’ve become friends. He still works as a DJ at the bar. He changed his name to “DJ the Survivor” or something like that.
Sometimes, he’ll text me: “Doctor, what are you doing? You want to come down to the bar?”
I’m like, “No. I don’t.”
It’s been more than a year, but I remember every detail. When you go into medicine, you dream that one day you’ll be able to say, “I saved somebody.”
He texted me a year later and told me he’s celebrating two birthdays now. He said, “I’m turning 1 year old today!”
I think about the value of life. How we can take it for granted. We think, I’m young, nothing is going to happen to me. But this guy was 39. He went to work and died that night.
I was able to help bring him back. That makes me thankful for every day.
Jose Valle Giler, MD, is a pulmonary, critical care, and sleep medicine physician at NCH Healthcare System in Naples, Florida.
A version of this article appeared on Medscape.com .
Emergencies happen anywhere, anytime, and sometimes, medical professionals find themselves in situations where they are the only ones who can help. Is There a Doctor in the House? is a series by this news organization that tells these stories.
It was my first night off after 12 days. It was a Friday night, and I went to a bar in Naples to get a beer with some friends. As it turned out, it wasn’t a night off after all.
As soon as we got inside, we heard over the speaker that they needed medical personnel and to please go to the left side of the bar. I thought it would be syncope or something like that.
I went over there and saw a woman holding up a man. He was basically leaning all over her. The light was low, and the music was pounding. I started to assess him and tried to get him to answer me. No response. I checked for pulses — nothing.
The woman helped me lower him to the floor. I checked again for a pulse. Still nothing. I said, “Call 911,” and started compressions.
The difficult part was the place was completely dark. I knew where his body was on the floor. I could see his chest. But I couldn’t see his face at all.
It was also extremely loud with the music thumping. After a while, they finally shut it off.
Pretty soon, the security personnel from the bar brought me an automated external defibrillator, and it showed the man was having V-fib arrest. I shocked him. Still no pulse. I continued with cardiopulmonary resuscitation (CPR).
I hadn’t noticed, but lots of people were crowding around us. Somebody came up and said, “He’s my friend. He has a 9-year-old daughter. He can’t die. Let me help with the compressions.” I was like, “Go for it.”
The guy started kind of pushing on the man’s abdomen. He had no idea how to do compressions. I said, “Okay, let me take over again.”
Out of the crowd, nobody else volunteered to help. No one asked me, “Hey, what can I do?” Meanwhile, I found out later that someone was filming the whole thing on their phone.
But what the guy said about the man’s young daughter stayed in my brain. I thought, we need to keep going.
I did more compressions and shocked him again. Still no pulse. At that point, the police and emergency medical services showed up. They checked, nothing had changed, so they got him into the ambulance.
I asked one of the paramedics, “Where are you taking him? I can call ahead.”
But he said, “That’s HIPAA. We can’t tell you.” They also wouldn’t let me go with him in the ambulance.
“I have an active Florida license, and I work in the ICU [intensive care unit],” I said.
“No, we need to follow our protocol,” he replied.
I understood that, but I just wanted to help.
It was around 10:30 PM by then, and I was drenched in sweat. I had to go home. The first thing I did after taking a shower was open the computer and check my system. I needed to find out what happened to the guy.
I was looking for admissions, and I didn’t see him. I called the main hospital downtown and the one in North Naples. I couldn’t find him anywhere. I stayed up until almost 1:00 AM checking for his name. At that point I thought, okay, maybe he died.
The next night, Saturday, I was home and got a call from one of my colleagues. “Hey, were you in a bar yesterday? Did you do CPR on somebody?”
“How did you know?” I said.
He said the paramedics had described me — “a tall doctor with glasses who was a nice guy.” It was funny that he knew that was me.
He told me, “The guy’s alive. He’s sick and needs to be put on dialysis, but he’s alive.”
Apparently, the guy had gone to the emergency department at North Naples, and the doctors in the emergency room (ER) worked on him for over an hour. They did continuous CPR and shocked him for close to 40 minutes. They finally got his pulse back, and after that, he was transferred to the main hospital ICU. They didn’t admit him at the ER, which was why I couldn’t find his name.
On Sunday, I was checking my patients’ charts for the ICU that coming week. And there he was. I saw his name and the documentation by the ED that CPR was provided by a critical care doctor in the field. He was still alive. That gave me so much joy.
So, the man I had helped became my patient. When I saw him on Monday, he was intubated and needed dialysis. I finally saw his face and thought, Oh, so that’s what you look like. I hadn’t realized he was only 39 years old.
When he was awake, I explained to him I was the doctor that provided CPR at the bar. He was very grateful, but of course, he didn’t remember anything.
Eventually, I met his daughter, and she just said, “Thank you for allowing me to have my dad.”
The funny part is that he broke his leg. Well, that’s not funny, but no one had any idea how it happened. That was his only complaint. He was asking me, “Doctor, how did you break my leg?”
“Hey, I have no idea how you broke your leg,” I replied. “I was trying to save your life.”
He was in the hospital for almost a month but made a full recovery. The amazing part: After all the evaluations, he has no neurological deficits. He’s back to a normal life now.
They never found a cause for the cardiac arrest. I mean, he had an ejection fraction of 10%. All my money was on something drug related, but that wasn’t the case. They’d done a cardiac cut, and there was no obstruction. They couldn’t find a reason.
We’ve become friends. He still works as a DJ at the bar. He changed his name to “DJ the Survivor” or something like that.
Sometimes, he’ll text me: “Doctor, what are you doing? You want to come down to the bar?”
I’m like, “No. I don’t.”
It’s been more than a year, but I remember every detail. When you go into medicine, you dream that one day you’ll be able to say, “I saved somebody.”
He texted me a year later and told me he’s celebrating two birthdays now. He said, “I’m turning 1 year old today!”
I think about the value of life. How we can take it for granted. We think, I’m young, nothing is going to happen to me. But this guy was 39. He went to work and died that night.
I was able to help bring him back. That makes me thankful for every day.
Jose Valle Giler, MD, is a pulmonary, critical care, and sleep medicine physician at NCH Healthcare System in Naples, Florida.
A version of this article appeared on Medscape.com .
Emergencies happen anywhere, anytime, and sometimes, medical professionals find themselves in situations where they are the only ones who can help. Is There a Doctor in the House? is a series by this news organization that tells these stories.
It was my first night off after 12 days. It was a Friday night, and I went to a bar in Naples to get a beer with some friends. As it turned out, it wasn’t a night off after all.
As soon as we got inside, we heard over the speaker that they needed medical personnel and to please go to the left side of the bar. I thought it would be syncope or something like that.
I went over there and saw a woman holding up a man. He was basically leaning all over her. The light was low, and the music was pounding. I started to assess him and tried to get him to answer me. No response. I checked for pulses — nothing.
The woman helped me lower him to the floor. I checked again for a pulse. Still nothing. I said, “Call 911,” and started compressions.
The difficult part was the place was completely dark. I knew where his body was on the floor. I could see his chest. But I couldn’t see his face at all.
It was also extremely loud with the music thumping. After a while, they finally shut it off.
Pretty soon, the security personnel from the bar brought me an automated external defibrillator, and it showed the man was having V-fib arrest. I shocked him. Still no pulse. I continued with cardiopulmonary resuscitation (CPR).
I hadn’t noticed, but lots of people were crowding around us. Somebody came up and said, “He’s my friend. He has a 9-year-old daughter. He can’t die. Let me help with the compressions.” I was like, “Go for it.”
The guy started kind of pushing on the man’s abdomen. He had no idea how to do compressions. I said, “Okay, let me take over again.”
Out of the crowd, nobody else volunteered to help. No one asked me, “Hey, what can I do?” Meanwhile, I found out later that someone was filming the whole thing on their phone.
But what the guy said about the man’s young daughter stayed in my brain. I thought, we need to keep going.
I did more compressions and shocked him again. Still no pulse. At that point, the police and emergency medical services showed up. They checked, nothing had changed, so they got him into the ambulance.
I asked one of the paramedics, “Where are you taking him? I can call ahead.”
But he said, “That’s HIPAA. We can’t tell you.” They also wouldn’t let me go with him in the ambulance.
“I have an active Florida license, and I work in the ICU [intensive care unit],” I said.
“No, we need to follow our protocol,” he replied.
I understood that, but I just wanted to help.
It was around 10:30 PM by then, and I was drenched in sweat. I had to go home. The first thing I did after taking a shower was open the computer and check my system. I needed to find out what happened to the guy.
I was looking for admissions, and I didn’t see him. I called the main hospital downtown and the one in North Naples. I couldn’t find him anywhere. I stayed up until almost 1:00 AM checking for his name. At that point I thought, okay, maybe he died.
The next night, Saturday, I was home and got a call from one of my colleagues. “Hey, were you in a bar yesterday? Did you do CPR on somebody?”
“How did you know?” I said.
He said the paramedics had described me — “a tall doctor with glasses who was a nice guy.” It was funny that he knew that was me.
He told me, “The guy’s alive. He’s sick and needs to be put on dialysis, but he’s alive.”
Apparently, the guy had gone to the emergency department at North Naples, and the doctors in the emergency room (ER) worked on him for over an hour. They did continuous CPR and shocked him for close to 40 minutes. They finally got his pulse back, and after that, he was transferred to the main hospital ICU. They didn’t admit him at the ER, which was why I couldn’t find his name.
On Sunday, I was checking my patients’ charts for the ICU that coming week. And there he was. I saw his name and the documentation by the ED that CPR was provided by a critical care doctor in the field. He was still alive. That gave me so much joy.
So, the man I had helped became my patient. When I saw him on Monday, he was intubated and needed dialysis. I finally saw his face and thought, Oh, so that’s what you look like. I hadn’t realized he was only 39 years old.
When he was awake, I explained to him I was the doctor that provided CPR at the bar. He was very grateful, but of course, he didn’t remember anything.
Eventually, I met his daughter, and she just said, “Thank you for allowing me to have my dad.”
The funny part is that he broke his leg. Well, that’s not funny, but no one had any idea how it happened. That was his only complaint. He was asking me, “Doctor, how did you break my leg?”
“Hey, I have no idea how you broke your leg,” I replied. “I was trying to save your life.”
He was in the hospital for almost a month but made a full recovery. The amazing part: After all the evaluations, he has no neurological deficits. He’s back to a normal life now.
They never found a cause for the cardiac arrest. I mean, he had an ejection fraction of 10%. All my money was on something drug related, but that wasn’t the case. They’d done a cardiac cut, and there was no obstruction. They couldn’t find a reason.
We’ve become friends. He still works as a DJ at the bar. He changed his name to “DJ the Survivor” or something like that.
Sometimes, he’ll text me: “Doctor, what are you doing? You want to come down to the bar?”
I’m like, “No. I don’t.”
It’s been more than a year, but I remember every detail. When you go into medicine, you dream that one day you’ll be able to say, “I saved somebody.”
He texted me a year later and told me he’s celebrating two birthdays now. He said, “I’m turning 1 year old today!”
I think about the value of life. How we can take it for granted. We think, I’m young, nothing is going to happen to me. But this guy was 39. He went to work and died that night.
I was able to help bring him back. That makes me thankful for every day.
Jose Valle Giler, MD, is a pulmonary, critical care, and sleep medicine physician at NCH Healthcare System in Naples, Florida.
A version of this article appeared on Medscape.com .
Complexity of hemodynamic assessment in patients with cirrhosis and septic shock
Critical Care Network
Nonrespiratory Critical Care Section
In patients with decompensated cirrhosis, there are multiple intrahepatic and extrahepatic factors contributing to hemodynamic alterations at baseline, including endothelial cell dysfunction, hepatic stellate cell activation promoting increase in vasoconstrictors, decrease in vasodilators, and angiogenesis leading to worsening of portal hypertension. Increased resistance to hepatic blood flow leads to increased production of nitric oxide and other vasodilators leading to splanchnic vasodilation, decreased effective blood volume, activation of the renin angiotensin system, sodium, and water retention. In addition to portal hypertension and splanchnic vasodilation, there is a decrease in systemic vascular resistance and hyperdynamic circulation with increased cardiac output. As cirrhosis progresses to the decompensated stage, patients may develop cirrhotic cardiomyopathy, characterized by impaired cardiac response to stress, manifesting as systolic and diastolic dysfunction, and electrophysiological abnormalities such as QT prolongation leading to hypotension and dysregulated response to fluid resuscitation.
Elevated lactate levels in acutely ill patients are an independent risk factor for mortality in patients with cirrhosis. However, lactate levels >2mmol/L need not necessarily define sepsis in these patients, as these patients have decreased lactate clearance. Understanding the intricate interplay between the cardiac pump, vascular tone, and afterload is essential in managing shock in these individuals. Aggressive volume resuscitation may not be well tolerated, emphasizing the need for frequent hemodynamic assessments and prompt initiation of vasopressors when indicated.
Critical Care Network
Nonrespiratory Critical Care Section
In patients with decompensated cirrhosis, there are multiple intrahepatic and extrahepatic factors contributing to hemodynamic alterations at baseline, including endothelial cell dysfunction, hepatic stellate cell activation promoting increase in vasoconstrictors, decrease in vasodilators, and angiogenesis leading to worsening of portal hypertension. Increased resistance to hepatic blood flow leads to increased production of nitric oxide and other vasodilators leading to splanchnic vasodilation, decreased effective blood volume, activation of the renin angiotensin system, sodium, and water retention. In addition to portal hypertension and splanchnic vasodilation, there is a decrease in systemic vascular resistance and hyperdynamic circulation with increased cardiac output. As cirrhosis progresses to the decompensated stage, patients may develop cirrhotic cardiomyopathy, characterized by impaired cardiac response to stress, manifesting as systolic and diastolic dysfunction, and electrophysiological abnormalities such as QT prolongation leading to hypotension and dysregulated response to fluid resuscitation.
Elevated lactate levels in acutely ill patients are an independent risk factor for mortality in patients with cirrhosis. However, lactate levels >2mmol/L need not necessarily define sepsis in these patients, as these patients have decreased lactate clearance. Understanding the intricate interplay between the cardiac pump, vascular tone, and afterload is essential in managing shock in these individuals. Aggressive volume resuscitation may not be well tolerated, emphasizing the need for frequent hemodynamic assessments and prompt initiation of vasopressors when indicated.
Critical Care Network
Nonrespiratory Critical Care Section
In patients with decompensated cirrhosis, there are multiple intrahepatic and extrahepatic factors contributing to hemodynamic alterations at baseline, including endothelial cell dysfunction, hepatic stellate cell activation promoting increase in vasoconstrictors, decrease in vasodilators, and angiogenesis leading to worsening of portal hypertension. Increased resistance to hepatic blood flow leads to increased production of nitric oxide and other vasodilators leading to splanchnic vasodilation, decreased effective blood volume, activation of the renin angiotensin system, sodium, and water retention. In addition to portal hypertension and splanchnic vasodilation, there is a decrease in systemic vascular resistance and hyperdynamic circulation with increased cardiac output. As cirrhosis progresses to the decompensated stage, patients may develop cirrhotic cardiomyopathy, characterized by impaired cardiac response to stress, manifesting as systolic and diastolic dysfunction, and electrophysiological abnormalities such as QT prolongation leading to hypotension and dysregulated response to fluid resuscitation.
Elevated lactate levels in acutely ill patients are an independent risk factor for mortality in patients with cirrhosis. However, lactate levels >2mmol/L need not necessarily define sepsis in these patients, as these patients have decreased lactate clearance. Understanding the intricate interplay between the cardiac pump, vascular tone, and afterload is essential in managing shock in these individuals. Aggressive volume resuscitation may not be well tolerated, emphasizing the need for frequent hemodynamic assessments and prompt initiation of vasopressors when indicated.
Empowering ICU physicians in MCS critical care
Pulmonary Vascular and Cardiovascular Network
Cardiovascular Medicine and Surgery Section
Intensive care physicians around the nation are pivotal in improving shock-related patient outcomes. Most intensive care units (academic and nonacademic) are currently managed by intensive care physicians, and a large majority of these physicians are either pulmonary/critical care, emergency medicine critical care, surgery critical care, or medicine/critical care.
There is lack of systematic training in cardiogenic shock across the board in these specialties as it relates to management of patients supported on extracorporeal membrane oxygenation (ECMO), left ventricular assist devices (LVADs), percutaneous devices, and intermediate devices such as centrimag devices.
By integrating comprehensive systematic training on cardiogenic shock recognition and management into educational initiatives, fellowship programs that are noncardiology-based can empower health care providers to make informed decisions and expedite life-saving interventions for patients in need of advanced cardiac support. Furthermore, the next generation of intensive care physicians may require ongoing education in the cardiac space, including additional training in point-of-care ultrasound, transesophageal echocardiography (TEE), and advanced hemodynamics, including management of alarms related to percutaneous and durable devices. Through continuous education and training both at conferences and at the simulation center in Glenview, Illinois, CHEST is especially suited to aid intensive care physicians to navigate the evolving landscape of mechanical circulatory support critical care and improve outcomes for patients in need of mechanical circulatory support.
Pulmonary Vascular and Cardiovascular Network
Cardiovascular Medicine and Surgery Section
Intensive care physicians around the nation are pivotal in improving shock-related patient outcomes. Most intensive care units (academic and nonacademic) are currently managed by intensive care physicians, and a large majority of these physicians are either pulmonary/critical care, emergency medicine critical care, surgery critical care, or medicine/critical care.
There is lack of systematic training in cardiogenic shock across the board in these specialties as it relates to management of patients supported on extracorporeal membrane oxygenation (ECMO), left ventricular assist devices (LVADs), percutaneous devices, and intermediate devices such as centrimag devices.
By integrating comprehensive systematic training on cardiogenic shock recognition and management into educational initiatives, fellowship programs that are noncardiology-based can empower health care providers to make informed decisions and expedite life-saving interventions for patients in need of advanced cardiac support. Furthermore, the next generation of intensive care physicians may require ongoing education in the cardiac space, including additional training in point-of-care ultrasound, transesophageal echocardiography (TEE), and advanced hemodynamics, including management of alarms related to percutaneous and durable devices. Through continuous education and training both at conferences and at the simulation center in Glenview, Illinois, CHEST is especially suited to aid intensive care physicians to navigate the evolving landscape of mechanical circulatory support critical care and improve outcomes for patients in need of mechanical circulatory support.
Pulmonary Vascular and Cardiovascular Network
Cardiovascular Medicine and Surgery Section
Intensive care physicians around the nation are pivotal in improving shock-related patient outcomes. Most intensive care units (academic and nonacademic) are currently managed by intensive care physicians, and a large majority of these physicians are either pulmonary/critical care, emergency medicine critical care, surgery critical care, or medicine/critical care.
There is lack of systematic training in cardiogenic shock across the board in these specialties as it relates to management of patients supported on extracorporeal membrane oxygenation (ECMO), left ventricular assist devices (LVADs), percutaneous devices, and intermediate devices such as centrimag devices.
By integrating comprehensive systematic training on cardiogenic shock recognition and management into educational initiatives, fellowship programs that are noncardiology-based can empower health care providers to make informed decisions and expedite life-saving interventions for patients in need of advanced cardiac support. Furthermore, the next generation of intensive care physicians may require ongoing education in the cardiac space, including additional training in point-of-care ultrasound, transesophageal echocardiography (TEE), and advanced hemodynamics, including management of alarms related to percutaneous and durable devices. Through continuous education and training both at conferences and at the simulation center in Glenview, Illinois, CHEST is especially suited to aid intensive care physicians to navigate the evolving landscape of mechanical circulatory support critical care and improve outcomes for patients in need of mechanical circulatory support.
A Prescription Checklist for Older Adults in ED
TOPLINE:
The geriatric emergency medication safety recommendations (GEMS-Rx) is the first expert consensus-based list identifying high-risk medication classes that should not be prescribed to older patients visiting the emergency department (ED).
METHODOLOGY:
- The American Geriatrics Society (AGS) has already established guidelines to identify potentially inappropriate medications in older adults; however, the criteria are centered on chronic conditions and long-term medication use and are unsuitable for managing ED prescriptions.
- In this study, the GEMS-Rx high-risk prescription list was prepared with a panel of 10 ED physicians with expertise in geriatrics and quality measurement and a pharmacist with expertise in geriatric pharmacotherapy and emergency medicine.
- They reviewed over 30 medication classes from the 2019 AGS Beers Criteria that were deemed inappropriate for use in older patients. Despite their not being included in the Beers list, the use of short- and long-acting opioids was also discussed.
- After three rounds of review and discussion, the panelists ranked each class of medication on a 5-point Likert scale, with a score of 1 indicating the lowest and 5 indicating the greatest need for avoiding a drug in an ED prescription.
TAKEAWAY:
- The first round suggested that first-generation antihistamines, metoclopramide, short-acting opioids, antipsychotics, barbiturates, skeletal muscle relaxants, and benzodiazepines should be avoided, with mean Likert scores ranging from 3.7 to 4.6.
- Although nonbenzodiazepine and benzodiazepine receptor agonist hypnotics (“Z-drugs”) were not initially considered owing to their low frequency of prescription in ED settings, the panelists finally included “Z” drugs and sulfonylureas in the GEMS-Rx list after the second and third rounds.
- The final list of high-risk medications to be avoided in ED settings that were prioritized included benzodiazepines, skeletal muscle relaxants, barbiturates, first-generation antipsychotics, first-generation antihistamines, “Z” drugs, metoclopramide, and sulfonylureas.
- However, seizure disorders, benzodiazepine withdrawal, ethanol withdrawal, severe generalized anxiety disorder, end-of-life care, allergic reactions, and ED visits for prescription refilling were deemed exceptional cases in which these high-risk medications could be prescribed.
IN PRACTICE:
“By combining expert consensus and evidence-based criteria, this list can serve as a resource to guide prescribing decisions and mitigate potential risks associated with medications at this crucial care transition. The incorporation of this emergency medicine-specific geriatric prescription list in a national quality measure has the potential to improve patient safety and enhance the quality of care for the millions of older adults who seek care in EDs each year,” the authors said.
SOURCE:
This study was led by Rachel M. Skains, MD, MSPH, Department of Emergency Medicine, University of Alabama at Birmingham, and published online in Annals of Emergency Medicine.
LIMITATIONS:
The GEMS-Rx list was prepared by physicians and pharmacists and may not have fully captured data regarding individual patient preferences, comorbidities, or other contextual factors. During the meetings, the panelists’ identities were not concealed from one another, which may have affected the conversations owing to response and social desirability bias. Furthermore, this list may not be generalizable to other settings because it was produced and intended for usage in US EDs.
DISCLOSURES:
This work was supported by the American College of Emergency Physicians. Some of the authors, including the lead author, declared being supported by various funding agencies. Few authors also declared serving in leadership positions for several sources.
A version of this article appeared on Medscape.com.
TOPLINE:
The geriatric emergency medication safety recommendations (GEMS-Rx) is the first expert consensus-based list identifying high-risk medication classes that should not be prescribed to older patients visiting the emergency department (ED).
METHODOLOGY:
- The American Geriatrics Society (AGS) has already established guidelines to identify potentially inappropriate medications in older adults; however, the criteria are centered on chronic conditions and long-term medication use and are unsuitable for managing ED prescriptions.
- In this study, the GEMS-Rx high-risk prescription list was prepared with a panel of 10 ED physicians with expertise in geriatrics and quality measurement and a pharmacist with expertise in geriatric pharmacotherapy and emergency medicine.
- They reviewed over 30 medication classes from the 2019 AGS Beers Criteria that were deemed inappropriate for use in older patients. Despite their not being included in the Beers list, the use of short- and long-acting opioids was also discussed.
- After three rounds of review and discussion, the panelists ranked each class of medication on a 5-point Likert scale, with a score of 1 indicating the lowest and 5 indicating the greatest need for avoiding a drug in an ED prescription.
TAKEAWAY:
- The first round suggested that first-generation antihistamines, metoclopramide, short-acting opioids, antipsychotics, barbiturates, skeletal muscle relaxants, and benzodiazepines should be avoided, with mean Likert scores ranging from 3.7 to 4.6.
- Although nonbenzodiazepine and benzodiazepine receptor agonist hypnotics (“Z-drugs”) were not initially considered owing to their low frequency of prescription in ED settings, the panelists finally included “Z” drugs and sulfonylureas in the GEMS-Rx list after the second and third rounds.
- The final list of high-risk medications to be avoided in ED settings that were prioritized included benzodiazepines, skeletal muscle relaxants, barbiturates, first-generation antipsychotics, first-generation antihistamines, “Z” drugs, metoclopramide, and sulfonylureas.
- However, seizure disorders, benzodiazepine withdrawal, ethanol withdrawal, severe generalized anxiety disorder, end-of-life care, allergic reactions, and ED visits for prescription refilling were deemed exceptional cases in which these high-risk medications could be prescribed.
IN PRACTICE:
“By combining expert consensus and evidence-based criteria, this list can serve as a resource to guide prescribing decisions and mitigate potential risks associated with medications at this crucial care transition. The incorporation of this emergency medicine-specific geriatric prescription list in a national quality measure has the potential to improve patient safety and enhance the quality of care for the millions of older adults who seek care in EDs each year,” the authors said.
SOURCE:
This study was led by Rachel M. Skains, MD, MSPH, Department of Emergency Medicine, University of Alabama at Birmingham, and published online in Annals of Emergency Medicine.
LIMITATIONS:
The GEMS-Rx list was prepared by physicians and pharmacists and may not have fully captured data regarding individual patient preferences, comorbidities, or other contextual factors. During the meetings, the panelists’ identities were not concealed from one another, which may have affected the conversations owing to response and social desirability bias. Furthermore, this list may not be generalizable to other settings because it was produced and intended for usage in US EDs.
DISCLOSURES:
This work was supported by the American College of Emergency Physicians. Some of the authors, including the lead author, declared being supported by various funding agencies. Few authors also declared serving in leadership positions for several sources.
A version of this article appeared on Medscape.com.
TOPLINE:
The geriatric emergency medication safety recommendations (GEMS-Rx) is the first expert consensus-based list identifying high-risk medication classes that should not be prescribed to older patients visiting the emergency department (ED).
METHODOLOGY:
- The American Geriatrics Society (AGS) has already established guidelines to identify potentially inappropriate medications in older adults; however, the criteria are centered on chronic conditions and long-term medication use and are unsuitable for managing ED prescriptions.
- In this study, the GEMS-Rx high-risk prescription list was prepared with a panel of 10 ED physicians with expertise in geriatrics and quality measurement and a pharmacist with expertise in geriatric pharmacotherapy and emergency medicine.
- They reviewed over 30 medication classes from the 2019 AGS Beers Criteria that were deemed inappropriate for use in older patients. Despite their not being included in the Beers list, the use of short- and long-acting opioids was also discussed.
- After three rounds of review and discussion, the panelists ranked each class of medication on a 5-point Likert scale, with a score of 1 indicating the lowest and 5 indicating the greatest need for avoiding a drug in an ED prescription.
TAKEAWAY:
- The first round suggested that first-generation antihistamines, metoclopramide, short-acting opioids, antipsychotics, barbiturates, skeletal muscle relaxants, and benzodiazepines should be avoided, with mean Likert scores ranging from 3.7 to 4.6.
- Although nonbenzodiazepine and benzodiazepine receptor agonist hypnotics (“Z-drugs”) were not initially considered owing to their low frequency of prescription in ED settings, the panelists finally included “Z” drugs and sulfonylureas in the GEMS-Rx list after the second and third rounds.
- The final list of high-risk medications to be avoided in ED settings that were prioritized included benzodiazepines, skeletal muscle relaxants, barbiturates, first-generation antipsychotics, first-generation antihistamines, “Z” drugs, metoclopramide, and sulfonylureas.
- However, seizure disorders, benzodiazepine withdrawal, ethanol withdrawal, severe generalized anxiety disorder, end-of-life care, allergic reactions, and ED visits for prescription refilling were deemed exceptional cases in which these high-risk medications could be prescribed.
IN PRACTICE:
“By combining expert consensus and evidence-based criteria, this list can serve as a resource to guide prescribing decisions and mitigate potential risks associated with medications at this crucial care transition. The incorporation of this emergency medicine-specific geriatric prescription list in a national quality measure has the potential to improve patient safety and enhance the quality of care for the millions of older adults who seek care in EDs each year,” the authors said.
SOURCE:
This study was led by Rachel M. Skains, MD, MSPH, Department of Emergency Medicine, University of Alabama at Birmingham, and published online in Annals of Emergency Medicine.
LIMITATIONS:
The GEMS-Rx list was prepared by physicians and pharmacists and may not have fully captured data regarding individual patient preferences, comorbidities, or other contextual factors. During the meetings, the panelists’ identities were not concealed from one another, which may have affected the conversations owing to response and social desirability bias. Furthermore, this list may not be generalizable to other settings because it was produced and intended for usage in US EDs.
DISCLOSURES:
This work was supported by the American College of Emergency Physicians. Some of the authors, including the lead author, declared being supported by various funding agencies. Few authors also declared serving in leadership positions for several sources.
A version of this article appeared on Medscape.com.
Compassionate extubation and beyond: Is there a need for more guidance in managing end-of-life in the intensive care unit?
Critical Care Network
Palliative and End-of-Life Care Section
For providers caring for critically ill patients, navigating death and dying in the intensive care unit (ICU) with proficiency and empathy is essential. Approximately 20% of deaths in the United States occur during or shortly after a stay in the ICU and approximately 40% of ICU deaths involve withdrawal of artificial life support (WOALS) or compassionate extubation.
This is a complex process that may involve advanced communication with family, expertise in mechanical ventilation, vasopressors, dialysis, and complex symptom management. Importantly, surrogate medical decision-making for a critically ill patient can be a challenging experience associated with anxiety and depression. How the team approaches WOALS can make a difference to both patients and decision-makers. Unfortunately, there is striking variation in practice and lack of guidance in navigating issues that arise at end-of-life in the ICU. One study of 2,814 hospitals in the US with ICU beds found that 52% had intensivists while 48% did not.2 This highlights the importance of developing resources focusing on end-of-life care in the ICU setting regardless of the providers’ educational training.
Important elements could include the role for protocol-based WOALS, use of oxygen, selection and dosing strategy of comfort-focused medications, establishing expectations, and addressing uncertainties. This would be meaningful in providing effective, ethical end-of-life care based on evidence-based strategies. While death may be unavoidable, a thoughtful approach can allow providers to bring dignity to the dying process and lessen the burden of an already difficult experience for patients and families alike.
References
1. Curtis JR, et al. Am J Respir Crit Care Med. 2012;186[7]:587-592.
2. Halpern NA, et al. Crit Care Med. 2019;47[4]:517-525.
Critical Care Network
Palliative and End-of-Life Care Section
For providers caring for critically ill patients, navigating death and dying in the intensive care unit (ICU) with proficiency and empathy is essential. Approximately 20% of deaths in the United States occur during or shortly after a stay in the ICU and approximately 40% of ICU deaths involve withdrawal of artificial life support (WOALS) or compassionate extubation.
This is a complex process that may involve advanced communication with family, expertise in mechanical ventilation, vasopressors, dialysis, and complex symptom management. Importantly, surrogate medical decision-making for a critically ill patient can be a challenging experience associated with anxiety and depression. How the team approaches WOALS can make a difference to both patients and decision-makers. Unfortunately, there is striking variation in practice and lack of guidance in navigating issues that arise at end-of-life in the ICU. One study of 2,814 hospitals in the US with ICU beds found that 52% had intensivists while 48% did not.2 This highlights the importance of developing resources focusing on end-of-life care in the ICU setting regardless of the providers’ educational training.
Important elements could include the role for protocol-based WOALS, use of oxygen, selection and dosing strategy of comfort-focused medications, establishing expectations, and addressing uncertainties. This would be meaningful in providing effective, ethical end-of-life care based on evidence-based strategies. While death may be unavoidable, a thoughtful approach can allow providers to bring dignity to the dying process and lessen the burden of an already difficult experience for patients and families alike.
References
1. Curtis JR, et al. Am J Respir Crit Care Med. 2012;186[7]:587-592.
2. Halpern NA, et al. Crit Care Med. 2019;47[4]:517-525.
Critical Care Network
Palliative and End-of-Life Care Section
For providers caring for critically ill patients, navigating death and dying in the intensive care unit (ICU) with proficiency and empathy is essential. Approximately 20% of deaths in the United States occur during or shortly after a stay in the ICU and approximately 40% of ICU deaths involve withdrawal of artificial life support (WOALS) or compassionate extubation.
This is a complex process that may involve advanced communication with family, expertise in mechanical ventilation, vasopressors, dialysis, and complex symptom management. Importantly, surrogate medical decision-making for a critically ill patient can be a challenging experience associated with anxiety and depression. How the team approaches WOALS can make a difference to both patients and decision-makers. Unfortunately, there is striking variation in practice and lack of guidance in navigating issues that arise at end-of-life in the ICU. One study of 2,814 hospitals in the US with ICU beds found that 52% had intensivists while 48% did not.2 This highlights the importance of developing resources focusing on end-of-life care in the ICU setting regardless of the providers’ educational training.
Important elements could include the role for protocol-based WOALS, use of oxygen, selection and dosing strategy of comfort-focused medications, establishing expectations, and addressing uncertainties. This would be meaningful in providing effective, ethical end-of-life care based on evidence-based strategies. While death may be unavoidable, a thoughtful approach can allow providers to bring dignity to the dying process and lessen the burden of an already difficult experience for patients and families alike.
References
1. Curtis JR, et al. Am J Respir Crit Care Med. 2012;186[7]:587-592.
2. Halpern NA, et al. Crit Care Med. 2019;47[4]:517-525.
Implementing a critical care TEE program at your institution
Starting from the ground up!
Bedside-focused cardiac ultrasound assessment, or cardiac point-of-care ultrasound (POCUS), has become common in intensive care units throughout the US and the world.
However, obtaining images adequate for decision making via standard transthoracic echo (TTE) is not possible in a significant number of patients; as high as 30% of critically ill patients, according to The American Society of Echocardiography (ASE) guidelines.1 Factors common to critically ill patients, such as invasive mechanical ventilation, external dressings, and limited mobility, contribute to poor image acquisition.
In almost all these cases, the factors limiting image acquisition can be eliminated by utilizing a transesophageal approach. In a recent study, researchers were able to demonstrate that adding transesophageal echocardiography (TEE) to TTE in critically ill patients yielded a new diagnosis or a change in management about 45% of the time.2
Using transesophageal ultrasound for a focused cardiac assessment in hemodynamically unstable patients is not new—and is often referred to as rescue TEE or resuscitative TEE. A broader term, transesophageal ultrasound, has also been used to include sonographic evaluation of the lungs in patients with poor acoustic windows. At my institution, we use the term critical care TEE to define TEE performed by a noncardiology-trained intensivist in an intubated critically ill patient.
Regardless of the term, the use of transesophageal ultrasound by the noncardiologist in the ICU appears to be a developing trend. As with other uses of POCUS, ultrasound machines continue to be able to “do more” at a lower price point. In 2024, several cart-based ultrasound machines are compatible with transesophageal probes and contain software packages capable of common cardiac measurements.
Despite this growing interest, intensivists are likely to encounter barriers to implementing critical care TEE. Our division recently implemented adding TEE to our practice. Our practice involves two separate systems: a Veterans Administration hospital and a university-based county hospital. Our division has integrated the use of TEE in the medical ICU at both institutions. Having navigated the process at both institutions, I can offer some guidance in navigating barriers.
The development of a critical care TEE program must start with a strong base in transthoracic cardiac POCUS, at least for the foreseeable future. Having a strong background in TTE gives learners a solid foundation in cardiac anatomy, cardiac function, and ultrasound properties. Obtaining testamur status or board certification in critical care echocardiography is not an absolute must but is a definite benefit. Having significant experience in TTE image acquisition and interpretation will flatten the learning curve for TEE. Interestingly, image acquisition in TEE is often easier than in TTE, so the paradigm of learning TTE before TEE may reverse in the years to come.
Two barriers often work together to create a vicious cycle that stops the development of a TEE program at its start. These barriers include the lack of training and lack of equipment, specifically a TEE probe. Those who do not understand the value of TEE may ask, “Why purchase equipment for a procedure that you do not yet know how to do?” The opposite question can also be asked, “Why get trained to do something you don’t have the equipment to perform?”
My best advice to break this cycle is to “dive in” to whichever barrier seems easier to overcome first. I started with obtaining knowledge and training. Obtaining training and education in a procedure that is historically not done in your specialty is challenging but is not impossible. It takes a combination of high levels of self-motivation and at least one colleague with the training to support you. I approached a cardiac anesthesiologist, whom I knew from the surgical ICU. Cardiologists can also be a resource, but working with cardiac anesthesiologists offers several advantages. TEEs done by cardiac anesthesiologists are similar to those done in ICU patients (ie, all patients are intubated and sedated). The procedures are also scheduled several days in advance, making it easier to integrate training into your daily work schedule. Lastly, the TEE probe remains in place for several hours, so repeating the probe manipulations again as a learner does not add additional risk to the patient. In my case, we somewhat arbitrarily agreed that I participate in 25 TEE exams. (CME courses, both online and in-person simulation, exist and greatly supplement self-study.)
Obtaining equipment is also a common barrier, though this has become less restrictive in the last several years. As previously mentioned, many cart-based ultrasound machines can accommodate a TEE probe. This changes the request from purchasing a new machine to “just a probe.” Despite the higher cost than most other probes, those in charge of purchasing are often more open to purchasing “a probe” than to purchasing an ultrasound machine.
Additionally, the purchasing decision regarding probes may fall to a different person than it does for an ultrasound machine. If available, POCUS image archiving into the medical record can help offset the cost of equipment, both by increasing revenue via billing and by demonstrating that equipment is being used. If initially declined, continue to ask and work to integrate the purchase into the next year’s budget. Inquire about the process of making a formal request and follow that process. This will often involve obtaining a quote or quotes from the ultrasound manufacturer(s).
Keep in mind that the probe will require a special storage cabinet specifically designed for TEE probes. It is prudent to include this in budget requests. If needed, the echocardiography lab can be a useful resource for additional information regarding the cabinet requirements. It is strongly recommended to discuss TEE probe models with sterile processing before any purchasing. If options are available, it is wise to choose a model the hospital already uses, as the cleaning protocol is well established. Our unit purchased a model that did not have an established protocol, which took nearly 6 months to develop. If probe options are limited, involving sterile processing early to start developing a protocol will help decrease delays.
Obtaining hospital privileges is also a common barrier, though this may not be as challenging as expected. Hospitals typically have well-outlined policies on obtaining privileges for established procedures. One of our hospital systems had four different options; the most straightforward required 20 hours of CME specific to TEE and 10 supervised cases by a proctor currently holding TEE privileges (see Table 1).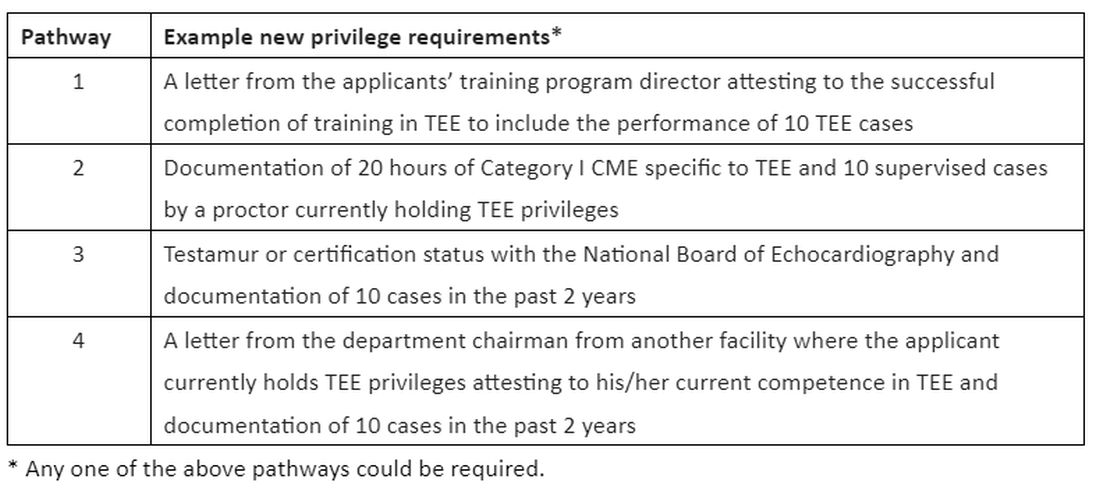
Discussions about obtaining privileges should involve your division chief, chair of medicine, and the cardiology division chief. Clearly outlining the plan to perform this procedure only in critically ill patients who are already intubated for other reasons made these conversations go much more smoothly. In the development of delineation of privileges, we used the term critical care TEE to clearly define this patient population. During these conversations, highlight the safety of the procedure; ASE guidelines3 estimate a severe complication rate of less than 1 in 10,000 cases and explain the anticipated benefits to critically ill patients.
In conclusion, at an institution that is already adept at the use of POCUS in the ICU, the additional of critical care TEE within 1 to 2 years is a very realistic achievement. It will undoubtedly require patience, persistence, and self-motivation, but the barriers are becoming smaller every day. Stay motivated!
Dr. Proud is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Pulmonary and Critical Care Medicine Program Director, UT Health San Antonio.
References:
1. Porter TR, Abdelmoneim S, Belcik FT, et al. Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography. J Am Soc Echocardiogr. 2024;27(8):797-810.
2. Si X, Ma J, Cao DY, et al. Transesophageal echocardiography instead or in addition to transthoracic echocardiography in evaluating haemodynamic problems in intubated critically ill patients. Ann Transl Med. 2020;8(12):785.
3. Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a cmprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardioraphy and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964.
Starting from the ground up!
Starting from the ground up!
Bedside-focused cardiac ultrasound assessment, or cardiac point-of-care ultrasound (POCUS), has become common in intensive care units throughout the US and the world.
However, obtaining images adequate for decision making via standard transthoracic echo (TTE) is not possible in a significant number of patients; as high as 30% of critically ill patients, according to The American Society of Echocardiography (ASE) guidelines.1 Factors common to critically ill patients, such as invasive mechanical ventilation, external dressings, and limited mobility, contribute to poor image acquisition.
In almost all these cases, the factors limiting image acquisition can be eliminated by utilizing a transesophageal approach. In a recent study, researchers were able to demonstrate that adding transesophageal echocardiography (TEE) to TTE in critically ill patients yielded a new diagnosis or a change in management about 45% of the time.2
Using transesophageal ultrasound for a focused cardiac assessment in hemodynamically unstable patients is not new—and is often referred to as rescue TEE or resuscitative TEE. A broader term, transesophageal ultrasound, has also been used to include sonographic evaluation of the lungs in patients with poor acoustic windows. At my institution, we use the term critical care TEE to define TEE performed by a noncardiology-trained intensivist in an intubated critically ill patient.
Regardless of the term, the use of transesophageal ultrasound by the noncardiologist in the ICU appears to be a developing trend. As with other uses of POCUS, ultrasound machines continue to be able to “do more” at a lower price point. In 2024, several cart-based ultrasound machines are compatible with transesophageal probes and contain software packages capable of common cardiac measurements.
Despite this growing interest, intensivists are likely to encounter barriers to implementing critical care TEE. Our division recently implemented adding TEE to our practice. Our practice involves two separate systems: a Veterans Administration hospital and a university-based county hospital. Our division has integrated the use of TEE in the medical ICU at both institutions. Having navigated the process at both institutions, I can offer some guidance in navigating barriers.
The development of a critical care TEE program must start with a strong base in transthoracic cardiac POCUS, at least for the foreseeable future. Having a strong background in TTE gives learners a solid foundation in cardiac anatomy, cardiac function, and ultrasound properties. Obtaining testamur status or board certification in critical care echocardiography is not an absolute must but is a definite benefit. Having significant experience in TTE image acquisition and interpretation will flatten the learning curve for TEE. Interestingly, image acquisition in TEE is often easier than in TTE, so the paradigm of learning TTE before TEE may reverse in the years to come.
Two barriers often work together to create a vicious cycle that stops the development of a TEE program at its start. These barriers include the lack of training and lack of equipment, specifically a TEE probe. Those who do not understand the value of TEE may ask, “Why purchase equipment for a procedure that you do not yet know how to do?” The opposite question can also be asked, “Why get trained to do something you don’t have the equipment to perform?”
My best advice to break this cycle is to “dive in” to whichever barrier seems easier to overcome first. I started with obtaining knowledge and training. Obtaining training and education in a procedure that is historically not done in your specialty is challenging but is not impossible. It takes a combination of high levels of self-motivation and at least one colleague with the training to support you. I approached a cardiac anesthesiologist, whom I knew from the surgical ICU. Cardiologists can also be a resource, but working with cardiac anesthesiologists offers several advantages. TEEs done by cardiac anesthesiologists are similar to those done in ICU patients (ie, all patients are intubated and sedated). The procedures are also scheduled several days in advance, making it easier to integrate training into your daily work schedule. Lastly, the TEE probe remains in place for several hours, so repeating the probe manipulations again as a learner does not add additional risk to the patient. In my case, we somewhat arbitrarily agreed that I participate in 25 TEE exams. (CME courses, both online and in-person simulation, exist and greatly supplement self-study.)
Obtaining equipment is also a common barrier, though this has become less restrictive in the last several years. As previously mentioned, many cart-based ultrasound machines can accommodate a TEE probe. This changes the request from purchasing a new machine to “just a probe.” Despite the higher cost than most other probes, those in charge of purchasing are often more open to purchasing “a probe” than to purchasing an ultrasound machine.
Additionally, the purchasing decision regarding probes may fall to a different person than it does for an ultrasound machine. If available, POCUS image archiving into the medical record can help offset the cost of equipment, both by increasing revenue via billing and by demonstrating that equipment is being used. If initially declined, continue to ask and work to integrate the purchase into the next year’s budget. Inquire about the process of making a formal request and follow that process. This will often involve obtaining a quote or quotes from the ultrasound manufacturer(s).
Keep in mind that the probe will require a special storage cabinet specifically designed for TEE probes. It is prudent to include this in budget requests. If needed, the echocardiography lab can be a useful resource for additional information regarding the cabinet requirements. It is strongly recommended to discuss TEE probe models with sterile processing before any purchasing. If options are available, it is wise to choose a model the hospital already uses, as the cleaning protocol is well established. Our unit purchased a model that did not have an established protocol, which took nearly 6 months to develop. If probe options are limited, involving sterile processing early to start developing a protocol will help decrease delays.
Obtaining hospital privileges is also a common barrier, though this may not be as challenging as expected. Hospitals typically have well-outlined policies on obtaining privileges for established procedures. One of our hospital systems had four different options; the most straightforward required 20 hours of CME specific to TEE and 10 supervised cases by a proctor currently holding TEE privileges (see Table 1).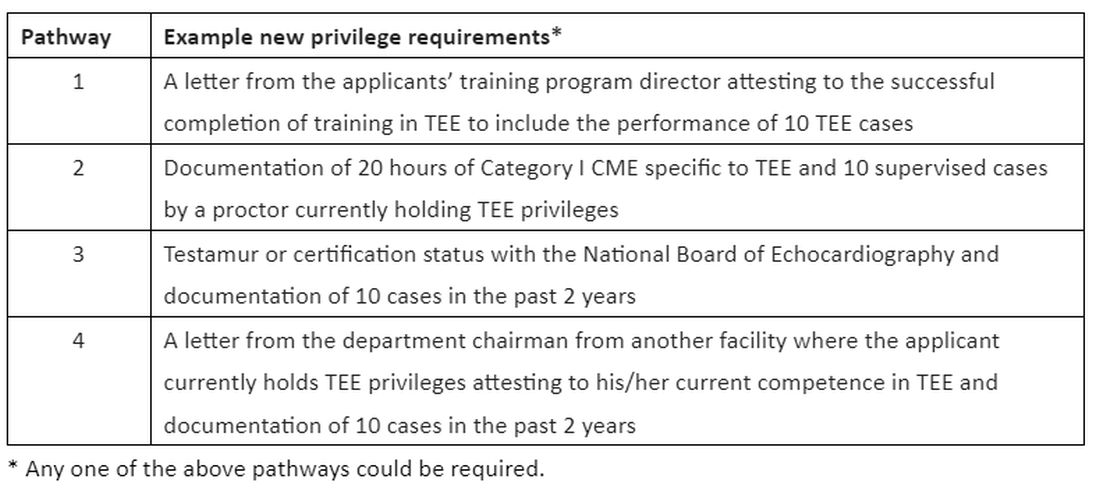
Discussions about obtaining privileges should involve your division chief, chair of medicine, and the cardiology division chief. Clearly outlining the plan to perform this procedure only in critically ill patients who are already intubated for other reasons made these conversations go much more smoothly. In the development of delineation of privileges, we used the term critical care TEE to clearly define this patient population. During these conversations, highlight the safety of the procedure; ASE guidelines3 estimate a severe complication rate of less than 1 in 10,000 cases and explain the anticipated benefits to critically ill patients.
In conclusion, at an institution that is already adept at the use of POCUS in the ICU, the additional of critical care TEE within 1 to 2 years is a very realistic achievement. It will undoubtedly require patience, persistence, and self-motivation, but the barriers are becoming smaller every day. Stay motivated!
Dr. Proud is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Pulmonary and Critical Care Medicine Program Director, UT Health San Antonio.
References:
1. Porter TR, Abdelmoneim S, Belcik FT, et al. Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography. J Am Soc Echocardiogr. 2024;27(8):797-810.
2. Si X, Ma J, Cao DY, et al. Transesophageal echocardiography instead or in addition to transthoracic echocardiography in evaluating haemodynamic problems in intubated critically ill patients. Ann Transl Med. 2020;8(12):785.
3. Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a cmprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardioraphy and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964.
Bedside-focused cardiac ultrasound assessment, or cardiac point-of-care ultrasound (POCUS), has become common in intensive care units throughout the US and the world.
However, obtaining images adequate for decision making via standard transthoracic echo (TTE) is not possible in a significant number of patients; as high as 30% of critically ill patients, according to The American Society of Echocardiography (ASE) guidelines.1 Factors common to critically ill patients, such as invasive mechanical ventilation, external dressings, and limited mobility, contribute to poor image acquisition.
In almost all these cases, the factors limiting image acquisition can be eliminated by utilizing a transesophageal approach. In a recent study, researchers were able to demonstrate that adding transesophageal echocardiography (TEE) to TTE in critically ill patients yielded a new diagnosis or a change in management about 45% of the time.2
Using transesophageal ultrasound for a focused cardiac assessment in hemodynamically unstable patients is not new—and is often referred to as rescue TEE or resuscitative TEE. A broader term, transesophageal ultrasound, has also been used to include sonographic evaluation of the lungs in patients with poor acoustic windows. At my institution, we use the term critical care TEE to define TEE performed by a noncardiology-trained intensivist in an intubated critically ill patient.
Regardless of the term, the use of transesophageal ultrasound by the noncardiologist in the ICU appears to be a developing trend. As with other uses of POCUS, ultrasound machines continue to be able to “do more” at a lower price point. In 2024, several cart-based ultrasound machines are compatible with transesophageal probes and contain software packages capable of common cardiac measurements.
Despite this growing interest, intensivists are likely to encounter barriers to implementing critical care TEE. Our division recently implemented adding TEE to our practice. Our practice involves two separate systems: a Veterans Administration hospital and a university-based county hospital. Our division has integrated the use of TEE in the medical ICU at both institutions. Having navigated the process at both institutions, I can offer some guidance in navigating barriers.
The development of a critical care TEE program must start with a strong base in transthoracic cardiac POCUS, at least for the foreseeable future. Having a strong background in TTE gives learners a solid foundation in cardiac anatomy, cardiac function, and ultrasound properties. Obtaining testamur status or board certification in critical care echocardiography is not an absolute must but is a definite benefit. Having significant experience in TTE image acquisition and interpretation will flatten the learning curve for TEE. Interestingly, image acquisition in TEE is often easier than in TTE, so the paradigm of learning TTE before TEE may reverse in the years to come.
Two barriers often work together to create a vicious cycle that stops the development of a TEE program at its start. These barriers include the lack of training and lack of equipment, specifically a TEE probe. Those who do not understand the value of TEE may ask, “Why purchase equipment for a procedure that you do not yet know how to do?” The opposite question can also be asked, “Why get trained to do something you don’t have the equipment to perform?”
My best advice to break this cycle is to “dive in” to whichever barrier seems easier to overcome first. I started with obtaining knowledge and training. Obtaining training and education in a procedure that is historically not done in your specialty is challenging but is not impossible. It takes a combination of high levels of self-motivation and at least one colleague with the training to support you. I approached a cardiac anesthesiologist, whom I knew from the surgical ICU. Cardiologists can also be a resource, but working with cardiac anesthesiologists offers several advantages. TEEs done by cardiac anesthesiologists are similar to those done in ICU patients (ie, all patients are intubated and sedated). The procedures are also scheduled several days in advance, making it easier to integrate training into your daily work schedule. Lastly, the TEE probe remains in place for several hours, so repeating the probe manipulations again as a learner does not add additional risk to the patient. In my case, we somewhat arbitrarily agreed that I participate in 25 TEE exams. (CME courses, both online and in-person simulation, exist and greatly supplement self-study.)
Obtaining equipment is also a common barrier, though this has become less restrictive in the last several years. As previously mentioned, many cart-based ultrasound machines can accommodate a TEE probe. This changes the request from purchasing a new machine to “just a probe.” Despite the higher cost than most other probes, those in charge of purchasing are often more open to purchasing “a probe” than to purchasing an ultrasound machine.
Additionally, the purchasing decision regarding probes may fall to a different person than it does for an ultrasound machine. If available, POCUS image archiving into the medical record can help offset the cost of equipment, both by increasing revenue via billing and by demonstrating that equipment is being used. If initially declined, continue to ask and work to integrate the purchase into the next year’s budget. Inquire about the process of making a formal request and follow that process. This will often involve obtaining a quote or quotes from the ultrasound manufacturer(s).
Keep in mind that the probe will require a special storage cabinet specifically designed for TEE probes. It is prudent to include this in budget requests. If needed, the echocardiography lab can be a useful resource for additional information regarding the cabinet requirements. It is strongly recommended to discuss TEE probe models with sterile processing before any purchasing. If options are available, it is wise to choose a model the hospital already uses, as the cleaning protocol is well established. Our unit purchased a model that did not have an established protocol, which took nearly 6 months to develop. If probe options are limited, involving sterile processing early to start developing a protocol will help decrease delays.
Obtaining hospital privileges is also a common barrier, though this may not be as challenging as expected. Hospitals typically have well-outlined policies on obtaining privileges for established procedures. One of our hospital systems had four different options; the most straightforward required 20 hours of CME specific to TEE and 10 supervised cases by a proctor currently holding TEE privileges (see Table 1).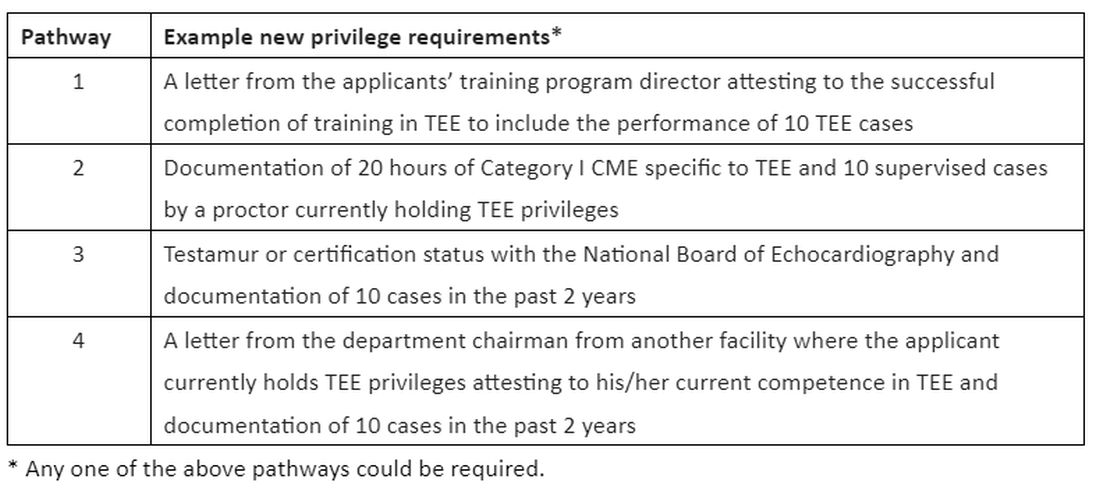
Discussions about obtaining privileges should involve your division chief, chair of medicine, and the cardiology division chief. Clearly outlining the plan to perform this procedure only in critically ill patients who are already intubated for other reasons made these conversations go much more smoothly. In the development of delineation of privileges, we used the term critical care TEE to clearly define this patient population. During these conversations, highlight the safety of the procedure; ASE guidelines3 estimate a severe complication rate of less than 1 in 10,000 cases and explain the anticipated benefits to critically ill patients.
In conclusion, at an institution that is already adept at the use of POCUS in the ICU, the additional of critical care TEE within 1 to 2 years is a very realistic achievement. It will undoubtedly require patience, persistence, and self-motivation, but the barriers are becoming smaller every day. Stay motivated!
Dr. Proud is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Pulmonary and Critical Care Medicine Program Director, UT Health San Antonio.
References:
1. Porter TR, Abdelmoneim S, Belcik FT, et al. Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography. J Am Soc Echocardiogr. 2024;27(8):797-810.
2. Si X, Ma J, Cao DY, et al. Transesophageal echocardiography instead or in addition to transthoracic echocardiography in evaluating haemodynamic problems in intubated critically ill patients. Ann Transl Med. 2020;8(12):785.
3. Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a cmprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardioraphy and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964.
A Military Nurse Saves a Life After a Brutal Rollover Crash
Emergencies happen anywhere and anytime, and sometimes, medical professionals find themselves in situations where they are the only ones who can help. Is There a Doctor in the House? is a series telling these stories.
A week earlier I’d had a heart surgery and was heading out for a post-op appointment when I saw it: I had a flat tire. It didn’t make sense. The tire was brand new, and there was no puncture. But it was flat.
I swapped out the flat for the spare and went off base to a tire shop. While I was there, my surgeon’s office called and rescheduled my appointment for a couple of hours later. That was lucky because by the time the tire was fixed, I had just enough time to get there.
The hospital is right near I-35 in San Antonio, Texas. I got off the freeway and onto the access road and paused to turn into the parking lot. That’s when I heard an enormous crash.
I saw a big poof of white smoke, and a car barreled off the freeway and came rolling down the embankment.
When the car hit the access road, I saw a woman ejected through the windshield. She bounced and landed in the road about 25 feet in front of me.
I put my car in park, grabbed my face mask and gloves, and started running toward her. But another vehicle — a truck towing a trailer — came from behind to drive around me. The driver didn’t realize what had happened and couldn’t stop in time…
The trailer ran over her.
I didn’t know if anyone could’ve survived that, but I went to her. I saw several other bystanders, but they were frozen in shock. I was praying, dear God, if she’s alive, let me do whatever I need to do to save her life.
It was a horrible scene. This poor lady was in a bloody heap in the middle of the road. Her right arm was twisted up under her neck so tightly, she was choking herself. So, the first thing I did was straighten her arm out to protect her airway.
I started yelling at people, “Call 9-1-1! Run to the hospital! Let them know there’s an accident out here, and I need help!”
The woman had a pulse, but it was super rapid. On first glance, she clearly had multiple fractures and a bad head bleed. With the sheer number of times she’d been injured, I didn’t know what was going on internally, but it was bad. She was gargling on her own blood and spitting it up. She was drowning.
A couple of technicians from the hospital came and brought me a tiny emergency kit. It had a blood pressure cuff and an oral airway. All the vital signs indicated the lady was going into shock. She’d lost a lot of blood on the pavement.
I was able to get the oral airway in. A few minutes later, a fire chief showed up. By now, the traffic had backed up so badly, the emergency vehicles couldn’t get in. But he managed to get there another way and gave me a cervical collar (C collar) and an Ambu bag.
I was hyper-focused on what I could do at that moment and what I needed to do next. Her stats were going down, but she still had a pulse. If she lost the pulse or went into a lethal rhythm, I’d have to start cardiopulmonary resuscitation (CPR). I asked the other people, but nobody else knew CPR, so I wouldn’t have help.
I could tell the lady had a pelvic fracture, and we needed to stabilize her. I directed people how to hold her neck safely and log-roll her flat on the ground. I also needed to put pressure on the back of her head because of all the bleeding. I got people to give me their clothes and tried to do that as I was bagging her.
The windows of her vehicle had all been blown out. I asked somebody to go find her purse with her ID. Then I noticed something …
My heart jumped into my stomach.
A car seat. There was an empty child’s car seat in the back of the car.
I started yelling at everyone, “Look for a baby! Go up and down the embankment and across the road. There might have been a baby in the car!”
But there wasn’t. Thank God. She hadn’t been driving with her child.
At that point, a paramedic came running from behind all the traffic. We did life support together until the ambulance finally arrived.
Emergency medical services got an intravenous line in and used medical anti-shock trousers. Thankfully, I already had the C collar on, and we’d been bagging her, so they could load her very quickly.
I got rid of my bloody gloves. I told a police officer I would come back. And then I went to my doctor’s appointment.
The window at my doctor’s office faced the access road, so the people there had seen all the traffic. They asked me what happened, and I said, “It was me. I saw it happen. I tried to help.” I was a little frazzled.
When I got back to the scene, the police and the fire chief kept thanking me for stopping. Why wouldn’t I stop? It was astounding to realize that they imagined somebody wouldn’t stop in a situation like this.
They told me the lady was alive. She was in the intensive care unit in critical condition, but she had survived. At that moment, I had this overwhelming feeling: God had put me in this exact place at the exact time to save her life.
Looking back, I think about how God ordered my steps. Without the mysterious flat tire, I would’ve gone to the hospital earlier. If my appointment hadn’t been rescheduled, I wouldn’t have been on the access road. All those events brought me there.
Several months later, the woman’s family contacted me and asked if we could meet. I found out more about her injuries. She’d had multiple skull fractures, facial fractures, and a broken jaw. Her upper arm was broken in three places. Her clavicle was broken. She had internal bleeding, a pelvic fracture, and a broken leg. She was 28 years old.
She’d had multiple surgeries, spent 2 months in the ICU, and another 3 months in intensive rehab. But she survived. It was incredible.
We all met up at a McDonald’s. First, her little son — who was the baby I thought might have been in the car — ran up to me and said, “Thank you for saving my mommy’s life.”
Then I turned, and there she was — a beautiful lady looking at me with awe and crying, saying, “It’s me.”
She obviously had gone through a transformation from all the injuries and the medications. She had a little bit of a speech delay, but mentally, she was there. She could walk.
She said, “You’re my angel. God put you there to save my life.” Her family all came up and hugged me. It was so beautiful.
She told me about the accident. She’d been speeding that day, zigzagging through lanes to get around the traffic. And she didn’t have her seatbelt on. She’d driven onto the shoulder to try to pass everyone, but it started narrowing. She clipped somebody’s bumper, went into a tailspin, and collided with a second vehicle, which caused her to flip over and down the embankment.
“God’s given me a new lease on life,” she said, “a fresh start. I will forever wear my seatbelt. And I’m going to do whatever I can to give back to other people because I don’t even feel like I deserve this.”
I just cried.
I’ve been a nurse for 29 years, first on the civilian side and later in the military. I’ve led codes and responded to trauma in a hospital setting or a deployed environment. I was well prepared to do what I did. But doing it under such stress with adrenaline bombarding me ... I’m amazed. I just think God’s hand was on me.
At that time, I was personally going through some things. After my heart surgery, I was in an emotional place where I didn’t feel loved or valued. But when I had that realization — when I knew that I was meant to be there to save her life, I also got the very clear message that I was valued and loved so much.
I know I have a very strong purpose. That day changed my life.
US Air Force Lt. Col. Anne Staley is the officer in charge of the Military Training Network, a division of the Defense Health Agency Education and Training Directorate in San Antonio, Texas.
A version of this article appeared on Medscape.com.
Emergencies happen anywhere and anytime, and sometimes, medical professionals find themselves in situations where they are the only ones who can help. Is There a Doctor in the House? is a series telling these stories.
A week earlier I’d had a heart surgery and was heading out for a post-op appointment when I saw it: I had a flat tire. It didn’t make sense. The tire was brand new, and there was no puncture. But it was flat.
I swapped out the flat for the spare and went off base to a tire shop. While I was there, my surgeon’s office called and rescheduled my appointment for a couple of hours later. That was lucky because by the time the tire was fixed, I had just enough time to get there.
The hospital is right near I-35 in San Antonio, Texas. I got off the freeway and onto the access road and paused to turn into the parking lot. That’s when I heard an enormous crash.
I saw a big poof of white smoke, and a car barreled off the freeway and came rolling down the embankment.
When the car hit the access road, I saw a woman ejected through the windshield. She bounced and landed in the road about 25 feet in front of me.
I put my car in park, grabbed my face mask and gloves, and started running toward her. But another vehicle — a truck towing a trailer — came from behind to drive around me. The driver didn’t realize what had happened and couldn’t stop in time…
The trailer ran over her.
I didn’t know if anyone could’ve survived that, but I went to her. I saw several other bystanders, but they were frozen in shock. I was praying, dear God, if she’s alive, let me do whatever I need to do to save her life.
It was a horrible scene. This poor lady was in a bloody heap in the middle of the road. Her right arm was twisted up under her neck so tightly, she was choking herself. So, the first thing I did was straighten her arm out to protect her airway.
I started yelling at people, “Call 9-1-1! Run to the hospital! Let them know there’s an accident out here, and I need help!”
The woman had a pulse, but it was super rapid. On first glance, she clearly had multiple fractures and a bad head bleed. With the sheer number of times she’d been injured, I didn’t know what was going on internally, but it was bad. She was gargling on her own blood and spitting it up. She was drowning.
A couple of technicians from the hospital came and brought me a tiny emergency kit. It had a blood pressure cuff and an oral airway. All the vital signs indicated the lady was going into shock. She’d lost a lot of blood on the pavement.
I was able to get the oral airway in. A few minutes later, a fire chief showed up. By now, the traffic had backed up so badly, the emergency vehicles couldn’t get in. But he managed to get there another way and gave me a cervical collar (C collar) and an Ambu bag.
I was hyper-focused on what I could do at that moment and what I needed to do next. Her stats were going down, but she still had a pulse. If she lost the pulse or went into a lethal rhythm, I’d have to start cardiopulmonary resuscitation (CPR). I asked the other people, but nobody else knew CPR, so I wouldn’t have help.
I could tell the lady had a pelvic fracture, and we needed to stabilize her. I directed people how to hold her neck safely and log-roll her flat on the ground. I also needed to put pressure on the back of her head because of all the bleeding. I got people to give me their clothes and tried to do that as I was bagging her.
The windows of her vehicle had all been blown out. I asked somebody to go find her purse with her ID. Then I noticed something …
My heart jumped into my stomach.
A car seat. There was an empty child’s car seat in the back of the car.
I started yelling at everyone, “Look for a baby! Go up and down the embankment and across the road. There might have been a baby in the car!”
But there wasn’t. Thank God. She hadn’t been driving with her child.
At that point, a paramedic came running from behind all the traffic. We did life support together until the ambulance finally arrived.
Emergency medical services got an intravenous line in and used medical anti-shock trousers. Thankfully, I already had the C collar on, and we’d been bagging her, so they could load her very quickly.
I got rid of my bloody gloves. I told a police officer I would come back. And then I went to my doctor’s appointment.
The window at my doctor’s office faced the access road, so the people there had seen all the traffic. They asked me what happened, and I said, “It was me. I saw it happen. I tried to help.” I was a little frazzled.
When I got back to the scene, the police and the fire chief kept thanking me for stopping. Why wouldn’t I stop? It was astounding to realize that they imagined somebody wouldn’t stop in a situation like this.
They told me the lady was alive. She was in the intensive care unit in critical condition, but she had survived. At that moment, I had this overwhelming feeling: God had put me in this exact place at the exact time to save her life.
Looking back, I think about how God ordered my steps. Without the mysterious flat tire, I would’ve gone to the hospital earlier. If my appointment hadn’t been rescheduled, I wouldn’t have been on the access road. All those events brought me there.
Several months later, the woman’s family contacted me and asked if we could meet. I found out more about her injuries. She’d had multiple skull fractures, facial fractures, and a broken jaw. Her upper arm was broken in three places. Her clavicle was broken. She had internal bleeding, a pelvic fracture, and a broken leg. She was 28 years old.
She’d had multiple surgeries, spent 2 months in the ICU, and another 3 months in intensive rehab. But she survived. It was incredible.
We all met up at a McDonald’s. First, her little son — who was the baby I thought might have been in the car — ran up to me and said, “Thank you for saving my mommy’s life.”
Then I turned, and there she was — a beautiful lady looking at me with awe and crying, saying, “It’s me.”
She obviously had gone through a transformation from all the injuries and the medications. She had a little bit of a speech delay, but mentally, she was there. She could walk.
She said, “You’re my angel. God put you there to save my life.” Her family all came up and hugged me. It was so beautiful.
She told me about the accident. She’d been speeding that day, zigzagging through lanes to get around the traffic. And she didn’t have her seatbelt on. She’d driven onto the shoulder to try to pass everyone, but it started narrowing. She clipped somebody’s bumper, went into a tailspin, and collided with a second vehicle, which caused her to flip over and down the embankment.
“God’s given me a new lease on life,” she said, “a fresh start. I will forever wear my seatbelt. And I’m going to do whatever I can to give back to other people because I don’t even feel like I deserve this.”
I just cried.
I’ve been a nurse for 29 years, first on the civilian side and later in the military. I’ve led codes and responded to trauma in a hospital setting or a deployed environment. I was well prepared to do what I did. But doing it under such stress with adrenaline bombarding me ... I’m amazed. I just think God’s hand was on me.
At that time, I was personally going through some things. After my heart surgery, I was in an emotional place where I didn’t feel loved or valued. But when I had that realization — when I knew that I was meant to be there to save her life, I also got the very clear message that I was valued and loved so much.
I know I have a very strong purpose. That day changed my life.
US Air Force Lt. Col. Anne Staley is the officer in charge of the Military Training Network, a division of the Defense Health Agency Education and Training Directorate in San Antonio, Texas.
A version of this article appeared on Medscape.com.
Emergencies happen anywhere and anytime, and sometimes, medical professionals find themselves in situations where they are the only ones who can help. Is There a Doctor in the House? is a series telling these stories.
A week earlier I’d had a heart surgery and was heading out for a post-op appointment when I saw it: I had a flat tire. It didn’t make sense. The tire was brand new, and there was no puncture. But it was flat.
I swapped out the flat for the spare and went off base to a tire shop. While I was there, my surgeon’s office called and rescheduled my appointment for a couple of hours later. That was lucky because by the time the tire was fixed, I had just enough time to get there.
The hospital is right near I-35 in San Antonio, Texas. I got off the freeway and onto the access road and paused to turn into the parking lot. That’s when I heard an enormous crash.
I saw a big poof of white smoke, and a car barreled off the freeway and came rolling down the embankment.
When the car hit the access road, I saw a woman ejected through the windshield. She bounced and landed in the road about 25 feet in front of me.
I put my car in park, grabbed my face mask and gloves, and started running toward her. But another vehicle — a truck towing a trailer — came from behind to drive around me. The driver didn’t realize what had happened and couldn’t stop in time…
The trailer ran over her.
I didn’t know if anyone could’ve survived that, but I went to her. I saw several other bystanders, but they were frozen in shock. I was praying, dear God, if she’s alive, let me do whatever I need to do to save her life.
It was a horrible scene. This poor lady was in a bloody heap in the middle of the road. Her right arm was twisted up under her neck so tightly, she was choking herself. So, the first thing I did was straighten her arm out to protect her airway.
I started yelling at people, “Call 9-1-1! Run to the hospital! Let them know there’s an accident out here, and I need help!”
The woman had a pulse, but it was super rapid. On first glance, she clearly had multiple fractures and a bad head bleed. With the sheer number of times she’d been injured, I didn’t know what was going on internally, but it was bad. She was gargling on her own blood and spitting it up. She was drowning.
A couple of technicians from the hospital came and brought me a tiny emergency kit. It had a blood pressure cuff and an oral airway. All the vital signs indicated the lady was going into shock. She’d lost a lot of blood on the pavement.
I was able to get the oral airway in. A few minutes later, a fire chief showed up. By now, the traffic had backed up so badly, the emergency vehicles couldn’t get in. But he managed to get there another way and gave me a cervical collar (C collar) and an Ambu bag.
I was hyper-focused on what I could do at that moment and what I needed to do next. Her stats were going down, but she still had a pulse. If she lost the pulse or went into a lethal rhythm, I’d have to start cardiopulmonary resuscitation (CPR). I asked the other people, but nobody else knew CPR, so I wouldn’t have help.
I could tell the lady had a pelvic fracture, and we needed to stabilize her. I directed people how to hold her neck safely and log-roll her flat on the ground. I also needed to put pressure on the back of her head because of all the bleeding. I got people to give me their clothes and tried to do that as I was bagging her.
The windows of her vehicle had all been blown out. I asked somebody to go find her purse with her ID. Then I noticed something …
My heart jumped into my stomach.
A car seat. There was an empty child’s car seat in the back of the car.
I started yelling at everyone, “Look for a baby! Go up and down the embankment and across the road. There might have been a baby in the car!”
But there wasn’t. Thank God. She hadn’t been driving with her child.
At that point, a paramedic came running from behind all the traffic. We did life support together until the ambulance finally arrived.
Emergency medical services got an intravenous line in and used medical anti-shock trousers. Thankfully, I already had the C collar on, and we’d been bagging her, so they could load her very quickly.
I got rid of my bloody gloves. I told a police officer I would come back. And then I went to my doctor’s appointment.
The window at my doctor’s office faced the access road, so the people there had seen all the traffic. They asked me what happened, and I said, “It was me. I saw it happen. I tried to help.” I was a little frazzled.
When I got back to the scene, the police and the fire chief kept thanking me for stopping. Why wouldn’t I stop? It was astounding to realize that they imagined somebody wouldn’t stop in a situation like this.
They told me the lady was alive. She was in the intensive care unit in critical condition, but she had survived. At that moment, I had this overwhelming feeling: God had put me in this exact place at the exact time to save her life.
Looking back, I think about how God ordered my steps. Without the mysterious flat tire, I would’ve gone to the hospital earlier. If my appointment hadn’t been rescheduled, I wouldn’t have been on the access road. All those events brought me there.
Several months later, the woman’s family contacted me and asked if we could meet. I found out more about her injuries. She’d had multiple skull fractures, facial fractures, and a broken jaw. Her upper arm was broken in three places. Her clavicle was broken. She had internal bleeding, a pelvic fracture, and a broken leg. She was 28 years old.
She’d had multiple surgeries, spent 2 months in the ICU, and another 3 months in intensive rehab. But she survived. It was incredible.
We all met up at a McDonald’s. First, her little son — who was the baby I thought might have been in the car — ran up to me and said, “Thank you for saving my mommy’s life.”
Then I turned, and there she was — a beautiful lady looking at me with awe and crying, saying, “It’s me.”
She obviously had gone through a transformation from all the injuries and the medications. She had a little bit of a speech delay, but mentally, she was there. She could walk.
She said, “You’re my angel. God put you there to save my life.” Her family all came up and hugged me. It was so beautiful.
She told me about the accident. She’d been speeding that day, zigzagging through lanes to get around the traffic. And she didn’t have her seatbelt on. She’d driven onto the shoulder to try to pass everyone, but it started narrowing. She clipped somebody’s bumper, went into a tailspin, and collided with a second vehicle, which caused her to flip over and down the embankment.
“God’s given me a new lease on life,” she said, “a fresh start. I will forever wear my seatbelt. And I’m going to do whatever I can to give back to other people because I don’t even feel like I deserve this.”
I just cried.
I’ve been a nurse for 29 years, first on the civilian side and later in the military. I’ve led codes and responded to trauma in a hospital setting or a deployed environment. I was well prepared to do what I did. But doing it under such stress with adrenaline bombarding me ... I’m amazed. I just think God’s hand was on me.
At that time, I was personally going through some things. After my heart surgery, I was in an emotional place where I didn’t feel loved or valued. But when I had that realization — when I knew that I was meant to be there to save her life, I also got the very clear message that I was valued and loved so much.
I know I have a very strong purpose. That day changed my life.
US Air Force Lt. Col. Anne Staley is the officer in charge of the Military Training Network, a division of the Defense Health Agency Education and Training Directorate in San Antonio, Texas.
A version of this article appeared on Medscape.com.
Should intensivists place PEG tubes in critically ill patients?
The practice of initiating early and adequate nutrition in critically ill patients is a cornerstone of ICU management. Adequate nutrition combats the dangerous catabolic state that accompanies critical illness. A few of the benefits of this practice are a decrease in disease severity with resultant lessened hospital and ICU lengths of stay, reduced infection rates, and a decrease in hospital mortality. Enteral nutrition (EN) is the route of nutritional support most associated with safe and effective provision of enhanced immunologic function and the ability to preserve the patient’s lean body mass while avoiding metabolic and infectious complications.
Since its inception in 1980, percutaneous endoscopic gastrostomy (PEG) tubes have become the preferred method for delivering EN in ICUs across the United States. When comparing PEG and nasogastric tubes (NGTs), evidence shows reduced bleeding events, less tube dislodgement, and decreased tube obstructions with a faster rate of recovery of previous swallowing function that prevents delays in medical care and increased mortality rate. Although PEG tubes do not entirely prevent acid reflux or aspiration events, they are positively correlated to significantly reduced rates of both which result in a survival benefit seen in a 2012 study (Psychiatry Clin Neurosci. 2012 Aug;66[5]:418).
The majority of PEG tubes placed in the United States has unquestionably shifted to the ICU patient population since 2014 according to the largest health care database search on this topic published in 2019 (Ann Am Thorac Soc. 2019 Jun;16[6]:724). The safety and efficacy of this procedure has only improved, yet the delayed timing of placement remains problematic and often exceeds what is medically necessary or financially feasible.
To understand this issue, it is important to consider that despite intensivists being globally recognized as procedurally sound with enhanced ultrasound expertise, their endoscopic experience is usually limited to bronchoscopy without formal training in upper gastrointestinal endoscopy. This is the leading theory to explain why intensivists are performing their own percutaneous tracheostomies but not gastrostomies. Fortunately, the FDA-approved Point of Care Ultrasound Magnet Aligned Gastrostomy (PUMA-G) System has shown analogous safety and efficacy when compared with the traditional endoscopically placed PEG tube technique (J Intensive Care Med. 2022 May;37[5]:641).
A case series was published in 2021 that included three intensivists who underwent a 3-hour cadaver-based training course for the PUMA-G System with a mandatory minimum successful placement of three gastric tubes (J Clin Ultrasound. 2021 Jan;49[1]:28). Once they demonstrated competence in the technique, the procedure was performed on mechanically ventilated and sedated patients without any reported complications peri-procedurally or over the next 30 days. The evidence that intensivists can use their current skillset to rapidly become competent in this ultrasound-guided bedside procedure is without question.
PEG tube placement by intensivists is a procedure that will undoubtedly benefit patients in the ICU and assist in offloading the operation costs of a significant number of critical care units and their associated organizations. This is an area ripe for growth with further education and research.
The practice of initiating early and adequate nutrition in critically ill patients is a cornerstone of ICU management. Adequate nutrition combats the dangerous catabolic state that accompanies critical illness. A few of the benefits of this practice are a decrease in disease severity with resultant lessened hospital and ICU lengths of stay, reduced infection rates, and a decrease in hospital mortality. Enteral nutrition (EN) is the route of nutritional support most associated with safe and effective provision of enhanced immunologic function and the ability to preserve the patient’s lean body mass while avoiding metabolic and infectious complications.
Since its inception in 1980, percutaneous endoscopic gastrostomy (PEG) tubes have become the preferred method for delivering EN in ICUs across the United States. When comparing PEG and nasogastric tubes (NGTs), evidence shows reduced bleeding events, less tube dislodgement, and decreased tube obstructions with a faster rate of recovery of previous swallowing function that prevents delays in medical care and increased mortality rate. Although PEG tubes do not entirely prevent acid reflux or aspiration events, they are positively correlated to significantly reduced rates of both which result in a survival benefit seen in a 2012 study (Psychiatry Clin Neurosci. 2012 Aug;66[5]:418).
The majority of PEG tubes placed in the United States has unquestionably shifted to the ICU patient population since 2014 according to the largest health care database search on this topic published in 2019 (Ann Am Thorac Soc. 2019 Jun;16[6]:724). The safety and efficacy of this procedure has only improved, yet the delayed timing of placement remains problematic and often exceeds what is medically necessary or financially feasible.
To understand this issue, it is important to consider that despite intensivists being globally recognized as procedurally sound with enhanced ultrasound expertise, their endoscopic experience is usually limited to bronchoscopy without formal training in upper gastrointestinal endoscopy. This is the leading theory to explain why intensivists are performing their own percutaneous tracheostomies but not gastrostomies. Fortunately, the FDA-approved Point of Care Ultrasound Magnet Aligned Gastrostomy (PUMA-G) System has shown analogous safety and efficacy when compared with the traditional endoscopically placed PEG tube technique (J Intensive Care Med. 2022 May;37[5]:641).
A case series was published in 2021 that included three intensivists who underwent a 3-hour cadaver-based training course for the PUMA-G System with a mandatory minimum successful placement of three gastric tubes (J Clin Ultrasound. 2021 Jan;49[1]:28). Once they demonstrated competence in the technique, the procedure was performed on mechanically ventilated and sedated patients without any reported complications peri-procedurally or over the next 30 days. The evidence that intensivists can use their current skillset to rapidly become competent in this ultrasound-guided bedside procedure is without question.
PEG tube placement by intensivists is a procedure that will undoubtedly benefit patients in the ICU and assist in offloading the operation costs of a significant number of critical care units and their associated organizations. This is an area ripe for growth with further education and research.
The practice of initiating early and adequate nutrition in critically ill patients is a cornerstone of ICU management. Adequate nutrition combats the dangerous catabolic state that accompanies critical illness. A few of the benefits of this practice are a decrease in disease severity with resultant lessened hospital and ICU lengths of stay, reduced infection rates, and a decrease in hospital mortality. Enteral nutrition (EN) is the route of nutritional support most associated with safe and effective provision of enhanced immunologic function and the ability to preserve the patient’s lean body mass while avoiding metabolic and infectious complications.
Since its inception in 1980, percutaneous endoscopic gastrostomy (PEG) tubes have become the preferred method for delivering EN in ICUs across the United States. When comparing PEG and nasogastric tubes (NGTs), evidence shows reduced bleeding events, less tube dislodgement, and decreased tube obstructions with a faster rate of recovery of previous swallowing function that prevents delays in medical care and increased mortality rate. Although PEG tubes do not entirely prevent acid reflux or aspiration events, they are positively correlated to significantly reduced rates of both which result in a survival benefit seen in a 2012 study (Psychiatry Clin Neurosci. 2012 Aug;66[5]:418).
The majority of PEG tubes placed in the United States has unquestionably shifted to the ICU patient population since 2014 according to the largest health care database search on this topic published in 2019 (Ann Am Thorac Soc. 2019 Jun;16[6]:724). The safety and efficacy of this procedure has only improved, yet the delayed timing of placement remains problematic and often exceeds what is medically necessary or financially feasible.
To understand this issue, it is important to consider that despite intensivists being globally recognized as procedurally sound with enhanced ultrasound expertise, their endoscopic experience is usually limited to bronchoscopy without formal training in upper gastrointestinal endoscopy. This is the leading theory to explain why intensivists are performing their own percutaneous tracheostomies but not gastrostomies. Fortunately, the FDA-approved Point of Care Ultrasound Magnet Aligned Gastrostomy (PUMA-G) System has shown analogous safety and efficacy when compared with the traditional endoscopically placed PEG tube technique (J Intensive Care Med. 2022 May;37[5]:641).
A case series was published in 2021 that included three intensivists who underwent a 3-hour cadaver-based training course for the PUMA-G System with a mandatory minimum successful placement of three gastric tubes (J Clin Ultrasound. 2021 Jan;49[1]:28). Once they demonstrated competence in the technique, the procedure was performed on mechanically ventilated and sedated patients without any reported complications peri-procedurally or over the next 30 days. The evidence that intensivists can use their current skillset to rapidly become competent in this ultrasound-guided bedside procedure is without question.
PEG tube placement by intensivists is a procedure that will undoubtedly benefit patients in the ICU and assist in offloading the operation costs of a significant number of critical care units and their associated organizations. This is an area ripe for growth with further education and research.