User login
FDA modifies safety label for Addyi
The Food and Drug Administration has issued a safety labeling change for flibanserin (Addyi), a treatment for premenopausal women with acquired, generalized hypoactive sexual desire disorder, according to a press release issued April 11 by the agency. Previously, the warning said women should abstain from alcohol entirely.
According to the release, the manufacturer, Sprout, had hoped the FDA would remove the boxed warning and contraindication entirely. However, based on a review of two postmarket research studies, the agency chose to order these modifications to the warnings instead.
The first postmarket study was missing information related to participants’ blood pressure, which FDA officials thought was critical in determining risk; it appeared that this resulted from safety precautions built into the trial. The concern was that not only did this absent information provide further evidence of an interaction but that women at home would not have the benefit of these safety precautions and could suffer serious outcomes, including falls, accidents, and bodily harm. The other postmarketing trial showed that delaying administration of flibanserin until at least 2 hours after consuming alcohol reduced the risk of serious hypotension and syncope.
It is recommended that flibanserin be taken at bedtime because of risks associated with hypotension and syncope, as well as risks associated with central nervous system depression (such as sleepiness). Furthermore, patients are encouraged to discontinue treatment with flibanserin if their hypoactive sexual desire disorder does not improve after 8 weeks. The most common adverse reactions include dizziness, sleepiness, nausea, fatigue, insomnia, and dry mouth.
Full prescribing information is available on the FDA website, as is the full release regarding these safety label modifications.
The Food and Drug Administration has issued a safety labeling change for flibanserin (Addyi), a treatment for premenopausal women with acquired, generalized hypoactive sexual desire disorder, according to a press release issued April 11 by the agency. Previously, the warning said women should abstain from alcohol entirely.
According to the release, the manufacturer, Sprout, had hoped the FDA would remove the boxed warning and contraindication entirely. However, based on a review of two postmarket research studies, the agency chose to order these modifications to the warnings instead.
The first postmarket study was missing information related to participants’ blood pressure, which FDA officials thought was critical in determining risk; it appeared that this resulted from safety precautions built into the trial. The concern was that not only did this absent information provide further evidence of an interaction but that women at home would not have the benefit of these safety precautions and could suffer serious outcomes, including falls, accidents, and bodily harm. The other postmarketing trial showed that delaying administration of flibanserin until at least 2 hours after consuming alcohol reduced the risk of serious hypotension and syncope.
It is recommended that flibanserin be taken at bedtime because of risks associated with hypotension and syncope, as well as risks associated with central nervous system depression (such as sleepiness). Furthermore, patients are encouraged to discontinue treatment with flibanserin if their hypoactive sexual desire disorder does not improve after 8 weeks. The most common adverse reactions include dizziness, sleepiness, nausea, fatigue, insomnia, and dry mouth.
Full prescribing information is available on the FDA website, as is the full release regarding these safety label modifications.
The Food and Drug Administration has issued a safety labeling change for flibanserin (Addyi), a treatment for premenopausal women with acquired, generalized hypoactive sexual desire disorder, according to a press release issued April 11 by the agency. Previously, the warning said women should abstain from alcohol entirely.
According to the release, the manufacturer, Sprout, had hoped the FDA would remove the boxed warning and contraindication entirely. However, based on a review of two postmarket research studies, the agency chose to order these modifications to the warnings instead.
The first postmarket study was missing information related to participants’ blood pressure, which FDA officials thought was critical in determining risk; it appeared that this resulted from safety precautions built into the trial. The concern was that not only did this absent information provide further evidence of an interaction but that women at home would not have the benefit of these safety precautions and could suffer serious outcomes, including falls, accidents, and bodily harm. The other postmarketing trial showed that delaying administration of flibanserin until at least 2 hours after consuming alcohol reduced the risk of serious hypotension and syncope.
It is recommended that flibanserin be taken at bedtime because of risks associated with hypotension and syncope, as well as risks associated with central nervous system depression (such as sleepiness). Furthermore, patients are encouraged to discontinue treatment with flibanserin if their hypoactive sexual desire disorder does not improve after 8 weeks. The most common adverse reactions include dizziness, sleepiness, nausea, fatigue, insomnia, and dry mouth.
Full prescribing information is available on the FDA website, as is the full release regarding these safety label modifications.
Seniors in long-term care face higher suicide risks
Seniors who move into and live in long-term care facilities are at increased risk of suicide, according to reporting by the PBS NewsHour and Kaiser Health News. The report focused on the story of Roland K. Tiedemann, a senior who, in his younger days, was an outdoorsman, traveled around the world, and served as a surrogate dad to his granddaughter. When his health deteriorated, he moved to a long-term care facility with his wife, who later was diagnosed with dementia. At age 89, Mr. Tiedemann, who was facing a third move into a facility that would take Medicaid, “locked his door ... and jumped to his death from his fourth floor window,” the report said. The death of Mr. Tiedemann led Julie A. Rickard, PhD, to start asking questions at his facility and working with other centers to identify the signs of depression. A few years earlier, after a “rash of suicides, mostly among young people,” Dr. Rickard had started developing the Suicide Prevention Coalition of North Central Washington. It is also important for families to ask whether suicide prevention and mental health protocols are in place at long-term care facilities. Ultimately, Dr. Rickard and Jane Davis – Mr. Tiedemann’s daughter – agree that stigma needs to be reduced so that residents feel free to talk their depression and anxiety. PBS NewsHour.
More and more people are using mental health apps, and a new study has found that few of those apps have a sound scientific basis for their claims. The researchers scoured iTunes and Google Play for 1,435 mental health apps. These were whittled to 73 of the most popular. The apps addressed common mental health disorders, including depression, anxiety, and substance abuse, as well as some less common illnesses, such as schizophrenia. Of the 73 apps, 47 claimed to be able to effectively diagnose the target condition, improve the user symptoms or mood, and bolster self-management. In about 40% of cases, the app site trotted out scientific language to buttress claims of effectiveness. However, when the researchers took a rigorous look at the science behind the apps, only one was based on a published study. Moreover, for about one-third of the apps, no supporting scientific at all could be found. Science speak did not translate into evidence-based science. The annual market for self-improvement products and apps, including those focusing on mental health, is $10 billion in the United States. Forbes.
Police officers trained in helping people with mental health problems can get positive results, a newspaper report shows. That’s what happened when Logan Elliott called Clive, Iowa, police to report that his fiancé had threatened suicide – and had had a prior attempt, according to the Des Moines Register. Mr. Elliott’s fiancé, Codii Lewis, was in a “depressive state,” was suffering from the loss of his dog, and was troubled by uncertainty regarding the cost of a procedure undertaken to confirm his gender as a transgender man; as a result, Mr. Lewis climbed onto a ledge. He streamed video of his encounter with the police on Facebook Live, and eventually, after kicking one of the officers, he was subdued and taken into custody. The training that Clive officers receive “calls for less aggressive behavior by police,” the article said. “It emphasizes de-escalation, especially when the subject may be suicidal. It doesn’t expect officers to be therapists or handle all mental health situations, but it does ask that they handle mental health situations differently” from the way they might handle other calls. People with mental illness that is untreated are 16 times more likely to be killed by law enforcement than are people without mental illness. Des Moines Register.
An exhibit now running at the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., is intended to put a human face on mental illness. The 99 Faces Project: Portraits Without Labels by Boston-area artist Lynda Michaud Cutrell presents photos of people with serious mental illnesses and those who love them, the New Hampshire Union Leader reported. Portraits were taken with the help of three photographers nationwide. The long list was trimmed to 99 that mirror the ethnic makeup of the U.S. population. The roster of individuals includes 33 with schizophrenia and 33 with bipolar disorder. The remaining 33 are “chronically normal” according to Ms. Cutrell. The viewer can’t tell the difference between the mentally affected individuals and those who are not; they look like people one encounters every day. And that’s the point. Marianne Barthel, director of the Dartmouth-Hitchcock Arts Program, hopes the exhibit leads to conversations that help “normalize mental health in our society, to recognize that the people you’re looking at in these images could be you or your family member,” the article said. Ms. Barthel also hopes that the exhibit, which runs until September, will help reduce the stigma around mental illness by showing that “there are people who are living successful lives with these illnesses.” One of the 99 faces is that of actress Glenn Close, who cofounded the organization Bring Change To Mind in 2010 after her sister was diagnosed with bipolar disorder and her nephew with schizoaffective disorder. New Hampshire Union Leader.
Deliberation about the use of the death penalty for a prisoner in Kansas has implications for those with mental illness who commit crimes. As the Topeka Capital-Journal reported, James Kahler was convicted of murdering his estranged wife, her grandmother, and his two teenage daughters in 2009. Two years later, he was sentenced to death, and several years later, the Kansas Supreme Court upheld that conviction. His guilt is not in question. What is at issue is his impairment. His lawyers had earlier argued that severe depression had made his grip on reality tenuous and that he could not be executed. Now comes the news that the U.S. Supreme Court will rule whether the decision by the state of Kansas to abolish insanity as a defense was constitutional under the 8th and 14th amendments. The high court’s ruling will have profound implications for people with mental illness. In addition to those in Kansas, under state laws in Alaska, Idaho, Montana, and Utah, “a traditional insanity defense in which a person must understand the difference between right and wrong before being found guilty of a crime isn’t allowed,” the report said. An accused can cite “mental disease or defect” as a partial defense. However, in such cases, it must be proven that the person had no intention of committing a crime. In their petition to the Supreme Court, his attorneys argued that he knew he was shooting people, but that he was so disturbed at the time that he could not stop himself. “A favorable decision would make it clear that the Constitution requires that a defendant be able to understand the difference between right and wrong before being found guilty, and, in cases like Mr. Kahler’s, put to death,” his defense attorney, Meryle Carver-Allmond, told the Capital-Journal. “We’re hopeful that, in taking Mr. Kahler’s case, the United States Supreme Court has indicated a desire to find that the Constitution requires better of us in our treatment of mentally ill defendants.” The Topeka Capital-Journal.
Seniors who move into and live in long-term care facilities are at increased risk of suicide, according to reporting by the PBS NewsHour and Kaiser Health News. The report focused on the story of Roland K. Tiedemann, a senior who, in his younger days, was an outdoorsman, traveled around the world, and served as a surrogate dad to his granddaughter. When his health deteriorated, he moved to a long-term care facility with his wife, who later was diagnosed with dementia. At age 89, Mr. Tiedemann, who was facing a third move into a facility that would take Medicaid, “locked his door ... and jumped to his death from his fourth floor window,” the report said. The death of Mr. Tiedemann led Julie A. Rickard, PhD, to start asking questions at his facility and working with other centers to identify the signs of depression. A few years earlier, after a “rash of suicides, mostly among young people,” Dr. Rickard had started developing the Suicide Prevention Coalition of North Central Washington. It is also important for families to ask whether suicide prevention and mental health protocols are in place at long-term care facilities. Ultimately, Dr. Rickard and Jane Davis – Mr. Tiedemann’s daughter – agree that stigma needs to be reduced so that residents feel free to talk their depression and anxiety. PBS NewsHour.
More and more people are using mental health apps, and a new study has found that few of those apps have a sound scientific basis for their claims. The researchers scoured iTunes and Google Play for 1,435 mental health apps. These were whittled to 73 of the most popular. The apps addressed common mental health disorders, including depression, anxiety, and substance abuse, as well as some less common illnesses, such as schizophrenia. Of the 73 apps, 47 claimed to be able to effectively diagnose the target condition, improve the user symptoms or mood, and bolster self-management. In about 40% of cases, the app site trotted out scientific language to buttress claims of effectiveness. However, when the researchers took a rigorous look at the science behind the apps, only one was based on a published study. Moreover, for about one-third of the apps, no supporting scientific at all could be found. Science speak did not translate into evidence-based science. The annual market for self-improvement products and apps, including those focusing on mental health, is $10 billion in the United States. Forbes.
Police officers trained in helping people with mental health problems can get positive results, a newspaper report shows. That’s what happened when Logan Elliott called Clive, Iowa, police to report that his fiancé had threatened suicide – and had had a prior attempt, according to the Des Moines Register. Mr. Elliott’s fiancé, Codii Lewis, was in a “depressive state,” was suffering from the loss of his dog, and was troubled by uncertainty regarding the cost of a procedure undertaken to confirm his gender as a transgender man; as a result, Mr. Lewis climbed onto a ledge. He streamed video of his encounter with the police on Facebook Live, and eventually, after kicking one of the officers, he was subdued and taken into custody. The training that Clive officers receive “calls for less aggressive behavior by police,” the article said. “It emphasizes de-escalation, especially when the subject may be suicidal. It doesn’t expect officers to be therapists or handle all mental health situations, but it does ask that they handle mental health situations differently” from the way they might handle other calls. People with mental illness that is untreated are 16 times more likely to be killed by law enforcement than are people without mental illness. Des Moines Register.
An exhibit now running at the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., is intended to put a human face on mental illness. The 99 Faces Project: Portraits Without Labels by Boston-area artist Lynda Michaud Cutrell presents photos of people with serious mental illnesses and those who love them, the New Hampshire Union Leader reported. Portraits were taken with the help of three photographers nationwide. The long list was trimmed to 99 that mirror the ethnic makeup of the U.S. population. The roster of individuals includes 33 with schizophrenia and 33 with bipolar disorder. The remaining 33 are “chronically normal” according to Ms. Cutrell. The viewer can’t tell the difference between the mentally affected individuals and those who are not; they look like people one encounters every day. And that’s the point. Marianne Barthel, director of the Dartmouth-Hitchcock Arts Program, hopes the exhibit leads to conversations that help “normalize mental health in our society, to recognize that the people you’re looking at in these images could be you or your family member,” the article said. Ms. Barthel also hopes that the exhibit, which runs until September, will help reduce the stigma around mental illness by showing that “there are people who are living successful lives with these illnesses.” One of the 99 faces is that of actress Glenn Close, who cofounded the organization Bring Change To Mind in 2010 after her sister was diagnosed with bipolar disorder and her nephew with schizoaffective disorder. New Hampshire Union Leader.
Deliberation about the use of the death penalty for a prisoner in Kansas has implications for those with mental illness who commit crimes. As the Topeka Capital-Journal reported, James Kahler was convicted of murdering his estranged wife, her grandmother, and his two teenage daughters in 2009. Two years later, he was sentenced to death, and several years later, the Kansas Supreme Court upheld that conviction. His guilt is not in question. What is at issue is his impairment. His lawyers had earlier argued that severe depression had made his grip on reality tenuous and that he could not be executed. Now comes the news that the U.S. Supreme Court will rule whether the decision by the state of Kansas to abolish insanity as a defense was constitutional under the 8th and 14th amendments. The high court’s ruling will have profound implications for people with mental illness. In addition to those in Kansas, under state laws in Alaska, Idaho, Montana, and Utah, “a traditional insanity defense in which a person must understand the difference between right and wrong before being found guilty of a crime isn’t allowed,” the report said. An accused can cite “mental disease or defect” as a partial defense. However, in such cases, it must be proven that the person had no intention of committing a crime. In their petition to the Supreme Court, his attorneys argued that he knew he was shooting people, but that he was so disturbed at the time that he could not stop himself. “A favorable decision would make it clear that the Constitution requires that a defendant be able to understand the difference between right and wrong before being found guilty, and, in cases like Mr. Kahler’s, put to death,” his defense attorney, Meryle Carver-Allmond, told the Capital-Journal. “We’re hopeful that, in taking Mr. Kahler’s case, the United States Supreme Court has indicated a desire to find that the Constitution requires better of us in our treatment of mentally ill defendants.” The Topeka Capital-Journal.
Seniors who move into and live in long-term care facilities are at increased risk of suicide, according to reporting by the PBS NewsHour and Kaiser Health News. The report focused on the story of Roland K. Tiedemann, a senior who, in his younger days, was an outdoorsman, traveled around the world, and served as a surrogate dad to his granddaughter. When his health deteriorated, he moved to a long-term care facility with his wife, who later was diagnosed with dementia. At age 89, Mr. Tiedemann, who was facing a third move into a facility that would take Medicaid, “locked his door ... and jumped to his death from his fourth floor window,” the report said. The death of Mr. Tiedemann led Julie A. Rickard, PhD, to start asking questions at his facility and working with other centers to identify the signs of depression. A few years earlier, after a “rash of suicides, mostly among young people,” Dr. Rickard had started developing the Suicide Prevention Coalition of North Central Washington. It is also important for families to ask whether suicide prevention and mental health protocols are in place at long-term care facilities. Ultimately, Dr. Rickard and Jane Davis – Mr. Tiedemann’s daughter – agree that stigma needs to be reduced so that residents feel free to talk their depression and anxiety. PBS NewsHour.
More and more people are using mental health apps, and a new study has found that few of those apps have a sound scientific basis for their claims. The researchers scoured iTunes and Google Play for 1,435 mental health apps. These were whittled to 73 of the most popular. The apps addressed common mental health disorders, including depression, anxiety, and substance abuse, as well as some less common illnesses, such as schizophrenia. Of the 73 apps, 47 claimed to be able to effectively diagnose the target condition, improve the user symptoms or mood, and bolster self-management. In about 40% of cases, the app site trotted out scientific language to buttress claims of effectiveness. However, when the researchers took a rigorous look at the science behind the apps, only one was based on a published study. Moreover, for about one-third of the apps, no supporting scientific at all could be found. Science speak did not translate into evidence-based science. The annual market for self-improvement products and apps, including those focusing on mental health, is $10 billion in the United States. Forbes.
Police officers trained in helping people with mental health problems can get positive results, a newspaper report shows. That’s what happened when Logan Elliott called Clive, Iowa, police to report that his fiancé had threatened suicide – and had had a prior attempt, according to the Des Moines Register. Mr. Elliott’s fiancé, Codii Lewis, was in a “depressive state,” was suffering from the loss of his dog, and was troubled by uncertainty regarding the cost of a procedure undertaken to confirm his gender as a transgender man; as a result, Mr. Lewis climbed onto a ledge. He streamed video of his encounter with the police on Facebook Live, and eventually, after kicking one of the officers, he was subdued and taken into custody. The training that Clive officers receive “calls for less aggressive behavior by police,” the article said. “It emphasizes de-escalation, especially when the subject may be suicidal. It doesn’t expect officers to be therapists or handle all mental health situations, but it does ask that they handle mental health situations differently” from the way they might handle other calls. People with mental illness that is untreated are 16 times more likely to be killed by law enforcement than are people without mental illness. Des Moines Register.
An exhibit now running at the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., is intended to put a human face on mental illness. The 99 Faces Project: Portraits Without Labels by Boston-area artist Lynda Michaud Cutrell presents photos of people with serious mental illnesses and those who love them, the New Hampshire Union Leader reported. Portraits were taken with the help of three photographers nationwide. The long list was trimmed to 99 that mirror the ethnic makeup of the U.S. population. The roster of individuals includes 33 with schizophrenia and 33 with bipolar disorder. The remaining 33 are “chronically normal” according to Ms. Cutrell. The viewer can’t tell the difference between the mentally affected individuals and those who are not; they look like people one encounters every day. And that’s the point. Marianne Barthel, director of the Dartmouth-Hitchcock Arts Program, hopes the exhibit leads to conversations that help “normalize mental health in our society, to recognize that the people you’re looking at in these images could be you or your family member,” the article said. Ms. Barthel also hopes that the exhibit, which runs until September, will help reduce the stigma around mental illness by showing that “there are people who are living successful lives with these illnesses.” One of the 99 faces is that of actress Glenn Close, who cofounded the organization Bring Change To Mind in 2010 after her sister was diagnosed with bipolar disorder and her nephew with schizoaffective disorder. New Hampshire Union Leader.
Deliberation about the use of the death penalty for a prisoner in Kansas has implications for those with mental illness who commit crimes. As the Topeka Capital-Journal reported, James Kahler was convicted of murdering his estranged wife, her grandmother, and his two teenage daughters in 2009. Two years later, he was sentenced to death, and several years later, the Kansas Supreme Court upheld that conviction. His guilt is not in question. What is at issue is his impairment. His lawyers had earlier argued that severe depression had made his grip on reality tenuous and that he could not be executed. Now comes the news that the U.S. Supreme Court will rule whether the decision by the state of Kansas to abolish insanity as a defense was constitutional under the 8th and 14th amendments. The high court’s ruling will have profound implications for people with mental illness. In addition to those in Kansas, under state laws in Alaska, Idaho, Montana, and Utah, “a traditional insanity defense in which a person must understand the difference between right and wrong before being found guilty of a crime isn’t allowed,” the report said. An accused can cite “mental disease or defect” as a partial defense. However, in such cases, it must be proven that the person had no intention of committing a crime. In their petition to the Supreme Court, his attorneys argued that he knew he was shooting people, but that he was so disturbed at the time that he could not stop himself. “A favorable decision would make it clear that the Constitution requires that a defendant be able to understand the difference between right and wrong before being found guilty, and, in cases like Mr. Kahler’s, put to death,” his defense attorney, Meryle Carver-Allmond, told the Capital-Journal. “We’re hopeful that, in taking Mr. Kahler’s case, the United States Supreme Court has indicated a desire to find that the Constitution requires better of us in our treatment of mentally ill defendants.” The Topeka Capital-Journal.
My patient will die
“You are the best doctor I ever had.” These were the words of my patient at our final session. I kissed Rosa on the cheek and embraced her as she left my office. And I said, “It is important to show the love.”
“This may be the last time I come to your office,” she said. When Rosa came through the door at the beginning of the session, I was taken aback. She had lost weight and was using a walker; her face was drawn and sallow. I knew she had a recent diagnosis of liver cancer and had been hospitalized. She told me: “I have 3 months to live.” The cancer was inoperable.
She sat in a chair close to me, and we reminisced about 20 years as doctor and patient. She also talked about the stents in her liver; when they blocked, the pain resulted in a revisit to the emergency department. She had help from home health aides for several hours a day. Rosa’s sister arrived from Puerto Rico to be here “for as long as it takes.”
When she started therapy, Rosa was a single mother who lived in the projects with her adolescent son, Wesley. Her husband had died of AIDS. Unemployed and depressed, she told me that an uncle had sexually abused her when she was a child. Over the years, she looked to me for support: When her son, Wesley, got shot in the leg on a basketball court; when Wesley married a woman who shunned her; when her nephew who stayed with her got arrested for selling drugs and she lost her apartment as a result. Rosa remained in New York, displaced and struggling to find a reasonable home. After Wesley married, he moved with his family to rural Pennsylvania.
Whenever Rosa called to set up a therapy session, we talked about her problems. I prescribed medication for her, and I directed her to proper medical care. Often, I encouraged her to improve her diet, lose weight, and exercise – but to no avail. Her health deteriorated. She had cardiac surgery, heart failure, diabetes, hypertension, and chronic obesity. All these illnesses became her concern. She attended clinics at the hospital.
Now she told me that she would miss her son and would not see her two young grandchildren grow up. Rosa took Wesley to a funeral home to select a coffin and a headstone. It was tough for both of them, but she wanted to spare Wesley the trouble of doing it alone. She reflected, “It was like hitting a concrete wall” when she discovered her terminal diagnosis.
Rosa is facing pain, saying goodbye, and death. During her meeting, her ordeal made me cry, but I tried to contain it. I have been her doctor for so long, not a member of her family, not a friend. Yet I love her.
“Just to be is a blessing. Just to live is holy.”
– Abraham Joshua Heschel
Dr. Cohen is in private practice and is a clinical assistant professor of psychiatry at Weill Cornell Medical Center of New York-Presbyterian Hospital, and psychiatric consultant at the Hospital for Special Surgery, also in New York. She made changes to the patient’s story to protect confidentiality.
“You are the best doctor I ever had.” These were the words of my patient at our final session. I kissed Rosa on the cheek and embraced her as she left my office. And I said, “It is important to show the love.”
“This may be the last time I come to your office,” she said. When Rosa came through the door at the beginning of the session, I was taken aback. She had lost weight and was using a walker; her face was drawn and sallow. I knew she had a recent diagnosis of liver cancer and had been hospitalized. She told me: “I have 3 months to live.” The cancer was inoperable.
She sat in a chair close to me, and we reminisced about 20 years as doctor and patient. She also talked about the stents in her liver; when they blocked, the pain resulted in a revisit to the emergency department. She had help from home health aides for several hours a day. Rosa’s sister arrived from Puerto Rico to be here “for as long as it takes.”
When she started therapy, Rosa was a single mother who lived in the projects with her adolescent son, Wesley. Her husband had died of AIDS. Unemployed and depressed, she told me that an uncle had sexually abused her when she was a child. Over the years, she looked to me for support: When her son, Wesley, got shot in the leg on a basketball court; when Wesley married a woman who shunned her; when her nephew who stayed with her got arrested for selling drugs and she lost her apartment as a result. Rosa remained in New York, displaced and struggling to find a reasonable home. After Wesley married, he moved with his family to rural Pennsylvania.
Whenever Rosa called to set up a therapy session, we talked about her problems. I prescribed medication for her, and I directed her to proper medical care. Often, I encouraged her to improve her diet, lose weight, and exercise – but to no avail. Her health deteriorated. She had cardiac surgery, heart failure, diabetes, hypertension, and chronic obesity. All these illnesses became her concern. She attended clinics at the hospital.
Now she told me that she would miss her son and would not see her two young grandchildren grow up. Rosa took Wesley to a funeral home to select a coffin and a headstone. It was tough for both of them, but she wanted to spare Wesley the trouble of doing it alone. She reflected, “It was like hitting a concrete wall” when she discovered her terminal diagnosis.
Rosa is facing pain, saying goodbye, and death. During her meeting, her ordeal made me cry, but I tried to contain it. I have been her doctor for so long, not a member of her family, not a friend. Yet I love her.
“Just to be is a blessing. Just to live is holy.”
– Abraham Joshua Heschel
Dr. Cohen is in private practice and is a clinical assistant professor of psychiatry at Weill Cornell Medical Center of New York-Presbyterian Hospital, and psychiatric consultant at the Hospital for Special Surgery, also in New York. She made changes to the patient’s story to protect confidentiality.
“You are the best doctor I ever had.” These were the words of my patient at our final session. I kissed Rosa on the cheek and embraced her as she left my office. And I said, “It is important to show the love.”
“This may be the last time I come to your office,” she said. When Rosa came through the door at the beginning of the session, I was taken aback. She had lost weight and was using a walker; her face was drawn and sallow. I knew she had a recent diagnosis of liver cancer and had been hospitalized. She told me: “I have 3 months to live.” The cancer was inoperable.
She sat in a chair close to me, and we reminisced about 20 years as doctor and patient. She also talked about the stents in her liver; when they blocked, the pain resulted in a revisit to the emergency department. She had help from home health aides for several hours a day. Rosa’s sister arrived from Puerto Rico to be here “for as long as it takes.”
When she started therapy, Rosa was a single mother who lived in the projects with her adolescent son, Wesley. Her husband had died of AIDS. Unemployed and depressed, she told me that an uncle had sexually abused her when she was a child. Over the years, she looked to me for support: When her son, Wesley, got shot in the leg on a basketball court; when Wesley married a woman who shunned her; when her nephew who stayed with her got arrested for selling drugs and she lost her apartment as a result. Rosa remained in New York, displaced and struggling to find a reasonable home. After Wesley married, he moved with his family to rural Pennsylvania.
Whenever Rosa called to set up a therapy session, we talked about her problems. I prescribed medication for her, and I directed her to proper medical care. Often, I encouraged her to improve her diet, lose weight, and exercise – but to no avail. Her health deteriorated. She had cardiac surgery, heart failure, diabetes, hypertension, and chronic obesity. All these illnesses became her concern. She attended clinics at the hospital.
Now she told me that she would miss her son and would not see her two young grandchildren grow up. Rosa took Wesley to a funeral home to select a coffin and a headstone. It was tough for both of them, but she wanted to spare Wesley the trouble of doing it alone. She reflected, “It was like hitting a concrete wall” when she discovered her terminal diagnosis.
Rosa is facing pain, saying goodbye, and death. During her meeting, her ordeal made me cry, but I tried to contain it. I have been her doctor for so long, not a member of her family, not a friend. Yet I love her.
“Just to be is a blessing. Just to live is holy.”
– Abraham Joshua Heschel
Dr. Cohen is in private practice and is a clinical assistant professor of psychiatry at Weill Cornell Medical Center of New York-Presbyterian Hospital, and psychiatric consultant at the Hospital for Special Surgery, also in New York. She made changes to the patient’s story to protect confidentiality.
Brexanolone approval ‘marks an important milestone’
In March 2019, the Food and Drug Administration approved a novel medication, Zulresso (brexanolone), for the treatment of postpartum depression. Brexanolone is the first FDA-approved medication for the treatment of postpartum depression, a serious illness that affects nearly one in nine women soon after giving birth.1
Mothers with postpartum depression experience feelings of sadness, irritability, and anxiety, as well as isolation from their loved ones (including their new baby) and exhaustion. The feelings of sadness and anxiety can be extreme, and can interfere with a woman’s ability to care for herself or her family. In some cases, these symptoms can be life threatening. Indeed, the most common cause of maternal death after childbirth in the developed world is suicide.2 Because of the severity of the symptoms and their impact on the family, postpartum depression usually requires treatment.
Until now, there have been no drugs specifically approved to treat postpartum depression. Commonly, postpartum depression is treated with medications that previously were approved for the treatment of major depressive disorder, despite limited evidence documenting their efficacy for postpartum depression. Other putative treatment alternatives include psychotherapy, estrogen therapy, and neuromodulation, such as electroconvulsive therapy and repetitive transcranial magnetic stimulation. Each of these treatments can take weeks or longer to take effect, time that is of elevated importance given the rapidly developing mother-infant relationship in the early postpartum period. Brexanolone addresses both the issue of efficacy and speed of onset, representing a major step forward in the care of women suffering from postpartum depression.
Importantly, the approval of brexanolone marks an important milestone for the psychiatric research community in general and the National Institute of Mental Health in particular, as it represents a compelling example of successful bench-to-bedside translation of basic neuroscience findings to benefit patients. As we have noted elsewhere,3 the research underlying the discovery of endogenous neurosteroids and their role in modulating GABA receptors laid the foundation for the development of brexanolone, an intravenous formulation of the neurosteroid allopregnanolone. The recognition that allopregnanolone was a protective factor induced by stress, that it derived from progesterone, and that its peripheral blood levels were dramatically reduced in the early postpartum period led to the hypothesis that it might be useful as a treatment for postpartum depression.
Sage Therapeutics took on the task of testing this hypothesis, designing a program, in consultation with the FDA, to test the efficacy of allopregnanolone in women with postpartum depression in a series of randomized, placebo-controlled studies assessing brexanolone. 4,5 It is a significant accomplishment of Sage Therapeutics to not only successfully complete the therapeutic program of studies (given past experience with difficulties recruiting these women for placebo-controlled treatment trials) but as well to demonstrate a robust therapeutic effect.
Although the FDA’s approval of a new and novel treatment is exciting for many women, there are still limitations to the broader use of brexanolone. It is delivered intravenously, requires an overnight stay in a certified medical center, and is likely to be considerably expensive, according to early reports – potentially limiting the access to the treatment. There also are potentially serious side effects, such as sedation, dizziness, or sudden loss of consciousness. Nonetheless, this is a promising first step and hopefully will spur further efforts to identify and optimize additional strategies to treat postpartum depression. In fact, other formulations of allopregnanolone and novel analogs to treat postpartum depression already are under study, including some that are orally bioavailable.6,7,8
Several important questions remain to be answered about both brexanolone and postpartum depression: What is the underlying mechanism through which allopregnanolone acts in the brain and reduces depressive symptoms? Is the mechanism unique to postpartum women, or might brexanolone also be effective in nonreproductive depressions in women and men? What causes postpartum depression, and what are the risk factors involved for women who develop this serious condition? Future work will focus on these and other important questions to the benefit of women who have suffered with this condition.
The FDA approval of brexanolone represents the second approval in a month of a new antidepressant treatment targeting different molecules in the brain. In early March 2019, the agency approved Spravato (esketamine) nasal spray as a therapy for treatment-resistant depression. Like brexanolone, esketamine is a fast-acting antidepressant that works through a novel mechanism, completely different from other antidepressants. These new treatment approvals are encouraging, as there has been a paucity for many years in approving new effective treatments for mood disorders.
However, treatment development in psychiatry still has a long way to go and the full underlying neurobiology of mood disorders, including postpartum depression, remains poorly understood. Many challenges are ahead of us in our efforts to develop new treatments and increase our understanding of mental illnesses. Nevertheless, the approval of brexanolone is an important milestone, giving hope to the many women who suffer from postpartum depression, and paving the way for the development of additional novel and effective medications to treat this serious and sometimes life-threatening condition.
Dr. Gordon is the director of the National Institute of Mental Health (NIMH), the lead federal agency for research on mental disorders. He oversees an extensive research portfolio of basic and clinical research that seeks to transform the understanding and treatment of mental illnesses, paving the way for prevention, recovery, and cure. Dr. Hillefors works at the NIMH and oversees the Translational Therapeutics Program in the division of translational research, focusing on the development of novel treatments and biomarkers and early phase clinical trials. She received her MD and PhD in neuroscience at the Karolinska Institute, Sweden. Dr. Schmidt joined the NIMH in 1986 after completing his psychiatric residency at the University of Toronto. He is the chief of the Section on Behavioral Endocrinology, within the Intramural Research Program at the NIMH, where his laboratory studies the relationship between hormones, stress, and mood – particularly in the areas of postpartum depression, severe premenstrual dysphoria, and perimenopausal depression.
References
1. J Psychiatric Res. 2018 Sep;104:235-48.
2. Br J Psychiatry. 2003 Oct;183:279-81.
3. NIMH Director’s Messages. 2019 Mar 20.
4. Lancet. 2017 Jul 29;390(10093):480-9.
5. Lancet. 2018 Sep 22; 392(10152):1058-70.
6. Sage Therapeutics News. 2019 Jan 7.
7. Marinus Pharmaceuticals. 2017 Jun 27.
8. ClinicalTrials.gov Identifier: NCT03460756. 2019 Mar.
In March 2019, the Food and Drug Administration approved a novel medication, Zulresso (brexanolone), for the treatment of postpartum depression. Brexanolone is the first FDA-approved medication for the treatment of postpartum depression, a serious illness that affects nearly one in nine women soon after giving birth.1
Mothers with postpartum depression experience feelings of sadness, irritability, and anxiety, as well as isolation from their loved ones (including their new baby) and exhaustion. The feelings of sadness and anxiety can be extreme, and can interfere with a woman’s ability to care for herself or her family. In some cases, these symptoms can be life threatening. Indeed, the most common cause of maternal death after childbirth in the developed world is suicide.2 Because of the severity of the symptoms and their impact on the family, postpartum depression usually requires treatment.
Until now, there have been no drugs specifically approved to treat postpartum depression. Commonly, postpartum depression is treated with medications that previously were approved for the treatment of major depressive disorder, despite limited evidence documenting their efficacy for postpartum depression. Other putative treatment alternatives include psychotherapy, estrogen therapy, and neuromodulation, such as electroconvulsive therapy and repetitive transcranial magnetic stimulation. Each of these treatments can take weeks or longer to take effect, time that is of elevated importance given the rapidly developing mother-infant relationship in the early postpartum period. Brexanolone addresses both the issue of efficacy and speed of onset, representing a major step forward in the care of women suffering from postpartum depression.
Importantly, the approval of brexanolone marks an important milestone for the psychiatric research community in general and the National Institute of Mental Health in particular, as it represents a compelling example of successful bench-to-bedside translation of basic neuroscience findings to benefit patients. As we have noted elsewhere,3 the research underlying the discovery of endogenous neurosteroids and their role in modulating GABA receptors laid the foundation for the development of brexanolone, an intravenous formulation of the neurosteroid allopregnanolone. The recognition that allopregnanolone was a protective factor induced by stress, that it derived from progesterone, and that its peripheral blood levels were dramatically reduced in the early postpartum period led to the hypothesis that it might be useful as a treatment for postpartum depression.
Sage Therapeutics took on the task of testing this hypothesis, designing a program, in consultation with the FDA, to test the efficacy of allopregnanolone in women with postpartum depression in a series of randomized, placebo-controlled studies assessing brexanolone. 4,5 It is a significant accomplishment of Sage Therapeutics to not only successfully complete the therapeutic program of studies (given past experience with difficulties recruiting these women for placebo-controlled treatment trials) but as well to demonstrate a robust therapeutic effect.
Although the FDA’s approval of a new and novel treatment is exciting for many women, there are still limitations to the broader use of brexanolone. It is delivered intravenously, requires an overnight stay in a certified medical center, and is likely to be considerably expensive, according to early reports – potentially limiting the access to the treatment. There also are potentially serious side effects, such as sedation, dizziness, or sudden loss of consciousness. Nonetheless, this is a promising first step and hopefully will spur further efforts to identify and optimize additional strategies to treat postpartum depression. In fact, other formulations of allopregnanolone and novel analogs to treat postpartum depression already are under study, including some that are orally bioavailable.6,7,8
Several important questions remain to be answered about both brexanolone and postpartum depression: What is the underlying mechanism through which allopregnanolone acts in the brain and reduces depressive symptoms? Is the mechanism unique to postpartum women, or might brexanolone also be effective in nonreproductive depressions in women and men? What causes postpartum depression, and what are the risk factors involved for women who develop this serious condition? Future work will focus on these and other important questions to the benefit of women who have suffered with this condition.
The FDA approval of brexanolone represents the second approval in a month of a new antidepressant treatment targeting different molecules in the brain. In early March 2019, the agency approved Spravato (esketamine) nasal spray as a therapy for treatment-resistant depression. Like brexanolone, esketamine is a fast-acting antidepressant that works through a novel mechanism, completely different from other antidepressants. These new treatment approvals are encouraging, as there has been a paucity for many years in approving new effective treatments for mood disorders.
However, treatment development in psychiatry still has a long way to go and the full underlying neurobiology of mood disorders, including postpartum depression, remains poorly understood. Many challenges are ahead of us in our efforts to develop new treatments and increase our understanding of mental illnesses. Nevertheless, the approval of brexanolone is an important milestone, giving hope to the many women who suffer from postpartum depression, and paving the way for the development of additional novel and effective medications to treat this serious and sometimes life-threatening condition.
Dr. Gordon is the director of the National Institute of Mental Health (NIMH), the lead federal agency for research on mental disorders. He oversees an extensive research portfolio of basic and clinical research that seeks to transform the understanding and treatment of mental illnesses, paving the way for prevention, recovery, and cure. Dr. Hillefors works at the NIMH and oversees the Translational Therapeutics Program in the division of translational research, focusing on the development of novel treatments and biomarkers and early phase clinical trials. She received her MD and PhD in neuroscience at the Karolinska Institute, Sweden. Dr. Schmidt joined the NIMH in 1986 after completing his psychiatric residency at the University of Toronto. He is the chief of the Section on Behavioral Endocrinology, within the Intramural Research Program at the NIMH, where his laboratory studies the relationship between hormones, stress, and mood – particularly in the areas of postpartum depression, severe premenstrual dysphoria, and perimenopausal depression.
References
1. J Psychiatric Res. 2018 Sep;104:235-48.
2. Br J Psychiatry. 2003 Oct;183:279-81.
3. NIMH Director’s Messages. 2019 Mar 20.
4. Lancet. 2017 Jul 29;390(10093):480-9.
5. Lancet. 2018 Sep 22; 392(10152):1058-70.
6. Sage Therapeutics News. 2019 Jan 7.
7. Marinus Pharmaceuticals. 2017 Jun 27.
8. ClinicalTrials.gov Identifier: NCT03460756. 2019 Mar.
In March 2019, the Food and Drug Administration approved a novel medication, Zulresso (brexanolone), for the treatment of postpartum depression. Brexanolone is the first FDA-approved medication for the treatment of postpartum depression, a serious illness that affects nearly one in nine women soon after giving birth.1
Mothers with postpartum depression experience feelings of sadness, irritability, and anxiety, as well as isolation from their loved ones (including their new baby) and exhaustion. The feelings of sadness and anxiety can be extreme, and can interfere with a woman’s ability to care for herself or her family. In some cases, these symptoms can be life threatening. Indeed, the most common cause of maternal death after childbirth in the developed world is suicide.2 Because of the severity of the symptoms and their impact on the family, postpartum depression usually requires treatment.
Until now, there have been no drugs specifically approved to treat postpartum depression. Commonly, postpartum depression is treated with medications that previously were approved for the treatment of major depressive disorder, despite limited evidence documenting their efficacy for postpartum depression. Other putative treatment alternatives include psychotherapy, estrogen therapy, and neuromodulation, such as electroconvulsive therapy and repetitive transcranial magnetic stimulation. Each of these treatments can take weeks or longer to take effect, time that is of elevated importance given the rapidly developing mother-infant relationship in the early postpartum period. Brexanolone addresses both the issue of efficacy and speed of onset, representing a major step forward in the care of women suffering from postpartum depression.
Importantly, the approval of brexanolone marks an important milestone for the psychiatric research community in general and the National Institute of Mental Health in particular, as it represents a compelling example of successful bench-to-bedside translation of basic neuroscience findings to benefit patients. As we have noted elsewhere,3 the research underlying the discovery of endogenous neurosteroids and their role in modulating GABA receptors laid the foundation for the development of brexanolone, an intravenous formulation of the neurosteroid allopregnanolone. The recognition that allopregnanolone was a protective factor induced by stress, that it derived from progesterone, and that its peripheral blood levels were dramatically reduced in the early postpartum period led to the hypothesis that it might be useful as a treatment for postpartum depression.
Sage Therapeutics took on the task of testing this hypothesis, designing a program, in consultation with the FDA, to test the efficacy of allopregnanolone in women with postpartum depression in a series of randomized, placebo-controlled studies assessing brexanolone. 4,5 It is a significant accomplishment of Sage Therapeutics to not only successfully complete the therapeutic program of studies (given past experience with difficulties recruiting these women for placebo-controlled treatment trials) but as well to demonstrate a robust therapeutic effect.
Although the FDA’s approval of a new and novel treatment is exciting for many women, there are still limitations to the broader use of brexanolone. It is delivered intravenously, requires an overnight stay in a certified medical center, and is likely to be considerably expensive, according to early reports – potentially limiting the access to the treatment. There also are potentially serious side effects, such as sedation, dizziness, or sudden loss of consciousness. Nonetheless, this is a promising first step and hopefully will spur further efforts to identify and optimize additional strategies to treat postpartum depression. In fact, other formulations of allopregnanolone and novel analogs to treat postpartum depression already are under study, including some that are orally bioavailable.6,7,8
Several important questions remain to be answered about both brexanolone and postpartum depression: What is the underlying mechanism through which allopregnanolone acts in the brain and reduces depressive symptoms? Is the mechanism unique to postpartum women, or might brexanolone also be effective in nonreproductive depressions in women and men? What causes postpartum depression, and what are the risk factors involved for women who develop this serious condition? Future work will focus on these and other important questions to the benefit of women who have suffered with this condition.
The FDA approval of brexanolone represents the second approval in a month of a new antidepressant treatment targeting different molecules in the brain. In early March 2019, the agency approved Spravato (esketamine) nasal spray as a therapy for treatment-resistant depression. Like brexanolone, esketamine is a fast-acting antidepressant that works through a novel mechanism, completely different from other antidepressants. These new treatment approvals are encouraging, as there has been a paucity for many years in approving new effective treatments for mood disorders.
However, treatment development in psychiatry still has a long way to go and the full underlying neurobiology of mood disorders, including postpartum depression, remains poorly understood. Many challenges are ahead of us in our efforts to develop new treatments and increase our understanding of mental illnesses. Nevertheless, the approval of brexanolone is an important milestone, giving hope to the many women who suffer from postpartum depression, and paving the way for the development of additional novel and effective medications to treat this serious and sometimes life-threatening condition.
Dr. Gordon is the director of the National Institute of Mental Health (NIMH), the lead federal agency for research on mental disorders. He oversees an extensive research portfolio of basic and clinical research that seeks to transform the understanding and treatment of mental illnesses, paving the way for prevention, recovery, and cure. Dr. Hillefors works at the NIMH and oversees the Translational Therapeutics Program in the division of translational research, focusing on the development of novel treatments and biomarkers and early phase clinical trials. She received her MD and PhD in neuroscience at the Karolinska Institute, Sweden. Dr. Schmidt joined the NIMH in 1986 after completing his psychiatric residency at the University of Toronto. He is the chief of the Section on Behavioral Endocrinology, within the Intramural Research Program at the NIMH, where his laboratory studies the relationship between hormones, stress, and mood – particularly in the areas of postpartum depression, severe premenstrual dysphoria, and perimenopausal depression.
References
1. J Psychiatric Res. 2018 Sep;104:235-48.
2. Br J Psychiatry. 2003 Oct;183:279-81.
3. NIMH Director’s Messages. 2019 Mar 20.
4. Lancet. 2017 Jul 29;390(10093):480-9.
5. Lancet. 2018 Sep 22; 392(10152):1058-70.
6. Sage Therapeutics News. 2019 Jan 7.
7. Marinus Pharmaceuticals. 2017 Jun 27.
8. ClinicalTrials.gov Identifier: NCT03460756. 2019 Mar.
Survivors offer ‘mass shooting grief 101’
People coping with the aftermath of mass shootings might find some solace from Sandy and Lonnie Phillips. The couple, whose daughter was gunned down in the 2012 slaughter in an Aurora, Colo., movie theater, travels the country to help those whose pain is raw begin processing their grief. Mr. and Mrs. Phillips, driven by compassion, hope that sharing their experience will help others. They have started a nonprofit organization called Survivors Empowered to offer advice and kinship in the wake of mass shootings.
Emergency department visits can prove disorienting for patients with physical illnesses. But for those with mental illness, such visits can feel not only disorienting but disconcerting – particularly if sedation or restraints are involved. “If you are living with schizophrenia or bipolar disorder, that is a really tough way to begin that road to recovery,” said Jack Rozel, MD, president of the American Association for Emergency Psychiatry (AAEP), in an interview with CNN. At about 100 locations across the country, psychiatric EDs staffed by psychiatrists and other physicians, nurses, and social workers are triaging and treating patients with mental illness. The goal is treatment and either release or referral to more specialized care within 24 hours. The approach is the brainchild of Scott Zeller, MD, vice president of acute psychiatry at Vituity and a past president of the AAEP. The physician-led organization provides staffing and consulting services to medical centers nationwide. Dr. Zeller hatched the idea of a psychiatric ED while working as chief of psychiatric emergency services at John George Psychiatric Hospital in San Leandro, Calif. “We need to treat people at the emergency level of care,” he said. “The vast majority of psychiatric emergencies can be resolved in less than 24 hours.” Dr. Zeller took the reins in transforming the center from a traditional ward, including the use of restraints, to a setting more like a living room that was supportive rather than institutional. The results included improved patient outcomes and cost savings – in part because of the reduced time spent in the ED. CNN.
In Buffalo, N.Y., a new memorial to be installed in the Buffalo and Erie County Naval and Military Park will honor veterans who were lost to suicide. Ground was broken recently for the Battle Within Memorial. The 8-feet-tall sculpture will portray one soldier carrying the empty outline of another soldier as a metaphor for help between comrades and the losses that can be tied to the fallout from combat. “It’s a compelling piece of steel,” because it is designed in such a way that allows viewers to see through it, said Paul Marzello, the park’s president and chief executive officer, in an interview with WBFO, a National Public Radio affiliate in Buffalo. “By looking through it you’ll be able to look, as you see through it, someone’s soul.” Among veterans and active duty personnel, an estimated 20 commit suicide each day, according to the military publication Stars and Stripes. One hope of supporters of The Battle Within Foundation, which is leading the project, is that the memorial will inspire those experiencing psychic pain to seek help.“It is our sincerest hope that this monument will in some way help build public awareness of this ongoing tragedy, provide a lifeline for the suffering, and honor our heroes for their service, no matter where they died,” said Mark Donnelly, PhD, president of the Battle Within Foundation. The unveiling is scheduled for May 27, 2019. WBFO.
The field of psychiatry needs to do a better job of helping some patients come off of psychiatric drugs, said Allen Frances, MD, chairperson of DSM-IV task force, in an interview with the New Yorker. This process of removing drugs, called “deprescribing,” “requires a great deal more skill, time, commitment, and knowledge of the patient than prescribing does.” Another psychiatrist quoted in the article, Giovanni A. Fava, MD, said he has struggled to publish research looking at what happens to patients when they stop taking antidepressants. Yet another psychiatrist quoted in the article, Swapnil Gupta, MD, MBBS, said that, for many patients, coming off their medications “is a loss of identity, a different way of living. Suddenly, everything that you are doing is yours – and not necessarily your medication.” The article chronicles the experiences of Laura Delano, a woman diagnosed with bipolar disorder and prescribed valproic acid (Depakote) while in high school. Over the next several years, Ms. Delano found herself taking numerous medications and with a different diagnosis. Eventually, she removed herself from her many medications, started a blog, and launched a website called The Withdrawal Project. The New Yorker.
The National Council for Behavioral Health and Lady Gaga’s Born This Way Foundation have teamed up to develop a Teen Mental Health First Aid pilot program designed to “enhance the mental health of young people,” according to a report on Washington’s WTOP radio. Eight U.S. high schools have been chosen to participate in the program, which will teach students about mental illnesses and addictions. It also will help teenagers respond to friends who might be struggling with a problem with mental health or addiction. The Teen Mental Health First Aid program, a five-step action plan, was adapted from an evidence-based training program from Australia. Researchers at Johns Hopkins University, Baltimore, will evaluate the pilot program to assess its effectiveness. The National Alliance on Mental Illness has reported than 20% of American adults and the same percentage of U.S. teens are living with mental health challenges. After the pilot study results are analyzed, the training will be made available to the public. WTOP.
People coping with the aftermath of mass shootings might find some solace from Sandy and Lonnie Phillips. The couple, whose daughter was gunned down in the 2012 slaughter in an Aurora, Colo., movie theater, travels the country to help those whose pain is raw begin processing their grief. Mr. and Mrs. Phillips, driven by compassion, hope that sharing their experience will help others. They have started a nonprofit organization called Survivors Empowered to offer advice and kinship in the wake of mass shootings.
Emergency department visits can prove disorienting for patients with physical illnesses. But for those with mental illness, such visits can feel not only disorienting but disconcerting – particularly if sedation or restraints are involved. “If you are living with schizophrenia or bipolar disorder, that is a really tough way to begin that road to recovery,” said Jack Rozel, MD, president of the American Association for Emergency Psychiatry (AAEP), in an interview with CNN. At about 100 locations across the country, psychiatric EDs staffed by psychiatrists and other physicians, nurses, and social workers are triaging and treating patients with mental illness. The goal is treatment and either release or referral to more specialized care within 24 hours. The approach is the brainchild of Scott Zeller, MD, vice president of acute psychiatry at Vituity and a past president of the AAEP. The physician-led organization provides staffing and consulting services to medical centers nationwide. Dr. Zeller hatched the idea of a psychiatric ED while working as chief of psychiatric emergency services at John George Psychiatric Hospital in San Leandro, Calif. “We need to treat people at the emergency level of care,” he said. “The vast majority of psychiatric emergencies can be resolved in less than 24 hours.” Dr. Zeller took the reins in transforming the center from a traditional ward, including the use of restraints, to a setting more like a living room that was supportive rather than institutional. The results included improved patient outcomes and cost savings – in part because of the reduced time spent in the ED. CNN.
In Buffalo, N.Y., a new memorial to be installed in the Buffalo and Erie County Naval and Military Park will honor veterans who were lost to suicide. Ground was broken recently for the Battle Within Memorial. The 8-feet-tall sculpture will portray one soldier carrying the empty outline of another soldier as a metaphor for help between comrades and the losses that can be tied to the fallout from combat. “It’s a compelling piece of steel,” because it is designed in such a way that allows viewers to see through it, said Paul Marzello, the park’s president and chief executive officer, in an interview with WBFO, a National Public Radio affiliate in Buffalo. “By looking through it you’ll be able to look, as you see through it, someone’s soul.” Among veterans and active duty personnel, an estimated 20 commit suicide each day, according to the military publication Stars and Stripes. One hope of supporters of The Battle Within Foundation, which is leading the project, is that the memorial will inspire those experiencing psychic pain to seek help.“It is our sincerest hope that this monument will in some way help build public awareness of this ongoing tragedy, provide a lifeline for the suffering, and honor our heroes for their service, no matter where they died,” said Mark Donnelly, PhD, president of the Battle Within Foundation. The unveiling is scheduled for May 27, 2019. WBFO.
The field of psychiatry needs to do a better job of helping some patients come off of psychiatric drugs, said Allen Frances, MD, chairperson of DSM-IV task force, in an interview with the New Yorker. This process of removing drugs, called “deprescribing,” “requires a great deal more skill, time, commitment, and knowledge of the patient than prescribing does.” Another psychiatrist quoted in the article, Giovanni A. Fava, MD, said he has struggled to publish research looking at what happens to patients when they stop taking antidepressants. Yet another psychiatrist quoted in the article, Swapnil Gupta, MD, MBBS, said that, for many patients, coming off their medications “is a loss of identity, a different way of living. Suddenly, everything that you are doing is yours – and not necessarily your medication.” The article chronicles the experiences of Laura Delano, a woman diagnosed with bipolar disorder and prescribed valproic acid (Depakote) while in high school. Over the next several years, Ms. Delano found herself taking numerous medications and with a different diagnosis. Eventually, she removed herself from her many medications, started a blog, and launched a website called The Withdrawal Project. The New Yorker.
The National Council for Behavioral Health and Lady Gaga’s Born This Way Foundation have teamed up to develop a Teen Mental Health First Aid pilot program designed to “enhance the mental health of young people,” according to a report on Washington’s WTOP radio. Eight U.S. high schools have been chosen to participate in the program, which will teach students about mental illnesses and addictions. It also will help teenagers respond to friends who might be struggling with a problem with mental health or addiction. The Teen Mental Health First Aid program, a five-step action plan, was adapted from an evidence-based training program from Australia. Researchers at Johns Hopkins University, Baltimore, will evaluate the pilot program to assess its effectiveness. The National Alliance on Mental Illness has reported than 20% of American adults and the same percentage of U.S. teens are living with mental health challenges. After the pilot study results are analyzed, the training will be made available to the public. WTOP.
People coping with the aftermath of mass shootings might find some solace from Sandy and Lonnie Phillips. The couple, whose daughter was gunned down in the 2012 slaughter in an Aurora, Colo., movie theater, travels the country to help those whose pain is raw begin processing their grief. Mr. and Mrs. Phillips, driven by compassion, hope that sharing their experience will help others. They have started a nonprofit organization called Survivors Empowered to offer advice and kinship in the wake of mass shootings.
Emergency department visits can prove disorienting for patients with physical illnesses. But for those with mental illness, such visits can feel not only disorienting but disconcerting – particularly if sedation or restraints are involved. “If you are living with schizophrenia or bipolar disorder, that is a really tough way to begin that road to recovery,” said Jack Rozel, MD, president of the American Association for Emergency Psychiatry (AAEP), in an interview with CNN. At about 100 locations across the country, psychiatric EDs staffed by psychiatrists and other physicians, nurses, and social workers are triaging and treating patients with mental illness. The goal is treatment and either release or referral to more specialized care within 24 hours. The approach is the brainchild of Scott Zeller, MD, vice president of acute psychiatry at Vituity and a past president of the AAEP. The physician-led organization provides staffing and consulting services to medical centers nationwide. Dr. Zeller hatched the idea of a psychiatric ED while working as chief of psychiatric emergency services at John George Psychiatric Hospital in San Leandro, Calif. “We need to treat people at the emergency level of care,” he said. “The vast majority of psychiatric emergencies can be resolved in less than 24 hours.” Dr. Zeller took the reins in transforming the center from a traditional ward, including the use of restraints, to a setting more like a living room that was supportive rather than institutional. The results included improved patient outcomes and cost savings – in part because of the reduced time spent in the ED. CNN.
In Buffalo, N.Y., a new memorial to be installed in the Buffalo and Erie County Naval and Military Park will honor veterans who were lost to suicide. Ground was broken recently for the Battle Within Memorial. The 8-feet-tall sculpture will portray one soldier carrying the empty outline of another soldier as a metaphor for help between comrades and the losses that can be tied to the fallout from combat. “It’s a compelling piece of steel,” because it is designed in such a way that allows viewers to see through it, said Paul Marzello, the park’s president and chief executive officer, in an interview with WBFO, a National Public Radio affiliate in Buffalo. “By looking through it you’ll be able to look, as you see through it, someone’s soul.” Among veterans and active duty personnel, an estimated 20 commit suicide each day, according to the military publication Stars and Stripes. One hope of supporters of The Battle Within Foundation, which is leading the project, is that the memorial will inspire those experiencing psychic pain to seek help.“It is our sincerest hope that this monument will in some way help build public awareness of this ongoing tragedy, provide a lifeline for the suffering, and honor our heroes for their service, no matter where they died,” said Mark Donnelly, PhD, president of the Battle Within Foundation. The unveiling is scheduled for May 27, 2019. WBFO.
The field of psychiatry needs to do a better job of helping some patients come off of psychiatric drugs, said Allen Frances, MD, chairperson of DSM-IV task force, in an interview with the New Yorker. This process of removing drugs, called “deprescribing,” “requires a great deal more skill, time, commitment, and knowledge of the patient than prescribing does.” Another psychiatrist quoted in the article, Giovanni A. Fava, MD, said he has struggled to publish research looking at what happens to patients when they stop taking antidepressants. Yet another psychiatrist quoted in the article, Swapnil Gupta, MD, MBBS, said that, for many patients, coming off their medications “is a loss of identity, a different way of living. Suddenly, everything that you are doing is yours – and not necessarily your medication.” The article chronicles the experiences of Laura Delano, a woman diagnosed with bipolar disorder and prescribed valproic acid (Depakote) while in high school. Over the next several years, Ms. Delano found herself taking numerous medications and with a different diagnosis. Eventually, she removed herself from her many medications, started a blog, and launched a website called The Withdrawal Project. The New Yorker.
The National Council for Behavioral Health and Lady Gaga’s Born This Way Foundation have teamed up to develop a Teen Mental Health First Aid pilot program designed to “enhance the mental health of young people,” according to a report on Washington’s WTOP radio. Eight U.S. high schools have been chosen to participate in the program, which will teach students about mental illnesses and addictions. It also will help teenagers respond to friends who might be struggling with a problem with mental health or addiction. The Teen Mental Health First Aid program, a five-step action plan, was adapted from an evidence-based training program from Australia. Researchers at Johns Hopkins University, Baltimore, will evaluate the pilot program to assess its effectiveness. The National Alliance on Mental Illness has reported than 20% of American adults and the same percentage of U.S. teens are living with mental health challenges. After the pilot study results are analyzed, the training will be made available to the public. WTOP.
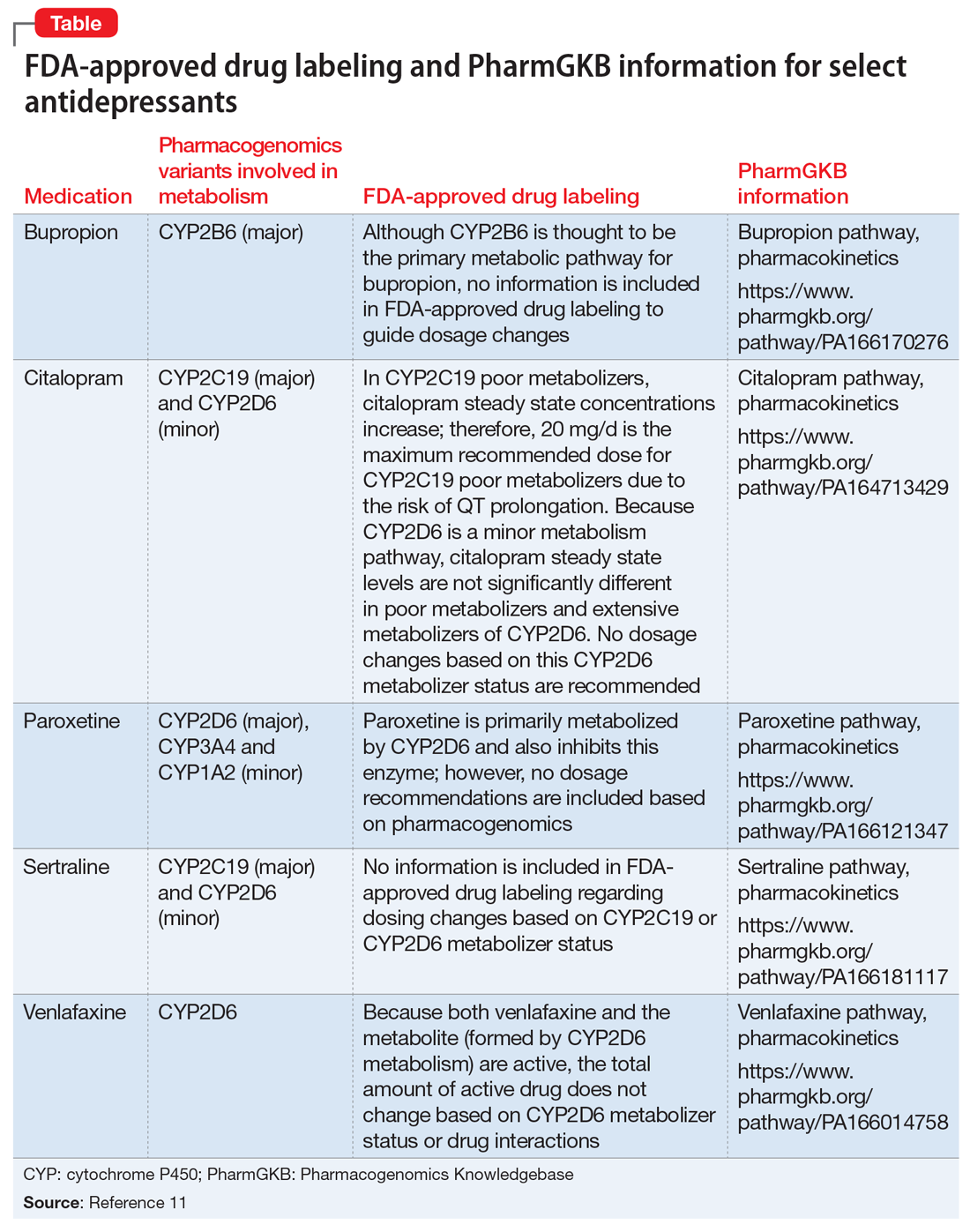
Pharmacogenomics testing: What the FDA says
Mr. R, age 30, is referred to you by his primary care physician, who diagnosed him with depression approximately 2 years ago. When he was first diagnosed, Mr. R was prescribed
Mr. R says that based on his primary care physician’s recommendation, he had undergone pharmacogenomics testing to help guide therapy. He presents the results to you, and you notice that he has the cytochrome P450 (CYP) 2C19 *2/*3 genotype and a CYP2D6*4/*5 genotype. Both are associated with a poor metabolism phenotype. Should you use these findings to determine which medication Mr. R should be treated with next?
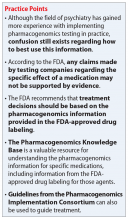
While the field of pharmacogenomics is not new, within the last few years this science has begun to transition into clinical practice. A recent meta-analysis found support for using pharmacogenomics testing results in clinical practice.1 This study included more than 1,700 patients who took part in 5 controlled trials that randomized participants to either pharmacogenetics-guided or unguided (ie, standard) treatment. Each participant was assessed using the Hamilton Depression Rating Scale-17 (HDRS-17) a minimum of 3 times over a minimum of 8 weeks.1 While the exact inclusion and exclusion criteria for each trial differed, they all defined remission of depression as achieving an HDRS-17 score ≤7. Overall, the authors concluded that based on the random-effects pooled risk ratio, there was a significant association between pharmacogenetics-guided prescribing and remission (relative risk = 1.71, 95% confidence interval [CI], 1.17 to 2.48; P = .005). The results of this meta-analysis are controversial, however, because all 5 studies were industry-funded, and interpretation of the testing results was based on proprietary algorithms.
Experts in the field and professional societies, such as the International Society of Psychiatric Genetics (ISPG), have issued policy statements on genetic testing within psychiatry.2,3 While the ISPG did not necessarily endorse use of pharmacogenomics in practice, they recommended that clinicians follow good medical practice and stay current on changes to drug labeling and adverse event reports.3 The ISPG also noted that useful but not exhaustive lists of pharmacogenetic tests are maintained by the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the US FDA.3
Laboratory developed vs direct-to-consumer tests
In a previous Savvy Psychopharmacology article,4 we had discussed the role of CPIC, but not the role of the FDA. This issue is key because there is a lack of clarity regarding pharmacogenomics tests and whether they are considered Class II devices by the FDA, which would require their review and approval. Until recently, the FDA was fairly quiet regarding pharmacogenomics tests because most of these tests were considered laboratory developed tests, which were regulated under the Clinic Laboratory Improvements Amendments program. The critical distinction of a laboratory developed test is that it is developed and performed in a single laboratory and is offered to patients only when prescribed by a clinician. Due to this distinction, laboratory developed pharmacogenomics tests did not need FDA 510(k) clearance, which is a premarket submission common for medical devices.
Direct-to-consumer pharmacogenomics tests are different in that the FDA has classified these platforms as medical devices; however, they are reviewed by the FDA only if they are being used for moderate- to high-risk medical purposes, or if the results of the testing may have a higher impact on medical care. As part of its review, the FDA examines test accuracy and reliably measures to determine if the measurement is predictive of a certain state of health and supported by what the company claims about the test and how well it works. Additionally, the FDA examines the company-provided descriptive information to ensure that consumers can easily understand it without the help of a clinician.5
Conflicting FDA statements
Recently the FDA issued 2 statements—one a policy statement and the other a safety communication—about laboratory developed tests and direct-to-consumer tests. The statements appear to contradict themselves, despite focusing on using pharmacogenomics testing in practice.
Continue to: The FDA's first statement
The FDA’s first statement. On October 31, 2018, the FDA released a policy statement that they had “permitted marketing, with special controls,” of the Personal Genome Service Pharmacogenetic Reports test through 23andMe (a direct-to-consumer genetic testing company) for 33 different variants within specific pharmacogenomic genes (CYP2C19, CYP2C9, CYP3A5, UGT1A1, DPYD, TPMT, SLC01B1, and CYP2D6) that may impact drug metabolism or response.6 As part of its review of this Personal Genome Service Pharmacogenetic Reports test, the FDA found that the company-provided data showed that the test is accurate and can correctly identify the 33 specific genetic variants. The FDA review also showed that the testing results were reproducible, and the test instructions and reports could be understood by consumers.
While the specific reports related to this testing are not yet available within 23andMe, this approval allows for greater oversight by the FDA with regard to the pharmacogenomics information provided through this company’s Personal Genome Service Pharmacogenetic Reports test. The FDA noted that this approval was only for adults age >185 and that consumers “should not use the test results to stop or change any medication.”6 Further, the FDA stated that the results of the direct-to-consumer test should be confirmed with independent pharmacogenomics testing before making any medical decision. Unfortunately, the FDA did not offer guidance on what would be an appropriate independent pharmacogenomics test, but it did provide a link to a list of FDA-approved nucleic acid–based tests, on which 23andMe’s Personal Genome Service Pharmacogenetic Reports test is included.7
The FDA’s second statement. On November 1, 2018, the FDA issued a separate safety communication that cautioned clinicians and patients that most of the current commercially available testing platforms for pharmacogenomics have not been FDA-reviewed, meaning that they may lack clinical evidence supporting their use.8 Further, the FDA safety communication stated, “Changing drug treatment based on the results from such a genetic test could lead to inappropriate treatment decisions and potentially serious health consequences for the patient.”8
Taken together, these FDA statements appear to support pharmacogenomics testing with approval of the 23andMe’s Personal Genome Service Pharmacogenetic Reports test but warn that the testing results should not be used to make treatment decisions, and that they should be verified. However, the FDA does not offer any guidance on what an appropriate testing platform would be
What the FDA advises
The FDA has provided some guidance to clinicians and patients regarding next steps for patients who are interested in having pharmacogenomics testing or who have already undergone testing. The FDA’s first point is that both clinicians and patients need to be aware that pharmacogenomics testing is not FDA-reviewed, that patients should discuss the results of their testing with their clinicians, and that they should not stop their medication based on the results of the testing. Additionally, the FDA recommends that clinicians and patients should be aware that any claims made by the testing companies regarding the specific effect of a medication may not be supported by evidence. Furthermore, the FDA strongly recommends that clinicians consult the FDA-approved drug label, or the label of the FDA-cleared or FDA-approved genetic test, for information regarding how genetic information should be used in making treatment decisions. The FDA recommends reviewing the Warning section, as well as the Indications and Usage, Dosage and Administration, or Use in Specific Populations sections of the FDA-approved drug labeling.
Continue to: Unfortunately, this information...
Unfortunately, this information might be difficult to locate due to the lack of consistency regarding where it is placed in the FDA-approved drug labeling. The Pharmacogenomics Knowledgebase (https://www.pharmgkb.org/) can help clinicians quickly identify information regarding medications, their metabolic pathways, CPIC dosing guidelines, and the FDA-approved drug labeling information.9 By searching for specific medications within the Pharmacogenomic Knowledge Base, information regarding the FDA-approved drug labeling can be easily found, which is important because currently >120 medications contain pharmacogenomics information in their FDA-approved drug labeling.10
CASE CONTINUED
Overall Mr. R’s pharmacogenomics testing results indicate that he has 2 genotypes that are associated with poor metabolism phenotypes and could result in reduced metabolism of medications that are metabolized by these CYP enzymes, leading to higher blood levels and an increased risk of adverse effects. The Table11 lists pharmacogenomics information from the FDA-approved drug labeling and from the Pharmacogenomics Knowledgebase for both the medications Mr. R has previously been prescribed and for several potential medications to consider.
It would be prudent to first discuss with Mr. R the FDA’s recent policy statement and safety communication. While you could recommend that he pursue additional pharmacogenomics testing, it is unclear which specific laboratory is available to conduct this confirmatory analysis.
Because Mr. R has had unsuccessful trials of several medications that primarily fall in the selective serotonin reuptake inhibitors class, it might be time to consider a medication from a different class. A quick review of the FDA-approved drug labeling for
Related Resources
- Gammal RS, Gardner KN, Burghardt KJ. Where to find guidance on using pharmacogenomics in psychiatric practice. Current Psychiatry. 2016;15(9):93-94.
- Clinical Pharmacogenomics Implementation Consortium. What is CPIC? https://www.pharmgkb.org/page/cpic.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Citalopram • Celexa
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
1. Bousman CA, Arandjelovic K, Mancuso SG, et al. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20(1):37-47.
2. Zubenko GS, Sommer BR, Cohen BM. Pharmacogenetics in psychiatry: a companion, rather than competitor, to protocol-based care-reply. JAMA Psychiatry. 2018;75(10):1090-1091.
3. International Society for Psychiatric Genetics. Genetic testing statement: genetic testing and psychiatric disorders: a statement from the International Society of Psychiatric Genetics. https://ispg.net/genetic-testing-statement/. Revised January 26, 2017. Accessed January 1, 2019.
4. Ellingrod VL, Ward KM. Using pharmacogenetics guidelines when prescribing: what’s available. Current Psychiatry. 2018;17(1):43-46.
5. U.S. Food and Drug Administration. Medical devices: direct-to-consumer tests. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm624726.htm. Published November 1, 2018. Accessed January 1, 2019.
6. U.S. Food and Drug Administration. FDA news releases: FDA authorizes first direct-to consumer test for detecting variants that may be associated with medication metabolism. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm624753.htm. Published October 31, 2018. Accessed January 1, 2019.
7. U.S. Food and Drug Administration. Medical devices: nucleic acid based tests. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm330711.htm. Published February 5, 2019. Accessed March 1, 2019.
8. U.S. Food and Drug Administration. Medical devices. The FDA warns against the use of many genetic tests with unapproved claims to predict patient response to specific medications: FDA Safety Communications. https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm624725.htm. Published November 1, 2018. Accessed January 1, 2019.
9. Whirl-Carrillo EM, McDonagh JM, Hebert L, et al. Pharmacogenomics knowledge for personalized medicine. Clin Pharmacol Ther. 2012;92(4):414-417.
10. U.S. Food and Drug Administration. Drugs. Table of pharmacogenomic biomarkers in drug labeling. https://www.fda.gov/Drugs/ScienceResearch/ucm572698.htm. Published August 3, 2018. Accessed January 1, 2019.
11. U.S. Food and Drug Administration. Drugs@FDA: FDA approved drug products. https://www.accessdata.fda.gov/scripts/cder/daf. Accessed March 4, 2019.
Mr. R, age 30, is referred to you by his primary care physician, who diagnosed him with depression approximately 2 years ago. When he was first diagnosed, Mr. R was prescribed
Mr. R says that based on his primary care physician’s recommendation, he had undergone pharmacogenomics testing to help guide therapy. He presents the results to you, and you notice that he has the cytochrome P450 (CYP) 2C19 *2/*3 genotype and a CYP2D6*4/*5 genotype. Both are associated with a poor metabolism phenotype. Should you use these findings to determine which medication Mr. R should be treated with next?
While the field of pharmacogenomics is not new, within the last few years this science has begun to transition into clinical practice. A recent meta-analysis found support for using pharmacogenomics testing results in clinical practice.1 This study included more than 1,700 patients who took part in 5 controlled trials that randomized participants to either pharmacogenetics-guided or unguided (ie, standard) treatment. Each participant was assessed using the Hamilton Depression Rating Scale-17 (HDRS-17) a minimum of 3 times over a minimum of 8 weeks.1 While the exact inclusion and exclusion criteria for each trial differed, they all defined remission of depression as achieving an HDRS-17 score ≤7. Overall, the authors concluded that based on the random-effects pooled risk ratio, there was a significant association between pharmacogenetics-guided prescribing and remission (relative risk = 1.71, 95% confidence interval [CI], 1.17 to 2.48; P = .005). The results of this meta-analysis are controversial, however, because all 5 studies were industry-funded, and interpretation of the testing results was based on proprietary algorithms.
Experts in the field and professional societies, such as the International Society of Psychiatric Genetics (ISPG), have issued policy statements on genetic testing within psychiatry.2,3 While the ISPG did not necessarily endorse use of pharmacogenomics in practice, they recommended that clinicians follow good medical practice and stay current on changes to drug labeling and adverse event reports.3 The ISPG also noted that useful but not exhaustive lists of pharmacogenetic tests are maintained by the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the US FDA.3
Laboratory developed vs direct-to-consumer tests
In a previous Savvy Psychopharmacology article,4 we had discussed the role of CPIC, but not the role of the FDA. This issue is key because there is a lack of clarity regarding pharmacogenomics tests and whether they are considered Class II devices by the FDA, which would require their review and approval. Until recently, the FDA was fairly quiet regarding pharmacogenomics tests because most of these tests were considered laboratory developed tests, which were regulated under the Clinic Laboratory Improvements Amendments program. The critical distinction of a laboratory developed test is that it is developed and performed in a single laboratory and is offered to patients only when prescribed by a clinician. Due to this distinction, laboratory developed pharmacogenomics tests did not need FDA 510(k) clearance, which is a premarket submission common for medical devices.
Direct-to-consumer pharmacogenomics tests are different in that the FDA has classified these platforms as medical devices; however, they are reviewed by the FDA only if they are being used for moderate- to high-risk medical purposes, or if the results of the testing may have a higher impact on medical care. As part of its review, the FDA examines test accuracy and reliably measures to determine if the measurement is predictive of a certain state of health and supported by what the company claims about the test and how well it works. Additionally, the FDA examines the company-provided descriptive information to ensure that consumers can easily understand it without the help of a clinician.5
Conflicting FDA statements
Recently the FDA issued 2 statements—one a policy statement and the other a safety communication—about laboratory developed tests and direct-to-consumer tests. The statements appear to contradict themselves, despite focusing on using pharmacogenomics testing in practice.
Continue to: The FDA's first statement
The FDA’s first statement. On October 31, 2018, the FDA released a policy statement that they had “permitted marketing, with special controls,” of the Personal Genome Service Pharmacogenetic Reports test through 23andMe (a direct-to-consumer genetic testing company) for 33 different variants within specific pharmacogenomic genes (CYP2C19, CYP2C9, CYP3A5, UGT1A1, DPYD, TPMT, SLC01B1, and CYP2D6) that may impact drug metabolism or response.6 As part of its review of this Personal Genome Service Pharmacogenetic Reports test, the FDA found that the company-provided data showed that the test is accurate and can correctly identify the 33 specific genetic variants. The FDA review also showed that the testing results were reproducible, and the test instructions and reports could be understood by consumers.
While the specific reports related to this testing are not yet available within 23andMe, this approval allows for greater oversight by the FDA with regard to the pharmacogenomics information provided through this company’s Personal Genome Service Pharmacogenetic Reports test. The FDA noted that this approval was only for adults age >185 and that consumers “should not use the test results to stop or change any medication.”6 Further, the FDA stated that the results of the direct-to-consumer test should be confirmed with independent pharmacogenomics testing before making any medical decision. Unfortunately, the FDA did not offer guidance on what would be an appropriate independent pharmacogenomics test, but it did provide a link to a list of FDA-approved nucleic acid–based tests, on which 23andMe’s Personal Genome Service Pharmacogenetic Reports test is included.7
The FDA’s second statement. On November 1, 2018, the FDA issued a separate safety communication that cautioned clinicians and patients that most of the current commercially available testing platforms for pharmacogenomics have not been FDA-reviewed, meaning that they may lack clinical evidence supporting their use.8 Further, the FDA safety communication stated, “Changing drug treatment based on the results from such a genetic test could lead to inappropriate treatment decisions and potentially serious health consequences for the patient.”8
Taken together, these FDA statements appear to support pharmacogenomics testing with approval of the 23andMe’s Personal Genome Service Pharmacogenetic Reports test but warn that the testing results should not be used to make treatment decisions, and that they should be verified. However, the FDA does not offer any guidance on what an appropriate testing platform would be
What the FDA advises
The FDA has provided some guidance to clinicians and patients regarding next steps for patients who are interested in having pharmacogenomics testing or who have already undergone testing. The FDA’s first point is that both clinicians and patients need to be aware that pharmacogenomics testing is not FDA-reviewed, that patients should discuss the results of their testing with their clinicians, and that they should not stop their medication based on the results of the testing. Additionally, the FDA recommends that clinicians and patients should be aware that any claims made by the testing companies regarding the specific effect of a medication may not be supported by evidence. Furthermore, the FDA strongly recommends that clinicians consult the FDA-approved drug label, or the label of the FDA-cleared or FDA-approved genetic test, for information regarding how genetic information should be used in making treatment decisions. The FDA recommends reviewing the Warning section, as well as the Indications and Usage, Dosage and Administration, or Use in Specific Populations sections of the FDA-approved drug labeling.
Continue to: Unfortunately, this information...
Unfortunately, this information might be difficult to locate due to the lack of consistency regarding where it is placed in the FDA-approved drug labeling. The Pharmacogenomics Knowledgebase (https://www.pharmgkb.org/) can help clinicians quickly identify information regarding medications, their metabolic pathways, CPIC dosing guidelines, and the FDA-approved drug labeling information.9 By searching for specific medications within the Pharmacogenomic Knowledge Base, information regarding the FDA-approved drug labeling can be easily found, which is important because currently >120 medications contain pharmacogenomics information in their FDA-approved drug labeling.10
CASE CONTINUED
Overall Mr. R’s pharmacogenomics testing results indicate that he has 2 genotypes that are associated with poor metabolism phenotypes and could result in reduced metabolism of medications that are metabolized by these CYP enzymes, leading to higher blood levels and an increased risk of adverse effects. The Table11 lists pharmacogenomics information from the FDA-approved drug labeling and from the Pharmacogenomics Knowledgebase for both the medications Mr. R has previously been prescribed and for several potential medications to consider.
It would be prudent to first discuss with Mr. R the FDA’s recent policy statement and safety communication. While you could recommend that he pursue additional pharmacogenomics testing, it is unclear which specific laboratory is available to conduct this confirmatory analysis.
Because Mr. R has had unsuccessful trials of several medications that primarily fall in the selective serotonin reuptake inhibitors class, it might be time to consider a medication from a different class. A quick review of the FDA-approved drug labeling for
Related Resources
- Gammal RS, Gardner KN, Burghardt KJ. Where to find guidance on using pharmacogenomics in psychiatric practice. Current Psychiatry. 2016;15(9):93-94.
- Clinical Pharmacogenomics Implementation Consortium. What is CPIC? https://www.pharmgkb.org/page/cpic.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Citalopram • Celexa
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
Mr. R, age 30, is referred to you by his primary care physician, who diagnosed him with depression approximately 2 years ago. When he was first diagnosed, Mr. R was prescribed
Mr. R says that based on his primary care physician’s recommendation, he had undergone pharmacogenomics testing to help guide therapy. He presents the results to you, and you notice that he has the cytochrome P450 (CYP) 2C19 *2/*3 genotype and a CYP2D6*4/*5 genotype. Both are associated with a poor metabolism phenotype. Should you use these findings to determine which medication Mr. R should be treated with next?
While the field of pharmacogenomics is not new, within the last few years this science has begun to transition into clinical practice. A recent meta-analysis found support for using pharmacogenomics testing results in clinical practice.1 This study included more than 1,700 patients who took part in 5 controlled trials that randomized participants to either pharmacogenetics-guided or unguided (ie, standard) treatment. Each participant was assessed using the Hamilton Depression Rating Scale-17 (HDRS-17) a minimum of 3 times over a minimum of 8 weeks.1 While the exact inclusion and exclusion criteria for each trial differed, they all defined remission of depression as achieving an HDRS-17 score ≤7. Overall, the authors concluded that based on the random-effects pooled risk ratio, there was a significant association between pharmacogenetics-guided prescribing and remission (relative risk = 1.71, 95% confidence interval [CI], 1.17 to 2.48; P = .005). The results of this meta-analysis are controversial, however, because all 5 studies were industry-funded, and interpretation of the testing results was based on proprietary algorithms.
Experts in the field and professional societies, such as the International Society of Psychiatric Genetics (ISPG), have issued policy statements on genetic testing within psychiatry.2,3 While the ISPG did not necessarily endorse use of pharmacogenomics in practice, they recommended that clinicians follow good medical practice and stay current on changes to drug labeling and adverse event reports.3 The ISPG also noted that useful but not exhaustive lists of pharmacogenetic tests are maintained by the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the US FDA.3
Laboratory developed vs direct-to-consumer tests
In a previous Savvy Psychopharmacology article,4 we had discussed the role of CPIC, but not the role of the FDA. This issue is key because there is a lack of clarity regarding pharmacogenomics tests and whether they are considered Class II devices by the FDA, which would require their review and approval. Until recently, the FDA was fairly quiet regarding pharmacogenomics tests because most of these tests were considered laboratory developed tests, which were regulated under the Clinic Laboratory Improvements Amendments program. The critical distinction of a laboratory developed test is that it is developed and performed in a single laboratory and is offered to patients only when prescribed by a clinician. Due to this distinction, laboratory developed pharmacogenomics tests did not need FDA 510(k) clearance, which is a premarket submission common for medical devices.
Direct-to-consumer pharmacogenomics tests are different in that the FDA has classified these platforms as medical devices; however, they are reviewed by the FDA only if they are being used for moderate- to high-risk medical purposes, or if the results of the testing may have a higher impact on medical care. As part of its review, the FDA examines test accuracy and reliably measures to determine if the measurement is predictive of a certain state of health and supported by what the company claims about the test and how well it works. Additionally, the FDA examines the company-provided descriptive information to ensure that consumers can easily understand it without the help of a clinician.5
Conflicting FDA statements
Recently the FDA issued 2 statements—one a policy statement and the other a safety communication—about laboratory developed tests and direct-to-consumer tests. The statements appear to contradict themselves, despite focusing on using pharmacogenomics testing in practice.
Continue to: The FDA's first statement
The FDA’s first statement. On October 31, 2018, the FDA released a policy statement that they had “permitted marketing, with special controls,” of the Personal Genome Service Pharmacogenetic Reports test through 23andMe (a direct-to-consumer genetic testing company) for 33 different variants within specific pharmacogenomic genes (CYP2C19, CYP2C9, CYP3A5, UGT1A1, DPYD, TPMT, SLC01B1, and CYP2D6) that may impact drug metabolism or response.6 As part of its review of this Personal Genome Service Pharmacogenetic Reports test, the FDA found that the company-provided data showed that the test is accurate and can correctly identify the 33 specific genetic variants. The FDA review also showed that the testing results were reproducible, and the test instructions and reports could be understood by consumers.
While the specific reports related to this testing are not yet available within 23andMe, this approval allows for greater oversight by the FDA with regard to the pharmacogenomics information provided through this company’s Personal Genome Service Pharmacogenetic Reports test. The FDA noted that this approval was only for adults age >185 and that consumers “should not use the test results to stop or change any medication.”6 Further, the FDA stated that the results of the direct-to-consumer test should be confirmed with independent pharmacogenomics testing before making any medical decision. Unfortunately, the FDA did not offer guidance on what would be an appropriate independent pharmacogenomics test, but it did provide a link to a list of FDA-approved nucleic acid–based tests, on which 23andMe’s Personal Genome Service Pharmacogenetic Reports test is included.7
The FDA’s second statement. On November 1, 2018, the FDA issued a separate safety communication that cautioned clinicians and patients that most of the current commercially available testing platforms for pharmacogenomics have not been FDA-reviewed, meaning that they may lack clinical evidence supporting their use.8 Further, the FDA safety communication stated, “Changing drug treatment based on the results from such a genetic test could lead to inappropriate treatment decisions and potentially serious health consequences for the patient.”8
Taken together, these FDA statements appear to support pharmacogenomics testing with approval of the 23andMe’s Personal Genome Service Pharmacogenetic Reports test but warn that the testing results should not be used to make treatment decisions, and that they should be verified. However, the FDA does not offer any guidance on what an appropriate testing platform would be
What the FDA advises
The FDA has provided some guidance to clinicians and patients regarding next steps for patients who are interested in having pharmacogenomics testing or who have already undergone testing. The FDA’s first point is that both clinicians and patients need to be aware that pharmacogenomics testing is not FDA-reviewed, that patients should discuss the results of their testing with their clinicians, and that they should not stop their medication based on the results of the testing. Additionally, the FDA recommends that clinicians and patients should be aware that any claims made by the testing companies regarding the specific effect of a medication may not be supported by evidence. Furthermore, the FDA strongly recommends that clinicians consult the FDA-approved drug label, or the label of the FDA-cleared or FDA-approved genetic test, for information regarding how genetic information should be used in making treatment decisions. The FDA recommends reviewing the Warning section, as well as the Indications and Usage, Dosage and Administration, or Use in Specific Populations sections of the FDA-approved drug labeling.
Continue to: Unfortunately, this information...
Unfortunately, this information might be difficult to locate due to the lack of consistency regarding where it is placed in the FDA-approved drug labeling. The Pharmacogenomics Knowledgebase (https://www.pharmgkb.org/) can help clinicians quickly identify information regarding medications, their metabolic pathways, CPIC dosing guidelines, and the FDA-approved drug labeling information.9 By searching for specific medications within the Pharmacogenomic Knowledge Base, information regarding the FDA-approved drug labeling can be easily found, which is important because currently >120 medications contain pharmacogenomics information in their FDA-approved drug labeling.10
CASE CONTINUED
Overall Mr. R’s pharmacogenomics testing results indicate that he has 2 genotypes that are associated with poor metabolism phenotypes and could result in reduced metabolism of medications that are metabolized by these CYP enzymes, leading to higher blood levels and an increased risk of adverse effects. The Table11 lists pharmacogenomics information from the FDA-approved drug labeling and from the Pharmacogenomics Knowledgebase for both the medications Mr. R has previously been prescribed and for several potential medications to consider.
It would be prudent to first discuss with Mr. R the FDA’s recent policy statement and safety communication. While you could recommend that he pursue additional pharmacogenomics testing, it is unclear which specific laboratory is available to conduct this confirmatory analysis.
Because Mr. R has had unsuccessful trials of several medications that primarily fall in the selective serotonin reuptake inhibitors class, it might be time to consider a medication from a different class. A quick review of the FDA-approved drug labeling for
Related Resources
- Gammal RS, Gardner KN, Burghardt KJ. Where to find guidance on using pharmacogenomics in psychiatric practice. Current Psychiatry. 2016;15(9):93-94.
- Clinical Pharmacogenomics Implementation Consortium. What is CPIC? https://www.pharmgkb.org/page/cpic.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Citalopram • Celexa
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
1. Bousman CA, Arandjelovic K, Mancuso SG, et al. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20(1):37-47.
2. Zubenko GS, Sommer BR, Cohen BM. Pharmacogenetics in psychiatry: a companion, rather than competitor, to protocol-based care-reply. JAMA Psychiatry. 2018;75(10):1090-1091.
3. International Society for Psychiatric Genetics. Genetic testing statement: genetic testing and psychiatric disorders: a statement from the International Society of Psychiatric Genetics. https://ispg.net/genetic-testing-statement/. Revised January 26, 2017. Accessed January 1, 2019.
4. Ellingrod VL, Ward KM. Using pharmacogenetics guidelines when prescribing: what’s available. Current Psychiatry. 2018;17(1):43-46.
5. U.S. Food and Drug Administration. Medical devices: direct-to-consumer tests. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm624726.htm. Published November 1, 2018. Accessed January 1, 2019.
6. U.S. Food and Drug Administration. FDA news releases: FDA authorizes first direct-to consumer test for detecting variants that may be associated with medication metabolism. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm624753.htm. Published October 31, 2018. Accessed January 1, 2019.
7. U.S. Food and Drug Administration. Medical devices: nucleic acid based tests. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm330711.htm. Published February 5, 2019. Accessed March 1, 2019.
8. U.S. Food and Drug Administration. Medical devices. The FDA warns against the use of many genetic tests with unapproved claims to predict patient response to specific medications: FDA Safety Communications. https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm624725.htm. Published November 1, 2018. Accessed January 1, 2019.
9. Whirl-Carrillo EM, McDonagh JM, Hebert L, et al. Pharmacogenomics knowledge for personalized medicine. Clin Pharmacol Ther. 2012;92(4):414-417.
10. U.S. Food and Drug Administration. Drugs. Table of pharmacogenomic biomarkers in drug labeling. https://www.fda.gov/Drugs/ScienceResearch/ucm572698.htm. Published August 3, 2018. Accessed January 1, 2019.
11. U.S. Food and Drug Administration. Drugs@FDA: FDA approved drug products. https://www.accessdata.fda.gov/scripts/cder/daf. Accessed March 4, 2019.
1. Bousman CA, Arandjelovic K, Mancuso SG, et al. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20(1):37-47.
2. Zubenko GS, Sommer BR, Cohen BM. Pharmacogenetics in psychiatry: a companion, rather than competitor, to protocol-based care-reply. JAMA Psychiatry. 2018;75(10):1090-1091.
3. International Society for Psychiatric Genetics. Genetic testing statement: genetic testing and psychiatric disorders: a statement from the International Society of Psychiatric Genetics. https://ispg.net/genetic-testing-statement/. Revised January 26, 2017. Accessed January 1, 2019.
4. Ellingrod VL, Ward KM. Using pharmacogenetics guidelines when prescribing: what’s available. Current Psychiatry. 2018;17(1):43-46.
5. U.S. Food and Drug Administration. Medical devices: direct-to-consumer tests. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm624726.htm. Published November 1, 2018. Accessed January 1, 2019.
6. U.S. Food and Drug Administration. FDA news releases: FDA authorizes first direct-to consumer test for detecting variants that may be associated with medication metabolism. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm624753.htm. Published October 31, 2018. Accessed January 1, 2019.
7. U.S. Food and Drug Administration. Medical devices: nucleic acid based tests. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm330711.htm. Published February 5, 2019. Accessed March 1, 2019.
8. U.S. Food and Drug Administration. Medical devices. The FDA warns against the use of many genetic tests with unapproved claims to predict patient response to specific medications: FDA Safety Communications. https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm624725.htm. Published November 1, 2018. Accessed January 1, 2019.
9. Whirl-Carrillo EM, McDonagh JM, Hebert L, et al. Pharmacogenomics knowledge for personalized medicine. Clin Pharmacol Ther. 2012;92(4):414-417.
10. U.S. Food and Drug Administration. Drugs. Table of pharmacogenomic biomarkers in drug labeling. https://www.fda.gov/Drugs/ScienceResearch/ucm572698.htm. Published August 3, 2018. Accessed January 1, 2019.
11. U.S. Food and Drug Administration. Drugs@FDA: FDA approved drug products. https://www.accessdata.fda.gov/scripts/cder/daf. Accessed March 4, 2019.
Performance-based pay linked to anxiety, depression
A study from researchers at Washington University in St. Louis and Aarhus University in Denmark charts the relationship of payment based on work done and employee mental health. According to phys.org, an aggregator of science, research, and technology news, performance-based pay is in place in 70% of U.S. companies. This means that employee income is based on a combination of bonuses, commission, profit sharing, and individual/team incentives, rather than guaranteed salaries. For some employees, performance-based pay can prove lucrative. But for others, such systems can lead to poor mental health.
The study, published in the Academy of Management Discoveries, charted the use of prescription medications for anxiety and depression by nearly 319,000 employees at about 1,300 companies in Denmark (2019 Feb 26. doi: 10.5465/amd.2018.0007). Those in lower-paid positions and older employees were most vulnerable.
“Basically, older workers seem to be driving all of this effect,” said coauthor Lamar Pierce, PhD, professor of organization and strategy, and associate dean at Washington University. “One, it’s harder for them to move, so they have less labor mobility. And, two, they have less flexibility: Learning new roles, adapting to change, they have more fully formed preferences at this point.”
A gender link also was evident; women were more likely to leave companies that adopted a pay-for-performance system. “Our study expands existing work by showing that the mental health costs of performance-based pay can be severe enough to necessitate pharmaceutical treatment,” the authors wrote.
Once a firm switched to the pay-for-performance system, the number of employees using anxiety and depression medications, which included Xanax and Zoloft, increased by 5.7%. The actual number of affected employees is almost certainly much higher, according to Dr. Pierce. Projecting the data to the United States, Dr. Pierce and his coauthor, Michael S. Dahl, PhD, estimated that 100,000 Americans could be affected.
“These types of mental health problems are incredibly costly to both the individual and firm. If this is reflective of a broader increase in stress and depression in employees, the costs are very high,” added Dr. Pierce. The study highlights the broader health and wellness implications of the companies’ compensation policies, he said. phys.org.
More and more people in the United States with severe mental illness and addictions reportedly are homeless, particularly in the Pacific Northwest and on the West Coast. Legislation aimed at addressing that problem is under discussion by Washington state lawmakers and appears to have broad support. The bill, which would authorize creation of a teaching hospital with 150 beds for people with mental illness, garnered unanimous support in the state’s House of Representatives and now has passed a Senate committee.
“The need for mental health care across our state has outgrown our facilities and our supply of trained health care professionals,” said State Sen. Annette Cleveland, chair of the Senate Health & Long Term Care Committee. “This important facility will address those needs head-on by expanding our physical capacity, enlarging our skilled workforce and increasing access through the use of telehealth services. The establishment of this dedicated behavioral health facility at the University of Washington would be the first of its kind in the nation.”
Jürgen Unützer, MD, MPH told KOMO News that the facility would be accredited and modern. “We would have a facility that’s from 2021 that’s state of the art, that’s approved, that’s a safe, welcoming environment where people would take their family members and say ‘this is a place that can give me some hope,’ ” said Dr. Unützer, who chairs the department of psychiatry and behavioral services at the University of Washington, Seattle.
The legislation, H.B. 1593, is part of efforts by Gov. Jay Inslee to tackle mental health issues in the state. The state’s aging mental health infrastructure has been losing federal funding, and patient safety issues have been identified at state-run mental health hospitals. KOMO News.
The New York Police Department recently reported a near-doubling of 911 calls by people the city refers to as “emotionally disturbed persons” over the past decade. Encounters between police and people in need reportedly have resulted in the deaths of 14 people over the last 3 years.
“There is a serious problem in New York City in the manner in which the NYPD interacts with mentally ill people,” said attorney Sanford Rubenstein, who is representing seven families whose family members with mental illness have been shot by police since 2016. “The training of police officers with regard to that interaction is limited and the number of patrol officers who have been trained is small. That is unacceptable.”
The problem was recognized years ago, and a plan was put in place by the city to provide mental health training to every police officer. Flash ahead 4 years and less than one-third of the police force has received any mental health training – just 11,970 of the 36,753 uniformed police officers. What’s more, teams of mental health workers and police that were formed 3 years ago to help intervene in responses to emotionally disturbed people have not been brought into the loop of the 911 system. The result has been 911 responses by officers not trained to deal with such situations and without the support of those who could help. The number of 911 calls related to emotionally disturbed people rose from just over 91,000 in 2009 to nearly 180,000 in 2018, averaging almost 500 every day. The calls are disproportionately from predominantly black and Hispanic precincts.
A 2014 announcement of “diversion centers,” where people with emotional disturbances could be brought by police instead of ferrying them to hospitals or jail, has failed to materialize. “[The problem] is overwhelming in the neighborhoods that I represent,” said Bronx council member Ritchie J. Torres. “Whether it be Tremont or Fordham – you can feel it and see it on the ground. ... You see chemically addicted, mentally ill people, who either are languishing on the street or being cycled in and out of the criminal justice system. And I’m wondering to myself, there has to be a better approach. This is insane.” New York Magazine.
Iowa Gov. Kim Reynolds has signed a comprehensive bill that, among other things, aims to make sweeping changes in the state’s mental health system. The new law also requires suicide prevention training for school personnel in the state. “This legislation was pushed over the finish line by individuals and families who knew firsthand the importance of having a robust mental health system,” Gov. Reynolds said. Critics contend that the legislation does not go far enough in several respects, including specifying where funding will come from and ensuring full access to care. Meanwhile, the governor announced plans to sign an executive order “establishing a platform to begin developing a children’s mental health system.” Des Moines Register.
Emergency room staff at AdventHealth hospitals in Orlando and neighboring Kissimmee, Fla., will begin assessing the mental health of patients as part of a pilot project with the University of Central Florida, according to reporting by 90.7 WMFE, a National Public Radio affiliate in central Florida. “How do we start providing that preventive care like we would with a typical chest pain patient? The same type of health care probably doesn’t apply to those patients with that mental health disorder,” said Robert Geissler, director of emergency services at AdventHealth Kissimmee. “And that’s why we’re trying to change the landscape with this particular project.” Similar programs in Michigan and Tennessee have helped curb suicides and lowered costs associated with mental health–related emergency care. As part of the AdventHealth program in Florida, emergency room staff will ask patients about feelings of hopelessness or despair as part of routine assessments. Patients deemed at high risk of suicide will be paired with counselors for the next 3 months, with daily calls and possibly house visits. Other mental health care resources in the community will be enlisted. 90.7 WMFE.
A study from researchers at Washington University in St. Louis and Aarhus University in Denmark charts the relationship of payment based on work done and employee mental health. According to phys.org, an aggregator of science, research, and technology news, performance-based pay is in place in 70% of U.S. companies. This means that employee income is based on a combination of bonuses, commission, profit sharing, and individual/team incentives, rather than guaranteed salaries. For some employees, performance-based pay can prove lucrative. But for others, such systems can lead to poor mental health.
The study, published in the Academy of Management Discoveries, charted the use of prescription medications for anxiety and depression by nearly 319,000 employees at about 1,300 companies in Denmark (2019 Feb 26. doi: 10.5465/amd.2018.0007). Those in lower-paid positions and older employees were most vulnerable.
“Basically, older workers seem to be driving all of this effect,” said coauthor Lamar Pierce, PhD, professor of organization and strategy, and associate dean at Washington University. “One, it’s harder for them to move, so they have less labor mobility. And, two, they have less flexibility: Learning new roles, adapting to change, they have more fully formed preferences at this point.”
A gender link also was evident; women were more likely to leave companies that adopted a pay-for-performance system. “Our study expands existing work by showing that the mental health costs of performance-based pay can be severe enough to necessitate pharmaceutical treatment,” the authors wrote.
Once a firm switched to the pay-for-performance system, the number of employees using anxiety and depression medications, which included Xanax and Zoloft, increased by 5.7%. The actual number of affected employees is almost certainly much higher, according to Dr. Pierce. Projecting the data to the United States, Dr. Pierce and his coauthor, Michael S. Dahl, PhD, estimated that 100,000 Americans could be affected.
“These types of mental health problems are incredibly costly to both the individual and firm. If this is reflective of a broader increase in stress and depression in employees, the costs are very high,” added Dr. Pierce. The study highlights the broader health and wellness implications of the companies’ compensation policies, he said. phys.org.
More and more people in the United States with severe mental illness and addictions reportedly are homeless, particularly in the Pacific Northwest and on the West Coast. Legislation aimed at addressing that problem is under discussion by Washington state lawmakers and appears to have broad support. The bill, which would authorize creation of a teaching hospital with 150 beds for people with mental illness, garnered unanimous support in the state’s House of Representatives and now has passed a Senate committee.
“The need for mental health care across our state has outgrown our facilities and our supply of trained health care professionals,” said State Sen. Annette Cleveland, chair of the Senate Health & Long Term Care Committee. “This important facility will address those needs head-on by expanding our physical capacity, enlarging our skilled workforce and increasing access through the use of telehealth services. The establishment of this dedicated behavioral health facility at the University of Washington would be the first of its kind in the nation.”
Jürgen Unützer, MD, MPH told KOMO News that the facility would be accredited and modern. “We would have a facility that’s from 2021 that’s state of the art, that’s approved, that’s a safe, welcoming environment where people would take their family members and say ‘this is a place that can give me some hope,’ ” said Dr. Unützer, who chairs the department of psychiatry and behavioral services at the University of Washington, Seattle.
The legislation, H.B. 1593, is part of efforts by Gov. Jay Inslee to tackle mental health issues in the state. The state’s aging mental health infrastructure has been losing federal funding, and patient safety issues have been identified at state-run mental health hospitals. KOMO News.
The New York Police Department recently reported a near-doubling of 911 calls by people the city refers to as “emotionally disturbed persons” over the past decade. Encounters between police and people in need reportedly have resulted in the deaths of 14 people over the last 3 years.
“There is a serious problem in New York City in the manner in which the NYPD interacts with mentally ill people,” said attorney Sanford Rubenstein, who is representing seven families whose family members with mental illness have been shot by police since 2016. “The training of police officers with regard to that interaction is limited and the number of patrol officers who have been trained is small. That is unacceptable.”
The problem was recognized years ago, and a plan was put in place by the city to provide mental health training to every police officer. Flash ahead 4 years and less than one-third of the police force has received any mental health training – just 11,970 of the 36,753 uniformed police officers. What’s more, teams of mental health workers and police that were formed 3 years ago to help intervene in responses to emotionally disturbed people have not been brought into the loop of the 911 system. The result has been 911 responses by officers not trained to deal with such situations and without the support of those who could help. The number of 911 calls related to emotionally disturbed people rose from just over 91,000 in 2009 to nearly 180,000 in 2018, averaging almost 500 every day. The calls are disproportionately from predominantly black and Hispanic precincts.
A 2014 announcement of “diversion centers,” where people with emotional disturbances could be brought by police instead of ferrying them to hospitals or jail, has failed to materialize. “[The problem] is overwhelming in the neighborhoods that I represent,” said Bronx council member Ritchie J. Torres. “Whether it be Tremont or Fordham – you can feel it and see it on the ground. ... You see chemically addicted, mentally ill people, who either are languishing on the street or being cycled in and out of the criminal justice system. And I’m wondering to myself, there has to be a better approach. This is insane.” New York Magazine.
Iowa Gov. Kim Reynolds has signed a comprehensive bill that, among other things, aims to make sweeping changes in the state’s mental health system. The new law also requires suicide prevention training for school personnel in the state. “This legislation was pushed over the finish line by individuals and families who knew firsthand the importance of having a robust mental health system,” Gov. Reynolds said. Critics contend that the legislation does not go far enough in several respects, including specifying where funding will come from and ensuring full access to care. Meanwhile, the governor announced plans to sign an executive order “establishing a platform to begin developing a children’s mental health system.” Des Moines Register.
Emergency room staff at AdventHealth hospitals in Orlando and neighboring Kissimmee, Fla., will begin assessing the mental health of patients as part of a pilot project with the University of Central Florida, according to reporting by 90.7 WMFE, a National Public Radio affiliate in central Florida. “How do we start providing that preventive care like we would with a typical chest pain patient? The same type of health care probably doesn’t apply to those patients with that mental health disorder,” said Robert Geissler, director of emergency services at AdventHealth Kissimmee. “And that’s why we’re trying to change the landscape with this particular project.” Similar programs in Michigan and Tennessee have helped curb suicides and lowered costs associated with mental health–related emergency care. As part of the AdventHealth program in Florida, emergency room staff will ask patients about feelings of hopelessness or despair as part of routine assessments. Patients deemed at high risk of suicide will be paired with counselors for the next 3 months, with daily calls and possibly house visits. Other mental health care resources in the community will be enlisted. 90.7 WMFE.
A study from researchers at Washington University in St. Louis and Aarhus University in Denmark charts the relationship of payment based on work done and employee mental health. According to phys.org, an aggregator of science, research, and technology news, performance-based pay is in place in 70% of U.S. companies. This means that employee income is based on a combination of bonuses, commission, profit sharing, and individual/team incentives, rather than guaranteed salaries. For some employees, performance-based pay can prove lucrative. But for others, such systems can lead to poor mental health.
The study, published in the Academy of Management Discoveries, charted the use of prescription medications for anxiety and depression by nearly 319,000 employees at about 1,300 companies in Denmark (2019 Feb 26. doi: 10.5465/amd.2018.0007). Those in lower-paid positions and older employees were most vulnerable.
“Basically, older workers seem to be driving all of this effect,” said coauthor Lamar Pierce, PhD, professor of organization and strategy, and associate dean at Washington University. “One, it’s harder for them to move, so they have less labor mobility. And, two, they have less flexibility: Learning new roles, adapting to change, they have more fully formed preferences at this point.”
A gender link also was evident; women were more likely to leave companies that adopted a pay-for-performance system. “Our study expands existing work by showing that the mental health costs of performance-based pay can be severe enough to necessitate pharmaceutical treatment,” the authors wrote.
Once a firm switched to the pay-for-performance system, the number of employees using anxiety and depression medications, which included Xanax and Zoloft, increased by 5.7%. The actual number of affected employees is almost certainly much higher, according to Dr. Pierce. Projecting the data to the United States, Dr. Pierce and his coauthor, Michael S. Dahl, PhD, estimated that 100,000 Americans could be affected.
“These types of mental health problems are incredibly costly to both the individual and firm. If this is reflective of a broader increase in stress and depression in employees, the costs are very high,” added Dr. Pierce. The study highlights the broader health and wellness implications of the companies’ compensation policies, he said. phys.org.
More and more people in the United States with severe mental illness and addictions reportedly are homeless, particularly in the Pacific Northwest and on the West Coast. Legislation aimed at addressing that problem is under discussion by Washington state lawmakers and appears to have broad support. The bill, which would authorize creation of a teaching hospital with 150 beds for people with mental illness, garnered unanimous support in the state’s House of Representatives and now has passed a Senate committee.
“The need for mental health care across our state has outgrown our facilities and our supply of trained health care professionals,” said State Sen. Annette Cleveland, chair of the Senate Health & Long Term Care Committee. “This important facility will address those needs head-on by expanding our physical capacity, enlarging our skilled workforce and increasing access through the use of telehealth services. The establishment of this dedicated behavioral health facility at the University of Washington would be the first of its kind in the nation.”
Jürgen Unützer, MD, MPH told KOMO News that the facility would be accredited and modern. “We would have a facility that’s from 2021 that’s state of the art, that’s approved, that’s a safe, welcoming environment where people would take their family members and say ‘this is a place that can give me some hope,’ ” said Dr. Unützer, who chairs the department of psychiatry and behavioral services at the University of Washington, Seattle.
The legislation, H.B. 1593, is part of efforts by Gov. Jay Inslee to tackle mental health issues in the state. The state’s aging mental health infrastructure has been losing federal funding, and patient safety issues have been identified at state-run mental health hospitals. KOMO News.
The New York Police Department recently reported a near-doubling of 911 calls by people the city refers to as “emotionally disturbed persons” over the past decade. Encounters between police and people in need reportedly have resulted in the deaths of 14 people over the last 3 years.
“There is a serious problem in New York City in the manner in which the NYPD interacts with mentally ill people,” said attorney Sanford Rubenstein, who is representing seven families whose family members with mental illness have been shot by police since 2016. “The training of police officers with regard to that interaction is limited and the number of patrol officers who have been trained is small. That is unacceptable.”
The problem was recognized years ago, and a plan was put in place by the city to provide mental health training to every police officer. Flash ahead 4 years and less than one-third of the police force has received any mental health training – just 11,970 of the 36,753 uniformed police officers. What’s more, teams of mental health workers and police that were formed 3 years ago to help intervene in responses to emotionally disturbed people have not been brought into the loop of the 911 system. The result has been 911 responses by officers not trained to deal with such situations and without the support of those who could help. The number of 911 calls related to emotionally disturbed people rose from just over 91,000 in 2009 to nearly 180,000 in 2018, averaging almost 500 every day. The calls are disproportionately from predominantly black and Hispanic precincts.
A 2014 announcement of “diversion centers,” where people with emotional disturbances could be brought by police instead of ferrying them to hospitals or jail, has failed to materialize. “[The problem] is overwhelming in the neighborhoods that I represent,” said Bronx council member Ritchie J. Torres. “Whether it be Tremont or Fordham – you can feel it and see it on the ground. ... You see chemically addicted, mentally ill people, who either are languishing on the street or being cycled in and out of the criminal justice system. And I’m wondering to myself, there has to be a better approach. This is insane.” New York Magazine.
Iowa Gov. Kim Reynolds has signed a comprehensive bill that, among other things, aims to make sweeping changes in the state’s mental health system. The new law also requires suicide prevention training for school personnel in the state. “This legislation was pushed over the finish line by individuals and families who knew firsthand the importance of having a robust mental health system,” Gov. Reynolds said. Critics contend that the legislation does not go far enough in several respects, including specifying where funding will come from and ensuring full access to care. Meanwhile, the governor announced plans to sign an executive order “establishing a platform to begin developing a children’s mental health system.” Des Moines Register.
Emergency room staff at AdventHealth hospitals in Orlando and neighboring Kissimmee, Fla., will begin assessing the mental health of patients as part of a pilot project with the University of Central Florida, according to reporting by 90.7 WMFE, a National Public Radio affiliate in central Florida. “How do we start providing that preventive care like we would with a typical chest pain patient? The same type of health care probably doesn’t apply to those patients with that mental health disorder,” said Robert Geissler, director of emergency services at AdventHealth Kissimmee. “And that’s why we’re trying to change the landscape with this particular project.” Similar programs in Michigan and Tennessee have helped curb suicides and lowered costs associated with mental health–related emergency care. As part of the AdventHealth program in Florida, emergency room staff will ask patients about feelings of hopelessness or despair as part of routine assessments. Patients deemed at high risk of suicide will be paired with counselors for the next 3 months, with daily calls and possibly house visits. Other mental health care resources in the community will be enlisted. 90.7 WMFE.
Do Collaborative Models Work for Mental Health in a General Clinical Setting?
Collaborative chronic care models (CCMs) are effective in serious mental illnesses, which has been shown in extensive randomized clinical trials. Much of their effectiveness comes from the emphasis on flexibility: They are implemented according to local needs, capabilities, and priorities. Collaborative chronic care models also provide support: for redesigned work roles that promote “anticipatory” continuous care, for self-management, and for clinical decision making at a local level.
In 2013, the VA Office of Mental Health and Suicide Prevention (OMHSP) began an initiative to enhance care coordination in general mental health clinics with mixed-diagnosis populations. It established interdisciplinary teams in each VA medical center throughout the US. Although providing centrally developed guidance, VAOMHSP gave facilities “broad latitude” to develop their team processes. In 2015, VAOMHSP adopted the CCM.
But most of the data on how well CCMs work for mental health conditions come from depression treatment in primary care—and the effects seem to be inconsistent. So researchers from Veterans Affairs Boston Healthcare System and others partnered with VAOMHSP to find out whether the CCM model would be effective in a general clinical setting.
They recruited 9 VA facilities for a 2-year study conducted in 3 waves. The implementation strategy was based on the premise that “health care is a complex adaptive system rather than a highly controlled machine.” That is, it would work best if local solutions for local challenges could be developed in accordance with evidence-based guidance. The multifaceted approach included an external facilitator who provided guidance and quality improvement expertise and an on-site internal facilitator to direct the implementation.
In the study, 5,596 veterans treated by outpatient general mental health teams were included in hospitalization analyses. A randomly selected sample of 1,050 (including 210 women) was identified for health status interviews.
The researchers found a “robust” and sustained reduction in mental health hospitalization. However, the effects on self-reported health outcomes were “limited,” the researchers say. The mental component score (the primary intervention outcome) did not change statistically significantly with implementation support in adjusted or unadjusted models, nor did other interview measures. The researchers say they saw no difference in the way veterans were treated between higher and lower implementing teams.
In post hoc analyses, though, patients with more complex problems, defined as receiving treatment for ≥ 3 mental health diagnoses in the previous year, did show statistically significant improvements in the facilitation year (by a magnitude of 0.31 SD). By contrast, those with ≤ 2 diagnoses declined nonsignificantly during the same time. The researchers note that other studies have found that CCM-based teams in patient-centered medical homes have also shown more benefit among higher morbidity patients.
Overall, the model was shown to be effectively implemented with “practical, scalable support” for clinicians. Another benefit was that teams performed better, the researchers found. They assessed team function at baseline and during the second 6 months on measures, including communication, cohesion, role clarity, and team primacy (prioritizing team over individual goals). The subscales showed high ratings for cohesion and communication at baseline, which did not change with implementation support. However, role clarity and team primacy improved significantly. The researchers conclude that under typical practice conditions CCMs can help the clinicians help the sickest patients.
Collaborative chronic care models (CCMs) are effective in serious mental illnesses, which has been shown in extensive randomized clinical trials. Much of their effectiveness comes from the emphasis on flexibility: They are implemented according to local needs, capabilities, and priorities. Collaborative chronic care models also provide support: for redesigned work roles that promote “anticipatory” continuous care, for self-management, and for clinical decision making at a local level.
In 2013, the VA Office of Mental Health and Suicide Prevention (OMHSP) began an initiative to enhance care coordination in general mental health clinics with mixed-diagnosis populations. It established interdisciplinary teams in each VA medical center throughout the US. Although providing centrally developed guidance, VAOMHSP gave facilities “broad latitude” to develop their team processes. In 2015, VAOMHSP adopted the CCM.
But most of the data on how well CCMs work for mental health conditions come from depression treatment in primary care—and the effects seem to be inconsistent. So researchers from Veterans Affairs Boston Healthcare System and others partnered with VAOMHSP to find out whether the CCM model would be effective in a general clinical setting.
They recruited 9 VA facilities for a 2-year study conducted in 3 waves. The implementation strategy was based on the premise that “health care is a complex adaptive system rather than a highly controlled machine.” That is, it would work best if local solutions for local challenges could be developed in accordance with evidence-based guidance. The multifaceted approach included an external facilitator who provided guidance and quality improvement expertise and an on-site internal facilitator to direct the implementation.
In the study, 5,596 veterans treated by outpatient general mental health teams were included in hospitalization analyses. A randomly selected sample of 1,050 (including 210 women) was identified for health status interviews.
The researchers found a “robust” and sustained reduction in mental health hospitalization. However, the effects on self-reported health outcomes were “limited,” the researchers say. The mental component score (the primary intervention outcome) did not change statistically significantly with implementation support in adjusted or unadjusted models, nor did other interview measures. The researchers say they saw no difference in the way veterans were treated between higher and lower implementing teams.
In post hoc analyses, though, patients with more complex problems, defined as receiving treatment for ≥ 3 mental health diagnoses in the previous year, did show statistically significant improvements in the facilitation year (by a magnitude of 0.31 SD). By contrast, those with ≤ 2 diagnoses declined nonsignificantly during the same time. The researchers note that other studies have found that CCM-based teams in patient-centered medical homes have also shown more benefit among higher morbidity patients.
Overall, the model was shown to be effectively implemented with “practical, scalable support” for clinicians. Another benefit was that teams performed better, the researchers found. They assessed team function at baseline and during the second 6 months on measures, including communication, cohesion, role clarity, and team primacy (prioritizing team over individual goals). The subscales showed high ratings for cohesion and communication at baseline, which did not change with implementation support. However, role clarity and team primacy improved significantly. The researchers conclude that under typical practice conditions CCMs can help the clinicians help the sickest patients.
Collaborative chronic care models (CCMs) are effective in serious mental illnesses, which has been shown in extensive randomized clinical trials. Much of their effectiveness comes from the emphasis on flexibility: They are implemented according to local needs, capabilities, and priorities. Collaborative chronic care models also provide support: for redesigned work roles that promote “anticipatory” continuous care, for self-management, and for clinical decision making at a local level.
In 2013, the VA Office of Mental Health and Suicide Prevention (OMHSP) began an initiative to enhance care coordination in general mental health clinics with mixed-diagnosis populations. It established interdisciplinary teams in each VA medical center throughout the US. Although providing centrally developed guidance, VAOMHSP gave facilities “broad latitude” to develop their team processes. In 2015, VAOMHSP adopted the CCM.
But most of the data on how well CCMs work for mental health conditions come from depression treatment in primary care—and the effects seem to be inconsistent. So researchers from Veterans Affairs Boston Healthcare System and others partnered with VAOMHSP to find out whether the CCM model would be effective in a general clinical setting.
They recruited 9 VA facilities for a 2-year study conducted in 3 waves. The implementation strategy was based on the premise that “health care is a complex adaptive system rather than a highly controlled machine.” That is, it would work best if local solutions for local challenges could be developed in accordance with evidence-based guidance. The multifaceted approach included an external facilitator who provided guidance and quality improvement expertise and an on-site internal facilitator to direct the implementation.
In the study, 5,596 veterans treated by outpatient general mental health teams were included in hospitalization analyses. A randomly selected sample of 1,050 (including 210 women) was identified for health status interviews.
The researchers found a “robust” and sustained reduction in mental health hospitalization. However, the effects on self-reported health outcomes were “limited,” the researchers say. The mental component score (the primary intervention outcome) did not change statistically significantly with implementation support in adjusted or unadjusted models, nor did other interview measures. The researchers say they saw no difference in the way veterans were treated between higher and lower implementing teams.
In post hoc analyses, though, patients with more complex problems, defined as receiving treatment for ≥ 3 mental health diagnoses in the previous year, did show statistically significant improvements in the facilitation year (by a magnitude of 0.31 SD). By contrast, those with ≤ 2 diagnoses declined nonsignificantly during the same time. The researchers note that other studies have found that CCM-based teams in patient-centered medical homes have also shown more benefit among higher morbidity patients.
Overall, the model was shown to be effectively implemented with “practical, scalable support” for clinicians. Another benefit was that teams performed better, the researchers found. They assessed team function at baseline and during the second 6 months on measures, including communication, cohesion, role clarity, and team primacy (prioritizing team over individual goals). The subscales showed high ratings for cohesion and communication at baseline, which did not change with implementation support. However, role clarity and team primacy improved significantly. The researchers conclude that under typical practice conditions CCMs can help the clinicians help the sickest patients.
Depression increasing among American teens, young adults
Time spent on social media is seen as partly to blame
Depression, suicidal thoughts, and mental distress appear to be on the rise among American teenagers and young adults, and a new study points to their use of social media as a cause. According to the study’s lead author, Jean M. Twenge, PhD, the findings might be evident of a generational shift in mental illness. The study looked at data from more than 200,000 adolescents aged 12-17 and nearly 400,000 young adults aged 18 and over from 2005 to 2017. During that time, reported symptoms consistent with major depression increased by 52% among the teens and 63% among the young adults. Girls were especially at risk, with one in five teenage girls having experienced major depression in 2017. In addition, by 2017, nearly three-quarters of young adults had experienced feelings of hopelessness about their lives. Meanwhile, the rate of suicide rose during that study period. Dr. Twenge said a major factor contributing to those trends is the plugged-in lifestyle of many teens and young adults. “Spending time on social media tends not to be in real time,” said Dr. Twenge, a psychologist at San Diego State University. “You’re not having a real-time conversation with someone – usually you’re not seeing their face, and you can’t give them a hug; it’s just not as emotionally fulfilling as seeing someone in person,” she said in an interview with National Public Radio. , according to Robert Crosnoe, PhD, a sociologist and adolescent health researcher from the University of Texas at Austin. “I think we are living in a time of great uncertainty, where people are unsure about the future of the country but also their own futures,” he said. “And that is anxiety provoking for anybody, but it’s especially true for young people whose whole future is ahead of them.” NPR.
Alexandra Valoras was a high school student who earned straight As and participated in extracurricular school activities like robotics and pastimes like snowboarding. On the outside, her future looked bright. But inside, Alexandra lived in a world of despair. Her journals revealed profound self-loathing and sadness. She repeatedly expressed a desire to end her own life, reported Jim Axelrod of CBS News. Alexandra is far from alone. The suicide rate for American teens her age is at a 40-year high. One reason is the pressure for perfection, with failure being viewed as catastrophic. “I don’t want this notebook to end, I love it more than myself (?) I need a place where there is no need for me to be perfect,” Alexandra wrote in one entry. “We have a culture that makes kids think that if they’re not perfect, they’re less than good,” said Scott White, a counselor at Alexandra’s high school. Not every person can reach them.” On March 18, 2018, Alexandra wrote her last entry. “What I will miss by dying tonight. The possibility of anything getting better.” She then tidied up her room, walked to an overpass, and jumped. She was 17 years old. Her parents, Dean and Alysia Valoras, shared their daughter’s journals with the hope of helping others. “The hurt, the sadness is evolving,” Mr. Valoras said in the report. “And now there is this thing called living, so that I am a good father, a good husband, a good person.” CBS Sunday Morning.
For college students, accessing mental health services can be a challenge – especially when cost is an issue. In an effort to address that problem Loyola University in New Orleans recently opened a clinic for low-income students in need of psychiatric services. The clinic, opened in February, hopes to serve about 50 patients each week and is open to students and community members. “I’m really stoked about working with this demographic. It’s a population that doesn’t make a lot of money. So you can go to this clinic, pay a small co-pay, and not have to rely on having health insurance,” said Sarah Zoghbi of the New Orleans Musicians’ Clinic & Assistance Foundation, one of the organizations providing support to the clinic. The clinic aims to address the gap in mental health services for the underinsured and uninsured in the area. And it’s sorely needed. Louisiana ranks 38th among the states for lower rates of access to care and higher prevalence of mental illness, according to the 2019 Mental Health America report. About 599,000 adults in Louisiana, about 17% of the population, have a mental illness. “It is our sincere hope to fill a gap in the community by providing high-quality services for those in need,” said the clinic’s director John Dewell, PhD. “No one will be turned away for lack of funds.” The Times-Picayune.
More and more video games are “tackling mental health issues,” Laura Parker wrote in the New York Times. “Mental health is becoming a more central narrative in our culture with efforts to normalize mental health challenges,” according to Eve Crevoshay, of Take This, a group that seeks to destigmatize mental illness within the video game industry. “With that trend comes response from creative industries, including games.” One of the games that Ms. Parker mentioned, called Sea of Solitude, is expected to publish this year. Another, called Celeste, examines depression and anxiety through a protagonist who tries to avoid obstacles. And yet another, called Hellblade, focuses on a warrior who deals with psychosis. Raffael Boccamazzo, PsyD, a psychotherapist who works as clinical director for Take This, said video games can be more effective at helping people bounce back “from negative moods than passive forms of media like TV or movies.” Take This provides resources, guidelines, and training about mental health on its website. The New York Times.
General offers of help to families in crisis are fine but might not get acted upon. It is better to offer something specific, and “the more specific, the better,” wrote Andrea Paterson in the Washington Post. “Not ‘Can I bring dinner sometime?’ Instead, something like, ‘I’d like to come over on Thursday and bring turkey chili.’ Ms. Paterson wrote that she came to that conclusion after her husband was diagnosed with stage 4 metastatic lung cancer in 2013. His death 4½ years later plunged Ms. Paterson and her sons “into crisis,” she wrote. Her tight network of friends and neighbors helped her cope, she said, and their concrete offers of help kept the family going. Such offers need not be earth shattering or monumental, she said. One of her “all-time favorites” was delightfully simple: “ ‘I’m having a cup of tea, watching Audrey learn to roller skate in the driveway. Come join me.’ Needless to say, I joined her.” Ms. Paterson shared several other specifics that might help families in crisis, such as getting a friend to set up a support network of helpers who can pick up prescriptions, meet repairmen, and so on. “Remember that what you offer doesn’t need to be expensive or extravagant,” Ms. Paterson wrote. “ ‘Tomorrow night we are watching the Super Bowl: Join us for tacos and ice cream.’ After all, no one can be in a crisis 24/7.” The Washington Post.
Time spent on social media is seen as partly to blame
Time spent on social media is seen as partly to blame
Depression, suicidal thoughts, and mental distress appear to be on the rise among American teenagers and young adults, and a new study points to their use of social media as a cause. According to the study’s lead author, Jean M. Twenge, PhD, the findings might be evident of a generational shift in mental illness. The study looked at data from more than 200,000 adolescents aged 12-17 and nearly 400,000 young adults aged 18 and over from 2005 to 2017. During that time, reported symptoms consistent with major depression increased by 52% among the teens and 63% among the young adults. Girls were especially at risk, with one in five teenage girls having experienced major depression in 2017. In addition, by 2017, nearly three-quarters of young adults had experienced feelings of hopelessness about their lives. Meanwhile, the rate of suicide rose during that study period. Dr. Twenge said a major factor contributing to those trends is the plugged-in lifestyle of many teens and young adults. “Spending time on social media tends not to be in real time,” said Dr. Twenge, a psychologist at San Diego State University. “You’re not having a real-time conversation with someone – usually you’re not seeing their face, and you can’t give them a hug; it’s just not as emotionally fulfilling as seeing someone in person,” she said in an interview with National Public Radio. , according to Robert Crosnoe, PhD, a sociologist and adolescent health researcher from the University of Texas at Austin. “I think we are living in a time of great uncertainty, where people are unsure about the future of the country but also their own futures,” he said. “And that is anxiety provoking for anybody, but it’s especially true for young people whose whole future is ahead of them.” NPR.
Alexandra Valoras was a high school student who earned straight As and participated in extracurricular school activities like robotics and pastimes like snowboarding. On the outside, her future looked bright. But inside, Alexandra lived in a world of despair. Her journals revealed profound self-loathing and sadness. She repeatedly expressed a desire to end her own life, reported Jim Axelrod of CBS News. Alexandra is far from alone. The suicide rate for American teens her age is at a 40-year high. One reason is the pressure for perfection, with failure being viewed as catastrophic. “I don’t want this notebook to end, I love it more than myself (?) I need a place where there is no need for me to be perfect,” Alexandra wrote in one entry. “We have a culture that makes kids think that if they’re not perfect, they’re less than good,” said Scott White, a counselor at Alexandra’s high school. Not every person can reach them.” On March 18, 2018, Alexandra wrote her last entry. “What I will miss by dying tonight. The possibility of anything getting better.” She then tidied up her room, walked to an overpass, and jumped. She was 17 years old. Her parents, Dean and Alysia Valoras, shared their daughter’s journals with the hope of helping others. “The hurt, the sadness is evolving,” Mr. Valoras said in the report. “And now there is this thing called living, so that I am a good father, a good husband, a good person.” CBS Sunday Morning.
For college students, accessing mental health services can be a challenge – especially when cost is an issue. In an effort to address that problem Loyola University in New Orleans recently opened a clinic for low-income students in need of psychiatric services. The clinic, opened in February, hopes to serve about 50 patients each week and is open to students and community members. “I’m really stoked about working with this demographic. It’s a population that doesn’t make a lot of money. So you can go to this clinic, pay a small co-pay, and not have to rely on having health insurance,” said Sarah Zoghbi of the New Orleans Musicians’ Clinic & Assistance Foundation, one of the organizations providing support to the clinic. The clinic aims to address the gap in mental health services for the underinsured and uninsured in the area. And it’s sorely needed. Louisiana ranks 38th among the states for lower rates of access to care and higher prevalence of mental illness, according to the 2019 Mental Health America report. About 599,000 adults in Louisiana, about 17% of the population, have a mental illness. “It is our sincere hope to fill a gap in the community by providing high-quality services for those in need,” said the clinic’s director John Dewell, PhD. “No one will be turned away for lack of funds.” The Times-Picayune.
More and more video games are “tackling mental health issues,” Laura Parker wrote in the New York Times. “Mental health is becoming a more central narrative in our culture with efforts to normalize mental health challenges,” according to Eve Crevoshay, of Take This, a group that seeks to destigmatize mental illness within the video game industry. “With that trend comes response from creative industries, including games.” One of the games that Ms. Parker mentioned, called Sea of Solitude, is expected to publish this year. Another, called Celeste, examines depression and anxiety through a protagonist who tries to avoid obstacles. And yet another, called Hellblade, focuses on a warrior who deals with psychosis. Raffael Boccamazzo, PsyD, a psychotherapist who works as clinical director for Take This, said video games can be more effective at helping people bounce back “from negative moods than passive forms of media like TV or movies.” Take This provides resources, guidelines, and training about mental health on its website. The New York Times.
General offers of help to families in crisis are fine but might not get acted upon. It is better to offer something specific, and “the more specific, the better,” wrote Andrea Paterson in the Washington Post. “Not ‘Can I bring dinner sometime?’ Instead, something like, ‘I’d like to come over on Thursday and bring turkey chili.’ Ms. Paterson wrote that she came to that conclusion after her husband was diagnosed with stage 4 metastatic lung cancer in 2013. His death 4½ years later plunged Ms. Paterson and her sons “into crisis,” she wrote. Her tight network of friends and neighbors helped her cope, she said, and their concrete offers of help kept the family going. Such offers need not be earth shattering or monumental, she said. One of her “all-time favorites” was delightfully simple: “ ‘I’m having a cup of tea, watching Audrey learn to roller skate in the driveway. Come join me.’ Needless to say, I joined her.” Ms. Paterson shared several other specifics that might help families in crisis, such as getting a friend to set up a support network of helpers who can pick up prescriptions, meet repairmen, and so on. “Remember that what you offer doesn’t need to be expensive or extravagant,” Ms. Paterson wrote. “ ‘Tomorrow night we are watching the Super Bowl: Join us for tacos and ice cream.’ After all, no one can be in a crisis 24/7.” The Washington Post.
Depression, suicidal thoughts, and mental distress appear to be on the rise among American teenagers and young adults, and a new study points to their use of social media as a cause. According to the study’s lead author, Jean M. Twenge, PhD, the findings might be evident of a generational shift in mental illness. The study looked at data from more than 200,000 adolescents aged 12-17 and nearly 400,000 young adults aged 18 and over from 2005 to 2017. During that time, reported symptoms consistent with major depression increased by 52% among the teens and 63% among the young adults. Girls were especially at risk, with one in five teenage girls having experienced major depression in 2017. In addition, by 2017, nearly three-quarters of young adults had experienced feelings of hopelessness about their lives. Meanwhile, the rate of suicide rose during that study period. Dr. Twenge said a major factor contributing to those trends is the plugged-in lifestyle of many teens and young adults. “Spending time on social media tends not to be in real time,” said Dr. Twenge, a psychologist at San Diego State University. “You’re not having a real-time conversation with someone – usually you’re not seeing their face, and you can’t give them a hug; it’s just not as emotionally fulfilling as seeing someone in person,” she said in an interview with National Public Radio. , according to Robert Crosnoe, PhD, a sociologist and adolescent health researcher from the University of Texas at Austin. “I think we are living in a time of great uncertainty, where people are unsure about the future of the country but also their own futures,” he said. “And that is anxiety provoking for anybody, but it’s especially true for young people whose whole future is ahead of them.” NPR.
Alexandra Valoras was a high school student who earned straight As and participated in extracurricular school activities like robotics and pastimes like snowboarding. On the outside, her future looked bright. But inside, Alexandra lived in a world of despair. Her journals revealed profound self-loathing and sadness. She repeatedly expressed a desire to end her own life, reported Jim Axelrod of CBS News. Alexandra is far from alone. The suicide rate for American teens her age is at a 40-year high. One reason is the pressure for perfection, with failure being viewed as catastrophic. “I don’t want this notebook to end, I love it more than myself (?) I need a place where there is no need for me to be perfect,” Alexandra wrote in one entry. “We have a culture that makes kids think that if they’re not perfect, they’re less than good,” said Scott White, a counselor at Alexandra’s high school. Not every person can reach them.” On March 18, 2018, Alexandra wrote her last entry. “What I will miss by dying tonight. The possibility of anything getting better.” She then tidied up her room, walked to an overpass, and jumped. She was 17 years old. Her parents, Dean and Alysia Valoras, shared their daughter’s journals with the hope of helping others. “The hurt, the sadness is evolving,” Mr. Valoras said in the report. “And now there is this thing called living, so that I am a good father, a good husband, a good person.” CBS Sunday Morning.
For college students, accessing mental health services can be a challenge – especially when cost is an issue. In an effort to address that problem Loyola University in New Orleans recently opened a clinic for low-income students in need of psychiatric services. The clinic, opened in February, hopes to serve about 50 patients each week and is open to students and community members. “I’m really stoked about working with this demographic. It’s a population that doesn’t make a lot of money. So you can go to this clinic, pay a small co-pay, and not have to rely on having health insurance,” said Sarah Zoghbi of the New Orleans Musicians’ Clinic & Assistance Foundation, one of the organizations providing support to the clinic. The clinic aims to address the gap in mental health services for the underinsured and uninsured in the area. And it’s sorely needed. Louisiana ranks 38th among the states for lower rates of access to care and higher prevalence of mental illness, according to the 2019 Mental Health America report. About 599,000 adults in Louisiana, about 17% of the population, have a mental illness. “It is our sincere hope to fill a gap in the community by providing high-quality services for those in need,” said the clinic’s director John Dewell, PhD. “No one will be turned away for lack of funds.” The Times-Picayune.
More and more video games are “tackling mental health issues,” Laura Parker wrote in the New York Times. “Mental health is becoming a more central narrative in our culture with efforts to normalize mental health challenges,” according to Eve Crevoshay, of Take This, a group that seeks to destigmatize mental illness within the video game industry. “With that trend comes response from creative industries, including games.” One of the games that Ms. Parker mentioned, called Sea of Solitude, is expected to publish this year. Another, called Celeste, examines depression and anxiety through a protagonist who tries to avoid obstacles. And yet another, called Hellblade, focuses on a warrior who deals with psychosis. Raffael Boccamazzo, PsyD, a psychotherapist who works as clinical director for Take This, said video games can be more effective at helping people bounce back “from negative moods than passive forms of media like TV or movies.” Take This provides resources, guidelines, and training about mental health on its website. The New York Times.
General offers of help to families in crisis are fine but might not get acted upon. It is better to offer something specific, and “the more specific, the better,” wrote Andrea Paterson in the Washington Post. “Not ‘Can I bring dinner sometime?’ Instead, something like, ‘I’d like to come over on Thursday and bring turkey chili.’ Ms. Paterson wrote that she came to that conclusion after her husband was diagnosed with stage 4 metastatic lung cancer in 2013. His death 4½ years later plunged Ms. Paterson and her sons “into crisis,” she wrote. Her tight network of friends and neighbors helped her cope, she said, and their concrete offers of help kept the family going. Such offers need not be earth shattering or monumental, she said. One of her “all-time favorites” was delightfully simple: “ ‘I’m having a cup of tea, watching Audrey learn to roller skate in the driveway. Come join me.’ Needless to say, I joined her.” Ms. Paterson shared several other specifics that might help families in crisis, such as getting a friend to set up a support network of helpers who can pick up prescriptions, meet repairmen, and so on. “Remember that what you offer doesn’t need to be expensive or extravagant,” Ms. Paterson wrote. “ ‘Tomorrow night we are watching the Super Bowl: Join us for tacos and ice cream.’ After all, no one can be in a crisis 24/7.” The Washington Post.
Depression: a changing concept in the age of ketamine
What does it mean to define an amalgamation of symptoms as a “psychiatric disorder?” Are psychiatric disorders an extreme variation of normative human behavior? Is human behavior simply an output phenotype of some neurologic chemical processes that become disordered in mental illness? Can depression be localized in the brain and subsequently turned on or off? If depression were to be localized in the brain, would it be an excess of a neurotransmitter, the depletion of a receptor, a malfunctioning neuron, an overactive connectome, poorly processed genetic material, or something as yet undefined? Those questions always have been present in our minds and influenced our understanding of patients, but a recent development in psychiatry raises questions about one of the few things we were historically confident about.
A part of our foundational understanding of depression was that it is not sadness, per se. One can be sad for any amount of time. It is not uncommon to feel sad for any variety of reasons, such as watching an adorable 60-second commercial for dog food.1 Those fleeting moments of sadness can even be empowering; they remind us about the things we care about and would be sad to miss.
Sadness in oneself can demonstrate the experience of empathic sadness for others. On the contrary, depression appears to have little apparent purpose, and instead results in a maladaptive way of coping that is all-consuming and often very damaging. Depression is not a mood but a state of being, something that is not defined by how one feels but who one is or has become because of the disorder. So it comes as somewhat of a surprise when we heard that ketamine could alleviate depression in minutes.2,3 As described by a ketamine expert, symptoms are relieved in “no less than an hour.”4 The surprise is not so much that a treatment would work but that improvement could be defined in such a short time frame.
Psychiatry has debated the definition of depression for its entire existence. There are many ways to tackle the concept of depression. A lot of the debate has been about the causes of depression. One example of the continued evolution of our understanding of depression is our prior categorization of depression as “exogenous” or “endogenous.”5 Exogenous depression was described as happening in the context of social stressors and as best treated with therapy. Endogenous depression was a supposedly truer form of depression as a disorder and was more biologically based. Patients suffering from endogenous depression were thought to have chemical abnormalities in the brain that could be alleviated by tricyclic antidepressants and subsequently SSRIs. Like many prior debates about depression, this one appears to be little discussed nowadays. A review of the use of the term “endogenous depression” in books shows an onset in the 1930s, a peak in the 1980s, and a rapid decline since.6
More recently, psychiatrists have defined depression using the DSM-5 criteria. Depression is thought to be the presence of at least five out of nine symptoms listed in the manual for a period of 2 weeks that cause significant distress or impairment.7 The DSM attempts to address criticism by providing information on its limitations and best use, and encourages clinical interpretation of symptoms. The DSM does not portray itself as a gold standard but rather as a tool for treatment planning and effective communication between peers. Furthermore, the National Institute on Mental Health is promoting an alternative understanding of depression using its own Research Domain Criteria, which attempt to provide a more objective understanding of the disorder based on biological rather than subjective correlates.
The growing literature on ketamine partly hinges on the belief that depression is something that can be redefined and changed at any moment. Many trials ask patients whether their depression remains in remission in the subsequent hours, days, and weeks following administration of the drug. However, one wonders if that is even possible. If a patient’s depression is alleviated in an hour, was it really clinical depression? Is it truly in remission? Contrary to our previous understanding, is depression, in reality, a switch that can be turned off by an infusion of an N-methyl-D-aspartate (NMDA)–receptor antagonist? Without minimizing the suffering of patients seeking ketamine or the relief provided to patients who benefit from the treatment, we simply are pointing out that the definition of depression did not account for this reported phenomenon of relatively instantaneous relief. The seemingly miraculous effects of ketamine suggest a new paradigm where any intervention – whether chemical, social, or psychological – could turn off the devastating effects of depression in an instant.
After all, the most widely used scale of depression, the nine-item Patient Health Questionnaire (PHQ-9) asks patients, “Over the last 2 weeks, how often have you been bothered by any of the following problems?” The highest answer one can give is “Nearly every day.” Are we incorrect to think that if one were suicidal every minute of the past 2 weeks, one would still score, nearly every day, even if one’s symptoms were relieved for the past hour? Thus, a maximum score of 27 would remain a 27 no matter what happened in the past hour.
We do realize that we are being overly literal. Ketamine makes some people feel better quickly, and researchers try to capture that effect by asking patients about their symptoms within short intervals. Furthermore, one has to start somewhere. After the infusion is a reasonable time to ask patients how they feel. We are also cognizant that many ketamine researchers do more long-term follow-ups and/or have recommended longer-term studies. Nonetheless,
Expanding our definition of depression to encompass experiences with short time frames may have unintended consequences. As living circumstances rarely change in minutes, the emphasis on rapid recovery makes the patients more in control of their reported experiences and thus their diagnoses. One cannot assess a patient’s impairment or disability from minute to minute. One is left with emphasizing the patient’s subjective symptoms and deemphasizing their relationships, goals, and daily functioning. How could one measure eating habits, hygiene, or participation in hobbies every hour? Another consequence of this reduced time frame is the expansion of a diagnosis that no longer requires the presence of symptoms for 2 weeks. Considering the already vast number of people diagnosed with depression,9,10 this small change may further expand the number diagnosed with a mood disorder. Perhaps to many practitioners and patients these arguments seem obtuse and fastidious, but there is a core failure in modern psychiatry to clearly differentiate the human condition from mental illness. Said failure has vast implications for psychiatric epidemiology, the sociological understanding of psychic suffering and suicide, as well as the overprescribing of psychotropic medications.
Ketamine is an exciting prospect to many psychiatrists who feel like we have had little advancement and few novel treatments in a long time; advertised breakthroughs in the treatment of depression since fluoxetine have not been particularly impressive. Furthermore, the concerns about potential ketamine abuse are not theoretical but a very real problem in some parts of the world.11,12 The concerns about abuse are worsened considering recent evidence that suggests that ketamine’s effect may be driven by its opiate rather than NMDA effects.13 While some have discussed those concerns, we think that the field also needs to address the fact that the debate about ketamine is also changing our definition of depression.
References
1. https://www.youtube.com/watch?v=MpcUN6XvGmk.
2. J Clin Psychiatry. 2016 Jun;77(6):e719-25.
3. Emerg (Tehran). 2014 Winter;2(1):36-9.
4. “Is esketamine the game-changer for depression we want?” Rolling Stone. 2019 Mar 11.
5. Psychol Med. 1971;1(3):191-6.
6. https://books.google.com/ngrams.
7. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). American Psychiatric Association, 2013.
8. Am J Psychiatry. 2014 Apr;171(4):395-7.
9. “Many people taking antidepressants discover they cannot quit.” New York Times. 2018 Apr 7.
10. “Antidepressants show greatest increase in number of prescription items dispensed.” National Health Service. 2015 Jul 5.
11. “The ketamine connection.” BBC News. 2015 Jul 10.
12. Front Psychiatry. 2018 Jul 17. doi: 10.33389/fpsyt.2018.00313.
13. Am J Psychiatry. 2018 Dec 1;175(2):1205-15.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. Among his writings is Coercion and the critical psychiatrist, chapter 7 in the new book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer Nature Switzerland, 2019, pp. 155-77). Dr. Lehman is an associate professor of psychiatry at UCSD. He is codirector of all Acute and Intensive Psychiatric Treatment at the VA Medical Center in San Diego, where he practices clinical psychiatry. He also is the course director for the UCSD third-year medical student psychiatry clerkship.
*This article was updated 3/25/2019.
What does it mean to define an amalgamation of symptoms as a “psychiatric disorder?” Are psychiatric disorders an extreme variation of normative human behavior? Is human behavior simply an output phenotype of some neurologic chemical processes that become disordered in mental illness? Can depression be localized in the brain and subsequently turned on or off? If depression were to be localized in the brain, would it be an excess of a neurotransmitter, the depletion of a receptor, a malfunctioning neuron, an overactive connectome, poorly processed genetic material, or something as yet undefined? Those questions always have been present in our minds and influenced our understanding of patients, but a recent development in psychiatry raises questions about one of the few things we were historically confident about.
A part of our foundational understanding of depression was that it is not sadness, per se. One can be sad for any amount of time. It is not uncommon to feel sad for any variety of reasons, such as watching an adorable 60-second commercial for dog food.1 Those fleeting moments of sadness can even be empowering; they remind us about the things we care about and would be sad to miss.
Sadness in oneself can demonstrate the experience of empathic sadness for others. On the contrary, depression appears to have little apparent purpose, and instead results in a maladaptive way of coping that is all-consuming and often very damaging. Depression is not a mood but a state of being, something that is not defined by how one feels but who one is or has become because of the disorder. So it comes as somewhat of a surprise when we heard that ketamine could alleviate depression in minutes.2,3 As described by a ketamine expert, symptoms are relieved in “no less than an hour.”4 The surprise is not so much that a treatment would work but that improvement could be defined in such a short time frame.
Psychiatry has debated the definition of depression for its entire existence. There are many ways to tackle the concept of depression. A lot of the debate has been about the causes of depression. One example of the continued evolution of our understanding of depression is our prior categorization of depression as “exogenous” or “endogenous.”5 Exogenous depression was described as happening in the context of social stressors and as best treated with therapy. Endogenous depression was a supposedly truer form of depression as a disorder and was more biologically based. Patients suffering from endogenous depression were thought to have chemical abnormalities in the brain that could be alleviated by tricyclic antidepressants and subsequently SSRIs. Like many prior debates about depression, this one appears to be little discussed nowadays. A review of the use of the term “endogenous depression” in books shows an onset in the 1930s, a peak in the 1980s, and a rapid decline since.6
More recently, psychiatrists have defined depression using the DSM-5 criteria. Depression is thought to be the presence of at least five out of nine symptoms listed in the manual for a period of 2 weeks that cause significant distress or impairment.7 The DSM attempts to address criticism by providing information on its limitations and best use, and encourages clinical interpretation of symptoms. The DSM does not portray itself as a gold standard but rather as a tool for treatment planning and effective communication between peers. Furthermore, the National Institute on Mental Health is promoting an alternative understanding of depression using its own Research Domain Criteria, which attempt to provide a more objective understanding of the disorder based on biological rather than subjective correlates.
The growing literature on ketamine partly hinges on the belief that depression is something that can be redefined and changed at any moment. Many trials ask patients whether their depression remains in remission in the subsequent hours, days, and weeks following administration of the drug. However, one wonders if that is even possible. If a patient’s depression is alleviated in an hour, was it really clinical depression? Is it truly in remission? Contrary to our previous understanding, is depression, in reality, a switch that can be turned off by an infusion of an N-methyl-D-aspartate (NMDA)–receptor antagonist? Without minimizing the suffering of patients seeking ketamine or the relief provided to patients who benefit from the treatment, we simply are pointing out that the definition of depression did not account for this reported phenomenon of relatively instantaneous relief. The seemingly miraculous effects of ketamine suggest a new paradigm where any intervention – whether chemical, social, or psychological – could turn off the devastating effects of depression in an instant.
After all, the most widely used scale of depression, the nine-item Patient Health Questionnaire (PHQ-9) asks patients, “Over the last 2 weeks, how often have you been bothered by any of the following problems?” The highest answer one can give is “Nearly every day.” Are we incorrect to think that if one were suicidal every minute of the past 2 weeks, one would still score, nearly every day, even if one’s symptoms were relieved for the past hour? Thus, a maximum score of 27 would remain a 27 no matter what happened in the past hour.
We do realize that we are being overly literal. Ketamine makes some people feel better quickly, and researchers try to capture that effect by asking patients about their symptoms within short intervals. Furthermore, one has to start somewhere. After the infusion is a reasonable time to ask patients how they feel. We are also cognizant that many ketamine researchers do more long-term follow-ups and/or have recommended longer-term studies. Nonetheless,
Expanding our definition of depression to encompass experiences with short time frames may have unintended consequences. As living circumstances rarely change in minutes, the emphasis on rapid recovery makes the patients more in control of their reported experiences and thus their diagnoses. One cannot assess a patient’s impairment or disability from minute to minute. One is left with emphasizing the patient’s subjective symptoms and deemphasizing their relationships, goals, and daily functioning. How could one measure eating habits, hygiene, or participation in hobbies every hour? Another consequence of this reduced time frame is the expansion of a diagnosis that no longer requires the presence of symptoms for 2 weeks. Considering the already vast number of people diagnosed with depression,9,10 this small change may further expand the number diagnosed with a mood disorder. Perhaps to many practitioners and patients these arguments seem obtuse and fastidious, but there is a core failure in modern psychiatry to clearly differentiate the human condition from mental illness. Said failure has vast implications for psychiatric epidemiology, the sociological understanding of psychic suffering and suicide, as well as the overprescribing of psychotropic medications.
Ketamine is an exciting prospect to many psychiatrists who feel like we have had little advancement and few novel treatments in a long time; advertised breakthroughs in the treatment of depression since fluoxetine have not been particularly impressive. Furthermore, the concerns about potential ketamine abuse are not theoretical but a very real problem in some parts of the world.11,12 The concerns about abuse are worsened considering recent evidence that suggests that ketamine’s effect may be driven by its opiate rather than NMDA effects.13 While some have discussed those concerns, we think that the field also needs to address the fact that the debate about ketamine is also changing our definition of depression.
References
1. https://www.youtube.com/watch?v=MpcUN6XvGmk.
2. J Clin Psychiatry. 2016 Jun;77(6):e719-25.
3. Emerg (Tehran). 2014 Winter;2(1):36-9.
4. “Is esketamine the game-changer for depression we want?” Rolling Stone. 2019 Mar 11.
5. Psychol Med. 1971;1(3):191-6.
6. https://books.google.com/ngrams.
7. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). American Psychiatric Association, 2013.
8. Am J Psychiatry. 2014 Apr;171(4):395-7.
9. “Many people taking antidepressants discover they cannot quit.” New York Times. 2018 Apr 7.
10. “Antidepressants show greatest increase in number of prescription items dispensed.” National Health Service. 2015 Jul 5.
11. “The ketamine connection.” BBC News. 2015 Jul 10.
12. Front Psychiatry. 2018 Jul 17. doi: 10.33389/fpsyt.2018.00313.
13. Am J Psychiatry. 2018 Dec 1;175(2):1205-15.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. Among his writings is Coercion and the critical psychiatrist, chapter 7 in the new book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer Nature Switzerland, 2019, pp. 155-77). Dr. Lehman is an associate professor of psychiatry at UCSD. He is codirector of all Acute and Intensive Psychiatric Treatment at the VA Medical Center in San Diego, where he practices clinical psychiatry. He also is the course director for the UCSD third-year medical student psychiatry clerkship.
*This article was updated 3/25/2019.
What does it mean to define an amalgamation of symptoms as a “psychiatric disorder?” Are psychiatric disorders an extreme variation of normative human behavior? Is human behavior simply an output phenotype of some neurologic chemical processes that become disordered in mental illness? Can depression be localized in the brain and subsequently turned on or off? If depression were to be localized in the brain, would it be an excess of a neurotransmitter, the depletion of a receptor, a malfunctioning neuron, an overactive connectome, poorly processed genetic material, or something as yet undefined? Those questions always have been present in our minds and influenced our understanding of patients, but a recent development in psychiatry raises questions about one of the few things we were historically confident about.
A part of our foundational understanding of depression was that it is not sadness, per se. One can be sad for any amount of time. It is not uncommon to feel sad for any variety of reasons, such as watching an adorable 60-second commercial for dog food.1 Those fleeting moments of sadness can even be empowering; they remind us about the things we care about and would be sad to miss.
Sadness in oneself can demonstrate the experience of empathic sadness for others. On the contrary, depression appears to have little apparent purpose, and instead results in a maladaptive way of coping that is all-consuming and often very damaging. Depression is not a mood but a state of being, something that is not defined by how one feels but who one is or has become because of the disorder. So it comes as somewhat of a surprise when we heard that ketamine could alleviate depression in minutes.2,3 As described by a ketamine expert, symptoms are relieved in “no less than an hour.”4 The surprise is not so much that a treatment would work but that improvement could be defined in such a short time frame.
Psychiatry has debated the definition of depression for its entire existence. There are many ways to tackle the concept of depression. A lot of the debate has been about the causes of depression. One example of the continued evolution of our understanding of depression is our prior categorization of depression as “exogenous” or “endogenous.”5 Exogenous depression was described as happening in the context of social stressors and as best treated with therapy. Endogenous depression was a supposedly truer form of depression as a disorder and was more biologically based. Patients suffering from endogenous depression were thought to have chemical abnormalities in the brain that could be alleviated by tricyclic antidepressants and subsequently SSRIs. Like many prior debates about depression, this one appears to be little discussed nowadays. A review of the use of the term “endogenous depression” in books shows an onset in the 1930s, a peak in the 1980s, and a rapid decline since.6
More recently, psychiatrists have defined depression using the DSM-5 criteria. Depression is thought to be the presence of at least five out of nine symptoms listed in the manual for a period of 2 weeks that cause significant distress or impairment.7 The DSM attempts to address criticism by providing information on its limitations and best use, and encourages clinical interpretation of symptoms. The DSM does not portray itself as a gold standard but rather as a tool for treatment planning and effective communication between peers. Furthermore, the National Institute on Mental Health is promoting an alternative understanding of depression using its own Research Domain Criteria, which attempt to provide a more objective understanding of the disorder based on biological rather than subjective correlates.
The growing literature on ketamine partly hinges on the belief that depression is something that can be redefined and changed at any moment. Many trials ask patients whether their depression remains in remission in the subsequent hours, days, and weeks following administration of the drug. However, one wonders if that is even possible. If a patient’s depression is alleviated in an hour, was it really clinical depression? Is it truly in remission? Contrary to our previous understanding, is depression, in reality, a switch that can be turned off by an infusion of an N-methyl-D-aspartate (NMDA)–receptor antagonist? Without minimizing the suffering of patients seeking ketamine or the relief provided to patients who benefit from the treatment, we simply are pointing out that the definition of depression did not account for this reported phenomenon of relatively instantaneous relief. The seemingly miraculous effects of ketamine suggest a new paradigm where any intervention – whether chemical, social, or psychological – could turn off the devastating effects of depression in an instant.
After all, the most widely used scale of depression, the nine-item Patient Health Questionnaire (PHQ-9) asks patients, “Over the last 2 weeks, how often have you been bothered by any of the following problems?” The highest answer one can give is “Nearly every day.” Are we incorrect to think that if one were suicidal every minute of the past 2 weeks, one would still score, nearly every day, even if one’s symptoms were relieved for the past hour? Thus, a maximum score of 27 would remain a 27 no matter what happened in the past hour.
We do realize that we are being overly literal. Ketamine makes some people feel better quickly, and researchers try to capture that effect by asking patients about their symptoms within short intervals. Furthermore, one has to start somewhere. After the infusion is a reasonable time to ask patients how they feel. We are also cognizant that many ketamine researchers do more long-term follow-ups and/or have recommended longer-term studies. Nonetheless,
Expanding our definition of depression to encompass experiences with short time frames may have unintended consequences. As living circumstances rarely change in minutes, the emphasis on rapid recovery makes the patients more in control of their reported experiences and thus their diagnoses. One cannot assess a patient’s impairment or disability from minute to minute. One is left with emphasizing the patient’s subjective symptoms and deemphasizing their relationships, goals, and daily functioning. How could one measure eating habits, hygiene, or participation in hobbies every hour? Another consequence of this reduced time frame is the expansion of a diagnosis that no longer requires the presence of symptoms for 2 weeks. Considering the already vast number of people diagnosed with depression,9,10 this small change may further expand the number diagnosed with a mood disorder. Perhaps to many practitioners and patients these arguments seem obtuse and fastidious, but there is a core failure in modern psychiatry to clearly differentiate the human condition from mental illness. Said failure has vast implications for psychiatric epidemiology, the sociological understanding of psychic suffering and suicide, as well as the overprescribing of psychotropic medications.
Ketamine is an exciting prospect to many psychiatrists who feel like we have had little advancement and few novel treatments in a long time; advertised breakthroughs in the treatment of depression since fluoxetine have not been particularly impressive. Furthermore, the concerns about potential ketamine abuse are not theoretical but a very real problem in some parts of the world.11,12 The concerns about abuse are worsened considering recent evidence that suggests that ketamine’s effect may be driven by its opiate rather than NMDA effects.13 While some have discussed those concerns, we think that the field also needs to address the fact that the debate about ketamine is also changing our definition of depression.
References
1. https://www.youtube.com/watch?v=MpcUN6XvGmk.
2. J Clin Psychiatry. 2016 Jun;77(6):e719-25.
3. Emerg (Tehran). 2014 Winter;2(1):36-9.
4. “Is esketamine the game-changer for depression we want?” Rolling Stone. 2019 Mar 11.
5. Psychol Med. 1971;1(3):191-6.
6. https://books.google.com/ngrams.
7. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). American Psychiatric Association, 2013.
8. Am J Psychiatry. 2014 Apr;171(4):395-7.
9. “Many people taking antidepressants discover they cannot quit.” New York Times. 2018 Apr 7.
10. “Antidepressants show greatest increase in number of prescription items dispensed.” National Health Service. 2015 Jul 5.
11. “The ketamine connection.” BBC News. 2015 Jul 10.
12. Front Psychiatry. 2018 Jul 17. doi: 10.33389/fpsyt.2018.00313.
13. Am J Psychiatry. 2018 Dec 1;175(2):1205-15.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. Among his writings is Coercion and the critical psychiatrist, chapter 7 in the new book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer Nature Switzerland, 2019, pp. 155-77). Dr. Lehman is an associate professor of psychiatry at UCSD. He is codirector of all Acute and Intensive Psychiatric Treatment at the VA Medical Center in San Diego, where he practices clinical psychiatry. He also is the course director for the UCSD third-year medical student psychiatry clerkship.
*This article was updated 3/25/2019.