User login
Wuhan virus: What clinicians need to know
As the Wuhan coronavirus story unfolds, , according to infectious disease experts.

“We are asking that of everyone with fever and respiratory symptoms who comes to our clinics, hospital, or emergency room. It’s a powerful screening tool,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn.
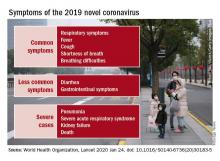
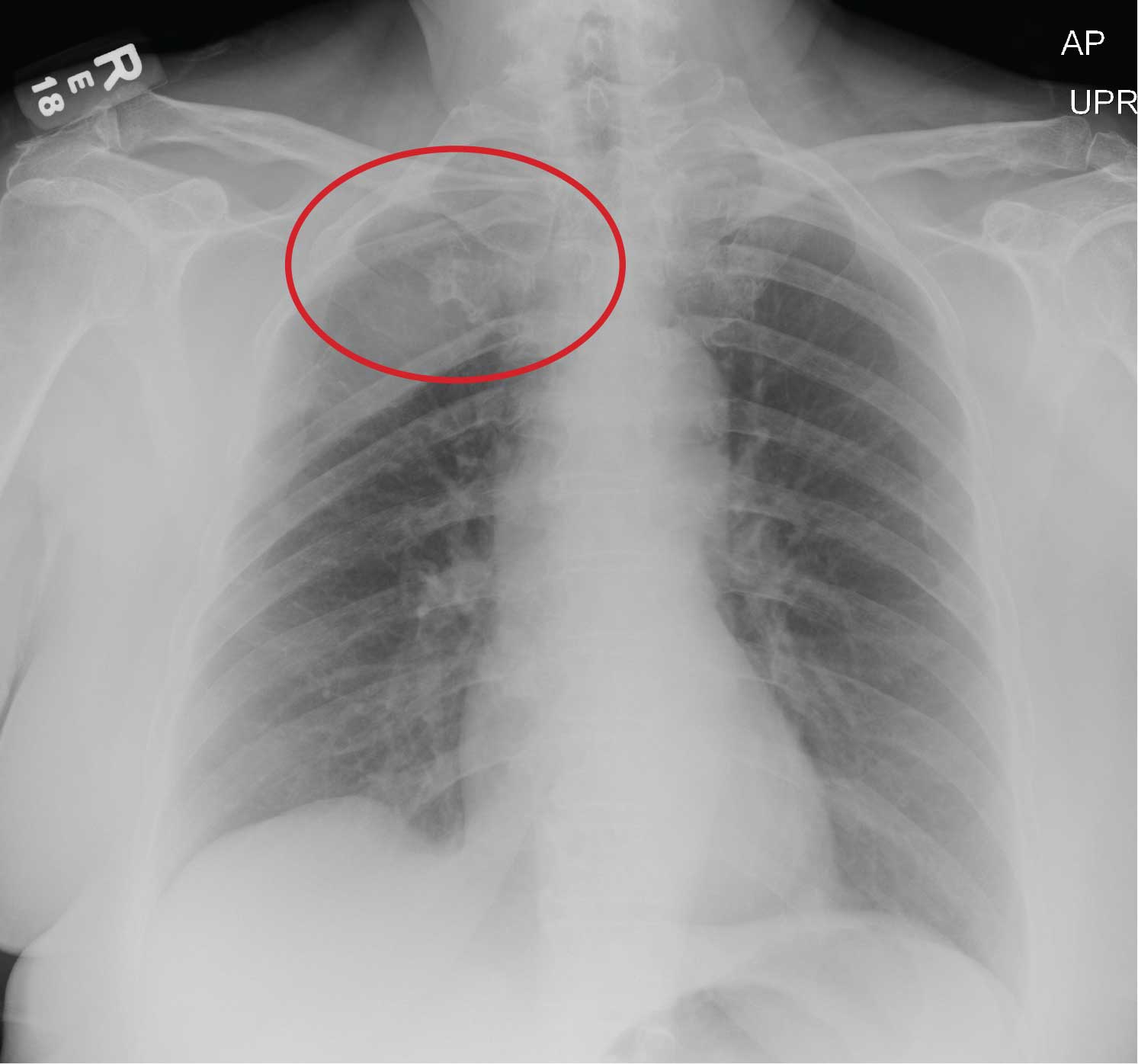
In addition to fever, common signs of infection include cough, shortness of breath, and breathing difficulties. Some patients have had diarrhea, vomiting, and other gastrointestinal symptoms. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure, and death. The incubation period appears to be up to 2 weeks, according to the World Health Organization (WHO).
If patients exhibit symptoms and either they or a close contact has returned from China recently, take standard airborne precautions and send specimens – a serum sample, oral and nasal pharyngeal swabs, and lower respiratory tract specimens if available – to the local health department, which will forward them to the Centers for Disease Control and Prevention (CDC) for testing. Turnaround time is 24-48 hours.
The 2019 Novel Coronavirus (2019-nCoV), identified as the cause of an outbreak of respiratory illness first detected in December in association with a live animal market in Wuhan, China, has been implicated in almost 2,000 cases and 56 deaths in that country. Cases have been reported in 13 countries besides China. Five cases of 2019-nCoV infection have been confirmed in the United States, all in people recently returned from Wuhan. As the virus spreads in China, however, it’s almost certain more cases will show up in the United States. Travel history is key, Dr. Schaffner and others said.
Plan and rehearse
The first step to prepare is to use the CDC’s Interim Guidance for Healthcare Professionals to make a written plan specific to your practice to respond to a potential case. The plan must include notifying the local health department, the CDC liaison for testing, and tracking down patient contacts.
“It’s not good enough to just download CDC’s guidance; use it to make your own local plan and know what to do 24/7,” said Daniel Lucey, MD, an infectious disease expert at Georgetown University Medical Center, Washington, D.C.
“Know who is on call at the health department on weekends and nights,” he said. Know where the patient is going to be isolated; figure out what to do if there’s more than one, and tests come back positive. Have masks on hand, and rehearse the response. “Make a coronavirus team, and absolutely have the nurses involved,” as well as other providers who may come into contact with a case, he added.
“You want to be able to do as well as your counterparts in Washington state and Chicago,” where the first two U.S. cases emerged. “They were prepared. They knew what to do,” Dr. Lucey said.
Those first two U.S. patients – a man in Everett, Wash., and a Chicago woman – developed symptoms after returning from Wuhan, a city of 11 million just over 400 miles inland from the port city of Shanghai. On Jan. 26 three more cases were confirmed by the CDC, two in California and one in Arizona, and each had recently traveled to Wuhan. All five patients remain hospitalized, and there’s no evidence they spread the infection further. There is also no evidence of human-to-human transmission of other cases exported from China to any other countries, according to the WHO.
WHO declined to declare a global health emergency – a Public Health Emergency of International Concern, in its parlance – on Jan. 23. The step would have triggered travel and trade restrictions in member states, including the United States. For now, at least, the group said it wasn’t warranted at this point.
Fatality rates
The focus right now is China. The outbreak has spread beyond Wuhan to other parts of the country, and there’s evidence of fourth-generation spread.
Transportation into and out of Wuhan and other cities has been curtailed, Lunar New Year festivals have been canceled, and the Shanghai Disneyland has been closed, among other measures taken by Chinese officials.
The government could be taking drastic measures in part to prevent the public criticism it took in the early 2000’s for the delayed response and lack of transparency during the global outbreak of another wildlife market coronavirus epidemic, severe acute respiratory syndrome (SARS). In a press conference Jan. 22, WHO officials commended the government’s containment efforts but did not say they recommended them.
According to WHO, serious cases in China have mostly been in people over 40 years old with significant comorbidities and have skewed towards men. Spread seems to be limited to family members, health care providers, and other close contacts, probably by respiratory droplets. If that pattern holds, WHO officials said, the outbreak is containable.
The fatality rate appears to be around 3%, a good deal lower than the 10% reported for SARS and much lower than the nearly 40% reported for Middle East respiratory syndrome (MERS), another recent coronavirus mutation from the animal trade.
The Wuhan virus fatality rate might drop as milder cases are detected and added to the denominator. “It definitely appears to be less severe than SARS and MERS,” said Amesh Adalja, MD, an infectious disease physician in Pittsburgh and emerging infectious disease researcher at Johns Hopkins University, Baltimore.
SARS: Lessons learned
In general, the world is much better equipped for coronavirus outbreaks than when SARS, in particular, emerged in 2003.
WHO officials in their press conference lauded China for it openness with the current outbreak, and for isolating and sequencing the virus immediately, which gave the world a diagnostic test in the first days of the outbreak, something that wasn’t available for SARS. China and other countries also are cooperating and working closely to contain the Wuhan virus.
“What we know today might change tomorrow, so we have to keep tuned in to new information, but we learned a lot from SARS,” Dr. Shaffner said. Overall, it’s likely “the impact on the United States of this new coronavirus is going to be trivial,” he predicted.
Dr. Lucey, however, recalled that the SARS outbreak in Toronto in 2003 started with one missed case. A woman returned asymptomatic from Hong Kong and spread the infection to her family members before she died. Her cause of death wasn’t immediately recognized, nor was the reason her family members were sick, since they hadn’t been to Hong Kong recently.
The infection ultimately spread to more than 200 people, about half of them health care workers. A few people died.
If a virus is sufficiently contagious, “it just takes one. You don’t want to be the one who misses that first patient,” Dr. Lucey said.
Currently, there are no antivirals or vaccines for coronaviruses; researchers are working on both, but for now, care is supportive.
This article was updated with new case numbers on 1/26/20.
As the Wuhan coronavirus story unfolds, , according to infectious disease experts.

“We are asking that of everyone with fever and respiratory symptoms who comes to our clinics, hospital, or emergency room. It’s a powerful screening tool,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn.
In addition to fever, common signs of infection include cough, shortness of breath, and breathing difficulties. Some patients have had diarrhea, vomiting, and other gastrointestinal symptoms. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure, and death. The incubation period appears to be up to 2 weeks, according to the World Health Organization (WHO).
If patients exhibit symptoms and either they or a close contact has returned from China recently, take standard airborne precautions and send specimens – a serum sample, oral and nasal pharyngeal swabs, and lower respiratory tract specimens if available – to the local health department, which will forward them to the Centers for Disease Control and Prevention (CDC) for testing. Turnaround time is 24-48 hours.
The 2019 Novel Coronavirus (2019-nCoV), identified as the cause of an outbreak of respiratory illness first detected in December in association with a live animal market in Wuhan, China, has been implicated in almost 2,000 cases and 56 deaths in that country. Cases have been reported in 13 countries besides China. Five cases of 2019-nCoV infection have been confirmed in the United States, all in people recently returned from Wuhan. As the virus spreads in China, however, it’s almost certain more cases will show up in the United States. Travel history is key, Dr. Schaffner and others said.
Plan and rehearse
The first step to prepare is to use the CDC’s Interim Guidance for Healthcare Professionals to make a written plan specific to your practice to respond to a potential case. The plan must include notifying the local health department, the CDC liaison for testing, and tracking down patient contacts.
“It’s not good enough to just download CDC’s guidance; use it to make your own local plan and know what to do 24/7,” said Daniel Lucey, MD, an infectious disease expert at Georgetown University Medical Center, Washington, D.C.
“Know who is on call at the health department on weekends and nights,” he said. Know where the patient is going to be isolated; figure out what to do if there’s more than one, and tests come back positive. Have masks on hand, and rehearse the response. “Make a coronavirus team, and absolutely have the nurses involved,” as well as other providers who may come into contact with a case, he added.
“You want to be able to do as well as your counterparts in Washington state and Chicago,” where the first two U.S. cases emerged. “They were prepared. They knew what to do,” Dr. Lucey said.
Those first two U.S. patients – a man in Everett, Wash., and a Chicago woman – developed symptoms after returning from Wuhan, a city of 11 million just over 400 miles inland from the port city of Shanghai. On Jan. 26 three more cases were confirmed by the CDC, two in California and one in Arizona, and each had recently traveled to Wuhan. All five patients remain hospitalized, and there’s no evidence they spread the infection further. There is also no evidence of human-to-human transmission of other cases exported from China to any other countries, according to the WHO.
WHO declined to declare a global health emergency – a Public Health Emergency of International Concern, in its parlance – on Jan. 23. The step would have triggered travel and trade restrictions in member states, including the United States. For now, at least, the group said it wasn’t warranted at this point.
Fatality rates
The focus right now is China. The outbreak has spread beyond Wuhan to other parts of the country, and there’s evidence of fourth-generation spread.
Transportation into and out of Wuhan and other cities has been curtailed, Lunar New Year festivals have been canceled, and the Shanghai Disneyland has been closed, among other measures taken by Chinese officials.
The government could be taking drastic measures in part to prevent the public criticism it took in the early 2000’s for the delayed response and lack of transparency during the global outbreak of another wildlife market coronavirus epidemic, severe acute respiratory syndrome (SARS). In a press conference Jan. 22, WHO officials commended the government’s containment efforts but did not say they recommended them.
According to WHO, serious cases in China have mostly been in people over 40 years old with significant comorbidities and have skewed towards men. Spread seems to be limited to family members, health care providers, and other close contacts, probably by respiratory droplets. If that pattern holds, WHO officials said, the outbreak is containable.
The fatality rate appears to be around 3%, a good deal lower than the 10% reported for SARS and much lower than the nearly 40% reported for Middle East respiratory syndrome (MERS), another recent coronavirus mutation from the animal trade.
The Wuhan virus fatality rate might drop as milder cases are detected and added to the denominator. “It definitely appears to be less severe than SARS and MERS,” said Amesh Adalja, MD, an infectious disease physician in Pittsburgh and emerging infectious disease researcher at Johns Hopkins University, Baltimore.
SARS: Lessons learned
In general, the world is much better equipped for coronavirus outbreaks than when SARS, in particular, emerged in 2003.
WHO officials in their press conference lauded China for it openness with the current outbreak, and for isolating and sequencing the virus immediately, which gave the world a diagnostic test in the first days of the outbreak, something that wasn’t available for SARS. China and other countries also are cooperating and working closely to contain the Wuhan virus.
“What we know today might change tomorrow, so we have to keep tuned in to new information, but we learned a lot from SARS,” Dr. Shaffner said. Overall, it’s likely “the impact on the United States of this new coronavirus is going to be trivial,” he predicted.
Dr. Lucey, however, recalled that the SARS outbreak in Toronto in 2003 started with one missed case. A woman returned asymptomatic from Hong Kong and spread the infection to her family members before she died. Her cause of death wasn’t immediately recognized, nor was the reason her family members were sick, since they hadn’t been to Hong Kong recently.
The infection ultimately spread to more than 200 people, about half of them health care workers. A few people died.
If a virus is sufficiently contagious, “it just takes one. You don’t want to be the one who misses that first patient,” Dr. Lucey said.
Currently, there are no antivirals or vaccines for coronaviruses; researchers are working on both, but for now, care is supportive.
This article was updated with new case numbers on 1/26/20.
As the Wuhan coronavirus story unfolds, , according to infectious disease experts.

“We are asking that of everyone with fever and respiratory symptoms who comes to our clinics, hospital, or emergency room. It’s a powerful screening tool,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn.
In addition to fever, common signs of infection include cough, shortness of breath, and breathing difficulties. Some patients have had diarrhea, vomiting, and other gastrointestinal symptoms. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure, and death. The incubation period appears to be up to 2 weeks, according to the World Health Organization (WHO).
If patients exhibit symptoms and either they or a close contact has returned from China recently, take standard airborne precautions and send specimens – a serum sample, oral and nasal pharyngeal swabs, and lower respiratory tract specimens if available – to the local health department, which will forward them to the Centers for Disease Control and Prevention (CDC) for testing. Turnaround time is 24-48 hours.
The 2019 Novel Coronavirus (2019-nCoV), identified as the cause of an outbreak of respiratory illness first detected in December in association with a live animal market in Wuhan, China, has been implicated in almost 2,000 cases and 56 deaths in that country. Cases have been reported in 13 countries besides China. Five cases of 2019-nCoV infection have been confirmed in the United States, all in people recently returned from Wuhan. As the virus spreads in China, however, it’s almost certain more cases will show up in the United States. Travel history is key, Dr. Schaffner and others said.
Plan and rehearse
The first step to prepare is to use the CDC’s Interim Guidance for Healthcare Professionals to make a written plan specific to your practice to respond to a potential case. The plan must include notifying the local health department, the CDC liaison for testing, and tracking down patient contacts.
“It’s not good enough to just download CDC’s guidance; use it to make your own local plan and know what to do 24/7,” said Daniel Lucey, MD, an infectious disease expert at Georgetown University Medical Center, Washington, D.C.
“Know who is on call at the health department on weekends and nights,” he said. Know where the patient is going to be isolated; figure out what to do if there’s more than one, and tests come back positive. Have masks on hand, and rehearse the response. “Make a coronavirus team, and absolutely have the nurses involved,” as well as other providers who may come into contact with a case, he added.
“You want to be able to do as well as your counterparts in Washington state and Chicago,” where the first two U.S. cases emerged. “They were prepared. They knew what to do,” Dr. Lucey said.
Those first two U.S. patients – a man in Everett, Wash., and a Chicago woman – developed symptoms after returning from Wuhan, a city of 11 million just over 400 miles inland from the port city of Shanghai. On Jan. 26 three more cases were confirmed by the CDC, two in California and one in Arizona, and each had recently traveled to Wuhan. All five patients remain hospitalized, and there’s no evidence they spread the infection further. There is also no evidence of human-to-human transmission of other cases exported from China to any other countries, according to the WHO.
WHO declined to declare a global health emergency – a Public Health Emergency of International Concern, in its parlance – on Jan. 23. The step would have triggered travel and trade restrictions in member states, including the United States. For now, at least, the group said it wasn’t warranted at this point.
Fatality rates
The focus right now is China. The outbreak has spread beyond Wuhan to other parts of the country, and there’s evidence of fourth-generation spread.
Transportation into and out of Wuhan and other cities has been curtailed, Lunar New Year festivals have been canceled, and the Shanghai Disneyland has been closed, among other measures taken by Chinese officials.
The government could be taking drastic measures in part to prevent the public criticism it took in the early 2000’s for the delayed response and lack of transparency during the global outbreak of another wildlife market coronavirus epidemic, severe acute respiratory syndrome (SARS). In a press conference Jan. 22, WHO officials commended the government’s containment efforts but did not say they recommended them.
According to WHO, serious cases in China have mostly been in people over 40 years old with significant comorbidities and have skewed towards men. Spread seems to be limited to family members, health care providers, and other close contacts, probably by respiratory droplets. If that pattern holds, WHO officials said, the outbreak is containable.
The fatality rate appears to be around 3%, a good deal lower than the 10% reported for SARS and much lower than the nearly 40% reported for Middle East respiratory syndrome (MERS), another recent coronavirus mutation from the animal trade.
The Wuhan virus fatality rate might drop as milder cases are detected and added to the denominator. “It definitely appears to be less severe than SARS and MERS,” said Amesh Adalja, MD, an infectious disease physician in Pittsburgh and emerging infectious disease researcher at Johns Hopkins University, Baltimore.
SARS: Lessons learned
In general, the world is much better equipped for coronavirus outbreaks than when SARS, in particular, emerged in 2003.
WHO officials in their press conference lauded China for it openness with the current outbreak, and for isolating and sequencing the virus immediately, which gave the world a diagnostic test in the first days of the outbreak, something that wasn’t available for SARS. China and other countries also are cooperating and working closely to contain the Wuhan virus.
“What we know today might change tomorrow, so we have to keep tuned in to new information, but we learned a lot from SARS,” Dr. Shaffner said. Overall, it’s likely “the impact on the United States of this new coronavirus is going to be trivial,” he predicted.
Dr. Lucey, however, recalled that the SARS outbreak in Toronto in 2003 started with one missed case. A woman returned asymptomatic from Hong Kong and spread the infection to her family members before she died. Her cause of death wasn’t immediately recognized, nor was the reason her family members were sick, since they hadn’t been to Hong Kong recently.
The infection ultimately spread to more than 200 people, about half of them health care workers. A few people died.
If a virus is sufficiently contagious, “it just takes one. You don’t want to be the one who misses that first patient,” Dr. Lucey said.
Currently, there are no antivirals or vaccines for coronaviruses; researchers are working on both, but for now, care is supportive.
This article was updated with new case numbers on 1/26/20.
FDA: Cybersecurity vulnerabilities identified in GE Healthcare monitoring devices
The Food and Drug Administration has issued a warning that certain GE Healthcare Clinical Information Central Stations and Telemetry Servers have cybersecurity vulnerabilities that may introduce risk to monitored patients.
silence alarms, generate false alarms, and interfere with alarms of patient monitors connected to these devices, according to an “Urgent Medical Device Correction” letter issued by GE Healthcare in November 2019.
The affected devices are the ApexPro Telemetry Server and CARESCAPE Telemetry Server, the CARESCAPE Central Station (CSCS) version 1, and the CIC Pro Clinical Information Center Central Station version 1. These devices are used in health care facilities for displaying information, such as the patient’s physiological parameters, and for monitoring patient status from a central location in a facility.
No adverse events related to the vulnerabilities have been reported to the FDA. Health care facility staff should update their devices when GE Healthcare issues a software patch that addresses the vulnerability, separate the network connecting patient monitors using affected devices from the rest of the hospital, and use firewalls and other means to minimize the risk of remote or local network attacks.
“The FDA takes reports of cybersecurity vulnerabilities in medical devices seriously and will continue to work with GE Healthcare as the firm develops software patches to correct these vulnerabilities as soon as possible. The FDA will continue to assess new information concerning the vulnerabilities and will keep the public informed if significant new information becomes available,” the FDA said in the Safety Communication.
The Food and Drug Administration has issued a warning that certain GE Healthcare Clinical Information Central Stations and Telemetry Servers have cybersecurity vulnerabilities that may introduce risk to monitored patients.
silence alarms, generate false alarms, and interfere with alarms of patient monitors connected to these devices, according to an “Urgent Medical Device Correction” letter issued by GE Healthcare in November 2019.
The affected devices are the ApexPro Telemetry Server and CARESCAPE Telemetry Server, the CARESCAPE Central Station (CSCS) version 1, and the CIC Pro Clinical Information Center Central Station version 1. These devices are used in health care facilities for displaying information, such as the patient’s physiological parameters, and for monitoring patient status from a central location in a facility.
No adverse events related to the vulnerabilities have been reported to the FDA. Health care facility staff should update their devices when GE Healthcare issues a software patch that addresses the vulnerability, separate the network connecting patient monitors using affected devices from the rest of the hospital, and use firewalls and other means to minimize the risk of remote or local network attacks.
“The FDA takes reports of cybersecurity vulnerabilities in medical devices seriously and will continue to work with GE Healthcare as the firm develops software patches to correct these vulnerabilities as soon as possible. The FDA will continue to assess new information concerning the vulnerabilities and will keep the public informed if significant new information becomes available,” the FDA said in the Safety Communication.
The Food and Drug Administration has issued a warning that certain GE Healthcare Clinical Information Central Stations and Telemetry Servers have cybersecurity vulnerabilities that may introduce risk to monitored patients.
silence alarms, generate false alarms, and interfere with alarms of patient monitors connected to these devices, according to an “Urgent Medical Device Correction” letter issued by GE Healthcare in November 2019.
The affected devices are the ApexPro Telemetry Server and CARESCAPE Telemetry Server, the CARESCAPE Central Station (CSCS) version 1, and the CIC Pro Clinical Information Center Central Station version 1. These devices are used in health care facilities for displaying information, such as the patient’s physiological parameters, and for monitoring patient status from a central location in a facility.
No adverse events related to the vulnerabilities have been reported to the FDA. Health care facility staff should update their devices when GE Healthcare issues a software patch that addresses the vulnerability, separate the network connecting patient monitors using affected devices from the rest of the hospital, and use firewalls and other means to minimize the risk of remote or local network attacks.
“The FDA takes reports of cybersecurity vulnerabilities in medical devices seriously and will continue to work with GE Healthcare as the firm develops software patches to correct these vulnerabilities as soon as possible. The FDA will continue to assess new information concerning the vulnerabilities and will keep the public informed if significant new information becomes available,” the FDA said in the Safety Communication.
Race, ethnicity may influence outcomes after supratentorial intracerebral hemorrhage
researchers reported Jan. 22 in Neurology.
“There has been considerable research on stroke in older people, but there is still much to be learned about stroke in younger people and how it affects people of different races and ethnicities,” study author Daniel Woo, MD, professor of neurology at the University of Cincinnati, said in a news release. “Our study found that, even when you account for factors that affect outcomes, such as how big the stroke is, race and ethnicity were still independent predictors of how well people would recover.”
A subset of ERICH participants
To examine predictors of functional outcome in young patients with ICH, researchers analyzed data from a subset of patients in the Ethnic/Racial Variations in Intracerebral Hemorrhage (ERICH) study. ERICH enrolled patients with nontraumatic ICHs at 42 sites in the United States. It included 1,000 non-Hispanic black patients, 1,000 non-Hispanic white patients, and 1,000 Hispanic patients. Participants self-reported race and ethnicity.
Lead author Laura C. Miyares from Yale School of Medicine in New Haven, Conn., and colleagues analyzed data from 418 patients in ERICH who were aged 18-49 years and had supratentorial ICH. The cohort had an average age of 43 years, and 69% were male. In this subset, 41% were black, 12% were white, and 47% were Hispanic.
The primary outcome was modified Rankin Scale (mRS) score 3 months after the ICH, and the investigators defined a poor outcome as a score of 4 or greater. At 3 months, 35% had a poor functional outcome. Approximately 18% were unable to walk without assistance and attend to their bodily needs (mRS 4); 8% were bedridden, incontinent, and required nursing care (mRS 5); and 10% had died (mRS 6).
The percentage of patients with a poor functional outcome was 52% among white patients, 35% among black patients, and 31% among Hispanic patients. In a univariable analysis, black patients had a 51% reduction in odds of a poor outcome, compared with white patients, and Hispanic patients had a 59% reduction.
“The association between race/ethnicity and 3-month post-ICH functional outcome remained significant after adjusting for age, sex, premorbid disability, ICH location, ICH volume, [intraventricular hemorrhage] extension, systolic blood pressure, and [Glasgow Coma Scale] score on admission,” the researchers said. “In multivariable analysis, using white patients as the reference category, black patients had a 58% reduction in the odds of poor functional outcome at 3 months and Hispanic patients had a 66% reduction in the same odds.”
Their analysis identified the importance of other risk factors as well. “The volume of the hematoma, the most powerful predictor of outcome in older patients with ICH, was also found to be the most significant predictor of poor outcome in young patients,” they said.
Vascular risks and oral anticoagulants
About 80% of the young adults with ICH had a history of diagnosed hypertension. In nearly half, the condition was untreated. “After hypertension, the most common stroke risk factors in the young were diabetes, high cholesterol, smoking, and alcohol abuse,” the authors said. “In combination, these results indicate that vascular risk factors, especially untreated, could explain a large proportion of cases of ICH in the young.”
“Our results also point to treatment with oral anticoagulants before hospitalization as a potential mediator of the effect of race/ethnicity on short-term functional outcomes,” they said. About 8% of the white patients used oral anticoagulants, compared with 4% of the black patients and 1% of the Hispanic patients. Oral anticoagulant treatment “is a known risk factor for ICH and an established predictor of poor outcome in this condition. However, because only a small proportion of enrolled young patients with ICH were on [oral anticoagulants] prior to presentation, these results should be further validated by future studies.”
The study’s limitations include the broad categorization of racial and ethnic groups, the fact that younger patients with supratentorial ICH were more likely to be black or Hispanic and less likely to be white, and the exclusion of a significant proportion of cases of young white patients with smaller ICH volumes because of missing data, the researchers noted. Although the cohort was large, researchers may need to study more patients to capture differences among racial and ethnic groups, the investigators said.
The association between race/ethnicity and functional outcome could relate to “distinct pathophysiologies of the initial bleed or unique mechanisms of secondary injury,” the researchers suggested. “Future studies are necessary to probe the potential biological and social mediators of these findings to elucidate the role of race/ethnicity in ICH severity and functional recovery, and to develop improved prognostication for a racially varied population.”
ERICH is supported by the National Institute of Neurological Disorders and Stroke. Authors disclosed grants from the government, professional societies, and a university.
SOURCE: Miyares LC et al. Neurology. 2020 Jan 22. doi: 10.1212/WNL.0000000000008930.
researchers reported Jan. 22 in Neurology.
“There has been considerable research on stroke in older people, but there is still much to be learned about stroke in younger people and how it affects people of different races and ethnicities,” study author Daniel Woo, MD, professor of neurology at the University of Cincinnati, said in a news release. “Our study found that, even when you account for factors that affect outcomes, such as how big the stroke is, race and ethnicity were still independent predictors of how well people would recover.”
A subset of ERICH participants
To examine predictors of functional outcome in young patients with ICH, researchers analyzed data from a subset of patients in the Ethnic/Racial Variations in Intracerebral Hemorrhage (ERICH) study. ERICH enrolled patients with nontraumatic ICHs at 42 sites in the United States. It included 1,000 non-Hispanic black patients, 1,000 non-Hispanic white patients, and 1,000 Hispanic patients. Participants self-reported race and ethnicity.
Lead author Laura C. Miyares from Yale School of Medicine in New Haven, Conn., and colleagues analyzed data from 418 patients in ERICH who were aged 18-49 years and had supratentorial ICH. The cohort had an average age of 43 years, and 69% were male. In this subset, 41% were black, 12% were white, and 47% were Hispanic.
The primary outcome was modified Rankin Scale (mRS) score 3 months after the ICH, and the investigators defined a poor outcome as a score of 4 or greater. At 3 months, 35% had a poor functional outcome. Approximately 18% were unable to walk without assistance and attend to their bodily needs (mRS 4); 8% were bedridden, incontinent, and required nursing care (mRS 5); and 10% had died (mRS 6).
The percentage of patients with a poor functional outcome was 52% among white patients, 35% among black patients, and 31% among Hispanic patients. In a univariable analysis, black patients had a 51% reduction in odds of a poor outcome, compared with white patients, and Hispanic patients had a 59% reduction.
“The association between race/ethnicity and 3-month post-ICH functional outcome remained significant after adjusting for age, sex, premorbid disability, ICH location, ICH volume, [intraventricular hemorrhage] extension, systolic blood pressure, and [Glasgow Coma Scale] score on admission,” the researchers said. “In multivariable analysis, using white patients as the reference category, black patients had a 58% reduction in the odds of poor functional outcome at 3 months and Hispanic patients had a 66% reduction in the same odds.”
Their analysis identified the importance of other risk factors as well. “The volume of the hematoma, the most powerful predictor of outcome in older patients with ICH, was also found to be the most significant predictor of poor outcome in young patients,” they said.
Vascular risks and oral anticoagulants
About 80% of the young adults with ICH had a history of diagnosed hypertension. In nearly half, the condition was untreated. “After hypertension, the most common stroke risk factors in the young were diabetes, high cholesterol, smoking, and alcohol abuse,” the authors said. “In combination, these results indicate that vascular risk factors, especially untreated, could explain a large proportion of cases of ICH in the young.”
“Our results also point to treatment with oral anticoagulants before hospitalization as a potential mediator of the effect of race/ethnicity on short-term functional outcomes,” they said. About 8% of the white patients used oral anticoagulants, compared with 4% of the black patients and 1% of the Hispanic patients. Oral anticoagulant treatment “is a known risk factor for ICH and an established predictor of poor outcome in this condition. However, because only a small proportion of enrolled young patients with ICH were on [oral anticoagulants] prior to presentation, these results should be further validated by future studies.”
The study’s limitations include the broad categorization of racial and ethnic groups, the fact that younger patients with supratentorial ICH were more likely to be black or Hispanic and less likely to be white, and the exclusion of a significant proportion of cases of young white patients with smaller ICH volumes because of missing data, the researchers noted. Although the cohort was large, researchers may need to study more patients to capture differences among racial and ethnic groups, the investigators said.
The association between race/ethnicity and functional outcome could relate to “distinct pathophysiologies of the initial bleed or unique mechanisms of secondary injury,” the researchers suggested. “Future studies are necessary to probe the potential biological and social mediators of these findings to elucidate the role of race/ethnicity in ICH severity and functional recovery, and to develop improved prognostication for a racially varied population.”
ERICH is supported by the National Institute of Neurological Disorders and Stroke. Authors disclosed grants from the government, professional societies, and a university.
SOURCE: Miyares LC et al. Neurology. 2020 Jan 22. doi: 10.1212/WNL.0000000000008930.
researchers reported Jan. 22 in Neurology.
“There has been considerable research on stroke in older people, but there is still much to be learned about stroke in younger people and how it affects people of different races and ethnicities,” study author Daniel Woo, MD, professor of neurology at the University of Cincinnati, said in a news release. “Our study found that, even when you account for factors that affect outcomes, such as how big the stroke is, race and ethnicity were still independent predictors of how well people would recover.”
A subset of ERICH participants
To examine predictors of functional outcome in young patients with ICH, researchers analyzed data from a subset of patients in the Ethnic/Racial Variations in Intracerebral Hemorrhage (ERICH) study. ERICH enrolled patients with nontraumatic ICHs at 42 sites in the United States. It included 1,000 non-Hispanic black patients, 1,000 non-Hispanic white patients, and 1,000 Hispanic patients. Participants self-reported race and ethnicity.
Lead author Laura C. Miyares from Yale School of Medicine in New Haven, Conn., and colleagues analyzed data from 418 patients in ERICH who were aged 18-49 years and had supratentorial ICH. The cohort had an average age of 43 years, and 69% were male. In this subset, 41% were black, 12% were white, and 47% were Hispanic.
The primary outcome was modified Rankin Scale (mRS) score 3 months after the ICH, and the investigators defined a poor outcome as a score of 4 or greater. At 3 months, 35% had a poor functional outcome. Approximately 18% were unable to walk without assistance and attend to their bodily needs (mRS 4); 8% were bedridden, incontinent, and required nursing care (mRS 5); and 10% had died (mRS 6).
The percentage of patients with a poor functional outcome was 52% among white patients, 35% among black patients, and 31% among Hispanic patients. In a univariable analysis, black patients had a 51% reduction in odds of a poor outcome, compared with white patients, and Hispanic patients had a 59% reduction.
“The association between race/ethnicity and 3-month post-ICH functional outcome remained significant after adjusting for age, sex, premorbid disability, ICH location, ICH volume, [intraventricular hemorrhage] extension, systolic blood pressure, and [Glasgow Coma Scale] score on admission,” the researchers said. “In multivariable analysis, using white patients as the reference category, black patients had a 58% reduction in the odds of poor functional outcome at 3 months and Hispanic patients had a 66% reduction in the same odds.”
Their analysis identified the importance of other risk factors as well. “The volume of the hematoma, the most powerful predictor of outcome in older patients with ICH, was also found to be the most significant predictor of poor outcome in young patients,” they said.
Vascular risks and oral anticoagulants
About 80% of the young adults with ICH had a history of diagnosed hypertension. In nearly half, the condition was untreated. “After hypertension, the most common stroke risk factors in the young were diabetes, high cholesterol, smoking, and alcohol abuse,” the authors said. “In combination, these results indicate that vascular risk factors, especially untreated, could explain a large proportion of cases of ICH in the young.”
“Our results also point to treatment with oral anticoagulants before hospitalization as a potential mediator of the effect of race/ethnicity on short-term functional outcomes,” they said. About 8% of the white patients used oral anticoagulants, compared with 4% of the black patients and 1% of the Hispanic patients. Oral anticoagulant treatment “is a known risk factor for ICH and an established predictor of poor outcome in this condition. However, because only a small proportion of enrolled young patients with ICH were on [oral anticoagulants] prior to presentation, these results should be further validated by future studies.”
The study’s limitations include the broad categorization of racial and ethnic groups, the fact that younger patients with supratentorial ICH were more likely to be black or Hispanic and less likely to be white, and the exclusion of a significant proportion of cases of young white patients with smaller ICH volumes because of missing data, the researchers noted. Although the cohort was large, researchers may need to study more patients to capture differences among racial and ethnic groups, the investigators said.
The association between race/ethnicity and functional outcome could relate to “distinct pathophysiologies of the initial bleed or unique mechanisms of secondary injury,” the researchers suggested. “Future studies are necessary to probe the potential biological and social mediators of these findings to elucidate the role of race/ethnicity in ICH severity and functional recovery, and to develop improved prognostication for a racially varied population.”
ERICH is supported by the National Institute of Neurological Disorders and Stroke. Authors disclosed grants from the government, professional societies, and a university.
SOURCE: Miyares LC et al. Neurology. 2020 Jan 22. doi: 10.1212/WNL.0000000000008930.
FROM NEUROLOGY
Key clinical point: Among young adults with supratentorial intracerebral hemorrhage (ICH), black race and Hispanic ethnicity are associated with better functional outcomes, compared with white race.
Major finding: In multivariable analysis, black patients had a 58% reduction in the odds of poor functional outcome at 3 months, compared with white patients, and Hispanic patients had a 66% reduction.
Study details: An analysis of data from a subset of 418 patients in the Ethnic/Racial Variations in Intracerebral Hemorrhage (ERICH) study.
Disclosures: ERICH is supported by the National Institute of Neurological Disorders and Stroke. Authors disclosed grants from the government, professional societies, and a university.
Source: Miyares LC et al. Neurology. 2020 Jan 22. doi: 10.1212/WNL.0000000000008930.
Dual e-cigarette and combustible tobacco use compound respiratory disease risk
according to recent longitudinal analysis published in the American Journal of Preventive Medicine.
E-cigarettes have been promoted as a safer alternative to combustible tobacco, and until recently, there has been little and conflicting evidence by which to test this hypothesis. This study conducted by Dharma N. Bhatta, PhD, and Stanton A. Glantz, PhD, of the Center for Tobacco Control Research and Education at the University of California, San Francisco, is one of the first longitudinal examinations of e-cigarette use and controlling for combustible tobacco use.
Dr. Bhatta and Dr. Glantz performed a multivariable, logistic regression analysis of adults enrolled in the nationally representative, population-based, longitudinal Population Assessment of Tobacco and Health study. The researchers analyzed the tobacco use of adults in the study in three waves, following them through wave 1 (September 2013 to December 2014), wave 2 (October 2014 to October 2015), and wave 3 (October 2015 to October 2016), analyzing the data between 2018 and 2019. Overall, wave 1 began with 32,320 participants, and 15.1% of adults reported respiratory disease at baseline.
Lung or respiratory disease was assessed by asking participants whether they had been told by a health professional that they had chronic obstructive pulmonary disease, chronic bronchitis, emphysema, or asthma. The researchers defined e-cigarette and combustible tobacco use as participants who never, currently, or formerly used e-cigarettes or smoked combustible tobacco. Participants who indicated they used e-cigarettes or combustible tobacco frequently or infrequently were placed in the current-user group, while past users were those participants who said they used to, but no longer use e-cigarettes or combustible tobacco.
The results showed former e-cigarette use (adjusted odds ratio, 1.34; 95% confidence interval, 1.23-1.46) and current e-cigarette use (aOR, 1.32; 95% CI, 1.17-1.49) were associated with an increased risk of having incident respiratory disease.
The data showed a not unexpected statistically significant association between former combustible tobacco use (aOR, 1.29; 95% CI, 1.14-1.47) as well as current combustible tobacco use (aOR, 1.61; 95% CI, 1.42-1.82) and incident respiratory disease risk.
There was a statistically significant association between respiratory disease and former or current e-cigarette use for adults who did not have respiratory disease at baseline, after adjusting for factors such as current combustible tobacco use, clinical variables, and demographic differences. Participants in wave 1 who reported former (aOR, 1.31; 95% CI, 1.07-1.60) or current e-cigarette use (aOR, 1.29; 95% CI, 1.03-1.61) had a significantly higher risk of developing incident respiratory disease in subsequent waves. There was also a statistically significant association between use of combustible tobacco and subsequent respiratory disease in later waves of the study (aOR, 2.56; 95% CI, 1.92-3.41), which the researchers noted was independent of the usual risks associated with combustible tobacco.
The investigators also looked at the link between dual use of e-cigarettes and combustible tobacco and respiratory disease risk. “The much more common pattern is dual use, in which an e-cigarette user continues to smoke combusted tobacco products at the same time (93.7% of e-cigarette users at wave 2 and 91.2% at wave 3 also used combustible tobacco; 73.3% of e-cigarette users at wave 2 and 64.9% at wave 3 also smoked cigarettes),” they wrote.
The odds of developing respiratory disease for participants who used both e-cigarettes and combustible tobacco were 3.30, compared with a participant who never used e-cigarettes, with similar results seen when comparing e-cigarettes and cigarettes.
“Although switching from combustible tobacco, including cigarettes, to e-cigarettes theoretically could reduce the risk of developing respiratory disease, current evidence indicates a high prevalence of dual use, which is associated with in-creased risk beyond combustible tobacco use,” the investigators wrote.
Harold J. Farber, MD, FCCP, professor of pediatrics in the pulmonary section at Baylor College of Medicine and Texas Children’s Hospital, both in Houston, said in an interview that the increased respiratory risk among dual users, who are likely using e-cigarettes and combustible tobacco together as a way to quit smoking, is particularly concerning.
“There is substantial reason to be concerned about efficacy of electronic cigarette products. Real-world observational studies have shown that, on average, tobacco smokers who use electronic cigarettes are less likely to stop smoking than those who do not use electronic cigarettes,” he said. “People who have stopped tobacco smoking but use electronic cigarettes are more likely to relapse to tobacco smoking than those who do not use electronic cigarettes.”
Dr. Farber noted that there are other Food and Drug Administration–approved medications for treating tobacco addiction. In addition, the World Health Organization, American Medical Association, Centers for Disease Control and Prevention, and FDA have all advised that e-cigarettes should not be used as smoking cessation aids, he said, especially in light of current outbreak of life-threatening e-cigarette and vaping lung injuries currently being investigated by the CDC and FDA.
“These study results suggest that the CDC reports of e-cigarette, or vaping, product use–associated lung injury are likely to be just the tip of the iceberg,” he said. “Although the CDC has identified vitamin E acetate–containing products as an important culprit, it is unlikely to be the only one. There are many substances in the emissions of e-cigarettes that have known irritant and/or toxic effects on the airways.”
Dr. Bhatta and Dr. Glantz acknowledged several limitations in their analysis, including the possibility of recall bias, not distinguishing between nondaily and daily e-cigarette or combustible tobacco use, and combining respiratory conditions together to achieve adequate power. The study shows an association, but the mechanism by which e-cigarettes may contribute to the development of lung disease remains under investigation.
This study was supported by grants from the National Institute on Drug Abuse; the National Cancer Institute; the FDA Center for Tobacco Products; the National Heart, Lung, and Blood Institute; and the University of California, San Francisco Helen Diller Family Comprehensive Cancer Center Global Cancer Program. Dr. Bhatta and Dr. Glantz reported no relevant conflicts of interest.
SOURCE: Bhatta DN, Glantz SA. Am J Prev Med. 2019 Dec 16. doi: 10.1016/j.amepre.2019.07.028.
according to recent longitudinal analysis published in the American Journal of Preventive Medicine.
E-cigarettes have been promoted as a safer alternative to combustible tobacco, and until recently, there has been little and conflicting evidence by which to test this hypothesis. This study conducted by Dharma N. Bhatta, PhD, and Stanton A. Glantz, PhD, of the Center for Tobacco Control Research and Education at the University of California, San Francisco, is one of the first longitudinal examinations of e-cigarette use and controlling for combustible tobacco use.
Dr. Bhatta and Dr. Glantz performed a multivariable, logistic regression analysis of adults enrolled in the nationally representative, population-based, longitudinal Population Assessment of Tobacco and Health study. The researchers analyzed the tobacco use of adults in the study in three waves, following them through wave 1 (September 2013 to December 2014), wave 2 (October 2014 to October 2015), and wave 3 (October 2015 to October 2016), analyzing the data between 2018 and 2019. Overall, wave 1 began with 32,320 participants, and 15.1% of adults reported respiratory disease at baseline.
Lung or respiratory disease was assessed by asking participants whether they had been told by a health professional that they had chronic obstructive pulmonary disease, chronic bronchitis, emphysema, or asthma. The researchers defined e-cigarette and combustible tobacco use as participants who never, currently, or formerly used e-cigarettes or smoked combustible tobacco. Participants who indicated they used e-cigarettes or combustible tobacco frequently or infrequently were placed in the current-user group, while past users were those participants who said they used to, but no longer use e-cigarettes or combustible tobacco.
The results showed former e-cigarette use (adjusted odds ratio, 1.34; 95% confidence interval, 1.23-1.46) and current e-cigarette use (aOR, 1.32; 95% CI, 1.17-1.49) were associated with an increased risk of having incident respiratory disease.
The data showed a not unexpected statistically significant association between former combustible tobacco use (aOR, 1.29; 95% CI, 1.14-1.47) as well as current combustible tobacco use (aOR, 1.61; 95% CI, 1.42-1.82) and incident respiratory disease risk.
There was a statistically significant association between respiratory disease and former or current e-cigarette use for adults who did not have respiratory disease at baseline, after adjusting for factors such as current combustible tobacco use, clinical variables, and demographic differences. Participants in wave 1 who reported former (aOR, 1.31; 95% CI, 1.07-1.60) or current e-cigarette use (aOR, 1.29; 95% CI, 1.03-1.61) had a significantly higher risk of developing incident respiratory disease in subsequent waves. There was also a statistically significant association between use of combustible tobacco and subsequent respiratory disease in later waves of the study (aOR, 2.56; 95% CI, 1.92-3.41), which the researchers noted was independent of the usual risks associated with combustible tobacco.
The investigators also looked at the link between dual use of e-cigarettes and combustible tobacco and respiratory disease risk. “The much more common pattern is dual use, in which an e-cigarette user continues to smoke combusted tobacco products at the same time (93.7% of e-cigarette users at wave 2 and 91.2% at wave 3 also used combustible tobacco; 73.3% of e-cigarette users at wave 2 and 64.9% at wave 3 also smoked cigarettes),” they wrote.
The odds of developing respiratory disease for participants who used both e-cigarettes and combustible tobacco were 3.30, compared with a participant who never used e-cigarettes, with similar results seen when comparing e-cigarettes and cigarettes.
“Although switching from combustible tobacco, including cigarettes, to e-cigarettes theoretically could reduce the risk of developing respiratory disease, current evidence indicates a high prevalence of dual use, which is associated with in-creased risk beyond combustible tobacco use,” the investigators wrote.
Harold J. Farber, MD, FCCP, professor of pediatrics in the pulmonary section at Baylor College of Medicine and Texas Children’s Hospital, both in Houston, said in an interview that the increased respiratory risk among dual users, who are likely using e-cigarettes and combustible tobacco together as a way to quit smoking, is particularly concerning.
“There is substantial reason to be concerned about efficacy of electronic cigarette products. Real-world observational studies have shown that, on average, tobacco smokers who use electronic cigarettes are less likely to stop smoking than those who do not use electronic cigarettes,” he said. “People who have stopped tobacco smoking but use electronic cigarettes are more likely to relapse to tobacco smoking than those who do not use electronic cigarettes.”
Dr. Farber noted that there are other Food and Drug Administration–approved medications for treating tobacco addiction. In addition, the World Health Organization, American Medical Association, Centers for Disease Control and Prevention, and FDA have all advised that e-cigarettes should not be used as smoking cessation aids, he said, especially in light of current outbreak of life-threatening e-cigarette and vaping lung injuries currently being investigated by the CDC and FDA.
“These study results suggest that the CDC reports of e-cigarette, or vaping, product use–associated lung injury are likely to be just the tip of the iceberg,” he said. “Although the CDC has identified vitamin E acetate–containing products as an important culprit, it is unlikely to be the only one. There are many substances in the emissions of e-cigarettes that have known irritant and/or toxic effects on the airways.”
Dr. Bhatta and Dr. Glantz acknowledged several limitations in their analysis, including the possibility of recall bias, not distinguishing between nondaily and daily e-cigarette or combustible tobacco use, and combining respiratory conditions together to achieve adequate power. The study shows an association, but the mechanism by which e-cigarettes may contribute to the development of lung disease remains under investigation.
This study was supported by grants from the National Institute on Drug Abuse; the National Cancer Institute; the FDA Center for Tobacco Products; the National Heart, Lung, and Blood Institute; and the University of California, San Francisco Helen Diller Family Comprehensive Cancer Center Global Cancer Program. Dr. Bhatta and Dr. Glantz reported no relevant conflicts of interest.
SOURCE: Bhatta DN, Glantz SA. Am J Prev Med. 2019 Dec 16. doi: 10.1016/j.amepre.2019.07.028.
according to recent longitudinal analysis published in the American Journal of Preventive Medicine.
E-cigarettes have been promoted as a safer alternative to combustible tobacco, and until recently, there has been little and conflicting evidence by which to test this hypothesis. This study conducted by Dharma N. Bhatta, PhD, and Stanton A. Glantz, PhD, of the Center for Tobacco Control Research and Education at the University of California, San Francisco, is one of the first longitudinal examinations of e-cigarette use and controlling for combustible tobacco use.
Dr. Bhatta and Dr. Glantz performed a multivariable, logistic regression analysis of adults enrolled in the nationally representative, population-based, longitudinal Population Assessment of Tobacco and Health study. The researchers analyzed the tobacco use of adults in the study in three waves, following them through wave 1 (September 2013 to December 2014), wave 2 (October 2014 to October 2015), and wave 3 (October 2015 to October 2016), analyzing the data between 2018 and 2019. Overall, wave 1 began with 32,320 participants, and 15.1% of adults reported respiratory disease at baseline.
Lung or respiratory disease was assessed by asking participants whether they had been told by a health professional that they had chronic obstructive pulmonary disease, chronic bronchitis, emphysema, or asthma. The researchers defined e-cigarette and combustible tobacco use as participants who never, currently, or formerly used e-cigarettes or smoked combustible tobacco. Participants who indicated they used e-cigarettes or combustible tobacco frequently or infrequently were placed in the current-user group, while past users were those participants who said they used to, but no longer use e-cigarettes or combustible tobacco.
The results showed former e-cigarette use (adjusted odds ratio, 1.34; 95% confidence interval, 1.23-1.46) and current e-cigarette use (aOR, 1.32; 95% CI, 1.17-1.49) were associated with an increased risk of having incident respiratory disease.
The data showed a not unexpected statistically significant association between former combustible tobacco use (aOR, 1.29; 95% CI, 1.14-1.47) as well as current combustible tobacco use (aOR, 1.61; 95% CI, 1.42-1.82) and incident respiratory disease risk.
There was a statistically significant association between respiratory disease and former or current e-cigarette use for adults who did not have respiratory disease at baseline, after adjusting for factors such as current combustible tobacco use, clinical variables, and demographic differences. Participants in wave 1 who reported former (aOR, 1.31; 95% CI, 1.07-1.60) or current e-cigarette use (aOR, 1.29; 95% CI, 1.03-1.61) had a significantly higher risk of developing incident respiratory disease in subsequent waves. There was also a statistically significant association between use of combustible tobacco and subsequent respiratory disease in later waves of the study (aOR, 2.56; 95% CI, 1.92-3.41), which the researchers noted was independent of the usual risks associated with combustible tobacco.
The investigators also looked at the link between dual use of e-cigarettes and combustible tobacco and respiratory disease risk. “The much more common pattern is dual use, in which an e-cigarette user continues to smoke combusted tobacco products at the same time (93.7% of e-cigarette users at wave 2 and 91.2% at wave 3 also used combustible tobacco; 73.3% of e-cigarette users at wave 2 and 64.9% at wave 3 also smoked cigarettes),” they wrote.
The odds of developing respiratory disease for participants who used both e-cigarettes and combustible tobacco were 3.30, compared with a participant who never used e-cigarettes, with similar results seen when comparing e-cigarettes and cigarettes.
“Although switching from combustible tobacco, including cigarettes, to e-cigarettes theoretically could reduce the risk of developing respiratory disease, current evidence indicates a high prevalence of dual use, which is associated with in-creased risk beyond combustible tobacco use,” the investigators wrote.
Harold J. Farber, MD, FCCP, professor of pediatrics in the pulmonary section at Baylor College of Medicine and Texas Children’s Hospital, both in Houston, said in an interview that the increased respiratory risk among dual users, who are likely using e-cigarettes and combustible tobacco together as a way to quit smoking, is particularly concerning.
“There is substantial reason to be concerned about efficacy of electronic cigarette products. Real-world observational studies have shown that, on average, tobacco smokers who use electronic cigarettes are less likely to stop smoking than those who do not use electronic cigarettes,” he said. “People who have stopped tobacco smoking but use electronic cigarettes are more likely to relapse to tobacco smoking than those who do not use electronic cigarettes.”
Dr. Farber noted that there are other Food and Drug Administration–approved medications for treating tobacco addiction. In addition, the World Health Organization, American Medical Association, Centers for Disease Control and Prevention, and FDA have all advised that e-cigarettes should not be used as smoking cessation aids, he said, especially in light of current outbreak of life-threatening e-cigarette and vaping lung injuries currently being investigated by the CDC and FDA.
“These study results suggest that the CDC reports of e-cigarette, or vaping, product use–associated lung injury are likely to be just the tip of the iceberg,” he said. “Although the CDC has identified vitamin E acetate–containing products as an important culprit, it is unlikely to be the only one. There are many substances in the emissions of e-cigarettes that have known irritant and/or toxic effects on the airways.”
Dr. Bhatta and Dr. Glantz acknowledged several limitations in their analysis, including the possibility of recall bias, not distinguishing between nondaily and daily e-cigarette or combustible tobacco use, and combining respiratory conditions together to achieve adequate power. The study shows an association, but the mechanism by which e-cigarettes may contribute to the development of lung disease remains under investigation.
This study was supported by grants from the National Institute on Drug Abuse; the National Cancer Institute; the FDA Center for Tobacco Products; the National Heart, Lung, and Blood Institute; and the University of California, San Francisco Helen Diller Family Comprehensive Cancer Center Global Cancer Program. Dr. Bhatta and Dr. Glantz reported no relevant conflicts of interest.
SOURCE: Bhatta DN, Glantz SA. Am J Prev Med. 2019 Dec 16. doi: 10.1016/j.amepre.2019.07.028.
FROM THE AMERICAN JOURNAL OF PREVENTIVE MEDICINE
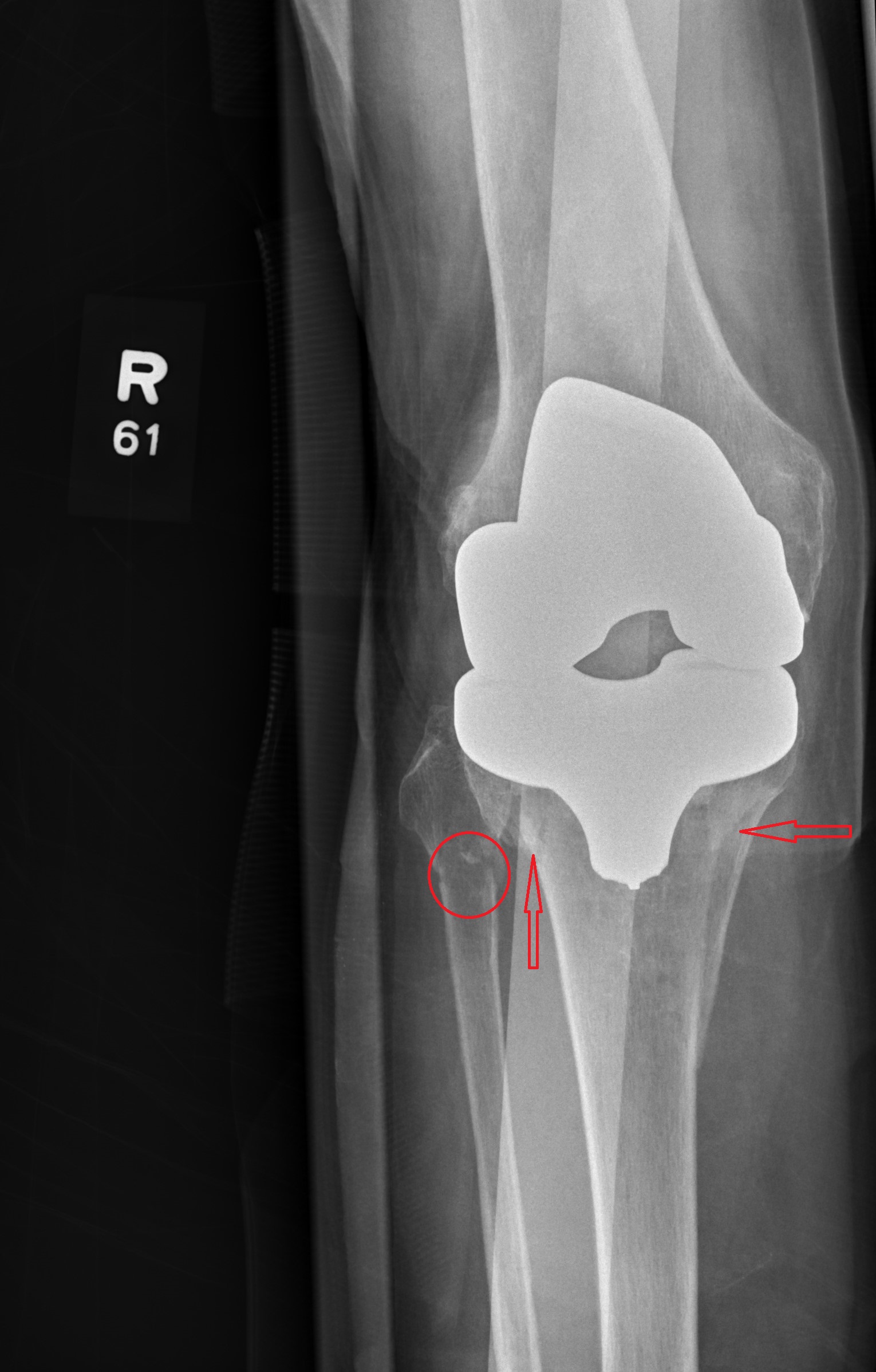
X-Ray Goes Knee Deep
Answer
The radiograph shows evidence of status post arthroplasty. There are no abnormalities within the prosthesis. However, the patient has a fracture of the proximal tibia that extends into the tibial plateau, as well as a nondisplaced fracture of the proximal fibula.
The patient was admitted and orthopedics consulted.
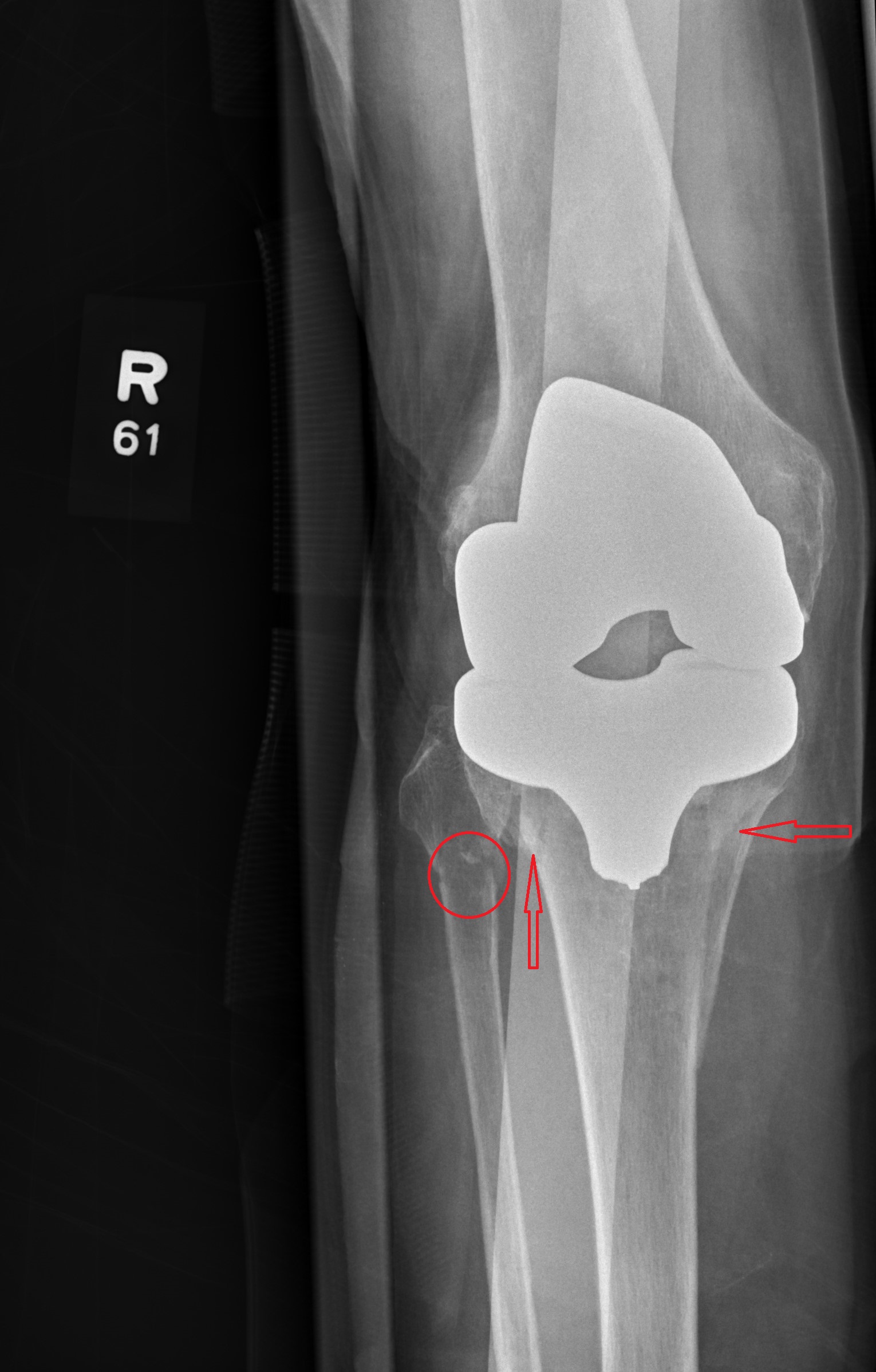
Answer
The radiograph shows evidence of status post arthroplasty. There are no abnormalities within the prosthesis. However, the patient has a fracture of the proximal tibia that extends into the tibial plateau, as well as a nondisplaced fracture of the proximal fibula.
The patient was admitted and orthopedics consulted.
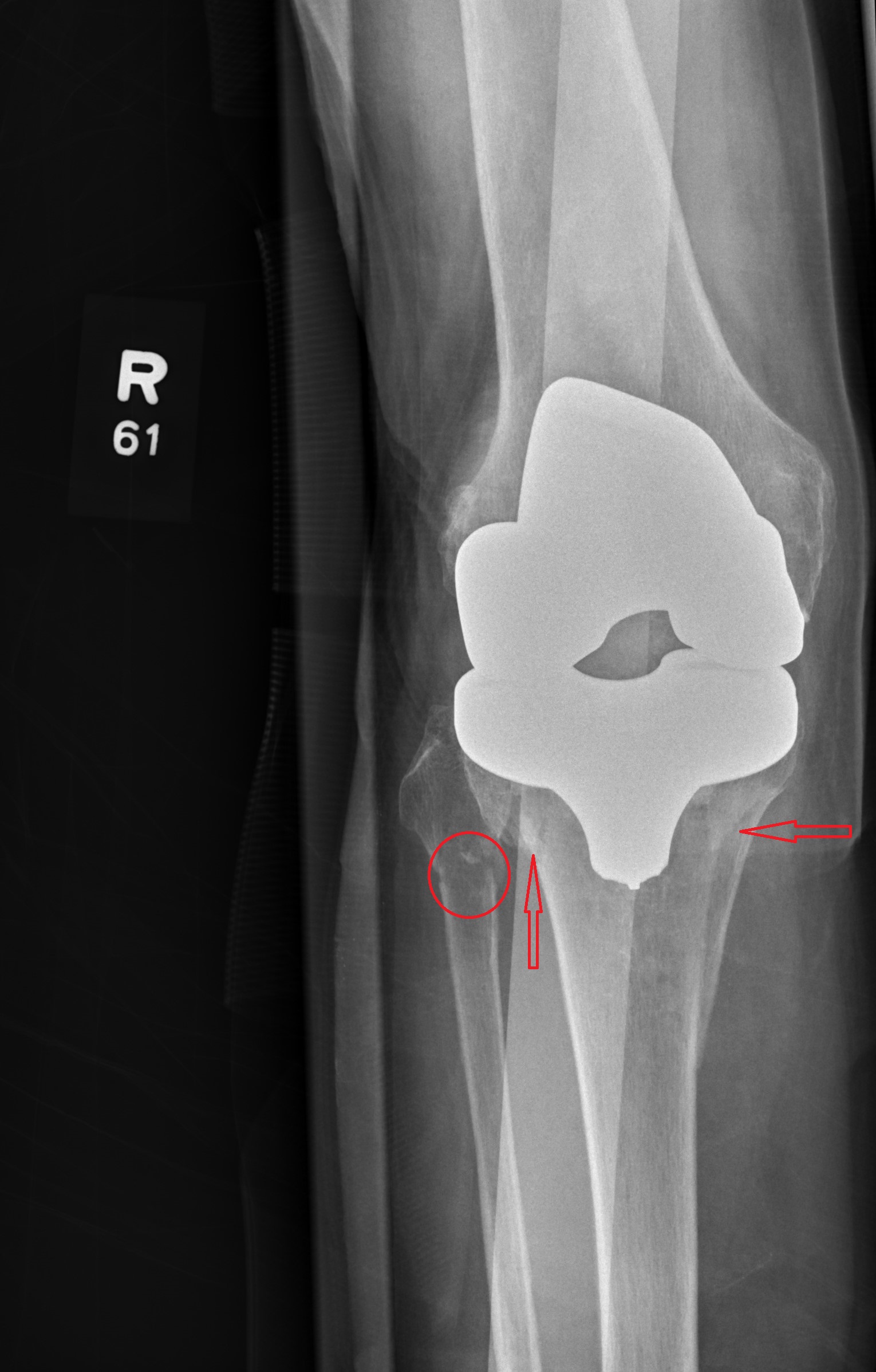
Answer
The radiograph shows evidence of status post arthroplasty. There are no abnormalities within the prosthesis. However, the patient has a fracture of the proximal tibia that extends into the tibial plateau, as well as a nondisplaced fracture of the proximal fibula.
The patient was admitted and orthopedics consulted.

Skip CTs for breakthrough seizures in chronic epilepsy
BALTIMORE – Head CTs for breakthrough seizures in chronic epilepsy are useful for known structural triggers such as brain tumors, but they don’t change management for most patients, according to a review from the SUNY Upstate Medical University, Syracuse, N.Y., emergency department.
“Nonselective use of ED neuroimaging in patients with no new neurological findings” and no known structural problem, is “very low yield, and increases the use of hospital resources and radiation exposure without impacting the immediate care,” concluded investigators led by Shahram Izadyar, MD, an epileptologist and associate professor of neurology at the university.
In short, CTs for breakthrough seizures – routine in many EDs – usually are a waste of time and money. Absent a known structural cause, “there really isn’t a reason to do imaging,” he said at the American Epilepsy Society annual meeting.
Dr. Izadyar wanted to look into the issue after noticing how common CTs were among his breakthrough patients. He and his team reviewed 90 adults with an established diagnosis of epilepsy and on at least one antiepileptic who presented to the university ED for breakthrough seizures during 2017-2018; 39 (43.3%) had head CTs, 51 (56.7%) did not.
CT changed management in three of the four patients (4.4%) who had a known brain tumor, leading, for instance, to steroids for increased tumor edema. The rest of the patients had nonfocal exams, and imaging had no impact on management.
There was no rhyme or reason why some people got CTs and others didn’t; it seemed to be dependent on the provider. Defensive medicine probably had something to do with it, as well as saving time by ordering a CT instead of doing a neurologic exam, Dr. Izadyar said.
People aren’t going to stop doing defensive medicine, but even a small reduction in unnecessary CTs would “be a positive change.” There’s the cost issue, but also the radiation exposure, which is considerable when people end up in the ED every few months for breakthrough seizures, he said.
There were no differences between the CT and no-CT groups in the suspected causes of breakthroughs (P = .93). About half the cases were probably because of noncompliance, about a quarter from sleep deprivation, and the rest from a change in seizure medication or some other issue.
Dr. Izadyar said the next step is taking the findings to his ED colleagues, and perhaps calculating how much money the university would save by skipping CTs in chronic epilepsy patients with no known structural problem.
There were slightly more men than women in the study, and the mean age was 38 years.
There was no industry funding, and the investigators didn’t have any relevant disclosures.
SOURCE: Ali S et al. AES 2019. Abstract 1.213.
BALTIMORE – Head CTs for breakthrough seizures in chronic epilepsy are useful for known structural triggers such as brain tumors, but they don’t change management for most patients, according to a review from the SUNY Upstate Medical University, Syracuse, N.Y., emergency department.
“Nonselective use of ED neuroimaging in patients with no new neurological findings” and no known structural problem, is “very low yield, and increases the use of hospital resources and radiation exposure without impacting the immediate care,” concluded investigators led by Shahram Izadyar, MD, an epileptologist and associate professor of neurology at the university.
In short, CTs for breakthrough seizures – routine in many EDs – usually are a waste of time and money. Absent a known structural cause, “there really isn’t a reason to do imaging,” he said at the American Epilepsy Society annual meeting.
Dr. Izadyar wanted to look into the issue after noticing how common CTs were among his breakthrough patients. He and his team reviewed 90 adults with an established diagnosis of epilepsy and on at least one antiepileptic who presented to the university ED for breakthrough seizures during 2017-2018; 39 (43.3%) had head CTs, 51 (56.7%) did not.
CT changed management in three of the four patients (4.4%) who had a known brain tumor, leading, for instance, to steroids for increased tumor edema. The rest of the patients had nonfocal exams, and imaging had no impact on management.
There was no rhyme or reason why some people got CTs and others didn’t; it seemed to be dependent on the provider. Defensive medicine probably had something to do with it, as well as saving time by ordering a CT instead of doing a neurologic exam, Dr. Izadyar said.
People aren’t going to stop doing defensive medicine, but even a small reduction in unnecessary CTs would “be a positive change.” There’s the cost issue, but also the radiation exposure, which is considerable when people end up in the ED every few months for breakthrough seizures, he said.
There were no differences between the CT and no-CT groups in the suspected causes of breakthroughs (P = .93). About half the cases were probably because of noncompliance, about a quarter from sleep deprivation, and the rest from a change in seizure medication or some other issue.
Dr. Izadyar said the next step is taking the findings to his ED colleagues, and perhaps calculating how much money the university would save by skipping CTs in chronic epilepsy patients with no known structural problem.
There were slightly more men than women in the study, and the mean age was 38 years.
There was no industry funding, and the investigators didn’t have any relevant disclosures.
SOURCE: Ali S et al. AES 2019. Abstract 1.213.
BALTIMORE – Head CTs for breakthrough seizures in chronic epilepsy are useful for known structural triggers such as brain tumors, but they don’t change management for most patients, according to a review from the SUNY Upstate Medical University, Syracuse, N.Y., emergency department.
“Nonselective use of ED neuroimaging in patients with no new neurological findings” and no known structural problem, is “very low yield, and increases the use of hospital resources and radiation exposure without impacting the immediate care,” concluded investigators led by Shahram Izadyar, MD, an epileptologist and associate professor of neurology at the university.
In short, CTs for breakthrough seizures – routine in many EDs – usually are a waste of time and money. Absent a known structural cause, “there really isn’t a reason to do imaging,” he said at the American Epilepsy Society annual meeting.
Dr. Izadyar wanted to look into the issue after noticing how common CTs were among his breakthrough patients. He and his team reviewed 90 adults with an established diagnosis of epilepsy and on at least one antiepileptic who presented to the university ED for breakthrough seizures during 2017-2018; 39 (43.3%) had head CTs, 51 (56.7%) did not.
CT changed management in three of the four patients (4.4%) who had a known brain tumor, leading, for instance, to steroids for increased tumor edema. The rest of the patients had nonfocal exams, and imaging had no impact on management.
There was no rhyme or reason why some people got CTs and others didn’t; it seemed to be dependent on the provider. Defensive medicine probably had something to do with it, as well as saving time by ordering a CT instead of doing a neurologic exam, Dr. Izadyar said.
People aren’t going to stop doing defensive medicine, but even a small reduction in unnecessary CTs would “be a positive change.” There’s the cost issue, but also the radiation exposure, which is considerable when people end up in the ED every few months for breakthrough seizures, he said.
There were no differences between the CT and no-CT groups in the suspected causes of breakthroughs (P = .93). About half the cases were probably because of noncompliance, about a quarter from sleep deprivation, and the rest from a change in seizure medication or some other issue.
Dr. Izadyar said the next step is taking the findings to his ED colleagues, and perhaps calculating how much money the university would save by skipping CTs in chronic epilepsy patients with no known structural problem.
There were slightly more men than women in the study, and the mean age was 38 years.
There was no industry funding, and the investigators didn’t have any relevant disclosures.
SOURCE: Ali S et al. AES 2019. Abstract 1.213.
REPORTING FROM AES 2019
Applying Robust Process Improvement Techniques to the Voluntary Inpatient Psychiatry Admission Process
From the Wake Forest School of Medicine (Ms. Newman), and Wake Forest Baptist Health, Department of Psychiatry and Behavioral Medicine (Dr. Kramer), Winston-Salem, NC.
Abstract
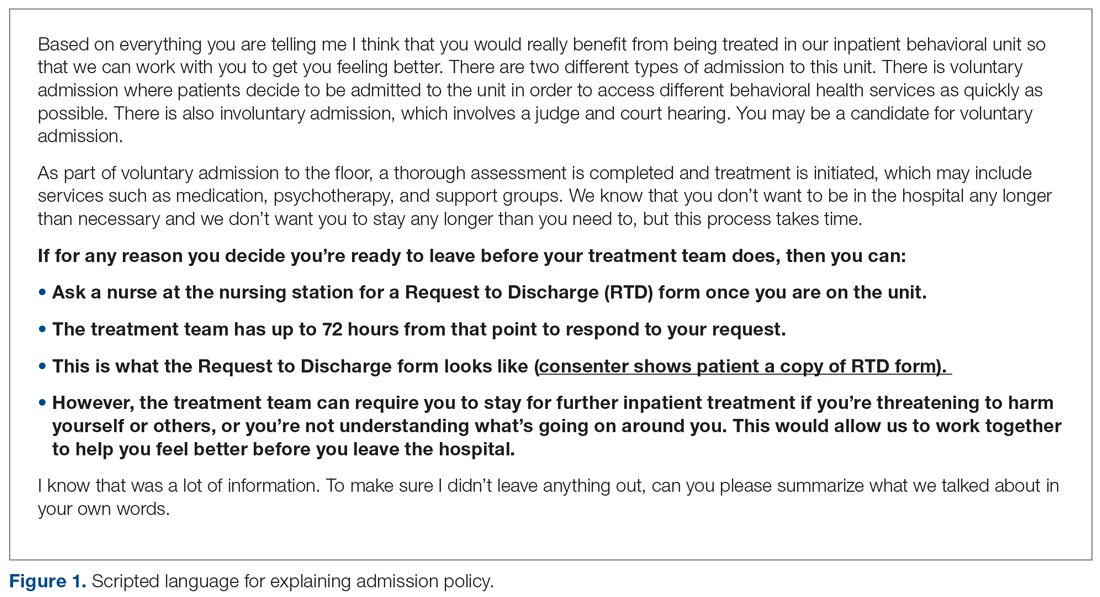
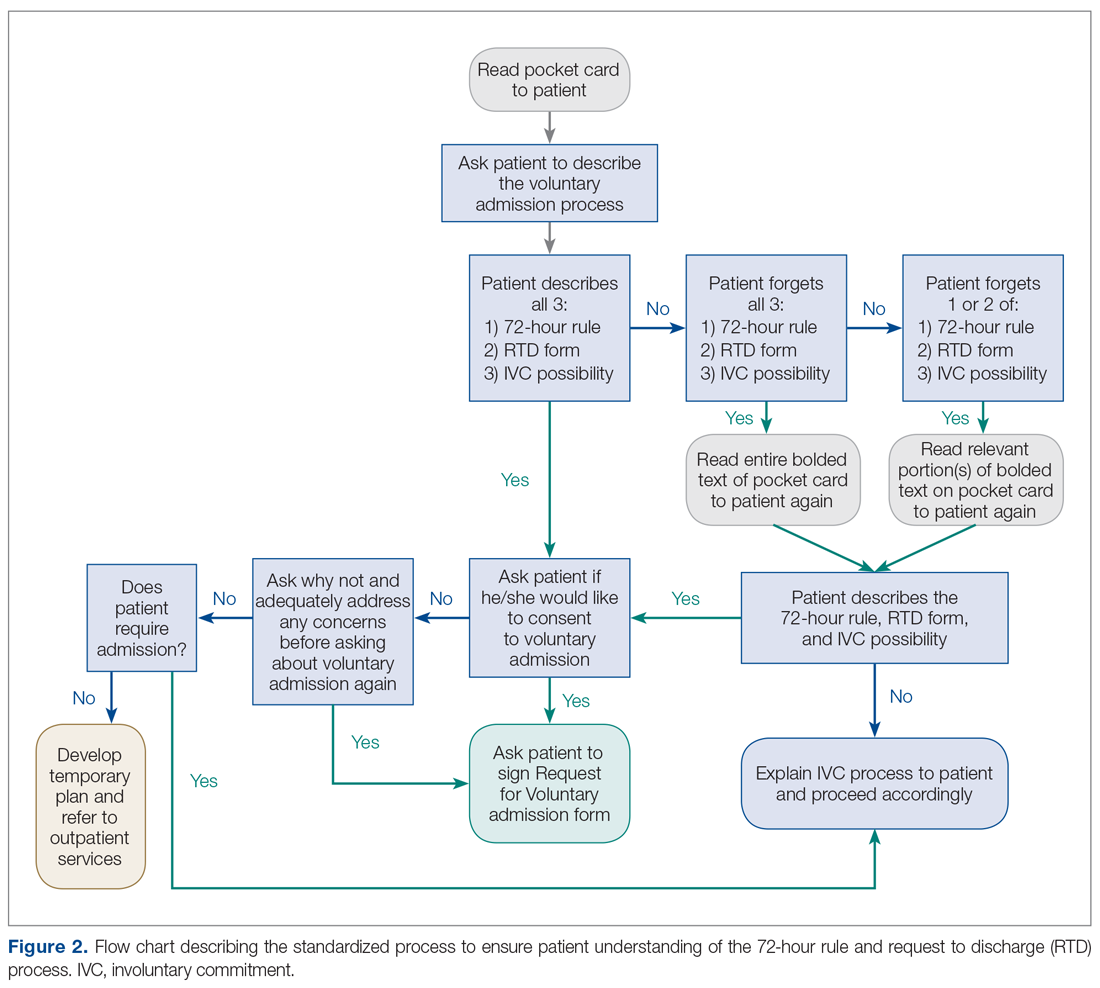
- Background: Adults voluntarily admitted to inpatient behavioral health units can ask to sign a Request to Discharge (RTD) form if they would like to be discharged before the treatment team agrees that discharge is appropriate. This gives the team 72 hours to determine whether the patient is safe to discharge or to involuntarily commit the patient to the unit. At 1 medical center, patients who were offered voluntary admission often lacked complete understanding of the “72-hour rule” and the early discharge procedure.
- Methods: Robust Process Improvement® techniques were implemented to improve the admission process. Flow charts, standardized scripts, and pocket cards were distributed to relevant staff. The Request for Voluntary Admission form was revised to emphasize the “72-hour rule” and the process for requesting a RTD form.
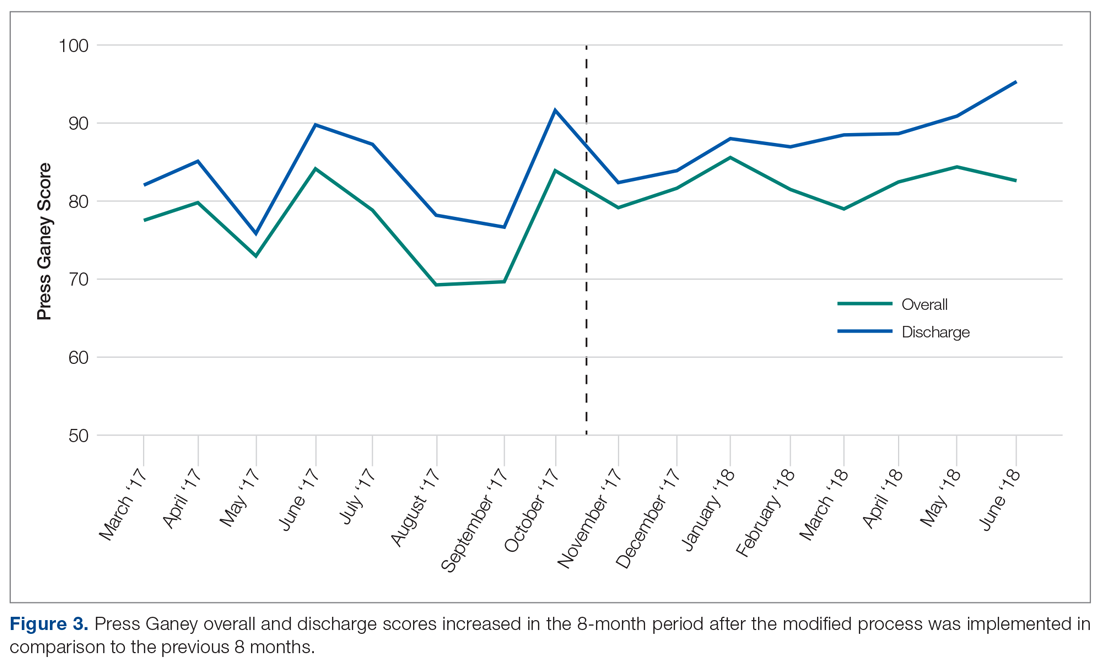
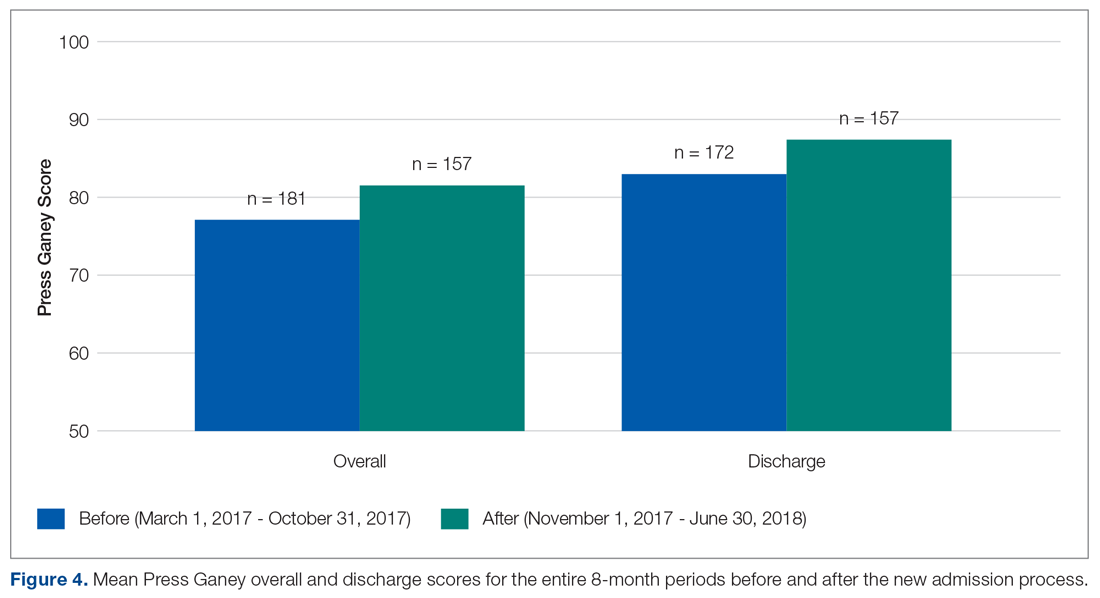
- Results: The unit’s average overall Press Ganey score improved from 77.1 to 81.6 (P = 0.003), while the average discharge score improved from 83.0 to 87.5 (P = 0.023) following implementation of the new process.
- Conclusion: Incorporating strategies such as an opportunity to “teach back” important information about the voluntary admission process (ie, what the 72-hour rule is, what the request to discharge form is, and the possibility of involuntary commitment) allows clinicians to assess capacity while simultaneously giving patients realistic expectations of the admission. These changes can lead to improvement in patient satisfaction.
Keywords: behavioral health; communication; patient satisfaction.
Communication is paramount within medical teams to improve outcomes and strengthen rapport with patients, particularly with psychiatric patients in acute crisis. Studies
While some forms of communication are required to protect the safety of patients and others around them, other forms are required to build strong relationships with patients. However, these 2 goals do not have to be mutually exclusive in the psychiatric hospital environment. Hospitals aim to improve patient satisfaction while simultaneously providing effective communication about treatment. Studies have indicated that communication during graduate medical training may decline due to “emotional and physical brutality” associated with residency training programs.4 To ameliorate this and emphasize communication education, accredited psychiatry residency programs require residents to use structured communication tools to achieve a level 2 in the Accreditation Council for Graduate Medical Education milestone project for the category of patient safety and health care team.5 These standardized processes allow all patients to receive the same important information related to their care while minimizing human error. Such communication skills aim to improve health care outcomes and satisfaction for patients while also training better physicians.
For legal and ethical reasons, the adult inpatient behavioral health units at major hospitals are highly regulated. In most states, a patient who is admitted to an adult inpatient behavioral health unit on a voluntary basis can ask to sign a request to discharge (RTD) form if he or she would like to be discharged from the hospital before the treatment team sees fit.6 In most jurisdictions, this action gives the treatment team 72 hours to determine whether the patient is safe to discharge. Within that time frame, the physician must either discharge the patient, or, if it is not safe to do so, involuntarily commit him or her to the unit. In most jurisdictions, this process is commonly referred to as the “72-hour rule.”
In North Carolina, state legislation Chapter 122C, Article 5, Part 2(b) specifies: “In 24-hour facilities the application shall acknowledge that the applicant may be held by the facility for a period of 72 hours after any written request for release that the applicant may make, and shall acknowledge that the 24-hour facility may have the legal right to petition for involuntary commitment of the applicant during that period. At the time of application, the facility shall tell the applicant about procedures for discharge.”7 This requirement can be somewhat confusing for both medical team members and patients alike.
As formerly practiced on the behavioral health unit described in this report, patients offered voluntary admission status to the inpatient behavioral unit often lacked complete understanding of the 72-hour rule and the process for requesting early discharge from the facility. We hypothesized that this led to the observed patient frustration and hostility, lack of trust in the treatment team, poor attendance and participation in group therapy activities, medication refusal, and overall decreased patient satisfaction. To address this issue, this pilot project was conducted to improve the voluntary admission process on the adult inpatient unit of a major academic medical center in North Carolina.
In April 2008, The Joint Commission’s Center for Transforming Healthcare embarked on an enterprise-wide initiative called Robust Process Improvement (RPI). RPI was developed as a blended approach in applying Six Sigma, Lean, and Change Management techniques to improve medical processes and procedures. RPI techniques were applied in this study to better define the problems related to inpatient behavioral health unit admission and discharge by collecting data, obtaining staff involvement, creating a solution, and monitoring for lasting benefit.
Methods
This quality improvement project took place at an 885-bed tertiary care academic medical center with Level 1 Trauma Center designation. Institutional Review Board approval was not required because this was performed as a quality improvement project rather than an experimental clinical trial and was not designed to create new generalizable knowledge.
The techniques used to improve outcomes on the inpatient behavioral health unit included Active Listening, Elevator Speech, Statistics, Cause and Effect Diagrams, development of a Communication Plan, Brainstorming, and Standard Work. Through interviews with physician assistants, nurses, and resident physicians conducted over a 1-month period, it became clear that there was confusion among patients surrounding the voluntary admission process, the process for requesting discharge, and the possibility of a voluntary admission being converted to an involuntary one. Active listening was used to better understand the opportunities for improvement from multiple perspectives through varying stages of the admission—from the consent process in the emergency department, admission to the unit, throughout the hospital stay, to the time of discharge. The following elevator speech was used to highlight the areas of confusion and the importance of implementing change with the team involved in implementing the new admission procedures:
Our project is about improving patient understanding of the voluntary admission process to the Adult Psychiatry Unit and the 72-hour rule. This is important because the present process leads to patient misunderstanding, discontent on the unit, resistance to provided therapies, and low Press Ganey satisfaction scores. Success will look like reduced patient confusion about the 72-hour rule, increased group participation, decreased patient-staff conflict, and improved Press Ganey scores. What we are asking from you is to use a standardized, scripted informed consent process, flow chart, and pocket card during the voluntary admission process.
Additionally, brainstorming sessions were conducted with physician assistants, nurses, and residents to discuss options to improve the process and elicit a list of barriers.
Data Gathering
Several metrics were tracked to further understand the issue. Overall Press Ganey scores, in addition to admission and discharge subsection scores, were tracked for the 8 months prior to implementing the quality improvement procedures (March 2017-October 2017). Additionally, the treatment team members answered survey questions related to perceived patient understanding at the beginning of training sessions in the 5-week period immediately prior to implementing the quality improvement procedures. This survey was administered using a 6-point Likert scale, ranging from 1 (never) to 6 (frequently), and included the following questions:
- How often do you have to explain: (a) Request for Voluntary Admission form, (b) 72-Hour Rule, (c) Request to Discharge form?
- How often is there confusion about the 72-hour rule and RTD form once admitted to the adult inpatient psychiatric unit?
- How often do you need to re-explain the 72-hour rule and RTD form once admitted to the adult inpatient psychiatric unit?
In-depth interviews were conducted with 4 resident physicians, 4 physician assistants, and 3 nurses to identify specific shortcomings of the admission procedure. A key finding from these interviews was that some patients tended not to understand that the treatment team had 72 hours to respond to the RTD application. Instead, several patients had indicated that they thought that they could immediately discharge themselves since they were on the unit “voluntarily” or that they could categorically discharge themselves after 72 hours of being admitted. This feedback was crucial in determining the next steps that could be taken to minimize confusion.
Process Changes
In preparation for this quality improvement project, the language and layout of the Request for Voluntary Admission form was revised and approved internally by the hospital’s Forms Committee to emphasize the 72-hour rule and the process for completing a RTD form. Additionally, these interviews indicated that it was difficult to track patients who were admitted voluntarily versus involuntarily. To rectify this problem, a field was added to the electronic medical record system to include current psychiatric admission status, allowing the selection to be either “Voluntary” or “Involuntary.” This new field in the electronic medical record system gives nurses the ability to easily update legal status daily as appropriate, which minimizes the risk of information not being effectively communicated at shift changes, while also allowing various members of the treatment team to be updated on the admission status of each patient.
After reviewing data and obtaining staff involvement related to the problem, a new psychiatric admission and consent process was created. The new consent and admission process was characterized by a standardized procedure and scripted language to present to candidates for voluntary admission. The standardized procedure begins with the admitting staff member reading scripted consent language from a pocket card that includes 3 key points describing the voluntary admission procedure (see script in Figure 1). The first key point is to describe the 72-hour rule. Next, the staff member describes the purpose of the RTD form and shows an example to the patient. Finally, the staff member responsible for consenting describes the possibility of the patient being required to remain on the unit involuntarily in the event that he or she wants to leave before the treatment team sees fit and is deemed to be a danger to himself or herself or others.
On the reverse side of the pocket card, an example of the RTD form is available to show to the patient. The subsequent teach-back procedure is summarized using the flow chart in Figure 2, and this was made available to staff who participate in the admission and discharge processes. After reading the consent script, the consenting staff member must ask the patient to recall the 3 key points. For each key point that the patient cannot recall, the relevant section of the scripted language is re-read to the patient, who is asked to explain it again. If the patient recalls the 3 key points, then he or she is deemed to have cognitive capacity and thus can become a candidate for voluntary admission.
Flow charts, scripts, and pocket cards were created and distributed to relevant physicians, physician assistants, and nurses who participate in the admission or discharge process. Additional copies of pocket cards were made available within the department. In October 2017, an attending psychiatrist and medical student trained psychiatry physician assistants, nurses, and resident physicians who participated in the admission process in the ED or patient care on the unit on how to use the new materials. The new process was first implemented on November 1, 2017.
Measurements
Press Ganey scores were compared for 8 months before and 8 months after implementing the new process to monitor changes from the patients’ perspective. Additionally, the treatment team members answered survey questions related to perceived patient understanding at the beginning of training sessions in mid-September through mid-October and again 5 weeks after the new process was implemented.
Results
The behavioral health unit’s Press Ganey (overall and discharge) scores increased during the 8-month period following implementation of the quality improvement project (Figure 3). There was a notable upward trend of overall and discharge Press Ganey scores on a month-by-month basis from November through April. In total, 181 Press Ganey score reports were available for the 6-month period prior to the new process versus 157 score reports after (Figure 4). The average overall Press Ganey score for respondents improved from 77.1 to 81.6 (P = 0.003), while the average discharge score improved from 83.0 to 87.5 (P = 0.023).
In recent months, the behavioral health discharge satisfaction score has become one of the highest performing aspects of the department according to Press Ganey reports. From April through June 2018, the department has performed in the 98th percentile or higher in “information about patient’s rights” during admission and “discharge instructions if help is needed.”
The survey related to perceived patient satisfaction and confusion also indicated significant improvement. Survey respondents indicated that there was less confusion about the 72-hour rule and RTD form after the quality improvement procedure was implemented (P = 0.039) and that fewer attempts to re-explain these concepts were required as well (P = 0.035).
Discussion
The Press Ganey scores for this unit indicated an improvement in patient satisfaction, in particular with the discharge process. While the overall Press Ganey scores on the inpatient behavioral health unit showed a significant improvement, it remained stagnant, around 80, during the 8-month period after implementing the new standardized admission process. However, the discharge score consistently improved over the same 8 months, from 82 to 95 in the most recent month. Also, the overall and discharge scores indicated a brief spike/improvement in October, immediately preceding the implementation of the new scripted language. Given the timeline, this spike is likely related to the ongoing meetings, trainings, and awareness of the upcoming process improvement.
With hospital and health system reimbursements becoming increasingly tied with patient outcomes, quality improvement efforts to improve patient care and satisfaction are of the utmost importance. In order to develop the rapport with patients needed for a high level of cooperation and excellent outcomes on an inpatient psychiatric unit, it is essential that all patients receive specific information about what the admission entails and what the options are for being discharged from the unit. Since a voluntary admission can be converted to an involuntary admission if a patient is deemed a threat to himself or herself or others despite already signing a RTD form, it is essential that this is not only discussed prior to admission, but that these details are explicitly checked for understanding. This allows the treatment team to assess for capacity and the patient to demonstrate informed consent. Differing expectations or understanding in what the voluntary admission or discharge process entails can lead to patient frustration and hostility, lack of trust in the treatment team, poor attendance and participation in group therapy activities, and medication refusal. Altogether, this can lead to longer inpatient stays, increased costs, decreased outcomes, and decreased patient satisfaction.
These initiatives were relatively easy to implement and are backed by evidence that they ultimately increased patient satisfaction. These findings could be extended to other institutions to improve the voluntary admission process and, ultimately, the patient experience. Additionally, the methods could be applied to other patient care processes within psychiatric facilities, and to improve other aspects of the patient care experience that have room for improvement, as illustrated by the department’s Press Ganey subsection scores, or areas that the treatment team would like to focus on.
Limitations
There are several limitations in the design and evaluation of this project. The assessment of patient understanding, especially in psychiatric patients, is very difficult to quantify. The principal measure of assessing patient understanding was limited to health care professional survey results. This may have led to a slight social desirability bias. An objective assessment of understanding directly from the patients was not readily attainable in our study, but future studies could look at this metric in addition to health care professional survey results.
Additionally, the overall Press Ganey scores may be influenced by factors beyond the admission process and the applied improvement procedures. It is difficult to discern whether there were any other factors that also contributed to the overall increase. However, the discharge score was a more direct measure specifically related to the modified procedures, and the temporal association of the intervention with the increased scores suggests that the intervention was responsible.
Conclusion
Standardization of the consent process ensures that all patients receive the necessary information every time in busy clinical settings. Incorporating an opportunity to “teach back” specific important information about the voluntary admission process, specifically what the 72-hour rule is, what the RTD form is, and the possibility of involuntary commitment, allows clinicians to assess capacity, while simultaneously allowing patients to have realistic expectations of the admission. Concise, standardized answers regarding these points minimizes variation in information being dispersed and decreases the possibility of omitting important information. At a major academic medical center, easy-to-implement quality improvement techniques significantly decreased patient confusion surrounding the 72-hour rule and the RTD form, along with the frequency in which these policies needed to be re-explained on the adult inpatient psychiatric unit. These changes ultimately led to improvement in patient satisfaction, as indicated by significant improvement in both overall and discharge patient satisfaction scores.
Corresponding author: Jennifer F. Newman, 475 Vine St., Winston-Salem, NC, 27101; jnewman9@u.rochester.edu.
Financial disclosures: None.
1. Redfern E, Brown R, Vincent C. Improving communication in the emergency department. Emerg Med J. 2009;26:658-661.
2. Payne CE, Stein JM, Leong T, Dressler DD. Avoiding handover fumbles: a controlled trial of a structured handover tool versus traditional handover methods. BMJ Qual Saf. 2012;21:925-932.
3. Weller J, Boyd M, Cumin D. Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J. 2014;90:149-154.
4. DiMatteo MR. The role of the physician in the emerging health care environment. Western J Med. 1998;168:328.
5. The Psychiatry Milestone Project. J Grad Med Educ. 2014;6(1 Suppl 1):284-304.
6. Garakani A, Shalenberg E, Burstin SC, et al. Voluntary psychiatric hospitalization and patient-driven requests for discharge: a statutory review and analysis of implications for the capacity to consent to voluntary hospitalization. Harv Rev Psychiatry. 2014;22:241-249.
7. Procedure for Admission and Discharge of Clients Act, 211 § 122C-211(2014).
From the Wake Forest School of Medicine (Ms. Newman), and Wake Forest Baptist Health, Department of Psychiatry and Behavioral Medicine (Dr. Kramer), Winston-Salem, NC.
Abstract
- Background: Adults voluntarily admitted to inpatient behavioral health units can ask to sign a Request to Discharge (RTD) form if they would like to be discharged before the treatment team agrees that discharge is appropriate. This gives the team 72 hours to determine whether the patient is safe to discharge or to involuntarily commit the patient to the unit. At 1 medical center, patients who were offered voluntary admission often lacked complete understanding of the “72-hour rule” and the early discharge procedure.
- Methods: Robust Process Improvement® techniques were implemented to improve the admission process. Flow charts, standardized scripts, and pocket cards were distributed to relevant staff. The Request for Voluntary Admission form was revised to emphasize the “72-hour rule” and the process for requesting a RTD form.
- Results: The unit’s average overall Press Ganey score improved from 77.1 to 81.6 (P = 0.003), while the average discharge score improved from 83.0 to 87.5 (P = 0.023) following implementation of the new process.
- Conclusion: Incorporating strategies such as an opportunity to “teach back” important information about the voluntary admission process (ie, what the 72-hour rule is, what the request to discharge form is, and the possibility of involuntary commitment) allows clinicians to assess capacity while simultaneously giving patients realistic expectations of the admission. These changes can lead to improvement in patient satisfaction.
Keywords: behavioral health; communication; patient satisfaction.
Communication is paramount within medical teams to improve outcomes and strengthen rapport with patients, particularly with psychiatric patients in acute crisis. Studies
While some forms of communication are required to protect the safety of patients and others around them, other forms are required to build strong relationships with patients. However, these 2 goals do not have to be mutually exclusive in the psychiatric hospital environment. Hospitals aim to improve patient satisfaction while simultaneously providing effective communication about treatment. Studies have indicated that communication during graduate medical training may decline due to “emotional and physical brutality” associated with residency training programs.4 To ameliorate this and emphasize communication education, accredited psychiatry residency programs require residents to use structured communication tools to achieve a level 2 in the Accreditation Council for Graduate Medical Education milestone project for the category of patient safety and health care team.5 These standardized processes allow all patients to receive the same important information related to their care while minimizing human error. Such communication skills aim to improve health care outcomes and satisfaction for patients while also training better physicians.
For legal and ethical reasons, the adult inpatient behavioral health units at major hospitals are highly regulated. In most states, a patient who is admitted to an adult inpatient behavioral health unit on a voluntary basis can ask to sign a request to discharge (RTD) form if he or she would like to be discharged from the hospital before the treatment team sees fit.6 In most jurisdictions, this action gives the treatment team 72 hours to determine whether the patient is safe to discharge. Within that time frame, the physician must either discharge the patient, or, if it is not safe to do so, involuntarily commit him or her to the unit. In most jurisdictions, this process is commonly referred to as the “72-hour rule.”
In North Carolina, state legislation Chapter 122C, Article 5, Part 2(b) specifies: “In 24-hour facilities the application shall acknowledge that the applicant may be held by the facility for a period of 72 hours after any written request for release that the applicant may make, and shall acknowledge that the 24-hour facility may have the legal right to petition for involuntary commitment of the applicant during that period. At the time of application, the facility shall tell the applicant about procedures for discharge.”7 This requirement can be somewhat confusing for both medical team members and patients alike.
As formerly practiced on the behavioral health unit described in this report, patients offered voluntary admission status to the inpatient behavioral unit often lacked complete understanding of the 72-hour rule and the process for requesting early discharge from the facility. We hypothesized that this led to the observed patient frustration and hostility, lack of trust in the treatment team, poor attendance and participation in group therapy activities, medication refusal, and overall decreased patient satisfaction. To address this issue, this pilot project was conducted to improve the voluntary admission process on the adult inpatient unit of a major academic medical center in North Carolina.
In April 2008, The Joint Commission’s Center for Transforming Healthcare embarked on an enterprise-wide initiative called Robust Process Improvement (RPI). RPI was developed as a blended approach in applying Six Sigma, Lean, and Change Management techniques to improve medical processes and procedures. RPI techniques were applied in this study to better define the problems related to inpatient behavioral health unit admission and discharge by collecting data, obtaining staff involvement, creating a solution, and monitoring for lasting benefit.
Methods
This quality improvement project took place at an 885-bed tertiary care academic medical center with Level 1 Trauma Center designation. Institutional Review Board approval was not required because this was performed as a quality improvement project rather than an experimental clinical trial and was not designed to create new generalizable knowledge.
The techniques used to improve outcomes on the inpatient behavioral health unit included Active Listening, Elevator Speech, Statistics, Cause and Effect Diagrams, development of a Communication Plan, Brainstorming, and Standard Work. Through interviews with physician assistants, nurses, and resident physicians conducted over a 1-month period, it became clear that there was confusion among patients surrounding the voluntary admission process, the process for requesting discharge, and the possibility of a voluntary admission being converted to an involuntary one. Active listening was used to better understand the opportunities for improvement from multiple perspectives through varying stages of the admission—from the consent process in the emergency department, admission to the unit, throughout the hospital stay, to the time of discharge. The following elevator speech was used to highlight the areas of confusion and the importance of implementing change with the team involved in implementing the new admission procedures:
Our project is about improving patient understanding of the voluntary admission process to the Adult Psychiatry Unit and the 72-hour rule. This is important because the present process leads to patient misunderstanding, discontent on the unit, resistance to provided therapies, and low Press Ganey satisfaction scores. Success will look like reduced patient confusion about the 72-hour rule, increased group participation, decreased patient-staff conflict, and improved Press Ganey scores. What we are asking from you is to use a standardized, scripted informed consent process, flow chart, and pocket card during the voluntary admission process.
Additionally, brainstorming sessions were conducted with physician assistants, nurses, and residents to discuss options to improve the process and elicit a list of barriers.
Data Gathering
Several metrics were tracked to further understand the issue. Overall Press Ganey scores, in addition to admission and discharge subsection scores, were tracked for the 8 months prior to implementing the quality improvement procedures (March 2017-October 2017). Additionally, the treatment team members answered survey questions related to perceived patient understanding at the beginning of training sessions in the 5-week period immediately prior to implementing the quality improvement procedures. This survey was administered using a 6-point Likert scale, ranging from 1 (never) to 6 (frequently), and included the following questions:
- How often do you have to explain: (a) Request for Voluntary Admission form, (b) 72-Hour Rule, (c) Request to Discharge form?
- How often is there confusion about the 72-hour rule and RTD form once admitted to the adult inpatient psychiatric unit?
- How often do you need to re-explain the 72-hour rule and RTD form once admitted to the adult inpatient psychiatric unit?
In-depth interviews were conducted with 4 resident physicians, 4 physician assistants, and 3 nurses to identify specific shortcomings of the admission procedure. A key finding from these interviews was that some patients tended not to understand that the treatment team had 72 hours to respond to the RTD application. Instead, several patients had indicated that they thought that they could immediately discharge themselves since they were on the unit “voluntarily” or that they could categorically discharge themselves after 72 hours of being admitted. This feedback was crucial in determining the next steps that could be taken to minimize confusion.
Process Changes
In preparation for this quality improvement project, the language and layout of the Request for Voluntary Admission form was revised and approved internally by the hospital’s Forms Committee to emphasize the 72-hour rule and the process for completing a RTD form. Additionally, these interviews indicated that it was difficult to track patients who were admitted voluntarily versus involuntarily. To rectify this problem, a field was added to the electronic medical record system to include current psychiatric admission status, allowing the selection to be either “Voluntary” or “Involuntary.” This new field in the electronic medical record system gives nurses the ability to easily update legal status daily as appropriate, which minimizes the risk of information not being effectively communicated at shift changes, while also allowing various members of the treatment team to be updated on the admission status of each patient.
After reviewing data and obtaining staff involvement related to the problem, a new psychiatric admission and consent process was created. The new consent and admission process was characterized by a standardized procedure and scripted language to present to candidates for voluntary admission. The standardized procedure begins with the admitting staff member reading scripted consent language from a pocket card that includes 3 key points describing the voluntary admission procedure (see script in Figure 1). The first key point is to describe the 72-hour rule. Next, the staff member describes the purpose of the RTD form and shows an example to the patient. Finally, the staff member responsible for consenting describes the possibility of the patient being required to remain on the unit involuntarily in the event that he or she wants to leave before the treatment team sees fit and is deemed to be a danger to himself or herself or others.
On the reverse side of the pocket card, an example of the RTD form is available to show to the patient. The subsequent teach-back procedure is summarized using the flow chart in Figure 2, and this was made available to staff who participate in the admission and discharge processes. After reading the consent script, the consenting staff member must ask the patient to recall the 3 key points. For each key point that the patient cannot recall, the relevant section of the scripted language is re-read to the patient, who is asked to explain it again. If the patient recalls the 3 key points, then he or she is deemed to have cognitive capacity and thus can become a candidate for voluntary admission.
Flow charts, scripts, and pocket cards were created and distributed to relevant physicians, physician assistants, and nurses who participate in the admission or discharge process. Additional copies of pocket cards were made available within the department. In October 2017, an attending psychiatrist and medical student trained psychiatry physician assistants, nurses, and resident physicians who participated in the admission process in the ED or patient care on the unit on how to use the new materials. The new process was first implemented on November 1, 2017.
Measurements
Press Ganey scores were compared for 8 months before and 8 months after implementing the new process to monitor changes from the patients’ perspective. Additionally, the treatment team members answered survey questions related to perceived patient understanding at the beginning of training sessions in mid-September through mid-October and again 5 weeks after the new process was implemented.
Results
The behavioral health unit’s Press Ganey (overall and discharge) scores increased during the 8-month period following implementation of the quality improvement project (Figure 3). There was a notable upward trend of overall and discharge Press Ganey scores on a month-by-month basis from November through April. In total, 181 Press Ganey score reports were available for the 6-month period prior to the new process versus 157 score reports after (Figure 4). The average overall Press Ganey score for respondents improved from 77.1 to 81.6 (P = 0.003), while the average discharge score improved from 83.0 to 87.5 (P = 0.023).
In recent months, the behavioral health discharge satisfaction score has become one of the highest performing aspects of the department according to Press Ganey reports. From April through June 2018, the department has performed in the 98th percentile or higher in “information about patient’s rights” during admission and “discharge instructions if help is needed.”
The survey related to perceived patient satisfaction and confusion also indicated significant improvement. Survey respondents indicated that there was less confusion about the 72-hour rule and RTD form after the quality improvement procedure was implemented (P = 0.039) and that fewer attempts to re-explain these concepts were required as well (P = 0.035).
Discussion
The Press Ganey scores for this unit indicated an improvement in patient satisfaction, in particular with the discharge process. While the overall Press Ganey scores on the inpatient behavioral health unit showed a significant improvement, it remained stagnant, around 80, during the 8-month period after implementing the new standardized admission process. However, the discharge score consistently improved over the same 8 months, from 82 to 95 in the most recent month. Also, the overall and discharge scores indicated a brief spike/improvement in October, immediately preceding the implementation of the new scripted language. Given the timeline, this spike is likely related to the ongoing meetings, trainings, and awareness of the upcoming process improvement.
With hospital and health system reimbursements becoming increasingly tied with patient outcomes, quality improvement efforts to improve patient care and satisfaction are of the utmost importance. In order to develop the rapport with patients needed for a high level of cooperation and excellent outcomes on an inpatient psychiatric unit, it is essential that all patients receive specific information about what the admission entails and what the options are for being discharged from the unit. Since a voluntary admission can be converted to an involuntary admission if a patient is deemed a threat to himself or herself or others despite already signing a RTD form, it is essential that this is not only discussed prior to admission, but that these details are explicitly checked for understanding. This allows the treatment team to assess for capacity and the patient to demonstrate informed consent. Differing expectations or understanding in what the voluntary admission or discharge process entails can lead to patient frustration and hostility, lack of trust in the treatment team, poor attendance and participation in group therapy activities, and medication refusal. Altogether, this can lead to longer inpatient stays, increased costs, decreased outcomes, and decreased patient satisfaction.
These initiatives were relatively easy to implement and are backed by evidence that they ultimately increased patient satisfaction. These findings could be extended to other institutions to improve the voluntary admission process and, ultimately, the patient experience. Additionally, the methods could be applied to other patient care processes within psychiatric facilities, and to improve other aspects of the patient care experience that have room for improvement, as illustrated by the department’s Press Ganey subsection scores, or areas that the treatment team would like to focus on.
Limitations
There are several limitations in the design and evaluation of this project. The assessment of patient understanding, especially in psychiatric patients, is very difficult to quantify. The principal measure of assessing patient understanding was limited to health care professional survey results. This may have led to a slight social desirability bias. An objective assessment of understanding directly from the patients was not readily attainable in our study, but future studies could look at this metric in addition to health care professional survey results.
Additionally, the overall Press Ganey scores may be influenced by factors beyond the admission process and the applied improvement procedures. It is difficult to discern whether there were any other factors that also contributed to the overall increase. However, the discharge score was a more direct measure specifically related to the modified procedures, and the temporal association of the intervention with the increased scores suggests that the intervention was responsible.
Conclusion
Standardization of the consent process ensures that all patients receive the necessary information every time in busy clinical settings. Incorporating an opportunity to “teach back” specific important information about the voluntary admission process, specifically what the 72-hour rule is, what the RTD form is, and the possibility of involuntary commitment, allows clinicians to assess capacity, while simultaneously allowing patients to have realistic expectations of the admission. Concise, standardized answers regarding these points minimizes variation in information being dispersed and decreases the possibility of omitting important information. At a major academic medical center, easy-to-implement quality improvement techniques significantly decreased patient confusion surrounding the 72-hour rule and the RTD form, along with the frequency in which these policies needed to be re-explained on the adult inpatient psychiatric unit. These changes ultimately led to improvement in patient satisfaction, as indicated by significant improvement in both overall and discharge patient satisfaction scores.
Corresponding author: Jennifer F. Newman, 475 Vine St., Winston-Salem, NC, 27101; jnewman9@u.rochester.edu.
Financial disclosures: None.
From the Wake Forest School of Medicine (Ms. Newman), and Wake Forest Baptist Health, Department of Psychiatry and Behavioral Medicine (Dr. Kramer), Winston-Salem, NC.
Abstract
- Background: Adults voluntarily admitted to inpatient behavioral health units can ask to sign a Request to Discharge (RTD) form if they would like to be discharged before the treatment team agrees that discharge is appropriate. This gives the team 72 hours to determine whether the patient is safe to discharge or to involuntarily commit the patient to the unit. At 1 medical center, patients who were offered voluntary admission often lacked complete understanding of the “72-hour rule” and the early discharge procedure.
- Methods: Robust Process Improvement® techniques were implemented to improve the admission process. Flow charts, standardized scripts, and pocket cards were distributed to relevant staff. The Request for Voluntary Admission form was revised to emphasize the “72-hour rule” and the process for requesting a RTD form.
- Results: The unit’s average overall Press Ganey score improved from 77.1 to 81.6 (P = 0.003), while the average discharge score improved from 83.0 to 87.5 (P = 0.023) following implementation of the new process.
- Conclusion: Incorporating strategies such as an opportunity to “teach back” important information about the voluntary admission process (ie, what the 72-hour rule is, what the request to discharge form is, and the possibility of involuntary commitment) allows clinicians to assess capacity while simultaneously giving patients realistic expectations of the admission. These changes can lead to improvement in patient satisfaction.
Keywords: behavioral health; communication; patient satisfaction.
Communication is paramount within medical teams to improve outcomes and strengthen rapport with patients, particularly with psychiatric patients in acute crisis. Studies
While some forms of communication are required to protect the safety of patients and others around them, other forms are required to build strong relationships with patients. However, these 2 goals do not have to be mutually exclusive in the psychiatric hospital environment. Hospitals aim to improve patient satisfaction while simultaneously providing effective communication about treatment. Studies have indicated that communication during graduate medical training may decline due to “emotional and physical brutality” associated with residency training programs.4 To ameliorate this and emphasize communication education, accredited psychiatry residency programs require residents to use structured communication tools to achieve a level 2 in the Accreditation Council for Graduate Medical Education milestone project for the category of patient safety and health care team.5 These standardized processes allow all patients to receive the same important information related to their care while minimizing human error. Such communication skills aim to improve health care outcomes and satisfaction for patients while also training better physicians.
For legal and ethical reasons, the adult inpatient behavioral health units at major hospitals are highly regulated. In most states, a patient who is admitted to an adult inpatient behavioral health unit on a voluntary basis can ask to sign a request to discharge (RTD) form if he or she would like to be discharged from the hospital before the treatment team sees fit.6 In most jurisdictions, this action gives the treatment team 72 hours to determine whether the patient is safe to discharge. Within that time frame, the physician must either discharge the patient, or, if it is not safe to do so, involuntarily commit him or her to the unit. In most jurisdictions, this process is commonly referred to as the “72-hour rule.”
In North Carolina, state legislation Chapter 122C, Article 5, Part 2(b) specifies: “In 24-hour facilities the application shall acknowledge that the applicant may be held by the facility for a period of 72 hours after any written request for release that the applicant may make, and shall acknowledge that the 24-hour facility may have the legal right to petition for involuntary commitment of the applicant during that period. At the time of application, the facility shall tell the applicant about procedures for discharge.”7 This requirement can be somewhat confusing for both medical team members and patients alike.
As formerly practiced on the behavioral health unit described in this report, patients offered voluntary admission status to the inpatient behavioral unit often lacked complete understanding of the 72-hour rule and the process for requesting early discharge from the facility. We hypothesized that this led to the observed patient frustration and hostility, lack of trust in the treatment team, poor attendance and participation in group therapy activities, medication refusal, and overall decreased patient satisfaction. To address this issue, this pilot project was conducted to improve the voluntary admission process on the adult inpatient unit of a major academic medical center in North Carolina.
In April 2008, The Joint Commission’s Center for Transforming Healthcare embarked on an enterprise-wide initiative called Robust Process Improvement (RPI). RPI was developed as a blended approach in applying Six Sigma, Lean, and Change Management techniques to improve medical processes and procedures. RPI techniques were applied in this study to better define the problems related to inpatient behavioral health unit admission and discharge by collecting data, obtaining staff involvement, creating a solution, and monitoring for lasting benefit.
Methods
This quality improvement project took place at an 885-bed tertiary care academic medical center with Level 1 Trauma Center designation. Institutional Review Board approval was not required because this was performed as a quality improvement project rather than an experimental clinical trial and was not designed to create new generalizable knowledge.
The techniques used to improve outcomes on the inpatient behavioral health unit included Active Listening, Elevator Speech, Statistics, Cause and Effect Diagrams, development of a Communication Plan, Brainstorming, and Standard Work. Through interviews with physician assistants, nurses, and resident physicians conducted over a 1-month period, it became clear that there was confusion among patients surrounding the voluntary admission process, the process for requesting discharge, and the possibility of a voluntary admission being converted to an involuntary one. Active listening was used to better understand the opportunities for improvement from multiple perspectives through varying stages of the admission—from the consent process in the emergency department, admission to the unit, throughout the hospital stay, to the time of discharge. The following elevator speech was used to highlight the areas of confusion and the importance of implementing change with the team involved in implementing the new admission procedures:
Our project is about improving patient understanding of the voluntary admission process to the Adult Psychiatry Unit and the 72-hour rule. This is important because the present process leads to patient misunderstanding, discontent on the unit, resistance to provided therapies, and low Press Ganey satisfaction scores. Success will look like reduced patient confusion about the 72-hour rule, increased group participation, decreased patient-staff conflict, and improved Press Ganey scores. What we are asking from you is to use a standardized, scripted informed consent process, flow chart, and pocket card during the voluntary admission process.
Additionally, brainstorming sessions were conducted with physician assistants, nurses, and residents to discuss options to improve the process and elicit a list of barriers.
Data Gathering
Several metrics were tracked to further understand the issue. Overall Press Ganey scores, in addition to admission and discharge subsection scores, were tracked for the 8 months prior to implementing the quality improvement procedures (March 2017-October 2017). Additionally, the treatment team members answered survey questions related to perceived patient understanding at the beginning of training sessions in the 5-week period immediately prior to implementing the quality improvement procedures. This survey was administered using a 6-point Likert scale, ranging from 1 (never) to 6 (frequently), and included the following questions:
- How often do you have to explain: (a) Request for Voluntary Admission form, (b) 72-Hour Rule, (c) Request to Discharge form?
- How often is there confusion about the 72-hour rule and RTD form once admitted to the adult inpatient psychiatric unit?
- How often do you need to re-explain the 72-hour rule and RTD form once admitted to the adult inpatient psychiatric unit?
In-depth interviews were conducted with 4 resident physicians, 4 physician assistants, and 3 nurses to identify specific shortcomings of the admission procedure. A key finding from these interviews was that some patients tended not to understand that the treatment team had 72 hours to respond to the RTD application. Instead, several patients had indicated that they thought that they could immediately discharge themselves since they were on the unit “voluntarily” or that they could categorically discharge themselves after 72 hours of being admitted. This feedback was crucial in determining the next steps that could be taken to minimize confusion.
Process Changes
In preparation for this quality improvement project, the language and layout of the Request for Voluntary Admission form was revised and approved internally by the hospital’s Forms Committee to emphasize the 72-hour rule and the process for completing a RTD form. Additionally, these interviews indicated that it was difficult to track patients who were admitted voluntarily versus involuntarily. To rectify this problem, a field was added to the electronic medical record system to include current psychiatric admission status, allowing the selection to be either “Voluntary” or “Involuntary.” This new field in the electronic medical record system gives nurses the ability to easily update legal status daily as appropriate, which minimizes the risk of information not being effectively communicated at shift changes, while also allowing various members of the treatment team to be updated on the admission status of each patient.
After reviewing data and obtaining staff involvement related to the problem, a new psychiatric admission and consent process was created. The new consent and admission process was characterized by a standardized procedure and scripted language to present to candidates for voluntary admission. The standardized procedure begins with the admitting staff member reading scripted consent language from a pocket card that includes 3 key points describing the voluntary admission procedure (see script in Figure 1). The first key point is to describe the 72-hour rule. Next, the staff member describes the purpose of the RTD form and shows an example to the patient. Finally, the staff member responsible for consenting describes the possibility of the patient being required to remain on the unit involuntarily in the event that he or she wants to leave before the treatment team sees fit and is deemed to be a danger to himself or herself or others.
On the reverse side of the pocket card, an example of the RTD form is available to show to the patient. The subsequent teach-back procedure is summarized using the flow chart in Figure 2, and this was made available to staff who participate in the admission and discharge processes. After reading the consent script, the consenting staff member must ask the patient to recall the 3 key points. For each key point that the patient cannot recall, the relevant section of the scripted language is re-read to the patient, who is asked to explain it again. If the patient recalls the 3 key points, then he or she is deemed to have cognitive capacity and thus can become a candidate for voluntary admission.
Flow charts, scripts, and pocket cards were created and distributed to relevant physicians, physician assistants, and nurses who participate in the admission or discharge process. Additional copies of pocket cards were made available within the department. In October 2017, an attending psychiatrist and medical student trained psychiatry physician assistants, nurses, and resident physicians who participated in the admission process in the ED or patient care on the unit on how to use the new materials. The new process was first implemented on November 1, 2017.
Measurements
Press Ganey scores were compared for 8 months before and 8 months after implementing the new process to monitor changes from the patients’ perspective. Additionally, the treatment team members answered survey questions related to perceived patient understanding at the beginning of training sessions in mid-September through mid-October and again 5 weeks after the new process was implemented.
Results
The behavioral health unit’s Press Ganey (overall and discharge) scores increased during the 8-month period following implementation of the quality improvement project (Figure 3). There was a notable upward trend of overall and discharge Press Ganey scores on a month-by-month basis from November through April. In total, 181 Press Ganey score reports were available for the 6-month period prior to the new process versus 157 score reports after (Figure 4). The average overall Press Ganey score for respondents improved from 77.1 to 81.6 (P = 0.003), while the average discharge score improved from 83.0 to 87.5 (P = 0.023).
In recent months, the behavioral health discharge satisfaction score has become one of the highest performing aspects of the department according to Press Ganey reports. From April through June 2018, the department has performed in the 98th percentile or higher in “information about patient’s rights” during admission and “discharge instructions if help is needed.”
The survey related to perceived patient satisfaction and confusion also indicated significant improvement. Survey respondents indicated that there was less confusion about the 72-hour rule and RTD form after the quality improvement procedure was implemented (P = 0.039) and that fewer attempts to re-explain these concepts were required as well (P = 0.035).
Discussion
The Press Ganey scores for this unit indicated an improvement in patient satisfaction, in particular with the discharge process. While the overall Press Ganey scores on the inpatient behavioral health unit showed a significant improvement, it remained stagnant, around 80, during the 8-month period after implementing the new standardized admission process. However, the discharge score consistently improved over the same 8 months, from 82 to 95 in the most recent month. Also, the overall and discharge scores indicated a brief spike/improvement in October, immediately preceding the implementation of the new scripted language. Given the timeline, this spike is likely related to the ongoing meetings, trainings, and awareness of the upcoming process improvement.
With hospital and health system reimbursements becoming increasingly tied with patient outcomes, quality improvement efforts to improve patient care and satisfaction are of the utmost importance. In order to develop the rapport with patients needed for a high level of cooperation and excellent outcomes on an inpatient psychiatric unit, it is essential that all patients receive specific information about what the admission entails and what the options are for being discharged from the unit. Since a voluntary admission can be converted to an involuntary admission if a patient is deemed a threat to himself or herself or others despite already signing a RTD form, it is essential that this is not only discussed prior to admission, but that these details are explicitly checked for understanding. This allows the treatment team to assess for capacity and the patient to demonstrate informed consent. Differing expectations or understanding in what the voluntary admission or discharge process entails can lead to patient frustration and hostility, lack of trust in the treatment team, poor attendance and participation in group therapy activities, and medication refusal. Altogether, this can lead to longer inpatient stays, increased costs, decreased outcomes, and decreased patient satisfaction.
These initiatives were relatively easy to implement and are backed by evidence that they ultimately increased patient satisfaction. These findings could be extended to other institutions to improve the voluntary admission process and, ultimately, the patient experience. Additionally, the methods could be applied to other patient care processes within psychiatric facilities, and to improve other aspects of the patient care experience that have room for improvement, as illustrated by the department’s Press Ganey subsection scores, or areas that the treatment team would like to focus on.
Limitations
There are several limitations in the design and evaluation of this project. The assessment of patient understanding, especially in psychiatric patients, is very difficult to quantify. The principal measure of assessing patient understanding was limited to health care professional survey results. This may have led to a slight social desirability bias. An objective assessment of understanding directly from the patients was not readily attainable in our study, but future studies could look at this metric in addition to health care professional survey results.
Additionally, the overall Press Ganey scores may be influenced by factors beyond the admission process and the applied improvement procedures. It is difficult to discern whether there were any other factors that also contributed to the overall increase. However, the discharge score was a more direct measure specifically related to the modified procedures, and the temporal association of the intervention with the increased scores suggests that the intervention was responsible.
Conclusion
Standardization of the consent process ensures that all patients receive the necessary information every time in busy clinical settings. Incorporating an opportunity to “teach back” specific important information about the voluntary admission process, specifically what the 72-hour rule is, what the RTD form is, and the possibility of involuntary commitment, allows clinicians to assess capacity, while simultaneously allowing patients to have realistic expectations of the admission. Concise, standardized answers regarding these points minimizes variation in information being dispersed and decreases the possibility of omitting important information. At a major academic medical center, easy-to-implement quality improvement techniques significantly decreased patient confusion surrounding the 72-hour rule and the RTD form, along with the frequency in which these policies needed to be re-explained on the adult inpatient psychiatric unit. These changes ultimately led to improvement in patient satisfaction, as indicated by significant improvement in both overall and discharge patient satisfaction scores.
Corresponding author: Jennifer F. Newman, 475 Vine St., Winston-Salem, NC, 27101; jnewman9@u.rochester.edu.
Financial disclosures: None.
1. Redfern E, Brown R, Vincent C. Improving communication in the emergency department. Emerg Med J. 2009;26:658-661.
2. Payne CE, Stein JM, Leong T, Dressler DD. Avoiding handover fumbles: a controlled trial of a structured handover tool versus traditional handover methods. BMJ Qual Saf. 2012;21:925-932.
3. Weller J, Boyd M, Cumin D. Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J. 2014;90:149-154.
4. DiMatteo MR. The role of the physician in the emerging health care environment. Western J Med. 1998;168:328.
5. The Psychiatry Milestone Project. J Grad Med Educ. 2014;6(1 Suppl 1):284-304.
6. Garakani A, Shalenberg E, Burstin SC, et al. Voluntary psychiatric hospitalization and patient-driven requests for discharge: a statutory review and analysis of implications for the capacity to consent to voluntary hospitalization. Harv Rev Psychiatry. 2014;22:241-249.
7. Procedure for Admission and Discharge of Clients Act, 211 § 122C-211(2014).
1. Redfern E, Brown R, Vincent C. Improving communication in the emergency department. Emerg Med J. 2009;26:658-661.
2. Payne CE, Stein JM, Leong T, Dressler DD. Avoiding handover fumbles: a controlled trial of a structured handover tool versus traditional handover methods. BMJ Qual Saf. 2012;21:925-932.
3. Weller J, Boyd M, Cumin D. Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J. 2014;90:149-154.
4. DiMatteo MR. The role of the physician in the emerging health care environment. Western J Med. 1998;168:328.
5. The Psychiatry Milestone Project. J Grad Med Educ. 2014;6(1 Suppl 1):284-304.
6. Garakani A, Shalenberg E, Burstin SC, et al. Voluntary psychiatric hospitalization and patient-driven requests for discharge: a statutory review and analysis of implications for the capacity to consent to voluntary hospitalization. Harv Rev Psychiatry. 2014;22:241-249.
7. Procedure for Admission and Discharge of Clients Act, 211 § 122C-211(2014).
Trial finds three drugs equally effective for established status epilepticus
according to a study published Nov. 27 in the New England Journal of Medicine. The effectiveness and safety of the intravenous medications do not differ significantly, the researchers wrote.
“Having three equally effective second-line intravenous medications means that the clinician may choose a drug that takes into account individual situations,” wrote Phil E.M. Smith, MD, in an accompanying editorial (doi: 10.1056/NEJMe1913775). Clinicians may consider “factors such as the presumed underlying cause of status epilepticus; coexisting conditions, including allergy, liver and renal disease, hypotension, propensity to cardiac arrhythmia, and alcohol and drug dependence; the currently prescribed antiepileptic treatment; the cost of the medication; and governmental agency drug approval,” said Dr. Smith, who is affiliated with University Hospital of Wales in Cardiff.
A gap in guidance
Evidence supports benzodiazepines as the initial treatment for status epilepticus, but these drugs do not work in up to a third of patients, said first study author Jaideep Kapur, MBBS, PhD, and colleagues. “Clinical guidelines emphasize the need for rapid control of benzodiazepine-refractory status epilepticus but do not provide guidance regarding the choice of medication on the basis of either efficacy or safety,” they wrote. Dr. Kapur is a professor of neurology and the director of UVA Brain Institute at University of Virginia in Charlottesville.
Levetiracetam, fosphenytoin, and valproate are the three most commonly used medications for benzodiazepine-refractory status epilepticus. The Food and Drug Administration has labeled fosphenytoin for this indication in adults, and none of the drugs is approved for children. To determine the superiority or inferiority of these medications, the researchers conducted the Established Status Epilepticus Treatment Trial (ESETT). The blinded, comparative-effectiveness trial enrolled 384 patients at 57 hospital EDs in the United States. Patients were aged 2 years or older, had received a generally accepted cumulative dose of benzodiazepines for generalized convulsive seizures lasting more than 5 minutes and continued to have persistent or recurrent convulsions between 5-30 minutes after the last dose of benzodiazepine.
Patients randomly received one of the three trial drugs, which “were identical in appearance, formulation, packaging, and administration,” the authors said. The primary outcome was absence of clinically apparent seizures and improving responsiveness at 60 minutes after the start of the infusion without administration of additional anticonvulsant medication. ED physicians determined the presence of seizure and improvement in responsiveness.
Trial was stopped for futility
The trial included 400 enrollments of 384 unique patients during 2015-2017. Sixteen patients were enrolled twice, and their second enrollments were not included in the intention-to-treat analysis. A planned interim analysis after 400 enrollments to assess the likelihood of success or futility found that the trial had met the futility criterion. “There was a 1% chance of showing a most effective or least effective treatment if the trial were to continue to the maximum sample size” of 795 patients, Dr. Kapur and coauthors wrote. The researchers continued enrollment in a pediatric subcohort for a planned subgroup analysis by age.
In all, 55% of the patients were male, 43% were black, and 16% were Hispanic. The population was 39% children and adolescents, 48% adults aged 18-65 years, and 13% older than 65 years. Most patients had a final diagnosis of status epilepticus (87%). Other final diagnoses included psychogenic nonepileptic seizures (10%).
At 60 minutes after treatment administration, absence of seizures and improved responsiveness occurred in 47% of patients who received levetiracetam, 45% who received fosphenytoin, and 46% who received valproate.
In 39 patients for whom the researchers had reliable information about time to seizure cessation, median time to seizure cessation numerically favored valproate (7 minutes for valproate vs. 10.5 minutes for levetiracetam vs. 11.7 minutes for fosphenytoin), but the number of patients was limited, the authors noted.
“Hypotension and endotracheal intubation were more frequent with fosphenytoin than with the other two drugs, and deaths were more frequent with levetiracetam, but these differences were not significant,” wrote Dr. Kapur and colleagues. Seven patients who received levetiracetam died, compared with three who received fosphenytoin and two who received valproate. Life-threatening hypotension occurred in 3.2% of patients who received fosphenytoin, compared with 1.6% who received valproate and 0.7% who received levetiracetam. Endotracheal intubation occurred in 26.4% or patients who received fosphenytoin, compared with 20% of patients in the levetiracetam group and 16.8% in the valproate group.
The trial’s limitations include the enrollment of patients with psychogenic nonepileptic seizures and the use of clinical instead of electroencephalographic criteria for the primary outcome measure, the investigators wrote.
Dr. Smith noted that third- and fourth-line management of status epilepticus is not supported by high-quality evidence, and further studies are needed. Given the evidence from ESETT, “the practical challenge for the management of status epilepticus remains the same as in the past: ensuring that clinicians are familiar with, and follow, a treatment protocol,” he said.
The trial was funded by the National Institute of Neurological Disorders and Stroke. Dr. Kapur had no financial disclosures. A coauthor holds a patent on intravenous carbamazepine and intellectual property on intravenous topiramate. Other coauthors have ties to pharmaceutical and medical device companies.
Dr. Smith is coeditor of Practical Neurology and a member of the U.K. National Institute for Health and Clinical Excellence (NICE) guidelines committee for epilepsy.
SOURCE: Kapur J et al. N Engl J Med. 2019 Nov 27. doi: 10.1056/NEJMoa1905795.
according to a study published Nov. 27 in the New England Journal of Medicine. The effectiveness and safety of the intravenous medications do not differ significantly, the researchers wrote.
“Having three equally effective second-line intravenous medications means that the clinician may choose a drug that takes into account individual situations,” wrote Phil E.M. Smith, MD, in an accompanying editorial (doi: 10.1056/NEJMe1913775). Clinicians may consider “factors such as the presumed underlying cause of status epilepticus; coexisting conditions, including allergy, liver and renal disease, hypotension, propensity to cardiac arrhythmia, and alcohol and drug dependence; the currently prescribed antiepileptic treatment; the cost of the medication; and governmental agency drug approval,” said Dr. Smith, who is affiliated with University Hospital of Wales in Cardiff.
A gap in guidance
Evidence supports benzodiazepines as the initial treatment for status epilepticus, but these drugs do not work in up to a third of patients, said first study author Jaideep Kapur, MBBS, PhD, and colleagues. “Clinical guidelines emphasize the need for rapid control of benzodiazepine-refractory status epilepticus but do not provide guidance regarding the choice of medication on the basis of either efficacy or safety,” they wrote. Dr. Kapur is a professor of neurology and the director of UVA Brain Institute at University of Virginia in Charlottesville.
Levetiracetam, fosphenytoin, and valproate are the three most commonly used medications for benzodiazepine-refractory status epilepticus. The Food and Drug Administration has labeled fosphenytoin for this indication in adults, and none of the drugs is approved for children. To determine the superiority or inferiority of these medications, the researchers conducted the Established Status Epilepticus Treatment Trial (ESETT). The blinded, comparative-effectiveness trial enrolled 384 patients at 57 hospital EDs in the United States. Patients were aged 2 years or older, had received a generally accepted cumulative dose of benzodiazepines for generalized convulsive seizures lasting more than 5 minutes and continued to have persistent or recurrent convulsions between 5-30 minutes after the last dose of benzodiazepine.
Patients randomly received one of the three trial drugs, which “were identical in appearance, formulation, packaging, and administration,” the authors said. The primary outcome was absence of clinically apparent seizures and improving responsiveness at 60 minutes after the start of the infusion without administration of additional anticonvulsant medication. ED physicians determined the presence of seizure and improvement in responsiveness.
Trial was stopped for futility
The trial included 400 enrollments of 384 unique patients during 2015-2017. Sixteen patients were enrolled twice, and their second enrollments were not included in the intention-to-treat analysis. A planned interim analysis after 400 enrollments to assess the likelihood of success or futility found that the trial had met the futility criterion. “There was a 1% chance of showing a most effective or least effective treatment if the trial were to continue to the maximum sample size” of 795 patients, Dr. Kapur and coauthors wrote. The researchers continued enrollment in a pediatric subcohort for a planned subgroup analysis by age.
In all, 55% of the patients were male, 43% were black, and 16% were Hispanic. The population was 39% children and adolescents, 48% adults aged 18-65 years, and 13% older than 65 years. Most patients had a final diagnosis of status epilepticus (87%). Other final diagnoses included psychogenic nonepileptic seizures (10%).
At 60 minutes after treatment administration, absence of seizures and improved responsiveness occurred in 47% of patients who received levetiracetam, 45% who received fosphenytoin, and 46% who received valproate.
In 39 patients for whom the researchers had reliable information about time to seizure cessation, median time to seizure cessation numerically favored valproate (7 minutes for valproate vs. 10.5 minutes for levetiracetam vs. 11.7 minutes for fosphenytoin), but the number of patients was limited, the authors noted.
“Hypotension and endotracheal intubation were more frequent with fosphenytoin than with the other two drugs, and deaths were more frequent with levetiracetam, but these differences were not significant,” wrote Dr. Kapur and colleagues. Seven patients who received levetiracetam died, compared with three who received fosphenytoin and two who received valproate. Life-threatening hypotension occurred in 3.2% of patients who received fosphenytoin, compared with 1.6% who received valproate and 0.7% who received levetiracetam. Endotracheal intubation occurred in 26.4% or patients who received fosphenytoin, compared with 20% of patients in the levetiracetam group and 16.8% in the valproate group.
The trial’s limitations include the enrollment of patients with psychogenic nonepileptic seizures and the use of clinical instead of electroencephalographic criteria for the primary outcome measure, the investigators wrote.
Dr. Smith noted that third- and fourth-line management of status epilepticus is not supported by high-quality evidence, and further studies are needed. Given the evidence from ESETT, “the practical challenge for the management of status epilepticus remains the same as in the past: ensuring that clinicians are familiar with, and follow, a treatment protocol,” he said.
The trial was funded by the National Institute of Neurological Disorders and Stroke. Dr. Kapur had no financial disclosures. A coauthor holds a patent on intravenous carbamazepine and intellectual property on intravenous topiramate. Other coauthors have ties to pharmaceutical and medical device companies.
Dr. Smith is coeditor of Practical Neurology and a member of the U.K. National Institute for Health and Clinical Excellence (NICE) guidelines committee for epilepsy.
SOURCE: Kapur J et al. N Engl J Med. 2019 Nov 27. doi: 10.1056/NEJMoa1905795.
according to a study published Nov. 27 in the New England Journal of Medicine. The effectiveness and safety of the intravenous medications do not differ significantly, the researchers wrote.
“Having three equally effective second-line intravenous medications means that the clinician may choose a drug that takes into account individual situations,” wrote Phil E.M. Smith, MD, in an accompanying editorial (doi: 10.1056/NEJMe1913775). Clinicians may consider “factors such as the presumed underlying cause of status epilepticus; coexisting conditions, including allergy, liver and renal disease, hypotension, propensity to cardiac arrhythmia, and alcohol and drug dependence; the currently prescribed antiepileptic treatment; the cost of the medication; and governmental agency drug approval,” said Dr. Smith, who is affiliated with University Hospital of Wales in Cardiff.
A gap in guidance
Evidence supports benzodiazepines as the initial treatment for status epilepticus, but these drugs do not work in up to a third of patients, said first study author Jaideep Kapur, MBBS, PhD, and colleagues. “Clinical guidelines emphasize the need for rapid control of benzodiazepine-refractory status epilepticus but do not provide guidance regarding the choice of medication on the basis of either efficacy or safety,” they wrote. Dr. Kapur is a professor of neurology and the director of UVA Brain Institute at University of Virginia in Charlottesville.
Levetiracetam, fosphenytoin, and valproate are the three most commonly used medications for benzodiazepine-refractory status epilepticus. The Food and Drug Administration has labeled fosphenytoin for this indication in adults, and none of the drugs is approved for children. To determine the superiority or inferiority of these medications, the researchers conducted the Established Status Epilepticus Treatment Trial (ESETT). The blinded, comparative-effectiveness trial enrolled 384 patients at 57 hospital EDs in the United States. Patients were aged 2 years or older, had received a generally accepted cumulative dose of benzodiazepines for generalized convulsive seizures lasting more than 5 minutes and continued to have persistent or recurrent convulsions between 5-30 minutes after the last dose of benzodiazepine.
Patients randomly received one of the three trial drugs, which “were identical in appearance, formulation, packaging, and administration,” the authors said. The primary outcome was absence of clinically apparent seizures and improving responsiveness at 60 minutes after the start of the infusion without administration of additional anticonvulsant medication. ED physicians determined the presence of seizure and improvement in responsiveness.
Trial was stopped for futility
The trial included 400 enrollments of 384 unique patients during 2015-2017. Sixteen patients were enrolled twice, and their second enrollments were not included in the intention-to-treat analysis. A planned interim analysis after 400 enrollments to assess the likelihood of success or futility found that the trial had met the futility criterion. “There was a 1% chance of showing a most effective or least effective treatment if the trial were to continue to the maximum sample size” of 795 patients, Dr. Kapur and coauthors wrote. The researchers continued enrollment in a pediatric subcohort for a planned subgroup analysis by age.
In all, 55% of the patients were male, 43% were black, and 16% were Hispanic. The population was 39% children and adolescents, 48% adults aged 18-65 years, and 13% older than 65 years. Most patients had a final diagnosis of status epilepticus (87%). Other final diagnoses included psychogenic nonepileptic seizures (10%).
At 60 minutes after treatment administration, absence of seizures and improved responsiveness occurred in 47% of patients who received levetiracetam, 45% who received fosphenytoin, and 46% who received valproate.
In 39 patients for whom the researchers had reliable information about time to seizure cessation, median time to seizure cessation numerically favored valproate (7 minutes for valproate vs. 10.5 minutes for levetiracetam vs. 11.7 minutes for fosphenytoin), but the number of patients was limited, the authors noted.
“Hypotension and endotracheal intubation were more frequent with fosphenytoin than with the other two drugs, and deaths were more frequent with levetiracetam, but these differences were not significant,” wrote Dr. Kapur and colleagues. Seven patients who received levetiracetam died, compared with three who received fosphenytoin and two who received valproate. Life-threatening hypotension occurred in 3.2% of patients who received fosphenytoin, compared with 1.6% who received valproate and 0.7% who received levetiracetam. Endotracheal intubation occurred in 26.4% or patients who received fosphenytoin, compared with 20% of patients in the levetiracetam group and 16.8% in the valproate group.
The trial’s limitations include the enrollment of patients with psychogenic nonepileptic seizures and the use of clinical instead of electroencephalographic criteria for the primary outcome measure, the investigators wrote.
Dr. Smith noted that third- and fourth-line management of status epilepticus is not supported by high-quality evidence, and further studies are needed. Given the evidence from ESETT, “the practical challenge for the management of status epilepticus remains the same as in the past: ensuring that clinicians are familiar with, and follow, a treatment protocol,” he said.
The trial was funded by the National Institute of Neurological Disorders and Stroke. Dr. Kapur had no financial disclosures. A coauthor holds a patent on intravenous carbamazepine and intellectual property on intravenous topiramate. Other coauthors have ties to pharmaceutical and medical device companies.
Dr. Smith is coeditor of Practical Neurology and a member of the U.K. National Institute for Health and Clinical Excellence (NICE) guidelines committee for epilepsy.
SOURCE: Kapur J et al. N Engl J Med. 2019 Nov 27. doi: 10.1056/NEJMoa1905795.
FROM NEJM
Key clinical point: Among children and adults with benzodiazepine-refractory status epilepticus, fosphenytoin, valproate, and levetiracetam each stop seizures by 60 minutes in approximately half of patients.
Major finding: Absence of seizures and improved responsiveness occurred in 47% of patients who received levetiracetam, 45% who received fosphenytoin, and 46% who received valproate.
Study details: The Established Status Epilepticus Treatment Trial (ESETT) was a blinded, comparative-effectiveness trial that enrolled 384 patients at 57 hospital EDs in the United States.
Disclosures: The trial was funded by the National Institute of Neurological Disorders and Stroke. Dr. Kapur had no financial disclosures. A coauthor holds a patent on intravenous carbamazepine and intellectual property on intravenous topiramate. Other coauthors have ties to pharmaceutical and medical device companies.
Source: Kapur J et al. N Engl J Med. 2019 Nov 27. doi: 10.1056/NEJMoa1905795.
Treating LDL to below 70 reduces recurrent stroke
PHILADELPHIA – Treating patients to a lower LDL target after an ischemic stroke of atherosclerotic origin resulted in fewer recurrent strokes or major cardiovascular events, compared with a higher LDL goal, even though the international trial was stopped early because of lack of funding.
“In the Treat Stroke to Target [TST] trial we showed that the group of patients with an atherosclerotic stroke achieving an LDL cholesterol of less than 70 mg/dL had 22% less recurrent ischemic stroke or other major vascular events than the group achieving a LDL cholesterol between 90 and 110 mg/dL,” lead author Pierre Amarenco, MD, chairman of the department of neurology and the stroke center at Bichat Hospital in Paris, said in an interview.
“We avoided more than one in recurrence in five,” he added.
The findings of the investigator-initiated trial were reported during a late-breaking research session at the American Heart Association scientific sessions and simultaneously published online Nov. 18 in the New England Journal of Medicine (doi: 10.1056/NEJMoa1910355).
Discussant Mitchell S.V. Elkind, MD, president-elect of the American Heart Association, called the TST findings “practice confirming” of a strategy many cardiologists already follow for stroke patients.
“The TST study is only the second trial that was done in neurology for stroke prevention using statins and lipid-lowering therapy, and that’s what makes it a hopeful and real advance,” he said in an interview.
To achieve the LDL-lowering goal, two-thirds of patients received a high-dose statin therapy while the remainder received both high-dose statin and ezetimibe (Zetia, Merck). There were no significant increases in intracranial hemorrhage observed between lower- and higher-target groups.
“Now guidelines should move to recommending a target LDL cholesterol of less than 70 mg/dL in all patients with a proven ischemic stroke of atherosclerotic origin,” said Dr. Amarenco, who is also a professor of neurology at Denis Diderot Paris University.
Rare lipid study following stroke
American Heart Association/American Stroke Association guidelines recommend intense statin therapy after an atherothrombotic stroke “but no target level is given to the practitioners,” Dr. Amarenco said. “In reality, most patients receive a reduced dose of statin.”
For example, despite 70% of patients receiving a statin, the average LDL cholesterol level was 92 mg/dL in a real-world registry.
The TST trial is the first major study to evaluate treating to target LDL levels in the ischemic stroke population since the SPARCL trial in 2006. SPARCL was the first randomized, controlled clinical trial to evaluate whether daily statin therapy could reduce the risk of stroke in patients who had suffered a stroke or transient ischemic attack (TIA).
SPARCL demonstrated a 16% risk reduction with atorvastatin 80 mg daily versus placebo, and further risk reduction of 33% among those with carotid stenosis, over 5 years. There was some concern about safety for a time; post-hoc analysis showed what appeared to be an increased risk for intracranial hemorrhage with statin treatment. Subsequent analyses seemed to suggest the finding may have been a chance one, however.
For the TST study, Dr. Amarenco and colleagues enrolled participants between March 2010 and December 2018 at one of 61 centers in France. In 2015, the study expanded to include 16 sites in South Korea.
Investigators evaluated participants after an ischemic stroke or a TIA with evidence of atherosclerosis. Blood pressure, smoking cessation, and diabetes were well controlled, he said.
Dr. Amarenco and colleagues randomly assigned 1,430 participants to the low–LDL cholesterol target group, less than 70 mg/dL, and another 1,430 to a high-LDL group with a target of 100 mg/dL.
Assessments were every 6 months and up to 1 year after the last patient joined the study.
Treatment with any available statin on the market was allowed. Ezetimibe could be added on top of statin therapy as necessary. A total of 55% were statin naive at study entry.
Study stopped early
The trial was stopped in May 2019 after allocated funds ran out. At this point, researchers had 277 events to analyze, although their initial goal was to reach 385.
The primary endpoint of this event-driven trial was a composite of nonfatal stroke, nonfatal MI, and unstable angina followed by urgent coronary revascularization; TIA followed by urgent carotid revascularization; or cardiovascular death, including sudden deaths.
The endpoint was experienced by 8.5% of participants in the lower-target group versus 10.9% of those in the higher-target group. This translated to a 22% relative risk reduction (adjusted hazard ratio, 0.78; 95% confidence interval, 0.68-0.98; P =.04).
A total of 86% of participants had an ischemic stroke confirmed by brain MRI or CT scan. In this group, the relative risk reduction was 33% – “meaning that we could avoid one-third of recurrent major vascular events,” Dr. Amarenco said.
Furthermore, targeting the lower LDL levels was associated with a relative risk reduction of 40% among those with diabetes.
Secondary outcomes not significant
The investigators used hierarchical testing to compare two outcomes at a time in a prespecified order. They planned to continue this strategy until a comparison emerged as nonsignificant.
This occurred right away when their first composite secondary endpoint comparison between nonfatal MI and urgent revascularization was found to be not significantly different between groups (P = .12).
The early ending “weakened the results of the trial, and the results should be taken with caution because of that,” Dr. Amarenco said.
In addition, the number of hemorrhagic strokes did not differ significantly between groups. There were 18 of these events in the lower-target group and 13 in the higher-target cohort.
That numerical increase in intracranial hemorrhage was “driven by the Korean patients. … and that is something we will report soon,” Dr. Amarenco said.
Interestingly, the researchers also evaluated how much time participants spent within the target LDL cholesterol range, averaged by study site. They found that 53% of the lower–LDL target group, for example, was in the therapeutic range on average during the study.
When Dr. Amarenco and colleagues looked at participants who managed to spend 50%-100% in the target range, the relative risk reduction was 36%.
“So we can hypothesize that, if we had used a more potent drug like PCSK9 inhibitors to be closer to 100% in the therapeutic range, we may have had a greater effect size,” Dr. Amarenco said.
“Our results suggest that LDL cholesterol is causally related to atherosclerosis and confirm that the lower the LDL cholesterol the better,” Dr. Amarenco said.
“Future trials should explore the efficacy and safety of lowering LDL cholesterol to very low levels such as less than 55 mg/dL or even 30 mg/dL (as obtained in the FOURIER trial) by using PCSK9 inhibitors or equivalent in patients with an ischemic stroke due to atherosclerotic disease,” Dr. Amarenco said.
‘Practice-confirming’ findings
The findings are also in line with secondary analyses of the WASID (Neurology. 1995 Aug;45[8]:1488-93) and SAMMPRIS trials, which should dispel some concerns that persist about taking LDL to such low levels that it increases risk of intracerebral hemorrhage, Dr. Amarenco noted.
However, TST, he said, didn’t provide clear answers on what specific subgroups of patients with a stroke history would benefit from aggressive lipid lowering.
“What is stroke without atherosclerotic disease?” he said. “Some people say small-vessel disease is also a form of atherosclerosis, and most patients with atrial fibrillation, which is increasingly recognized as a cause of stroke, are also going to have atherosclerosis of the heart as well as the brain and blood vessels.
“Many, many stroke patients will fall into this category,” Dr. Elkind said, “and the question is, should they be treated more aggressively with lipid lowering?”
“The results of this study fit pretty nicely into the rubric of the AHA cholesterol guidelines,” said Donald M. Lloyd-Jones, MD, chairman, department of preventive medicine at Northwestern University Feinberg School of Medicine, Chicago, and chair of the AHA’s 2019 Council on Scientific Sessions Programming. Dr. Lloyd-Jones was also a member of the guideline committee.
Stroke patients are not “garden variety coronary patients,” he said. “The concern about intracerebral hemorrhage continues to be something that we wonder about: Should we be driving our stroke patients as low as our coronary patients? I think these data will certainly help us.”
Consideration for future guidelines
The study would have been more helpful if it provided more detail about the treatment regimens used, Jennifer Robinson, MD, director of the prevention intervention center, department of epidemiology, University of Iowa, said in an interview.
“What was the dose intensity of statins the patients were on?” Dr. Robinson said. “Part of our struggle has been to convince people to use high-intensity statins – get the maximum from statins that are generic now and cost saving in even very low-risk primary prevention patients.”
She said that a third of patients in TST also took ezetimibe with the statin “makes sense” because of its generic status.
Nonetheless, Dr. Robinson said, TST adds to the evidence that LDL of 100 mg/dL is not good enough, that high-intensity statin therapy is superior to a moderate regimen and that adding a nonstatin – ezetimibe in TST – can derive added benefit.
The TST findings may give guideline writers direction going forward, she said. “We really need to start thinking about the potential for net benefit from added therapy, whether it’s from intensifying LDL lowering, adding icosapent ethyl (Vascepa, Amarin), which seems to have remarkable benefits, or SGLT2 inhibitor,” she said.
“There are a lot of options,” Dr. Robinson said. “We need to have an outlook beyond just treating to target with what really is the best maximized accepted therapy.”
TST was funded primarily by French Government, but also with grants from Pfizer, Astra Zeneca and Merck. Dr. Amarenco disclosed that he is a consultant or advisor to Modest, Sanofi, Bristol-Myers Squibb, and Amgen; receives honoraria from Modest, Amgen, Kowa, Shing Poon, Kowa, Bayer, GSK, Fibrogen, and AstraZeneca. He also receives research grants from Pfizer, Astra Zeneca, Sanofi, BMS, Merck, Boston Scientific, and the French Government.
This article also appears on Medscape.com.
SOURCE: Amarenco P. ACC 2019, Late Breaking Science 6 session.
PHILADELPHIA – Treating patients to a lower LDL target after an ischemic stroke of atherosclerotic origin resulted in fewer recurrent strokes or major cardiovascular events, compared with a higher LDL goal, even though the international trial was stopped early because of lack of funding.
“In the Treat Stroke to Target [TST] trial we showed that the group of patients with an atherosclerotic stroke achieving an LDL cholesterol of less than 70 mg/dL had 22% less recurrent ischemic stroke or other major vascular events than the group achieving a LDL cholesterol between 90 and 110 mg/dL,” lead author Pierre Amarenco, MD, chairman of the department of neurology and the stroke center at Bichat Hospital in Paris, said in an interview.
“We avoided more than one in recurrence in five,” he added.
The findings of the investigator-initiated trial were reported during a late-breaking research session at the American Heart Association scientific sessions and simultaneously published online Nov. 18 in the New England Journal of Medicine (doi: 10.1056/NEJMoa1910355).
Discussant Mitchell S.V. Elkind, MD, president-elect of the American Heart Association, called the TST findings “practice confirming” of a strategy many cardiologists already follow for stroke patients.
“The TST study is only the second trial that was done in neurology for stroke prevention using statins and lipid-lowering therapy, and that’s what makes it a hopeful and real advance,” he said in an interview.
To achieve the LDL-lowering goal, two-thirds of patients received a high-dose statin therapy while the remainder received both high-dose statin and ezetimibe (Zetia, Merck). There were no significant increases in intracranial hemorrhage observed between lower- and higher-target groups.
“Now guidelines should move to recommending a target LDL cholesterol of less than 70 mg/dL in all patients with a proven ischemic stroke of atherosclerotic origin,” said Dr. Amarenco, who is also a professor of neurology at Denis Diderot Paris University.
Rare lipid study following stroke
American Heart Association/American Stroke Association guidelines recommend intense statin therapy after an atherothrombotic stroke “but no target level is given to the practitioners,” Dr. Amarenco said. “In reality, most patients receive a reduced dose of statin.”
For example, despite 70% of patients receiving a statin, the average LDL cholesterol level was 92 mg/dL in a real-world registry.
The TST trial is the first major study to evaluate treating to target LDL levels in the ischemic stroke population since the SPARCL trial in 2006. SPARCL was the first randomized, controlled clinical trial to evaluate whether daily statin therapy could reduce the risk of stroke in patients who had suffered a stroke or transient ischemic attack (TIA).
SPARCL demonstrated a 16% risk reduction with atorvastatin 80 mg daily versus placebo, and further risk reduction of 33% among those with carotid stenosis, over 5 years. There was some concern about safety for a time; post-hoc analysis showed what appeared to be an increased risk for intracranial hemorrhage with statin treatment. Subsequent analyses seemed to suggest the finding may have been a chance one, however.
For the TST study, Dr. Amarenco and colleagues enrolled participants between March 2010 and December 2018 at one of 61 centers in France. In 2015, the study expanded to include 16 sites in South Korea.
Investigators evaluated participants after an ischemic stroke or a TIA with evidence of atherosclerosis. Blood pressure, smoking cessation, and diabetes were well controlled, he said.
Dr. Amarenco and colleagues randomly assigned 1,430 participants to the low–LDL cholesterol target group, less than 70 mg/dL, and another 1,430 to a high-LDL group with a target of 100 mg/dL.
Assessments were every 6 months and up to 1 year after the last patient joined the study.
Treatment with any available statin on the market was allowed. Ezetimibe could be added on top of statin therapy as necessary. A total of 55% were statin naive at study entry.
Study stopped early
The trial was stopped in May 2019 after allocated funds ran out. At this point, researchers had 277 events to analyze, although their initial goal was to reach 385.
The primary endpoint of this event-driven trial was a composite of nonfatal stroke, nonfatal MI, and unstable angina followed by urgent coronary revascularization; TIA followed by urgent carotid revascularization; or cardiovascular death, including sudden deaths.
The endpoint was experienced by 8.5% of participants in the lower-target group versus 10.9% of those in the higher-target group. This translated to a 22% relative risk reduction (adjusted hazard ratio, 0.78; 95% confidence interval, 0.68-0.98; P =.04).
A total of 86% of participants had an ischemic stroke confirmed by brain MRI or CT scan. In this group, the relative risk reduction was 33% – “meaning that we could avoid one-third of recurrent major vascular events,” Dr. Amarenco said.
Furthermore, targeting the lower LDL levels was associated with a relative risk reduction of 40% among those with diabetes.
Secondary outcomes not significant
The investigators used hierarchical testing to compare two outcomes at a time in a prespecified order. They planned to continue this strategy until a comparison emerged as nonsignificant.
This occurred right away when their first composite secondary endpoint comparison between nonfatal MI and urgent revascularization was found to be not significantly different between groups (P = .12).
The early ending “weakened the results of the trial, and the results should be taken with caution because of that,” Dr. Amarenco said.
In addition, the number of hemorrhagic strokes did not differ significantly between groups. There were 18 of these events in the lower-target group and 13 in the higher-target cohort.
That numerical increase in intracranial hemorrhage was “driven by the Korean patients. … and that is something we will report soon,” Dr. Amarenco said.
Interestingly, the researchers also evaluated how much time participants spent within the target LDL cholesterol range, averaged by study site. They found that 53% of the lower–LDL target group, for example, was in the therapeutic range on average during the study.
When Dr. Amarenco and colleagues looked at participants who managed to spend 50%-100% in the target range, the relative risk reduction was 36%.
“So we can hypothesize that, if we had used a more potent drug like PCSK9 inhibitors to be closer to 100% in the therapeutic range, we may have had a greater effect size,” Dr. Amarenco said.
“Our results suggest that LDL cholesterol is causally related to atherosclerosis and confirm that the lower the LDL cholesterol the better,” Dr. Amarenco said.
“Future trials should explore the efficacy and safety of lowering LDL cholesterol to very low levels such as less than 55 mg/dL or even 30 mg/dL (as obtained in the FOURIER trial) by using PCSK9 inhibitors or equivalent in patients with an ischemic stroke due to atherosclerotic disease,” Dr. Amarenco said.
‘Practice-confirming’ findings
The findings are also in line with secondary analyses of the WASID (Neurology. 1995 Aug;45[8]:1488-93) and SAMMPRIS trials, which should dispel some concerns that persist about taking LDL to such low levels that it increases risk of intracerebral hemorrhage, Dr. Amarenco noted.
However, TST, he said, didn’t provide clear answers on what specific subgroups of patients with a stroke history would benefit from aggressive lipid lowering.
“What is stroke without atherosclerotic disease?” he said. “Some people say small-vessel disease is also a form of atherosclerosis, and most patients with atrial fibrillation, which is increasingly recognized as a cause of stroke, are also going to have atherosclerosis of the heart as well as the brain and blood vessels.
“Many, many stroke patients will fall into this category,” Dr. Elkind said, “and the question is, should they be treated more aggressively with lipid lowering?”
“The results of this study fit pretty nicely into the rubric of the AHA cholesterol guidelines,” said Donald M. Lloyd-Jones, MD, chairman, department of preventive medicine at Northwestern University Feinberg School of Medicine, Chicago, and chair of the AHA’s 2019 Council on Scientific Sessions Programming. Dr. Lloyd-Jones was also a member of the guideline committee.
Stroke patients are not “garden variety coronary patients,” he said. “The concern about intracerebral hemorrhage continues to be something that we wonder about: Should we be driving our stroke patients as low as our coronary patients? I think these data will certainly help us.”
Consideration for future guidelines
The study would have been more helpful if it provided more detail about the treatment regimens used, Jennifer Robinson, MD, director of the prevention intervention center, department of epidemiology, University of Iowa, said in an interview.
“What was the dose intensity of statins the patients were on?” Dr. Robinson said. “Part of our struggle has been to convince people to use high-intensity statins – get the maximum from statins that are generic now and cost saving in even very low-risk primary prevention patients.”
She said that a third of patients in TST also took ezetimibe with the statin “makes sense” because of its generic status.
Nonetheless, Dr. Robinson said, TST adds to the evidence that LDL of 100 mg/dL is not good enough, that high-intensity statin therapy is superior to a moderate regimen and that adding a nonstatin – ezetimibe in TST – can derive added benefit.
The TST findings may give guideline writers direction going forward, she said. “We really need to start thinking about the potential for net benefit from added therapy, whether it’s from intensifying LDL lowering, adding icosapent ethyl (Vascepa, Amarin), which seems to have remarkable benefits, or SGLT2 inhibitor,” she said.
“There are a lot of options,” Dr. Robinson said. “We need to have an outlook beyond just treating to target with what really is the best maximized accepted therapy.”
TST was funded primarily by French Government, but also with grants from Pfizer, Astra Zeneca and Merck. Dr. Amarenco disclosed that he is a consultant or advisor to Modest, Sanofi, Bristol-Myers Squibb, and Amgen; receives honoraria from Modest, Amgen, Kowa, Shing Poon, Kowa, Bayer, GSK, Fibrogen, and AstraZeneca. He also receives research grants from Pfizer, Astra Zeneca, Sanofi, BMS, Merck, Boston Scientific, and the French Government.
This article also appears on Medscape.com.
SOURCE: Amarenco P. ACC 2019, Late Breaking Science 6 session.
PHILADELPHIA – Treating patients to a lower LDL target after an ischemic stroke of atherosclerotic origin resulted in fewer recurrent strokes or major cardiovascular events, compared with a higher LDL goal, even though the international trial was stopped early because of lack of funding.
“In the Treat Stroke to Target [TST] trial we showed that the group of patients with an atherosclerotic stroke achieving an LDL cholesterol of less than 70 mg/dL had 22% less recurrent ischemic stroke or other major vascular events than the group achieving a LDL cholesterol between 90 and 110 mg/dL,” lead author Pierre Amarenco, MD, chairman of the department of neurology and the stroke center at Bichat Hospital in Paris, said in an interview.
“We avoided more than one in recurrence in five,” he added.
The findings of the investigator-initiated trial were reported during a late-breaking research session at the American Heart Association scientific sessions and simultaneously published online Nov. 18 in the New England Journal of Medicine (doi: 10.1056/NEJMoa1910355).
Discussant Mitchell S.V. Elkind, MD, president-elect of the American Heart Association, called the TST findings “practice confirming” of a strategy many cardiologists already follow for stroke patients.
“The TST study is only the second trial that was done in neurology for stroke prevention using statins and lipid-lowering therapy, and that’s what makes it a hopeful and real advance,” he said in an interview.
To achieve the LDL-lowering goal, two-thirds of patients received a high-dose statin therapy while the remainder received both high-dose statin and ezetimibe (Zetia, Merck). There were no significant increases in intracranial hemorrhage observed between lower- and higher-target groups.
“Now guidelines should move to recommending a target LDL cholesterol of less than 70 mg/dL in all patients with a proven ischemic stroke of atherosclerotic origin,” said Dr. Amarenco, who is also a professor of neurology at Denis Diderot Paris University.
Rare lipid study following stroke
American Heart Association/American Stroke Association guidelines recommend intense statin therapy after an atherothrombotic stroke “but no target level is given to the practitioners,” Dr. Amarenco said. “In reality, most patients receive a reduced dose of statin.”
For example, despite 70% of patients receiving a statin, the average LDL cholesterol level was 92 mg/dL in a real-world registry.
The TST trial is the first major study to evaluate treating to target LDL levels in the ischemic stroke population since the SPARCL trial in 2006. SPARCL was the first randomized, controlled clinical trial to evaluate whether daily statin therapy could reduce the risk of stroke in patients who had suffered a stroke or transient ischemic attack (TIA).
SPARCL demonstrated a 16% risk reduction with atorvastatin 80 mg daily versus placebo, and further risk reduction of 33% among those with carotid stenosis, over 5 years. There was some concern about safety for a time; post-hoc analysis showed what appeared to be an increased risk for intracranial hemorrhage with statin treatment. Subsequent analyses seemed to suggest the finding may have been a chance one, however.
For the TST study, Dr. Amarenco and colleagues enrolled participants between March 2010 and December 2018 at one of 61 centers in France. In 2015, the study expanded to include 16 sites in South Korea.
Investigators evaluated participants after an ischemic stroke or a TIA with evidence of atherosclerosis. Blood pressure, smoking cessation, and diabetes were well controlled, he said.
Dr. Amarenco and colleagues randomly assigned 1,430 participants to the low–LDL cholesterol target group, less than 70 mg/dL, and another 1,430 to a high-LDL group with a target of 100 mg/dL.
Assessments were every 6 months and up to 1 year after the last patient joined the study.
Treatment with any available statin on the market was allowed. Ezetimibe could be added on top of statin therapy as necessary. A total of 55% were statin naive at study entry.
Study stopped early
The trial was stopped in May 2019 after allocated funds ran out. At this point, researchers had 277 events to analyze, although their initial goal was to reach 385.
The primary endpoint of this event-driven trial was a composite of nonfatal stroke, nonfatal MI, and unstable angina followed by urgent coronary revascularization; TIA followed by urgent carotid revascularization; or cardiovascular death, including sudden deaths.
The endpoint was experienced by 8.5% of participants in the lower-target group versus 10.9% of those in the higher-target group. This translated to a 22% relative risk reduction (adjusted hazard ratio, 0.78; 95% confidence interval, 0.68-0.98; P =.04).
A total of 86% of participants had an ischemic stroke confirmed by brain MRI or CT scan. In this group, the relative risk reduction was 33% – “meaning that we could avoid one-third of recurrent major vascular events,” Dr. Amarenco said.
Furthermore, targeting the lower LDL levels was associated with a relative risk reduction of 40% among those with diabetes.
Secondary outcomes not significant
The investigators used hierarchical testing to compare two outcomes at a time in a prespecified order. They planned to continue this strategy until a comparison emerged as nonsignificant.
This occurred right away when their first composite secondary endpoint comparison between nonfatal MI and urgent revascularization was found to be not significantly different between groups (P = .12).
The early ending “weakened the results of the trial, and the results should be taken with caution because of that,” Dr. Amarenco said.
In addition, the number of hemorrhagic strokes did not differ significantly between groups. There were 18 of these events in the lower-target group and 13 in the higher-target cohort.
That numerical increase in intracranial hemorrhage was “driven by the Korean patients. … and that is something we will report soon,” Dr. Amarenco said.
Interestingly, the researchers also evaluated how much time participants spent within the target LDL cholesterol range, averaged by study site. They found that 53% of the lower–LDL target group, for example, was in the therapeutic range on average during the study.
When Dr. Amarenco and colleagues looked at participants who managed to spend 50%-100% in the target range, the relative risk reduction was 36%.
“So we can hypothesize that, if we had used a more potent drug like PCSK9 inhibitors to be closer to 100% in the therapeutic range, we may have had a greater effect size,” Dr. Amarenco said.
“Our results suggest that LDL cholesterol is causally related to atherosclerosis and confirm that the lower the LDL cholesterol the better,” Dr. Amarenco said.
“Future trials should explore the efficacy and safety of lowering LDL cholesterol to very low levels such as less than 55 mg/dL or even 30 mg/dL (as obtained in the FOURIER trial) by using PCSK9 inhibitors or equivalent in patients with an ischemic stroke due to atherosclerotic disease,” Dr. Amarenco said.
‘Practice-confirming’ findings
The findings are also in line with secondary analyses of the WASID (Neurology. 1995 Aug;45[8]:1488-93) and SAMMPRIS trials, which should dispel some concerns that persist about taking LDL to such low levels that it increases risk of intracerebral hemorrhage, Dr. Amarenco noted.
However, TST, he said, didn’t provide clear answers on what specific subgroups of patients with a stroke history would benefit from aggressive lipid lowering.
“What is stroke without atherosclerotic disease?” he said. “Some people say small-vessel disease is also a form of atherosclerosis, and most patients with atrial fibrillation, which is increasingly recognized as a cause of stroke, are also going to have atherosclerosis of the heart as well as the brain and blood vessels.
“Many, many stroke patients will fall into this category,” Dr. Elkind said, “and the question is, should they be treated more aggressively with lipid lowering?”
“The results of this study fit pretty nicely into the rubric of the AHA cholesterol guidelines,” said Donald M. Lloyd-Jones, MD, chairman, department of preventive medicine at Northwestern University Feinberg School of Medicine, Chicago, and chair of the AHA’s 2019 Council on Scientific Sessions Programming. Dr. Lloyd-Jones was also a member of the guideline committee.
Stroke patients are not “garden variety coronary patients,” he said. “The concern about intracerebral hemorrhage continues to be something that we wonder about: Should we be driving our stroke patients as low as our coronary patients? I think these data will certainly help us.”
Consideration for future guidelines
The study would have been more helpful if it provided more detail about the treatment regimens used, Jennifer Robinson, MD, director of the prevention intervention center, department of epidemiology, University of Iowa, said in an interview.
“What was the dose intensity of statins the patients were on?” Dr. Robinson said. “Part of our struggle has been to convince people to use high-intensity statins – get the maximum from statins that are generic now and cost saving in even very low-risk primary prevention patients.”
She said that a third of patients in TST also took ezetimibe with the statin “makes sense” because of its generic status.
Nonetheless, Dr. Robinson said, TST adds to the evidence that LDL of 100 mg/dL is not good enough, that high-intensity statin therapy is superior to a moderate regimen and that adding a nonstatin – ezetimibe in TST – can derive added benefit.
The TST findings may give guideline writers direction going forward, she said. “We really need to start thinking about the potential for net benefit from added therapy, whether it’s from intensifying LDL lowering, adding icosapent ethyl (Vascepa, Amarin), which seems to have remarkable benefits, or SGLT2 inhibitor,” she said.
“There are a lot of options,” Dr. Robinson said. “We need to have an outlook beyond just treating to target with what really is the best maximized accepted therapy.”
TST was funded primarily by French Government, but also with grants from Pfizer, Astra Zeneca and Merck. Dr. Amarenco disclosed that he is a consultant or advisor to Modest, Sanofi, Bristol-Myers Squibb, and Amgen; receives honoraria from Modest, Amgen, Kowa, Shing Poon, Kowa, Bayer, GSK, Fibrogen, and AstraZeneca. He also receives research grants from Pfizer, Astra Zeneca, Sanofi, BMS, Merck, Boston Scientific, and the French Government.
This article also appears on Medscape.com.
SOURCE: Amarenco P. ACC 2019, Late Breaking Science 6 session.
REPORTING FROM AHA 2019
Is It More Than a Cold?
ANSWER
The radiograph does not demonstrate any evidence of infiltrate or pleural effusion. However, of note is a rather large lytic lesion involving the posterior aspect of the right fourth rib. This finding is very concerning for either a primary bone neoplasm or (more likely) a metastatic one.
The patient denied any history of cancer. She was promptly referred to Hematology/Oncology for further evaluation and workup. At last update, she had undergone a bone marrow biopsy, with preliminary pathology results suggestive of a plasma cell neoplasm.
ANSWER
The radiograph does not demonstrate any evidence of infiltrate or pleural effusion. However, of note is a rather large lytic lesion involving the posterior aspect of the right fourth rib. This finding is very concerning for either a primary bone neoplasm or (more likely) a metastatic one.
The patient denied any history of cancer. She was promptly referred to Hematology/Oncology for further evaluation and workup. At last update, she had undergone a bone marrow biopsy, with preliminary pathology results suggestive of a plasma cell neoplasm.
ANSWER
The radiograph does not demonstrate any evidence of infiltrate or pleural effusion. However, of note is a rather large lytic lesion involving the posterior aspect of the right fourth rib. This finding is very concerning for either a primary bone neoplasm or (more likely) a metastatic one.
The patient denied any history of cancer. She was promptly referred to Hematology/Oncology for further evaluation and workup. At last update, she had undergone a bone marrow biopsy, with preliminary pathology results suggestive of a plasma cell neoplasm.
A 70-year-old woman presents to the urgent care clinic with a week-long history of cold and cough that she feels is getting worse. She reports subjective fever and chills, as well as an occasional pain in the right side of her chest when she breathes. She has been taking OTC products with limited relief.
Her medical history is significant for mild hypertension. She denies smoking. On physical exam, you note an elderly female in no obvious distress. She is afebrile, with normal vital signs. Pulse oximetry reveals an O2 saturation of 98% on room air. Auscultation of her lungs demonstrates a little bit of mid bronchial congestion and perhaps some bibasilar crackles.
You order a complete blood count as well as a chest radiograph (shown). What is your impression?