User login
ACES Act to Study Cancer in Aviators Is Now Law
A bipartisan bill establishing research directives aimed at revealing cancer risks among military aviators and aircrews recently became law.
Spearheaded by Sen. Mark Kelly (D-AZ) and Sen. Tom Cotton (R-AR), as well as Rep. August Pfluger (R-TX-11) and Rep. Jimmy Panetta (D-CA-19), all of whom are veterans, the Aviator Cancer Examination Study (ACES) Act was signed into law on August 14. The ACES Act will address cancer rates among Army, Navy, Air Force, and Marine Corps aircrew members by directing the Secretary of the US Department of Veterans Affairs to study cancer incidence and mortality rates among these populations.
Military aviators and aircrews face a 15% to 24% higher rate of cancer compared with the general US population, including a 75% higher rate of melanoma, 31% higher rate of thyroid cancer, 20% higher rate of prostate cancer, and 11% higher rate of female breast cancer, with potential links to non-Hodgkin lymphoma and testicular cancer. These individuals are also diagnosed earlier in life, at the median age of 55 years compared with 67 years. However, further investigation is still needed to understand why.
“By better understanding the correlation between aviator service and cancer, we can better assist our military and provide more adequate care for our veterans,” Kelly said.
Some reasons for the higher rates of cancer in aviators seem clear, such as the association between dioxin exposure and cancer. In a study of cancer incidence and mortality in Air Force veterans of the Vietnam War, incidence of melanoma and prostate cancer was increased among White veterans who sprayed herbicides during Operation Ranch Hand. The risk of cancer at any site, prostate cancer, and melanoma was increased in the highest dioxin exposure category among veterans who spent ≤ 2 years in Southeast Asia.
However, some links between these veterans and increased cancer rates are less clear. In a review of 28 studies (including 18 studies in military settings), slight evidence was found for associations between jet fuel exposure and various outcomes including cancer. Cosmic ionizing radiation (CIR) exposure is another possible cause. Several epidemiological studies have documented elevated incidence and mortality for several cancers in flight crews, but a link between them and CIR exposure has not been established.
Certain occupations have been associated with increased risk of testicular germ cell tumors, including aircraft maintenance, military pilots, fighter pilots, and aircrews. Those associations led to hypotheses that job-related chemical exposures (eg, per- and polyfluoroalkyl substances, solvents, paints, hydrocarbons in degreasing/lubricating agents, lubricating oils) may increase risk. A study of young active-duty Air Force servicemen found that pilots and men with aircraft maintenance jobs had elevated tenosynovial giant cell tumor risk, but indicates that further research is needed to “elucidate specific occupational exposures underlying these associations.”
“As a former Navy pilot, there are certain risks that we know and accept come with our service, but we know far less about the health risks that are affecting many aviators and aircrews years later,” Kelly said in a statement. “Veteran aviators and aircrews deserve answers about the correlation between their job and cancer risks so we can reduce those risks for future pilots. Getting this across the finish line has been a bipartisan effort from the start, and I’m proud to see this bill become law so we can deliver real answers and accountability for those who served.”
“The ACES Act is now the law of the land,” Cotton added. “We owe it to past, present, and future aviators in the armed forces to study the prevalence of cancer among this group of veterans.”
The ACES Act complements Kelly’s bipartisan Counting Veterans’ Cancer Act, which requires Veterans Health Administration facilities to share cancer data with state cancer registries, thereby guaranteeing their inclusion in the national registries. Key provisions of the Counting Veterans’ Cancer Act were included in the first government funding package of fiscal year 2024.
A bipartisan bill establishing research directives aimed at revealing cancer risks among military aviators and aircrews recently became law.
Spearheaded by Sen. Mark Kelly (D-AZ) and Sen. Tom Cotton (R-AR), as well as Rep. August Pfluger (R-TX-11) and Rep. Jimmy Panetta (D-CA-19), all of whom are veterans, the Aviator Cancer Examination Study (ACES) Act was signed into law on August 14. The ACES Act will address cancer rates among Army, Navy, Air Force, and Marine Corps aircrew members by directing the Secretary of the US Department of Veterans Affairs to study cancer incidence and mortality rates among these populations.
Military aviators and aircrews face a 15% to 24% higher rate of cancer compared with the general US population, including a 75% higher rate of melanoma, 31% higher rate of thyroid cancer, 20% higher rate of prostate cancer, and 11% higher rate of female breast cancer, with potential links to non-Hodgkin lymphoma and testicular cancer. These individuals are also diagnosed earlier in life, at the median age of 55 years compared with 67 years. However, further investigation is still needed to understand why.
“By better understanding the correlation between aviator service and cancer, we can better assist our military and provide more adequate care for our veterans,” Kelly said.
Some reasons for the higher rates of cancer in aviators seem clear, such as the association between dioxin exposure and cancer. In a study of cancer incidence and mortality in Air Force veterans of the Vietnam War, incidence of melanoma and prostate cancer was increased among White veterans who sprayed herbicides during Operation Ranch Hand. The risk of cancer at any site, prostate cancer, and melanoma was increased in the highest dioxin exposure category among veterans who spent ≤ 2 years in Southeast Asia.
However, some links between these veterans and increased cancer rates are less clear. In a review of 28 studies (including 18 studies in military settings), slight evidence was found for associations between jet fuel exposure and various outcomes including cancer. Cosmic ionizing radiation (CIR) exposure is another possible cause. Several epidemiological studies have documented elevated incidence and mortality for several cancers in flight crews, but a link between them and CIR exposure has not been established.
Certain occupations have been associated with increased risk of testicular germ cell tumors, including aircraft maintenance, military pilots, fighter pilots, and aircrews. Those associations led to hypotheses that job-related chemical exposures (eg, per- and polyfluoroalkyl substances, solvents, paints, hydrocarbons in degreasing/lubricating agents, lubricating oils) may increase risk. A study of young active-duty Air Force servicemen found that pilots and men with aircraft maintenance jobs had elevated tenosynovial giant cell tumor risk, but indicates that further research is needed to “elucidate specific occupational exposures underlying these associations.”
“As a former Navy pilot, there are certain risks that we know and accept come with our service, but we know far less about the health risks that are affecting many aviators and aircrews years later,” Kelly said in a statement. “Veteran aviators and aircrews deserve answers about the correlation between their job and cancer risks so we can reduce those risks for future pilots. Getting this across the finish line has been a bipartisan effort from the start, and I’m proud to see this bill become law so we can deliver real answers and accountability for those who served.”
“The ACES Act is now the law of the land,” Cotton added. “We owe it to past, present, and future aviators in the armed forces to study the prevalence of cancer among this group of veterans.”
The ACES Act complements Kelly’s bipartisan Counting Veterans’ Cancer Act, which requires Veterans Health Administration facilities to share cancer data with state cancer registries, thereby guaranteeing their inclusion in the national registries. Key provisions of the Counting Veterans’ Cancer Act were included in the first government funding package of fiscal year 2024.
A bipartisan bill establishing research directives aimed at revealing cancer risks among military aviators and aircrews recently became law.
Spearheaded by Sen. Mark Kelly (D-AZ) and Sen. Tom Cotton (R-AR), as well as Rep. August Pfluger (R-TX-11) and Rep. Jimmy Panetta (D-CA-19), all of whom are veterans, the Aviator Cancer Examination Study (ACES) Act was signed into law on August 14. The ACES Act will address cancer rates among Army, Navy, Air Force, and Marine Corps aircrew members by directing the Secretary of the US Department of Veterans Affairs to study cancer incidence and mortality rates among these populations.
Military aviators and aircrews face a 15% to 24% higher rate of cancer compared with the general US population, including a 75% higher rate of melanoma, 31% higher rate of thyroid cancer, 20% higher rate of prostate cancer, and 11% higher rate of female breast cancer, with potential links to non-Hodgkin lymphoma and testicular cancer. These individuals are also diagnosed earlier in life, at the median age of 55 years compared with 67 years. However, further investigation is still needed to understand why.
“By better understanding the correlation between aviator service and cancer, we can better assist our military and provide more adequate care for our veterans,” Kelly said.
Some reasons for the higher rates of cancer in aviators seem clear, such as the association between dioxin exposure and cancer. In a study of cancer incidence and mortality in Air Force veterans of the Vietnam War, incidence of melanoma and prostate cancer was increased among White veterans who sprayed herbicides during Operation Ranch Hand. The risk of cancer at any site, prostate cancer, and melanoma was increased in the highest dioxin exposure category among veterans who spent ≤ 2 years in Southeast Asia.
However, some links between these veterans and increased cancer rates are less clear. In a review of 28 studies (including 18 studies in military settings), slight evidence was found for associations between jet fuel exposure and various outcomes including cancer. Cosmic ionizing radiation (CIR) exposure is another possible cause. Several epidemiological studies have documented elevated incidence and mortality for several cancers in flight crews, but a link between them and CIR exposure has not been established.
Certain occupations have been associated with increased risk of testicular germ cell tumors, including aircraft maintenance, military pilots, fighter pilots, and aircrews. Those associations led to hypotheses that job-related chemical exposures (eg, per- and polyfluoroalkyl substances, solvents, paints, hydrocarbons in degreasing/lubricating agents, lubricating oils) may increase risk. A study of young active-duty Air Force servicemen found that pilots and men with aircraft maintenance jobs had elevated tenosynovial giant cell tumor risk, but indicates that further research is needed to “elucidate specific occupational exposures underlying these associations.”
“As a former Navy pilot, there are certain risks that we know and accept come with our service, but we know far less about the health risks that are affecting many aviators and aircrews years later,” Kelly said in a statement. “Veteran aviators and aircrews deserve answers about the correlation between their job and cancer risks so we can reduce those risks for future pilots. Getting this across the finish line has been a bipartisan effort from the start, and I’m proud to see this bill become law so we can deliver real answers and accountability for those who served.”
“The ACES Act is now the law of the land,” Cotton added. “We owe it to past, present, and future aviators in the armed forces to study the prevalence of cancer among this group of veterans.”
The ACES Act complements Kelly’s bipartisan Counting Veterans’ Cancer Act, which requires Veterans Health Administration facilities to share cancer data with state cancer registries, thereby guaranteeing their inclusion in the national registries. Key provisions of the Counting Veterans’ Cancer Act were included in the first government funding package of fiscal year 2024.
Housing Program Expansion Opens Doors to More Veterans
TOPLINE:Expanding United States Department of Housing and Urban Development-Veterans Affairs Supportive Housing (HUD-VASH) eligibility to veterans with other-than-honorable (OTH) discharge significantly increased their program enrollments without impacting services for those with honorable discharge. Emergency department visits increased for honorable discharge veterans while hospitalizations rose for both groups.
METHODOLOGY:
- A quality improvement study following SQUIRE 2.0 reporting guidelines analyzed data from 129,873 veterans enrolled in HUD-VASH between June 1, 2019, and September 30, 2021.
- Analysis included 127,876 veterans (98.5%) with honorable/general discharge and 1997 veterans (1.5%) with OTH discharge, with a mean age of 53.7 years.
- Researchers utilized an interrupted time series design to compare program enrollments and healthcare utilization before (June 2019-December 2020) and after (January 2021-September 2021) policy implementation.
- Data linkage between the Homeless Operations and Management Evaluation System database and VA Corporate Data Warehouse enabled tracking of emergency department visits, hospitalizations, and primary care visits.
TAKEAWAY:
- Monthly HUD-VASH enrollments showed a significant increase for OTH veterans after the policy change (difference in slopes, 1.90; 95% confidence interval [CI], 1.28-2.52), while honorable/general veterans experienced a non-significant increase (difference in slopes, 9.23; 95% CI, −20.35-38.79).
- Emergency department visits demonstrated a significant increase for honorable/general veterans (change in slope, 0.24; 95% CI, 0.12-0.35) but not for OTH veterans (change in slope, 0.08;
95% CI, −0.12-0.28). - Hospitalizations significantly increased for both OTH veterans (change in slope, 0.098; 95% CI, 0.009-0.170) and honorable/general veterans (change in slope, 0.078; 95% CI, 0.004-0.060).
- Primary care visits showed no significant changes for either group after the policy implementation (OTH: change in slope, −0.12; 95% CI, −0.65-0.42; honorable/general: change in slope, 0.20;
95% CI, −0.13-0.53).
IN PRACTICE:“Expanding HUD-VASH eligibility increased access to housing and social support for OTH veterans without disrupting services for those with honorable discharges,” the authors reported. “Efforts should focus on improving access to connecting OTH veterans with clinical services outside of HUD-VASH.”
SOURCE:The study was led by Thomas F. Nubong, MD, Center of Innovation for Long-Term Services and Supports, Providence Veterans Affairs Medical Center in Providence. It was published online on August 5 in JAMA Network Open.
LIMITATIONS: According to the authors, the study period overlapped with the COVID-19 pandemic, potentially affecting results. Additionally, staff training on the policy change varied across US Department of Veterans Affairs (VA) sites, introducing implementation inconsistencies. The single-group interrupted time series design, while effective for tracking temporal trends, limited formal comparisons between discharge groups.
DISCLOSURES: The analyses were conducted under the VA Homeless Programs Office with operational funding support. Jack Tsai, PhD, and Eric Jutkowitz, PhD, reported being principal investigators of a VA Merit study on the Impact of COVID-19 for the HUD-VASH program. James L. Rudolph, MD, reported receiving grants from Icosavax outside the submitted work and being a United States government employee.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
TOPLINE:Expanding United States Department of Housing and Urban Development-Veterans Affairs Supportive Housing (HUD-VASH) eligibility to veterans with other-than-honorable (OTH) discharge significantly increased their program enrollments without impacting services for those with honorable discharge. Emergency department visits increased for honorable discharge veterans while hospitalizations rose for both groups.
METHODOLOGY:
- A quality improvement study following SQUIRE 2.0 reporting guidelines analyzed data from 129,873 veterans enrolled in HUD-VASH between June 1, 2019, and September 30, 2021.
- Analysis included 127,876 veterans (98.5%) with honorable/general discharge and 1997 veterans (1.5%) with OTH discharge, with a mean age of 53.7 years.
- Researchers utilized an interrupted time series design to compare program enrollments and healthcare utilization before (June 2019-December 2020) and after (January 2021-September 2021) policy implementation.
- Data linkage between the Homeless Operations and Management Evaluation System database and VA Corporate Data Warehouse enabled tracking of emergency department visits, hospitalizations, and primary care visits.
TAKEAWAY:
- Monthly HUD-VASH enrollments showed a significant increase for OTH veterans after the policy change (difference in slopes, 1.90; 95% confidence interval [CI], 1.28-2.52), while honorable/general veterans experienced a non-significant increase (difference in slopes, 9.23; 95% CI, −20.35-38.79).
- Emergency department visits demonstrated a significant increase for honorable/general veterans (change in slope, 0.24; 95% CI, 0.12-0.35) but not for OTH veterans (change in slope, 0.08;
95% CI, −0.12-0.28). - Hospitalizations significantly increased for both OTH veterans (change in slope, 0.098; 95% CI, 0.009-0.170) and honorable/general veterans (change in slope, 0.078; 95% CI, 0.004-0.060).
- Primary care visits showed no significant changes for either group after the policy implementation (OTH: change in slope, −0.12; 95% CI, −0.65-0.42; honorable/general: change in slope, 0.20;
95% CI, −0.13-0.53).
IN PRACTICE:“Expanding HUD-VASH eligibility increased access to housing and social support for OTH veterans without disrupting services for those with honorable discharges,” the authors reported. “Efforts should focus on improving access to connecting OTH veterans with clinical services outside of HUD-VASH.”
SOURCE:The study was led by Thomas F. Nubong, MD, Center of Innovation for Long-Term Services and Supports, Providence Veterans Affairs Medical Center in Providence. It was published online on August 5 in JAMA Network Open.
LIMITATIONS: According to the authors, the study period overlapped with the COVID-19 pandemic, potentially affecting results. Additionally, staff training on the policy change varied across US Department of Veterans Affairs (VA) sites, introducing implementation inconsistencies. The single-group interrupted time series design, while effective for tracking temporal trends, limited formal comparisons between discharge groups.
DISCLOSURES: The analyses were conducted under the VA Homeless Programs Office with operational funding support. Jack Tsai, PhD, and Eric Jutkowitz, PhD, reported being principal investigators of a VA Merit study on the Impact of COVID-19 for the HUD-VASH program. James L. Rudolph, MD, reported receiving grants from Icosavax outside the submitted work and being a United States government employee.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
TOPLINE:Expanding United States Department of Housing and Urban Development-Veterans Affairs Supportive Housing (HUD-VASH) eligibility to veterans with other-than-honorable (OTH) discharge significantly increased their program enrollments without impacting services for those with honorable discharge. Emergency department visits increased for honorable discharge veterans while hospitalizations rose for both groups.
METHODOLOGY:
- A quality improvement study following SQUIRE 2.0 reporting guidelines analyzed data from 129,873 veterans enrolled in HUD-VASH between June 1, 2019, and September 30, 2021.
- Analysis included 127,876 veterans (98.5%) with honorable/general discharge and 1997 veterans (1.5%) with OTH discharge, with a mean age of 53.7 years.
- Researchers utilized an interrupted time series design to compare program enrollments and healthcare utilization before (June 2019-December 2020) and after (January 2021-September 2021) policy implementation.
- Data linkage between the Homeless Operations and Management Evaluation System database and VA Corporate Data Warehouse enabled tracking of emergency department visits, hospitalizations, and primary care visits.
TAKEAWAY:
- Monthly HUD-VASH enrollments showed a significant increase for OTH veterans after the policy change (difference in slopes, 1.90; 95% confidence interval [CI], 1.28-2.52), while honorable/general veterans experienced a non-significant increase (difference in slopes, 9.23; 95% CI, −20.35-38.79).
- Emergency department visits demonstrated a significant increase for honorable/general veterans (change in slope, 0.24; 95% CI, 0.12-0.35) but not for OTH veterans (change in slope, 0.08;
95% CI, −0.12-0.28). - Hospitalizations significantly increased for both OTH veterans (change in slope, 0.098; 95% CI, 0.009-0.170) and honorable/general veterans (change in slope, 0.078; 95% CI, 0.004-0.060).
- Primary care visits showed no significant changes for either group after the policy implementation (OTH: change in slope, −0.12; 95% CI, −0.65-0.42; honorable/general: change in slope, 0.20;
95% CI, −0.13-0.53).
IN PRACTICE:“Expanding HUD-VASH eligibility increased access to housing and social support for OTH veterans without disrupting services for those with honorable discharges,” the authors reported. “Efforts should focus on improving access to connecting OTH veterans with clinical services outside of HUD-VASH.”
SOURCE:The study was led by Thomas F. Nubong, MD, Center of Innovation for Long-Term Services and Supports, Providence Veterans Affairs Medical Center in Providence. It was published online on August 5 in JAMA Network Open.
LIMITATIONS: According to the authors, the study period overlapped with the COVID-19 pandemic, potentially affecting results. Additionally, staff training on the policy change varied across US Department of Veterans Affairs (VA) sites, introducing implementation inconsistencies. The single-group interrupted time series design, while effective for tracking temporal trends, limited formal comparisons between discharge groups.
DISCLOSURES: The analyses were conducted under the VA Homeless Programs Office with operational funding support. Jack Tsai, PhD, and Eric Jutkowitz, PhD, reported being principal investigators of a VA Merit study on the Impact of COVID-19 for the HUD-VASH program. James L. Rudolph, MD, reported receiving grants from Icosavax outside the submitted work and being a United States government employee.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Critical Access for Veterans Bill Would Undermine VA Care
The Critical Access for Veterans Care Act, S.1868, introduced in May by Senators Kevin Cramer (R-ND) and Tim Sheehy (R-MT), would fundamentally reshape how veterans living in rural communities access private health care. The legislation establishes a new paradigm impacting veterans enrolled in US Department of Veterans Affairs (VA) health care who reside within 35 miles of any Centers for Medicare & Medicaid Services-designated Critical Access Hospital (CAH) or affiliated clinic. The bill would allow veterans unprecedented autonomy to self-refer directly to these facilities.
However, despite its seemingly straightforward title, the bill will not expedite care delivery, reduce travel burdens, or enhance network critical care capacity for veterans living in rural areas. Instead, the bill would further privatize veteran health care delivery by permitting veterans within this geographic radius to independently pursue care at CAHs and clinics without prior authorization. The legislation would establish a parallel referral system that erodes the Veterans Community Care Program (VCCP) eligibility determinations that were meticulously developed under the VA MISSION Act of 2018.
Some lawmakers have repeatedly pushed to eliminate VA's authorization role in the past 6 years, seeking to grant unrestricted private sector access to various veteran populations, particularly those requiring mental health services. Sponsors of the current bill are explicitly pursuing this same objective, characterizing VA authorization as an “unnecessary roadblock” that should be removed. However, this characterization misrepresents the actual function and value of the authorization process.
Over the past 6 years, provisions in the VA MISSION Act and other laws for predetermining veteran eligibility for private care have provided veterans with broad access while maintaining oversight and accountability. Enrolled veterans may receive comprehensive emergency medical and psychiatric care at any health care facility, including CAHs. They are guaranteed unrestricted walk-in urgent care access anywhere in the country. Veterans can also obtain outpatient and inpatient services through VCCP clinicians when they meet the following established access criteria: VA facilities exceed 30-minute travel times for primary and mental health services or 60 minutes for specialty care, or when appointment wait times surpass 20 days for primary/mental health care or 28 days for specialty services. Nearly half of covered veterans used this option in FY2023.
This bill does more than upend the established paradigm of VCCP eligibility requirements: it also eliminates the critical function of utilization review and accountability. Its passage would establish a dangerous precedent. By eliminating drive time and wait time eligibility standards and simultaneously removing VA’s ability to manage use, the bill generates powerful political momentum to extend identical provisions to all enrolled veterans. Furthermore, this legislation could specifically precipitate the downsizing or closure of VA community-based outpatient clinics (CBOCs) in areas served by CAHs. North Dakota, for example, operates 5 CBOCs that could be affected. Veterans who live in rural areas within the standard 30- to 60-minute drive time of a CBOC and can secure appointments within the established 20- to 28-day timeframes would no longer be subject to the same eligibility criteria that govern all covered veterans.
The Veterans Healthcare Policy Institute (VHPI) has serious reservations about legislation that eliminates VA's indispensable authorization and referral functions for supplemental private care. Founded in 2016, the VHPI is a nonprofit, nonpartisan organization dedicated to analyzing health care, disability compensation, and benefits for US veterans and their families. It provides fact-based research to educate the public and improve care quality both within and outside the VA.
New initiatives threaten to drastically reduce veterans' health and disability benefits through staff cuts and service reductions that will limit access to earned benefits and life-sustaining health care. Attacks against the VA also threaten to erode the training that produces new cohorts of health professionals, dramatically exacerbating the nation’s already dire shortages of physicians, nurses, psychologists and social workers.
VHPI’s coverage of Veterans Health Administration downsizing within rural health care provides important context. Starting with a comprehensive 15-page white paper published in 2024, VHPI has consistently highlighted how veterans living in rural communities face the same health care access challenges as all rural Americans—living in regions with severe shortages of health care facilities, professionals, and support staff. Lawmakers who assume veterans living in rural areas will experience shorter wait times and drive distances through private sector care fundamentally misunderstand these systemic issues
VHPI is committed to rigorously scrutinize policies that may compromise high quality care for veterans, especially those living in rural areas. The organization recently examined the flawed assumptions underlying these misguided policies. On August 12, VHPI released an in-depth analysis of private sector clinicians’ capacity to care for veterans in across all 50 states titled “Veterans’ Health Care Choice—Myth or Reality? A State- by- State Reality Check of the False Promise of VA Privatization.” This analysis revealed that, in most states, and in all rural states, the private sector system was struggling to meet even the basic needs of non-veterans. As one long time VA expert stated, to imagine that the system could absorb an influx of millions of veterans – particularly when new cuts to Medicaid and other healthcare funding are implemented, is “delusional.”
Russell Lemle and Suzanne Gordon are senior policy analysts at the Veterans Healthcare Policy Institute. Suzanne Gordon is author of Wounds of War.
The Critical Access for Veterans Care Act, S.1868, introduced in May by Senators Kevin Cramer (R-ND) and Tim Sheehy (R-MT), would fundamentally reshape how veterans living in rural communities access private health care. The legislation establishes a new paradigm impacting veterans enrolled in US Department of Veterans Affairs (VA) health care who reside within 35 miles of any Centers for Medicare & Medicaid Services-designated Critical Access Hospital (CAH) or affiliated clinic. The bill would allow veterans unprecedented autonomy to self-refer directly to these facilities.
However, despite its seemingly straightforward title, the bill will not expedite care delivery, reduce travel burdens, or enhance network critical care capacity for veterans living in rural areas. Instead, the bill would further privatize veteran health care delivery by permitting veterans within this geographic radius to independently pursue care at CAHs and clinics without prior authorization. The legislation would establish a parallel referral system that erodes the Veterans Community Care Program (VCCP) eligibility determinations that were meticulously developed under the VA MISSION Act of 2018.
Some lawmakers have repeatedly pushed to eliminate VA's authorization role in the past 6 years, seeking to grant unrestricted private sector access to various veteran populations, particularly those requiring mental health services. Sponsors of the current bill are explicitly pursuing this same objective, characterizing VA authorization as an “unnecessary roadblock” that should be removed. However, this characterization misrepresents the actual function and value of the authorization process.
Over the past 6 years, provisions in the VA MISSION Act and other laws for predetermining veteran eligibility for private care have provided veterans with broad access while maintaining oversight and accountability. Enrolled veterans may receive comprehensive emergency medical and psychiatric care at any health care facility, including CAHs. They are guaranteed unrestricted walk-in urgent care access anywhere in the country. Veterans can also obtain outpatient and inpatient services through VCCP clinicians when they meet the following established access criteria: VA facilities exceed 30-minute travel times for primary and mental health services or 60 minutes for specialty care, or when appointment wait times surpass 20 days for primary/mental health care or 28 days for specialty services. Nearly half of covered veterans used this option in FY2023.
This bill does more than upend the established paradigm of VCCP eligibility requirements: it also eliminates the critical function of utilization review and accountability. Its passage would establish a dangerous precedent. By eliminating drive time and wait time eligibility standards and simultaneously removing VA’s ability to manage use, the bill generates powerful political momentum to extend identical provisions to all enrolled veterans. Furthermore, this legislation could specifically precipitate the downsizing or closure of VA community-based outpatient clinics (CBOCs) in areas served by CAHs. North Dakota, for example, operates 5 CBOCs that could be affected. Veterans who live in rural areas within the standard 30- to 60-minute drive time of a CBOC and can secure appointments within the established 20- to 28-day timeframes would no longer be subject to the same eligibility criteria that govern all covered veterans.
The Veterans Healthcare Policy Institute (VHPI) has serious reservations about legislation that eliminates VA's indispensable authorization and referral functions for supplemental private care. Founded in 2016, the VHPI is a nonprofit, nonpartisan organization dedicated to analyzing health care, disability compensation, and benefits for US veterans and their families. It provides fact-based research to educate the public and improve care quality both within and outside the VA.
New initiatives threaten to drastically reduce veterans' health and disability benefits through staff cuts and service reductions that will limit access to earned benefits and life-sustaining health care. Attacks against the VA also threaten to erode the training that produces new cohorts of health professionals, dramatically exacerbating the nation’s already dire shortages of physicians, nurses, psychologists and social workers.
VHPI’s coverage of Veterans Health Administration downsizing within rural health care provides important context. Starting with a comprehensive 15-page white paper published in 2024, VHPI has consistently highlighted how veterans living in rural communities face the same health care access challenges as all rural Americans—living in regions with severe shortages of health care facilities, professionals, and support staff. Lawmakers who assume veterans living in rural areas will experience shorter wait times and drive distances through private sector care fundamentally misunderstand these systemic issues
VHPI is committed to rigorously scrutinize policies that may compromise high quality care for veterans, especially those living in rural areas. The organization recently examined the flawed assumptions underlying these misguided policies. On August 12, VHPI released an in-depth analysis of private sector clinicians’ capacity to care for veterans in across all 50 states titled “Veterans’ Health Care Choice—Myth or Reality? A State- by- State Reality Check of the False Promise of VA Privatization.” This analysis revealed that, in most states, and in all rural states, the private sector system was struggling to meet even the basic needs of non-veterans. As one long time VA expert stated, to imagine that the system could absorb an influx of millions of veterans – particularly when new cuts to Medicaid and other healthcare funding are implemented, is “delusional.”
Russell Lemle and Suzanne Gordon are senior policy analysts at the Veterans Healthcare Policy Institute. Suzanne Gordon is author of Wounds of War.
The Critical Access for Veterans Care Act, S.1868, introduced in May by Senators Kevin Cramer (R-ND) and Tim Sheehy (R-MT), would fundamentally reshape how veterans living in rural communities access private health care. The legislation establishes a new paradigm impacting veterans enrolled in US Department of Veterans Affairs (VA) health care who reside within 35 miles of any Centers for Medicare & Medicaid Services-designated Critical Access Hospital (CAH) or affiliated clinic. The bill would allow veterans unprecedented autonomy to self-refer directly to these facilities.
However, despite its seemingly straightforward title, the bill will not expedite care delivery, reduce travel burdens, or enhance network critical care capacity for veterans living in rural areas. Instead, the bill would further privatize veteran health care delivery by permitting veterans within this geographic radius to independently pursue care at CAHs and clinics without prior authorization. The legislation would establish a parallel referral system that erodes the Veterans Community Care Program (VCCP) eligibility determinations that were meticulously developed under the VA MISSION Act of 2018.
Some lawmakers have repeatedly pushed to eliminate VA's authorization role in the past 6 years, seeking to grant unrestricted private sector access to various veteran populations, particularly those requiring mental health services. Sponsors of the current bill are explicitly pursuing this same objective, characterizing VA authorization as an “unnecessary roadblock” that should be removed. However, this characterization misrepresents the actual function and value of the authorization process.
Over the past 6 years, provisions in the VA MISSION Act and other laws for predetermining veteran eligibility for private care have provided veterans with broad access while maintaining oversight and accountability. Enrolled veterans may receive comprehensive emergency medical and psychiatric care at any health care facility, including CAHs. They are guaranteed unrestricted walk-in urgent care access anywhere in the country. Veterans can also obtain outpatient and inpatient services through VCCP clinicians when they meet the following established access criteria: VA facilities exceed 30-minute travel times for primary and mental health services or 60 minutes for specialty care, or when appointment wait times surpass 20 days for primary/mental health care or 28 days for specialty services. Nearly half of covered veterans used this option in FY2023.
This bill does more than upend the established paradigm of VCCP eligibility requirements: it also eliminates the critical function of utilization review and accountability. Its passage would establish a dangerous precedent. By eliminating drive time and wait time eligibility standards and simultaneously removing VA’s ability to manage use, the bill generates powerful political momentum to extend identical provisions to all enrolled veterans. Furthermore, this legislation could specifically precipitate the downsizing or closure of VA community-based outpatient clinics (CBOCs) in areas served by CAHs. North Dakota, for example, operates 5 CBOCs that could be affected. Veterans who live in rural areas within the standard 30- to 60-minute drive time of a CBOC and can secure appointments within the established 20- to 28-day timeframes would no longer be subject to the same eligibility criteria that govern all covered veterans.
The Veterans Healthcare Policy Institute (VHPI) has serious reservations about legislation that eliminates VA's indispensable authorization and referral functions for supplemental private care. Founded in 2016, the VHPI is a nonprofit, nonpartisan organization dedicated to analyzing health care, disability compensation, and benefits for US veterans and their families. It provides fact-based research to educate the public and improve care quality both within and outside the VA.
New initiatives threaten to drastically reduce veterans' health and disability benefits through staff cuts and service reductions that will limit access to earned benefits and life-sustaining health care. Attacks against the VA also threaten to erode the training that produces new cohorts of health professionals, dramatically exacerbating the nation’s already dire shortages of physicians, nurses, psychologists and social workers.
VHPI’s coverage of Veterans Health Administration downsizing within rural health care provides important context. Starting with a comprehensive 15-page white paper published in 2024, VHPI has consistently highlighted how veterans living in rural communities face the same health care access challenges as all rural Americans—living in regions with severe shortages of health care facilities, professionals, and support staff. Lawmakers who assume veterans living in rural areas will experience shorter wait times and drive distances through private sector care fundamentally misunderstand these systemic issues
VHPI is committed to rigorously scrutinize policies that may compromise high quality care for veterans, especially those living in rural areas. The organization recently examined the flawed assumptions underlying these misguided policies. On August 12, VHPI released an in-depth analysis of private sector clinicians’ capacity to care for veterans in across all 50 states titled “Veterans’ Health Care Choice—Myth or Reality? A State- by- State Reality Check of the False Promise of VA Privatization.” This analysis revealed that, in most states, and in all rural states, the private sector system was struggling to meet even the basic needs of non-veterans. As one long time VA expert stated, to imagine that the system could absorb an influx of millions of veterans – particularly when new cuts to Medicaid and other healthcare funding are implemented, is “delusional.”
Russell Lemle and Suzanne Gordon are senior policy analysts at the Veterans Healthcare Policy Institute. Suzanne Gordon is author of Wounds of War.
VA To Lose 30K Positions Via Attrition, No RIFs Planned
The initial plan to reduce the US Department of Veterans Affairs (VA) workforce by 15%—roughly 83,000 employees—has been revised. The VA announced that it expected to reduce its workforce by 30,000 positions through normal attrition, early retirements, and resignations by the end of fiscal year 2025, “eliminating the need for a large-scale reduction-in-force.” Most of the positions will not be replaced due to the federal hiring freeze, which has been extended for 3 months.
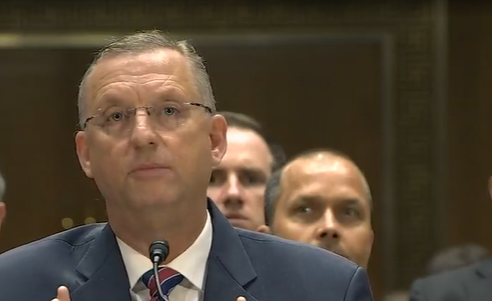
“Since March, we’ve been conducting a holistic review of the department centered on reducing bureaucracy and improving services to Veterans,” VA Secretary Doug Collins said in a press release. “A department-wide RIF is off the table, but that doesn’t mean we’re done improving VA.”
About 17,000 VA employees have left their jobs as of June 1. From now and Sept. 30, the department expects another reduction of nearly 12,000. Pete Kasperowicz, a VA spokesperson, said there would not be any reductions beyond the 30,000 planned.
The VA says it has multiple safeguards in place to ensure the reductions do not impact veteran care or benefits. All VA mission-critical positions are exempt from the voluntary early retirement authority and deferred resignation program, and > 350,000 positions are exempt from the federal hiring freeze.
The release noted several other improvements regarding VA performance in 2025, among them that the disability claims backlog has been reduced by 30% and a record 2 million disability claims have been processed by June. More than 60,000 VA employees have also returned to the office, according to the release.
“As a result of our efforts, VA is headed in the right direction – both in terms of staff levels and customer service,” Collins said. “Our review has resulted in a host of new ideas for better serving Veterans that we will continue to pursue.”
The initial plan to reduce the US Department of Veterans Affairs (VA) workforce by 15%—roughly 83,000 employees—has been revised. The VA announced that it expected to reduce its workforce by 30,000 positions through normal attrition, early retirements, and resignations by the end of fiscal year 2025, “eliminating the need for a large-scale reduction-in-force.” Most of the positions will not be replaced due to the federal hiring freeze, which has been extended for 3 months.
“Since March, we’ve been conducting a holistic review of the department centered on reducing bureaucracy and improving services to Veterans,” VA Secretary Doug Collins said in a press release. “A department-wide RIF is off the table, but that doesn’t mean we’re done improving VA.”
About 17,000 VA employees have left their jobs as of June 1. From now and Sept. 30, the department expects another reduction of nearly 12,000. Pete Kasperowicz, a VA spokesperson, said there would not be any reductions beyond the 30,000 planned.
The VA says it has multiple safeguards in place to ensure the reductions do not impact veteran care or benefits. All VA mission-critical positions are exempt from the voluntary early retirement authority and deferred resignation program, and > 350,000 positions are exempt from the federal hiring freeze.
The release noted several other improvements regarding VA performance in 2025, among them that the disability claims backlog has been reduced by 30% and a record 2 million disability claims have been processed by June. More than 60,000 VA employees have also returned to the office, according to the release.
“As a result of our efforts, VA is headed in the right direction – both in terms of staff levels and customer service,” Collins said. “Our review has resulted in a host of new ideas for better serving Veterans that we will continue to pursue.”
The initial plan to reduce the US Department of Veterans Affairs (VA) workforce by 15%—roughly 83,000 employees—has been revised. The VA announced that it expected to reduce its workforce by 30,000 positions through normal attrition, early retirements, and resignations by the end of fiscal year 2025, “eliminating the need for a large-scale reduction-in-force.” Most of the positions will not be replaced due to the federal hiring freeze, which has been extended for 3 months.
“Since March, we’ve been conducting a holistic review of the department centered on reducing bureaucracy and improving services to Veterans,” VA Secretary Doug Collins said in a press release. “A department-wide RIF is off the table, but that doesn’t mean we’re done improving VA.”
About 17,000 VA employees have left their jobs as of June 1. From now and Sept. 30, the department expects another reduction of nearly 12,000. Pete Kasperowicz, a VA spokesperson, said there would not be any reductions beyond the 30,000 planned.
The VA says it has multiple safeguards in place to ensure the reductions do not impact veteran care or benefits. All VA mission-critical positions are exempt from the voluntary early retirement authority and deferred resignation program, and > 350,000 positions are exempt from the federal hiring freeze.
The release noted several other improvements regarding VA performance in 2025, among them that the disability claims backlog has been reduced by 30% and a record 2 million disability claims have been processed by June. More than 60,000 VA employees have also returned to the office, according to the release.
“As a result of our efforts, VA is headed in the right direction – both in terms of staff levels and customer service,” Collins said. “Our review has resulted in a host of new ideas for better serving Veterans that we will continue to pursue.”
OIG Report Reveals Lapses in VA Retention and Recruitment Process
The Veterans Health Administration (VHA) paid about $828 million in recruitment and retention incentives from 2020 to 2023, but the process for providing an estimated $340.9 million of that was not “effectively governed” according to a recent US Department of Veterans Affairs (VA) Office of Inspector General (OIG) investigation.
About one-third of incentives were missing forms or signatures, or lacked sufficient justification, for the payments to about 130,000 VHA employees. In the report, the OIG notes the VHA has faced “long-standing challenges related to occupational shortages,” adding that a shortage occupation designation does not mean there are actual shortages at a facility.
“Most shortage occupations continue to experience annual net growth and are not critically understaffed in most facilities,” the report says.
More than 85% of incentive monies in 2022 and 2023 were paid to employees in occupations on staffing shortage lists. OIG estimated the VHA paid incentives to 38,800 employees (about 30%) where the award justification could not be verified or was insufficient.
Amplified by the COVID-19 pandemic and the PACT Act, the need to recruit and retain employees peaked in 2021, when record numbers of health care workers left their jobs. An October 2021 survey of 1000 medical professionals found nearly 1 in 5 health care workers quit during the pandemic, with most citing stress and burnout, and an additional 31% were considering quitting. When the PACT Act was signed into law in August 2022, it created thousands of newly benefits-eligible veterans.
In May 2022, the VA reported it needed to hire 52,000 employees annually for the next 5 years to keep up. In response, the VA released a 10-step plan to support recruitment and retention, focusing on raising wages when possible and finding other incentives when it wasn’t (ie, relocation bonuses or greater flexibility for remote work). The OIG report acknowledged the pandemic exacerbated VHA’s recruitment and retention challenges.
By 2024, the VA had not only reduced employee turnover by 20% over the prior 2 years, but had also exceeded its hiring goals. The VHA workforce grew by 7.4% in fiscal year 2023, its highest rate of growth in > 15 years.
VA officials must retain the documentation for incentives for 6 years so the process can be reconstructed if necessary. However, the OIG report noted “numerous instances” where documentation couldn’t be produced and therefore could not determine whether the incentives complied with policy.
The report also identified 28 employees who received retention incentive payments long after their award period had expired. The VA paid about $4.6 million for incentives that should have been terminated. The VA reported that it is pursuing debt collection for 27 of the 28 employees.
Only if the “identified weaknesses” are addressed will the VHA have assurance that incentives are being used effectively, the OIG said. Its recommendations included enforcing quality control checks and establishing accountability measures. The OIG also recommended establishing oversight procedures to review retention incentives annually, recertify them if appropriate, or terminate them.
The Veterans Health Administration (VHA) paid about $828 million in recruitment and retention incentives from 2020 to 2023, but the process for providing an estimated $340.9 million of that was not “effectively governed” according to a recent US Department of Veterans Affairs (VA) Office of Inspector General (OIG) investigation.
About one-third of incentives were missing forms or signatures, or lacked sufficient justification, for the payments to about 130,000 VHA employees. In the report, the OIG notes the VHA has faced “long-standing challenges related to occupational shortages,” adding that a shortage occupation designation does not mean there are actual shortages at a facility.
“Most shortage occupations continue to experience annual net growth and are not critically understaffed in most facilities,” the report says.
More than 85% of incentive monies in 2022 and 2023 were paid to employees in occupations on staffing shortage lists. OIG estimated the VHA paid incentives to 38,800 employees (about 30%) where the award justification could not be verified or was insufficient.
Amplified by the COVID-19 pandemic and the PACT Act, the need to recruit and retain employees peaked in 2021, when record numbers of health care workers left their jobs. An October 2021 survey of 1000 medical professionals found nearly 1 in 5 health care workers quit during the pandemic, with most citing stress and burnout, and an additional 31% were considering quitting. When the PACT Act was signed into law in August 2022, it created thousands of newly benefits-eligible veterans.
In May 2022, the VA reported it needed to hire 52,000 employees annually for the next 5 years to keep up. In response, the VA released a 10-step plan to support recruitment and retention, focusing on raising wages when possible and finding other incentives when it wasn’t (ie, relocation bonuses or greater flexibility for remote work). The OIG report acknowledged the pandemic exacerbated VHA’s recruitment and retention challenges.
By 2024, the VA had not only reduced employee turnover by 20% over the prior 2 years, but had also exceeded its hiring goals. The VHA workforce grew by 7.4% in fiscal year 2023, its highest rate of growth in > 15 years.
VA officials must retain the documentation for incentives for 6 years so the process can be reconstructed if necessary. However, the OIG report noted “numerous instances” where documentation couldn’t be produced and therefore could not determine whether the incentives complied with policy.
The report also identified 28 employees who received retention incentive payments long after their award period had expired. The VA paid about $4.6 million for incentives that should have been terminated. The VA reported that it is pursuing debt collection for 27 of the 28 employees.
Only if the “identified weaknesses” are addressed will the VHA have assurance that incentives are being used effectively, the OIG said. Its recommendations included enforcing quality control checks and establishing accountability measures. The OIG also recommended establishing oversight procedures to review retention incentives annually, recertify them if appropriate, or terminate them.
The Veterans Health Administration (VHA) paid about $828 million in recruitment and retention incentives from 2020 to 2023, but the process for providing an estimated $340.9 million of that was not “effectively governed” according to a recent US Department of Veterans Affairs (VA) Office of Inspector General (OIG) investigation.
About one-third of incentives were missing forms or signatures, or lacked sufficient justification, for the payments to about 130,000 VHA employees. In the report, the OIG notes the VHA has faced “long-standing challenges related to occupational shortages,” adding that a shortage occupation designation does not mean there are actual shortages at a facility.
“Most shortage occupations continue to experience annual net growth and are not critically understaffed in most facilities,” the report says.
More than 85% of incentive monies in 2022 and 2023 were paid to employees in occupations on staffing shortage lists. OIG estimated the VHA paid incentives to 38,800 employees (about 30%) where the award justification could not be verified or was insufficient.
Amplified by the COVID-19 pandemic and the PACT Act, the need to recruit and retain employees peaked in 2021, when record numbers of health care workers left their jobs. An October 2021 survey of 1000 medical professionals found nearly 1 in 5 health care workers quit during the pandemic, with most citing stress and burnout, and an additional 31% were considering quitting. When the PACT Act was signed into law in August 2022, it created thousands of newly benefits-eligible veterans.
In May 2022, the VA reported it needed to hire 52,000 employees annually for the next 5 years to keep up. In response, the VA released a 10-step plan to support recruitment and retention, focusing on raising wages when possible and finding other incentives when it wasn’t (ie, relocation bonuses or greater flexibility for remote work). The OIG report acknowledged the pandemic exacerbated VHA’s recruitment and retention challenges.
By 2024, the VA had not only reduced employee turnover by 20% over the prior 2 years, but had also exceeded its hiring goals. The VHA workforce grew by 7.4% in fiscal year 2023, its highest rate of growth in > 15 years.
VA officials must retain the documentation for incentives for 6 years so the process can be reconstructed if necessary. However, the OIG report noted “numerous instances” where documentation couldn’t be produced and therefore could not determine whether the incentives complied with policy.
The report also identified 28 employees who received retention incentive payments long after their award period had expired. The VA paid about $4.6 million for incentives that should have been terminated. The VA reported that it is pursuing debt collection for 27 of the 28 employees.
Only if the “identified weaknesses” are addressed will the VHA have assurance that incentives are being used effectively, the OIG said. Its recommendations included enforcing quality control checks and establishing accountability measures. The OIG also recommended establishing oversight procedures to review retention incentives annually, recertify them if appropriate, or terminate them.
2026 VA Budget Bill Narrowly Passed by House Appropriations Committee
2026 VA Budget Bill Narrowly Passed by House Appropriations Committee
The US House Appropriations Committee approved a $453 billion budget to fund the US Department of Veterans (VA), military construction, and other programs in 2026 by a 36-27 vote. The bill includes $34 billion proposed for community care programs, an increase of > 50% from 2025 community care funding levels.
The discretionary funding would also send $2.5 billion to the VA electronic health records modernization program. Mandatory spending includes $53 billion for the Toxic Exposures Fund, which supports benefits and health care costs associated with the PACT Act.
Although VA budget bills are typically bipartisan in nature, this bill passed by a much narrower margin than is typical. Rep. Debbie Wasserman Schultz (D-FL), ranking member of the Military Construction, Veterans Affairs and Related Agencies Appropriations Subcommittee, said the bill “diverts far too many resources away from the vital, VA-based care that veterans consistently tell us they want, and it pushes them into pricier, subpar corporate hospitals.”
Committee Democrats offered dozens of amendments. All amendments were rejected except for a modification that would block staff reductions at the Veterans Crisis Line and other VA suicide prevention programs.
The bill now moves to the full House of Representatives for consideration. House leaders have not yet announced when that vote will take place; the House is in recess the week of June 16, 2025.
The committee also released the Fiscal Year 2026 Military Construction, Veterans Affairs, and Related Agencies Bill, which would spend > $83 million, a 22% increase over the 2025.
The US House Appropriations Committee approved a $453 billion budget to fund the US Department of Veterans (VA), military construction, and other programs in 2026 by a 36-27 vote. The bill includes $34 billion proposed for community care programs, an increase of > 50% from 2025 community care funding levels.
The discretionary funding would also send $2.5 billion to the VA electronic health records modernization program. Mandatory spending includes $53 billion for the Toxic Exposures Fund, which supports benefits and health care costs associated with the PACT Act.
Although VA budget bills are typically bipartisan in nature, this bill passed by a much narrower margin than is typical. Rep. Debbie Wasserman Schultz (D-FL), ranking member of the Military Construction, Veterans Affairs and Related Agencies Appropriations Subcommittee, said the bill “diverts far too many resources away from the vital, VA-based care that veterans consistently tell us they want, and it pushes them into pricier, subpar corporate hospitals.”
Committee Democrats offered dozens of amendments. All amendments were rejected except for a modification that would block staff reductions at the Veterans Crisis Line and other VA suicide prevention programs.
The bill now moves to the full House of Representatives for consideration. House leaders have not yet announced when that vote will take place; the House is in recess the week of June 16, 2025.
The committee also released the Fiscal Year 2026 Military Construction, Veterans Affairs, and Related Agencies Bill, which would spend > $83 million, a 22% increase over the 2025.
The US House Appropriations Committee approved a $453 billion budget to fund the US Department of Veterans (VA), military construction, and other programs in 2026 by a 36-27 vote. The bill includes $34 billion proposed for community care programs, an increase of > 50% from 2025 community care funding levels.
The discretionary funding would also send $2.5 billion to the VA electronic health records modernization program. Mandatory spending includes $53 billion for the Toxic Exposures Fund, which supports benefits and health care costs associated with the PACT Act.
Although VA budget bills are typically bipartisan in nature, this bill passed by a much narrower margin than is typical. Rep. Debbie Wasserman Schultz (D-FL), ranking member of the Military Construction, Veterans Affairs and Related Agencies Appropriations Subcommittee, said the bill “diverts far too many resources away from the vital, VA-based care that veterans consistently tell us they want, and it pushes them into pricier, subpar corporate hospitals.”
Committee Democrats offered dozens of amendments. All amendments were rejected except for a modification that would block staff reductions at the Veterans Crisis Line and other VA suicide prevention programs.
The bill now moves to the full House of Representatives for consideration. House leaders have not yet announced when that vote will take place; the House is in recess the week of June 16, 2025.
The committee also released the Fiscal Year 2026 Military Construction, Veterans Affairs, and Related Agencies Bill, which would spend > $83 million, a 22% increase over the 2025.
2026 VA Budget Bill Narrowly Passed by House Appropriations Committee
2026 VA Budget Bill Narrowly Passed by House Appropriations Committee
VA to Allow Veteran Referrals to Community Care Without Second Review
VA to Allow Veteran Referrals to Community Care Without Second Review
Veterans enrolled in the US Department of Veterans Affairs (VA) who have been referred to Community Care no longer need a second review from a VA clinician according to a new policy. The provision implements language from the Senator Elizabeth Dole 21st Century Veterans Healthcare and Benefits Improvement Act. VA officials hope that it will speed up access to community care.
The move expands on the 2019 MISSION Act, which allows eligible veterans to access health care from non-VA clinicians that is paid for by the VA when it is in their “best medical interest.” Those decisions, however, were not considered final until reviewed by a second VA doctor.
The Dole Act prohibits VA administrators from overriding a VA doctor’s referral for a patient to receive outside care. According to the law, the ban on administrative review will remain in place for 2 years, after which the VA must report on its effects to Congress. The VA announced it would begin training employees to ensure the community care referral process is followed in compliance with the Dole Act.
Analysis from the Veterans Healthcare Policy Institute claims the best medical interest criterion “is to be considered when a veteran's health and/or well-being would be compromised if they were not able to be seen in the community for the requested clinical service.”
During a March hearing, Rep. Julia Brownley (D-CA), ranking Democrat on the House Veterans’ Affairs subcommittee on health, said any veteran who seeks residential treatment should get it, but noted the VA has not developed a fee schedule for community treatment centers. In at least 1 case, she said, the department was charged up to $6000 a day for 1 patient. Brownley also noted that the VA doesn't track the timeliness or quality of medical care in community residential treatment facilities.
“We have no way of knowing the level of treatment or support they are getting,” she said. “We must find a balance between community care and VA direct care. In my opinion, we have not found that balance when it comes to residential rehabilitation treatment facilities.”
At the same hearing, chair of the House Veterans Affairs health subcommittee Rep. Mariannette Miller-Meeks (R-IA) said more change is needed—specifically to ensure that veterans also can access private residential substance abuse treatment centers. Some, she said, “are told they cannot access community care unless a VA facility fails to meet a 20-day threshold—forcing them to wait, even when immediate, alternative options exist."
The House of Representatives passed H.R. 1969, the No Wrong Door for Veterans Act, in May, which expands the VA suicide prevention grant program. However, the Senate has yet to take up the legislation. “I’ve seen firsthand how difficult it can be for veterans in crisis to navigate a complicated system when every second counts,” Miller-Meeks said. “The No Wrong Door for Veterans Act ensures that our heroes are never turned away or left without help. It streamlines access, strengthens coordination, and reaffirms our promise to those who served.”
Veterans enrolled in the US Department of Veterans Affairs (VA) who have been referred to Community Care no longer need a second review from a VA clinician according to a new policy. The provision implements language from the Senator Elizabeth Dole 21st Century Veterans Healthcare and Benefits Improvement Act. VA officials hope that it will speed up access to community care.
The move expands on the 2019 MISSION Act, which allows eligible veterans to access health care from non-VA clinicians that is paid for by the VA when it is in their “best medical interest.” Those decisions, however, were not considered final until reviewed by a second VA doctor.
The Dole Act prohibits VA administrators from overriding a VA doctor’s referral for a patient to receive outside care. According to the law, the ban on administrative review will remain in place for 2 years, after which the VA must report on its effects to Congress. The VA announced it would begin training employees to ensure the community care referral process is followed in compliance with the Dole Act.
Analysis from the Veterans Healthcare Policy Institute claims the best medical interest criterion “is to be considered when a veteran's health and/or well-being would be compromised if they were not able to be seen in the community for the requested clinical service.”
During a March hearing, Rep. Julia Brownley (D-CA), ranking Democrat on the House Veterans’ Affairs subcommittee on health, said any veteran who seeks residential treatment should get it, but noted the VA has not developed a fee schedule for community treatment centers. In at least 1 case, she said, the department was charged up to $6000 a day for 1 patient. Brownley also noted that the VA doesn't track the timeliness or quality of medical care in community residential treatment facilities.
“We have no way of knowing the level of treatment or support they are getting,” she said. “We must find a balance between community care and VA direct care. In my opinion, we have not found that balance when it comes to residential rehabilitation treatment facilities.”
At the same hearing, chair of the House Veterans Affairs health subcommittee Rep. Mariannette Miller-Meeks (R-IA) said more change is needed—specifically to ensure that veterans also can access private residential substance abuse treatment centers. Some, she said, “are told they cannot access community care unless a VA facility fails to meet a 20-day threshold—forcing them to wait, even when immediate, alternative options exist."
The House of Representatives passed H.R. 1969, the No Wrong Door for Veterans Act, in May, which expands the VA suicide prevention grant program. However, the Senate has yet to take up the legislation. “I’ve seen firsthand how difficult it can be for veterans in crisis to navigate a complicated system when every second counts,” Miller-Meeks said. “The No Wrong Door for Veterans Act ensures that our heroes are never turned away or left without help. It streamlines access, strengthens coordination, and reaffirms our promise to those who served.”
Veterans enrolled in the US Department of Veterans Affairs (VA) who have been referred to Community Care no longer need a second review from a VA clinician according to a new policy. The provision implements language from the Senator Elizabeth Dole 21st Century Veterans Healthcare and Benefits Improvement Act. VA officials hope that it will speed up access to community care.
The move expands on the 2019 MISSION Act, which allows eligible veterans to access health care from non-VA clinicians that is paid for by the VA when it is in their “best medical interest.” Those decisions, however, were not considered final until reviewed by a second VA doctor.
The Dole Act prohibits VA administrators from overriding a VA doctor’s referral for a patient to receive outside care. According to the law, the ban on administrative review will remain in place for 2 years, after which the VA must report on its effects to Congress. The VA announced it would begin training employees to ensure the community care referral process is followed in compliance with the Dole Act.
Analysis from the Veterans Healthcare Policy Institute claims the best medical interest criterion “is to be considered when a veteran's health and/or well-being would be compromised if they were not able to be seen in the community for the requested clinical service.”
During a March hearing, Rep. Julia Brownley (D-CA), ranking Democrat on the House Veterans’ Affairs subcommittee on health, said any veteran who seeks residential treatment should get it, but noted the VA has not developed a fee schedule for community treatment centers. In at least 1 case, she said, the department was charged up to $6000 a day for 1 patient. Brownley also noted that the VA doesn't track the timeliness or quality of medical care in community residential treatment facilities.
“We have no way of knowing the level of treatment or support they are getting,” she said. “We must find a balance between community care and VA direct care. In my opinion, we have not found that balance when it comes to residential rehabilitation treatment facilities.”
At the same hearing, chair of the House Veterans Affairs health subcommittee Rep. Mariannette Miller-Meeks (R-IA) said more change is needed—specifically to ensure that veterans also can access private residential substance abuse treatment centers. Some, she said, “are told they cannot access community care unless a VA facility fails to meet a 20-day threshold—forcing them to wait, even when immediate, alternative options exist."
The House of Representatives passed H.R. 1969, the No Wrong Door for Veterans Act, in May, which expands the VA suicide prevention grant program. However, the Senate has yet to take up the legislation. “I’ve seen firsthand how difficult it can be for veterans in crisis to navigate a complicated system when every second counts,” Miller-Meeks said. “The No Wrong Door for Veterans Act ensures that our heroes are never turned away or left without help. It streamlines access, strengthens coordination, and reaffirms our promise to those who served.”
VA to Allow Veteran Referrals to Community Care Without Second Review
VA to Allow Veteran Referrals to Community Care Without Second Review
Suicide Prevention Grant Program Reauthorized
Suicide Prevention Grant Program Reauthorized
Community-based organizations that provide suicide-prevention services can now access about $52.5 million in US Department of Veterans Affairs (VA) grants. The grant is part of the 3-year Staff Sergeant Fox Suicide Prevention Grant Program, which honors Parker Gordon Fox, a sniper instructor at the U.S. Army Infantry School at Fort Benning, Georgia, who died by suicide in 2020. In consecutive Congressional hearings, lawmakers called for the reauthorization of the program to address gaps in VA care.
“It has been a game-changer for so many veterans,” Sen. Richard Blumenthal (D-CT) said.
The money provides or coordinates primarily nonclinical suicide prevention services, including outreach and linkage to VA and community resources. Services also may include baseline mental health screenings, case management and peer support, education on suicide risk, VA benefits assistance, and emergency clinical services.
Since its inception in 2022, the program has awarded $157.5 million to 95 organizations in 43 states, US territories, and tribal lands. Speaking before the House Committee on Veterans’ Affairs on May 15, VA Secretary Doug Collins praised the Fox program for bringing “different voices into the conversation,” but added it wasn’t enough. He noted that the veteran suicide rate has not changed since 2008, despite the VA annually spending $588 million on suicide prevention over the past few years.
In an op-ed, Russell Lemle, a senior policy analyst at the Veterans Healthcare Policy Institute, disputed Collins' characterization of veteran suicides. Between 2008 and 2022 (the last year for which complete data is available), US deaths by suicide increased 37% while the number of veteran deaths by suicide fell 2%. “This data collection was the single best part of the program,” he argued, calling for reauthorization to continue requiring data-targeted solutions.
According to a 2024 VA interim report on the Fox grant program, grantees had completed > 16,590 outreach contacts and engaged 3204 participants as of September 30, 2023. An additional 864 individuals were onboarding at the time of the report.
The current version of the grant program requires grantees to use validated tools, including the VA Data Collection Tool, and other assessments furnished by VA to determine the effectiveness of the suicide prevention services. They must also provide each participant with a satisfaction survey and submit periodic and annual financial and performance reports.
Despite the Trump administration’s cuts and cancellations to the federal workforce and federal programs, Collins told the Senate committee he is firmly on the side of working with community-based organizations like the Fox grant program to broaden the VA’s reach: “I want to use grants and programs like [the Fox grant program] to reach out beyond the scope of where we’re currently reaching, to say how can we actually touch the veteran that’s not being touched right now by these programs,” Collins said. “We’ve got to do better at using the grants, using our programs to go outside the normal bubble and use others to help get the word out.”
Grant applications are due in July and VA will choose awardees in September. Organizations can apply for grants worth up to $750,000 and may apply to renew awards from year to year throughout the length of the program.
Community-based organizations that provide suicide-prevention services can now access about $52.5 million in US Department of Veterans Affairs (VA) grants. The grant is part of the 3-year Staff Sergeant Fox Suicide Prevention Grant Program, which honors Parker Gordon Fox, a sniper instructor at the U.S. Army Infantry School at Fort Benning, Georgia, who died by suicide in 2020. In consecutive Congressional hearings, lawmakers called for the reauthorization of the program to address gaps in VA care.
“It has been a game-changer for so many veterans,” Sen. Richard Blumenthal (D-CT) said.
The money provides or coordinates primarily nonclinical suicide prevention services, including outreach and linkage to VA and community resources. Services also may include baseline mental health screenings, case management and peer support, education on suicide risk, VA benefits assistance, and emergency clinical services.
Since its inception in 2022, the program has awarded $157.5 million to 95 organizations in 43 states, US territories, and tribal lands. Speaking before the House Committee on Veterans’ Affairs on May 15, VA Secretary Doug Collins praised the Fox program for bringing “different voices into the conversation,” but added it wasn’t enough. He noted that the veteran suicide rate has not changed since 2008, despite the VA annually spending $588 million on suicide prevention over the past few years.
In an op-ed, Russell Lemle, a senior policy analyst at the Veterans Healthcare Policy Institute, disputed Collins' characterization of veteran suicides. Between 2008 and 2022 (the last year for which complete data is available), US deaths by suicide increased 37% while the number of veteran deaths by suicide fell 2%. “This data collection was the single best part of the program,” he argued, calling for reauthorization to continue requiring data-targeted solutions.
According to a 2024 VA interim report on the Fox grant program, grantees had completed > 16,590 outreach contacts and engaged 3204 participants as of September 30, 2023. An additional 864 individuals were onboarding at the time of the report.
The current version of the grant program requires grantees to use validated tools, including the VA Data Collection Tool, and other assessments furnished by VA to determine the effectiveness of the suicide prevention services. They must also provide each participant with a satisfaction survey and submit periodic and annual financial and performance reports.
Despite the Trump administration’s cuts and cancellations to the federal workforce and federal programs, Collins told the Senate committee he is firmly on the side of working with community-based organizations like the Fox grant program to broaden the VA’s reach: “I want to use grants and programs like [the Fox grant program] to reach out beyond the scope of where we’re currently reaching, to say how can we actually touch the veteran that’s not being touched right now by these programs,” Collins said. “We’ve got to do better at using the grants, using our programs to go outside the normal bubble and use others to help get the word out.”
Grant applications are due in July and VA will choose awardees in September. Organizations can apply for grants worth up to $750,000 and may apply to renew awards from year to year throughout the length of the program.
Community-based organizations that provide suicide-prevention services can now access about $52.5 million in US Department of Veterans Affairs (VA) grants. The grant is part of the 3-year Staff Sergeant Fox Suicide Prevention Grant Program, which honors Parker Gordon Fox, a sniper instructor at the U.S. Army Infantry School at Fort Benning, Georgia, who died by suicide in 2020. In consecutive Congressional hearings, lawmakers called for the reauthorization of the program to address gaps in VA care.
“It has been a game-changer for so many veterans,” Sen. Richard Blumenthal (D-CT) said.
The money provides or coordinates primarily nonclinical suicide prevention services, including outreach and linkage to VA and community resources. Services also may include baseline mental health screenings, case management and peer support, education on suicide risk, VA benefits assistance, and emergency clinical services.
Since its inception in 2022, the program has awarded $157.5 million to 95 organizations in 43 states, US territories, and tribal lands. Speaking before the House Committee on Veterans’ Affairs on May 15, VA Secretary Doug Collins praised the Fox program for bringing “different voices into the conversation,” but added it wasn’t enough. He noted that the veteran suicide rate has not changed since 2008, despite the VA annually spending $588 million on suicide prevention over the past few years.
In an op-ed, Russell Lemle, a senior policy analyst at the Veterans Healthcare Policy Institute, disputed Collins' characterization of veteran suicides. Between 2008 and 2022 (the last year for which complete data is available), US deaths by suicide increased 37% while the number of veteran deaths by suicide fell 2%. “This data collection was the single best part of the program,” he argued, calling for reauthorization to continue requiring data-targeted solutions.
According to a 2024 VA interim report on the Fox grant program, grantees had completed > 16,590 outreach contacts and engaged 3204 participants as of September 30, 2023. An additional 864 individuals were onboarding at the time of the report.
The current version of the grant program requires grantees to use validated tools, including the VA Data Collection Tool, and other assessments furnished by VA to determine the effectiveness of the suicide prevention services. They must also provide each participant with a satisfaction survey and submit periodic and annual financial and performance reports.
Despite the Trump administration’s cuts and cancellations to the federal workforce and federal programs, Collins told the Senate committee he is firmly on the side of working with community-based organizations like the Fox grant program to broaden the VA’s reach: “I want to use grants and programs like [the Fox grant program] to reach out beyond the scope of where we’re currently reaching, to say how can we actually touch the veteran that’s not being touched right now by these programs,” Collins said. “We’ve got to do better at using the grants, using our programs to go outside the normal bubble and use others to help get the word out.”
Grant applications are due in July and VA will choose awardees in September. Organizations can apply for grants worth up to $750,000 and may apply to renew awards from year to year throughout the length of the program.
Suicide Prevention Grant Program Reauthorized
Suicide Prevention Grant Program Reauthorized
Collins Lays Out Plans to Reduce VA by 15% in Congressional Hearings
Collins Lays Out Plans to Reduce VA by 15% in Senate Hearing
US Department of Veterans Affairs (VA) Secretary Doug Collins testified in US House of Representatives and US Senate committees hearings that bringing staff numbers down to fiscal year 2019 figures was simply a goal: “Our goal, as we look at it, as everything goes forward, is a 15% decrease,” he told the senators. “It’s a goal. You have to start somewhere.”
“It’s a process we’re going through and I’m not going to work out a process in front of a committee or anywhere else,” Collins testified in the Senate on May 6, adding that it would be “incompetence” or “malpractice” to do so before time. “[When] we’re doing something as large as we are in an organization as sensitive on this Hill, it would not be right for us to do that in public. It would not be right for us to just come out and say here’s everything that we got and then have everybody scared because in the end it may not be the final decision.”
“We’re going to come to the best possible decision we can for the veterans in this country so they can have a VA system that actually works,” Collins argued in the Senate. “The VA’s been an issue for a long time. We’re trying to not make it an issue anymore.”
Collins later told a House committee on May 15 that VA was conducting a thorough review of department structure and staffing across the enterpise. "Our goal is to increase productivity and efficiency and to eliminate waste and bureaucracy improving health care delivery and benefits to our veterans. We are going to maintain VA essential jobs like doctors and nurses and claims processors" but eliminate positions it deemed "nonmission-critical" and consolidating areas of "overlap and waste."
Senate ranking member Richard Blumenthal (D-CT) and Chairman Jerry Moran (R-KS) both placed an emphasis on accountability for responsible resizing at the hearing.
“The department is at a critical juncture,” Moran said. “Perhaps that’s always true, and I want to hear from you that the changes under way at the VA are backed by data, informed by veteran demand, focused on improving outcomes for men and women the VA serves, and will be carried out in close coordination with this committee, as well as with veterans, VA staff, and veteran organizations.” Moran stressed that cutting should be about right-sizing, done carefully, and while treating people “with gratitude and respect.”
Blumenthal was more direct in his criticism of the approach: “You cannot slash and trash the VA without eliminating those essential positions which provide access and availability of health care. It simply cannot be done,” he told Collins.
In response, Collins replied, “You have stated on several occasions already that I am saying we are going to fire 83,000 employees. That is wrong.” Collins insisted that the VA was “looking at a goal of how many employees we have and how many employees that are actually working in the front line taking care. I have doctors and nurses right now that do not see patients. Is that helping veteran health care?”
Collins defended the actions of the VA and spoke about challenges he was “constantly fighting” in the early weeks of his tenure. “We’ve been hit by a barrage of false rumors, innuendo, disinformation, speculation implying firing doctors and nurses, and forcing staff to work in closets and showers and that there’s chaos in the department, none of which have been backed up. Why? Because we canceled some contracts that worked for the VA that we should be doing in-house and we let go of less than one half of one percent of nonmission critical employees.”
The Trump Administration offered federal employees the option of resigning, which purportedly will go toward meeting the 15% target. NPR reported that VA employees have since shared data showing that 11,273 agency employees nationwide have applied for deferred resignation. Most of those employees are nurses (about 1300), medical support assistants (about 800), and social workers (about 300).
Collins stressed that the aim of restructuring was to protect veterans’ health care. By getting rid of DEI initiatives, the VA saved $14 million, which he said was redirected to veterans with disabilities who need prosthetics.
Sen. Bernie Sanders (D-VT) addressed concerns about the existing shortage of clinicians at the VA, asking Collins what he was doing to bring in more doctors, nurses, and social workers. In addition to moving doctors and nurses from nonpatient care to patient care, Collins said, he planned to work with Congress to make salaries more competitive.
But money and adding more employees are not always the solution, Collins said. For example, he said, the VA has been spending $588 million a year veteran suicide research, its top clinical priority. Yet, he said there has not been a significant decrease in veteran suicide rates since 2008.
The most recent VA suicide report, released in 2024, indicates suicide rates have remained steady since 2001. However, in 2022, the number of suicides among veterans (6407) was actually lower than in 12 of the previous 14 years.
According to media reports, congressional lawmakers, and union officials, Veteran Crisis Line (VCL) staff were among the 2400 probationary employees fired in February. In a Feb. 20 video, Collins accused Democrats of spreading lies and insisted no one who answered the phone was fired.
Later, in a letter to senators, Collins admitted that 24 VCL support staff were “erroneously” sent termination notices. The firings were later reversed, Collins said, and all VCL employees had been reinstated at the same position they previously held. “Ensuring the VCL is always accessible 24/7 is one of the department’s top priorities,” Collins insisted.
Collins shared his approval of keeping and expanding VA programs and studies on psychedelic treatments for patients with posttraumatic stress disorder and traumatic brain injury. He also spoke to the proposed 2026 budget calling for a $5.4 billion increase for the VA. If approved, that money would be targeted for medical care and homelessness.
US Department of Veterans Affairs (VA) Secretary Doug Collins testified in US House of Representatives and US Senate committees hearings that bringing staff numbers down to fiscal year 2019 figures was simply a goal: “Our goal, as we look at it, as everything goes forward, is a 15% decrease,” he told the senators. “It’s a goal. You have to start somewhere.”
“It’s a process we’re going through and I’m not going to work out a process in front of a committee or anywhere else,” Collins testified in the Senate on May 6, adding that it would be “incompetence” or “malpractice” to do so before time. “[When] we’re doing something as large as we are in an organization as sensitive on this Hill, it would not be right for us to do that in public. It would not be right for us to just come out and say here’s everything that we got and then have everybody scared because in the end it may not be the final decision.”
“We’re going to come to the best possible decision we can for the veterans in this country so they can have a VA system that actually works,” Collins argued in the Senate. “The VA’s been an issue for a long time. We’re trying to not make it an issue anymore.”
Collins later told a House committee on May 15 that VA was conducting a thorough review of department structure and staffing across the enterpise. "Our goal is to increase productivity and efficiency and to eliminate waste and bureaucracy improving health care delivery and benefits to our veterans. We are going to maintain VA essential jobs like doctors and nurses and claims processors" but eliminate positions it deemed "nonmission-critical" and consolidating areas of "overlap and waste."
Senate ranking member Richard Blumenthal (D-CT) and Chairman Jerry Moran (R-KS) both placed an emphasis on accountability for responsible resizing at the hearing.
“The department is at a critical juncture,” Moran said. “Perhaps that’s always true, and I want to hear from you that the changes under way at the VA are backed by data, informed by veteran demand, focused on improving outcomes for men and women the VA serves, and will be carried out in close coordination with this committee, as well as with veterans, VA staff, and veteran organizations.” Moran stressed that cutting should be about right-sizing, done carefully, and while treating people “with gratitude and respect.”
Blumenthal was more direct in his criticism of the approach: “You cannot slash and trash the VA without eliminating those essential positions which provide access and availability of health care. It simply cannot be done,” he told Collins.
In response, Collins replied, “You have stated on several occasions already that I am saying we are going to fire 83,000 employees. That is wrong.” Collins insisted that the VA was “looking at a goal of how many employees we have and how many employees that are actually working in the front line taking care. I have doctors and nurses right now that do not see patients. Is that helping veteran health care?”
Collins defended the actions of the VA and spoke about challenges he was “constantly fighting” in the early weeks of his tenure. “We’ve been hit by a barrage of false rumors, innuendo, disinformation, speculation implying firing doctors and nurses, and forcing staff to work in closets and showers and that there’s chaos in the department, none of which have been backed up. Why? Because we canceled some contracts that worked for the VA that we should be doing in-house and we let go of less than one half of one percent of nonmission critical employees.”
The Trump Administration offered federal employees the option of resigning, which purportedly will go toward meeting the 15% target. NPR reported that VA employees have since shared data showing that 11,273 agency employees nationwide have applied for deferred resignation. Most of those employees are nurses (about 1300), medical support assistants (about 800), and social workers (about 300).
Collins stressed that the aim of restructuring was to protect veterans’ health care. By getting rid of DEI initiatives, the VA saved $14 million, which he said was redirected to veterans with disabilities who need prosthetics.
Sen. Bernie Sanders (D-VT) addressed concerns about the existing shortage of clinicians at the VA, asking Collins what he was doing to bring in more doctors, nurses, and social workers. In addition to moving doctors and nurses from nonpatient care to patient care, Collins said, he planned to work with Congress to make salaries more competitive.
But money and adding more employees are not always the solution, Collins said. For example, he said, the VA has been spending $588 million a year veteran suicide research, its top clinical priority. Yet, he said there has not been a significant decrease in veteran suicide rates since 2008.
The most recent VA suicide report, released in 2024, indicates suicide rates have remained steady since 2001. However, in 2022, the number of suicides among veterans (6407) was actually lower than in 12 of the previous 14 years.
According to media reports, congressional lawmakers, and union officials, Veteran Crisis Line (VCL) staff were among the 2400 probationary employees fired in February. In a Feb. 20 video, Collins accused Democrats of spreading lies and insisted no one who answered the phone was fired.
Later, in a letter to senators, Collins admitted that 24 VCL support staff were “erroneously” sent termination notices. The firings were later reversed, Collins said, and all VCL employees had been reinstated at the same position they previously held. “Ensuring the VCL is always accessible 24/7 is one of the department’s top priorities,” Collins insisted.
Collins shared his approval of keeping and expanding VA programs and studies on psychedelic treatments for patients with posttraumatic stress disorder and traumatic brain injury. He also spoke to the proposed 2026 budget calling for a $5.4 billion increase for the VA. If approved, that money would be targeted for medical care and homelessness.
US Department of Veterans Affairs (VA) Secretary Doug Collins testified in US House of Representatives and US Senate committees hearings that bringing staff numbers down to fiscal year 2019 figures was simply a goal: “Our goal, as we look at it, as everything goes forward, is a 15% decrease,” he told the senators. “It’s a goal. You have to start somewhere.”
“It’s a process we’re going through and I’m not going to work out a process in front of a committee or anywhere else,” Collins testified in the Senate on May 6, adding that it would be “incompetence” or “malpractice” to do so before time. “[When] we’re doing something as large as we are in an organization as sensitive on this Hill, it would not be right for us to do that in public. It would not be right for us to just come out and say here’s everything that we got and then have everybody scared because in the end it may not be the final decision.”
“We’re going to come to the best possible decision we can for the veterans in this country so they can have a VA system that actually works,” Collins argued in the Senate. “The VA’s been an issue for a long time. We’re trying to not make it an issue anymore.”
Collins later told a House committee on May 15 that VA was conducting a thorough review of department structure and staffing across the enterpise. "Our goal is to increase productivity and efficiency and to eliminate waste and bureaucracy improving health care delivery and benefits to our veterans. We are going to maintain VA essential jobs like doctors and nurses and claims processors" but eliminate positions it deemed "nonmission-critical" and consolidating areas of "overlap and waste."
Senate ranking member Richard Blumenthal (D-CT) and Chairman Jerry Moran (R-KS) both placed an emphasis on accountability for responsible resizing at the hearing.
“The department is at a critical juncture,” Moran said. “Perhaps that’s always true, and I want to hear from you that the changes under way at the VA are backed by data, informed by veteran demand, focused on improving outcomes for men and women the VA serves, and will be carried out in close coordination with this committee, as well as with veterans, VA staff, and veteran organizations.” Moran stressed that cutting should be about right-sizing, done carefully, and while treating people “with gratitude and respect.”
Blumenthal was more direct in his criticism of the approach: “You cannot slash and trash the VA without eliminating those essential positions which provide access and availability of health care. It simply cannot be done,” he told Collins.
In response, Collins replied, “You have stated on several occasions already that I am saying we are going to fire 83,000 employees. That is wrong.” Collins insisted that the VA was “looking at a goal of how many employees we have and how many employees that are actually working in the front line taking care. I have doctors and nurses right now that do not see patients. Is that helping veteran health care?”
Collins defended the actions of the VA and spoke about challenges he was “constantly fighting” in the early weeks of his tenure. “We’ve been hit by a barrage of false rumors, innuendo, disinformation, speculation implying firing doctors and nurses, and forcing staff to work in closets and showers and that there’s chaos in the department, none of which have been backed up. Why? Because we canceled some contracts that worked for the VA that we should be doing in-house and we let go of less than one half of one percent of nonmission critical employees.”
The Trump Administration offered federal employees the option of resigning, which purportedly will go toward meeting the 15% target. NPR reported that VA employees have since shared data showing that 11,273 agency employees nationwide have applied for deferred resignation. Most of those employees are nurses (about 1300), medical support assistants (about 800), and social workers (about 300).
Collins stressed that the aim of restructuring was to protect veterans’ health care. By getting rid of DEI initiatives, the VA saved $14 million, which he said was redirected to veterans with disabilities who need prosthetics.
Sen. Bernie Sanders (D-VT) addressed concerns about the existing shortage of clinicians at the VA, asking Collins what he was doing to bring in more doctors, nurses, and social workers. In addition to moving doctors and nurses from nonpatient care to patient care, Collins said, he planned to work with Congress to make salaries more competitive.
But money and adding more employees are not always the solution, Collins said. For example, he said, the VA has been spending $588 million a year veteran suicide research, its top clinical priority. Yet, he said there has not been a significant decrease in veteran suicide rates since 2008.
The most recent VA suicide report, released in 2024, indicates suicide rates have remained steady since 2001. However, in 2022, the number of suicides among veterans (6407) was actually lower than in 12 of the previous 14 years.
According to media reports, congressional lawmakers, and union officials, Veteran Crisis Line (VCL) staff were among the 2400 probationary employees fired in February. In a Feb. 20 video, Collins accused Democrats of spreading lies and insisted no one who answered the phone was fired.
Later, in a letter to senators, Collins admitted that 24 VCL support staff were “erroneously” sent termination notices. The firings were later reversed, Collins said, and all VCL employees had been reinstated at the same position they previously held. “Ensuring the VCL is always accessible 24/7 is one of the department’s top priorities,” Collins insisted.
Collins shared his approval of keeping and expanding VA programs and studies on psychedelic treatments for patients with posttraumatic stress disorder and traumatic brain injury. He also spoke to the proposed 2026 budget calling for a $5.4 billion increase for the VA. If approved, that money would be targeted for medical care and homelessness.
Collins Lays Out Plans to Reduce VA by 15% in Senate Hearing
Collins Lays Out Plans to Reduce VA by 15% in Senate Hearing
Multiagent AI Systems in Health Care: Envisioning Next-Generation Intelligence
Artificial intelligence (AI) is rapidly evolving, with large language models (LLMs) marking a significant milestone in processing and generating human-like responses to natural language prompts. However, this advancement only signals the beginning of a more profound transformation in AI capabilities. The development of AI agents represents a new paradigm at the forefront of this evolution.
BACKGROUND
AI agents represent a leap forward from traditional LLM applications. While definitions may vary slightly among technology developers, the core concept remains: these agents are autonomous software entities designed to interact with their environment, make independent decisions, and execute tasks based on predefined goals.1-3 What sets AI agents apart is their combination of sophisticated components within structured architectures. At their core, AI agents incorporate an LLM for response generation, which is augmented by a suite of tools to optimize workflow and complete tasks, memory capabilities for personalized interactions, and autonomous reasoning. This combination allows AI agents to plan, create subtasks, gather information, and learn iteratively from their own experiences or other AI agents.
The true potential of this technology becomes apparent when multiple AI agents collaborate within multiagent AI systems. This concept introduces a new level of flexibility and capability in tackling complex tasks. Autogen, CrewAI, and LangChain offer various agent network configurations, including hierarchical, sequential, conditional, or even parallel task execution.4-6 This adaptability opens up a world of possibilities across various industries, but perhaps nowhere is the potential impact more exciting and profound than in health care.
AI agents in health care present an opportunity to revolutionize patient care, streamline administrative processes, and support complex clinical decision-making. This review examines 3 scenarios that illustrate the impact of AI agents in health care: a hypothetical sepsis management system, chronic disease management, and hospital patient flow optimization. This article will provide a detailed look at the technical implementation challenges, including the integration with existing health care IT systems, data privacy considerations, and the crucial role of explainable AI in maintaining trust and transparency.
It is challenging to implement AI agents in health care. Concerns include ensuring data quality and mitigating bias, seamlessly integrating these systems into existing clinical workflows, and navigating the complex ethical considerations that arise when deploying autonomous systems in health care. The integration with Internet of Things (IoT) devices for real-time patient data monitoring and the development of more sophisticated natural language interfaces to enhance future human-AI collaboration.
The adoption of AI agents in health care is only beginning, and it promises to be transformative. As AI continues to evolve, a comprehensive understanding of its applications, limitations, and ethical considerations is essential. This report provides a comprehensive overview of the current state, potential applications, and future directions of AI agents in health care, offering insights valuable to researchers, clinicians, and policymakers.
MultiAgent AI architecture
Sepsis Management
Despite advancements in broad-spectrum antibiotics, imaging, and life support systems, mortality rates associated with sepsis remain high. The complexity of optimizing care in clinical settings has hindered progress in managing sepsis. Previous attempts to develop predictive sepsis models have proven challenging.7 This report proposes a multiagent AI system designed to enhance comprehensive patient monitoring and care through coordinated AI-driven interventions.
Data Collection and Integration Agent. Powered by a controlled vocabulary to specify all data, the primary function for the data collection and integration agent is to clean, transform, and organize patient data from structured and unstructured sources. This agent prepares succinct summaries of consultant notes and formats data for human and machine consumption. All numerical data are presented graphically, including relevant historical data trends. The agent also digitally captures all orders in a structured format using a specified controlled vocabulary. This structured data feed supports the output of other agents, including documentation, treatment planning, and risk stratification, while also supplying the data structures for future training.
Diagnostic Agent. Critical illness is characterized by multiple abnormalities across a wide array of tests, ranging from plain chest X-ray, computed tomography (CT), blood cell composition, plasma chemistry, and microscopic evaluation of specimens. Additionally, life support parameters provide insights into disease severity and can inform management recommendations. These data offer a wide array of visual and numerical data to be used as input for computation, recommendation, and further training. For example, to evaluate fluid overload on chest X-rays or tissue histopathology slides, an AI agent can leverage deep learning models such as convolutional neural networks and vision transformers to analyze images like radiographs and histopathology slides.8,9 Recurrent neural networks or transformer models process sequential data like time-series vital signs. The agent also implements ensemble methods that combine multiple machine learning algorithms to enhance diagnostic accuracy.
Risk Stratification Agent. This assesses severity and predicts potential outcomes. Morbidity and mortality risks are calculated using an established scoring system and individualized based on the history of other agents’ conditional patients. These are presented graphically, with major risk factors highlighted for explainability.
Treatment Recommendation Agent. Using a reinforcement learning framework supplemented by up-to-date clinical guidelines, this system leverages historical data structured with standardized vocabulary to analyze patients with similar clinical features. Training is also conducted on the patient’s physiological data. All recommendations are presented via a dedicated user interface in a readable format, along with recommendations for editable, orderable items, references, and full-text snippets from previous research. Stop rules end computing if confidence in recommendations is too broad or no clear pathway can be computed with certainty, prompting human mitigation.
Resource Management Agent. This agent coordinates hospital resources using constraint programming techniques for optimal resource allocation, uses queueing theory models to predict and manage patient flow, and implements genetic algorithms for complex scheduling problems.10,11
Monitoring and Alert Agent. By tracking patients’ progress and alerting staff to changes, this agent uses anomaly detection algorithms to identify unusual patterns in patient data and implement time-series forecasting models, such as autoregressive integrated moving average and prophet, to predict future patient states. The agent also uses stream-processing techniques for real-time data analysis.12,13
Documentation and Reporting Agent. This agent maintains comprehensive medical records and generates reports. It employs advanced natural language processing techniques for automated report generation, uses advanced LLMs fine-tuned on medical corpora for narrative creation, and implements information-retrieval techniques to efficiently query patient records.
CLINICAL CASE STUDIES
To illustrate the functionality of a multiagent system, this report examines its application for managing sepsis. The data collection and integration agent continuously aggregates patient data from various sources, normalizing and timestamping it for consistent processing. The diagnostic agent analyzes this integrated data in real time, applying sepsis criteria and utilizing a deep learning model trained on a large sepsis dataset to detect subtle patterns.
The risk stratification agent calculates severity scores, such as the Sepsis-related Organ Failure Assessment (SOFA), quick SOFA (qSOFA), and Acute Physiology and Chronic Health Evaluation II, upon detecting a possible sepsis case.14 It predicts the likelihood of specific outcomes and estimates the potential trajectory of the patient’s condition for the next 24 to 48 hours. Based on this assessment, the treatment recommendation agent suggests an initial treatment plan, including appropriate antibiotics, fluid resuscitation protocols, and vasopressor recommendations, recommendations when indicated.
Concurrently, the resource management agent checks the availability of necessary resources and prioritizes allocation based on the severity. The monitoring agent tracks the patient’s response to interventions in real time, alerting the care team to any concerning changes or lack of expected improvement. Throughout this process, the documentation agent ensures that all actions, responses, and outcomes are meticulously recorded in a structured format and generates real-time updates for the patient’s electronic health record (EHR) and preparing summary reports for handoffs between care teams.
Administrative Workflow Support
Modern health care operations are resource-intensive, requiring coordination of advanced imaging, procedures, laboratory testing, and professional consultations.15 AI-powered health care administrative workflow systems are revolutionizing how medical facilities coordinate patient care. For patients with chronic cough, these systems seamlessly integrate scheduling, imaging, diagnostics, and follow-up care into a cohesive process that reduces administrative burden while improving patient outcomes. Through an intuitive interface and automated assistance, health care practitioners (HCPs) can track patient progress from initial consultation through diagnosis and treatment.
The process begins when an HCP enters a patient into the system, which triggers an automated CT scan scheduling system. The system considers factors like urgency, facility availability, and patient preferences to suggest optimal appointment times. Once imaging is complete, AI agents analyze the radiology reports, extract key findings, and generate structured summaries that highlight critical information such as “mild bronchial wall thickening with patchy ground-glass opacities” or “findings consistent with chronic bronchitis.”
Based on these findings, the system automatically generates evidence-based recommendations for follow-up care, such as pulmonology consultations or follow-up imaging in 3 months. These recommendations are presented to the ordering clinician, along with suggested appointment slots for specialist consultations. The system then manages the coordination of multiple appointments, ensuring each step in the patient’s care plan is properly sequenced and scheduled.
The entire process is monitored through a comprehensive dashboard that provides real-time updates on patient status, appointment schedules, and clinical recommendations. HCPs can track which patients require immediate attention, view upcoming appointments, and monitor the progress of ongoing care plans.
Multiagent AI Operation Optimization
Hospitals are complex entities that must function at different scales and respond in an agile, timely manner at all hours, deploying staff at various positions.16 A system of AI agents can receive signals from sensors monitoring foot traffic in the emergency department and trauma unit, as well as the availability of operating room staff, equipment, and intensive care unit beds. Smart sensors enable this monitoring through IoT networks. These networks benefit from advances in adaptive and consensus networking algorithms, along with recent advances in bioengineering and biocomputing.17
For example, in the case of imaging for suspected abdominal obstruction, an AI agent tasked with scheduling CTs could time the patient’s arrival based on acuity. Another AI agent could alert staff transporting the patient to the CT appointment, with the next location contingent on a clinical decision to proceed to the operating room. Yet another AI agent could summarize radiology interpretations and alert the surgery and anesthesia teams to a potential case, while others could notify operating room staff of equipment needs or reserve a bed. In this paradigm, AI agents facilitate more precise and timely communication between multiple staff members.
TECHNICAL IMPLEMENTATION
Large Language Models
Each agent uses a different LLM optimized for its specific task. For example, the diagnostic agent uses an LLM pretrained on a large corpus of biomedical literature and fine-tuned on a dataset of confirmed sepsis cases and their presentations.18 It implements few-shot learning techniques to adapt to rare or atypical presentations. The treatment recommendation agent also uses an LLM, employing a retrieval-augmented generation approach to access the latest clinical guidelines during inference. The documentation agent uses another advanced language model, fine-tuned on a large corpus of high-quality medical documentation, implementing controlled text generation techniques and utilizing a separate smaller model for real-time error checking and correction.
Interagent Quality Control
Agents learn from their own experience and the experience of other agents. They are equipped with user-defined rule-based and model-based systems for quality assurance, with clear stopping rules for human involvement and mitigation.
Sophisticated quality control measures bolster the system’s reliability, including ensemble techniques for result comparison, redundancy for critical tasks, and automatic human review for disagreements above a certain threshold. Each agent provides a calibrated confidence score with its output, used to weigh inputs in downstream tasks and trigger additional checks for low-confidence outputs.
A dedicated quality control agent monitors output from all agents, employing both supervised and unsupervised anomaly detection techniques. Feedback loops allow agents to evaluate the quality and utility of information received from other agents. The system implements a multiarmed bandit approach to dynamically adjust the influence of different agents based on their performance and periodically retrains agent models using federated learning techniques.19
Electronic Health Record Integration
Seamless EHR integration is crucial for practical implementation. The system has secure application programming interface access to various EHR platforms, implements OAuth 2.0 for authentication, and use HTTPS with perfect forward secrecy for all communications.20 It works with HL7 FHIR to ensure interoperability and uses SNOMED CT for clinical terminology to ensure semantic interoperability across different EHRs.21,22
The system implements a multilevel approval system for write-backs to EHRs, with different thresholds based on the information’s criticality. It uses digital signatures to ensure the integrity and nonrepudiation of AI-generated entries and implements blockchain technology to create an immutable and distributed ledger of all AI system actions.23
Decision Transparency
To ensure transparency in decision-making processes, the system applies techniques (eg, local interpretable model-agnostic explanations and Shapley additive explanations) to provide insights into agent decision-making processes.24-26 It provides customized visualizations for different stakeholders and allows users to explore alternative decision paths through what-if scenario modeling.27
The system provides calibrated confidence indicators for each recommendation or decision, implementing a novel confidence calibration agent that continuously monitors and adjusts confidence scores based on observed outcomes.
Continuous Learning and Adaptation
The system employs several techniques to remain current with evolving medical knowledge. Federated learning includes information from diverse datasets across multiple institutions without compromising patient privacy.28 A/B testing is used to safely deploy and compare new agent versions in controlled settings, implementing multiarmed bandit algorithms to efficiently explore new models while minimizing potential negative impacts. Human-in-the-loop learning and active learning techniques are used to incorporate feedback from HCPs and efficiently solicit expert input on the most informative data.29
CLINICAL IMPLICATIONS
The implementation of multiagent AI systems in health care has several potential benefits: enhanced diagnostic accuracy, personalized treatment, improved efficiency, continuous monitoring, and resource optimization. A recent review of AI sepsis predictive models exhibited superior results to standard clinical scoring methods like qSOFA.30 In oncology, such systems can result in more tailored treatments, enhancing outcomes.31 The implementation of an ambient dictation system can improve workflow and prevent HCP burnout.32
ETHICAL CONSIDERATIONS AND AI OVERSIGHT
Integrating AI agents into health care raises significant ethical considerations that must be carefully addressed to ensure equitable and effective care delivery. One primary concern involves cultural and linguistic competency, as AI systems may struggle with cultural nuances, idioms, and context-specific communication patterns. This becomes particularly challenging in regions with diverse ethnic populations or immigrant communities, where medical terminology may not have direct translations and cultural beliefs significantly influence health care decisions. AI systems also may inherit and amplify existing biases in health care delivery, whether through HCP bias reflected in training data, patient bias affecting acceptance of AI-assisted care, or demographic underrepresentation during system development.
AI agents present unique opportunities for improving health care access and outcomes through community engagement, though such initiatives require thoughtful implementation. Predictive analytics can identify high-risk individuals within communities who may benefit from preventive care, while analysis of social determinants of health can enable more targeted interventions. However, these capabilities must be balanced with privacy concerns and the risk of surveillance, particularly in communities that distrust health care institutions. The potential for AI to bridge health care gaps must be weighed against the need to maintain cultural sensitivity and community trust.
The governance and oversight of health care AI systems requires a multistakeholder approach with clear lines of responsibility and accountability. This includes involvement from government health care agencies, professional medical associations, ethics boards, and independent auditors, all working together to establish and enforce standards while monitoring system performance and addressing potential biases. Health care organizations must maintain transparent policies about AI use, implement regular monitoring and evaluation protocols, and establish precise mechanisms for patient feedback and grievance resolution. Ongoing assessment and adjustment of these systems, informed by community feedback and outcomes data, will be crucial for their ethical implementation, ensuring that AI agents complement, rather than replace, human judgment and cultural sensitivity.
FUTURE DIRECTIONS
Despite the potential benefits, implementing multiagent AI systems in health care faces significant challenges that require careful consideration. Beyond the fundamental issues such as data quality and bias mitigation, health care organizations struggle with fragmented systems, inconsistent data formats, and varying quality. Technical infrastructure requirements are substantial, particularly in rural or underserved areas that lack robust networks and cybersecurity. HCPs already face significant cognitive load and time pressures, making integrating AI agents into existing workflows particularly challenging. There is also the critical issue of transparency and interpretability, as health care decisions require clear reasoning and accountability that many black-box AI systems struggle to provide.
The legal landscape introduces another layer of complexity, particularly regarding liability, consent, and privacy questions. When AI agents contribute to medical decisions, establishing clear lines of responsibility becomes crucial. There are also serious concerns about algorithmic fairness and the potential for AI systems to perpetuate or amplify existing inequities. The cost of implementation remains a significant barrier, requiring substantial investment in technology, training, and ongoing maintenance while ensuring resources are not diverted from direct patient care. Moreover, HCPs may resist adoption due to concerns about job security, loss of autonomy, or skepticism about AI capabilities while paradoxically facing risks of overreliance on AI systems that could lead to the degradation of human clinical skills.
Addressing these challenges requires a multifaceted approach that combines technical solutions with organizational and policy changes. Health care organizations must implement rigorous data validation processes and interoperability standards while developing hybrid models that balance sophisticated AI capabilities with interpretable techniques. Extensive research and iterative design processes, with direct input from HCPs, are essential for successful integration. Establishing independent ethics boards to oversee system development and deployment, conducting multicenter randomized controlled trials, and creating clear regulatory frameworks will ensure safe and effective implementation. Success will ultimately depend on ongoing collaboration between technology developers, HCPs, policymakers, and patients, maintaining a steady focus on improving patient care and outcomes while carefully navigating the complex challenges of AI integration in health care.33-35
As multiagent AI systems in health care evolve, several exciting directions emerge. These include the integration of IoT and wearable devices, the development of more sophisticated natural language interfaces, and applying these systems to predictive maintenance of medical equipment.
CONCLUSIONS
The advent of multiagent AI systems in health care represents a paradigm shift in the approach to patient care, clinical decision making, and health care management. While these systems offer immense potential to transform health care delivery, their development and implementation must be guided by rigorous scientific validation, ethical considerations, and a patient-centered approach. The ultimate goal remains clear: harnessing the power of AI to improve patient outcomes, enhance the efficiency of health care delivery, and ultimately advance the health and well-being of patients.
Amazon Web Services, Inc. What are AI agents? Agents in artificial intelligence explained. Accessed April 7, 2025. https://aws.amazon.com/what-is/ai-agents/
Gutowska A. What are AI agents? IBM. Accessed April 7, 2025. https://www.ibm.com/think/topics/ai-agents
Agent AI. Microsoft Research. Accessed April 7, 2025. https://www.microsoft.com/en-us/research/project/agent-ai
Microsoft. AutoGen. Accessed April 7, 2025. https://microsoft.github.io/autogen/
Crew AI. The Leading Multi-Agent Platform. CrewAI. Accessed April 7, 2025. https://www.crewai.com/
LangChain. Accessed April 7, 2025. https://www.langchain.com/
Wong A, Otles E, Donnelly JP, et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern Med. 2021;181(8):1065-1070. doi:10.1001/jamainternmed.2021.2626
Willemink MJ, Roth HR, Sandfort V. Toward foundational deep learning models for medical imaging in the new era of transformer networks. Radiol Artif Intell. 2022;4(6):e210284. doi:10.1148/ryai.210284
Waqas A, Bui MM, Glassy EF, et al. Revolutionizing digital pathology with the power of generative artificial intelligence and foundation models. Lab Invest. 2023;103(11):100255. doi:10.1016/j.labinv.2023.100255
Moreno-Carrillo A, Arenas LMÁ, Fonseca JA, Caicedo CA, Tovar SV, Muñoz-Velandia OM. Application of queuing theory to optimize the triage process in a tertiary emergency care (“ER”) department. J Emerg Trauma Shock. 2019;12(4):268-273. doi:10.4103/JETS.JETS_42_19
Pongcharoen P, Hicks C, Braiden PM, Stewardson DJ. Determining optimum genetic algorithm parameters for scheduling the manufacturing and assembly of complex products. Int J Prod Econ. 2002;78(3):311-322. doi:10.1016/S0925-5273(02)00104-4
Sardar I, Akbar MA, Leiva V, Alsanad A, Mishra P. Machine learning and automatic ARIMA/Prophet models-based forecasting of COVID-19: methodology, evaluation, and case study in SAARC countries. Stoch Environ Res Risk Assess. 2023;37(1):345-359. doi:10.1007/s00477-022-02307-x
Samosir J, Indrawan-Santiago M, Haghighi PD. An evaluation of data stream processing systems for data driven applications. Procedia Comput Sci. 2016;80:439-449. doi:10.1016/j.procs.2016.05.322
Asmarawati TP, Suryantoro SD, Rosyid AN, et al. Predictive value of sequential organ failure assessment, quick sequential organ failure assessment, acute physiology and chronic health evaluation II, and new early warning signs scores estimate mortality of COVID-19 patients requiring intensive care unit. Indian J Crit Care Med. 2022;26(4):466-473. doi:10.5005/jp-journals-10071-24170
Khan S, Vandermorris A, Shepherd J, et al. Embracing uncertainty, managing complexity: applying complexity thinking principles to transformation efforts in healthcare systems. BMC Health Serv Res. 2018;18(1):192. doi:10.1186/s12913-018-2994-0
Plsek PE, Greenhalgh T. The challenge of complexity in health care. BMJ. 2001;323(7313):625-628. doi:10.1136/bmj.323.7313.625
Kouchaki S, Ding X, Sanei S. AI- and IoT-enabled solutions for healthcare. Sensors. 2024;24(8):2607. doi:10.3390/s24082607
Saab K, Tu T, Weng WH, et al. Capabilities of Gemini Models in Medicine. arXiv. doi:10.48550/arXiv.2404.18416
Villar SS, Bowden J, Wason J. Multi-armed bandit models for the optimal design of clinical trials: benefits and challenges. Stat Sci. 2015;30(2):199-215. doi:10.1214/14-STS504
Auth0. What is OAuth 2.0. Accessed April 7, 2025. https://auth0.com/intro-to-iam/what-is-oauth-2
HL7. Welcome to FHIR. Updated March 26, 2025. Accessed April 7, 2025. https://www.hl7.org/fhir/
SNOMED International. Accessed April 7, 2025. https://www.snomed.org
Hasselgren A, Kralevska K, Gligoroski D, Pedersen SA, Faxvaag A. Blockchain in healthcare and health sciences—a scoping review. Int J Med Inf. 2020;134:104040. doi:10.1016/j.ijmedinf.2019.104040
Ribeiro MT, Singh S, Guestrin C. “Why Should I Trust You?”: Explaining the predictions of any classifier. In: Proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining. 2016:1135-1144. doi:10.1145/2939672.2939778
Ekanayake IU, Meddage DPP, Rathnayake U. A novel approach to explain the black-box nature of machine learning in compressive strength predictions of concrete using Shapley additive explanations (SHAP). Case Stud Constr Mater. 2022;16:e01059. doi:10.1016/j.cscm.2022.e01059
Alabi RO, Elmusrati M, Leivo I, Almangush A, Mäkitie AA. Machine learning explainability in nasopharyngeal cancer survival using LIME and SHAP. Sci Rep. 2023;13(1):8984. doi:10.1038/s41598-023-35795-0
Otto E, Culakova E, Meng S, et al. Overview of sankey flow diagrams: focusing on symptom trajectories in older adults with advanced cancer. J Geriatr Oncol. 2022;13(5):742-746. doi:10.1016/j.jgo.2021.12.017
Fereidooni H, Marchal S, Miettinen M, et al. SAFELearn: secure aggregation for private federated learning. In: 2021 IEEE security and privacy workshops (SPW). 2021:56-62. doi:10.1109/SPW53761.2021.00017
Linton DL, Pangle WM, Wyatt KH, Powell KN, Sherwood RE. Identifying key features of effective active learning: the effects of writing and peer discussion. Life Sci Educ. 2014;13(3):469-477. doi:10.1187/cbe.13-12-0242
Yang HS. Machine learning for sepsis prediction: prospects and challenges. Clin Chem. 2024;70(3):465-467. doi:10.1093/clinchem/hvae006
Liao J, Li X, Gan Y, et al. Artificial intelligence assists precision medicine in cancer treatment. Front Oncol. 2023;12. doi:10.3389/fonc.2022.998222
Tierney AA, Gayre G, Hoberman B, et al. Ambient artificial intelligence scribes to alleviate the burden of clinical documentation. NEJM Catal. 2024;5(3):CAT.23.0404. doi:10.1056/CAT.23.0404
Borkowski AA, Jakey CE, Thomas LB, Viswanadhan N, Mastorides SM. Establishing a hospital artificial intelligence committee to improve patient care. Fed Pract. 2022;39(8):334-336. doi:10.12788/fp.0299
Isaacks DB, Borkowski AA. Implementing trustworthy AI in VA high reliability health care organizations. Fed Pract.2024;41(2):40-43. doi:10.12788/fp.0454
Han R, Acosta JN, Shakeri Z, Ioannidis JPA, Topol EJ, Rajpurkar P. Randomized controlled trials evaluating artificial intelligence in clinical practice: a scoping review. Lancet Digit Health. 2024;6(5):e367-e373. doi:10.1016/S2589-7500(24)00047-5
Artificial intelligence (AI) is rapidly evolving, with large language models (LLMs) marking a significant milestone in processing and generating human-like responses to natural language prompts. However, this advancement only signals the beginning of a more profound transformation in AI capabilities. The development of AI agents represents a new paradigm at the forefront of this evolution.
BACKGROUND
AI agents represent a leap forward from traditional LLM applications. While definitions may vary slightly among technology developers, the core concept remains: these agents are autonomous software entities designed to interact with their environment, make independent decisions, and execute tasks based on predefined goals.1-3 What sets AI agents apart is their combination of sophisticated components within structured architectures. At their core, AI agents incorporate an LLM for response generation, which is augmented by a suite of tools to optimize workflow and complete tasks, memory capabilities for personalized interactions, and autonomous reasoning. This combination allows AI agents to plan, create subtasks, gather information, and learn iteratively from their own experiences or other AI agents.
The true potential of this technology becomes apparent when multiple AI agents collaborate within multiagent AI systems. This concept introduces a new level of flexibility and capability in tackling complex tasks. Autogen, CrewAI, and LangChain offer various agent network configurations, including hierarchical, sequential, conditional, or even parallel task execution.4-6 This adaptability opens up a world of possibilities across various industries, but perhaps nowhere is the potential impact more exciting and profound than in health care.
AI agents in health care present an opportunity to revolutionize patient care, streamline administrative processes, and support complex clinical decision-making. This review examines 3 scenarios that illustrate the impact of AI agents in health care: a hypothetical sepsis management system, chronic disease management, and hospital patient flow optimization. This article will provide a detailed look at the technical implementation challenges, including the integration with existing health care IT systems, data privacy considerations, and the crucial role of explainable AI in maintaining trust and transparency.
It is challenging to implement AI agents in health care. Concerns include ensuring data quality and mitigating bias, seamlessly integrating these systems into existing clinical workflows, and navigating the complex ethical considerations that arise when deploying autonomous systems in health care. The integration with Internet of Things (IoT) devices for real-time patient data monitoring and the development of more sophisticated natural language interfaces to enhance future human-AI collaboration.
The adoption of AI agents in health care is only beginning, and it promises to be transformative. As AI continues to evolve, a comprehensive understanding of its applications, limitations, and ethical considerations is essential. This report provides a comprehensive overview of the current state, potential applications, and future directions of AI agents in health care, offering insights valuable to researchers, clinicians, and policymakers.
MultiAgent AI architecture
Sepsis Management
Despite advancements in broad-spectrum antibiotics, imaging, and life support systems, mortality rates associated with sepsis remain high. The complexity of optimizing care in clinical settings has hindered progress in managing sepsis. Previous attempts to develop predictive sepsis models have proven challenging.7 This report proposes a multiagent AI system designed to enhance comprehensive patient monitoring and care through coordinated AI-driven interventions.
Data Collection and Integration Agent. Powered by a controlled vocabulary to specify all data, the primary function for the data collection and integration agent is to clean, transform, and organize patient data from structured and unstructured sources. This agent prepares succinct summaries of consultant notes and formats data for human and machine consumption. All numerical data are presented graphically, including relevant historical data trends. The agent also digitally captures all orders in a structured format using a specified controlled vocabulary. This structured data feed supports the output of other agents, including documentation, treatment planning, and risk stratification, while also supplying the data structures for future training.
Diagnostic Agent. Critical illness is characterized by multiple abnormalities across a wide array of tests, ranging from plain chest X-ray, computed tomography (CT), blood cell composition, plasma chemistry, and microscopic evaluation of specimens. Additionally, life support parameters provide insights into disease severity and can inform management recommendations. These data offer a wide array of visual and numerical data to be used as input for computation, recommendation, and further training. For example, to evaluate fluid overload on chest X-rays or tissue histopathology slides, an AI agent can leverage deep learning models such as convolutional neural networks and vision transformers to analyze images like radiographs and histopathology slides.8,9 Recurrent neural networks or transformer models process sequential data like time-series vital signs. The agent also implements ensemble methods that combine multiple machine learning algorithms to enhance diagnostic accuracy.
Risk Stratification Agent. This assesses severity and predicts potential outcomes. Morbidity and mortality risks are calculated using an established scoring system and individualized based on the history of other agents’ conditional patients. These are presented graphically, with major risk factors highlighted for explainability.
Treatment Recommendation Agent. Using a reinforcement learning framework supplemented by up-to-date clinical guidelines, this system leverages historical data structured with standardized vocabulary to analyze patients with similar clinical features. Training is also conducted on the patient’s physiological data. All recommendations are presented via a dedicated user interface in a readable format, along with recommendations for editable, orderable items, references, and full-text snippets from previous research. Stop rules end computing if confidence in recommendations is too broad or no clear pathway can be computed with certainty, prompting human mitigation.
Resource Management Agent. This agent coordinates hospital resources using constraint programming techniques for optimal resource allocation, uses queueing theory models to predict and manage patient flow, and implements genetic algorithms for complex scheduling problems.10,11
Monitoring and Alert Agent. By tracking patients’ progress and alerting staff to changes, this agent uses anomaly detection algorithms to identify unusual patterns in patient data and implement time-series forecasting models, such as autoregressive integrated moving average and prophet, to predict future patient states. The agent also uses stream-processing techniques for real-time data analysis.12,13
Documentation and Reporting Agent. This agent maintains comprehensive medical records and generates reports. It employs advanced natural language processing techniques for automated report generation, uses advanced LLMs fine-tuned on medical corpora for narrative creation, and implements information-retrieval techniques to efficiently query patient records.
CLINICAL CASE STUDIES
To illustrate the functionality of a multiagent system, this report examines its application for managing sepsis. The data collection and integration agent continuously aggregates patient data from various sources, normalizing and timestamping it for consistent processing. The diagnostic agent analyzes this integrated data in real time, applying sepsis criteria and utilizing a deep learning model trained on a large sepsis dataset to detect subtle patterns.
The risk stratification agent calculates severity scores, such as the Sepsis-related Organ Failure Assessment (SOFA), quick SOFA (qSOFA), and Acute Physiology and Chronic Health Evaluation II, upon detecting a possible sepsis case.14 It predicts the likelihood of specific outcomes and estimates the potential trajectory of the patient’s condition for the next 24 to 48 hours. Based on this assessment, the treatment recommendation agent suggests an initial treatment plan, including appropriate antibiotics, fluid resuscitation protocols, and vasopressor recommendations, recommendations when indicated.
Concurrently, the resource management agent checks the availability of necessary resources and prioritizes allocation based on the severity. The monitoring agent tracks the patient’s response to interventions in real time, alerting the care team to any concerning changes or lack of expected improvement. Throughout this process, the documentation agent ensures that all actions, responses, and outcomes are meticulously recorded in a structured format and generates real-time updates for the patient’s electronic health record (EHR) and preparing summary reports for handoffs between care teams.
Administrative Workflow Support
Modern health care operations are resource-intensive, requiring coordination of advanced imaging, procedures, laboratory testing, and professional consultations.15 AI-powered health care administrative workflow systems are revolutionizing how medical facilities coordinate patient care. For patients with chronic cough, these systems seamlessly integrate scheduling, imaging, diagnostics, and follow-up care into a cohesive process that reduces administrative burden while improving patient outcomes. Through an intuitive interface and automated assistance, health care practitioners (HCPs) can track patient progress from initial consultation through diagnosis and treatment.
The process begins when an HCP enters a patient into the system, which triggers an automated CT scan scheduling system. The system considers factors like urgency, facility availability, and patient preferences to suggest optimal appointment times. Once imaging is complete, AI agents analyze the radiology reports, extract key findings, and generate structured summaries that highlight critical information such as “mild bronchial wall thickening with patchy ground-glass opacities” or “findings consistent with chronic bronchitis.”
Based on these findings, the system automatically generates evidence-based recommendations for follow-up care, such as pulmonology consultations or follow-up imaging in 3 months. These recommendations are presented to the ordering clinician, along with suggested appointment slots for specialist consultations. The system then manages the coordination of multiple appointments, ensuring each step in the patient’s care plan is properly sequenced and scheduled.
The entire process is monitored through a comprehensive dashboard that provides real-time updates on patient status, appointment schedules, and clinical recommendations. HCPs can track which patients require immediate attention, view upcoming appointments, and monitor the progress of ongoing care plans.
Multiagent AI Operation Optimization
Hospitals are complex entities that must function at different scales and respond in an agile, timely manner at all hours, deploying staff at various positions.16 A system of AI agents can receive signals from sensors monitoring foot traffic in the emergency department and trauma unit, as well as the availability of operating room staff, equipment, and intensive care unit beds. Smart sensors enable this monitoring through IoT networks. These networks benefit from advances in adaptive and consensus networking algorithms, along with recent advances in bioengineering and biocomputing.17
For example, in the case of imaging for suspected abdominal obstruction, an AI agent tasked with scheduling CTs could time the patient’s arrival based on acuity. Another AI agent could alert staff transporting the patient to the CT appointment, with the next location contingent on a clinical decision to proceed to the operating room. Yet another AI agent could summarize radiology interpretations and alert the surgery and anesthesia teams to a potential case, while others could notify operating room staff of equipment needs or reserve a bed. In this paradigm, AI agents facilitate more precise and timely communication between multiple staff members.
TECHNICAL IMPLEMENTATION
Large Language Models
Each agent uses a different LLM optimized for its specific task. For example, the diagnostic agent uses an LLM pretrained on a large corpus of biomedical literature and fine-tuned on a dataset of confirmed sepsis cases and their presentations.18 It implements few-shot learning techniques to adapt to rare or atypical presentations. The treatment recommendation agent also uses an LLM, employing a retrieval-augmented generation approach to access the latest clinical guidelines during inference. The documentation agent uses another advanced language model, fine-tuned on a large corpus of high-quality medical documentation, implementing controlled text generation techniques and utilizing a separate smaller model for real-time error checking and correction.
Interagent Quality Control
Agents learn from their own experience and the experience of other agents. They are equipped with user-defined rule-based and model-based systems for quality assurance, with clear stopping rules for human involvement and mitigation.
Sophisticated quality control measures bolster the system’s reliability, including ensemble techniques for result comparison, redundancy for critical tasks, and automatic human review for disagreements above a certain threshold. Each agent provides a calibrated confidence score with its output, used to weigh inputs in downstream tasks and trigger additional checks for low-confidence outputs.
A dedicated quality control agent monitors output from all agents, employing both supervised and unsupervised anomaly detection techniques. Feedback loops allow agents to evaluate the quality and utility of information received from other agents. The system implements a multiarmed bandit approach to dynamically adjust the influence of different agents based on their performance and periodically retrains agent models using federated learning techniques.19
Electronic Health Record Integration
Seamless EHR integration is crucial for practical implementation. The system has secure application programming interface access to various EHR platforms, implements OAuth 2.0 for authentication, and use HTTPS with perfect forward secrecy for all communications.20 It works with HL7 FHIR to ensure interoperability and uses SNOMED CT for clinical terminology to ensure semantic interoperability across different EHRs.21,22
The system implements a multilevel approval system for write-backs to EHRs, with different thresholds based on the information’s criticality. It uses digital signatures to ensure the integrity and nonrepudiation of AI-generated entries and implements blockchain technology to create an immutable and distributed ledger of all AI system actions.23
Decision Transparency
To ensure transparency in decision-making processes, the system applies techniques (eg, local interpretable model-agnostic explanations and Shapley additive explanations) to provide insights into agent decision-making processes.24-26 It provides customized visualizations for different stakeholders and allows users to explore alternative decision paths through what-if scenario modeling.27
The system provides calibrated confidence indicators for each recommendation or decision, implementing a novel confidence calibration agent that continuously monitors and adjusts confidence scores based on observed outcomes.
Continuous Learning and Adaptation
The system employs several techniques to remain current with evolving medical knowledge. Federated learning includes information from diverse datasets across multiple institutions without compromising patient privacy.28 A/B testing is used to safely deploy and compare new agent versions in controlled settings, implementing multiarmed bandit algorithms to efficiently explore new models while minimizing potential negative impacts. Human-in-the-loop learning and active learning techniques are used to incorporate feedback from HCPs and efficiently solicit expert input on the most informative data.29
CLINICAL IMPLICATIONS
The implementation of multiagent AI systems in health care has several potential benefits: enhanced diagnostic accuracy, personalized treatment, improved efficiency, continuous monitoring, and resource optimization. A recent review of AI sepsis predictive models exhibited superior results to standard clinical scoring methods like qSOFA.30 In oncology, such systems can result in more tailored treatments, enhancing outcomes.31 The implementation of an ambient dictation system can improve workflow and prevent HCP burnout.32
ETHICAL CONSIDERATIONS AND AI OVERSIGHT
Integrating AI agents into health care raises significant ethical considerations that must be carefully addressed to ensure equitable and effective care delivery. One primary concern involves cultural and linguistic competency, as AI systems may struggle with cultural nuances, idioms, and context-specific communication patterns. This becomes particularly challenging in regions with diverse ethnic populations or immigrant communities, where medical terminology may not have direct translations and cultural beliefs significantly influence health care decisions. AI systems also may inherit and amplify existing biases in health care delivery, whether through HCP bias reflected in training data, patient bias affecting acceptance of AI-assisted care, or demographic underrepresentation during system development.
AI agents present unique opportunities for improving health care access and outcomes through community engagement, though such initiatives require thoughtful implementation. Predictive analytics can identify high-risk individuals within communities who may benefit from preventive care, while analysis of social determinants of health can enable more targeted interventions. However, these capabilities must be balanced with privacy concerns and the risk of surveillance, particularly in communities that distrust health care institutions. The potential for AI to bridge health care gaps must be weighed against the need to maintain cultural sensitivity and community trust.
The governance and oversight of health care AI systems requires a multistakeholder approach with clear lines of responsibility and accountability. This includes involvement from government health care agencies, professional medical associations, ethics boards, and independent auditors, all working together to establish and enforce standards while monitoring system performance and addressing potential biases. Health care organizations must maintain transparent policies about AI use, implement regular monitoring and evaluation protocols, and establish precise mechanisms for patient feedback and grievance resolution. Ongoing assessment and adjustment of these systems, informed by community feedback and outcomes data, will be crucial for their ethical implementation, ensuring that AI agents complement, rather than replace, human judgment and cultural sensitivity.
FUTURE DIRECTIONS
Despite the potential benefits, implementing multiagent AI systems in health care faces significant challenges that require careful consideration. Beyond the fundamental issues such as data quality and bias mitigation, health care organizations struggle with fragmented systems, inconsistent data formats, and varying quality. Technical infrastructure requirements are substantial, particularly in rural or underserved areas that lack robust networks and cybersecurity. HCPs already face significant cognitive load and time pressures, making integrating AI agents into existing workflows particularly challenging. There is also the critical issue of transparency and interpretability, as health care decisions require clear reasoning and accountability that many black-box AI systems struggle to provide.
The legal landscape introduces another layer of complexity, particularly regarding liability, consent, and privacy questions. When AI agents contribute to medical decisions, establishing clear lines of responsibility becomes crucial. There are also serious concerns about algorithmic fairness and the potential for AI systems to perpetuate or amplify existing inequities. The cost of implementation remains a significant barrier, requiring substantial investment in technology, training, and ongoing maintenance while ensuring resources are not diverted from direct patient care. Moreover, HCPs may resist adoption due to concerns about job security, loss of autonomy, or skepticism about AI capabilities while paradoxically facing risks of overreliance on AI systems that could lead to the degradation of human clinical skills.
Addressing these challenges requires a multifaceted approach that combines technical solutions with organizational and policy changes. Health care organizations must implement rigorous data validation processes and interoperability standards while developing hybrid models that balance sophisticated AI capabilities with interpretable techniques. Extensive research and iterative design processes, with direct input from HCPs, are essential for successful integration. Establishing independent ethics boards to oversee system development and deployment, conducting multicenter randomized controlled trials, and creating clear regulatory frameworks will ensure safe and effective implementation. Success will ultimately depend on ongoing collaboration between technology developers, HCPs, policymakers, and patients, maintaining a steady focus on improving patient care and outcomes while carefully navigating the complex challenges of AI integration in health care.33-35
As multiagent AI systems in health care evolve, several exciting directions emerge. These include the integration of IoT and wearable devices, the development of more sophisticated natural language interfaces, and applying these systems to predictive maintenance of medical equipment.
CONCLUSIONS
The advent of multiagent AI systems in health care represents a paradigm shift in the approach to patient care, clinical decision making, and health care management. While these systems offer immense potential to transform health care delivery, their development and implementation must be guided by rigorous scientific validation, ethical considerations, and a patient-centered approach. The ultimate goal remains clear: harnessing the power of AI to improve patient outcomes, enhance the efficiency of health care delivery, and ultimately advance the health and well-being of patients.
Artificial intelligence (AI) is rapidly evolving, with large language models (LLMs) marking a significant milestone in processing and generating human-like responses to natural language prompts. However, this advancement only signals the beginning of a more profound transformation in AI capabilities. The development of AI agents represents a new paradigm at the forefront of this evolution.
BACKGROUND
AI agents represent a leap forward from traditional LLM applications. While definitions may vary slightly among technology developers, the core concept remains: these agents are autonomous software entities designed to interact with their environment, make independent decisions, and execute tasks based on predefined goals.1-3 What sets AI agents apart is their combination of sophisticated components within structured architectures. At their core, AI agents incorporate an LLM for response generation, which is augmented by a suite of tools to optimize workflow and complete tasks, memory capabilities for personalized interactions, and autonomous reasoning. This combination allows AI agents to plan, create subtasks, gather information, and learn iteratively from their own experiences or other AI agents.
The true potential of this technology becomes apparent when multiple AI agents collaborate within multiagent AI systems. This concept introduces a new level of flexibility and capability in tackling complex tasks. Autogen, CrewAI, and LangChain offer various agent network configurations, including hierarchical, sequential, conditional, or even parallel task execution.4-6 This adaptability opens up a world of possibilities across various industries, but perhaps nowhere is the potential impact more exciting and profound than in health care.
AI agents in health care present an opportunity to revolutionize patient care, streamline administrative processes, and support complex clinical decision-making. This review examines 3 scenarios that illustrate the impact of AI agents in health care: a hypothetical sepsis management system, chronic disease management, and hospital patient flow optimization. This article will provide a detailed look at the technical implementation challenges, including the integration with existing health care IT systems, data privacy considerations, and the crucial role of explainable AI in maintaining trust and transparency.
It is challenging to implement AI agents in health care. Concerns include ensuring data quality and mitigating bias, seamlessly integrating these systems into existing clinical workflows, and navigating the complex ethical considerations that arise when deploying autonomous systems in health care. The integration with Internet of Things (IoT) devices for real-time patient data monitoring and the development of more sophisticated natural language interfaces to enhance future human-AI collaboration.
The adoption of AI agents in health care is only beginning, and it promises to be transformative. As AI continues to evolve, a comprehensive understanding of its applications, limitations, and ethical considerations is essential. This report provides a comprehensive overview of the current state, potential applications, and future directions of AI agents in health care, offering insights valuable to researchers, clinicians, and policymakers.
MultiAgent AI architecture
Sepsis Management
Despite advancements in broad-spectrum antibiotics, imaging, and life support systems, mortality rates associated with sepsis remain high. The complexity of optimizing care in clinical settings has hindered progress in managing sepsis. Previous attempts to develop predictive sepsis models have proven challenging.7 This report proposes a multiagent AI system designed to enhance comprehensive patient monitoring and care through coordinated AI-driven interventions.
Data Collection and Integration Agent. Powered by a controlled vocabulary to specify all data, the primary function for the data collection and integration agent is to clean, transform, and organize patient data from structured and unstructured sources. This agent prepares succinct summaries of consultant notes and formats data for human and machine consumption. All numerical data are presented graphically, including relevant historical data trends. The agent also digitally captures all orders in a structured format using a specified controlled vocabulary. This structured data feed supports the output of other agents, including documentation, treatment planning, and risk stratification, while also supplying the data structures for future training.
Diagnostic Agent. Critical illness is characterized by multiple abnormalities across a wide array of tests, ranging from plain chest X-ray, computed tomography (CT), blood cell composition, plasma chemistry, and microscopic evaluation of specimens. Additionally, life support parameters provide insights into disease severity and can inform management recommendations. These data offer a wide array of visual and numerical data to be used as input for computation, recommendation, and further training. For example, to evaluate fluid overload on chest X-rays or tissue histopathology slides, an AI agent can leverage deep learning models such as convolutional neural networks and vision transformers to analyze images like radiographs and histopathology slides.8,9 Recurrent neural networks or transformer models process sequential data like time-series vital signs. The agent also implements ensemble methods that combine multiple machine learning algorithms to enhance diagnostic accuracy.
Risk Stratification Agent. This assesses severity and predicts potential outcomes. Morbidity and mortality risks are calculated using an established scoring system and individualized based on the history of other agents’ conditional patients. These are presented graphically, with major risk factors highlighted for explainability.
Treatment Recommendation Agent. Using a reinforcement learning framework supplemented by up-to-date clinical guidelines, this system leverages historical data structured with standardized vocabulary to analyze patients with similar clinical features. Training is also conducted on the patient’s physiological data. All recommendations are presented via a dedicated user interface in a readable format, along with recommendations for editable, orderable items, references, and full-text snippets from previous research. Stop rules end computing if confidence in recommendations is too broad or no clear pathway can be computed with certainty, prompting human mitigation.
Resource Management Agent. This agent coordinates hospital resources using constraint programming techniques for optimal resource allocation, uses queueing theory models to predict and manage patient flow, and implements genetic algorithms for complex scheduling problems.10,11
Monitoring and Alert Agent. By tracking patients’ progress and alerting staff to changes, this agent uses anomaly detection algorithms to identify unusual patterns in patient data and implement time-series forecasting models, such as autoregressive integrated moving average and prophet, to predict future patient states. The agent also uses stream-processing techniques for real-time data analysis.12,13
Documentation and Reporting Agent. This agent maintains comprehensive medical records and generates reports. It employs advanced natural language processing techniques for automated report generation, uses advanced LLMs fine-tuned on medical corpora for narrative creation, and implements information-retrieval techniques to efficiently query patient records.
CLINICAL CASE STUDIES
To illustrate the functionality of a multiagent system, this report examines its application for managing sepsis. The data collection and integration agent continuously aggregates patient data from various sources, normalizing and timestamping it for consistent processing. The diagnostic agent analyzes this integrated data in real time, applying sepsis criteria and utilizing a deep learning model trained on a large sepsis dataset to detect subtle patterns.
The risk stratification agent calculates severity scores, such as the Sepsis-related Organ Failure Assessment (SOFA), quick SOFA (qSOFA), and Acute Physiology and Chronic Health Evaluation II, upon detecting a possible sepsis case.14 It predicts the likelihood of specific outcomes and estimates the potential trajectory of the patient’s condition for the next 24 to 48 hours. Based on this assessment, the treatment recommendation agent suggests an initial treatment plan, including appropriate antibiotics, fluid resuscitation protocols, and vasopressor recommendations, recommendations when indicated.
Concurrently, the resource management agent checks the availability of necessary resources and prioritizes allocation based on the severity. The monitoring agent tracks the patient’s response to interventions in real time, alerting the care team to any concerning changes or lack of expected improvement. Throughout this process, the documentation agent ensures that all actions, responses, and outcomes are meticulously recorded in a structured format and generates real-time updates for the patient’s electronic health record (EHR) and preparing summary reports for handoffs between care teams.
Administrative Workflow Support
Modern health care operations are resource-intensive, requiring coordination of advanced imaging, procedures, laboratory testing, and professional consultations.15 AI-powered health care administrative workflow systems are revolutionizing how medical facilities coordinate patient care. For patients with chronic cough, these systems seamlessly integrate scheduling, imaging, diagnostics, and follow-up care into a cohesive process that reduces administrative burden while improving patient outcomes. Through an intuitive interface and automated assistance, health care practitioners (HCPs) can track patient progress from initial consultation through diagnosis and treatment.
The process begins when an HCP enters a patient into the system, which triggers an automated CT scan scheduling system. The system considers factors like urgency, facility availability, and patient preferences to suggest optimal appointment times. Once imaging is complete, AI agents analyze the radiology reports, extract key findings, and generate structured summaries that highlight critical information such as “mild bronchial wall thickening with patchy ground-glass opacities” or “findings consistent with chronic bronchitis.”
Based on these findings, the system automatically generates evidence-based recommendations for follow-up care, such as pulmonology consultations or follow-up imaging in 3 months. These recommendations are presented to the ordering clinician, along with suggested appointment slots for specialist consultations. The system then manages the coordination of multiple appointments, ensuring each step in the patient’s care plan is properly sequenced and scheduled.
The entire process is monitored through a comprehensive dashboard that provides real-time updates on patient status, appointment schedules, and clinical recommendations. HCPs can track which patients require immediate attention, view upcoming appointments, and monitor the progress of ongoing care plans.
Multiagent AI Operation Optimization
Hospitals are complex entities that must function at different scales and respond in an agile, timely manner at all hours, deploying staff at various positions.16 A system of AI agents can receive signals from sensors monitoring foot traffic in the emergency department and trauma unit, as well as the availability of operating room staff, equipment, and intensive care unit beds. Smart sensors enable this monitoring through IoT networks. These networks benefit from advances in adaptive and consensus networking algorithms, along with recent advances in bioengineering and biocomputing.17
For example, in the case of imaging for suspected abdominal obstruction, an AI agent tasked with scheduling CTs could time the patient’s arrival based on acuity. Another AI agent could alert staff transporting the patient to the CT appointment, with the next location contingent on a clinical decision to proceed to the operating room. Yet another AI agent could summarize radiology interpretations and alert the surgery and anesthesia teams to a potential case, while others could notify operating room staff of equipment needs or reserve a bed. In this paradigm, AI agents facilitate more precise and timely communication between multiple staff members.
TECHNICAL IMPLEMENTATION
Large Language Models
Each agent uses a different LLM optimized for its specific task. For example, the diagnostic agent uses an LLM pretrained on a large corpus of biomedical literature and fine-tuned on a dataset of confirmed sepsis cases and their presentations.18 It implements few-shot learning techniques to adapt to rare or atypical presentations. The treatment recommendation agent also uses an LLM, employing a retrieval-augmented generation approach to access the latest clinical guidelines during inference. The documentation agent uses another advanced language model, fine-tuned on a large corpus of high-quality medical documentation, implementing controlled text generation techniques and utilizing a separate smaller model for real-time error checking and correction.
Interagent Quality Control
Agents learn from their own experience and the experience of other agents. They are equipped with user-defined rule-based and model-based systems for quality assurance, with clear stopping rules for human involvement and mitigation.
Sophisticated quality control measures bolster the system’s reliability, including ensemble techniques for result comparison, redundancy for critical tasks, and automatic human review for disagreements above a certain threshold. Each agent provides a calibrated confidence score with its output, used to weigh inputs in downstream tasks and trigger additional checks for low-confidence outputs.
A dedicated quality control agent monitors output from all agents, employing both supervised and unsupervised anomaly detection techniques. Feedback loops allow agents to evaluate the quality and utility of information received from other agents. The system implements a multiarmed bandit approach to dynamically adjust the influence of different agents based on their performance and periodically retrains agent models using federated learning techniques.19
Electronic Health Record Integration
Seamless EHR integration is crucial for practical implementation. The system has secure application programming interface access to various EHR platforms, implements OAuth 2.0 for authentication, and use HTTPS with perfect forward secrecy for all communications.20 It works with HL7 FHIR to ensure interoperability and uses SNOMED CT for clinical terminology to ensure semantic interoperability across different EHRs.21,22
The system implements a multilevel approval system for write-backs to EHRs, with different thresholds based on the information’s criticality. It uses digital signatures to ensure the integrity and nonrepudiation of AI-generated entries and implements blockchain technology to create an immutable and distributed ledger of all AI system actions.23
Decision Transparency
To ensure transparency in decision-making processes, the system applies techniques (eg, local interpretable model-agnostic explanations and Shapley additive explanations) to provide insights into agent decision-making processes.24-26 It provides customized visualizations for different stakeholders and allows users to explore alternative decision paths through what-if scenario modeling.27
The system provides calibrated confidence indicators for each recommendation or decision, implementing a novel confidence calibration agent that continuously monitors and adjusts confidence scores based on observed outcomes.
Continuous Learning and Adaptation
The system employs several techniques to remain current with evolving medical knowledge. Federated learning includes information from diverse datasets across multiple institutions without compromising patient privacy.28 A/B testing is used to safely deploy and compare new agent versions in controlled settings, implementing multiarmed bandit algorithms to efficiently explore new models while minimizing potential negative impacts. Human-in-the-loop learning and active learning techniques are used to incorporate feedback from HCPs and efficiently solicit expert input on the most informative data.29
CLINICAL IMPLICATIONS
The implementation of multiagent AI systems in health care has several potential benefits: enhanced diagnostic accuracy, personalized treatment, improved efficiency, continuous monitoring, and resource optimization. A recent review of AI sepsis predictive models exhibited superior results to standard clinical scoring methods like qSOFA.30 In oncology, such systems can result in more tailored treatments, enhancing outcomes.31 The implementation of an ambient dictation system can improve workflow and prevent HCP burnout.32
ETHICAL CONSIDERATIONS AND AI OVERSIGHT
Integrating AI agents into health care raises significant ethical considerations that must be carefully addressed to ensure equitable and effective care delivery. One primary concern involves cultural and linguistic competency, as AI systems may struggle with cultural nuances, idioms, and context-specific communication patterns. This becomes particularly challenging in regions with diverse ethnic populations or immigrant communities, where medical terminology may not have direct translations and cultural beliefs significantly influence health care decisions. AI systems also may inherit and amplify existing biases in health care delivery, whether through HCP bias reflected in training data, patient bias affecting acceptance of AI-assisted care, or demographic underrepresentation during system development.
AI agents present unique opportunities for improving health care access and outcomes through community engagement, though such initiatives require thoughtful implementation. Predictive analytics can identify high-risk individuals within communities who may benefit from preventive care, while analysis of social determinants of health can enable more targeted interventions. However, these capabilities must be balanced with privacy concerns and the risk of surveillance, particularly in communities that distrust health care institutions. The potential for AI to bridge health care gaps must be weighed against the need to maintain cultural sensitivity and community trust.
The governance and oversight of health care AI systems requires a multistakeholder approach with clear lines of responsibility and accountability. This includes involvement from government health care agencies, professional medical associations, ethics boards, and independent auditors, all working together to establish and enforce standards while monitoring system performance and addressing potential biases. Health care organizations must maintain transparent policies about AI use, implement regular monitoring and evaluation protocols, and establish precise mechanisms for patient feedback and grievance resolution. Ongoing assessment and adjustment of these systems, informed by community feedback and outcomes data, will be crucial for their ethical implementation, ensuring that AI agents complement, rather than replace, human judgment and cultural sensitivity.
FUTURE DIRECTIONS
Despite the potential benefits, implementing multiagent AI systems in health care faces significant challenges that require careful consideration. Beyond the fundamental issues such as data quality and bias mitigation, health care organizations struggle with fragmented systems, inconsistent data formats, and varying quality. Technical infrastructure requirements are substantial, particularly in rural or underserved areas that lack robust networks and cybersecurity. HCPs already face significant cognitive load and time pressures, making integrating AI agents into existing workflows particularly challenging. There is also the critical issue of transparency and interpretability, as health care decisions require clear reasoning and accountability that many black-box AI systems struggle to provide.
The legal landscape introduces another layer of complexity, particularly regarding liability, consent, and privacy questions. When AI agents contribute to medical decisions, establishing clear lines of responsibility becomes crucial. There are also serious concerns about algorithmic fairness and the potential for AI systems to perpetuate or amplify existing inequities. The cost of implementation remains a significant barrier, requiring substantial investment in technology, training, and ongoing maintenance while ensuring resources are not diverted from direct patient care. Moreover, HCPs may resist adoption due to concerns about job security, loss of autonomy, or skepticism about AI capabilities while paradoxically facing risks of overreliance on AI systems that could lead to the degradation of human clinical skills.
Addressing these challenges requires a multifaceted approach that combines technical solutions with organizational and policy changes. Health care organizations must implement rigorous data validation processes and interoperability standards while developing hybrid models that balance sophisticated AI capabilities with interpretable techniques. Extensive research and iterative design processes, with direct input from HCPs, are essential for successful integration. Establishing independent ethics boards to oversee system development and deployment, conducting multicenter randomized controlled trials, and creating clear regulatory frameworks will ensure safe and effective implementation. Success will ultimately depend on ongoing collaboration between technology developers, HCPs, policymakers, and patients, maintaining a steady focus on improving patient care and outcomes while carefully navigating the complex challenges of AI integration in health care.33-35
As multiagent AI systems in health care evolve, several exciting directions emerge. These include the integration of IoT and wearable devices, the development of more sophisticated natural language interfaces, and applying these systems to predictive maintenance of medical equipment.
CONCLUSIONS
The advent of multiagent AI systems in health care represents a paradigm shift in the approach to patient care, clinical decision making, and health care management. While these systems offer immense potential to transform health care delivery, their development and implementation must be guided by rigorous scientific validation, ethical considerations, and a patient-centered approach. The ultimate goal remains clear: harnessing the power of AI to improve patient outcomes, enhance the efficiency of health care delivery, and ultimately advance the health and well-being of patients.
Amazon Web Services, Inc. What are AI agents? Agents in artificial intelligence explained. Accessed April 7, 2025. https://aws.amazon.com/what-is/ai-agents/
Gutowska A. What are AI agents? IBM. Accessed April 7, 2025. https://www.ibm.com/think/topics/ai-agents
Agent AI. Microsoft Research. Accessed April 7, 2025. https://www.microsoft.com/en-us/research/project/agent-ai
Microsoft. AutoGen. Accessed April 7, 2025. https://microsoft.github.io/autogen/
Crew AI. The Leading Multi-Agent Platform. CrewAI. Accessed April 7, 2025. https://www.crewai.com/
LangChain. Accessed April 7, 2025. https://www.langchain.com/
Wong A, Otles E, Donnelly JP, et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern Med. 2021;181(8):1065-1070. doi:10.1001/jamainternmed.2021.2626
Willemink MJ, Roth HR, Sandfort V. Toward foundational deep learning models for medical imaging in the new era of transformer networks. Radiol Artif Intell. 2022;4(6):e210284. doi:10.1148/ryai.210284
Waqas A, Bui MM, Glassy EF, et al. Revolutionizing digital pathology with the power of generative artificial intelligence and foundation models. Lab Invest. 2023;103(11):100255. doi:10.1016/j.labinv.2023.100255
Moreno-Carrillo A, Arenas LMÁ, Fonseca JA, Caicedo CA, Tovar SV, Muñoz-Velandia OM. Application of queuing theory to optimize the triage process in a tertiary emergency care (“ER”) department. J Emerg Trauma Shock. 2019;12(4):268-273. doi:10.4103/JETS.JETS_42_19
Pongcharoen P, Hicks C, Braiden PM, Stewardson DJ. Determining optimum genetic algorithm parameters for scheduling the manufacturing and assembly of complex products. Int J Prod Econ. 2002;78(3):311-322. doi:10.1016/S0925-5273(02)00104-4
Sardar I, Akbar MA, Leiva V, Alsanad A, Mishra P. Machine learning and automatic ARIMA/Prophet models-based forecasting of COVID-19: methodology, evaluation, and case study in SAARC countries. Stoch Environ Res Risk Assess. 2023;37(1):345-359. doi:10.1007/s00477-022-02307-x
Samosir J, Indrawan-Santiago M, Haghighi PD. An evaluation of data stream processing systems for data driven applications. Procedia Comput Sci. 2016;80:439-449. doi:10.1016/j.procs.2016.05.322
Asmarawati TP, Suryantoro SD, Rosyid AN, et al. Predictive value of sequential organ failure assessment, quick sequential organ failure assessment, acute physiology and chronic health evaluation II, and new early warning signs scores estimate mortality of COVID-19 patients requiring intensive care unit. Indian J Crit Care Med. 2022;26(4):466-473. doi:10.5005/jp-journals-10071-24170
Khan S, Vandermorris A, Shepherd J, et al. Embracing uncertainty, managing complexity: applying complexity thinking principles to transformation efforts in healthcare systems. BMC Health Serv Res. 2018;18(1):192. doi:10.1186/s12913-018-2994-0
Plsek PE, Greenhalgh T. The challenge of complexity in health care. BMJ. 2001;323(7313):625-628. doi:10.1136/bmj.323.7313.625
Kouchaki S, Ding X, Sanei S. AI- and IoT-enabled solutions for healthcare. Sensors. 2024;24(8):2607. doi:10.3390/s24082607
Saab K, Tu T, Weng WH, et al. Capabilities of Gemini Models in Medicine. arXiv. doi:10.48550/arXiv.2404.18416
Villar SS, Bowden J, Wason J. Multi-armed bandit models for the optimal design of clinical trials: benefits and challenges. Stat Sci. 2015;30(2):199-215. doi:10.1214/14-STS504
Auth0. What is OAuth 2.0. Accessed April 7, 2025. https://auth0.com/intro-to-iam/what-is-oauth-2
HL7. Welcome to FHIR. Updated March 26, 2025. Accessed April 7, 2025. https://www.hl7.org/fhir/
SNOMED International. Accessed April 7, 2025. https://www.snomed.org
Hasselgren A, Kralevska K, Gligoroski D, Pedersen SA, Faxvaag A. Blockchain in healthcare and health sciences—a scoping review. Int J Med Inf. 2020;134:104040. doi:10.1016/j.ijmedinf.2019.104040
Ribeiro MT, Singh S, Guestrin C. “Why Should I Trust You?”: Explaining the predictions of any classifier. In: Proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining. 2016:1135-1144. doi:10.1145/2939672.2939778
Ekanayake IU, Meddage DPP, Rathnayake U. A novel approach to explain the black-box nature of machine learning in compressive strength predictions of concrete using Shapley additive explanations (SHAP). Case Stud Constr Mater. 2022;16:e01059. doi:10.1016/j.cscm.2022.e01059
Alabi RO, Elmusrati M, Leivo I, Almangush A, Mäkitie AA. Machine learning explainability in nasopharyngeal cancer survival using LIME and SHAP. Sci Rep. 2023;13(1):8984. doi:10.1038/s41598-023-35795-0
Otto E, Culakova E, Meng S, et al. Overview of sankey flow diagrams: focusing on symptom trajectories in older adults with advanced cancer. J Geriatr Oncol. 2022;13(5):742-746. doi:10.1016/j.jgo.2021.12.017
Fereidooni H, Marchal S, Miettinen M, et al. SAFELearn: secure aggregation for private federated learning. In: 2021 IEEE security and privacy workshops (SPW). 2021:56-62. doi:10.1109/SPW53761.2021.00017
Linton DL, Pangle WM, Wyatt KH, Powell KN, Sherwood RE. Identifying key features of effective active learning: the effects of writing and peer discussion. Life Sci Educ. 2014;13(3):469-477. doi:10.1187/cbe.13-12-0242
Yang HS. Machine learning for sepsis prediction: prospects and challenges. Clin Chem. 2024;70(3):465-467. doi:10.1093/clinchem/hvae006
Liao J, Li X, Gan Y, et al. Artificial intelligence assists precision medicine in cancer treatment. Front Oncol. 2023;12. doi:10.3389/fonc.2022.998222
Tierney AA, Gayre G, Hoberman B, et al. Ambient artificial intelligence scribes to alleviate the burden of clinical documentation. NEJM Catal. 2024;5(3):CAT.23.0404. doi:10.1056/CAT.23.0404
Borkowski AA, Jakey CE, Thomas LB, Viswanadhan N, Mastorides SM. Establishing a hospital artificial intelligence committee to improve patient care. Fed Pract. 2022;39(8):334-336. doi:10.12788/fp.0299
Isaacks DB, Borkowski AA. Implementing trustworthy AI in VA high reliability health care organizations. Fed Pract.2024;41(2):40-43. doi:10.12788/fp.0454
Han R, Acosta JN, Shakeri Z, Ioannidis JPA, Topol EJ, Rajpurkar P. Randomized controlled trials evaluating artificial intelligence in clinical practice: a scoping review. Lancet Digit Health. 2024;6(5):e367-e373. doi:10.1016/S2589-7500(24)00047-5
Amazon Web Services, Inc. What are AI agents? Agents in artificial intelligence explained. Accessed April 7, 2025. https://aws.amazon.com/what-is/ai-agents/
Gutowska A. What are AI agents? IBM. Accessed April 7, 2025. https://www.ibm.com/think/topics/ai-agents
Agent AI. Microsoft Research. Accessed April 7, 2025. https://www.microsoft.com/en-us/research/project/agent-ai
Microsoft. AutoGen. Accessed April 7, 2025. https://microsoft.github.io/autogen/
Crew AI. The Leading Multi-Agent Platform. CrewAI. Accessed April 7, 2025. https://www.crewai.com/
LangChain. Accessed April 7, 2025. https://www.langchain.com/
Wong A, Otles E, Donnelly JP, et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern Med. 2021;181(8):1065-1070. doi:10.1001/jamainternmed.2021.2626
Willemink MJ, Roth HR, Sandfort V. Toward foundational deep learning models for medical imaging in the new era of transformer networks. Radiol Artif Intell. 2022;4(6):e210284. doi:10.1148/ryai.210284
Waqas A, Bui MM, Glassy EF, et al. Revolutionizing digital pathology with the power of generative artificial intelligence and foundation models. Lab Invest. 2023;103(11):100255. doi:10.1016/j.labinv.2023.100255
Moreno-Carrillo A, Arenas LMÁ, Fonseca JA, Caicedo CA, Tovar SV, Muñoz-Velandia OM. Application of queuing theory to optimize the triage process in a tertiary emergency care (“ER”) department. J Emerg Trauma Shock. 2019;12(4):268-273. doi:10.4103/JETS.JETS_42_19
Pongcharoen P, Hicks C, Braiden PM, Stewardson DJ. Determining optimum genetic algorithm parameters for scheduling the manufacturing and assembly of complex products. Int J Prod Econ. 2002;78(3):311-322. doi:10.1016/S0925-5273(02)00104-4
Sardar I, Akbar MA, Leiva V, Alsanad A, Mishra P. Machine learning and automatic ARIMA/Prophet models-based forecasting of COVID-19: methodology, evaluation, and case study in SAARC countries. Stoch Environ Res Risk Assess. 2023;37(1):345-359. doi:10.1007/s00477-022-02307-x
Samosir J, Indrawan-Santiago M, Haghighi PD. An evaluation of data stream processing systems for data driven applications. Procedia Comput Sci. 2016;80:439-449. doi:10.1016/j.procs.2016.05.322
Asmarawati TP, Suryantoro SD, Rosyid AN, et al. Predictive value of sequential organ failure assessment, quick sequential organ failure assessment, acute physiology and chronic health evaluation II, and new early warning signs scores estimate mortality of COVID-19 patients requiring intensive care unit. Indian J Crit Care Med. 2022;26(4):466-473. doi:10.5005/jp-journals-10071-24170
Khan S, Vandermorris A, Shepherd J, et al. Embracing uncertainty, managing complexity: applying complexity thinking principles to transformation efforts in healthcare systems. BMC Health Serv Res. 2018;18(1):192. doi:10.1186/s12913-018-2994-0
Plsek PE, Greenhalgh T. The challenge of complexity in health care. BMJ. 2001;323(7313):625-628. doi:10.1136/bmj.323.7313.625
Kouchaki S, Ding X, Sanei S. AI- and IoT-enabled solutions for healthcare. Sensors. 2024;24(8):2607. doi:10.3390/s24082607
Saab K, Tu T, Weng WH, et al. Capabilities of Gemini Models in Medicine. arXiv. doi:10.48550/arXiv.2404.18416
Villar SS, Bowden J, Wason J. Multi-armed bandit models for the optimal design of clinical trials: benefits and challenges. Stat Sci. 2015;30(2):199-215. doi:10.1214/14-STS504
Auth0. What is OAuth 2.0. Accessed April 7, 2025. https://auth0.com/intro-to-iam/what-is-oauth-2
HL7. Welcome to FHIR. Updated March 26, 2025. Accessed April 7, 2025. https://www.hl7.org/fhir/
SNOMED International. Accessed April 7, 2025. https://www.snomed.org
Hasselgren A, Kralevska K, Gligoroski D, Pedersen SA, Faxvaag A. Blockchain in healthcare and health sciences—a scoping review. Int J Med Inf. 2020;134:104040. doi:10.1016/j.ijmedinf.2019.104040
Ribeiro MT, Singh S, Guestrin C. “Why Should I Trust You?”: Explaining the predictions of any classifier. In: Proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining. 2016:1135-1144. doi:10.1145/2939672.2939778
Ekanayake IU, Meddage DPP, Rathnayake U. A novel approach to explain the black-box nature of machine learning in compressive strength predictions of concrete using Shapley additive explanations (SHAP). Case Stud Constr Mater. 2022;16:e01059. doi:10.1016/j.cscm.2022.e01059
Alabi RO, Elmusrati M, Leivo I, Almangush A, Mäkitie AA. Machine learning explainability in nasopharyngeal cancer survival using LIME and SHAP. Sci Rep. 2023;13(1):8984. doi:10.1038/s41598-023-35795-0
Otto E, Culakova E, Meng S, et al. Overview of sankey flow diagrams: focusing on symptom trajectories in older adults with advanced cancer. J Geriatr Oncol. 2022;13(5):742-746. doi:10.1016/j.jgo.2021.12.017
Fereidooni H, Marchal S, Miettinen M, et al. SAFELearn: secure aggregation for private federated learning. In: 2021 IEEE security and privacy workshops (SPW). 2021:56-62. doi:10.1109/SPW53761.2021.00017
Linton DL, Pangle WM, Wyatt KH, Powell KN, Sherwood RE. Identifying key features of effective active learning: the effects of writing and peer discussion. Life Sci Educ. 2014;13(3):469-477. doi:10.1187/cbe.13-12-0242
Yang HS. Machine learning for sepsis prediction: prospects and challenges. Clin Chem. 2024;70(3):465-467. doi:10.1093/clinchem/hvae006
Liao J, Li X, Gan Y, et al. Artificial intelligence assists precision medicine in cancer treatment. Front Oncol. 2023;12. doi:10.3389/fonc.2022.998222
Tierney AA, Gayre G, Hoberman B, et al. Ambient artificial intelligence scribes to alleviate the burden of clinical documentation. NEJM Catal. 2024;5(3):CAT.23.0404. doi:10.1056/CAT.23.0404
Borkowski AA, Jakey CE, Thomas LB, Viswanadhan N, Mastorides SM. Establishing a hospital artificial intelligence committee to improve patient care. Fed Pract. 2022;39(8):334-336. doi:10.12788/fp.0299
Isaacks DB, Borkowski AA. Implementing trustworthy AI in VA high reliability health care organizations. Fed Pract.2024;41(2):40-43. doi:10.12788/fp.0454
Han R, Acosta JN, Shakeri Z, Ioannidis JPA, Topol EJ, Rajpurkar P. Randomized controlled trials evaluating artificial intelligence in clinical practice: a scoping review. Lancet Digit Health. 2024;6(5):e367-e373. doi:10.1016/S2589-7500(24)00047-5